Advanced Cryopreservation Techniques for Mesenchymal Stem Cells: A Comprehensive Guide for Clinical Translation
This article provides a comprehensive analysis of current cryopreservation methodologies for Mesenchymal Stem Cells (MSCs), essential 'off-the-shelf' therapeutics for regenerative medicine and immunomodulation.
Advanced Cryopreservation Techniques for Mesenchymal Stem Cells: A Comprehensive Guide for Clinical Translation
Abstract
This article provides a comprehensive analysis of current cryopreservation methodologies for Mesenchymal Stem Cells (MSCs), essential 'off-the-shelf' therapeutics for regenerative medicine and immunomodulation. We explore foundational principles of cryoinjury and cryoprotection, detail established and emerging preservation protocols including slow freezing and vitrification, and address critical challenges in post-thaw viability and functionality. The content systematically compares cryoprotectant solutions, including DMSO-containing and DMSO-free alternatives, and evaluates functional recovery of cryopreserved MSCs through preclinical and clinical lenses. This resource equips researchers, scientists, and drug development professionals with the knowledge to optimize MSC cryopreservation for enhanced clinical efficacy and manufacturing scalability.
The Science of MSC Cryopreservation: Principles, Challenges, and Clinical Imperatives
Mesenchymal stem cells (MSCs) have emerged as a cornerstone of regenerative medicine and cell-based therapies due to their unique biological properties, versatility, and clinical safety profile [1]. First identified in bone marrow by Friedenstein and colleagues in the 1960s, MSCs are non-hematopoietic, multipotent stem cells that can differentiate into various mesodermal lineages including osteoblasts, chondrocytes, and adipocytes [2] [1]. Their therapeutic potential extends beyond differentiation capacity to include potent immunomodulatory functions and paracrine signaling activities that make them attractive candidates for treating a broad spectrum of human diseases, from autoimmune disorders and inflammatory conditions to orthopedic injuries and degenerative diseases [1]. The positioning of MSCs within regenerative medicine has been further refined by advancements in cryopreservation techniques, which enable long-term preservation of cell functionality for clinical applications [3].
This application note provides a comprehensive framework for defining MSCs according to international standards, detailing their therapeutic mechanisms, and presenting optimized protocols for their characterization and cryopreservation. Special emphasis is placed on integrating these cells into regenerative medicine research, with practical guidance for maintaining cell quality and potency throughout the preservation process.
Defining MSCs: International Identification Criteria
Minimal Defining Criteria
The International Society for Cellular Therapy (ISCT) has established minimal criteria to standardize the definition of human MSCs across the scientific community, encompassing plastic adherence, specific surface marker expression, and multilineage differentiation potential [1] [3].
Table 1: Minimal Criteria for Defining Human MSCs According to ISCT
| Criterion Category | Specific Requirements | Purpose/Significance |
|---|---|---|
| Plastic Adherence | Must adhere to plastic surfaces under standard culture conditions | Distinguishes MSCs from hematopoietic and other non-adherent cell populations [1] [3] |
| Surface Marker Expression (Positive) | ||
| CD105 (Endoglin) | ≥95% expression | Type I membrane glycoprotein essential for cell migration and angiogenesis [1] |
| CD90 (Thy-1) | ≥95% expression | N-glycosylated glycosylphosphatidylinositol mediating cell-cell and cell-ECM interactions [1] |
| CD73 (5'-ectonucleotidase) | ≥95% expression | Catalyzes AMP hydrolysis to adenosine; role in cell signaling within bone marrow [1] |
| Surface Marker Expression (Negative) | ≤2% expression (combined) | |
| CD45 | Marker for white blood cells [1] | |
| CD34 | Biomarker for hematopoietic stem and endothelial cells [1] | |
| CD14/CD11b | Expressed on monocytes and macrophages [1] | |
| CD79α/CD19 | Markers of B cells [1] | |
| HLA-DR | MHC class II molecule with strong immunogenic properties [1] | |
| Multilineage Differentiation | Must demonstrate in vitro differentiation into: | Confirms functional multipotency [1] [3] |
| Osteoblasts | Mineralized matrix formation (Alizarin Red S staining) | |
| Adipocytes | Lipid droplet accumulation (Oil Red O staining) | |
| Chondrocytes | Proteoglycan-rich matrix (Alcian Blue staining) |
Additional Stemness Markers
Beyond the ISCT minimum criteria, MSCs typically express transcription factors associated with stemness, including octamer-binding transcription factor 4 (OCT-4) and homeobox protein NANOG [2]. These intracellular markers help maintain the pluripotent state and self-renewal capacity of MSCs.
MSC Identification Workflow
The following diagram illustrates the standardized workflow for identifying and characterizing MSCs according to ISCT criteria:
Therapeutic Mechanisms of MSCs
Immunomodulatory Properties
MSCs exhibit remarkable immunomodulatory capabilities that are crucial for their therapeutic effects. These functions are primarily mediated through cell-cell interactions, cytokine secretion, and soluble factors [2]. The immunomodulatory behavior of MSCs is not static but depends on the surrounding microenvironment, particularly the levels of inflammatory cytokines.
Table 2: Immunomodulatory Functions of MSCs
| Immune Cell Target | Mechanism of Action | Key Soluble Factors/Pathways | Therapeutic Outcome |
|---|---|---|---|
| T Lymphocytes | Suppress activation and proliferation; promote Treg induction [2] | TGF-β, HGF, IDO, PGE2, NO [2] | Reduced inflammatory response; promoted immune tolerance [2] |
| Macrophages | Promote polarization from pro-inflammatory M1 to anti-inflammatory M2 phenotype [2] | PGE2, TSG-6, IL-6 [2] | Enhanced tissue repair; resolution of inflammation [2] |
| Dendritic Cells | Inhibit differentiation and maturation of DC precursors [2] | PGE2 [2] | Reduced antigen presentation and T cell activation [2] |
| B Lymphocytes | Trigger proliferation, activation and IgG secretion [2] | IDO [2] | Modulation of humoral immunity [2] |
| Neutrophils | Recruitment to inflammation sites under low cytokine conditions [2] | CXCL9, CXCL10, CXCL11 [2] | Phagocytosis and pathogen clearance [2] |
Context-Dependent Immunomodulation
The immunomodulatory function of MSCs demonstrates remarkable plasticity based on the inflammatory milieu. This "polarization" phenomenon means MSCs can exhibit either pro-inflammatory or anti-inflammatory properties depending on cytokine levels in their microenvironment [2]:
- Pro-inflammatory phenotype: Occurs at low levels of IFN-γ and TNF-α, where MSCs produce chemokines (MIP-1α/β, RANTES, CXCL9, CXCL10) that activate T cells and promote M1 macrophage proliferation [2].
- Anti-inflammatory phenotype: Dominates under high levels of IFN-γ and TNF-α, where MSCs secrete immunosuppressive factors (TGF-β, HGF, IDO, PGE2, NO) that inhibit T lymphocyte activation and promote Treg induction [2].
The following diagram illustrates how environmental cues dictate MSC immunomodulatory polarization:
Paracrine and Autocrine Activities
The therapeutic effects of MSCs are largely mediated through their secretome - the bioactive molecules they release, including growth factors, cytokines, chemokines, and extracellular vesicles [1]. A key autocrine mechanism involves prostaglandin E2 (PGE2) signaling, which maintains self-renewal capacity and contributes to immunomodulation [2]. The COX-2/PGE2 axis represents a crucial pathway influencing cell cycle, proliferation, and viability through EP receptor activation [2].
MSCs can be isolated from various tissues, with each source offering distinct advantages and limitations for specific therapeutic applications.
Table 3: Comparison of Primary MSC Sources and Characteristics
| Tissue Source | Key Advantages | Limitations/Considerations | Therapeutic Specialization |
|---|---|---|---|
| Bone Marrow (BM-MSCs) | Most extensively studied; high differentiation potential; strong immunomodulatory effects [1] | Invasive harvesting procedure; declining cell quality with donor age [1] | Orthopedic applications; graft-versus-host disease (GVHD) [1] |
| Adipose Tissue (AD-MSCs) | Easier to harvest in large quantities; less invasive collection; comparable therapeutic properties [1] | Variable quality based on donor health and BMI [2] | Plastic and reconstructive surgery; aesthetic medicine [1] |
| Umbilical Cord (UC-MSCs) | Enhanced proliferation capacity; lower immunogenicity; suitable for allogeneic transplantation [1] | Ethical considerations; limited availability [1] | Immunological disorders; allogeneic "off-the-shelf" therapies [1] [4] |
| Dental Pulp (DP-SCs) | Accessible source; unique regenerative properties [1] | Limited cell numbers; specialized isolation protocols [1] | Dental and craniofacial regeneration [1] |
| Placenta (P-MSCs) | High proliferation potential; immunomodulatory capacity [1] | Ethical considerations; potential contamination risk [1] | Obstetric and gynecological applications [1] |
Source-Dependent Functional Variation
The therapeutic efficacy of MSCs varies significantly depending on their tissue of origin. Comparative studies have revealed that:
- Umbilical cord-derived MSCs significantly improve diabetic abnormalities and diabetic nephropathy compared to bone marrow-derived MSCs [2].
- Wharton's jelly-derived MSCs show superior regenerative profiles for skin therapy in Systemic Sclerosis, promoting fibroblast-mediated wound healing and VEGF expression more effectively than BM-MSCs [4].
- Clonogenicity and function of placenta MSCs (P-MSCs) were found superior to cord MSCs (C-MSCs) in some studies [2].
Cryopreservation Protocols for MSCs
Cryopreservation Methods
Effective cryopreservation is essential for maintaining MSC viability and functionality for clinical applications. The two primary techniques are slow freezing and vitrification, each with distinct mechanisms and applications [3].
Table 4: Comparison of MSC Cryopreservation Methods
| Parameter | Slow Freezing | Vitrification |
|---|---|---|
| Mechanism | Gradual dehydration to minimize intracellular ice crystal formation [3] | Ultra-rapid cooling to achieve glassy solid state without ice formation [3] |
| Cooling Rate | Controlled rate (typically -1°C/min to -3°C/min) [3] | Extremely rapid (direct immersion in liquid nitrogen) [3] |
| CPA Concentration | Low (e.g., 10% DMSO) [3] | High (mixtures of permeating CPAs) [3] |
| Survival Rate | 70-80% cell survival [3] | Variable; technique-dependent |
| Technical Complexity | Simple; easy to operate; minimal contamination risk [3] | Higher technical skill required |
| Recommended Use | Clinical and laboratory MSC cryopreservation [3] | Specialized applications; limited clinical use |
Standardized Slow Freezing Protocol
The following protocol represents the recommended method for clinical and laboratory cryopreservation of MSCs [3]:
Materials:
- Cryopreservation medium: Culture medium supplemented with 10% DMSO or commercial DMSO-free cryopreservation solution (e.g., PRIME-XV FreezIS DMSO-Free)
- Controlled-rate freezer
- Cryogenic vials
- Liquid nitrogen storage system
Procedure:
- Harvesting: Harvest MSCs at 80-90% confluence using standard trypsinization protocol.
- Preparation: Centrifuge cell suspension and resuspend in cryopreservation medium at 1-5 × 10^6 cells/mL.
- Aliquoting: Dispense 1 mL aliquots into cryogenic vials.
- Equilibration: Hold vials at 4°C for 30-60 minutes.
- Cooling Phase 1: Transfer to mechanical freezer at -20°C to -80°C for 2-24 hours.
- Cooling Phase 2: Place in vapor phase of liquid nitrogen (-135°C) for 24 hours.
- Long-term Storage: Transfer to liquid nitrogen (-196°C) for long-term preservation.
Thawing Protocol:
- Rapidly thaw cryovials in a 37°C water bath with gentle agitation until only a small ice crystal remains.
- Decontaminate vial exterior with 70% ethanol.
- Transfer cell suspension to pre-warmed complete culture medium.
- Centrifuge at 300 × g for 5 minutes to remove cryoprotectant.
- Resuspend in fresh culture medium and plate at desired density.
Impact of Cryopreservation on MSC Functionality
Cryopreservation can significantly affect MSC properties and functionality. Key considerations include:
- Cell Recovery: Post-thaw viability should exceed 70% for clinical applications [3].
- Differentiation Potential: Cryopreserved MSCs should maintain trilineage differentiation capacity.
- Immunophenotype: Surface marker expression (CD73, CD90, CD105) should remain stable after thawing.
- Metabolic Activity: Temporary reduction in metabolic activity is normal immediately post-thaw.
Recent advances in DMSO-free cryopreservation solutions (e.g., PRIME-XV FreezIS) have demonstrated comparable cell recovery and post-thaw proliferative capacity while eliminating DMSO toxicity concerns [5]. These solutions have shown promise in nonclinical animal trials as nontoxic alternatives for cell therapy applications [5].
Application Notes: MSC Cryopreservation in Research and Therapy
Quality Control Assessment
Comprehensive quality control assessment should be performed both pre-cryopreservation and post-thaw to ensure MSC functionality:
Table 5: Quality Control Parameters for Cryopreserved MSCs
| Assessment Parameter | Pre-Cryopreservation | Post-Thaw (24-48h) | Acceptance Criteria |
|---|---|---|---|
| Viability | >95% (trypan blue exclusion) | >70% | Maintain minimum viability threshold |
| Immunophenotype | ≥95% positive for CD73, CD90, CD105 | ≥95% positive for same markers | Consistent phenotype expression |
| ≤2% positive for CD45, CD34, HLA-DR | ≤2% positive for same markers | Absence of hematopoietic contamination | |
| Doubling Time | 24-72 hours (source-dependent) | Within 20% of pre-freeze value | Maintain proliferative capacity |
| Differentiation Potential | Positive for osteo, adipo, chondro | Positive for all three lineages | Maintain multipotency |
| Microbiological Safety | Negative for mycoplasma, bacteria, fungi | N/A | Sterility assurance |
Clinical Dosing Considerations
Optimizing MSC dose is critical for therapeutic efficacy. Recent meta-analyses in knee osteoarthritis treatment reveal that:
- Doses of ≤ 25 million cells were associated with statistically significant improvement in WOMAC scores [6].
- Higher doses (> 25 million cells) did not demonstrate additional benefit [6].
- Meta-regression confirmed no significant dose-response relationship, supporting the use of lower, more efficient doses [6].
These findings highlight the importance of dose optimization in MSC therapy development, particularly considering that excessive cell administration in hypoxic environments (like intra-articular spaces) may lead to increased cell death due to resource competition [6].
The Scientist's Toolkit: Essential Research Reagents
Table 6: Essential Research Reagents for MSC Characterization and Cryopreservation
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Culture Media | PRIME-XV MSC Expansion XSFM [5], α-MEM supplemented with FCS [4] | Expansion while maintaining stemness; large-scale culture |
| Cryopreservation Solutions | PRIME-XV FreezIS DMSO-Free [5], DMSO-containing solutions [3] | Maintain viability and functionality during freezing/thawing |
| Surface Marker Antibodies | CD73, CD90, CD105, CD45, CD34, HLA-DR [1] [3] | Flow cytometric verification of MSC identity |
| Differentiation Kits | Osteogenic: Dexamethasone, β-glycerophosphate, ascorbate [1] | In vitro trilineage differentiation confirmation |
| Chondrogenic: TGF-β, dexamethasone, ascorbate [1] | ||
| Adipogenic: IBMX, dexamethasone, indomethacin [1] | ||
| Characterization Stains | Alizarin Red S (osteogenesis), Oil Red O (adipogenesis), Alcian Blue (chondrogenesis) [1] | Visualization and quantification of differentiation |
| CRISPR/Cas9 Components | Cas9 nucleases, guide RNAs, delivery vectors [7] | Genetic engineering to enhance therapeutic properties |
| Aurora A inhibitor 1 | Aurora A Inhibitor 1 is a potent, selective compound for cancer research. It targets the Aurora A kinase pathway. For Research Use Only. Not for human use. | |
| 5'-Methylthioadenosine-13C6 | 5'-Methylthioadenosine-13C6, MF:C11H15N5O3S, MW:303.29 g/mol | Chemical Reagent |
The comprehensive characterization and proper cryopreservation of MSCs are fundamental to advancing their applications in regenerative medicine. Adherence to ISCT criteria provides essential standardization, while understanding source-dependent functional variations enables researchers to select optimal MSC types for specific therapeutic applications. The integration of robust cryopreservation protocols ensures maintenance of MSC viability, functionality, and therapeutic potential, supporting the development of reproducible and effective cell-based therapies. As MSC research continues to evolve, particularly with emerging technologies like CRISPR-based genetic engineering [7] and cell-free approaches using MSC secretomes [4], the foundational principles outlined in this application note will remain critical for ensuring scientific rigor and therapeutic efficacy.
The Critical Role of Cryopreservation in Enabling 'Off-the-Shelf' Cell Therapies
The advent of cell-based therapies has marked a significant revolution in regenerative medicine and oncology. Among these, therapies utilizing Mesenchymal Stem Cells (MSCs) have demonstrated exceptional promise due to their immunomodulatory properties, multi-lineage differentiation potential, and tropism towards injured tissues and tumors [3] [8]. However, a major challenge limiting their widespread clinical application is the need for readily available, therapeutically competent cell products. 'Off-the-shelf' cell therapies—characterized by their immediate availability for treatment—are emerging as a pivotal solution, and cryopreservation is the foundational technology enabling this paradigm [9]. By allowing long-term storage of MSC-based products without compromising their biological functionality, cryopreservation facilitates the creation of cell biobanks, ensures quality control, and standardizes therapeutic protocols, thereby transforming the landscape of regenerative medicine [3] [8]. This Application Note delineates the critical methodologies, quantitative outcomes, and standardized protocols underpinning the successful cryopreservation of MSCs for off-the-shelf applications.
Impact of Cryopreservation on MSC Function: Quantitative Analysis
Successful development of off-the-shelf therapies depends on the post-thaw retention of MSC viability and function. Recent studies provide robust quantitative data on the effects of cryopreservation on key MSC properties, confirming their suitability for clinical applications.
Table 1: Post-Thaw Functional Analysis of Cryopreserved MSCs
| Functional Assay | Test System | Key Findings | Significance for Therapy |
|---|---|---|---|
| Cell Viability | Slow freezing with CPAs [3] | ~70-80% cell survival rate | Provides sufficient viable cell numbers for therapeutic doses. |
| Proliferation Capacity | Colony Forming Units (CFU-f) of BMAC frozen at -80°C [10] | Preserved after 4 weeks of cryopreservation | Indicates retention of self-renewal capability, crucial for tissue regeneration. |
| Multilineage Differentiation | Chondrogenic, osteogenic, adipogenic induction of frozen BMAC [10] | Capacity preserved post-thaw | Maintains therapeutic potential for repairing diverse tissues like cartilage and bone. |
| In Vivo Cartilage Repair | OA rat model treated with frozen BMAC [10] | Significantly improved histology scores vs. control; equivalent to fresh BMAC | Confirms functional efficacy in a disease model, validating clinical relevance. |
| Anti-Cancer Efficacy | HCC model with engineered, frozen-thawed MSCs [9] | >80% tumor growth inhibition; potent anti-cancer effect post-thaw | Critical for off-the-shelf oncology applications, as functionality is retained despite cold-chain transport. |
The data demonstrates that cryopreservation is not merely a storage technique but a integral process that can be optimized to maintain, and reliably deliver, the critical functions of MSCs for clinical use.
Experimental Protocols for MSC Cryopreservation
The following section details standardized protocols for the cryopreservation and thawing of MSCs, critical for ensuring consistent and high-quality results in research and clinical settings.
Standardized Slow Freezing Protocol
The slow freezing method is the most widely adopted technique for MSC cryopreservation due to its operational simplicity and efficacy [3].
Step 1: Cell Harvest and Preparation
- Harvest MSCs at 80-90% confluence (e.g., at passage 2-4). Wash with PBS and dissociate using a standard reagent like trypsin-EDTA.
- Resuspend the cell pellet in a pre-chilled (4°C) cryoprotective medium. A typical formulation is 90% autologous plasma or fetal bovine serum (FBS) and 10% Dimethyl Sulfoxide (DMSO) [10]. Cell density should be adjusted to (1 \times 10^6) to (5 \times 10^6) cells/mL [10].
Step 2: Controlled-Rate Freezing
- Aliquot the cell suspension into cryogenic vials.
- Immediately place the vials in a controlled-rate freezing device or an isopropanol-based freezing container (e.g., "Mr. Frosty") to achieve an approximate cooling rate of -1°C/min [10].
- Transfer the container to a -80°C freezer for a minimum of 4 weeks (or as required) [10].
Step 3: Long-Term Storage
- After 24 hours, promptly transfer the cryovials to a liquid nitrogen storage tank (-196°C) for long-term preservation [3].
Optimized Thawing and Post-Thaw Handling Protocol
Rapid and careful thawing is crucial to maximize cell viability and recovery.
Step 1: Rapid Thawing
Step 2: CPA Removal
- Gently transfer the thawed cell suspension to a sterile tube containing a pre-warmed culture medium (e.g., α-MEM with 20% FBS) to gradually dilute the DMSO.
- Centrifuge the cell suspension at 300-400 × g for 5-10 minutes to pellet the cells [10].
- Carefully aspirate the supernatant containing the cryoprotectant.
Step 3: Cell Viability Assessment and Culture
- Resuspend the cell pellet in fresh, complete culture medium.
- Count the cells and assess viability using a method such as Trypan Blue exclusion.
- Plate the cells at the desired density for expansion or direct experimentation. A post-thaw viability of 70-80% is typically expected with optimized protocols [3].
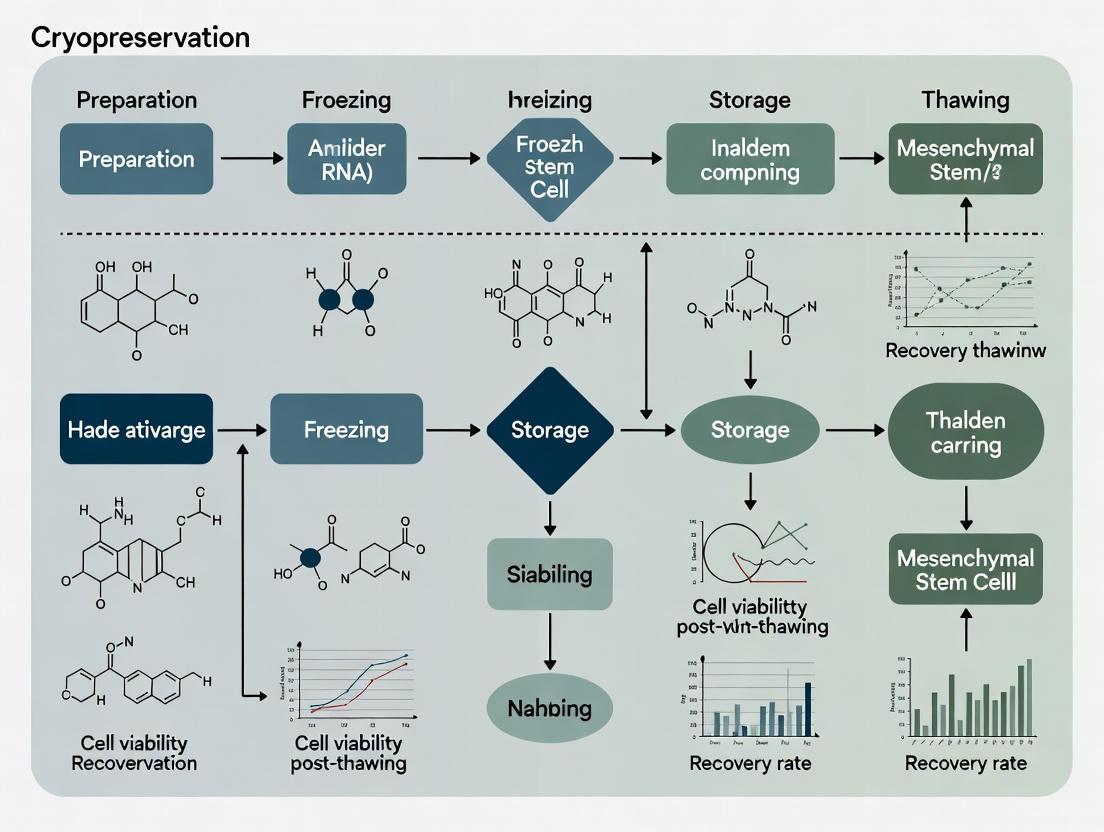
Diagram 1: MSC cryopreservation and thawing workflow.
Essential Reagents and Materials
The consistency of cryopreservation outcomes is heavily dependent on the quality and selection of reagents.
Table 2: Research Reagent Solutions for MSC Cryopreservation
| Reagent/Material | Function/Description | Example Formulation/Catalog |
|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Penetrating (endocellular) cryoprotectant; reduces intracellular ice crystal formation. | Cell culture grade, sterile-filtered. Often used at 10% (v/v) in plasma/FBS [10]. |
| Autologous Plasma / FBS | Serves as the base medium for cryoprotectant; provides proteins and nutrients that stabilize the cell membrane. | 90% (v/v) in final freezing medium [10]. |
| Sucrose / Trehalose | Non-penetrating (exocellular) cryoprotectant; stabilizes cell membranes and mitigates osmotic shock. | Often used at 0.1M concentration in combination with DMSO [11] [8]. |
| Programmable Freezer / Passive Cooler | Provides controlled cooling rate critical for the slow freezing method. | e.g., "Mr. Frosty" isopropanol chamber (~-1°C/min) or advanced programmable freezers [10]. |
| Cryogenic Vials | Secure, leak-proof containers designed for ultra-low temperature storage. | Internally-threaded, sterile vials rated for liquid nitrogen. |
| Liquid Nitrogen Storage System | Provides long-term storage at -196°C, ensuring metabolic stasis. | Vapor-phase storage is often preferred to minimize contamination risks. |
Mechanisms and Workflow: From Cryopreservation to Clinical Application
Cryopreservation's role extends beyond simple storage; it enables a streamlined workflow from cell biobanking to clinical administration. The underlying mechanisms involve protecting cells from the lethal effects of ice crystal formation and osmotic stress during the freezing and thawing processes [8]. Cryoprotective Agents (CPAs) like DMSO and sucrose are fundamental to this protection.
Diagram 2: Off-the-shelf therapy workflow and cryopreservation mechanisms.
Cryopreservation is the critical enabler for the practical and commercial viability of off-the-shelf MSC therapies. By implementing robust, standardized protocols for freezing and thawing—supported by a comprehensive understanding of cryoprotectant mechanisms and their impact on cell function—researchers and clinicians can ensure the reliable delivery of safe and potent cell products. The quantitative data confirms that cryopreserved MSCs can retain their therapeutic efficacy, from in vitro proliferation to in vivo disease modification. As the field advances, continued optimization of these protocols, particularly in reducing the reliance on potentially toxic CPAs like DMSO, will further enhance the safety and efficacy profile of these transformative off-the-shelf treatments.
Cryopreservation is a fundamental technique for the long-term storage of biological specimens, including mesenchymal stem cells (MSCs), which are vital for cell-based therapeutics, regenerative medicine, and drug development [12]. At cryopreserved temperatures (typically -80°C or -196°C), chemical and biological reactions are significantly reduced or halted, enabling long-term preservation [12]. However, the freezing and thawing processes introduce significant risks of cryoinjury, primarily through ice crystal formation and osmotic stress [12] [13]. These physical and chemical damages can compromise cell viability, functionality, and therapeutic potential, presenting major challenges for clinical and research applications [14]. For MSC research, understanding and mitigating cryoinjury is paramount to ensuring that post-thaw cells retain their critical properties, including immunomodulatory function, multipotent differentiation capacity, and anti-inflammatory properties [14] [15]. This Application Note details the mechanisms of cryoinjury and provides optimized protocols to minimize damage, framed within the context of advancing MSC-based therapies.
Fundamental Mechanisms of Cryoinjury
Cryoinjury during the freeze-thaw cycle manifests through two interconnected mechanisms: physical damage from ice crystals and physiological damage from osmotic imbalances.
Ice Crystal Formation and Growth
The phase transition of water from liquid to solid is a primary cause of cellular damage. Ice crystal formation occurs in both extracellular and intracellular compartments, with specific consequences for each [12].
- Extracellular Ice Formation: During slow freezing, ice crystals first form in the extracellular solution. This leads to mechanical damage by distorting and compressing cells and tissues. Furthermore, the exclusion of solutes from the growing ice lattice results in a progressive increase in the solute concentration of the remaining unfrozen extracellular fluid [12] [16].
- Intracellular Ice Formation (IIF): At higher cooling rates, intracellular water does not have sufficient time to exit the cell osmotically. This results in the supercooling of the intracellular solution and eventual nucleation of ice crystals within the cell. IIF is almost universally fatal, causing irreversible damage to intracellular organelles and disrupting the plasma membrane [12] [13].
- Recrystallization during Thawing: During the warming process, especially at slow warming rates, small, unstable ice crystals can merge to form larger, more damaging crystals. This process, known as recrystallization, exacerbates mechanical damage to cellular structures [12].
Osmotic Stress and Solute Effects
The formation of extracellular ice initiates a cascade of osmotic events that pose a significant threat to cell survival [13].
- Cell Dehydration: As extracellular ice forms, the unfrozen extracellular solution becomes hypertonic. To maintain equilibrium, water moves out of the cell down its chemical potential gradient, leading to cellular dehydration and shrinkage. Excessive dehydration can cause a critical reduction in cell volume and damage to the plasma membrane [12].
- Solution-Effect Injury: The progressive concentration of electrolytes and other solutes in the unfrozen fraction can damage cells through denaturation of proteins and destabilization of lipid membranes. This is termed "solution-effect" injury [12] [13].
- Oxidative Stress: The cryopreservation process can also generate reactive oxygen species (ROS), leading to oxidative damage of lipids, proteins, and nucleic acids, further compromising cell function post-thaw [13].
The following diagram illustrates the interconnected pathways of cryoinjury during the freezing process.
Diagram 1: Pathways of Cryoinjury During Freezing. Slow cooling primarily leads to dehydration injury, while rapid cooling causes intracellular ice formation. Both pathways can result in fatal cell damage. Node colors indicate process stages (yellow), injury mechanisms (red), and outcomes (gray).
Quantitative Analysis of Cryoinjury and Recovery
The effect of cryopreservation on MSC function is quantifiable. Post-thaw analyses reveal significant alterations in phenotype and function, while an acclimation period can facilitate recovery.
Table 1: Functional Recovery of MSCs After a 24-Hour Post-Thaw Acclimation Period [14]
| Parameter | Freshly Thawed (FT) MSCs | Thawed + 24h Acclimation (TT) MSCs | Measurement Method |
|---|---|---|---|
| Viability & Apoptosis | Significantly increased apoptosis | Significantly reduced apoptosis | Annexin V/PI flow cytometry |
| Proliferation | Decreased cell proliferation | Restored clonogenic capacity | Metabolic activity assay (Resazurin), clonogenic assay |
| Phenotype | Decreased CD44 and CD105 surface markers | Marker expression maintained | Flow cytometry immunophenotyping |
| Gene Expression | Decreased key regenerative genes | Upregulation of angiogenic and anti-inflammatory genes | Gene expression analysis |
| Immunomodulation | Maintained ability to arrest T-cell proliferation | Significantly more potent T-cell proliferation arrest | T-cell co-culture assay |
| Anti-inflammatory Function | Diminished IFN-γ secretion | Maintained anti-inflammatory properties | Cytokine secretion assay (IFN-γ) |
Optimizing cryopreservation conditions is critical for maximizing post-thaw viability. Data from systematic cell banking analyses provide insights into the impact of storage duration and revival methods.
Table 2: Impact of Storage Duration and Revival Method on Cell Attachment [17]
| Condition | Optimal Performance | Key Findings |
|---|---|---|
| Storage Duration | 0-6 months | Fibroblasts stored for 0-6 months showed the highest number of vials with optimal cell attachment (>60%) after 24 hours. |
| Revival Method | Direct seeding | The direct revival method (thaw and direct seed) resulted in a higher number of vials with optimal cell attachment compared to the indirect method (thaw, centrifuge, then seed). |
| Cell Type | Fibroblasts | Fibroblast cells showed better post-thaw attachment performance compared to other cell types like keratinocytes, respiratory epithelial cells, and bone marrow MSCs under identical conditions. |
| Cryomedium | FBS + 10% DMSO | This classic cryomedium formulation yielded superior results in cell attachment analysis compared to commercial medium alternatives. |
Experimental Protocols for Assessing Cryoinjury
This section provides detailed methodologies for key experiments cited in this note, allowing for the direct assessment of cryoinjury and the validation of cryopreservation protocols for MSCs.
Protocol: Post-Thaw Viability and Apoptosis Assay
This protocol assesses immediate cryoinjury by quantifying cell viability and apoptosis immediately after thawing and after a recovery period [14].
- Cell Preparation: Obtain cryopreserved MSCs (e.g., bone marrow-derived, P3-P5). Create three experimental groups:
- FC (Fresh Cells): Cells in continuous culture, harvested for a baseline.
- FT (Freshly Thawed): Vials thawed and used immediately.
- TT (Thawed + Time): Vials thawed and acclimated in standard culture flasks for 24 hours prior to analysis.
- Thawing: Rapidly thaw frozen vials by gentle agitation in a 37°C water bath for approximately 1-2 minutes.
- Cell Washing: For the FT group, immediately after thawing, transfer the cell suspension to a centrifuge tube containing pre-warmed complete culture medium. Centrifuge at 5000 rpm for 5 minutes. Aspirate the supernatant containing DMSO and resuspend the cell pellet in fresh medium.
- Staining: Resuspend 1.5 x 10^6 cells/mL in 1X Annexin V binding buffer. Incubate with Annexin V-FITC for 10 minutes in the dark. Add Propidium Iodide (PI) immediately before analysis.
- Flow Cytometry Analysis: Analyze cells using a flow cytometer (e.g., BD FACSCelesta) within 1 hour.
- Viable Cells: Annexin V-FITC negative, PI negative.
- Early Apoptotic: Annexin V-FITC positive, PI negative.
- Late Apoptotic/Necrotic: Annexin V-FITC positive, PI positive.
- Data Interpretation: Compare the percentage of viable and apoptotic cells between the FT, TT, and FC groups. A successful protocol should show a significant reduction in apoptotic cells in the TT group compared to the FT group.
Protocol: TTC-Based Cell Viability Assay for Cryopreserved Samples
The 2,3,5-Triphenyltetrazolium Chloride (TTC) assay is a colorimetric method used to quantify the viability of cell masses, such as embryogenic callus, and can be adapted for 3D MSC cultures [18].
- Sample Preparation: After thawing and any planned acclimation period, collect the cells or tissue. For adherent MSCs, this may require trypsinization and formation of a pellet.
- TTC Incubation: Prepare a 0.5% (w/v) TTC solution in an appropriate buffer (e.g., phosphate-buffered saline). Completely immerse the cell sample in the TTC solution. Incubate in the dark at 25°C for 24 hours.
- Termination and Extraction: After incubation, remove the TTC solution and wash the sample. To extract the red formazan product, add an organic solvent like 95% ethanol or dimethyl sulfoxide to the sample and incubate for several hours.
- Spectrophotometric Quantification: Transfer the extracted formazan solution to a cuvette and measure the absorbance at a wavelength of 485-500 nm using a spectrophotometer.
- Data Interpretation: The absorbance value is directly proportional to the activity of dehydrogenases in viable cells and thus to the viability of the sample. Compare absorbance values between different cryopreservation treatment groups to identify the optimal conditions.
The workflow for a comprehensive cryopreservation and assessment study is outlined below.
Diagram 2: Workflow for Cryopreservation and Post-Thaw Assessment of MSCs. The diagram outlines the key steps from cell preparation through to the battery of quality control and functional assays used to quantify cryoinjury and validate recovery.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for MSC Cryopreservation Studies
| Reagent/Material | Function/Application | Example & Notes |
|---|---|---|
| Permeable Cryoprotectant | Penetrates cell membrane, reduces intracellular ice formation, suppresses freezing point. | Dimethyl Sulfoxide (DMSO): Used at 5-10% (v/v) final concentration. Cytotoxic at high concentrations/temperatures [13] [17]. |
| Non-Permeable Cryoprotectant | Induces protective dehydration, stabilizes membranes, modulates ice crystal growth. | Sucrose/Trehalose: Often used at 0.2-0.4 mol∙L−1; helps reduce required DMSO concentration [13] [18]. Polyethylene Glycol (PEG): Used as an additive in cryoprotectant cocktails [18]. |
| Serum/Protein Additive | Provides undefined growth factors and proteins that enhance membrane stability and cell survival. | Fetal Bovine Serum (FBS): Commonly used at 80-90% in cryomedium (e.g., 90% FBS + 10% DMSO) [14]. Human Platelet Lysate (HPL): Xeno-free alternative for clinical applications [17]. |
| Commercial Cryomedium | Chemically defined, serum-free formulations for standardized and regulatory-compliant workflows. | CryoStor: Pre-mixed, serum-free solution designed to minimize ice formation and improve post-thaw recovery [17]. |
| Viability Assay Reagents | Quantify cell survival and apoptosis post-thaw. | Annexin V/Propidium Iodide (PI): Distinguishes viable, early apoptotic, and late apoptotic/necrotic cells via flow cytometry [14]. Trypan Blue: Standard dye exclusion test for immediate post-thaw viability count [17]. |
| Metabolic Activity Probe | Assesses functional potency and proliferation capacity of revived cells. | Resazurin (e.g., Vybrant Assay): Reduced by viable cells to fluorescent resorufin; measured over time to track growth [14]. |
| Controlled-Rate Freezer | Provides reproducible, optimal cooling rate (typically -1°C/min) to minimize ice crystal damage. | "Mr. Frosty" or "CoolCell": Isopropanol-based freezing containers that approximate -1°C/min when placed at -80°C [17]. |
| Cox-2-IN-11 | Cox-2-IN-11, MF:C12H12OS3, MW:268.4 g/mol | Chemical Reagent |
| PI3K-IN-28 | PI3K-IN-28, MF:C26H16F9N3O3S2, MW:653.5 g/mol | Chemical Reagent |
Cryopreservation is an indispensable tool in biomedical research, enabling the long-term storage of biological materials such as mesenchymal stem cells (MSCs) at ultra-low temperatures. The success of cryopreservation hinges critically on cryoprotectant agents (CPAs), which mitigate damage caused by ice formation, osmotic stress, and dehydration during freezing and thawing cycles. CPAs are broadly categorized into two classes based on their ability to cross cell membranes: penetrating (permeating) and non-penetrating (non-permeating) agents [19].
Penetrating CPAs are typically small, neutral molecules that diffuse across cell membranes, protecting both the intracellular and extracellular environments. In contrast, non-penetrating CPAs are larger molecules or polymers that remain outside cells, providing protection through extracellular mechanisms [20] [21]. For advanced therapies like MSC-based treatments, where preserving cell viability, differentiation potential, and functionality post-thaw is paramount, understanding the distinct mechanisms of these CPA classes is essential for developing optimized cryopreservation protocols. This document details their mechanisms, applications, and provides specific protocols for MSC research.
Mechanisms of Action
The protective effects of CPAs during freezing and thawing are mediated through several key mechanisms. While both CPA classes utilize some similar principles, their specific applications and effects differ significantly due to their membrane permeability.
Core Protective Mechanisms
- Colligative Protection: Both CPA classes depress the freezing point of aqueous solutions and reduce the fraction of water that turns into ice at any given temperature. This directly limits ice crystal formation and growth, thereby minimizing mechanical damage to cellular structures [20].
- Vitrification: At high concentrations, CPAs can form an amorphous, glass-like state instead of crystalline ice during cooling. This vitrified matrix immobilizes water and biomolecules, preventing the destructive processes of ice crystallization and recrystallization [22] [20].
- Water Replacement: This mechanism is particularly associated with disaccharides like trehalose and sucrose. As water is removed during freezing, these molecules can form hydrogen bonds with the polar head groups of phospholipids and proteins, effectively replacing water molecules and maintaining the structural integrity of membranes and macromolecules in a dehydrated state [23] [21].
- Preferential Exclusion: Non-penetrating CPAs, such as sugars and polymers, are often excluded from the hydration layer of proteins and membrane surfaces. This stabilization forces proteins into a more compact, native conformation, preventing denaturation and aggregation during freeze-induced concentration of solutes [20].
Penetrating CPA Mechanisms
Penetrating CPAs like dimethyl sulfoxide (DMSO) and glycerol protect cells from the inside. Their ability to cross the plasma membrane is crucial for preventing lethal intracellular ice formation (IIF). By equilibrating across the membrane, they reduce the osmotic differential between the intra- and extracellular compartments during freezing. This minimizes cell dehydration and shrinkage, as water is less driven out of the cell to equilibrate with the increasingly concentrated external environment [22] [24]. Intracellular CPAs also increase the viscosity of the cytoplasmic solution, which hinders the nucleation and growth of ice crystals within the cell [19].
Non-Penetrating CPA Mechanisms
Non-penetrating CPAs, including trehalose, sucrose, and hydroxyethyl starch, operate primarily in the extracellular space. They create a hypertonic environment that promotes gentle, protective cell dehydration before freezing, thereby reducing the amount of freezable water inside the cell and the risk of IIF [22] [23]. Furthermore, they contribute significantly to the formation of a stable glassy (vitrified) matrix extracellularly, which mechanically suppresses ice crystal growth and protects the outer surface of the cell membrane [22] [20]. Some polymers, such as polyampholytes, also demonstrate strong ice recrystallization inhibition (IRI) activity, preventing small ice crystals from merging into larger, more damaging ones during temperature fluctuations [22].
Table 1: Comparison of Common Penetrating and Non-Penetrating CPAs
| CPA | Class | Primary Mechanism | Typical Conc. in MSC Research | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| DMSO | Penetrating | Colligative action, intracellular vitrification, water replacement [20] | 5-10% | High efficacy, rapid membrane penetration [25] [21] | Dose-dependent cytotoxicity, can alter differentiation [25] [21] |
| Glycerol | Penetrating | Colligative action, intracellular water replacement [20] | 5-10% | Lower toxicity than DMSO [26] | Slower permeation, requires careful removal [21] |
| Trehalose | Non-Penetrating | Water replacement, preferential exclusion, extracellular vitrification [20] [21] | 50-250 mM (with delivery tech) | Biocompatible, FDA-approved, stabilizes membranes [21] | Poor membrane permeation in mammalian cells [21] |
| Sucrose | Non-Penetrating | Preferential exclusion, extracellular vitrification [20] [24] | 0.1-0.5 M | Common in lyophilized formulations [20] | Used alone, offers limited cryoprotection for cells |
Application Notes for Mesenchymal Stem Cell Research
The choice and application of CPAs are critical for maintaining the viability, multipotency, and functionality of MSCs post-thaw.
Efficacy and Toxicity Considerations
DMSO remains the most widely used and effective CPA for MSCs, often at concentrations of 10% [25]. However, its cytotoxicity is a significant concern. Toxicity is concentration-dependent and can manifest as reduced cell viability, impaired proliferation, and altered differentiation potential [25] [26]. When administered to patients in cell therapy products, DMSO has been associated with infusion-related reactions, although current doses in MSC therapies are typically 2.5-30 times lower than the 1 g/kg level accepted in hematopoietic stem cell transplantation [25]. Strategies to mitigate DMSO toxicity include using lower concentrations (e.g., 5%) or combining it with non-penetrating CPAs to create synergistic effects that reduce the required DMSO dose [20] [24].
Advanced Strategies: Combining CPAs and Innovative Delivery
A promising strategy is the use of CPA cocktails that combine penetrating and non-penetrating agents. For example, formulations containing DMSO with trehalose or sucrose have shown improved post-thaw recovery for various cell types, as they leverage both intracellular and extracellular protection mechanisms [24]. Furthermore, because mammalian cells lack transporters for trehalose, advanced delivery methods are required for it to exert intracellular effects. A recent breakthrough uses ultrasound with microbubbles (UMT) to temporarily porate the MSC membrane, allowing trehalose to enter the cell [21]. This technique has demonstrated high cryoprotective capability while avoiding the cytotoxicity associated with DMSO, successfully preserving MSC viability and multipotency [21].
Experimental Protocols
Protocol 1: Standard Cryopreservation of MSCs with DMSO
This protocol describes a standard method for cryopreserving MSCs using a controlled-rate freezer and a DMSO-based cryoprotectant solution [25] [24].
Research Reagent Solutions:
- Growth Medium: DMEM supplemented with 10% FBS and 1% penicillin/streptomycin.
- Cryopreservation Solution: 90% (v/v) FBS and 10% (v/v) DMSO. Prepare fresh and keep at 4°C before use.
Procedure:
- Cell Preparation: Harvest MSCs at 80-90% confluency using a standard trypsinization procedure. Centrifuge the cell suspension and resuspend the pellet in cold Growth Medium to create a concentrated cell suspension (e.g., 1-2 x 10^7 cells/mL).
- CPA Addition: Slowly and dropwise, add an equal volume of cold Cryopreservation Solution to the cell suspension while gently swirling the tube, resulting in a final concentration of 5 x 10^6 cells/mL in 5% DMSO and 45% FBS. This slow addition minimizes osmotic shock.
- Aliquoting: Immediately aliquot the cell-CPA mixture into pre-chilled cryogenic vials (e.g., 1 mL per vial).
- Controlled-Rate Freezing:
- Place the vials in a controlled-rate freezer.
- Cool from room temperature to -40°C at a rate of -1°C per minute.
- Then cool from -40°C to -90°C at a rate of -10°C per minute.
- Transfer and Storage: After freezing, quickly transfer the vials to a liquid nitrogen storage tank for long-term preservation at ≤ -150°C.
Protocol 2: Ultrasound-Mediated Delivery of Trehalose for MSC Cryopreservation
This advanced protocol outlines a method for delivering the non-penetrating CPA trehalose into MSCs using ultrasound and microbubbles, enabling DMSO-free or DMSO-reduced cryopreservation [21].
Research Reagent Solutions:
- Trehalose Solution: D-(+)-Trehalose dihydrate dissolved in DMEM without phenol red at concentrations of 50, 100, 250, 500, 750, and 1000 mM.
- Microbubble Suspension: Commercial SonoVue microbubbles, resuspended according to manufacturer's instructions.
- Cell Suspension: MSCs resuspended in DMEM without phenol red at a density of 1 x 10^6 cells/mL.
Procedure:
- Sample Preparation: In a 2.0 mL Eppendorf tube, combine 1 mL of the Cell Suspension, 1% (v/v) of the Microbubble Suspension, and the desired volume of Trehalose Solution to achieve the final target concentration.
- Ultrasound Exposure:
- Place the sample tube in a holder within a degassed water bath maintained at 35 ± 1°C.
- Expose the sample to focused ultrasound using the following optimized parameters [21]:
- Frequency: 0.5 MHz
- Peak Negative Pressure: 0.25 MPa
- Pulse Length: 100 ms
- Pulse Repetition Period: 2 s
- Total Exposure Duration: 5 minutes
- Monitor cavitation signals passively to ensure stable bubble activity.
- Post-Treatment Processing: After exposure, let the samples stand for 2 minutes to allow microbubbles to dissipate. The cells are now loaded with trehalose and ready for cryopreservation.
- Cryopreservation: Aliquot the treated cell suspension into cryovials and freeze using the controlled-rate freezing procedure described in Protocol 1.
- Thawing and Assessment: Rapidly thaw the vials in a 37°C water bath. Dilute the cell suspension in a step-wise manner with warm culture medium to reduce osmotic shock. Assess cell viability, membrane integrity, and, crucially, multipotency (ability to differentiate into adipocytes, osteocytes, and chondrocytes).
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for CPA Studies
| Reagent / Material | Function in CPA Research | Example Application |
|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Penetrating CPA; gold standard for cell cryopreservation [25]. | Positive control in efficacy studies; component of standard cryopreservation media for MSCs [25]. |
| D-(+)-Trehalose Dihydrate | Non-penetrating CPA; stabilizes membranes and proteins via water replacement [21]. | Investigational CPA for DMSO-free protocols, often requiring delivery technology like UMT [21]. |
| SonoVue Microbubbles | Ultrasound contrast agent; nucleates cavitation for membrane poration [21]. | Essential for ultrasound-mediated intracellular delivery of impermeable CPAs like trehalose [21]. |
| Fetal Bovine Serum (FBS) | Protein source; provides additional undefined protective elements in cryomedium. | Base component (e.g., 90%) of many standard cryopreservation solutions [21]. |
| Controlled-Rate Freezer | Equipment; ensures reproducible and optimal cooling rates for cell survival. | Standardized freezing from +4°C to -90°C for sensitive cell types like MSCs [24]. |
| Egfr-IN-9 | Egfr-IN-9|Potent EGFR Inhibitor for Research | Egfr-IN-9 is a potent EGFR kinase inhibitor for cancer research. This product is For Research Use Only and is not intended for diagnostic or therapeutic use. |
| Etifoxine-d5 | Etifoxine-d5, MF:C17H17ClN2O, MW:305.8 g/mol | Chemical Reagent |
Workflow and Mechanism Diagrams
CPA Mechanisms and MSC Cryopreservation Workflow
Mechanisms of Cryoprotection
The transition of mesenchymal stem/stromal cell (MSC)-based therapies from research to clinical application faces a critical bottleneck: the need for effective cryopreservation that maintains both cellular viability and critical therapeutic functions. Cryopreservation enables the establishment of cell banks, provides time for quality control testing, and facilitates off-the-shelf availability for acute treatment scenarios [27] [28] [29]. However, the freezing and thawing processes can significantly impair the very properties that make MSCs therapeutically valuable—specifically, their immunomodulatory capabilities and multilineage differentiation potential. This application note examines the key challenges in preserving these essential functions and provides detailed protocols to enhance post-thaw recovery for preclinical and clinical applications.
Critical Challenges in Functional Preservation
Temporal Dynamics of Post-Thaw Recovery
The immediate post-thaw period represents a critical window where MSCs exhibit significant functional impairments that may not be reflected in basic viability metrics. Research demonstrates that although viability may recover within 24 hours after thawing, metabolic activity and adhesion potential remain substantially compromised during this period [30]. This recovery timeline has profound implications for therapeutic applications, particularly those requiring immediate MSC functionality upon administration.
Table 1: Temporal Recovery Profile of Key MSC Attributes Post-Thaw
| Time Post-Thaw | Viability | Apoptosis Level | Metabolic Activity | Adhesion Potential | Immunomodulatory Capacity |
|---|---|---|---|---|---|
| Immediate (0 h) | Significantly reduced | Significantly elevated | Substantially impaired | Substantially impaired | Variable impairment |
| 2-4 hours | Beginning to recover | Remains elevated | Impaired | Impaired | Likely impaired |
| 24 hours | Recovered to near baseline | Reduced but may remain above baseline | Remains lower than fresh cells | Remains lower than fresh cells | Recovering |
| Beyond 24 hours | Normalized | Normalized | Variable recovery | Variable recovery | Context-dependent recovery |
Compromised Immunomodulatory Potency
The immunomodulatory functions of MSCs, mediated through paracrine signaling and direct cell contact, are particularly vulnerable to cryopreservation-induced damage. These functions include sensing the inflammatory environment and responding by either promoting or suppressing immune responses through complex interactions with T-cells, B-cells, macrophages, dendritic cells, and neutrophils [31]. Studies indicate that the actin cytoskeleton of freshly thawed MSCs is disrupted, leading to reduced adhesion to endothelium and potentially poor engraftment following intravenous infusion [29]. Furthermore, freshly thawed MSCs may exhibit diminished response to interferon-γ (IFN-γ), a key cytokine that licenses their immunosuppressive functions [29].
Impact on Multilineage Differentiation Capacity
The defining characteristic of MSCs—their ability to differentiate into osteogenic, adipogenic, and chondrogenic lineages—can be variably affected by cryopreservation. Quantitative assessments have demonstrated that cryopreservation reduces colony-forming unit ability and differentially affects adipogenic and osteogenic differentiation potentials across cell lines from different donors [30]. This variability introduces significant challenges for standardized therapeutic applications where consistent differentiation potential is essential.
Strategic Solutions and Protocols
Advanced Cryoprotectant Strategies
DMSO-Free Cryoprotectant Formulations
Recent multicenter studies have demonstrated that DMSO-free solutions containing sucrose, glycerol, and isoleucine (SGI) can provide cryoprotection comparable to traditional DMSO-containing solutions [27]. The international collaborative study found no significant differences in cell viability, recovery, immunophenotype, or gene expression profiles between MSCs cryopreserved with SGI versus DMSO-containing solutions.
Table 2: Comparison of Cryoprotectant Solutions
| Cryoprotectant Solution | Composition | Post-Thaw Viability | Cell Recovery | Immunophenotype Preservation | Differentiation Potential | Clinical Concerns |
|---|---|---|---|---|---|---|
| Traditional DMSO | 5-10% DMSO in serum | Variable (70-95%) | Variable | Maintained | Variable impact | DMSO toxicity in patients [28] [32] |
| Sucrose-Glycerol-Isoleucine (SGI) | Sucrose + Glycerol + Isoleucine | Comparable to DMSO | Comparable to DMSO | Maintained | Comparable to DMSO | Reduced toxicity risk |
| Trehalose-Based (UMT) | Trehalose delivered via ultrasound + microbubbles | >90% with optimized protocol | High with optimized protocol | Maintained | Multipotency preserved | No cytotoxic CPAs [21] |
Novel Intracellular Delivery Methods
For non-penetrating cryoprotectants like trehalose to be effective, they must be present on both sides of the cell membrane. Advanced delivery methods have been developed to facilitate intracellular trehalose transport:
Ultrasound-Mediated Trehalose Delivery Protocol [21]:
- Prepare cell suspension at density of 1 × 10^6 cells/ml in trehalose solution (50-1000 mM in DMEM without phenol red)
- Add 1% (v/v) SonoVue microbubbles
- Expose to ultrasound parameters: 0.5 MHz frequency, 0.25 MPa peak negative pressure, 100 ms pulse length, 2 s pulse repetition period
- Optimal exposure time: 5 minutes
- Post-treatment, cryopreserve cells using standard protocols
This method achieves intracellular trehalose delivery through temporary membrane poration, enhancing cryoprotection while avoiding cytotoxic agents.
Controlled Ice Nucleation Protocols
Uncontrolled ice nucleation during freezing creates significant temperature instability, contributing to cellular damage. Implementing controlled nucleation using medical-grade ice nucleation devices (IND) standardizes the freezing process and improves post-thaw recovery [33].
Ice Nucleation Protocol for Cryovials [33]:
- Prepare MSC suspension in cryoprotectant solution at recommended concentration
- Transfer to cryovials (1.0 mL per vial)
- Place IND in contact with cryovial solution
- Use controlled-rate freezer programmed to cool at -1°C/min
- Activate IND at -5°C to initiate controlled ice nucleation
- Continue cooling to -80°C before transfer to liquid nitrogen for storage
Ice Nucleation Protocol for 96-Well Plates [33]:
- Seed MSCs in 96-well plates at desired density
- Add cryopreservation solution to wells
- Place IND array into plate wells
- Freeze in controlled-rate freezer at -1°C/min
- For adhered cells, use IND with slow thaw for greatest metabolic activity post-thaw
Optimized Thawing and Recovery Methods
The thawing process is equally critical for functional preservation. Research indicates that the method and timing of post-thaw processing significantly impact functional recovery:
Standardized Thawing Protocol [30] [32]:
- Rapidly thaw cryovials in 37°C water bath with gentle agitation until small ice crystal remains
- Transfer cell suspension to pre-warmed complete medium (9:1 dilution ratio)
- Centrifuge at 200g for 5 minutes at room temperature to remove cryoprotectant
- Resuspend pellet in fresh complete medium
- For immediate use: Assess viability and administer
- For recovery: Seed at 5,000 cells/cm² and allow 24-48 hours recovery before functional assessment
Post-Thaw Quality Assessment Framework
Comprehensive Functional Assessment Protocol
Rigorous post-thaw assessment is essential to ensure MSC functionality. A tiered approach evaluating both immediate and recovered cellular functions provides the most accurate prediction of therapeutic potential.
Immunomodulatory Potency Assessment [29] [31]:
- IFN-γ Responsiveness: Stimulate with IFN-γ (50 ng/mL) for 24-72 hours and measure IDO expression via Western blot or kynurenine production assay
- T-cell Suppression Assay: Co-culture MSCs with activated human PBMCs at ratios of 1:3, 1:6, and 1:12 (MSC:PBMC) for 3-5 days
- Measure PBMC proliferation via 3H-thymidine incorporation or CFSE dilution
- Cytokine Secretion Profile: Analyze PGE2, TGF-β, HGF, and IL-6 production via ELISA under stimulated conditions
- Macrophage Polarization Assay: Assess ability to induce M2 phenotype in primary macrophages through CD206/CD163 expression
Multilineage Differentiation Assessment [30]:
- Osteogenic Differentiation: Culture in osteoinductive medium (DMEM, 10% FBS, 0.1 μM dexamethasone, 10 mM β-glycerophosphate, 50 μM ascorbate-2-phosphate) for 21 days
- Assessment: Alizarin Red S staining for mineralized matrix, osteocalcin expression via RT-PCR
- Adipogenic Differentiation: Culture in adipogenic medium (DMEM, 10% FBS, 1 μM dexamethasone, 0.5 mM isobutylmethylxanthine, 10 μg/mL insulin, 200 μM indomethacin) for 14-21 days
- Assessment: Oil Red O staining for lipid vacuoles, PPAR-γ expression via RT-PCR
- Chondrogenic Differentiation: Pellet culture in chondrogenic medium (DMEM, 1% ITS, 50 μg/mL ascorbate-2-phosphate, 40 μg/mL proline, 100 μg/mL sodium pyruvate, 0.1 μM dexamethasone, 10 ng/mL TGF-β3) for 21 days
- Assessment: Safranin O staining for proteoglycans, collagen type II expression
Essential Quality Control Metrics
Table 3: Post-Thaw Quality Control Parameters
| Assessment Category | Specific Parameters | Acceptance Criteria | Assessment Timing |
|---|---|---|---|
| Viability & Recovery | Membrane integrity (Trypan blue, PI exclusion) | >80% viability | 0h, 24h post-thaw |
| Apoptosis level (Annexin V/PI) | <15% early/late apoptosis | 0h, 24h post-thaw | |
| Metabolic activity (XTT, MTT) | >70% of fresh control | 24h, 48h, 72h post-thaw | |
| Immunophenotype | CD73, CD90, CD105 expression | >90% positive | 24h post-thaw |
| CD14, CD20, CD34, CD45 expression | <5% positive | 24h post-thaw | |
| Immunomodulatory Function | IDO expression after IFN-γ stimulation | Comparable to fresh control | 48h post-stimulation |
| T-cell suppression | >50% suppression at 1:6 ratio | 3-5 days co-culture | |
| Differentiation Potential | Osteogenic (Alizarin Red) | Positive staining | 21 days differentiation |
| Adipogenic (Oil Red O) | Positive staining | 14-21 days differentiation | |
| Chondrogenic (Safranin O) | Positive staining | 21 days differentiation |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for MSC Cryopreservation Studies
| Category | Specific Reagent/Device | Function/Purpose | Application Notes |
|---|---|---|---|
| Cryoprotectants | DMSO (Cell Culture Grade) | Penetrating CPA, prevents intracellular ice formation | Use at 5-10% final concentration; associated with toxicity concerns [28] |
| Trehalose (Dihydrate) | Non-penetrating CPA, stabilizes membranes | Requires intracellular delivery (UMT) for optimal efficacy [21] | |
| Sucrose-Glycerol-Isoleucine (SGI) | DMSO-free CPA alternative | Multicenter study shows comparable performance to DMSO [27] | |
| Ice Nucleation Devices | Medical Grade IND | Controls ice formation temperature | Reduces freezing process variability; improves reproducibility [33] |
| Assessment Reagents | IFN-γ (Recombinant) | Stimulates immunomodulatory IDO pathway | Essential for potency assessment; use at 50 ng/mL [29] |
| IDO Antibodies/Kynurenine Assay | Measures immunomodulatory response | Critical for functional potency validation [29] | |
| Osteo/Adipo/Chondro Induction Kits | Assess multilineage differentiation potential | Quality control for stemness preservation [30] | |
| Delivery Systems | Ultrasound + Microbubbles (SonoVue) | Facilitates intracellular trehalose delivery | Enables use of non-penetrating CPAs [21] |
| Cell Culture | MSC-qualified FBS | Supports MSC growth and maintenance | Maintains differentiation potential during expansion |
| Axl-IN-4 | Axl-IN-4|AXL Inhibitor|For Research Use Only | Axl-IN-4 is a potent AXL kinase inhibitor. It is for Research Use Only (RUO) and not for diagnostic or therapeutic applications. | Bench Chemicals |
| Zanamivir-Cholesterol Conjugate | Zanamivir-Cholesterol Conjugate|Long-Acting NA Inhibitor | Zanamivir-Cholesterol Conjugate is a long-acting neuraminidase inhibitor with potent efficacy against drug-resistant influenza. For Research Use Only. Not for human use. | Bench Chemicals |
Preserving the immunomodulatory properties and multilineage differentiation potential of MSCs post-thaw requires a multifaceted approach addressing cryoprotectant composition, freezing kinetics, and post-thaw recovery conditions. The protocols and assessment frameworks presented herein provide researchers with standardized methods to ensure functional preservation of cryopreserved MSCs. As MSC therapies continue to advance through clinical development, robust cryopreservation methodologies that maintain critical cellular functions will be essential for delivering consistent, potent, and reliable therapeutic products. Future directions should focus on further optimization of DMSO-free cryoprotectant formulations, standardization of ice nucleation control across different container formats, and development of rapid potency assays that can predict in vivo therapeutic efficacy.
Practical Protocols: Implementing Slow Freezing, Vitrification, and Novel Techniques
Slow freezing is a foundational technique in the cryopreservation of mesenchymal stem cells (MSCs), enabling their long-term storage for research and clinical applications in regenerative medicine [3] [8]. This method operates on the principle of controlled-rate cooling to facilitate gradual cellular dehydration, thereby minimizing the lethal formation of intracellular ice crystals [3] [13]. The successful cryopreservation of MSCs is paramount for establishing biobanks, ensuring the immediate availability of quality-controlled cells for therapeutic use, and avoiding the genetic alterations associated with continuous cell passaging [3] [8] [34]. This protocol details the standardized methodology for the slow freezing of MSCs, framed within the broader context of optimizing cryopreservation techniques for advanced biomedical research.
Core Principles of Slow Freezing
The slow freezing process is designed to protect cells from the two primary mechanisms of cryoinjury: intracellular ice formation and solution-effects injury [13]. During controlled cooling, the extracellular solution freezes first. This increases the concentration of solutes in the unfrozen extracellular fluid, creating an osmotic gradient that draws water out of the cell passively, leading to gradual cellular dehydration [3] [13]. This dehydration is critical as it reduces the amount of water available inside the cell to form damaging ice crystals upon further cooling [3].
The role of Cryoprotective Agents (CPAs) is to further mitigate these damaging effects. They are broadly classified into two categories:
- Penetrating (Endocellular) CPAs: Low molecular weight compounds like Dimethyl Sulfoxide (DMSO) and glycerol that enter the cell. They depress the freezing point of water, reduce the fraction of water that turns to ice, and minimize "solution-effects" injury by diluting the intracellular electrolyte concentration [8] [34] [13].
- Non-Penetrating (Exocellular) CPAs: Macromolecules or sugars like sucrose, trehalose, and hydroxyethyl starch that remain outside the cell. They enhance dehydration by increasing the osmotic pressure of the extracellular solution and help stabilize the cell membrane [8] [34] [13].
The following diagram illustrates the sequential workflow and the underlying protective mechanisms of a standard slow freezing process for MSCs.
Quantitative Data on Cryopreservation Outcomes
The efficacy of slow freezing is influenced by the specific CPAs used. Traditional agents like DMSO are effective but can be cytotoxic, driving research into alternative and combination solutions. The table below summarizes post-thaw cell viability and recovery data from key studies comparing different cryoprotectant formulations.
Table 1: Comparison of Cryoprotectant Solutions for MSC Slow Freezing
| Cryoprotectant Solution | Reported Post-Thaw Viability | Reported Cell Recovery | Key Study Findings |
|---|---|---|---|
| 10% DMSO (Standard Control) | Baseline for comparison | Baseline for comparison | Considered the traditional standard, but carries risk of cytotoxicity and patient side effects [27] [13]. |
| Sucrose/Glycerol/Isoleucine (SGI) | Comparable to DMSO controls | Comparable to DMSO controls | DMSO-free, multicentre study showed comparable viability, recovery, and preserved immunophenotype [27]. |
| Zwitterion/DMSO (10/15) | Not specified | 151% relative to commercial CPA | Emerging CPA combination; showed superior cell recovery in spheroid cryopreservation models [35]. |
| 5% DMSO + Trehalose | Not specified | Not specified | Non-permeating CPAs like trehalose allow reduction of DMSO concentration, mitigating toxicity [13]. |
The cooling rate is another critical parameter that must be optimized for different cell types. The table below collates evidence on the impact of cooling rates on post-thaw outcomes from various biological models.
Table 2: Impact of Cooling Rate on Post-Thaw Outcomes in Various Models
| Cell Type / Model | Cooling Rate | Post-Thaw Outcome | Reference |
|---|---|---|---|
| Sheep Spermatogonial Stem Cells | 1°C/min (from 0°C to -10°C) | Significantly higher viability, proliferation, and stemness activity compared to faster rates [36]. | [36] |
| Umbilical Cord Blood Mononuclear Cells | 2°C/min | 75.5% viability | [37] |
| General MSC Protocol | -1°C/min to -3°C/min | Standard recommended rate for slow freezing of MSCs [13]. | [13] |
Standardized Slow Freezing Protocol for MSCs
Reagent Preparation
- Cryoprotectant Media Formulation: Prepare a solution of 10% (v/v) DMSO in Fetal Bovine Serum (FBS) or your standard culture medium. Alternatively, a DMSO-free solution containing Sucrose-Glycerol-Isoleucine (SGI) can be used [27]. The solution must be sterile and kept cold (2-8°C) before use.
- Other Reagents: Phosphate-Buffered Saline (PBS), trypsin/EDTA or other cell dissociation reagent, complete culture medium.
Equipment List
- Programmable Rate-Controlled Freezer or Isopropanol-based Freezing Chamber
- Liquid Nitrogen Storage Tank
- Cryogenic Vials
- Centrifuge
- Water Bath (37°C)
- Laminar Flow Hood
- Inverted Microscope
Step-by-Step Procedure
- Cell Harvesting: Culture MSCs to 70-80% confluence. Wash the cell monolayer with PBS and dissociate using an appropriate enzyme. Inactivate the enzyme using complete culture medium [13].
- Cell Counting and Centrifugation: Perform a cell count and centrifuge the cell suspension (e.g., 300 x g for 10 minutes). Aspirate and discard the supernatant.
- CPA Addition and Aliquotting: Resuspend the cell pellet in cold cryoprotectant media to a concentration of 1-5 x 10^6 cells/mL. Gently mix to create a homogeneous suspension. Aliquot the cell suspension into cryogenic vials (e.g., 1 mL/vial) [3] [13].
- Controlled-Rate Freezing:
- Using a Programmable Freezer: Place the cryovials in the freezer and initiate a program with a cooling rate of -1°C/min to -3°C/min from 4°C down to at least -40°C to -80°C [13] [36].
- Using an Isopropanol Chamber: Place the cryovials in the chamber and transfer it to a -80°C mechanical freezer for 24 hours. The isopropanol provides an approximate cooling rate of -1°C/min, which is suitable for many cell types [36].
- Long-Term Storage: After the controlled freezing step, immediately transfer the cryovials to a liquid nitrogen storage tank for long-term preservation at -150°C to -196°C [3] [8].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for MSC Slow Freezing
| Item | Function / Rationale | Example / Note |
|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Penetrating CPA; gold standard for intracellular protection [8] [13]. | Use clinical grade; typically used at 5-10% (v/v) [27] [13]. |
| Sucrose | Non-penetrating CPA; promotes extracellular vitrification and osmotic dehydration [8] [13]. | Often used in combination with penetrating CPAs to reduce their required concentration [38] [13]. |
| Trehalose | Non-penetrating CPA; stabilizes cell membranes and proteins in a dry state [13]. | A natural disaccharide; investigated as a component of DMSO-free formulations [13]. |
| Fetal Bovine Serum (FBS) | Base medium component; provides proteins and nutrients. | Can be replaced with human serum albumin or serum-free alternatives for clinical applications. |
| Programmable Freezer | Equipment for controlled-rate cooling; ensures consistent, reproducible freezing kinetics. | Critical for protocol standardization; alternatives are isopropanol chambers [36]. |
| Liquid Nitrogen Storage | Provides ultra-low temperature environment (-196°C) for long-term metabolic stasis of cells [3] [8]. | Requires continuous monitoring and maintenance. |
| eIF4A3-IN-6 | eIF4A3-IN-6, MF:C26H25N3O5, MW:459.5 g/mol | Chemical Reagent |
| (S)-3-Hydroxy Midostaurin | (S)-3-Hydroxy Midostaurin, CAS:945260-14-0, MF:C35H30N4O5, MW:586.6 g/mol | Chemical Reagent |
Quality Control and Post-Thaw Assessment
Rigorous quality control is essential after thawing cryopreserved MSCs. Key parameters to assess include:
- Viability: Use trypan blue exclusion or flow cytometry-based assays (e.g., Annexin V/PI) to determine the percentage of live cells. A viability of >70-80% is generally considered acceptable, though this can vary [3] [13].
- Cell Recovery: Calculate the percentage of cells recovered post-thaw compared to the number initially cryopreserved.
- Functionality Assessments:
- Proliferation Potential: Assess growth kinetics and population doubling time over several passages [36].
- Immunophenotype: Verify the expression of characteristic MSC surface markers (CD73, CD90, CD105) and lack of hematopoietic markers via flow cytometry [27] [34].
- Differentiation Potential: Confirm the trilineage differentiation capacity (osteogenic, adipogenic, chondrogenic) post-thaw [34].
- Metabolic Activity: Use assays like MTT or AlamarBlue to assess metabolic function [36].
Slow freezing remains a cornerstone technique for the preservation of MSCs, vital for both basic research and clinical therapy. Its success hinges on the precise interplay between controlled cooling rates and the protective action of cryoprotectants. While DMSO-based protocols are widely established, ongoing research into DMSO-free solutions, such as those containing SGI or novel zwitterions, shows promising results for reducing toxicity without compromising cell viability and function [27] [35]. Standardization of this methodology, coupled with comprehensive post-thaw quality control, is critical for ensuring the reliable and effective use of mesenchymal stem cells in the advancing field of regenerative medicine.
Vitrification has emerged as a pivotal cryopreservation technology for mesenchymal stem cells (MSCs), enabling long-term storage by solidifying cellular materials into a glassy state without deleterious ice crystal formation [39]. This process necessitates the use of high concentrations of cryoprotective agents (CPAs)—typically ranging from 6 to 8 M—to suppress ice nucleation and facilitate an amorphous vitreous solid during cooling to cryogenic temperatures [39] [3]. For MSC research and subsequent clinical applications in drug development, mastering vitrification is essential for creating viable biobanks that preserve cell functionality, potency, and differentiation capacity post-thaw [40] [8]. This protocol outlines detailed methodologies for the vitrification of MSCs, emphasizing practical application for scientists engaged in regenerative medicine and therapeutic development.
Post-Vitrification Cell Viability and Functionality
Table 1: Viability and Functional Outcomes of Vitrified MSCs
| Parameter | Vitrification Performance | Comparative Slow-Freezing Performance | Assessment Method |
|---|---|---|---|
| Cell Viability | 89.4% ± 4.2% [39] | 93.2% ± 1.2% [39] | Flow cytometry, Live/Dead staining |
| Proliferation Capacity | No significant difference in population doubling time up to 5 passages [39] | No significant difference in population doubling time up to 5 passages [39] | Population doubling time assay |
| Apoptosis Induction | No significant increase in TUNEL+ cells [39] | Comparable baseline levels [39] | TUNEL assay |
| Oxidative Stress | No significant increase in intracellular ROS [39] | Comparable baseline levels [39] | ROS detection assay |
| Multipotency Retention | Preserved adipogenic, chondrogenic, and osteogenic differentiation [39] | Preserved adipogenic, chondrogenic, and osteogenic differentiation [39] | Lineage-specific staining (Oil Red O, Alcian Blue, Von Kossa) |
| Surface Marker Profile | Maintained positive expression of CD44, CD73, CD90, CD105; negative for CD31, CD34 [39] | Maintained positive expression of CD44, CD73, CD90, CD105; negative for CD31, CD34 [39] | Flow cytometry |
3D Spheroid and Apoptosis Gene Expression
Table 2: Gene Expression and 3D Spheroid Survival Post-Cryopreservation
| Parameter | Vitrification Result | Slow-Freezing Result | Implications |
|---|---|---|---|
| Single-Cell Gene Expression | No significant changes in apoptosis/oxidative stress genes [39] | No significant changes in apoptosis/oxidative stress genes [39] | Low cytotoxicity at single-cell level |
| Spheroid Bax/Bcl-2 Ratio | Lower ratio [39] | Higher ratio [39] | Reduced apoptotic signaling in vitrified spheroids |
| Spheroid p53 Expression | Lower upregulation [39] | Significant increase [39] | Reduced cryo-damage-induced apoptosis in vitrified spheroids |
| Spheroid Core Viability (200-900μm) | High viability, mild cell death [39] | Excessive cell death in core region [39] | Superior CPA permeation in vitrified spheroids |
| Spheroid Bcl-xL Expression | Considerably upregulated [39] | Lower expression [39] | Enhanced anti-apoptotic signaling |
Cryoprotectant Formulations and Efficacy
Table 3: Cryoprotectant Agent (CPA) Composition and Performance
| CPA Formulation | Composition | Reported Cell Viability | Advantages & Notes |
|---|---|---|---|
| Standard Penetrating CPA | ~6-8 M DMSO, EG, and/or PG [39] [3] | 89.4% ± 4.2% [39] | Effective ice suppression; potential osmotic/toxicity risks |
| DMSO-Free Solution (SGI) | Sucrose, Glycerol, Isoleucine [27] | Comparable to DMSO controls [27] | Reduced patient toxicity risks; suitable for clinical applications |
| Trehalose with Ultrasound | 50-1000 mM Trehalose + Microbubbles [21] | Preserved membrane integrity & multipotency [21] | Non-toxic, FDA-approved; requires ultrasonication for delivery |
Experimental Protocols
Protocol 1: Conventional Vitrification of 2D MSC Monolayers
Principle: This protocol utilizes high concentrations of permeating CPAs to achieve a glassy state during rapid cooling, preventing intracellular ice crystallization.
Materials:
- Cells: Human adipose-derived MSCs (passage 3-5)
- Base Solution: Dulbecco's Phosphate-Buffered Saline (DPBS) supplemented with 20% serum
- CPA Stock Solution: 8 M DMSO and Ethylene Glycol (EG) in a 1:1 ratio in base solution
- Equilibration Solution: 2 M DMSO + 2 M EG in base solution
- Vitrification Solution: 4 M DMSO + 4 M EG + 0.5 M sucrose in base solution
- Dilution Solution: 1 M sucrose in base solution
- Washing Solution: Base solution only
- Equipment: Cryotubes, programmable freezer, liquid nitrogen storage tank, 37°C water bath
Procedure:
- Cell Preparation: Harvest MSCs at 80-90% confluence using standard trypsinization. Centrifuge and resuspend in base solution at a concentration of 1-2 x 10^6 cells/mL.
- CPA Equilibration: Incubate the cell suspension in an equal volume of Equilibration Solution for 10 minutes at room temperature (20-22°C). This step minimizes osmotic shock.
- Vitrification Solution Loading: Centrifuge the cell suspension and resuspend in a pre-cooled Vitrification Solution. Incubate for 1 minute at 4°C. Critical Step: Keep the exposure time short due to high CPA toxicity.
- Rapid Cooling: Quickly aliquot 0.5 mL of the cell suspension into pre-cooled cryotubes and plunge directly into liquid nitrogen. Ensure rapid cooling rates exceed -20,000°C/min to ensure a glassy state.
- Storage: Transfer cryotubes to a liquid nitrogen storage tank (-196°C) for long-term preservation.
- Rapid Warming: For thawing, rapidly retrieve the cryotube and immediately immerse it in a 37°C water bath with gentle agitation for 60-90 seconds.
- CPA Removal and Cell Recovery:
- Step 1: Immediately transfer the thawed suspension to 10 volumes of pre-warmed (37°C) Dilution Solution. Incubate for 5 minutes.
- Step 2: Centrifuge at 300 x g for 5 minutes. Gently resuspend the cell pellet in Washing Solution.
- Step 3: Centrifuge again and resuspend in complete culture medium for subsequent culture and analysis [39] [3].
Protocol 2: Vitrification of 3D MSC Spheroids
Principle: This protocol is optimized for size-controlled MSC spheroids, addressing CPA permeation challenges in 3D structures to prevent core ice crystal formation.
Materials:
- Spheroid Generation: Low-adherence U-bottom 96-well plates or hanging drop platforms
- CPA Solutions: Similar to Protocol 1, with adjusted sucrose concentrations
- Assessment Tools: Confocal microscopy with Live/Dead staining (Calcein-AM/Ethidium homodimer-1)
Procedure:
- Spheroid Fabrication: Seed 1,000-5,000 MSCs per well in low-adherence U-bottom plates. Centrifuge at 300 x g for 5 minutes to aggregate cells. Culture for 3-5 days to form compact spheroids of defined size (200-900 μm).
- CPA Equilibration: Carefully transfer spheroids using wide-bore pipettes through increasing concentrations of CPA (e.g., 2 M, then 4 M) in base solution, allowing 5-10 minutes per step at room temperature.
- Vitrification Loading: Incubate spheroids in the final Vitrification Solution (4 M DMSO + 4 M EG + 0.8 M sucrose) for 2-3 minutes at 4°C.
- Rapid Cooling: Using specialized vitrification carriers (e.g., Cryotop), submerge spheroids directly into liquid nitrogen.
- Rapid Warming: Rapidly warm by plunging the carrier into 37°C Washing Solution.
- Stepwise CPA Removal: Transfer spheroids sequentially through decreasing sucrose concentrations (1.0 M, 0.5 M, 0.25 M) in base solution, incubating for 5 minutes in each, before a final wash in culture medium [39].
Protocol 3: DMSO-Free Vitrification Using Ultrasonication-Assisted Trehalose Delivery
Principle: This novel technique uses ultrasound and microbubbles to deliver non-penetrating trehalose intracellularly, avoiding the toxicity associated with traditional CPAs.
Materials:
- CPA: 250-500 mM trehalose in DMEM without phenol red [21]
- Microbubbles: SonoVue microbubbles (1% v/v)
- Ultrasound System: 500 kHz focused ultrasound source, passive cavitation detector (PCD)
- Exposure Chamber: Maintained at 35 ± 1°C
Procedure:
- Cell Preparation: Suspend MSCs at 1 x 10^6 cells/mL in trehalose solution containing 1% (v/v) microbubbles.
- Ultrasound Exposure: Place the cell suspension in the focus of the ultrasound source. Expose to ultrasound (0.25 MPa peak negative pressure, 100 ms pulse length, 2 s pulse repetition period) for 5 minutes. Monitor cavitation activity with the PCD to ensure stable, non-inertial cavitation.
- Post-Treatment Processing: After exposure, let the cell suspension stand for 2 minutes to allow microbubble dissipation.
- Vitrification and Storage: Centrifuge and resuspend cells in a fresh trehalose-based vitrification solution. Aliquot into cryotubes and plunge into liquid nitrogen.
- Thawing and Assessment: Rapidly warm in a 37°C water bath. Centrifuge to remove trehalose and resuspend in culture medium. Assess viability, membrane integrity, and multipotency [21].
Workflow and Mechanism Diagrams
Diagram 1: Experimental workflow for MSC vitrification, outlining key phases from cell preparation to post-thaw analysis.
Diagram 2: Mechanism of CPA action in vitrification, illustrating molecular interactions leading to the glassy state.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Reagents for MSC Vitrification
| Category | Specific Item | Function & Application Notes |
|---|---|---|
| Primary Cryoprotectants | Dimethyl Sulfoxide (DMSO) | Penetrating CPA; industry standard but cytotoxic at high concentrations [8] |
| Ethylene Glycol (EG) | Penetrating CPA; often used in combination with DMSO [39] | |
| Propylene Glycol (PG) | Penetrating CPA; alternative to DMSO and EG [3] | |
| DMSO-Free Alternatives | Trehalose | Non-penetrating, biocompatible disaccharide; requires ultrasonication for intracellular delivery [21] |
| Sucrose | Non-penetrating CPA; commonly used in osmotic buffering and dilution solutions [8] [27] | |
| SGI Solution (Sucrose, Glycerol, Isoleucine) | DMSO-free clinical-grade alternative; reduces patient toxicity risks [27] | |
| Specialized Equipment | Programmable Freezer | Enables controlled-rate cooling for protocol standardization |
| Cryogenic Storage Tank | Liquid nitrogen tank for long-term storage at -196°C | |
| Ultrasonication System with Microbubbles | Facilitates intracellular delivery of non-penetrating CPAs like trehalose [21] | |
| Low-Adherence Plates | Essential for 3D MSC spheroid formation | |
| Viability Assessment Tools | Live/Dead Staining (Calcein-AM/ETH) | Fluorescent discrimination of live vs. dead cells post-thaw |
| Flow Cytometry | Quantifies viability and confirms MSC surface marker profile | |
| TUNEL Assay Kit | Detects apoptotic DNA fragmentation | |
| ROS Detection Assay | Measures reactive oxygen species generation post-thaw | |
| Ido1-IN-17 | Ido1-IN-17, MF:C28H32BrClFN5O2, MW:604.9 g/mol | Chemical Reagent |
| Hypoxanthine-13C5 | Hypoxanthine-13C5, MF:C5H4N4O, MW:141.08 g/mol | Chemical Reagent |
Vitrification represents a robust and effective methodology for the cryopreservation of MSCs in both 2D and 3D culture formats. While traditional protocols using high concentrations of penetrating CPAs like DMSO remain effective, recent advances in DMSO-free solutions and novel delivery methods for non-penetrating agents like trehalose offer promising avenues for reducing cytotoxicity and enhancing clinical safety [21] [27]. The critical parameters for success include precise control of cooling/warming rates, careful management of CPA addition and removal to mitigate osmotic stress, and thorough post-thaw validation of cell quality and functionality. By adhering to these detailed protocols and leveraging the provided toolkit, researchers can reliably establish MSC biobanks to support advanced therapeutic development and regenerative medicine applications.
Within the field of mesenchymal stem cell (MSC) research, effective cryopreservation is a critical gateway to clinical application. It enables the storage and off-the-shelf availability of these therapeutic cells, ensuring they remain viable and functional from the manufacturing facility to the patient bedside [28]. The choice of cryoprotective agent (CPA) formulation is paramount, directly impacting cell recovery, viability, and potency post-thaw. This application note provides a detailed comparison of the traditional cornerstone of cryopreservation—Dimethyl Sulfoxide (DMSO)-based and serum-containing media—against emerging, defined alternatives. Framed within the context of standardizing MSC research for clinical translation, this document offers structured data and actionable protocols to guide researchers and therapy developers in making informed, reproducible decisions for their cryopreservation strategies.
Comparative Analysis of CPA Formulations
The landscape of CPA formulations is broadly divided between well-established, traditional media and modern, defined alternatives. The tables below summarize the key characteristics, components, and performance metrics of these formulations.
Table 1: Composition and Key Characteristics of Major CPA Formulations
| Formulation Type | Key Components | Mechanism of Action | Advantages | Disadvantages & Risks |
|---|---|---|---|---|
| DMSO-Based Media [28] [27] | 5-10% (v/v) DMSO, Base carrier medium (e.g., saline or culture medium) | Penetrating CPA; reduces intracellular ice formation by disrupting ice crystal growth [28]. | • High cell viability & recovery across diverse cell types [41]• Rapid membrane penetration [41]• Long-standing history of use & extensive protocol validation | • Patient toxicity risks (e.g., infusion reactions) [28] [27]• Cytotoxic effects on cells during long-term exposure [21]• Requires careful removal (washing) post-thaw |
| Serum-Containing Media [41] | 10% DMSO, 20-90% Fetal Bovine Serum (FBS), Base culture medium | Serum provides growth factors, proteins, and antioxidants; supports membrane integrity and minimizes ice crystal damage [41]. | • Superior cellular protection from extracellular ice• Established efficacy & widespread researcher familiarity [41] | • High batch-to-batch variability of serum [42]• Risk of xenogenic immunogenicity & pathogen transmission [42]• Not suitable for clinical-grade GMP manufacturing |
| Serum-Free/Defined Media [42] [43] | DMSO or DMSO-free CPAs, Human Serum Albumin (HSA) or recombinant proteins, Chemically defined supplements | Replaces animal components with defined, xeno-free alternatives; mechanism of cryoprotection is CPA-dependent. | • GMP-compliant & suitable for clinical applications [42]• Reduced contamination risk & batch variability [43]• Enhanced product consistency & safety profile | • Can be more expensive than traditional media• May require optimization for specific MSC sources• Formulation-specific efficacy |
| DMSO-Free Alternatives [27] [21] | Sucrose, Trehalose, Glycerol, Isoleucine, Polymers (e.g., PVP, HES) | Non-penetrating CPAs; function extracellularly to suppress ice formation and stabilize cell membranes via osmotic dehydration and hydrogen bonding [21]. | • Eliminates DMSO-related toxicity concerns [27] [44]• Biocompatible and natural (e.g., trehalose) [21] | • Often requires advanced delivery methods (e.g., electroporation, ultrasound) for intracellular delivery [28] [21]• Cryoprotective efficacy can be cell-type dependent |
Table 2: Summary of Experimental Outcomes from Comparative Studies
| Study Focus | Tested Formulations | Key Performance Metrics | Results Summary |
|---|---|---|---|
| International Multicenter Study on DMSO-Free Formulation [27] | • Test: Sucrose-Glycerol-Isoleucine (SGI)• Control: Standard DMSO-containing solutions (5-10%) | • Cell Viability• Cell Recovery• Immunophenotype (CD73, CD90, CD105)• Gene Expression Profile | SGI solution demonstrated comparable results to DMSO-containing controls in cell viability, recovery, and immunophenotype across multiple international centers. |
| Ultrasound-Mediated Trehalose Delivery [21] | • Test: 50-1000 mM Trehalose + Microbubbles + Ultrasound• Control: Conventional 10% DMSO + FBS | • Post-thaw Viability• Membrane Integrity• Preservation of Multipotency (chondrogenic, osteogenic, adipogenic differentiation) | Optimized trehalose concentration (250-500 mM) delivered via ultrasound achieved similar cryopreservation outcomes to DMSO-based methods, successfully preserving MSC multipotency. |
| GMP-Validation of Serum-Free Media [42] | • Test: MSC-Brew GMP Medium (Serum-Free)• Control: Standard Media with FBS | • Post-thaw Viability (>95%)• Doubling Time• Colony-Forming Unit (CFU) Assay• Sterility and Endotoxin Testing | Cells cultured and cryopreserved in the serum-free, GMP-compliant medium showed enhanced proliferation rates, high post-thaw viability, and maintained sterility and marker expression for up to 180 days. |
| Toxicology Study on DMSO in Sepsis Models [44] | • Test: Cryopreserved MSCs with 5% DMSO (Diluted)• Control: Washed MSCs (DMSO removed) | • Cell Recovery & Apoptosis• Potency (phagocytosis rescue)• In-vivo mortality, body weight, organ injury | No DMSO-related adverse effects were detected in murine sepsis models. MSCs with 5% DMSO showed higher cell recovery and equivalent potency compared to washed MSCs. |
Detailed Experimental Protocols
Protocol 1: Cryopreservation of MSCs Using Standard DMSO/Serum-Based Media
This protocol outlines the conventional method for cryopreserving MSCs using a formulation containing 10% DMSO and serum, which remains a common benchmark in research settings [28] [42].
- Principle: Slow, controlled freezing in the presence of a penetrating cryoprotectant (DMSO) and extracellular protective agents (serum) to minimize intracellular ice crystallization and mitigate freeze-induced cell damage.
- Materials:
- Research Reagent Solutions:
- Culture Medium: e.g., MEM α, supplemented with 10% FBS and gentamicin [42].
- Trypsin-EDTA solution: For cell detachment.
- CPA Freezing Medium: 50% Culture Medium, 40% FBS, 10% DMSO. Prepare fresh and keep chilled (2-8°C) before use.
- Equipment: Controlled-rate freezer, -80°C freezer, liquid nitrogen storage tank, cryogenic vials, centrifuge, hemocytometer.
- Research Reagent Solutions:
- Step-by-Step Procedure:
- Cell Harvest: Culture MSCs to 80-90% confluency. Wash the cell layer with PBS and detach using a suitable concentration of trypsin-EDTA. Neutralize the trypsin with complete culture medium.
- Cell Counting and Centrifugation: Count the cell suspension using a hemocytometer or automated cell counter. Centrifuge the cell suspension at 300 × g for 10 minutes. Aspirate and discard the supernatant completely [42].
- Resuspension in CPA Medium: Resuspend the cell pellet in chilled CPA Freezing Medium to a final concentration of 1-5 × 10^6 cells/mL. Gently mix the suspension to ensure uniform cell distribution without creating bubbles.
- Aliquoting: Immediately aliquot the cell suspension into cryogenic vials (e.g., 1 mL per vial).
- Controlled-Rate Freezing: Place the cryovials in a controlled-rate freezer. Program the freezer to cool at a rate of -1°C per minute from room temperature to -40°C, followed by a rapid cool down to -100°C [28]. Alternatively, use a "Mr. Frosty" isopropanol-filled chamber, which provides an approximate cooling rate of -1°C/min when placed at -80°C overnight.
- Long-Term Storage: Transfer the cryovials to the vapor phase of a liquid nitrogen storage tank (-135°C to -150°C) for long-term preservation.
Protocol 2: Cryopreservation of MSCs Using a Defined, DMSO-Free SGI Formulation
This protocol describes the use of a sucrose-glycerol-isoleucine (SGI)-based, DMSO-free cryopreservation solution, validated in an international multicenter study [27].
- Principle: Utilizes a combination of non-penetrating (sucrose) and penetrating (glycerol) cryoprotectants, along with isoleucine, to provide extracellular and intracellular protection without the use of DMSO or serum.
- Materials:
- Research Reagent Solutions:
- Base Solution: Physiological saline or a simple buffer like PBS.
- SGI Cryoprotectant Solution: Sucrose (e.g., 30 mM), Glycerol (e.g., 5%), L-Isoleucine (e.g., 7.5 mM) in the base solution [27]. Filter-sterilize and store at 2-8°C.
- Equipment: Same as Protocol 1.
- Research Reagent Solutions:
- Step-by-Step Procedure:
- Cell Harvest and Counting: Follow Steps 1 and 2 from Protocol 1 to obtain a concentrated cell pellet.
- Resuspension in SGI Medium: Gently resuspend the cell pellet in the pre-chilled SGI Cryoprotectant Solution to a final concentration of 1-5 × 10^6 cells/mL.
- Aliquoting and Freezing: Aliquot the cell suspension into cryovials. Proceed with controlled-rate freezing using the same parameters as in Protocol 1 (i.e., -1°C/min to -40°C) [27].
- Long-Term Storage: Transfer the vials to liquid nitrogen for long-term storage.
Protocol 3: Advanced Intracellular Delivery of Trehalose via Ultrasound
For research into novel CPA delivery systems, this protocol details the use of ultrasound and microbubbles to facilitate the intracellular loading of trehalose, a non-penetrating sugar [21].
- Principle: Ultrasound-induced cavitation of microbubbles creates transient, non-lethal pores in the cell membrane, allowing the diffusion of trehalose into the cytoplasm to provide intracellular cryoprotection.
- Materials:
- Research Reagent Solutions:
- Trehalose Solution: 250-500 mM D-(+)-Trehalose dihydrate in DMEM without phenol red [21].
- Microbubble Contrast Agent: e.g., SonoVue.
- Cell Culture Medium: Standard MSC growth medium.
- Equipment: Ultrasound system with a focused source (e.g., 500 kHz), passive cavitation detector (PCD) for monitoring, sample chamber, water bath heater.
- Research Reagent Solutions:
- Step-by-Step Procedure:
- Sample Preparation: Harvest and count MSCs as before. Prepare a cell suspension at a density of 1 × 10^6 cells/mL in the trehalose solution. Add 1% (v/v) of the microbubble suspension to the cell-trehalose mixture [21].
- Ultrasound Exposure Setup: Transfer the sample to an Eppendorf tube or custom chamber. Position the sample in the focus of the ultrasound transducer within a degassed water bath maintained at 35°C.
- Sonication Parameters: Expose the sample to ultrasound using parameters such as: 0.5 MHz frequency, 0.25 MPa peak negative pressure, 100 ms pulse length, 2 s pulse repetition period, for 5 minutes total exposure [21]. Monitor cavitation signals with the PCD.
- Post-Sonication Processing: After sonication, let the sample rest for 5 minutes. Centrifuge the cells gently (200 × g for 5 min) to remove the trehalose solution and microbubbles.
- Cryopreservation: Resuspend the trehalose-loaded cells in a suitable carrier medium (e.g., PBS with 1% HSA) for freezing. Proceed with controlled-rate freezing and storage as described in previous protocols.
Visualizing the Experimental Workflows
The following diagrams illustrate the key procedural pathways for the protocols described above.
Conventional vs. DMSO-Free Cryopreservation Workflow
Ultrasound-Mediated Trehalose Delivery Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for MSC Cryopreservation Research
| Reagent / Material | Function / Role | Example Use-Case & Notes |
|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Penetrating cryoprotectant that enters the cell to prevent intracellular ice formation. | Gold standard CPA; used at 5-10% (v/v) [28] [41]. Requires caution due to potential cellular and patient toxicity. |
| Fetal Bovine Serum (FBS) | Provides a complex mixture of proteins, growth factors, and antioxidants for extracellular protection. | Common component in research-grade freezing media [41]. Batch variability and regulatory concerns limit clinical use. |
| Recombinant Human Serum Albumin (rHSA) | Animal-origin-free protein stabilizer and osmotic regulator; replaces FBS in GMP-compliant media. | Critical for clinical translation; reduces contamination risk and batch variability (e.g., Optibumin 25) [41]. |
| Trehalose | Non-penetrating, biocompatible disaccharide that stabilizes cell membranes during dehydration/freezing. | DMSO-free alternative; requires assisted delivery (e.g., ultrasound, electroporation) for intracellular efficacy [21]. |
| Sucrose | Non-penetrating CPA; acts as an osmotic balancer and helps stabilize the extracellular environment. | Component of many DMSO-free formulations, such as the SGI solution [27]. |
| GMP-Compliant, Serum-Free Media | Chemically defined, xeno-free basal media (e.g., MSC-Brew, MesenCult-ACF Plus) for cell culture and cryopreservation. | Essential for manufacturing clinically applicable MSCs; supports cell growth and maintains phenotype while ensuring safety [42]. |
| Microbubble Contrast Agent | Ultrasound contrast agent (e.g., SonoVue) that cavitates under acoustic pressure to permeabilize cell membranes. | Enables intracellular delivery of impermeable CPAs like trehalose in advanced cryopreservation protocols [21]. |
| Atg7-IN-1 | Atg7-IN-1, MF:C17H19FN6O5S2, MW:470.5 g/mol | Chemical Reagent |
| 21-Desacetyldeflazacort-D5 | 21-Desacetyldeflazacort-D5, MF:C23H29NO5, MW:404.5 g/mol | Chemical Reagent |
The advancement of mesenchymal stromal/stem cell (MSC)-based therapies is critically dependent on reliable, safe, and effective cryopreservation methods that facilitate "off-the-shelf" availability. Cryopreservation enables long-term storage, rigorous quality control, and timely delivery of cellular products, which is essential for both clinical applications and commercial viability [45] [46]. For decades, dimethyl sulfoxide (DMSO) has been the predominant cryoprotectant for MSCs, leveraging its ability to penetrate cells and suppress ice crystal formation. However, a growing body of evidence indicates that DMSO poses significant challenges, including concentration-dependent cytotoxicity, induction of unwanted cell differentiation, and the potential to cause adverse reactions in patients, ranging from nausea and chills to more severe cardiovascular or neurological events [47] [48] [46]. These concerns have catalyzed the field to develop safer, DMSO-free cryopreservation strategies.
Innovative solutions are emerging that replace DMSO with combinations of biologically compatible molecules. Among the most promising is a novel cryoprotectant solution comprising Sucrose, Glycerol, and Isoleucine (SGI) in a Plasmalyte A base, which has demonstrated comparable performance to traditional DMSO-containing formulas in an international multicenter study [49]. Concurrently, several clinical-grade, commercially available DMSO-free solutions are being rigorously evaluated. This application note details the composition, efficacy, and practical protocols for implementing these DMSO-free alternatives, providing researchers and drug development professionals with the tools to integrate these innovations into their MSC research and therapeutic product development workflows.
Sucrose-Glycerol-Isoleucine (SGI): A Novel DMSO-Free Formulation
Composition and Rationale
The SGI formulation is a scientifically engineered, serum-free solution designed to provide comprehensive cryoprotection through the synergistic action of its components.
- Sucrose: A non-penetrating disaccharide that acts as an osmotic buffer, stabilizing the cell membrane and mitigating dehydration-induced damage during freezing.
- Glycerol: A penetrating cryoprotectant that enters the cell, disrupting ice crystal formation and reducing intracellular freezing points. Its lower toxicity profile compared to DMSO makes it a favorable alternative.
- Isoleucine: An amino acid that may contribute to membrane stabilization and provide additional osmotic support, enhancing the overall resilience of cells during the freeze-thaw cycle.
- Plasmalyte A Base: A balanced, physiological solution that provides a stable ionic and pH environment, minimizing osmotic and chemical stress.
Key Experimental Findings from Multicenter Validation
A pivotal international multicenter study conducted under the PACT/BEST Collaborative compared this SGI solution against standard in-house DMSO-containing cryoprotectants (typically 5-10% DMSO) from seven participating centers [49]. The results provide strong evidence for its application in MSC cryopreservation.
Table 1: Post-Thaw Performance of MSCs Cryopreserved with SGI vs. DMSO-Based Solutions
| Parameter | Pre-Cryopreservation (Baseline) | SGI Solution (Post-Thaw) | DMSO-Based Solutions (Post-Thaw) | Statistical Significance |
|---|---|---|---|---|
| Viability | 94.3% (95% CI: 87.2-100%) | 82.9% (decrease of 11.4%) | 89.8% (decrease of 4.5%) | P < 0.001 for SGI decrease; P=0.049 for DMSO decrease |
| Recovery of Viable MSCs | Not Applicable | 92.9% (95% CI: 85.7-100.0%) | 87.3% (5.6% lower than SGI) | P < 0.013 |
| Immunophenotype | Conformed to ISCT criteria | No significant difference from pre-freeze or DMSO-preserved cells | No significant difference from pre-freeze profile | Not Significant |
| Global Gene Expression | Baseline Profile | Comparable to pre-freeze and DMSO-preserved cells | Comparable to pre-freeze profile | Not Significant |
The data indicates that while the immediate post-thaw viability of MSCs cryopreserved in SGI was slightly lower than those preserved in DMSO, the SGI solution enabled a significantly higher recovery of viable cells. Critically, the cells retained their defining surface markers (CD73, CD90, CD105) and global gene expression profiles, confirming that the formulation maintains core cellular identity and is unlikely to induce unwanted phenotypic changes [49]. The average viability above 80% is generally considered clinically acceptable, positioning SGI as a viable candidate for further development and application.
Beyond the investigational SGI formulation, several commercial, GMP-grade, DMSO-free cryopreservation solutions are available. These products offer researchers standardized, regulatory-compliant options, though their performance can vary.
Table 2: Commercially Available DMSO-Free Cryopreservation Solutions for MSCs
| Product Name | Key Components | Reported Performance on MSCs | Key Characteristics |
|---|---|---|---|
| CryoScarless (CSL) | Not fully disclosed | Provides the second-best post-thaw viability and recovery after CPP-STEM in a CB HSC study; suitable for storage at -80°C or in LN₂ [48]. | Xenogeneic- and serum-free formulation. |
| CryoProtectPureSTEM (CPP-STEM) | Balanced salt base, glycol derivatives, non-toxic protein components of xenogenic origin [48]. | In a CB HSC study, provided post-thaw viability, recovery, and potency equal or superior to DMSO; supported equivalent short- and long-term engraftment kinetics [48]. | DMSO- and serum-free; performance with MSCs is promising but requires further direct validation. |
| Pentaisomaltose (PIM) | Pentaisomaltose (a sugar alcohol), Albumin [48]. | Similar recovery of CD34+ cells and CFUs compared to 10% DMSO in PBSC grafts; supported similar long-term engraftment [48] [28]. | Primarily studied for hematopoietic stem cells. |
| StemCell Keep | Polyampholyte-based [47]. | Effective for cryopreservation of human iPSCs, ESCs, and MSCs; mechanism involves adsorption onto the cell membrane for surface protection [47]. | Protein- and DMSO-free. |
A direct comparative study of cryopreservation solutions highlighted the importance of formulation over the mere presence or absence of DMSO. MSCs cryopreserved in solutions with 10% DMSO (NutriFreez and PHD10) displayed comparable viabilities and recoveries up to 6 hours after thawing. In contrast, a solution containing only 5% DMSO (CryoStor CS5) showed a decreasing trend in both viability and recovery over the same period. Furthermore, MSCs cryopreserved in NutriFreez and PHD10 exhibited significantly better post-thaw proliferative capacity after a 6-day culture compared to those in other solutions [45] [50]. This underscores that a simple reduction of DMSO concentration without careful reformulation can be detrimental, and that well-designed DMSO-free solutions can match or exceed the performance of some DMSO-containing standards.
The Scientist's Toolkit: Essential Reagents for DMSO-Free Cryopreservation
Transitioning to DMSO-free protocols requires a specific set of reagents and materials. The following table outlines the core components of a toolkit for implementing the SGI protocol and working with other advanced cryopreservation solutions.
Table 3: Research Reagent Solutions for DMSO-Free MSC Cryopreservation
| Reagent/Material | Function/Description | Example/Note |
|---|---|---|
| Plasmalyte A | A balanced salt solution used as a physiological base for in-house cryomedium formulation. Provides ionic and pH stability. | Often used as a diluent and base for solutions like PHD10 and SGI [49] [45]. |
| Human Serum Albumin (HA) | Provides colloidal osmotic pressure, stabilizes cell membranes, and reduces mechanical stress during freezing and thawing. | Used at 5% in clinical-grade formulations like PHD10 [45]. |
| Sucrose | Non-penetrating cryoprotectant that dehydrates cells and minimizes osmotic shock. | A key component of the SGI formulation and many other DMSO-free strategies [49] [51]. |
| Glycerol | Penetrating cryoprotectant with lower cytotoxicity than DMSO. Modulates ice crystal formation. | Used in the SGI formulation (concentration not fully disclosed) and other combinations [49] [51]. |
| L-Isoleucine | An amino acid that may act as an osmolyte and contribute to membrane stabilization during cryopreservation. | A distinctive component of the SGI formulation [49]. |
| Commercial DMSO-Free Media | Pre-formulated, regulatory-compliant solutions offering standardization and convenience. | Examples include CryoScarless, CryoProtectPureSTEM, and StemCell Keep [47] [48]. |
| Controlled-Rate Freezer | Equipment that ensures a consistent, optimized cooling rate (typically -1°C/min to -3°C/min), which is critical for high cell viability and recovery. | Essential for reproducible slow-freezing protocols [49] [3]. |
| Dicoumarol-d8 | Dicoumarol-d8 Stable Isotope | |
| Ret-IN-11 | Ret-IN-11 | Ret-IN-11 is a potent RET kinase inhibitor for cancer research. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
Detailed Experimental Protocols
Protocol 1: Cryopreservation of MSCs Using the SGI Formulation
The following protocol is adapted from the methodology of the international multicenter study [49].
Workflow Overview:
Step-by-Step Methodology:
Preparation of SGI Cryomedium:
- Prepare the DMSO-free cryopreservation solution containing precise concentrations of sucrose, glycerol, and isoleucine in a base of Plasmalyte A. The exact molarities may be proprietary, but the formulation is known to be effective for clinical-grade MSC preservation [49].
- Sterile-filter the solution (0.22 µm) and store it at 4°C until use.
Cell Harvest and Resuspension:
- Harvest MSCs from culture using standard trypsinization or non-enzymatic methods.
- Perform a viable cell count and centrifuge to form a cell pellet.
- Resuspend the cell pellet in the pre-chilled SGI cryomedium to a final concentration suitable for your application (e.g., 3-9 million cells/mL, as tested in similar studies [45]).
Aliquoting and Freezing:
- Quickly aliquot the cell suspension into cryogenic vials or freezing bags.
- Transfer the aliquots to a controlled-rate freezer.
- Initiate a slow-freezing program. A typical protocol involves cooling at a rate of -1°C to -3°C per minute until reaching at least -40°C, followed by a more rapid cooling phase before transfer to liquid nitrogen for long-term storage [49] [3].
Storage:
- Store the vials or bags in the vapor or liquid phase of liquid nitrogen (below -150°C) for a minimum of one week before thawing and assessment.
Protocol 2: Post-Thaw Viability and Functional Assessment
Evaluating the success of cryopreservation requires a multi-parametric approach beyond immediate viability.
Workflow Overview:
Step-by-Step Methodology:
Thawing and Sample Preparation:
- Rapidly thaw a vial of cryopreserved MSCs by gently agitating it in a 37°C water bath for approximately 2 minutes or until the last ice crystal disappears [45] [3].
- To mitigate the osmotic stress of direct dilution, consider a stepwise dilution or a single wash step using a solution like Plasmalyte A supplemented with 5% Human Albumin (PLA/5% HA) [45]. Note that washing can lead to cell loss and should be optimized for each protocol.
Viability and Recovery Assessment:
- Viability: Perform cell counts using the Trypan Blue exclusion method immediately post-thaw (0-hour) and at subsequent time points (e.g., 2, 4, 6 hours) to assess stability. For a more nuanced view of cell health, use Annexin V/Propidium Iodide (PI) staining followed by flow cytometry to distinguish between live, early apoptotic, and dead cells [45] [50].
- Recovery: Calculate the percentage recovery of viable cells using the formula: (Total number of live cells post-thaw / Number of cells originally cryopreserved) × 100%.
Immunophenotype Analysis:
- Confirm that the thawed MSCs retain their characteristic surface marker profile as defined by the International Society for Cellular Therapy (ISCT).
- Stain cells with fluorescently conjugated antibodies against positive markers (e.g., CD73, CD90, CD105) and negative markers (e.g., CD45, CD34, CD14) and analyze by flow cytometry. The profile should be comparable to pre-freeze cells and those cryopreserved in DMSO [49] [45].
Functional Potency Assays:
- Proliferation Capacity: Seed thawed MSCs at a low density and culture for 4-6 days. Perform cell counts at the end of the culture period to assess regrowth potential. Studies show that cells preserved in optimal formulations (like NutriFreez/PHD10) exhibit far better proliferative capacity than those in suboptimal ones [45].
- Immunomodulatory Function: Validate functionality using assays such as:
- T-cell Proliferation Inhibition: Co-culture thawed MSCs with activated peripheral blood mononuclear cells (PBMCs) and measure the suppression of T-cell proliferation using methods like CFSE dilution.
- Monocytic Phagocytosis: Assess the ability of thawed MSCs to enhance the phagocytic activity of monocytes, a key immunomodulatory mechanism [45] [50]. No significant differences should be observed between MSCs cryopreserved in the best DMSO-free and DMSO-containing solutions.
The SGI formulation represents a significant breakthrough in DMSO-free cryopreservation, demonstrating that a carefully balanced combination of sucrose, glycerol, and isoleucine can provide post-thaw recovery and functional characteristics that are comparable, and in some aspects superior, to traditional DMSO-based methods. The existence of multiple commercial clinical-grade alternatives further expands the toolkit available to researchers and clinicians.
Future work should focus on refining these formulations to close the small gap in immediate post-thaw viability and on conducting rigorous in vivo functional studies to confirm the long-term therapeutic potency of MSCs preserved with these novel solutions. As the field moves towards greater standardization and safety, the adoption of such DMSO-free protocols will be instrumental in realizing the full clinical and commercial potential of MSC-based therapies.
The transition of Mesenchymal Stem Cell (MSC) therapies from conventional 2D cultures to complex three-dimensional (3D) spheroids and tissue constructs represents a significant advancement in regenerative medicine. These 3D models more accurately mimic the native tissue microenvironment, preserving critical cell-cell and cell-extracellular matrix interactions that govern physiological function [52]. However, this architectural complexity introduces substantial challenges for cryopreservation, as conventional protocols optimized for single-cell suspensions often lead to unacceptable losses in viability, structural integrity, and functionality upon thawing [52] [53]. The preservation of these sophisticated constructs is not merely about keeping cells alive; it is about maintaining their structured biofunctionality. The core challenge lies in managing ice crystal formation, cryoprotectant agent (CPA) diffusion, and thermal gradients within a dense, multicellular structure, where cell-cell contacts can facilitate intracellular ice formation and where diffusion limitations can create zones of variable CPA concentration [52] [34]. This document provides detailed application notes and protocols, framed within a broader thesis on cryopreservation techniques for MSC research, to empower researchers and therapy developers in establishing robust preservation workflows for 3D MSC products.
Theoretical Foundations: Key Phenomena Governing 3D Cryopreservation Success
The cryopreservation outcome of 3D MSC constructs is governed by interconnected thermodynamic and biochemical phenomena. Understanding these is crucial for protocol optimization.
Mass Transfer and Osmotic Behavior: Unlike single cells in suspension, MSC spheroids exhibit significantly different mass transfer properties. Research on L929 cell spheroids has demonstrated that the packing of cells substantially reduces osmotic water transport across the plasma membrane, and permeability coefficients for water and CPAs like dimethyl sulfoxide (Me₂SO) are highest for individual cells and decrease significantly for cells located deeper within the spheroid [52]. This necessitates longer equilibration times. Furthermore, the osmotically inactive volume of a spheroid (αsph), a critical parameter for predicting volumetric changes during freezing, is considerably larger than that of its constituent single cells (αcell). For example, for 3-day cultivated MSC spheroids, αsph was found to be 0.684, compared to αcell of 0.367, due to the space occupied by cell-cell contacts and the developing extracellular matrix [52].
Ice Formation Dynamics: The presence of intercellular contacts fundamentally alters ice nucleation behavior. Evidence indicates that intracellular ice forms at significantly lower cooling rates in spheroids and tissues than in single-cell suspensions, as ice can propagate from one cell to its neighbors through membrane contacts [52] [53]. This makes rapid cooling protocols riskier for 3D constructs. Therefore, a cooling rate of 1°C/min, which promotes protective dehydration over intracellular ice formation, is most commonly employed in slow freezing protocols for spheroids [54] [52].
Cryoprotectant Cytotoxicity: The universal use of Meâ‚‚SO (DMSO) as a penetrating CPA presents a major clinical hurdle. While intravenous administration of DMSO is common for some cell therapies, it is associated with adverse events [54]. More critically, for novel administration routes directly into organs like the brain or eye, even low concentrations of DMSO (0.5-1%) can cause significant cytotoxicity [54]. This creates a pressing need for post-thaw washing, which introduces risks of contamination and shear stress, complicating the path to "off-the-shelf" therapies [54]. The scientific premise of recent advances is to either reduce DMSO to minimal levels or replace it entirely with less toxic alternatives.
Experimental Protocols for 3D MSC Construct Cryopreservation
Protocol 1: Slow Freezing of MSC Spheroids with Optimized Media
This protocol is designed for the cryopreservation of pre-formed MSC spheroids using clinically relevant freezing media.
- Aim: To preserve MSC spheroids with high viability, maintained phenotype, and minimal DMSO-related toxicity.
Materials:
- MSC Spheroids: Pre-formed using your method of choice (e.g., hanging drop, ultra-low attachment plates).
- Cryopreservation Media: Compare commercial GMP-grade media. CryoStor10 (CS10) has shown superior results in maintaining viability and morphology [55].
- Control Medium (CM): Dulbecco's Modified Eagle's Medium (DMEM) with 20% Fetal Bovine Serum (FBS) and 10% DMSO.
- Equipment: Programmable freezer, -80°C mechanical freezer, liquid nitrogen storage tank, 37°C water bath or automated thawing device.
Methodology:
- Equilibration: After spheroid formation, carefully aspirate the culture medium. Resuspend the spheroids in the selected cryopreservation medium (e.g., CS10, SCB, RFM) or CM. Gently pipette to ensure even distribution.
- Aliquoting: Transfer the spheroid suspension into cryovials (e.g., 1 mL/vial).
- Freezing: Place the cryovials in a controlled-rate freezer. Initiate the following slow-freezing profile:
- Start at 4°C.
- Cool at a rate of -1°C/min down to -40°C to -50°C.
- Hold for 10-15 minutes.
- Rapidly transfer the vials to the vapor phase of a liquid nitrogen tank (below -130°C) for long-term storage.
- Thawing: When needed, rapidly retrieve a vial and thaw it by gentle agitation in a 37°C water bath until only a small ice crystal remains (approx. 2-3 minutes).
- Post-Thaw Handling: Immediately transfer the thawed suspension to a centrifuge tube containing pre-warmed culture medium. Gently centrifuge (e.g., 300-400 x g for 5 minutes) to pellet the spheroids. Aspirate the supernatant containing the CPA and resuspend the spheroids in fresh culture medium for subsequent analysis or application.
Key Analysis Endpoints:
- Viability: Assess using LIVE/DEAD assay or Annexin V/Propidium Iodide staining. CS10 has demonstrated relatively higher post-thaw viability compared to CM and other media [55].
- Morphology: Use scanning electron microscopy (SEM) to check for preserved spheroid surface architecture.
- Phenotype: Verify the retention of MSC surface markers (CD105, CD73, CD90) and the absence of hematopoietic markers via flow cytometry.
- Functionality: Test differentiation potential (osteogenic, adipogenic, chondrogenic) and gene expression of stemness markers (e.g., OCT4, NANOG) post-thaw.
Protocol 2: Hydrogel Microencapsulation for Low-DMSO Cryopreservation
This innovative protocol uses alginate hydrogel microcapsules to physically protect MSCs, enabling a drastic reduction in DMSO concentration.
- Aim: To cryopreserve MSCs with high efficiency using DMSO concentrations at or below 2.5%, mitigating CPA toxicity.
Materials:
- Cells: Human Umbilical Cord MSCs (hUC-MSCs).
- Hydrogel Components: Sodium Alginate, Calcium Chloride (CaClâ‚‚) solution, Mannitol, Hydroxypropyl methylcellulose.
- Core Solution: Mannitol and hydroxypropyl methylcellulose in sterile water.
- Equipment: High-voltage electrostatic coaxial spraying device, infusion pumps, coaxial needle assembly.
Methodology:
- Cell Preparation: Culture hUC-MSCs to 80% confluence. Trypsinize, centrifuge, and collect the cell pellet. Keep on ice.
- Core Solution Preparation: On ice, mix the core solution with Type I collagen and 0.1 mol/L NaOH. Resuspend the hUC-MSCs pellet in this solution to form the "core" of the future microcapsules.
- Microencapsulation:
- Load the cell-containing core solution into a syringe on an infusion pump connected to the inner lumen of a coaxial needle.
- Load the sodium alginate shell solution into another syringe on a pump connected to the outer lumen.
- Place a beaker with CaClâ‚‚ crosslinking solution below the needle.
- Apply a high voltage (e.g., 6 kV) for electrostatic spraying. Adjust the flow rates (e.g., core: 25 μL/min, shell: 75 μL/min).
- The liquid forms microdroplets that fall into the CaClâ‚‚ solution, instantly gelling into solid microcapsules encapsulating the cells.
- Cryopreservation: Harvest the microcapsules and resuspend them in a freezing medium containing a low concentration of 2.5% (v/v) DMSO. Transfer to cryovials and freeze using a standard slow-freeze protocol (as in Protocol 1).
- Thawing and Use: Thaw rapidly at 37°C. The microcapsules can be directly cultured or implanted, as alginate is biocompatible and biodegradable, or the cells can be released if needed [56].
Key Analysis Endpoints:
- Viability: Cell viability within microcapsules post-thaw should meet or exceed the 70% clinical threshold [56].
- Functionality: Confirm retained multidifferentiation potential (osteogenic, adipogenic, chondrogenic).
- Stemness: Assess enhanced expression of stemness-related genes (e.g., SOX2, OCT4) compared to 2D-cultured controls.
Data Presentation and Analysis
The following tables consolidate quantitative data from recent studies to facilitate comparison of different strategies.
Table 1: Comparison of Commercial Cryopreservation Media for MSC Spheroids [55]
| Media Name | Key Composition | Post-Thaw Viability | Morphology Preservation | Phenotype Retention |
|---|---|---|---|---|
| CryoStor10 (CS10) | Proprietary, GMP-grade | Relatively Higher | Well-preserved (via SEM) | Similar to non-frozen control |
| Stem-Cellbanker (SCB) | Proprietary, GMP-grade | Relatively Higher | Good | Data not specified |
| Recovery Cell Culture Freezing Media (RFM) | Proprietary | Lower than CS10/SCB | Data not specified | Data not specified |
| Conventional Medium (CM) | 10% DMSO, 20% FBS | Lower | Less preserved | Data not specified |
Table 2: Performance of Hydrogel Microencapsulation Cryopreservation with Low DMSO [56]
| DMSO Concentration | Encapsulation Status | Post-Thaw Viability | Stemness Gene Expression | Differentiation Potential |
|---|---|---|---|---|
| 10.0% | Non-encapsulated (2D) | High (Baseline) | Baseline | Baseline |
| 5.0% | Non-encapsulated (2D) | Reduced | Data not specified | Data not specified |
| 2.5% | Non-encapsulated (2D) | <70% (Below clinical threshold) | Data not specified | Data not specified |
| 2.5% | Alginate Microencapsulated | ≥70% (Meets clinical threshold) | Enhanced | Retained |
| 1.0% | Alginate Microencapsulated | <70% | Data not specified | Data not specified |
| 0% | Alginate Microencapsulated | Very Low | Data not specified | Data not specified |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for 3D MSC Cryopreservation Research
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| GMP-Grade Cryopreservation Media | Ready-to-use, optimized media for clinical translation. Provides a controlled baseline. | CryoStor10 (CS10), Stem-Cellbanker (SCB) [55] |
| Penetrating Cryoprotectants | Low molecular weight CPAs that enter cells, reducing intracellular ice formation. | Dimethyl Sulfoxide (DMSO), Glycerol, Ethylene Glycol (EG) [34] |
| Non-Penetrating Cryoprotectants | Macromolecules that protect cells extracellularly, enabling DMSO reduction. | Sucrose, Trehalose, Hyaluronic Acid (HMW-HA), Polyvinyl alcohol (PVA) [34] [53] |
| Hydrogel Biomaterials | Form 3D scaffolds and microcapsules for structural support and cryoprotection. | Alginate, Hyaluronic Acid (MeHA), Matrigel, Chitosan [56] [53] [57] |
| Programmable Freezer | Provides precise, reproducible control over cooling rates for slow freezing. | Capable of a -1°C/min ramp from 4°C to -50°C [54] |
| High-Throughput Microencapsulation System | Generates uniform, size-controlled cell-laden hydrogel microbeads. | Microfluidic devices, High-voltage electrostatic coaxial sprayers [56] [57] |
| Lsd1-IN-12 | Lsd1-IN-12, MF:C16H16N2O, MW:252.31 g/mol | Chemical Reagent |
| Anti-inflammatory agent 22 | Anti-inflammatory agent 22, MF:C22H16O6, MW:376.4 g/mol | Chemical Reagent |
Signaling Pathways and Workflow Visualization
The experimental workflow for cryopreserving 3D MSC constructs integrates multiple steps, from preparation to analysis. The following diagram outlines this generalized, optimized workflow.
Optimized Workflow for 3D MSC Cryopreservation
Emerging research suggests that the protective effect of certain biomaterials like Hyaluronic Acid (HA) during cryopreservation may involve the modulation of specific intracellular signaling pathways, particularly those regulating cytoskeletal integrity and apoptosis. The diagram below illustrates this hypothesized mechanism.
Cryoprotective Signaling Pathway Modulation
Within the broader framework of cryopreservation techniques for mesenchymal stem cell (MSC) research, the thawing and post-thaw recovery process is a critical determinant of experimental success and therapeutic efficacy. Cryopreserved MSCs are an indispensable resource for regenerative medicine and drug development, enabling long-term storage and off-the-shelf availability for research and clinical applications [3] [8]. However, the process of thawing poses significant risks to cell viability and function, including osmotic shock, mechanical damage from ice recrystallization, and toxicity from cryoprotective agents (CPAs) such as dimethyl sulfoxide (DMSO) [13] [58]. A meticulously optimized thawing protocol is therefore not merely a final step but a crucial procedure to ensure that the robust biological properties of MSCs—including their immunomodulatory capacity and differentiation potential—are preserved for downstream applications [59]. This application note provides a detailed, evidence-based protocol for the rapid warming, CPA removal, and post-thaw recovery of MSCs, designed to deliver high cell viability and functional integrity for the most demanding research and development settings.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table catalogues essential reagents and materials required for the execution of the thawing and recovery protocols described herein.
Table 1: Essential Reagents and Materials for MSC Thawing and Recovery
| Item | Function/Description | Key Considerations for Use |
|---|---|---|
| Water Bath | Provides a stable 37°C environment for rapid vial thawing. | Must be clean and validated to prevent microbial contamination of vials [58]. |
| Dulbecco's Phosphate-Buffered Saline (DPBS) | A balanced salt solution used for washing cells and diluting CPA-containing media. | Provides an isotonic buffer to maintain osmotic balance during CPA removal [59]. |
| Complete Culture Medium | Growth medium (e.g., Alpha-MEM) supplemented with Fetal Bovine Serum (FBS) and antibiotics. | Serum can help stabilize cell membranes post-thaw. Pre-warm to 37°C before use [59]. |
| Dimethyl Sulfoxide (DMSO) | The most common penetrating CPA requiring removal post-thaw. | Use clinical-grade (e.g., CryoSure) for therapeutic applications to ensure purity and safety [59]. |
| Human Serum Albumin (HSA) | A non-penetrating CPA and macromolecular additive. | Helps mitigate osmotic shock during CPA addition and removal; used at 2% in freezing solutions [59]. |
| Polyethylene Glycol (PEG) | A non-penetrating polymer CPA. | Can be used in combination with reduced DMSO concentrations to lower overall CPA toxicity [59]. |
| Trypan Blue or AO/PI Stains | Viability stains for assessing membrane integrity post-thaw. | Use for a quick assessment of viability before plating or further expansion [60]. |
| Antitubercular agent-10 | Antitubercular agent-10|Research Compound | Antitubercular agent-10 is a small molecule inhibitor for infectious disease research. This product is for Research Use Only (RUO). Not for human or veterinary use. |
| Myricetin-13C3 | Myricetin-13C3, MF:C15H10O8, MW:321.21 g/mol | Chemical Reagent |
Critical Parameters for Optimized Thawing
Successful recovery of cryopreserved MSCs hinges on the precise control of several physical and chemical parameters. The quantitative values summarized in the table below are derived from established protocols and empirical research.
Table 2: Quantitative Parameters for MSC Thawing and Recovery
| Parameter | Optimal Value or Condition | Rationale & Consequences of Deviation |
|---|---|---|
| Thawing Rate | Rapid, >100°C/min, in a 37°C water bath until ice crystals just disappear [3]. | Prevents damaging ice recrystallization inside the cell. Slow thawing promotes ice crystal growth and cell death. |
| CPA Removal | Centrifugation after gradual dilution of CPA [3] [13]. | Prevents "osmotic shock" and excessive cell swelling, which can cause lysis. |
| Post-Thaw Cell Seeding Density | 2x10^5 - 1x10^6 viable cells per well of a 6-well plate [58]. | Too high density can lead to nutrient depletion; too low density can impair growth due to lack of paracrine signaling. |
| Post-Thaw Assessment Timing | 24-48 hours after plating [58]. | Allows cells to recover metabolically and attach, providing a more accurate assessment of functional viability. |
| DMSO Concentration in Infusate | As low as possible; residual DMSO is associated with patient adverse effects [13] [28]. | High DMSO concentrations in final products can cause adverse reactions in patients, including allergic responses [3] [13]. |
The following workflow diagram outlines the logical sequence and decision points in the post-thaw recovery process, from vial removal to final assessment.
Detailed Experimental Protocol: Thawing and Recovery of Cryopreserved MSCs
This step-by-step protocol is designed to maximize the recovery of viable, functional MSCs after cryopreservation. All steps should be performed under sterile conditions in a biological safety cabinet unless otherwise specified.
Materials and Pre-Thaw Preparation
- Cryopreserved MSC Vial: Ensure the vial is clearly labeled and stored in the vapor phase of liquid nitrogen (-140°C to -180°C) until the moment of thawing [58].
- Pre-warmed Media: Thaw complete culture medium (e.g., Alpha-MEM with 10% FBS, 1% GlutaMAX, 1% penicillin/streptomycin) and store in a 37°C water bath or incubator until use [59].
- Dilution Medium: Prepare a dilution medium, which can be complete culture medium or DPBS supplemented with 2-5% HSA or FBS. The protein supplement helps stabilize cells during the osmotic stress of CPA removal [59].
- Equipment: Ensure access to a 37°C water bath, a centrifuge with a swinging-bucket rotor, and a haemocytometer or automated cell counter.
Step-by-Step Thawing and CPA Removal
- Rapid Thawing: Remove the cryovial from liquid nitrogen storage and immediately transfer it to a 37°C water bath. Submerge the vial just below the cap level and gently agitate it until only a small ice crystal remains (typically 2-3 minutes). It is critical to work quickly to minimize the time CPAs spend at elevated temperatures, which increases their toxicity [3] [58].
- Decontamination: Wipe the exterior of the vial thoroughly with 70% ethanol before placing it inside the biological safety cabinet.
- Gradual Dilution: Gently transfer the thawed cell suspension from the vial using a pipette into a 15 mL conical tube containing 10 mL of pre-warmed dilution medium. It is crucial to add the cell suspension dropwise to the dilution medium while gently swirling the tube. This slow dilution gradually reduces the extracellular DMSO concentration, preventing a massive and rapid influx of water into the cells that would cause osmotic lysis [13] [60].
- Centrifugation: Cap the tube and centrifuge at 200-300 x g for 5-10 minutes to pellet the cells. Using lower g-forces minimizes mechanical damage to the already stressed cells [58].
- Supernatant Removal: Carefully decant or aspirate the supernatant, which contains the diluted but potentially still toxic CPAs.
- Resuspension: Gently resuspend the cell pellet in 1-2 mL of fresh, pre-warmed complete culture medium. Avoid vigorous pipetting to prevent shearing the cells.
- Cell Counting and Viability Assessment: Mix a small aliquot of the cell suspension with Trypan Blue stain (typically 1:1) and count using a haemocytometer or automated cell counter. Calculate the total viable cell count and percentage viability. This provides a critical baseline for seeding and assessing the success of the thaw.
Post-Thaw Recovery and Culture
- Seeding: Seed the cells at the recommended density (e.g., 2x10^5 - 1x10^6 viable cells per well of a 6-well plate) in pre-warmed complete culture medium. Seeding at an appropriate density is vital for successful attachment and proliferation [58].
- Incubation: Place the culture vessel in a 37°C, 5% CO₂ incubator and allow the cells to attach undisturbed for at least 24-48 hours.
- Initial Medium Change: After 24 hours, consider replacing the culture medium to remove any non-adherent, dead cells and residual CPA traces. This can improve the health of the adherent, viable population.
- Functional Assessment: Between 24 and 48 hours post-thaw, assess cell morphology, confluence, and viability. Functional assays, such as immunomodulatory potency or differentiation potential, should be conducted once the cells have fully recovered and are actively proliferating, typically after the first passage [59].
Troubleshooting Common Thawing Issues
Even with a robust protocol, challenges can arise. The following table addresses common problems and offers evidence-based solutions.
Table 3: Troubleshooting Guide for MSC Thawing and Recovery
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Low Post-Thaw Viability | Slow or inconsistent thawing; improper CPA removal. | Ensure a consistent 37°C water bath and thaw rapidly. Always dilute the CPA dropwise with gentle mixing [58] [60]. |
| Poor Cell Attachment | Cryoinjury from the freezing process; old or over-confluent pre-freeze culture. | Ensure cells are frozen at a healthy, low passage number and 70-80% confluence. Allow 48 hours for attachment before assessing [58]. |
| High Background Contamination | Water bath contamination; non-sterile technique. | Use sterile, sealed containers in the water bath or validated dry-warming devices. Wipe vials thoroughly with ethanol before opening [3]. |
| Reduced Immunomodulatory Function | Loss of surface markers or metabolic activity due to cryopreservation stress. | Optimize the entire cryopreservation chain, including the freezing solution. Some studies suggest using combinations of CPAs (e.g., PEG with reduced DMSO) can better preserve function [59]. |
The thawing process is a critical gateway to unlocking the full potential of cryopreserved mesenchymal stem cells for research and therapy. By rigorously adhering to the principles of rapid warming, controlled CPA removal, and gentle post-thaw handling as outlined in this application note, scientists can significantly enhance the recovery of viable, functional MSCs. The standardized protocols and troubleshooting guidance provided here serve as a foundational resource for ensuring experimental reproducibility and advancing the development of reliable MSC-based applications. As the field progresses, continued optimization of these thawing processes, particularly through the development of less toxic CPA cocktails and automated thawing systems, will further improve the consistency and therapeutic efficacy of mesenchymal stem cell products.
Overcoming Limitations: Strategies for Enhanced Viability, Functionality, and Safety
In the field of mesenchymal stem cell (MSC) research, effective cryopreservation is paramount for ensuring the availability of viable, functional cells for therapeutic applications. A significant challenge in this process is managing the inherent toxicity of cryoprotective agents (CPAs), primarily dimethyl sulfoxide (DMSO), and the osmotic stress incurred during CPA addition and removal [3]. This application note details two synergistic strategies—mathematically optimized osmotic stress management and the use of reduced DMSO or DMSO-free cryopreservation formulations. These protocols, developed within the context of advanced MSC research, are designed to minimize cellular damage, maintain post-thaw functionality, and enhance the safety profile of cryopreserved MSC products for drug development and clinical applications.
Quantitative Data on Cryopreservation Formulations
The following tables summarize key quantitative data from recent studies evaluating different CPA strategies for MSC cryopreservation, focusing on reduced-DMSO and DMSO-free formulations.
Table 1: Performance of Low-DMSO Cryopreservation Formulations
| DMSO Concentration (%) | Additional Key Components | Cell Viability / Recovery | Key Findings | Source (Cell Type) |
|---|---|---|---|---|
| 2.5% | 10% Alginate Microcapsule | ≥70% viability | Meets clinical threshold; retains phenotype & differentiation potential. | [56] (hUC-MSCs) |
| 5%, 2.5%, 1% | 2.5%-10% Recombinant Albumin | Maintained viability vs. control | Recombinant albumin (Optibumin) enables effective cryopreservation at DMSO levels as low as 1%. | [61] (UC-MSCs) |
| 5% | 5% PEG, 2% HSA | High viability & function | Supported immunomodulatory function of fucosylated MSCs. | [59] (BMMSCs/AdMSCs) |
| 7.5% | 2.5% PEG, 2% HSA | High viability & function | Propylene glycol (PG)-based solution supporting fucosylated MSC function. | [59] (BMMSCs/AdMSCs) |
Table 2: Performance of DMSO-Free Cryopreservation Formulations
| Key Components | Comparative Control | Cell Viability / Recovery | Key Findings | Source (Cell Type) |
|---|---|---|---|---|
| Sucrose, Glycerol, Isoleucine (SGI) | In-house DMSO solutions | Comparable average viability and recovery across 7 centers | No loss in proliferative capacity or immunophenotype. | [27] (MSCs, Multicenter) |
| Proprietary DMSO-Free Solution (FreezIS) | Commercial DMSO solution | Similar viability and viable cell density | Nontoxic in nonclinical trials; supports post-thaw proliferation. | [5] (MSCs) |
| Saline with 7.5% Propylene Glycol, 2.5% PEG, 2% HSA | DMSO-containing solutions | High viability & function | Effective for fucosylated MSCs, offers a DMSO-free alternative. | [59] (BMMSCs/AdMSCs) |
Experimental Protocols
Protocol 1: Toxicity-Cost-Optimized CPA Equilibration
This protocol uses a numerical model to minimize cumulative CPA toxicity and osmotic damage during tissue equilibration, moving beyond traditional step-wise methods [62].
- Principle: The optimal CPA addition strategy is determined by minimizing a toxicity cost function,
J_tox = ∫ C_CPA^α dt, whereC_CPAis the intracellular CPA concentration andαis a phenomenological rate parameter (empirically determined to be ~1.6 for endothelial cells), while respecting cell-specific osmotic tolerance limits [62]. - Measurement of Tissue Diffusivity:
- Procedure: Tissue samples (e.g., skin, fibroid, myometrium) are exposed to CPA solutions. The solute diffusivity (
D) is determined by fitting mass transport data to a diffusion model,∂u/∂t = div · D grad u[62]. - Example Data: Measured propylene glycol diffusivities were 0.6 × 10â»â¶ cm²/s (skin), 1.2 × 10â»â¶ cm²/s (fibroid), and 1.3 × 10â»â¶ cm²/s (myometrium) [62].
- Procedure: Tissue samples (e.g., skin, fibroid, myometrium) are exposed to CPA solutions. The solute diffusivity (
- Numerical Optimization:
- Inputs: Incorporate the measured tissue diffusivity (
D), cell-specific hydraulic conductivity (L_p), solute permeability (P_s), and osmotic tolerance limits into the combined mass transport and cell volume model [62]. - Output: The model generates a time-varying CPA concentration profile for the external bath that minimizes the combined toxic and osmotic damage cost function during loading to the desired final intracellular concentration [62].
- Inputs: Incorporate the measured tissue diffusivity (
The following workflow diagram illustrates the complete experimental procedure for implementing the toxicity-cost-optimized CPA equilibration protocol.
Protocol 2: Hydrogel Microencapsulation for Low-DMSO Cryopreservation
This protocol details the use of alginate hydrogel microcapsules to enable effective cryopreservation of MSCs with low concentrations of DMSO [56].
- Cell Culture: Culture human umbilical cord MSCs (hUC-MSCs) in complete medium (DMEM/F12 with 10% FBS, 1% penicillin/streptomycin) at 37°C with 5% CO₂ [56].
- Preparation of Hydrogel Microcapsules:
- Core Solution Preparation: On ice, mix 0.68 g mannitol and 0.15 g hydroxypropyl methylcellulose in sterile water. Add NaOH, Type I collagen from rat tail, and sterile water in appropriate proportions. Resuspend the hUC-MSCs pellet in this core solution [56].
- Shell Solution: Prepare a sodium alginate solution (0.46 g mannitol, 0.2 g sodium alginate in sterile water) [56].
- Encapsulation via Electrostatic Spraying:
- Use a custom coaxial needle assembly connected to two infusion pumps.
- Load the cell-containing core solution and the alginate shell solution into separate syringes.
- Set the flow rates to 25 μL/min (core) and 75 μL/min (shell).
- Apply a high voltage (6 kV) for electrostatic spraying.
- Collect the formed microdroplets in a calcium chloride solution (6.0 g in sterile water) for rapid gelation to form microspheres.
- Collect the microspheres, centrifuge at 600 rpm for 5 min, and resuspend in complete culture medium for further culture [56].
- Low-DMSO Cryopreservation:
- Cryomedium Preparation: Prepare freezing medium containing a final concentration of 2.5% (v/v) DMSO in culture medium.
- Freezing: Mix the microencapsulated MSCs with the cryomedium. Use a controlled-rate freezer or a
Mr. Frostydevice to freeze the cells at -80°C before transfer to liquid nitrogen for long-term storage [56].
- Post-Thaw Analysis:
- Thaw cells rapidly in a 37°C water bath.
- Assess cell viability, phenotype (via surface marker expression), and multilineage differentiation potential to confirm retained functionality [56].
Protocol 3: DMSO-Free Cryopreservation of MSCs
This protocol is adapted from an international multicenter study validating a DMSO-free solution for MSC cryopreservation [27].
- DMSO-Free Solution (SGI) Preparation: The cryoprotectant solution contains sucrose, glycerol, and isoleucine as key components [27].
- Cell Preparation and Cryopreservation:
- Harvest MSCs at the desired passage and concentration.
- Resuspend the cell pellet in the pre-chilled SGI cryopreservation solution.
- Aliquot the cell suspension into cryovials.
- Freeze the cells using a controlled-rate freezer, following a custom freezing protocol [27].
- Store the cryovials in liquid nitrogen.
- Thawing and Post-Thaw Analysis:
- Rapidly thaw the cryovials in a 37°C water bath.
- Note: The SGI study did not indicate a requirement for specialized post-thaw washing to remove the CPA [27].
- Evaluate cell viability and recovery. Assess immunophenotype (expression of CD105, CD73, CD90) and differentiation potential to ensure cryopreservation has not altered fundamental MSC properties [27].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Mitigating CPA Toxicity in MSC Cryopreservation
| Reagent / Material | Function & Application Note |
|---|---|
| Dimethyl Sulfoxide (DMSO) | Penetrating CPA; the current gold standard. Use clinical-grade DMSO and aim to minimize concentration (e.g., to 2.5-5%) to reduce cytotoxicity and patient side effects [46] [63]. |
| Propylene Glycol (PG) | Penetrating CPA; can be used as a component in low-DMSO or DMSO-free freezing solutions. Shown to be effective in formulations for fucosylated MSCs [59]. |
| Sucrose | Non-penetrating CPA; acts as an osmotic buffer and helps stabilize cell membranes. A key component in the validated DMSO-free SGI formulation [27]. |
| Recombinant Human Albumin (e.g., Optibumin) | Animal-origin-free protein additive; stabilizes cell membranes, reduces apoptosis, and enables effective low-DMSO (1-2.5%) cryopreservation, enhancing regulatory compliance [61]. |
| Polyethylene Glycol (PEG) | Polymer additive; can inhibit ice recrystallization and modify membrane fluidity. Used in combination with other CPAs in low-toxicity formulations [59]. |
| Sodium Alginate | Biomaterial for forming hydrogel microcapsules; provides a 3D protective environment for cells, physically shields against ice crystal damage, and enables a significant reduction in required DMSO concentration [56]. |
| Fucosyltransferase VII (FTVII) & GDP-fucose | Critical reagents for the exofucosylation of MSCs to enhance their homing potential to inflammatory sites. Their use prior to cryopreservation requires subsequent validation of retained function post-thaw [59]. |
| Controlled-Rate Freezer | Essential equipment for implementing slow freezing protocols with highly reproducible cooling rates, minimizing intra- and extracellular ice crystal formation and ensuring consistent post-thaw outcomes [3] [63]. |
| Ddx3-IN-2 | Ddx3-IN-2, MF:C20H23N5O, MW:349.4 g/mol |
Workflow for Formulation Selection
The following decision diagram outlines a logical pathway for selecting the appropriate cryopreservation strategy based on research goals and regulatory constraints.
Optimizing Cooling and Warming Rates to Minimize Ice Recrystallization Damage
Ice recrystallization is a major cause of cellular damage during cryopreservation, particularly impacting the viability and functionality of sensitive cell types like mesenchymal stem cells (MSCs). This process involves the growth of large ice crystals at the expense of smaller ones during warming phases, leading to mechanical stress and compromised cell membranes [64]. For MSC-based therapies in regenerative medicine, where post-thaw viability and metabolic function are critical, controlling ice recrystallization through optimized thermal protocols is essential [65] [1]. This Application Note provides detailed, evidence-based protocols and data tables to guide researchers in minimizing cryoinjury through optimized cooling and warming rate strategies.
Fundamental Principles and Key Variables
The success of cryopreservation hinges on navigating the phase transitions of water and cryoprotective agent (CPA) solutions. Two critical parameters define these transitions:
- Critical Cooling Rate (CCR): The minimum cooling rate required to avoid ice crystallization and achieve vitrification (formation of a glassy, amorphous state) [66].
- Critical Warming Rate (CWR): The minimum warming rate required to prevent ice formation (devitrification) and recrystallization during the return to physiological temperatures. The CWR is typically one to two orders of magnitude higher than the CCR for the same solution [66].
These rates are primarily determined by the CPA formulation and concentration. Lower CPA concentrations generally require higher CCRs and even higher CWRs to avoid ice formation [66]. The relationship between cooling rate, warming rate, and cell survival is illustrated below.
Diagram 1: Impact of Cooling and Warming Rates on Cryopreservation Outcome. The pathway to high cell survival depends on meeting or exceeding both the Critical Cooling Rate (CCR) and Critical Warming Rate (CWR).
Quantitative Data on Critical Rates for Common CPAs
Selecting appropriate cooling and warming rates requires knowledge of the specific CCR and CWR for the CPA formulation in use. The following table summarizes published data for common CPAs and CPA cocktails relevant to biobanking and cell therapy.
Table 1: Critical Cooling and Warming Rates for Common Cryoprotectants
| Cryoprotectant Formulation | Concentration | Critical Cooling Rate (CCR) | Critical Warming Rate (CWR) | Primary Application Context |
|---|---|---|---|---|
| DP6 [66] | 6 M | 40 °C/min | 189 °C/min | Tissue & Organ Vitrification |
| VS55 [66] | 8.4 M | 2.5 °C/min | 50 °C/min | Tissue & Organ Vitrification |
| M22 [66] | 9.3 M | 0.1 °C/min | 0.4 °C/min | Tissue & Organ Vitrification |
| DMSO (extrapolated) [66] | 5-6 M (approx. 40% w/w) | ~1-10 °C/min | ~100-1000 °C/min | Cell Suspensions (Slow Freezing) |
| 15% Glycerol (with IRI) [64] | 15% v/v | ~1 °C/min (controlled) | Not Specified | Red Blood Cell Model |
For MSC cryopreservation, slow freezing protocols often use cooling rates around -1 °C/min in the presence of permeating CPAs like DMSO, followed by storage in liquid nitrogen vapor [67]. However, the warming rate is equally critical; for example, a warming rate of 45°C/min is established as good practice for some cell types, though evidence points to the need for optimization for specific cells like T cells [67].
Experimental Protocols
Protocol A: Determining Post-Thaw Viability of MSCs Using a Standard Slow Freezing Method
This protocol is adapted from methods used for adipose-derived MSC (ADSC) cryopreservation and industry survey findings [65] [67].
1. Materials
- Cells: Confluent culture of MSCs (Passage 3-5).
- Freezing Medium: Culture medium supplemented with 10% FBS and 5-10% DMSO. For optimized formulations, include exocellular cryoprotectants like 2% PEG, 3% trehalose, and 2% BSA [65].
- Equipment: Controlled-rate freezer (CRF), cryogenic vials, isopropanol freezing chamber (if CRF is unavailable), water bath (37°C).
2. Cell Harvest and Preparation
- Harvest MSCs using standard trypsinization procedure.
- Centrifuge and resuspend cell pellet in pre-chilled (4°C) freezing medium at a density of 0.5-1 x 10^6 cells/mL.
- Aliquot 1 mL of cell suspension into labeled cryogenic vials. Keep vials on ice.
3. Controlled-Rate Freezing
- Place vials in a controlled-rate freezer.
- Initiate the following freeze curve:
- Cool from 4°C to -5°C at a rate of -2°C/min.
- Hold at -5°C for 5-10 minutes (seeding step to induce controlled extracellular ice nucleation).
- Resume cooling from -5°C to -40°C at a rate of -1°C/min.
- Cool from -40°C to -100°C at a rate of -5°C/min.
- Alternatively, use an isopropanol freezing chamber pre-equilibrated at room temperature. Place vials in the chamber and store at -80°C for 24 hours.
- Transfer vials to long-term storage in liquid nitrogen.
4. Thawing and Viability Assessment
- Rapidly warm a cryovial by gently swirling it in a 37°C water bath for ~2 minutes until only a small ice crystal remains.
- Decontaminate the vial with 70% ethanol and transfer its contents to a sterile tube.
- Slowly add 9 mL of pre-warmed culture medium drop-wise while gently agitating to dilute the CPA and minimize osmotic shock.
- Centrifuge, aspirate supernatant, and resuspend the cell pellet in fresh culture medium.
- Determine post-thaw viability using Trypan Blue exclusion or an automated cell counter.
- Plate cells for functional assays (e.g., clonogenic assay, metabolic activity, differentiation potential) as required.
Protocol B: Assessing Ice Recrystallization Inhibition (IRI) Activity
This protocol uses the "splat cooling" method to quantitatively assess the IRI activity of novel cryoprotectants, such as small molecules or proteins, which is vital for developing improved freezing media [64] [68].
1. Materials
- Test Solution: Phosphate-buffered saline (PBS) containing the candidate IRI compound at the desired concentration.
- Equipment: Two pre-cooled (-80°C) metal blocks, glass slides, microscope with cold stage and camera.
2. Sample Preparation and Freezing
- Pipette a 10 µL droplet of the test solution onto the center of a clean glass slide.
- Release the slide horizontally from a height of ~1.5 meters onto a pre-cooled metal block, causing the droplet to splat into a thin wafer that freezes instantly.
3. Annealing and Image Acquisition
- Transfer the splatted sample onto a second pre-cooled metal block held at a constant sub-zero temperature (e.g., -8°C to -10°C) in the microscope's cold stage.
- Allow the sample to anneal (temper) for 30-90 minutes. During this period, ice recrystallization will occur in samples lacking IRI activity.
- Capture multiple bright-field images of the ice crystals within the annealed sample at 10x or 20x magnification.
4. Data Analysis
- Use image analysis software (e.g., ImageJ) to measure the mean ice crystal area in each micrograph.
- Calculate the % Ice Recrystallization Inhibition (% IRI) by comparing the mean crystal size in the test sample to a PBS-only control.
- A potent IRI will maintain significantly smaller ice crystals compared to the control after the annealing period.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Cryopreservation and IRI Research
| Reagent Category | Example(s) | Function / Rationale |
|---|---|---|
| Permeating CPAs | Dimethyl Sulfoxide (DMSO), Glycerol, Ethylene Glycol | Penetrate the cell, reducing intracellular ice formation by colligatively depressing the freezing point and allowing time for cell dehydration [69]. |
| Non-Permeating CPAs | Fetal Bovine Serum (FBS), Trehalose, Polyethylene Glycol (PEG), Dextran, Bovine Serum Albumin (BSA) | Remain outside the cell, mitigating osmotic shock and "solution effects." Can help stabilize cell membranes [65]. |
| Ice Recrystallization Inhibitors (IRIs) | Small molecule carbohydrate derivatives (e.g., compounds 3-5 [64]), Plant proteins (e.g., TaIRI-2, TaENO [68]) | Do not prevent initial ice formation but inhibit the growth of large, damaging ice crystals during the thawing process, a major source of cryoinjury [64] [68]. |
| Viability & Function Assays | Trypan Blue, Fluorescent live/dead stains, MTT/XTT, Clonogenic (CFU-F) Assay, Oxidative Stress & Apoptosis Kits | Assess post-thaw cell health, recovery, and functional capacity, which are the ultimate metrics for protocol success [65]. |
Optimizing cooling and warming rates is not merely a technical exercise but a fundamental requirement for ensuring the high viability and functionality of cryopreserved MSCs. The protocols and data provided here underscore that careful attention to both the Critical Cooling Rate and the more demanding Critical Warming Rate is essential to mitigate the damaging effects of ice recrystallization. Incorporating novel Ice Recrystallization Inhibitors into CPA formulations presents a promising strategy to reduce dependence on high concentrations of traditional CPAs like DMSO, thereby minimizing toxicity and oxidative stress [65] [64]. As the field of regenerative medicine advances, the development of tailored, species-specific, and even cell-type-specific cryopreservation protocols will be paramount for the effective biobanking and clinical translation of MSC-based therapies.
This application note addresses the critical challenge of post-thaw cell loss in mesenchymal stem cell (MSC) research and therapy. We provide a comprehensive analysis of the fundamental mechanisms underlying cryoinjury and present optimized, clinically compatible protocols to significantly enhance post-thaw recovery rates and membrane integrity. The strategies outlined herein—including specific thawing solutions, cell cycle synchronization, and optimized handling parameters—enable researchers and therapy developers to achieve >90% post-thaw viability with preserved immunomodulatory potency, facilitating more reliable and effective MSC applications in regenerative medicine.
Cryopreservation serves as a pivotal technology bridging the spatiotemporal gap between MSC production and clinical application, enabling "off-the-shelf" availability for acute treatments [70]. However, conventional cryopreservation methods substantially compromise MSC viability and function through multiple injury mechanisms including osmotic stress, intracellular ice crystal formation, and prolonged exposure to cytotoxic cryoprotectants [67] [71]. Quantitative assessments reveal that cryopreservation reduces cell viability, increases apoptosis, and impairs metabolic activity and adhesion potential, with some attributes requiring more than 24 hours for partial recovery [72]. This application note delineates evidence-based strategies to mitigate these challenges, focusing specifically on improving post-thaw recovery rates and maintaining membrane integrity through optimized protocols compatible with clinical translation.
Fundamental Mechanisms of Cryoinjury
Understanding the cellular and molecular mechanisms of cryoinjury is essential for developing effective countermeasures. Recent research has identified several key injury pathways:
Cell Cycle-Dependent Cryosensitivity
A groundbreaking discovery reveals that S-phase MSCs exhibit exquisite sensitivity to cryoinjury, demonstrating heightened levels of delayed apoptosis post-thaw and reduced immunomodulatory function [73]. The cryopreservation and thawing processes induce double-stranded breaks in labile replicating DNA, triggering apoptotic cascades that substantially diminish post-thaw recovery and functionality.
Membrane Integrity Compromise
The freeze-thaw process disrupts membrane integrity through several mechanisms:
- Ice crystal formation physically damages membrane structures
- Osmotic stress during cryoprotectant addition/removal causes membrane stretching and compression
- Cold-induced phase transitions in membrane lipids increase fragility
Apoptotic Pathway Activation
Cryopreservation activates mitochondrial apoptotic pathways, characterized by cytochrome c release and caspase activation [71]. Research indicates that MSCs in 3D spheroid configurations activate the AKT-cytochrome c-caspase anti-apoptotic cascade during preservation, conferring enhanced resistance to cold shock stress [71].
Quantitative Assessment of Post-Thaw Recovery
Systematic evaluation of post-thaw MSC attributes reveals specific temporal patterns of recovery and persistent functional impairments that must be addressed through optimized protocols.
Table 1: Temporal Recovery Profile of Cryopreserved MSCs
| Time Post-Thaw | Viability Recovery | Apoptosis Level | Metabolic Activity | Adhesion Potential |
|---|---|---|---|---|
| Immediate (0h) | 70-85% | Significantly Increased | 50-70% of Fresh | 40-60% of Fresh |
| 2-4 hours | 75-80% | Peak Apoptosis | 60-75% of Fresh | 50-70% of Fresh |
| 24 hours | 85-90% | Reduced but Elevated | 70-85% of Fresh | 70-80% of Fresh |
| Beyond 24h | >90% (Variable) | Near Baseline | Variable by Cell Line | Variable by Cell Line |
Data compiled from [72] [74] demonstrates that while viability recovers within 24 hours, metabolic activity and adhesion potential remain compromised, indicating the need for specialized recovery solutions.
Optimized Protocols for Enhanced Post-Thaw Recovery
Thawing and Reconstitution Solution Optimization
The composition of thawing and reconstitution solutions critically determines initial cell recovery and membrane integrity. Research demonstrates that protein-free thawing solutions result in up to 50% cell loss [70].
Table 2: Efficacy Comparison of Reconstitution Solutions for Post-Thaw MSC Stability
| Solution Composition | Immediate Viability (%) | 4-Hour Viability (%) | Cell Loss After 4h | Recommended Use |
|---|---|---|---|---|
| Protein-Free Saline | 65-75% | 50-65% | >40% | Not Recommended |
| PBS (Protein-Free) | 70-80% | 55-70% | >40% | Not Recommended |
| Culture Medium | 75-85% | 60-75% | >40% | Limited Applications |
| Isotonic Saline + 2% HSA | 90-95% | 85-92% | <10% | Optimal Performance |
| Ringer's Acetate + 2% HSA | 88-94% | 84-90% | <10% | Excellent Alternative |
Data from [70] indicates that isotonic saline supplemented with 2% human serum albumin (HSA) provides optimal post-thaw stability, maintaining >90% viability with minimal cell loss for at least 4 hours at room temperature.
Step-by-Step Thawing and Reconstitution Protocol
Materials Required:
- Pre-warmed water bath (37°C)
- Clinical-grade human serum albumin (HSA)
- Isotonic saline or Ringer's acetate
- Centrifuge with appropriate carriers
- Sterile pipettes and tubes
Procedure:
- Rapid Thawing: Remove vial from liquid nitrogen and immediately place in 37°C water bath with gentle agitation until only a small ice crystal remains (approximately 1-2 minutes).
Dilution: Transfer cell suspension to 15mL conical tube containing 10mL pre-warmed thawing solution (isotonic saline with 2% HSA). Add dropwise with gentle mixing.
Centrifugation: Centrifuge at 300-400g for 5 minutes at room temperature to pellet cells.
Reconstitution: Discard supernatant and resuspend cell pellet in preferred administration solution at optimal concentration (>10^5 cells/mL).
Storage: Use immediately or store in isotonic saline with 2% HSA for up to 4 hours at room temperature.
Critical Considerations:
- Cell Concentration: Diluting MSCs to <10^5/mL in protein-free vehicles results in instant cell loss (>40%) and reduced viability (<80%) [70]
- Temperature Control: Maintain reconstituted cells at room temperature; avoid refrigeration
- Time Sensitivity: Complete administration within 4 hours of reconstitution for optimal viability
Cell Cycle Synchronization Protocol
To mitigate S-phase specific cryoinjury, implement cell cycle synchronization prior to cryopreservation:
Materials:
- Serum-free medium or medium with reduced growth factors
- Standard culture equipment
Procedure:
- Culture MSCs to 70-80% confluence following standard protocols
- Replace complete medium with serum-free medium or medium containing reduced growth factors (0.5-1% FBS/hPL instead of 5-10%)
- Incubate for 24-48 hours at 37°C, 5% CO₂
- Harvest cells for cryopreservation using standard protocols
- Confirm cell cycle arrest via flow cytometry (optional)
Validation: This growth factor deprivation strategy blocks cell cycle progression at G0/G1, greatly reducing post-thaw dysfunction by preventing apoptosis induced by double-stranded breaks in replicating DNA [73]. Viability, clonal growth, and T cell suppression function are preserved at pre-cryopreservation levels.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Optimized MSC Cryopreservation
| Reagent | Function | Recommended Specifications | Alternative Options |
|---|---|---|---|
| Human Serum Albumin (HSA) | Prevents thawing and dilution-induced cell loss; stabilizes membranes | Clinical grade, 2% in isotonic solutions | Plasmanate, recombinant albumin |
| Dimethyl Sulfoxide (DMSO) | Cryoprotectant; penetrates cells to prevent ice formation | GMP-grade, 10% final concentration | Glycerol (less effective for MSCs) |
| Isotonic Saline | Reconstitution solution; maintains osmotic balance | Clinical grade, sterile | Ringer's acetate, PlasmaLyte |
| Cryostor CS10 | Commercial cryopreservation medium | cGMP-manufactured, serum-free | STEM-CELLBANKER, CryoStor |
| Human Platelet Lysate (hPL) | Culture expansion supplement; xeno-free | GMP-grade, pathogen inactivated | FBS (research use only) |
| Polyethylene Glycol (PEG) | Deep supercooling additive; inhibits ice nucleation | 35 kD, 5% (w/v) in UW solution | - |
Functional Validation of Post-Thaw MSCs
Ensuring post-thaw MSCs retain therapeutic efficacy is paramount. Comparative studies demonstrate that thawed MSCs show comparable immunomodulatory potency to cultured cells both in vitro and in vivo [74].
Key Functional Assessments:
- Immunomodulatory Potency: Thawed and cultured MSCs equally suppress proliferation of activated T cells and enhance phagocytosis of monocytes
- Barrier Function Restoration: Both fresh and thawed MSCs significantly decrease endothelial cell permeability after LPS-induced injury
- In Vivo Efficacy: In polymicrobial septic animals, thawed MSCs significantly improve phagocytic ability of peritoneal lavage cells and reduce plasma levels of lactate and inflammatory cytokines comparably to fresh cells [74]
Phenotypic Stability: Despite higher levels of apoptotic cells beyond 4 hours post-thaw, MSC surface marker profiles (CD73, CD90, CD105 positive; CD14, CD19, CD34, CD45, HLA-DR negative) remain unchanged [74].
Advanced Techniques: Deep Supercooling as an Alternative Approach
For specialized applications, deep supercooling (DSC) presents an alternative preservation method that avoids conventional cryoprotectants. This technique preserves MSC spheroids at −12°C without ice formation for up to 7 days through surface sealing with heavy paraffin oil [71].
Advantages:
- Eliminates cytotoxic cryoprotectants
- Maintains high cell viability, energy levels, and differentiation capacity
- Particularly effective for 3D MSC spheroids which exhibit enhanced resistance to cold shock stress
Mechanism: 3D MSC spheroids possess close cell-cell interactions via N-cadherin that activate the AKT-cytochrome c-caspase anti-apoptotic cascade during preservation [71].
This application note provides evidence-based protocols to substantially mitigate post-thaw cell loss in MSC applications. The key findings can be summarized as:
- Protein supplementation with 2% HSA in isotonic solutions prevents up to 50% of thawing-related cell loss
- Cell cycle synchronization through serum starvation prior to freezing protects replication-vulnerable S-phase cells
- Optimal cell concentration maintenance (>10^5 cells/mL) prevents dilution-induced apoptosis
- Simple isotonic saline with HSA ensures >90% viability with minimal cell loss for at least 4 hours post-thaw
Implementation of these optimized protocols will enhance reproducibility across different laboratories and clinical trials, improving standardization in the field of MSC-based therapies while ensuring high cell recovery, viability, and functional potency.
Cryopreservation represents a critical processing step in the development of "off-the-shelf" mesenchymal stem cell (MSC)-based therapies, enabling long-term storage and distribution of cellular products [70] [3]. However, the freezing and thawing processes can induce substantial changes in MSC phenotype and function, potentially compromising therapeutic efficacy [14] [3]. This application note provides detailed methodologies for validating two critical quality attributes—immunophenotype and immunomodulatory potency—following MSC cryopreservation. Implementation of these standardized assessment protocols ensures that cryopreserved MSC products maintain their critical biological properties prior to clinical administration, supporting the advancement of reliable cellular therapies.
The Impact of Cryopreservation on MSC Function
Temporal Dynamics of Functional Recovery
Research demonstrates that cryopreservation significantly impacts MSC biology, but these effects are often transient. Freshly thawed MSCs (FT MSCs) exhibit multiple functional deficiencies immediately post-thaw, including reduced surface marker expression, increased apoptosis, diminished proliferative capacity, and impaired immunomodulatory function [14] [75]. However, a 24-hour acclimation period in standard culture conditions allows MSCs to recover most of their functional potency, a critical consideration for both research and clinical applications [14] [75].
Table 1: Functional Comparison of Freshly Thawed vs. Acclimated MSCs
| Functional Parameter | Freshly Thawed MSCs | 24-hour Acclimated MSCs |
|---|---|---|
| Viability/Apoptosis | Significantly increased apoptosis [14] | Significantly reduced apoptosis [14] |
| Surface Marker Expression | Decreased CD44 and CD105 [14] | Normalized expression patterns [14] |
| Proliferative Capacity | Decreased cell proliferation [14] | Improved proliferative capacity [14] |
| Metabolic Activity | Significantly increased [14] | Normalized metabolic activity [14] |
| Immunomodulatory Gene Expression | Decreased key regenerative genes [14] | Upregulation of angiogenic and anti-inflammatory genes [14] |
| T-cell Suppression | Maintained but less potent [14] | Significantly more potent arrest of T-cell proliferation [14] |
Optimized Thawing and Reconstitution for Functional Preservation
The thawing and reconstitution process significantly impacts post-thaw MSC recovery and function. Key considerations include:
- Protein Requirement: Thawing cryopreserved MSCs in protein-free solutions can result in up to 50% cell loss [70] [76].
- Solution Composition: Isotonic saline with 2% Human Serum Albumin (HSA) provides superior MSC stability compared to protein-free vehicles or PBS [70] [76].
- Cell Concentration: Reconstituting MSCs to concentrations below 10âµ/mL in protein-free vehicles causes instant cell loss (>40%) and reduced viability (<80%) [70] [76].
Immunophenotype Assessment Protocol
Surface Marker Staining and Analysis
This protocol evaluates adherence to International Society for Cellular Therapy (ISCT) criteria by assessing positive (CD73, CD90, CD105) and negative (CD34, CD45, HLA-DR) marker expression [14] [1].
Materials:
- MSC Analysis Kit (BD Biosciences) or equivalent antibody cocktails
- Flow cytometry staining buffer (1% BSA in PBS)
- Fc block (BioLegend)
- Flow cytometer (e.g., BD FACSCanto II or FACSCelesta)
Procedure:
- Cell Preparation: Harvest and wash MSCs to achieve a concentration of 1×10ⶠcells/mL in staining buffer.
- Fc Blocking: Incubate cells with Fc block for 10 minutes at room temperature to reduce non-specific binding.
- Antibody Staining:
- Prepare antibody cocktail containing positive markers (CD90-FITC, CD105-PerCP-Cy5.5, CD73-APC) and negative markers (CD45-PE, CD34-PE, CD11b-PE, CD19-PE, HLA-DR-PE).
- Add CD44-PE and CD142-PE antibodies in separate tubes for additional characterization.
- Incubate cells with antibodies for 20 minutes at 22°C in the dark.
- Washing and Analysis: Wash cells to remove excess antibodies and resuspend in staining buffer for flow cytometry analysis.
- Data Analysis: Analyze using FACSDiva software, determining the percentage of cells expressing each marker. ISCT-compliant MSCs should express ≥95% positive markers and ≤2% negative markers [1].
Table 2: Key Surface Markers for MSC Immunophenotyping
| Marker | Expression | Biological Function | ISCT Criteria |
|---|---|---|---|
| CD73 | Positive [1] | 5'-exonuclease, catalyzes AMP hydrolysis [1] | ≥95% [1] |
| CD90 | Positive [1] | Cell-cell and cell-ECM interactions [1] | ≥95% [1] |
| CD105 | Positive [1] | Type I membrane glycoprotein, angiogenesis [1] | ≥95% [1] |
| CD44 | Positive [14] | Hyaluronic acid receptor, cell adhesion | Not specified |
| CD34 | Negative [1] | Hematopoietic stem cell marker [1] | ≤2% [1] |
| CD45 | Negative [1] | White blood cell marker [1] | ≤2% [1] |
| HLA-DR | Negative [1] | MHC class II, immunogenicity [1] | ≤2% [1] |
Immunomodulatory Potency Assay
Standardized PBMC Proliferation Inhibition Assay
This protocol measures MSC potency through their capacity to inhibit T-cell proliferation, a key immunomodulatory mechanism [14] [77].
Materials:
- Cryopreserved pooled PBMCs (from 3-5 donors)
- Carboxyfluorescein succinimidyl ester (CFSE)
- T-cell activation reagents (CD3/CD28 dynabeads or PMA/ionomycin)
- Flow cytometry equipment
- Cell culture medium
Procedure:
- PBMC Pool Preparation:
- CFSE Labeling: Incubate PBMCs with CFSE according to manufacturer's instructions.
- Co-culture Setup:
- Plate MSCs in 96-well plates at varying densities (e.g., 1:3, 1:6, 1:12 MSC:PBMC ratios).
- Add CFSE-labeled PBMCs (e.g., 1×10ⵠcells/well).
- Activate PBMCs with CD3/CD28 dynabeads or PMA/ionomycin.
- Include controls: unstimulated PBMCs and activated PBMCs without MSCs.
- Incubation: Culture for 3-5 days at 37°C, 5% CO₂.
- Flow Cytometry Analysis: Harvest cells and analyze CFSE dilution by flow cytometry to determine PBMC proliferation.
- Potency Calculation:
- Calculate % inhibition = [1 - (Proliferation with MSCs / Proliferation without MSCs)] × 100
- Establish release criteria (e.g., >30% inhibition) based on product specifications [77].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Post-Thaw MSC Functional Assessment
| Reagent/Category | Specific Examples | Function & Importance |
|---|---|---|
| Cryopreservation Media | CryoStor CS10 [70] | Serum-free, GMP-compatible cryopreservation medium |
| Thawing/Reconstitution Solutions | Isotonic saline + 2% HSA [70] [76] | Prevents cell loss during thawing and reconstitution |
| Flow Cytometry Antibodies | CD73, CD90, CD105, CD34, CD45, HLA-DR [14] [1] | ISCT-defined immunophenotype characterization |
| Viability Assessment | 7-AAD, Annexin V/PI [14] [70] | Distinguishes viable, early apoptotic, and dead cells |
| Functional Assay Reagents | CFSE, CD3/CD28 dynabeads [77] | Tracks lymphocyte proliferation and activation |
| Standardized PBMC Reagents | Cryopreserved PBMC pools (3-5 donors) [77] | Reduces donor variability in potency assays |
Comprehensive post-thaw assessment of MSC immunophenotype and immunomodulatory potency is essential for ensuring the quality and efficacy of cellular therapies. The protocols detailed in this application note provide standardized methodologies for validating these critical quality attributes, enabling researchers and drug development professionals to reliably characterize cryopreserved MSC products. Implementation of these assessment strategies supports the development of consistent, potent MSC-based therapies with predictable clinical performance, ultimately advancing the field of regenerative medicine.
The field of regenerative medicine is increasingly reliant on the consistent and reliable supply of high-quality mesenchymal stem cells (MSCs). Clinical biobanking serves as the critical infrastructure supporting this supply chain, ensuring that cellular products maintain their therapeutic potential from donor to patient. Adherence to Good Manufacturing Practice (GMP) standards is not merely a regulatory formality but a fundamental requirement to guarantee the safety, identity, purity, and potency of banked MSCs throughout their lifecycle [78] [79]. The transition from research-scale preservation to clinically scalable biobanking introduces complex challenges in standardization, quality control, and regulatory alignment that must be systematically addressed through optimized protocols and rigorous operational discipline.
The growing market for GMP-grade cryopreservation solutions, projected to expand at a CAGR of 4.4% from 2025 to 2032, reflects the increasing importance of standardized, quality-assured biobanking practices in supporting cell therapies and regenerative medicine applications [78]. This application note establishes detailed protocols and evidence-based strategies for implementing scalable, GMP-compliant biobanking processes specifically tailored for MSC-based therapeutics, with emphasis on maintaining critical quality attributes during cryopreservation and post-thaw recovery.
Quantitative Analysis of Cryopreservation Impact on MSCs
A critical component of GMP-compliant biobanking is the thorough characterization of how cryopreservation affects MSC quality and functionality. The following table summarizes key findings from recent studies on cryopreserved MSC products, providing benchmark data for protocol validation and quality control.
Table 1: Functional Assessment of Cryopreserved MSC Products - Experimental Data Summary
| Study Model | Cryopreservation Method | Post-Thaw Viability | Functional Assessment | Key Findings |
|---|---|---|---|---|
| Human BMAC [10] | Slow freeze (-80°C) in 10% DMSO/autologous plasma | Not explicitly quantified | CFU-f assay, multilineage differentiation, in vivo cartilage repair | Preserved proliferation and multilineage differentiation capacity; No significant difference in cartilage repair efficacy between fresh and frozen BMAC in OA rat model |
| iPSC-Derived Therapies [54] | 1°C/min cooling in Me2SO (5-10%) with post-thaw wash | Variable (protocol-dependent) | Clinical trial meta-analysis | 100% of preclinical iPSC therapy studies (12/12) used Me2SO with post-thaw wash; 32% (18/57) clinical trials disclosed cryopreservation method |
| General MSC Cryopreservation [3] | Slow freezing (-1°C/min) with CPAs | 70-80% | In vitro functionality, differentiation potential | Success depends on cooling rate control, CPA optimization, and thawing consistency; DMSO cytotoxicity requires careful washing |
The data demonstrates that while cryopreservation can maintain MSC functionality when properly optimized, significant variability exists across protocols and cell sources. The BMAC study is particularly noteworthy as it provides direct evidence of functional equivalence between fresh and frozen products in a disease model, supporting the feasibility of single-harvest, multiple-injection approaches that enhance patient comfort and treatment accessibility [10]. These quantitative benchmarks enable evidence-based protocol establishment and quality monitoring in clinical biobanking operations.
GMP Compliance Framework for Clinical Biobanking
Regulatory Foundations and Quality Systems
GMP-compliant biobanking operates within a comprehensive regulatory ecosystem that demands meticulous documentation, robust quality systems, and adherence to standardized protocols. The core principles of GMP focus on ensuring product safety and efficacy through controlled processes, validated methods, and thorough traceability [78] [80]. Several key regulatory trends are currently shaping the landscape for advanced therapy medicinal products (ATMPs):
- Regulatory Modernization and Divergence: Global regulatory agencies are modernizing at different paces, creating a complex landscape of regional requirements. The EU's Pharma Package (2025) introduces modulated exclusivity and supply resilience obligations, while ICH E6(R3) guidelines shift clinical trial oversight toward risk-based models [80].
- Advanced Therapy Frameworks: Regulators are expanding bespoke frameworks addressing manufacturing consistency, long-term follow-up, and ethical use for advanced therapies [80].
- Quality Management Integration: Effective biobanking requires integration of quality systems covering document control, deviation management, change control, and supplier qualification [79].
The establishment of a Pharmaceutical Quality System (PQS) aligned with ICH Q10 principles provides the foundation for GMP compliance, emphasizing product and process understanding, quality risk management, and knowledge management throughout the product lifecycle.
Essential Documentation and Traceability
Comprehensive documentation constitutes the primary evidence of GMP compliance and product quality. The following documentation framework is essential for clinical MSC biobanking:
- Banking Protocols and SOPs: Detailed, validated procedures for every aspect of the banking process, from donor screening to final product storage and distribution [79].
- Batch Records: Complete documentation of each banking procedure, including all materials, equipment, and personnel involved [78].
- Quality Control Records: Comprehensive testing data supporting product release, including viability, identity, purity, potency, and safety parameters [79].
- Temperature Monitoring Documentation: Continuous monitoring records with defined alert and action limits for all storage units [81].
- Chain of Identity Systems: Robust systems ensuring unambiguous sample identification throughout the banking process [79].
The integration of digital platforms with built-in compliance features enhances traceability and reduces documentation errors. Automated data logging systems provide complete audit trails that streamline regulatory compliance and reduce administrative burdens [81].
Cryopreservation Protocols for Clinical-Grade MSCs
Slow Freezing Method for MSC Biobanking
Slow freezing represents the current gold standard for clinical MSC cryopreservation due to its robustness, scalability, and compatibility with GMP requirements [3]. The following protocol details a validated approach for GMP-compliant MSC banking:
Table 2: GMP-Compliant Slow Freezing Protocol for MSCs
| Process Step | Parameters | GMP Considerations | Quality Metrics |
|---|---|---|---|
| Pre-freeze Processing | Harvest at exponential growth phase; Wash and resuspend in isotonic base medium | Use of GMP-grade reagents; Defined passage number; In-process viability >90% | Cell concentration: 1-10×10ⶠcells/mL; Vitality >90% |
| Cryomedium Formulation | 5-10% DMSO in serum-free cryopreservation medium or autologous plasma | GMP-grade DMSO; Defined formulation; Quality testing on final medium | Endotoxin <0.5 EU/mL; Sterility negative |
| Cooling Rate Control | Controlled-rate freezing at -1°C/min to -40°C; -5°C/min to -80°C; Transfer to LN₂ | Validated freezing program; Temperature monitoring; Qualification of equipment | Documented cooling profile; No deviations |
| Long-term Storage | Vapor phase liquid nitrogen (-150°C to -196°C) | Validated storage system; Continuous temperature monitoring; Backup systems | Temperature stability ±5°C; Secure chain of custody |
| Thawing & Wash | Rapid thawing (37°C water bath); DMSO removal by dilution/centrifugation | Controlled process; GMP-grade wash solutions; Closed systems | Post-thaw viability >70%; Sterility maintenance |
The critical mechanisms of slow freezing include gradual cellular dehydration, controlled extracellular ice formation, and minimization of intracellular ice crystals through optimized cooling rates [3]. The pre-freeze processing phase requires particular attention, as cells should be harvested during exponential growth phase, just before entering stationary phase, to maximize viability and uniformity after thawing [79]. Standardized culture media and reagents across all banking operations significantly enhance reproducibility and compliance [79].
Cryoprotectant Strategies and DMSO Reduction
Cryoprotective agents (CPAs) are essential for preventing freezing damage but introduce safety concerns, particularly with dimethyl sulfoxide (DMSO), which has documented cytotoxicity and potential for adverse reactions in patients [54] [3]. A strategic approach to CPA selection includes:
- Penetrating CPAs: Low molecular weight compounds like DMSO, glycerol, and ethylene glycol that penetrate cells and reduce ice crystal formation [8].
- Non-Penetrating CPAs: Macromolecules like sucrose, trehalose, and hydroxyethyl starch that protect cells extracellularly through osmotic buffering and membrane stabilization [8].
- CPA Cocktails: Balanced formulations combining penetrating and non-penetrating agents at reduced concentrations to minimize toxicity while maintaining efficacy [54].
For clinical applications where direct administration without washing is preferred (such as novel administration routes including intracerebral or epicardial injection), developing Meâ‚‚SO-free cryopreservation media becomes critical [54]. However, such formulations typically require optimization of freezing profiles to enhance performance, as they may yield suboptimal post-thaw viability with conventional slow-freeze protocols [54].
Implementation Workflow and Visual Guide
Comprehensive Biobanking Workflow
The following diagram illustrates the complete workflow for GMP-compliant MSC biobanking, integrating both technical and quality management components:
Cryoprotectant Mechanism of Action
Understanding how cryoprotectants function at the cellular level is essential for protocol optimization and troubleshooting:
Essential Reagents and Materials for GMP-Compliant Biobanking
The selection of appropriate reagents and materials is critical for maintaining GMP compliance and ensuring product quality. The following table details essential components for clinical-grade MSC biobanking:
Table 3: Essential Research Reagent Solutions for GMP-Compliant MSC Biobanking
| Reagent Category | Specific Examples | Function | GMP Requirements |
|---|---|---|---|
| Basal Media | Serum-free MSC expansion media | Cell growth and maintenance | Defined formulation; Certificate of Analysis (CoA); Endotoxin testing |
| Cryoprotectants | DMSO, glycerol, trehalose, sucrose | Protect cells from freezing damage | Pharmaceutical grade; High purity; Sterile filtration |
| Cryopreservation Media | GMP-grade formulated media | Provide optimized environment for freezing | Serum-free; Defined composition; Lot consistency |
| Storage Containers | Cryogenic vials, cryobags | Secure containment during storage | Biocompatible; Validated cryogenic performance; Leak-proof |
| Quality Control Reagents | Flow cytometry antibodies, viability assays | Assessment of critical quality attributes | Validated for intended use; Precise specificity and sensitivity |
The migration toward serum-free, xeno-free formulations represents a key trend in clinical-grade biobanking, eliminating variability and safety concerns associated with serum-containing media [78] [3]. Additionally, the integration of GMP-grade cryopreservation media, as opposed to "home-brew" formulations, ensures reproducibility and regulatory alignment essential for commercial CGT manufacturing [79].
The successful implementation of scalable, GMP-compliant biobanking for MSCs requires integrated consideration of scientific, technical, and regulatory factors. The protocols and frameworks presented in this application note provide a foundation for establishing robust banking operations that can support the advancing field of MSC-based therapies. As the industry evolves, several emerging trends will shape the future of clinical biobanking:
- DMSO-Reduced and Xeno-Free Formulations: Continued development of safer, more defined cryopreservation media that eliminate components of concern [54] [3].
- Advanced Monitoring and Digital Integration: Implementation of AI-assisted monitoring systems that provide predictive analytics and continuous surveillance of sample integrity [81] [82].
- Standardization and Global Harmonization: Efforts to establish universally accepted standards for cryopreservation protocols and quality assessment [80] [83].
- Advanced Storage Technologies: Development of hybrid storage systems combining mechanical freezers with vapor-phase liquid nitrogen modules for enhanced flexibility and reliability [82].
The convergence of optimized cryopreservation protocols with rigorous quality systems creates a pathway toward truly scalable, clinically compliant MSC biobanking that can reliably support the regenerative medicine ecosystem and accelerate the delivery of transformative therapies to patients.
The advancement of mesenchymal stem cell (MSC) therapies in regenerative medicine is critically dependent on reliable cryopreservation protocols that maintain cell viability, phenotype, and functionality post-thaw [1]. Traditional cryopreservation methods often rely on high concentrations of dimethyl sulfoxide (DMSO), which can induce cellular toxicity and adverse reactions in patients [27] [56]. This document details novel approaches in biophysical optimization and cell-specific cryopreservation, providing application notes and structured protocols to enhance the quality and translational potential of MSC-based products. These methodologies are framed within a broader thesis on improving cryopreservation techniques for MSC research and clinical application, addressing the need for standardized, safe, and efficient preservation strategies [3] [27].
Application Notes: Current Landscape and Emerging Solutions
The Challenge of DMSO in Clinical Applications
While DMSO remains a widely used cryoprotective agent (CPA), its clinical application presents significant challenges. Studies have documented adverse reactions in patients, including nausea, vomiting, arrhythmias, and neurotoxicity, following the transfusion of stem cells containing DMSO [3] [56]. Furthermore, DMSO toxicity can compromise cell membrane integrity and the actin cytoskeleton during the freeze-thaw cycle [27]. These concerns have accelerated research into DMSO-reduction and DMSO-free strategies to improve the safety profile of MSC therapies without compromising post-thaw cell quality.
Quantitative Analysis of Cryoprotectant Solutions
Recent multicenter studies have validated alternative cryoprotectant solutions that can effectively replace traditional DMSO-containing formulations. The table below summarizes key performance data from a comparative international study of a novel DMSO-free solution versus standard DMSO-containing controls [27].
Table 1: Viability and Recovery of MSCs Cryopreserved with Different Solutions
| Cryoprotectant Solution | Average Post-Thaw Viability (%) | Average Cell Recovery (%) | Key Components |
|---|---|---|---|
| DMSO-Free (SGI Solution) | 84.2 | 71.2 | Sucrose, Glycerol, Isoleucine |
| In-House DMSO Controls | 86.1 | 72.6 | DMSO (concentration varied by site) |
| Fresh MSC Control (Unfrozen) | 95.0 | 100.0 | N/A |
The data demonstrates that the DMSO-free SGI solution yields comparable post-thaw viability and cell recovery to traditional DMSO-based protocols, establishing it as a viable and safer alternative for clinical-grade MSC cryopreservation [27].
Advanced Biophysical Optimization Strategies
Biophysical optimization involves engineering the physical environment during freezing to minimize cryo-injury. Two primary techniques dominate this field:
- Slow Freezing: This controlled-rate freezing method allows for gradual cellular dehydration, minimizing the formation of lethal intracellular ice crystals [3]. The cooling rate is typically maintained below -3°C/min, often using a programmable freezer to ensure consistency [3]. This method is considered the gold standard for clinical and laboratory MSC cryopreservation due to its operational simplicity and low contamination risk [3].
- Vitrification: This ultra-rapid cooling technique solidifies the cellular suspension into a glass-like state without ice crystal formation [3] [56]. It can be achieved through equilibrium methods, balancing cells with specific CPA formulations, or non-equilibrium methods, which rely on extremely high cooling rates and high CPA concentrations [3]. While promising, vitrification faces challenges related to the toxicity of high CPA concentrations and stringent sample volume limitations [56].
Table 2: Comparison of Primary Cryopreservation Methods for MSCs
| Parameter | Slow Freezing | Vitrification |
|---|---|---|
| Mechanism | Gradual dehydration; controlled ice formation | Ultra-rapid cooling; glassy solid state |
| CPA Concentration | Low to Moderate | High |
| Cooling Rate | Slow (e.g., -1°C/min to -3°C/min) | Very Rapid (e.g., >20,000°C/min) |
| Primary Risk | Extracellular ice crystal damage | CPA toxicity; devitrification during thawing |
| Ease of Use | High; easily scalable | Low; technically demanding, small volumes |
Hydrogel Microencapsulation: A 3D Biophysical Shield
Hydrogel microencapsulation represents a groundbreaking biophysical approach to cryopreservation. This technology involves encapsulating MSCs within a three-dimensional (3D) alginate-based hydrogel matrix before freezing [56]. The hydrogel structure acts as a physical barrier, mitigating ice crystal damage and reducing osmotic stress during the freeze-thaw process. Research has demonstrated that this technique enables effective cryopreservation of MSCs with DMSO concentrations as low as 2.5%, while maintaining cell viability above the 70% clinical threshold [56]. Furthermore, cryopreserved microencapsulated MSCs retain their phenotype, differentiation potential, and exhibit enhanced expression of stemness genes, making this a highly promising strategy for clinical applications [56].
Experimental Protocols
Protocol 1: DMSO-Free Cryopreservation of MSCs Using SGI Solution
This protocol is adapted from an international multicenter study that validated the performance of a sucrose-glycerol-isoleucine (SGI) solution against traditional DMSO-based cryoprotectants [27].
Objective: To cryopreserve MSCs using a DMSO-free solution that maintains high cell viability, recovery, and phenotype post-thaw.
Materials:
- Research Reagent Solutions:
- Confluent MSC Culture (Passage 3-5).
- Cryovials.
- Programmable Freezer or Isopropanol Freezing Chamber.
- Liquid Nitrogen Storage System.
Methodology:
- Cell Harvesting: Harvest MSCs at 80-90% confluency using standard trypsinization techniques. Centrifuge the cell suspension and resuspend the pellet in complete culture medium to achieve a final concentration of 1-5 x 10^6 cells/mL.
- CPA Addition: Gently mix the cell suspension with an equal volume of SGI cryoprotectant solution, achieving a 1:1 dilution. The final cell concentration for cryopreservation will be 0.5-2.5 x 10^6 cells/mL.
- Aliquoting: Dispense 1 mL of the cell-CPA mixture into each cryovial.
- Controlled-Rate Freezing:
- Place the cryovials in a programmable freezer and initiate the cooling cycle.
- Alternatively, place cryovials in an isopropanol freezing chamber and store at -80°C for 24 hours.
- Long-Term Storage: After 24 hours, promptly transfer the cryovials to a liquid nitrogen storage tank (-135°C to -196°C) for long-term preservation.
- Thawing and Assessment:
- Rapidly thaw cryovials in a 37°C water bath until only a small ice crystal remains.
- Gently transfer the cell suspension to a tube containing pre-warmed complete culture medium to dilute the CPA.
- Centrifuge to remove the CPA and resuspend the cell pellet in fresh medium.
- Determine post-thaw viability using Trypan Blue exclusion and perform flow cytometry for standard MSC surface markers (CD73, CD90, CD105) to confirm phenotype [27].
DMSO-Free Cryopreservation Workflow
Protocol 2: Hydrogel Microencapsulation for Low-DMSO Cryopreservation
This protocol leverages hydrogel microcapsules to shield MSCs, enabling a significant reduction in DMSO concentration [56].
Objective: To cryopreserve MSCs using alginate hydrogel microencapsulation with ≤2.5% DMSO, preserving cell viability and multipotency.
Materials:
- Research Reagent Solutions:
- Human Umbilical Cord MSCs (hUC-MSCs) or other MSC types.
- High-Voltage Electrostatic Coaxial Spraying Device.
- Cryovials.
- Liquid Nitrogen Storage System.
Methodology:
- Cell Preparation: Harvest hUC-MSCs and centrifuge to obtain a cell pellet.
- Microsphere Core Formation: Resuspend the cell pellet in the core solution on ice. This creates the cell-loaded core fluid for encapsulation.
- Hydrogel Encapsulation:
- Load the cell-core solution into a syringe connected to the inner lumen of a coaxial needle assembly.
- Load the sodium alginate shell solution into another syringe connected to the outer lumen.
- Use an electrostatic sprayer (e.g., at 6 kV) to generate microdroplets that fall into a calcium chloride solution, where they instantly gel into microcapsules [56].
- Post-Encapsulation Culture: Collect the microcapsules, wash, and transfer to a culture flask for a short incubation (e.g., 2-4 hours) in complete medium.
- Cryopreservation:
- Transfer microcapsules to cryovials and suspend in the low-DMSO cryomedium (2.5% DMSO).
- Freeze the cryovials using a slow freezing protocol (as in Protocol 1, Step 4) and store in liquid nitrogen.
- Thawing and Analysis:
- Rapidly thaw microcapsules in a 37°C water bath.
- Wash to remove cryomedium and dissolve alginate microcapsules with a chelating agent (e.g., sodium citrate) to release cells for analysis [56].
- Assess viability, perform CFU assays, and induce osteogenic and adipogenic differentiation to confirm multipotency.
Hydrogel Microencapsulation Cryopreservation Workflow
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and their critical functions in advanced MSC cryopreservation protocols.
Table 3: Essential Reagents for Advanced MSC Cryopreservation Research
| Reagent/Material | Function | Application Notes |
|---|---|---|
| SGI Cryoprotectant | DMSO-free CPA; provides osmotic stability and membrane protection [27]. | Multicenter-validated; suitable for clinical-grade manufacturing. |
| Alginate Hydrogel | Forms a 3D microcapsule for physical cell shielding during freezing [56]. | Enables radical DMSO reduction; requires specialized equipment for encapsulation. |
| MSC-Brew GMP Medium | Animal component-free culture medium [42]. | Ensures GMP compliance; reduces batch-to-batch variability and immunogenicity risks. |
| Programmable Freezer | Provides controlled, reproducible cooling rates for slow freezing [3]. | Critical for protocol standardization and minimizing ice crystal damage. |
The future of MSC cryopreservation lies in the meticulous integration of novel biophysical and biochemical strategies. The protocols and data presented herein demonstrate that DMSO-free solutions and hydrogel microencapsulation are no longer experimental concepts but are viable, validated approaches that can significantly enhance the safety and efficacy profile of MSC-based therapies. Adopting these optimized, cell-specific protocols, alongside GMP-compliant reagents, is essential for any research or drug development program aimed at successful clinical translation. Continued innovation in this field will undoubtedly focus on further refining these techniques, automating processes, and developing integrated platforms that ensure the delivery of potent and reliable MSC products from the manufacturing suite to the patient.
Evidence-Based Analysis: Functional Recovery and Clinical Efficacy of Cryopreserved MSCs
Mesenchymal stem cells (MSCs) represent a cornerstone of regenerative medicine due to their multipotent differentiation capacity, immunomodulatory properties, and therapeutic potential for treating inflammatory diseases [1]. The transition from preclinical research to clinical applications necessitates reliable cryopreservation techniques to create "off-the-shelf" therapies available for immediate use [84]. This application note systematically examines the current evidence regarding functional differences between freshly cultured and cryopreserved MSCs through structured analysis of quantitative potency data, detailed experimental protocols, and mechanistic insights to guide robust research and development.
Quantitative Analysis of MSC Potency Attributes
Comprehensive Potency Outcome Comparison
Table 1: Summary of In Vivo Efficacy and In Vitro Potency Outcomes from Systematic Review
| Category | Total Experiments | Significantly Different Outcomes | Percentage | Direction of Favored Outcome |
|---|---|---|---|---|
| In Vivo Preclinical Efficacy | 257 | 6 | 2.3% | 2 fresh, 4 cryopreserved |
| In Vitro Potency Measures | 68 | 9 | 13% | 7 fresh, 2 cryopreserved |
Analysis of 18 comparative preclinical studies reveals that the overwhelming majority (97.7%) of in vivo efficacy outcomes showed no statistically significant difference between freshly cultured and cryopreserved MSCs across 101 distinct outcome measures [84]. The limited significantly different outcomes demonstrated no consistent directional favorability. In vitro potency assessments showed greater variability, with 13% of experiments reaching statistical significance, predominantly favoring freshly cultured MSCs [84]. This discrepancy between in vivo and in vitro results suggests that standardized cryopreservation protocols largely preserve therapeutic functionality despite potential alterations in specific in vitro assays.
Functional Equivalence in Specific Applications
Table 2: Functional Properties of Fresh vs. Cryopreserved MSCs in Orthopedic Applications
| Functional Attribute | Fresh BMAC | Cryopreserved BMAC | Significance |
|---|---|---|---|
| Proliferation Capacity | Maintained | Preserved after 4 weeks at -80°C | No significant difference |
| Multilineage Differentiation | Present | Similarly maintained | No significant difference |
| Histological Cartilage Improvement | Significant vs. control | Significant vs. control | No significant difference between groups |
| CFU-f Formation | Present | Preserved post-thaw | Comparable colony counts |
Recent investigation into bone marrow aspirate concentrate (BMAC) demonstrates functional equivalence between fresh and cryopreserved products. After four weeks of storage at -80°C, cryopreserved BMAC maintained equivalent proliferation capacity, multilineage differentiation potential, and cartilage repair capability in a rat osteoarthritis model [10]. The preserved functional attributes support the feasibility of single harvest approaches with cryopreserved aliquots for multiple treatments, potentially reducing patient burden and enhancing clinical utility.
Experimental Protocols for Potency Assessment
Standardized Cryopreservation and Thawing Methodology
Protocol: Cryopreservation of MSCs for Functional Studies
- Cell Preparation: Culture MSCs to 70-80% confluence in standard growth medium (αMEM with 20% FBS, 1% Penicillin/Streptomycin, and 10 ng/mL FGF-2) [10].
- Harvesting: Detach cells using standard trypsinization, neutralize with serum-containing medium, and centrifuge at 300-400 × g for 5 minutes.
- Cryopreservation Formulation: Resuspend cell pellet at 1×10^6 cells/mL in cryoprotectant medium comprising 10% dimethyl sulfoxide (DMSO) and 90% autologous plasma or serum-free commercial cryopreservation medium [10].
- Freezing Protocol: Aliquot cell suspension into cryovessels and use controlled-rate freezing container (~-1°C/min) or programmable freezer. Transfer to long-term storage at -80°C or liquid nitrogen after complete solidification.
- Thawing and Recovery: Rapidly thaw cryovials in 37°C water bath (≤2 minutes). Immediately dilute with pre-warmed culture medium, centrifuge at 300 × g for 5 minutes to remove DMSO, and resuspend in fresh culture medium [10].
- Post-Thaw Culture: Plate cells at appropriate density and allow 24-hour recovery before functional assays, as cryopreserved MSCs may require this period to regain full functionality [84].
Comprehensive Potency Assay Workflow
Figure 1: Experimental workflow for comparative assessment of fresh versus cryopreserved MSC potency attributes.
Critical Parameters for Potency Assessment
Immunomodulatory Potency Assays:
- T cell Suppression Assay: Co-culture MSCs with activated peripheral blood mononuclear cells (PBMCs) at varying ratios (1:10 to 1:100 MSC:PBMC). Quantify T cell proliferation via CFSE dilution or 3H-thymidine incorporation after 3-5 days [84] [1].
- Macrophage Polarization: Assess MSC-mediated shift from M1 to M2 macrophages using flow cytometry analysis of surface markers (CD206, CD80) and cytokine secretion profiles (IL-10, IL-12) [1].
- Cytokine Secretion Profiling: Quantify immunomodulatory factors (IDO, PGE2, TSG-6, IL-6, HGF, TGF-β) in conditioned media using ELISA or multiplex immunoassays under basal and inflammatory priming conditions (IFN-γ, TNF-α) [84] [85].
Differentiation Capacity Assessment:
- Osteogenic Differentiation: Culture in induction medium (DMEM, 10% FBS, 0.1μM dexamethasone, 10mM β-glycerophosphate, 50μM ascorbate-2-phosphate) for 2-3 weeks. Assess mineralization via Alizarin Red S staining and quantify osteogenic markers (Runx2, Osteocalcin) by qPCR [85] [10].
- Chondrogenic Differentiation: Pellet culture in defined medium (DMEM, 1% ITS, 100nM dexamethasone, 50μM ascorbate-2-phosphate, 40μg/mL proline, 10ng/mL TGF-β3) for 3 weeks. Analyze glycosaminoglycan content via Safranin O staining and chondrogenic genes (SOX9, COL2A1) expression [85].
- Adipogenic Differentiation: Induce with medium (DMEM, 10% FBS, 1μM dexamethasone, 0.5mM IBMX, 10μg/mL insulin, 200μM indomethacin) for 2-3 weeks. Visualize lipid vacuoles with Oil Red O staining and quantify adipogenic markers (PPARγ, C/EBPα) [85].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for MSC Potency Studies
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| Culture Media | αMEM, DMEM with 20% FBS | Baseline MSC expansion and maintenance |
| Cryoprotectants | DMSO (10%), Autologous plasma | Cell preservation during freezing |
| Differentiation Kits | Osteo/Chondro/Adipogenic induction media | Multilineage differentiation capacity assessment |
| Immunophenotyping Antibodies | CD73, CD90, CD105, CD34, CD45, HLA-DR | MSC characterization per ISCT criteria |
| Cytokine Detection | ELISA kits for IDO, PGE2, TSG-6 | Quantification of immunomodulatory factors |
| Cell Viability Assays | CFSE, 7-AAD, Annexin V | Post-thaw recovery and apoptosis assessment |
| Inflammation Priming Agents | IFN-γ, TNF-α | MSC licensing for enhanced immunomodulation |
Mechanistic Insights and Technical Considerations
Molecular Pathways in MSC Cryopreservation
Figure 2: Molecular and cellular pathways affected by cryopreservation and recovery in MSCs.
The molecular mechanisms underlying MSC functional preservation after cryopreservation involve complex stress response pathways. Cryopreservation induces immediate physical stresses including intracellular ice formation, membrane disruption, and osmotic imbalance, potentially triggering apoptotic pathways [84]. The 24-hour recovery period allows for cellular repair, restoration of mitochondrial function, and re-establishment of secretory profiles [84] [86]. Interestingly, elevated apoptosis in cryopreserved MSCs may potentially enhance immunomodulatory effects through efferocytosis mechanisms, where phagocytic clearance of apoptotic MSCs by immune cells contributes to anti-inflammatory responses [87].
Critical Technical Considerations
Cryopreservation Protocol Variability: The systematic review by Dave et al. identified substantial methodological heterogeneity across studies, with cryopreservation duration rarely reported and viability rates ranging from 60-97% [84] [87]. This variability underscores the necessity for standardized reporting of cryopreservation parameters including freezing rate, cryoprotectant concentration, storage duration, and thawing methods to enable valid cross-study comparisons.
Source-Dependent Functional Differences: Emerging evidence suggests that MSC potency following cryopreservation may vary depending on tissue source. Recent research indicates that Prrx1-lineage MSCs from white adipose tissue demonstrate superior in vitro differentiation potential and contain more primitive adipose stem cells compared to Dermo1-lineage MSCs [85]. Such source-specific variations highlight the importance of careful MSC population selection for specific therapeutic applications.
Comprehensive analysis of current evidence indicates that properly executed cryopreservation protocols generally preserve the critical functional attributes of MSCs, with the majority of in vivo efficacy outcomes (97.7%) showing no significant difference between freshly cultured and cryopreserved products [84]. The observed discrepancies in specific in vitro potency measures (13% significantly different) underscore the importance of standardized cryopreservation methodologies and systematic potency assessment using biologically relevant functional assays. Implementation of the detailed protocols and analytical frameworks presented in this application note will enhance reproducibility and reliability in MSC-based therapeutic development, ultimately supporting the clinical translation of cryopreserved MSC products as readily available "off-the-shelf" therapies for inflammatory and degenerative conditions.
Within the broader context of a thesis on cryopreservation techniques for mesenchymal stem cell (MSC) research, establishing robust preclinical models to validate the anti-inflammatory efficacy of MSC-based therapies is a critical foundational step. The therapeutic potential of MSCs is largely mediated through their potent immunomodulatory and anti-inflammatory properties [1]. Before these cells can be cryopreserved, distributed, and utilized in therapeutic applications, their biological functionality must be confirmed using reliable and predictive in vivo models of inflammation. This application note synthesizes systematic review findings on the most prevalent and effective in vivo models used to evaluate anti-inflammatory efficacy, providing detailed protocols to standardize assessment methods for MSC research and development.
Systematic Review of Key In Vivo Inflammation Models
The selection of an appropriate in vivo model is necessary to demonstrate the effectiveness and elucidate the mechanisms of action of agents under assessment, identifying a drug with real potential to render therapeutic effects on humans [88]. The following table summarizes the primary in vivo inflammation models used in preclinical research, detailing their induction mechanisms and the specific inflammatory pathways they activate.
Table 1: Summary of Primary In Vivo Inflammation Models for Preclinical Evaluation
| Model Name | Inducing Agent | Type of Inflammation | Key Measured Outcomes | Inflammatory Pathways Involved |
|---|---|---|---|---|
| Carrageenan-Induced Paw Edema [88] | Carrageenan (sulfated polysaccharide) | Acute | Paw volume increase, leukocyte infiltration, pro-inflammatory cytokine levels (TNF-α, IL-6) | COX-2 activation, prostaglandin release, NF-κB signaling |
| TPA-Induced Ear Edema [88] | 12-O-tetradecanoylphorbol-13-acetate (TPA) | Acute | Ear thickness, ear weight, myeloperoxidase (MPO) activity | Protein kinase C (PKC) activation, leukocyte infiltration |
| Complete Freund’s Adjuvant (CFA)-Induced Arthritis [88] | Heat-killed Mycobacterium tuberculosis (in mineral oil) | Chronic | Paw volume, joint inflammation, radiographic joint damage, cytokine levels | Th1 immune response, TNF-α, IL-1β, IL-6, IL-23/IL-17 pathways [88] |
| Carrageenan-Induced Peritonitis [88] | Carrageenan | Acute | Peritoneal exudate volume, leukocyte count and type in exudate | Neutrophil and macrophage migration, chemokine production |
| Formalin-Induced Paw Edema [88] | Formalin solution | Acute (biphasic) | Paw licking/biting behavior (early neurogenic phase), paw volume (late inflammatory phase) | Direct tissue irritation, neurogenic inflammation, cytokine-mediated phase |
| Cotton Pellet-Induced Granuloma [88] | Subcutaneous cotton pellet implantation | Chronic (Granulomatous) | Granuloma tissue dry weight, hydroxyproline content (for fibrosis) | Foreign-body reaction, chronic granulomatous inflammation, fibroblast proliferation |
Quantitative data from a meta-analysis on resveratrol demonstrates the efficacy that can be measured in such models, showing significant reductions in key inflammatory markers: TNF-α content (SMD = -1.58) and IL-6 content (SMD = -2.16) [89] [90]. These findings underscore the sensitivity of these models in detecting the anti-inflammatory effects of therapeutic agents.
Detailed Experimental Protocols
Below are standardized operational protocols for two highly reproducible and widely used models: the Carrageenan-Induced Paw Edema model for acute inflammation and the CFA-Induced Arthritis model for chronic inflammation.
Protocol 1: Carrageenan-Induced Paw Edema (Acute Inflammation)
This is a highly sensitive and reproducible test used to estimate the potential anti-inflammatory impact of natural and synthetic compounds [88].
- Objective: To evaluate the efficacy of therapeutic agents in attenuating acute inflammation.
- Materials:
- Animals: Typically rats or mice (e.g., Wistar rats, 150-200g).
- Inducing Agent: 1% λ-carrageenan solution in sterile saline.
- Equipment: Plethysmometer (for paw volume measurement), syringes (1mL), 26-30G needles.
- Procedure:
- Acclimatization: House animals for at least 5-7 days under standard conditions with ad libitum access to food and water.
- Baseline Measurement: Measure the initial volume of the right hind paw of each animal using a plethysmometer.
- Pre-treatment: Administer the test compound (e.g., MSC-derived conditioned medium, cryopreserved MSC suspension) or vehicle control via a predetermined route (e.g., intravenous, intraperitoneal) at a suitable time point prior to carrageenan injection.
- Induction of Inflammation: Subcutaneously inject 100 µL of 1% carrageenan solution into the plantar surface of the pre-measured right hind paw.
- Post-injection Measurement: Measure the paw volume again at regular intervals (e.g., 1, 2, 3, 4, 5, and 24 hours) post-carrageenan injection.
- Tissue Collection: At the endpoint, animals are euthanized, and paw tissue can be collected for biochemical analysis (e.g., myeloperoxidase activity, cytokine levels like TNF-α and IL-6) or histopathology.
- Data Analysis:
- Calculate the increase in paw volume (edema) at each time point relative to the baseline.
- Express the anti-inflammatory activity as the percentage inhibition of edema in treated groups compared to the control group.
- Statistical analysis (e.g., ANOVA) should be performed to determine significance.
Protocol 2: CFA-Induced Arthritis (Chronic Inflammation)
This model is a gold standard for studying chronic inflammatory and autoimmune conditions like rheumatoid arthritis [88].
- Objective: To assess the therapeutic potential of agents against chronic, immune-mediated inflammatory disease.
- Materials:
- Animals: Rats (e.g., Lewis rats) or mice (e.g., DBA/1).
- Inducing Agent: Complete Freund's Adjuvant (CFA), containing heat-killed Mycobacterium tuberculosis.
- Equipment: Calipers (for joint diameter), syringes, needles, apparatus for behavioral tests (e.g., incapacitance tester).
- Procedure:
- Acclimatization: As described in Protocol 1.
- Induction of Arthritis: Intradermally inject 100-200 µL of CFA into the base of the tail or a footpad. A low dose (e.g., 0.1-0.5 mg/rat) is typically sufficient.
- Treatment Regimen: Administer the test product (e.g., cryopreserved and thawed MSCs) after the onset of clinical signs (typically around day 10-14 post-CFA). Treatment can continue for several days or weeks.
- Monitoring and Scoring: Monitor animals regularly and score for clinical signs of arthritis. Quantitative measurements include:
- Paw Volume/Thickness: Measured using plethysmometer or calipers.
- Clinical Arthritis Score: A semi-quantitative score (e.g., 0-4 per paw) for redness, swelling, and deformity.
- Weight Bearing: Assessed using an incapacitance tester to measure pain.
- Termination and Analysis: At the endpoint (e.g., day 21-28), euthanize animals and collect blood (for serum cytokine analysis), joints, and spleens for histopathological, radiological, and immunological analysis.
- Data Analysis:
- Analyze clinical scores, paw volumes, and weight-bearing data over time using repeated-measures ANOVA.
- Histopathological scoring of joint sections for inflammation, pannus formation, cartilage damage, and bone resorption.
- Measure serum levels of pro-inflammatory cytokines (e.g., TNF-α, IL-6, IL-17) and rheumatoid factor.
Signaling Pathways in Inflammation
The efficacy of therapeutic interventions in these models is often mediated through the modulation of key inflammatory signaling pathways. The diagram below illustrates the central NF-κB pathway, a critical regulator of the immune response.
Figure 1: NF-κB Inflammatory Signaling Pathway. This pathway is a primary target for many anti-inflammatory therapies, including MSC-based treatments. Activation leads to the production of key cytokines measured in preclinical models [88] [89].
Another pathway frequently investigated in the context of fibrosis and chronic inflammation is the TGF-β/Smad pathway, which can be targeted by anti-fibrotic agents.
Figure 2: TGF-β/Smad Pro-fibrotic Signaling Pathway. This pathway is central to the development of chronic inflammation and tissue fibrosis, and its inhibition is a key mechanism of action for effective therapies [89] [90].
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential reagents and materials required for establishing and evaluating these in vivo inflammation models.
Table 2: Essential Research Reagents for In Vivo Inflammation Studies
| Reagent/Material | Function and Application | Example Use Case |
|---|---|---|
| λ-Carrageenan [88] | Sulfated polysaccharide used to induce acute, localized inflammation. Activates innate immune response via NLRP3 inflammasome and cytokine release. | Induction of paw edema and peritonitis models. |
| Complete Freund's Adjuvant (CFA) [88] | Immunopotentiator containing inactivated mycobacteria in oil. Used to induce a potent, chronic T-cell-mediated immune response. | Induction of rheumatoid arthritis models and other autoimmune conditions. |
| Cryopreserved MSCs [1] [3] | Therapeutic cellular product with immunomodulatory properties. Their post-thaw viability and function are critical test variables. | Intravenous or intraperitoneal administration to assess therapeutic effect on inflammation. |
| Dimethyl Sulfoxide (DMSO) [3] | Cryoprotective agent (CPA) used to protect cells (like MSCs) from ice crystal formation during freezing. Requires careful removal post-thaw. | Component of freezing media for MSC cryopreservation. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Analytical tool for quantifying specific proteins (e.g., cytokines TNF-α, IL-6) in serum, tissue homogenates, or cell culture supernatant. | Measurement of inflammatory biomarkers in collected biological samples. |
| Plethysmometer | Instrument that uses water displacement to measure the volume of a rodent's paw with high precision. | Primary outcome measurement in the carrageenan-induced paw edema model. |
Cryopreservation is a critical unit operation in the mesenchymal stem cell (MSC) supply chain, enabling off-the-shelf availability for clinical applications in regenerative medicine and immunotherapy. The choice of cryoprotectant directly impacts post-thaw viability, recovery, phenotypic stability, and ultimately, therapeutic efficacy [50]. For decades, dimethyl sulfoxide (DMSO) has been the predominant cryoprotectant due to its ability to penetrate cells and suppress ice crystal formation [28]. However, concerns regarding its potential toxicity to both cells and patients have driven the development of DMSO-free formulations [27] [91]. This application note provides a structured, data-driven comparison of four cryoprotectant solutions: the DMSO-containing CryoStor CS10 (CS10), and the DMSO-free alternatives Stem-Cellbanker (SCB), Recovery Cell Culture Freezing Media (RFM), and a sucrose-glycerol-isoleucine (SGI) formulation.
Quantitative Performance Comparison
The following tables consolidate key quantitative findings from recent, multi-center studies to facilitate direct comparison of the cryoprotectants.
Table 1: Post-Thaw Viability and Recovery of MSCs Cryopreserved in Different Media
| Cryoprotectant | Key Composition | Post-Thaw Viability (%) | Post-Thaw Cell Recovery | References |
|---|---|---|---|---|
| CryoStor CS10 | 10% DMSO | ~85-95% (Trypan Blue) | Comparable to other 10% DMSO solutions | [55] [50] |
| Stem-Cellbanker (SCB) | DMSO-free (proprietary) | Relatively high (LIVE/DEAD assay) | Information not specified | [55] |
| Recovery RFM | DMSO-free (proprietary) | Lower than CS10 and SCB | Information not specified | [55] |
| SGI Formulation | Sucrose, Glycerol, Isoleucine | ~80% (Flow cytometry) | ~70% | [27] |
| NutriFreez | 10% DMSO | Comparable to PHD10 and CS10 | Maintained up to 6 hours post-thaw | [50] |
| PHD10 | Plasmalyte A, 5% HA, 10% DMSO | Comparable to NutriFreez and CS10 | Maintained up to 6 hours post-thaw | [50] |
Table 2: Functional and Phenotypic Assessment of Post-Thaw MSCs
| Cryoprotectant | Phenotype (Surface Marker Expression) | Immunomodulatory Potency (T-cell Inhibition) | Proliferative Capacity Post-Thaw | References |
|---|---|---|---|---|
| CryoStor CS10 | Preserved (CD73, CD90, CD105) | Information not specified | Significantly reduced (10-fold less) | [55] [50] |
| Stem-Cellbanker (SCB) | Preserved | Information not specified | Information not specified | [55] |
| Recovery RFM | Information not specified | Information not specified | Information not specified | [55] |
| SGI Formulation | Preserved (CD73, CD90, CD105) | Comparable to DMSO-controls | Information not specified | [27] |
| NutriFreez | Preserved | Comparable to PHD10 | Similar to PHD10 | [50] |
| PHD10 | Preserved | Comparable to NutriFreez | Similar to NutriFreez | [50] |
Detailed Experimental Protocols
Multicenter Comparison of SGI vs. DMSO-Containing Solutions
This protocol summarizes the methodology of an international, multi-center study that compared a novel DMSO-free SGI formulation against institution-specific DMSO-containing solutions [27].
- Cell Culture and Preparation: MSCs were isolated from bone marrow aspirates from a single donor per center and expanded in culture. Upon reaching confluence, cells were harvested for cryopreservation.
- Cryopreservation Formulations:
- Test Solution: SGI solution (Sucrose, Glycerol, Isoleucine).
- Control Solutions: Each participating center used its own standard DMSO-containing cryomedium (e.g., 5-10% DMSO in culture medium or other base solutions).
- Freezing Protocol: The final MSC suspension was aliquoted into cryovials. The cryovials were placed in an isopropanol-based freezing container (e.g., "Mr. Frosty") and transferred to a -80°C freezer for at least 24 hours to facilitate a controlled cooling rate of approximately -1°C/min. After slow freezing, vials were transferred to liquid nitrogen for long-term storage.
- Thawing and Assessment: After storage, vials were thawed rapidly in a 37°C water bath. Cell viability was measured using flow cytometry, and recovery was calculated. The immunophenotype of MSCs was analyzed via flow cytometry for standard positive (CD73, CD90, CD105) and negative markers. A subset of centers also performed gene expression profiling.
Head-to-Head Comparison of CS10, SCB, and RFM for MSC Spheroids
This protocol details a study designed to evaluate three GMP-grade cryoprotectants for preserving MSC spheroids, a critical format for regenerative medicine [55].
- Spheroid Generation: MSCs were cultured in 3D conditions to form spheroids.
- Cryopreservation Formulations:
- Tested Media: CryoStor CS10 (CS10), Stem-Cellbanker (SCB), and Recovery Cell Culture Freezing Media (RFM).
- Control: Conventional freezing medium (CM: DMEM with 20% FBS and 10% DMSO).
- Freezing and Storage: Spheroids were suspended in the respective cryomedia and subjected to a freeze/thaw cycle. The specific freezing method was not detailed, but storage lasted for 2 months.
- Post-Thaw Analysis:
- Viability: Assessed using LIVE/DEAD assays and Annexin V/Propidium Iodide staining.
- Morphology: Examined using scanning electron microscopy (SEM).
- Stemness: Evaluated through gene expression analysis of stem cell and MSC markers.
Protocol for High-Concentration Cryopreservation and Post-Thaw Dilution
This protocol investigates the impact of cryopreserving MSCs at high concentrations, a common clinical practice to minimize infusion volume, and the effect of post-thaw dilution [50].
- Cell Culture: Bone marrow-derived MSCs were cultured and harvested at passage 4.
- Cryopreservation Formulations and Concentrations: Cells were cryopreserved at three concentrations: 3, 6, and 9 million cells/mL (M/mL) in four different solutions: NutriFreez (10% DMSO), PHD10 (Plasmalyte A/5% Human Albumin/10% DMSO), CryoStor CS5 (5% DMSO), and CryoStor CS10 (10% DMSO).
- Freezing and Storage: Vials were frozen and stored in liquid nitrogen for over one week.
- Thawing and Dilution:
- Vials were thawed in a 37°C water bath for 2 minutes.
- Cells cryopreserved at 3 M/mL were assessed without dilution.
- Cells cryopreserved at 6 M/mL were diluted 1:1 with Plasmalyte A/5% HA.
- Cells cryopreserved at 9 M/mL were diluted 1:2 to achieve a uniform final concentration of 3 M/mL.
- Time-Course Assessment: Cell viability (Trypan blue exclusion) and apoptosis (Annexin V/PI staining) were measured immediately post-thaw (0h) and monitored over 6 hours at room temperature.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials and Reagents for Cryopreservation Studies
| Item | Function/Description | Example Products / Components |
|---|---|---|
| Base Cryoprotectants | Primary agents for protecting cells during freeze-thaw cycle. | CryoStor CS10/CS5, Stem-Cellbanker, Recovery RFM, SGI Solution, NutriFreez |
| In-House Media Components | For formulating custom cryopreservation solutions. | DMSO, Sucrose, Glycerol, Isoleucine, Plasmalyte A, Human Albumin (HA) |
| Cell Staining & Viability Kits | To assess cell survival, apoptosis, and death post-thaw. | LIVE/DEAD Assay Kit, Annexin V/Propidium Iodide (PI) Kit, Trypan Blue, Acridine Orange (AO)/DAPI |
| Freezing Containers | To provide a controlled cooling rate (~ -1°C/min) for slow freezing. | Mr. Frosty Freezing Container |
| Controlled-Rate Freezer | Advanced equipment for programmable, reproducible freezing profiles. | Various manufacturers |
| Automated Thawing System | Ensures consistent and rapid thawing of cryovials. | ThawSTAR Automated Thawing System |
| Hematology Analyzer | To count and characterize cells, e.g., platelets in BMAC samples. | Ruby Automated Hematology Analyzer |
Experimental Workflow and Decision Pathway
The following diagram illustrates a generalized workflow for conducting a head-to-head cryoprotectant comparison study, integrating key steps from the cited protocols.
Cryoprotectant Comparison Workflow
The data from recent studies indicate that DMSO-free formulations, particularly the SGI solution and Stem-Cellbanker, have reached a stage of development where their performance is comparable to, and in some cases may surpass, traditional DMSO-based media like CryoStor CS10 [27] [55]. The selection of an optimal cryoprotectant is not one-size-fits-all but depends on the specific research or clinical application requirements. Key considerations include the necessity of completely eliminating DMSO due to patient safety concerns, the format of the cells (e.g., 2D monolayers vs. 3D spheroids), the required post-thaw shelf life before administration, and the critical quality attributes (CQAs) such as viability, recovery, and functional potency. The protocols and data presented here provide a foundation for researchers to make an evidence-based selection and to design robust validation studies for their specific MSC-based products.
Cryopreservation serves as a critical step in the manufacturing and clinical deployment of Mesenchymal Stem Cell (MSC)-based therapies, enabling long-term storage and "off-the-shelf" availability [92] [93]. However, the freezing and thawing processes can potentially compromise critical therapeutic functions of MSCs. This application note details the specific impacts of cryopreservation on the core therapeutic mechanisms of MSCs—paracrine signaling, immunomodulation, and engraftment potential—and provides standardized protocols for the assessment and mitigation of these effects, framed within the broader context of cryopreservation research.
Quantitative Impact of Cryopreservation on MSC Therapeutic Attributes
The following tables summarize the quantitative findings from key studies on the temporal recovery of MSC attributes post-thaw and the comparative potency of fresh versus cryopreserved products.
Table 1: Temporal Recovery of Key MSC Attributes Post-Thaw (Based on [30])
| Cell Attribute | Immediately Post-Thaw (0 h) | 4 Hours Post-Thaw | 24 Hours Post-Thaw | Beyond 24 Hours (Long-Term) |
|---|---|---|---|---|
| Viability | Significantly reduced | Begins recovery | Recovers to near-baseline | Maintained |
| Apoptosis Level | Significantly increased | Peak level | Decreased, but may remain elevated | Normalizes |
| Metabolic Activity | Significantly impaired | Remains impaired | Remains lower than fresh cells | Variable recovery by cell line |
| Adhesion Potential | Significantly impaired | Remains impaired | Remains lower than fresh cells | Variable recovery by cell line |
| Immunophenotype | Minimal change (CD44, CD105 may decrease [14]) | Minimal change | Minimal change | Stable |
| CFU-F Ability | Not Applicable (Assayed later) | Not Applicable | Not Applicable | Reduced in some cell lines |
| Differentiation Potential | Maintained (osteogenic, chondrogenic) [14] | Maintained | Maintained | Variably affected (adipogenic, osteogenic) |
Table 2: Comparative Summary of Fresh vs. Thawed MSC Functional Potency (Based on [14] [94] [74])
| Functional Attribute | Freshly Cultured MSCs (FC) | Freshly Thawed MSCs (FT, 0h) | Thawed & Acclimated MSCs (TT, 24h) | In Vivo Outcome |
|---|---|---|---|---|
| T-cell Suppression | Potent | Potent, but may be reduced [94] or comparable [74] | Potent; significantly more potent than FT [14] | Improved outcomes with fresh cells in some studies [94] |
| Anti-inflammatory Gene Expression | Baseline | Significantly decreased [14] | Upregulated [14] | - |
| Angiogenic Gene Expression | Baseline | Decreased [14] | Upregulated [14] | - |
| Apoptosis | Baseline | Significantly increased [14] [74] | Significantly reduced [14] | - |
| Complement Activation & IBMIR | Lower | Increased, leading to faster serum-mediated elimination [94] | Not Reported | Potential for reduced engraftment [94] |
| Phagocytosis Enhancement | Effective | Comparable to Fresh [74] | Not Tested | Comparable improvement in bacterial clearance (FT vs. FC) [74] |
Experimental Protocols for Assessing Therapeutic Mechanisms
Below are detailed protocols for key experiments cited in the analysis of cryopreservation's impact.
Protocol: Assessing Post-Thaw Viability and Apoptosis Over Time
This protocol is designed to quantitatively measure the recovery of cryopreserved MSCs, as performed in [30].
- Key Reagents: hBM-MSCs, Cryopreservation Medium (FBS + 10% DMSO), Phosphate-Buffered Saline (PBS), Trypsin-EDTA, Annexin V Binding Buffer, Annexin V-FITC, Propidium Iodide (PI), Flow Cytometry Staining Buffer.
- Procedure:
- Cell Thawing: Rapidly thaw cryopreserved vials in a 37°C water bath for 1 minute. Transfer cell suspension to pre-warmed complete medium to dilute DMSO. Centrifuge at 200g for 5 minutes. Discard supernatant and resuspend cells in fresh complete medium.
- Time-Point Seeding: Immediately after thawing and counting, seed cells for the "0 h" time point. For subsequent time points (e.g., 2 h, 4 h, 24 h), first incubate the resuspended cells in a humidified incubator (37°C, 5% CO₂) for the respective duration before seeding.
- Viability & Apoptosis Staining: At each time point, harvest cells and wash with PBS. Resuspend ~1.5 x 10ⵠcells in 100 µL of Annexin V Binding Buffer. Add 5 µL of Annexin V-FITC and 5 µL of PI solution. Incubate for 15 minutes in the dark at room temperature.
- Analysis: Add 400 µL of binding buffer to each tube and analyze immediately using flow cytometry. Use unstained and single-stained controls for compensation. Cell populations are defined as: Viable (Annexin Vâ»/PIâ»), Early Apoptotic (Annexin Vâº/PIâ»), Late Apoptotic/Necrotic (Annexin Vâº/PIâº).
Protocol: In Vitro T-cell Suppression Assay
This protocol evaluates the immunomodulatory capacity of MSCs post-thaw, a critical quality potency assay [14] [74].
- Key Reagents: MSCs (FC, FT, TT), Peripheral Blood Mononuclear Cells (PBMCs) from healthy donor, CD3/CD28 T-cell Activation Dynabeads, CellTrace CFSE Cell Proliferation Kit, Roswell Park Memorial Institute (RPMI) 1640 medium supplemented with 10% FBS, Flow Cytometry Staining Buffer.
- Procedure:
- MSC Preparation: Seed MSCs from the different groups (FC, FT, TT) in a flat-bottom tissue culture plate and allow to adhere overnight (for FC and TT). For the FT group, seed cells immediately after thawing.
- PBMC Preparation & Labeling: Isolate PBMCs via density gradient centrifugation. Label PBMCs with CFSE according to the manufacturer's instructions.
- Co-culture Setup: Activate CFSE-labeled PBMCs with CD3/CD28 beads at a recommended ratio (e.g., 1 bead per cell). Add activated PBMCs to the MSC monolayers at a defined ratio (e.g., 10:1 PBMCs:MSCs). Include controls for non-activated PBMCs and activated PBMCs without MSCs.
- Incubation & Analysis: Co-culture for 5 days in a 37°C incubator. Harvest non-adherent cells and analyze CFSE dilution of CD3⺠T cells using flow cytometry. The percentage inhibition of proliferation is calculated relative to the activated PBMC-only control.
Protocol: Assessing MSC-Mediated Enhancement of Monocyte Phagocytosis
This assay tests the ability of MSCs to modulate innate immune function, relevant for applications in sepsis and ARDS [74].
- Key Reagents: MSCs (FC, FT), CD14⺠Monocytes (isolated from PBMCs), Fluorescently-labeled E. coli particles or BioParticles, Lipopolysaccharides (LPS), Flow Cytometry Staining Buffer.
- Procedure:
- Co-culture Setup: Seed MSCs (FC or FT) and allow to adhere. Isolate CD14⺠monocytes using magnetic-activated cell sorting (MACS). Add monocytes to the MSC cultures. Treat co-cultures with LPS to induce an inflammatory injury and impair monocyte function.
- Phagocytosis Assay: After 24 hours of co-culture, add pHrodo Red E. coli BioParticles (which fluoresce intensely in phagolysosomes) to the cells. Incubate for 1-2 hours.
- Analysis: Harvest monocytes, wash, and analyze by flow cytometry. The phagocytic activity is reported as the percentage of CD14⺠cells that are positive for pHrodo Red fluorescence, or as the mean fluorescence intensity (MFI). Compare results to LPS-injured monocytes without MSC co-culture.
Visualization of Signaling Pathways and Experimental Workflows
Diagram 1: Impact of Cryopreservation on MSC Therapeutic Mechanisms and Recovery Pathway. This workflow illustrates the cascade from cryopreservation stress through functional impairment, and the potential for recovery via a post-thaw acclimation period.
Diagram 2: Mechanisms of Reduced Engraftment and Rapid Clearance of Freshly Thawed MSCs. This diagram details the pathway linking post-thaw cellular damage to activation of the innate immune system and subsequent poor engraftment.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for MSC Cryopreservation and Potency Studies
| Reagent / Material | Function / Application | Example Usage in Protocols |
|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Penetrating cryoprotectant; prevents intracellular ice crystal formation. | Standard component of cryopreservation medium at 5-10% concentration [14] [3]. |
| Fetal Bovine Serum (FBS) | Provides extracellular protein support, enhancing membrane stability during freeze-thaw. | Common base (90%) for cryopreservation medium [14] [30]. |
| Human Platelet Lysate (hPL) | Xeno-free alternative to FBS in cryopreservation and culture media. | Used in serum-free freezing media formulations for clinical applications [93]. |
| Annexin V / Propidium Iodide (PI) | Fluorescent dyes for flow cytometric detection of apoptosis (early/late) and necrosis. | Critical for assessing post-thaw cell death and recovery over time (Protocol 3.1) [14] [30]. |
| CD3/CD28 Activation Beads | Polyclonal activators of T-cells via TCR and co-stimulatory pathways. | Used to stimulate PBMCs in T-cell suppression assays (Protocol 3.2) [74]. |
| CellTrace CFSE | Fluorescent cell dye that dilutes with each cell division, tracking proliferation. | Labels PBMCs to quantify T-cell proliferation inhibition by MSCs (Protocol 3.2) [74]. |
| pHrodo BioParticles | pH-sensitive fluorescent particles; fluorescence increases upon phagocytosis. | Used to quantitatively measure monocyte/phagocyte functional capacity (Protocol 3.3) [74]. |
| Rho-associated kinase (ROCK) inhibitor | Small molecule inhibitor (e.g., Y-27632) that reduces apoptosis and improves cell survival. | Added post-thaw to culture media to enhance attachment and viability of cryopreserved MSCs [93]. |
The data conclusively demonstrate that cryopreservation induces a transient but significant impairment of MSC therapeutic attributes, particularly in the first 4-24 hours post-thaw. The core mechanisms of paracrine signaling and immunomodulation are compromised, and engraftment potential is reduced due to enhanced complement activation and clearance [94] [30].
For clinical applications requiring immediate administration (e.g., acute sepsis), the use of freshly thawed MSCs is supported by evidence showing retained critical immunomodulatory functions [74]. However, for conditions where sustained in vivo activity is crucial, implementing a 24-hour post-thaw acclimation period in standard culture conditions is a highly recommended strategy to "reactivate" MSCs, restore their functional potency, and maximize therapeutic efficacy [14] [30]. This protocol should be integrated into the therapeutic manufacturing pipeline to ensure delivery of a maximally potent cell product.
Cryopreservation serves as a pivotal process in the translational pathway of mesenchymal stem cell (MSC)-based therapies, enabling long-term storage and distribution while maintaining critical quality attributes. The biosafety assessment of cryopreserved MSC products encompasses a comprehensive evaluation of genomic stability, functional potency, and clinical safety profiles to ensure patient safety and therapeutic efficacy. As the field advances toward standardized clinical applications, understanding the impact of cryopreservation methodologies on MSC biology becomes paramount for regulatory compliance and manufacturing consistency [3] [67]. This application note provides a structured framework for evaluating biosafety parameters of cryopreserved MSC products within the broader context of cryopreservation techniques for mesenchymal stem cell research.
Current challenges in cryopreservation include maintaining post-thaw viability, differentiation capacity, and immunomodulatory properties while minimizing cryopreservation-induced stress responses. The International Society for Cell & Gene Therapy (ISCT) has identified cryopreservation scaling as a major industry hurdle, with 22% of experts citing "ability to process at large scale" as the most significant challenge [67]. This document addresses these challenges by providing standardized protocols for biosafety assessment, focusing specifically on genomic stability and clinical safety profiling essential for preclinical and clinical development.
Current Cryopreservation Methodologies and Biosafety Implications
Cryopreservation Techniques in MSC Research
Two primary techniques dominate MSC cryopreservation: slow freezing and vitrification. Slow freezing, characterized by controlled cooling rates typically at -1°C/min to -3°C/min, facilitates gradual cellular dehydration and minimizes intracellular ice crystal formation [3]. This method remains the gold standard for clinical MSC cryopreservation due to its operational simplicity and reduced contamination risk. Approximately 70-80% of cells survive when employing this gradual freezing procedure [3]. In contrast, vitrification employs high cooling rates and high concentrations of cryoprotectant agents (CPAs) to achieve a glass-like state without ice formation, though its application is limited by CPA toxicity and sample volume constraints [3] [56].
Industry surveys reveal that 87% of cell therapy developers utilize controlled-rate freezing for cryopreservation, while only 13% rely on passive freezing methods, predominantly for early-stage clinical development (up to phase II) [67]. This preference stems from the enhanced process control afforded by controlled-rate freezers, which allow definition of critical parameters including cooling rate before nucleation, temperature of ice nucleation, and final sample temperature before transfer to cryogenic storage [67].
Cryoprotectant Agents: Composition and Safety Concerns
Cryoprotectant agents are essential components of cryopreservation protocols, categorized as penetrating (e.g., dimethyl sulfoxide - DMSO) or non-penetrating (e.g., sucrose, trehalose). DMSO has remained the most widely utilized penetrating CPA despite well-documented toxicity concerns including cellular stress, differentiation alterations, and adverse clinical reactions in patients [27] [3]. Clinical manifestations of DMSO toxicity include nausea, vomiting, arrhythmias, neurotoxicity, and respiratory depression [56].
Recent advancements focus on DMSO reduction or elimination through novel formulations. A 2024 international multicenter study demonstrated that a DMSO-free solution containing sucrose, glycerol, and isoleucine (SGI) achieved comparable results to traditional DMSO-containing cryoprotectants in preserving MSC viability, recovery, and immunophenotype [27]. Additionally, hydrogel microencapsulation technology has enabled effective cryopreservation with DMSO concentrations as low as 2.5% while sustaining cell viability above the 70% clinical threshold [56].
Table 1: Comparison of Cryopreservation Methods for MSCs
| Parameter | Slow Freezing | Vitrification | Novel Approaches |
|---|---|---|---|
| Cooling Rate | -1°C/min to -3°C/min | > -1000°C/min | Variable |
| CPA Concentration | Low (5-10% DMSO) | High (≥30% total CPA) | Low (≤2.5% DMSO with biomaterials) |
| Ice Formation | Extracellular, minimal intracellular | None (glassy state) | Controlled extracellular |
| Cell Viability | 70-80% | Variable (technique-dependent) | >70% with optimized protocols |
| Clinical Translation | High | Limited | Emerging |
| Scalability | Excellent | Limited by sample volume | Promising |
Comprehensive Biosafety Assessment Framework
Genomic Stability Assessment
3.1.1 Cytogenetic Analysis Genomic integrity represents a fundamental biosafety parameter for cryopreserved MSC products. Standard cytogenetic analysis should include G-banding karyotyping to detect chromosomal abnormalities at a resolution of 5-10 Mb. For higher resolution detection of submicroscopic alterations, array Comparative Genomic Hybridization (aCGH) or Single Nucleotide Polymorphism (SNP) arrays provide comprehensive assessment of copy number variations. The experimental protocol involves:
- Culturing post-thaw MSCs for 10-14 population doublings
- Cell harvesting during logarithmic growth phase (60-70% confluence)
- Metaphase arrest using colcemid (0.1 μg/mL for 45-60 minutes)
- Hypotonic treatment (0.075 M KCl for 20 minutes at 37°C)
- Fixation with 3:1 methanol:acetic acid
- Slide preparation and banding analysis of ≥20 metaphase spreads per sample [95]
3.1.2 DNA Damage Response Assays DNA damage response should be evaluated through γH2AX foci quantification via immunofluorescence microscopy. This assay detects double-strand breaks, with >10 foci per cell indicating significant genotoxic stress. Additional assessment should include comet assays under alkaline conditions (pH>13) to detect single and double-strand breaks, with analysis of ≥100 cells per sample using automated scoring systems [95].
Tumorigenicity and Teratogenicity Testing
3.2.1 In Vitro Transformation Assays Soft agar colony formation assays provide a sensitive measure of anchorage-independent growth, a hallmark of cellular transformation. The methodology includes:
- Preparing base agar layer (0.5-0.6% agar in complete medium)
- Seeding 1×10ⴠpost-thaw MSCs in top agar layer (0.3% agar)
- Culturing for 3-4 weeks with medium replenishment twice weekly
- Staining with iodonitrotetrazolium chloride and counting colonies >50μm A positive control (transformed cell line) should form >100 colonies, while test MSC samples should demonstrate <5 colonies per 1×10ⴠcells plated [95].
3.2.2 In Vivo Tumorigenicity Models The gold standard for tumorigenicity assessment involves subcutaneous implantation of 1×10ⷠpost-thaw MSCs into immunodeficient mice (NOD/SCID or NSG strains). Animals should be monitored for 16-24 weeks, with biweekly palpation for nodule formation. Terminal analysis includes:
- Histopathological examination of implantation sites and major organs
- Immunohistochemistry for human-specific markers (e.g., HLA, mitochondria)
- Assessment of metastatic potential through human Alu sequence PCR in distant organs [95]
Functional Potency and Immunomodulatory Capacity
3.3.1 Multilineage Differentiation Potential Post-thaw differentiation capacity should be evaluated through standardized in vitro assays:
- Osteogenic differentiation: 21-day culture in induction media containing 10mM β-glycerophosphate, 50μM ascorbate-2-phosphate, and 100nM dexamethasone, with mineralization quantified by Alizarin Red S staining
- Adipogenic differentiation: 14-day culture in media containing 1μM dexamethasone, 0.5mM isobutylmethylxanthine, 50μM indomethacin, with lipid accumulation visualized by Oil Red O staining
- Chondrogenic differentiation: 21-day pellet culture in media containing 10ng/mL TGF-β3, 50μM ascorbate-2-phosphate, with proteoglycan deposition assessed by Safranin O staining [96] [97]
3.3.2 Immunomodulatory Function Immunosuppressive capacity should be evaluated through mixed lymphocyte reactions (MLR) or T-cell proliferation assays:
- Isculating peripheral blood mononuclear cells (PBMCs) from ≥3 healthy donors
- Labeling responder PBMCs with CFSE (1μM)
- Stimulating with mitogens (PHA, 5μg/mL) or allogeneic PBMCs
- Coculturing with post-thaw MSCs at ratios from 1:1 to 1:10 (MSC:PBMC)
- Quantifying T-cell proliferation after 5 days by flow cytometry Functional MSCs should suppress T-cell proliferation by ≥30% at 1:10 ratio [96] [98]
Table 2: Biosafety Assessment Parameters for Cryopreserved MSC Products
| Assessment Category | Specific Tests | Acceptance Criteria | Regulatory Reference |
|---|---|---|---|
| Genomic Stability | Karyotyping (G-banding) | Normal diploid karyotype in ≥20 metaphases | FDA/EMA guidelines |
| aCGH/SNP array | No clinically significant CNVs | ISCT standards | |
| γH2AX foci assay | <10 foci/nucleus | ICH S2(R1) | |
| Tumorigenic Potential | Soft agar colony formation | <5 colonies/10â´ cells | WHO guidelines |
| In vivo tumorigenicity (mouse model) | No tumor formation at 16 weeks | FDA guidance | |
| Functional Potency | Trilineage differentiation | Positive staining in ≥2 lineages | ISCT minimal criteria |
| Immunosuppression assay | ≥30% inhibition of T-cell proliferation | Ph. Eur. 5.2.3 | |
| Cell Quality | Viability (flow cytometry) | ≥70% post-thaw viability | USP <1046> |
| Sterility (bacterial/fungal) | No microbial growth after 14 days | Ph. Eur. 2.6.27 | |
| Mycoplasma (PCR/culture) | Negative | FDA CBER guidance |
Experimental Protocols for Biosafety Profiling
Post-Thaw Viability and Recovery Assessment
Materials:
- Cryopreserved MSC aliquots
- Complete culture medium (α-MEM with 20% FBS, 1% penicillin/streptomycin, 10ng/mL FGF-2)
- DMSO removal solution (5% dextrose-40 or 0.9% NaCl with 5% human serum albumin)
- Flow cytometry reagents (Annexin V-FITC, 7-AAD, or propidium iodide)
- Automated cell counter
Protocol:
- Rapidly thaw cryovials in a 37°C water bath with gentle agitation until only a small ice crystal remains (approximately 2-3 minutes)
- Transfer cell suspension to 15mL conical tube containing pre-warmed DMSO removal solution using a drop-wise method (first mL over 1 minute, remaining volume over 3-5 minutes)
- Centrifuge at 300×g for 5 minutes and carefully aspirate supernatant
- Resuspend cell pellet in complete culture medium and perform cell counting
- Assess viability using dual staining with Annexin V-FITC and 7-AAD per manufacturer's instructions
- Plate cells at 5×10³ cells/cm² for recovery assessment and calculate population doubling time over 3 passages [3] [97]
Acceptance Criteria: Post-thaw viability ≥70% by flow cytometry and recovery of ≥80% proliferative capacity within 3 passages compared to pre-freeze controls.
Senescence-Associated Beta-Galactosidase Staining
Cellular senescence represents a critical quality attribute impacted by cryopreservation stress. The protocol includes:
- Seeding post-thaw MSCs at 5×10³ cells/cm² in 6-well plates
- Culturing for 24 hours until 60-70% confluence
- Fixing cells with 2% formaldehyde/0.2% glutaraldehyde for 5 minutes at room temperature
- Staining with X-gal solution (1mg/mL at pH 6.0) for 16 hours at 37°C in a dry incubator without CO₂
- Quantifying senescent cells (blue staining) by counting ≥500 cells across multiple fields Acceptable thresholds: <15% SA-β-gal positive cells in early-passage cultures [3].
Biodistribution Assessment Using qPCR
For preclinical development, biodistribution analysis tracks cell fate post-transplantation:
- Isolating genomic DNA from target tissues (lung, liver, spleen, brain, gonads)
- Performing qPCR with species-specific primers (e.g., human Alu sequences in mouse tissues)
- Generating standard curves using known mixtures of human and mouse DNA
- Expressing results as human DNA equivalents per μg of total tissue DNA
- Monitoring at multiple timepoints (24 hours, 1 week, 1 month post-administration) [95]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Cryopreservation Biosafety Studies
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Cryoprotectants | DMSO, Sucrose-Glycerol-Isoleucine (SGI), Trehalose | Prevent intracellular ice formation, reduce freezing point | DMSO concentration optimization (2.5-10%); toxicity profiling essential |
| Cell Viability Assays | Annexin V/7-AAD, CFSE, Calcein-AM/EthD-1 | Distinguish live/apoptotic/necrotic populations; functional metabolism | Combine with flow cytometry for quantitative analysis |
| Differentiation Kits | Osteogenic: Ascorbate-2-phosphate, β-glycerophosphate; Adipogenic: IBMX, Indomethacin | Assess multipotency retention post-thaw | Include positive controls; quantify with image analysis |
| Genomic Stability Tools | G-banding kits, aCGH platforms, γH2AX antibodies | Detect chromosomal abnormalities, DNA damage | Establish baseline for donor-specific variations |
| Immunomodulation Assays | CFSE, PHA, MLR kits, IFN-γ ELISA | Quantify immunosuppressive capacity | Use multiple donor PBMCs for robustness |
| Biomaterial Scaffolds | Alginate hydrogels, 3D bioprinting matrices | Enhance post-thaw recovery, mimic niche | Sterility and endotoxin testing critical |
Technological Advances and Future Perspectives
Recent technological innovations address critical challenges in MSC cryopreservation biosafety. Hydrogel microencapsulation represents a promising approach, with studies demonstrating that alginate-based microcapsules enable effective cryopreservation with only 2.5% DMSO while maintaining viability above the 70% clinical threshold [56]. These biomaterial-based strategies provide physical protection during freezing and thawing cycles, potentially reducing cryoinjury and preserving functionality.
Advanced controlled-rate freezing systems incorporating temperature profiling and real-time monitoring enhance process consistency. Industry surveys indicate that nearly 30% of organizations rely on vendor expertise for system qualification, highlighting the need for standardized protocols [67]. The implementation of freeze curve analysis as part of quality control provides critical process data, though current practice shows limited use of this information in product release decisions.
Emerging evidence supports the functional equivalence of properly cryopreserved MSCs compared to fresh counterparts. A 2025 study demonstrated that BMAC cryopreserved at -80°C for four weeks maintained equivalent proliferation capacity, multilineage differentiation potential, and in vivo cartilage repair capability compared to fresh controls [97]. These findings validate strategic approaches involving single harvest with cryopreserved storage for multiple administrations, potentially reducing patient burden.
Future directions include the development of DMSO-free cryopreservation formulations standardized across manufacturing platforms, integration of omics technologies for comprehensive biosafety profiling, and establishment of correlations between process parameters and critical quality attributes to enable quality-by-design approaches in MSC cryopreservation.
Visualizing Biosafety Assessment Workflows
Biosafety Assessment Workflow
Cryopreservation Impact Pathways
Quantitative Data on Cryopreservation Impact
The following tables consolidate key quantitative findings from recent studies on the impact of cryopreservation on Mesenchymal Stem Cells (MSCs).
Table 1: Impact of Cryopreservation on hBM-MSC Attributes (Short-Term Recovery) [72]
| Cell Attribute | Immediate Post-Thaw (0h) | 4 Hours Post-Thaw | 24 Hours Post-Thaw |
|---|---|---|---|
| Viability | Reduced | Began to recover | Recovered to near-baseline |
| Apoptosis Level | Significantly Increased | Remained Elevated | Decreased, but above fresh cell levels |
| Metabolic Activity | Impaired | Impaired | Remained lower than fresh cells |
| Adhesion Potential | Impaired | Impaired | Remained lower than fresh cells |
Table 2: Impact of Cryopreservation on hBM-MSC Attributes (Long-Term Function) [72]
| Cell Attribute | Impact of Cryopreservation |
|---|---|
| Proliferation Rate | No significant difference observed compared to fresh cells. |
| Colony-Forming Unit (CFU-F) Ability | Reduced in two out of three tested cell lines. |
| Adipogenic & Osteogenic Differentiation | Variably affected across different cell lines; no consistent trend. |
Table 3: Functional Equivalence of Fresh vs. Frozen Bone Marrow Aspirate Concentrate (BMAC) [10]
| Assay Type | Fresh BMAC | BMAC Frozen for 4 Weeks at -80°C |
|---|---|---|
| MSC Proliferation | Preserved | Preserved; no significant difference from fresh |
| Multilineage Differentiation | Preserved | Preserved; similar capacity to fresh BMAC |
| In Vivo Cartilage Repair (OA Rat Model) | Improved histological score | Improved histological score; no significant difference from fresh BMAC |
Detailed Experimental Protocols
This protocol details the methodology for quantifying the recovery of human Bone Marrow-derived MSCs (hBM-MSCs) at critical time points after thawing.
- 1. Cell Culture:
- Culture hBM-MSCs in Dulbecco’s Modified Eagle Medium (DMEM) supplemented with 10% (v/v) Fetal Bovine Serum (FBS).
- Maintain cultures at 37°C and 5% CO2 in a humidified incubator.
- Seed cells at a density of 5,000 cells per square centimeter and passage them upon reaching confluence.
- 2. Cryopreservation:
- At the target passage (e.g., P4), detach cells and centrifuge at 200 × g.
- Count cells and resuspend them at a concentration of 1 × 10^6 cells per milliliter in FBS supplemented with 10% (v/v) DMSO.
- Aliquot 1 mL of cell suspension into cryogenic vials.
- Place vials in a controlled-rate freezing container (e.g., "Mr. Frosty") filled with isopropyl alcohol and store at -80°C for 24 hours to achieve a cooling rate of approximately -1°C/min.
- After 24 hours, transfer vials to liquid nitrogen for long-term storage (minimum 1 week).
- 3. Thawing and Post-Thaw Analysis:
- Rapidly thaw vials in a 40°C water bath for exactly 1 minute.
- Dilute the cell suspension drop-wise with pre-warmed complete medium (9 mL).
- Centrifuge at 200 × g for 5 minutes to remove the DMSO-containing supernatant.
- Resuspend the cell pellet in fresh complete medium and count cells.
- Immediate Assays (0h): Use cells directly for viability, apoptosis, and other assays.
- Recovery Period Assays: Incubate aliquots of cells in fresh complete medium for 2, 4, or 24 hours in a humidified incubator before performing subsequent assays.
This protocol outlines the collaborative study design for comparing DMSO-containing and DMSO-free cryoprotectant solutions across multiple manufacturing centers.
- 1. Cell Preparation and Cryopreservation:
- Each participating center uses MSCs isolated and expanded from a single donor according to their local, established protocols.
- Cells are cryopreserved in two different solutions:
- Test Solution: SGI solution (a DMSO-free solution containing Sucrose, Glycerol, and Isoleucine).
- Control Solution: The center's standard in-house DMSO-containing cryoprotectant solution.
- For each solution, at least three cryovials are prepared as measurement replicates.
- 2. Thawing and Analysis:
- Vials are thawed and analyzed for key quality attributes. Specific assays include:
- Cell Viability: Measured using flow cytometry or similar methods.
- Cell Recovery: Calculated as the percentage of viable cells recovered post-thaw compared to the number frozen.
- Immunophenotype: Confirmation of standard MSC surface markers (e.g., CD73, CD90, CD105) and lack of hematopoietic markers via flow cytometry.
- Gene Expression Profile: Analysis of key genes to assess cellular function and stability.
- Vials are thawed and analyzed for key quality attributes. Specific assays include:
This protocol describes the process for testing the functional equivalence of frozen BMAC in cartilage repair.
- 1. BMAC Collection and Processing:
- Obtain bone marrow aspirate from patients and process it to create BMAC, enriching for mononuclear cells and MSCs.
- 2. Cryopreservation of BMAC:
- Centrifuge fresh BMAC at 1500 × g for 10 minutes.
- Collect the buffy coat and resuspend it in a cryoprotectant medium consisting of 10% DMSO and 90% autologous plasma.
- Freeze the cells using a controlled-rate freezing container and store at -80°C for a defined period (e.g., 4 weeks).
- 3. In Vitro Functional Assays:
- Colony Forming Unit-fibroblast (CFU-f) Assay: Seed mononuclear cells from fresh and frozen BMAC and culture for 14 days. Fix, stain with crystal violet, and manually count colonies containing >100 cells.
- Multilineage Differentiation: Culture MSCs from fresh and frozen BMAC in osteogenic and adipogenic induction media. Assess differentiation potential using standard staining protocols (e.g., Alizarin Red for osteogenesis, Oil Red O for adipogenesis).
- 4. In Vivo Cartilage Repair Assessment:
- Use an osteoarthritis (OA) rat model.
- Compare the therapeutic effects of fresh BMAC, frozen BMAC, and a control (e.g., PBS).
- Evaluate cartilage repair by scoring histological sections of the tibial plateau cartilage using established scoring systems (e.g., ICRS histology score).
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Cryopreservation Studies
| Reagent / Material | Function and Application in Cryopreservation |
|---|---|
| Dimethyl Sulfoxide (DMSO) | A standard penetrating cryoprotective agent (CPA) that prevents intracellular ice crystal formation. Used at concentrations around 10% (v/v) [72] [27]. |
| SGI Solution (Sucrose, Glycerol, Isoleucine) | A DMSO-free, non-penetrating CPA alternative. Reduces risks associated with DMSO toxicity in clinical applications [27]. |
| Autologous Plasma | Serves as a natural, patient-specific base for cryoprotectant solutions. Used to resuspend cells in BMAC freezing protocols, often with DMSO [10]. |
| Fetal Bovine Serum (FBS) | Common component of cell culture and freezing media. Provides proteins and other molecules that can stabilize cell membranes during freezing [72]. |
| Controlled-Rate Freezer (or "Mr. Frosty") | A device that ensures a consistent, optimal cooling rate (typically -1°C/min) to maximize cell viability during the freezing process [72] [10]. |
| Ficoll Gradient | A solution used for density gradient centrifugation to isolate mononuclear cells (including MSCs) from bone marrow aspirate or BMAC prior to culture or analysis [10]. |
Experimental Workflow and Pathway Visualizations
The following diagrams, generated using Graphviz DOT language, illustrate key experimental workflows and logical relationships described in the protocols.
Conclusion
Cryopreservation is no longer a mere storage step but a critical determinant of therapeutic success for MSC-based therapies. While significant advancements have been made in protocol standardization and DMSO-free cryoprotectant development, challenges remain in perfectly preserving the nuanced functionality of these living drugs. The future of MSC cryopreservation lies in the development of cell-specific, precision protocols that account for source tissue and intended clinical application. Continued innovation in cryoprotectant engineering, combined with robust functional validation, will be paramount to fully realizing the potential of 'off-the-shelf' MSC products in regenerative medicine and beyond, ultimately ensuring that these promising therapies deliver consistent, safe, and efficacious clinical outcomes.
References
- 1. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 2. Identifying the Therapeutic Significance of Mesenchymal Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7291143/]
- 3. Effects, methods and limits of the cryopreservation on ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03954-3]
- 4. Cell-free regenerative medicine: identifying the best source ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1518412/full]
- 5. Advancing Key Processes of the MSC Therapy ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925001902]
- 6. Efficacy of a single intra-articular injection of mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398016/]
- 7. CRISPR-mediated engineering of mesenchymal stromal/stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574024/]
- 8. Cryostorage of Mesenchymal Stem Cells and Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9454587/]
- 9. Evaluating the potential of off-the-shelf engineered ... [https://www.sciencedirect.com/science/article/pii/S0753332224015622]
- 10. Short-Term Cryopreservation Preserved the Function of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524150/]
- 11. Optimization of freezing and thawing protocols for human ... [https://www.sciencedirect.com/science/article/pii/S0011224025000513]
- 12. Ice Inhibition for Cryopreservation: Materials, Strategies, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7967093/]
- 13. Principles and Protocols For Post-Cryopreservation Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9113563/]
- 14. Cryopreserved mesenchymal stem cells regain functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6716839/]
- 15. Comparison of freshly cultured versus cryopreserved ... [https://elifesciences.org/articles/75053]
- 16. Cryopreservation of brain cell structure: a review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11753176/]
- 17. Optimisation of cryopreservation conditions, including storage ... [https://bmcmolcellbiol.biomedcentral.com/articles/10.1186/s12860-024-00516-6]
- 18. A Cryopreservation and Regeneration Protocol for ... [https://www.mdpi.com/2223-7747/14/20/3127]
- 19. Chemical approaches to cryopreservation [https://www.nature.com/articles/s41570-022-00407-4]
- 20. Optimization for Biopharma Stability... | allanchem.com Cryoprotectant [https://allanchem.com/cryoprotectant-optimization-for-biopharma-stability/]
- 21. Mesenchymal stem cell cryopreservation with cavitation- ... [https://www.nature.com/articles/s44172-024-00265-6]
- 22. Molecular mechanisms cell cryopreservation with polyampholytes... of [https://www.nature.com/articles/s43246-021-00118-1?error=cookies_not_supported&code=96690885-df93-4e5a-b03f-14fecdc86523]
- 23. A Closer Look at the Potential Mechanisms of Action ... [https://www.mdpi.com/2076-2607/13/2/435]
- 24. Proteomic approach for evaluating cryoprotectant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12048564/]
- 25. Dimethyl sulfoxide in cryopreserved mesenchymal stromal ... [https://pubmed.ncbi.nlm.nih.gov/40826088/]
- 26. Frontiers | Comprehensive overview of the toxicities of small-molecule... [https://www.frontiersin.org/journals/toxicology/articles/10.3389/ftox.2025.1477822/full]
- 27. Cryopreservation of mesenchymal stem/stromal cells using ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324924007734]
- 28. Dimethyl sulfoxide in cryopreserved mesenchymal stromal cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362920/]
- 29. Cryopreserved Mesenchymal Stromal Cells Maintain ... [https://www.nature.com/articles/srep26463]
- 30. Quantitative assessment of the impact of cryopreservation on ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-02054-2]
- 31. Recent advances to enhance the immunomodulatory potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9537745/]
- 32. Principles and Protocols For Post-Cryopreservation Quality ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.907943/full]
- 33. Cryopreservation of Mesenchymal Stem Cells Using ... [https://www.mdpi.com/1422-0067/21/22/8579]
- 34. Cryostorage of Mesenchymal Stem Cells and Biomedical ... [https://www.mdpi.com/2073-4409/11/17/2691]
- 35. Cryopreservation of tissues by slow-freezing using an ... [https://www.nature.com/articles/s41598-022-23913-3]
- 36. Comparison of different freezing rates on post-thaw viability ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224025000094]
- 37. A comparison of cryopreservation methods: Slow-cooling vs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3196719/]
- 38. Comparative analysis between slow freezing and ultra ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6210620/]
- 39. Vitrification for cryopreservation of 2D and 3D stem cells culture using high concentration of cryoprotective agents - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7449025/]
- 40. Cryopreservation of Human Stem Cells for Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3088734/]
- 41. Cell Freezing Media Market Size & Opportunities, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/cell-freezing-media-market]
- 42. Optimizing mesenchymal stem cell therapy: from isolation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12054297/]
- 43. Cell Freezing Media Market to Grow 8.6% CAGR till 2035 [https://www.towardshealthcare.com/insights/cell-freezing-media-market-sizing]
- 44. A Potency and Toxicology Study on the Tolerability ... [https://www.sciencedirect.com/science/article/pii/S2329050125002062]
- 45. Key quality parameter comparison of mesenchymal stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11324487/]
- 46. Dimethyl sulfoxide in cryopreserved mesenchymal stromal cell ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06807-6]
- 47. Strategies in developing dimethyl sulfoxide (DMSO)-free ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.1030965/full]
- 48. Dimethyl sulfoxide-free cryopreservation solutions for ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324921007805]
- 49. Cryopreservation of mesenchymal stem/stromal cells using a ... [https://pubmed.ncbi.nlm.nih.gov/39066775/]
- 50. Key quality parameter comparison of mesenchymal stem ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1412811/full]
- 51. Table 1 Strategies for the DMSO-free cryopreservation of ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06807-6/tables/1]
- 52. Theory-based cryopreservation mode of mesenchymal ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224024000610]
- 53. Advances in Cryopreservation Strategies for 3D ... [https://www.mdpi.com/1422-0067/26/14/6908]
- 54. Optimizing cryopreservation strategies for scalable cell therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC11659802/]
- 55. Comparison of Cryopreservation Media for Mesenchymal ... [https://pubmed.ncbi.nlm.nih.gov/38011543/]
- 56. Hydrogel microcapsulation technology reduces the DMSO ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12639263/]
- 57. Cryopreserving 3D cell culture models of Alzheimer's ... [https://www.nature.com/articles/s41598-025-94810-8]
- 58. Cryopreservation of Cells: Dos and Don'ts [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/the-dos-and-donts-of-cryopreservation.html]
- 59. Optimizing cryopreservation conditions for use of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1385691/full]
- 60. Cryopreservation and Recovery of Primary Cells [https://www.intechopen.com/online-first/1231876]
- 61. Low-DMSO Cryopreservation of MSCs with Optibumin 25 ... [https://invitria.com/resources/low-dmso-cryopreservation-of-mscs-with-optibumin-25-recombinant-albumin/]
- 62. A toxicity function approach to optimal cost equilibration in... CPA [https://pmc.ncbi.nlm.nih.gov/articles/PMC8183460/]
- 63. Risks of Protein and DMSO in... - Atlantis Bioscience Pte Ltd [https://www.atlantisbioscience.com/blog/risks-dmso-protein-cryopreservation-cell-gene-therapy/]
- 64. Small molecule ice recrystallization inhibitors mitigate red ... [https://www.nature.com/articles/srep23619]
- 65. Species-specific optimisation of cryopreservation media for ... [https://pubmed.ncbi.nlm.nih.gov/39921190/]
- 66. CRITICAL COOLING AND WARMING RATES AS A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10186587/]
- 67. Cryopreservation - Key Survey Findings from the ISCT ... [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/05/28/cryopreservation-key-survey-findings-from-the-isct]
- 68. Inhibition of ice recrystallization and cryoprotective activity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4838640/]
- 69. The principal variables of cryopreservation: solutions, ... [https://www.sciencedirect.com/science/article/pii/S0015028211010429]
- 70. Reconstitution and post-thaw storage of cryopreserved human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10154666/]
- 71. Deep-supercooling preservation of stem cell spheroids for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11751798/]
- 72. Quantitative assessment of the impact of cryopreservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7734731/]
- 73. Identification of a fundamental cryoinjury mechanism in ... [https://www.sciencedirect.com/science/article/pii/S0011224023000913]
- 74. Thawed Mesenchymal Stem Cell Product Shows ... [https://www.nature.com/articles/s41598-019-54462-x]
- 75. Cryopreserved Mesenchymal Stem Cells Regain ... [https://pubmed.ncbi.nlm.nih.gov/31464641/]
- 76. Reconstitution and post-thaw storage of cryopreserved ... [https://www.sciencedirect.com/science/article/pii/S2352320423000275]
- 77. Optimized reagents for immunopotency assays on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10148700/]
- 78. GMP Grade Cryopreservation Medium Market Analysis ... [https://www.linkedin.com/pulse/gmp-grade-cryopreservation-medium-market-ayxbc]
- 79. Cryopreservation: Key to Scalable & Global Cell Therapy ... [https://www.atlantisbioscience.com/blog/cryopreservation-in-cell-therapy-enabling-scalability-quality-and-global-distribution/?srsltid=AfmBOop7678oJgze5FdTcOB0JR-wzk98ycRnGI3DtunZb6OLLAQdhh50]
- 80. Regulatory strategy reimagined: Three trends accelerating ... [https://www.drugdiscoverytrends.com/regulatory-strategy-reimagined-three-trends-accelerating-drug-development/]
- 81. Cryopreservation & Platelet Storage Technologies Market ... [https://www.towardshealthcare.com/insights/cryopreservation-and-platelet-storage-technologies-market-sizing]
- 82. Cryopreservation & Platelet Storage Technologies Market [https://www.globenewswire.com/news-release/2025/10/15/3167303/0/en/Cryopreservation-Platelet-Storage-Technologies-Market.html]
- 83. The current state of biobanking [https://www.ddw-online.com/the-current-state-of-biobanking-36067-202508/]
- 84. Comparison of freshly cultured versus cryopreserved ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9286731/]
- 85. Comparison studies identify mesenchymal stromal cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10984924/]
- 86. Comparison of freshly cultured versus freshly thawed ... [https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-020-01437-z]
- 87. Peer review in Comparison of freshly cultured versus ... [https://elifesciences.org/articles/75053/peer-reviews]
- 88. Models in vivo and in vitro for the study of acute and ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576924008129]
- 89. Protective effects and mechanism of resveratrol in animal ... [https://pubmed.ncbi.nlm.nih.gov/41089832/]
- 90. Protective effects and mechanism of resveratrol in animal ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1666698/full]
- 91. Cryopreservation with DMSO affects the DNA integrity ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224024000026]
- 92. Impact of Cryopreservation and Freeze-Thawing on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9045030/]
- 93. The impact of cryopreservation on bone marrow-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6883667/]
- 94. Do Cryopreserved Mesenchymal Stromal Cells Display ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4381870/]
- 95. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 96. Validated methods for isolation and qualification of ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06972-8]
- 97. Short-Term Cryopreservation Preserved the Function of ... [https://www.mdpi.com/2073-4409/14/19/1569]
- 98. From bench to bedside: translating mesenchymal stem cell ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1639439/full]