Bridging the Gap: Validating iPSC Disease Phenotypes with Clinical Data for Robust Disease Modeling and Drug Development
This article provides a comprehensive overview of the strategies and challenges in validating disease phenotypes in induced pluripotent stem cell (iPSC) models against real-world clinical data.
Bridging the Gap: Validating iPSC Disease Phenotypes with Clinical Data for Robust Disease Modeling and Drug Development
Abstract
This article provides a comprehensive overview of the strategies and challenges in validating disease phenotypes in induced pluripotent stem cell (iPSC) models against real-world clinical data. Aimed at researchers, scientists, and drug development professionals, it explores the foundational principles of iPSC-based disease modeling, details advanced methodological approaches for creating clinically relevant phenotypes, and addresses key troubleshooting and optimization challenges. Furthermore, it examines cutting-edge validation frameworks, including the use of AI and large-scale clinical data, to enhance the predictive accuracy and translational value of iPSC models for therapeutic discovery and personalized medicine.
The Foundation of iPSC Disease Modeling: From Cellular Reprogramming to Clinical Phenotypes
The development of induced pluripotent stem cell (iPSC) technology represents a transformative breakthrough in regenerative medicine and disease modeling. iPSCs are a type of pluripotent stem cell generated directly from somatic cells through the introduction of specific reprogramming factors, effectively reversing the developmental clock of specialized cells back to an embryonic-like state [1] [2]. This technology, pioneered by Shinya Yamanaka and Kazutoshi Takahashi in 2006, demonstrated that the forced expression of four transcription factors (Oct4, Sox2, Klf4, and c-Myc, collectively known as Yamanaka factors or OSKM) could convert mouse fibroblasts into pluripotent stem cells [1] [3] [2].
The core principle of iPSC generation rests on the fundamental understanding that while somatic cells harbor complete genetic information, phenotypic diversity is achieved through reversible epigenetic mechanisms rather than irreversible genetic changes [1]. This concept was initially demonstrated through seminal somatic cell nuclear transfer (SCNT) experiments by John Gurdon, which showed that nuclei from differentiated cells could support full embryonic development when transferred into enucleated eggs [1] [3]. The iPSC technology builds upon this principle, offering a powerful platform for disease modeling, drug screening, and cell therapy applications while bypassing the ethical concerns associated with embryonic stem cells [1] [3] [2].
Molecular Mechanisms of Reprogramming
Key Transcription Factors and Their Roles
The reprogramming of somatic cells to pluripotency involves profound remodeling of chromatin structure and the epigenome, orchestrated by core transcription factors [1] [3]. Each factor plays distinct yet interconnected roles in resetting cellular identity:
- Oct4 (Pou5f1): A POU-family transcription factor crucial for maintaining pluripotency. Oct4 deletion leads to spontaneous differentiation into trophoblast cells, demonstrating its essential role in preserving the pluripotent state [2]. It forms core regulatory circuits with Sox2 and Nanog to activate pluripotency-associated genes [3].
- Sox2: An SRY-box transcription factor that partners with Oct4 to bind composite SOX-OCT motifs in enhancers and promoters of pluripotency genes. This partnership enables the activation of a broad network of genes essential for establishing pluripotency [3] [2].
- Klf4: A Krüppel-like factor that supports reprogramming through multiple mechanisms, including activation of epithelial genes during mesenchymal-to-epithelial transition (MET) and reinforcement of the pluripotency network through interaction with Oct4 and Sox2 [3].
- c-Myc: A proto-oncogene that enhances reprogramming efficiency by binding broadly to somatic genome regions with open chromatin, facilitating access for other reprogramming factors to their target genes. It primarily promotes cell cycle progression and metabolic changes conducive to reprogramming [3].
Alternative factor combinations have also proven effective, with Thomson and colleagues demonstrating successful reprogramming using OCT4, SOX2, NANOG, and LIN28 [1] [2]. The specific combination used can influence reprogramming efficiency and the quality of resulting iPSCs.
Phases of Reprogramming
The process of somatic cell reprogramming occurs through a sequential series of molecular events characterized by two main transcriptional waves [1] [3]:
Early Phase Events: The initial reprogramming stage begins with OSKM factors binding to somatic cell genomes, where c-Myc facilitates access to closed chromatin regions [3]. This binding initiates:
- Silencing of somatic genes including Thy1, Snai1, Snai2, Zeb1, and Zeb2 surface markers [3]
- Activation of early pluripotency-associated genes [1]
- Initiation of mesenchymal-to-epithelial transition (MET), characterized by upregulation of epithelial genes (Cdh1, Epcam, Ocln) and downregulation of mesenchymal markers [1] [3]
Late Phase Events: The subsequent stage establishes stable pluripotency through:
- Activation of core pluripotency circuitry including Nanog, Sall4, Utf1, and endogenous Sox2 [3]
- Epigenetic resetting with establishment of ESC-like chromatin modifications [1] [3]
- Morphological transformation into compact, ESC-like colonies with high nuclear-to-cytoplasmic ratios [1]
- Formation of autoregulatory loops that maintain the pluripotent state without continuous transgene expression [3]
The complete reprogramming process is typically slow and inefficient, taking 3-4 weeks for human cells with efficiencies around 0.01-0.1% for most methods [2]. The low efficiency reflects significant barriers including activation of p53-dependent senescence pathways and the stochastic nature of epigenetic remodeling [3].
Comparative Analysis of Reprogramming Methods
Integration-Based vs. Non-Integration Methods
Various reprogramming methods have been developed, each with distinct advantages and limitations for research and therapeutic applications. These methods can be broadly categorized into integrating and non-integrating systems [3].
Quantitative Comparison of Major Non-Integrating Methods
Recent comparative studies have provided quantitative data on the performance of the most commonly used non-integrating reprogramming methods [4].
Table 1: Comparison of Major Non-Integrating Reprogramming Methods
| Method | Reprogramming Efficiency* | Key Factors Delivered | Genomic Integration | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Sendai Virus (SeV) | 0.1-1% | OSKM | No | High efficiency, works with multiple cell types, well-defined clearance | Viral method, potential immunogenicity |
| Episomal Vectors | 0.04-0.3% | Oct4, Sox2, Lin28, Klf4, L-Myc (+ p53 suppression) | No (extra-chromosomal) | Virus-free, transgene-free iPSCs | Lower efficiency, requires electroporation |
| Synthetic mRNA | 0.5-2% | OSKM modified mRNAs | No | High efficiency, precise control, no vector design needed | Requires multiple transfections, potential immune activation |
| Protein Transduction | <0.001% | Recombinant OSKM proteins | No | Completely footprint-free, minimal safety concerns | Very low efficiency, technically challenging |
*Efficiency range represents percentage of starting somatic cells that become iPSC colonies [5] [4]
A 2025 comparative analysis examining reprogramming success rates across different source materials found that Sendai virus reprogramming yielded significantly higher success rates compared to episomal methods [4]. The study also demonstrated that source material (fibroblasts, LCLs, or PBMCs) did not significantly impact success rates, highlighting the robustness of viral delivery systems [4].
Experimental Protocols for iPSC Generation
Sendai Virus Reprogramming Protocol
The Sendai virus (SeV) system represents one of the most efficient non-integrating reprogramming methods. Below is a detailed protocol based on the CytoTune Sendai Reprogramming Kit [4]:
Day 0: Preparation and Plating
- Culture source cells (e.g., fibroblasts, PBMCs) in appropriate medium
- Ensure cells are 70-90% confluent at time of transduction
- Prepare essential supplements including 10μM Y-27632 (ROCK inhibitor)
Day 1: Viral Transduction
- Dilute CytoTune viruses in appropriate culture medium
- Remove culture medium from cells and add virus-containing medium
- Incubate cells for 24 hours at 37°C, 5% CO2
Day 2: Medium Replacement
- Remove virus-containing medium and replace with fresh culture medium
- Culture cells for additional 6 days with medium changes every other day
- Monitor transduction efficiency via GFP expression if using reporter constructs
Day 7: Harvest and Replate
- Harvest transduced cells using appropriate dissociation reagent
- Replate cells onto feeder layers or extracellular matrix-coated plates (e.g., Matrigel)
- Switch to hiPSC culture medium supplemented with ROCK inhibitor
Days 10-30: Colony Selection and Expansion
- Continue culture with daily medium changes
- Monitor emergence of ESC-like colonies with defined borders, high nuclear-to-cytoplasmic ratio
- Mechanically pick individual colonies between days 21-30
- Expand clonal lines and validate pluripotency
Episomal Reprogramming Protocol
The episomal reprogramming method provides a non-viral alternative for generating footprint-free iPSCs [5]:
Day 0: Nucleofection Preparation
- Culture source cells to 75-90% confluency
- Prepare episomal vector mixture containing OCT4, SOX2, LIN28, KLF4, L-MYC, and p53 suppression factors [5]
- Harvest cells and resuspend in nucleofection solution
Day 1: Nucleofection
- Perform nucleofection using Amaxa Nucleofector II device (Program U-015 for LCLs, U-023 for fibroblasts) [4]
- Plate transfected cells in culture medium
- Culture under hypoxic conditions (5% O2) to enhance efficiency [4]
Days 2-7: Post-Transfection Culture
- Change medium every other day
- Monitor transfection efficiency via GFP expression if using reporter constructs
- Avoid antibiotic use during this critical period [5]
Days 7-14: Replating
- Harvest transfected cells and replate at appropriate density on feeder cells or extracellular matrix
- Switch to hiPSC culture medium
Days 14-35: Colony Selection
- Identify and manually pick at least 24 candidate colonies for expansion [4]
- Expand clonal lines and confirm loss of episomal vectors (typically after ~5 passages) [5]
- Validate pluripotency markers and differentiation potential
The Scientist's Toolkit: Essential Research Reagents
Table 2: Essential Reagents for iPSC Generation and Characterization
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | CytoTune Sendai Viruses, Epi5 Episomal Vectors [5] [4] | Deliver OSKM transcription factors | Sendai: high efficiency; Episomal: integration-free |
| Cell Culture Media | mTeSR1, Essential 8, DMEM/F12 with KSR | Support iPSC growth and maintenance | Defined, xeno-free formulations preferred |
| Culture Supplements | Y-27632 (ROCK inhibitor), bFGF, L-ascorbic acid | Enhance cell survival, promote pluripotency | ROCK inhibitor critical post-thaw and during passaging |
| Extracellular Matrices | Matrigel, Geltrex, Vitronectin, Laminin-521 | Provide substrate for feeder-free culture | Mimic basement membrane for cell attachment |
| Characterization Antibodies | Anti-OCT4, SOX2, NANOG, SSEA-4, TRA-1-60 | Confirm pluripotency marker expression | Essential for quality control of iPSC lines |
| Differentiation Inducers | BMP4, Activin A, CHIR99021, Retinoic acid | Direct differentiation to specific lineages | Used for functional validation of pluripotency |
| Quality Control Assays | Karyotyping, STR profiling, Mycoplasma testing | Ensure genetic integrity and sterility | Critical for biobanking and therapeutic applications |
Applications in Disease Modeling and Clinical Validation
iPSC technology has revolutionized approaches to disease modeling and drug discovery by enabling the generation of patient-specific disease models [1] [3]. The ability to differentiate iPSCs into various cell types allows researchers to recapitulate disease phenotypes in vitro, providing powerful platforms for:
Mechanistic Studies of Pathogenesis: iPSCs derived from patients with genetic disorders can be differentiated into affected cell types to study disease mechanisms. For example, iPSCs from spinal muscular atrophy patients have been differentiated into neurons to model disease-specific phenotypes [3]. Similarly, iPSCs have been extensively applied to study diabetes pathogenesis through differentiation into pancreatic β-cells [6].
Drug Screening and Toxicity Testing: iPSC-derived cells enable high-throughput screening of compound libraries using human cells with disease-relevant genetic backgrounds. This approach is particularly valuable for neurological disorders and cardiac conditions, where species-specific differences limit the predictive value of animal models [1].
Clinical Applications and Cell Therapy: The potential to generate autologous cells for transplantation represents one of the most promising applications of iPSC technology. Significant progress has been made in developing iPSC-derived cells for retinal diseases, Parkinson's disease, and myocardial infarction [1]. A 2020 review highlighted successes in animal models, including correction of sickle cell anemia in mice through autologous iPSC therapy [3].
The integration of CRISPR/Cas9 gene editing with iPSC technology has further enhanced its utility by enabling precise genetic corrections in patient-specific iPSCs, facilitating both functional studies and development of therapeutic approaches [3]. As the field advances, the validation of iPSC disease phenotypes with clinical data remains essential for establishing the relevance and predictive value of these innovative cellular models [6].
The Promise of Patient-Specific iPSCs for Disease Modeling and Personalized Medicine
The advent of induced pluripotent stem cells (iPSCs) has catalyzed a transformative shift in biomedical research and therapeutic development. First established by Shinya Yamanaka and colleagues in 2006, iPSC technology enables the reprogramming of adult somatic cells into a pluripotent state through the introduction of specific transcription factors, classically OCT4, SOX2, KLF4, and c-MYC (OSKM) [1] [7]. This groundbreaking discovery, which earned Yamanaka the Nobel Prize in Physiology or Medicine in 2012, provided an ethically acceptable alternative to embryonic stem cells while offering unprecedented access to patient-specific human cells for research [8]. The fundamental promise of patient-specific iPSCs lies in their capacity to capture the unique genetic background of individual patients, thereby enabling the development of personalized disease models that more accurately recapitulate human pathophysiology than traditional animal models or immortalized cell lines [9].
The application of iPSC technology within personalized medicine represents a convergence of stem cell biology, genomics, and drug discovery. By generating pluripotent stem cells from patients with known genetic variants and clinical histories, researchers can differentiate these cells into the specific cell types affected in various diseases—neurons for neurodegenerative disorders, cardiomyocytes for cardiac conditions, or hepatocytes for metabolic diseases [8] [1]. These patient-derived cellular models retain the donor's complete genetic information, providing a powerful platform for elucidating disease mechanisms, identifying novel therapeutic targets, screening drug candidates, and developing personalized treatment strategies [8] [10] [9]. This approach is particularly valuable for rare genetic diseases, which collectively affect millions worldwide but often lack adequate models for research and therapeutic development [11].
This review will objectively compare the performance of iPSC-based disease modeling against traditional approaches, examining its validation against clinical data across multiple disease contexts. We will present structured experimental data, detailed methodologies, and analytical frameworks that demonstrate how patient-specific iPSCs are reshaping our approach to understanding and treating human disease.
Comparative Analysis of Disease Modeling Platforms
To objectively evaluate the performance of patient-specific iPSCs against traditional disease modeling approaches, we have summarized key comparative metrics across multiple dimensions in the table below.
Table 1: Performance Comparison of Disease Modeling Platforms
| Model Characteristic | Patient-Specific iPSCs | Animal Models | Immortalized Cell Lines |
|---|---|---|---|
| Genetic Relevance | Carries patient's complete genotype; preserves disease-associated variants [9] | Species-specific genetic background; human transgenes often overexpressed [12] | Cancer-derived; extensively mutated; non-physiological gene expression [9] |
| Phenotypic Predictive Value | Recapitulates patient-specific disease phenotypes (e.g., neuronal degeneration, cardiac arrhythmia) [12] | Limited translation of therapeutic efficacy (∼95% failure rate in ALS trials) [12] | Poor correlation with human tissue responses; missing complex physiology [9] |
| Scalability for Screening | Indefinite expansion potential; compatible with HTS formats (384-/1536-well plates) [9] | Low-throughput; time-consuming and expensive | High-throughput capable but physiologically irrelevant [9] |
| Clinical Correlation | Transcriptomic profiles match human post-mortem tissue; donor phenotype correlations [12] | Species-specific pathophysiology; different drug metabolism [13] | No clinical correlation possible |
| Temporal Resolution | Enables longitudinal monitoring of disease progression in human cells [12] | Requires terminal timepoints; limited longitudinal assessment | Continuous culture but non-physiological aging |
| Multi-system Modeling | Emerging 3D organoid systems with multiple cell types [1] [11] | Intact organism with systemic physiology | Limited to single cell types |
The comparative advantage of iPSC-based models is particularly evident in their ability to model complex, sporadic diseases that have proven resistant to traditional modeling approaches. A landmark study utilizing a library of iPSCs from 100 patients with sporadic amyotrophic lateral sclerosis (SALS) demonstrated that patient-derived motor neurons recapitulated key disease features including reduced survival and accelerated neurite degeneration that correlated with donor survival time—a critical validation against clinical data [12]. This model also successfully predicted the clinical failure of 97% of drugs previously tested in ALS trials, demonstrating superior predictive validity compared to traditional transgenic models [12].
Similarly, in cardiovascular disease, iPSC-derived cardiomyocytes from patients with hereditary arrhythmogenic disorders have replicated electrophysiological abnormalities observed in patients, enabling both mechanistic studies and drug screening [8] [7]. The capacity to capture patient-specific drug responses represents a particular strength of iPSC technology, addressing a fundamental limitation of traditional one-size-fits-all therapeutic development [10].
Experimental Validation of iPSC Disease Models
The scientific credibility of iPSC-based disease modeling depends on rigorous validation against clinical data. The table below summarizes key validation approaches and representative findings from recent studies across multiple disease contexts.
Table 2: Experimental Validation of iPSC Disease Models Against Clinical Data
| Disease Area | Validation Methodology | Key Correlation with Clinical Data | Reference |
|---|---|---|---|
| Sporadic ALS | Longitudinal survival analysis of motor neurons from 100 SALS patients | Neurite degeneration rate correlated with donor survival time (p<0.001) [12] | [12] |
| Epilepsy | RNA-seq of CLCNKB-mutant iPSCs vs. control lines | Identification of differentially expressed genes previously implicated in epilepsy phenotypes [14] | [14] |
| Parkinson's Disease | Transplantation of iPSC-derived dopaminergic neurons in clinical trials | Graft survival, dopamine production, and absence of tumors in patients (Phase I/II) [7] | [7] |
| Cardiovascular Disease | Drug screening using iPSC-cardiomyocytes from congenital arrhythmia patients | Recapitulation of patient-specific drug responses (e.g., KCNQ1 mutation responses) [8] | [8] [10] |
| Diabetes | Differentiation of iPSCs to insulin-producing β-cells | Reversal of hyperglycemia in animal models; recapitulation of autoimmune destruction with T-cells [8] [6] | [8] [6] |
| Rare Diseases (NPH) | Kidney organoids from NPHP1-deficient iPSCs | Cyst formation consistent with patient renal pathology; reversal with gene correction [11] | [11] |
Detailed Experimental Protocol: Large-Scale Drug Screening in iPSC-Derived Motor Neurons
To illustrate the methodological rigor required for robust iPSC-based disease modeling, we detail the experimental protocol from the landmark SALS study [12], which exemplifies the comprehensive approach needed to validate disease phenotypes against clinical data:
1. iPSC Library Generation and Quality Control
- Somatic Cell Source: Dermal fibroblasts isolated from skin biopsies of 100 SALS patients and 25 healthy controls [12]
- Reprogramming Method: Non-integrating episomal vectors delivered via automated robotics platform to maximize uniformity [12]
- Quality Control Measures: Genomic integrity verification (karyotyping), pluripotency confirmation (immunocytochemistry for canonical markers), and trilineage differentiation potential [12]
- Clinical Annotation: Comprehensive donor clinical data including ALS subtype, site of onset, age of onset, ALSFRS-R progression rate, and survival time [12]
2. Motor Neuron Differentiation and Characterization
- Protocol: Five-stage spinal motor neuron differentiation adapted from established protocols with optimized maturation conditions [12]
- Purity Assessment: Immunocytochemistry for cell-type-specific markers demonstrating >92% purity for motor neurons (ChAT+, MNX1/HB9+, Tuj1+) with minimal contamination from astrocytes (<0.12%) and microglia (<0.04%) [12]
- Functional Assessment: Electrophysiological measurements to confirm neuronal activity and pharmacological response to riluzole [12]
3. Phenotypic Screening and Longitudinal Analysis
- Live-Cell Imaging: Daily monitoring using virally delivered motor neuron-specific reporter (HB9-turbo) in conjunction with automated image acquisition [12]
- Quantitative Metrics: Survival curves, neurite degeneration rates, and correlation with donor clinical parameters [12]
- Transcriptomic Profiling: RNA sequencing to compare SALS motor neurons with controls and post-mortem spinal cord tissue [12]
4. Drug Screening and Validation
- Compound Library: >100 drugs previously tested in ALS clinical trials [12]
- Screening Format: High-throughput assessment of motor neuron survival [12]
- Hit Validation: Combinatorial testing of effective drugs across multiple SALS donors to account for population heterogeneity [12]
This comprehensive protocol demonstrates the multi-layered validation approach required to establish iPSC-based models with strong clinical correlation. The study's findings were particularly significant for demonstrating that only 3% of drugs that showed efficacy in traditional ALS models rescued motor neuron survival across the SALS donor population, mirroring the high failure rate of these compounds in clinical trials [12].
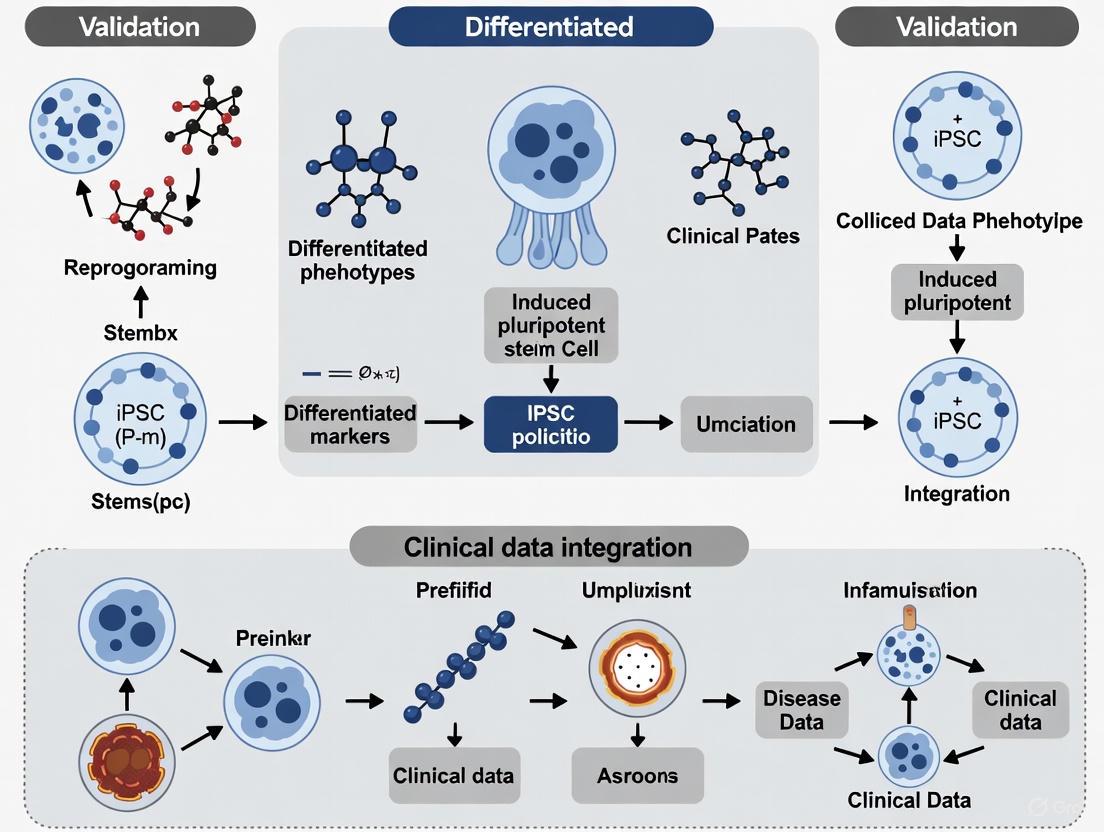
Visualization of iPSC Workflow and Signaling
To better understand the technical workflow and molecular mechanisms underlying iPSC-based disease modeling, the following diagrams provide visual representations of key processes.
Diagram 1: iPSC Technology Workflow from Somatic Cells to Disease Modeling. This diagram illustrates the sequential process of generating patient-specific disease models, beginning with somatic cell isolation from various accessible tissues, through reprogramming using OSKM factors or non-integrating methods, expansion of pluripotent cells, and directed differentiation into disease-relevant cell types for modeling and therapeutic development [8] [1] [7].
Diagram 2: Molecular Mechanisms of Somatic Cell Reprogramming. This diagram outlines the key molecular events during iPSC generation, highlighting the two-phase process where early reprogramming involves stochastic silencing of somatic genes and chromatin remodeling, while late reprogramming features deterministic activation of the pluripotency network and epigenetic resetting, culminating in stabilization of the pluripotent state [1].
Research Reagent Solutions for iPSC-Based Disease Modeling
The successful implementation of iPSC technology requires specialized reagents and platforms. The table below details essential research tools and their applications in patient-specific disease modeling.
Table 3: Essential Research Reagents and Platforms for iPSC-Based Disease Modeling
| Reagent Category | Specific Product/Platform | Function and Application | Key Features |
|---|---|---|---|
| Reprogramming Systems | CytoTune-iPS Sendai Reprogramming Kit [14] | Non-integrating reprogramming of somatic cells | Leave-no-trace methodology; high efficiency [7] |
| Culture Systems | mTeSR1/Matrigel culture system [14] | Maintenance of pluripotent iPSCs | Defined, feeder-free conditions; enhanced reproducibility [8] |
| Differentiation Kits | iCell Cardiomyocytes [13] | Directed differentiation to specific lineages | High-purity, functionally mature cells; batch consistency [13] |
| Gene Editing Tools | CRISPR-Cas9 systems [7] | Generation of isogenic controls; disease mutation correction | Precise genetic modification; creation of paired cell lines [7] |
| Characterization Assays | Pluripotency marker antibodies [8] | Quality control of iPSCs and differentiated cells | Verification of pluripotent state (OCT4, NANOG) [8] |
| Specialized Media | Maturation supplements for cardiomyocytes [9] | Enhanced functional maturation of differentiated cells | Promotion of adult-like phenotypes; improved drug response [9] |
| Automation Platforms | opti-ox precision cell programming [13] | Large-scale, consistent differentiation | Industrial-scale production; exceptional purity [13] |
The selection of appropriate reagents and platforms is critical for generating reproducible, high-quality iPSC models. Commercial providers have optimized systems for specific applications, such as Ncardia's cardiomyocytes for cardiac safety pharmacology, FUJIFILM CDI's iCell products for various lineages, and bit.bio's opti-ox technology for consistent differentiation at scale [13]. These standardized platforms are increasingly important for reducing technical variability and enabling more direct comparison of results across different laboratories and studies.
For genetic studies, CRISPR-Cas9 gene editing systems have become indispensable for generating isogenic control lines—where disease-causing mutations are corrected in patient-derived iPSCs or introduced into healthy iPSCs [7]. This powerful approach controls for genetic background variability and enables definitive establishment of genotype-phenotype relationships, as demonstrated in studies of Parkinson's disease where correction of LRRK2 mutations rescued mitochondrial dysfunction in patient-derived neurons [7].
Patient-specific iPSCs have emerged as a transformative platform for disease modeling and therapeutic development, offering unprecedented ability to capture human genetic diversity and recapitulate disease pathophysiology in vitro. The rigorous validation of iPSC-derived disease models against clinical data—as demonstrated by correlations between in vitro phenotypes and patient outcomes—establishes their growing value in the biomedical research toolkit [12] [14].
While challenges remain in standardization, functional maturation, and cost, the continuous refinement of differentiation protocols, the development of more complex multi-cellular systems including organoids, and the integration of emerging technologies like AI-guided differentiation and high-content screening are rapidly advancing the field [7] [9]. The ongoing clinical translation of iPSC-based therapies for conditions like Parkinson's disease and geographic atrophy further validates the fundamental utility of this platform [7].
As the field progresses toward more physiologically relevant in vitro models and larger-scale biobanking efforts, patient-specific iPSCs are poised to become an increasingly central component of personalized medicine, enabling not only improved drug development efficiency but ultimately the creation of truly individualized therapeutic approaches based on a patient's unique cellular responses.
Induced pluripotent stem cell (iPSC) technology has revolutionized biomedical research by providing a platform for creating patient-specific disease models. By reprogramming somatic cells into pluripotent stem cells, researchers can generate disease-relevant cell types to study pathogenesis and test therapeutic interventions. This guide compares the application of iPSC technology across three key disease areas—neurological, cardiac, and metabolic disorders—highlighting successful studies that have bridged the gap between in vitro modeling and clinical validation.
Neurological Disorders: Amyotrophic Lateral Sclerosis (ALS)
Experimental Protocol and Workflow
A landmark 2025 study established a robust framework for modeling sporadic ALS (SALS) using iPSCs [12]. Researchers generated an iPSC library from 100 SALS patients and 25 healthy controls. A five-stage protocol differentiated iPSCs into spinal motor neurons with high purity (92.44% ± 1.66%) [12]. Key steps included:
- Fibroblast Isolation and Reprogramming: Skin biopsies from donors were reprogrammed using non-integrating episomal vectors on an automated robotics platform to ensure uniformity [12].
- Motor Neuron Differentiation: Adapted from an established spinal motor neuron differentiation protocol with optimized maturation conditions [12].
- Phenotypic Screening: Cultures were monitored daily using live-cell imaging with a motor neuron-specific reporter (HB9-turboGFP) [12].
- Longitudinal Analysis: Automated image analysis quantified motor neuron survival and neurite degeneration over time [12].
The following workflow diagram illustrates the key stages of this large-scale screening approach:
Key Findings and Clinical Validation
This study demonstrated that SALS motor neurons recapitulated key disease features, including reduced survival and accelerated neurite degeneration that correlated with donor survival time [12]. Transcriptional profiling aligned with postmortem spinal cord tissues from ALS patients, validating the model's pathophysiological relevance [12].
In drug screening, the model showed remarkable predictive value for clinical outcomes. When testing over 100 drugs previously evaluated in ALS clinical trials, 97% failed to rescue motor neuron survival, mirroring their clinical trial failures [12]. The study identified a promising therapeutic combination of baricitinib, memantine, and riluzole that significantly improved motor neuron survival across the heterogeneous SALS donor population [12].
Research Reagent Solutions
Table: Key Research Reagents for iPSC-Based ALS Modeling
| Reagent/Solution | Function | Example Product/Description |
|---|---|---|
| Non-integrating Episomal Vectors | Reprogramming somatic cells without genomic integration | Episomal plasmids containing OCT4, SOX2, KLF4, c-MYC [12] |
| Motor Neuron Differentiation Kit | Directing iPSCs toward spinal motor neuron fate | Commercial kits or established 5-stage protocols [12] |
| HB9-turboGFP Reporter | Labeling motor neurons for live-cell imaging | Viral vector with motor neuron-specific promoter [12] |
| Cell Culture Matrices | Providing substrate for cell attachment and growth | Matrigel-coated plates [15] |
| Neuronal Maintenance Media | Supporting motor neuron survival and maturation | Optimized culture medium with specific growth factors [12] |
Metabolic Disorders: Fatty Acid Oxidation Disorders & Barth Syndrome
Experimental Approach
iPSC models have advanced the study of metabolic cardiomyopathies, particularly long-chain fatty acid oxidation disorders (lcFAODs) and Barth syndrome (BTHS) [16]. These disorders disrupt cardiac energy metabolism through three primary mechanisms: toxic metabolite accumulation, excessive substrate storage, and energy deficiency [16]. Research protocols typically involve:
- Patient iPSC Generation: Somatic cells from patients with specific mutations are reprogrammed to iPSCs [16].
- Cardiomyocyte Differentiation: iPSCs are differentiated into cardiomyocytes using specific biochemical cues [16].
- Metabolic and Functional Analysis: Researchers assess mitochondrial function, fatty acid oxidation rates, and contractile properties [16].
The diagram below illustrates how inherited metabolic defects lead to cardiac dysfunction:
Disease Modeling Successes
iPSC-cardiomyocytes from lcFAOD patients have revealed disease-specific alterations in mitochondrial morphology and function, enabling drug screening to identify compounds that restore metabolic balance [16]. For Barth syndrome, caused by TAFAZZIN mutations, iPSC models have elucidated the link between defective cardiolipin remodeling and mitochondrial inefficiency, providing a platform for testing potential interventions [16].
Research Reagent Solutions
Table: Essential Reagents for Metabolic Cardiomyopathy Research
| Reagent/Solution | Function | Application Example |
|---|---|---|
| Definitive Endoderm Induction Kits | First step in cardiac differentiation | STEMdiff Definitive Endoderm Kit [15] |
| Cardiac Differentiation Media | Directing iPSCs to cardiomyocyte lineage | Media with stage-specific growth factors [16] |
| Metabolic Substrates | Assessing energy pathway function | Labeled fatty acids for oxidation studies [16] |
| Mitochondrial Dyes | Visualizing and quantifying mitochondrial function | TMRE, JC-1 for membrane potential [16] |
| Calcium Indicators | Measuring calcium handling in cardiomyocytes | Fura-2, Fluo-4 for functional assessment [16] |
Cardiac Disorders: Disease Modeling & Drug Screening
Methodological Advances
iPSC-derived cardiomyocytes have become valuable for modeling inherited cardiac conditions and screening for drug-induced toxicity [17]. Key methodological considerations include:
- Maturation Strategies: iPSC-derived cardiomyocytes often resemble neonatal cells, requiring advanced maturation protocols to better model adult disease [17].
- 3D Culture Systems: Engineered heart tissues provide more physiological relevance than 2D cultures [17].
- Metabolic Maturation: Optimizing culture conditions to promote adult-like metabolic phenotypes [16].
Applications and Outcomes
In drug discovery, iPSC-cardiomyocytes have been extensively used for preclinical cardiotoxicity screening, particularly for predicting arrhythmogenic potential [13]. Companies like Fujifilm CDI and Ncardia have industrialized iPSC-derived cardiomyocyte production for high-throughput safety pharmacology [13]. For disease modeling, iPSC-cardiomyocytes from patients with hereditary cardiomyopathies have revealed disease mechanisms and enabled patient-specific drug testing [16].
Comparative Analysis of iPSC Models Across Disease Areas
Table: Quantitative Comparison of iPSC Disease Modeling Success
| Parameter | Neurological (ALS) | Metabolic (lcFAODs/BTHS) | Cardiac (Channelopathies/CM) |
|---|---|---|---|
| Sample Size in Key Studies | 100 SALS patients [12] | Multiple cell lines per disorder [16] | Varies (often 5-20 patients) [17] |
| Differentiation Efficiency | 92.44% ± 1.66% motor neurons [12] | High purity achievable [16] | High purity, but maturation limited [17] |
| Key Phenotypes Recapitulated | Reduced survival, neurite degeneration [12] | Mitochondrial dysfunction, metabolic alterations [16] | Arrhythmias, contractile dysfunction [17] |
| Clinical Predictive Value | 97% accurate for clinical trial failures [12] | Pathophysiological mechanisms confirmed [16] | Strong for cardiotoxicity prediction [13] |
| Therapeutic Discovery | Identified effective drug combination [12] | Targets for metabolic correction identified [16] | Patient-specific drug responses [16] |
iPSC technology has generated clinically relevant models across neurological, cardiac, and metabolic disorders, with the most compelling successes emerging from studies that incorporate large patient cohorts and rigorous clinical validation. The SALS model demonstrates the power of iPSCs to predict clinical trial outcomes and identify new therapeutic combinations. In metabolic and cardiac disorders, iPSCs have uncovered disease mechanisms and provided platforms for drug screening. Future directions include improving cellular maturation, developing more complex multicellular models, and integrating artificial intelligence to enhance phenotypic analysis and predictive accuracy [18]. As these technologies advance, iPSC-based disease models will play an increasingly central role in bridging the gap between preclinical research and clinical application.
In the decade and a half since their discovery, induced pluripotent stem cells (iPSCs) have revolutionized biomedical research, offering unprecedented opportunities for disease modeling, drug discovery, and regenerative medicine [1]. The ability to reprogram adult somatic cells into a pluripotent state and differentiate them into virtually any cell type provides a powerful platform for studying human diseases in vitro [19]. However, as the field matures and approaches clinical translation, a critical validation gap has emerged: the disconnect between iPSC-derived disease phenotypes observed in laboratory settings and the actual clinical manifestations in human patients. This gap represents a significant challenge for realizing the full potential of iPSC technology in therapeutic development, necessitating robust strategies to ensure that in vitro models faithfully recapitulate in vivo disease biology.
The Nature of the Validation Gap in iPSC Research
The validation gap in iPSC research stems from multiple technical and biological challenges that limit the physiological relevance of iPSC-derived models. A primary concern is the immaturity of iPSC-derived cells, which often resemble fetal rather than adult phenotypes, posing particular challenges for modeling late-onset diseases like neurodegenerative disorders [20]. This cellular immaturity means that disease-relevant pathways active in adult patients may not be fully functional in vitro, potentially leading to false negatives in drug screening or incomplete disease modeling.
Another significant factor is the inherent variability in iPSC models. Research has demonstrated that genetic background differences between iPSC donors contribute substantial variation, which can obscure disease-specific phenotypes [21]. This problem is exacerbated by differences in reprogramming methods, differentiation protocols, and culture conditions across laboratories. A power analysis of published iPSC studies reveals that many are underpowered to detect realistic effect sizes given this variability, leading to unreliable results and difficulties in replicating findings [21].
The structural simplicity of many iPSC models further contributes to the validation gap. While 2D monocultures offer experimental convenience, they lack the cellular diversity and complex tissue architecture of human organs [22]. This limitation is particularly relevant for diseases where non-cell-autonomous mechanisms—interactions between different cell types—play crucial roles in pathogenesis.
Table 1: Key Factors Contributing to the Validation Gap in iPSC Disease Modeling
| Factor | Impact on Validation | Potential Solutions |
|---|---|---|
| Cellular Immaturity | Limited relevance for late-onset diseases; incomplete phenotype development | Prolonged culture, metabolic maturation, 3D culture systems |
| Donor Variability | Difficulty distinguishing disease-specific effects from background genetic variation | Isogenic controls, larger cohort sizes, multi-line studies |
| Model Simplicity | Inability to capture tissue-level and non-cell-autonomous disease mechanisms | Co-culture systems, 3D organoids, engineered microenvironments |
| Technical Variability | Poor reproducibility across laboratories and experiments | Standardized protocols, quality control metrics, automated systems |
Quantitative Evidence of the Validation Challenge
Recent systematic analyses have quantified the scope of the validation challenge in iPSC-based modeling. A 2023 study examining statistical power in iPSC-based brain disease research found that most published case-control studies are significantly underpowered due to high variability between lines [21]. The analysis demonstrated that for a realistic effect size (Cohen's d = 1.0) with data variance similar to actual iPSC-derived neurons, a case-control study would require approximately 20 lines per group to achieve 80% power—far more than the typical 3-10 lines used in most published studies.
This power analysis further revealed that studies using isogenic lines consistently demonstrate higher statistical power than case-control designs comparing unrelated patients and controls [21]. For the same effect size, an isogenic pair design might require only 5-7 pairs to achieve similar power, representing a 3-4 fold increase in efficiency. This finding highlights the importance of appropriate experimental design in bridging the validation gap.
Table 2: Statistical Power Comparison for Different iPSC Study Designs
| Study Design | Sample Size Required for 80% Power | Relative Efficiency | Key Limitations |
|---|---|---|---|
| Case-Control (Unrelated Lines) | ~20 lines per group | 1x | High genetic background variation |
| Single Isogenic Pair | 1 pair (2 lines) | Limited generalizability | Restricted to single genetic context |
| Multiple Isogenic Pairs | ~5-7 pairs | 3-4x | Requires gene editing for each pair |
Strategies for Bridging the Validation Gap
Isogenic Controls as a Validation Tool
The use of isogenic controls represents one of the most powerful approaches for addressing the validation gap. By comparing iPSC-derived cells that differ only at a specific disease-relevant locus, researchers can isolate the effects of a particular mutation while controlling for background genetic variation [21]. This strategy was effectively demonstrated in a Huntington's disease model where introduction of a 50 CAG repeat expansion in the HTT gene of a control line enabled clear identification of disease-related phenotypes, including transcriptional changes and electrophysiological abnormalities [23].
The generation of isogenic lines typically involves CRISPR-Cas9 genome editing to introduce or correct disease-associated mutations in well-characterized iPSC lines [7]. This approach has been successfully applied to numerous conditions, including Parkinson's disease, where correction of the A53T SNCA mutation in patient-derived iPSCs enabled researchers to confirm that observed pathological features were mutation-dependent [7].
Advanced Model Systems: From 2D to 3D
Bridging the validation gap requires moving beyond simple 2D cultures to more physiologically relevant model systems. Cerebral organoids have emerged as a promising platform that better recapitulates the cellular diversity and spatial organization of human tissues [22]. These 3D structures contain multiple neural cell types and have demonstrated the ability to model disease features not observable in 2D cultures, such as the neurofibrillary tangles and β-amyloid plaques characteristic of Alzheimer's disease pathology [22].
The development of co-culture systems further addresses the validation gap by enabling investigation of non-cell-autonomous disease mechanisms [22]. For example, wild-type neural progenitor cells show reduced proliferation when co-cultured with PS1-mutant microglia compared to wild-type microglia, demonstrating how intercellular interactions contribute to Alzheimer's disease pathogenesis [22].
Multi-Omics and Phenotypic Characterization
Comprehensive validation requires thorough molecular and functional characterization of iPSC-derived models. Multi-omics approaches—including transcriptomics, proteomics, and epigenomics—provide robust benchmarks for assessing how closely iPSC-derived cells resemble their in vivo counterparts [21]. For instance, proteomic analysis of iPSC-derived neurons has revealed significant variation between lines, highlighting the importance of thorough characterization [21].
Functional validation through electrophysiological analysis remains crucial for neuronal models. In the validated Huntington's model, multi-electrode array (MEA) measurements demonstrated altered neuronal activity in HTT-mutant neurons compared to isogenic controls, providing functional correlation with molecular changes [23].
Diagram 1: Comprehensive Workflow for Validating iPSC Disease Models. This workflow integrates isogenic control generation, advanced model systems, multi-omics characterization, and clinical correlation to bridge the validation gap.
Experimental Protocols for Validation
Protocol 1: Generation and Validation of Isogenic Pairs
- Starting Material Selection: Begin with a well-characterized, high-quality iPSC line with normal karyotype and robust differentiation potential [23].
- CRISPR-Cas9 Design: Design guide RNAs targeting the locus of interest with minimal off-target effects. Include repair templates with desired modifications and appropriate selection markers.
- Electroporation: Deliver CRISPR components to iPSCs using nucleofection under optimized conditions.
- Clonal Selection: Isolate single cells and expand clonal lines. Screen for successful editing using PCR, sequencing, and functional assays.
- Off-Target Assessment: Perform whole-genome sequencing or targeted analysis of predicted off-target sites to confirm specificity.
- Pluripotency Confirmation: Verify that edited lines maintain pluripotency markers and differentiation potential.
- Banking: Create master and working cell banks of validated isogenic pairs.
Protocol 2: Multi-Omics Characterization of Disease Phenotypes
- Sample Preparation: Differentiate isogenic control and disease lines simultaneously using standardized protocols with appropriate sample replication.
- Transcriptomic Analysis:
- RNA extraction with quality control (RIN > 8.0)
- Bulk or single-cell RNA sequencing with minimum 20 million reads per sample
- Differential expression analysis with correction for multiple comparisons
- Proteomic Profiling:
- Protein extraction and quantification
- LC-MS/MS analysis using SWATH or label-free quantification
- Pathway enrichment analysis of differentially expressed proteins
- Functional Validation:
- Electrophysiological assessment (patch clamp or MEA for neuronal models)
- Metabolic assays (ATP production, mitochondrial function)
- Cellular imaging (immunocytochemistry, live-cell imaging)
- Data Integration: Correlate omics datasets with functional measurements to identify coherent disease signatures.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for iPSC Model Validation
| Reagent/Solution | Function | Application in Validation |
|---|---|---|
| CRISPR-Cas9 Systems | Precise genome editing | Generation of isogenic controls; introduction of disease mutations |
| Non-integrating Reprogramming Vectors (e.g., Sendai virus, mRNA) | Footprint-free iPSC generation | Production of clinically relevant iPSC lines with minimal genomic alterations |
| Defined Differentiation Kits | Directed differentiation to specific lineages | Standardized production of target cell types across experiments |
| Organoid Culture Matrices (e.g., Matrigel) | 3D support structure | Generation of complex tissue models with improved physiological relevance |
| Multi-Electrode Arrays (MEA) | Network-level electrophysiological recording | Functional validation of neuronal models |
| Multiplex Immunocytochemistry Antibody Panels | Protein expression analysis | Characterization of cellular identity and maturity |
| Bulk/Single-cell RNA-seq Kits | Transcriptomic profiling | Molecular validation of disease phenotypes |
As iPSC technology continues to evolve, several emerging approaches show promise for further bridging the validation gap. Artificial intelligence and machine learning are being applied to improve differentiation protocols, predict cellular behavior, and identify subtle disease phenotypes that might escape conventional analysis [24]. These computational approaches can extract more information from complex datasets, enhancing the predictive value of iPSC models.
The integration of high-content screening with multi-omics readouts enables comprehensive phenotyping that captures the multidimensional nature of human diseases [24]. As these technologies become more accessible, they will support more rigorous validation of iPSC models against clinical benchmarks.
Furthermore, the establishment of standardized validation frameworks across the field will promote consistency and reproducibility. Organizations like the International Society for Stem Cell Research (ISSCR) provide guidelines for stem cell research and clinical translation that emphasize rigor, oversight, and transparency [25]. Adherence to these principles strengthens the validity of iPSC-based findings.
In conclusion, while a significant validation gap currently exists between iPSC disease models and clinical reality, the research community has developed powerful strategies to address this challenge. Through the implementation of isogenic controls, advanced model systems, comprehensive molecular and functional characterization, and correlation with clinical data, researchers can enhance the predictive value of iPSC models. As these approaches become standardized and widely adopted, iPSC technology will increasingly fulfill its promise to accelerate drug discovery and development, ultimately leading to more effective therapies for patients.
Methodologies for Generating and Characterizing Clinically Relevant iPSC Phenotypes
The generation of induced pluripotent stem cells (iPSCs) represents one of the most significant breakthroughs in modern regenerative medicine and disease modeling. Since the pioneering work of Takahashi and Yamanaka in 2006-2007, the field has evolved from a basic proof-of-concept to a sophisticated technological platform with profound implications for drug discovery and therapeutic development [1] [7]. The core challenge in iPSC generation has centered on optimizing the balance between two critical parameters: reprogramming efficiency (the percentage of somatic cells successfully converted to pluripotency) and safety profile (minimizing risks associated with genomic instability and tumorigenicity) [26] [27]. This comparison guide provides an objective analysis of contemporary reprogramming methodologies, their performance metrics, and their application in validating disease phenotypes against clinical data—a crucial consideration for researchers and drug development professionals seeking physiologically relevant models.
Comparative Analysis of Reprogramming Techniques
Current reprogramming methods span multiple technological approaches, each with distinct advantages and limitations for clinical translation and disease modeling applications.
Table 1: Comparison of Major Reprogramming Techniques
| Method | Reprogramming Factors Delivered | Efficiency Range | Genomic Integration | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|
| Retroviral/Lentiviral | OSKM (Oct4, Sox2, Klf4, c-Myc) [1] | 0.01%-0.1% [26] | Yes | High efficiency for difficult-to-reprogram cells; well-established protocol | Significant tumorigenicity risk; silencing issues; unsuitable for clinical applications |
| Episomal Vectors | OSKM, sometimes with additional factors (e.g., LIN28, NANOG) [7] | ~0.001% [7] | No | Non-integrating; relatively simple implementation | Low efficiency; potential vector persistence in some cells |
| Sendai Virus | OSKM [7] | 0.1%-1% [7] | No | High efficiency; robust reprogramming; cytoplasmic RNA virus | Viral vector requires dilution through cell division; potential immunogenicity |
| mRNA Reprogramming | OSKMNL (Oct4, Sox2, Klf4, c-Myc, Nanog, Lin28) with immune evasion factors [27] | Up to 4% (fibroblasts); 0.5% (PBMCs) [27] | No | Highest safety profile; precise temporal control; xeno-free conditions | Requires daily transfections; potential immune activation without modifiers |
| Chemical Reprogramming | Small molecule cocktails [1] [28] | Not fully quantified | No | Completely non-genetic; potentially scalable | Complex multi-stage process; efficiency optimization ongoing |
The data reveals a clear inverse relationship between integration risk and reprogramming efficiency in earlier methods, with newer approaches like mRNA reprogramming successfully breaking this trade-off by achieving both high efficiency and excellent safety profiles [27].
Table 2: Experimental Performance Metrics in Disease Modeling Applications
| Method | Typical Reprogramming Time | Teratoma Formation Risk | Genetic Stability | Suitable for Clinical Applications | Best Applications |
|---|---|---|---|---|---|
| Retroviral/Lentiviral | 2-3 weeks [1] | High | Low due to insertional mutagenesis | No | Basic research; mechanistic studies |
| Episomal Vectors | 3-4 weeks [7] | Moderate | Moderate | Preclinical | Disease modeling with isogenic controls |
| Sendai Virus | 3-4 weeks [7] | Low | High | With rigorous clearance testing | Disease modeling; drug screening |
| mRNA Reprogramming | 10-14 days [27] | Very Low | Very High | Yes, with GMP compliance | Clinical-grade iPSCs; personalized medicine |
| Chemical Reprogramming | Not fully established | Potentially Low | Potentially High | Under investigation | Future therapeutic applications |
Molecular Mechanisms and Signaling Pathways
The reprogramming process involves profound remodeling of the chromatin structure and epigenome, transitioning through distinct molecular phases [1]. The early phase is characterized by the silencing of somatic genes and activation of early pluripotency-associated genes, while the late phase involves stabilization of the pluripotency network [1]. Mesenchymal-to-epithelial transition (MET) represents a critical bottleneck in this process, coordinated by suppression of pro-epithelial-to-mesenchymal transition (EMT) signals like TGF-β signaling [26].
The molecular roadmap above illustrates the phased progression from somatic to pluripotent state, highlighting key barriers and enhancers that impact efficiency. Research has identified specific strategies to modulate these pathways, including depletion of barriers like p53, p21, and Mbd3, or overexpression of enhancing genes such as FOXH1 and GLIS1 [26]. Understanding these mechanisms enables researchers to select reprogramming methods that optimally navigate this complex landscape.
Experimental Protocols for High-Efficiency Reprogramming
mRNA Reprogramming Protocol
The mRNA reprogramming approach represents one of the most advanced methods for generating clinical-grade iPSCs, combining high efficiency with an excellent safety profile [27]. The following protocol is adapted from commercial mRNA reprogramming kits with optimization for research applications:
Day 0: Plate neonatal or adult human fibroblasts on iMatrix-511-coated wells at a density of 10,000-20,000 cells per cm² in fibroblast culture medium [27].
Days 1-4: Perform daily transfections with StemRNA 3rd Gen Reprogramming Factor mRNAs (OSKMNL - Oct4, Sox2, Klf4, c-Myc, Nanog, Lin28) combined with immune evasion factors (EKB) using a suitable transfection reagent. Incubate cells in NutriStem hPSC XF medium at 37°C with 5% O₂ (hypoxic conditions) to enhance colony yields [27].
Days 5-14: Change medium daily without additional transfections. Monitor emerging iPSC colonies daily for morphology changes characteristic of pluripotent cells [27].
Days 10-14: Identify and manually pick compact iPSC colonies with defined borders and high nucleus-to-cytoplasm ratio for further expansion and characterization [27].
Protocol for Enhancing Reprogramming Efficiency
Several strategic enhancements can significantly improve reprogramming outcomes across different methods:
Hypoxic Conditions: Maintain cultures at 5% O₂ throughout reprogramming to enhance colony yields by reducing oxidative stress [27].
Small Molecule Supplementation: Add vitamin C (ascorbic acid) to culture media to enhance reprogramming efficiency through epigenetic modulation, particularly as a co-factor for histone and DNA demethylases [26].
Barrier Inhibition: Implement transient inhibition of reprogramming barriers such as p53 or TGF-β signaling using small molecule inhibitors (e.g., A83-01 for TGF-β inhibition) during early reprogramming phases to enhance efficiency [26].
MET Promotion: Enhance mesenchymal-to-epithelial transition by supplementing with small molecules that promote this critical early reprogramming event [26].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Advanced Reprogramming
| Reagent Category | Specific Examples | Function in Reprogramming | Application Notes |
|---|---|---|---|
| Reprogramming Factors | StemRNA 3rd Gen mRNA cocktail (OSKMNL + EKB) [27] | Core factors inducing pluripotency; immune evasion | Enables high-efficiency, integration-free reprogramming |
| Culture Matrices | iMatrix-511, Corning Matrigel [27] | Provides extracellular matrix support for cell attachment and signaling | Critical for colony formation and expansion |
| Culture Media | NutriStem hPSC XF Medium [27] | Defined, xeno-free medium supporting reprogramming and pluripotency | Eliminates batch-to-batch variability |
| Small Molecule Enhancers | Vitamin C, TGF-β inhibitors, MAPK inhibitors [26] | Modulates signaling pathways to enhance efficiency | Particularly valuable for difficult-to-reprogram cell types |
| Efficiency Reporters | Fbxo15-β-gal/neo reporter system [1] | Enables quantification and selection of reprogrammed cells | Essential for method optimization and quality control |
Disease Modeling Applications and Clinical Validation
Advanced reprogramming techniques have enabled unprecedented opportunities for disease modeling and drug discovery. The capacity to generate patient-specific iPSCs provides a biologically matched resource for studying disease mechanisms and screening therapeutic compounds [19] [29].
The workflow above illustrates how advanced reprogramming enables the generation of disease models that can be rigorously validated against clinical data. A landmark study demonstrating this approach involved generating an iPSC library from 100 sporadic ALS (SALS) patients and conducting population-wide phenotypic screening [12]. The resulting motor neurons recapitulated key disease aspects including reduced survival, accelerated neurite degeneration correlating with donor survival, transcriptional dysregulation, and appropriate pharmacological rescue by riluzole [12]. This validation against clinical outcomes establishes the pathophysiological relevance of iPSC models for drug development.
Similar approaches have been successfully applied across numerous disease areas:
Neurological Disorders: iPSC-derived dopaminergic neurons from Parkinson's patients show impaired mitochondrial function, increased oxidative stress, and α-synuclein accumulation [29].
Cardiac Diseases: iPSC-derived cardiomyocytes from patients with familial long-QT syndrome demonstrate prolonged action potentials, mirroring the clinical electrophysiological abnormality [19].
Metabolic Disorders: Hepatocyte-like cells derived from patients with α1-antitrypsin deficiency recapitulate the pathological phenotype with aggregation of misfolded protein in the endoplasmic reticulum [29].
The field of iPSC reprogramming continues to evolve with several emerging trends shaping future applications. Partial reprogramming approaches are gaining attention for their potential to achieve cellular rejuvenation without complete dedifferentiation, potentially offering therapeutic applications for age-related diseases [28]. Chemical reprogramming using entirely non-genetic methods represents another frontier, though efficiency and protocol standardization remain challenging [28]. For disease modeling, the progression from two-dimensional cultures to complex three-dimensional organoids and multi-organ systems enables more physiologically relevant studies of tissue-level interactions and disease pathophysiology [19] [29].
The integration of CRISPR-Cas9 genome editing with iPSC technology has further enhanced disease modeling capabilities, allowing creation of isogenic controls that differ only at disease-relevant loci, thereby eliminating confounding genetic background effects [7] [29]. Additionally, artificial intelligence and machine learning are being applied to improve standardization, quality control, and differentiation outcome prediction in iPSC manufacturing [7].
In conclusion, the ongoing refinement of reprogramming techniques has progressively enhanced both efficiency and safety profiles, with mRNA reprogramming currently representing the optimal balance for many research and clinical applications. The rigorous validation of disease phenotypes against clinical data ensures the physiological relevance of iPSC models, positioning this technology as an indispensable platform for drug discovery and the development of personalized medicine approaches. As standardization improves and protocols become more accessible, these advanced reprogramming techniques will continue to transform our approach to disease modeling and therapeutic development.
The advent of induced pluripotent stem cell (iPSC) technology has revolutionized regenerative medicine by providing a platform for disease modeling, drug screening, and potential cell therapies. A critical challenge in this field is achieving precision differentiation—generating functionally mature, patient-specific somatic cells that accurately recapitulate native physiology and disease phenotypes. This guide provides a comparative analysis of experimental protocols for differentiating iPSCs into three therapeutically crucial cell types: cardiomyocytes, neurons, and pancreatic beta-cells, with a specific focus on validating resulting disease models against clinical data.
Experimental Protocols for Precision Differentiation
Cardiomyocyte Differentiation
Overview: Efficient cardiac differentiation requires stage-specific manipulation of developmental signaling pathways to guide iPSCs through mesoderm, cardiac mesoderm, and cardiomyocyte progenitor stages, ultimately yielding functional cardiomyocytes.
- Key Signaling Pathways: The Wnt/β-catenin pathway requires precise temporal regulation—initial activation promotes mesoderm commitment, while subsequent inhibition drives cardiac specification. Concurrent BMP (Bone Morphogenetic Protein) and Nodal/Activin A signaling further enhance cardiac progenitor formation [30] [31].
- Maturation Challenges: hiPSC-derived cardiomyocytes (hiPSC-CMs) typically exhibit an immature fetal-like phenotype, characterized by a rounded morphology, poorly organized sarcomeres, lack of T-tubules, and a reliance on glycolytic metabolism rather than mitochondrial oxidative phosphorylation [30].
- Advanced Maturation Protocol: A robust method for enhancing maturation involves culturing cells on a biomimetic fibronectin-Matrigel composite extracellular matrix (ECM). This is combined with precise small-molecule modulation of key signaling pathways, resulting in significantly improved sarcomere organization, contractile function, and electrophysiological properties that more closely resemble adult cardiomyocytes [32].
Neuronal Differentiation
Overview: Neuronal differentiation leverages fundamental developmental principles, where morphogen gradients pattern iPSCs toward specific neural fates, followed by terminal differentiation into diverse neuronal subtypes.
- Dual Strategies: Two primary methods exist:
- Transcription Factor Overexpression: Direct introduction of lineage-specific transcription factors (e.g., Ngn2 for motor neurons) instructs rapid neuronal conversion [33].
- Small Molecule-Mediated Induction: Sequential use of small molecules modulates key pathways (SMAD, Wnt, SHH) to direct neural induction and subtype specification in a more scalable manner [33] [1].
- Subtype Specification: The specific combination of morphogens determines the neuronal subtype. For example, dopaminergic neurons require activation of SHH (Sonic Hedgehog) and FGF8 (Fibroblast Growth Factor 8) to establish a midbrain identity, while motor neuron generation depends on caudalizing (retinoic acid) and ventralizing (SHH) signals [33].
- Current Challenges: Key hurdles include achieving high purity and functional maturity of specific neuronal subtypes, and ensuring the long-term survival and functional integration of transplanted neurons in vivo [33].
Pancreatic Beta-Cell Differentiation
Overview: Generating glucose-responsive insulin-producing cells (IPCs) involves mimicking pancreatic organogenesis by guiding iPSCs through definitive endoderm, primitive gut tube, pancreatic progenitor, and endocrine progenitor stages.
- Key Markers and Real-Time Monitoring: A powerful approach for protocol optimization involves using a Pdx1-mRFP/Insulin-hrGFP dual-reporter iPSC line. This allows for real-time monitoring of two key transcription factors: Pdx1 (pancreatic progenitor marker) and Insulin (beta-cell hormone) [34].
- Protocol Enhancements: Studies demonstrate that 3D induction protocols significantly improve the efficiency of pancreatic progenitor specification and yield more mature IPCs compared to traditional 2D cultures. Furthermore, treatments that promote DNA demethylation can enhance differentiation efficiency by remodeling the epigenetic landscape [34].
- Functional Maturity: The ultimate goal is to generate beta-cells that exhibit glucose-stimulated insulin secretion, express key maturity markers (e.g., MAFA, NKX6.1), and contain insulin granules, achieving functional parity with primary human islet beta-cells [34].
The diagram below summarizes the core signaling pathways and key markers involved in differentiating iPSCs into these three target cell types.
Comparative Analysis of Differentiation Outcomes and Functional Validation
The table below provides a detailed, quantitative comparison of the typical yields, key maturity markers, and functional characteristics achieved by contemporary differentiation protocols for each target cell type.
Table 1: Quantitative Comparison of iPSC Differentiation Outcomes
| Differentiation Aspect | Cardiomyocytes | Neurons (Dopaminergic) | Beta-Cells |
|---|---|---|---|
| Differentiation Efficiency | High purity: >90% cTnT+ reported [30] | ~50-80% TUJ1+; ~30-60% TH+ for dopaminergic [33] | Variable; 10-30% Insulin+ without sorting [34] |
| Key Structural Markers | cTnT, α-actinin, MLC2v, βMHC [30] | TUJ1, MAP2, Tyrosine Hydroxylase (TH) [33] | PDX1, NKX6.1, C-peptide, Insulin [34] |
| Critical Functional Assays | Contractility analysis, Ca2+ transients, MEA for electrophysiology [30] [32] | Electrophysiology (patch clamp), dopamine release, synaptic activity [33] | Glucose-Stimulated Insulin Secretion (GSIS), C-peptide secretion [34] |
| In Vivo Validation | Engraftment in rodent/ primate MI models; EHM allografts in macaques/human [31] | Functional improvement in PD rodent/ primate models; dopamine release [35] [36] | Glucose correction in diabetic rodent models; reversal of hyperglycemia [34] |
| Primary Limitation | Immature phenotype, fetal gene expression, lack of T-tubules [30] [31] | Subtype purity, functional integration post-transplantation, synaptic complexity [33] | Functional immaturity, inconsistent GSIS, polyhormonal cells [34] |
The Scientist's Toolkit: Essential Research Reagents
Successful precision differentiation relies on a core set of high-quality reagents and tools. The following table details essential components for establishing these protocols in a research setting.
Table 2: Key Research Reagent Solutions for iPSC Differentiation
| Reagent / Tool | Primary Function | Application Across Cell Types |
|---|---|---|
| Yamanaka Factor Reprogramming Tools | Non-integrating methods (e.g., Sendai virus, mRNA) to generate clinical-grade iPSCs [37] [36] | Foundational step for creating patient-specific lines for all cell types. |
| Small Molecule Pathway Modulators | Precise temporal control of key pathways (Wnt, BMP, TGF-β, SHH, RA) [33] [1] [32] | Core component of all differentiation protocols (e.g., CHIR99021 for Wnt activation). |
| Extracellular Matrix (ECM) Components | Provide biophysical and biochemical cues for cell adhesion, survival, and differentiation (e.g., Vitronectin, Matrigel, Fibronectin composites) [32] | Used in all protocols; composite matrices enhance cardiomyocyte maturation [32]. |
| Reporter Cell Lines | Enable real-time monitoring of differentiation efficiency via lineage-specific fluorescent proteins (e.g., PDX1-mRFP/Insulin-hrGFP) [34] | Critical for protocol optimization, especially for beta-cells and neuronal subtypes. |
| Cell Surface Markers for Purification | Antibodies against proteins like CD34 (hematopoietic) or CD142 (pancreatic progenitors) for isolating specific populations [38] | Used to enrich target populations (e.g., CD34+ progenitors) to increase purity. |
The precision differentiation of iPSCs into cardiomyocytes, neurons, and beta-cells has progressed remarkably, moving from proof-of-concept to the development of sophisticated protocols capable of generating cells with increasing structural and functional maturity. The consistent theme across all three lineages is that functional maturation remains the primary bottleneck, whether it involves achieving adult-like metabolic and electrophysiological properties in cardiomyocytes, robust synaptic integration of neurons, or fully glucose-responsive insulin secretion in beta-cells. Overcoming these hurdles requires a multi-faceted approach, integrating advanced engineering strategies like 3D culture, biochemical stimulation, and genetic tools to guide cells toward a more complete mature state. As these technologies mature and converge with advancements in gene editing and biomaterials, the path toward clinically relevant disease modeling, high-fidelity drug screening, and effective autologous cell therapies becomes increasingly attainable.
In the landscape of modern biomedical research, the quest for physiologically relevant models that narrow the divide between conventional two-dimensional (2D) cell cultures and dynamic living systems has driven the rise of organoid technology [39]. Traditional 2D culture systems, while simple and cost-effective, differ substantially from original tumors in various aspects, including the tumor microenvironment, cell metabolism, and gene expression profiles [40]. These models fail to faithfully recapitulate human-specific responses, leading to poor predictive value and high attrition rates in clinical trials [41]. For many years, scientists have recognized that depending on the physiological processes studied, these simplified models often lack the intricate interactions found in native tissues, such as tissue-specific architecture, cell-extracellular matrix interactions, spatial organization, and diversity of cell types that are essential for tissue functionality [42].
Three-dimensional organoids represent a revolutionary advancement in disease modeling, offering miniature, in vitro models of human organs grown from stem cells or tissue samples [39] [43]. These systems preserve patient-specific genetic, epigenetic, and phenotypic features, providing unprecedented opportunities for personalized disease modeling and drug response prediction [41]. The convergence of stem cell and organoid technologies has catalyzed the emergence of next-generation preclinical platforms, particularly in the context of precision medicine and the validation of iPSC disease phenotypes against clinical data [41] [44]. As the field progresses, organoids are rapidly becoming indispensable tools for researchers seeking to bridge the translational gap between preclinical findings and clinical applications.
Fundamental Differences Between 2D and 3D Model Systems
Structural and Functional Limitations of 2D Cultures
Conventional 2D cell cultures, in which cells grow as a flat monolayer on plastic surfaces, present several critical limitations for disease modeling and drug development. The artificial environment fails to replicate the complex three-dimensional architecture of human tissues, leading to altered cell morphology, polarization, and signaling [40] [42]. In 2D systems, cell-extracellular matrix interactions are fundamentally different, gene expression profiles are significantly altered, and critical tissue-specific functions are often lost [40]. These limitations substantially reduce the predictive power of 2D models for human physiological responses.
The simplification of the cellular environment in 2D cultures results in abnormal cell differentiation, proliferation, and drug metabolism patterns. For instance, 2D-cultured cells typically exhibit uniform exposure to oxygen, nutrients, and therapeutic agents—a condition rarely found in human tissues or tumors where gradient distributions create microenvironments with distinct cellular behaviors [42]. This lack of physiological relevance contributes to the high failure rates observed in drug development, where promising results from 2D models frequently fail to translate to clinical success [41].
Advantages of 3D Organoid Models
Organoids are three-dimensional, self-organizing structures derived from stem cells that closely mimic the cytoarchitecture and functional characteristics of native human organs [41]. These advanced models offer several significant advantages over traditional 2D systems:
- Architectural Complexity: Organoids replicate the spatial organization, cellular heterogeneity, and tissue-specific structures of original organs, including crypt-villus architecture in intestinal organoids and bile canaliculi in hepatic organoids [41].
- Functional Fidelity: They preserve key physiological functions, such as polarized secretion, metabolic activity, and electrical signaling patterns, more accurately reflecting in vivo conditions [43].
- Patient Specificity: Patient-derived organoids (PDOs) retain the genetic, epigenetic, and phenotypic features of the donor tissue, enabling personalized disease modeling and drug testing [39] [41].
- Microenvironment Recapitulation: 3D organoids better model the tumor microenvironment, including gradients of oxygen, nutrients, and therapeutic agents that influence drug penetration and efficacy [40] [42].
Table 1: Comparative Analysis of 2D vs. 3D Organoid Culture Systems
| Characteristic | 2D Culture Systems | 3D Organoid Models |
|---|---|---|
| Spatial Architecture | Monolayer, flat growth | 3D structure, tissue-like organization |
| Cell-Cell Interactions | Limited to horizontal contacts | Multi-directional, physiologically relevant |
| Extracellular Matrix | Artificial or absent | Natural or biomimetic matrix present |
| Proliferation Patterns | Uniform | Heterogeneous, with growth gradients |
| Gene Expression | Altered, dedifferentiated | Tissue-specific, differentiated |
| Drug Response | Typically more sensitive | More physiologically relevant resistance |
| Metabolic Activity | Homogeneous | Zoned, with metabolic heterogeneity |
| Predictive Value for Clinical Response | Limited (~5% translation) | Enhanced, with demonstrated correlation |
Experimental Validation: Direct Comparisons of 2D and 3D Systems
Methodological Approaches for Comparative Studies
Robust comparative analyses between 2D and 3D models require standardized protocols for generating and evaluating both systems. For pancreatic cancer research, studies have established conditionally reprogrammed cell (CRC) lines under 2D conditions before transitioning to 3D organoid cultures using a Matrigel-based platform without organoid-specific medium components to preserve intrinsic molecular subtypes [40]. This approach allows direct comparison using isogenic cell populations, eliminating genetic variability as a confounding factor.
Key methodological considerations include:
- Matrix Selection: Matrigel is commonly used for 3D organoid culture, providing a basement membrane-rich environment that supports self-organization and polarity [40].
- Medium Composition: Avoidance of niche factors like Wnt3a, R-Spondin-1, and Noggin in some protocols preserves original molecular subtypes and disease phenotypes [40].
- Characterization Techniques: Morphological, molecular, and drug sensitivity analyses are performed to compare responses between 2D and 3D systems and correlate with clinical outcomes [40].
- Viability Assessment: Advanced imaging techniques like brightfield live-cell imaging with label-free segmentation algorithms enable accurate growth rate calculations and drug response quantification [45].
Quantitative Evidence of Enhanced Predictive Power
Recent studies provide compelling quantitative evidence supporting the superior predictive value of 3D organoid models. In pancreatic cancer research, drug response profiling of standard chemotherapies (gemcitabine plus nab-paclitaxel and FOLFIRINOX) demonstrated that 3D organoids more accurately mirrored patient clinical responses than 2D cultures [40]. Notably, the IC50 values for the 3D organoids were generally higher, reflecting the structural complexity and drug penetration barriers observed in vivo [40].
For neurodegenerative disease modeling, brain organoids have enabled the study of patient-specific cellular phenotypes that correlate with clinical data. A significant advancement demonstrated that iPSC-derived astrocytes from Alzheimer's patients exhibited morphology changes that stratified with clinical biomarker levels (CSF YKL-40), allowing correlation between cellular phenotypes and patient clinical presentation [44]. This approach enables patient stratification by providing cellular models that reflect the heterogeneity of complex disorders.
Table 2: Quantitative Comparison of Drug Response in 2D vs. 3D Models
| Parameter | 2D Culture Findings | 3D Organoid Findings | Clinical Correlation |
|---|---|---|---|
| IC50 Values | Generally lower, indicating higher drug sensitivity | Higher values, reflecting in vivo-like drug resistance | 3D values closer to clinical response doses [40] |
| Heterogeneity | Homogeneous response across population | Variable response mimicking patient variability | Recapitulates inter-patient variability in clinical trials [41] [45] |
| Therapeutic Window | Overestimated for many compounds | More accurate prediction of efficacy/toxicity balance | Better predicts clinical success/failure [39] |
| Mechanistic Insights | Limited to cell-autonomous effects | Reveals microenvironment-mediated resistance | Explains clinical drug resistance mechanisms [40] [42] |
| Growth Rate Metrics | Traditional metrics division-dependent | Normalized Organoid Growth Rate (NOGR) accounts for variability | More biologically relevant drug sensitivity assessment [45] |
Technical Approaches for Robust Organoid Culture
Essential Reagents and Methodologies
Successful organoid culture requires specific reagents and techniques that support three-dimensional growth and self-organization. The research toolkit for organoid generation includes several critical components:
Table 3: Essential Research Reagent Solutions for Organoid Culture
| Reagent/Cultureware | Function | Example Applications |
|---|---|---|
| Matrigel Matrix | Basement membrane extract providing 3D scaffold | Supports polarization and self-organization of epithelial organoids [40] |
| Stem Cell Sources | iPSCs, embryonic stem cells, or adult stem cells | Starting material for generating various organoid types [41] [43] |
| ROCK Inhibitor (Y-27632) | Prevents anoikis in dissociated cells | Enhances survival during initial plating and passaging [40] |
| Tissue-Specific Media Formulations | Defined combinations of growth factors and inhibitors | Directs differentiation toward specific lineages (e.g., neural, hepatic, intestinal) [39] [41] |
| Low-Adhesion Plates | Prevents cell attachment to promote 3D aggregation | Enables spheroid formation in suspension cultures [42] |
| CRISPR-Cas9 Systems | Genome editing for disease modeling or correction | Creating isogenic controls or introducing disease mutations [39] [7] |
Advanced Imaging and Analysis Workflows
Modern organoid research employs sophisticated imaging and analysis pipelines to extract meaningful quantitative data. The OrBITS (Organoid Brightfield Identification-based Therapy Screening) platform utilizes label-free bulk and single-organoid deep learning-based segmentation from brightfield images [45]. This approach enables non-invasive monitoring of organoid growth and viability without fluorescent markers, preserving sample integrity for longitudinal studies.
The Normalized Organoid Growth Rate (NOGR) metric represents a significant advancement over traditional assessment methods. Specifically developed for brightfield imaging-based assays, NOGR more effectively captures cytostatic and cytotoxic drug effects compared to conventional metrics like IC50 or relative viability [45]. This is particularly valuable for distinguishing between growth inhibition and actual cell death—a critical distinction in therapeutic development that is often obscured in 2D models.
Applications in Disease Modeling and Precision Medicine
Neurodegenerative Disease Modeling
Brain organoids have emerged as powerful tools for studying neurodegenerative diseases, providing insights into human-specific aspects of brain development and pathology that cannot be effectively modeled in animals [43]. These 3D models recapitulate key cellular and molecular aspects of conditions like Alzheimer's and Parkinson's disease, offering a platform for studying disease mechanisms and potential therapeutic strategies [43].
Recent advances demonstrate the utility of iPSC-derived brain cell types in modeling disease heterogeneity and correlating cellular phenotypes with clinical data. For Alzheimer's disease, iPSC-derived astrocytes from patient panels exhibit structural changes that stratify with clinical biomarker levels (CSF YKL-40), enabling correlation between cellular phenotypes and patient clinical presentation [44]. This approach provides valuable models for patient stratification and personalized therapeutic development.
Cancer Research and Drug Screening
In oncology, patient-derived tumor organoids (PDTOs) have shown remarkable fidelity to original tumors, retaining histological and genomic features, including intratumoral heterogeneity and drug resistance patterns [41]. These models are increasingly used for medium-throughput drug screening, offering real-time insight into individual responses to chemotherapy, targeted agents, or immunotherapies [41].
Pancreatic cancer research exemplifies the translational potential of organoid technology. Studies using patient-derived organoids to study KRAS inhibition and chemotherapy resistance have identified novel therapeutic vulnerabilities [46]. Similarly, in colorectal cancer, organoid models have been successfully used to evaluate morphological and viability characteristics across multiple cell lines, providing insights into tumor-stroma interactions in a 3D setting [42].
Current Challenges and Future Directions
Despite significant advances, organoid technology faces several challenges that must be addressed to maximize its potential. Limitations include variability in organoid generation, lack of vascularization, difficulties in large-scale production, and incomplete recapitulation of the tumor microenvironment, particularly immune cells and stromal components [39] [41] [43]. Batch-to-batch variability in matrices like Matrigel and differences in protocol implementation across laboratories also present hurdles to standardization [41].
Future developments are focusing on several key areas:
- Vascularization and Immune Integration: Strategies to incorporate endothelial cells and immune components to better model complex tissue interactions [39].
- Standardization and Scalability: Development of automated, high-throughput platforms for large-scale organoid production and screening [41] [45].
- Multi-omics Integration: Combining organoid technology with genomic, transcriptomic, and proteomic analyses for comprehensive disease characterization [39] [41].
- Organ-on-Chip Technologies: Integrating organoids with microfluidic systems to model inter-organ crosstalk and systemic drug responses [39] [41].
- Artificial Intelligence Applications: Leveraging AI for image analysis, phenotype classification, and correlation with clinical data [44] [45].
As these advancements mature, organoid technology is poised to become an increasingly central component of biomedical research, drug development, and precision medicine, offering more human-relevant, ethical, and individualized approaches to understanding and treating complex diseases.
The transition from traditional 2D cultures to sophisticated 3D organoid models represents a paradigm shift in complex disease modeling. Organoids bridge the critical gap between simplified monolayer cultures and in vivo physiology, offering unprecedented opportunities to model human diseases with enhanced physiological relevance. The demonstrated ability of patient-derived organoids to recapitulate clinical drug responses and their growing utility in correlating cellular phenotypes with patient clinical data underscore their transformative potential in personalized medicine and drug development.
While challenges remain in standardization, vascularization, and immune integration, ongoing interdisciplinary innovations are rapidly addressing these limitations. As organoid technology continues to evolve, integrated with advances in microfluidics, genetic engineering, and artificial intelligence, it promises to accelerate the development of safer, more effective therapeutics and advance our fundamental understanding of human biology and disease mechanisms. For researchers and drug development professionals, embracing and refining these sophisticated 3D models is essential for advancing translational research and bringing precision medicine approaches to clinical practice.
High-Content Phenotypic Screening and Multi-Omics Characterization
The convergence of high-content phenotypic screening and multi-omics technologies is revolutionizing the validation of disease-specific phenotypes in induced pluripotent stem cell (iPSC) models. This integrated approach provides a powerful framework for bridging in vitro observations with clinical relevance, a central challenge in translational research. High-content imaging delivers rich, quantitative data on cellular morphology and structure, while multi-omics analyses—encompassing proteomics, lipidomics, and metabolomics—supply a deep molecular context for these observed phenotypes [47] [48]. For researchers using iPSC-derived neurons and other cell types to model human diseases, this multi-faceted strategy is indispensable for confirming that the in vitro phenotypes accurately reflect human disease biology, thereby strengthening the predictive value of iPSC-based platforms for drug discovery and mechanistic studies [47] [1] [49].
Core Technology Comparisons
The following section provides a detailed, data-driven comparison of the primary technologies used for phenotypic and molecular characterization.
High-Content Phenotypic Screening Platforms
Table 1: Comparison of High-Content Screening and Image Analysis Platforms
| Platform / Assay | Key Measurable Parameters | Typical Throughput | Key Advantages | Common Applications in iPSC Validation |
|---|---|---|---|---|
| Cell Painting Assay [48] | ~280+ features/cell (Intensity, Texture, Shape, Spatial relationships between organelles) | Medium-to-High (96/384-well) | Unbiased, comprehensive morphological profiling; Detects subtle phenotypes | Mechanism of Action (MoA) identification, toxicity assessment, phenotypic hit triage |
| Confocal HCA (e.g., ImageXpress Micro Confocal) [48] | 3D Z-stacks, co-localization, intensity quantification | Medium (Confocal), High (Widefield) | Superior image resolution and optical sectioning | Detailed analysis of complex 3D models (e.g., organoids), sub-cellular localization |
| Semantic Segmentation (e.g., SINAP in IN Carta) [48] | Object identification accuracy, segmentation precision | Software-dependent (post-acquisition) | Improved feature detection with pre-trained or user-trained deep learning models | Robust nuclei/cell detection in heterogeneous iPSC-derived cultures |
| Semiconductor Microplate Platform [50] | Label-free assessment of cell morphology and function | High (96-well) | Label-free, functional electrical impedance data | Long-term, non-invasive monitoring of iPSC-derived cell health and function |
Multi-Omics Characterization Technologies
Table 2: Comparison of Omics Technologies for iPSC Phenotype Validation
| Omics Layer | Technology Examples | Key Outputs | Role in iPSC Phenotype Validation | Typical Coverage/Sensitivity |
|---|---|---|---|---|
| Proteomics [47] | LC-MS/MS (Data Independent Acquisition), UHPLC-MS/MS | Protein identification/quantification, signaling states, post-translational modifications | Confirms protein-level changes underlying morphological phenotypes; identifies therapeutic targets | Up to ~5,000 proteins with platforms like Olink/Somalogic [51] |
| Lipidomics [47] | UHPLC-MS/MS with deuterated internal standards | Lipid species identification and quantification (e.g., cardiolipins, fatty acids) | Reveals metabolic stress, membrane composition changes, disease-specific lipid signatures | Hundreds of lipid species across multiple classes |
| Metabolomics [47] | UHPLC-MS/MS with internal standards (e.g., 13C515N folic acid) | Identification/quantification of cellular metabolites (amino acids, carbohydrates) | Provides a snapshot of cellular metabolic activity and energy status | Dozens to hundreds of central carbon metabolites |
| Transcriptomics [49] | RNA-Seq, single-cell RNA-Seq | Global gene expression patterns, pathway activation | Links morphological changes to transcriptional rewiring; essential for developmental stage validation | Genome-wide |
Detailed Experimental Protocols
This section outlines the core methodologies for generating reproducible data in integrated phenotypic and multi-omics studies.
High-Content Phenotypic Profiling Using the Cell Painting Assay
The following workflow is adapted from established protocols for unbiased morphological profiling [48].
- Cell Culture and Seeding: Plate iPSC-derived cells (e.g., cortical neurons [47]) in a Matrigel-coated 384-well μClear plate at an optimized density (e.g., 2,000 cells/well in 40 μL of culture medium). Incubate at 37°C for 24 hours to allow for cell attachment.
- Perturbation and Treatment: Replace the medium with a low-serum version (e.g., 2% FBS) prior to compound addition. Treat cells with the experimental compounds in a dilution series (e.g., 7-point, 1:3). Include DMSO vehicle controls and relevant positive/negative controls in quadruplicate wells. Incubate for a specified duration (e.g., 24 hours).
- Staining and Fixation:
- Live-Cell Staining: Stain live cells with 500 nM MitoTracker DeepRed for 30 minutes at 37°C in the dark to label mitochondria.
- Fixation: Fix cells with 3.2% paraformaldehyde (PFA) for 20 minutes.
- Permeabilization and Staining: Permeabilize cells with 0.1% Triton X-100 for 20 minutes. Prepare a master staining solution in a blocking buffer (1X HBSS, 1% BSA) containing: 5 μL/mL phalloidin (F-actin), 100 μg/mL Concanavalin A (endoplasmic reticulum), 5 μg/mL Hoechst (nuclei), 1.5 μg/mL Wheat Germ Agglutinin (WGA, Golgi apparatus), and 3 μM SYTO 14 (RNA/nucleoli). Incubate cells with the staining solution for 30 minutes at room temperature in the dark. Perform three wash steps with 1X HBSS.
- Image Acquisition: Acquire images using a high-content imaging system (e.g., ImageXpress Micro Confocal) with a 20x objective. Acquire a small Z-stack (e.g., 3 images) and use a best-focus projection. Utilize filter sets for DAPI (Hoechst), FITC (SYTO 14), TRITC (Con A/WGA), Texas Red (Phalloidin), and Cy5 (MitoTracker). Acquire at least 4 fields of view per well to ensure statistical robustness.
- Feature Extraction and Analysis:
- Image Analysis: Use software (e.g., IN Carta) with a semantic segmentation module (SINAP) for robust identification of nuclei, cytoplasm, and organelles (mitochondria, ER, actin). Extract ~280 measurements per cell related to intensity, texture, shape, and spatial relationships.
- Data Processing: Export single-cell data and upload to an analysis platform (e.g., HC StratoMineR). Perform quality control (e.g., remove wells with <50 cells), data transformation, and feature scaling.
- Phenotypic Profiling: Use Principal Component Analysis (PCA) for dimensionality reduction. Calculate a "distance score" from the principal components to quantify the phenotypic effect of each treatment. Use this score for hit selection and hierarchical clustering to group compounds with similar mechanisms of action.
Integrated Multi-Omics Sample Preparation from iPSCs
This protocol enables the concurrent extraction of proteins, lipids, and metabolites from a single iPSC sample, ensuring integrated analysis from the same biological source [47].
- Cell Harvesting: Wash iPSCs or iPSC-derived neurons (e.g., day 14 i3Neurons [47]) gently with ice-cold PBS. Quench and harvest cells by adding 350 μL of an ice-cold methanol/water mixture (5:2, v/v) directly onto the culture plate and scraping. Transfer the lysate to a 2 mL tube. Repeat this step and combine the lysates.
- Simultaneous Extraction of Proteins, Lipids, and Metabolites (Folch Method):
- Add pre-defined internal standards to the sample: deuterated lipid standards (e.g., EquiSplash mix) for lipidomics and 13C515N folic acid for metabolomics.
- Sonicate the sample tubes on ice for 2 minutes.
- Add 1 mL of HPLC-grade chloroform to each sample, followed by incubation on ice for 1 hour with frequent vortexing.
- Centrifuge the samples at 12,700 rpm at 4°C for 15 minutes. This will separate the mixture into three phases: a bottom chloroform layer (lipids), an interphase (proteins), and a top aqueous layer (metabolites).
- Fraction Separation and Preparation:
- Lipid Fraction: Carefully transfer the bottom chloroform layer to a new tube. Dry under a gentle stream of nitrogen or in a SpeedVac.
- Metabolite Fraction: Transfer the top aqueous layer to a separate tube. Dry using a SpeedVac.
- Protein Pellet: Retain the protein pellet in the original tube and allow it to air dry.
- Sample Preparation for LC-MS/MS:
- Proteomics: Reconstitute the protein pellet in 8 M urea lysis buffer. Reduce, alkylate, and digest proteins using trypsin/Lys-C. Desalt the resulting peptides.
- Lipidomics: Reconstitute the dried lipid extract in 150 μL of methanol/chloroform/water (18:1:1, v/v/v).
- Metabolomics: Reconstitute the dried metabolite extract in 35 μL of water with 0.1% formic acid.
- Data Acquisition: Analyze the fractions using respective LC-MS/MS methods (e.g., 210-min gradient on a Q-Exactive HF-X Orbitrap MS for proteomics; UHPLC-MS/MS for lipidomics and metabolomics).
Visualizing Integrated Workflows and Biological Relationships
The following diagrams, generated using Graphviz DOT language, illustrate the core experimental workflows and data integration logic.
Integrated Phenotypic & Multi-Omics Workflow
Integrated Phenotypic and Multi-Omics Workflow for iPSC Validation
Multi-Omics Data Integration Logic
Multi-Omics Data Integration and Analysis Logic
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Reagents and Materials for Integrated Screening
| Item Name | Function / Role | Example Application / Note |
|---|---|---|
| iPSC Line (e.g., i3Neuron) [47] | Provides a pure, scalable population of human neurons for consistent screening. | Engineered with doxycycline-inducible NGN2 for rapid, synchronized differentiation. |
| Cell Painting Dye Set [48] | Comprehensively labels major organelles for unbiased morphological profiling. | Includes: MitoTracker (mitochondria), Phalloidin (actin), Con A (ER), WGA (Golgi), SYTO 14 (RNA), Hoechst (nuclei). |
| Matrigel / PLO Coating [47] [48] | Provides a biologically relevant substrate for cell attachment and growth. | Essential for robust plating of sensitive iPSC-derived cells in multi-well plates. |
| Deuterated Internal Standards [47] | Enables accurate quantification in mass spectrometry-based omics. | Added during extraction to correct for technical variability (e.g., EquiSplash for lipids). |
| Trypsin/Lys-C Mix [47] | Enzymatically digests proteins into peptides for proteomic analysis. | Key reagent for sample preparation in bottom-up proteomics workflows. |
| FAIR Data Management Platform [49] | Stores, organizes, and shares large-scale imaging and omics data. | Critical for reproducibility and collaborative analysis of multi-modal datasets. |
| AI/ML Analysis Platform (e.g., PhenAID) [49] | Integrates multimodal data to identify patterns, predict MoA, and validate phenotypes. | Bridges the gap between complex data and actionable biological insights. |
Overcoming Barriers: Troubleshooting Phenotypic Variability and Optimization Strategies
Tumorigenicity Risk in iPSC-Derived Therapies
A primary safety concern for clinical application of induced pluripotent stem cells (iPSCs) is their potential for tumorigenicity. This risk arises from two main sources: the presence of residual undifferentiated cells in the final product and the genetic and epigenetic instability acquired during reprogramming or culture [52]. Tumorigenicity evaluation must be an integral part of the safety assessment for any cell-based therapy, with strategies tailored to the specific product's risk profile.
Regulatory Considerations and Risk Assessment
Global regulatory agencies acknowledge that tumorigenicity risk is influenced by multiple factors, including cell source, phenotype, differentiation status, proliferative capacity, and ex vivo processing methods [52]. While a unified global regulatory consensus on technical implementation is still evolving, evaluation strategies generally focus on in vivo and in vitro methods to assess this risk before clinical trials.
Table 1: Tumorigenicity Evaluation Methods for iPSC-Based Products
| Method Type | Specific Method | Key Measured Parameters | Considerations |
|---|---|---|---|
| In Vivo Assays | Teratoma Formation Assay [53] | Formation of tissues from three germ layers; histopathological analysis | Gold standard for pluripotency; requires immune-deficient mice |
| Tumor Formation Studies | Monitoring for abnormal growth following implantation | Long observation periods; species-specific limitations | |
| In Vitro Assays | Karyotyping & Genomic Analysis [53] | Chromosomal number and structure abnormalities | Detects gross abnormalities but not single nucleotide changes |
| Residual Undifferentiated Cell Quantification | Flow cytometry for pluripotency markers (e.g., Tra-1-60, SSEA-4) [53] | Critical for final product release testing | |
| Functional Assays | Soft Agar Colony Formation | Anchorage-independent growth potential | Correlates with tumorigenic potential |
Experimental Protocol: Teratoma Formation Assay
The teratoma formation assay is a standard method to evaluate the differentiation potential and tumorigenic risk of iPSC lines and their derivatives [53].
Detailed Protocol:
- Cell Preparation: Harvest iPSCs or differentiated cells (typically 2×10^6 cells) and resuspend in 50μl of PBS/Matrigel mixture [53].
- Implantation: Inject the cell suspension subcutaneously or under appropriate tissue capsules into immunodeficient mice (e.g., CAnN.Cg-Foxn1 nu/CrljOri mice).
- Observation Period: Monitor for 10-12 weeks, observing for palpable mass formation.
- Histopathological Analysis: Excise formed teratomas, fix in formaldehyde, process for paraffin embedding, section at 5μm thickness, and perform hematoxylin and eosin staining.
- Evaluation: Assess for the presence of differentiated tissues from all three germ layers (ectoderm, mesoderm, and endoderm) as evidence of pluripotency, and specifically screen for any malignant components.
Genomic Instability in iPSC Generation and Culture
Genomic instability represents a critical challenge in iPSC-based therapies, as mutations acquired during reprogramming or extended culture can compromise safety and efficacy. A systematic investigation revealed that genomic alterations occur throughout the iPSC lifecycle—from reprogramming through differentiation and passaging [53].
Reprogramming Method Impacts Genomic Integrity
The choice of reprogramming method significantly influences the genomic stability of resulting iPSCs. Sendai virus (SV) and episomal vector (Epi) methods demonstrate markedly different genomic instability profiles:
Table 2: Genomic Alterations in iPSCs by Reprogramming Method
| Reprogramming Method | CNA Frequency during Reprogramming | SNV Occurrence | Key Observations |
|---|---|---|---|
| Sendai Virus (SV) | 100% of cell lines showed CNAs [53] | Observed during passaging and differentiation [53] | Higher genomic instability; upregulation of chromosomal instability genes in late passages |
| Episomal Vectors (Epi) | 40% of cell lines showed CNAs [53] | No SNVs detected [53] | Lower frequency of genomic alterations |
| Overall Findings | Total of 10 CNAs and 5 SNVs observed across all phases [53] | TP53 mutations identified as particularly concerning [53] | Careful genomic scrutiny essential for clinical preparation |
Experimental Protocol: Comprehensive Genomic Analysis
A multi-technique approach provides the most complete assessment of genomic integrity in iPSC lines [53].
Detailed Protocol:
- Chromosome Analysis: Perform standard G-banding karyotyping to identify gross chromosomal abnormalities at a resolution of approximately 5-10 Mb.
- Chromosomal Microarray: Use array-based comparative genomic hybridization (aCGH) or SNP arrays to detect copy number variations (CNVs) and copy number alterations (CNAs) at higher resolution.
- Short Tandem Repeat (STR) Analysis: Authenticate cell lines and monitor for cross-contamination.
- Next-Generation Sequencing (NGS): Implement whole genome or targeted sequencing to identify single nucleotide variations (SNVs), with particular attention to cancer-associated genes like TP53 [53].
- Gene Expression Analysis: Utilize RNA sequencing or qPCR to assess expression of chromosomal instability-related genes, especially in late-passage cells.
Batch Effects and Quality Control Standardization
Batch effects introduce significant variability in iPSC differentiation outcomes and pose a major challenge for reproducible disease modeling and clinical translation [35]. These inconsistencies arise from differences in reprogramming techniques, donor genetic variability, culture conditions, and differentiation protocol implementation.
The persistence of embryonic or fetal identity in derived tissues and background genetic variability of iPSC lines create pervasive barriers to consistent differentiation outcomes [19]. Commercial cell providers now offer QC-verified batches to address these concerns, and efforts to benchmark electrophysiological performance or gene expression signatures are underway, though not yet universal [9].
Table 3: Strategies to Mitigate Batch Effects in iPSC Research
| Strategy Category | Specific Approach | Implementation | Outcome |
|---|---|---|---|
| Genetic Standardization | Isogenic Controls [29] | CRISPR/Cas9 correction or introduction of mutations | Controls for genetic background; enables direct phenotype-genotype correlation |
| Process Control | Automated Culture Systems [35] | Robotic maintenance and differentiation | Reduces operator-dependent variability |
| Analytical Correction | AI/ML Quality Control [35] | Automated colony morphology classification; differentiation outcome prediction | Enhances standardization and reproducibility in manufacturing |
| Characterization | Functional Biomarkers | Electrophysiological profiling; metabolic assays | Confirms functional maturity beyond molecular markers |
Experimental Protocol: Establishing Isogenic Controls
CRISPR/Cas9 genome editing has become an essential tool for creating isogenic controls that minimize batch effects by controlling for genetic background [35].
Detailed Protocol:
- Guide RNA Design: Design sgRNAs flanking the mutation of interest, considering off-target potential and efficiency.
- Repair Template Construction: Generate a single-stranded oligodeoxynucleotide (ssODN) or plasmid donor template containing the desired correction or mutation with appropriate homologous arms.
- Electroporation: Deliver ribonucleoprotein complexes (Cas9 protein + sgRNA) and repair template to iPSCs using specialized systems (e.g., Neon Transfection System) [53].
- Clone Isolation and Expansion: Plate at clonal density, manually pick colonies, and expand in quality-controlled culture conditions.
- Genotypic Validation: Confirm precise genome editing via Sanger sequencing, PCR analysis, and elimination of off-target edits through whole-genome sequencing.
- Phenotypic Validation: Ensure pluripotency maintenance through immunocytochemistry for markers (OCT4, Nanog, SSEA-4) [53] and teratoma formation assays [53].
Research Reagent Solutions
Table 4: Essential Research Reagents for iPSC Quality Control
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Reprogramming Systems | CytoTune-iPS 2.0 Sendai Reprogramming Kit; Episomal iPS reprogramming vectors [53] | Non-integrating reprogramming of somatic cells to pluripotency |
| Pluripotency Validation Antibodies | OCT3/4, Nanog, Tra-1-81, SSEA-3, Tra-1-60, SSEA-4 [53] | Immunocytochemical confirmation of pluripotent state |
| Differentiation Kits | STEMdiff Mesenchymal Progenitor Kit [53] | Directed differentiation to specific lineages |
| Culture Media | mTeSR1; MesenCult-ACF Medium [53] | Maintenance of pluripotency or support of differentiated cells |
| Genomic Analysis Kits | Chromosomal Microarray kits; NGS library preparation kits | Detection of CNAs, SNVs, and other genomic alterations |
| Cell Characterization Kits | ALP Staining Kit (Vector Red) [53]; Mycoplasma Detection Kit [53] | Assessment of pluripotency and routine quality control |
Visualizing Experimental Workflows
Tumorigenicity Risk Assessment Workflow
Tumorigenicity Risk Assessment Workflow
Genomic Screening Pipeline
Comprehensive Genomic Screening Pipeline
Standardizing Protocols for Manufacturing, Quality Control, and Potency Assays
The promise of induced pluripotent stem cell (iPSC) technologies in modeling human diseases and developing personalized regenerative treatments is fundamentally dependent on the standardization of manufacturing, quality control, and potency assays [35]. iPSCs, generated by reprogramming adult somatic cells into a pluripotent state, provide a versatile platform for creating patient-specific cellular models that are biologically matched and reduce the risk of immune rejection [35]. However, the translational potential of these technologies has been hampered by significant challenges in standardization, including variability in differentiation outcomes, genetic and epigenetic abnormalities, and the risk of tumor formation [35]. Perhaps most critically, the lack of reliable, standardized potency assays has limited the ability to ensure consistent biological activity across product lots, creating a major barrier to clinical application [54] [55].
This guide objectively compares current approaches and methodologies for standardizing iPSC-based workflows, with a specific focus on validating disease phenotypes against clinical data. We present comparative experimental data and detailed protocols to enable researchers to implement robust, reproducible systems for iPSC-based drug discovery and development.
Comparative Analysis of iPSC Phenotypic Screening Platforms
Large-scale phenotypic screening of iPSC-derived cells has emerged as a powerful approach for disease modeling and therapeutic discovery, particularly for complex, sporadic diseases. The table below compares key performance metrics from recent studies, highlighting the impact of standardization on experimental outcomes.
Table 1: Performance Comparison of iPSC Phenotypic Screening Platforms
| Screening Platform & Study Focus | Scale (Donors) | Key Performance Metrics | Clinical Correlation Findings | Limitations & Challenges |
|---|---|---|---|---|
| SALS Motor Neuron Survival [12] | 100 SALS patients, 25 controls | • Accelerated neurite degeneration correlated with donor survival (p<0.01).• Transcriptional profile matched post-mortem spinal cord.• 97% of clinically failed drugs also failed in the model. |
Donor survival time correlated with in vitro neurite degeneration rate. | Requires highly optimized, standardized differentiation protocol to maintain phenotype. |
| Population-wide ALS Phenotyping [12] | 100 SALS, 11 monogenic ALS, 25 controls | • High-purity motor neurons (92.44% ± 1.66%).• Successful pharmacological rescue with riluzole.• Identified a potential 3-drug combinatorial therapy. | Recapitulated donor clinical heterogeneity (onset age, progression rate). | Cell-autonomous system may not fully capture non-cell-autonomous disease mechanisms. |
| Answer ALS Consortium [12] | ~1,000 iPSC lines | • No significant motor neuron survival deficit reported.• No clear separation in transcriptomic profiles between SALS and controls. | Limited correlation between in vitro model and clinical disease pathophysiology. | Lack of robust, standardized phenotyping protocol across a large donor cohort. |
Experimental Protocols for Validating iPSC Disease Phenotypes
Protocol: Large-Scale Phenotypic Screening of iPSC-Derived Motor Neurons
This protocol, adapted from a large-scale sporadic Amyotrophic Lateral Sclerosis (SALS) study, details a standardized workflow for generating and phenotyping iPSC-derived motor neurons to validate disease phenotypes against clinical data [12].
- iPSC Library Generation and Quality Control: Donor fibroblasts are reprogrammed using non-integrating episomal vectors on an automated robotics platform to maximize output and uniformity [12]. All generated lines must undergo rigorous quality control:
- Standardized Motor Neuron Differentiation: A five-stage protocol adapted from established spinal motor neuron differentiation methods is used [12] [35]. Key steps include:
- Culture Purity Validation: Immunostaining for markers like ChAT, MNX1/HB9, and Tuj1. The protocol yields
92.44% ± 1.66%pure motor neuron cultures with minimal contamination from astrocytes (0.12%) and microglia (0.04%) [12].
- Culture Purity Validation: Immunostaining for markers like ChAT, MNX1/HB9, and Tuj1. The protocol yields
- Longitudinal Live-Cell Imaging and Phenotyping: Cultures are monitored daily using live-cell imaging coupled with a virally delivered, non-integrating, motor neuron-specific reporter (HB9-turbo) [12]. Key quantitative phenotypes assessed are:
- Neurite Degeneration: Measured via automated image analysis.
- Cell Survival: Tracked over time.
- Clinical Correlation Analysis: In vitro phenotypes (e.g., rate of neurite degeneration) are statistically correlated with donor clinical data, such as survival time from onset, using appropriate correlation coefficients [12].
- Pharmacological Validation: The model is validated by testing drugs with known clinical efficacy (e.g., riluzole) to confirm it recapitulates expected therapeutic responses [12].
The workflow for this protocol is standardized to ensure reproducibility across a large number of cell lines.
Protocol: Implementing a Potency Assurance Strategy for CGT Products
For iPSC-derived cell and gene therapy (CGT) products, the FDA's recent draft guidance recommends a holistic Potency Assurance Strategy rather than relying on a single potency test. This strategy integrates quality by design and risk management principles from ICH Q8-Q13 [54] [56].
- Define Quality Target Product Profile (QTPP): Based on the product's Mechanism of Action (MOA), intended clinical indication, and route of administration [56].
- Identify Potency-Related Critical Quality Attributes (CQAs): Use product characterization studies, prior knowledge, and nonclinical/clinical data to identify CQAs critical for the therapeutic effect [56]. For a complex product, multiple CQAs may be needed to fully reflect potency [54].
- Risk Assessment and Control Strategy:
- Risk Assessment: Conduct a formal risk assessment (per ICH Q9) for each potency-related CQA, considering the entire process from manufacturing to administration [56].
- Control of Materials: Strictly control critical raw materials, especially biological activities like growth factors, and evaluate all contact materials (e.g., container closure systems) for potential impact on potency [54] [55].
- Process Parameters: Identify and control Critical Process Parameters (CPPs) that impact CQAs. Implement In-Process Controls (IPCs) like viability and phenotype characterization [54] [55].
- Potency Assay Selection and Validation: The strategy must include at least one bioassay for lot release [54] [56].
- Assay Qualification/Validation: Assays must be precise, accurate, specific, and robust. Qualification is needed for early clinical stages, with full validation for product licensing [56] [57].
- Reference Standards: Use authenticated reference strains or USP Bioassay Reference Standards to ensure comparability and reproducibility [58] [59].
The following diagram illustrates the core logic of building a potency assurance strategy.
The Scientist's Toolkit: Essential Reagents and Materials
Successful standardization requires carefully selected and controlled reagents. The following table details key solutions used in the featured experimental protocols.
Table 2: Essential Research Reagent Solutions for Standardized iPSC Workflows
| Reagent / Material | Function & Application | Key Considerations for Standardization |
|---|---|---|
| Non-Integrating Reprogramming Vectors (e.g., episomal, Sendai virus, mRNA) | Reprogram somatic cells into iPSCs without genomic integration, enhancing clinical safety [35]. | Use of GMP-grade materials is critical for clinical translation. Avoids insertional mutagenesis risk. |
| Reference Strains & Standards | Ensure comparability and reproducibility of bioassays (e.g., antibiotic potency, iPSC differentiation) [58] [59]. | Must be internationally recognized, regularly traced to source, and verified for activity (e.g., per USP, ChP) [58]. |
| GMP-Grade Culture Media & Supplements (e.g., FBS, platelet lysate) | Support the robust and consistent expansion and differentiation of iPSCs and derived cells [57]. | Strict quality control and batch-to-batch consistency are vital to minimize variability in differentiation outcomes. |
| Critical Raw Materials (e.g., growth factors, cytokines) | Direct lineage specification and maturation during differentiation protocols. | Biological activity is a key parameter. Requires strict acceptance criteria and testing before use in manufacturing [54] [55]. |
| Validated Assay Reagents | Used in quality control and potency assays (e.g., immunophenotyping, qPCR, ELISA). | Reagents must be qualified for specificity and precision. New lots of critical reagents can cause shifts in assay results [59] [57]. |
Regulatory and Quality Considerations for Standardization
Evolving Regulatory Landscape for Potency Assays
The regulatory framework for potency assurance, particularly for CGT products, is evolving. The U.S. FDA's 2023 draft guidance on "Potency Assurance for Cellular and Gene Therapy Products" marks a significant shift from the 2011 guidance, promoting a holistic, risk-based strategy over a narrow focus on the assay itself [54] [55] [56].
- The Potency Assurance Strategy: This overarching concept incorporates principles from ICH Q8-Q13, emphasizing that consistent potency is achieved through comprehensive product and process understanding and a robust control strategy, not just by final product testing [54] [56].
- Focus on Manufacturing Controls: The guidance highlights the importance of Critical Process Parameters (CPPs), in-process testing, and control of critical raw materials and contact materials as essential elements for ensuring consistent potency [54] [55].
- Assay Development: The guidance advises using at least one bioassay for lot release, which should be based on a risk assessment. It encourages avoiding animal-based assays where possible due to variability and aligning with the 3Rs (Replacement, Reduction, Refinement) [54] [55]. It also notes that the assay does not need to fully reflect the complex MOA but should effectively mitigate the risk to product potency [54].
Analytical Method Validation in a GMP Context
For iPSC-derived products classified as Advanced Therapy Medicinal Products (ATMPs), manufacturing must comply with Good Manufacturing Practice (GMP) rules, which include validating analytical methods used for quality control [57].
- Validation Parameters: Per ICH Q2(R1) guidelines, key parameters for method validation include accuracy, precision (repeatability and intermediate precision), specificity, detection limit, linearity, and range [57].
- Risk-Based Approach: For investigational ATMPs in early phases, demonstration of method suitability may be sufficient, though a risk-based approach often justifies full validation of release methods to ensure product quality and safety [57].
- Challenges with Complex Products: Validating methods for cellular products presents unique challenges due to their intrinsic biological variability and the lack of compendial methods. This often requires customized validation strategies and well-characterized reference samples [57].
The standardization of manufacturing, quality control, and potency assays is the linchpin for translating iPSC technologies from research tools into reliable platforms for drug discovery and clinical application. As demonstrated by large-scale studies in diseases like ALS, the implementation of rigorously optimized and standardized protocols is a prerequisite for generating disease-relevant phenotypes that correlate with clinical data [12]. Furthermore, the evolving regulatory landscape underscores the necessity of adopting a holistic, science- and risk-based potency assurance strategy that encompasses the entire product lifecycle, from raw material control to final product release [54] [56]. By integrating the comparative data, experimental protocols, and standardized toolkits outlined in this guide, researchers and drug development professionals can significantly enhance the reproducibility, reliability, and clinical translatability of their iPSC-based research.
The Role of AI and Machine Learning in Predicting Differentiation Outcomes and Analyzing Complex Datasets
The integration of artificial intelligence (AI) and machine learning (ML) with induced pluripotent stem cell (iPSC) technology is fundamentally transforming disease modeling and drug discovery. This synergy is particularly crucial for validating iPSC-derived disease phenotypes against clinical data, a core challenge in translational research. AI systems excel at analyzing the massive, multi-modal datasets generated in stem cell research—including genomic, proteomic, and image-based data—to uncover hidden biological patterns [18]. By leveraging these capabilities, researchers can now make more accurate predictions about stem cell behavior, optimize differentiation protocols, and generate more clinically relevant disease models that truly capture the complex polygenic nature of conditions like Alzheimer's disease [60].
AI/ML Paradigms in Stem Cell Research
Core Approaches and Their Applications
Multiple AI/ML paradigms have been established to address specific challenges in stem cell biology. Table 1 summarizes the primary approaches, their functions, and applications in iPSC research.
Table 1: Core AI/ML Approaches in iPSC Research
| AI/ML Approach | Primary Function | Specific Applications in iPSC Research |
|---|---|---|
| Convolutional Neural Networks (CNNs) [61] [18] | Image analysis and pattern recognition | Automated analysis of iPSC colony morphology, real-time monitoring of differentiation, and quality assessment of derived cells like cardiomyocytes. |
| Deep Learning (DL) & Generative Models [62] [18] | Modeling complex non-linear relationships and generating new data | Predicting successful cellular reprogramming, generating novel molecular structures, and forecasting differentiation outcomes from omics data. |
| Supervised ML (e.g., SVM, Random Forest) [61] | Classification and regression based on labeled data | Classifying cell types, predicting iPSC pluripotency, and identifying genetic stability from defined parameters. |
| Predictive Modeling & Digital Twins [63] | Simulating biological processes and disease progression | Creating in silico models of disease progression for clinical trials, predicting patient-specific treatment responses. |
Experimental Workflow for AI-Driven Phenotype Validation
The following diagram illustrates the integrated workflow for applying AI/ML to validate iPSC disease models against clinical data, a process central to the thesis of bridging cellular models and human disease.
AI-iPSC Clinical Validation Workflow
Quantitative Performance of AI/ML Models
Performance Metrics for Key Tasks
The effectiveness of AI/ML in predicting differentiation outcomes and analyzing complex datasets is demonstrated through quantitative performance metrics across various tasks. Table 2 consolidates experimental data from multiple studies, providing a comparative overview of model performance.
Table 2: Performance Metrics of AI/ML Models in Stem Cell Applications
| Application Area | AI/ML Technique | Key Performance Metric | Reported Outcome | Experimental Context |
|---|---|---|---|---|
| Cellular Reprogramming | Convolutional Neural Networks (CNN) [18] | Prediction Accuracy | High accuracy in identifying iPSCs with successful reprogramming potential | Analysis of time-lapse bright-field microscopy images to track morphological changes. |
| Lineage Differentiation | Deep Learning (DL) [18] | Differentiation Outcome Prediction | Improved protocol efficiency and consistency | Multi-omics data integration to forecast differentiation trajectories to target cell types. |
| Quality Control | Deep Learning [18] | Classification Accuracy | High precision in distinguishing healthy vs. abnormal iPSC colonies | Automated imaging analysis of colony morphology, structure, and viability. |
| Polygenic Risk Assessment | Polygenic Risk Score (PRS) Models [60] | Disease Prediction Accuracy | 84% accuracy in predicting individual's risk of developing Alzheimer's disease | Analysis of >70 genetic variants from genome-wide association studies (GWAS). |
| Clinical Trial Optimization | Digital Twin Generators [63] | Trial Efficiency | Significant reduction in control arm size and faster patient recruitment | AI-driven models of disease progression for Phase III trials in Alzheimer's disease. |
Case Study: AI-Driven iPSC Resource for Alzheimer's Disease
A landmark study creating the IPMAR resource (iPSC Platform to Model Alzheimer's Disease Risk) exemplifies AI's power in analyzing complex genetic datasets for disease modeling. Researchers generated 109 iPSC lines from donors selected based on polygenic risk scores (PRS), capturing extremes of genetic risk for common Alzheimer's disease [60]. The resource includes:
- 90 lines with extremes of global AD PRS (34 LOAD, 29 EOAD, 27 low-risk controls)
- 19 lines with extremes of complement pathway-specific PRS (9 high-risk, 10 low-risk)
- Rich associated datasets including clinical, longitudinal, and genetic data
This resource enables researchers to stratify individuals based on specific genetic risk profiles and correlate these with functional cellular assays, paving the way for personalized medicine approaches in Alzheimer's disease [60].
Detailed Experimental Protocols
Protocol 1: AI-Driven Quality Control of iPSC Colonies
This protocol details the use of convolutional neural networks (CNNs) for automated quality assessment of iPSC cultures, a critical step for ensuring reproducible differentiation outcomes [18].
Materials:
- High-resolution microscope with time-lapse capability
- Computing infrastructure with GPU acceleration
- Label-free imaging capability (phase contrast, bright-field microscopy)
Methodology:
- Image Acquisition: Capture time-lapse bright-field microscopy images of developing iPSC colonies at regular intervals (e.g., every 2-4 hours) over the reprogramming or differentiation period.
- Data Preprocessing: Apply normalization and standardization techniques to ensure consistent image quality across samples [64].
- Model Training: Train CNN architectures (e.g., ResNet, VGG) on manually annotated images to classify colonies based on morphological features associated with pluripotency, genetic stability, and differentiation potential.
- Feature Identification: The model learns to identify key morphological characteristics including colony boundaries, cell density, and structural organization that correlate with quality metrics.
- Validation: Implement k-fold cross-validation (typically k=5 or k=10) to assess model performance and prevent overfitting [64] [65].
- Deployment: Integrate the trained model into an automated system for real-time monitoring and quality assessment of iPSC cultures.
Protocol 2: Predictive Modeling of Differentiation Outcomes Using Multi-Omics Data
This protocol describes a comprehensive approach to predicting iPSC differentiation outcomes by integrating multiple data modalities through deep learning models [18].
Materials:
- Transcriptomic data (RNA-seq)
- Epigenomic data (ATAC-seq, ChIP-seq)
- Proteomic data (mass spectrometry)
- High-performance computing cluster
Methodology:
- Data Collection: Generate transcriptomic, epigenomic, and proteomic profiles at multiple time points during differentiation protocols.
- Data Integration: Apply data normalization and feature selection techniques to create a unified multi-omics dataset [64].
- Model Architecture: Implement a multi-modal deep learning framework that can process different data types through separate input branches that merge in later layers.
- Training Regimen: Train models using stratified k-fold cross-validation to predict differentiation efficiency and terminal cell type characteristics.
- Interpretability Analysis: Apply model-agnostic interpretation tools like SHAP (SHapley Additive exPlanations) to identify the most influential features driving predictions [65].
- Experimental Validation: Correlate model predictions with functional assays of differentiated cells (e.g., electrophysiology for neurons, beating for cardiomyocytes).
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3 catalogs key reagents and computational tools essential for implementing AI-driven iPSC research, with explanations of their specific functions in the experimental workflow.
Table 3: Essential Research Reagents and Computational Tools for AI-iPSC Integration
| Tool/Reagent Category | Specific Examples | Function in AI-iPSC Workflow |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (Yamanaka factors) [18] | Foundation for generating patient-specific iPSC lines that retain donor genetic information for disease modeling. |
| Differentiation Kits | Commercial neural, cardiac, hepatic differentiation kits | Provide standardized protocols that generate consistent cellular backgrounds for AI model training and validation. |
| Multi-Omics Assays | RNA-seq kits, ATAC-seq kits, mass spectrometry reagents | Generate complex molecular datasets that serve as input features for AI/ML predictive models of cell fate. |
| Quality Control Assays | Pluripotency markers (e.g., NANOG), viability stains, karyotyping kits | Generate ground-truth data for training and validating AI-based quality control systems. |
| AI/ML Frameworks | TensorFlow, PyTorch, Scikit-learn [64] [65] | Provide foundational algorithms and architectures for building custom predictive models from iPSC data. |
| Model Interpretation Tools | SHAP, LIME, Explainable Boosting Machines (EBM) [65] | Enable interpretation of "black box" AI models to extract biologically meaningful insights from predictions. |
| Validation Platforms | Galileo, custom cross-validation pipelines [64] | Assess model performance, detect overfitting, and ensure generalizability before experimental deployment. |
AI Model Validation Framework for iPSC Applications
Critical Validation Dimensions
Given the high-stakes applications in disease modeling and drug discovery, rigorous validation of AI/ML models for iPSC research is essential. The following framework outlines key dimensions that must be addressed [65]:
- Data Appropriateness: Ensure training data comprehensively represents the biological variability expected in real-world applications, with proper handling of missing data and outliers [64].
- Methodology and Model Testing: Implement computationally intensive validation methods like k-fold cross-validation and leave-one-out cross-validation (LOOCV) to assess model stability [65].
- Conceptual Soundness and Interpretability: Apply model-agnostic interpretation tools (SHAP, LIME) to validate that feature importance aligns with biological knowledge [65].
- Ongoing Monitoring and Governance: Establish continuous monitoring for model performance degradation (model drift) as new data becomes available [64] [65].
The integration of AI and ML with iPSC technology represents a paradigm shift in how researchers approach disease modeling and drug discovery. By leveraging these powerful computational tools to analyze complex datasets and predict differentiation outcomes, scientists can create more clinically relevant models that better bridge the gap between cellular phenotypes and human disease. As these methodologies continue to mature, they promise to accelerate the development of personalized regenerative therapies and enhance our fundamental understanding of disease mechanisms.
Navigating Regulatory and Scalability Hurdles for Clinical Translation
The derivation of induced pluripotent stem cells (iPSCs) represents a transformative milestone in regenerative medicine, offering unprecedented opportunities for patient-specific therapies, disease modeling, and drug discovery [1]. By reprogramming adult somatic cells into a pluripotent state using defined transcription factors, researchers can generate patient-specific cells capable of differentiating into nearly any tissue type [7]. This technology provides a versatile platform for developing biologically matched therapies that circumvent ethical concerns associated with embryonic stem cells while potentially reducing immune rejection risks [7] [66].
Despite this considerable promise, translating iPSC technologies from laboratory research to routine clinical applications has proven challenging [7]. The journey from preclinical validation to approved therapies faces significant practical and biological barriers, including tumorigenic risks, manufacturing complexities, and regulatory uncertainties [67] [66]. Furthermore, critical questions around long-term engraftment, tissue integration, and immune tolerance remain unresolved [7]. This comparison guide examines the current state of iPSC clinical translation, analyzing key hurdles and presenting objective data to inform researchers and drug development professionals working to advance iPSC-based therapies toward clinical application.
Regulatory Pathways for iPSC-Based Therapies
The regulatory landscape for iPSC-based products is complex, requiring careful navigation of agency requirements and quality standards. Regulatory approval pathways demand rigorous attention to product characterization, safety profiling, and manufacturing consistency [66].
Table 1: Comparison of Autologous vs. Allogeneic iPSC Approaches
| Parameter | Autologous iPSCs | Allogeneic iPSCs |
|---|---|---|
| Immune Compatibility | High (patient-specific) | Variable (may require immune suppression) |
| Manufacturing Timeline | Long (3-6 months per patient) | Short (using pre-established cell banks) |
| Scalability | Low (patient-specific batches) | High (large-scale production possible) |
| Quality Control | Variable (per patient batch) | Consistent (master cell banks) |
| Cost Considerations | High (personalized manufacturing) | Lower (economies of scale) |
| Regulatory Pathway | Complex (multiple products) | Simplified (single product) |
| Clinical Examples | Parkinson's disease trials [7] | Retinal disorders, platelet products [67] |
A critical regulatory requirement is the implementation of Good Manufacturing Practices (GMP)-compliant production systems early in development [66]. This involves establishing defined culture systems that avoid chemically undefined media or materials of animal origin, which carry risks of transmitting xenopathogens [66]. Regulatory submissions must include rigorous quality controls documenting viability, function, purity, and sterility for each manufactured cell batch, with certificates of analysis generated for all product lots certified for clinical use [66].
Figure 1: iPSC Clinical Translation Regulatory Pathway
For preclinical studies, regulatory agencies require comprehensive biodistribution testing and tumorigenicity assessments [66]. These studies evaluate product safety, off-target effects, and the potential for teratoma formation from residual undifferentiated cells within transplanted products [66]. Advanced imaging technologies including positron emission tomography (PET), magnetic resonance imaging (MRI), and bioluminescence imaging (BLI) have improved monitoring of transplanted grafts, enabling spatiotemporal mapping of transplanted cells for both long-term and short-term safety studies required by regulatory agencies [66].
Scalability and Manufacturing Challenges
The transition from research-scale to clinical-grade iPSC manufacturing presents substantial scalability challenges that must be addressed through technological innovation and process optimization.
Table 2: Scalability Challenges in iPSC Manufacturing
| Manufacturing Stage | Research Scale | Clinical Scale | Solutions |
|---|---|---|---|
| Reprogramming | Viral vectors, variable efficiency | Non-integrating methods, defined efficiency [7] | Episomal plasmids, mRNA, Sendai virus [7] |
| Cell Expansion | Manual culture, limited scale | Automated bioreactors, monitoring systems [7] | Scale-out technologies, process controls |
| Differentiation | Variable protocols, fetal characteristics [29] | Standardized protocols, mature phenotypes | 3D culture, organoid systems, metabolic maturation [19] |
| Quality Control | Periodic sampling, limited assays | In-line monitoring, comprehensive characterization [66] | Genomic stability tests, potency assays, sterility testing |
| Storage & Distribution | Short-term, local use | Cryopreserved, stable inventory | Master/working cell banks, validated cryopreservation |
Recent advances in automation and artificial intelligence are enhancing standardization in iPSC manufacturing [7]. AI-guided differentiation and automated colony morphology classification systems are being applied to improve quality control and reproducibility [7]. Additionally, mathematical modeling of differentiation processes enables in silico optimization of protocols, potentially reducing extensive experimentation needs [68]. For example, modeling iPSC differentiation to definitive endoderm has predicted optimal differentiation periods of 1.9-2.4 days and ideal plating densities near 300,000 cells per well for maximum yield efficiency [68].
Manufacturing scalability differs significantly between autologous and allogeneic approaches [66]. Allogeneic therapies benefit from established master cell banks that enable large-scale, cost-effective production runs, while autologous approaches require patient-specific manufacturing with inherent scalability limitations [66]. The choice between these approaches depends on multiple factors including target disease, clinical urgency, and cost considerations [7].
Clinical Trial Landscape and Evidence Base
The clinical evidence base for iPSC therapies is emerging but remains limited, with early studies demonstrating feasibility while highlighting the need for more robust controlled trials.
Table 3: Published Clinical Studies of iPSC-Derived Therapies
| Medical Condition | Cell Product | Study Design | Patients Treated | Key Outcomes |
|---|---|---|---|---|
| Parkinson's Disease | Dopaminergic progenitors [7] | Phase I/II | Not specified | Cell survival, dopamine production, no tumors [7] |
| Geographic Atrophy (AMD) | RPE product (Eyecyte-RPE) [7] | IND approval | Not specified | Approved in India (2024) [7] |
| Retinitis Pigmentosa | Retinal organoid [67] | Uncontrolled | 1 | Stable survival for 2 years [67] |
| Bullous Keratopathy | Corneal endothelial cell substitute [67] | First-in-human | 5 | Improved corneal transparency [67] |
| B-cell Lymphoma | CD19 CAR-NK cells [67] | Phase I | Not specified | First iPSC-derived CAR clinical trial [67] |
| Heart Failure | Cardiovascular cell secretome [67] | Case report | 1 | First use of secretome approach [67] |
A systematic scoping review identified only 10 published clinical studies and 22 ongoing registered trials utilizing iPSCs across various conditions including cardiac diseases, ocular disorders, cancer, and graft-versus-host disease [67]. Published studies were predominantly small and uncontrolled, with only two studies enrolling more than four patients and a total of just 115 patients treated across all published studies [67]. This limited evidence base precludes definitive conclusions about safety or efficacy and highlights the early stage of clinical translation for iPSC-based therapies.
The variability among studies and ongoing trials complicates the understanding of iPSC therapeutic potential [67]. Studies show considerable differences in design, medical conditions examined, cell sources for iPSC generation, and specific iPSC-derived cell products administered [67]. While iPSC characterization was generally aligned with criteria established by the International Society for Stem Cell Research, standardized outcome reporting and adherence to consistent cell product characterization criteria would enhance comparability between studies and potentially accelerate development [67].
Experimental Protocols for iPSC Validation
Tumorigenicity Risk Assessment
Purpose: Evaluate potential for teratoma formation or uncontrolled proliferation from residual undifferentiated iPSCs or incorrectly specified cells in the final product [66].
Methodology:
- In vitro pluripotency testing: Flow cytometry for pluripotency markers (OCT4, SOX2, NANOG)
- In vivo tumor formation assay: Transplant cell product into immunodeficient mice (e.g., NSG mice)
- Long-term monitoring: Serial bioluminescence imaging (BLI) if reporter genes are introduced
- Histopathological analysis: Post-mortem examination for teratoma formation or abnormal growth
Key Parameters: Minimum sensitivity threshold for detecting undifferentiated cells, duration of monitoring (typically 12-20 weeks), cell dose escalation [66].
Genomic Stability Assessment
Purpose: Identify genetic and epigenetic abnormalities acquired during reprogramming or long-term culture that may impact product safety [7].
Methodology:
- Karyotyping: G-banding analysis for chromosomal abnormalities
- Copy number variation (CNV) analysis: Array comparative genomic hybridization (aCGH) or SNP microarray
- Whole genome sequencing: Identification of point mutations and small insertions/deletions
- Epigenetic profiling: DNA methylation analysis at key developmental loci
Quality Thresholds: Normal karyotype, absence of recurrent reprogramming-associated mutations (e.g., TP53), stable epigenetic patterns comparable to normal tissues [7].
Functional Potency Assays
Purpose: Demonstrate biological activity of the differentiated cell product relevant to its intended mechanism of action.
Methodology:
- Cell-type specific marker expression: Flow cytometry or immunocytochemistry for lineage-specific proteins
- Functional characterization:
- Cardiomyocytes: Multi-electrode array (MEA) for electrophysiology [69]
- Neurons: Calcium imaging or patch clamp for electrical activity
- Hepatocytes: Cytochrome P450 activity, albumin secretion
- In vivo efficacy: Animal models of target disease demonstrating functional improvement
Validation Criteria: Quantitative potency measures with predefined acceptance criteria, correlation with intended biological effect [69].
Research Reagent Solutions for iPSC Translation
Table 4: Essential Research Reagents for iPSC Clinical Translation
| Reagent Category | Specific Examples | Function | Clinical-Grade Considerations |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, C-MYC (OSKM) [1] | Somatic cell reprogramming | Non-integrating delivery methods (episomal, mRNA, Sendai) [7] |
| Culture Matrices | Matrigel, recombinant laminin, synthemax | Extracellular matrix support | Xeno-free, defined composition, GMP-grade [66] |
| Cell Culture Media | mTeSR, StemFit, E8 medium [68] | Pluripotency maintenance | Chemically defined, xeno-free, lot-to-lot consistency |
| Differentiation Inducers | Growth factors (Activin A, BMP4, FGF), small molecules [68] | Lineage specification | GMP-grade, purity documentation, concentration optimization |
| Cell Dissociation Agents | Accutase, TrypLE, recombinant enzymes | Passaging and harvesting | Animal origin-free, minimal enzymatic damage |
| Cryopreservation Media | DMSO-based formulations | Cell banking | Defined composition, controlled-rate freezing compatibility |
The clinical translation of iPSC technologies stands at a pivotal juncture, with demonstrated feasibility in early-stage trials but significant hurdles remaining before widespread clinical adoption. Success will require coordinated advances across multiple domains: manufacturing technologies to ensure scalable, cost-effective production; regulatory science to establish efficient yet rigorous evaluation pathways; and clinical research to generate robust evidence of safety and efficacy.
The ongoing transition from autologous to allogeneic approaches may address critical scalability challenges, while innovations in gene editing, bioengineering, and machine learning promise to enhance product quality and consistency [7]. Furthermore, the development of increasingly complex 3D models, including organoids and organ-on-chip systems, provides more physiologically relevant platforms for validating disease phenotypes and predicting clinical responses [19] [29].
As the field progresses, researchers and developers must prioritize standardized characterization, rigorous safety assessment, and transparent reporting to build the robust evidence base needed for regulatory approval and clinical adoption. With continued interdisciplinary collaboration and strategic focus on addressing key translational challenges, iPSC-based therapies hold tremendous potential to revolutionize treatment for a broad spectrum of human diseases.
Validation Frameworks: Correlating iPSC Phenotypes with Clinical and Population Data
The successful use of induced pluripotent stem cells (iPSCs) in disease modeling, drug screening, and regenerative medicine hinges on the rigorous validation of these cells and their derivatives. As iPSC technologies move closer to clinical application, establishing comprehensive validation benchmarks that span molecular characterization to functional outputs becomes increasingly critical. This guide compares current approaches and methodologies for validating iPSC disease phenotypes, providing researchers with a framework for ensuring model fidelity and clinical relevance.
Core Validation Benchmarks for iPSC Lines
Before iPSCs can be utilized for disease modeling or therapeutic development, they must pass a series of quality control measures to ensure their safety, genetic integrity, and functional capacity. The table below outlines four fundamental benchmarks for validating newly generated iPSC lines.
Table 1: Core Validation Benchmarks for iPSC Lines
| Benchmark Category | Key Parameters Assessed | Common Methodologies | Acceptance Criteria |
|---|---|---|---|
| Viability & Sterility | Microbial contamination (e.g., Mycoplasma), cell viability [70] | Mycoplasma testing, sterility filters [70] | Absence of microbial contamination; high cell viability [70] |
| Genetic Integrity | Chromosomal abnormalities, culture-induced mutations [70] | G-banded karyotyping, identity verification (e.g., SNPTrace Panel) [70] | Normal karyotype; confirmation of donor identity [70] |
| Stemness | Expression of pluripotency markers (e.g., Oct4, Tra-1-60) [70] | Quantitative methods like FACS analysis, Pluritest assay [70] | High expression of markers over a large cell population [70] |
| Pluripotency | Capacity to differentiate into three germ layers (Ecto-, Endo-, Mesoderm) [70] | Embryoid body (EB) formation, gene expression analysis (qPCR), hPSC Scorecard [70] | Expression of genes specific to all three germ layers [70] |
For clinical applications, these benchmarks must be validated under Good Manufacturing Practice (GMP) standards. For instance, one study established that a minimum of 20,000 cells (120 ng genomic DNA) is required for accurate residual episomal vector testing, and assessing markers of the undifferentiated state should show expression of at least three individual markers on 75% of cells [71].
Advanced Molecular Characterization Techniques
Beyond basic validation, novel technologies are enabling deeper molecular phenotyping of iPSCs and their derivatives, which is crucial for accurate disease modeling.
Single-Cell Multi-Omic Profiling
Recent advances allow for the simultaneous profiling of genomic DNA and RNA in thousands of single cells. Single-cell DNA–RNA sequencing (SDR-seq) is a scalable method that can accurately determine the zygosity of coding and noncoding variants alongside associated gene expression changes [72]. This technology is particularly powerful for linking precise genotypes to disease-relevant cellular states in iPSC models [72].
Polygenic Risk Stratification
For modeling complex polygenic diseases like Alzheimer's, simply using patient-derived iPSCs is insufficient. The IPMAR Resource exemplifies a new benchmark by selecting donor iPSCs based on extreme polygenic risk scores (PRS) [60]. This resource includes lines from patients with high-risk late-onset AD, high-risk early-onset AD, and low-risk controls, enabling researchers to stratify individuals based on specific genetic risk profiles and study associated molecular dysfunctions [60].
Figure 1: Workflow for generating genetically stratified iPSC resources for complex disease modeling, as demonstrated in the IPMAR Resource for Alzheimer's disease [60].
Functional Phenotyping of iPSC-Derived Models
The ultimate validation of an iPSC-based disease model lies in its ability to recapitulate functional disease phenotypes. The following table compares key functional assays and their applications across different disease contexts.
Table 2: Functional Phenotyping Assays for iPSC-Derived Models
| Functional Assay | Measured Output | Disease Context | Key Findings |
|---|---|---|---|
| Longitudinal Live-Cell Imaging | Neuronal survival, neurite degeneration, correlation with donor survival [12] | Sporadic ALS (SALS) [12] | Motor neurons from SALS patients showed reduced survival and accelerated neurite degeneration correlating with donor survival [12] |
| Electrophysiological Profiling | Neuronal activity, network function [12] | SALS [12] | SALS motor neurons exhibited electrophysiological abnormalities rescued by riluzole [12] |
| Pharmacological Challenge | Response to approved therapeutics; high-throughput drug screening [12] | SALS [12] | 97% of drugs previously tested in ALS clinical trials failed to mitigate neurodegeneration; riluzole efficacy was recapitulated [12] |
| Transcriptomic Profiling | Disease-specific gene expression signatures [12] | SALS [12] | Transcriptional profiling of SALS motor neurons identified significant differential expression consistent with postmortem spinal cord tissues [12] |
Protocol: Longitudinal Live-Cell Imaging of iPSC-Derived Motor Neurons
The following methodology, adapted from a large-scale sporadic ALS study, details a robust protocol for assessing motor neuron health [12]:
Motor Neuron Differentiation: Adapt a well-established spinal motor neuron differentiation protocol with extensively optimized maturation conditions. A five-stage protocol generates high-purity cultures of mature motor neurons [12].
Cell Type Validation: Confirm culture purity using immunostaining and highly stringent quantification criteria. Target >90% of cells co-expressing choline acetyltransferase (ChAT), motor neuron and pancreas homeobox 1 (MNX1/HB9), and β-tubulin III (Tuj1) [12].
Live-Cell Reporter System: Implement a virally delivered, non-integrating, motor neuron-specific reporter (e.g., HB9-turbo) for specific tracking of motor neurons in mixed cultures [12].
Image Acquisition and Analysis: Monitor cultures daily using automated live-cell imaging. Implement highly stringent quantification criteria to objectively assess motor neuron survival and neurite degeneration over time [12].
This pipeline successfully demonstrated reduced survival and accelerated neurite degeneration in SALS motor neurons compared to healthy controls, establishing a critical functional benchmark for ALS modeling [12].
Experimental Design for Process Optimization
Optimizing iPSC differentiation protocols presents a significant challenge due to the myriad of possible culture conditions. Traditional "one factor at a time" (OFAT) approaches are inefficient for navigating this complex parameter space [73].
Figure 2: Hierarchy of Design of Experiments (DOE) approaches for optimizing iPSC differentiation, ranging from simple but inefficient OFAT to sophisticated modeling with RSM [73].
Statistical Design of Experiments (DOE) approaches enable efficient screening and optimization of differentiation protocols. The table below compares major DOE methodologies relevant to iPSC research.
Table 3: Design of Experiments (DOE) Approaches for iPSC Differentiation Optimization
| DOE Method | Key Principle | Advantages | Limitations |
|---|---|---|---|
| One Factor at a Time (OFAT) | Vary one factor while holding others constant [73] | Simple, intuitive [73] | Inefficient; misses interaction effects; poor reproducibility [73] |
| Full Factorial Design | Test all possible combinations of factors and levels [73] | Estimates all main and interaction effects [73] | Number of experimental runs becomes prohibitive with many factors [73] |
| Fractional Factorial Design | Test a carefully chosen subset of full factorial combinations [73] | Estimates main and two-order interactions with fewer runs [73] | Risk of missing optimal conditions decreases with lower "resolution" [73] |
| Orthogonal Array Design | Use fixed arrays to assess multiple factors with multiple levels [73] | High experimental efficiency; robust parameter design capability [73] | Limited ability to model complex response surfaces [73] |
| Response Surface Methodology (RSM) | Model relationship between factors and responses [73] | Powerful optimization capability; identifies optimal conditions [73] | Limited to small number of factors; sensitive to outliers [73] |
These DOE approaches are increasingly recommended by regulatory authorities like the FDA and EMA for pharmaceutical product development, making them essential for clinical translation of iPSC-based therapies [73].
The Scientist's Toolkit: Essential Research Reagents and Solutions
The following table details key reagents and tools used in advanced iPSC validation and disease modeling studies.
Table 4: Essential Research Reagents for iPSC Validation and Disease Modeling
| Reagent/Solution | Function | Application Example |
|---|---|---|
| Pluritest Assay | Molecular assay to confirm undifferentiated state of pluripotent stem cells using global gene expression data [70] | Assessment of stemness in iPSCs as part of quality control pipeline [70] |
| hPSC Scorecard | Molecular assay that uses gene expression profiling to quantitatively assess the differentiation potential of pluripotent stem cells [70] | Analysis of trilineage differentiation potential in GMP-compliant iPSC quality control [70] [71] |
| HB9-turbo Reporter | Motor neuron-specific fluorescent reporter delivered via non-integrating virus [12] | Specific tracking of motor neuron survival and health in longitudinal live-cell imaging studies [12] |
| SNPTrace Panel | Panel of single nucleotide polymorphisms used for cell line identity verification [70] | Confirm donor identity and monitor for cross-contamination between cell lines [70] |
| SDR-seq Platform | Single-cell DNA–RNA sequencing technology enabling simultaneous genotype and phenotype analysis [72] | Linking precise genetic variants to gene expression changes in iPSC models [72] |
The validation of iPSC disease phenotypes requires a multi-layered approach spanning from molecular markers to functional outputs. As the field progresses toward clinical translation, benchmarks are evolving from basic quality control checks to sophisticated functional assays that better recapitulate disease pathology. The emergence of large-scale, genetically stratified iPSC resources, combined with advanced functional phenotyping and robust experimental design, is paving the way for more predictive disease models and successful therapeutic development. Researchers must select validation benchmarks appropriate for their specific disease context and intended application, whether for basic disease mechanism discovery or clinical translation.
Leveraging Large-Scale Clinical Data and Biobanks for Robust Correlation
The integration of large-scale clinical data from biobanks with induced pluripotent stem cell (iPSC) technology represents a transformative approach for validating disease phenotypes and accelerating therapeutic development. iPSCs, generated by reprogramming adult somatic cells to an embryonic stem cell-like state, provide an unlimited source of patient-specific cells that can be differentiated into various specialized cell types, including neurons and cardiomyocytes [1] [74]. This technology has created unprecedented opportunities for modeling human diseases in vitro, particularly for conditions affecting tissues that are difficult to access in patients, such as neurodegenerative disorders [75] [76].
The true power of iPSC-based disease modeling emerges when these cellular models are correlated with large-scale clinical data from biobanks—organized collections of human biological samples linked to comprehensive personal and health information [77] [78]. Major biobanks worldwide, including the UK Biobank (500,000 participants) and the All of Us Research Program (1 million+ participants), integrate electronic health records, genetic data, imaging, and lifestyle information, creating rich datasets for research [79] [80]. When combined with iPSC technology, these resources enable researchers to bridge the gap between in vitro observations and clinical manifestations, validating disease-specific phenotypes across different genetic backgrounds and establishing more reliable platforms for drug discovery and development.
Table 1: Key Large-Scale Biobanks and Their Research Applications
| Biobank Name | Sample Size | Primary Data Types | Key Strengths | Notable iPSC Applications |
|---|---|---|---|---|
| UK Biobank | 500,000 participants [79] | EHRs, genetic data, imaging, lifestyle surveys [79] | Extensive phenotyping, longitudinal data | Validating cellular phenotypes from patient-derived iPSCs with clinical disease progression [77] |
| All of Us Research Program | 1 million+ participants [79] | EHRs, whole genome sequencing, survey data, wearable device data [79] | Focus on populations underrepresented in biomedical research | Replicating pharmacogenetic findings across diverse populations [80] |
| Taiwan Biobank | 200,000+ participants [79] | Lifestyle surveys, National Health Insurance records, genomic data [79] | Integration with national health insurance database | Population-specific disease variant characterization |
| China Kadoorie Biobank | 512,000+ participants [79] | Health insurance records, lifestyle surveys, genomic data [79] | Large population-based cohort with long follow-up | Environmental and genetic interaction studies |
| 45 and Up Study | 250,000+ participants [79] | Clinical/hospital records, pharmacy data, cancer registry [79] | Long-term follow-up data | Age-related disease modeling |
Table 2: iPSC-Specific Biobanks and Their Applications
| iPSC Resource | Scope | Key Features | Disease Applications | Validation Capabilities |
|---|---|---|---|---|
| ALS iPSC Biobank [75] | 35 iPSC lines from patients with ALS-related mutations (TARDBP, FUS, ANXA11, etc.) | Open-access, patient-derived lines with healthy controls | Amyotrophic lateral sclerosis, neurodegenerative diseases | Confirmation of cytoplasmic FUS mislocalization and reduced neurite outgrowth [75] |
| EBiSC [74] | Standardized, high-quality iPSC lines | Large repertoire of genetically diverse cell lines | Drug development, disease modeling | Standardized panels for pharmacogenetics and safety testing |
Experimental Approaches for Validating iPSC Disease Phenotypes with Clinical Data
Recapitulating Disease Phenotypes in iPSC-Derived Cells
The fundamental validation of iPSC disease models begins with demonstrating that cellular phenotypes observed in vitro correspond to clinical manifestations in patients. In proof-of-concept studies using FUS-ALS patient-derived iPSCs, researchers differentiated these cells into motor neurons and observed significant disease-relevant abnormalities, including increased cytoplasmic FUS protein localization and reduced neurite outgrowth compared to healthy controls [75]. These cellular phenotypes mirror the motor neuron degeneration characteristic of ALS patients, providing face validity for the model system.
For rare diseases, which collectively affect hundreds of millions worldwide but often lack effective treatments, iPSC models offer particularly valuable insights [81]. For example, in Juvenile Nephronophthisis (NPH), a genetic kidney disease, researchers developed patient-derived iPSCs and differentiated them into kidney organoids, successfully recapitulating disease-specific features including abnormal cell proliferation and renal cyst formation [81]. Importantly, these phenotypes were reversed upon reintroduction of the functional NPHP1 gene, demonstrating the specificity of the model and validating the disease mechanism [81].
Leveraging Biobank Data for Pharmacogenetic Validation
Large-scale biobanks linked to electronic health records provide powerful resources for validating iPSC-based observations regarding drug responses and treatment efficacy. A recent study leveraging UK Biobank and All of Us data demonstrated this approach by analyzing the genetic underpinnings of cardiometabolic drug responses [80]. Researchers extracted clinical and medication prescription data from EHRs to conduct genome-wide association studies on drug response outcomes, including lipid response to statins and HbA1c response to metformin.
The study successfully recovered previously reported pharmacogenetic signals, including variants in APOE, LPA, and SLCO1B1 associated with statin response, while also identifying a novel rare variant association in GIMAP5 with HbA1c response to metformin [80]. Crucially, these associations were treatment-specific and not associated with biomarker progression in medication-naive individuals, strengthening their validity as true pharmacogenetic markers. This approach demonstrates how biobank data can confirm molecular mechanisms initially observed in iPSC-derived cells, bridging cellular models with patient responses.
Methodological Protocols for Robust Correlation Studies
Table 3: Key Experimental Protocols for iPSC-Biobank Correlation Studies
| Protocol Step | Methodological Details | Quality Controls | Application Example |
|---|---|---|---|
| iPSC Generation from Biobank Samples | Reprogramming via nucleofection with plasmids expressing OCT3/4, L-MYC, KLF4, SV40LT, LIN28, SOX2, and shRNA-p53 [75] | Pluripotency marker verification, karyotype analysis, differentiation potential | Generation of 35 ALS patient-derived iPSC lines from the UK MND Collections [75] |
| Differentiation to Target Cell Types | Chemically defined conditions or doxycycline-inducible transcription factor systems (e.g., 2 weeks for motor neurons) [75] | Cell-type specific marker expression, functional assessment | FUS-ALS iPSCs differentiated into functionally active motor neurons [75] |
| Phenotypic Characterization | Immunocytochemistry, functional assays, transcriptomics, measurement of morphological parameters (e.g., neurite outgrowth) [75] | Comparison to isogenic controls, multiple cell line analysis | Quantification of cytoplasmic FUS protein and neurite outgrowth in FUS-ALS motor neurons [75] |
| Biobank EHR Data Extraction | Structured query development for medication prescriptions, biomarker measurements, diagnostic codes [80] | Consistency checks across data sources, handling of missing data | Extraction of lipid levels before and after statin initiation from UK Biobank primary care records [80] |
| Genetic Association Analysis | GWAS and rare variant burden tests on drug response phenotypes [80] | Population stratification control, replication in independent cohorts | Discovery in UK Biobank (N=18,753 for statin response), replication in All of Us [80] |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Research Reagents and Platforms for iPSC-Biobank Integration Studies
| Research Tool Category | Specific Examples | Function and Application | Considerations for Selection |
|---|---|---|---|
| iPSC Reprogramming Systems | CytoTune-iPS Sendai Reprogramming Kit, Episomal plasmids [75] [82] | Non-integrating reprogramming of somatic cells to pluripotency | Integration-free methods preferred for clinical applications; efficiency varies by cell type |
| Differentiation Kits | Commercial motor neuron differentiation kits, Cardiomyocyte differentiation kits | Directed differentiation of iPSCs into specific cell lineages | Batch-to-batch consistency crucial for reproducible disease modeling |
| Gene Editing Tools | CRISPR/Cas9 systems, TALENs [74] | Generation of isogenic controls and introduction of disease mutations | Essential for controlling for genetic background effects in disease modeling |
| Biobank Data Access Platforms | UK Biobank Research Analysis Platform, All of Us Researcher Workbench | Secure computational environments for analyzing biobank data | Data use agreements required; variable computational resources needed |
| Quality Control Assays | Pluripotency markers (Nanog, Oct4), Trilineage differentiation assays, Karyotyping | Verification of iPSC line quality and stability | Regular testing recommended throughout culture period to monitor stability |
Research Applications and Impact Assessment
Enhancing Drug Discovery and Development
The integration of iPSC models with biobank data significantly enhances drug discovery by providing more physiologically relevant human cellular systems for compound screening. iPSC-derived cells enable the creation of "disease-in-a-dish" models that can be used for phenotypic screens to identify drug compounds with desirable effects on disease-relevant cellular phenotypes [74]. This approach is particularly valuable for neurodegenerative diseases like Alzheimer's and Parkinson's, where animal models often fail to fully recapitulate human disease pathology [76].
Furthermore, combining iPSC technology with biobank genetic data enables target validation in more physiologically relevant contexts instead of studying drug actions on purified targets in isolation [74]. For example, iPSC-derived neurons from Alzheimer's patients have been used to screen anti-amyloid beta compounds, demonstrating reduced amyloid plaque deposition in patient-derived cortical neurons [76]. This validation step is crucial for de-risking drug development programs before advancing to costly clinical trials.
Advancing Precision Medicine Initiatives
The combination of patient-derived iPSCs and extensive biobank data holds particular promise for advancing precision medicine. By generating iPSCs from patients with diverse genetic backgrounds and correlating their cellular drug responses with genetic variants identified in biobanks, researchers can identify molecular signatures that predict individual patient responses to medications [74]. This approach enables stratification of patient populations and development of targeted treatments tailored to individual molecular profiles.
The power of this strategy is exemplified by recent research using iPSC-derived cardiomyocytes to model cardiac channelopathies like long QT syndrome [76]. These studies have revealed how specific mutations in ion channel genes (KCNQ1, KCNH2, SCN5A) affect channel function and response to pharmacological agents, enabling the testing of personalized therapeutic approaches [76]. When correlated with clinical data from biobanks regarding arrhythmia risk and drug responses in patients carrying these mutations, such models become powerful tools for personalizing treatment strategies.
The strategic integration of large-scale clinical data from biobanks with iPSC-based disease models represents a powerful paradigm for validating disease mechanisms and advancing therapeutic development. This approach enables researchers to move beyond correlation to establish causal relationships between genetic variants, cellular phenotypes, and clinical disease manifestations. As both technologies continue to evolve—with biobanks expanding in scale and diversity, and iPSC methodologies advancing in maturation and complexity—their combined potential to transform biomedical research will only increase.
Future developments will likely focus on enhancing the maturity and complexity of iPSC-derived models through co-culture systems and organoid technologies, better recapitulating tissue-level organization and cell-cell interactions [76]. Simultaneously, biobanks will continue to expand their data types to include multi-omics profiling and real-world evidence from digital health technologies. Together, these advancements will create increasingly robust platforms for understanding human disease biology and accelerating the development of novel therapeutics, ultimately enabling more personalized and effective healthcare interventions.
In modern healthcare, a significant challenge lies in predicting the future trajectory of complex diseases. Artificial intelligence (AI), particularly transformer-based models, is emerging as a powerful tool to address this challenge by learning patterns from longitudinal patient data to forecast disease progression. These models analyze a patient's past and current health states to predict, and ultimately help change, their future clinical course [83]. The potential of this approach is profoundly relevant for validating disease phenotypes derived from induced pluripotent stem cell (iPSC) models. By comparing the in vitro phenotypes observed in patient-derived cells with the in silico trajectories predicted from real-world clinical data, researchers can strengthen the biological relevance of their iPSC models, creating a powerful, closed-loop framework for understanding human disease [19] [84].
This guide provides an objective comparison of transformer-based predictive models against other analytical methods, detailing their performance, experimental protocols, and application in bridging iPSC research with clinical validation.
Comparative Analysis of Modeling Approaches
Various AI and machine learning methodologies can be applied to patient trajectory data. The table below compares Transformer models against other established approaches.
Table 1: Comparison of Modeling Approaches for Disease Trajectory Forecasting
| Model Type | Key Mechanism | Representative Models | Strengths | Weaknesses |
|---|---|---|---|---|
| Transformer-Based | Self-attention to weigh importance of all past events in a sequence [83] [85] | Delphi, CLIMAT [83] [85] | High accuracy for complex, long-range dependencies; models full disease spectrum [83] | Computationally intensive; requires very large datasets [83] |
| Recurrent Neural Networks (RNNs) | Processes data sequentially, maintaining a hidden state of past information [85] | LSTM, GRU [85] | Effective for time-series data; accounts for temporal order [85] | Struggles with very long sequences; gradient vanishing/exploding [85] |
| Fully-Connected Networks (FCNs) | Dense layers of connections between inputs and outputs [85] | Standard feedforward neural networks [85] | Simple and fast to implement and train [85] | Treats inputs as independent; ignores temporal dependencies [85] |
| Hawkes Process | Statistical model where past events influence the rate of future events [86] | Custom point process models [86] | Interpretable; mathematically sound for event sequences [86] | Can be outperformed in accuracy by more complex sequential models [86] |
Performance Benchmarking: Transformers in Action
In head-to-head comparisons, transformer architectures have demonstrated state-of-the-art performance in forecasting the progression of degenerative diseases.
Table 2: Quantitative Performance Comparison on Specific Disease Forecasting Tasks
| Disease / Task | Transformer Model (Performance) | Best Non-Transformer Model (Performance) | Performance Metric |
|---|---|---|---|
| General Multi-Disease Prediction | Delphi-2M [83] | Age- and Sex-Stratified Incidence (Epidemiological Baseline) [83] | Average AUC: ~0.76 [83] |
| Knee Osteoarthritis Prognosis | CLIMATv2 [85] | LSTM-based Model [85] | Higher Balanced Accuracy [85] |
| Alzheimer's Disease Clinical Status Forecast | CLIMATv2 [85] | GRU-based Model [85] | Higher Balanced Accuracy & Better Calibration [85] |
Key Experimental Findings
- Delphi-2M's Broad Predictive Power: Trained on data from 402,799 UK Biobank participants, Delphi-2M can predict the rates of over 1,000 diseases simultaneously. Its generative nature allows it to sample synthetic future health trajectories for up to 20 years, providing individualized estimates of potential disease burden [83].
- CLIMATv2's Clinical Inspiration: The CLIMAT framework mimics the clinical decision-making process between a radiologist (analyzing imaging data) and a general practitioner (integrating this analysis with other clinical data). This multi-agent, transformer-based design has shown superior performance and better calibration in forecasting the progression of knee osteoarthritis and Alzheimer's disease [85].
Experimental Protocols for Transformer Models
Implementing a transformer-based disease forecasting model involves a structured workflow. The following diagram outlines the key stages from data preparation to clinical application.
Diagram 1: Experimental workflow for transformer-based disease trajectory forecasting and integration with iPSC validation.
Detailed Methodologies
Data Preprocessing and Feature Engineering
The first critical step involves converting raw, heterogeneous health data into a sequence format that a transformer model can process.
- Tokenization of Medical Events: Medical concepts, such as diagnoses (represented by ICD-10 codes), medications, and clinical measurements, are mapped to discrete tokens, analogous to words in a sentence. A typical vocabulary may include over 1,250 distinct tokens [83].
- Encoding Temporal Information: Unlike text, health events occur on a continuous time axis. To handle this, standard positional encodings used in NLP are replaced with an encoding of continuous age using sine and cosine basis functions. This allows the model to understand the precise timing of events in a patient's life [83].
- Handling of Auxiliary Data: Non-temporal patient information, such as sex, body mass index (BMI), and smoking status, is also incorporated as special input tokens. These factors are used to condition the predictions but are typically not predicted by the model itself [83].
Model Architecture and Training Specifications
The core of the approach involves adapting the transformer architecture for longitudinal health data.
- Architecture Modifications: The standard GPT-2 architecture is modified with three key extensions:
- Continuous Time Encoding: Replaces discrete positional encoding [83].
- Time-to-Event Prediction Head: Adds an output head to predict the time to the next event using an exponential waiting time model, in addition to predicting the event itself [83].
- Causal Attention Masking: The causal attention mask is amended to also mask tokens recorded at the same time, ensuring the model learns from past events only [83].
- Training Regime: Models are trained using a held-out portion of the data (e.g., 20% of the cohort) for validation and hyperparameter optimization. Training leverages large-scale population datasets, such as the UK Biobank (~400,000 participants) or Danish disease registries (~1.9 million individuals) [83].
- Loss Function: The model is trained to minimize a loss function like cross-entropy for the next token prediction. Novel loss functions like the Calibrated Loss based on Upper Bound (CLUB) have been introduced to improve the calibration of predictions, ensuring that the predicted probabilities of outcomes more accurately reflect their true likelihoods [85].
Pathway to Phenotype Validation: Integrating AI with iPSC Models
The predictions generated by transformer models are not endpoints; they serve as a clinical benchmark for validating findings from in vitro disease models. The diagram below illustrates this integrative validation loop.
Diagram 2: Integrative loop for validating iPSC disease phenotypes with AI-powered clinical predictions.
Application to Neurodevelopmental Disorders
This integrative approach is particularly powerful for complex disorders like Autism Spectrum Disorder (ASD).
- iPSC Model Observations: iPSCs from donors with ASD can be differentiated into neurons, revealing phenotypes such as reduced synaptic density, altered neurite outgrowth, and transcriptional changes [87] [84]. For monogenic forms like Timothy Syndrome, neurons show defects in calcium signaling and neurotransmitter expression [87].
- Transformer Model Correlation: A model like Delphi can analyze the longitudinal health records of individuals with ASD, predicting their elevated risk for specific co-morbidities such as epilepsy or intellectual disability over time [83]. When the cellular phenotype (e.g., neuronal excitability) aligns with the predicted clinical trajectory (e.g., higher risk of seizures), confidence in the biological relevance of the iPSC model is significantly increased [84].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successfully implementing this research requires a combination of computational tools and biological reagents.
Table 3: Essential Resources for AI-iPSC Integration Research
| Category | Item / Solution | Specific Function in Workflow |
|---|---|---|
| Data & Compute | UK Biobank / Danish Disease Registry-scale data [83] | Training and validation of transformer models on large, longitudinal patient datasets. |
| Graphics Processing Units (GPUs) [88] | Accelerates the training and inference of complex deep learning models like transformers. | |
| Software & Models | Transformer Architectures (GPT-2, custom) [83] | Core model for learning temporal dependencies and generating predictions from sequence data. |
| CLIMAT Framework [85] | Specialized, clinically-inspired transformer for multi-modal data (images + clinical variables). | |
| CRISPR/Cas9 System [89] [35] | Gene editing tool for creating isogenic control lines in iPSC experiments, crucial for validating the causal role of genetic variants. | |
| Biological Reagents | Patient-Derived iPSCs [87] [19] [84] | Foundation for generating disease-relevant cell types (e.g., neurons) that preserve the patient's genetic background. |
| Directed Differentiation Protocols [19] | Methods to differentiate iPSCs into specific target cells (e.g., dopaminergic neurons, cortical neurons). | |
| 3D Organoid Culture Systems [19] | Advanced cell culture techniques to create complex, multi-cellular structures that better model human tissue and disease pathophysiology. |
The translation of induced pluripotent stem cell (iPSC) technology from a research tool to a clinical application represents a pivotal advancement in regenerative medicine. The ability to reprogram adult somatic cells into pluripotent stem cells and differentiate them into various cell types has opened new avenues for disease modeling, drug screening, and cell-based therapies. This guide objectively compares the clinical validation of iPSC-derived therapies across three therapeutic areas: Parkinson's disease, macular degeneration, and cardiac disease. We examine the experimental data, methodologies, and clinical outcomes that demonstrate the progress and remaining challenges in validating iPSC-based phenotypic responses against clinical data, providing researchers and drug development professionals with a critical analysis of the current landscape.
iPSC Technology: Mechanisms and Workflows
Historical Development and Key Mechanisms
The discovery of iPSC technology by Shinya Yamanaka in 2006, using four transcription factors (OCT4, SOX2, KLF4, and c-MYC) to reprogram mouse fibroblasts into pluripotent stem cells, marked a transformative milestone in regenerative medicine [1] [35]. This achievement was quickly extended to human cells in 2007, generating patient-specific iPSCs from adult fibroblasts [1]. The molecular mechanisms of somatic cell reprogramming involve extensive transcriptional and epigenetic remodeling, generally occurring in two phases: an early phase where somatic identity is suppressed, and a late phase characterized by stabilization of the pluripotency network [35]. Critical events include chromatin opening, DNA demethylation at key regulatory genes, and mesenchymal-to-epithelial transition (MET) [1] [35].
Core Differentiation Workflow
The following diagram illustrates the generalized workflow for deriving clinically relevant cell types from iPSCs, as applied in the case studies discussed in this guide:
Case Study 1: Parkinson's Disease
Experimental Protocol and Clinical Trial Design
A landmark Phase I/II trial published in 2025 investigated the safety and efficacy of allogeneic iPSC-derived dopaminergic progenitors for Parkinson's disease [90]. The trial enrolled seven patients aged 50-69 at Kyoto University Hospital who received bilateral transplantation of dopaminergic progenitors derived from a clinical-grade human iPSC line (QHJI01s04) established from a healthy donor with a homozygous HLA haplotype matching 17% of the Japanese population [90].
The experimental methodology involved:
- iPSC Differentiation: Dopaminergic progenitors were induced using a previously established protocol with CORIN+ cell sorting on days 11-13 to enrich for floor plate markers [90].
- Quality Control: The final product contained approximately 60% dopaminergic progenitors and 40% dopaminergic neurons, with no TPH2-expressing serotonergic neurons detected [90].
- Transplantation: Patients received bilateral transplantation into the putamen using a neurosurgical navigation system, with three patients receiving low-dose (2.1-2.6 × 10^6 cells per hemisphere) and four receiving high-dose (5.3-5.5 × 10^6 cells per hemisphere) [90].
- Immunosuppression: Tacrolimus was administered (0.06 mg/kg twice daily) with target trough levels of 5-10 ng/mL, reduced by half at 12 months and discontinued at 15 months [90].
- Follow-up: Patients were monitored for 24 months, with primary outcomes focusing on safety and adverse events, and secondary outcomes assessing motor symptom changes and dopamine production [90].
Clinical Validation and Outcomes
Table 1: Clinical Outcomes from Parkinson's Disease Trial [90]
| Parameter | Baseline | 24-Month Follow-up | Change | Notes |
|---|---|---|---|---|
| MDS-UPDRS Part III OFF Score | 46.5 points | 37.0 points | -9.5 points (-20.4%) | Average of 6 patients |
| MDS-UPDRS Part III ON Score | 12.0 points | 7.7 points | -4.3 points (-35.7%) | Average of 6 patients |
| Hoehn & Yahr Stage Improvement | - | - | 4 patients showed improvement | OFF state assessment |
| 18F-DOPA PET Ki Values | Baseline | 24-month | +44.7% increase | Putamen uptake |
| Serious Adverse Events | - | - | None reported | 73 mild-moderate events |
The clinical data demonstrated compelling validation of the iPSC-derived dopaminergic phenotype. The increased 18F-DOPA uptake on PET imaging confirmed functional dopamine production by the grafted cells, correlating with clinical improvements in motor function [90]. This represents a direct validation of the predicted phenotypic functionality of the iPSC-derived dopaminergic neurons when transplanted into the human brain.
Case Study 2: Macular Degeneration
Experimental Protocol and Clinical Development
The application of iPSC technology for macular degeneration has progressed through several key clinical studies. The first cellular therapy involving transplant of iPSCs into humans was initiated in 2013 at the RIKEN Center in Kobe, Japan, led by Dr. Masayo Takahashi, investigating the safety of iPSC-derived retinal pigment epithelial (RPE) cell sheets in patients with age-related macular degeneration [91].
The experimental approach typically involves:
- iPSC Derivation: Patient-specific or allogeneic iPSCs are generated from dermal fibroblasts or peripheral blood mononuclear cells.
- RPE Differentiation: iPSCs are directed to differentiate into RPE cells using specific growth factors and culture conditions that mimic retinal development.
- Sheet Formation: RPE cells are organized into monolayer sheets on specialized scaffolds.
- Transplantation: The RPE sheets are surgically implanted into the subretinal space to replace damaged retinal pigment epithelium.
More recently, Eyecyte-RPE, an iPSC-derived RPE product, received IND approval in India in 2024 for geographic atrophy associated with AMD, representing an important step toward scalable and cost-effective cell therapy approaches [35].
Clinical Validation and Outcomes
While comprehensive quantitative clinical data from larger trials is still emerging, early studies have demonstrated:
- Safety: The initial RIKEN trial established the feasibility and safety of autologous iPSC-RPE transplantation [91].
- Engraftment: Histological evidence from preliminary studies suggests survival and integration of transplanted RPE cells.
- Function: Some studies have reported stabilization or modest improvement in visual acuity in treated patients.
The progression from autologous to allogeneic approaches addresses scalability challenges while maintaining therapeutic potential, though comprehensive quantitative outcomes from larger trials are still forthcoming.
Case Study 3: Cardiac Disease
Experimental Protocols and Clinical Applications
iPSC applications in cardiac disease have primarily focused on disease modeling and drug screening, with therapeutic applications advancing through preclinical and early clinical stages. The differentiation protocols typically involve:
- Cardiomyocyte Differentiation: iPSCs are directed toward cardiac lineage using sequential activation and inhibition of Wnt signaling pathways, along with other cardiogenic factors.
- Purification: Metabolic selection or genetic markers are used to enrich for cardiomyocytes.
- Maturation: Various electrical, mechanical, and hormonal stimuli are applied to promote maturation of cardiomyocytes.
- Delivery: For therapeutic applications, cells are typically delivered as suspensions or engineered tissue patches.
Recent advances have enabled chamber-specific cardiac cell generation, allowing for more precise disease modeling of atrial and ventricular conditions [92].
Clinical Validation and Outcomes
The therapeutic application of iPSC-derived cardiomyocytes is still in earlier stages compared to neurological and retinal applications. Key developments include:
- Preclinical Validation: Studies in non-human primates have demonstrated that iPSC-derived cardiomyocyte patches can improve cardiac performance, though they have also revealed challenges such as transient arrhythmias [35].
- Disease Modeling: iPSC-derived cardiomyocytes have been successfully used to model inherited arrhythmia syndromes, recapitulate disease phenotypes, and predict drug responses [92].
- Safety Demonstrations: Research has confirmed the capacity of iPSC-derived cardiomyocytes to exhibit proper electrophysiological properties and contractile function.
The clinical validation in cardiac applications has thus far been strongest for disease modeling and drug screening applications, with therapeutic validation primarily from preclinical models.
Comparative Analysis of Clinical Validation
Table 2: Cross-Case Comparison of iPSC Clinical Validation Status
| Parameter | Parkinson's Disease | Macular Degeneration | Cardiac Disease |
|---|---|---|---|
| Highest Clinical Phase | Phase I/II Completed | Phase I/II Completed | Preclinical/Early Clinical |
| Quantitative Functional Data | Strong (PET, Motor Scores) | Limited/Qualitative | Preclinical Only |
| Safety Profile | No serious adverse events | No serious adverse events | Arrhythmia concerns in primates |
| Phenotypic Validation | Direct correlation with clinical improvement | Evidence of engraftment | Functional in vitro & animal models |
| Sample Size (Current Data) | 7 patients | Limited published data | Primarily preclinical models |
| Durability of Effect | 24 months demonstrated | Limited long-term data | Unknown |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for iPSC Differentiation and Validation
| Reagent/Category | Function | Example Applications |
|---|---|---|
| Reprogramming Factors | Induce pluripotency (OCT4, SOX2, KLF4, c-MYC) | Initial iPSC generation [1] |
| CORIN Antibodies | Sort floor plate-derived dopaminergic progenitors | Parkinson's disease protocols [90] |
| Small Molecule Inhibitors | Direct differentiation (Wnt, TGF-β, BMP pathways) | Cardiomyocyte differentiation [92] |
| Matrigel/ECM Substrates | Provide 3D scaffolding for organoid development | Retinal organoid formation [29] |
| Tacrolimus | Immunosuppression for allogeneic transplants | Clinical trial immunosuppression [90] |
| CRISPR/Cas9 Systems | Genetic modification for isogenic controls | Disease modeling & correction [35] |
Signaling Pathways and Experimental Workflows
The following diagram illustrates the key signaling pathways involved in directing iPSC differentiation toward therapeutically relevant cell types, highlighting critical regulatory nodes:
The clinical validation of iPSC-derived phenotypes across these three therapeutic areas demonstrates both substantial progress and remaining challenges. The Parkinson's disease trial provides the most comprehensive clinical validation to date, with quantitative imaging and functional data directly correlating iPSC-derived dopaminergic neurons with clinical improvement. The macular degeneration applications have established safety and feasibility, though more extensive quantitative outcomes are needed. Cardiac applications show strong preclinical validation with therapeutic applications still in earlier stages.
For researchers and drug development professionals, these case studies highlight the critical importance of rigorous phenotypic characterization, robust differentiation protocols, and comprehensive functional validation in the clinical translation of iPSC-based therapies. The successful validation of iPSC-derived dopaminergic neurons in Parkinson's disease represents a milestone for the field and provides a roadmap for similar validation in other therapeutic areas. As the technology advances, with improvements in differentiation efficiency, safety profiling, and scalable manufacturing, the clinical validation of iPSC-based therapies is poised to expand across multiple disease areas.
Conclusion
The successful validation of iPSC disease phenotypes with clinical data is the crucial bridge connecting innovative stem cell research to tangible clinical applications. While significant challenges remain in standardization, scalability, and safety, the convergence of advanced reprogramming techniques, sophisticated differentiation protocols, and powerful AI-driven analytical tools is rapidly closing the validation gap. The future of the field lies in fostering collaborative ecosystems that integrate deep clinical phenotyping with robust iPSC modeling. This synergy will not only enhance the predictive power of these models for drug discovery and toxicity screening but will also accelerate the development of safe and effective, patient-specific regenerative therapies, ultimately paving the way for a new era in precision medicine.
References
- 1. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 2. Induced pluripotent stem cell [https://en.wikipedia.org/wiki/Induced_pluripotent_stem_cell]
- 3. Induced Pluripotent Stem Cells: Reprogramming Platforms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7194323/]
- 4. Human iPSC Success: The Impact of Approaches... Reprogramming [https://pmc.ncbi.nlm.nih.gov/articles/PMC11756937/]
- 5. Epi5™ Episomal iPSC Kit 1 kit | Contact Us | Invitrogen Reprogramming [https://www.thermofisher.com/order/catalog/product/A15960]
- 6. Global research dynamics in the induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12272591/]
- 7. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 8. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590075/]
- 9. Stem cell disease modeling: A new era for drug discovery [https://www.abcam.com/en-us/stories/articles/stem-cell-disease-modeling]
- 10. Patient and Disease–Specific Induced Pluripotent Stem ... [https://www.sciencedirect.com/science/article/pii/S0031699724009451]
- 11. Editorial: Studying rare diseases using induced pluripotent ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1686438/full]
- 12. Large-scale drug screening in iPSC-derived motor neurons ... [https://www.nature.com/articles/s41593-025-02118-7]
- 13. How Human iPSCs are Revolutionizing Drug Discovery in ... [https://bioinformant.com/ipsc-drug-discovery/]
- 14. Development of patient-specific iPSC-based epilepsy models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12209222/]
- 15. In silico modeling of directed differentiation of induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12404646/]
- 16. Metabolic cardiomyopathies: untangling clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12603204/]
- 17. Cardiac repair and regeneration: cell therapy, in vivo ... [https://www.nature.com/articles/s12276-025-01549-3]
- 18. Smarter stem cells: how AI is supercharging iPSC technology [https://link.springer.com/article/10.1007/s00441-025-03999-7]
- 19. Induced pluripotent stem cells in disease modelling and drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6584039/]
- 20. Key Challenges in Clinical iPSC Applications [https://www.reprocell.com/blog/key-challenges-in-clinical-ipsc-applications-how-reprocell-helps-you-succeed]
- 21. Power and optimal study design in iPSC-based brain ... [https://www.nature.com/articles/s41380-022-01866-3]
- 22. Phenotyping Neurodegeneration in Human iPSCs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9237961/]
- 23. Genotype and phenotype validation of an isogenic human ... [https://www.bit.bio/resources/posters/huntingtons-htt50cag-phenotype-poster-mar23]
- 24. Smarter stem cells: how AI is supercharging iPSC technology [https://pubmed.ncbi.nlm.nih.gov/40804204/]
- 25. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 26. Reprogramming barriers and enhancers: strategies to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4642739/]
- 27. Why mRNA Reprogramming Is the Key to Safer and Faster ... [https://www.reprocell.com/blog/why-mrna-reprogramming-is-the-key-to-safer-and-faster-ipsc-generation]
- 28. The long and winding road of reprogramming-induced ... [https://www.nature.com/articles/s41467-024-46020-5]
- 29. Modeling human diseases with induced pluripotent stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC5868991/]
- 30. Human induced pluripotent stem cell-derived ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1687840/full]
- 31. Recent Advances of Pluripotent Stem Cell-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12654378/]
- 32. Enhanced cardiomyocyte differentiation and repair through ... [https://www.sciencedirect.com/science/article/pii/S0753332225008364]
- 33. Progression of differentiation of iPSCs into specific ... [https://www.sciencedirect.com/science/article/abs/pii/S0301468125000362]
- 34. Real-time observation of pancreatic beta from... cell differentiation [https://pmc.ncbi.nlm.nih.gov/articles/PMC6614661/]
- 35. Clinical translation of human iPSC technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12498231/]
- 36. Pluripotent Stem Cells: Recent Advances and Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025069/]
- 37. Induced pluripotent stem cells : An overview | Abcam [https://www.abcam.com/en-us/knowledge-center/stem-cells/induced-pluripotent-stem-cells]
- 38. Direct Comparison of Four Hematopoietic Differentiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7486192/]
- 39. Organoids as predictive platforms: advancing disease ... [https://www.sciencedirect.com/science/article/abs/pii/S016836592500834X]
- 40. Establishing 3D organoid models from patient-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131615/]
- 41. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 42. Comparative analysis of 3D-culture techniques for ... [https://www.nature.com/articles/s41598-025-13588-x]
- 43. Modeling neurodegenerative diseases with brain organoids [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1663286/full]
- 44. Comment on “Changes in iPSC-Astrocyte Morphology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12202090/]
- 45. Development and validation of the Normalized Organoid ... [https://www.nature.com/articles/s42003-024-07329-5]
- 46. 3D Cell Culture Summit Roadshow 2025 [https://www.corning.com/worldwide/en/products/life-sciences/news-events/events/2025/09/3d-summit-2025.html]
- 47. Multiomics Evaluation of Human iPSCs and iPSC-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11799864/]
- 48. High-Content Phenotypic Profiling with Cell Painting Assay [https://www.moleculardevices.com/en/assets/app-note/dd/img/high-content-phenotypic-profiling-using-the-cell-painting-assay]
- 49. The Future of Drug Discovery: Integrating Phenotypic Data with Omics and AI - Ardigen | Top AI-Powered CRO for Drug Discovery & Clinical Trials [https://ardigen.com/the-future-of-drug-discovery-integrating-phenotypic-data-with-omics-and-ai/]
- 50. Phenotypic screening | Nature Communications [https://www.nature.com/subjects/phenotypic-screening/ncomms]
- 51. Machine learning and multi-omics integration: advancing cardiovascular translational research and clinical practice | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06425-2]
- 52. Global regulatory considerations and practices for ... [https://www.sciencedirect.com/science/article/pii/S0273230024002101]
- 53. Tracing genomic instability in induced mesenchymal ... [https://www.nature.com/articles/s12276-025-01439-8]
- 54. Potency assurance for CGT products: an assessment of FDA’s new draft guidance :: Parexel [https://www.parexel.com/insights/blog/potency-assurance-for-cgt-products-an-assessment-of-fdas-new-draft-guidance]
- 55. FDA Issues Draft Guidance For Cell & Gene Therapy Potency Assurance [https://www.cellandgene.com/doc/fda-issues-draft-guidance-for-cell-gene-therapy-potency-assurance-0001]
- 56. Potency of Cell and Gene Medicinal Products: New FDA Guideline [https://www.dlrcgroup.com/potency-of-cell-and-gene-medicinal-products-new-fda-guideline/]
- 57. Tips and Tricks for Validation of Quality Control Analytical Methods in Good Manufacturing Practice Mesenchymal Stromal Cell Production - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6142742/]
- 58. Reliable Antibiotic Potency Testing for Pharmaceutical Development and Quality Control | SGS [https://www.sgs.com/en/news/2025/11/reliable-antibiotic-potency-testing-for-pharmaceutical-development-and-quality-control]
- 59. USP Bioassay Reference Standards [https://www.usp.org/biologics/bioassays]
- 60. Modeling common Alzheimer's disease with high and low ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12365843/]
- 61. A literature review: machine learning-based stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11193562/]
- 62. Transformative Role of Artificial Intelligence in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406033/]
- 63. How AI will reshape pharma in 2025 [https://www.drugtargetreview.com/article/154981/how-ai-will-reshape-pharma-by-2025/]
- 64. AI Model Validation: Best Practices for Accuracy & Reliability [https://galileo.ai/blog/best-practices-for-ai-model-validation-in-machine-learning]
- 65. AI/ML Model Validation Framework [https://towardsdatascience.com/ai-ml-model-validation-framework-13dd3f10e824/]
- 66. JCI - Hurdles to clinical translation of human induced pluripotent stem cells [https://www.jci.org/articles/view/80575]
- 67. The emerging promise of induced pluripotent stem cells in ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925008461]
- 68. In silico modeling of directed differentiation of induced ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013407]
- 69. Cell-based drug discovery: Why human iPSC-derived ... [https://www.bit.bio/blog/cell-based-drug-discovery-with-human-ipsc-models]
- 70. Stem Cells: 4 Benchmarks to master when working with iPSCs [https://sampled.com/a-guide-to-validating-stem-cells/]
- 71. Validating human induced pluripotent stem cell-specific ... [https://www.sciencedirect.com/science/article/pii/S1465324924006108]
- 72. Functional phenotyping of genomic variants using joint ... [https://www.nature.com/articles/s41592-025-02805-0]
- 73. Clever Experimental Designs: Shortcuts for Better iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8700474/]
- 74. About iPSC Research amd Applications · EBiSC [https://ebisc.org/about/ipsc_research]
- 75. Generation of an Open-Access Patient-Derived iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10218399/]
- 76. Utility of iPSC-Derived Cells for Disease Modeling, Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9180434/]
- 77. Quantifying the impact of biobanks and cohort studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037000/]
- 78. Understanding the value of biobank attributes to ... [https://www.nature.com/articles/s41598-023-49394-6]
- 79. Time to use large-scale biobank databases in health policy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12393043/]
- 80. Leveraging large-scale biobank EHRs to enhance ... [https://www.nature.com/articles/s41467-025-58152-3]
- 81. Studying rare diseases using induced pluripotent stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12450901/]
- 82. Induced Pluripotent Stem Cells as a Disease Modeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3343213/]
- 83. Learning the natural history of human disease with ... [https://www.nature.com/articles/s41586-025-09529-3]
- 84. The use of iPSC technology for modeling Autism Spectrum ... [https://www.sciencedirect.com/science/article/abs/pii/S0969996119301342]
- 85. Clinically-Inspired Multi-Agent Transformers for Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10880139/]
- 86. Analyzing Patient Trajectories With Artificial Intelligence - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8686456/]
- 87. Modeling autism spectrum disorders with human neurons - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4975680/]
- 88. Machine Learning in Clinical Trials: A Primer with Applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10228463/]
- 89. Modeling Parkinson's Disease Using Induced Pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7091557/]
- 90. Phase I/II trial of iPS-cell-derived dopaminergic cells for ... [https://www.nature.com/articles/s41586-025-08700-0]
- 91. Induced Pluripotent Stem Cell (iPSC) Industry Trends for ... [https://bioinformant.com/ipsc-industry-trends/]
- 92. The role of iPSC research for insight into inherited ... [https://www.sciencedirect.com/science/article/pii/S1547527125025172]