Cellular Adaptation to Hypoxia: Molecular Mechanisms, Therapeutic Strategies, and Clinical Translation
This article provides a comprehensive analysis of the molecular pathways and therapeutic strategies for improving cell survival in hypoxic environments, a critical challenge in cancer biology, regenerative medicine, and ischemic...
Cellular Adaptation to Hypoxia: Molecular Mechanisms, Therapeutic Strategies, and Clinical Translation
Abstract
This article provides a comprehensive analysis of the molecular pathways and therapeutic strategies for improving cell survival in hypoxic environments, a critical challenge in cancer biology, regenerative medicine, and ischemic diseases. We explore foundational mechanisms including HIF-mediated signaling and metabolic reprogramming, examine methodological approaches for hypoxia targeting and imaging, discuss optimization strategies to overcome therapeutic resistance, and review validation techniques for assessing intervention efficacy. Designed for researchers, scientists, and drug development professionals, this review synthesizes current evidence from molecular pathways to clinical applications, offering insights for developing novel therapeutic interventions targeting hypoxic microenvironments.
Molecular Mechanisms of Cellular Adaptation to Hypoxia
Frequently Asked Questions (FAQ)
Q1: Why do I detect HIF-1α but not HIF-2α in my acute hypoxia experiments? This is likely due to the "HIF switch" – a temporal regulation where HIF-1α responds to acute hypoxia, while HIF-2α dominates during chronic hypoxia [1]. HIF-1α protein is rapidly stabilized under acute hypoxia (e.g., hours), driving the initial cellular response [1]. Confirm the duration of hypoxic exposure; HIF-2α stabilization often requires longer periods (e.g., 48-72 hours) [1].
Q2: My HIF-α western blots are inconclusive under normoxia. What could be wrong? Under normoxic conditions, HIF-α subunits have an extremely short half-life (approximately 5 to 8 minutes) due to continuous proteasomal degradation [1]. Inconclusive results are likely because the protein is degraded rapidly. To detect it, you must inhibit the degradation pathway. Use specific prolyl hydroxylase domain (PHD) enzyme inhibitors (e.g, FG-4592) or proteasome inhibitors (e.g., MG-132) in your normoxic cultures to artificially stabilize the HIF-α subunits for detection [1].
Q3: My cell viability decreases under hypoxia when I expect increased survival. Why? The role of HIF is highly context-dependent. While HIF can promote survival through metabolic reprogramming and angiogenesis, it can also directly induce apoptosis under certain conditions [2]. HIF-1α can upregulate pro-apoptotic genes like BNIP3 and modulate the BCL2 family proteins, activating both death receptor and mitochondrial apoptosis pathways [2]. Check the cell type, hypoxia severity, and duration. In some primary cells like fibroblasts, HIF-1α upregulation is a direct cause of apoptosis [2].
Q4: Why do I see different HIF target gene expression in different cell lines? HIF-1α and HIF-2α, while similar, have non-redundant and sometimes opposing functions and can regulate distinct sets of target genes [1] [3] [4]. This specificity arises from:
- Cell-type specific expression: HIF-2α expression is more cell-type-specific than HIF-1α [4].
- Different DNA binding preferences: HIF-1α tends to bind to HRE motifs near promoter regions, whereas HIF-2α binding is often more distal [1].
- Crosstalk and antagonism: In some immune cells, HIF-2α represses HIF-1α expression, and its deletion can lead to a hyper-inflammatory phenotype driven by HIF-1α [3].
Troubleshooting Guide
| Problem | Potential Cause | Suggested Solution |
|---|---|---|
| Poor HIF-α detection in hypoxia | Inefficient hypoxia induction; degradation still occurring | Validate O₂ levels with an analyzer; use a chemical hypoxia mimetic like CoCl₂ [2]. |
| No upregulation of known HIF target genes | Inefficient HIF transcriptional activity; off-target effects | Check for functional HIF complex using a HRE-luciferase reporter assay; confirm siRNA/shRNA knockdown efficiency [2]. |
| Contradictory results in functional assays | Overlooked HIF-1α/HIF-2α specificity; non-canonical regulation | Analyze isoforms separately; test for oxygen-independent regulation (e.g., via inflammatory cytokines like TNF-α or IL-6) [1]. |
| Unstable Treg cell function in hypoxia studies | Disruption of HIF-2α, crucial for Treg suppressive function | Focus on HIF-2α specific knockout or inhibition; assess HIF-1α levels, as its upregulation can impair Treg function upon HIF-2α loss [3]. |
Key Quantitative Data on HIF Regulation
Table 1: Key Regulatory Proteins and Their Affinities for HIF-α Subunits
| Regulatory Protein / Enzyme | Primary Function | Notable Preference / Effect |
|---|---|---|
| PHD2 | Prolyl hydroxylation of HIF-α, targeting it for degradation | Primarily targets HIF-1α [1]. |
| PHD3 | Prolyl hydroxylation of HIF-α, targeting it for degradation | Displays greater affinity for HIF-2α than HIF-1α [1]. |
| FIH | Asparaginyl hydroxylation, inhibits HIF transactivation | Hydroxylates N803 in HIF-1α and N847 in HIF-2α [1]. |
| pVHL | E3 ubiquitin ligase recognizing hydroxylated HIF-α | Binds and ubiquitinates both HIF-1α and HIF-2α for proteasomal degradation [1]. |
Table 2: Experimental Parameters for HIF Stabilization and Detection
| Experimental Condition | HIF-1α Protein Half-Life | HIF-2α Protein Half-Life | Primary Functional Role |
|---|---|---|---|
| Normoxia (21% O₂) | ~5-8 minutes [1] | ~5-8 minutes [1] | Rapid degradation, negligible activity. |
| Acute Hypoxia (2-24 h) | Rapidly stabilized, dominant isoform [1] | Lower levels | Metabolic shift to glycolysis; initiation of angiogenesis [1]. |
| Chronic Hypoxia (48-72 h) | Levels may decrease | Stabilized, dominant isoform [1] | Sustains vascular remodeling and maturation genes [1]. |
Detailed Experimental Protocol: Analyzing HIF-1α-Induced Apoptosis
This protocol is adapted from a study investigating HIF-1α-mediated apoptosis in human uterosacral ligament fibroblasts (hUSLFs) [2].
Objective: To investigate the mechanisms of HIF-1α-induced apoptosis via both death receptor and mitochondrial pathways.
Materials:
- Cell Line: Primary human fibroblasts or other relevant cell type.
- HIF Inducer: Cobalt Chloride (CoCl₂), prepared in sterile PBS or culture medium.
- Gene Silencing: siRNA targeting HIF-1α and non-targeting negative control.
- Transfection Reagent: Lipofectamine 2000 or equivalent.
- Key Assays: MTT assay kit, Annexin V-FITC/PI apoptosis detection kit, JC-1 mitochondrial membrane potential assay kit, Western blot reagents.
- Antibodies for Western Blot: Anti-HIF-1α, Anti-Cleaved Caspase-3, -8, -9, Anti-BNIP3, Anti-Bcl-2, Anti-Bax, Anti-Cytochrome C.
Methodology:
- Cell Culture and Treatment:
- Culture cells in appropriate medium. For hypoxia mimetic treatment, expose cells to a range of CoCl₂ concentrations (e.g., 0-300 μM) for 24-72 hours [2]. Determine the IC₅₀ using an MTT assay.
- Gene Silencing:
- Transfect cells with HIF-1α-specific siRNA or negative control siRNA using Lipofectamine 2000 according to the manufacturer's instructions. Incubate for 24-48 hours before subsequent experiments [2].
- Measuring Apoptosis:
- Flow Cytometry: Use an Annexin V-FITC/PI staining kit. Analyze stained cells on a flow cytometer. HIF-1α induction should increase the percentage of Annexin V-positive cells [2].
- TUNEL Assay: Fix cells and incubate with TUNEL reaction mixture to label DNA strand breaks. Counterstain with DAPI and visualize under a fluorescence microscope [2].
- Analyzing Mitochondrial Pathway:
- Mitochondrial Membrane Potential (ΔΨm): Use the JC-1 dye. Healthy mitochondria with high ΔΨm show red fluorescence; apoptotic cells with low ΔΨm show green fluorescence. Measure the red/green fluorescence ratio. HIF-1α induction should decrease the ratio, indicating loss of ΔΨm [2].
- Western Blot: Analyze protein lysates for key mitochondrial pathway indicators: upregulation of BNIP3, Bax, and cytosolic Cytochrome C; downregulation of Bcl-2; and cleavage/activation of Caspase-9 [2].
- Analyzing Death Receptor Pathway:
- Western Blot: Analyze protein lysates for key death receptor pathway indicators: upregulation of TRAIL, DR5, and Fas; downregulation of c-FLIP and DcR2; and cleavage/activation of Caspase-8 [2].
- Execution Phase:
- Western Blot: Confirm the final stage of apoptosis by detecting cleaved Caspase-3 in all HIF-1α-induced samples. This effect should be reversed by HIF-1α knockdown [2].
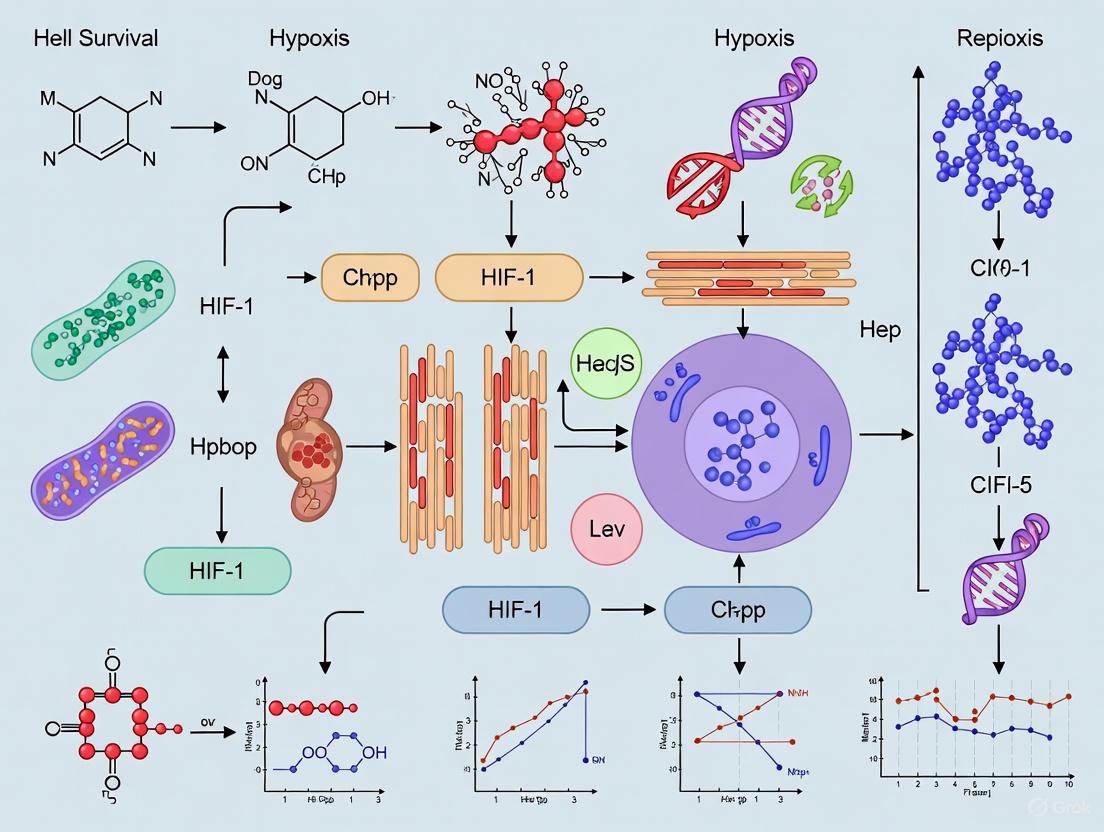
Signaling Pathway Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for HIF Pathway Research
| Reagent / Tool | Function / Mechanism | Example Application |
|---|---|---|
| CoCl₂ (Cobalt Chloride) | Chemical hypoxia mimetic; inhibits PHD enzymes, stabilizing HIF-α [2]. | Inducing HIF-1α in cell culture (e.g., at 150-200 μM for 24h) to study apoptosis [2]. |
| siRNA / shRNA (HIF-1α or HIF-2α) | Isoform-specific gene silencing to delineate unique functions. | Validating the specific role of HIF-1α in apoptosis by knocking it down and observing rescued cell viability [2]. |
| PHD Inhibitors (e.g., FG-4592) | Selective inhibition of PHD enzymes, stabilizing HIF-α under normoxia. | Investigating the therapeutic potential of HIF stabilization, such as in erythropoiesis. |
| HIF-2α Specific Inhibitors | Pharmacological inhibition of HIF-2α activity (e.g., PT2385). | Selectively targeting HIF-2α in cancer models or to modulate Treg cell function [3]. |
| HRE-Luciferase Reporter | Plasmid containing HRE sequences driving luciferase gene; measures HIF transcriptional activity. | Quantifying the functional output of HIF stabilization in different cell types or under drug treatment. |
| Antibodies: HIF-1α / HIF-2α | Detecting protein levels and localization via Western Blot or IF. | Confirming HIF-α stabilization in hypoxia vs. normoxia and its knockdown efficiency. |
| Antibodies: Cleaved Caspases | Detecting activation of apoptosis executioners. | Confirming apoptosis induction via HIF-1α and identifying the pathway involved [2]. |
| JC-1 Dye | Fluorescent probe for measuring mitochondrial membrane potential (ΔΨm). | Demonstrating HIF-1α's role in initiating the intrinsic apoptosis pathway [2]. |
Frequently Asked Questions (FAQs)
Q1: Why do cells shift from oxidative phosphorylation to glycolysis under hypoxic conditions? This metabolic reprogramming, known as the Warburg effect in cancer cells, occurs because oxygen availability becomes limited for efficient oxidative phosphorylation (OXPHOS). Cells adapt by upregulating glycolysis to generate ATP more rapidly, though less efficiently (2 ATP/glucose vs ~36 ATP/glucose via OXPHOS). This shift is primarily mediated by hypoxia-inducible factors (HIFs) that transcriptionally activate glycolytic enzymes and suppress mitochondrial activity [5] [6]. Glycolysis also provides metabolic intermediates for biosynthesis, supporting cell survival and proliferation in low-oxygen environments [5] [7].
Q2: What is the role of HIF-1α in hypoxic metabolic reprogramming? HIF-1α is the master regulator of cellular response to hypoxia. Under low oxygen:
- HIF-1α stabilizes and translocates to the nucleus
- Activates transcription of genes involved in glycolysis, angiogenesis, and cell survival
- Upregulates glucose transporters (GLUT1) and glycolytic enzymes (HK, PFK, LDHA)
- Suppresses mitochondrial metabolism by activating PDK1, which inhibits pyruvate dehydrogenase (PDH), reducing pyruvate entry into TCA cycle [6] [8] [7].
Q3: How do mitochondrial adaptations support cell survival during hypoxia? Mitochondria undergo functional adaptations to optimize limited oxygen utilization:
- Metabolic Flexibility: Shift to consuming alternative fuels like glutamine and fatty acids [7]
- Reduced ROS Production: Decreased electron transport chain activity lowers reactive oxygen species generation [8]
- Fission/Fusion Dynamics: Increased mitochondrial fission supports quality control and metabolic adaptation [5]
- Mitochondrial Biogenesis: In chronic hypoxia, sirtuin-mediated biogenesis helps maintain mitochondrial mass [9].
Q4: What experimental methods can assess metabolic shifts in hypoxic cells? Key methodologies include:
- Metabolomics: CE-TOFMS for comprehensive analysis of water-soluble metabolites [7]
- Seahorse Analyzer: Measures oxygen consumption rate (OCR) and extracellular acidification rate (ECAR) in real-time
- Flow Cytometry: Evaluates mitochondrial membrane potential, ROS production, and surface marker expression [10]
- Transcriptomics: RNA sequencing identifies HIF-target genes and metabolic pathway alterations [10].
Q5: How can we therapeutically target hypoxic cells? Emerging strategies include:
- HIF Inhibitors: Direct targeting of HIF-1α stability or activity [6]
- Metabolic Modulators: PIM3 kinase inhibition reverses hypoxia-induced T-cell dysfunction [10]
- Combination Therapies: Glycolytic inhibitors with conventional chemotherapeutics [7]
- Hypoxia-Activated Prodrugs: Selective targeting of hypoxic tumor regions [6].
Troubleshooting Common Experimental Challenges
Problem: Inconsistent metabolic responses in hypoxic cell cultures Potential Causes and Solutions:
- Oxygen Fluctuations: Use tri-gas incubators with continuous O₂ monitoring instead of anaerobic chambers [10]
- Improper Hypoxia Duration: Optimize exposure time (typically <48 hours for protective responses, avoiding senescence from prolonged exposure) [11]
- Cell Density Effects: Maintain consistent seeding density to prevent nutrient/gradient variations
- Validation Method: Verify hypoxia response via HIF-1α western blotting or HIF-reporter assays.
Problem: Poor cell survival post-hypoxic exposure Intervention Strategies:
- Preconditioning: Gradually acclimatize cells to hypoxia using stepped oxygen reduction [11]
- Metabolic Support: Supplement with pyruvate, glutamine, or fatty acids to support alternative energy pathways [7]
- Antioxidants: Add low-dose antioxidants to mitigate hypoxic burst of ROS during reoxygenation [8]
- Culture Optimization: Use specialized media formulations designed for hypoxic conditions.
Problem: Variable results in metabolic flux assays Technical Considerations:
- Normalization Issues: Normalize OCR/ECAR measurements to cell count, protein content, and mitochondrial DNA
- Substrate Concentration: Optimize glucose and glutamine concentrations in assay media [7]
- Hypoxia Equilibration: Allow sufficient time for medium gas equilibrium before assays (typically 2-4 hours)
- Control Validation: Include normoxic controls treated with HIF stabilizers (e.g., CoCl₂, DMOG) to distinguish HIF-specific effects.
Table 1: Metabolic Pathway Efficiency Comparison
| Parameter | Oxidative Phosphorylation | Glycolysis |
|---|---|---|
| ATP Yield per Glucose | ~36 molecules [5] | 2 molecules [5] |
| ATP Production Rate | Slower [5] | Faster [5] |
| Oxygen Requirement | High [8] | None [8] |
| Metabolic Intermediates | Limited | Abundant (for biosynthesis) [5] |
Table 2: Hypoxia-Induced Gene Expression Changes
| Gene | Function | Hypoxia Response | Experimental Validation |
|---|---|---|---|
| HIF-1α | Master hypoxia regulator | Stabilized/upregulated [11] [6] | Western blot, immunofluorescence [11] |
| VEGF | Angiogenesis | Upregulated [11] | ELISA, qPCR [11] |
| GLUT1 | Glucose transport | Upregulated [6] | Flow cytometry, glucose uptake assays [7] |
| PDK1 | Mitochondrial gatekeeper | Upregulated [7] | qPCR, enzyme activity assays [7] |
| BNIP3 | Mitophagy | Upregulated [5] | Immunoblotting, confocal microscopy [5] |
Detailed Experimental Protocols
Protocol 1: HIF-1α Stabilization and Detection
Based on mesenchymal stem cell preconditioning [11]
Materials:
- Tri-gas incubator (1-5% O₂, 5% CO₂, balance N₂)
- Anti-HIF-1α antibody (mouse monoclonal)
- Proteasome inhibitor (MG132, optional)
- Lysis buffer (RIPA with protease inhibitors)
Methodology:
- Culture cells to 70-80% confluence in standard conditions
- Transfer to hypoxic chamber (1-5% O₂) for 2-48 hours based on cell type optimization
- For protein detection, lyse cells directly in hypoxic workstation to prevent reoxygenation
- Perform western blotting with HIF-1α antibodies
- For immunofluorescence, fix cells immediately post-hypoxia with 4% PFA
Technical Notes:
- Include normoxic controls (21% O₂) cultured in parallel
- Use HIF-1α stabilizers (CoCl₂ 100-200μM) as positive controls
- Optimal hypoxia duration varies by cell type (MSCs: <48 hours [11])
Protocol 2: Metabolic Flux Analysis Under Hypoxia
Adapted from CAR-T cell studies [10]
Materials:
- Seahorse XF Analyzer with hypoxia module
- XF Glycolysis Stress Test Kit
- XF Mito Stress Test Kit
- Substrate-limited media (XF Base Medium)
Procedure:
- Culture cells under normoxic or hypoxic conditions for 24-72 hours
- Seed 20,000-50,000 cells/well in Seahorse plates
- Equilibrate in non-buffered assay medium in hypoxic chamber (1% O₂) for 1 hour
- Load plates into hypoxia module maintaining 1% O₂ throughout assay
- For glycolysis stress test: sequentially inject glucose, oligomycin, and 2-DG
- For mitochondrial stress test: sequentially inject oligomycin, FCCP, and rotenone/antimycin A
Data Interpretation:
- Compare basal and maximal glycolytic capacity via ECAR
- Assess mitochondrial function through ATP-linked respiration and spare respiratory capacity via OCR
- Normalize data to protein content or cell number
Research Reagent Solutions
Table 3: Essential Reagents for Hypoxia Metabolism Research
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| HIF Stabilizers | CoCl₂, DMOG, FG-4592 | Chemical hypoxia mimetics; induce HIF signaling without chamber | Concentration optimization critical; off-target effects possible [6] |
| Glycolytic Inhibitors | 2-DG, 3-bromopyruvate, WZB117 | Target glucose metabolism; probe glycolytic dependence | Compensatory OXPHOS upregulation may occur [7] |
| Mitochondrial Modulators | Oligomycin, FCCP, rotenone | Assess mitochondrial function in stress tests | Titrate carefully; cell type-specific toxicity [10] |
| Metabolic Sensors | MitoTracker Red, 2-NBDG, MitoSOX | Measure mitochondrial mass, glucose uptake, ROS | Validate with appropriate controls; consider probe stability in hypoxia [5] |
| Hypoxia Markers | Pimonidazole, HIF-1α antibodies | Detect hypoxic regions in tissues/cells | Pimonidazole requires in vivo injection; antibody validation essential [11] |
Metabolic Pathway Diagrams
HIF-1α Signaling Pathway in Hypoxia
Experimental Workflow for Metabolic Reprogramming Studies
Frequently Asked Questions (FAQs)
Q1: What is the core function of SREBP1 in cancer cells facing metabolic stress? A1: SREBP1 is a master transcription factor that orchestrates de novo lipogenesis, a critical adaptive response for cancer cell survival under stress conditions like hypoxia. It upregulates key enzymes for fatty acid synthesis, providing lipids for membrane biogenesis, energy production via Fatty Acid Oxidation (FAO), and protection from oxidative damage [12] [13] [14]. In hypoxic triple-negative breast cancer (TNBC), SREBP1-mediated lipogenesis and autophagy work together to promote cell survival by facilitating ATP production through FAO [13] [15].
Q2: Why is targeting SREBP1 a promising strategy against therapy-resistant cancers? A2: Research shows that resistant cancer cells often sustain SREBP1-dependent lipogenesis to maintain survival, irrespective of the original resistance mechanism. For example, in BRAF-therapy-resistant melanoma, resistant cells restore lipogenesis to protect from ROS-induced damage. Pharmacological inhibition of SREBP1 sensitizes these resistant cells to targeted therapy, highlighting its role as a key downstream mediator of resistance [14]. In TNBC, high SREBP1 expression is associated with a worse prognosis, further underscoring its therapeutic potential [13].
Q3: How does the hypoxic tumor microenvironment activate SREBP1? A3: Hypoxia can activate SREBP1 through multiple signaling pathways. Key upstream regulators include:
- PI3K/Akt/mTOR Pathway: Hyperactive Akt and mTORC1 can induce the synthesis and proteolytic activation of SREBP1, leading to lipid accumulation [12].
- EGFR Signaling: Promotes SCAP glycosylation, reducing its association with Insig proteins and leading to SREBP1 proteolytic activation [12].
- Transcriptional and Post-translational Regulation: Hypoxia can influence SREBP1 expression and activation via pathways involving HIF-1α, c-Myc, and O-GlcNAcylation [12] [16].
Q4: What are the key downstream effectors of SREBP1 that drive cancer progression? A4: SREBP1 transcriptionally activates a suite of lipogenic enzymes, including:
- ACLY (ATP Citrate Lyase): Generates acetyl-CoA in the cytoplasm.
- ACC (Acetyl-CoA Carboxylase): Catalyzes the first committed step in fatty acid synthesis.
- FASN (Fatty Acid Synthase): The rate-limiting enzyme for de novo fatty acid synthesis.
- SCD (Stearoyl-CoA Desaturase): Introduces double bonds into fatty acids, generating monounsaturated fatty acids critical for membrane fluidity and function [12] [14].
Troubleshooting Guide: Common Experimental Issues
Table 1: Troubleshooting SREBP1-Related Experiments
| Problem Phenomenon | Potential Cause | Suggested Solution |
|---|---|---|
| Low cell viability in hypoxic conditions despite SREBP1 activation. | Lipogenesis is occurring, but cells lack machinery to utilize lipids for energy. | Co-assess autophagy markers (e.g., LC3-I/II) and fatty acid oxidation (FAO) rates. Supplementing with an autophagy inducer (e.g., Rapamycin) may restore viability [13]. |
| Inconsistent SREBP1 target gene expression under hypoxia across cell lines. | Cell-type specific regulation; differences in culture conditions (e.g., serum concentration, cell density). | Standardize culture conditions. Use multiple cell models (e.g., TNBC vs. ER+). Confirm SREBP1 activation status via Western Blot for mature SREBP1 and not just mRNA [12] [16]. |
| Therapy-resistant cells remain viable after SREBP1 inhibition. | Existence of compensatory survival pathways or incomplete inhibition. | Combine SREBP1 inhibitors (e.g., Fatostatin) with other targeted agents (e.g., BRAF inhibitors). Validate inhibition by monitoring multiple downstream lipogenic enzymes [14]. |
| Failure to replicate hypoxic lipid droplet accumulation. | Insufficient hypoxic exposure; altered balance between lipid synthesis and uptake. | Ensure proper hypoxia induction (e.g., 1% O2 for 48 hours). Quantify lipid droplets with Nile Red staining and check expression of lipid uptake proteins like FABPs [13] [16]. |
Table 2: Quantitative Data on SREBP1 Inhibition in Hypoxic TNBC Models
| Experimental Metric | Normoxic MDA-MB-231 | Hypoxic MDA-MB-231 | Hypoxic MDA-MB-231 + SREBP1 Inhibition (Fatostatin/siRNA) | Restoration with Rapamycin (Autophagy Inducer) |
|---|---|---|---|---|
| Cell Viability/Proliferation | Baseline | Markedly Increased [13] | Reduced [13] | Restored [13] |
| ATP Production | Baseline | Maintained or Increased | Reduced [13] | Restored [13] |
| Expression of Lipogenic Enzymes (e.g., FASN) | Baseline | Increased [13] | Decreased [13] | Not Reported |
| Expression of Autophagy Markers | Baseline | Increased [13] | Decreased [13] | Increased (by induction) |
| Fatty Acid Oxidation (FAO) | Baseline | Increased [13] | Decreased [13] | Not Reported |
Detailed Experimental Protocols
Protocol 1: Assessing SREBP1 Function in Hypoxia-Induced Lipogenesis
Objective: To evaluate the role of SREBP1 in mediating lipogenesis and cell survival under hypoxic conditions. Materials:
- Cell lines: Triple-negative breast cancer MDA-MB-231 cells [13].
- Reagents: SREBP1 inhibitor (e.g., Fatostatin, 5-15 µM), autophagy inducer (Rapamycin, 0.1-10 µM) [13].
- Equipment: Hypoxic chamber (1% O2, 5% CO2, 95% N2 at 37°C) [13].
Methodology:
- Hypoxia Induction: Culture MDA-MB-231 cells in a sealed hypoxic incubator chamber at 1% O2 for 48 hours. Maintain control cells under normoxia (21% O2) [13].
- Pharmacological Inhibition: Treat cells with Fatostatin or vehicle control under hypoxic conditions for 48 hours [13].
- Rescue Experiments: Co-treat hypoxic cells with Fatostatin and Rapamycin to test if inducing autophagy can bypass the need for SREBP1 [13].
- Downstream Analysis:
- Viability Assay: Use MTT or trypan blue exclusion assays to quantify cell viability and proliferation [13].
- Lipid Quantification: Stain neutral lipids with Nile Red and quantify via immunofluorescence [13].
- Gene Expression: Analyze mRNA levels of SREBP1 targets (ACLY, ACC, FASN, SCD) and FAO-related enzymes by RT-qPCR [13].
- Metabolic Analysis: Measure ATP production and FAO rates using specific commercial assay kits [13].
Protocol 2: Validating SREBP1 as a Target to Overcome Therapy Resistance
Objective: To determine if SREBP1 inhibition can re-sensitize therapy-resistant cancer cells to targeted agents. Materials:
- Cell lines: BRAF-mutant, therapy-resistant melanoma cell lines (e.g., 451lu R, M249 R) [14].
- Reagents: BRAF inhibitor (e.g., Vemurafenib), SREBP1 inhibitor (e.g., Fatostatin).
Methodology:
- Combination Treatment: Treat resistant cells with Vemurafenib, Fatostatin, or a combination thereof.
- Lipogenesis Measurement: Assess de novo lipogenesis by tracking 14C-acetate incorporation into lipids or using isotopomer spectral analysis for palmitate synthesis [14].
- Lipidomics: Perform mass spectrometry-based phospholipidome analysis to monitor shifts from saturated/mono-unsaturated to poly-unsaturated membrane lipids, a hallmark of lipogenesis inhibition [14].
- Viability & Apoptosis: Measure cell death and viability using Annexin V/PI staining and cell viability assays [14].
Signaling Pathways and Experimental Workflows
SREBP1 Activation and Lipogenesis Signaling Pathway
Experimental Workflow for Hypoxia & SREBP1 Studies
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for SREBP1 and Lipogenesis Research
| Reagent Name | Function/Application | Example Usage in Context |
|---|---|---|
| Fatostatin | Chemical inhibitor of SREBP1 activation. | Used at 5-15 µM to block SREBP1 processing and function, validating its role in hypoxic survival and therapy resistance [13] [14]. |
| siRNA/shRNA vs. SREBP1 | Genetic tool for knocking down SREBP1 expression. | Confirms phenotypic effects of pharmacological inhibition and rules off-target effects [13]. |
| Rapamycin | Inducer of autophagy (mTORC1 inhibitor). | Used at 0.1-10 µM as a rescue agent to test if autophagy can compensate for loss of SREBP1-mediated lipogenesis [13]. |
| Vemurafenib | BRAF(V600E) inhibitor. | Used in melanoma studies to create therapeutic stress; combination with SREBP1 inhibitors overcomes resistance [14]. |
| Nile Red Stain | Fluorescent dye for neutral lipid detection. | Quantifies intracellular lipid droplet accumulation under hypoxia or after SREBP1 inhibition [13]. |
| Antibodies: mSREBP1, FASN, LC3 | Protein detection by Western Blot/IF. | mSREBP1 antibody detects the active, nuclear form. LC3 antibodies monitor autophagy activation [13] [14]. |
Troubleshooting Guide: Hypoxia-Induced Autophagy
This guide addresses common experimental challenges in monitoring and modulating autophagy in hypoxic environments.
Table 1: Troubleshooting Common Experimental Issues
| Problem & Phenomenon | Potential Causes | Recommended Solutions & Verification Methods |
|---|---|---|
| Inconsistent LC3B-II/I ratio (e.g., no change or decrease under hypoxia) [17]: Conflicting results in Western blot analysis of this key autophagy marker. | 1. Incomplete autophagy flux measurement.2. Hypoxia level or duration insufficient to trigger a response.3. Cell-type specific variations in autophagic response. | 1. Use lysosomal inhibitors (e.g., Chloroquine (CQ), Bafilomycin A1) to block degradation and measure accumulated LC3B-II [18].2. Verify HIF-1α stabilization as a positive control for hypoxia response [19].3. Titrate hypoxia exposure time and oxygen concentration (e.g., 1% O₂) [18]. |
| Lack of expected protective effect: Cell death occurs despite autophagy induction under hypoxia. | 1. Excessive or prolonged autophagy leading to autophagic cell death.2. Concurrent activation of apoptotic pathways.3. Autophagy is functioning as a survival mechanism for damaged cells that should be eliminated. | 1. Assess cell viability and apoptosis markers (e.g., caspase-3 cleavage) alongside autophagy markers [19].2. Modulate autophagy genetically (e.g., siRNA against ATG5/7) or pharmacologically to determine its precise role [20]. |
| Poor reproducibility of hypoxic conditions: Variable results between experiments or lab members. | 1. Inconsistent O₂ levels in hypoxic chambers.2. Variations in media pre-equilibration time.3. Differences in cell density affecting local oxygen microenvironments. | 1. Calibrate and log O₂ and CO₂ levels continuously using in-chamber sensors.2. Standardize protocol for media pre-equilibration in the hypoxic environment (e.g., 4-6 hours) [18].3. Maintain consistent cell seeding density and media volume across experiments. |
Frequently Asked Questions (FAQs)
Q1: Does hypoxia always activate autophagy in all cell types? No, the effect of hypoxia on autophagy is context-dependent. While hypoxia often induces autophagy as a pro-survival response, some studies report its attenuation. For instance, one study found that systemic hypoxia during exercise tended to attenuate the autophagy marker LC3B-II/I ratio in human peripheral blood mononuclear cells (PBMCs) [17]. The outcome depends on the cell type, severity and duration of hypoxia, and the overall cellular stress context [19] [20].
Q2: What is the most reliable method to confirm functional autophagy flux under hypoxia? The gold standard is to measure autophagy flux, not just marker levels. This involves comparing samples with and without lysosomal inhibitors. An increase in LC3B-II levels in inhibitor-treated samples confirms that autophagy is being initiated and that autophagosomes are being formed and degraded. Simply measuring a single LC3B-II value can be misleading [18] [20].
Q3: How does HIF-1α activation relate to autophagy induction under hypoxia? HIF-1α is a master regulator of the hypoxic response and can induce autophagy through several pathways. A key mechanism is the transcriptional upregulation of BNIP3 and BNIP3L/NIX. These proteins disrupt the inhibitory interaction between Bcl-2 and Beclin-1, freeing Beclin-1 to initiate autophagosome formation [19]. Furthermore, hypoxia and HIF-1α can inhibit mTOR, a major suppressor of autophagy [19] [20].
Q4: Why is autophagy considered a "double-edged sword" in hypoxic cancer environments? Autophagy can act as both a tumor suppressor and a tumor promoter. Initially, it can suppress tumorigenesis by removing damaged organelles and proteins. However, in established tumors, hypoxia-induced autophagy can be a critical survival mechanism for cancer cells, allowing them to recycle nutrients and survive low-oxygen conditions, thereby promoting tumor growth and resistance to therapy [19] [20].
Core Signaling Pathways & Experimental Workflows
Key Molecular Pathway of Hypoxia-Induced Autophagy
The following diagram illustrates the primary signaling pathway through which hypoxia activates autophagy, centered on HIF-1α stabilization.
Standard Experimental Workflow for Analysis
This workflow outlines a standard protocol for investigating hypoxia-induced autophagy in cell culture models.
Detailed Experimental Protocol
Title: Assessing Autophagy Flux in Human Trophoblast Cells (HTR8/SVneo) Under Hypoxic Conditions.
Background: This protocol is adapted from a study investigating the protective role of autophagy in preeclampsia [18]. It details the use of chemical modulators to assess autophagic flux in response to hypoxia (1% O₂).
Materials:
- HTR8/SVneo cell line (or other relevant cell type)
- Hypoxic chamber/tri-gas incubator (for 1% O₂, 5% CO₂, balance N₂)
- Normoxic incubator (20% O₂, 5% CO₂)
- Chloroquine (CQ)
- Rapamycin (optional inducer)
- ox-LDL (optional stress inducer)
- Lysis buffer, reagents for Western Blot (antibodies against LC3B, p62, HIF-1α)
Method Steps:
- Cell Culture & Group Setup: Culture HTR8/SVneo cells in standard DMEM with 10% FBS. Seed cells at a consistent density and allow to adhere. Divide cells into the following experimental groups:
- Control: Normoxia
- Hypoxia: 1% O₂
- Hypoxia + CQ: 1% O₂ + 40 μM Chloroquine (12h incubation) [18]
- Normoxia + CQ: (Important control for basal flux)
- (Optional groups: Hypoxia + ox-LDL, Hypoxia + Rapamycin)
Hypoxia Exposure & Treatment: Place plates in the pre-equilibrated hypoxic chamber (1% O₂). Maintain control plates in the normoxic incubator (20% O₂). For CQ-treated groups, add the inhibitor for the final 12 hours of the hypoxia exposure period.
Sample Collection & Analysis: After the treatment period (e.g., 24-48h), lyse cells directly in the plate. Perform Western Blot analysis for:
- LC3B: Compare LC3B-II levels. A increase in the Hypoxia+CQ group vs. Hypoxia alone confirms increased autophagic flux.
- p62/SQSTM1: Levels should decrease with autophagy induction but accumulate when flux is blocked (e.g., in CQ groups).
- HIF-1α: Verify hypoxic response.
Key Quantitative Data from Reference Study [18]: Table: Autophagy Marker Changes in HTR8/SVneo Cells Under Hypoxia & Modulation
| Experimental Group | LC3B-II Protein Level (vs. Control) | p62 Protein Level (vs. Control) | Interpretation |
|---|---|---|---|
| Hypoxia (1% O₂) | Increased | Decreased | Successful autophagy induction and flux. |
| Hypoxia + Chloroquine | Further Increased | Increased | Autophagic flux is blocked, confirming ongoing activity in hypoxia. |
| ox-LDL Treatment | Unchanged/Decreased | Increased | Impaired autophagy. |
| ox-LDL + Hypoxia | Increased | Decreased | Hypoxia rescues ox-LDL-impaired autophagy. |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Studying Hypoxia and Autophagy
| Reagent / Material | Function & Application in Research | Key Considerations |
|---|---|---|
| Tri-Gas Incubator | Creates a controlled, sustained hypoxic environment (e.g., 1% O₂). | Essential for physiological studies vs. chemical hypoxia mimetics. Requires regular calibration [18]. |
| Cobalt Chloride (CoCl₂) | A chemical mimetic of hypoxia that stabilizes HIF-1α. | Useful for preliminary, low-cost screens but does not replicate all aspects of true hypoxia [19]. |
| Chloroquine (CQ) / Bafilomycin A1 | Lysosomal inhibitors that block autophagic degradation, allowing flux measurement. | Critical for distinguishing between increased autophagosome synthesis vs. blocked degradation [18]. |
| Antibody: LC3B | Detects the lipidated form (LC3B-II) associated with autophagosomes via Western Blot or IF. | Monitor the LC3B-II/I ratio and total LC3B-II levels with and without inhibitors [17]. |
| Antibody: HIF-1α | Confirms activation of the hypoxic response pathway. | Serves as a positive control for hypoxia experiments. Has a short half-life under normoxia [19]. |
| Antibody: p62/SQSTM1 | Marks cargo targeted for autophagy; levels typically inversely correlate with autophagic activity. | Accumulation indicates blocked autophagy; degradation suggests active flux. Always interpret with LC3B data [17] [20]. |
Frequently Asked Questions (FAQs)
Q1: What are the most common histone modifications induced by hypoxia, and what are their functional outcomes? Hypoxia triggers specific, activating histone modifications. Key changes include increases in H3K4me3, H3K9ac, H3K14ac, and H3K27ac, which are associated with open chromatin and active gene transcription. In contrast, repressive marks like H3K9me3 and H3K27me3 often remain unchanged. These activating modifications are found within regulatory regions of genes essential for cellular adaptation, such as those involved in metabolism and fiber cell formation, and directly regulate their expression [21].
Q2: How does hypoxia lead to changes in transcription start site (TSS) selection, and what is the functional impact? Hypoxia causes pervasive transcription start site (TSS) switching, a process largely driven by changes in H3K4me3 distribution and nucleosome repositioning. This switching remodels the 5' untranslated region (5'UTR) of mRNAs, which in turn selectively alters their translation efficiency, independent of changes in the overall mRNA abundance. This mechanism enhances the synthesis of key proteins like pyruvate dehydrogenase kinase 1 (PDK1), which is crucial for metabolic adaptation to low oxygen [22].
Q3: Can hypoxia-induced epigenetic changes persist after normal oxygen levels are restored? Yes, hypoxic exposure can create a "hypoxic memory" where a subset of epigenetic alterations persists even after reoxygenation. These persistent changes, including stable DNA methylation patterns, histone modifications, and altered non-coding RNA expression, can drive long-term gene expression programs that contribute to the progression of chronic diseases, such as the transition from acute kidney injury to chronic kidney disease [23].
Q4: What is the role of metabolic factors in hypoxia-induced epigenetic remodeling? Cellular metabolism and epigenetics are tightly intertwined. Key metabolites such as S-adenosylmethionine (SAM) and acetyl-CoA serve as essential substrates for epigenetic enzymes. SAM is the primary methyl donor for DNA and histone methyltransferases, while acetyl-CoA is the acetyl group donor for histone acetyltransferases. In hypoxia, metabolic reprogramming can alter the availability of these metabolites, thereby directly influencing the epigenetic landscape and gene expression in cancer and other diseases [24].
Troubleshooting Experimental Challenges
Table: Common Issues in Hypoxia Epigenetics Research
| Problem | Potential Cause | Solution |
|---|---|---|
| High Background in CUT&RUN | Non-specific antibody binding or incomplete washing. | Optimize antibody concentration and include high-stringency wash steps. Validate antibodies with relevant negative control regions [21]. |
| Poor Polysome Profile | Ribosome degradation or improper lysis buffer preparation. | Use fresh cycloheximide in experiments, prepare buffers fresh, and avoid RNA degradation by using RNase inhibitors [22]. |
| Low Cell Viability in Prolonged Hypoxia | Excessive metabolic stress or buildup of toxic metabolites. | Optimize the duration of hypoxia exposure and cell density. Consider using specialized media formulations designed for hypoxic culture [21] [22]. |
| Inconsistent H3K4me3 ChIP-qPCR Results | Variable cross-linking efficiency or chromatin fragmentation. | Standardize cross-linking time and temperature. Calibrate sonication conditions to achieve consistent fragment sizes (200–500 bp) [22]. |
Detailed Experimental Protocols
Protocol 1: Analyzing Histone Modifications in Hypoxia (Based on Chick Lens Model)
This protocol outlines the process for detecting global changes in histone modifications in response to hypoxia [21].
Cell Culture & Hypoxic Exposure:
- Culture E13 chick lenses or your chosen cell line.
- Place the experimental group in a hypoxic chamber set to 1% O₂, 5% CO₂, at 37°C. The control group remains in a normoxic incubator (21% O₂).
- Expose for the desired duration (e.g., 24-48 hours).
Acid Extraction of Histones:
- Wash cells with ice-cold PBS.
- Lyse cells in a suitable buffer and isolate nuclei.
- Resuspend the nuclear pellet in 0.2 M H₂SO₄ and incubate on a rotator at 4°C for 2-4 hours.
- Centrifuge at high speed. Collect the supernatant containing the acid-soluble histones.
- Precipitate histones by adding 100% trichloroacetic acid (TCA) to a final concentration of 25%. Incubate on ice for 1 hour.
- Pellet histones by centrifugation, wash with ice-cold acetone, and air-dry.
- Resuspend the histone pellet in nuclease-free water.
Analysis:
- Quantify histone modifications via Western Blotting using specific antibodies against H3K4me3, H3K27ac, etc., with total histone H3 as a loading control.
- For genome-wide localization, perform CUT&RUN or ChIP-seq using the extracted histones/chromatin.
Protocol 2: Profiling the Translatome Under Hypoxia
This protocol describes how to identify changes in mRNA translation efficiency during hypoxic stress [22].
Hypoxic Treatment and Lysate Preparation:
- Culture T47D or H9 cells. Treat experimental cells with hypoxia (0.5-1% O₂) for 24-48 hours, keeping controls in normoxia.
- Before harvesting, treat cells with 100 µg/mL cycloheximide for 10 minutes to arrest ribosomes.
- Wash, scrape, and lyse cells in a polysome lysis buffer containing cycloheximide and RNase inhibitors.
Polysome Profiling:
- Layer the lysate onto a 10-50% sucrose density gradient.
- Centrifuge at high speed (e.g., 35,000 rpm in an SW41 rotor for 2-3 hours) to separate ribosomal complexes by size.
- Fractionate the gradient using a density gradient fractionation system while monitoring absorbance at 254 nm to obtain profiles of monosomes (80S) and polysomes.
RNA Extraction and Sequencing:
- Isolate total RNA from the "heavy polysome" fractions (typically >3 ribosomes) and from the total cell lysate input.
- Prepare libraries and perform RNA-seq on both the total and polysome-associated RNA samples.
Data Analysis:
- Use bioinformatics tools like anota2seq to compare total mRNA levels to polysome-associated mRNA levels. This identifies transcripts with altered translation efficiency ("translation" mode) or those where mRNA changes are buffered at the translational level ("offsetting" mode) [22].
The Scientist's Toolkit: Key Research Reagents
Table: Essential Reagents for Hypoxia Epigenetics
| Reagent / Tool | Function / Utility | Key Example |
|---|---|---|
| KDM5 Inhibitors | Pharmacologically inhibits H3K4 demethylases, mimicking hypoxia-induced H3K4me3 accumulation and TSS switching. | Used to demonstrate that H3K4me3 changes can drive 5'UTR remodeling independently of HIF [22]. |
| HDAC Inhibitors (HDACis) | Block histone deacetylase activity, leading to increased histone acetylation. Used to probe the role of acetylation in gene activation. | Vorinostat (FDA-approved for cancer); used in research to study PAH [23] [25]. |
| HAT Inhibitors | Inhibit histone acetyltransferases, preventing histone acetylation. Useful for establishing the necessity of acetylation for specific hypoxic responses. | Used to test the requirement for H3K27ac in hypoxia-induced gene expression [21]. |
| Hypoxia Mimetics | Chemicals that stabilize HIF-α (e.g., by inhibiting PHDs) to activate hypoxic signaling in normoxic conditions. | Cobalt chloride (CoCl₂), Dimethyloxalylglycine (DMOG) [21]. |
| CUT&RUN / ChIP-seq Kits | For genome-wide mapping of histone modifications and transcription factor binding sites. | Used to identify hypoxia-specific localization of H3K4me3 and H3K27ac near gene promoters [21]. |
| nanoCAGE Sequencing | Precisely maps transcription start sites (TSS) and identifies 5'UTR isoforms, crucial for studying TSS switching. | Used to reveal pervasive 5'UTR remodeling under hypoxia in T47D and H9 cells [22]. |
Signaling Pathways and Workflows
Hypoxia-Induced Chromatin Remodeling Pathway
Experimental Workflow for Hypoxia Epigenetics
Therapeutic Targeting and Intervention Strategies
This technical support center is designed for researchers investigating Hypoxia-Inducible Factor (HIF) pathway inhibitors to enhance cell survival under hypoxic conditions. The HIF pathway serves as the master regulator of cellular adaptation to low oxygen, coordinating responses in angiogenesis, metabolic reprogramming, and cell survival [26] [27]. In the tumor microenvironment, hypoxia creates a stressful setting that triggers these adaptive changes, but prolonged hypoxia can lead to cell death [27]. Targeting this pathway requires precise methodological approaches and troubleshooting of common experimental challenges.
Troubleshooting Guides
Problem 1: Inconsistent HIF-α Stabilization in Normoxic Cell Cultures
Issue: Unexpected HIF-α subunit stabilization under normal oxygen conditions (21% O₂), complicating experimental results.
Explanation: While HIF-α is typically degraded under normoxia, several oxygen-independent mechanisms can trigger its stabilization, potentially confounding experimental outcomes in studies aimed at improving cell survival [28].
Solution:
- Verify Genetic Background: Check for mutations in key regulatory genes, particularly in renal carcinoma cell lines (e.g., 786-O, RCC4). Inactivation of the Von Hippel-Lindau (VHL) tumor suppressor gene leads to constitutive HIF-α stabilization even under normoxia [29] [30]. Use VHL-deficient cells with and without functional VHL reintroduction for controlled experiments.
- Check Metabolite Accumulation: Assess the accumulation of metabolites that inhibit Prolyl Hydroxylase Domain (PHD) enzymes, such as fumarate, succinate, or (R)-2-hydroxyglutarate. These can result from mutations in genes like FH, SDH, or IDH1/2 [27] [28]. Metabolomic profiling can identify these interfering compounds.
- Confirm Pathway Activation Status: Investigate the activation of oncogenic signaling pathways. The PI3K/AKT/mTOR and MAPK/ERK pathways can increase HIF-1α translation and protein levels independently of oxygen tension [29] [28]. Use specific pathway inhibitors as controls.
- Validate Hydroxylation Status: Employ hydroxylation-specific antibodies to distinguish between hydroxylated (targeted for degradation) and non-hydroxylated (stable) forms of HIF-α [28].
Problem 2: Off-Target Effects in HIF Inhibition Assays
Issue: Small molecule inhibitors intended to target HIF produce effects unrelated to HIF pathway inhibition.
Explanation: Many reported HIF inhibitors act through indirect or undetermined mechanisms, such as general effects on transcription, translation, or receptor tyrosine kinase signaling, rather than direct targeting of HIF subunits [26] [27].
Solution:
- Utilize Direct Binding Assays: For HIF-2α inhibitors (e.g., Belzutifan, PT2385), use AlphaScreen protein-protein interaction assays to confirm direct disruption of the HIF-2α/ARNT heterodimerization [30]. Isothermal Titration Calorimetry (ITC) can quantitatively measure binding affinity to the HIF-2α PAS-B domain [30].
- Employ Comprehensive Controls: Include structurally related but inactive analogs as negative controls when available. For instance, use the inactive (S)-enantiomer of a compound to verify that observed effects are specific to the active (R)-enantiomer that binds the target [30].
- Perform Transcriptional Validation: Quantify mRNA expression of known HIF target genes (e.g., VEGFA, SLC2A1/GLUT1, BNIP3) via RT-qPCR to confirm that the inhibitor specifically blocks HIF-mediated transcription [26].
- Monitor Isoform Specificity: Differentiate between HIF-1 and HIF-2 inhibition. Use isoform-specific reporter gene assays and monitor expression of isoform-preferential target genes to determine selectivity and avoid misinterpretation of effects [26] [29].
Problem 3: Poor Cellular Activity in HIF-PHD Inhibitor Studies
Issue: HIF Prolyl Hydroxylase (HIF-PHD) inhibitors fail to stabilize HIF-α or induce target genes in cellular models.
Explanation: HIF-PHD inhibitors (e.g., Roxadustat, Vadadustat) are 2-oxoglutarate (2-OG) competitors and their efficacy can be reduced by high intracellular concentrations of 2-OG or insufficient cellular uptake [31] [32] [33].
Solution:
- Modify Cell Culture Conditions: Reduce the concentration of 2-OG and other TCA cycle intermediates (e.g., succinate, fumarate) in the culture medium, as they can compete with the inhibitor [27].
- Confirm Iron Availability: Ensure adequate intracellular Fe²⁺ levels, as PHDs are iron-dependent dioxygenases. Iron chelation can mimic hypoxia and confound results; conversely, iron supplementation may reduce inhibitor efficacy [27] [28].
- Use a Positive Hypoxia Control: Always include a hypoxic chamber (e.g., 1% O₂) or a known chemical hypoxia mimetic (e.g., CoCl₂, DMOG) as a positive control to verify the responsiveness of your cellular system.
- Optimize Dosing and Timing: Perform time-course and dose-response experiments. HIF-1α and HIF-2α have distinct stabilization kinetics—HIF-1α responds rapidly to acute hypoxia/HIF-PHD inhibition, while HIF-2α accumulates gradually during prolonged exposure [29].
Frequently Asked Questions (FAQs)
Q1: What are the key considerations for choosing between HIF-1 vs. HIF-2 selective inhibition?
A: The choice depends on your biological context and research goals. HIF-1α is often associated with acute hypoxia response, metabolic switch to glycolysis (regulating GLUT1, HK2), and cell autonomy, while HIF-2α is prominent in chronic hypoxia, erythropoiesis (regulating EPO), and specific cancers like ccRCC [29] [32] [30]. In ccRCC with VHL loss, HIF-2α often acts as the primary oncoprotein, making it a preferred target [26] [30]. For broader therapeutic impact in most cancers, dual inhibition may be desirable, but this must be balanced against potential safety concerns, as complete HIF pathway blockade could have systemic toxicities [26].
Q2: How do I validate the specificity of a direct HIF-2α inhibitor like Belzutifan in my experiments?
A: To validate specificity:
- Binding Site Mutants: Use cell lines engineered with point mutations in the HIF-2α PAS-B domain (e.g., Cys255, Asp237, Asno247, Met252, Met263, Gln277, Met279) that disrupt inhibitor binding. Resistance in these mutants indicates on-target activity [30].
- Heterodimerization Assays: Monitor the formation of the HIF-2α/ARNT complex via co-immunoprecipitation in the presence of the inhibitor. Effective compounds should disrupt this interaction without affecting the protein levels of individual subunits [30].
- Target Gene Analysis: Measure the transcript levels of HIF-2-preferential target genes (e.g., EPO, VEGFA, CCND1) versus HIF-1-preferential genes (e.g., PGK1, LDHA) to confirm selective HIF-2 blockade [26] [29].
Q3: What are the primary mechanisms of acquired resistance to HIF-2α inhibitors?
A: A key mechanism involves missense mutations in the HIF-2α PAS-B domain that sterically hinder drug binding while preserving the protein's ability to dimerize with ARNT and activate transcription [30]. Commonly reported mutations affect residues like Met252, Gln277, and Met279. Using second-generation inhibitors (e.g., PT2399, compound 12) with different binding modes or developing HIF-2α degraders (PROTACs) that operate independently of the binding pocket are potential strategies to overcome this resistance [30].
Q4: Can HIF-PHD inhibitors have effects beyond erythropoiesis that are relevant to cell survival research?
A: Yes. HIF-PHD inhibitors significantly reshape the immune landscape and modulate inflammation by stabilizing HIF-α in immune cells [32]. This includes recalibrating macrophage polarization from a pro-inflammatory M1 towards a pro-resolution M2 phenotype, altering neutrophil lifespan and function, and enhancing NK cell cytotoxicity [32]. These immunomodulatory effects can profoundly influence tumor cell survival and the response to immunotherapy in the hypoxic niche.
Table 1: Potency and Selectivity Profiles of Representative HIF-2α Inhibitors
| Compound Name | Chemical Class | Target | Binding Affinity (K_D) / Potency (IC₅₀) | Key Characteristics |
|---|---|---|---|---|
| Belzutifan (PT2977) | Tetrazole | HIF-2α PAS-B | K_D: ~30 nM [30] | FDA-approved for ccRCC; disrupts heterodimerization with ARNT. |
| PT2385 | Tetrazole | HIF-2α PAS-B | K_D: ~90 nM [30] | First-generation inhibitor; predecessor to Belzutifan. |
| Compound 12 | Bicyclic | HIF-2α PAS-B | IC₅₀: 0.8 nM (AlphaScreen) [30] | High potency; structurally distinct from tetrazole series. |
| Compound 16 | Cycloalkyl[c]thiophene | HIF-2α PAS-B | IC₅₀: 2 nM (AlphaScreen) [30] | Developed via bioisosteric replacement of PT2385 scaffold. |
Table 2: Experimental Readouts for Verifying HIF Pathway Modulation
| Experimental Goal | Key Assays | Critical Controls | Potential Pitfalls |
|---|---|---|---|
| Confirm HIF-α Stabilization | Western Blot (whole cell lysates), Immunofluorescence | Normoxia (21% O₂) vs. Hypoxia (1% O₂); VHL-reconstituted cells [28]. | Poor antibody specificity; failure to detect rapid protein turnover. |
| Measure Transcriptional Activity | RT-qPCR of target genes (e.g., VEGFA, BNIP3), HRE-Luciferase Reporter Assay | Null-reporter (HRE-mutated); isoform-specific knockdown [26] [27]. | Non-specific effects on transcription/translation; hypoxia-mimicking conditions. |
| Validate Direct Target Engagement | AlphaScreen/Co-IP (heterodimer disruption), ITC, X-ray Crystallography | Binding-site mutants; inactive enantiomers [30]. | Compound aggregation; interference with assay components. |
| Assess Functional Outcome | Cell proliferation/apoptosis under hypoxia, Spheroid growth in 3D culture, Xenograft models | Paired isogenic cell lines; in vivo imaging [26] [27]. | Off-target effects dominating the phenotype; inadequate hypoxia models. |
HIF Signaling Pathway and Inhibitor Mechanisms
The diagram below illustrates the core HIF signaling pathway and the mechanisms of action for the main classes of inhibitors under both normoxic and hypoxic conditions.
Experimental Protocols
Protocol 1: Validating Direct HIF-2α Inhibitor Mechanism
Objective: Confirm that a candidate small molecule directly disrupts HIF-2α/ARNT heterodimerization.
Materials:
- Purified recombinant HIF-2α PAS-B domain protein and ARNT PAS-B domain protein.
- AlphaScreen His-Tag Detection Kit (PerkinElmer).
- Test compound (e.g., Belzutifan) and a structurally related inactive control.
- Plate reader capable of AlphaScreen measurement.
Method:
- Complex Formation: In a white opaque plate, mix His-tagged HIF-2α PAS-B domain and GST-tagged ARNT PAS-B domain at optimized concentrations in assay buffer.
- Inhibitor Incubation: Pre-incubate the HIF-2α protein with a serial dilution of the test compound or DMSO control for 60 minutes.
- Detection: Add the AlphaScreen donor and acceptor beads according to the manufacturer's protocol. Incubate the plate in the dark for 1-2 hours.
- Measurement: Read the AlphaScreen signal. A decrease in signal intensity relative to the DMSO control indicates disruption of the protein-protein interaction.
- Data Analysis: Plot signal vs. inhibitor concentration to calculate an IC₅₀ value. Compare the potency of your compound to a known inhibitor like PT2385 as a benchmark [30].
Protocol 2: Assessing HIF-Mediated Cell Survival Under Chronic Hypoxia
Objective: Quantify the effect of HIF pathway inhibition on cancer cell viability during prolonged hypoxia.
Materials:
- Appropriate cancer cell line (e.g., RCC4 for VHL-null, HCT116 for VHL-wildtype).
- Hypoxia workstation (capable of maintaining 0.5-1% O₂).
- HIF inhibitor (HIF-2α specific or HIF-PHD inhibitor) and vehicle control.
- Cell Titer-Glo 3D Cell Viability Assay (Promega).
Method:
- Culture Setup: Seed cells in 96-well plates at a density ensuring sub-confluence at the assay endpoint.
- Inhibitor Treatment: After cell attachment, add a dose range of the HIF inhibitor or vehicle control.
- Hypoxic Exposure: Transfer plates to the hypoxia workstation (0.5-1% O₂, 5% CO₂, balance N₂). Maintain a normoxic control plate in a standard incubator.
- Viability Assessment: After 72-96 hours, equilibrate plates to room temperature under hypoxia. Add Cell Titer-Glo reagent and measure luminescence according to the manufacturer's instructions.
- Data Analysis: Normalize luminescence readings to the normoxic vehicle control. Plot dose-response curves to determine the inhibitor's effect on survival specifically under hypoxic stress [26] [27].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for HIF Pathway Research
| Reagent Category | Specific Examples | Primary Function in Research |
|---|---|---|
| Cell Lines (VHL-deficient) | 786-O, RCC4 | Model constitutive HIF-2α stabilization; study oncogenic HIF signaling. |
| Cell Lines (Isogenic Pairs) | RCC4±VHL, HCT116±VHL | Control for genetic background; isolate VHL/HIF-specific phenotypes. |
| Direct HIF-2α Inhibitors | Belzutifan (PT2977), PT2385, PT2399 | Tool compounds for selective disruption of HIF-2α/ARNT dimerization. |
| HIF-PHD Inhibitors | Roxadustat (FG-4592), DMOG, IOX2 | Stabilize HIF-α pharmacologically; mimic hypoxic response in normoxia. |
| Hydroxylation-Specific Antibodies | Anti-HIF-1α (Pro402-OH), Anti-HIF-1α (Asn803-OH) | Distinguish active vs. inactive HIF-α; assess PHD/FIH activity. |
| HRE Reporter Constructs | HRE-Luciferase plasmids (pan-HIF, HIF-1 specific, HIF-2 specific) | Quantify HIF transcriptional activity and isoform specificity. |
| PROTAC Molecules | HIF-2α degraders (e.g., compound 25, 26) [30] | Induce targeted degradation of HIF-2α; useful for studying protein function and overcoming resistance. |
FAQs: Metabolic Modulation in Hypoxia Research
Q1: Why does hypoxia cause a metabolic shift away from mitochondrial oxidative phosphorylation? Under hypoxic conditions, the limited oxygen availability directly impairs the function of the electron transport chain (ETC), which relies on oxygen as the final electron acceptor. This disruption makes aerobic ATP production via oxidative phosphorylation inefficient. Consequently, cells undergo a metabolic reprogramming to prioritize ATP-generating pathways that are less dependent on oxygen, primarily through a shift to anaerobic glycolysis [8] [34].
Q2: What are the key metabolic differences between species adapted to high-altitude versus low-altitude habitats when exposed to hypoxia? Research on rodent species from different altitudes reveals distinct metabolic strategies for hypoxia adaptation. The high-altitude native Qinghai vole (Neodon fuscus) sustains its energy supply by regulating fatty acid oxidation under low-oxygen conditions. In contrast, species accustomed to lower altitudes, like the Brandt's vole (Lasiopodomys brandtii) and the Kunming mouse (Mus musculus), rely more on aerobic oxidation and anaerobic glycolysis of glucose, respectively, for energy maintenance during hypoxia [35].
Q3: How does an elevated NADH/NAD+ ratio under ETC dysfunction or hypoxia lead to metabolic derangements? Mitochondrial ETC dysfunction or hypoxia increases the cellular NADH/NAD+ ratio because the ETC is critical for oxidizing NADH back to NAD+. This elevated ratio inhibits key NADH-generating metabolic reactions. For instance, it can suppress the activity of enzymes like glyceraldehyde 3-phosphate dehydrogenase (GAPDH) in glycolysis, causing a bottleneck and forcing a rewiring of glucose metabolism to regenerate NAD+ through pathways like lactate fermentation [36].
Q4: What is the role of HIF-1α in hypoxic metabolic reprogramming? Hypoxia-inducible factor-1α (HIF-1α) is a master regulator of the cellular response to low oxygen. Under hypoxia, HIF-1α stabilizes and orchestrates the transcription of genes that promote a shift toward glycolytic metabolism. This includes upregulating glucose transporters (GLUTs), glycolytic enzymes, and pyruvate dehydrogenase kinase 1 (PDK1). PDK1 inhibits pyruvate dehydrogenase (PDH), thereby reducing the flow of pyruvate into the mitochondrial TCA cycle and favoring its conversion to lactate [37] [34].
Q5: Can modulating fatty acid oxidation be a viable strategy to improve cell survival in hypoxia? Evidence from naturally adapted high-altitude species suggests that yes, sustaining fatty acid oxidation (FAO) is a viable hypoxic survival strategy. In these species, a regulated FAO pathway appears to serve as an efficient energy source. Therefore, in a research context, promoting FAO—for example, by modulating key regulators like PPARα—could represent a therapeutic strategy to enhance cellular energy production and improve survival in low-oxygen environments [35].
Troubleshooting Guides
Issue 1: Inconsistent Metabolic Shift to Glycolysis Under Experimental Hypoxia
Problem: Cells in your hypoxia model do not show a consistent or robust increase in glycolysis, as measured by extracellular acidification rate (ECAR) or lactate production.
- Potential Cause and Solution:
- Cause: Inadequate stabilization of HIF-1α. The hypoxic conditions might not be sufficiently low or prolonged to prevent HIF-1α degradation.
- Solution: Verify the oxygen concentration in your chamber (e.g., 1% O₂ or lower) and the duration of exposure. Confirm HIF-1α stabilization via Western blot [34].
- Cause: Cell-type specific responses. Some primary cells or differentiated tissues may have a less plastic metabolism.
- Solution: Include a positive control, such as a cancer cell line known to exhibit the Warburg effect. Consider using chemical HIF stabilizers (e.g., PHD inhibitors) to validate your setup [37].
Issue 2: Difficulty in Tracing Metabolic Rewiring Using Isotope-Labeled Glucose
Problem: When using ( [U^{-13}C] )-glucose or other labeled tracers in hypoxic cells, the expected labeling patterns in glycolytic intermediates or TCA cycle metabolites are not observed.
- Potential Cause and Solution:
- Cause: Insufficient tracer concentration or incubation time.
- Solution: Ensure the tracer fully replaces unlabeled glucose in the medium. Perform a time-course experiment to determine the optimal incubation period for label incorporation into your metabolites of interest [36].
- Cause: High background of unlabeled metabolites from internal stores (e.g., glycogen).
- Solution: Pre-incubate cells in glucose-free media for a period to deplete intracellular glycogen stores before adding the labeled glucose tracer [36].
Issue 3: Failure to Recapitulate High-Altitude Adaptation Phenotypes in Model Systems
Problem: Your cellular or animal model does not show the enhanced fatty acid oxidation capacity seen in high-altitude adapted species.
- Potential Cause and Solution:
- Cause: The model system lacks the genetic or regulatory architecture of adapted species.
- Solution: Consider a comparative approach using multiple cell types or species. Alternatively, use genetic engineering tools (e.g., CRISPR) to overexpress key regulatory genes identified in adapted species, such as those involved in fatty acid oxidation, in your model system [35].
- Cause: The acute hypoxia exposure time is too short to induce the adaptive metabolic pathway.
- Solution: Extend the duration of hypoxic exposure or consider using intermittent hypoxia protocols that may better mimic certain physiological conditions and induce adaptive responses [35].
Experimental Protocols for Key Methodologies
Protocol 1: Measuring the NADH/NAD+ Ratio and Rewiring of Glucose Metabolism in Hypoxic Cells
This protocol is adapted from methods used to analyze metabolic derangements resulting from ETC inhibition, which shares features with hypoxia [36].
Key Resources:
| REAGENT or RESOURCE | SOURCE | IDENTIFIER |
|---|---|---|
| [4-(^2)H]-glucose | Cambridge Isotope laboratories | cat# DLM-9294-PK |
| [3-(^2)H]-glucose | Cambridge Isotope laboratories | cat# DLM-9294-PK |
| [U-(^{13})C]-glucose | Sigma-Aldrich | cat# 389374 |
| Antimycin A (ETC inhibitor) | Sigma-Aldrich | cat# A8674 |
| Extraction buffer | Prepared Fresh | 80% methanol |
Procedure:
- Preparation: Pre-condition cells in glucose-free medium if necessary. Prepare tracing media: glucose-free DMEM supplemented with 10% dialyzed FBS and 10 mM of the respective labeled glucose (( [U^{-13}C] ), ( [4-^2H] ), or ( [3-^2H] )) [36].
- Hypoxia & Tracer Incubation: Place cells in a hypoxia chamber (e.g., 1% O₂) with the prepared tracing medium. Include ETC inhibitors (e.g., Antimycin A) if used to exacerbate the hypoxic effect.
- Metabolite Extraction: After incubation (e.g., 24h), quickly remove media and wash cells with cold saline. Add pre-chilled 80% methanol extraction buffer to the cell plate, then scrape and collect the homogenate.
- Sample Processing: Incubate extracts on ice, then centrifuge at 15,000 g at 4°C for 20 min. Collect the supernatant and dilute if necessary before LC-MS/MS analysis [36].
- Data Analysis: The deuterium from ( [4-^2H] )-glucose traces electron transfer from glycolytic NADH, while ( [3-^2H] )-glucose traces the oxidative pentose phosphate pathway. ( [U^{-13}C] )-glucose is used to trace the fate of glucose carbons [36].
Protocol 2: Quasi-Targeted Metabolomics of Skeletal Muscle Under Hypoxia
This protocol is based on a study investigating metabolic patterns in rodent skeletal muscle under hypoxia [35].
Procedure:
- Sample Collection: After exposing animals to normoxia or hypoxia (e.g., 10% O₂ for 48h), dissect skeletal muscle tissues. Rinse with sterile saline, snap-freeze in liquid nitrogen, and store at -80°C.
- Metabolite Extraction: Homogenize 100 mg of frozen tissue in liquid nitrogen. Add 500 µL of pre-chilled 80% methanol with 0.1% formic acid, vortex thoroughly, and incubate on ice.
- Sample Processing: Centrifuge the homogenate at 15,000 g at 4°C for 20 min. Dilute a portion of the supernatant to a final methanol concentration of 53% using LC-MS-grade water. Centrifuge again and inject the supernatant into the LC-MS/MS system for analysis [35].
- Quality Control: Generate quality control (QC) samples by pooling equal volumes from each experimental sample to ensure analytical consistency [35].
Data Presentation
Table 1: Species-Specific Metabolic Adaptations to Hypoxia
Table summarizing the distinct metabolic strategies employed by three rodent species from different altitudes when exposed to hypoxia, based on transcriptomic and metabolomic data [35].
| Species | Native Altitude | Preferred Energy Pathway in Hypoxia | Key Adaptive Features |
|---|---|---|---|
| Qinghai vole (Neodon fuscus) | 3700-4800 m | Fatty Acid Oxidation | Superior adaptation to regulate fatty acid oxidation for energy. |
| Brandt's vole (Lasiopodomys brandtii) | < 2000 m | Aerobic Glucose Oxidation | Relies on more efficient aerobic mechanisms where possible. |
| Kunming mouse (Mus musculus) | Low altitude | Anaerobic Glycolysis | Shifts to glycolysis, leading to potential lactate accumulation. |
Table 2: Key Metabolites and Ratios as Indicators of NADH/NAD+ Redox State
Table listing metabolites that can serve as sensitive indicators of an elevated NADH/NAD+ ratio in tissues and plasma, useful for assessing hypoxic impact [36].
| Metabolite / Ratio | Direction of Change in High NADH/NAD+ | Functional Significance |
|---|---|---|
| Lactate/Pyruvate Ratio | Increases | A classic reflection of the cytosolic NADH/NAD+ ratio. |
| α-Hydroxybutyrate | Increases | A sensitive marker of altered redox state and glutathione synthesis. |
| Alanine | Increases | Indicates a shift in aminotransferase reactions. |
| Aspartate | Decreases | Reflects inhibition of malate-aspartate shuttle activity. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Hypoxic Metabolism Research
| Reagent / Tool | Function / Application | Example |
|---|---|---|
| Chemical ETC Inhibitors | To induce mitochondrial dysfunction and mimic/amplify hypoxic metabolic effects. | Antimycin A, Piericidin A [36]. |
| Stable Isotope-Labeled Metabolites | To trace metabolic pathway fluxes and fates of nutrients (e.g., glucose, glutamine). | [U-(^{13})C]-Glucose, [4-(^2)H]-Glucose, [3-(^2)H]-Glucose [36]. |
| HIF Stabilizers (PHD Inhibitors) | To chemically simulate hypoxia by preventing HIF-1α degradation, independent of O₂ level. | Dimethyloxallylglycine (DMOG), Roxadustat. |
| NAD+/NADH Quantification Kits | To directly measure the cellular redox state, a central parameter in hypoxic metabolism. | Commercial colorimetric or LC-MS based kits [36]. |
| Extraction Buffers for Metabolomics | To quench metabolism and extract intracellular metabolites for LC-MS/MS analysis. | Pre-chilled 80% Methanol with 0.1% Formic Acid [35] [36]. |
Metabolic Pathway Visualizations
Troubleshooting Guide: FAQs on Hypoxia-Activated Prodrugs (HAPs) Research
FAQ 1: Why does my HAP show high efficacy in vitro but fails in in vivo models?
Answer: This common issue often stems from inadequate consideration of the tumor microenvironment (TME) and pharmacokinetics.
- Potential Cause 1: Insufficient or heterogeneous hypoxia in the tumor model. HAPs require severe hypoxia (<1.3% O₂ or <10 mmHg) for efficient activation [38] [39]. The level and distribution of hypoxia can vary significantly between in vitro setups and in vivo tumors, and even between different in vivo models [40].
- Solution: Characterize the hypoxic fraction of your in vivo tumor model before initiating therapy. Use techniques like pimonidazole immunohistochemistry or [18F]-FAZA/[18F]-MISO PET imaging to confirm the presence and extent of hypoxia [41] [40].
- Potential Cause 2: Inadequate prodrug penetration or rapid systemic clearance. The disorganized tumor vasculature can hinder drug delivery to hypoxic regions, which are often distant from blood vessels [38].
- Solution: Investigate the pharmacokinetics and biodistribution of your HAP. Consider modifying the dosing schedule or exploring formulations that enhance tumor delivery.
FAQ 2: My HAP is toxic to well-oxygenated cells in culture. What could be the reason?
Answer: Off-target, oxygen-independent activation is a frequent challenge.
- Potential Cause 1: Activation by reductases expressed in normoxic cells. Some prodrugs, like PR-104, can be activated by enzymes such as aldo-keto reductase 1C3 (AKR1C3) regardless of oxygen levels [38].
- Solution: Quantify the expression of potential activating reductases (e.g., AKR1C3, Cytochrome P450 oxidoreductase) in your cell lines. Use inhibitors or genetic knockdown to confirm the specific reductase responsible for the off-target activation [38] [42].
- Potential Cause 2: The prodrug has a high K-value (oxygen concentration that halves its cytotoxic potency), meaning it is activated under moderately hypoxic conditions that might be present in some in vitro settings or even in normal tissues like the bone marrow [38].
- Solution: Determine the K-value for your HAP. A lower K-value indicates activation under more severe hypoxia and potentially a better therapeutic window [38].
FAQ 3: How can I enhance the efficacy of a HAP in a resistant tumor model?
Answer: Consider combination therapies that increase the hypoxic fraction or target complementary pathways.
- Strategy 1: Modulate Tumor Oxygenation. Use vasodilators (e.g., hydralazine) to induce a "vascular steal" effect, transiently reducing tumor blood flow and oxygen supply. Alternatively, use metabolic sensitizers (e.g., pyruvate) to increase cellular oxygen consumption, thereby expanding the hypoxic region [39].
- Solution Protocol: Administer the vasodilator or sensitizer shortly before the HAP to create a window of maximum hypoxia for prodrug activation. Mathematical modeling can help optimize the timing [39].
- Strategy 2: Combine with Conventional Therapies. HAPs target hypoxic cells that are resistant to radiotherapy and many chemotherapies. Combining a HAP with these agents can lead to synergistic cell killing [43] [42].
- Solution Protocol: Standard chemotherapeutics (e.g., gemcitabine, docetaxel, cisplatin) or radiotherapy can be administered in sequence with the HAP. This approach targets both the oxygenated and hypoxic compartments of the tumor [41] [43].
Experimental Protocols for Key HAP Assays
Protocol 1: Verifying Hypoxia-Selective Cytotoxicity In Vitro
Objective: To confirm that the cytotoxic activity of a prodrug is significantly enhanced under hypoxic conditions.
Materials:
- Hypoxia workstation/chamber for maintaining low O₂ (e.g., 0.1-1% O₂).
- Normoxic cell culture incubator (21% O₂).
- Appropriate cell lines.
- HAP stock solution and vehicle control.
- Cell viability assay kit (e.g., MTT, clonogenic assay).
Methodology:
- Cell Seeding: Seed cells in multiple well-plates at a density that will be sub-confluent at the time of analysis.
- Pre-equilibration: Place one set of plates in the hypoxic chamber and another in the normoxic incubator for 24 hours to pre-equilibrate the cells to their respective oxygen conditions.
- Drug Treatment: Add a range of HAP concentrations and controls to the plates inside the hypoxia chamber to avoid oxygen exposure. Transfer the hypoxic treatment plates back to the hypoxia chamber and the normoxic plates to the normoxic incubator.
- Incubation: Incubate for a predetermined time (e.g., 4-72 hours, depending on the drug and cell type).
- Viability Assessment:
- For acute cytotoxicity: Perform a viability assay (e.g., MTT) immediately after treatment.
- For long-term clonogenic survival: Trypsinize the cells, re-seed at low density in normoxic conditions, and allow colonies to form for 7-14 days before staining and counting.
- Data Analysis: Calculate IC₅₀ values for both hypoxic and normoxic conditions. A true HAP should show a significantly lower IC₅₀ (e.g., 10- to 100-fold) under hypoxia [43].
Protocol 2: Testing HAP Combination with Transient Hypoxia Modulators
Objective: To evaluate if a vasodilator or metabolic sensitizer can improve the efficacy of a HAP in an in vivo model.
Materials:
- Mouse tumor model (e.g., subcutaneous xenograft).
- HAP, Vasodilator (e.g., Hydralazine), Metabolic Sensitizer (e.g., Pyruvate).
- Pimonidazole HCl or access to hypoxia PET imaging.
Methodology:
- Tumor Hypoxia Characterization: Randomize tumor-bearing mice and use pimonidazole or PET imaging in a subset to establish baseline hypoxia.
- Treatment Groups: Divide mice into groups:
- Group 1: Vehicle control
- Group 2: HAP monotherapy
- Group 3: Vasodilator/Sensitizer monotherapy
- Group 4: HAP + Vasodilator/Sensitizer (with varying timings)
- Drug Administration:
- For vasodilator combination: Administer vasodilator intravenously 15-30 minutes before HAP injection. This timing allows for the reduction in tumor blood flow to establish hypoxia [39].
- For metabolic sensitizer combination: Administer sensitizer shortly (e.g., 5-15 minutes) before or concurrently with HAP to elevate oxygen consumption during drug exposure [39].
- Efficacy Endpoints: Monitor tumor growth over time. At endpoint, harvest tumors for analysis (e.g., immunohistochemistry for hypoxia markers, apoptosis, DNA damage).
Quantitative Data on Hypoxia-Activated Prodrugs
Table 1: Clinically Evaluated Hypoxia-Activated Prodrugs and Key Properties
| Prodrug (Class) | Active Cytotoxin | Mechanism of Action | Key Clinical Trial Findings & Status |
|---|---|---|---|
| Tirapazamine (TPZ) (Benzotriazine dioxide) | Oxidative radical | DNA single/double-strand breaks [42] | Phase III trials in HNSCC & NSCLC showed no overall survival benefit; hampered by toxicity (muscle cramps, ototoxicity) [38] [40]. |
| PR-104 (Dinitrobenzamide mustard) | DNA cross-linking nitrogen mustard | DNA interstrand cross-links [38] | Phase I/II trials showed dose-limiting myelosuppression (neutropenia, thrombocytopenia); activation by AKR1C3 causes off-target toxicity [38]. |
| Evofosfamide (TH-302) (2-Nitroimidazole mustard) | Bromo-isophosphoramide mustard (Br-IPM) | DNA cross-linking [43] | Phase III in pancreatic cancer & sarcoma failed primary survival endpoints; preclinical data shows strong hypoxia-selective cytotoxicity [38] [40] [43]. |
| AQ4N (Banoxantrone) (Aliphatic N-oxide) | AQ4 (topoisomerase II inhibitor) | DNA intercalation and topoisomerase II inhibition [42] | Early-phase trials demonstrated safety and evidence of hypoxia-targeted activation in tumors; limited single-agent efficacy [42]. |
Table 2: Research Reagent Solutions for HAP Studies
| Reagent / Tool | Function / Application | Specific Examples |
|---|---|---|
| Hypoxia Markers (Exogenous) | Directly labels hypoxic cells in tissue sections for histological validation. | Pimonidazole, EF5 [41] [40] |
| Hypoxia PET Tracers | Non-invasive imaging to detect and quantify tumor hypoxia in vivo. | [18F]-FMISO, [18F]-FAZA, [18F]-HX4 [41] [40] |
| Hypoxia Gene Signatures | mRNA-based assessment of hypoxic tumor status from biopsy samples. | 15-gene signature, 26-gene signature [41] [40] |
| HIF-1α Inhibitors | Tool compounds to dissect the role of HIF-1 pathway in HAP response and resistance. | Chetomin (disrupts HIF-1α/p300 interaction) [41] |
| 3D Culture Models | In vitro systems that mimic the diffusion gradients (oxygen, nutrients, drug) of in vivo tumors. | Multicellular Tumor Spheroids (MCTS), Multicellular Layers (MCL) [43] [44] |
Signaling Pathways and Experimental Workflows
HIF-1α Stabilization and HAP Activation Pathway
Diagram Title: HIF-1α Pathway and HAP Activation Mechanism
Workflow for Validating a Hypoxia-Activated Prodrug
Diagram Title: HAP Preclinical Validation Workflow
Fundamental Concepts & Mechanisms
What is hypoxia preconditioning (HPC) and what is its primary purpose in cell therapy? Hypoxia preconditioning is a technique where cells (like stem cells) are exposed to brief, non-lethal periods of low oxygen before transplantation. The primary purpose is to induce an adaptive, protective response, making the cells more resilient to the severe hypoxia and other stresses they will encounter in the damaged target tissue, such as an infarcted heart or injured spinal cord. This "warning signal" prepares the organism for more harmful conditions, ultimately increasing cell survival and the therapeutic efficacy of the treatment [45].
What are the key molecular mechanisms activated by HPC? The core molecular response to HPC is orchestrated by the Hypoxia-Inducible Factor (HIF) pathway [46] [45] [47].
- Under normal oxygen (Normoxia): HIF-1α is continuously produced but rapidly degraded by prolyl hydroxylase domain enzymes (PHDs), which mark it for destruction by the VHL E3 ubiquitin ligase complex [47].
- Under low oxygen (Hypoxia): PHD activity is inhibited. This stabilizes HIF-1α, allowing it to accumulate, translocate to the nucleus, and dimerize with HIF-1β. This complex then binds to Hypoxia Response Elements (HREs) in DNA, activating a transcriptional program for cellular adaptation [47]. This program includes:
The diagram below illustrates this central signaling pathway.
Optimized Protocols & Parameters
What are the critical parameters for optimizing HPC? Successful HPC depends on carefully balancing oxygen concentration, exposure duration, and cell culture status. The optimal parameters can vary by cell type, but general guidelines from the literature are summarized in the table below.
Table 1: Key Experimental Parameters for Hypoxia Preconditioning
| Parameter | Optimal Range / Condition | Key Findings & Considerations |
|---|---|---|
| Oxygen Concentration | 0.5% - 5% O₂ [48] [46] [50] | 0.5% O₂ was optimal for rat MSCs, mimicking the severe ischemia of an infarct zone [48]. 5% O₂ is commonly used for human umbilical cord MSCs [50]. |
| Exposure Duration | 6 - 24 hours [48] [49] | A 6-hour exposure was optimal for mouse cardiac progenitor cells, while 24 hours was best for rat MSCs. Longer exposures (e.g., 72 hours) can be detrimental [48] [49]. |
| Cell Passage & State | Low passage (P3-P8) cells, cultured under normoxia post-thaw [48] [51] | Cryopreserved MSCs that were cultured for at least one passage after thawing responded better to HPC than freshly thawed cells [48]. |
| Key Readouts / Biomarkers | ↑ HIF-1α, CXCR4, p-Akt, Bcl-2, VEGF [48] [49] | These markers indicate successful activation of pro-survival and pro-angiogenic pathways. A reduction in apoptosis upon subsequent severe stress is a key functional readout [48]. |
Can you provide a detailed experimental protocol for HPC of mesenchymal stem cells (MSCs)? The following workflow details a standard protocol for hypoxic preconditioning of MSCs, based on established methodologies [48] [50].
Detailed Methodology:
- Cell Culture Post-Thaw: Thaw cryopreserved MSCs and culture them in standard normoxic conditions (21% O₂, 5% CO₂) using complete growth medium (e.g., DMEM with 10% FBS) for at least one passage. This allows cells to recover from cryopreservation stress [48].
- Preparation for HPC: When cells reach 80-90% confluence, detach them using a standard cell-detachment solution like Accutase. Plate the cells at the desired density for your experiment [48].
- Hypoxic Exposure: Once cells have adhered and reached 80-90% confluence again, place the culture dishes in a specialized environmental chamber (e.g., a C-Chamber) housed within a standard CO₂ incubator. Flush the chamber with a pre-mixed gas containing the desired low oxygen concentration (e.g., 0.5% or 5% O₂), 5% CO₂, and the balance N₂. Maintain the cells in this hypoxic environment for the predetermined optimal time (e.g., 24 hours) [48] [50].
- Harvesting and Validation: After the hypoxic exposure, harvest the cells for transplantation or downstream analysis. Confirm the success of HPC by measuring key biomarkers, such as increased protein levels of HIF-1α, phosphorylated Akt (p-Akt), and VEGF via Western blot or ELISA [48]. A functional validation involves subjecting the cells to severe hypoxia (e.g., 0.1% O₂) and measuring apoptosis (e.g., via Annexin V assay), which should be significantly reduced in HPC cells compared to controls [48].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Tools for Hypoxia Preconditioning Research
| Item | Function / Description | Examples & Citations |
|---|---|---|
| Hypoxia Chambers/Workstations | Creates a controlled, humidified low-O₂ environment for cell culture. | Modular incubator chambers; C-Chambers [48] [45]. |
| Gas Mixture | Pre-mixed gas to establish hypoxic conditions in the chamber. | 0.5% or 5% O₂, 5% CO₂, balanced N₂ [48] [50]. |
| HIF Stabilizers (Chemical Mimetics) | Pharmacologically inhibits PHDs, stabilizing HIF-1α under normoxia. Used as an alternative to physical hypoxia. | Cobalt Chloride (CoCl₂), Desferrioxamine (DFO), Dimethyloxaloylglycine (DMOG) [45] [47]. |
| HIF-1α Inducers & Inhibitors | Tools to manipulate the HIF pathway to establish causality. | Inducer: FG-4592 (Roxadustat) [52]. Inhibitor: small interfering RNA (siRNA-HIF-1α) [52]. |
| CXCR4 Antagonist | Blocks the SDF-1α/CXCR4 axis to investigate its role in HPC-induced cell migration and survival. | AMD3100 (Plerixafor) [49]. |
| Key Antibodies for Validation | Essential for Western blot, ELISA, and ICC to confirm HPC success. | Antibodies against HIF-1α, p-Akt (Ser473), Bcl-2, VEGF, CXCR4, Caspase-3 [48] [52] [49]. |
| Apoptosis Detection Kits | To functionally validate the enhanced survival of HPC-cells. | Annexin V-FITC/PI apoptosis detection kit [48]. TUNEL assay kit [52]. |
Troubleshooting Common Experimental Issues
FAQ 1: I cannot detect HIF-1α specific bands in my Western blots from hypoxic cells. What could be wrong? This is a common challenge due to the rapid degradation of HIF-1α upon re-exposure to oxygen [47].
- Solution:
- Rapid Lysis: Prepare cell lysates as quickly as possible after the hypoxic exposure. It is ideal to lyse the cells directly inside the hypoxic chamber or use a method that allows for immediate denaturation [47].
- Fractionate: Analyze HIF-1α in nuclear-cytoplasmic fractions instead of whole cell lysates. The active, transcriptionally active pool of HIF-1α accumulates in the nucleus, and fractionation enriches for this pool, enhancing detection. Use Lamin B as a loading control for nuclear fractions [47].
- Use Positive Controls: Always include a positive control, such as lysates from cells treated with a chemical HIF stabilizer like CoCl₂ (100-300 µM for 4-6 hours) [47].
- Band Expectation: Be aware that the theoretical molecular weight of HIF-1α is ~93kDa, but the post-translationally modified (and detectable) protein typically runs at 110-130 kDa [47].
FAQ 2: My HPC-cells are not showing improved survival in vivo. What factors should I check?
- Solution:
- Verify Passage Number: Ensure you are using low-passage cells (e.g., passages 3-8). Higher passage cells may lose their responsiveness to preconditioning and their therapeutic potency [51].
- Confirm Pre-culture Condition: Do not use freshly thawed cells directly for HPC. Data shows that cryopreserved MSCs cultured under normoxia for at least one passage before HPC respond more effectively, showing decreased apoptosis and enhanced expression of functional proteins [48].
- Check Exposure Duration: Re-evaluate the duration of hypoxic exposure. An optimal time window exists (e.g., 6-24 hours), and prolonged hypoxia (e.g., 72 hours) can be detrimental and fail to induce the prosurvival phenotype [48].
- In Vivo Model Timing: Consider the timing of cell delivery relative to the HPC protocol. The adaptive effects of normobaric hypoxia preconditioning can last up to 72 hours, so transplanting cells within this window is crucial [45].
FAQ 3: Beyond whole cells, are there other therapeutic approaches using HPC? Yes, a rapidly growing area is the use of cell-free therapies derived from HPC-cells.
- Solution: Extracellular Vesicles (EVs). The secretome of MSCs, particularly EVs, is a key mediator of their therapeutic effect. HPC significantly alters the protein cargo of MSC-derived EVs, enriching them with factors that enhance tissue repair. For example, hypoxic MSC-EVs show superior efficacy in treating renal ischemia-reperfusion injury, in part due to an accumulation of antioxidant proteins like GSTO1 [46] [50]. This approach offers advantages such as lower immunogenicity and better biological safety compared to whole-cell transplants [46].
Hypoxia, characterized by inadequate oxygen levels in tissues, is a fundamental feature of the microenvironment in many solid tumors and ischemic diseases. For researchers focused on improving cell survival in hypoxic environments, accurately detecting and monitoring hypoxia is paramount. Hypoxia can substantially impact clinical outcomes by promoting tumor invasion, metastasis, immune escape, and therapy resistance [53]. When intracellular oxygen content decreases, it triggers a complex cellular response, primarily mediated by hypoxia-inducible factors (HIFs), which regulate the expression of hundreds of genes involved in cell metabolism, proliferation, and survival [54].
The development of non-invasive imaging biomarkers for hypoxia has become a critical tool in both basic research and clinical translation. These biomarkers allow for repeated assessment of hypoxia dynamics without invasive procedures, enabling the evaluation of therapeutic interventions aimed at improving cell survival. This technical support guide provides detailed methodologies and troubleshooting advice for researchers utilizing these advanced technologies in their investigations of hypoxic environments.
Key Hypoxia Imaging Modalities and Biomarkers
Major Imaging Techniques for Hypoxia Detection
Table 1: Comparison of Major Hypoxia Imaging Techniques
| Technique | Signal Measured | Advantages | Limitations | Resolution | Cost |
|---|---|---|---|---|---|
| PET/CT | Positrons from radiotracers | High sensitivity and specificity | Radioactive; Limited spatial resolution; Low signal-to-noise ratio (SNR) | ~5 mm | High [53] |
| MRI | Magnetic resonance signals | High spatial resolution; No ionizing radiation | Lower sensitivity for molecular targets; Complex quantitative analysis | ~1 mm | High [53] |
| Optical Molecular Imaging | Fluorescence, phosphorescence, or bioluminescence | Real-time imaging; High sensitivity; Lower cost | Limited penetration depth; Visible/NIR-I only | ~1-3 mm | Low-Medium [53] |
| Phosphorescence Lifetime Imaging | Oxygen-induced luminescence quenching | Real-time; Quantitative; Available to detect cyclic hypoxia | Poor biocompatibility; Low penetration depth | ~1-3 mm | Medium [53] |
Design Strategies for Hypoxia-Targeted Probes
Table 2: Probe Design Strategies for Hypoxia Imaging
| Category | Mechanism | Representative Probes | Advantages | Disadvantages |
|---|---|---|---|---|
| Physical | Direct oxygen sensing via luminescence quenching | PpyPt NPs, PtTFPP/PtOEP | Real-time; Quantitative; Detects cyclic hypoxia | Poor biocompatibility; Low penetration depth [53] |
| Biological | Enzyme-activated (NTRs, AzoRs) or receptor-targeted (CAIX) | 18F-FMISO, 18F-FAZA, 18F-HX4, CAIX-800 | High specificity; Good stability; Easy accessibility | Off-target activation; Limited sensitivity [53] |
| Chemical | Detection of hypoxia-relevant compounds (pH, H₂O₂, H₂S) | Ir-D, Au@Pt-Se NPs, CD-950 | High sensitivity; Good specificity; High SNR | Cross-reactivity; Complex synthesis [53] |
Experimental Protocols for Hypoxia Detection
Protocol: In Vitro Hypoxia Induction and Validation for Cell Survival Studies
Purpose: To establish controlled hypoxic conditions for evaluating cell survival and therapeutic interventions.
Materials:
- Hypoxia chamber (e.g., PEEK chamber with gas-permeable foil) [55]
- Gas mixtures: 94.5% N₂, 5% CO₂, 0.5% O₂ (hypoxia); 95% N₂, 5% CO₂ (anoxia) [55]
- Oxygen microsensor (e.g., Needle-Type optical O₂ microsensor) [55]
- Cell culture reagents and equipment
Procedure:
- Chamber Setup: Seed cells in appropriate vessels and place in the hypoxia chamber.
- Gassing: Connect pre-mixed gas to chamber inlet. Gas for 2 hours at 200 mL/min flow rate to achieve stable oxygen concentration [55].
- Oxygen Validation: Use oxygen microsensor to verify pO₂ levels in cell culture medium.
- Experimental Treatment: Apply therapeutic interventions while maintaining hypoxic conditions.
- Assessment: Perform clonogenic survival assays, metabolic activity tests, or molecular analyses.
Troubleshooting:
- Inconsistent hypoxia: Verify gas mixture composition and chamber seals.
- Cell death during gassing: Ensure chamber maintains 37°C and 5% CO₂ throughout experiment.
- Variable results: Pre-equilibrate all solutions to hypoxic conditions before use.
Protocol: Validation of Hypoxia Imaging Biomarkers
Purpose: To confirm that imaging signals correlate with actual hypoxia levels in experimental models.
Materials:
- Hypoxia imaging probe appropriate for your model system
- Imaging equipment (PET, MRI, or optical imaging system)
- Reference standard for hypoxia validation (e.g., pimonidazole immunohistochemistry)
- Oxygen measuring system (e.g., OxyLite fiber optic probe)
Procedure:
- Model Preparation: Establish tumor xenografts or other disease models.
- Probe Administration: Inject hypoxia-specific probe according to established protocols.
- Image Acquisition: Perform imaging at optimal time points post-injection.
- Tissue Collection: Harvest tissues immediately after imaging.
- Validation: Correlate imaging signals with ex vivo analyses (IHC, Western blot for HIF-1α, pimonidazole staining).
Troubleshooting:
- High background signal: Optimize timing between probe administration and imaging.
- Poor target-to-background ratio: Consider probe dosage adjustment or alternative probes.
- Inconsistent results: Standardize animal preparation and anesthesia protocols.
HIF Signaling Pathway in Hypoxia Response
Diagram 1: HIF Signaling Pathway in Hypoxia Response. This diagram illustrates the central hypoxia response pathway mediated by HIF transcription factors, which regulates key processes in cell survival under low oxygen conditions [54].
Frequently Asked Questions (FAQs)
Q1: What oxygen concentration constitutes "hypoxia" in cell culture compared to physiological conditions?
A: In cell culture, the "true" normoxic oxygen condition in a standard incubator at 37°C with 5% CO₂ is approximately 18.6% O₂ (141 mmHg pO₂), not the commonly cited 20-21% found in room air [56]. Physiologically, tissue oxygen levels vary significantly:
- Normal tissue pO₂: ~40-60 mmHg
- Mild hypoxia: ~10-20 mmHg
- Severe hypoxia: <10 mmHg
- Anoxia: 0 mmHg
For in vitro experiments, hypoxia is typically induced at 0.5-2% O₂ (∼4-15 mmHg) to mimic tumor microenvironments [55] [56].
Q2: Why do my hypoxia imaging results show high variability between experiments?
A: Variability can arise from multiple sources:
- Temporal fluctuations: Hypoxia is often cyclic, not constant, leading to dynamic changes in imaging signals [53].
- Probe kinetics: Uneven delivery or clearance of imaging probes can create heterogeneity.
- Technical factors: Inconsistent imaging parameters, anesthesia effects in animal models, or improper probe handling.
- Biological heterogeneity: Natural variations in hypoxia patterns between subjects or even within the same tumor over time.
Solution: Implement rigorous standardization of experimental protocols, include internal controls, use multiple animals/subjects per group, and consider complementary validation methods.
Q3: How do I choose between different hypoxia imaging biomarkers for my specific research application?
A: Selection depends on your research question and model system:
- For high sensitivity and quantification: PET tracers (18F-FMISO, 18F-FAZA) are preferred despite higher cost [53].
- For high spatial resolution and anatomical correlation: MRI-based methods are optimal [53].
- For real-time monitoring in accessible models: Optical imaging probes provide excellent temporal resolution [57] [53].
- For hypoxia mechanism studies: CAIX-targeted probes specifically report on HIF pathway activation [53].
Consider your required balance between spatial resolution, temporal resolution, sensitivity, cost, and compatibility with your experimental model.
Q4: What are the key validation methods to confirm that my imaging signal truly represents hypoxia?
A: A multi-modal validation approach is recommended:
- Molecular validation: Immunohistochemistry for HIF-1α, CAIX, or GLUT1 expression [53] [54].
- Histochemical validation: Pimonidazole staining as a gold standard hypoxia marker.
- Direct measurement: Oxygen-sensitive electrodes or probes (where feasible) [55].
- Correlative imaging: Using multiple imaging biomarkers with different mechanisms to confirm findings.
Research Reagent Solutions
Table 3: Essential Research Reagents for Hypoxia Studies
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Hypoxia Chambers | Custom PEEK chambers with gas-permeable membranes [55] | Controlled induction of hypoxic conditions for cell culture | Ensure precise oxygen control; Validate with microsensors |
| Chemical Hypoxia Mimetics | Cobalt chloride, Deferoxamine | Induce HIF stabilization under normoxic conditions | May not fully replicate true hypoxia; Useful for initial screening |
| Oxygen Sensing Probes | PreSens optical O₂ microsensors [55] | Direct measurement of oxygen concentration | Essential for validation; Different probe sizes for various applications |
| PET Radiotracers | 18F-FMISO, 18F-FAZA, 18F-HX4 [53] | Non-invasive hypoxia detection in vivo | Require specialized facilities; Excellent for translational studies |
| Optical Imaging Probes | Dual-lock fluorescent probes, Ratiometric oxygen probes [53] | Real-time hypoxia monitoring in transparent models | Limited penetration depth; High sensitivity |
| Hydrogel-Based Systems | Oxygen-releasing microparticles (CPO-PCL) [58] | Maintain cell viability in severely hypoxic conditions | Control oxygen release kinetics; Minimize ROS production |
| Wearable Sensors | Integrated lactate-oxygenation sensors [57] | Simultaneous monitoring of metabolic and oxygenation changes | Emerging technology; Excellent for continuous monitoring |
Advanced Methodologies for Enhanced Hypoxia Research
Protocol: Oxygen-Releasing Hydrogels for Cell Survival in Severe Hypoxia
Purpose: To sustain cell viability under severely hypoxic conditions using oxygen-generating biomaterials.
Materials:
- Calcium peroxide (CPO)
- Polycaprolactone (PCL)
- Gelatin methacryloyl (GelMA)
- Electrospray equipment
- Crosslinking equipment
Procedure:
- OMP Fabrication: Create oxygen-releasing microparticles (OMPs) by electrospraying PCL (10% w/v) and CPO (0.5-5% w/v) in chloroform [58].
- Hydrogel Preparation: Mix OMPs with GelMA hydrogel precursor at optimized concentration.
- Cell Encapsulation: Suspend cells in hydrogel-OMP mixture and crosslink.
- Hypoxia Challenge: Culture constructs in severely hypoxic or anoxic conditions.
- Assessment: Monitor cell viability, metabolic activity, and proliferation over time.
Troubleshooting:
- Cytotoxicity: Optimize CPO concentration and encapsulation efficiency to minimize reactive oxygen species generation.
- Oxygen burst release: Ensure complete PCL encapsulation of CPO to control release kinetics.
- Inadequate oxygen duration: Increase OMP concentration or optimize polymer thickness.
Emerging Technologies: Dual-Modality Sensing Approaches
Recent advances in hypoxia detection include integrated sensing platforms that simultaneously monitor multiple parameters. For example, wearable devices that combine colorimetric lactate biosensors with near-infrared (NIR) tissue oxygenation sensors provide complementary metabolic and oxygenation data [57]. These systems are particularly valuable for monitoring dynamic changes in hypoxia and the resulting metabolic adaptations.
The field is also moving toward "dual-lock" fluorescent probes that require activation by two different hypoxia-associated biomarkers, significantly enhancing specificity by reducing false positives [53]. Similarly, ratiometric probes with built-in self-calibration capabilities improve quantitative accuracy by accounting for technical variations in signal acquisition [53].
Overcoming Challenges in Hypoxia-Targeted Interventions
Addressing Tumor Microenvironment-Mediated Therapy Resistance
Frequently Asked Questions
Q1: What makes the Tumor Microenvironment (TME) a key contributor to therapy resistance? The TME is a complex ecosystem where cancer cells interact with various stromal components, creating physical and functional barriers that reduce treatment efficacy. Key mechanisms include:
- Physical barriers: Dense extracellular matrix (ECM) and abnormal vasculature impede drug penetration [59] [60].
- Cellular barriers: Immunosuppressive cells like M2 macrophages, myeloid-derived suppressor cells (MDSCs), and cancer-associated fibroblasts (CAFs) create an environment that protects tumor cells [61] [62].
- Metabolic competition: Tumor cells and immune cells compete for nutrients, constraining anti-tumor immune responses [62].
- Hypoxia: Low oxygen conditions activate HIF signaling pathways that promote survival mechanisms and resistance to chemotherapy and radiation [6].
Q2: Why do some tumors not respond to immunotherapy? "Cold" tumors characterized by minimal T-cell infiltration often resist immunotherapy due to:
- Immune exclusion: Hostile stroma prevents lymphocyte infiltration despite potential immunogenicity [59].
- Immunosuppressive networks: Regulatory T cells, tumor-associated macrophages, and myeloid-derived suppressor cells create an inhibitory milieu [61].
- Metabolic reprogramming: Hypoxia-driven shifts to anaerobic metabolism acidify the TME, suppressing immune function [6] [62].
- Checkpoint molecule expression: PD-1/PD-L1 interactions and other checkpoint pathways inhibit anti-tumor immunity [62].
Q3: What experimental models best capture TME-mediated resistance?
- Advanced in vivo models: Immunocompetent mouse models that recapitulate human TME components, including stromal heterogeneity and immune cell infiltrates [60].
- Computational models: Agent-based pharmacokinetic models simulating perivascular niche dynamics to optimize treatment timing [60].
- 3D culture systems: Models incorporating ECM components and multiple cell types to better mimic human disease TME [59] [60].
Q4: How can we overcome hypoxia-mediated resistance?
- HIF pathway inhibition: Target HIF-1α stabilization or downstream signaling [6].
- Metabolic modulators: Compounds that counter hypoxia-induced glycolytic shifts [61] [6].
- Vascular normalizing agents: Improve oxygen and drug delivery by remodeling abnormal tumor vasculature [61] [60].
- Hypoxia-activated prodrugs: Agents specifically activated in low-oxygen environments [6].
Troubleshooting Guides
Problem: Poor Drug Penetration in Dense Tumor Stroma
Potential Causes and Solutions:
| Cause | Diagnostic Approach | Solution |
|---|---|---|
| Excessive ECM deposition | Histology for collagen/fibronectin; stiffness measurements | Stromal-targeting agents (e.g., pan-lysyl oxidase inhibitors) [59] |
| CAF-mediated barrier | CAF marker analysis (α-SMA, FAP); single-cell RNA sequencing | Hedgehog pathway inhibition; CAF reprogramming strategies [59] |
| High interstitial fluid pressure | Pressure measurement; perfusion imaging | VEGF inhibition; angiotensin receptor blockers [60] |
Experimental Protocol: Evaluating Stromal Modulation
- Establish stroma-rich model: Use patient-derived xenografts or engineered co-cultures with high CAF content.
- Administer stromal-targeting agent: Test inhibitors against LOX, FAK, or TGF-β.
- Assess penetration: Use fluorescently-labeled therapeutics or mass spectrometry imaging.
- Evaluate efficacy: Measure tumor growth inhibition and correlate with stromal changes.
Problem: Immunosuppressive TME in "Cold" Tumors
Potential Causes and Solutions:
| Cause | Diagnostic Approach | Solution |
|---|---|---|
| Myeloid suppression | Flow cytometry for MDSCs/M2 macrophages; cytokine profiling | CSF-1R inhibitors; CCR2 antagonists; PI3K-γ inhibitors [61] |
| T-cell exclusion | Spatial transcriptomics; multiplex IHC for T-cell positioning | STING agonists; CXCR4 antagonists; tumor vaccines [61] [63] |
| Metabolic suppression | Metabolite profiling; hypoxia markers; pH mapping | Metabolic modulators (e.g., ARG1 inhibitors); pH buffers [62] |
Experimental Protocol: "Cold-to-Hot" Transformation
- Baseline characterization: Perform single-cell RNA sequencing and spatial transcriptomics to map immune populations.
- Combination therapy: Implement ICI plus TME-modifying agent (e.g., anti-PD-1 + CSF-1R inhibitor).
- Monitor immune infiltration: Use serial imaging and flow cytometry to track CD8+ T-cell influx.
- Assess functional immunity: Measure cytokine production and tumor cell killing.
Problem: Hypoxia-Mediated Treatment Resistance
Potential Causes and Solutions:
| Cause | Diagnostic Approach | Solution |
|---|---|---|
| HIF pathway activation | HIF-1α IHC; hypoxia gene signatures; pimonidazole staining | HIF inhibitors; hypoxia-activated prodrugs; hyperbaric oxygen [6] |
| Metabolic reprogramming | FDG-PET; lactate measurement; metabolic flux analysis | Glycolysis inhibitors; mitochondrial optimizers [6] [62] |
| Angiogenic dysfunction | CD31 IHC; perfusion imaging; vessel maturity assessment | VEGF/VEGFR targeting; angiopoietin-2 inhibitors [6] [60] |
Experimental Protocol: Targeting Hypoxic Adaptation
- Quantify hypoxia: Use pimonidazole staining or hypoxia-sensitive reporters.
- Modulate hypoxia response: Apply HIF inhibitors or hypoxia-activated prodrugs.
- Measure functional effects: Assess cell viability, DNA damage, and apoptosis in hypoxic vs. normoxic regions.
- Validate in vivo: Use window chamber models or hypoxia reporters in animal models.
TME-Targeting Therapeutic Approaches
Table: Strategies to Overcome TME-Mediated Resistance
| Resistance Mechanism | Therapeutic Class | Example Agents | Key Targets |
|---|---|---|---|
| Immunosuppression | Immune checkpoint inhibitors | Anti-PD-1/PD-L1 antibodies | PD-1, PD-L1 [62] |
| Myeloid-targeting agents | CSF-1R inhibitors | CSF-1R [61] | |
| Stromal barriers | ECM-modifying agents | LOX inhibitors | Lysyl oxidase [59] |
| CAF-targeting therapies | FAP-targeting agents | Fibroblast activation protein [59] | |
| Hypoxia | HIF pathway inhibitors | HIF-1α inhibitors | HIF-1α [6] |
| Vascular normalizing agents | Bevacizumab | VEGF-A [6] [59] | |
| Metabolic dysregulation | Metabolic modulators | Dichloroacetate | Pyruvate dehydrogenase kinase [62] |
Research Reagent Solutions
Table: Essential Reagents for TME Research
| Category | Reagent | Function/Application |
|---|---|---|
| Hypoxia Modeling | Hypoxia chambers/incubators | Maintain precise low-oxygen conditions for cell culture [6] |
| Pimonidazole HCl | Hypoxia marker for immunohistochemistry [6] | |
| HIF-1α antibodies | Detect hypoxia-inducible factor stabilization [6] | |
| Stromal Analysis | CAF markers (α-SMA, FAP) | Identify and quantify cancer-associated fibroblasts [59] |
| Collagen quantification assays | Measure ECM deposition and remodeling [59] [60] | |
| Matrix metalloproteinase assays | Evaluate ECM degradation capacity [60] | |
| Immune Monitoring | Multiplex IHC panels | Spatial analysis of immune cell distributions [64] |
| Cytokine profiling arrays | Measure immunosuppressive factors [61] | |
| MDSC isolation kits | Isolate and characterize myeloid-derived suppressor cells [61] | |
| Metabolic Analysis | Extracellular flux analyzers | Measure glycolytic and mitochondrial function [62] |
| Lactate assay kits | Quantify glycolytic activity [62] | |
| Metabolite detection kits | Profile TME nutrient availability and waste products [62] |
Signaling Pathways and Experimental Workflows
HIF-1α Signaling Pathway in Hypoxic TME
Experimental Workflow for Hypoxia Research
Key Technical Considerations
Model Selection: Choose TME models that faithfully recapitulate human stromal heterogeneity, which varies significantly between organ sites [59].
TME Monitoring: Incorporate real-time TME assessment tools such as spatial transcriptomics and single-cell sequencing to track dynamic changes during therapy [61] [64].
Combination Strategies: Design therapies that simultaneously target multiple TME components (e.g., ICIs + vascular normalizers + metabolic modulators) [61].
Treatment Timing: Computational models suggest optimal timing, such as administering chemotherapy 1 hour before radiation, can significantly improve outcomes [60].
Hypoxia Preconditioning: For cell-based therapies, preconditioning MSCs in hypoxic conditions (<48 hours) enhances their survival and regenerative potential without causing senescence [11].
Optimizing Drug Delivery to Hypoxic Regions
Frequently Asked Questions (FAQs)
1. What are the primary physiological barriers that limit drug delivery to hypoxic regions? Hypoxic regions within tumors are characterized by several physiological barriers that collectively impede effective drug delivery. These include:
- Abnormal Vasculature: Tumor blood vessels are tortuous, leaky, and poorly organized, leading to uneven blood flow and drug delivery [34] [65].
- Increased Interstitial Fluid Pressure (IFP): The combination of leaky blood vessels and a lack of functional lymphatic drainage causes fluid to accumulate in the tumor, raising the pressure inside the tissue. This high IFP acts as a barrier, opposing the inflow of therapeutics from the bloodstream [65].
- Dense Extracellular Matrix (ECM): The space between cells is filled with a dense network of proteins and other molecules that physically block the diffusion of drugs, especially larger nanoparticles [66] [67].
- Distance from Blood Vessels: Hypoxic cells are often located far from functional blood vessels (over 100-200 µm), a distance that exceeds the effective diffusion range of many drugs [34] [68].
2. How can I confirm that my drug is being selectively activated in hypoxic zones? Selective activation in hypoxia can be confirmed using several methodological approaches:
- Hypoxia-Activated Prodrugs (HAPs): Design or use prodrugs that are chemically reduced and activated only under low oxygen conditions. Examples include Tirapazamine and Quinone-based prodrugs like EO9 [69] [70].
- Hypoxia Markers: Co-administer or conjugate your drug to hypoxia-specific markers such as EF5 or Pimonidazole. These compounds form adducts with macromolecules in hypoxic cells, which can then be detected via immunohistochemistry on tumor sections, allowing you to correlate drug activity with hypoxic regions [68].
- In Vitro Validation: Always validate the hypoxia-selective cytotoxicity of your drug candidate using in vitro cell culture models under controlled normoxic (~18.6% O₂ at sea level) and hypoxic (typically 0.1-2% O₂) conditions [69] [56].
3. My nanoparticles are failing to penetrate deep into the tumor. What strategies can improve their distribution? Improving nanoparticle penetration requires overcoming both biological and physical barriers:
- Biomimetic Coating: Camouflage nanoparticles with cancer cell membranes (e.g., Lung Cancer Cell Membrane-mimicking Nanocarriers, LCCMNs) to improve their circulation time and enhance tumor-specific accumulation [67].
- Modulate Liposome Composition: Systematically optimize the lipid composition (e.g., ratios of phosphatidylcholine, sphingomyelin, cholesterol) and acyl chain structures to enhance membrane fluidity, stability, and tumor permeability [67].
- External Physical Stimulation: Employ Low-Intensity Pulsed Ultrasound (LIPUS). Optimized LIPUS parameters (e.g., 45% duty cycle, 0.5 W/cm² intensity) can create unidirectional fluid flow, significantly enhancing the penetration of both free drugs and liposomal nanoparticles into hypoxic regions [71] [72].
4. Are there non-invasive methods to measure tumor hypoxia in my experimental models? Yes, non-invasive imaging techniques are critical for longitudinal studies:
- PET Imaging with Hypoxia Tracers: Use positron emission tomography (PET) scanners with hypoxia-sensitive radiotracers such as 18F-FMISO or 18F-EF5. These compounds accumulate in viable hypoxic cells and allow for spatial mapping and quantitative analysis of hypoxia within tumors [68].
- Transparent Tumor Imaging (CLARITY): For ex-vivo 3D analysis, use tissue optical clearing methods like CLARITY on intact tumors. This technique enables high-resolution 3D visualization and quantification of drug distribution, apoptotic cells, and blood vessels in relation to hypoxic regions without physical sectioning [72].
Troubleshooting Guides
Problem: Inconsistent or Poor Drug Activation in Hypoxic Regions
| Potential Cause | Recommended Solution | Experimental Protocol to Verify |
|---|---|---|
| Insufficient hypoxia | Utilize 3D cell culture models (spheroids) to better mimic the physiological hypoxic gradient found in solid tumors. | Protocol: Spheroid Drug Response Assay.1. Generate spheroids from your target cancer cell line using low-attachment plates or the hanging drop method.2. Allow spheroids to grow to 400-500 µm in diameter to ensure a hypoxic core develops.3. Treat spheroids with your HAP and a hypoxia marker (e.g., EF5).4. Analyze spheroid sections for cell death (via TUNEL or Caspase-3 staining) and co-localize with the hypoxia marker signal to confirm selective killing in the hypoxic core [66]. |
| Rapid drug clearance | Reformulate the drug using nanocarriers (e.g., liposomes, polymeric NPs) to improve pharmacokinetics and enhance the EPR (Enhanced Permeability and Retention) effect. | Protocol: Pharmacokinetic (PK) and Biodistribution Study.1. Administer your drug (free or nano-formulated) to tumor-bearing mice.2. Collect blood and tissue samples (tumor, liver, kidney, spleen) at multiple time points.3. Use HPLC-MS or fluorescence imaging to quantify drug concentration in each sample.4. Calculate key PK parameters (half-life, AUC) and determine the tumor-to-muscle ratio to assess targeted accumulation [67]. |
| Off-target activation | Ensure your prodrug design leverages hypoxia-specific bioreductive mechanisms, such as the one-electron reduction of nitroimidazoles or quinones, which is reversible in normoxic conditions. | Protocol: *In Vitro Hypoxia-Normoxia Cytotoxicity Screen.*1. Culture cells in specialized incubators that maintain precise O₂ control (e.g., 20% O₂ for normoxia, 1% O₂ for hypoxia).2. Treat cells with a range of drug concentrations under both conditions for 24-72 hours.3. Assess cell viability using an MTT or CellTiter-Glo assay.4. Calculate the Hypoxic Cytotoxicity Ratio (HCR): IC₅₀ (Normoxia) / IC₅₀ (Hypoxia). A successful HAP will have an HCR significantly greater than 1 [69]. |
| Potential Cause | Recommended Solution | Experimental Protocol to Verify |
|---|---|---|
| High Interstitial Fluid Pressure (IFP) | Implement vascular normalization strategies. Administer low-dose anti-angiogenic agents (e.g., anti-VEGF antibodies) to prune abnormal vessels and reduce IFP, thereby improving drug perfusion. | Protocol: IFP Measurement and Drug Uptake.1. Implant tumor models subcutaneously in mice.2. Treat a group with a vascular normalizing agent (e.g., DC101 antibody).3. Measure IFP in anesthetized mice using a specialized needle probe and pressure transducer system.4. Administer a fluorescently labeled drug or nanoparticle.5. Image tumors ex vivo to quantify and compare drug distribution and intensity between treated and control groups [65]. |
| Inefficient nanoparticle design | Develop biomimetic or size-tunable nanoparticles. Use the natural lipid coating technology to create cell-membrane camouflaged nanocarriers that evade the immune system and have enhanced tumor-homing capabilities. | Protocol: Evaluating Nanoparticle Penetration.1. Prepare nanoparticles loaded with a fluorescent dye (e.g., Rhodamine) with optimized lipid composition.2. Treat tumor-bearing mice and harvest tumors.3. Use the CLARITY tissue clearing method on intact tumors to render them transparent.4. Image the entire tumor using confocal or light-sheet microscopy.5. Perform 3D analysis to measure the distance of nanoparticle signals from the nearest blood vessel, quantifying penetration into hypoxic, vessel-distant areas [67] [72]. |
| Physical penetration barriers | Integrate external physical methods to enhance delivery. Apply Low-Intensity Pulsed Ultrasound (LIPUS) to induce unidirectional fluid flow and sonoporation, mechanically pushing drugs deeper into the tumor tissue. | Protocol: LIPUS-Assisted Drug Delivery.1. Systemically administer the therapeutic agent to your animal model.2. Apply LIPUS directly to the tumor region using optimized parameters: Duty Cycle (DC): 45%, Spatial-peak temporal-average intensity (Ispta): 0.5 W/cm², for a duration of 5-10 minutes.3. Ensure proper coupling using an ultrasound gel.4. Quantify the enhancement by comparing drug penetration depth and anti-tumor efficacy (e.g., tumor growth inhibition, apoptosis) with a non-LIPUS control group [71] [72]. |
Quantitative Data for Experimental Planning
Table 1: Optimized Parameters for LIPUS-Enhanced Drug Delivery
| Parameter | Optimal Value | Experimental Impact | Citation |
|---|---|---|---|
| Duty Cycle (DC) | 45% | More significant effect on drug penetration and efficacy than intensity alone. | [72] |
| Spatial-peak temporal-average intensity (Iₛₚₜₐ) | 0.5 W/cm² | Efficacy saturated at values above this intensity under a 45% DC. | [72] |
| Liposome Penetration Enhancement | ~1.8-fold increase | LIPUS improved the penetration depth of liposomal nanoparticles into hypoxic regions. | [71] [72] |
| Therapeutic Outcome | ~5-fold increase in apoptosis | LIPUS-assisted chemotherapy resulted in a fivefold increase in apoptotic cancer cell death. | [72] |
Table 2: Key Characteristics of Hypoxia-Activated Prodrug (HAP) Strategies
| Strategy | Mechanism of Activation | Key Challenge | Citation |
|---|---|---|---|
| Nitroimidazole-based HAPs | One-electron reduction in hypoxia forms cytotoxic radicals; reaction is reversed by O₂. | Coupling between drug activation and dynamic oxygen consumption by viable cells. | [69] [70] |
| Quinone-based HAPs (e.g., EO9, RH1) | Enzymatic reduction (by NQO1 or one-electron reductases) triggers aziridine ring opening for DNA alkylation. | Efficacy depends on the expression levels of specific reductase enzymes in the tumor. | [69] |
| Bioreductive Nanoparticles | Hypoxia-responsive linkers in nanocarriers degrade in low O₂, releasing the encapsulated drug. | Ensuring the nanoparticle itself can penetrate the hypoxic region before activation. | [66] [67] |
Signaling Pathways and Experimental Workflows
Diagram 1: The HIF-1 Signaling Pathway in Tumor Hypoxia and Its Impact on Therapy. This diagram illustrates how low oxygen (hypoxia) leads to the stabilization of the HIF-1α transcription factor, which drives the expression of genes that promote abnormal vasculature, drug resistance, and metabolic changes, ultimately creating barriers to effective treatment [34].
Diagram 2: Integrated Workflow for Evaluating Hypoxia-Targeted Drug Delivery. This workflow outlines key steps from nanoparticle design and in vitro testing to in vivo evaluation, incorporating critical techniques like hypoxia imaging and LIPUS application for enhancing and assessing drug delivery efficacy [66] [72].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Hypoxia Drug Delivery Research
| Item | Function/Application | Key Consideration |
|---|---|---|
| Hypoxia-Activated Prodrugs (HAPs) | Provide selective cytotoxicity in low-oxygen environments. Tirapazamine and Quinone-based agents (e.g., EO9) are classic examples. | Validate the Hypoxic Cytotoxicity Ratio (HCR) in your specific cell models, as efficacy is dependent on the local reductase enzyme profile [69] [70]. |
| Hypoxia Markers (EF5, Pimonidazole) | Enable detection and visualization of hypoxic regions in cells and tissues via immunohistochemistry or flow cytometry. | Crucial for correlating drug activity with hypoxia in experimental models. EF5 can also be used for non-invasive PET imaging [68]. |
| Biomimetic Lipid Components | Serve as building blocks for constructing nanocarriers (e.g., LCCMNs) with enhanced biocompatibility and tumor-targeting properties. | Systematic optimization of lipid ratios (e.g., PC, SM, Chol) and acyl chain structures is required to maximize circulation time and tumor penetration [67]. |
| LIPUS Device | A non-invasive instrument that applies specific ultrasound parameters to enhance drug penetration physically. | Parameter optimization is critical. Key settings include Duty Cycle (45%) and Intensity (0.5 W/cm²) for effective, safe treatment [71] [72]. |
| Tissue Optical Clearing Reagents (CLARITY) | A set of chemicals used to render tissues transparent for high-resolution 3D imaging of drug distribution, vasculature, and hypoxia. | Allows for quantitative analysis of drug penetration relative to blood vessels in an intact tumor without physical sectioning artifacts [72]. |
Mitigating Immunosuppressive Effects of Chronic Hypoxia
Chronic hypoxia, a defining hallmark of the solid tumor microenvironment (TME), drives immunosuppression and is a major cause of resistance to cancer immunotherapy [73] [34]. This phenomenon results from an imbalance between the high oxygen demand of rapidly proliferating cancer cells and the inadequate supply from abnormal tumor vasculature [73]. This technical resource details the mechanisms by which hypoxia subverts anti-tumor immunity and provides actionable experimental strategies to counteract these effects, supporting the broader research goal of improving cell survival and function in hypoxic environments.
FAQ: Key Mechanisms of Hypoxia-Induced Immunosuppression
Q1: What are the primary mechanisms through which chronic hypoxia creates an immunosuppressive tumor microenvironment?
Chronic hypoxia fosters immunosuppression through several interconnected mechanisms, masterfully regulated by the stabilization of Hypoxia-Inducible Factor-1α (HIF-1α) [73] [34].
- Polarization of Macrophages: Hypoxia reprograms tumor-associated macrophages (TAMs) towards a pro-tumorigenic M2 phenotype. This is driven by factors like lactate and succinate released by hypoxic tumor cells, which activate the HIF-1α, Hedgehog, and mTOR signaling pathways in macrophages. M2 macrophages suppress T-cell function and promote tissue repair and angiogenesis [73].
- T cell Exhaustion and Dysfunction: The hypoxic TME impairs the infiltration and cytotoxic function of CD8+ T cells while promoting their exhaustion. It also enhances the accumulation of immunosuppressive regulatory T cells (Tregs) [73] [74].
- Metabolite Accumulation: Hypoxia leads to the buildup of immunosuppressive metabolites like adenosine and lactate, which directly inhibit effector T cell function and foster acidosis [74].
- Upregulation of Immune Checkpoints: Hypoxia can induce the expression of immune checkpoint molecules like PD-L1 on tumor and immune cells, further driving T cell exhaustion [73].
FAQ: Experimental Models & Reagents
Q2: How can I accurately model chronic hypoxia in vitro, and what key reagents are essential?
Modeling chronic hypoxia requires precise control of oxygen levels and the use of specific biochemical tools.
- Physiological Hypoxia Chambers: For the most accurate simulation, use a tri-gas cell culture incubator that controls O₂, CO₂, and N₂. The "true" normoxic O₂ concentration in a standard humidified (37°C, 5% CO₂) incubator at sea level is approximately 18.6%, not the 20.9% found in room air [56]. For chronic hypoxia, researchers often use conditions between 0.5% to 5% O₂ for 24 hours to several days [75].
- Hypoxia Mimetics: These chemicals inhibit HIF-1α degradation, mimicking hypoxic conditions under normal oxygen levels. They are useful but do not replicate all aspects of true hypoxia.
Table 1: Essential Research Reagents for Hypoxia and HIF Research
| Reagent / Tool | Function / Target | Key Application Notes |
|---|---|---|
| Deferoxamine (DFO) | HIF-1α stabilizer (Iron chelator) | Mimics hypoxia; suppresses p53-mediated apoptosis [76]. |
| Cobalt Chloride (CoCl₂) | HIF-1α/HIF-2α stabilizer | Common positive control for HIF induction in Western blots [75]. |
| DMOG | PHD inhibitor (HIF stabilizer) | Used to probe HIF-dependent signaling [75]. |
| HIF-1 Alpha Antibody | Detects HIF-1α protein | Expect bands at ~110-130 kDa due to PTMs; rapid sample processing is critical [75]. |
| HIF-2 Alpha/EPAS1 Antibody | Specific detection of HIF-2α | Crucial for studying chronic hypoxia; should not cross-react with HIF-1α [75]. |
| Nuclear Extraction Kit | Fractionates cellular components | Recommended for detecting active, nuclear-localized HIF [75]. |
Troubleshooting Guide: HIF Detection and Analysis
Q3: I cannot detect HIF-1α in my Western blots, even from cells subjected to hypoxia or treated with CoCl₂. What could be wrong?
HIF-1α is notoriously labile, and its detection requires optimized protocols. Below is a workflow diagram summarizing the critical steps for successful detection, followed by a detailed troubleshooting table.
Table 2: Troubleshooting HIF Detection in Western Blot
| Problem | Potential Cause | Solution |
|---|---|---|
| Weak or no signal | HIF-1α degradation under normoxia; even overexpressed HIF-1α is degraded in oxygen [75]. | Scrape cells directly into lysis buffer immediately after hypoxia exposure. Use proteasome inhibitors (e.g., MG132) in lysis buffer. |
| Non-specific bands | Protein degradation. | Optimize lysis speed and include protease inhibitors. Expect the main band at 110-130 kDa; lower bands may be degradation products [75]. |
| High background | Antibody concentration too high or non-specific binding. | Titrate the primary antibody. Use a HIF-1α-specific antibody that does not cross-react with HIF-2α [75]. |
| Inconsistent results | Analyzing whole cell lysates. | Prepare nuclear and cytoplasmic fractions. HIF-1α translocates to the nucleus upon stabilization; fractionation enriches the target protein [75]. Use Lamin B1 or Histone H3 as a nuclear loading control. |
Advanced Techniques: Targeting Hypoxia to Boost Immunity
Q4: What are some advanced experimental strategies to mitigate hypoxia and its immunosuppressive effects?
Emerging approaches focus on normalizing the tumor vasculature, directly targeting HIF pathways, and using novel physical methods.
- Tumor Vascular Normalization: Using low-dose anti-angiogenic agents (e.g., Bevacizumab) can "normalize" the chaotic tumor vasculature, improving perfusion, alleviating hypoxia, and enhancing immune cell infiltration [74]. This reduces immunosuppressive factors like VEGF, TGF-β1, and IL-10 [74].
- Sononeoperfusion: A novel physical method where low mechanical index ultrasound-stimulated microbubble cavitation (USMC) is used to enhance tumor blood perfusion. This "sononeoperfusion" effect ameliorates hypoxia, downregulates HIF-1α and VEGF, and reduces the accumulation of Tregs, MDSCs, and M2-TAMs. It synergizes with anti-PD-L1 therapy to promote CD8+ T cell infiltration and function [74].
- Hypoxia-Activated Prodrugs (HAPs) and HIF Inhibitors: These therapeutic agents are designed to be activated specifically in hypoxic regions or to directly inhibit the HIF signaling pathway, thereby disrupting the primary mechanism of hypoxia adaptation [73] [34].
The following diagram illustrates the core hypoxia signaling pathway and the points where experimental interventions can take effect.
Quantitative Data & Experimental Parameters
Q5: What quantitative data and specific parameters are critical for designing experiments on chronic hypoxia?
Precise control and measurement are paramount. The following table consolidates key quantitative data from the literature.
Table 3: Key Quantitative Data and Experimental Parameters in Hypoxia Research
| Parameter | Typical Range / Value | Context and Significance |
|---|---|---|
| Physiological Normoxia (in vitro) | ~18.6% O₂ (at sea level) | Actual O₂ in standard humidified (37°C, 5% CO₂) incubators [56]. |
| Hypoxia (in vitro) | 0.1% - 5% O₂ | Common range for experimental hypoxia; <0.1% is often termed "anoxia" [75]. |
| Chronic Hypoxia Duration | 24 hours - several days | Used to model long-term adaptation [75]. |
| HIF-1α vs. HIF-2α Activity | HIF-1α: active 2-24h (<0.1% O₂)\nHIF-2α: active up to 2-3 days (<5% O₂) | HIF-1α drives the initial response; HIF-2α sustains the response during chronic hypoxia [75]. |
| Oxygen Enhancement Ratio (OER) | 1 - 3 | Ratio of radiation dose needed for equal effect under hypoxia vs. normoxia. Decreases with high-LET radiation [55]. |
| Hypoxic Tumor pO₂ | <10 mmHg | Measured in patient tumors (e.g., pancreatic, breast, cervical cancer); indicates severe hypoxia [34]. |
| Sononeoperfusion (USMC) Parameters | MI: 0.29, PNP: 0.43 MPa\nFrequency: 3 MHz, Time: 10 min | Example parameters for effective perfusion enhancement and hypoxia alleviation in mouse models [74]. |
Troubleshooting Guides and FAQs
FAQ 1: Why are my cancer models showing increased resistance to therapy under hypoxic conditions?
Hypoxia within the tumor microenvironment is a major contributor to therapy resistance. The lack of oxygen leads to several adaptive changes in cancer cells:
- Molecular Adaptation: Hypoxia stabilizes Hypoxia-Inducible Factors (HIFs), which regulate over 1,000 genes responsible for cancer progression, metabolic reprogramming, and therapy resistance [77].
- Suppressed Apoptosis: Under hypoxic conditions, the stabilization of the p53 protein is reversed. This leads to decreased levels of downstream pro-apoptotic proteins like Bax, Bid, and Puma, suppressing the mitochondrial apoptotic pathway and making cells resistant to drugs like cisplatin and doxorubicin [76].
- Metabolic Shift: Cells switch their energy production from oxygen-dependent pathways to glycolysis for survival. The enzyme PDK1, which facilitates this switch, is more efficiently produced under hypoxia due to changes in gene regulation [78].
FAQ 2: How can I effectively model hypoxic conditions in my in vitro experiments for therapy testing?
Choosing the right model is critical for generating physiologically relevant data. Below is a comparison of common methods.
| Method | Mechanism | Best For | Key Considerations |
|---|---|---|---|
| Chemical Hypoxia (e.g., Deferoxamine) | Iron chelator that mimics hypoxia by inhibiting HIF prolyl hydroxylases [76]. | High-throughput screening; acute hypoxia studies. | Concentration and exposure time must be optimized to avoid off-target effects. |
| Low-O2 Incubators | Physically maintains a controlled gas environment (e.g., 1% O2) [77]. | Long-term chronic hypoxia studies; most physiologically direct method. | Requires specialized equipment; recovery of cells for analysis can introduce artifacts. |
| Hypobaric Chambers | Reduces partial pressure of oxygen (pO2) to simulate high-altitude conditions [79]. | Studying hypobaric hypoxia (e.g., for altitude-related research). | Less common for standard tumor biology; equipment can be bulky. |
FAQ 3: What are the key mechanisms by which combination therapies overcome hypoxia-induced resistance?
Combination strategies target the tumor through multiple, synergistic mechanisms:
- Spatial Cooperation and Radiation Sensitization: In chemoradiotherapy (CRT), chemotherapy can sensitize cancer cells to radiation through several interactions, including inhibiting cellular repair of radiation damage and eliminating hypoxic cells [80].
- Immunogenic Cell Death (ICD): Both radiotherapy and certain chemotherapies can induce ICD. This process involves the release of damage-associated molecular patterns (DAMPs), which act as danger signals to activate dendritic cells and initiate a potent anti-tumor immune response [81].
- Targeting Hypoxia Signaling: Emerging research focuses on inhibiting key survival pathways under hypoxia. For example, targeting the kinase ULK1, which is essential for cell survival under hypoxia by regulating autophagy and organelle turnover, can enhance cell death in hypoxic tumor regions [82].
FAQ 4: My experimental results show high variance in cell death assays under hypoxia. What could be the cause?
Variability can arise from several sources related to hypoxia modeling:
- Inconsistent Hypoxic Exposure: Ensure the hypoxic environment (in incubators or chambers) is stable and well-calibrated. Frequent opening of the chamber can cause significant O2 fluctuations.
- Cell Line-Specific Responses: Different cancer cell lines have varying degrees of innate hypoxia tolerance. For instance, the aggressive MDA-MB-231 breast cancer line shows less significant reduction in proliferation under hypoxia compared to the MCF-7 line [77].
- Assay Timing: Hypoxia induces a complex sequence of adaptive responses. Measuring cell death too early may not capture full adaptation, while measuring too late may miss initial apoptotic waves. Data shows apoptotic activity (Caspase-3/7) is significantly increased in all breast cell lines after 5 days of hypoxia [77].
The following tables consolidate key quantitative findings from recent research on hypoxia and therapy responses.
Table 1: Impact of Long-Term Hypoxia (5 Days) on Breast Cell Lines [77]
| Cell Line | Malignancy | Change in Cell Number (Hypoxia vs. Normoxia) | Change in Metabolic Activity | Apoptotic Cells (% Increase) |
|---|---|---|---|---|
| MDA-MB-231 | High (Metastatic) | Not Significant | Not Significant | Significant (p < 0.01) |
| MCF-7 | Low (Adenocarcinoma) | Significant Decrease | Significant Decrease | Significant (p < 0.01) |
| MCF-10A | Non-Malignant | Significant Decrease | Significant Decrease | Significant (p < 0.01) |
Table 2: Key Molecular Changes in Breast Cell Lines Under Hypoxia [77]
| Cell Line | Vimentin (Mesenchymal Marker) | E-Cadherin (Epithelial Marker) | Extravasation Rate |
|---|---|---|---|
| MDA-MB-231 | Significant Increase | Low (No Significant Change) | Increased |
| MCF-7 | Low (No Significant Change) | Significant Decrease | Increased |
| MCF-10A | Significant Increase | Low (No Significant Change) | Increased |
| Note: Hypoxia increased the extravasation potential of all lines, which was reversed by HIF-1α knockdown. |
Experimental Protocols
Protocol 1: Assessing the Impact of Hypoxia on Chemotherapy-Induced Apoptosis
This protocol is adapted from studies on HCT116 colon carcinoma and other cell lines [76].
- Cell Preparation: Seed your cancer cell line of interest (e.g., HCT116) in multiple culture plates.
- Hypoxia Induction: Once cells adhere, place experimental groups in a hypoxic incubator (1% O2) or treat with a hypoxic mimetic like Deferoxamine (e.g., 100-200 µM). Maintain control groups in normoxia (21% O2).
- Chemotherapy Treatment: After 24-48 hours of pre-conditioning, add chemotherapeutic agents (e.g., Cisplatin, Doxorubicin) at relevant IC50 concentrations to both hypoxic and normoxic groups.
- Analysis (After 24-72h of drug exposure):
- Cell Death: Quantify dead cells by counting trypan-blue-positive cells in the supernatant or by measuring the SubG1 population via flow cytometry.
- Apoptotic Markers: Analyze key apoptotic markers by Western blotting: Cytochrome c release from mitochondria, Caspase-3 cleavage, and expression levels of p53 and pro-apoptotic proteins (Bax, Bid, Puma).
Protocol 2: Evaluating Combination Therapy Efficacy in a 3D Microvascular Extravasation Model
This protocol is based on a microfluidic model used to study breast cancer cell lines [77].
- Device Preparation: Use a microfluidic chip to create a 3D microvascular network. Seed human umbilical vein endothelial cells (HUVECs) in the central channel and allow them to form perfusable vessel-like structures over 4-7 days.
- Cell Pre-conditioning: Pre-condition your cancer cells (e.g., MDA-MB-231, MCF-7) under hypoxic (1% O2) or normoxic conditions for 72 hours. For inhibition studies, transfert cells with HIF-1α siRNA prior to hypoxia exposure.
- Extravasation Assay: Introduce the pre-conditioned cancer cells into the microvascular network. Allow the cells to circulate, adhere to the endothelium, and extravasate over 24-48 hours.
- Fixation and Staining: Fix the device and stain for F-actin (e.g., Phalloidin) and nuclei (DAPI) to visualize the different stages of transmigration.
- Quantification: Image the entire network using confocal microscopy. Quantify the extravasation rate by calculating the percentage of total added cells that have fully migrated through the endothelial barrier.
Signaling Pathways and Experimental Workflows
Hypoxia-Induced Therapy Resistance Pathway
Therapy Efficacy Testing Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Hypoxia and Combination Therapy Research
| Reagent / Tool | Function / Mechanism | Example Application |
|---|---|---|
| Deferoxamine (DFO) | Hypoxia mimetic; iron chelator that stabilizes HIF-1α by inhibiting prolyl hydroxylases [76]. | Inducing hypoxic conditions in normoxic cell cultures to study HIF signaling. |
| HIF-1α siRNA | Silences HIF-1α gene expression to inhibit the master regulator of hypoxic response [77]. | Validating the specific role of HIF-1α in hypoxia-induced therapy resistance or extravasation. |
| ULK1 Inhibitor | Blocks ULK1 kinase activity, which is essential for autophagy and cell survival under hypoxia [82]. | Testing combination strategies to target hypoxic cell survival pathways. |
| Anti-Galectin-1 Antibody | Neutralizes Galectin-1, an immunosuppressive protein upregulated by hypoxia and radiation [82]. | Combining with radiotherapy and immunotherapy to enhance T-cell infiltration and tumor killing. |
| 3D Microfluidic Chips | Provides a physiologically relevant in vitro model with human cell-derived microvessels [77]. | Studying the critical steps of metastasis, such as extravasation, in a controlled microenvironment. |
Timing and Dosing Considerations for Hypoxia-Targeting Agents
Frequently Asked Questions (FAQs)
General Principles
What makes timing and dosing particularly challenging for hypoxia-targeting agents? The primary challenge is the spatial and temporal heterogeneity of tumor hypoxia [83]. Hypoxic regions are not static; they can experience acute (cycling) or chronic hypoxia, and their location can shift over time and in response to treatment [84] [83]. Furthermore, the abnormal tumor vasculature impedes uniform drug delivery, making it difficult to achieve effective concentrations in the target regions [85]. Dosing must balance efficacy with toxicity, especially for agents like nitroimidazoles, where dose-limiting toxicities such as peripheral neuropathy have hampered clinical success [84].
How can I determine if my in vitro hypoxia model is clinically relevant? Clinical data suggests that the overall median pO2 in many solid tumors is around 10 mm Hg, with approximately 20-30% of the tumor volume having a pO2 of less than 2.5 mm Hg [84]. The majority of hypoxic cells often experience mild to moderate hypoxia (0.5% to 10% pO2) rather than severe hypoxia (approx. 0.1% pO2) [84]. When designing experiments, using a range of oxygen concentrations within these clinically observed levels, rather than only near-anoxia (0.1%), will yield more translatable results.
Agent-Specific Queries
For Hypoxic Cell Radiosensitizers like Nimorazole, when should it be administered relative to radiation? Administration must be timed so that the drug is present within the tumor at the time of radiation delivery [84]. The mechanism of action involves the drug undergoing bioreductive activation under hypoxic conditions, creating reactive intermediates that "fix" the DNA damage caused by radiation. If the drug is not present at the moment of irradiation, this radiosensitization effect is lost.
What is the key dosing consideration for Hypoxic Cytotoxins like Tirapazamine? Tirapazamine is a prodrug activated under hypoxic conditions to form a cytotoxic species [84]. A critical consideration is patient stratification. Clinical trials failed to show an overall benefit, but a subset analysis revealed that patients with p16-negative oropharyngeal cancer and those with hypoxic tumors confirmed by 18F-MISO-PET imaging showed a trend toward improved outcomes [84]. This underscores the importance of using biomarkers to identify patients with hypoxic tumors who are most likely to respond.
For Oxygen Consumption Rate (OCR) Reducers like Metformin, what are the timing implications? Agents that reduce a tumor's oxygen consumption rate (e.g., Metformin, Nelfinavir) aim to re-oxygenate the tumor microenvironment [84]. The dosing schedule should be designed to ensure a sustained reduction in OCR at the time of other treatments, such as radiotherapy. Preclinical models indicate that even a 30% decrease in O2 consumption can significantly reduce the hypoxic fraction [84]. The therapeutic effect comes from improved oxygenation, not a direct cytotoxic effect, so the agent must be dosed to maintain this physiological change during the entire course of concomitant therapy.
How does Hyperthermia (HT) influence timing for combination therapies? Mild hyperthermia (39–43°C) can improve tumor oxygenation by increasing blood flow and decreasing oxygen consumption [85]. Studies show that applying HT before radiation yields a greater anti-tumor effect than applying it after, because the increased oxygenation sensitizes the cells to radiation [85]. Recent clinical data also suggests that a short time interval between HT and radiation results in better patient outcomes [85].
Troubleshooting Common Experimental Issues
Issue: Inconsistent results with a hypoxia-activated prodrug in a mouse model.
- Potential Cause: Inadequate characterization of the hypoxic fraction in your model. The level and distribution of hypoxia can vary significantly between tumor models and even within the same model over time.
- Solution:
- Stratify your animals: Use a hypoxia imaging biomarker like 18F-FAZA or 18F-MISO PET to group animals based on their level of tumor hypoxia before treatment [84] [83].
- Validate hypoxia ex vivo: After sacrifice, analyze tumor sections using immunohistochemistry for exogenous (e.g., pimonidazole adducts) or endogenous (e.g., CA-IX, HIF-1α) hypoxia markers to confirm the presence of hypoxia in the regions of interest.
Issue: A drug that reduces OCR works in some cell lines but not in vivo.
- Potential Cause: The in vivo tumor microenvironment may have compensating factors not present in 2D culture, such as interactions with stromal cells or different metabolic dependencies.
- Solution:
- Confirm target engagement: Verify that your drug is indeed hitting its intended target (e.g., mitochondrial complex I) in the in vivo setting.
- Measure functional outcome: Directly measure the change in tumor oxygenation following drug administration. This can be done using oxygen electrodes or, non-invasively, with BOLD-MRI [83]. A positive change in oxygenation confirms the drug is having the desired physiological effect.
Issue: Failure to replicate a published radiosensitization protocol using carbogen breathing.
- Potential Cause: Inconsistent timing and duration of gas breathing relative to irradiation. The effect of carbogen is transient and requires precise synchronization.
- Solution: Standardize the breathing protocol. Pre-clinical and clinical studies (like the ARCON trials) specify that animals or patients should breathe the gas for a defined period (e.g., 10-30 minutes) before and then throughout the duration of the radiation session to ensure adequate oxygen delivery at the time of irradiation [85].
Experimental Protocols & Data Tables
Protocol 1: Assessing the Timing for an OCR-Reducing Agent with Radiotherapy
Objective: To determine the optimal pre-treatment window for administering an OCR-reducing agent (e.g., Metformin) prior to focal irradiation.
Materials:
- Orthotopic or subcutaneous tumor model.
- OCR-reducing agent (e.g., Metformin, dissolved in saline).
- Irradiator.
- Hypoxia marker (e.g., Pimonidazole HCl).
Method:
- Grouping: Randomize tumor-bearing mice into several groups (n≥5):
- Group 1: Vehicle control.
- Group 2: Radiation alone.
- Group 3: Agent administered 1 hour before radiation.
- Group 4: Agent administered 4 hours before radiation.
- Group 5: Agent administered 24 hours before radiation.
- Hypoxia Labeling: Inject pimonidazole (60 mg/kg, i.p.) 1 hour before sacrifice to label hypoxic regions present at the time of irradiation.
- Treatment:
- Administer the OCR-reducing agent at the specified time points before a single dose of radiation (e.g., 5-10 Gy).
- Analysis:
- Sacrifice animals 24 hours post-irradiation.
- Harvest tumors, fix, and section.
- Perform immunohistochemistry for pimonidazole adducts and a DNA double-strand break marker (e.g., γH2AX).
- Quantify the hypoxic fraction (pimonidazole-positive area) and the number of γH2AX foci in both normoxic (pimonidazole-negative) and hypoxic (pimonidazole-positive) regions.
Expected Outcome: The optimal pre-treatment time will be the one that shows the greatest reduction in pimonidazole staining (indicating re-oxygenation) and the highest level of DNA damage within the previously hypoxic regions.
Protocol 2: Validating Hypoxia-Agent Delivery with Immunohistochemistry
Objective: To confirm that a systemically administered agent reaches its hypoxic target.
Materials:
- Hypoxia-activated prodrug or fluorescently-labeled hypoxia-targeting molecule.
- Pimonidazole HCl.
- Antibodies for pimonidazole and the drug (or its tag).
Method:
- Co-injection: Administer the hypoxia-targeting agent and pimonidazole simultaneously to tumor-bearing mice.
- Tumor Harvest: Sacrifice animals at a predetermined time post-injection (based on the agent's pharmacokinetics).
- Immunofluorescence: Process tumor sections for double-labeling immunofluorescence using antibodies against pimonidazole and the agent.
- Imaging & Analysis: Acquire high-resolution confocal images. Quantify the co-localization coefficient (e.g., Pearson's correlation) between the pimonidazole signal and the agent's signal.
Expected Outcome: Successful delivery and activation/retention will be demonstrated by a high degree of co-localization between the agent and the pimonidazole hypoxia marker.
Quantitative Data Tables
Table 1: Dosing and Timing of Select Hypoxia-Targeting Agents in Preclinical Studies
| Agent Class | Example Agent | Typical Preclinical Dosing | Critical Timing Consideration | Key Rationale |
|---|---|---|---|---|
| OCR Reducer | Metformin | 50-300 mg/kg, daily oral gavage [84] | Administer 1-4 hours before radiation [84] | Allows time for reduced oxygen consumption to increase tumor pO2, sensitizing hypoxic cells. |
| Hypoxic Cytotoxin | Tirapazamine | 10-30 mg/kg, i.p., single or multiple doses [84] | Administer 30-60 mins before radiation or chemo [84] | Ensures active cytotoxic species is present during/after radiation-induced DNA damage. |
| PI3K/HIF Inhibitor | Nelfinavir | 50-100 mg/kg, oral, daily [84] | Chronic dosing (days) to achieve stable inhibition [84] | Targets upstream signaling (PI3K/Akt) that supports HIF activity and hypoxic survival. |
| Adjuvant: Mild Hyperthermia | -- | 40.5-41.5°C for 30-60 mins [85] | Apply immediately before radiation (<1 hour) [85] | Maximizes radiosensitization from HT-induced increased blood flow and reduced oxygen consumption. |
Table 2: Clinical Evidence for Timing and Patient Stratification
| Trial / Agent | Cancer Type | Dosing & Timing Strategy | Outcome & Key Insight |
|---|---|---|---|
| HeadSTART (Phase III) Tirapazamine [84] | Advanced HNSCC | Tirapazamine + Cisplatin + Radiotherapy | No overall benefit. But a subset of p16-negative patients and those with MISO-PET hypoxic tumors showed improved locoregional control [84]. |
| ARCON Trials [85] | Laryngeal and Bladder Cancer | Accelerated Radiotherapy with Carbogen and Nicotinamide | Improved patient survival and outcome. Demonstrates the efficacy of targeting both acute (via Nicotinamide) and chronic (via Carbogen) hypoxia. |
| Metformin Analysis (Retrospective) [84] | Localized Prostate Cancer | Patients on metformin during radiotherapy | Reduction in biochemical relapse. Correlative data supporting the hypothesis that metformin improves radiotherapy response, potentially via reduced OCR. |
Signaling Pathways & Experimental Workflows
Diagram 1: Molecular Pathways of Hypoxia and Therapeutic Intervention Points
This diagram illustrates the core hypoxia response pathway and the points at which different classes of therapeutic agents intervene.
Diagram 2: Experimental Workflow for Dosing and Timing Optimization
This workflow outlines a systematic approach to determining the optimal dosing schedule and timing for a hypoxia-targeting agent in a preclinical setting.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Hypoxia-Timing Research
| Reagent / Material | Function & Application in Timing Studies |
|---|---|
| Pimonidazole HCl | Exogenous hypoxia marker. Injected at specific times before sacrifice. Its adducts form in hypoxic cells (pO2 < 10 mm Hg) and are detected by IHC, providing a snapshot of hypoxia at the time of injection [84]. |
| 18F-FAZA / 18F-MISO PET Tracers | Non-invasive imaging biomarkers for hypoxia. Used to monitor changes in hypoxic volume over time and in response to treatment. Critical for patient/animal stratification and for assessing the re-oxygenation effect of OCR reducers [84] [83]. |
| Hypoxia Gene Signatures (e.g., Buffa, Ragnum) | Gene expression-based hypoxia quantification. Pan-cancer analyses suggest the Buffa/mean and Ragnum/interquartile mean signatures are among the most promising for patient stratification in clinical trials [86]. Useful for classifying tumors without fresh tracer injection. |
| Anti-CA-IX / Anti-HIF-1α Antibodies | Detect endogenous hypoxia markers via IHC. CA-IX is a stable, hypoxia-induced protein useful for labeling chronically hypoxic regions. Provides complementary data to pimonidazole [83]. |
| Oxygen Microelectrodes | Direct, quantitative measurement of tissue oxygen tension (pO2). Provides a gold-standard validation for hypoxia markers and the physiological impact of OCR-reducing agents, though it is an invasive technique [84]. |
| Carbogen Gas (95% O2, 5% CO2) | Used to increase oxygen delivery and combat diffusion-limited chronic hypoxia. Timing is critical: must be breathed before and during radiation for effective radiosensitization [85]. |
| Nicotinamide | A vitamin B3 derivative. Thought to reduce acute (perfusion-limited) hypoxia by inhibiting transient vascular shutdown. Used in combination with carbogen in the ARCON protocol [85]. |
Assessment Models and Efficacy Evaluation
Researchers can induce hypoxia in vitro through physical systems that control the ambient environment or chemical agents that mimic hypoxic signaling. The choice of method depends on the research goals, required level of hypoxia, and experimental constraints.
Table 1: Comparison of Major Hypoxia Induction Methods
| Method | Mechanism of Action | Typical Oxygen Levels | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Chamber Systems | Physical control of gas composition in a sealed environment | Typically 0.1-5% O₂ [87] | • Creates true oxygen deprivation [87]• Compatible with various cell types• Allows chronic exposure studies | • Long equilibration times (~24 hours) [87]• Restricted real-time imaging [87]• Imposes uniform hypoxia, lacking physiological gradients [87] |
| Chemical Inducers (CoCl₂) | Mimics hypoxia by stabilizing HIF-1α and HIF-2α [87] | Does not alter physical O₂ environment [87] | • Fast induction of hypoxic response [87]• Accessible to labs without specialized equipment [87]• Compatible with real-time imaging | • Produces pseudohypoxia rather than true O₂ deprivation [87]• Does not fully replicate hypoxic transcriptional program [87]• Potential chemical toxicity |
| Chemical Inducers (DMOG) | Competitive inhibitor of prolyl hydroxylases [87] | Does not alter physical O₂ environment [87] | • Fast induction [87]• Accessible technique [87] | • Generates pseudohypoxia [87]• Chemical-specific side effects• Limited physiological relevance |
| Self-Generation Systems | Cellular oxygen consumption creates natural gradients [87] | Can reach 0.2% O₂ in core areas [87] | • Creates physiological O₂ gradients [87]• Enables real-time hypoxia monitoring [87]• Rapid environmental transitions | • Requires specialized equipment [87]• More complex setup [87]• Limited commercial availability |
Frequently Asked Questions and Troubleshooting
Chamber System Troubleshooting
Problem: Slow equilibration time in hypoxia chamber
- Solution: Pre-equilibrate culture media in the hypoxic environment for 4-6 hours before adding to cells. Ensure chamber seals properly and check gas cylinder pressures. Use real-time oxygen sensors to verify internal conditions [87].
Problem: Inconsistent hypoxia levels across chamber
- Solution: Avoid overcrowding of plates and ensure adequate space between culture vessels for gas circulation. Use fans in larger chambers and consider a smaller chamber for more uniform conditions [87].
Problem: Difficulty performing real-time imaging during hypoxia
- Solution: Consider alternative systems that allow hypoxia maintenance during imaging, such as microfluidic devices with gas control or self-generation systems that don't require sealed chambers [87] [88].
Problem: Cell death under chronic hypoxia
- Solution: Gradually acclimate cells to low oxygen conditions by stepwise reduction of O₂ levels. Optimize media composition and consider using specialized hypoxic media formulations. Reduce serum concentration if necessary.
Chemical Inducer Troubleshooting
Problem: Inconsistent HIF-1α stabilization with CoCl₂
- Solution: Prepare fresh CoCl₂ solutions for each experiment and optimize concentration (typically 100-300 μM) and treatment duration (4-6 hours). Confirm hypoxic response using positive controls [89].
Problem: Chemical toxicity observed with DMOG
- Solution: Titrate concentration (common range: 0.5-1 mM) and exposure time. Include viability assays and consider alternative inducers like desferrioxamine (DFO) for sensitive cell types [89].
Problem: Lack of expected hypoxic gene expression
- Solution: Verify that your chemical inducer is functioning with positive control antibodies for HIF-1α. Ensure chemical inducers are not expired and are properly stored. Remember that chemical inducers create pseudohypoxia and may not replicate the full hypoxic transcriptome [87] [89].
Problem: Difficulty detecting HIF-1α by Western blot
- Solution: HIF-1α degrades rapidly upon oxygen exposure. Prepare lysates quickly using pre-chilled buffers in a hypoxic environment. Use proteasome inhibitors (MG132) in lysis buffer. Analyze nuclear fractions rather than whole cell lysates for better detection [89].
General Experimental Considerations
How do I validate successful hypoxia induction?
- Monitor HIF-1α stabilization via Western blot (expect bands at 110-130 kDa) [89]
- Measure expression of hypoxic target genes (VEGF, CA9, GLUT1) via qPCR [89]
- Use chemical oxygen sensors or probe-based systems for physical hypoxia confirmation [87]
What oxygen concentration should I use?
- Mild hypoxia: 1-5% O₂
- Severe hypoxia: 0.1-1% O₂
- Anoxia: <0.1% O₂
- Choose based on your biological question and cell type [90]
How long should hypoxia exposure be?
- Acute hypoxia: 2-24 hours (typically studied with HIF-1α) [89]
- Chronic hypoxia: 24+ hours (typically studied with HIF-2α) [89]
- The duration affects which HIF-α isoforms are active and downstream pathways
Detailed Experimental Protocols
Protocol: Self-Generation of Hypoxia with Real-Time Monitoring
This protocol enables creation of physiological oxygen gradients through cellular oxygen consumption, allowing real-time monitoring of hypoxia development [87].
Table 2: Key Reagents for Hypoxia Self-Generation System
| Reagent/Equipment | Specification | Function |
|---|---|---|
| Phosphorescent film (PtTFPP/PFPE) | Spin-coated on coverslips [87] | Real-time oxygen sensing via phosphorescence quenching [87] |
| Acrylic plug with micropillars | 100 μm diameter pillars, 100 μm spacing [87] | Limits oxygen exchange, creates diffusion barrier [87] |
| Gas-permeable culture dish | 25 mm diameter | Allows oxygen diffusion for gradient formation [87] |
| PC3-GFP cells | Metastatic prostate cancer line | Model cell line for hypoxia studies [87] |
| Time-lapse imaging system | With appropriate filters | Captures phosphorescence signals for O₂ mapping [87] |
Step-by-Step Procedure:
Phosphorescent Film Calibration:
- Synthesize PtTFPP/PFPE films by dissolving PtTFPP (5 mg/g PFPE) in DCM with ABVN initiator (0.5% w/w) [87]
- Spin-coat onto 25 mm glass coverslips at 1000 RPM for 30 seconds [87]
- Cure films at 75°C for 10 hours under nitrogen atmosphere [87]
- Calibrate films under known O₂ concentrations (0.2%, 1%, 5%, 21%) [87]
System Assembly:
- Plate PC3-GFP cells (or other cell types) on gas-permeable dishes containing calibrated phosphorescent films [87]
- Culture in complete RPMI 1640 medium at 37°C, 5% CO₂ until 70-80% confluent [87]
- Gently place acrylic plug with adhesive pillars over cell monolayer [87]
- Ensure even contact without compressing cells [87]
Hypoxia Development and Imaging:
O₂ Gradient Mapping:
Protocol: Microfluidic Hypoxia System for Cardiac Research
This advanced protocol uses microfluidic technology to create spatially controlled hypoxia zones, ideal for studying ischemia-reperfusion and cardiac regeneration [88].
System Setup:
- Fabricate PDMS microfluidic device with six rectangular chambers (3 × 35 mm) [88]
- Integrate polyurethane nanofibrous mats with Fe₃O₄ magnetic nanoparticles [88]
- Differentiate iPSCs into cardiomyocytes (iPSC-CMs) using established protocols [88]
- Seed iPSC-CMs into microfluidic chambers at appropriate density [88]
Hypoxia Induction:
- Design two-zone holder with separate gas controls [88]
- Create "hypoxia zone" by introducing nitrogen or oxygen-scavenging reagents [88]
- Maintain "normoxia zone" with standard culture conditions [88]
- Use oxygen sensors to verify zone-specific O₂ concentrations [88]
Regeneration Assessment:
- Co-culture hypoxia-damaged iPSC-CMs with naïve iPSCs [88]
- Monitor cardiac troponin T (cTnT) expression as regeneration marker [88]
- Assess functional recovery through contraction analysis [88]
Research Reagent Solutions
Table 3: Essential Reagents for Hypoxia Research
| Reagent Category | Specific Examples | Application Notes |
|---|---|---|
| HIF Stabilizers | CoCl₂, DMOG, DFO [87] [89] | Use for rapid HIF induction without specialized equipment; optimal concentrations vary by cell type [87] [89] |
| HIF Inhibitors | LW6, Bay-876 [91] | LW6 targets HIF-1α degradation; Bay-876 blocks glycolytic pathway [91] |
| Antibodies | HIF-1α (NB100-105), HIF-2α (NB100-122), HIF-3α (NB100-252) [89] | HIF-1α runs at 110-130 kDa; nuclear fractionation recommended for better detection [89] |
| Oxygen Sensors | PtTFPP/PFPE films, commercial probe systems [87] | Enable real-time oxygen monitoring; require calibration [87] |
| Cell Lines | PC3-GFP, dHL-60 (differentiated), iPSC-CMs [87] [91] [88] | Choose based on research focus: cancer (PC3), neutrophil (dHL-60), cardiac (iPSC-CMs) [87] [91] [88] |
Signaling Pathways and Workflows
Diagram 1: HIF Signaling Pathway in Normoxia and Hypoxia
Diagram 2: Experimental Workflow for Hypoxia Studies
Animal Models for Studying Physiological and Pathological Hypoxia
FAQs: Selecting and Implementing Animal Models for Hypoxia Research
What are the main types of hypoxia models, and how do I choose? Your choice should be guided by the specific human condition or physiological state you aim to replicate. The two primary categories are exogenous (environmental) and endogenous (within the body) hypoxia [92] [79].
- Exogenous Hypoxia: Achieved by reducing the oxygen content in the inspired air.
- Chronic Sustained Hypoxia (CSH): Continuous low oxygen, modeling chronic lung disease or permanent residence at high altitude [93].
- Chronic Intermittent Hypoxia (CIH): Recurring cycles of low oxygen and reoxygenation, modeling obstructive sleep apnea [93].
Which animal species is most appropriate for hypoxia research? Rats are the most prevalent models, with mice also being widely used [92]. The choice often depends on a balance between physiological relevance and practical considerations.
Table 1: Comparison of Common Animal Models in Hypoxia Research
| Animal Model | Key Advantages | Common Hypoxia Applications | Notable Considerations |
|---|---|---|---|
| Rats (e.g., Sprague-Dawley, Wistar) | Size allows for easier surgical procedures and repeated sampling; physiology is well-characterized; reactions to hypoxia are better known [92]. | High-altitude studies (hypobaric chambers); CSH and CIH models for pulmonary and metabolic diseases [92] [93]. | Different strains show varying tolerance; Sprague-Dawley and Wistar are the most common [92]. |
| Mice | Lower cost; availability of transgenic strains to study specific genetic pathways [92]. | Studies requiring genetic manipulation; models of cancer and neurodegenerative diseases [94] [76]. | Degree of vascular remodeling in response to CSH is typically less than in rats [93]. |
| Wild/Nontraditional Species (e.g., Naked Mole Rats, Deep-Diving Seals) | Exhibit extreme natural adaptations to hypoxia; can reveal unique protective mechanisms [95]. | Identifying evolutionary adaptations and novel therapeutic targets for ischemia-reperfusion injury or extreme hypoxia [95]. | Not commercially standardized; require specialized husbandry and research protocols [95]. |
My results are inconsistent. Could the rat strain be a factor? Yes. Different rat strains demonstrate noticeable differences in their physiological and adaptive responses to hypoxia [92]. For example, Sprague-Dawley and Wistar rats have different critical lethal altitudes and high hypoxia tolerance times [92]. Always specify the strain used in your methodology and be cautious when comparing results across different strains.
How does chronic intermittent hypoxia (CIH) affect physiology differently from chronic sustained hypoxia (CSH)? The pattern of oxygen deprivation drives fundamentally different physiological outcomes [93].
Table 2: Physiological Effects of Chronic Sustained vs. Intermittent Hypoxia
| Hypoxia Model | Cardiovascular Effects | Metabolic Effects | Model of Human Condition |
|---|---|---|---|
| Chronic Sustained Hypoxia (CSH) | Reliably induces pulmonary hypertension (PH); variable effects on systemic blood pressure [93]. | Appears to have protective effects on glucose metabolism [93]. | Chronic lung/heart disease; high-altitude residence [93]. |
| Chronic Intermittent Hypoxia (CIH) | Increases systemic blood pressure; associated with endothelial dysfunction [93]. | Maladaptive changes including glucose dysregulation and progression of non-alcoholic fatty liver disease [93]. | Obstructive Sleep Apnea (OSA) [93]. |
Troubleshooting Common Experimental Issues
Unexpected High Mortality in Hypoxia Chamber
- Problem: Animals are dying during a hypoxia exposure protocol that should be sublethal.
- Solution:
- Verify Strain Tolerance: Check the literature for your specific strain's critical hypoxia thresholds. For instance, Sprague-Dawley rats generally have a critical lethal altitude between 9250–10668 m, while Wistar rats can tolerate slightly higher altitudes [92].
- Calibrate Equipment: Ensure the oxygen sensor and pressure regulators (for hypobaric chambers) are accurately calibrated. A small error can make the exposure more severe than intended.
- Gradual Acclimatization: Do not place animals directly into the target hypoxia. Implement a step-wise reduction in oxygen or pressure over several days to allow for physiological acclimatization [92].
Inconsistent Molecular Readouts After Hypoxia Exposure
- Problem: High variability in the measurement of biomarkers like HIF-1α between animals in the same treatment group.
- Solution:
- Control for Timing: HIF-1α protein stabilizes rapidly but is also degraded quickly upon reoxygenation. Standardize the time between the end of hypoxia exposure and tissue collection across all subjects [93] [76].
- Standardize Sample Processing: Process tissue samples in an environment that maintains the hypoxic condition (e.g., using anaerobic chambers) to prevent reoxygenation artifacts before analysis.
Failure to Observe Expected Protective or Pathological Phenotype
- Problem: After a hypoxia pre-conditioning protocol, animals do not show increased tolerance to a subsequent severe insult.
- Solution:
- Optimize the "Dose" of Hypoxia: The protective effect of pre-conditioning is highly dependent on the severity and duration of the hypoxic stimulus. A regimen that is too mild may not trigger adaptation, while one that is too severe causes damage. Systemically test different durations (e.g., 1-4 hours) and oxygen concentrations (e.g., 8-12% O₂) [79].
- Confirm Functional Endpoints: Use functional tests (e.g., pole test for motor function, measurements of pulmonary arterial pressure) in addition to molecular biomarkers to confirm the phenotype [94].
The Scientist's Toolkit: Key Reagent Solutions
Table 3: Essential Reagents and Materials for Hypoxia Research
| Item | Function/Application | Example Use Case |
|---|---|---|
| Hypobaric or Normobaric Chambers | Creates a controlled low-oxygen environment for housing animals [92]. | Modeling high-altitude exposure (hypobaric) or diseases like COPD (normobaric) [92] [93]. |
| Oxygen Controller | Precisely monitors and regulates the oxygen concentration within a chamber [92]. | Maintaining a stable FiO₂ (e.g., 10% for severe CSH) for the duration of the experiment [93]. |
| Hypoxia-Inducible Factor (HIF) Stabilizers (e.g., Deferoxamine) | Chemical mimetics that inhibit HIF prolyl hydroxylases, stabilizing HIF-1α even under normoxic conditions [76]. | Studying HIF-dependent pathways in cell culture without a hypoxia chamber; used to model hypoxia-induced drug resistance in cancer cells [76]. |
| p53 Knock-out Models | Genetic tools to dissect the role of p53 in hypoxia-induced apoptosis [76]. | Demonstrating that hypoxia-mediated suppression of apoptosis under low oxygen is p53-dependent [76]. |
| Antibodies for Hypoxia Markers (e.g., HIF-1α, pimonidazole adducts) | Detecting and quantifying hypoxia at the cellular and tissue level. | Immunohistochemistry or Western blot to confirm hypoxic regions in tissue sections or cell cultures. |
Experimental Workflow and Key Signaling Pathways
Diagram 1: Typical Workflow for a Hypoxia Pre-conditioning and Challenge Experiment
This diagram outlines a common experimental design used to investigate the protective effects of moderate hypoxia against a subsequent, more severe hypoxic or ischemic insult.
Diagram 2: Simplified HIF-1α Signaling Pathway in Hypoxia
This pathway is central to most cellular responses to low oxygen, influencing metabolism, angiogenesis, and cell survival.
Diagram 3: Contrasting Pathogenic vs. Protective Hypoxia Outcomes
The ultimate effect of hypoxia on cells and tissues depends on the severity, duration, and pattern of exposure, determining whether the outcome is pathological damage or adaptive protection.
FAQs: Hypoxia Imaging Modalities
1. What are the primary imaging modalities for detecting tumor hypoxia, and how do they differ? The primary non-invasive modalities are Positron Emission Tomography (PET), Magnetic Resonance Imaging (MRI), and emerging Optical Molecular Imaging (OMI). They differ in their fundamental mechanism for detecting hypoxia, what they directly measure, their spatial resolution, and their sensitivity [53] [96].
- PET uses radioactive tracers that are biologically reduced and trapped in hypoxic cells, providing a direct measure of tissue hypoxia at the cellular level. It offers high sensitivity but limited spatial resolution [97] [98].
- MRI techniques measure physiological consequences of hypoxia, such as changes in blood oxygenation, perfusion, or water diffusion. MRI provides excellent soft-tissue contrast and high spatial resolution but often offers an indirect assessment of hypoxia [97] [96].
- Optical Imaging uses probes that are activated by hypoxia-related analytes (e.g., enzymes, pH). It allows for real-time imaging and high sensitivity but has very limited tissue penetration depth, making it more suitable for superficial tumors or intraoperative use [53] [99].
2. Why is quantifying hypoxia important in cancer research and drug development? Hypoxia is a key factor in tumor aggressiveness and treatment resistance. It promotes genetic instability, metastasis, and immune escape [97] [96]. Crucially, hypoxic cells are up to 3 times more resistant to radiation therapy because oxygen is essential for fixing radiation-induced DNA damage [97] [100]. Hypoxia also confers resistance to many chemotherapeutic agents [96]. Therefore, accurately quantifying hypoxia is essential for prognostic stratification, tailoring radiotherapy doses (e.g., dose painting), and developing new hypoxia-activated prodrugs (HAPs) [53] [101].
3. What are the advantages and limitations of the most common PET tracers for hypoxia? The most common PET tracers are nitroimidazole-based compounds and copper-based agents, each with distinct pharmacokinetics [97] [98].
Table: Comparison of Common Hypoxia-Specific PET Tracers
| Tracer | Mechanism | Key Advantages | Key Limitations |
|---|---|---|---|
| [18F]-FMISO [ [97] [98] | Nitroimidazole derivative; bioreduced and trapped in hypoxic cells. | The most widely used and validated tracer; considered a gold standard. | Slow clearance from normoxic tissues leads to a low tumor-to-background ratio; requires late imaging (2-3 hours post-injection). |
| [18F]-FAZA [ [53] [98] | Nitroimidazole derivative; more hydrophilic than FMISO. | Faster clearance from normoxic tissues, providing a better tumor-to-background ratio. | Less clinical experience compared to FMISO. |
| [64Cu]-ATSM [ [97] [98] | Copper diacetyl-bis(N4-methylthiosemicarbazone); reduced and trapped in hypoxic cells. | Very high tumor-to-background contrast; rapid imaging possible. | Retention mechanism may be influenced by factors beyond pO2 (e.g., thiol levels); reliability may vary by tumor type. |
4. Can MRI truly quantify hypoxia, and what are its main techniques? While MRI does not directly measure oxygen concentration like some PET tracers, quantitative MRI parameters can identify and characterize hypoxic tumor subvolumes [101]. The main techniques include:
- Blood Oxygen Level Dependent (BOLD): Measures changes in deoxyhemoglobin, serving as a proxy for blood oxygenation. It is sensitive to acute hypoxia but does not directly measure tissue oxygenation and can be influenced by blood flow and volume [97] [102].
- Dynamic Contrast-Enhanced (DCE-MRI): Tracks the inflow of a gadolinium-based contrast agent to assess tumor perfusion and permeability, which are related to oxygen delivery [97] [101].
- Diffusion-Weighted Imaging (DWI): Calculates the Apparent Diffusion Coefficient (ADC), which reflects cellularity. Hypoxic regions can show restricted diffusion due to cellular proliferation or, conversely, increased diffusion near necrotic areas [97] [101].
- Quantitative T1 and T2 Mapping: These relaxometry techniques measure intrinsic tissue properties. Studies have shown significant differences in T1 and T2 values between hypoxic and normoxic tumor subvolumes defined by [18F]-FMISO PET, suggesting they can help characterize the hypoxic microenvironment [101].
5. What are the biggest challenges in hypoxia imaging, and what future directions are promising? Key challenges include the spatial and temporal heterogeneity of hypoxia (cyclic hypoxia), the low resolution and signal-to-noise ratio of some PET techniques, and the indirect nature of many MRI methods [97] [53] [98].
Promising future directions focus on:
- Multimodal Imaging: Combining PET/MRI to leverage the high hypoxia specificity of PET with the high anatomical and functional resolution of MRI [103] [101].
- Novel Probe Design: Developing dual-lock or ratiometric probes that require two hypoxia-associated biomarkers for activation, improving specificity [53] [99].
- Machine Learning: Applying models to analyze multiparametric data from PET and MRI to improve the accuracy of hypoxia maps [53].
Troubleshooting Guides
Issue 1: Poor Tumor-to-Background Contrast in Hypoxia PET Imaging
Problem: Your PET image shows low signal differentiation between the tumor and surrounding normal tissue, making it difficult to define hypoxic sub-volumes.
Possible Causes and Solutions:
- Cause: Incorrect Imaging Timepoint. Nitroimidazole tracers like [18F]-FMISO require sufficient time to clear from normoxic tissues.
- Cause: Low Tracer Specificity or High Lipophilicity. [18F]-FMISO is relatively lipophilic, leading to slower clearance.
- Cause: Underlying Poor Perfusion. Hypoxic regions often have poor blood flow, which can limit tracer delivery and create a false negative.
Issue 2: Interpreting Discrepancies Between PET and MRI Hypoxia Readings
Problem: The suspected hypoxic region identified by MRI (e.g., BOLD or DWI) does not align with the region highlighted by a hypoxia-specific PET tracer.
Explanation and Resolution: This is common because PET and MRI measure different physiological aspects.
- Explanation: A BOLD-MRI signal primarily reflects vascular oxygenation, while a hypoxia PET tracer reflects tissue oxygenation at the cellular level. A region could have well-oxygenated blood but poor oxygen diffusion to the tissue, leading to a positive PET signal but a negative BOLD result [97] [102].
- Resolution:
- Do not treat the techniques as interchangeable. Understand that each modality provides a different piece of the puzzle.
- Use multimodal registration. Fuse the PET and MRI images to visually and quantitatively compare the different biological maps [104] [101].
- Leverage quantitative MRI. Instead of relying solely on BOLD, use a multiparametric approach. Studies show that quantitative parameters like ADC (from DWI), T1 max, and T2 max can show significant differences between hypoxic and normoxic subvolumes defined by [18F]-FMISO PET [101].
Issue 3: Challenges with Imaging Cyclic (Intermittent) Hypoxia
Problem: Hypoxia is a dynamic phenomenon, and a single static image may not capture its transient nature, leading to an incomplete assessment.
Possible Causes and Solutions:
- Cause: Static Imaging Snapshots. A single PET or MRI scan provides information at one moment in time and may miss fluctuations in oxygenation that occur over minutes to hours [53] [96].
- Solution:
- For PET: This is challenging due to radiation dose and tracer pharmacokinetics. A dynamic PET acquisition (scanning from the moment of injection) can provide kinetic parameters (like the trapping rate constant, k3) that may be more robust than a single static image [98].
- For MRI/Optical: Use techniques capable of real-time or repeated monitoring.
- BOLD-MRI can be performed before and after a carbogen challenge (breathing a gas with high oxygen and CO2 content) to assess vascular function and hypoxia [102].
- Optical Imaging probes, particularly those based on phosphorescence lifetime quenching, are excellent for real-time mapping of cyclic hypoxia due to their rapid response [53] [99].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents and Materials for Hypoxia Imaging Research
| Item | Function/Application | Examples & Notes |
|---|---|---|
| Nitroimidazole Tracers | PET imaging; become irreversibly trapped in hypoxic cells. | [18F]-FMISO: Gold standard [ [97] [98]. [18F]-FAZA: Improved clearance [ [53] [98]. [18F]-HX4: Clinical promise [ [53] [96]. |
| Copper-based Tracers | PET imaging; reduced and trapped in hypoxic environments. | [64Cu]-ATSM: Very high contrast; mechanism may be complex and tumor-dependent [ [97] [98]. |
| Pimonidazole | Hypoxia immunohistochemistry; bioreductive marker for ex vivo validation. | Used to stain hypoxic regions in excised tissue; can be conjugated to antibodies (e.g., FITC) for fluorescence imaging to validate in vivo findings [ [104]. |
| Phosphorescent Probes | Optical imaging; direct pO2 sensing via O2 quenching of luminescence. | PpyPt NPs, Rhenium-diimine complexes: Used for real-time phosphorescence lifetime imaging (PLI) of cyclic hypoxia [ [53] [99]. |
| Dual-Lock/Fluorescent Probes | Optical imaging; detect multiple hypoxia-associated analytes for high specificity. | Probes activated by two biomarkers (e.g., NTRs and pH) to minimize off-target signals and improve signal-to-background ratio [ [53]. |
| CAIX-Targeting Agents | PET/SPECT/Optical imaging; target carbonic anhydrase IX, a hypoxia-induced enzyme. | [89Zr]-girentuximab, CAIX-800: Provide an indirect, stable method for identifying hypoxic conditions [ [97] [53] [99]. |
Experimental Workflows and Pathways
Diagram 1: Workflow for Multimodal Hypoxia Validation
This diagram outlines a practical methodology for cross-validating in vivo imaging findings with ex vivo biology, crucial for confirming experimental results.
Diagram 2: Molecular Pathways & Probe Mechanisms in Hypoxia
This chart illustrates the cellular response to hypoxia and the activation mechanisms of different classes of imaging probes.
Foundational Principles of Biomarker Validation
What is the difference between biomarker discovery and validation?
Biomarker discovery is the initial identification of a measurable characteristic that indicates normal or pathogenic biological processes or responses to an intervention [105]. Validation is the subsequent process that determines the performance of the discovered biomarker is credible, reliable, and reproducible for its intended use [106] [107]. It establishes how well the biomarker measures, represents, or predicts a specific biological process or clinical outcome.
Why is clear intended use critical before starting validation?
A precisely defined intended use statement guides the appropriate level and scope of validation required [106]. It must specify:
- Intended patient population and specimen type
- Test purpose and what the results will inform
- Associated risks and benefits to patients
- Testing delivery model (local vs. central) Higher degrees of validation evidence are required for biomarkers posing greater patient risks [106].
What are the key stages in the biomarker validation process?
The validation pipeline typically progresses through these key stages [106]:
| Validation Stage | Primary Objective | Regulatory Context |
|---|---|---|
| Analytical Method Development | Develop reliable test method for the biomarker | Research Use Only (RUO) |
| Retrospective Clinical Validation | Assess performance in archived clinical samples | Observational Study |
| Investigational Use Validation | Inform treatment decisions in clinical trials | Investigational Device Exemption (IDE) |
| Marketing Approval | Demonstrate safety/effectiveness for clinical use | FDA PMA/510(k); EU IVDR |
| Post-Market Surveillance | Monitor real-world performance | Ongoing regulatory compliance |
Biomarker Validation in Hypoxia Research
How does the hypoxic tumor microenvironment impact biomarker validation?
Hypoxia creates unique challenges for biomarker validation due to its dynamic effects on cellular processes. Hypoxia-inducible factors (HIF-1 and HIF-2) stabilize under low oxygen and activate gene programs for angiogenesis, glycolysis, and metastasis [6]. This biological complexity means hypoxia-related biomarkers must be validated across varying oxygen tensions and should account for HIF-driven molecular adaptations.
What are key considerations for validating hypoxia-related gene signatures?
When working with hypoxia-related gene signatures like those identified in diminished ovarian reserve (FANCI, KAT2A, TACC3, TPX2, VHL, WSB1) [108] or solid tumors [109]:
- Confirm hypoxia-specific expression patterns across multiple independent cohorts
- Validate analytical performance across different specimen types (tissue, blood, etc.)
- Establish clinical relevance to hypoxic response through correlation with known hypoxia markers
- Ensure reproducibility across different laboratory environments and platforms
Experimental Protocols & Methodologies
What is a standard workflow for validating prognostic gene signatures?
The following workflow illustrates the key stages for robust validation of prognostic gene signatures, integrating computational and clinical approaches:
What statistical methods are essential for biomarker validation?
Appropriate statistical methods must be selected based on the biomarker's intended use and study design [105]:
| Biomarker Type | Primary Statistical Test | Key Performance Metrics |
|---|---|---|
| Prognostic | Main effect test of association between biomarker and outcome | Hazard ratios, Kaplan-Meier curves, log-rank test |
| Predictive | Interaction test between treatment and biomarker | Interaction p-value, stratified hazard ratios |
| Diagnostic | Receiver Operating Characteristic (ROC) analysis | Sensitivity, Specificity, AUC (Area Under Curve) |
For high-dimensional biomarker data, control of multiple comparisons using false discovery rate (FDR) methods is essential [105].
How are hypoxia-related signaling pathways assessed in validation studies?
The HIF pathway serves as the central regulator of cellular response to hypoxia and is frequently assessed in validation studies:
The Scientist's Toolkit
What essential reagents and platforms are needed for biomarker validation?
| Reagent/Platform | Function in Validation | Application Notes |
|---|---|---|
| Archived Clinical Specimens | Provide biologically relevant samples for retrospective validation | Ensure diversity and represent target population; assess specimen stability [106] |
| Hypoxia Chamber/Culture System | Create controlled low-oxygen environments for experimental models | Essential for validating hypoxia-specific biomarkers [108] [6] |
| qPCR Assays | Quantify gene expression of candidate biomarkers | Gold standard for transcriptional biomarkers; requires normalization genes [108] |
| Western Blot Reagents | Detect and quantify protein-level biomarkers | Validates translation of gene signatures to protein expression [108] |
| Immunohistochemistry Kits | Spatial validation of biomarkers in tissue context | Provides tissue architecture context; semi-quantitative |
| ELISA Assays | Quantify soluble biomarkers in biofluids | High-throughput option for clinical translation |
| Flow Cytometry Antibodies | Analyze biomarker expression at single-cell level | Essential for heterogeneous samples like tumor microenvironments |
| NGS Platforms | Validate genomic and transcriptomic biomarkers | Provides comprehensive molecular profiling [105] |
How should researchers approach data quality and integration in validation studies?
Effective validation requires rigorous data quality control and integration strategies [110]:
- Apply data-type specific quality metrics (e.g., fastQC for NGS data, arrayQualityMetrics for microarrays)
- Implement batch effect correction methods to address technical variability
- Use appropriate data integration strategies (early, intermediate, or late integration) for multi-omics data
- Compare multiple outcome definitions to address lack of clarity or information loss
Troubleshooting Common Validation Challenges
How can I address poor reproducibility across validation cohorts?
Poor reproducibility often stems from technical and biological variability. Mitigation strategies include [107]:
- Standardize operating procedures across all participating sites
- Implement randomization and blinding during specimen analysis to prevent bias [105]
- Use pre-planned statistical analysis plans to avoid data-driven conclusions [105]
- Validate across multiple independent cohorts with diverse patient populations
What should I do when my biomarker shows poor clinical utility?
When a biomarker is analytically valid but lacks clinical utility [107]:
- Re-evaluate the intended use and target population definition
- Assess if clinical workflow integration is feasible (turnaround time, sample requirements)
- Compare against existing standard of care biomarkers to demonstrate added value
- Consider whether a multi-biomarker panel might perform better than a single biomarker [105]
How can I avoid machine learning pitfalls in biomarker validation?
When using machine learning for biomarker development [107]:
- Address overfitting by using separate discovery and validation cohorts
- Manage high-dimensional data through appropriate feature selection methods
- Recognize and mitigate biases in training data that could affect generalizability
- Combine machine learning with classical statistics to balance prediction and interpretability
What are solutions for biomarker validation in hypoxic environments?
Specific challenges in hypoxia research require specialized approaches [108] [6]:
- Model System Validation: Confirm hypoxic conditions (measure pO2, HIF-1α stabilization)
- Temporal Considerations: Account for acute vs. chronic hypoxia timelines in experimental design
- Microenvironment Complexity: Use appropriate models that capture tumor microenvironment heterogeneity
- Metabolic Adaptation: Assess both HIF-dependent and HIF-independent pathways to hypoxia adaptation
Comparative Analysis of Hypoxia-Targeting Modalities Across Disease Models
Frequently Asked Questions (FAQs)
Q1: What is the central molecular regulator of cellular response to hypoxia, and why is it a key therapeutic target?
A1: The central molecular regulator is Hypoxia-Inducible Factor 1-alpha (HIF-1α). It is a master transcription factor that orchestrates cellular adaptation to low oxygen conditions. Under hypoxia, HIF-1α stabilizes and translocates to the nucleus, where it dimerizes with HIF-1β and binds to Hypoxia-Response Elements (HREs), activating a genetic program for survival [111] [6]. This program includes upregulating genes for angiogenesis (e.g., VEGF), metabolic shift to glycolysis, and cell proliferation [6]. In diseases like cancer and chronic graft-versus-host disease (cGVHD), HIF-1α promotes pathological processes such as tumor survival, metastasis, fibrosis, and inflammation [111] [6]. Therefore, targeting HIF-1α or its downstream pathways offers a strategic approach to disrupt these disease mechanisms.
Q2: What are the primary pathophysiological changes in a hypoxic tumor microenvironment that can be exploited for imaging or therapy?
A2: Hypoxia creates a unique tumor microenvironment with several key characteristics [112]:
- Acidic pH (Acidosis): HIF-1 upregulates glucose transporters and glycolytic enzymes, leading to lactate production and secretion, which acidifies the extracellular matrix [112].
- Aberrant Levels of Reactive Species: This includes elevated reactive oxygen species (e.g., H₂O₂, •OH), reactive nitrogen species (e.g., NO•, ONOO⁻), and reactive sulfur species (e.g., H₂S) due to altered cellular metabolism and enzyme activity [112].
- Elevated Redox Buffers: As a defense mechanism, hypoxic cells increase production of antioxidants like glutathione and NADPH to manage oxidative stress [112].
- Inorganic Ion Imbalance: Changes in concentrations of ions like Ca²⁺ and PO₄³⁻ occur due to incomplete cellular respiration [112]. These distinct biochemical changes provide targets for responsive imaging probes and therapeutic agents.
Q3: How can researchers experimentally enhance the survival of stem cells transplanted into a hypoxic environment?
A3: A key methodology is hypoxic preconditioning (HPC). This involves exposing stem cells to a brief, controlled period of hypoxia before transplantation to prime them for the harsh conditions of the ischemic site. For example, research on rat mesenchymal stem cells (MSCs) has shown that preconditioning at 0.5% oxygen for 24 hours is optimal. This HPC protocol significantly reduces apoptosis upon subsequent severe hypoxia exposure by upregulating pro-survival proteins (p-Akt, Bcl-2, survivin) and pro-angiogenic factors (VEGF) [48]. It is critical that cells are cultured under normoxia for at least one passage after thawing before HPC, as directly using cryopreserved cells diminishes the protective effect [48].
Troubleshooting Guides
Issue 1: Low Engraftment and Survival of Transplanted Cells in Hypoxic Niches
Problem: A significant proportion of therapeutic cells die within days of transplantation into an ischemic area, limiting treatment efficacy [48].
Solution: Implement a Hypoxic Preconditioning Protocol.
- Step 1: Culture your cells (e.g., MSCs) under standard normoxic conditions (21% O₂) for at least one passage after thawing to ensure metabolic recovery [48].
- Step 2: Precondition the cells by transferring them to a hypoxic chamber with 0.5% O₂ for 24 hours. Avoid longer exposures (e.g., 72 hours), as this can diminish the pro-survival effect [48].
- Step 3: Post-HPC, validate success by checking for upregulated markers before transplantation. Use immunoblotting to confirm increased levels of HIF-1α, p-Akt, survivin, and VEGF [48].
- Step 4: Proceed with transplantation. Studies in rat infarct models show that HPC-MSCs have better retention and improve functional outcomes [48].
Issue 2: Off-Target Effects During HIF-1α Pathway Modulation
Problem: Systemic administration of HIF-1α inhibitors or activators causes unintended effects in healthy, normoxic tissues.
Solution: Utilize Nanotherapeutic and Targeted Delivery Systems.
- Investigate Smart Nanocarriers: Develop or use nanoparticle-based systems designed to release their payload (e.g., HIF-1α inhibitors) specifically in the hypoxic tissue. These systems can be engineered to respond to the low pH or high reactive species levels in the target microenvironment [111] [6].
- Employ Dual-Mode Imaging Probes: To precisely monitor and validate targeting, use dual-mode imaging probes that are activated by hypoxia-associated conditions (e.g., low pH, high H₂O₂). This allows for orthogonal validation of the drug's location and effect, helping to refine delivery parameters [112]. This approach is crucial for balancing therapeutic effects, such as suppressing cGVHD while preserving the graft-versus-leukemia activity in allo-HSCT patients [111].
Table 1: Efficacy of Hypoxic Preconditioning in Mesenchymal Stem Cells (MSCs) This table summarizes key experimental data from a study on optimizing MSC survival [48].
| Preconditioning Parameter | Measurement / Outcome | Optimal Value / Finding | Key Upregulated Markers (vs. Normoxic Controls) |
|---|---|---|---|
| Oxygen Concentration | 0.5% O₂ | 0.5% | HIF-1α, VEGF, p-Akt (Ser473), Survivin |
| Exposure Duration | 24, 48, 72 hours | 24 hours | Highest levels of pro-survival and pro-angiogenic proteins |
| Cell State Post-Thaw | Direct vs. cultured | Normoxic culture for ≥1 passage | Effective response to HPC; stable protein expression |
| Functional Outcome | Apoptosis under severe hypoxia (0.1% O₂) | Significantly reduced apoptosis | Lower cytochrome c, caspase-3, caspase-7 activation |
Table 2: Hypoxia-Associated Pathophysiological Changes and Targeting Strategies This table synthesizes key targets within the hypoxic microenvironment for imaging and therapeutic intervention [6] [112].
| Microenvironment Change | Key Biomarkers / Chemicals | Associated Imaging Modalities | Therapeutic Intervention Strategies |
|---|---|---|---|
| Acidic pH (Acidosis) | Lactate, H⁺ ions | MRI, Optical Imaging | pH-responsive drug delivery systems; buffer agents |
| Elevated Reactive Oxygen Species | H₂O₂, •OH, O₂•⁻ | Photoacoustic, MRI, EPR | ROS-scavenging nanoparticles; pro-oxidant therapies |
| Elevated Reactive Nitrogen Species | NO•, ONOO⁻ | SPECT, PET | NOS inhibitors; ONOO⁻-responsive probes |
| Redox Imbalance | Glutathione, NADPH | MRI, Fluorescence | Glutathione inhibitors; redox-sensitive nanocarriers |
| HIF-1α Pathway Activation | HIF-1α, VEGF | PET, SPECT, Optical | HIF-1α inhibitors (e.g., small molecules); nanotherapeutics |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Hypoxia Research A curated list of key reagents used in the featured experiments and field [48] [112].
| Reagent / Material | Function / Application | Specific Example |
|---|---|---|
| HIF-1α Antibody | Detection and quantification of HIF-1α protein stabilization via Western Blot/Immunoblot. | Anti-HIF-1α antibody (e.g., from Chemicon) [48]. |
| Pro-Survival & Apoptosis Markers | Evaluating the efficacy of hypoxic preconditioning. | Antibodies against p-Akt, survivin, Bcl-2, cytochrome c, caspase-3, caspase-7 [48]. |
| Pro-Angiogenic Factor ELISA Kit | Quantifying secretion of angiogenic factors like VEGF. | Rat VEGF ELISA Kit [48]. |
| Hypoxia Chamber / Workstation | Maintaining precise, low-oxygen culture conditions for experiments. | C-Chamber with ProOx Model C21 (BioSpherix) for 0.5% O₂ [48]. |
| Dual-Mode Imaging Probes | Non-invasive detection and characterization of hypoxic regions. | Probes responsive to pH, H₂O₂, or ONOO⁻ for modalities like MRI/PET or CT/Fluorescence [112]. |
Experimental Workflow and Signaling Pathways
HPC Workflow for Cell Survival
HIF-1α Signaling in Hypoxia
Conclusion
The intricate molecular networks governing cellular adaptation to hypoxia present both challenges and opportunities for therapeutic intervention. Key takeaways include the central role of HIF signaling in coordinating survival responses, the critical importance of metabolic reprogramming through pathways like SREBP1-mediated lipogenesis, and the potential of autophagy as a therapeutic target. Future directions should focus on developing more sophisticated hypoxia imaging technologies, validating predictive biomarkers for patient stratification, and designing smart combination therapies that target both hypoxic cells and their immunosuppressive microenvironment. The translation of hypoxia-targeting strategies requires multidisciplinary approaches integrating molecular biology, imaging sciences, and clinical trial design to ultimately improve outcomes in cancer, ischemic diseases, and regenerative medicine applications.
References
- 1. The Distinct Role of HIF-1α and HIF-2α in Hypoxia and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071368/]
- 2. Hypoxia-Inducible Factor 1-α (HIF-1α) Induces Apoptosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6289032/]
- 3. HIF-2α is indispensable for regulatory T cell function [https://www.nature.com/articles/s41467-020-18731-y]
- 4. HIF-1 and HIF-2 Transcription Factors - Similar but Not ... [https://www.sciencedirect.com/science/article/pii/S1016847823129165]
- 5. Oxidative and Glycolytic Metabolism - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12345780/]
- 6. Hypoxia-Driven Metabolic and Molecular Reprogramming [https://www.sciencedirect.com/science/article/abs/pii/S0344033825004649]
- 7. Glycolytic suppression dramatically changes the ... - Nature [https://www.nature.com/articles/s41598-019-55296-3]
- 8. The regulation of cell metabolism by hypoxia and hypercapnia [https://pmc.ncbi.nlm.nih.gov/articles/PMC11923829/]
- 9. Metabolic reprogramming in ischemic stroke [https://www.nature.com/articles/s41419-025-08114-w]
- 10. Metabolic reprogramming through PIM3 inhibition reverses ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590754/]
- 11. Hypoxia-induced metabolic reprogramming in mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183037/]
- 12. Targeting SREBP-1-Mediated Lipogenesis as Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9330218/]
- 13. Hypoxia‑induced SREBP1‑mediated lipogenesis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11837466/]
- 14. Sustained SREBP-1-dependent lipogenesis as a key ... [https://www.nature.com/articles/s41467-018-04664-0]
- 15. Hypoxia‑induced SREBP1‑mediated lipogenesis and ... [https://pubmed.ncbi.nlm.nih.gov/39975955/]
- 16. Lipid metabolism in cancer cells under metabolic stress [https://www.nature.com/articles/s41416-019-0451-4]
- 17. Systemic hypoxia appears to attenuate autophagy in ... [https://www.nature.com/articles/s41598-025-21430-7]
- 18. Autophagy Activation by Hypoxia Regulates Angiogenesis ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2021.709751/full]
- 19. Role of Hypoxia-Mediated Autophagy in Tumor Cell Death ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7866864/]
- 20. Hypoxia-associated autophagy flux dysregulation in ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383524002167]
- 21. Hypoxia-Driven Histone Modifications Govern Gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12510386/]
- 22. Epigenetic alterations facilitate transcriptional and ... [https://www.nature.com/articles/s41556-025-01786-8]
- 23. Epigenetic memories induced by hypoxia in AKI-to-CKD ... [https://link.springer.com/article/10.1007/s10157-025-02745-1]
- 24. The emerging intertwined activities of metabolism and ... [https://www.nature.com/articles/s12276-025-01537-7]
- 25. Editorial: Exploring the role of epigenetic modifications in ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1618278/full]
- 26. Development of small molecule inhibitors of hypoxia ... [https://www.sciencedirect.com/science/article/abs/pii/S0031699725074836]
- 27. Hypoxia inducible factor pathway inhibitors as anticancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3871878/]
- 28. Regulatory mechanisms of hypoxia‐inducible factor 1 activity [https://pmc.ncbi.nlm.nih.gov/articles/PMC5834787/]
- 29. Hypoxia Inducible Factor-2α (HIF-2α) Pathway Inhibitors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12228116/]
- 30. Recent progress in the development of hypoxia-inducible ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523424005257]
- 31. Hypoxia-inducible factor–prolyl hydroxylase inhibitors in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7983025/]
- 32. Hypoxia-Inducible Factor Prolyl Hydroxylase (HIF-PHD) ... [https://www.mdpi.com/2673-5261/6/4/25]
- 33. Recent advance of hypoxia-inducible factor prolyl ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523425006725]
- 34. Hypoxic microenvironment in cancer [https://www.nature.com/articles/s41392-023-01332-8]
- 35. Variation in metabolic pattern regulation under hypoxic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12487112/]
- 36. Protocols for analyzing metabolic derangements caused by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8784396/]
- 37. The role of HIF-1α in hypoxic metabolic reprogramming ... [https://www.sciencedirect.com/science/article/pii/S104366182500074X]
- 38. Hypoxia-activated prodrugs and (lack of) clinical progress [https://pmc.ncbi.nlm.nih.gov/articles/PMC6357685/]
- 39. Exploring chronic and transient tumor hypoxia for ... [https://www.nature.com/articles/s41540-023-00327-z]
- 40. Hypoxia-activated prodrugs: paths forward in the era of ... [https://www.nature.com/articles/bjc201679]
- 41. Hypoxia-activated prodrugs in cancer therapy - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5433896/]
- 42. Targeting Hypoxia: Hypoxia-Activated Prodrugs in Cancer ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.700407/full]
- 43. The Hypoxia-Activated Prodrug TH-302: Exploiting ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2021.636892/full]
- 44. Hypoxia-activated prodrug SN30000 in multicellular tumour ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1006469]
- 45. Hypoxic preconditioning — A nonpharmacological approach ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7690942/]
- 46. Role of hypoxia preconditioning in therapeutic potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9350626/]
- 47. Frequently Asked Questions about Hypoxia Research & HIFs [https://www.novusbio.com/support/hypoxia-and-hif-faqs?srsltid=AfmBOorBrPXyNWE61iWYwJKRjRuxPOcY6dFUB9R33hDKQYf-puE17h-b]
- 48. Hypoxic preconditioning induces the expression of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3006322/]
- 49. Role of Stromal Cell Derived Factor-1α–CXCR4 Axis [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0037948]
- 50. Enhanced therapeutic effects of hypoxia-preconditioned ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04166-z]
- 51. - Hypoxia human bone marrow-derived mesenchymal... preconditioning [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02497-1]
- 52. Hypoxia preconditioning promotes bone marrow ... [https://www.nature.com/articles/s41419-019-1410-y]
- 53. Imaging hypoxia for head and neck cancer: current status ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12374539/]
- 54. Hypoxia signaling in human health and diseases [https://www.nature.com/articles/s41392-022-01080-1]
- 55. Influence of acute hypoxia and radiation quality on cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3700520/]
- 56. Frequently asked questions in hypoxia research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5045069/]
- 57. Detecting Hypoxia Through the Non-Invasive and ... [https://www.mdpi.com/2079-6374/14/12/584]
- 58. Survival and Proliferation under Severely Hypoxic ... [https://www.mdpi.com/2079-4983/12/2/30]
- 59. The tumor microenvironment as the missing piece in cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288999/]
- 60. The tumor microenvironment in therapy resistance [https://www.frontiersin.org/journals/lab-on-a-chip-technologies/articles/10.3389/frlct.2024.1420233/full]
- 61. strategies for Cold-to-Hot tumor transformation [https://pubmed.ncbi.nlm.nih.gov/40342732/]
- 62. Role of tumor microenvironment in cancer progression and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10242329/]
- 63. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 64. 3 things to know about the tumor microenvironment [https://www.mdanderson.org/cancerwise/what-is-the-tumor-microenvironment-3-things-to-know.h00-159460056.html]
- 65. Overview of Methods for Overcoming Hindrance to Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4512202/]
- 66. Prospects for hypoxia-based drug delivery platforms for the ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365922008239]
- 67. Biomimetic lipid nanocarriers overcome hypoxia barriers in ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925007102]
- 68. Optimizing Hypoxia Detection and Treatment Strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4365940/]
- 69. Hypoxia-targeted drug delivery - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6361706/]
- 70. Mathematical modeling and sensitivity analysis of hypoxia- ... [https://arxiv.org/html/2507.15642v2]
- 71. low-intensity pulsed ultrasound (LIPUS)-driven deep ... [https://pubmed.ncbi.nlm.nih.gov/39744223/]
- 72. low-intensity pulsed ultrasound (LIPUS)-driven deep ... [https://www.thno.org/v15p0030.htm]
- 73. Targeting the hypoxia signaling pathway with nanomedicine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462398/]
- 74. Alleviating Tumor Hypoxia and Immunosuppression via... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11635779/]
- 75. FAQs - Hypoxia and HIFs [https://www.bio-techne.com/research-areas/hypoxia/hypoxia-and-hif-faqs]
- 76. Modeling hypoxia facilitates cancer cell survival through ... [https://www.sciencedirect.com/science/article/pii/S0009279721001897]
- 77. A 3D microvascular network model to study the impact of ... [https://www.nature.com/articles/s41598-018-36381-5]
- 78. Epigenetic changes help cells adapt to low oxygen levels [https://news.ki.se/epigenetic-changes-help-cells-adapt-to-low-oxygen-levels]
- 79. Experimental Modeling of Damaging and Protective Hypoxia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9773672/]
- 80. Chemoradiotherapy in Cancer Treatment: Rationale and ... [https://ar.iiarjournals.org/content/41/1/1]
- 81. Combination strategies to maximize the benefits of cancer ... [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-021-01164-5]
- 82. Researchers working on novel strategies to improve ... [https://www.aacrmeetingnews.org/news/researchers-working-on-novel-strategies-to-improve-radiation-therapy/]
- 83. The Role of Imaging Biomarkers to Guide Pharmacological ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.853568/full]
- 84. A Novel Approach to Targeting Hypoxia and Improving ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4418024/]
- 85. Targeting Hypoxia: Revival of Old Remedies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8615589/]
- 86. A landmark evaluation of hypoxia gene expression ... [https://www.sciencedirect.com/science/article/pii/S2666979X25000205]
- 87. Protocol to model tumor hypoxia in vitro using real-time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597275/]
- 88. A novel holder and microfluidic system for spatially controlled ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00460h]
- 89. Frequently Asked Questions about Hypoxia Research & HIFs [https://www.novusbio.com/support/hypoxia-and-hif-faqs?srsltid=AfmBOorm9wrZfPxl5YPgvpnuRfAStD9Rg-xZKu0Eqfp76Ia1f4PHDsRu]
- 90. Hypoxia [https://www.bio-techne.com/research-areas/hypoxia]
- 91. In vitro study: HIF-1α-dependent glycolysis enhances ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1583587/full]
- 92. Hypoxia modeling techniques: A review - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC9877323/]
- 93. The Cardiovascular and Metabolic Effects of Chronic ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2022.873522/full]
- 94. Hypoxia ameliorates neurodegeneration and movement ... [https://www.nature.com/articles/s41593-025-02010-4]
- 95. Lessons in immune adaptations to hypoxia revealed by ... [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-023-01788-8]
- 96. Functional Imaging of Hypoxia: PET and MRI [https://www.mdpi.com/2072-6694/15/13/3336]
- 97. Advances in PET and MRI imaging of tumor hypoxia - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9947663/]
- 98. PET of Hypoxia: Current and Future Perspectives [https://jnm.snmjournals.org/content/53/8/1171]
- 99. Imaging hypoxia for head and neck cancer: current status, ... [https://www.thno.org/v15p8012.htm]
- 100. Advances in PET and MRI imaging of tumor hypoxia [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2023.1055062/full]
- 101. Quantitative MRI to Characterize Hypoxic Tumors in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10047588/]
- 102. Cancers - Functional Imaging of Hypoxia: PET and MRI [https://www.mdpi.com/2072-6694/15/13/3336/review_report]
- 103. PET-MRI: Challenges and new directions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2934593/]
- 104. A practical method for multimodal registration and ... [https://www.nature.com/articles/s41598-020-74459-1]
- 105. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 106. A Guide to Biomarker Validation [https://sonraianalytics.com/a-guide-to-biomarker-validation/]
- 107. Biomarker Validation: Avoiding Misleading Results [https://www.fiosgenomics.com/biomarker-validation-avoiding-misleading-results/]
- 108. Identification of hypoxia-related diagnostic biomarkers and ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1626992/full]
- 109. Efficient discovery of robust prognostic biomarkers and ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383525000667]
- 110. Ten quick tips for biomarker discovery and validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9371329/]
- 111. Frontiers | Targeting -inducible factor 1α in chronic... hypoxia [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1605669/full]
- 112. Dual- Mode Tumor Imaging Using Probes That Are Responsive to... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9313010/]