Adult Stem Cells from Somatic Tissues: A 2025 Guide to Bone Marrow and Adipose Sources for Research and Therapy
This article provides a comprehensive analysis of adult stem cells sourced from bone marrow and adipose tissue, tailored for researchers and drug development professionals.
Adult Stem Cells from Somatic Tissues: A 2025 Guide to Bone Marrow and Adipose Sources for Research and Therapy
Abstract
This article provides a comprehensive analysis of adult stem cells sourced from bone marrow and adipose tissue, tailored for researchers and drug development professionals. It covers the foundational biology and niches of these somatic stem cells, detailed methodologies for isolation and characterization, and strategies for troubleshooting and optimizing culture systems. The content also includes a critical validation and comparative analysis of Hematopoietic Stem Cells (HSCs) and Mesenchymal Stem Cells (MSCs) from these sources, reviewing their therapeutic applications in approved treatments and ongoing clinical trials. The scope is designed to serve as a key resource for preclinical and translational research efforts.
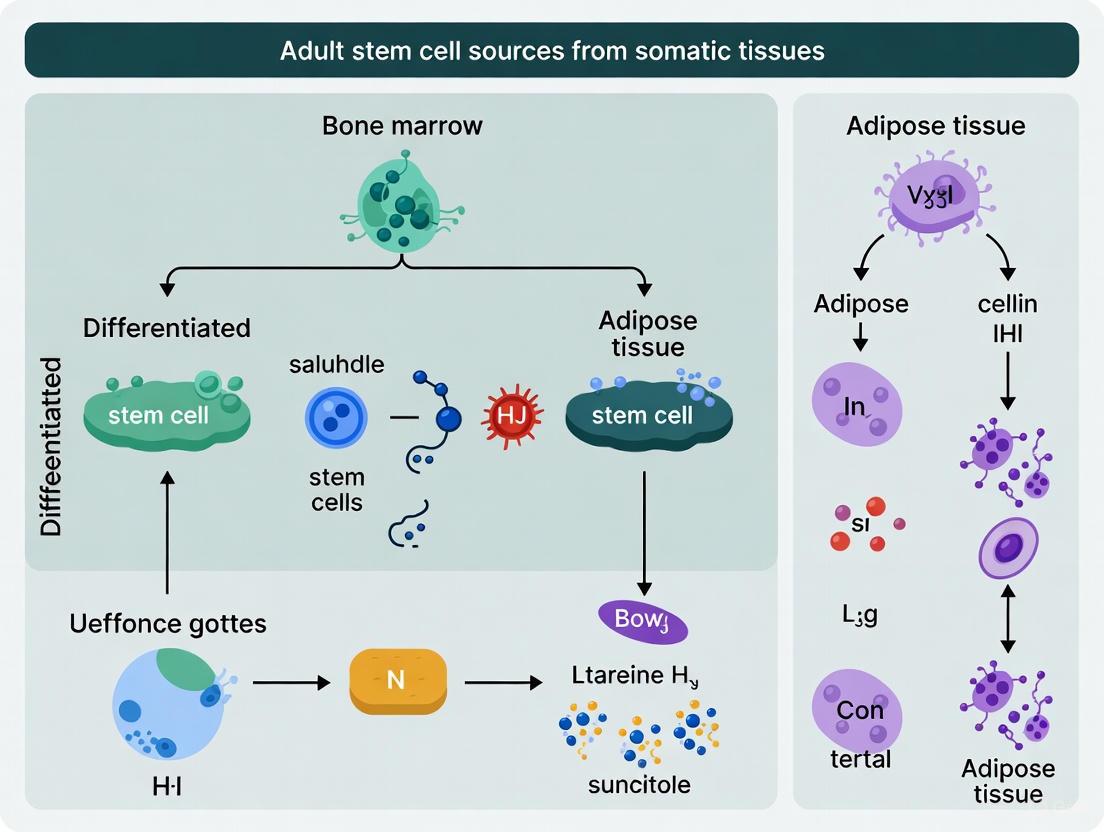
The Biology of Adult Stem Cells: Exploring Bone Marrow and Adipose Niches
Adult stem cells (ASCs), also known as somatic stem cells, are undifferentiated cells found throughout the body after embryonic development. These remarkable cells serve as a fundamental biological resource for tissue maintenance and repair, residing in specific niches within various vascularized organs and tissues [1]. Their primary function involves replacing cells lost through normal physiological turnover, injury, or disease, making them essential for long-term tissue homeostasis [1]. Unlike embryonic stem cells which are pluripotent, adult stem cells are generally considered multipotent, meaning they can differentiate into multiple—but not all—cell types, typically those related to their tissue of origin [2] [3].
The historical understanding of ASCs has evolved significantly, with their initial identification in tissues with high turnover rates like blood and skin. Contemporary research has revealed their presence in virtually all vascularized tissues, including those with limited regenerative capacity such as neural and cardiac tissues [1] [3]. This widespread distribution underscores their critical role in organismal maintenance and positions them as crucial therapeutic targets in regenerative medicine. ASCs maintain their populations through self-renewal while also producing progenitor cells that undergo differentiation to maintain tissue-specific cellular composition [1].
Defining Properties of Adult Stem Cells
Self-Renewal Capability
Self-renewal represents the capacity of adult stem cells to divide and generate identical copies of themselves throughout an organism's lifespan. This property allows ASC populations to maintain their numbers without depletion, ensuring a continuous reservoir for tissue maintenance [1]. The self-renewal process is tightly regulated by both intrinsic genetic programs and extrinsic signals from the specialized microenvironment, or niche, where these cells reside [1] [4].
The mechanism of stem cell division is particularly sophisticated. When ASCs divide, they can produce daughter cells that either become new stem cells (self-renewal) or specialized cells (differentiation) with tissue-specific functions [1]. This balance between self-renewal and differentiation is critical for tissue homeostasis, and its dysregulation can lead to either tissue degeneration or hyperproliferative disorders. While ASC populations are typically maintained throughout adulthood, research indicates that their function and numbers can decrease with advancing age, potentially impacting regenerative capacity [1].
Multipotency and Differentiation Capacity
Multipotency refers to the ability of adult stem cells to differentiate into multiple, but limited, specialized cell types within their lineage [2] [3]. This property distinguishes them from pluripotent embryonic stem cells, which can generate all cell types of the three germ layers. The differentiation potential of ASCs is typically restricted to cell types relevant to their tissue of origin, reflecting their specialized roles in tissue maintenance [3].
The multipotent nature of ASCs enables them to generate transit-amplifying cells—progeny that undergo several rounds of division before terminal differentiation [4]. This mechanism allows a single stem cell to produce numerous differentiated cells, efficiently maintaining or repairing tissues. The process of lineage commitment involves complex molecular regulation, with niche-derived signals playing instructive roles in fate determination [4]. For instance, in the Drosophila ovary model, Wnt and Hedgehog signaling pathways have been shown to coordinate progenitor cell fate decisions, demonstrating how extrinsic cues guide multipotent cells toward specific lineages [4].
Table 1: Core Functional Properties of Adult Stem Cells
| Property | Functional Significance | Biological Mechanism |
|---|---|---|
| Self-Renewal | Maintains stem cell population throughout life | Asymmetric cell division; regulated by niche signals |
| Multipotency | Generates multiple cell types of native tissue | Lineage-restricted differentiation capacity |
| Quiescence | Prevents exhaustion of stem cell pool | Reversible cell cycle arrest; activated by damage signals |
| Niche Interaction | Regulates stem cell behavior and fate | Response to paracrine signaling and cell-cell contact |
Major Types and Locations of Adult Stem Cells
Adult stem cells reside in specific anatomical locations, or niches, within various tissues throughout the body. These specialized microenvironments provide the signals necessary to maintain stem cell properties while regulating their activity according to tissue needs [4]. Different types of ASCs exhibit distinct differentiation potentials tailored to their tissue contexts.
Hematopoietic Stem Cells (HSCs)
Hematopoietic stem cells reside primarily in the bone marrow and are responsible for the continuous regeneration of all blood cell lineages throughout life [1] [2]. These cells represent one of the most thoroughly characterized adult stem cell populations and form the biological basis for bone marrow transplantation therapy. HSCs give rise to the complete repertoire of blood cells, including erythrocytes (red blood cells), leukocytes (white blood cells), and platelets [1] [3]. Their proper function is essential for immune competence, oxygen transport, and clotting mechanisms.
Mesenchymal Stem Cells (MSCs)
Mesenchymal stem cells represent a heterogeneous population of stromal cells that can differentiate into various mesodermal lineages, including osteoblasts (bone cells), chondrocytes (cartilage cells), and adipocytes (fat cells) [1]. According to the International Society for Cellular Therapy (ISCT), defining standards for human MSCs includes plastic adherence in standard culture, specific surface antigen expression (CD105+, CD73+, CD90+, with ≤2% expression of hematopoietic markers CD45, CD34, CD14 or CD11b, CD79a or CD19, and HLA-DR), and in vitro differentiation into osteoblasts, adipocytes, and chondroblasts [1]. MSCs have been isolated from multiple tissues, including bone marrow, adipose tissue, umbilical cord, placenta, and dental pulp [1].
Tissue-Specific Stem Cells
Beyond HSCs and MSCs, numerous specialized adult stem cells exist in specific tissues:
- Neural Stem Cells (NSCs): Located in specific brain areas, including the hippocampus and subventricular zone, NSCs can generate the brain's major cell types: neurons, astrocytes, and oligodendrocytes [1].
- Epithelial Stem Cells: Found in the lining of the digestive tract and the basal layer of the epidermis, these cells continually regenerate these protective barriers throughout life [1].
- Skeletal Muscle Stem Cells (Satellite Cells): Residing in a quiescent state beneath the basal lamina of muscle fibers, these cells activate in response to injury to repair and regenerate skeletal muscle [1].
- Adipose-Derived Stem Cells (ADSCs): Located in fat tissue, ADSCs can differentiate into various cell types, including adipocytes, cartilage cells, and bone cells [1].
Table 2: Major Adult Stem Cell Types and Their Characteristics
| Stem Cell Type | Primary Location | Differentiation Potential | Key Functions |
|---|---|---|---|
| Hematopoietic (HSCs) | Bone marrow, umbilical cord blood | All blood cell lineages | Immune cell production, oxygen transport |
| Mesenchymal (MSCs) | Bone marrow, adipose tissue, dental pulp | Osteoblasts, chondrocytes, adipocytes | Skeletal tissue maintenance, immunomodulation |
| Neural (NSCs) | Hippocampus, subventricular zone | Neurons, astrocytes, oligodendrocytes | Limited neural repair, brain homeostasis |
| Epithelial | Skin basal layer, intestinal crypts | Keratinocytes, intestinal epithelial cells | Skin renewal, gut lining regeneration |
| Muscle Satellite | Skeletal muscle tissue | Myoblasts, muscle fibers | Muscle repair and regeneration |
Research Methodologies and Experimental Approaches
Lineage Commitment Assessment
Advanced imaging and spectroscopic techniques enable researchers to characterize stem cell differentiation with minimal perturbation. Broadband Coherent Anti-Stokes Raman Scattering (BCARS) microscopy has emerged as a powerful label-free method for quantifying lineage commitment in individual stem cells [5]. This approach allows for non-invasive, quantitative characterization of stem cell differentiation without the need for fluorescent labels or cell destruction, preserving cellular integrity for further analysis.
The BCARS methodology involves several key steps. First, stem cells are cultured under differentiation-inducing conditions (e.g., adipogenic or osteogenic media) alongside controls in basal media. After a differentiation period (typically 2 weeks), cells are fixed and analyzed using BCARS microscopy, which provides hyperspectral imaging data with high spatial resolution [5]. The acquired spectra are processed through several computational steps: noise reduction via singular value decomposition, time-domain Kramers-Kronig transform to retrieve Raman susceptibility spectra, and calculation of second derivatives of individual spectra. This process generates chemical maps that reveal phenotypic commitment at single-cell resolution based on intrinsic biochemical composition [5].
Signaling Pathway Analysis
Understanding how niche signals coordinate adult stem cell fate decisions requires precise analysis of signaling pathway activity. Quantitative microscopy approaches using pathway-specific reporters enable researchers to monitor signaling dynamics in progenitor cells [4]. For example, in the Drosophila ovary model, reporters for Wnt, Hedgehog (Hh), and Notch pathways have revealed how multiple niche signals specify progenitor cell fate [4].
Experimental approaches for signaling analysis typically involve:
- Reporter constructs expressing fluorescent proteins under the control of pathway-responsive elements
- Quantitative image analysis of signal intensity and distribution within tissue contexts
- Genetic manipulation through loss-of-function and gain-of-function experiments
- Correlation with differentiation markers to establish causal relationships between signaling activity and cell fate decisions [4]
These methodologies have revealed that Wnt signaling transiently inhibits expression of the main body cell fate determinant Eya in the Drosophila ovary, biasing cells toward polar and stalk fates when hyperactivated. Meanwhile, Hh signaling independently controls the proliferation to differentiation transition, demonstrating how multiple niche signals coordinate to pattern cell fates [4].
Diagram 1: Niche signaling in stem cell fate. Multiple niche-derived signals (Wnt, Hh, Notch) act on stem and progenitor cells to coordinate self-renewal and differentiation decisions during tissue maintenance.
Advanced Research Reagents and Experimental Tools
Essential Research Reagents
Cutting-edge research on adult stem cells requires specialized reagents and tools that enable precise manipulation and analysis. The following table details key research reagent solutions essential for experimental work in this field:
Table 3: Key Research Reagent Solutions for Adult Stem Cell Research
| Reagent/Tool | Function | Application Examples |
|---|---|---|
| BCARS Microscopy | Label-free chemical imaging based on Raman scattering | Quantifying lineage commitment in individual hMSCs [5] |
| Pathway Reporters (e.g., fz3-RFP) | Monitoring signaling pathway activity in live cells | Visualizing Wnt signaling gradients in germarium [4] |
| Defined Culture Media | Maintaining stemness or inducing specific differentiation | Adipogenic, osteogenic, and basal media for hMSC differentiation [5] |
| Surface Marker Antibodies | Identification and isolation of stem cell populations | CD105, CD73, CD90 for MSCs; CD45, CD34 negative selection [1] |
| Genetic Tools (RNAi, CRISPR) | Manipulating gene expression in stem cells | Knockdown of β-catenin to validate Wnt reporter specificity [4] |
Experimental Workflow
A typical experimental workflow for characterizing adult stem cell differentiation involves multiple coordinated steps from cell isolation through quantitative analysis. The following diagram illustrates a generalized approach for studying lineage commitment:
Diagram 2: Stem cell differentiation workflow. Key steps include cell isolation, expansion in culture, differentiation induction, and label-free analysis using BCARS microscopy, with validation through conventional staining methods.
Emerging Concepts and Clinical Relevance
Muse Cells: A Unique ASC Population
Recent research has identified a unique subpopulation of ASCs called Multilineage-differentiating stress-enduring (Muse) cells. These cells are naturally present in various connective tissues, including bone marrow, adipose tissue, dermis, and peripheral blood [6]. Muse cells exhibit several remarkable properties that distinguish them from conventional mesenchymal stromal cells, including stress tolerance, spontaneous differentiation into tri-germ layer lineages, and non-tumorigenicity [6].
Unlike induced pluripotent stem cells (iPSCs) which require artificial reprogramming, Muse cells are naturally pluripotent-like without genetic modification. They demonstrate targeted homing to injured tissues through the S1P-S1PR2 axis, where they contribute to regeneration through direct differentiation and paracrine effects [6]. Clinical trials with Muse cells have shown promise for treating conditions including stroke, myocardial infarction, and osteoarthritis, highlighting their therapeutic potential while maintaining a favorable safety profile [6].
Therapeutic Mechanisms
Adult stem cells exert their therapeutic effects through multiple coordinated mechanisms [2]:
- Differentiation: Replacement of lost or damaged cells in diseased organs
- Paracrine signaling: Promotion of healing through secreted bioactive factors
- Immunomodulation: Control of autoimmune and inflammatory responses
- Homing & Migration: Targeted movement to sites of injury
- Engraftment & Integration: Functional incorporation into host tissues
- Anti-apoptotic & Anti-fibrotic: Reduction of cell death and pathological scarring
These mechanisms collectively enable ASCs to function as "biological drugs" with dynamic responsiveness to local environmental cues. Unlike conventional pharmaceuticals, stem cells can sense signals from injured tissues, adapt to their microenvironment, and execute appropriate regenerative responses [2]. This adaptability positions ASC-based therapies as promising approaches for conditions with complex pathologies, including neurodegenerative disorders, cardiovascular diseases, and autoimmune conditions [2] [3].
Adult stem cells, defined by their capacities for self-renewal and multipotency, represent foundational components of tissue maintenance and repair throughout postnatal life. Residing in specialized niches within diverse somatic tissues, these cells respond to physiological demands and pathological challenges by generating appropriate progeny while maintaining their own populations. Ongoing research continues to elucidate the complex regulatory networks that control ASC behavior, including niche-derived signals, intracellular pathways, and systemic factors.
The characterization of various ASC populations—from well-established hematopoietic and mesenchymal stem cells to newly identified Muse cells—has revealed both shared principles and unique specializations. Advanced research methodologies, including label-free imaging and single-cell analysis, provide increasingly sophisticated tools for probing ASC biology with minimal perturbation. As our understanding of these remarkable cells deepens, so too does their potential for clinical application in regenerative medicine, offering promising avenues for addressing numerous debilitating conditions that currently lack effective treatments.
The bone marrow (BM) represents a quintessential adult stem cell somatic tissue source, harboring two primary populations: Hematopoietic Stem Cells (HSCs) and Mesenchymal Stromal Cells (MSCs). These cells reside within a specialized microenvironment known as the "niche," a dynamic structural and functional unit that regulates stem cell fate decisions including quiescence, self-renewal, differentiation, and mobilization [7] [8]. The HSCs are rare, multipotent cells responsible for the lifelong production of all blood and immune cells, while MSCs are multipotent stromal cells that can differentiate into osteoblasts, adipocytes, and chondrocytes, and provide critical physical and metabolic support for hematopoiesis [8]. This intricate cellular cooperation establishes the bone marrow as a foundational reservoir in somatic stem cell biology with profound implications for regenerative medicine, disease pathogenesis, and therapeutic development.
Characterization of Bone Marrow Resident Stem Cells
Hematopoietic Stem Cells (HSCs)
HSCs exist in a carefully regulated hierarchy within the bone marrow. Long-term HSCs (LT-HSCs) possess durable self-renewal capacity and offer lifelong multilineage reconstitution potential. These give rise to short-term HSCs (ST-HSCs), which exhibit limited self-renewal but robust short-term engraftment capacity. Further down the hierarchy are the multipotent progenitors (MPPs), which lack self-renewal capability but retain multilineage differentiation potential, eventually yielding lineage-restricted progenitors [8]. The functional integrity of HSCs is paramount for successful Hematopoietic Stem Cell Transplantation (HSCT), a curative treatment for genetic blood disorders and hematological malignancies [8].
Table 1: Hematopoietic Stem and Progenitor Cell Populations
| Cell Population | Surface Phenotype | Function | Self-Renewal Capacity |
|---|---|---|---|
| LT-HSC | CD150+ CD48− Lin− Sca−1+ c-Kit+ [9] | Lifelong, multilineage reconstitution | High |
| ST-HSC | Lin− Sca-1+ c-Kit+ (LSK) [9] [8] | Short-term multilineage reconstitution | Limited |
| MPP | Lin− Sca-1+ c-Kit+ (LSK) [8] | Multilineage differentiation | None |
| CMP | Lin− CD127− Sca-1− c-Kit+ CD34+ FcγR− [9] | Myeloid lineage commitment | None |
| CLP | Lin− CD127+ Sca-1+ c-Kit+ [9] | Lymphoid lineage commitment | None |
Mesenchymal Stromal Cells (MSCs)
MSCs are an exceptionally rare cell population, comprising only 0.01% to 0.001% of the total cells in BM [8]. According to the International Society for Cellular Therapy (ISCT), human MSCs must adhere to plastic under standard culture conditions; express surface antigens CD105, CD73, and CD90 (>95%); lack expression of CD45, CD34, CD14/CD11b, CD79α/CD19, and HLA-DR (<2%); and possess tri-lineage differentiation potential (adipogenic, osteogenic, chondrogenic) [10] [8]. Within the BM niche, two distinct MSC populations play complementary roles: Nestin-positive (Nestin⁺) MSCs, located in perivascular regions, are crucial for maintaining HSC quiescence and retention, while leptin receptor-positive (LepR⁺) MSCs constitute a significant portion of the adult BM stroma and support HSC homing, localization, and maintenance [8].
Table 2: Key Surface Markers for Mesenchymal Stromal Cell Characterization
| Surface Marker | Other Name | Expression in AD-MSCs | Function |
|---|---|---|---|
| CD10 | MME | Positive [10] | Membrane metalloendopeptidase |
| CD13 | ANPEP | Positive [10] | Alanyl aminopeptidase |
| CD29 | ITGB1 | Positive [10] | Integrin subunit beta 1 (cell adhesion) |
| CD44 | CD44 | Positive [10] | Cell adhesion and migration |
| CD73 | NT5E | Positive [10] | 5'-nucleotidase ecto |
| CD90 | THY1 | Positive [10] | Thy-1 cell surface antigen |
| CD105 | ENG | Positive [10] | Endoglin |
| CD106 | VCAM1 | Positive [10] | Vascular cell adhesion molecule 1 |
| CD45 | PTPRC | Negative [10] [8] | Hematopoietic lineage marker |
| CD34 | CD34 | Variable (early culture) [10] | Hematopoietic progenitor marker |
The Bone Marrow Microenvironment: A Dynamic Interactive Niche
The bone marrow microenvironment is a complex, multi-cellular structure where various niche components secrete signaling molecules that collectively regulate HSC fate. The vascular niche,
involving sinusoidal endothelial cells (SECs) and arterial endothelial cells (AECs), facilitates HSPC trafficking and maintains quiescence, respectively [8]. The perivascular niche,
anchored by MSCs, is a primary site for HSC maintenance. Key cellular components include:
- Mesenchymal Stromal Cells (MSCs): LepR⁺ MSCs are major producers of CXC-chemokine ligand 12 (CXCL12) and Stem Cell Factor (SCF), both essential for HSC maintenance [8].
- Endothelial Cells: Sinusoidal endothelial cells regulate HSPC trafficking, while arterial endothelial cells maintain HSPC quiescence and reactive oxygen species (ROS) levels [8].
- Osteoblasts: Bone-lining cells at the endosteum anchor HSPCs and secrete regulatory cytokines that enhance hematopoiesis [8].
- Sympathetic Nervous System: Innervates the BM, modulating osteoblast activity and CXCL12 expression to regulate HSPC dynamics, particularly in response to stress [8].
- Megakaryocytes: Platelet-producing cells that release factors like platelet factor 4 (PF4) and TGF-β1 to help maintain HSC quiescence [8].
Figure 1: Cellular Interactions in the Bone Marrow Niche. HSCs receive critical signals from various niche components including MSCs, osteoblasts, endothelial cells, megakaryocytes, and the sympathetic nervous system.
Recent Advances and Experimental Approaches
Reversal of HSC Aging through Lysosomal Targeting
A groundbreaking 2025 study revealed that aging in blood-forming stem cells is not irreversible. Researchers discovered that lysosomes in aged HSCs become hyper-acidic, depleted, damaged, and abnormally activated, disrupting metabolic and epigenetic stability. By suppressing this hyperactivation with a specific vacuolar ATPase inhibitor, lysosomal integrity and blood-forming stem cell function were restored. Remarkably, ex vivo treatment of old stem cells with this lysosomal inhibitor boosted their in vivo blood-forming capacity more than eightfold. This restoration also dampened harmful inflammatory pathways by improving lysosomal processing of mitochondrial DNA and reducing activation of the cGAS-STING immune signaling pathway, a key driver of inflammation and aging in stem cells [11].
Figure 2: HSC Aging Reversal via Lysosomal Modulation. Targeting lysosomal hyperactivity with a vacuolar ATPase inhibitor restores function in aged HSCs.
Bone Marrow Adipose Tissue as a Metabolic Regulator
Bone marrow adipose tissue (MAT) has emerged as a significant component of the hematopoietic microenvironment, remodeling in various metabolic conditions including obesity, diabetes, caloric restriction, and aging. MAT-derived Stem Cell Factor (SCF) is essential for hematopoiesis at steady state and upon metabolic stresses. Genetic ablation of the Kitl gene (encoding SCF) from adipocytes and bone marrow stroma cells using Adipoq-Cre and Osx1-Cre mouse models diminished hematopoietic stem and progenitor cells and myeloid progenitors in the bone marrow, leading to macrocytic anemia. The composition and differentiation of hematopoietic progenitor cells dynamically responded to metabolic challenges including high-fat diet, β3-adrenergic activation, thermoneutrality, and aging, responses that were largely impaired in adipocyte-specific SCF knockout mice [9].
Novel Transplant Protocols Using Antibody-Based Conditioning
A Phase 1 clinical trial demonstrated a breakthrough in stem cell transplantation by replacing toxic chemotherapy or radiation with an antibody-based conditioning regimen. Patients received briquilimab, an antibody against CD117 (c-Kit) on the surface of blood-forming stem cells, which eliminated host HSCs without toxic side effects. This approach, combined with T-cell-depleted haploidentical transplants from parents, successfully treated three children with Fanconi anemia—a genetic disease that makes standard transplant extremely risky. All three patients achieved nearly 100% donor chimerism two years post-transplant, far exceeding the initial goal of 1% donor chimerism, demonstrating the efficacy of this less toxic approach [12].
Table 3: Key Research Reagent Solutions for Bone Marrow Stem Cell Research
| Reagent/Cell Type | Function/Application | Example Use Case |
|---|---|---|
| Briquilimab (anti-CD117) | Antibody targeting c-Kit on HSCs; enables chemotherapy-free transplant conditioning [12] | Replaces toxic busulfan chemotherapy in stem cell transplantation protocols |
| Collagenase Type I | Enzyme for tissue dissociation during stromal vascular fraction (SVF) isolation [10] | Digestion of adipose tissue to isolate AD-MSCs from lipoaspirate |
| AMD3100 (Plerixafor) | CXCR4 receptor antagonist that mobilizes HSPCs from bone marrow [8] | Clinical mobilization of HSPCs for collection via apheresis |
| G-CSF | Granulocyte-colony stimulating factor cytokine [8] | Mobilization of HSPCs from bone marrow to peripheral blood |
| Vacuolar ATPase Inhibitor | Suppresses lysosomal hyperacidity in aged HSCs [11] | Ex vivo rejuvenation of aged hematopoietic stem cells |
| CD34+ Selection | Enrichment for blood-forming stem cells from donor tissue [12] | Generating stem cell-rich grafts for transplantation |
Experimental Protocols for Bone Marrow Stem Cell Research
Isolation and Culture of Adipose-Derived MSCs (AD-MSCs)
Protocol Source: [10]
- Tissue Harvesting: Collect adipose tissue during surgery or liposuction. Wash the tissue several times in phosphate-buffered saline (PBS).
- Digestion: Digest the tissue at 37°C with 0.075% collagenase type I for approximately 30-60 minutes.
- Enzyme Neutralization: Neutralize collagenase activity with DMEM medium containing 10% fetal bovine serum (FBS).
- Centrifugation: Centrifuge at 1200× g for 10 minutes to obtain a high-density stromal vascular fraction (SVF) pellet.
- Red Blood Cell Lysis: Suspend the pellet in 160 mM NH4Cl and incubate for 10 minutes at room temperature to lyse red blood cells.
- Plating: Clean pellets by repeated centrifugation in neutralizing medium, then place in plastic culture flasks with appropriate medium (e.g., DMEM/F12 with 10% FBS).
- Expansion: Culture at 37°C with 5% CO2, changing medium every 2-3 days. AD-MSCs typically retain their phenotype until passage 6.
Flow Cytometry Analysis of Hematopoietic Stem and Progenitor Cells
Protocol Source: [9]
- Bone Marrow Cell Isolation: Flush bone marrow from femurs in Ca2+ and Mg2+ free PBS with 1% heat-inactivated bovine serum.
- Cell Suspension Preparation: Dissociate cells to a single-cell suspension by gently passing through a 25-gauge needle and filtering through a 70-μm nylon mesh.
- Red Blood Cell Lysis: Remove red blood cells using ammonium-chloride-potassium lysing buffer.
- Antibody Staining: Stain cells with a cocktail of biotin-conjugated lineage antibodies (CD3e, B220, Ter119, Mac-1, Gr-1, CD4, CD5, CD8) followed by Streptavidin-AF488.
- Progenitor Panel Staining: Subsequently stain with CD127-APC, c-Kit-APC-eFluor780, Sca-1-Super Bright 436, CD34-PE, and FcγR-PerCP-eFluor710.
- HSC Staining: For LT-HSC identification, include CD150-BV605 and CD48-BUV395.
- Analysis: Perform multicolor analysis on a flow cytometer (e.g., BD LSRII). Identify populations as follows:
- HSPC: Lin−Sca-1+c-Kit+ (LSK)
- LT-HSC: CD150+CD48−Lin−Sca−1+c-Kit+
- Myeloid Progenitor: Lin−CD127−Sca-1−c-Kit+
- CLP: Lin−CD127+Sca-1+c-Kit+
Figure 3: Workflow for Hematopoietic Stem Cell Isolation. Complex multicolor flow cytometry enables identification of HSC subpopulations.
Clinical Implications and Future Directions
The interplay between HSCs and MSCs in the bone marrow reservoir has profound clinical implications. The ability to reverse HSC aging [11] and develop non-toxic conditioning regimens [12] opens new avenues for treating age-related blood disorders and making stem cell transplantation accessible to more vulnerable populations. Furthermore, understanding bone marrow adipose tissue as a metabolic sensor and regulator of hematopoiesis provides insights into the hematopoietic complications of metabolic diseases [9].
Ongoing research is exploring how lysosomal dysfunction in old stem cells may contribute to the formation of leukemic stem cells, potentially linking normal stem cell aging to cancer development [11]. The reauthorization of the Stem Cell Therapeutic and Research Act in 2025, with funding of $33 million annually for the C.W. Bill Young Cell Transplantation Program and $23 million annually for the National Cord Blood Inventory, ensures continued support for these life-saving programs and the research that underpins them [13].
As single-cell transcriptomic methods advance, they deliver unprecedented insight into gene expression profiles of individual cells, helping to deconstruct cellular hierarchy and differentiation trajectories, and to understand cell-cell interactions within the bone marrow microenvironment [14]. These technologies will further illuminate the complex dynamics of bone marrow as a stem cell reservoir, driving the next generation of somatic stem cell therapies.
Adipose-derived stem cells (ASCs), also referred to as adipose-derived adult stem (ADAS) cells, have emerged as a pivotal tool in regenerative medicine and tissue engineering. As a type of mesenchymal stem cell (MSC) residing in adipose tissue, ASCs fulfill the critical requirements for an ideal stem cell source: they are abundantly available, can be harvested with minimal morbidity, differentiate reliably down multiple pathways, and can be transplanted safely and efficiously [15]. Within the broader context of adult stem cell research, ASCs present a compelling alternative to bone marrow-derived mesenchymal stem cells (BMSCs), primarily due to their accessibility and superior yield from a readily available tissue source [16]. The ease of procurement via minimally invasive liposuction procedures, coupled with a differentiation capacity that is not adversely affected by donor age, positions ASCs as a frontrunner for autologous cell-based therapies [16] [17]. This technical guide provides an in-depth examination of ASC isolation, characterization, and comparative analysis with other somatic tissue sources, specifically tailored for researchers and drug development professionals.
Isolation of Adipose-Derived Stem Cells
The isolation of ASCs from adipose tissue is a standardized process that leverages their physiological presence within the stromal vascular fraction (SVF) of fat. The procedure hinges on the breakdown of the extracellular matrix to release the cellular components, followed by their separation and culture.
Standard Enzymatic Isolation Protocol
The most widely utilized method for isolating ASCs relies on enzymatic digestion of lipoaspirated or excised adipose tissue [16] [17]. The following protocol is adapted from established methodologies [18] [19]:
- Tissue Collection and Washing: Subcutaneous adipose tissue is obtained via liposuction or direct surgical excision. The tissue is extensively washed with sterile phosphate-buffered saline (PBS) containing antibiotics (e.g., 1-5% penicillin/streptomycin) to remove blood cells and contaminants [19].
- Enzymatic Digestion: The washed adipose tissue is minced and digested with 0.1% to 0.2% collagenase type I (or type IV) in PBS for 30-60 minutes at 37°C with constant agitation. Collagenase hydrolyzes collagen, breaking down the tissue structure and releasing the cellular components [18] [19].
- Digestion Neutralization: The collagenase activity is neutralized by adding an equal volume of culture medium, typically Dulbecco's Modified Eagle's Medium (DMEM) supplemented with 10% fetal bovine serum (FBS) [19]. For clinical-scale expansion, FBS is often replaced with human platelet lysate (hPL) to avoid xenogeneic components and comply with Good Manufacturing Practice guidelines [16] [18].
- Centrifugation and Separation: The neutralized cell suspension is centrifuged (e.g., 1200-1800 rpm for 5-10 minutes). This separates the mixture into three layers: a top layer of mature adipocytes (floating), an intermediate aqueous layer, and a pellet containing the SVF cells, including ASCs, preadipocytes, endothelial cells, and pericytes [16] [17] [19].
- Pellet Washing and Plating: The SVF pellet is resuspended in culture medium, filtered through a 70-100 μm cell strainer to remove debris, and centrifuged again. The final pellet is resuspended and plated in culture flasks [19].
- In vitro Expansion: The plated cells are maintained at 37°C in a humidified atmosphere with 5% CO2. After 24-48 hours, non-adherent cells are removed by washing with PBS. The adherent cells, which include the ASC population, are allowed to proliferate, with the medium changed twice weekly. Upon reaching 80-90% confluence, cells are passaged using trypsin/EDTA [18] [19].
The diagram below illustrates this core isolation workflow.
Characterization of ASCs
Proper characterization of ASCs is essential to confirm their identity and functional potency before experimental or clinical use. This involves assessing immunophenotype, differentiation potential, and proliferative capacity.
Immunophenotypic Characterization by Flow Cytometry
According to the International Society for Cellular Therapy (ISCT) criteria for MSCs, ASCs must express a specific set of surface markers and lack expression of hematopoietic markers [19]. Analysis is performed using flow cytometry on cells at passage 3-5.
- Cell Preparation: Harvest ASCs using trypsin/EDTA and wash with PBS. Use approximately 4 × 10^5 cells per sample [19].
- Staining: Incubate cells with fluorescently conjugated antibodies against target surface markers for 30 minutes in the dark at 4°C. Include unstained and isotype control samples for gating and background subtraction [18] [19].
- Analysis: Analyze the stained cells using a flow cytometer, collecting data for at least 50,000 events. The population of interest should demonstrate high expression (≥90%) of typical MSC markers and low expression (≤2%) of hematopoietic markers [19].
Table 1: Key Surface Markers for ASC Characterization
| Marker | Expression in ASCs | Function / Significance | Reference |
|---|---|---|---|
| CD73 | Positive (≥90%) | Ecto-5'-nucleotidase; MSC-defining marker | [16] [19] |
| CD90 | Positive (≥90%) | Thy-1 cell surface antigen; MSC-defining marker | [16] [19] |
| CD105 | Positive (≥90%) | Endoglin; MSC-defining marker | [16] [19] |
| CD44 | Positive | Hyaluronic acid receptor | [16] |
| CD166 | Positive | Activated Leukocyte Cell Adhesion Molecule | [16] |
| CD34 | Variable/Low | Hematopoietic progenitor cell marker; often negative in cultured ASCs but present in SVF | [16] [17] [19] |
| CD45 | Negative (≤2%) | Pan-hematopoietic marker | [16] [19] |
| CD14 | Negative (≤2%) | Monocyte/macrophage marker | [19] |
| CD19 | Negative (≤2%) | B-cell marker | [19] |
| HLA-DR | Negative (≤2%) | Major Histocompatibility Complex Class II | [19] |
| Stro-1 | Low | Mesenchymal progenitor marker; often lower in ASCs vs. BMSCs | [19] |
| CD49d | High | Alpha-4 integrin; often higher in ASCs vs. BMSCs | [19] |
Tri-Lineage Differentiation Potential
A defining functional characteristic of ASCs is their ability to differentiate into multiple mesodermal lineages. The following protocols induce osteogenic, adipogenic, and chondrogenic differentiation.
- Baseline: Plate ASCs at a density of 3-5 x 10^3 cells/cm² in growth medium (DMEM + 10% FBS/hPL) for 24 hours before switching to differentiation media [18] [19].
- Staining and Analysis: Differentiated cells are fixed and stained after 14-21 days. Adipogenic cultures are stained with Oil Red O to visualize lipid vesicles. Osteogenic cultures are stained with Alizarin Red S to detect calcium deposits. Chondrogenic pellets are sectioned and stained with Alcian Blue or Safranin O to visualize sulfated glycosaminoglycans in the extracellular matrix [19]. Quantitative reverse transcription polymerase chain reaction (qRT-PCR) can be used to measure the expression of lineage-specific genes.
Table 2: Standard In vitro Differentiation Protocols for ASCs
| Lineage | Induction Medium Components | Key Markers / Stains | Incubation Period |
|---|---|---|---|
| Adipogenic | 0.5 mM IBMX, 1 μM dexamethasone, 10 μM insulin, 200 μM indomethacin [19] | Oil Red O (lipid vesicles), PPAR-γ, FABP4 [19] | 14-21 days |
| Osteogenic | 0.1 μM dexamethasone, 10 mM β-glycerophosphate, 50 μM ascorbic acid-2-phosphate [19] | Alizarin Red S (calcium deposition), Alkaline Phosphatase (ALP) activity, Osteopontin, Runx2 [18] [19] | 14-21 days |
| Chondrogenic | Pellet culture in 0.1 μM dexamethasone, 1% ITS+ premix, 50 μg/mL ascorbic acid-2-phosphate, 10 ng/mL TGF-β3, 40 μg/mL proline [19] | Alcian Blue / Safranin O (proteoglycans), Collagen type II, Aggrecan, SOX9 [19] | 21-28 days |
ASCs vs. Bone Marrow-Derived MSCs: A Donor-Matched Comparison
Within the landscape of adult stem cell sources, bone marrow has been the traditional gold standard. However, direct, donor-matched comparisons reveal critical biological differences that inform source selection for specific applications.
Table 3: Donor-Matched Comparison of ASCs and BMSCs [18] [19]
| Parameter | Adipose-Derived Stem Cells (ASCs) | Bone Marrow-Derived MSCs (BMSCs) |
|---|---|---|
| Tissue Harvest | Minimally invasive (liposuction); abundant source [15] [16] | Highly invasive (bone marrow aspiration); limited source [16] [19] |
| Cell Yield | High (~500,000 stem cells per 1g of adipose tissue) [15] | Low (~100-1000 stem cells per 1mL of marrow) [19] |
| Proliferation Rate | Significantly higher population doublings [18] [19] | Lower proliferation capacity, higher senescence [16] [19] |
| Effect of Donor Age | No significant decline in proliferation with age [16] | Proliferation and differentiation potential decline with age [16] |
| Osteogenic Potential | Moderate | Superior (earlier/higher ALP activity, calcium deposition) [18] [19] |
| Chondrogenic Potential | Moderate | Superior (higher collagen type II production) [18] |
| Adipogenic Potential | Superior (more and larger lipid vesicles) [19] | Moderate |
| Immunomodulatory Effects | More potent inhibitory effects on immune cells [18] | Potent, but may be less so than ASCs in some assays [18] |
| Secretome Profile | Higher secretion of bFGF, IFN-γ, IGF-1 [18] | Higher secretion of HGF and SDF-1 [18] |
The following diagram summarizes the key comparative advantages of each cell source, derived from the donor-matched data.
The Scientist's Toolkit: Essential Research Reagents
This section details the key reagents and materials required for the isolation, expansion, and characterization of ASCs, forming a core toolkit for researchers in this field.
Table 4: Essential Research Reagents for ASC Isolation and Characterization
| Reagent / Material | Function / Application | Notes & Considerations |
|---|---|---|
| Collagenase Type I/IV | Enzymatic digestion of adipose tissue to release the Stromal Vascular Fraction (SVF). | Concentration (0.1-0.2%) and incubation time (30-60 min) must be optimized to maximize cell viability and yield [18] [19]. |
| Culture Medium (DMEM) | Basal medium for cell growth and expansion. | Often supplemented with glucose and glutamine. |
| Fetal Bovine Serum (FBS) | Standard serum supplement for in vitro cell culture, providing growth factors and adhesion factors. | Clinical Caution: Use of xenogeneic FBS is undesirable for clinical applications due to risk of pathogen transmission and immune reaction [18]. |
| Human Platelet Lysate (hPL) | Human-derived, xeno-free alternative to FBS for clinical-scale expansion. | Promotes faster proliferation; compliant with Good Manufacturing Practice (GMP) guidelines [16] [18]. |
| Antibiotics (Pen/Strep) | Added to wash buffers and media to prevent bacterial contamination during isolation and initial culture. | Typically used at 1% concentration. |
| Trypsin/EDTA | Enzymatic detachment of adherent cells for subculturing (passaging) and cell counting. | |
| Flow Cytometry Antibodies | Immunophenotypic characterization of ASCs (e.g., CD73, CD90, CD105, CD45, CD34). | Crucial for confirming MSC identity as per ISCT criteria [19]. |
| Tri-lineage Differentiation Kits | Defined media supplements for inducing osteogenic, adipogenic, and chondrogenic differentiation. | Commercially available kits ensure reproducibility. Key components include dexamethasone, IBMX, insulin, ascorbic acid, and TGF-β3 [19]. |
| Lineage-Specific Stains | Histochemical validation of differentiation (Oil Red O, Alizarin Red S, Alcian Blue). | Allows for qualitative and semi-quantitative analysis of differentiation efficiency. |
Adipose tissue represents a highly accessible and abundant source of multipotent mesenchymal stem cells. The detailed protocols for isolation and characterization outlined in this guide provide a reliable foundation for research and development. The critical comparison with BMSCs underscores a fundamental principle: the choice of stem cell source must be systematically considered based on the specific clinical or experimental application [18]. ASCs hold distinct advantages in proliferative capacity, immunomodulatory function, and ease of harvest, making them particularly suitable for applications in soft tissue regeneration, immunomodulation, and chronic wound healing [15] [16]. The field continues to advance rapidly, with ongoing clinical trials exploring the efficacy of ASCs and their derivatives, such as the stromal vascular fraction (SVF) and exosomes, across a spectrum of medical conditions [20]. Future efforts must prioritize international collaboration, large-scale trials, and the resolution of standardization challenges to fully realize the therapeutic potential of ASCs in regenerative medicine [20].
The bone marrow (BM) microenvironment constitutes a sophisticated regulatory niche that is fundamental to the maintenance of adult stem cells, the support of hematopoiesis, and the regulation of bone remodeling. This specialized milieu facilitates intricate signaling crosstalk between hematopoietic stem cells (HSCs) and mesenchymal stem cells (MSCs), orchestrated by cytokines, growth factors, and extracellular matrix components [21]. Within this context, bone marrow adipose tissue (BMAT) has transitioned from being perceived as an inert space-filler to being recognized as a dynamic endocrine organ that actively participates in metabolic and regenerative processes [21] [22]. The bone marrow adipose tissue constitutes approximately 10% of total adipose mass and can occupy up to 70% of bone marrow volume in adults, underscoring its significant physical presence within the niche [21]. This whitepaper provides an in-depth analysis of the bone marrow and adipose microenvironments, focusing on their anatomical and functional intricacies, with specific emphasis on their relevance to adult stem cell research for scientists and drug development professionals.
Anatomical and Functional Organization of Bone Marrow Niches
The bone marrow stroma is organized into distinct yet interconnected functional niches that regulate stem cell fate decisions through precise spatial positioning of signaling cues and cellular interactions.
Endosteal and Vascular Niches: Comparative Analysis
The endosteal and vascular niches represent two principal microenvironments within bone marrow that maintain HSCs through distinct mechanistic approaches.
Table 1: Characteristics of Major Bone Marrow Niches
| Feature | Endosteal Niche | Vascular Niche |
|---|---|---|
| Location | Bone-lining surface | Surrounding arterioles and sinusoids |
| Oxygenation | Markedly hypoxic [21] | Relatively oxygen-rich [21] |
| Key Molecular Factors | HIF-1α, Osteopontin, Ang-1 [21] | CXCL12, SCF, Nitric Oxide, IL-6 [21] |
| Primary HSC Function | Maintenance in deep quiescence [21] | Cycling, differentiation, and mobilization [21] |
| Stromal Cell Types | Osteoblasts, bone-lining cells | LepR+ perivascular stromal cells, Endothelial cells [21] |
The vascular niche itself comprises specialized endothelial cell subpopulations, including type-L (sinusoidal), type-H (arteriole-associated), and arterial endothelial cells, which coordinate hematopoietic function through differential secretion of angiocrine factors [21]. Bone marrow adipocytes (BMAs) strategically position themselves between these regions, engaging with both niches and exhibiting remarkable functional plasticity depending on their specific location and physiological context [21].
Bone Marrow Adipose Tissue: A Unique Adipose Depot
Bone marrow adipose tissue exhibits distinct characteristics that differentiate it from classical white (WAT) or brown adipose tissue (BAT). BMAs demonstrate unique metabolic properties, including reduced insulin-stimulated glucose uptake due to lower GLUT4 expression and resistance to cold-induced glucose uptake [21]. During highly anabolic phases such as puberty or fracture repair, BMAs can transiently exhibit a brown adipocyte-like phenotype, expressing transcription factors such as PR domain-containing 16 (Prdm16) and Forkhead box C2, along with marker genes including PGC1α, Dio2, β3AR, and UCP1, thereby establishing a microenvironment conducive to osteogenesis [21].
Table 2: Functional Roles of Bone Marrow Adipocytes in Homeostasis
| Function | Mechanism | Impact on Niche |
|---|---|---|
| Metabolic Regulation | Lipolysis in response to metabolic stimuli; FFAs release via HSL and ATGL activation [21] | Systemic energy balance; local lipid availability |
| Osteogenic Modulation | Secretion of leptin and adiponectin (positive effect); RANKL secretion (negative effect) [21] | Context-dependent bone formation or resorption |
| Hematopoietic Support | Sequestration of excess lipids to reduce lipotoxic stress [21] | Protection of HSCs and osteoblasts from lipid-induced damage |
| Endocrine Signaling | Production of adipokines, cytokines, and chemokines [21] | Paracrine and systemic signaling |
Methodological Approaches for Investigating Bone Marrow Niches
Experimental Models and Isolation Techniques
Investigating the bone marrow microenvironment requires specialized methodological approaches that account for the unique properties of BMAs and their surrounding cellular constituents. The Bone Marrow Adiposity Society (BMAS) has highlighted the critical challenge of methodological variability and has established consensus recommendations to standardize isolation, storage, and characterization protocols for BMAT and bone marrow adipocytes (BMAds) [22]. Key considerations include:
- Site-Specificity: BMAT demonstrates significant heterogeneity across different skeletal sites (e.g., long bones vs. vertebrae) and between species, necessitating careful experimental design and interpretation [22].
- Isolation Techniques: Standardized protocols for BMAds isolation are essential for generating reproducible data in downstream applications, including high-throughput omics analyses [22].
- Functional Assays: Lipidomic analyses of BMAds in murine osteoporosis models have revealed significant alterations in lipid species, particularly increases in acylcarnitine and fatty acids (e.g., arachidonic acid), which contribute to mitochondrial dysfunction in neighboring cells [23].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Bone Marrow Adiposity Research
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Staining & Detection | Oil Red O (ORO), Alkaline Phosphatase (ALP), Hematoxylin & Eosin (H&E), Senescence-associated β-galactosidase (SA-β-gal) [23] | Visualization of lipids, osteogenic differentiation, general histology, senescence detection |
| Cell Culture Models | BMSC adipogenic/osteogenic induction, MC3T3-E1 osteoblast line [23] | In vitro modeling of differentiation and cell crosstalk |
| Molecular Probes | JC-1 (mitochondrial membrane potential), MitoSOX (mitochondrial superoxide) [23] | Assessment of mitochondrial function and oxidative stress |
| Lipid Modulators | GW1929 (fatty acid agonist), GW9662 (fatty acid antagonist) [23] | Experimental manipulation of lipid signaling pathways |
| Nanoparticle Systems | CZP@LC nanoplatform (Cu/Zn-ZIF8 loaded with PG3@LC) [23] | Targeted interference with adipocyte lipid metabolism |
Signaling Pathways in Bone Marrow Niches
The following diagrams, created using DOT language, illustrate key signaling pathways and experimental workflows relevant to bone marrow adipocyte research. The color palette adheres to the specified guidelines, ensuring sufficient contrast for readability.
Signaling Pathways Governing MSC Fate Decisions
Diagram 1: Aging skews MSC fate toward adipogenesis via altered Wnt/β-catenin and PPARγ signaling, exacerbated by oxidative stress and senescence-associated secretory phenotype (SASP) factors [21].
BMAd Lipid Crosstalk Experimental Workflow
Diagram 2: Experimental workflow for identifying and targeting BMAd-derived lipid crosstalk that induces osteoblast senescence in osteoporosis [23].
Pathophysiological Implications and Therapeutic Targeting
Dysregulation of the bone marrow microenvironment contributes significantly to disease pathogenesis, particularly in aging and metabolic disorders. Age-related transformations shift MSC differentiation from osteogenesis toward adipogenesis, altering secretory profiles and impairing endothelial function, which destabilizes the vascular niche and reduces hematopoietic stem cell support [21]. This culminates in clinical manifestations of bone fragility and disrupted hematopoiesis.
In osteoporosis, BMAds accumulate and secrete excessive lipids, including polyunsaturated fatty acids like arachidonic acid (AA). These lipids induce mitochondrial dysfunction and senescence in neighboring osteoblasts, creating a vicious cycle that further impairs bone formation [23]. Therapeutic strategies are emerging that target these pathological mechanisms. For instance, the CZP@LC nanoplatform—a polycation-loaded biomimetic dual-site framework—specifically targets BMAds in osteoporotic conditions to interfere with pathological lipid crosstalk [23]. This approach mitigates mitochondrial dysfunction in bone marrow cells, prevents senescence accumulation, and restores osteogenesis, demonstrating the potential of targeting BMAd-mediated pathways for therapeutic benefit [23].
The bone marrow and adipose microenvironments represent complex, dynamic niches where specialized anatomical structures govern stem cell fate through precise molecular signaling. Bone marrow adipocytes function as active participants in metabolic regulation, hematopoietic support, and bone homeostasis, rather than passive space-fillers. The ongoing standardization of experimental methods by organizations like BMAS, coupled with emerging technologies such as targeted nanotherapies that modulate adipocyte lipid metabolism, promises to accelerate both our fundamental understanding and therapeutic manipulation of these critical somatic stem cell niches. Future research focusing on the specific signaling molecules and metabolic pathways identified in this whitepaper will undoubtedly yield novel interventions for a range of degenerative, metabolic, and hematopoietic disorders.
Adult stem cells are undifferentiated cells found throughout the body after development, possessing the dual abilities of self-renewal and differentiation into specialized cell types [1]. They serve as fundamental units for maintaining tissue homeostasis and facilitating repair following injury. Within the context of somatic tissue sources, mesenchymal stem cells (MSCs) derived from bone marrow (BM-MSCs) and adipose tissue (Adipose-Derived Stem Cells, ADSCs) represent two of the most extensively researched populations in regenerative medicine [1] [24]. These cells reside in highly specialized microenvironments known as stem cell niches, which integrate structural, biochemical, and mechanical cues to precisely regulate stem cell behavior, including quiescence, self-renewal, and differentiation [25]. The core functions of these adult stem cells—maintenance of tissue homeostasis, orchestration of repair processes, and dynamic immunomodulation—are not solely determined by their intrinsic genetic programs but are profoundly influenced by these niche interactions [25]. This whitepaper provides an in-depth technical analysis of these core functions, framed within contemporary research on bone marrow and adipose-derived stem cells.
Core Functions of Adult Stem Cells
The therapeutic potential of BM-MSCs and ADSCs is realized through three principal, interconnected biological functions: sustained tissue homeostasis, coordinated response to injury, and sophisticated immunomodulation.
Tissue Homeostasis
The primary role of adult stem cells in healthy tissue is to maintain homeostasis by ensuring a continuous, balanced replacement of cells lost to normal turnover.
- Cell Replacement and Tissue Maintenance: Adult stem cells systematically replace cells lost through normal wear and tear, injury, or disease, thanks to their self-renewal and differentiation abilities [1]. This is essential for the homeostasis of organs with high turnover rates. For instance, hematopoietic stem cells (HSCs) in the bone marrow niche give rise to all blood cell lineages, thereby maintaining the circulatory system [1] [26].
- Metabolic and Endocrine Regulation: Beyond simple cell replacement, stem cells and their niche constituents actively participate in systemic metabolic regulation. Bone marrow adipocytes (BMAs), which share a common mesenchymal origin with BM-MSCs, are now recognized as a dynamic endocrine organ [26]. They secrete factors like adiponectin and free fatty acids (FFAs) that support HSC homeostasis and modulate bone metabolism [26].
- Niche Maintenance and Signaling: Stem cells also contribute to the integrity of their own niche. Through paracrine signaling and direct cell-cell contact, they help maintain the supportive function of neighboring cells, such as endothelial cells, osteoblasts, and immune cells, creating a stable microenvironment for sustained tissue function [25].
Tissue Repair and Regeneration
Upon tissue damage, the normally quiescent stem cell niche becomes activated, initiating a complex repair program.
- Activation and Proliferation: Signals from the injured microenvironment, including released cytokines and growth factors, activate resident stem cells, prompting them to exit quiescence and proliferate [1] [25].
- Differentiation and Matrix Remodeling: The progeny of activated stem cells differentiate to replace lost cell types. MSCs can differentiate into osteoblasts, chondrocytes, and adipocytes to repair mesodermal tissues [1]. Furthermore, they secrete enzymes and factors that remodel the extracellular matrix (ECM), clearing debris and facilitating the formation of new tissue scaffolding [24].
- Paracrine-Mediated Repair: A significant mechanism of stem cell-mediated repair is through robust paracrine activity. Stem cells secrete a cocktail of bioactive molecules—including growth factors, cytokines, and chemokines—that act on resident cells to promote angiogenesis, suppress apoptosis, and stimulate the proliferation of local progenitor cells [24]. This "bystander effect" is often more critical for repair than the direct differentiation of the stem cells themselves [24].
Immunomodulation
A defining feature of MSCs from both bone marrow and adipose tissue is their potent capacity to modulate immune responses, a function critical in both homeostasis and repair.
- Anti-inflammatory Effects: In inflammatory disease models, such as experimental autoimmune encephalomyelitis (EAE), administration of BM-MSCs, ADSCs, or the stromal vascular fraction (SVF) from adipose tissue significantly reduces serum levels of pro-inflammatory cytokines like IFNγ and IL-12 [27]. This indicates a systemic anti-inflammatory effect.
- Cell-to-Cell Immune Regulation: MSCs interact directly and indirectly with a wide range of immune cells. They can suppress the proliferation and activation of T-cells, inhibit B-cell function, modulate dendritic cell maturation, and drive macrophages toward an anti-inflammatory (M2) phenotype [25] [27]. This re-establishment of a balanced immune environment is crucial for the resolution of inflammation and progression to the repair phase following injury.
- Dynamic Niche Interactions: The immunomodulatory function is not static; it is influenced by signals from the inflammatory niche. In turn, MSCs alter the niche through their secretome. For example, in obesity, adipose tissue macrophages shift toward a pro-inflammatory state, which disrupts the niche homeostasis. Weight loss can partially reverse this senescence and inflammation, demonstrating the dynamic reciprocity between stem cells, immune cells, and their niche [28].
Table 1: Comparative Analysis of Immunomodulatory Effects in an EAE Model
| Cell Therapy | Clinical Score Amelioration | Reduction in IFNγ | Reduction in IL-12 | Reduction in Inflammatory Infiltrates |
|---|---|---|---|---|
| Bone Marrow MSCs (BM-MSCs) | Significant | Comparable to other groups | Significant | Significant |
| Adipose-Derived Stem Cells (ASCs) | Significant | Comparable to other groups | Significant | Significant |
| Stromal Vascular Fraction (SVF) | Significant (as effective as ASCs/BM-MSCs) | Comparable to other groups | Significant (more than BM-MSCs/ASCs) | Significant |
Experimental Models and Methodologies
Investigating the core functions of adult stem cells requires robust and standardized experimental protocols. The following methodologies are central to the field.
Protocol 1: Comparative Functional Analysis in Disease Models
This protocol, adapted from a study comparing ADSCs and BM-MSCs in an EAE model, outlines the key steps for evaluating therapeutic efficacy [27].
Protocol 2: Isolation and Characterization of Bone Marrow Adipocytes
Studying the bone marrow niche requires specialized methods for isolating its most abundant cell type, the bone marrow adipocyte (BMA) [29] [22].
- Tissue Processing: Bone marrow samples are obtained from long bones (e.g., tibia, femur) or vertebrae. The marrow is flushed and subjected to collagenase digestion to liberate the cellular components.
- Adipocyte Isolation: The digested marrow is centrifuged. Mature adipocytes float to the top due to their high lipid content, forming a distinct layer that can be purified from the stromal vascular pellet [29].
- Characterization: Isolated BMAs are characterized using:
- Standardization Challenge: A key challenge in the field is the lack of widely adopted standardized protocols, which the Bone Marrow Adiposity Society (BMAS) is working to address [29] [22].
Key Signaling Pathways Regulating Stem Cell Fate
The core functions of adult stem cells are governed by a set of highly conserved signaling pathways. These pathways integrate signals from the niche to dictate cell fate decisions.
Table 2: Research Reagent Solutions for Stem Cell Niche Studies
| Research Reagent / Tool | Primary Function in Experimentation |
|---|---|
| Collagenase Type I | Enzymatic digestion of tissues (adipose, bone marrow) to isolate stem cells and adipocytes [27]. |
| Stromal Vascular Fraction (SVF) | The heterogeneous, non-expanded cellular fraction from adipose tissue used directly in therapy, containing ADSCs, endothelial cells, and immune cells [27]. |
| Fetal Bovine Serum (FBS) | A key, though ill-defined, component of culture media for the ex vivo expansion of MSCs; subject to replacement efforts for clinical use [27]. |
| CD105, CD73, CD90 Antibodies | Surface antigen markers used for the immunophenotypic identification and definition of human MSCs via flow cytometry [1]. |
| Osteogenic/Adipogenic Induction Media | Defined media containing specific factors (e.g., dexamethasone, ascorbate for osteogenesis; insulin, IBMX for adipogenesis) to assess MSC multipotency in vitro [1]. |
| Spatial Transcriptomics | A high-resolution omics technology that maps gene expression data onto tissue architecture, allowing the study of cells within their native niche context [28]. |
BM-MSCs and ADSCs are central to a sophisticated biological system that maintains tissue integrity, responds to injury, and calibrates immune responses. Their core functions are inseparable from the dynamic regulatory control of their native niches in bone marrow and adipose tissue. While these cells share broad functional characteristics, critical differences in their abundance, accessibility, and specific responses to pathological cues make them uniquely suited for different therapeutic applications. The future of regenerative medicine lies in moving beyond a purely stem-cell-centric view. Success will depend on treating the stem cell and its niche as an inseparable therapeutic unit. Advancements in high-resolution niche mapping, the development of niche-mimetic engineered scaffolds, and the execution of niche-targeted clinical trials will be pivotal in unlocking the full regenerative potential of adult stem cells for treating degenerative diseases, injuries, and immune dysregulation.
From Lab to Clinic: Isolation, Characterization, and Therapeutic Applications
Within the context of research on adult stem cell somatic tissue sources, particularly bone marrow adipose tissue and subcutaneous adipose tissue, standardized and reproducible tissue processing is a critical foundation for experimental success. The isolation of specific cell populations, including mesenchymal stem cells and mature adipocytes, from these complex tissues is a fundamental step for investigating their role in physiology, disease, and regenerative medicine. The techniques of collagenase digestion and differential centrifugation form the cornerstone of this isolation process. This guide details the current, optimized protocols for processing adipose and bone marrow tissues, providing structured data, methodological details, and visual workflows to support researchers in generating high-quality, comparable data in the field of stem cell research.
Core Principles of Tissue Dissociation
The primary objective of tissue dissociation is to liberate individual cells from the dense extracellular matrix that holds them in place, while maximizing cell viability and preserving biological function. For adipose and bone marrow tissues, this presents unique challenges due to their high lipid content and complex stromal networks.
- Enzymatic Action: Collagenase, a matrix-degrading enzyme, specifically targets and hydrolyzes collagen, a major structural component of the extracellular matrix. This action disrupts the tissue architecture, releasing intact adipocytes, stromal cells, and the vascular fraction.
- Mechanical Assistance: Enzymatic digestion is typically augmented by mechanical disruption, such as mincing tissue with scissors, to increase the surface area for enzyme action and improve dissociation efficiency.
- Fractional Separation: Following dissociation, differential centrifugation exploits differences in cell size and density to separate buoyant adipocytes from the pelleted stromal vascular fraction, which contains a heterogeneous mix of cells including adipose-derived stem cells, endothelial cells, and immune cells.
Experimental Protocols & Methodologies
Collagenase Digestion of Human Lipoaspirate
This protocol is adapted from studies investigating the optimization of fat graft processing and is suitable for isolating cells from subcutaneous adipose tissue [30].
Materials:
- Tissue Source: Human lipoaspirate from elective liposuction procedures.
- Collagenase Solution: 0.1% (weight/volume) Collagenase Type I in a digestion buffer containing 2.5% BSA, 20 mM HEPES, and cations (e.g., CaCl₂) to maintain enzymatic activity.
- Equipment: 37°C water bath or incubator, centrifuge, sterile tubes and pipettes.
Step-by-Step Procedure:
- Tissue Preparation: Wash the lipoaspirate with phosphate-buffered saline to remove blood cell contaminants and local anesthetics.
- Digestion: Incubate the adipose tissue at a concentration of 1 g tissue per 1 mL of collagenase-containing digestion buffer.
- Agitation: Place the tissue-enzyme mixture in a 37°C water bath, agitating every 5 minutes to ensure uniform digestion.
- Digestion Duration: Digest for a standardized period. Studies indicate that a duration of 30 to 40 minutes is optimal, as longer digestion times (e.g., 60 minutes) significantly decrease the viability of both adipocytes and stromal cells [30].
- Reaction Termination: After digestion, wash the tissue digest three times with PBS to remove residual collagenase.
Differential Centrifugation for Cell Fractionation
Following collagenase digestion, differential centrifugation is used to separate different cell populations based on their buoyancy.
Step-by-Step Procedure:
- Initial Low-Speed Spin: Centrifuge the digested tissue mixture at a low g-force (e.g., 300 × g for 10 minutes) [30] [31].
- Fraction Separation: Following this spin, three distinct layers will form:
- Top Layer: Mature, lipid-filled adipocytes (floating).
- Middle Layer: Aqueous solution of collagenase and buffer.
- Bottom Pellet: The stromal vascular fraction, containing ADSCs, pericytes, endothelial cells, and immune cells.
- Pellet Washing: Carefully aspirate the supernatant and resuspend the SVF pellet in a wash buffer. Repeat centrifugation at the same low speed to remove remaining contaminants.
- High-Speed Clearing Spin: For protocols isolating extracellular vesicles from the digested supernatant, subsequent high-speed centrifugation (e.g., 2000 × g for 20 minutes) is used to remove cellular debris [31].
Isolation of Cells from Bone Marrow Adipose Tissue
Bone marrow adipose tissue presents distinct challenges due to its location and complex microenvironment. A perfusion-based dissociation is often required for intact tissue.
Key Considerations:
- Two-Step Perfusion: For intact bone or liver tissue, a two-step perfusion process is highly effective. The tissue is first perfused with a calcium-free buffer, followed by perfusion with a collagenase solution [31].
- Optimal Digestion Time: For mouse liver, an optimal treatment time for collagenase dissolution is 7 to 10 minutes. A shorter duration causes incomplete dissolution, while a longer duration may cause tissue damage [31].
- Standardization Need: The Bone Marrow Adiposity Society (BMAS) has highlighted that methods for isolating BMAT or bone marrow adipocytes are highly variable and has advocated for widely adopted standardized protocols to improve reproducibility [29].
Table 1: Impact of Collagenase Digestion Time on Cell Viability
| Digestion Time (Minutes) | Adipocyte Viability (Human) | Stromal Cell Viability (Human) | Key Findings |
|---|---|---|---|
| 30 | High | High | Recommended starting point for optimal yield and viability [30] |
| 40 | High | High | Common clinical protocol duration; maintains high viability [32] |
| 50-60 | Significantly Decreased | Significantly Decreased | Prolonged exposure detrimental to both cell types [30] |
Table 2: Differential Centrifugation Parameters for Subcellular Fractionation
| Centrifugation Speed & Duration | Pelleted Components | Supernatant Contains | Typical Application |
|---|---|---|---|
| 50 × g for 10 min [31] | Large cell clusters, undigested tissue | Single cells, small debris | Initial clarification of tissue digest |
| 300 × g for 10 min [30] [31] | Stromal Vascular Fraction (SVF) | Mature adipocytes, lipids | Standard SVF isolation from adipose tissue |
| 2000 × g for 20 min [31] | Cellular debris, apoptotic bodies | Smaller vesicles, organelles | Clearing supernatant for downstream EV isolation |
The following tables consolidate key quantitative findings from the literature to guide protocol optimization.
Table 3: Comparison of Tissue Digestion Protocols from Recent Research
| Tissue Type | Protocol Name/Type | Key Enzymes & Concentrations | Incubation Conditions | Reported Outcome |
|---|---|---|---|---|
| Human Adipose Tissue | Standard Collagenase Digestion [30] | 0.1% Collagenase Type I | 37°C, 30-60 min | Digestion >50 min decreases adipocyte & stromal cell viability. |
| Gut Mucosa | One-Step Collagenase [33] | Collagenase (type not specified) | 37°C | Time-efficient; cell viability and composition comparable to gold standard. |
| Gut Mucosa | Two-Step Collagenase (Gold Standard) [33] | EDTA + Collagenase | 37°C (fraction-specific) | Sequential isolation of epithelial and lamina propria cells. |
| Human Breast Cancer Biopsy | Method 5 (Optimized) [34] | 1.6 mg/mL Collagenase IV + 0.14 mg/mL Hyaluronidase | Overnight, 37°C | Highly effective for establishing primary cell cultures. |
| Mouse Liver | Two-Step Perfusion [31] | Collagenase Type IV | 37°C, 7-10 min perfusion | Optimal for tissue dissociation and high EV yield. |
The Scientist's Toolkit: Essential Research Reagents
This table lists critical reagents and their functions for successfully executing these isolation protocols.
Table 4: Essential Reagents for Tissue Dissociation and Cell Isolation
| Reagent / Material | Function / Purpose | Example & Notes |
|---|---|---|
| Collagenase Type I/IV | Enzymatic digestion of collagen in extracellular matrix. | Worthington Biochemical or Serva brands; type and concentration must be optimized per tissue [30] [34]. |
| Hyaluronidase | Degrades hyaluronic acid in the extracellular matrix. | Often used in combination with collagenase for enhanced tissue dissociation [34]. |
| Bovine Serum Albumin | Acts as a carrier protein and reduces non-specific cell adhesion and enzyme inhibition. | Typically used at 2.5-5% in digestion buffers [30]. |
| HEPES Buffer | Maintains stable pH during the digestion process outside a CO₂ incubator. | Crucial for ensuring consistent enzyme activity [30]. |
| Calcium Chloride | Cofactor for collagenase enzyme activity. | Essential for maximal enzymatic efficiency [30]. |
| Phosphate Buffered Saline | Washing and dilution medium; maintains osmotic balance. | Used for washing tissue pre-digestion and terminating the reaction post-digestion. |
| DMEM/F12 Medium | Base medium for cell suspension and culture post-isolation. | Often supplemented with serum for initial plating of isolated cells [34]. |
Workflow and Signaling Pathway Visualization
The diagram below illustrates the standard workflow for processing adipose tissue to isolate key cellular fractions, integrating both enzymatic and mechanical steps.
The following diagram outlines the hypothesized signaling pathways and cellular interactions within the bone marrow niche, based on current research.
The bone marrow stroma and adipose tissue represent two pivotal somatic tissue sources in adult stem cell research, harboring distinct yet crucial stem cell populations: mesenchymal stromal cells (MSCs) and hematopoietic stem cells (HSCs). These cells are fundamental to regenerative medicine, tissue engineering, and therapeutic development. Their isolation and characterization rely heavily on the precise identification of unique cell surface antigen profiles. For researchers and drug development professionals, accurately defining these phenotypic markers is not merely a procedural step but a cornerstone for ensuring experimental reproducibility, therapeutic efficacy, and safety. The International Society for Cellular Therapy (ISCT) established minimal criteria to define human MSCs, requiring ≥95% of the population to express CD105, CD73, and CD90, while lacking expression of hematopoietic markers such as CD45, CD34, CD14, CD11b, and HLA-DR [35] [36]. This whitepaper provides an in-depth technical guide to the surface antigen profiles of MSCs and HSCs, focusing on their functional significance, standardized characterization methodologies, and critical considerations for research within the context of adult stem cell investigations involving bone marrow and adipose tissue.
Phenotypic Marker Profiles for Mesenchymal Stromal Cells (MSCs)
Core Positive Marker Definition and Functions
The triad of CD105, CD73, and CD90 forms the core of the immunophenotypic definition of culture-expanded MSCs as per ISCT guidelines. Their individual biological functions and expression patterns are detailed below.
Table 1: Core Positive Surface Markers for Human MSCs
| Marker | Alternative Name | Primary Function | Expression Specificity |
|---|---|---|---|
| CD105 | Endoglin | Accessory receptor for TGF-β superfamily ligands [37]. | Highly expressed on vascular endothelial cells; expressed at low levels on freshly isolated adipose-derived MSCs, increasing with culture [37]. |
| CD73 | Ecto-5'-nucleotidase | Converts extracellular AMP to adenosine [37]. | Expressed on lymphocytes, endothelial cells, and fibroblasts; specific epitopes (SH3, SH4) may be MSC-specific [37]. |
| CD90 | Thy-1 | GPI-linked protein involved in cell-cell and cell-matrix interactions [37]. | Expressed on endothelial cells, fibroblasts, HSCs, and neurons; species-specific antibody reactivity is a concern [37]. |
In addition to the core positive markers, MSCs are also frequently characterized by the presence of other molecules, including CD44, CD29, CD166, and CD146 [35] [36]. It is critical to note that the expression of these markers can be dynamic. For instance, CD34 is a positive marker for native MSCs in adipose tissue's stromal vascular fraction and in bone marrow, but its expression is typically lost upon in vitro culture [38] [37] [35].
Essential Negative Markers and Hematopoietic Exclusion
The definitive immunophenotypic profile of MSCs requires the absence of markers associated with other lineages, particularly the hematopoietic lineage. This exclusion is vital for ensuring population purity in experimental and therapeutic applications.
Table 2: Key Negative Surface Markers for Human MSCs
| Marker | Typically Identifies | Importance in MSC Definition |
|---|---|---|
| CD45 | Pan-leukocyte marker [35] | Primary marker for excluding hematopoietic cells [39] [35]. |
| CD34 | Hematopoietic stem/progenitor cells, endothelial cells [37] | A controversial marker; positive on native MSCs in some tissues (e.g., adipose) but generally negative on culture-expanded MSCs [38] [37]. |
| CD14/CD11b | Monocytes, macrophages, granulocytes [35] | Further excludes the myeloid lineage [36]. |
| CD19/CD79a | B cells [35] | Excludes the lymphoid B-cell lineage [36]. |
| HLA-DR | MHC Class II molecules | Indicates an immunologically activated state; should be absent on undifferentiated MSCs [35]. |
Tissue-Specific and Functional Subpopulation Markers
While the ISCT criteria provide a foundational definition, the MSC population is heterogeneous. Advanced research has identified additional markers that define functional subpopulations or indicate "stemness."
- STRO-1: This antigen, identified from CD34+ bone marrow cells, is used to isolate a primitive stromal precursor population but has been shown to be an endothelial antigen [37] [35].
- CD271 (LNGFR): The low-affinity nerve growth factor receptor is a marker for prospective isolation of bone marrow MSCs with high colony-forming efficiency [40].
- CD146 (MCAM): This marker identifies a perivascular subset of MSCs and is associated with in vivo bone formation potential [35] [40]. The ratio of CD271+/CD146+ and CD271+/CD146- subsets changes with donor age [40].
- SSEA-1 & CD49a: In mouse models, SSEA-1 identifies a primitive mesenchymal population, while CD49a is used for prospective isolation [35].
Phenotypic Marker Profiles for Hematopoietic Stem Cells (HSCs)
Core Defining Markers for Human HSCs
The classical and most consistently used marker for human hematopoietic stem and progenitor cells (HSPCs) is CD34, a transmembrane sialomucin [37]. The CD34+ fraction of bone marrow or umbilical cord blood is enriched for cells capable of reconstituting the hematopoietic system. However, it is crucial to recognize that the CD34+ population is heterogeneous and contains various lineage-committed progenitors alongside the true, multipotent HSCs. Furthermore, some studies suggest the existence of primitive CD34- HSCs, indicating phenotypic heterogeneity within this compartment [37].
Additional Markers for HSC Enrichment and Isolation
To isolate a more purified HSC population, CD34 is typically used in combination with other markers, most notably the absence of lineage commitment markers.
- Lineage Negativity (Lin-): A cocktail of antibodies against mature blood cell lineage markers (e.g., CD3, CD14, CD19, CD56) is used to exclude committed cells.
- CD90 (Thy-1) and CD38: Primitive HSCs are often characterized as CD34+CD38-CD90+ [35].
- CD45: While a pan-hematopoietic marker, its expression level (dim) can be used in conjunction with other markers for identification.
Table 3: Key Surface Markers for Human HSCs
| Marker | Expression on HSCs | Function and Notes |
|---|---|---|
| CD34 | Positive | Primary marker for enrichment; function may be adhesive/anti-adhesive [37]. |
| CD45 | Positive (dim) | Pan-hematopoietic marker; used to confirm hematopoietic origin. |
| CD90 (Thy-1) | Positive on a primitive subset | Used to further refine the CD34+ population [35]. |
| CD38 | Negative on most primitive HSCs | Expression increases with differentiation. |
| Lineage Markers | Negative | Cocktail (CD3, CD14, CD19, CD56, etc.) excludes mature blood cells. |
Experimental Protocols for Marker Analysis
Standard Flow Cytometry Protocol for MSC Characterization
Flow cytometry is the gold-standard technology for the immunophenotypic characterization of MSCs and HSCs. The following protocol is adapted for the analysis of cultured human MSCs according to ISCT criteria [39] [41].
1. Cell Preparation and Staining
- Harvest MSCs (e.g., at passage 3-5) using a standard detachment reagent like trypsin/EDTA.
- Wash cells twice with FACS Buffer (e.g., PBS + 1-2% FBS) and resuspend to a concentration of 1-5 x 10^7 cells/mL.
- Distribute 100 µL of cell suspension per flow cytometry tube.
- Add the recommended concentration of fluorochrome-conjugated antibodies. A typical panel includes:
- Positive markers: Anti-CD73, CD90, CD105.
- Negative markers: Anti-CD45, CD34, CD14, CD19.
- Viability dye: To exclude dead cells.
- Incubate for 20-30 minutes at 4°C in the dark.
- Wash cells twice with FACS Buffer to remove unbound antibody and resuspend in a fixed volume (e.g., 300-500 µL) for analysis.
2. Flow Cytometric Acquisition and Analysis
- Use a standard flow cytometer equipped with lasers and filters appropriate for the fluorochromes used.
- Create a forward scatter (FSC) vs. side scatter (SSC) plot to gate on the main cell population, excluding debris.
- Use a viability dye to gate on live cells.
- Apply fluorescence minus one (FMO) controls or isotype controls to set positive staining boundaries accurately.
- Acquire a minimum of 10,000 events per sample within the live cell gate.
- Analyze the data to determine the percentage of cells positive for each marker. According to ISCT criteria, ≥95% of the MSC population must express CD73, CD90, and CD105, while ≤2% should express the negative markers [35].
Isolation of MSCs from Bone Marrow Aspirate
For the isolation of MSCs directly from tissue sources like bone marrow, a common method involves density gradient centrifugation followed by plastic adherence [35].
1. Density Gradient Centrifugation
- Dilute the bone marrow aspirate with an equal volume of PBS.
- Carefully layer the diluted sample over a Ficoll-Paque density gradient medium.
- Centrifuge at 400 x g for 30-40 minutes at room temperature with the brake off.
- After centrifugation, carefully aspirate the mononuclear cell (MNC) layer at the interface.
- Wash the MNCs twice with PBS or culture medium.
2. Plastic Adherence and Culture
- Resuspend the MNCs in complete MSC expansion medium (e.g., DMEM supplemented with 10% FBS, 100 U/mL penicillin, and 100 µg/mL streptomycin).
- Seed the cells into tissue culture flasks at a density of 1-2 x 10^5 cells/cm².
- Incubate the cultures at 37°C in a humidified atmosphere with 5% CO₂.
- After 48-72 hours, remove the non-adherent cells (primarily hematopoietic cells) by changing the medium.
- Continue to refresh the medium every 3-4 days until the adherent MSCs reach 70-80% confluence, then passage them.
This method leverages the defining plastic adherence property of MSCs to separate them from the hematopoietic majority in the bone marrow.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents for MSC and HSC Research
| Reagent / Tool | Function / Application | Example from Literature |
|---|---|---|
| Ficoll-Paque | Density gradient medium for isolation of mononuclear cells from bone marrow or blood [39]. | Used in initial separation of BM-MNCs for subsequent MSC culture [39] [40]. |
| Flow Cytometry Antibody Panels | Multiparametric immunophenotypic characterization of cells. | Pre-configured hMSC characterization panels (e.g., CD45/CD73/CD90/CD105) are commercially available [41]. |
| Stem Cell Culture Media | Ex vivo expansion of MSCs while preserving stemness. | Studies compare media like DMEM-F12, M199, and commercial formulations for optimal expansion [42]. |
| Collagenase Type I | Enzymatic digestion of tissues (e.g., adipose tissue) to isolate the stromal vascular fraction (SVF) [42]. | Used for dissociating lipoaspirate samples to obtain ASCs [42]. |
| CD271 & CD146 Antibodies | Prospective isolation of MSC subpopulations via fluorescence-activated cell sorting (FACS) [40]. | Used to identify distinct CFU-F-containing subsets in human bone marrow that change with age [40]. |
Visualization of Experimental Workflows and Cellular Relationships
Workflow for MSC Characterization from Bone Marrow
MSC and HSC Phenotypic Relationships in Bone Marrow
Critical Considerations and Technical Caveats
- Marker Specificity and Dynamics: No single marker is unique to MSCs. CD73, CD90, and CD105 are expressed by other cell types, including fibroblasts and endothelial cells [37]. Furthermore, marker expression can change with in vitro passage; for example, CD34 is expressed on native adipose-derived MSCs but is lost in culture [38] [37].
- Species Differences: Phenotypic markers for MSCs show significant variation between species. The CD34+CD45-CD31- phenotype is used for mouse MSC isolation, which differs markedly from the human ISCT criteria [35].
- Functional Validation: Surface marker expression alone is insufficient to define MSCs. The ISCT mandates functional validation of trilineage differentiation potential (adiopogenic, osteogenic, chondrogenic) in vitro [35].
- Tissue Source Variability: The composition and potency of MSCs can vary based on the tissue of origin (e.g., bone marrow vs. adipose tissue), influencing marker expression and differentiation capacity [38] [35].
The precise definition of surface antigen profiles for MSCs (CD105+, CD73+, CD90+) and HSCs (primarily CD34+) is a non-negotiable standard in somatic stem cell research. Adherence to the ISCT criteria for MSCs, coupled with an understanding of the more established markers for HSCs, provides a robust framework for the isolation, characterization, and functional study of these cells. As research progresses, the discovery of more specific markers and subpopulation signatures will further refine our understanding of these complex cellular systems, enhancing their application in drug development and clinical therapies. Researchers must remain vigilant of the technical caveats, including marker dynamics and species differences, to ensure the generation of high-quality, reproducible data.
In the field of regenerative medicine, the trilineage differentiation potential of adult stem cells—specifically into adipogenic, osteogenic, and chondrogenic lineages—serves as a fundamental functional criterion for defining multipotent mesenchymal stromal cells (MSCs) [43] [44]. This potential is not only a key identifier but also a critical measure of cell potency for developing therapies for degenerative conditions such as osteoporosis, osteoarthritis, and soft tissue defects [45] [2]. Somatic tissue sources, particularly bone marrow and adipose tissue, are the most prevalent and clinically relevant reservoirs for these MSCs [1] [44].
This technical guide provides a detailed framework for validating MSC potency through standardized in vitro differentiation assays. It is structured to support researchers and drug development professionals in establishing robust, reproducible protocols that can quantitatively assess differentiation efficiency, a necessity for both quality control in clinical manufacturing and rigorous preclinical research [46] [43].
Core Principles of Trilineage Differentiation
The commitment of MSCs to adipogenic, osteogenic, or chondrogenic fates is governed by complex and often reciprocal signaling pathways. A key regulatory principle is the balance between adipogenesis and osteogenesis; factors and conditions that stimulate one lineage typically inhibit the other [44]. This balance is crucial for maintaining tissue homeostasis, such as in bone marrow, where an shift toward adipogenesis at the expense of osteogenesis is associated with bone loss and osteoporosis [44].
Understanding these regulatory networks is essential for designing effective differentiation protocols and accurately interpreting assay results. The cascades involve an initial downregulation of stemness genes, followed by the sequential activation of lineage-specific transcription factors and the subsequent synthesis of characteristic extracellular matrices [44]. The tables and diagram below summarize the key molecular features and signaling activities that define the pluripotent state and these specific differentiated lineages.
Table 1: Key Molecular Markers for Assessing Trilineage Differentiation
| Lineage | Key Upregulated Genes | Critical Transcription Factors | Characteristic Output |
|---|---|---|---|
| Adipogenesis | FABP4, PPARγ [46] [43] | PPARγ [44] | Lipid droplet accumulation [46] |
| Osteogenesis | Col11a1 [43] | RUNX2 [43] | Calcium deposition / Mineralization [45] |
| Chondrogenesis | ACAN (Aggrecan) [43] | SOX9 [43] | Proteoglycan synthesis [45] |
Table 2: Signal Transduction Pathway (STP) Activity Profiles Quantitative STP activity measurement reveals distinct profiles for pluripotent and differentiated cells [47].
| Cell State / Lineage | Active Pathways | Inactive Pathways |
|---|---|---|
| Pluripotency (qPAP) | PI3K, MAPK, Hedgehog, Notch, TGFβ, NFκB [47] | Wnt [47] |
| Intestinal Progenitors | PI3K, Wnt, Notch [47] | - |
Figure 1: MSC Differentiation Pathways and Regulatory Balance. Differentiation from a pluripotent state is driven by specific cues and marked by key genes. A state of reciprocal inhibition exists between the adipogenic and osteogenic lineages [44].
Experimental Protocols
This section provides detailed, step-by-step methodologies for inducing and analyzing trilineage differentiation. Standardization of these protocols is critical for obtaining reproducible and comparable results across different cell sources and laboratories [43].
Adipogenic Differentiation Protocol
The process of adipogenesis transforms spindle-shaped MSCs into cells laden with lipid droplets, which can be visualized and quantified using specific stains.
- Cell Seeding: Plate MSCs (passages 3-6 are typically suitable [43]) at a confluency of >95% in standard expansion medium (e.g., DMEM with 10% FBS) [48]. High cell density is a critical trigger for adipogenic commitment.
- Induction: Once cells reach confluence, replace the expansion medium with Adipogenic Induction Medium. A standard formulation includes:
- DMEM base medium.
- 0.5 mM 3-isobutyl-1-methylxanthine (IBMX).
- 1 μM Dexamethasone.
- 10 μg/mL Insulin [48].
- Maintenance: Culture the cells for up to 21 days, changing the medium every 2-3 days [48] [46].
- Analysis: Adipogenic differentiation can be assessed through:
- Oil Red O Staining: Stains neutral lipids in the droplets red [48].
- Nile Red Staining & Fluorescence: A quantitative alternative that can be measured using flow cytometry or a fluorescent microplate reader. The fluorescence intensity can be normalized to DNA content (e.g., using DAPI) for a quantitative measure of adipogenesis [46].
- Gene Expression Analysis: Quantify the upregulation of adipogenic genes like FABP4 (which can increase 100 to 5000-fold) and PPARγ via qRT-PCR [46] [43].
Osteogenic Differentiation Protocol
Osteogenic differentiation leads to the deposition of a mineralized matrix, a key characteristic of bone-forming osteoblasts.
- Cell Seeding: Plate MSCs at a density that allows them to reach ~70% confluency within 24 hours [45].
- Induction: Replace the medium with Osteogenic Induction Medium. A typical formulation contains:
- Maintenance: Culture the cells for 12-21 days, refreshing the medium every 2-3 days [45] [48].
- Analysis: Osteogenesis is confirmed by detecting calcium deposits and osteogenic gene expression.
Chondrogenic Differentiation Protocol
Chondrogenesis is typically induced using a pellet or micromass culture system to mimic the condensed environment of developing cartilage.
- Pellet Formation: Transfer 250,000 to 1 million MSCs into a 15 mL polypropylene tube. Centrifuge at 1000 rpm for 5 minutes to form a pelleted micromass at the bottom of the tube [45] [48].
- Induction: Carefully remove the supernatant and add Chondrogenic Induction Medium without disrupting the pellet. The medium is often composed of:
- Maintenance: Culture the pellets for 21-28 days, refreshing the medium every 2-3 days. The pellets should be left undisturbed as much as possible [45].
- Analysis: Chondrogenic output is assessed by:
- Safranin-O Staining: Stains proteoglycans in the cartilage matrix a deep orange-red, indicating successful differentiation [45].
- Alcian Blue Staining: Stains sulfated glycosaminoglycans (GAGs) blue [48].
- Pellet Size Measurement: Increased pellet size over the culture period indicates matrix deposition and expansion [45].
- Gene Expression Analysis: Quantify the upregulation of ACAN (Aggrecan) via qRT-PCR [43].
Figure 2: Experimental Workflow for Trilineage Differentiation. The schematic outlines the key steps for directing MSCs through adipogenic, osteogenic, and chondrogenic lineages, highlighting specific culture durations, induction factors, and analysis methods for each pathway [45] [48] [43].
Quantitative Assessment & Data Analysis
Moving beyond qualitative staining, robust validation requires quantitative techniques that provide objective, numerical data on differentiation efficiency. This is essential for comparing cell populations, optimizing protocols, and establishing release criteria for clinical-grade cells.
Table 3: Quantitative Methods for Assessing Differentiation Efficiency
| Method | Target | Application | Key Advantage |
|---|---|---|---|
| Nile Red / DAPI Microplate Assay [46] | Neutral Lipids (Adipogenesis) | Fluorescence measurement of lipid content normalized to DNA. | High-throughput, quantitative; provides a single numerical value (Nile Red/DAPI ratio). |
| Alizarin Red Extraction & Quantification [45] | Calcium Deposits (Osteogenesis) | Colorimetric measurement of extracted dye from mineralized matrix. | Semi-quantitative to quantitative; overcomes subjectivity of visual scoring. |
| Pellet Size Measurement [45] | Matrix Deposition (Chondrogenesis) | Microscopic measurement of pellet diameter increase over time. | Simple quantitative metric of overall cartilage matrix production. |
| qRT-PCR for Lineage Genes [43] | Gene Expression (All Lineages) | Quantification of fold-change in key markers (FABP4, Col11a1, ACAN). | Highly specific and sensitive; detects early molecular commitment. |
| Flow Cytometry for Intracellular Proteins [46] | Protein Expression (e.g., FABP4) | Single-cell analysis of protein accumulation in differentiated cells. | Reveals heterogeneity within a culture population. |
The Scientist's Toolkit: Key Research Reagent Solutions
A successful differentiation experiment relies on a suite of well-defined reagents and tools. The table below catalogues essential materials and their functions, forming a core toolkit for researchers in this field.
Table 4: Essential Reagents and Tools for Trilineage Differentiation Assays
| Category | Item | Function / Application |
|---|---|---|
| Induction Factors | Dexamethasone [48] | A synthetic glucocorticoid used in all three differentiation protocols to promote cell commitment. |
| IBMX [48] | A phosphodiesterase inhibitor that raises intracellular cAMP levels, primarily used to induce adipogenesis. | |
| Insulin [48] | Promotes lipid accumulation in adipogenesis and supports chondrogenesis. | |
| TGF-β3 [48] | A key morphogen for inducing chondrogenic differentiation in pellet cultures. | |
| Ascorbic-2-Phosphate [45] [48] | A stable form of Vitamin C essential for collagen synthesis in osteogenesis and chondrogenesis. | |
| Glycerol Phosphate [45] [48] | A source of organic phosphate that promotes hydroxyapatite crystal formation and matrix mineralization in osteogenesis. | |
| Staining & Detection | Oil Red O [48] | A lysochrome (fat-soluble dye) used to stain neutral lipids and triglycerides in adipocytes. |
| Alizarin Red S [45] [48] | An anthraquinone dye that chelates calcium ions, staining calcium deposits in osteogenic cultures. | |
| Safranin-O [45] | A cationic dye that binds to proteoglycans and glycosaminoglycans in cartilaginous matrix. | |
| Nile Red [46] | A fluorescent dye for detecting intracellular lipid droplets, suitable for quantitative fluorescence assays. | |
| Molecular Biology | qRT-PCR Kits [43] | For quantitative measurement of lineage-specific gene expression markers (e.g., FABP4, ACAN, Col11a1). |
| CD Markers (CD34, CD146, CD271) [45] | Antibodies for magnetic-activated cell sorting (MACS) to isolate specific stem cell subpopulations with enhanced differentiation potential. | |
| Cell Culture | MACS Separation System [45] | Technology for the positive selection and enrichment of specific cell types using magnetic beads, useful for purifying progenitor populations. |
Advanced Research Considerations
As the field progresses, several advanced considerations are crucial for enhancing the relevance and application of differentiation assays.
Impact of Cell Source and Heterogeneity: The differentiation potential of MSCs is not uniform. Studies show that specific subpopulations within a tissue source have varying capacities. For instance, in microfragmented adipose tissue, CD146+ stem cells demonstrate superior osteogenic potential (higher calcium deposition), while CD271+ cells show superior chondrogenic potential (increased proteoglycan formation) [45]. The donor-specific heterogeneity in the abundance of these potent subsets can significantly impact clinical outcomes [45].
Transcriptomic Profiling: High-throughput techniques like RNA-seq are revolutionizing our understanding of differentiation. They allow for the analysis of the entire transcriptome, including mRNAs, miRNAs, and lncRNAs, at different time points during differentiation [44]. This systems-level approach helps depict the complex regulatory networks and identify novel key molecules and signaling pathways driving lineage commitment.
Assay Standardization and High-Throughput Methods: There is a growing need for standardized, quantitative methods to ensure reproducibility across labs, especially for clinical translation. Fluorescence-based microplate assays (e.g., Nile Red/DAPI) and standardized qRT-PCR protocols offer robust, quantitative alternatives to subjective staining scores [46] [43]. These methods are vital for the quality control of manufactured MSC batches [46].
Mesenchymal Stem/Stromal Cells (MSCs) represent a cornerstone of regenerative medicine, offering immense therapeutic potential due to their multipotent differentiation capacity, immunomodulatory properties, and paracrine activity. Originally identified in bone marrow, MSCs have since been isolated from various tissues, including adipose tissue, umbilical cord, and dental pulp [49] [50]. The International Society for Cellular Therapy (ISCT) establishes minimum criteria for defining MSCs: adherence to plastic, specific surface marker expression (CD73+, CD90+, CD105+, CD34-, CD45-, CD11b-, CD14-, CD19-, HLA-DR-), and tri-lineage differentiation potential into osteoblasts, adipocytes, and chondroblasts in vitro [49] [50]. This technical guide delineates the core therapeutic mechanisms of MSCs—differentiation, paracrine signaling, and immunomodulation—within the specific context of adult stem cell sources, particularly bone marrow and adipose tissue, providing methodologies and analytical frameworks for research and drug development.
Core Therapeutic Mechanisms of MSCs
Multilineage Differentiation Capacity
MSCs demonstrate a well-documented capacity to differentiate into multiple mesodermal lineages, including osteoblasts, chondrocytes, and adipocytes, which forms a fundamental mechanism for direct tissue repair and regeneration [49] [50]. The differentiation process is tightly regulated by key transcription factors and signaling pathways. Adipogenic differentiation is controlled by PPARγ (Peroxisome Proliferator-Activated Receptor gamma) and C/EBPs (CCAAT/enhancer-binding proteins), while osteogenic differentiation is governed by Runx2 [51] [21]. This adipogenic program is mutually exclusive with the osteoblastogenic program in Bone Marrow MSCs (BM-MSCs), creating a dynamic equilibrium within the bone marrow microenvironment [51]. Furthermore, the field recognizes the phenomenon of dedifferentiation, where mature bone marrow adipocytes can revert to their multipotent stem cell state, thereby contributing to the MSC pool and niche homeostasis, a process of particular interest in haematological malignancies [51].
Table 1: Key Transcription Factors in MSC Differentiation
| Transcription Factor | Primary Role | Associated Signaling Pathways |
|---|---|---|
| PPARγ | Master regulator of adipogenesis; controls fat cell development | TGF-β/BMP, WNT, SHH, NOTCH, FGFs [51] |
| C/EBPs | Works with PPARγ to promote adipocyte commitment | TGF-β/BMP, WNT, SHH, NOTCH, FGFs [51] |
| Runx2 | Master regulator of osteogenesis; drives bone formation | WNT/β-catenin, BMP [21] |
| Sox9 | Essential for chondrogenesis (cartilage formation) | TGF-β/Smad [21] |
The therapeutic application of differentiation is exemplified in treating orthopedic injuries. For instance, adipose-derived stem cell (ADSC) spheroids, pre-differentiated toward bone cells and combined with β-tricalcium phosphate, have successfully promoted spine fracture repair in rat models, demonstrating enhanced bone regeneration and strength [52].
Paracrine Signaling and Secretome Activity
The therapeutic benefits of MSCs are largely mediated through their paracrine activity rather than direct differentiation and engraftment [53] [54]. The MSC secretome—comprising growth factors, cytokines, chemokines, and extracellular vesicles (EVs)—exerts proliferative, anti-apoptotic, and anti-inflammatory effects on injured tissues [49] [54] [55].
Table 2: Key Components of the MSC Secretome and Their Functions
| Secretome Component | Primary Function | Experimental Evidence |
|---|---|---|
| VEGF, FGF, HGF | Promotes angiogenesis and cell proliferation | 2- to 7-fold increase in co-culture with injured cells [54] |
| PGE2 (Prostaglandin E2) | Inhibits NF-κB, shifts macrophages to anti-inflammatory M2 phenotype | Reduces pro-inflammatory factors (IL-1β, TNF-α) [55] |
| TSG-6 (TNF-α-stimulated gene 6) | Potent anti-inflammatory protein, inhibits NF-κB and TLR2 pathways | Improves inflammatory microenvironment in OA and disc degeneration [55] |
| IL-10 | Anti-inflammatory cytokine, inhibits p38 MAPK pathway | Suppresses neutrophil-driven inflammation [55] |
| Extracellular Vesicles/Exosomes | Carry proteins, lipids, and nucleic acids (e.g., lncRNA-KLF3-AS1) | Inhibit chondrocyte apoptosis and promote proliferation in OA [55] |
The paracrine effect is highly context-dependent. The injured tissue microenvironment influences the composition of the MSC secretome, which in turn regulates local cellular responses such as survival, proliferation, and migration [53]. Administration of MSC-conditioned medium (MSC-CM) alone has been shown to recapitulate the therapeutic benefits of whole MSC transplantation in models of acute organ injury, underscoring the paramount importance of paracrine mechanisms [54].
Immunomodulatory Properties
MSCs possess remarkable immunomodulatory capabilities, interacting with both innate and adaptive immune cells to suppress excessive inflammation and promote a transition to tissue repair [49] [50] [55]. They modulate the function of T cells, B cells, dendritic cells, and macrophages through both direct cell-cell contact and the release of soluble factors [50] [55]. A key mechanism involves inducing a phenotypic shift in macrophages from a pro-inflammatory M1 state to an anti-inflammatory, tissue-reparative M2 state, facilitated by the secretion of PGE2 and IDO (Indoleamine 2,3-dioxygenase) [55]. Furthermore, MSCs can inhibit the activation and proliferation of pro-inflammatory T cells and suppress the antigen-presenting capacity of dendritic cells [50]. The immunomodulatory effects are not constitutive but are licensed by inflammatory cytokines such as IFN-γ present in the disease microenvironment [55]. In osteoarthritis (OA), for example, BMSC paracrine signals inhibit the NF-κB pathway, a master regulator of inflammation, thereby reducing levels of TNF-α, IL-1β, and IL-6, which are key drivers of cartilage degradation [55].
Experimental Methodologies for MSC Research
Isolation and Characterization of Bone Marrow Adipose Tissue (BMAT) and Adipocytes
The Bone Marrow Adiposity Society (BMAS) provides updated consensus protocols for the experimental analysis of BMAT and Bone Marrow Adipocytes (BMAds) to harmonize research in this field [29] [22]. Key technical considerations include:
- Standardized Isolation: BMAS working groups recommend specific protocols for the isolation and purification of human BMAds to ensure reproducibility. A critical step is the careful removal of hematopoietic cells to obtain a pure adipocyte population [29].
- High-Throughput Omics: State-of-the-art characterization employs single-cell and spatial transcriptomics to unravel the molecular, cellular, and spatial organization of the bone marrow niche. This allows for the identification of distinct adipocyte subpopulations with unique functions [29].
- Biobanking: Standardized protocols for the storage and preservation of BMAT and BMAds are crucial for maintaining cell viability and molecular integrity for downstream experiments [29] [22].
Tracking and Evaluating MSC Homing
Homing—the migration of MSCs to sites of injury—is a critical first step for their therapeutic action. Experimental evaluation involves:
- Delivery Methods: Studies compare direct (local) administration (e.g., intra-articular, intraspinal) with systemic (usually intravenous) administration. Direct delivery avoids pulmonary entrapment and ensures higher local cell concentration, while systemic delivery relies on chemotactic gradients [49].
- Cell Tracking: In vivo tracking of administered MSCs is achieved using labeled cells (e.g., GFP+, dye-labeled) or advanced imaging techniques to monitor their migration, engraftment, and survival at the injury site [53].
- Homing Assays: The homing process can be broken down into distinct phases—adhesion, activation, entrapment, diapedesis, and migration—which can be studied in vitro using transwell systems with chemotactic gradients or in vivo in animal models of disease [49].
Research Reagent Solutions Toolkit
Table 3: Essential Reagents for MSC and BMAT Research
| Reagent / Tool | Primary Function | Specific Examples & Applications |
|---|---|---|
| Surface Marker Antibodies | Identification and purification of MSCs via flow cytometry | CD73, CD90, CD105 (positive); CD34, CD45, HLA-DR (negative) [49] [50] |
| Differentiation Inducers | Directing MSC lineage commitment in vitro | Dexamethasone (adiopgenic & osteogenic); 1,25-dihydroxyvitamin D3 (osteogenic) [50] |
| Cytokines & Growth Factors | Modulating MSC function and paracrine secretion | Wnt3a, TGF-β1, FIZZ1 (for dedifferentiation studies) [51]; TNF-α, IFN-γ (to license immunomodulation) [55] |
| Signaling Pathway Modulators | Investigating molecular mechanisms | Agonists/Antagonists for TGF-β/BMP, WNT, NOTCH, and PPARγ pathways [51] [21] |
| 3D Culture Scaffolds | Enhancing therapeutic efficacy and mimicking niche | β-tricalcium phosphate (for bone repair), synthetic polymers for spheroid formation [49] [52] |
Signaling Pathway Visualizations
MSC Mechanisms Overview
BMA Dedifferentiation Process
MSC Paracrine in Osteoarthritis
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) represents a potentially curative intervention for aggressive hematologic malignancies. However, its therapeutic efficacy is frequently compromised by graft-versus-host disease (GVHD), a serious complication wherein donor immune cells attack recipient tissues. GVHD manifests in two primary forms: an acute variant (aGVHD), typically occurring within 100 days post-transplant, and a chronic form (cGVHD), which can persist long-term and significantly impair quality of life. Despite advances in prophylactic regimens, GVHD remains a major cause of morbidity and non-relapse mortality, driving an urgent need for more effective therapeutic strategies.
The bone marrow microenvironment, particularly bone marrow adipose tissue (BMAT), is increasingly recognized as a critical player in transplant biology. BMAT, once considered a passive space-filler, is now understood as a dynamic endocrine organ that influences hematopoiesis, immune regulation, and bone homeostasis [26]. Its proximity to hematopoietic stem cells and progenitor cells within the marrow cavity positions it as a key modulator of post-transplant recovery and immune reconstitution. Age-related shifts in mesenchymal stem cell differentiation towards adipogenesis over osteogenesis can alter the bone marrow niche, potentially affecting HSC function and immune cell dynamics post-transplant [26]. This review examines the current landscape of FDA-approved GVHD therapies and active clinical trials, framing these developments within the broader context of bone marrow adipose research and its implications for transplant medicine.
FDA-Approved Therapies for Chronic Graft-Versus-Host Disease
The therapeutic arsenal for chronic GVHD has expanded substantially over the past decade. The U.S. Food and Drug Administration (FDA) has approved four primary drugs for cGVHD, each targeting distinct signaling pathways and cellular mechanisms involved in its pathogenesis [56].
Table 1: FDA-Approved Therapies for Chronic Graft-Versus-Host Disease (cGVHD)
| Drug Name | Molecular Target | Key Mechanism of Action | Clinical Context for Approval |
|---|---|---|---|
| Ibrutinib | Bruton's tyrosine kinase (BTK) | Inhibits B-cell receptor and macrophage signaling pathways involved in cGVHD pathogenesis. | Approved for cGVHD after failure of one or more lines of systemic therapy. |
| Ruxolitinib | JAK1 and JAK2 | Modulates inflammatory cytokine signaling via the JAK-STAT pathway. | Approved for cGVHD after failure of one or more lines of systemic therapy. |
| Belumosudil (KD025) | ROCK2 | Selective ROCK2 inhibitor; downregulates pro-inflammatory T helper 17 cells and upregulates regulatory T cells. | Approved for cGVHD after failure of at least two prior lines of systemic therapy. [57] |
| Axatilimab | CSF-1R | Targets colony-stimulating factor-1 receptor on macrophages, implicated in the fibrotic processes of cGVHD. | Approved for cGVHD. [56] |
These agents exemplify a shift towards targeted immunomodulation, moving beyond broad-spectrum immunosuppression. Their development underscores the importance of understanding the specific cellular and molecular drivers of GVHD, including potential interactions with the bone marrow microenvironment.
Breakthrough FDA Approval: Ryoncil (remestemcel-L) for Steroid-Refractory Acute GVHD
In a landmark decision in January 2025, the FDA approved the first mesenchymal stromal cell (MSC) therapy, remestemcel-L-rknd (Ryoncil), for the treatment of steroid-refractory acute GVHD (SR-aGVHD) in pediatric patients aged two months and older [58]. This approval, facilitated through fast track, orphan drug, and priority review designations, marks a significant advancement in the cellular therapy landscape.
The approval was based on a single-arm study of 54 pediatric patients with SR-aGVHD following allo-HSCT. The primary efficacy endpoints were overall response rate (ORR) at day 28 and the duration of that response. The trial demonstrated an ORR of 70% (95% CI: 56.4, 82.0), which included a complete response (CR) rate of 30% and a partial response (PR) rate of 41%. The median duration of response—measured from day 28 until disease progression, initiation of new systemic therapy, or mortality—was 54 days [58]. The safety profile was manageable, with the most frequently reported non-laboratory adverse reactions including viral and bacterial infections, fever, bleeding, swelling, abdominal pain, and hypertension.
This therapy leverages the potent immunomodulatory properties of MSCs, which are stromal cells residing in the perivascular niche of the bone marrow that can differentiate into adipocytes, osteoblasts, and chondrocytes [26]. The connection to bone marrow adipose research is direct, as MSCs are the progenitor cells for bone marrow adipocytes. The efficacy of remestemcel-L underscores the therapeutic potential of harnessing cellular components native to the bone marrow microenvironment to re-establish immune tolerance.
Active Clinical Trials in Graft-Versus-Host Disease
The clinical pipeline for GVHD is robust, featuring numerous investigational agents across various phases of development. These trials explore new mechanisms of action, combination therapies, and strategies for both prevention and treatment. Major academic centers, including Mayo Clinic, Dana-Farber, UCSF, and UCSD, are actively contributing to this research [59] [57] [60].
Table 2: Selected Active Clinical Trials for Graft-Versus-Host Disease (2025)
| Trial Intervention / Focus | Phase | Condition | Key Mechanism / Objective | Location / Identifier |
|---|---|---|---|---|
| Itacitinib (GRAVITAS-301) [59] | Phase 3 | aGVHD | JAK1 inhibitor combined with corticosteroids as first-line treatment for Grade II-IV aGVHD. | Mayo Clinic |
| Itolizumab (EQUATOR) [59] [57] | Phase 3 | aGVHD | Anti-CD6 monoclonal antibody combined with corticosteroids for first-line treatment of high-grade aGVHD. | Mayo Clinic, Dana-Farber (22-190) |
| Steroid-free Treatment (BMT CTN 1501) [59] | Phase 2 | aGVHD | Evaluates sirolimus vs. prednisone for standard-risk aGVHD using novel biomarker-based risk stratification. | Mayo Clinic |
| Axatilimab [59] [61] | Phase 2/3 | cGVHD | Anti-CSF-1R inhibitor for recurrent or refractory cGVHD; also in combination with corticosteroids as initial treatment. | UCSD, Mayo Clinic, Jacksonville |
| Belumosudil Combination [60] | Phase 3 | cGVHD | Tests belumosudil (ROCK2 inhibitor) in combination with corticosteroids for newly diagnosed moderate or severe cGVHD. | UCSF |
| Natalizumab [59] | Phase 2 | aGVHD | Assesses safety & efficacy of natalizumab + standard steroids for high-risk aGVHD. | Mayo Clinic |
| T-reg Enriched Cells [57] | Pilot/Phase 1 | Relapse/GVHD | Uses Treg-enriched cells in haploidentical transplant to enhance graft-vs-leukemia effect while controlling GVHD. | Dana-Farber (20-336) |
| Biomarker Verification (ABLE 2.0) [60] | N/A | cGVHD | Validates a pediatric prognostic biomarker algorithm to predict risk for later cGVHD development. | UCSF |
These trials reflect several key trends in GVHD research: a move towards risk-adapted therapy using biomarker stratification (e.g., BMT CTN 1501, ABLE 2.0), the exploration of novel pathways beyond calcineurin inhibition (e.g., JAK/STAT, ROCK2), and the strategic manipulation of cellular populations (e.g., T-regs, NK cells) to separate the graft-versus-tumor effect from GVHD [59] [57].
Experimental Methodologies in Bone Marrow Adiposity Research
Understanding the bone marrow microenvironment, including BMAT, is crucial for advancing GVHD research. The Bone Marrow Adiposity Society (BMAS) has established consensus views and standardized protocols for the isolation and characterization of BMAT and bone marrow adipocytes (BMAds) to harmonize research in the field [29] [22].
Key Experimental Workflow for BMAT Isolation and Analysis
The following diagram outlines a generalized, state-of-the-art workflow for the experimental analysis of bone marrow adipose tissue, based on BMAS recommendations.
The Scientist's Toolkit: Essential Reagents for BMAT Research
Table 3: Key Research Reagent Solutions for Bone Marrow Adipose Tissue Studies
| Reagent / Material | Primary Function in BMAT Research | Specific Examples / Notes |
|---|---|---|
| Collagenase Enzymes | Digest the extracellular matrix and surrounding bone tissue to liberate bone marrow adipocytes (BMAds) and stromal vascular fraction from intact marrow. | Type I, II, or IV collagenase; concentration and digestion time must be optimized for specific bone sites and species. [29] [22] |
| Density Gradient Media | Purify isolated BMAds from other bone marrow cells based on their buoyant density. | Percoll or similar media; creates a gradient for separation during centrifugation. [22] |
| Adipocyte Culture Media | Support the in vitro maintenance, differentiation, and study of BMAds and their precursors. | Typically contains fetal bovine serum, insulin, dexamethasone, and IBMX (for differentiation). [29] |
| Antibody Panels | Characterize BMAd cell surface markers and intracellular proteins via flow cytometry and immunofluorescence. | Targets include PPARγ, FABP4, Perilipin; markers for MSC progenitors (CD73, CD90, CD105). [26] |
| Deep-Learning Algorithms | Large-scale, non-invasive quantification of bone marrow fat fraction (BMFF) from medical images. | Applied to MRI datasets (e.g., UK Biobank) to measure BMFF in spine, femoral head, hip, and diaphysis. [62] |
These standardized methods and reagents are vital for generating reproducible data on BMAT biology. The application of high-throughput omics approaches (transcriptomics, proteomics, lipidomics) to these carefully prepared samples is revealing the unique molecular signature of BMAds and their complex roles in health and disease [29] [62] [22].
Signaling Pathways at the Interface of BMAT and GVHD Pathobiology
The pathophysiology of GVHD involves a complex cascade of immune activation, inflammation, and tissue damage. Key signaling pathways implicated in GVHD are also influenced by, and may influence, the bone marrow adipose niche. The following diagram integrates these interconnected pathways.
This schematic illustrates how BMAT is not a passive bystander but may actively participate in the immune dysregulation of GVHD. Aging or stressed BMAs can adopt a pro-inflammatory phenotype, secreting cytokines like IL-6 and TNF-α that may exacerbate the "inflammatory storm" driving GVHD pathogenesis [26]. Conversely, the intense inflammatory milieu of GVHD can alter BMAT function, creating a potential feedback loop. Approved and investigational drugs (Ruxolitinib, Belumosudil, Ibrutinib, Axatilimab) target key nodes in these immune pathways, highlighting their clinical relevance.
The landscape of GVHD therapy is rapidly evolving, marked by the approval of targeted small molecules and the groundbreaking validation of cellular therapy with Ryoncil. These clinical advances, however, represent a beginning rather than an endpoint. The integration of bone marrow adipose biology into the conceptual framework of transplant immunology opens up new frontiers for research and therapeutic development. Future efforts should focus on several key areas:
- Mechanistic Crosstalk: Delineating the precise molecular mechanisms by which BMAT and its secreted factors (adipokines, FFAs) influence alloreactive T-cells, regulatory T-cells, and other immune effectors involved in GVHD.
- Biomarker Discovery: Validating BMAT-related molecules or imaging signatures (e.g., bone marrow fat fraction from MRI) as biomarkers for predicting GVHD risk, severity, or response to therapy [62] [60].
- Therapeutic Targeting: Exploring whether modulating BMAT function—through pharmacological, nutritional, or lifestyle interventions—can improve transplant outcomes and reduce GVHD incidence.
- Combination Strategies: Designing rational combination therapies that simultaneously target pathological immune responses and favorably modulate the bone marrow niche to promote tolerance and tissue repair.
The ongoing clinical trials highlighted in this review reflect a maturation of the field towards precision medicine in GVHD management. By continuing to dissect the complex interplay between the immune system and the bone marrow microenvironment, particularly the adipose compartment, researchers and clinicians can develop more effective and less toxic strategies to separate graft-versus-host disease from the desirable graft-versus-tumor effect, ultimately improving survival and quality of life for transplant recipients.
Navigating Research Hurdles: Scalability, Standardization, and Functional Assays
In the evolving field of regenerative medicine, adult stem cells from somatic tissue sources like bone marrow and adipose tissue represent a cornerstone for therapeutic development. However, the inherent heterogeneity of these cells presents a significant challenge for clinical translation. Donor-specific factors—including age, health status, and anatomical tissue source—profoundly impact the biological efficacy and therapeutic potential of stem cell populations. This whitepaper synthesizes current research to delineate the effects of these donor variables on cell quality, providing researchers and drug development professionals with a detailed guide to navigating and mitigating this variability for robust experimental and clinical outcomes.
Quantifying the Impact of Donor Characteristics
The quality and functional potency of adult stem cells are not uniform; they are significantly influenced by the donor's physiological context. The quantitative and qualitative impacts of key donor characteristics are summarized in the table below.
Table 1: Impact of Donor Characteristics on Adult Stem Cell Quality
| Donor Characteristic | Impact on Proliferation | Impact on Differentiation Potential | Key Supporting Evidence |
|---|---|---|---|
| Age | Proliferation capacity decreases with age; fetal/calf cells show higher population doublings [63]. | Differentiation potential becomes restricted with age; chondrogenic and osteogenic potential often decline [63]. | Bovine AT-MSCs from younger donors surpassed 30 population doublings; older donors showed reduced viability [63]. |
| Health Status (Obesity/Diabetes) | Impaired ASC functionality and reduced cell viability [64]. | Adipogenic and other lineage potentials are compromised [64]. | Metabolic conditions alter the adipose tissue microenvironment, impairing ASC functionality for grafting [64]. |
| Tissue Source (Anatomical Site) | Varies based on vascularity and cellular composition of the harvest site [64]. | Lineage preference (e.g., adipogenic, osteogenic) varies by source [1] [64]. | Fat from different body regions varies in stem cell content, affecting graft viability and integration [64]. |
| Breed/Species | Breed-specific proliferation rates observed (e.g., bovine Holstein Friesian vs. Belgian Blue) [63]. | Breed significantly affects lineage potential (e.g., osteogenic differentiation) [63]. | Belgian Blue bovine MSCs showed superior osteogenic differentiation vs. Holstein Friesian [63]. |
Experimental Protocols for Assessing Donor Variability
Rigorous and standardized in vitro assays are critical for quantifying donor-dependent differences in stem cell quality. The following protocols are essential for comprehensive cell characterization.
Isolation and Culture of Adipose-Derived Mesenchymal Stromal Cells (ASCs)
This protocol is adapted from methods used to isolate bovine MSCs [63].
- Tissue Collection and Transport: Subcutaneous adipose tissue is collected and transported to the laboratory in a sterile container, typically within 1-2 hours post-collection.
- Enzymatic Digestion: The tissue is dissected into small pieces (~1 mm³) and digested in a solution of 1 mg/mL Liberase in a culture medium for 6 hours at 38.5°C in a humidified 5% CO₂ atmosphere.
- Stromal Vascular Fraction (SVF) Isolation: The digest is filtered through a 70 μm cell strainer to remove debris. The filtrate is centrifuged, and the resulting cell pellet, containing the SVF, is resuspended in culture medium.
- Plastic Adherence Selection: The cell suspension is seeded into culture flasks. After 24 hours, non-adherent cells are removed by replacing the medium. The adherent cells are cultured and passaged upon reaching 70-90% confluency using trypsin-EDTA [64] [63].
Tri-Lineage Differentiation Assays
These assays confirm the multipotency of isolated MSCs, a key defining criterion.
- Adipogenic Differentiation: Cells are cultured in induction media containing dexamethasone, indomethacin, and insulin. Differentiation is confirmed by intracellular lipid droplet accumulation, visualized by Oil Red O staining [63].
- Osteogenic Differentiation: Cells are cultured in media containing dexamethasone and β-glycerophosphate. Differentiation is confirmed by calcium deposition, visualized by Alizarin Red S staining [63].
- Chondrogenic Differentiation: Pellet cultures are maintained in media containing TGF-β. Differentiation is confirmed by sulfated proteoglycan detection in the extracellular matrix using Alcian Blue staining [63].
Assessment of Proliferation and Senescence
- Population Doubling (PD) Assays: Cell concentration and viability are determined at each passage using a hemocytometer and trypan blue exclusion. Population doublings are calculated to track long-term proliferation capacity [63].
- Senescence-Associated β-Galactosidase (SA-β-gal) Staining: Cells are fixed and incubated with a chromogenic substrate at pH 6.0. Senescent cells are identified by the presence of blue cytoplasmic staining [63].
Immunophenotyping by Flow Cytometry
Cells are harvested and incubated with fluorescently conjugated antibodies against specific surface markers. Analysis is performed using flow cytometry. Human MSCs are defined by positive expression of CD73, CD90, and CD105, and negative expression of hematopoietic markers (CD11b, CD14, CD19, CD34, CD45, HLA-DR) [64] [63].
Signaling Pathways and Molecular Mechanisms
The functional properties of stem cells, from homing to differentiation, are governed by complex molecular pathways. Understanding these is key to manipulating cell behavior.
Diagram 1: Muse cell homing to damaged tissue via S1P-S1PR2 axis.
The Scientist's Toolkit: Key Research Reagent Solutions
A selection of critical reagents and their functions, as derived from the experimental protocols, is provided below to aid in experimental design.
Table 2: Essential Research Reagents for Stem Cell Characterization
| Reagent / Tool | Function in Experimental Protocol |
|---|---|
| Liberase | Enzyme blend for enzymatic digestion of adipose tissue to isolate the stromal vascular fraction (SVF) [63]. |
| Tri-lineage Differentiation Kits | Pre-formulated media supplements for inducing adipogenic, osteogenic, and chondrogenic differentiation in vitro [63]. |
| Flow Cytometry Antibody Panels | Fluorescently conjugated antibodies against CD73, CD90, CD105, CD34, CD45, etc., for immunophenotyping and assessing cell purity [64] [63]. |
| SA-β-gal Staining Kit | Chemical assay for detecting senescence-associated β-galactosidase activity to identify senescent cells [63]. |
| Growth Factors (VEGF, FGF, HGF) | Proteins used in culture media to direct differentiation of ASCs into specific lineages like endothelial cells or hepatocytes [64]. |
The systematic investigation of donor variability is not merely an academic exercise but a fundamental prerequisite for the advancement of reproducible and efficacious adult stem cell therapies. Factors such as donor age, health status, and tissue source directly dictate critical cell qualities like proliferation, differentiation potential, and secretory profile. By adopting standardized, rigorous experimental protocols and leveraging emerging cell populations like Muse cells, the field can progress from merely acknowledging heterogeneity to actively controlling for it. This will ultimately enable the selection of optimal cell sources and the development of personalized, predictable regenerative treatments grounded in a deep understanding of donor-specific biological determinants.
The journey of adult stem cells from somatic tissues like bone marrow and adipose tissue to clinical applications hinges on the ability to expand them in vitro without compromising their fundamental biological properties. Achieving this requires a delicate balance: providing the necessary signals for robust proliferation while meticulously preserving therapeutic potency. For researchers and drug development professionals, optimizing this process is not merely a technical exercise but a critical determinant of translational success. This guide details evidence-based strategies for developing culture systems that support the scalable expansion of adult stem cells while maintaining the functional characteristics that define their clinical utility, directly supporting the broader thesis that these somatic tissue sources are viable foundations for advanced regenerative therapies.
The challenge is multifaceted. Adult stem cells, including Mesenchymal Stem Cells (MSCs) and Hematopoietic Stem Cells (HSCs), are integral to the body's maintenance and repair mechanisms, capable of self-renewal and differentiation into specialized cell types [1]. However, their function and number can decrease with age, and their behavior in vitro is profoundly influenced by culture conditions [1]. A poorly designed culture system can lead to replicative senescence, unwanted differentiation, or a gradual loss of in vivo efficacy, even in the face of successful numerical expansion. Therefore, the modern paradigm of culture optimization is intrinsically linked to the measurement of potency—the "specific ability or capacity of the product to affect a given result" [65]. This guide integrates culture methodology with potency assessment, providing a comprehensive framework for quality-driven stem cell expansion.
Foundational Principles: Potency and the Cellular Environment
Defining Potency for Cell Therapies
In the context of cell-based Advanced Therapy Medicinal Products (ATMPs), potency is a Critical Quality Attribute (CQA) that must be measured for each lot to ensure the therapy will have its intended clinical effect [65] [66]. Unlike simple identity or purity tests, a potency assay must quantify the therapy's functional activity in direct alignment with its Mechanism of Action (MoA) [65]. For adult stem cells, this MoA can be multifaceted, involving:
- Direct Differentiation into target cells like osteoblasts, chondrocytes, or adipocytes [1] [67].
- Paracrine Signaling through the secretion of bioactive factors that promote healing and repair [2].
- Immunomodulation by controlling autoimmune and inflammatory responses [2].
- Homing and Migration to sites of injury [2].
A robust potency assay is not just a regulatory requirement; it is an essential tool that guides process development, ensures consistent efficacy, and smooths the path to approval [65].
The Impact of the Physiochemical Niche
Moving away from traditional two-dimensional (2D) monolayers to more physiologically relevant systems is a cornerstone of modern culture optimization. Simplified 2D conditions often decrease the reliability and usefulness of data, as they fail to recapitulate the in vivo microenvironment [68]. Research shows that a three-dimensional (3D) culture environment can foster a "healthier," more realistic tissue model. For instance, a developed 3D bone marrow adipose tissue (BMAT) model exhibited less-inflammatory gene expression profiles compared to 2D culture, as supported by microarray data and KEGG pathway analysis [68]. This demonstrates that 3D systems can better mimic the in vivo niche, influencing cell signaling, differentiation potential, and overall function—key components of potency.
Table 1: Key Differences Between 2D and 3D Culture Systems
| Feature | 2D Culture System | 3D Culture System |
|---|---|---|
| Cell-ECM Interactions | Limited, unnatural polarity | Complex, biomimetic |
| Oxygen & Nutrient Gradients | Uniform | Physiologically relevant gradients |
| Cell-Cell Signaling | Primarily lateral | Omnidirectional, more in vivo-like |
| Differentiation Potential | May be limited or aberrant | Enhanced, often more controlled and relevant |
| Inflammatory Profile | Can be higher (as seen in BMAT model) | Can be lower, more representative of native tissue [68] |
Strategic Framework for Culture Optimization
Advanced Culture Platforms and Scaffolds
The choice of scaffold is critical for 3D culture. Ideal scaffolds are biocompatible, porous, and provide mechanical support that guides tissue development. For bone marrow-derived MSCs, porous silk fibroin scaffolds with pores of 500–600 microns have been successfully used to create stable 3D BMAT models that can be cultured for at least three months in vitro [68]. Similarly, in bone regeneration studies, a hybrid scaffold of β-Tricalcium Phosphate (β-TCP) and Recombinant Collagen Peptide (RCP) fabricated using 3D printing technology provided an internal structure suitable for cell loading, growth, and colonization [69]. The RCP coating was specifically designed to promote bone replacement, showing how scaffold functionalization can direct stem cell fate and potency.
Monitoring Differentiation Status and Timing
The timing of cell transplantation or harvest is a critical variable. A study optimizing bone marrow cell culture for bone regeneration found that the differentiation status of the cells profoundly impacted outcomes. The research employed alkaline phosphatase (ALP) staining, alizarin red staining, and real-time RT-PCR for markers like Runx2, Alp, Col1a1, and Bglap to track osteoblastic differentiation [69]. The results demonstrated that cells cultured for 7 days—characterized by peak Runx2 and Alp expression and prominent ALP staining (indicating a pre-maturation state)—were the most efficient for bone regeneration upon transplantation. In contrast, cells cultured for 14 days, which showed mineralization (alizarin red staining) and high expression of later markers, were less effective [69]. This underscores that for some applications, propagating a progenitor-like state is more therapeutically valuable than driving full terminal differentiation in vitro.
Diagram 1: Culture duration optimization workflow.
Cell Substrate Selection for Potency Assays
The foundation of any potency assay is a relevant and reproducible cellular response. The choice of cell substrate directly impacts the assay's relevance to the MoA, sensitivity, and reproducibility [70].
- Primary Cells: These are often the gold standard for biological relevance, as they accurately represent in vivo conditions. However, they present challenges for potency assays due to donor-to-donor variability, limited lifespan, and the need for repeated collections, which can compromise assay consistency [70].
- Immortalized Cells: These cells offer indefinite proliferation, ensuring a consistent and scalable source of material. Their drawback is that the genetic alterations required for immortality can lead to reduced physiological relevance and potential chromosomal aberrations, which may not fully reflect the complexity of native tissue [70].
- Engineered Cells: These provide a flexible and powerful solution, especially for complex MoAs. They can be customized to express specific receptors or reporter constructs. The main challenge is ensuring stable and reproducible expression of the introduced genetic material over successive passages, which may require advanced techniques like CRISPR/Cas9-based genome editing [70].
Table 2: Functional Potency Assays for Different Stem Cell Mechanisms of Action
| Mechanism of Action | Example Potency Assay | Measurable Readout | Applicable Cell Types |
|---|---|---|---|
| Direct Differentiation | In vitro trilineage differentiation | Quantification of adipogenic (Oil Red O), osteogenic (Alizarin Red), and chondrogenic (Alcian Blue) stains [1] | MSCs |
| Immunomodulation | Co-culture with activated immune cells (e.g., PBMCs) | Suppression of T-cell proliferation (e.g., via CFSE dilution) or reduction of pro-inflammatory cytokine (e.g., IFN-γ) secretion [66] [2] | MSCs |
| Paracrine Signaling | Conditioned media bioassay on target cells | Promotion of endothelial cell tube formation; stimulation of fibroblast migration in a scratch assay | MSCs, Adipose-derived cells |
| Cytotoxicity (for immune cells) | Co-culture with target cells | Measurement of target cell lysis (e.g., 51Cr release, flow cytometry with live/dead dyes) or induction of degranulation (CD107a) [66] | CAR-T, NK cells |
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for Culture and Potency Assessment
| Reagent / Material | Function | Example in Context |
|---|---|---|
| Silk Fibroin Scaffolds | Provides a biocompatible, porous 3D structure for cell growth and tissue formation. | Used to create a stable 3D bone marrow adipose tissue (BMAT) model for studying adipocyte-tumor interactions [68]. |
| β-TCP/RCP Hybrid Scaffold | A synthetic bone graft material that supports osteoblast progenitor cell attachment and bone regeneration. | 3D-printed scaffold used for transplanting pre-cultured bone marrow cells, leading to efficient bone formation in vivo [69]. |
| Recombinant Collagen Peptide (RCP) | Coating material that enhances cell attachment and promotes tissue-specific regeneration (e.g., bone). | Coated onto β-TCP scaffolds to improve bone replacement outcomes [69]. |
| Custom Cell Mimics (e.g., TruCytes) | Standardized, engineered cells used as reference materials in potency assays to ensure consistency and reproducibility. | Enable early development of MoA-relevant potency assays (e.g., measuring IFN-γ from CAR-T cells) before final clinical material is available [65]. |
| Adipogenic Induction Cocktail | A mixture of compounds to direct stem cell differentiation into adipocytes. | Typically contains IBMX, indomethacin, dexamethasone, and insulin, as used for differentiating human MSCs into BMAs [68]. |
| Master Cell Bank (MCB) & Working Cell Bank (WCB) | A tiered system of cryopreserved, well-characterized cells that ensures a consistent and reliable source for assays and manufacturing. | Critical for providing a reproducible foundation for potency assays and reducing variability between experimental runs [70]. |
Integrated Experimental Protocols
Protocol: Establishing a 3D Bone Marrow Adipose Tissue Model
This protocol is adapted from research aimed at creating a physiologically relevant model for studying the bone marrow niche and its role in disease [68].
Scaffold Preparation:
- Utilize porous, aqueous 6.5% (wt/wt) silk fibroin scaffolds with pore sizes of 500–600 microns.
- Cut scaffolds into cylinders (e.g., 5 mm diameter x 3 mm height).
- Autoclave for sterilization.
- Pre-soak scaffolds in culture media containing 10% FBS and 1% Penicillin-Streptomycin-Fungizone one day prior to cell seeding.
Cell Isolation and Expansion:
- Isolate primary human Mesenchymal Stromal Cells (MSCs) from cancellous bone marrow obtained from surgical waste (e.g., total hip arthroplasty) via IRB-approved protocols.
- Isolate MSCs by plastic surface adherence in expansion media: DMEM supplemented with 10% FBS, 2 mM L-glutamine, and 1X Antibiotic-Antimycotic.
- Culture until approximately 50% confluency, remove non-adherent cells, and expand MSCs for use at passage 2-4.
3D Seeding and Culture:
- Seed MSCs onto the pre-soaked silk scaffolds at a density of approximately 1 x 10^6 cells per scaffold in a minimal volume (~20 μL) to facilitate cell attachment.
- After 2 hours, add sufficient media to the wells to fully cover the scaffolds.
- Allow cells to expand on the scaffolds until they appear evenly spread throughout the structure (typically 1-10 days).
Adipogenic Differentiation:
- Switch the media to adipogenic induction media once the scaffolds are confluent.
- For human MSCs, use basal hMSC media supplemented with 500 μM IBMX, 50 μM indomethacin, 1 μM dexamethasone, and 1 μM insulin.
- Maintain cultures, with regular media changes, for up to several weeks to form a mature BMAT model. The model can be stably cultured for at least 3 months in vitro.
Protocol: Optimizing Pre-culture Duration for Bone Regeneration
This protocol outlines the key steps to determine the optimal culture period for bone marrow cells before transplantation onto a scaffold, a critical factor for maximizing therapeutic efficacy [69].
Cell Culture and Differentiation:
- Isolate bone marrow cells from the tibia and femora of mice (e.g., C57BL/6J).
- Subject the cells to osteogenic culture for varying durations (e.g., 4, 7, and 14 days).
Monitoring Differentiation Status:
- Alkaline Phosphatase (ALP) Staining: Perform at each time point to identify early osteogenic differentiation. The most prominent staining is often observed at the intermediate time point (e.g., day 7).
- Alizarin Red Staining: Perform to detect late-stage mineralization and calcium deposition, which should be positive at longer culture durations (e.g., day 14).
- Real-time RT-PCR Analysis: Quantify expression of key osteogenic markers:
- Early/Mid Markers: Runx2 (peak expression often at day 7), Alp (peak expression often at day 7).
- Late Markers: Col1a1 (peak expression often at day 14), Bglap (Osteocalcin, peak expression often at day 14).
Flow Cytometry Analysis:
- Analyze changes in the abundance of other cell populations, such as endothelial cells and monocytes, over the culture period. This provides a broader understanding of the cellular composition being transplanted.
In Vivo Validation:
- Load cells from each culture time point (4, 7, 14 days) onto the scaffold (e.g., β-TCP/RCP).
- Implant the cell-scaffold constructs subcutaneously or subperiosteally into an animal model (e.g., mice).
- Harvest grafts after a set period (e.g., 8 weeks) and evaluate them histologically for bone formation. The time point that shows the most prominent osteogenesis in vivo (e.g., day 7 in the cited study) is identified as the optimal pre-culture duration.
Diagram 2: Potency assay development strategy.
Optimizing culture systems for adult stem cells derived from bone marrow and adipose tissue requires an integrated, Quality-by-Design (QbD) approach. This involves strategically selecting culture platforms—favoring 3D over 2D where possible—and fine-tuning process parameters like culture duration based on functional readouts of differentiation status. Crucially, this optimization cannot be performed in a vacuum. It must be guided by robust, MoA-relevant potency assays that are developed early in the process and use well-characterized cell substrates to ensure consistency and regulatory compliance [65] [70]. By treating potency not as a final release checkpoint but as a central guide for process development, researchers can de-risk their programs and accelerate the translation of high-quality, effective adult stem cell therapies from the bench to the bedside.
The field of regenerative medicine is poised to revolutionize treatment for a wide range of diseases through the application of adult stem cells derived from somatic tissues such as bone marrow and adipose tissue. These cells, particularly mesenchymal stem/stromal cells (MSCs), possess remarkable regenerative and immunomodulatory properties that make them attractive therapeutic candidates [71]. However, a significant translational barrier exists: the transition from laboratory-scale research to large-scale production under Good Manufacturing Practice (GMP) standards [72].
This challenge is particularly acute for adult stem cell therapies because most clinical applications require millions to hundreds of millions of cells per dose, while the initial frequency of MSCs in native tissues is remarkably low—approximately one MSC per 10⁴–10⁵ mononuclear cells in bone marrow or per 10²–10³ cells from lipoaspirate [71]. Furthermore, the autologous nature of many therapies means manufacturing processes must accommodate patient-specific variations while maintaining consistency, quality, and safety [73]. This technical guide examines the core scalability challenges and presents solutions for GMP-compliant production of adult stem cells from bone marrow and adipose tissue sources, providing researchers and drug development professionals with practical frameworks for navigating this critical transition.
Core Scalability Challenges in Adult Stem Cell Manufacturing
Process Design and Scale-Up Limitations
Traditional planar culture systems, such as flasks and multi-layered vessels, present significant limitations for large-scale production. These systems require substantial manual manipulation, extensive incubator space, and are characterized by open processing steps that increase contamination risks [71]. The labor-intensive nature of these systems makes them economically unviable for commercial-scale production and challenges the reproducibility required by regulatory authorities [74]. Additionally, planar systems demonstrate limited scalability—achieving clinically relevant cell numbers often necessitates multiple passages that may compromise cell quality, as studies have reported decrements in proliferation and differentiation capacity of MSCs in late passages [71].
Biological and Donor Variability
A fundamental challenge in scaling adult stem cell production lies in their inherent biological heterogeneity. MSCs from different tissue sources (bone marrow versus adipose) exhibit distinct growth kinetics and functional properties [75]. Furthermore, donor-specific factors including age, health status, and tissue source significantly impact cell expansion potential [73]. One study investigating adipose-derived stem cells from different donors found notable differences in cell size and maximum achievable cell densities, which would directly impact lot-to-lot consistency in manufacturing [73]. For autologous therapies, this variability is compounded as each batch represents a unique product, requiring manufacturing processes robust enough to accommodate biological diversity while maintaining critical quality attributes.
Culture Medium and Supplement Standardization
The transition from research-grade to GMP-compliant manufacturing necessitates eliminating poorly defined components, most notably fetal bovine serum (FBS). While FBS has been a staple in research-scale cultures, its lot-to-lot variability and potential for xenogenic immunogenic reactions make it unsuitable for clinical production [71] [73]. The field is increasingly shifting toward serum-free or human-derived supplements like human platelet lysate (hPL), but this transition requires re-optimization of expansion protocols and validation of consistent cell quality [71]. Additionally, the qualification and sourcing of raw materials must comply with stringent regulatory standards, adding complexity to supply chain management.
Analytical and Quality Control Demands
As stem cell production scales, maintaining rigorous quality control becomes increasingly challenging yet essential. According to International Society for Cellular Therapy (ISCT) guidelines, MSCs must demonstrate plastic adherence, specific surface marker expression (CD105+, CD73+, CD90+, CD45-, CD34-, CD14-, CD11b-, CD79α-, HLA-DR-), and trilineage differentiation potential [71]. Beyond these identity criteria, manufacturers must establish potency assays, monitor genetic stability, and ensure absence of microbial contamination throughout the process [71] [74]. Implementing these analytical methods in a manner that keeps pace with production scale without creating bottlenecks represents a significant operational challenge.
Table 1: Key Challenges in Scaling Adult Stem Cell Production
| Challenge Category | Specific Limitations | Impact on Manufacturing |
|---|---|---|
| Process Design | Planar culture systems; Manual operations; Limited scale-up capacity | Labor intensive; Space inefficient; Contamination risk; Poor reproducibility |
| Biological Variability | Donor age and health status; Tissue source differences; Passage-dependent changes | Lot-to-lot inconsistency; Unpredictable expansion yields; Variable product quality |
| Culture Components | FBS variability and safety concerns; Component qualification; Supply chain management | Regulatory non-compliance; Immunogenic risks; Process instability |
| Quality Control | Complex identity testing; Potency assay development; Microbial contamination monitoring | Production bottlenecks; Extended release timelines; Increased costs |
Automated Manufacturing Platforms for Scalable GMP Production
Advanced bioreactor systems and automated platforms have emerged as essential solutions for overcoming traditional scalability limitations. These closed, integrated systems minimize manual intervention, enhance reproducibility, and provide the monitoring and control capabilities necessary for GMP compliance [71].
Comparative Analysis of Automated Expansion Systems
Table 2: Automated Bioreactor Systems for MSC Expansion
| System | Technology | Scale/Capacity | Reported Yield | Key Features |
|---|---|---|---|---|
| Quantum Cell Expansion System | Hollow fiber bioreactor | 21,000 cm² surface area | 100-276 × 10⁶ BM-MSCs in 7-day expansion [71] | Continuous medium exchange; Programmable gas control; Reduced open manipulations from 54,400 to 133 steps [71] |
| CliniMACS Prodigy | Integrated cell processing with adherent cell culture | Multi-layer vessels | >29-50 × 10⁶ equine MSCs at P0 [71] | Automated from isolation to harvest; Closed system; GMP-compliant medium available |
| Microcarrier-based Bioreactors | Stirred-tank with microcarriers | Scalable from 1-100 L | Varies with vessel size and MC density | Homogeneous culture environment; Monitoring and control of parameters; Scalable platform technology [73] |
| Hollow Fiber Bioreactors | Intracapillary cell growth | Up to 10⁹ cells [73] | High cell densities in small footprint | High surface-to-volume ratio; Continuous perfusion; Simulates in vivo microenvironment |
Implementation Considerations for Automated Platforms
Selecting an appropriate automated platform requires careful consideration of multiple factors. The Quantum system has demonstrated effectiveness in maintaining immunomodulatory function of expanded MSCs, with studies showing preserved ability to suppress T-lymphocyte activation in vitro [71]. Similarly, microcarrier-based systems in stirred bioreactors have proven effective for expanding adipose-derived stem cells under xeno-free conditions, with comparable growth between static and dynamically mixed conditions [73]. Process integration is another critical consideration—while some systems focus exclusively on expansion, others like the CliniMACS Prodigy offer complete integration from cell isolation through harvest, reducing processing steps and contamination risks [71].
Experimental Protocols for Scalable GMP-Compliant Expansion
Microcarrier-Based Expansion of Adipose-Derived Stem Cells
This protocol outlines a GMP-compliant approach for expanding human Adipose Tissue Stem Cells (hASCs) using microcarrier technology in dynamically mixed systems [73].
Materials and Reagents:
- Subcutaneous adipose tissue (abdominal region, obtained with ethical approval)
- Collagenase AB (0.28 Wünsch Unit/mL)
- Serum-free, xeno-free culture medium
- Human albumin (1% in PBS)
- Microcarriers (100-300 μm, suitable for hASC attachment)
- Stirred bioreactor system
Procedure:
- Tissue Processing: Wash adipose tissue in PBS, separate from skin tissue, and homogenize using a blender (10-15 seconds for 100-400g of fat tissue).
- Enzymatic Digestion: Digest tissue with collagenase solution for 45 minutes at 37°C with gentle agitation.
- Reaction Termination: Add PBS supplemented with 1% human albumin to stop enzymatic reaction.
- Cell Seeding: Isolate Stromal Vascular Fraction (SVF) by centrifugation and seed onto microcarriers at appropriate density in serum-free medium.
- Dynamic Expansion: Culture in stirred bioreactor system with controlled parameters (mixing speed: 49 rpm for 10 g/L microcarriers, power input per volume: 0.63 W/m³, nominal shear stress: 4.96 × 10⁻³ Pa).
- Monitoring: Sample regularly for cell counting, viability assessment, and metabolite analysis (glucose, lactate).
- Harvesting: Harvest cells when densities reach 0.41-0.56 × 10⁵ hASCs/cm² (end of exponential growth phase) using appropriate detachment protocol.
Critical Process Parameters:
- Maintain cells below hyperconfluent state to preserve stemness
- Monitor glucose and lactate levels to guide feeding strategies
- Control hydrodynamic stresses to avoid negative effects on cell growth
- Determine harvest timing based on growth phase rather than fixed timelines
Process Analytical Technologies and Quality Control
Implementing robust monitoring throughout the expansion process is essential for GMP compliance. The following analytical approaches should be integrated:
Growth and Metabolic Monitoring:
- Regular cell counting and viability assessment (trypan blue exclusion or automated methods)
- Glucose consumption and lactate production rates to monitor metabolic activity
- Lactate dehydrogenase (LDH) release as indicator of cell damage
- Morphological evaluation through microscopy
Quality Attribute Verification:
- Flow cytometry for surface marker expression (CD105, CD73, CD90, with absence of hematopoietic markers)
- Trilineage differentiation potential (adipogenic, chondrogenic, osteogenic) following ISCT guidelines
- Karyotyping or other genetic stability assessment at appropriate passages
- Endotoxin and mycoplasma testing
- Sterility testing per pharmacopeial methods
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for GMP-Compliant Stem Cell Expansion
| Reagent/Material | Function | GMP-Compliant Options |
|---|---|---|
| Culture Medium | Provides nutrients, growth factors, and physiological environment | Serum-free, xeno-free formulations; MSC-Brew GMP [71] |
| Growth Supplements | Enhances cell attachment, proliferation, and viability | Human platelet lysate (hPL); Defined growth factor cocktails |
| Microcarriers | Provides surface for cell attachment in 3D bioreactor systems | Polystyrene, gelatin, or natural polymer-based; 100-300 μm range [73] |
| Dissociation Reagents | Detaches cells from culture surfaces for passaging or harvest | Animal origin-free enzymes; Xeno-free trypsin alternatives |
| Cryopreservation Media | Preserves cell viability during frozen storage | Defined formulations with DMSO or DMSO-free alternatives; Serum-free cryoprotectants |
| Coating Substrates | Enhances cell attachment to bioreactor surfaces | Recombinant human adhesion proteins (fibronectin, vitronectin) [71] |
Visualization of Manufacturing Workflows and Relationships
Scalable GMP Manufacturing Workflow
Scale-Up Decision Pathway
Transitioning from laboratory-scale to large-scale GMP production of adult stem cells requires a systematic approach that addresses both technical and regulatory challenges. The implementation of automated bioreactor systems, adoption of defined culture components, and development of robust monitoring strategies form the foundation for successful scale-up. As the field advances, emerging technologies including artificial intelligence, advanced process analytical technologies, and continuous bioprocessing offer promising avenues for further enhancing the consistency, efficiency, and scalability of adult stem cell manufacturing. By adopting these frameworks and learning from successful implementations, researchers and drug development professionals can overcome critical scalability challenges and accelerate the delivery of transformative stem cell therapies to patients.
In the development of Advanced Therapy Medicinal Products (ATMPs), including those derived from adult somatic stem cell sources like bone marrow and adipose tissue, potency testing represents a fundamental critical quality attribute that separates biological medicinal products from those based on small molecules [76]. According to international regulatory guidance, potency is defined as the quantitative measure of biological activity linked to the relevant biological properties of the product, with assay results ideally correlating with clinical response [76]. For stem cell therapies, this represents a significant challenge as these "living drugs" possess complex and often pleiotropic mechanisms of action that cannot be fully characterized by surface markers alone [2] [76].
The regulatory imperative for robust potency assays is clear. The U.S. FDA requires quantitative functional potency assays for product release, while EU regulators may allow surrogate assays for release testing when correlated with functional characterization assays [76]. This regulatory landscape demands sophisticated validation approaches that capture the multifaceted biological functions of stem cells, particularly as the field advances toward later-stage clinical trials and commercial applications for bone marrow-derived mesenchymal stem/stromal cells (BM-MSCs) and adipose-derived stem cells (ASCs) [76] [77].
Key Functional Mechanisms to Assess
Stem cells exert their therapeutic effects through multiple interconnected mechanisms that must be captured in a comprehensive potency testing strategy. The table below summarizes the primary mechanisms and corresponding assessment approaches for adult stem cells from bone marrow and adipose sources.
Table 1: Key Functional Mechanisms and Assessment Approaches for Adult Stem Cell Potency
| Functional Mechanism | Biological Significance | Example Assessment Methods |
|---|---|---|
| Immunomodulation | Controls autoimmune/inflammatory responses; crucial for treating conditions like Crohn's disease and multiple sclerosis [2]. | T-cell proliferation suppression; cytokine secretion profiling (e.g., IFN-γ, IL-10) [78] [77]. |
| Paracrine Signaling | Promotes healing through secreted factors; important for heart failure and wound healing [2]. | Multiplex analysis of secreted factors (VEGF, HGF, FGF); conditioned media bioassays [78] [77]. |
| Differentiation Capacity | Replaces lost/damaged cells; relevant for osteoarthritis and spinal cord injury [2]. | Trilineage differentiation (adiopogenic, osteogenic, chondrogenic) with quantitative endpoint analysis [1] [79]. |
| Homing & Migration | Enables travel to injury sites; critical for stroke and rheumatoid arthritis applications [2]. | Transwell migration assays toward injury-related chemokine gradients (e.g., SDF-1) [77]. |
| Vasculogenic Support | Promotes blood vessel formation; essential for tissue engineering and ischemic conditions [80]. | Microfluidic co-culture with endothelial cells; vessel formation and stability quantification [80]. |
Each mechanism represents a potential axis for potency assay development, with the most comprehensive strategies incorporating multiple assays to capture the complex functional identity of stem cell products [76] [77].
Advanced In Vitro Potency Assay Platforms
3D Microfluidic Systems
Traditional 2D culture systems often fail to adequately predict clinical efficacy, leading to the development of advanced 3D models that better emulate in vivo conditions [78]. Recent work has demonstrated a microfluidic on-chip 3D system for evaluating patient-derived bone marrow aspirate concentrate (BMAC) samples from a Phase 3 multicenter trial for knee osteoarthritis (NCT03818737) [78].
This system utilizes a poly(dimethylsiloxane) (PDMS) microfluidic device with a cell-laden synthetic hydrogel (PEG-4MAL hydrogel presenting cell-adhesive RGD peptide) that is perfused with media at physiological flow rates (1.0 μL/min, approximating interstitial fluid velocity) [78]. When BMAC samples were cultured in this system with a customized osteoarthritis simulated synovial fluid (simSF), they exhibited elevated levels of immunomodulatory and trophic proteins compared to 2D culture [78]. Most importantly, secreted analyte data from the 3D system showed higher correlative power with patient pain scores and improved prediction of clinical outcomes compared to 2D assays [78].
Table 2: Comparison of 2D vs. 3D Microfluidic Potency Assay Platforms
| Parameter | Traditional 2D Assay | 3D Microfluidic System |
|---|---|---|
| Structural Complexity | Monolayer on plastic | 3D hydrogel matrix with perfusable channels |
| Mechanical Cues | Rigid, flat surface | Tunable matrix stiffness and fluid shear stress |
| Soluble Factor Gradients | Limited by diffusion | Controlled perfusion establishes physiological gradients |
| Secretory Profile | Baseline levels of analytes | Elevated immunomodulatory and trophic factors |
| Clinical Predictive Power | Limited correlation | Improved prediction of patient pain scores (VAS/KOOS) |
| Assay Duration | Typically several days | Rapid 24-hour perfusion culture |
Co-culture Models for Vasculogenic Potency Assessment
The ability of MSCs to support vascularization is a critical function for many regenerative applications. Recent research comparing the vasculogenic potency of BM-MSCs and ASCs in microfluidic chips revealed significant differences in their capacity to support microvascular network formation [80].
In this assay, MSCs are co-cultured with endothelial cells (such as HUVECs) in a fibrin hydrogel within a perfusable microfluidic chip (DAX-1; Aim Biotech) [80]. Both BM-MSCs and ASCs supported the formation of interconnected microvascular networks, but with distinct phenotypes: BM-MSCs induced formation of fully perfusable microvasculature with larger vessel area and length, while ASCs resulted in partially perfusable networks [80]. BM-MSCs also demonstrated superior pericyte characteristics with significantly higher expression of endothelial and pericyte-specific genes, as well as genes involved in vasculature maturation [80].
Diagram 1: Vasculogenic Potency Assay Workflow. This microfluidic co-culture system enables quantitative comparison of vasculogenic support capacity between different MSC sources.
Standardized Methodologies for Functional Validation
Immunomodulatory Potency Assessment
The immunomodulatory capacity of MSCs represents one of their most therapeutically relevant functions. A robust potency assay should evaluate the T cell suppression capability through co-culture systems [77]. The standard protocol involves:
- Isolate peripheral blood mononuclear cells (PBMCs) from healthy donors by density gradient centrifugation
- Activate T-cells using anti-CD3/CD28 antibodies or mitogens like phytohemagglutinin (PHA)
- Co-culture activated T-cells with MSCs at varying ratios (typically 1:10 to 1:100 MSC:T-cell ratios)
- Quantify T-cell proliferation via 3H-thymidine incorporation, CFSE dilution, or flow cytometric analysis of proliferation markers (Ki-67)
- Analyze cytokine profile in supernatant using multiplex ELISA (measuring IFN-γ, TNF-α, IL-10, TGF-β)
This functional assessment directly measures a key mechanism of action for MSCs in treating inflammatory and autoimmune conditions [2] [77].
Trilineage Differentiation Capacity
The multipotency of MSCs remains a cornerstone of their functional characterization, with the International Society for Cell & Gene Therapy (ISCT) recommending differentiation toward osteogenic, adipogenic, and chondrogenic lineages as a release criterion [79]. Standardized protocols include:
Adipogenic Differentiation:
- Induction Media: DMEM high glucose with 10% FBS, 1 μM dexamethasone, 0.5 mM IBMX, 10 μg/mL insulin, 200 μM indomethacin
- Duration: 14-21 days
- Validation: Oil Red O staining of lipid droplets, quantification after extraction, expression of PPARγ and FABP4
Osteogenic Differentiation:
- Induction Media: DMEM low glucose with 10% FBS, 0.1 μM dexamethasone, 10 mM β-glycerophosphate, 50 μM ascorbate-2-phosphate
- Duration: 21-28 days
- Validation: Alizarin Red S staining of mineralized matrix, quantitative calcium measurement, expression of Runx2 and osteocalcin
Chondrogenic Differentiation:
- Pellet Culture: 2.5×10^5 cells centrifuged in 15 mL polypropylene tube
- Induction Media: DMEM high glucose with 1% ITS+1, 0.1 μM dexamethasone, 50 μg/mL ascorbate-2-phosphate, 40 μg/mL proline, 10 ng/mL TGF-β3
- Duration: 21-28 days
- Validation: Alcian blue or Safranin O staining of proteoglycans, collagen type II immunohistochemistry
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for Stem Cell Potency Assays
| Reagent/Category | Specific Examples | Application in Potency Testing |
|---|---|---|
| Microfluidic Systems | DAX-1 chip (Aim Biotech), PDMS devices | 3D culture with perfusion for enhanced physiological relevance [78] [80] |
| Hydrogel Matrices | PEG-4MAL, Fibrin, Collagen I | 3D cell encapsulation with tunable biochemical/mechanical properties [78] [80] |
| Differentiation Kits | STEMPRO Adipogenesis/Osteogenesis/Chondrogenesis Kits | Standardized trilineage differentiation capacity assessment [79] |
| Cytokine Arrays | Luminex multiplex arrays, ELISA kits | Quantitative analysis of secretory function (VEGF, HGF, IL-6, etc.) [77] |
| Cell Tracking Dyes | CFSE, CellTracker dyes | Monitoring cell proliferation, migration, and persistence [77] |
| Flow Cytometry Antibodies | CD73, CD90, CD105, CD45, CD34, HLA-DR | Immunophenotype verification per ISCT criteria [79] |
Implementation Strategy for Comprehensive Potency Assessment
Developing a robust potency assay strategy requires systematic implementation across the product development lifecycle. For early-phase clinical trials, qualified methods are generally accepted, while validated methods must be in place for commercial production and pivotal trials [76]. A tiered approach is recommended:
- Mechanism of Action (MoA) Mapping: Identify all relevant MoAs for the specific clinical indication
- Assay Selection: Choose appropriate biological and surrogate assays for each MoA
- Matrix Development: Establish correlation between different assay readouts
- Validation: Demonstrate assay precision, accuracy, linearity, and robustness
- Clinical Correlation: Where possible, establish relationship between potency measures and clinical outcomes
The most successful implementations often employ a potency assay matrix that combines multiple complementary assays to fully capture the biological activity of complex cell therapy products [76] [77]. This is particularly important for products like BMAC, which contains heterogeneous cell populations with multiple potential mechanisms of action [78].
The evolution of potency testing beyond surface markers to robust functional assays represents a critical maturation in the stem cell therapy field. The advent of advanced platforms like 3D microfluidic systems that better predict clinical outcomes marks significant progress toward reliable product characterization [78]. As the field continues to advance, the implementation of comprehensive potency assessment strategies that capture the multifaceted nature of stem cell function will be essential for successful clinical translation of bone marrow and adipose-derived stem cell therapies.
Adult stem cells, particularly those derived from bone marrow and adipose tissue, represent a cornerstone of modern regenerative medicine and drug development research. Their multipotent differentiation capacity, relatively accessible somatic sources, and lower ethical concerns compared to embryonic stem cells make them highly promising for therapeutic applications [2] [67]. Mesenchymal stem cells (MSCs) from these sources can differentiate into adipocytes, chondrocytes, myocytes, cardiomyocytes, and osteoblasts, contributing to tissue maintenance and repair [81] [67]. However, the translational pathway from laboratory research to clinical application is fraught with technical challenges. A significant hurdle is the lack of standardized protocols for isolation, culture, and differentiation, leading to inconsistent results and difficulties in comparing data across studies [24] [81]. This guide identifies common pitfalls encountered at each stage of working with bone marrow and adipose-derived stem cells and provides evidence-based solutions to enhance protocol reliability and experimental reproducibility.
Isolation Pitfalls and Solutions
The initial isolation of stem cells from tissue sources is a critical step that can define the success of subsequent experiments. Inconsistencies here can compromise cell quality, purity, and functionality.
Tissue Acquisition and Pre-processing
- Pitfall 1: Inconsistent Donor Selection and Tissue Sampling: The functional properties of stem cells can vary significantly depending on the donor's age, health status, and the specific anatomical site of tissue harvest [2] [24]. For bone marrow, MSCs harvested from different bones of the same individual differ in regenerative potential and cell concentration [24]. For adipose tissue, subcutaneous and visceral fat depots contain adipocytes with different secretome, endocrine regulation, and proliferation rates [24].
- Solution: Implement strict donor screening criteria and document all donor metadata. Standardize the anatomical source for tissue harvesting (e.g., iliac crest for bone marrow, subcutaneous abdominal region for adipose tissue). For adipose-derived stem cells (ADSCs), specify whether white, brown, or beige adipose tissue was used, as their biological properties differ [24].
- Pitfall 2: Suboptimal Tissue Transport and Processing Delays: Extended time between tissue harvest and processing can lead to decreased cell viability and increased senescence due to ischemia and temperature fluctuations.
- Solution: Minimize the ischemic time by pre-establishing a streamlined workflow. Transport tissue in a sterile, temperature-controlled preservation solution validated for the specific tissue type.
Cell Harvesting Techniques
- Pitfall 3: Over-digestion with Enzymes: The use of collagenase for digesting adipose tissue or bone marrow is necessary to free stromal cells but can be detrimental if overly aggressive. Excessive enzyme concentration or prolonged incubation time can damage surface receptors and impair cell function [82].
- Solution: Perform enzyme titration and time-course experiments for each new batch of collagenase to determine the minimal effective concentration and duration. Routinely validate the activity of enzymatic batches.
- Pitfall 4: Inadequate RBC and Debris Removal: Failure to effectively remove red blood cells (RBCs) and tissue debris can inhibit the growth of the target stem cell population and lead to inaccurate cell counts.
- Solution: Incorporate a density gradient centrifugation step (e.g., using Ficoll-Paque or Percoll) following enzymatic digestion to efficiently separate mononuclear cells from RBCs and debris [82]. For adipose tissue, thorough washing of the lipoaspirate with sterile buffer before digestion is crucial.
Culture Pitfalls and Solutions
Once isolated, maintaining stem cells in culture requires careful attention to their microenvironment to preserve their undifferentiated state, multipotency, and genomic stability.
Media and Supplementation
- Pitfall 1: Serum Batch Variability: The use of fetal bovine serum (FBS) as a media supplement introduces significant variability due to differences in growth factor and hormone composition between batches. This is a major contributor to poor inter-laboratory reproducibility [81].
- Solution: Where possible, transition to defined, xeno-free culture media. If FBS is necessary, perform a multi-batch qualification test based on the specific MSC application (e.g., proliferation rate, differentiation potential) and create a large, single-batch stock to be used for an entire research program [81].
- Pitfall 2: Unoptimized Seeding Density: Seeding cells at too low or too high a density can trigger spontaneous differentiation, senescence, or lead to contact inhibition that alters cell morphology and function.
- Solution: Determine the optimal seeding density for your specific cell type and application. For bone marrow-MSCs (BM-MSCs), a common range is 1,000-5,000 cells/cm². Adherence to plastic is a defining characteristic of MSCs, and this density supports proper adherence and expansion [82].
Passage and Maintenance
- Pitfall 3: High Passage-Induced Senescence: Repeated passaging can lead to cellular senescence, characterized by altered morphology (e.g., enlarged, flattened cells), slowed proliferation, and reduced differentiation capacity [81].
- Solution: Establish a maximum passage number for your experiments (e.g., passage 4-6 for many MSC applications). Monitor senescence-associated biomarkers (e.g., β-galactosidase activity) regularly. Use cryopreserved low-passage cell stocks to ensure consistency.
- Pitfall 4: Mycoplasma Contamination: Mycoplasma contamination is a common, often undetected, problem that can alter cell behavior, metabolism, and viability, leading to unreliable data.
- Solution: Implement a strict routine testing protocol for mycoplasma using PCR-based or enzymatic assays. Practice aseptic technique and quarantine new cell lines until tested.
Table 1: Troubleshooting Common Culture Problems
| Problem | Potential Causes | Solutions |
|---|---|---|
| Slow Proliferation | High passage number, suboptimal serum, low seeding density, microbial contamination | Use low-passage cells, qualify serum batches, optimize seeding density, test for contamination [81] |
| Spontaneous Differentiation | High cell density, inappropriate media, serum factors | Maintain subconfluent cultures, use fresh differentiation-inducing media only when needed, try defined media [67] |
| Altered Morphology | Senescence, contamination, over-trypsinization | Monitor passage number, check for contamination, standardize passaging protocol [81] |
| Poor Attachment | Over-passaging, damaged surface receptors from over-trypsinization, low quality coating matrix | Reduce passaging frequency, optimize trypsinization time/temperature, ensure proper surface coating [82] |
Differentiation Pitfalls and Solutions
Directing stem cells toward a specific lineage is a complex process. Failure to achieve efficient and homogeneous differentiation undermines the validity of disease modeling and therapeutic applications.
Protocol Optimization and Validation
- Pitfall 1: Inefficient Differentiation Due to Cell Source or Status: The differentiation potential is not the same for all types of stem cells and depends on their source and stage of development [2]. BM-MSCs and ADSCs may exhibit varying efficiencies when directed toward osteogenic or chondrogenic lineages.
- Solution: Pre-screen your cell source for its potency toward the desired lineage. Do not assume all MSC sources are equivalent. Ensure cells are healthy, proliferating, and at an appropriate passage number before initiating differentiation.
- Pitfall 2: Inadequate Induction Cocktails and Timing: Using suboptimal concentrations of inducing agents (e.g., dexamethasone, ascorbate, IBMX) or incorrect temporal sequences can result in incomplete, heterogeneous, or off-target differentiation.
- Solution: Do not rely solely on published protocols without internal optimization. Perform dose-response and time-course experiments for critical inducing factors. The differentiation capability (into adipocytes, chondrocytes, and osteoblasts) is a defining criterion for MSCs and must be rigorously validated [82].
Confirmation and Characterization
- Pitfall 3: Over-reliance on Single Markers: Assessing differentiation success based on a single molecular marker (e.g., Oil Red O for adipocytes) can be misleading, as it may not confirm functional maturity or could represent an intermediate state.
- Solution: Implement a multi-parametric validation strategy. Combine histological staining, gene expression analysis (RT-qPCR for multiple lineage-specific genes), protein detection (immunocytochemistry/western blot), and, where possible, functional assays (e.g., calcium handling for cardiomyocytes) [83].
- Pitfall 4: Heterogeneous Cell Populations: Even with an optimized protocol, the resulting cell population is often a mix of fully differentiated, partially differentiated, and undifferentiated cells, which can confound experimental outcomes.
- Solution: Consider fluorescence-activated cell sorting (FACS) using cell surface markers specific for the target differentiated cell type to isolate a pure population for downstream applications.
Table 2: Key Markers for Validating MSC Differentiation
| Lineage | Induction Factors (Examples) | Key Validation Markers |
|---|---|---|
| Osteogenic | Dexamethasone, β-glycerophosphate, Ascorbate | Alkaline Phosphatase (ALP), Osteocalcin (OCN), Mineralization (Alizarin Red staining) [81] |
| Chondrogenic | TGF-β, Dexamethasone, Ascorbate | Aggrecan (ACAN), Collagen Type II (COL2A1), Sulfated Glycosaminoglycans (sGAG) deposition [81] |
| Adipogenic | Dexamethasone, IBMX, Indomethacin, Insulin | Peroxisome Proliferator-Activated Receptor γ (PPARγ), Fatty Acid Binding Protein 4 (FABP4), Lipid droplets (Oil Red O staining) [81] |
The Scientist's Toolkit: Research Reagent Solutions
Selecting the right reagents is fundamental for reproducibility. The following table details essential materials and their critical functions in adult stem cell research.
Table 3: Essential Research Reagents for Adult Stem Cell Work
| Reagent / Material | Function | Technical Considerations |
|---|---|---|
| Collagenase Type I/II | Enzymatic digestion of tissue (adipose, bone marrow) to release stromal vascular fraction. | Batch variability is high; requires activity testing and titration to avoid cytotoxicity [24] [82]. |
| Density Gradient Medium (e.g., Ficoll-Paque) | Isolation of mononuclear cells by density gradient centrifugation. | Critical for removing red blood cells and debris; density and centrifugation parameters must be standardized [82]. |
| Defined, Xeno-Free Media | Serum-free culture medium for expansion and differentiation. | Eliminates batch variability and ethical concerns of FBS; supports clinical translation [81]. |
| Flow Cytometry Antibodies | Immunophenotyping for MSC surface markers (e.g., CD73, CD90, CD105; lack of CD34, CD45). | Essential for confirming cell identity and purity per ISCT criteria; panel design is critical [82]. |
| Lineage-Specific Induction Factors | Directing differentiation toward osteogenic, chondrogenic, adipogenic, etc. lineages. | Cocktails require optimization for each cell source; common factors: TGF-β, BMPs, dexamethasone, ascorbate [81] [67]. |
Workflow and Signaling Visualization
Understanding the experimental workflow and the key signaling pathways involved in differentiation is crucial for intelligent troubleshooting. The diagram below outlines a generalized pathway from tissue isolation to characterized differentiation.
The following diagram summarizes the key signaling pathways that are often manipulated to direct MSCs toward common mesodermal lineages.
Navigating the complexities of adult stem cell research requires a meticulous and critical approach to protocol design and execution. The pitfalls in isolating, culturing, and differentiating BM-MSCs and ADSCs are significant, but they can be systematically addressed through rigorous standardization, validation, and a deep understanding of cell biology. By adopting the solutions outlined in this guide—such as qualifying reagent batches, monitoring cellular senescence, and implementing multi-parametric differentiation validation—researchers can significantly enhance the reliability and reproducibility of their data. As the field progresses, the move toward defined, xeno-free culture systems and the development of more precise differentiation protocols will be paramount in fully realizing the therapeutic potential of these powerful somatic cells in regenerative medicine and drug development.
Benchmarking Somatic Sources: A Comparative Analysis of Efficacy and Clinical Potential
The field of regenerative medicine has identified Mesenchymal Stem Cells (MSCs) as a cornerstone for developing novel therapeutic strategies. While MSCs can be isolated from various tissues, bone marrow (BM) and adipose (fat) tissue have emerged as the two most prevalent and clinically relevant sources. The choice between Bone Marrow-derived MSCs (BM-MSCs) and Adipose-derived MSCs (ADSCs) has significant implications for research methodology, therapeutic efficacy, and clinical translation. This whitepaper provides a systematic, technical comparison of BM-MSCs and ADSCs, focusing on their biological properties, immunomodulatory capacities, differentiation potential, and practical considerations for drug development and clinical application. Framed within a broader thesis on adult stem cell somatic tissue sources, this analysis aims to equip researchers and scientists with the quantitative data and experimental insights necessary to select the most appropriate cell source for specific biomedical applications.
Core Biological Properties and Practical Considerations
The fundamental characteristics of MSCs, including their isolation, expansion, and basic biology, vary significantly between bone marrow and adipose sources. These differences directly influence experimental design and clinical strategy.
Table 1: Comparative Characteristics of BM-MSCs and ADSCs [84] [85] [86]
| Parameter | Adipose-Derived MSCs (ADSCs) | Bone Marrow-Derived MSCs (BM-MSCs) | Key Implications |
|---|---|---|---|
| Harvest Site & Method | Subcutaneous fat via minimally invasive liposuction [86] | Iliac crest via bone marrow aspiration (more invasive) [86] | ADSC harvest is generally considered a less invasive procedure [84]. |
| Cell Yield (per mL tissue) | ~500,000–2,000,000 [86] | ~5,000–100,000 [86] | ADSCs offer a substantially higher initial yield, reducing the need for extensive in vitro expansion [85]. |
| Proliferation Rate | Higher [86] | Moderate [86] | ADSCs typically expand faster in culture, potentially shortening preparation time. |
| Metabolic Activity | Higher [85] | Lower [85] | Correlated with increased cytokine secretion in ADSCs [85]. |
| Key Markers in Tumor Tropism | Contribute to α-SMA+ vascular and fibrovascular stroma [87] | Contribute to FSP+/FAP+ Tumor-Associated Fibroblasts (TAFs) [87] | Suggests discriminative recruitment into tumor microenvironments based on origin [87]. |
Figure 1: Comparative Isolation and Culture Workflow for BM-MSCs and ADSCs.
Immunomodulatory Properties: A Quantitative and Functional Analysis
The immunomodulatory capacity of MSCs is a key therapeutic mechanism. Direct comparative studies reveal both qualitative similarities and important quantitative differences between BM-MSCs and ADSCs.
Comparative Potency and Cytokine Secretion
A systematic study comparing MSCs from age-matched donors found that while both cell types suppress the proliferation of stimulated peripheral blood mononuclear cells (PBMCs) and inhibit the differentiation of monocyte-derived immature dendritic cells (iDCs), ADSCs showed more potent immunomodulatory effects at equal cell numbers [85]. This enhanced potency is correlated with a higher baseline secretion of key immunomodulatory cytokines.
Table 2: Immunomodulatory Profile Comparison [85]
| Aspect | Adipose-Derived MSCs (ADSCs) | Bone Marrow-Derived MSCs (BM-MSCs) |
|---|---|---|
| Overall Immunosuppression | Potent effects at lower cell numbers [85] | Potent effects at higher cell numbers [85] |
| Key Cytokine Secretion | Higher levels of IL-6 and TGF-β1 [85] | Lower levels of IL-6 and TGF-β1 [85] |
| Functional Consequence | More potent suppression of PBMC proliferation [85] | Less potent suppression of PBMC proliferation [85] |
Experimental Protocol: PBMC Proliferation Suppression Assay
This protocol is a standard method for quantifying the immunomodulatory capacity of MSCs in vitro [85].
- MSC Plating: Plate MSCs (BM-MSCs or ADSCs) in graded doses in a 96-well flat-bottomed plate in DMEM-LG supplemented with 10% Fetal Calf Serum (FCS). Allow cells to adhere overnight.
- PBMC Stimulation: Isolate PBMCs from healthy donors using a Ficoll-Paque density gradient. Add PBMCs (1.0 × 10^5/well) to the MSC cultures and stimulate them with human T-activator CD3/CD28 Dynabeads at a bead-to-PBMC ratio of 1:5.
- Incubation and Measurement: Culture the co-cultures for 5 days. For the final 6-18 hours, pulse the cells with [³H]-thymidine.
- Data Analysis: Harvest the cells onto a filtermat and measure incorporated [³H]-thymidine using a β-scintillation counter. The percentage of suppression is calculated by comparing proliferation in co-cultures to proliferation of PBMCs alone.
Differentiation Potential and Therapeutic Efficacy
The functional capacity of MSCs is also defined by their ability to differentiate into various lineages and promote tissue regeneration in disease models.
Table 3: Differentiation Potential and Therapeutic Evidence [86] [84]
| Parameter | Adipose-Derived MSCs (ADSCs) | Bone Marrow-Derived MSCs (BM-MSCs) |
|---|---|---|
| Chondrogenic Differentiation | Moderate [86] | Strong [86] |
| Adipogenic Differentiation | High (native tissue origin) | Lower |
| Osteogenic Differentiation | Established protocol [85] | Established protocol [85] |
| Research Volume (PubMed) | Lower (e.g., 27 results for "stroke") [84] | Higher (e.g., 205 results for "stroke") [84] |
| Representative Therapeutic Finding | Effective for immunomodulatory therapy; potential alternative with lower cell numbers needed [85] | Efficacy in treating stroke, myocardial infarction, ALS, type I diabetes is "essentially settled science" [84] |
Figure 2: Differentiation Potential of BM-MSCs vs. ADSCs.
The Scientist's Toolkit: Essential Reagents and Materials
Successful isolation, culture, and characterization of MSCs require a standardized set of reagents and tools. The following table details essential items for working with both BM-MSCs and ADSCs.
Table 4: Key Research Reagent Solutions for MSC Research [85] [9]
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Ficoll-Paque | Density gradient medium for isolating mononuclear cells from bone marrow aspirates. | Critical first step for BM-MSC isolation; not typically needed for ADSC isolation from Stromal Vascular Fraction (SVF). |
| Collagenase (Type I/II) | Enzymatic digestion of extracellular matrix in adipose tissue to release the SVF. | Essential for liberating ADSCs from lipoaspirate samples; concentration and incubation time must be optimized. |
| DMEM-LG (Low Glucose) | Basal culture medium for MSC expansion. | Preferred over high-glucose DMEM for maintaining MSC stemness and preventing spontaneous differentiation. |
| Fetal Calf Serum (FCS) | Essential supplement for cell culture media providing growth factors and adhesion proteins. | Batch testing is crucial due to variability. Some protocols use Human Serum for clinical-grade expansions. |
| CD14 Microbeads (MACS) | Magnetic-activated cell sorting for purification of monocytes from PBMCs. | Used in co-culture experiments to isolate specific immune cell populations for functional assays [85]. |
| Osteo-/Adipogenic Induction Kits | Defined media cocktails containing inducing agents for lineage-specific differentiation. | Used for in vitro trilineage differentiation assays to confirm MSC multipotency. |
| Flow Cytometry Antibodies | Characterization of MSC surface marker profile (e.g., CD73, CD90, CD105) and immunophenotyping. | Essential for quality control and confirming MSC identity according to International Society for Cellular Therapy criteria. |
The choice between BM-MSCs and ADSCs is not a matter of one source being universally superior, but rather of selecting the right tool for a specific application. BM-MSCs are supported by a more extensive history of clinical research and may exhibit superior chondrogenic potential, making them a strong candidate for skeletal repair. ADSCs, in contrast, offer significant practical advantages in terms of harvest yield, proliferation rate, and potent immunomodulatory effects, positioning them as a highly efficient and accessible alternative for therapies leveraging paracrine signaling and immune regulation.
Future research should focus on standardizing isolation and characterization protocols across labs, conducting more direct, prospective comparative studies in specific disease models, and elucidating the precise mechanisms behind their functional differences. As the field progresses toward personalized medicine, understanding the unique advantages of each somatic tissue source will be paramount for developing effective, evidence-based regenerative therapies.
Within the field of regenerative medicine, adult mesenchymal stem cells (MSCs) are pivotal for their therapeutic potential. These cells are isolated from various somatic tissues, with bone marrow (BM) and adipose tissue (AT) being the most extensively studied and utilized sources [18] [1]. The choice of tissue source is not trivial, as it profoundly impacts the yield, expansion kinetics, and functional potency of the resulting MSCs, which in turn influences the feasibility and efficacy of clinical applications. For drug development professionals and translational scientists, a systematic understanding of the quantitative and kinetic differences between BM- and AT-derived MSCs is essential for rational experimental design and therapeutic development. This whitepaper synthesizes current research to provide a direct, data-driven comparison of these two prominent cell sources, focusing on the metrics that matter most for industrial and clinical translation: initial yield, proliferative capacity, and growth kinetics.
Isolation Yield and Proliferation Rates
The initial cell yield from tissue harvest and the subsequent proliferative capacity in culture are critical determinants for achieving the cell numbers required for therapy or research. The data indicate significant source-dependent variation.
Table 1: Quantitative Comparison of Yield and Proliferation between ATMSCs and BMMSCs
| Metric | Adipose-derived MSCs (ATMSCs) | Bone Marrow-derived MSCs (BMMSCs) | Notes & Context |
|---|---|---|---|
| Typical Isolation Yield | ~1 in 30 to 1 in 1,000 nucleated cells [88] | ~1 in 50,000 to 1 in 1,000,000 nucleated cells [88] | Yield from raw tissue; AT provides a substantially higher initial number of MSCs. |
| Proliferative Potential | Greater proliferative potential [18] | Lower proliferative potential compared to ATMSCs [18] | Assessed under identical culture conditions (e.g., human platelet lysate-supplemented medium). |
| Population Doubling | Higher cumulative population doubling (CPD) [18] | Lower CPD in serial passage studies [18] | Indicates a greater expansion capacity over multiple passages. |
| CFU-F Efficiency | No significant difference observed from BMMSCs [18] | No significant difference observed from ATMSCs [18] | Colony-forming unit-fibroblast efficiency reflects clonogenic potential. |
Experimental Evidence from Comparative Studies
A direct head-to-head comparison of BMMSCs and ATMSCs cultured under human platelet lysate (hPL) conditions confirmed that while both cell types exhibit a similar fibroblast-like morphology and standard MSC surface marker expression (CD105+, CD73+, CD90+), ATMSCs possess a significantly greater proliferative potential [18]. This study involved serial passaging of cells, with population doubling (PD) calculated at each passage using the formula PD = log10(Nh) / log10(2), where Nh is the harvested cell number and Np is the plated cell number. Cumulative population doubling (CPD) was then used to track total expansion capacity, clearly demonstrating the advantage of the adipose source [18].
Further supporting this, a study on peripheral nerve regeneration noted that the yield and proliferative ability of ATMSCs are greater than those of BMMSCs [89]. This makes AT an attractive source for applications requiring large cell numbers, as it is more accessible and provides a higher stromal cell yield with lower patient morbidity during harvest [89] [88].
Detailed Experimental Protocols for Comparison
To ensure reproducible and valid comparisons between MSC sources, standardized experimental workflows are crucial. The following protocols are adapted from key studies that directly compared BMMSCs and ATMSCs.
Protocol 1: Isolation and Expansion for Proliferation Kinetics
This protocol is designed for the direct comparison of proliferation rates and long-term expansion potential [18] [89].
Tissue Harvesting:
- Bone Marrow: Collect BM aspirates (e.g., 25 mL) from human donors. Isolate mononuclear cells via density gradient centrifugation (e.g., over a lymphoprep gradient). Plate the mononuclear cells at a high density (e.g., 2 × 10^5/cm²) [18].
- Adipose Tissue: Obtain lipoaspirate tissues (e.g., 25 mL). Wash extensively with PBS and digest with an equal volume of 0.2% collagenase type IV at 37°C for 30-40 minutes. Centrifuge the digest to obtain a stromal vascular fraction (SVF) pellet. Plate the viable SVF cells (e.g., 1 × 10^6) [18] [89].
Cell Culture:
- Culture both cell types in a standardized medium, such as Iscove’s Modified Dulbecco’s Medium (IMDM) supplemented with 5% human platelet lysate (hPL) and 2 U/mL heparin [18].
- Maintain cultures at 37°C with 5% CO₂. Replace the medium twice weekly.
- Upon reaching 80-90% confluence, harvest cells using trypsin-EDTA and replate at a standardized seeding density (e.g., 2,000 cells/cm²) for serial passaging [18].
Proliferation Assay:
- At each passage, harvest and count the cells when they reach 80-90% confluence.
- Calculate the Population Doubling (PD) for each passage using the formula:
PD = [log10(Nh) - log10(Np)] / log10(2)whereNhis the number of cells harvested andNpis the number of cells plated. - Calculate the Cumulative Population Doubling (CPD) by summing the PD of all passages [18].
Protocol 2: Colony-Forming Unit Fibroblast (CFU-F) Assay
This assay evaluates the clonogenic potential of freshly isolated MSCs, a key indicator of stemness [18].
- Cell Preparation and Plating: After the initial expansion (e.g., Passage 1), create a single-cell suspension of both BMMSCs and ATMSCs. Plate the cells in six-well culture plates at a low density (e.g., 1 × 10^3 cells per well) in IMDM supplemented with 5% hPL [18].
- Culture and Fixation: Incubate the plates for 14 days, changing the medium periodically. Do not disturb the colonies during medium changes. On day 14, carefully remove the medium, wash the cell layer with PBS, and fix with methanol for 10-15 minutes [18].
- Staining and Counting: Stain the fixed cells with crystal violet for 20-30 minutes. Gently rinse off the excess stain with water and allow the plates to air dry. Count only the distinct colonies composed of 50 or more cells under a microscope [18].
The experimental workflow for the direct comparison of MSC sources, from isolation to functional assay, is outlined below.
Molecular Mechanisms Underlying Proliferative Differences
The observed kinetic differences between BMMSCs and ATMSCs are rooted in distinct molecular and signaling pathways that regulate cell cycle progression, senescence, and differentiation commitment.
Signaling Pathways and Genetic Regulators
Senescence and Differentiation Bias: A major limitation in using autologous MSCs, particularly BMMSCs, is cellular senescence. Senescent MSCs exhibit reduced proliferation, impaired colony-forming ability, and a marked decline in osteogenic potential. With aging and in in vitro culture, there is a shift in the bone marrow microenvironment where mesenchymal and adipocyte progenitors undergo quantitative and qualitative transformations, favoring adipogenesis over osteogenesis [26]. This is regulated by altered signaling through pathways like Wnt/β-catenin, Notch, and PPARγ [26]. The adipogenic bias can inherently limit the proliferative capacity of the osteo-lineage cells.
Non-coding RNA Regulation: Recent research highlights the role of non-coding RNAs in fine-tuning MSC proliferation and differentiation. For instance, CircRNA_1809 has been identified as a promoter of osteogenic differentiation in BMMSCs. It functions as a competing endogenous RNA (ceRNA) by sponging miR-370-3p, which subsequently upregulates the expression of Kitlg, a gene critical for osteogenesis [90]. Disruption in such regulatory networks can differentially impact the maintenance of proliferative, undifferentiated states in MSCs from various sources.
Secreted Factors and Immunomodulation: The secretome profile—the collection of growth factors, cytokines, and chemokines secreted by cells—differs between BMMSCs and ATMSCs. Under identical hPL culture conditions, differences were observed in the secretion of basic fibroblast growth factor (bFGF), interferon-γ (IFN-γ), insulin-like growth factor-1 (IGF-1), stem cell-derived factor-1 (SDF-1), and hepatocyte growth factor (HGF) [18]. These factors create distinct autocrine and paracrine signaling environments that can directly influence proliferation and immunomodulatory potency, with ATMSCs often exhibiting more potent immunomodulatory effects [18].
The core signaling pathways that influence the proliferation and differentiation of MSCs within the bone marrow niche are summarized below.
The Scientist's Toolkit: Essential Research Reagents
Successful experimentation in MSC research relies on a foundation of key reagents and materials. The following table details essential components for the isolation, culture, and characterization of MSCs from bone marrow and adipose tissue.
Table 2: Key Research Reagent Solutions for MSC Studies
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Digestive Enzymes | Collagenase Type IV, Collagenase I [18] [89] | Breaks down the extracellular matrix to liberate stromal cells from adipose tissue (Collagenase IV) or bone marrow fragments. |
| Culture Media | Iscove’s Modified Dulbecco’s Medium (IMDM), Dulbecco’s Modified Eagle’s Medium (DMEM) [18] [88] | The basal nutrient medium for cell growth and expansion. |
| Media Supplements | Fetal Bovine Serum (FBS), Human Platelet Lysate (hPL) [18] | Provides essential growth factors, hormones, and attachment factors. hPL is a xeno-free alternative to FBS for clinical-grade expansion. |
| Characterization Antibodies | Anti-CD105, Anti-CD73, Anti-CD90, Anti-CD45, Anti-CD34 [18] [89] [91] | Used in flow cytometry to confirm the immunophenotype of MSCs (positive for CD105, CD73, CD90; negative for CD45, CD34). |
| Osteogenic Induction Supplements | Dexamethasone, Ascorbic Acid 2-Phosphate, β-Glycerophosphate [88] | Components of standard osteogenic differentiation media, inducing MSC differentiation into osteoblast lineage. |
| Analysis Kits | Alkaline Phosphatase (ALP) Assay Kit, Calcium Content Assay Kit [88] | Quantify activity of ALP (an early osteogenic marker) and calcium deposition (a late marker of mineralization), respectively. |
The direct comparison between adipose tissue and bone marrow as sources for MSCs reveals a clear trade-off that must be considered within the context of a specific research or therapeutic goal. Adipose tissue emerges as the superior source when the primary requirement is a high yield of cells with robust and sustained proliferative capacity. This makes ATMSCs particularly advantageous for applications requiring rapid expansion to large clinical-scale numbers. Conversely, bone marrow-derived MSCs, while more challenging to obtain in quantity, may be preferred for applications where enhanced osteogenic or chondrogenic differentiation potential is the critical factor [18]. The choice is not merely a matter of preference but a strategic decision. Understanding the quantitative and kinetic profiles of these somatic tissue sources, as detailed in this whitepaper, enables researchers and drug developers to systematically select the optimal cell source for their specific pathway to clinical application.
The therapeutic application of mesenchymal stem cells (MSCs) has undergone a fundamental shift. Initially valued for their differentiation potential, their capacity for tissue repair and regeneration is now largely attributed to their paracrine activity [92] [93]. MSCs secrete a complex array of bioactive molecules, collectively known as the secretome, which includes soluble factors (growth factors, cytokines, chemokines) and extracellular vesicles (EVs), particularly exosomes [94] [95]. These components act as sophisticated messengers, orchestrating processes such as angiogenesis, immunomodulation, and cell survival in recipient cells [96].
The composition of the secretome is not universal; it varies significantly with the MSC tissue source. For regenerative medicine, the two most clinically relevant somatic tissues are bone marrow (BM) and adipose tissue (AT) [18]. This technical guide provides a comparative analysis of the paracrine factor expression and exosome secretion profiles of BM-MSCs and AT-MSCs, framing the discussion within the context of selecting the optimal cell source for specific therapeutic applications in drug development and clinical research.
Comparative Analysis of Soluble Paracrine Factors
A head-to-head comparison of the soluble factors secreted by BM-MSCs and AT-MSCs reveals distinct profiles that inform their therapeutic specializations.
Table 1: Comparative Secretion of Key Soluble Factors by BM-MSCs and AT-MSCs
| Factor Category | Specific Factor | BM-MSC Secretion | AT-MSC Secretion | Primary Functional Implication |
|---|---|---|---|---|
| Angiogenic Factors | VEGF-A | High [92] [94] | Comparable/High [92] [94] | Promotes blood vessel formation |
| VEGF-D | Lower [92] [97] | Higher [92] [97] | Supports endothelial tubulogenesis | |
| HGF | Higher [18] | Lower [18] | Angiogenesis & tissue morphogenesis | |
| bFGF (FGF-2) | Comparable [92] | Higher [18] | Cell proliferation & angiogenesis | |
| Immunomodulatory & Other Factors | IGF-1 | Lower [18] | Higher [92] [18] [97] | Metabolic regulation & growth promotion |
| TGF-β | Higher [94] | Lower [94] | Immunosuppression & matrix synthesis | |
| SDF-1 | Higher [18] | Lower [18] | Stem cell homing & recruitment | |
| IL-8 | Lower [97] | Higher [97] | Neutrophil chemotaxis & angiogenesis | |
| PGE2 | Higher [94] | Lower [94] | Immunomodulation |
- AT-MSCs demonstrate a pronounced profile for promoting angiogenesis and cell proliferation, characterized by significantly higher expression of VEGF-D, IGF-1, and bFGF [92] [18] [97]. Functional assays confirm that the conditioned medium from human AT-MSCs (ASCs) leads to increased endothelial tubulogenesis, driven primarily by VEGF-A and VEGF-D [92].
- BM-MSCs show a stronger signature for immunomodulation and stem cell homing, secreting higher levels of TGF-β, HGF, and SDF-1 [18] [94]. This aligns with observations of their potent effects in modulating the immune response and recruiting other repair cells to injury sites.
Characterization and Cargo of MSC-Derived Exosomes
Exosomes are nano-sized (30–150 nm) extracellular vesicles derived from the endosomal system, specifically from multivesicular bodies (MVBs) that fuse with the plasma membrane [98] [95]. They are lipid-bilayer enclosed vesicles that carry a functional cargo of proteins, lipids, nucleic acids (mRNA, miRNA), and other bioactive molecules from their parent cell [99] [98].
Table 2: Characteristics of Exosomes from BM-MSCs vs. AT-MSCs
| Characteristic | BM-MSC Exosomes | AT-MSC Exosomes |
|---|---|---|
| General Production | Higher quantity under standard culture conditions [94] | Lower quantity under standard culture conditions [94] |
| Key Cargo Components | Proteins related to metabolic processes & regulation of biological processes [94] [93] | Distinct protein profile, potentially enriched for different regenerative pathways [94] |
| Common Markers | CD9, CD63, CD81 (present on surface, used for identification/isolation) [100] [98] | CD9, CD63, CD81 (present on surface, used for identification/isolation) [100] [98] |
| Functional Overlap | Shared core proteins & functional annotations with AT-MSC exosomes for tissue regeneration [93] | Shared core proteins & functional annotations with BM-MSC exosomes for tissue regeneration [93] |
Proteomic analyses reveal that while there is a substantial overlap in the core protein composition and functional annotations of exosomes from both sources, quantitative and qualitative differences exist [94] [93]. For instance, a study in canine species found that exosomes from BM-MSCs contained a greater number of proteins involved in the regulation of metabolic and biological processes compared to those from AT-MSCs [94]. The internalization of these exosomes by recipient cells is a regulated process, facilitated by adhesion signaling and specific endocytic pathways involving molecules like galectin-3 and lysosome-associated membrane protein-2C [100].
Diagram 1: Exosome Biogenesis and Uptake Pathway. Illustrates the formation of exosomes from multivesicular bodies in the donor cell and their subsequent internalization by a recipient cell, leading to functional changes.
Experimental Protocols for Secretome Analysis
Primary Cell Culture and Standardization
To ensure a valid comparative analysis, MSCs from different sources must be cultured under identical, standardized conditions [92] [18].
- Cell Source: Human BM-MSCs can be obtained commercially or isolated from bone marrow aspirates via density gradient centrifugation. Human AT-MSCs are typically isolated from lipoaspirate tissue via collagenase digestion and centrifugation to obtain the stromal vascular fraction [92] [18].
- Culture Medium: Use a base medium such as Dulbecco's Modified Eagle Medium (DMEM) low-glucose or Iscove’s Modified Dulbecco’s Medium (IMDM). For clinical relevance, supplement with 5%-10% human Platelet Lysate (hPL) instead of fetal bovine serum (FBS) to avoid xenogeneic immune reactions and to better mimic human physiological conditions [18].
- Cell Passaging: Harvest cells at 80-90% confluence using trypsin-EDTA and replate at a standardized density (e.g., 2,000 cells/cm²) [18]. Use cells within specific passages (e.g., P3-P6) to avoid senescence-related changes in the secretome.
Analysis of Soluble Factor Secretion
- Conditioned Media (CM) Collection:
- Culture MSCs until 70-80% confluent.
- Wash cells thoroughly with PBS to remove serum/residual proteins.
- Incubate with serum-free medium for 24-48 hours.
- Collect the CM and centrifuge at 2,000 × g for 10 minutes to remove cells and debris. Aliquot and store at -80°C [92].
- Protein Quantification:
- Enzyme-Linked Immunosorbent Assay (ELISA): The gold standard for quantifying specific soluble factors (e.g., VEGF, IGF-1, HGF) in CM using specific antibody pairs [92] [18].
- Multiplex Bead-Based Assays (e.g., Luminex): Enable high-throughput, simultaneous quantification of dozens of analytes from a small volume of CM [18] [94].
Isolation and Characterization of Exosomes
Several techniques are available for exosome isolation, each with advantages and limitations.
Table 3: Common Techniques for Exosome Isolation
| Method | Principle | Advantages | Disadvantages |
|---|---|---|---|
| Ultracentrifugation | Sequential centrifugation steps based on size/density | Widely used; no reagent requirement | Time-consuming; can cause vesicle aggregation/damage [100] [98] |
| Size Exclusion Chromatography (SEC) | Separates particles by size through a porous column | Preserves vesicle integrity & function; good purity | May not fully separate from similar-sized proteins [98] |
| Tangential Flow Filtration (TFF) | Uses tangential flow across membranes for size-based separation | Scalable for industrial/manufacturing use | Requires specialized equipment [98] |
| Immunoaffinity Capture | Uses antibodies against exosome surface markers (CD9, CD63, CD81) | High specificity and purity | Lower yield; captures only specific subpopulations [98] |
- Characterization Workflow: Isolated exosomes must be characterized using a combination of techniques:
- Nanoparticle Tracking Analysis (NTA): Determines particle size distribution and concentration [95].
- Transmission Electron Microscopy (TEM): Provides visual confirmation of classic cup-shaped morphology [100] [95].
- Western Blot: Confirms the presence of positive markers (CD9, CD63, CD81, TSG101) and the absence of negative markers (e.g., calnexin) [100] [98].
Diagram 2: Experimental Workflow for Secretome Analysis. Outlines the key steps from cell culture and conditioned media collection to exosome isolation, characterization, and functional validation.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 4: Essential Reagents and Kits for Secretome Research
| Item | Function/Application | Example/Brief Explanation |
|---|---|---|
| Human Platelet Lysate (hPL) | Serum supplement for clinical-grade MSC culture | Xeno-free alternative to FBS; promotes MSC expansion [18]. |
| Collagenase, Type I/IV | Enzymatic digestion of adipose tissue | Liberates AT-MSCs from the stromal vascular fraction [92] [18]. |
| Lymphoprep / Ficoll-Paque | Density gradient medium | Isolation of mononuclear cells from bone marrow aspirates [18]. |
| CD9/CD63/CD81 Antibodies | Exosome characterization & isolation | Used for Western Blot, Immunoaffinity Capture, and flow cytometry [100] [98]. |
| ELISA Kits | Quantification of soluble factors | Target-specific kits for VEGF, IGF-1, HGF, etc. [92] [18]. |
| Total Exosome Isolation Kits | Precipitation-based isolation from CM | Simplified, column-based isolation methods [98]. |
| NTA System (e.g., NanoSight) | Particle size & concentration analysis | Characterizes exosome preparation according to MISEV guidelines [95]. |
| TEM with Negative Staining | Morphological analysis of exosomes | Validates the cup-shaped structure of isolated vesicles [100] [95]. |
The choice between BM-MSCs and AT-MSCs is not a matter of superiority, but of strategic alignment with therapeutic goals. AT-MSCs, with their robust pro-angiogenic and proliferative secretome, high IGF-1 and VEGF-D expression, and superior proliferative capacity, may be the preferred source for therapies targeting wound healing, cardiovascular ischemia, and conditions requiring rapid vascularization [92] [18]. Conversely, BM-MSCs, with their strong immunomodulatory profile, high secretion of HGF and SDF-1, and potent osteogenic/chondrogenic potential, appear better suited for applications in immune disorders, bone/cartilage regeneration, and therapies leveraging stem cell homing [18] [96].
The future of MSC-based therapeutics is increasingly leaning toward cell-free approaches utilizing purified secretome components or engineered exosomes [93] [95]. Understanding the nuanced differences cataloged in this analysis is paramount for researchers and drug development professionals to rationally select the ideal somatic tissue source, optimize production protocols, and develop highly effective, targeted regenerative medicines.
Within regenerative medicine, the functional efficacy of mesenchymal stem cells (MSCs) is primarily governed by two core properties: their capacity for multi-lineage differentiation and their potent immunomodulatory activity. These metrics are critically influenced by the somatic tissue source from which the cells are derived. This whitepaper provides a technical analysis of the functional efficacy of bone marrow-derived MSCs (BM-MSCs) and adipose-derived MSCs (AD-MSCs), the two most prevalent adult stem cell sources. It synthesizes current quantitative data on their differentiation potential and immunomodulatory signatures, details standardized experimental protocols for their assessment, and diagrams the key signaling pathways involved. The objective is to equip researchers and drug development professionals with a structured framework for the quantitative evaluation and selection of MSC sources for specific therapeutic applications.
Mesenchymal stem cells (MSCs) are defined by the International Society for Cellular Therapy (ISCT) as plastic-adherent cells expressing specific surface markers (CD73, CD90, CD105) and lacking hematopoietic markers, with the capacity to differentiate into osteogenic, chondrogenic, and adipogenic lineages in vitro [50]. While MSCs can be isolated from various tissues, bone marrow and adipose tissue represent the most extensively studied adult somatic sources for clinical and research applications [86] [50].
The "functional efficacy" of these cells is not a unitary metric but a composite of specific biological competencies. For the purposes of this guide, functional efficacy is quantified through two primary axes:
- Differentiation Potential: The ability to undergo commitment and differentiate into specific mesodermal lineages—osteogenic, chondrogenic, and adipogenic—which is crucial for structural tissue regeneration.
- Immunomodulatory Strength: The capacity to modulate immune responses through paracrine signaling and direct cell-cell contact, primarily via the secretion of soluble factors and extracellular vesicles that alter the behavior of immune cells [50].
Both axes are significantly impacted by the tissue of origin, necessitating a direct comparative analysis to inform pre-clinical and clinical development.
Quantitative Comparison of AD-MSCs and BM-MSCs
A comparative analysis of peer-reviewed studies and clinical data reveals distinct functional profiles for AD-MSCs and BM-MSCs. The table below summarizes key quantitative and qualitative efficacy metrics.
Table 1: Comparative Functional Efficacy Metrics of AD-MSCs and BM-MSCs
| Parameter | Adipose-Derived MSCs (AD-MSCs) | Bone Marrow-Derived MSCs (BM-MSCs) | References |
|---|---|---|---|
| Harvest Site & Cell Yield | Subcutaneous fat (liposuction); ~500,000–2,000,000 cells/mL | Iliac crest (aspiration); ~5,000–100,000 cells/mL | [86] |
| Proliferation Rate | Higher | Moderate | [86] |
| Chondrogenic Differentiation | Moderate | Strong / Superior | [86] [101] |
| Osteogenic Differentiation | Moderate | Strong | [50] |
| Adipogenic Differentiation | Strong (native tissue environment) | Moderate | [50] |
| Key Immunomodulatory Factors | Strong secretome; IL-10, TGF-β, PGE2 | Moderate secretome; upregulation of IL-10 demonstrated in specific models | [86] [101] [102] |
| Key Pro-inflammatory Targets | Downregulates TNF-α | Downregulates TNF-α and MMP-13 | [101] |
| Performance in Aged Microenvironment | Maintained cell yield and phenotype | Reduced proliferation and differentiation potential | [86] [101] |
The data indicates that BM-MSCs demonstrate superior chondrogenic and osteogenic potential, making them a preferred source for skeletal repair [86] [101]. Conversely, AD-MSCs offer a significant practical advantage in cell yield and proliferative capacity, and their immunomodulatory secretome is often more robust, though BM-MSCs have shown superior immunomodulatory outcomes in specific inflammatory models, such as septic arthritis [101].
Experimental Protocols for Assessing Differentiation Potential
Standardized, reproducible assays are critical for the accurate evaluation of MSC differentiation. The following protocols are adapted from established methodologies.
Adipogenesis Assay Protocol
This protocol is optimized for human BM-MSCs (hBM-MSCs) but is applicable to AD-MSCs with minimal adjustments [103].
Research Reagent Solutions:
- Induction Medium: Dulbecco's Modified Eagle Medium (DMEM) high glucose, 10% Fetal Bovine Serum (FBS), 1% Penicillin-Streptomycin (P/S), 1 µM Dexamethasone (induces differentiation), 0.5 mM 3-Isobutyl-1-methylxanthine (IBMX, raises cAMP levels), 10 µg/mL Insulin (promotes lipid accumulation), 200 µM Indomethacin (PPARγ agonist).
- Maintenance Medium: DMEM high glucose, 10% FBS, 1% P/S, 10 µg/mL Insulin.
- Staining Solution: Oil Red O (ORO) in 60% isopropanol (stains neutral lipids).
- Fluorescence Detection: Nile Red solution or BODIPY 493/503 (alternative neutral lipid dyes), Hoechst 33342 (nuclear counterstain).
Detailed Methodology:
- Cell Seeding: Seed hBM-MSCs at a standardized density of 2.0 x 10^4 cells/cm² in basal growth medium (DMEM + 10% FBS + 1% P/S). Allow cells to adhere for 24 hours.
- Induction Cycle: Replace the medium with Adipogenic Induction Medium. Incubate for 3 days.
- Maintenance Cycle: Replace the medium with Adipogenic Maintenance Medium. Incubate for 1-3 days.
- Cycle Repetition: Repeat steps 2 and 3 for a total of 3-5 cycles to ensure robust adipogenic differentiation.
- Staining and Quantification:
- Wash cells with Phosphate Buffered Saline (PBS) and fix with 4% Paraformaldehyde (PFA) for 20 minutes.
- Wash with PBS and incubate with pre-filtered 0.3% Oil Red O working solution for 30-60 minutes.
- Wash extensively with distilled water to remove unbound dye.
- For quantification, elute the bound ORO dye with 100% isopropanol and measure the absorbance at 520 nm. Alternatively, use fluorescence-based quantification with Nile Red, normalized to cell count via Hoechst staining.
Diagram 1: Adipogenesis assay workflow
Chondrogenesis & Osteogenesis Assay Protocols
Chondrogenic Differentiation:
- Method: Pellet or micromass culture system to mimic cell-cell interactions of cartilage development.
- Induction Medium: DMEM high glucose, 1% ITS+ Premix, 1% P/S, 50 µg/mL Ascorbate-2-phosphate, 40 µg/mL Proline, 100 nM Dexamethasone, 10 ng/mL Transforming Growth Factor-beta 3 (TGF-β3).
- Analysis: Histological sectioning and staining with Toluidine Blue (proteoglycans) or Alcian Blue (glycosaminoglycans, GAGs). Immunohistochemistry for Collagen Type II (COL2A1) [101].
Osteogenic Differentiation:
- Induction Medium: DMEM low glucose, 10% FBS, 1% P/S, 50 µg/mL Ascorbate-2-phosphate, 10 mM β-glycerophosphate, 100 nM Dexamethasone.
- Analysis: Staining with 2% Alizarin Red S (ARS) to detect calcium deposits. Quantify by eluting ARS with cetylpyridinium chloride and measuring absorbance at 562 nm.
Experimental Protocols for Quantifying Immunomodulatory Strength
The immunomodulatory capacity of MSCs is primarily assessed by their ability to suppress immune cell activation and their secretome profile.
In Vitro T-cell Proliferation Suppression Assay
This assay measures the functional ability of MSCs to suppress the activation of peripheral blood mononuclear cells (PBMCs).
Research Reagent Solutions:
- Mitogen: Phytohemagglutinin (PHA).
- Co-culture System: Transwell inserts to separate MSCs from PBMCs (paracrine-only effect) or direct contact co-culture.
- Proliferation Dye: Carboxyfluorescein succinimidyl ester (CFSE).
- Cell Separation: Ficoll-Paque gradient for PBMC isolation.
Detailed Methodology:
- PBMC Isolation: Isolate PBMCs from human blood using density-gradient centrifugation with Ficoll-Paque.
- PBMC Labeling: Resuspend PBMCs in PBS containing 1-5 µM CFSE and incubate for 20 minutes. Quench the reaction with 5 volumes of FBS.
- Co-culture Setup: Seed MSCs (e.g., BM-MSC1 or AD-MSC1) in a 24-well plate and allow to adhere overnight. Add CFSE-labeled PBMCs to the wells at a defined MSC:PBMC ratio (e.g., 1:10). Add PHA to stimulate T-cell proliferation.
- Controls: Include wells with PBMCs + PHA but without MSCs (maximum proliferation control), and PBMCs without PHA (background proliferation control).
- Analysis: After 3-5 days, harvest PBMCs and analyze CFSE fluorescence intensity by flow cytometry. The degree of suppression is calculated by the reduction in the proportion of CFSE-low (proliferated) cells in co-culture wells compared to the maximum proliferation control.
Secretome Analysis via ELISA/Multiplex Assay
Quantifying the cytokine profile of MSC-conditioned media provides a direct measure of immunomodulatory strength.
Detailed Methodology:
- Conditioned Media Collection: Culture MSCs under standard or inflammatory conditions (e.g., primed with IFN-γ). After 24-48 hours, collect the supernatant and centrifuge to remove cells and debris.
- Analysis: Use Enzyme-Linked Immunosorbent Assay (ELISA) or multiplex bead-based arrays (e.g., Luminex) to quantify concentrations of key immunomodulatory factors.
Diagram 2: Immunomodulation assay workflow
Signaling Pathways Governing Functional Efficacy
The differential functional outcomes of AD-MSCs and BM-MSCs are orchestrated by distinct intracellular signaling pathways.
Key Signaling Pathways in Immunomodulation
The immunomodulatory effects are largely mediated by paracrine factors that signal through specific pathways in immune cells.
Diagram 3: MSC immunomodulation signaling pathways
Pathway Description: Inflammatory signals from the microenvironment, such as IFN-γ released by activated T-cells, prime MSCs to upregulate the secretion of immunosuppressive factors like IDO, PGE2, and IL-10 [102]. These factors act on immune cells: PGE2 and TGF-β can inhibit T-cell proliferation and cytotoxicity, while IL-10 promotes the activity of regulatory T-cells (T-regs), creating a feedback loop that dampens the immune response [101] [102]. BM-MSCs in specific models, such as septic arthritis, have demonstrated a significant upregulation of IL-10 and downregulation of pro-inflammatory TNF-α, correlating with superior therapeutic outcomes [101].
Key Signaling in Chondrogenic Differentiation
The TGF-β superfamily signaling is the master regulator of chondrogenesis.
Pathway Description: TGF-β (e.g., TGF-β3) binds to its receptor on the MSC surface, initiating an intracellular signaling cascade. The canonical pathway involves the phosphorylation of SMAD2/3 proteins, which complex with SMAD4 and translocate to the nucleus. This complex activates the transcription of key chondrogenic genes, including Collagen Type II Alpha 1 (COL2A1) and Aggrecan (ACAN), which are essential components of the cartilage extracellular matrix [101]. The superior chondrogenic potential of BM-MSCs is linked to a more robust activation of this pathway and higher subsequent expression of markers like COL2A1 compared to AD-MSCs [86] [101].
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs critical reagents required for the experimental protocols described in this whitepaper.
Table 2: Essential Research Reagents for MSC Functional Assays
| Reagent/Category | Specific Examples | Function in Assay |
|---|---|---|
| Cell Culture Media | DMEM (high/low glucose), Alpha-MEM, Fetal Bovine Serum (FBS), Penicillin-Streptomycin (P/S) | Base nutrition and support for MSC growth and differentiation. |
| Differentiation Inducers | Dexamethasone, IBMX, Insulin, Indomethacin, β-glycerophosphate, Ascorbate-2-phosphate, TGF-β3 | Specific chemical and biological cues to direct lineage commitment. |
| Staining & Detection | Oil Red O, Alizarin Red S, Alcian Blue/Toluidine Blue, Nile Red / BODIPY, CFSE, Antibodies (CD73, CD90, CD105) | Visualize and quantify differentiation outcomes or track cell proliferation. |
| Immunoassay Kits | ELISA Kits (for IL-10, TGF-β, TNF-α, PGE2), Multiplex Bead Arrays | Quantify concentrations of immunomodulatory factors in conditioned media. |
| Cell Separation | Ficoll-Paque, Transwell inserts, Immunomagnetic separation kits (e.g., for CD34+ selection) | Isolate specific cell populations (e.g., PBMCs) or create co-culture systems. |
The choice between AD-MSCs and BM-MSCs is not a matter of overall superiority but of aligning source-specific functional strengths with therapeutic goals. BM-MSCs are the metric benchmark for orthopaedic applications requiring robust chondrogenesis and osteogenesis, and they have demonstrated potent immunomodulation in specific inflammatory disease models [86] [101]. AD-MSCs present a compelling alternative where high cell yield, rapid expansion, and a broad-spectrum secretome are prioritized, such as in trophic tissue support and modulating systemic inflammation [86] [102]. A deep understanding of these functional efficacy metrics, coupled with standardized experimental protocols for their assessment, is fundamental for advancing rational, evidence-based MSC therapies from the laboratory to the clinic.
The field of regenerative medicine is witnessing a significant paradigm shift with the emergence of induced pluripotent stem cell-derived mesenchymal stromal cells (iMSCs). This innovation addresses critical limitations of primary mesenchymal stem cells (MSCs) sourced from traditional adult tissues like bone marrow and adipose tissue. While bone marrow-derived MSCs (BM-MSCs) have long been the research gold standard, their clinical application faces challenges including low cell numbers (approximately 0.001-0.002% in bone marrow), donor-dependent heterogeneity, and reduced proliferative capacity with age [104] [24]. Adipose-derived stem cells (ADSCs), though more abundant (containing approximately 500-fold more MSCs than bone marrow), still exhibit source-related variability that complicates standardized therapeutic development [104] [105].
iMSCs represent a technologically advanced alternative, generated through the directed differentiation of induced pluripotent stem cells (iPSCs). This approach offers a potentially unlimited cell source with enhanced consistency, scalability, and reduced batch-to-batch variability [104] [106]. By 2025, industry assessments projected that a single iPSC bank could theoretically produce over 29 million clinical doses of iMSC therapy, highlighting their transformative potential for large-scale therapeutic applications [106]. Furthermore, iMSCs closely mimic the biological properties of tissue-derived MSCs, including their immunomodulatory functions and regenerative capacities, while overcoming the fundamental limitations of donor dependency and senescence that have long constrained primary MSC therapies [107] [104] [106].
Technical Comparison: iMSCs Versus Tissue-Derived MSCs
Extensive proteomic and functional analyses reveal both similarities and distinctive signatures across MSC sources. The table below provides a systematic comparison of the key characteristics.
Table 1: Comparative Analysis of MSC Sources and Characteristics
| Characteristic | Bone Marrow MSCs (BM-MSCs) | Adipose-Derived MSCs (ADSCs) | Umbilical Cord MSCs (UC-MSCs) | iPSC-Derived MSCs (iMSCs) |
|---|---|---|---|---|
| Tissue Availability | Low (invasive harvest) [24] | High (minimally invasive) [105] [24] | Limited (natal source) [24] | Unlimited (differentiated from iPSCs) [104] |
| Relative MSC Yield | Very Low (0.001-0.002%) [104] | High (~1% of SVF) [102] [104] | Variable [24] | Unlimited scale-up potential [104] [106] |
| Proliferative Capacity | Limited, senescence-prone [104] | Moderate [24] | High [24] | Superior, sustained [104] [106] |
| Secretome Profile | Enriched in fibrotic/ECM proteins [107] | Pro-angiogenic, anti-inflammatory [102] | Proteins for proliferative potential [107] | Customizable, defined [107] |
| Key Advantages | Extensive research history [24] | Abundant source, ease of harvest [105] | Proliferative capacity [24] | Scalability, consistency, defined origin [104] |
| Primary Limitations | Donor age dependency, invasiveness [104] [24] | Donor variability [24] | Limited source availability [24] | Complex manufacturing, newer technology [108] |
Functional Secretome and Immunomodulatory Profiles
Under inflammatory licensing, iMSCs demonstrate a remarkable capacity to shift their secretory profile. Resting secretomes are typically defined by extracellular matrix (ECM) and pro-regenerative proteins, while licensed secretomes become enriched with chemotactic and immunomodulatory proteins like IDO, which increased more than 10-fold post-licensing in one comprehensive study [107]. Research directly comparing iMSCs to primary human umbilical cord MSCs (hUCMSCs) has demonstrated that iMSCs exhibit comparable immunomodulatory potency, effectively inhibiting T-cell proliferation by 94.6% in direct contact co-cultures and inducing anti-inflammatory macrophage polarization [106]. Furthermore, the extracellular vesicles (EVs) derived from iMSCs display similar immunomodulatory and pro-regenerative potential, with their efficacy significantly enhanced when parent iMSCs are primed with pro-inflammatory cytokines [106].
Experimental Validation: Key Methodologies and Protocols
Standardized In Vitro iMSC Characterization Workflow
Robust experimental validation is essential for characterizing iMSCs. The following workflow outlines the key processes from differentiation to functional assessment.
Diagram 1: iMSC characterization workflow. The process begins with iPSC culture, proceeds through directed differentiation, and culminates in rigorous phenotypic and functional validation.
Detailed Experimental Protocols
Inflammatory Licensing and Immunophenotyping
To validate iMSC response to inflammatory cues, researchers employ a standardized licensing protocol. Cells are exposed to a cytokine cocktail—typically 15 ng/mL IFN-γ and 15 ng/mL TNF-α for 48 hours—following International Society for Cell & Gene Therapy (ISCT) recommendations for immune functional assays [107]. Successful licensing is confirmed through:
- Flow Cytometry Analysis: Measurement of upregulated surface markers HLA-ABC and HLA-DR. Post-licensing, >98% of iMSCs should express both markers, a significant increase from the low baseline expression (1.5-14% for HLA-ABC in resting iMSCs) [107].
- Immunomodulatory Factor Secretion: Quantification of indoleamine 2,3-dioxygenase (IDO) in conditioned medium via ELISA. Effective licensing typically induces a >10-fold increase in IDO secretion, confirming acquisition of an immunosuppressive MSC2 phenotype [107].
Immunomodulatory Potency Assays
Functional validation of iMSCs requires rigorous immune cell interaction assays. The following protocols are considered gold standard:
T-cell Proliferation Suppression Assay:
- Co-culture Setup: iMSCs are co-cultured with anti-CD2/CD3/CD28 bead-stimulated peripheral blood mononuclear cells (PBMCs) for 5 days in two formats: direct cell-to-cell contact and indirect contact using transwell inserts [106].
- Quantification: T-cell proliferation is measured via CD3+ cell counts after the co-culture period. Percentage inhibition is calculated relative to activated PBMCs cultured alone. Benchmark iMSCs demonstrate ~94.6% suppression in direct contact and ~49.3% in indirect contact conditions, comparable to primary hUCMSCs [106].
- Cytokine Analysis: ELISA measurement of TNF-α levels in co-culture supernatants confirms immunomodulation, with effective iMSCs typically reducing TNF-α by >90% [106].
Macrophage Polarization Assay:
- Monocyte Isolation: CD14+ monocytes are isolated from PBMCs and cultured in transwells above iMSC monolayers [106].
- Polarization Assessment: Monocyte differentiation toward M2 (anti-inflammatory) phenotypes is evaluated via surface marker expression (CD206, CD163) and cytokine secretion profiling (increased IL-10, decreased TNF-α) [106].
Extracellular Vesicle (EV) Functional Analysis
The therapeutic potential of iMSC-derived EVs is assessed through:
- In Vitro Scratch Assay: iMSC-EVs are applied to monolayer cultures, and wound closure rates are measured to quantify pro-regenerative potential [106].
- Priming Strategies: Enhancement of EV efficacy through parental iMSC pre-treatment with pro-inflammatory cytokines (e.g., IFN-γ, TNF-α), which significantly boosts their immunomodulatory capacity [106].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for iMSC Characterization and Functional Analysis
| Reagent/Category | Specific Examples | Research Function | Experimental Application Notes |
|---|---|---|---|
| Differentiation Media | Specific cytokine cocktails | Directs iPSC differentiation toward MSC lineage | Protocols vary; often use BMP, FGF, TGF-β pathway modulators |
| Flow Cytometry Antibodies | CD73, CD90, CD105, CD34, CD45, HLA-DR, HLA-ABC | Confirms MSC phenotype & licensing status | Post-licensing, >98% cells should be HLA-ABC+/HLA-DR+ [107] |
| Inflammatory Cytokines | IFN-γ, TNF-α | Induces inflammatory licensing (MSC2 phenotype) | Standard: 15 ng/mL each for 48h per ISCT recommendations [107] |
| Cell Culture Inserts | Transwell permeable supports | Enables contact-independent co-culture | Critical for distinguishing paracrine vs. contact-dependent effects |
| Immune Cell Isolation Kits | CD14+ monocyte isolation, Pan T-cell isolation | Prepares immune cells for co-culture assays | Enables assessment of macrophage polarization & T-cell suppression |
| ELISA Kits | IDO, TNF-α, IL-10 | Quantifies immunomodulatory soluble factors | IDO increase >10-fold confirms successful licensing [107] |
| EV Isolation Kits | Size-exclusion chromatography, precipitation | Harvests iMSC-EVs for functional studies | iMSC-EVs show enhanced effects after parental cell priming [106] |
Regulatory Roadmaps and Clinical Translation
Current Global Regulatory Landscape for MSC Therapies
The regulatory pathway for cell therapies continues to evolve, with distinct geographic variations in approval frameworks. As of 2025, the global landscape includes 12 approved MSC-based therapies, concentrated primarily in South Korea (5 products), Japan (2 products), and the European Union (2 products) [109]. Notably, the U.S. Food and Drug Administration (FDA) had not yet granted full approval for any MSC therapy, though several products were under active review [109]. The first FDA-approved MSC product, Ryoncil (remestemcel-L), received approval in December 2024 for pediatric steroid-refractory acute graft-versus-host disease, marking a pivotal regulatory milestone [108].
The clinical trial ecosystem for MSCs remains robust, with over 1,670 registered trials on ClinicalTrials.gov as of 2025. Nearly 75% of these studies focus on regenerative medicine product development, reflecting strong continued interest in MSC therapeutic applications [109]. The distribution of MSC sources in current clinical trials includes bone marrow, adipose tissue, umbilical cord, and increasingly, iMSCs [109].
iMSC-Specific Regulatory Considerations and Development Pathways
For iMSC-based products, regulatory strategy must address several unique considerations. The following diagram outlines the key stages and decision points in the development pathway.
Diagram 2: iMSC therapy development pathway. The journey from cell bank establishment to regulatory approval requires rigorous characterization at each stage, with particular emphasis on the defined differentiation process.
Key regulatory mechanisms facilitating iMSC development include:
- Expedited FDA Designations: Programs such as the Regenerative Medicine Advanced Therapy (RMAT) designation and Fast Track status can accelerate development for iMSC products addressing unmet medical needs [108].
- Drug Master Files (DMFs): The submission of Type II DMFs for clinical-grade iPSC lines (as demonstrated by REPROCELL in 2025) provides comprehensive regulatory documentation that developers can reference in their Investigational New Drug (IND) applications, thereby streamlining submissions [108].
- Clinical Trial Authorization Distinction: Researchers must distinguish between FDA-authorized trials (via IND clearance) and FDA-approved products (via Biologics License Application). As of 2025, several iMSC programs had received IND clearance to proceed with clinical trials, including CYP-001 for graft-versus-host disease and Fertilo, the first iPSC-based therapy to enter U.S. Phase III trials [108].
iPSC-derived MSCs represent a transformative approach in the field of regenerative medicine, effectively addressing the fundamental limitations of donor dependency, heterogeneity, and scalability that have hampered traditional tissue-derived MSCs. The robust experimental frameworks for characterizing iMSCs—encompassing inflammatory licensing, immunomodulatory potency assays, and extracellular vesicle functionality—provide researchers with validated tools to advance this promising platform.
The regulatory landscape is progressively adapting to accommodate these complex therapeutic products, with a clear pathway from master cell bank establishment through clinical development to market authorization. As the field matures, future developments will likely focus on optimizing differentiation protocols for enhanced consistency, implementing advanced bioengineering strategies to boost iMSC functionality, and establishing universal standards for iMSC characterization and quality control. With over 1,670 clinical trials investigating MSC therapies and projections suggesting 50 globally approved MSC-based products by 2040, iMSCs are positioned to play an increasingly prominent role in realizing the full potential of cell-based regenerative therapies [109].
Conclusion
Bone marrow and adipose tissue remain indispensable and highly complementary sources of adult stem cells for regenerative medicine. While bone marrow is the established source for hematopoietic reconstitution, adipose tissue offers superior accessibility and yield for mesenchymal stromal cell applications. The successful clinical translation of these 'living drugs,' as evidenced by recent FDA approvals, hinges on overcoming key challenges in standardization, scalable manufacturing, and rigorous functional validation. Future research must focus on refining isolation and expansion protocols, developing advanced potency assays, and leveraging new technologies like iMSCs to fully realize the potential of somatic stem cells in creating robust, off-the-shelf therapies for a wider range of diseases.
References
- 1. Adult Stem Cells: Explained (2025) [https://www.dvcstem.com/post/adult-stem-cells]
- 2. Stem cells as biological drugs for incurable diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505543/]
- 3. recent developments and future prospects in stem-cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634165/]
- 4. Quantitative microscopy of the Drosophila ovary shows ... [https://www.nature.com/articles/s41467-017-01322-9]
- 5. Quantitative, Label-Free Characterization of Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4074749/]
- 6. The promising role of muse cells in regenerative medicine [https://www.sciencedirect.com/science/article/abs/pii/S0024320525006605]
- 7. Interactions of Hematopoietic and Associated ... [https://pubmed.ncbi.nlm.nih.gov/41009600/]
- 8. Exploring MSC and HSPC interactions: new frontiers in ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04753-0]
- 9. Bone marrow adipose tissue-derived stem cell factor mediates ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6717592/]
- 10. Adipose-Derived Mesenchymal Stromal Cells in Basic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9962639/]
- 11. Mount Sinai Scientists Reverse Aging in Blood Stem Cells ... [https://www.mountsinai.org/about/newsroom/2025/mount-sinai-scientists-reverse-aging-in-blood-stem-cells-by-targeting-lysosomal-dysfunction]
- 12. Stem cell transplant without toxic preparation successfully ... [https://med.stanford.edu/news/all-news/2025/07/stem-cell-transplant.html]
- 13. Stem Cell Therapeutic and Research Reauthorization Act of ... [http://matsui.house.gov/media/press-releases/matsui-smith-and-colleagues-introduce-stem-cell-therapeutic-and-research]
- 14. Adipose-derived mesenchymal stromal cells in clinical trials [https://www.sciencedirect.com/science/article/pii/S0024320524003515]
- 15. Human adipose-derived stem cells: isolation ... [https://pubmed.ncbi.nlm.nih.gov/19432707/]
- 16. Adipose Tissue-Derived Stem Cells in Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5040903/]
- 17. Adipose tissue stem cells in regenerative medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5880231/]
- 18. Comparative analysis of human mesenchymal stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4453294/]
- 19. Adipose-derived and bone marrow mesenchymal stem cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-018-0914-1]
- 20. Bridging the gap: clinical translation of adipose-derived stem ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04405-3]
- 21. Bone marrow adipocytes: key players in vascular niches ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12367753/]
- 22. Experimental analysis of bone marrow adipose tissue and ... [https://www.sciencedirect.com/science/article/pii/S2352187225000385]
- 23. Remodeling adipocytes' lipid metabolism with a polycation ... [https://www.nature.com/articles/s41467-025-63376-4]
- 24. Current progress and limitations of research regarding the therapeutic use of adipose-derived stem cells: literature review | Journal of Umm Al-Qura University for Applied Sciences [https://link.springer.com/article/10.1007/s43994-024-00147-9]
- 25. Stem-Cell Niches in Health and Disease: Microenvironmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249023/]
- 26. Bone marrow adipocytes: key players in vascular niches, ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1633801/full]
- 27. Comparison of human adult stem cells from adipose tissue and bone marrow in the treatment of experimental autoimmune encephalomyelitis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4054950/]
- 28. Selective remodelling of the adipose niche in obesity and ... [https://www.nature.com/articles/s41586-025-09233-2]
- 29. An update from the bone marrow adiposity society (BMAS) [https://pubmed.ncbi.nlm.nih.gov/40837072/]
- 30. Differential effects of processing time and duration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4676560/]
- 31. Isolation of Tissue Extracellular Vesicles from the Liver [https://www.jove.com/t/58649/isolation-of-tissue-extracellular-vesicles-from-the-liver]
- 32. Use of collagenase to isolate adipose tissue-derived stem ... [https://www.stemcelltherjournal.com/journals/jsctt/jsctt-aid1026.php]
- 33. Gut mucosa dissociation protocols influence cell type ... [https://www.nature.com/articles/s41598-022-13812-y]
- 34. optimising methods for primary cell culture isolation [https://cancerci.biomedcentral.com/articles/10.1186/s12935-023-03190-4]
- 35. Mesenchymal Stromal Cells: Markers, Isolation and Culture ... [https://www.stemcell.com/mesenchymal-cells-lp.html]
- 36. Adult Mesenchymal Stem Cells and Cell Surface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3178966/]
- 37. Commonly Used Mesenchymal Stem Cell Markers and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3839663/]
- 38. Adipose-derived mesenchymal stromal/stem cells - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4131268/]
- 39. MSC surface markers (CD44, CD73, and CD90) can identify human MSC-derived extracellular vesicles by conventional flow cytometry - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4709865/]
- 40. The composition of the mesenchymal stromal cell ... [https://haematologica.org/article/view/6203]
- 41. hMSC CD45/CD73/CD90/CD105 Antibody Panel [https://www.stemcell.com/products/msc-characterization-antibody-panel.html]
- 42. Human adipose-derived mesenchymal stem cells in vitro [https://www.sciencedirect.com/science/article/abs/pii/S1465324910703716]
- 43. A new protocol for validation of Chondro, Adipo and Osteo ... [https://www.sciencedirect.com/science/article/abs/pii/S0040816622001951]
- 44. Adipogenesis, Osteogenesis, and Chondrogenesis of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2020.00561/full]
- 45. Chondrogenic and Osteogenic In Vitro Differentiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11856665/]
- 46. Assay validation for the assessment of adipogenesis ... [https://www.sciencedirect.com/science/article/pii/S146532491200014X]
- 47. Stem Cell Research [https://www.sciencedirect.com/science/article/pii/S1873506122000976]
- 48. 4.4. Multilineage Differentiation (Adipogenesis ... [https://bio-protocol.org/exchange/minidetail?id=9067339&type=30]
- 49. Mesenchymal Stem/Stromal Cells and Their Paracrine Activity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8875256/]
- 50. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 51. Bone marrow mesenchymal stem cells and adipocytes in ... [https://www.frontiersin.org/journals/oncology-reviews/articles/10.3389/or.2025.1704345/full]
- 52. Adipose tissue stem cells show promise in treating ... [https://www.news-medical.net/news/20251105/Adipose-tissue-stem-cells-show-promise-in-treating-osteoporotic-vertebral-fractures.aspx]
- 53. Mesenchymal stem cells: paracrine signaling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2902653/]
- 54. Paracrine mechanisms of proliferative, anti-apoptotic and ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324913006464]
- 55. Immunoregulatory paracrine effect of mesenchymal stem ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1411507/full]
- 56. FDA-approved therapies for chronic GVHD [https://pubmed.ncbi.nlm.nih.gov/39786434/]
- 57. Stem Cell Transplant Clinical Trials and Research [https://www.dana-farber.org/cancer-care/treatment/stem-cell-transplantation/clinical-trials-research]
- 58. FDA Approves First MSC Therapy to Treat GvHD [https://www.aabb.org/news-resources/news/article/2025/01/02/fda-approves-first-msc-therapy-to-treat-gvhd]
- 59. Graft-Versus-Host Disease Clinical Trials [https://www.mayo.edu/research/clinical-trials/diseases-conditions/graft-versus-host-disease]
- 60. UCSF Graft Versus Host Disease Clinical Trials for 2025 [https://clinicaltrials.ucsf.edu/graft-versus-host-disease]
- 61. UCSD Graft Versus Host Disease Clinical Trials for 2025 [https://clinicaltrials.ucsd.edu/graft-versus-host-disease]
- 62. Clinical implications of bone marrow adiposity identified by ... [https://www.nature.com/articles/s41467-025-63395-1]
- 63. Donor age and breed determine mesenchymal stromal cell ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04236-2]
- 64. Donor variability in adipose tissue-derived stem cells [https://www.explorationpub.com/Journals/em/Article/1001243]
- 65. How Potency Assay Strategy Can Accelerate Cell Therapy ... [https://slingshotbio.com/how-potency-assay-strategy-can-accelerate-cell-therapy-development/]
- 66. Potency assays and biomarkers for cell-based advanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10288881/]
- 67. Stem Cells in Regenerative Medicine: A Journey from Adult ... [https://www.mdpi.com/1422-0067/26/17/8255]
- 68. Development of a 3D Bone Marrow Adipose Tissue Model [https://pmc.ncbi.nlm.nih.gov/articles/PMC6062483/]
- 69. Optimization of culture duration of bone marrow cells ... [https://www.sciencedirect.com/science/article/pii/S2352320420300225]
- 70. Cells as Substrates for Potency Assay [https://rouken.bio/scientific-resources/insights/cells-as-substrates-for-potency-assays-a-critical-tool-in-biopharmaceutical-development]
- 71. Automated Manufacturing Processes and Platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11872983/]
- 72. Current challenges and future directions of ATMPs in ... [https://www.sciencedirect.com/science/article/pii/S2352320425001506]
- 73. An Approach towards a GMP Compliant In-Vitro Expansion ... [https://www.mdpi.com/2306-5354/7/3/77]
- 74. Current good manufacturing practice considerations for ... [https://www.sciencedirect.com/science/article/pii/S2666534421000118]
- 75. Adipose-Derived Stem Cells for Regenerative Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5679280/]
- 76. Potency testing of cell and gene therapy products [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2023.1190016/full]
- 77. Potency assays for human adipose-derived stem cells as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9188073/]
- 78. On-chip 3D potency assay for prediction of clinical ... [https://www.nature.com/articles/s41467-025-60158-w]
- 79. Validated methods for isolation and qualification of ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06972-8]
- 80. Vasculogenic Potency of Bone Marrow [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.764237/full]
- 81. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 82. Validated methods for isolation and qualification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12403454/]
- 83. Adult stem cell sources for skeletal and smooth muscle tissue ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-02835-x]
- 84. Bone marrow vs. adipose MSCs - Research Article [https://www.foreverlabs.com/articles/blog/bone-marrow-vs-adipose-mscs]
- 85. Adipose Tissue-Derived Multipotent Stromal Cells Have a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3673757/]
- 86. Comparative Study of Adipose-Derived and Bone Marrow ... [https://www.genesispub.org/comparative-study-of-adipose-derived-and-bone-marrow-derived-mesenchyme-stem-cells-for-intervertebral-disc-regeneration-in-patients-with-degenerative-disc-disease]
- 87. Origins of the Tumor Microenvironment [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0030563]
- 88. A Comparative Study of Osteogenic Differentiation Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4204190/]
- 89. A comparison of the use of adipose-derived and bone marrow ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-01661-3]
- 90. CircRNA_1809 promotes the osteogenic differentiation of ... [https://www.nature.com/articles/s41598-025-03711-3]
- 91. Categories, applications, and potential of stem cells in ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1606100/full]
- 92. Comparative Analysis of Paracrine Factor Expression ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3411362/]
- 93. A systematic review of mesenchymal stem cell secretome [https://www.sciencedirect.com/science/article/abs/pii/S8756328224002588]
- 94. Comparative analysis and characterization of soluble ... [https://www.sciencedirect.com/science/article/pii/S0165242718303350]
- 95. Unlocking the potential of EXOs in regenerative medicine [https://www.sciencedirect.com/science/article/abs/pii/S0040816625003489]
- 96. Comparative analysis of mouse bone marrow and adipose ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-02110-x]
- 97. Comparative analysis of paracrine factor expression in ... [https://pubmed.ncbi.nlm.nih.gov/22188562/]
- 98. Stem cell derived exosome trilogy: an epic comparison of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04440-0]
- 99. Exosomes Digest (1/4 July 2025) - Vita Motus [https://vitamotusag.com/exosomes-digest/exosomes-digest-1-4-july-2025/]
- 100. Uptake of small extracellular vesicles by recipient cells is ... [https://www.nature.com/articles/s41467-025-57617-9]
- 101. The effect of therapeutic potential and safety of bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12654889/]
- 102. Evolution of cell therapies derived from adipose tissue [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382222/]
- 103. Development and characterization of a standardized ... [https://www.sciencedirect.com/science/article/pii/S3050620425000247]
- 104. Induced Mesenchymal Stem Cells: An Emerging Source for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11943107/]
- 105. Adipose derived stem cells – Sources, differentiation ... [https://www.sciencedirect.com/science/article/pii/S0753332225002306]
- 106. Unveiling the Immunomodulatory and regenerative potential of... [https://www.nature.com/articles/s41598-024-75956-3?error=cookies_not_supported&code=94417d5f-2f90-4d63-ba49-6b79788d9937]
- 107. Proteomic profiling of iPSC and tissue- derived MSC secretomes reveal... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11794695/]
- 108. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 109. Mesenchymal Stem Cells/Medicinal Signaling Cells Advances... [https://www.businesswire.com/news/home/20251009529610/en/Mesenchymal-Stem-CellsMedicinal-Signaling-Cells-Advances-Applications-Report-2025-1670-Trials-12-Approvals-Worldwide-and-Path-to-50-Approvals-by-2040---ResearchAndMarkets.com]