Strategies for Preventing Teratoma Formation in Pluripotent Stem Cell Therapies: A 2025 Review of Safety Assessment and Risk Mitigation
This article provides a comprehensive analysis of current strategies and emerging technologies for mitigating teratoma formation risk in human pluripotent stem cell (hPSC)-derived therapies.
Strategies for Preventing Teratoma Formation in Pluripotent Stem Cell Therapies: A 2025 Review of Safety Assessment and Risk Mitigation
Abstract
This article provides a comprehensive analysis of current strategies and emerging technologies for mitigating teratoma formation risk in human pluripotent stem cell (hPSC)-derived therapies. Tailored for researchers, scientists, and drug development professionals, it covers the foundational biology of tumorigenic risk, explores innovative methods for eliminating residual undifferentiated hPSCs, addresses key challenges in safety assessment, and evaluates advanced validation techniques. The content synthesizes the latest 2025 consensus recommendations and research to offer a practical framework for enhancing the safety profile of hPSC-derived cell therapy products, supporting the advancement of rigorous, internationally harmonized safety protocols in regenerative medicine.
Understanding Teratoma Risk: The Biological Basis of Tumorigenicity in Pluripotent Stem Cells
Why are undifferentiated human pluripotent stem cells (hPSCs) considered tumorigenic?
The tumorigenic risk of hPSCs is intrinsically linked to the fundamental properties of pluripotency and self-renewal. The core issue is that even a small number of residual undifferentiated hPSCs in a differentiated cell product can form tumors upon transplantation [1] [2].
- Pluripotency and Tumorigenicity are Historically Linked: The earliest research on highly pluripotent stem cells was conducted on embryonic carcinoma cells (EC) derived from teratocarcinomas. When embryonic stem cells (ESCs) were later isolated, they shared not only pluripotency with these EC cells but also their robust tumorigenicity, as both readily form teratomas [1].
- The Teratoma Assay Paradox: The standard assay to demonstrate a cell's pluripotency—the teratoma assay—is itself a tumor formation assay. This underscores the strong biological link between "stemness" and tumorigenic potential. The formation of a benign teratoma from transplanted cells is clear evidence of their pluripotency but also highlights a significant safety risk for clinical applications [1].
- Minimal Cell Number Required: Preclinical models have shown that transplanting even 10,000 or fewer undifferentiated hPSCs can be sufficient to form a teratoma in vivo. When considering therapies where billions of differentiated cells are transplanted into a patient, even a tiny residual undifferentiated population of 0.001% could be therapeutically unacceptable, necessitating a depletion of undifferentiated hPSCs by a factor of 10,000 to 1,000,000 (5- to 6-log reduction) to ensure safety [2].
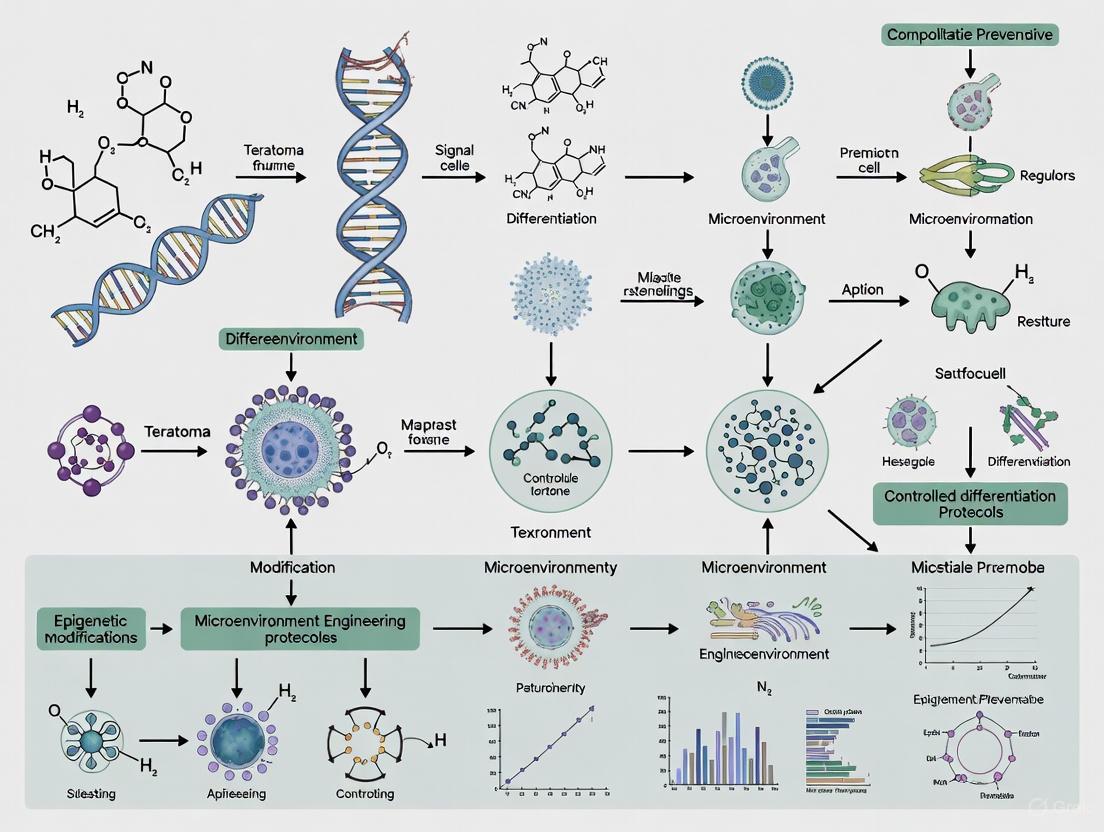
The following diagram illustrates the fundamental relationship between the defining properties of hPSCs and their clinical safety risk.
What is the molecular basis for the tumorigenicity of hPSCs?
The molecular programs that govern pluripotency and self-renewal in stem cells are co-opted in many human tumors. Key pluripotency transcription factors are either established oncogenes or are strongly linked to tumorigenesis [1].
Table 1: Key Molecular Links Between Pluripotency and Tumorigenicity
| Gene/Factor | Role in Pluripotency | Role in Tumorigenesis |
|---|---|---|
| c-MYC | Essential for normal signaling in mESC; dramatically boosts iPSC generation efficiency [1]. | A classic proto-oncogene; elevated expression may have a role in all human cancer [1]. |
| KLF4 | One of the four original Yamanaka factors for reprogramming; required for ESC pluripotency and self-renewal [1]. | An established oncogene in various contexts [1]. |
| NANOG | A master transcription factor critical for maintaining pluripotency [2]. | Linked to tumorigenesis; expressed in certain cancer cells [1]. |
| SOX2 | Essential transcription factor for the pluripotent state. | Linked to tumorigenesis in various cancers [1]. |
| OCT3/4 | Core pluripotency transcription factor. | Associated with tumorigenic processes [1]. |
This shared molecular machinery creates a significant challenge: reducing the tumorigenic potential of hPSCs by targeting these factors may inevitably reduce their essential "stemness" and pluripotency, which are the very properties needed for regenerative therapies [1].
What strategies exist to mitigate the risk of teratoma formation?
Mitigation strategies focus on two main areas: ensuring the purity of the differentiated cell product and developing safety switches to eliminate unwanted cells.
Table 2: Strategies for Mitigating hPSC Tumorigenicity
| Strategy Category | Specific Method | Mechanism of Action | Key Advantage |
|---|---|---|---|
| Cell Product Purity | Improved differentiation protocols | Reduces the number of residual undifferentiated hPSCs in the final therapeutic product. | Addresses the problem at its source. |
| Cell Surface Marker-Based Depletion | Antibody-mediated removal (e.g., against SSEA-3, TRA-1-60) [2]. | Physically removes undifferentiated hPSCs that express specific surface markers. | Well-established methodology. |
| Genetic Safety Switches | NANOG-promoter driven iCaspase9 [2] | A "suicide gene" is inserted into the NANOG locus. Undifferentiated cells expressing NANOG undergo apoptosis upon administration of a small molecule drug (AP20187). | Highly specific to the pluripotent state; achieves >1,000,000-fold depletion of hPSCs [2]. |
| Genetic Safety Switches | ACTB-promoter driven safety systems (e.g., iCaspase9, TK) [2]. | A suicide gene expressed in all cells derived from the engineered hPSC line. Allows elimination of the entire cell product if adverse events (e.g., tumors from mis-differentiated cells) occur. | Provides a broad "kill-switch" for the entire therapy if needed. |
The following workflow diagrams two key experimental approaches for implementing and validating these genetic safeguards.
What are the key experimental protocols for assessing tumorigenicity?
Teratoma Assay Protocol
The teratoma assay is the gold-standard functional test for both pluripotency and tumorigenic potential [1].
- Cell Preparation: Harvest the hPSC population or differentiated cell product to be tested. A positive control of known undifferentiated hPSCs and a negative control (e.g., fibroblasts) should be included.
- Transplantation: Inject cells into an immunodeficient mouse host (e.g., NSG or NOG mice). Common sites are the testis capsule, kidney capsule, or subcutaneous space.
- Monitoring: Palpate the injection site regularly for tumor formation over a period of 8-20 weeks.
- Histological Analysis:
- Sacrifice the animal and harvest the resulting tumor or graft.
- Fix the tissue in formalin and embed in paraffin.
- Section and stain with Hematoxylin and Eosin (H&E).
- Examine microscopically for the presence of differentiated tissues derived from all three embryonic germ layers: ectoderm (e.g., neural tissue, keratinocytes), mesoderm (e.g., cartilage, bone, muscle), and endoderm (e.g., gut-like epithelial tissues).
This protocol validates a specific safeguard to remove residual undifferentiated cells.
- Cell Line Engineering:
- Use CRISPR/Cas9 RNP and AAV6-based genome editing to knock-in an inducible Caspase9 (iCaspase9)-YFP cassette downstream of the stop codon in the NANOG gene, separated by T2A "self-cleaving" peptide sequences.
- Create a biallelic knock-in to prevent escape.
- Validate the knock-in and confirm normal pluripotency and karyotype.
- In Vitro Specificity and Potency Testing:
- Differentiate the engineered hPSCs into target lineages (e.g., liver progenitors, bone progenitors, forebrain progenitors).
- Treat both undifferentiated and differentiated cultures with the small molecule inducer AP20187 (at 1 nM concentration for 24 hours).
- Quantify cell death via flow cytometry (Annexin V/propidium iodide staining) or cell viability assays.
- Expected Outcome: >1,000,000-fold depletion of undifferentiated hPSCs, with >95% survival of the differentiated progeny.
- In Vivo Teratoma Prevention Assay:
- Mix a small number of undifferentiated NANOG-iCaspase9 hPSCs (e.g., 10,000) with a large number of their differentiated progeny.
- Transplant the mixture into immunodeficient mice.
- Administer AP20187 or a vehicle control to the animals.
- Monitor for teratoma formation over time. The experimental group receiving AP20187 should show a significant reduction or complete absence of teratomas compared to the control group.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying hPSC Tumorigenicity and Safety
| Reagent / Tool | Function / Application | Example(s) |
|---|---|---|
| Pluripotency Surface Markers | Identification and sorting of undifferentiated hPSCs via flow cytometry or antibody-mediated depletion. | SSEA-3, SSEA-4, TRA-1-60, TRA-1-81 [2]. |
| CRISPR/Cas9 System | Genome editing to insert safety switches (e.g., iCaspase9) into specific genetic loci (e.g., NANOG). | Cas9 ribonucleoprotein (RNP) with AAV6 donor template [2]. |
| Inducible Safety Switches | Genetically encoded systems for targeted cell ablation. | iCaspase9 (activated by AP20187); Herpes Simplex Virus Thymidine Kinase (HSV-TK, activated by Ganciclovir) [2]. |
| Small Molecule Inducers | Activation of inducible safety switches in vitro and in vivo. | AP20187 (for iCaspase9); Ganciclovir (for HSV-TK) [2]. |
| Immunodeficient Mouse Models | In vivo hosts for teratoma formation assays and safety switch validation. | NSG (NOD-scid-gamma), NOG mice [1] [2]. |
| Clinical-Grade iPSC Lines | GMP-compliant, well-characterized starting material for therapy development, referenced in regulatory submissions. | StemRNA Clinical Seed iPSCs (REPROCELL) [3]. |
Frequently Asked Questions (FAQs)
Q: Are there any clinical data on the safety of hPSC-derived therapies regarding tumorigenicity? A: Yes, the clinical landscape is expanding. As of late 2024, a major review of 115 global clinical trials involving PSC-derived products, which had dosed over 1,200 patients, reported no significant class-wide safety concerns [3]. Specific trials, such as a Phase I/II trial of iPSC-derived dopaminergic progenitors for Parkinson's disease published in 2025, reported no tumor formation in patients [4]. This suggests that with careful manufacturing and quality control, the tumorigenicity risk can be managed.
Q: Can't we just use surface markers to remove all undifferentiated hPSCs from a cell product? A: While surface markers are a valuable tool, a significant challenge is specificity. Many surface markers traditionally used to identify undifferentiated hPSCs (e.g., SSEA-3, TRA-1-60) are also expressed at lower levels on various differentiated cell types that might be part of the therapeutic product [2]. Using these markers for negative selection could therefore inadvertently deplete a portion of the desired therapeutic cells. Genetic safeguards driven by highly specific pluripotency gene promoters (like NANOG) offer a more precise alternative for targeting the undifferentiated state.
Q: What is the difference between a teratoma and a malignant tumor? A: A teratoma is a benign tumor containing a disorganized mixture of tissues from all three germ layers (ectoderm, mesoderm, endoderm). It is the most common tumor type formed by pluripotent stem cells. However, hPSCs can also form malignant tumors, such as teratocarcinomas, which contain both differentiated tissues and undifferentiated, proliferative stem cells that can invade other tissues. Furthermore, if hPSCs acquire genetic abnormalities in culture, their differentiated progeny could potentially form other types of cancers [1] [2].
Q: Where can I find the latest best practices for developing hPSC-based therapies? A: The International Society for Stem Cell Research (ISSCR) provides comprehensive and regularly updated guidance. Their "Best Practices for the Development of Pluripotent Stem Cell-Derived Therapies" document covers key principles from cell line selection and manufacturing to preclinical studies and regulatory considerations [5] [6]. This is an essential resource for any researcher translating hPSC science towards the clinic.
FAQs: Addressing Core Research Challenges
Q1: What is the primary cellular mechanism that initiates teratoma formation in hPSC-based therapies? Teratoma formation is primarily initiated by the presence of residual undifferentiated human pluripotent stem cells (hPSCs) within the differentiated cell product. Even very small quantities of these cells are sufficient; studies demonstrate that the transplantation of as few as 10,000 undifferentiated hPSCs can lead to teratoma formation in immunodeficient mouse models [7] [2]. These residual hPSCs escape differentiation protocols and, once transplanted, utilize their innate pluripotency to form complex tumors containing tissues from all three embryonic germ layers (ectoderm, mesoderm, and endoderm) [8].
Q2: How do the unique apoptotic pathways in hPSCs present a target for preventing teratomas? Research has revealed that hPSCs possess a unique apoptotic machinery characterized by a biased expression profile of pro- and anti-apoptotic genes. While many pro-apoptotic genes are upregulated, the survival of hPSCs is highly dependent on a few key anti-apoptotic factors, notably survivin (encoded by BIRC5) and Bcl10. These factors are highly expressed in undifferentiated hPSCs but are sharply downregulated upon differentiation. This dependency creates a vulnerability that can be therapeutically targeted. Using small-molecule inhibitors to block these anti-apoptotic factors selectively triggers the intrinsic apoptotic pathway in hPSCs, while sparing differentiated cells [9].
Q3: What are the most sensitive methods for detecting residual hPSCs in a cell therapy product? Sensitive detection is critical for risk assessment. Current consensus recommends in vitro assays over conventional in vivo teratoma assays due to their superior sensitivity and faster results. Key methods include:
- Digital PCR (dPCR) for hPSC-specific RNA: This method allows for the absolute quantification of pluripotency-associated transcripts with high precision.
- Highly Efficient Culture (HEC) Assay: This assay is designed to maximize the opportunity for any residual hPSC to proliferate and form colonies in culture, thereby confirming their presence. These in vitro methods provide a more practical and sensitive framework for evaluating the teratoma formation risk of hPSC-derived cell therapy products before clinical use [10] [11].
Q4: Can you provide a proven experimental protocol for evaluating teratoma risk in vivo? The in vivo teratoma assay remains a gold standard for demonstrating pluripotency and assessing tumorigenic risk.
- Cell Preparation: Prepare a monocellular suspension of your hPSC-derived cell product. It is crucial to include a positive control group of undifferentiated hPSCs.
- Animal Model: Use immunodeficient mice, such as NOD/SCID gamma (NSG) mice, to prevent immune rejection of the human cells.
- Transplantation: Systemically inject (e.g., intravenous) or inject the cells into an ectopic site (e.g., subcutaneous, intramuscular) [12] [8]. The number of cells injected should reflect the clinical dose.
- Monitoring: Observe the animals for a period of 12 to 24 weeks. Teratomas can form as early as 5 weeks post-injection [12].
- Endpoint Analysis: Perform necropsy on animals showing signs of tumor growth or at the study endpoint. Excised tumors are fixed, sectioned, and stained with hematoxylin and eosin (H&E) for histological confirmation of trilineage differentiation (ectoderm, mesoderm, endoderm) [8].
Troubleshooting Guides
Issue: Inconsistent Results in Selective hPSC Elimination with Small Molecules
Problem: A researcher is using quercetin to eliminate residual hPSCs from a differentiated neuronal cell population, but the results are inconsistent, with some batches showing poor hPSC death.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Insufficient Drug Exposure | - Check drug concentration and treatment duration.- Use a validated viability assay (e.g., flow cytometry for Annexin V/PI) on a defined co-culture of hPSCs and differentiated cells. | - Optimize the dose and duration. For quercetin, a single treatment sufficient to induce complete cell death of hPSCs is required [9]. |
| Variable Differentiation Efficiency | - Quantify the percentage of undifferentiated cells pre- and post-treatment using flow cytometry for pluripotency markers (OCT4, NANOG). | - Improve the differentiation protocol to minimize initial hPSC residue before applying the purge. |
| Loss of Differentiated Cell Function | - Assess the functionality of the differentiated neurons (e.g., electrophysiology, marker expression) post-treatment. | - Confirm the selective toxicity of the chosen molecule. Consider switching to another specific inhibitor like YM155 (survivin inhibitor) or digoxin (cardiac glycoside), which have shown minimal impact on certain differentiated cells [12] [7]. |
Issue: Failure to Prevent Teratoma Formation After Cell Transplantation
Problem: Despite a pre-transplantation purge step, teratomas still form in animal models after transplantation of an hPSC-derived hepatic progenitor product.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Insufficient Purging Efficiency | - Spike a known number of luciferase-expressing hPSCs into your product, apply the purge, and use bioluminescence to quantify remaining cells. | - Increase the log-reduction capacity of your purge. A >5-log depletion of hPSCs is likely needed for a billion-cell product [2]. Consider orthogonal safeguards like a NANOG-iCaspase9 suicide gene system, which can achieve >1 million-fold depletion [2]. |
| Purging Method is Not Pluripotent-Specific | - Validate the expression profile of your target (e.g., survivin) in both hPSCs and the therapeutic hepatic progenitors. | - Use a target with higher specificity to the pluripotent state. NANOG is a more specific marker than survivin, which can be expressed in some differentiated progeny [2]. |
| Teratoma from Wrong Differentiated Lineage | - Perform detailed histopathology on the formed teratoma to confirm it originated from pluripotent cells (disorganized tissues) versus a monomorphic tumor from a progenitor. | - This indicates a differentiation protocol issue, not a purge failure. The solution is to improve the lineage specification and purity of the differentiated product [2]. |
Summarized Quantitative Data
Table 1: Efficacy of Small-Molecule Compounds in Selective hPSC Elimination
| Compound | Primary Target | Effective Concentration (in vitro) | hPSC Viability Reduction | Key Differentiated Cells Spared | Citation |
|---|---|---|---|---|---|
| Quercetin | Survivin | Not fully quantified | Selective and complete cell death | Dopamine neurons, Smooth muscle cells | [9] |
| YM155 | Survivin | Not fully quantified | Efficient killing | Human CD34+ hematopoietic cells | [12] |
| Digoxin | Na+/K+-ATPase | 2.5 μM | ~70% (Annexin V/PI+) | Human bone marrow mesenchymal stem cells (hBMMSCs), hESC-derived MSCs, neurons | [7] |
| Lanatoside C | Na+/K+-ATPase | 2.5 μM | ~82% (Annexin V/PI+) | Human bone marrow mesenchymal stem cells (hBMMSCs), hESC-derived MSCs, neurons | [7] |
Table 2: Performance of Genetic Safeguard Systems for hPSC-Derived Therapies
| System Name | Genetic Basis | Inducing Molecule | Depletion Efficiency | Key Advantage |
|---|---|---|---|---|
| NANOG-iCaspase9 | iCaspase9 knocked into NANOG locus | AP20187 (1 nM) | 1.75 x 10^6-fold (>>5-log) | Extreme specificity and potency against undifferentiated state [2] |
| ACTB-iCaspase9 | iCaspase9 under constitutive ACTB promoter | AP20187 | Kills all engineered cells | "Global off-switch" for the entire cell product in case of adverse events [2] |
| Embryonic-specific TK | Thymidine Kinase under pmiR-302/367 promoter | Ganciclovir (GCV) | Less efficient than iCaspase-9 | Specific to pluripotent state [12] |
Experimental Protocols
Protocol: Selective Elimination of Residual hPSCs using YM155
Application: Purging residual hiPSCs from a differentiated hematopoietic cell population before transplantation [12].
Materials:
- YM155 survivin inhibitor
- Differentiated cell population (e.g., hPSC-derived CD34+ cells)
- Appropriate cell culture medium (e.g., StemSpan for CD34+ cells)
- Flow cytometry equipment and antibodies for pluripotency markers (e.g., TRA-1-60, SSEA4)
Procedure:
- Harvest Cells: Gently harvest the differentiated cell population, which contains residual hiPSCs, into a single-cell suspension.
- Drug Treatment: Seed the cells in culture plates and add YM155 at the optimized concentration. A vehicle control (e.g., DMSO) must be included.
- Incubation: Incubate the cells with YM155 for a defined period (e.g., 24 hours). The specific duration and concentration require internal optimization.
- Assessment & Transplantation:
- Viability Check: Assess cell viability using trypan blue exclusion.
- Pluripotency Marker Analysis: Analyze the cells by flow cytometry for pluripotency surface markers (e.g., TRA-1-60) to quantify the reduction in the hPSC population.
- Functional Assay: The purged cell product is now ready for downstream functional assays or transplantation into animal models. Studies show this treatment eradicates teratoma formation in NSG mice without compromising the engraftment capacity of human CD34+ cells [12].
Protocol: Validating Purging Efficiency with a NANOG-iCaspase9 Safeguard System
Application: To achieve a ultra-high, specific log-reduction of undifferentiated hPSCs from any hPSC-derived cell product [2].
Materials:
- Genome-edited hPSC line with biallelic NANOG-iCaspase9 knock-in
- Inducer molecule AP20187
- Control differentiated cells (e.g., forebrain progenitors, bone progenitors, liver progenitors)
Procedure:
- Differentiate Engineered Cells: Differentiate the NANOG-iCaspase9 hPSCs into the desired therapeutic progenitor or cell type.
- Spike-in Experiment (Optional but recommended): For a rigorous validation, mix a known number of undifferentiated NANOG-iCaspase9 hPSCs (e.g., 1%) with the differentiated cell product.
- Inducer Treatment: Treat the cell mixture with 1 nM AP20187 for 24 hours.
- Quantify Depletion:
- In vitro Colony Assay: Plate the treated cells under hPSC-self-renewal conditions and count the number of alkaline phosphatase-positive colonies after 7-10 days. Compare to an untreated control.
- In vivo Teratoma Assay: Transplant the AP20187-treated cell product into immunodeficient mice. The result should be a complete absence of teratoma formation over the observation period, demonstrating the efficacy of the safeguard [2].
Pathway and Workflow Visualizations
hPSC-Specific Apoptosis Pathway
Diagram 1: Molecular mechanism of small molecule-induced hPSC apoptosis.
Teratoma Risk Mitigation Workflow
Diagram 2: Integrated workflow for teratoma risk mitigation.
The Scientist's Toolkit
Table 3: Essential Research Reagents for Teratoma Prevention Studies
| Reagent / Tool | Function / Application | Key Notes |
|---|---|---|
| YM155 | Small-molecule survivin inhibitor; selectively induces apoptosis in hPSCs. | Validated for purging hiPSCs from hematopoietic progenitors without toxicity to CD34+ cells [12]. |
| Digoxin | FDA-approved cardiac glycoside; inhibits Na+/K+-ATPase, cytotoxic to hPSCs. | Kills hESCs but spares differentiated MSCs and neurons; prevents teratoma formation in vivo [7]. |
| AP20187 | Dimerizing drug; induces apoptosis in cells engineered with iCaspase9. | Used with NANOG-iCaspase9 system for ultra-specific, high-efficiency hPSC depletion [2]. |
| Anti-TRA-1-60 Antibody | Cell surface marker for undifferentiated hPSCs; used for FACS analysis/sorting. | Critical for quantifying residual hPSC populations before and after purging interventions. |
| NSG (NOD/SCID/IL2rg-/-) Mice | Immunodeficient mouse model for in vivo teratoma assays. | The gold-standard model for assessing the tumorigenic potential of hPSC-derived products [12] [8]. |
| Digital PCR (dPCR) | Highly sensitive nucleic acid quantification for detecting trace levels of hPSC-specific RNA. | An essential in vitro method with superior sensitivity for residual hPSC detection in final products [10] [11]. |
The Critical Role of Rigorous Safety Assessment in Clinical Translation
Technical Support Center: Preventing Teratoma Formation in Pluripotent Stem Cell Therapies
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary safety concern associated with pluripotent stem cell-derived therapies? The primary safety concern is teratoma formation, a type of tumor arising from residual undifferentiated human pluripotent stem cells (hPSCs) that may persist in the differentiated cell product. Even a small number of residual hPSCs (10,000 or fewer) can form a teratoma in vivo [2]. Systemic injection of hiPSCs has been shown to produce multisite teratomas in immune-deficient mice in as little as 5 weeks [12].
FAQ 2: What methods can be used to purge residual undifferentiated hPSCs before transplantation? Two primary methods are compared in recent research:
- Suicide Gene Systems: These involve engineering hPSCs to express a suicide gene, such as inducible Caspase-9 (iCaspase-9), under the control of a pluripotency-specific promoter (e.g.,
pmiR-302/367orNANOG). Administration of a small molecule prodrug (AP20187) activates the suicide mechanism in undifferentiated cells [12] [2]. - Small Molecule Inhibitors: Using chemicals that specifically kill pluripotent cells, such as the survivin inhibitor YM155. This molecule exploits the fact that hiPSCs fully rely on survivin for survival [12].
FAQ 3: How efficient are these purging methods? Efficiency varies significantly between approaches:
- The NANOG-iCaspase-9 suicide gene system can deplete undifferentiated hPSCs by over 1.75 million-fold (10^6) in vitro [2].
- The survivin inhibitor YM155 was found to be more efficient at killing hiPSCs than the iCaspase-9/AP20187 system and fully eradicated teratoma formation in immune-deficient mice [12].
FAQ 4: Is there toxicity to therapeutic cells with these purging methods? Yes, this is a critical consideration. Research indicates:
- The iCaspase-9/AP20187 system showed nonspecific toxicity on human CD34+ hematopoietic stem cells, strongly impairing their repopulation capability in adoptive transfers [12].
- In contrast, the survivin inhibitor YM155 demonstrated no toxicity on CD34+ cells, either in vitro or in adoptive transfers, making it a more suitable candidate for hematological applications [12].
FAQ 5: What are the best practices for detecting residual hPSCs in a cell therapy product? In vitro assays are increasingly favored for their sensitivity and efficiency.
- Digital PCR (dPCR) for detecting hPSC-specific RNA and the highly efficient culture (HEC) assay offer superior detection sensitivity compared to conventional in vivo teratoma assays in mice [10].
- Validating these in vitro assays for each specific product is essential for confident safety assessment [10].
Troubleshooting Guides
Problem 1: Excessive differentiation in hPSC cultures, leading to heterogeneity and challenges in purifying the target cell type.
- Potential Causes & Solutions:
- Cause: Old or improperly stored cell culture medium.
- Solution: Ensure complete cell culture medium (e.g., mTeSR Plus) kept at 2-8°C is less than 2 weeks old [13].
- Cause: Overgrown colonies or uneven cell aggregate sizes during passaging.
- Solution: Passage cultures when colonies are large and compact but before they overgrow. Ensure cell aggregates generated during passaging are evenly sized [13].
- Cause: Cultures are exposed to suboptimal conditions outside the incubator for extended periods.
- Solution: Minimize time culture plates are out of the incubator (aim for less than 15 minutes at a time) [13].
Problem 2: Differentiated cell product is still contaminated with residual pluripotent cells after a purging procedure.
- Potential Causes & Solutions:
- Cause: The purging method lacks sufficient specificity or efficiency for your cell line.
- Solution: Consider switching from a suicide gene/prodrug system to a small molecule inhibitor like YM155, which showed higher efficiency in killing hiPSCs without compromising therapeutic CD34+ cells [12]. Alternatively, implement a genome-edited orthogonal safeguard system that combines multiple safety switches for more robust control [2].
- Cause: The promoter driving the suicide gene is not sufficiently specific to the pluripotent state.
- Solution: Use a promoter with high specificity to undifferentiated cells, such as the NANOG promoter, which is sharply downregulated upon differentiation, unlike other potential markers [2].
Problem 3: Low cell viability or attachment after passaging and purging treatments.
- Potential Causes & Solutions:
- Cause: Excessive manipulation or overly harsh dissociation reagents.
- Solution: Reduce pipetting of cell aggregates and optimize incubation time with passaging reagents (e.g., ReLeSR) for your specific cell line [13] [14].
- Cause: Nonspecific toxicity from the purging agent on differentiated cells.
- Solution: If using a suicide gene/prodrug, titrate the prodrug (e.g., AP20187) to the lowest effective concentration. For iCaspase-9, 1 nM AP20187 was optimal, as higher concentrations can downregulate NANOG and reduce system efficiency [2]. If toxicity persists, evaluate alternative agents like YM155 [12].
- Cause: Incorrect plating density or matrix coating.
- Solution: Plate a higher number of cell aggregates initially and ensure you are using the correct tissue culture-treated or non-treated plates for your specific coating matrix (e.g., Vitronectin XF, Matrigel) [13] [14].
Table 1: Comparison of Purging Methods for Residual Undifferentiated hPSCs
| Method | Mechanism | Reported Efficiency | Key Advantages | Key Limitations & Toxicity |
|---|---|---|---|---|
| Survivin Inhibitor (YM155) | Chemical inhibition of survivin, essential for hPSC survival. | More efficient than iCaspase-9/AP20187; eradicated teratomas in vivo [12]. | No toxicity on CD34+ hematopoietic stem cells; does not require genetic modification [12]. | Specificity for other therapeutically relevant differentiated cell types should be verified per product. |
| iCaspase-9 Suicide Gene | Genetically engineered iCaspase-9 under pluripotency promoter; activated by AP20187 prodrug. | >10^6-fold depletion of hPSCs in vitro with NANOG promoter [2]. | Highly specific and rapid apoptosis; potential for inducible control in vivo [2]. | Nonspecific toxicity of AP20187 prodrug on CD34+ cells, impairing hematopoiesis [12]. |
| Thymidine Kinase (TK) | Genetically engineered TK; activated by ganciclovir prodrug. | Less efficient and rapid than iCaspase-9 [12]. | Well-established "suicide gene" system. | Requires extended in vitro treatment; not suitable for all cell types. |
Table 2: Sensitivity of Assays for Detecting Residual Undifferentiated hPSCs
| Assay Type | Key Examples | Relative Sensitivity | Key Considerations |
|---|---|---|---|
| In Vitro Assays | Digital PCR (dPCR) for hPSC-specific RNA; Highly Efficient Culture (HEC) Assay [10]. | Superior sensitivity compared to in vivo models [10]. | Requires rigorous validation for each product; faster and more cost-effective than in vivo studies [10]. |
| In Vivo Assays | Teratoma assay in immune-deficient mice (e.g., NSG, NOG) [12] [10]. | Conventional standard, but less sensitive than advanced in vitro methods [10]. | Time-consuming (can take 5+ weeks [12]), expensive, and has ethical considerations regarding animal use. |
Experimental Protocols
Protocol 1: In Vitro Purging of Residual hPSCs Using a Survivin Inhibitor This protocol is adapted from findings that YM155 efficiently kills hiPSCs without harming CD34+ hematopoietic stem cells [12].
- Preparation: Differentiate your hPSC line into the desired therapeutic cell population (e.g., hematopoietic progenitors).
- Treatment: At the final stage of differentiation, add the survivin inhibitor YM155 to the culture medium. The optimal concentration and duration must be determined empirically for your specific cell product but were effective in eliminating teratoma risk in pre-clinical models [12].
- Washing: After treatment, wash the cells thoroughly to remove the inhibitor.
- Assessment: Use a highly sensitive assay (e.g., digital PCR for pluripotency markers) to quantify the depletion of residual undifferentiated hPSCs. Validate the functional capacity of the purified therapeutic cell product (e.g., through colony-forming assays for hematopoietic cells).
Protocol 2: Validating a Genome-Edited Safety Switch (NANOG-iCaspase9) This protocol outlines the key steps for implementing and testing the orthogonal safeguard system described by [2].
- Cell Line Engineering:
- Use Cas9 RNP and AAV6-based genome editing to knock-in an iCaspase9 cassette and a fluorescent reporter (e.g., YFP) downstream of the stop codon in the NANOG gene locus, separated by T2A peptides.
- Generate a clonal hPSC line with biallelic integration to prevent escape.
- Validate the edited line for normal karyotype, pluripotency marker expression, and tri-lineage differentiation potential.
- In Vitro Purging Test:
- Differentiate the engineered hPSCs into your target cell type (e.g., liver, bone, or forebrain progenitors).
- Treat the differentiated cell population with 1 nM AP20187 for 24 hours to activate iCaspase9 in any residual NANOG-positive (undifferentiated) cells.
- Measure the depletion of undifferentiated hPSCs using flow cytometry for the reporter (YFP) or pluripotency markers. This system achieved a >10^6-fold depletion [2].
- In Vivo Safety Test:
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Teratoma Risk Assessment and Mitigation
| Research Reagent | Function/Brief Explanation | Example Use Case |
|---|---|---|
| Survivin Inhibitor (YM155) | Small molecule that selectively kills pluripotent stem cells by inhibiting survivin (BIRC5), a protein critical for hPSC survival [12]. | Purging residual hiPSCs from a differentiated hematopoietic cell product prior to transplantation [12]. |
| AP20187 | Small molecule dimerizer drug used to activate the inducible Caspase-9 (iCaspase-9) suicide gene system [12] [2]. | Eliminating undifferentiated hPSCs from a culture of NANOG-iCaspase9 engineered cells [2]. |
| ROCK Inhibitor (Y-27632) | Increases survival of dissociated hPSCs and improves cell viability after passaging or thawing [14]. | Adding to culture medium for 18-24 hours after passaging or thawing hPSCs to reduce apoptosis [14]. |
| Essential 8 Medium | A defined, feeder-free culture medium optimized for the growth and maintenance of human pluripotent stem cells [14]. | Routine culture of hiPSCs to maintain a pluripotent state before initiating differentiation protocols. |
| Geltrex / Matrigel / Vitronectin XF | Extracellular matrix proteins used to coat culture vessels, providing a substrate that supports hPSC attachment and growth in feeder-free conditions [13] [14]. | Coating tissue culture plates to create a suitable surface for plating and maintaining hPSCs. |
Experimental Workflow and Safety Switch Diagrams
Diagram 1: Teratoma risk mitigation workflow for hPSC therapies.
Diagram 2: Genome-edited safety switch mechanism for hPSC purge.
Current Regulatory Expectations for Tumorigenicity Risk Evaluation
Teratoma formation represents a significant safety concern in the development of pluripotent stem cell-derived therapies. As human pluripotent stem cells (hPSCs) can form these complex tumors containing multiple tissue types, regulatory agencies worldwide require rigorous assessment of tumorigenicity risk before clinical application. This technical support guide examines current regulatory expectations and provides practical methodologies for evaluating and mitigating teratoma formation risk in hPSC-derived cell therapy products (CTPs).
FAQ: Regulatory Framework and Testing Requirements
What is the current regulatory position on in vivo versus in vitro tumorigenicity testing?
Regulatory thinking has evolved significantly, with a 2025 consensus recommendation from the Health and Environmental Sciences Institute's International Cell Therapy Committee highlighting that in vitro assays such as digital PCR (dPCR) detection of hPSC-specific RNA and highly efficient culture (HEC) assays offer superior detection sensitivity compared to conventional in vivo models [10] [15] [11]. While traditional in vivo tumorigenicity assays in immunodeficient mice (e.g., NOD/SCID, NSG) remain part of some regulatory frameworks, there is growing recognition that these models have limitations in predicting human clinical outcomes [15].
How should we approach tumorigenicity testing for products targeting hematologic applications?
For hematologic applications, research demonstrates that systemic injection of hiPSCs produces multisite teratomas in immune-deficient mice as soon as 5 weeks after injection [12]. This finding underscores the critical importance of purging residual undifferentiated PSCs before administration. When considering purge strategies, studies indicate that survivin inhibitor YM155 was more efficient than AP20187/iCaspase-9 for killing hiPSCs without toxicity on CD34+ cells, both in vitro and in adoptive transfers [12].
What are the key regulatory guidelines governing stem cell-based medicinal products?
Regulatory agencies employ a risk-based approach that varies by region [16]. The International Council for Harmonisation (ICH) guidelines form the foundation, with recent updates including:
- ICH E6(R3) Good Clinical Practice (effective July 2025 in EU) emphasizes risk-based quality management and technological innovation in clinical trials [17] [18] [19]
- Regional guidelines specific to advanced therapy medicinal products (ATMPs) in the EU, regenerative medical products in Japan, and biological products in the US [16]
- Product-specific technical guidance for various hPSC-derived CTPs including retinal pigment epithelial cells and articular cartilage regeneration products [16]
Experimental Protocols for Tumorigenicity Assessment
Highly Efficient Culture (HEC) Assay for Residual Undifferentiated hPSCs
The HEC assay provides a sensitive in vitro method for detecting residual undifferentiated hPSCs in final products [10] [11].
Materials and Reagents:
- Rho kinase inhibitor (ROCKi) supplemented culture medium
- Matrigel-coated culture vessels
- Pluripotency markers (e.g., anti-TRA-1-60, anti-SSEA4 antibodies)
- Culture conditions optimized for hPSC growth (mTeSR or equivalent)
Procedure:
- Prepare serial dilutions of the test CTP sample
- Plate cells in ROCKi-supplemented medium on Matrigel-coated plates
- Culture for 14-21 days with regular medium changes
- Score colonies for pluripotent morphology and confirm with immunocytochemistry
- Calculate the frequency of undifferentiated hPSCs based on colony formation
Validation Parameters:
- Limit of detection (LOD) established using spiked samples
- Inter- and intra-assay precision
- Specificity against differentiated cell types
Digital PCR (dPCR) for hPSC-Specific Markers
dPCR offers a highly sensitive molecular method for quantifying residual undifferentiated hPSCs [10] [11].
Workflow:
Key Pluripotency Markers:
- mRNA transcripts: NANOG, POUSF1 (OCT4), SOX2
- Long non-coding RNAs: specific to pluripotent state
- Micro-RNAs: miR-302 family, miR-367
Validation Requirements:
- Establish detection limit with spike-in experiments
- Demonstrate specificity across differentiated lineages
- Determine linear dynamic range
- Assess interference from matrix effects
In Vivo Tumorigenicity Assay in Immunodeficient Mice
While in vitro methods are increasingly preferred, understanding traditional in vivo approaches remains important [10] [12] [20].
Animal Models:
- NOD.Cg-PrkdcscidIL2rgtm1Wjl (NSG) mice
- NOD.Cg-PrkdcscidIL2rgtm1Sug (NOG) mice
- Other severe combined immunodeficiency (SCID) models
Experimental Design:
- Test groups: CTP, positive control (hPSCs), negative control (fully differentiated cells)
- Cell doses: Maximum feasible dose (MFD) plus lower doses
- Route of administration: product-specific (subcutaneous, intramuscular, intravenous)
- Observation period: minimum 12-16 weeks
- Endpoints: palpation, imaging, necropsy, histopathology
Comparative Analysis of Detection Methods
Table 1: Sensitivity Comparison of Tumorigenicity Assessment Methods
| Method | Detection Limit | Time Required | Key Advantages | Regulatory Acceptance |
|---|---|---|---|---|
| In vivo tumorigenicity | ~1×10⁴ cells [20] | 12-16 weeks | Whole-system assessment | Traditional standard |
| Highly Efficient Culture (HEC) | ~1×10⁻⁶ [10] | 2-3 weeks | Functional assessment of pluripotency | Increasing acceptance |
| Digital PCR | ~1×10⁻⁶ [10] [11] | 2-3 days | Quantitative, high-throughput | Supported by recent consensus |
| Flow Cytometry | ~1×10⁻⁴ | Hours | Rapid, single-cell resolution | Complementary technique |
Research Reagent Solutions
Table 2: Essential Reagents for Tumorigenicity Risk Assessment
| Reagent/Category | Specific Examples | Application | Considerations |
|---|---|---|---|
| Pluripotency Markers | Anti-TRA-1-60, Anti-SSEA4, Anti-OCT4 | Immunodetection of residual hPSCs | Specificity for undifferentiated state |
| Molecular Assays | dPCR assays for NANOG, POUSF1 | Quantitative residual hPSC detection | Primer/probe validation critical |
| Culture Reagents | ROCK inhibitor, mTeSR medium | HEC assay | Optimize for sensitive detection |
| Animal Models | NSG, NOG mice | In vivo tumorigenicity | Institutional animal care protocols |
| Control Materials | Reference hPSCs, Differentiated cells | Assay qualification | Well-characterized biospecimens |
Troubleshooting Guides
Problem: Inconsistent Results in HEC Assay
Potential Causes and Solutions:
- Cause: Variability in culture conditions
- Solution: Standardize matrix coating procedures and qualify all culture reagents
- Cause: Suboptimal ROCKi concentration
- Solution: Titrate ROCKi (typically 5-10 μM) using positive control hPSCs
- Cause: Overgrowth of differentiated cells
- Solution: Include selective agents or use morphological criteria early in culture
Problem: High Background in dPCR Assay
Potential Causes and Solutions:
- Cause: RNA degradation
- Solution: Implement rigorous RNA quality control (RIN >8.0)
- Cause: Non-specific amplification
- Solution: Optimize primer annealing temperature and validate specificity
- Cause: Inhibitors in sample matrix
- Solution: Include internal controls and optimize nucleic acid purification
Problem: Variable Teratoma Formation in Animal Models
Potential Causes and Solutions:
- Cause: Immunodeficient mouse strain variability
- Solution: Use consistent strain source and monitor immune leakage
- Cause: Injection technique variability
- Solution: Standardize cell preparation and injection protocols across operators
- Cause: Cell viability issues
- Solution: Minimize time between cell preparation and implantation
Risk Mitigation Strategies
Genetic Safety Switches
Engineering hPSCs with suicide genes provides a safety strategy for eliminating teratoma-initiating cells [12] [20].
Approaches:
- Herpes simplex virus thymidine kinase (HSV-TK) + ganciclovir [20]
- Integrated into NANOG locus via homologous recombination
- Enables selective elimination of undifferentiated cells
- Inducible caspase-9 (iCaspase-9) + AP20187 [12]
- Controlled by pluripotency-specific promoters (pmiR-302/367)
- Demonstrated efficacy in vitro but showed toxicity to CD34+ cells
Small Molecule Inhibitors
Survivin inhibitor YM155 [12]:
- Shows high efficiency in eliminating hiPSCs
- No observed toxicity to CD34+ hematopoietic cells
- Effectively prevents teratoma formation in immunodeficient mice
The regulatory landscape for tumorigenicity risk assessment of hPSC-derived therapies is rapidly evolving toward more sensitive, human-relevant in vitro methods. A comprehensive testing strategy should integrate orthogonal methods including highly sensitive molecular assays (dPCR), functional culture assays (HEC), and appropriate in vivo models when justified. Implementation of risk mitigation strategies such as genetic safety switches or small molecule purging approaches can further enhance product safety. As regulatory thinking continues to advance, maintaining awareness of updated guidelines and consensus recommendations is essential for successful development of safe hPSC-based therapies.
Proactive Prevention: Strategies for Eliminating Residual Pluripotent Stem Cells
Targeting hPSC-Specific Surface Markers for Selective Cell Removal
FAQ: Addressing Researcher Questions on PSC Removal Strategies
Q1: What are the key cell surface markers used to identify and target human pluripotent stem cells (hPSCs) for removal?
The most well-characterized cell surface markers for identifying undifferentiated hPSCs are the glycolipid antigens SSEA3 and SSEA4, and the glycoprotein antigens TRA-1-60 and TRA-1-81 [21] [22]. These markers were initially identified on human embryonic carcinoma cells and are also expressed by the inner cell mass of pre-implantation human embryos, providing a reliable signature of the pluripotent state [21]. Monitoring these markers provides a standardized measure of cell status and is fundamental for comparing different cell lines and culture conditions [22].
Q2: Why is it critical to remove residual undifferentiated hPSCs from differentiated cell populations intended for therapy?
Residual undifferentiated hPSCs possess unlimited self-renewal capacity and are intrinsically tumorigenic, capable of forming teratomas (benign tumors containing tissues from all three germ layers) upon transplantation [23] [10]. Studies have shown that even a very small number of residual undifferentiated cells—in some cases, as few as 20 to 100 undifferentiated stem cells within a population of differentiated cells—can eventually lead to teratoma formation [23] [12]. A clinical case report documented the occurrence of a rapidly growing, metastatic immature teratoma in a patient who received autologous iPSC-derived pancreatic beta cells, underscoring this critical safety risk [23].
Q3: What are the primary strategic approaches for eliminating residual hPSCs?
The main strategies can be categorized as follows:
- Pharmacological: Using small-molecule compounds that induce selective apoptosis in hPSCs.
- Immunological: Employing antibodies or antibody-drug conjugates that target hPSC-specific surface markers.
- Genetic: Engineering hPSCs with "safety switches" or suicide genes that can be activated to eliminate the cells.
- Physical Separation: Using fluorescence-activated cell sorting (FACS) or magnetic-activated cell sorting (MACS) to deplete marker-positive hPSCs from a mixed population [23] [12] [2].
Q4: What are common challenges when using cell surface markers for hPSC depletion, and how can they be troubleshooted?
| Challenge | Potential Cause | Troubleshooting Solutions |
|---|---|---|
| Low Purity Post-Depletion | Inefficient antibody binding; incomplete cell separation. | Optimize antibody concentration and incubation time; use a combination of markers (e.g., SSEA-3, TRA-1-60) for more robust depletion; validate separation efficiency with flow cytometry [12] [22]. |
| Low Viability of Target Cell Population | Excessive mechanical stress during FACS; cytotoxicity from the depletion method. | Use gentler sorting settings; consider magnetic bead-based separation (MACS) as a lower-stress alternative; test viability post-sorting and adjust protocols accordingly [12]. |
| Incomplete hPSC Elimination & Teratoma Formation | Low sensitivity of the detection or elimination method; presence of hPSCs that do not express the targeted marker. | Employ highly sensitive in vitro assays (e.g., digital PCR, highly efficient culture assays) to detect residual hPSCs; consider a multi-pronged approach combining surface marker depletion with a pharmacological agent [10]. |
| Unexpected Toxicity to Differentiated Cells | The targeted surface marker or pathway is also expressed at low levels in the therapeutic cell population. | Thoroughly validate marker specificity for undifferentiated cells across your specific differentiated cell types; consider alternative, more specific targets like Dsg2 [24] [2]. |
Troubleshooting Guide: Experimental Issues in hPSC Removal
Problem: Inconsistent results in antibody-based targeting of hPSCs.
- Solution 1: Validate Antibody Specificity and Titer. Not all antibodies perform equally. Confirm the specificity of your antibody for the intended target (e.g., SSEA-4, TRA-1-60) using appropriate positive (undifferentiated hPSCs) and negative (fully differentiated somatic cells) controls. Perform a titration experiment to determine the optimal antibody concentration that maximizes signal-to-noise ratio [21] [22].
- Solution 2: Account for Pluripotency State Heterogeneity. hPSC cultures can contain subpopulations in different pluripotent states (naïve vs. primed), which express different surface markers. For instance, naïve hPSCs may express SSEA-4 differently than primed cells. Characterize your starting cell population and ensure your chosen markers are appropriate for the specific pluripotent state you are targeting [22] [25].
Problem: Differentiated cell product is compromised after hPSC removal treatment.
- Solution 1: Titrate Drug Concentrations and Exposure Time. When using small-molecule inhibitors or antibody-drug conjugates, a dose-response and time-course experiment is essential. The goal is to find a window where hPSCs are effectively killed while differentiated cells remain viable and functional [12] [24].
- Solution 2: Implement a "Safety Switch" as a Contingency. For critical applications, use hPSCs that have been genetically engineered with an inducible "safety switch," such as iCaspase9 under a pluripotency-specific promoter (e.g., NANOG). This provides a fail-safe mechanism to eliminate the entire cell product, including any potentially contaminating hPSCs, after transplantation if adverse events arise [2].
Experimental Protocol: Selective Elimination of hPSCs Using an Anti-Dsg2 Antibody-Drug Conjugate
This protocol is adapted from Park et al. (2020) and outlines a method for selectively eliminating undifferentiated hPSCs by targeting the highly specific surface marker Desmoglein 2 (Dsg2) with a doxorubicin (DOX) conjugate [24].
1. Principle The monoclonal antibody K6-1 specifically targets Dsg2, which is highly expressed on undifferentiated hPSCs but at low levels in differentiated somatic cells. Conjugating this antibody to the chemotherapeutic drug doxorubicin creates a targeted delivery system (K6-1-DOX). The conjugate is selectively internalized by Dsg2-positive hPSCs, leading to intracellular DOX release and apoptosis, while sparing Dsg2-negative differentiated cells [24].
2. Reagents
- Purified Anti-Dsg2 Antibody (K6-1)
- Doxorubicin (DOX)
- Conjugation buffer
- hPSC culture (undifferentiated control)
- Differentiated somatic cell culture (negative control)
- Cell culture media
3. Step-by-Step Procedure 1. Preparation of ADC: Conjugate the K6-1 antibody to doxorubicin via a chemical linker. Purify the K6-1-DOX conjugate and characterize it using HPLC or SDS-PAGE to confirm conjugation efficiency and stability [24]. 2. In Vitro Treatment: * Culture undifferentiated hPSCs and the differentiated cell product of interest. * Treat cells with varying concentrations of K6-1-DOX (e.g., 0.1 - 10 µM) for 24-72 hours. * Include control groups: untreated cells, cells treated with unconjugated DOX, and cells treated with an irrelevant antibody-DOX conjugate. 3. Assessment of Cytotoxicity: * Measure cell viability using assays like MTT or CellTiter-Glo. * Analyze apoptosis via flow cytometry for Annexin V/propidium iodide staining. * Confirm selective elimination by quantifying the depletion of pluripotency marker-positive cells (e.g., via flow cytometry for OCT4 or NANOG) in the mixed population. 4. In Vivo Validation (Teratoma Assay): * Pre-treat a sample of hPSCs with K6-1-DOX or a control. * Inject the treated cells into immunodeficient mice (e.g., NSG). * Monitor the mice for teratoma formation over 8-16 weeks. Effective elimination should result in no teratomas in the K6-1-DOX group, while control groups should develop tumors [24].
Research Reagent Solutions: Essential Materials for hPSC Removal Studies
| Reagent / Tool | Function / Application | Key Considerations |
|---|---|---|
| Anti-SSEA-3/-4, TRA-1-60/-81 Antibodies [21] | Immunophenotyping and physical depletion (FACS/MACS) of undifferentiated hPSCs. | Standard panel for defining pluripotent state; efficiency can be affected by marker heterogeneity. |
| Anti-Dsg2 Antibody (K6-1) [24] | Target for highly specific antibody-drug conjugates against hPSCs. | Reported to be highly differentially expressed in hPSCs vs. somatic tissues. |
| Survivin Inhibitor (YM155) [12] | Small molecule that induces selective apoptosis in hPSCs. | Can be toxic to some differentiated cell types (e.g., hematopoietic stem cells); requires careful titration [12] [2]. |
| Inducible Caspase 9 (iCasp9) System [2] | Genetically encoded "safety switch" activated by small molecule AP20187. | Can be placed under a pluripotency-specific promoter (e.g., NANOG) for selective killing or a ubiquitous promoter for total product elimination. |
| PluriTest Assay [cite[1]] | Bioinformatic tool to assess pluripotency and identity of hPSCs based on gene expression. | Useful for quality control and verifying the undifferentiated state of cells pre- and post-removal strategies. |
Workflow Diagram: Strategic Approaches to Eliminate Residual hPSCs
The diagram below illustrates the logical decision-making process for selecting an hPSC removal strategy based on experimental or therapeutic goals.
Optimizing Differentiation Protocols to Minimize Undifferentiated Cell Populations
Troubleshooting Guides & FAQs
Frequently Asked Questions
FAQ 1: Why is it critical to minimize undifferentiated hPSC populations in cell therapy products? Even a small number of residual undifferentiated human pluripotent stem cells (hPSCs) can form teratomas in vivo. Studies have shown that as few as 10,000 undifferentiated hPSCs can generate these tumors, which presents a significant safety risk for clinical therapies. When transplanting billions of hPSC-derived cells, even a 0.001% residual undifferentiated cell contamination could be therapeutically unacceptable [2] [26].
FAQ 2: What are the primary methods for eliminating residual undifferentiated hPSCs? There are three predominant strategies:
- Physical separation based on pluripotent-specific cell surface antigens (e.g., depletion of SSEA-4+, TRA-1-60+ cells).
- Chemical elimination using small molecules that selectively induce apoptosis in pluripotent cells (e.g., survivin inhibitors like YM155).
- Genetic safeguards involving genome-edited suicide genes (e.g., inducible Caspase-9 under a NANOG promoter) that can be activated before transplantation [12] [2] [26].
FAQ 3: My hPSC cultures are showing excessive spontaneous differentiation (>20%). What could be the cause? Excessive differentiation in maintenance cultures can be caused by several factors:
- Using culture medium that has been stored at 2-8°C for more than two weeks.
- Allowing the culture plate to remain outside the incubator for extended periods (>15 minutes).
- Overgrown colonies or unevenly sized cell aggregates after passaging.
- Insufficient colony density after passaging [13].
- Cells located on the rim of colonies lacking cell-to-cell contact, which can trigger spontaneous differentiation [27].
FAQ 4: How can culture conditions influence the differentiation potential of PSCs? The culture medium can alter the differentiation potential of PSCs. Cells cultured in medium that supports the glycolytic pathway tend to maintain high expression of CHD7 and retain strong differentiation potential. In contrast, culture conditions that support mitochondrial function can reduce CHD7 levels and compromise differentiation capability [27].
Troubleshooting Common Problems
Problem: Low cell attachment after passaging during differentiation protocols.
- Potential Solutions [13]:
- Plate a higher number of cell aggregates initially (e.g., 2-3 times higher) to maintain a more densely confluent culture.
- Work quickly after cells are treated with passaging reagents to minimize the duration that cell aggregates are in suspension.
- Reduce the incubation time with passaging reagents, as your specific cell line may be more sensitive.
- Do not excessively pipette to break up cell aggregates. Instead, increase the incubation time with the passaging reagent by 1-2 minutes to allow natural dissociation.
- Ensure you are using the correct culture plate type (non-tissue culture-treated for certain coatings like Vitronectin XF; tissue culture-treated for others like Matrigel).
Problem: Differentiated cells detach along with colonies when using passaging reagents like ReLeSR.
- Potential Solutions [13]:
- Decrease the incubation time with the reagent by 1-2 minutes.
- Decrease the incubation temperature to room temperature (15-25°C).
Problem: Cell aggregates obtained during passaging are too large for optimal differentiation.
- Potential Solutions [13]:
- Increase the incubation time with the dissociation reagent.
- Increase pipetting of the cell aggregates to break them up, but avoid generating a single-cell suspension.
- Add a wash step using D-PBS (without Ca++ and Mg++) before adding the non-enzymatic passaging reagents.
Quantitative Data & Safety Strategies
The following table summarizes and compares key strategies for eliminating tumorigenic hPSCs, a critical step for safe cell therapy [12] [2] [26].
Table 1: Comparison of Strategies for Eliminating Tumorigenic Pluripotent Stem Cells
| Strategy | Mechanism of Action | Reported Efficacy | Key Advantages | Key Limitations / Toxicities |
|---|---|---|---|---|
| Survivin Inhibition (YM155) | Chemical inhibitor of survivin (BIRC5), an protein essential for hPSC survival. | Efficiently kills hiPSCs; purge fully eradicated teratoma formation in mice [12]. | More efficient than iCaspase-9/AP20187 for killing hiPSCs; No toxicity on CD34+ hematopoietic stem cells in vitro and in adoptive transfers [12]. | Broad expression of survivin in some differentiated cell types may limit specificity [2]. |
| Inducible Caspase-9 (iCaspase-9) | Genetically engineered "suicide gene" activated by a small molecule (AP20187), triggering apoptosis. | >106-fold depletion of undifferentiated hPSCs [2]. | Highly specific, rapid, and irreversible apoptosis; Biallelic knock-in prevents escape [2]. | Nonspecific toxicity of prodrug AP20187 on some cell types (e.g., CD34+ cells), impairing human hematopoiesis [12]. Higher AP20187 concentrations can downregulate NANOG [2]. |
| Thymidine Kinase (TK) | Viral/ bacterial enzyme that converts prodrug ganciclovir (GCV) into a toxic nucleotide analog. | Successful ablation of teratomas in various models [12] [2]. | Well-established system. | Requires extended in vitro treatment for full efficacy; potential for bystander effect [12]. |
| NANOG-iCasp9 Orthogonal Safeguard | Genome-edited iCaspase-9 knocked into endogenous NANOG locus, specific to pluripotent state. | 1.75 x 106-fold depletion of undifferentiated hPSCs; prevented teratoma formation [2]. | Highly specific to undifferentiated state; faithful to endogenous NANOG downregulation; safeguards cannot be silenced without loss of pluripotency [2]. | Requires genome editing; optimal at low AP20187 doses (1 nM) [2]. |
Table 2: Key Reagents for Targeting Undifferentiated hPSCs
| Reagent / Method | Function in Elimination Strategy | Experimental Consideration |
|---|---|---|
| YM155 | Small molecule survivin inhibitor; selectively induces apoptosis in undifferentiated hPSCs. | Demonstrated efficiency in purging hiPSCs without toxicity to CD34+ hematopoietic stem cells [12]. |
| AP20187 | Small molecule dimerizer drug; activates the inducible Caspase-9 (iCaspase-9) suicide gene. | Can exhibit non-specific toxicity on certain cell types, including hematopoietic CD34+ cells [12]. Optimal dose for NANOG-iCaspase9 is 1 nM [2]. |
| Ganciclovir (GCV) | Prodrug; converted to a toxic compound by thymidine kinase (TK), killing transduced cells. | Less efficient and rapid than iCaspase-9/AP20187 system; may require longer treatment duration [12]. |
| Anti-SSEA-4 / TRA-1-60 Antibodies | Antibodies for cell surface markers; used for fluorescence-activated cell sorting (FACS) to deplete undifferentiated cells. | Results can be affected by gating strategy; procedure can be time-consuming and expensive, and may affect viability of therapeutic cells [12] [26]. |
| Geltrex/Matrigel | Extracellular matrix (ECM) coating; provides a more in vivo-like environment that can enhance differentiation efficiency. | Implementation of Geltrex in a pancreatic differentiation protocol significantly enhanced the expression of pancreatic markers in dental stem cells [28]. |
Detailed Experimental Protocols
Protocol 1: Purging Residual hPSCs with Survivin Inhibitor YM155
This protocol is adapted from methods used to eliminate hiPSCs before grafting in hematopoietic contexts [12].
- Preparation: Differentiate your hiPSCs toward the desired lineage using your established protocol.
- Treatment: At the end of the differentiation process, treat the heterogeneous cell population containing residual hiPSCs with a survivin inhibitor (e.g., YM155) at a determined optimal concentration.
- Note: The exact concentration and duration should be determined empirically for each cell line and differentiation protocol. In the cited study, YM155 was more efficient than AP20187/iCaspase-9 at killing hiPSCs.
- Assessment: After treatment, assess the viability of both the target differentiated cells and the residual hiPSCs.
Protocol 2: Using a Genome-Edited NANOG-iCaspase9 Safeguard
This protocol outlines the use of an orthogonal safety switch to selectively eliminate undifferentiated hPSCs [2].
- Cell Line Generation: Engineer hPSC lines to biallelically express an inducible Caspase9 (iCaspase9) cassette downstream of the endogenous NANOG coding sequence using CRISPR/Cas9 RNP and AAV6-mediated genome editing. The construct should use T2A peptides to separate NANOG, iCaspase9, and a fluorescent reporter (e.g., YFP).
- Validation: Validate the edited cell lines for normal pluripotency, karyotype, and differentiation potential. Confirm that YFP (reporting iCaspase9 expression) is uniformly expressed in undifferentiated cells and extinguished upon differentiation.
- Pre-transplantation Purging: Before transplanting differentiated cell products, treat the cell culture with 1 nM AP20187 for 12-24 hours to selectively eliminate any residual NANOG-positive (undifferentiated) cells.
- Confirmation: Confirm the depletion efficiency via flow cytometry for pluripotency markers and functional in vivo teratoma assays in immunodeficient mice.
Signaling Pathways & Experimental Workflows
Diagram: Orthogonal Safeguard Strategy for hPSC Therapy Safety
Diagram 1: Orthogonal Safeguard Strategy for hPSC Therapy Safety. This workflow shows two distinct, drug-inducible safety switches integrated into hPSCs. Strategy 1 (NANOG-iCaspase9) is activated before transplantation to selectively eliminate residual undifferentiated cells. Strategy 2 (ACTB-TK/iCaspase9) acts as a master "off-switch" for the entire graft if adverse events occur after transplantation [2].
Diagram: Strategic Workflow to Minimize Teratoma Risk
Diagram 2: Strategic Workflow to Minimize Teratoma Risk. A multi-step approach is critical for ensuring the safety of hPSC-derived therapies. This involves optimizing the initial differentiation, maintaining culture quality to prevent spontaneous differentiation, actively purging residual pluripotent cells, and rigorously validating the final product [12] [28] [13].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions
| Reagent / Tool | Function | Application Note |
|---|---|---|
| Geltrex/Matrigel | Extracellular matrix providing a complex 3D environment for enhanced differentiation. | Significantly enhanced the expression of pancreatic markers (Foxa-2, Sox-17, PDX-1) in dental stem cell differentiation protocols [28]. |
| Survivin Inhibitor (YM155) | Small molecule that selectively targets survivin, a protein highly relied upon by hPSCs for survival. | A key chemical for purging residual hiPSCs; shown to be efficient and non-toxic to CD34+ hematopoietic stem cells [12]. |
| AP20187 | Bioactive dimerizer drug used to activate the inducible Caspase-9 (iCaspase9) suicide gene. | The optimal dose for systems like NANOG-iCaspase9 is 1 nM; higher concentrations can downregulate NANOG [2]. |
| Gentle Cell Dissociation Reagent | Enzyme-free solution for passaging hPSCs as clumps, preserving cell viability and surface markers. | Critical for maintaining healthy cultures; over-incubation or excessive pipetting can result in overly small aggregates or single cells, which may not be ideal for some differentiation protocols [13]. |
| mTeSR Plus / Essential 8 Media | Defined, feeder-free culture media for the maintenance of undifferentiated hPSCs. | The quality and freshness of the culture medium is paramount; old medium can lead to excessive spontaneous differentiation [13] [27]. |
| Anti-Pluripotency Markers (SSEA-4, TRA-1-60) | Antibodies for detecting undifferentiated hPSCs via flow cytometry or immunocytochemistry. | Used for quality control to quantify residual undifferentiated cells before and after purging strategies. Results can be sensitive to gating strategies [12] [26]. |
FAQs: miRNA and Genetic Circuits in Teratoma Prevention
Q1: How do miRNA-based strategies specifically prevent teratoma formation in pluripotent stem cell therapies? miRNA-based strategies leverage the natural role of microRNAs in post-transcriptional regulation to eliminate residual undifferentiated human pluripotent stem cells (hPSCs) from differentiated cell therapy products. These strategies typically target hPSC-specific markers or pathways essential for pluripotency. For instance, introducing miRNAs that trigger the degradation of core pluripotency transcripts (like c-Myc) or promoting the expression of pro-differentiation miRNAs can selectively remove tumorigenic cells, thereby mitigating the risk of teratoma formation upon transplantation [30] [26].
Q2: What is the primary technical challenge in validating miRNA-target interactions for a novel genetic circuit? The primary challenge lies in the accurate prediction and experimental validation of miRNA-target interactions. Computational predictions suggest a single miRNA can regulate hundreds of mRNA molecules, but these interactions are highly dependent on cellular context, miRNA abundance, and the presence of competing endogenous RNAs (ceRNAs). False positives are common, and validation requires rigorous methodologies beyond bioinformatics, such as overexpression or knockdown experiments combined with high-throughput sequencing to confirm the specific degradation of the target transcript [31].
Q3: My genetic circuit for cell sorting shows perfect performance in vitro, but how do I assess its in vivo efficacy against teratoma formation? The most stringent assay for assessing teratoma risk is in vivo teratoma formation. This involves transplanting your cell therapy product into immunodeficient mouse models (e.g., SCID, NOD) and monitoring for tumor formation over time. This method provides a comprehensive, biologically relevant assessment of the product's safety. Additionally, highly sensitive in vitro assays like digital PCR (dPCR) for residual hPSC-specific RNA can be used to quantify the remaining undifferentiated cells in your product before transplantation, providing a complementary safety checkpoint [32] [10].
Q4: Why might my miRNA expression data from high-throughput sequencing be unreliable, and how can I improve it? RNA sequencing data for miRNA can be unreliable due to several factors:
- Low RNA Quality: Degraded RNA can generate fragments that are mis-annotated as miRNAs [31].
- Low Abundance Targets: miRNAs expressed at very low levels or in a temporally restricted manner may have few mapped reads, making their validation difficult [31].
- Inconsistent Processing Guidelines: Without stringent bioinformatics pipelines that check for features like 3' overhangs and 5' end compatibility with the miRNA processing machinery, many false-positive miRNAs can be annotated [31]. To improve reliability, ensure high-quality RNA input, use enrichment strategies for small RNAs, and adhere to established miRNA annotation guidelines that require multiple lines of evidence [31].
Troubleshooting Guides
Table 1: Troubleshooting miRNA Detection and Quantification
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Low or no amplification signal for abundant miRNA targets. | Insufficient RNA input or suboptimal reverse transcription efficiency. | Titrate total RNA input up to 250 ng. Double the amount of reverse transcriptase enzyme to 6.6 U/µL [33]. |
| Multiple peaks in melt curve analysis (SYBR Green assays). | - Contaminating genomic DNA.- High primer concentration leading to primer-dimers.- Non-specific amplification. | - DNase-treat the RNA sample.- Optimize forward primer concentration to ~200 nM.- Check primer specificity and ensure a positive control is included [33]. |
| Amplification in No-Template Control (NTC) with Ct < 38. | - Reagent contamination.- Contamination from plasmids or artificial templates in the lab. | - Change reagents and use dedicated equipment.- Decontaminate surfaces with a DNA degradation solution. Work in a separate location if necessary [33]. |
| Inconsistent results from highly multiplexed miRNA profiling (e.g., Megaplex). | A subset of assays inherently exhibits lower NTC Ct values in large multiplex pools. | Consider these assays semi-quantitative in the multiplex format. Validate significant fold-changes using corresponding individual TaqMan MicroRNA Assays [33]. |
Table 2: Troubleshooting Genetic Circuit Performance
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Genetic circuit fails to activate cell sorting mechanism in a subset of cells. | Heterogeneous expression of circuit components or variable cellular state. | Implement a dual-reporter system to identify and isolate cells with correct circuit function. Optimize delivery method (e.g., lentiviral vs. mRNA transfection) for more consistent expression. |
| High false-positive rate in cell sorting, removing differentiated cells. | Promoter leakiness or non-specific activity of the genetic circuit's sensor. | Use a more specific hPSC-specific promoter (e.g., with enhanced epigenetic silencing upon differentiation). Incorporate additional logic gates (AND gates) that require multiple hPSC markers for activation. |
| Differentiated cell product shows reduced viability or function after sorting. | Off-target effects of the cell-killing mechanism (e.g., toxin gene) or persistent low-level activity. | Employ a "suicide switch" that can be activated only for a limited time post-sorting. Validate the absence of off-target transcript degradation using RNA-Seq on the final product. |
Experimental Protocols
Protocol 1: Highly SensitiveIn VitroDetection of Residual hPSCs
This protocol uses digital PCR (dPCR) to quantify trace amounts of residual undifferentiated hPSCs in a differentiated cell therapy product, a key safety assessment [10].
- RNA Extraction: Isolve total RNA from the cell therapy product using a column-based method that enriches for small RNAs. Determine RNA concentration and quality (e.g., RIN > 8.0).
- cDNA Synthesis: Convert RNA to cDNA using a reverse transcription kit suitable for a wide dynamic range. Include controls without reverse transcriptase (-RT) to detect genomic DNA contamination.
- dPCR Setup: Prepare the dPCR reaction mix using probes specific to hPSC markers (e.g., NANOG, POUSF1/OCT4). Include a reference gene for normalization.
- Partitioning and Amplification: Load the reaction mix into a dPCR chip or droplet generator to partition the sample into thousands of individual reactions. Perform PCR amplification.
- Analysis: Use the dPCR analyzer to count the positive and negative partitions. Calculate the absolute copy number of the hPSC-specific transcript and the reference gene per ng of total RNA. The limit of detection (LOD) for this method is superior to traditional qPCR [10].
Protocol 2:In VivoTeratoma Formation Assay
This is the "gold standard" assay to evaluate the tumorigenic potential of your cell product in an in vivo model [32].
- Cell Preparation: Harvest hPSCs or your final cell therapy product. Prepare a single-cell suspension in an appropriate buffer (e.g., PBS) mixed with Matrigel to enhance engraftment.
- Animal Model: Use immunodeficient mouse strains (e.g., Nu/Nu nude, NOD-SCID) to prevent immune rejection. Anesthetize the mice using an isoflurane system.
- Cell Transplantation: Inject cells subcutaneously, intramuscularly, or into an organ-specific site (e.g., intramyocardial). The critical cell number varies by site; for example, ~1×10⁵ cells may be needed for intramyocardial injection, while as few as 1×10⁴ may suffice for skeletal muscle [32].
- Monitoring: Monitor mice for teratoma formation over 12-20 weeks. For cells expressing reporters (e.g., luciferase), use bioluminescence imaging (BLI) for non-invasive, longitudinal tracking.
- Histological Analysis: Upon endpoint, resect the resulting teratomas. Fix, section, and stain with H&E. Confirm the presence of tissues derived from all three germ layers (ectoderm, mesoderm, and endoderm) to validate pluripotency [32].
Data Presentation
Table 3: Key RNA Degradation Pathways in Pluripotent Stem Cells
This table summarizes the core machinery that can be harnessed by miRNA strategies and genetic circuits to degrade pluripotency transcripts [30].
| Degradation Pathway | Key Complex/Enzyme | Direction | Primary Role in PSCs |
|---|---|---|---|
| Deadenylation-dependent decay | CCR4-NOT, PAN2-PAN3 | 3' → 5' | Shortens the poly(A) tail, marking RNAs for decay; fine-tunes transcript abundance. |
| 5'→3' exonucleolytic decay | XRN1 (exonuclease), DCP1/DCP2 (decapping) | 5' → 3' | Mediates transcript clearance after decapping; maintains pluripotency network responsiveness. |
| 3'→5' decay (RNA exosome) | Exosome complex (with TRAMP/NEXT/PAXT) | 3' → 5' | Major nuclease for nuclear and cytoplasmic RNA surveillance; degrades misprocessed RNAs. |
| Nonsense-Mediated Decay (NMD) | UPF1, SMG1, SMG6 | Specialized | Quality control; also actively degrades transcripts of core pluripotency factors like c-Myc. |
| miRNA-mediated decay | RISC (Ago2, TRBP, Dicer) | Specialized | Selectively degrades or represses target mRNAs through sequence-specific binding. |
Pathway and Workflow Visualizations
Diagram 1: miRNA Biogenesis and Function
Diagram Title: miRNA Biogenesis, Processing, and Mechanism of Action
Diagram Title: Integrated Strategy for Teratoma Risk Mitigation
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions
| Item | Function/Application |
|---|---|
| TaqMan MicroRNA Assays | For sensitive and specific quantification of individual mature miRNA levels from total RNA [33]. |
| NCode VILO miRNA cDNA Synthesis Kit | A specialized kit for reverse transcribing miRNA, ideal for use with SYBR Green-based detection methods [33]. |
| Matrigel | Used to suspend cells for transplantation in teratoma formation assays, enhancing engraftment efficiency [32]. |
| Immunodeficient Mouse Models (e.g., Nu/Nu, SCID, NSG) | In vivo hosts for teratoma assays, as they do not reject transplanted human cells [32]. |
| Digital PCR (dPCR) Systems | Provides absolute quantification of residual hPSC-specific markers with high sensitivity, crucial for product safety release [10]. |
| Rho Kinase Inhibitor (ROCKi) | Improves the survival and viability of hPSCs during single-cell passaging and preparation for assays [10]. |
FAQs: Core Principles and Method Selection
1. Why is the physical removal of residual hPSCs from differentiated cell products critical for therapy? Human pluripotent stem cells (hPSCs), including induced pluripotent stem cells (iPSCs), possess unlimited self-renewal capacity. Even a small number of residual undifferentiated hPSCs contaminating a therapeutic cell product can lead to teratoma formation post-transplantation. This tumorigenic risk is a major clinical hurdle for hPSC-based regenerative medicine. The goal of purging is to eliminate these residual undifferentiated cells to ensure patient safety [26] [23].
2. What is the fundamental difference between FACS and MACS?
- FACS (Fluorescence-Activated Cell Sorting) is a laser-based technology that analyzes and sorts individual cells based on fluorescent labeling of specific cell markers. It allows for multiparameter sorting (using multiple markers simultaneously) and provides high-resolution separation based on antigen density [34].
- MACS (Magnetic-Activated Cell Sorting) uses superparamagnetic beads conjugated to antibodies. Cells labeled with these beads are retained in a magnetic column, while unlabeled cells flow through. It is primarily a bulk separation method, ideal for positive selection or depletion of cell populations [34].
3. How do I decide whether to use FACS or MACS for my hPSC depletion experiment? The choice depends on your experimental requirements for purity, recovery, throughput, and technical resources.
Table 1: Choosing Between FACS and MACS for hPSC Purging
| Criterion | FACS | MACS |
|---|---|---|
| Purity | High (can exceed 95%) [34] | High for enrichment, but may require consecutive cycles for highest purity [34] |
| Cell Viability | Can be lower due to high shear stress | Generally higher; gentler process with lower shear stress [34] |
| Throughput & Speed | Lower throughput; processes thousands of cells per second serially | High throughput; fast and simple, processing bulk samples quickly [34] |
| Multiparameter Capability | Excellent; allows sorting based on multiple surface markers and light scatter | Limited; typically suited for one or two markers per separation run |
| Complexity & Cost | High; requires expensive instrumentation and trained personnel | Lower; simpler technology, lower cost, easier to use [34] |
| Clinical Applicability | Less common for direct clinical cell processing | Approved for certain clinical applications (e.g., CD34+ cell enrichment) [34] |
4. What are the key surface markers for identifying and removing undifferentiated hPSCs? Several cell surface markers are highly expressed on undifferentiated hPSCs and can be targeted for their removal. It is often beneficial to use a combination of markers to improve the specificity of depletion.
Table 2: Key Surface Markers for Depleting Undifferentiated hPSCs
| Marker | Description | Role in Purging |
|---|---|---|
| SSEA-5 | Glycolipid antigen prevalent on hPSCs | Part of antibody panels for removing teratoma-forming cells [35]. |
| TRA-1-60 | Glycoprotein marker specific for pluripotency | Used in flow cytometry-based identification and removal; requires cell fixation which limits live-cell sorting [35]. |
| TRA-1-81 | Glycoprotein marker closely related to TRA-1-60 | Similar uses and limitations as TRA-1-60 [35]. |
| EpCAM (CD326) | Epithelial cell adhesion molecule, a reference stem cell marker | Useful for immunophenotyping and isolating live hPSC populations [35]. |
| Integrin α6 (CD49f) | Cell adhesion receptor, a marker for multipotency | Prevalent on hPSCs and used for their identification and isolation [35]. |
| c-Kit (CD117) | Receptor tyrosine kinase | A stem cell-prevalent marker used in immunophenotyping panels [35]. |
| SSEA-4 | Glycolipid antigen | Used in complex protocols for depleting undifferentiated iPSCs (e.g., alongside TRA-1-60) [12]. |
Troubleshooting Guides
Problem 1: Low Cell Viability After Sorting
Potential Causes and Solutions:
- Cause: Excessive shear stress during sorting, particularly in FACS.
- Solution: Ensure the instrument nozzle size is appropriate for your cell type. For large or fragile cells, use a larger nozzle diameter (e.g., 100-130 µm) to lower pressure and shear stress. Using a cell-friendly buffer containing EDTA rather than trypsin can also help [35].
- Cause: Prolonged processing time or holding cells at high densities on ice.
- Solution: Minimize the time between cell preparation and sorting. Keep cells cold but process quickly. After sorting, plate cells immediately in recovery medium.
- Cause: Apoptosis due to the single-cell dissociation process.
Problem 2: Inadequate Purity of the Sorted Population
Potential Causes and Solutions:
- Cause: Insufficient specificity of the antibody panel.
- Solution: Many markers once thought to be hPSC-specific are also expressed on some differentiated progeny [2]. Validate your antibody panel on both undifferentiated hPSCs and the target differentiated cell type. Use a combination of positive markers (e.g., SSEA-5, TRA-1-60) and negative markers for the desired cell type.
- Cause: Gating strategy errors in FACS.
- Solution: Include appropriate controls: unstained cells, cells with isotype antibodies, and a sample of your differentiated cell product to set accurate gates and exclude autofluorescence.
- Cause: Overloading the MACS column.
- Solution: Do not exceed the recommended cell number for the column size. If very high purity is required, consider performing a second, consecutive round of MACS separation, which can achieve purity comparable to FACS for some applications [34].
Problem 3: Low Yield or Recovery of Target Cells
Potential Causes and Solutions:
- Cause: Overly stringent gating in FACS, excluding viable cells.
- Solution: Re-evaluate gates using control samples. Slightly widening gates during the initial sort can improve yield, though it may slightly compromise purity.
- Cause: Inefficient elution in MACS.
- Solution: For positive selection, after removing the column from the magnetic field, use a plunger and ample buffer to vigorously flush out all labeled cells. Ensure the column is not clogged.
- Cause: Cell loss during pre-sort washing and centrifugation steps.
- Solution: Use low-protein-binding tubes and filter pipette tips. Avoid excessive centrifugation force and resuspend pellets gently but thoroughly.
Experimental Protocols
Detailed Protocol: Depleting Residual hPSCs via MACS
This protocol uses negative selection to remove undifferentiated hPSCs (marked by SSEA-4 and TRA-1-60) from a differentiated cell population, sparing the target therapeutic cells.
Materials:
- Differentiated Cell Suspension: A single-cell suspension of your hPSC-derived product.
- MACS Microbeads: Anti-SSEA-4 and Anti-TRA-1-60 MicroBeads (or a cocktail).
- MACS Buffer: D-PBS, pH 7.2, supplemented with 0.5% BSA and 2 mM EDTA.
- MACS Separator & Columns: Choose a column (e.g., LS Columns) based on the total cell number.
- Cell Culture Reagents: D-PBS, ACCUTASE or a suitable cell dissociation reagent, and recovery culture medium with ROCK inhibitor.
Procedure:
- Prepare Cell Suspension: Create a single-cell suspension from your differentiated culture using ACCUTASE. Wash cells once with MACS buffer and pass them through a 30-40 µm pre-separation filter to remove cell clumps.
- Count Cells: Perform a viable cell count using Trypan Blue exclusion.
- Label with Microbeads: Resuspend up to 10^7 cells in 90 µL of cold MACS buffer. Add 10 µL of each anti-SSEA-4 and Anti-TRA-1-60 MicroBeads. Mix well and incubate for 15 minutes in the refrigerator (2-8°C).
- Wash Cells: Add 1-2 mL of MACS buffer, centrifuge at 300 x g for 5 minutes, and decant the supernatant.
- Prepare MACS Column: Place the column in the magnetic field of the MACS Separator. Rinse the column with 3 mL of MACS buffer.
- Apply Cell Suspension: Resuspend the cell pellet in 500 µL to 1 mL of MACS buffer. Apply the cell suspension onto the column. Collect the unlabeled, flow-through fraction (this is your hPSC-depleted product).
- Wash Column: Add 3 x 3 mL of MACS buffer to the column, collecting each wash with the flow-through fraction.
- Analyze and Culture: Count the cells in the flow-through. To assess depletion efficiency, analyze an aliquot of the pre-sort and post-sort populations by flow cytometry for pluripotency markers (e.g., OCT4). Plate the hPSC-depleted cells in recovery medium supplemented with Y-27632.
Detailed Protocol: Purging Residual hPSCs via FACS
This protocol provides high-purity depletion by using a combination of pluripotency surface markers and a viability dye.
Materials:
- Differentiated Cell Suspension: As described in the MACS protocol.
- Antibodies: Fluorescently-conjugated antibodies against hPSC markers (e.g., Anti-SSEA-5-PE, Anti-TRA-1-60-Alexa Fluor 647).
- Viability Dye: e.g., DAPI or Propidium Iodide (PI).
- FACS Buffer: D-PBS with 1-2% FBS or BSA.
- FACS Sorter: A sorter capable of detecting the chosen fluorophores.
Procedure:
- Prepare Single-Cell Suspension: Follow steps 1 and 2 from the MACS protocol.
- Stain for Viability: Resuspend cells in FACS buffer containing a viability dye (e.g., 1 µg/mL DAPI) and incubate for 5-10 minutes on ice.
- Stain with Antibodies: Add the fluorescently-labeled antibodies against hPSC surface markers. Incubate for 20-30 minutes on ice in the dark.
- Wash and Resuspend: Wash cells twice with FACS buffer to remove unbound antibody. Finally, resuspend cells in FACS buffer at a concentration suitable for sorting (e.g., 5-10 x 10^6 cells/mL). Pass the suspension through a cell strainer snap cap.
- Set Up FACS Sorter:
- Use unstained cells and single-color controls to set up compensation and photomultiplier tube (PMT) voltages.
- Create a scatter gate (FSC-A vs. SSC-A) to exclude debris.
- Create a single-cell gate (FSC-H vs. FSC-A) to exclude doublets.
- Create a viability gate to exclude DAPI-positive (dead) cells.
- Finally, create a sort gate that excludes the cells positive for the pluripotency surface markers (SSEA-5, TRA-1-60).
- Sort and Collect: Sort the viable, marker-negative population into a tube containing collection medium. Keep collected cells on ice.
- Post-Sort Analysis and Culture: Perform a post-sort analysis of the collected fraction to confirm purity. Plate the cells in recovery medium with Y-27632.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for hPSC Purging
| Reagent / Kit | Function | Application Note |
|---|---|---|
| ROCK Inhibitor (Y-27632) | Improves survival of dissociated hPSCs; reduces apoptosis. | Critical for enhancing cell viability after FACS/MACS sorting. Add to culture medium before and after sorting [36] [37]. |
| ACCUTASE | Enzyme blend for gentle cell dissociation. | Generates high-quality single-cell suspensions from hPSC cultures, essential for accurate sorting [35] [37]. |
| MACS Microbeads & Columns | Magnetic beads and separation columns for MACS. | Ideal for rapid, high-throughput depletion of residual hPSCs. The CliniMACS system is designed for clinical-scale processing [34]. |
| hPSC Surface Marker Antibody Panels | Antibodies for markers like SSEA-5, TRA-1-60, EpCAM. | Used for immunophenotyping and sorting live hPSCs. Kits are available for characterization, but fixation-free antibodies are needed for sorting [35]. |
| Annexin V Apoptosis Detection Kits | Detects apoptotic cells early in the cell death process. | Useful for troubleshooting and quantifying apoptosis-induced cell death after the sorting process. |
| Defined Culture Media (e.g., E8, StemFlex) | Chemically defined media for hPSC maintenance. | Provides a consistent environment for culturing cells pre- and post-sort, reducing variability [36]. |
Safety Validation: Assessing Purging Efficiency
After performing FACS or MACS, it is crucial to validate the efficiency of hPSC depletion. The following workflow outlines the key methods used for safety validation, progressing from in vitro checks to more stringent in vivo testing.
Validation Workflow for hPSC Depletion
- Flow Cytometry: Re-analyze the sorted cell population for the same pluripotency surface markers used for sorting. This provides a direct measure of marker-positive cell reduction [38] [35].
- qPCR/dPCR: Use quantitative PCR (qPCR) or more sensitive digital PCR (dPCR) to detect RNA transcripts of core pluripotency factors (e.g., OCT4, NANOG). This method has superior detection sensitivity and is suitable for quality control [10].
- Highly Efficient Culture (HEC) Assay: This in vitro assay tests the functional capacity of any residual hPSCs to form colonies under conditions that favor pluripotent cell growth. It is a highly sensitive functional test for residual undifferentiated cells [10].
- In Vivo Teratoma Assay: The gold standard test. The final cell product is transplanted into immunodeficient mice (e.g., NSG or NOG mice), which are monitored for teratoma formation over an extended period (e.g., 12-20 weeks). The absence of tumors provides the highest confidence in product safety [10] [23].
Overcoming Assessment Challenges: Limitations of Traditional Teratoma Assays and Modern Solutions
Critical Limitations of In Vivo Teratoma Assays in Immunocompromised Mice
Frequently Asked Questions
FAQ 1: What are the primary limitations of the in vivo teratoma assay for assessing pluripotency and tumorigenicity?
The in vivo teratoma assay, historically considered the "gold standard" for assessing pluripotent stem cell (PSC) pluripotency and tumorigenicity, faces several critical limitations [39] [40]:
- Ethical and Resource Concerns: The assay is labor-intensive, time-consuming, costly, and raises ethical issues due to its reliance on animal models [39] [40].
- Lack of Standardization: There is significant variation in how the assay is conducted between different laboratories. Key variables like the immunodeficient mouse strain used, the site of cell injection (e.g., subcutaneous, kidney capsule), the number of cells injected, and the duration of the experiment are not standardized, which can impact the reliability and reproducibility of the results [39] [40].
- Qualitative and Subjective Readouts: The assessment primarily relies on qualitative histological examination to identify tissues from the three germ layers. This introduces subjectivity and makes it difficult to perform quantitative comparisons between different PSC lines [39].
- Limited Sensitivity in Clinically Relevant Models: While the assay can be highly sensitive in optimized conditions (e.g., with specific injection sites and extracellular matrix supports), its sensitivity drops significantly when using clinical-grade cell formulations and transplantation sites. This limits its predictive value for actual therapeutic scenarios [10] [41].
- Questionable Predictive Value for Human Immune Response: The assay is performed in immunodeficient mice, which lack a functional immune system to reject the human cells. This may overstate the tumorigenic risk in human patients who have competent immune systems [42]. Research shows that even using "humanised" mice with a reconstituted human immune system does not increase the assay's sensitivity, indicating that the immunodeficient mouse model itself may not accurately represent the human clinical situation [42].
FAQ 2: What are the key protocol variations in the teratoma assay that affect its outcome and reliability?
The teratoma assay lacks a universal standard operating procedure, and multiple protocol variables are known to influence the formation and composition of teratomas, leading to inter-laboratory inconsistencies [39] [41].
Table: Key Protocol Variables in the Teratoma Assay and Their Impact
| Protocol Variable | Common Variations | Impact on Assay Outcome |
|---|---|---|
| Mouse Strain | NOD/SCID, NSG, NOG, others [10] [42] | Degree of immunodeficiency affects engraftment success and tumor growth rate [10]. |
| Injection Site | Subcutaneous, Intramuscular, Kidney Capsule, Testis [39] [41] | The kidney capsule is often reported as the most sensitive site, while subcutaneous is less sensitive [41]. |
| Cell Preparation | Co-injection with Matrigel, single-cell suspension vs. clusters [41] | The use of Matrigel can significantly enhance teratoma formation efficiency, potentially skewing sensitivity estimates [41]. |
| Injected Cell Number | Wide range reported (e.g., 10^5 to 10^7 cells) [40] | Higher cell numbers can force teratoma formation, potentially masking subtle differences in pluripotent strength [39]. |
| Assay Duration | Typically 8-20 weeks, but highly variable [40] | Insufficient time may not allow for full differentiation and teratoma development, complicating data interpretation [39]. |
FAQ 3: What in vitro alternatives are available to replace or supplement the in vivo teratoma assay?
Driven by the need for more robust, scalable, and ethical testing methods, as well as the 3R principles (Replacement, Reduction, and Refinement of animal use), several in vitro assays have been developed [10] [39] [41]. These can be broadly categorized as follows:
- Molecular Methods: These techniques detect residual undifferentiated PSCs by targeting specific molecules highly expressed in the pluripotent state.
- Digital PCR (dPCR): Used to detect PSC-specific RNA markers (e.g., LIN28A). It is highly sensitive and robust, capable of detecting very low levels of residual PSCs, and is suitable for quantitative quality control [10] [41].
- Flow Cytometry: Detects PSC-specific surface proteins (e.g., SSEA-4, TRA-1-60). While rapid, its sensitivity is generally lower than molecular methods like dPCR [41].
- Functional/Culture-Based Methods: These assays test the functional capacity of residual PSCs to proliferate.
- Highly Efficient Culture (HEC) Assay: This method places the cell therapy product in a culture condition that selectively promotes the expansion of any residual undifferentiated PSCs. The resulting colonies are then stained (e.g., for Alkaline Phosphatase) and counted. It is highly sensitive and does not rely on a single specific marker [10] [41].
- Bioinformatic Tools: Tools like PluriTest (assesses pluripotency based on transcriptomic data) and ScoreCard (assesses differentiation potential into the three germ layers) can be used for initial line characterization, though they may not be universally accepted by regulatory bodies for final safety assessment [39] [40].
Table: Comparison of Key In Vitro Alternatives to the Teratoma Assay
| Method | Target | Key Advantage | Key Disadvantage | Reported Sensitivity |
|---|---|---|---|---|
| In Vivo Teratoma Assay | Functional pluripotency & malignancy | Provides histological data on complex tissue formation [39] | Low throughput, costly, variable, ethical concerns [40] | Varies widely with protocol (e.g., ~0.0002% in optimized models) [41] |
| Digital PCR (dPCR) | PSC-specific RNA (e.g., LIN28A) | High sensitivity, quantitative, robust [10] | Marker may not be universal for all cell types [41] | Very high; more sensitive than most in vivo models [10] |
| Highly Efficient Culture (HEC) | Functional proliferation of residual PSCs | Does not depend on a single marker; highly sensitive [10] | Longer duration (e.g., 7 days); may not suit all products [41] | Very high; can detect 0.0005% spiked PSCs [41] |
| Flow Cytometry | PSC-specific surface markers | Fast and relatively inexpensive [41] | Lower sensitivity compared to dPCR and HEC [41] | Lower than dPCR and HEC [41] |
FAQ 4: What are the current regulatory and industry perspectives on moving away from the in vivo assay?
There is a growing consensus within the scientific and regulatory communities that validated in vitro assays should be prioritized. The Health and Environmental Sciences Institute's International Cell Therapy Committee recommends that with a properly validated and highly sensitive in vitro method (like dPCR or HEC), in vitro assays can replace in vivo assays for evaluating the teratoma formation risk of PSC-derived cell therapy products [10] [41]. International multi-center studies are underway to standardize and validate these in vitro methods, aiming for globally harmonized procedures [10]. However, it is important to note that for now, regulatory authorities may still require in vivo data for the final safety assessment of clinical products, particularly to assess malignancy risk, for which in vitro assays are still in development [40] [42].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents and Models for Teratoma Risk Assessment Research
| Reagent / Model | Function / Application | Key Considerations |
|---|---|---|
| NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) Mice | The most commonly used immunodeficient model for the in vivo teratoma assay [42]. | Provides a highly immunocompromised environment for efficient engraftment of human cells. However, it may overestimate tumorigenic risk [42]. |
| Matrigel | Basement membrane extract. Often co-injected with cells to enhance engraftment and teratoma formation efficiency [41]. | Improves assay sensitivity but is a variable biological product and its use may not reflect clinical delivery methods [41]. |
| AP20187 (AP20) | A small molecule dimerizer drug used to activate the inducible Caspase 9 (iCasp9) suicide gene system [2]. | Used in engineered safeguard systems to selectively eliminate undifferentiated PSCs in vitro or ablate the entire cell product in vivo in case of adverse events [2]. |
| YM155 | A small molecule inhibitor of Survivin (BIRC5) [12]. | Can be used to selectively kill undifferentiated PSCs that highly depend on Survivin for survival. However, its specificity must be verified as it can sometimes be toxic to differentiated progeny [12] [2]. |
| Anti-SSEA-4 / TRA-1-60 Antibodies | Antibodies for detecting pluripotency-associated surface markers via flow cytometry or immunocytochemistry [12] [2]. | Useful for qualitative assessment of pluripotent state, but expression can be downregulated rapidly upon differentiation and sensitivity for residual cell detection is limited [41]. |
| LIN28A Assay Primers | Primers for qPCR or dPCR to detect PSC-specific RNA expression [10] [41]. | LIN28A is a commonly used marker for sensitive molecular detection of residual PSCs, though its applicability across all differentiated cell types should be confirmed [41]. |
Experimental Pathways and Workflows
The following diagrams illustrate the core concepts and experimental strategies discussed in this guide.
Diagram 1: Multifaceted Limitations of the In Vivo Teratoma Assay
Diagram 2: Orthogonal Safeguard Strategy for Cell Therapy Safety
This diagram outlines a genome-editing approach to incorporate two independent safety switches directly into pluripotent stem cells, addressing two major risks of cell therapy [2].
Teratoma formation represents one of the most significant safety concerns in pluripotent stem cell (PSC)-derived therapies. As the field advances toward clinical applications, addressing variability through standardized protocols and reporting has become increasingly critical. Current regulatory frameworks require rigorous safety assessments, but the lack of harmonized methods can lead to inconsistent risk evaluation across different laboratories and product development programs [10] [15]. This technical support center provides actionable guidance and troubleshooting resources to help researchers implement robust, standardized approaches for teratoma risk assessment.
FAQs: Teratoma Risk Assessment
What are the key limitations of traditional in vivo teratoma assays?
Traditional in vivo tumorigenicity assays, which involve transplanting cells into immunodeficient mice, present several significant limitations:
- Translational relevance concerns: These models assume human cells will behave similarly in animal hosts as in the human physiological environment, which may not accurately predict clinical behavior [15].
- Variable sensitivity: Detection sensitivity can be inconsistent across different laboratories and animal models [10].
- Lengthy duration: These assays typically require extended timeframes (weeks to months) to obtain results [10].
- Ethical considerations: The use of large numbers of animals raises ethical concerns and aligns with efforts to implement the 3Rs (Replacement, Reduction, and Refinement) in research [10].
Which emerging in vitro methods offer superior sensitivity for detecting residual undifferentiated hPSCs?
Emerging in vitro technologies demonstrate significantly enhanced detection capabilities for residual undifferentiated human pluripotent stem cells (hPSCs):
| Method | Reported Sensitivity | Key Advantages |
|---|---|---|
| Digital PCR (dPCR) for hPSC-specific RNA | Superior to conventional methods | High sensitivity and reproducibility; enables absolute quantification of target sequences [10] [15] |
| Highly Efficient Culture (HEC) Assay | Superior to conventional methods | Exceptional sensitivity for detecting rare undifferentiated cells through optimized culture conditions [10] [15] |
| Flow Cytometry with Specific Lectins | Varies with markers used | Allows detection of pluripotency-associated surface markers; requires validated antibody panels [10] |
Multi-site validation studies have demonstrated that these in vitro approaches provide significantly greater sensitivity and reproducibility compared to traditional in vivo methods [15].
What are the essential elements for validating in vitro assays for teratoma risk assessment?
When implementing in vitro assays for product quality control, several key validation parameters must be addressed:
- Limit of Detection (LOD): Establish the minimum number of undifferentiated hPSCs that can be reliably detected in a background of differentiated cells [10].
- Specificity: Demonstrate the assay does not cross-react with differentiated cell types present in the final product [10].
- Robustness and Reproducibility: Validate performance across different operators, equipment, and days [10].
- Standardized Reference Materials: Use well-characterized hPSC lines as positive controls to enable cross-laboratory comparisons [10].
Troubleshooting Guides
Problem: Inconsistent Results in Teratoma Risk Assessment Between Laboratories
Potential Causes and Solutions:
| Issue | Root Cause | Solution |
|---|---|---|
| Variable assay sensitivity | Differing experimental protocols and acceptance criteria | Implement standardized protocols from recognized organizations like ISSCR and HESI [5] [15] |
| Lack of reference materials | No common positive controls for assay calibration | Establish well-characterized hPSC lines as reference standards for cross-laboratory comparison [10] |
| Inadequate reporting | Missing critical methodological details | Adhere to ISSCR Standards for reporting basic characterization, pluripotency, and genomic information [6] [43] |
Problem: Poor Detection Sensitivity for Residual Undifferentiated hPSCs
Troubleshooting Steps:
- Verify assay detection limits using spiking experiments with known numbers of hPSCs in differentiated cell populations [10].
- Implement orthogonal methods to confirm results (e.g., combine molecular and cellular detection approaches) [10].
- Optimize sample preparation to ensure representative sampling and avoid cell loss during processing [10].
- Validate with appropriate controls including known positive and negative samples in each assay run [10].
Experimental Protocols for Teratoma Risk Assessment
Highly Efficient Culture (HEC) Assay for Detecting Residual Undifferentiated hPSCs
Principle: This method uses optimized culture conditions to maximize the proliferation potential of residual undifferentiated hPSCs, enabling detection of very rare cells within a differentiated cell population.
Materials:
- Test article (hPSC-derived cell product)
- Appropriate hPSC culture medium (e.g., StemFlex, mTeSR1, or E8) [44]
- Rho kinase inhibitor (Y-27632) for enhanced cell survival [44]
- Matrigel-coated or feeder-dependent culture vessels
- Positive control (known number of hPSCs)
- Negative control (fully differentiated cells)
Procedure:
- Sample Preparation: Dissociate the cell product to single cells using Accutase or similar enzyme solution [44].
- Plating: Plate cells at multiple densities in hPSC culture conditions supplemented with Rho kinase inhibitor.
- Culture Maintenance: Culture for 14-21 days with regular medium changes every 24-48 hours.
- Colony Identification: Monitor for emergence of hPSC colonies characterized by compact morphology, high nucleus-to-cytoplasm ratio, and distinct colony edges.
- Characterization: Confirm pluripotency of colonies through staining for markers like TRA-1-60, TRA-1-81, or SSEA-4 [10].
- Quantification: Calculate the frequency of undifferentiated hPSCs based on colony numbers and initial plating density.
Troubleshooting Note: If no colonies are detected, verify assay sensitivity by spiking with a low number (10-100) of hPSCs into differentiated cells to confirm detectability.
Digital PCR (dPCR) Protocol for hPSC-Specific Markers
Principle: dPCR partitions samples into thousands of individual reactions, enabling absolute quantification of rare hPSC-specific transcripts without standard curves.
Materials:
- RNA extracted from cell product
- dPCR system and compatible reagents
- Primers/probes for hPSC-specific markers (e.g., NANOG, POUSF1)
- Reverse transcription kit
- Nuclease-free water and tubes
Procedure:
- RNA Extraction: Isolate high-quality RNA from the test sample using validated methods.
- cDNA Synthesis: Convert RNA to cDNA using reverse transcriptase with random hexamers and/or gene-specific primers.
- Reaction Setup: Prepare dPCR reaction mix according to manufacturer's instructions.
- Partitioning: Load samples into dPCR chip or cartridge for partitioning.
- Amplification: Run amplification protocol with appropriate cycling conditions.
- Analysis: Quantify positive and negative partitions to calculate absolute copy numbers of target transcripts.
Validation: Establish limit of detection (LOD) and limit of quantification (LOQ) using serial dilutions of hPSC RNA in differentiated cell RNA.
Research Reagent Solutions
Essential materials and tools for standardized teratoma risk assessment:
| Reagent/Tool | Function | Examples/Specifications |
|---|---|---|
| StemRNA Clinical iPSC Seed Clones | Standardized starting material for consistent results | GMP-compliant, comprehensive regulatory documentation [3] |
| Pluripotency Markers | Detection of undifferentiated hPSCs | TRA-1-60, SSEA-4, NANOG, POUSF1 [10] [2] |
| CRISPRa Systems (e.g., SAM-TET1) | Verification of silent gene reporters | Enables rapid validation without cell state transitions; available through Addgene [44] |
| Defined Culture Media | Consistent maintenance of hPSCs | StemFlex, mTeSR1, E8 medium [44] |
| Genetic Safeguards | Inducible safety switches for PSC-derived therapies | NANOG-iCaspase9 system for selective ablation of undifferentiated hPSCs [2] |
Teratoma Risk Assessment Workflow
Genetic Safety Switch Mechanism
Implementing standardized protocols and reporting frameworks is essential for advancing safe PSC-based therapies. By adopting consensus recommendations from organizations like HESI and ISSCR, utilizing sensitive in vitro assays, and incorporating genetic safeguards where appropriate, researchers can significantly reduce variability in teratoma risk assessment [10] [5] [15]. These approaches not only enhance product safety but also facilitate regulatory evaluation and accelerate the development of much-needed regenerative therapies.
Enhancing Detection Sensitivity for Rare Residual Undifferentiated Cells
Frequently Asked Questions (FAQs)
1. What are the key markers for identifying residual undifferentiated pluripotent stem cells? Residual undifferentiated human pluripotent stem cells (hPSCs) are typically identified using specific pluripotency markers. Key intracellular transcription factors include OCT4 (POU5F1) and NANOG, which are essential for maintaining self-renewal and pluripotency [45]. Important cell surface markers comprise SSEA-4 (Stage-Specific Embryonic Antigen-4) and TRA-1-60 (Tumor-related antigen 1-60), which are downregulated upon differentiation [12] [45]. The expression of these markers must be tightly linked to the pluripotent state for accurate detection [2].
2. Why is detecting rare residual undifferentiated cells critical for therapy development? Detecting these cells is paramount for patient safety. hPSCs are intrinsically tumorigenic, and even a small number of residual undifferentiated cells (as few as 10,000) can lead to teratoma formation after transplantation [12] [2] [11]. Teratomas are tumors that can contain tissues from all three germ layers. Therefore, rigorous assessment and mitigation of this risk are prerequisites for clinical application, with some studies suggesting a need for a greater than 1-million-fold (6-log) depletion of hPSCs to ensure safety in a billion-cell product [2].
3. What are the advantages of in vitro assays over in vivo teratoma assays for detection? Traditional in vivo teratoma assays, which involve injecting cells into immunodeficient mice and monitoring for tumor formation, are time-consuming (taking weeks to months), expensive, and low-throughput. Modern in vitro assays, such as highly efficient culture assays and digital PCR (dPCR) for hPSC-specific RNA, offer superior detection sensitivity, faster results, and are more suitable for quality control in a manufacturing setting [11].
4. How can I improve the sensitivity of my flow cytometry assay for rare cell detection? Improving flow cytometry sensitivity for rare event analysis involves several strategic considerations:
- Antigen Density Matching: Pair bright fluorophores with low-abundance (scarce) antigens and dimmer fluorophores with highly expressed antigens to prevent signal masking [46].
- Cell Enrichment: Use pre-enrichment techniques, such as magnetic-activated cell sorting (MACS) with antibody-conjugated beads, to increase the relative concentration of the target rare cell population before flow analysis [46].
- Panel Design: Utilize tools like fluorescence spectral viewers to minimize spectral overlap and design panels that allow for clear discrimination of multiple markers [46].
5. Are there non-invasive methods for monitoring pluripotent stem cell cultures? Yes, label-free imaging approaches combined with machine learning (AI) are emerging as powerful non-invasive tools. These methods use bright-field microscopy images of live cells to predict the expression of pluripotency markers like OCT4 and NANOG. Deep learning models (e.g., Bright2Nuc) can analyze these images to infer cell states, track differentiation, and segment nuclei without the need for fluorescent staining, which can be cytotoxic and requires cell fixation [47] [45].
Troubleshooting Guides
Problem: Low Sensitivity in Detecting Residual Pluripotent Cells
Potential Causes and Solutions:
Cause: Inadequate Marker Specificity
- Solution: Validate the specificity of your markers across differentiated cell types. Some historically used markers (e.g., survivin) are also expressed in differentiated progeny. NANOG has been shown to be one of the most specific transcription factors for the pluripotent state, sharply downregulating within 24-48 hours of differentiation [2].
- Action: Consider implementing a genetic safety switch (e.g., NANOG-promoter driven iCaspase9) that not only detects but also selectively eliminates undifferentiated cells upon addition of a small molecule inducer (AP20187), achieving over 1-million-fold depletion [2].
Cause: Insufficient Limit of Detection (LOD) in Current Assay
- Solution: Transition to more sensitive analytical techniques. The table below compares common methods.
| Method | Key Principle | Reported Sensitivity | Advantages | Disadvantages |
|---|---|---|---|---|
| In Vivo Teratoma Assay | Cell injection into immunodeficient mice; tumor monitoring [12] [11] | ~10,000 cells [2] | Gold standard for functional tumorigenicity | Low-throughput, long duration (weeks-months), expensive [11] |
| Flow Cytometry | Antibody-based detection of surface/intracellular markers [12] [48] | Varies (e.g., 0.1-1%) | Quantitative, multi-parameter | Sensitivity limited by sample size; requires specific markers [46] |
| Digital PCR (dPCR) | Absolute quantification of hPSC-specific RNA/DNA targets without a standard curve [11] | Superior sensitivity [11] | High sensitivity, precise, reproducible | Requires known target sequences |
| Highly Efficient Culture Assay | In vitro culture under conditions that favor hPSC outgrowth [11] | Superior sensitivity [11] | Highly sensitive, in vitro format | May not detect all pluripotent states |
Problem: High Background or Poor Viability in Flow Cytometry
Potential Causes and Solutions:
Cause: Suboptimal Fluorophore Selection
- Solution: Adhere to best practices for fluorophore selection. Match fluorophore brightness to antigen density. Ensure the fluorophore's excitation/emission maxima are compatible with your cytometer's lasers and detectors. Utilize tools like spectral viewers to manage Stokes shift and avoid spectral overlap in multi-parameter panels [46].
- Action: For intracellular staining of transcription factors (e.g., OCT4, NANOG), ensure fixation and permeabilization protocols are rigorously optimized to preserve epitopes and cell integrity [46].
Cause: Cytotoxicity from Staining or Imaging
- Solution: For long-term or repeated monitoring, adopt label-free imaging technologies. Using bright-field microscopy and AI models eliminates the need for fluorescent stains, reducing phototoxicity and preserving cell viability for subsequent therapeutic use [45].
Advanced Workflow: Integrating Detection and Purging
For comprehensive risk mitigation, a robust workflow integrates sensitive detection with effective purging strategies. The following diagram illustrates the logical decision pathway for ensuring cell product safety.
Research Reagent Solutions
This table details key reagents and their functions in the detection and mitigation of residual undifferentiated cells.
| Reagent / Tool | Function / Target | Key Application Note |
|---|---|---|
| Anti-SSEA-4 / TRA-1-60 Antibodies | Binds to surface glycans on hPSCs [12] [45] | Used in flow cytometry or immunostaining for identification and quantification of undifferentiated cells. |
| Anti-OCT4 / NANOG Antibodies | Binds to core pluripotency transcription factors [45] | Requires cell permeabilization for intracellular staining. Essential for validating pluripotent state. |
| YM155 | Small molecule inhibitor of Survivin (BIRC5) [12] | Efficiently kills hPSCs; showed less toxicity on CD34+ hematopoietic stem cells compared to suicide gene prodrugs in one study [12]. |
| iCaspase-9 / AP20187 System | Genetically encoded "safety switch"; AP20187 induces dimerization and apoptosis [12] [2] | When driven by a pluripotency-specific promoter (e.g., NANOG), can achieve >10^6-fold depletion of hPSCs [2]. |
| Bright2Nuc (AI Model) | Predicts nuclear staining from bright-field images [47] | Enables label-free, non-invasive tracking of cell state and nuclei in 3D cultures, reducing analytical cell loss. |
Integrating Quality-by-Design Principles into Manufacturing Processes
FAQs: QbD Core Principles and Application
What is Quality-by-Design (QbD) and why is it critical for stem cell therapy? Quality-by-Design is a systematic, risk-based approach to development that begins with predefined objectives and emphasizes product and process understanding and control [49]. It aims to build quality into the product and process from the beginning, rather than relying solely on end-product testing [50]. For pluripotent stem cell therapies, this is paramount for preventing teratoma formation, as it ensures process consistency and identifies critical parameters controlling undifferentiated cell populations.
How does QbD differ from traditional quality assurance methods? Traditional quality assurance often relies on fixed processes and end-product testing (quality by testing). QbD shifts the focus to building quality in during the design and development stages. It uses statistical, analytical, and risk-management methodologies to understand and control the manufacturing process, ensuring the finished medicine consistently meets its predefined quality characteristics [50] [51]. This proactive approach is essential for managing the complexity and variability inherent in living cell products.
Which regulatory guidelines support the implementation of QbD? The International Council for Harmonisation (ICH) guidelines provide the primary framework:
- ICH Q8 (R2): Pharmaceutical Development
- ICH Q9: Quality Risk Management
- ICH Q10: Pharmaceutical Quality System
- ICH Q11: Development and Manufacture of Drug Substances [49] [50] [51] Regulatory agencies like the EMA and FDA encourage applications that include QbD elements [50].
FAQs: QbD Implementation for Teratoma Prevention
What are the key QbD elements for a pluripotent stem cell therapy process? A QbD framework consists of several key elements applied iteratively [49]:
- Quality Target Product Profile (QTPP): A prospective summary of the quality characteristics of the drug product.
- Critical Quality Attributes (CQAs): Physical, chemical, biological, or microbiological properties or characteristics that must be within an appropriate limit, range, or distribution to ensure the desired product quality.
- Critical Material Attributes (CMAs) & Critical Process Parameters (CPPs): Material and process parameters that must be controlled to ensure the CQAs are met.
- Control Strategy: A set of controls derived from current understanding of the product and process, ensuring process performance and product quality.
- Process Capability & Continual Improvement: Ongoing monitoring and refinement to increase process capability and reduce variability.
How is a QTPP defined for a therapy targeting teratoma prevention? The Quality Target Product Profile (QTPP) is the foundation of development, outlining the desired quality characteristics of the final therapy based on safety and efficacy needs [49]. For a therapy aiming to prevent teratoma formation, the QTPP would include specific safety-related targets.
Table: Example QTPP for a Pluripotent Stem Cell-Based Therapy
| QTPP Element | Target | Rationale for Teratoma Prevention |
|---|---|---|
| Dosage Form | Suspension for injection | Suitable for targeted delivery. |
| Route of Administration | Localized (e.g., intramuscular, intraocular) | Limits systemic exposure of cells. |
| Dosage Strength | X million viable cells/dose | Established as efficacious with minimal teratoma risk. |
| Purity (Viable Cell Fraction) | ≥ 90% | Ensures consistent dosing and process control. |
| Product-Specific Purity (Residual Undifferentiated Cells) | ≤ 0.01% | Critical safety CQA to directly minimize teratoma risk. |
| Potency (Functional Marker Expression) | ≥ Y units | Ensures therapeutic cells are properly differentiated and functional. |
| Container Closure System | Pre-filled, cryogenic vial | Maintains cell viability and sterility. |
What CQAs are most critical for mitigating teratoma risk? A CQA is critical if falling outside its acceptable limit poses a significant risk to patient safety [49]. The most relevant CQAs for teratoma prevention are:
- Residual Undifferentiated Cell Count: The proportion of pluripotent cells remaining in the final product is a direct measure of teratoma risk.
- Potency: A measure of the desired biological function of the differentiated cell population. A high potency indicates successful differentiation away from a pluripotent, tumorigenic state.
- Identity/Purity of Target Differentiated Cell Population: Specific markers confirming the presence of the desired, terminally differentiated cell type and the absence of other lineages.
- Viability: Impacts both efficacy and safety, as non-viable cells can cause inflammatory reactions.
Troubleshooting Guides
Problem: High Variability in Residual Undifferentiated Cell Levels Between Batches
Potential Root Causes:
- Inconsistent raw materials (e.g., growth factors, differentiation inductors).
- Uncontrolled critical process parameters during differentiation.
- Inadequate in-process monitoring and control.
Investigational Experiments and Protocols:
Table: Experiment to Identify CPPs Affecting Residual Pluripotent Cells
| Factor | Low Level | High Level | CQA Measured |
|---|---|---|---|
| Concentration of Differentiation Factor A | 10 ng/mL | 50 ng/mL | % Pluripotency Marker (e.g., OCT4) |
| Duration of Differentiation Phase 1 | 72 hours | 120 hours | % Target Differentiated Cell Marker |
| Cell Seeding Density | 0.5 x 10^5/cm² | 2.0 x 10^5/cm² | Viability, % Pluripotency Marker |
| Experiment Design: | A Design of Experiment (DoE) approach, such as a Full or Fractional Factorial design, should be used to efficiently study these factors and their interactions [49] [52]. |
Protocol 1: DoE for Process Optimization
- Define Factors and Ranges: Based on prior knowledge and risk assessment, select process parameters (like those above) and their realistic operating ranges.
- Generate DoE Matrix: Use statistical software to create an experimental run list.
- Execute Runs: Perform the differentiation process according to the DoE matrix.
- Analyze CQAs: For each run, measure the CQAs (e.g., % pluripotency markers via flow cytometry).
- Statistical Analysis: Build a model to identify which factors (CPPs) and interactions significantly impact the CQAs. Establish a "design space" [49].
Solution: Based on the DoE results, refine the process and establish a control strategy. This may include:
- Tightening acceptance criteria on raw materials (CMAs) [49].
- Defining proven acceptable ranges for the identified CPPs (e.g., Differentiation Factor A concentration: 30-40 ng/mL).
- Implementing in-process checks (e.g., monitor a differentiation marker at a key step) as part of a Process Analytical Technology (PAT) strategy [49] [50].
Problem: Low Potency and Incomplete Differentiation
Potential Root Causes:
- Inadequate or unstable differentiation signals.
- Unoptimized cell culture environment (e.g., substrate, media components).
- Underlying genetic instability of the pluripotent stem cell line.
Investigational Experiments and Protocols:
Protocol 2: Characterization of Differentiation Efficiency
- Flow Cytometry: Harvest cells at the end of the differentiation process. Stain cells with antibodies against pluripotency markers (e.g., OCT4, NANOG), early progenitor markers, and terminal differentiation markers. This provides a quantitative profile of the cell population.
- qPCR Analysis: Measure the expression levels of pluripotency and differentiation marker genes relative to a housekeeping gene. This sensitive technique can detect low levels of undifferentiated cells.
- Functional Assay: Perform an assay specific to the target cell type's function (e.g., glucose-stimulated insulin secretion for beta cells, electrophysiology for cardiomyocytes).
- In Vivo Teratoma Assay: The gold standard for safety. Inject a sample of the final product into immunocompromised mice (e.g., NOG/SCID) and monitor for tumor formation over 12-20 weeks. This validates the findings from your in vitro assays.
Solution:
- Re-evaluate and optimize the differentiation protocol, focusing on the timing and concentration of key morphogens.
- Ensure the use of qualified, consistent raw materials (CMAs).
- Implement the functional assay and a surrogate marker (e.g., via flow cytometry) as part of the potency release test for the final product.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for QbD-Driven Stem Cell Process Development
| Item | Function in Teratoma Prevention | Example(s) |
|---|---|---|
| Pluripotency Markers | Quantify residual undifferentiated cells; define a CQA. | Antibodies against OCT4, SOX2, NANOG (for flow cytometry/immunocytochemistry). |
| Differentiation Markers | Confirm successful differentiation; define identity/purity CQAs. | Antibodies against target cell-specific proteins (e.g., TUJ1 for neurons, MHC for cardiomyocytes). |
| Defined Culture Media | Provides consistent, reproducible differentiation signals; a key CMA. | Commercially available, serum-free differentiation kits or custom formulations. |
| Growth Factors & Small Molecules | Directs cell fate away from pluripotency; critical CMAs. | Recombinant proteins (BMP, FGF, Activin A), small molecule inhibitors (e.g., CHIR99021). |
| Cell Selection Kits | Physically remove residual undifferentiated cells. | Magnetic-activated cell sorting (MACS) or Fluorescence-activated cell sorting (FACS) kits for specific surface markers. |
Process Visualization
The following diagram illustrates the systematic QbD workflow for developing a stem cell therapy process with integrated risk control points for teratoma prevention.
Diagram Title: QbD Workflow for Teratoma Prevention
The following diagram outlines a high-level manufacturing process for a pluripotent stem cell therapy, highlighting critical control points where monitoring and control are essential to minimize teratoma risk.
Diagram Title: Stem Cell Manufacturing with Critical Controls
Advanced Safety Validation: Comparing In Vitro and In Vivo Assays for Teratoma Risk Assessment
Troubleshooting Guides
Digital PCR (dPCR) Troubleshooting
Problem: Inaccurate quantification or failed run
| Problem Category | Specific Issue | Potential Cause | Solution |
|---|---|---|---|
| Sample & Assay Setup | Sample not in "digital range" | Target concentration too high, leading to signal saturation [53] | Serially dilute the sample and re-run to ensure some partitions are positive and some are negative [54]. |
| Poor partitioning | Improper droplet generation or chip loading; presence of inhibitors or viscous samples [53] | Ensure sample is properly homogenized and free of particulates. Verify partitioning quality according to platform specifications. | |
| Data Analysis | Software threshold setting error | Automatic threshold incorrectly distinguishing positive and negative partitions [54] | Manually review and set the fluorescence threshold in the analysis software to correctly classify partitions [54]. |
| High variation between replicates | Inconsistent partition volume or poor technique [53] | Use calibrated equipment, ensure consistent pipetting technique, and create sufficient technical replicates. |
Problem: Low sensitivity for detecting rare undifferentiated cells
| Specific Issue | Potential Cause | Solution |
|---|---|---|
| Cannot detect low-level targets (e.g., <0.001% hiPSCs) | Insufficient number of partitions analyzed; suboptimal assay design [55] | Use a dPCR platform that generates a high number of partitions (e.g., >20,000 droplets). Validate assay using a spike-in experiment with known ratios of hiPSCs in differentiated cells [55]. |
| High background noise | Non-specific amplification or probe degradation [53] | Re-design primers/probes for greater specificity, particularly for the pluripotency marker (e.g., LIN28). Aliquot reagents to avoid freeze-thaw cycles. |
Highly Efficient Culture (HEC) Troubleshooting
Problem: Excessive spontaneous differentiation in hPSC cultures
| Problem Category | Specific Issue | Potential Cause | Solution |
|---|---|---|---|
| Culture Environment | Differentiation >20% | Culture medium is outdated or improperly prepared [13] | Ensure complete culture medium is less than 2 weeks old when stored at 2-8°C [13]. |
| Overgrowth of colonies or low colony density during passaging [13] | Passage cultures when colonies are large and dense but before they begin to differentiate in the center. Plate an even, optimal density of cell aggregates [13]. | ||
| Handling Technique | Culture plate out of incubator for extended periods [13] | Minimize time outside the incubator to less than 15 minutes at a time [13]. | |
| Passaging Process | Cell aggregates too large or too small | Incorrect incubation time or pipetting force with dissociation reagent [13] | For larger aggregates, increase incubation time by 1-2 minutes and pipette more. For smaller aggregates, decrease incubation time and minimize manipulation [13]. |
Problem: Low cell attachment or viability after passaging
| Specific Issue | Potential Cause | Solution |
|---|---|---|
| Significant cell death post-passage | Excessive scraping or harsh pipetting [13] | Use gentle, non-enzymatic passaging reagents and minimize scraping. Optimize pipetting to break colonies into small, uniform aggregates without creating single cells. |
| Poor attachment to culture vessel | Incorrect plate coating; matrix degradation | Ensure the use of non-tissue culture-treated plates with specific coatings like Vitronectin. Confirm that the coating solution is fresh and applied correctly [13]. |
Frequently Asked Questions (FAQs)
Q1: Why is digital PCR considered superior to qPCR for detecting residual undifferentiated stem cells in a therapeutic product? dPCR provides absolute quantification without needing a standard curve and is more resistant to PCR inhibitors, offering higher sensitivity and precision for rare target detection [53]. This is critical for teratoma risk prevention, as it can detect contamination levels as low as 0.001% hiPSCs (approximately 1 hiPSC in 100,000 cardiomyocytes) [55].
Q2: What is the most sensitive molecular target for detecting residual hiPSCs using dPCR? LIN28 mRNA is a highly sensitive and specific marker for undifferentiated hiPSCs. A ddPCR assay targeting LIN28 can robustly detect 0.001% undifferentiated hiPSCs mixed with hiPSC-derived cardiomyocytes, and LIN28 expression is negligible in most mature human tissues [55].
Q3: My hPSC cultures are prone to differentiation. What are the key factors to stabilize the culture? Maintaining culture stability requires attention to detail:
- Medium Quality: Use fresh, pre-warmed medium less than two weeks old [13].
- Passaging: Passage at the right confluence and generate evenly sized cell aggregates [13].
- Environmental Control: Minimize time outside the incubator and maintain stable temperature, humidity, and CO₂ levels [13].
- Routine Inspection: Manually remove any areas of spontaneous differentiation before passaging.
Q4: How can I physically remove undifferentiated cells from a differentiated cell population? While fluorescence-activated cell sorting (FACS) can be used to deplete cells expressing pluripotency surface markers (e.g., SSEA-4, TRA-1-60), the results can be variable and may affect the viability of the therapeutic HSC population [12]. The sensitivity and specificity of this method may be lower than genetic or pharmacological approaches.
Q5: Besides sensitive detection, what are other strategies to eliminate residual undifferentiated cells? Two main strategies are:
- Pharmacological Inhibition: Using small molecules like the survivin inhibitor YM155 can selectively kill undifferentiated hiPSCs without toxic effects on differentiated hematopoietic CD34+ cells, effectively preventing teratoma formation in vivo [12].
- Genetic "Safeguards": Genome editing can introduce drug-inducible "suicide genes" like iCaspase-9 under the control of a pluripotency-specific promoter (e.g., NANOG). Adding the dimerizer drug AP20187 activates caspase-9, selectively eliminating undifferentiated hPSCs with high efficiency (>10⁶-fold depletion) [2].
Sensitivity of Teratoma Prevention and Detection Methods
| Method | Target / Principle | Key Performance Metric | Reference |
|---|---|---|---|
| ddPCR (Detection) | LIN28 mRNA expression | Detection sensitivity of 0.001% hiPSCs in a differentiated cell population. | [55] |
| Survivin Inhibitor (Purging) | YM155, targets survivin (BIRC5) | Efficiently kills hiPSCs; no toxicity on CD34+ cells; fully eradicated teratoma formation in vivo. | [12] |
| NANOG-iCaspase9 (Purging) | Drug-inducible suicide gene under NANOG promoter | Depleted undifferentiated hPSCs by >1.75 million-fold; spare differentiated progeny. | [2] |
Experimental Protocols
Protocol 1: Detection of Residual Undifferentiated hiPSCs via Droplet Digital PCR
This protocol is adapted from a study demonstrating highly sensitive detection of residual hiPSCs in cardiomyocyte preparations [55].
1. Sample Preparation:
- Cell Mixing Experiment: Mix known numbers of undifferentiated hiPSCs with hiPSC-derived cardiomyocytes (or your target differentiated cell type) to create a standard curve (e.g., 1%, 0.1%, 0.01%, 0.001% hiPSCs).
- RNA Extraction: Lyse the cell mixtures and extract total RNA using a column-based or magnetic bead-based method. Include a DNase treatment step to remove genomic DNA contamination.
- cDNA Synthesis: Convert equal amounts of total RNA (e.g., 1 µg) into cDNA using a reverse transcriptase kit with random hexamers and/or oligo-dT primers.
2. ddPCR Reaction Setup:
- Assay Design: Use a TaqMan-based probe and primer set targeting a pluripotency-specific gene, such as LIN28 [55].
- Reaction Mix: Prepare the ddPCR reaction mix according to the manufacturer's instructions (e.g., Bio-Rad QX200 system). A typical 20 µL reaction includes:
- ddPCR Supermix for Probes (no dUTP)
- LIN28 primer-probe assay (900 nM primers, 250 nM probe final concentration)
- cDNA template (up to 100 ng of input RNA equivalent)
- Nuclease-free water
- Droplet Generation: Transfer the reaction mix to a DG8 cartridge for droplet generation. Each sample will generate approximately 20,000 nanoliter-sized droplets [53].
3. PCR Amplification and Reading:
- PCR Cycling: Transfer the generated droplets to a 96-well PCR plate. Seal the plate and run on a conventional thermal cycler using optimized cycling conditions for your assay.
- Droplet Reading: After PCR, place the plate in a droplet reader. The reader will flow droplets one-by-one past a fluorescence detector, classifying each as positive or negative [53].
4. Data Analysis:
- The software uses Poisson statistics to calculate the absolute concentration of the LIN28 target (copies/µL) in the original reaction.
- The percentage of residual hiPSCs can be calculated based on the standard curve generated from the spiked samples.
Protocol 2: Purging Undifferentiated hiPSCs with a Survivin Inhibitor
This protocol is adapted from a study comparing purge strategies for hematopoietic applications [12].
1. In Vitro Treatment:
- Cell Culture: Maintain the heterogeneous cell population (differentiated product contaminated with residual hiPSCs) in its appropriate culture medium.
- Drug Administration: Add the survivin inhibitor YM155 at a determined optimal concentration (e.g., in the nanomolar range) to the culture medium [12].
- Incubation: Incubate the cells with the inhibitor for a specified period (e.g., 24-48 hours).
- Wash and Analyze: After treatment, wash the cells thoroughly with PBS to remove the drug. Assess cell viability and the remaining number of undifferentiated cells (e.g., via flow cytometry for pluripotency markers or a ddPCR LIN28 assay).
2. Validation of Purging Efficiency:
- In Vivo Teratoma Assay: The gold standard for validating purge efficiency is to transplant the treated cell product into immunodeficient mice (e.g., NSG mice) and monitor for teratoma formation over several weeks. An effective purge with YM155 should result in no teratoma formation, unlike untreated controls [12].
Experimental Workflow and Signaling Pathways
Workflow for Ensuring Cell Product Safety
Pluripotency Pathway and Intervention Targets
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Teratoma Prevention Research |
|---|---|
| Bio-Rad QX200 Droplet Digital PCR System | A widely used platform for absolute quantification of nucleic acids; enables highly sensitive detection of rare undifferentiated cells via targets like LIN28 [53] [55]. |
| LIN28 Primer-Probe Assay | A TaqMan-based assay targeting the LIN28 mRNA, a highly sensitive and specific marker for residual hiPSCs used in quality control ddPCR assays [55]. |
| Survivin Inhibitor (YM155) | A small molecule that selectively induces apoptosis in undifferentiated hiPSCs by inhibiting survivin (BIRC5), used to purge contaminated cell products before transplantation [12]. |
| Inducible Caspase-9 (iCaspase-9) System | A genetically encoded "safety switch." When expressed under a pluripotency-specific promoter (e.g., NANOG), it allows for drug-induced (AP20187) ablation of undifferentiated hPSCs with high specificity [2]. |
| mTeSR Plus Medium | A defined, feeder-free culture medium for maintaining human pluripotent stem cells, helping to maintain a stable, undifferentiated state and reduce spontaneous differentiation [13]. |
| ReLeSR | A non-enzymatic, gentle passaging reagent for hPSCs that promotes the formation of uniform cell aggregates, critical for maintaining healthy, undifferentiated cultures [13]. |
| Vitronectin XF | A defined, human recombinant matrix used for coating culture vessels to support the attachment and growth of hPSCs under feeder-free conditions [13]. |
Frequently Asked Questions (FAQs)
FAQ 1: Why are my in vitro assay results poor predictors of in vivo teratoma formation?
In vitro assays are conducted in a controlled, simplified environment outside a living organism, while in vivo assays operate within the complexity of a whole, living system. [56] This fundamental difference means that initial in vitro measurements can be poor predictors of subsequent in vivo behavior. [57] [58] Key reasons include:
- Lack of Systemic Complexity: In vitro models cannot replicate the full physiological environment, including immune responses, systemic metabolic processes, and complex organ-system interactions present in a living organism. [56] [59] For teratoma formation, this means the fate of residual undifferentiated human pluripotent stem cells (hPSCs) may not be accurately modeled in a dish.
- Assay Sensitivity Limitations: The limit of detection (LOD) of your in vitro assay may be insufficient. If the assay cannot detect very low levels of residual hPSCs, it will fail to predict teratoma risk, as even a small number of hPSCs (10,000 or fewer) can form a teratoma in vivo. [10] [2]
- Dynamic Changes Post-Implantation: The process of implantation itself can alter the properties of the material being tested. For example, electrode implantation changes electrochemical impedance, and similar unforeseen interactions can occur with transplanted cells. [57] [58]
FAQ 2: What are the most sensitive methods for detecting residual hPSCs to prevent teratoma formation?
The following table summarizes and compares the key methods for detecting residual hPSCs, which is critical for evaluating teratoma risk. [10]
| Method | Technology Type | Key Performance Metric (Sensitivity) | Pros | Cons |
|---|---|---|---|---|
| In Vivo Teratoma Assay | Animal Model (e.g., NSG mice) | The tumor-producing dose at the 50% end-point (TPD50) | The historical "gold standard"; provides a whole-organism context. [10] | Time-consuming (can take months), costly, less quantitative, ethical concerns. [10] |
| Highly Efficient Culture (HEC) Assay | In Vitro Culture | High sensitivity; can detect very low numbers of hPSCs. | Superior sensitivity, faster and more cost-effective than in vivo assays. [10] | Still requires a cell culture period; may not capture all in vivo influences. |
| Digital PCR (dPCR) | In Vitro Molecular | High sensitivity for detecting hPSC-specific RNA/DNA. | Superior sensitivity, quantitative, high-throughput capability. [10] | Requires knowledge of specific hPSC markers; does not assess functional tumorigenicity. |
| Flow Cytometry | In Vitro Cell Surface Marker | Limited by antibody specificity and gating strategy. | Relatively fast and accessible. | Lower sensitivity; results affected by gating; can compromise cell viability. [12] |
| Suicide Gene Switch (e.g., NANOG-iCaspase9) | Genetically Engineered Safeguard | >10^6-fold depletion of undifferentiated hPSCs. [2] | Extremely effective and specific purge of pluripotent cells; can be induced pre-transplantation. [2] | Requires genetic modification of the stem cell line. |
| Small Molecule Inhibitors (e.g., YM155) | In Vitro Chemical | Kills hPSCs, but specificity can be an issue. [12] | No genetic modification required. | Potential for toxicity on differentiated therapeutic cells, compromising the product. [12] |
FAQ 3: How do I validate that my in vitro safety assay is robust enough for clinical translation?
Robust validation is essential to ensure your assay is "fit for purpose." The process involves several stages, as outlined in the Assay Guidance Manual: [60]
- Pre-Study Validation: This occurs before the assay is used routinely. You must define and demonstrate key performance parameters such as:
- Sensitivity and Specificity: The assay's ability to correctly identify true positives and true negatives. [61]
- Reproducibility: The consistency of results across multiple runs and operators.
- Assay Robustness (Z' factor): A statistical measure (Z') that assesses the quality and suitability of an assay for high-throughput screening. A Z' score between 0.5 and 1.0 is considered excellent. [62]
- In-Study Validation: This involves ongoing monitoring of the assay's performance during its routine use. This includes running control samples (e.g., known numbers of hPSCs) with each assay batch to create control charts that track stability over time. [60]
- Cross-Validation: When transferring the assay to a new laboratory or making a substantive change to the protocol, a formal comparison (cross-validation) must be performed to ensure results are consistent with the original method. [60]
Troubleshooting Guides
Problem: Low In Vitro / In Vivo Correlation in Teratoma Risk Assessment
Possible Causes and Solutions:
- Cause 1: Inadequate Sensitivity of the In Vitro Assay.
- Solution: Replace low-sensitivity methods (e.g., standard flow cytometry) with more sensitive ones. Implement a highly efficient culture (HEC) assay or digital PCR (dPCR) for residual hPSC detection, as these have shown superior sensitivity compared to traditional in vivo assays. [10]
- Cause 2: The In Vitro Assay Lacks a Complex Physiological Environment.
- Solution: There is no perfect in vitro replacement for the in vivo environment. The current best practice is to use a tiered testing strategy. Use highly sensitive in vitro assays for initial, rapid screening of your cell therapy products. Then, reserve more resource-intensive in vivo assays for final validation of selected candidates, as recommended by international consensus committees. [10]
- Cause 3: Poor Assay Robustness and High Variability.
- Solution: Statistically validate your assay's robustness using the Z' factor. A low Z' score (<0.5) indicates high variability and an unreliable assay. Optimize assay conditions (e.g., cell density, incubation times, reagent concentrations) to achieve a Z' score of 0.5 or higher. [62] Ensure proper study design, including randomization and adequate sample size. [60]
Problem: Choosing a Strategy to Eliminate Residual hPSCs
Decision Guide: This flowchart outlines the decision process for selecting a strategy to purge residual undifferentiated hPSCs, a critical step in preventing teratoma formation.
Problem: Interpreting Dose-Response Data from In Vitro Safety Assays
Key Metrics to Calculate: When testing small molecule inhibitors for purging hPSCs, correctly interpreting the dose-response curve is critical.
- IC50 Value: This is the concentration of a drug that produces 50% of its maximal inhibitory response. A lower IC50 indicates a more potent compound. [62] For example, the suicide gene activator AP20187 has an IC50 of 0.065 nM for killing NANOG-iCaspase9 hPSCs. [2]
- Signal-to-Background (S/B) or Fold-Activation: This ratio indicates the strength of your assay's functional response. A high S/B ratio is desirable as it indicates a strong signal above the background noise. [62]
- Toxicity Separation Index (TSI): A more advanced, continuous metric (ranging from 0.5 to 1.0) that quantifies how well a test differentiates between toxic and non-toxic compounds. A TSI of 1.0 indicates perfect separation. [61] Use this to evaluate whether your purging agent selectively kills hPSCs while sparing the differentiated therapeutic cells.
The Scientist's Toolkit: Essential Reagents & Materials
The following table lists key reagents and materials used in developing and validating safety strategies for pluripotent stem cell therapies.
| Research Reagent | Function / Explanation | Example Application in Teratoma Prevention |
|---|---|---|
| NSG (NOD-scid IL2Rγnull) Mice | An immunodeficient mouse strain used for in vivo teratoma assays. Lacks adaptive immunity and natural killer cells, allowing engraftment of human cells. [12] | The standard model for assessing the tumorigenic potential of hPSC-derived cell therapy products by injecting them and monitoring for teratoma formation. [10] |
| Inducible Caspase 9 (iCaspase9) | A "suicide gene" system. A modified Caspase 9 protein is activated by a small molecule drug (AP20187), triggering rapid apoptosis in the cells expressing it. [2] | Knocked into the NANOG locus to create a safety switch. Administering AP20187 before transplantation selectively kills any residual undifferentiated hPSCs, preventing teratomas. [2] |
| AP20187 | A small molecule, dimerizing drug that is biologically inert. It acts as the specific activator for the iCaspase9 system. [2] | Used in vitro to activate the NANOG-iCaspase9 safety switch in a cell therapy product, purging it of teratoma-initiating cells prior to transplantation. [2] |
| YM155 | A small molecule inhibitor of survivin (BIRC5), a protein highly expressed in pluripotent stem cells and critical for their survival. [12] | Tested as a chemical purge agent to eliminate residual hiPSCs from differentiated cell populations before transplantation in hematopoietic applications. [12] |
| Rho Kinase Inhibitor (Y-27632) | A small molecule that improves the survival and cloning efficiency of human pluripotent stem cells by inhibiting apoptosis. [10] | Used in Highly Efficient Culture (HEC) assays to support the growth of very low numbers of residual hPSCs, thereby increasing the assay's detection sensitivity. [10] |
| Anti-SSEA-4 / TRA-1-60 Antibodies | Antibodies targeting cell surface markers highly expressed on undifferentiated pluripotent stem cells. [12] | Used in flow cytometry or magnetic-activated cell sorting (MACS) to detect or deplete residual undifferentiated hPSCs from a differentiated cell product. [12] |
For researchers and drug development professionals working with pluripotent stem cell (PSC)-derived therapies, multi-site validation studies are a critical component of the pathway to clinical application. These studies are designed to establish the robustness and reproducibility of analytical methods and experimental findings across different laboratories, equipment, and personnel. In the specific context of preventing teratoma formation, these studies take on heightened importance due to the serious safety implications of residual undifferentiated human PSCs (hPSCs) in cell therapy products (CTPs). The fundamental goal is to ensure that safety assays yield consistent, reliable results regardless of where they are performed, thereby building confidence in the safety profile of hPSC-derived therapies among regulators and the scientific community [10] [15].
A recent consensus recommendation from the Health and Environmental Sciences Institute's (HESI) International Cell Therapy Committee has emphasized the critical role of multi-site validation for teratoma risk assessment. These studies directly address challenges such as inter-laboratory variability, protocol implementation differences, and analytical sensitivity thresholds. By validating methods across multiple sites, researchers can distinguish between true biological signals and artifacts introduced by specific laboratory conditions or techniques, ultimately ensuring that teratoma risk assessments are accurate and dependable [10] [11] [15].
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: Why is multi-site validation particularly important for teratoma risk assessment assays?
Multi-site validation is crucial because it demonstrates that your teratoma risk assessment methods produce consistent and reliable results across different laboratory environments, instruments, and operators. This process confirms the robustness of your assay protocol and ensures that the detection sensitivity for residual undifferentiated hPSCs meets required safety thresholds regardless of where the testing is performed. For regulatory approval, evidence from multi-site studies significantly strengthens the case that your cell therapy product can be consistently manufactured with acceptable teratoma risk [10] [15].
Q2: What are the key parameters to establish when designing a multi-site validation study for teratoma assays?
When designing a multi-site validation study, you should focus on establishing these core parameters:
- Limit of Detection (LOD): The lowest number of undifferentiated hPSCs that can be reliably detected in a background of differentiated cells across all participating sites.
- Inter-site Reproducibility: The consistency of results obtained when the same samples are tested at different participating laboratories.
- Inter-operator Reproducibility: The consistency of results obtained when different trained personnel execute the same protocol.
- Inter-equipment Reproducibility: The consistency of results obtained when using equivalent equipment from different manufacturers across sites. The HESI Committee's multi-site validation studies found that modern in vitro assays, particularly digital PCR (dPCR) and highly efficient culture (HEC) assays, demonstrated superior sensitivity and reproducibility compared to traditional in vivo methods [10] [15].
Q3: What is the difference between inter-rater reliability (IRR) and inter-user reproducibility (IUR) in validation studies?
Inter-rater reliability (IRR) refers to the consistency of results when the same data or images are interpreted by different raters or analysts. For example, in a recent multi-site ultrasound study, IRR was measured by having multiple physicians interpret the same VExUS images, achieving a Kappa Statistic of 0.71 [63]. In contrast, inter-user reproducibility (IUR) assesses the consistency of results when different operators collect data from the same subject or sample using the same protocol. In the same study, IUR was evaluated by having different ultrasonographers perform sequential scans on the same patients, yielding a Kappa Statistic of 0.63 [63]. Both metrics are essential for validating that your teratoma detection method produces consistent results regardless of who performs the assay or interprets the data.
Q4: How do we address the challenge of protocol drift across multiple sites during a long-term validation study?
Protocol drift can be mitigated through several strategies:
- Implement a centralized training program for all site personnel before study initiation, with standardized training materials and competency assessment.
- Establish a reference standard or control samples that are regularly tested by all sites to monitor consistency.
- Schedule regular cross-site meetings to discuss protocol nuances and address questions.
- Utilize a centralized data monitoring system with predefined quality control checkpoints to identify deviations early.
- Consider using a structured schema-driven framework like ReproSchema, which standardizes data collection procedures and enhances reproducibility across different research settings [64].
Q5: What are the advantages of in vitro over in vivo assays for multi-site teratoma risk validation?
Recent consensus recommendations strongly favor in vitro assays for multi-site teratoma risk validation due to their superior detection sensitivity, better reproducibility, and reduced ethical concerns. Specifically, droplet digital PCR (dPCR) for detecting hPSC-specific RNA and highly efficient culture (HEC) assays have demonstrated significantly greater sensitivity and inter-site consistency compared to traditional in vivo teratoma assays in immunodeficient mice. Additionally, in vitro methods eliminate the biological variability introduced by different animal housing conditions, immune status, and monitoring techniques across sites, which can complicate the interpretation of multi-site validation data [10] [11] [15].
Troubleshooting Guides
Problem: Inconsistent results for the same sample across different validation sites.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Protocol interpretation differences | - Conduct site visits to observe technique- Review raw data and intermediate results | - Create detailed video protocol with critical step emphasis- Establish reference standards for expected values at key steps |
| Reagent lot variability | - Audit reagent sources and lot numbers across sites- Test critical reagents with control samples | - Centralize sourcing for critical reagents- Implement within-lot and between-lot quality control testing |
| Equipment calibration differences | - Verify calibration records for all instruments- Run standardized reference samples on all equipment | - Establish equipment qualification requirements before study initiation- Implement cross-site calibration verification program |
| Environmental condition variations | - Monitor and record temperature, humidity, CO₂ levels | - Define acceptable ranges for critical environmental parameters- Implement environmental monitoring with alerts |
Problem: Poor inter-rater reliability in subjective assessment components.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Ambiguous scoring criteria | - Conduct blinded re-scoring of samples by multiple raters- Analyze specific items with greatest disagreement | - Refine scoring rubric with explicit examples and boundary cases- Create extensive image library with reference scores |
| Insufficient rater training | - Assess inter-rater agreement before and after training- Identify raters with consistent scoring deviations | - Implement centralized training with competency certification- Establish ongoing calibration sessions with reference samples |
| Rater fatigue or cognitive bias | - Analyze scoring patterns over time and sequence- Monitor for drift from reference standards | - Implement random quality control samples in scoring workflow- Establish reasonable daily scoring limits and mandatory breaks |
Problem: Inadequate detection sensitivity for residual hPSCs across sites.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Sample processing losses | - Track recovery rates using spike-in controls- Compare results from split samples processed differently | - Optimize and standardize sample handling procedures- Implement process controls to monitor cell loss |
| Insufficient assay sensitivity | - Perform limit of detection studies at each site- Compare signal-to-noise ratios across sites | - Transition to more sensitive methods (e.g., dPCR, HEC assays)- Pre-concentrate samples or amplify targets |
| Background interference | - Analyze differentiated cell matrix effects- Test assay performance with various cell type mixtures | - Modify purification or enrichment steps- Develop strategies to reduce background signal |
Experimental Protocols & Methodologies
Multi-site Validation Framework for Teratoma Risk Assays
The diagram below illustrates a comprehensive workflow for designing, executing, and analyzing multi-site validation studies for teratoma risk assessment assays:
This structured approach ensures that all participating sites adhere to identical protocols and quality standards, enabling meaningful comparison of results across locations. The framework emphasizes pre-study harmonization, concurrent execution, and centralized analysis to minimize inter-site variability [10] [63] [15].
In Vitro vs. In Vivo Teratoma Assay Comparison
The following workflow compares the experimental processes for traditional in vivo versus emerging in vitro teratoma assay methods:
Recent multi-site validation studies demonstrate that in vitro methods provide significant advantages for inter-laboratory reproducibility due to their quantitative nature, reduced biological variability, and higher sensitivity for detecting residual hPSCs [10] [15].
Quantitative Comparison of Teratoma Risk Assessment Methods
The table below summarizes the performance characteristics of different teratoma risk assessment methods based on multi-site validation studies:
| Method Type | Specific Assay | Detection Sensitivity | Time to Result | Inter-site Reproducibility | Key Advantages | |
|---|---|---|---|---|---|---|
| In Vivo | Traditional teratoma assay in immunodeficient mice | Low (variable, depends on animal model) | 5+ weeks | Moderate to Low | Provides biological context; Historical regulatory acceptance | |
| In Vitro | Digital PCR (dPCR) | High (precise detection of hPSC-specific RNA) | 1-2 days | High | Quantitative; Highly sensitive; Minimal biological variability | |
| In Vitro | Highly Efficient Culture (HEC) | Very High (can detect single residual hPSCs) | 2-3 weeks | High | Extreme sensitivity; Functional assessment of pluripotency | |
| In Vitro | Flow cytometry (SSEA-4, TRA-1-60) | Moderate | 1 day | Moderate | Rapid; Can be combined with other analyses | [10] [12] [11] |
Survivin Inhibition Teratoma Prevention Protocol
For researchers investigating pharmacological approaches to eliminate residual hPSCs, the following detailed protocol is based on published methodology that demonstrated complete eradication of teratoma formation in immune-deficient mice:
Principle: Survivin inhibitor YM155 selectively induces apoptosis in undifferentiated hPSCs while sparing differentiated cells, including hematopoietic stem cells, providing a safety purge method for cell therapy products.
Reagents and Equipment:
- Survivin inhibitor YM155 (commercially available)
- hPSC culture medium and differentiation medium
- Cell therapy product (differentiated cell population)
- Flow cytometer with appropriate antibodies for pluripotency markers (SSEA-4, TRA-1-60)
- Cell culture incubator (37°C, 5% CO₂)
- Animal model for teratoma assay (e.g., NSG mice)
Procedure:
- Prepare cell therapy product according to your established differentiation protocol.
- Treat with YM155 at optimized concentration (typically 100-500 nM) for 24-48 hours in culture.
- Assess purity post-treatment using flow cytometry for pluripotency markers (SSEA-4, TRA-1-60) to confirm depletion of undifferentiated hPSCs.
- Validate functionality of the purified differentiated cell population using appropriate functional assays.
- Confirm teratoma prevention by injecting the purified cell product into immunodeficient mice (e.g., NSG) and monitor for tumor formation for 12+ weeks.
Critical Steps and Troubleshooting:
- Dose optimization: Perform dose-response curve with YM155 (0-1000 nM) using mixed cultures of hPSCs and differentiated cells to establish the minimal concentration that eliminates hPSCs while preserving differentiated cell viability and function.
- Treatment timing: The optimal treatment duration is typically 24-48 hours; longer exposures may adversely affect differentiated cells.
- Validation: Always include appropriate controls (untreated mixed populations) in teratoma assays to confirm the effectiveness of the purge.
- Safety profiling: Conduct comprehensive functional assessment of the therapeutic cell population post-treatment to ensure YM155 exposure hasn't compromised therapeutic efficacy.
This method has been shown to be more efficient than suicide gene approaches (such as iCaspase-9/AP20187) for eliminating hPSCs without toxicity to hematopoietic stem cells, making it particularly suitable for therapies where preserving stem cell function is essential [12].
The Scientist's Toolkit: Research Reagent Solutions
The table below provides essential materials and reagents for implementing teratoma risk assessment and prevention strategies:
| Reagent/Assay | Specific Examples | Primary Function | Application Notes | |
|---|---|---|---|---|
| hPSC Detection | Digital PCR (dPCR) for pluripotency markers | Quantitative detection of residual hPSCs | Provides superior sensitivity and reproducibility for multi-site studies; targets include hPSC-specific RNA transcripts | |
| hPSC Detection | Highly Efficient Culture (HEC) Assay | Functional assessment of teratoma-forming cells | Can detect single residual hPSCs; requires specialized culture conditions | |
| hPSC Elimination | Survivin Inhibitor (YM155) | Selective elimination of undifferentiated hPSCs | Effective purging agent; no toxicity to hematopoietic stem cells at working concentrations | |
| hPSC Elimination | Inducible Caspase-9 (iCaspase-9)/AP20187 | Suicide gene system for hPSC elimination | Genetic modification required; potential toxicity to some differentiated cells | |
| Pluripotency Markers | Anti-SSEA-4, TRA-1-60 antibodies | Identification of undifferentiated hPSCs by flow cytometry | Standard characterization; sensitivity limitations for rare cell detection | |
| Animal Models | NSG, NOG mice | In vivo teratoma formation assessment | Required for traditional tumorigenicity testing; significant inter-site variability | [10] [12] [11] |
Framework for Assay Validation and Implementation in Quality Control
Core Concepts: The Role of Assay Validation in Preventing Teratoma Formation
Why is a validated quality control framework critical for pluripotent stem cell therapies?
A robust quality control (QC) framework is fundamental to ensuring the safety of pluripotent stem cell-derived therapies by preventing teratoma formation. Human pluripotent stem cells (hPSCs), including induced pluripotent stem cells (hiPSCs), are intrinsically tumorigenic, and even a small number of residual undifferentiated cells—as few as 10,000—can form teratomas in vivo [2]. The primary goal of QC assays in this context is to detect and quantify these residual undifferentiated hPSCs with high sensitivity and specificity before the cell therapy product is released [10]. Implementing a validated QC framework is not merely a regulatory formality; it is a crucial risk mitigation strategy to ensure that cell therapy products (CTPs) are safe for patient administration [65].
What are the key pillars of an effective QC system for cell-based therapies?
An effective QC system is built on several key pillars, which together provide confidence in the product's safety, identity, purity, and potency [66]. These include:
- Identity Testing: Confirming the identity of the cell product and the absence of residual undifferentiated cells.
- Purity Testing: Ensuring the product is free from unwanted impurities, which includes residual undifferentiated hPSCs.
- Potency Testing: Measuring the biological activity of the therapeutic cells, which is directly linked to the intended clinical effect.
- Analytical Validation: Demonstrating that the test methods used for QC are suitable for their intended purpose, proving they are reliable, reproducible, and accurate [67].
Validation Parameters & Methodologies
What specific parameters must be validated for a teratoma-risk assay?
For any analytical method used in quality control, a set of core performance characteristics must be formally validated. The table below summarizes these key parameters and their definitions.
Table 1: Key Validation Parameters for Quality Control Assays
| Validation Parameter | Definition and Importance |
|---|---|
| Specificity | The ability to unequivocally assess the analyte in the presence of other components. This is crucial for distinguishing undifferentiated hPSCs from differentiated cell types in a heterogeneous product [65] [2]. |
| Sensitivity | The lowest amount of an analyte that can be reliably detected. For teratoma risk, this defines the assay's limit in detecting rare residual hPSCs [10]. |
| Accuracy | The closeness of agreement between a test result and the accepted reference value. It indicates how correct the measurement of residual hPSCs is [68]. |
| Precision | The closeness of agreement between a series of measurements from multiple sampling. It includes repeatability (same operator, same day) and intermediate precision (different days, different analysts) [69]. |
| Limit of Detection (LOD) | The lowest concentration of an analyte that can be detected, but not necessarily quantified. It is often calculated as the mean blank value + [3.29 * (standard deviation)] [69]. |
| Limit of Quantitation (LOQ) | The lowest concentration of an analyte that can be quantified with acceptable precision and accuracy. A common definition is the lowest concentration where the assay imprecision (% CV) is less than 20% [69]. |
| Linearity and Range | The interval over which the analytical procedure has a directly proportional response. This confirms the assay works accurately across a specified range of analyte concentrations [69]. |
| Robustness | A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters, indicating its reliability during normal usage [68]. |
The following workflow outlines the typical lifecycle of an analytical method, from initial design to continuous monitoring, which should be applied to teratoma-risk assays.
What is a detailed experimental protocol for validating a quantitative PCR (qPCR) assay for residual undifferentiated hiPSCs?
Objective: To validate a qPCR assay for detecting a pluripotency marker gene (e.g., NANOG) to quantify residual hiPSCs in a differentiated cell therapy product. Materials:
- Genomic DNA: From pure hiPSCs (for standard curve) and from the final cell product.
- Primers/Probes: Specifically designed for the pluripotency marker.
- qPCR Instrument: Calibrated and qualified.
- Reagents: Master mix for probe-based qPCR.
Methodology:
- Assay Specificity: Test the primer/probe set against genomic DNA from the fully differentiated target cell type (the therapeutic product) to ensure no false-positive signal. Test against DNA from other related cell types that might be present.
- Standard Curve and Linearity: Prepare a serial dilution of pure hiPSC genomic DNA in a background of differentiated cell DNA. The range should cover from below the expected LOD to above the maximum expected level. Run each dilution in replicate. The correlation coefficient (R²) should be >0.98 [69].
- LOD and LOQ Determination:
- LOD: Perform replicate measurements (n≥10) of a blank sample (differentiated cell DNA only). Calculate the LOD as: Mean(blank) + 3.29 * SD(blank) [69].
- LOQ: Using low-concentration samples near the LOD, calculate the LOQ as the lowest concentration at which the % Coefficient of Variation (CV) is ≤20% [69].
- Precision (Repeatability and Intermediate Precision):
- Repeatability: Have one analyst run the same sample (with a known quantity of residual hiPSCs) multiple times on the same day.
- Intermediate Precision: Have a second analyst run the same sample on a different day and/or with a different instrument.
- Calculate the % CV for both studies. Acceptance criteria should be predefined (e.g., % CV <25% for the LOQ, <15% for higher concentrations) [67].
- Accuracy/Recovery: Spike known numbers of hiPSCs into the differentiated cell product. Extract DNA and run the qPCR assay. Calculate the percentage recovery of the spiked hiPSCs.
Troubleshooting Guides & FAQs
FAQ 1: Our assay's standard curve is linear, but experimental sample dilutions are not. What could be the cause?
Problem: This is a classic sign of interfering substances in the sample matrix. The standard curve, prepared in a clean buffer, may perform well, but components in the biological sample (e.g., from digested tissue or culture media) can inhibit or interfere with the assay chemistry at high concentrations [69].
Solution:
- Perform a Minimum Required Dilution (MRD): Dilute the sample until the interference is eliminated and linearity is restored. The MRD must be determined during method validation and applied to all test samples [69].
- Purify the Sample: If dilution is not feasible, introduce a sample purification or clean-up step (e.g., column purification for DNA/RNA, precipitation for proteins) to remove the interfering substances.
- Use a Standard Additive: For some assays, adding a competing substance to the standard curve matrix can help mimic the sample and improve accuracy.
FAQ 2: How do we set a scientifically justified acceptance criterion for a flow cytometry assay measuring pluripotency markers?
Problem: Simply having a "positive" signal is insufficient for batch release. A validated assay requires a quantitative cutoff.
Solution:
- Base the criterion on Validation Data: The acceptance criterion must be grounded in the assay's validated performance. For example, one validated approach for hiPSC release is to require "the expression of at least three individual markers on at least 75% of the cells" [65].
- Use Appropriate Controls: When using multi-color flow cytometry panels, a Fluorescence Minus One (FMO) control is advised to set gates accurately and account for fluorescent spread, ensuring the specificity of the measurement [65].
- Correlate with Functional Data: Where possible, correlate the flow cytometry result with a functional assay, such as a teratoma assay or an in vitro differentiation potential assay, to confirm that cells below the cutoff are not tumorigenic.
FAQ 3: What is the best strategy to confirm our assay can achieve a sufficient log-reduction in undifferentiated cells to mitigate teratoma risk?
Problem: The assay must be sensitive enough to ensure a several-log reduction of hPSCs, as a 5-log depletion may be required for products with billions of cells [2].
Solution:
- Spike-In/Log-Reduction Studies: During validation, perform a spike-in experiment where you introduce a known, high number of hiPSCs into your final cell product. Treat the product with your purification or depletion process (e.g., a survivin inhibitor, magnetic bead sorting). Use your validated QC assay (e.g., dPCR, highly sensitive culture assay) to quantify the remaining hiPSCs post-treatment.
- Calculate the Log-Reduction: The log-reduction is calculated as: Log10(Initial hPSC Count / Final hPSC Count). A successful validation will demonstrate that your process and QC control can consistently achieve a pre-defined log-reduction (e.g., >4-log or >6-log) [2].
The diagram below illustrates a multi-layered safety and validation strategy that integrates directly validated QC assays with orthogonal safety mechanisms.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Teratoma-Risk QC Assays
| Reagent / Material | Function in QC and Validation | Key Considerations |
|---|---|---|
| Digital PCR (dPCR) | Absolute quantification of residual hiPSCs by targeting pluripotency-specific RNA/DNA. Offers superior sensitivity and precision over qPCR for low-abundance targets [10]. | Ideal for validating the LOD of other methods. Requires highly specific primers/probes. |
| Flow Cytometry Antibodies (e.g., anti-SSEA-4, TRA-1-60) | Detection of pluripotency-associated surface markers on individual cells. Provides information on the percentage of residual undifferentiated cells [65]. | Specificity must be validated for the specific cell product. FMO controls are critical [65]. |
| Highly Efficient Culture (HEC) Assay | In vitro functional assay that expands rare residual hiPSCs to form colonies, confirming their tumorigenic potential. | Considered a highly sensitive "gold standard" but can be time-consuming (2-3 weeks) [10]. |
| Survivin Inhibitor (YM155) | Small molecule chemical that selectively kills pluripotent stem cells by targeting the survivin protein, which is critical for hPSC survival [12]. | Used as a purge strategy prior to transplantation. Must be validated for lack of toxicity on the therapeutic differentiated cells [12]. |
| Inducible Caspase-9 (iCaspase-9) System | Genetically engineered "safety switch" under control of a pluripotency-specific promoter (e.g., NANOG). Administration of a small molecule (AP20187) triggers apoptosis specifically in undifferentiated cells [2]. | Provides a highly specific and effective (>1e6-fold depletion) safeguard. Requires genetic modification of the master cell line [2]. |
| Genomic DNA Extraction Kits | Preparation of high-quality, high-molecular-weight DNA for PCR-based assays. | Yield, purity, and absence of inhibitors are critical for assay performance, especially for sensitive LOD/LOQ. |
Conclusion
Preventing teratoma formation requires a multi-faceted approach integrating advanced cell purification technologies, sensitive detection methods, and rigorous validation frameworks. The field is moving decisively toward highly sensitive in vitro assays like digital PCR and HEC, which offer superior detection capabilities over traditional in vivo models. Future directions will focus on international harmonization of safety assessment protocols, development of next-generation biosensors for real-time monitoring, and AI-guided manufacturing controls. These advances, supported by ongoing multi-site validation studies and consensus recommendations, are paving the way for safer clinical translation of hPSC-derived therapies, ultimately increasing confidence in their therapeutic application while systematically addressing one of regenerative medicine's most significant safety challenges.
References
- 1. Deconstructing Stem Cell Tumorigenicity: A Roadmap to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2733374/]
- 2. Improving the safety of human pluripotent stem cell ... [https://www.nature.com/articles/s41467-020-16455-7]
- 3. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 4. Clinical translation of human iPSC technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12498231/]
- 5. The ISSCR Launches Roadmap for Developing Pluripotent ... [https://www.isscr.org/isscr-news/the-isscr-launches-best-practices]
- 6. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 7. Elimination of undifferentiated human embryonic stem cells ... [https://www.nature.com/articles/s41598-017-05616-2]
- 8. Teratomas produced from human pluripotent stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5338735/]
- 9. Inhibition of pluripotent stem cell-derived teratoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3761568/]
- 10. Evaluating teratoma formation risk of pluripotent stem cell- ... [https://www.sciencedirect.com/science/article/pii/S146532492500684X]
- 11. Evaluating teratoma formation risk of pluripotent stem cell ... [https://pubmed.ncbi.nlm.nih.gov/40392167/]
- 12. Preventing Pluripotent Cell Teratoma in Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5442801/]
- 13. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 14. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/hk/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 15. Evaluating teratoma formation risk of pluripotent stem cell- ... [https://hesiglobal.org/publication/evaluating-teratoma-formation-risk-of-pluripotent-stem-cell-derived-cell-therapy-products-a-consensus-recommendation-from-the-health-and-environmental-sciences-institutes-international-cell/]
- 16. Country-specific regulation and international ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10444560/]
- 17. ICH E6 Good clinical practice - Scientific guideline [https://www.ema.europa.eu/en/ich-e6-good-clinical-practice-scientific-guideline]
- 18. ICH E6(R3) Explained: A Guide to the 2025 GCP Update [https://intuitionlabs.ai/articles/ich-e6-r3-gcp-guidelines-2025]
- 19. ICH GCP E6 has arrived: Are we ready? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12591519/]
- 20. A Scalable Approach to Prevent Teratoma Formation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3463330/]
- 21. PSC Gene and Cell Surface Marker Expression | Cell Quality [https://www.stemcell.com/psc-cell-quality/gene-marker-expression]
- 22. The application of cell surface markers to demarcate distinct ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6983944/]
- 23. Elimination of tumorigenic pluripotent stem cells from their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277835/]
- 24. Selective elimination of human pluripotent stem cells by ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961220305111]
- 25. Cell surface markers for the identification and study of ... [https://www.sciencedirect.com/science/article/pii/S1873506117302477]
- 26. Elimination of tumorigenic pluripotent stem cells from their ... [https://www.sciencedirect.com/science/article/pii/S221367112500147X]
- 27. Improving the differentiation potential of pluripotent stem ... [https://www.nature.com/articles/s41598-022-18400-8]
- 28. Optimization of differentiation protocols of dental tissues stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9487116/]
- 29. Using Advanced Cell Culture Techniques to Differentiate ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.667246/full]
- 30. RNA Degradation in Pluripotent Stem Cells - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563098/]
- 31. Challenges in microRNAs' targetome prediction and validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC6585557/]
- 32. Teratoma formation: A tool for monitoring pluripotency in stem ... [https://www.ncbi.nlm.nih.gov/books/NBK133287/]
- 33. miRNA and pri-miRNA Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/real-time-digital-PCR-applications-support-center/mirna-and-noncoding-rna-support/mirna-and-noncoding-rna-support-troubleshooting.html]
- 34. Magnetic-Activated Cell Sorting - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/magnetic-activated-cell-sorting]
- 35. Immunophenotyping of Live Human Pluripotent Stem Cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5903271/]
- 36. Efficient and safe single-cell cloning of human pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11009857/]
- 37. Using Single-Cell hPSCs for Intestinal Organoid ... [https://www.stemcell.com/intestinal-organoid-differentation-from-single-cells.html]
- 38. Label-Free and High-Throughput Removal of Residual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11016845/]
- 39. Evaluating Strategies to Assess the Differentiation Potential of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11762643/]
- 40. Teratoma Assay for Testing Pluripotency and Malignancy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9967860/]
- 41. 综述:评估多能干细胞衍生细胞治疗产品的畸胎瘤形成风险 [https://www.ebiotrade.com/newsf/2025-5/20250507181017714.htm]
- 42. Humanised Mice and Immunodeficient Mice (NSG) Are ... [https://www.mdpi.com/1422-0067/23/9/4680]
- 43. ISSCR Standards for Human Stem Cell Use in Research [https://www.stemcell.com/psc-cell-quality/isscr-standards]
- 44. Protocol to rapidly verify silent gene reporter in human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12596206/]
- 45. Noninvasive, label-free image approaches to predict ... [https://www.nature.com/articles/s41598-024-66591-z]
- 46. Newsletter: Cellular Markers for Flow Cytometry Analysis [https://fluorofinder.com/newsletter-cellular-markers-for-flow-cytometry-analysis/]
- 47. Label-free imaging of 3D pluripotent stem cell differentiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10391578/]
- 48. Flow cytometry markers guide [https://www.abcam.com/en-us/knowledge-center/flow-cytometry/flow-cytometry-markers]
- 49. Understanding Pharmaceutical Quality by Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4070262/]
- 50. Quality by design | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/quality-design]
- 51. Quality by design [https://en.wikipedia.org/wiki/Quality_by_design]
- 52. Process Development Considerations for Cell Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4572896/]
- 53. The Role of Digital PCR in Enhancing Diagnostic Power ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11311727/]
- 54. Digital PCR Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/real-time-digital-PCR-applications-support-center/digital-pcr-support/digital-pcr-support-troubleshooting.html]
- 55. Highly sensitive droplet digital PCR method for detection of ... [https://www.sciencedirect.com/science/article/pii/S2352320415000498]
- 56. In Vivo vs. In Vitro Models: Key Differences and ... [https://liveonbiolabs.com/in-vivo-vs-in-vitro-models/]
- 57. Comparison of the In Vitro and In Vivo Electrochemical ... [https://pubmed.ncbi.nlm.nih.gov/35056268/]
- 58. Comparison of the In Vitro and In Vivo Electrochemical ... [https://www.mdpi.com/2072-666X/13/1/103]
- 59. In Vivo vs. In Vitro: Choosing the Right Experimental Model ... [https://www.cusabio.com/c-21169.html?srsltid=AfmBOoocLI6PWcFkaXU2iEmaTr3wHoD5dq51fdSswWr74dPm6ayu-gdn]
- 60. In Vivo Assay Guidelines - Assay Guidance Manual - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK92013/]
- 61. Performance metrics of in vitro tests - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6785777/]
- 62. Understanding Assay Performance Metrics [https://indigobiosciences.com/understanding-assay-performance-metrics/]
- 63. Reliability and reproducibility of the venous excess ultrasound... [https://ccforum.biomedcentral.com/articles/10.1186/s13054-024-04961-9]
- 64. Journal of Medical Internet Research - Standardizing Survey Data... [https://www.jmir.org/2025/1/e63343]
- 65. Validating human induced pluripotent stem cell-specific ... [https://www.sciencedirect.com/science/article/pii/S1465324924006108]
- 66. The Essential Need for a Validated Potency Assay for Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8599250/]
- 67. Points to Consider in Quality Control Method Validation ... [https://www.bioprocessintl.com/qa-qc/points-to-consider-in-quality-control-method-validation-and-transfer]
- 68. Pharma Quality Control in Drug Development and ... [https://amsbiopharma.com/pharma-quality-control-strategies/]
- 69. Analytical Validation and Quality Control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10264544/]