Assessing the Safety Profile of Stem Cell-Based Therapies: From Foundational Risks to Clinical Validation
This article provides a comprehensive safety profile assessment of stem cell-based therapies for researchers, scientists, and drug development professionals.
Assessing the Safety Profile of Stem Cell-Based Therapies: From Foundational Risks to Clinical Validation
Abstract
This article provides a comprehensive safety profile assessment of stem cell-based therapies for researchers, scientists, and drug development professionals. It systematically explores the foundational biological risks, including tumorigenicity and immunogenicity, and details methodological frameworks for risk management from manufacturing to clinical application. The content further addresses troubleshooting for persistent challenges like long-term safety and standardization, and validates findings through meta-analyses and long-term clinical studies. By synthesizing current evidence and regulatory perspectives, this review aims to support the safe and ethical translation of stem cell technologies into clinical practice.
Understanding Fundamental Safety Risks in Stem Cell Therapeutics
The transition of benign teratomas into malignant neoplasms represents a critical junction in understanding tumorigenesis, with profound implications for the safety profiling of stem cell-based therapies. Although mature cystic teratomas (MCTs) are typically benign, containing differentiated tissues from all three germ layers, 1-3% undergo malignant transformation (MT) into aggressive cancers, defined as germ cell tumors with somatic malignancy (GCTSM) [1] [2]. This progression underscores the latent risks associated with pluripotent and totipotent cells, which are central to regenerative medicine. This guide systematically compares the pathological features, experimental models, and safety assessment protocols essential for evaluating the tumorigenic potential of cellular products, providing a foundational framework for researchers and drug development professionals to mitigate oncogenic risk.
Teratomas are unique tumors composed of various somatic tissues, often resembling disordered organogenesis. Their study is indispensable for stem cell research for two primary reasons: they are a recognized risk factor in pluripotent stem cell transplantation, and they provide a natural model for investigating malignant transformation. MCTs, the most common ovarian germ cell tumors, are generally benign [2]. However, in rare cases, somatic tissues within the teratoma can acquire malignant characteristics, transforming into carcinomas (e.g., squamous cell carcinoma, adenocarcinoma) or sarcomas [1] [3]. The World Health Organization (WHO) classifies these aggressive entities as GCTSM, which are associated with a poor prognosis and a median patient survival of approximately nine months [1]. This paradigm highlights the critical need for rigorous biosafety assessments to identify and eliminate potentially tumorigenic cells from therapeutic products.
Comparative Analysis of Malignant Transformation
Incidence and Common Histological Subtypes
Malignant transformation is a rare but serious event. The following table summarizes the key data and common malignant outcomes based on clinical case studies and literature reviews.
Table 1: Incidence and Common Malignant Subtypes in Teratoma Transformation
| Feature | Mature Cystic Teratoma (MCT) [1] [2] | Transformed GCTSM [1] [3] [2] |
|---|---|---|
| Overall Incidence of MT | 1% - 3% of cases | N/A |
| Most Common Malignancy | Squamous Cell Carcinoma (∼88% of MT cases) | Sarcomas (e.g., rhabdomyosarcoma), Adenocarcinomas |
| Other Reported Malignancies | Adenocarcinoma, sarcoma, carcinoid, melanoma [2] | Carcinosarcoma, primitive neuroectodermal tumors |
| Key Risk Factors | Advanced age (post-menopausal), large tumor size, rapid growth [2] | Prior chemotherapy or radiotherapy can induce transformation [1] |
Pathophysiological Mechanisms and Diagnostic Markers
The mechanism driving malignant transformation is multifaceted. One hypothesis involves the malignant degeneration of a single tissue component within a pre-existing benign teratoma over a long natural history, a phenomenon more common in older patients [1]. Alternatively, chemotherapy or radiotherapy for a prior germ cell tumor can induce transformation in a part of the teratoma, a scenario more frequently observed in younger individuals [1].
Diagnosis relies on a combination of histopathology and immunohistochemistry (IHC). IHC markers are crucial for identifying the lineage of the malignant component:
- Carcinoma Identification: Pancytokeratin (PCK) and cytokeratin (CK) markers like CK7 and CK20 help differentiate adenocarcinoma phenotypes [3].
- Sarcomatous Components: Vimentin is a broad mesenchymal marker [1].
- Melanoma: Melan-A is a specific marker for melanocytic differentiation, as demonstrated in a rare case of testicular teratoma transforming into melanoma in a red deer [4].
- Immature Elements: S100 protein can highlight neural/glial tissues and is used to identify immature neuroectodermal components [4].
Serum biomarkers, while less specific, can support clinical suspicion. Elevations in SCC-Ag may be seen in squamous cell carcinoma transformation, and carcinoembryonic antigen (CEA) or CA 19-9 can be elevated, particularly in adenocarcinomas [3] [2].
Experimental Models for Assessing Tumorigenic Potential
A robust biosafety assessment for cell therapies must evaluate the risks of oncogenicity, tumorigenicity, and teratogenicity [5]. The following workflow and table detail the standard and emerging models used in this evaluation.
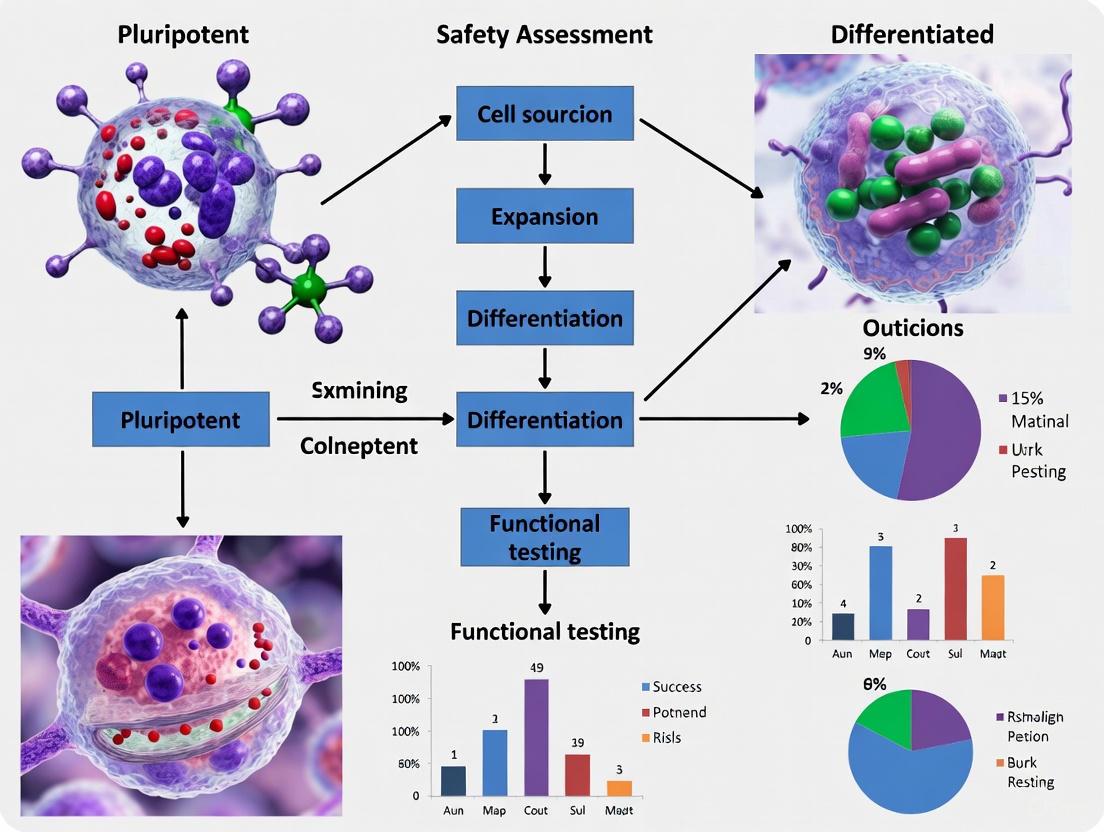
Diagram 1: Experimental workflow for assessing the tumorigenic potential of cell products, integrating in vitro, in vivo, and advanced technological approaches.
Table 2: Key Experimental Models for Tumorigenicity and Oncogenicity Assessment [5] [6] [7]
| Model Type | Key Application | Critical Readouts | Advantages | Limitations |
|---|---|---|---|---|
| In Vivo Teratoma Assay | Gold standard for testing the pluripotency and safety of stem cell lines by assessing their ability to form differentiated tissues. | Histopathological identification of tissues from the three germ layers; presence of immature or malignant components. | Directly assesses differentiation potential and latent tumorigenicity. | Time-consuming (weeks to months), expensive, requires animal facilities. |
| In Vivo Tumorigenicity in Immunocompromised Mice | General safety test for any cell product to assess its potential to form tumors in vivo. | Palpable mass formation, tumor histology, metastasis, animal survival. | Models the complex in vivo environment; provides data on tumor growth and aggression. | Does not fully replicate human immune system; false negatives are possible. |
| Patient-Derived Xenograft (PDX) Models | Retains key features of the original tumor (gene expression, histopathology, drug response) better than cell line models. | Tumor growth rate, drug response, molecular signature fidelity. | High clinical relevance; excellent for studying tumor biology and personalized therapy. | Success rate is variable; expensive and time-consuming to establish. |
| 3D Organoid Models | Emerging platform for high-throughput drug screening and studying tumor heterogeneity and CSC biology. | Organoid morphology, growth patterns, response to therapeutic agents. | Recapitulates tumor architecture and cell-cell interactions; derived from patient tissue. | May lack full tumor microenvironment components (e.g., immune cells, vasculature). |
The Scientist's Toolkit: Essential Reagents and Assays
A comprehensive biosafety assessment requires a suite of well-characterized reagents and analytical methods.
Table 3: Essential Research Reagent Solutions for Tumorigenicity Assessment
| Reagent / Assay Name | Primary Function in Research | Key Application in Safety Context |
|---|---|---|
| Immunohistochemistry (IHC) Antibodies (e.g., Pancytokeratin, Vimentin, Melan-A, S100) | To identify specific protein markers within tissue sections, determining cell lineage and differentiation status. | Critical for characterizing the cellular composition of teratomas and identifying the histological type of any malignant transformation [1] [4]. |
| CD44 & CD133 Antibodies | To isolate and identify cancer stem cell (CSC) populations via flow cytometry or cell sorting. | Used to assess the presence of putative CSCs in a cell product, which are associated with tumor initiation and therapy resistance [7]. |
| Soft Agar Colony Formation Assay | To measure anchorage-independent cell growth, a hallmark of cellular transformation. | An in vitro test to screen for the tumorigenic potential of a cell product before committing to more complex in vivo studies [5]. |
| PCR and Sequencing Reagents | To analyze genomic stability, detect mutations, and assess oncogene activation. | Used for quality control of cell products, checking for genetic abnormalities that could predispose to tumorigenesis [5]. |
| Single-Cell RNA Sequencing Kits | To profile the transcriptome of individual cells, revealing population heterogeneity and rare cell states. | Identifies the presence of stem-like or aberrant subpopulations within a therapeutic cell product that might be missed by bulk analysis [7]. |
Emerging Technologies and Future Perspectives
The field is rapidly evolving with new technologies enhancing the precision of safety assessments. Single-cell sequencing and spatial transcriptomics are revolutionizing our understanding of CSC heterogeneity and its role in tumorigenesis [7]. AI-driven multiomics analysis is being leveraged to identify stemness indices and predict oncogenic risk from complex datasets [7]. Furthermore, CRISPR-based functional screens in sophisticated models like PDX and organoids are powerful tools for identifying genetic drivers of malignant transformation and therapy resistance [6] [7].
These technological advances are paving the way for novel therapeutic strategies aimed at eliminating CSCs, such as dual metabolic inhibition and engineered immune cells (CAR-T, CAR-NK) [5] [7]. The integration of these rigorous safety assessments during product development is paramount for the successful and responsible translation of stem cell-based therapies into clinical practice.
The malignant transformation of teratomas serves as a powerful, natural model for studying the tumorigenic potential inherent in pluripotent cells. For researchers and clinicians developing stem cell-based therapies, a deep understanding of this process is non-negotiable. A meticulous biosafety strategy—combining the standard in vivo assays detailed here with cutting-edge molecular profiling and in vitro screens—forms the bedrock of risk mitigation. As the field advances, the continued refinement of these assessment protocols, guided by insights from both clinical pathology and preclinical models, will ensure that the remarkable therapeutic potential of regenerative medicine is realized with an uncompromising commitment to patient safety.
Human leukocyte antigen (HLA) matching stands as a cornerstone determinant of success in allogeneic hematopoietic stem cell transplantation (HSCT), directly influencing the critical balance between graft rejection and graft-versus-host disease (GVHD). The HLA system, encoded by the major histocompatibility complex (MHC) on chromosome 6p21.3, comprises highly polymorphic cell surface proteins essential for immune recognition [8]. These proteins function as sentinels of the immune system, presenting peptide antigens to T cells and enabling discrimination between self and non-self [8]. In transplantation, HLA molecules serve as the primary targets for alloreactive T-cell responses, making their compatibility between donor and recipient a fundamental prerequisite for engraftment and long-term transplant success.
The clinical significance of HLA compatibility is underscored by its profound impact on transplant outcomes. Histocompatibility barriers can trigger two primary immunologic complications: graft rejection, where recipient immune cells destroy donor cells, and GVHD, where donor immune cells attack recipient tissues [8] [9]. Both processes involve complex cellular interactions mediated by T-cell recognition of disparate HLA molecules, making sophisticated HLA matching strategies essential for navigating immunogenicity in stem cell-based therapies. This guide examines current HLA matching approaches, their associated outcomes, and emerging technologies that are expanding compatible donor options for patients requiring HSCT.
HLA System: Genetics and Polymorphism
Molecular Structure and Function
The HLA system is categorized into two primary classes of molecules with distinct structures and functions. Class I HLA molecules (HLA-A, -B, and -C) are expressed on nearly all nucleated cells and consist of a polymorphic α-chain non-covalently associated with β2-microglobulin. These molecules present endogenous peptides to CD8+ cytotoxic T cells, facilitating the identification and elimination of infected or malignant cells [8]. The peptide-binding groove of class I molecules is formed by the α1 and α2 domains, which contain the highest concentration of polymorphic residues that determine antigen binding specificity and T-cell receptor recognition [8].
Class II HLA molecules (HLA-DR, -DQ, and -DP) exhibit a more restricted expression pattern, primarily on professional antigen-presenting cells such as dendritic cells, macrophages, and B cells. These molecules comprise α and β chains that form a peptide-binding groove, presenting exogenous antigens to CD4+ helper T cells to initiate and modulate immune responses [8]. Beyond these classical HLA molecules, the HLA region also includes non-classical class Ib genes (HLA-E, -F, -G) and class III genes encoding complement components, tumor necrosis factor, and heat shock proteins that contribute to immune regulation [8].
Extreme Genetic Polymorphism
The HLA gene system represents the most polymorphic region in the human genome, creating significant challenges for donor-recipient matching. This polymorphism arose evolutionarily to provide populations with diverse immune recognition capabilities against pathogens. As of 2024, the number of identified HLA alleles has expanded dramatically to over 20,000 variants across classical HLA loci [8] [9]. The distribution of known alleles across major HLA loci demonstrates the scale of this diversity:
Table 1: HLA Allele Diversity Across Major Loci
| HLA Locus | Class | Number of Identified Alleles |
|---|---|---|
| HLA-A | I | >2,000 |
| HLA-B | I | >2,600 |
| HLA-C | I | >1,500 |
| HLA-DRB1 | II | >1,200 |
| HLA-DQB1 | II | >700 |
| HLA-DPB1 | II | >600 |
This remarkable diversity means that unrelated individuals rarely share identical HLA profiles, making the probability of finding a perfectly matched unrelated donor in the general population exceptionally low [9]. The polymorphism is concentrated in the exons encoding the antigen-binding clefts of HLA molecules, particularly affecting amino acid residues that contact presented peptides or T-cell receptors, thereby directly influencing allorecognition [8].
HLA Typing Technologies: Resolution and Clinical Applications
Evolution of Typing Methodologies
HLA typing technologies have evolved substantially from serological approaches to high-resolution molecular methods, dramatically improving matching precision. Serological typing, which utilized antibodies to detect HLA antigens on cell surfaces, was limited by reagent availability, cross-reactivity, and inability to distinguish many allelic variants [9]. The development of DNA-based typing methods revolutionized the field by enabling direct characterization of HLA genes rather than their protein products.
Early molecular techniques included sequence-specific oligonucleotide probe (SSOP) and sequence-specific primer (SSP) PCR, which identified known polymorphisms but had limited resolution for distinguishing closely related alleles [8] [10]. Sanger sequencing-based typing (SBT) provided higher resolution but faced challenges with phase ambiguity, where the cis/trans alignment of polymorphisms in heterozygous samples remained uncertain [8]. The contemporary gold standard, next-generation sequencing (NGS), overcomes these limitations by providing clonal sequencing that resolves phase ambiguity and enables complete characterization of HLA genes across their entire coding regions [8] [10].
Next-Generation Sequencing and Beyond
NGS technologies offer unprecedented resolution for HLA typing through massively parallel sequencing of long DNA fragments. The key advantage of NGS lies in its ability to generate millions of sequencing reads that span entire HLA genes, enabling comprehensive variant detection and haplotype phasing without ambiguity [8]. Third-generation sequencing platforms like Pacific Biosciences (PacBio) single-molecule real-time (SMRT) sequencing and Oxford Nanopore Technologies (ONT) further advance this capability by generating ultra-long reads that seamlessly cover extensive genomic regions, including introns and regulatory elements [8].
The implementation of NGS in clinical HLA typing has significantly improved donor selection accuracy while reducing ambiguous assignments that previously complicated transplant matching. These technological advances provide the resolution necessary to implement permissible mismatch strategies and identify potentially immunogenic disparities that might be missed by lower-resolution methods [8] [10]. The workflow below illustrates the NGS-based HLA typing process:
Diagram 1: NGS HLA Typing Workflow
Donor Matching Strategies and Clinical Outcomes
Conventional Matching Algorithms
Traditional donor selection for HSCT prioritized matching at specific HLA loci based on their demonstrated impact on clinical outcomes. Current international guidelines from the World Marrow Donor Association (WMDA) and European Society for Blood and Marrow Transplantation (EBMT) recommend high-resolution typing for HLA-A, -B, -C, and -DRB1, often referred to as the 8/8 match when fully matched [10]. Some centers also consider HLA-DQB1 and -DPB1 matching, expanding to a 10/10 or 12/12 match paradigm [8] [10].
The relationship between HLA matching and transplant outcomes follows a dose-response pattern, where increasing disparity correlates with higher risks of complications. A matched sibling donor (MSD) remains the ideal source, associated with the most favorable outcomes, but is only available for approximately 30% of patients [11] [12]. For patients without a matched sibling, matched unrelated donors (MUD) from registry databases represent the next preferred option, with outcomes comparable to MSD when fully matched at 8/8 loci [10] [12].
Mismatched Unrelated Donor Transplants
For the substantial proportion of patients, particularly those from ethnically diverse backgrounds, who cannot find a fully matched donor, mismatched unrelated donors (MMUD) have emerged as a viable alternative. Recent studies demonstrate that MMUD HSCT with appropriate conditioning and GVHD prophylaxis can achieve outcomes approaching those of matched transplants [10] [12].
Key findings from clinical trials investigating MMUD transplants include:
Table 2: Outcomes of Mismatched Unrelated Donor Transplants
| Study / Trial | Matching Level | Patients | Overall Survival | Acute GVHD (II-IV) | Non-Relapse Mortality |
|---|---|---|---|---|---|
| 15-MMUD Trial [10] | 4/8 - 7/8 | 80 | 72% (1-year, MAC)79% (1-year, RIC) | 36% | 22% |
| Meta-analysis [12] | Mostly 7/8 | 3,336 | 63.9% (1-year)42.1% (3-year) | 36.4% | 22.6% |
| ACCESS Trial (Interim) [10] | 4/8 - 7/8 | 84 | 84% (1-year, MAC)79% (1-year, RIC) | Not reported | Not reported |
The introduction of post-transplant cyclophosphamide (PTCy) as GVHD prophylaxis has been instrumental in improving MMUD outcomes by selectively eliminating alloreactive T-cells in the early post-transplant period [10]. This approach has demonstrated particular success in bridging the donor availability gap for ethnic and racial minorities, who have historically faced significantly lower probabilities of finding matched unrelated donors [10] [12].
Non-Sibling Family Donors and Outcomes
Extended family searches represent another strategy for identifying suitable donors, particularly in populations with high rates of consanguinity. Matched family donors (MFD) include parents, children, cousins, uncles, aunts, and grandparents who share HLA haplotypes with the recipient [11]. While these donors expand the potential donor pool, outcomes differ from traditional sibling transplants.
A retrospective analysis comparing MFD to matched sibling donor (MSD) transplants demonstrated that while MFD expands donor options, it carries increased risks. The study reported significantly higher complications in the MFD group including viral infections (p<0.05), acute GVHD (p<0.05), and graft rejection (p<0.05) [11]. Both event-free survival (EFS) and overall survival (OS) at three years were significantly lower in the MFD cohort compared to MSD (EFS: 58% vs. 80%, p=0.003; OS: 61% vs. 82%, p=0.002) [11]. These differences were partially attributed to older donor age in the MFD group (median 36-40 years) compared to MSD (median 12 years), highlighting the impact of donor characteristics beyond HLA matching alone [11].
The following diagram illustrates the comparative outcomes between different donor types:
Diagram 2: Donor Types and Outcome Profiles
Experimental Approaches to Overcome HLA Barriers
Genetic Engineering of Cell Products
Innovative genetic engineering approaches are being developed to circumvent HLA barriers altogether. CRISPR-Cas9 genome editing technology enables the creation of "hypoimmunogenic" cell products that evade allorecognition by disrupting key molecules in HLA presentation pathways [13]. A multifaceted approach involves:
- Disruption of B2M (beta-2-microglobulin): Prevents surface expression of HLA class I molecules, eliminating recognition by host CD8+ T cells [13]
- Disruption of CIITA (class II transactivator): Abrogates HLA class II expression, preventing CD4+ T cell recognition [13]
- HLA-E fusion protein expression: Engineered HLA-E/B2M fusion molecules engage NK cell inhibitory receptors (NKG2A), preventing "missing-self" activation and attack by natural killer cells [13]
This combined engineering approach generates cellular therapeutics that resist both T-cell and NK-cell mediated rejection while retaining their intended therapeutic function. Studies with regulatory T cells (Tregs) demonstrate that such engineered cells maintain FOXP3 stability, suppressive function, and the ability to prolong graft survival in humanized mouse models [13].
Permissible Mismatch Strategies
Research has identified that not all HLA mismatches carry equal immunogenic potential. The concept of "permissible mismatches" refers to specific HLA disparities that do not significantly increase risks of GVHD or graft failure despite being technically mismatched [9]. Factors influencing permissibility include:
- The specific HLA locus involved (some loci tolerate mismatch better than others)
- The degree of molecular similarity between the mismatched alleles
- The direction of mismatch in the host-versus-graft versus graft-versus-host directions
- The presence of non-inherited maternal antigens that may induce tolerance
Retrospective analyses by Petersdorf et al. identified that mismatches for HLA-C and HLA-DP are frequently permissible in certain contexts, whereas HLA-DRB1 mismatches typically carry higher risk [9]. Similarly, McGlave's research demonstrated that HLA-DQ and DP mismatches may have minimal impact on transplantation efficacy compared to DRB1 mismatches [9]. These findings enable transplant physicians to prioritize donors with permissible mismatches when fully matched donors are unavailable, significantly expanding the donor pool without substantially increasing risks.
The Scientist's Toolkit: Essential Research Reagents and Methods
Table 3: Key Research Reagents and Experimental Tools for HLA and Rejection Studies
| Reagent/Technology | Application | Experimental Function |
|---|---|---|
| Next-Generation Sequencers (Illumina, PacBio, Nanopore) [8] | High-resolution HLA typing | Enables comprehensive allele-level typing with phasing capability across entire HLA genes |
| CRISPR-Cas9 Systems [13] | HLA engineering | Facilitates targeted disruption of B2M, CIITA and insertion of HLA-E transgenes |
| Flow Cytometry Panels (anti-CD3, CD4, CD8, CD25, CD56) [13] | Immune monitoring | Quantifies T-cell and NK-cell populations; assesses alloreactive immune responses |
| PTCy (Post-Transplant Cyclophosphamide) [10] | GVHD prophylaxis | Selective elimination of alloreactive T-cells; enables mismatched transplantation |
| Anti-thymocyte globulin (ATG) [11] | In vivo T-cell depletion | Reduces alloreactive T-cells in conditioning; modulates GVHD risk |
| Humanized Mouse Models (NSG, NOG strains) [13] | In vivo functional assays | Provides human immune system context for evaluating graft rejection mechanisms |
| Cytokine Detection Assays (ELISA, Luminex) [5] | Immunogenicity assessment | Measures inflammatory mediators associated with alloreactive responses |
| qPCR Biodistribution Assays [5] | Cell tracking | Monitors persistence and distribution of administered cellular products |
The landscape of HLA matching and immunogenicity management in stem cell transplantation continues to evolve with significant implications for both basic research and clinical practice. The traditional paradigm of requiring perfect HLA matches has progressively shifted toward more nuanced approaches that incorporate permissible mismatches, advanced GVHD prophylaxis, and engineered cellular products. These developments collectively expand access to transplantation for patients across diverse ethnic backgrounds who historically faced limited donor options.
For researchers and drug development professionals, several key principles emerge. First, the resolution of HLA typing matters—high-resolution NGS methods provide the necessary detail to inform donor selection and predict alloreactivity risks. Second, post-transplant cyclophosphamide has emerged as a powerful tool for managing the immunologic challenges of HLA-mismatched transplantation. Finally, genetic engineering approaches that ablate HLA expression while controlling NK cell responses represent a promising frontier for creating universally compatible "off-the-shelf" cellular therapeutics.
As these technologies mature, the field moves closer to the goal of making stem cell transplantation accessible to all patients in need, regardless of HLA barriers. Future research directions will likely focus on refining mismatch permissibility algorithms, optimizing combination immunosuppression regimens, and developing next-generation engineered cell products with enhanced persistence and function in allogeneic environments.
Ethical and Safety Boundaries in hESC and iPSC Clinical Translation
The translation of human pluripotent stem cells from laboratory research to clinical therapies represents one of the most promising yet challenging frontiers in regenerative medicine. Among these, human Embryonic Stem Cells (hESCs) and induced Pluripotent Stem Cells (iPSCs) stand as the two primary pillars of this therapeutic landscape [14]. hESCs, derived from the inner cell mass of blastocysts, possess the quintessential benchmark for pluripotency but are accompanied by significant ethical controversies and allogeneic immune rejection concerns [14] [15]. In parallel, iPSCs, generated through the reprogramming of somatic cells, offer a patient-specific alternative that circumvents embryo destruction yet introduce distinct safety considerations, particularly regarding genetic instability and tumorigenicity [16] [17]. For researchers, scientists, and drug development professionals navigating this complex field, a rigorous comparative assessment of their safety profiles is fundamental to guiding therapeutic development. This analysis objectively examines the ethical and safety boundaries of both cell types within the framework of clinical translation, providing experimental data and methodologies essential for informed research and development decisions.
Comparative Ethical and Safety Profiles: hESCs vs. iPSCs
The ethical and safety considerations for hESCs and iPSCs diverge significantly, influencing their applicability for specific clinical and research purposes. Table 1 provides a systematic comparison of these critical parameters, offering a foundation for risk-benefit analysis in therapeutic development.
Table 1: Comparative Analysis of Ethical and Safety Profiles for hESCs and iPSCs
| Parameter | Human Embryonic Stem Cells (hESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Ethical Status | Contentious; involves destruction of human embryos [14] | Largely resolved; derived from somatic cells, avoiding embryo use [16] [14] |
| Source Material | Surplus IVF embryos [14] [15] | Patient-specific somatic cells (e.g., skin, blood) [16] [18] |
| Immunogenicity | High risk of allogeneic immune rejection [14] | Low risk with autologous use; allogeneic use requires immune matching [16] |
| Tumorigenicity Risk | Teratoma formation from residual undifferentiated cells [14] | Teratoma formation; additional risk from integrating vectors and oncogene reactivation (e.g., c-MYC) [16] [14] [18] |
| Genetic Stability | Generally stable karyotype [14] | Higher risk of genetic and epigenetic abnormalities from reprogramming [16] [17] |
| Key Safety Mechanism | Purity of differentiated cell population [14] | Use of non-integrating reprogramming methods [16] [18] |
| Regulatory Oversight | Stringent; involves embryo research oversight committees [15] | Complex; focuses on manufacturing and safety of reprogrammed cells [16] |
The ethical landscape is distinctly polarized. hESC research remains ethically contentious in many jurisdictions because it necessitates the destruction of human embryos, raising profound questions about the onset of human personhood [14] [15]. In contrast, iPSCs were hailed as an ethical solution, as they are derived from a simple somatic cell biopsy (e.g., skin or blood), completely bypassing the need for embryos [16] [14]. However, iPSCs are not without ethical challenges, as their unlimited differentiation potential raises concerns about their use in human reproductive cloning or the generation of human-animal chimeras [14].
From a safety perspective, the risk of tumor formation is a primary barrier to clinical translation for both cell types. For hESCs, the predominant risk is teratoma formation from residual undifferentiated cells that escape purification before transplantation [14]. iPSCs carry this same risk, compounded by the potential for insertional mutagenesis if integrating viral vectors are used for reprogramming, and the possible reactivation of oncogenes like c-MYC, one of the original Yamanaka factors [16] [18]. Furthermore, the reprogramming process itself can induce genetic and epigenetic abnormalities, creating unique safety challenges for iPSCs that are not as prevalent in hESCs [16] [17].
Experimental Assessment of Safety and Efficacy
Robust preclinical safety assessment is a non-negotiable prerequisite for clinical translation. Regulatory agencies like the FDA and EMA require comprehensive data packages that rigorously evaluate multiple risk domains before approving first-in-human trials [5]. The following section outlines core experimental protocols and data for assessing the safety of hESC and iPSC-based products.
Key Safety Assessment Protocols
A practice-oriented biosafety framework for cell therapy must evaluate several key principles: toxicity, oncogenicity/tumorigenicity/teratogenicity, immunogenicity, biodistribution, and overall cell product quality [5]. The methodologies for these assessments are detailed below.
Tumorigenicity and Teratoma Assay
Objective: To evaluate the potential of the stem cell product to form unwanted growths, including teratomas or tumors, in vivo.
- Methodology: The gold-standard assay involves the transplantation of the cell product into immunocompromised mice (e.g., NOD-scid or NSG strains) via a clinically relevant route (e.g., subcutaneous, intramuscular, or into the target organ) [5].
- Controls: Inclusion of known pluripotent stem cells (positive control) and fully differentiated, non-tumorigenic cells (negative control) is critical for assay validation.
- Endpoint Monitoring: Animals are monitored for up to 6 months for palpable mass formation. The study concludes with histopathological examination of the transplantation site and major organs to identify any ectopic tissue growth or neoplasms [5].
- Data Interpretation: The presence of tissues derived from all three germ layers (ectoderm, mesoderm, endoderm) confirms teratoma formation, indicating residual pluripotent cells in the product.
Biodistribution and Long-Term Engraftment
Objective: To track the migration, persistence, and fate of administered cells in the body over time.
- Methodology: Cells are labeled with a traceable marker prior to transplantation. Common methods include:
- Lentiviral Luciferase/GFP Labeling: Enables real-time in vivo bioluminescence imaging (BLI) to monitor cell location and survival longitudinally [5].
- Quantum Dots or Radioactive Labels (e.g., for PET/MRI): Used for advanced anatomical and functional imaging [5].
- qPCR for Human-Specific Sequences: A highly sensitive method to quantify human cell presence in rodent tissues post-mortem [5].
- Experimental Timeline: Analyses are performed at multiple time points (e.g., 24 hours, 1 week, 1 month, 3 months) after administration to assess initial homing and long-term persistence.
- Safety Signal: The presence of cells in non-target organs, particularly the gonads, represents a critical safety risk and must be thoroughly investigated.
In Vitro Genetic Stability Assessment
Objective: To identify genetic and epigenetic abnormalities acquired during the reprogramming (iPSCs) or long-term culture (hESCs and iPSCs) processes.
- Methodology:
- Karyotyping (G-banding): Detects gross chromosomal abnormalities (e.g., aneuploidy, translocations) [16].
- Whole Genome Sequencing (WGS): Identifies single nucleotide variants (SNVs), small insertions/deletions (indels), and copy number variations (CNVs) [16].
- Targeted Sequencing of Cancer-Related Genes: Focuses on genes known to be frequently mutated in stem cells or cancers (e.g., TP53) [16] [17].
- Quality Threshold: Cell lines with significant genomic alterations are deemed unsuitable for clinical use.
Supporting Quantitative Safety Data
Table 2 summarizes exemplar quantitative data from preclinical studies, highlighting the type of evidence required to support the safety of an investigational cell product.
Table 2: Preclinical Safety and Efficacy Data from Representative Studies
| Cell Type / Product | Disease Model | Key Efficacy Result | Critical Safety Finding | Citation (Example) |
|---|---|---|---|---|
| iPSC-derived Dopaminergic Neurons | Parkinson's Disease (Non-Human Primate) | Improved motor function; dopamine production | No tumor formation in grafted brains after 2 years | [16] |
| iPSC-derived Cardiomyocytes | Myocardial Infarction (Primate) | Improved cardiac contractility | Transient arrhythmias post-transplantation | [16] |
| Allogeneic iPSC-derived RPE Cells | Geographic Atrophy (Clinical Trial) | Phase I/II trial showed feasibility | No severe adverse events related to cells in initial patients | [16] |
| Fetal Neural Stem Cells | Ataxia Telangiectasia (Human) | N/A | Donor-derived glioneuronal neoplasm in one patient | [19] |
Methodological Workflows and Signaling Pathways
The journey from somatic cell to clinical-grade therapeutic involves a series of complex, tightly regulated steps. The following diagrams, generated using Graphviz, visualize the core workflows and molecular pathways that underpin the development of hESC and iPSC therapies.
Ethical Oversight and Clinical Translation Workflow
This diagram outlines the critical decision points and oversight requirements for translating hESC and iPSC research into clinical applications.
Core Pluripotency Signaling and Reprogramming Network
The reprogramming of somatic cells to iPSCs and the maintenance of pluripotency in both iPSCs and hESCs are governed by a core molecular network. This pathway illustrates the key transcription factors and their functional interactions.
The Scientist's Toolkit: Essential Research Reagents
The development and safety assessment of hESC and iPSC therapies rely on a suite of critical reagents and tools. Table 3 catalogs these essential materials, providing researchers with a reference for constructing their experimental workflows.
Table 3: Key Research Reagents and Materials for hESC/iPSC Research
| Reagent/Material | Function/Purpose | Application in hESC/iPSC Work |
|---|---|---|
| Yamanaka Factor Plasmids | Deliver OCT4, SOX2, KLF4, c-MYC genes for reprogramming. | Generation of iPSCs from somatic cells [18]. |
| Non-Integrating Vectors (e.g., Sendai Virus, Episomal Plasmids) | Safer delivery of reprogramming factors; vectors do not integrate into host genome. | Clinical-grade iPSC generation to minimize tumorigenicity risk [16] [18]. |
| CRISPR/Cas9 System | Precision genome editing for gene correction or insertion of reporter genes. | Creating isogenic controls, correcting disease-causing mutations in patient iPSCs [16]. |
| Matrigel / Defined Synthetic Matrices | Provides a substrate that mimics the extracellular matrix for cell growth. | Feeder-free culture of hESCs and iPSCs, improving reproducibility and scalability [16]. |
| Flow Cytometry Antibodies | Detect specific cell surface (e.g., TRA-1-60, SSEA4) or intracellular markers. | Assessing pluripotency, purifying differentiated cell populations, checking for residual undifferentiated cells [5]. |
| In Vivo Imaging Substrates (e.g., D-Luciferin) | Reacts with luciferase enzyme in labeled cells to produce light. | Monitoring cell survival, biodistribution, and tumor formation in animal models via bioluminescence imaging [5]. |
| HLA Typing Kits | Identify specific human leukocyte antigen (HLA) profiles. | Creating HLA-matched iPSC banks for allogeneic therapy with reduced immunogenicity [16] [17]. |
The clinical translation of both hESCs and iPSCs is bounded by a complex framework of ethical considerations and safety hurdles that demand meticulous management. hESCs continue to be challenged by persistent ethical debates and the biological reality of allogeneic rejection, whereas iPSCs, while resolving the central ethical dilemma, present a potentially more intricate safety profile due to the inherent uncertainties of cellular reprogramming and the risks of genomic instability [16] [14] [17]. For the research and development community, the path forward is not a matter of choosing one cell type as universally superior, but of making context-dependent decisions guided by rigorous comparative data. The future of safe and effective stem cell therapies hinges on unwavering commitment to robust preclinical safety assessment, adherence to evolving international guidelines [15], and the continuous integration of technological innovations such as CRISPR-based quality control and AI-driven manufacturing [16]. By systematically addressing these ethical and safety boundaries, the field can responsibly unlock the immense therapeutic potential of human pluripotent stem cells.
Microbiological Risks in Cell Collection, Manipulation, and Banking
The field of stem cell-based therapies represents a revolutionary approach to treating numerous incurable diseases, from neurodegenerative disorders to spinal cord injuries. As these advanced therapies progress toward clinical application, ensuring their microbiological safety has become paramount for regulatory approval and patient welfare. The safety profile assessment of these biological products demands rigorous evaluation of potential contamination risks throughout the entire pipeline—from initial cell collection through manipulation and long-term banking. Recent clinical advances, including the Q-Cell study investigating human glial-restricted progenitor cell transplantation for transverse myelitis patients, highlight the transitional progress from preclinical models to human trials, where microbiological safety is a fundamental concern [20].
Microbiological risks in stem cell products present unique challenges compared to conventional pharmaceuticals. These living products cannot undergo terminal sterilization, making preventative control strategies essential throughout manufacturing. Contamination may originate from multiple sources: donor tissues, reagents of animal origin, the processing environment, or handling procedures. Such contamination can compromise product efficacy, lead to transmission of infectious diseases to recipients, and potentially cause serious adverse events. This comprehensive analysis compares current microbiological risk assessment methodologies, control technologies, and experimental data to establish a framework for safety profiling in stem cell-based therapy research and development.
Quantitative Analysis of Microbiological Risks Across SoHO Products
Microbial Risk Classification and Assessment Data
The Microbiological Risk Classification and Assessment tool (MiRCA), developed by the European Directorate for the Quality of Medicines & HealthCare (EDQM), provides a standardized approach for evaluating contamination risks during the procurement and processing of Substances of Human Origin (SoHO). A comprehensive 2025 study analyzed 7,881 SoHO products to determine risk values across different product categories, offering comparative quantitative data essential for safety prioritization [21].
Table 1: Microbiological Risk Assessment of SoHO Products Using MiRCA Tool
| SoHO Product Type | Procurement Risk Value | Processing Risk Value | Total Risk Value (out of 695) | Post-Processing Contamination Rate |
|---|---|---|---|---|
| Femoral Heads (Living Donor) | 6.2 | 8.2 | 14.4 | Not Specified |
| Vascular Tissue (Deceased Donor) | 68.1 | 85.3 | 153.4 | Not Specified |
| Tendons & Ligaments (Deceased Donor) | 70.5 | 82.9 | 153.4 | Not Specified |
| Fascia Lata (Deceased Donor) | 68.8 | 84.6 | 153.4 | Not Specified |
| Hematopoietic Progenitor Cells (HPC) | 75.3 | 85.7 | 161.0 | Not Specified |
| Donor Lymphocytes (DL) | 70.1 | 80.2 | 150.3 | Not Specified |
| Cord Blood (CB) | 74.5 | 86.8 | 161.3 | Not Specified |
| Human Breast Milk | Not Assessed | 172.5 | 172.5 | 11.6% |
The data reveals striking differences in microbiological risk profiles across SoHO product types. Femoral heads procured from living donors demonstrated the lowest overall risk value (14.4/695), attributable to controlled surgical procurement conditions and effective decontamination protocols. In contrast, cell-based products like hematopoietic progenitor cells and cord blood showed significantly higher risk values (approximately 161/695), reflecting their complex processing requirements and heightened susceptibility to contamination during manipulation [21]. Most notably, human breast milk processing presented the highest contamination risk (172.5/695) with an 11.6% post-processing contamination rate, underscoring the particular challenges associated with non-sterile origin substances.
Microbial Contamination Screening Standards
International standards establish definitive testing requirements for microbiological screening of tissues and cells. The following table summarizes key testing methodologies and acceptance criteria across different biological products based on current guidelines [22].
Table 2: Microbiological Screening Standards for Tissues and Cells
| Product Category | Screening Methodology | Critical Pathogens | Acceptance Criteria | Disposition of Contaminated Products |
|---|---|---|---|---|
| Solid Tissues | Swab culture, bone chips, enrichment liquid cultures | Clostridium spp., Streptococcus pyogenes, Staphylococcus aureus | No highly virulent pathogens | Discard or terminal sterilization (gamma irradiation) |
| Cardiovascular Tissues | Additional testing for Mycobacterium spp. | Mycobacterium spp. | No mycobacterial contamination | Discard if positive |
| Cord Blood | Aerobic/anaerobic bacterial and fungal cultures (European Pharmacopoeia 2.6.27) | Broad spectrum bacteria and fungi | No microbial growth | Discard if positive |
| Stem Cell Products (PBSC, bone marrow) | Aerobic/anaerobic bacterial and fungal cultures (European Pharmacopoeia 2.6.27) | Bacteria and fungi to species level | Identification to species level | Trend analysis, antimicrobial susceptibility testing |
| Cryopreserved Skin Allografts | Pre/post-decontamination cultures | Non-pathogenic bacteria | No pathogenic bacteria | Can be transplanted if non-pathogenic bacteria present |
The screening requirements highlight a risk-based approach to microbiological safety. While all contaminated cord blood units must be discarded, cryopreserved skin allografts with non-pathogenic bacteria may be transplanted, recognizing the clinical risk-benefit balance [22]. For stem cell products, identification to species level and antimicrobial susceptibility testing are mandatory, enabling informed clinical decisions regarding prophylactic antibiotic therapy when implantation of contaminated products is medically justified.
Experimental Protocols for Microbiological Risk Assessment
Donor Screening and Testing Protocol
Comprehensive donor screening represents the primary defense against microbiological contamination in stem cell products. The following protocol details the standardized methodology for evaluating donor eligibility [23]:
Donor Medical History Review: Conduct extensive review of medical records and lifestyle questionnaires to identify risk factors for transmissible diseases. This evaluation must be approved by qualified clinical advisors trained in banking procedures.
Serological Testing: Perform initial screening using FDA-approved serological tests including:
- HIV-1 and HIV-2 antibody detection
- Hepatitis B surface antigen (HBsAg)
- Hepatitis C virus (HCV) antibody
- Treponema pallidum (syphilis) specific antibody
Nucleic Acid Amplification Testing (NAT): Implement polymerase chain reaction (PCR)-based testing to detect viral genomic material during the "window period" of infections when antibodies may not be detectable. This is particularly critical for HIV and HCV, where individuals may be viraemic for months before seroconversion.
Additional Testing for Leukocyte-Rich Products: For stem cell products containing significant leukocyte populations, include:
- Human T-cell lymphotrophic virus (HTLV-I and HTLV-II) antibody testing
- Cytomegalovirus (CMV) antibody testing
- Toxoplasma antibody testing (for specific transplant scenarios)
Prion Disease Assessment: Evaluate risk factors for transmissible spongiform encephalopathies (TSEs) including Creutzfeldt-Jakob Disease (CJD) using validated assays as they become available.
This multi-layered testing approach significantly reduces the risk of undetected viremia in donor tissues. Research indicates that the addition of NAT methods to routine screening can substantially reduce infection risk for recipients of stem cell products [23].
Environmental Monitoring and Processing Control Protocol
Maintaining controlled environments during cell processing is essential for preventing contamination introduction. The following protocol details the environmental monitoring strategy employed in tissue establishments [21]:
Cleanroom Specifications: Process cells and tissues in Class A cleanrooms with Class B background environments. For stem cell banking facilities, implement minimally Class D background environments. Regularly verify cleanliness grades through:
- Particle counting
- Aeroscopy (air sampling)
- Environmental surface swabs
Microbiological Monitoring: Conduct routine environmental monitoring through:
- Active air sampling using volumetric collection methods
- Surface monitoring of critical work areas via contact plates and swabs
- Personnel monitoring (glove prints) during aseptic operations
- Use of nutrient-rich media for bacteria and Sabouraud dextrose agar for fungi
Decontamination Procedures: Implement tissue-specific decontamination protocols:
- Musculoskeletal tissues: Single application of 10% Betadine solution
- Vascular tissues: Antibiotic cocktail immersion (ciprofloxacin 3 µg/mL, amikacin 12 µg/mL, metronidazole 12 µg/mL, and vancomycin 12 µg/mL in Custodiol CE solution)
Process Validation: Validate all aseptic processes through media fills that simulate actual production conditions, including all manual interventions and worst-case scenarios.
Water Quality Monitoring: Use purified water meeting compendial standards for both processing and cleanroom cleaning, with regular microbial and endotoxin testing.
This comprehensive environmental monitoring protocol provides essential data for trend analysis and early detection of potential contamination issues before product compromise occurs.
Diagram 1: Microbiological Risk Assessment Workflow for Stem Cell Banking. This diagram illustrates the systematic approach to identifying, classifying, and mitigating contamination risks throughout the cell banking process, highlighting three critical assessment components.
Essential Research Reagent Solutions for Microbiological Control
Implementing effective microbiological control in stem cell banking requires specialized reagents and materials. The following table details essential solutions and their applications in contamination prevention [23] [21].
Table 3: Essential Research Reagents for Microbiological Control in Stem Cell Banking
| Reagent Category | Specific Examples | Function & Application | Risk Mitigated |
|---|---|---|---|
| Antibiotic Cocktails | Ciprofloxacin (3 µg/mL), Amikacin (12 µg/mL), Metronidazole (12 µg/mL), Vancomycin (12 µg/mL) | Decontamination of vascular tissues during processing | Bacterial contamination from procurement |
| Antimycotic Agents | Amphotericin B, Nystatin | Prevention of fungal contamination in cell cultures | Fungal contamination during manipulation |
| Decontamination Solutions | 10% Betadine (Povidone-iodine) | Surface decontamination of musculoskeletal tissues | Environmental bacterial contamination |
| Culture Media Additives | Recombinant proteins, Small molecule compounds | Replacement of animal-derived components in stem cell culture | Adventitious virus contamination from animal sera |
| Preservation Solutions | CryoSure-DMSO, Albutein, Plasmalyte with glucose | Cryopreservation of cell therapy products | Microbial growth during storage |
| Microbiological Culture Media | Fluid thioglycollate medium, Tryptic soy broth, Sabouraud dextrose agar | Sterility testing according to European Pharmacopoeia 2.6.27 | Undetected bacterial and fungal contamination |
| Nucleic Acid Testing Reagents | PCR kits for HIV, HBV, HCV, NAT reagents | Detection of viral genomic material in donor samples | Window period viral infections |
The selection of appropriate reagent solutions directly impacts the effectiveness of microbiological control strategies. Particularly critical is the transition toward xeno-free culture systems using recombinant proteins and defined components to eliminate the risk of contamination from animal-derived products like fetal bovine serum, which may introduce bovine viral diarrhea virus or other animal pathogens [23] [24].
Diagram 2: Critical Control Points in Stem Cell Manufacturing. This workflow identifies key stages where microbiological controls must be implemented to prevent contamination, highlighting four essential control points where testing and monitoring are critical.
Emerging Technologies and Future Directions
The field of microbiological safety for stem cell-based therapies continues to evolve with several promising technological developments:
Advanced Detection Methods: Next-generation sequencing and metagenomic approaches are being validated for comprehensive detection of microbial contaminants, including unexpected or novel pathogens that escape conventional testing protocols. These molecular techniques offer the potential for broader detection spectra without prior knowledge of potential contaminants [23].
Automated Closed Processing Systems: To minimize human-derived contamination, automated bioreactor systems with closed processing pathways are increasingly being adopted. These systems reduce manual interventions and associated contamination risks while improving process standardization across different product batches [24].
Pathogen Reduction Technologies: Novel technologies for pathogen inactivation in cellular products are under development, including photochemical treatment methods and non-thermal plasma applications. While maintaining cell viability and function, these approaches could provide an additional safety layer for stem cell products [23].
Artificial Intelligence in Risk Prediction: Machine learning algorithms are being applied to contamination event data to predict potential failure modes before they occur. These predictive models can analyze environmental monitoring trends, personnel practices, and equipment performance to identify emerging risks proactively [24].
The integration of these advanced technologies with established microbiological control frameworks will continue to enhance the safety profile of stem cell-based therapies, supporting their transition from investigational applications to standardized clinical treatments.
Microbiological risk management in cell collection, manipulation, and banking represents a critical component of safety assessment for stem cell-based therapies. The comparative data presented demonstrates significant variation in contamination risks across different product types, with cell-based products generally presenting higher risk profiles than solid tissues. Implementation of comprehensive donor screening, stringent environmental controls, and rigorous product testing protocols forms the foundation of an effective safety strategy.
The ongoing development of the Q-Cell study and similar clinical trials for stem cell applications highlights the successful translation of these safety protocols to human therapies [20]. As the field advances toward more complex stem cell engineering approaches, including gene-edited products and combination therapies, microbiological risk assessment methodologies must similarly evolve to address emerging challenges. Through continued refinement of detection methods, processing technologies, and regulatory standards, the field can ensure that stem cell-based therapies realize their transformative potential while maintaining the highest standards of patient safety.
Methodological Frameworks for Risk Assessment and Management
The development of safe and effective stem cell-based therapies relies heavily on rigorous product characterization, a process governed by international scientific standards and national regulatory requirements. The International Society for Stem Cell Research (ISSCR) provides comprehensive ethical and scientific guidelines for stem cell research and clinical translation, while the U.S. Food and Drug Administration (FDA) enforces specific regulatory pathways for product approval [15] [25]. These frameworks, though distinct in their origin and scope, share the common objective of ensuring that cellular products are sufficiently characterized to guarantee their identity, purity, potency, and safety before human use.
For researchers and drug development professionals, navigating these guidelines is essential for successful translation from laboratory research to clinical application. The ISSCR's guidelines, updated in 2025, emphasize oversight mechanisms and ethical principles that underpin responsible research practices [15] [26]. Concurrently, the FDA's focus on Chemistry, Manufacturing, and Controls has intensified, with recent data showing that 74% of Complete Response Letters issued between 2020 and 2024 were driven by quality or manufacturing deficiencies [27]. This article provides a detailed comparison of these frameworks, with a specific focus on their requirements for product characterization, to support the safety profile assessment of stem cell-based therapies.
Comparative Analysis of FDA and ISSCR Guidelines
Core Principles and Scope
The ISSCR Guidelines and FDA regulatory requirements, while complementary, differ in their foundational principles and areas of emphasis. The table below summarizes their core characteristics:
Table 1: Core Principles and Scope of FDA and ISSCR Guidelines
| Aspect | FDA Regulatory Framework | ISSCR Guidelines |
|---|---|---|
| Primary Focus | Regulatory approval for marketing; Safety and efficacy in human subjects [25] [27] | Ethical research conduct; Scientific rigor; Oversight standards [15] |
| Legal Status | Legally binding requirements for product approval in the U.S. [25] | Internationally recognized, ethics-based guidelines; Inform policy but do not supersede law [15] |
| Key Emphasis | Chemistry, Manufacturing, and Controls; Preclinical toxicology; Clinical trial design [27] | Ethical principles; Institutional oversight; Transparency; Social justice [15] |
| Product Scope | "Substantially manipulated" cells or those for "non-homologous use" [25] | All stem cell research and clinical translation, including embryo models [15] [26] |
| Recent Updates | Increasing CMC stringency; Requiring potency assays in early trials [27] | 2025 update focused on stem cell-based embryo models (SCBEMs) [26] |
Specific Requirements for Product Characterization
Both frameworks mandate thorough product characterization, though they articulate these requirements with different specificity. The following table compares key characterization requirements:
Table 2: Comparative Product Characterization Requirements
| Characterization Parameter | FDA Regulatory Expectations | ISSCR Guideline Recommendations |
|---|---|---|
| Identity/Purity | Validated analytical methods; Defined acceptance criteria; Documentation of cellular identity [27] | Verification of cellular authenticity; Population purity; Standardized operating procedures [25] |
| Potency | Potency assays required, even in early-stage trials; Quantitative measures of biological activity [27] | Assessment of functional activity; Confirmation of differentiation potential; Criteria for therapeutic efficacy [25] |
| Viability | Quantitative viability data at time of release; Correlation with efficacy [5] | Measurement of post-implantation viability; Cell survival rates in target tissues [5] |
| Genomic Stability | Assessment of genetic and epigenetic changes during culture; Monitoring for malignant transformation [25] | Analysis of genomic stability during cell culture; Evolving understanding of genetic and epigenetic status [25] |
| Tumorigenicity | In vitro and in vivo assessment in immunocompromised animals; Long-term follow-up [5] | Evaluation of oncogenic potential; Particularly crucial for pluripotent cells [5] |
| Biodistribution | Tracking of cell movement using qPCR and imaging (PET, MRI); Monitoring cell fate over time [5] | Analysis of biodistribution patterns; Understanding cell movement post-transplantation [5] |
| Manufacturing Quality | GMP conditions; Validated processes; Comprehensive quality control systems [25] [27] | Quality control systems; Standard operating procedures; GMP conditions when possible [25] |
A critical area of alignment between both frameworks is the emphasis on rigorous manufacturing standards. The FDA increasingly focuses on Chemistry, Manufacturing, and Controls strategy, with gaps in this area becoming a leading cause of therapy rejection [27]. Similarly, the ISSCR recommends that manufacturing be performed under Good Manufacturing Practice (GMP) conditions and subject to rigorous, independent oversight [25].
Experimental Protocols for Safety and Characterization Assessment
Comprehensive Product Characterization Workflow
The assessment of stem cell-based products requires an integrated approach to evaluate multiple safety and characterization parameters. The following workflow diagram illustrates the key experimental phases and decision points in this process:
Detailed Methodologies for Key Characterization Assays
Tumorigenicity and Oncogenicity Assessment
The risk of malignant transformation is a primary safety concern for stem cell-based products, particularly those with proliferative capacity or derived from pluripotent stem cells. The ISSCR highlights the importance of evaluating oncogenic potential, while the FDA requires rigorous tumorigenicity assessment [5] [25]. A comprehensive assessment includes:
- In vitro transformation assays: Soft agar colony formation assays to assess anchorage-independent growth potential; focus formation assays in permissive cell lines.
- In vivo tumorigenicity studies: Administration of cells to immunocompromised animals (e.g., nude mice, NSG mice) at multiple doses via relevant routes; long-term observation (at least 16 weeks) for tumor formation; histopathological examination of any masses [5].
- Genetic stability monitoring: Karyotype analysis to detect chromosomal abnormalities; PCR-based assays for specific oncogenic mutations; comparative genomic hybridization to identify copy number variations [25].
These assays should be performed on cells at various passages, including at the end of production, to assess whether extended culture increases tumorigenic risk. Current regulatory expectations include using highly sensitive methods capable of detecting low-frequency genetic abnormalities in heterogeneous cell populations.
Biodistribution and Cell Fate Tracking
Understanding the migration, engraftment, and persistence of administered cells is critical for assessing both safety and mechanism of action. The FDA emphasizes biodistribution studies using sensitive tracking methods [5]. Key methodologies include:
- Quantitative PCR (qPCR): For species-specific sequences (e.g., Alu repeats for human cells in animal models); enables quantification of cell number in various tissues over time [5].
- Molecular imaging: Positron Emission Tomography with radiolabeled cells; Magnetic Resonance Imaging with contrast agents; bioluminescence imaging with luciferase-expressing cells [5].
- Histological analysis: Immunohistochemistry with species-specific or cell-type-specific antibodies; in situ hybridization for human-specific sequences.
These studies should be conducted in relevant animal models of the target disease, with sampling at multiple time points to understand both short-term trafficking and long-term persistence. Biodistribution data directly informs toxicity studies by identifying tissues for detailed histopathological examination.
Potency Assay Development
Potency assays represent a particularly challenging aspect of product characterization, as they must quantitatively measure the biological function responsible for the product's therapeutic effect. Both FDA and ISSCR guidelines emphasize the importance of relevant, quantitative potency assays [25] [27]. Development strategies include:
- Mechanism-based assays: If the mechanism of action is known (e.g., secretion of specific trophic factors, immunomodulatory activity, differentiation into specific lineages), develop quantitative assays measuring these functions.
- Multi-assay approaches: When a single mechanism isn't definitive, employ a matrix of assays measuring different aspects of biological activity.
- Progressive validation: Begin with research-grade assays during early development and transition to validated, GMP-compliant assays as products approach licensure.
The FDA now expects inclusion of potency assays even in early-stage clinical trials, representing a significant elevation of regulatory standards [27]. These assays must be scientifically justified, demonstrate suitability for their intended purpose, and be stability-indicating.
Essential Research Reagents and Materials
The following table details key reagents and materials essential for implementing the characterization protocols aligned with regulatory standards:
Table 3: Essential Research Reagents for Stem Cell Product Characterization
| Reagent/Material | Primary Function | Application in Characterization | Regulatory Consideration |
|---|---|---|---|
| eTeSR Medium | hPSC maintenance medium | Genetic stability assessment during long-term culture [28] | Supports consistency in cell expansion |
| STEMmatrix BME | Basement membrane matrix | Supports feeder-free expansion and differentiation [28] | hPSC-qualified for reproducibility |
| Alvetex Advanced | 3D cell culture scaffold | Enhanced organoid and tissue model generation [28] | Improves assay physiological relevance |
| Maestro MEA System | Electrophysiological assessment | Functional potency testing of electrically active cells (e.g., cardiomyocytes, neurons) [28] | Provides quantitative functional data |
| ImmunoCult-XF Medium | Serum-free cell culture medium | Expansion of T-cells and other immune cells for immunogenicity assessment [28] | GMP-grade available for manufacturing |
| StemSpan-AOF | Animal origin-free medium | Culture of hematopoietic cells without animal-derived components [28] | Reduces contamination risk for clinical use |
| Flow Cytometry Antibodies | Cell surface and intracellular marker detection | Identity, purity, and differentiation status determination [5] [25] | Requires validation for characterization assays |
| qPCR Assays | Nucleic acid quantification | Genetic stability, biodistribution, and identity testing [5] | Must be validated for sensitivity and specificity |
The FDA regulations and ISSCR guidelines, while distinct in authority and scope, provide complementary frameworks for ensuring the thorough characterization of stem cell-based therapies. The FDA's rigorous CMC requirements establish legally enforceable standards for product quality, while the ISSCR's ethical and scientific guidelines provide foundational principles for responsible research conduct [15] [27]. A comprehensive safety assessment strategy must integrate both frameworks, addressing detailed manufacturing controls while upholding broader ethical responsibilities.
For researchers and developers, successful navigation of this landscape requires early and strategic planning for product characterization. Key recommendations include: engaging with regulatory agencies during early development phases; investing in robust, validated analytical methods; implementing quality-by-design principles throughout process development; and maintaining thorough documentation of all characterization data. As noted in recent FDA rejections, deficiencies in manufacturing and characterization now represent the most significant barrier to approval, underscoring the critical importance of these activities [27].
The continued evolution of both regulatory frameworks will likely place even greater emphasis on comprehensive product characterization. Developers should anticipate increasing expectations for advanced potency assays, high-resolution genetic stability assessment, and thorough understanding of cell fate and mechanisms of action. By adopting the most rigorous elements of both FDA and ISSCR frameworks, developers can maximize both regulatory success and, more importantly, patient safety.
The field of stem cell-based therapies holds transformative potential for treating a wide range of intractable diseases, from neurodegenerative disorders to heart disease. However, this promise is tempered by significant safety concerns that must be rigorously addressed through comprehensive preclinical assessment. The safety profile assessment of stem cell-based therapies research depends on a triad of fundamental assays: karyotyping for genetic stability, pluripotency tests for differentiation potential, and in vivo models for systemic safety and tumorigenicity. These assays form the cornerstone of regulatory submissions and clinical translation, ensuring that cellular products meet stringent safety criteria before human administration. As the industry evolves—with the global digital karyotyping market projected to grow from $1.17 billion in 2024 to $1.29 billion in 2025—so too do the technologies and methodologies underpinning these critical safety assessments [29]. This guide provides a comparative analysis of these essential preclinical safety assays, offering researchers objective performance data and standardized protocols for implementation.
Karyotyping and Genetic Stability Assessment
Technology Comparison and Detection Capabilities
Karyotyping remains a fundamental requirement for assessing the genomic stability of stem cell lines, particularly crucial for pluripotent stem cells which may acquire chromosomal abnormalities during culture or reprogramming. Traditional karyotyping has evolved to include advanced molecular techniques that offer varying resolutions, detection capabilities, and throughput characteristics.
Table 1: Comparative Analysis of Karyotyping Technologies in Stem Cell Safety Assessment
| Technology | Resolution | Key Strengths | Key Limitations | Optimal Use Cases |
|---|---|---|---|---|
| Traditional Karyotyping (G-banding) | ~5-10 Mb | Detects balanced translocations, inversions; established gold standard | Low resolution; requires cell culture; labor-intensive | Routine screening; initial characterization |
| Digital Karyotyping | ~1-5 Mb | Automated analysis; high-throughput capability; AI integration | Limited detection of balanced rearrangements | High-volume screening; QC in manufacturing |
| CNV-Sequencing (CNV-Seq) | ~1-100 Kb | High-resolution for copy number variations; culture-independent | Cannot detect balanced translocations | Comprehensive aneuploidy/CNV detection |
| Chromosomal Microarray (CMA) | ~10-100 Kb | Genome-wide CNV detection; no culture requirement | Limited to unbalanced alterations | When combined with karyotyping for maximal detection |
Recent comparative studies demonstrate the complementary value of these technologies. In a 2024 study comparing CNV-Seq with traditional karyotyping across 177 amniotic fluid samples, CNV-Seq identified chromosomal abnormalities in 26.0% of cases compared to 22.6% with karyotyping. CNV-Seq showed 100% concordance for common aneuploidies (trisomy 21, 18, 13, monosomy X, and 47, XXY) while additionally detecting three mosaic cases and 13 clinically significant CNVs missed by karyotyping [30]. Similarly, a 2025 study on congenital heart disease diagnoses found that CMA identified pathogenic CNVs in 4.42% of cases with normal karyotypes, providing incremental diagnostic value [31].
Experimental Protocols for Karyotyping Assays
Protocol 1: Traditional G-Banding Karyotyping
Sample Requirements: Actively dividing stem cells at 70-80% confluence Procedure:
- Cell Culture & Mitotic Arrest: Treat cells with colchicine (0.1 µg/mL final concentration) for 45-90 minutes to arrest cells in metaphase
- Hypotonic Treatment: Expose cells to pre-warmed 0.075M KCl for 15-20 minutes at 37°C
- Fixation: Apply fresh Carnoy's fixative (3:1 methanol:glacial acetic acid) with three changes over 30 minutes
- Slide Preparation: Drop cell suspension onto clean, wet slides and air dry
- Trypsin-Giemsa Banding (G-banding):
- Treat slides with trypsin solution (0.025-0.05%) for 30-60 seconds
- Stain with 4% Giemsa solution for 5-7 minutes
- Rinse gently with distilled water and air dry
- Microscopy & Analysis: Image 15-20 metaphase spreads per sample using automated systems (e.g., GSL-120, Leica Microsystems) following the 2016 International System of Human Cytogenetic Nomenclature [30] [31]
Protocol 2: CNV-Sequencing for Stem Cell Lines
Sample Requirements: High-quality genomic DNA (≥50 ng) from stem cell cultures Procedure:
- DNA Extraction & QC: Isolate genomic DNA using validated kits (e.g., QIAamp DNA Mini Kit), ensuring DNA integrity number (DIN) ≥7.0
- Library Preparation: Use library prep kits (e.g., NEBNext Ultra II DNA Library Prep Kit for Illumina) with unique dual indexing
- Sequencing: Run on high-throughput platforms (e.g., Illumina NextSeq 500) targeting 5-10 million reads per sample
- Bioinformatic Analysis:
- Align sequences to reference genome (hg38/GRCh38)
- Call CNVs using specialized algorithms with ≥3 consecutive probes and log2 ratio ≥0.3
- Annotate variants using DECIPHER, ClinGen, and ACMG guidelines [30]
Figure 1: Integrated Workflow for Comprehensive Genetic Assessment of Stem Cell Lines
Pluripotency Assessment Technologies
Comparative Performance of Pluripotency Assays
Pluripotency testing verifies the differentiation capacity of stem cells, a critical safety parameter that ensures cells cannot form inappropriate tissues or teratomas upon transplantation. Current methods vary significantly in their complexity, standardization, and predictive value.
Table 2: Comparison of Pluripotency Assessment Methods for Stem Cell Safety Evaluation
| Assay Type | Key Readouts | Throughput | Standardization Level | Regulatory Acceptance |
|---|---|---|---|---|
| Embryoid Body (EB) Formation | Spontaneous trilineage differentiation | Medium | Low (stochastic) | Established, but variable |
| Directed Trilineage Differentiation | Specific germ layer markers | Medium-High | Medium | Increasing adoption |
| Teratoma Formation | Tissue formation in vivo | Low | Low (variable histology) | Declining due to ethical concerns |
| Marker-Based qPCR (hiPSCore) | 12-gene expression signature | High | High (quantitative) | Emerging with validation |
Recent technological advances are addressing longstanding limitations in pluripotency assessment. The 2024 development of "hiPSCore"—a machine learning-based scoring system utilizing 12 validated marker genes—represents a significant advancement toward standardization. This system, trained on 15 iPSC lines and validated on 10 additional lines, accurately classifies pluripotent and differentiated cells while predicting their potential to form specialized 2D cells and 3D organoids [32]. The identified markers include CNMD, NANOG, and SPP1 for pluripotency; CER1, EOMES, and GATA6 for endoderm; APLNR, HAND1, and HOXB7 for mesoderm; and HES5, PAMR1, and PAX6 for ectoderm [32].
Experimental Protocols for Pluripotency Assessment
Protocol 1: Directed Trilineage Differentiation with Flow Cytometry Validation
Materials:
- Commercially available directed differentiation kits (e.g., Thermo Fisher Scientific)
- Flow cytometry antibodies: Oct3/4, SSEA-4 (pluripotency); CXCR4, SOX17 (endoderm); PAX6, SOX2 (ectoderm); CD140b, T/BRACHYURY (mesoderm) Procedure:
- Pluripotency Baseline: Confirm >95% expression of pluripotency markers prior to differentiation
- Directed Differentiation: Follow manufacturer protocols for each germ layer lineage
- Flow Cytometry Analysis:
- Harvest cells with enzyme-free dissociation buffer
- Fix and permeabilize cells using intracellular staining protocols
- Incubate with fluorochrome-conjugated antibodies (30 minutes, 4°C)
- Analyze on flow cytometer, collecting ≥10,000 events per sample
- Establish positive thresholds using isotype controls [32]
Protocol 2: qPCR-Based Pluripotency Assessment (hiPSCore Method)
Materials:
- RNA extraction kit (e.g., RNeasy Plus Mini Kit)
- cDNA synthesis kit (e.g., High-Capacity cDNA Reverse Transcription Kit)
- qPCR reagents and validated primer sets for 12 marker genes Procedure:
- RNA Extraction & QC: Isolve total RNA, verify integrity (RIN ≥9.0)
- cDNA Synthesis: Convert 500ng-1μg RNA to cDNA using reverse transcriptase
- qPCR Setup:
- Prepare reactions in triplicate with SYBR Green master mix
- Run on real-time PCR system with cycling conditions: 95°C for 10min, followed by 40 cycles of 95°C for 15sec and 60°C for 1min
- Include no-template controls and inter-run calibrators
- Data Analysis:
- Calculate ΔΔCt values using housekeeping genes (GAPDH, HPRT1)
- Input normalized expression values into hiPSCore algorithm for classification [32]
Figure 2: Standardized Workflow for qPCR-Based Pluripotency Assessment
In Vivo Models for Tumorigenicity and Biodistribution
Comprehensive Safety Assessment in Animal Models
In vivo models provide irreplaceable data on systemic safety, tumorigenic potential, and biodistribution patterns of stem cell therapies—critical considerations for regulatory approval. These assessments typically utilize immunocompromised rodents to accommodate human cell transplantation and long-term observation.
Table 3: In Vivo Models for Stem Cell Therapy Safety Assessment
| Model Type | Key Safety Endpoints | Study Duration | Detection Methods | Predictive Value |
|---|---|---|---|---|
| Subcutaneous Transplantation | Teratoma formation, histopathology | 12-20 weeks | Palpation, caliper measurement, H&E staining | High for pluripotency-related risks |
| Intramuscular Transplantation | Ectopic tissue formation, local invasion | 12-20 weeks | Histology, immunohistochemistry | Medium-High |
| Biodistribution Models | Organ-specific engraftment, migration | 2-12 weeks | qPCR, bioluminescence, PET imaging | Essential for route-specific safety |
| Toxicity Pharmacology | Systemic toxicity, organ function | 4-26 weeks | Clinical pathology, histopathology | Required for IND applications |
As of December 2024, more than 1,200 patients have been dosed with human pluripotent stem cell (hPSC) products, accumulating to >10¹¹ clinically administered cells. Current data from clinical trials "so far showing no generalizable safety concerns," validating the predictive value of these preclinical models when properly implemented [33]. A comprehensive 2025 review outlines essential biosafety principles for cell therapy, including toxicity, oncogenicity/tumorigenicity/teratogenicity, immunogenicity, biodistribution, and cell product quality assessment [5].
Experimental Protocols for In Vivo Safety Assessment
Protocol 1: Tumorigenicity Assay in Immunocompromised Mice
Animals: NOD-scid gamma (NSG) or similar immunocompromised mice, 6-8 weeks old Test Article: Stem cell preparation (≥1×10⁶ cells per site) with positive control (known tumorigenic cells) Procedure:
- Cell Preparation: Harvest cells at >90% viability, resuspend in appropriate matrix (e.g., Matrigel diluted 1:1 with saline)
- Transplantation:
- Subcutaneous route: Bilateral flank injections, 100μL per site
- Intramuscular route: Hind limb injections, 50μL per site
- Clinical Observations:
- Daily for first week, then twice weekly for general health
- Weekly palpation for mass formation
- Biweekly body weight measurements
- Termination Criteria:
- Tumors reaching 1.5cm diameter or 10% body weight
- Study conclusion at 16-20 weeks
- Histopathological Analysis:
- Necropsy with gross examination
- H&E staining of tumors and major organs
- Immunohistochemistry for human-specific markers (e.g., STEM121) and lineage markers [5]
Protocol 2: Biodistribution Study Using qPCR
Animals: Immunocompromised rodents appropriate for administration route Test Article: Stem cells administered via clinically relevant route Procedure:
- Study Design: Include multiple timepoints (e.g., 24h, 1wk, 1mo, 3mo) with n=5-8 per group
- Tissue Collection: Harvest major organs (brain, heart, lungs, liver, spleen, kidneys, gonads, injection site)
- DNA Extraction: Isolve genomic DNA from ~25mg tissue using commercial kits
- qPCR Analysis:
- Use human-specific Alu sequence primers: Forward 5'-ACGCCTGTAATCCCAGCACTT-3', Reverse 5'-TCGCCCAGGCTGGAGTGCA-3'
- Run standard curve with known human cell numbers spiked into mouse tissue
- Calculate human cell equivalents per μg total DNA
- Data Interpretation: Compare levels across timepoints and tissues to assess clearance/persistence [5]
Research Reagent Solutions for Safety Assessment
Table 4: Essential Research Reagents for Stem Cell Safety Assessment
| Reagent Category | Specific Products | Manufacturer Examples | Primary Applications |
|---|---|---|---|
| Karyotyping Systems | MetaSight G200, GSL-120 | Hangzhou Diagens, Leica Microsystems | Automated metaphase capture, analysis |
| CNV Detection Kits | CytoScan, SurePrint G3 | Agilent, Thermo Fisher | Chromosomal microarray analysis |
| Pluripotency Antibodies | Oct3/4, SSEA-4, Nanog | BD Biosciences, Thermo Fisher | Flow cytometry, immunocytochemistry |
| Directed Differentiation Kits | Trilineage differentiation kits | Thermo Fisher, STEMCELL Technologies | Controlled germ layer specification |
| qPCR Assays | TaqMan hPSC Scorecard | Thermo Fisher | Pluripotency assessment |
| In Vivo Imaging Agents | Luciferin, IVISense | PerkinElmer | Biodistribution tracking |
| Cell Culture Media | mTeSR, StemFlex | STEMCELL Technologies | Undifferentiated stem cell maintenance |
The market for these research tools is expanding rapidly, with companies increasingly focusing on technological innovation. For instance, the recent launch of the MetaSight G200 system—which captures intelligent metaphase images and completes slide scanning in four minutes—exemplifies the trend toward automation and standardization in karyotyping [29]. Similarly, the development of the hiPSCore algorithm represents the integration of machine learning into routine pluripotency assessment [32].
A comprehensive safety assessment strategy for stem cell-based therapies requires the integrated application of karyotyping, pluripotency testing, and in vivo models. Our comparative analysis demonstrates that while traditional methods remain valuable, emerging technologies—particularly AI-enhanced karyotyping platforms, standardized qPCR-based pluripotency assays, and sensitive biodistribution tracking—are significantly improving the accuracy, efficiency, and predictive value of preclinical safety assessment. The expanding clinical trial landscape, with 116 approved hPSC clinical trials testing 83 products as of December 2024, underscores the successful translation of these safety assessment paradigms [33]. As regulatory frameworks continue to evolve across different regions [34], the standardized implementation of these core assays will remain essential for ensuring the safety of stem cell therapies while facilitating their progression to clinical application.
In the rapidly advancing field of stem cell-based therapies, the safety profile of these novel biological products is paramount. A robust Current Good Manufacturing Practice (cGMP) framework and a comprehensive quality control (QC) strategy are not merely regulatory hurdles but are fundamental to ensuring the identity, purity, potency, and safety of cellular products, thereby protecting patient welfare and validating clinical research outcomes [35] [36]. This guide objectively compares the foundational elements of cGMP systems against less rigorous approaches and details the experimental protocols that underpin the safety assessment of stem cell therapies.
cGMP vs. Non-GMP: A Critical Comparison for Cell Therapy
For researchers transitioning from basic science to translational medicine, understanding the practical implementation of cGMP is the first step. The following table compares the minimum cGMP requirements against typical non-GMP research practices, highlighting the critical differences that ensure product quality and safety.
| Feature | cGMP-Compliant Approach (Ensuring Product Quality) | Typical Basic Research Approach (For Discovery) |
|---|---|---|
| Core Philosophy | Quality is built into every step of the process (Quality by Design) [37] [38]. Relies on in-process controls and a validated, reproducible system. | Quality is often assessed only at the end-point through testing; processes may be variable and are not always validated. |
| Facility & Environment | Purpose-designed cleanrooms with controlled air purity (ISO Class 5-7), temperature, humidity, and pressure to prevent contamination [39]. | Standard labs without stringent environmental controls or monitoring. |
| Personnel & Training | Staff are formally trained and qualified for specific procedures (e.g., aseptic technique) with maintained records [39] [37]. | Training is often informal and on-the-job; records may not be systematically kept. |
| Documentation & Traceability | Comprehensive, controlled documentation for all activities (SOPS, batch records, deviations). Full traceability from raw materials to final product [36] [40]. | Notebook entries are sufficient; methods can change frequently without formal documentation or change control. |
| Raw Materials | Materials are qualified and tested to meet strict specifications. Sourced from approved suppliers with certificates of analysis [36] [38]. | Materials are often used as supplied without additional qualification testing; focus is primarily on scientific grade. |
| Process & Equipment Controls | Equipment is qualified, calibrated, and maintained according to strict schedules. Manufacturing processes are validated to consistently produce a product that meets its specs [36] [37]. | Equipment use and maintenance can be ad-hoc. Processes are often optimized for speed or yield, not necessarily consistency. |
| Quality Control (QC) Testing | Mandatory and rigorous testing for identity, purity, potency, viability, and sterility for every product batch before release [39] [5]. | Testing is performed intermittently to answer specific research questions, not for routine batch release. |
| Laboratory Controls | Relies on validated analytical methods and a reliable quality control laboratory [36] [37]. | Methods are often not fully validated; results are for research use only. |
The "C" in cGMP stands for "current," emphasizing that manufacturers must employ up-to-date technologies and systems to comply with the regulation, as practices that were adequate decades ago may be insufficient by today's standards [36] [38]. This is particularly critical in cell therapy, where the product is often living, cannot be terminally sterilized, and has a short shelf-life, making quality-by-design the only viable path [39] [5].
Essential Analytical Methods for Cell Product Characterization
A core component of cGMP is the rigorous quality control testing of the cellular product. The following experimental protocols are standard for assessing the critical quality attributes of stem cell-based therapies. The table below summarizes the key assays, their functions, and the regulatory standards that guide their implementation.
| Test Category | Key Analytical Methods | Critical Parameters Measured | Purpose in Safety & Identity Assessment |
|---|---|---|---|
| Identity & Purity | Flow Cytometry, PCR, Karyotyping | Surface marker profile (e.g., CD73+, CD90+, CD105+ for MSCs), Genetic identity, Purity of cell population [39] [5] | Confirms the correct cell product and absence of unintended cell types. |
| Potency | In Vitro Differentiation Assays (e.g., osteogenic, adipogenic, chondrogenic), Cytokine Secretion Assays | Differentiation capacity, Immunomodulatory activity (e.g., IDO activity, PGE2 secretion) [39] [41] | Measures the biological activity responsible for the therapeutic effect. |
| Viability & Quantity | Trypan Blue Exclusion, Automated Cell Counting | Total cell number, Percent viability [5] | Ensures delivery of a sufficient dose of live, functional cells. |
| Safety (Sterility) | BacT/ALERT, Mycoplasma PCR, Endotoxin (LAL) Assay | Absence of bacteria, fungi, mycoplasma, and endotoxins [39] [5] | Prevents administration of a contaminated product. |
| Safety (Tumorigenicity) | Soft Agar Colony Formation, In Vivo Teratoma Assay (in immunodeficient mice) | Anchorage-independent growth, Teratoma formation [5] | Assesses the risk of malignant transformation, crucial for pluripotent stem cells. |
| Genetic Stability | Karyotype (G-banding), Whole Genome Sequencing | Chromosomal abnormalities, Mutations [5] | Monitors genomic integrity after cell expansion and manipulation. |
Detailed Experimental Protocols
1. Flow Cytometry for Cell Identity and Purity
- Objective: To quantitatively determine the presence and absence of specific cell surface markers, confirming the identity and purity of the cell population [5].
- Protocol:
- Cell Harvesting: Dissociate cells into a single-cell suspension using a non-enzymatic agent like EDTA or a gentle enzyme to preserve surface epitopes.
- Staining: Aliquot cells into tubes. Incubate with fluorochrome-conjugated antibodies against target markers (e.g., CD73, CD90, CD105 for MSCs) and appropriate isotype controls. Keep one aliquot unstained for autofluorescence control.
- Washing & Fixation: Wash cells with a buffer like PBS containing 1-2% FBS to remove unbound antibody. Cells may be fixed with a 1-4% paraformaldehyde solution if analysis is not immediate.
- Data Acquisition: Analyze cells on a flow cytometer, collecting a minimum of 10,000 events per sample.
- Analysis: Use software to gate on viable cells based on forward/side scatter and a viability dye. The percentage of positive cells for each marker is calculated against the isotype control. A product may be deemed acceptable if, for example, >95% of cells express the positive markers and <5% express negative markers (e.g., hematopoietic markers CD34, CD45) [5].
2. In Vitro Trilineage Differentiation Potency Assay (for MSCs)
- Objective: To demonstrate the functional capacity of Mesenchymal Stem/Stromal Cells (MSCs) to differentiate into osteocytes, adipocytes, and chondrocytes, a key measure of potency [41].
- Protocol:
- Osteogenic Differentiation:
- Seed MSCs at a defined density (e.g., 20,000 cells/cm²) in growth medium until confluent.
- Replace with osteogenic induction medium (containing Dexamethasone, Ascorbic Acid, and β-Glycerophosphate).
- Culture for 21 days, changing the medium twice weekly.
- Analysis: Fix cells and stain with 2% Alizarin Red S to detect calcium deposits (mineralization).
- Adipogenic Differentiation:
- Seed MSCs at a high density (e.g., 50,000 cells/cm²) in growth medium until confluent.
- Replace with adipogenic induction medium (containing Insulin, Dexamethasone, Indomethacin, and IBMX).
- Culture for 14-21 days, changing the medium twice weekly.
- Analysis: Fix cells and stain with Oil Red O to detect lipid vacuoles.
- Chondrogenic Differentiation:
- Pellet 250,000 MSCs in a conical tube via centrifugation.
- Culture the pellet in chondrogenic induction medium (containing TGF-β3 and Dexamethasone).
- Culture for 21-28 days.
- Analysis: Fix pellet, embed in paraffin, section, and stain with Toluidine Blue or Safranin O to detect proteoglycans.
- Osteogenic Differentiation:
3. Sterility Testing with BacT/ALERT
- Objective: To detect the presence of viable aerobic and anaerobic microorganisms in the final cell therapy product [39] [5].
- Protocol:
- Sample Collection: Aseptically withdraw a representative sample (e.g., 5-10 mL) from the final product container.
- Inoculation: Inoculate the sample into both BacT/ALERT iAST (aerobic) and iNST (anaerobic) culture bottles.
- Incubation & Monitoring: Load the bottles into the BacT/ALERT instrument, which incubates them at 35±1.5°C and continuously monitors for CO2 production, a sign of microbial growth.
- Duration: The test is typically run for 14 days, as required by pharmacopoeial standards (e.g., USP <71>, Ph. Eur. 2.6.1).
- Interpretation: A bottle that flags as positive indicates a potential contamination. The contents must be subcultured for identification. The product is released only if all bottles show no growth throughout the incubation period. For products with short shelf-lives, rapid microbiological methods with shorter read-out times may be employed as an alternative [39].
The Scientist's Toolkit: Essential Reagents for cGMP-Compliant Research
Transitioning to translational work requires carefully selecting reagents that meet regulatory scrutiny. The following table details critical materials and their cGMP-quality considerations.
| Research Reagent / Material | Function in Cell Therapy Manufacturing | cGMP-Grade Considerations |
|---|---|---|
| Cell Culture Media | Provides nutrients and environment for cell growth/sustenance. | Must be xeno-free (animal-origin free) or human-derived with full traceability and testing for adventitious agents. Requires a Certificate of Analysis (CoA) [39] [42]. |
| Growth Factors & Cytokines | Directs stem cell differentiation and expansion. | Recombinant human proteins are preferred over animal-sourced. Must be sourced from qualified suppliers with CoA confirming identity, purity, potency, and absence of endotoxins [5]. |
| Attachment Substrates | Provides a surface for adherent cells to grow. | Defined substrates (e.g., recombinant laminin) are preferred over poorly defined ones (e.g., Matrigel). Rigorous testing for bioburden and endotoxins is critical [5]. |
| Gene Editing Reagents | Used for genetic modification (e.g., CRISPR nucleases, mRNAs). | Plasmids or mRNAs must be manufactured in a cGMP facility. Testing includes sterility, endotoxin, and full sequence verification [42]. |
| Primary Cells & Cell Lines | The starting material for the therapy (e.g., iPSCs, MSCs). | Must be sourced from qualified donors with extensive infectious disease testing. Master Cell Banks are created and fully characterized for identity, purity, potency, and sterility [39] [42]. |
| Critical Assay Kits | Used for quality control testing (e.g., endotoxin, mycoplasma). | Must be qualified for use with the specific cell product. Use of compendial methods (e.g., USP, Ph. Eur.) is strongly recommended [37]. |
cGMP Workflow for Cell Therapy Manufacturing
The logical flow of a cGMP-compliant manufacturing process for a stem cell therapy, from donor to final product, can be visualized as a series of controlled and verified stages. The diagram below maps this critical pathway.
Biosafety Assessment: From In Vitro to Clinical Trials
The cGMP framework is inextricably linked to the comprehensive biosafety assessment required for regulatory approval. This assessment extends beyond quality control to include specific preclinical safety studies, the workflow of which is illustrated below.
For cell therapy products, the preclinical safety assessment is critical for identifying potential risks. Key methodologies include [5]:
- Biodistribution Studies: These studies track the migration, persistence, and potential accumulation of cells in non-target tissues following administration. This is typically assessed in immunocompromised animal models using quantitative PCR (qPCR) for human-specific DNA sequences or molecular imaging techniques like bioluminescence imaging (BLI) or positron emission tomography (PET).
- Tumorigenicity Studies: This assesses the risk of unwanted cell growth or malignant transformation. For pluripotent stem cell (PSC)-derived products, the gold standard is the in vivo teratoma assay, where cells are injected into immunocompromised mice and monitored for the formation of tumors containing tissues from all three germ layers. For adult stem cells like MSCs, in vitro assays like soft agar colony formation are used to detect anchorage-independent growth, a hallmark of transformation.
- Toxicity and Immunogenicity Studies: General toxicity studies monitor for adverse effects, including clinical observations, clinical pathology (blood counts, clinical chemistry), and detailed histopathology of major organs. Immunogenicity assessment evaluates the potential for the cell product to provoke an immune response in the recipient, which is crucial for allogeneic therapies.
The journey from a research concept to a clinically applicable stem cell therapy is complex and heavily dependent on a cGMP and quality control framework. This system, built on the principles of Quality by Design, rigorous documentation, and controlled processes, is not a constraint but an enabler. It provides the structure necessary to ensure that the cellular product administered to a patient is consistently what it is purported to be—pure, potent, and safe. For researchers and drug developers, a deep integration of these principles from the earliest stages of development is the most effective strategy for successfully translating promising science into safe and effective therapies.
The safety profile assessment of stem cell-based therapies represents a critical and distinct challenge within pharmaceutical development. Unlike traditional small-molecule drugs, stem cell therapies are characterized by their complex biological nature, potential for proliferation and differentiation, and persistence within the recipient, necessitating specialized clinical trial designs for safety monitoring [25]. These living products introduce unique risks, including uncontrolled cellular growth, immunological reactions, and donor-derived transmissions, which require vigilant and prolonged observation [25] [43]. The International Society for Stem Cell Research (ISSCR) emphasizes that given the uncertain nature of this therapeutic modality, rigorous and expert oversight is essential to protect research participants and ensure the credible development of the field [25].
This guide objectively compares monitoring methodologies and frameworks against conventional clinical trial approaches, providing researchers with structured data and protocols to enhance safety assessment integrity. The focus is on practical, implementable strategies for detecting, evaluating, and reporting adverse events throughout the trial lifecycle and beyond, with particular emphasis on managing the extended timelines required for long-term follow-up (LTFU).
Comparative Analysis of Safety Monitoring Frameworks
Key Definitions and Regulatory Classifications
A fundamental understanding of specific safety terminologies and regulatory classifications is the foundation of effective monitoring. Stem cell-based products, particularly those that are substantially manipulated or used in a non-homologous manner, are typically regulated as Advanced Therapy Medicinal Products (ATMPs) by agencies like the FDA and EMA [25]. This classification triggers specific requirements for safety monitoring and reporting.
Table 1: Key Safety Event Definitions in Clinical Trials
| Term | Definition | Special Considerations for Stem Cell Trials |
|---|---|---|
| Adverse Event (AE) | Any untoward medical occurrence in a clinical trial participant [44]. | Requires careful assessment to distinguish from underlying disease progression or expected inflammatory response to administration. |
| Serious Adverse Event (SAE) | An AE that results in death, is life-threatening, requires inpatient hospitalization, prolongs existing hospitalization, results in persistent disability, or is a congenital anomaly [44]. | Of particular concern are SAEs potentially linked to cell proliferation (e.g., tumor formation) or ectopic tissue formation. |
| Suspected Unexpected Serious Adverse Reaction (SUSAR) | A serious adverse event that is both unexpected and believed to be caused by the investigational product [44]. | "Unexpected" means not listed in the Investigator's Brochure. For novel cell therapies, the list of expected events may evolve rapidly. |
| Unanticipated Problem (UP) | An incident that is unexpected, related to participation in the research, and suggests that the research places subjects at greater risk [44]. | Can include manufacturing deviations that affect product quality and thus patient safety [45]. |
| Protocol Deviation | Any change or departure from the study design or procedures in the protocol [45]. | Important protocol deviations are those that might significantly affect data completeness/accuracy or a subject's rights, safety, or well-being [45]. |
Quantitative Safety Outcomes in Recent Stem Cell Trials
Current clinical data reveals distinct safety trends across different stem cell therapy applications. The following table summarizes quantitative safety data from recent clinical trials, providing a basis for comparing the safety profiles of different approaches.
Table 2: Comparative Safety and Efficacy Outcomes from Recent Stem Cell Clinical Trials
| Therapeutic Area | Cell Type / Therapy | Key Efficacy Metric(s) | Reported Adverse Events & Safety Profile | Reference Context |
|---|---|---|---|---|
| Autoimmune Diseases (Crohn's, SLE, Scleroderma) | Mesenchymal Stem Cells (MSCs), Hematopoietic Stem Cells (HSCs) | Clinical remission rates categorized as Low (≤50%), Middle (>50-75%), or High (>75%) across 244 global trials [46]. | Short-term tolerability of stem cell infusions reported as favorable; concerns regarding allogeneic MSC immune rejection and need for long-term safety data [46]. | Systematic Review of trials (2006-2025) |
| Knee Osteoarthritis | Not Specified | Improvement in pain and mobility, leading to enhanced quality of life and occupational participation [47]. | Not explicitly quantified in the available excerpt. Pain reduction was a primary motive for seeking treatment [47]. | Observational Study (n=32) |
| Oncology & Degenerative Diseases | MSCs, Engineered Immune Cells | 40-60% improvement in WOMAC scores (degenerative diseases); 78% ctDNA clearance (oncology, p<0.001) [43]. | Cytokine Release Syndrome (CRS) noted as a key risk for engineered cell products (e.g., CAR-T); immune effector cell-associated neurotoxicity syndrome (ICANS) [43]. | Review of Clinical Trials in China |
| Various Degenerative Conditions | Mesenchymal Stem Cells (MSCs) | ~80% success rate reported for joint repair and autoimmune/inflammatory conditions; 87.5% of patients reported sustained improvement within 3 months [48]. | Risks associated with cell culture (accumulation of mutations, genomic instability) and potential for malignant transformation, especially with prolonged passage [25] [48]. | Clinic-Based Data Analysis |
Methodologies for Adverse Event Monitoring
Core Monitoring Procedures and Workflows
A systematic workflow for AE monitoring is vital for ensuring participant safety and data quality. The following diagram illustrates the integrated safety monitoring pathway from event detection to reporting, highlighting critical decision points.
Integrated Safety Monitoring Pathway
The Principal Investigator (PI) bears ultimate responsibility for protecting participant safety, but a trained team is essential for execution [44]. Clinical Research Coordinators (CRCs) often handle initial data collection, but evaluation of safety events (assessing severity, relatedness, expectedness) must be performed by the PI or a qualified Sub-Investigator (Sub-I), not by coordinators [44]. Sources of safety information are diverse and must be proactively monitored, including direct participant reports, investigator observations during study procedures, clinically significant abnormal findings from labs or imaging, and reports from non-study medical encounters [44].
The Scientist's Toolkit: Essential Reagents and Materials for Safety Assessment
Table 3: Key Research Reagent Solutions for Stem Cell Safety Assessment
| Item / Reagent | Function in Safety Assessment | Specific Application Example |
|---|---|---|
| Donor Screening Assays | To screen donors and/or resulting cell banks for infectious diseases and other risk factors, mitigating transmission risk [25]. | FDA/EMA-compliant blood tests for adventitious agents; medical history collection [25]. |
| Cell Bank Characterization Kits | To ensure the absence of adventitious agents when donor screening is not possible (e.g., hESC lines) [25]. | PCR-based or other validated tests for pathogens on master and working cell banks [25]. |
| Genomic Stability Assays | To detect genetic and epigenetic changes accumulated during cell culture expansion that could lead to altered function or malignancy [25]. | Karyotyping, FISH, or increasingly, single-cell omics to assess genomic integrity [43]. |
| Flow Cytometry Panels | To characterize cellular composition, identity, purity, and potency of the final product—critical for dose consistency and safety [25]. | Purity checks for MSC surface markers (e.g., CD73+, CD90+, CD105+); absence of hematopoietic markers [48]. |
| Cytokine Release Syndrome (CRS) Management Protocols | To monitor and manage immune-related adverse events common with engineered immune cell therapies [43]. | Tocilizumab (IL-6R antagonist); C-reactive protein (CRP) monitoring [43]. |
| Common Terminology Criteria for Adverse Events (CTCAE) | A standardized scale for grading AE severity, often mandated by protocols for objectivity [44]. | Grading AEs from 1 (Mild) to 5 (Death) to ensure consistent reporting across sites [44]. |
Protocols for Long-Term Follow-Up (LTFU)
Rationale and Design for Extended Monitoring
Long-term follow-up is a cornerstone of stem cell therapy safety assessment, justified by the unique biological properties of these products. The proliferative capacity and potential for delayed adverse effects, such as tumorigenicity or late-onset immunological complications, make LTFU not merely prudent but a regulatory expectation [25] [43]. The ISSCR guidelines explicitly note that stem cells can proliferate in culture for extended periods, and this very capacity carries risks that may only manifest years after administration [25].
Effective LTFU study design should incorporate:
- Predefined Duration: Follow-up periods of 5-15 years are common, with the specific timeframe justified by the product's mechanism of action and preclinical data [43].
- Systematic Data Collection Points: Establishing clear schedules for follow-up contacts (e.g., annually) balances data collection burden with participant retention.
- Robust Participant Retention Strategies: These may include flexible follow-up methods (remote monitoring, telehealth, electronic patient-reported outcomes (ePRO)), regular communication, and tracking systems for participant location [49].
- Integration with National Registries: Where available, linking with disease or transplant registries can help capture long-term outcomes and mitigate loss to follow-up [46].
LTFU Data Collection and Technology Integration
Modern LTFU programs leverage technology to enhance efficiency and data quality. The integration of mobile apps and wearable devices allows for continuous, real-time tracking of key health indicators relevant to stem cell transplantation, such as vital signs, activity levels, and patient-reported symptoms [49]. This real-time data can enable earlier detection of potential late-onset complications.
Furthermore, secure data transmission platforms are critical for managing the vast amount of longitudinal data generated. These platforms facilitate the tracking of complex data points, including HLA match details, conditioning regimens, and long-term immunosuppression protocols, while ensuring patient confidentiality through robust data protection measures [49]. The LTFU data collection should be comprehensive, focusing not only on survival and major adverse events but also on long-term quality of life, functional status, and the potential need for re-intervention.
Analysis of Protocol Deviations and Their Impact on Safety
Defining and Managing Protocol Deviations
The FDA's 2025 draft guidance on clinical trial protocol deviations provides a critical framework for classifying events that may impact data integrity or participant safety [45]. A protocol deviation is defined as "any change, divergence, or departure from the study design or procedures defined in the protocol." A critical subset of these are important protocol deviations, which are those that "might significantly affect the completeness, accuracy, and/or reliability of the study data or that might significantly affect a subject's rights, safety, or well-being" [45].
For stem cell trials, examples of important protocol deviations impacting safety include:
- Failing to administer the investigational product in accordance with protocol requirements (e.g., incorrect dose, route, or preparation) [45].
- Failing to conduct study procedures designed to assess safety (e.g., omitting scheduled safety lab assessments or imaging) [45].
- Enrolling a subject in violation of key eligibility criteria designed to ensure the safety of the participant population [45].
- Deviations in the cell handling process, such as a temperature excursion during transport or an error in product thawing, that could compromise product quality and safety [43].
Sponsors are recommended to pre-specify in the protocol which deviations will be considered "important" and to train investigators on this classification. Furthermore, sponsors or investigators should conduct root-cause analyses of any recurrent protocol deviations to prevent recurrence [45]. This is especially critical in stem cell trials where process consistency is directly linked to product safety.
The safety profile assessment of stem cell-based therapies demands a specialized and vigilant approach to clinical trial design, particularly concerning adverse event monitoring and long-term follow-up. The dynamic regulatory landscape, exemplified by the recent FDA draft guidance on protocol deviations, underscores the ongoing evolution of standards to ensure patient safety and data integrity [45]. As the field advances, future efforts will likely prioritize several key areas:
- Standardization of LTFU Protocols: Developing universally accepted standards for the duration, frequency, and data elements of LTFU will facilitate cross-trial comparisons and meta-analyses [25].
- Advanced Safety Biomarkers: Research into predictive biomarkers for specific stem cell-related risks, such as tumorigenicity or immunogenicity, will enable more proactive safety monitoring [43] [48].
- Integration of Real-World Data (RWD): Leveraging data from electronic health records, patient registries, and digital health technologies will complement traditional clinical trial safety data and provide insights into long-term outcomes in broader patient populations [49] [46].
By adhering to rigorous, evidence-based monitoring frameworks and embracing technological and regulatory advancements, researchers can navigate the complex safety landscape of stem cell-based therapies, ultimately ensuring their responsible translation into safe and effective clinical applications.
Addressing Persistent Challenges and Optimizing Safety Protocols
The application of human pluripotent stem cells (hPSCs), including induced pluripotent stem cells (iPSCs), in regenerative medicine represents a frontier in treating life-threatening diseases. These cells possess unique self-renewal and multi-lineage differentiation capabilities, making them invaluable for generating therapeutic cell types to treat conditions such as Parkinson's disease, macular degeneration, heart failure, and diabetes mellitus [50]. However, the tumorigenic risk posed by residual undifferentiated hPSCs remains a formidable obstacle to clinical implementation [50]. The same cellular features that make pluripotent stem cells valuable for biomedical applications can also lead to tumor formation, specifically teratomas—benign tumors composed of randomly distributed differentiated structures arising from all three germ layers [50].
Even with prolonged differentiation procedures, some undifferentiated PSCs may persist, and transplantation of differentiated cells derived from both mouse and human PSCs can still lead to tumor formation [50]. A recent clinical case report highlighted this concern, describing the occurrence of an immature teratoma in a patient who received an intramuscular injection of autologous iPSC-derived pancreatic beta cells for diabetes treatment [50]. The tumor contained OCT4- and SOX2-positive cells, grew rapidly, showed strong vascularization, and was unresponsive to chemotherapy. This case underscores the critical need to develop efficient hPSC removal strategies and implement strict quality control measures for all iPSC-based therapies [50].
This guide comprehensively compares the two principal approaches for mitigating tumorigenic risk: (1) purification strategies that eliminate residual undifferentiated cells prior to transplantation, and (2) suicide gene strategies that enable post-transplantation ablation of problematic cells. We provide experimental data, methodological details, and analytical frameworks to inform safety protocol selection for preclinical and clinical development.
Purification Strategies: Pre-Transplantation Safeguards
Purification strategies focus on removing residual undifferentiated pluripotent stem cells from differentiated cell populations before transplantation. These approaches primarily target hPSC-specific surface markers or physiological characteristics [50].
Key Methodologies and Experimental Evidence
Table 1: Comparison of Major Purification Strategies for Tumor Risk Mitigation
| Strategy Type | Specific Method | Target | Removal Efficiency | Advantages | Limitations |
|---|---|---|---|---|---|
| Small Molecules | Not specified in results | hPSC-specific pathways | Varies by compound | Clinically viable; Scalable | Potential off-target effects on differentiated cells [50] |
| MicroRNAs (miRNAs) | miRNA-based targeting | Pluripotency factors | High in some studies | Specificity; Natural regulatory mechanisms | Delivery challenges; Stability issues [50] |
| Antibody-Based | Cell sorting (e.g., FACS, MACS) | hPSC-specific surface markers | High with optimized markers | High specificity; Well-established protocols | Requires cell dissociation; Potential loss of target cells [50] |
| Pharmacological | Small-molecule inhibitors | Pluripotency pathways | Dependent on timing/dose | Non-genetic; Temporary treatment | Cytotoxicity risk; Incomplete elimination [50] |
Experimental Assessment of Purification Efficiency
Robust assessment of purification strategy effectiveness is essential. Researchers employ several standardized methods to evaluate the efficiency of pluripotent stem cell elimination:
- In vitro assays: Quantitative PCR for pluripotency genes (OCT4, NANOG, SOX2), flow cytometry for hPSC-specific surface markers (SSEA-4, TRA-1-60, TRA-1-81), and immunocytochemistry for intracellular pluripotency factors [50].
- In vivo teratoma assays: The gold standard for assessing tumorigenic potential, involving injection of cell populations into immunodeficient mice (e.g., NOD/SCID or NSG strains) with monitoring for tumor formation over several weeks to months [50] [51].
- Genetic stability monitoring: Karyotyping and genomic analysis to detect chromosomal abnormalities (e.g., trisomy 20, trisomy 12q) that may increase tumorigenic potential [50].
Studies have demonstrated that even 20-100 undifferentiated murine ESCs within a population of differentiated cells can lead to teratoma formation in mouse models, though the direct applicability to hPSCs requires further investigation [50].
Suicide Gene Strategies: Post-Transplantation Safety Switches
Suicide gene strategies involve genetically engineering therapeutic cells to express "safety switch" genes that allow selective ablation of the transplanted cells if adverse effects, such as tumor formation or unacceptable toxicity, occur after transplantation [52] [53] [54].
Major Suicide Gene Systems: Mechanisms and Applications
Table 2: Comparison of Leading Suicide Gene Systems
| System | Origin | Activating Agent | Mechanism of Action | Activation Kinetics | Clinical Validation |
|---|---|---|---|---|---|
| HSV-TK | Viral | Ganciclovir (GCV) | Phosphorylates GCV → DNA chain termination & apoptosis [54] | Slow (3-5 days) [55] | Phase I-III trials [56] |
| Inducible Caspase 9 (iCasp9) | Human | AP1903/Chemical Dimerizer | Caspase cascade activation → Apoptosis [52] [54] | Rapid (<30 minutes) [55] [54] | Phase I trials [52] |
| CD20-Based | Human | Rituximab/Anti-CD20 mAb | Antibody-dependent cellular cytotoxicity & complement activation [55] [54] | Rapid (hours) [55] | Preclinical models [52] [55] |
| RQR8 | Engineered Human | Rituximab | Combined CD20 mimotope & CD34 selector → Cell elimination [52] | Rapid (hours) | Preclinical models [52] |
| Mutant TMPK (mTMPK) | Engineered Human | AZT/Zidovudine | Enhanced phosphorylation of AZT → DNA chain termination [55] | Intermediate | Preclinical models [55] |
Key Signaling Pathways in Suicide Gene Systems
The following diagram illustrates the core apoptotic pathways activated by major suicide gene systems:
Experimental Evidence and Clinical Validation
iCasp9 Clinical Performance
In a phase I clinical trial, recipients of haploidentical hematopoietic stem cell transplantation for hematological malignancies received escalating doses of ΔiC9-modified T cells. When patients developed acute graft-versus-host disease (GVHD), administration of a single dose of 0.4 mg/kg AP1903 resulted in apoptosis of ≥90% of ΔiC9-modified T cells within 30 minutes, followed by rapid and permanent abrogation of GVHD [52]. Remarkably, residual ΔiC9-modified T cells were able to re-expand and contained pathogen-specific precursors, suggesting preserved immune function in non-eliminated cells [52].
HSV-TK System in Parkinsonian Models
A study utilizing a hPSC line carrying a FailSafe suicide gene (thymidine kinase linked to cyclinD1) demonstrated robust ventral midbrain specification in vitro and formed functional neural grafts upon transplantation in a Parkinsonian rat model [53]. Activation of the suicide gene by ganciclovir administration resulted in significantly smaller grafts without affecting the total yield of dopamine neurons or their capacity to innervate the host brain and reverse motor deficits at six months. This approach effectively reduced non-dopamine neuronal, glial, and proliferative populations that may pose adverse influences on graft and host function [53].
Combinatorial Suicide Gene Approaches
Research has explored combining multiple suicide genes to overcome limitations of individual systems. One study tested a two-suicide gene system combining ΔiC9 with an inducible caspase 8 (ΔiC8) or with the RQR8 compact suicide gene [52]. Jurkat cells co-transduced to co-express both systems showed enhanced elimination with superior reduction in cell regrowth when both systems were activated simultaneously compared to individual activation [52].
Clinical Trial of Suicide Gene Therapy for GBM
A first-in-human, phase I clinical trial investigated suicide gene therapy using allogeneic adipose tissue-derived mesenchymal stem cells (ADSCs) carrying the HSV-TK gene in patients with recurrent glioblastoma multiforme (GBM) [56]. The therapy demonstrated a favorable safety profile with a median overall survival of 16.0 months and median progression-free survival of 11.0 months. Among 12 patients, 8 showed partial response and 4 showed stable disease, supporting further investigation in phase II/III trials [56].
Comparative Analysis: Strategic Considerations for Therapeutic Development
Integration with Differentiation Protocols
The timing and duration of suicide gene activation require careful optimization based on cell cycle kinetics of target cells. Research comparing undifferentiated PSCs and ventral midbrain neural progenitors revealed that total cell cycle length significantly increased in maturing cultures (PSCs: 16±0.4h, VM: 33±0.6h), while the proportion of time spent in S phase was significantly reduced (PSCs: 55%, VM: 44%) [53]. These differences impact susceptibility to suicide gene systems like HSV-TK/GCV that incorporate during DNA replication, necessitating prolonged GCV administration (10 days) for complete elimination of neural progenitors compared to undifferentiated PSCs (5 days) [53].
Addressing Limitations and Enhancing Efficacy
Table 3: Strategies to Overcome Limitations of Tumor-Risk Mitigation Approaches
| Approach | Limitations | Mitigation Strategies |
|---|---|---|
| Purification Methods | Incomplete removal; Potential damage to differentiated cells; Does not address late-emerging risks | Combine multiple methods; Regular monitoring for genetic instability; Use with suicide genes as backup |
| HSV-TK System | Immunogenic; Slow kinetics; Interferes with ganciclovir use for CMV [55] [54] | Use in immunocompromised settings; Codon optimization; Prolonged drug administration [56] |
| iCasp9 System | Incomplete elimination (90-95%); Potential resistance mechanisms [52] | Combinatorial approaches; BCL-2 inhibition; Repeated/heightened dimerizer doses [52] |
| CD20/RQR8 System | Depletes endogenous B-cells; Limited clinical validation [55] [54] | Transient B-cell depletion; Codon optimization; Combination with other systems [52] [55] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Tumorigenicity Mitigation Studies
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| Suicide Gene Activators | AP1903/Rimiducid (iCasp9), Ganciclovir (HSV-TK), Rituximab (CD20/RQR8) | Small molecules or antibodies that activate suicide gene systems [52] [54] [56] |
| Pluripotency Markers | Anti-OCT4, Anti-SOX2, Anti-NANOG, Anti-SSEA-4, Anti-TRA-1-60, Anti-TRA-1-81 | Identify residual undifferentiated PSCs via flow cytometry, ICC [50] |
| Cell Line Engineering | SFG retroviral vector, Lentiviral vectors, PiggyBac transposon system | Deliver suicide genes or reporter constructs to therapeutic cells [52] [55] [57] |
| Apoptosis Detection | Anti-active Caspase-3, Annexin V, Propidium Iodide | Validate suicide gene efficacy through apoptosis measurement [52] [54] |
| In Vivo Models | Immunodeficient mice (NSG, NOD/SCID), Parkinsonian rat model | Assess teratoma formation and therapeutic efficacy [50] [53] |
Mitigating tumorigenicity requires a multi-layered approach that combines rigorous pre-transplantation purification with post-transplantation safety switches. The experimental data presented in this guide demonstrates that no single method provides complete protection, but strategic integration of complementary approaches can significantly enhance safety profiles. Purification strategies using small molecules, miRNAs, or antibody-based methods can reduce initial tumorigenic load, while suicide gene systems like iCasp9 and HSV-TK provide a crucial safety net against unexpected proliferation or malignant transformation after transplantation.
The choice of specific strategies must be tailored to the particular therapeutic application, considering the differentiation protocol efficiency, target cell characteristics, and clinical context. As the field advances, innovations in genetic engineering, such as combinatorial suicide gene systems and enhanced targeting approaches, promise to further strengthen the safety framework for stem cell-based therapies, accelerating their translation to clinical practice.
Optimizing Delivery Routes and Dosing to Minimize Adverse Events
The advancement of stem cell-based therapies, particularly those utilizing mesenchymal stem cells (MSCs), has introduced a new class of "living biodrugs" with immense therapeutic potential for conditions ranging from heart failure to acute kidney injury and neurological disorders [41]. Unlike conventional pharmaceuticals, these living biologic agents present unique challenges in determining optimal delivery routes and dosing regimens to maximize efficacy while minimizing adverse events. Safety concerns including thromboembolism, fibrosis, and complications related to cell processing have been reported, highlighting the critical need for precise administration protocols [58]. This comparative guide examines current evidence and experimental data on delivery methods and dosing strategies, providing researchers and drug development professionals with evidence-based frameworks for optimizing the safety profiles of stem cell-based therapies.
Comparative Analysis of Delivery Routes: Safety and Efficacy Profiles
Route-Dependent Safety Outcomes in Cardiac Applications
The route of administration significantly influences both the safety profile and therapeutic efficacy of MSC therapies, particularly in cardiovascular applications. A 2024 systematic review and meta-analysis of phase II randomized controlled trials (RCTs) in heart failure patients revealed that all delivery methods demonstrated safety, with no significant difference in serious adverse events (SAEs) compared to controls (RR: 0.84, 95%CI: 0.66-1.05, P = 0.11) [59]. However, subgroup analysis revealed important route-specific safety distinctions, with transendocardial injection (TESI) showing a significant reduction in serious adverse events (RR = 0.71, 95%CI: 0.54-0.95, P = 0.04) [59].
Table 1: Safety and Efficacy of MSC Delivery Routes in Heart Failure
| Delivery Route | Safety Profile (SAEs) | LVEF Improvement | 6MWD Improvement | Key Advantages | Reported Risks |
|---|---|---|---|---|---|
| Transendocardial (TESI) | RR: 0.71 (0.54-0.95)* | Not significant | Data insufficient | Site-directed delivery; Bypasses pulmonary circulation | Minimal procedural risk |
| Intracoronary (IC) | No significant difference | WMD: 7.26% (5.61-8.92)* | WMD: 115.0m (91.5-138.5)* | Direct coronary access; Clinically established | Potential microvascular obstruction |
| Intravenous (IV) | No significant difference | Not significant | Data insufficient | Minimally invasive; Systemic distribution | Pulmonary first-pass effect; Lung entrapment |
| Transepicardial (TEPI) | Data insufficient | Data insufficient | Data insufficient | Direct visual guidance; Precision delivery | Surgical invasiveness |
*Statistically significant
Route Selection for Renal Applications
In renal applications, the choice of administration route significantly impacts cell engraftment and potential adverse events. Intravenous administration, while minimally invasive, results in significant pulmonary first-pass effect, with cells trapped in lung tissue and potentially causing complications [60]. One study reported that intravenous delivery required higher cell doses to achieve therapeutic effects at the target site, consequently increasing the risk of pulmonary embolism and thrombotic events [60]. Intra-arterial delivery bypasses the pulmonary filter but carries risks of cell embolism and increased procedural trauma [60].
Local administration approaches for renal conditions, including renal cortex injection and subcapsular implantation, have demonstrated enhanced safety profiles in preclinical models. These methods enable precise cell delivery to the target tissue while minimizing systemic distribution and associated risks [60]. In animal models of acute kidney injury, local administration demonstrated improved renal function recovery, attenuated tubular injury and fibrosis, with no identifiable safety concerns [60].
Dose-Response Relationships: Balancing Efficacy and Safety
Dose-Dependent Safety and Efficacy in Heart Failure
Establishing a dose-response relationship is critical for optimizing MSC therapies, with recent evidence challenging conventional "more is better" assumptions. A 2024 systematic review and meta-analysis of RCTs involving 1,098 heart failure patients revealed a superior safety and efficacy profile for lower-dose MSC treatments [61]. When studies were categorized as low-dose (<100 million cells) or high-dose (≥100 million cells), low-dose treatment demonstrated a more significant protective effect against mortality and major adverse cardiac events (MACE) [61].
Table 2: Dose-Response Relationship in Heart Failure with Reduced EF
| Dose Category | Cell Quantity | LVEF Change | 6-MWD Improvement | Safety Profile | Recommendation Level |
|---|---|---|---|---|---|
| Low Dose | <100 million cells | WMD: 3.01% (0.65-5.38%)* | 26.74m (3.74-49.74m)* | Superior protective effect | First-line consideration |
| High Dose | ≥100 million cells | WMD: -0.48% (-2.14-1.18) | 36.73m (6.74-66.72m)* | Higher event rates | Conditional use |
| Excluding ADRCs | <100 million cells | Significant improvement | Data insufficient | Better safety profile | Recommended refinement |
*Statistically significant
Functional capacity improvements, as measured by the 6-minute walk distance (6-MWD), were observed in both low-dose (26.74m, 95% CI: 3.74-49.74m) and high-dose (36.73m, 95% CI: 6.74-66.72m) groups [61]. The exclusion of studies using adipose-derived regenerative cells (ADRCs) further enhanced safety outcomes and significant LVEF improvements, suggesting that cell source modifications can optimize the therapeutic window [61].
Dose Optimization Principles Across Applications
The dose-response relationship varies significantly based on cell type, administration route, and disease pathology. A landscape analysis of oncology therapies reveals that compounds approved at maximum tolerated dose (MTD) demonstrated lower dose intensity and higher dose modifications due to adverse events compared to those approved below MTD [62]. This highlights the importance of dose optimization to balance efficacy with tolerability.
In MSC applications, overdosing has been associated with increased thromboembolic risk via release of procoagulant tissue factor [58]. Case reports describe inflammatory-associated thromboembolism in kidney transplant patients following umbilical cord-derived MSC infusion, emphasizing the critical relationship between cell quantity and adverse events [58]. Conversely, insufficient dosing may yield subtherapeutic effects, underscoring the need for precise dose titration.
Experimental Protocols and Methodologies
Preclinical Assessment of Delivery Routes
Renal Local Administration Protocol (as implemented in animal models of acute kidney injury) [60]:
- Animal Preparation: Anesthetize using approved institutional protocols (e.g., ketamine/xylazine for rodents)
- Surgical Exposure: Perform flank incision to expose the kidney under aseptic conditions
- Cell Injection: Slowly administer MSC suspension (50-100μL containing 1-2×10^6 cells) using insulin syringe with 29G needle
- Injection Sites: Multiple cortical sites avoiding major vessels, or subcapsular space
- Hemostasis: Apply gentle pressure with sterile sponge post-injection
- Closure: Standard surgical wound closure
- Monitoring: Assess renal function (serum creatinine, BUN) at 24, 48, and 72 hours post-procedure
This method has demonstrated improved cell retention, enhanced therapeutic potential, and reduced risks of lung infarction and mortality compared to systemic routes [60].
Clinical Dose-Finding Study Design
Phase II RCT Dose-Escalation Methodology (as implemented in heart failure trials) [61]:
- Study Design: Randomized, double-blind, placebo-controlled trial
- Dose Cohorts: Predefined low-dose (<100 million cells) and high-dose (≥100 million cells) groups
- Administration: Uniform delivery route (typically intracoronary or transendocardial) across dose groups
- Endpoint Assessment:
- Safety: Death and MACEs recorded throughout study duration
- Efficacy: LVEF measured by cardiac MRI or echocardiography at baseline and 6-12 months
- Functional Capacity: 6-MWD performed at standardized intervals
- Biomarkers: pro-BNP levels serially measured
- Statistical Analysis: Pre-specified subgroup analysis by dose category using random-effects models
This methodology enables direct comparison of dose-dependent effects while controlling for confounding variables.
Visualization of Optimization Strategies
Delivery Route Selection Algorithm
Dose Optimization Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Delivery and Dosing Optimization
| Reagent/Material | Function | Application Examples | Safety Considerations |
|---|---|---|---|
| Fetal Bovine Serum (FBS) | Cell culture supplement | MSC expansion | Risk of xeno-contamination; Use human serum alternatives |
| Human Serum Albumin | Cryopreservation medium | Cell storage | Reduced immune reactions vs. FBS |
| Procoagulant Tissue Factor Assay | Safety screening | Thrombosis risk assessment | Critical for high-dose formulations |
| Chromosomal Aberration Test | Genetic stability check | Cell processing QC | Essential after long-term culture |
| Mycoplasma Detection Kit | Contamination screening | Cell banking | Overdosed antibiotics increase risk |
| Hydrogel Scaffolds | 3D culture & delivery | Enhanced cell retention | Improves survival post-administration |
| Population PK/PD Models | Dose-exposure relationship | Trial simulation | Predicts optimal dosing regimens |
Optimizing delivery routes and dosing strategies represents a critical pathway toward enhancing the safety profile of stem cell-based therapies. The evidence indicates that route selection should be disease-specific, with transendocardial and local administration approaches offering superior safety profiles for cardiac and renal applications, respectively. Perhaps counterintuitively, lower MSC doses (<100 million cells) demonstrate superior safety and efficacy in heart failure treatment compared to higher doses, challenging conventional dosing paradigms.
Future optimization efforts should incorporate patient-specific factors, cell source variations, and advanced delivery technologies to further refine the therapeutic window. The continued standardization of dosing protocols and route selection criteria will accelerate the clinical translation of stem cell therapies while maintaining the paramount importance of patient safety.
Standardizing Manufacturing to Overcome Heterogeneity and Contamination
The therapeutic potential of stem cell-based interventions is vast, offering promising strategies for conditions previously considered untreatable, from neurological disorders like Parkinson's disease to cardiovascular diseases and autoimmune conditions [5] [63]. However, this promise is tempered by significant safety challenges, primarily stemming from two interconnected issues: cellular heterogeneity and contamination risks. These challenges represent the most significant barriers to the widespread clinical translation of stem cell therapies [5] [64].
Product heterogeneity refers to the natural biological variation in stem cell populations, which can lead to inconsistent therapeutic outcomes and unpredictable safety profiles. Meanwhile, contamination risks encompass microbial infection, cross-contamination, and the introduction of unintended cell types during manufacturing [5] [63]. The dual challenges of heterogeneity and contamination are intrinsically linked to manufacturing processes, underscoring why standardized production protocols form the cornerstone of biosafety in stem cell-based therapies [5].
This article objectively compares standardized versus non-standardized manufacturing approaches, providing experimental data and methodologies relevant to researchers, scientists, and drug development professionals working to enhance the safety profile of stem cell-based therapies.
Cellular heterogeneity manifests at multiple levels, including genetic variation, differential differentiation potential, and functional characteristics across cell populations. Without proper controls, this heterogeneity can lead to varied potency, unpredictable engraftment, and serious safety complications, including tumor formation [5] [64].
Comparative Analysis of Heterogeneity Control Methods
Table 1: Experimental Comparison of Heterogeneity Control Strategies in Stem Cell Manufacturing
| Control Strategy | Experimental Approach | Key Parameters Measured | Data Outcome (Standardized vs. Non-standardized) | Reference Technique |
|---|---|---|---|---|
| Cell Sorting & Characterization | Flow cytometry for surface marker expression | Percentage of target cell population (e.g., CD73+, CD90+, CD105+ for MSCs) | 95.2% ± 2.1% vs. 72.8% ± 15.3% | Flow cytometry with specific antibody panels [5] |
| Genetic Stability Monitoring | Karyotyping and genetic analysis | Chromosomal abnormalities per passage | < 0.5% abnormalities at P10 vs. 3.8% abnormalities at P10 | G-banding karyotype analysis [5] [64] |
| Differentiation Potential Assessment | Trilineage differentiation assays | Adipogenic, chondrogenic, osteogenic differentiation efficiency | Consistent >85% differentiation vs. highly variable (45-90%) differentiation | Histochemical staining (Oil Red O, Alcian Blue, Alizarin Red) [5] |
| Biodistribution Tracking | Quantitative PCR and imaging techniques | Cell migration to non-target sites | Predictable distribution vs. unexpected migration patterns | qPCR for species-specific genes, PET, MRI [5] |
Detailed Experimental Protocol: Cell Population Purity Assessment
Objective: To determine the percentage of target stem cell population in a final product using flow cytometry.
Materials:
- Single-cell suspension of stem cell product
- Fluorescently labeled antibodies against target surface markers (e.g., CD73, CD90, CD105 for MSCs)
- Isotype control antibodies
- Flow cytometry buffer (PBS with 1-2% FBS)
- Flow cytometer with appropriate laser and detector configuration
Methodology:
- Prepare single-cell suspension at concentration of 1×10^7 cells/mL
- Aliquot 100 μL of cell suspension per test tube
- Add predetermined optimal concentration of fluorescent antibodies to experimental tubes and isotype controls to control tubes
- Incubate for 30 minutes at 4°C in the dark
- Wash cells twice with flow cytometry buffer
- Resuspend cells in 300-500 μL buffer for analysis
- Acquire data on flow cytometer, collecting at least 10,000 events per sample
- Analyze data using forward versus side scatter gating to exclude debris and doublets, followed by fluorescence analysis for target markers
Quality Threshold: Products for clinical use should demonstrate >90% purity for target cell population markers [5].
Contamination Control: Methodologies and Standards
Contamination in stem cell products represents a critical safety concern, encompassing microbial contamination (bacteria, fungi, viruses, mycoplasma), cross-contamination with other cell lines, and introduction of unintended cell types during differentiation.
Comprehensive Contamination Testing Framework
Table 2: Experimental Framework for Contamination Control in Stem Cell Manufacturing
| Contamination Type | Detection Method | Standardized Protocol | Acceptance Criteria | Experimental Evidence |
|---|---|---|---|---|
| Sterility (Bacteria/Fungi) | Automated culture systems (e.g., BACTEC) | 14-day incubation in multiple media | No growth in any test system | Sterility failure rate: <1% vs. 5-15% in non-standardized approaches [5] |
| Mycoplasma | PCR-based detection and culture methods | Nucleic acid extraction and amplification with positive controls | Negative by both methods | Detection sensitivity: 1-10 CFU with standardized PCR vs. 100-1000 CFU with culture alone [5] |
| Endotoxin | Limulus Amebocyte Lysate (LAL) test | Kinetic chromogenic method with standard curve | <0.5 EU/mL for parenteral administration | Coefficient of variation: <10% with standardized method vs. 15-25% with gel-clot method [5] |
| Viral Contamination | PCR for specific viruses (HIV, Hepatitis B/C, herpes viruses) | Multiplex PCR with internal controls | Negative for specified pathogens | False negative rate: <0.1% with standardized multiplex PCR vs. 1-5% with individual assays [65] |
| Cell Line Cross-Contamination | Short Tandem Repeat (STR) profiling | Analysis of 8-16 core loci with reference database | Match to reference cell line with >80% similarity | Cross-contamination detection: 100% with standardized STR vs. unable to detect with morphology alone [5] |
Detailed Experimental Protocol: Mycoplasma Detection by PCR
Objective: To detect mycoplasma contamination in stem cell cultures using PCR-based method.
Materials:
- DNA extraction kit (commercial system recommended)
- Mycoplasma PCR detection kit (including primers, controls, and master mix)
- Sterile phosphate-buffered saline (PBS)
- Thermal cycler
- Gel electrophoresis equipment or real-time PCR detection system
Methodology:
- Collect approximately 1×10^6 cells by centrifugation (300 × g for 5 minutes)
- Wash cell pellet with sterile PBS and resuspend in 200 μL PBS
- Extract DNA according to manufacturer's protocol, including positive and negative extraction controls
- Prepare PCR reaction mix according to detection kit instructions:
- 12.5 μL master mix
- 2.5 μL mycoplasma primer mix
- 5 μL template DNA
- 5 μL nuclease-free water
- Include the following controls in each run:
- Positive control (provided in kit)
- Negative template control (nuclease-free water)
- Negative extraction control
- Internal amplification control (if available)
- Run PCR with the following cycling conditions:
- Initial denaturation: 95°C for 2 minutes
- 35 cycles of: 95°C for 30 seconds, 60°C for 30 seconds, 72°C for 30 seconds
- Final extension: 72°C for 5 minutes
- Analyze results by gel electrophoresis (expected band ~500 bp) or real-time detection
Interpretation: Samples showing amplification at the expected size are considered positive for mycoplasma contamination and should be discarded immediately to prevent spread [5].
Biosafety Assessment: Standardized versus Non-Standardized Approaches
Rigorous biosafety assessment is essential for stem cell therapies, with standardized manufacturing protocols significantly enhancing the predictive value of these assessments.
Tumorigenicity Risk Assessment
The risk of tumor formation represents one of the most significant safety concerns for stem cell therapies, particularly those involving pluripotent stem cells [5] [64].
Experimental Approaches for Tumorigenicity Assessment:
- In vitro soft agar colony formation assay: Measures anchorage-independent growth potential
- In vivo tumor formation in immunodeficient mice: Gold standard for assessing teratoma/tumor formation potential
- Genetic stability monitoring: Regular karyotyping and genetic analysis to detect abnormalities
Standardized Protocol: In Vivo Tumorigenicity Assay
- Animal Model: Immunocompromised mice (e.g., NOD-scid IL2Rγnull)
- Cell Administration: 1×10^7 cells per animal via subcutaneous or intramuscular injection
- Observation Period: 16-24 weeks with regular palpation for tumor formation
- Endpoint Analysis: Histopathological examination of suspected masses and key organs
Experimental Evidence: Studies demonstrate that standardized manufacturing with rigorous quality controls reduces tumorigenic potential from approximately 15% to less than 1% in pluripotent stem cell-derived products [5] [64].
Biodistribution and Long-Term Fate Analysis
Understanding the migration, engraftment, and persistence of administered stem cells is critical for predicting and preventing off-target effects.
Standardized Tracking Methodologies:
- Quantitative PCR: For species-specific genes in xenograft models
- Bioluminescence Imaging: Using luciferase-transduced cells
- Magnetic Resonance Imaging (MRI): With iron oxide-labeled cells
- Positron Emission Tomography (PET): Using radiolabeled tracers
Experimental Evidence: Standardized manufacturing results in more predictable biodistribution patterns, with >85% of cells remaining at the administration site versus highly variable distribution (30-90%) with non-standardized approaches [5].
Visualization: Standardized Manufacturing Workflow for Stem Cell Therapies
The following diagram illustrates the integrated approach required for standardized stem cell manufacturing, highlighting critical control points for managing heterogeneity and contamination risks.
This workflow emphasizes the staged approach with critical control points where specific heterogeneity and contamination checks must be implemented and passed before proceeding to the next manufacturing stage.
The Scientist's Toolkit: Essential Reagents and Materials
Implementing standardized manufacturing requires specific research reagents and materials designed to maintain consistency and prevent contamination.
Table 3: Essential Research Reagent Solutions for Standardized Stem Cell Manufacturing
| Reagent Category | Specific Examples | Function in Standardization | Key Quality Parameters |
|---|---|---|---|
| Defined Culture Media | Xeno-free MSC medium, E8 medium for pluripotent cells | Eliminates batch-to-batch variability of serum-containing media | Certificate of analysis with component concentrations, endotoxin levels <0.5 EU/mL [5] |
| Characterized Growth Factors | Recombinant FGF-2, TGF-β, BMP proteins | Maintains consistent differentiation inhibition/induction | Purity >95% by SDS-PAGE, biological activity confirmed by dose-response curves [5] |
| Cell Separation Reagents | Fluorescent antibody panels, magnetic bead separation kits | Ensures reproducible isolation of target cell populations | Lot-to-lot consistency validation, >90% efficiency in separation protocols [5] |
| Quality Control Assays | Mycoplasma detection kits, sterility testing systems | Standardized contamination screening | Validation against reference standards, inclusion of appropriate controls [5] [65] |
| Cryopreservation Solutions | Defined cryoprotectant formulations | Maintains cell viability and function post-thaw | Post-thaw viability >80%, maintained differentiation capacity [5] |
Standardized manufacturing protocols represent a fundamental requirement for overcoming the dual challenges of heterogeneity and contamination in stem cell-based therapies. The experimental data and methodologies presented demonstrate quantitatively superior outcomes across critical safety parameters—including product consistency, contamination control, and tumorigenicity risk reduction—when standardized approaches are implemented.
As the field advances toward broader clinical application, adherence to rigorous standards such as those outlined in the ISSCR Guidelines for Stem Cell Research and Clinical Translation becomes increasingly vital [15]. The comparative data presented in this analysis provides researchers and drug development professionals with evidence-based guidance for implementing manufacturing protocols that maximize safety profiles without compromising therapeutic potential.
Future directions will likely involve further refinement of real-time monitoring technologies, advanced analytical methods for characterizing cellular heterogeneity, and international harmonization of manufacturing standards to ensure consistent safety profiles across global therapeutic development programs.
A major hurdle in transitioning stem cell therapies from the laboratory to the clinic is the robust immune-mediated rejection of allogeneic cells. The human immune system is programmed to recognize and destroy cells displaying foreign markers, primarily human leukocyte antigens (HLAs). These highly polymorphic cell surface proteins, encoded by the major histocompatibility complex (MHC), are the primary triggers of graft rejection. When transplanted allogeneic cells present mismatched HLA molecules, they activate both the adaptive immune system (T cells and B cells) and innate immune system (Natural Killer cells), leading to the destruction of the therapeutic graft [66] [67].
Overcoming this immunogenicity is critical for the success and scalability of regenerative medicine. Two dominant, complementary strategies have emerged to address this challenge: the creation of HLA-engineered universal donor cells and the establishment of banks of HLA-matched stem cell lines. This guide objectively compares the leading approaches for managing immunogenicity, detailing their underlying mechanisms, experimental protocols, and the critical safety considerations that must be addressed for clinical application. This analysis is framed within the essential, broader context of biosafety assessment for stem cell-based therapies, which demands rigorous evaluation of toxicity, tumorigenicity, and immunogenicity [5] [68].
Strategic Approaches to Immune Evasion
The core objective of immune evasion strategies is to prevent host immune cells from recognizing donor cells as foreign. The table below summarizes the key characteristics of the primary approaches.
Table 1: Comparison of Strategies for Managing Immunogenicity in Stem Cell Therapies
| Strategy | Core Principle | Key Genetic Targets | Primary Immune Cells Evaded | Major Advantages | Major Challenges & Risks |
|---|---|---|---|---|---|
| HLA Homozygous Cell Banks | Banking iPSC lines with common homozygous HLA haplotypes to serve a large population with partial matches [69]. | Natural HLA haplotypes (no engineering). | Alloreactive T cells (with a sufficient match). | Utilizes non-engineered, genetically stable cells; simpler regulatory path. | Limited population coverage with a finite number of lines; requires extensive banking logistics [70]. |
| MHC Class I Knockout (KO) | Prevents CD8+ T cell recognition by eliminating surface expression of HLA-A, -B, and -C [66] [69]. | B2M (most common) or direct KO of HLA-A, -B, -C. | CD8+ Cytotoxic T cells. | Highly effective against T cell cytotoxicity. | Triggers "missing-self" response, leading to NK cell-mediated lysis [66] [71]. |
| MHC Class II Knockout | Prevents CD4+ T cell help and activation by eliminating HLA class II expression [66]. | CIITA (master regulator of Class II) [66]. | CD4+ Helper T cells. | Disrupts a critical axis for adaptive immune activation. | Does not protect from CD8+ T or NK cell responses. |
| Multi-Target KO (Class I & II) | Synergistic targeting to evade both key T cell populations [66] [70]. | B2M + CIITA or HLA-A/B + HLA-DRA [66] [70]. | CD8+ and CD4+ T cells. | Broader protection against adaptive immunity. | NK cell-mediated lysis remains a significant problem [66]. |
| "Hypoimmune" Cells (KO + Transgene) | A multi-pronged approach combining HLA deletion with expression of immunosuppressive transgenes [72]. | B2M/CIITA KO + HLA-G, PD-L1, PD-L2, CD47. | T cells, NK cells, macrophages. | Comprehensive evasion of innate and adaptive immunity. | Higher genetic complexity; potential for immunogenicity of transgenes; increased tumorigenicity risk [72]. |
Experimental Protocols for Generating Universal Cells
Generation of HLA Class I/II Double-Knockout iPSCs
A 2025 study detailed a protocol for creating triple-knockout iPSCs by disrupting HLA-A, HLA-B, and HLA-DRA genes using CRISPR-Cas9 in a heterozygous iPSC line [70]. This method targets the polymorphic HLA-A and HLA-B directly, while KO of the non-polymorphic HLA-DRA gene disrupts the structure of all MHC class II molecules (DR, DQ, DP), a more efficient approach than targeting individual DRB genes [70].
Detailed Workflow:
- Guide RNA (gRNA) Design and Validation: Design and validate high-efficiency gRNAs for HLA-A, HLA-B, and HLA-DRA genes.
- Electroporation: On Day 0, prepare CRISPR-Cas9 ribonucleoprotein (RNP) complexes by combining 80 µg of each gRNA with 4 µg/µL of Cas9 nuclease. Electroporate 1 million iPSCs (e.g., YiP3 cell line) using a system like the Lonza 4D-Nucleofector (Program CA-137) [70].
- Single-Cell Cloning: Days 3-5: Harvest transfected cells and perform single-cell sorting via flow cytometry into 96-well plates.
- Clone Expansion and Genotyping: Culture single-cell clones and expand them. Between days 11-28, screen clones by PCR and Sanger sequencing to identify those with bi-allelic knockout of all three target genes. The final candidate clone (e.g., "Clone A7") is selected [70].
- Validation:
- Pluripotency: Confirm expression of markers like OCT4, SOX2, and NANOG via mRNA and protein analysis.
- Karyotyping: Perform G-bandning to ensure no chromosomal abnormalities were introduced.
- In Vitro Differentiation: Use a trilineage differentiation kit to confirm differentiation potential into ectoderm, mesoderm, and endoderm.
- Immunogenicity Assay: Co-culture engineered iPSCs with human peripheral blood mononuclear cells (PBMCs) and monitor T cell (especially effector memory T cell) proliferation to confirm reduced immunogenicity [70].
The following workflow diagram summarizes the key steps in this gene-editing protocol:
Engineering of Hypoimmunogenic Cells with Immune Modulators
A 2024 study adopted a more complex strategy, creating HLA class Ia/II DKO iPSCs and further arming them with immunomodulatory transgenes and a safety switch [72].
Detailed Workflow:
- Generation of HLA Class Ia/II DKO iPSCs:
- Sequentially electroporate iPSCs with Cas9 RNP complexes targeting HLA-A, -B, and -C genes. Screen clones via flow cytometry (reduced HLA class I staining after IFN-γ stimulation) and in vitro Cas9 cleavage assays to identify homozygous mutants [72].
- Electroporate the selected HLA class Ia KO clone with RNP targeting RFXANK, a gene critical for MHC class II expression. Screen for homozygous KO clones as above [72].
- Introduction of Transgenes:
- Use a piggyBac transposon system to introduce expression cassettes for the following into the HLA class Ia/II DKO iPSCs:
- β-2-microglobulin (B2M): To enhance surface expression of HLA-G.
- HLA-G: A non-polymorphic HLA class I molecule that inhibits NK and T cell cytotoxicity [66] [72].
- PD-L1 and PD-L2: Immune checkpoint molecules that suppress T cell activation.
- RapaCasp9: A rapamycin-activated caspase-9 suicide gene safety switch to allow for ablation of the cells in case of adverse events [72].
- Use a piggyBac transposon system to introduce expression cassettes for the following into the HLA class Ia/II DKO iPSCs:
- Validation:
- Confirm transgene expression and pluripotency.
- Differentiate the engineered "HyPSCs" into target cells like hematopoietic progenitor cells (HPCs) and endothelial cells.
- Perform mixed lymphocyte reactions and NK cell cytotoxicity assays to demonstrate evasion of both innate and adaptive immunity.
- Validate the RapaCasp9 safety switch by administering rapamycin and confirming apoptosis in vitro and in vivo [72].
Quantitative Data and Comparative Efficacy
The performance of these strategies is quantitatively assessed through a variety of immune functional assays. The table below summarizes typical experimental data from key studies.
Table 2: Experimental Immune Evasion Data for Different Engineered Cell Products
| Cell Type / Strategy | Experimental Model | Key Outcome Measures | Result | Source |
|---|---|---|---|---|
| B2M KO ESC (MHC I KO) | Mixed Leukocyte Reaction (MLR) | CD8+ T cell response | Significant reduction | [69] |
| B2M KO ESC | In Vitro Killing Assay | CD8+ T cell-mediated killing | <1% of control | [66] |
| β2M-HLA-G Fusion iPSC | NK Cell Cytotoxicity Assay | NK-mediated lysis | Resistant | [66] |
| HLA-A/B/DRA KO iPSC (Clone A7) | Immunogenicity Assay | Effector Memory T cell proliferation | Absent | [70] |
| HyPSC (KO + HLA-G/PD-L1/PD-L2) | NK Cell Cytotoxicity Assay | NK-mediated lysis | Evaded | [72] |
| HyPSC (KO + HLA-G/PD-L1/PD-L2) | Mixed Lymphocyte Reaction | T cell proliferation | Suppressed | [72] |
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents and their applications for research in HLA engineering and immunogenicity assessment.
Table 3: Key Research Reagents for HLA Engineering and Immune Evasion Studies
| Research Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| CRISPR-Cas9 System (RNP) | Knocking out HLA genes (B2M, CIITA, HLA-A/B) with high precision and reduced off-target effects. | Generation of HLA class I/II DKO iPSCs [70] [72]. |
| Adeno-Associated Virus (AAV) Vectors | High-efficiency gene targeting for creating homozygous knockouts or inserting transgenes without nucleases. | Derivation of HLA-homozygous ESCs via mitotic recombination [69]. |
| PiggyBac Transposon System | Stable integration of large genetic cargo (e.g., multiple transgenes) for creating "hypoimmune" cells. | Introducing HLA-G, PD-L1, PD-L2, and RapaCasp9 into DKO iPSCs [72]. |
| Flow Cytometry Antibodies | Detecting surface expression of HLA molecules (e.g., pan-HLA class I, HLA-G), pluripotency markers, and immune cell markers. | Validating HLA knockout efficiency and characterizing differentiated cell products [70] [72]. |
| Interferon-gamma (IFN-γ) | Upregulating MHC expression to test the robustness of HLA knockout under inflammatory conditions. | Stress-testing engineered cells to ensure no aberrant HLA expression [70] [72]. |
| Mixed Leukocyte Reaction (MLR) | In vitro co-culture assay to measure T cell activation and proliferation against donor cells. | Quantifying the immunogenicity of engineered stem cells or their derivatives [69] [72]. |
| Rapamycin | Pharmacological inducer of dimerization to activate the RapaCasp9 safety switch. | Testing the efficacy of the suicide gene system to ablate engineered cells [72]. |
Integrated Safety Assessment within a Biosafety Framework
The pursuit of universal donor cells must be contextualized within a comprehensive biosafety framework. The very modifications that confer immune evasion also present unique risks that must be mitigated [5] [68].
- Tumorigenicity and Oncogenicity: The deletion of MHC class I molecules is a known mechanism used by cancers to evade immune surveillance [71]. Therefore, hypoimmunogenic cells risk forming teratomas or tumors if any undifferentiated pluripotent cells remain after transplantation. Furthermore, the use of integrating vectors for transgenes and the potential for off-target effects from gene-editing nucleases like Cas9 could disrupt tumor suppressor genes or activate oncogenes [5] [72].
- Risk Mitigation Strategies:
- Safety Switches: Incorporating inducible suicide genes like RapaCasp9 or HSV-TK provides a controllable mechanism to eliminate the transplanted cells in case of unforeseen adverse events, such as teratoma formation [72].
- Biodistribution Studies: Using quantitative PCR (qPCR) and medical imaging (e.g., PET, MRI) in preclinical models to track the location, persistence, and potential proliferation of engineered cells after transplantation is a regulatory requirement [5] [68].
- Rigorous Product Quality Control: Final cell products must be thoroughly tested for sterility, identity, potency, viability, and genetic stability before clinical use, aligning with Quality-by-Design principles [5] [68].
The following diagram illustrates the critical relationship between immune evasion strategies and the essential components of a comprehensive safety assessment.
The field of managing immunogenicity for stem cell therapies is rapidly advancing, with strategies ranging from elegantly simple single-gene knockouts to sophisticated multi-gene engineered "hypoimmune" cells. The choice of strategy involves a critical trade-off between the degree of immune protection and the complexity of engineering and associated safety risks. HLA-matched cell banks offer a potentially safer, non-engineered path but with logistical and coverage limitations. In contrast, universal engineered cells promise true "off-the-shelf" availability but demand exceptionally rigorous biosafety profiles, including robust suicide gene systems.
For researchers and drug developers, the path forward requires a balanced approach. The selection of an immunogenicity management strategy must be guided by the specific clinical indication, target cell type, and duration of therapy. Crucially, from the earliest stages of development, these therapies must be designed and evaluated within a holistic biosafety framework that proactively addresses the unique risks of tumorigenicity and uncontrolled proliferation. As gene-editing technologies and our understanding of immunology continue to mature, the goal of safe, effective, and universally compatible stem cell therapies moves closer to reality.
Validating Safety Through Clinical Evidence and Comparative Analysis
Meta-Analysis of MSC Therapy Safety Across 62 Clinical Trials
Mesenchymal stem cell (MSC) therapy has emerged as a cornerstone of regenerative medicine, offering promising therapeutic potential for a diverse range of diseases. As the number of clinical trials investigating MSCs continues to grow, a rigorous and comprehensive assessment of their safety profile becomes increasingly critical for researchers, clinicians, and regulatory bodies. While individual clinical trials provide valuable insights, they are often limited by sample size and specific patient populations. Meta-analyses of multiple trials offer a more powerful approach to identifying safety signals and quantifying risks. This review synthesizes safety data from a comprehensive meta-analysis of 62 clinical trials to provide a definitive safety profile of MSC-based therapies, examining the frequency and nature of adverse events across different medical conditions, delivery routes, and cell sources. The findings provide the scientific community with an evidence-based foundation for guiding future clinical trial design and therapeutic applications.
Methodology of the Meta-Analysis
Search Strategy and Study Selection
Inclusion Criteria:
- Population: Patients with any of approximately 20 different diseases, as covered by the included trials.
- Intervention: Administration of any MSC product, regardless of dose, route of delivery, or tissue source.
- Comparison: Placebo control or standard of care.
- Outcomes: Reported data on adverse events (AEs) and/or serious adverse events (SAEs).
- Study Design: Randomized controlled trials only.
The screening process involved deduplication, title and abstract review, and full-text assessment for eligibility, ensuring the final analysis included only high-quality, relevant studies for a robust safety evaluation [73].
Data Extraction and Quality Assessment
Data extraction was performed systematically to capture all relevant safety and study characteristics. Key extracted information included:
- Trial demographics: Author, year, clinical field, and disease condition.
- Intervention details: MSC tissue source, cell dosage, preparation method, and route of administration.
- Safety outcomes: Total number of AEs and SAEs, specific event types, and their frequency in both treatment and control groups.
To assess the risk of bias in the included individual studies, standard tools such as the Cochrane Collaboration's Risk of Bias tool were utilized. This step was critical for evaluating the internal validity of the trials and the overall strength of the evidence synthesized in the meta-analysis [74] [75].
Quantitative Safety Profile of MSC Therapy
The meta-analysis of 62 randomized clinical trials, encompassing data from 3,546 participants, provides a robust, large-scale assessment of the safety of MSC administration [73]. The findings demonstrate that MSC therapies are generally safe and well-tolerated across a spectrum of diseases and patient populations.
Overall Safety and Tolerability: The analysis concluded that the administration of MSCs was not associated with a significant increase in serious adverse events (SAEs) compared to control groups. This overarching finding reinforces the favorable safety profile of MSCs that has been observed in numerous smaller studies [76].
The table below summarizes the comprehensive safety data from the meta-analysis, detailing the frequency of both common, non-serious adverse events and serious adverse events.
Table 1: Comprehensive Safety Profile of MSC Therapy from Meta-Analysis of 62 Trials (n=3,546 participants)
| Safety Outcome | Event Type | Frequency / Findings | Clinical Significance |
|---|---|---|---|
| Serious Adverse Events (SAEs) | Overall Incidence | No significant increase vs. control [73] | MSC therapy was not associated with an elevated risk of major safety concerns. |
| Common Non-Serious Adverse Events | Transient Fever | Most frequently reported [73] | Mild, self-resolving reaction likely related to cell infusion. |
| Administration Site Reactions | Common [73] | Includes discomfort, swelling, or redness; typically mild and temporary. | |
| Constipation | Reported [73] | Generally mild and manageable. | |
| Fatigue | Reported [73] | Typically transient. | |
| Sleeplessness | Reported [73] | Typically transient. | |
| Specific Risk Assessments | Oncogenic Risk | No cardiac-related cancer cases reported in AMI trials [74] | No short-term signal for cancer risk; longer follow-up recommended. |
| Immunogenicity | Low immunogenicity; some immune recognition with repeated allogeneic doses [73] | Supports general safety of allogeneic use, but caution advised for repeated administration. |
The analysis specifically investigated the oncogenic risk of MSC therapy. In the context of acute myocardial infarction (AMI), no cardiac-related cancer cases were reported in any study group, though the authors noted that longer follow-up is necessary to fully assess potential long-term oncogenic risks [74]. Furthermore, the immunogenicity of MSCs was explored. While MSCs are historically considered to have low immunogenicity, which supports the feasibility of allogeneic transplantation, the analysis noted that repeated intra-articular injections of allogeneic MSCs in an animal model triggered an adverse clinical response, suggesting that immune recognition by the host can occur in certain scenarios [73].
Experimental Protocols for Safety Assessment
The established safety profile of MSCs is underpinned by rigorous preclinical and clinical experimental protocols designed to identify potential risks. Regulatory agencies, such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), provide guidelines for the biosafety assessment of cell-based medicinal products [5].
Preclinical Safety and Toxicity Assessment
Before clinical administration, MSC products undergo extensive preclinical testing. General toxicity studies aim to determine the relationship between cell dose and adverse effects, often with a primary endpoint of structural tissue changes at post-mortem examination. These studies assess both acute and chronic toxicity in animal models [5].
The experimental workflow involves:
- In Vivo Monitoring: Animals are closely monitored for mortality, clinical signs, behavioral changes, and weight fluctuations.
- Laboratory Analysis: Blood and urine are collected for analysis, including complete blood count, clinical biochemistry (liver enzymes, renal function markers, electrolytes), and metabolic panels [5].
- Histopathological Examination: A critical component of toxicity analysis. A multi-organ histopathological assessment is performed, with particular attention to the transplantation site and organs where biodistribution studies indicate cellular accumulation. This examines cell death, immune cell infiltration, and other pathological signs [5].
Table 2: Key Research Reagent Solutions for MSC Safety and Efficacy Assessment
| Research Reagent / Tool | Primary Function in MSC Research |
|---|---|
| Flow Cytometry Antibodies (CD73, CD90, CD105, CD34, CD45, HLA-DR) | Characterizing MSC cell surface marker expression to verify identity and purity according to ISCT criteria [77]. |
| Differentiation Induction Media (Osteogenic, Chondrogenic, Adipogenic) | Assessing the multipotent differentiation potential of MSCs, a key defining property, in vitro [77] [73]. |
| Cell Culture Media & Supplements (e.g., Fetal Bovine Serum, Growth Factors) | Expanding and maintaining MSCs in culture while preserving their viability, potency, and genetic stability [5] [73]. |
| Quantitative PCR (qPCR) | Quantifying cell biodistribution and persistence in animal models by detecting human-specific DNA sequences in animal tissues [5]. |
| Cytokine/Chemokine Analysis Kits (ELISA, Multiplex Arrays) | Profiling the MSC secretome and measuring immunomodulatory factors in vitro or in patient sera post-treatment [77] [75]. |
Clinical Safety Monitoring
In clinical trials, safety monitoring is continuous and systematic. The protocol involves:
- Adverse Event Tracking: All AEs and SAEs are recorded from the time of cell administration through the follow-up period, with their relationship to the investigational product assessed.
- Laboratory Investigations: Serial blood tests (hematology, clinical chemistry) and vital sign measurements are performed to detect subclinical toxicity.
- Imaging: Techniques like magnetic resonance imaging (MRI) or positron emission tomography (PET) may be used to monitor for ectopic tissue formation or unexpected biodistribution [5].
- Long-Term Follow-Up: Particularly for cell therapies, long-term monitoring is essential to assess risks of delayed adverse events, such as tumorigenicity or teratogenicity [74] [5].
The following diagram illustrates the integrated experimental workflow for a comprehensive biosafety assessment of an MSC product, from preclinical development to clinical application.
Analysis of Safety Across Clinical Applications
The safety profile of MSCs must be evaluated within the context of their specific clinical application, as the underlying disease and route of administration can influence risk.
Cardiovascular Disease: A meta-analysis of 15 trials (1,218 participants) for acute myocardial infarction found stem cell therapy was associated with fewer adverse events than controls (OR 0.66), supporting its short-to-mid-term safety [74]. The therapy showed no significant effect on most efficacy parameters in the short term but demonstrated potential long-term benefits for left ventricular ejection fraction, underscoring a positive risk-benefit ratio [74].
Acute Respiratory Distress Syndrome (ARDS): A separate meta-analysis of 48 studies (1,773 patients) investigated MSCs and their derived extracellular vesicles for ARDS. It found a significant reduction in all-cause mortality within one month and no significant differences in AEs or SAEs between the treatment and control groups, indicating the therapy is well-tolerated in this critically ill population [75].
Immune-Mediated Diseases: The potent immunomodulatory properties of MSCs make them attractive for conditions like graft-versus-host disease (GVHD). The recent FDA approval of an MSC product (Rexlemestrocel-L) for pediatric steroid-refractory acute GVHD is a landmark that confirms the favorable safety and efficacy profile of MSCs in a rigorous regulatory context [5] [76].
This synthesis of meta-analytic evidence firmly establishes that MSC-based therapies exhibit a favorable and predictable safety profile across hundreds of patients and numerous disease states. The most common adverse events are transient and mild, with no significant increase in serious adverse events compared to control groups. This compelling safety data, combined with the recent regulatory approvals for MSC products, provides strong justification for the continued clinical development of these promising therapies.
However, several challenges must be addressed to advance the field. Efficacy has been inconsistent across trials, partly due to heterogeneity in cell sources, production methods, dosing, and administration protocols [76] [73]. Future research must prioritize the standardization of MSC products and trial designs. Furthermore, while short-term safety is well-documented, long-term follow-up remains essential to fully rule out delayed risks, such as oncogenicity [74] [5]. The field is also evolving towards enhancement strategies, including the genetic modification or preconditioning of MSCs to boost their therapeutic potency, and exploring cell-free therapies using MSC-derived extracellular vesicles, which may offer a similarly beneficial profile with a potentially improved safety and regulatory pathway [73]. For researchers and clinicians, these findings affirm that MSC therapy can be pursued within well-designed clinical trials with a high degree of confidence in its patient safety.
The transition of stem cell-based therapies from experimental treatments to established clinical interventions hinges on the availability of robust long-term safety data. For researchers and drug development professionals, understanding the extended safety profile of these "living drugs" is paramount, as their biological activity and persistence within the body present unique challenges not encountered with conventional pharmaceuticals [78]. Unlike traditional drugs that are metabolized and excreted, stem cells can potentially persist, migrate, or exhibit unforeseen behaviors over extended periods, necessitating rigorous long-term monitoring [78]. This analysis synthesizes the most current five-year and extended follow-up data for various stem cell therapies in autoimmune diseases, providing a critical evaluation of their safety profiles and the methodological frameworks used for their assessment.
The fundamental distinction of stem cells as biological drugs lies in their dynamic nature. They are not inert compounds but viable entities capable of responding to environmental cues through complex mechanisms including paracrine signaling, immunomodulation, and functional integration into host tissues [78]. While these mechanisms underpin their therapeutic potential, they also introduce theoretical risks such as unintended cell differentiation, improper tissue integration, or immune-mediated rejection of allogeneic cells over the long term. Consequently, regulatory bodies like the International Society for Stem Cell Research (ISSCR) emphasize thorough long-term follow-up in their guidelines to ensure patient welfare and data integrity [15]. This review objectively compares the available long-term safety data across different stem cell platforms to inform future research and clinical development.
Comparative Analysis of Long-Term Safety Outcomes
Long-term studies are increasingly validating the favorable safety profile of stem cell therapies in autoimmune diseases. The table below summarizes key quantitative safety outcomes from recent clinical studies with extended follow-up periods.
Table 1: Long-Term Safety and Efficacy Outcomes in Stem Cell Therapy Clinical Studies
| Therapy & Disease | Study Duration (Median/Mean) | Key Safety Findings | Efficacy Correlates | Citation |
|---|---|---|---|---|
| UCMSC Infusion (CLV-100) in Healthy Subjects | 5-year follow-up | No treatment-related adverse events; no tumorigenicity; stable organ function parameters. | Sustained, dose-dependent immunomodulatory (anti-inflammatory) effect. | [79] |
| Autologous HCT in Severe Systemic Sclerosis | 9.1 years (range 0.5–14.3) | Overall survival: 94.2%; Treatment-related mortality: 5.8% (1/17 patients). | Significant improvement in mRSS (31 to 7); stabilization/improvement of lung function. | [80] |
| UCMSC in Systemic Lupus Erythematosus (Chinese Population) | 6-year follow-up | Potentially safe over medium-term. | (Data focused on safety outcome). | [79] |
| UCMSC in Ischemic Stroke (South Korean Study) | 5-year follow-up | Potentially safe over medium-term. | (Data focused on safety outcome). | [79] |
The data demonstrates that with appropriate patient selection and management, stem cell therapies can exhibit a manageable long-term safety profile. The 94.2% overall survival rate over nearly a decade in severe Systemic Sclerosis patients treated with autologous HCT is particularly notable, indicating durable efficacy without late-onset toxicity in most patients [80]. Furthermore, the complete absence of tumorigenicity or major health issues in the 5-year healthy volunteer study of UCMSCs (CLV-100) provides strong reassurance regarding the oncogenic safety of this specific allogeneic product [79].
Detailed Experimental Protocols for Safety Monitoring
To ensure the reliability of long-term data, consistent and comprehensive monitoring protocols are essential. The following methodologies are representative of high-quality safety assessment in the field.
Protocol for Medium-Term Safety Follow-Up (5 Years)
A 2025 follow-up study on Umbilical Cord-derived Mesenchymal Stem Cells (CLV-100) established a robust protocol for monitoring healthy subjects over five years [79].
- Study Design & Subjects: This was a 5-year follow-up of a Phase I study involving 11 healthy volunteers who had previously received a single intravenous infusion of allogeneic UCMSCs at either a low dose (65 million cells) or a high dose (130 million cells). All subjects were retained for the long-term follow-up, demonstrating the feasibility of complete long-term data collection.
- Primary Safety Endpoints: The assessment focused on clinical and subclinical outcomes, including:
- Death, hospitalization, and related adverse events.
- Cancer incidence, with levels of cancer markers tracked.
- Assessment Methods:
- Clinical Consultations: Comprehensive medical history review and physical examination.
- Laboratory Testing: Full blood count, renal and liver function tests.
- Inflammatory Biomarker Quantification: Serum levels of pro-inflammatory cytokines (IL-6, TNF-α) and anti-inflammatory factors (IL-1Ra, TGF-β, HGF, VEGF) were measured using multiplex array kits and ELISA to track sustained immunomodulatory effects [79].
Protocol for Long-Term Efficacy and Safety in Disease-Specific Cohorts
A July 2025 study on autologous hematopoietic cell transplantation (HCT) for severe Systemic Sclerosis provides a model for long-term assessment in a patient population with a median follow-up of 9.1 years [80].
- Patient Selection: Eligibility was restricted to patients with severe, refractory disease (mRSS ≥15 with organ involvement) but excluded those with advanced, irreversible organ damage (severe heart failure, pulmonary hypertension, severe respiratory failure). This highlights the critical importance of stringent patient selection in managing long-term risks and outcomes.
- Transplantation Protocol:
- Mobilization: Cyclophosphamide (4 g/m²) and G-CSF.
- Conditioning: Immunoablation with cyclophosphamide (50 mg/kg/d for 4 days) and anti-thymocyte globulin (2.5 mg/kg/d for 3 days).
- Reinfusion: Cryopreserved peripheral blood stem cells with a target CD34+ count of 4 × 10⁶ cells/kg.
- Long-Term Endpoints:
- Safety: Treatment-related mortality (TRM), overall survival, and the need for additional immunosuppressive drugs post-transplant.
- Efficacy: Response was defined as a >25% improvement in the modified Rodnan Skin Score (mRSS), subjective improvement in gastrointestinal symptoms, and objective assessment of lung function (FEV1, DLCO) via HRCT [80].
Mechanisms of Action and Safety Considerations
The long-term safety of a stem cell therapy is intrinsically linked to its mechanism of action. The primary therapeutic strategies—systemic immunomodulation and immune system reset—carry distinct risk profiles.
Diagram: Mechanistic Pathways and Associated Long-Term Safety Considerations of Different Cell Therapies.
As illustrated, Mesenchymal Stem Cells (MSCs), particularly those derived from umbilical cord (UCMSCs), primarily exert their effect through paracrine signaling, secreting factors like TGF-β, PGE2, and IDO to modulate the immune environment without long-term engraftment [81] [78] [79]. This transient mechanism is associated with a favorable long-term safety profile, as confirmed by the 5-year healthy volunteer study [79]. In contrast, Autologous Hematopoietic Cell Transplantation (HCT) employs a more aggressive mechanism of immune system ablation and reconstitution, aiming for a durable "immune reset." This approach carries a higher, yet manageable, risk profile, including treatment-related mortality, which underscores the necessity for careful patient selection [80]. Emerging therapies like CAR-T cells for autoimmunity use targeted B-cell depletion. Notably, early data suggests that in autoimmune settings, CAR-T cells exhibit limited persistence, which may reduce long-term risks of immunodeficiency and represents a significant safety advantage over their application in oncology [82] [83].
The Scientist's Toolkit: Essential Research Reagents
The rigorous evaluation of long-term safety in clinical trials depends on a standardized set of research tools and biological materials. The following table details key reagents and their functions in monitoring safety and mechanisms of action.
Table 2: Key Research Reagent Solutions for Long-Term Safety Monitoring
| Reagent / Material | Primary Function in Safety & Efficacy Assessment |
|---|---|
| UCMSCs (e.g., CLV-100) | The investigational cellular product itself; used to assess cell source impact on long-term safety and immunomodulatory potency [79]. |
| Anti-thymocyte globulin (ATG) | Immunoablative agent used in conditioning regimens (e.g., for HCT) to deplete T-cells; critical for evaluating regimen-related toxicity and long-term immune reconstitution [80]. |
| Cyclophosphamide | Chemotherapeutic/immunosuppressive agent used for stem cell mobilization and conditioning; its dosing is a key variable in short and long-term toxicity profiles [80]. |
| Multiplex Array Kits (e.g., R&D System) | Simultaneously quantify panels of serum cytokines (e.g., IL-6, TNF-α, IL-1Ra, VEGF, HGF) to track persistent immunomodulatory effects and inflammatory status over time [79]. |
| ELISA Kits (e.g., for TGF-β) | Quantify specific soluble factors in serum or plasma; essential for validating anti-inflammatory activity and monitoring specific pathway engagement [79]. |
The accumulation of five-year and extended follow-up data represents a critical step in maturing the field of stem cell therapy for autoimmune diseases. Current evidence, while still growing, indicates that certain stem cell-based interventions, particularly UCMSC infusions and autologous HCT, can exhibit a acceptable long-term safety profile when administered to appropriately selected patients under rigorous protocols. The consistent reporting of stable organ function, absence of tumorigenicity, and sustained immunomodulation provides a strong foundation for the continued clinical development of these therapies.
Future efforts must focus on standardizing long-term monitoring protocols across clinical trials to facilitate robust meta-analyses. Furthermore, research should prioritize identifying biomarkers predictive of long-term safety and efficacy, which will enable more precise patient stratification. As newer therapies like allogeneic CAR-T cells for autoimmunity enter clinical testing, applying these rigorous long-term assessment frameworks from the outset will be essential. The ultimate goal is to build a comprehensive safety database that not only secures regulatory approval but also earns the trust of the clinical community and patients, thereby fulfilling the transformative promise of stem cell-based biological drugs.
{#title}
Comparative Safety Profiles: MSCs vs. Pluripotent Stem Cell-Derived Products
Stem cell-based therapies represent a frontier in regenerative medicine, offering potential treatments for a range of diseases and injuries. The safety profile of these cellular products is a paramount concern that directly influences their clinical translation and regulatory approval. Among the various cell types under investigation, Mesenchymal Stem/Stromal Cells (MSCs) and pluripotent stem cell (PSC)-derived products, which include products derived from both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), are two of the most prominent categories. MSCs are multipotent adult stem cells with known immunomodulatory properties, while PSCs are defined by their ability to differentiate into any cell type in the body. This inherent biological difference underpins distinct safety considerations for each platform. This guide provides a comparative analysis of their safety profiles, grounded in current preclinical and clinical data, and details the experimental protocols essential for their thorough biosafety assessment [5] [84].
The table below summarizes the core safety considerations for MSCs and pluripotent stem cell-derived products, providing a high-level comparison for researchers and developers.
Table 1: Core Safety Profile Comparison: MSCs vs. Pluripotent Stem Cell-Derived Products
| Safety Parameter | Mesenchymal Stem/Stromal Cells (MSCs) | Pluripotent Stem Cell (PSC)-Derived Products (iPSC/ESC) |
|---|---|---|
| Tumorigenicity Risk | Generally considered low. MSCs are non-tumorigenic and do not form teratomas. The primary concern is potential malignant transformation after long-term culture in vitro [77]. | A primary safety concern. PSCs themselves are tumorigenic and can form teratomas. The risk with their derivatives hinges on the persistence of undifferentiated pluripotent cells in the final product [85] [84] [16]. |
| Immunogenicity | Low immunogenicity; often used in allogeneic settings due to immunomodulatory properties. Conflicting data exists on post-transplantation immune recognition [77] [86]. | A complex profile. Autologous iPSC-derived products are theoretically immune-tolerant. However, allogeneic PSC-products may require immunosuppression. Aberrant gene expression in differentiated cells can also provoke immune responses [85] [16]. |
| Biodistribution & Engraftment | Often show limited long-term engraftment. Therapeutic effects are frequently attributed to paracrine signaling. Cells can lodge in off-target sites like lungs after IV infusion [5]. | Designed for stable engraftment and integration into host tissue (e.g., retina, brain). Must be carefully controlled to prevent ectopic tissue formation or integration into incorrect locations [33]. |
| Genetic Stability | Can accumulate chromosomal abnormalities during in vitro expansion, potentially impacting function and safety [5]. | Reprogramming and differentiation processes can introduce genetic and epigenetic abnormalities, a key concern for clinical application [84] [16]. |
| Clinical Safety Record | Extensive clinical use with a generally favorable safety profile. Meta-analyses report no significant increase in serious adverse events (SAEs) compared to controls in conditions like ARDS [86]. | A more limited but growing clinical record. As of late 2024, over 1,200 patients have been dosed with PSC-derived products across 116 trials, with data so far "showing no generalizable safety concerns" [33]. |
Detailed Safety Analysis and Key Experimental Assays
A robust safety assessment requires a suite of specialized assays designed to address the specific risks associated with each cell type. The following section outlines critical experimental protocols for evaluating tumorigenicity, immunogenicity, and overall product quality.
Tumorigenicity Assessment
a) In Vitro Transformation Assays:
- Objective: To screen for early signs of malignant transformation in cell cultures.
- Protocol:
- Soft Agar Colony Formation Assay: Cells are suspended in a semi-solid soft agar medium and cultured for 3-4 weeks. This assay tests for anchorage-independent growth, a hallmark of oncogenic transformation.
- Proliferation Kinetics: Monitor population doubling times and saturation density over serial passages. A significant decrease in doubling time can indicate uncontrolled growth.
- Genomic DNA Analysis: Isolate genomic DNA from late-passage cells and perform whole-genome sequencing or targeted sequencing of oncogenes and tumor suppressor genes to identify mutations.
- Interpretation: Formation of colonies in soft agar or acquisition of deleterious mutations signals a potential tumorigenic risk [5].
b) In Vivo Tumorigenicity Models:
- Objective: To assess the potential for tumor formation in vivo.
- Protocol:
- Animal Model: Use immunodeficient mice (e.g., NOD/SCID, NSG) to prevent immune rejection of human cells.
- Cell Transplantation: Implant the cell product at a dose significantly higher than the intended clinical dose, often via subcutaneous, intramuscular, or a clinically relevant route.
- Observation Period: Monitor animals for up to 6 months for signs of tumor formation at the injection site or distant locations.
- Terminal Analysis: Perform necropsy and histopathological examination (H&E staining) of the implantation site and major organs to identify teratomas or other tumors.
- Interpretation: The presence of tumors containing cells from multiple germ layers confirms the presence of residual pluripotent cells in PSC-derived products [5] [84].
Immunogenicity Profiling
a) In Vitro Immune Cell Activation Assays:
- Objective: To evaluate the potential of the cell product to provoke an immune response.
- Protocol:
- Co-culture Setup: Co-culture the stem cell product with allogeneic or autologous human peripheral blood mononuclear cells (PBMCs).
- Immune Cell Analysis: Use flow cytometry to quantify the activation and proliferation of key immune cell populations, including:
- T-cells: Measure activation markers (CD69, CD25) and proliferation via dye dilution.
- NK Cells: Assess expression of activation receptors (NKG2D) and cytotoxic activity.
- Dendritic Cells/Macrophages: Monitor maturation markers (CD80, CD86, HLA-DR).
- Cytokine Profiling: Collect culture supernatants and use multiplex ELISA or Luminex assays to quantify pro-inflammatory cytokines (e.g., IFN-γ, TNF-α, IL-6) [5].
b) HLA Typing and Expression Analysis:
- Objective: To determine the immunogenic potential related to donor-recipient matching.
- Protocol:
- DNA-based HLA Typing: Use PCR-based sequencing to determine the HLA class I and II alleles of the cell product.
- Flow Cytometry: Analyze the surface expression of HLA class I and II molecules on the cell product, noting that MSCs typically have low HLA class II expression [5].
Product Quality and Characterization
Rigorous quality control is the foundation of safety. The following assays are mandatory for releasing any cellular product for clinical use, forming the basis of a Chemistry, Manufacturing, and Controls (CMC) dossier. Table 2: Critical Quality Control Assays for Stem Cell-Based Products
| Assay Category | Specific Test | Methodology | Purpose & Acceptance Criteria |
|---|---|---|---|
| Identity | Surface Marker Profiling | Flow Cytometry | MSCs: ≥95% positive for CD73, CD90, CD105; ≤2% positive for CD34, CD45, HLA-DR [77].PSC-Derived: Profile specific to target cell type (e.g., tyrosine hydroxylase for dopaminergic neurons). |
| Potency | Functional Assay | In vitro differentiation (MSCs) or functional readout (PSC). | MSCs: Demonstrated ability to differentiate into osteocytes, adipocytes, and chondrocytes [77].PSC-Derived: Assay relevant to therapeutic mechanism (e.g., glucose-stimulated insulin secretion for beta cells). |
| Purity/Viability | Viability | Trypan Blue Exclusion or Automated Cell Counter | Determine the percentage of live cells pre-transplantation. |
| Safety | Sterility | BacT/ALERT or similar microbiological culture | Confirms absence of bacterial and fungal contaminants. |
| Mycoplasma | PCR or culture-based methods | Confirms absence of mycoplasma contamination. | |
| Endotoxin | Limulus Amebocyte Lysate (LAL) Assay | Quantifies endotoxin levels, which must be below regulatory limits. |
Diagram 1: Comprehensive Safety Assessment Workflow for Stem Cell Products. This diagram outlines the key experimental pathways for evaluating tumorigenicity, immunogenicity, and product quality.
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists key reagents and tools required to perform the critical safety assays described in this guide.
Table 3: Essential Research Reagent Solutions for Stem Cell Safety Assessment
| Reagent / Solution | Function / Application | Key Considerations |
|---|---|---|
| Immunodeficient Mice (e.g., NSG) | In vivo tumorigenicity studies. Provides a permissive environment for assessing human cell growth and tumor formation. | Strain selection (e.g., NOD/SCID, NSG) impacts engraftment efficiency and study duration. |
| Flow Cytometry Antibodies | Cell identity (CD73, CD90, CD105) and immune cell profiling (CD3, CD4, CD8, CD56, CD69). | Validation for specific cell types (human vs. mouse) is critical. Multicolor panel design requires compensation controls. |
| Soft Agar | Semi-solid medium for anchorage-independent growth assay, a hallmark of transformation. | Requires careful preparation to create distinct top and bottom layers. |
| Cell Culture Media & Supplements | Expansion and maintenance of stem cells and differentiated derivatives. | Use of defined, xeno-free media (e.g., with human platelet lysate) is preferred for clinical-grade cells [85]. |
| PCR/QPCR Reagents | HLA genotyping, mycoplasma testing, and analysis of gene expression. | Assays must be highly sensitive and specific, especially for detecting low-level contaminants. |
| LAL Endotoxin Assay Kit | Quantification of bacterial endotoxins in the final cell product. | A critical release criterion; levels must be below the threshold set by regulatory authorities. |
| CRISPR-Cas9 System | Gene editing tool used to correct disease-causing mutations in iPSCs or to create "kill switches" for added safety [16]. | Off-target effects must be thoroughly evaluated using whole-genome sequencing. |
The safety landscapes for MSC and pluripotent stem cell-derived therapies are distinct yet converging on the need for rigorous, standardized assessment. MSCs present a generally favorable safety profile in the near term, with risks centered on administration-related events and cell quality. In contrast, PSC-derived products carry a more complex risk profile, dominated by the inherent tumorigenicity of undifferentiated cells, but clinical data from over 1,200 patients to date is encouraging, showing no generalized safety concerns [86] [33]. For both platforms, a comprehensive biosafety assessment—encompassing detailed tumorigenicity studies, immunogenicity profiling, and stringent quality control—is non-negotiable for successful clinical translation. The experimental protocols and tools outlined in this guide provide a foundational framework for researchers and drug development professionals to ensure that the transformative potential of stem cell therapies is realized with the highest possible safety standards.
Stem cell-based therapies represent a paradigm shift in regenerative medicine, offering potential strategies for conditions previously considered untreatable. However, their therapeutic promise is inextricably linked to a complex safety profile that varies significantly by disease pathology and patient population. This guide provides a comparative assessment of the risk-benefit landscape for stem cell therapies across three distinct clinical contexts: stroke, rheumatoid arthritis (RA), and aging. The assessment is framed within a rigorous biosafety framework that prioritizes operational principles including toxicity, tumorigenicity, immunogenicity, biodistribution, and cell product quality [5]. For researchers and drug development professionals, understanding these disease-specific nuances is critical for designing clinically relevant preclinical studies and mitigating patient risk during clinical translation.
Disease Burden and Current Treatment Landscape
The global burden of target diseases profoundly influences the risk tolerance and benefit expectations for novel stem cell therapies. The following table summarizes key epidemiological and current treatment limitations for stroke, rheumatoid arthritis, and aging-related decline.
Table 1: Disease Burden and Current Treatment Landscape
| Disease Area | Global Burden & Epidemiology | Limitations of Standard Care |
|---|---|---|
| Stroke | - Incidence: ~12 million new cases/year globally [87]- Leading Cause: Second leading cause of death and third leading cause of death and disability combined worldwide [87]- Economic Impact: ~$890 billion annually (0.66% of global GDP) [87] | - Limited time window for acute thrombolytics- No approved therapies to regenerate damaged brain tissue or fully restore lost function- High prevalence of long-term disability among survivors |
| Rheumatoid Arthritis (RA) | - Information not fully available in search results- Known to be a chronic autoimmune disorder causing joint inflammation and damage | - Current treatments (e.g., DMARDs, biologics) focus on symptom suppression and slowing disease progression rather than cure- Can have significant side effects and variable efficacy |
| Aging | - Aging brain shows reduced plasticity, impaired recovery from injury, and chronic "inflammaging" [88]- Associated with BBB disruption, pericyte loss, and endothelial dysfunction [88] | - No interventions currently reverse fundamental aging processes- Treatments are typically symptomatic and manage age-related comorbidities |
Stem Cell Mechanisms and Therapeutic Potential
The proposed mechanism of action of stem cell therapies differs based on both the cell type and the pathological environment of the target disease. Mesenchymal stem cells (MSCs) are a primary focus in many applications due to their multipotency, immunomodulatory properties, and relative ease of isolation [89].
Key Therapeutic Mechanisms of Mesenchymal Stem Cells (MSCs)
MSCs are thought to promote repair and recovery through multiple parallel mechanisms rather than solely through cell replacement. The diagram below illustrates the primary therapeutic mechanisms of MSCs in the context of neurological injury and aging.
Diagram 1: Multimodal Mechanisms of MSCs. MSCs promote recovery through secretion of trophic factors, immunomodulation, promotion of vascularization, and reducing inflammation, leading to functional tissue repair.
In the aging brain, these mechanisms are particularly relevant. The aged brain environment is characterized by increased inflammation ("inflammaging"), reduced neurogenesis, and blood-brain barrier (BBB) dysfunction [88]. MSC therapy aims to counteract these processes by secreting factors that promote a restorative microenvironment, protecting existing neurons, and stimulating the growth of new blood vessels to improve cerebral blood flow [88] [89].
The evidence base for stem cell therapies varies considerably across different disease indications. The table below summarizes key efficacy findings from preclinical and clinical studies, highlighting the stage of development for each application.
Table 2: Summary of Preclinical and Clinical Evidence for Stem Cell Therapies
| Disease / Application | Key Efficacy Findings (Preclinical) | Key Efficacy Findings (Clinical) | Overall Stage of Development |
|---|---|---|---|
| Stroke | - MSC transplantation in mice reduces infarct size and enhances neurological function [89].- Leads to brain cell growth and functional recovery in mouse models [90]. | - Meta-analysis of 26 RCTs (n=1,527) shows significant improvements in neurological function and daily living activities [89].- MSC therapy appears safe, with no significant increase in adverse events reported [89]. | Early Clinical Trials (Promising Phase I/II results) |
| Aging & Age-Related Decline | - Studies suggest potential to modulate age-related processes like chronic inflammation and reduced plasticity [88]. | - Direct clinical evidence for anti-aging applications is limited and primarily exploratory.- Data often extrapolated from studies on age-related diseases. | Preclinical / Early Concept |
| Rheumatoid Arthritis (RA) | Information on RA-specific stem cell studies was not available in the provided search results. | Information on RA-specific stem cell studies was not available in the provided search results. | Information not available |
Comprehensive Risk and Biosafety Assessment
A rigorous biosafety assessment is the cornerstone of responsible clinical translation. The risks associated with stem cell-based therapies are multifaceted and must be evaluated using a systematic, practice-oriented framework [5].
Core Biosafety Principles and Assessment Methodologies
The following workflow outlines the critical components of a biosafety assessment and the standard methodologies employed to address each risk category.
Diagram 2: Biosafety Assessment Framework. A comprehensive safety profile for a cell therapy product is built by evaluating core risk principles using specific preclinical methodologies.
Disease-Specific Risk Considerations
The manifestation of these general risks is highly dependent on the patient population and disease pathophysiology.
Stroke: For therapies involving intracranial administration, the injection procedure itself carries risks, such as hemorrhagic retinopathy or ocular hypertension, as seen in early trials for macular degeneration [5]. The inflammatory environment of the acute stroke brain may also heighten the risk of immunogenic reactions despite the immune-privileged status of MSCs [5] [88].
Aging: The aged population presents unique challenges. Age-related immunosenescence may alter expected immunogenic responses to allogeneic cells [88]. Furthermore, the aging microenvironment, with its accumulation of epigenetic alterations and oxidative stress, could potentially increase the risk of malignant transformation of transplanted cells, necessitating rigorous long-term tumorigenicity studies in relevant aged animal models [5] [88].
Experimental Protocols and Research Toolkit
Translating a stem cell therapy from bench to bedside requires a standardized set of experimental protocols and reagents to ensure data reproducibility and rigorous safety assessment.
Detailed Methodologies for Key Experiments
Biodistribution Assessment via qPCR
- Objective: To track the migration and persistence of administered cells in target and non-target tissues over time.
- Protocol:
- Sample Collection: At predetermined time points post-treatment, collect tissues of interest (e.g., brain, liver, lungs, spleen, gonads) and homogenize.
- DNA Extraction: Isolate total genomic DNA from homogenized tissues using a commercial kit.
- qPCR Setup: Perform qPCR reactions using primers specific to a unique sequence present in the administered human cells (e.g., Alu repeat elements for human cells in a mouse model).
- Quantification: Use a standard curve generated from known quantities of the cell product to calculate the number of human cells per microgram of host tissue DNA. This allows for quantitative comparison of cell presence across different organs and time points [5].
Tumorigenicity Testing in Immunocompromised Models
- Objective: To evaluate the potential for the cell product to form abnormal growths or tumors.
- Protocol:
- Animal Model: Utilize immunodeficient mice (e.g., nude mice or NSG mice) to prevent rejection of human cells.
- Cell Administration: Implant the test stem cell product subcutaneously or into a clinically relevant site (e.g., brain parenchyma for a CNS therapy). Include a positive control group (e.g., injection of a known tumorigenic cell line) and a negative control group (e.g., vehicle injection).
- Observation Period: Monitor animals for an extended period (e.g., 6 months or longer) for signs of ill health and palpate for mass formation.
- Terminal Analysis: At study endpoint, perform a necropsy. Weigh organs and conduct a thorough histopathological examination of the injection site and major organs for any evidence of tumor formation or ectopic tissue growth [5].
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and their applications in stem cell therapy development and biosafety assessment.
Table 3: Essential Research Reagents for Stem Cell Therapy Development
| Research Reagent / Tool | Primary Function in R&D | Application Context |
|---|---|---|
| qPCR Probes/Primers for Human-Specific Sequences | Quantify biodistribution of human cells in animal models by amplifying unique genomic markers [5]. | Biodistribution Studies |
| Immunodeficient Mouse Models | Provide an in vivo environment for assessing tumorigenicity and long-term safety of human cell products without immune rejection [5]. | Tumorigenicity Studies |
| Flow Cytometry Antibodies | Characterize cell surface marker identity (e.g., CD73, CD90, CD105 for MSCs), assess purity, and analyze immune cell populations in toxicology studies [5]. | Product Identity, Purity, Immunogenicity |
| Cell Culture Media & Supplements | Expand and maintain stem cell populations under defined conditions, ensuring product quality and genetic stability during manufacturing [5]. | Cell Product Manufacturing |
| Molecular Probes for Imaging | Label cells for in vivo tracking using modalities like PET or MRI to monitor initial localization and medium-term persistence [5]. | Biodistribution & Cell Fate |
The risk-benefit profile of stem cell-based therapies is inherently disease-specific, shaped by the underlying pathology, patient population, and mode of delivery. Stroke therapies, while addressing a massive unmet medical need, require meticulous assessment of neurological toxicity, biodistribution to sensitive brain regions, and procedure-related risks. For applications in aging, the altered physiology of the aged host—marked by inflammaging, immunosenescence, and a potentially pro-oncogenic microenvironment—demands tailored safety studies that go beyond standard young adult models. A comprehensive biosafety framework, integrating rigorous product quality control with disease-relevant preclinical models and carefully designed clinical trials, is essential for the ethical and successful translation of these promising therapies. Future research must focus on generating robust, comparative safety data to illuminate these disease-specific risk-benefit equations further.
Conclusion
The safety profile of stem cell-based therapies is increasingly defined by robust preclinical and clinical data, revealing a generally favorable risk-benefit ratio for well-characterized products like MSCs, though unique risks for pluripotent cells remain. Successful clinical translation hinges on rigorous adherence to evolving regulatory frameworks, standardized manufacturing, and comprehensive long-term patient monitoring. Future directions must prioritize overcoming tumorigenicity concerns, optimizing combination strategies, and developing globally harmonized safety standards to fully realize the therapeutic potential of stem cells while ensuring patient safety remains paramount.
References
- 1. Malignant Transformation of Mature Cystic Teratoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12612795/]
- 2. Mature cystic teratoma and their malignant transformation [https://www.sciencedirect.com/science/article/abs/pii/S0748798325000691]
- 3. Malignant transformations in mature cystic teratomas [https://www.spandidos-publications.com/10.3892/mi.2025.251?text=fulltext]
- 4. Case Report: Testicular teratoma with malignant ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1699289/full]
- 5. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 6. Patient-derived xenograft models: Current status ... [https://www.sciencedirect.com/science/article/pii/S2352304225000091]
- 7. Cancer stem cells: landscape, challenges and emerging ... [https://www.nature.com/articles/s41392-025-02360-2]
- 8. Advancements in HLA Typing Techniques and Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11175610/]
- 9. The Advanced HLA Typing Strategies for Hematopoietic Stem ... Cell [https://www.intechopen.com/chapters/42655]
- 10. HLA Typing For HSCT New Research Indicates Expanded ... [https://www.cellandgene.com/doc/hla-typing-for-hsct-new-research-indicates-expanded-patient-compatibility-0001]
- 11. Outcomes Following Allogeneic Stem Cell Transplantation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6369069/]
- 12. Outcomes with mismatched unrelated donor allogeneic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.1005042/full]
- 13. HLA matching or CRISPR editing of HLA class I/II enables ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518618/]
- 14. Ethical and Safety Issues of Stem -Based Therapy Cell [https://pubmed.ncbi.nlm.nih.gov/29333086/]
- 15. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 16. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 17. Clinical translation of human iPSC technologies [https://pubmed.ncbi.nlm.nih.gov/41059336/]
- 18. Induced pluripotent stem - Wikipedia cell [https://en.wikipedia.org/wiki/Induced_pluripotent_stem_cell]
- 19. New perspectives in human therapeutic research stem cell [https://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-7-29]
- 20. Q-Cell 研究——2025 年最新进展| SRNA 博客 [https://wearesrna.org/zh-CN/blog/q-cell-2025/]
- 21. Microbiological risk assessment during the procurement ... [https://www.nature.com/articles/s41598-025-24496-5]
- 22. 9.6: Recommended standards for microbiological screening [https://www.transfusionguidelines.org/red-book/chapter-9-microbiology-tests-for-donors-and-donations-general-specifications-for-laboratory-test-procedures/9-6-recommended-standards-for-microbiological-screening]
- 23. Microbiological control in stem cell banks - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7080164/]
- 24. 2025年干细胞技术发展的方向 - 上海逐典生物科技有限公司 [https://www.chaselection.com/newsinfo/591.html]
- 25. 3. Clinical Translation of Stem Cell-based Interventions [https://www.isscr.org/guidelines/clinical-translation-of-stem-cell-based-interventions]
- 26. The ISSCR Releases Targeted Update to the Guidelines ... [https://www.isscr.org/isscr-news/the-isscr-releases-targeted-update-to-the-guidelines-for-stem-cell-research-and-clinical-translation]
- 27. Why gene and cell therapies are stalling at the FDA [https://www.drugdiscoverynews.com/why-gene-and-cell-therapies-are-stalling-at-the-fda-16527]
- 28. ISSCR 2025: Quality Is Our Common Language [https://www.stemcell.com/virtual-conference-exhibition/isscr]
- 29. Digital Karyotyping Market Report 2025 [https://www.researchandmarkets.com/reports/6178309/digital-karyotyping-market-report?srsltid=AfmBOooFPyR9qgmsObMLIdSRaBrleCQYOhrTuV3nvyjDUPYCzmRFHL55]
- 30. Comparative Efficacy of CNV-Sequencing and Karyotyping ... [https://bmrat.org/index.php/BMRAT/article/view/908]
- 31. Complementary role of echocardiography, karyotyping ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428034/]
- 32. Reassessment of marker genes in human induced ... [https://www.nature.com/articles/s41467-024-52922-1]
- 33. Pluripotent stem-cell-derived therapies in clinical trial [https://pubmed.ncbi.nlm.nih.gov/39753110/]
- 34. Comparative analysis of regulations and studies on stem cell ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04065-9]
- 35. Current Good Manufacturing Practice (CGMP) Regulations [https://www.fda.gov/drugs/pharmaceutical-quality-resources/current-good-manufacturing-practice-cgmp-regulations]
- 36. Facts About the Current Good Manufacturing Practice ... [https://www.fda.gov/drugs/pharmaceutical-quality-resources/facts-about-current-good-manufacturing-practice-cgmp]
- 37. Current Good Manufacturing Practice (cGMP): An Overview ... [https://www.chromatographyonline.com/view/current-good-manufacturing-practice-cgmp-an-overview-for-the-analytical-chemist]
- 38. What is cGMP in the pharma industry? 7 experts explain [https://www.qualio.com/blog/what-is-cgmp-in-the-pharmaceutical-industry]
- 39. Cell therapy: cGMP facilities and manufacturing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3666518/]
- 40. Current Good Manufacturing Practices (cGMP) [https://www.qualityze.com/blogs/cGMP-role-in-quality]
- 41. Stem cell-based therapy for human diseases [https://www.nature.com/articles/s41392-022-01134-4]
- 42. cGMP Cell Therapy Manufacturing Services [https://appliedstemcell.com/ipsc-cgmp-manufacturing/]
- 43. Overview of Cellular Therapeutics Clinical Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193569/]
- 44. UUSOP-14: Clinical Trial Safety Assessment and Reporting [https://qualitycompliance.research.utah.edu/sop-library/uu-sop-14.php]
- 45. Clinical Trial Protocol Deviations: A New FDA Draft ... [https://www.ropesgray.com/en/insights/alerts/2025/01/clinical-trial-protocol-deviations-a-new-fda-draft-guidance-to-ring-in-the-new-year]
- 46. Global clinical trials on stem cell therapy for autoimmune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1616231/full]
- 47. Examining the relationship between stem cell treatment ... [https://www.sciencedirect.com/science/article/abs/pii/S1360859224005928]
- 48. Stem Cell Success Rate: Evaluated (2025) [https://www.dvcstem.com/post/stem-cell-success-rate]
- 49. Stem Cell Therapy Success Rates Hit 78%: New Research ... [https://globalrph.com/2025/03/stem-cell-therapy-success-rates-hit-78-new-research-reveals-breakthrough-results/]
- 50. Elimination of tumorigenic pluripotent stem cells from their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277835/]
- 51. Deconstructing Stem Cell Tumorigenicity: A Roadmap to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2733374/]
- 52. Combinatorial suicide gene strategies for the safety of cell ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.975233/full]
- 53. Human stem cells harboring a suicide gene improve the ... [https://www.nature.com/articles/s41467-021-23125-9]
- 54. Improving the safety of cell therapy products by suicide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4245885/]
- 55. Comparison of Different Suicide-Gene Strategies for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4015080/]
- 56. Suicide gene therapy using allogeneic adipose tissue-derived ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-04213-4]
- 57. Possible Strategies to Reduce the Tumorigenic Risk of ... [https://www.mdpi.com/1422-0067/25/10/5177]
- 58. Adverse events, side effects and complications in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9659480/]
- 59. Establishing delivery route-dependent safety and efficacy of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11235206/]
- 60. Optimization strategies of mesenchymal stem cell-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10150535/]
- 61. Dose-response relationship of MSCs as living Bio-drugs in ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03713-4]
- 62. Landscape analysis of adverse events and dose intensity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11700039/]
- 63. Stem Cell Therapy Safety and Risks [https://www.medtravellers.com/stem-cell-therapy-safety-and-risks/]
- 64. Ethical and Safety Considerations in Stem Cell-Based ... [https://www.intechopen.com/chapters/84169]
- 65. Frequently Asked Questions About Safety and Guarantees [https://www.startstemcells.com/frequently-asked-questions-about-safety-and-guarantees.html]
- 66. Universal cell donor lines: A review of the current research [https://pmc.ncbi.nlm.nih.gov/articles/PMC10679649/]
- 67. Immunogenicity and allogenicity: a challenge of stem cell ... [https://pubmed.ncbi.nlm.nih.gov/20559977/]
- 68. Safety Assessment of Stem Cell-Based Therapies [https://www.mdpi.com/2073-4409/14/21/1660]
- 69. HLA Engineering of Human Pluripotent Stem Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3677304/]
- 70. Generation of hypoimmunogenic universal iPS cells ... [https://www.nature.com/articles/s12276-025-01422-3]
- 71. Comparing the Benefits and Drawbacks of Stem Cell Therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10767552/]
- 72. Hypoimmunogenic human iPSCs expressing HLA-G, PD-L1 ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03810-4]
- 73. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 74. Safety and efficacy of stem cell therapy in acute myocardial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12207128/]
- 75. Efficacy and safety of mesenchymal stem/stromal cells and ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04644-4]
- 76. Mesenchymal stromal cell therapy: Progress to date and ... [https://pubmed.ncbi.nlm.nih.gov/39916329/]
- 77. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 78. Stem cells as biological drugs for incurable diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505543/]
- 79. Umbilical Cord-derived Mesenchymal Stem Cells (CLV- ... [https://link.springer.com/article/10.1007/s40883-025-00384-2]
- 80. Safety and long-term efficacy of autologous hematopoietic cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12301330/]
- 81. Global clinical trials on stem cell therapy for autoimmune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12328461/]
- 82. Innovations in immunotherapy for autoimmune diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485509/]
- 83. CAR-T cell therapy embarks on autoimmune disease [https://www.nature.com/articles/s41409-024-02429-6]
- 84. Stem cell therapy: a revolutionary cure or a pandora's box [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04334-1]
- 85. Natural vs. Induced Pluripotent Stem Cell Therapies [https://esmed.org/natural-vs-induced-pluripotent-stem-cell-therapies/]
- 86. Efficacy and safety of mesenchymal stem/stromal cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12481956/]
- 87. World Stroke Organization: Global Stroke Fact Sheet 2025 [https://pmc.ncbi.nlm.nih.gov/articles/PMC11786524/]
- 88. Advances in brain remodeling, stem cell therapies, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12254094/]
- 89. Stem Cell Therapy: A Stroke Recovery Breakthrough in ... [https://www.dvcstem.com/post/stem-cell-therapy-stroke]
- 90. Stem cell transplant for stroke leads to brain cell growth and ... [https://keck.usc.edu/news/stem-cell-transplant-for-stroke-leads-to-brain-cell-growth-and-functional-recovery-in-mice/]