Beyond the Dish: Evaluating the Physiological Relevance of iPSC-Derived Tissues for Disease Modeling and Drug Discovery
This article provides a comprehensive evaluation of the physiological relevance of tissues derived from human induced pluripotent stem cells (iPSCs) for biomedical research.
Beyond the Dish: Evaluating the Physiological Relevance of iPSC-Derived Tissues for Disease Modeling and Drug Discovery
Abstract
This article provides a comprehensive evaluation of the physiological relevance of tissues derived from human induced pluripotent stem cells (iPSCs) for biomedical research. It explores the foundational principles of iPSC technology, details advanced methodologies for generating physiologically representative models like engineered tissues and organoids, and addresses key challenges in maturation, reproducibility, and scalability. The content critically examines validation strategies, including comparative transcriptomic analyses and functional assays, to benchmark these models against native human physiology. Aimed at researchers, scientists, and drug development professionals, this review synthesizes current advancements and persistent gaps, offering a roadmap for leveraging iPSC-derived tissues to enhance drug discovery and clinical translation.
The iPSC Revolution: Foundations for Modeling Human Physiology
The field of somatic cell reprogramming was revolutionized in 2006 when Takahashi and Yamanaka demonstrated that introducing four specific transcription factors—OCT4, SOX2, KLF4, and c-MYC (collectively known as the OSKM factors)—could reprogram mouse fibroblasts into induced pluripotent stem cells (iPSCs) [1] [2]. This groundbreaking discovery proved that mature, differentiated cells could be returned to a pluripotent state without controversial embryonic sources, earning Shinya Yamanaka and John Gurdon the 2012 Nobel Prize in Physiology or Medicine [2]. The subsequent derivation of human iPSCs in 2007 opened unprecedented opportunities for disease modeling, drug screening, and regenerative medicine [3] [2].
The fundamental principle underlying reprogramming is that somatic cells maintain a complete genetic code despite differentiation, with cellular identity being determined by reversible epigenetic mechanisms rather than irreversible genetic changes [2] [4]. Reprogramming essentially reverses the developmental process, erasing somatic epigenetic memory and reestablishing the pluripotent state through profound remodeling of chromatin structure, DNA methylation patterns, and gene expression profiles [2]. This process involves two broad phases: an early stochastic phase where somatic genes are silenced and early pluripotency genes activated, followed by a more deterministic phase where late pluripotency genes are established [2].
Core Reprogramming Methodologies: A Comparative Analysis
Reprogramming Factor Combinations
The original OSKM factors remain the foundation for most reprogramming approaches, but significant optimizations have been developed to address safety concerns and improve efficiency. Research has revealed that the c-MYC component, while enhancing efficiency, acts as an oncogene and poses significant tumorigenic risks [1]. Subsequent studies have identified alternative factor combinations that minimize this risk while maintaining reprogramming capability.
Table 1: Comparative Analysis of Reprogramming Factor Combinations
| Factor Combination | Components | Efficiency | Safety Profile | Key Advantages | Primary Applications |
|---|---|---|---|---|---|
| OSKM | OCT4, SOX2, KLF4, c-MYC | High | Lower (oncogenic c-MYC) | Gold standard, well-characterized | Basic research, early proof-of-concept studies |
| OSK | OCT4, SOX2, KLF4 | Moderate | Higher (c-MYC free) | Reduced tumorigenic risk | Preclinical therapeutic development |
| OSNL | OCT4, SOX2, NANOG, LIN28 | Moderate | Higher (c-MYC free) | Alternative non-oncogenic combination | Disease modeling, therapeutic applications |
| L-Myc variant | OCT4, SOX2, KLF4, L-MYC | High | Higher (reduced oncogenicity) | Family member with lower tumorigenic potential | Clinical translation, safety-sensitive applications |
| OCT4-only (specific contexts) | OCT4 alone in neural stem cells | Variable | High (minimal factors) | Demonstrates OCT4's pivotal role | Mechanistic studies, specialized applications |
Alternative factors have been identified that can substitute for components of the original OSKM combination. KLF2 and KLF5 can replace KLF4, while SOX1 and SOX3 can substitute for SOX2 [1]. Similarly, L-MYC and N-MYC can replace c-MYC with reduced oncogenic risk [1]. Beyond transcription factor family members, other genes and small molecules can enhance or replace core factors. Nuclear receptor NR5A2 can substitute for OCT4, while the small molecule RepSox can replace SOX2 in reprogramming cocktails [1]. Additional factors like Esrrb and Glis1 can serve as alternatives to c-MYC, addressing safety concerns while maintaining efficiency [1].
Delivery Systems for Reprogramming Factors
The method used to deliver reprogramming factors significantly impacts the genomic integrity, safety profile, and clinical potential of resulting iPSCs. Initial approaches relied on integrating viral vectors, raising concerns about insertional mutagenesis and tumorigenesis. The field has subsequently developed numerous non-integrating delivery methods to enhance safety profiles.
Table 2: Comparison of Reprogramming Factor Delivery Systems
| Delivery Method | Genetic Integration | Efficiency | Safety Profile | Technical Complexity | Clearance/Duration |
|---|---|---|---|---|---|
| Retrovirus | Yes (random) | High | Low (insertional mutagenesis) | Moderate | Persistent expression |
| Lentivirus | Yes (random) | High | Low (insertional mutagenesis) | Moderate | Persistent expression |
| Sendai Virus | No (episomal) | High | High | Moderate | Cleared by passage 10 [5] |
| Adenovirus | No (episomal) | Low | High | High | Transient (weeks) |
| Episomal Plasmid | No (episomal) | Low to moderate | High | Low | Lost with cell divisions |
| Synthetic mRNA | No | Moderate | High | High (requires multiple transfection) | Transient (days) |
| Recombinant Protein | No | Very low | High | High (requires multiple treatment) | Transient (hours/days) |
Integration-free methods like Sendai virus reprogramming have become particularly valuable for generating clinically relevant iPSCs. This approach preserves genomic integrity while maintaining high reprogramming efficiency, with the viral vector typically cleared by passage 10 [5]. The resulting iPSCs demonstrate normal karyotypes and proper differentiation into all three germ layers, making them suitable for regenerative medicine applications [5].
Chemical Reprogramming Approaches
A fundamentally different approach involves using only small molecules to induce pluripotency, eliminating the need for genetic manipulation entirely. Fully chemical reprogramming of murine fibroblasts was first achieved in 2013 using seven small-molecule compounds [2], and the approach has since been adapted for human cells.
Recent advances have demonstrated robust chemical reprogramming methods for human blood cells, achieving efficient generation of human chemically induced pluripotent stem (hCiPS) cells from both cord blood and adult peripheral blood mononuclear cells [6]. This method works with both fresh and cryopreserved blood cells across different donors and can generate over 100 hCiPS colonies from a single drop of fingerstick blood [6]. Chemical reprogramming operates through fundamentally different molecular pathways compared to transcription factor-based approaches, often involving a stepwise process with transient activation of regenerative programs that mimic a reversed developmental pathway [6].
Chemical reprogramming offers several advantages: small molecules are easily synthesized and standardized, the approach avoids genetic modification entirely, and it can achieve high efficiency with minimally invasive cell sources like blood [6]. These characteristics make chemical reprogramming particularly promising for clinical applications where safety and standardization are paramount.
Experimental Protocols for iPSC Generation and Validation
Sendai Virus Reprogramming Protocol
The Sendai virus (SeV) system represents one of the most widely used non-integrating methods for generating clinical-grade iPSCs. The following protocol outlines the key steps for efficient reprogramming of human peripheral blood mononuclear cells (PBMCs):
Initial Cell Preparation and Expansion
- Isolate PBMCs from whole blood using density gradient centrifugation
- Culture PBMCs in expansion medium supplemented with cytokines (SCF, IL-3, IL-6, EPO) for 7-10 days to establish erythroid progenitor cells (EPCs) [6]
- Maintain cells at a density of 0.5-1×10^6 cells/mL in tissue culture plates at 37°C, 5% CO₂
Viral Transduction
- Harvest expanded EPCs and seed at 1×10^5 cells per well in 6-well plates coated with retronectin
- Transduce cells with CytoTune-iPS 2.0 Sendai Reprogramming Kit containing SeV vectors encoding OCT4, SOX2, KLF4, and c-MYC at an MOI of 3-5
- Centrifuge plates at 1000×g for 30 minutes to enhance viral attachment (spinoculation)
- Incubate at 37°C for 24 hours, then replace with fresh expansion medium
Transition to Pluripotency Conditions
- 24 hours post-transduction, transfer transduced cells to feeder-free culture vessels pre-coated with recombinant human vitronectin
- Transition culture medium to Essential 8 Flex medium supplemented with small molecule enhancers (e.g., 0.5mM sodium butyrate, 0.5mM valproic acid)
- Change medium daily and monitor for emergence of compact, ESC-like colonies (typically 14-21 days post-transduction)
Colony Picking and Expansion
- Manually pick individual iPSC colonies based on morphological criteria (high nucleus-to-cytoplasm ratio, distinct borders) between days 21-28
- Transfer colonies to 96-well plates pre-coated with vitronectin using collagenase IV treatment
- Expand clonal lines through sequential passaging and bank at early passages (P3-P5)
Figure 1: Sendai Virus Reprogramming Workflow
Chemical Reprogramming Protocol for Blood Cells
For chemical reprogramming of human blood cells, the following optimized protocol has demonstrated high efficiency across multiple donors:
Blood Cell Preparation
- Isolate mononuclear cells from cord blood (CBMCs) or peripheral blood (PBMCs) using Ficoll density gradient centrifugation
- Culture cells in erythroid progenitor cell (EPC) medium consisting of StemSpan SFEM II supplemented with EPO (2 U/mL), SCF (100 ng/mL), IL-3 (10 ng/mL), and dexamethasone (1µM) for 7 days
- Passage cells every 2-3 days maintaining density at 0.5-1×10^6 cells/mL
Chemical Reprogramming Induction
- Seed 5×10^4 EPCs per well in 12-well plates pre-coated with laminin-521
- Initiate reprogramming using stage-specific small molecule combinations:
- Stage 1 (Days 0-7): VPA (0.5mM), CHIR99021 (3µM), 616452 (2µM), Forskolin (10µM) in EPC medium
- Stage 2 (Days 7-21): VPA (0.5mM), CHIR99021 (3µM), 616452 (2µM), Forskolin (10µM), DZNep (0.5µM), TTNPB (1µM) in pluripotency induction medium
- Stage 3 (Days 21+): VPA (0.5mM), CHIR99021 (3µM), 616452 (2µM) in Essential 8 Flex medium
- Change medium every other day and monitor for adherent cell emergence and colony formation
hCiPS Colony Expansion
- Manually pick emerging colonies between days 28-35 based on compact morphology and well-defined borders
- Transfer to vitronectin-coated plates in Essential 8 Flex medium
- Passage using EDTA solution (0.5mM) every 5-7 days at 70-80% confluence
Quality Control and Validation Assays
Rigorous characterization is essential to confirm pluripotency and genomic integrity of generated iPSCs:
Pluripotency Marker Validation
- Immunocytochemistry: Fix cells with 4% PFA, permeabilize with 0.1% Triton X-100, and stain for nuclear pluripotency markers (OCT4, SOX2, NANOG) and surface markers (SSEA-4, TRA-1-60, TRA-1-81) [5]
- qPCR Analysis: Isolve RNA using TRIzol, synthesize cDNA, and perform quantitative PCR for endogenous pluripotency genes (POUSF1, SOX2, NANOG) with normalization to housekeeping genes (GAPDH, HPRT1)
Trilineage Differentiation Capacity
- Embryoid Body Formation: Harvest iPSCs with collagenase IV, culture in suspension in differentiation medium (DMEM/F12 with 20% FBS, 1% NEAA, 1mM L-glutamine) for 7 days
- Directed Differentiation: Differentiate iPSCs into representative lineages:
- Ectoderm: Neural induction using dual SMAD inhibition (dorsomorphin 1µM, SB431542 10µM) for 10 days, followed by immunostaining for PAX6 and NESTIN [5]
- Mesoderm: Mesodermal induction with BMP4 (50ng/mL) and Activin A (100ng/mL) for 5 days, analyze for BRACHYURY and NKX2.5 expression [5]
- Endoderm: Definitive endoderm differentiation using Activin A (100ng/mL) and CHIR99021 (3µM) for 5 days, validate with FOXA2 and SOX17 immunostaining [5]
Genomic Integrity Assessment
- Karyotype Analysis: Perform G-banding chromosomal analysis at 400-550 band resolution to confirm normal karyotype (46,XX or 46,XY) [5]
- Sendai Clearance Testing: Confirm absence of SeV genome by RT-PCR targeting SeV RNA using primers for the KOSM genes at passage 10 [5]
- Mycoplasma Testing: Regular mycoplasma screening using PCR-based detection methods
Molecular Mechanisms of Reprogramming
Signaling Pathways in Pluripotency Acquisition
The reprogramming process involves coordinated activation and suppression of multiple signaling pathways that collectively establish and maintain the pluripotent state. Understanding these pathways is essential for optimizing reprogramming efficiency and directing differentiation.
Wnt/β-Catenin Signaling The Wnt pathway plays a dual role in reprogramming, with precise temporal control being critical for success. In the canonical Wnt/β-catenin pathway, Wnt ligands bind to Frizzled receptors and LRP5/6 co-receptors, disrupting the β-catenin destruction complex (Axin, APC, GSK3β, CK1α) [7]. This prevents β-catenin phosphorylation and degradation, allowing its accumulation and translocation to the nucleus where it partners with TCF/LEF transcription factors to activate pluripotency genes [7]. Small molecule GSK3β inhibitors like CHIR99021 enhance reprogramming by stabilizing β-catenin, particularly during the early stages [1] [6].
TGF-β/SMAD Signaling The TGF-β pathway supports pluripotency through multiple mechanisms. Signaling through SMAD2/3 activated by TGF-β, Activin A, and Nodal supports self-renewal of primed pluripotent stem cells [8]. Simultaneously, BMP-activated SMAD1/5/8 signaling must be carefully balanced, as BMP promotes differentiation in most contexts but supports self-renewal in specific stem cell types [8]. Small molecule TGF-β pathway inhibitors (SB431542, A83-01) are commonly used in reprogramming to overcome epigenetic barriers and enhance mesenchymal-to-epithelial transition (MET) [1].
Additional Signaling Pathways Multiple other pathways contribute to establishing pluripotency. Hedgehog signaling can potentiate Wnt pathway activity and is essential for embryonic development [7]. Notch signaling regulates cell fate decisions through cell-cell communication and can influence reprogramming efficiency [8]. The Hippo pathway interacts with Wnt signaling through β-catenin and YAP/TAZ interactions, forming a complex regulatory network important for tissue size control and stem cell maintenance [7].
Figure 2: Key Signaling Pathways in Pluripotency
Epigenetic Remodeling During Reprogramming
Reprogramming involves comprehensive epigenetic remodeling to erase somatic memory and establish a pluripotent epigenome. Key changes include:
DNA Methylation Dynamics Pluripotent stem cells exhibit unique DNA methylation patterns characterized by global hypomethylation with focal hypermethylation at specific regulatory elements [4]. During reprogramming, somatic cell methylation patterns are erased through active and passive demethylation processes, followed by establishment of pluripotency-specific patterns. Studies comparing iPSCs from related donors demonstrate that iPSCs maintain donor-specific DNA methylation patterns even after reprogramming, indicating that some epigenetic variation persists despite comprehensive remodeling [4].
Histone Modification Changes The chromatin landscape undergoes dramatic reorganization during reprogramming. Somatic-specific histone marks (H3K9me3, H3K27me3) are removed from pluripotency genes, while activating marks (H3K4me3, H3K27ac) are established. Histone modifiers including SUV39H1, YY1, DOT1L, and Jhdm1a/1b significantly influence reprogramming efficiency [1]. Small molecule epigenetic modulators such as histone deacetylase inhibitors (valproic acid, sodium butyrate, trichostatin A) and DNA methyltransferase inhibitors (5-aza-cytidine, RG108) enhance reprogramming by facilitating epigenetic plasticity [1].
Chromatin Accessibility Changes Reprogramming involves widespread alterations in chromatin accessibility, with closed chromatin regions in somatic cells becoming accessible in pluripotent states. ATAC-seq analyses reveal that epigenetic variation increases as cells differentiate, while the direct relationship with genetic variation becomes stronger in iPSCs compared to differentiated cells [4]. This suggests that reprogramming creates a ground state with stronger genetic control over epigenetic patterns, which then diversifies during differentiation.
Essential Research Reagents and Tools
Table 3: Essential Research Reagents for iPSC Generation and Characterization
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC/L-MYC | Core transcription factors for pluripotency induction | L-MYC reduces tumorigenic risk compared to c-MYC [1] |
| Delivery Systems | CytoTune-iPS 2.0 Sendai Virus, Episomal plasmids, Synthetic mRNA | Factor delivery with varying integration profiles | Sendai virus offers high efficiency with clearance by passage 10 [5] |
| Small Molecule Enhancers | VPA, Sodium butyrate, Trichostatin A, CHIR99021, RepSox, 616452 | Epigenetic modulators and signaling pathway inhibitors | Significantly improve efficiency (up to 6.5-fold with VPA + 8-Br-cAMP) [1] |
| Culture Matrices | Vitronectin, Laminin-521, Matrigel | Extracellular matrix support for pluripotency | Defined matrices (vitronectin) preferred for clinical applications |
| Pluripotency Media | Essential 8, mTeSR1, Pluripotency induction medium | Support iPSC self-renewal and expansion | Chemically defined formulations enhance reproducibility |
| Characterization Antibodies | OCT4, SOX2, NANOG, SSEA-4, TRA-1-60, TRA-1-81 | Pluripotency marker validation | Combined immunocytochemistry and flow cytometry for validation [5] |
| Differentiation Reagents | BMP4, Activin A, CHIR99021, dorsomorphin, SB431542 | Directed differentiation into three germ layers | SMAD inhibition critical for neural ectoderm differentiation [5] |
| Quality Control Assays | G-banding karyotyping, Mycoplasma PCR, SeV clearance testing | Genomic integrity and safety validation | Mandatory for clinical-grade iPSC lines [5] |
The journey from somatic cells to pluripotency has evolved dramatically since the initial discovery of iPSCs in 2006. The core reprogramming principles now encompass diverse methodologies including integration-free factor delivery, chemical reprogramming, and precise modulation of signaling pathways. Current approaches prioritize safety through non-integrating methods and reduced reliance on oncogenic factors while maintaining high efficiency through small molecule enhancers and optimized culture conditions.
The physiological relevance of iPSC-derived tissues continues to improve through better understanding of reprogramming mechanisms, particularly the epigenetic remodeling processes that create a authentic pluripotent state. As reprogramming protocols become more standardized and efficient, iPSC technology is poised to advance numerous applications including disease modeling, drug screening, and regenerative medicine. The ongoing development of chemically defined, xeno-free systems will further enhance the translational potential of iPSC-derived tissues for clinical applications.
The advent of induced pluripotent stem cells (iPSCs) has revolutionized regenerative medicine and in vitro disease modeling. First introduced in 2006 by Shinya Yamanaka and colleagues, iPSCs are generated by reprogramming somatic cells to a pluripotent state through the transient overexpression of key transcription factors, most commonly Oct4, Sox2, Klf4, and c-Myc (OSKM) [2] [9]. Unlike human embryonic stem cells (hESCs), iPSC derivation does not require the destruction of human embryos, circumventing ethical concerns while providing an invaluable reservoir of patient-specific pluripotent cells [10] [9]. However, the critical challenge remains thoroughly validating the pluripotency of the iPSC starting platform to ensure these cells possess the differentiation capacity and functional equivalence necessary for reliable research and clinical applications. This guide objectively compares the key markers and validation methodologies for confirming true pluripotent status in iPSCs, providing researchers with a framework for rigorous quality assessment.
Core Pluripotency Markers: Molecular Signatures of iPSCs
The molecular profile of fully reprogrammed iPSCs closely resembles that of hESCs, characterized by specific surface antigens, transcription factors, and enzymatic activities.
Table 1: Key Molecular Markers for Validating iPSC Pluripotency
| Marker Category | Specific Markers | Detection Method | Acceptance Criterion |
|---|---|---|---|
| Surface Antigens | SSEA-4, TRA-1-60, TRA-1-81 [11] | Flow Cytometry, Immunocytochemistry | Expression on ≥75% of the cell population [12] |
| Transcription Factors | Oct3/4, Sox2, Nanog [9] [11] | Immunocytochemistry, RNA Analysis | Nuclear expression, significant transcriptional upregulation |
| Enzymatic Activity | Alkaline Phosphatase (AP) [9] | Colorimetric or Fluorescent Assay | High enzymatic activity visually detectable in colonies |
The expression of these core markers is regulated by an interconnected autoregulatory loop, with Oct4 and Sox2 playing particularly pivotal roles in establishing and maintaining the pluripotent state [9]. The validation of these markers should be performed using standardized assays. For flow cytometry, the use of a fluorescence minus one (FMO) control is advised to ensure accurate gating and control for fluorescent spread [12].
Functional Validation of Pluripotency: Beyond Molecular Markers
While molecular marker expression is necessary, it is insufficient alone to confirm full pluripotency. Functional assays are required to demonstrate the fundamental capacity of iPSCs to differentiate into derivatives of all three embryonic germ layers.
In Vitro Trilineage Differentiation
The gold standard in vitro assay involves differentiating iPSCs into ectoderm, mesoderm, and endoderm lineages, typically via embryoid body (EB) formation [10]. The directed differentiation potential can be assessed with a lineage scorecard, with a proposed detection limit of at least two out of three positive lineage-specific markers for each germ layer being a suitable criterion for validation [12].
In Vivo Teratoma Formation
The injection of iPSCs into immunodeficient mice leads to the formation of teratomas—complex tumors containing tissues from all three germ layers, such as neural tissue (ectoderm), cartilage (mesoderm), and epithelial structures (endoderm) [10]. This assay remains a rigorous, though time-consuming, test of functional pluripotency.
Epigenetic Landscape and Pluripotency Assessment
The reprogramming process involves profound remodeling of the epigenome to reset the somatic cell's epigenetic memory and establish a pluripotent state [2]. While global DNA methylation patterns between hiPSCs and hESCs are largely similar, studies have reported subtly different methylated regions [10]. Some differences are attributed to epigenetic memory—a persistence of epigenetic marks from the somatic cell of origin [10]. However, these differences tend to diminish with continuous cell passaging [10]. Analysis of global histone modification patterns (e.g., H3K4me3, H3K27me3) provides additional insight into the epigenetic state of the pluripotency network.
iPSCs vs. ESCs: A Comparative Analysis of Pluripotency
The equivalence between iPSCs and the "gold standard" hESCs has been extensively debated. Overall, the molecular and functional profiles of iPSCs and hESCs are remarkably similar, though not always identical [10] [13].
Table 2: Comparative Analysis of Pluripotency in hESCs and hiPSCs
| Characteristic | Human Embryonic Stem Cells (hESCs) | Human Induced Pluripotent Stem Cells (hiPSCs) |
|---|---|---|
| Origin | Inner cell mass of the blastocyst [10] | Reprogrammed somatic cells [9] |
| Ethical Considerations | Controversial due to embryo destruction [10] [9] | Ethically favorable; no embryos required [9] [11] |
| Genetic Background | Unique per line | Can be patient-specific [10] |
| Transcriptional Profile | Reference "gold standard" [10] | Largely similar, but subtle differences and increased variability reported [10] [13] |
| Epigenetic State | Established pluripotent epigenome | May retain epigenetic memory of cell of origin; can acquire aberrant methylation [10] |
| Functional Differentiation | Robust, high yield of differentiated progeny [10] | Can be variable and less efficient for some lineages (e.g., neural, cardiovascular) [10] |
| Tumorigenicity Risk | Teratoma formation | Teratoma formation; potential risk from integrating reprogramming vectors [9] |
Some studies comparing isogenic cell lines (those with the same genetic background) have found minimal differences in gene expression and methylation profiles between hiPSCs and hESCs, suggesting that many reported discrepancies may be due to genetic variation rather than the reprogramming process itself [14]. Furthermore, a 2017 study demonstrated equivalent neuronal differentiation potential between genetically unmatched hESCs and integration-free hiPSCs, with the derived motor neurons showing similar functionality in a neural muscular junction assay [13].
Quality Control in GMP-Compliant iPSC Production
For clinical applications, validation under Good Manufacturing Practice (GMP) standards is essential. Key validated parameters for GMP batch release include the absence of residual reprogramming vectors and demonstration of directed differentiation potential [12]. Screening for residual episomal vectors should occur between passages eight and ten, as testing at earlier passages might lead to unnecessary rejection of lines that have not yet fully cleared the vectors [12]. A minimum input of 20,000 cells (120 ng of genomic DNA) is recommended for the accurate determination of residual vectors [12].
The Scientist's Toolkit: Essential Reagents for iPSC Validation
Table 3: Key Research Reagent Solutions for iPSC Validation
| Reagent/Category | Example Product(s) | Primary Function in Validation |
|---|---|---|
| Defined Culture Medium | Essential 8, mTeSR Plus [11] | Maintains iPSCs in a stable, undifferentiated state for consistent analysis. |
| Extracellular Matrix | Vitronectin, ES-Matrigel [11] | Provides a defined, xeno-free substrate for robust iPSC growth. |
| Reprogramming Vectors | ReproRNA-OKSGM, Episomal Vectors [9] [15] | Non-integrating systems for footprint-free iPSC generation. |
| Flow Cytometry Antibodies | Anti-SSEA-4, Anti-TRA-1-60 [12] [11] | Quantifies expression of key pluripotency surface markers. |
| Immunocytochemistry Antibodies | Anti-OCT4, Anti-NANOG [13] [11] | Visualizes nuclear localization of core pluripotency factors. |
| Trilineage Differentiation Kits | Commercially available directed differentiation kits | Provides a standardized system for functional validation of differentiation potential. |
| qPCR Assays | Pluripotency TaqMan Gene Expression Panels | Enables quantitative transcriptional analysis of pluripotency genes. |
Critical Considerations for Robust Validation
- Reprogramming Method: The choice of reprogramming vector (integrating vs. non-integrating) can significantly impact the genomic integrity and transcriptional profile of the resulting iPSCs [9]. Non-integrating methods are preferred for clinical applications.
- Genetic Background: The donor's genetic background is a major source of variability. Using isogenic controls is ideal for comparative studies [10] [14].
- Clonal Variation: Not all iPSC clones from the same reprogramming experiment are equal. Multiple clones should be characterized to select the most suitable line [10].
- Passage Number: Epigenetic memory tends to fade with passaging, and residual reprogramming factors are diluted. Use mid-passage cells for validation to ensure a stable phenotype [10] [12].
Validating the pluripotent starting platform of iPSCs is a multi-faceted process that requires assessing molecular markers, functional differentiation capacity, and epigenetic status. While iPSCs demonstrate immense versatility and hold great promise for regenerative medicine and disease modeling, their equivalence to hESCs can be variable. A rigorous, standardized validation workflow incorporating the key markers and assays outlined in this guide is essential for researchers to ensure the quality and physiological relevance of their iPSC-derived tissues. As the field advances, the development of more refined "scorecards" and GMP-compliant quality control tests will further solidify iPSCs as a reliable and powerful tool for research and therapy.
A critical challenge in modern regenerative medicine and drug development is the efficient generation of physiologically relevant human tissues. Induced pluripotent stem cells (iPSCs), with their capacity for unlimited self-renewal and ability to differentiate into any cell type, offer an unparalleled platform to address this challenge [2] [16]. However, the differentiation potential and functional maturity of the resulting tissues are highly dependent on the specific protocols and conditions employed. This guide objectively compares prominent differentiation strategies by analyzing key experimental data, providing researchers with a foundation for selecting and optimizing protocols for specific applications.
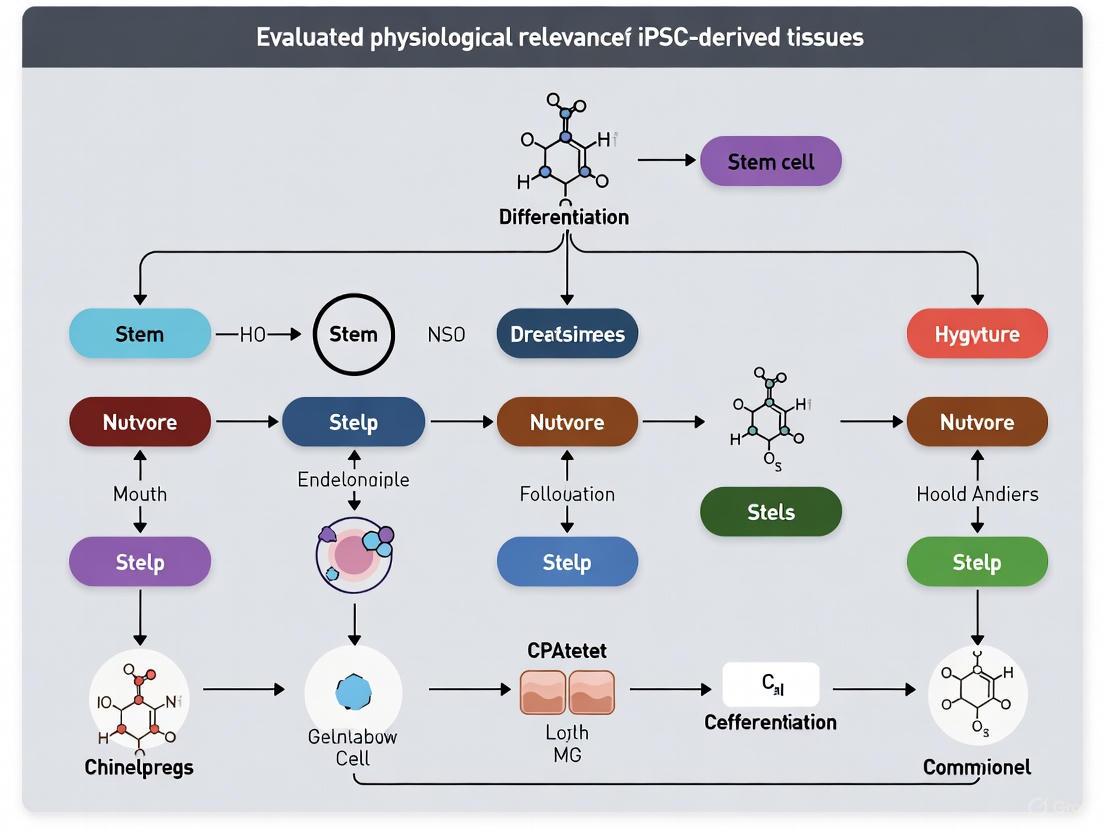
Key Signaling Pathways Governing iPSC Differentiation
The directed differentiation of iPSCs recapitulates embryonic development, relying on the precise activation or inhibition of key signaling pathways to guide cell fate. The following diagram illustrates the primary pathways involved in this process.
The activation of these pathways is context-dependent, varying with the timing, duration, and combination of signals. For example, BMP signaling has been identified as a key controller in the differentiation of neural crest cells and ectodermal placode cells, while FGF/BMP signaling cooperation is crucial for thyroid lineage specification [17] [18]. Similarly, Wnt and TGF-β signaling are instrumental in steering cells toward definitive endoderm, the precursor for liver, pancreas, and lung tissues [19].
Comparative Analysis of Cardiomyocyte Differentiation Protocols
The choice of pre-culture medium before initiating differentiation is a critical variable influencing the efficiency and outcome of iPSC-directed differentiation. Recent research has systematically evaluated this effect on the generation of cardiomyocytes.
Table 1: Impact of Pre-culture Medium on Cardiac Troponin T (cTnT) Positivity in Differentiated Cells
| Pre-culture Medium Type | Description | cTnT+ Cell Population (%) |
|---|---|---|
| StemFit AK03 (No. 1) | Standard pluripotency maintenance medium | 84% |
| Similar to E8 Medium (No. 3) | Low-nutrient, albumin-free formulation | 89% |
| Similar to E8 Medium (No. 2) | Low-nutrient, albumin-free formulation | 91% |
| Similar to EB Formation Medium (No. 5) | High-nutrient medium with KnockOut Serum Replacement (KOSR) | 95% |
Data adapted from a 2025 study investigating seven variations of pre-culture media [20].
The data demonstrates that medium composition directly impacts differentiation yield. Media approximating the high-nutrient environment of Embryoid Body (EB) Formation medium, which contains growth factors and proteins like albumin and transferrin, yielded the highest efficiency of cardiomyocyte differentiation (95% cTnT+ cells) [20]. This suggests that a nutrient-rich pre-culture environment may better prepare iPSCs for the subsequent stress of differentiation induction. Furthermore, the same study found that tissues derived using E8-like medium precursors exhibited higher protein expression levels of atrial natriuretic peptide (ANP), indicating not only higher yield but also enhanced tissue maturation [20].
Experimental Protocols for Directing iPSC Differentiation
Protocol 1: Directed Differentiation into Thyroid Follicular Cells
This protocol recapitulates developmental stages to derive thyroid follicular cells (TFCs) without exogenous transcription factors [18].
- Maintenance and Seeding: Culture human iPSCs on a suitable substrate (e.g., Matrigel) in a maintenance medium like mTeSR-1 or StemFit. Prior to differentiation, passage cells as single cells using an enzyme like TrypLE Select and plate them at an appropriate density, often with a Rho-associated protein kinase (ROCK) inhibitor (e.g., Y-27632) to enhance survival.
- Definitive Endoderm Induction: Replace the maintenance medium with an endoderm induction medium. This typically involves activating key signaling pathways, notably WNT and TGF-β/Activin A signaling, for a defined period (e.g., 3-5 days) to specify the definitive endoderm lineage.
- Anterior Foregut Endoderm Induction: Following definitive endoderm formation, pattern the cells toward anterior foregut endoderm. This stage often uses a combination of growth factors and small-molecule inhibitors, such as BMP and TGF-β inhibitors, alongside FGF signaling activation.
- Thyroid Lineage Specification and Maturation: Specify the thyroid lineage using a combination of Fibroblast Growth Factor (FGF) and Bone Morphogenetic Protein (BMP) signaling. Subsequent maturation into functional TFCs involves culture in a medium containing hormones such as TSH and IGF-1 to promote the formation of thyroid follicles capable of expressing thyroglobulin and thyroid hormones.
Protocol 2: Single-Step Direct Conversion into Functional Neurons
This alternative approach bypasses multi-stage differentiation by forced expression of a single neurogenic transcription factor, Neurogenin-2 (NGN2), to rapidly convert human ESCs and iPSCs into functional induced neuronal (iN) cells with nearly 100% yield and purity in under two weeks [21].
- Genetic Modification: Engineer the iPSC line to allow for inducible expression of the human NGN2 gene. This is typically achieved by lentiviral transduction or targeted integration of the NGN2 transgene under a doxycycline-inducible promoter.
- Induction and Culture: Initiate neuronal conversion by adding doxycycline to the culture medium. Cells are subsequently cultured in a neuronal induction medium supplemented with specific neurotrophic factors (e.g., BDNF, NT-3).
- Maturation and Purification: Within days, cells downregulate pluripotency markers and begin expressing neuronal proteins. After one week, cells can be replated onto supportive substrates (e.g., poly-D-lysine, laminin) and maintained in neuronal maturation media. The high purity of the culture often eliminates the need for further cell sorting.
This method produces neurons that form mature pre- and postsynaptic specializations, exhibit spontaneous network activity, and integrate synaptically upon transplantation into mouse brain [21].
The Scientist's Toolkit: Essential Reagents for iPSC Differentiation
Successful differentiation relies on a core set of reagents and materials. The table below details essential components for the protocols discussed.
Table 2: Key Research Reagent Solutions for iPSC Differentiation
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| StemFit AK03 / mTeSR Plus | Chemically defined medium for maintenance of iPSC pluripotency. | Pre-culture of iPSCs prior to initiation of differentiation [20]. |
| Essential 8 Medium | Low-nutrient, albumin-free medium for selective culture of iPSCs. | Pre-culture medium shown to support high-efficiency cardiac differentiation [20]. |
| iMatrix-511 / Laminin-521 | Recombinant laminin-based substrate for coating culture vessels. | Provides a defined surface for iPSC attachment and growth, supporting differentiation [20]. |
| Y-27632 (ROCK Inhibitor) | Small molecule that inhibits Rho-associated kinase. | Significantly improves survival of iPSCs after single-cell passaging [19]. |
| CHIR 99021 | Small molecule inhibitor of Glycogen Synthase Kinase-3 (GSK-3). | Activates Wnt/β-catenin signaling; used in definitive endoderm and cardiomyocyte induction [20]. |
| Recombinant FGF2 (bFGF) | Growth factor that activates FGF signaling pathways. | Critical for maintaining pluripotency and for directing differentiation into mesoderm and endoderm lineages [18]. |
| Recombinant BMP4 | Growth factor that activates BMP signaling pathways. | Used in conjunction with FGF for thyroid lineage specification from anterior foregut endoderm [18]. |
| Doxycycline | Small molecule used for inducing gene expression. | Required for activating transgene expression (e.g., NGN2) in inducible direct conversion systems [21]. |
Enhancing Functional Maturity through Biomimetic Culture Systems
Achieving a mature, adult-like phenotype in iPSC-derived cells remains a significant hurdle. Simple 2D monocultures often yield immature, fetal-like cells. Advanced culture systems that better mimic the in vivo environment have shown great promise in overcoming this limitation.
- 3D Co-culture Systems: Research demonstrates that hiPSC-derived cardiomyocytes (hiPSC-CMs) co-cultured with human coronary artery endothelial cells in a 3D gelatin methacryloyl (GelMA) hydrogel show significantly higher expression of cardiac maturation markers compared to standard 2D monocultures. Omics analysis confirmed the upregulation of pathways related to cardiac differentiation and contraction in the 3D system [22].
- Paracrine and Direct Contact Signaling: The functional maturation of hiPSC-CMs is further enhanced by co-culture with hiPSC-derived cardiac fibroblasts (hiPSC-CFs). This improvement is driven by a mechanism that requires both paracrine signaling (soluble factors) and direct cellular interactions. While conditioned medium from hiPSC-CFs improved some contractile properties, full functional maturation with enhanced contractile strain and kinetics required direct contact [22].
The following workflow summarizes the strategic options for generating functionally mature tissues from iPSCs, integrating the protocols and maturation strategies discussed.
The selection of a differentiation pathway is a fundamental decision that determines the physiological relevance and utility of the resulting iPSC-derived tissues. As the data indicates, protocol variables like pre-culture medium can alter differentiation efficiency by over 10% [20]. Furthermore, the choice between multi-stage directed differentiation and direct conversion trades off the recapitulation of development for speed and purity [18] [21]. For disease modeling and drug screening, the emergence of complex 3D co-culture systems is proving essential for driving cells beyond a fetal-like state into a more mature, adult phenotype that yields more predictive and translatable data [22]. By quantitatively comparing these approaches, researchers can make informed decisions to generate high-quality, functionally mature human tissues that advance the fields of regenerative medicine and therapeutic development.
The advent of Induced Pluripotent Stem Cell (iPSC) technology has revolutionized regenerative medicine and drug discovery by providing unprecedented access to human cell types for research and therapeutic applications. iPSCs are laboratory-made pluripotent stem cells produced by reprogramming somatic cells through the expression of specific pluripotency genes, a process first discovered in 2006 by Shinya Yamanaka's lab [23] [2]. Within this field, two distinct cellular source paradigms have emerged: patient-specific (autologous) approaches, which utilize cells derived from the same individual receiving the therapy, and allogeneic approaches, which employ cells from donor-derived sources manufactured for "off-the-shelf" use [24]. The choice between these paradigms represents a critical strategic decision for researchers and drug development professionals, with significant implications for physiological relevance, immune compatibility, manufacturing scalability, and clinical applicability. This comparison guide objectively examines the technical and practical considerations for both approaches within the context of evaluating physiological relevance in iPSC-derived tissue research.
Comparative Analysis: Key Parameters for Research and Development
The table below summarizes the core characteristics of patient-specific versus allogeneic iPSC sources across parameters critical for research and therapeutic development.
Table 1: Comprehensive Comparison of Patient-Specific and Allogeneic iPSC Sources
| Parameter | Patient-Specific (Autologous) iPSCs | Allogeneic iPSCs |
|---|---|---|
| Definition | iPSCs derived from and genetically identical to the patient/research subject [25] | iPSCs derived from a healthy donor, designed for universal application [24] |
| Immune Compatibility | High; minimal immune response upon transplantation [25] | Variable; requires immune suppression or HLA matching to prevent rejection [25] [26] |
| Physiological Relevance for Disease Modeling | Excellent for modeling patient-specific disease mechanisms and genetic backgrounds [23] [3] | Limited for personalized genetics; suitable for general disease mechanisms or when created with specific mutations [23] |
| Manufacturing Scalability | Low; individualized production runs are resource-intensive [24] | High; single, well-characterized cell bank can supply multiple patients or studies [26] [24] |
| Production Timeline & Cost | Timeline: Several months [24]Cost: High per unit [24] | Timeline: Immediate from cell bank [24]Cost: Lower per unit [24] |
| Batch-to-Batch Variability | High variability between individual patients/donors [26] | Low variability from a master cell bank [24] |
| Ideal Applications | Personalized medicine, disease modeling with patient genetics, cell therapies without immunosuppression [25] [3] | High-throughput drug screening, toxicology studies, off-the-shelf cell therapies [23] [26] |
Experimental Evidence: Immune Response and Functional Outcomes
Direct comparative studies, particularly in immunologically competent models, provide the most compelling data for evaluating these two cellular sources.
Key Findings from a Primate Transplantation Study
A seminal 2013 study directly compared autologous and allogeneic transplantation of iPSC-derived neurons into the brains of non-human primates without immunosuppression [25]. The experimental workflow and key outcomes of this critical study are detailed below.
Figure 1: Experimental workflow and key findings from the direct comparison of autologous and allogeneic iPSC-derived neural transplants in non-human primates [25].
Detailed Experimental Protocol
Cell Source and iPSC Generation: Fibroblasts or peripheral blood mononuclear cells (PBMCs) were obtained from four cynomolgus monkeys. iPSCs were generated using either retroviral vectors (for fibroblasts) or non-integrating episomal vectors (for PBMCs) [25].
Dopaminergic Neuron Differentiation: Selected iPSC clones were differentiated into neural cells using a growth factor-based protocol. Dissociated iPSCs were incubated in ultralow-attachment plates with BMP and Activin/NODAL signaling inhibitors to initiate neural induction. Midbrain dopaminergic (DA) neuron fate was induced by sequential addition of purmorphamine/FGF8 and FGF2/FGF20. The resulting cells expressed characteristic midbrain DA markers (LMX1A, FOXA2, TH, PITX3) [25].
Major Histocompatibility Complex (MHC) Mismatch Verification: Prior to transplantation, genotyping of MHC (Major Histocompatibility Complex) class I alleles was performed to confirm mismatch between donor and recipient animals in the allogeneic group [25].
Transplantation and Monitoring: Each animal received six stereotactic injections of iPSC-derived neural cells into the left striatum. Animals were observed for 3.5–4 months without immunosuppression. Monitoring included:
- PET imaging: Using [11C]PK11195 to visualize microglial activation [25].
- Serum cytokine analysis: Measuring IFN-γ levels as an indicator of systemic immune activation [25].
- Histological and immunofluorescence analysis: Post-mortem examination of graft survival and immune cell infiltration using markers for microglia (IBA-1), MHC class II, pan-leukocytes (CD45), T-cells (CD3), and cytotoxic T-cells (CD8) [25].
Quantitative Outcomes
The table below summarizes the key quantitative findings from this direct comparison study.
Table 2: Quantitative Outcomes from Primate iPSC-Derived Neuron Transplantation Study [25]
| Outcome Measure | Autologous Grafts | Allogeneic Grafts |
|---|---|---|
| Microglia Activation (IBA-1+ cells) | Minimal | Significantly higher |
| MHC Class II Expression | Low | Elevated, co-localized with host microglia |
| Leukocyte Infiltration (CD45+ cells) | Minimal | Significant accumulation |
| T-cell Infiltration (CD3+ cells) | Minimal | Present, ~60% were CD8+ cytotoxic T-cells |
| Dopaminergic Neuron Survival | 4,428 ± 1,130 neurons/tract | 2,247 ± 641 neurons/tract |
| PET [11C]PK11195 Uptake | No apparent uptake | Increased in 1 of 2 allografted animals at 3 months |
Implications for Research and Therapy
This direct comparison demonstrates that even in an immunologically privileged site like the brain, allogeneic grafts trigger a measurable acquired immune response that negatively impacts cell survival compared to autologous grafts [25]. For research requiring long-term engraftment or modeling of complex tissue environments, patient-specific cells may provide superior physiological relevance by avoiding these confounding immune responses.
The Scientist's Toolkit: Essential Reagents for iPSC Research
The table below catalogs key reagents and their applications in developing and differentiating patient-specific and allogeneic iPSCs.
Table 3: Essential Research Reagents for iPSC-Derived Tissue Research
| Reagent/Category | Function/Application | Examples/Specifics |
|---|---|---|
| Reprogramming Factors | Convert somatic cells to pluripotent state | OCT4, SOX2, KLF4, c-MYC (OSKM) [2] |
| Non-Integrating Vectors | Safer reprogramming for clinical applications | Sendai virus, episomal plasmids [3] |
| Neural Induction Media | Direct differentiation toward neural lineages | BMP/Activin/NODAL inhibitors [25] |
| Patterning Factors | Specify regional identity (e.g., midbrain) | Purmorphamine (SHH agonist), FGF8, FGF20 [25] |
| Cell Characterization Antibodies | Validate pluripotency and differentiation | Anti-OCT4, NANOG (pluripotency); Anti-TH, FOXA2, LMX1A (dopaminergic neurons) [25] |
| Immune Monitoring Reagents | Assess host immune response | Anti-IBA1 (microglia), anti-CD45 (leukocytes), anti-CD3 (T cells) [25] |
| GMP-Grade Materials | Clinical-grade manufacturing | cGMP-compliant cytokines, xeno-free matrices [24] |
Manufacturing and Scalability Considerations
The manufacturing pipeline differs significantly between patient-specific and allogeneic approaches, impacting their suitability for various research applications.
Figure 2: Comparative manufacturing workflows for patient-specific versus allogeneic iPSC-derived products, highlighting the scalability advantage of allogeneic approaches [24].
Manufacturing Protocols and Quality Control
Allogeneic iPSC Bank Establishment: For allogeneic products, a Master Cell Bank (MCB) is established from a single, well-characterized iPSC clone [24]. This process requires:
- Donor eligibility determination: Comprehensive health screening and infectious disease testing of the cell donor [24].
- Extensive characterization: Testing for sterility, mycoplasma, adventitious viruses, pluripotency, and genomic stability [24].
- cGMP compliance: All materials and processes must adhere to Current Good Manufacturing Practices, with animal-origin-free reagents preferred [24].
Patient-Specific iPSC Generation: For autologous products, the process begins anew for each patient/research subject, with more limited quality control focused on sterility, identity, and differentiation potential [24].
Purification Strategies: To ensure safety, particularly for removing residual undifferentiated iPSCs that could form teratomas, purification using specific surface markers is employed. Magnetic bead-based separation is often preferred over FACS for better compliance with closed-system manufacturing requirements [24].
The choice between patient-specific and allogeneic iPSC sources represents a fundamental trade-off between immune compatibility and manufacturing scalability. Patient-specific iPSCs offer the critical advantage of minimizing immune rejection, thereby providing more physiologically relevant models for long-term engraftment studies and enabling autologous therapies without immunosuppression [25]. Conversely, allogeneic iPSCs provide scalable, cost-effective "off-the-shelf" products suitable for high-throughput drug screening and broader therapeutic applications [23] [24].
Emerging technologies are blurring the distinction between these paradigms. CRISPR-Cas9 genome editing enables correction of disease-causing mutations in patient-specific iPSCs [3], while also allowing creation of "universal donor" allogeneic cells through knockout of HLA genes [26]. Similarly, iPSC-derived organoids are being applied to both patient-specific disease modeling and allogeneic drug screening platforms [27]. The optimal choice depends fundamentally on the research question or clinical application, with the critical advantage going to patient-specific sources when immune compatibility is paramount, and to allogeneic sources when scalability and standardization are primary concerns.
Building Better Models: Advanced Fabrication of iPSC-Derived Tissues
The transition from two-dimensional (2D) to three-dimensional (3D) cellular models represents a paradigm shift in cardiovascular research, drug discovery, and regenerative medicine. While 2D cultures of human pluripotent stem cell-derived cardiomyocytes (hPSC-CMs) have provided valuable insights, they inherently lack the structural complexity and cell-cell interactions found in native heart tissue [28]. This limitation has driven the development of more physiologically relevant models, primarily cardiac organoids and engineered heart tissues (EHTs), which better mimic the human heart's microenvironment.
The fundamental challenge in using hPSC-derived cardiomyocytes is their typically immature state, which limits their applications for disease modeling and drug screening [29]. Even extended culture periods up to one year fail to achieve maturity equivalent to in vivo conditions, indicating that either standard culture conditions are inhibitory or critical maturation stimuli are absent [29]. This maturation gap has significant implications for predicting human cardiac responses and remains a central consideration in evaluating the physiological relevance of iPSC-derived tissues.
Comparative Analysis of 3D Cardiac Models
Defining Characteristics and Applications
Cardiac organoids and EHTs represent complementary approaches with distinct design philosophies, fabrication methods, and application strengths, as summarized in Table 1.
Table 1: Key Characteristics of 3D Cardiac Models
| Feature | Cardiac Organoids | Engineered Heart Tissues (EHTs) |
|---|---|---|
| Formation Principle | Self-organization from stem/progenitor cells [30] | Bioengineering approaches with predefined architecture [28] [31] |
| Cellular Complexity | Multiple cardiac cell types (CMs, ECs, fibroblasts) [30] [29] | Primarily cardiomyocytes, often with engineered non-myocyte components [31] |
| Structural Fidelity | Recapitulates developmental cardiac structures [30] | Recapitulates adult cardiac tissue alignment and mechanics [31] |
| Primary Applications | Disease modeling, developmental biology, drug screening [30] | Drug safety testing (cardiotoxicity), regenerative therapy patches [28] [31] |
| Key Advantages | Patient-specific modeling, complex cell-cell interactions [30] | Controlled architecture, tunable mechanical properties, direct functional measurements [31] |
| Limitations | Size limitation due to lack of vasculature, variability [32] | Limited innate cellular complexity, requires external support [31] |
Quantitative Functional Comparison
Functional performance metrics provide critical insights for researchers selecting appropriate models for specific applications. Table 2 compares key parameters across different cardiac models.
Table 2: Quantitative Functional Comparison of Cardiac Models
| Parameter | 2D Cardiac Cultures | Cardiac Organoids | Engineered Heart Tissues | Native Adult Heart |
|---|---|---|---|---|
| Contractile Force | Not measurable | ~1-2 mN [29] | 1-5 mN [31] | >1000 mN |
| Maturation Markers (TNNI3/TNNI1 ratio) | <5% [29] | ~18% (SF-hCOs) to higher with directed maturation [29] | Varies with protocol, typically higher than 2D | ~100% |
| Spontaneous Beat Rate (bpm) | 30-60 [29] | 30-90 (DM-hCOs: reduced rate) [29] | 60-120 (often paced) | 60-100 (sinus rhythm) |
| Metabolic Capacity | Glycolytic dominance [29] | Intermediate, can be enhanced [29] | Can be enhanced via fatty acid supplementation [29] | Oxidative phosphorylation |
| Drug Response Predictive Value | Moderate (limited for chronic toxicity) [28] | High for disease-specific mechanisms [30] [29] | High for acute electrophysiology and contractility [28] | N/A |
Experimental Protocols for Advanced 3D Cardiac Models
Directed Maturation Protocol for Cardiac Organoids (DM-hCOs)
A recent breakthrough in cardiac organoid maturation addresses the critical limitation of immaturity in hPSC-derived models [29]. The directed maturation protocol incorporates specific pathway activators to drive cardiomyocytes toward a more adult-like state, as visualized in Figure 1.
Figure 1: Directed maturation workflow for cardiac organoids. This protocol enhances maturity through transient activation of AMPK and ERR pathways [29].
The protocol builds upon a serum-free hCO foundation with two key additions:
- CHIR99021 (2 μM) during the first 2 days of hCO formation to enhance Wnt signaling
- Transient 4-day treatment with DY131 (3 μM) and MK8722 (10 μM) to activate estrogen-related receptors (ERR) and AMP-activated protein kinase (AMPK), respectively [29]
This combinatorial approach induces metabolic switching to oxidative phosphorylation and enhances expression of mature sarcomeric proteins, including cardiac troponin I (cTnI). Phosphoproteomic analysis reveals that this treatment shares 48.2% of differentially regulated phosphosites with electrical pacing, including key cardiac regulators such as phospholamban (PLN S16/T17), which enhances sarcoplasmic reticulum calcium cycling [29].
Vascularized Cardiac Organoid Generation
A significant limitation of traditional organoids is the lack of functional vasculature, restricting their size and maturity. A recent Stanford Medicine protocol has overcome this challenge through optimized differentiation conditions that simultaneously generate multiple cardiac cell types [32].
Table 3: Essential Reagents for Vascularized Cardiac Organoid Formation
| Reagent Category | Specific Examples | Function | Protocol Timing |
|---|---|---|---|
| Pluripotency Maintenance | Small molecules for stem cell culture | Maintain starting cell pluripotency | Pre-differentiation |
| Mesoderm Induction | CHIR99021, BMP4 | Direct differentiation toward cardiac mesoderm | Days 0-3 |
| Cardiac Specification | Wnt inhibitors, FGFs | Promote cardiac progenitor formation | Days 3-5 |
| Vascular Induction | VEGFA, specific growth factor combinations | Enhance endothelial and smooth muscle differentiation | Days 5-10+ |
| Metabolic Maturation | Palmitate, linoleate, oleate | Promote oxidative metabolism | Days 17-22 |
| Maturation Agonists | DY131 (ERRβ/γ), MK8722 (AMPK) | Enhance transcriptional and metabolic maturity | Days 24-28 |
The winning "condition 32" from their screening of 34 different recipes produced organoids containing 15-17 different cell types, comparable to a six-week embryonic heart, with organized doughnut-shaped structures featuring cardiomyocytes and smooth muscle cells inside and an outer layer of endothelial cells forming branched, tubular vessels [32]. This self-organization approximates early embryonic development conditions, making these vascularized organoids valuable models for studying early human development.
3D Bioprinting of Engineered Heart Tissues
Bioprinting represents a bioengineering approach to creating EHTs with precise architectural control. The process involves several key stages, each with specific technical requirements, as shown in Figure 2.
Figure 2: 3D bioprinting workflow for engineered heart tissues. Multiple printing modalities offer different trade-offs in resolution, speed, and biocompatibility [31].
Key bioprinting modalities each present distinct advantages for cardiac applications:
- Extrusion-based: Most common, good for high cell density, but lower resolution [31]
- Jetting-based (inkjet, laser-assisted, electrohydrodynamic): Higher resolution, suitable for precise cellular patterning [31]
- Light-based (stereolithography - SLA, digital light processing - DLP): High resolution, but potential UV toxicity [31]
- Volumetric: Emerging technique for rapid 3D fabrication [31]
Bioink design has evolved toward natural-synthetic hybrids combining bioactive components (decellularized extracellular matrix - dECM, collagen, fibrin) with synthetic tunability (gelatin methacryloyl - GelMA, polyethylene glycol - PEG, methacrylated hyaluronic acid - MeHA) [31]. Conductive components are often incorporated to enhance electrical coupling between cardiomyocytes.
Application Case Studies in Disease Modeling and Drug Discovery
Modeling Inherited Cardiomyopathies
Cardiac organoids have demonstrated significant utility in modeling complex inherited heart diseases. When derived from human pluripotent stem cells with mutations in calsequestrin 2 (CASQ2) and ryanodine receptor 2 (RYR2), directed maturation hCOs (DM-hCOs) exhibit a pronounced pro-arrhythmia phenotype, effectively recapitulating key features of catecholaminergic polymorphic ventricular tachycardia (CPVT) [29].
Similarly, modeling of cardiomyopathy caused by a desmoplakin (DSP) mutation resulted in fibrosis and cardiac dysfunction in DM-hCOs. This model led to the identification of INCB054329, a bromodomain and extra-terminal inhibitor, as a potential therapeutic compound mitigating the desmoplakin-related functional defect [29]. These findings establish matured cardiac organoids as versatile platforms for applications in cardiac biology, disease modeling, and drug screening.
Vascularized Organoids for Developmental Studies
The incorporation of functional vasculature enables novel applications in developmental biology and toxicology. When vascularized cardiac organoids were exposed to fentanyl, researchers observed increased blood vessel formation [32]. This finding demonstrates the potential of these models for studying how substances affect developing cardiovascular systems during early pregnancy, a period that is difficult to study in humans for ethical reasons.
The vascularized organoids also provide insights into diseases involving abnormal endothelial-epithelial interactions. For instance, using patient-derived iPSCs with FOXF1 mutations (causing alveolar capillary dysplasia with pulmonary venous misalignment), vascularized lung organoids revealed primary endothelial defects and secondary epithelial abnormalities that could not be modeled in traditional epithelial-only organoids [33].
Drug Screening and Cardiotoxicity Testing
Engineered heart tissues offer significant advantages for pharmaceutical screening through their reproducible contractile function and electrophysiological properties. Heart-on-a-chip (HoC) technologies developed using microfluidic chip-based platforms enable real-time monitoring of contraction and electrical activity, providing multifaceted information essential for capturing natural tissue responses to pharmacological compounds [28].
The enhanced maturation achieved in DM-hCOs makes them particularly valuable for drug testing, as they more accurately recapitulate adult human cardiac drug responses compared to traditional 2D cultures [29]. These advanced models can detect subtle contractile abnormalities and pro-arrhythmic effects that might be missed in less mature systems, potentially reducing late-stage drug attrition due to cardiotoxicity.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Key Research Reagent Solutions for 3D Cardiac Tissue Engineering
| Reagent Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Stem Cell Sources | Human iPSCs, ESCs | Starting cell material for differentiation | Patient-specific vs. standardized lines; genetic stability |
| Induction Factors | CHIR99021 (Wnt activator), BMP4 | Mesoderm induction and cardiac patterning | Concentration and timing critical for efficiency |
| Maturation Agonists | DY131 (ERRβ/γ), MK8722 (AMPK) | Enhance metabolic and functional maturity | Transient application sufficient for sustained effects |
| Metabolic Substrates | Palmitate, oleate, linoleate | Promote oxidative metabolic maturation | Fatty acid composition influences maturation outcomes |
| Matrix Materials | Matrigel, fibrin, collagen, synthetic hybrids | Provide 3D structural support | Defined vs. complex matrices; mechanical properties |
| Vascular Induction | VEGFA, FGF, specific combinatorial factors | Promote endothelial and smooth muscle differentiation | Multiple cell type coordination required |
| Functional Assessment | Calcium dyes, contractile force sensors | Evaluate electrophysiology and mechanical function | Real-time monitoring capabilities |
The evolution from 2D cultures to 3D cardiac organoids and engineered heart tissues represents significant progress in cardiovascular research. While both approaches enhance physiological relevance compared to traditional 2D systems, they offer complementary strengths: cardiac organoids excel in cellular complexity and disease modeling, whereas EHTs provide superior control over architecture and functional measurements.
Current research is focused on addressing remaining limitations, particularly in achieving full maturity and vascularization. The development of vascularized organoids that can connect to host circulation marks a critical step toward potential regenerative applications [32]. Similarly, directed maturation protocols that activate specific signaling pathways demonstrate that strategic interventions can substantially enhance functional maturity [29].
As these technologies continue to advance, they promise to accelerate drug discovery through more predictive human-relevant models and potentially enable patient-specific regenerative therapies for cardiovascular disease, the leading cause of death worldwide [34]. The integration of these platforms with emerging technologies like 3D bioprinting, organ-on-chip systems, and single-cell genomics will further enhance their utility for both basic research and translational applications.
In the field of tissue engineering and regenerative medicine, the extracellular matrix (ECM) serves as the fundamental architectural blueprint for cellular life. This non-cellular, three-dimensional network of macromolecules provides not only structural support but also critical biochemical and biomechanical cues that regulate cell behavior, signaling, and tissue development [35]. The growing emphasis on developing physiologically relevant human in vitro models, particularly those utilizing human induced pluripotent stem cells (hiPSCs), has intensified the need for advanced scaffold systems that can accurately replicate the native ECM microenvironment [36]. Such systems are crucial for applications spanning drug development, disease modeling, and cellular therapeutics, where biological accuracy directly impacts translatability and predictive power.
The native ECM is a dynamic, complex structure whose composition varies across tissues and developmental stages. Its main components include collagens, elastin, laminin, fibronectin, proteoglycans, and glycosaminoglycans [35]. Furthermore, the ECM acts as a reservoir for various growth factors such as FGF, EGF, VEGF, and TGF-β, releasing them in a tightly regulated manner to guide processes including stem cell differentiation, angiogenesis, and tissue repair [35]. Beyond biochemistry, physical properties like ECM stiffness play a pivotal role in mechanotransduction, directly affecting cell fate decisions and lineage specification [35]. This multifaceted role makes the ECM an essential template for scaffold design, driving the development of innovative materials that can support the maintenance, expansion, and differentiation of hiPSCs in a biologically natural manner [36].
Categories of ECM-Mimetic Scaffolds
Scaffolds for tissue engineering are broadly classified into three categories based on their origin and composition: natural, synthetic, and hybrid. Each offers distinct advantages and limitations for replicating the native ECM.
Natural Scaffolds
Natural scaffolds are derived from biological sources and closely replicate the composition of native ECM, preserving structural integrity and biochemical cues essential for cellular functions [35].
- Decellularized ECM (dECM): Produced by removing cellular components and antigens from tissues or organs while preserving the native ECM structure and bioactive factors. This process minimizes immune and inflammatory responses while maintaining critical cues for cell adhesion, proliferation, and differentiation [35]. Decellularization techniques include chemical, enzymatic, and physical methods [35].
- Matrigel: A basement membrane extract derived from Engelbreth-Holm-Swarm (EHS) mouse sarcoma, composed primarily of laminin, collagen IV, and entactin [37]. Despite its widespread use, Matrigel suffers from batch-to-batch variability, undefined composition, limited mechanical tunability, and ethical concerns regarding its tumor-derived, animal-based origin [37].
- Other Natural Polymers: Materials including hyaluronic acid, alginate, collagen, and chitosan are also used, but they often present challenges such as low mechanical strength, uncontrollable degradation, and potential immunogenicity [38].
Synthetic Scaffolds
Synthetic scaffolds are composed of lab-engineered polymers, enabling precise control over mechanical properties including strength, stiffness, elasticity, and porosity [35]. This category offers superior reproducibility, scalability, and tunability compared to natural materials.
- Thermoresponsive Polymers: Platforms such as poly(N-isopropylacrylamide) (pNIPAM) allow for non-invasive cell harvesting through temperature-induced hydration changes, facilitating the creation of contiguous cell sheets with preserved cell-cell junctions and deposited ECM [39].
- Functionalized Synthetic Hydrogels: Customizable polymers can be engineered with specific bioactive motifs (e.g., RGD peptides, vitronectin, fibronectin) to enhance cell adhesion, proliferation, and differentiation [40]. For example, a thermoresponsive terpolymer of NiPAAm, VPBA, and PEGMMA has demonstrated effective support for hiPSC pluripotency and robust cardiac differentiation [40].
- Conductive Polymers: Materials like polyaniline (PANI), polythiophene (PTh), and polypyrrole (PPy) can be used to create electroconductive scaffolds that regulate biological functions such as cell adhesion, migration, differentiation, and DNA synthesis, which is particularly beneficial for electrically excitable tissues [41].
Hybrid Scaffolds
Hybrid composites integrate both natural ECM components and synthetic materials, aiming to merge the bioactivity of biological components with the mechanical strength and processability of synthetic ones [35]. This approach offers a promising compromise for various tissue engineering applications.
- Nanomaterial-Enhanced Hydrogels: The integration of nanomaterials (e.g., carbon nanotubes, gold nanoparticles, graphene) into hydrogels can reinforce mechanical properties, enable conductivity, and introduce dynamic responsiveness [37].
- Functionalized Natural Scaffolds: Natural ECM scaffolds can be engineered with bioactive molecules to enhance their performance. For instance, collagen-based scaffolds have been functionalized with a dermatan sulfate molecule conjugated with collagen-binding and integrin-targeting peptides (LXW7-DS-SILY) to significantly improve endothelial progenitor cell attachment, growth, and neovascularization in diabetic wound healing [42].
Table 1: Comparison of Major Scaffold Categories for Tissue Engineering
| Category | Key Examples | Advantages | Disadvantages |
|---|---|---|---|
| Natural Scaffolds | Decellularized ECM (dECM), Matrigel, Collagen, Hyaluronic Acid | High bioactivity, innate cellular recognition, superior biocompatibility [35] | Batch-to-batch variability (e.g., Matrigel), poor mechanical properties, limited tunability, risk of immunogenicity [37] |
| Synthetic Scaffolds | pNIPAM, PEG-based hydrogels, Polyacrylamide, PANI-based polymers | Excellent reproducibility, tunable mechanical/chemical properties, scalable manufacturing [35] [40] | Typically lack innate bioactivity, may require complex functionalization, potential for inflammatory degradation by-products [35] [38] |
| Hybrid Scaffolds | Nano-enhanced hydrogels, peptide-functionalized ECM | Balanced bioactivity and mechanical control, customizable functionality [35] [37] | Increased complexity in design and fabrication, potential nanomaterial cytotoxicity, higher production costs [37] |
Key Scaffold Fabrication Techniques and Design Innovations
Multiple fabrication techniques are employed to create scaffolds that address specific mechanical, physicochemical, and biological requirements of target tissues [35].
Decellularization
This process involves the removal of cellular material from native tissues, leaving behind a complex, tissue-specific ECM scaffold. Techniques can be chemical, enzymatic, or physical, often used in combination [35]. A key advancement is the creation of ECM scaffolds with aligned microchannels (ECM-C) using sacrificial templates implanted in vivo. This method produces scaffolds with guided microchannels that promote oriented cell growth and enhanced vascularization upon implantation [38].
Electrospinning
This technique uses high voltage to fabricate micro- or nano-scale fibrous scaffolds that morphologically resemble native collagen fibers. It is applicable to a wide range of materials and produces scaffolds with a high surface-to-volume ratio and porosity, facilitating nutrient transport and cell-matrix communication [41]. For example, conductive nanofibrous scaffolds for skin tissue engineering have been created from polyaniline-grafted tragacanth gum and poly(vinyl alcohol) [41].
Multidimensional Bioprinting
3D, 4D, 5D, and 6D bioprinting technologies enable the layer-by-layer fabrication of complex structures using bioinks that incorporate ECM-derived components or synthetic polymers. This allows for precise spatial control over cell placement and scaffold architecture [35]. A significant challenge in this area is the limited availability of bioinks that adequately mimic the sophisticated biochemical and mechanical properties of the native ECM [43].
In Vivo Scaffold Engineering
An innovative approach involves using the body as a bioreactor. Sacrificial templates are implanted subcutaneously, where the host's body forms a vascularized tissue capsule around them. The template is then removed and the newly formed ECM is decellularized, resulting in an ECM scaffold with an innate and organized microarchitecture that supports cell infiltration and vascularization [38].
Quantitative Performance Comparison of Scaffold Platforms
Experimental data from recent studies provides a quantitative basis for comparing the performance of different scaffold platforms.
Table 2: Experimental Performance Data of Selected Scaffold Systems
| Scaffold Type & Material | Key Experimental Findings | Cell Type / Assay | Reference |
|---|---|---|---|
| Synthetic Terpolymer (NiPAAm-based) | Cardiac differentiation efficiency: ~65% cTnT+ and ~25% cTnI+ cells; superior to Matrigel, Cultrex, and VitroGel controls [40] | hiPSCs / Flow Cytometry | [40] |
| ECM with Microchannels (ECM-C) | Porosity: 74.4 ± 2.1%; Anisotropy: 0.89 ± 0.12; Significant improvement in cell migration velocity and Euclidean distance vs. control scaffolds [38] | L6, RSC96, A10 cell lines / Cell Tracking | [38] |
| Conductive Nanofiber (TG-g-PANI/PVA) | Electrical Conductivity: 1.07 × 10⁻⁵ S/cm; Hemolysis Rate: <2%; HSA Protein Adsorption: 49 μg/mg [41] | L929 mouse fibroblasts / MTT, Hemolysis Assay | [41] |
| Functionalized SIS (LXW7-DS-SILY) | Significant improvement in wound healing, neovascularization, and collagen fibrillogenesis in a diabetic rat ischemic model vs. unfunctionalized SIS [42] | ZDF Rat EPCs / In Vivo Wound Model | [42] |
Detailed Experimental Protocols
To ensure reproducibility and provide practical insights, here are detailed methodologies for key experiments cited in this guide.
Protocol: Evaluating hiPSC Cardiac Differentiation on Synthetic Terpolymers
This protocol is adapted from studies demonstrating enhanced cardiomyocyte differentiation using functionalized synthetic scaffolds [40].
- Scaffold Preparation and Functionalization: Synthesize the thermoresponsive terpolymer via free-radical polymerization of NiPAAm, VPBA, and PEGMMA monomers. Dissolve the sterile terpolymer in cold DI water to form a working solution. Coat culture surfaces and incubate at 37°C to form a stable layer. Functionalize by adsorbing bioactive molecules (e.g., RGD peptides, vitronectin, fibronectin) onto the polymer surface.
- hiPSC Culture and Seeding: Maintain hiPSCs in feeder-free conditions using defined culture media. Dissociate cells into a single-cell suspension and seed at an optimized density onto the functionalized terpolymer surfaces in culture media supplemented with a Rho-associated kinase (ROCK) inhibitor.
- Cardiac Differentiation Induction: Upon reaching confluence, initiate differentiation using a standardized cardiac-directed protocol, such as sequential modulation of the Wnt/β-catenin signaling pathway with CHIR99021 and IWP-4 small molecules in a defined, serum-free medium.
- Analysis of Differentiation Efficiency: Between days 10-15 of differentiation, harvest the cells for analysis.
- Flow Cytometry: Fix and permeabilize cells. Stain with fluorescently conjugated antibodies against cardiac-specific troponins (cTnT and cTnI). Analyze using flow cytometry to quantify the percentage of cardiomyocytes.
- Immunofluorescence: Fix cells and stain for cardiac markers (e.g., cTnT, α-actinin). Use DAPI for nuclear counterstaining. Image with confocal microscopy to assess sarcomeric organization and contractile structures.
- Gene Expression Analysis: Extract total RNA and perform reverse transcription quantitative PCR (RT-qPCR) to evaluate the expression of key cardiac genes (e.g., NKX2-5, MYH6, TNNT2).
Protocol: Assessing Cell Guidance in ECM Scaffolds with Microchannels
This protocol outlines methods to quantify the guided cell behavior on anisotropic ECM-C scaffolds, as demonstrated in [38].
- Scaffold Preparation: Prepare ECM-C scaffolds using the in vivo sacrificial template method [38]. Briefly, implant aligned polycaprolactone (PCL) microfiber membranes subcutaneously in rats. After 4 weeks, explant the cellularized constructs, remove the PCL template by leaching, and decellularize using a combination of SDS and nucleases.
- Cell Seeding: Seed relevant cell types (e.g., skeletal muscle L6 cells, Schwann RSC96 cells, or vascular smooth muscle A10 cells) onto the ECM-C scaffolds and control scaffolds (e.g., non-porous decellularized capsules) at a defined density.
- Live-Cell Imaging and Tracking: 24 hours post-seeding, place the scaffolds in a live-cell imaging system maintained at 37°C and 5% CO₂. Acquire time-lapse images at regular intervals (e.g., every 10 minutes for 12-24 hours).
- Data Analysis: Track individual cell movements using cell tracking software.
- Velocity: Calculate the mean velocity of cells from their tracks.
- Euclidean Distance: Measure the straight-line distance from the start to the end point of each cell track.
- Directionality: Calculate the ratio of the Euclidean distance to the total path length traveled.
- Cell Orientation and Circularity: From fixed endpoint images, stain actin cytoskeletons (e.g., with phalloidin) and nuclei (DAPI). Use image analysis software to measure the orientation angle of cells relative to the scaffold's microchannels and the circularity of nuclei.
Signaling Pathways in ECM-Mediated Cell Regulation
The extracellular matrix influences cell fate through complex biochemical and mechanotransduction pathways. The following diagram illustrates the key signaling mechanisms by which an engineered ECM scaffold directs hiPSC behavior, culminating in cardiac differentiation.
Diagram Title: ECM Scaffold Signaling in hiPSC Cardiac Differentiation
The Scientist's Toolkit: Key Research Reagents and Materials
Successful replication of advanced scaffold studies requires specific reagents and materials. The following table details essential components for the featured experiments.
Table 3: Essential Research Reagents for ECM-Mimetic Scaffold Studies
| Reagent / Material | Function / Application | Example from Research |
|---|---|---|
| Thermoresponsive Terpolymer | Synthetic matrix for hiPSC culture and differentiation; enables non-invasive cell harvest [40]. | NiPAAm-VPBA-PEGMMA terpolymer for maintenance of hiPSC pluripotency and cardiac differentiation [40]. |
| Functionalization Peptides | Confer bioactivity to synthetic or natural scaffolds by providing specific cell-binding motifs. | RGD peptides (for integrin binding), LXW7 cyclic peptide (binds integrin αvβ3), SILY peptide (binds collagen) [40] [42]. |
| Conductive Copolymer | Imparts electrical conductivity to scaffolds, regulating functions of electrically excitable cells. | Polyaniline-grafted tragacanth gum (TG-g-PANI) used in electrospun nanofibrous skin scaffolds [41]. |
| Decellularized ECM (dECM) | Provides a natural, bioactive, and tissue-specific scaffold; can be derived from tissues or in vivo engineered. | ECM scaffolds with parallel microchannels (ECM-C) for guided tissue regeneration [38]. Porcine SIS scaffold for wound healing applications [42]. |
| Cardiac Differentiation Kit | Defined media and small molecules for directed differentiation of hiPSCs to cardiomyocytes. | Small molecule modulators of Wnt signaling (e.g., CHIR99021, IWP-4) [40] [43]. |
| Antibodies for Characterization | Essential for quantifying differentiation efficiency and cell phenotype via flow cytometry and immunofluorescence. | Antibodies against cardiac Troponin T (cTnT), Troponin I (cTnI), and NKX2-5 [40] [43]. |
The pursuit of physiologically relevant hiPSC-derived tissues is intrinsically linked to the development of advanced scaffold materials that faithfully mimic the native extracellular matrix. While natural matrices like Matrigel have been instrumental historically, their shortcomings in reproducibility and tunability are driving the field toward defined, synthetic, and hybrid platforms. Quantitative data demonstrates that these advanced scaffolds can not only match but surpass the performance of traditional matrices in key metrics like differentiation efficiency and guidance of complex tissue morphogenesis [40] [38].
Future progress will depend on overcoming several key challenges. Vascularization remains a primary obstacle for engineering thick, clinically relevant tissues; integrating sacrificial bioprinting techniques with pro-angiogenic functionalization represents a promising strategy [43]. Furthermore, as the field moves beyond structural mimicry, the next generation of "smart" scaffolds will need to incorporate dynamic responsiveness, capable of altering their properties in response to environmental cues or delivering biological signals in a spatiotemporally controlled manner [37]. Finally, the translation of these technologies will require rigorous standardization, scalability, and comprehensive in vivo validation to ensure biosafety and functional fidelity [43]. By continuing to refine the complex dialogue between cells and their engineered surroundings, researchers can unlock the full potential of hiPSC technology for regenerative medicine, disease modeling, and drug development.
The transition from traditional two-dimensional (2D) static cultures to three-dimensional (3D) dynamic systems represents a paradigm shift in tissue engineering and regenerative medicine. Bioreactors have emerged as fundamental tools in this transition, providing the precise environmental control necessary to direct cell fate and generate functional tissues in vitro. Unlike static cultures that merely sustain cells, advanced bioreactor systems actively impose mechanical and electrical cues that mimic the dynamic physiological environment of native tissues. This capability is particularly crucial for the maturation of induced pluripotent stem cell (iPSC)-derived tissues, which often remain developmentally immature without appropriate biophysical stimulation [36] [44].
The physiological relevance of engineered tissues is directly dependent on their exposure to biomimetic conditioning during development. Tissues such as cardiac muscle, skeletal muscle, tendons, and ligaments naturally develop under specific regimes of mechanical strain, fluid shear stress, and electrical activity. Recapitulating these complex biophysical signals in vitro requires sophisticated bioreactor systems capable of delivering tunable, quantifiable, and reproducible stimuli. This guide provides a systematic comparison of bioreactor technologies for applying mechanical and electrical cues, with specific emphasis on their application to iPSC-derived tissue models. We evaluate system configurations, performance parameters, and experimental outcomes to assist researchers in selecting appropriate dynamic culture platforms for their specific applications [45] [44].
Bioreactor Systems for Mechanical Stimulation
Fundamental Principles and Bioreactor Configurations
Mechanical stimulation in bioreactors primarily encompasses cyclic stretch, compression, and fluid-induced shear stress. Each modality targets specific tissue types and cellular responses. The effectiveness of mechanical conditioning depends on precise control over multiple parameters including strain magnitude, frequency, duration, and waveform pattern (e.g., sinusoidal, triangular, or square) [45].
The molecular mechanisms through which cells perceive and respond to mechanical forces involve mechanotransduction pathways that convert physical stimuli into biochemical signals. As illustrated below, these pathways involve force transmission through cell-matrix adhesions and cytoskeletal elements, ultimately activating transcription factors that regulate genes responsible for tissue maturation and function [46].
Comparative Analysis of Mechanical Bioreactor Systems
Different bioreactor configurations have been developed to address specific mechanical conditioning requirements. The table below provides a systematic comparison of the primary bioreactor types used for mechanical stimulation, their operational principles, and key applications.
Table 1: Comparison of Bioreactor Systems for Mechanical Stimulation
| Bioreactor Type | Mechanism of Action | Strain Parameters | Key Applications | Limitations |
|---|---|---|---|---|
| Stretch Bioreactors | Uniaxial or biaxial tensile strain applied to elastic membranes or 3D constructs | • Amplitude: 2-15% strain• Frequency: 0.5-2 Hz• Duration: Days to weeks• Waveform: Sinusoidal, triangular | Cardiac tissue engineering, blood vessels, tendons, ligaments, skin | Primarily for tensile strain applications; may require custom-designed scaffolds |
| Compression Bioreactors | Axial compressive forces applied directly to 3D constructs | • Amplitude: 1-20% compression• Frequency: 0.1-1 Hz• Dynamic or static loading regimes | Cartilage, bone, intervertebral disc tissue engineering | Potential for necrotic core formation in large constructs without perfusion |
| Perfusion Systems | Continuous medium flow through porous scaffolds generating fluid shear stress | • Flow rate: 0.1-10 mL/min• Shear stress: 0.1-30 mPa• Continuous or oscillatory flow | Bone, cartilage, engineered liver tissue, large 3D constructs | Limited control over macroscopic mechanical strain; primarily enhances mass transfer |
| Stirred-Tank Bioreactors | Agitation-induced hydrodynamic forces on suspended cells or microcarriers | • Agitation rate: 20-200 rpm• Impeller design determines shear profile• Scalable from mL to L volumes | iPSC expansion as aggregates, cartilage, bone marrow models | Heterogeneous shear distribution; potential for damaging high-shear zones |
The selection of appropriate mechanical stimulation parameters must align with the target tissue's physiological environment. For example, cardiac tissue engineering typically employs cyclic stretch parameters that mimic the diastolic filling of ventricles (5-15% strain, 1-2 Hz), while tendon and ligament applications often utilize higher strain magnitudes (5-20%) at lower frequencies (0.1-1 Hz) to simulate physiological loading patterns [45].
Systems for Electrical Stimulation
Principles and Implementation Strategies
Electrical stimulation in bioreactor systems delivers pulsatile electrical fields that mimic the native electrophysiological environment of excitable tissues. This approach is particularly critical for proper maturation and functional assembly of cardiac tissues, neuronal networks, and skeletal muscle constructs. The applied electrical fields promote cell-cell coupling, synchronize contractile activity, and enhance the expression of key functional proteins [44].
The implementation of electrical stimulation requires specialized bioreactor designs incorporating electrode configurations that generate uniform electric fields across the developing tissue constructs. Electrode materials must be biocompatible, corrosion-resistant, and capable of delivering controlled stimulus waveforms without detrimental electrochemical reactions. Commonly used materials include platinum, stainless steel, and conductive polymers that can be integrated into tissue culture chambers [44].
Comparative Analysis of Electrical Stimulation Platforms
Electrical stimulation systems vary in their configuration, programmability, and integration with other bioreactor functions. The table below compares key platform characteristics and their applications in tissue engineering.
Table 2: Comparison of Electrical Stimulation Platforms for Tissue Engineering
| Platform Characteristics | Carbon Rod Electrodes | Platinum Wire Electrodes | Microfabricated Electrode Arrays | Conductive Scaffolds |
|---|---|---|---|---|
| Field Configuration | Uniform field between parallel electrodes | Localized field around wire placement | Patterned, multi-directional fields | Integrated 3D field throughout scaffold |
| Stimulation Parameters | • Voltage: 2-10 V• Frequency: 1-5 Hz• Duration: 1-10 ms pulses | • Voltage: 1-5 V• Frequency: 1-3 Hz• Duration: 1-5 ms pulses | • Voltage: 0.1-3 V• Frequency: 0.1-100 Hz• Duration: 0.1-5 ms pulses | • Voltage: 0.5-5 V• Frequency: 0.5-5 Hz• Continuous or pulsed |
| Key Applications | Cardiac tissue engineering, skeletal muscle maturation | Cardiac patches, neuronal stimulation | High-throughput screening, neural interfaces, micro-tissues | Myocardial repair, nerve guidance conduits |
| Technical Considerations | Simple setup, scalable, potential for pH shifts at electrodes | Biologically inert, stable performance, higher cost | High spatial resolution, complex fabrication, limited scalability | Integrated construct design, material conductivity limitations |
Experimental Validation and Protocol Implementation
Standardized Workflow for Bioreactor Conditioning
Implementing mechanical or electrical stimulation in tissue engineering requires a systematic approach from construct preparation through final analysis. The workflow below outlines the key stages in a standardized bioreactor conditioning protocol, particularly applicable to iPSC-derived tissues.
Representative Experimental Protocol: Cardiac Tissue Maturation
The following detailed protocol exemplifies the application of combined mechanical and electrical stimulation for engineering functionally mature cardiac tissues from iPSC-derived cardiomyocytes, based on established methodologies with performance metrics [45] [44].
Objective: To generate mature, functional cardiac tissue constructs from iPSC-derived cardiomyocytes through cyclic mechanical stretch conditioning.
Materials and Reagents:
- Scaffold: Decellularized human skin (d-HuSk) or engineered collagen/ fibrin hydrogels
- Cells: iPSC-derived cardiomyocytes (iPSC-CMs) at >90% purity
- Culture Medium: Cardiomyocyte maintenance medium supplemented with growth factors
- Bioreactor System: Tunable stretch bioreactor with environmental control
- Analysis Reagents: RNA isolation kit, qPCR reagents, immunohistochemistry supplies
Methodology:
- Construct Preparation: Seed iPSC-CMs onto d-HuSk scaffolds at 5×10^6 cells/cm² density. Maintain in static culture for 5 days to allow cell attachment and initial matrix interaction.
- Bioreactor Loading: Transfer cell-seeded constructs to stretch bioreactor chambers. Calibrate displacement sensors to verify target strain amplitudes.
- Conditioning Protocol: Apply uniaxial cyclic stretch with the following regimen:
- Days 1-3: 5% strain at 0.5 Hz for 30 minutes twice daily
- Days 4-7: 7% strain at 1 Hz for 1 hour twice daily
- Days 8-14: 10% strain at 1.5 Hz for 2 hours twice daily
- Environmental Control: Maintain temperature at 37°C, pH at 7.4, and dissolved oxygen at 40-60% throughout the conditioning period.
- Monitoring: Record real-time contractile activity and force generation using integrated force transducers.
- Endpoint Analysis: Assess structural maturation (sarcomere organization, connexin-43 distribution), molecular markers (qPCR for cardiac genes), and functional output (contractile force, electrical conduction velocity).
Validation Metrics: Successful cardiac tissue maturation typically demonstrates a 3-5 fold increase in contractile force, enhanced sarcomeric organization, and elevated expression of maturation markers (MYH6/MYH7 ratio, cTnl, SERCA2a) compared to static controls [45].
Research Reagent Solutions for Dynamic Culture Systems
The successful implementation of bioreactor-based conditioning protocols requires specific reagents and materials optimized for dynamic culture environments. The following table details essential research solutions for mechanical and electrical stimulation studies.
Table 3: Essential Research Reagents and Materials for Dynamic Culture Systems
| Reagent/Material | Function | Application Examples | Technical Considerations |
|---|---|---|---|
| Synthetic Peptide Hydrogels (e.g., PGmatrix) | Defined 3D culture matrix for iPSC expansion and differentiation | Physiologically relevant 3D culture of hiPSCs, supporting pluripotency maintenance and directed differentiation | Superior to animal-derived matrices; enables better control over mechanical properties and composition [36] |
| Decellularized Extracellular Matrix (dECM) | Biological scaffold with native composition and architecture | Cardiac tissue engineering (d-HuSk), vessel, cartilage, and bone regeneration | Maintains native biomechanical and biochemical cues; requires sterilization and potential antigen removal [45] |
| iPSC-Derived Cell Lines | Patient-specific or disease-specific cell sources | Disease modeling, drug screening, autologous tissue engineering | Requires efficient differentiation protocols; potential for epigenetic memory affecting differentiation bias [2] |
| Programmable Bioreactor Systems | Precise delivery of mechanical/electrical stimuli | Customizable stretch, compression, or electrical stimulation regimens | System compatibility with sterile culture; real-time monitoring capability; scalability limitations [45] |
| Real-Time Monitoring Sensors | Continuous assessment of culture parameters | Dissolved oxygen, pH, glucose, lactate, contractile force measurements | Requires calibration; potential for drift during long-term cultures; non-invasive sensors preferred [44] |
| Cloud-Based Data Analytics Platforms | Analysis of high-throughput bioreactor data | Compare experimental conditions, identify process interactions, optimize protocols | Enables comparison between experiments; custom overlays of process parameters; group runs by condition [47] |
The strategic imposition of mechanical and electrical cues through advanced bioreactor systems represents a cornerstone in the pursuit of physiologically relevant iPSC-derived tissues. The comparative data presented in this guide demonstrates that dynamic culture systems consistently outperform static cultures across multiple tissue types, particularly in achieving structural organization, functional maturation, and molecular marker expression profiles reminiscent of native tissues.
For researchers implementing these technologies, successful outcomes depend on careful parameter selection aligned with target tissue physiology, systematic validation of maturation endpoints, and iterative optimization of stimulation regimens. The integration of real-time monitoring and automated control systems further enhances reproducibility and enables more sophisticated conditioning protocols. As the field advances, the convergence of mechanical and electrical stimulation modalities with biochemical cues in multi-parameter bioreactor systems will likely yield further improvements in tissue fidelity, ultimately bridging the gap between engineered constructs and native human tissues for both therapeutic applications and predictive drug screening platforms.
The quest for physiologically relevant models in biomedical research has long been a driving force in pharmaceutical development. Traditional two-dimensional (2D) cell cultures and animal models have proven insufficient for accurately predicting human-specific responses, contributing to high attrition rates in clinical trials [48] [49]. Induced pluripotent stem cell (iPSC) technology has emerged as a transformative platform, enabling the generation of patient-specific cells that recapitulate disease phenotypes in a human context. This review objectively compares the performance of various iPSC-derived tissue models across different experimental paradigms, highlighting their physiological relevance through direct comparison of experimental outcomes, scalability, and predictive validity.
Fundamental Principles of iPSC Technology
Induced pluripotent stem cells (iPSCs) are generated by reprogramming somatic cells to a pluripotent state through the expression of specific transcription factors, primarily OCT4, SOX2, KLF4, and c-MYC (OSKM) [2]. This groundbreaking technology, pioneered by Shinya Yamanaka, has fundamentally transformed biomedical research by providing unlimited access to patient-specific cells [23] [2]. The reprogramming process involves profound remodeling of the chromatin structure and epigenome, effectively reversing the developmental clock to create cells with embryonic stem cell-like properties [2].
iPSCs can be differentiated into virtually any somatic cell type using lineage-specific protocols, providing unprecedented opportunities for disease modeling, drug screening, and regenerative medicine [49] [2]. The technology is particularly valuable because it preserves the genetic background of the donor, enabling researchers to study disease mechanisms and drug responses in a personalized context [50]. Furthermore, the advent of CRISPR/Cas9 genome editing has facilitated the generation of isogenic control lines, allowing precise correlation of genetic mutations with disease phenotypes without confounding genetic background effects [48].
Comparative Advantages of iPSC Platforms
Table: Performance Comparison of Disease Modeling Platforms
| Model Type | Genetic Relevance | Physiological Complexity | Scalability | Human Predictivity |
|---|---|---|---|---|
| Animal Models | Low (interspecies differences) | High (systemic context) | Moderate | Variable, often poor |
| 2D Cell Cultures | High (if human-derived) | Low | High | Limited |
| iPSC 2D Models | High (patient-specific) | Moderate | High | Good for cell-autonomous effects |
| iPSC 3D Organoids | High (patient-specific) | High | Moderate | Excellent |
| iPSC Organ-on-Chip | High (patient-specific) | High (includes fluid flow) | Low-Moderate | Potentially superior |
Case Study 1: Large-Scale Drug Screening in Sporadic ALS
Experimental Protocol and Model System
A recent landmark study demonstrated the power of iPSC technology for modeling sporadic amyotrophic lateral sclerosis (SALS) and conducting large-scale drug screening [51]. Researchers established a curated iPSC library from 100 patients with SALS, 11 suspected monogenic cases, and 25 healthy controls. Fibroblasts isolated from skin biopsies were reprogrammed using non-integrating episomal vectors via an automated robotics platform to ensure uniformity [51].
Key Methodology Steps:
- iPSC Generation: Footprint-free reprogramming using episomal vectors
- Quality Control: Genomic integrity verification, pluripotency confirmation, trilineage differentiation potential assessment
- Motor Neuron Differentiation: Five-stage protocol adapted from established spinal motor neuron differentiation methods
- Phenotypic Screening: Longitudinal live-cell imaging with motor neuron-specific reporters
- Drug Screening: Testing of 100+ compounds that had previously entered ALS clinical trials
The differentiation protocol generated highly enriched spinal motor neuron cultures with 92.44% ± 1.66% purity, characterized by co-expression of choline acetyltransferase (ChAT), motor neuron and pancreas homeobox 1 (MNX1/HB9), and β-tubulin III (Tuj1) [51]. This reductionist system enabled focused assessment of cell-autonomous effects in ALS.
Performance Outcomes and Validation
The iPSC-derived SALS motor neurons successfully recapitulated key disease pathologies, including significantly reduced survival and accelerated neurite degeneration compared to healthy controls [51]. Importantly, the severity of neurite degeneration in vitro correlated with donor survival time, establishing the physiological relevance of the model.
In drug screening, the model demonstrated remarkable predictive validity: less than 5% of the 100+ compounds tested showed efficacy in rescuing motor neuron survival across SALS donors, reflecting the high failure rate observed in clinical trials [51]. The study identified a promising therapeutic combination of riluzole, memantine, and baricitinib that significantly increased SALS motor neuron survival, representing the first therapeutic candidates validated across the heterogeneous SALS population using an iPSC model.
Table: Key Results from Large-Scale ALS Drug Screening
| Parameter | Control Motor Neurons | SALS Motor Neurons | Response to Combination Therapy |
|---|---|---|---|
| Neuronal Survival | Normal | Significantly reduced | Significant improvement |
| Neurite Degeneration | Normal rate | Accelerated | Reduced degeneration |
| Response to Riluzole | N/A | Rescue of survival and electrophysiological abnormalities | Enhanced effect in combination |
| Drug Screening Predictive Value | N/A | 97% of clinically failed drugs showed no efficacy | N/A |
Case Study 2: Immunocompetent Skin Model for Sensitization Testing
Experimental Protocol and Model System
An advanced immunocompetent skin model constructed entirely from iPSC-derived cell types represents a significant innovation in dermatological research and toxicology testing [52]. This model integrates iPSC-derived fibroblasts (iPSC-FB), keratinocytes (iPSC-KC), and dendritic cells (iPSC-DC) into a three-dimensional construct that recapitulates the layered architecture and immune competence of human skin.
Key Methodology Steps:
- Cell Differentiation: Generation of iPSC-FB, iPSC-KC, and iPSC-DC from the same iPSC line
- 3D Construct Assembly: Sequential layering of iPSC-FB in collagen matrix (dermal layer) and iPSC-KC (epidermal layer)
- Immune Component Integration: Incorporation of iPSC-DC into the construct
- Model Validation: Treatment with well-characterized skin sensitizers of varying potency
- Response Assessment: Measurement of cytokine secretion and dendritic cell activation markers
Unlike previous models that partially incorporated immune cells, this system enabled full integration of iPSC-DC without baseline activation, a significant advancement that more accurately mimics human skin physiology [52].
Performance in Toxicological Assessment
The iPSC-derived immunocompetent skin model successfully replicated physiological responses to skin sensitizers, detecting compounds across a range of potencies from extreme to weak sensitizers [52]. The model addressed multiple key events in the Adverse Outcome Pathway (AOP) for skin sensitization simultaneously, including keratinocyte activation (key event 2) and dendritic cell activation (key event 3).
When treated with sensitizing chemicals, the model demonstrated characteristic immune activation with upregulated surface markers (CD86, CD80, CD40) and secretion of pro-inflammatory cytokines including IL-1β, TNF-α, and IL-18 [52]. This comprehensive response profile enabled more accurate prediction of sensitization potential compared to traditional single-event assays like KeratinoSens and h-CLAT.
Case Study 3: Cardiac Disease Modeling and Drug Screening
Experimental Protocol and Model System
iPSC-derived cardiomyocytes (iPSC-CMs) have become a cornerstone of cardiac safety pharmacology and disease modeling [48] [50]. Advanced models have evolved from simple 2D monolayers to complex three-dimensional engineered heart tissues (EHTs) that better recapitulate cardiac physiology.
Key Methodology Steps for EHT Generation:
- Cardiomyocyte Differentiation: Directed differentiation of iPSCs using small molecules and growth factors
- Non-Myocyte Inclusion: Incorporation of iPSC-derived endothelial cells, smooth muscle cells, and fibroblasts
- 3D Scaffold Seeding: Use of hydrogels (collagen, fibrin, Matrigel) or decellularized tissue extracts as scaffolds
- Maturation: Application of mechanical stress and electrical stimulation to promote adult-like phenotypes
- Phenotypic Screening: Assessment of contractile function, electrophysiology, and hypertrophic responses
These EHTs resemble the native myocardial microenvironment and recapitulate coordinated contractile and electrophysiological interactions among heterogeneous cell types and extracellular matrix components [48].
Enhanced Predictive Capacity
iPSC-based cardiac models have demonstrated superior performance in predicting cardiotoxicity compared to traditional models. For example, iPSC-derived cardiomyocytes have been used to detect cardiotoxic effects of chemotherapeutics such as doxorubicin, which may not be readily observed in non-human systems [49]. Furthermore, disease-specific models such as those for dilated cardiomyopathy and arrhythmogenic right ventricular dysplasia/cardiomyopathy have identified cardiac phenotypes crucial to pathogenesis that were not apparent in animal models [48].
The incorporation of patient-specific genetic backgrounds has enabled the identification of individualized susceptibility to drug-induced cardiotoxicity, particularly for chemotherapeutic agents like tyrosine kinase inhibitors [50]. This personalized approach allows for better risk stratification and therapeutic decision-making.
The Scientist's Toolkit: Essential Research Reagents
Table: Key Reagent Solutions for iPSC-Based Disease Modeling and Drug Screening
| Reagent Category | Specific Examples | Function | Performance Considerations |
|---|---|---|---|
| Reprogramming Systems | Episomal vectors, Sendai virus, mRNA | Footprint-free somatic cell reprogramming | Sendai virus: high efficiency; Episomal: completely DNA-free |
| Differentiation Kits | Commercial cardiomyocyte, neuronal, hepatocyte kits | Directed differentiation to specific lineages | Variability in efficiency and maturity between vendors |
| Extracellular Matrices | Matrigel, laminin-521, synthetic hydrogels | 3D culture support and differentiation | Matrigel: biologically active but variable; Synthetic: defined composition |
| Genome Editing Tools | CRISPR/Cas9 systems, base editors | Generation of isogenic controls and disease mutations | CRISPR: high efficiency but potential off-target effects |
| Characterization Antibodies | Pluripotency markers (Nanog, OCT4), lineage-specific markers | Quality control of iPSCs and differentiated cells | Essential for validating model fidelity |
| Functional Assays | Calcium imaging dyes, multi-electrode arrays, contractility measurements | Assessment of functional phenotypes | Critical for evaluating physiological relevance |
Technological Advances and Future Directions
The field of iPSC-based disease modeling continues to evolve with several emerging technologies enhancing physiological relevance. Organ-on-chip systems that combine iPSC-derived tissues with microfluidic perfusion provide finer control over tissue-tissue interactions and incorporation of physical forces like shear stress and mechanical strain [48]. These systems enable the creation of multi-organ platforms that can model systemic drug responses.
Recent advances in single-cell technologies have revealed that iPSC-derived cells often exhibit immature, fetal-like characteristics [48] [22]. To address this limitation, researchers have developed enhanced maturation protocols incorporating biochemical cues, mechanical stimulation, and 3D microenvironmental support. For example, co-culture of iPSC-derived cardiomyocytes with cardiac fibroblasts in 3D hydrogels has demonstrated improved maturation markers and functional properties compared to 2D monocultures [22].
The integration of artificial intelligence with iPSC-based screening platforms represents another frontier in drug discovery. AI-driven approaches can identify complex patterns in high-content screening data from iPSC-derived models, potentially accelerating target identification and compound optimization [53]. Several AI-designed therapeutics identified using these approaches have already entered clinical trials, demonstrating the synergy between iPSC technology and computational methods [53].
iPSC-derived tissue models have established themselves as indispensable tools for disease modeling and drug screening, offering superior physiological relevance compared to traditional 2D cultures and animal models. The case studies presented herein demonstrate that iPSC platforms can successfully recapitulate disease-specific phenotypes, exhibit high predictive validity in drug screening, and provide insights into human-specific disease mechanisms. While challenges remain regarding cellular maturation and standardization, ongoing technological innovations continue to enhance the fidelity and utility of these models. As the field progresses, iPSC-based approaches are poised to become central components of drug discovery pipelines and personalized medicine strategies, ultimately improving the efficiency of therapeutic development and the predictability of clinical outcomes.
Visual Appendix: Experimental Workflows and Signaling Pathways
iPSC-Based Drug Screening Workflow
Skin Sensitization Adverse Outcome Pathway
Bridging the Relevance Gap: Overcoming Technical and Biological Hurdles
The transformative potential of human induced pluripotent stem cell-derived cardiomyocytes (iPSC-CMs) in regenerative medicine, drug development, and disease modeling is significantly hampered by one persistent challenge: their characteristic immature phenotype. Despite sharing the genomic blueprint of their donors, iPSC-CMs generated using current protocols typically resemble fetal cardiomyocytes rather than adult cells. This immaturity manifests through disorganized sarcomeres, underdeveloped mitochondrial networks, altered metabolic activity, and deficient electrophysiological properties, which collectively limit their predictive accuracy in drug screening and therapeutic efficacy upon transplantation [54] [55]. Overcoming this barrier is critical for unlocking the full potential of iPSC technology in cardiovascular research and therapy. This guide objectively compares the most advanced maturation strategies emerging from recent research, evaluating their efficacy based on key structural, metabolic, and functional outcomes.
Strategic Approaches to Cardiac Maturation
Metabolic Maturation Strategies
Objective: To drive the metabolic shift from glycolytic metabolism toward fatty acid oxidation, mimicking the transition that occurs in postnatal cardiac development.
Key Interventions:
- Fatty Acid Supplementation: Culture media enriched with lipids and fatty acids (e.g., palmitate, oleate) to provide substrates for mitochondrial β-oxidation [56] [57].
- Hormonal Signaling: Triiodothyronine (T3) treatment to stimulate mitochondrial biogenesis and oxidative phosphorylation [54].
- PGC-1α Activation: Genetic or pharmacological activation of peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α), a master regulator of mitochondrial biogenesis [57].
Experimental Evidence: Transcriptome analyses reveal that metabolic preconditioning significantly upregulates genes involved in the tricarboxylic acid (TCA) cycle, electron transport chain, and fatty acid oxidation. iPSC-CMs subjected to these conditions demonstrate a marked increase in mitochondrial density, cristae formation, and ATP production via oxidative phosphorylation, moving their metabolic profile closer to adult cardiomyocytes [56] [57].
Structural Maturation via Biomechanical Cues
Objective: To replicate the structured in vivo myocardial environment and promote sarcomere alignment, T-tubule development, and gap junction formation.
Key Interventions:
- Nanopatterning (NP): Culture surfaces engineered with micro- and nano-scale patterns (e.g., linear gratings) to guide cell and sarcomere alignment [56].
- 3D Engineered Heart Tissues (EHTs): Embedding iPSC-CMs within three-dimensional biomaterial scaffolds (e.g., collagen, fibrin) to provide physiological cell-matrix interactions [54] [55].
- Substrate Stiffness Tuning: Using hydrogels with stiffness values mimicking native myocardial tissue (≈10 kPa) to promote hypertrophic growth and sarcomerogenesis [54].
Experimental Evidence: Immunostaining reveals that nanopatterning alone significantly enhances the organization of α-actinin-positive sarcomeres into aligned myofibrils and promotes the peripheral localization of connexin 43 (Cx43) at gap junctions. When combined with 3D culture, these approaches foster the development of T-tubule-like structures and mature calcium handling, which are critical for excitation-contraction coupling [56] [55].
Functional Maturation through Electromechanical Stimulation
Objective: To mimic the continuous electromechanical workload of the native heart, thereby driving functional adaptation and maturation.
Key Interventions:
- Electrical Pacing (ES): Application of defined electrical field stimulation, often following a "training regime" of progressively increasing frequency (e.g., from 2 Hz to 6 Hz) [56] [54].
- Mechanical Stretching: Subjecting 3D engineered tissues to uniaxial or cyclic stretch to simulate hemodynamic loading [54].
Experimental Evidence: Electrically paced tissues exhibit a more negative resting membrane potential, significantly increased maximum upstroke velocity (Vmax), and the emergence of a distinct "notch-and-dome" action potential morphology, characteristic of adult ventricular myocytes. Furthermore, these tissues demonstrate a positive force-frequency relationship (FFR) and enhanced conduction velocity, indicating advanced electrophysiological maturity [56] [54].
Table 1: Quantitative Comparison of Maturation Outcomes Across Different Strategies
| Maturation Strategy | Sarcomere Length (µm) | Resting Membrane Potential (mV) | Conduction Velocity (cm/s) | Key Markers of Maturity |
|---|---|---|---|---|
| Standard 2D Culture | ~1.6 | -44.1 ± 9.8 | 12.5 ± 5.8 | Spontaneous beating, disorganized sarcomeres |
| Metabolic Medium (MM) | ~1.7 | -49.7 ± 8.5 | 22.3 ± 3.7 | Increased Ito density, improved Ca2+ handling |
| MM + Nanopatterning (NP) | ~1.8 | -58.2 ± 7.4 | 25.6 ± 4.3 | Aligned myofibrils, membrane-localized Cx43 |
| MM + NP + Electrostimulation (ES) | ~1.8 | -65.6 ± 8.5 | 27.8 ± 7.3 | Notch-and-dome AP, T-tubule-like structures, oxidative metabolism |
Integrated Experimental Workflow for Maximal Maturation
The most potent results are achieved not by applying stimuli in isolation, but by integrating them in a synergistic manner. A representative, high-efficacy protocol from recent literature is detailed below.
Detailed Integrated Protocol
This protocol systematically combines metabolic, structural, and electrical cues [56].
Step 1: Cell Culture and Differentiation
- Use iPSCs from at least 3 healthy donors to account for biological variability.
- Differentiate iPSCs into ventricular-like cardiomyocytes using a standard directed differentiation protocol.
- On day 15 post-differentiation, harvest iPSC-CMs for maturation induction.
Step 2: Metabolic Priming and Structural Alignment
- Plate the cells on nanopatterned surfaces coated with a suitable extracellular matrix protein (e.g., fibronectin, laminin). The patterns typically consist of linear grooves with a width and pitch in the micron range.
- Culture the cells in a lipid-enriched maturation medium (MM). This medium is based on a standard basal medium (e.g., RPMI 1640) supplemented with B-27, lipids (e.g., a combination of fatty acids like palmitate and oleate conjugated to albumin), and a high concentration of calcium (≥2-3 mM) [56].
Step 3: Application of Electromechanical Cues
- After 3-5 days of culture on nanopatterned surfaces in MM, initiate electrical stimulation.
- Use a commercial or custom-built pacing system with carbon electrodes.
- Apply a monophasic rectangular pulse with parameters typically set at 2 Hz, 5-7 V, and 2 ms pulse duration.
- Maintain this stimulation regimen for a minimum of 2-4 weeks, with medium changes every 2-3 days.
Signaling Pathways in Integrated Maturation
The integrated maturation protocol activates multiple interconnected signaling pathways that drive the maturation process. The diagram below illustrates the logical relationships and key signaling pathways activated by different stimuli.
Diagram: Signaling Pathways Activated by Integrated Maturation. External stimuli (yellow) activate specific intracellular signaling pathways (blue), leading to distinct mature phenotypes (green). ES: Electrostimulation; NP: Nanopatterning.
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of advanced maturation protocols requires specific, high-quality reagents. The table below catalogs key solutions used in the featured experiments.
Table 2: Key Research Reagent Solutions for iPSC-CM Maturation
| Reagent/Material | Function in Maturation Protocol | Example Product/Composition |
|---|---|---|
| Lipid-Enriched Maturation Medium | Shifts metabolism from glycolysis to fatty acid oxidation; provides essential nutrients. | Base medium (e.g., RPMI) supplemented with B-27, albumin-conjugated lipids (palmitate, oleate), and high Ca²⁺ (≥2mM) [56]. |
| Nanopatterned Culture Surfaces | Provides topographical cues for cell and sarcomere alignment, mimicking native tissue anisotropy. | Cyclic olefin polymer or polystyrene substrates with micro- (1-2 µm) or nano-scale (200-800 nm) ridge/groove patterns [56]. |
| Electrical Stimulation System | Delivers controlled electrical pulses to mimic in vivo pacing; improves electrophysiology and E-C coupling. | C-Pace EP Culture Pacer (IonOptix) or custom setups with carbon electrodes, generating 2-6 Hz, 5-7 V, 2 ms pulses [56] [54]. |
| 3D Hydrogel Scaffolds | Creates a physiologically relevant 3D environment for tissue formation; transmits mechanical force. | Fibrin or collagen-based hydrogels mixed with iPSC-CMs to form Engineered Heart Tissues (EHTs) [54] [55]. |
| Hormone Supplements | Activates nuclear hormone receptors to drive maturation-associated gene programs. | Triiodothyronine (T3 hormone), Dexamethasone [54]. |
Impact on Pharmacological Response
The ultimate validation of maturation efficacy is a physiological response to cardioactive drugs. Immature iPSC-CMs often exhibit aberrant responses; for instance, verapamil (an L-type calcium channel blocker) abolishes beating in immature models at clinically relevant concentrations, which does not reflect its safe profile in adult patients [56]. Maturation directly addresses this discrepancy.
Evidence of Improved Predictive Power: Systematic drug testing on iPSC-CMs matured using the combined (MM+NP+ES) approach reveals a pharmacological profile more closely aligned with adult cardiomyocytes. This includes more mature calcium handling, appropriate sensitivity to hERG channel blockers, and a normalized response to multichannel blockers like verapamil, thereby enhancing the predictive accuracy for pro-arrhythmic risk and cardiotoxicity screening [56] [55].
The immaturity of iPSC-CMs remains a significant hurdle, but the integration of metabolic, structural, and electromechanical stimuli presents a powerful and validated solution. Data consistently demonstrates that no single factor is sufficient; maximal maturation is a synergistic outcome. The combined regimen of lipid-enriched metabolic medium, nanopatterned surfaces, and chronic electrical pacing currently sets the benchmark, producing cardiomyocytes with adult-like electrophysiology, structured contractile machinery, and oxidative metabolic capacity. This progression directly translates to more physiologically relevant and predictive models for drug discovery and safety pharmacology, marking a critical step toward reliable regenerative therapies and personalized medicine.
The advent of Induced Pluripotent Stem Cell (iPSC) technologies has fundamentally transformed in vitro modeling of human diseases and development, offering unprecedented access to otherwise inaccessible human cell types, particularly in neurology [58] [2]. However, this powerful platform faces a formidable obstacle: inherent variability that can confound experimental reproducibility and compromise the meaningful interpretation of data. Without due consideration, the thousands of human iPSC lines generated over the past decade inevitably affect the reproducibility of iPSC-based experiments [58]. Differences between donor individuals, the genetic stability of the lines themselves, and technical experimental variability collectively impact critical parameters including differentiation potency, cellular heterogeneity, morphology, and transcript abundance [58]. This article provides a comprehensive comparison of the sources of this variability, the methodologies for its detection, and the strategic approaches required to ensure genetic stability and reproducibility, thereby enabling iPSC-derived tissues to achieve their full potential in research and therapeutic applications.
iPSC derivation and differentiation are multistep processes where small variations at each stage can accumulate, generating significantly different outcomes [58]. Understanding the distinct origins of this variability is the first step toward controlling it.
Genetic Background and Donor-Specific Effects
The genetic background of the donor is the most significant contributor to heterogeneity at the iPSC stage, surpassing other non-genetic factors like culture conditions or sex [58]. Systematic phenotyping initiatives, such as the Human Induced Pluripotent Stem Cells Initiative (HipSci), have reported that 5-46% of the variation in iPSC phenotypes is attributable to inter-individual differences [58]. Consequently, iPSC lines derived from the same individual are consistently more similar to each other in terms of gene expression, expression quantitative trait loci (eQTLs), and DNA methylation patterns than lines from different donors [58]. This inherent genetic diversity, while valuable for studying population-wide effects, presents a substantial challenge for reproducible disease modeling, especially for complex disorders with polygenic risk.
Genetic Instability During Culture and Differentiation
A paramount concern in the development of stem cell-based therapies is the occurrence of unintended genetic modifications during the expansion and differentiation of iPSCs, which can lead to tumorigenicity [59]. Conventional cytogenetic methods like karyotyping can miss subtle abnormalities. For instance, while karyotyping may show a normal result, higher-resolution methods like CytoScanHD chip analysis can uncover critical findings such as a 1.7 Mbps gain in genomic copy numbers at chromosome 20q11.21, encompassing the cancer-related gene ASXL1 [59]. Whole-exome and targeted sequencing of iPSC-derived cardiomyocytes further reveal specific single-nucleotide variants and insertions/deletions in genes like KMT2C, BCOR, and MUC4, which are classified as tier 1 variants in the COSMIC database and can persist through passaging and differentiation [59]. This demonstrates that the pluripotent state and the stresses of culture can select for mutations that confer a growth advantage.
Experimental and Technical Heterogeneity
Even after controlling for genotype, substantial experimental heterogeneity remains [58]. This technical variability arises from multiple sources:
- Protocol Differences: Variations in reprogramming methods, differentiation protocols (including the specific combinations and concentrations of small molecules like CHIR99021 or growth factors like retinoic acid), and culture conditions can lead to drastically different outcomes [58] [60].
- Cellular Maturity: Most current iPSC differentiation protocols produce immature or fetal-like cells, which may not fully recapitulate adult disease phenotypes [58].
- Model Complexity: While 3D organoids better mimic native tissue architecture, they introduce additional challenges in scalability, reproducibility, and variability in maturation levels between individual organoids [27] [61].
Table 1: Key Sources of Variability in iPSC Models
| Variability Source | Impact on Model System | Quantitative Evidence |
|---|---|---|
| Donor Genetic Background | Affects gene expression, differentiation potency, and eQTLs. | Accounts for 5-46% of phenotypic variation [58]. |
| Genetic Instability | Acquisition of subclonal mutations; potential for tumorigenicity. | Copy number gain at 20q11.21; specific mutations in KMT2C and BCOR identified [59]. |
| Differentiation Protocol | Impacts cellular heterogeneity, maturity, and functional output. | Prolonged protocols can lead to detachment and failed differentiation in late-passage cells [59]. |
| Model System (2D vs. 3D) | 2D models lack physiological architecture; 3D organoids face reproducibility challenges. | 2D cultures lose tissue morphology and cell-cell interactions; 3D organoids show batch-to-batch variability [27] [61]. |
Advanced Methodologies for Detecting and Quantifying Variability
Ensuring the genetic stability of iPSCs and their derivatives requires a suite of complementary analytical techniques, ranging from conventional cytogenetics to ultra-sensitive molecular assays.
Genetic Stability Testing Workflow
A robust assessment of genetic stability involves a tiered approach. The workflow typically begins with the generation and differentiation of iPSCs across multiple batches to account for passage-dependent effects [59]. Functional validation of the differentiated cells (e.g., cardiomyocytes) is crucial, confirmed via gene expression markers like TNNT2 and MYH7 [59]. Genetic analysis then proceeds from a macro- to a micro-scale, as detailed in the experimental protocol below.
Experimental Protocol 1: Assessment of Genetic Stability in iPSC-Derived Cardiomyocytes
- Objective: To systematically identify genetic variations arising during the expansion of hiPSCs and their differentiation into cardiomyocytes (CMs) [59].
- Materials:
- Human iPSCs (cultured across early, intermediate, and late passages).
- Standard culture reagents and cardiomyocyte differentiation kits.
- Tools for molecular biology: RT-qPCR systems, reagents for G-banding karyotyping, CytoScanHD microarrays, Next-Generation Sequencer (for WES and targeted sequencing), droplet digital PCR (ddPCR) system.
- Method Steps:
- Differentiation: Differentiate multiple batches of hiPSCs at different passages (early, intermediate, late) into CMs. Monitor for functional contractile beating and sheet formation [59].
- Quality Control: Confirm successful differentiation using RT-qPCR to analyze the downregulation of pluripotency genes (e.g., POU5F1) and upregulation of cardiac markers (e.g., TNNT2, MYL2, MYH7) [59].
- Cytogenetic Analysis:
- High-Resolution Sequencing:
- Perform Whole-Exome Sequencing (WES) to identify single base-pair variants and small indels across all exons. Analyze data with tools like the Variant Effect Predictor (VEP) and cross-reference with COSMIC [59].
- Perform Targeted Sequencing on a panel of 344 cancer-related genes to deeply interrogate loci of high concern [59].
- Variant Validation: Validate identified mutations (e.g., in KMT2C and BCOR) using droplet digital PCR (ddPCR). This method is validated per ICH guidelines for specificity, precision, and robustness, offering absolute quantification and higher sensitivity than conventional qPCR, thus avoiding false positives [59].
- Expected Outcome: Identification of persistent genetic variants (CNVs and single nucleotide variants) that may pose a tumorigenic risk, enabling a comprehensive safety profile of the iPSC-derived therapeutic product [59].
Statistical and Bioinformatic Tools for Accounting for Variation
Beyond laboratory techniques, statistical models are essential to disentangle wanted biological signals from unwanted technical noise.
- Principal Component Analysis (PCA): A statistical approach that uses orthogonal transformation to identify principal components that capture the majority of variation in the data, often used to visualize batch effects or donor-driven clustering [58].
- Probabilistic Estimation of Expression Residuals (PEER): Based on factor analysis, PEER identifies hidden factors (e.g., technical artifacts or unknown confounders) that explain much of the expression variability in transcriptomic datasets [58].
- Removal of Unwanted Variation (RUV): A normalization method that explicitly identifies and removes unwanted sources of variation within omics readouts, thereby enhancing the detection of true biological differences [58].
Strategic Approaches to Taming Variability
Addressing the challenge of variability requires a multi-pronged strategy that encompasses experimental design, quality control, and technological innovation.
Robust Experimental Design and Quality Control
The foundation of reproducible iPSC research is a rigorous and well-documented quality control (QC) regimen. Key elements include:
- Use of Isogenic Controls: Engineering isogenic iPSC lines that differ only at a specific disease-relevant locus provides a genetically identical control, powerfully controlling for background genetic effects [58] [62].
- Standardized Protocols and "Rosetta Lines": Adoption of standardized culture and differentiation protocols across laboratories minimizes technical divergence. The use of a common reference or "Rosetta" iPSC line enables researchers to directly address and calibrate experimental variation between different laboratory environments [58].
- Comprehensive Cell Banking: To mitigate the effects of genetic drift and accumulated mutations over time, creating large, early-passage master cell banks is essential. Working within a low passage number range helps ensure consistency [59].
Leveraging Complex Models and Analytical Integration
While increasing model complexity can introduce variability, it is also the key to achieving physiological relevance. Strategies to harness this complexity include:
- Incorporating Non-Neural Cell Types in Brain Models: Co-culturing iPSC-derived neurons with microglia and astrocytes helps recapitulate the native brain microenvironment, providing more relevant insights into disease mechanisms [62].
- Integration with Patient Biophysical Data: A frontier in the field is the integration of high-resolution cellular phenotyping data from iPSC models with patient-derived biophysical data, such as quantitative neuroimaging. This synergy, potentially powered by generative AI modeling, can bridge the gap between cellular phenotypes and clinical presentation, creating predictive models for personalized medicine [62].
Table 2: The Scientist's Toolkit: Key Reagents and Methods for Managing Variability
| Tool Category | Specific Example | Function in Managing Variability |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) [2] [62] | Fundamental for inducing pluripotency; consistency in reprogramming method is crucial. |
| Small Molecule Inhibitors/Activators | CHIR99021 (Wnt activator), DMH-1 (BMP inhibitor), SB431542 (TGF-β inhibitor) [60] [61] | Direct differentiation toward specific lineages (e.g., motor neurons); precise concentrations are vital for protocol reproducibility. |
| Genetic Analysis Kits & Reagents | CytoScanHD Chip, WES Kit, Targeted Sequencing Panel, ddPCR Supermix [59] | Enable detection of genetic variants at different levels of resolution, ensuring genetic stability and product safety. |
| Bioinformatic Tools | Principal Component Analysis (PCA), Probabilistic Estimation of Expression Residuals (PEER) [58] | Statistical methods to identify, visualize, and correct for unwanted sources of technical and biological variation in large datasets. |
The promise of iPSC-derived models in revolutionizing disease research and regenerative medicine is undeniable. However, realizing this potential hinges on the community's ability to systematically "tame variability." This requires a concerted effort to acknowledge and understand the multifaceted sources of heterogeneity, from donor genetics and genetic instability to technical artifacts. As reviewed, the scientific toolkit for this task is powerful and expanding, encompassing sensitive molecular assays like ddPCR, sophisticated bioinformatic normalization methods, and robust experimental designs employing isogenic controls. The path forward lies not in eliminating all variation, but in rigorously controlling for it through standardized quality control and leveraging advanced analytical and modeling approaches to extract meaningful, reproducible biological insights. By adopting these strategies, researchers can ensure that iPSC-based models fulfill their destiny as reliable, physiologically relevant, and transformative tools for biomedical science.
The approval of induced pluripotent stem cell (iPSC)-based therapies for clinical trials is becoming a reality after more than two decades of research and development [63]. These therapies offer a versatile platform for regenerative medicine, disease modeling, and drug discovery by enabling the generation of patient-specific cells capable of differentiating into nearly any tissue type [3]. However, manufacturing these therapies at the scale required for patient treatment and clinical trial enabling activities remains a significant challenge [63]. The global iPSC market, expected to reach US$4.69 Billion by 2033 from US$2.01 Billion in 2024, reflects both the promise and substantial scaling challenges facing this field [64]. This guide objectively compares current manufacturing approaches within the broader context of evaluating the physiological relevance of iPSC-derived tissues, providing researchers and drug development professionals with critical insights into scalable manufacturing technologies.
Key Manufacturing Challenges in iPSC Clinical Translation
Translating iPSC technologies from research to clinical application presents multiple interconnected manufacturing challenges that impact both scalability and therapeutic efficacy. The table below summarizes these primary challenges and their implications for clinical translation.
Table 1: Key Challenges in Scaling iPSC Manufacturing for Clinical Translation
| Challenge Category | Specific Manufacturing Hurdles | Impact on Clinical Translation |
|---|---|---|
| Process Standardization | Variability in differentiation outcomes, lack of harmonized quality control measures [63] [3] | Reduced batch-to-batch consistency and product reliability |
| Genetic Stability | Genetic and epigenetic abnormalities during reprogramming and expansion [3] | Potential tumorigenicity and safety concerns in patients |
| Manufacturing Systems | Limited scalability of 2D culture systems, complex transition to 3D bioreactors [63] | Inability to produce sufficient cell quantities for widespread clinical use |
| Regulatory Compliance | Stringent GMP requirements, lengthy approval timelines [64] [3] | Increased development costs and delayed market access |
| Cost Management | High production costs, complex manufacturing processes [64] | Limited economic viability and accessibility of final therapies |
Beyond these technical challenges, reliable scale-up under Good Manufacturing Practice (GMP) conditions remains a major hurdle, with critical questions around long-term engraftment, tissue integration, and immune tolerance still unresolved [3]. These factors collectively impact not only manufacturing scalability but also the physiological relevance and predictive value of iPSC-derived tissues for research and clinical applications.
Comparative Analysis of Scalable Manufacturing Technologies
Expansion and Differentiation Platforms
Different expansion and differentiation systems offer varying advantages for scaling iPSC manufacturing. The selection of appropriate technologies depends on the specific cell type required, scale needs, and ultimate application (research vs. clinical use).
Table 2: Comparison of Scalable Technologies for iPSC Expansion and Differentiation
| Technology Platform | Compatibility with GMP | Maximum Scalability | Key Applications | Limitations |
|---|---|---|---|---|
| 2D Static Culture | Limited (open systems) [63] | Laboratory scale (≤ 100 cm²) [63] | Research, early differentiation | Labor-intensive, surface area limitations |
| Multi-layer Vessels | Moderate (controlled environment) [63] | Pilot scale (≤ 3000 cm²) [63] | Process development, small-batch production | Limited process monitoring capabilities |
| Suspension Bioreactors | High (closed systems) [63] | Industrial scale (≥ 2000 L) [63] | Large-scale production of cardiomyocytes, neural progenitors | Requires optimization for each cell type |
| Microcarrier-based Systems | High (with appropriate controls) [63] | Commercial scale (≥ 2000 L) [63] | MSC production, 3D tissue formation | Cell harvesting challenges, potential clumping |
Process Analytical Technologies for Quality Control
Implementing robust Process Analytical Technology (PAT) is essential for monitoring Critical Process Parameters (CPPs) and Critical Quality Attributes (CQAs) in scalable iPSC manufacturing. The integration of these technologies enables real-time quality control and ensures product consistency.
Table 3: Process Analytical Technologies for iPSC Manufacturing Monitoring
| Monitoring Technology | Measured Parameters | Implementation Complexity | Scalability |
|---|---|---|---|
| In-line pH/Oxygen Sensors | Metabolic activity, culture condition maintenance [63] | Low (standard in bioreactors) | Highly scalable |
| Automated Microscopy | Cell morphology, confluence, differentiation status [63] | Medium (requires integration) | Moderate |
| Flow Cytometry Sampling | Surface marker expression, population purity [63] | High (requires aseptic sampling) | Limited at production scale |
| Metabolite Analysis | Nutrient consumption, waste product accumulation [63] | Medium (automated systems available) | Highly scalable |
| AI-Based Morphology Classification | Colony characteristics, early quality assessment [3] | High (specialized algorithms needed) | Highly scalable |
Experimental Protocols for Scalability Assessment
Protocol: Bioreactor Expansion of iPSCs
Objective: Establish scalable expansion of iPSCs in suspension bioreactor systems. Materials: Clinical-grade iPSC line, sterile single-use bioreactor vessel, defined culture medium, microcarriers (if applicable), sampling system, pH and dissolved oxygen sensors. Methodology:
- Pre-culture iPSCs in 2D system to establish baseline growth characteristics
- Adapt cells to suspension culture through progressive passage series
- Inoculate bioreactor at optimal cell density (determined empirically)
- Maintain culture parameters: pH 7.2-7.4, dissolved oxygen 30-60%, temperature 37°C
- Implement fed-batch or perfusion feeding strategy based on metabolite data
- Monitor cell density, viability, and pluripotency marker expression daily
- Harvest cells at predetermined density and assess quality attributes Quality Controls: Flow cytometry for pluripotency markers (OCT4, SOX2, NANOG), karyotype analysis, viability assessment, sterility testing [63] [3].
Protocol: Automated Differentiation in Bioreactor Systems
Objective: Achieve consistent, large-scale differentiation of iPSCs to target cell types. Materials: Expanded iPSCs, stirred-tank bioreactor, differentiation media components, growth factors, sampling system, process control software. Methodology:
- Seed iPSCs at optimized density for differentiation initiation
- Programmed, timed addition of differentiation factors through automated pumps
- Continuous monitoring of oxygen consumption rate as indicator of metabolic shifts
- Daily sampling for marker expression analysis (flow cytometry, PCR)
- Adjustment of mixing speed to maintain cell suspension while minimizing shear stress
- Process termination based on predefined differentiation markers
- Final cell harvest and purification using appropriate separation technologies Quality Controls: Assessment of target cell purity, functional characterization, genomic stability testing, residual undifferentiated cell quantification [63].
iPSC Clinical Manufacturing Workflow
The following diagram illustrates the complete workflow for manufacturing clinically applicable iPSC-derived tissues, from somatic cell reprogramming to final product release.
Critical Path to Clinical Translation
The pathway from research development to clinical application requires navigating specific stages with distinct scalability considerations and regulatory requirements.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful scaling of iPSC manufacturing requires specialized reagents and materials designed to maintain cell quality and differentiation potential throughout the expansion process.
Table 4: Essential Research Reagents for Scalable iPSC Manufacturing
| Reagent/Material | Function | Scalability Considerations |
|---|---|---|
| Chemically Defined Medium | Supports iPSC growth without undefined components [63] | Enables consistent large-scale production; reduces batch variability |
| Non-integrating Reprogramming Vectors | Generates iPSCs without genomic integration [3] | Critical for clinical compliance; reduces tumorigenicity risk |
| GMP-grade Extracellular Matrices | Provides surface for 2D cell attachment and growth [63] | Must be qualified for clinical use; impacts cell morphology and function |
| Xeno-free Differentiation Factors | Directs cell fate toward specific lineages [63] | Essential for clinical applications; eliminates animal-derived components |
| Cell Dissociation Enzymes | Enables cell passaging and harvesting [63] | Impacts cell viability and recovery; must be serum-free and defined |
| Cryopreservation Media | Maintains cell viability during frozen storage [64] | Critical for cell banking; formulation affects post-thaw recovery |
| Quality Control Assays | Assesses identity, purity, and potency [63] [3] | Must be validated and scalable for lot release testing |
Achieving true scalability in iPSC manufacturing for clinical translation requires addressing multiple interconnected challenges through technological innovation, process optimization, and quality-by-design approaches. The comparison of current technologies reveals a clear progression from research-scale 2D systems to industrial-scale bioreactor platforms, each with distinct advantages and limitations. Emerging technologies such as AI-guided differentiation [3], process analytical technologies [63], and automated closed-system manufacturing are progressively addressing key bottlenecks in scaling, quality control, and cost reduction. As the field advances toward more widespread clinical testing and commercial application, the integration of these technologies with robust regulatory frameworks will be essential for realizing the full potential of iPSC-based therapies in regenerative medicine. The ongoing clinical trials in areas such as Parkinson's disease, retinal disorders, and cardiac conditions [3] provide promising evidence that these scalability challenges can be overcome through continued interdisciplinary collaboration and innovation.
The pursuit of physiological relevance in human induced pluripotent stem cell (iPSC)-derived tissues represents a central challenge in modern biomedical research. Traditional two-dimensional (2D) monolayer cultures often fail to recapitulate the complex architecture and functionality of native human tissues, limiting their predictive value in disease modeling and drug development [48]. This guide objectively evaluates an integrated technological framework combining three-dimensional (3D) biomanufacturing, artificial intelligence (AI)-enhanced gene editing, and personalized differentiation protocols. By comparing this unified approach against conventional methods, we provide researchers with a data-driven analysis of tools that are reshaping preclinical research.
The Foundational Shift from 2D to Physiologically Relevant 3D Systems
The limitations of 2D culture systems have become increasingly apparent as researchers seek more human-relevant models. While 2D monolayers have served as initial platforms for iPSC differentiation, they lack the complex, heterotypic environment where cells normally reside in vivo [48]. Parenchymal cells in living organs exist within a sophisticated 3D environment supported by organized extracellular matrix (ECM) and multiple cell types. For example, in the human heart, cardiomyocytes represent only approximately 30% of total cells, with the remainder consisting of vascular smooth muscle cells, endothelial cells, fibroblasts, and leukocytes [48]. Without dynamic, reciprocal support from ECM and surrounding cells, 2D models lack essential information regarding cell-cell communications and cell-matrix mechanics.
Advanced 3D systems address these limitations through two primary approaches: engineered tissue constructs using biomaterial scaffolds and self-organizing organoids [48]. The transition to 3D culture demonstrates measurable improvements in cellular maturity, functionality, and transcriptional profiles, as quantified in the table below comparing 2D and 3D cardiac differentiation.
Table 1: Quantitative Comparison of 2D Monolayer vs. 3D Suspension Culture for iPSC-Derived Cardiomyocyte Production
| Parameter | 2D Monolayer Differentiation | 3D Suspension Bioreactor |
|---|---|---|
| Yield (cells/mL) | Lower, scales linearly with plate area [65] | ~1.21 million [65] |
| Purity (% TNNT2+) | High intra- and inter-batch variability [65] | ~94% [65] |
| Functional Maturity | Higher spontaneous beating rate, fetal-like [48] [65] | More mature functional properties, lower beating rate [65] |
| Onset of Contraction | Differentiation day 7 [65] | Differentiation day 5 [65] |
| Batch-to-Batch Reproducibility | Significant variation [65] | High reproducibility across lines and batches [65] |
| Ventricular Identity | Lower expression of markers (e.g., MYH7, MYL2) [65] | Higher expression; 83.4% positive for MLC2v [65] |
| Cryopreservation Viability | Reported negative impact on function [65] | >90% viability post-recovery [65] |
Experimental Protocol: 3D Suspension Cardiac Differentiation
The following methodology outlines the optimized bioreactor protocol for generating iPSC-derived cardiomyocytes (hiPSC-CMs) in suspension, as validated by extensive morphological and functional characterization [65]:
- Input Cell Quality Control: Begin with quality-controlled master cell banks of hiPSCs. Verify pluripotency marker SSEA4 expression exceeds 70% via FACS analysis, as values below this threshold predict failed differentiation [65].
- Embryoid Body (EB) Formation: Culture hiPSCs in a stirred-tank bioreactor that monitors and adjusts temperature, O₂, CO₂, and pH. Allow cells to spontaneously aggregate into EBs [65].
- Mesoderm Induction: Monitor EB diameter. Initiate differentiation by adding 7 µM CHIR99021 (a Wnt pathway activator) when EB diameter reaches 100 µm (typically at 24 hours). EBs smaller than 100 µm may disintegrate, while those larger than 300 µm differentiate less efficiently due to diffusion limits [65].
- Cardiac Specification: Incubate with CHIR99021 for 24 hours, followed by a 24-hour gap with no treatment. Subsequently, add 5 µM IWR-1 (a Wnt pathway inhibitor) for 48 hours to promote cardiac specification [65].
- Maturation and Harvesting: Maintain cells in culture for a total of 15 days. The resulting cardiomyocytes (bCMs) can be cryopreserved with high recovery viability (>90%) [65].
Diagram: Workflow for 3D Suspension Cardiac Differentiation
AI and Gene Editing as Enabling Technologies
The integration of artificial intelligence and precision gene editing has created a synergistic toolkit that enhances both the efficiency and accuracy of iPSC-based research.
AI-Augmented Genome Editing
AI models are critically improving CRISPR-based genome editing by bringing enhanced precision, efficiency, and affordability [66]. These systems assist researchers in multiple facets of experimental design:
- gRNA Design Optimization: AI tools like DeepCRISPR, CRISTA, and DeepHF predict optimal guide RNAs (gRNAs) by factoring in genomic context, Cas protein type, desired mutation, on-target/off-target scores, and potential impacts on gene function and cell phenotype [66].
- Outcome Prediction: Machine learning algorithms, such as SPROUT, can predict the repair outcomes of gene editing in primary cells with high accuracy, allowing researchers to design experiments that maximize the desired editing outcome [66].
- End-to-End Experiment Planning: Advanced AI agent systems, such as CRISPR-GPT, leverage large language models (LLMs) to automate and enhance the entire gene-editing workflow. This AI co-pilot can assist with selecting CRISPR systems (e.g., Cas9, Cas12a, dCas9), recommending delivery methods, designing gRNAs, predicting off-target effects, selecting experimental protocols, and planning validation assays [67].
Table 2: Essential Research Reagent Solutions for Integrated iPSC Research
| Category | Specific Tool/Reagent | Function in Integrated Workflow |
|---|---|---|
| CRISPR System | CRISPR-Cas9, CRISPR-Cas12a, base editors, prime editors [66] [67] | Introduces precise genetic modifications for disease modeling or gene correction. |
| AI Design Tool | CRISPR-GPT, DeepCRISPR, CRISTA [66] [67] | Plans experiments, designs high-efficiency gRNAs, and predicts off-target effects. |
| 3D Culture Matrix | Synthetic peptide hydrogels (e.g., PGmatrix), Matrigel, defined polymers [36] | Provides a physiologically relevant 3D microenvironment for cell growth and differentiation. |
| Differentiation Inducer | Small molecules (e.g., CHIR99021, IWR-1) [65] | Directs lineage-specific differentiation more cost-effectively than growth factors. |
| Bioreactor System | Stirred-tank, vertical-wheel, wave bioreactors [36] [65] | Enables scalable 3D cell production with controlled parameters (O₂, pH, temperature). |
Experimental Protocol: AI-Guided Gene Knockout
The following protocol exemplifies an end-to-end AI-guided workflow for knocking out a target gene in a human cell line, demonstrating how AI integrates into the experimental process [67]:
- Experiment Planning (AI Meta-Mode): Input a freestyle request (e.g., "Knock out the human TGFβR1 gene in A549 lung cancer cells") into the AI agent (e.g., CRISPR-GPT). The AI Planner decomposes this request into a sequence of tasks: CRISPR system selection, delivery method recommendation, gRNA design, and protocol selection [67].
- CRISPR System Selection: The AI agent, leveraging expert guidelines and published literature, selects an appropriate system. For knockout, CRISPR-Cas12a may be recommended [67].
- gRNA Design and Validation: The AI Task executor designs specific gRNAs for the target gene, predicts their on-target efficiency and potential off-target sites using integrated tools, and returns the optimized sequences [67].
- Wet-Lab Execution: Junior researchers, following the AI-generated protocol, perform the experiment. This includes:
- Culturing the target cell line (e.g., A549).
- Transfecting or transducing cells with the CRISPR machinery.
- Validating knockout efficiency via genomic DNA sequencing (e.g., T7E1 assay or NGS) and confirming phenotypical changes at the protein level (e.g., Western blot) [67].
Integrated Workflow and Comparative Analysis
The true power of these technologies is realized through their integration into a seamless workflow. This unified approach begins with patient-specific somatic cells, which are reprogrammed into iPSCs. AI-assisted gene editing then corrects mutations or introduces disease-relevant variants, followed by AI-optimized differentiation protocols within physiological 3D environments to generate mature, functional tissues [36] [67].
Diagram: Integrated Workflow for Physiologically Relevant iPSC Research
This integrated framework offers significant advantages over traditional, siloed approaches. The combination of 3D biomanufacturing, AI, and gene editing directly addresses the core challenge of physiological relevance by producing tissues with enhanced maturity, complexity, and patient-specificity. For pharmaceutical researchers and scientists, this toolkit enables more accurate disease modeling, more predictive toxicology screening, and a robust pathway toward personalized cell therapies [2] [49].
Benchmarking Fidelity: Strategies for Validating Physiological Relevance
The emergence of human induced pluripotent stem cell (iPSC) technology has introduced a powerful tool for modeling human development and disease, with particular value for accessing living human cell types that are otherwise difficult to study, such as neurons and vascular smooth muscle cells [2] [68] [69]. However, a significant challenge remains in determining how closely iPSC-derived tissues resemble their native in vivo counterparts, which is essential for ensuring their physiological relevance in research and drug development [69]. Multi-omics validation—specifically the integrated application of transcriptomic and proteomic profiling—provides a comprehensive solution to this challenge by enabling researchers to simultaneously examine the molecular state of cells at both the gene expression and functional protein levels [68].
Transcriptomics reveals the RNA-level blueprint of cellular identity, while proteomics directly characterizes the functional effector molecules that execute cellular processes, including critical post-translational modifications that cannot be detected through nucleic acid analysis alone [70] [71]. The integration of these approaches is particularly crucial in iPSC-derived tissues because mRNA expression levels do not always correlate directly with protein abundance due to complex post-transcriptional regulation [68]. This review provides a comparative analysis of current transcriptomic and proteomic profiling platforms, evaluates their performance in validating iPSC-derived tissues, and offers practical methodological guidance for implementing multi-omics validation in stem cell research.
Platform Comparisons: Transcriptomic and Proteomic Profiling Technologies
High-Throughput Transcriptomic Sequencing Platforms
Table 1: Comparison of High-Throughput Transcriptomic Sequencing Platforms
| Platform | Technology Principle | Read Type | Accuracy & Sensitivity | Applications in iPSC Research | Considerations |
|---|---|---|---|---|---|
| Illumina | Sequencing-by-Synthesis (SBS) | Short-read | High accuracy and sensitivity [72] | Single-cell RNA-seq of heterogeneous iPSC differentiations [72] | Higher cost per sample; industry standard for accuracy |
| MGI Tech | DNA Nanoball (DNB) sequencing | Short-read | Similar accuracy and sensitivity to Illumina [72] | Large-scale iPSC differentiation studies requiring high throughput [72] | Lower cost alternative; suitable for high-throughput applications |
| PacBio | Single Molecule Real-Time (SMRT) | Long-read | Lower per-read accuracy but better for isoform detection | Full-length transcript sequencing for alternative splicing analysis | Higher error rate but detects structural variants |
| Oxford Nanopore | Nanopore sensing | Long-read | Moderate accuracy; real-time sequencing | Direct RNA sequencing; rapid analysis of iPSC derivatives | Portable options available; lower equipment cost |
Mass Spectrometry-Based Proteomic Platforms
Table 2: Comparison of Quantitative Proteomics Methods
| Method | Quantification Approach | Multiplexing Capacity | Advantages | Limitations | iPSC Application Examples |
|---|---|---|---|---|---|
| Label-Free Quantification (LFQ) | Spectral counting or ion intensity [70] | Unlimited samples | Simple sample preparation; no chemical labeling required [70] | Higher variability between runs; requires more replicates [70] | Global proteome profiling of iPSCs vs. neurons [68] |
| SILAC (Stable Isotope Labeling with Amino Acids in Cell Culture) | Metabolic labeling with heavy isotopes [70] | 2-3 conditions | High accuracy; minimal technical variation [70] | Requires specialized media; not suitable for all cell types [70] | Comparative studies of iPSC differentiation stages |
| TMT/iTRAQ (Isobaric Tagging) | Chemical tagging post-digestion [70] | Up to 16-18 samples | High multiplexing capability; applicable to any sample type [70] | Ratio compression due to co-isolated peptides [70] | Parallel analysis of multiple iPSC lines or conditions |
| Data-Independent Acquisition (DIA) | Fragment ion libraries of all peptides | Unlimited samples | Comprehensive data recording; high reproducibility | Complex data analysis; requires spectral libraries | Longitudinal studies of iPSC differentiation |
Emerging and Specialized Proteomic Technologies
Table 3: Emerging Proteomic Technologies for Specialized Applications
| Technology | Principle | Throughput | Sensitivity | Best Use Cases in iPSC Research |
|---|---|---|---|---|
| Protein Pathway Array (PPA) | Antibody-based detection of signaling proteins [71] | Medium | High for targeted proteins | Mapping signaling networks in iPSC-derived cells [71] |
| Proximity Ligation Assay (Olink) | Paired antibody recognition with DNA amplification [71] | High | Exceptional (fg-pg/mL) | Validation of key biomarkers in iPSC disease models |
| SIMOA | Single molecule array technology [71] | Medium | Ultra-high (single molecule detection) | Detecting low-abundance proteins in iPSC-derived neuronal media |
| Luminex | Bead-based immunoassay with fluorescent barcoding [71] | High | High for targeted panels | Screening cytokine secretion in iPSC-derived immune cells |
Experimental Design and Methodologies for Multi-Omics Validation
Integrated Workflow for Multi-Omics Analysis of iPSC-Derived Tissues
The successful implementation of multi-omics validation requires careful experimental design that preserves sample integrity while enabling comprehensive molecular profiling. The following workflow diagram illustrates a robust approach for parallel transcriptomic and proteomic analysis of iPSC-derived tissues:
Detailed Methodological Protocols
Sample Preparation for Parallel Transcriptomic and Proteomic Analysis
Optimal sample preparation is critical for preserving molecular integrity and ensuring accurate multi-omics measurements. For integrated proteomics, lipidomics, and metabolomics analyses, researchers should follow these standardized procedures [68]:
Cell Harvesting: Gently wash cells twice with ice-cold phosphate-buffered saline (PBS) to remove media contaminants. For a typical multi-omics analysis, harvest at least 2 million cells per biological replicate to ensure sufficient material for all analyses.
Simultaneous Metabolite, Lipid, and Protein Extraction: Immediately add 350 μL of ice-cold methanol/water mixture (5:2 v/v, HPLC grade) directly onto the cell culture plate and scrape cells into pre-chilled 2 mL tubes. Repeat this step once and combine to minimize cell loss.
Phase Separation: Add 1 mL of HPLC-grade chloroform to each sample, followed by incubation on ice for 1 hour with frequent vortexing. Centrifuge at 12,700 rpm at 4°C for 15 minutes to separate phases.
Fraction Collection: Carefully transfer the bottom chloroform layer (containing lipids) and top aqueous layer (containing metabolites) to separate tubes. Retain the protein pellet in the original tube for processing.
Protein Processing for Proteomics: Reconstitute dried protein pellets in lysis buffer (8 M urea, 50 mM ammonium bicarbonate, 150 mM sodium chloride). After protein concentration measurement, reduce proteins with 5 mM tris(2-carboxyethyl)phosphine (TCEP) for 40 minutes at 37°C, alkylate with 15 mM iodoacetamide (IAA) for 30 minutes at 37°C in the dark, and quench with 5 mM dithiothreitol (DTT) for 10 minutes at 37°C. Dilute urea concentration below 1 M with 50 mM ammonium bicarbonate before digesting with trypsin/Lys-C mix (1:30, w:w) for 16 hours at 37°C.
LC-MS/MS Analysis for Proteomic Profiling
For comprehensive proteomic coverage, the following liquid chromatography-mass spectrometry parameters are recommended [68]:
- Chromatography System: Dionex Ultimate 3000 RSLCnano or equivalent
- Column: Easy-Spray PepMap RSLC C18 column (2 μm, 100 Å, 75 μm × 50 cm)
- Mobile Phase: A: 0.1% formic acid in water; B: 0.1% formic acid in acetonitrile
- Gradient: 210 minutes with temperature maintained at 55°C
- Mass Spectrometer: Q-Exactive HF-X Orbitrap or similar high-resolution instrument
- MS Settings: MS1 scan range: m/z 400-1000; Resolution: 60,000; AGC target: 1e6; Maximum injection time: 60 ms
Transcriptomic Library Preparation and Sequencing
For transcriptomic analysis, particularly single-cell RNA sequencing of heterogeneous iPSC differentiations:
Library Preparation: Use standardized kits such as the 10x Genomics Chromium platform for single-cell applications or Illumina TruSeq for bulk RNA sequencing.
Quality Control: Ensure RNA Integrity Number (RIN) > 8.5 for bulk RNA-seq and viability >80% for single-cell preparations.
Sequencing Parameters: Aim for minimum coverage of 20-30 million reads per sample for bulk RNA-seq and 50,000 reads per cell for single-cell RNA-seq.
Platform Selection: Both Illumina and MGI Tech platforms produce similar results for clustering and gene expression analyses, with choice depending on cost and throughput requirements [72].
Applications in iPSC-Derived Tissue Validation
Characterizing iPSC-Derived Neurons
Multi-omics approaches have been successfully applied to validate the molecular identity of iPSC-derived neurons. A comprehensive proteomics, lipidomics, and metabolomics comparison between human iPSCs and iPSC-derived glutamatergic neurons revealed distinct molecular profiles consistent with neuronal maturation [68]. Proteins related to mitosis, DNA replication, and pluripotency were highly enriched in iPSCs, while synaptic proteins, neurotransmitters, and axon guidance pathways were significantly upregulated in neurons [68]. This molecular validation provides confidence that iPSC-derived neurons recapitulate key features of native neurons, making them suitable for modeling neurological disorders and screening neuroactive compounds.
In disease modeling applications, multi-omics validation has been particularly valuable for understanding how genetic mutations affect molecular networks. For example, in progranulin (PGRN) deficiency modeling, integrated multi-omics revealed that neurons were more susceptible to PGRN loss than iPSCs, consistent with the neurological symptoms observed in patients with GRN mutations [68]. This approach identified altered pathways in neuroinflammation, purine metabolism, and neurite outgrowth, providing a comprehensive view of disease mechanisms.
Validating iPSC-Derived Smooth Muscle Cells
The validation of iPSC-derived smooth muscle cells (iPSC-SMCs) presents unique challenges due to the diverse embryonic origins and inherent phenotypic plasticity of SMCs in vivo [69]. Transcriptomic and proteomic profiling has been essential for verifying that differentiation protocols produce SMCs with the appropriate lineage specification. Researchers have developed lineage-specific differentiation protocols that generate SMCs via neuroectodermal, paraxial mesoderm, and lateral plate mesoderm intermediates, each requiring validation of distinct molecular markers [69].
Proteomic analysis has been particularly important for confirming the expression of both early (ACTA2, TAGLN, CNN1) and late (SMTN, MYH11) markers of SMC differentiation [69]. Additionally, multi-omics approaches have revealed origin-specific phenotypes, such as the requirement for the transcriptional co-activator MKL2 in neuroectoderm-to-SMC differentiation but not in mesoderm-to-SMC differentiation [69]. These molecular validations ensure that iPSC-SMCs recapitulate the functional diversity of native vascular smooth muscle cells.
Evaluating Stem Cell-Derived Platelets
Comparative multi-omics analysis has revealed important similarities and differences between stem cell-derived platelets and their native counterparts. Transcriptomic and proteomic profiling of mouse embryonic platelets demonstrated that they exhibit reduced classic immune-regulatory and procoagulant features but enhanced development-supporting traits compared to adult platelets [73]. Notably, human iPSC-derived platelets were found to closely resemble embryonic platelets both molecularly and functionally, sharing similar multi-omics signatures and demonstrating superior regenerative potential in wound healing applications [73]. This molecular characterization is essential for developing platelet-based therapies with tailored clinical applications.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Essential Research Reagents and Platforms for Multi-Omics Validation
| Category | Specific Product/Platform | Key Features | Application in iPSC Validation |
|---|---|---|---|
| Stem Cell Culture | Essential 8 Medium | Defined, xeno-free maintenance | Human iPSC culture [68] |
| Neuronal Differentiation | i3Neuron Technology | Dox-inducible NGN2; pure cortical neurons | Rapid, consistent neuronal differentiation [68] |
| SMC Differentiation | Lineage-specific protocols | TGFβ1 and PDGF-BB induction | Generation of origin-specific smooth muscle cells [69] |
| Proteomics Sample Prep | Sequencing-grade trypsin | High specificity cleavage | Protein digestion for LC-MS/MS [74] |
| Protein Quantification | BCA or Bradford Assay | Colorimetric quantification | Total protein measurement pre-MS [68] |
| Chromatography | C18 reversed-phase columns | High-resolution separation | Peptide separation pre-MS [74] |
| Mass Spectrometry | Orbitrap-based instruments | High mass accuracy and resolution | Protein identification and quantification [68] |
| RNA Sequencing | Illumina NovaSeq Series | High-throughput sequencing | Transcriptome profiling [72] |
| Bioinformatics | Python/R packages | Statistical analysis and visualization | Multi-omics data integration [75] |
Data Integration and Bioinformatics Strategies
The true power of multi-omics approaches lies in the integrated analysis of complementary datasets to extract biologically meaningful insights. Effective integration requires specialized bioinformatics approaches:
Multi-Step Bioinformatics Pipeline: Implement comprehensive pipelines that integrate differential expression analysis, protein-protein interaction network construction, and functional enrichment analysis to identify key hub genes and proteins associated with cellular identity and function [75].
Pathway-Centric Integration: Focus on mapping multi-omics data onto biological pathways rather than analyzing individual molecules in isolation. This approach recognizes that diseases and developmental processes involve coordinated changes across multiple molecular layers [68].
Network-Based Multi-Omics Integration: Perceive biological systems as interconnected networks where each omics layer contributes to uncovering authentic connections within molecular networks [68]. This approach helps identify central regulators of cellular phenotype that may not be apparent from single-omics analyses.
Temporal Integration: For differentiation time courses, incorporate temporal patterns of expression across omics layers to identify sequential molecular events that drive cellular maturation and specialization.
The following diagram illustrates the key bioinformatics workflow for integrating and interpreting multi-omics data:
Multi-omics validation through integrated transcriptomic and proteomic profiling provides an essential framework for establishing the physiological relevance of iPSC-derived tissues. As the technology continues to advance, with improvements in sequencing sensitivity, mass spectrometry accuracy, and bioinformatic integration tools, these approaches will become increasingly accessible and powerful. The ongoing development of standardized validation protocols and reference datasets for specific iPSC-derived cell types will further enhance reproducibility and reliability across the field. By implementing comprehensive multi-omics validation strategies, researchers can confidently utilize iPSC-derived tissues to model human development and disease, accelerate drug discovery, and advance toward personalized medicine applications.
The advent of human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs) has revolutionized cardiovascular research, offering an unprecedented human-relevant platform for disease modeling, drug development, and regenerative medicine [76]. However, the physiological relevance of findings from these models hinges on a critical factor: their functional maturity. hiPSC-CMs typically exhibit a fetal-like phenotype characterized by structural, metabolic, and electrophysiological immaturity, which limits their ability to fully recapitulate adult human cardiac physiology [76] [77] [78]. This limitation underscores the necessity for rigorous functional benchmarking to validate these models and interpret experimental data accurately.
Functional benchmarking provides standardized metrics to assess how closely hiPSC-CMs mimic adult human cardiomyocytes across three fundamental domains: electrophysiology, contractility, and metabolic activity. The establishment of consensus benchmarks enables researchers to evaluate the efficacy of maturation strategies, compare results across different laboratories and protocols, and ultimately enhance the predictive power of hiPSC-CM-based assays [76]. This guide provides a comprehensive comparison of current benchmarking methodologies, quantitative data on mature phenotypes, and detailed experimental protocols to support the standardization of functional assessments in cardiac research.
Electrophysiological Benchmarking
Key Parameters and Experimental Data
Electrophysiological benchmarking assesses the ion channel activity, action potential properties, and conduction characteristics that underpin the heart's rhythmic contractions. Adult cardiomyocytes exhibit distinct electrophysiological signatures that are often blunted in immature hiPSC-CMs [76].
Table 1: Key Electrophysiological Benchmarking Parameters for hiPSC-CMs
| Parameter | Adult Cardiomyocyte Benchmark | Typical Immature hiPSC-CM Phenotype | Primary Experimental Assay |
|---|---|---|---|
| Resting Membrane Potential | ~ -90 mV [76] | > -80 mV [76] | Patch-Clamp Electrophysiology |
| Action Potential Amplitude | ~ 100-110 mV [76] | Reduced amplitude | Patch-Clamp Electrophysiology |
| Action Potential Duration (APD90) | ~ 230-300 ms [76] | Highly variable, often longer | Patch-Clamp Electrophysiology |
| Upstroke Velocity (dV/dtmax) | ~ 250-300 V/s [76] | Significantly slower | Patch-Clamp Electrophysiology |
| Conduction Velocity | 30-100 cm/s [76] | Typically < 40 cm/s [76] | Microelectrode Array (MEA) |
| Spontaneous Beating | Low to zero [76] | High, spontaneous activity | Microscopy, MEA |
Detailed Experimental Protocols
Patch-Clamp Electrophysiology for Action Potential Characterization
The patch-clamp technique is the gold standard for detailed characterization of action potential parameters and individual ion currents at the single-cell level.
- Cell Preparation: hiPSC-CMs are dissociated into single cells and plated on glass coverslips compatible with the patch-clamp setup. Cells should be used within 1-3 days after plating to ensure optimal health and attachment.
- Solution Configuration:
- External Solution: Contains (in mM): 140 NaCl, 5.4 KCl, 1.8 CaCl₂, 1 MgCl₂, 10 HEPES, 10 Glucose; pH adjusted to 7.4 with NaOH.
- Internal (Pipette) Solution: Contains (in mM): 120 K-Aspartate, 20 KCl, 10 NaCl, 5 MgATP, 10 HEPES, 0.1 EGTA; pH adjusted to 7.2 with KOH.
- Recording Procedure: The whole-cell patch-clamp configuration is established. To record action potentials, cells are current-clamped. A brief depolarizing current stimulus is applied to elicit an action potential. Key parameters (Resting Membrane Potential, Amplitude, APD90, dV/dtmax) are measured from the resulting trace. For voltage-clamp recordings of specific ion currents, tailored voltage protocols and pharmacological inhibitors are used to isolate currents (e.g., INa, ICaL, IKr).
Microelectrode Array (MEA) for Field Potential and Conduction Analysis
MEA recordings provide a non-invasive method to assess the field potential, which is the extracellular correlate of the action potential, and can be used to derive conduction velocity in syncytia or engineered tissues.
- Sample Preparation: hiPSC-CMs are cultured as a monolayer or 3D tissue on MEA plates containing a grid of embedded electrodes. The system should be placed in a cell culture incubator with controlled temperature and CO₂.
- Data Acquisition: Spontaneous or paced electrical activity is recorded from all electrodes simultaneously. The Field Potential Duration (FPD), which correlates with APD, and the beat period are measured.
- Conduction Velocity Calculation: The activation time for each electrode is determined from the maximum slope of the field potential. A propagation map is created, and conduction velocity is calculated from the distance between electrodes and the difference in their activation times.
Diagram 1: Electrophysiology assessment workflow, showing parallel paths for Patch-Clamp and MEA methods.
Contractility and Mechanical Force Benchmarking
Key Parameters and Experimental Data
Contractile function is a direct measure of a cardiomyocyte's primary purpose: to generate force. Mature adult cardiomyocytes produce significantly more force than their immature counterparts and exhibit a positive force-frequency relationship, a hallmark of maturity that is often reversed in hiPSC-CMs [76].
Table 2: Key Contractility Benchmarking Parameters for hiPSC-CMs
| Parameter | Adult Cardiomyocyte Benchmark | Typical Immature hiPSC-CM Phenotype | Primary Experimental Assay |
|---|---|---|---|
| Contractile Stress | 25-44 mN/mm² [76] | Significantly lower [76] | Engineered Heart Tissue (EHT) Force Transduction |
| Sarcomere Length | ~ 2.0 - 2.2 μm [76] | Shorter, disorganized | Fluorescence Microscopy (e.g., α-actinin staining) |
| Force-Frequency Relationship | Positive (Bowditch effect) | Negative or Flat | EHT with Pacing |
| Twitch Kinetics | Fast contraction/relaxation | Slower kinetics | Video-based Motion Analysis |
Detailed Experimental Protocols
Engineered Heart Tissue (EHT) and Force Transduction
EHTs are 3D constructs that allow for the direct measurement of contractile force, providing a more physiologically relevant context than 2D monolayers.
- EHT Fabrication:
- A mixture of hiPSC-CMs and human cardiac fibroblasts (in a ratio such as 4:1) is combined with a hydrogel matrix, commonly fibrin or collagen.
- The cell-hydrogel mix is cast into custom molds containing flexible silicone posts or between two attachment points. The gel polymerizes, forming a 3D tissue strip suspended between the posts.
- Tissues are maintained in culture with continuous medium perfusion or rocking to enhance nutrient delivery and maturation.
- Force Measurement:
- Spontaneous Force: The EHT is placed on a setup where the deflection of the posts is tracked via video microscopy. The contractile force is calculated from the post deflection and its known stiffness using Hooke's law (Force = Stiffness × Deflection).
- Paced Force-Frequency Relationship: EHTs are electrically paced at increasing frequencies (e.g., 0.5 Hz to 2.0 Hz). The developed force at each frequency is recorded. A positive force-frequency relationship (increased force with increased pacing rate) is a key indicator of maturity.
Sarcomere Imaging and Structural Analysis
The organization of sarcomeres, the fundamental contractile units, is a critical structural correlate of function.
- Immunostaining: hiPSC-CMs are fixed and stained for sarcomeric proteins such as α-actinin (Z-discs) and cardiac Troponin I (cTnI) or T (cTnT).
- Imaging and Analysis: High-resolution confocal microscopy is used to capture images. The regularity of the striated pattern is assessed qualitatively. Quantitative analysis can be performed using fast Fourier transform (FFT) to determine the periodicity of the striations, which corresponds to the average sarcomere length. The transition from slow skeletal troponin I (ssTnI) to cardiac troponin I (cTnI) is also a recognized marker of structural maturation [77].
Metabolic Activity Benchmarking
Key Parameters and Experimental Data
The heart is a metabolic powerhouse, and a shift from glycolysis to fatty acid oxidation (FAO) is a cornerstone of postnatal cardiac maturation. Immature hiPSC-CMs rely predominantly on glycolysis for ATP production, whereas adult cardiomyocytes derive >70% of their energy from FAO [76] [78].
Table 3: Key Metabolic Benchmarking Parameters for hiPSC-CMs
| Parameter | Adult Cardiomyocyte Benchmark | Typical Immature hiPSC-CM Phenotype | Primary Experimental Assay |
|---|---|---|---|
| Primary Energy Source | Fatty Acid Oxidation (>70%) [76] [78] | Aerobic Glycolysis [78] | Metabolic Flux Analysis |
| Mitochondrial Content | ~30% of cell volume [76] | Lower density, underdeveloped | Electron Microscopy |
| Glycolytic Rate | Low (adult) | High | Seahorse XF Analyzer |
| Oxidative Capacity | High | Low | Seahorse XF Analyzer |
Detailed Experimental Protocols
Seahorse XF Analyzer for Metabolic Flux Analysis
The Seahorse XF Analyzer measures the extracellular acidification rate (ECAR, a proxy for glycolysis) and the oxygen consumption rate (OCR, a proxy for oxidative phosphorylation) in real-time.
- Cell Preparation: hiPSC-CMs are seeded as a monolayer in specialized Seahorse XF microplates. For maturation studies, cells are often cultured in media supplemented with fatty acids (e.g., palmitate conjugated to BSA) and hormones (e.g., triiodothyronine T3, dexamethasone) to promote metabolic maturity [77] [78].
- Assay Media: On the day of the assay, culture medium is replaced with XF assay medium (bicarbonate-free, pH 7.4), supplemented with specific substrates:
- Glycolytic Rate Assay: Contains 2 mM Glutamine.
- MitoStress Test: Contains 10 mM Glucose, 1 mM Pyruvate, and 2 mM L-Glutamine.
- Drug Injections and Data Interpretation (MitoStress Test):
- Basal Measurement: OCR and ECAR are measured.
- Oligomycin (ATP synthase inhibitor): Injected to reveal the portion of OCR linked to ATP production. A drop in OCR indicates ATP-linked respiration.
- FCCP (mitochondrial uncoupler): Injected to induce maximum respiratory capacity. A strong response indicates a high reserve capacity.
- Rotenone & Antimycin A (Complex I & III inhibitors): Injected to shut down mitochondrial respiration. The remaining OCR is non-mitochondrial. Key parameters are calculated: Basal Respiration, ATP-linked Respiration, Maximal Respiration, and Spare Respiratory Capacity.
Assessment of Metabolic Substrate Utilization
Tracking the metabolism of specific substrates like fatty acids provides direct evidence of metabolic maturation.
- Radioactive or Stable Isotope Tracers: hiPSC-CMs are incubated with culture medium containing traceable substrates, such as 13C-labeled palmitate (for FAO) or 13C-labeled glucose.
- Analysis: The production of 13CO₂ or the incorporation of the label into TCA cycle intermediates is measured using mass spectrometry. A high rate of labeled palmitate oxidation directly confirms functional fatty acid beta-oxidation.
Diagram 2: Key stimuli that promote cardiomyocyte maturation and the resulting functional outcomes.
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Key Research Reagent Solutions for hiPSC-CM Functional Benchmarking
| Reagent/Material | Function | Example Use Case |
|---|---|---|
| STEMdiff Ventricular Cardiomyocyte Differentiation Kit | Directed differentiation of hiPSCs to ventricular-like CMs. | Generating a consistent and pure starting population of hiPSC-CMs for functional studies [77]. |
| Metabolic Maturation Media (e.g., MM-1) | Media supplemented with T3, dexamethasone, IGF-1, lipids to promote oxidative metabolism. | Shifting hiPSC-CM metabolism from glycolysis to fatty acid oxidation [77]. |
| Fibrin/Collagen Hydrogel | Biocompatible matrix for 3D Engineered Heart Tissue (EHT) formation. | Creating 3D tissue constructs for contractile force measurements [65]. |
| Patch-Clamp Electrophysiology Rig | Setup for high-fidelity recording of action potentials and ion currents. | Gold-standard assessment of single-cell electrophysiological parameters [76]. |
| Microelectrode Array (MEA) System | Non-invasive platform for recording field potentials and conduction velocity. | Assessing electrophysiological synchronization and drug responses in monolayers/tissues [79]. |
| Seahorse XF Analyzer | Instrument for real-time measurement of cellular metabolic flux. | Quantifying glycolytic rates and mitochondrial oxidative function [78]. |
| Antibodies (cTnT, α-actinin, cTnI) | Immunostaining of sarcomeric and cardiac-specific proteins. | Visualizing and quantifying sarcomere structure and organization [77] [65]. |
Comprehensive functional benchmarking across electrophysiological, contractile, and metabolic domains is not merely a quality control step but a fundamental requirement for establishing the physiological relevance of hiPSC-derived cardiac tissues. The data and protocols outlined in this guide provide a framework for researchers to quantitatively evaluate their models against adult human benchmarks. As the field progresses, the adoption of standardized benchmarking practices, potentially combined with advanced computational modeling [80] [81], will be crucial for improving the predictive accuracy of hiPSC-CM platforms in drug discovery, disease modeling, and the development of regenerative therapies. The integration of multi-parametric assessments is key to generating truly mature and functionally representative human cardiac cells in vitro.
The evaluation of physiological relevance is a cornerstone of biomedical research, dictating the translational potential of experimental findings. For decades, primary human tissues have served as the gold standard for in vitro studies due to their native architecture, mature functionality, and preservation of donor-specific characteristics. The advent of induced pluripotent stem cell (iPSC) technology has introduced a powerful alternative, offering an unlimited source of human cells through the reprogramming of somatic cells back to a pluripotent state [2]. This breakthrough has created unprecedented opportunities for disease modeling, drug screening, and regenerative medicine.
However, a critical question remains: how closely do iPSC-derived tissues mimic their primary human tissue counterparts? This comparison guide objectively examines the performance of iPSC-derived tissues against primary human tissues, providing researchers and drug development professionals with a rigorous evaluation of their respective advantages, limitations, and appropriate applications. We synthesize comparative experimental data across multiple tissue types and provide detailed methodologies to inform experimental design and interpretation within the broader context of physiological relevance evaluation.
Physiological and Functional Comparison Across Tissue Types
Neural Tissues
Table 1: Comparison of iPSC-Derived Neurons versus Primary Human Neurons
| Parameter | iPSC-Derived Cortical Neurons | Primary Fetal Cortical Neurons | Experimental Evidence |
|---|---|---|---|
| Neuronal Identity | 93.6% expressed neuronal markers (MAP2, NCAM1, TUBB3) [82] | Closely resembled by iPSC-derived neurons at single-cell level [82] | Single-cell RT-qPCR and RNA-seq |
| Glutamatergic Synapse Genes | 63.9-70.3% expressed GRIA1, DLG4, SYN1 [82] | Similar expression patterns observed [82] | Single-cell multiplex RT-qPCR |
| Cortical Layer Identity | 68.4% assignable using canonical markers; co-expression of deep/upper layer markers [82] | Similar co-expression patterns observed, suggesting marker limitations [82] | Immunostaining for TBR1, CUX1, BCL11B |
| Functional Maturation | Repetitive firing and spontaneous synaptic activity after ~85 days [82] [83] | Electrically active with mature network activity | Microelectrode arrays (MEA) |
| Developmental Stage | Resemble fetal rather than adult cortical neurons [82] | Fetal developmental stage | Single-cell RNA-seq clustering analysis |
| GABAergic Neurons | 23.9% expressed GAD1 [82] | Proportion similar to fetal development | Correlation with SLC17A7 (r = -0.10) |
Research demonstrates that iPSC-derived cortical neurons show striking resemblance to primary fetal cortical neurons at the single-cell transcriptome level, clustering closely with fetal rather than adult neurons [82]. However, these cells exhibit functional immaturity compared to adult brain tissue, with considerably less expression of synaptic or ion channel-related pathways [82]. The assignment of cortical layer identity using canonical markers presents challenges, as a subpopulation of iPSC-derived neurons co-expresses canonical fetal deep and upper cortical layer markers—a phenomenon that appears concordant with data from primary cells [82].
In comparative performance analyses, iPSC-derived neural progenitor cells (NPCs) in 3D neurosphere cultures first differentiate into βIII-Tubulin+ neurons, suggesting an earlier developmental stage than primary human NPCs, which first differentiate into Nestin+ and/or GFAP+ radial glia-like cells [83]. Despite this immaturity, iPSC-derived neuronal networks become electrically active on microelectrode arrays after approximately 85 days in culture and show similar sensitivity to developmental neurotoxic compounds like methylmercury chloride in migration assays [83].
Cardiac Tissues
Table 2: Comparison of iPSC-Derived Cardiomyocytes versus Primary Adult Human Cardiomyocytes
| Parameter | iPSC-Derived Cardiomyocytes | Adult Human Primary Cardiomyocytes | Experimental Evidence |
|---|---|---|---|
| Cell Phenotype | Mixed/unreliable population [84] | Pure/reliable rod-shaped cells [84] | Morphological analysis |
| Sarcomeric Structure | Disorganized [84] | Highly organized [84] | Immunofluorescence |
| T-Tubule Structure | Deficient [84] | Abundant [84] | Electron microscopy |
| Contraction Pattern | Spontaneous beating [84] | Requires electrical pacing [84] | Calcium imaging & MEA |
| Excitation-Contraction | Immature calcium handling; negative force-frequency relationship [84] | Mature calcium handling; positive force-frequency relationship [84] | Sarcomere shortening & calcium transient assays |
| Inotropic Responses | Potential for "false inotropy" and "false margin" [84] | Predictive of clinical outcomes [84] | Pharmacological testing with reference compounds |
| Ion Channel Expression | Under- or over-expressed versus physiological levels [84] | Physiological expression patterns [84] | Patch clamp & transcriptomics |
| Pro-arrhythmia Prediction | Limited specificity in risk prediction [84] | 96% sensitivity, 100% specificity [84] | Multiparametric mechanistic profiling |
The structural and functional differences between iPSC-derived cardiomyocytes and adult human primary cardiomyocytes have significant implications for drug discovery and safety pharmacology. iPSC-derived cardiomyocytes have a disorganized sarcomere structure resembling fetal and neonatal cardiomyocytes, unlike the highly organized, aligned sarcomeres in adult primary cells [84]. This structural immaturity translates to functional differences, including spontaneous contraction rather than paced beating, and divergent calcium handling properties [84].
These differences lead to potentially misleading pharmacological responses. Studies have documented "false inotropy" where compounds appear to increase contractility in iPSC-derived cardiomyocytes through mechanisms that don't translate to adult human cells, and "false margin" where safety margins appear larger than they are in mature human cardiomyocytes [84]. Adult human primary cardiomyocytes demonstrate superior predictive value for pro-arrhythmia risk, with 96% sensitivity and 100% specificity when testing clinical reference compounds, outperforming iPSC-derived models [84].
Metabolic Tissues and Other Cell Types
In hepatocyte differentiation, the transcriptional pattern and metabolic profiles of iPSC-derived hepatocytes have been shown to mimic fetal rather than adult hepatocytes [48]. This immaturity presents challenges for modeling adult-onset diseases and conducting drug metabolism studies that require mature enzymatic activity. Similar limitations have been observed across other cell types, though protocols continue to be refined.
For pancreatic β-cell generation for diabetes research, iPSC differentiation protocols have advanced significantly, with current research focusing on enhancing immune evasion mechanisms and gene therapy to improve cell survival and function after transplantation [85]. However, complete functional maturation comparable to primary human islet cells remains a challenge, particularly regarding glucose-responsive insulin secretion.
Experimental Design and Methodological Considerations
iPSC Differentiation and Characterization Workflows
The process of generating and validating iPSC-derived tissues involves multiple critical steps that influence their physiological relevance. The following diagram illustrates a typical workflow for the generation and characterization of iPSC-derived tissues for comparison with primary tissues:
Detailed Experimental Protocols for Comparative Studies
Neural Differentiation and Cortical Layer Marker Analysis
Objective: To generate iPSC-derived cortical neurons and assess their similarity to primary fetal neurons through cortical layer identity marker expression.
Methods:
- iPSC Neural Induction: Use dual SMAD inhibition with small molecules (e.g., noggin, SB431542) for neural induction [82]. Culture cells in neural induction medium (NIM) for enhanced neuronal performance compared to noggin-only protocols [83].
- Neuronal Differentiation: Plate neuroepithelial cells for final differentiation and maintain for extended periods (typically 81-180 days) to allow functional maturation [82].
- Immunostaining: Fix cells and stain for deep layer markers (TBR1, BCL11B/CTIP2) and upper layer markers (CUX1, POU3F2/BRN2, SATB2) [82]. Compare staining patterns with primary fetal brain sections.
- Single-Cell Transcriptomics: Perform multiplex single-cell RT-qPCR or RNA-seq on 96 genes important for neuronal function and cortical layer identity [82]. Include housekeeping genes (GAPDH) and negative controls.
- Functional Assessment: Record electrophysiological activity using microelectrode arrays (MEAs) after ≥85 days of differentiation [83]. Assess repetitive firing capability in response to depolarization and spontaneous synaptic activity [82].
Key Considerations: The protocol requires prolonged differentiation periods to achieve functional maturity. Patchy expression of cortical layer markers in individual cells is expected; assignment of laminar identity may require multivariate analysis of multiple markers [82].
Cardiac Functional Maturity Assessment
Objective: To compare the functional properties and pharmacological responses of iPSC-derived cardiomyocytes versus adult human primary cardiomyocytes.
Methods:
- Cell Sources: Obtain commercially available iPSC-derived cardiomyocytes or differentiate in-house using established protocols. Acquire adult human primary cardiomyocytes from ethically consented donor hearts [84].
- Structural Analysis: Fix and stain for sarcomeric proteins (α-actinin, troponin) to assess sarcomere organization. Use high-resolution imaging to compare structural maturity [84].
- Calcium Handling: Load cells with calcium-sensitive dyes (e.g., Fluo-4) and record transients. Analyze kinetics including rise time, decay time, and amplitude [84].
- Contractility Assessment: Use video-based edge detection or micropost arrays to measure sarcomere shortening or contraction force. For iPSC-derived cardiomyocytes, pace electrically at 1-2 Hz to override spontaneous beating [84].
- Pharmacological Profiling: Test reference inotropic compounds (positive: isoproterenol, milrinone; negative: verapamil, propranolol) across concentration ranges. Generate concentration-response curves for sarcomere shortening and calcium transient parameters [84].
- Pro-arrhythmia Assessment: Use multi-electrode arrays (MEAs) to measure field potentials. Challenge with pro-arrhythmic compounds (e.g., E-4031, cisapride) and assess for early afterdepolarizations and repolarization abnormalities [84].
Key Considerations: Account for the spontaneous beating of iPSC-derived cardiomyocytes by implementing electrical pacing. Be aware of the potential for "false inotropy" and "false margin" in iPSC-derived models [84]. Primary adult cardiomyocytes have limited viability in culture, requiring rapid experimental execution.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Experimental Solutions for Comparative Studies
| Reagent Category | Specific Examples | Function & Application | Considerations |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, C-MYC (OSKM) [2] [86] | Reprogram somatic cells to pluripotency | C-MYC omission reduces tumorigenic risk but lowers efficiency [86] |
| Neural Induction Agents | Dual SMAD inhibitors (noggin, SB431542) [82] | Direct differentiation toward neural lineage | NIM protocol may yield higher performance than noggin alone [83] |
| Cardiac Differentiation | Growth factors (BMP4, FGF2), small molecules (CHIR99021, IWP2) | Specify mesodermal and cardiac lineage | Protocol efficiency varies by iPSC line; may require optimization |
| 3D Culture Systems | Matrigel, synthetic hydrogels, decellularized scaffolds [48] | Provide three-dimensional growth environment | Enhances maturation and tissue-like organization compared to 2D |
| Characterization Antibodies | TBR1, BCL11B (deep layer); CUX1, SATB2 (upper layer) [82] | Identify cortical layer identity in neurons | Co-expression of markers common; may reflect biological reality [82] |
| Functional Assay Reagents | Calcium-sensitive dyes (Fluo-4), microelectrode arrays [84] | Assess electrophysiology and signaling | MEA enables non-invasive long-term functional monitoring |
| Maturation Enhancers | Thyroid hormone (T3), glucocorticoids [84] | Promote adult-like phenotype in derived cells | Critical for modeling adult-onset diseases |
The comparative analysis reveals that iPSC-derived tissues demonstrate remarkable similarity to primary fetal tissues at the transcriptional and structural levels, making them invaluable for studying developmental processes, modeling genetic diseases, and conducting drug screening in a human context. However, they frequently exhibit functional immaturity compared to adult primary tissues, which can limit their predictive value for adult physiology and disease.
Primary human tissues remain the gold standard for physiological relevance when studying adult biology and disease mechanisms, particularly for applications requiring mature function such as predictive toxicology and pharmacology. However, their limited availability, donor-to-donor variability, and inability to model genetic diseases in isogenic backgrounds present significant constraints.
The strategic integration of both systems—using iPSC-derived tissues for their scalability, genetic tractability, and human specificity, while validating key findings with primary tissues for physiological relevance—represents the most robust approach for advancing biomedical research and drug development. As differentiation protocols continue to improve and maturation strategies evolve, the fidelity of iPSC-derived tissues is expected to increase, potentially narrowing the gap with primary tissues in the coming years.
Utilizing Isogenic Controls to Isulate Disease-Specific Phenotypes
A critical challenge in modern biomedical research is the accurate identification of disease-specific phenotypes amidst the confounding variable of human genetic diversity. Isogenic controls—genetically identical cell lines that differ only at a specific, disease-causing locus—have emerged as a powerful solution. This guide evaluates the performance of isogenic human induced pluripotent stem cell (iPSC) models against traditional non-isogenic models, focusing on their physiological relevance in disease modeling and drug discovery.
The Critical Role of Isogenic Controls in Phenotype Isolation
In disease modeling, a "perfect" control is essential for isolating the phenotypic consequences of a single genetic mutation. Isogenic human disease models are families of cells engineered to model patient genetics in vitro, accompanied by a genetically matched 'normal' control cell, creating an isogenic system to research disease biology [87].
The core advantage lies in eliminating genetic background noise. Patient-derived iPSCs, while valuable, contain the entire genetic history of the donor, which can obscure subtle disease phenotypes. This is particularly relevant for late-age onset disorders where in vitro phenotypes are predicted to be subtle and susceptible to significant effects from genetic background variations [88] [89]. Generating isogenic pairs—where a disease-causing point mutation is either introduced into a healthy cell line or corrected in a patient-derived cell line—provides a genetically defined condition. This allows researchers to attribute any observed differences in phenotype directly to the mutation under investigation, rather than to unrelated genetic variations between different donors [88] [89].
Experimental Protocol: Establishing an Isogenic Cardiac Arrhythmia Model
A robust protocol for modeling cardiac arrhythmias using isogenic iPSCs demonstrates the application of this technology [90]. The workflow below outlines the key steps from cell line engineering to phenotypic validation.
Experimental Workflow: From Gene Editing to 3D Phenotyping
Detailed Methodologies
- Precision Gene Editing: To model specific long QT syndrome (LQTS) and short QT syndrome (SQTS) mutations in the KCNH2 gene, researchers used CRISPR-Cas9 with single-strand oligonucleotide (ssODN) repair templates. This approach aimed to recreate the specific N588D (LQTS) and N588K (SQTS) point mutations in the well-characterized 409B2 hiPSC line. A key technique involved using a combination of ssODNs carrying the patient missense mutation and a silent "PAM-blocking" mutation to prevent Cas9 re-cleavage and reliably generate compound heterozygous variants [90].
- 3D Cardiac Tissue Formation: Differentiated hiPSC-derived cardiomyocytes (CMs) and mesenchymal cells (MCs) were combined to form 3D cardiac tissue sheets (CTSs). These 3D structures, consisting of 5-6 cell layers, provide a more physiologically relevant environment compared to 2D monolayers (1-2 cell layers) and are essential for reproducing complex arrhythmic events like Torsade de Pointes (TdP) [90].
- Phenotypic Assessment: Electrophysiological properties were measured using multielectrode arrays (MEAs) to record the extracellular field potential (FP) from both 2D monolayers and 3D CTSs. The field potential duration corrected by Fridericia's formula (FPDcF), which corresponds to the QT interval in a clinical electrocardiogram (ECG), was a key quantitative metric. The phenotypic fidelity of the models was further tested by challenging the tissues with hERG channel blockers to induce arrhythmic events [90].
Performance Comparison: Isogenic vs. Non-Isogenic Models
The following tables summarize quantitative data and key findings from a direct comparison of isogenic and non-isogenic approaches, based on the described cardiac arrhythmia study [90].
Table 1: Quantitative Electrophysiological Phenotyping in 2D Monolayers
| Cell Model | Field Potential Duration (FPDcF) | Comparison to Control | Phenotypic Interpretation |
|---|---|---|---|
| Isogenic Control (409B2) | 231 ± 24 ms | Baseline | Normal QT interval |
| Isogenic LQT Mutant (N588D) | 323 ± 21 ms | Prolonged (p < 0.05) | Recapitulates Long QT Syndrome |
| Isogenic SQT Mutant (N588K) | 82 ± 18 ms | Shortened (p < 0.05) | Recapitulates Short QT Syndrome |
| Non-Isogenic Patient iPSCs | High Variability | Confounded by genetic background | Inconsistent phenotype isolation |
Table 2: Functional Outcomes in 3D Tissue Models
| Model Feature | Isogenic 3D Cardiac Tissues | Non-Isogenic/2D Models |
|---|---|---|
| Structural Complexity | 5-6 cell layers; recapitulates tissue-level structure | 1-2 cell layers; simplistic |
| Arrhythmia Induction | Differential susceptibility to TdP-like events upon hERG blockade | Often fail to exhibit authentic arrhythmic events |
| Phenotypic Validation | Strong, clinically consistent response | Poor validation in vitro |
| Data Confidence | High: phenotypes attributed to specific mutation | Low: phenotypes influenced by multiple genetic factors |
Molecular Pathways and Workflow Logic
The rationale for using isogenic controls is rooted in the need to map genotype to phenotype with high fidelity. The following diagram illustrates the logical pathway from genetic perturbation to conclusive phenotypic readout, highlighting where isogenic controls provide critical clarity.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of isogenic models relies on a suite of specialized reagents and tools.
Table 3: Essential Reagents for Isogenic iPSC Disease Modeling
| Research Reagent | Function in Experimental Protocol | Example Application in Featured Study |
|---|---|---|
| CRISPR-Cas9 System | Induces targeted double-strand breaks in DNA for precise gene editing. | Introduction of N588D/K mutations into the KCNH2 gene in healthy hiPSCs [90] [89]. |
| ssODN (single-strand Oligonucleotide) | Serves as a repair template for Homology-Directed Repair (HDR) to introduce specific point mutations. | Delivering the exact nucleotide change to create the LQTS and SQTS mutations [90]. |
| Isogenic hiPSC Pairs | The core experimental and control material; a healthy line and its mutant derivative. | 409B2 parent line vs. engineered LQT26 (N588D) and SQT22 (N588K) clones [90]. |
| Cardiac Differentiation Kit | Directs hiPSCs to differentiate into cardiomyocytes. | Generating hiPSC-derived cardiomyocytes (hiPSC-CMs) from all isogenic lines for phenotyping [90]. |
| Multielectrode Array (MEA) | Records extracellular field potentials to assess electrophysiological function non-invasively. | Measuring FPDcF from spontaneously beating 2D monolayers and 3D CTSs [90] [91]. |
| hERG Channel Blocker | Pharmacological agent used to challenge the system and probe for latent arrhythmogenic tendencies. | Inducing Torsade de Pointes (TdP)-like waveforms in 3D tissues to validate disease phenotype [90]. |
The experimental data demonstrate that the combination of isogenic controls and advanced 3D tissue modeling robustly isolates disease-specific phenotypes that are often masked in non-isogenic or 2D systems. Isogenic models provide a direct causal link between genotype and phenotype, leading to high data confidence and strong, clinically consistent validation in vitro. This approach overcomes the critical limitation of genetic variability, enabling more accurate disease modeling, predictive toxicology screening, and the development of targeted therapeutics with greater translational potential [90] [91] [92].
Conclusion
The physiological relevance of iPSC-derived tissues has progressed dramatically, transforming them from a novel tool into an indispensable platform for human-specific disease modeling and drug discovery. The convergence of advanced bioengineering, such as 3D organoids and EHTs, with rigorous validation frameworks and emerging technologies like AI and CRISPR, is systematically closing the gap between in vitro models and in vivo human physiology. Future success hinges on standardizing maturation protocols, improving scalability under cGMP, and fostering regulatory convergence. By continuing to enhance the fidelity of these models, the scientific community can accelerate the development of safer, more effective therapeutics and realize the full potential of personalized regenerative medicine.
References
- 1. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 2. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 3. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 4. iPSCs and iPSC-derived cells as a model of human ... [https://www.nature.com/articles/s41467-025-56569-4]
- 5. Generation and validation of a iPSC line from a healthy ... [https://www.sciencedirect.com/science/article/pii/S1873506125001941]
- 6. Chemical reprogramming of human blood cells to ... [https://www.sciencedirect.com/science/article/abs/pii/S1934590925002607]
- 7. Wnt signaling pathways in biology and disease [https://www.nature.com/articles/s41392-025-02142-w]
- 8. Pharmacological modulation of stem cells signaling pathway ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04438-8]
- 9. Induced Pluripotent Stem Cells: Reprogramming Platforms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7194323/]
- 10. Comparison of Human Induced Pluripotent and Embryonic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3070108/]
- 11. Engineered iPSC‐derived natural killer cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12246386/]
- 12. Validating human induced pluripotent stem cell-specific ... [https://www.sciencedirect.com/science/article/pii/S1465324924006108]
- 13. Genetically unmatched human iPSC and ESC exhibit ... [https://www.nature.com/articles/s41598-017-17882-1]
- 14. Comparison of the molecular profiles of human embryonic ... [https://www.sciencedirect.com/science/article/pii/S1873506113001724]
- 15. Reprogramming of Pluripotent Stem Cells [https://www.stemcell.com/technical-resources/area-of-interest/pluripotent-stem-cell-research/reprogramming/overview.html]
- 16. Induced Pluripotent Stem Cells (iPSCs)—Roles in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8467501/]
- 17. Pluripotent Stem Cells: Recent Advances and Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025069/]
- 18. Protocol for directed differentiation of human induced ... [https://www.sciencedirect.com/science/article/pii/S2666166725003855]
- 19. In silico modeling of directed differentiation of induced ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013407]
- 20. Effect of iPS cell culture medium on the differentiation ... [https://www.nature.com/articles/s41598-025-13259-x]
- 21. Rapid Single-Step Induction of Functional Neurons from ... [https://www.sciencedirect.com/science/article/pii/S0896627313004492]
- 22. Editorial: Role of induced pluripotent stem cells (iPSCs) in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1734717/full]
- 23. Induced Pluripotent Stem Cell (iPSC) Industry Trends for ... [https://bioinformant.com/ipsc-industry-trends/]
- 24. Development of allogeneic iPS cell‐based therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC9906386/]
- 25. Direct Comparison of Autologous and Allogeneic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3849265/]
- 26. Engineering the next generation of allogeneic CAR cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277817/]
- 27. iPSC-derived and Patient-Derived Organoids: Applications ... [https://www.sciencedirect.com/science/article/pii/S2666027X24000501]
- 28. Development and application of 3D cardiac tissues derived ... [https://www.sciencedirect.com/science/article/pii/S1347436724000557]
- 29. Maturation of human cardiac organoids enables complex ... [https://www.nature.com/articles/s44161-025-00669-3]
- 30. Cardiac organoids: a new tool for disease modeling and ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1537730/full]
- 31. 3D Bioprinting Functional Engineered Heart Tissues [https://www.mdpi.com/1422-0067/26/21/10707]
- 32. Advance in creating organoids could aid research, lead to ... [https://med.stanford.edu/news/all-news/2025/06/heart-organoid.html]
- 33. 华人团队首次从iPSC构建出高度血管化的肺和肠道类器官 ... [https://news.bioon.com/article/fcc5885924e8.html]
- 34. Advances in 3D Organoid Models for Stem Cell-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10049446/]
- 35. Design and Applications of Extracellular Matrix Scaffolds in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293650/]
- 36. Physiological Relevant 3D Biomanufacturing of Pluripotent ... [https://link.springer.com/article/10.1007/s40778-025-00250-5]
- 37. Extracellular-Matrix-Mimetic Hydrogels by Using ... [https://www.mdpi.com/1422-0067/26/11/4987]
- 38. In vivo engineered extracellular matrix scaffolds with ... [https://www.nature.com/articles/s41467-019-12545-3]
- 39. Scaffold-free cell-based tissue engineering therapies [https://www.nature.com/articles/s41536-021-00133-3]
- 40. Synthetic thermoresponsive scaffolds for the expansion and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402885/]
- 41. Extracellular matrix-mimetic electrically conductive ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813023029367]
- 42. Bioactive extracellular matrix scaffolds engineered with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8636679/]
- 43. Advances and Prospects in Using Induced Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11951483/]
- 44. Bioreactor design and validation for manufacturing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8870603/]
- 45. Compact and tunable stretch bioreactor advancing tissue ... [https://www.sciencedirect.com/science/article/abs/pii/S1350453320301168]
- 46. Dynamic intracellular mechanical cues facilitate collective ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8091894/]
- 47. Analyze High-Throughput Bioreactor Data in the Cloud [https://www.culturebiosciences.com/resources/analyze-all-your-high-throughput-bioreactor-data-in-the-cloud]
- 48. Modeling human diseases with induced pluripotent stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC5868991/]
- 49. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 50. Patient and Disease–Specific Induced Pluripotent Stem ... [https://www.sciencedirect.com/science/article/pii/S0031699724009451]
- 51. Large-scale drug screening in iPSC-derived motor neurons ... [https://www.nature.com/articles/s41593-025-02118-7]
- 52. Development of an iPSC-derived immunocompetent skin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12056326/]
- 53. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 54. Strategies for Improving the Maturity of Human Induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6392006/]
- 55. Progress in engineering functional cardiac tissues from ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706125006762]
- 56. Comprehensive promotion of iPSC-CM maturation by ... [https://www.nature.com/articles/s41467-025-58044-6]
- 57. Enhancing Mitochondrial Maturation in iPSC- ... [https://www.mdpi.com/2673-6411/5/3/23]
- 58. Addressing variability in iPSC-derived models of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6994963/]
- 59. Assessment of Genetic Stability in Human Induced ... [https://www.mdpi.com/1422-0067/25/2/1101]
- 60. Quantitative comparison of the mRNA content of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7876496/]
- 61. iPSC-derived and Patient-Derived Organoids - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12020925/]
- 62. Advances in physiological and clinical relevance of hiPSC ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2024.1478572/full]
- 63. Scaling up pluripotent stem cell-based therapies [https://www.sciencedirect.com/science/article/pii/S1465324925006784]
- 64. Induced Pluripotent Stem Cells (iPSCs) Market Prospects ... [https://www.businesswire.com/news/home/20251111238841/en/Induced-Pluripotent-Stem-Cells-iPSCs-Market-Prospects-2025-2033-Industry-Gains-Traction-with-Rising-Investments-and-Collaborations---ResearchAndMarkets.com]
- 65. Efficient and reproducible generation of human iPSC ... [https://www.nature.com/articles/s41467-024-50224-0]
- 66. Advancing genome editing with artificial intelligence [https://pmc.ncbi.nlm.nih.gov/articles/PMC10800897/]
- 67. CRISPR-GPT for agentic automation of gene-editing ... [https://www.nature.com/articles/s41551-025-01463-z]
- 68. Multiomics Evaluation of Human iPSCs and iPSC-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11799864/]
- 69. Use of iPSC-Derived Smooth Muscle Cells to Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11209779/]
- 70. Finding a vocation for validation: taking proteomics beyond ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9906375/]
- 71. High-throughput proteomics: a methodological mini-review [https://www.nature.com/articles/s41374-022-00830-7]
- 72. Validation of single-cell transcriptomic profiles from ... [https://pubmed.ncbi.nlm.nih.gov/40490970/]
- 73. Enhanced regenerative and developmental potential of ... [https://www.sciencedirect.com/science/article/pii/S2666379125003702]
- 74. Proteome Profiling - BGI Mass Spec, NGS, Multi-omics ... [https://www.bgi.com/global/service/proteome-profiling]
- 75. Transcriptomic profiling and bioinformatics-driven statistical ... [https://www.sciencedirect.com/science/article/pii/S037811192500383X]
- 76. Induced pluripotent stem cell-derived cardiomyocyte in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12376733/]
- 77. Metabolic Culture Medium Enhances Maturation of Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346743/]
- 78. Characterization of cardiac metabolism in iPSC-derived ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-03021-9]
- 79. Human induced pluripotent stem cell-derived closed-loop ... [https://www.sciencedirect.com/science/article/pii/S258900422400213X]
- 80. Computational modeling of cardiac electrophysiology and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11381036/]
- 81. Benchmarking electrophysiological models of human atrial ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2012.00487/full]
- 82. Assessing similarity to primary tissue and cortical layer identity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4754051/]
- 83. Comparative performance analysis of human iPSC-derived ... [https://www.sciencedirect.com/science/article/pii/S1873506117302167]
- 84. Stem Cells Comparison to Human Cardiomyocytes [https://anabios.com/stem-cells-comparison/]
- 85. Global research dynamics in the induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12272591/]
- 86. A Comparative View on Human Somatic Cell Sources for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4241335/]
- 87. Isogenic human disease models [https://en.wikipedia.org/wiki/Isogenic_human_disease_models]
- 88. Generation of Isogenic Pluripotent Stem Cells Differing ... [https://www.sciencedirect.com/science/article/pii/S0092867411006611]
- 89. Genomic Editing Tools to Model Human Diseases with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4216528/]
- 90. Modeling mutation-specific arrhythmogenic phenotypes in ... [https://www.nature.com/articles/s41598-024-52871-1]
- 91. Cell-based drug discovery: Why human iPSC-derived ... [https://www.bit.bio/blog/cell-based-drug-discovery-with-human-ipsc-models]
- 92. Stem cell disease modeling: A new era for drug discovery [https://www.abcam.com/en-us/stories/articles/stem-cell-disease-modeling]