2D vs 3D Cell Culture: A Comprehensive Efficacy Comparison for Predictive Preclinical Research
This article provides a systematic comparison of two-dimensional (2D) and three-dimensional (3D) cell culture systems, analyzing their efficacy in mimicking in vivo conditions for biomedical research and drug development.
2D vs 3D Cell Culture: A Comprehensive Efficacy Comparison for Predictive Preclinical Research
Abstract
This article provides a systematic comparison of two-dimensional (2D) and three-dimensional (3D) cell culture systems, analyzing their efficacy in mimicking in vivo conditions for biomedical research and drug development. It covers foundational biological differences, practical methodologies, key challenges with optimization strategies, and rigorous validation through comparative studies. Aimed at researchers, scientists, and drug development professionals, the content synthesizes current evidence demonstrating that 3D models more accurately recapitulate tissue architecture, cell-cell interactions, gene expression, and drug response, thereby offering more physiologically relevant and predictive data for reducing costly late-stage drug failures.
Beyond the Monolayer: How 3D Architecture Reshapes Cell Behavior and Biology
Core Principles and Fundamental Differences
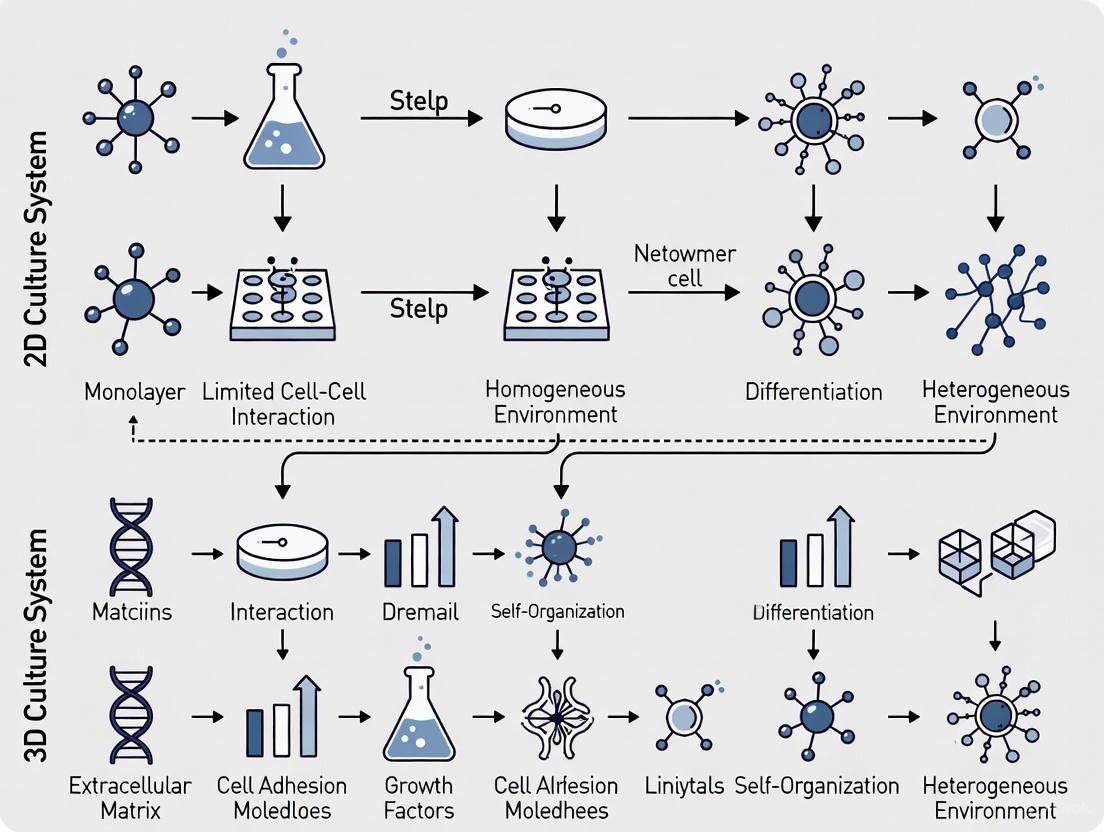
Cell culture is a foundational tool in biomedical research, and the choice between two-dimensional (2D) and three-dimensional (3D) systems fundamentally shapes experimental outcomes. A 2D culture involves growing cells as a single, adherent layer on a flat, rigid plastic or glass surface [1] [2]. This simple and reproducible method has been the standard for decades. In contrast, a 3D culture system allows cells to grow in all three spatial dimensions, facilitating cell-cell and cell-extracellular matrix (ECM) interactions that more closely mimic the architectural and functional complexity of living tissues [1] [3].
The core principle distinguishing these models is their physiological relevance. In vivo, cells reside within a complex 3D microenvironment, surrounded by other cells and an ECM that provides biochemical and mechanical cues [4]. The spatial arrangement in 3D cultures influences critical processes such as cell differentiation, proliferation, gene expression, and responsiveness to stimuli—aspects that are fundamentally altered in 2D monolayers [1]. The table below summarizes the key characteristics of each system.
Table 1: Fundamental Comparison of 2D and 3D Cell Culture Systems
| Characteristic | 2D Culture | 3D Culture | Key References |
|---|---|---|---|
| Spatial Architecture | Monolayer; flat and spread | Multi-layered; tissue-like structure | [1] [2] |
| Cell-ECM Interactions | Disturbed; single plane of attachment | Physiologically representative; natural polarity | [1] [3] |
| Microenvironment | Uniform nutrient and oxygen access | Creates nutrient, oxygen, and metabolic gradients | [1] [5] |
| Gene & Protein Expression | Altered compared to in vivo | More closely resembles in vivo profiles | [1] [6] |
| Proliferation Rate | Generally high | Often reduced, more akin to in vivo tissues | [7] |
| Cost & Technical Ease | Low-cost, simple, highly reproducible | More expensive, time-consuming, and complex | [1] [8] |
| Throughput & Standardization | Excellent for high-throughput screening | Lower throughput; standardization can be challenging | [8] [4] |
Experimental Data and Efficacy Comparison
Drug Response and Resistance
A critical area where 2D and 3D models diverge significantly is in drug testing. Studies consistently show that 3D cultures exhibit higher innate resistance to both targeted therapies and classical chemotherapeutic agents, providing a more accurate prediction of clinical outcomes [7] [5].
In a pivotal study using HER2-positive breast cancer cell lines (BT474, HCC1954, EFM192A), researchers directly compared the efficacy of the targeted drug neratinib and the chemotherapeutic docetaxel in 2D versus 3D cultures (the latter formed using the poly-HEMA forced-floating method) [7]. The results were striking, as summarized in the table below.
Table 2: Comparative Drug Efficacy in 2D vs. 3D Breast Cancer Models (Data adapted from [7])
| Cell Line | Treatment | Cell Survival in 2D | Cell Survival in 3D | Difference (3D vs 2D) |
|---|---|---|---|---|
| BT474 | Neratinib | 62.7% | 90.8% | +28.1% |
| HCC1954 | Neratinib | 64.7% | 77.3% | +12.6% |
| EFM192A | Neratinib | 59.7% | 86.8% | +27.1% |
| BT474 | Docetaxel | 60.3% | 91.0% | +30.7% |
| HCC1954 | Docetaxel | 52.3% | 101.6% | +49.0% |
| EFM192A | Docetaxel | 46.2% | 96.2% | +50.0% |
This innate resistance in 3D models is facilitated by several physiological factors:
- Altered Protein Expression: The study found increased expression of proteins involved in cell survival (e.g., Akt) and drug transporters associated with resistance in 3D cultures [7].
- Enhanced Drug Metabolism: Activity of the drug-metabolizing enzyme CYP3A4 was substantially increased in 3D cultures compared to their 2D counterparts [7].
- Diffusion Barriers: The compact architecture of 3D spheroids creates gradients of oxygen, nutrients, and waste, which can limit drug penetration to the core of the structure, mimicking the hypoxic core of solid tumors [1] [5].
Cell Viability and Morphology
The same breast cancer study also quantified fundamental differences in cell viability and morphology. After 6 days of culture, the viability of 3D spheroids was significantly lower than that of 2D monolayers: BT474 3D viability was 41.6% of its 2D control, HCC1954 was 18.4%, and EFM192A was 44.0% [7]. This reflects a more physiologically relevant proliferation rate.
Morphologically, cells in 3D culture form tight spheroids, often surrounded by a self-secreted extracellular matrix, which is a stark contrast to the flat, spread-out appearance of cells in 2D monolayers [7]. This restored 3D morphology directly impacts cellular signaling and function.
Experimental Workflow for Drug Efficacy
Methodologies for Key 3D Culture Techniques
The creation of 3D models can be broadly classified into scaffold-based and scaffold-free techniques, each with specific protocols and applications [5] [3].
Scaffold-Based Techniques
Scaffolds provide a physical 3D structure that supports cell attachment and growth.
- Hydrogel-Based Cultures: Hydrogels are water-swollen polymer networks that mimic the native ECM [3]. A common protocol using Matrigel involves liquefying the Matrigel on ice, mixing it with a cell suspension, and then plating the mixture. Upon incubation at 37°C, the Matrigel solidifies, embedding the cells in a 3D protein-rich environment [1]. Natural hydrogels (e.g., collagen, alginate) and synthetic hydrogels (e.g., Polyethylene Glycol - PEG) are also widely used, with the latter offering greater control over mechanical properties [6] [3].
- Polymeric Hard Material-Based Scaffolds: These are rigid, porous structures made from biodegradable materials like polylactic acid (PLA) or polycaprolactone (PCL) [6] [3]. Cells are seeded onto these scaffolds and migrate into the pores, where they attach, grow, and form 3D tissues.
Scaffold-Free Techniques
These methods rely on the innate ability of cells to self-assemble.
- The Hanging Drop Method: This technique involves suspending a droplet of cell culture medium, containing a known number of cells, from the lid of a culture dish. Gravity causes the cells to aggregate at the bottom of the droplet, forming a single spheroid [5].
- Ultra-Low Attachment (ULA) Plates: These plates are manufactured with a covalently bound hydrogel surface that prevents protein and cell attachment. When seeded into ULA plates, cells are forced to aggregate and form spheroids [1] [5].
- Magnetic Levitation: In this advanced technique, cells are first incubated with magnetic nanoparticles. When exposed to an external magnetic field, the cells are levitated and gathered to form a dense 3D spheroid at the air-media interface [5].
Table 3: Essential Research Reagents for 3D Cell Culture (Compiled from [1] [6] [9])
| Reagent Category | Specific Examples | Function in 3D Culture |
|---|---|---|
| Natural Hydrogels | Matrigel, Collagen, Alginate, Fibrin | Provide a biologically active, ECM-like matrix for cell embedding and growth. |
| Synthetic Hydrogels | Polyethylene Glycol (PEG), PLA, PCL | Offer tunable stiffness and porosity with minimal batch-to-batch variability. |
| Scaffold Materials | Polymeric scaffolds (e.g., PCL, PLA), Glass microfibers | Provide a rigid, porous 3D structure for cell attachment and tissue formation. |
| Specialized Cultureware | Ultra-Low Attachment (ULA) Plates, Hanging Drop Plates | Prevent cell adhesion, forcing cells to self-assemble into spheroids. |
| Bioinks for 3D Bioprinting | Gelatin Methacryloyl (GelMA), Alginate-based bioinks, Cell-laden hydrogels | Serve as printable materials for the precise spatial patterning of cells and biomaterials. |
Molecular Mechanisms and Signaling Pathways
The differential response to drugs and stimuli in 2D versus 3D systems is rooted in profound changes at the molecular level. The 3D architecture restores physiological signaling that is lost in 2D monolayers.
Molecular Basis for Drug Resistance in 3D Models
Key molecular differences include:
- Gene Expression and Splicing: Cells in 3D culture exhibit gene expression and mRNA splicing patterns that are more representative of in vivo tissues, unlike the altered profiles found in 2D cultures [1].
- Activation of Survival Pathways: Research has demonstrated that components of critical cell survival pathways, such as Akt and Erk, show increased expression in 3D cultures compared to 2D, contributing to enhanced cell survival and drug resistance [7].
- Metabolic Changes: The gradient-driven microenvironment within 3D spheroids can lead to areas of hypoxia, which alters cellular metabolism and further contributes to a drug-resistant phenotype [5].
The choice between 2D and 3D culture systems is not a matter of one being universally superior, but of selecting the appropriate tool for the research question. 2D cultures remain invaluable for high-throughput screening, genetic manipulations, and basic research where simplicity, low cost, and reproducibility are paramount [8]. However, the evidence is clear that 3D culture systems provide a superior model for preclinical research demanding physiological accuracy, particularly in drug discovery, cancer biology, and personalized medicine [7] [5] [3]. Their ability to mimic the tissue microenvironment, including critical cell-ECM interactions, gradient formation, and more in vivo-like molecular profiles, makes them indispensable for bridging the translational gap between traditional cell culture and animal models, ultimately leading to more predictive and successful clinical outcomes.
Cell culture systems are indispensable tools in basic and clinical in vitro research. The classically preferred model is a static dish culture system which mainly generates adherent two-dimensional (2D) cell monolayers [2]. However, such culture systems do not reflect the situation in vivo, where cells grow within a complex three-dimensional (3D) microenvironment and where vascular perfusion continuously supplies and removes metabolites and catabolites, respectively [2]. This article provides a comprehensive comparison of cell-cell and cell-extracellular matrix (ECM) interactions within these fundamentally different culture environments, framing the analysis within the broader context of efficacy comparison for research and drug development applications.
It is now well-established that cells behave structurally and functionally different when seeded on thin 2D surface-coated substrate versus a thick layer of polymeric 3D molecules, which more closely mimics their natural environment [2]. The spatial arrangement of cells significantly affects how they interact with each other and their surroundings, ultimately influencing experimental outcomes in drug discovery, toxicity testing, and basic biological research [7]. This comparison aims to objectively evaluate the performance of both systems based on current scientific evidence.
Core Biological Differences: Interaction Complexities in 2D vs 3D Environments
Fundamental Architecture and Cellular Interactions
The fundamental distinction between these culture systems lies in their spatial organization and the resulting biological interactions. In 2D cultures, cells are grown attached to tissue culture-grade plastic as a single layer, which imposes artificial polarity and limits natural cell-cell contacts [2] [8]. Conversely, 3D cultures allow cells to grow in all directions, enabling them to form more physiologically relevant structures such as spheroids and organoids [8].
Cell-cell interactions in these systems differ substantially. In 3D environments, cells exhibit proximity to other cells on all sides, creating more natural communication networks through direct contact and signaling molecules [2]. These interactions are mediated by transmembrane adhesion receptors that bind to specific extracellular ligand partners and link receptor cytoplasmic domains to intracellular cytoskeletal systems via protein complexes [10]. The spatial arrangement in 3D cultures facilitates the formation of more natural cell adhesion complexes, including adherens junctions, desmosomes, and gap junctions, which are critical for tissue function [11].
Cell-ECM interactions represent another crucial distinction. In vivo, cells interact continuously with a complex ECM that regulates essential biological functions like cell migration, apoptosis, transcription regulation, and receptor expression [6]. While 3D cultures replicate these interactions through natural or synthetic matrices, 2D cultures provide only a flat, rigid surface that fundamentally alters how cells engage with their substrate [2] [6]. This difference significantly impacts cytoskeletal organization, mechanical signaling, and overall cell behavior.
Molecular and Structural Implications
The dimensional context profoundly influences molecular and structural characteristics at the cellular level. Research demonstrates that cells in 3D culture exhibit more authentic gene expression profiles and protein expression patterns compared to their 2D counterparts [6]. For example, immortalized human hepatocyte HepG2 cells grown in traditional 2D culture lose substantial amounts of CYP450 enzyme mRNA and activity—critical components for drug metabolism—while 3D culture using an ECM hydrogel restores these phenotypic characteristics [7].
Structural complexity also markedly differs between the systems. Three-dimensional cultures exhibit a higher degree of structural organization and homeostasis analogous to tissues and organs in vivo [2]. This includes the development of natural gradients of oxygen, pH, and nutrients that influence cellular behavior and drug responses [8]. The cytoarchitecture in 3D cultures more accurately represents in vivo conditions, with cells establishing more natural polarity and functional organization [2].
Diagram 1: Comparative molecular pathways in 2D versus 3D culture systems showing how the initial environment leads to fundamentally different cellular outcomes.
Experimental Data Comparison: Quantitative Performance Metrics
Drug Response and Resistance Profiles
Substantial evidence demonstrates that 3D cell cultures exhibit drug response profiles that more closely resemble in vivo conditions compared to 2D models. This is particularly evident in cancer research, where 3D models better replicate the resistance mechanisms observed in solid tumors.
A study using HER2-positive breast cancer cell lines (BT474, HCC1954, EFM192A) revealed significant differences in response to both targeted therapy and classical chemotherapy between 2D and 3D cultures [7]. When treated with the HER-targeted drug neratinib, 2D cultured cells showed significantly reduced cell survival (62.7±1.2% for BT474) compared to 3D cultures (90.8±4.5% for BT474), indicating substantially increased resistance in the 3D models [7]. Similarly, when exposed to the chemotherapeutic agent docetaxel, 2D cultures of BT474 cells demonstrated 60.3±8.7% survival compared to 91±5.9% in 3D cultures [7].
Table 1: Comparative Drug Response in 2D vs 3D Breast Cancer Cultures
| Cell Line | Drug Treatment | Cell Survival in 2D (%) | Cell Survival in 3D (%) | Difference |
|---|---|---|---|---|
| BT474 | Neratinib | 62.7 ± 1.2 | 90.8 ± 4.5 | 28.1 ± 5.4 |
| BT474 | Docetaxel | 60.3 ± 8.7 | 91.0 ± 5.9 | 30.7 ± 2.8 |
| HCC1954 | Neratinib | 64.7 ± 3.9 | 77.3 ± 6.9 | 12.6 ± 5.3 |
| HCC1954 | Docetaxel | 52.3 ± 8.5 | 101.6 ± 5.7 | 49.0 ± 3.1 |
| EFM192A | Neratinib | 59.7 ± 2.1 | 86.8 ± 0.6 | 27.1 ± 2.7 |
| EFM192A | Docetaxel | 46.2 ± 2.6 | 96.2 ± 1.9 | 50.0 ± 2.5 |
The increased resistance observed in 3D cultures has been attributed to several factors, including altered expression of proteins involved in cell survival, increased activity of drug transporters associated with resistance, and enhanced drug metabolizing enzyme activity [7]. Specifically, research shows that activity of CYP3A4, a crucial drug-metabolizing enzyme, is substantially increased in 3D compared to 2D cultures [7].
Viability, Phenotypic, and Functional Comparisons
Beyond drug response, significant differences exist in basic cellular functions between 2D and 3D systems. Studies consistently show that cell viability measures differ substantially between the two formats, with 3D cultures often exhibiting lower ATP levels—a standard viability metric—compared to 2D cultures when measured at the same time points [7].
After 6 days of culture seeded at identical densities, BT474 3D cell viability was only 41.6±5.9% of that measured in BT474 2D cells. Similarly, HCC1954 3D cell viability was only 18.4±1.5% of that measured in 2D cultures, and EFM192A 3D cell viability was 44±3.7% of their 2D counterparts [7]. These differences likely reflect distinct metabolic states and proliferation rates rather than simply indicating poorer health in 3D cultures.
Morphological examinations using scanning electron microscopy reveal substantial differences between 2D and 3D cultured cells [7]. While cells in 2D culture typically spread out to form monolayers with characteristic flattened morphology, the same cells grown in 3D conditions form structured spheroids with complex surface features. Some cell lines in 3D culture appear to secrete significant extracellular matrix that smoothens the spheroid surface and creates pores, making individual cells difficult to distinguish—a characteristic more reminiscent of in vivo tissue architecture [7].
Table 2: Functional and Structural Comparison of 2D vs 3D Culture Systems
| Parameter | 2D Culture | 3D Culture | Biological Significance |
|---|---|---|---|
| Cell Viability (ATP levels) | Higher (reference) | 18-44% of 2D levels [7] | Different metabolic state in 3D |
| Drug Metabolizing Enzyme Activity | Reduced CYP activity | Substantially increased CYP3A4 [7] | Better prediction of drug metabolism |
| Expression of Survival Proteins | Lower | Increased Akt expression [7] | Enhanced survival signaling in 3D |
| Cell Morphology | Flat, spread monolayers | Structured spheroids with ECM [7] | Better tissue representation |
| Gene Expression Profile | Artificial | More physiologically relevant [6] | Better translational potential |
| Spatial Organization | Single layer, artificial polarity | Natural architecture, gradients [8] | Recreation of tissue context |
Methodological Approaches: Experimental Implementation
3D Culture Techniques and Technologies
Three-dimensional cell culture technologies can be broadly divided into two categories: scaffold-based and scaffold-free techniques [6]. The choice between these approaches depends on several parameters, including the nature of the cells (cell line vs primary cells, tissue origin) and the research objectives.
Scaffold-based techniques utilize supportive matrices that facilitate three-dimensional growth. These include:
- Hydrogel-based scaffolds: Natural or synthetic polymer networks that swell in water, allowing cell embedding or surface coating. These can be further categorized as ECM protein-based hydrogels (e.g., Matrigel, collagen), natural hydrogels (e.g., alginate, chitosan), or synthetic hydrogels (e.g., PEG-based) [6].
- Polymeric hard material-based scaffolds: Fibrous or spongeous structures made from materials such as polystyrene (ideal for imaging due to transparency) or biodegradable polymers like polycaprolactone [6].
Scaffold-free techniques rely on cellular self-assembly to form structures known as spheroids—non-adherent cell aggregates that mimic solid tissues [6]. These systems enable cells to secrete their own ECM and establish natural nutrient and oxygen gradients. Scaffold-free approaches include:
- Hanging drop methods: Utilizing gravitational forces and surface tension to encourage cell aggregation [8].
- Ultra-low attachment plates: Specially treated surfaces that prevent cell adhesion, promoting spheroid formation [8].
- Rotary bioreactors: Systems that use continuous motion to maintain cells in suspension, facilitating aggregate formation [2].
Diagram 2: Decision pathway for selecting appropriate 3D culture methodologies based on research objectives and technical requirements.
The Scientist's Toolkit: Essential Research Reagents and Materials
Implementing robust 3D culture systems requires specific reagents and materials that differ from traditional 2D approaches. The following table details key solutions and their applications in establishing physiologically relevant 3D microenvironments.
Table 3: Essential Research Reagents for 3D Cell Culture Applications
| Reagent/Material | Type | Primary Function | Research Applications |
|---|---|---|---|
| Poly-HEMA | Scaffold-free | Prevents cell adhesion to promote spheroid formation [7] | Forced-floating 3D culture methods |
| Basement Membrane Extracts (e.g., Matrigel) | ECM-based hydrogel | Provides complex ECM environment for cell embedding | Organoid culture, angiogenesis assays |
| Alginate Hydrogels | Natural hydrogel | Tunable 3D matrix for cell encapsulation | Cell migration studies, tissue engineering |
| Polyethylene Glycol (PEG) Hydrogels | Synthetic hydrogel | Defined, customizable ECM microenvironment | Mechanobiology studies, drug screening |
| Ultra-Low Attachment Plates | Scaffold-free surface | Prevents cell attachment, enables spheroid formation | High-throughput drug screening, toxicity testing |
| Hanging Drop Plates | Scaffold-free platform | Gravity-assisted spheroid formation | Multicellular tumor spheroid generation |
| Rotary Wall Vessels | Bioreactor system | Maintains cells in suspension by constant motion | Large-scale 3D culture, tissue modeling |
Research Applications: Context-Specific System Selection
Appropriate Use Cases for 2D Culture Systems
Despite the physiological advantages of 3D models, 2D culture systems remain valuable for specific research applications where their simplicity, cost-effectiveness, and compatibility with high-throughput workflows provide practical benefits [8].
Appropriate use cases for 2D culture include:
- High-throughput screening (HTS) applications: Early-stage compound screening where thousands of molecules need rapid evaluation [8].
- Basic cytotoxicity assessments: Initial evaluation of compound toxicity using standardized protocols [8].
- Genetic manipulation studies: Techniques such as CRISPR-Cas9 gene editing where accessibility and efficiency are prioritized [8].
- Receptor-ligand interaction studies: Investigation of specific molecular interactions without complex tissue context [8].
- Large-scale cell production: Applications requiring substantial biomass where cost and scalability are primary concerns.
A tiered approach is often most efficient, using 2D systems for initial screening followed by 3D models for validation and more sophisticated studies [8]. This strategy leverages the strengths of both systems while managing resource constraints.
Applications Benefitting from 3D Culture Models
Three-dimensional culture systems provide particular value in research contexts where tissue architecture, cell-cell interactions, and physiological gradients significantly influence biological outcomes [8]. These applications typically prioritize physiological relevance over throughput and cost considerations.
Key applications where 3D cultures excel include:
- Cancer research and drug development: Especially for solid tumors where the microenvironment influences drug penetration, resistance mechanisms, and cellular responses [8] [7].
- Stem cell differentiation and organoid development: Where three-dimensional context supports proper tissue-specific differentiation and function [8].
- Toxicology and safety pharmacology: Particularly for organs like the liver where metabolizing enzyme function is crucial and better maintained in 3D cultures [6] [7].
- Infectious disease modeling: Studying host-pathogen interactions in tissue-like environments [8].
- Personalized medicine approaches: Using patient-derived organoids to match therapies to individual patients, as demonstrated by institutions like Memorial Sloan Kettering Cancer Center [8].
Leading research organizations and pharmaceutical companies have incorporated 3D models into their workflows. For example, Roche uses 3D tumor spheroids to model hypoxic tumor cores and test immunotherapies, while Emulate Inc. deploys liver-on-chip platforms for preclinical hepatotoxicity screening [8].
The comparison between 2D and 3D culture systems reveals a complex landscape where each approach offers distinct advantages and limitations. Two-dimensional cultures provide simplicity, cost-effectiveness, and compatibility with high-throughput workflows, making them suitable for initial screening and specific molecular studies. However, their limitations in replicating in vivo physiology, particularly regarding cell-cell and cell-ECM interactions, can compromise translational relevance.
Three-dimensional culture systems demonstrate superior performance in modeling tissue architecture, drug resistance, metabolic function, and cellular differentiation. The experimental data clearly shows that 3D models generate different—and often more physiologically relevant—responses to therapeutic agents, gene expression profiles, and functional outcomes. These advantages come with increased complexity, cost, and technical challenges that must be considered in experimental planning.
The evolving landscape of cell culture technologies suggests a future of integrated approaches rather than exclusive adoption of either system. Hybrid workflows that strategically employ both 2D and 3D models at different stages of research, combined with advanced analytics and possibly AI integration, represent the most promising path forward [8]. As regulatory bodies increasingly recognize data from 3D models in drug submissions, the strategic implementation of these physiologically relevant systems will continue to grow in importance throughout biomedical research and drug development.
For decades, two-dimensional (2D) cell culture has been a fundamental tool in biological research, yet it imposes artificial constraints that fundamentally alter cellular architecture. In traditional 2D systems, cells are forced to adhere and spread on rigid, flat plastic or glass surfaces, resulting in unnatural flattened morphologies and disrupted polarity [8] [12]. This environment fails to recapitulate the complex three-dimensional architecture of living tissues, where cells interact with neighbors and the extracellular matrix (ECM) in all dimensions.
The shift to three-dimensional (3D) cell culture represents a paradigm shift in experimental biology. These systems allow cells to grow and interact in a spatial context that closely mimics the in vivo microenvironment, thereby preserving essential morphological characteristics and establishing proper apical-basal polarity found in native tissues [13] [12]. This guide provides an objective comparison of how 3D culture systems maintain natural cellular structure compared to traditional 2D methods, supported by experimental data and protocols for researchers and drug development professionals.
Fundamental Differences in Cellular Architecture
Morphological Characteristics Across Culture Models
The table below summarizes the key differences in cellular morphology and polarity between 2D and 3D culture systems.
Table 1: Comparative Analysis of Cellular Morphology and Polarity in 2D vs. 3D Culture Systems
| Feature | 2D Culture | 3D Culture |
|---|---|---|
| Cell Shape | Flattened, stretched morphology [8] | Natural, tissue-like 3D architecture [13] |
| Polarity | Often disrupted or partially formed [12] | Proper apical-basal polarization [12] |
| Cell-Cell Interactions | Limited to peripheral contacts [12] | Multi-faceted, natural adhesion patterns [14] |
| Cell-ECM Interactions | Single plane, unnatural binding [15] | Natural, spatially organized ECM binding [13] |
| Spatial Organization | Monolayer, forced 2D arrangement [8] | Self-organizing, tissue-like structures [14] |
| Gene Expression | Altered due to unnatural substrate [8] | In vivo-like expression profiles [8] |
| Proliferation Rate | Typically faster, unregulated [12] | Physiologically relevant rates [12] |
| Nutrient/Oxygen Access | Uniform, non-physiological [14] | Gradient-dependent, physiologically accurate [8] |
Quantitative Assessment of Structural Features
Experimental data reveals measurable differences in structural preservation between culture systems.
Table 2: Experimental Measurements of Structural Preservation in Culture Models
| Parameter | 2D Culture Findings | 3D Culture Findings | Experimental Evidence |
|---|---|---|---|
| Cytoskeletal Organization | Stress fibers prominent; abnormal actin distribution [12] | Natural cytoskeletal arrangement; tissue-specific architecture [12] | Immunofluorescence imaging [12] |
| Differentiation Markers | Reduced expression of tissue-specific markers [15] | Enhanced expression of functional differentiation markers [15] | Gene expression analysis (qPCR) [8] |
| Cell Viability in Core | Not applicable (monolayer) | Viable cells throughout structure with possible necrotic core in large spheroids (>300μm) [16] | Live/dead staining and confocal microscopy [16] |
| Drug Penetration | Uniform access; overestimated efficacy [8] | Gradient penetration; predictive of in vivo response [8] | Chemotherapy drug testing in cancer spheroids [8] |
| Tight Junction Formation | Irregular junctional protein localization [12] | Proper tight junction assembly and function [12] | Transmission electron microscopy [12] |
Experimental Protocols for Structural Analysis
Protocol 1: 3D Spheroid Formation and Morphological Analysis
Objective: To generate and characterize 3D spheroids using scaffold-free methods for morphological assessment.
Materials:
- Nunclon Sphera 96-well U-bottom plates (Thermo Fisher Scientific) [16]
- Appropriate cell culture medium (e.g., Gibco 3D culture media) [16]
- Cell lines of interest (e.g., HepG2, A549) [16]
- Phosphate Buffered Saline (PBS)
- Centrifuge
- Inverted microscope or high-content analysis system (e.g., CellInsight CX7) [16]
Methodology:
- Cell Seeding: Prepare single-cell suspension at optimal density (e.g., 5,000 cells/well for A549 in 96-well plate) [16].
- Spheroid Formation: Centrifuge plate at low speed (300-500 × g) for 5 minutes to aggregate cells at well bottom [16].
- Culture Maintenance: Incubate at 37°C, 5% CO₂ for 3-7 days, with half-medium changes every 2-3 days [16].
- Morphological Assessment:
- Image spheroids daily using brightfield microscopy to monitor size and structure [16].
- For detailed analysis, use high-content imaging systems to measure diameter, volume, and circularity [16].
- For internal structure analysis, use clearing reagents (e.g., CytoVista) followed by fluorescence imaging [16].
Expected Results: Formation of compact, spherical structures with cell-cell interactions throughout. Size depends on initial seeding density and culture duration.
Protocol 2: Immunofluorescence Analysis of Cell Polarity in 3D Models
Objective: To visualize and quantify establishment of apical-basal polarity in 3D cultures.
Materials:
- 3D spheroids/organoids (7-14 days in culture)
- Fixation solution (e.g., 4% paraformaldehyde)
- Permeabilization buffer (e.g., 0.1-0.5% Triton X-100)
- Blocking solution (e.g., 1-5% BSA in PBS)
- Primary antibodies for polarity markers (e.g., ZO-1, Par3, aPKC)
- Fluorescently-labeled secondary antibodies
- Nuclear stain (e.g., DAPI)
- Mounting medium (e.g., ProLong Glass Antifade Mountant) [16]
- Confocal microscope
Methodology:
- Fixation: Fix spheroids with 4% PFA for 30-60 minutes at room temperature.
- Permeabilization and Blocking: Permeabilize with 0.3% Triton X-15 for 30 minutes, then block with 3% BSA for 2 hours.
- Antibody Staining: Incubate with primary antibodies overnight at 4°C, followed by secondary antibodies for 2-4 hours at room temperature.
- Mounting and Imaging: Mount spheroids using anti-fade mounting medium and image using confocal microscopy with z-stack acquisition [16].
Expected Results: Distinct localization of polarity proteins at appropriate membrane domains, demonstrating proper apical-basal polarization in 3D models compared to disrupted patterns in 2D cultures.
Research Reagent Solutions for 3D Culture
Table 3: Essential Research Reagents for 3D Cell Culture and Structural Analysis
| Reagent Category | Specific Products | Function in 3D Culture |
|---|---|---|
| Scaffold Systems | Matrigel, Geltrex, Collagen, VitroGel [16] [17] | Provides extracellular matrix mimicry for cell attachment and morphogenesis |
| Scaffold-Free Platforms | Nunclon Sphera plates, Hanging drop plates, Ultra-low attachment surfaces [16] | Enables self-assembly of spheroids through minimized cell-surface adhesion |
| Specialized Media | Gibco 3D culture media, Organoid differentiation media [16] | Provides optimized nutrients and signaling molecules for 3D growth |
| Imaging Reagents | CytoVista 3D Culture Clearing Agent, ProLong Glass Antifade Mountant [16] | Enables deep imaging within 3D structures by reducing light scattering |
| Analysis Tools | CellInsight CX7 HCA System, EVOS cell imaging systems [16] | Allows quantitative analysis of size, morphology, and protein localization |
Signaling Pathways in Morphology and Polarity Establishment
The following diagram illustrates key signaling pathways regulating morphology and polarity in 3D cultures, highlighting differences from 2D systems.
Impact on Predictive Value in Drug Development
The preservation of natural morphology and polarity in 3D cultures significantly enhances their predictive value in pharmaceutical research. Cells cultured in 3D exhibit more physiological gene expression profiles, drug metabolism, and toxicity responses compared to 2D cultures [8] [15]. For instance, hepatocytes in 3D culture maintain cytochrome P450 expression and metabolic function that rapidly declines in 2D conditions [15]. This preservation of tissue-specific functionality makes 3D models particularly valuable for preclinical testing.
In cancer research, 3D tumor spheroids develop physiological barriers to drug penetration, including hypoxic cores and compact tissue architecture, providing more accurate prediction of chemotherapeutic efficacy [8] [18]. Studies have demonstrated that drugs showing promise in 2D models often fail in clinical trials due to this discrepancy, with 3D cultures potentially bridging this translational gap [8].
The evidence comprehensively demonstrates that 3D cell culture systems preserve natural cellular morphology and polarity far more effectively than traditional 2D methods. By enabling cells to establish proper three-dimensional architecture, cell-cell interactions, and apical-basal polarization, these systems provide more physiologically relevant models for basic research and drug development. While 2D cultures remain valuable for high-throughput screening and certain mechanistic studies, 3D systems offer superior structural and functional mimicry of in vivo tissues.
The research community is increasingly adopting hybrid approaches, leveraging the strengths of both systems while recognizing that 3D culture represents a fundamental advancement in preserving natural cellular structure. As technologies mature and become more accessible, 3D culture systems are poised to significantly enhance the predictive power of in vitro research and accelerate the development of more effective therapeutics.
In the realm of cancer biology and drug development, the transition from two-dimensional (2D) to three-dimensional (3D) cell culture systems represents a critical advancement in preclinical modeling. While traditional 2D monolayers have served as fundamental tools for decades, they lack the architectural complexity and microenvironmental cues present in living tissues [1]. Nutrient and oxygen gradients emerge as defining characteristics of 3D spheroids, creating physiological heterogeneity that closely mimics the avascular regions of solid tumors [19] [20].
These gradients are not merely technical observations; they are fundamental to recapitulating the tumor microenvironment (TME). In vivo, tumors develop complex spatial organizations where access to oxygen and nutrients varies significantly from the well-perfused periphery to the often nutrient-deprived and hypoxic core [19]. This spatial heterogeneity drives differential cellular behaviors, gene expression profiles, and drug responses—none of which can be adequately modeled in 2D cultures where cells experience uniform exposure to media components [8] [1]. The emergence of these natural gradients in 3D spheroids enables researchers to study critical phenomena such as drug penetration, hypoxia-induced signaling, and the development of therapeutic resistance mechanisms that mirror clinical responses [19] [7].
This guide objectively compares the capabilities of 2D and 3D culture systems in modeling these vital physiological parameters, providing experimental data and methodologies that highlight the superior predictive power of gradient-containing 3D models in preclinical research.
Comparative Analysis of 2D and 3D Culture Systems
Fundamental Structural Differences
The structural basis for gradient formation fundamentally differs between 2D and 3D culture systems, originating from their distinct spatial organizations:
- 2D Monolayers: Cells grow as a single layer attached to a flat plastic or glass surface, with uniform access to oxygen and nutrients dissolved in the culture medium [1]. This homogeneous environment fails to create the variable conditions that cells experience in solid tissues and tumors.
- 3D Spheroids: Cells aggregate into three-dimensional structures, typically ranging from hundreds to thousands of cells. In these configurations, the physical limitations of diffusion create natural gradients from the periphery to the core [19] [20]. Cells in outer regions experience higher concentrations of oxygen and nutrients, while those in inner regions progressively encounter metabolic waste accumulation, nutrient deprivation, and hypoxia [19].
Table 1: Fundamental Differences Between 2D and 3D Culture Systems
| Feature | 2D Culture System | 3D Spheroid System |
|---|---|---|
| Spatial Architecture | Monolayer; flat morphology | Three-dimensional; tissue-like structure |
| Gradient Formation | Uniform nutrient/oxygen access | Physiological nutrient/oxygen gradients |
| Cell-Cell Interactions | Limited to peripheral contacts in a single plane | Extensive, multi-directional interactions mimicking tissues |
| Cell-ECM Interactions | Limited to 2D surface binding | Natural 3D ECM integration and remodeling |
| Proliferation Patterns | Homogeneous proliferation throughout | Zonal proliferation (outer layer) and quiescence (inner layer) |
| Drug Penetration | Immediate, uniform drug access | Limited, gradient-dependent penetration mimicking in vivo tumors |
| Gene Expression Profile | Often altered, less representative of in vivo tissue | Better preserves in vivo-like gene expression patterns |
| Predictive Value for Drug Response | Limited; overestimates efficacy | Higher; better predicts clinical drug responses including resistance |
Quantitative Comparison of Microenvironmental Parameters
The structural differences between 2D and 3D systems translate into quantitatively distinct microenvironmental conditions that significantly impact cellular behavior and drug response. Research has systematically documented these variations:
Table 2: Quantitative Differences in Microenvironment and Drug Response Between 2D and 3D Cultures
| Parameter | 2D Culture | 3D Spheroid | Experimental Evidence |
|---|---|---|---|
| Oxygen Gradient | Homogeneous distribution | Hypoxic core (<3% O₂); normoxic periphery | Spheroids cultured at 3% O₂ exhibited reduced dimensions and increased necrosis [21] |
| Glucose Concentration Threshold for Necrosis | Not applicable | ~0.08 mM (critical threshold for necrosis) | COMSOL-based multiphysics model of HER2-positive BT-474 spheroids identified this critical threshold [22] |
| Drug Resistance (Docetaxel) | 40-54% cell survival reduction | Minimal reduction (4-9% survival reduction) | HER2-positive breast cancer cell lines showed significantly reduced efficacy in 3D systems [7] |
| Drug Resistance (Neratinib) | 37-40% cell survival reduction | 9-23% survival reduction | Targeted therapy showed reduced efficacy in 3D cultures of HER2-positive breast cancer cells [7] |
| Cell Viability (ATP levels) | 100% (reference) | 18-44% of 2D levels | Significantly lower metabolic activity in 3D cultures across multiple cell lines [7] |
| CYP3A4 Enzyme Activity | Lower baseline activity | Substantially increased activity | Enhanced drug metabolism capability in 3D cultures better mimicking hepatic function [7] |
The data demonstrate that 3D spheroids develop a heterogeneous cellular landscape with distinct zonation: an outer proliferative zone, an intermediate quiescent zone, and an inner necrotic core, each characterized by unique microenvironmental conditions and cellular behaviors [19] [20]. This architectural complexity directly contributes to the enhanced drug resistance observed in 3D systems, more accurately reflecting clinical treatment challenges.
Experimental Evidence: Gradient Formation and Impact
Methodologies for Studying Gradients in 3D Spheroids
Spheroid Formation Techniques
Researchers employ various established methods to generate 3D spheroids for gradient studies:
- Hanging Drop Technique: Cells aggregate spontaneously in liquid droplets suspended from plate lids, forming uniform spheroids without external scaffold interference [8] [23].
- Ultra-Low Attachment Plates: Specialized polymer-coated surfaces prevent cell attachment, forcing cells to aggregate in the well bottom under standard culture conditions [18] [23].
- Agitation-Based Methods: Bioreactors with constant rotation maintain cells in suspension, promoting aggregation through continuous gentle mixing [23].
- Scaffold-Based Systems: Natural (e.g., Matrigel, collagen) or synthetic polymers provide structural support that facilitates 3D organization and cell-ECM interactions [24] [23].
Gradient Visualization and Quantification Methods
Advanced technologies enable direct observation and measurement of gradients:
- Time-Lapse Microscopy with Viability Stains: Fluorescent markers (e.g., propidium iodide for necrosis, Calcein-AM for viability) track spheroid development and zone formation over time [21] [20].
- Single-Cell RNA Sequencing: Reveals differential gene expression across spheroid zones, identifying upregulation of hypoxia-responsive genes (e.g., HIF-1α) and extracellular matrix components in inner regions [21].
- Microfluidic Chemotaxis Chambers: Specialized devices generate controlled nutrient gradients, allowing real-time monitoring of spheroid responses to defined microenvironmental conditions [20].
- Multiphysics Computational Modeling: COMSOL-based simulations integrate growth dynamics, nutrient diffusion, uptake kinetics, and porosity evolution to predict gradient formation and its effects [22].
Impact of Culture Conditions on Gradient Formation
Experimental evidence demonstrates that specific culture parameters significantly influence gradient development and spheroid characteristics:
- Oxygen Concentration: Spheroids cultured at 3% O₂ exhibited reduced dimensions and increased necrosis compared to those under standard oxygen conditions [21].
- Serum Concentration: Serum levels above 10% promoted dense spheroid formation with distinct necrotic and proliferative zones, while serum-free conditions led to spheroid shrinkage and increased cell detachment [21].
- Initial Seeding Density: The number of cells initially seeded directly correlates with final spheroid size, impacting nutrient diffusion distances and consequent gradient steepness [21].
Diagram 1: Impact of culture conditions on spheroid gradient formation and functional outcomes. External factors influence microgradient development, which establishes distinct structural zones that ultimately drive clinically relevant functional outcomes.
The Researcher's Toolkit: Essential Reagents and Methodologies
Establishing reliable 3D spheroid models requires specific materials and approaches designed to support three-dimensional growth and gradient formation. The following table summarizes key solutions and their applications in spheroid research:
Table 3: Essential Research Reagents and Solutions for Spheroid Gradient Studies
| Reagent/Solution | Function in Spheroid Research | Application Notes |
|---|---|---|
| Ultra-Low Attachment Plates | Prevents cell adhesion, promotes 3D aggregation | Polystyrene plates with covalently bound hydrogel coating; essential for scaffold-free spheroid formation [1] [23] |
| Basement Membrane Matrix (e.g., Matrigel) | Provides natural scaffold for cell invasion and signaling | Contains endogenous bioactive factors; influences spheroid morphology and gene expression [24] [23] |
| Natural Hydrogels (Collagen, Alginate) | Creates 3D ECM-mimetic environment for spheroid embedding | Collagen I at 2mg/mL concentration used in chemotaxis chambers to study invasion [20] |
| Synthetic Hydrogels (PEG, PLA) | Provides defined, customizable scaffold with controlled properties | Offers higher consistency and reproducibility than natural hydrogels; minimal bioactive interference [23] |
| Fetal Bovine Serum (FBS) | Source of growth factors and chemoattractants | Concentrations of 10-20% promote dense spheroid formation; serum-free conditions induce shrinkage [21] [20] |
| Chemotaxis Chambers | Generates stable nutrient gradients for invasion studies | Microfluidic devices with porous membranes create controlled FBS gradients (0-100%) [20] |
| Viability Assay Kits | Quantifies live/dead cells across spheroid zones | ATP-based assays show 60-80% lower viability in 3D vs 2D cultures [8] [7] |
Standardized Protocol: Establishing Gradient-Containing Spheroids
Based on methodologies from the cited research, the following protocol represents a standardized approach for generating spheroids with physiological nutrient and oxygen gradients:
- Coating Preparation: Create a 1% agarose solution in ultrapure water and add to 48-well plates (100μL/well). Allow polymerization at room temperature to form non-adhesive surfaces.
- Cell Seeding: Harvest and count cells from 2D cultures. Seed at optimized density (e.g., 2×10³ cells/well for CT26 colon carcinoma cells) in complete medium.
- Spheroid Formation: Incubate plates under standard conditions (37°C, 5% CO₂) for 5-7 days without disturbance to allow compact spheroid formation.
- Medium Optimization: Use medium with 10% FBS for optimal structure; adjust glucose concentration to physiological levels (5.5 mM) rather than standard high-glucose formulations.
- Gradient Development: Monitor daily until spheroids reach 200-500μm diameter, indicating established nutrient/oxygen gradients.
Gradient Quantification and Validation
- Viability Staining: Incubate spheroids with propidium iodide (necrotic core) and Calcein-AM (viable cells) for 30 minutes at 37°C.
- Image Analysis: Capture fluorescent images using confocal microscopy; quantify spatial distribution of live/dead cells using software like AnaSP [21].
- Oxygen Gradient Confirmation: Measure hypoxia using HIF-1α immunostaining or hypoxyprobe markers.
- Gene Expression Analysis: Process spheroids for single-cell RNA sequencing to identify gradient-dependent gene expression patterns (e.g., ECM genes COL18A1, MUC5B in inner zones) [21].
The evidence comprehensively demonstrates that nutrient and oxygen gradients in 3D spheroids are not experimental artifacts but rather defining features that create physiological heterogeneity mirroring in vivo conditions. These gradients drive the formation of distinct cellular zones with divergent proliferation profiles, metabolic activities, and drug sensitivities—fundamental characteristics of solid tumors that cannot be recaptured in 2D monolayers [19] [20].
The functional significance of these gradients extends beyond morphological mimicry to enhanced predictive validity in drug development. The dramatically different drug responses observed between 2D and 3D systems, with 3D spheroids consistently showing greater resistance to both targeted therapies and classical chemotherapeutics, directly reflect the gradient-induced heterogeneity that complicates clinical cancer treatment [7]. Furthermore, the preservation of more physiological gene expression patterns, metabolic enzyme activity, and cellular signaling pathways in 3D gradient systems underscores their superior biological relevance [21] [7].
For researchers and drug development professionals, the implication is clear: incorporating 3D spheroid models with established nutrient and oxygen gradients provides essential preclinical data that better predicts clinical outcomes. While 2D systems retain value for high-throughput initial screening, gradient-containing 3D models offer indispensable insight into drug penetration, mechanism of action in heterogeneous microenvironments, and resistance development—ultimately strengthening the translational pipeline and potentially reducing late-stage drug attrition rates.
For decades, two-dimensional (2D) cell culture has been a fundamental workhorse in biological research, providing a straightforward and low-cost method to maintain cells and perform experiments [8]. However, this approach involves growing cells in a single layer on flat surfaces, which does not reflect the essential features of tumor tissues found in living organisms [25]. The limitations of 2D culture have prompted the development of three-dimensional (3D) models that more accurately mimic the complex and dynamic cell-cell communications and cell-matrix interactions occurring in native tissue microenvironments [2] [25].
The transition from 2D to 3D culture systems represents more than just a technical shift—it introduces a fundamental biological variable that significantly influences cellular behavior, particularly gene expression and splicing patterns. Cells in the body naturally reside within a complex three-dimensional architecture where they interact with their surroundings on all sides, creating gradients of oxygen, nutrients, and signaling molecules [2]. This spatial organization is crucial for maintaining proper cellular function and tissue homeostasis, elements that are largely lost in traditional 2D cultures.
This comparison guide examines the profound transcriptomic shifts that occur when cells transition from 2D to 3D microenvironments, providing researchers with an evidence-based framework for selecting appropriate culture systems based on their experimental goals. We present quantitative data, experimental methodologies, and practical resources to support informed decision-making in cancer research and drug development.
Fundamental Differences Between 2D and 3D Culture Systems
Structural and Microenvironmental Contrasts
The structural differences between 2D and 3D culture systems create fundamentally distinct microenvironments that dramatically influence cellular behavior. In 2D cultures, cells are forced to adapt to an unnatural flat, rigid surface where they form monolayers with disrupted cell polarity and altered morphology [26]. This environment exposes the entire cell surface to the culture medium, creating uniform conditions without gradients. In contrast, 3D cultures allow cells to grow in all directions, forming complex structures that more closely resemble native tissues [2] [27].
Table 1: Core Characteristics of 2D vs. 3D Culture Systems
| Feature | 2D Culture | 3D Culture |
|---|---|---|
| Growth Pattern | Monolayer on flat surfaces | Multilayer, expanding in all directions |
| Cell-Matrix Interactions | Limited, unnatural adhesion | Complex, biomimetic adhesion |
| Spatial Organization | Uniform, two-dimensional | Three-dimensional with spatial gradients |
| Cell-Cell Contacts | Limited to peripheral contacts | Omni-directional, as found in vivo |
| Microenvironment | Homogeneous nutrient and oxygen distribution | Heterogeneous, creating nutrient/oxygen gradients |
| Physiological Relevance | Low, does not reflect natural tissue architecture | High, better mimics native tissue organization |
The 3D microenvironment enables the formation of critical physiological features such as oxygen gradients, pH gradients, and nutrient gradients that significantly influence cellular behavior and gene expression profiles [8]. These gradients are particularly important in cancer research, as they recreate the conditions found in solid tumors, including hypoxic regions that drive tumor progression and drug resistance [25].
Technical Implementation of 3D Culture Systems
Three-dimensional cultures can be established using several technical approaches, each with distinct advantages and applications:
- Scaffold-based methods: Utilize biological or synthetic materials to provide structural support. These include hydrogels, polymeric hard materials, and decellularized extracellular matrix (dECM) scaffolds that provide mechanical support and cell adhesion sites [28] [27].
- Scaffold-free methods: Rely on the self-aggregation properties of cells. The hanging drop technique is a well-established scaffold-free approach that uses gravitational and surface tension forces to facilitate natural cellular aggregate formation [8] [27].
- Bioreactor systems: Employ dynamic culture conditions to enhance nutrient distribution and waste removal. Examples include spinner flasks, rotating wall vessels, and orbital shakers that prevent cells from adhering to surfaces, keeping cells and spheroids in suspension [27] [25].
- Microfluidic platforms: Create precisely controlled microenvironments for culturing organoids and other 3D structures, allowing for sophisticated manipulation of culture conditions [29].
Transcriptomic Differences Between 2D and 3D Cultures
Gene Expression and Splicing Alterations
The structural and microenvironmental differences between 2D and 3D culture systems trigger profound transcriptomic changes that significantly impact cellular function and drug response. Cells in 3D cultures exhibit gene expression profiles that more closely resemble in vivo conditions compared to their 2D counterparts [8].
Table 2: Transcriptomic Differences Between 2D and 3D Cultures
| Transcriptomic Feature | 2D Culture Characteristics | 3D Culture Characteristics | Functional Implications |
|---|---|---|---|
| Gene Expression Fidelity | Altered gene expression patterns compared to in vivo [2] | Better gene expression profiles resembling in vivo conditions [8] | More clinically relevant drug response predictions |
| DNA Damage Response Pathways | Standard response to DNA damage | Upregulation of MRE11 and associated DNA damage repair pathways [30] | Enhanced genomic stability mechanisms |
| Metabolic Pathway Activity | Uniform metabolic activity | Increased metabolic activity at center of microregions [31] | Better modeling of tumor metabolic heterogeneity |
| Immune-Related Signaling | Limited immune marker expression | Increased antigen presentation along microregion edges [31] | More accurate immunotherapy response modeling |
| Oncogenic Pathway Activation | Altered oncogene expression | Differential activity in pathways like MYC [31] | Better recapitulation of cancer driver mechanisms |
| Alternative Splicing Patterns | Simplified splicing profiles | Complex, tissue-specific splicing patterns | Enhanced functional proteome diversity |
Research has demonstrated that 3D cultures exhibit a higher degree of structural complexity and homeostasis analogous to tissues and organs [2]. A comprehensive study examining 131 tumour sections across 6 cancer types using spatial transcriptomics revealed that tumor microregions show distinct spatial organization with varied genetic activities, including increased metabolic activity at the center and elevated antigen presentation along the leading edges [31]. These patterns are not observed in 2D systems due to their uniform microenvironment.
Key Molecular Pathways Differentially Regulated in 3D Microenvironments
The transcriptomic shifts in 3D environments activate several crucial molecular pathways with significant implications for cancer biology and therapeutic development:
Diagram 1: Transcriptomic Pathways in 3D Microenvironments. This diagram illustrates key molecular pathways differentially regulated in 3D culture systems, showing how microenvironment-induced changes in gene expression and splicing influence clinically relevant cellular behaviors.
One particularly important pathway differentially regulated in 3D environments involves MRE11, a critical component of the MRE11-RAD50-NBS1 (MRN) complex responsible for recognizing and repairing DNA double-strand breaks [30]. Studies in hepatocellular carcinoma (HCC) have demonstrated that high MRE11 expression is strongly associated with poor prognosis and regulates immune responses within the tumor microenvironment, facilitating immune evasion via the cGAS-STING pathway and HGF-MET axis [30]. This pathway activation is more accurately modeled in 3D culture systems that maintain appropriate cell-cell interactions and spatial organization.
Experimental Evidence and Methodologies
Key Experimental Protocols for Transcriptomic Analysis
To accurately assess transcriptomic differences between 2D and 3D culture systems, researchers employ several sophisticated methodological approaches:
Spatial Transcriptomics Protocol:
- Tissue Preparation: Fresh tumor tissues are collected and embedded in Optimal Cutting Temperature (OCT) compound for cryosectioning [31].
- Sectioning: Tissues are cut into thin sections (typically 10-20 μm) and placed on specialized glass slides containing barcoded capture areas.
- Staining and Imaging: Sections are stained with Haematoxylin and Eosin (H&E) for histological analysis and imaged [31].
- Permeabilization: Tissue sections are permeabilized to release mRNA molecules which bind to spatially barcoded capture probes.
- Library Preparation: cDNA libraries are synthesized, amplified, and prepared for sequencing.
- Sequencing and Data Analysis: Libraries are sequenced, and bioinformatic tools are used to map transcriptomic data back to spatial locations.
Single-Cell RNA Sequencing Protocol:
- Cell Dissociation: 3D structures are dissociated into single-cell suspensions using enzymatic and mechanical methods [30].
- Cell Viability Assessment: Cell viability is confirmed using trypan blue exclusion or similar methods.
- Single-Cell Capture: Cells are loaded into microfluidic devices for single-cell barcoding.
- Reverse Transcription and Amplification: mRNA is reverse transcribed and cDNA is amplified.
- Library Preparation and Sequencing: Libraries are prepared using platform-specific protocols and sequenced.
- Bioinformatic Analysis: Data processing, normalization, clustering, and trajectory inference are performed.
3D Culture Models for Drug Response Evaluation:
- Model Establishment: Patient-derived cancer cells (PDCCs) are cultured in 3D matrices such as decellularized extracellular matrix (dECM) scaffolds [28] or as organoids [29].
- Drug Treatment: Compounds are applied at clinically relevant concentrations, often in gradient doses.
- Viability Assessment: Cell viability is measured using assays optimized for 3D structures (e.g., ATP-based assays, resazurin reduction).
- Transcriptomic Analysis: Treated and control samples are processed for bulk or single-cell RNA sequencing.
- Pathway Analysis: Differentially expressed genes are analyzed for enriched pathways and biological processes.
Quantitative Evidence from Comparative Studies
Substantial experimental evidence demonstrates the profound transcriptomic differences between 2D and 3D culture systems:
Drug Resistance Mechanisms: Transcriptomic analysis of 3D tumor models reveals upregulation of multidrug resistance (MDR) proteins through specific cellular signaling pathways, including those activated by hypoxia, low nutrient supply, and low pH [25]. These conditions are naturally recreated in 3D models but are largely absent in 2D systems.
Tumor Microregion Heterogeneity: Spatial transcriptomic studies of 3D tumor models have identified distinct "tumor microregions" - spatially distinct cancer cell clusters separated by stromal areas that vary in size and density among cancer types [31]. These microregions exhibit differential gene expression patterns, with increased metabolic activity at the center and increased antigen presentation along the leading edges.
Immune Interaction Signatures: Analysis of 3D tumor models co-cultured with immune cells has revealed dynamic remodeling of the tumor microenvironment under immunotherapy, with high MRE11 expression facilitating epithelial-mesenchymal transition (EMT) and extensive remodeling of the tumor microenvironment [30].
Implications for Drug Discovery and Development
Drug Response and Resistance Mechanisms
The transcriptomic shifts observed in 3D culture systems have profound implications for drug discovery and development, particularly in predicting clinical efficacy:
Table 3: Drug Response Differences Between 2D and 3D Cultures
| Parameter | 2D Culture Response | 3D Culture Response | Clinical Relevance |
|---|---|---|---|
| Drug Sensitivity | Generally hypersensitive | More resistant, resembling in vivo responses | Better prediction of clinical efficacy |
| Drug Penetration | Uniform exposure throughout cells | Gradient penetration, creating sanctuary sites | Models physiological drug distribution barriers |
| IC50 Values | Typically lower | Higher, more clinically relevant | Improved dose selection for clinical trials |
| Multidrug Resistance | Limited expression of MDR proteins | Upregulated MDR expression in hypoxic regions | Recapitulates clinical resistance mechanisms |
| Combination Therapy Effects | Often overestimated | More predictive of clinical outcomes | Better prioritization of combination regimens |
| Immunotherapy Response | Limited predictive value | Models immune-tumor interactions | Enhanced immuno-oncology drug screening |
Compared to 2D cultures, cells in 3D generally exhibit a reduced sensitivity to chemotherapeutic agents, providing a more accurate prediction of clinical drug response [25]. This difference stems from multiple factors, including the presence of physiological barriers to drug penetration, altered proliferation kinetics, and the development of microenvironment-induced resistance mechanisms.
Applications in Personalized Medicine
The enhanced physiological relevance of 3D culture systems, particularly those derived from patient samples, enables more effective personalized medicine approaches:
Patient-Derived Organoids (PDOs): These 3D structures retain the genetic and phenotypic characteristics of the patient's original tumor and can more accurately reflect tumor biology than traditional cell lines [29]. They allow for functional testing of patients' cancer cells against various therapeutic options.
Therapeutic Biomarker Discovery: The transcriptomic profiles generated from 3D cultures have proven more reliable for identifying predictive biomarkers of drug response. For instance, MRE11 expression patterns in 3D hepatocellular carcinoma models have been identified as promising biomarkers for diagnosis and potential targets for personalized immunotherapy [30].
Treatment Selection Guidance: Prominent cancer centers like Memorial Sloan Kettering Cancer Center (MSKCC) now use patient-derived organoids to match therapies to drug-resistant pancreatic cancer patients, demonstrating the clinical utility of 3D culture systems [8].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Implementing robust comparisons between 2D and 3D culture systems requires specific reagents and technical platforms:
Table 4: Essential Research Reagents and Platforms for Transcriptomic Studies
| Category | Specific Products/Platforms | Application in Transcriptomic Studies |
|---|---|---|
| 3D Scaffold Systems | Decellularized ECM (dECM) scaffolds [28], Hydrogels (Matrigel, collagen) | Provide biomechanical and biochemical cues for proper 3D gene expression |
| Spatial Transcriptomics | 10X Genomics Visium, Nanostring GeoMx | Enable spatial mapping of gene expression patterns in 3D structures |
| Single-Cell RNA Sequencing | 10X Genomics Chromium, BD Rhapsody | Resolve cellular heterogeneity within 3D cultures |
| Cell Culture Platforms | Ultra-low attachment plates, Hanging drop plates, Microfluidic chips (OrganoPlate) | Facilitate formation and maintenance of 3D structures |
| Extracellular Matrix Components | Laminin, Fibronectin, Collagen I/IV | Recreate tissue-specific microenvironment for proper signaling |
| Analysis Tools | Seurat, Scanpy, stCancer package, GEPIA2 | Process and interpret transcriptomic data from 3D models |
The selection of appropriate reagents and platforms is critical for generating reliable, reproducible data when comparing 2D and 3D systems. For instance, decellularized extracellular matrix (dECM) scaffolds have been shown to create complex microenvironments that better maintain native gene expression profiles compared to basic protein matrices typically employed in 2D or simpler 3D culture systems [28].
The transition from 2D to 3D cell culture systems represents far more than a technical advancement—it constitutes a fundamental shift in how researchers model biological systems. The transcriptomic differences between these systems are profound and well-documented, with 3D environments promoting gene expression and splicing patterns that more closely resemble in vivo conditions. These differences significantly impact drug response profiles, mechanistic studies of disease processes, and the predictive accuracy of preclinical models.
For researchers and drug development professionals, the choice between 2D and 3D culture systems should be guided by specific research objectives. While 2D systems remain valuable for high-throughput screening and certain reductionist experimental approaches, 3D models provide essential physiological context for studies requiring clinical relevance. The optimal approach for many research programs involves a complementary strategy, using 2D systems for initial screening followed by 3D models for validation and mechanistic studies.
As technological advancements continue to improve the accessibility and reproducibility of 3D culture systems, their adoption is expected to grow, ultimately enhancing the translation of basic research findings into clinical applications. Strategic integration of 3D models into research workflows will support both improved understanding of disease mechanisms and the discovery of more effective, personalized therapeutic interventions.
Implementing 3D Models: Techniques and Their Transformative Applications in Biomedicine
The transition from traditional two-dimensional (2D) to three-dimensional (3D) cell culture represents a fundamental evolution in biomedical research. While 2D cultures, where cells grow as monolayers on flat plastic surfaces, have been the workhorse of laboratories for decades, they present significant limitations [2]. Cells in 2D exhibit altered gene expression, increased drug sensitivity, and cannot replicate the complex architecture and cell-cell interactions found in living tissues [2] [32]. In contrast, 3D cell culture systems bridge the gap between simple 2D cultures and complex in vivo environments, enabling cells to grow in all directions, form natural gradients of oxygen and nutrients, and establish cell-matrix interactions that closely mimic the physiological conditions of human tissues and organs [2] [33]. This enhanced biological relevance is crucial for applications in drug discovery, disease modeling, and regenerative medicine [32].
The foundation of most 3D culture systems is the scaffold—a material that provides structural and biochemical support for cell attachment, proliferation, and organization. This guide objectively compares the performance of the predominant scaffold-based techniques: the naturally-derived Matrigel, various hydrogel systems, and emerging synthetic polymer scaffolds, providing a clear analysis of their efficacy within the broader thesis of 2D versus 3D culture system research.
The Gold Standard and Its Limitations: Matrigel
Matrigel, a basement membrane matrix extracted from Engelbreth-Holm-Swarm (EHS) mouse sarcoma, has been the "gold standard" scaffold for 3D cell culture for over four decades [34] [35]. Its main components are laminin (~60%), collagen IV (~30%), entactin (~8%), and the heparin sulfate proteoglycan perlecan [34]. This composition, rich in bioactive molecules like laminin-derived peptides IKVAV and YIGSR, provides a naturally favorable environment for a myriad of applications, including stem cell culture, regenerative medicine, and organoid assembly [34] [35]. Matrigel is a thermosensitive hydrogel, existing as a liquid at 4°C and forming a gel at 37°C, facilitating easy cell encapsulation [36].
Documented Limitations and Performance Issues
Despite its widespread use, Matrigel's suitability for rigorous, reproducible research is hampered by several critical limitations:
- Complex and Ill-Defined Composition: Matrigel contains a complex mixture of over 1,800 proteins, including growth factors (e.g., TGF-β, FGFs) and enzymes (e.g., MMPs), which vary between batches and are not fully characterized [34] [35]. This introduces significant experimental uncertainty.
- Batch-to-Batch Variability: Variations in the mechanical and biochemical properties within a single batch and between different batches lead to a lack of reproducibility in cell culture experiments [34] [35] [37].
- Animal-Derived Nature: As a murine sarcoma-derived product, Matrigel presents a risk of xenogenic contaminants, limiting its use for therapeutic cell manufacturing and raising concerns for clinical translation [34] [37].
- Limited Tunability: Its composition is not conducive to physical or biochemical manipulation, making it difficult to fine-tune the matrix to probe specific cell behaviors or achieve defined biological outcomes [34] [35].
Synthetic Scaffold Alternatives: A Designed Approach
To overcome the limitations of Matrigel, significant research efforts have focused on developing synthetic and defined scaffolds. These materials aim to provide a xenogenic-free, chemically defined, and highly tunable environment for 3D cell culture [34] [35].
Synthetic Hydrogels
Synthetic hydrogels are three-dimensional networks of hydrophilic polymers that absorb large amounts of water, mimicking the natural extracellular matrix (ECM) [38]. They are highly designable and can be classified by their source (natural, synthetic, semi-synthetic), durability (durable, biodegradable), and responsiveness to environmental stimuli (smart hydrogels) [38]. Common synthetic polymers include polyethylene glycol (PEG), polyacrylamide (PAA), and PLGA-PEG-PLGA triblock copolymers [34] [37] [39].
- Advantages: Their primary advantage is the independent control over mechanical properties (e.g., stiffness, viscoelasticity) and biochemical cues (e.g., adhesion ligands, growth factors) [40] [39]. For instance, PEG hydrogels functionalized with RGD peptides (a common cell-adhesion motif) have been successfully used for intestinal organoid culture and to study cancer cell dissemination [34] [40].
- Performance Data: A 2025 study developed a fully synthetic injectable gel scaffold (PLGA-PEG-PLGA/LAPONITE/L-Arg@NU-1000) for skeletal muscle regeneration. In vivo experiments demonstrated that its tissue regeneration efficiency was higher than that of Matrigel, as judged by histological analysis including MYH3 immunofluorescent staining [37].
Recombinant Protein and Peptide Hydrogels
These scaffolds strive to combine the bioactivity of natural components with the definition and reproducibility of synthetic systems.
- Recombinant Protein Hydrogels: These are composed of engineered proteins, such as recombinant elastin or laminin, produced in controlled systems (e.g., E. coli), ensuring a defined and consistent composition [36].
- Self-Assembling Peptide (SAP) Hydrogels: These are made from short peptide sequences that spontaneously organize into nanofibers under specific physiological conditions, forming a hydrogel scaffold [36]. They can be functionalized with bioactive epitopes (e.g., IKVAV) to direct cell behavior [34].
Comparative Performance Analysis
The table below summarizes key performance characteristics of Matrigel, synthetic hydrogels, and peptide-based scaffolds, highlighting their comparative efficacy.
Table 1: Comprehensive Comparison of Scaffold-Based 3D Culture Techniques
| Feature | Matrigel | Synthetic Hydrogels (e.g., PEG, PAA) | Peptide Hydrogels |
|---|---|---|---|
| Composition & Definition | Complex, ill-defined, >1800 proteins [34] [35] | Chemically defined, reproducible [34] | Chemically defined, reproducible [36] |
| Batch-to-Batch Variability | High, a major source of irreproducibility [34] [35] | Low, highly reproducible [34] | Very low, highly reproducible [36] |
| Origin & Safety | Mouse sarcoma, xenogenic, not clinically translatable [34] [37] | Synthetic, xenogenic-free, better clinical potential [34] [37] | Synthetic, xenogenic-free, good clinical potential [36] |
| Tunability of Properties | Very low, difficult to manipulate [34] | Very high, independent control over mechanics and biochemistry [40] [39] | High, can engineer peptide sequences [34] |
| Bioactivity | High, but uncontrolled and variable [34] | Customizable via incorporation of specific ligands (e.g., RGD, IKVAV) [34] [40] | Customizable via peptide design [34] |
| Typical Applications | Stem cell culture, organoids, angiogenesis assays [34] [35] | Organoid culture, regenerative medicine, mechanistic studies [34] [37] [39] | Neural tissue engineering, 3D cell culture [34] |
| Documented Performance | Excellent growth but inconsistent results; promotes epithelial dissemination in cancer models [40] | Equivalent or superior to Matrigel in stem cell culture and organoid formation; induced dissemination at intermediate adhesion/rigidity [34] [40] [37] | Promotes neural stem cell differentiation; can direct specific cell behaviors [34] |
The following diagram illustrates the fundamental logical relationship between the choice of scaffold material and the key considerations in 3D cell culture.
Diagram 1: Scaffold Selection Logic
Experimental Protocols and Data Generation
Example Protocol: Culturing Intestinal Organoids in PEG-Based Hydrogels
The following workflow details a method for creating synthetic hydrogel environments for organoid culture, as an alternative to Matrigel [34].
Table 2: Key Reagents for PEG Hydrogel Organoid Culture
| Reagent / Material | Function in Protocol |
|---|---|
| 4-Arm PEG-VS (PEG-vinyl sulfone) | Macromer that forms the backbone of the hydrogel network through covalent crosslinking. |
| Peptide Crosslinker (e.g., GCGPQG↓IWGQCG) | MMP-degradable crosslinker; allows cells to remodel and invade the matrix. |
| Adhesion Peptide (e.g., CRGDS) | Provides integrin-binding sites for cell attachment and survival. |
| Laminin-Derived Peptides | Provides specific bioactive cues to support stemness and differentiation. |
| Factor XIIIa | Enzyme that catalyzes the crosslinking reaction between PEG-VS and peptides. |
| Intestinal Stem Cells | Primary cells or progenitor cells used to generate organoids. |
Step-by-Step Workflow:
- Hydrogel Precursor Preparation: Dissolve 4-arm PEG-VS macromer at a concentration of 1-5 mM in a cell-compatible buffer (e.g., Tris-EDTA, pH 7.6). Separately, prepare solutions of the MMP-degradable peptide crosslinker (2-4 mM) and the adhesion peptide (e.g., RGD, 1-2 mM) [34].
- Cell Suspension: Harvest and resuspend intestinal stem cells in the PEG-VS solution at the desired density (e.g., 1-5 x 10^5 cells/mL).
- Crosslinking Initiation: Combine the cell-PEG-VS suspension with the peptide crosslinker and adhesion peptide solutions. Immediately add Factor XIIIa enzyme (2-3 U/mL final concentration) to initiate gelation. Mix rapidly but gently.
- Gelation: Quickly pipet the mixture into the desired culture vessel (e.g., multi-well plate). The gelation process typically occurs within 10-30 minutes at 37°C.
- Culture Maintenance: After full gelation, overlay the hydrogel with organoid-specific culture medium. Change the medium every 2-3 days.
- Analysis: Organoid growth and morphology can be monitored via microscopy. For endpoint analysis, hydrogels can be degraded (if possible) to release organoids for sequencing, or fixed and processed for immunohistochemistry.
Representative Experimental Data
Quantitative data from the literature demonstrates the performance of synthetic scaffolds against the benchmark of Matrigel.
Table 3: Comparative Experimental Data: Synthetic vs. Matrigel
| Application / Cell Type | Scaffold Material | Key Performance Metric vs. Matrigel | Citation |
|---|---|---|---|
| Skeletal Muscle Regeneration | PLGA-PEG-PLGA/LAPONITE/L-Arg@NU-1000 | Higher regeneration efficiency in vivo based on histological scoring (MYH3, H&E staining) [37] | [37] |
| Mammary Epithelial Cell Dissemination | RGD-functionalized PEG hydrogel | Induced dissemination at intermediate adhesion/rigidity; Matrigel did not induce dissemination [40] | [40] |
| Human Pluripotent Stem Cell (hPSC) Culture | Synthetic polymer surfaces (e.g., PMEDSAH) | Supported long-term 2D culture and maintenance of hPSCs [34] | [34] |
| Mouse Neuroepithelial Tubule Organoids | PEG hydrogel with laminin peptides | Supported the formation of brain organoids [34] | [34] |
The relationship between scaffold properties and cellular responses is a key area of investigation, particularly in cancer research.
Diagram 2: Mechanical Property Effects
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs key materials and their functions for researchers establishing scaffold-based 3D cultures, particularly with synthetic systems.
Table 4: Research Reagent Solutions for 3D Scaffold Culture
| Reagent / Material | Category | Primary Function in 3D Culture |
|---|---|---|
| Matrigel / BME | Natural, Tumor-Derived | Provides a complex, bioactive basement membrane matrix for general organoid and stem cell culture. |
| PEG-based Macromers | Synthetic Hydrogel | Serves as a chemically defined, inert backbone for creating customizable hydrogels. |
| RGD Peptide | Biochemical Cue | The quintessential integrin-binding peptide, added to synthetic hydrogels to promote cell adhesion. |
| MMP-Sensitive Peptides | Functional Crosslinker | Allows cell-mediated degradation and remodeling of the hydrogel, critical for invasion and growth. |
| LAPONITE | Nanomaterial | Clay nanoparticle used to enhance the mechanical properties and printability of hydrogels. |
| Recombinant Laminins | Defined Natural Protein | Provides a defined source of key basement membrane proteins for specific differentiation cues. |
| Self-Assembling Peptides | Peptide Hydrogel | Forms nanofiber scaffolds that mimic the physical nanostructure of native ECM. |
The objective comparison of scaffold-based techniques reveals a clear trajectory in 3D cell culture research. While Matrigel remains a prevalent tool due to its ease of use and high initial bioactivity, its inherent limitations in definition, reproducibility, and tunability pose significant challenges for rigorous scientific inquiry and clinical translation. Synthetic alternatives, particularly advanced hydrogels and peptide scaffolds, have demonstrated equivalent or even superior performance in specific applications such as stem cell culture, organoid formation, and tissue regeneration [34] [37]. The defining advantage of synthetic systems is their customizability, which allows researchers to deconstruct the complex microenvironment into specific mechanical and biochemical parameters. This capability is fundamental to advancing the broader thesis of 3D culture systems: to create more predictive and human-relevant models that bridge the gap between traditional 2D cultures and in vivo physiology, thereby accelerating drug discovery and regenerative medicine.
The transition from two-dimensional (2D) to three-dimensional (3D) cell culture represents a paradigm shift in biomedical research. Traditional 2D culture, where cells grow as monolayers on flat surfaces, fails to replicate the complex in vivo cellular microenvironment [6] [41]. Cells in the body reside within a three-dimensional extracellular matrix, interacting with neighboring cells in all dimensions, which profoundly influences their gene expression, differentiation, and response to stimuli [41] [42]. This limitation of 2D culture often leads to data that does not fully translate to clinical outcomes [6]. Scaffold-free 3D methods have emerged as powerful tools that encourage cells to self-assemble into structures like spheroids, restoring cell-cell interactions and physiological relevance without the use of artificial matrices, thus providing a more accurate model for drug screening, cancer research, and toxicology studies [6] [41].
Scaffold-free methods rely on the innate ability of cells to aggregate. The three primary techniques—hanging drop, ultra-low attachment plates, and agitation-based methods—achieve this by preventing cell attachment to a substrate, thereby encouraging spheroid formation.
Comparative Analysis of Scaffold-Free Methods
A direct comparison of the hanging drop and ULA plate methods using the RT4 human bladder cancer cell line provides robust, quantitative data for researchers.
Table 1: Quantitative Comparison of Hanging Drop vs. ULA Plates for RT4 Bladder Cancer Spheroids [43]
| Parameter | Hanging Drop Method | Ultra-Low Attachment (ULA) Plate Method |
|---|---|---|
| Optimal Seeding Concentration | 2.5 - 3.75 x 10⁴ cells/mL | 0.5 - 1.25 x 10⁴ cells/mL |
| Typical Spheroid Diameter | ~300-500 μm (at optimal concentration) | ~300-500 μm (at optimal concentration) |
| Spheroidization Time | ~48 hours | ~48 hours |
| Response to Doxorubicin (IC₅₀) | 0.83 μg/mL | 1.00 μg/mL |
| Resistance vs. 2D Culture | Higher | Higher |
| Ease of Use & Throughput | Medium (requires transfer for assays) | High (straightforward, suitable for HTS) |
Table 2: Summary of General Method Characteristics, Advantages, and Limitations
| Method | Principle | Key Advantages | Key Limitations |
|---|---|---|---|
| Hanging Drop [44] [43] [45] | Gravity-enforced cell aggregation at the liquid-air interface. | High spheroid uniformity; Minimal mechanical stress; Cost-effective. | Lower throughput; Manual medium replenishment; Potential droplet coalescence. |
| Ultra-Low Attachment (ULA) Plates [46] [43] [47] | Hydrophilic polymer coating minimizes cell adhesion, enabling spheroid formation in wells. | Simple, standardized protocol; Amenable to high-throughput screening and automation. | Plate-to-plate variability in coating quality; Potential for multiple spheroids per well. |
| Agitation-Based Methods [42] | Constant motion prevents cell attachment to vessel surfaces. | Suitable for large-scale spheroid and suspension culture; Can produce larger spheroids. | Shear stress on cells; Requires specialized equipment (e.g., spinner flasks, bioreactors). |
Detailed Experimental Protocols
Protocol 1: Hanging Drop Method for Spheroid Formation
The hanging drop technique is a cornerstone scaffold-free method that utilizes gravity to form highly uniform spheroids [44].
Detailed Methodology:
- Cell Suspension Preparation: Harvest and resuspend cells in appropriate culture medium. Cell density must be optimized for each cell type. For primary buffalo hepatocytes, this method has proven effective for maintaining liver-specific functions [48]. For the RT4 bladder cancer cell line, a concentration of 2.5 - 3.75 x 10⁴ cells/mL is optimal [43].
- Droplet Dispensing: Pipette droplets of cell suspension onto the inner surface of a Petri dish lid. Typical volumes range from 20-40 μL [43] [45].
- Inversion and Culture: Carefully invert the lid and place it over the bottom of the Petri dish, which contains phosphate-buffered saline (PBS) or culture medium to maintain humidity [45] [48].
- Incubation: Culture the dish in a standard humidified incubator (37°C, 5% CO₂) for several days. Cells will aggregate at the bottom of the droplet and form a single spheroid.
- Medium Exchange (Optional): For long-term cultures, partially refresh the medium by carefully removing and adding small volumes to the droplet every 2-3 days [43].
- Spheroid Harvesting: To use spheroids in assays, wash them from the droplet by pipetting medium over the drop [43].
Modernization with SpheroMold: Recent innovations address traditional challenges like droplet coalescence. The SpheroMold is a 3D-printed polydimethylsiloxane (PDMS) support attached to a Petri dish lid. Its defined holes act as physical barriers, preventing droplet fusion during handling, allowing for a higher density of drops per unit area, and enabling the use of larger medium volumes to reduce feeding frequency [45].
Protocol 2: Spheroid Formation Using Ultra-Low Attachment Plates
The forced floating method using ULA plates is one of the simplest and most widely adopted techniques for generating spheroids [43].
Detailed Methodology:
- Plate Selection: Choose ULA plates with a round (U-) bottom profile to encourage the formation of a single, centered spheroid per well [47].
- Cell Seeding: Prepare a single-cell suspension and seed cells directly into the ULA plates. The working volume is typically 100-200 μL per well for a 96-well plate [46] [43] [47].
- Centrifugation (Optional): A brief, low-speed centrifugation (e.g., 1000 rpm for 3-5 minutes) can help gather all cells at the bottom of the well, promoting uniform aggregation.
- Incubation and Monitoring: Place the plate in the incubator. Spheroids typically form within 24-48 hours. As shown in a comparative study, U87-MG glioblastoma cells can form compact, round spheroids in U-bottom ULA plates within 48 hours [47].
- Medium Exchange: For long-term culture, carefully remove half of the medium and replace it with fresh medium every 2-3 days, taking care not to disrupt the spheroid.
Critical Consideration - Plate Selection: The choice of ULA plate significantly impacts experimental outcomes. A 2024 study benchmarking ten different ULA microplates for primary human and canine hepatocytes found differences in spheroid size, geometry, reproducibility, and function. Plates from Corning and Biofloat showed the best overall performance, with high viability and the most physiologically relevant phenotypes [46].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for Scaffold-Free 3D Culture
| Item | Function & Importance | Example Brands/Notes |
|---|---|---|
| ULA Plates, U-Bottom | Provides a chemically modified surface to inhibit cell attachment, forcing cells to aggregate into spheroids within the well. The U-bottom shape guides a single spheroid formation. | Corning, Biofloat, VitroPrime [46] [47] |
| Hanging Drop Plates | Specialty plates with engineered lids or supports to simplify the creation and maintenance of multiple hanging drops, reducing manual error. | Perfecta3D [43] |
| PDMS (Polydimethylsiloxane) | A biocompatible silicone used to create custom supports like the SpheroMold to modernize the traditional hanging drop method. | Sylgard 184 [45] |
| Poly-HEMA | A polymer used to coat standard cultureware to create a non-adhesive surface, a cost-effective alternative to commercial ULA plates. | Sigma-Aldrich [48] |
| Spheroid Analysis Hydrogel | A ready-to-use hydrogel matrix for embedding pre-formed spheroids to conduct invasion assays and study cell migration. | VitroGel [47] |
The choice among hanging drop, ultra-low attachment plates, and agitation methods is not one of absolute superiority but of strategic application. Hanging drop excels in generating highly uniform spheroids for fundamental biological studies where consistency is paramount. Ultra-low attachment plates offer a robust, straightforward, and scalable solution ideal for high-throughput drug screening and toxicology assays. Agitation-based methods are best suited for large-scale production of spheroids or when cultivating more complex organoid structures. As the data demonstrates, these scaffold-free systems collectively provide a critical bridge between simplistic 2D monolayers and complex in vivo environments, enabling more physiologically relevant and predictive research in drug development and disease modeling.
For decades, biomedical research has relied on two-dimensional (2D) cell cultures and animal models for drug discovery and disease modeling. However, these traditional models suffer from significant limitations. 2D cell cultures, where cells grow as a monolayer on plastic surfaces, fail to replicate the complex three-dimensional microenvironment of human tissues, leading to altered cell morphology, polarity, and gene expression [26]. Conversely, animal models, while providing a complex physiological system, are often poor predictors of human outcomes due to interspecies differences in metabolism, genetics, and disease progression [49] [50]. These limitations contribute to high drug candidate failure rates in clinical trials, highlighting an urgent need for more predictive and human-relevant research models [51].
The emergence of advanced three-dimensional (3D) culture systems represents a transformative approach that bridges the gap between conventional 2D cultures and in vivo human physiology. Among these, bioreactors, organ-on-a-chip (OOC) platforms, and 3D bioprinting have gained prominence for their ability to mimic the structural, mechanical, and biochemical features of native tissues [49] [51]. These systems better recapitulate critical physiological aspects such as diffusion kinetics, cell-cell and cell-matrix interactions, and inclusion of stromal components, ultimately leading to more accurate predictions of human drug responses and disease mechanisms [52]. This guide provides a comprehensive comparison of these advanced systems, focusing on their efficacy relative to traditional methods, with supporting experimental data and methodologies.
Fundamental Limitations of 2D Culture Systems
Traditional 2D cell culture systems, while simple and well-established, distort crucial aspects of cellular physiology. Cells cultured in 2D lack the natural 3D architecture of tissues, which disrupts normal cell polarity, mechanical cues, biochemical gradients, and cell-cell communication networks [26] [49]. These alterations significantly impact cell behavior, differentiation, and response to therapeutic agents, ultimately reducing the predictive power of drug screening assays. Research demonstrates substantial differences in drug response between cells cultured in 2D versus 3D formats, with 3D cultures showing greater resistance to chemotherapeutic agents—a phenomenon also observed in clinical settings [49] [50].
Advanced 3D Systems: Key Technologies and Benefits
Table 1: Comparison of Advanced 3D Cell Culture Systems
| Technology | Key Features | Primary Advantages | Common Applications | Reported Efficacy Improvements |
|---|---|---|---|---|
| Organ-on-a-Chip (OOC) | Microfluidic devices containing living human cells that simulate organ-level physiology [49] [51]. | Provides dynamic microenvironments with physiological fluid flow and mechanical forces; enables multi-organ integration [49]. | Disease modeling, drug toxicity testing, pharmacokinetic studies [49]. | Better prediction of human drug-induced pulmonary edema compared to static cultures [50]. |
| 3D Bioprinting | Automated fabrication of 3D tissue constructs via layer-by-layer deposition of bioinks containing cells and biomaterials [53] [54]. | Enables precise spatial control over multiple cell types and extracellular matrix components; customizable architecture [55] [54]. | Tissue engineering, high-throughput drug screening, disease modeling [53] [52]. | Significantly enhanced liver function in 3D-bioprinted liver-on-a-chip compared to conventional cultures [55]. |
| Bioreactors | Controlled systems that provide essential physiological conditions (e.g., perfusion, mechanical stimulation) for 3D tissue maturation [53] [56]. | Maintains nutrient supply and waste removal in thick constructs; mimics physiological mechanical cues [56]. | Organoid culture, tissue engineering, stem cell differentiation [56]. | Improved cell viability and reduced core necrosis in perfused neural organoids [56]. |
The relationship between these technologies and their position in the evolution of preclinical models can be visualized as a progressive increase in physiological relevance.
Experimental Data and Performance Comparison
Quantitative Comparison of 2D vs 3D Systems
Substantial experimental evidence demonstrates the superior performance of advanced 3D systems compared to traditional 2D cultures across multiple parameters. The data below summarizes key comparative findings from published studies.
Table 2: Experimental Comparison of 2D vs 3D Culture Systems in Drug Discovery
| Parameter | 2D Culture Performance | 3D System Performance | Experimental Context | Source |
|---|---|---|---|---|
| Drug Sensitivity | Increased sensitivity to chemotherapeutics; does not replicate clinical resistance patterns [49]. | Greater resistance to chemotherapeutics; better mimics in vivo tumor response [49] [50]. | Cancer cell response to various chemotherapeutic agents [49]. | Arch Med Sci (2018) [26] |
| Liver Function | Rapid decline in metabolic activity; limited lifespan [55]. | Significantly enhanced and sustained albumin production, urea synthesis, and cytochrome P450 activity [55]. | 3D-bioprinted liver-on-a-chip with spatial heterogeneity [55]. | Lab Chip (2016) [55] |
| Cell Viability in Thick Tissues | Not applicable for thick constructs. | High cell viability maintained in constructs >400μm through perfusion; reduced core necrosis [56]. | Neural organoids in perfused 3D-printed bioreactor over 7 days [56]. | Biomicrofluidics (2021) [56] |
| Predictive Value for Human Toxicity | Poor correlation with human clinical outcomes [49]. | Successfully predicted drug-induced pulmonary edema in lung-on-a-chip model [50]. | Lung-on-a-chip model exposed to toxic compounds [50]. | Nat Rev Drug Discov (2015) [50] |
Detailed Experimental Protocols
Protocol: One-Step Fabrication of 3D-Bioprinted Liver-on-a-Chip
This methodology, adapted from a study demonstrating significantly enhanced liver function, outlines the integrated fabrication of a liver-on-a-chip platform using 3D bioprinting technology [55].
- Bioink Preparation: Prepare a composite bioink containing primary human hepatocytes, hepatic stellate cells, and endothelial cells in a suitable biomaterial matrix (e.g., gelatin-based hydrogel with low protein absorption properties) [55].
- 3D Bioprinting Process:
- Utilize a pressure-assisted extrusion bioprinting system.
- Load the bioink into a sterile printing cartridge.
- Set printing parameters: extrusion pressure 15-25 kPa, printing speed 5-10 mm/s, nozzle diameter 100-200 μm.
- Print the tissue construct directly within the microfluidic chip in a single-step process, creating spatially heterogeneous patterns mimicking the liver lobule architecture [55].
- Chip Perfusion and Culture:
- Connect the printed chip to a perfusion system providing continuous medium flow at 0.1-0.5 mL/hour to mimic blood flow.
- Maintain at 37°C, 5% CO₂.
- Allow tissue maturation for 7-14 days with constant perfusion [55].
- Functional Assessment:
- Albumin Secretion: Quantify using ELISA from collected effluent medium weekly.
- Urea Synthesis: Measure urea concentration in the medium using colorimetric assays.
- Cytochrome P450 Activity: Assess using substrate-based assays (e.g., CYP3A4 activity with luciferin-IPA) [55].
Protocol: High-Throughput Drug Screening Using 3D-Bioprinted Models
This protocol, synthesized from multiple sources, describes the use of 3D-bioprinted constructs for compound screening, a method shown to improve preclinical drug efficacy predictions [49] [52].
- Array Fabrication:
- Compound Treatment:
- After tissue maturation (typically 3-7 days), add drug candidates to wells using automated liquid handling.
- Include a range of concentrations (e.g., 0.1 nM - 100 μM) and appropriate controls.
- Incubate for a predetermined period (e.g., 72 hours) [52].
- Viability and Efficacy Assessment:
- Data Analysis:
- Calculate IC₅₀ values for each compound.
- Compare dose-response curves between 2D and 3D models.
- Use imaging analysis software to quantify morphological changes [52].
The workflow for establishing and testing these advanced models involves multiple coordinated steps, from design to functional analysis.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of advanced 3D culture systems requires specific materials and reagents. The following table details key components and their functions based on protocols cited in the literature.
Table 3: Essential Research Reagents and Materials for Advanced 3D Systems
| Material/Reagent | Function | Example Applications | Notes & Considerations |
|---|---|---|---|
| Bioinks (Natural) | Scaffold materials providing structural support and biochemical cues; often include gelatin, collagen, hyaluronic acid, or basement membrane extracts [53] [54]. | General tissue fabrication, soft organ models (liver, kidney) [53]. | High biocompatibility but variable mechanical properties; may require crosslinking. |
| Bioinks (Synthetic) | Precisely tunable polymers (e.g., PEG, PCL, PLGA) offering controlled mechanical properties and degradation rates [53] [54]. | Structures requiring specific stiffness (bone, cartilage); high-resolution printing [53]. | May lack natural bioactive motifs; often functionalized with RGD or other peptides. |
| Polydimethylsiloxane (PDMS) | Elastomeric polymer used for fabricating microfluidic chips and organ-on-a-chip devices [49] [51]. | Transparent microfluidic devices allowing real-time imaging [49]. | Excellent transparency and gas permeability; can absorb small hydrophobic molecules. |
| Perfusion Bioreactors | Systems providing continuous medium flow, nutrient supply, and waste removal for 3D tissue constructs [56]. | Long-term culture of thick tissue constructs and organoids [56]. | Mimics vascular flow; prevents necrosis in tissue cores; parameters (shear stress, flow rate) must be optimized. |
| Cell Viability Assays (3D-optimized) | ATP-based quantification methods (e.g., CellTiter-Glo 3D) adapted for penetration into 3D structures [52]. | Drug screening workflows for 3D-bioprinted tissues and spheroids [52]. | Standard MTT assays may not penetrate deeply; require validation for 3D models. |
The comprehensive comparison presented in this guide demonstrates the clear efficacy advantages of advanced 3D systems—bioreactors, organ-on-a-chip platforms, and 3D bioprinting—over traditional 2D cultures. These technologies successfully address critical limitations of conventional models by providing more physiologically relevant microenvironments that better maintain native cell functionality, enhance tissue-specific functions, and ultimately yield more predictive data for human drug responses [55] [49] [50].
The integration of these technologies represents the most promising future direction. The combination of 3D bioprinting's architectural control with organ-on-a-chip's dynamic perfusion capabilities creates synergistic effects, enabling the fabrication of complex, vascularized tissue models with high physiological relevance [51] [57]. Furthermore, the ongoing development of 4D bioprinting, where printed structures can change shape or functionality over time in response to stimuli, promises even more dynamic models that can mimic developmental and pathological processes [53]. As these technologies continue to mature, they are poised to significantly transform the drug discovery pipeline, reduce reliance on animal models, and accelerate the development of safer, more effective therapeutics.
The high failure rate of drug candidates in clinical trials, often due to safety concerns like liver toxicity or a lack of efficacy, presents a major challenge in pharmaceutical development [58]. A significant factor in this failure is the overreliance on traditional two-dimensional (2D) cell cultures for preclinical testing, which are poor predictors of human physiology [59]. This guide provides an objective comparison between 2D and three-dimensional (3D) cell culture systems, focusing on their performance in high-content screening (HCS) and toxicity testing for drug discovery. We will summarize quantitative experimental data, detail essential methodologies, and provide the tools needed to implement more predictive 3D models.
2D vs. 3D Cell Culture: A Fundamental Paradigm Shift
Cell culture is a cornerstone of drug discovery and cancer research. While 2D culture, where cells grow in a single layer on flat surfaces, has been the standard method for decades, 3D culture—where cells grow in all directions to form tissue-like structures—offers a more physiologically relevant alternative [60] [2].
The core difference lies in the tumor microenvironment (TME). In the body, tumors are complex, three-dimensional ecosystems, not flat sheets of cells. The 3D models, such as multicellular tumor spheroids (MCTS), better represent this reality by recapitulating critical tissue-like properties, including spatial architecture, cell-cell interactions, and the formation of physiological gradients (e.g., oxygen, nutrients, pH) [8] [59]. The table below summarizes the key distinctions.
Table 1: Fundamental Characteristics of 2D vs. 3D Cell Cultures
| Characteristic | 2D Cell Culture | 3D Cell Culture | Key References |
|---|---|---|---|
| Cell Morphology & Shape | Flat and elongated; forced to grow as a monolayer. | Natural cell shape is preserved; cells form 3D aggregates/spheroids with multiple layers. | [60] [2] |
| Cell-Cell & Cell-ECM Interactions | Limited and less accurate; lack of spatial organization. | Common and physiologically relevant; enable complex communication. | [8] [60] |
| Exposure to Nutrients/Growth Factors | Uniform; all cells are exposed to the same conditions. | Gradients form; core cells may receive less oxygen and nutrients, mimicking tumor cores. | [60] [61] |
| Gene & Protein Expression | Often vastly different from in vivo models. | Resemble expression levels found in cells in vivo. | [60] [61] |
| Drug Sensitivity & Resistance | Often overestimate efficacy; little resistance to drugs. | More accurately represent in vivo responses; show greater drug resistance. | [8] [60] |
| Differentiation | Poor | Well-differentiated | [60] |
| Cost & Infrastructure | Inexpensive; standard protocols and equipment. | More expensive; often requires specialized equipment and expertise. | [8] [60] |
| Data Analysis & Replicability | Highly replicable and easily interpretable. | Can be difficult to replicate and interpret; requires advanced software (e.g., AI). | [60] [15] |
Quantitative Comparison: Experimental Data from the Literature
Direct comparisons in rigorous studies demonstrate how the choice of culture model can dramatically alter experimental outcomes. The data below highlight differences in proliferation, cell death, gene expression, and, most critically, response to therapeutic agents.
Table 2: Experimental Data Comparing 2D and 3D Culture Responses
| Experimental Parameter | Findings in 2D Culture | Findings in 3D Culture | Study Details |
|---|---|---|---|
| Cell Proliferation Rate | Rapid, unnatural proliferation pace. | Significantly slower and more realistic proliferation pattern over time (p < 0.01). | Colorectal cancer (CRC) cell lines; MTS assay [61]. |
| Cell Death Profile (Apoptosis) | Higher baseline of apoptotic cells. | Different death phase profile; fewer cells in early and late apoptosis stages. | CRC cell lines; Flow cytometry with Annexin V/PI staining [61]. |
| Drug Response (IC50) | Generally lower IC50 values, indicating higher potency. | Higher IC50 values, demonstrating increased resistance. For example, 3D spheroids showed resistance to 5-FU, Cisplatin, and Doxorubicin. | CRC cell lines; treated with 5-fluorouracil, cisplatin, and doxorubicin [61]. |
| Transcriptomic Profile | Significant dissimilarity (p-adj < 0.05) involving thousands of up/down-regulated genes compared to 3D and patient samples (FFPE). | Shared significant similarity in gene expression and methylation patterns with patient-derived FFPE samples. | RNA sequencing and bioinformatic analysis of five CRC cell lines [61]. |
| Hepatotoxicity (IC50) | Not applicable (data best derived from 3D). | iCell Hepatocytes 2.0 in 3D spheroids yielded IC50 values for known toxins: - Methyl mercury: 2.82 µM - Staurosporine: 0.91 µM - Doxorubicin·HCl: 5.69 µM | High-content 3D toxicity assay with iPSC-derived hepatocytes [62]. |
Essential Workflows and Protocols for 3D Spheroid Screening
Implementing a robust 3D screening model requires standardized protocols. The following section details a proven methodology for forming, treating, and analyzing hepatocyte spheroids for toxicity assessment, adaptable for various cell types.
Workflow Diagram: 3D Spheroid Toxicity Screening
The diagram below outlines the key stages of a high-content 3D toxicity screening assay.
Detailed Experimental Protocol
The workflow is based on established methods for using human iPSC-derived hepatocytes (e.g., iCell Hepatocytes 2.0) to form 3D liver spheroids for toxicity assessment [62] [59].
Step 1: Spheroid Formation
- Pre-culture: Thaw and maintain cryopreserved human iPSC-derived hepatocytes according to the manufacturer's protocol in 2D format for 7 days to recover and mature.
- Detachment & Seeding: Detach cells using Accutase. Mix the cell suspension with a Geltrex solution and plate into low-attachment spheroid plates (e.g., from Corning or InSphero) at a density of 1,000 cells/well.
- Centrifugation: Centrifuge the plate at 300 x g for 2 minutes to settle the cells and remove bubbles.
- Incubation: Incubate the plate in a humidified incubator at 37°C and 5% CO₂. Spheroids typically form within 24–48 hours [62].
Step 2: Compound Treatment
- After spheroid formation, add hepatotoxic test compounds to the culture medium.
- Incubate the spheroids with the compounds for a defined period, typically 72 hours, to assess chronic effects [62].
Step 3: Viability Staining (No-Wash Protocol)
- Prepare a dye mixture in sterile phosphate-buffered saline (PBS). A common multiparametric mix includes:
- 2 μM Calcein AM (green, for live cells)
- 3 μM Ethidium Homodimer-1 (EthD-1, red, for dead cells)
- 10 μM Hoechst 33342 (blue, for nuclei)
- Add the dye solution directly to the spheroid cultures and incubate for 2 hours. The "no-wash" protocol minimizes spheroid loss and displacement [62].
- Alternative Stains: For mechanistic studies, use CellEvent Caspase-3/7 (apoptosis) or MitoTracker Orange (mitochondrial integrity) [62] [59].
- Prepare a dye mixture in sterile phosphate-buffered saline (PBS). A common multiparametric mix includes:
Step 4: High-Content Imaging
Step 5: 3D Image Analysis
- Perform analysis using high-content analysis software (e.g., MetaXpress).
- Use the "Find Spherical Objects" function to define the spheroids and individual cells. Set parameters for the approximate size (e.g., 100-300 μm width for spheroids) and fluorescence intensity threshold.
- Connect objects across Z-planes using "Connect by Best Match" to segment and score nuclei and cytoplasm in the 3D volume without double-counting [62].
Step 6: Multiparametric Quantification
- Quantify key phenotypic features for each spheroid, including:
- Viability: Number of Calcein AM-positive (live) and EthD-1-positive (dead) cells.
- Morphology: Spheroid volume, diameter, and roundness.
- Fluorescence Intensity: Average and integrated intensity for all channels.
- Mechanistic Markers: Intensity of Caspase 3/7 (apoptosis) or MitoTracker (mitochondrial health) [62].
- Fit dose-response data to calculate IC50 values for different parameters, providing a rich profile of compound toxicity [62] [59].
- Quantify key phenotypic features for each spheroid, including:
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of 3D HCS relies on a suite of specialized reagents and tools. The following table catalogues key materials used in the featured protocols.
Table 3: Essential Reagents and Tools for 3D High-Content Screening
| Item Name | Function/Application | Specific Example(s) |
|---|---|---|
| iPSC-Derived Cells | Provides a biologically relevant, human-based cell source that retains metabolic function better than cell lines. | iCell Hepatocytes 2.0 (Cellular Dynamics International) [62]. |
| Ultra-Low Attachment (ULA) Plates | Prevents cell attachment, forcing cells to aggregate and form spheroids. Essential for scaffold-free spheroid production. | Corning Spheroid Plates, Nunclon Sphera plates, InSphero GravityTRAP ULA plates [59] [61]. |
| Extracellular Matrix (ECM) Substitute | Provides a scaffold that mimics the in vivo cellular environment for scaffold-based 3D cultures. | Geltrex, Matrigel, synthetic hydrogels (e.g., PEG-based) [62] [60]. |
| Viability/Cytotoxicity Dyes | Multiplexed staining to simultaneously identify live cells, dead cells, and nuclei within 3D structures. | Calcein AM (live), Ethidium Homodimer-1 (EthD-1, dead), Hoechst 33342 (nuclei) [62] [59]. |
| Mechanistic Fluorescent Probes | Investigate specific mechanisms of toxicity, such as apoptosis or mitochondrial dysfunction. | CellEvent Caspase-3/7 (apoptosis), MitoTracker Orange (mitochondrial membrane potential), LysoTracker (lysosomal mass) [62] [59]. |
| Confocal High-Content Imager | Automated microscope capable of acquiring sharp images at different Z-planes through 3D samples. | ImageXpress Micro Confocal System (Molecular Devices), Opera Phenix (PerkinElmer) [62] [63]. |
| 3D Image Analysis Software | Software designed to segment, analyze, and quantify complex 3D image data. | MetaXpress (Molecular Devices), Harmony (PerkinElmer), IN Carta (GE) [62] [63]. |
Visualizing Data Analysis and Biological Complexity in 3D
The power of 3D HCS lies in its ability to deconvolute complex biological phenomena. The diagram below illustrates how multiple quantitative parameters are extracted from a single 3D spheroid to build a comprehensive toxicity profile.
The transition from 2D to 3D cell culture models represents a fundamental evolution in preclinical drug discovery. As the comparative data and protocols in this guide demonstrate, 3D systems—particularly when combined with high-content imaging and analysis—provide a more physiologically relevant and predictive platform for assessing compound efficacy and toxicity [62] [61]. While 2D cultures remain useful for high-throughput primary screening due to their simplicity and low cost, 3D models excel in contexts where tissue architecture, realistic drug penetration, and long-term metabolic stability are critical for accurate decision-making [8] [15].
The future of drug discovery is not a binary choice but a strategic integration of both models. A tiered approach using 2D for high-volume screening and 3D for lead validation and mechanistic studies is becoming the standard in advanced laboratories [8]. This strategy, augmented by AI-driven image analysis and patient-derived organoids, is poised to bridge the long-standing gap between in vitro models and human clinical outcomes, ultimately reducing attrition rates and delivering safer, more effective therapeutics to patients [15] [58].
In the pursuit of precision oncology, the transition from traditional two-dimensional (2D) cell cultures to three-dimensional (3D) patient-derived organoids (PDOs) represents a paradigm shift in preclinical modeling. Traditional 2D cultures, where cells grow as monolayers on flat plastic surfaces, have long been the workhorse of cancer research due to their simplicity, low cost, and compatibility with high-throughput screening [2] [8]. However, these models fundamentally lack the physiological context of human tumors, as they cannot replicate critical features like the tumor microenvironment (TME), cellular heterogeneity, and spatial organization [64] [65]. This limitation often translates to poor clinical predictability, with many compounds showing efficacy in 2D models failing in human trials [8] [66].
Patient-derived organoids have emerged as transformative tools that bridge this translational gap. PDOs are 3D in vitro models derived directly from patient tumor tissue that recapitulate the histological, genetic, and phenotypic features of their parental tumors [67] [68]. By preserving patient-specific characteristics and incorporating essential cell-cell and cell-matrix interactions, PDOs provide a more physiologically relevant platform for therapy selection, drug screening, and biomarker discovery in personalized treatment regimens [68] [66]. The establishment of living PDO biobanks from diverse cancer types and patient populations further enhances their utility for both basic research and clinical applications [67].
This guide provides a comprehensive comparison between 2D culture systems and 3D PDO models, focusing on their respective capabilities for therapy selection in personalized medicine. We present experimental data, methodological protocols, and analytical frameworks to help researchers select the most appropriate model system for their specific applications.
Physiological and Functional Comparison: 2D Models Versus 3D PDOs
Key Structural and Functional Differences
The table below summarizes the fundamental differences between 2D cultures and 3D PDOs that impact their utility in therapy selection:
Table 1: Fundamental Differences Between 2D Cultures and 3D PDOs
| Characteristic | 2D Cell Culture | 3D Patient-Derived Organoids | References |
|---|---|---|---|
| Support for cell growth | Plastic/glass surfaces | Extracellular matrix (e.g., Matrigel, hydrogels) | [2] [64] |
| Cellular architecture | Monolayer, flattened morphology | 3D structure preserving tissue architecture | [64] [65] |
| Cell-cell & cell-matrix interactions | Limited primarily to horizontal contacts | Complex, multi-directional interactions mimicking in vivo conditions | [64] [65] |
| Tumor microenvironment | Lacks stromal and immune components | Retains some native TME elements; can be co-cultured with immune/stromal cells | [68] [69] |
| Cellular heterogeneity | Homogeneous, often clonal | Heterogeneous, containing multiple cell types | [67] [65] |
| Gene expression profiles | Altered due to artificial substrate | More closely mirrors in vivo expression patterns | [65] |
| Drug response predictability | Often overestimates efficacy; poor clinical correlation | Better predicts patient response; high clinical correlation | [70] [68] |
| Nutrient and oxygen gradients | Uniform exposure | Physiological gradients forming hypoxic cores etc. | [2] [8] |
Predictive Performance in Drug Response
Quantitative comparisons of drug response between 2D and 3D models consistently demonstrate the superior predictive value of PDOs for clinical outcomes:
Table 2: Drug Response Comparison Between 2D Cultures and 3D PDOs
| Parameter | 2D Cell Culture | 3D Patient-Derived Organoids | Clinical Correlation | References |
|---|---|---|---|---|
| Drug sensitivity | Increased sensitivity; IC~50~ values often lower | Reduced sensitivity; more resistant profile | PDO responses correlate with patient outcomes (80-100% in various studies) | [70] [65] |
| Drug penetration | Direct, unimpeded access to all cells | Limited penetration; barrier effects similar to in vivo tumors | Recapitulates drug distribution challenges in solid tumors | [8] [71] |
| Therapeutic index | Overestimated | More accurately predicted | Better predicts efficacy-toxicity balance | [70] |
| Resistance mechanisms | Limited representation of innate and acquired resistance | Models multiple resistance pathways (hypoxia, CSCs, stroma-mediated) | Closer mimicry of clinical resistance patterns | [68] [65] |
| High-throughput screening | Excellent compatibility; low cost per compound | More complex but increasingly adaptable to HTS formats | PDO biobanks enable population-wide therapeutic profiling | [70] [67] |
Establishing Patient-Derived Organoid Models: Methodological Framework
Core Protocol for PDO Generation
The successful establishment of PDOs requires careful attention to tissue processing, matrix selection, and culture conditions. The following protocol outlines the key steps:
Tissue Acquisition and Processing: Obtain fresh tumor tissue from surgical resection or biopsy under sterile conditions. Mechanically dissociate into small fragments (0.5-2 mm³) followed by enzymatic digestion using collagenase/hyaluronidase solutions at 37°C for 30-90 minutes [67] [69].
Cell Isolation and Seeding: Filter digested tissue through 70-100μm strainers to obtain single-cell suspensions or small clusters. Centrifuge and resuspend in appropriate organoid medium supplemented with tissue-specific growth factors [68] [69].
3D Embedding and Culture:
- Option A (Matrigel Embedding): Mix cell suspension with Basement Membrane Extract (e.g., Matrigel, Cultrex) at 1:1-1:3 ratio. Plate as droplets in pre-warmed culture plates and polymerize at 37°C for 20-30 minutes. Overlay with organoid culture medium [68] [69].
- Option B (Suspension Culture): Seed cells in ultra-low attachment plates with agitation to promote spheroid formation [65] [71].
Culture Maintenance: Refresh medium every 2-4 days, monitoring organoid formation and growth. Passage organoids every 1-4 weeks by mechanical/ enzymatic dissociation and re-seeding in fresh matrix [67].
Cryopreservation: Harvest organoids, resuspend in freezing medium (e.g., 90% FBS + 10% DMSO), and gradually freeze to -80°C before transferring to liquid nitrogen for long-term storage [67].
Advanced PDO Culture Systems for Immunotherapy Applications
For immunotherapy applications, standard PDO protocols require modifications to incorporate immune components:
Advanced PDO Culture Systems for Immunotherapy
Air-Liquid Interface (ALI) Culture: Maintains endogenous stromal and immune components from original tumor tissue by culturing tumor fragments in collagen gels at the air-liquid interface, preserving autologous TME complexity [69].
Microfluidic 3D Culture: Enables high-throughput generation of micro-organospheres with controlled fluid flow, allowing real-time assessment of immune cell trafficking and tumor-immune interactions [68] [69].
3D Bioprinting: Precisely positions multiple cell types (tumor cells, fibroblasts, immune cells) in spatially defined patterns to recreate tissue-scale organization and cell-cell interactions [65] [69].
The Scientist's Toolkit: Essential Reagents and Platforms for PDO Research
Successful implementation of PDO technology requires specialized reagents and equipment. The following table details essential solutions for establishing robust PDO workflows:
Table 3: Essential Research Reagent Solutions for PDO Generation and Analysis
| Category | Specific Products/Platforms | Function and Application | References |
|---|---|---|---|
| Extracellular Matrices | Matrigel, Cultrex BME, Collagen I, Synthetic hydrogels | Provide 3D scaffold for organoid growth; mimic native extracellular matrix | [64] [65] |
| Specialized Media | IntestiCult, STEMdiff, customized media with tissue-specific factors | Support stem cell maintenance and differentiation; enable tissue-specific growth | [67] [68] |
| Culture Platforms | Ultra-low attachment plates, Transwell systems, Microfluidic chips | Facilitate 3D structure formation; enable advanced culture configurations | [65] [69] |
| Analysis Tools | IN Carta Image Analysis Software, CellXpress.ai Automated Culture System | Automated image analysis and data processing; scalable organoid production | [70] |
| Molecular Characterization Kits | Single-cell RNA sequencing, Multiplex immunofluorescence, ATP-based viability assays | Comprehensive profiling of heterogeneity and drug response | [67] [68] |
Experimental Design for Therapy Selection: A Comparative Workflow
To illustrate the application of PDOs in therapy selection, the following diagram outlines a comprehensive experimental workflow that integrates both 2D and 3D approaches:
Therapy Selection Workflow Using PDOs
This integrated approach leverages the strengths of both systems:
Initial High-Throughput Screening in 2D: Rapidly screen large compound libraries using 2D cultures to identify candidate therapeutics [8] [71].
Validation in 3D PDO Models: Test promising candidates from 2D screens against patient-matched PDOs to assess efficacy in a more physiologically relevant context [70].
Multi-Omics Profiling: Integrate genomic, transcriptomic, and proteomic analyses of PDOs to identify biomarkers predictive of treatment response [67] [66].
Clinical Correlation: Compare PDO drug responses with patient outcomes to validate predictive accuracy and refine selection algorithms [68].
This tiered approach balances efficiency with physiological relevance, enabling comprehensive therapeutic profiling while conserving valuable patient-derived materials.
The integration of patient-derived organoids into personalized medicine represents a significant advancement over traditional 2D models for therapy selection. While 2D cultures remain valuable for initial high-throughput screening and basic mechanistic studies, their limitations in predicting clinical responses are well-documented [70] [66]. PDOs address many of these limitations by preserving patient-specific tumor characteristics, cellular heterogeneity, and aspects of the tumor microenvironment that significantly influence treatment response [67] [68].
The future of PDO technology lies in further enhancing model complexity through incorporation of immune components, stromal cells, and vascular elements [69], standardization of culture protocols [67], and integration with advanced analytical platforms including artificial intelligence and multi-omics approaches [70] [66]. As these innovations mature and PDO biobanks expand to encompass broader patient diversity, these models will play an increasingly central role in guiding therapeutic decisions and advancing precision oncology.
For researchers embarking on PDO-based studies, a hybrid approach that strategically employs both 2D and 3D systems often provides the most practical and informative path forward, leveraging the distinct advantages of each platform while maximizing resources and translational potential.
The fidelity of in vitro disease models profoundly impacts the translation of research findings to clinical success. For decades, two-dimensional (2D) cell culture has been the standard tool for investigating disease mechanisms and therapeutic responses. However, the recognition that cells grown in flat monolayers differ significantly from their in vivo counterparts has driven the adoption of three-dimensional (3D) culture systems [2] [64]. These 3D models—including spheroids, organoids, and organs-on-chips—provide a more physiologically relevant context by recapitulating critical aspects of the native tissue microenvironment, such as cell-cell and cell-extracellular matrix (ECM) interactions, nutrient and oxygen gradients, and spatial architecture [65] [1]. This guide provides an objective comparison of 2D and 3D culture systems, focusing on their efficacy in modeling cancer, neurodegenerative, and infectious diseases, supported by experimental data and detailed protocols.
Physiological and Functional Comparison
The core difference between 2D and 3D culture systems lies in their spatial geometry, which dictates cellular morphology, signaling, and function. In 2D cultures, cells adhere to a flat, rigid plastic surface, forcing them to adopt an unnatural flattened morphology and disrupting their inherent polarity [64] [1]. In contrast, 3D cultures allow cells to grow in all directions, forming complex structures that mimic natural tissues. This fundamental difference manifests in several key physiological aspects, summarized in the table below.
Table 1: Key Physiological Differences Between 2D and 3D Culture Systems
| Characteristic | 2D Culture | 3D Culture | References |
|---|---|---|---|
| Spatial Architecture | Monolayer; forced 2D expansion | Multicellular structures (spheroids, organoids); tissue-like architecture | [65] [1] |
| Cell Morphology & Polarity | Altered, flattened morphology; loss of native polarity | Preserved natural morphology and polarity | [64] [1] |
| Cell-Cell & Cell-ECM Interactions | Limited to a single plane;缺乏复杂的相互作用 | Complex 3D interactions; mimics in vivo microenvironment | [65] [64] [72] |
| Gene Expression & Signaling | Altered gene expression, splicing, and signal transduction | In vivo-like gene expression profiles and signaling pathways | [65] [1] |
| Tumor Microenvironment (TME) | Cannot model stromal, immune, or vascular interactions | Can incorporate fibroblasts, immune cells, and vasculature | [65] [72] |
| Drug Penetration & Response | Homogeneous drug exposure; typically higher sensitivity | Diffusion barriers; gradients of oxygen/nutrients; drug resistance | [65] [8] [1] |
| Proliferation & Metabolism | Uniform, high proliferation rate | Heterogeneous proliferation; inner layers may be quiescent or apoptotic | [64] [1] |
The following diagram illustrates the structural and micro-environmental consequences of these differences, particularly in the context of a tumor spheroid.
Diagram 1: Structural and micro-environmental differences between 2D and 3D culture systems, highlighting the key factors that lead to differing biological outcomes.
Efficacy in Disease Modeling
Cancer Research
Cancer research has greatly benefited from 3D models, as they effectively mimic the complex structure and pathophysiology of solid tumors.
Table 2: Comparison of 2D vs. 3D Models in Cancer Research
| Application | 2D Model Performance | 3D Model Performance | Supporting Evidence |
|---|---|---|---|
| Drug Screening & Response | Overestimates efficacy; fails to predict clinical failure due to lack of penetration barriers. | Predicts drug resistance; models diffusion and hypoxic cores. HeLa spheroids show increased resistance vs. 2D counterparts [65]. | [65] [8] |
| Tumor Microenvironment (TME) | Limited to monoculture; cannot model stromal interactions. | Enables co-culture with fibroblasts and immune cells; models cell-ECM interactions driving invasion [65] [72]. | [65] [64] |
| Metastasis & Invasion | Poorly recapitulates due to lack of 3D ECM for cells to invade. | Allows study of invasion into ECM (e.g., Matrigel); models key steps in metastasis [1]. | [1] |
| Gene Expression & Tumor Heterogeneity | Altered expression; selective pressure reduces heterogeneity. | Retains original tumor heterogeneity; expression profiles closer to patient tumors [65]. | [65] [1] |
Neurodegenerative Disease Research
While the search results provided less direct data on neurodegenerative models, the general principles of 3D culture are highly relevant. The ability to model the complex cell-cell interactions in the brain—between neurons, astrocytes, and microglia—is a significant advantage of 3D systems. Brain organoids derived from induced pluripotent stem cells (iPSCs) can model the 3D architecture of brain regions and have been used to study Alzheimer's disease and Parkinson's disease [8] [73]. The formation of nutrient and oxygen gradients in 3D can also help model the stressful microenvironments that contribute to neurodegeneration.
Infectious Disease Research
3D models are revolutionizing the study of host-pathogen interactions by providing a more realistic tissue barrier for infection.
- Viral Infections: The NIH and Harvard have used brain organoids to model Zika virus infection and its impact on fetal development, something that was not possible with 2D cultures [8]. Similarly, lung organoids have been deployed to study SARS-CoV-2 infection and pathogenesis [8].
- Barrier Integrity & Pathogen Invasion: 3D models and organ-on-a-chip systems that incorporate epithelial layers allow for the study of barrier integrity and how pathogens breach these barriers [73] [74]. The inclusion of flow in some microphysiological systems further enhances the modeling of how infections spread.
Experimental Data and Protocols
Key Experimental Comparisons
Quantitative data consistently shows that 3D cultures provide a more clinically predictive model for drug testing.
Table 3: Experimental Data Comparison: Drug Response in 2D vs. 3D
| Experiment Description | 2D Culture Results | 3D Culture Results | Implications & References |
|---|---|---|---|
| Cytotoxicity Assay (e.g., Doxorubicin on SW-480 cells) | High sensitivity to treatment; significant cell death [8]. | Reduced sensitivity; higher viability post-treatment [8]. | 3D models mimic the drug resistance observed in in vivo tumors. [64] [8] |
| Gene Expression Analysis | Downregulation of tissue-specific genes; altered mRNA splicing [1]. | Expression of genes (e.g., SLC2A1, ALDOC, PFKFB4) associated with in vivo drug resistance [65]. | 3D cultures maintain a more in vivo-like transcriptome, explaining phenotypic differences. [65] |
| Morphological Analysis | Altered, spread-out cell morphology [1]. | Preservation of native tissue morphology and polarity [1]. | Confirms the more physiologically relevant structure of 3D models. [64] [1] |
Detailed Experimental Protocols
This scaffold-free technique is popular for its simplicity and ability to produce spheroids of uniform size.
- Cell Preparation: Create a single-cell suspension of your cancer cell line (e.g., HCT-116, MCF-7) using standard trypsinization. Centrifuge and resuspend the cells in complete growth medium at a concentration of 1-5 x 10^5 cells/mL (optimization may be required).
- Dispensing Droplets: Using a pipette, dispense 20-30 µL droplets of the cell suspension onto the inner surface of a Petri dish lid. Space the droplets evenly to prevent coalescence.
- Inversion and Culture: Carefully invert the lid and place it over the base of the dish, which contains PBS or medium to maintain humidity. The droplets will now be hanging from the lid.
- Incubation: Place the assembled dish in a 37°C, 5% CO2 incubator for 48-72 hours. Gravity will cause the cells to settle at the bottom of the droplet and self-assemble into a single spheroid.
- Harvesting: To harvest, carefully place the lid right-side-up and pipette the spheroids out of the droplets. They can now be used for drug treatment or analysis.
This method is widely used for cultivating organoids that require ECM support for growth and differentiation.
- Thawing Matrigel: Slowly thaw Corning Matrigel matrix on ice overnight at 4°C. Pre-chill all tips and tubes to prevent premature gelling.
- Cell Embedding: Gently mix your single-cell suspension with the cold, liquid Matrigel on ice. A typical final concentration is 2-5 x 10^4 cells/mL in Matrigel.
- Plating: Pipette 50-100 µL of the cell-Matrigel mixture into the center of each well of a pre-warmed 24-well plate.
- Gelation: Incubate the plate at 37°C for 20-30 minutes to allow the Matrigel to polymerize and form a solid gel.
- Overlaying Medium: After polymerization, carefully add 500 µL of pre-warmed complete growth medium (often supplemented with specific growth factors like EGF, Noggin, and R-spondin for organoid culture) on top of the gel.
- Maintenance: Culture the plate in a 37°C, 5% CO2 incubator, replacing the medium every 2-3 days. Organoids will form and grow within the Matrigel dome over 1-2 weeks.
The Scientist's Toolkit: Essential Reagents and Materials
Success in 3D cell culture relies on specialized reagents and tools. The following table lists key solutions for setting up and analyzing 3D models.
Table 4: Key Research Reagent Solutions for 3D Cell Culture
| Item | Function/Description | Example Products/Brands |
|---|---|---|
| Basement Membrane Matrix | A natural ECM hydrogel derived from mouse sarcoma, rich in laminin, collagen IV, and growth factors. Provides a scaffold for organoid growth and differentiation. | Corning Matrigel Matrix [65] [73] |
| Ultra-Low Attachment (ULA) Plates | Plates with a covalently bound hydrogel surface that inhibits cell attachment, promoting cell aggregation and spheroid formation in suspension. | Corning Spheroid Microplates, MilliporeSigma Millicell Microwell Plates [71] [73] |
| Hanging Drop Plates | Plates designed with micro-wells to facilitate the hanging drop method, enabling high-throughput production of uniform spheroids. | - |
| Hydrogels (Synthetic) | Defined, xeno-free synthetic polymers that serve as customizable scaffolds, offering greater batch-to-batch consistency than animal-derived matrices. | PEG-based hydrogels, QGel [64] |
| Tissue Clearing Reagents | Chemical solutions that render 3D samples transparent, enabling deep-tissue imaging and analysis without the need for physical sectioning. | Visikol HISTO-M, Corning 3D Clear Tissue Clearing Reagent [73] |
| Microphysiological Systems | Microfluidic chips that house 3D cell cultures under dynamic flow conditions, allowing for the modeling of multi-organ interactions and vascular perfusion. | Organ-on-a-chip systems (e.g., from Emulate Inc., Mimetas OrganoPlate) [8] [74] |
The choice between 2D and 3D culture systems is strategic and should be dictated by the specific research question. 2D cultures remain a powerful, cost-effective tool for high-throughput initial screening, genetic manipulation, and foundational studies where simplicity and reproducibility are paramount [71]. However, for disease modeling that demands physiological relevance—such as predicting clinical drug response, studying complex cell-ECM interactions, or modeling the tumor microenvironment—3D cultures are unequivocally superior [65] [64]. The future of preclinical research lies not in choosing one over the other, but in implementing integrated, tiered workflows that leverage the speed of 2D for discovery and the fidelity of 3D for validation, ultimately accelerating the development of more effective therapies.
Navigating the Challenges: Practical Solutions for Robust 3D Culture Workflows
The transition from traditional two-dimensional (2D) to three-dimensional (3D) cell culture systems represents a paradigm shift in biomedical research, offering more physiologically relevant models that better mimic in vivo conditions. While 2D cultures—where cells grow in a single layer on flat surfaces—have been the workhorse of laboratories for decades due to their simplicity and cost-effectiveness, they cannot accurately represent the intricate cellular environments of living organisms [75]. The emergence of 3D systems, including spheroids, organoids, and organ-on-chip technologies, responds to the critical need for models that more faithfully replicate human physiology, particularly for drug development and disease modeling applications [76]. However, this transition introduces significant challenges across four key dimensions: cost structures, throughput capabilities, standardization protocols, and reproducibility metrics. This article provides a comprehensive comparison of these critical parameters to guide researchers in selecting appropriate model systems for their specific applications.
Comparative Analysis of Economic and Operational Parameters
The choice between 2D and 3D culture systems involves significant trade-offs between physiological relevance and practical laboratory considerations. The table below provides a detailed comparison of key parameters based on current technologies and market data.
Table 1: Comprehensive Comparison of 2D vs. 3D Cell Culture Systems
| Parameter | 2D Cell Culture | 3D Cell Culture |
|---|---|---|
| Initial Setup Cost | Low (basic plasticware, standard media) [8] | High (specialized scaffolds, matrices, equipment) [77] [8] |
| Per-Experiment Cost | Low [75] | Significantly higher (2-5x) [8] |
| Throughput Capacity | High (compatible with 384/1536-well formats) [15] | Moderate to low (96-384 well formats with limitations) [70] |
| Technical Complexity | Low (well-established protocols) [75] | High (requires specialized expertise) [77] |
| Experimental Duration | Shorter (days) [8] | Longer (weeks to months) [78] [8] |
| Standardization Status | High (decades of protocol refinement) [75] | Moderate and evolving [76] |
| Reproducibility Between Labs | High [75] | Challenging due to protocol variability [76] [77] |
| Regulatory Acceptance | Well-established [79] | Growing but not yet universal [79] |
| Scalability | Excellent for industrial applications [75] | Limited by current technologies [76] |
| Personnel Training Requirements | Minimal to moderate [75] | Extensive and specialized [77] |
Economic Considerations in Model Selection
Cost Structures and Infrastructure Investment
The financial implications of adopting 3D culture systems extend beyond consumables to encompass infrastructure and specialized personnel requirements. While basic 2D culture requires only standard tissue culture flasks/plates and conventional media, 3D systems demand significant investment in scaffolds (hydrogels, polymeric scaffolds), extracellular matrix mimics (such as Corning Matrigel), and specialized equipment [75] [80]. The market data reflects this divergence, with the global 3D cell culture market projected to grow from USD $2.20 billion in 2024 to USD $6.92 billion by 2035, demonstrating increased adoption despite higher costs [81]. This growth is fueled by recognition that while 3D models have higher upfront costs, they may reduce expensive late-stage drug failures by providing more predictive data early in development pipelines [70].
Throughput Limitations and Technical Barriers
Throughput capacity remains a significant differentiator between culture platforms. The simplicity of 2D systems enables compatibility with high-density plate formats (up to 1536-well), automated liquid handling, and streamlined imaging and analysis workflows [15]. In contrast, 3D models present substantial throughput challenges, particularly for complex organoid systems that may require weeks to mature and often demand low-attachment surface plates, hanging drop methods, or magnetic levitation approaches [75]. Analysis presents additional bottlenecks, as traditional microscopy and analysis algorithms designed for 2D monolayers struggle with the optical density and spatial complexity of 3D structures [70]. Advanced solutions such as high-content confocal imaging, tissue clearing techniques, and artificial intelligence-based analysis platforms are emerging to address these limitations but further increase cost and complexity [70].
Table 2: Technical Requirements for Advanced 3D Culture Applications
| Research Application | Recommended 3D Model | Specialized Equipment Needed | Technical Considerations |
|---|---|---|---|
| High-Throughput Drug Screening | Spheroids in ULA plates [75] | Automated liquid handlers, high-content imagers [70] | Balance between throughput and physiological relevance |
| Patient-Derived Tumor Models | Organoids in hydrogel matrices [80] | Advanced ECM materials (e.g., Matrigel) [80] | Preservation of tumor heterogeneity and microenvironment |
| Tissue Engineering | Scaffold-based systems [75] | Bioreactors, 3D bioprinters [81] | Mechanical support and nutrient diffusion management |
| Metabolic Studies | Microfluidic 3D cultures [78] | Organ-on-chip platforms [77] | Real-time monitoring of metabolite gradients |
Standardization and Reproducibility Challenges
Protocol Variability and Quality Control
Standardization represents perhaps the most significant hurdle in 3D cell culture adoption. Traditional 2D systems benefit from decades of protocol refinement, standardized reagents, and well-characterized cell lines, contributing to high inter-laboratory reproducibility [75]. In contrast, 3D systems exhibit substantial variability in scaffold fabrication, cell sourcing, and culture conditions [76]. Natural hydrogels such as Matrigel display batch-to-batch variability in protein composition, while differences in cell seeding densities, spheroid sizes, and organoid differentiation protocols introduce additional variability that complicates cross-study comparisons [76]. Robust quality control measures including standardized cell counting methods, validated ECM lots, and controlled environmental conditions are essential to minimize technical variability [76].
Experimental Design for Reproducible 3D Culture
The following workflow diagram illustrates a standardized approach to establishing reproducible 3D culture systems, highlighting critical control points that impact experimental outcomes:
Diagram 1: Standardized 3D Culture Workflow. This workflow highlights critical control points for ensuring reproducibility in 3D culture systems, from cell sourcing through data analysis.
Essential Research Reagent Solutions
The successful implementation of 3D culture systems requires specialized materials and reagents that define the cellular microenvironment. The following table details key components and their functions in establishing physiologically relevant models.
Table 3: Essential Research Reagents for 3D Cell Culture Systems
| Reagent Category | Specific Examples | Function & Application | Key Considerations |
|---|---|---|---|
| Scaffold Matrices | Corning Matrigel, collagen hydrogels, synthetic PEG-based polymers [75] | Provide 3D structural support mimicking native ECM; essential for organoid development and cell differentiation | Batch-to-batch variability (natural matrices); tunable stiffness (synthetic polymers) [76] |
| Specialized Cultureware | Ultra-low attachment (ULA) plates, hanging drop plates, microfluidic chips [75] [81] | Enable spheroid formation without artificial scaffolds; permit controlled fluid flow and nutrient gradients | Throughput limitations; compatibility with existing laboratory equipment [70] |
| Cell Culture Media | Defined organoid media, specialized differentiation cocktails [70] | Support stem cell maintenance and directed differentiation; maintain tissue-specific functions | Proprietary formulations; requirement for specific growth factor supplements |
| Analysis Reagents | Tissue-clearing reagents, 3D viability assays, extracellular flux sensors [70] | Enable visualization and functional assessment within dense 3D structures; measure metabolic gradients | Compatibility with 3D structures; penetration depth limitations |
Strategic Implementation Approaches
Hybrid Workflows for Balanced Efficiency and Relevance
Progressive research programs are adopting integrated approaches that leverage the complementary strengths of both 2D and 3D systems rather than treating them as mutually exclusive options [8]. A tiered strategy employs 2D cultures for initial high-throughput screening of compound libraries, followed by focused evaluation of lead candidates in more physiologically relevant 3D models [70] [15]. This hybrid approach balances the cost-effectiveness and scalability of 2D systems with the enhanced predictive power of 3D models, optimizing resource allocation while maximizing the biological relevance of key findings [15] [8].
Emerging Solutions and Future Directions
The 3D cell culture landscape is rapidly evolving to address current limitations. Automation technologies are reducing variability through standardized liquid handling and culture processes [70] [77]. Advanced computational methods, including artificial intelligence and machine learning, are enabling more sophisticated analysis of complex 3D data sets [70] [8]. Regulatory agencies are increasingly recognizing data from human-relevant 3D models, with the FDA and EMA providing guidelines that encourage the use of these systems in safety and efficacy testing [79]. Additionally, industry-academic collaborations are accelerating the development of standardized protocols and reference materials to improve inter-laboratory reproducibility [81] [79].
The selection between 2D and 3D culture systems involves navigating a complex landscape of technical and practical considerations. While 3D models offer superior physiological relevance that can enhance the predictive power of preclinical research, they require significant investment in specialized reagents, equipment, and personnel training. The decision framework should consider research objectives, available resources, and required throughput. For target identification and large-scale compound screening, 2D systems remain efficient and cost-effective. For advanced disease modeling, toxicity assessment, and therapeutic validation, 3D systems provide invaluable biological context that often justifies their additional complexity and cost. As technologies mature and standardization improves, integrated approaches that strategically employ both systems throughout the research pipeline will likely yield the most efficient path to biologically meaningful and clinically relevant discoveries.
The evolution from two-dimensional (2D) to three-dimensional (3D) cell culture models represents a paradigm shift in biomedical research, particularly in oncology and drug development. Traditional 2D culture systems, where cells grow as monolayers on flat plastic surfaces, have been a fundamental technique for decades. However, they fundamentally fail to replicate the complex architectural and functional characteristics of living tissues [65] [2]. As a result, data obtained from 2D models often poorly predict clinical responses, as they lack critical cell-cell and cell-matrix interactions, and cannot mimic the inherent heterogeneity of in vivo tumors, which comprise diverse cell types including cancer stem cells, stromal cells, and immune cells [65].
In contrast, 3D culture systems, including organoids and spheroids, provide a microenvironment that more closely resembles in vivo conditions. These models preserve the architectural characteristics, gene expression profiles, signaling pathways, and drug sensitivities of primary tissues [65]. This advancement has created an urgent need for sophisticated imaging and analysis techniques capable of visualizing and quantifying these complex 3D structures. The transition necessitates moving beyond conventional 2D microscopy to technologies that can non-destructively resolve internal structures, capture volumetric data, and provide accurate quantitative metrics in three dimensions [82] [2].
Comparative Analysis of 2D and 3D Imaging Technologies
The selection of an appropriate imaging technology depends heavily on the research objectives, balancing factors such as resolution, penetration depth, and sample processing requirements. The table below provides a comprehensive comparison of key imaging modalities used in the analysis of 3D biological structures.
Table 1: Comparison of Imaging Technologies for 3D Structure Analysis
| Technology | Key Principle | Max Resolution | Penetration Depth | Sample Preparation | Key Advantages | Main Limitations |
|---|---|---|---|---|---|---|
| Confocal Microscopy | Laser scanning with spatial filtering | ~200 nm | ~100-200 µm | Fluorescent labeling required | Optical sectioning, live-cell imaging | Limited penetration, photobleaching |
| Light Sheet Fluorescence Microscopy (LSFM) | Orthogonal illumination with detection | ~300 nm | Several mm | Fluorescent labeling required | High speed, low phototoxicity | Specialized setups, scattering in dense samples |
| Micro-CT (X-ray) | X-ray transmission and computed reconstruction | ~0.5-10 µm | Several cm | Minimal (often non-destructive) | True volumetric imaging, quantitative data | Limited soft tissue contrast, resolution vs. sample size trade-off |
| FIBSEM | Sequential milling and imaging with ion/electron beams | ~4-10 nm | Limited by destructive sectioning | Extensive (resin embedding, staining) | Ultra-high resolution, 3D tomography | Destructive, time-consuming, small volumes |
| MRI | Nuclear magnetic resonance signals | ~10-100 µm | Unlimited | Typically non-destructive | Excellent soft tissue contrast, deep penetration | Lower resolution, expensive, long acquisition times |
Advanced 3D Imaging Modalities
3D X-ray Imaging (Micro-CT)
X-ray computed tomography (Micro-CT) provides a non-destructive method for visualizing the internal structure of materials and biological samples in three dimensions. This technology generates true volumetric imaging, allowing comprehensive internal analysis without the need for extensive sample preparation [82]. Unlike destructive techniques, Micro-CT preserves sample integrity, enabling further analysis or testing after imaging. Modern systems offer high throughput capabilities, rapidly acquiring data for multiple samples, and provide quantitative data on the size, shape, and distribution of internal features [82]. The main limitation lies in spatial resolution, which is typically lower than electron microscopy techniques, making it complementary to rather than a replacement for higher-resolution methods [82].
Focused Ion Beam Scanning Electron Microscopy (FIBSEM)
FIBSEM represents a high-resolution 3D imaging and milling technique that uses a focused beam of ions to analyze and modify materials at micro and nano scales [82]. This method excels in performing serial sectioning of samples to create high-resolution images of internal structures and is particularly valuable for preparing thin lamellae for subsequent transmission electron microscopy. FIBSEM enables 3D tomography by sequentially milling away layers and capturing images at each step, providing an extremely detailed view of internal ultrastructure [82]. However, as an inherently destructive technique that involves material removal, it compromises sample integrity and can be time-consuming, especially for complex samples or large areas [82].
Table 2: Performance Metrics for 3D Imaging Technologies in Biological Applications
| Application Scenario | Recommended Technology | Typical Resolution | Processing Time | Quantitative Capabilities |
|---|---|---|---|---|
| Tumor Spheroid Volume Analysis | Confocal Microscopy | 200-300 nm | Minutes to hours | Good for fluorescent markers |
| Organoid Vascularization | Light Sheet Microscopy | 300-500 nm | Minutes | Excellent for large, cleared samples |
| Bone Tissue Engineering | Micro-CT | 1-10 µm | Hours | Excellent for mineralization |
| Subcellular Organelle Mapping | FIBSEM | 4-10 nm | Days | Excellent for ultrastructure |
| Soft Tissue Morphometry | MRI | 50-100 µm | Hours to days | Good for tissue classification |
Experimental Protocols for 3D Structure Analysis
Protocol 1: Volumetric Analysis of Tumor Spheroids Using Light Sheet Microscopy
Principle: This protocol utilizes orthogonal plane illumination to rapidly capture optical sections of intact 3D spheroids with minimal phototoxicity, enabling accurate volume quantification and morphological characterization.
Materials:
- Tumor spheroids (500-800 µm diameter)
- Fibrin or Matrigel matrix for embedding
- Optical clearing reagent (e.g., CUBIC, ScaleS)
- Light sheet fluorescence microscope
- Nuclear staining dye (e.g., Hoechst 33342)
- Viability indicator (e.g., Calcein AM)
Procedure:
- Spheroids Preparation: Culture tumor cell lines in low-adhesion U-bottom plates for 5-7 days to form spheroids.
- Staining: Incubate spheroids with nuclear stain (5 µg/mL) and viability indicator (1 µM) for 2 hours at 37°C.
- Embedding: Transfer individual spheroids to 1.5 mm diameter capillaries and embed in fibrin gel (10 mg/mL).
- Clearing: Immerse samples in clearing reagent for 48 hours at 4°C with gentle agitation.
- Image Acquisition: Mount capillaries in light sheet microscope and acquire z-stacks with 2 µm step size.
- Data Analysis: Reconstruct 3D volumes and quantify using segmentation algorithms.
Quantification Metrics:
- Spheroid volume (µm³)
- Necrotic core ratio (%)
- Surface irregularity index
- Cell density (cells/µm³)
Protocol 2: High-Resolution Ultrastructural Analysis Using FIBSEM
Principle: This protocol employs sequential ion beam milling and SEM imaging to reconstruct nanoscale architecture of 3D cellular structures, providing unprecedented detail of subcellular organization.
Materials:
- 3D cultured cells or small tissue explants
- Glutaraldehyde (2.5%) and osmium tetroxide (1%) fixatives
- Uranyl acetate and lead citrate stains
- Dehydration series ethanol (30-100%)
- Epoxy resin embedding medium
- Conductive silver paint
- FIBSEM system with gallium ion source
Procedure:
- Fixation: Immerse samples in glutaraldehyde in 0.1M cacodylate buffer for 2 hours at 4°C.
- Post-fixation: Treat with osmium tetroxide for 1 hour to enhance contrast.
- Staining: En bloc staining with uranyl acetate (2%) for 30 minutes.
- Dehydration: Sequential ethanol dehydration (30%, 50%, 70%, 90%, 100%).
- Embedding: Infiltrate with epoxy resin and polymerize at 60°C for 48 hours.
- Mounting: Trim resin block and apply conductive paint to edges.
- FIBSEM Imaging: Set ion beam to 30kV, 1-3 nA for sequential milling at 10-20 nm increments.
- Image Stack Reconstruction: Align sequential images and generate 3D model.
Quantification Metrics:
- Organelle volume and distribution
- Membrane surface areas
- Inter-organelle distances
- Vesicle counts and size distributions
Diagram Title: FIBSEM 3D Ultrastructural Analysis Workflow
Signaling Pathways in 3D Microenvironments and Their Analysis
The transition from 2D to 3D culture systems significantly alters cellular signaling pathways, which can be visualized and quantified through appropriate imaging techniques. Key pathways affected include:
Hippo Signaling Pathway: In 2D cultures, cell spreading inhibits the Hippo pathway, allowing YAP/TAZ translocation to the nucleus and promoting proliferation. In 3D environments, restricted cell spreading activates the Hippo pathway, sequestering YAP/TAZ in the cytoplasm and reducing proliferation - more accurately reflecting in vivo conditions [65].
Integrin-Mediated Signaling: Focal adhesion formation differs substantially between 2D and 3D contexts. In 3D matrices, integrins engage with extracellular matrix components in a more physiological manner, activating different signaling cascades including FAK/Src and ILK/PI3K pathways that influence cell survival, migration, and differentiation [65].
Hypoxia-Inducible Factor (HIF) Pathway: The development of oxygen gradients in 3D structures larger than 200-300 µm creates hypoxic cores that stabilize HIF-1α, activating genes promoting angiogenesis, metabolic adaptation, and drug resistance - a critical phenomenon absent in 2D monolayers [65].
Diagram Title: Key Signaling Pathways in 3D Microenvironments
The Scientist's Toolkit: Essential Reagents and Materials
Successful imaging and analysis of complex 3D structures requires specialized reagents and materials optimized for three-dimensional contexts. The following table details essential components for 3D imaging workflows.
Table 3: Essential Research Reagents and Materials for 3D Structure Imaging and Analysis
| Category | Specific Product/Technology | Function in 3D Analysis | Compatibility |
|---|---|---|---|
| Scaffold Materials | Matrigel, Laminin-rich ECM | Provides physiological 3D microenvironment for cell growth | Light microscopy, FIBSEM |
| Synthetic Hydrogels | PEG-based, Hyaluronic acid | Tunable mechanical properties for mechanotransduction studies | Most imaging modalities |
| Clearing Reagents | CUBIC, ScaleS, CLARITY | Reduces light scattering for deep tissue imaging | Light sheet, confocal microscopy |
| Fluorescent Labels | CellTracker, Phalloidin, DAPI | Visualizes cellular and structural components | Fluorescence microscopy |
| Viability Indicators | Calcein AM, Propidium Iodide | Distinguishes live/dead cells in 3D constructs | Live-cell imaging |
| Embedding Media | Epoxy resin, Optimal Cutting Temperature (OCT) compound | Supports sample structure for sectioning | FIBSEM, Micro-CT |
| Contrast Agents | Osmium tetroxide, Lead citrate | Enhances electron density for EM | SEM, FIBSEM, TEM |
| X-ray Contrast | Phosphotungstic acid, Iodine-based | Improves soft tissue contrast in Micro-CT | Micro-CT |
Quantitative Comparison of 2D vs 3D Culture Systems
The biological differences between 2D and 3D culture systems have profound implications for research outcomes, particularly in drug development and disease modeling. The table below summarizes key quantitative differences observed between these systems.
Table 4: Experimental Data Comparison: 2D vs 3D Culture Systems
| Parameter | 2D Culture Performance | 3D Culture Performance | Experimental Evidence |
|---|---|---|---|
| Drug IC50 Values | 10-1000x lower | Clinically relevant concentrations | Chemotherapy agents show significantly higher resistance in 3D models [65] |
| Gene Expression Profiles | Altered expression patterns | Closer to in vivo tissues | Transcriptome analysis shows 3D cultures maintain differentiation markers [65] |
| Proliferation Rates | High, uniform | Heterogeneous, gradient-dependent | Ki67 staining shows proliferation gradients in 3D spheroids [2] |
| Apoptosis Resistance | Lower | Higher, especially in core regions | Caspase-3 staining shows reduced apoptosis in 3D cultures [65] |
| Glucose Consumption | Uniform across population | Gradient formation | FRET-based sensors show metabolic heterogeneity [2] |
| Oxygen Consumption | Uniform | Hypoxic core development | pimonidazole staining confirms hypoxia in spheroids >200µm [65] |
Impact on Drug Screening Outcomes
The differences between 2D and 3D systems have particularly significant implications for drug discovery. Studies consistently demonstrate that 3D culture models exhibit increased resistance to chemotherapeutic agents, more accurately reflecting clinical responses [65]. For example, HeLa spheroids show enhanced resistance compared to their 2D counterparts due to factors including cytoskeletal reorganization, overexpression of specific genes (SLC2A1, ALDOC, and PFKFB4) driving drug resistance, and the ability to model tumor microenvironment complexity through co-culture with fibroblasts [65]. This improved predictive power makes 3D models invaluable for preclinical drug screening.
Integrated Workflow for Comprehensive 3D Analysis
A multi-modal approach combining complementary techniques provides the most comprehensive analysis of complex 3D structures. The following workflow integrates multiple technologies to maximize information extraction while preserving sample integrity.
Diagram Title: Multi-Modal 3D Structure Analysis Workflow
This integrated approach begins with non-destructive screening using techniques like light sheet microscopy or Micro-CT to identify regions of interest while preserving sample integrity [82]. Subsequently, targeted high-resolution analysis using FIBSEM provides nanometer-scale details of selected regions [82]. Finally, correlative analysis combines datasets from multiple modalities to generate comprehensive quantitative 3D models that span from macroscopic to ultrastructural levels.
The evolution from 2D to 3D culture systems represents more than a technical improvement - it constitutes a fundamental transformation in how we model biological complexity. This paradigm shift demands equally advanced imaging and analysis techniques capable of resolving and quantifying complex 3D structures. No single imaging technology provides a complete solution; rather, the most powerful approaches integrate multiple complementary modalities that span resolution scales from macroscopic to nanoscopic.
The future of 3D structure analysis lies in the continued development of correlative workflows that seamlessly combine non-destructive screening methods with targeted high-resolution techniques. As 3D models become increasingly sophisticated - incorporating multiple cell types, vascular networks, and immune components - advanced imaging technologies will be indispensable for validating these systems and extracting meaningful quantitative data. For researchers in drug development and disease modeling, mastering these imaging technologies is no longer optional but essential for generating clinically relevant data and advancing our understanding of complex biological systems.
In the realm of three-dimensional (3D) cell culture, spheroids have emerged as a pivotal model that bridges the gap between conventional two-dimensional (2D) monolayers and complex in vivo environments. These self-assembled cellular aggregates replicate critical aspects of tissue physiology that are absent in 2D systems, including complex cell-cell interactions, physiological nutrient gradients, and spatially organized metabolic zones [83]. The very structure that grants spheroids their physiological relevance also creates their fundamental challenge: managing the diffusion of nutrients and removal of metabolic waste throughout their entire volume.
As spheroids increase in size, they develop distinct microenvironments with varying cellular states. The outer layers typically contain proliferating cells with ample access to oxygen and nutrients, while the core region becomes progressively deprived of these essential elements, potentially leading to quiescent, hypoxic, or even necrotic zones [84]. This phenomenon directly mirrors the diffusion limitations observed in solid tumors and tissues, making understanding and optimizing these processes essential for creating physiologically relevant models [83] [84]. This guide examines the key factors influencing nutrient diffusion and waste removal in spheroids, providing direct comparisons with 2D systems and offering practical strategies for optimizing spheroid viability for research and drug development applications.
Fundamental Differences Between 2D and 3D Systems
The microenvironment in 2D cell culture is fundamentally different from that in 3D spheroids. In traditional monolayers, cells are attached to a flat, rigid substrate and are uniformly exposed to the culture medium, resulting in largely homogeneous growth conditions without significant diffusion barriers [85] [86]. This configuration simplifies nutrient delivery and waste removal but fails to recapitulate the spatial organization and diffusion dynamics of living tissues.
In contrast, 3D spheroids exhibit complex diffusion dynamics where nutrients and oxygen must permeate through multiple cell layers to reach the core, while metabolic wastes must travel outward to be removed [84]. This creates overlapping gradients that influence cellular behavior, gene expression, and drug sensitivity in ways that more closely mimic in vivo conditions [83] [86]. The table below summarizes the key differences between these systems:
Table 1: Comparison of Nutrient and Waste Management in 2D vs. 3D Culture Systems
| Parameter | 2D Monolayer Culture | 3D Spheroid Culture |
|---|---|---|
| Nutrient Access | Uniform and unrestricted access to nutrients [85] | Diffusion-limited; creates concentration gradients [83] [84] |
| Waste Accumulation | Easily removed with medium changes [74] | Accumulates in the core, creating metabolic gradients [84] |
| Oxygen Availability | Homogeneous, often hyperoxic [86] | Gradient-dependent; can lead to hypoxic cores [83] [84] |
| Cell Morphology | Flat, stretched morphology [84] | Natural, in vivo-like shape [84] |
| Proliferation Zones | Uniform proliferation [84] | Zonal proliferation: outer proliferating, inner quiescent/hypoxic [84] |
| Drug Response | Direct exposure; no penetration barrier [83] | Diffusion-limited penetration; better predicts in vivo efficacy [83] |
Critical Factors Affecting Spheroid Viability
Spheroid Size and Structure
The diameter of spheroids directly impacts their internal diffusion dynamics. Smaller spheroids (typically <200 μm) generally maintain good viability throughout their structure due to sufficient nutrient penetration [84]. As spheroids grow larger (500-1000 μm), they develop characteristic zoning with proliferating cells at the periphery, quiescent cells in intermediate layers, and potentially necrotic cores when critical diffusion limits are exceeded [84]. The structural integrity of spheroids also varies by cell type, with some forming compact, highly organized aggregates while others develop looser structures that may alter diffusion characteristics [87].
Culture Media Composition
Media formulation significantly influences spheroid growth and viability. A recent large-scale study analyzing over 32,000 spheroids demonstrated that media composition directly alters growth and death profiles [88]. For instance, HEK 293T spheroids grown in RPMI 1640 showed increased cell death signals compared to other media types, attributed to differences in glucose and calcium levels across DMEM, DMEM/F12, and RPMI formulations [88]. These components affect spheroid size, shape, and viability, highlighting the need to consider how standard media diverge from physiological conditions.
Oxygen Tension
Oxygen availability is a critical factor in spheroid viability. Spheroids cultured under physiological hypoxic conditions (3% O₂) exhibited decreased dimensions, reduced viability, and lower ATP content compared to those under standard culture conditions [88]. This oxygen gradient mimics the tumor microenvironment and influences cellular metabolism, but must be carefully controlled to prevent excessive cell death in the core regions.
Serum Concentration
Serum concentration in culture media directly affects spheroid architecture. Research with MCF-7 spheroids demonstrated that low or serum-free conditions caused spheroids to shrink significantly and display increased cell detachment [88]. In contrast, 10-20% fetal bovine serum produced compact, viable spheroids with distinct necrotic and proliferative zones, offering a balance between cell growth and physiological relevance [88].
Table 2: Impact of Culture Conditions on Spheroid Viability Parameters
| Culture Condition | Optimal Range | Impact on Spheroid Viability | Experimental Evidence |
|---|---|---|---|
| Initial Seeding Density | Cell line-dependent | Affects final spheroid size and structural stability; very high densities may cause rupture [88] | Spheroids from 6,000-7,000 cells were largest but unstable; lower densities produced more stable spheroids [88] |
| Oxygen Level | Physiologically relevant (e.g., 3% O₂) | Hypoxic conditions decrease dimensions and viability but better mimic tumor microenvironment [88] | Hypoxia (3% O₂) decreased equivalent diameter, volume, and viability compared to normoxia [88] |
| Serum Concentration | 10-20% FBS | Essential for compact architecture; low serum causes shrinkage and cell detachment [88] | 0.5-1% FBS peaked cell death; 10-20% FBS produced viable spheroids with distinct zones [88] |
| Media Formulation | Cell line-specific | Varying glucose, calcium significantly affect size, shape, viability [88] | HEK 293T in RPMI 1640 showed increased death vs. other media [88] |
Experimental Approaches and Methodologies
Spheroid Formation Techniques
Various methods exist for generating spheroids, each with distinct advantages for managing diffusion:
Hanging Drop Method: This scaffold-free technique uses gravity to concentrate cells at the bottom of suspended droplets, promoting self-assembly into spheroids [83] [45]. The method produces relatively uniform spheroids but can be limited by throughput and the risk of droplet coalescence during handling [83]. Modern innovations like the 3D-printed SpheroMold address these limitations by providing physical barriers that prevent droplet fusion and enable higher density cultures [45].
Ultra-Low Attachment (ULA) Plates: These plates feature specially treated surfaces that prevent cell attachment, forcing cells to aggregate and form spheroids in a high-throughput manner [87]. This approach is particularly useful for large-scale screening studies and allows control over spheroid size through initial seeding density [88] [87].
Scaffold-Based Systems: Natural or synthetic hydrogels (e.g., Matrigel, collagen, PEG) provide a 3D extracellular matrix (ECM) that supports spheroid formation and can influence diffusion characteristics [83] [84]. The composition and density of these matrices can be tuned to mimic specific tissue environments.
Assessment Methods for Viability and Diffusion
Histological Analysis: Traditional embedding, sectioning, and staining techniques reveal the internal architecture of spheroids, including necrotic cores and proliferative zones [89]. Advanced microarray approaches now enable parallel processing of up to 96 spheroids on a single slide, improving efficiency and reproducibility [89].
Viability Assays: The CellTiter-Glo 3D assay measures ATP content as an indicator of metabolic activity and cell health [88]. This luminescent approach is particularly valuable for dense 3D structures where other assays may underperform. Viability can also be assessed using fluorescence-based live/dead stains (e.g., calcein AM/ethidium homodimer-1) followed by confocal microscopy to visualize the spatial distribution of live and dead cells [45] [90].
Morphometric Analysis: High-throughput image analysis using software like AnaSP and ReViSP can extract quantitative metrics (compactness, solidity, sphericity) from thousands of spheroids, correlating morphological features with culture conditions [88] [87]. Large-scale image atlases like SLiMIA provide reference datasets for method development and optimization [87].
Diagram 1: Comprehensive workflow for assessing spheroid viability and diffusion characteristics.
The Researcher's Toolkit: Essential Reagents and Tools
Table 3: Essential Research Tools for Spheroid Culture and Analysis
| Tool/Reagent | Primary Function | Application Notes |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Prevents cell attachment, enabling spheroid self-assembly [87] | Available in 96-well and 384-well formats; suitable for high-throughput screening [87] |
| Extracellular Matrix (ECM) Hydrogels | Provides 3D scaffold mimicking natural tissue environment [83] | Natural (e.g., Matrigel, collagen) or synthetic (e.g., PEG); composition affects diffusion [83] |
| CellTiter-Glo 3D Assay | Measures ATP content as indicator of metabolic activity [88] | Optimized for penetration into dense 3D structures; compatible with luminescence readers [88] |
| 3D-Tips with Mesh Barrier | Enables media changes without spheroid aspiration [90] | 40-μm pores retain spheroids; significantly reduces loss compared to standard methods [90] |
| Hanging Drop Array Plates | Forms spheroids using gravity in suspended droplets [83] [45] | Produces uniform spheroids; modern designs prevent droplet coalescence [45] |
| AnaSP/ReViSP Software | Quantifies spheroid morphometrics from images [88] | Analyzes parameters like compactness, solidity, sphericity; enables high-throughput analysis [88] |
| Microarray Embedding System | Parallel processing of multiple spheroids for histology [89] | Enables sectioning/staining of up to 96 spheroids on single slide [89] |
Optimizing nutrient diffusion and waste removal in spheroids requires a multifaceted approach that balances physiological relevance with practical experimental constraints. Key strategies include:
- Controlling spheroid size through initial seeding density to maintain optimal diffusion characteristics
- Matching media composition to cell type-specific requirements and physiological conditions
- Implementing physiologically relevant oxygen levels to better mimic in vivo environments
- Selecting appropriate formation methods based on throughput needs and analytical requirements
- Utilizing specialized tools like 3D-tips and viability assays optimized for 3D cultures
The structural complexity of spheroids that creates diffusion challenges is precisely what makes them valuable for drug development and disease modeling. By implementing the optimization strategies outlined in this guide, researchers can enhance spheroid viability and functionality, creating more predictive models that better bridge the gap between traditional 2D culture and in vivo systems. As the field advances, standardized approaches to managing nutrient diffusion and waste removal will be crucial for improving reproducibility and translational potential in 3D cell culture research.
In the pursuit of more predictive and scalable cell-based assays, the research community is increasingly moving beyond the simplistic dichotomy of 2D versus 3D culture systems. While traditional two-dimensional (2D) monolayers offer proven scalability and procedural simplicity, three-dimensional (3D) cultures provide superior physiological relevance by mimicking native tissue architecture [91] [8]. This has created a strategic imperative for hybrid 2D/3D workflows that leverage the respective strengths of each system to accelerate research and development timelines without compromising biological accuracy.
The limitations of relying exclusively on either approach are well-documented. Traditional 2D cultures, grown on flat surfaces like flasks and multi-well plates, often fail to replicate critical cell-cell interactions and spatial organization found in living tissues [8]. This can lead to misleading data, particularly in drug discovery where compounds that appear efficacious in 2D models frequently fail in clinical trials [8]. Conversely, 3D cultures—including spheroids, organoids, and scaffold-based systems—while offering more realistic tissue microenvironment simulation, present significant challenges for scaling, monitoring, and cell harvesting [91].
This comparative guide examines integrated strategies that combine the speed and throughput of 2D systems with the biological realism of 3D models. By objectively analyzing performance data and providing detailed experimental protocols, we aim to equip researchers with practical frameworks for implementing tiered workflow approaches that maximize both efficiency and predictive power in biomedical research and drug development.
The strategic selection between 2D, 3D, and hybrid approaches requires a clear understanding of their relative performance across key parameters essential for scalable expansion. The data below, synthesized from current literature and vendor specifications, provides a quantitative foundation for this decision-making process.
Table 1: Comprehensive Comparison of 2D, 3D, and Hybrid Culture Systems for Scalable Expansion
| Performance Parameter | Traditional 2D Systems | Advanced 3D Systems | Hybrid 2D/3D Workflow |
|---|---|---|---|
| Cell Proliferation Rate | High, but can lead to unintended differentiation [92] | Variable; often slower due to diffusion limitations | Optimized via initial 2D expansion followed by 3D culture |
| Scalability | Highly scalable using multi-layer stacks and roller bottles [91] | Challenging for scaffold-based systems; easier with suspension spheroids [91] | High; uses 2D for master cell banks, 3D for application testing |
| Gene Expression Fidelity | Often deviates from in vivo profiles [8] | More accurately mimics in vivo conditions [8] | Context-dependent; can match specific experimental phases to optimal system |
| Drug Response Prediction | Poor predictive value for solid tumors (often overestimates efficacy) [8] | High predictive value; replicates tumor microenvironment and drug resistance [8] | High; uses 3D for final validation after initial 2D screening |
| Cost Efficiency | Low cost per vessel; high labor intensity at scale [91] | Higher reagent costs; potentially lower labor [8] | Balanced; reduces costly 3D reagents for initial screening stages |
| Throughput | Excellent for High-Throughput Screening (HTS) [8] | Moderate; improving with new technologies like microfluidics [93] | High; maintains HTS compatibility for early stages |
| Reproducibility | High with standardized protocols [91] | Can be variable; depends on matrix consistency and spheroid formation method | High through process standardization across systems |
| Cell Harvesting Efficiency | Simple and efficient using enzymatic methods [91] | Difficult, especially from fixed-bed bioreactors; requires enzymatic digestion [91] | Flexible; harvesting strategy tailored to culture phase |
| Technical Complexity | Low; well-established protocols [8] | High; requires optimization of multiple parameters (e.g., scaffold, media) [91] | Moderate; requires expertise in both systems and transition points |
Table 2: Experimental Outcome Comparison in Key Research Applications
| Application Area | 2D Culture Performance | 3D Culture Performance | Hybrid Workflow Advantage |
|---|---|---|---|
| Cancer Research & Drug Testing | Limited value; fails to model hypoxic tumor core and cell-ECM interactions [8] | High physiological relevance; models tumor microenvironments, hypoxia, and drug penetration gradients [8] [93] | Enables rapid screening of compound libraries in 2D followed by validation in pathologically relevant 3D models |
| Toxicology & Safety Pharmacology | Useful for basic cytotoxicity assessment but overestimates toxicity for some compounds [8] | More accurate prediction of human responses; used for liver and skin toxicity models [94] [8] | Tiered testing improves predictivity while managing resource constraints |
| Stem Cell Expansion & Differentiation | Risk of phenotypic drift and loss of pluripotency markers during scale-up [91] [92] | Maintains pluripotency and enables better differentiation into complex tissue structures [92] | Facilitates large-scale expansion of high-quality stem cells with maintained pluripotency for regenerative medicine |
| Personalized Medicine | Limited clinical predictive value using patient-derived cells | High predictive value using Patient-Derived Organoids (PDOs) for therapy selection [94] [8] | Streamlines process by using 2D for initial cell expansion from patient biopsies before 3D organoid generation for drug testing |
Experimental Protocols for Hybrid Workflow Implementation
Tiered Drug Screening Protocol
This protocol outlines a standardized approach for leveraging both 2D and 3D systems in a complementary fashion for more efficient and predictive drug screening.
Phase 1: High-Throughput 2D Screening
- Objective: Rapidly screen large compound libraries to identify potential hits.
- Methodology:
- Seed cells (e.g., cancer cell lines) in 96-well or 384-well plates at a standardized density (e.g., 10,000 cells/well for a 96-well plate) [95].
- After 24 hours, treat with a concentration range (e.g., 0.4-50 μM) of compounds [95].
- After 72 hours of incubation, assess cell viability using a colorimetric assay like MTT [95].
- Data Analysis: Normalize data to untreated controls and calculate IC₅₀ values. Select the most promising 10-20% of compounds for advancement.
Phase 2: Validation in 3D Models
- Objective: Confirm efficacy of hits in a physiologically relevant 3D context.
- Methodology:
- Generate 3D spheroids using ultra-low attachment plates or hydrogel embedding (e.g., VitroGel). For printing, use a density of 3,000 cells/well in a PEG-based hydrogel [95].
- Allow 7 days for spheroid maturation and establishment of relevant tissue architecture [95].
- Treat mature spheroids with the hit compounds identified from Phase 1.
- After 72 hours, assess viability using 3D-optimized assays like CellTiter-Glo 3D [95].
- Data Analysis: Compare dose-response curves and IC₅₀ values between 2D and 3D models. Compounds showing efficacy in both systems, or which demonstrate unique activity in the 3D model, are selected for further development.
Scalable Expansion of Human Pluripotent Stem Cells (hPSCs)
This protocol details a seamless transition from 2D culture to 3D scale-up for the production of high-quality hPSCs, addressing common challenges of consistency and yield.
Stage 1: 2D Culture for Master Cell Banks
- Objective: Maintain genetic stability and create a master cell bank.
- Methodology:
- Culture hPSCs on traditional 2D surfaces (e.g., Matrigel-coated plates) with defined media.
- Passage cells at 70-80% confluence using standard enzymatic (e.g., Accutase) or non-enzymatic methods.
- Cryopreserve a large, characterized master cell bank.
Stage 2: Transition to 3D Static Suspension Culture
- Objective: Achieve high-yield expansion while preserving pluripotency.
- Methodology (using a system like VitroGel STEM):
- Thaw and Mix: Thaw cells from liquid nitrogen and directly mix with the xeno-free hydrogel solution. This eliminates the need for matrix coating, reducing preparation time from hours to ~5 minutes [92].
- Culture: Plate the cell-hydrogel mixture in standard tissue culture vessels. The hydrogel supports the formation and growth of uniform 3D spheroids [92].
- Maintain: Culture for 7-day cycles, monitoring spheroid growth and morphology. Spheroids should display characteristics like shallow craters, indicating high expression of hPSC markers and healthy expansion [92].
- Harvest: After the expansion cycle, recover cells using a non-enzymatic harvesting solution (e.g., VitroGel Organoid Recovery Solution) or simple centrifugation. This avoids the complications of retrieving cells from rigid scaffolds [92].
Diagram 1: hPSC 3D Scale-Up Workflow.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of hybrid 2D/3D strategies relies on access to specialized reagents and materials. The following table details key solutions that facilitate the transition between culture systems and support scalable expansion.
Table 3: Key Research Reagent Solutions for Hybrid 2D/3D Workflows
| Reagent/Material | Function in Hybrid Workflow | Specific Application Example |
|---|---|---|
| VitroGel STEM | Xeno-free, synthetic hydrogel for 3D static suspension culture; enables direct transition from thawed or 2D cells. | Scalable expansion of hPSCs directly from liquid nitrogen, maintaining pluripotency and enabling easy harvest [92]. |
| Ultra-Low Attachment (ULA) Plates | Surface treatment that inhibits cell attachment, forcing cells to self-assemble into spheroids in a scaffold-free manner. | Generation of uniform multicellular tumor spheroids (MCTS) for medium-throughput drug screening [8]. |
| PeptiGels / Other Hydrogels | Tunable synthetic or natural polymer scaffolds that provide a biomimetic 3D extracellular matrix (ECM) for cell growth. | Creating a tissue-specific microenvironment for organoid culture or studying cell-ECM interactions in cancer invasion [93]. |
| CellTiter-Glo 3D | Luminescent assay optimized for quantifying ATP in 3D cell cultures, overcoming penetration limitations of other assays. | Measuring cell viability and compound efficacy in dense 3D spheroids and organoids post-2D screening [95]. |
| Non-Enzymatic Harvesting Solutions | Gently dissociates cells from hydrogels or animal-based ECM without damaging surface proteins via enzymatic digestion. | Recovering viable hPSCs or organoids from 3D hydrogels like VitroGel for downstream analysis or re-plating [92]. |
| Microfluidic Chips (Organ-on-a-Chip) | Devices that create controlled microenvironments with fluid flow, allowing for more advanced modeling of organ-level physiology. | Advanced toxicity testing and disease modeling (e.g., liver-on-chip for hepatotoxicity) after initial 3D hit confirmation [8] [93]. |
The future of cell-based research and development lies not in choosing between 2D and 3D systems, but in strategically integrating them. The hybrid workflows and comparative data presented in this guide demonstrate that a tiered approach effectively balances operational efficiency with biological relevance. By using 2D cultures for high-throughput tasks like initial compound screening and master cell bank generation, and reserving more complex 3D models for validation and specialized studies, research teams can optimize resource allocation and improve the predictive power of their preclinical data.
The ongoing integration of automation, AI-driven data analysis, and standardized reagent systems like xeno-free hydrogels is making these hybrid workflows increasingly accessible and reproducible [93] [92]. As the field evolves, the adoption of such flexible, multi-model strategies will be crucial for accelerating the translation of basic research into effective therapies, ultimately bridging the gap between flat biology and real-world clinical outcomes.
The foundation of reliable in vitro research rests upon selecting a cell culture system that accurately mirrors the complexity of living tissue while providing robust experimental control. For decades, two-dimensional (2D) culture on flat plastic surfaces has been the standard workhorse in biological research [64] [74]. However, the recognition that cells behave fundamentally differently when grown in three-dimensional (3D) environments has driven a paradigm shift toward matrix-based 3D culture systems [2] [72]. This guide provides an objective comparison of 2D and 3D culture matrices, evaluating their performance across key biological parameters to inform selection for specific research applications.
Fundamental Differences Between 2D and 3D Culture Environments
The core distinction between these systems lies in their spatial architecture and how this influences cell behavior. In 2D culture, cells adhere to a rigid, flat surface, forming a monolayer where all cells experience uniform exposure to nutrients and experimental treatments [2] [96]. Conversely, 3D culture allows cells to grow in all directions within a matrix scaffold, establishing natural gradients of oxygen, nutrients, and signaling molecules that closely mimic the in vivo tissue microenvironment [8] [71].
This architectural difference profoundly impacts cellular physiology. Cells in 3D matrices maintain native morphology and establish more realistic cell-cell and cell-matrix interactions [64] [72]. They develop complex cytoarchitecture including polarization and natural tissue organization absent in 2D systems [2]. The 3D environment also recapitulates physiochemical gradients such as hypoxia in inner layers of cell spheroids, which is crucial for studying tumor biology and drug penetration [61] [8].
Table 1: Core Characteristics of 2D vs. 3D Culture Systems
| Characteristic | 2D Culture | 3D Culture |
|---|---|---|
| Spatial Organization | Monolayer on flat surface | Three-dimensional structure in matrix |
| Cell-Matrix Interactions | Limited to basal surface | Omni-directional, physiologically relevant |
| Microenvironment | Homogeneous nutrient and gas exposure | Heterogeneous with natural gradients |
| Cell Morphology | Altered, flattened morphology | Preserved native architecture |
| Physiological Relevance | Low; altered gene expression | High; mimics in vivo conditions |
| Drug Sensitivity | Typically overestimated | More predictive of in vivo response |
Experimental Evidence: Quantitative Performance Comparisons
Recent comparative studies provide compelling data on the functional differences between these culture systems. A 2023 study comparing 2D and 3D colorectal cancer models demonstrated significant differences in multiple parameters essential for predictive research [61].
In proliferation assays, cells in 3D culture showed significantly different growth kinetics compared to 2D monolayers (p < 0.01) [61]. Perhaps more notably, apoptosis analysis revealed distinct cell death phase profiles between the two systems [61]. This has direct implications for therapeutic development, as cells in 3D matrices better replicate the drug resistance observed in clinical tumors due to limited penetration and microenvironmental protection [64] [61].
Gene expression analyses further highlight fundamental biological differences. Transcriptomic studies using RNA sequencing have identified thousands of significantly differentially expressed genes (p-adj < 0.05) between 2D and 3D cultures across multiple cell lines [61]. These expression differences span critical pathways including those governing cell differentiation, proliferation, and ECM interaction [61]. Epigenetically, 3D cultures more closely match patient-derived samples (FFPE), sharing similar methylation patterns and microRNA expression profiles, while 2D cultures show elevated methylation rates and altered microRNA expression [61].
Table 2: Experimental Data Comparison from Colorectal Cancer Study
| Parameter | 2D Culture | 3D Culture | Significance |
|---|---|---|---|
| Proliferation Pattern | Standard monolayer growth | Significant difference over time | p < 0.01 |
| Response to 5-FU, Cisplatin, Doxorubicin | Uniform sensitivity | Heterogeneous response with resistance | p < 0.01 |
| Methylation Pattern | Elevated rate | Matched patient FFPE samples | Differentiated |
| microRNA Expression | Altered profile | Matched patient FFPE samples | Differentiated |
| Differentially Expressed Genes | Thousands up/down-regulated vs 3D | Thousands up/down-regulated vs 2D | p-adj < 0.05 |
Technical Implementation: Methodologies and Protocols
Establishing 3D Culture Models
Implementing 3D culture systems requires specific methodologies that differ substantially from traditional 2D approaches. The two primary strategies include scaffold-based and scaffold-free techniques [64] [73].
Scaffold-Based Methods utilize natural or synthetic matrices to provide structural support that mimics the extracellular matrix (ECM). Common approaches include:
- Hydrogels: Natural (e.g., Matrigel, collagen, alginate) or synthetic polymers that form hydrated networks supporting cell growth and differentiation [64] [72].
- Polymeric Hard Scaffolds: Rigid porous structures made from synthetic materials like PLA or PGA that provide mechanical support for specific tissues [96].
- Decellularized ECM: Native tissue ECM with cellular components removed, preserving native biochemical and structural cues [64].
Scaffold-Free Methods rely on cell self-assembly without exogenous matrix support:
- Hanging Drop Technique: Cells aggregate by gravity in suspended droplets to form uniform spheroids [73] [74].
- Low-Attachment Plates: Specialized U-bottom wells with ultra-low attachment surfaces promote spontaneous spheroid formation [61] [71].
- Rotary Bioreactors: Continuous motion prevents adhesion and promotes aggregate formation through constant agitation [2] [96].
Protocol: Generating 3D Spheroids Using Low-Attachment Plates
The following protocol, adapted from the colorectal cancer comparison study, details standardized spheroid formation [61]:
- Cell Preparation: Harvest and count cells using standard trypsinization procedures.
- Seeding: Prepare cell suspension at 5×10³ cells/200µL complete media per well. Aliquot 200µL into individual wells of Nunclon Sphera super-low attachment U-bottom 96-well microplates.
- Culture Maintenance: Maintain spheroids in complete medium at 37°C, 5% CO₂ with humidification.
- Media Changes: Perform three consecutive 75% medium changes every 24 hours to maintain nutrient supply while preserving spheroid integrity.
- Monitoring: Observe spheroid formation daily; compact, spherical structures typically form within 72 hours.
This method produces uniform, reproducible spheroids suitable for high-throughput drug screening and mechanistic studies.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of 3D culture systems requires specific reagents and materials that differ from traditional 2D culture. The following table details essential solutions for establishing robust 3D culture models:
Table 3: Essential Research Reagent Solutions for 3D Culture
| Product Category | Example Products | Function & Application |
|---|---|---|
| Low-Attachment Plates | Nunclon Sphera U-bottom plates, Millicell Microwell plates | Promote spheroid formation through specialized surface chemistry and geometry |
| ECM Matrices | Corning Matrigel, collagen hydrogels, synthetic PEG-based hydrogels | Provide bioactive scaffold mimicking native extracellular matrix |
| Tissue Clearing Reagents | Visikol HISTO-M, Corning 3D clear tissue clearing reagent | Enable deep imaging of 3D structures without physical sectioning |
| Specialized Media Supplements | Growth factors, differentiation cocktails, ECM components | Direct specialized cell differentiation and maintain tissue-specific functions |
| Automated Culture Systems | Corning Matribot bioprinter, rotary bioreactors | Enable precise, reproducible scaffold seeding and long-term culture maintenance |
Decision Framework: Selecting the Appropriate Culture System
The choice between 2D and 3D culture systems should be guided by research objectives, resource constraints, and the specific biological questions being addressed. The following decision pathway provides a systematic approach to selection:
When to Prioritize 2D Culture
2D systems remain the appropriate choice for:
- High-throughput compound screening in early drug discovery phases [8] [71]
- Genetic manipulation studies (e.g., CRISPR screens) requiring uniform cell access [8]
- Basic pathway analysis and receptor-ligand interaction studies [8] [71]
- Resource-limited settings or when extensive historical comparison data exists [74] [71]
When to Invest in 3D Culture
3D systems provide superior value for:
- Tumor microenvironment modeling including hypoxia and drug penetration studies [61] [8]
- Stem cell differentiation and organoid development [8] [73]
- Toxicology and safety pharmacology assessment with human-relevant models [8] [73]
- Personalized medicine approaches using patient-derived organoids [8] [73]
- Studies of complex diseases like cancer, Alzheimer's, and metabolic disorders [8]
The most effective research strategies often integrate both 2D and 3D culture systems rather than treating them as mutually exclusive alternatives. A tiered approach using 2D for primary screening followed by 3D validation of lead candidates leverages the strengths of both systems [8] [71]. This hybrid model balances the practical advantages of 2D culture—speed, cost-effectiveness, and experimental simplicity—with the physiological relevance of 3D systems that better predict clinical outcomes [61] [72].
As the field advances, emerging technologies like organ-on-a-chip systems, automated 3D culture platforms, and AI-driven analysis of complex 3D data are further bridging the gap between in vitro models and human physiology [8] [73]. The strategic selection and implementation of appropriate culture matrices—balancing biological relevance with experimental control—remains fundamental to generating clinically predictive data and advancing biomedical discovery.
Evidence-Based Analysis: Quantifying the Superior Predictive Power of 3D Cultures
The efficacy of chemotherapy is a cornerstone of cancer treatment, yet its success is often limited by the development of drug resistance. Preclinical models that accurately predict therapeutic response are therefore fundamental to advancing oncology research and drug development. For decades, traditional two-dimensional (2D) cell culture, where cells grow in a single layer on flat plastic surfaces, has been the standard experimental system. While valued for its simplicity, low cost, and compatibility with high-throughput screening, the 2D model has a significant limitation: it fails to replicate the complex three-dimensional architecture of human tumors [65] [8]. This oversimplified environment alters cancer cell biology, leading to data that often does not translate well to the clinical setting [65].
In response to these limitations, three-dimensional (3D) culture systems have emerged as a transformative technology. These models, including spheroids and organoids, allow cells to grow and interact in all directions, more closely mimicking the structural and functional complexity of in vivo tumors [65] [8]. They recapitulate critical tumor features such as gradients of oxygen and nutrients, cell-cell and cell-extracellular matrix (ECM) interactions, and the presence of hypoxic cores [8] [97]. This review provides a comparative analysis of 2D and 3D culture systems, focusing on their performance in evaluating chemotherapy efficacy and resistance mechanisms. By synthesizing experimental data and case studies, we aim to guide researchers in selecting the most appropriate model for their scientific inquiries.
Comparative Performance: 2D vs. 3D Models in Key Assays
Substantial evidence demonstrates that cancer cells cultured in 2D and 3D systems exhibit markedly different behaviors in terms of drug sensitivity, proliferation, gene expression, and cell death. The tables below summarize these key differences based on experimental data.
Table 1: Comparative Drug Response in 2D vs. 3D Cultures
| Cancer Type | Chemotherapeutic Agent | Response in 2D | Response in 3D | Fold-Resistance in 3D | Study Reference |
|---|---|---|---|---|---|
| Head and Neck (HNSCC) | Cisplatin | Sensitive | Decreased sensitivity | Varies by cell line [97] | [97] |
| Head and Neck (HNSCC) | Cetuximab (anti-EGFR) | Sensitive | Decreased sensitivity | Varies by cell line [97] | [97] |
| Colorectal Cancer | 5-Fluorouracil, Cisplatin, Doxorubicin | Higher sensitivity | Significantly more resistant | Significant (p<0.01) [61] | [61] |
| Glioblastoma | Alkylating Chemotherapies (e.g., Temozolomide) | More sensitive | Increased resistance | Mediated by ECM [98] | [98] |
Table 2: Biological Characteristics of 2D vs. 3D Cultures
| Characteristic | 2D Culture | 3D Culture | Research Implication |
|---|---|---|---|
| Cell Proliferation | High, uniform rate [61] | Heterogeneous; slower in spheroid core [97] [61] | Better models tumor growth kinetics |
| Gene Expression | Altered; does not mimic in vivo [65] | More in vivo-like; upregulation of stemness genes (NANOG, SOX2) [97] | More accurate transcriptomic data |
| Apoptosis Profile | Higher baseline apoptosis [61] | More live cells, fewer early/late apoptotic cells [61] | Reflects survival mechanisms in tumors |
| Tumor Microenvironment | Lacks ECM and spatial organization [65] | Self-assembled ECM; cell-matrix interactions [98] [8] | Critical for studying drug penetration and resistance |
Experimental Protocols for Evaluating Drug Response
To ensure the reliability and reproducibility of comparative studies, standardized protocols are essential. Below are detailed methodologies for assessing chemotherapy efficacy in both 2D and 3D systems.
Protocol 1: Generating 3D Spheroids for Drug Screening
This protocol is adapted from studies on Head and Neck Squamous Cell Carcinoma (HNSCC) and colorectal cancer [97] [61].
- Step 1: Spheroid Formation. Seed 6,000-8,000 cells per well in a 96-well, ultra-low attachment (ULA), round-bottomed plate. The ULA surface prevents cell attachment, forcing them to aggregate and form a single spheroid per well [97].
- Step 2: Culture and Maturation. Culture the plates under standard conditions (37°C, 5% CO2) for a period of 3 to 7 days to allow for spheroid consolidation and maturation. Change 75% of the medium every 24-48 hours to maintain nutrient levels [61].
- Step 3: Drug Treatment. After spheroids have formed, add the chemotherapeutic agent directly to the well. Studies often use a range of concentrations (e.g., Cisplatin at 1, 2, and 4 µg/ml) to establish a dose-response curve [97].
- Step 4: Incubation and Assessment. Incubate the spheroids with the drug for the desired period (e.g., 7 days). Viability can then be assessed using assays like the MTS or CellTiter 96 AQueous One Solution assay [97] [61]. For spheroids, it is often necessary to dissociate them into a single-cell suspension using trypsin before performing the viability assay to ensure accurate readings [97].
Protocol 2: Direct Comparison of 2D and 3D Drug Sensitivity
This protocol outlines a parallel experiment to directly compare efficacy across models [61].
- Step 1: Parallel Culture. Culture the same cell line in both 2D (standard tissue culture plates) and 3D (ULA plates) formats. The initial cell seeding density should be equivalent (e.g., 5x10^3 cells/well) [61].
- Step 2: Synchronized Treatment. After the 3D spheroids have matured (e.g., 72 hours), treat both 2D monolayers and 3D spheroids with identical concentrations of the chemotherapeutic drug(s) [61].
- Step 3: Viability Assay. Following a standardized incubation period, measure cell viability. A common method is the colorimetric MTS assay, which measures the metabolic activity of cells. The bio-reduction of MTS into soluble formazan is detected by measuring absorbance at 490 nm [61].
- Step 4: Data Analysis. Calculate the IC50 (half-maximal inhibitory concentration) for both 2D and 3D cultures. The fold-resistance of the 3D model can be determined using the formula: Fold Resistance = IC50 (3D) / IC50 (2D) [99].
Mechanisms Underlying Differential Drug Responses
The increased resistance to chemotherapy observed in 3D models is not an artifact but a consequence of their ability to replicate key resistance mechanisms found in human tumors. The following diagram synthesizes the major mechanisms involved.
Diagram: Mechanisms of Drug Resistance in 3D Tumor Spheroids. The 3D architecture activates multiple, interconnected resistance pathways, including extracellular matrix (ECM)-mediated survival signaling, induction of a hypoxic core, increased activity of drug efflux pumps, and enrichment of cancer stem cells (CSCs), collectively leading to treatment failure.
The diagram above illustrates several core mechanisms:
- Extracellular Matrix (ECM) Interactions: In scaffold-based 3D cultures, engagement with ECM components like hyaluronic acid (HA) through receptors such as CD44 and integrins activates pro-survival signaling pathways, notably Src. This signaling inhibits the expression of pro-apoptotic factors, enabling cancer cells to withstand chemotherapy-induced damage [98].
- The Hypoxic Core and Metabolic Adaptation: As spheroids grow, diffusion limitations create an inner core that is depleted of oxygen and nutrients. This hypoxia stabilizes Hypoxia-Inducible Factor-alpha (HIF-α), which drives a metabolic switch to glycolysis (the Warburg effect) and activates genes that promote cell survival, angiogenesis, and invasion [100] [97]. This environment also favors the emergence of a mutator phenotype, increasing genetic instability and cancer progression [100].
- Efflux Pump Upregulation: A well-established mechanism of multidrug resistance (MDR) is the overexpression of ATP-binding cassette (ABC) transporters, such as P-glycoprotein (P-gp), multidrug resistance proteins (MRPs), and breast cancer resistance protein (BCRP). These proteins use ATP to actively pump a wide range of chemotherapeutic drugs out of the cell, reducing intracellular concentrations and, thus, efficacy [100] [101].
- Cancer Stem Cell (CSC) Enrichment and Altered Gene Expression: 3D cultures have been shown to enrich for cells with a CSC-like phenotype, which are inherently more resistant to therapy and can drive tumor recurrence [97]. This is coupled with a significant reprogramming of the cellular transcriptome. Studies report thousands of genes being differentially expressed in 3D cultures compared to 2D, including the upregulation of stemness markers like NANOG and SOX2, which contributes to the observed drug resistance [97] [61].
The Scientist's Toolkit: Essential Reagents and Platforms
Selecting the appropriate tools is critical for establishing robust 2D and 3D culture models. The table below lists key solutions and their applications.
Table 3: Research Reagent Solutions for 2D and 3D Culture
| Reagent / Platform | Function | Application Context |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Prevents cell attachment, enabling spheroid self-assembly. | Scaffold-free 3D spheroid formation (e.g., hanging drop, ULA round-bottom plates) [97] [61]. |
| Matrigel / Basement Membrane Extract | A complex, reconstituted ECM providing biochemical and structural support. | Scaffold-based 3D organoid culture for stem cell maintenance and differentiation [65]. |
| Hyaluronic Acid (HA) Scaffolds | Bioengineered ECM component to model specific tissue environments. | Studying ECM-mediated drug resistance, particularly in brain tumors (glioblastoma) [98]. |
| CellTiter 96 AQueous MTS Assay | Colorimetric method to quantify metabolically active (viable) cells. | Standardized cell viability and proliferation assessment in 2D and dissociated 3D cultures [97] [61]. |
| Organoid-on-a-Chip (OoC) | Microfluidic device integrating 3D models with dynamic flow. | Advanced TME modeling, drug permeability studies, and high-throughput screening under physiologically relevant flow conditions [102]. |
| Annexin V FITC / PI Apoptosis Kit | Fluorescent staining to distinguish live, early apoptotic, late apoptotic, and necrotic cells. | Flow cytometry-based analysis of drug-induced programmed cell death [61]. |
The evidence from direct comparative studies is clear: 3D cell culture models provide a more physiologically relevant and predictive platform for evaluating chemotherapy efficacy and resistance mechanisms than traditional 2D monolayers. The data generated from 3D systems—from transcriptomic profiles to IC50 values—align more closely with clinical behavior, including the robust modeling of drug resistance that so often limits treatment success in patients [97] [61].
The choice between models is not necessarily binary. A tiered, strategic approach is increasingly adopted by leading laboratories: utilizing 2D models for high-throughput initial screening due to their speed and low cost, followed by validation in 3D models for their predictive power and physiological relevance [8]. The future of preclinical oncology research lies in the continued refinement of these 3D technologies—such as vascularized organoid-on-a-chip systems and patient-derived organoids—and their integration into hybrid workflows that combine the strengths of both 2D and 3D paradigms to accelerate the development of more effective cancer therapies [65] [8] [102].
In vitro cell culture models are fundamental tools for investigating cancer biology and evaluating potential therapeutics. For decades, two-dimensional (2D) culture has been the standard methodology, but its limitations in mimicking the complex in vivo tumor environment have driven the adoption of three-dimensional (3D) models. In colorectal cancer (CRC) research, this transition is particularly significant because tumor behavior is heavily influenced by the tumor microenvironment (TME), which includes cell-cell interactions, extracellular matrix (ECM) components, and spatial organization that 2D systems cannot replicate [103]. The shift to 3D cultures represents a critical advancement in bridging the gap between traditional in vitro models and in vivo physiology, offering more physiologically relevant data for proliferation and apoptosis studies.
This guide provides a direct comparison of 2D and 3D culture systems for evaluating proliferation and apoptosis in colorectal cancer research. We present experimental data, detailed methodologies, and analytical frameworks to help researchers select appropriate models for specific applications, particularly in drug development workflows where predictive accuracy is paramount for successful clinical translation.
Comparative Performance: Proliferation and Apoptosis in 2D vs. 3D Models
Quantitative Differences in Proliferation and Apoptosis
Table 1: Direct comparison of proliferation and apoptosis metrics between 2D and 3D colorectal cancer models
| Parameter | 2D Culture Characteristics | 3D Culture Characteristics | Experimental Evidence |
|---|---|---|---|
| Proliferation Rate | Higher and more uniform proliferation [104] | Heterogeneous proliferation with significantly (p < 0.01) different patterns over time [104] | MTS/PMS colorimetric assay across five CRC cell lines [104] |
| Proliferation Distribution | Homogeneous Ki-67 expression [105] | Varied Ki-67-positive cells in epithelial CRAC cells; unchanged high proliferation in mesenchymal cells [105] | Immunocytochemical analysis of epithelial vs. mesenchymal CRC cell lines [105] |
| Apoptosis Baseline | Higher baseline apoptosis in standard conditions [104] | Significantly different cell death phase profile [104] | FITC Annexin V/PI staining with flow cytometry [104] |
| Drug-Induced Apoptosis | SN-38 induced significant apoptosis with caspase-3/7 activation [106] | Dramatically diminished apoptosis and anti-proliferation effects of SN-38 [106] | Caspase-Glo 3/7 assay after drug exposure in HCT116 cells [106] |
| Spatial Apoptosis Patterns | Uniform drug-induced cell death [106] | Sorafenib induced significant apoptosis primarily in center of spheroids [106] | Cell death localization analysis in 3D spheroids [106] |
| Gene Expression | Altered microRNA expression; elevated methylation rate [104] | miRNA expression and methylation patterns similar to FFPE patient samples [104] | RNA sequencing and bioinformatic analysis [104] |
Drug Response and Resistance Profiles
Table 2: Comparative drug response data between 2D and 3D colorectal cancer models
| Therapeutic Agent | Response in 2D Models | Response in 3D Models | Implications for Drug Development |
|---|---|---|---|
| 5-Fluorouracil (5-FU) | Standard concentration-response curve [104] | Significant (p < 0.01) difference in responsiveness [104] | 3D models reveal resistance mechanisms missed in 2D screens |
| Cisplatin | Conventional IC50 values achievable [104] | Significant (p < 0.01) difference in responsiveness [104] | Better prediction of clinical efficacy for platinum-based therapies |
| Doxorubicin | Expected cytotoxicity profile [104] | Significant (p < 0.01) difference in responsiveness [104] | Improved modeling of anthracycline responses in solid tumors |
| SN-38 (Irinotecan metabolite) | Significant apoptosis with caspase-3/7 activation [106] | Dramatically diminished apoptosis effects [106] | 3D models identify inherent chemoresistance in spatial contexts |
| Sorafenib | Induced cell death without caspase activation [106] | Significant apoptosis in spheroid centers; distinct cell death pathways [106] | Reveals context-dependent mechanisms of kinase inhibitors |
Experimental Protocols for Direct Comparison
Standardized Proliferation Assay Protocol
The CellTiter 96 AQueous Non-Radioactive Cell Proliferation Assay (MTS assay) provides a standardized method for comparing proliferation between 2D and 3D cultures [104]:
- Cell Culture Setup: Plate five colorectal adenocarcinoma cell lines (Caco-2, HCT-116, LS174T, SW-480, HCT-8) in both 2D and 3D formats at identical initial densities (5 × 10³ cells/well). For 3D cultures, use Nunclon Sphera super-low attachment U-bottom 96-well microplates.
- Incubation Conditions: Maintain cultures under identical conditions (37°C, 5% CO₂, humidified atmosphere) with three consecutive 75% medium changes every 24 hours for 3D cultures.
- MTS Reagent Application: At desired timepoints, add 20µL of tetrazolium/phenazine methosulfate mixture (MTS/PMS, 20:1 v/v) to each well containing 100µL of culture medium.
- Signal Development and Detection: Incubate plate for 4 hours at 37°C, then measure absorbance at 490nm using an ELISA plate reader. The bio-reduction of MTS into soluble formazan by metabolically active cells provides a quantitative proliferation measure.
- Data Analysis: Compare proliferation curves between 2D and 3D cultures across multiple time points. Statistical analysis typically shows significant (p < 0.01) differences in proliferation patterns.
Comparative Apoptosis Analysis Protocol
The FITC Annexin V Apoptosis Detection Protocol enables direct comparison of apoptotic states [104]:
- Cell Harvesting: After incubation periods (24h for 2D, 72h for 3D), harvest cells using gentle trypsinization. For 3D spheroids, additional mechanical dissociation may be required.
- Washing and Preparation: Wash cells twice with ice-cold Hanks Balanced Salt Solution (HBSS) and collect by centrifugation (10min, 1200rpm, ambient temperature). Resuspend at 1 × 10⁶ cells mL⁻¹ in Annexin-binding buffer.
- Staining: Aliquot 100µL cell suspension and stain with 5µL FITC-labeled Annexin V and 5µL propidium iodide (PI) for 15min at room temperature protected from light.
- Analysis: Add 400µL binding buffer, mix gently, and analyze using a fluorescence-activated cell flow cytometer (e.g., FACSCalibur). Use FacsDiva software (Version 5.0.3) or equivalent for data analysis.
- Population Discrimination: Identify four distinct cell populations: (1) live cells (Annexin negative/PI negative), (2) early apoptotic cells (Annexin positive/PI negative), (3) late apoptotic cells (Annexin positive/PI positive), and (4) necrotic cells (Annexin negative/PI positive).
3D Spheroid Formation and Drug Treatment Protocol
For consistent 3D culture generation and drug testing [106]:
- Spheroid Formation: Harvest pre-cultured CRC cells and seed into 24 or 96-well NanoCulture plates at 1 × 10⁴ cells mL⁻¹ density. Incubate at 37°C in 5% CO₂ for 7 days to form mature spheroids.
- Drug Exposure: Prepare compound solutions at three times desired final concentration in medium. Add 50µL to 7-day-old spheroids in 100µL existing medium.
- Viability Assessment: After 72h drug exposure, measure cell viability using ATP-based assays (e.g., TOYO INK CA50). Add 50µL reagent per well, incubate 10min at 37°C with shaking, then measure luminescence.
- Caspase Activity Measurement: Use Caspase-Glo 3/7 assay systems to quantify apoptosis activation in both 2D and 3D formats after drug treatment.
- Morphological Analysis: For structural assessment, harvest spheroids, embed in collagen gels, fix with paraformaldehyde, and process for paraffin sectioning and H&E staining.
Molecular Mechanisms: Signaling Pathways in 2D vs. 3D Environments
Epithelial-Mesenchymal Transition (EMT) Differences
The expression patterns of epithelial and mesenchymal markers significantly differ between 2D and 3D cultures, influencing both proliferation and apoptosis responses [105]:
- In 2D cultures, CRC cell lines exhibit distinct epithelial or mesenchymal characteristics with corresponding E-cadherin (epithelial marker) and vimentin (mesenchymal marker) expression patterns.
- In 3D cultures, mesenchymal cells from 2D cultures show reduced vimentin mRNA levels, indicating a shift in gene expression profiles.
- Membrane localization of E-cadherin becomes more pronounced in 3D cultures for most cell lines, enhancing cell-cell adhesion mechanisms.
- These phenotypic differences directly impact proliferative capacity and apoptotic susceptibility, particularly in response to therapeutic agents.
miRNA Regulation and JAK-STAT Signaling
The microRNA expression profiles differ significantly between 2D and 3D environments, with important implications for proliferation and apoptosis regulation [104] [107]:
- miR-198 expression is significantly reduced in CRC cell lines compared to normal colon cells, and its overexpression inhibits CRC cell proliferation while promoting apoptosis.
- miR-198 exerts these effects by targeting ADAM28 and subsequently blocking the JAK-STAT signaling pathway, a critical regulator of cell survival and proliferation.
- 3D cultures demonstrate miRNA expression patterns more closely resembling those found in formalin-fixed paraffin-embedded (FFPE) patient samples than 2D cultures.
- The epigenetic regulation through methylation patterns also differs, with 2D cells showing elevation in methylation rate compared to 3D cultures and patient samples.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key research reagents and their applications in 2D/3D comparative studies
| Reagent/Catalog Item | Primary Function | Application in 2D/3D Comparison |
|---|---|---|
| Nunclon Sphera U-bottom Plates | Facilitate 3D spheroid formation | Provide low-attachment surface for consistent 3D spheroid generation [104] |
| CellTiter 96 AQueous MTS Assay | Measure metabolic activity/proliferation | Quantitative comparison of proliferation rates between 2D and 3D cultures [104] |
| FITC Annexin V Apoptosis Kit | Detect phosphatidylserine externalization | Standardized apoptosis measurement across culture formats [104] |
| Caspase-Glo 3/7 Assay System | Measure caspase activation | Apoptosis pathway analysis in drug treatment studies [106] |
| NanoCulture Plates | 3D spheroid formation | Alternative 3D culture platform for drug sensitivity testing [106] |
| Type I Collagen | Extracellular matrix component | Scaffold-based 3D model construction [108] |
| Anti-E-cadherin Antibodies | Epithelial marker detection | EMT status assessment in different culture conditions [105] |
| Anti-vimentin Antibodies | Mesenchymal marker detection | Mesenchymal character evaluation across models [105] |
| Polycaprolactone (PCL) | 3D scaffold material | 3D bioprinting and scaffold-based model systems [108] |
The comparative data presented in this guide demonstrates that 3D culture systems provide distinct advantages for colorectal cancer research, particularly in modeling the complex interplay between proliferation and apoptosis that occurs in vivo. The heterogeneous proliferation patterns, spatially distinct apoptosis responses, and enhanced drug resistance observed in 3D models more closely mirror clinical tumor behavior than traditional 2D systems.
However, 2D cultures remain valuable for high-throughput screening, mechanistic studies with reduced complexity, and initial drug discovery phases. The optimal approach involves strategic integration of both systems: using 2D models for initial screening and 3D models for validation and more physiologically relevant assessment of drug efficacy and resistance mechanisms. This integrated methodology ultimately enhances the predictive accuracy of preclinical cancer research and improves translation success in drug development pipelines.
The process of drug development is notoriously lengthy, expensive, and marked by high failure rates. A significant contributing factor is the poor predictive power of traditional preclinical models, leading to a translational gap between laboratory results and clinical outcomes. Historically, drug discovery has relied heavily on two-dimensional (2D) cell cultures grown as monolayers on plastic surfaces. While these 2D models are valuable for their simplicity, cost-effectiveness, and compatibility with high-throughput screening, they lack the physiological relevance needed to accurately predict drug efficacy and toxicity in humans [2] [109]. Consequently, over 90% of new anticancer compounds fail in clinical trials, often due to insufficient effectiveness or unexpected toxicity that was not captured during preclinical testing [109] [110].
The fundamental limitation of 2D culture is its inability to mimic the complex three-dimensional architecture and cellular microenvironment found in living tissues [111]. In vivo, cells exist within a sophisticated extracellular matrix (ECM), engage in intricate cell-cell and cell-ECM interactions, and are exposed to gradients of oxygen, nutrients, and signaling molecules. These critical factors influence key aspects of cell behavior, including gene expression, proliferation, differentiation, and drug response [2] [61]. The growing recognition of these limitations has accelerated the development and adoption of three-dimensional (3D) cell culture models, which are increasingly recognized as a crucial technology for bridging the translational gap in drug development.
Fundamental Limitations of 2D Models in Predicting In Vivo Outcomes
Cells cultured in 2D monolayers exhibit significant alterations in morphology, signaling, and function compared to their in vivo counterparts. On flat, rigid plastic surfaces, cells are forced into an unnatural state of hyper-flattening, which disrupts their native polarity and cytoskeletal organization [109]. This aberrant morphology has profound downstream effects, including altered gene expression profiles, disrupted cell communication, and changed metabolic activities [2] [61].
Perhaps the most critical shortcoming of 2D cultures in oncology research is their failure to replicate the tumor microenvironment (TME). The TME is a complex ecosystem comprising cancer cells, stromal cells, immune components, and the extracellular matrix, all of which interact dynamically to influence tumor progression and treatment response [109] [110]. In 2D cultures, the absence of this spatial architecture eliminates crucial phenomena such as:
- Nutrient and oxygen gradients that create distinct proliferative, quiescent, and necrotic zones
- Cell-ECM interactions that activate pro-survival signaling pathways
- Physical barriers to drug penetration that limit compound efficacy in solid tumors [112] [110]
These limitations collectively contribute to the consistently observed overestimation of drug efficacy in 2D models compared to in vivo results, a discrepancy that becomes painfully apparent during costly late-stage clinical failures.
Table 1: Key Physiological Differences Between 2D Cultures, 3D Cultures, and In Vivo Conditions
| Parameter | 2D Culture | 3D Culture | In Vivo Environment |
|---|---|---|---|
| Cell Morphology & Polarity | Altered, forced flattening; loss of native polarity | Preserved tissue-specific architecture and polarity | Native morphology and polarization maintained |
| Cell-Cell & Cell-ECM Interactions | Limited to 2D plane; unnatural adhesion | Complex 3D interactions; natural adhesion molecules | Highly complex and dynamic interactions |
| Gene Expression Profile | Significantly altered mRNA splicing and expression | More representative of in vivo expression patterns | Tissue- and context-specific expression |
| Drug Response | Uniform exposure; typically overestimates efficacy | Gradients and penetration barriers; more predictive resistance | Complex pharmacokinetics/pharmacodynamics |
| Tumor Microenvironment | Absent | Can incorporate multiple cell types and ECM | Fully present with stromal and immune components |
| Metabolic Environment | Homogeneous nutrient and oxygen access | Heterogeneous; creates metabolic zones | Vascularized; highly heterogeneous |
How 3D Cultures Better Recapitulate In Vivo Physiology
Three-dimensional cell culture systems bridge the gap between conventional 2D cultures and in vivo models by recreating critical aspects of tissue physiology that determine drug responses. The enhanced predictive validity of 3D models stems from their ability to replicate the structural and functional complexity of human tissues through several key mechanisms.
Architectural and Microenvironmental Fidelity
In 3D cultures, cells can assemble into complex structures that closely mimic the microarchitecture of native tissues. This spatial organization enables the formation of physiological cell-cell contacts and interactions with the surrounding extracellular matrix that are essential for maintaining tissue-specific functions [2] [111]. These interactions activate signaling pathways that regulate cell survival, proliferation, and differentiation in ways that cannot be replicated in 2D environments. Furthermore, 3D cultures naturally develop metabolic and oxygen gradients due to the limited diffusion distance of gases and nutrients within the cellular mass [112] [110]. This results in the establishment of heterogeneous microenvironments with distinct proliferative, quiescent, and necrotic zones – a hallmark of solid tumors that significantly influences drug sensitivity and the emergence of resistant cell populations [112].
Molecular and Functional Relevance
At the molecular level, 3D cultures demonstrate gene expression profiles, signaling activities, and metabolic states that more closely resemble in vivo conditions than their 2D counterparts. Transcriptomic analyses have revealed that thousands of genes are differentially expressed between 2D and 3D culture systems, with 3D models showing remarkable similarity to original tumor tissues in pathways related to cell adhesion, ECM-receptor interactions, and hypoxia response [61]. This molecular fidelity translates to more physiologically relevant drug responses, including the development of resistance mechanisms observed in clinical settings, such as:
- Upregulation of drug efflux transporters
- Enhanced DNA repair capacity
- Activation of pro-survival signaling pathways [109] [111]
The preservation of these critical features makes 3D cultures superior predictors of in vivo drug behavior, enabling more accurate preclinical assessment of compound efficacy and safety.
Diagram 1: The role of 3D culture systems in bridging the translational gap between traditional 2D models and in vivo biology.
Direct Experimental Evidence: Benchmarking 3D Models Against In Vivo Data
Drug Response Correlations
Compelling evidence for the superior predictive value of 3D models comes from direct comparisons of drug responses between in vitro and in vivo systems. A comprehensive study on prostate cancer cell lines (PC-3, LNCaP, and DU145) demonstrated that cells cultured in 3D formats showed significantly higher resistance to paclitaxel and docetaxel compared to 2D cultures, more closely mirroring the treatment response patterns observed in patients [113]. Similarly, research on HCT116 colon carcinoma cells revealed that 3D multicellular tumor spheroids (MCTS) provided upfront information on anticancer drug effects that was tantamount to that obtained from animal xenograft studies [112]. This enhanced predictive power is largely attributed to the replication of physical barriers to drug penetration in 3D models, which is a critical determinant of efficacy in solid tumors but entirely absent in monolayer cultures.
Molecular and Phenotypic Validation
At the molecular level, benchmarking studies have shown remarkable concordance between 3D models and original tumors. A sophisticated transcriptomic analysis comparing 2D and 3D cultures of colorectal cancer cell lines with patient-derived formalin-fixed paraffin-embedded (FFPE) tissues revealed that 3D cultures and FFPE samples shared similar methylation patterns and microRNA expression, while 2D cultures showed significant alterations [61]. Furthermore, the gene expression profiles of 3D cultures demonstrated greater similarity to in vivo tumors across multiple pathways controlling cell proliferation, death, and differentiation. These molecular parallels translate to functional equivalences, as 3D models successfully recapitulate critical in vivo phenotypes such as:
- Hypoxic cores with activated hypoxia-inducible factor (HIF) signaling
- Metabolic heterogeneity and zone-specific proliferation rates
- Stem cell populations with enhanced drug efflux capability
- Invasion and migration patterns reflective of metastatic potential [112] [61] [109]
Table 2: Experimental Evidence Benchmarking 3D Models Against In Vivo Data
| Study Type | Experimental Findings | Clinical/In Vivo Correlation | Citation |
|---|---|---|---|
| Prostate Cancer Drug Response | 3D cultures showed higher resistance to paclitaxel and docetaxel vs. 2D | Mirrored the treatment response patterns observed in patients | [113] |
| Colon Cancer Molecular Profiling | 3D cultures shared methylation patterns and miRNA expression with patient FFPE samples | Close molecular similarity to original human tumors | [61] |
| HDAC Inhibitor Testing | 3D spheroid response to Troxbam and Troxham compounds was equivalent to animal studies | Provided information tantamount to animal xenograft data | [112] |
| Multicellular Tumor Spheroid | Reduced drug susceptibility in spheroid cores due to penetration barriers | Recapitulated limited drug penetration in poorly vascularized tumor regions | [110] |
| Transcriptomic Analysis | Thousands of genes differentially expressed between 2D and 3D; 3D more similar to in vivo | Gene expression fidelity enhancing predictive value for drug response | [61] |
Essential 3D Culture Methodologies and Protocols
The successful implementation of 3D culture models requires careful selection of appropriate methodologies based on research objectives and available resources. The two primary categories of 3D culture systems are scaffold-free and scaffold-based approaches, each with distinct advantages and applications.
Scaffold-Free Methods
Scaffold-free techniques rely on the innate ability of cells to self-assemble into 3D structures when prevented from adhering to a surface:
- Hanging Drop Method: Cells are seeded in droplets on the underside of a culture dish lid, where surface tension maintains the droplet formation. Cells accumulate at the liquid-air interface and form spheroids within 48-72 hours [112] [110]. This method produces uniform, tightly packed spheroids without requiring artificial matrices but has limitations for high-throughput applications and medium exchange.
- Ultra-Low Attachment Plates: These specially treated plates prevent cell adhesion, forcing cells to aggregate and form spheroids. Also known as the forced floating method, this approach is more amenable to standardized assays and medium changes compared to the hanging drop technique [61] [110].
- Liquid-Overlay Technique: Culture wells are coated with non-adhesive materials like poly-HEMA or agarose to prevent attachment, promoting spheroid formation through centrifugation or spontaneous aggregation [110].
Scaffold-Based Methods
Scaffold-based approaches provide a physical support structure that mimics the native extracellular matrix:
- Hydrogels: Natural (e.g., Matrigel, collagen, alginate) or synthetic (e.g., PEG, PVA) hydrogels provide a hydrous, biocompatible environment that supports cell growth and organization [114] [115]. Hydrogels are particularly valuable for studying cell-ECM interactions and creating tissue-specific microenvironments.
- Bioreactors: Systems like spinner flasks and rotational wall vessels maintain cells in suspension through constant agitation, promoting aggregation into spheroids [110]. These systems enable large-scale production of 3D cultures but may impose shear stress on cells.
- 3D Bioprinting: This advanced technique deposits cells and support materials in precise spatial arrangements to create complex tissue architectures with defined geometry and cellular composition [114] [110].
Table 3: Comparison of Common 3D Culture Techniques
| Method | Principle | Advantages | Limitations | Best Applications |
|---|---|---|---|---|
| Hanging Drop | Cell self-assembly in surface tension-maintained droplets | Uniform spheroid size, no scaffold interference | Difficult medium changes, low throughput | Initial drug screening, developmental studies |
| Ultra-Low Attachment Plates | Forced aggregation on non-adhesive surfaces | Easy handling, compatible with standard assays | Limited size control, minimal ECM interaction | High-throughput compound screening |
| Hydrogels | Cell encapsulation in ECM-mimetic matrices | Tissue-like stiffness, biochemical cues | Batch variability (natural hydrogels), cost | Disease modeling, migration studies |
| Bioreactors | Constant agitation prevents adhesion | Large-scale production, long-term culture | Shear stress potential, size heterogeneity | Large-scale tissue engineering, bioprocessing |
| 3D Bioprinting | Layer-by-layer deposition of bioinks | Architectural control, multicellular structures | Technical complexity, specialized equipment | Complex tissue models, vascularized constructs |
The Scientist's Toolkit: Essential Reagents and Materials
Implementing robust and reproducible 3D culture systems requires access to specialized reagents and materials. The following table details essential components for establishing these advanced models in a research setting.
Table 4: Essential Research Reagent Solutions for 3D Cell Culture
| Reagent/Material | Function | Examples/Specifications | Key Considerations |
|---|---|---|---|
| Basement Membrane Matrix | Natural hydrogel scaffold providing ECM components | Matrigel, collagen I, alginate | Batch variability; growth factor content may affect results |
| Synthetic Hydrogels | Defined, tunable scaffold with controllable properties | PEG, PVA, polyacrylamide | Reproducible mechanical properties; may lack biological cues |
| Ultra-Low Attachment Plates | Prevent cell adhesion to promote spheroid formation | U-bottom spheroid microplates, poly-HEMA coated plates | Well geometry determines spheroid size and uniformity |
| Hanging Drop Plates | Facilitate spheroid formation through gravity | 384-well hanging drop array plates | Compatible with automated liquid handling systems |
| Specialized Culture Media | Support 3D growth and maintain phenotype | Defined media with appropriate growth factors | May require optimization for specific 3D applications |
| Oxygen-Sensing Probes | Monitor gradient formation in 3D structures | Luminescent or fluorescent oxygen sensors | Essential for validating hypoxic core development |
| Viability Assay Kits | Assess cell health and compound toxicity in 3D | ATP-based, resazurin reduction, live/dead staining | Must be optimized for penetration in 3D structures |
| * Tissue Dissociation Kits* | Recover cells from 3D structures for analysis | Enzyme cocktails (collagenase, dispase, trypsin) | Optimization required to balance yield and viability |
The compelling body of evidence demonstrates that 3D cell culture models represent a significant advancement over traditional 2D systems for predicting in vivo outcomes in drug discovery and development. By more accurately recapitulating critical features of native tissues—including 3D architecture, cell-ECM interactions, gradient formation, and physiological gene expression patterns—3D models provide a more physiologically relevant platform for evaluating compound efficacy, toxicity, and mechanism of action [61] [109]. The enhanced predictive validity of these models has the potential to substantially reduce late-stage drug attrition rates by identifying promising candidates and eliminating poor performers earlier in the development process.
Looking forward, the integration of 3D culture systems with other advanced technologies promises to further enhance their utility and predictive power. The emergence of organ-on-a-chip platforms that incorporate fluid flow and mechanical stimulation, patient-derived organoids that capture inter-individual heterogeneity, and 3D bioprinting approaches that enable precise control over cellular spatial organization represent the next frontier in preclinical model development [114] [109] [110]. Furthermore, the adoption of artificial intelligence and machine learning for analyzing the complex multidimensional data generated by 3D systems will accelerate the extraction of biologically meaningful insights. As these technologies mature and standardization improves, 3D culture models are poised to become an indispensable component of the drug development pipeline, ultimately bridging the translational gap and delivering more effective therapies to patients with greater efficiency.
In vitro cell culture is a cornerstone of biological research, drug discovery, and cancer biology. For decades, two-dimensional (2D) culture has been the standard method due to its simplicity and cost-effectiveness [1]. However, the recognition that cells grown in monolayers on plastic surfaces exhibit significant differences in morphology, polarity, and signaling compared to their in vivo counterparts has driven the adoption of three-dimensional (3D) culture systems [1] [5]. These differences extend to the epigenetic level, particularly affecting DNA methylation and microRNA expression—key regulatory mechanisms that control gene expression without altering the DNA sequence itself [116].
The broader thesis of this efficacy comparison is that 3D culture systems more faithfully recapitulate the epigenetic landscape of human tissues and tumors, thereby providing more translationally relevant data for drug development and disease modeling. This guide objectively compares the performance of 2D and 3D culture systems by synthesizing current experimental data on methylation and microRNA patterns, with a specific focus on their fidelity to patient-derived tissues.
Comparative Analysis of Epigenetic Fidelity
DNA Methylation Patterns
DNA methylation, the addition of a methyl group to cytosine bases in CpG dinucleotides, is a fundamental epigenetic mark frequently altered in human cancers [116]. The cellular microenvironment, including cell-cell and cell-extracellular matrix (ECM) interactions, profoundly influences these patterns.
Table 1: Comparative Fidelity of DNA Methylation Patterns
| Culture System | Fidelity to Patient Tissue | Key Characteristics | Supporting Evidence |
|---|---|---|---|
| 2D Culture | Low | • Elevated global methylation rates [61]• Altered patterns due to unlimited O₂/nutrient access [1]• Disrupted methylation maintenance enzymes [116] | Colorectal cancer cell lines showed significant elevation in methylation rate compared to patient FFPE samples [61]. |
| 3D Culture | High | • Shares near-identical methylation pattern with patient FFPE tissue [61]• Better maintains original tumor methylation class [117]• Recapitulates in vivo-like hypoxia-driven methylation [118] [119] | In pediatric brain tumors, 3D cultures were significantly more consistent with the methylation class of the parental tumor than 2D cultures [117]. |
microRNA Expression Profiles
microRNAs (miRNAs) are small non-coding RNAs that post-transcriptionally regulate gene expression. Their expression is highly sensitive to cellular context and architecture, making the culture environment a critical variable in experimental outcomes.
Table 2: Comparative Fidelity of microRNA Expression Patterns
| Culture System | Fidelity to Patient Tissue | Key Characteristics | Supporting Evidence |
|---|---|---|---|
| 2D Culture | Low | • Altered microRNA expression relative to in vivo conditions [61]• Does not mimic the gradient-dependent expression found in tumors [1] | In colorectal cancer models, 2D cells showed altered microRNA expression compared to patient samples [61]. |
| 3D Culture | High | • Expression profile closely aligned with patient FFPE tissue [61]• Mirrors the heterogeneous expression found in tumor masses [1] | A study on five colorectal cancer cell lines found 3D cultures and patient FFPE samples shared the same microRNA expression, while 2D cells were altered [61]. |
Experimental Protocols for Assessing Epigenetic Fidelity
To ensure the reliability and reproducibility of epigenetic studies, standardized protocols for generating 3D models and analyzing epigenetic marks are essential. Below are detailed methodologies from key cited studies.
Protocol 1: Establishing 3D Spheroid Cultures for Epigenetic Analysis
This protocol is adapted from a 2023 comparative study in colorectal cancer [61].
- Cell Seeding: Prepare a single-cell suspension. Add an aliquot of 200 µL of cell suspension (5 × 10³ cells) into individual wells of a Nunclon Sphera super-low attachment U-bottom 96-well microplate.
- Culture Maintenance: Maintain spheroids in a complete cell culture medium (e.g., DMEM supplemented with 10% FBS) under standard conditions (37 °C, 5% CO₂, humidified atmosphere).
- Medium Changes: Perform three consecutive 75% medium changes every 24 hours to maintain nutrient levels and remove waste.
- Harvesting: Spheroids are typically ready for analysis after 7 days of culture, once they have formed compact 3D structures.
Protocol 2: DNA Methylation Analysis via Cell-free DNA (cfDNA) or Tissue DNA
This protocol is based on work for genome-scale methylation analysis from patient plasma and tissues [120].
- DNA Extraction:
- For plasma cfDNA: Isolate cell-free DNA from patient plasma using a commercial cfDNA extraction kit. Input as little as 6-10 ng of cfDNA can be sufficient.
- For tissue/Cells: Extract genomic DNA from formalin-fixed paraffin-embedded (FFPE) patient tissues, 2D-cultured cells, or 3D spheroids using standard phenol-chloroform or commercial kits.
- Bisulfite Conversion: Treat the purified DNA with sodium bisulfite using a kit such as the EZ DNA Methylation-Lightning Kit. This conversion changes unmethylated cytosines to uracils, while methylated cytosines remain unchanged.
- Library Preparation & Sequencing: Perform library preparation for bisulfite sequencing. The cited studies used Cell-free Reduced Representation Bisulfite Sequencing (cfRRBS) or RRBS to generate genome-scale methylation libraries, which enrich for CpG-rich regions and provide high-quality data from low-input samples [120].
- Bioinformatic Analysis: Process sequencing data through a dedicated bioinformatics pipeline. This typically includes:
- Alignment to a reference genome.
- Differential methylation analysis to identify regions discriminatory between sample groups (e.g., cancer vs. control, 2D vs. 3D).
- Validation of findings with targeted methods like pyrosequencing.
Signaling Pathways and Molecular Mechanisms
The microenvironment in 3D cultures activates specific signaling pathways that drive a more in vivo-like epigenetic state. Key pathways include hypoxia signaling, metabolic reprogramming, and organogenesis-related signaling.
As illustrated, the 3D microenvironment initiates a cascade of molecular events:
- Hypoxia Response: The inner core of 3D spheroids experiences reduced oxygen, leading to HIF1α stabilization [118] [119]. This mimics the hypoxic nature of solid tumors and influences the activity of epigenetic modifiers, including DNA methyltransferases (DNMTs) and TET enzymes responsible for DNA demethylation [116] [118].
- Activation of Developmental Pathways: 3D culture specifically upregulates TGF-β-SMAD signaling, a pathway critical for organogenesis and tumorigenesis [118] [119]. This signaling directly and indirectly (e.g., through microRNA) reshapes the epigenetic landscape.
- Metabolic Reprogramming: Cells in 3D cultures downregulate oxidative phosphorylation (OXPHOS) and undergo other metabolic shifts [118]. These changes affect metabolites like α-ketoglutarate, a essential cofactor for TET enzymes, thereby directly linking metabolism to DNA methylation status.
The Scientist's Toolkit: Essential Research Reagents
Success in 3D culture and epigenetic analysis relies on specialized reagents and tools. The following table details key solutions used in the featured experiments.
Table 3: Research Reagent Solutions for 3D Epigenetic Studies
| Reagent / Solution | Function in Research | Example Application in Cited Studies |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Prevents cell adhesion, forcing self-aggregation into spheroids. | Used for 3D spheroid formation of colorectal cancer cell lines (e.g., Caco-2, HCT-116) [61]. |
| Matrigel / Hydrogels | Provides a scaffold mimicking the extracellular matrix (ECM). | Used in "cultures in gel-like substances" to enable 3D interactions and tissue-like structure formation [1]. |
| Reduced Representation Bisulfite Sequencing (RRBS) Kits | Enables genome-scale DNA methylation analysis from low-input DNA. | Used to generate methylomes from patient cfDNA, FFPE tissues, and cell lines [120] [61]. |
| Nunclon Sphera U-bottom Plates | A specific brand of ULA plate designed for consistent spheroid formation. | The specified platform for 3D culture in the colorectal cancer comparison study [61]. |
| Fetal Bovine Serum (FBS) | Standard supplement for cell culture media, providing growth factors. | Note: Serum can be a source of epigenetic divergence; serum-free conditions are often preferred for higher fidelity [117]. |
The collective experimental data strongly demonstrates that 3D cell culture systems surpass traditional 2D monolayers in preserving the epigenetic fidelity of source tissues. The evidence shows that 3D models maintain DNA methylation patterns and microRNA expression profiles that are nearly identical to those found in patient-derived FFPE samples, whereas 2D cultures exhibit significant and widespread epigenetic alterations [61] [117].
For researchers in drug development and cancer biology, transitioning to 3D models is no longer just an option but a necessity for generating pre-clinical data with greater predictive power. The use of 3D cultures that more accurately mimic the tumor microenvironment, including its gradients, cell-cell interactions, and metabolic heterogeneity, will reduce the high attrition rates in drug discovery pipelines and provide deeper insights into the epigenetic mechanisms driving human disease.
Three-dimensional (3D) cell culture systems are increasingly demonstrating their value in de-risking the drug development process by providing more physiologically relevant human tissue models. When evaluated against the traditional two-dimensional (2D) monolayer culture, 3D models show a higher predictive power for clinical outcomes, despite higher initial costs. This cost-benefit analysis positions 3D cell culture not as an expense, but as a strategic investment to mitigate the enormous financial losses from late-stage clinical trial failures, which can cost hundreds of millions of dollars per failed drug and are often attributable to a lack of clinical efficacy or unacceptable toxicity that was not predicted by 2D models or animal studies [121] [122].
The pharmaceutical industry faces a critical challenge: the exorbitant cost and high failure rate of bringing new therapeutics to market. A single drug requires an investment of US$1-2 billion and an average of 10-15 years of research and development, yet only one in every 5,000-10,000 candidates ultimately receives FDA approval [121]. A significant cause of attrition is the poor predictive value of existing preclinical models, including 2D cell cultures and animal studies, for human Absorption, Distribution, Metabolism, Excretion, and Toxicological (ADME-Tox) profiles [121]. Approximately 90% of compounds fail during clinical development, with many failing in the most expensive Phase III trials due to a lack of efficacy or unforeseen toxicity [122]. This analysis directly compares 2D and 3D cell culture systems, quantifying their respective costs and benefits within the critical context of improving predictive accuracy and reducing catastrophic late-stage trial failures.
Comparative Analysis: 2D vs. 3D Cell Culture Systems
Fundamental Differences and Physiological Relevance
Cells in the human body exist in a complex three-dimensional microenvironment, surrounded by other cells and an extracellular matrix (ECM). This architecture is crucial for proper cell function, signaling, and response to stimuli.
- 2D Cell Culture: This traditional method involves growing cells as a monolayer on flat, rigid plastic surfaces. This environment forces cells to adapt an unnatural, flattened morphology and disrupts native cell-cell and cell-ECM interactions [64] [122]. Consequently, cellular processes such as gene expression, proliferation, differentiation, and drug response are significantly altered [122].
- 3D Cell Culture: These systems permit cells to grow and interact in all three dimensions, more accurately mimicking the in vivo tissue architecture. This can be achieved using scaffold-based techniques (e.g., hydrogels, polymeric supports) or scaffold-free techniques (e.g., spheroids, organoids) [123] [5]. The 3D environment restores physiologically relevant cell polarization, complex cell signaling, and the formation of nutrient and oxygen gradients, leading to more in vivo-like cellular behavior and drug responses [64] [123].
The table below summarizes the core characteristics that differentiate these two systems.
Table 1: Key Characteristics of 2D vs. 3D Cell Culture Models
| Characteristic | 2D Cell Culture | 3D Cell Culture | Key References |
|---|---|---|---|
| Growth Environment | Flat, rigid plastic surfaces | 3D scaffold (e.g., hydrogel) or scaffold-free aggregate | [64] [122] |
| Cell Morphology | Flat, stretched | Natural, histotypic 3D structure | [64] [122] |
| Cell-Cell & Cell-ECM Interactions | Limited, primarily 2D | Complex, physiologically relevant 3D interactions | [64] [123] |
| Nutrient/Gradient Exposure | Homogeneous | Heterogeneous (mimicking in vivo tissue) | [64] |
| Proliferation Rate | Often higher, unregulated | More controlled, similar to in vivo rates | [122] |
| Gene & Protein Expression | Altered due to unnatural environment | More closely mirrors expression in human tissues | [123] |
| Drug Sensitivity/Predictivity | Often hypersensitive, less predictive | More resistant and predictive of in vivo response | [64] [70] |
| Tissue Differentiation | Moderate to poor | Well-differentiated | [64] |
| Cellular Heterogeneity | Primarily proliferating cells | Mixed populations (proliferating, quiescent, necrotic) | [122] |
Quantitative Data and Experimental Evidence
The superior physiological relevance of 3D cultures translates into tangible, quantifiable differences in experimental outcomes, particularly in drug discovery.
Table 2: Comparative Experimental Data from 2D and 3D Models
| Experimental Endpoint | 2D Model Performance | 3D Model Performance | Implications for Drug Discovery | |
|---|---|---|---|---|
| Predictive Accuracy for In Vivo Efficacy | Low; many compounds active in 2D fail in clinics | Higher; better recapitulation of drug resistance and tumor microenvironment | Reduces false positives, failing ineffective compounds earlier | [122] [70] |
| Drug Penetration & Resistance | All cells equally exposed; does not model penetration | Models physical and metabolic barriers to drug penetration | Identifies compounds with poor tissue penetration early | [122] |
| Toxicology (e.g., Hepatotoxicity) | May overlook toxicity due to altered metabolism | Improved prediction of human-relevant toxicology (e.g., liver toxicity) | Reduces false negatives, flagging toxic compounds earlier | [121] [70] |
| Metabolic Function (e.g., CYP450 in hepatocytes) | Declines rapidly within days in culture | Retained for significantly longer (weeks) | Provides more reliable data for drug metabolism studies | [15] |
| Tumor Modeling | Homogenous, proliferating cells | Heterogeneous cell populations, including hypoxic and necrotic cores | Better model for screening oncology drugs | [122] |
Supporting Experimental Data:
- A study comparing breast cancer cell lines (JIMT1) found that proliferation rates in 3D culture were highly dependent on the scaffold material, growing 1.86-fold faster in Matrigel but 7.2-fold slower on synthetic polyHEMA compared to 2D, highlighting how the 3D microenvironment directly influences cellular behavior [122].
- Research has consistently shown that cells in 3D cultures, such as various endometrial and colorectal cancer cell lines, exhibit significantly reduced proliferation rates compared to their 2D counterparts, which is more representative of in vivo tumor growth [122].
- In high-content screening, drugs tested in 3D models frequently show reduced efficacy compared to 2D, a phenomenon that aligns with clinical observations of drug resistance, thereby providing a more realistic and valuable screening platform [70].
Cost-Benefit Analysis Framed Against Clinical Trial Attrition
The Cost of Failure: A Compelling Case for Change
The primary financial burden in drug development is the cost of failure, particularly in late-stage clinical trials. With only about 10% of compounds successfully progressing through clinical development, the industry spends hundreds of millions annually on failed drug development [121] [122]. A significant portion of these failures is attributed to data from 2D monolayer cultures and animal models that did not accurately predict human response [122]. Investing in more predictive models earlier in the pipeline, while seemingly costly upfront, is a powerful strategy to reduce this astronomical attrition rate.
Direct and Indirect Cost Comparison
Table 3: Comprehensive Cost-Benefit Analysis of 2D vs. 3D Cell Culture
| Cost & Benefit Factor | 2D Cell Culture | 3D Cell Culture | Analysis & Net Impact |
|---|---|---|---|
| Direct Costs | |||
| Setup & Materials | Low cost; well-established, inexpensive plastics | Higher cost; specialized matrices (e.g., Matrigel), microplates, scaffolds | Higher direct cost for 3D. |
| Labor & Expertise | Low to moderate; standard, widely taught protocols | Higher; requires specialized technical expertise and training | Higher operational cost for 3D. |
| Assay & Screening | Low cost per well; easy analysis | Higher cost per well; may require advanced imaging/AI analysis | Higher screening cost for 3D. |
| Indirect & Strategic Benefits | |||
| Predictive Power for Efficacy | Low; high false positive rate | High; more clinically relevant responses | Major strategic benefit for 3D. Reduces Phase II/III efficacy failures. |
| Predictive Power for Toxicity | Low; altered metabolism can mask toxicity | Higher; retains metabolic function, better toxicology models | Major strategic benefit for 3D. Reduces Phase III safety failures. |
| Throughput & Speed | High; ideal for initial high-throughput screening (HTS) | Lower throughput; better for secondary screening of lead candidates | Benefit for 2D in early HTS; 3D adds value downstream. |
| Reduction of Animal Studies | Limited | Significant potential; more human-relevant data | Strategic and ethical benefit for 3D. |
| Long-Term Financial Impact | High Risk: Lower upfront cost is offset by high risk of late-stage clinical failure. | High Investment, High Return: Higher upfront cost is an investment to de-risk late-stage failures, saving hundreds of millions per failed drug. | The high cost of 3D culture is justified as an insurance policy against catastrophic trial failure. |
Practical Implementation: Protocols and Tools for the Lab
Experimental Workflow: From 2D Screening to 3D Validation
A common and effective strategy is to use 2D and 3D models in tandem, leveraging the strengths of each at different stages of the drug discovery pipeline. The following diagram illustrates a proposed integrated workflow.
Detailed Protocol: Establishing a 3D Spheroid Drug Sensitivity Assay
Aim: To evaluate the efficacy of a lead compound on a cancer cell line using a 3D spheroid model and compare it to traditional 2D monolayer response.
Materials (The Scientist's Toolkit): Table 4: Essential Research Reagents and Materials for 3D Spheroid Culture
| Item | Function/Benefit | Example Products/Types | |
|---|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Prevents cell adhesion, forcing cells to aggregate and form spheroids. Essential for scaffold-free methods. | Corning Spheroid Microplates, Nunclon Sphera | [123] [5] |
| Hydrogel/ECM Matrix | Provides a biologically active 3D scaffold that mimics the native extracellular matrix for cell growth and signaling. | BD Matrigel, Cultrex BME, Collagen I, synthetic PEG hydrogels | [64] [122] [5] |
| Hanging Drop Plate | Uses gravity to enable cell aggregation into highly uniform spheroids in a droplet of media. | GravityPLUS Hanging Drop Plates | [5] |
| Specialized Culture Media | Formulated to support the metabolic needs of dense 3D structures and may include factors to promote differentiation. | Organoid growth media, custom formulations | [70] |
| High-Content Imaging System | Confocal or spinning disk systems capable of optical sectioning to visualize the interior of 3D structures. | ImageXpress Confocal HT.ai, Lionheart FX | [70] |
| Automated Liquid Handler | Ensures precision and reproducibility when dispensing viscous matrices and setting up assays in microplates. | Platforms from Tecan, Hamilton, Beckman Coulter | [70] |
Methodology:
- Spheroid Generation:
- Scaffold-free (ULA method): Harvest and count cells. Seed a pre-optimized cell density (e.g., 1,000-5,000 cells/well) in a 96-well U-bottom ULA plate in 100-200 µL of complete media. Centrifuge the plate at low speed (e.g., 500 x g for 5 minutes) to aggregate cells at the well bottom. Incubate for 72-96 hours to allow for compact spheroid formation [123].
- Scaffold-based (Embedded method): Mix cells with a chilled hydrogel, such as Matrigel, at a recommended ratio (e.g., 1:1). Pipette the cell-matrix mixture into a pre-warmed culture plate and allow it to polymerize at 37°C for 30 minutes. Overlay with complete media [122].
Drug Treatment:
- Once spheroids are formed (typically after 3 days), add serially diluted compounds to the wells. Include vehicle controls (e.g., DMSO). Ensure gentle pipetting to avoid disrupting the spheroids.
Incubation and Endpoint Analysis:
- Incubate for a predetermined period (e.g., 72-144 hours). Monitor spheroid health and morphology daily using a brightfield microscope.
- Viability Assay: At the endpoint, perform a cell viability assay (e.g., CellTiter-Glo 3D). Note that standard ATP-based assays may require longer incubation times and shaking for adequate reagent penetration in 3D models.
- High-Content Imaging & Analysis: Fix and stain spheroids with dyes for live/dead cells (e.g., Calcein AM/Propidium Iodide) and a nuclear stain (e.g., Hoechst). Acquire z-stack images using a confocal high-content imager. Use advanced software (e.g., IN Carta) with AI to quantify spheroid volume, viability, and morphology changes [70].
Signaling Pathway Alterations in 3D Microenvironments
The 3D architecture fundamentally alters how cells perceive their environment, leading to changes in critical signaling pathways that govern growth, survival, and drug response. These differences explain why drug efficacy often differs between 2D and 3D models.
The transition from 2D to 3D cell culture is not merely a technical upgrade but a necessary strategic evolution in biomedical research and drug discovery. While 2D systems remain valuable for high-throughput primary screening and certain mechanistic studies due to their simplicity and low cost, their limitations in predicting human clinical outcomes are profound and financially crippling at later stages.
The higher initial costs of 3D culture systems are a justifiable investment when weighed against the potential savings from avoiding a single late-stage clinical trial failure. The enhanced predictive power of 3D models for both drug efficacy and toxicity provides a more reliable and human-relevant dataset for making critical go/no-go decisions earlier in the development pipeline. As technologies such as organ-on-a-chip systems, automated bioreactors, and AI-driven image analysis continue to mature, the scalability, reproducibility, and integration of 3D models will only improve, further solidifying their role as an indispensable tool for reducing attrition and bringing safer, more effective medicines to patients faster [70] [5].
Conclusion
The comparative analysis unequivocally demonstrates that 3D cell culture systems offer a paradigm shift in preclinical research, providing a more physiologically relevant context that 2D monolayers cannot replicate. Key takeaways confirm that 3D models excel in mimicking the tumor microenvironment, tissue-specific architecture, and heterogeneous drug responses, leading to more predictive data for human outcomes. Future directions point toward the integration of hybrid 2D/3D workflows for efficiency, the widespread adoption of patient-derived organoids for personalized oncology, and the increasing incorporation of AI and machine learning for complex data analysis. As regulatory bodies like the FDA increasingly consider 3D data, these advanced models are poised to significantly reduce attrition rates in drug development, lower reliance on animal models, and accelerate the delivery of effective therapies to patients.
References
- 1. and 2 cell D – a 3 of different types of cancer... D cultures comparison [https://pmc.ncbi.nlm.nih.gov/articles/PMC6040128/]
- 2. and 2 Cell D 3 D Culture Comparison [https://www.news-medical.net/life-sciences/2D-and-3D-Cell-Culture-Comparison.aspx]
- 3. cell 3 : Models and applications | Abcam D culture [https://www.abcam.com/en-us/knowledge-center/cell-culture/3d-cell-culture]
- 4. 3D vs 2D Cell Culture: Key Insights and Advantages [https://www.mimetas.com/en/blogs/345/3d-cell-culture-vs--traditional-2d-cell-culture-explained.html]
- 5. Frontiers | Is It Time to Start Transitioning From 2D to 3D Cell Culture? [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2020.00033/full]
- 6. Cell 3 Tools and Techniques D Culture [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/3d-cell-culture/3d-cell-culture-technology]
- 7. The relevance of using 3 cell D , in addition to cultures ... 2 D monolayer [https://pmc.ncbi.nlm.nih.gov/articles/PMC5216757/]
- 8. Cell 3 : Which Model Suits Your Lab in D ? vs 2 D Culture 2025 [https://www.pharmanow.live/knowledge-hub/research/3d-vs-2d-cell-culture-comparison]
- 9. Bioink Selection for 3D Bioprinting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/3d-cell-culture/3d-bioprinting-bioinks]
- 10. – Cell and cell –matrix cell - PMC interactions [https://pmc.ncbi.nlm.nih.gov/articles/PMC3302741/]
- 11. - Cell Adhesion and Cell - Cell Flashcards | Quizlet ECM interactions [https://quizlet.com/416106993/cell-cell-adhesion-and-cell-ecm-interactions-flash-cards/]
- 12. Three-Dimensional Cell Culture: A Breakthrough in Vivo [https://www.mdpi.com/1422-0067/16/3/5517]
- 13. Perspective of 3D culture in medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC11693738/]
- 14. Role of three-dimensional cell culture in therapeutics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10042111/]
- 15. 2D vs 3D Cell Culture: Choosing the Right Model [https://www.tempobioscience.com/2d-vs-3d-cell-culture-choosing-the-right-model-by-tempo-bioscience/]
- 16. 5 steps to creating 3D cell culture models [https://www.thermofisher.com/us/en/home/life-science/cell-culture/organoids-spheroids-3d-cell-culture/5-steps-creating-3d-cell-models.html]
- 17. 3d Cell Culture Market Trends, Share and Forecast, 2025- ... [https://www.coherentmarketinsights.com/market-insight/3d-cell-culture-market-534]
- 18. Comparison of two-dimensional and three- ... [https://www.sciencedirect.com/science/article/pii/S2405580824002024]
- 19. Three-Dimensional Spheroids as In Vitro Preclinical Models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7762220/]
- 20. Gradient-induced instability in tumour spheroids unveils ... [https://www.nature.com/articles/s41598-024-69570-6]
- 21. Influence of experimental variables on spheroid attributes [https://www.nature.com/articles/s41598-025-92037-1]
- 22. Integrating simulation and experimental validation of ... [https://www.sciencedirect.com/science/article/pii/S0928098725003677]
- 23. 3D Cell Culture Methods and Applications [https://elveflow.com/microfluidic-reviews/3d-cell-culture-methods-and-applications-a-short-review/]
- 24. Comparison of 3D culture systems on mesenchymal stem cell ... [https://pubmed.ncbi.nlm.nih.gov/41077855/]
- 25. Three-Dimensional In Vitro Tumor Models for Cancer Research and Drug Evaluation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4171250/]
- 26. and 2 cell D - a 3 of different types of cancer... D cultures comparison [https://pubmed.ncbi.nlm.nih.gov/30002710/]
- 27. How do cells cultured in 2 and D differ? - Eppendorf Taiwan 3 D [https://www.eppendorf.com/tw-en/lab-academy/life-science/cell-biology/how-do-cells-cultured-in-2d-and-3d-differ-a-dimension-shift/%20]
- 28. Construction of 3D tumor in vitro models with an immune microenvironment exhibiting similar tumor properties and biomimetic physiological functionality - Biomaterials Science (RSC Publishing) [https://pubs.rsc.org/en/content/articlelanding/2025/bm/d4bm00754a]
- 29. Frontiers | Advancements and challenges in culturing patient-derived cancer cells for personalized therapeutics [https://www.frontiersin.org/journals/lab-on-a-chip-technologies/articles/10.3389/frlct.2025.1663420/full]
- 30. Elucidating the dynamic tumor microenvironment through deep... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03931-7]
- 31. Tumour evolution and microenvironment interactions in 2 and... D [https://pmc.ncbi.nlm.nih.gov/articles/PMC11525187/]
- 32. - Scaffold cell based models in cancer 3 | Journal of... D culture research [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-024-00994-y]
- 33. Cell 3 Tools and D Culture Techniques [https://www.sigmaaldrich.com/NI/es/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/3d-cell-culture/3d-cell-culture-technology]
- 34. alternatives to Synthetic - PMC Matrigel [https://pmc.ncbi.nlm.nih.gov/articles/PMC7500703/]
- 35. alternatives to Synthetic | Nature Reviews Materials Matrigel [https://www.nature.com/articles/s41578-020-0199-8?error=cookies_not_supported&code=73570dc5-e034-4ee8-b1ff-8b314e629045]
- 36. Frontiers | Organoid scaffold materials: research and application [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1637456/full]
- 37. MOFs—Combining Fully Synthetic Injectable Hydrogel Scaffolds Exhibiting Higher Skeletal Muscle Regenerative Efficiency than Matrigel [https://www.mdpi.com/2310-2861/11/7/514]
- 38. Hydrogel scaffolds for tissue engineering: Progress and challenges - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3963751/]
- 39. Effects of hydrogel stiffness and viscoelasticity on organoid culture... [https://molmed.biomedcentral.com/articles/10.1186/s10020-025-01131-7]
- 40. The independent roles of mechanical, structural and adhesion characteristics of 3D hydrogels on the regulation of cancer invasion and dissemination - PubMed [https://pubmed.ncbi.nlm.nih.gov/24044993/]
- 41. Three-Dimensional Cell Culture Methods | Encyclopedia MDPI [https://encyclopedia.pub/entry/40202]
- 42. How do cells cultured in 2 and D differ? A dimension shift... 3 D [https://www.eppendorf.com/rs-en/lab-academy/life-science/cell-biology/how-do-cells-cultured-in-2d-and-3d-differ-a-dimension-shift/]
- 43. Frontiers | Comparative Analysis of 3D Bladder Tumor Spheroids... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2017.00605/full]
- 44. Principles of Hanging Drop Method (Spheroid Formation) in Cell Culture - PubMed [https://pubmed.ncbi.nlm.nih.gov/38411887/]
- 45. Frontiers | SpheroMold: modernizing the hanging drop method for spheroid culture [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2024.1397153/full]
- 46. The choice of ultra-low attachment plates impacts primary human and primary canine hepatocyte spheroid formation, phenotypes, and function - PubMed [https://pubmed.ncbi.nlm.nih.gov/38403411/]
- 47. VitroPrime™ Ultra-Low Attachment Plates | 3D Spheroid [https://www.thewellbio.com/product/vitroprime-ultra-low-attachment-u-bottom/]
- 48. Hanging Drop, A Best Three-Dimensional (3D) Culture Method for Primary Buffalo and Sheep Hepatocytes | Scientific Reports [https://www.nature.com/articles/s41598-017-01355-6]
- 49. 3D-bioprinted all-inclusive bioanalytical platforms for cell studies | Scientific Reports [https://www.nature.com/articles/s41598-020-71452-6]
- 50. (PDF) Comparative of 3Dimensional ( Efficacy ) Cell 3 ... D Culture [https://www.academia.edu/144456380/Comparative_Efficacy_of_3Dimensional_3D_Cell_Culture_Organoids_Vs_2Dimensional_2D_Cell_Cultures_Vs_Experimental_Animal_Models_In_Disease_modeling_Drug_development_And_Drug_Toxicity_Testing]
- 51. 3D Printing Techniques and Their Applications to Organ-on-a-Chip Platforms: A Systematic Review [https://www.mdpi.com/1424-8220/21/9/3304]
- 52. 3D bioprinting for high-throughput screening: Drug screening, disease modeling, and precision medicine applications - PubMed [https://pubmed.ncbi.nlm.nih.gov/33738018/]
- 53. 3D Bioprinting: An attractive alternative to traditional organ transplantation [https://www.engineegroup.us/articles/ABSE-5-112.php]
- 54. Frontiers | 3 at the Frontier of Regenerative Medicine... D Bioprinting [https://www.frontiersin.org/journals/medical-technology/articles/10.3389/fmedt.2020.607648/full]
- 55. One-step fabrication of an organ - on - a - chip with spatial heterogeneity... [https://pubmed.ncbi.nlm.nih.gov/27302471/]
- 56. Scientists grow human neocortex using cheap 3 printed D bioreactor [https://3dprintingindustry.com/news/scientists-grow-human-neocortex-using-cheap-3d-printed-bioreactor-188207/]
- 57. Frontiers | Recent Advances in Additive Manufacturing and 3D Bioprinting for Organs-On-A-Chip and Microphysiological Systems [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.837087/full]
- 58. AI-assisted high - content imaging and toxicity using liver... screening [https://www.selectscience.net/video/ai-assisted-high-content-imaging-and-toxicity-screening-using-liver-organoids]
- 59. Frontiers | High-Content Monitoring of Drug Effects in a 3D Spheroid Model [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2017.00293/full]
- 60. Is It Time to Start Transitioning From 2D to 3D Cell Culture? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7067892/]
- 61. Comparative analysis between 2D and 3D colorectal cancer culture models for insights into cellular morphological and transcriptomic variations | Scientific Reports [https://www.nature.com/articles/s41598-023-45144-w]
- 62. - High using iPSC-derived Hepatocyte... Content 3 D Toxicity Screening [https://www.moleculardevices.com/en/assets/app-note/dd/img/high-content-3d-toxicity-assay-using-ipsc-derived-hepatocyte-spheroids]
- 63. Review of High-content Screening Applications in Toxicology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7011178/]
- 64. 3D Cell Culture Systems: Tumor Application, Advantages, and Disadvantages - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8618305/]
- 65. Insights on the differences between two‑ and three‑dimensional culture ... [https://www.spandidos-publications.com/10.3892/ijmm.2025.5626?text=fulltext]
- 66. Frontiers | Advances in precision oncology using patient-derived organoids and functional biomaterials [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1670328/full]
- 67. Patient-Derived Organoid Biobanks for Translational Research and Precision Medicine: Challenges and Future Perspectives [https://www.mdpi.com/2075-4426/15/8/394]
- 68. Frontiers | Transforming cancer treatment: integrating patient - derived ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1563198/full]
- 69. - Patient tumor derived for cancer immunotherapy: organoids ... culture [https://link.springer.com/article/10.1007/s10637-025-01523-w]
- 70. vs 3 Cell Lines in Drug Discovery & Disease Modeling D Organoids 2 D [https://www.moleculardevices.com/lab-notes/3d-biology/3d-organoids-vs-2d-cell-lines-drug-discovery]
- 71. 2D vs 3D Cell Culture: Advantages, Limitations, and Lab Setup – AstorScientific [https://www.astorscientific.us/blogs/news/2d-vs-3d-cell-culture]
- 72. 3D Cell Culture Systems: Tumor Application, Advantages, and Disadvantages | MDPI [https://www.mdpi.com/1422-0067/22/22/12200]
- 73. vs 2 Cell D | FluoroFinder 3 D Cultures [https://fluorofinder.com/2d-vs-3d-cell-cultures/]
- 74. Versus 3D Cell 2 : D and Disadvantages Cultures Advantages [https://www.mimetas.com/en/blogs/315/2d-versus-3d-cell-cultures-advantages-and-disadvantages.html]
- 75. 3D vs. 2D Culture Systems: A Comprehensive Comparison ... [https://www.creative-biolabs.com/3d-biology/3d-vs-2d-culture-systems.htm]
- 76. Three-Dimensional Culture System: A New Frontier in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292892/]
- 77. USA 3D Cell Culture Market Size and Forecasts 2031 [https://mobilityforesights.com/product/usa-3d-cell-culture-market]
- 78. 2D versus 3D tumor-on-chip models to study the impact of ... [https://www.nature.com/articles/s41598-025-03504-8]
- 79. 3D Cell Culture Market Report and Forecast 2025-2034 [https://www.researchandmarkets.com/reports/6100920/3d-cell-culture-market-report-forecast?srsltid=AfmBOooqwI_TKP9afvOJkJG3alqCFzfka1ZDQhAy-j6y7sTWiUbFWd9O]
- 80. 3D Cell Culture Summit Roadshow 2025 [https://www.corning.com/worldwide/en/products/life-sciences/news-events/events/2025/09/3d-summit-2025.html]
- 81. Top 30 Global 3D Cell Culture Market Analysis and ... [https://www.sphericalinsights.com/blogs/top-30-companies-in-global-3d-cell-culture-market-2025-2035-competitive-analysis-and-forecast]
- 82. Semiconductor Failure Analysis: Comparing ZEISS 3 X-Ray and... D [https://www.zeiss.co.uk/microscopy/l/campaigns/2025/3d-x-ray-microscopy-vs-2d-microscopy.html]
- 83. as a Type of Three-Dimensional Cell Spheroids —Examples... Cultures [https://pmc.ncbi.nlm.nih.gov/articles/PMC7503223/]
- 84. 2D & 3D cell cultures | PPT [https://www.slideshare.net/slideshow/2d-3d-cell-cultures/238781436]
- 85. Modeling Physiological Events in 2D vs. 3D Cell Culture - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5545611/]
- 86. A Comparison of 2D vs 3D Cell Culture | Emulate Blog [https://emulatebio.com/2d-vs-3d-cell-culture-models/]
- 87. The Spheroid Light Microscopy Image Atlas for morphometrical analysis of three-dimensional cell cultures | Scientific Data [https://www.nature.com/articles/s41597-025-04441-x]
- 88. What 32,000 3D Spheroids Revealed About Culture Conditions - Promega Connections [https://www.promegaconnections.com/what-32000-3d-spheroids-revealed-about-culture-conditions/]
- 89. Microarray Embedding/Sectioning for Parallel Analysis of 3 Cell... D [https://www.nature.com/articles/s41598-019-52007-w?error=cookies_not_supported]
- 90. -tips: user-friendly mesh barrier pipette tips for 3 - D 3 D spheroid culture [https://jbioleng.biomedcentral.com/articles/10.1186/s13036-019-0210-3]
- 91. 2D vs 3D cell culture: What’s best for scalable biopharmaceutical production? - Green Elephant Biotech [https://greenelephantbiotech.com/blog/2d-vs-3d-cell-culture-what-s-best-for-scalable-biopharmaceutical-production/]
- 92. Cell Culture and Scale-up of Human Pluripotent Stem Cells [https://www.thewellbio.com/applications/in-vitro/stem-cells/]
- 93. Cell 3 Market: Comprehensive Analysis... - PharmiWeb.com d Culture [https://www.pharmiweb.com/press-release/2025-02-12/3d-cell-culture-market-comprehensive-analysis-and-forecast-2025-2035]
- 94. Cell 3 in the Real World: 5 Uses You'll Actually See... D Culture System [https://www.linkedin.com/pulse/3d-cell-culture-system-real-world-5-uses-youll-actually-4pvxf]
- 95. A comparative analysis of 2D and 3D experimental data for the identification of the parameters of computational models | Scientific Reports [https://www.nature.com/articles/s41598-023-42486-3]
- 96. How do cells cultured in 2 and D differ? - Eppendorf Lithuania 3 D [https://www.eppendorf.com/lt-en/lab-academy/life-science/cell-biology/how-do-cells-cultured-in-2d-and-3d-differ-a-dimension-shift/%20]
- 97. The effect of 2 and 3D cell D on treatment response, EMT... cultures [https://cancerci.biomedcentral.com/articles/10.1186/s12935-019-0733-1]
- 98. Bioengineered scaffolds for 3D culture demonstrate extracellular matrix-mediated mechanisms of chemotherapy resistance in glioblastoma - PubMed [https://pubmed.ncbi.nlm.nih.gov/31028838/]
- 99. In vitro Development of Chemotherapy and Targeted Therapy Drug-Resistant Cancer Cell Lines: A Practical Guide with Case Studies - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3944788/]
- 100. Emerging Therapeutic Strategies to Overcome Drug Resistance in Cancer Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11240358/]
- 101. Understanding and overcoming multidrug resistance in cancer | Nature Reviews Clinical Oncology [https://www.nature.com/articles/s41571-025-01059-1]
- 102. https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1643230/xml [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1643230/xml]
- 103. Frontiers | In vitro 3D modeling of colorectal cancer: the pivotal role of the extracellular matrix, stroma and immune modulation [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1545017/full]
- 104. analysis between Comparative and 2 ... D 3 D colorectal cancer culture [https://pmc.ncbi.nlm.nih.gov/articles/PMC10603139/]
- 105. Morphological and functional analysis of colorectal cell lines in... cancer [https://www.nature.com/articles/s41598-025-87660-x?error=cookies_not_supported&code=dd589de4-c9c6-4ea1-97a6-d34691ae9ea9]
- 106. Analysis of Sensitivity and Cell Death Pathways Mediated by... [https://scialert.net/fulltext/?doi=ijcr.2018.1.12]
- 107. MiR-198 affects the proliferation and apoptosis of colorectal cancer through regulation of ADAM28/JAK-STAT signaling pathway [https://www.europeanreview.org/article/17106]
- 108. 3D printed in vitro tumor tissue model of colorectal cancer - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7667682/]
- 109. Three-Dimensional In Vitro Cell Cultures as a Feasible and Promising Alternative to Two-Dimensional and Animal Models in Cancer Research [https://www.ijbs.com/v20p5293.htm]
- 110. Recent advances in 3D cell culture models in cancer drug development | Journal of Pharmaceutical Investigation [https://link.springer.com/article/10.1007/s40005-025-00740-y]
- 111. Frontiers | Three-Dimensional in Vitro Cell Culture Models in Drug Discovery and Drug Repositioning [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2018.00006/full]
- 112. 3D cell cultures, as a surrogate for animal models, enhance the diagnostic value of preclinical in vitro investigations by adding information on the tumour microenvironment: a comparative study of new dual-mode HDAC inhibitors | Investigational New Drugs [https://link.springer.com/article/10.1007/s10637-022-01280-0]
- 113. Comparative Assay of 2 and D Cell 3 Models: Proliferation... D Culture [https://pubmed.ncbi.nlm.nih.gov/29623827/]
- 114. Three-Dimensional In Vitro Cell Culture Models for Efficient Drug Discovery: Progress So Far and Future Prospects - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9412659/]
- 115. Two-Dimensional ( 2 ) and Three-Dimensional ( D ) Cell... | IntechOpen 3 D [https://www.intechopen.com/chapters/64565]
- 116. Reprogramming of the Genome-Wide DNA Methylation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10093594/]
- 117. Evaluating cell culture reliability in pediatric brain tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11026496/]
- 118. The context-dependent epigenetic and organogenesis ... [https://elifesciences.org/reviewed-preprints/101299v2]
- 119. The context-dependent epigenetic and organogenesis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11160912/]
- 120. Clinical cancer epigenetics [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-025-01948-3]
- 121. Role of in vitro two-dimensional ( 2 ) and three-dimensional... D [https://pmc.ncbi.nlm.nih.gov/articles/PMC9909725/]
- 122. -Dimensional Cell Three and Their Applications in... Culture Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC4026212/]
- 123. 3D cell culture - Wikipedia [https://en.wikipedia.org/wiki/3D_cell_culture]