Biomaterial Scaffolds for Stem Cell Delivery: Engineering the Niche for Regenerative Medicine
This article provides a comprehensive overview of the latest advancements in biomaterial scaffolds for stem cell delivery, a cornerstone of regenerative medicine.
Biomaterial Scaffolds for Stem Cell Delivery: Engineering the Niche for Regenerative Medicine
Abstract
This article provides a comprehensive overview of the latest advancements in biomaterial scaffolds for stem cell delivery, a cornerstone of regenerative medicine. Tailored for researchers, scientists, and drug development professionals, it explores the foundational principles of creating cell-instructive microenvironments. It delves into the diverse portfolio of natural, synthetic, and composite biomaterials, their applications in bone, wound, and neural tissue engineering, and the critical challenges of ensuring cell survival, integration, and safety. The content further synthesizes validation strategies and comparative study outcomes, offering a roadmap for translating scaffold-based stem cell therapies from the laboratory to the clinic.
The Blueprint of Life: How Biomaterial Scaffolds Create Stem Cell Niches
The stem cell niche constitutes a specialized temporal and spatial organization that provides the anatomical and functional interactions critical for stem cell fate determination [1] [2]. This dynamic microenvironment integrates cellular contacts, molecular signals, and biophysical cues to regulate stem cell self-renewal, quiescence, and differentiation [1]. Within the context of biomaterial scaffolds for therapeutic delivery, understanding native niche biology provides an essential blueprint for engineering synthetic microenvironments that can maintain stem cell potency and function after transplantation. This application note delineates the core components of physiological stem cell niches and provides detailed protocols for their replication in biomaterial design, offering researchers a framework for developing more effective stem cell-based therapies.
The concept of the stem cell niche was first hypothesized by Schofield as a specialized microenvironment required for stem cell maintenance [2]. The initial experimental demonstration emerged from studies of the C. elegans distal tip cell (DTC), a single mesenchymal cell that provides the essential microenvironment for germline stem cell (GSC) maintenance through Notch signaling [2]. This foundational concept has since expanded to encompass diverse tissue systems, with niches identified in bone marrow, intestinal crypts, skeletal muscle, and neural tissues [1] [2] [3].
Stem cell niches function not merely as passive support structures but as active agents of feedback control and coordination among tissue compartments [2]. They protect stem cells from damage while enabling responsiveness to physiological demands for cell replacement and repair. The emerging understanding of niche biology reveals that aged or altered niches significantly contribute to the decline in stem cell function associated with aging and disease, highlighting the therapeutic potential of niche-targeted interventions [1].
Table 1: Core Components of the Stem Cell Niche
| Component Category | Specific Elements | Functional Role |
|---|---|---|
| Cellular Elements | Mesenchymal, endothelial, immune cells, Paneth cells (intestine) | Structural support, secretion of regulatory factors, immune modulation [1] [2] |
| Extracellular Matrix (ECM) | Integrins, laminin, fibronectin, collagen, proteoglycans | Structural scaffolding, mechanical cues, growth factor reservoir [1] [3] |
| Signaling Molecules | Wnt, Notch, TGF-β, FGF, chemokines | Regulation of self-renewal, quiescence, differentiation decisions [1] [2] |
| Biophysical Cues | Matrix stiffness, shear stress, oxygen tension, temperature | Influence on stem cell metabolism, proliferation, and lineage commitment [1] |
Analytical Methods for Niche Characterization
Protocol: Isolation of Niche-Specific Stem Cells and Stromal Components
This protocol details the isolation of Lgr5+ intestinal stem cells and their associated Paneth cells, which constitute a well-defined niche unit [2].
Materials and Reagents
- Lgr5-EGFP-IRES-CreERT2 mice (Jackson Laboratory, Stock #008875) - for identification of Lgr5+ stem cells
- Collagenase/Dispase solution (1-2 mg/mL in PBS) - for tissue dissociation
- Fluorescence-activated cell sorting (FACS) buffers (PBS with 2% FBS)
- Anti-CD24 antibody (eBioscience, cat. #11-0242-82) - for Paneth cell identification
- Intestinal epithelial cell culture medium:
- Advanced DMEM/F12
- 1x N2 supplement
- 1x B27 supplement
- 1mM N-acetylcysteine
- 50 ng/mL EGF
Procedure
Tissue Harvest and Dissociation:
- Euthanize Lgr5-EGFP mouse and immediately extract small intestine.
- Open intestine longitudinally, wash with cold PBS, and mince into 2-4 mm fragments.
- Incubate tissue fragments in collagenase/dispase solution for 30-45 minutes at 37°C with gentle agitation.
- Pipette tissue digest vigorously every 10 minutes to facilitate dissociation.
- Pass cell suspension through 70μm cell strainer to remove undigested fragments.
Cell Sorting:
- Centrifuge cell suspension at 400 x g for 5 minutes and resuspend in FACS buffer.
- Incubate with anti-CD24 antibody (1:100 dilution) for 20 minutes on ice.
- Wash cells twice with FACS buffer and resuspend at 10-20 x 10⁶ cells/mL.
- Sort using FACS:
- Lgr5+ stem cells: EGFP+ CD24- population
- Paneth cells: EGFP- CD24hi population
- Collect sorted populations in ice-cooled collection tubes containing culture medium.
Validation:
- Assess purity by re-analyzing sorted populations.
- Confirm functional capacity of Lgr5+ cells by organoid formation assay.
Technical Notes
- Maintain cells at 4°C throughout the isolation process when possible to preserve viability.
- For optimal organoid formation, plate Lgr5+ cells in combination with Paneth cells (1:1 ratio) in Matrigel.
- This protocol can be adapted for other niche systems by modifying dissociation enzymes and surface markers.
Protocol: 3D Co-culture System for Hematopoietic Stem Cell Niche Modeling
This protocol establishes a biomimetic microenvironment for studying human hematopoietic stem/progenitor cells (HSPCs) and mesenchymal stromal cells (MSCs) [4].
Materials and Reagents
- Porous poly(ε-caprolactone) (PCL) scaffolds (prepared by thermal fiber bonding) [5]
- Human bone marrow-derived MSCs (Lonza, cat. #PT-2501)
- Human CD34+ HSPCs (StemCell Technologies, cat. #70002)
- HSC expansion medium:
- StemSpan SFEM II
- 100 ng/mL SCF
- 100 ng/mL TPO
- 50 ng/mL FGF-2
- 3D bioreactor system (optional, for perfusion culture)
Procedure
Scaffold Preparation:
- Sterilize PCL scaffolds (5mm diameter x 2mm thickness) in 70% ethanol for 30 minutes.
- Wash thoroughly with PBS and pre-condition in expansion medium for 2 hours at 37°C.
Cell Seeding:
- Seed MSCs at density of 1x10⁵ cells/scaffold and culture for 7 days to establish stromal layer.
- Subsequently seed CD34+ HSPCs at density of 5x10⁴ cells/scaffold.
- Maintain co-cultures in expansion medium with medium changes every 2-3 days.
Analysis:
- After 14 days, assess HSPC expansion by flow cytometry using CD34 and CD45 markers.
- Evaluate colony-forming potential by methylcellulose assay.
- Analyze spatial organization by confocal microscopy of immunostained scaffolds.
Technical Notes
- Scaffold porosity and stiffness can be modified to mimic specific niche properties.
- Incorporation of niche-specific cytokines (e.g., CXCL12) can enhance niche functionality.
- This 3D co-culture system more accurately recapitulates the bone marrow microenvironment compared to traditional 2D cultures.
Biomaterial Scaffolds as Synthetic Niches
The translation of stem cell therapies faces significant challenges, including poor cell survival, limited engraftment, and phenotypic instability following transplantation [5] [6]. Biomaterial scaffolds designed to replicate key aspects of native niches offer promising solutions to these limitations by providing tailored microenvironments that support stem cell function.
Table 2: Biomaterial Classes for Synthetic Niche Engineering
| Biomaterial Class | Examples | Advantages | Stem Cell Applications |
|---|---|---|---|
| Natural Polymers | Collagen, chitosan, alginate, hyaluronan, gelatin, silk fibroin | Innate biocompatibility, bioactive motifs, enzymatic degradation [5] | Neural repair, mesenchymal stem cell delivery, cartilage regeneration [5] |
| Synthetic Biodegradable Polymers | Poly(L-lactic acid), poly(glycolic acid), polycaprolactone, polyphosphoester | Tunable mechanical properties, controlled degradation rates, reproducible manufacture [5] | Hematopoietic stem cell expansion, cardiac tissue engineering [4] |
| Conductive Polymers | Polypyrrole, polythiophene, polyaniline | Electrical signal conduction, enhanced neurite outgrowth, neural cell activation [5] | Neural tissue engineering, rehabilitation after nerve injury [5] |
| Hybrid Systems | Protein-functionalized synthetic polymers, polymer-ceramic composites | Combinatorial advantages, multifunctionality, graded properties | Bone regeneration, osteogenic differentiation [6] |
Diagram: Native vs. Engineered Niche Signaling Pathways
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Stem Cell Niche Research and Engineering
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Stem Cell Markers | Lgr5-EGFP mice, CD34 antibodies, Pax7 antibodies | Identification and isolation of specific stem cell populations [2] [3] |
| Niche Signaling Modulators | Recombinant Wnt3a, Dll4-Fc, R-spondin-1, Noggin | Activation or inhibition of key niche signaling pathways [2] |
| Matrix Proteins | Laminin-521, Collagen IV, Fibronectin, Matrigel | Recreation of basal lamina components for stem cell support [1] [3] |
| Biomaterial Polymers | Polycaprolactone, chitosan, alginate, hyaluronic acid | Scaffold fabrication with tunable physical and biochemical properties [5] |
| Protease-Sensitive Linkers | MMP-cleavable peptides, heparin-binding domains | Creation of dynamically responsive matrices that remodel with cells [6] |
| Cytokine Delivery Systems | PLGA microparticles, affinity-based release systems | Spatiotemporal control of morphogen presentation in synthetic niches [6] |
Application Notes for Therapeutic Scaffold Design
Protocol: Biomaterial Scaffold for Neural Stem Cell Delivery
This protocol details the fabrication of an electrically conductive scaffold for neural stem cell (NSC) delivery to overcome limitations in neural repair [5].
Materials and Reagents
- Polycaprolactone (PCL) (Sigma-Aldrich, cat. #440744) - structural polymer
- Polypyrrole (PPy) (Sigma-Aldrich, cat. #577030) - conductive component
- Nerve growth factor (NGF) (PeproTech, cat. #450-01) - neurotrophic factor
- Electrospinning apparatus with high-voltage power supply
- Neural stem cell culture derived from human induced pluripotent stem cells
Procedure
Polymer Solution Preparation:
- Prepare 12% (w/v) PCL solution in 1,1,1,3,3,3-hexafluoro-2-propanol.
- Add 3% (w/w) PPy relative to PCL mass and stir for 24 hours to ensure complete dissolution.
- Incorporate NGF (50 μg/mL) into the polymer solution immediately before electrospinning.
Scaffold Fabrication:
- Load polymer solution into 5mL syringe with 21G blunt needle.
- Set electrospinning parameters:
- Flow rate: 1.0 mL/hour
- Voltage: 15 kV
- Collector distance: 15 cm
- Collector rotation speed: 1000 rpm
- Collect aligned nanofibers on mandrel collector for 4 hours.
- Cross-link scaffolds with genipin (0.5% w/v) for 12 hours to stabilize structure.
Cell Seeding and Implantation:
- Sterilize scaffolds in 70% ethanol for 2 hours and UV irradiate for 30 minutes per side.
- Seed NSCs at density of 1x10⁶ cells/scaffold in neuronal differentiation medium.
- Culture for 7 days with medium changes every 2 days before in vivo implantation.
- For neural injury models, implant NSC-seeded scaffolds at lesion site using microsurgical techniques.
Technical Notes
- Scaffold conductivity can be modulated by varying PPy content (1-5% w/w).
- Alignment of nanofibers guides directional neurite outgrowth.
- Controlled release of NGF enhances NSC survival and differentiation.
- This scaffold design has applications in spinal cord injury and neurodegenerative disease models.
Developmental Transitions in Niche Composition
Understanding how niches change during development provides critical insights for designing age-appropriate therapeutic scaffolds. The transition from emerging fetal niches to adult niches involves significant changes in ECM composition, signaling networks, and cellular interactions [3].
Application in Aging and Disease
Aged niches display altered signaling profiles, modified ECM composition, and chronic inflammatory states that contribute to declining stem cell function [1]. Niche-targeted interventions represent promising strategies for rejuvenating stem cell function in age-related diseases. Biomaterial scaffolds can be designed to counteract age-related niche dysfunction through:
Delivery of Youthful Systemic Factors: Scaffolds can release factors present in young niches but diminished in aged environments.
Reduction of Senescent Cells: Incorporation of senolytics or modifiers of senescence-associated secretory phenotype (SASP).
ECM Rejuvenation: Provision of embryonic ECM components that restore regenerative capacity [3].
Inflammation Modulation: Controlled release of anti-inflammatory cytokines to counteract chronic inflammation in aged niches.
The stem cell niche represents a dynamic, multi-component signaling center that exerts precise control over stem cell fate decisions. As a design template, native niche biology informs the development of biomaterial scaffolds that can maintain stem cell potency and direct therapeutic outcomes after transplantation. The protocols and application notes provided here offer researchers a foundation for designing synthetic niches tailored to specific stem cell types and therapeutic applications.
Future directions in the field include the development of four-dimensional scaffolds that dynamically change their properties in response to environmental cues, the integration of multiple niche cells to recreate tissue-level complexity, and the personalization of scaffolds based on patient-specific niche characteristics. As understanding of niche biology continues to evolve, so too will the sophistication of biomaterial scaffolds, ultimately enhancing the efficacy and reliability of stem cell-based therapies.
Core Principles of the Bottom-Up Approach
The "bottom-up" paradigm in biomaterial design represents a fundamental shift from traditional methods. This approach prioritizes a deep understanding of the fundamental biological properties and microenvironmental needs of stem cells first, then engineering cell-instructive biomaterials specifically to support them [7]. Unlike conventional strategies that adapt cells to pre-existing materials, this framework designs biomaterials from the molecular level upward to address critical clinical translation challenges [7]. These challenges include differentiation variability, incomplete matching of induced pluripotent stem cells (iPSCs) to somatic counterparts, functional maturity of derived cells, and poor survival of therapeutic cell populations like endothelial colony-forming cells (ECFCs) and multipotent mesenchymal stromal cells (MSCs) in hostile in vivo niches [7].
The "bottom" refers to the essential biological and microenvironmental requirements of stem cells, such as specific mechanical cues (e.g., matrix stiffness), biochemical gradients (e.g., morphogens), and precise cell-cell interactions [7]. The "up" represents the subsequent development of biomaterial platforms tailored to these specific requirements. By mirroring native stem cell niches, these tailored biomaterials significantly enhance differentiation fidelity, reprogramming efficiency, and functional tissue integration, offering a transformative roadmap for regenerative medicine [7].
Quantitative Characterization of Scaffolds and Cellular Response
A critical component of the bottom-up approach is the rigorous, quantitative characterization of both the scaffold's physical properties and the biological response of the encapsulated cells. The tables below summarize key parameters and methods.
Table 1: Quantitative Characterization of 3D Scaffold Architecture via Micro-CT
| Parameter | Description | Significance for Bone Tissue Engineering | Example Measurement |
|---|---|---|---|
| Macropore Size | Primary pore diameter; spherical pores ~500 µm in bioactive glass foams [8]. | Provides space for cell migration, tissue ingrowth, and vascularization [8]. | >500 µm [8] |
| Interconnect Size | Diameter of windows connecting adjacent macropores; distinct from pore throats [8]. | Dominates nutrient diffusion, cell communication, and tissue perfusion; critical for viability [8]. | >100 µm (minimum for bone ingrowth) [8] |
| Percentage Porosity | Volume fraction of void space within the scaffold [8]. | Influences total cell loading capacity and ultimate tissue volume [8]. | 85-92% (e.g., bioactive glass scaffolds) [8] |
| Permeability | Measure of fluid flow through the porous network; can be predicted from µCT data [8]. | Informs optimization of bioreactor conditions for cell culture and nutrient delivery [8]. | Modeled from 3D pore structure [8] |
Table 2: Direct Quantitative Analysis of Cells within 3D Scaffolds
| Analysis Type | Measured Parameter | Technical Basis | Key Advantage |
|---|---|---|---|
| Cell Density/Distribution [9] | Number of cells per mm³ of scaffold; spatial distribution. | Fluorescence staining of nuclei (Hoechst 33342) and wide-field microscopy with Z-stack imaging [9]. | Direct cell counting within the intact 3D structure, avoiding destructive processing and associated cell loss [9]. |
| Proliferative Activity [9] | Dynamics of cell population growth over time. | Time-course analysis of cell nucleus counts within scaffold fragments using the above method [9]. | Enables assessment of cell cycle progression and expansion potential within the actual 3D microenvironment [9]. |
| Cell Viability [9] | Ratio of live to dead cells. | Sequential use of membrane-permeant (Hoechst 33342) and membrane-impermeant (Propidium Iodide) DNA dyes [9]. | Provides a direct viability metric within the scaffold, superior to indirect metabolic assays like MTT [9]. |
Detailed Experimental Protocols
Protocol: Non-Destructive 3D Analysis of Scaffold Architecture using Micro-CT
This protocol enables the quantitative, non-destructive 3D analysis of pore and interconnect size distributions, which are critical parameters for scaffold design [8].
- Step 1: Image Acquisition. Scaffolds are imaged using high-resolution X-ray micro-computed tomography (μCT). Acquire 3D images of the scaffold structure with sufficient resolution to resolve the smallest interconnects of interest (e.g., ~100 µm) [8].
- Step 2: Image Thresholding. Process the μCT images to distinguish between the solid scaffold material and the pore space. Apply a global threshold to create a binary (black and white) 3D image [8].
- Step 3: Pore & Interconnect Identification. Apply custom algorithms to the binary 3D image stack.
- Pore Identification: Use a combination of 3D distance mapping and watershed segmentation to identify and label individual pore cavities [8].
- Interconnect Identification: Apply a separate algorithm to detect the regions of open space that connect adjacent pores, treating them as distinct structural features [8].
- Step 4: Size Distribution Calculation. For each identified pore and interconnect, calculate its size. Generate full distributions (e.g., pore diameter, interconnect length) for the entire scaffold volume [8].
- Step 5: Validation. Validate the μCT-based size distributions against established methods such as mercury intrusion porosimetry (MIP) and manual 3D image analysis to ensure accuracy [8].
Micro-CT Analysis Workflow
Protocol: Direct Quantitative Analysis of Cells within a 3D Scaffold
This method allows for the direct counting of cell nuclei within an opaque, 3D scaffold, enabling accurate assessment of cell density, distribution, proliferation, and viability without destructive processing [9].
- Step 1: Sample Preparation and Staining.
- Place a scaffold fragment (≥ 0.64 cm²) into a well of a 24-well fluorescence plate with opaque walls.
- Add 1 µL of Hoechst 33342 solution (10 µg/mL) per 2 mL of culture medium in the well.
- Incubate for 30 minutes at 37°C.
- Remove the dye medium and wash the scaffold fragment twice with PBS (2 mL per wash, 10-minute incubations) [9].
- Step 2: Data Visualization and Z-Stack Acquisition.
- Add 0.3-1.0 mL of PBS to the well to prevent drying.
- Transfer the plate to a wide-field fluorescence imager (e.g., Cytation 5) equipped with a Z-stack function.
- For each field of view, acquire images at multiple focal planes along the Z-axis to a depth of ≤ 530 µm. Use a 4x or 10x objective.
- The instrument software synthesizes the in-focus portions of each layer into a single, fully focused "stitched" Z-stack image for each field of view. Acquire at least 10 such images per sample [9].
- Step 3: Image Processing and Nuclei Counting.
- Process the stitched Z-stack images using image analysis software (e.g., Gen5).
- Apply a fluorescence intensity threshold filter (e.g., >7000 relative units) to count only brightly stained nuclei and to help separate closely spaced nuclei.
- Apply an object area filter (e.g., <30 µm²) to exclude non-nuclear artifacts or unseparated clusters.
- Visually confirm via a "mask" function that all nuclei are counted correctly and adjust filter thresholds if necessary for new scaffold types [9].
- Step 4: Quantitative Analysis.
- For each sample, calculate the average number of cells (N) from the ≥10 stitched Z-stack images.
- Calculate the number of cells per mm³ (K) using the formula: K = N / (B * C * D * 10⁻⁹) where B, C, and D are the dimensions (in µm) of the analyzed field of view along the X, Y, and Z axes, respectively [9].
- Step 5: Assessing Viability (Optional).
- Follow the staining procedure using a combination of Hoechst 33342 (stains all nuclei) and Propidium Iodide (PI, stains only nuclei of dead cells with compromised membranes).
- Acquire Z-stacks for both fluorescence channels and count the total nuclei (Hoechst) and dead nuclei (PI). Calculate viability as: (Total Nuclei - PI-positive Nuclei) / Total Nuclei [9].
Cell Quantification Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Bottom-Up Scaffold Analysis
| Item | Function/Description | Application Note |
|---|---|---|
| Hoechst 33342 [9] | Cell-permeant fluorescent dye that binds double-stranded DNA. | Enables live-cell nuclear staining for direct quantification within intact 3D scaffolds without the need for fixation [9]. |
| Propidium Iodide (PI) [9] | Cell-impermeant fluorescent DNA dye. | Used in conjunction with Hoechst to identify dead cells with compromised plasma membranes in viability assays [9]. |
| Bioactive Glass (70S30C) [8] | Sol-gel derived foam scaffold (70 mol% SiO₂, 30 mol% CaO). | Example of an osteoconductive and bioactive scaffold material that stimulates bone cell activity and bonds to bone [8]. |
| Wide-Field Fluorescence Imager with Z-Stack [9] | Microscope system capable of acquiring images at multiple Z-planes and synthesizing fully focused images. | Essential for quantitative analysis in opaque 3D scaffolds, as it overcomes the limitations of light microscopy through optical sectioning [9]. |
| Image Analysis Software (e.g., Gen5) [9] | Software for processing stitched Z-stack images and applying counting filters. | Allows for automated, high-throughput counting using customizable filters for fluorescence intensity and object area to ensure accuracy [9]. |
The field of regenerative medicine is increasingly focused on combining advanced stem cell types with sophisticated biomaterial scaffolds to direct tissue repair and regeneration. For researchers and drug development professionals, understanding the unique properties and clinical translation pathways of induced pluripotent stem cells (iPSCs), mesenchymal stem cells (MSCs), and endothelial colony-forming cells (ECFCs) is crucial for designing next-generation therapies. These cells represent the most promising "key players" in clinical development, each offering distinct advantages and facing specific challenges. Critically, their therapeutic potential is profoundly influenced by their interaction with the three-dimensional biomaterial scaffold microenvironment, which provides essential physical and biochemical cues for cell survival, differentiation, and functional integration. This application note provides a structured comparison of these cell types, detailed experimental protocols aligned with their clinical applications, and essential tools for integrating them with scaffold-based delivery systems.
Stem Cell Profiles at a Glance
Table 1: Comparative Overview of Key Stem Cell Players for Scaffold-Based Therapies
| Feature | Induced Pluripotent Stem Cells (iPSCs) | Mesenchymal Stem Cells (MSCs) | Endothelial Colony-Forming Cells (ECFCs) |
|---|---|---|---|
| Origin | Reprogrammed somatic cells (e.g., skin fibroblasts) [10] | Multiple tissues: bone marrow, adipose tissue, umbilical cord [11] [12] | Cord blood, peripheral blood, vessel wall [13] |
| Key Markers | OCT4, SOX2, KLF4, c-MYC (reprogramming factors) [10] | CD73, CD90, CD105+; CD34, CD45, HLA-DR- [11] [12] | CD34, CD31, VEGFR2+; CD45, CD14- [13] |
| Differentiation Potential | Pluripotent (all three germ layers) [10] | Multipotent (mesodermal lineages: osteo-, chondro-, adipo-genic) [11] | Committed progenitor (endothelial lineage) [13] |
| Primary Mechanism of Action | Cell replacement via differentiation into target somatic cells [14] [10] | Paracrine signaling (growth factors, extracellular vesicles), immunomodulation [11] [15] | Blood vessel formation and direct vascular integration [13] [16] |
| Clinical Trial Landscape | 10 published studies, 22 ongoing trials (cardiac, ocular, cancer) [14] [10] | Over 10 approved therapies globally (GVHD, Crohn's, osteoarthritis) [11] [12] | No clinical trials to date; promising preclinical data [13] |
| Key Challenge for Delivery | Tumorigenicity risk from undifferentiated cells; need for precise lineage commitment within scaffold [10] | Variable potency based on donor age and tissue source; ensuring retention and survival post-transplantation [11] [12] | Very low frequency in blood; maintaining robust angiogenic function in diseased microenvironments [13] [16] |
| Scaffold Design Implication | Requires sophisticated, spatially defined cues for precise differentiation. | Ideal for incorporation into hydrogels and 3D-printed scaffolds that enhance paracrine effects. | Needs pro-angiogenic microenvironments and micro-patterning to guide vascular network formation. |
Detailed Clinical Applications & Experimental Protocols
Induced Pluripotent Stem Cells (iPSCs)
iPSCs are reprogrammed adult cells that have been returned to an embryonic-like pluripotent state, capable of differentiating into any cell type in the body [10]. Their application is emerging in clinical trials for conditions like cardiac disease, ocular disorders, and cancer, with 10 published clinical studies and 22 ongoing registered trials as of early 2025 [14] [10]. A primary challenge is the risk of tumorigenicity, which necessitates rigorous purification of the differentiated cell product before transplantation [10].
Protocol 1: In Vitro Differentiation of iPSCs into Cardiomyocytes for Cardiac Patch Therapy This protocol is adapted from preclinical studies underpinning current clinical efforts for heart failure [17] [10].
- Objective: To generate a functional cardiac patch by seeding iPSC-derived cardiomyocytes onto a biomimetic scaffold.
- Materials:
- Cells: Human iPSC line.
- Basal Medium: RPMI 1640.
- Small Molecules: CHIR99021 (GSK-3 inhibitor), IWP-4 (Wnt inhibitor).
- Supplements: B-27 Supplement (with and without insulin).
- Scaffold: 3D porous elastomer patch (e.g., PGS/GelMA composite).
- Procedure:
- Maintenance: Culture iPSCs in essential 8 medium on Matrigel-coated plates until 80-90% confluent.
- Mesoderm Induction (Day 0-2): Dissociate iPSCs into single cells and seed onto the 3D scaffold at a high density (5-10 x 10^6 cells/cm³). Switch to RPMI/B-27 minus insulin medium supplemented with 6-12 µM CHIR99021.
- Cardiac Progenitor Induction (Day 2-5): Replace medium with RPMI/B-27 minus insulin containing 5 µM IWP-4.
- Cardiomyocyte Maturation (Day 5-30+): On day 5, change to RPMI/B-27 with insulin. Refresh the medium every 2-3 days. Spontaneous contractions are typically observed between days 8-12. Maintain the construct for up to 30 days to promote metabolic and functional maturation.
- Quality Control: Analyze by flow cytometry for cardiac Troponin T (cTnT) expression (>80% purity expected). Perform electrophysiological assessment via patch clamp or microelectrode array (MEA).
Mesenchymal Stem Cells (MSCs)
MSCs are multipotent stromal cells with potent immunomodulatory and tissue-repair capabilities, primarily mediated through paracrine secretion of bioactive molecules and extracellular vesicles [11] [15]. With over ten approved therapies worldwide for conditions like graft-versus-host disease (GVHD) and Crohn's disease fistulas, they are the most clinically advanced cell type discussed here [11] [12].
Protocol 2: Seeding and Tri-Lineage Differentiation of MSCs in a 3D Biomimetic Scaffold This protocol is foundational for bone and soft tissue engineering applications [18] [19].
- Objective: To evaluate the multipotency of MSCs within a 3D scaffold environment by inducing osteogenic, chondrogenic, and adipogenic differentiation.
- Materials:
- Cells: Bone marrow-derived MSCs (BMSCs).
- Scaffold: 3D-printed bilayered scaffold (e.g., vECM/GelMA/SF bioink) [19].
- Basal Medium: Dulbecco's Modified Eagle Medium (DMEM) with 10% FBS.
- Induction Media: Commercial osteogenic, chondrogenic, and adipogenic differentiation kits.
- Procedure:
- Cell Seeding: Trypsinize P3-P5 BMSCs and resuspend in basal medium. Seed cells drop-wise onto the sterilized 3D scaffold at a density of 1x10^6 cells/cm³. Allow 4 hours for attachment in an incubator before adding more medium.
- Osteogenic Differentiation: Culture scaffold in osteogenic medium for 21 days. Refresh medium twice weekly. Analysis: Fix and stain with 2% Alizarin Red S to detect calcium deposits.
- Chondrogenic Differentiation: Culture scaffold in chondrogenic medium in a pellet culture system for 21 days. Analysis: Fix, section, and stain with 1% Alcian Blue to detect sulfated glycosaminoglycans.
- Adipogenic Differentiation: Culture scaffold in adipogenic medium for 21 days. Refresh medium twice weekly. Analysis: Fix and stain with 0.5% Oil Red O to visualize lipid vacuoles.
- Quality Control: Confirm MSC phenotype prior to seeding via flow cytometry for CD73, CD90, CD105 (≥95% positive) and CD34, CD45, HLA-DR (≤2% positive) [11] [12].
Endothelial Colony-Forming Cells (ECFCs)
ECFCs are true endothelial progenitors with high proliferative potential and the ability to form de novo blood vessels in vivo [13]. They are a promising tool for vascularizing engineered tissues, though no clinical trials have been conducted yet. A major barrier is their low frequency in peripheral blood (approximately 1.7 cells per 10^8 mononuclear cells) and donor-specific heterogeneity [13] [16].
Protocol 3: Isolation, Expansion, and Tubulogenesis Assay of ECFCs for Vascularization This protocol is critical for pre-clinical assessment of ECFC functionality in creating vascular networks [13].
- Objective: To isolate ECFCs from human umbilical cord blood and evaluate their in vitro vessel-forming capability on a basement membrane matrix.
- Materials:
- Cell Source: Human umbilical cord blood collected in CPDA-1 bags.
- Coating Substrate: Rat tail collagen I.
- Culture Medium: EGM-2 MV BulletKit (Lonza).
- Tubulogenesis Substrate: Growth Factor Reduced (GFR) Matrigel.
- Antibodies: for flow cytometry (CD31, CD34, CD45, CD14, VEGFR2).
- Procedure:
- Isolation: Isolate mononuclear cells from cord blood via density gradient centrifugation (Ficoll-Paque). Plate 1-5x10^7 cells per well of a collagen I-coated 6-well plate in EGM-2 medium.
- Expansion: After 24 hours, gently wash away non-adherent cells. Refresh medium daily for the first week, then every other day thereafter. Colonies with cobblestone morphology (ECFCs) appear in 5-14 days. Expand by trypsinizing and re-plating at 1:3 ratio.
- Phenotyping: Characterize cells at P2-P4 by flow cytometry. ECFCs should be >95% positive for CD31, CD34, and VEGFR2, and >95% negative for CD45 and CD14 [13].
- Tubulogenesis Assay: Thaw GFR Matrigel on ice and coat a 96-well plate (50 µL/well). Polymerize at 37°C for 30 min. Seed 1x10^4 ECFCs per well in EGM-2. Incubate for 6-18 hours and image under a microscope. Quantify total tube length, number of branches, and meshes per field.
- Quality Control: Only use ECFCs with a confirmed phenotype and high tubulogenesis capacity (e.g., >5000 µm total tube length per field) for scaffold vascularization studies.
Visualizing the Experimental Workflow
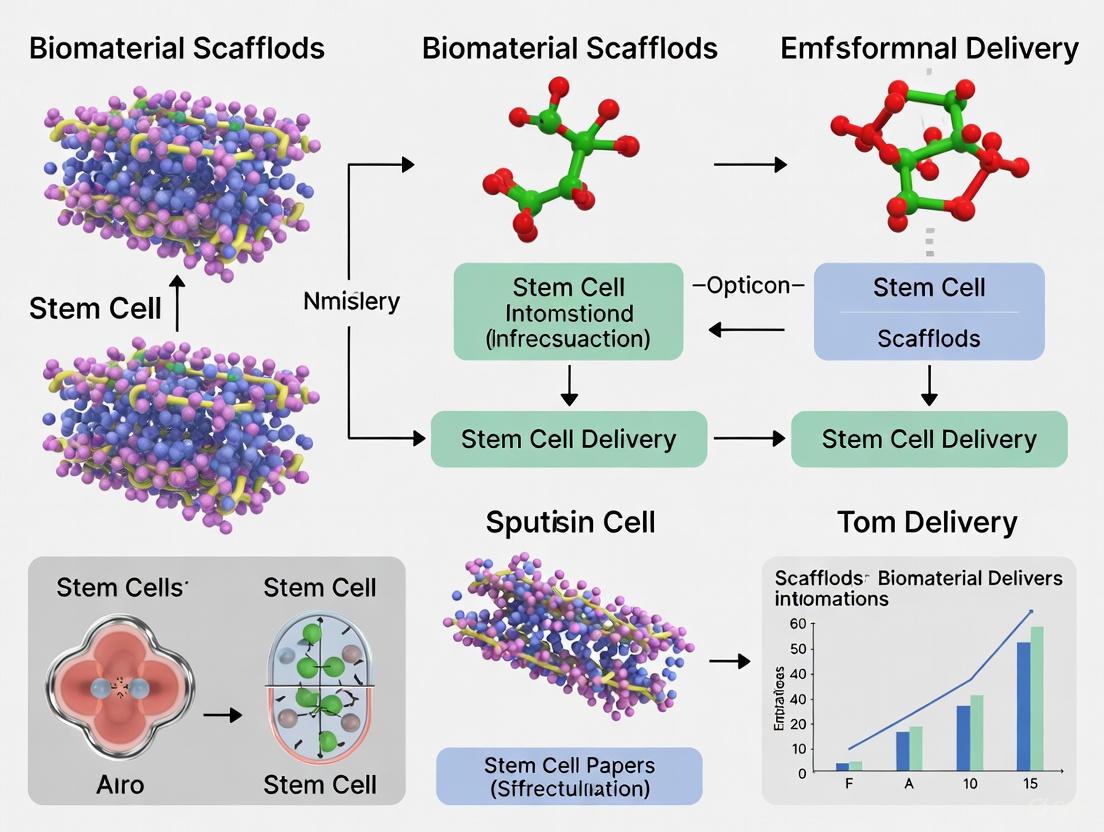
The following diagram illustrates the core workflow for developing a stem cell-based tissue construct, integrating the protocols for iPSCs, MSCs, and ECFCs.
Diagram 1: Stem Cell-Based Construct Development Workflow (52 characters)
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagent Solutions for Stem Cell and Scaffold Research
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| Collagen I | Substrate for cell adhesion and culture; promotes ECFC isolation and expansion. | Coating culture flasks for primary ECFC isolation from blood [13]. |
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable hydrogel; provides tunable mechanical properties and bioactivity for 3D printing. | Component of bioink for 3D-printed bilayered vaginal scaffolds [19]. |
| Decellularized Extracellular Matrix (dECM) | Provides native tissue-specific biochemical and structural cues to scaffolds. | Porcine vaginal ECM (vECM) used in composite bioinks to mimic native tissue microenvironment [19]. |
| EGM-2 MV BulletKit | Specialized medium optimized for growth and maintenance of microvascular endothelial cells. | Culture and expansion of ECFCs after isolation [13]. |
| Small Molecule Inhibitors (CHIR99021, IWP-4) | Direct stem cell differentiation by modulating key signaling pathways (e.g., Wnt). | Sequential use for directed differentiation of iPSCs to cardiomyocytes [10]. |
| Flow Cytometry Antibodies (CD73, CD90, CD105, CD31, CD34, CD45) | Cell surface marker identification for phenotypic characterization and purity assessment. | Confirming MSC (CD73+/CD90+/CD105+) and ECFC (CD31+/CD34+/CD45-) phenotypes [11] [12] [13]. |
| Alizarin Red S, Alcian Blue, Oil Red O | Histochemical stains for detecting calcium (bone), proteoglycans (cartilage), and lipids (fat). | Assessing tri-lineage differentiation potential of MSCs in 2D or 3D culture [19]. |
iPSCs, MSCs, and ECFCs each offer a unique and powerful set of tools for addressing different challenges in regenerative medicine. The successful clinical translation of these cells is inextricably linked to their effective integration with advanced biomaterial scaffolds. These scaffolds are not merely passive carriers; they are active microenvironments that can be engineered to enhance cell survival, direct fate, and ultimately, improve therapeutic outcomes. By leveraging the structured data, detailed protocols, and reagent guidance provided, researchers can accelerate the development of sophisticated, safe, and effective stem cell-scaffold therapies for a wide range of debilitating diseases.
In the field of regenerative medicine and stem cell delivery, biomaterial scaffolds serve a dual purpose that extends far beyond passive structural support. While their three-dimensional architecture provides the physical framework for cell attachment and tissue formation, emerging research reveals their equally critical role in active biological signaling. These dynamic scaffolds modulate cellular behavior by presenting precise biochemical and biophysical cues that guide stem cell survival, proliferation, migration, and differentiation [5] [20]. This complex functionality makes scaffolds indispensable for overcoming the significant challenges in therapeutic stem cell delivery, including poor cell survival, limited retention at target sites, and uncontrolled differentiation [21] [22]. The evolution of scaffold design now focuses on engineering these materials to replicate key aspects of the native extracellular matrix, creating microenvironments that can direct stem cell fate toward specific therapeutic outcomes for conditions ranging from spinal cord injury to retinal degeneration [5] [21].
Core Scaffold Functions
Structural Support Functions
The structural properties of scaffolds establish the fundamental basis for their performance in stem cell delivery applications. These physical characteristics determine how scaffolds interact with both host tissues and delivered cells.
Table 1: Essential Structural Properties of Biomaterial Scaffolds for Stem Cell Delivery
| Property | Functional Role | Ideal Parameters | Impact on Stem Cells |
|---|---|---|---|
| Biocompatibility | Enables integration without adverse immune response | Non-toxic, non-immunogenic | Supports cell survival and function [20] |
| Biodegradability | Temporary support that transfers load to new tissue | Rate matches tissue regeneration | Prevents long-term interference with regenerated tissue [20] |
| Mechanical Strength | Withstands physiological forces during healing | Similar to target tissue | Influences stem cell differentiation pathways [20] |
| Porosity & Pore Size | Enables cell infiltration, vascularization, nutrient waste exchange | High interconnectivity, tissue-specific pore size (e.g., ~95μm for neural repair) | Facilitates 3D colonization, tissue integration [20] [22] |
The interconnected porosity of scaffolds is particularly critical for stem cell applications, as it enables three-dimensional cell distribution, vascular ingrowth, and efficient diffusion of nutrients and signaling molecules [20]. For example, porous collagen-based scaffolds (PCSs) with mean pore diameters of approximately 95μm have demonstrated excellent support for neural stem cell infiltration and distribution in spinal cord injury models [22]. The mechanical properties of scaffolds must be carefully matched to the target tissue, as these physical cues significantly influence stem cell differentiation decisions through mechanotransduction pathways [5].
Dynamic Signaling Functions
Beyond physical support, advanced scaffolds actively participate in biological signaling through multiple mechanisms. These dynamic functions enable precise control over stem cell behavior and tissue regeneration processes.
Table 2: Scaffold-Mediated Signaling Mechanisms in Stem Cell Delivery
| Signaling Mechanism | Key Components | Biological Effects | Experimental Evidence |
|---|---|---|---|
| Biochemical Signaling | Incorporated growth factors, adhesion peptides (RGD), glycosaminoglycans (Chondroitin-6-sulfate) | Enhanced neuronal differentiation of NSCs; guided axonal elongation [22] | |
| Electroconductive Signaling | Polypyrrole, Polyaniline, Polythiophene polymers | Enhanced neurite outgrowth; improved nerve signal propagation [5] | |
| Mechanotransduction | Stiffness-tuned matrices, surface topography | Regulation of neurite repair via TRPV1, Piezo, VGCC ion channels [5] | |
| Immunomodulation | Controlled cytokine release (IL-4, IL-13), scaffold microstructure | Polarization of macrophages to anti-inflammatory M2 phenotype; reduced astrogliosis [6] [22] |
Scaffolds functionalized with specific biochemical cues can significantly enhance therapeutic outcomes. For instance, collagen-glycosaminoglycan (CG) scaffolds containing chondroitin-6-sulfate promoted significantly greater oligodendrocyte differentiation from neural stem cells compared to two-dimensional culture controls (36.3% vs 23.0%) [22]. Similarly, electroconductive polymers like polypyrrole facilitate electrical signal propagation that enhances neurite outgrowth and neuronal activation, making them particularly valuable for neural tissue engineering applications [5].
The integration of these signaling modalities enables scaffolds to function as sophisticated extracellular matrix analogs that can dynamically regulate the stem cell microenvironment. This is particularly evident in immune cell engineering, where scaffold properties can be tuned to control the polarization of therapeutic macrophages or enhance the persistence of delivered T-cells in cancer immunotherapy [6].
Application Notes: Scaffold Design for Specific Therapeutic Applications
Neural Tissue Engineering
In neural repair, scaffold design requires careful consideration of both the inhibitory CNS environment and the specific needs of neuronal cell types. Porous collagen-based scaffolds have demonstrated remarkable success in promoting recovery after spinal cord injury, with studies showing that mice receiving NSC-seeded PCS grafts achieved locomotion performance statistically indistinguishable from uninjured animals within 12 weeks post-injury [22]. The porous architecture of these scaffolds enables robust axonal elongation through the lesion site while reducing inhibitory astrogliosis. Furthermore, the inclusion of glycosaminoglycans like chondroitin-6-sulfate in scaffold composition significantly influences neural stem cell differentiation patterns, promoting oligodendrocyte lineage commitment which is crucial for remyelination strategies [22].
Retinal Tissue Engineering
Retinal repair presents unique challenges due to the delicate sensory tissue structure and the need for precise cellular layering. Scaffolds for retinal progenitor cell (RPC) delivery have evolved into three principal designs: microcylinder scaffolds that mimic vertical retinal organization, fibrous scaffolds that replicate extracellular matrix microstructure, and hydrogel scaffolds that match retinal mechanical properties [21]. Thin microcylinder scaffolds (5-6μm thickness) with precisely engineered pores (10-25μm diameter) have demonstrated 20-fold increases in transplanted cell retention compared to non-structured films while minimizing retinal deformation during implantation [21]. Biodegradable polyesters like PLGA, PCL, and PGS are particularly advantageous for subretinal implantation due to their tunable degradation profiles, with PGS offering superior mechanical matching to native retinal tissue [21].
Immune Cell Engineering
Scaffolds have emerged as powerful platforms for enhancing the efficacy of adoptive immune cell therapies, including CAR-T cells, dendritic cells, and macrophages. Biomaterial scaffolds can address critical limitations in these living drugs by providing localized delivery, maintaining therapeutic phenotypes, and enhancing cell viability [6]. For example, alginate-based hydrogels have been used to create injectable scaffolds that support dendritic cell survival and function for vaccination applications, while porous polymer scaffolds can enhance CAR-T cell expansion and persistence through sustained cytokine presentation [6]. The scaffold microenvironment can be precisely engineered to control immune cell polarization, as demonstrated by decellularized matrix scaffolds that drive macrophages toward regenerative phenotypes for spinal cord repair [6].
Experimental Protocols
Protocol: Neural Stem Cell Seeding and Differentiation in Porous Collagen Scaffolds
This protocol describes the methodology for preparing, seeding, and differentiating neural stem cells within porous collagen-based scaffolds (PCS) for neural tissue engineering applications, based on established procedures with demonstrated efficacy in spinal cord injury models [22].
Materials Required
- Porous collagen or collagen-glycosaminoglycan scaffolds (0.5% mass fraction, ~95μm mean pore diameter)
- Embryonic neural stem cells (NSCs)
- Poly-D-lysine and laminin for 2D control surfaces
- Complete NSC medium: DMEM/F-12 supplemented with B27, N2, EGF (20ng/mL), FGF2 (20ng/mL)
- Differentiation medium: DMEM/F-12 with B27, N2, 1% FBS, BDNF (10ng/mL), GDNF (10ng/mL)
- Fixation solution: 4% paraformaldehyde in PBS
- Immunostaining antibodies: Nestin, Tuj1 (neurons), GFAP (astrocytes), Olig2 (oligodendrocytes)
Procedure
- Scaffold Preparation: Hydrate sterile PCS samples in PBS for 2 hours, then equilibrate in complete medium for 24 hours before cell seeding.
- NSC Expansion: Culture NSCs as neurospheres in complete medium for 5-7 days, then dissociate to single-cell suspension using Accutase.
- 3D Seeding: pipette 50μL of NSC suspension (5×10^6 cells/mL) onto each hydrated PCS (5mm diameter × 2mm thickness). Centrifuge at 300×g for 5 minutes to enhance cell infiltration into scaffold pores.
- Pre-implantation Culture: Maintain seeded scaffolds in complete medium for 3 days to allow cell attachment and initial proliferation.
- Differentiation Induction: Switch to differentiation medium for 4-7 days, refreshing medium every 2-3 days.
- Analysis: Fix constructs with 4% PFA for immunostaining and confocal microscopy analysis.
Technical Notes
- Seeding efficiency typically exceeds 80% with the centrifugation method.
- Scaffold degradation should be minimal during the 7-10 day culture period.
- >99% of cells should express nestin at 3 days post-seeding, confirming maintenance of stemness.
Protocol: Retinal Progenitor Cell Delivery Using Thin Microcylinder Scaffolds
This protocol details the fabrication, cell seeding, and subretinal implantation of thin microcylinder scaffolds for retinal progenitor cell delivery, optimized to minimize retinal damage while maximizing cell retention and integration [21].
Materials Required
- Polycaprolactone (PCL) or poly(glycerol sebacate) (PGS) resin
- Polydimethylsiloxane (PDMS) negative molds with microcylinder architecture
- Retinal progenitor cells (RPCs) or photoreceptor precursors
- Poly-D-lysine and laminin coating solutions
- Subretinal implantation surgical instruments
- Animal model (e.g., rhodopsin knockout mice for degeneration models)
Procedure
- Scaffold Fabrication: Create PCL scaffolds by solvent casting over PDMS negatives with 25μm diameter pores. For PGS scaffolds, cure pre-polymer at 120°C under vacuum using PDMS molds with 50μm diameter pores separated 175μm apart.
- Surface Modification: Treat scaffolds with oxygen plasma, then coat with poly-D-lysine (50μg/mL, 2 hours) followed by laminin (10μg/mL, 4 hours) to enhance cell adhesion.
- Cell Seeding: Apply RPC suspension (10μL at 1×10^5 cells/μL) to scaffold surface, then centrifuge at 200×g for 3 minutes to drive cells into pores.
- Pre-implantation Culture: Maintain seeded scaffolds in retinal differentiation medium for 5-7 days before implantation.
- Scaffold Implantation: For PGS scaffolds, roll the flexible scaffold and load into a 1mm internal diameter needle for subretinal injection. For rigid scaffolds, use specialized implantation tools.
- Outcome Assessment: Evaluate cell integration, photoreceptor outer segment formation, and functional recovery at 4-8 weeks post-implantation.
Technical Notes
- Scaffold thickness should not exceed 50μm to minimize retinal detachment and damage.
- PGS scaffolds offer superior mechanical compatibility with retinal tissue but require laminin coating for cell adhesion.
- Expect 20-fold increases in cell retention compared to bolus injection methods.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Scaffold-Based Stem Cell Research
| Category/Reagent | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Natural Polymers | Collagen, Chitosan, Alginate, Hyaluronan, Silk Fibroin, Gelatin | Biocompatible ECM analogs; support cell adhesion and infiltration | Batch variability; potential immunogenicity; tunable degradation [5] [20] |
| Synthetic Polymers | PLA, PLGA, PCL, Polyphosphoester, Polyurethane | Reproducible properties; controllable biodegradation; mechanical strength | Hydrophobicity may require surface modification [5] [20] |
| Conductive Polymers | Polypyrrole, Polyaniline, Polythiophene | Enhance neurite outgrowth; support electrical signaling in neural tissues | Requires composite formation for biodegradability [5] |
| Surface Modifiers | Poly-D-Lysine, Laminin, RGD Peptides | Enhance cell-scaffold adhesion; promote specific integrin signaling | Coating density affects cell behavior; stability concerns [21] [22] |
| Fabrication Technologies | Solvent Casting/Particle Leaching, Electrospinning, Freeze Drying, 3D Printing | Create controlled pore architectures; nanofibrous structures; patient-specific designs | Equipment cost; resolution limitations; scalability challenges [23] |
The selection of appropriate biomaterials and fabrication methods is critical for developing effective scaffold-based stem cell delivery systems. Natural polymers like collagen and chitosan offer excellent biocompatibility and biological recognition but may exhibit batch-to-batch variability. Synthetic polymers such as PLGA and PCL provide more consistent mechanical and degradation properties but often require surface modification to enhance cell adhesion [5] [20]. Conductive polymers represent a specialized class of materials particularly valuable for neural applications, where they support the electrical activity essential for neuronal function and network formation [5]. Surface modification with adhesion proteins like laminin is frequently necessary to promote sufficient stem cell attachment and retention, especially for synthetic materials [21] [22].
A Materials Toolkit: From Natural Polymers to 3D-Printed Constructs
The development of biomaterial scaffolds for stem cell delivery represents a cornerstone of modern regenerative medicine. Among the various options, natural biomaterials—specifically collagen, fibrin, and decellularized extracellular matrix (dECM)—provide unparalleled advantages as they inherently recapitulate critical aspects of the native tissue microenvironment. These materials are not merely passive structural supports but active participants in regulating stem cell behavior through tissue-specific biochemical composition, mechanical cues, and spatial organization. The integration of stem cells with these biomaterials aims to overcome significant clinical translation challenges, including poor cell survival post-transplantation, insufficient control over differentiation, and limited functional integration with host tissues [24] [25].
Decellularized ECM scaffolds, in particular, have emerged as a premier platform because they preserve the complex tapestry of native tissue structure, including a diverse array of collagens, proteoglycans, glycosaminoglycans (GAGs), and sequestered growth factors [26] [27]. This preserved complexity creates a biomimetic template that promotes cell integration, immunomodulation, and constructive tissue remodeling, making it ideally suited for hosting and delivering therapeutic stem cells [26]. This application note provides a current overview of the properties and applications of these key natural biomaterials, with a specific focus on dECM, and details standardized protocols for their utilization in stem cell research.
Application Notes: Properties and Comparative Analysis
Key Characteristics of Natural Biomaterials
Decellularized Extracellular Matrix (dECM) is derived from tissues or organs through processes that remove cellular material while preserving the intricate native ECM structure and composition. The primary strength of dECM lies in its tissue-specific bioactivity; it naturally contains a complex mixture of structural proteins (e.g., collagens, elastin), proteoglycans, and signaling molecules (e.g., growth factors) that mimic the in vivo stem cell niche [26] [27]. This composition provides inherent cell-instructive cues that can direct stem cell fate. However, a common limitation of pure dECM is its inherent mechanical weakness and poor tunability, which can be addressed through crosslinking or combination with synthetic materials [26] [28].
Collagen, particularly Type I, is the most abundant protein in the human ECM and a fundamental component of many tissues. It is highly biocompatible, biodegradable, and contains cell adhesion motifs (e.g., RGD sequences) that support cell attachment and proliferation [29]. While collagen hydrogels can self-assemble, they often lack the mechanical strength and complexity of full native ECM.
Fibrin is a natural polymer formed from fibrinogen and thrombin during the wound healing process. It serves as an excellent provisional matrix and is widely used as a clinical sealant. Fibrin's key advantages include its injectability and its role in promoting cell migration and angiogenesis. However, its rapid degradation rate and relatively weak mechanics often require stabilization.
Quantitative Comparison of Biomaterial Properties
The following table summarizes the key properties of these natural biomaterials, with a specific focus on data derived from dECM sources.
Table 1: Comparative Properties of Natural Biomaterials for Stem Cell Delivery
| Property | Decellularized ECM (dECM) | Collagen (Type I) | Fibrin |
|---|---|---|---|
| Key Composition | Complex, tissue-specific mix of collagens, GAGs, proteoglycans, glycoproteins, growth factors [26] [27] | Primarily collagen type I fibrils [29] | Fibrin polymer network |
| Mechanical Properties (Elastic Modulus) | Wide range, tissue-dependent (e.g., Skin ECM ~highest; Birth ECM ~lowest) [29] | Tunable, typically lower; varies with concentration & crosslinking | Soft, weak; degrades rapidly |
| Gelation Kinetics | Significantly slower than pure collagen control [29] | Rapid, temperature-dependent self-assembly | Very rapid, enzyme-mediated (thrombin) |
| Degradation Profile | Biodegradable; rate depends on tissue source, crosslinking [26] | Biodegradable via collagenases; rate is tunable | Rapid; requires protease inhibitors (e.g., aprotinin) for stabilization |
| Key Advantages | Tissue-specific bioactivity, inherent complexity, immunomodulatory potential [26] [25] | Excellent biocompatibility, well-established protocols, abundant cell adhesion sites | Injectable, promotes angiogenesis, clinically approved as sealant |
Tissue-Specific dECM Composition and Applications
dECM is not a single material but a class of materials whose properties vary significantly with the tissue of origin. This tissue-specificity is crucial for selecting the appropriate scaffold for a given stem cell application.
Table 2: Tissue-Specific Properties and Applications of dECM Scaffolds
| Tissue Source | Key ECM Components | Stem Cell Applications | Notable Findings |
|---|---|---|---|
| Tendon | ~70% Collagen I (dry weight); Decorin, Fibromodulin, COMP, Tenascin-C [27] | Tendon stem/progenitor cell delivery for musculoskeletal repair | Promotes directional cell alignment and tenogenic differentiation; composite dECM-hydrogels enhance injectability and mechanical recovery in rabbit Achilles tendon models [27]. |
| Skin | Collagen I, III; High elastin content [29] | Mesenchymal stromal cell (MSC) delivery for wound healing | Skin-derived Methacryloyl-functionalized dECM (MA-dECM) showed a 30-fold increase in elastic modulus and significantly accelerated wound closure and vascularization in mice [28]. |
| Skeletal Muscle | Collagen IV, Laminin, Fibronectin [30] | Satellite cell or myoblast delivery for volumetric muscle loss (VML) | Heparinized muscle dECM scaffolds enabled sustained release of PDGF, FGF, and VEGF from PRP, enhancing angiogenesis and host cell migration in a VML model [30]. |
| Birth Tissues (e.g., Umbilical Cord) | Collagen content comparable to pure collagen control [29] | Cord-tissue MSC (CMSC) encapsulation and delivery | Birth ECM hydrogels supported the highest metabolic activity of encapsulated CMSCs compared to other human ECM sources [29]. |
Experimental Protocols
Protocol 1: Fabrication of Granular MA-dECM Hydrogels for 3D Bioprinting
This protocol describes the modification of skin-derived dECM into a photo-crosslinkable, granular hydrogel compatible with extrusion 3D printing and stem cell encapsulation, based on a recent study [28].
Workflow Overview:
Materials & Reagents:
- Acellular dECM: Derived from porcine or human skin, solubilized via enzymatic digestion.
- Methacrylic anhydride (MA): For introducing photo-crosslinkable functional groups.
- Photoinitiator: Irgacure 2959 or Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP).
- Phosphate Buffered Saline (PBS): For washing and solution preparation.
- UV Light Source: (365-405 nm) for crosslinking.
Step-by-Step Procedure:
- Methacryloyl Functionalization: React the solubilized dECM solution with methacrylic anhydride (e.g., 0.5% v/v) under controlled pH (e.g., 8.0) for several hours at 4°C. Terminate the reaction and dialyze extensively against distilled water to remove unreacted monomers. Lyophilize the resulting MA-dECMA to a porous foam for storage.
- Precursor Hydrogel Formation: Dissolve the lyophilized MA-dECM powder in a cell culture-compatible solvent (e.g., PBS) at a desired concentration (e.g., 3-5% w/v). Add the photoinitiator (e.g., 0.1% w/v LAP) and sterilize the solution by filtration.
- Primary Crosslinking & Granulation: Expose the MA-dECM precursor solution to UV light (e.g., 5-10 mW/cm² for 1-5 minutes) to form a bulk hydrogel. Mechanically fragment this bulk hydrogel through a mesh or sieve to create a slurry of granular microgels.
- 3D Bioprinting and Cell Encapsulation:
- Option A (Cell Seeding on Scaffold): Seed the granular hydrogel with a suspension of stem cells (e.g., MSCs, endothelial colony-forming cells) and allow for cell attachment.
- Option B (Cell Encapsulation in Bulk): Mix the stem cell suspension directly with the MA-dECM precursor solution before primary crosslinking in step 3.
- Load the cell-laden granular hydrogel or precursor into a bioprinter cartridge. Extrude the material through a nozzle to create 3D structures.
- Secondary Stabilization: After printing, expose the entire construct to a second, longer UV crosslinking cycle (e.g., 10-20 mW/cm² for 5-10 minutes) to stabilize the structure and fuse the microgels.
Notes: The granular form exhibits shear-thinning behavior, enabling smooth extrusion, and self-heals after the shear force is removed. The mechanical properties of the final construct can be tuned by varying the MA-dECM concentration, UV intensity, and exposure time [28].
Protocol 2: Heparinization of dECM Scaffolds for Sustained Growth Factor Delivery
This protocol outlines a method to functionalize dECM scaffolds with heparin, creating an affinity-based system for the controlled release of growth factors, which can be used to enhance the paracrine signaling of delivered stem cells or recruit host cells [30].
Workflow Overview:
Materials & Reagents:
- Macroporous dECM Scaffold: Fabricated from skeletal muscle or other tissues via decellularization, freeze-drying, and crosslinking.
- Heparin Sodium: From porcine intestinal mucosa or other biological sources.
- Crosslinkers: 1-ethyl-3-(3-dimethylaminopropyl)carbodiimide (EDC) and N-hydroxysuccinimide (NHS).
- Platelet-Rich Plasma (PRP) or EVs: As a source of growth factors (e.g., PDGF, FGF, VEGF).
- Toluidine Blue: For qualitative assessment of heparin conjugation.
Step-by-Step Procedure:
- Scaffold Fabrication: Decellularize the source tissue (e.g., skeletal muscle) using a combination of detergents (e.g., SDS, Triton X-100), enzymes, and washes. Confirm decellularization by quantifying DNA content (<50 ng/mg dry tissue) and preserving ECM components like collagen and GAGs. Create a macroporous scaffold using a freeze-drying technique.
- EDC/NHS Crosslinking: Hydrate the dECM scaffold in a MES buffer solution. Incubate the scaffold with a fresh EDC/NHS solution (e.g., 20mM EDC, 10mM NHS) for 2-4 hours at room temperature to activate carboxyl groups on the ECM. Rinse thoroughly to remove excess crosslinkers.
- Heparin Conjugation: Transfer the activated scaffold to a heparin solution (e.g., 1 mg/mL in PBS). Incubate for 12-24 hours at 4°C to allow covalent conjugation between the amine groups on heparin and the activated carboxyl groups on the scaffold. Wash extensively with PBS to remove unbound heparin.
- Verification of Heparinization: Qualitatively confirm successful conjugation using Toluidine Blue staining. Heparin-bound scaffolds (DSMS-H) will show a deeper blue color compared to the background color of control scaffolds (DSMS) [30].
- Loading of Bioactive Molecules: Incubate the heparinized scaffold (DSMS-H) with the growth factor source, such as PRP or a solution of extracellular vesicles (EVs). The negatively charged heparin molecules will electrostatically bind and retain positively charged growth factors.
- Release Kinetics Assessment: To characterize the release profile, immerse the loaded scaffold in PBS at 37°C under gentle agitation. Collect supernatant at predetermined time points and quantify the concentration of specific growth factors (e.g., PDGF-BB, FGF2, VEGF) using ELISA. The heparinized scaffold is expected to show a significantly reduced burst release and a more sustained release profile over several days compared to a non-heparinized control [30].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for dECM and Stem Cell Research
| Reagent / Material | Function / Application | Example Use in Protocols |
|---|---|---|
| Sodium Dodecyl Sulfate (SDS) | Ionic detergent for effective decellularization; disrupts lipid membranes and dissociates DNA from proteins [26] | Primary detergent in tissue decellularization protocols (e.g., for skeletal muscle, tendon). Requires careful concentration control and thorough washing to avoid cytotoxicity [30] [31]. |
| Triton X-100 | Non-ionic detergent for delipidation and removal of residual ionic detergents [26] | Used in sequence with SDS for more complete decellularization and removal of detergent residues [31]. |
| Methacrylic Anhydride (MA) | Introduces photo-polymerizable methacryloyl groups into biomolecules like dECM or gelatin [28] | Key reagent for creating MA-dECM or GelMA, enabling UV-light-mediated crosslinking for mechanical tunability and shape fidelity in 3D bioprinting [28]. |
| EDC / NHS Crosslinker | Zero-length crosslinker that forms amide bonds between carboxyl and amine groups without becoming part of the linkage [30] | Used to enhance the mechanical integrity of dECM scaffolds and to conjugate molecules (e.g., heparin) to the dECM by targeting their amine groups [30]. |
| Heparin Sodium | Highly sulfated glycosaminoglycan with high affinity for a wide range of growth factors [30] | Immobilized on dECM scaffolds to create an affinity-based system for the sustained and controlled delivery of growth factors from PRP or other sources [30]. |
| Irgacure 2959 / LAP | Photoinitiators that generate radicals upon UV/Violet light exposure to initiate polymerization [28] | Essential for crosslinking methacrylated materials (MA-dECM, GelMA). LAP offers better water solubility and biocompatibility than Irgacure 2959. |
Signaling Pathways in Biomaterial-Stem Cell Interactions
The therapeutic success of stem cell-laden biomaterials is largely governed by the activation of specific intracellular signaling pathways triggered by cell-material interactions. The following diagram summarizes the key pathways involved.
Key Signaling Pathways Activated by Natural Biomaterials:
Pathway Description: Stem cells adhere to natural biomaterials primarily via integrin receptors that recognize specific ligands (e.g., RGD sequences) present in the scaffold [26]. This adhesion leads to the formation of focal adhesion complexes and the activation of Focal Adhesion Kinase (FAK). FAK activation initiates several downstream pathways:
- The MAPK/ERK pathway is crucial for promoting cell proliferation and survival [26].
- The PI3K/Akt pathway further enhances survival signals and plays a key role in lineage specification and differentiation [26] [24].
- Mechanotransduction pathways are activated as cells sense and respond to the mechanical properties (e.g., elasticity, stiffness) of the biomaterial scaffold, directly influencing stem cell fate decisions and guiding cytoskeletal organization [26] [25].
Furthermore, growth factors sequestered and presented by the dECM (e.g., VEGF, TGF-β, FGF) bind to their respective tyrosine kinase receptors, synergizing with integrin signaling to amplify these pro-regenerative signals and guide functional tissue formation [26] [30].
The regeneration of critical-sized bone defects remains a significant clinical challenge, with an estimated 2.2 million bone graft procedures performed annually worldwide [32]. Within the context of biomaterial scaffolds for stem cell delivery research, synthetic and ceramic scaffolds provide an essential foundation for bone tissue engineering. These constructs address the limitations of natural bone grafts by offering tunable properties, consistent quality, and osteoconductive surfaces that guide cellular behavior and tissue formation [33] [32].
Synthetic polymers, particularly poly(lactic-co-glycolic acid) (PLGA), provide exceptional versatility through tunable mechanical properties, degradation rates, and scaffold architecture. When combined with osteoconductive ceramic materials such as hydroxyapatite (HA) and β-tricalcium phosphate (β-TCP), these composite scaffolds create a biomimetic microenvironment that supports stem cell viability, differentiation, and ultimately, functional bone regeneration [34]. This application note details the quantitative performance, experimental protocols, and biological mechanisms of these advanced scaffold systems to facilitate their effective implementation in regenerative medicine research.
Quantitative Performance of Composite Scaffolds
The performance of composite scaffolds is critically dependent on their composition and fabrication methodology. The quantitative data below highlight the impact of material selection and production technique on key scaffold properties.
Table 1: Comparative Performance of Bone Graft Materials and Scaffolds
| Material Type | Osteoconductivity | Osteoinductivity | Compressive Strength (MPa) | Degradation Time | Key Advantages |
|---|---|---|---|---|---|
| Autograft | High | High | N/A (Native Tissue) | N/A | Gold standard, biological properties |
| Allograft | Moderate | Variable | Variable | 6-18 months | Availability |
| β-TCP Ceramics | High | Moderate | 1-10 [32] | 6-24 months [32] | Bioresorbable, osteoconductive |
| PLGA Polymers | Low | Low | 0.5-5 [34] | 1-12 months [34] | Tunable degradation |
| PLGA-HA Composite | High | Enhanced | 2-15 [34] | 3-18 months | Balanced properties |
Advanced fabrication technologies significantly impact scaffold characteristics and performance. Automated manufacturing methods, particularly 3D bioprinting, have demonstrated substantial improvements over traditional approaches.
Table 2: Impact of Fabrication Method on PLGA-HA Scaffold Properties
| Parameter | Manual Casting | Automated 3D Bioprinting | Improvement Factor |
|---|---|---|---|
| Processing Time (per scaffold) | 10 min 51 sec | 2 min [34] | 5.4x faster |
| Material Retention (average weight) | 0.01169 g [34] | 0.02354 g [34] | 2x greater |
| Inter-batch Reproducibility | Low [34] | High [34] | Significant improvement |
| Structural Complexity | Limited [34] | High (controlled porosity) [34] | Enhanced design control |
| Coating Uniformity | Variable [34] | Consistent [34] | Improved homogeneity |
Experimental Protocols
Automated Fabrication of PLGA-HA Composite Scaffolds
This protocol describes the automated fabrication of PLGA-HA composite scaffolds using 3D bioprinting technology, enabling high reproducibility and precise architectural control [34].
Materials Required
- Poly(dl-lactide-co-glycolide) (PLGA)
- Hydroxyapatite nanoparticles (nHA)
- Chloroform
- Borosilicate glass vials with polypropylene lids
- Polyvinyl alcohol (PVA) filament for mold printing
- Lulzbot bioprinter with 2.5 mL and 5 mL syringes
- Autodesk Inventor software
- CURA Lulzbot Edition slicer software
- Bambu Carbon X1 3D printer
- Precision laboratory scale
- Magnetic stirrer
- Probe sonicator
Procedure
PVA Mold Fabrication
- Design the scaffold mold using CAD software (e.g., Autodesk Inventor)
- Generate G-code and fabricate PVA molds using an Ender 3D printer
- Store PVA molds under controlled humidity conditions
- Weigh and record individual mold weights before use
PLGA-HA Solution Preparation
- Calibrate an empty borosilicate glass vial on a precision scale
- Add chloroform (5.92 g) to the vial, accounting for evaporation
- Weigh 100 mg of PLGA (stored at -15 to -18°C) and add to chloroform
- Insert magnetic stirring bar and seal vial with parafilm
- Stir on a magnetic stirrer (without heat) for ≥3 hours until complete dissolution
- Slowly add hydroxyapatite nanoparticles while dispersing with a probe sonicator for 2-3 minutes to ensure even distribution
Automated Casting via 3D Bioprinting
- Design the casting path using 3D CAD software
- Load PLGA-HA solution into bioprinter syringe (2.5 mL or 5 mL capacity)
- Calibrate the Lulzbot bioprinter
- Set extrusion parameters: rate of 4 mm/s, layer height of 2 mm
- Execute automated casting process (approximately 5 min 11 sec for 4 molds with 2.5 mL syringe; 3 min 46 sec with 5 mL syringe)
- Allow solvent evaporation under controlled conditions
Quality Assessment
- Verify chemical composition using Fourier Transform Infrared Spectroscopy (FTIR)
- Analyze pore structure and morphology using Scanning Electron Microscopy (SEM)
- Assess mechanical properties through compression testing
Troubleshooting Notes
- Chloroform volatility: Use weight-based measurements instead of volume-based
- Material handling: Use borosilicate glass and polypropylene to prevent chemical reactions
- Scalability: Implement 3D-printed mesh filters for high-throughput experimentation
In Vitro Assessment of Scaffold-Cell Interactions
This protocol details the evaluation of cell-scaffold interactions using mesenchymal stem cells, critical for assessing the regenerative potential of fabricated constructs [35] [36].
Materials Required
- Mesenchymal stem cells (bone marrow, adipose, or umbilical cord-derived)
- Cell culture media (Dulbecco's Modified Eagle Medium with 10% FBS)
- Resazurin sodium salt (for viability assay)
- Phosphate-buffered saline (PBS)
- Fixation solution (2.5% glutaraldehyde in 0.1 M sodium cacodylate buffer)
- Primary antibodies (CD73, CD90, CD105 for MSC characterization)
- Fluorescence-activated cell sorting (FACS) equipment
Procedure
Cell Seeding on Scaffolds
- Sterilize scaffolds (UV irradiation or ethanol treatment)
- Pre-wet scaffolds in culture media for 2-4 hours
- Seed MSCs at density of 50,000-100,000 cells per scaffold
- Allow cell attachment for 4-6 hours before adding additional media
Viability and Proliferation Assessment
- Prepare resazurin working solution (10% in culture media)
- Incubate cell-scaffold constructs with resazurin for 2-4 hours at 37°C
- Measure fluorescence (560EX/590EM) at 24, 48, and 72 hours
- Calculate cell numbers based on standard curve
Immunophenotyping via Flow Cytometry
- Harvest cells from scaffolds using collagenase/trypsin treatment
- Wash cells with PBS and aliquot 100,000 cells per tube
- Incubate with antibodies against CD73, CD90, CD105 (positive markers) and CD34, CD45 (negative markers)
- Fix cells with 2% paraformaldehyde
- Analyze using flow cytometry to confirm MSC phenotype
Microscopic Evaluation
- Fix cell-scaffold constructs with 2.5% glutaraldehyde
- Process for SEM: dehydrate through ethanol series, critical point dry, sputter coat with gold/palladium
- Image using SEM to assess cell morphology and integration
Biological Mechanisms and Signaling Pathways
The regenerative capacity of composite scaffolds is mediated through specific biological mechanisms that direct cellular behavior and tissue formation. The following diagram illustrates the key signaling pathways activated by synthetic and ceramic scaffolds to promote osteogenic differentiation of mesenchymal stem cells.
Diagram 1: Signaling pathways in scaffold-mediated bone regeneration. Ceramic components (HA/β-TCP) promote osteoconduction and BMP-2 upregulation, driving MSC differentiation toward osteogenic lineage through RUNX2 activation. Tunable polymers enhance cell adhesion and modulate degradation, influencing the RANKL/OPG balance critical for bone remodeling. β-TCP additionally promotes macrophage polarization toward anti-inflammatory M2 phenotype, creating a favorable regenerative microenvironment.
The molecular mechanisms underlying scaffold-mediated osteogenesis involve complex interactions between multiple signaling pathways. HA and β-TCP ceramics directly stimulate osteogenic differentiation by activating the bone morphogenetic protein (BMP) signaling pathway, particularly upregulating BMP-2 expression [32]. This activation occurs through calcium-sensing receptors (CaSR) on mesenchymal stem cells, leading to downstream SMAD phosphorylation and translocation to the nucleus where they activate transcription of osteogenic genes including RUNX2, the master regulator of osteoblast differentiation [32] [36].
Simultaneously, scaffold topography and mechanical properties activate Wnt/β-catenin signaling, which synergizes with BMP signaling to enhance osteogenic commitment while suppressing adipogenic differentiation [32]. The controlled degradation of polymer components regulates the local release of calcium and phosphate ions, which further promotes osteoblast mineralization through activation of calcium-sensing receptors and alkaline phosphatase activity [32].
An additional crucial mechanism involves immunomodulation, where β-TCP scaffolds promote the polarization of macrophages toward the anti-inflammatory M2 phenotype [32]. This transition from pro-inflammatory M1 to regenerative M2 macrophages enhances BMP-2 expression while reducing pro-inflammatory cytokine production, creating a microenvironment conducive to bone formation rather than fibrosis [32] [36].
The following workflow diagram illustrates the integrated experimental approach for developing and evaluating synthetic and ceramic scaffolds for bone regeneration applications.
Diagram 2: Integrated workflow for scaffold development and evaluation. The process begins with strategic material selection and scaffold design, proceeds through automated or manual fabrication, and culminates in comprehensive physical, biological, and molecular characterization to optimize scaffold performance for bone regeneration applications.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of scaffold-based bone regeneration research requires specific materials and reagents with defined functions. The following table details essential components for designing, fabricating, and evaluating synthetic and ceramic scaffolds.
Table 3: Essential Research Reagents for Scaffold-Based Bone Regeneration Studies
| Category | Specific Reagents/Materials | Function/Application | Key Considerations |
|---|---|---|---|
| Polymer Materials | PLGA, PCL, PEG | Structural scaffold matrix; tunable degradation | Varying copolymer ratios affect degradation rate [34] |
| Ceramic Components | Hydroxyapatite (HA), β-TCP | Osteoconduction; enhancing compressive strength | Nanoparticles improve distribution [32] [34] |
| Solvents | Chloroform, Hexafluoroisopropanol | Polymer dissolution for processing | Weight-based measurement improves accuracy [34] |
| Fabrication Aids | PVA (mold material), Borosilicate glass vials | Support structures; chemical compatibility | Prevents reaction with solvents [34] |
| Cell Sources | BM-MSCs, AD-MSCs, UC-MSCs | Osteogenic differentiation potential | Source affects proliferation and potency [36] |
| Characterization Tools | FTIR, SEM, Flow cytometer | Material and biological assessment | Automated analysis enhances reproducibility [37] |
| Osteogenic Assays | Alkaline phosphatase, Osteocalcin | Differentiation status monitoring | Multiple timepoints recommended [36] |
Synthetic and ceramic composite scaffolds represent a advanced platform for stem cell delivery in bone regeneration research. The integration of tunable polymers like PLGA with osteoconductive ceramics such as HA and β-TCP creates a biomimetic microenvironment that supports mesenchymal stem cell viability, osteogenic differentiation, and ultimately, functional bone tissue formation. The automated fabrication protocols, quantitative performance data, and biological mechanisms detailed in this application note provide researchers with the essential tools to implement these advanced scaffold systems in their regenerative medicine programs. As the field evolves, the convergence of biomaterial science, stem cell biology, and manufacturing technology will continue to enhance the precision and clinical translatability of scaffold-based bone regeneration strategies.
The field of regenerative medicine is being transformed by advanced fabrication technologies that enable precise control over the cellular microenvironment. Among these, 3D bioprinting and injectable hydrogel systems represent two complementary platforms for creating biomimetic scaffolds for stem cell delivery. These technologies address critical challenges in tissue engineering, including the replication of native tissue architecture, provision of mechanical support, and sustained presentation of biological cues. Within the context of biomaterial scaffolds for stem cell research, 3D bioprinting offers unparalleled spatial control for constructing complex, hierarchically organized tissues, while injectable hydrogels provide minimally invasive delivery capabilities for therapeutic cells and biomolecules [38] [39]. This document presents detailed application notes and experimental protocols to guide researchers in leveraging these advanced fabrication methods for stem cell delivery applications.
3D Bioprinting Systems
3D bioprinting is defined as a technique for fabricating biomimetic structures using cell-laden biomaterials deposited in predefined patterns through a layer-by-layer process [40]. This technology enables the creation of complex 3D constructs with precisely controlled architectures, including pore size, geometry, and distribution, which are critical parameters influencing cellular behavior such as nutrient diffusion, cell adhesion, migration, and differentiation [40]. The fundamental principle involves the additive manufacturing of bioinks—hydrogel materials encapsulating cells and bioactive factors—according to digital designs, typically generated from computer-aided design (CAD) models or medical imaging data.
Key applications in stem cell research include:
- Tissue-Specific Constructs: Creation of multi-layered, multi-cellular tissues mimicking native组织结构, such as endothelial-epithelial barriers for disease modeling [41].
- Personalized Disease Models: Using patient-derived induced pluripotent stem cells (iPSCs) to generate patient-specific tissue models for drug screening and disease mechanism studies [42].
- High-Throughput Screening: Fabrication of standardized, reproducible tissue constructs for evaluating drug efficacy and toxicity in physiologically relevant environments [43].
Injectable Hydrogel Systems
Injectable hydrogels represent a distinct class of biomaterials that undergo sol-gel transition in response to physiological stimuli such as temperature, pH, or ionic strength [39]. These systems can be administered in a minimally invasive manner as liquids that transform into stable gels at the target site, creating a biomimetic microenvironment for encapsulated cells and facilitating sustained release of therapeutic agents [44] [38]. Their "smart" characteristics enable precise localization and controlled presentation of biological cues, making them particularly valuable for therapeutic delivery and regeneration applications.
Key applications in stem cell delivery include:
- Minimally Invasive Cell Therapy: Delivery of mesenchymal stem cells (MSCs) for intervertebral disc regeneration, as demonstrated by Chen et al., where hydrogel microspheres supported nucleus pulposus-like differentiation [45].
- Sustained Biomolecule Release: Controlled delivery of anti-tuberculosis drugs (Rifampicin and Isoniazid) over extended periods (6-10 days) to improve treatment compliance [44].
- Inflammation Modulation: Peptide-functionalized hydrogels that modulate local inflammatory environments to enhance stem cell survival and differentiation [45].
Table 1: Comparative Analysis of 3D Bioprinting and Injectable Hydrogel Technologies
| Parameter | 3D Bioprinting | Injectable Hydrogels |
|---|---|---|
| Spatial Control | High (micrometer-scale precision) | Low to moderate |
| Structural Complexity | High (complex 3D architectures) | Moderate (limited by injection and gelation) |
| Invasiveness | Typically requires implantation | Minimally invasive |
| Gelation Mechanism | Photo-crosslinking, thermal, ionic | Temperature, pH, ionic strength |
| Primary Applications | Tissue constructs, disease models, organ printing | Cell delivery, drug release, soft tissue regeneration |
| Representative Materials | GelMA, collagen, hyaluronic acid | Poloxamer, chitosan, Carbopol |
| Typical Cell Density | High (10^6 - 10^7 cells/mL) | Moderate (10^5 - 10^6 cells/mL) |
Experimental Protocols
Protocol 1: Design and Bioprinting of Multi-Layered 3D Constructs
This protocol describes the fabrication of 3D models with two cell lineage layers to recreate multi-cell constructs, adaptable for various stem cell types including primary cells, commercial cell lines, and induced pluripotent stem cells (iPSCs) [41].
Major Step 1: 3D Model Design
- Software Setup: Download and install TinkerCAD (https://www.tinkercad.com/) and create a new account [41].
- Geometry Creation:
- Select basic shapes from the shapes menu (cylindrical form recommended)
- Modify length and width to 10.0 mm using white squares at vertices
- Set height to 1.0 mm (must be a multiple of layer height for slicing)
- Multi-Layer Design:
- Copy-paste the initial object
- Use the mouse's left button to drag the new object to fit the first object
- Lift one object 1 mm above the other using the dark arrow in the middle
- Export each object separately as .STL files ("Bottom" and "Top")
Major Step 2: Slicing Setup
- Software Installation: Download Prusa Slicer (https://www.prusa3d.com/page/prusaslicer_424/) and install, then set mode to "Expert" for additional features [41].
- Print Settings Configuration:
- Layers and perimeters: Set layer height and first layer height to 0.2 mm
- Configure Vertical Shells to 0
- Set Horizontal shells, Solid Layers, Top, and Bottom to 0
- Infill Parameters:
- Fill density: 50%
- Fill Pattern: Rectilinear
- Combine infill every: 1
- Solid Infill and Fill Angle: 0 and 90, respectively
- Skirt and Brim: Set Loops and Brim width to 0
Major Step 3: Bioink Preparation and Bioprinting
- GelMA/Geltrex Bioink Formulation:
- Prepare GelMA according to established protocols, controlling methacrylate degree for tailored properties [41]
- Mix with Geltrex (basement membrane extract) to enhance bioactivity
- Incorporate stem cells at appropriate density (typically 1-5×10^6 cells/mL)
- Bioprinting Execution:
- Load bioink into printing cartridges
- Execute bioprinting using optimized parameters for your specific bioprinter
- Perform photo-crosslinking (typically UV light, 5-30 seconds) to stabilize structure
Protocol 2: Formulation and Characterization of Injectable Thermo-responsive Hydrogels
This protocol outlines the development of an injectable in-situ gel system for sustained delivery, optimized for stem cell encapsulation and release [44].
Major Step 1: Hydrogel Formulation
- Polymer Solution Preparation:
- Use cold process method to prepare hydrogel solutions
- Combine Poloxamer 407, Carbopol 940, and HPMC at varying concentrations
- Dissolve polymers in cold buffer solution (4°C) to facilitate hydration
- Stir continuously until clear solution forms
- Stem Cell Encapsulation:
- Suspend stem cells in polymer solution at low temperature (4°C) where solution remains liquid
- Maintain homogeneous cell distribution by gentle mixing
Major Step 2: Physicochemical Characterization
- Gelation Temperature:
- Use vial inversion method or rheological analysis
- Optimal gelation temperature: ~26°C for physiological compatibility [44]
- Viscosity Measurements:
- Measure sol viscosity at room temperature (target: ~238 cP)
- Measure gel viscosity at physiological temperature (target: ~1700 cP) [44]
- Morphological Analysis:
- Use scanning electron microscopy (SEM) to examine network structure
- Confirm porous, interconnected architecture
Major Step 3: In Vitro Cell Compatibility and Release Studies
- Cell Viability Assessment:
- Culture encapsulated stem cells for predetermined time points
- Assess viability using Live/Dead staining (calcein-AM/propidium iodide)
- Perform MTT assay to quantify metabolic activity [46]
- Release Kinetics:
- For drug delivery applications, monitor release in phosphate buffer pH 7.4
- Sample at predetermined intervals and analyze via HPLC or spectrophotometry
Table 2: Key Characterization Parameters for Injectable Hydrogel Systems
| Parameter | Target Value | Analytical Method | Significance |
|---|---|---|---|
| Gelation Temperature | 26-37°C | Vial inversion method, rheology | Determines in vivo gelation behavior |
| Sol Viscosity | 200-300 cP | Rheometry | Ensures injectability through standard needles |
| Gel Viscosity | 1500-2000 cP | Rheometry | Affects mechanical integrity and release kinetics |
| Gelation Time | 30 seconds - 5 minutes | Visual observation, rheology | Critical for clinical application |
| Swelling Ratio | 50-90% | Gravimetric analysis | Influences mechanical properties and degradation |
| Drug Release Duration | 6-10 days | In vitro release studies | Determines dosing frequency for therapeutics |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for 3D Bioprinting and Injectable Hydrogel Research
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Gelatin Methacrylate (GelMA) | Photocrosslinkable bioink for 3D bioprinting | Varying methacrylation degrees (30-80%); tunable mechanical properties [41] |
| Poloxamer 407 | Thermo-responsive polymer for injectable hydrogels | Forms gels at physiological temperatures; FDA-approved [44] |
| Chitosan | Natural polymer for smart injectable hydrogels | Biocompatible, biodegradable; pH-responsive gelation [39] |
| Carbopol 940 | Polymeric additive for viscosity modulation | Enhances gel strength and sustained release properties [44] |
| Photoinitiators | Crosslinking activation for photopolymerizable hydrogels | Irgacure 2959, LAP; concentration 0.05-0.2% w/v [41] |
| Geltrex | Basement membrane extract for bioink enhancement | Contains laminin, collagen IV; improves cell adhesion and viability [41] |
| Gelatin from porcine skin | Bioink component for cell support | Provides RGD sequences for cell adhesion [41] |
| Methacrylic anhydride | Synthesis of methacrylated polymers | Used for functionalization of natural polymers [41] |
Signaling Pathways and Experimental Workflows
Signaling Pathways in Stem Cell Differentiation Within Hydrogel Microenvironments
Injectable hydrogel microspheres functionalized with bioactive peptides can modulate specific signaling pathways to direct stem cell differentiation. The following diagram illustrates the pathway activated by Wnt5a-mimetic peptide Foxy5 in promoting nucleus pulposus-like differentiation of BMSCs, relevant for intervertebral disc regeneration [45]:
Stem Cell Differentiation Signaling
Experimental Workflow for 3D Bioprinting and Hydrogel Characterization
The following workflow illustrates the integrated process for designing, fabricating, and characterizing 3D bioprinted constructs and injectable hydrogels for stem cell delivery:
Experimental Workflow
Advanced fabrication technologies including 3D bioprinting and injectable hydrogel systems provide powerful platforms for creating biomaterial scaffolds tailored for stem cell delivery. The protocols and application notes presented here offer researchers detailed methodologies for implementing these technologies in their investigations. As the field progresses, integration of these approaches with emerging technologies such as artificial intelligence for design optimization [47] and advanced biomaterials with enhanced bioactivity will further expand their potential in regenerative medicine and therapeutic development.
Bone Regeneration
Application Note
Bone regeneration remains a significant clinical challenge, particularly for critical-sized defects, non-union fractures, and patients with compromised healing capacity. Functionalized mesenchymal stem cells (MSCs) delivered via advanced biomaterial scaffolds have emerged as a transformative strategy to overcome the limitations of naive MSCs, which often exhibit poor survival, low engraftment rates, and inconsistent osteogenic potential after transplantation. [48]
The therapeutic efficacy of MSCs is rooted in their dual capacity for direct differentiation into osteoblasts and powerful paracrine signaling. These cells secrete bone morphogenetic proteins (BMPs), vascular endothelial growth factor (VEGF), and other factors that collectively promote angiogenesis, immunomodulation, and extracellular matrix remodeling—all critical processes in the bone regeneration cascade. [48] Key signaling pathways governing this process include Wnt/β-catenin for osteoblast maturation and RUNX2 as the master transcription factor for osteogenic lineage commitment. [48]
Recent advances focus on enhancing MSC performance through genetic preconditioning, chemical modification, or integration with nanoparticles to boost their bone-forming potential. Furthermore, the physical design of the delivery scaffold itself, particularly its shape conformity to the bone defect, has been identified as a fundamentally important factor significantly enhancing bone regeneration efficacy. [49]
Table 1: Quantitative Analysis of Scaffold Performance in Bone Regeneration
| Scaffold Type | Experimental Model | Key Metrics | Results | Source |
|---|---|---|---|---|
| HA/PLGA/Bleed | Rat calvarial critical-size defect (8mm) | Histomorphometry (Collagen-I), Histology, Immunoexpression (Rank-L) | Superior collagen-I fiber formation vs. HA/PLGA; Increased biomaterial degradation & bone remodeling. [50] | [50] |
| PBN/BMP/5-aza-dC | Beagle mandibular 3-wall defect | Bone Volume/Total Volume (BV/TV), Bone Mineral Density (BMD) | BV/TV: 75.95 ± 0.86%; BMD: 0.85 ± 0.01 at 8 weeks; Significant increase from 4 to 8 weeks. [51] | |
| Scaffolds with Linearly Increasing Shape Conformity | Rat calvaria defect | New Bone Volume (Micro-CT), Histology | Increased shape conformity linearly correlated with increased new bone volume and more centralized bone regeneration. [49] |
Experimental Protocol: Evaluating Composite Scaffolds in a Rat Calvarial Defect Model
Objective: To assess the bone regenerative capacity of a novel hydroxyapatite/poly(lactic-co-glycolic) acid/hemostatic polysaccharide (HA/PLGA/Bleed) scaffold compared to HA/PLGA and empty controls. [50]
Materials:
- Animals: Male Wistar rats (280 ± 20 g).
- Scaffolds: HA/PLGA (30% HA + 70% PLGA) and HA/PLGA/Bleed (2.4% HA + 5.6% PLGA + 92% Bleed), 1.5 mm thick, 8 mm diameter. [50]
- Equipment: Trephine drill (8 mm diameter), micromotor, suture materials, formalin, EDTA for decalcification.
Methodology:
- Surgical Creation of Defect: Anesthetize rats. Make a 1.5 cm incision along the skullcap, and create a critical-sized bone defect using an 8-mm trephine drill with constant saline irrigation to prevent thermal necrosis. [50]
- Implantation: Randomly assign animals to groups: Control (empty defect), BG1 (implanted with HA/PLGA scaffold), BG2 (implanted with HA/PLGA/Bleed scaffold). [50]
- Post-operative Care: Administer analgesic and monitor for infection. Euthanize cohorts at 15, 30, and 60 days post-operation. [50]
- Sample Analysis:
- Histopathology: Fix bone samples in formalin, decalcify in EDTA, embed in paraffin, section (5 µm), and stain with Hematoxylin and Eosin (H&E) for morphological assessment. [50]
- Immunohistochemistry: Stain sections for Collagen-I (Col-1) and receptor activator of nuclear factor kappa-Β ligand (Rank-L) to evaluate extracellular matrix formation and bone remodeling activity, respectively. [50]
- Data Analysis: Use non-parametric statistical tests (e.g., Mann-Whitney) with a significance level of p ≤ 0.05. [50]
Signaling Pathway: MSC-Mediated Bone Regeneration
The Scientist's Toolkit: Key Reagents for Bone Regeneration Studies
Table 2: Essential Research Reagents for Bone Tissue Engineering
| Reagent / Material | Function & Application | Key Characteristics |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Therapeutically active cell source for bone regeneration. [48] | Multipotent; sourced from bone marrow (BM-MSC), adipose tissue (AD-MSC), or umbilical cord (UC-MSC); potent paracrine signaling and osteogenic differentiation capacity. [48] |
| Hydroxyapatite (HA) | Osteoconductive mineral component of scaffolds. [50] | Mimics natural bone mineral; provides calcium and phosphate; supports osteoblast adhesion and growth. [50] |
| Poly(lactic-co-glycolic) acid (PLGA) | Synthetic, biodegradable polymer for scaffold fabrication. [50] | Provides mechanical stability and structural integrity; tunable degradation rate. [50] |
| Bone Morphogenetic Protein-2 (BMP-2) | Potent osteoinductive growth factor. [51] | Drives osteogenic differentiation of MSCs; often requires sustained delivery systems to mitigate side effects. [51] |
| 3D Bioprinted Scaffold | Structural platform for cell delivery and tissue guidance. [49] [51] | Enables customization and precise shape conformity to defect; can be functionalized with bioactive molecules. [49] [51] |
Wound Healing
Application Note
The paradigm of immune cells as "living drugs" is revolutionizing therapeutic strategies for complex wounds. Adoptive cell therapies, including T cells, macrophages, and dendritic cells (DCs), offer unprecedented potential. However, their clinical translation is hindered by inherent complexities: poor delivery to target tissues, difficulty in maintaining therapeutic phenotypes in vivo, and limited persistence. [6]
Biomaterial scaffolds are being engineered to overcome these barriers by creating protective microenvironments that enhance the viability, function, and localized delivery of therapeutic immune cells. For example, scaffold-based delivery of tumor-infiltrating lymphocytes (TILs) and chimeric antigen receptor (CAR) T cells has been shown to enhance their anti-tumor efficacy, a principle that can be adapted to modulate chronic wound inflammation. [6]
Alginate hydrogels and other porous, biodegradable materials have proven effective as delivery vehicles for dendritic cells, promoting sustained immunomodulatory activity. Similarly, scaffolds designed to recruit endogenous immune cells to the wound site are under active investigation, offering a cell-free alternative that leverages the body's own repair mechanisms. [6]
Experimental Protocol: Biomaterial-Mediated Immune Cell Delivery
Objective: To utilize a biomaterial scaffold for the targeted delivery and recruitment of therapeutic immune cells to a wound site. [6]
Materials:
- Immune Cells: T cells, macrophages, or dendritic cells, expanded and potentially engineered ex vivo.
- Scaffold Material: Biodegradable hydrogel (e.g., alginate, collagen) or porous polymer scaffold.
- Molecular Cues: Cytokines (e.g., IL-2), chemokines, or antigens to be loaded into the scaffold.
- Animal Model: Immunocompetent mouse or other appropriate wound healing model.
Methodology:
- Scaffold Fabrication and Functionalization: Prepare the scaffold from the chosen biomaterial (e.g., via cross-linking, 3D printing). Load it with selected immune cells and/or molecular cues (cytokines, chemokines) that promote cell survival and function. [6]
- Implantation/Application: Apply the cell-laden scaffold directly to the wound site in the animal model. For cell recruitment strategies, implant the scaffold loaded only with chemoattractants to mobilize the host's endogenous immune cells. [6]
- In Vivo Monitoring: Track immune cell persistence, phenotype, and functional activity at the wound site over time using non-invasive imaging (e.g., bioluminescence) and subsequent tissue analysis. [6]
- Efficacy Assessment: Analyze wound closure rates, levels of key inflammatory and regenerative biomarkers, and histology of the healed tissue to evaluate the quality and functionality of the regenerated skin. [6]
Signaling Workflow: Scaffold-Guided Immune Modulation in Wound Healing
Neurological Repair
Application Note
The central nervous system (CNS) has a limited capacity for self-repair following injury or degeneration. Stem cell-based therapies, particularly using mesenchymal stem cells (MSCs), hold promise but face the critical challenge of surviving and integrating within the harsh, inflammatory environment of the injured brain or spinal cord. [5]
Biomaterial scaffolds are being reframed from simple physical "pathways" to multifunctional "platforms" that can actively coordinate the complex process of neural repair. [52] These scaffolds are designed to guide neuronal migration, support axonal regeneration, and enhance the survival and integration of transplanted stem cells. [52] [5] For spinal cord injury (SCI), 3D polymeric scaffolds aim to restore structural integrity and provide directional cues for axonal growth across the lesion. [53]
Conductive polymers, such as polypyrrole and graphene oxide, are particularly promising as they carry electrical impulses that help stimulate neurite outgrowth and restore nerve signal transmission. [5] [53] Combining these with synthetic polymers like PLGA-PEG and bioactive ceramics like hydroxyapatite creates nanocomposite scaffolds with improved biocompatibility, mechanical matching to neural tissue, and enhanced cellular adhesion. [53]
Experimental Protocol: 3D Bioprinting a Nanocomposite Scaffold for Spinal Cord Injury
Objective: To fabricate and evaluate a multifunctional 3D-bioprinted scaffold for supporting axonal regeneration after spinal cord injury. [53]
Materials:
- Polymers: PLGA-PEG copolymer as the primary scaffold material. [53]
- Conductive Nanomaterial: Graphene oxide (GO) to enhance electrical conductivity and cellular interactions. [53]
- Bioactive Ceramic: Hydroxyapatite (HA) to improve biocompatibility and bioactivity. [53]
- Bioink: Alginate-gelatin hydrogel for encapsulating cells or biomolecules.
- 3D Bioprinter: A bioprinter capable of extruding the composite bioink.
Methodology:
- Ink Formulation: Synthesize and characterize the nanocomposite ink by combining PLGA-PEG, GO, and HA. Disperse the components uniformly to ensure printability and functionality. [53]
- Scaffold Design and Printing: Design a 3D scaffold model with micro-architecture that mimics the aligned structure of the spinal cord. Use the bioprinter to fabricate the scaffold, optimizing parameters like pressure, speed, and temperature. [53]
- Scaffold Characterization: Assess the scaffold's mechanical properties (e.g., flexibility, compliance), porosity, degradation profile, and electrical conductivity in vitro. [53]
- In Vitro Testing: Seed the scaffold with neural stem cells or MSCs. Evaluate cell viability, proliferation, and differentiation into neuronal lineages. Assess neurite outgrowth and alignment along the scaffold's structure. [53]
- In Vivo Evaluation: Implant the scaffold into a rodent model of spinal cord injury (e.g., hemisection or contusion). Monitor functional recovery over time using behavioral assays (e.g., Basso Mouse Scale) and conduct post-mortem histological analysis to confirm axonal regeneration and integration with host tissue. [53]
Signaling Pathway: Stem Cell & Scaffold-Mediated Neural Repair
The Scientist's Toolkit: Key Reagents for Neural Repair Studies
Table 3: Essential Research Reagents for Neural Tissue Engineering
| Reagent / Material | Function & Application | Key Characteristics |
|---|---|---|
| Conductive Polymers (e.g., Polypyrrole, Graphene Oxide) | Key component of scaffolds to enhance electrical signaling. [5] [53] | Supports neurite outgrowth and neuronal activity by carrying electrical impulses; often integrated into composite scaffolds. [5] [53] |
| PLGA-PEG Copolymer | Synthetic polymer base for creating flexible, biodegradable scaffolds. [53] | Offers mechanical stability and tunable degradation; PEG moiety can improve biocompatibility and reduce protein adsorption. [53] |
| Neurotrophic Factors (NGF, BDNF, GDNF) | Bioactive signaling molecules for neuronal survival and growth. [5] | Critical for supporting stem cell differentiation and axon guidance; often delivered in a controlled manner from the scaffold. [5] |
| Natural Polymers (Chitosan, Alginate, Collagen) | Hydrogel base for bioinks and cell encapsulation. [5] | Generally biocompatible and can be modified with cell-adhesion peptides; provide a soft, hydrated environment for cells. [5] |
| Neural Stem Cells (NSCs) / MSCs | Therapeutic cell source for repopulating damaged neural circuits. [5] | NSCs have innate neural differentiation potential; MSCs are attractive for their paracrine immunomodulatory and trophic effects. [5] |
Navigating Clinical Hurdles: Safety, Integration, and Functional Maturity
Addressing Low Cell Retention and Survival in Hostile Microenvironments
A significant bottleneck in the clinical translation of stem cell therapies is the massive loss of transplanted cells at the delivery site. In the context of a hostile microenvironment, such as ischemic myocardium or brain tissue, transplanted cells face numerous challenges leading to poor retention and survival. Studies indicate that when stem cells are transplanted as a simple suspension in saline or media, cell retention can be as low as 11% after 90 minutes, dropping to a mere 0.6% within 24 hours [54]. This catastrophic cell loss is attributed to several factors, including mechanical washout, exposure to ischemia and inflammation, leakage from the injection site, and a specific form of programmed cell death called anoikis, which is triggered by the disruption of cell-extracellular matrix (ECM) interactions during cell harvesting [55] [54]. This application note, framed within broader research on biomaterial scaffolds, details quantitative evidence and provides actionable protocols to overcome these barriers.
Quantitative Analysis of the Problem and Biomaterial Solutions
The following tables summarize the key quantitative data on cell retention challenges and the demonstrated efficacy of various biomaterial-based intervention strategies.
Table 1: Documented Cell Retention Rates Following Direct Injection
| Cell Type | Delivery Method | Host Model | Initial Retention | Retention at 24 Hours | Reference |
|---|---|---|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Intramyocardial Injection (Saline) | Infarcted Rat/Porcine Heart | ~11% | ~0.6% | [54] |
| Bone Marrow Stem Cells (BMSCs) | Intracoronary Infusion | Human Acute Myocardial Infarction | - | No improvement in LV function at 4 months | [55] |
Table 2: Efficacy of Biomaterial-Based Strategies in Preclinical Models
| Biomaterial Strategy | Cell Type | Disease Model | Key Outcome & Improvement | Reference |
|---|---|---|---|---|
| Collagen Matrix Patch | BMSCs | Human MI (MAGNUM Phase I Trial) | ↑ Infarct thickness; ↓ LV end-diastolic volume vs. cell-only | [55] |
| Shear-Thinning Hydrogel | Adipose-derived Stem Cells (ASCs) | In vitro Injection Model | 47% higher cell viability at Day 3 post-injection vs. saline | [55] |
| Nanopatterned Cell Patch | Cardiosphere-derived Cells | Rat MI Model | Enhanced cell retention & viability; preserved myocardial thickness | [55] |
| Smooth Muscle Cell-Endothelial Progenitor Cell Sheet | Smooth Muscle Cells, EPCs | Rodent Ischemic Cardiomyopathy | Significant increase in functional microvasculature and myocardial function | [55] |
Classifying Biomaterial Scaffolds for Stem Cell Delivery
Biomaterial-based strategies to enhance stem cell delivery are broadly classified into two categories, each with distinct mechanisms of action.
Injectable Biomaterials
Injectable systems, primarily hydrogels, are designed for minimally invasive delivery. They protect cells from mechanical shear and extensional forces during injection and provide a supportive ECM-like environment upon gelation in situ [55] [56]. Key subtypes include:
- Shear-Thinning Hydrogels: These hydrogels flow as a fluid under the mechanical stress of injection but rapidly self-heal to form a solid gel once deposited, creating "plug flow" that centralizes and protects cells [55] [56]. Examples include alginate and hyaluronic acid (HA).
- Stimuli-Responsive Hydrogels: These materials undergo a sol-gel transition in response to physiological stimuli such as body temperature (thermo-responsive) or local pH (pH-sensitive) [56].
- Microcarriers and Microcapsules: These provide a large surface area for cell attachment and facilitate better diffusion of nutrients and waste, enhancing survival of the encapsulated cells [56].
Implantable Scaffolds
Implantable scaffolds, such as cardiac patches, are typically seeded with cells ex vivo and then surgically attached to the target tissue. They provide a well-defined 3D structure that prevents anoikis and supports long-term cell survival and differentiation [55]. A key challenge is ensuring adequate graft perfusion and thickness, which can limit translation for acute conditions due to the invasive implantation procedure [55].
Detailed Experimental Protocols
Protocol: Assessing Stem Cell Viability Post-Needle Injection Using a Shear-Thinning Hydrogel
This protocol evaluates the protective effect of a biomaterial during the injection process itself [55] [56].
Objective: To quantify and compare the viability of stem cells after being injected through a standard needle using a saline vehicle versus a shear-thinning hydrogel.
Materials:
- Cells: Human Adipose-Derived Stem Cells (ASCs) or Mesenchymal Stem Cells (MSCs).
- Hydrogel: Engineered shear-thinning hydrogel (e.g., alginate or hyaluronic acid-based).
- Control Vehicle: Phosphate-Buffered Saline (PBS).
- Equipment: 1 mL syringes, 26G-32G needles, cell culture incubator, live/dead viability/cytotoxicity kit (e.g., Calcein-AM/Ethidium homodimer-1), fluorescence microscope, hemocytometer or automated cell counter.
Method:
- Cell Preparation: Harvest and concentrate cells to 5 x 10^6 cells/mL.
- Vehicle Preparation: Gently mix the cell pellet with either:
- Experimental Group: 1 mL of shear-thinning hydrogel precursor.
- Control Group: 1 mL of PBS.
- Injection Simulation:
- Load each cell suspension into a 1 mL syringe fitted with a 27G needle.
- Eject the suspension into a sterile microcentrifuge tube at a controlled, slow flow rate (e.g., 5-10 µL/min) using a syringe pump.
- Viability Assessment:
- Incubate the ejected samples for 1 hour at 37°C to allow hydrogel gelation.
- For hydrogel samples, add a chelating agent (e.g., EDTA for alginate) to liquefy the gel for cell counting.
- Mix a 50 µL aliquot of each sample with 50 µL of live/dead stain.
- Incubate for 30 minutes in the dark.
- Count live (green) and dead (red) cells using a hemocytometer under a fluorescence microscope or an automated cell counter with fluorescence capability.
- Data Analysis: Calculate percentage viability as (Number of live cells / Total number of cells) x 100. Compare the hydrogel group to the PBS control using a Student's t-test.
Protocol: In Vivo Evaluation of a Biomaterial-Enhanced Stem Cell Therapy in a Rodent MI Model
This protocol assesses the functional improvement of a cell-seeded biomaterial in a disease model [55] [54].
Objective: To determine the effect of a cell-laden hydrogel on cardiac function and cell engraftment in a rodent model of myocardial infarction.
Materials:
- Animals: Adult Sprague-Dawley rats.
- Surgical Supplies: Equipment for left anterior descending (LAD) coronary artery ligation, small animal ventilator, echocardiography system.
- Test Articles:
- Group 1: ASCs in shear-thinning hydrogel.
- Group 2: ASCs in PBS (cell-only control).
- Group 3: Hydrogel only (material control).
- Group 4: Sham operation.
- Histology: Antibodies for specific cell markers (e.g., cardiac Troponin T, CD31), TUNEL assay kit.
Method:
- MI Induction and Treatment: Anesthetize rats and perform LAD ligation to induce MI. Immediately after ligation, randomly assign animals to treatment groups and perform intramyocardial injections at the infarct border zone.
- Functional Assessment: Perform transthoracic echocardiography pre-surgery and at 4 weeks post-treatment. Measure Left Ventricular End-Diastolic Volume (LVEDV) and Ejection Fraction (EF).
- Tissue Harvest and Analysis: At 4 weeks, euthanize animals and harvest hearts.
- Histology: Section hearts and stain with Masson's Trichrome to quantify infarct size and fibrosis. Perform immunofluorescence staining to identify transplanted cells (pre-labeled with a cell tracker or expressing a reporter like GFP) and assess differentiation and angiogenesis.
- Cell Engraftment Quantification: Use fluorescence imaging or quantitative PCR for a human-specific gene to determine the number of retained human cells.
- Data Analysis: Compare functional parameters (LVEDV, EF) and structural parameters (infarct size, cell engraftment) between groups using one-way ANOVA with post-hoc testing.
Workflow for Developing a Biomaterial-Based Therapy
The path from concept to preclinical validation involves a series of interconnected steps, as outlined below.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Biomaterial-Enhanced Stem Cell Research
| Item | Function/Application | Example & Notes |
|---|---|---|
| Alginate | Base polymer for ionic cross-linking; forms shear-thinning hydrogels. | Use high-G content for stiffer gels; cross-link with Ca²⁺ ions. |
| Hyaluronic Acid (HA) | Native ECM component; can be modified to form injectable hydrogels. | Often functionalized with methacrylate groups (MeHA) for photo-cross-linking. |
| Polyethylene Glycol (PEG) | Synthetic, "blank slate" polymer; highly tunable mechanical properties. | Functionalized with maleimide or vinyl sulfone groups for bio-orthogonal click chemistry. |
| RGD Peptide | Cell-adhesive ligand; incorporated into biomaterials to prevent anoikis. | Crucial for promoting integrin-mediated cell adhesion and survival. |
| Live/Dead Viability Assay | Quantifies cell survival after injection or within a 3D construct. | Calcein-AM (live, green) / EthD-1 (dead, red) is the standard. |
| Bioluminescence Imaging (BLI) | Non-invasive, longitudinal tracking of cell retention in live animals. | Requires cells transduced with a luciferase reporter gene. |
| Shear-Thinning Hydrogel Kit | Ready-to-use system for testing cell delivery protection. | Commercial kits (e.g., HyStem-C) can accelerate initial proof-of-concept studies. |
The integration of stem cells with advanced biomaterial scaffolds represents a paradigm shift in regenerative medicine, directly addressing the critical challenge of low cell retention and survival. The quantitative data and detailed protocols provided here underscore the efficacy of this approach, from protecting cells during injection to supporting their long-term engraftment and function. By employing these strategies, researchers can significantly enhance the therapeutic potential of stem cells, paving the way for more effective and reliable clinical applications.
The application of induced pluripotent stem cells (iPSCs) in regenerative medicine represents a paradigm shift, offering the potential for patient-specific cell therapies. However, the clinical translation of iPSC-based treatments is significantly hampered by two primary safety concerns: their inherent tumorigenic potential and the risk of immune rejection upon transplantation. iPSCs, similar to embryonic stem cells (ESCs), possess the capacity for self-renewal and differentiation into virtually all cell types, which also renders them capable of forming teratomas or teratocarcinomas if undifferentiated cells remain in the graft [57]. Furthermore, the assumption that autologous iPSCs would be immune-privileged has been challenged by studies demonstrating that even syngeneic iPSCs can elicit an immune response, leading to graft rejection [57] [58].
Biomaterial scaffolds are increasingly investigated as a strategic delivery system to mitigate these risks. These scaffolds provide a three-dimensional environment that can enhance the survival, integration, and directed differentiation of transplanted cells while acting as a protective barrier against the host immune system. This application note details the critical risks associated with iPSC therapies and provides structured protocols and data for their mitigation within the context of biomaterial scaffold research.
Quantitative Risk Profiling of iPSC-Based Therapies
Tumorigenicity and Survival Rates
The risk of tumor formation from stem cell grafts is a primary determinant of survival in animal models. A comparative study transplanting different stem cell types into syngeneic mouse brains provided stark quantitative evidence of this risk [58].
Table 1: Survival Rates and Tumorigenicity Post-Stem Cell Transplantation in Mouse Brain
| Stem Cell Type Grafted | Survival Rate at 14 Days | Survival Rate at 28 Days | Evidence of Tumor Formation |
|---|---|---|---|
| iPSCs | ~60% | <15% | Yes (Malignant to Benign Teratomas) |
| ESCs | ~50% | <10% | Yes (Malignant to Benign Teratomas) |
| iNSCs | ~100% | ~100% | No |
| NSCs | ~100% | ~100% | No |
| MSCs | ~100% | ~100% | No |
The data underscores the high tumorigenic risk associated with pluripotent cells (iPSCs and ESCs), leading to massive animal death within 28 days. In contrast, induced Neural Stem Cells (iNSCs), Neural Stem Cells (NSCs), and Mesenchymal Stem Cells (MSCs) showed no evidence of tumor formation and allowed for long-term survival, presenting them as safer alternatives for cell-based therapies [58].
Immunogenicity and Host Immune Response
The immunogenicity of stem cell grafts is closely linked to their tumorigenicity. Immune cell infiltration is a hallmark of graft rejection and is profoundly more significant in response to tumor-forming pluripotent cells.
Table 2: Immune Cell Infiltration in Mouse Brain Following Stem Cell Transplantation
| Stem Cell Type Grafted | CD11b+ Microglia/Macrophages | CD3+ T Cells | CD19+ B Cells | Correlation with Tumor Grade |
|---|---|---|---|---|
| iPSCs (G3 Tumors) | Massive Infiltration | Massive Infiltration | Massive Infiltration | Strong Positive |
| ESCs (G3 Tumors) | Massive Infiltration | Massive Infiltration | Massive Infiltration | Strong Positive |
| iPSCs/ESCs (G1/G2 Tumors) | Moderate Infiltration | Moderate Infiltration | Moderate Infiltration | Positive |
| iNSCs / NSCs / MSCs | Minimal to None | Minimal to None | Minimal to None | Not Applicable |
This immune response is driven by the recognition of foreign antigens. A key finding is the elevated levels of chemokines in the brain tissue and serum of mice that developed tumors from ESC or iPSC grafts. This chemokine release is positively correlated with the activation of the NF-κB signaling pathway, creating a pro-inflammatory feedback loop that exacerbates immune rejection and tissue damage [58].
Molecular Mechanisms of Immunogenicity
MHC Expression and Its Regulation
The immunogenicity of PSCs and their derivatives is largely governed by the expression of Major Histocompatibility Complex (MHC) molecules.
- Undifferentiated PSCs: Exhibit a state of immune privilege, characterized by low or absent surface expression of MHC class I molecules and a complete absence of MHC class II antigens and co-stimulatory molecules (CD80, CD86) [57].
- Upon Differentiation: A significant upsurge in MHC class I expression is typically observed. This increased immunogenicity poses a substantial barrier to the survival of transplanted differentiated cells [57].
- Epigenetic Control: The expression of these immune molecules is tightly regulated by epigenetic mechanisms. In undifferentiated human ESCs and iPSCs, the genes for MHC class II and its master regulator, CIITA, are silenced via heavy DNA methylation. In contrast, MHC class I genes undergo demethylation and activating histone modifications (e.g., H3K4me3) during differentiation, facilitating their expression and increasing susceptibility to T-cell-mediated rejection [57].
Signaling Pathways in Immune Rejection
The following diagram illustrates the key molecular and cellular interactions in the tumorigenicity and immune rejection of iPSC grafts.
Experimental Protocols for Risk Assessment
Protocol: In Vivo Tumorigenicity Assay
Objective: To evaluate the tumor-forming potential of iPSCs or their derivatives post-transplantation in an immunocompetent syngeneic model [58].
Cell Preparation:
- Harvest iPSCs, control ESCs (positive control), and iNSCs/NSCs (negative control) using standard methods.
- Prepare a single-cell suspension at a concentration of 1x10^5 to 1x10^6 cells/µL in a sterile, cold buffer suitable for injection (e.g., PBS with low glucose).
Animal Model and Transplantation:
- Use immunocompetent, syngeneic adult mice (e.g., C57BL/6).
- Anesthetize the animals and secure them in a stereotaxic apparatus.
- Using a micro-syringe, perform an intracerebral (or site-specific) injection of the cell suspension (e.g., 2-5 µL) into the target region (e.g., motor cortex). The coordinates should be predetermined based on a mouse brain atlas.
- Include a sham-surgery control group injected with vehicle only.
Post-Operative Monitoring:
- Monitor animals daily for survival and general health.
- Observe for specific neurological or behavioral deficits that may indicate tumor growth.
- Maintain the cohort for a predetermined endpoint (e.g., 28 days for acute tumorigenicity, 24 weeks for long-term survival).
Histopathological Analysis:
- At endpoint, perfuse animals transcardially with PBS followed by 4% paraformaldehyde (PFA).
- Extract brains, post-fix in PFA, and embed in paraffin.
- Section tissues serially (5-7 µm thickness) throughout the injection site and stain with Hematoxylin and Eosin (H&E).
- Have blinded, board-certified pathologists grade tumors based on established criteria, assessing malignancy, tissue destruction, and immune cell infiltration [58].
Protocol: Assessment of Graft-Induced Immunogenicity
Objective: To characterize the type and extent of host immune cell infiltration in response to the transplanted graft [58].
Tissue Preparation:
- Follow the animal model and transplantation steps from Protocol 4.1.
- At the desired timepoints (e.g., 7, 14, 28 days post-transplant), harvest the graft site and surrounding tissue.
Immunofluorescence Staining:
- Generate cryosections or deparaffinized sections of the tissue.
- Perform antigen retrieval if required.
- Block sections with an appropriate serum (e.g., 5% normal goat serum) for 1 hour at room temperature.
- Incubate sections overnight at 4°C with primary antibodies against:
- CD11b (for microglia/macrophages)
- CD3 (pan-T cell marker)
- CD4 (helper T cells)
- CD8 (cytotoxic T cells)
- CD19 (B cells)
- The following day, incubate with fluorophore-conjugated secondary antibodies for 1 hour at room temperature, protected from light.
- Counterstain nuclei with DAPI and mount with an anti-fade medium.
Imaging and Quantification:
- Acquire high-resolution images using confocal laser scanning microscopy (CLSM).
- Use image analysis software to count the number of specific immune-positive cells in standardized fields of view within and around the graft site.
- Statistically compare the density of infiltrated immune cells between experimental groups (e.g., iPSC vs. iNSC grafts).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for iPSC Safety Research
| Research Reagent / Material | Function and Application in Risk Mitigation Studies |
|---|---|
| Porous Collagen-Based Scaffolds (PCS) | A biomaterial used to deliver and protect NSCs at injury sites; shown to enhance neuronal differentiation, axonal elongation, and locomotion recovery in spinal cord injury models while reducing astrogliosis [22]. |
| Biomimetic Scaffolds (Porous, Hydrogel, Nanofibrous) | Used for seeding and delivering MSCs or MSC-derived exosomes; enhances cell shelf life and exosome stability, providing a conducive 3D environment for wound healing and immunomodulation [59]. |
| Flow Cytometry Antibody Panels (CD29, CD44, CD14, CD34, CD45) | For the identification and characterization of MSCs based on positive (CD29, CD44) and negative (CD14, CD34, CD45) surface marker expression [58]. |
| Immunofluorescence Antibodies (Nanog, Nestin, Sox2, GFAP, Tuj1, Olig2) | Key for characterizing stem cell identity (Nanog for pluripotency, Nestin for NSCs) and tracking differentiation outcomes (GFAP for astrocytes, Tuj1 for neurons, Olig2 for oligodendrocytes) in vitro and in vivo [22] [58]. |
| Cytokine/Chemokine Multiplex Assays | To quantify elevated levels of pro-inflammatory chemokines and cytokines (e.g., in serum or tissue homogenates) associated with tumor formation and immune rejection, such as in response to iPSC/ESC grafts [58]. |
Concluding Remarks
The journey of iPSCs from the laboratory to the clinic is contingent upon rigorously addressing the dual challenges of tumorigenicity and immunogenicity. The data and protocols outlined herein provide a framework for researchers to systematically evaluate these risks. The integration of biomaterial scaffolds, such as porous collagen-based matrices, presents a highly promising strategy to enhance graft survival, direct cell fate, and shield transplanted cells from immune surveillance. Future work must focus on optimizing scaffold design—tailoring composition, porosity, and degradation kinetics—and combining them with safer cell sources like iNSCs to develop robust and clinically viable regenerative therapies.
Overcoming Differentiation Variability and Epigenetic Memory
The therapeutic application of induced pluripotent stem cells (iPSCs) is fundamentally constrained by two interconnected biological challenges: differentiation variability and epigenetic memory. Differentiation variability refers to the inconsistent efficiency with which iPSC lines generate desired, functionally mature somatic cells. A major contributor to this inconsistency is epigenetic memory—the residual epigenetic signatures (DNA methylation, histone modifications) inherited from the parental somatic cell, which can create a lineage-specific bias, favoring differentiation back into the original cell type [7] [60]. Within the context of biomaterial scaffolds for stem cell delivery, these challenges are exacerbated as the scaffold microenvironment must not only support cell survival and engraftment but also actively counteract these inherent variabilities to ensure reproducible and safe therapeutic outcomes. This Application Note details protocols and strategies, centered on a novel "bottom-up" biomaterial design paradigm, to directly overcome these barriers [7] [24].
The tables below summarize the core problems and the corresponding biomaterial-based intervention strategies.
Table 1: Impact of Epigenetic Memory on iPSC Differentiation. Adapted from [7] [61] [60].
| Challenge | Underlying Mechanism | Impact on Differentiation |
|---|---|---|
| Lineage Bias | Retention of parental somatic cell epigenetic marks (e.g., DNA methylation, H3K27me3) [7] [60]. | iPSCs show preferential differentiation toward their tissue of origin, leading to heterogeneous cell populations [7]. |
| Incomplete Maturation | Failure to fully activate mature cell gene networks (e.g., MAFA, NKX6.1 in β-cells) and silence "disallowed" genes [60]. | Derived cells exhibit immature functionality, such as low amplitude Glucose-Stimulated Insulin Secretion (GSIS) [60]. |
| Inter-Donor Variability | Differences in the epigenetic background of the source cells from different donors [7]. | Significant line-to-line variation in differentiation efficiency and functional maturity [7] [60]. |
Table 2: Biomaterial Strategies to Modulate Epigenetic Memory and Enhance Differentiation. Based on [7] [61] [24].
| Biomaterial Strategy | Target Epigenetic Mechanism | Expected Outcome |
|---|---|---|
| Tailored Mechanical Cues | Modulation of chromatin remodeling via mechanotransduction pathways [7]. | Promotes erasure of somatic memory and acquisition of new lineage-specific epigenetic states. |
| Spatial Patterning of Epigenetic Inhibitors/Activators | Localized delivery of small molecules targeting DNMTs (e.g., 5-Azacytidine) or EZH2 inhibitors [61]. | Resets epigenetic memory and reduces lineage bias, improving differentiation fidelity. |
| Dynamic Biochemical Gradients | Control of signaling pathways (Wnt, TGF-β, BMP) that interact with the epigenetic machinery [7] [61]. | Guides coordinated epigenetic and transcriptional changes for precise lineage specification. |
Experimental Protocols
Protocol: Epigenetic Reset of Human iPSCs Using Biomaterial-Assisted Culture
This protocol describes a method to reduce lineage-restricting epigenetic memory in iPSCs prior to differentiation, using a biomaterial substrate engineered to deliver mechanical and biochemical cues.
I. Materials
- Human iPSCs with known parental somatic cell origin.
- Engineered Hydrogel Substrate: Synthesize a hyaluronic acid-based hydrogel tuned to a stiffness of ~1 kPa to mimic the mechanical properties of a naive epiblast [7].
- EZH2 Inhibitor Solution: Prepare a 10 mM stock solution of GSK126 or DZNep in DMSO [61].
- Standard iPSC culture reagents: mTeSR Plus medium, Vitronectin, DPBS, Accutase.
II. Procedure
Biomaterial Functionalization:
- Mix the hydrogel precursor solution according to manufacturer's instructions.
- For experimental group: Supplement the hydrogel solution with the EZH2 inhibitor to a final working concentration of 1 µM before polymerization.
- For control group: Use hydrogel supplemented with an equivalent volume of vehicle (DMSO).
- Pipette the solution into culture plates and allow to polymerize at 37°C for 30 minutes.
Cell Seeding and Culture:
- Harvest human iPSCs as single cells using Accutase. Neutralize with DMEM/F-12 + 10% FBS and count.
- Seed cells at a density of 15,000 cells/cm² onto the functionalized and control hydrogels in mTeSR Plus medium containing 10 µM Y-27632 (ROCK inhibitor).
- Refresh the medium daily for 5-7 days, ensuring the experimental group is maintained in medium containing 1 µM EZH2 inhibitor.
Assessment of Epigenetic Reset:
- Day 7: Harvest cells for analysis.
- Immunofluorescence: Stain for H3K27me3. A successful reset should show a significant reduction in global H3K27me3 levels in the experimental group compared to the vehicle control [61].
- qPCR: Analyze the expression of lineage-specific genes from the parental cell type. Reduced expression indicates diminished epigenetic memory.
- Flow Cytometry: Assess the homogeneity of pluripotency markers (OCT4, NANOG). Increased homogeneity suggests a more naive population.
Protocol: Directed Differentiation of iPSCs to Pancreatic β-Cells on a 3D Biomaterial Scaffold
This protocol leverages a staged, biomaterial-guided approach to direct epigenetically reset iPSCs into functionally mature pancreatic β-cells, overcoming inherent maturation barriers.
I. Materials
- "Reset" iPSCs from Protocol 3.1.
- 3D Porous Scaffold: Use a Polycaprolactone (PCL) scaffold fabricated via electrospinning, with a fiber diameter of 1-2 µm and porosity >90% to facilitate high cell loading and mass transport [5].
- Differentiation Media: Prepare a series of basal media (e.g., MCDB131) supplemented with stage-specific factors as outlined below [60].
II. Procedure
Scaffold Preparation and Cell Seeding:
- Sterilize PCL scaffolds in 70% ethanol for 30 minutes, followed by extensive washing with DPBS.
- Pre-condition scaffolds in basal medium for 2 hours at 37°C.
- Seed a single-cell suspension of reset iPSCs at a high density (5-10 million cells per scaffold) onto the pre-conditioned scaffolds using a centrifugal force method to ensure efficient infiltration.
Staged Differentiation in 3D Culture: The following stages are conducted with the scaffold immersed in the respective media, which are changed every 2-3 days.
- Stage 1: Definitive Endoderm (Days 1-3). Culture in media containing Activin A (100 ng/mL) and CHIR99021 (3 µM) to induce definitive endoderm commitment [60].
- Stage 2: Primitive Gut Tube (Days 4-7). Switch to media with FGF10 (50 ng/mL) and KAAD-cyclopamine (0.25 µM).
- Stage 3: Pancreatic Progenitors (Days 8-12). Use media supplemented with Retinoic Acid (2 µM), Noggin (50 ng/mL), and SB431542 (10 µM) to promote pancreatic fate.
- Stage 4: Pancreatic β-Cell Maturation (Days 13-30). Culture in media containing T3 (1 µM), ALK5i II (10 µM), and Betalin-1 (10 µM) to drive final functional maturation.
Functional Characterization:
- Glucose-Stimulated Insulin Secretion (GSIS) Assay (Day 30):
- Pre-incubate scaffolds in low glucose (2.8 mM) Krebs buffer for 1 hour.
- Stimulate with high glucose (20 mM) Krebs buffer for 1 hour.
- Collect supernatants and measure insulin secretion via ELISA. A mature functionality is indicated by a Stimulation Index (high glucose/low glucose) >2 [60].
- Immunohistochemistry: Section scaffolds and stain for key maturity markers: PDX1, NKX6.1, INSulin, and MAFA. Co-localization of these markers indicates a mature β-cell phenotype.
- Glucose-Stimulated Insulin Secretion (GSIS) Assay (Day 30):
Visualization of Strategies and Workflows
The following diagrams illustrate the core concepts and experimental workflows.
Diagram 1: Overcoming Epigenetic Memory with Biomaterials.
Diagram 2: Experimental Workflow for Functional Cell Generation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Implementing the Protocols.
| Item | Function/Application | Example/Catalog Note |
|---|---|---|
| Hyaluronic Acid-Based Hydrogel | A tunable biomaterial for 2D culture that provides mechanical and biochemical cues to influence cell fate and epigenetics [7]. | Select a system (e.g., HyStem) that allows for user-defined stiffness modulation (0.5 - 5 kPa). |
| EZH2 Inhibitor (GSK126) | A small molecule inhibitor that targets the histone methyltransferase EZH2, reducing H3K27me3 levels to help erase epigenetic memory [61]. | Reconstitute in DMSO for a 10 mM stock; use at 0.5-1 µM working concentration in culture. |
| Electrospun PCL Scaffold | A synthetic, biodegradable 3D scaffold providing structural support and high surface area for 3D cell culture and tissue formation [5]. | Source or fabricate scaffolds with high porosity (>90%) and fiber diameters in the 1-2 µm range. |
| Staged Differentiation Factors Kit | A collection of recombinant proteins and small molecules for the precise, multi-stage differentiation of iPSCs into specific lineages like pancreatic β-cells [60]. | Look for kits that include Activin A, CHIR99021, FGF10, Retinoic Acid, and T3 for endodermal lineages. |
| Glucose-Stimulated Insulin Secretion (GSIS) Assay Kit | A critical functional assay to validate the maturity and glucose-responsive function of derived β-cells [60]. | Ensure the kit includes low/high glucose buffers and a sensitive, specific insulin ELISA. |
The integration of a "bottom-up" biomaterial design philosophy—which prioritizes the fundamental biological needs of stem cells—provides a powerful and necessary framework for tackling the persistent challenges of differentiation variability and epigenetic memory [7] [24]. The protocols and strategies outlined here demonstrate that by engineering biomaterial scaffolds to actively manipulate the epigenetic landscape and guide differentiation through physiologically relevant cues, researchers can significantly enhance the fidelity, efficiency, and functional maturity of iPSC-derived cells. This approach is indispensable for advancing the clinical translation of reliable and safe stem cell-based therapies.
Biomaterial scaffolds are engineered structures designed to support, control, and stimulate the regeneration of biological tissues. Within the context of stem cell delivery for regenerative medicine, these scaffolds serve as temporary three-dimensional frameworks that mimic the native extracellular matrix (ECM). The efficacy of a scaffold is largely determined by three critical optimization levers: its mechanical properties, which must match the target tissue to avoid stress shielding and provide appropriate cues for cellular development; its architectural porosity, which facilitates nutrient diffusion, waste removal, and cell migration; and its biofunctionalization, which provides biochemical signals to direct stem cell fate. This document provides detailed application notes and experimental protocols for the characterization and optimization of these fundamental parameters to advance research in biomaterial scaffolds for stem cell delivery.
Optimization of Mechanical Properties
The mechanical properties of a scaffold—including its elastic modulus, tensile strength, and degradation rate—are paramount as they directly influence stem cell adhesion, proliferation, differentiation, and overall functionality. An inappropriate mechanical environment can lead to implant failure or poor therapeutic outcomes.
Key Biomaterials and Their Mechanical Characteristics
The choice of material forms the foundation of a scaffold's mechanical behavior. Both natural and synthetic polymers are widely used, each offering distinct advantages.
Table 1: Characteristics of Common Biomaterials for Scaffold Fabrication
| Material Class | Example Materials | Key Mechanical & Biological Properties | Advantages | Limitations |
|---|---|---|---|---|
| Natural Polymers | Collagen, Gelatin, Chitosan, Alginate, Hyaluronan, Silk Fibroin [5] | Elastic, biocompatible, biodegradable, often contain cell-adhesion motifs. | High biocompatibility; inherent bioactivity. | Batch-to-batch variability; lower mechanical strength. |
| Synthetic Polymers | Poly(L-lactic acid) (PLLA), Poly(glycolic acid) (PGA), Polycaprolactone (PCL), Poly(lactic-co-glycolic acid) (PLGA) [5] [62] | Tunable mechanical strength and degradation rate (e.g., via molecular weight and copolymer ratio). | Reproducible and tunable properties. | Typically hydrophobic; lack of natural bioactivity. |
| Conductive Polymers | Polypyrrole, Polythiophene, Polyaniline [5] | Conduct electricity; can enhance neurite outgrowth and cell activity under electrical stimulation. | Enables electrical stimulation for neural and cardiac applications. | Processing can be challenging; biocompatibility varies. |
Protocol: Fabrication and Mechanical Testing of PLGA-based Porous Scaffolds
This protocol details the creation of a composite scaffold using PLGA and nano-hydroxyapatite (nHA) through thermally induced phase separation, a method that yields highly porous structures suitable for bone tissue engineering [62].
Materials:
- PLGA (Lactide:Glycolide = 80:20)
- nano-Hydroxyapatite (nHA)
- 1,4-Dioxane (solvent)
- Liquid Nitrogen or -20°C Freezer
- Freeze Dryer
Procedure:
- Dissolution: Dissolve 720 mg of PLGA in 12 mL of 1,4-dioxane in a glass vial under magnetic stirring for 30 minutes.
- Dispersion: Add 360 mg of nHA to the PLGA solution. Use an ultrasonic homogenizer to disperse the nHA completely for 10 minutes to avoid agglomeration.
- Casting: Pour the homogeneous PLGA/nHA/1,4-dioxane mixture into a polytetrafluoroethylene (PTFE) mold.
- Phase Separation: Rapidly transfer the mold to a -20°C freezer and incubate overnight to allow for complete thermally induced phase separation.
- Lyophilization: Transfer the frozen scaffold to a freeze dryer. Lyophilize for at least 48 hours to sublime the 1,4-dioxane solvent crystals, resulting in a dry, porous scaffold.
- Sterilization: Sterilize the final scaffold using Gamma irradiation (e.g., 25 kGy Co⁶⁰) prior to in vivo use [62].
Mechanical Characterization:
- Elastic Modulus and Tensile Strength: Perform uniaxial tensile testing using a standard mechanical tester. Cut scaffolds into dog-bone-shaped specimens. Measure the stress-strain curve at a constant strain rate (e.g., 1 mm/min) until failure. The elastic modulus is calculated from the linear slope of the stress-strain curve.
- Compressive Strength: For scaffolds intended for load-bearing applications (e.g., bone), perform compressive testing on cylindrical samples.
Control of Scaffold Porosity
Porosity and pore interconnectivity are critical for vascularization, nutrient diffusion, and tissue in-growth. The ideal scaffold should have a high, interconnected porosity to facilitate these processes while maintaining mechanical integrity.
Additive Manufacturing Technologies for Porosity Control
Additive manufacturing (AM) enables precise control over pore size, shape, and distribution, allowing for the fabrication of scaffolds with customized architectures.
Table 2: Additive Manufacturing Technologies for Porous Scaffold Fabrication [63]
| Technology | Resolution (μm) | Applicable Materials | Key Advantages | Key Disadvantages |
|---|---|---|---|---|
| Selective Laser Sintering (SLS) | 76 - 100 | Polymers, Metals, Alloys | Complex geometry; no support structures needed; high powder reuse. | Low energy efficiency; relatively low part density. |
| Selective Laser Melting (SLM) | 80 - 250 | Metals and Alloys (e.g., Ti, Ta) [63] | Complex geometry; high density parts with mechanical properties comparable to forged material. | High cost; residual stress; rough surface finish. |
| Electron Beam Melting (EBM) | 50 - 100 | Metals and Alloys (e.g., Ti alloys, Co-Cr) | High energy efficiency; operates in vacuum; good for reactive metals. | High cost; rough surface finish; limited material selection. |
Protocol: Porosity Measurement via Liquid Displacement
This is a common method for determining the overall porosity of a scaffold [62].
Materials:
- Scaffold sample
- Anhydrous Ethanol
- Density bottle or graduated cylinder
- Analytical balance
Procedure:
- Weigh the dry scaffold (W).
- Immerse the scaffold in a known volume (V1) of ethanol in a graduated cylinder in a vacuum desiccator. Apply a vacuum for 15-20 minutes to force the ethanol into the pores, ensuring full infiltration.
- After releasing the vacuum, record the new total volume (V2) (scaffold + ethanol).
- Remove the ethanol-impregnated scaffold and record the remaining ethanol volume (V3).
- Calculations:
- Volume of the scaffold skeleton, Vs = V2 - V3
- Total volume of the scaffold, Vt = V2 - V1
- Porosity (%) = [(Vt - Vs) / Vt] × 100
Strategies for Biofunctionalization
Biofunctionalization involves modifying a scaffold's surface or bulk material with biochemical cues to direct specific cellular responses, such as stem cell adhesion, proliferation, and differentiation.
Incorporation of Growth Factors and Cytokines
A powerful strategy is the controlled delivery of growth factors. This can be achieved using a multi-carrier system to protect the bioactive molecules and control their release kinetics.
Protocol: Fabrication of ADM-Loaded Chitosan Microsphere-Scaffold Composite [62]
This protocol describes the incorporation of Adrenomedullin (ADM), an osteogenic and angiogenic peptide, into a PLGA/nHA scaffold via chitosan microspheres.
Part A: Preparation of Chitosan Microspheres (Emulsion-Ionic Cross-linking)
- Dissolve 900 mg of chitosan in 29 mL of 2% (v/v) aqueous acetic acid.
- Dissolve 1 mg of ADM in 1 mL of 2% (v/v) acetic acid and add it to the chitosan solution.
- Pour this mixture into 300 mL of liquid paraffin containing 2% (w/v) Span-80 emulsifier. Stir mechanically at 400-600 rpm for 2 hours to form a water-in-oil emulsion.
- Slowly add 70 mL of 5% (w/v) tripolyphosphate (TPP) solution dropwise to cross-link the chitosan. Continue stirring for 4 hours.
- Collect the microspheres by centrifugation, and wash repeatedly with petroleum ether, isopropyl alcohol, and distilled water.
- Lyophilize the microspheres to obtain a dry powder.
Part B: Composite Scaffold Fabrication
- Follow the PLGA/nHA scaffold fabrication protocol from Section 2.2.
- After dispersing the nHA in the PLGA/1,4-dioxane solution, add 240 mg of the ADM-loaded chitosan microspheres.
- Agitate the mixture to disperse the microspheres uniformly before casting and freeze-drying.
Part C: In Vitro Release Study
- Immerse the composite scaffold in 10 mL of simulated body fluid (SBF) at 37°C under dynamic conditions (e.g., shaking incubator).
- At predetermined time intervals, withdraw the release medium and replace it with fresh SBF.
- Analyze the concentration of released ADM in the collected medium using High-Performance Liquid Chromatography (HPLC) to characterize the release profile over several weeks [62].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Biomaterial Scaffold Research and Stem Cell Delivery
| Reagent / Material | Function and Application in Research |
|---|---|
| PLGA | A synthetic, biodegradable copolymer used as the primary scaffold material; its degradation rate and mechanical properties can be tuned by altering the lactide:glycolide ratio [62]. |
| Chitosan | A natural polymer used to form microspheres for the controlled delivery of peptides/proteins due to its biocompatibility, biodegradability, and strong adhesion [62]. |
| nano-Hydroxyapatite (nHA) | A ceramic material that mimics the mineral component of bone; incorporated into polymer scaffolds to improve osteoconductivity and mechanical strength [62]. |
| Adrenomedullin (ADM) | A multifunctional growth factor peptide with demonstrated osteogenic and pro-angiogenic effects, used as a model bioactive molecule for bone tissue engineering [62]. |
| Mesenchymal Stem Cells (MSCs) | A primary adult stem cell type used in therapeutic delivery for their multi-lineage differentiation potential, immunomodulatory properties, and relative ease of isolation from bone marrow, adipose tissue, or umbilical cord [5]. |
| Nerve Growth Factor (NGF) | A neurotrophic factor used to functionalize scaffolds for neural tissue engineering applications to promote neurite outgrowth and neuronal survival [5]. |
Visualization of Experimental Workflows and Signaling
Microsphere-Scaffold Composite Fabrication Workflow
Key Signaling Pathways in Neuronal Repair
Bench-to-Bedside Translation: In Vivo Models and Biomaterial Performance
In vivo models are indispensable for evaluating the safety and efficacy of novel biomaterial scaffolds for stem cell delivery. This document provides detailed application notes and standardized protocols for two critical areas of preclinical research: rodent cutaneous wound models and large bone defect studies. The content is structured to offer drug development professionals a clear framework for designing, executing, and interpreting in vivo validation experiments, ensuring data quality, reproducibility, and translational relevance.
Rodent Cutaneous Wound Healing Models
Rodent models are extensively used to study the mechanisms of wound healing and to test the therapeutic potential of stem cell-laden scaffolds for treating chronic non-healing wounds [64]. These models provide valuable mechanistic insights into how experimental interventions, such as biomaterial scaffolds, affect the complex wound healing process [64].
Model Selection and Key Considerations
Selecting an appropriate wound model is crucial for generating meaningful, translatable data. The table below summarizes the most frequently used rodent wound models and their primary applications [65] [64].
Table 1: Common Rodent Wound Models for Scaffold and Stem Cell Testing
| Model Type | Species/Strain | Induction Method | Simulated Human Condition | Key Research Applications |
|---|---|---|---|---|
| Excisional | Mice (e.g., C57BL/6, nude mice), Rats | Full-thickness skin removal | Acute wounds, Diabetic ulcers | Assessing wound closure kinetics, re-epithelialization, granulation tissue formation [66] |
| Diabetic | Genetically diabetic (db/db) mice, Streptozotocin (STZ)-induced | Chemical (STZ) or genetic mutation | Diabetic foot ulcers (DFUs) | Studying impaired healing in hyperglycemic conditions; testing pro-healing interventions [64] |
| Ischemic | Mice, Rats | Magnetic pressure-induced, ligation | Ischemic wounds, Pressure ulcers | Evaluating angiogenesis and healing in a low-oxygen microenvironment [65] [64] |
| Burns | Mice, Rats | Contact with heated metal rod | Thermal burn injuries | Investigating burn wound progression, infection control, and scar management [64] |
Critical Biological Variables: Data obtained from these models can vary considerably depending on species, strain, sex, age, hair cycling, and microbiome diversity [64]. For instance, the use of immunodeficient nude mice is essential for testing human-derived stem cells like Fetal Skin-Derived Stem Cells (FSSCs) to prevent xenogeneic rejection [66].
Experimental Protocol: Excisional Wound Model in Nude Mice
The following protocol is adapted from a study investigating fetal skin-derived stem cells (FSSCs) and can be adapted for evaluating biomaterial scaffolds [66].
Objective: To assess the efficacy of a novel stem cell-seeded scaffold in accelerating full-thickness cutaneous wound healing.
Materials:
- Animals: Female BALB/c nude mice (8-10 weeks old).
- Test Article: Scaffold containing therapeutic stem cells (e.g., FSSCs, ADSCs).
- Anesthesia: Isoflurane (3-5% for induction, 1-2% for maintenance).
- Surgical Supplies: Clippers, depilatory cream, povidone-iodine solution, surgical marker, biopsy punch (e.g., 6-8 mm), forceps, scissors, sutures or silicone splints, wound dressing.
- Analysis Tools: Digital camera for planimetry, histological equipment, immunohistochemistry reagents (e.g., for CD31, VEGF, Collagen I/III).
Procedure:
- Pre-operative Preparation:
- House mice under a 12-hour light/dark cycle with ad libitum access to food and water.
- Acclimate animals for at least one week prior to surgery.
- Obtain approval from the relevant Institutional Animal Care and Use Committee (IACUC).
Wound Creation (Day 0):
- Anesthetize the mouse and confirm depth of anesthesia by absence of pedal reflex.
- Shave the dorsal hair and apply depilatory cream to ensure a clean surgical field.
- Disinfect the skin with povidone-iodine solution.
- Using a biopsy punch, create one or two full-thickness excisional wounds on the mid-dorsum, ensuring the panniculus carnosus muscle is removed.
- (Optional) Secure a silicone splint around the wound with sutures to prevent contraction, thereby better modeling human healing which primarily involves re-epithelialization.
- Apply the test articles:
- Treatment Group: Stem cell-seeded scaffold.
- Control Groups: Empty scaffold, sham operation, or commercial standard of care.
- Cover the wound with a transparent semi-occlusive dressing.
Post-operative Monitoring:
- Monitor animals daily for signs of infection, distress, and wound appearance.
- Capture standardized digital photographs of the wounds at regular intervals (e.g., days 0, 3, 7, 14) with a reference scale for planimetric analysis.
Endpoint Analysis (e.g., Day 14):
- Wound Closure Measurement: Calculate the percentage of wound closure from images using image analysis software (e.g., ImageJ).
- Histological Analysis: Euthanize the animal, harvest the wound tissue with a margin of surrounding healthy skin, and fix in formalin.
- Process and embed tissue in paraffin.
- Section and stain with H&E for general morphology and Masson's Trichrome for collagen deposition.
- Perform immunohistochemistry for CD31 (to quantify angiogenesis) and Vascular Endothelial Growth Factor (VEGF).
- Analysis of Inflammatory Mediators: Use ELISA or multiplex assays on tissue homogenates to quantify cytokine levels (e.g., TNF-α, IL-6, IL-10) [66].
The experimental workflow for establishing and analyzing the wound model is summarized below.
Figure 1: Workflow for Rodent Excisional Wound Healing Study.
Large Bone Defect Studies
Large (critical-sized) bone defects cannot heal spontaneously within an animal's lifetime and represent a major clinical challenge. Preclinical models are essential for testing 3D-printed biomaterial scaffolds designed to provide mechanical support and orchestrate the bone regeneration process [67] [68] [69].
Model Selection and Key Considerations
The choice of animal model and defect location is critical and depends on the scaffold's intended clinical application and required load-bearing capacity.
Table 2: Common Preclinical Models for Large Bone Defect Repair
| Defect Location | Species | Defect Size (Critical) | Key Evaluations | Translational Relevance |
|---|---|---|---|---|
| Femoral Segmental | Rat, Rabbit, Sheep, Goat | 6-8 mm (Rat), 20 mm (Rabbit) >30 mm (Large) | Torsional biomechanical testing, μCT, histology | High-load bearing reconstruction (e.g., trauma, oncology) [68] |
| Cranial | Mouse, Rat, Rabbit | 4-8 mm (Rat) | μCT for bone volume/tissue volume (BV/TV), histology | Low-load bearing applications; craniofacial reconstruction [69] |
| Tibial / Tibial Plateau | Rabbit, Human (RCT) | Not specified | Radiographic fusion rate, scaffold density | Common site for clinical fractures; relevant for pivotal trials [68] |
| Radius Segmental | Rabbit, Dog, Sheep | 15-20 mm (Rabbit) | Radiography, biomechanics, scaffold degradation | Orthopedic repair of non-weight bearing long bones [68] |
Scaffold Design Requirements: An ideal bone scaffold must balance multiple properties [69]:
- Biocompatibility: No adverse immune reactions.
- Hierarchical Porosity: Interconnected macropores (>100 μm, ideally >300 μm) for cell migration and vascularization, plus micropores for nutrient exchange [69].
- Mechanical Properties: Compressive strength and elastic modulus should be tailored to match the target bone (e.g., cortical bone has a compressive strength of 50-200 MPa) [69].
- Osteoconductivity & Bioactivity: Ability to support bone ingrowth, often enhanced with components like β-TCP or magnesium (Mg) ions [68].
Experimental Protocol: Segmental Bone Defect in Rabbit Femur
This protocol outlines the evaluation of a 3D-printed composite scaffold in a rabbit femoral segmental defect, a common model for bridging the gap between small rodents and human clinical trials [68].
Objective: To determine the efficacy of a novel osteogenic scaffold (e.g., Mg-PLGA-β-TCP composite) in promoting bridging and biomechanical recovery of a critical-sized femoral defect.
Materials:
- Animals: Skeletally mature New Zealand White Rabbits.
- Test Article: 3D-printed scaffold (e.g., Mg-PLGA-β-TCP composite "Bongolle") [68].
- Control Article: Commercial porous β-TCP scaffold or autograft.
- Anesthesia: Ketamine/Xylazine or Isoflurane.
- Surgical Supplies: Clippers, antiseptics, surgical drapes, oscillating saw with custom jig, internal fixation plate and screws, saline irrigation, sutures.
- Analysis Tools: X-ray system, micro-Computed Tomography (μCT) scanner, biomechanical tester, histological equipment.
Procedure:
- Pre-operative Preparation:
- Acclimate animals and obtain IACUC approval.
- Pre-design and sterilize scaffolds to match the defect size.
Surgical Procedure (Day 0):
- Induce anesthesia and administer pre-operative analgesics.
- Position the animal laterally and prepare the hindlimb for aseptic surgery.
- Make a lateral skin incision and dissect musculature to expose the femoral mid-shaft.
- Stabilize the femur with a custom plate.
- Using an oscillating saw and a jig to protect soft tissues, create a critical-sized segmental defect (e.g., 15-20 mm).
- Continuously irrigate with saline to prevent thermal necrosis.
- Implant the test or control scaffold into the defect.
- Close the fascial and skin layers in sequence.
Post-operative Care:
- Provide analgesia for a minimum of 48-72 hours.
- Monitor animals daily for weight-bearing, signs of pain, and infection.
- Perform radiographic assessments at defined intervals (e.g., 2, 6, 12 weeks).
Endpoint Analysis (e.g., 12 or 24 weeks):
- Radiography/μCT: Assess bone union using a scoring system. Quantify 3D bone formation via μCT (Bone Volume/Tissue Volume - BV/TV, Trabecular Number/Thickness). In clinical RCTs, radiographic density changes (e.g., +9.29% at 12 weeks) indicate scaffold fusion and new bone formation [68].
- Biomechanical Testing: Test the excised femur in torsion to failure. Compare torsional stiffness and maximum torque to the intact contralateral limb.
- Histomorphometry: Process undecalcified bone sections (e.g., embedded in PMMA) for staining (e.g., Van Gieson, Stevenel's Blue). Quantify the percentage of new bone ingrowth within scaffold pores and bone-scaffold contact.
The multi-faceted evaluation strategy for bone defect repair is illustrated below.
Figure 2: Multi-Modal Analysis of Bone Defect Repair.
The Scientist's Toolkit: Essential Research Reagents and Materials
This section details key reagents and materials crucial for the successful execution of the protocols described above.
Table 3: Essential Research Reagents and Materials for In Vivo Validation
| Item | Function/Application | Example Use Case |
|---|---|---|
| Fetal Skin-Derived Stem Cells (FSSCs) | High-potency, low-immunogenicity stem cell source for wound healing. Promotes collagen secretion and angiogenesis [66]. | Seeding onto polymeric scaffolds for enhanced wound repair in nude mouse models [66]. |
| 3D-Printed Mg-PLGA-β-TCP Composite Scaffold | Bioadaptive, biodegradable bone graft substitute. Mg ions promote osteogenesis and angiogenesis; PLGA/β-TCP provides structure and osteoconductivity [68]. | Filling critical-sized segmental defects in rabbit femurs or tibiae to test bone regeneration [68]. |
| Low-Temperature Rapid Prototyping (LT-RP) | 3D printing technology enabling fabrication of complex scaffold architectures without compromising bioactivity of temperature-sensitive materials (e.g., growth factors, Mg) [68]. | Manufacturing patient-specific composite scaffolds (e.g., Bongolle) with precise pore size and mechanical properties [68]. |
| Anti-CD31 Antibody (PECAM-1) | Immunohistochemistry marker for identifying vascular endothelial cells, used to quantify angiogenesis (microvessel density) in healed wounds or regenerated bone [66]. | Staining sections from harvested wound or bone tissue to assess the pro-angiogenic effect of a therapeutic intervention [66]. |
| WRAHPS Guidelines Checklist | Standardized reporting framework for preclinical wound studies. Ensures comprehensive documentation of animal model variables, wounding procedures, and outcomes for reproducibility and regulatory compliance [64]. | Designing and reporting a study on a novel scaffold for diabetic wound healing to ensure all critical experimental details are captured [64]. |
Robust in vivo validation using standardized protocols is the cornerstone of translational research in regenerative medicine. The rodent wound and large bone defect models detailed herein, when executed with careful attention to model selection, surgical precision, and comprehensive analytical endpoints, provide critical proof-of-concept data for novel biomaterial scaffolds. Adherence to reporting guidelines like WRAHPS ensures data integrity and reproducibility, ultimately accelerating the development of safe and effective stem cell-based therapies for clinical application.
The field of regenerative medicine increasingly relies on advanced biomaterial scaffolds to deliver stem cells and promote tissue repair. Among the most prominent options are collagen scaffolds and decellularized xenografts, each offering a distinct set of advantages and challenges. Collagen scaffolds are fabricated from the most abundant protein in the mammalian extracellular matrix (ECM), providing a familiar, albeit simplified, microenvironment for cells [70]. Decellularized xenografts, derived from animal tissues, aim to preserve the complex, native three-dimensional architecture and biochemical composition of the original organ or tissue, such as the compositional-mechanical gradient of osteochondral tissue [71]. This application note provides a comparative analysis of these two platforms, framed within the context of biomaterial scaffolds for stem cell delivery research. It includes structured data, detailed experimental protocols, and visual tools to guide researchers and scientists in selecting and utilizing the appropriate scaffold for their specific therapeutic applications.
Fundamental Characteristics and Comparison
The core of the selection process lies in understanding the inherent properties of each scaffold type. The table below summarizes the key characteristics of collagen scaffolds and decellularized xenografts from a materials science and biological perspective.
Table 1: Comparative Analysis of Scaffold Fundamental Characteristics
| Characteristic | Collagen Scaffolds | Decellularized Xenografts |
|---|---|---|
| Source & Composition | Primarily Type I collagen; can be derived from mammalian tendon/skin (bovine, porcine) or marine sources [70]. A simplified, often single-protein system. | Tissue-specific ECM from xenogeneic sources (e.g., porcine, bovine); retains a complex mixture of structural proteins (collagens, elastin), proteoglycans, and GAGs [71] [72]. |
| Structural Bio-mimicry | Can be engineered into various architectures (sponges, hydrogels) but is a homogenized mimic of native ECM [70]. | Superiorly recapitulates the native 3D porous architecture and tissue-specific gradient structures of the source tissue [71]. |
| Bioactivity & Signaling | Excellent biocompatibility; contains RGD-like sequences that support cell adhesion via integrins [70]. Lacks the full spectrum of native ECM bio-cues. | Provides a tissue-specific microenvironment with retained native growth factors and bioactive cues that actively regulate cell fate [72] [73]. |
| Mechanical Properties | Generally poor mechanical strength; requires cross-linking or composite formation for load-bearing applications [73] [74]. | Inherits the mechanical properties of the native tissue, offering superior initial strength and structural stability for load-bearing tissues [71] [74]. |
| Immunogenicity | Low immunogenicity, especially with the use of atelocollagen (telopeptides removed) [70] [73]. | Risk of immune rejection due to residual cellular material (e.g., DNA, galactose-α-1,3-galactose) if decellularization is incomplete [71] [72]. |
| Key Advantage | High biocompatibility, tunable physical properties, and established commercial availability. | Unparalleled structural and biochemical complexity that mimics the native stem cell niche. |
| Primary Challenge | Simplistic composition that does not fully replicate the native ECM; weak mechanical properties. | Risk of immunogenicity; potential loss of ECM integrity during decellularization; batch-to-batch variability [71] [72]. |
Experimental Protocols for Evaluation
To standardize research and development, the following protocols outline key methodologies for evaluating the performance of these scaffolds in a stem cell delivery context.
Protocol: In Vitro Recellularization and Chondrogenic Differentiation
This protocol is adapted from studies using decellularized scaffolds for cartilage tissue engineering and can be applied to both scaffold types with minor modifications [75] [76].
Objective: To assess the efficiency of stem cell seeding, viability, and subsequent differentiation into chondrocytes within a 3D scaffold.
Materials:
- Scaffold: Sterile collagen-based scaffold or decellularized xenograft (e.g., osteochondral scaffold).
- Cells: Human Wharton's Jelly-derived Mesenchymal Stem Cells (hWJ-MSCs) or other relevant MSCs.
- Culture Media: Expansion medium (e.g., α-MEM with 10% FBS), Chondrogenic differentiation medium (e.g., containing TGF-β3, dexamethasone, ascorbate-2-phosphate, and ITS+ premix).
Procedure:
- Scaffold Pre-conditioning: Hydrate the scaffold in PBS or basal culture medium for 2-4 hours.
- Cell Seeding:
- Harvest hWJ-MSCs and resuspend at a density of 7 × 10^5 cells/mL in culture medium or a neutral carrier hydrogel [75].
- Carefully pipet the cell suspension onto the scaffold. Use a low-speed centrifugation (e.g., 400 × g for 5 minutes) to enhance cell infiltration if the scaffold is dense.
- In Vitro Culture:
- Maintain the cell-scaffold constructs in expansion medium for 24-48 hours to allow for cell attachment.
- Switch to chondrogenic differentiation medium for 3-4 weeks, changing the medium every 2-3 days.
- Analysis:
- Cell Viability: At 7 days, assess using a Live/Dead assay kit. Viability should exceed 95% on a high-quality scaffold [76].
- Histology: Fix constructs in 4% paraformaldehyde, embed in paraffin, section, and stain.
- H&E: For general cell distribution and morphology.
- Alcian Blue: To detect sulfated glycosaminoglycans (GAGs), a key component of cartilage matrix [76].
- Immunohistochemistry (IHC): Stain for chondrogenic markers such as Collagen Type II and Aggrecan [75].
- Gene Expression: Perform qRT-PCR to analyze the transcriptional upregulation of chondrogenic markers (e.g., COL2A1, ACAN, SOX9) compared to undifferentiated controls.
Protocol: Quantitative Analysis of Decellularization Efficiency
This protocol is critical for quality control of in-house or commercially sourced decellularized xenografts [76].
Objective: To quantify the removal of cellular material and retention of ECM components post-decellularization.
Materials:
- Native (control) tissue and Decellularized tissue.
- DNA Quantification Kit (e.g., PicoGreen), Protein Quantification Kit (e.g., Bradford assay).
- Reagents for H&E staining.
Procedure:
- Histological Evaluation (H&E Staining):
- Process native and decellularized tissues for paraffin sectioning and H&E staining.
- Evaluation: Visually confirm the absence of nuclear material (stained blue/purple by hematoxylin) in the decellularized tissue. Only empty lacunae should remain [76].
- Quantitative DNA Assessment:
- Digest weighed samples of native and decellularized tissues with proteinase K.
- Extract DNA and quantify using a fluorescent DNA-binding dye.
- Evaluation: The decellularized tissue should show a significant reduction in DNA content. A common benchmark is less than 50 ng of double-stranded DNA per mg of dry weight of ECM [76].
- ECM Component Retention (Bradford Assay):
- Digest tissue samples and subject them to a Bradford assay to determine total protein concentration.
- Evaluation: Compare the protein content of the decellularized tissue to the native control. A high retention percentage (e.g., >50%) indicates successful preservation of the ECM protein components [76].
Signaling Pathways in Scaffold-Cell Interactions
The biochemical and mechanical cues presented by scaffolds activate specific signaling pathways that direct stem cell fate. The diagram below illustrates the key pathways mediated by collagen and complex dECM.
The Scientist's Toolkit: Essential Research Reagents
Successful experimentation requires a suite of reliable reagents and materials. The following table lists essential solutions for working with collagen and decellularized xenograft scaffolds.
Table 2: Key Research Reagent Solutions for Scaffold-Based Studies
| Reagent / Material | Function & Application | Specific Example / Note |
|---|---|---|
| Type I Collagen Solution | Base material for fabricating custom collagen scaffolds; forms hydrogels at physiological pH and temperature [70]. | Rat tail tendon-derived (e.g., Gibco, A10483-01); concentration typically 3-5 mg/mL [75]. |
| Methacrylated Gelatin (GelMA) | A photocrosslinkable derivative of gelatin; allows for creating scaffolds with tunable mechanical properties via UV light [73]. | Used in biofabrication (e.g., 3D bioprinting) to create complex, cell-laden structures. |
| Gellan Gum | A polysaccharide used as a base bioink; gels in the presence of cations; often combined with dECM to improve bioprintability [76]. | Provides structural integrity for 3D-bioprinted constructs when mixed with dECM hydrogels. |
| Chondrogenic Differentiation Kit | A predefined media formulation to direct MSCs down a chondrogenic lineage in 3D culture. | Typically contains TGF-β3, a crucial inducer of chondrogenesis. |
| Live/Dead Viability/Cytotoxicity Kit | To quantitatively assess cell survival within the 3D scaffold post-seeding and during culture. | Uses calcein-AM (labels live cells green) and ethidium homodimer-1 (labels dead cells red). |
| Anti-Collagen Type II Antibody | A primary antibody for IHC; confirms successful chondrogenic differentiation by detecting a cartilage-specific collagen. | A positive stain indicates the production of a mature cartilage matrix. |
| PicoGreen dsDNA Quantitation Kit | A highly sensitive fluorescent assay for quantifying residual DNA in decellularized tissues. | Essential for validating the efficiency of a decellularization protocol [76]. |
The choice between collagen scaffolds and decellularized xenografts is not a matter of one being universally superior, but rather which is optimal for a specific research or therapeutic goal. Collagen scaffolds offer a controlled, tunable, and highly biocompatible platform, ideal for fundamental studies of cell-matrix interactions and for applications where simplicity and regulatory approval pathways are advantageous. In contrast, decellularized xenografts provide an unmatched level of biological complexity that can significantly enhance stem cell differentiation and functional tissue formation, particularly in complex tissue engineering scenarios like integrated osteochondral repair, albeit with the challenges of ensuring complete decellularization and managing immunogenicity. The ongoing convergence of these technologies—such as incorporating decellularized matrix components into designer collagen scaffolds—represents the future of sophisticated biomimetic scaffold design for stem cell delivery.
The efficacy of stem cell-based therapies using biomaterial scaffolds is fundamentally determined by three critical biological outcomes: successful angiogenesis to restore blood supply, minimal scarring for functional tissue restoration, and robust stem cell engraftment for sustained regenerative activity. This application note provides a standardized framework of quantitative metrics and detailed protocols to reliably assess these outcomes in preclinical research, enabling more reproducible and translatable evaluation of novel biomaterial scaffolds for stem cell delivery.
Quantifying Angiogenesis
Angiogenesis, the formation of new microvasculature, is essential for delivering oxygen and nutrients to regenerating tissue and transplanted cells. The following methods provide quantitative in vitro and in vivo assessment.
In Vitro Tube Formation Assay
This standard assay quantifies the ability of endothelial cells to form capillary-like structures on a basement membrane matrix, modeling the early stages of vasculogenesis [77].
Protocol:
- Matrix Preparation: Thaw Growth Factor Reduced Matrigel on ice overnight at 4°C. Pre-chill a 96-well plate and pipette tips.
- Matrix Coating: Add 50 µL of Matrigel to each well using pre-chilled tips. Incubate the plate for 30-60 minutes at 37°C to allow polymerization.
- Cell Seeding: Trypsinize and resuspend Human Umbilical Vein Endothelial Cells (HUVECs) at a density of (1.0 \times 10^5) to (2.0 \times 10^5) cells/mL in complete endothelial cell medium. Seed 50,000-100,000 cells per well on the polymerized Matrigel.
- Treatment & Incubation: Add pro-angiogenic factors (e.g., VEGF, FGF-2) or conditioned media from stem cell-seeded scaffolds to the wells. Incubate the plate for 4-18 hours at 37°C, 5% CO₂.
- Imaging & Analysis: Capture images (at least 3-5 random fields per well) using an inverted phase-contrast microscope at 40x-100x magnification. Analyze images with automated software (e.g., ImageJ with Angiogenesis Analyzer plugin) to quantify the parameters listed in Table 1.
Table 1: Key Quantitative Metrics for In Vitro Angiogenesis Assays
| Parameter | Description | Indication |
|---|---|---|
| Total Tube Length | Sum length of all capillary-like structures in pixels or µm. | Measures overall network complexity. |
| Number of Branches | Count of branch points in the tubular network. | Induces branching morphogenesis. |
| Number of Nodes | Count of master segments, branches, and isolated segments. | Reflects network connectivity and maturity. |
| Total Mesh Area | Total area enclosed by the tubular network. | Represents the potential for perfusion. |
In Vivo Assessment of Functional Vasculature
For studies involving animal models, functional assessment of new blood vessels is crucial. Implant biomaterial scaffolds subcutaneously or in targeted defect models, then analyze after 1-4 weeks.
Protocol:
- Perfusion with Dyed Lectin or Resin: Inject animals intravenously with FITC-labeled Lycopersicon esculentum (Tomato) Lectin (100 µL of 1 mg/mL solution) or a radio-opaque resin (e.g., Microfil) 10-20 minutes before sacrifice.
- Tissue Harvest and Processing: Excise the implant and surrounding tissue. For lectin-perfused samples, snap-freeze in O.C.T. compound for cryosectioning. For resin-perfused samples, fix in 4% PFA and dehydrate in ethanol for creating tissue clears.
- Imaging and Analysis:
- Immunofluorescence Staining: Section frozen tissue (8-12 µm thickness). Stain with antibodies against CD31 (Platelet Endothelial Cell Adhesion Molecule) and α-SMA (Alpha-Smooth Muscle Actin). Use appropriate fluorescent secondary antibodies and counterstain with DAPI.
- Image Acquisition: Capture confocal microscopy images (5-10 random fields per sample) or scan entire sections using a slide scanner.
- Quantification: Use image analysis software to calculate vessel density (CD31+ area / total area), vessel diameter, and the percentage of mature vessels (α-SMA+ and CD31+ co-staining).
Table 2: Key Quantitative Metrics for In Vivo Angiogenesis
| Parameter | Description | Indication |
|---|---|---|
| Vessel Density | Percentage of tissue area positive for endothelial markers (e.g., CD31). | Quantifies the extent of new vessel formation. |
| Perfused Vessel Density | Percentage of tissue area containing lectin-positive vessels. | Measures the fraction of functional, blood-perfused vessels. |
| Vessel Maturation Index | Ratio of α-SMA+ vessels to total CD31+ vessels. | Indicates vessel stability and functional maturity. |
| Hemoglobin Content | Drabkin’s method assay on homogenized implant tissue. | Provides a biochemical measure of total blood content. |
The diagram below illustrates the key signaling pathways and cellular events in angiogenesis that these assays measure.
Angiogenesis Signaling Pathway
Assessing Scarring and Fibrosis
Excessive scarring, characterized by aberrant collagen deposition and myofibroblast activity, impairs functional tissue recovery. The following methods quantify scar formation.
Histological Scoring of Scar Tissue
This qualitative-to-semiquantitative assessment provides a standardized evaluation of scar tissue architecture.
Protocol:
- Tissue Sectioning: Cut paraffin-embedded tissue sections to 5 µm thickness and mount on slides.
- Staining:
- Masson's Trichrome: Differentiates collagen (stained blue) from muscle/cytoplasm (stained red).
- Picrosirius Red: Stains collagen and, when viewed under polarized light, differentiates thick, mature (red/orange) collagen fibers from thin, newly synthesized (green) fibers.
- Scoring: Have at least two independent, blinded pathologists score the sections. A modified version of the Fleiss & Cahn scale can be used, as detailed in Table 3.
Table 3: Histological Scoring System for Scarring
| Parameter | Score 0 (Normal) | Score 1 (Mild) | Score 2 (Moderate) | Score 3 (Severe) |
|---|---|---|---|---|
| Collagen Density & Organization | Basket-weave pattern, loose organization | Mildly increased density, slightly disorganized | Moderately increased density, disorganized | Dense, hyalinized collagen bundles |
| Collagen Fiber Maturity | Predominantly thin, green fibers (Picrosirius Red) | Mix of green and orange/red fibers | Predominantly orange/red, thick fibers | Dense, thick, bright red fibers |
| Fibroblast/Hypercellularity | Normal fibroblast density | Mild increase | Moderate increase | Marked hypercellularity |
Quantitative Molecular Analysis
This provides objective, numerical data on key pro-fibrotic pathways.
Protocol:
- Protein Extraction: Homogenize implant tissue in RIPA buffer containing protease and phosphatase inhibitors. Centrifuge at 14,000 x g for 15 minutes at 4°C and collect the supernatant.
- Western Blotting:
- Separate 20-30 µg of total protein via SDS-PAGE and transfer to a PVDF membrane.
- Probe membranes with primary antibodies against: α-SMA (myofibroblast marker), TGF-β1 (key pro-fibrotic cytokine), Phospho-Smad2/3 (downstream of TGF-β), and Collagen I.
- Use GAPDH or β-Actin as a loading control.
- Quantify band intensity using densitometry software and normalize to loading controls.
- Hydroxyproline Assay:
- Hydrolyze a known weight of tissue in 6N HCl at 110°C for 16-18 hours.
- Neutralize the hydrolysate and use a Hydroxyproline Assay Kit (e.g., Sigma-Aldrich MAK008) according to the manufacturer's instructions.
- Calculate total collagen content based on the assumption that hydroxyproline constitutes about 12.5-14% of collagen by weight.
The core pathway driving fibrosis can be summarized as follows:
Core Scarring Signaling Pathway
Measuring Stem Cell Engraftment
The survival, retention, and integration of transplanted stem cells within the host tissue—collectively termed engraftment—is a primary determinant of therapeutic success [78]. The hostile post-transplantation microenvironment often leads to massive cell death, with studies indicating up to 90% of transplanted cells can undergo apoptosis within the initial days [78].
Tracking Cell Viability and Retention
Protocol:
- Cell Labeling: Prior to transplantation, label stem cells with a fluorescent cell tracker (e.g., CM-DiI, CFSE) or a luminescent reporter (e.g., luciferase for bioluminescence imaging). For genetic labels, use lentiviral transduction to express eGFP or Luc2.
- In Vivo Imaging:
- For bioluminescence, inject animals intraperitoneally with D-luciferin (150 mg/kg) and image 10-15 minutes later using an IVIS Spectrum or similar in vivo imaging system.
- For fluorescence, use a fluorescence imager. Acquire images at predetermined time points (e.g., day 1, 3, 7, 14 post-transplantation).
- Quantification: Draw regions of interest (ROIs) around the implant site and quantify total flux (photons/second) for bioluminescence or radiant efficiency for fluorescence. Plot values over time to generate a cell survival/retention curve.
Histological Engraftment Analysis
Protocol:
- Tissue Sectioning: Prepare frozen or paraffin-embedded sections of the implant site.
- Immunofluorescence Staining: Co-stain sections with:
- An antibody against the human-specific marker (e.g., anti-human Nucleoantigen, anti-human Mitochondria) to identify transplanted cells.
- An antibody against a relevant tissue-specific marker (e.g., CD31 for endothelium, α-SMA for smooth muscle, Vimentin for fibroblasts) to assess differentiation and integration.
- DAPI for nuclear counterstain.
- Imaging and Analysis: Use confocal microscopy to capture z-stack images. Quantify:
- Engraftment Efficiency: (Number of human-positive cells / Total number of cells (DAPI+)) × 100%.
- Integration Index: Percentage of human-positive cells that are in direct contact with host cells or are co-expressing a tissue-specific marker.
The critical challenges and engineering strategies to improve engraftment are multifaceted, targeting different causes of cell death.
Strategies to Overcome Engraftment Barriers
Table 4: Key Metrics for Stem Cell Engraftment
| Metric | Method of Measurement | Significance |
|---|---|---|
| Short-Term Cell Survival | In vivo bioluminescence/fluorescence imaging over 1-7 days. | Indicates initial resilience to transplantation stress. |
| Long-Term Cell Retention | In vivo imaging and histology at 2-8 weeks. | Measures persistence of the transplanted cell population. |
| Spatial Distribution | Histology: dispersion of labeled cells within the scaffold and host tissue. | Assesses cell migration and integration. |
| Functional Integration | Histology: co-localization of cell label with host-specific markers. | Confirms participation in tissue structure and function. |
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Reagents for Quantifying Regenerative Outcomes
| Reagent / Kit | Supplier Examples | Primary Function |
|---|---|---|
| Extracellular Matrix (Matrigel) | Corning, Thermo Fisher Scientific | Basement membrane matrix for in vitro tube formation assays. |
| HUVECs & Endothelial Cell Media | Lonza, PromoCell | Primary cells and optimized media for angiogenesis studies. |
| Angiogenesis Assay Kits | Thermo Fisher, Abcam, Bio-Techne | Pre-optimized kits for tube formation, migration, and proliferation. |
| Luminescent Cell Viability Assay | Promega (CellTiter-Glo) | Quantifying metabolically active cells in 3D scaffolds. |
| In Vivo Imaging System (IVIS) | PerkinElmer | Non-invasive tracking of luciferase-expressing cells. |
| Hydroxyproline Assay Kit | Sigma-Aldrich, Abcam | Colorimetric quantification of total collagen content in tissue. |
| Multiplex ELISA Kits | Bio-Techne, Thermo Fisher | Simultaneous quantification of multiple angiogenic/fibrotic biomarkers (VEGF, FGF, TGF-β, etc.) from tissue lysates or plasma [79]. |
| Oxygen-Generating Nanoparticles | Research-scale synthesis | Sustained oxygen release to enhance cell survival in ischemic environments [78]. |
| Fluorescent Cell Linkers (e.g., CM-DiI) | Thermo Fisher Scientific | Stable, long-term labeling of cells for in vivo tracking and histology. |
The transition of biomaterial scaffolds for stem cell delivery from a laboratory concept to a clinical therapy is a complex process governed by rigorous clinical trials and specific regulatory pathways. For researchers and drug development professionals, navigating this translational landscape is critical to successfully bringing new therapies to patients. This application note provides a structured overview of the clinical trial phases and regulatory frameworks applicable to scaffold-based stem cell products, which are often classified as Advanced Therapy Medicinal Products (ATMPs). It also details essential experimental protocols for generating robust preclinical data required for regulatory submissions, ensuring a more efficient and compliant translation from bench to bedside.
The Clinical Translation Pathway
The journey of a biomaterial-scaffold combination product from the laboratory to clinical application follows a defined, multi-stage process. The flowchart below illustrates the key stages from discovery through regulatory approval, highlighting the iterative "learn and confirm" cycle of clinical development.
Clinical trials for scaffold-based stem cell therapies are designed to systematically evaluate safety and efficacy in humans. Each phase has distinct objectives and characteristics, as summarized in the table below.
Table 1: Key Characteristics of Clinical Trial Phases for Scaffold-Based Therapies
| Phase | Primary Objective | Typical Sample Size | Key Endpoints | Considerations for Scaffold-Based Therapies |
|---|---|---|---|---|
| Phase I [80] | Initial safety & tolerability | 20-80 participants [81] | Incidence of adverse events, maximum tolerated dose | Scaffold biodegradation rate, local inflammatory response, initial cell viability and engraftment. |
| Phase II [80] | Preliminary efficacy & further safety | Several dozen to hundreds | Biomarker response, functional clinical outcome, dose-ranging | Optimizing cell-scaffold dose, assessing scaffold integration with host tissue, functional improvement. |
| Phase III [80] | Confirmatory efficacy, monitor side effects | Hundreds to thousands | Definitive clinical outcome measures (e.g., survival, pain score) | Demonstrating superiority over standard of care; large-scale, consistent GMP manufacturing of scaffold-cell product. |
| Phase IV (Post-Marketing) [80] | Long-term effectiveness & safety in general population | Thousands | Long-term adverse events, real-world outcomes | Long-term scaffold degradation products, delayed immune responses, durability of therapeutic effect. |
Navigating Regulatory Pathways
In the United States, clinical investigation of a novel biomaterial-scaffold stem cell therapy typically requires an Investigational New Drug (IND) application submitted to the Food and Drug Administration (FDA) [82] [81]. The FDA offers several pathways to facilitate clinical translation.
Table 2: Key U.S. Regulatory Pathways for Clinical Translation
| Pathway | Scope / Purpose | Preclinical Data Requirements | Limitations / Key Features |
|---|---|---|---|
| Traditional IND [81] | Therapeutic or diagnostic use; no restriction on participant numbers. | Robust data required: dosimetry, toxicology, and pharmacologic safety in two species (rodent and non-rodent). | The standard path to market; requires full Chemistry, Manufacturing, and Controls (CMC) data and cGMP manufacturing. |
| Exploratory IND (eIND) [81] | Basic research only; limited to microdose levels (<30 participants). | Reduced burden: preclinical evaluation in a single species; no genotoxicity data required. | Not for therapeutic use; must be withdrawn after initial microdose studies; a bridge to a full IND. |
| RDRC Program [81] | Basic research on approved radiotracers to study physiology/pathophysiology. | Uses existing safety data of the approved tracer; no first-in-human trials. | Not applicable to novel scaffold or cell products; only for research on already-approved agents. |
| Expedited Programs (e.g., RMAT) [82] | Accelerates development for serious conditions where preliminary evidence suggests an advantage. | Same as traditional IND, but with potential for more flexible data requirements and increased FDA interaction. | Can combine phases of development; available for regenerative medicine therapies, including certain cell-scaffold products. |
Adherence to ethical guidelines is paramount. The International Society for Stem Cell Research (ISSCR) emphasizes principles such as the primacy of patient welfare, rigorous independent peer review, and transparency throughout the research and development process [83]. Furthermore, a "bottom-up" biomaterial design approach—which prioritizes the fundamental biological needs of stem cells from the molecular level upward—is increasingly recognized as key to enhancing the therapeutic efficacy and clinical translation of these complex products [7] [24].
Essential Protocols for Preclinical Data Generation
Robust and standardized preclinical data is the foundation of a successful IND application. The following protocols outline key experiments for characterizing the scaffold and demonstrating the safety and function of the stem cell-scaffold construct.
Protocol: In Vitro Characterization of Biomaterial Scaffolds
This protocol details the assessment of critical physical and chemical properties of the biomaterial scaffold that influence its performance and biocompatibility.
Material Properties Analysis
- Porosity and Pore Architecture: Use micro-computed tomography (µCT) to obtain 3D reconstructions of the scaffold. Calculate the total porosity and analyze the pore size distribution, interconnectivity, and tortuosity.
- Mechanical Testing: Perform uniaxial compression testing on hydrated scaffolds (n≥5) using a universal testing machine. Calculate the compressive modulus from the linear elastic region of the stress-strain curve.
- Degradation Profiling: Sterilize and incubate pre-weighed scaffolds (Ws) in phosphate-buffered saline (PBS) at 37°C, pH 7.4. At predetermined timepoints, remove samples (n=3), dry thoroughly, and re-weigh (Wd). Calculate the mass loss percentage:
[(Ws - Wd) / Ws] * 100. Analyze the supernatant for degradation products via high-performance liquid chromatography (HPLC).
Stem Cell-Scaffold Interaction Assays
- Cell Seeding: Seed passage 4-6 human Bone Marrow-derived Mesenchymal Stromal Cells (hBM-MSCs) onto scaffolds at a density of 1x10^6 cells/scaffold. Allow 4 hours for attachment in a minimal volume of growth medium before submerging.
- Viability and Proliferation: At days 1, 3, and 7, assess cell viability using a Live/Dead assay (Calcein-AM and Ethidium homodimer-1) and visualize via confocal microscopy. Quantify metabolic activity using an AlamarBlue or MTS assay according to manufacturer instructions.
- Lineage-Specific Differentiation:
- Osteogenic: Culture in osteogenic induction medium (containing β-glycerophosphate, ascorbic acid, and dexamethasone) for 21 days. Assess mineralization by Alizarin Red S staining and quantify dye elution.
- Chondrogenic: Culture pellet cultures or scaffolds in chondrogenic induction medium (with TGF-β3) for 28 days. Analyze sulfated glycosaminoglycan (sGAG) content via a DMMB assay and collagen type II deposition by immunohistochemistry.
Protocol: In Vivo Safety and Efficacy Testing in a Rodent Model
This protocol describes a standard procedure for evaluating the safety and preliminary efficacy of the stem cell-laden scaffold in a relevant animal model, such as a rat critical-sized bone defect.
Surgical Implantation
- Animal Model: Use 12-week-old immunocompromised rats (e.g., NIH-III nude rats) to prevent allo-rejection (n=8-10 per group).
- Defect Creation and Implantation: Anesthetize the animal and create a 5-mm critical-sized segmental defect in the femur. Randomize animals to receive one of the following:
- Group 1: hBM-MSC-laden scaffold (test article).
- Group 2: Acellular scaffold (scaffold control).
- Group 3: Empty defect (negative control).
- Group 4: Autograft (positive control).
- Fixate the implant using an internal plate or external fixator and close the surgical site.
Post-Op Monitoring and Analysis
- Safety and Humane Endpoints: Monitor animals daily for the first week, then twice weekly for signs of pain, distress, infection, or lameness. Weigh animals weekly. Any animal showing severe, unalleviated pain or >20% body weight loss must be euthanized immediately.
- Terminal Analysis (8-12 weeks post-op): Euthanize all remaining animals.
- Radiographic and µCT Analysis: Harvest the operated and contralateral limbs. Perform high-resolution µCT scanning to quantify bone volume/total volume (BV/TV) and trabecular number at the defect site.
- Histological Processing and Staining: Decalcify explants, embed in paraffin, and section. Perform Hematoxylin and Eosin (H&E) staining for general morphology, and Safranin O/Fast Green or Masson's Trichrome staining for cartilage and collagen deposition, respectively.
- Toxicology: Collect major organs (liver, kidney, spleen, lung, heart) for histopathological examination to assess any systemic toxicity or ectopic tissue formation.
The Scientist's Toolkit: Key Reagents and Materials
The table below lists essential materials and their functions for developing and testing biomaterial scaffolds for stem cell delivery.
Table 3: Essential Research Reagents for Scaffold-Based Stem Cell Therapy Development
| Item/Category | Function & Rationale | Example(s) |
|---|---|---|
| Biomaterial Polymers | Provides the 3D structural support for cells; mechanical and chemical properties dictate cell fate and in vivo performance. | Synthetic (PLA, PLGA, PEG); Natural (alginate, chitosan, collagen, decellularized ECM) [84]. |
| Stem Cell Lines | The therapeutic "living" component; source must be well-characterized and quality-controlled. | Induced Pluripotent Stem Cells (iPSCs), Mesenchymal Stromal Cells (MSCs), Embryonic Stem Cells (ESCs) [7] [24]. |
| Lineage Induction Media | Directs stem cell differentiation within the scaffold toward a desired phenotype for functional tissue repair. | Osteogenic (Dexamethasone, β-glycerophosphate); Chondrogenic (TGF-β); Adipogenic (IBMX, Indomethacin) [24]. |
| In Vivo Animal Model | Provides a biologically relevant system for evaluating safety, biocompatibility, and preliminary efficacy before human trials. | Immunocompromised mice (for human cell studies); rat critical-sized defect models; large animal (sheep, pig) models. |
| cGMP Manufacturing Suite | Ensures the scaffold and final cell-scaffold product are manufactured consistently, safely, and with high quality for clinical use. | ISO 5 (Class A) cleanrooms, validated equipment, and documented procedures per cGMP guidelines [81]. |
The successful clinical translation of biomaterial scaffolds for stem cell delivery is a multidisciplinary endeavor that depends on a deep understanding of both biological science and regulatory science. By systematically following defined clinical trial phases, engaging with regulatory agencies early, and employing robust preclinical protocols, researchers can effectively navigate the path from discovery to clinical application. Adopting a strategic approach to translation is the key to unlocking the immense therapeutic potential of these advanced combination products for patients.
Conclusion
The integration of biomaterial scaffolds with stem cells represents a paradigm shift in regenerative medicine, moving from passive cell delivery to active, instructive tissue regeneration. The key takeaway is that a 'bottom-up' design philosophy—which tailors the scaffold's mechanical, chemical, and spatial properties to the fundamental needs of specific stem cells—is crucial for overcoming clinical translation barriers. Future progress hinges on developing smarter, dynamic materials that can precisely modulate the therapeutic microenvironment. The convergence of biomaterials with advanced technologies like 3D bioprinting and AI-driven design promises to unlock the next generation of personalized, off-the-shelf regenerative therapies, ultimately reshaping treatment for a wide array of degenerative diseases and injuries.
References
- 1. Targeting the stem cell niche micro-environment as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10235764/]
- 2. What does the concept of the stem cell niche really mean today? [https://pmc.ncbi.nlm.nih.gov/articles/PMC3298504/]
- 3. The emergence of the stem cell niche - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9868094/]
- 4. Stem Cell Niche: Methods and Protocols [https://link.springer.com/book/10.1007/978-1-4939-9508-0]
- 5. Exploration of biomaterial and stem cell-based strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574274/]
- 6. Biomaterial scaffolds for therapeutic immune cell ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925006947]
- 7. Bottom-up Biomaterial strategies for creating tailored stem ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1581292/full]
- 8. Non-destructive quantitative 3D analysis for the ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961206009616]
- 9. Quantitative analysis of cells encapsulated in a scaffold - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7897707/]
- 10. The emerging promise of induced pluripotent stem cells in ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925008461]
- 11. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 12. Mesenchymal stem cells: opening a new chapter in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465317/]
- 13. Recent advances in endothelial colony-forming cells [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05108-8]
- 14. The emerging promise of induced pluripotent stem cells in ... [https://pubmed.ncbi.nlm.nih.gov/41160002/]
- 15. Mesenchymal stem cells in treating human diseases [https://pubmed.ncbi.nlm.nih.gov/40841367/]
- 16. Unlocking the potential of endothelial progenitor cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12497398/]
- 17. Current status and new horizons in stem cell therapy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406451/]
- 18. Stem Cell Scaffolds: A Comparative Study of Biocompatible ... [https://www.hilarispublisher.com/open-access/stem-cell-scaffolds-a-comparative-study-of-biocompatible-materials-115324.html]
- 19. Biomimetic 3D-printed bilayered scaffold with stem cell ... [https://www.sciencedirect.com/science/article/pii/S2772950825004534]
- 20. The biomaterialist's task: scaffold biomaterials and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4295700/]
- 21. Scaffolds and stem cells: delivery of cell transplants for retinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3622368/]
- 22. Neural stem cell delivery via porous collagen scaffolds ... [https://www.nature.com/articles/s41536-020-0097-0]
- 23. Various manufacturing methods and ideal properties of ... [https://www.sciencedirect.com/science/article/pii/S2772810222000113]
- 24. Bottom-up Biomaterial strategies for creating tailored stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12129962/]
- 25. Exploration of biomaterial and stem cell-based strategies for ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07266-9]
- 26. Acellular Extracellular Matrix Scaffolds in Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565388/]
- 27. Research Progress on the Preparation and Application of ... [https://www.mdpi.com/1467-3045/47/4/251]
- 28. Fabrication of granular decellularized extracellular matrix ... [https://www.sciencedirect.com/science/article/pii/S1742706125007172]
- 29. A Comprehensive Comparison of Human ECM Properties ... [https://www.mdpi.com/2079-4983/14/7/363]
- 30. Controlled delivery of PRP from decellularized extracellular ... [https://www.nature.com/articles/s41598-025-92319-8]
- 31. Biocompatibility of decellularized spinach leaves [https://www.nature.com/articles/s44385-025-00028-8]
- 32. Enhancing Bone Repair with β-TCP-Based Composite Scaffolds [https://pmc.ncbi.nlm.nih.gov/articles/PMC12273726/]
- 33. Advances in smart hybrid scaffolds: A strategic approach ... [https://www.sciencedirect.com/science/article/pii/S2666138125000039]
- 34. Enhancing Bone Scaffold Fabrication: A Comparative ... [https://link.springer.com/article/10.1007/s10439-025-03752-9]
- 35. Comparison of cell‐scaffold interactions in a biological and a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11725368/]
- 36. Functionalized mesenchymal stem cells for enhanced bone ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04699-3]
- 37. Modern experimental methods for assessing the effectiveness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318997/]
- 38. Recent advances and challenges of injectable hydrogels in ... [https://www.sciencedirect.com/science/article/abs/pii/S016836592500642X]
- 39. Chitosan based smart injectable hydrogels for biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595387/]
- 40. Recent Advances in 3D Bioprinting of Porous Scaffolds for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12470888/]
- 41. Protocol for designing and bioprinting multi-layered ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10436237/]
- 42. Advanced 3D biomaterials and bioprinting strategies for in ... [https://www.sciencedirect.com/science/article/pii/S2949723X25000212]
- 43. 3D bioprinting of bioproduction cell lines [https://www.sciencedirect.com/science/article/pii/S2405886625000399]
- 44. Development and optimization of an injectable in-situ gel ... [https://www.nature.com/articles/s41598-025-05644-3]
- 45. Injectable hydrogel microspheres promoting inflammation ... [https://pubmed.ncbi.nlm.nih.gov/39938720/]
- 46. 3D collagen nanofiber scaffold with adipose derived stem ... [https://www.nature.com/articles/s41598-025-04763-1]
- 47. Artificial intelligence for design strategies of tissue ... [https://www.sciencedirect.com/science/article/pii/S2667325825004832]
- 48. Functionalized mesenchymal stem cells for enhanced bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577075/]
- 49. Quantitative analysis of bone regeneration efficacy as ... [https://www.sciencedirect.com/science/article/pii/S0264127523004884]
- 50. Comparison of two different biomaterials in the bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8291905/]
- 51. Improved bone regeneration with bone targeted scaffold [https://www.nature.com/articles/s41598-025-12497-3]
- 52. From pathways to platforms: Scaffold-based strategies to ... [https://www.sciencedirect.com/science/article/pii/S3050562325002363]
- 53. Functional Bioink and 3D Bioprinting Tissue Scaffold ... [https://pubmed.ncbi.nlm.nih.gov/41239033/]
- 54. Insight on stem cell preconditioning and instructive ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961216300412]
- 55. Stem Cell Therapy: Healing or Hype? Why Stem Cell Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5947316/]
- 56. Biomaterials to enhance stem cell transplantation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10169090/]
- 57. Immunogenicity and Tumorigenicity of Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3873036/]
- 58. Tumourigenicity and Immunogenicity of Induced Neural ... [https://www.nature.com/articles/srep29955]
- 59. Biomimetic scaffolds loaded with mesenchymal stem cells ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04012-8]
- 60. Epigenetic memory as crucial contributing factor in ... [https://link.springer.com/article/10.1007/s00441-025-03952-8]
- 61. Epigenetic crosstalk between stem cells and tumors [https://pmc.ncbi.nlm.nih.gov/articles/PMC12444435/]
- 62. Adrenomedullin delivery in microsphere-scaffold composite ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4124888/]
- 63. Metal Material, Properties and Design Methods of Porous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8033174/]
- 64. The Wound Reporting in Animal and Human Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11621255/]
- 65. Modeling Wound Chronicity In Vivo: The Translational ... [https://www.sciencedirect.com/science/article/pii/S0022202X2400006X]
- 66. Rapid cutaneous wound healing in nude mice by fetal skin ... [https://www.frontiersin.org/articles/10.3389/fmed.2025.1557973/full]
- 67. Advances in 3D-Printed scaffolds for bone defect repair [https://pubmed.ncbi.nlm.nih.gov/41311982/]
- 68. A prospective and multi-center randomized controlled trial [https://www.sciencedirect.com/science/article/abs/pii/S0142961225006702]
- 69. Advances in 3D-printed scaffold technologies for bone defect ... [https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/s12938-025-01381-w]
- 70. Recent Advances in the Development and Application of Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071569/]
- 71. Xenogeneic decellularized materials for integrated ... [https://www.sciencedirect.com/science/article/pii/S2590093525000499]
- 72. Decellularized extracellular matrix biomaterials for ... [https://www.sciencedirect.com/science/article/pii/S2452199X23003006]
- 73. Decellularized Cell‐Secreted Extracellular Matrices as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11934908/]
- 74. Scaffolding in tissue engineering: general approaches and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2587658/]
- 75. Fabrication of 3D Collagen-Based Decellularized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12446596/]
- 76. The introduction and evaluation of novel decellularized ... [https://www.nature.com/articles/s41598-025-11559-w]
- 77. Human In Vitro and Ex Vivo Models in Angiogenesis ... [https://bmrat.org/index.php/BMRAT/article/view/972]
- 78. Modulation of Stem Cell Survival and Engraftment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439257/]
- 79. PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12332904/]
- 80. Translational Science [https://www.eurogct.org/research-pathways/research-and-innovation/translational-science]
- 81. Pathways and challenges in the clinical translational of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634559/]
- 82. Regulatory Paths to Market - Drugs & Biologics [https://sc-ctsi.org/resources/regulatory-resources/drugs-biologics/regulatory-paths-to-market]
- 83. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 84. Integrating Drug Delivery with Tissue Regeneration [https://pubs.rsc.org/en/content/articlelanding/2025/tb/d5tb01338k]