Comparative Biodistribution of Cell Therapies: Analytical Methods, Regulatory Insights, and Clinical Implications
This article provides a comprehensive analysis of comparative biodistribution assessment for cell therapy products (CTPs), a critical component for evaluating their safety and efficacy.
Comparative Biodistribution of Cell Therapies: Analytical Methods, Regulatory Insights, and Clinical Implications
Abstract
This article provides a comprehensive analysis of comparative biodistribution assessment for cell therapy products (CTPs), a critical component for evaluating their safety and efficacy. Aimed at researchers, scientists, and drug development professionals, it explores the foundational regulatory requirements from agencies like the FDA, EMA, and PMDA, compares established and emerging analytical methodologies such as qPCR, ddPCR, and imaging techniques, addresses key troubleshooting and optimization challenges in delivery and dosing, and outlines validation strategies for robust, multi-site studies. By synthesizing current trends and best practices, this review serves as a vital resource for the non-clinical and clinical development of CTPs.
The Critical Role of Biodistribution in Cell Therapy: Purposes and Regulatory Landscapes
Biodistribution studies are a cornerstone in the preclinical development of Cell Therapy Products (CTPs), providing critical data on the in vivo journey of therapeutic cells post-administration. These studies assess the distribution, persistence, and clearance of a cellular agent from the administration site to both targeted and non-targeted tissues and biological fluids [1]. For CTPs, often called "living drugs," understanding this cellular kinetics is not merely a regulatory checkbox but a fundamental component for interpreting pharmacological responses, potential toxicities, and overall efficacy [2]. The biodistribution profile of adoptive T cell therapies, for instance, has been shown to directly influence clinical outcomes, highlighting its pivotal role in translating promising laboratory research into safe and effective patient treatments [2].
The regulatory requirement for these studies is driven by the need to ensure patient safety. By identifying off-target tissue accumulation and assessing the risk of germline transmission, biodistribution studies help de-risk clinical trials [3] [1]. Furthermore, they provide essential context for interpreting findings from other preclinical studies, such as toxicology and pharmacology, creating a comprehensive safety profile for new CTPs [3].
Regulatory Framework and Guidelines
The regulatory landscape for biodistribution studies of CTPs is complex and evolving, with guidelines issued by the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA). These guidelines generally advise a per-product approach, meaning the specific requirements are tailored to the unique aspects of each therapy [3]. Generally, biodistribution studies are required for CTPs to initiate first-in-human studies, especially when they involve new cell types, significant formulation changes, or novel routes of administration [3] [1].
Regulatory bodies strongly advise developers to request assistance before initiating preclinical studies [3]. The goal of these studies is to characterize the presence, persistence, and clearance of the drug product at a molecular level in both target and non-target tissues [3]. While not always mandatory, assessing the distribution of the therapeutic cells, their carrier/delivery system, and individual components may be requested [3]. Although these studies do not always have to comply with Good Laboratory Practice (GLP), the analytical techniques used, such as quantitative PCR (qPCR), must be rigorously validated to ensure data reliability [3] [1].
Table 1: Key Regulatory Considerations for Biodistribution Studies
| Aspect | Regulatory Consideration | Reference |
|---|---|---|
| General Requirement | Often required for CTPs; decided on a per-product basis. | [3] [1] |
| Study Goal | Characterize presence, persistence, and clearance in target and non-target tissues. | [3] |
| Animal Model | Should be as relevant as possible to the expected human situation. | [3] |
| GLP Compliance | Preclinical biodistribution studies do not have to comply with GLP. | [3] |
| Data Reliance | Studies may be avoided by referring to previous data for identical components. | [3] |
Key Methodologies for Biodistribution Assessment
A multi-faceted approach is required to fully characterize the biodistribution of CTPs. The current gold standard and most widely recommended method by the FDA is the quantitative polymerase chain reaction (qPCR) assay [1]. This method sensitively quantifies the number of vector copies (for gene therapies) or human cell DNA (for cellular therapies) present in animal tissue samples and biological fluids.
Core Workflow: qPCR for Biodistribution
The standard workflow involves several critical steps, from sample collection to data analysis, each contributing to the final biodistribution profile.
Diagram 1: Experimental qPCR Workflow
- CTP Administration and Tissue Harvesting: The CTP is administered to animal models via the intended clinical route. At predetermined time points, animals are sacrificed, and a wide panel of tissues (e.g., target organs, liver, spleen, gonads) and biological fluids (e.g., blood, urine, saliva) are collected [1].
- DNA Isolation: Genomic DNA is isolated from all collected samples. The DNA extraction method must be evaluated for its recovery rate and potential PCR inhibition effects to ensure accurate quantification [1].
- qPCR Analysis: The isolated DNA is used as a template in a qPCR reaction with primers and a probe specific to the therapeutic vector or human-specific DNA sequences (e.g., Alu repeats). The assay must be developed and validated for sensitivity and target-specificity. The FDA often requires a sensitivity of ≤ 50 copies per microgram of host DNA [1].
- Absolute Quantification: The quantity of the therapeutic agent in each sample is determined using a standard curve. For gene therapies, this reports the viral copy number per microgram of genomic DNA. For cell therapies, it quantifies the number of human cells distributed to animal organs [1].
Complementary and Emerging Techniques
While qPCR is a powerful and sensitive tool for quantifying DNA, it primarily confirms the physical presence of the therapeutic agent's genetic material. It does not directly confirm cell viability, protein expression, or functional activity. Therefore, a layered approach using complementary techniques is often necessary.
- Quantitative Reverse Transcription PCR (RT-qPCR): This technique is used for transgene expression profiling in tissues. It requires RNA isolation and converts RNA into cDNA, allowing for the quantification of mRNA expression levels, providing insight into whether the delivered genetic material is functionally active [1].
- Imaging Techniques: Modalities like in vivo fluorescence imaging (FLI) and bioluminescence imaging (BLI) offer real-time, non-invasive spatial data on cell location and persistence. These are invaluable for longitudinal studies within the same animal but may offer less quantitative granularity than qPCR [3].
- Mass Spectrometry (MS): MS-based assays can detect and quantify the therapeutic protein product encoded by the mRNA or transgene, moving beyond genetic material to assess functional output [3].
Table 2: Comparison of Biodistribution Assessment Techniques
| Technique | Measured Analyte | Key Advantages | Key Limitations |
|---|---|---|---|
| qPCR | DNA (Vector or human-specific) | High sensitivity, quantitative, gold standard, GLP-validatable. | Does not confirm cell viability or protein expression. |
| RT-qPCR | RNA (Transgene expression) | Assesses functional activity (transcription). | Does not confirm protein translation or function. |
| In Vivo Imaging | Light-emitting probes | Real-time, longitudinal, non-invasive, provides spatial context. | Lower resolution and quantitative precision compared to qPCR. |
| Mass Spectrometry | Protein product | Directly quantifies the functional protein product. | Complex method development; may have lower sensitivity for some targets. |
Comparative Analysis of Cell Therapy Products
Biodistribution profiles are not one-size-fits-all; they vary significantly between different types of CTPs. Understanding these differences is crucial for product development and regulatory strategy.
Adoptive T Cell Therapies vs. Stem Cell Therapies
Adoptive T cell therapies (such as CAR-T) and stem cell therapies (like MSCs) represent two major classes of CTPs with distinct biological functions and, consequently, different biodistribution fates. CAR-T cells are engineered to target specific antigens, ideally leading to their accumulation and expansion in tissues where that antigen is expressed, such as tumor sites [2]. In contrast, mesenchymal stem cells (MSCs) are often attracted to sites of inflammation and tissue injury, and a significant portion intravenously administered is often initially trapped in the lungs before redistributing to organs like the liver and spleen [1].
The persistence of these cells also differs markedly. CAR-T cells can persist for years in the host, leading to durable remissions, a phenomenon directly linked to their clinical efficacy [2]. MSCs, however, are often short-lived and may not engraft long-term, which can be a limitation for chronic conditions but may be sufficient for their primary mechanism of action via transient immunomodulation and paracrine signaling.
Impact of Administration Route
The route of administration is a critical factor shaping the biodistribution profile. The following diagram illustrates how different routes dictate the initial journey and eventual fate of a CTP within the body.
Diagram 2: Administration Route Impact
- Intravenous (IV) Injection: This leads to the most widespread distribution. Cells enter the systemic circulation, often resulting in initial accumulation in filtering organs like the lungs, liver, and spleen. This is common for CAR-T therapies targeting hematological malignancies [2] [1].
- Local/Intratumoral (IT) Injection: This route aims to maximize delivery to the target site (e.g., a solid tumor) while minimizing systemic exposure and off-target effects. However, some leakage into the circulation is often still detectable [2].
- Intraperitoneal (IP) Injection: This results in regional distribution within the peritoneal cavity, making it relevant for cancers like ovarian cancer. Cells may subsequently drain via the portal system to the liver [1].
Successfully conducting a biodistribution study requires a suite of specialized reagents and instruments. The following table details key solutions and their functions in a typical qPCR-based workflow.
Table 3: Key Research Reagent Solutions for Biodistribution Studies
| Tool / Reagent | Function in Biodistribution Studies |
|---|---|
| qPCR Instrument | Precisely amplifies and quantifies target DNA sequences in real-time. Instruments like the QuantStudio 6 Flex are capable of high-throughput 384-well analyses [1]. |
| Sequence-Specific Primers & Probes | Bind exclusively to the therapeutic vector's DNA or human-specific DNA sequences (e.g., Alu repeats), enabling specific detection of the CTP against the background of host animal DNA [1]. |
| DNA Standards for Quantification | Serially diluted plasmid DNA (for vector copies) or human cell DNA (for cell counts) used to generate a standard curve. This curve allows for the absolute quantification of the target in unknown samples [1]. |
| DNA/RNA Isolation Kits | Specialized kits for the efficient extraction of high-quality, inhibitor-free nucleic acids from a wide variety of tissue types and biological fluids [1]. |
| Animal Disease Models | Relevant in vivo models (e.g., immunodeficient mice for human cell tracking) that mimic the human disease state are crucial for generating clinically predictive biodistribution data [3]. |
Biodistribution studies provide an indispensable roadmap of CTP fate in the body, directly informing safety and efficacy from the lab to the clinic. A thorough understanding of regulatory guidelines, a strategic choice of sensitive and validated methodologies like qPCR, and the use of relevant animal models are all critical. As the CTP landscape expands into new territories, particularly solid tumors, the insights gained from sophisticated biodistribution assessments will be paramount in overcoming biological barriers, enhancing tumor penetration, and ultimately engineering the next generation of effective and safe "living drugs."
The development of advanced therapies, including cell and gene therapies, is a rapidly evolving field that presents unique regulatory challenges. Regulatory agencies worldwide have established specific frameworks to ensure the safety, quality, and efficacy of these innovative products while facilitating their development for serious conditions with unmet medical needs. The U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), and Japan's Pharmaceuticals and Medical Devices Agency (PMDA) represent three major regulatory systems with distinct yet increasingly convergent approaches to overseeing advanced therapy medicinal products (ATMPs). Understanding the similarities and differences among these frameworks is crucial for researchers, scientists, and drug development professionals working in the global landscape, particularly in critical areas like biodistribution assessment which directly informs product safety and biological activity.
The regulatory environment for these therapies continues to evolve rapidly. As of 2025, both the FDA and Japan have introduced significant updates to their regulatory guidance. The FDA has issued new draft guidance on expedited programs for regenerative medicine therapies, while Japan has amended its Act on the Safety of Regenerative Medicine to expand its scope to include in vivo gene therapy, with these changes taking effect in May 2025 [4] [5]. This dynamic regulatory landscape necessitates ongoing attention from researchers and developers in the field of cell and gene therapies.
Comparative Analysis of Regulatory Frameworks
Each regulatory agency operates within its distinct legal framework and utilizes specific terminology for advanced therapies. The FDA regulates these products as cellular and gene therapy (CGT) products under the Center for Biologics Evaluation and Research (CBER) [6]. The EMA classifies them as advanced therapy medicinal products (ATMPs), which include gene therapy medicines, somatic-cell therapy medicines, and tissue-engineered medicines [7] [8]. Japan's PMDA operates under a dual framework consisting of the Act on the Safety of Regenerative Medicine (ASRM), which governs the provision of regenerative medicine, and the Pharmaceuticals, Medical Devices, and Other Therapeutic Products Act (PMD Act), which regulates the commercialization of regenerative medical products [9]. Japan defines regenerative medical products as processed live human/animal cells (beyond minimal manipulation) intended for reconstruction/repair of body structures/functions or treatment/prevention of disease, plus gene therapy products (excluding prophylactic vaccines against infectious diseases) [9].
Table 1: Fundamental Regulatory Characteristics of FDA, EMA, and PMDA
| Characteristic | FDA (USA) | EMA (Europe) | PMDA (Japan) |
|---|---|---|---|
| Primary Legal Framework | Federal Food, Drug, and Cosmetic Act; Public Health Service Act | European Union Directives and Regulations | Act on the Safety of Regenerative Medicine (ASRM) & Pharmaceuticals and Medical Devices Act (PMD Act) |
| Product Category | Cellular and Gene Therapy (CGT) Products | Advanced Therapy Medicinal Products (ATMPs) | Regenerative Medical Products |
| Risk Classification | Case-based risk assessment | Case-based risk assessment | Three-tiered classification (Class I-III, with Class I highest risk) |
| Expedited Programs | Regenerative Medicine Advanced Therapy (RMAT) | Priority Medicines (PRIME) | Conditional/Time-limited Approval, Priority Review |
| Key Recent Updates | New draft guidances (2025) on expedited programs, innovative trial designs, and postapproval data collection [6] [5] | New multidisciplinary guideline on clinical-stage ATMPs effective July 2025 [10] | Amended ASRM effective May 2025, expanding scope to include in vivo gene therapy in Class I [4] |
Early-Phase Clinical Trial Design Considerations
The approach to early-phase clinical trials for advanced therapies reveals both convergence and unique regional emphases among the three agencies. A comparative analysis of guidelines reveals that all three agencies share common objectives for early-phase trials: safety evaluation, preliminary evidence of effectiveness gathering, and dose exploration [8]. The FDA additionally emphasizes feasibility assessment of the product administration process [8]. Regarding safety considerations specific to CGT products, the FDA provides the most detailed guidance, highlighting potential issues such as delayed infusion reactions, autoimmunity, graft failure, graft-versus-host disease (GvHD), new malignancies, transmission of infectious agents from a donor, and viral reactivation [8].
For monitoring and follow-up, both the FDA and EMA emphasize the need for long-term follow-up due to the potential for delayed adverse events. The FDA recommends at least one year or more of follow-up for each subject in early-phase trials, while the PMDA advises setting an appropriate follow-up period based on the type of gene therapy product, with specific mention that products with chromosomal integration vectors warrant particularly extended observation [8]. The FDA's 2025 draft guidance on "Innovative Designs for Clinical Trials of Cellular and Gene Therapy Products in Small Populations" further encourages flexibility in trial design for rare diseases, including the use of innovative designs comparing multiple investigational agents and the potential use of natural history data as historical controls when populations are adequately matched [11] [5].
Chemistry, Manufacturing, and Controls (CMC) Requirements
CMC requirements represent a critical component of advanced therapy development, with significant regulatory convergence but also important distinctions. The FDA generally adopts a graduated, phase-appropriate approach to Good Manufacturing Practice (GMP) compliance, with full verification typically occurring during pre-license inspection [10]. In contrast, the EMA's guideline on clinical-stage ATMPs emphasizes that GMP compliance is a prerequisite for clinical trials at both exploratory and pivotal stages, achieved partly through mandatory self-inspections [10].
For allogeneic donor eligibility determination, the FDA maintains more prescriptive requirements regarding donor screening and testing for infectious diseases, including specified tests, laboratory qualifications, and restrictions on pooling human cells or tissue from multiple donors [10]. The EMA acknowledges the importance of guarding against communicable disease transmission but provides more general guidance, reminding sponsors that requirements must comply with relevant EU and member state-specific legal requirements [10]. This divergence can create challenges for global developers using cellular starting materials obtained from donors screened under one jurisdiction's requirements for development in another region.
Table 2: Key CMC and Non-Clinical Requirements Across Agencies
| Requirement Area | FDA | EMA | PMDA |
|---|---|---|---|
| GMP Compliance | Phase-appropriate approach; verification at BLA stage | Prerequisite for clinical trials; mandatory self-inspections | Alignment with international standards; specific quality and safety guidelines |
| Donor Eligibility | Prescriptive requirements for screening and testing; restrictions on donor pooling | Compliance with EU and member state laws; general guidance on risk management | Detailed standards for biological raw materials; specific guidelines for different cell types |
| Potency Assurance | Dedicated guidance (2023) on demonstrating potency | Covered in overarching ATMP guidelines; product-specific requirements | Integrated into product-specific guidelines; focus on quantitative metrics |
| Biodistribution Assessment | Required as part of nonclinical assessment; long-term monitoring | ICH S12 guideline on nonclinical biodistribution | Required in nonclinical studies; tumorigenicity assessment for iPSC-derived products |
| Tumorigenicity Testing | Recommended for relevant cell types (e.g., pluripotent cells) | Addressed in reflection papers on stem cells and genetically modified cells | Detailed points to consider document for iPSC-based products |
Biodistribution Assessment in Regulatory Context
Regulatory Expectations for Biodistribution Studies
Biodistribution assessment represents a critical component of the nonclinical safety evaluation for advanced therapies, particularly within the context of comparative analysis across regulatory agencies. These studies are essential for understanding the migration, persistence, and fate of cellular products within the body, directly informing potential safety concerns such as ectopic tissue formation or unwanted engraftment [12]. The EMA has established a dedicated guideline (ICH S12) on nonclinical biodistribution considerations for gene therapy products, providing specific recommendations for these products [7]. While the FDA and PMDA may not have standalone biodistribution guidelines, they address these requirements within broader nonclinical guidance documents.
The PMDA has published specific "Points to consider" documents for efficient conduct of consultations on quality and safety from the early stages of development for both cellular and tissue-based products and gene therapy products [9]. These documents highlight the importance of biodistribution assessment, particularly for products with potential for widespread distribution or persistence. Furthermore, the PMDA emphasizes the need for tumorigenicity testing and genomic stability evaluation for human cell-based therapeutic products, especially those derived from induced pluripotent stem cells (iPSCs) [9]. The FDA's guidance on "Preclinical Assessment of Investigational Cellular and Gene Therapy Products" outlines similar expectations for biodistribution studies to support initial clinical trials.
Methodologies for Biodistribution Assessment
Regulatory agencies generally accept multiple methodological approaches for assessing biodistribution, with the choice dependent on product characteristics and scientific rationale. Commonly employed techniques include quantitative polymerase chain reaction (qPCR) for sensitive detection of cell-specific DNA sequences and imaging techniques such as positron emission tomography (PET) and magnetic resonance imaging (MRI) to monitor spatial distribution and persistence over time [12]. These methodologies enable researchers to track the movement and fate of administered cellular products in relevant animal models.
The design of biodistribution studies should incorporate multiple time points to understand both short-term trafficking and long-term persistence patterns. For products with potential for integration or genotoxic effects, longer duration studies may be necessary to assess potential risks. The selection of animal models should be scientifically justified, considering factors such as immunocompatibility with the human cell product and biological relevance to the intended clinical application. Immunodeficient animal models are often employed to permit engraftment and persistence of human cells, enabling more meaningful assessment of distribution patterns [12].
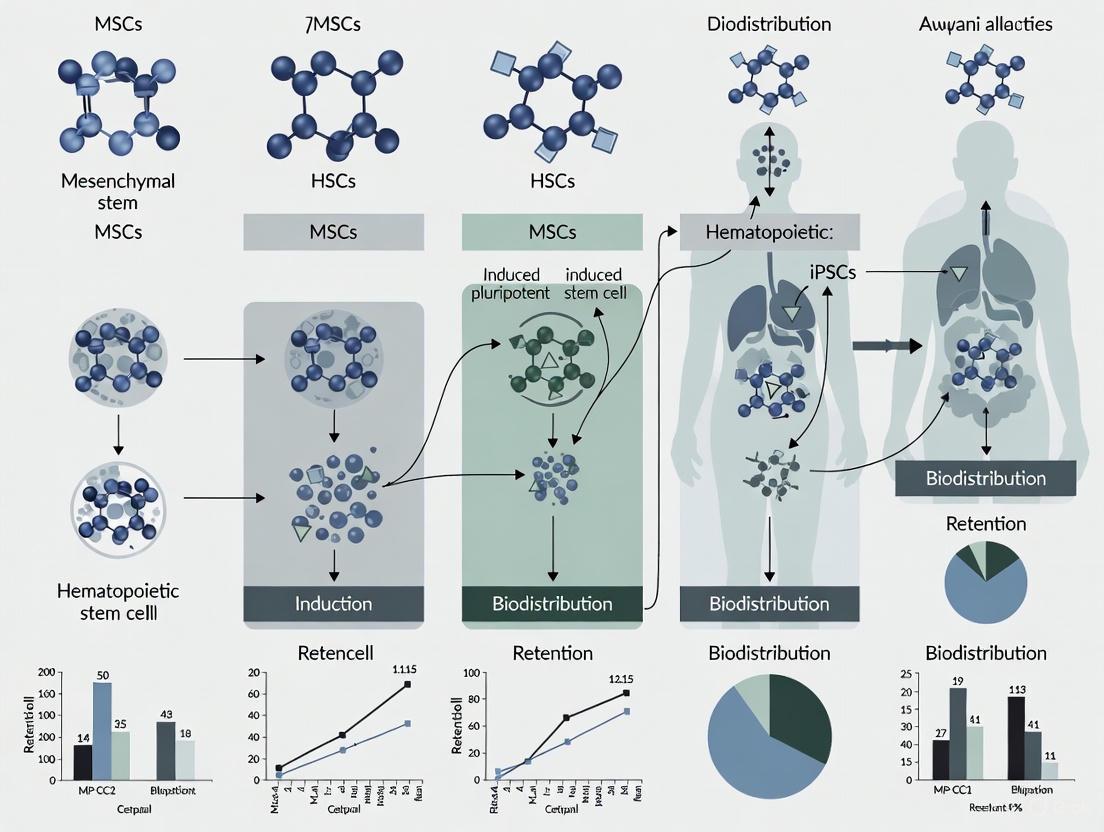
Figure 1: Biodistribution Assessment Workflow - This diagram illustrates the key stages in designing and conducting biodistribution studies for regulatory submissions, from initial model selection through data integration.
Comparative Analysis of Biodistribution Requirements
When comparing biodistribution requirements across regulatory agencies, a pattern of general alignment with regional nuances emerges. All three major agencies recognize the fundamental importance of understanding the in vivo distribution and persistence of cell-based products. However, the degree of specificity and emphasis on particular aspects may vary based on the product type and previous regulatory experience with similar modalities.
The FDA typically expects sponsors to provide comprehensive biodistribution data as part of the nonclinical package supporting initial clinical trials, with particular attention to products with potential for widespread distribution or targeting sensitive tissues. The EMA's ICH S12 guideline provides more detailed recommendations specific to gene therapy products, including considerations for vector shedding and environmental risk assessment [7]. Japan's PMDA incorporates biodistribution assessment within its broader framework for ensuring quality and safety of regenerative medical products, with specific considerations for products derived from iPSCs and other pluripotent cell sources [9]. For these higher-risk products, the PMDA emphasizes the need for thorough assessment of oncogenic potential and teratogenic effects, particularly when working with pluripotent cells that have the capacity to differentiate into various tissue types [12].
Essential Research Reagents and Methodologies
The conduct of robust biodistribution studies and other critical nonclinical assessments requires specialized research reagents and methodologies. The selection and validation of these tools are essential for generating reliable data acceptable to regulatory agencies. The following section outlines key components of the "scientist's toolkit" for biodistribution assessment and related safety studies, with particular relevance to comparative regulatory analysis.
Table 3: Essential Research Reagents and Methods for Biodistribution & Safety Assessment
| Reagent/Methodology | Primary Function | Regulatory Application | Considerations |
|---|---|---|---|
| Quantitative PCR (qPCR) | Sensitive detection of cell-specific DNA sequences to quantify biodistribution | Tracking and persistence of human cells in animal models; required by all agencies | Target human-specific sequences (e.g., Alu repeats); establish detection limits |
| Molecular Imaging Agents | Enable non-invasive monitoring of spatial and temporal distribution | Longitudinal assessment without sacrificing animals; accepted across agencies | Consider label stability, effect on cell viability/function |
| Immunodeficient Animal Models | Permit engraftment and persistence of human cells | Essential for meaningful biodistribution studies; used for all agencies | Select appropriate level of immunodeficiency; consider biological relevance |
| Flow Cytometry Reagents | Characterize cell identity, viability, and phenotypic changes | Product quality assessment; potency; immunogenicity evaluation | Validate antibody panels for specific cell types; include viability markers |
| Cytokine Analysis Kits | Quantify immune responses and inflammatory mediators | Immunogenicity assessment; safety pharmacology; required by all agencies | Multiplex platforms efficient for comprehensive profiling |
| Genomic Stability Assays | Detect chromosomal abnormalities and genetic changes | Tumorigenicity risk assessment; especially critical for PMDA for iPSC products | Karyotyping, FISH, CNV analysis; multiple methods recommended |
The selection of appropriate analytical methods should be guided by phase-appropriate validation principles, with increasing rigor required as product development advances. Regulatory agencies emphasize the importance of assay validation according to International Conference on Harmonisation (ICH) guidelines, including parameters such as accuracy, precision, linearity, range, specificity, and robustness [12]. For cell-specific assays, additional considerations include matrix effects from biological specimens and stability of cellular analytes under various storage and processing conditions. The implementation of quality-by-design principles in assay development helps ensure reproducible and reliable data across the product development lifecycle.
The comparative analysis of FDA, EMA, and PMDA guidelines for advanced therapies reveals a landscape of significant convergence with persistent regional distinctions. All three agencies have established specialized frameworks to address the unique challenges posed by cell and gene therapies, with particular attention to nonclinical safety assessment including biodistribution, tumorigenicity, and long-term monitoring. The ongoing revisions to regulatory guidelines across these jurisdictions demonstrate a responsive approach to the rapid scientific advancements in this field.
For researchers and drug development professionals, understanding both the commonalities and differences among these regulatory systems is essential for efficient global development strategy. Key areas of alignment include the general principles for biodistribution assessment, the importance of phase-appropriate product characterization, and the need for long-term follow-up to monitor delayed adverse events. Remaining differences in areas such as donor eligibility requirements and the timing of GMP compliance necessitate strategic planning for global development programs. As the field continues to evolve, ongoing regulatory convergence initiatives and increased international harmonization offer the promise of more efficient development pathways for these innovative therapies, potentially accelerating patient access to transformative treatments for serious conditions with unmet medical needs.
Biodistribution assessment is a cornerstone in the safety evaluation of cell-based therapies, providing critical insights into the travel and fate of therapeutic cells within a recipient's body. This distribution pattern is fundamentally linked to two paramount safety concerns: tumorigenicity and off-target effects. Tumorigenicity refers to the potential of administered cells to form abnormal growths, including teratomas or malignant tumors [12] [13]. Off-target effects, on the other hand, encompass unintended consequences in tissues other than the target organ, which can result from misplaced cell differentiation or inappropriate paracrine signaling [14]. For researchers and drug development professionals, understanding this link is not merely an academic exercise but a practical necessity for de-risking novel therapies. A therapy's biodistribution profile directly influences its risk blueprint; cells that migrate to or persist in sensitive anatomical compartments can pose significantly different safety challenges than those confined to the target site. This guide provides a comparative analysis of how different cell therapy platforms manage these interconnected risks, supported by experimental data and methodologies essential for robust preclinical safety assessment.
Comparative Analysis of Biodistribution-Linked Risks Across Cell Therapy Platforms
The inherent biological properties of different cell types dictate their biodistribution after administration and, consequently, their unique risk profiles. The table below provides a structured comparison of major cell therapy classes, highlighting how their distribution patterns correlate with specific safety concerns.
Table 1: Comparative Biodistribution and Linked Critical Risks of Cell Therapies
| Cell Therapy Platform | Primary Biodistribution Pattern | Linked Tumorigenicity Risk | Linked Off-Target/Immunogenicity Risk | Supporting Evidence Summary |
|---|---|---|---|---|
| Pluripotent Stem Cells (iPSCs/ESCs) | Widespread dissemination possible; potential for ectopic engraftment in organs like liver, spleen, and gonads [12]. | High due to potential residual undifferentiated cells with uncontrolled proliferative capacity [13]. | Risk of aberrant differentiation in non-target tissues (teratogenicity) [12]. | |
| Mesenchymal Stem/Stromal Cells (MSCs) | Often initially trapped in lungs post-IV injection; can home to sites of inflammation or injury [12]. | Low to Moderate; some reports of spontaneous transformation in long-term cultures, but generally considered low risk [12]. | Potential for off-target immunomodulation; may support tumor growth in microenvironment [12]. | |
| CAR-T Cells | Predominantly in lymphoid tissues, bone marrow, and sites of target antigen expression (e.g., tumors) [15]. | Low (Direct) but emerging concern for secondary T-cell cancers potentially linked to viral vector integration [15]. | High (On-target, off-tumor) toxicity if target antigen is expressed on healthy tissues [15]. | |
| Hematopoietic Stem Cells (HSCs) | Primary engraftment in bone marrow niche following intravenous infusion [12]. | Low for properly differentiated and characterized products. | Graft-versus-host disease (GvHD) from allogeneic transplants is a major immunogenic risk [12]. |
Essential Experimental Methodologies for Risk Assessment
A thorough investigation of the biodistribution-tumorigenicity axis requires a suite of complementary experimental protocols. The following section details key methodologies cited in recent literature and regulatory guidelines.
Quantitative Biodistribution Assessment
Objective: To quantitatively track the movement, persistence, and accumulation of therapeutic cells in target and non-target tissues over a defined period.
Protocol Details:
- Technology: Quantitative Polymerase Chain Reaction (qPCR) is a gold standard, especially for human-specific Alu sequences or other unique genetic markers in animal models [12].
- Procedure:
- Administration: The cell therapy product is administered to immunocompromised animal models (e.g., NSG mice) via the intended clinical route (e.g., intravenous, intramuscular).
- Tissue Collection: At predetermined timepoints (e.g., 24 hours, 1 week, 1 month, 3 months), animals are euthanized, and a comprehensive panel of organs (e.g., liver, lungs, spleen, gonads, brain, and injection site) is harvested.
- DNA Extraction: Genomic DNA is isolated from each tissue sample using validated kits.
- qPCR Analysis: DNA samples are analyzed via qPCR using primers and probes specific to the human genetic marker. A standard curve is generated from known quantities of the cell product to allow absolute quantification.
- Data Expression: Results are typically reported as vector genomes or cell equivalents per microgram of total DNA [12].
Supporting Imaging Techniques:
- Bioluminescence Imaging (BLI): Requires cells engineered to express luciferase. After injection of the substrate (e.g., D-luciferin), light emission is captured, providing a semi-quantitative, whole-body view of cell location and viability over time [12].
- Positron Emission Tomography (PET) / Magnetic Resonance Imaging (MRI): Used for deeper tissue imaging. Cells can be labeled with radioactive tracers (e.g., [18F]FDG for PET) or superparamagnetic iron oxide particles (for MRI) to monitor their homing and distribution non-invasively [12] [16].
Tumorigenicity and Oncogenicity Testing
Objective: To evaluate the potential of the cell product to form tumors in vivo, either from overgrowth or from malignant transformation.
Protocol Details:
- In Vivo Models: The most definitive assessments require long-term studies in immunodeficient animals with compromised abilities to reject human cells (e.g., NOD-scid IL2Rγnull mice) [12] [13].
- Study Design:
- Groups: Animals are divided into at least three groups: test article (the cell therapy product), a negative control (e.g., fully differentiated cells), and a positive control (e.g., undifferentiated pluripotent cells known to form teratomas).
- Administration: Cells are implanted at a high dose, often via a route that ensures high local concentration, such as subcutaneous or intramuscular injection.
- Observation Period: Animals are monitored for an extended period, typically 6-12 months, for palpable mass formation or signs of ill health.
- Necropsy and Histopathology: A full necropsy is performed. Tissues are examined grossly and microscopically (histopathology) for evidence of tumor formation. Suspected tumors are analyzed to determine their cell origin (host vs. donor) and histological type [13].
Supporting In Vitro Assays:
- Soft Agar Colony Formation Assay: Tests for anchorage-independent growth, a hallmark of cellular transformation.
- Karyotyping and Genomic Stability Analysis: Identifies chromosomal abnormalities that could predispose cells to tumorigenicity [12].
Investigating Off-Target Effects and Immunogenicity
Objective: To identify unintended biological consequences in non-target tissues and assess immune responses triggered by the therapy.
Protocol Details:
- For Off-Target Toxicity:
- Clinical Observations: Animals in biodistribution and tumorigenicity studies are closely monitored for behavioral changes, weight loss, and other signs of toxicity.
- Clinical Pathology: Blood samples are analyzed for hematology and clinical chemistry parameters (e.g., liver enzymes like ALT and AST, kidney markers like creatinine and BUN) to detect organ dysfunction [12].
- Histopathology: A comprehensive histological examination of all major organs is conducted to identify any cellular damage, inflammation, or abnormal tissue architecture not related to tumor formation [12].
- For Immunogenicity:
- Cytokine Profiling: Serum or plasma is analyzed using multiplex immunoassays (e.g., Luminex) to measure levels of cytokines (e.g., IL-6, IFN-γ) associated with immune activation, such as Cytokine Release Syndrome (CRS) [14].
- Immune Cell Phenotyping: Flow cytometry is performed on blood or tissue samples to characterize immune cell populations (e.g., T-cells, NK cells, macrophages) and their activation states in response to the therapy [12].
Figure 1: Integrated experimental workflow for assessing biodistribution-linked critical risks, showing the parallel evaluation pathways that feed into a comprehensive risk assessment.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful execution of the aforementioned experimental protocols relies on a suite of specialized reagents and tools. The table below catalogs essential solutions for researchers in this field.
Table 2: Essential Research Reagents for Biodistribution and Risk Assessment Studies
| Research Reagent / Solution | Primary Function | Key Considerations for Selection |
|---|---|---|
| Immunodeficient Mouse Models (e.g., NSG, NOG) | In vivo host for human cell engraftment and tumorigenicity studies. | Degree of immunodeficiency (T, B, NK cell deficiency), lifespan, cost, and susceptibility to radiation. |
| qPCR Kits for Human-Specific Sequences (e.g., Alu, LINE-1) | Quantitative biodistribution analysis in animal tissues. | Specificity for human DNA, sensitivity (limit of detection), and efficiency on complex tissue lysates. |
| Bioluminescence/Luciferase Reporter Systems | Non-invasive, longitudinal tracking of cell fate in vivo. | Signal brightness, stability in cell type, potential immunogenicity in immunocompetent models. |
| MRI Contrast Agents (e.g., SPIO nanoparticles) | Deep-tissue anatomical imaging and cell tracking via MRI. | Biocompatibility, labeling efficiency, persistence in cells, and potential impact on cell function. |
| Flow Cytometry Antibody Panels | Immunophenotyping of donor and host immune cells. | Multiplexing capability, host (e.g., mouse) cross-reactivity, and specificity for activation markers. |
| Cytokine Multiplex Assays | Profiling a broad spectrum of inflammatory mediators in serum/plasma. | Number of analytes, dynamic range, sample volume requirements, and species specificity. |
The relationship between biodistribution and critical safety risks is a fundamental aspect of cell therapy development that cannot be overlooked. As the data and methodologies outlined in this guide demonstrate, a proactive and integrated safety assessment strategy is paramount. This involves employing quantitative biodistribution studies (e.g., qPCR, imaging) in tandem with sensitive tumorigenicity assays and comprehensive off-target effect analyses from the earliest stages of product development. The field is evolving towards more predictive tools, including AI-driven safety modeling and advanced molecular assays for detecting genotoxicity [14] [17]. Furthermore, regulatory expectations are intensifying globally, emphasizing the need for standardized, rigorous approaches to these evaluations [13] [17]. For researchers, mastering the link between where cells go and what risks they may pose is not just about ensuring regulatory approval; it is about building a solid scientific foundation for the next generation of safe and effective cell therapies.
In the field of cell therapy, successful treatment outcomes hinge on the dynamic behaviors of administered therapeutic cells. Survival, engraftment, proliferation, and migration represent four fundamental parameters that collectively determine the efficacy and safety of cell-based therapies. These interconnected processes govern the journey of therapeutic cells from administration to functional integration within target tissues. A comprehensive understanding of these parameters enables researchers to optimize therapeutic protocols, predict clinical outcomes, and design more effective cell therapy products. This guide provides a comparative analysis of these essential parameters across different cell types, supported by experimental data and methodological insights crucial for drug development professionals.
Parameter Definitions and Biological Significance
Cell Survival
Cell survival refers to the viability and persistence of administered therapeutic cells in the host environment following transplantation. This parameter is crucial because acute donor cell death significantly limits therapeutic efficacy across multiple cell types [18]. The survival capacity varies substantially between cell types, with studies showing that within the first 3 weeks post-transplantation, mesenchymal stem cells (MSCs), skeletal myoblasts (SkMb), and fibroblasts (Fibro) experience significant cell death, while bone marrow mononuclear cells (MN) demonstrate more favorable survival patterns [18]. For MSCs specifically, studies in fibrotic liver models show that a large number die within 1 day after transplantation, with surviving cells nearly completely disappearing within 11 days [19]. Improving cell survival remains a primary focus in cell therapy optimization, as survival rates directly impact the number of cells available for engraftment and subsequent therapeutic functions.
Engraftment
Engraftment describes the process by which transplanted cells integrate structurally and functionally into the host tissue, establishing a stable presence. This parameter is distinct from mere survival as it involves successful incorporation into the tissue architecture. Engraftment efficiency is closely tied to cell survival, as only surviving cells can successfully engraft [19]. Research indicates that engraftment plateaus can occur at higher transplantation doses, where the total number of engrafted human cells never exceeds the initial dose, suggesting that donor cell expansion is inversely regulated by target niche parameters and/or transplantation density [20]. The relationship between administration route and engraftment efficiency is particularly important in systemic delivery, where cells must navigate through the circulation to reach target tissues.
Proliferation
Proliferation encompasses the capacity of transplanted cells to divide and expand their population after administration. This parameter is critical for achieving sufficient cell numbers to exert therapeutic effects, especially when initial engraftment numbers are low. However, studies have revealed an inverse correlation between transplantation dose and donor cell proliferation, suggesting that proliferation is tightly regulated by microenvironmental factors and niche availability [20]. Regardless of transplantation dose, research on human neural stem cells indicates that only a small proportion of transplanted cells remain mitotic after engraftment [20]. This highlights the complex balance between achieving therapeutic cell numbers and avoiding uncontrolled expansion that could lead to tumorigenicity.
Migration
Migration refers to the directed movement of transplanted cells from the administration site to target tissues, a process particularly crucial for systemically administered therapies. Also described as "homing," this parameter involves a coordinated multi-step process similar to leukocyte migration to inflammatory sites [19]. The migration process can be divided into distinct phases: rolling, activation, adhesion, crawling, and transendothelial migration [19]. Different cell types utilize various molecular mechanisms for migration; for instance, MSC rolling is facilitated by CD24 as a P-selectin ligand and CD29/VCAM-1 interactions with liver sinusoidal endothelial cells [19]. Effective migration ensures that sufficient numbers of therapeutic cells reach the intended site of injury or disease to exert their beneficial effects.
Comparative Analysis Across Cell Types
Table 1: Comparative Performance of Different Cell Types in Cardiac Therapy Models
| Cell Type | Survival Pattern | Engraftment Efficiency | Proliferation Capacity | Migration/Homing | Functional Outcome |
|---|---|---|---|---|---|
| Bone Marrow Mononuclear Cells (MN) | Significantly better; cardiac signals present at 6 weeks [18] | Favorable; confirmed by TaqMan PCR [18] | Not specifically reported | Not specifically reported | Significant preservation of fractional shortening, least ventricular dilatation [18] |
| Mesenchymal Stem Cells (MSC) | Significant death within 3 weeks [18] | Limited by poor survival [18] | Not specifically reported | Depends on CD29/VCAM-1 interactions [19] | Less robust functional preservation compared to MN [18] |
| Skeletal Myoblasts (SkMb) | Significant death within 3 weeks [18] | Limited by poor survival [18] | Can proliferate but risk of uncontrolled growth [21] | Not specifically reported | Limited functional preservation [18] |
| Fibroblasts (Fibro) | Significant death within 3 weeks [18] | Limited by poor survival [18] | Not specifically reported | Not specifically reported | Limited functional preservation [18] |
| Neural Stem Cells (NSC) | Varies with transplantation niche [20] | Plateaus at higher doses [20] | Inversely correlated with transplantation dose [20] | Not specifically reported | Not specifically reported |
Table 2: Key Molecular Mechanisms Governing Cell Behavior
| Parameter | Critical Molecular Mediators | Function in Cell Therapy |
|---|---|---|
| Survival | Oxidative stress resistance pathways [19] | Determines initial cell retention and persistence |
| Engraftment | Integrins, adhesion molecules [19] | Enables structural integration into host tissue |
| Proliferation | Mitotic signaling pathways [20] | Controls population expansion post-transplantation |
| Migration/Homing | Selectins (P-selectin), chemokine receptors (CXCR4), adhesion molecules (VCAM-1/CD29) [19] | Directs cells to target tissues following systemic administration |
Methodologies for Assessment
Tracking Cell Survival
- Bioluminescence Imaging (BLI): Non-invasive, quantitative method using firefly luciferase (Fluc) reporter genes; validated with strong correlation between Fluc expression and cell number (r² > 0.93) [18]
- TaqMan PCR: Ex vivo quantification using species-specific or sex-specific genetic markers (e.g., male-derived cells in female recipients via Sry gene detection) [18]
- Reporter Gene Imaging: Includes bioluminescence and fluorescence proteins for repetitive, non-invasive monitoring of cell viability [22]
Assessing Engraftment and Proliferation
- Droplet Digital PCR: Highly sensitive method for quantifying donor cell presence in host tissues; validated for biodistribution studies [23]
- Histological Analysis: Direct visualization of engrafted cells in tissue sections using immunohistochemistry or fluorescence tagging [18]
- Quantitative PCR (qPCR): Standard regulatory-recommended method for biodistribution studies; can detect ≤50 copies/μg host DNA [24] [25]
Monitoring Migration and Biodistribution
- Radionuclide Imaging (PET/SPECT): High sensitivity tracking using 111In-oxyquinoline or 99mTc-labeled cells; allows clinical translation [22]
- Magnetic Resonance Imaging (MRI): Uses superparamagnetic iron oxide particles for anatomical localization; suitable for 3D imaging [22]
- Spatial Multiomics: Emerging technology enabling detection of multiple RNA and protein targets simultaneously in tissue sections; useful for characterizing migratory cells [26]
Visualizing the Integrated Cell Journey
The following diagram illustrates the sequential relationship between the four key parameters in determining ultimate therapy efficacy:
Diagram 1: The sequential relationship between key parameters in cell therapy efficacy. The journey begins with cell survival and migration, which enable engraftment, creating a foundation for proliferation that collectively determines therapeutic efficacy.
Research Reagent Solutions
Table 3: Essential Research Tools for Parameter Assessment
| Reagent/Technology | Primary Application | Key Features |
|---|---|---|
| Firefly Luciferase (Fluc)/GFP Reporter System [18] | Longitudinal survival tracking | Enables non-invasive bioluminescence imaging and histological validation |
| Droplet Digital PCR [23] | Sensitive biodistribution quantification | Absolute quantification without standard curves; high precision |
| Quantitative PCR (qPCR) [24] [25] | Biodistribution and engraftment assessment | Regulatory-accepted; detects low copy numbers (≤50 copies/μg DNA) |
| Superparamagnetic Iron Oxide Particles [22] | MRI-based cell tracking | Suitable for 3D anatomical localization; low concentration detection |
| Radionuclide Tracers (111In-oxine, 99mTc) [22] | Clinical cell tracking | High sensitivity; clinically translatable |
| RNAscope Multiomic LS Assay [26] | Spatial characterization of migrated cells | Multiplex RNA/protein detection in tissue sections |
The comparative analysis of survival, engraftment, proliferation, and migration across different cell types reveals distinct advantages and limitations that inform therapeutic applications. Bone marrow mononuclear cells demonstrate superior survival characteristics translating to enhanced functional preservation in cardiac models, while other cell types face significant attrition barriers. The inverse relationship between transplantation dose and proliferation observed in neural stem cells highlights the complex regulation of cell expansion post-administration. Effective migration relies on conserved molecular mechanisms including selectin-mediated rolling and chemokine-directed activation. The integrated assessment of these four parameters through advanced imaging, molecular, and spatial technologies provides the comprehensive understanding necessary to optimize cell therapy products and predict their clinical behavior. As the field advances, strategies to enhance cell survival and direct migratory potential will be crucial for maximizing therapeutic efficacy across diverse medical applications.
Analytical Toolkits for Biodistribution: From qPCR to Advanced Imaging
Evaluating the biodistribution (BD) of cell therapy products (CTPs) is a critical component of non-clinical safety and efficacy assessment. BD data clarify cell survival time, engraftment, and distribution sites after administration, providing vital insights for predicting clinical outcomes [27]. Among the techniques available for this purpose, quantitative polymerase chain reaction (qPCR) and droplet digital PCR (ddPCR) have emerged as powerful tools for the sensitive detection and quantification of nucleic acids from administered CTPs within host tissues. These molecular biology tools are employed throughout the development pipeline, from preclinical bio-distribution studies for gene therapies to corresponding clinical development such as shedding and cellular kinetics [28]. This guide provides an objective comparison of qPCR and ddPCR performance, supported by experimental data relevant to biodistribution assessment.
Quantitative PCR (qPCR)
Quantitative PCR (qPCR), also known as real-time PCR, has been the gold standard for nucleic acid detection and quantification for years. It is a relative quantification method that monitors the amplification of a target DNA sequence in real time using fluorescent reporters. The quantification cycle (Cq) at which the fluorescence crosses a threshold is used, in conjunction with a standard curve, to determine the initial template concentration [29]. This method is valued for its speed, sensitivity, ease of use, and well-established guidelines.
Droplet Digital PCR (ddPCR)
Droplet Digital PCR (ddPCR) is a more recent technology that provides absolute quantification of nucleic acid molecules without the need for a standard curve. The reaction mixture is partitioned into thousands of nanoliter-sized droplets, and PCR amplification occurs within each individual droplet. After endpoint PCR, droplets are analyzed to count the positive and negative reactions, allowing for absolute quantification of the target molecule using Poisson statistics [30] [31]. This partitioning makes ddPCR less susceptible to PCR inhibitors and capable of higher precision, especially for low-abundance targets [29].
Direct Performance Comparison: Experimental Data
Multiple studies have directly compared the performance of qPCR and ddPCR, providing robust data to inform platform selection. The table below summarizes key performance characteristics based on empirical evidence.
Table 1: Experimental Performance Comparison of qPCR and ddPCR
| Performance Characteristic | qPCR | Droplet Digital PCR | Supporting Experimental Context |
|---|---|---|---|
| Quantification Method | Relative (ΔΔCq); requires standard curve [29] | Absolute (copies per μL); no standard curve [29] [30] | Fundamental operational difference |
| Detection Sensitivity | Best for moderate-to-high abundance targets (Cq < 30-35) [29] | Superior for low-abundance targets (down to ~0.5 copies/μL) [29] [31] | LOD for ndPCR: 0.39 copies/μL; ddPCR: 0.17 copies/μL [31] |
| Precision | Good for mid/high expression levels (>twofold changes) [29] | Higher precision; reliable detection of <1.5-fold changes [29] | CVs for ddPCR: 6-13%; qPCR: generally higher for low-abundance targets [31] |
| Accuracy in BD Studies | Accurate within a dynamic range, but relative | High accuracy for absolute copy number | In vitro BD validation showed accuracy (relative error) generally within ±50% for both [27] |
| Impact of Inhibitors | Susceptible; may require extra optimization [29] | More resilient due to endpoint analysis [29] | dPCR is less affected by PCR inhibitors in complex matrices like respiratory samples [32] |
| Multiplexing Capability | Requires validation for matched amplification efficiency [29] | Simplified multiplex development; minimal optimization [29] | Both platforms demonstrated robust performance in singleplex and multiplex formats [29] |
Further data from a gene expression study highlights ddPCR's advantage in detecting subtle changes. When measuring the low-abundance target BCL2, qPCR did not identify a statistically significant fold change, whereas ddPCR resolved a significant 2.07-fold difference with tighter error bars, demonstrating greater precision and sensitivity [29].
In the critical context of biodistribution, a multi-facility study demonstrated that both qPCR and ddPCR are fit-for-purpose. The study, which used the primate-specific Alu gene to track human mesenchymal stem cells (hMSCs) in immunodeficient mice, found that both methods exhibited similar accuracy (relative error generally within ±50%) and precision (coefficient of variation generally less than 50%). The resulting tissue distribution profiles were consistent across all facilities, identifying the lungs as the site of highest cell distribution [27].
Experimental Protocols for Biodistribution Analysis
The following workflow outlines a typical protocol for a biodistribution study of human cells in a mouse model using qPCR and ddPCR. This methodology is adapted from a study that successfully compared both techniques across multiple facilities [27].
Detailed Methodology
1. In Vivo Administration and Sample Collection:
- Animal Model: Immunodeficient mice are commonly used in non-clinical tumorigenicity and biodistribution studies to prevent rejection of human-derived CTPs [27].
- Cell Administration: A known number of human mesenchymal stem cells (hMSCs) or other CTPs are administered via a defined route (e.g., intravenous) [27].
- Tissue Harvest: At predetermined time points post-administration (e.g., 1, 4, and 24 hours), target tissues (e.g., lungs, liver, spleen, gonads) are collected. All tissues should be snap-frozen or preserved appropriately to prevent nucleic acid degradation.
2. Nucleic Acid Extraction:
- Homogenization: Tissues are homogenized in lysis buffer using bead-beating or other mechanical methods to ensure complete cell disruption.
- DNA Extraction: Genomic DNA is purified from the homogenates using commercial kits (e.g., MagMax Viral/Pathogen kit on a KingFisher Flex system) [32]. The extraction should include an RNase step if quantifying DNA targets. The quality and concentration of the extracted DNA should be assessed via spectrophotometry or fluorometry.
3. Assay Setup and Partitioning:
- Primer/Probe Design: Assays must be specific to the administered CTP and not cross-react with the host's genome. A common approach is to target a species-specific sequence, such as the primate-specific Alu gene for human cells in a rodent background [27]. Software is typically used for design, focusing on creating primers/probes that span a unique modification junction for maximum specificity.
- Reaction Setup:
- For qPCR, the reaction mix contains DNA template, primer-probe mix, and a master mix suitable for real-time PCR. The mix is loaded directly into a qPCR plate.
- For ddPCR, an analogous reaction mix is prepared. This mix is then loaded into a droplet generator (e.g., Bio-Rad's QX200) which partitions the sample into ~20,000 nanoliter-sized droplets, or into a nanoplate-based system (e.g., QIAGEN's QIAcuity) [32] [31].
4. Amplification and Analysis:
- Amplification:
- qPCR is run on a real-time thermocycler (e.g., Bio-Rad CFX Opus). The amplification is monitored in real-time, and Cq values are determined by the instrument's software [29].
- ddPCR involves endpoint PCR on a thermal cycler. After cycling, the plate or droplets are transferred to a reader that counts the positive and negative partitions [31].
- Quantification and Normalization:
- qPCR relies on a standard curve, created from serially diluted samples with known copy numbers, to convert Cq values into relative quantities. Data are often normalized to a reference gene [29].
- ddPCR uses Poisson statistics to calculate the absolute concentration in copies per microliter of input directly from the fraction of positive partitions, without a standard curve [30]. Results can be reported as copies per microgram of total DNA to normalize for tissue input differences.
Essential Research Reagent Solutions
The table below details key reagents and materials required for implementing these assays, particularly in a biodistribution context.
Table 2: Key Research Reagents and Materials for qPCR/ddPCR Biodistribution Studies
| Reagent / Material | Function / Description | Example Products / Targets |
|---|---|---|
| Species-Specific Primers/Probes | Enables specific detection of administered CTPs in a host background by targeting unique genomic sequences. | Primate-specific Alu sequence for human cells in mouse tissues [27] |
| Nucleic Acid Extraction Kits | For purification of high-quality, inhibitor-free DNA from complex tissue matrices; critical for assay robustness. | MagMax Viral/Pathogen kit (Thermo Fisher) [32]; High Pure Viral Nucleic Acid Kit (Roche) [33] |
| PCR Master Mixes | Optimized buffers, enzymes, and dNTPs tailored for either qPCR or ddPCR workflows. | Bio-Rad ddPCR Supermix; QIAGEN QIAcuity Probe PCR Kit; various RT-qPCR buffers [29] [33] |
| Digital PCR Partitioning Systems | Creates thousands of individual reactions for absolute quantification. | Droplet-based (Bio-Rad QX200); Nanoplate-based (QIAGEN QIAcuity) [32] [31] |
| Reference Gene Assays | Used for normalization in qPCR to account for variations in DNA input and extraction efficiency. | Pre-optimized assays for genes like ACTB, PGK1 (e.g., Bio-Rad PrimePCR Reference Gene Panel) [29] |
| Positive Control Templates | Synthetic DNA or plasmid containing the target sequence, used for standard curves (qPCR) and assay validation. | Synthesized DNA fragments [30]; Plasmid DNA controls |
The choice between qPCR and ddPCR for biodistribution studies is not a matter of one being universally superior, but rather of selecting the right tool for the specific experimental question and context.
- qPCR remains a powerful and efficient choice for moderate-to-high abundance targets where sample throughput and established workflows are priorities. Its reliance on a standard curve is manageable when suitable reference materials are available [29].
- ddPCR offers distinct advantages for applications requiring absolute quantification, high precision for low-abundance targets, or detection of subtle fold-changes (e.g., less than two-fold). Its resilience to inhibitors and simplified multiplexing are significant benefits when working with complex tissue samples [29] [30].
For cell therapy biodistribution, where quantifying low levels of engraftment in distant tissues is often the goal, ddPCR's superior sensitivity and precision make it an increasingly attractive platform. However, as demonstrated in multi-facility studies, both methods can generate reliable and comparable biodistribution profiles when properly validated [27]. The decision should be guided by the required level of sensitivity, the available sample quantity and quality, and the specific regulatory and project needs.
The development of effective cell therapies hinges on the ability to non-invasively monitor the fate of administered cells in living subjects. Biodistribution studies, which track the journey, persistence, and localization of therapeutic cells, are essential for predicting and assessing both the efficacy and toxicity of Cell Therapy Products (CTPs) [24]. Without this capability, the post-administration phase becomes a "black box," making it difficult to understand inconsistent clinical results, optimize delivery methods, or determine why some patients respond to treatment while others do not [34] [35]. Molecular imaging provides a powerful solution to this challenge by enabling the real-time, quantitative tracking of cells in vivo. This guide objectively compares the performance of four primary imaging modalities—PET, SPECT, MRI, and Optical Imaging—within the context of comparative biodistribution assessment for cell therapy research.
Comparative Analysis of Imaging Modalities
The table below provides a quantitative comparison of the key technical and performance characteristics of each imaging modality for cell tracking.
Table 1: Performance Comparison of In Vivo Imaging Modalities for Cell Tracking
| Modality | Spatial Resolution | Detection Sensitivity | Tissue Penetration | Quantitative Ability | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|---|
| PET | 1-2 mm [34] | High (picomolar) [36] | Unlimited | Excellent, absolute quantification possible [37] | Whole-body scanning, high sensitivity, quantifiable, clinically translatable [36] | Radiation exposure, requires cyclotron, lower spatial resolution than MRI [38] |
| SPECT | 1-2 mm [34] | High (picomolar) [36] | Unlimited | Good | Multiple probe imaging, clinically translatable [36] | Radiation exposure, generally lower resolution and sensitivity than PET [39] |
| MRI | 25-100 µm [40] | Low (micromolar); requires 10³ - 10⁴ cells [40] | Unlimited | Challenging for direct labels | Excellent soft-tissue contrast, high spatial resolution, anatomical and functional data [40] | Low sensitivity for cell detection, potential contrast agent artifacts, contraindicated for patients with implants [34] |
| Optical Imaging | 2-3 mm [36] | High (nanomolar for fluorescence) [36] | Limited (1-2 cm) [22] | Semi-quantitative | High throughput, low cost, versatile probe options [36] | Limited tissue penetration, significant light scatter, primarily preclinical use [22] [36] |
Experimental Protocols for Cell Tracking
Understanding the practical implementation of each modality is crucial for experimental design. The following section details standard methodologies for labeling and tracking cells in vivo.
Radionuclide Imaging (PET/SPECT)
Radionuclide imaging uses radioactive isotopes to label cells, allowing for highly sensitive detection after administration.
Cell Labeling Protocol (Direct Labeling):
- Isolate and culture the therapeutic cells of interest (e.g., T cells, mesenchymal stem cells).
- Incubate cells with the radiotracer in a buffered solution. Common tracers include:
- Wash cells thoroughly to remove unincorporated radioactivity.
- Resuspend in administration medium and validate cell viability and function post-labeling.
In Vivo Tracking:
- Administer labeled cells to the subject via the chosen route (e.g., intravenous, intracoronary).
- Image at multiple time points using a PET or SPECT scanner, often co-registered with CT for anatomical reference.
- Key Data Output: Quantification of percentage injected dose (%ID) retained in target tissues (e.g., 4.7% of injected endothelial progenitor cells in infarcted myocardium [34]) and longitudinal biodistribution maps.
Magnetic Resonance Imaging (MRI)
MRI tracks cells by detecting contrast agents that alter the magnetic properties of water protons in tissues.
Cell Labeling Protocol (Direct Labeling with SPIOs):
- Isolate and culture target cells.
- Introduce contrast agents via co-incubation, often with transfection agents to boost uptake. Common agents are:
- Wash and resuspend cells for administration.
In Vivo Tracking:
- Image subjects using T2/T2*-weighted sequences for SPIO-labeled cells. The "blooming artifact" of the dark signal amplifies detectability, allowing for the visualization of as few as 10³ cells [40].
- Key Data Output: High-resolution 3D anatomical maps showing the location of cell clusters as hypointense signal regions. The number of cells required for detection is typically higher than for nuclear methods (e.g., 10⁷ to 10⁸ for confident detection in swine hearts [34]).
Optical Imaging
Optical imaging uses light-emitting probes to track cells, but its use in humans is limited by tissue penetration.
Cell Labeling Protocol:
- Label cells ex vivo using one of two primary methods:
- Fluorescent Dyes (e.g., DiR, Cy5.5): Cells are incubated with lipophilic dyes that incorporate into cell membranes [36].
- Reporter Genes (e.g., Firefly Luciferase): Cells are genetically engineered to express light-producing enzymes. The substrate (e.g., D-luciferin) is administered systemically before imaging [22].
- Wash and administer the labeled cells.
- Label cells ex vivo using one of two primary methods:
In Vivo Tracking:
- For fluorescence imaging, illuminate the subject at the specific excitation wavelength and detect the emitted light. Near-infrared (NIR) dyes are preferred for deeper tissue penetration [36].
- For bioluminescence imaging, administer the substrate and detect the resulting bioluminescent signal without the need for excitation light, resulting in very low background [36].
- Key Data Output: 2D images showing relative signal intensity, which can be quantified as photons/second or radiant efficiency to estimate cell location and number, albeit with limited depth information.
The following diagram illustrates the core experimental workflow for labeling and tracking cells, which is common across modalities, while highlighting specific agent-modality pairings.
The Scientist's Toolkit: Essential Research Reagents
Successful cell tracking experiments rely on a suite of specialized reagents and materials. The table below lists key solutions and their functions in the context of biodistribution studies.
Table 2: Key Research Reagent Solutions for Cell Tracking Experiments
| Reagent/Material | Function in Cell Tracking | Examples & Notes |
|---|---|---|
| Superparamagnetic Iron Oxide (SPIO) | MRI contrast agent for direct cell labeling; creates negative contrast. | Feridex; high sensitivity but causes "blooming" artifact on images [34] [40]. |
| Radionuclide Tracers | Direct cell labeling for PET/SPECT imaging; provides high detection sensitivity. | [¹¹¹In]Oxyquinoline, ⁹⁹mTc-HMPAO, ¹⁸F-FDG; potential radiotoxic effects on cell function must be assessed [34] [22]. |
| Reporter Genes | Genetic constructs for indirect, long-term cell labeling; signal correlates with cell number/viability. | Firefly Luciferase (bioluminescence), Herpes Simplex Virus Thymidine Kinase (HSV-tk for PET); requires genetic modification [22]. |
| Near-Infrared (NIR) Dyes | Fluorescent probes for direct optical cell labeling; deeper tissue penetration than visible light. | DiR, Cy5.5, Cy7; used for in vivo and ex vivo validation imaging [41] [36]. |
| Transfection Agents | Enhance uptake of labeling agents (e.g., SPIOs) into cells during ex vivo culture. | Cationic liposomes or polymers; improves labeling efficiency but requires toxicity testing [40]. |
| Multimodal Nanoparticles | Single agent enabling detection by multiple modalities (e.g., MRI + fluorescence). | Perfluorocarbon (PFC) nanoparticles visible via ¹⁹F MRI and fluorescence; reduces regulatory burden [35]. |
No single imaging modality is perfect for all cell tracking scenarios. The choice depends on the specific research question, balancing the need for sensitivity, resolution, quantification, depth penetration, and clinical translation. MRI excels in providing high-resolution anatomical context for localized cell grafts. PET offers superior quantitative sensitivity for whole-body biodistribution and tracking over days to weeks. SPECT allows for simultaneous tracking of multiple probes. Optical Imaging remains a powerful, cost-effective tool for preclinical proof-of-concept studies.
The future of cell tracking lies in multimodal imaging and the development of novel, versatile agents. Combining modalities, such as PET-MRI or agents visible in both MRI and optical imaging, leverages the strengths of each technology [37] [35]. Furthermore, the integration of artificial intelligence for image analysis and partial volume correction is set to improve the quantitative accuracy of techniques like PET and SPECT [39]. As cell therapies continue to evolve, robust, broadly applicable imaging platforms will be indispensable for optimizing their design, validating their efficacy, and ensuring their safety in patients.
The comparative assessment of biodistribution is a critical component in the non-clinical safety and efficacy evaluation of cell therapy products (CTPs). It clarifies the cell survival time, engraftment, and distribution site, which are crucial for predicting clinical outcomes based on non-clinical studies [27]. However, the absence of a standardized international protocol for these assessments leads to methodological variability, posing significant challenges in the drug approval process [23]. This guide provides an objective comparison of two principal quantitative methods—quantitative Polymerase Chain Reaction (qPCR) and droplet digital PCR (ddPCR)—used in biodistribution studies, focusing on their sensitivity, specificity, and throughput. The analysis is framed within a broader thesis on comparative biodistribution assessment, offering researchers a data-driven framework for method selection in the development of CTPs, such as induced pluripotent stem cell (iPSC)-derived pancreatic islet cells [23].
Biodistribution studies are pivotal for elucidating the fate and tumorigenicity risk of CTPs. The fundamental goal is to detect and quantify the presence of human-derived cells within various mouse tissues following administration. The lack of standardized protocols can result in inconsistent and unreliable data, complicating the interpretation of results and hindering regulatory approval [23]. Two primary nucleic acid amplification techniques have been adapted to meet this challenge:
- Quantitative Polymerase Chain Reaction (qPCR): This method relies on the relative quantification of a target DNA sequence against a standard curve. It provides amplification data in real-time, allowing for the quantification of the initial amount of target DNA in a sample. Its established workflow and higher throughput make it a common choice in many laboratories.
- Droplet Digital PCR (ddPCR): This is an absolute quantification method that partitions a single PCR reaction into thousands of nanoliter-sized droplets. Each droplet acts as an individual PCR reactor. By counting the positive and negative droplets at the end of the amplification, the initial concentration of the target DNA can be calculated without the need for a standard curve, potentially offering greater precision and sensitivity for low-abundance targets.
The selection between these methods directly impacts the reliability of biodistribution data, influencing critical decisions on product safety and clinical translation.
Performance Comparison: qPCR vs. ddPCR
A direct comparison of qPCR and ddPCR performance is essential for informed method selection. The following table summarizes their key characteristics based on standardized evaluations.
Table 1: Performance Comparison of qPCR and ddPCR in Biodistribution Studies
| Performance Metric | qPCR | ddPCR |
|---|---|---|
| Quantification Principle | Relative (requires standard curve) | Absolute (no standard curve) |
| Accuracy (Relative Error) | Generally within ±50% [27] | Generally within ±50% [27] |
| Precision (Coefficient of Variation) | Generally <50% [27] | Generally <50% [27] |
| Sensitivity | High | Potentially higher for low-copy targets |
| Tolerance to PCR Inhibitors | Moderate | High |
| Throughput | Higher | Lower |
| Multiplexing Capability | Well-established | Developing |
| Data Output | Cq (Cycle of quantification) value | Copy number per microliter |
The table indicates that while both methods demonstrated comparable accuracy and precision in a multi-facility validation study, their underlying principles and operational strengths differ [27]. The choice between them often involves a trade-off between the absolute quantification and inhibitor tolerance of ddPCR and the higher throughput and easier multiplexing of qPCR.
Supporting Experimental Data
A key multi-facility study provides concrete experimental data supporting this comparison. The study aimed to standardize biodistribution assays and conducted in vivo BD studies after the intravenous administration of human mesenchymal stem cells (hMSCs) to immunodeficient mice [27].
- Experimental Findings: The biodistribution of hMSCs was evaluated at seven facilities (qPCR at three facilities; ddPCR at four facilities). The results revealed similar tissue distribution profiles across all facilities, irrespective of the quantification method used. The lungs showed the highest cell distribution among the tissues tested, a finding consistently reported by both qPCR and ddPCR platforms [27].
- Interpretation: This demonstrates that both methods can generate congruent biodistribution profiles in a real-world research setting. The conclusion was that both qPCR and ddPCR methods, using a protocol targeting primate-specific Alu sequences, are suitable for the BD evaluation of CTPs [27].
Detailed Experimental Protocols
To ensure reproducibility and reliability in biodistribution studies, detailed and standardized protocols are necessary. The following workflows outline the core methodologies for both qPCR and ddPCR, from sample preparation to data analysis.
Core Workflow for Biodistribution Assessment
The general process for conducting a biodistribution study is method-agnostic in its initial stages. The diagram below illustrates the shared workflow.
Diagram 1: Generic BD Study Workflow.
qPCR Experimental Protocol
The qPCR method provides relative quantification based on a standard curve. The specific protocol is detailed below.
Diagram 2: qPCR Quantification Workflow.
Detailed Methodology:
- Standard Curve Preparation: A standard is created using a known number of human cells spiked into control mouse tissues. Genomic DNA (gDNA) is extracted, and a series of dilutions is prepared to generate a standard curve for relative quantification [27].
- qPCR Reaction Setup: The reaction mix includes the gDNA sample, primers and a probe specific to a human-specific repetitive element (e.g., LINE1 [23] or Alu [27]), and a qPCR master mix containing DNA polymerase, dNTPs, and buffer.
- Amplification and Data Acquisition: The plate is run in a real-time PCR instrument. The cycle threshold (Cq) value for each reaction is determined.
- Data Analysis: The Cq values of the test samples are interpolated from the standard curve to determine the quantity of human DNA, which is then correlated to cell number.
ddPCR Experimental Protocol
The ddPCR protocol differs fundamentally in its partitioning step, enabling absolute quantification.
Diagram 3: ddPCR Quantification Workflow.
Detailed Methodology:
- Reaction Setup: The reaction mixture is prepared similarly to qPCR, containing the gDNA sample, human-specific primers and probe, and a ddPCR supermix.
- Droplet Generation: The reaction mixture is partitioned into approximately 20,000 nanoliter-sized oil-emulsion droplets using a droplet generator.
- Endpoint Amplification: The droplet emulsion is transferred to a PCR plate and amplified to endpoint in a thermal cycler.
- Droplet Reading and Analysis: The plate is read in a droplet reader, which flows each droplet past a fluorescent detector. Droplets are counted as positive (containing the target sequence) or negative.
- Absolute Quantification: The concentration of the target DNA in the original sample is calculated based on the fraction of positive droplets using Poisson distribution statistics, providing an absolute count without a standard curve.
The Scientist's Toolkit
A successful biodistribution study relies on specific reagents and instruments. The following table details key materials and their functions.
Table 2: Essential Research Reagents and Tools for Biodistribution Studies
| Item | Function/Description |
|---|---|
| Immunodeficient Mice | An in vivo model system that does not reject transplanted human cells, allowing for the study of human CTP biodistribution and persistence over time [23] [27]. |
| Human-Specific Primers/Probes | Oligonucleotides designed to target sequences unique to the human genome (e.g., LINE1 [23], Alu [27]), enabling specific detection of human cells within a mouse tissue background. |
| Droplet Digital PCR (ddPCR) System | An instrument platform that partitions samples into droplets for absolute nucleic acid quantification, offering high precision for low-abundance targets and tolerance to PCR inhibitors [27]. |
| Real-Time PCR Thermocycler | An instrument used for qPCR that monitors the amplification of a targeted DNA molecule in real-time, providing a relative measure of the starting quantity. |
| Nucleic Acid Extraction Kits | Reagents for the isolation and purification of high-quality genomic DNA from complex tissue samples, a critical step for downstream PCR analysis. |
| Cell Therapy Product (CTP) | The investigational product, such as iPSC-derived pancreatic islet cells, whose biodistribution and persistence are being evaluated [23]. |
The objective comparison between qPCR and ddPCR reveals that both methods are validated for biodistribution assessment of CTPs, demonstrating comparable accuracy and precision in a multi-facility setting [27]. The decision to use one over the other hinges on the specific requirements of the study. qPCR offers higher throughput and a more established workflow, making it suitable for studies where relative quantification is sufficient and sample numbers are high. In contrast, ddPCR provides absolute quantification without a standard curve, exhibits superior tolerance to PCR inhibitors, and may offer enhanced sensitivity for detecting very low levels of engraftment, which is critical for assessing tumorigenic risk [23] [27]. Therefore, the selection criteria should balance the need for absolute quantification and sensitivity (favoring ddPCR) against the demands of throughput and operational familiarity (favoring qPCR), all within the specific context of the cell therapy product and the key questions of the non-clinical study.
The advancement of mesenchymal stromal cell (MSC)-based therapies relies critically on understanding their pharmacokinetics, particularly their biodistribution—the journey and final destination of cells within the body after administration [42]. For cell-based products, which are "living drugs," biodistribution data are essential for evaluating safety, potential toxicity, and mechanisms of efficacy [43] [44]. Regulatory guidelines for Advanced Therapy Medicinal Products (ATMPs) explicitly request robust nonclinical biodistribution data before progression to large clinical trials [44].
Among the available techniques, quantitative polymerase chain reaction (qPCR) has emerged as a cornerstone method for its sensitivity and specificity in detecting human cells in animal tissues. This case study provides a multi-site evaluation of PCR-based methodologies, objectively comparing their performance with other established techniques in the context of MSC biodistribution assessment. We frame this comparison within the broader thesis that a holistic understanding of MSC cellular kinetics is a translational challenge that must be overcome to improve the clinical efficacy and regulatory approval of MSC therapies [42].
MSC Biodistribution Fundamentals
The Critical Role of Administration Route
The distribution pattern of MSCs in vivo is profoundly influenced by the route of administration, a key variable that must be considered when designing biodistribution studies.
| Route of Administration | Systemic Distribution | Primary Organs of Interest | Key Characteristics |
|---|---|---|---|
| Intravenous (IV) | Yes | Lungs, Liver, Spleen, Kidneys | Initial trapping in the lungs (first capillary filter), followed by redistribution [45]. |
| Intraarterial (IA) | Yes | Heart, Brain, Kidneys, Liver | Bypasses the pulmonary filter, leading to wider initial distribution [45]. |
| Local Injection (IM, IA, etc.) | No or Limited | Site of Injection | Cells primarily remain at the injection site; minimal systemic distribution [45]. |
| Intrathecal | No (Cranial migration possible) | Central Nervous System | Limited systemic biodistribution; cells distribute within the CNS [45]. |
Standard Biodistribution Profile
Across numerous studies, a consistent profile emerges for intravenously infused MSCs. Cells initially accumulate in the lungs before redistributing, primarily to the liver and spleen, with lower levels often detected in the kidneys [45] [43] [44]. The persistence of MSCs in tissues is generally short, with most studies reporting a rapid decline in detectable cells within days to a few weeks post-infusion [44]. This pattern appears consistent between animal models and humans, underscoring the value of preclinical data [45].
Comparative Analysis of Biodistribution Methodologies
Biodistribution studies employ a suite of complementary techniques. The workflow typically begins with in vivo imaging for longitudinal tracking, followed by ex vivo analysis of harvested tissues using methods like qPCR and immunohistochemistry to confirm and quantify cell presence.
Quantitative Performance Comparison
The selection of a detection method involves critical trade-offs between sensitivity, specificity, and the type of information provided. The following table summarizes the key characteristics of each major technology.
| Method | Sensitivity | Key Advantage | Primary Limitation | Spatial Information |
|---|---|---|---|---|
| qPCR | High (can detect <10 cells/µg tissue) [43] | Quantification, cost-effective, detects genetic material [43] | Cannot distinguish live/dead cells [43] | No |
| Bioluminescence Imaging (BLI) | Moderate (declines rapidly) [43] | Specific detection, safe, no radiation [43] | Limited tissue penetration, signal intensity [43] | Yes (but low resolution) |
| Positron Emission Tomography (PET) | High | Whole-body tracking, long-term potential [43] | Radioactivity, detects debris from dead cells [43] | Yes |
| Immunohistochemistry (IHC) | Moderate | Visual confirmation, spatial context, cell morphology [44] | Relies on antigen abundance/quality [43] | Yes |
| Flow Cytometry | High | Single-cell analysis, phenotyping | Requires single-cell suspensions, no tissue context | No |
A 2025 study utilizing multiple techniques on the same model system provided direct, quantitative comparisons. The data demonstrated that while all methods confirmed the lung as the primary site of MSC accumulation after IV injection, discrepancies were noted for secondary organs like the liver and kidney, largely due to the varying abilities to detect live versus dead cells [43].
Multi-Site Experimental Evaluation of PCR
Core Experimental Protocol
A robust, GLP-compliant biodistribution study for an allogeneic bone marrow-derived MSC product (MC0518) exemplifies the standard protocol for PCR-based assessment [44].
- Animal Model: NOD/SCID/IL2Rγnull (NSG) immuno-deficient mice.
- Dosing Regimen: Repeat intravenous doses of 1 x 10^6 human MSCs per animal, once weekly for 6 weeks.
- Tissue Collection: Animals were euthanized at predefined timepoints (24 hours, 1 week, and 4 weeks after the final dose). A comprehensive set of over 20 tissues and organs was collected.
- Nucleic Acid Extraction: Genomic DNA is extracted from homogenized tissue samples.
- qPCR Analysis: Detection of human-specific Alu sequences or other unique genomic markers (e.g., human DNA β-actin) using TaqMan probes. Results are quantified against a standard curve of known human cell numbers spiked into control mouse tissue [44].
Key Findings from PCR-Centric Studies
The application of this protocol yielded critical insights:
- Persistence: PCR analysis confirmed short persistence of human MSCs in mouse tissues, with levels declining dramatically by 24 hours post-infusion and becoming undetectable in most organs beyond that point [44].
- Biodistribution Pattern: The primary distribution was to the lungs, with occasional low-level distribution to other organs, consistent with the known profile [44].
- Method Validation: The study highlighted that combining qPCR with a second method like in situ hybridization (ISH) is crucial for reliable interpretation. While qPCR is highly sensitive, ISH provides visual confirmation of cell presence and morphology, helping to rule out false positives from non-specific amplification [44].
The Scientist's Toolkit: Essential Research Reagents
Successful execution of MSC biodistribution studies requires a suite of specialized reagents and tools.
| Reagent / Tool | Function / Application | Example / Note |
|---|---|---|
| qPCR Assay for Human DNA | Detects and quantifies human-specific genetic sequences in animal tissue. | Primers/Probes for Alu repeats or human-specific gene loci (e.g., β-actin) [43] [44]. |
| Immunodeficient Mouse Model | Prevents xenogeneic rejection of human cells, allowing for longer persistence studies. | NOD/SCID/IL2Rγnull (NSG) mice are a standard model [44]. |
| Cryopreservation Medium | Vehicle for cell dosing and control groups. | Often 10% DMSO + 5% Human Serum Albumin in saline [44]. |
| In Situ Hybridization Probe | Validates qPCR data and provides spatial context by staining for human-specific RNA/DNA in tissue sections. | Complements qPCR findings [44]. |
| Luciferase Lentivirus | Engineers MSCs for bioluminescence imaging (BLI). | GV260 is an example; requires puromycin selection [43]. |
| Radiolabel (89Zr-oxine) | Labels MSCs for Positron Emission Tomography (PET) tracking. | Requires high radiochemical purity (≥90%) [43]. |
Synthesizing Multi-Method Results
No single method provides a complete picture of MSC fate in vivo. The most accurate interpretation comes from integrating data from multiple platforms [43] [44]. For instance, a 2025 study showed:
- PET imaging detected signals in the liver and kidney shortly after injection, which may represent the clearance of dead cell debris [43].
- qPCR can detect the genetic material of these dead cells.
- IHC staining for a human-specific cell surface marker (e.g., hCD73) can confirm the presence of intact, viable MSCs [43].
This integrated approach clarifies that while MSCs are initially trapped in the lungs, dead cells and their components are subsequently processed and cleared by organs like the liver and kidneys.
This multi-site evaluation confirms that qPCR is a highly sensitive, quantitative, and cost-effective core method for MSC biodistribution studies, making it indispensable for regulatory submissions. Its primary limitation—the inability to distinguish between live and dead cells—necessitates its use within a complementary methodological framework.
Future advancements in the field will depend on the development of more precise techniques that can reliably identify viable MSCs, dead MSCs, and even host cells that have engulfed MSC material in vivo [43]. Until then, the combination of qPCR with imaging and histological methods represents the gold standard for generating comprehensive and reliable biodistribution data, thereby de-risking the clinical translation of MSC-based therapies.
Primer and Probe Design Best Practices for Targeted Biodistribution Assays
Accurate assessment of biodistribution—how a therapeutic agent disperses throughout an organism—is a fundamental requirement in the development of cell and gene therapies. For viral vector-based vaccines and other advanced therapy medicinal products, regulatory agencies mandate thorough preclinical evaluation to determine distribution patterns not only in target tissues but also in non-target tissues and gonadal tissues to assess risks of unintended incorporation [46]. Polymerase chain reaction (PCR)-based methods have emerged as the gold standard for this quantification due to their exceptional sensitivity and specificity. The reliability of these biodistribution studies hinges entirely on the meticulous design and validation of the primers and probes used to detect the therapeutic agent. These oligonucleotides must simultaneously satisfy stringent biochemical requirements for efficient amplification while fulfilling regulatory expectations for assay validation. This guide provides a comprehensive comparison of quantitative PCR (qPCR) and digital PCR (dPCR) methodologies for biodistribution assessment, detailing best practices for primer and probe design based on both foundational principles and recent experimental data.
Technology Comparison: qPCR vs. dPCR for Biodistribution
The selection of an appropriate PCR platform is a critical first step in designing a targeted biodistribution assay. While both qPCR and dPCR serve to quantify nucleic acids, they differ substantially in their underlying mechanisms, performance characteristics, and suitability for specific applications within biodistribution studies.
Table 1: Comparative Analysis of qPCR and dPCR for Biodistribution Assessment
| Parameter | Quantitative PCR (qPCR) | Digital PCR (dPCR) |
|---|---|---|
| Quantification Method | Relative quantification against a standard curve | Absolute quantification by endpoint counting of positive partitions |
| Lower Limit of Quantification (LLOQ) | 48 copies/reaction [46] | 12 copies/reaction [46] |
| Precision | Good | Higher than qPCR [46] |
| Accuracy & Precision in Validation | Meets pre-defined acceptance criteria [46] | Meets pre-defined acceptance criteria [46] |
| Sensitivity | Sufficient for most tissue analyses | Superior, beneficial for low-copy-number samples |
| Dependence on Calibration Curve | Required, potential source of variability | Not required, reduces reference material dependence |
| Optimal Application | High-abundance targets, routine analysis | Low-abundance targets, samples with PCR inhibitors, requiring absolute quantification |
Experimental data from a recent systematic comparison validates the performance of both technologies. In a model adenoviral vector vaccine study, both dPCR and qPCR met pre-defined acceptance criteria for intra- and inter-run accuracy and precision. Cross-validation demonstrated similar quantitative results between the two methods, though dPCR provided a four-fold lower limit of detection (12 copies/reaction for dPCR versus 48 copies/reaction for qPCR) [46]. This enhanced sensitivity makes dPCR particularly valuable for analyzing samples where the therapeutic agent is expected to be present at very low levels, such as gonadal tissues or blood at later time points. Furthermore, dPCR's absolute quantification nature eliminates the need for a standard curve, which can be a source of variability and simplifies the analytical process.
Experimental Protocol for Cross-Platform Validation
The following workflow, derived from validated studies, ensures robust cross-platform compatibility:
- Primer/Probe Design: Design primers and probes targeting a unique junction region (e.g., between the viral vector and transgene) to ensure specificity [46].
- DNA Extraction Optimization: Extract DNA from tissues (e.g., blood, liver, testis) and excreta. Optimize the protocol by adjusting starting sample amount and proteinase K concentration (e.g., up to 40 μL) to achieve recovery rates >70% [46].
- Reaction Setup:
- Thermocycling: Use platform-specific annealing temperatures (e.g., 52°C for dPCR and 58°C for qPCR for the same primer set) [46].
- Data Analysis: Quantify vector copy number in total DNA extract and express as copies per μg of genomic DNA or copies per diploid genome.
Figure 1: Experimental workflow for cross-platform PCR validation in biodistribution studies.
Primer and Probe Design: Core Principles and Protocols
The success of any PCR-based biodistribution assay is fundamentally determined by the biochemical properties of its primers and probes. Adherence to established design principles is paramount for achieving high sensitivity, specificity, and reproducibility.
Foundational Design Guidelines
Table 2: Essential Design Criteria for Primers and Probes
| Parameter | Primers | Hydrolysis (TaqMan) Probes |
|---|---|---|
| Length | 18–30 bases [47] | 20–30 bases (for single-quenched); can be longer with double-quenching [47] |
| Melting Temperature (Tm) | 60–64°C (ideal 62°C) [47] | 5–10°C higher than primers [47] |
| Tm Difference Between Primers | ≤ 2°C [47] | Not Applicable |
| GC Content | 35–65% (ideal 50%) [47] | 35–65% (ideal 50%) [47] |
| Annealing Temperature (Ta) | ~5°C below primer Tm [47] | Assay Ta should be ≤ 5°C below lower primer Tm [47] |
| Specificity Check | BLAST analysis for unique target sequence [47] | BLAST analysis, avoid overlap with primer-binding site [47] |
Advanced Considerations for Biodistribution Assays
Beyond these foundational guidelines, specific strategies are required for biodistribution studies to address unique challenges:
- Amplicon Location and Genomic DNA Discrimination: When analyzing gene therapies, design assays to span an exon-exon junction. This design reduces false-positive signals from residual genomic DNA (gDNA) contamination, as the intron-spanning amplicon will not be efficiently amplified from gDNA [47]. Treating RNA samples with DNase I is also recommended practice.
- Amplicon Length: Shorter amplicons (70–150 base pairs) are typically more efficiently amplified under standard cycling conditions. While longer amplicons (up to 500 bases) are possible, they require extended extension times [47].
- Avoiding Secondary Structures: Screen all oligonucleotides for self-dimers, heterodimers, and hairpins. The free energy (ΔG) of any predicted secondary structure should be weaker (more positive) than –9.0 kcal/mol to prevent interference with the reaction [47]. Tools like the IDT OligoAnalyzer are indispensable for this analysis.
- Probe Quenching Strategy: For hydrolysis probes, double-quenched probes that incorporate an internal quencher (e.g., ZEN or TAO) are recommended over single-quenched probes. They provide lower background fluorescence, resulting in higher signal-to-noise ratios, which is particularly beneficial for detecting low-abundance targets [47].
Figure 2: Logical workflow for designing specific and efficient primers and probes.
A successful biodistribution study relies on a suite of carefully selected reagents and tools. The following table details key solutions referenced in the development and validation of PCR assays for this application.
Table 3: Essential Research Reagent Solutions for Biodistribution PCR Assays
| Research Reagent | Function / Application | Experimental Context / Example |
|---|---|---|
| PrimerQuest Tool (IDT) | Designs highly customized qPCR assays and PCR primers based on input parameters [47]. | Used for in silico design of primers/probes targeting specific junctions (e.g., Ad-HKU1S) with optimized Tm and length [46]. |
| OligoAnalyzer Tool (IDT) | Analyzes oligonucleotide properties: Tm, hairpins, dimers, and mismatches [47]. | Critical for screening designed primers/probes to ensure ΔG of secondary structures > -9.0 kcal/mol [47]. |
| DNeasy Blood & Tissue Kit (QIAGEN) | Extracts genomic DNA from various biological samples for PCR analysis. | Used in biodistribution studies; protocol often optimized by increasing Proteinase K and adjusting sample input to achieve >70% recovery [46]. |
| Isolink Kit (Mallinckrodt) | Provides chemistry for generating [[99mTc(H₂O)₃(CO)₃]⁺ for radiolabeling. | While used for radiolabeling nanobodies in imaging-based biodistribution studies, it highlights alternative biodistribution techniques [48]. |
| Double-Quenched Probes (e.g., with ZEN/TAO) | Fluorescent hydrolysis probes with internal quencher for lower background and higher signal [47]. | Recommended over single-quenched probes for qPCR biodistribution assays to improve sensitivity for low-copy-number detection [47]. |
| DNase I (RNase-free) | Enzyme that degrades DNA to remove genomic DNA contamination from RNA samples. | Recommended pre-treatment step before reverse transcription when quantifying RNA, to prevent false positives from genomic DNA [47]. |
The precision of biodistribution data for cell and gene therapies is inextricably linked to the quality of the underlying PCR assay. A rigorous approach that incorporates cross-validation of qPCR and dPCR platforms, adherence to robust primer and probe design principles, and meticulous attention to experimental protocols is essential. By following the best practices and comparative data outlined in this guide—from leveraging the absolute quantification of dPCR for sensitive applications to implementing exon-junction spans and double-quenched probes—researchers can generate reliable, reproducible, and regulatory-ready biodistribution data. This foundation is critical for accurately assessing the safety and efficacy profiles of next-generation therapeutic products.
Overcoming Biodistribution Hurdles: Infusion Strategies and Technical Challenges
The efficacy of advanced cell therapies, particularly for solid tumors, is profoundly influenced by their delivery route. While intravenous (IV) infusion represents the standard for hematological malignancies, its effectiveness in solid tumors is limited by biological barriers that restrict cell trafficking to tumor sites, often resulting in poor tumor infiltration and systemic toxicities [49] [50]. Local-regional delivery strategies aim to overcome these hurdles by administering therapies directly into or near the tumor tissue, thereby enhancing local bioavailability and reducing systemic exposure [51] [50]. This guide provides a comparative assessment of IV and local-regional delivery, framing the analysis within the critical context of biodistribution and its impact on therapeutic outcomes for researchers and drug development professionals.
Comparative Biodistribution and Performance of Administration Routes
The choice of administration route directly determines the biodistribution profile of a cell therapy, which in turn dictates its safety and efficacy. The table below summarizes the core characteristics, advantages, and limitations of intravenous versus local-regional delivery.
Table 1: Comparative Analysis of Intravenous vs. Local-Regional Delivery for Solid Tumors
| Feature | Intravenous (IV) Delivery | Local-Regional Delivery |
|---|---|---|
| Definition | Systemic infusion into the bloodstream [49]. | Direct administration into a body cavity or tumor site (e.g., intraperitoneal, intratumoral) [49] [50]. |
| Theoretical Biodistribution | Whole-body circulation; widespread dissemination [49]. | High initial concentration at the target site with gradual systemic dissipation [50]. |
| Typical Tumor Infiltration | Often poor due to vascular and stromal barriers [49]. | Potentially high, as it bypasses circulation and homing steps [50]. |
| Key Advantages | Suitable for disseminated/metastatic disease; standardized procedure [49]. | Higher local bioactive concentration; reduced systemic toxicities; access to tumor-draining lymph nodes [50]. |
| Major Limitations | Limited tumor penetration; "on-target, off-tumor" toxicity; cytokine release syndrome (CRS) [49] [52]. | Invasiveness; technically challenging; limited to accessible tumors [50]. |
| Representative Clinical Context | Standard for approved CAR-T products (e.g., for lymphoma) [49]. | Investigational for solid tumors (e.g., ovarian cancer via intraperitoneal delivery) [49]. |
The efficacy of a delivery route is context-dependent. For instance, in a study on Type 2 Diabetic rats using human umbilical cord mesenchymal stem cells (UCMSCs), tail vein (IV) injection proved more effective in restoring glucose homeostasis and pancreatic function than intraperitoneal or direct pancreas injection [53]. This highlights that IV delivery can be optimal when the therapeutic mechanism requires broad systemic engagement. In contrast, for localized solid tumors, direct injection is often superior. Preclinical models demonstrate that local delivery achieves higher functional concentrations at the target site, which is crucial for agents like cytokines (e.g., IL-12) that have narrow therapeutic windows due to systemic toxicity [52] [50].
Experimental Models and Assessment Methodologies
Robust preclinical models are essential for quantifying the biodistribution and efficacy of different administration routes. The following workflow outlines a standard experimental approach for this comparative assessment.
Diagram 1: Workflow for comparative assessment of administration routes in preclinical models.
Detailed Experimental Protocols
1. In Vivo Therapy Administration and Monitoring:
- Animal Models: Utilize immunocompetent or humanized mouse models with established subcutaneous or orthotopic solid tumors. Models should be selected based on their relevance to the human cancer type and the therapy's mechanism of action (e.g., prostate or ovarian cancer models for CAR-T studies) [52].
- Administration: Randomize animals into groups receiving the same cell therapy product via different routes (e.g., IV tail vein injection vs. intratumoral or intraperitoneal injection). The dose and formulation must be identical across groups to ensure a direct comparison [53] [52].
- Longitudinal Monitoring: Track tumor volume regularly using caliper measurements or in vivo imaging (e.g., bioluminescence). Monitor animal body weight and overall health as indicators of systemic toxicity [52].
2. Terminal Biodistribution and Efficacy Analysis:
- Biodistribution Quantification: At the endpoint, harvest major organs (e.g., liver, lungs, spleen) and tumors. Quantify the presence of the therapeutic cells in these tissues using methods like quantitative polymerase chain reaction (qPCR) for specific transgenes (e.g., CAR transgene), flow cytometry, or immunohistochemistry [52].
- Tumor Microenvironment (TME) Interrogation: Process tumor tissue for single-cell suspensions and analyze by flow cytometry. Key markers include T cell activation (4-1BB), exhaustion (PD-1, TIM-3, LAG3), and persistence. Cytokine levels (e.g., IFN-γ) can be measured in tumor homogenates or serum via ELISA, with local delivery expected to show higher concentrations in the TME and lower systemic levels [52].
- Histopathological Examination: Analyze tissue sections (e.g., H&E staining) to assess tumor cell death, immune cell infiltration, and potential damage to normal organs, providing critical safety data [53] [52].
Engineering Strategies to Overcome Delivery Hurdles
Innovative engineering approaches are being developed to augment the efficacy of both IV and local-regional delivery. A prominent strategy involves arming cell therapies to actively modify the tumor microenvironment.
Diagram 2: Mechanism of engineered CAR-T cells secreting tumor-localizing fusion proteins.
As illustrated, CAR-T cells can be engineered to secrete bifunctional fusion proteins, such as an anti-PD-L1 antibody (αPD-L1) fused to a cytokine like IL-12 (αPD-L1–IL-12) [52]. This design leverages the natural upregulation of PD-L1 in the TME in response to IFN-γ. The secreted fusion protein binds to PD-L1 on tumor cells, simultaneously blocking an inhibitory checkpoint and anchoring the potent IL-12 cytokine directly within the tumor. This localized action promotes a pro-inflammatory TME and enhances CAR-T cell function, while minimizing the systemic exposure to IL-12 that typically causes severe toxicity [52]. In preclinical models, this strategy demonstrated superior safety and durable antitumor efficacy compared to CAR-T cells alone or those secreting non-tumor-targeted cytokines [52].
The Scientist's Toolkit: Key Research Reagents
The following table catalogues essential reagents and materials for conducting comparative biodistribution and efficacy studies.
Table 2: Essential Research Reagents for Administration Route Studies
| Research Reagent / Material | Function and Application in Experiments |
|---|---|
| Syngeneic/Xenograft Tumor Models | In vivo platforms for evaluating therapy trafficking and antitumor activity in an intact biological system [52]. |
| Anti-PD-L1 Antibody | Key reagent for engineering fusion proteins or for use as a combination therapy; used to block PD-1/PD-L1 inhibitory axis [52]. |
| Cytokine ELISA Kits | Quantify cytokine concentrations (e.g., IFN-γ, IL-12) in serum and tumor homogenates to assess immune activation and toxicity [53] [52]. |
| Flow Cytometry Antibodies | Profile immune cell populations, activation (4-1BB), and exhaustion markers (PD-1, TIM-3, LAG3) in blood and tumors [52]. |
| qPCR Reagents | Quantify biodistribution and persistence of genetically modified cells (e.g., CAR transgene copy number) in various tissues [52]. |
| Recombinant Oncolytic Adenovirus | Tool for studying localized virotherapy; can be engineered for selective replication in cancer cells [54]. |
The optimization of administration routes is a critical determinant in the success of solid tumor immunotherapies. Intravenous delivery offers a systemic approach for disseminated disease but is frequently hampered by inefficient tumor infiltration and dose-limiting toxicities. Local-regional strategies enhance intratumoral bioavailability and improve the therapeutic index by focusing potency at the disease site, though they are more invasive. The choice is not universally prescriptive but must be guided by the therapeutic agent's mechanism, the tumor's anatomic location, and the disease's metastatic burden. Future progress hinges on integrating delivery route optimization with advanced cellular engineering, such as designing cells to secrete tumor-localizing immunomodulators, to fully unlock the potential of cell therapies for solid cancers.
Chimeric antigen receptor (CAR) T-cell therapy has revolutionized the treatment of hematological malignancies, achieving impressive clinical outcomes for patients with refractory or relapsed diseases. However, this remarkable efficacy is counterbalanced by significant safety concerns, primarily cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS). The infusion dose of CAR-T cells represents a critical therapeutic variable that profoundly influences both treatment efficacy and toxicity severity. This guide examines current dosing strategies, their physiological underpinnings, and the experimental approaches used to optimize the balance between therapeutic benefit and adverse event management for researchers and drug development professionals.
Clinical Dosing Landscape and Efficacy-Toxicity Correlation
Substantial clinical evidence demonstrates the direct relationship between CAR-T cell dosing, therapeutic efficacy, and toxicity profiles. The table below summarizes approved CAR-T products and their associated dosing, efficacy, and toxicity metrics based on clinical trial data.
Table 1: Clinical Dosing, Efficacy, and Toxicity Profiles of Approved CAR-T Therapies
| CAR-T Therapy | Target | Cancer Type | Dose | ORR/CR (%) | CRS Any/Grade ≥3 (%) | ICANS Any/Grade ≥3 (%) |
|---|---|---|---|---|---|---|
| Axicabtagene ciloleucel | CD19 | DLBCL, FL | 2 × 10^6 cells/kg (max 200M) | - | 77/46 [55] | 40/13 [55] |
| Brexucabtagene autoleucel | CD19 | MCL | 2 × 10^6 cells/kg (max 200M) | - | - | - |
| Brexucabtagene autoleucel | CD19 | B-ALL | 1 × 10^6 cells/kg (max 100M) | - | - | - |
| Tisagenlecleucel | CD19 | B-ALL | 0.2-5 × 10^6 cells/kg (≤50 kg); 10-250 × 10^6 cells (>50 kg) | 81/60 [55] | 77/46 [55] | 40/13 [55] |
Higher tumor burden has been consistently identified as a predictor for increased CRS severity, necessitating careful dose optimization based on individual patient factors [55]. The variation in dosing strategies between products highlights the product-specific approach required to balance efficacy with manageable toxicity profiles.
Mechanisms Linking Dosing to Toxicity: Pathophysiological Foundations
Understanding the mechanistic pathways connecting CAR-T cell activation to toxicity manifestations is essential for developing improved dosing strategies. The following diagram illustrates the key cellular and molecular events in CRS and ICANS pathogenesis.
Diagram 1: CRS and ICANS Pathogenesis (25 words): illustrates cytokine-mediated toxicity pathways initiated by CAR-T cell activation and macrophage involvement
The pathophysiology begins when infused CAR-T cells recognize target antigens, triggering activation and proliferation [56]. Activated CAR-T cells induce pyroptosis in target tumor cells through perforin/granzyme-mediated cleavage of gasdermin proteins (GSDME/GSDMB), leading to cellular swelling and lysis [57]. This pyroptosis releases damage-associated molecular patterns (DAMPs) including HMGB1, ATP, and dsDNA, which activate bystander immune cells—particularly macrophages and monocytes [57]. These activated macrophages then produce massive quantities of proinflammatory cytokines including IL-6, IL-1, IFN-γ, and GM-CSF, creating the cytokine storm characteristic of CRS [55] [57]. Subsequent endothelial activation promotes blood-brain barrier disruption, allowing inflammatory cytokines and immune cells to enter the CNS, culminating in ICANS [55] [57]. Higher CAR-T cell doses intensify this cascade by increasing the magnitude of initial tumor cell killing and subsequent immune activation.
Methodologies for Biodistribution and Toxicity Assessment
Comprehensive evaluation of CAR-T cell biodistribution and toxicity mechanisms requires sophisticated experimental approaches. The table below outlines key methodologies and their applications in cell therapy research.
Table 2: Experimental Approaches for Biodistribution and Safety Assessment
| Methodology | Application | Key Insights Provided |
|---|---|---|
| Droplet Digital PCR | Biodistribution tracking | Quantifies human-specific LINE1 sequences across tissues; validated for sensitivity and specificity [23] |
| Multiplex Immunofluorescence (RNAscope Multiomic LS) | Spatial multiomics | Detects up to 6 RNA/protein targets simultaneously; identifies immune cell subtypes and functional states in tissue [26] |
| PET Imaging (18F-DOPA) | Graft survival monitoring | Measures metabolic activity and functional engraftment of therapeutic cells in target tissues [58] |
| Cytokine Profiling | CRS monitoring | Quantifies IL-6, IL-1, IFN-γ, GM-CSF levels; correlates with toxicity severity [55] [57] |
| Histopathological Analysis | Tissue toxicity assessment | Evaluates immune cell infiltration, cellular damage, and structural changes at administration sites and distant organs [12] |
These methodologies enable researchers to establish comprehensive safety profiles by tracking CAR-T cell migration, persistence, and functional status while monitoring associated tissue damage and systemic inflammatory responses.
Innovative Dosing Strategies for Optimized Risk-Benefit Ratio
Fractionated Dosing Regimens
Multiple infusion techniques administer the total CAR-T cell dose in fractions over several days rather than as a single bolus. This approach allows clinicians to monitor initial toxicity and adjust subsequent dosing accordingly, potentially mitigating severe CRS and ICANS while maintaining therapeutic efficacy [56].
Locoregional Delivery
For solid tumors, direct administration routes (intraperitoneal, intrathoracic, hepatic artery injection) enhance tumor site delivery while minimizing systemic exposure and associated toxicities [56]. This strategy reduces the required effective dose by bypassing systemic circulation hurdles.
Biomaterial-Assisted Delivery
Advanced biomaterial systems can localize and sustain CAR-T cell activity at target sites, potentially reducing the dose needed for efficacy by protecting cells from the suppressive tumor microenvironment and prolonging their functional persistence [56].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for CAR-T Biodistribution and Toxicity Studies
| Reagent/Technology | Function | Experimental Application |
|---|---|---|
| Anti-IL-6R Antibody (Tocilizumab) | IL-6 receptor blockade | CRS management; mechanistic studies of IL-6 pathway [55] |
| Human-Specific LINE1 Probes | Genomic DNA detection | Biodistribution tracking in animal models via ddPCR [23] |
| RNAscope Multiomic LS Assay | Multiplex RNA/protein detection | Spatial profiling of immune cell infiltration and activation states [26] |
| GM-CSF Neutralizing Antibodies (Lenzilumab) | GM-CSF pathway inhibition | Investigational toxicity mitigation in ZUMA-19 trial [55] |
| Corticosteroids (Dexamethasone) | Broad anti-inflammatory | ICANS management; study of immunosuppressive effects on CAR-T efficacy [55] |
The optimization of CAR-T cell infusion dosing strategies remains a dynamic area of research requiring meticulous balance between achieving therapeutic efficacy and managing treatment-emergent toxicities. Current evidence indicates that product-specific dosing, fractionated administration schedules, and novel delivery approaches can significantly influence this therapeutic window. Comprehensive biodistribution assessment using sensitive molecular and imaging technologies provides critical insights into CAR-T cell pharmacokinetics and pharmacodynamics, enabling more rational dose selection. As CAR-T therapy expands to new indications, continued refinement of dosing paradigms integrated with toxicity management protocols will be essential to maximize clinical benefits while ensuring patient safety. Future directions include personalized dosing algorithms based on patient-specific risk factors and the development of next-generation CAR constructs with improved safety profiles.
Addressing Variable Transduction Efficiency in Viral-Based Cell Therapies
Viral transduction serves as the cornerstone of modern immune cell therapy manufacturing, enabling the delivery of therapeutic genes that empower immune cells to combat cancer and other diseases. However, this process is plagued by significant variability in efficiency, which directly impacts therapeutic efficacy and consistency. Transduction efficiency, measured as the percentage of cells successfully expressing the transgene, represents a primary Critical Quality Attribute (CQA) for cell therapy products and directly correlates with clinical outcomes [59]. In clinical CAR-T cell manufacturing, transduction efficiencies typically demonstrate considerable variability, ranging between 30-70% [59]. This variability presents a formidable challenge for therapy developers, who must balance achieving adequate transgene expression with maintaining product safety and functionality.
The persistence of variable efficiency stems from the complex interplay of multiple factors, including cell quality (activation state, donor variability), viral vector properties (titre, envelope pseudotyping), and process parameters (cell-vector interaction, incubation time, enhancers) [59]. Much of the foundational process knowledge remains proprietary to leading institutions and pharmaceutical companies, creating significant hurdles for early-stage therapy developers lacking resources for extensive empirical optimization [59]. This comparative analysis examines the current landscape of viral transduction systems, their performance characteristics, and optimization methodologies to support more robust and reproducible cell therapy manufacturing.
Comparative Analysis of Viral Vector Systems
Viral vector selection represents one of the most critical determinants of transduction success, with each platform offering distinct trade-offs in efficiency, safety, and applicability across different immune cell types. The four most clinically advanced viral vector systems each possess unique characteristics that influence their performance in immune cell engineering.
Table 1: Comparative Performance of Viral Vector Systems in Immune Cell Transduction
| Vector System | Transduction Efficiency | Integration Profile | Payload Capacity | Primary Immune Cell Applications | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| Lentiviral Vectors (LVs) | High in T cells; Variable in NK cells/DCs | Stable integration in dividing and non-dividing cells | ~8 kb | T cells, NK cells, Dendritic cells | Broad tropism (especially with VSV-G pseudotyping); Relatively safe SIN designs | Insertional mutagenesis risk; Immunogenicity concerns; Complex manufacturing |
| Gamma-retroviruses (γRVs) | High in activated T cells; Low in NK cells | Stable integration only in dividing cells | ~8 kb | T cells | Robust, stable transgene integration; Backbone of early CAR-T therapies | Requires cell proliferation; Higher insertional mutagenesis risk; Poor NK cell tropism |
| Adenoviruses (AVs) | High across immune cell types | Non-integrating (transient) | ~8 kb | Dendritic cells, Macrophages | High transduction efficiency; Rapid production; Suitable for vaccine applications | Pronounced immunogenicity; Limited payload capacity; Unsuitable for most cell therapies |
| Adeno-Associated Viruses (AAVs) | Variable (cell-type dependent) | Non-integrating (predominantly episomal) | ~4.7 kb | Dendritic cells, T cells (with engineered capsids) | Favorable safety profile; Low immunogenicity; Transduces non-dividing cells | Small payload capacity; Requires innovative approaches for cell therapy applications |
Lentiviral Vectors: The Current Gold Standard
Lentiviral vectors have emerged as the leading platform for immune cell therapy due to their ability to achieve stable genomic integration in both dividing and non-dividing cells [59]. This characteristic is particularly valuable for long-term persistence of therapeutic cells, as demonstrated in FDA-approved CAR-T cell therapies [59]. Their broad tropism, enabled by pseudotyping with vesicular stomatitis virus-G (VSV-G) envelope proteins, allows efficient transduction of diverse immune cell types [59]. Modern self-inactivating (SIN) designs with improved integration site profiling have significantly mitigated early concerns about insertional mutagenesis [59].
Recent innovations in LV engineering focus on enhancing specificity and safety for emerging applications like in vivo CAR-T generation. Retargeted systems utilizing engineered envelopes from viruses like Nipah (NiV) and Measles virus (MV) demonstrate improved specificity for T-cell subsets while reducing off-target transduction [60]. For instance, CD8-targeted NiV-pseudotyped LVs and CD4-targeted MV-LVs have achieved high specificity in preclinical models, with the latter generating CAR-T cells with superior anti-tumor activity compared to CD8-targeted approaches [60]. These advances position LVs for both ex vivo and in vivo applications, though challenges regarding immunogenicity and manufacturing complexity persist [60].
Emerging Alternatives and Niche Applications
While LVs dominate the current landscape, other viral systems offer valuable capabilities for specific applications. Gamma-retroviruses remain historically significant as the backbone of early CAR-T therapies but require target cells to be actively proliferating and exhibit poor tropism for NK cells due to receptor incompatibility [59]. Adeno-associated viruses have gained attention for their favorable safety profile and ability to transduce non-dividing cells, making them suitable for delicate immune cell targets like dendritic cells [59]. However, their small payload capacity (~4.7 kb) has traditionally limited their use in cell therapy, though innovative approaches combining AAV with CRISPR systems or transposons are expanding their potential [59].
Non-viral delivery systems, particularly lipid nanoparticles (LNPs), present a transformative alternative to viral vectors by effectively addressing critical challenges such as immunogenicity and insertional mutagenesis [61]. LNPs enable in vivo delivery of mRNA encoding CARs directly into circulating T cells, bypassing the need for ex vivo cell manipulation [61]. Preclinical studies have demonstrated that intravenous administration of LNPs carrying prostate-specific membrane antigen (PSMA)-targeting CAR mRNA led to short-term but functionally effective CAR expression in circulating T cells [61]. This approach is now advancing to clinical trials (NCT04538599) for patients with metastatic solid tumors, representing a significant shift toward non-viral, in vivo CAR engineering technologies [61].
Key Process Parameters and Optimization Strategies
Achieving consistent, high-efficiency transduction requires meticulous optimization of critical process parameters across multiple dimensions. The following experimental approaches represent evidence-based strategies for enhancing transduction outcomes across different immune cell types.
Vector and Cell Preparation Methodologies
Cell Activation and Conditioning Protocols:
- T-cell Activation: Stimulate T cells with CD3/CD28 agonists for 24-48 hours prior to transduction to upregulate viral receptor expression and promote cell cycling [59]. Supplement culture media with cytokine cocktails (e.g., IL-2, IL-7, or IL-15) to support expansion, survival, and function post-transduction [59].
- NK-cell Conditioning: Address low baseline transduction efficiency by implementing cytokine pre-stimulation (e.g., IL-15) to enhance cell survival and counteract innate antiviral mechanisms [59]. Consider higher viral titres or tropism-engineered vectors to overcome intrinsic resistance [59].
- Cell Quality Assessment: Perform viability assessment (>80% recommended) using trypan blue exclusion or Annexin V/7-AAD staining analyzed by flow cytometry before transduction initiation [59].
Vector Selection and Titration:
- Pseudotyping Strategy: Select envelope proteins based on target cell type. VSV-G provides broad tropism, while cell-specific pseudotypes (e.g., CD3-targeted, CD8-targeted) enhance specificity, particularly for in vivo applications [60].
- MOI Optimization: Titrate multiplicity of infection (MOI) to balance efficiency and safety. For clinical CAR-T manufacturing, optimize MOI to achieve target transduction efficiency while maintaining vector copy number (VCN) below 5 copies per cell [59]. Lower MOI ranges typically reduce the incidence of high VCN cells [59].
- Vector Quality Control: Determine functional titre via transgene expression analysis and confirm absence of replication-competent viruses through appropriate assays [59].
Transduction Execution and Enhancement
Transduction Methodology:
- Standard Transduction Protocol: Resuspend pre-activated cells at 0.5-1×10^6 cells/mL in appropriate growth medium supplemented with cytokines and transduction enhancers. Add viral vector at optimized MOI and incubate for 16-24 hours at 37°C, 5% CO₂ [59] [62].
- Spinoculation: Enhance cell-vector contact by centrifugation at 800-1200×g for 30-120 minutes at 32°C immediately following vector addition [59]. This physical method significantly improves transduction efficiency across multiple cell types.
- Transduction Enhancers: Incorporate additives such as protamine sulfate (4μg/mL) or poloxamers (e.g., LentiBOOST at 1mg/mL) to increase transduction efficiency without significant toxicity [59] [62].
Post-transduction Processing:
- Media Exchange: Replace vector-containing media 16-24 hours post-transduction to remove excess vector and reduce toxicity.
- Cell Expansion Culture: Continue culture in appropriate cytokine-supplemented media for 7-14 days to allow transgene expression and cell expansion while monitoring viability and growth kinetics.
Table 2: Optimization Strategies for Specific Challenges in Viral Transduction
| Challenge | Optimization Approach | Experimental Evidence | Expected Outcome |
|---|---|---|---|
| Low Transduction Efficiency | Spinoculation + Transduction enhancers (e.g., LentiBOOST) | Clinical CAR-T manufacturing shows 30-70% efficiency ranges [59] | 1.5-3 fold improvement in transduction efficiency |
| High VCN (>5 copies/cell) | MOI reduction; Vector engineering with SIN designs | Lower MOI ranges reduce multiple integration events [59] | VCN maintained below safety threshold of 5 copies/cell |
| Poor Cell Viability Post-transduction | Reduced transduction duration; Culture supplementation with IL-2/IL-7/IL-15 | Annexin V/7-AAD staining for viability assessment [59] | Maintain viability >70% post-transduction |
| Cell-type Specific Transduction | Envelope pseudotyping (e.g., CD3-targeted LVs, NK-tropic vectors) | CD4-targeted MV-LVs achieved ~60% transduction of CD4+ lymphocytes [60] | Cell subset-specific transduction with reduced off-target effects |
| In Vivo Application | Tropism-modified vectors with targeting moieties (scFvs, VHHs, DARPins) | CD7-targeted LVs successfully transduced T and NK cells in preclinical models [63] | Specific in vivo engineering of target immune cells |
Analytical Methods for Transduction Assessment
Rigorous analytical assessment is essential for characterizing transduced cells and ensuring they meet critical quality attributes for therapeutic application. The following methodologies represent standard approaches for evaluating transduction outcomes.
Efficiency and Genomic Integration Analysis
Transduction Efficiency Measurement:
- Flow Cytometry: The primary method for assessing transduction efficiency via detection of surface-expressed transgene (e.g., CAR expression) or reporter proteins (e.g., GFP). Protocol: Harvest cells 72-96 hours post-transduction, stain with fluorochrome-conjugated antibodies against transgene markers, and analyze by flow cytometry. Include appropriate isotype controls and unstained controls [59].
- Functional Assays: Measure cytokine secretion (IFN-γ, IL-2) upon antigen-specific stimulation using ELISpot or intracellular cytokine staining to confirm functional transgene expression [59].
Vector Copy Number (VCN) Determination:
- Droplet Digital PCR (ddPCR): The gold standard method for VCN quantification due to superior precision without reliance on standard curves [59]. Protocol: Extract genomic DNA from transduced cells (minimum 1×10^5 cells), digest with restriction enzymes, and partition into ~20,000 droplets with transgene-specific and reference gene (e.g., RNase P) assays. Calculate VCN as (transgene copies/reference gene copies) × ploidy factor [59].
- qPCR Alternative: When ddPCR is unavailable, use quantitative PCR with standard curve method, though with recognition of lower precision compared to ddPCR.
Functional and Safety Assessments
Cell Functionality Evaluation:
- Cytotoxicity Assays: Measure target cell lysis capacity in co-culture assays using flow cytometry-based killing assays or real-time cytotoxicity measurements (e.g., xCELLigence systems) [59].
- Proliferation and Expansion Capacity: Monitor cell growth kinetics post-transduction and calculate population doublings. Perform CFU assays for stem/progenitor cells by plating transduced cells in semi-solid methocult medium and enumerating colonies after 14 days [62].
Product Safety Assessment:
- Replication-Competent Virus Testing: Perform appropriate assays to confirm absence of replication-competent lentivirus (RCL) or other relevant replication-competent viruses depending on vector system [59].
- Insertion Site Analysis: Utilize next-generation sequencing-based methods (e.g., LAM-PCR, UD-PCR) to monitor genomic integration profiles and assess potential genotoxic risks [59].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Viral Transduction Optimization
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Transduction Enhancers | Protamine Sulfate, LentiBOOST, Polybrene | Enhance viral attachment and entry | Concentration optimization required to balance efficiency and toxicity |
| Cytokine Supplements | IL-2, IL-7, IL-15, SCF, FLT3L, TPO | Support cell survival, proliferation, and function | Cell-type specific formulations; T cells: IL-2/IL-7/IL-15; HSC: SCF/FLT3L/TPO [59] [62] |
| Cell Activation Reagents | Anti-CD3/CD28 antibodies, Concanavalin A | Activate target cells to enhance transduction | Critical for retroviral transduction; 24-48 hour pre-stimulation recommended |
| Vector Quantification Assays | p24 ELISA, qPCR titration, functional titre assays | Measure vector concentration and functionality | Functional titre most relevant for predicting transduction efficiency |
| Analysis Reagents | Fluorochrome-conjugated antibodies, Annexin V/7-AAD, DNA extraction kits | Assess transduction efficiency, viability, and VCN | Flow cytometry panels should include viability markers and lineage markers |
Visualizing Transduction Optimization Workflows
Decision Framework for Vector Selection
Advanced Pseudotyping Strategies for Lentiviral Vectors
The field of viral-based cell therapies continues to evolve with promising innovations aimed at addressing the persistent challenge of variable transduction efficiency. Emerging approaches include advanced pseudotyping strategies utilizing engineered envelopes from viruses like Nipah and Measles that demonstrate improved specificity for T-cell subsets [60], in vivo transduction platforms that generate CAR-T cells directly within patients [60] [64], and nanoparticle-based delivery systems that offer alternatives to viral vectors with reduced immunogenicity and simplified manufacturing [61]. The ongoing refinement of these technologies, coupled with robust analytical methods and standardized processes, promises to enhance the consistency, safety, and accessibility of viral-based cell therapies, ultimately expanding their therapeutic potential across a broader range of diseases.
The therapeutic targeting of solid tumors, particularly those within the central nervous system, represents one of the most formidable challenges in oncology. Two primary obstacles collectively undermine treatment efficacy: the blood-brain barrier (BBB) and the immunosuppressive tumor microenvironment (TME). The BBB serves as a highly selective physiological barrier that severely restricts drug delivery to brain tumors, while the TME creates an immunosuppressive niche that actively inhibits effector immune cell function. Together, these barriers significantly limit the effectiveness of cell-based immunotherapies and other targeted approaches for solid tumors [65] [66]. Understanding and overcoming these dual barriers is critical for advancing the treatment of glioblastoma, other brain tumors, and solid malignancies elsewhere in the body.
This review examines the comparative challenges posed by the BBB and immunosuppressive TME in the context of cell therapy biodistribution and efficacy. We analyze current strategic approaches, present experimental data on emerging technologies, and provide detailed methodologies for evaluating therapeutic success. The integration of advanced drug delivery platforms with innovative cell engineering strategies offers promising avenues to overcome these barriers and improve patient outcomes.
The Blood-Brain Barrier: Structure, Function, and Therapeutic Implications
Physiological Structure of the BBB
The blood-brain barrier is a sophisticated multicellular structure that maintains the sensitive internal environment of the brain through three sequentially arranged barriers: the glycocalyx, endothelium, and extravascular compartment [67]. A continuous layer of non-fenestrated capillary endothelial cells connected by tight junctions forms the core of this barrier, supported by pericytes embedded in the basal membrane and astrocyte end-foot processes [66]. The glycocalyx, a 300-nm thick gel-like structure on the luminal membrane consisting of proteoglycans and glycosaminoglycans, serves as an initial sieve-like barrier to large molecules [67].
The endothelial cells create an approximately 200-nm thick wall characterized by limited pinocytic vesicles and robust intercellular connections that severely restrict solute transport. Transport across this endothelial layer occurs primarily through two mechanisms: paracellular diffusion (limited by tight junctions) and transcellular transport (including diffusion, carrier-mediated transport, receptor-mediated transcytosis, and active efflux) [67]. This complex structure effectively prevents the passage of most blood-borne proteins, drugs, and inflammatory cells into the brain parenchyma.
The Blood-Brain Tumor Barrier (BBTB) in Malignancy
Brain tumors, particularly high-grade gliomas, often cause degradation and dysfunction of the BBB, resulting in what is termed the blood-brain tumor barrier (BBTB). This pathological barrier features heterogeneous increases in vascular permeability throughout the tumor mass and surrounding tissue [67]. However, this breakdown is often incomplete and irregular, creating regions with variable barrier integrity. The BBTB remains more competent in low-grade gliomas and at the invasive borders of high-grade gliomas, complicating uniform drug delivery to all tumor regions [67]. This heterogeneity represents a significant challenge for therapeutic agents that rely on vascular delivery, including both chemotherapeutic drugs and cellular therapies.
The Immunosuppressive Tumor Microenvironment: Mechanisms of Therapy Resistance
Cellular and Molecular Components of the TME
The solid tumor microenvironment creates multiple immunosuppressive barriers that collectively inhibit effective anti-tumor immunity. Immunosuppressive cell populations including regulatory T cells (Tregs), tumor-associated macrophages (TAMs), and myeloid-derived suppressor cells (MDSCs) produce various mediators such as TGF-β, IL-10, and VEGF that inhibit dendritic cell maturation and cytotoxic T-cell function [68]. Physical barriers within the TME include dense extracellular matrix (ECM) deposition and fibrosis that obstruct immune cell infiltration, while aberrant tumor vasculature limits immune cell entry and migration [68].
Metabolic alterations further compromise immune function through hypoxia-induced adaptation, lactate production, acidification, and nutrient depletion. The accumulation of metabolites including lactate, adenosine, and kynurenine directly suppresses cytotoxic T-cell activation, proliferation, and effector functions [68]. These immunological, physical, and metabolic barriers collectively create an environment that neutralizes adoptive cell therapies and other immunotherapeutic approaches.
Impact on Cell Therapy Efficacy
Cell-based immunotherapies including CAR-T, CAR-NK, and TCR-T cells face significant challenges penetrating the TME and maintaining effector function. The hostile conditions within solid tumors effectively neutralize T-cell function through multiple mechanisms including immune checkpoint upregulation, metabolic suppression, and physical exclusion [69]. CAR-T cells specifically demonstrate limited efficacy against solid tumors despite their remarkable success in hematologic malignancies, largely due to these TME barriers combined with insufficient tumor infiltration [70]. The solid TME performs immunosuppressive functions through various routes including regulatory immune cells, hypoxia, immune checkpoint upregulation, and secretion of immunosuppressive mediators that collectively induce CAR-T inactivation [70].
Comparative Assessment of Therapeutic Platforms and Strategies
Emerging Platforms for BBB Penetration
Table 1: Strategies for Overcoming the Blood-Brain Barrier
| Strategy | Mechanism of Action | Therapeutic Platform | Key Findings | Limitations |
|---|---|---|---|---|
| Focused Ultrasound | Temporarily disrupts BBB using sound waves with microbubbles | Drug delivery enhancement | Non-invasive, reversible opening; enhances drug penetration [71] | Requires specialized equipment; potential for off-target effects |
| Nanoparticle Systems | Utilizes transcytosis pathways; can be functionalized with targeting ligands | Various nanocarriers, viral-like particles, cell-based systems | Can be engineered for specific transport mechanisms; multifunctional capacity [66] | Potential immunogenicity; scaling challenges |
| Vascular Normalization | Restores abnormal tumor vasculature to improve perfusion | VEGF inhibitors (e.g., bevacizumab) | Improves immune cell infiltration; enhances drug delivery [68] | Requires careful dosing to avoid excessive normalization |
| Receptor-Mediated Transcytosis | Exploits natural transport pathways (transferrin, insulin receptors) | Antibody-based therapies, engineered proteins | Utilizes endogenous transport mechanisms [67] | Limited payload capacity; potential receptor competition |
Table 2: Approaches for Modifying the Immunosuppressive TME
| Approach | Molecular Target | Therapeutic Platform | Impact on TME | Clinical Status |
|---|---|---|---|---|
| Immune Checkpoint Blockade | PD-1/PD-L1, CTLA-4 | ICIs combined with cell therapies | Reverses T-cell exhaustion; enhances effector function [52] | Clinical trials with mixed results |
| Cytokine Engineering | IL-12, IL-15, TGF-β | Armored CAR-T cells | Reprograms local immune environment; enhances persistence [52] | Preclinical and early clinical development |
| Metabolic Modulation | IDO1, adenosine pathway | Small molecule inhibitors | Alleviates metabolic suppression of T cells [71] | IDO1 inhibitors in clinical trials |
| ECM Remodeling | Hyaluronan, collagen | Enzymatic approaches (e.g., hyaluronidase) | Reduces physical barriers; improves cell infiltration [68] | Limited success in clinical trials |
| Vascular Normalization | VEGF/VEGFR | Anti-angiogenic therapies | Improves perfusion and immune cell infiltration [68] | Approved agents repurposed for combination therapy |
Advanced Cell Engineering Strategies
Innovative engineering approaches are emerging to enhance cell therapy efficacy against solid tumors. A novel strategy involves CAR-T cells engineered to secrete bifunctional fusion proteins combining interleukin-12 (IL-12) with a PD-L1 blocker [69] [52]. This design exploits the high PD-L1 expression typically found in tumor environments, ensuring that IL-12 accumulates specifically at tumor sites rather than circulating systemically. In mouse models, these modified CAR-T cells demonstrated potent anti-tumor efficacy against both prostate and ovarian cancers while avoiding the organ toxicity associated with systemic IL-12 administration [69].
Alternative engineering approaches include CAR-T cells equipped with other immunomodulatory partners including TGFβ traps and IL-15 complexes. However, comparative studies have demonstrated superior safety and efficacy profiles for the αPD-L1-IL-12 engineered constructs relative to other combinations [52]. These armored CAR-T cells show improved trafficking, tumor infiltration, and localized IFNγ production with reduced systemic inflammation-associated toxicities.
Experimental Models and Assessment Methodologies
Biodistribution Assessment for Cell Therapies
Evaluating the biodistribution (BD) of cell therapy products is essential for predicting and assessing their efficacy and toxicity profiles in non-clinical and clinical studies [72]. BD studies employ various analytical methods including quantitative polymerase chain reaction (qPCR) and imaging techniques such as PET, SPECT, and MRI. These approaches enable researchers to track the migration, persistence, and tissue distribution of administered cellular therapies, providing critical insights into their pharmacodynamic properties.
The unique "live cell" nature of CAR-T therapies presents distinctive challenges for biodistribution assessment, as these products display complex patterns of cellular kinetics involving initial fast diffusion, short-term proliferation and expansion, contraction, and enduring persistence [70]. Quantitative systems pharmacology (QSP) models have emerged as valuable tools for integrating CAR-T-related pathophysiological and pharmacological mechanisms with multiscale experimental data to advance our understanding of these multiphasic behaviors [70].
In Vitro Functional Assays for TME Engagement
Table 3: Key Functional Assays for Evaluating Cell Therapy-TME Interactions
| Assay Type | Experimental Readout | Information Gained | Key Methodological Considerations |
|---|---|---|---|
| Repetitive Tumor Challenge | Tumor cell killing, T cell expansion, cytokine secretion | Sustained effector function, persistence | Multiple rounds of tumor co-culture at set E:T ratios; flow cytometry analysis [52] |
| PD-L1 Binding Assay | Mean fluorescence intensity (MFI) | Fusion protein functionality, target engagement | Induction of PD-L1 expression via conditioned media; assessment of binding competition [52] |
| Cytokine Secretion Profiling | IFNγ, IL-2, other cytokines via ELISA | Activation status, functional potency | Time-course measurements during co-culture; correlation with cytotoxic activity |
| Migration and Invasion | Cell movement through ECM barriers | Trafficking potential, matrix penetration | Transwell systems with ECM coatings; measurement of migratory kinetics |
In Vivo Models for Therapeutic Evaluation
Animal models, particularly immunocompetent mouse models of prostate and ovarian cancer, have been instrumental in evaluating the safety and efficacy of engineered cell therapies against solid tumors [52]. These models allow researchers to assess not only direct anti-tumor effects but also the impact on the broader TME, including immune cell infiltration, cytokine milieu changes, and stromal remodeling. The use of syngeneic models with intact immune systems is particularly valuable for understanding the complex interactions between administered therapies and endogenous immunity.
In vivo evaluation typically includes measurements of tumor volume regression, survival benefit, cytokine release syndrome assessment, and detailed immunohistochemical analysis of tumor tissues following treatment. For brain tumor models, additional considerations include intracranial implantation techniques and specialized imaging approaches to monitor blood-brain barrier penetration and intratumoral distribution.
Table 4: Key Research Reagent Solutions for Solid Tumor Immunotherapy
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Engineered Cell Lines | PSCA-positive murine prostate cancer lines (PTEN-Kras hPSCA), RM9 | In vitro and in vivo tumor challenge models | Ensure consistent antigen expression; validate tumorigenic potential [52] |
| CAR Constructs | PSCA-CAR, CLDN18.2-CAR, HER2-CAR | Therapeutic effector cell engineering | Optimize transduction efficiency; confirm surface expression and function |
| Fusion Proteins | αPD-L1–IL-12, αPD-L1–TGFβtrap, αPD-L1–IL-15 | Armoring strategies for enhanced function | Validate binding specificity; confirm cytokine bioactivity [52] |
| Flow Cytometry Panel | mCD19t, CD4/CD8, PD-1, LAG-3, TIM-3, 4-1BB | Phenotypic characterization of engineered cells | Multicolor panel design; include viability staining; establish gating strategies [52] |
| Cytokine Detection | IFNγ ELISA, multiplex cytokine arrays | Functional assessment of immune activation | Establish standard curves; optimize sample collection time points [52] |
Signaling Pathways and Experimental Workflows
The following diagrams visualize key signaling pathways and experimental workflows relevant to solid tumor targeting strategies.
CAR-T Cell Activation and TME Engagement Mechanism
Diagram 1: CAR-T cell activation and TME engagement mechanism. Engineered CAR-T cells recognize tumor antigens via CAR receptors while secreting αPD-L1–IL-12 fusion proteins that bind PD-L1 and stimulate IL-12 receptors, leading to IFNγ production and TME remodeling [52].
Blood-Brain Barrier Structure and Transport Mechanisms
Diagram 2: Blood-brain barrier structure and transport mechanisms. The BBB consists of sequential barriers including the glycocalyx, endothelial cells with tight junctions, and astrocyte end-feet, with multiple transport mechanisms governing molecular passage [66] [67].
In Vitro Repetitive Tumor Challenge Assay Workflow
Diagram 3: In vitro repetitive tumor challenge assay workflow. This experimental approach evaluates CAR-T cell persistence and function through multiple rounds of tumor cell co-culture and analysis over time [52].
The challenges posed by the blood-brain barrier and immunosuppressive tumor microenvironment in solid tumor targeting represent significant but not insurmountable obstacles. Current research demonstrates that integrated approaches combining advanced cell engineering, strategic barrier modulation, and sophisticated delivery platforms hold substantial promise for overcoming these limitations. The development of armored CAR-T cells capable of locally modifying their microenvironment while resisting immunosuppressive signals represents a particularly promising direction.
Future progress will likely depend on continued innovation in biodistribution assessment techniques, including improved imaging modalities and computational modeling approaches that can better predict in vivo behavior of cellular therapies. Additionally, personalized strategies that account for interpatient heterogeneity in both BBB integrity and TME composition will be essential for maximizing therapeutic efficacy. As these advanced technologies mature and converge, they offer the potential to dramatically improve outcomes for patients with solid tumors, including those within the central nervous system that have traditionally been most resistant to treatment.
In the development and manufacturing of gene-modified cell therapies, controlling critical process parameters is essential for ensuring product safety and efficacy. Two of the most critical parameters are Vector Copy Number (VCN), which measures the number of integrated viral vector genomes per cell, and cell viability, which indicates the health and potency of the final product. Within the context of comparative biodistribution assessment, understanding these parameters is paramount for evaluating the tumorigenic risks and long-term persistence of therapeutic cells. This guide provides an objective comparison of the leading methodologies for VCN determination, detailing their experimental protocols, performance characteristics, and applications in characterizing cell therapy products.
Methodological Comparison for Vector Copy Number Determination
The accurate determination of VCN can be approached through population-average or single-cell analysis methods, each with distinct advantages and limitations.
Population-Average Vector Copy Number (pVCN) Analysis
Population-average methods provide a bulk measurement of VCN from extracted genomic DNA (gDNA). The established reference standard employs quantitative PCR (qPCR) with clonal Jurkat cell lines containing defined copies (1 to 4) of an integrated reference lentiviral vector [73]. These cell lines are engineered to be renewable and demonstrate stable VCN over long-term culture, making them a sustainable source of reference material [73].
Key Experimental Protocol for qPCR-based pVCN [73]:
- DNA Source: Genomic DNA extracted from bulk transduced cells.
- Target Sequences: Assays target specific regions of the integrated lentiviral genome (e.g., a synthetic C-frag ID tag,
gag, or RRE sequence). - Normalization: The viral target is normalized to a single-copy human reference gene (e.g.,
RPPH1,PTBP2, orRPL32) in separate or duplexed qPCR reactions. - Calculation: VCN is calculated based on the relative quantification of the viral target to the reference gene.
This method has demonstrated robust performance across independent laboratories and different qPCR instruments, showing high concordance in results [73].
Single-Cell Vector Copy Number (scVCN) Analysis
Single-cell methods have emerged to address the limitation of pVCN, which can mask significant cell-to-cell heterogeneity. A novel method utilizes droplet digital PCR (ddPCR) to quantify VCN in individual, isolated cells [74].
Key Experimental Protocol for ddPCR-based scVCN [74]:
- Single-Cell Isolation: Live, single cells are isolated into individual wells.
- Preamplification: Due to the low amount of DNA in a single cell, a targeted preamplification step is performed on selected lentiviral and human reference gene targets. This step is critical for generating sufficient template and has been optimized to minimize PCR bias, with targeted amplification kits outperforming whole-genome amplification kits [74].
- Droplet Digital PCR: The preamplified material is partitioned into thousands of nanoliter-sized droplets for a duplexed ddPCR reaction. This allows for the absolute quantification of both viral and reference gene targets without the need for a standard curve.
- Data Analysis: A Bayesian statistical framework is applied to the ddPCR data to estimate VCN integers with maximum likelihood scores for each cell, distinguishing transduced (VCN ≥1) from non-transduced (VCN=0) cells [74].
Comparative Performance Data
The table below summarizes quantitative data on the performance of the described VCN measurement techniques.
Table 1: Comparative Performance of VCN Determination Methods
| Methodological Feature | Population qPCR (Bulk gDNA) | Single-Cell ddPCR |
|---|---|---|
| Measured Output | Average VCN across the cell population [74] | VCN distribution per cell, including % transduced cells [74] |
| Theoretical Basis | Relative quantification against a reference gene [73] | Absolute quantification via Poisson statistics [74] |
| Key Performance | Concordant results across labs & instruments; CV ~2-7% [73] | Identifies cell-to-cell variability; Consistent with population data [74] |
| Required DNA Input | 25 ng - 125 ng per qPCR reaction [73] | Genomic DNA from a single cell (preamplified) [74] |
| Reference Standard | Defined VCN Jurkat cell lines (1-4 copies) [73] | Bayesian probability framework [74] |
| Information on Heterogeneity | No, obscures underlying distribution [74] | Yes, reveals distribution and rare high-VCN clones [74] |
Application in Biodistribution and Tumorigenicity Risk Assessment
Biodistribution studies are crucial for elucidating the fate and tumorigenicity risk of cell therapy products (CTPs). The single-cell VCN method provides a high-resolution tool for product characterization that can complement biodistribution studies [74]. A case study on iPSC-derived pancreatic islet cells highlights the importance of long-term biodistribution assessment, demonstrating that cells can remain localized at the transplantation site for one year with no migration to other organs, suggesting minimal tumorigenicity risk [23]. The ability of the scVCN assay to identify cell clones with a high number of vector integrations is directly relevant to safety assessments, as these clones could pose a greater risk of insertional mutagenesis if they persist and replicate following transplantation [74].
Experimental Workflow and Signaling Pathways
The following diagram illustrates the logical workflow for selecting a VCN analysis method based on the critical quality attributes of a cell therapy product.
The Scientist's Toolkit: Essential Research Reagents
The table below details key reagents and materials essential for conducting VCN and viability studies in cell therapy products.
Table 2: Essential Research Reagents for VCN and Cell Therapy Characterization
| Reagent/Material | Function & Application |
|---|---|
| Defined VCN Reference Standard Cell Lines | Renewable clonal cell lines (e.g., Jurkat with 1-4 LV copies) for accurate validation and calibration of qPCR VCN assays [73]. |
| Primer/Probe Sets for Viral Targets | Hydrolysis probes and primers for qPCR/ddPCR, targeting conserved lentiviral regions (e.g., RRE, WPRE, synthetic tags) to quantify integrated vector genomes [73] [74]. |
| Primer/Probe Sets for Reference Genes | Assays for single-copy human genes (e.g., RPPH1, TERT, RPL32) used for normalization in VCN calculations to account for genomic DNA input [73] [74]. |
| Targeted Preamplification Kits | Critical for single-cell VCN analysis via ddPCR; enables unbiased amplification of multiple specific targets from the minimal DNA of a single cell prior to partitioning [74]. |
| Droplet Digital PCR (ddPCR) System | Platform for absolute quantification of nucleic acids without a standard curve; essential for scVCN analysis and highly precise pVCN measurements [74]. |
| Human-Specific LINE1 Assay | ddPCR assay for biodistribution studies; quantifies human DNA in animal tissue to track the persistence and location of administered human cell therapies [23]. |
Ensuring Data Reliability: Validation Frameworks and Cross-Method Comparisons
Industry Best Practices for Validating qPCR and dPCR Biodistribution Assays
Within the evolving landscape of cell and gene therapy (CGT), biodistribution (BD) studies are indispensable for preclinical safety assessment, required by regulatory authorities worldwide [24] [1]. These studies evaluate the distribution, persistence, and clearance of administered cell therapy products (CTPs) from the site of administration to both target and non-target tissues [75] [46]. The data gleaned is crucial for predicting efficacy, understanding the mechanism of action, and identifying potential safety risks, such as ectopic tissue formation or tumorigenicity from undifferentiated cells [24].
Quantitative Polymerase Chain Reaction (qPCR) and digital PCR (dPCR) have emerged as the cornerstone analytical techniques for BD studies, enabling the sensitive and specific detection of administered CTPs within a complex biological background [27] [75]. However, a significant challenge persists: the absence of internationally unified regulatory guidance on assay validation [75] [46] [76]. This guide objectively compares the performance of qPCR and dPCR and synthesizes current industry best practices for their validation, providing a critical resource for researchers and drug development professionals navigating this complex field.
Comparative Performance: qPCR vs. dPCR
The choice between qPCR and dPCR is fundamental to BD study design. The table below summarizes a direct comparison of their key performance characteristics based on recent cross-industry studies and validation data.
Table 1: Performance Comparison of qPCR and dPCR in Biodistribution Assays
| Performance Characteristic | qPCR | dPCR |
|---|---|---|
| Sensitivity (Lower Limit of Quantification) | ~48 copies/reaction [46] | ~12 copies/reaction [46] |
| Accuracy (Relative Error) | Generally within ±50% [27] | Meets pre-defined criteria (e.g., ±50%) [77] [46] |
| Precision (Coefficient of Variation) | Generally <50% [27] | Higher precision than qPCR [46] [78] |
| Dynamic Range | Wide (e.g., 5-6 logs) [75] | Wide but can be constrained at high target concentrations |
| Quantification Method | Relative to a standard curve [75] | Absolute, without a standard curve [46] |
| Key Advantage | Well-established, wide dynamic range | Superior sensitivity and precision, absolute quantification |
| Common Application | BD studies with moderate sensitivity requirements [27] | Low-level persistence, shedding, CAR-T monitoring [78] |
Analysis of Experimental Data
Cross-validation studies demonstrate that while both methods can provide reliable data, their performance profiles differ. A multi-facility study using the primate-specific Alu gene to track human mesenchymal stem cells (hMSCs) in mice found that both qPCR and droplet digital PCR (ddPCR) showed similar accuracy (relative error generally within ±50%) and precision (coefficient of variation generally less than 50%) [27]. The tissue distribution profiles generated across seven facilities were consistent, successfully identifying the lungs as the primary site of cell distribution [27].
However, dPCR consistently demonstrates a sensitivity advantage. In a study quantifying an adenoviral vector vaccine, the lower limit of quantitation (LLOQ) for dPCR was set at 12 copies/reaction, compared to 48 copies/reaction for qPCR [46]. This enhanced sensitivity is particularly valuable for applications like monitoring Chimeric Antigen Receptor T-cell (CAR-T) persistence, where dPCR achieved a sensitivity of 0.01%, outperforming flow cytometry (0.1%) and qPCR (1%) [78]. Furthermore, dPCR's absolute quantification eliminates the need for a standard curve, reducing variability and potential matrix effects associated with curve-based quantification in qPCR [46].
Best Practices in Assay Validation
Despite the lack of formalized regulatory guidelines, a scientific consensus on best practices for validating qPCR and dPCR methods is emerging from industry experts and white papers [79] [76]. The goal of validation is to demonstrate that the assay is "fit-for-purpose"—reliable, reproducible, and sensitive enough to support safety assessments.
The following workflow outlines the key stages in developing and validating a robust PCR assay for biodistribution studies.
Figure 1: PCR Assay Development and Validation Workflow.
Core Validation Parameters and Acceptance Criteria
Based on the workflow above, the "Assay Validation" stage is critical. The table below details the core parameters and proposed acceptance criteria, drawing from recent literature and cross-industry recommendations [77] [46] [76].
Table 2: Key Validation Parameters and Proposed Acceptance Criteria
| Validation Parameter | Description | Proposed Acceptance Criteria |
|---|---|---|
| Accuracy | Closeness of measured value to true value | ±50% relative error for quality control (QC) samples [27] [46] |
| Precision | Repeatability of measurements | <50% coefficient of variation (CV) for QC samples [27] [46] |
| Sensitivity (LLOQ) | Lowest quantity reliably quantified | LLOQ should be defined (e.g., 50 copies/μg DNA) and meet accuracy/precision criteria [46] [1] |
| Specificity/Selectivity | Ability to measure target in intended matrix | No amplification in negative controls; >70% recovery from spiked matrix [46] |
| Linearity/Dynamic Range | Range over which results are linearly proportional | Minimum of 4-5 orders of magnitude with R² > 0.98 [75] |
For DNA-based BD assays, a probe-based qPCR (e.g., TaqMan) is recommended due to superior specificity over dye-based methods [75]. A typical qPCR reaction mixture includes sequence-specific primers and a probe, master mix, and up to 1,000 ng of sample genomic DNA [75]. The DNA extraction method must be rigorously optimized for recovery; one study improved recovery rates from below 60% to over 70% by adjusting sample input amounts and proteinase K volume [46].
Essential Protocols and Research Reagent Solutions
Detailed Protocol: qPCR Biodistribution Assay
This protocol outlines the key steps for performing a probe-based qPCR assay for BD studies, adapted from published methodologies [27] [75] [1].
- Sample DNA Extraction: Extract genomic DNA from tissues (e.g., liver, lung, spleen, gonads), blood, and excreta using a commercial kit (e.g., DNeasy Blood and Tissue Kit). The method must be optimized and validated for recovery rate and the absence of PCR inhibitors [46].
- Standard Curve Preparation: Prepare a standard curve using serial dilutions (e.g., 10-fold) of the reference standard (e.g., plasmid containing the target sequence or genomic DNA from the administered cells) spiked into naive matrix DNA (gDNA from untreated animals). A range from 10 to 10^8 copies is typical [75] [1].
- qPCR Reaction Setup: Assemble reactions in a 96-well or 384-well plate. A 50 μL reaction may contain:
- qPCR Run Conditions: Perform amplification on a real-time PCR instrument (e.g., QuantStudio) using the following cycling conditions:
- Enzyme Activation: 95°C for 10 min (1 cycle)
- Denaturation: 95°C for 15 sec
- Annealing/Extension: 60°C for 30-60 sec (40 cycles) [75].
- Data Analysis: The software generates a standard curve from the Ct values of the standards. The copy number in unknown samples is interpolated from this curve using the sample's Ct value [75].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table catalogues essential materials and their functions for successfully executing BD PCR assays.
Table 3: Essential Reagents and Materials for Biodistribution PCR Assays
| Item | Function/Description | Example Use Case |
|---|---|---|
| Species-Specific Primers/Probes | Enables specific detection of human cells in animal tissue; e.g., Alu sequences for human cell tracking [27]. | Quantifying human mesenchymal stem cells (hMSCs) in mouse tissues [27]. |
| Commercial Master Mix | Pre-mixed solution containing DNA polymerase, dNTPs, and optimized buffers for efficient amplification. | Probe-based qPCR using TaqMan universal master mix II [75]. |
| Genomic DNA Extraction Kit | For isolating high-quality, inhibitor-free DNA from complex biological matrices (tissues, blood, excreta). | Using the DNeasy Blood & Tissue Kit with optimized proteinase K steps for improved recovery [46]. |
| Reference Standard DNA | A known quantity of the target sequence (plasmid or cell DNA) used to construct the standard curve for absolute quantification. | Serially diluted linearized plasmid or human T-cell DNA spiked into mouse gDNA [46] [1]. |
| Digital PCR System | Instrumentation that partitions samples into thousands of nanoreactions for absolute nucleic acid quantification without a standard curve. | Using the QX200 or QuantStudio 3D system for high-sensitivity detection of viral vectors or rare cell events [46] [78]. |
The selection between qPCR and dPCR is not a matter of one being universally superior, but rather of choosing the right tool for the specific context of the BD study. The following diagram provides a logical framework for this decision-making process.
Figure 2: qPCR vs. dPCR Selection Framework.
In conclusion, qPCR remains a robust and widely accepted workhorse for many BD studies, particularly where targets are expected at moderate to high levels and a well-defined standard is available [27]. In contrast, dPCR offers compelling advantages for studies demanding the highest sensitivity, absolute quantification, and superior precision, such as monitoring long-term, low-level cell persistence or vector shedding [46] [78].
The regulatory landscape for BD assays is still evolving, with an increasing push for harmonization of validation criteria [76]. By adhering to the emerging best practices outlined in this guide—rigorous assay design, thorough validation of key parameters, and strategic selection of the PCR technology—researchers can generate high-quality, reliable biodistribution data that robustly supports the safety assessment of innovative cell and gene therapies.
Biodistribution studies are fundamental in the development of cell therapy products (CTPs), providing critical data on their travel, accumulation, and persistence within the body. This information is essential for predicting and assessing both efficacy and toxicity profiles during non-clinical and clinical development [72]. For adoptive T cell therapies (TCTs)—a class of "living drugs" that includes CAR-T cells, TCR-T cells, and tumor-infiltrating lymphocytes (TILs)—understanding cellular kinetics (CK) and biodistribution is particularly crucial. These parameters directly influence clinical outcomes, as the anti-tumor effects of CAR-T and TCR-T cells have been correlated with their expansion and persistence in patients [80]. Unlike traditional pharmaceuticals, TCTs can self-replicate, challenging conventional dose-exposure relationships and necessitating specialized analytical frameworks to define the acceptance criteria—accuracy, precision, and limits of quantification (LOQ)—that ensure data reliability [80].
This guide objectively compares the performance of key bioanalytical methods used in biodistribution studies, supporting scientists in selecting and validating appropriate techniques for their specific research context.
Core Analytical Methodologies and Experimental Protocols
A range of methods is employed to quantify biodistribution, each with distinct strengths and limitations. The following section details the experimental protocols for several key techniques.
Quantitative Polymerase Chain Reaction (qPCR)
qPCR is a primary method for quantifying the biodistribution of engineered CTPs, especially those with known genetic modifications.
- Experimental Protocol (qPCR for TCT Biodistribution): DNA is first extracted from homogenized tissues (e.g., blood, spleen, tumor). Specific primers and probes are then designed to target the unique transgene sequence (e.g., the CAR transgene or a specific TCR sequence). A standard curve is generated using serial dilutions of a plasmid containing the target sequence, with known copy numbers. The quantitative cycle (Cq) values from the tissue samples are interpolated from this standard curve to determine the vector copy number (VCN) per microgram of DNA or per cell. This protocol allows for the sensitive tracking of engineered cells in various organs [72] [80].
Radiotracing with Trichloroacetic Acid (TCA) Precipitation
Radiotracing offers exceptional sensitivity but can be confounded by the release of free radiolabel from biodegradable carriers. A refined method using TCA precipitation corrects for this.
- Experimental Protocol (TCA Precipitation for Accurate Radiotracing): After administering the radiolabeled (e.g., ¹²⁵I) product and collecting tissues, homogenates are prepared. An equal volume of 20% (w/v) TCA is added to the homogenate to precipitate proteins, nucleic acids, and larger carrier structures. The sample is vortexed and centrifuged, separating the precipitate (containing the carrier-bound radiolabel) from the supernatant (containing the free radiolabel). The radioactivity in both fractions is measured using a gamma counter. The signal from the free radiolabel in the supernatant is subtracted from the total signal to obtain the corrected biodistribution data specific to the carrier [81].
Imaging Mass Cytometry (IMC)
IMC is an innovative technology that combines mass spectrometry with spatial histology, allowing for the detection of metal-doped particles or metal-tagged antibodies at a cellular resolution.
- Experimental Protocol (IMC for Metal-doped Particles): Fresh-frozen or FFPE tissue sections are mounted on slides. For detecting metal-doped nanoplastics, as demonstrated in a recent mouse model study, the tissue is analyzed directly. Alternatively, tissues can be stained with antibodies conjugated to heavy metal isotopes to identify specific cell phenotypes. The slides are then ablated by a UV laser, and the vaporized material is atomized and ionized in a plasma. The ions are filtered and analyzed by time-of-flight (TOF) mass spectrometry. The spatial coordinates (x, y) of the ions are recorded, generating a highly multiplexed image that maps the distribution of the metal tags across the tissue [82].
Inductively Coupled Plasma Mass Spectrometry (ICP-MS)
ICP-MS is a highly sensitive technique for quantifying trace metals, which can be applied to study metal-doped model particles.
- Experimental Protocol (ICP-MS for Metal-doped Nanoplastics): Biological samples are completely digested using strong acids (e.g., nitric acid) in a microwave digester, transforming the solid tissue into a liquid matrix. The digested solution is introduced into the ICP-MS, where it is atomized and ionized in a high-temperature argon plasma. The resulting ions are separated by their mass-to-charge ratio and quantified. For bulk analysis, this provides the total metal content in a sample. In single-particle mode (spICP-MS), it can detect and count individual metal-doped nanoparticles [82].
Table 1: Comparison of Quantitative Bioanalytical Techniques in Biodistribution Studies.
| Technique | Measured Endpoint | Key Strengths | Key Limitations | Common Applications |
|---|---|---|---|---|
| qPCR | Vector Copy Number (VCN) | High sensitivity, quantitative, widely accessible | Requires specific genetic tag, loses spatial information | Tracking engineered CTPs (CAR-T, TCR-T) [72] [80] |
| Radiotracing (with TCA) | % Injected Dose per gram (%ID/g) | Extremely high sensitivity, standardized quantitation | Requires radioactive handling, potential for free label release [81] | Biodistribution of drug delivery systems & carriers [81] |
| Imaging Mass Cytometry (IMC) | Spatial distribution of metal tags | High multiplexing, cellular resolution, no signal quenching | Low throughput, destructive to sample, complex data analysis | Detection of metal-doped particles, high-plex tissue phenotyping [82] |
| ICP-MS | Total metal concentration | Ultra-sensitive for metals, can be used for single-particle analysis | Destructive, requires metal-doped model particles, loses spatial context | Quantifying metal-doped model nanoplastics in tissues [82] |
| X-ray Fluorescence Imaging (XFI) | Spatial distribution of medium/high-Z elements | Non-destructive, provides 3D spatial data, penetrates thick tissues | Lower sensitivity vs. ICP-MS/IMC, requires synchrotron source | Pre-screening for spatial distribution of metal-doped particles [82] |
Defining and Comparing Key Acceptance Criteria
The reliability of biodistribution data hinges on rigorously defining and validating analytical method parameters. Accuracy, precision, and the limit of quantification are the foundational pillars of this validation.
Accuracy
Accuracy defines how close a measured value is to the true value. It is paramount for ensuring that biodistribution data reflects the actual presence of the therapy in a tissue.
- In Radiotracing: The TCA precipitation method is a specific approach to improve accuracy. It corrects for confounding signals from free radiolabel (e.g., ¹²⁵I) that may detach from the carrier in vivo. This method was validated by spiking samples with known amounts of free radiolabel, which was then detected and separated with ≥85% accuracy, ensuring the final biodistribution data accurately reflects the carrier [81].
- In Mass Spectrometry Methods: For techniques like ICP-MS and IMC using metal-doped particles, accuracy is validated against certified reference materials and by spike-and-recovery experiments in relevant biological matrices (e.g., liver homogenate). This confirms that the sample preparation and analysis do not alter the quantitation of the metal tag [82].
Precision
Precision describes the reproducibility of measurements, typically reported as repeatability (intra-assay) and intermediate precision (inter-assay).
- In qPCR: Precision is demonstrated by low variability (% coefficient of variation) in vector copy number measurements across multiple replicates of the same sample, run within the same plate and across different days by different analysts. This is critical for reliably tracking changes in CTP persistence over time [72] [80].
- In spICP-MS: Precision is reflected in the consistent measurement of nanoparticle concentration and size distribution in repeated analyses of a homogeneous sample. High precision is necessary to make confident conclusions about particle accumulation in different organs [82].
Limit of Quantification (LOQ)
The LOQ is the lowest concentration of an analyte that can be quantitatively determined with acceptable levels of accuracy and precision.
- For qPCR: The LOQ is determined during assay validation and is the lowest copy number on the standard curve that can be reliably distinguished from background with a defined precision (e.g., CV < 25-35%). This defines the threshold for reporting a tissue as positive for the CTP [72].
- For Radiotracing and ICP-MS: These methods boast exceptionally low LOQs, often in the parts-per-billion range or lower, due to the inherent sensitivity of detecting radioactive decay and metal ions, respectively [82] [81]. This allows for detecting very low levels of CTPs or carriers in distant or hard-to-transduce tissues.
Table 2: Typical Performance Characteristics of Bioanalytical Techniques.
| Technique | Reported/Inferred LOQ | Key Factors Influencing Precision | Key Factors Influencing Accuracy |
|---|---|---|---|
| qPCR | ~10-100 copies (assay dependent) | Replicate variability, pipetting accuracy, inhibitor presence in sample [72] | Specificity of primers/probes, efficiency of DNA extraction, standard curve integrity [80] |
| Radiotracing | Sub-%ID/g (e.g., for ¹²⁵I) [81] | Counting statistics of radioactive decay, instrument drift | Presence of free radiolabel, quenching, geometry of sample during counting [81] |
| IMC | Not explicitly stated; high sensitivity [82] | Laser ablation stability, tissue heterogeneity, ion detection efficiency | Antibody specificity (if used), metal tag leaching, sample preparation artifacts |
| ICP-MS | sub-ppb for Pd [82] | Sample introduction stability, plasma fluctuations, matrix effects | Complete sample digestion, isobaric interferences, calibration drift |
| XFI | ~ppm for Pd [82] | X-ray beam stability, counting time per pixel | Self-absorption effects, sample thickness, overlap of emission lines |
An Integrated Workflow for Robust Biodistribution Analysis
No single analytical method is perfect. Therefore, an integrated workflow that leverages the strengths of complementary techniques provides the most comprehensive picture of CTP biodistribution. A recent study on nanoplastics exemplifies this powerful approach, using a combination of X-ray fluorescence imaging (XFI), ICP-MS, and IMC to track metal-doped particles in mice [82].
Diagram 1: A multi-technique workflow for biodistribution analysis.
In this workflow, non-destructive XFI scanning first provides a macroscopic overview of particle distribution, guiding the selection of regions of interest (ROIs) for deeper analysis [82]. Subsequently, bulk digestion and ICP-MS analysis of tissue samples deliver highly sensitive, quantitative data on total particle load across many samples. Finally, IMC is applied to the pre-identified ROIs to achieve cellular-resolution mapping, confirming particle uptake at the single-cell level. This synergistic approach minimizes time investment while maximizing the depth of information obtained, from organ-level distribution to nanoscale cellular interactions [82].
The Scientist's Toolkit: Essential Research Reagent Solutions
Selecting the appropriate reagents and materials is critical for the success of any biodistribution study. The table below details key solutions used in the featured methodologies.
Table 3: Essential Research Reagent Solutions for Biodistribution Studies.
| Reagent / Material | Function / Description | Application Context |
|---|---|---|
| Metal-doped Model Particles | Nanoplastics (e.g., Polystyrene) doped with rare elements (e.g., Palladium). Act as tracers to circumvent analytical challenges of unlabeled particles. [82] | Used as a proxy for environmental nanoplastics or model drug carriers in ICP-MS, XFI, and IMC studies. [82] |
| qPCR Assay Kits | Pre-optimized master mixes, primers, and probes for detecting specific transgenes (e.g., CAR, TCR) or species-specific DNA sequences. | Standardized quantification of engineered CTP biodistribution and persistence via DNA extraction from tissues. [72] [80] |
| Antibody-Metal Conjugates | Antibodies specific to cellular proteins (e.g., CD3, GFAP) covalently linked to heavy metal isotopes (e.g., ¹⁶³Dy, ¹⁷⁶Yb). | Enables highly multiplexed, spatial phenotyping of tissues and co-localization of CTPs using Imaging Mass Cytometry (IMC). [82] |
| Trichloroacetic Acid (TCA) | A precipitating agent used to separate large, radiolabeled structures (proteins, nucleic acids, carriers) from free radiolabel in solution. [81] | Critical for correcting biodistribution data in radiotracing studies by removing the confounding signal from degraded or free radiolabel. [81] |
| Cell-Specific Promoters | Genetic regulatory sequences (e.g., gfaABCD1405 for astrocytes, p546 for neurons) that restrict transgene expression to specific cell types. [83] | Used in AAV-mediated gene therapy to control biodistribution and expression of reporter genes or therapeutic proteins at the tissue and cellular level. [83] |
The accurate assessment of cell therapy biodistribution relies on a foundation of rigorously defined acceptance criteria. As demonstrated, no single analytical method universally excels across all dimensions of accuracy, precision, sensitivity, and spatial resolution. The choice between qPCR, radiotracing, and advanced mass spectrometry-based techniques like IMC and ICP-MS depends on the specific research question, the nature of the cell therapy product, and the required level of quantitative versus spatial information.
The emerging trend is toward integrated, complementary workflows. By combining techniques—using a non-destructive imaging method for initial screening, a bulk mass spectrometry method for sensitive quantification, and a high-resolution spatial technique for cellular confirmation—researchers can overcome the limitations of any single method. This multi-faceted approach, governed by clear acceptance criteria, provides the comprehensive and reliable biodistribution data essential for optimizing the efficacy and safety of next-generation cell therapies.
The therapeutic efficacy of cell therapies is intrinsically linked to their ability to reach target tissues in sufficient quantities while minimizing off-target accumulation. Tissue uptake and background ratios (TBR) have consequently emerged as critical quantitative metrics for comparing the performance of different cell therapy platforms. These metrics provide researchers with standardized parameters to objectively evaluate biodistribution patterns, enabling direct comparisons across diverse therapeutic platforms, including mesenchymal stromal cells (MSCs), chimeric antigen receptor (CAR) T cells, and viral vector-mediated gene therapies [42] [80].
For cell-based "living drugs," traditional pharmacokinetic principles often do not apply, as these therapies can actively expand, persist, or be cleared within the patient [80]. This complex kinetic behavior makes accurate measurement of tissue uptake particularly challenging yet vital for understanding product quality, potency, and stability. This guide provides a structured framework for the comparative assessment of tissue uptake and TBR across major cell therapy modalities, synthesizing current methodologies, experimental data, and standardized protocols to facilitate cross-platform evaluation.
Comparative Landscape of Cell Therapy Biodistribution
Quantitative Biodistribution Profiles
The following table summarizes key biodistribution characteristics and primary quantification methods for major cell therapy classes, highlighting their distinct distribution profiles and the technologies used to measure them.
Table 1: Comparative Biodistribution of Cell Therapy Platforms
| Therapy Platform | Primary Target Tissues | Key Quantitative Metrics | Primary Detection Methods | Major Uptake Challenges |
|---|---|---|---|---|
| MSC Therapy [42] | Lung, Liver, Spleen; Inflamed sites | Biodistribution coefficient; Persistence time; Organ-specific retention (%) | Optical imaging (BLI, FII); PCR; Radioactive labeling (e.g., 89Zr) | Significant pulmonary first-pass effect; Poor persistence in target tissues |
| CAR-T Cell Therapy [80] | Blood, Bone Marrow, Spleen, Lymph nodes; Tumor sites | Peak expansion (cells/μL); Area under the curve (AUC); Tumor penetration index | Flow cytometry; ddPCR; Quantitative PCR (qPCR) | Limited solid tumor penetration; T cell exhaustion in tumor microenvironment |
| rAAV Gene Therapy [84] [83] | Liver, CNS (serotype-dependent), Muscle, Heart | Vector genomes per cell (vg/cell); Transduction efficiency (%); Cellular uptake rate | Droplet digital PCR (ddPCR); Next-generation sequencing; Immunohistochemistry | Pre-existing immunity; Off-target transduction; Capsid uptake efficiency |
Tissue Uptake and Background Ratios Across Modalities
Direct comparison of tissue uptake metrics reveals fundamental differences in how various cell therapy platforms distribute throughout the body. For 89Zr-labeled monoclonal antibodies, a critical distinction must be made between total tissue uptake and target-mediated uptake, with studies showing that 38% of spleen uptake at 144 hours post-injection can be attributed to nonspecific antibody catabolism rather than target engagement [85]. This highlights the importance of applying correction factors to distinguish specific from non-specific uptake, a consideration that extends to other therapeutic platforms.
For mesenchymal stromal cells (MSCs), systemic administration results in a characteristic pulmonary first-pass effect, with the lungs sequestering 50-60% of intravenously infused cells immediately following administration [42]. This substantial background accumulation in non-target tissues presents a significant challenge for achieving therapeutic concentrations at disease sites. The kinetics of MSC persistence further compounds this challenge, with less than 5% of locally administered cells typically remaining at the injection site within hours after transplantation [42].
Adoptive T cell therapies exhibit markedly different distribution patterns, with peak expansion in blood and lymphoid tissues occurring days to weeks after infusion. Clinical studies have established clear correlations between CAR-T cell expansion/persistence and therapeutic efficacy, particularly in hematological malignancies [80]. Unlike MSCs, CAR-T cells demonstrate minimal lung entrapment but face significant barriers in penetrating solid tumors, resulting in unfavorable tumor-to-background ratios in these indications.
For recombinant AAV (rAAV) vectors, tissue uptake is highly dependent on serotype and administration route. Recent advances in promoter design, such as the novel truncated GFAP promoter (gfa1405) for astrocyte-specific expression, have improved target-to-background ratios in CNS-directed therapies [83]. Quantitative assessment of rAAV uptake has been revolutionized by ddPCR technology, which provides absolute quantitation of vector genomes with significantly improved precision over traditional TCID50 methods [84].
Experimental Protocols for Uptake Quantification
89Zr-mAb PET Correction Protocol for Specific Uptake
Accurate quantification of specific tissue uptake for labeled therapeutics requires correction for non-specific background accumulation. The following protocol, adapted from studies with 89Zr-labeled monoclonal antibodies, provides a robust framework for this correction [85]:
- Sample Collection: Obtain plasma samples concurrent with PET imaging acquisition, ideally at multiple time points post-injection (e.g., 24, 72, 144 hours) to characterize exposure.
- Tissue Activity Measurement: Quantify tissue uptake from PET images using standardized uptake value (SUV) or percentage injected dose (%ID) within precisely defined volumes of interest.
- Plasma Activity Measurement: Measure 89Zr concentration in plasma samples using a gamma counter, correcting for decay.
- Calculate Total Tissue Exposure: Determine the area under the plasma concentration-time curve (AUCplasma) from time zero to the imaging timepoint using non-compartmental analysis.
- Apply Correction Formula: Calculate the corrected tissue-to-plasma ratio (cTPR) using the established equation:
- cTPR = (Ctissue - [KNAC, tissue × AUCplasma]) / Cplasma
- Where Ctissue is tissue concentration (Bq/mL), KNAC, tissue is the tissue-specific net rate of irreversible uptake due to nonspecific antibody catabolism (μL·g⁻¹·h⁻¹), AUCplasma is total plasma exposure (Bq·mL⁻¹·h), and Cplasma is plasma concentration at imaging time (Bq/g).
- Interpret Results: Compare cTPR values to established baseline TPR (bTPR) values for the same tissue. A cTPR exceeding bTPR indicates presence of target-mediated uptake.
This methodology highlights the critical importance of accounting for nonspecific catabolism and residualization of labels, which significantly impacts background signal across multiple therapeutic platforms.
ddPCR Protocol for rAAV Cellular Uptake Quantification
The following protocol details a highly precise method for quantifying recombinant AAV (rAAV) cellular uptake using droplet digital PCR (ddPCR), which has demonstrated superior precision compared to traditional TCID50 methods [84]:
- Cell Line Preparation: Utilize a stable AAV receptor (AAVR) cell line to ensure consistent viral entry across experiments and serotypes.
- Virus Transduction: Incubate cells with rAAV vectors at varying multiplicities of infection (MOI) for 24-48 hours under standard culture conditions.
- Genomic DNA Extraction: Harvest cells and extract genomic DNA using a column-based or magnetic bead-based method, ensuring minimal DNA fragmentation.
- Droplet Digital PCR Setup:
- Prepare reaction mix containing digested genomic DNA, ddPCR supermix, and target-specific primers/probes for the transgene.
- Include reference gene primers/probes for normalization.
- Generate droplets using a droplet generator.
- PCR Amplification: Perform endpoint PCR on the droplet emulsion using the following cycling conditions:
- 95°C for 10 minutes (enzyme activation)
- 40 cycles of: 94°C for 30 seconds and 60°C for 60 seconds (amplification)
- 98°C for 10 minutes (enzyme deactivation)
- 4°C hold
- Droplet Reading and Analysis:
- Read droplets using a droplet reader to quantify positive and negative droplets.
- Calculate vector genomes per cell using the formula:
- Vector genomes/cell = (Concentration of target gene × Dilution factor × Reaction volume) / (Number of cells input × Concentration of reference gene)
- Data Interpretation: Compare uptake efficiency across different serotypes, promoters, or formulation conditions to identify optimal parameters for specific target tissues.
This method provides absolute quantitation of rAAV uptake without requiring standard curves, offering a robust platform for comparing viral vector uptake across experimental conditions.
Molecular Mechanisms Governing Tissue Homing and Uptake
MSC Homing Signaling Pathway
The tissue homing process for systemically administered mesenchymal stromal cells involves a coordinated multi-step mechanism that parallels leukocyte trafficking [42]:
CRISPR-Enhanced CAR T Cell Screening Workflow
The CELLFIE platform represents a systematic approach to enhancing CAR T cell function through targeted genetic modifications [86]:
Essential Research Reagent Solutions
The following table catalogues critical reagents and technologies for quantifying tissue uptake and background ratios across different cell therapy platforms.
Table 2: Essential Research Reagents for Uptake and TBR Assessment
| Reagent/Technology | Primary Application | Key Function in Uptake Studies | Performance Advantages |
|---|---|---|---|
| 89Zr Radiolabeling [85] | mAb PET Imaging; Cell Tracking | Enables quantitative PET imaging and pharmacokinetic modeling | Residualizing property allows cumulative uptake measurement; High sensitivity |
| CROP-seq-CAR Vector [86] | CRISPR CAR T Cell Screening | Simultaneous delivery of CAR and gRNA for pooled functional screens | Links gRNA identity to phenotypic readouts; Enables genome-wide screens in primary T cells |
| Droplet Digital PCR [84] | rAAV Quantitation; CAR T Cell Kinetics | Absolute quantitation of vector genomes and cellular kinetics | Superior precision vs. TCID50; No standard curves required; Absolute quantification |
| Aiforia AI Platform [87] | Scaffold-Based Cell Therapy Imaging | Automated cell counting in complex 3D environments | Overcomes challenges of dynamic backgrounds; High correlation with manual counts (r²=0.96) |
| Cell-Specific Promoters [83] | AAV-Mediated Gene Therapy | Restricts transgene expression to specific cell populations | Reduces off-target expression; Improves therapeutic index; gfa1405 for astrocyte specificity |
| CRISPR Editors (mRNA) [86] | Primary Immune Cell Engineering | Enables efficient gene knockout in hard-to-transfect cells | High editing efficiency (>80%); Flexible platform for diverse editors |
The comparative analysis of tissue uptake and background ratios across cell therapy platforms reveals both platform-specific challenges and unifying principles for optimization. The data demonstrates that correction for nonspecific uptake is essential for accurate interpretation of biodistribution studies, whether assessing 89Zr-mAb accumulation or MSC persistence [85] [42]. Furthermore, the integration of advanced quantification technologies like ddPCR and AI-based image analysis provides the precision necessary to distinguish subtle differences in uptake efficiency [84] [87].
The development of CRISPR screening platforms like CELLFIE represents a paradigm shift in cell therapy optimization, enabling systematic identification of genetic modifications that enhance therapeutic performance [86]. Similarly, the refinement of cell-specific promoters for viral vector therapies addresses the critical challenge of off-target expression, directly improving tumor-to-background ratios [83]. These technological advances, coupled with standardized quantitative frameworks for comparing uptake metrics across platforms, will accelerate the development of next-generation cell therapies with optimized biodistribution profiles and enhanced therapeutic efficacy.
For researchers engaged in cross-platform therapy development, the consistent application of these quantitative uptake metrics and correction methodologies will enable more meaningful comparisons across diverse therapeutic modalities, ultimately facilitating the selection of optimal platforms for specific disease indications.
In the field of cell therapy research, the inability to replicate scientific findings has emerged as a prevalent issue of great scientific and public concern. An alarmingly high estimate of 50–80% of preclinical studies fail to replicate, hindering scientific credibility and progress while preventing pharmacotherapeutic development [88] [89]. Multi-site study validation has emerged as a powerful methodological approach to address this challenge by systematically evaluating whether experimental results can be reproduced across different research environments, personnel, and equipment.
For biodistribution assessment of cell therapies, multi-site validation is particularly crucial. These studies are essential for predicting and assessing the efficacy and toxicity profiles of cell therapy products (CTPs), especially regarding tumorigenicity risks associated with undifferentiated pluripotent stem cells [24]. The lack of standardized biodistribution study protocols has led to inconsistent and unreliable results, posing significant challenges in the drug approval process [90]. Multi-site validation provides a framework for establishing robust, standardized protocols that generate reproducible data across different laboratories, thereby enhancing the reliability of biodistribution assessments for regulatory decision-making and clinical translation.
The Reproducibility Challenge in Scientific Research
Root Causes of Irreproducibility
The reproducibility crisis in preclinical research stems from multiple interconnected factors. Phenotypic plasticity—the ability of living organisms to change in response to their environment—presents a fundamental challenge. Even in highly standardized environments, phenotypes in control animals can fluctuate unexpectedly between batches, making it difficult to reproduce original findings [91]. Additional drivers include unrecognized variables in complex experimental models, poor documentation of procedures, selective reporting of positive findings, misinterpretation of technical noise as biological signal, and cognitive biases in research combined with flaws in the academic incentive system [89].
Traditional approaches to addressing variability have focused on excessive standardization of animal strains, housing, husbandry, and testing environments. However, this approach has limitations, as it results in more homogeneous study populations that generate spurious results representative only of specific standardized conditions, thereby paradoxically hampering replicability across different laboratory environments [88]. Gene-environment interactions can substantially affect animal behavior, and laboratories differ in numerous factors including personnel, odors, noise, and microbiota, creating substantial variation in phenotypes between laboratories even when studying the same genetic strain of animals [88].
Consequences for Cell Therapy Development
The implications of poor reproducibility are particularly acute for cell therapy development. Biodistribution studies are required by regulatory authorities including the FDA, EMA, and Japan's PMDA to evaluate the preclinical safety of viral/vector or cellular agents [24] [25]. Inconsistent findings in these studies can lead to:
- Misguided clinical trial designs based on unreliable preclinical data
- Failure to identify potential safety risks such as ectopic tissue formation or tumorigenicity
- Inaccurate assessment of engraftment efficiency and persistence of administered cells
- Reduced regulatory confidence in submitted data, potentially delaying clinical translation
Multi-Site Study Design Fundamentals
Core Principles and Methodologies
Multi-site study validation operates on the principle that embracing environmental and methodological variability across research sites, rather than attempting to eliminate it, leads to more robust and reproducible findings. This approach involves coordinated standardization of key experimental elements while allowing for necessary variation in other aspects. A successful multi-site validation requires harmonization of several critical components:
- Apparatus standardization: Using identical equipment across participating sites
- Protocol alignment: Implementing the same experimental procedures and timing
- Reagent consistency: Utilizing the same batch of critical reagents, such as test compounds
- Operational definitions: Establishing clear criteria for outcome measures across all sites
- Centralized data analysis: Processing data at a single location to minimize analytical variability
The fundamental insight behind multi-site validation is that reproducing findings across different laboratories with inherent environmental variations provides stronger evidence for the robustness of an experimental effect than replication within a single highly standardized environment [88] [91].
Quantitative Evidence Supporting Multi-Site Approaches
Recent research has demonstrated the superior performance of multi-site designs compared to single-site studies. Through simulations utilizing real data across 13 interventions in animal models of stroke, myocardial infarction, and breast cancer, scientists found that reproducibility substantially increased as the number of laboratories increased, with the most significant improvement occurring when moving from one to two sites [91]. This improvement came without necessarily increasing the total number of animals tested, addressing ethical concerns about animal use while enhancing scientific rigor.
Table 1: Impact of Multi-Site Designs on Reproducibility Metrics
| Experimental Design | Reproducibility Rate | Effect Size Accuracy | Sensitivity |
|---|---|---|---|
| Single-site (highly standardized) | Low | Often inflated | High in narrow context |
| Two-site design | Substantially improved | More accurate | Maintained with proper power |
| Multi-site (3+ sites) | Highest | Most accurate | Slightly reduced but more meaningful |
The improvement in reproducibility stems from increased accuracy and reduction in variability of effect size estimates, resulting in fewer outlier experiments. While there is a small penalty in the form of larger confidence intervals, this more accurately reflects the true uncertainty when treatment effects are considered in a broader biological context [91].
Biodistribution Assessment: A Case Study in Standardization
Regulatory Framework for Biodistribution Studies
Biodistribution studies for cell therapy products are viewed differently by various regulatory agencies, though all recognize their importance. The FDA views biodistribution studies as essential for determining "cell fate"—assessing survival/engraftment, distribution, differentiation/integration, and tumorigenicity of administered cells [24]. The EMA defines their purpose as assessing adverse events arising from risk factors specific to cell therapies, including survival/engraftment, proliferation, differentiation, migration, and tumorigenicity [24]. Japan's PMDA focuses on using biodistribution data to predict efficacy and safety and demonstrate the rationality of the administration method/route [24].
Despite these nuanced differences in perspective, all regulatory bodies agree on the fundamental need to understand where administered cells localize, how long they persist, and whether they migrate to non-target tissues. This information is critical for interpreting efficacy results and identifying potential safety concerns, particularly the risk of tumor formation from undifferentiated cells in pluripotent stem cell-derived products [24] [90].
Analytical Methods for Biodistribution Assessment
The current gold standard method for biodistribution assessment of cell therapies is quantitative polymerase chain reaction (qPCR) targeting species-specific or human-specific DNA sequences. This approach allows researchers to quantify the number of human cells present in various animal tissues following administration [24] [90] [25]. More recently, droplet digital PCR (ddPCR) has emerged as an alternative offering absolute quantification without the need for standard curves, potentially improving reproducibility across sites [90].
Table 2: Comparison of Biodistribution Assessment Methods
| Method | Sensitivity | Quantification Capability | Multi-Site Reproducibility | Limitations |
|---|---|---|---|---|
| qPCR | High (≤50 copies/μg DNA) | Relative quantification | Moderate (requires standardized calibration) | PCR inhibition effects, requires standard curves |
| ddPCR | High | Absolute quantification | Potentially higher | Higher cost, newer methodology |
| Imaging (PET/SPECT) | Variable | Semi-quantitative | Challenging (equipment variation) | Requires cell labeling, radiation exposure |
| Fluorescence Imaging | Moderate | Semi-quantitative | Low (signal attenuation issues) | Limited to superficial tissues, signal dilution with cell division |
In addition to molecular methods, various imaging technologies are used for non-invasive tracking of administered cells, including in vivo imaging systems (IVIS) with fluorescence labeling, positron emission tomography (PET), single photon emission computed tomography (SPECT), and magnetic resonance imaging (MRI) [24]. Each method has advantages and limitations, with the optimal approach depending on the specific research question, cell type, and administration route.
Successful Implementation: Key Research Examples
Shank2 Knockout Rat Model Study
A landmark multi-center study investigating a Shank2 knockout (KO) rat model for autism spectrum disorders demonstrates the power of coordinated standardization. Three research facilities reliably observed identical behavioral phenotypes in KO rats compared to their wild-type littermates, including hyperactivity and repetitive behaviors [88]. Furthermore, all sites documented the same dose-dependent attenuation of these phenotypes following acute injections of a selective mGluR1 antagonist.
The study's success relied on several harmonization strategies: using identical PhenoTyper behavioral assessment chambers at all sites, implementing the same EthoVision XT video tracking software, administering test compounds from the same chemical batch, and following aligned operational definitions of behavioral categories [88]. This coordinated approach enabled high replicability of both the baseline phenotype and pharmacological response across all three research centers, despite differences in location and personnel.
iPSC-Derived Pancreatic Islet Cell Biodistribution
A case study on the biodistribution of iPSC-derived pancreatic islet cells illustrates the application of multi-site validation principles to cell therapy products. Researchers optimized a droplet digital PCR method targeting human-specific LINE1 sequences and validated its quantitativity across different tissues using a single calibration curve [90]. This standardized approach allowed them to perform a long-term biodistribution study in immunodeficient mice that demonstrated the cells remained localized at the transplantation site for one year, with no migration to other organs [90].
This study provides valuable insights into the standardization of biodistribution protocols for iPSC-derived CTPs, suggesting that robust, reproducible results can be achieved through methodological harmonization. The findings also highlight the potential for some CTPs to exhibit favorable biodistribution profiles with minimal off-target localization, reducing tumorigenicity concerns [90].
Practical Implementation Framework
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementing robust multi-site biodistribution studies requires specific reagents and methodologies standardized across participating laboratories. The table below details essential research reagent solutions for ensuring reproducibility in cell therapy biodistribution assessment.
Table 3: Essential Research Reagent Solutions for Biodistribution Studies
| Reagent/Method | Function in Biodistribution Assessment | Standardization Requirements |
|---|---|---|
| Species-specific qPCR/ddPCR Assays | Quantification of human cells in animal tissues | Identical primer/probe sequences, standardized calibration curves |
| Digital PCR Systems | Absolute quantification of target DNA without standard curves | Same platform or cross-validated protocols |
| Reference DNA Standards | Calibration curve generation for qPCR | Common source material across all sites |
| DNA/RNA Isolation Kits | Nucleic acid extraction from various tissue types | Identical kits and protocols to minimize variability |
| Internal Control Genes | Assessment of DNA quality and PCR inhibition | Same control genes across all laboratories |
Experimental Protocol for Multi-Site Biodistribution Assessment
A standardized protocol for multi-site biodistribution assessment of cell therapy products should include the following key steps:
Sample Collection and Processing
- Standardized tissue collection schedule (e.g., 24h, 1wk, 1mo, 3mo post-administration)
- Identical tissue preservation methods across sites (e.g., flash-freezing in liquid N₂)
- Centralized or harmonized DNA/RNA extraction protocols
Molecular Analysis
- Quantitative PCR using validated species-specific assays
- Inclusion of internal control genes to assess DNA quality
- Use of standardized reference materials for calibration curves
- Implementation of negative and positive controls in each run
Data Analysis and Reporting
- Centralized data processing where possible
- Standardized calculation methods for vector copy numbers or cell numbers
- Harmonized statistical approaches for comparing across tissues and timepoints
- Unified reporting templates for regulatory submissions
This workflow can be visualized as a sequential process with quality checkpoints at each stage to ensure consistency across participating sites.
Analysis of Quantitative Multi-Site Performance Data
Reproducibility Metrics Across Fields
Evidence from multiple scientific disciplines demonstrates that multi-site designs significantly improve reproducibility metrics. In neuroimaging, brain-wide association studies (BWAS) have shown that sample sizes of thousands are required for reproducible findings, with effect sizes in small samples (n=25) having 99% confidence intervals of r±0.52, indicating severe inflation by chance [92]. At typical sample sizes (n=25), two independent population subsamples can reach opposite conclusions about the same brain-behaviour association solely due to sampling variability [92].
In primate research, proficiency testing for detection of specific pathogen-free viruses showed that through multi-year efforts with shared proficiency samples, testing percent agreement increased from as low as 67.1% for SRV testing in 2010 to 92.1% in 2019 [93]. Similarly, in proteomics, a multilaboratory study assessing multiple reaction monitoring (MRM) assays demonstrated that these assays could be highly reproducible within and across laboratories and instrument platforms when using common materials and standardized protocols [94].
Table 4: Quantitative Reproducibility Improvements Through Multi-Site Validation
| Field | Single-Site Reproducibility | Multi-Site Reproducibility | Key Standardization Factors |
|---|---|---|---|
| Primate Pathogen Detection | 67.1% agreement (2010) | 92.1% agreement (2019) | Shared proficiency samples, standardized assays [93] |
| Preclinical Behavior (Shank2 Model) | Variable single-site results | High replicability across 3 sites | Identical apparatus, protocol, compound batch [88] |
| Proteomics (MRM Assays) | Not reported | High intra- and inter-lab reproducibility | Common materials, standardized protocols [94] |
| MRI T2 Quantification | Intra-site CV: 3.15-8.49% | Inter-site CV: 14.16% | Centralized processing, standardized sequences [95] |
Sample Size Considerations for Biodistribution Studies
The relationship between sample size and reproducibility has important implications for designing biodistribution studies. Research has demonstrated that reproducibility substantially increases as sample sizes grow into the thousands, with replication rates beginning to improve and effect size inflation decreasing accordingly [92]. For biodistribution studies, this suggests that smaller experiments may produce unreliable estimates of cell trafficking patterns, potentially missing important off-target localization or overestimating engraftment efficiency.
Rather than conducting underpowered single-site studies, a more efficient approach involves implementing multi-site designs where each site processes a manageable number of animals, but the combined data provides sufficient statistical power for robust conclusions. This strategy aligns with ethical principles of using the minimum number of animals necessary to answer scientific questions, while recognizing that too few animals can also be wasteful if they produce irreproducible results [91].
Multi-site study validation represents a paradigm shift in how we approach reproducibility in cell therapy research, particularly for critical assessments like biodistribution. Rather than attempting to eliminate all environmental variation through excessive standardization, this approach strategically embraces and controls for variability across sites, producing more robust and generalizable findings. The evidence from multiple fields consistently demonstrates that multi-laboratory designs significantly enhance reproducibility without necessarily increasing total sample sizes, addressing both scientific and ethical considerations.
For cell therapy developers, implementing multi-site validation strategies for biodistribution assessment can strengthen regulatory submissions by providing higher-confidence safety data. As the field advances, further method harmonization—particularly around qPCR/ddPCR protocols, reference materials, and data reporting standards—will continue to improve reproducibility. Ultimately, adopting multi-site validation as a standard practice for critical preclinical studies will accelerate the development of safe and effective cell therapies by providing more reliable data for decision-making throughout the drug development pipeline.
Tailoring Validation Strategies for BD, Persistence, and Shedding
Biodistribution (BD), persistence, and shedding studies are fundamental components in the non-clinical and clinical development of cell and gene therapies (CGTs). They investigate the distribution, persistence, and clearance of therapy products in vivo, encompassing both target and non-target sites [43]. These studies provide essential data for selecting appropriate animal models, routes of administration, and assay methodologies, while also assessing potential risks and informing clinical trial design [43]. The accurate characterization of these parameters is critical for predicting and evaluating both the efficacy and toxicity profiles of CGTs [96].
This guide provides a comparative overview of the key analytical methods—quantitative PCR (qPCR), digital PCR (dPCR), and in vivo imaging—used to support these studies. It outlines tailored validation strategies, presents comparative performance data, and details essential experimental protocols to help researchers select and implement the most appropriate bioanalytical strategies for their CGT programs.
Method Comparison: qPCR, dPCR, and Imaging
The choice of analytical method profoundly impacts the quality and interpretation of BD, persistence, and shedding data. Each technique offers distinct advantages and limitations. The following table provides a structured comparison of these key methodologies.
Table 1: Comparison of Key Analytical Methods for BD, Persistence, and Shedding
| Method | Key Strengths | Key Limitations | Optimal Context of Use |
|---|---|---|---|
| qPCR | High sensitivity (can detect as few as 10 target cells/μg tissue) [43]; Cost-effective; Well-established workflows [43]. | Unable to differentiate between live and dead cells [43]; Requires a standard curve for quantification. | High-throughput quantification of vector genomes or cellular DNA in many samples; Shedding studies. |
| dPCR | Absolute quantification without a standard curve; High precision and tolerance for suboptimal PCR efficiency [97]; Robust performance in complex matrices. | Higher cost per sample than qPCR; Limited dynamic range compared to qPCR. | Absolute quantification of low-abundance targets; Situations where a reliable standard curve is difficult to generate. |
| Bioluminescence Imaging | Provides real-time, whole-body spatial and temporal data; Enables longitudinal studies in a single subject; Safe (non-radioactive). | Rapid signal decline limits long-term tracking [43]; Low signal intensity can hinder detection of small cell populations [43]. | Short-term, real-time tracking of cell homing and initial engraftment. |
| Radioisotope Imaging (e.g., 89Zr-PET/CT) | Enables long-term quantitative tracking [43]; High sensitivity and anatomical context. | Cannot distinguish signal from live cells, dead cells, or freed radioisotope (shedding) [43]; Requires specialized facilities and radiation safety protocols. | Long-term, quantitative tracking of cell fate; Understanding overall cell clearance kinetics. |
A recent study on human umbilical cord-derived mesenchymal stem cells (hUC-MSCs) highlights how these methods can be integrated. The research demonstrated a primary biodistribution pattern of lung > liver > kidney >> spleen after intravenous injection in mice [43]. However, it also revealed critical methodological limitations: for instance, while 89Zr-PET/CT showed persistent signals in the liver and kidney, this was likely due to the accumulation of dead cells and freed radioisotopes, obscuring the true fate of viable MSCs [43]. This underscores the necessity of a multi-method approach to accurately interpret results.
Experimental Protocols for Key Assays
PCR-Based Assay Development and Validation
Both qPCR and dPCR are cornerstone techniques for quantifying vector genomes, transgene expression, and cellular kinetics in CGTs [97]. The following workflow outlines the critical stages in developing and validating a robust PCR assay.
Diagram Title: PCR Assay Development and Validation Workflow
Primer and Probe Design: The process begins with careful in silico design of primers and probes using specialized software (e.g., PrimerQuest, Primer3). A critical step is ensuring specificity for the therapeutic transgene or vector sequence, which can be preliminarily assessed with tools like NCBI's Primer-Blast against the host genome [97]. To confer specificity for a vector-derived transcript over an endogenous one, the assay should target the junction between the transgene and a neighboring vector component (e.g., a promoter or untranslated region) [97]. It is recommended to design and empirically screen at least three candidate primer/probe sets in the relevant biological matrices (e.g., target tissues from pre-clinical species and humans) to identify the best performer [97].
Method Validation: Given the absence of specific regulatory guidance for molecular assays, validation parameters and acceptance criteria should be pre-defined based on the assay's Context of Use (COU) and referred literature [97] [77]. Key validation parameters include the Lower Limit of Quantification (LLOQ), which can be as low as 12 copies per reaction for dPCR and 48 copies per reaction for qPCR, and intra- and inter-run accuracy and precision [77] [97]. Cross-validation between dPCR and qPCR platforms is also recommended to ensure quantitative results are comparable [97].
Integrated Imaging and PCR Workflow for Cell Therapies
For cell-based products, combining imaging with PCR provides a more comprehensive understanding of cell fate in vivo. The protocol below, adapted from a study on hUC-MSCs, outlines this integrated approach.
Table 2: Key Research Reagent Solutions for Cell Tracking Studies
| Reagent / Material | Function in the Experiment |
|---|---|
| Luciferase-Transduced Cells (Luc-MSCs) | Generates bioluminescent signal for real-time, non-invasive tracking of live cells using imaging systems. |
| 89Zr-Oxine | A radioactive tracer with a long half-life (~78.4 hrs) for labeling cells for long-term tracking via PET/CT imaging [43]. |
| Primers/Probes for Species-Specific DNA (e.g., Alu-seq) | Enables highly sensitive detection and quantification of human cell DNA in mouse tissues using qPCR/dPCR [43]. |
| Antibodies for Multiplex IHC (e.g., anti-hCD73) | Allows visual identification and localization of human cells within tissue sections via microscopy, confirming cell presence and phenotype. |
| Naïve Host Genomic DNA (gDNA) | Serves as a critical negative control matrix during PCR assay development to empirically test primer/probe specificity and avoid off-target amplification [97]. |
Diagram Title: Integrated Cell Therapy Biodistribution Workflow
Cell Preparation and Administration: hUC-MSCs are engineered to express luciferase (creating "Luc-MSCs") for bioluminescence imaging and/or labeled with 89Zr-oxine for PET/CT tracking [43]. The 89Zr-oxine must be synthesized and tested for radiochemical purity (≥90%) prior to cell labeling [43]. These prepared cells are then administered to immunodeficient mouse models (e.g., NCG mice) via the clinically relevant route, such as intravenous injection [43].
Longitudinal Imaging and Terminal Analysis: Animals undergo longitudinal imaging over a period of days or weeks. 89Zr-PET/CT typically enables longer tracking (e.g., up to 14 days), while bioluminescence signals may decline more rapidly (e.g., by 7 days) [43]. At terminal time points, tissues are collected for further analysis. This includes qPCR or dPCR on tissue homogenates to quantify human-specific DNA sequences (e.g., Alu elements) with high sensitivity, and multiplex immunohistochemistry (mIHC) to visually confirm the presence and location of human cells (e.g., using an anti-hCD73 antibody) within tissue architecture [43].
Selecting and validating the right analytical strategies for biodistribution, persistence, and shedding is not a one-size-fits-all process. The optimal approach depends on the specific therapeutic product, the critical questions being asked, and the stage of development. As demonstrated, qPCR/dPCR and imaging techniques provide complementary data, and an integrated strategy often yields the most reliable interpretation of cell and gene therapy fate in vivo.
A thorough understanding of each method's strengths and weaknesses—such as qPCR's inability to distinguish live from dead cells or the potential for radioisotope shedding in 89Zr-studies—is essential for designing robust studies and meeting regulatory expectations. By applying the tailored validation strategies and experimental protocols outlined in this guide, researchers can generate the high-quality, reliable data needed to advance the development of safe and effective cell and gene therapies.
Conclusion
The comparative assessment of cell therapy biodistribution is a cornerstone for successful clinical translation, integrating rigorous regulatory science with sophisticated analytical methods. The harmonization of PCR-based techniques and the strategic application of imaging provide a multi-faceted understanding of cell fate. Optimizing delivery routes and infusion protocols is paramount to enhancing therapeutic index and managing safety risks. Future efforts must focus on establishing international consensus on method standardization, developing novel imaging probes for better resolution, and creating integrated pharmacokinetic-pharmacodynamic (PK/PD) models to predict clinical outcomes from non-clinical biodistribution data. Ultimately, a deep understanding of biodistribution will accelerate the development of safer and more effective precision cell therapies.
References
- 1. Biodistribution studies for Cell and Gene Therapy Products [https://content.noblelifesci.com/blog/biodistribution-studies-for-cell-and-gene-therapy-products]
- 2. Cellular Kinetics and Biodistribution of Adoptive T Cell ... [https://pubmed.ncbi.nlm.nih.gov/40032717/]
- 3. Regulatory guidelines and preclinical tools to study the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8957368/]
- 4. Detailed revisions to the subordinate regulation following ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12221229/]
- 5. FDA Publishes New Draft Guidance on Regenerative ... [https://www.hklaw.com/en/insights/publications/2025/10/fda-publishes-new-draft-guidance-on-regenerative-medicine-therapies]
- 6. Cellular & Gene Therapy Guidances | FDA [https://www.fda.gov/vaccines-blood-biologics/biologics-guidances/cellular-gene-therapy-guidances]
- 7. Guidelines relevant for advanced therapy medicinal products [https://www.ema.europa.eu/en/human-regulatory-overview/advanced-therapy-medicinal-products-overview/guidelines-relevant-advanced-therapy-medicinal-products]
- 8. Comparison of international guidelines for early-phase clinical trials of cellular and gene therapy products - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8979759/]
- 9. Regenerative Medical Products [https://www.pmda.go.jp/english/review-services/reviews/0003.html]
- 10. EMA Guideline On Clinical-Stage ATMPs Comes Into Effect [https://www.cellandgene.com/doc/ema-guideline-on-clinical-stage-atmps-comes-into-effect-on-the-verge-of-convergence-0001]
- 11. Innovative Designs for Clinical Trials of Cellular and Gene ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/innovative-designs-clinical-trials-cellular-and-gene-therapy-products-small-populations]
- 12. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 13. Global regulatory considerations and practices for ... [https://www.sciencedirect.com/science/article/pii/S0273230024002101]
- 14. Pharmacovigilance in Cell and Gene Therapy: Evolving ... [https://link.springer.com/article/10.1007/s40264-025-01596-9]
- 15. CAR T-Cell Therapies: Pharmacovigilance Challenges [https://www.pei.de/EN/newsroom/press-releases/year/2025/01-car-t-cell-therapies-pharmacovigilance-challenges.html]
- 16. Advances in Optical Contrast Agents for Medical Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC11942650/]
- 17. Top 10 Industry Predictions for 2025 [https://www.cryoport.com/bio-blog-top-10-industry-predictions-for-2025/]
- 18. Comparison of Different Adult Stem Cell Types for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3657517/]
- 19. Enhancing mesenchymal stem cell survival and homing ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03476-4]
- 20. Transplantation dose alters the dynamics of human neural ... [https://www.sciencedirect.com/science/article/pii/S1873506115000926]
- 21. Genetic Enhancement of Stem Cell Engraftment, Survival and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2668244/]
- 22. Comparison of Imaging Techniques for Tracking Cardiac Stem ... [https://jnm.snmjournals.org/content/48/12/1916]
- 23. A pancreatic islet cell case study [https://pubmed.ncbi.nlm.nih.gov/40777725/]
- 24. Biodistribution studies for cell therapy products [https://pmc.ncbi.nlm.nih.gov/articles/PMC8282960/]
- 25. Biodistribution Studies for Cell and Gene Therapy Products [https://noblelifesci.com/cell-and-gene-therapy-biodistribution-studies/]
- 26. RNAscope Multiomic LS in Cell Therapy - ASGCT 2025 [https://www.bio-techne.com/resources/literature/cell-therapy-biodistribution-assessment-using-spatial-multiomics]
- 27. Using qPCR and ddPCR to study biodistribution of cell ... [https://www.sciencedirect.com/science/article/pii/S1465324924008648]
- 28. The new frontier: qPCR vs ddPCR for cell and gene therapies [https://www.bioanalysis-zone.com/podcasts/the-new-frontier-qpcr-vs-ddpcr-for-cell-and-gene-therapies/]
- 29. qPCR vs. ddPCR: Which Is Best for You? [https://www.bioradiations.com/qpcr-vs-ddpcr-assays-select-the-best-gene-expression-analysis-method-for-your-application1125/]
- 30. Clinical validation of a multiplex droplet digital PCR for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9358819/]
- 31. Comparing the precision of two digital PCR applications for ... [https://www.nature.com/articles/s41598-025-13143-8]
- 32. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 33. Comparative evaluation of six nucleic acid amplification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8140580/]
- 34. Comparison of Different Imaging Techniques for Tracking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3638042/]
- 35. Broadly-applicable imaging platforms are necessary for ... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/155/broadlyapplicable-imaging-platforms-are-necessary-for-optimizing-cell-therapies-in-solid-tumors]
- 36. In vivo exosome imaging: applications of diverse ... [https://www.bmbreports.org/journal/view.html?doi=10.5483/BMBRep.2025-0060]
- 37. Hybrid PET-optical imaging using targeted probes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2867879/]
- 38. Recent Breakthroughs in PET-CT Multimodality Imaging [https://www.mdpi.com/2306-5354/11/12/1213]
- 39. Critical review of partial volume correction methods in PET ... [https://link.springer.com/article/10.1007/s00259-025-07612-5]
- 40. A primer on in vivo cell tracking using MRI [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2023.1193459/full]
- 41. Mapping Drug Biodistribution: Tracing the Journey to ... [https://biocytogen.com/blogs/biodistribution-in-drug-development]
- 42. Pharmacokinetic characteristics of mesenchymal stem cells ... [https://www.nature.com/articles/s41392-024-01936-8]
- 43. Biodistribution and persistence of human umbilical cord ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11881841/]
- 44. Non-clinical assessment of safety, biodistribution and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8649581/]
- 45. Biodistribution of Mesenchymal Stromal Cells after ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8268414/]
- 46. Method validation and assessment of the biodistribution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12395528/]
- 47. Rules and Tips for PCR & qPCR Primer Design | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/how-to-design-primers-and-probes-for-pcr-and-qpcr/]
- 48. Comparison of the Biodistribution and Tumor Targeting of Two ... [https://jnm.snmjournals.org/content/49/5/788]
- 49. Infusion and delivery strategies to maximize the efficacy of ... [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-024-00542-2]
- 50. Intratumoural administration and tumour tissue targeting of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8130796/]
- 51. Locoregional drug delivery for cancer therapy: Preclinical ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365924000877]
- 52. Solid tumour CAR-T cells engineered with fusion proteins ... [https://www.nature.com/articles/s41551-025-01509-2]
- 53. Effect of administration routes on the efficacy of human ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1536655/full]
- 54. Neutralizing monoclonal antibodies improve biodistribution of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193558/]
- 55. CAR-T Cell Therapy: the Efficacy and Toxicity Balance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10505056/]
- 56. Infusion and delivery strategies to maximize the efficacy of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11282638/]
- 57. Mechanisms of cytokine release syndrome and neurotoxicity ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-021-02148-6]
- 58. Phase I trial of hES cell-derived dopaminergic neurons for ... [https://www.nature.com/articles/s41586-025-08845-y]
- 59. Optimizing viral transduction in immune cell therapy ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06524-0]
- 60. In vivo CAR cell therapy: from bench to bedside [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-025-01759-2]
- 61. Clinical trials of nanoparticle-enhanced CAR-T and NK cell ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1655693/full]
- 62. Preclinical evaluation of lentiviral gene therapy for ... [https://www.nature.com/articles/s41434-025-00547-4]
- 63. Targeted in vivo delivery of genetic medicines utilizing an ... [https://www.sciencedirect.com/science/article/pii/S1525001625004873]
- 64. In vivo production of CAR T cell: Opportunities and challenges [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357247/]
- 65. Cell-based immunotherapies for solid tumors: advances, ... [https://pubmed.ncbi.nlm.nih.gov/40356763/]
- 66. Overcoming the blood – brain for the therapy of malignant brain... barrier [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-022-01610-7]
- 67. Frontiers | Blood - Brain , Barrier - Blood , and... Brain Tumor Barrier [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2020.00739/full]
- 68. Targeting tumor microenvironmental barriers to enhance ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1672601/full]
- 69. CAR-T Design Outsmarts Solid Tumor Defenses [https://www.regmednet.com/car-t-design-outsmarts-solid-tumor-defenses/]
- 70. Mechanistic data-informed multiscale quantitative systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12516987/]
- 71. 7 Latest Advances in Brain Research and Treatment ( Tumor ) 2025 [https://int.livhospital.com/7-latest-advances-in-brain-tumor-research-and-treatment-2025/]
- 72. Review Biodistribution studies for cell therapy products [https://www.sciencedirect.com/science/article/pii/S235232042100050X]
- 73. Reference standards for accurate validation and ... [https://www.nature.com/articles/s41598-020-79698-w]
- 74. Vector Copy Distribution at a Single-Cell Level Enhances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7217927/]
- 75. qPCR and qRT-PCR analysis: Regulatory points to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7786041/]
- 76. Recommendations for Method Development and ... [https://pubmed.ncbi.nlm.nih.gov/38316745/]
- 77. Method validation and assessment of the biodistribution ... [https://www.sciencedirect.com/science/article/pii/S2329050125001445]
- 78. Digital PCR Improves Sensitivity and Quantification in ... [https://www.sciencedirect.com/science/article/pii/S2666636723024119]
- 79. Best practices in qPCR and dPCR validation in regulated ... [https://www.bioanalysis-zone.com/best-practices-in-qpcr-and-dpcr-validation-in-regulated-bioanalytical-laboratories/]
- 80. Cellular Kinetics and Biodistribution of Adoptive T Cell ... [https://link.springer.com/article/10.1208/s12248-025-01017-w]
- 81. A method to improve quantitative radiotracing‐based analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8126812/]
- 82. advancing analytical techniques using metal-doped plastics [https://www.nature.com/articles/s42003-025-08709-1]
- 83. Comparative analysis of cell-specific promoters in AAV9 ... [https://pubmed.ncbi.nlm.nih.gov/41036104/]
- 84. A Highly Precise Method for the Quantitation of rAAV ... [https://pubmed.ncbi.nlm.nih.gov/40432593/]
- 85. 89Zr-mAb uptake interpretation requires the use of tissue to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474831/]
- 86. Systematic discovery of CRISPR-boosted CAR T cell ... [https://www.nature.com/articles/s41586-025-09507-9]
- 87. Using artificial intelligence to improve cell therapy assays [https://www.sciencedirect.com/science/article/abs/pii/S0040816625003210]
- 88. Reproducibility via coordinated standardization: a multi-center study in a Shank2 genetic rat model for Autism Spectrum Disorders | Scientific Reports [https://www.nature.com/articles/s41598-019-47981-0]
- 89. Reproducibility of research and preclinical validation: problems and solutions | Nature Reviews Clinical Oncology [https://www.nature.com/articles/nrclinonc.2013.171]
- 90. Considerations in Biodistribution Evaluation of iPSC ... [https://www.sciencedirect.com/science/article/pii/S2329050125001330]
- 91. Reproducible preclinical research—Is embracing variability the answer? - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5837077/]
- 92. Reproducible brain-wide association studies require ... [https://www.nature.com/articles/s41586-022-04492-9]
- 93. Multi-site proficiency testing for validation and standardization of assays to detect specific pathogen-free viruses, coronaviruses, and other agents in nonhuman primates - PubMed [https://pubmed.ncbi.nlm.nih.gov/35426147/]
- 94. Multi-site assessment of the precision and reproducibility of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2855883/]
- 95. Reproducibility of T1ρ and T2 quantification in a multi- ... [https://www.sciencedirect.com/science/article/pii/S1063458422008974]
- 96. Biodistribution studies for cell products: Current status... | CoLab therapy [https://colab.ws/articles/10.1016%2Fj.reth.2021.06.005]
- 97. Recommendations for Method Development and Validation of qPCR... [https://link.springer.com/article/10.1208/s12248-023-00880-9]