CRISPR-Cas9 and iPSCs: Revolutionizing Disease Modeling for Drug Discovery and Personalized Medicine
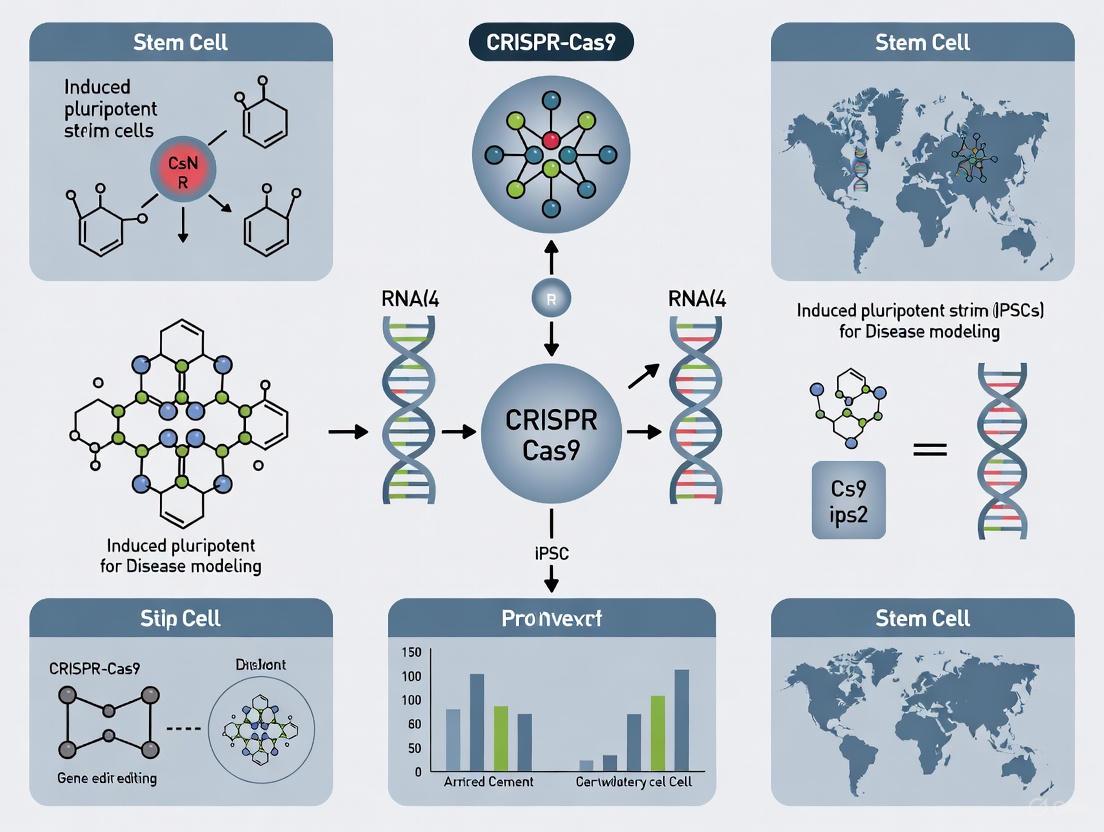
This article explores the powerful synergy between CRISPR-Cas9 gene editing and induced pluripotent stem cell (iPSC) technology, a combination that is revolutionizing disease modeling and therapeutic development.
CRISPR-Cas9 and iPSCs: Revolutionizing Disease Modeling for Drug Discovery and Personalized Medicine
Abstract
This article explores the powerful synergy between CRISPR-Cas9 gene editing and induced pluripotent stem cell (iPSC) technology, a combination that is revolutionizing disease modeling and therapeutic development. We provide a comprehensive analysis for researchers and drug development professionals, covering the foundational principles of reprogramming somatic cells into pluripotent stem cells and the mechanics of CRISPR-Cas9. The article details advanced methodologies for creating precise genetic disease models, including isogenic cell lines and complex 3D organoids, and addresses critical troubleshooting strategies for overcoming challenges in editing efficiency and genomic stability. Finally, we examine the rigorous validation of these models through functional assays and their application in high-throughput drug screening, toxicology testing, and ongoing clinical trials, highlighting the transformative impact on biomedical research and the path toward clinical translation.
Building Blocks: Understanding iPSC Reprogramming and CRISPR-Cas9 Mechanics
The discovery of induced pluripotent stem cells (iPSCs) by Shinya Yamanaka in 2006 marked a transformative milestone in regenerative medicine and biological research. By introducing four specific transcription factors—OCT4, SOX2, KLF4, and c-MYC (collectively known as the OSKM or Yamanaka factors)—his team demonstrated that somatic cells could be reprogrammed back to a pluripotent state [1]. This groundbreaking achievement proved that specialized adult cells carry the complete genetic code to revert to an embryonic-like state, capable of differentiating into virtually any cell type in the body [2] [3]. The iPSC technology effectively bypasses the ethical controversies associated with embryonic stem cells while providing an unlimited source of patient-specific cells for disease modeling, drug screening, and therapeutic development [3] [4].
The molecular machinery behind iPSC reprogramming involves profound remodeling of the epigenome. During the reprogramming process, somatic genes are progressively silenced while pluripotency-associated genes are activated through two major phases: an early stochastic phase and a late deterministic phase [1]. This process reverses the developmental clock, erasing somatic cell epigenetic memory and reestablishing the open chromatin configuration characteristic of pluripotent cells [1]. The resulting iPSCs closely resemble embryonic stem cells (ESCs) in their gene expression profiles, differentiation potential, and self-renewal capacity, making them invaluable tools for both basic research and clinical applications [3] [4].
Core Reprogramming Methodologies
Evolution of Reprogramming Factors
The original Yamanaka factors have undergone significant optimization to enhance safety and efficiency. Research has revealed that the oncogenic potential of c-MYC presents significant risks to iPSC stability and safety, prompting investigations into alternative factors [2]. Subsequent studies demonstrated that somatic cell reprogramming could be achieved using OCT4, SOX2, and KLF4 without c-MYC, though with reduced efficiency [2]. Alternative factor combinations have also been successfully employed, including OCT4, SOX2, NANOG, and LIN28 (OSNL), which eliminate c-MYC entirely [2] [1].
Factor substitution studies have identified several family members that can replace their original counterparts: KLF2 and KLF5 can substitute for KLF4; SOX1 and SOX3 can replace SOX2; and L-MYC and N-MYC can stand in for c-MYC [2]. Beyond direct family members, other genes and small molecules have shown reprogramming potential. For instance, NR5A2 can replace OCT4 when combined with SOX2 and KLF4, while the small molecule RepSox can effectively substitute for SOX2 [2]. Additional factors like Esrrb and Glis1 have also served as viable alternatives to c-MYC in somatic cell reprogramming [2].
Delivery Systems for Reprogramming
The method of introducing reprogramming factors into somatic cells significantly impacts the safety and quality of resulting iPSCs. Early approaches utilized integrating viral vectors, particularly retroviruses and lentiviruses, which raised concerns about insertional mutagenesis and tumorigenicity [3]. In response, researchers have developed numerous non-integrating delivery systems that minimize genomic alteration risks [3].
Table 1: Comparison of iPSC Reprogramming Delivery Systems
| Vector Type | Genetic Material | Genomic Integration | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Retrovirus | DNA | Yes | High efficiency | Integrates into genome; reactivation of transgenes |
| Lentivirus | DNA | Yes | Can infect non-dividing cells | Integration risks; variable silencing |
| Sendai Virus | RNA | No | High efficiency; non-integrating | Requires dilution; persistent for ~10 passages |
| Adenovirus | DNA | No | Non-integrating; good efficiency | Technically challenging; lower efficiency |
| Episomal Plasmid | DNA | No | Non-integrating; simple delivery | Low efficiency; requires multiple transfections |
| Synthetic mRNA | RNA | No | Non-integrating; high efficiency | Requires multiple transfections; immune stimulation |
| Recombinant Protein | Protein | No | Completely non-integrating | Very low efficiency; technically demanding |
Significant progress has been made in chemical reprogramming methods, which utilize defined small molecule combinations to induce pluripotency without genetic manipulation [2]. This approach represents a breakthrough in iPSC generation safety, substantially enhancing their clinical application potential. Chemical reprogramming activates early embryonic developmental genes and reveals a highly plastic intermediate cell state with enhanced chromatin accessibility [2].
Enhanced Reprogramming with Small Molecules
Small molecules that modulate epigenetic barriers and signaling pathways have proven highly effective in enhancing reprogramming efficiency. These compounds include DNA methyltransferase inhibitors (5-aza-cytidine, RG108), histone deacetylase inhibitors (sodium butyrate, trichostatin A, valproic acid), and histone methylation regulators (Neplanocin A) [2]. The combination of 8-Bromoadenosine 3′,5′-cyclic monophosphate (8-Br-cAMP) with valproic acid has demonstrated a 6.5-fold increase in human fibroblast reprogramming efficiency [2].
Diagram 1: Key Molecular Transitions During iPSC Reprogramming
Integration of CRISPR-Cas9 with iPSC Technology
CRISPR-Cas9 Fundamentals for iPSC Engineering
The CRISPR-Cas9 system has revolutionized genetic engineering in iPSCs by providing a precise, efficient, and scalable platform for targeted genome modifications [5] [6]. This two-component system consists of a Cas9 nuclease and a synthetic guide RNA (sgRNA) containing a 20-base variable domain that mediates DNA-binding specificity [5]. When Cas9 scans the genome, the sgRNA base-pairs with complementary DNA sequences, and upon detecting a perfect match followed by a 3' protospacer adjacent motif (PAM), Cas9 creates a blunt-ended double-strand break three base pairs 5' to the PAM [5].
In iPSC research, CRISPR-Cas9 enables the creation of precise disease models through gene knock-outs, knock-ins, and point mutations [5] [6]. The technology facilitates the generation of isogenic cell lines—genetically identical except for specific disease-relevant mutations—which are critical for distinguishing phenotypic differences attributable to genetic variants from background genetic variability [5]. This precision makes CRISPR-edited iPSCs particularly valuable for disease modeling and drug discovery applications [6].
Protocol: CRISPR-Cas9 Mediated Gene Knockout in iPSCs
Experimental Principle This protocol outlines the methodology for generating gene-specific knockouts in human iPSCs using the CRISPR-Cas9 system. Gene knockout is achieved through non-homologous end joining (NHEJ) repair of Cas9-induced double-strand breaks, which often introduces insertion/deletion (indel) mutations that disrupt gene function [5].
Materials and Reagents
Table 2: Essential Reagents for CRISPR-Cas9 in iPSCs
| Reagent Category | Specific Examples | Function | Notes |
|---|---|---|---|
| sgRNA Design Tools | CHOPCHOP, CRISPR Design Tool | Identifies optimal sgRNA sequences | Select guides with high on-target, low off-target activity |
| Expression Vectors | px330, pSpCas9(BB) | Delivers Cas9 and sgRNA to cells | May include selection markers (GFP, puromycin) |
| iPSC Culture Media | mTeSR, E8 medium | Maintains pluripotency during editing | Use defined, xeno-free formulations |
| Transfection Reagents | Lipofectamine Stem, Electroporation | Introduces CRISPR components into cells | Optimize for specific iPSC lines |
| Selection Agents | Puromycin, G418 | Enriches for successfully transfected cells | Determine kill curve for each cell line |
| Genomic DNA Extraction | DNeasy Blood & Tissue Kit | Isolates DNA for genotyping | Critical for validation steps |
| Validation Primers | Target-specific designs | Amplifies edited genomic regions | Design flanking the target site |
| Sequencing Tools | Sanger sequencing, NGS | Confirms editing efficiency and specificity | Barcoded deep sequencing recommended |
Step-by-Step Procedure
sgRNA Design and Cloning
- Design sgRNAs using online tools (CHOPCHOP, CRISPR Design Tool) targeting early exons of the gene of interest
- Select guides with high predicted on-target activity and minimal off-target effects
- Clone validated sgRNA sequences into appropriate expression vectors (e.g., px330) containing Cas9 and selection markers
- Verify constructs by Sanger sequencing before transfection [5]
iPSC Culture and Transfection
- Maintain human iPSCs in feeder-free conditions using defined culture media (e.g., mTeSR or E8)
- Passage cells as small clumps using EDTA or enzyme-free dissociation reagents
- Transfect iPSCs at 70-80% confluence using optimized methods (lipofection or electroporation)
- Include untransfected controls and empty vector controls [5]
Selection and Single-Cell Cloning
- Begin antibiotic selection (e.g., 0.5-1 μg/mL puromycin) 48 hours post-transfection
- Maintain selection for 3-5 days until control cells are completely dead
- Harvest surviving cells and seed at clonal density (1-10 cells/cm²)
- Manually pick individual colonies after 10-14 days for expansion [5]
Genotype Validation
- Extract genomic DNA from expanded clones using commercial kits
- PCR-amplify the target region using flanking primers
- Analyze editing efficiency via T7E1 or SURVEYOR mismatch assays
- Confirm indels in candidate clones by Sanger sequencing
- Verify pluripotency maintenance through immunostaining for markers (OCT4, NANOG, SOX2) [5]
Troubleshooting Notes
- Low editing efficiency: Optimize sgRNA design and transfection parameters
- Poor clone survival: Reduce selection stringency and improve single-cell survival supplements
- Off-target effects: Design multiple sgRNAs and use validated controls
- Pluripotency loss: Regularly monitor stem cell morphology and marker expression
Applications in Disease Modeling and Drug Development
Protocol: Establishing iPSC-Derived Disease Models
Experimental Principle Patient-specific iPSCs can be differentiated into disease-relevant cell types to model human pathologies in vitro. When combined with CRISPR-Cas9 gene editing, isogenic pairs of cell lines can be generated that differ only at the disease-causing locus, enabling precise mechanistic studies [5] [6].
Materials and Reagents
- Patient-derived iPSCs with disease-causing mutations
- CRISPR-Cas9 components for genetic correction
- Differentiation media specific to target cell type
- Cell type-specific antibodies for characterization
- Functional assay reagents (e.g., electrophysiology, calcium imaging)
Step-by-Step Procedure
iPSC Line Generation and Genetic Correction
- Derive iPSCs from patient somatic cells (fibroblasts or blood cells) using non-integrating methods
- Establish isogenic control line by correcting disease mutation using CRISPR-Cas9 with ssODN donor template
- Validate genetic correction through sequencing and off-target analysis
- Confirm pluripotency and normal karyotype before differentiation [6]
Directed Differentiation to Target Cell Type
- Adapt published differentiation protocols for specific cell types (neurons, cardiomyocytes, hepatocytes)
- Optimize timing and cytokine concentrations for your specific iPSC lines
- Monitor differentiation efficiency through time-course marker expression
- Purify target cells using fluorescence-activated cell sorting (FACS) or magnetic sorting when possible
Phenotypic Characterization
- Assess disease-specific morphological changes through immunocytochemistry
- Evaluate functional deficits using cell-type appropriate assays
- Perform transcriptomic and proteomic analyses to identify molecular pathways
- Compare patient, corrected isogenic control, and healthy lines in parallel experiments
Application Example: Neurodegenerative Disease Modeling In Parkinson's disease research, iPSCs from patients carrying LRRK2 or PARK2 mutations have been differentiated into dopaminergic neurons. After CRISPR-mediated correction, the neurons exhibited improved mitochondrial function and nuclear envelope integrity, demonstrating the value of this approach for mechanistic studies [3]. Similarly, in Alzheimer's disease, researchers have used CRISPR to introduce PSEN1 E280A mutations into iPSCs, then differentiated them into neural cells to create precision models for AD research [6].
High-Throughput Drug Screening Platforms
iPSC-derived cellular models have become invaluable tools for drug discovery and toxicity testing. The ability to generate human cardiomyocytes, hepatocytes, and neurons from iPSCs provides physiologically relevant systems for evaluating drug efficacy and safety [4] [6]. CRISPR-edited iPSCs further enhance these platforms by enabling the introduction of specific disease mutations or reporter genes that facilitate high-throughput screening [6].
Table 3: Applications of CRISPR-iPSC Platforms in Drug Development
| Application Area | iPSC-Derived Cell Type | CRISPR Modification | Readout | Notable Example |
|---|---|---|---|---|
| Cardiotoxicity Screening | Cardiomyocytes | Knock-in of calcium indicators | Calcium handling, beat rate | Identification of pro-arrhythmic compounds |
| Neurodegenerative Disease | Cortical neurons | Introduction of disease mutations | Tau phosphorylation, axon transport | Screening of tauopathy therapeutics |
| Metabolic Disorders | Hepatocytes | Reporter knock-in at metabolic genes | Lipid accumulation, glucose uptake | Steatosis drug screening |
| Monogenic Diseases | Disease-relevant cells | Correction of patient mutations | Functional rescue | Dyskeratosis congenita (PAPD5 inhibitors) |
| Cancer Immunotherapy | T-cells, NK cells | Knockout of immune checkpoints | Tumor cell killing | Hypoimmunogenic CAR-T cells |
A notable example of this approach comes from screening for dyskeratosis congenita (DC) therapeutics, where researchers used CRISPR-iPSC platforms to identify small-molecule PAPD5 inhibitors that restore telomerase activity in patient-derived cells [6]. Treatment with the inhibitor BCH001 demonstrated dose-dependent telomere extension in CRISPR knockout iPSCs, highlighting the power of this combined platform for discovering novel therapeutics [6].
Diagram 2: Integrated CRISPR-iPSC Workflow for Drug Discovery
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of iPSC and CRISPR technologies requires access to specialized reagents and platforms. The following table summarizes key solutions and their applications in iPSC-based research.
Table 4: Essential Research Reagent Solutions for iPSC and CRISPR Work
| Reagent Category | Specific Product Examples | Primary Function | Application Notes |
|---|---|---|---|
| Reprogramming Kits | CytoTune Sendai Virus, Episomal Vectors | Somatic cell reprogramming to iPSCs | Non-integrating methods preferred for clinical applications |
| iPSC Culture Media | mTeSR, StemFlex, E8 medium | Maintain pluripotency and support expansion | Defined, xeno-free formulations ensure consistency |
| CRISPR Nucleases | Wild-type Cas9, HiFi Cas9, Cas12a | Induce targeted DNA breaks for genome editing | High-fidelity variants reduce off-target effects |
| Delivery Systems | Lipofectamine Stem, Neon Electroporation | Introduce CRISPR components into iPSCs | Optimized for sensitive stem cell lines |
| Differentiation Kits | Cardiomyocyte, Neural, Hepatocyte Kits | Direct iPSCs toward specific lineages | Protocol optimization often required for different lines |
| Characterization Antibodies | OCT4, NANOG, TRA-1-60, Cell-type markers | Assess pluripotency and differentiation | Essential for quality control throughout projects |
| Cell Banking Reagents | CryoStor, Synth-a-Freeze | Long-term preservation of edited lines | Use controlled-rate freezing for high viability |
Major market players have developed specialized platforms to support these research needs. FUJIFILM CDI (formerly Cellular Dynamics International) dominates as the world's largest manufacturer of human cells from iPSCs, while companies like REPROCELL, Evotec, and Ncardia provide specialized iPSC-derived cells and services [4]. For custom disease modeling, bit.bio offers opti-ox powered human-iPSC derived cells with specific mutations, providing consistent, defined products for drug discovery workflows [4].
Scaling and Automation in iPSC Production
The translation of iPSC technologies from research tools to clinical applications requires scalable manufacturing approaches that maintain quality and reproducibility [7]. Traditional manual iPSC production methods, while flexible and widely used in academic settings, are being supplemented and replaced by automated systems that enhance consistency and throughput [8].
Automated platforms integrate reprogramming, expansion, and differentiation into closed workflows that minimize human error and variability [7] [8]. These systems are particularly valuable for clinical-grade manufacturing where adherence to Good Manufacturing Practice (GMP) standards is essential [7]. The adoption of process analytical technologies (PAT) and quality by design (QbD) approaches further enhances the robustness of iPSC production processes [7].
The global iPSC production market reflects this transition, with automated platforms representing the fastest-growing product category [8]. Biotechnology companies and contract manufacturing organizations are increasingly implementing these systems to accelerate the translation of iPSC-based therapies from research to clinical applications [8]. This scalable manufacturing infrastructure will be critical for realizing the full potential of iPSC technologies in regenerative medicine and drug development.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and CRISPR-associated protein 9 (Cas9) system constitutes a revolutionary gene-editing technology derived from a natural adaptive immune system in bacteria and archaea [9]. This powerful molecular machinery enables researchers to make precise, targeted modifications to DNA sequences across diverse biological systems, including induced pluripotent stem cells (iPSCs) [10]. The core system consists of two fundamental components: the Cas9 nuclease, which acts as a molecular "scissors" to cut DNA, and a guide RNA (gRNA), which functions as a programmable "GPS" to direct Cas9 to specific genomic locations [9]. When combined with iPSC technology, CRISPR-Cas9 provides an unprecedented platform for creating highly accurate human disease models, facilitating drug discovery, and advancing personalized medicine approaches [11] [10].
The application of CRISPR-Cas9 in iPSC-based disease modeling has transformed biomedical research by enabling the creation of isogenic cell lines that differ only at specific pathogenic loci, thereby eliminating confounding genetic background effects [10]. This technical advancement is particularly valuable for studying neurological disorders, cardiovascular diseases, and rare genetic conditions where patient-derived cells may be difficult to obtain or maintain in culture [12] [10]. As the field progresses, understanding the core principles of gRNA design, Cas9 function, and subsequent DNA repair mechanisms becomes essential for optimizing editing efficiency and precision in iPSC-based research models.
Core Components of the CRISPR-Cas9 System
Guide RNA (gRNA)
The guide RNA is a synthetic fusion molecule comprising two distinct RNA components: the CRISPR RNA (crRNA), which contains a ~20 nucleotide spacer sequence complementary to the target DNA site, and the trans-activating CRISPR RNA (tracrRNA), which serves as a scaffolding backbone that facilitates Cas9 binding [9]. These two elements are typically combined into a single-guide RNA (sgRNA) for experimental simplicity. The sgRNA directs Cas9 to a specific genomic locus through Watson-Crick base pairing between its spacer sequence and the target DNA [9].
Critical design considerations for functional gRNAs include:
- Specificity: The 20-nucleotide targeting sequence must be unique to the intended genomic locus to minimize off-target effects
- Protospacer Adjacent Motif (PAM): The target site must be immediately adjacent to a 5'-NGG-3' PAM sequence for Streptococcus pyogenes Cas9 (SpCas9)
- GC content: Optimal gRNAs typically contain 40-60% GC content for stable DNA binding
- Genomic context: Accessibility of the target chromatin region can significantly impact editing efficiency
Advances in computational tools and machine learning approaches have enhanced gRNA design parameters, leading to improved on-target efficiency and reduced off-target effects [13]. For iPSC applications, highly specific gRNAs are particularly critical due to the potential for clonal expansion and the need to maintain genomic integrity throughout differentiation protocols.
Cas9 Nuclease
The Cas9 protein is a multifunctional RNA-guided DNA endonuclease that induces double-strand breaks (DSBs) in target DNA sequences. Upon gRNA-mediated recognition of the target site, Cas9 undergoes conformational changes that position its nuclease domains (RuvC and HNH) to cleave opposite strands of the DNA duplex, generating blunt-ended DSBs approximately 3-4 nucleotides upstream of the PAM sequence [9].
Key Cas9 variants for specialized applications:
| Cas9 Variant | Attributes | Primary Applications in iPSC Research |
|---|---|---|
| Wild-type SpCas9 | High activity, broad compatibility | General gene knockout studies |
| High-fidelity Cas9 (e.g., SpCas9-HF1) | Reduced off-target cleavage | Therapeutic modeling where specificity is critical |
| Catalytically dead Cas9 (dCas9) | DNA binding without cleavage | Gene regulation (CRISPRi/a), epigenetic editing |
| Nickase Cas9 (nCas9) | Single-strand DNA cleavage | Base editing with reduced indel formation |
| Artificial intelligence-designed editors (e.g., OpenCRISPR-1) | Enhanced specificity, novel PAM preferences | Expanding targetable genomic loci [13] |
The large size of Cas9 cDNA (~4.2 kb) presents challenges for delivery via size-constrained vectors such as adeno-associated viruses (AAVs), necessitating the use of alternative delivery methods or compact Cas variants in certain experimental contexts [9].
DNA Repair Pathways and Editing Outcomes
Following Cas9-mediated DNA cleavage, cellular repair mechanisms are activated to resolve the double-strand break. The competing pathways and their resulting outcomes determine the ultimate genetic modification achieved through CRISPR editing. In the context of iPSC disease modeling, understanding and controlling these pathways is essential for generating predictable editing results.
Non-Homologous End Joining (NHEJ)
Non-homologous end joining is the dominant DNA repair pathway in mammalian cells, particularly in non-cycling cells. This error-prone mechanism directly ligates broken DNA ends without requiring a template, often resulting in small insertions or deletions (indels) at the cleavage site [9]. When these indels occur within protein-coding exons, they frequently produce frameshift mutations that disrupt gene function, making NHEJ particularly valuable for gene knockout studies in iPSC models [10].
Recent research has revealed that postmitotic cells, including neurons and cardiomyocytes derived from iPSCs, exhibit distinct NHEJ characteristics compared to dividing cells [12]. These nondividing cells demonstrate prolonged DSB repair kinetics, with indel accumulation continuing for up to two weeks post-editing, and favor classical NHEJ repair with a narrower distribution of smaller indels compared to their dividing counterparts [12] [14].
Homology-Directed Repair (HDR)
Homology-directed repair is a precise, template-dependent repair pathway that operates primarily during the S and G2 phases of the cell cycle. HDR requires a donor DNA template containing homologous sequences flanking the target site and can be harnessed to introduce specific nucleotide changes, insert reporter genes, or correct pathogenic mutations in iPSCs [9].
A significant challenge in HDR-based editing is the relatively low efficiency of this pathway compared to NHEJ, particularly in iPSCs. Researchers have developed several strategies to enhance HDR efficiency, including:
- Cell cycle synchronization to enrich for cells in S/G2 phase
- Timed delivery of CRISPR components during peak HDR activity
- Pharmacological inhibition of key NHEJ proteins (with important caveats regarding genomic integrity)
- Cas9 fusion proteins that recruit HDR-enhancing factors
It is important to note that recent studies have revealed that many strategies to enhance HDR, particularly pharmacological inhibition of DNA-PKcs, can inadvertently increase the frequency of large-scale structural variations, including kilobase- to megabase-scale deletions and chromosomal translocations [15]. These findings highlight the critical need for comprehensive genomic integrity assessment following editing, especially for therapeutic applications.
Alternative Repair Pathways
Beyond classical NHEJ and HDR, mammalian cells employ additional repair mechanisms including microhomology-mediated end joining (MMEJ) and single-strand annealing (SSA). These pathways are particularly relevant in dividing cells, where MMEJ contributes significantly to CRISPR editing outcomes [12]. Recent evidence indicates that postmitotic cells substantially downregulate MMEJ activity compared to their dividing counterparts, leading to different distributions of editing outcomes [12].
The following diagram illustrates the competitive relationship between these major DNA repair pathways following Cas9-induced double-strand breaks:
Competing DNA Repair Pathways After CRISPR-Cas9 Cleavage
Quantitative Analysis of CRISPR-Cas9 Editing Outcomes
Understanding the efficiency and distribution of editing outcomes is crucial for experimental design and interpretation in iPSC-based disease modeling. The following tables summarize key quantitative findings from recent studies investigating CRISPR-Cas9 editing across different cellular contexts.
DNA Repair Kinetics in Dividing vs. Nondividing Cells
Recent research has revealed significant differences in how dividing and nondividing cells process CRISPR-induced DNA damage, with important implications for editing strategies in iPSC-derived differentiated cells [12].
| Cell Type | Repair Kinetics (Time to Indel Plateau) | Predominant Repair Pathway | Characteristic Indel Distribution |
|---|---|---|---|
| Dividing Cells (iPSCs, activated T cells) | 1-3 days | MMEJ > NHEJ | Broad range, larger deletions |
| Nondividing Cells (iPSC-derived neurons, cardiomyocytes, resting T cells) | Up to 14-16 days | NHEJ > MMEJ | Narrow distribution, smaller indels |
| Postmitotic Human Neurons | 2 weeks | NHEJ (95% of outcomes) | Small indels (<10 bp) predominant |
DNA Repair Pathway Manipulation Outcomes
Chemical and genetic manipulation of DNA repair pathways can shift editing outcomes, but these approaches must be used with caution due to potential genotoxic consequences [12] [15].
| Intervention | Intended Effect | Actual Outcome | Genomic Safety Concerns |
|---|---|---|---|
| DNA-PKcs inhibitors (e.g., AZD7648) | Enhance HDR by suppressing NHEJ | Increased kilobase- to megabase-scale deletions; thousand-fold increase in chromosomal translocations | High risk of extensive structural variations [15] |
| 53BP1 inhibition | Enhance HDR | Improved precise editing without increased translocation frequency | Lower genomic risk profile [15] |
| RRM2 inhibition (in neurons) | Shift outcome distribution | Increased deletion size and overall indel efficiency | Cell type-specific effects requiring validation [14] |
| p53 suppression | Reduce apoptosis in edited cells | Decreased large chromosomal aberrations | Potential selection for p53-deficient clones with oncogenic potential [15] |
Experimental Protocols for CRISPR-iPSC Disease Modeling
Protocol 1: Generation of Isogenic iPSC Lines via CRISPR-Cas9
This protocol describes the complete workflow for creating precisely edited iPSC lines for disease modeling applications, incorporating both HDR-based precise editing and NHEJ-mediated gene disruption approaches [10].
Materials Required:
- Human iPSCs (patient-derived or control lines)
- CRISPR-Cas9 components (Cas9 protein or expression vector, sgRNA)
- Electroporation system (e.g., Neon Transfection System)
- Single-cell dissociation reagent
- iPSC culture medium with Rho-associated kinase (ROCK) inhibitor
- Genomic DNA extraction kit
- PCR reagents and sequencing primers
- Purified donor template for HDR (ssODN or dsDNA)
Step-by-Step Procedure:
sgRNA Design and Validation (3-5 days)
- Design sgRNAs using computational tools (e.g., CRISPick, CHOPCHOP)
- Select target sites with high on-target and low off-target scores
- Validate sgRNA efficiency in a surrogate system (e.g., HEK293 cells) using T7E1 assay or next-generation sequencing
CRISPR Component Delivery (1 day)
- Prepare ribonucleoprotein (RNP) complex by mixing 10 µg Cas9 protein with 5 µg sgRNA in opti-MEM, incubate at room temperature for 15 minutes
- Dissociate iPSCs to single cells using Accutase or similar enzyme
- Electroporate 1×10^6 iPSCs with RNP complex using manufacturer's recommended settings
- For HDR: Include 5 µL of 100 µM ssODN donor template in electroporation mixture
- Plate transfected cells at appropriate density in medium containing ROCK inhibitor
Clonal Isolation and Expansion (14-21 days)
- After 48-72 hours, dissociate and seed cells at low density (100-500 cells per 10 cm dish) for clonal formation
- Allow 10-14 days for distinct colony formation with regular medium changes
- Manually pick 96-192 well-isolated colonies using sterile pipette tips
- Transfer to 96-well plate format for expansion and screening
Genotypic Screening and Validation (7-10 days)
- Extract genomic DNA from expanded clones using commercial kits
- Perform PCR amplification of target region
- Analyze editing efficiency via Sanger sequencing or next-generation sequencing
- For HDR edits: Screen using restriction fragment length polymorphism (RFLP) if possible, followed by sequencing confirmation
- Expand positively identified clones for banking and further characterization
Quality Control and Characterization (14-21 days)
- Validate pluripotency markers via immunocytochemistry (OCT4, SOX2, NANOG)
- Confirm normal karyotype via G-banding analysis
- Verify absence of off-target edits at top predicted sites
- Assess differentiation potential through embryoid body formation
Protocol 2: DNA Repair Pathway Analysis in iPSC-Derived Neurons
This specialized protocol addresses the unique challenges of CRISPR editing in postmitotic cells, based on recent findings of distinct repair mechanisms in nondividing cell types [12] [14].
Materials Required:
- iPSC-derived neurons (≥30 days differentiation)
- Virus-like particles (VLPs) containing Cas9 RNP (VSVG/BRL-pseudotyped)
- Neuronal culture medium
- DNA extraction kit suitable for low cell numbers
- Next-generation sequencing library preparation kit
- RNA extraction and qRT-PCR reagents
- RRM2 inhibitors (optional, for repair pathway modulation)
Step-by-Step Procedure:
Neuronal Differentiation and Validation (30-60 days)
- Differentiate iPSCs to cortical neurons using established protocols
- Validate neuronal purity via immunostaining (NeuN, MAP2) and functional assays
- Confirm postmitotic status via Ki67 negativity
CRISPR Delivery via VLPs (1 day)
- Transduce neurons with VSVG/BRL-pseudotyped FMLV VLPs containing Cas9 RNP
- Use multiplicity of infection (MOI) optimized for >80% transduction efficiency
- Include untransduced controls and GFP-only VLP controls
Time-Course Analysis of Editing Outcomes (1-16 days)
- Harvest cells at multiple time points (days 1, 2, 4, 7, 11, 14, 16) post-transduction
- Extract genomic DNA and amplify target locus
- Prepare next-generation sequencing libraries
- Sequence with sufficient depth (>100,000 reads per sample) to detect rare variants
DNA Repair Pathway Characterization (3-7 days)
- Analyze sequencing data for indel spectrum and size distribution
- Quantify ratio of insertions to deletions as indicator of pathway bias
- Compare outcomes to isogenic dividing cells (iPSCs) edited with same sgRNA
- Perform transcriptomic analysis (RNA-seq) to identify differentially expressed DNA repair genes
Repair Pathway Modulation (Optional, 7-14 days)
- Treat neurons with RRM2 inhibitors (e.g., siRNAs) 24 hours pre-transduction
- Repeat editing and analysis to assess shifts in outcome distribution
- Evaluate effects on neuronal viability and functionality
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of CRISPR-iPSC disease modeling requires carefully selected reagents and tools. The following table summarizes essential materials and their applications.
| Reagent Category | Specific Examples | Function in CRISPR-iPSC Workflow |
|---|---|---|
| CRISPR Nucleases | Wild-type SpCas9, HiFi Cas9, OpenCRISPR-1 [13] | Inducing targeted DNA breaks with varying specificity profiles |
| Delivery Tools | Electroporation systems, lipid nanoparticles [16], virus-like particles (VLPs) [12] | Introducing CRISPR components into hard-to-transfect iPSCs and neurons |
| iPSC Culture Reagents | mTeSR1 medium, Rho kinase inhibitor, recombinant laminin-521 | Maintaining pluripotency and supporting single-cell survival after editing |
| DNA Repair Modulators | DNA-PKcs inhibitors, 53BP1 inhibitors, RRM2 inhibitors [12] [15] | Shifting repair pathway balance (use with caution due to genotoxic risks) |
| Validation Tools | Next-generation sequencing kits, T7 endonuclease I, digital PCR systems | Assessing on-target efficiency, detecting off-target effects, and quantifying editing outcomes |
| iPSC Differentiation Kits | Commercial neuronal, cardiac, or hepatic differentiation kits | Generating disease-relevant cell types from edited iPSCs for phenotypic analysis |
| Control Reagents | Validated control gRNAs, isogenic control cell lines, targeting and non-targeting donors | Establishing experimental baselines and controlling for technical variability |
The integration of CRISPR-Cas9 technology with iPSC-based disease modeling has created unprecedented opportunities for studying human diseases in physiologically relevant systems. The core principles of gRNA design, Cas9 function, and DNA repair pathway manipulation form the foundation for generating accurate genetic models that recapitulate disease pathogenesis. Recent advances in understanding cell-type-specific repair mechanisms, particularly in nondividing cells like neurons, have highlighted the importance of tailoring editing strategies to specific experimental contexts [12] [14].
As the field progresses, several key considerations emerge for researchers employing CRISPR-iPSC platforms. First, the choice of editing approach (NHEJ-mediated knockout vs. HDR-mediated precise editing) must align with experimental goals while considering the inherent limitations of each method. Second, the delivery method must be optimized for the specific cell type, with virus-like particles showing particular promise for hard-to-transfect differentiated cells [12]. Third, comprehensive genotypic and phenotypic validation remains essential, especially given the potential for large structural variations that may escape detection by conventional screening methods [15].
The rapid evolution of CRISPR technology, including the development of AI-designed editors [13] and improved delivery systems [16], continues to expand the capabilities of iPSC-based disease modeling. By applying the core principles and protocols outlined in this document, researchers can leverage these powerful tools to advance our understanding of disease mechanisms and accelerate the development of novel therapeutic strategies.
The convergence of induced pluripotent stem cell (iPSC) technology and CRISPR-Cas9 gene editing represents a transformative paradigm in biomedical research and disease modeling. Both technologies are Nobel Prize-winning breakthroughs that have individually reshaped their respective fields. When combined, they create a powerful platform that addresses long-standing challenges in human disease modeling, particularly for neurological disorders, genetic diseases, and complex multifactorial conditions. This synergy enables researchers to establish isogenic cell lines that differ only in specific disease-causing mutations, providing unprecedented precision in unraveling disease mechanisms while controlling for genetic background variability [10] [17].
The fundamental compatibility between these technologies stems from their complementary strengths. iPSCs provide a patient-specific, ethically acceptable, and infinitely expandable source of human cells that can be differentiated into virtually any cell type, from neurons to cardiomyocytes [18] [6]. Meanwhile, CRISPR-Cas9 offers an efficient, highly precise, and programmable genome editing system that can introduce, correct, or study disease-relevant mutations in these patient-derived cells [19] [20]. This combination has accelerated the development of increasingly sophisticated disease models, from simple 2D cultures to complex 3D organoid systems that better recapitulate human tissue architecture and pathophysiology [11] [10].
Scientific Foundation: Core Technologies and Their Convergence
Induced Pluripotent Stem Cells (iPSCs)
iPSCs are reprogrammed somatic cells that have been returned to an embryonic-like pluripotent state, first generated by Dr. Shinya Yamanaka in 2006 [18] [1]. The reprogramming process involves introducing a specific set of pluripotency-related transcription factors - originally Oct4, Klf4, Sox2, and c-Myc (OKSM, known as Yamanaka factors) - into differentiated cells such as skin fibroblasts or blood cells [6] [1]. These reprogrammed cells acquire two essential characteristics: self-renewal capacity (the ability to divide indefinitely) and pluripotency (the potential to differentiate into any cell type of the body) [1].
The revolutionary aspect of iPSC technology lies in its ability to generate patient-specific stem cells without the ethical concerns associated with embryonic stem cells (ESCs) [18] [6]. From a disease modeling perspective, iPSCs offer two critical advantages: (1) they retain the complete genetic background of the donor, including all polymorphisms and variations that might influence disease manifestation; and (2) they can be differentiated into disease-relevant cell types that are otherwise inaccessible in living patients, such as specific neuronal subtypes, cardiomyocytes, or hepatocytes [1] [17]. This has been particularly valuable for studying neurological disorders, where primary human neural tissue is rarely available for research [17].
CRISPR-Cas9 Genome Editing System
The CRISPR-Cas9 system is an adaptive immune mechanism derived from bacteria that has been repurposed as a highly versatile genome editing tool [19] [20]. The system consists of two core components: the Cas9 nuclease, which creates double-strand breaks in DNA, and a guide RNA (gRNA), which directs Cas9 to a specific genomic sequence complementary to its 20-nucleotide targeting region [19]. The requirement for a protospacer adjacent motif (PAM) sequence immediately downstream of the target site ensures additional specificity [19].
When introduced into cells, the CRISPR-Cas9 complex induces double-strand breaks (DSBs) at predetermined genomic locations [20]. The cell then activates one of two primary DNA repair pathways: non-homologous end joining (NHEJ), which often results in small insertions or deletions (indels) that disrupt gene function; or homology-directed repair (HDR), which uses a donor DNA template to precisely edit or introduce specific sequences [20]. The efficiency, simplicity, and low cost of CRISPR-Cas9 have made it the preferred genome editing technology for most research applications, superseding earlier methods like zinc finger nucleases (ZFNs) and transcription activator-like effector nucleases (TALENs) [19] [18].
Technological Synergy for Disease Modeling
The powerful synergy between iPSCs and CRISPR emerges from their complementary capabilities in disease modeling applications. CRISPR-mediated genome editing addresses a fundamental limitation of patient-derived iPSCs: the genetic variability between different donor lines, which can confound the identification of phenotype-genotype relationships [10] [17]. By using CRISPR to introduce specific disease-causing mutations into healthy control iPSCs, or conversely to correct mutations in patient-derived iPSCs, researchers can create isogenic pairs that differ only at the locus of interest while sharing an identical genetic background [10] [17]. This precise control enables unambiguous attribution of observed phenotypic differences to the specific genetic manipulation [17].
Table 1: Advantages of Combining iPSC and CRISPR Technologies for Disease Modeling
| Aspect | iPSC Technology Contribution | CRISPR Technology Contribution | Combined Advantage |
|---|---|---|---|
| Genetic Background | Provides patient-specific genetic context | Enables creation of isogenic controls | Isolates mutation-specific effects from background genetic variation |
| Disease Relevance | Retains complete patient genome with all disease-modifying variants | Allows introduction or correction of specific pathogenic mutations | Models both monogenic and complex polygenic disorders |
| Cell Source | Unlimited source of human cells; differentiation into relevant cell types | Permits genetic modification of otherwise inaccessible cell types | Humanized models of diseases affecting inaccessible tissues (e.g., brain, heart) |
| Experimental Scale | Suitable for high-throughput screening | Enables genome-wide CRISPR screens | Powerful platform for drug discovery and genetic screening |
| Therapeutic Development | Source for autologous cell therapy | Allows correction of mutations for regenerative medicine | Combined gene and cell therapy approaches |
Applications in Disease Modeling and Drug Development
Neurological Disorders
The CRISPR-iPSC platform has proven particularly valuable for modeling neurological disorders, which have been challenging to study due to limited access to human neuronal tissue and species-specific differences in brain physiology [19] [17]. iPSC-derived neurons, astrocytes, and brain organoids have been used to model a wide range of conditions, including Alzheimer's disease (AD), Parkinson's disease (PD), Huntington's disease (HD), amyotrophic lateral sclerosis (ALS), and neurodevelopmental disorders [19] [21] [17].
For Alzheimer's disease research, CRISPR-iPSC approaches have been used to introduce mutations in genes such as APP, PSEN1, and PSEN2 into control iPSCs, or to correct these mutations in patient-derived cells [6] [21]. These models have successfully recapitulated key aspects of AD pathology, including Aβ deposition, tau phosphorylation, and neuronal dysfunction [10] [21]. The 2021 Inducible Pluripotent Stem Cell Neurodegeneration Initiative (iNDI) represents a landmark large-scale application of this approach, generating 250 CRISPR-engineered iPSC clones to model Alzheimer's Disease and Related Dementias (ADRD) [6].
In Parkinson's disease research, isogenic iPSC lines have been created with mutations in the LRRK2 gene (including G2019S), which is associated with inherited forms of PD [6] [10]. These models have revealed disease-relevant phenotypes including mitochondrial dysfunction, dopaminergic neuron vulnerability, and impaired protein handling [10]. Similarly, for amyotrophic lateral sclerosis, iPSC-derived motor neurons with mutations in SOD1, TARDBP, and C9orf72 genes have shown abnormalities in axonal transport, RNA homeostasis, and stress granule formation [10].
Cardiovascular and Metabolic Diseases
CRISPR-iPSC technology has advanced the modeling of cardiovascular diseases by enabling the generation of human cardiomyocytes with specific disease-causing mutations [6]. These models have been particularly valuable for studying channelopathies such as long QT syndrome, where mutations in genes like KCNQ1 and SCN5A disrupt cardiac electrical activity [10]. iPSC-derived cardiomyocytes with these mutations recapitulate the prolonged action potential duration and arrhythmogenic potential observed in patients, providing a human-relevant platform for drug screening and safety assessment [6] [10].
In the metabolic disease domain, CRISPR-iPSC models have been applied to conditions such as familial hypercholesterolemia, Wilson's disease, and glycogen storage diseases [6] [10]. A proof-of-concept study in 2017 demonstrated that CRISPR-Cas9 could correct pathogenic mutations in the LDLR gene in iPSCs derived from patients with homozygous familial hypercholesterolemia (HoFH) [6]. After differentiation into hepatocytes, the corrected cells showed normal function, suggesting potential for future regenerative medicine applications [6].
Rare Genetic Disorders
The precision of CRISPR editing makes the CRISPR-iPSC platform particularly suited for modeling rare genetic disorders, which often result from specific point mutations or small indels in single genes [20]. Notable examples include Duchenne muscular dystrophy (DMD), sickle cell disease (SCD), β-thalassemia, and cystic fibrosis (CF) [20].
For Duchenne muscular dystrophy, researchers have used CRISPR in patient-derived iPSCs to implement exon skipping strategies that remove mutated exons and restore the reading frame of the dystrophin protein [20]. When differentiated into skeletal muscle progenitor cells, these edited cells expressed truncated but functional dystrophin and exhibited improved contractile function [20]. Similarly, for cystic fibrosis caused by the common ΔF508 mutation in the CFTR gene, CRISPR-mediated correction in iPSCs restored CFTR protein localization and chloride channel function in differentiated airway epithelial cells [20].
Table 2: Representative Disease Models Using CRISPR-iPSC Technology
| Disease Category | Target Genes | Cellular Model | Key Phenotypes Recapitulated |
|---|---|---|---|
| Alzheimer's Disease | APP, PSEN1, PSEN2 | Neurons, Brain Organoids | Aβ deposition, tau phosphorylation, neuronal dysfunction [6] [21] |
| Parkinson's Disease | LRRK2, GBA | Dopaminergic Neurons | Mitochondrial dysfunction, dopaminergic neuron vulnerability [6] [10] |
| Amyotrophic Lateral Sclerosis | SOD1, TARDBP, C9orf72 | Motor Neurons | Axonal transport defects, RNA homeostasis abnormalities, stress granule formation [10] |
| Long QT Syndrome | KCNQ1, SCN5A | Cardiomyocytes | Prolonged action potential, arrhythmogenicity [10] |
| Duchenne Muscular Dystrophy | DMD | Skeletal Muscle Cells | Dystrophin deficiency, impaired contractile function [20] |
| Cystic Fibrosis | CFTR | Airway Epithelial Cells | Defective chloride channel function, mucus secretion abnormalities [20] |
| Hereditary Sensory & Autonomic Neuropathy | NTRK1 | Dorsal Root Ganglia Organoids | Reduced sensory neurons, premature gliogenesis, impaired axonal outgrowth [22] |
Drug Discovery and Development
The CRISPR-iPSC platform has transformed early-stage drug discovery by providing human-relevant disease models for target identification, compound screening, and toxicity assessment [10]. The ability to generate large libraries of iPSCs with specific genetic modifications enables high-throughput screening (HTS) campaigns that identify potential therapeutic targets or compounds that reverse disease phenotypes [6] [10].
In one notable application, researchers used CRISPR-iPSC-derived neurons with GBA mutations (associated with Parkinson's disease) to screen for small molecules that could restore GCase enzyme activity and lysosomal function [10]. Identified hits showed efficacy in subsequent animal models, demonstrating the predictive value of this approach [10]. Similarly, in cystic fibrosis research, lung organoids derived from CFTR mutant iPSCs have been used to identify small molecules that correct the defective chloride channel function caused by the ΔF508 mutation [10].
The platform also excels in drug toxicity assessment, particularly for cardiotoxicity and hepatotoxicity [10]. iPSC-derived cardiomyocytes can be used to monitor changes in cardiac electrical activity in response to drug candidates, while iPSC-derived hepatocytes enable assessment of drug metabolism and toxicity accumulation [10]. By introducing polymorphisms in drug metabolism genes (such as CYP2D6 and CYP3A5) using CRISPR, researchers can further model how genetic variation affects drug responses across different individuals [10].
Experimental Protocols and Methodologies
Generation of Isogenic iPSC Lines Using CRISPR-Cas9
The creation of isogenic iPSC lines is a fundamental application of CRISPR technology in disease modeling. The following protocol outlines the key steps for introducing a specific mutation into control iPSCs or correcting a mutation in patient-derived iPSCs [10] [20]:
gRNA Design and Synthesis: Design 2-3 gRNAs targeting the genomic region of interest. Select gRNAs with high on-target efficiency and minimal off-target potential using computational prediction tools. Synthesize gRNAs as chemically modified synthetic RNAs for enhanced stability [20].
Donor Template Design: For HDR-mediated precise editing, design a single-stranded oligodeoxynucleotide (ssODN) donor template containing the desired edit along with homologous arms (typically 90-120 nucleotides each). Incorporate silent mutations in the PAM sequence or protospacer to prevent re-cutting of edited alleles [20].
iPSC Culture and Preparation: Culture iPSCs in feeder-free conditions using defined essential 8 medium. Passage cells as small clumps using EDTA dissociation. One day before editing, passage cells as single cells using Accutase and seed at optimal density for transfection [18].
CRISPR-Cas9 Delivery: Transfect iPSCs with ribonucleoprotein (RNP) complexes formed by pre-incubating Cas9 protein with synthetic gRNA. Use electroporation systems optimized for stem cells (e.g., Neon Transfection System). Include the ssODN donor template for HDR-mediated editing [20].
Clonal Selection and Expansion: After transfection, allow cells to recover for 48 hours, then dissociate to single cells and seed at clonal density. Isolate individual colonies after 10-14 days and expand in 96-well plates [20].
Genotypic Validation: Screen clones by PCR amplification of the target region and Sanger sequencing. For comprehensive analysis, use next-generation sequencing of the target locus to identify on-target edits and rule out random integration of the donor template [20].
Off-Target Assessment: Perform off-target analysis using GUIDE-seq or CIRCLE-seq for the selected gRNAs. Alternatively, whole-genome sequencing of edited clones provides the most comprehensive assessment of potential off-target effects [20].
Pluripotency and Karyotype Validation: Confirm that edited clones maintain pluripotency markers (OCT4, NANOG, SOX2) and normal karyotype before differentiation studies [20].
Differentiation into Disease-Relevant Cell Types
Following genetic modification, iPSCs are differentiated into cell types relevant to the disease being modeled. The following protocols describe differentiation into neuronal lineages and organoids, which are commonly used in neurological disease modeling [17]:
Neuronal Differentiation (2D Monoculture):
- Neural Induction: Transfer iPSCs to low-attachment plates to form embryoid bodies in neural induction medium containing dual SMAD inhibitors (LDN-193189 and SB431542) for 10-14 days [17].
- Neural Progenitor Cell (NPC) Expansion: Plate neural rosettes on poly-ornithine/laminin-coated dishes in NPC medium containing bFGF and EGF. Expand NPCs for 2-3 passages [17].
- Neuronal Differentiation: Dissociate NPCs and plate at high density in neuronal differentiation medium (NDM) containing BDNF, GDNF, cAMP, and ascorbic acid. Culture for 4-6 weeks with weekly half-medium changes, monitoring maturation by morphological changes and neuronal marker expression [17].
Cerebral Organoid Generation (3D Model):
- Embryoid Body Formation: Dissociate iPSCs to single cells and aggregate in low-attachment U-bottom plates in essential 6 medium with hLIF and CHIR99021 (4,000-10,000 cells per well) [17].
- Neural Induction: After 5 days, transfer embryoid bodies to Matrigel droplets in neural induction medium with dual SMAD inhibitors for 5 days [17].
- Organoid Maturation: Embed Matrigel-embedded organoids in spinning bioreactors or orbital shakers in neuronal differentiation medium. Culture for several months with regular medium changes, allowing complex neural tissue development [17].
Phenotypic Characterization and Functional Assays
Comprehensive phenotypic characterization is essential for validating disease models. The following assays are commonly used to assess pathological hallmarks in CRISPR-iPSC-derived models:
Molecular and Biochemical Assays:
- Immunocytochemistry: Fix cells with 4% PFA, permeabilize with 0.1% Triton X-100, and stain with primary antibodies against cell-type-specific markers (e.g., TUJ1 for neurons, GFAP for astrocytes) and disease-relevant proteins (e.g., Aβ, p-tau) [21] [17].
- Western Blotting: Analyze protein expression and post-translational modifications using SDS-PAGE and specific antibodies. Particularly useful for quantifying pathogenic protein species (e.g., Aβ42/Aβ40 ratio, phosphorylated tau) [21].
- ELISA: Quantify secreted factors or pathogenic proteins in conditioned media or cell lysates using commercial ELISA kits (e.g., for Aβ peptides) [21].
Functional Assays:
- Electrophysiology: Perform whole-cell patch clamping on neurons to assess action potential firing, synaptic activity, and channel function. For cardiomyocytes, use multi-electrode arrays (MEAs) to record field potentials and detect arrhythmogenic activity [10] [17].
- Calcium Imaging: Load cells with fluorescent calcium indicators (e.g., Fluo-4 AM) and monitor calcium transients using live-cell imaging to assess neural network activity or cardiomyocyte contraction [17].
- Metabolic Assays: Measure mitochondrial function using Seahorse Analyzer to assess oxygen consumption rates (OCR) and extracellular acidification rates (ECAR) [10] [21].
Research Reagent Solutions and Technical Tools
Successful implementation of CRISPR-iPSC disease modeling requires specific reagents and technical tools. The following table summarizes essential components and their functions in the experimental workflow:
Table 3: Essential Research Reagents and Tools for CRISPR-iPSC Disease Modeling
| Reagent/Tool Category | Specific Examples | Function and Application | Technical Notes |
|---|---|---|---|
| iPSC Culture | Essential 8 Medium, Matrigel, RevitaCell, Accutase | Maintenance of pluripotency, cell passaging, and recovery after editing | Use defined, xeno-free matrices and media for clinical relevance [18] |
| CRISPR Components | High-fidelity Cas9 (eSpCas9, HiFi-Cas9), synthetic sgRNA, ssODN donors | Genome editing with reduced off-target effects, precise HDR-mediated editing | RNP complexes show higher efficiency and reduced off-target effects compared to plasmid DNA [20] |
| Delivery Systems | Neon Transfection System, Amaxa Nucleofector | Efficient introduction of CRISPR components into iPSCs | Optimization of program settings and solution conditions is essential for high viability [20] |
| Differentiation Reagents | SMAD inhibitors (LDN-193189, SB431542), patterning factors (SHH, FGF8, BMP) | Directed differentiation into specific neural subtypes and regional identities | Concentration and timing of patterning factors determine regional specificity [17] |
| Characterization Tools | Pluripotency markers (OCT4, NANOG, SOX2), neuronal markers (TUJ1, MAP2), disease-relevant antibodies | Validation of pluripotency, differentiation efficiency, and disease phenotypes | Use multiple markers for comprehensive characterization [20] [17] |
| Quality Control Assays | Karyotyping, whole-genome sequencing, GUIDE-seq, mitochondrial sequencing | Assessment of genomic integrity, off-target effects, and genetic stability | Regular monitoring is essential for long-term culture and clinical applications [20] |
Technical Challenges and Solutions
Despite its transformative potential, the CRISPR-iPSC platform faces several technical challenges that researchers must address for robust experimental outcomes:
Editing Efficiency and HDR Limitations
A primary challenge in CRISPR-iPSC editing is the relatively low efficiency of homology-directed repair (HDR), which is necessary for precise gene correction or knock-in [18]. iPSCs predominantly use the non-homologous end joining (NHEJ) pathway, especially outside the S/G2 phases of the cell cycle [18]. Several strategies can enhance HDR efficiency:
- Cell Cycle Synchronization: Treat iPSCs with cell cycle inhibitors such as nocodazole or thymidine to enrich for S/G2 phases where HDR is more active [18].
- Chemical Enhancers: Include small molecule HDR enhancers such as SCR7 (an NHEJ inhibitor) or RS-1 (a RAD51 stimulator) during and after editing [20].
- NHEJ Inhibition: Transiently inhibit key NHEJ factors such as DNA ligase IV using chemical inhibitors to shift the balance toward HDR [20].
- Cas9 Variants: Use high-fidelity Cas9 variants and optimize delivery as RNP complexes to reduce cytotoxicity and improve editing efficiency [20].
Off-Target Effects and Genomic Instability
Off-target effects remain a concern for CRISPR editing, particularly for therapeutic applications [10] [20]. Additionally, long-term culture of iPSCs can lead to genomic instability and the emergence of karyotypic abnormalities [20]. Mitigation strategies include:
- Computational gRNA Design: Use advanced algorithms to select gRNAs with minimal predicted off-target sites [20].
- High-Fidelity Cas9 Variants: Employ engineered Cas9 proteins with reduced off-target activity (e.g., eSpCas9, SpCas9-HF1) [20].
- Comprehensive Off-Target Assessment: Implement high-throughput methods like GUIDE-seq, Digenome-seq, or CIRCLE-seq to empirically identify off-target sites [20].
- Regular Genomic Monitoring: Perform frequent karyotyping and genomic analysis to detect chromosomal abnormalities in cultured iPSCs [20].
Differentiation Variability and Model Maturation
iPSC differentiation protocols often yield heterogeneous cell populations with variable maturity, which can complicate phenotypic analysis [10] [17]. This is particularly challenging for neurological disease modeling, where human neurons require extended time to mature fully [17]. Addressing these challenges:
- Protocol Standardization: Use well-established, defined differentiation protocols with quality control checkpoints [17].
- Cell Sorting: Implement fluorescence-activated cell sorting (FACS) to purify specific cell populations using surface markers [17].
- Extended Maturation: Allow extended culture periods (3-6 months for neurons) to achieve more adult-like phenotypes [17].
- Assembloid Approaches: Combine region-specific organoids to create more complex models that better recapitulate tissue interactions [22] [17].
Visualization of Workflows and Signaling Pathways
CRISPR-iPSC Disease Modeling Workflow
The following diagram illustrates the complete workflow for creating disease models using CRISPR-edited iPSCs, from initial reprogramming to phenotypic analysis:
CRISPR-iPSC Disease Modeling Workflow
CRISPR-Cas9 Genome Editing Mechanism
This diagram details the molecular mechanism of CRISPR-Cas9 genome editing and the two primary DNA repair pathways exploited for different types of genetic modifications:
CRISPR-Cas9 Genome Editing Mechanism
The convergence of iPSC and CRISPR technologies has fundamentally transformed disease modeling approaches, enabling unprecedented precision in studying human genetic disorders. The ability to create isogenic cell lines that differ only in specific disease-causing mutations has resolved the long-standing challenge of genetic background variability in human disease studies [10] [17]. This platform has proven particularly valuable for neurological disorders, where human-specific pathophysiology is difficult to recapitulate in animal models [21] [17].
Future developments in this field will likely focus on enhancing model complexity and physiological relevance through advanced 3D organoid and assembloid systems [22] [17]. The integration of multiple cell types (neurons, glia, vascular cells) in these models will better recapitulate the tissue microenvironment and enable study of cell-cell interactions in disease pathogenesis [22] [17]. Similarly, the development of cryopreserved, pre-differentiated cells and standardized differentiation protocols will improve reproducibility and accessibility of these models across research laboratories [10].
Technological advancements in genome editing will continue to expand the capabilities of the CRISPR-iPSC platform. Base editing and prime editing systems offer more precise genetic modifications without double-strand breaks, potentially reducing off-target effects and improving safety profiles [20]. The combination of CRISPR screening with iPSC-based disease models enables systematic functional genomics in disease-relevant human cell types, accelerating target identification and validation [10] [17].
From a therapeutic perspective, the path toward clinical translation of CRISPR-iPSC-based approaches is becoming increasingly clear. The recent development of hypoimmunogenic iPSCs that evade immune recognition brings "off-the-shelf" allogeneic cell therapies closer to reality [6]. As protocols for in vivo delivery of CRISPR components improve, the potential for direct therapeutic genome editing in human patients continues to grow [21] [20].
In conclusion, the powerful synergy between iPSC and CRISPR technologies has created a robust platform for disease modeling that combines human physiological relevance with genetic precision. This convergence has accelerated our understanding of disease mechanisms and continues to drive innovation in drug discovery and therapeutic development. As both technologies evolve and integrate with other emerging approaches like single-cell omics, artificial intelligence, and advanced bioengineering, they will undoubtedly remain at the forefront of biomedical research and precision medicine.
The discovery of induced pluripotent stem cells (iPSCs) marked a paradigm shift in regenerative medicine, disease modeling, and drug discovery. This technology, which allows for the reprogramming of somatic cells into a pluripotent state, has evolved rapidly from a foundational scientific breakthrough to a platform for generating clinical-grade cell therapies. The convergence of iPSC technology with CRISPR-Cas9 gene editing has further revolutionized their application, enabling the creation of precise human disease models for research [1] [23]. This Application Note traces the key developmental milestones of iPSC technology and provides detailed protocols for their application in disease modeling research, specifically framed within the context of CRISPR-Cas9 gene editing.
Historical Milestones in iPSC Technology
The development of iPSC technology represents a synthesis of decades of research in nuclear reprogramming, stem cell biology, and transcription factor function [24]. The key historical milestones are summarized in the table below.
Table 1: Key Historical Milestones in iPSC Development
| Year | Milestone | Key Finding/Outcome | Significance | References |
|---|---|---|---|---|
| 1962 | Somatic Cell Nuclear Transfer (SCNT) | John Gurdon demonstrated that a nucleus from a differentiated frog intestinal cell could support development of a tadpole. | Established that cellular differentiation involves reversible epigenetic changes, not irreversible genetic alterations. | [1] [24] |
| 1981 | Isolation of Mouse ESCs | Martin Evans, Matthew Kaufman, and Gail Martin isolated pluripotent stem cells from mouse embryos. | Provided the first in vitro model of pluripotency and a reference point for reprogramming. | [1] [24] |
| 1987 | Transcription Factor-Mediated Reprogramming | Ectopic expression of MyoD was shown to convert fibroblasts into myoblasts. | Established the principle that transcription factors are master regulators of cell fate. | [24] |
| 2006 | Discovery of Mouse iPSCs | Kazutoshi Takahashi and Shinya Yamanaka reprogrammed mouse fibroblasts to pluripotency using four factors (Oct3/4, Sox2, c-Myc, Klf4). | Demonstrated that pluripotency can be induced in somatic cells by defined factors. | [25] [1] |
| 2007 | Generation of Human iPSCs & Alternative Factors | Yamanaka's group and James Thomson's group independently generated human iPSCs using OSKM and OCT4, SOX2, NANOG, LIN28, respectively. | Made patient-specific human pluripotent stem cells a reality, avoiding ethical concerns of human ESCs. | [1] [23] |
| 2008-2013 | Development of Non-Integrating Methods | Successive development of methods using episomal vectors, Sendai virus, synthetic mRNA, and fully chemical reprogramming. | Addressed safety concerns of insertional mutagenesis, enabling a path toward clinical applications. | [23] |
| 2012-Present | Integration with CRISPR-Cas9 | CRISPR-Cas9 enabled precise gene editing in iPSCs for creating isogenic disease models and correcting mutations. | Powered highly accurate human disease modeling and the development of precision cell therapies. | [21] [10] [23] |
| 2014-Present | Clinical Trials & HLA-Haplobanks | Initiation of first-in-human iPSC clinical trial for macular degeneration and development of "haplobanks" of HLA-matched iPSCs. | Marked the transition of iPSC technology from the lab to the clinic, addressing immunocompatibility. | [26] [23] |
The intellectual framework for iPSC technology was built upon earlier pioneering work. The German evolutionary biologist August Weismann proposed that heritable information is irreversibly restricted during somatic cell development [1]. This view was famously illustrated by Conrad Waddington's "epigenetic landscape" model in 1957, which depicted cell differentiation as a ball rolling downhill into increasingly stable, specialized valleys [1]. The subsequent SCNT experiments by Gurdon directly challenged this notion of irreversibility, demonstrating that the genome of a specialized cell retains the totipotent capacity to direct embryonic development when exposed to the appropriate cytoplasmic environment of an oocyte [1] [24]. This established the principle of cellular plasticity, which is the fundamental concept underlying cellular reprogramming.
The subsequent derivation of embryonic stem cell (ESC) lines from mice and humans provided a critical in vitro system for studying pluripotency [1] [24]. Cell fusion experiments, in which somatic cells were fused with ESCs, yielded hybrid cells that were pluripotent, providing strong evidence that ESCs contained dominant factors capable of reprogramming a somatic cell nucleus [24]. The final conceptual piece was provided by transdifferentiation studies, which showed that the forced expression of lineage-specific transcription factors could directly convert one somatic cell type into another [24]. This established that transcription factors are powerful enough to override a cell's established epigenetic state and drive a new cell fate.
The pivotal 2006 discovery by Takahashi and Yamanaka synthesized these three principles [25]. They systematically tested 24 candidate genes important for ESC function and successfully narrowed down the minimal set required for reprogramming mouse fibroblasts to four transcription factors: Oct3/4, Sox2, Klf4, and c-Myc (OSKM) [25] [1]. The resulting cells, termed induced pluripotent stem cells (iPSCs), exhibited the morphology, gene expression, and functional capacity (including teratoma formation and germline transmission) of ESCs [25]. This work earned Shinya Yamanaka and John Gurdon the 2012 Nobel Prize in Physiology or Medicine.
The Scientist's Toolkit: Essential Reagents for iPSC Research
The following table catalogs key reagents and materials essential for working with iPSCs, particularly in the context of gene editing and disease modeling.
Table 2: Key Research Reagent Solutions for iPSC Generation and Gene Editing
| Reagent Category | Specific Examples | Function/Application | Technical Notes | |
|---|---|---|---|---|
| Reprogramming Factors | Oct3/4, Sox2, Klf4, c-Myc (OSKM); OCT4, SOX2, NANOG, LIN28 | Ectopic expression reprograms somatic cells to a pluripotent state. | Can be delivered via integrating (retrovirus, lentivirus) or non-integrating methods (Sendai virus, mRNA, episomal vectors). | [25] [1] [23] |
| CRISPR-Cas9 System | Cas9 Nuclease, sgRNA, HDR donor template, Base Editors | Introduces or corrects disease-relevant mutations in iPSCs to create isogenic controls. | High-fidelity Cas variants reduce off-target effects. HDR is used for precise edits, while NHEJ creates knockouts. | [21] [10] [23] |
| Culture Matrices | Matrigel, Vitronectin, Laminin-521 | Provides a defined, xeno-free substrate for the attachment and growth of iPSCs and ESCs. | Critical for replacing mouse feeder cells (MEFs) to transition to clinically compliant cultures. | [27] [26] |
| Cell Culture Media | mTeSR, StemFit, Essential 8 | Chemically defined, feeder-free media formulations that support the self-renewal of iPSCs. | Maintains pluripotency and genomic stability over long-term culture. | [27] |
| Differentiation Induction Kits | Commercially available kits for neurons, cardiomyocytes, hepatocytes | Provides optimized protocols and reagents to direct iPSC differentiation into specific somatic lineages. | Ensures reproducibility and efficiency in generating disease-relevant cell types for modeling. | [28] [10] |
| Quality Control Assays | Karyotyping, Pluritest, Immunofluorescence (OCT4, NANOG, SSEA-4), Trilineage Differentiation In Vivo (Teratoma Assay) | Validates pluripotent state, genomic integrity, and differentiation potential of iPSC lines. | Mandatory for confirming the quality of parental and gene-edited clonal lines before experimentation. | [27] [23] |
Core Protocols for CRISPR-iPSC Disease Modeling
Protocol 1: Generation of Clinical-Grade iPSCs from Somatic Cells
This protocol outlines a method for generating integration-free human iPSCs using non-integrating vectors, suitable for subsequent clinical applications [27] [23].
Materials:
- Source Cells: Human dermal fibroblasts or peripheral blood mononuclear cells (PBMCs).
- Reprogramming Vector: CytoTune-iPS Sendai Virus Kit (non-integrating) or equivalent mRNA/episomal system.
- Culture Vessels: Matrigel-coated 6-well plates.
- Cell Culture Media: Fibroblast or PBMC growth medium, feeder-free iPSC maintenance medium (e.g., mTeSR1).
- Other Reagents: Rock inhibitor (Y-27632).
Procedure:
- Source Cell Preparation: Culture source cells to ~80% confluency. Ensure high viability (>90%).
- Viral Transduction: Calculate the appropriate multiplicity of infection (MOI). Add the Sendai virus vectors containing OSKM to the cell culture medium. Incubate for 24 hours.
- Media Change: After 24 hours, replace the virus-containing medium with fresh growth medium.
- Passaging and Plating: 5-7 days post-transduction, harvest the transduced cells using enzymatic dissociation. Plate the cells onto Matrigel-coated plates at a high density in medium supplemented with Rock inhibitor to enhance survival.
- Switch to iPSC Medium: 24 hours after replating, replace the growth medium with feeder-free iPSC maintenance medium. Continue feeding with iPSC medium every day.
- Colony Picking: After 3-4 weeks, distinct ESC-like colonies will emerge. Manually pick and expand individual clones into separate wells.
- Characterization: Validate bona fide iPSC status through immunocytochemistry (OCT4, NANOG, SSEA-4), PCR for the loss of the Sendai virus genome, and pluripotency tests (e.g., in vitro trilineage differentiation). Perform routine karyotyping.
Protocol 2: CRISPR-Cas9 Mediated Generation of Isogenic iPSC Lines
This protocol describes the use of CRISPR-Cas9 to correct a disease-causing mutation in patient-derived iPSCs, creating a genetically matched, isogenic control line [21] [10] [23].
Materials:
- Cells: Patient-derived iPSCs harboring a known pathogenic mutation.
- CRISPR Components: Plasmid or ribonucleoprotein (RNP) complex of Cas9 and target-specific sgRNA.
- Donor Template: Single-stranded oligodeoxynucleotide (ssODN) or double-stranded DNA donor containing the corrected sequence and silent restriction site.
- Transfection Reagent: Electroporation system (e.g., Neon) or chemical transfection reagent.
- Culture Media: iPSC maintenance medium with Rock inhibitor.
Procedure:
- Design and Preparation: Design sgRNA to target the genomic region near the mutation. Design an HDR donor template with the desired correction and a silent marker (e.g., novel restriction site).
- Delivery: Co-transfect patient iPSCs with the CRISPR-Cas9 complex (as plasmid or RNP) and the HDR donor template using electroporation.
- Recovery and Expansion: Plate transfected cells at low density in iPSC medium with Rock inhibitor. Allow cells to recover and expand for 5-7 days.
- Single-Cell Cloning: Harvest cells and seed at clonal density (<1 cell/well) in 96-well plates. Expand individual clones.
- Genotype Screening: Screen expanded clones by PCR and restriction fragment length polymorphism (RFLP) analysis (using the silent marker) to identify correctly edited clones.
- Sequence Validation: Sanger sequence the targeted genomic locus of candidate clones to confirm precise correction and rule off-target events.
- Quality Control: Bank the validated isogenic corrected clone and its mutant (parental) counterpart. Perform comparative karyotyping and pluripotency checks to ensure the editing process did not introduce unintended abnormalities.
Protocol 3: Phenotypic Screening of iPSC-Derived Neurons for Alzheimer's Disease Research
This protocol applies the isogenic iPSC lines to model Alzheimer's disease (AD) by differentiating them into neurons and assessing key pathological phenotypes [21] [28] [10].
Materials:
- iPSC Lines: Isogenic pair (e.g., with and without a mutation in APP or PSEN1).
- Differentiation Reagents: Neural induction medium, neuronal maturation supplements (e.g., BDNF, GDNF).
- Assay Kits: ELISA kits for Aβ40/42, antibodies for phospho-Tau and total Tau, immunocytochemistry reagents.
- Cell Culture: Matrigel-coated plates for 2D culture or low-attachment plates for 3D organoid formation.
Procedure:
- Neural Differentiation: Differentiate the isogenic iPSC pairs into cortical neurons using a standardized, multi-step protocol involving dual SMAD inhibition. For more complex modeling, generate 3D cerebral organoids.
- Sample Collection: Collect conditioned medium from mature neurons (e.g., at day 60-90 of differentiation) for secretome analysis.
- Aβ ELISA: Measure the concentration of Aβ40 and Aβ42 peptides in the conditioned medium using commercial ELISA kits. Calculate the Aβ42/Aβ40 ratio, a key indicator of pathogenicity.
- Tau Phosphorylation Analysis: Lyse a parallel set of neurons. Perform western blotting or immunofluorescence using antibodies specific for phosphorylated Tau (e.g., at Ser202/Thr205) and total Tau. Quantify the ratio of p-Tau to total Tau.
- Functional and Survival Assays: Perform additional assays as relevant, such as electrophysiology to measure neuronal activity, RNA sequencing to profile transcriptomic changes, or TUNEL staining to assess apoptosis.
- Data Analysis and Validation: Compare all phenotypic data between the mutant and isogenic control lines. Statistical significance confirms the mutation-specific phenotype, validating the model for subsequent drug screening.
Visualization of the Integrated CRISPR-iPSC Workflow
The entire process, from somatic cell to disease model and therapeutic application, is summarized in the following workflow.
Discussion and Future Perspectives
The journey from Yamanaka's initial discovery to the current era of clinical-grade iPSCs and CRISPR-engineered disease models has been remarkably rapid [23]. The integration of these technologies provides an unprecedented platform for studying human disease mechanisms in a patient-specific context, performing high-throughput drug screening, and developing personalized cell therapies [28] [10]. The ability to create isogenic controls via CRISPR-Cas9 is particularly powerful, as it eliminates the confounding effects of genetic background, allowing researchers to attribute phenotypic differences directly to the disease-causing mutation [21] [23].
Despite the immense progress, challenges remain. Genomic instability in iPSCs, potential off-target effects of CRISPR editing, and the functional immaturity of some iPSC-derived cell types compared to their adult human counterparts are key technical hurdles [21] [27] [10]. Furthermore, the high cost and complexity of manufacturing clinical-grade iPSC-derived products under Good Manufacturing Practice (GMP) conditions present significant translational barriers [27].
Future directions will focus on addressing these limitations through the development of more precise gene-editing tools (e.g., base and prime editing), improved differentiation protocols to generate more mature and complex tissue models (e.g., multi-cell type organoids), and the implementation of automation and artificial intelligence (AI) to standardize production and analyze complex phenotypic data [28] [10]. The ongoing establishment of HLA-matched iPSC "haplobanks," such as the one reported by Yamanaka's group matching ~40% of the Japanese population, will be crucial for scaling up allogeneic cell therapies [26]. As these technologies continue to mature, the CRISPR-iPSC platform is poised to remain a cornerstone of biomedical research and regenerative medicine for the foreseeable future.
From Theory to Lab Bench: Engineering Precise Genetic Disease Models with CRISPR-iPSCs
The combination of induced pluripotent stem cell (iPSC) technology and CRISPR-Cas9 gene editing has revolutionized the creation of human disease models for research and drug development [21] [10]. This application note details a standardized workflow for generating genetically engineered, patient-specific differentiated cells. This protocol provides researchers with a strategic framework for producing highly physiologically relevant in vitro models that recapitulate disease pathology, enabling precise investigation of molecular mechanisms and high-throughput drug screening [29] [10].
The comprehensive pathway from somatic cell to engineered differentiated cell type involves multiple critical stages, each requiring optimization for maximum efficiency and fidelity. The entire process, from patient cell collection to final characterization, typically spans 12-16 weeks. The schematic below illustrates this integrated workflow.
Detailed Experimental Protocols
Patient Somatic Cell Collection and iPSC Reprogramming
Objective: To obtain and reprogram patient somatic cells into induced pluripotent stem cells (iPSCs) while maintaining genetic integrity.
Materials:
- Source Tissue: Skin biopsy (fibroblasts) or peripheral blood mononuclear cells (PBMCs)
- Reprogramming Factors: OCT4, SOX2, KLF4, c-MYC (OSKM) or alternatives (OSKL, OSNL) [2]
- Delivery System: Non-integrating Sendai virus, episomal plasmids, or mRNA [2]
- Culture Medium: Essential 8 or mTeSR for maintenance [30]
Procedure:
- Cell Isolation: Process skin biopsy via enzymatic digestion (collagenase) to isolate fibroblasts or isolate PBMCs from blood using density gradient centrifugation.
- Culture Expansion: Expand somatic cells in appropriate medium (DMEM + 10% FBS for fibroblasts; RPMI + serum for PBMCs) for 2-3 passages.
- Reprogramming Factor Delivery:
- Prepare Sendai virus particles (CytoTune iPS 2.0 Sendai Kit) at appropriate MOI
- Infect 1×10^5 somatic cells in 6-well plate
- Incubate for 24 hours, then replace with fresh medium
- iPSC Colony Picking:
- After 14-21 days, identify and manually pick embryonic stem cell-like colonies
- Transfer to Matrigel-coated plates with mTeSR1 medium
- Expand and bank at passage 5-10
Quality Control:
- Confirm pluripotency via immunocytochemistry (OCT4, NANOG, SOX2)
- Perform karyotype analysis to ensure genomic integrity
- Verify absence of residual reprogramming vectors via PCR
CRISPR-Cas9 Mediated Gene Editing in iPSCs
Objective: To introduce precise genetic modifications in iPSCs while maintaining pluripotency and genomic integrity.
Materials:
- Nuclease: Alt-R S.p. HiFi Cas9 V3 or Cas12a Ultra (IDT) [31]
- Delivery Method: 4D Nucleofector System (Lonza) with P4 Primary Cell Solution [31]
- Donor Template: Single-stranded oligodeoxynucleotide (ssODN) or plasmid donor
Optimized Sequential Delivery Protocol (adapted from [31]):
Table 1: Sequential Delivery Protocol Timeline
| Day | Procedure | Key Parameters |
|---|---|---|
| -2 | Medium change to richer alternative | Use StemFlex medium |
| 0 | First nucleofection: donor plasmid | 3×10^6 cells, program CA-167 |
| 0 | Post-nucleofection recovery | 10 min in RPMI, 37°C |
| 1 | Second nucleofection: RNP complex | Same cell count and program |
| 1-3 | Cold shock incubation | 32°C |
| 4-7 | Return to standard culture | 37°C, 5% CO₂ |
| 8+ | Clone screening and expansion | Limiting dilution |
Detailed Steps:
- Guide RNA Design:
- Design gRNAs with minimal off-target potential using tools like CRISPOR
- Include on-target scoring >60 and verify specificity against reference genome
- RNP Complex Formation:
- Complex 60 pmol Cas9 protein with 120 pmol sgRNA in nucleofection buffer
- Incubate 10-20 minutes at room temperature
- Donor Plasmid Preparation:
- For knock-ins, design donor with ~800 bp homology arms
- Include silent mutations in PAM region to prevent re-cutting
- Sequential Nucleofection:
- Day 0: Nucleofect 3×10^6 iPSCs with 5-10 µg donor plasmid
- Recover cells in RPMI medium for 10 minutes, then plate in StemFlex
- Day 1: Harvest cells, nucleofect with pre-formed RNP complexes
- Immediately after nucleofection, transfer cells to 32°C incubator for 48-72 hours
Clone Isolation and Validation
Objective: To isolate isogenic clones with desired genetic modifications and confirm genomic integrity.
Procedure:
- Single-Cell Cloning:
- After editing, dissociate to single cells using Accutase
- Plate at limiting dilution (0.5-1 cell/well) in 96-well plates
- Include ROCK inhibitor Y-27632 (10 µM) for first 48 hours [30]
- Genotypic Screening:
- Extract genomic DNA from expanded clones
- Perform PCR amplification of target locus
- Confirm edits via Sanger sequencing or next-generation sequencing
- Off-Target Assessment:
- Utilize GUIDE-seq or CIRCLE-seq for unbiased off-target detection [32]
- Sequence top 5-10 computationally predicted off-target sites
- Phenotypic Confirmation:
- Verify pluripotency remains intact post-editing
- Confirm normal karyotype via G-banding analysis
- Exclude clones with abnormal morphology
Directed Differentiation to Target Cell Type
Objective: To differentiate genetically engineered iPSCs into relevant somatic cell types for disease modeling.
Neural Differentiation Protocol (adapted from [30]):
Table 2: Neural Differentiation Timeline
| Stage | Days | Medium | Key Components |
|---|---|---|---|
| Neural Induction | 0-7 | Neural Induction Medium | Dual SMAD inhibitors |
| NSC Expansion | 7-30 | NPM Medium | bFGF (20 ng/ml), EGF (20 ng/ml) |
| Terminal Differentiation | 30-51 | N2B27 Medium | No growth factors |
Detailed Steps:
- Neural Induction:
- Dissociate iPSCs to single cells and plate at 1×10^5 cells/cm²
- Culture in Neural Induction Medium with Dual SMAD inhibitors (SB431542 and LDN193189)
- Change medium daily for 7 days
- Neural Stem Cell (NSC) Expansion:
- Passage emerging NSCs using Accutase
- Maintain in NPM medium supplemented with bFGF and EGF
- Passage every 5-7 days at 1:3-1:6 ratio
- Terminal Differentiation:
- Plate NSCs at 4×10^4 cells/cm² on Matrigel-coated surfaces
- Culture in N2B27 medium without growth factors
- Maintain for 21 days with 50% medium changes every 2-3 days
- Characterization:
- Analyze neuronal markers (TUJ1, MAP2) via immunocytochemistry
- Assess synaptic function via calcium imaging or electrophysiology
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents and Their Applications
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC | Somatic cell reprogramming | c-MYC replacement (L-MYC) reduces tumorigenic risk [2] |
| CRISPR Nucleases | S.p. HiFi Cas9 V3, A.s. Cas12a Ultra | Genome editing | HiFi Cas9 reduces off-target effects [32] [31] |
| Delivery Systems | 4D Nucleofector, Lipofectamine Stem | Component delivery | Nucleofection superior for RNP delivery in iPSCs [31] |
| Culture Media | mTeSR1, StemFlex, Neural Induction | Cell maintenance and differentiation | StemFlex enhances editing efficiency [31] |
| Selection Agents | Puromycin, Geneticin, Flow cytometry | Clone enrichment | Avoid in GMP applications; use screening instead [31] |
| Characterization Tools | Flow cytometry, NGS, Immunocytochemistry | Quality assessment | Single-cell sequencing detects editing heterogeneity [33] |
Critical Factors for Success
Technical Optimization Strategies
Enhancing HDR Efficiency:
- Synchronize cell cycle in S/G2 phases using cell cycle inhibitors
- Utilize small molecules (RS-1, SCR7) to enhance HDR
- Optimize cold shock duration (48-72 hours at 32°C) [31]
Maintaining Pluripotency:
- Daily visual inspection to remove spontaneously differentiated areas
- Maintain cells in log-phase growth with regular passaging
- Use defined, feeder-free culture systems [18]
Ensuring Genomic Integrity:
- Regular karyotyping at expansion stages
- Limit total passages to prevent culture-acquired mutations
- Use genomic stability assays (CNV analysis)
Troubleshooting Common Challenges
Table 4: Troubleshooting Guide
| Problem | Potential Causes | Solutions |
|---|---|---|
| Low reprogramming efficiency | Poor somatic cell quality, Suboptimal factor delivery | Use early-passage somatic cells, Optimize viral titer or mRNA concentration |
| Poor editing efficiency | Inefficient delivery, Low HDR rates | Implement sequential delivery, Add HDR enhancers, Optimize gRNA design |
| Low cell survival post-nucleofection | Electroporation toxicity, Poor recovery | Use RPMI recovery step, Optimize nucleofection program, Plate at high density |
| Spontaneous differentiation | Suboptimal culture conditions, Over-confluence | Daily monitoring, Remove differentiated areas, Optimize passaging schedule |
| Genomic instability | Extended culture, Clonal selection | Limit passages, Bank early, Multiple clone characterization |
This application note provides a comprehensive framework for implementing a robust workflow from patient somatic cells to genetically engineered differentiated cell types. The strategic integration of optimized reprogramming, sequential CRISPR editing, and directed differentiation enables generation of physiologically relevant human disease models. The protocols detailed herein emphasize efficiency, reproducibility, and quality control—critical considerations for research and drug development applications. As the field advances, further refinements in editing precision and differentiation protocols will continue to enhance the fidelity and utility of these powerful models for understanding disease mechanisms and developing novel therapeutics.
The advent of human induced pluripotent stem cell (iPSC) technology has revolutionized disease modeling by enabling the establishment of cellular models from individual patients [34]. However, phenotypic variability arising from differing genetic backgrounds across iPSC lines can confound data interpretation [35]. Isogenic controls—genetically identical cell lines that differ only at a specific, disease-relevant locus—represent the gold standard for addressing this challenge [34] [36].
The combination of iPSC technology with CRISPR/Cas9 genome editing has provided an unprecedented ability to repair putative causative alleles in patient lines or introduce disease alleles into healthy "wild-type" cell lines [34]. This generates isogenic cell pairs that differ in a single genetic change, enabling researchers to precisely assess the molecular and cellular phenotypes resulting from that specific abnormality [34]. This approach establishes the true causative lesion, which is often impossible to ascertain from human genetic studies alone [34].
This application note details the methodology, experimental design, and practical implementation of creating and validating isogenic controls for disease mechanism studies, providing researchers with a framework for generating robust, interpretable disease models.
The Critical Role of Isogenic Controls in Disease Modeling
Overcoming Limitations of Traditional Models
Traditional disease models, including animal models and patient-derived primary cells, present significant limitations for studying human disease mechanisms. Approximately 20% of human genes lack identifiable one-to-one orthologues in mice, and even apparent orthologous genes can play different roles in different species [34]. Furthermore, primary cell cultures from patients are often challenging to maintain for extended periods and typically consist of heterogeneous cell populations that complicate analysis [34].
iPSC technology enables the derivation of clinically relevant cell types that would normally be inaccessible, such as neuronal or cardiac cells [34] [35]. Nevertheless, without isogenic controls, the varying genetic backgrounds of different iPSC lines can obscure disease-specific phenotypes [35]. Isogenic controls eliminate this confounder, ensuring that observed phenotypic differences can be confidently attributed to the introduced genetic modification.
Applications of Isogenic Control Lines
Isogenic cell lines serve multiple critical functions in biomedical research:
- Causative Mutation Validation: Precisely linking specific genetic mutations to cellular phenotypes [34]
- Drug Screening Platforms: Enabling high-throughput genetic and pharmacological screens to understand pathological mechanisms and develop novel therapeutics [34]
- Pathway Analysis: Facilitating detailed analysis of disease mechanisms without the noise of genetic background effects [35]
- Therapeutic Development: Providing optimized cellular models for developing and testing cellular or molecular gene therapies [34]
Quantitative Analysis of Editing Efficiency in Recent Studies
Recent advances in CRISPR/Cas9 editing protocols have dramatically improved the efficiency of generating isogenic controls. The table below summarizes editing efficiencies achieved with different approaches across multiple studies.
Table 1: Efficiency of CRISPR/Cas9 genome editing in generating isogenic controls
| Study/Application | Gene Target | Editing Type | Base Efficiency | Optimized Protocol Efficiency | Fold Improvement |
|---|---|---|---|---|---|
| SNP introduction [37] | EIF2AK3 (rs867529) | Point mutation | 2.8% | 59.5% | 21x |
| SNP introduction [37] | EIF2AK3 (rs13045) | Point mutation | 4% | 25% | 6x |
| APOE Christchurch mutation [37] | APOE | Point mutation | - | 49-99% (bulk), 94-100% (clones) | - |
| PSEN1 E280A reversion [37] | PSEN1 | Point mutation | - | 97-98% (bulk), 100% (clones) | - |
| Provirus deletion [38] | SLCO1B3 | Large deletion (4.2 kb) | 29% (wtCas9) | 69% (HiFi Cas9) | 2.4x |
| Stargardt disease modeling [36] | ABCA4 | Variant correction | Successful generation | Normal karyotype, no off-targets | - |
High-Efficiency Protocol for Generating Isogenic Controls
The following diagram illustrates the comprehensive workflow for generating isogenic controls using CRISPR/Cas9 in iPSCs:
Detailed Experimental Procedures
iPSC Culture and Maintenance
iPSCs are maintained in feeder-free conditions using specific culture media and matrices:
- Culture Medium: Use StemFlex (Gibco #A334901) or mTeSR Plus (STEMCELL Technology #100-0276) [37]
- Basal Matrix: Matrigel (Corning #47743-706) at a dilution of 1:400 in cold basic DMEM (final protein concentration ~25.8-26.5 μg/mL) [39] [37]
- Passaging: Use ReLeSR (STEMCELL Technologies #100-0484) for routine maintenance splitting [37]
- Coating Protocol: Add 2 mL coating medium per well of a 6-well plate, incubate at 4°C for 12 hours or at 37°C for 30 minutes [39]
gRNA Design and Molecular Cloning
Effective gRNA design is critical for successful genome editing:
- Target Selection: Choose a target site with the Cas9 cleavage site located less than 10 nucleotides from the intended mutation [37]
- PAM Consideration: For SpCas9, the PAM sequence is 5'-NGG-3' [40]
- Specificity Enhancement: Introduce silent "blocking" mutations in the repair template to prevent Cas9 re-cleavage after editing [35]
- Cloning: Clone sgRNAs into appropriate vectors such as pSpCas9(BB)-2A-GFP (PX458) from Addgene using BsmBI digestion [41]
Nucleofection and HDR Enhancement
This optimized protocol achieves high efficiency homologous directed repair (HDR):
- Timing: Perform nucleofection when iPSCs reach 80-90% confluency [37]
- Pre-treatment: Change to cloning media (StemFlex with 1% RevitaCell and 10% CloneR) 1 hour before nucleofection [37]
- RNP Complex Formation: Combine 0.6 μM guide RNA (IDT) and 0.85 μg/μL of Alt-R S.p. HiFi Cas9 Nuclease V3 (IDT #10810559), incubate at room temperature for 20-30 minutes [37]
- Electroporation Mix: Combine 0.5 μg pmaxGFP (LONZA #V4XP-3032), 5 μM single-strand oligonucleotide (ssODN) repair template, and the prepared RNP complex [37]
- HDR Enhancement: Co-transfect with 50 ng/μL pCXLE-hOCT3/4-shp53-F (Addgene #27077) for p53 knockdown [37]
- Additional Enhancers: Include HDR enhancer (IDT), electroporation enhancer (IDT), and CloneR (STEMCELL Technologies) to improve cell survivability and HDR rates [37]
Single-Cell Cloning and Validation
After nucleofection, single-cell cloning is essential for establishing pure isogenic lines:
- Single-Cell Dilution: Plate cells at low density in cloning medium containing pro-survival supplements [37] [38]
- Clone Expansion: Pick and expand individual colonies for genomic DNA extraction and characterization [38]
- Genotypic Validation: Use Sanger sequencing, restriction fragment length polymorphism (RFLP), or next-generation sequencing to confirm edits [41] [37]
- Karyotyping: Perform G-banding analysis to ensure chromosomal integrity [37]
- Pluripotency Confirmation: Verify that edited lines maintain pluripotent characteristics [36]
Molecular Engineering Strategies
The following diagram illustrates the molecular strategy for introducing specific mutations using CRISPR/Cas9 and repair templates:
Essential Reagents and Research Tools
Successful generation of isogenic controls requires specific reagents and tools. The table below catalogues essential solutions and their applications.
Table 2: Essential research reagents for generating isogenic controls in iPSCs
| Reagent Category | Specific Product | Application/Function | Key Features |
|---|---|---|---|
| CRISPR Nucleases | Alt-R S.p. HiFi Cas9 Nuclease V3 (IDT) [37] | High-fidelity genome editing | Reduced off-target effects |
| Wildtype SpCas9 [38] | Standard genome editing | Higher efficiency for challenging edits | |
| gRNA Delivery | pSpCas9(BB)-2A-GFP (PX458, Addgene) [41] [40] | All-in-one Cas9 and gRNA expression | GFP reporter for transfection efficiency |
| HDR Enhancement | pCXLE-hOCT3/4-shp53-F (Addgene) [37] | p53 knockdown | Improves HDR efficiency and cell survival |
| HDR Enhancer (IDT) [37] | Enhances homology-directed repair | Increases precise editing rates | |
| Cell Survival | CloneR (STEMCELL Technologies) [37] | Enhances single-cell survival | Critical for clonal expansion |
| RevitaCell (Gibco) [37] | Supports cell recovery post-electroporation | Improves viability after transfection | |
| ROCK inhibitor [37] | Prevents apoptosis in single cells | Standard for iPSC single-cell culture | |
| Validation Tools | T7 Endonuclease I [41] [38] | Detection of INDEL mutations | Mismatch cleavage assay |
| Digital PCR [38] | Absolute quantification of editing | High sensitivity for precise efficiency measurement | |
| ICE Analysis (Synthego) [37] | Sequencing-based efficiency quantification | Accurate measurement of HDR rates from NGS data |
Advanced Applications and Case Studies
Cardiac Arrhythmia Modeling
A compelling application of isogenic controls appears in the study of inherited cardiac arrhythmias. Researchers introduced N588D and N588K mutations in the KCNH2 gene, which cause long QT syndrome (LQTS) and short QT syndrome (SQTS) respectively, into a well-characterized iPSC line [35]. Electrophysiological analysis of derived cardiomyocytes showed significantly prolonged repolarization for LQTS mutants (323 ± 21 ms) and shortened repolarization for SQTS mutants (82 ± 18 ms) compared to isogenic controls (231 ± 24 ms) [35]. When formatted into 3D cardiac tissue sheets, these isogenic lines demonstrated differential susceptibility to arrhythmic events upon pharmacological challenge, faithfully recapitulating clinical disease phenotypes [35].
Overcoming Cas9 Silencing with SLEEK Technology
A significant technical challenge in using iPSCs for disease modeling is Cas9 silencing during differentiation, even when integrated into safe harbor loci like AAVS1 [39]. The SLEEK (Selection by Essential Gene Exon Knocking) technology overcomes this by inserting Cas9-EGFP into exon 9 of the GAPDH gene, using a recoded exon that preserves the GAPDH amino acid sequence [39]. This approach leverages the endogenous GAPDH promoter to drive robust, sustained Cas9-EGFP expression while enabling negative selection against non-edited cells through disruption of GAPDH function [39]. Edited iPSC-Cas9-EGFP cells maintain typical pluripotency and normal karyotype, providing a versatile platform for efficient genome editing throughout differentiation [39].
Validation and Quality Control
Rigorous validation of isogenic controls is essential for generating reliable research data. The following quality control measures should be implemented:
- Genomic Validation: Confirm intended edits via Sanger sequencing and verify absence of random integration [36] [37]
- Karyotypic Analysis: Perform G-banding analysis to ensure chromosomal integrity after editing [36] [37]
- Off-Target Assessment: Use whole genome sequencing or targeted approaches to verify absence of unintended edits [37]
- Pluripotency Confirmation: Demonstrate that edited lines maintain expression of pluripotency markers and differentiation potential [36]
- Line Identity Verification: Confirm isogenic relationship through STR profiling or SNP analysis [35]
Advanced quantification methods like qEva-CRISPR provide sensitive, quantitative evaluation of CRISPR/Cas9-mediated modifications, enabling simultaneous analysis of multiple targets and detection of all mutation types, including point mutations and large deletions [41]. Digital PCR offers absolute quantification of editing efficiencies, with demonstrated sensitivity for detecting large deletions in challenging models like chicken primordial germ cells [38].
The generation of isogenic controls through CRISPR/Cas9 genome editing represents a transformative approach for disease mechanism studies. By controlling for genetic background variability, these precision models enable researchers to confidently attribute phenotypic differences to specific genetic alterations. The optimized protocols detailed herein, incorporating p53 inhibition and pro-survival factors, can achieve homologous recombination rates exceeding 90%, dramatically reducing the time and resources required to create these critical research tools [37].
As demonstrated in disease modeling applications ranging from Stargardt disease to cardiac arrhythmias, isogenic controls provide the foundation for rigorous mechanistic studies, drug discovery platforms, and therapeutic development [36] [35]. The continued refinement of genome editing technologies, including high-fidelity Cas variants and innovative approaches to prevent silencing, will further enhance the efficiency and accessibility of these methods, empowering researchers to create increasingly sophisticated models of human disease [39] [38].
Application Note: CRISPR-Cas9 in iPSCs for Modeling Neurodegenerative Diseases
The convergence of Clustered Regularly Interspaced Short Palindromic Repeats/CRISPR-associated protein 9 (CRISPR-Cas9) gene editing with human-induced pluripotent stem cell (iPSC) technology has revolutionized the modeling of neurodegenerative diseases [21] [10]. This integrated platform enables researchers to create genetically precise, patient-specific cellular models that recapitulate key pathological features of Alzheimer's disease (AD), Parkinson's disease (PD), and Amyotrophic Lateral Sclerosis (ALS) in vitro [42] [43]. By constructing isogenic iPSC lines—where the genetic background is identical except for specific disease-relevant mutations—researchers can isolate the functional consequences of pathogenic variants while minimizing confounding genetic factors [44] [10]. This approach has become indispensable for studying disease mechanisms, identifying therapeutic targets, and conducting high-throughput drug screening.
Key Advantages and Applications
The CRISPR-iPSC platform offers several distinct advantages for neurodegenerative disease research. It enables the study of patient-specific mutations in disease-relevant cell types, such as neurons, astrocytes, and microglia, which are otherwise inaccessible in living patients [42] [43]. The technology facilitates the creation of 3D organoid models that better mimic the complexity of human brain tissue compared to traditional 2D cultures [21] [10]. Furthermore, isogenic iPSC pairs provide controlled experimental systems for evaluating candidate therapeutics and assessing toxicity in human cells [10]. These applications are transforming our approach to understanding and treating neurodegenerative diseases by providing more physiologically relevant human models.
Disease-Specific Modeling Applications
Alzheimer's Disease Modeling
CRISPR-Cas9 and iPSC technologies have advanced Alzheimer's disease modeling by enabling precise introduction of pathogenic mutations in genes such as APP, PSEN1, PSEN2, and APOE into human pluripotent stem cells [21] [43]. These edited cells can be differentiated into neurons, astrocytes, and microglia to study amyloid-beta processing, tau phosphorylation, neuroinflammation, and oxidative stress in a human genetic context [21]. The National Institutes of Health's Induced Pluripotent Stem Cell Neurodegenerative Disease Initiative (iNDI) represents a large-scale effort to model over 100 mutations associated with Alzheimer's disease and related dementias in standardized isogenic iPSC lines [44]. This resource will provide the research community with rigorously validated cellular models for studying AD mechanisms and screening therapeutic compounds.
Table 1: Key Genetic Targets for CRISPR-Cas9 Editing in Alzheimer's Disease Models
| Gene Target | Mutation Type | Pathological Consequence | iPSC-Derived Cell Types |
|---|---|---|---|
| APP | Various missense mutations | Altered Aβ production and aggregation | Neurons, astrocytes |
| PSEN1 | Pathogenic variants | Dysregulated γ-secretase activity | Neurons, cerebral organoids |
| PSEN2 | Pathogenic variants | Impaired γ-secretase function | Neurons, microglia |
| APOE | ε4 allele | Increased Aβ accumulation and neuroinflammation | Astrocytes, microglia |
Parkinson's Disease Modeling
In Parkinson's disease research, CRISPR-iPSC platforms have been utilized to model both familial and sporadic forms of the disease [10] [45]. Key genetic targets include LRRK2 (particularly the G2019S mutation), PRKN, PINK1, and SNCA, which have been introduced into iPSCs via CRISPR-Cas9 editing [10] [45]. The resulting dopaminergic neurons exhibit disease-relevant phenotypes such as mitochondrial dysfunction, increased susceptibility to oxidative stress, and impaired mitophagy [45]. A notable advancement came from researchers who used CRISPR/Cas9-mediated PINK1 deletion to generate a non-human primate model that recapitulated the human Parkinson's phenotype with neuronal loss in the substantia nigra [45]. These models provide valuable platforms for studying selective neuronal vulnerability and screening potential neuroprotective compounds.
Table 2: Parkinson's Disease Genes for CRISPR-iPSC Modeling
| Gene | CRISPR Application | Resulting Phenotypes in iPSC-Derived Dopaminergic Neurons |
|---|---|---|
| LRRK2 | Introduction of G2019S mutation | Mitochondrial dysfunction, increased oxidative stress |
| PRKN | Knockout or patient mutation | Impaired mitophagy, mitochondrial accumulation |
| PINK1 | Knockout or patient mutation | Defective mitochondrial quality control |
| SNCA | Introduction of multiplication mutations | α-synuclein aggregation, synaptic dysfunction |
Amyotrophic Lateral Sclerosis Modeling
ALS modeling has benefited significantly from CRISPR-iPSC technology, particularly for studying mutations in C9orf72, SOD1, TARDBP (encoding TDP-43), and FUS [46]. CRISPR-Cas9 enables the introduction of these mutations into iPSCs, which can then be differentiated into motor neurons to investigate disease mechanisms [46]. These motor neurons exhibit ALS-relevant pathologies including axonal transport defects, RNA metabolism abnormalities, stress granule formation, and increased vulnerability to excitotoxicity [46] [10]. The platform has been instrumental in identifying novel therapeutic targets and conducting functional genetic screens to understand selective vulnerability in ALS [46].
Experimental Protocols
Protocol 1: Generation of Isogenic iPSC Lines Using CRISPR-Cas9
Objective: To introduce a specific disease-associated mutation into a control iPSC line or correct a mutation in a patient-derived iPSC line to create an isogenic pair.
Materials:
- Healthy donor or patient-derived iPSCs
- CRISPR-Cas9 components (Cas9 nuclease, sgRNA)
- Single-stranded oligodeoxynucleotide (ssODN) donor template for HDR
- Electroporation system
- mTeSR1 or similar defined iPSC culture medium
- Matrigel or laminin-521 coated culture plates
- CloneR2 or similar cloning supplement
- PCR reagents for genotyping
- Sequencing primers
Procedure:
sgRNA Design and Validation: Design sgRNAs flanking the target site using computational tools. Select guides with high on-target efficiency and minimal off-target potential based on prediction algorithms [21] [10].
Donor Template Design: For point mutations, design an ssODN donor template containing the desired mutation along with homologous arms (typically 60-90 nt each side). Include silent mutations in the PAM site when possible to prevent re-cutting [10].
CRISPR-Cas9 Transfection: Combine 5μg of Cas9 protein, 2μg of sgRNA, and 2μL of 100μM ssODN donor template. Introduce the ribonucleoprotein complex into 1×10^6 iPSCs using electroporation (1400V, 10ms pulse width, 3 pulses) [10].
Single-Cell Cloning: At 48 hours post-transfection, dissociate iPSCs to single cells using Accutase. Plate at clonal density (500-1000 cells/10cm dish) in mTeSR1 supplemented with CloneR2. Identify and manually pick individual colonies after 10-14 days [44].
Genotypic Validation: Expand clones and screen for precise editing using PCR amplification of the target locus followed by Sanger sequencing. Confirm the absence of random integration of plasmid DNA [44].
Quality Control: Perform karyotype analysis (G-banding) to confirm genomic integrity. For lead clones, conduct whole-genome sequencing to rule off-target effects. Verify pluripotency through flow cytometry for markers (Oct4, Nanog, SSEA-4) and trilineage differentiation potential [42] [44].
Protocol 2: Differentiation of iPSCs to Disease-Relevant Neural Cells
Objective: To differentiate CRISPR-edited iPSCs into neuronal cell types relevant to neurodegenerative disease pathology.
Materials:
- Validated iPSC clones
- Neural induction medium (DMEM/F12, N2 supplement, non-essential amino acids)
- Neural differentiation medium (Neurobasal, B27 supplement)
- Small molecules (SB431542, LDN193189, CHIR99021)
- Growth factors (BDNF, GDNF, TGF-β3, ascorbic acid)
- Laminin and poly-ornithine coated plates
- Immunocytochemistry reagents
Procedure for Dopaminergic Neuron Differentiation (for PD models):
Neural Induction: Culture iPSCs to 80% confluence. Switch to neural induction medium supplemented with 10μM SB431542 and 100nM LDN193189. Change medium daily for 10-12 days until neural rosettes form [45].
Neural Precursor Cell (NPC) Expansion: Manually pick rosettes and plate on laminin/poly-ornithine coated dishes in NPC medium (DMEM/F12 with N2 supplement, B27 supplement, and 20ng/mL FGF2). Expand for 2 passages [45].
Dopaminergic Differentiation: Plate NPCs at 50,000 cells/cm² in neural differentiation medium supplemented with 100ng/mL FGF8, 100ng/mL SHH, 10ng/mL BDNF, 10ng/mL GDNF, 200μM ascorbic acid, and 500μM dbcAMP. Differentiate for 28-35 days with medium changes every other day [45].
Characterization: Fix cells and immunostain for tyrosine hydroxylase (TH), FOXA2, and β-tubulin III to confirm dopaminergic identity. Analyze electrophysiological properties using patch clamping to verify functional maturity [45].
Procedure for Cortical Neuron Differentiation (for AD models):
Neurogenin-2 (Ngn2) Induction: Transduce iPSCs with lentivirus containing Ngn2 and rtTA. Select with puromycin for 3 days. Induce Ngn2 expression with 2μg/mL doxycycline for 5 days [44].
Neuronal Maturation: Plate induced neurons on poly-D-lysine/laminin coated plates in neuronal medium (Neurobasal with B27, BDNF, NT-3, and laminin). Maintain for 21-28 days with half-medium changes every 3-4 days [44].
Characterization: Verify cortical identity through immunostaining for TBR1, CTIP2, and SATB2. Assess synaptic function through staining for PSD-95 and synapsin-1 [44].
Protocol 3: Phenotypic Screening in CRISPR-Edited Neural Models
Objective: To quantify disease-relevant phenotypes in CRISPR-edited iPSC-derived neural cells for mechanistic studies and drug screening.
Materials:
- CRISPR-edited iPSC-derived neural cells
- Cell-based assay reagents (ATP lite, Ca^2+ indicators, ROS probes)
- Immunocytochemistry supplies
- High-content imaging system
- Microelectrode array (MEA) system for electrophysiology
Procedure for Mitochondrial Function Assessment (for PD/ALS models):
Mitochondrial Membrane Potential: Load cells with 100nM Tetramethylrhodamine Methyl Ester (TMRM) in culture medium for 30 minutes at 37°C. Image using fluorescence microscopy (excitation/emission: 548/573nm). Quantify fluorescence intensity per cell [45].
ATP Production: Lyse 10,000 cells and measure ATP levels using luciferase-based assay according to manufacturer's protocol. Normalize to total protein content [45].
Reactive Oxygen Species (ROS) Measurement: Incubate cells with 5μM CM-H2DCFDA for 30 minutes. Wash and measure fluorescence (excitation/emission: 495/529nm). Treat with 100μM H2O2 for 1 hour as positive control [21].
Procedure for Amyloid-β and Tau Pathology Assessment (for AD models):
Aβ ELISA: Collect conditioned medium from 30-day cortical neurons. Concentrate 10x using centrifugal filters. Measure Aβ40 and Aβ42 levels using sandwich ELISA according to manufacturer's protocol. Calculate Aβ42/Aβ40 ratio [21].
Tau Phosphorylation Analysis: Lyse cells in RIPA buffer with phosphatase inhibitors. Separate 20μg protein by SDS-PAGE. Transfer to PVDF membrane and immunoblot for total tau (tau5) and phosphorylated tau (AT8, pS422). Quantify band intensity [21].
High-Content Imaging of Pathology: Fix cells and immunostain for Aβ (6E10 antibody) and phosphorylated tau (AT8). Counterstain with DAPI. Acquire 20 images per well using automated microscopy. Quantify aggregate number and size using image analysis software [21].
Visualization of Experimental Workflows
Isogenic iPSC Line Generation
Neural Differentiation and Phenotyping
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for CRISPR-iPSC Neurodegenerative Disease Modeling
| Reagent Category | Specific Products | Function in Experimental Workflow |
|---|---|---|
| iPSC Culture | mTeSR1, Essential 8 Medium | Maintain pluripotency and self-renewal of iPSCs |
| CRISPR Components | Synthetic sgRNA, HiFi Cas9, ssODN donors | Precise genome editing with reduced off-target effects |
| Cell Dissociation | Accutase, ReLeSR | Gentle passage and single-cell cloning of iPSCs |
| Neural Induction | SMAD inhibitors (SB431542, LDN193189) | Efficient conversion of iPSCs to neural lineage |
| Neural Differentiation | BDNF, GDNF, NT-3, ascorbic acid | Promote maturation and survival of neurons |
| Cell Characterization | Antibodies to Oct4, Nanog, TRA-1-60 | Validate pluripotent state pre-differentiation |
| Neuronal Markers | Antibodies to β-tubulin III, MAP2, synapsin | Confirm neuronal identity and maturity |
| Disease Markers | Antibodies to Aβ, p-tau, α-synuclein | Detect and quantify disease-relevant pathology |
| Viability Assays | ATP-lite, TMRM, CM-H2DCFDA | Measure cell health, mitochondrial function, ROS |
| Quality Control | Karyostat assays, Mycoplasma detection | Ensure genomic integrity and culture purity |
Technical Considerations and Quality Control
Addressing Technical Challenges
Successful implementation of CRISPR-iPSC neurodegenerative disease models requires careful attention to several technical challenges. Off-target effects remain a primary concern, which can be mitigated by using high-fidelity Cas9 variants and computational prediction of off-target sites [10]. The complexity of neural differentiation protocols introduces variability that can be addressed through standardized procedures and quality control checkpoints [42]. Genomic instability during extended iPSC culture necessitates regular karyotyping and monitoring of copy number variations [42] [44]. The iNDI project has established rigorous quality control measures including trio sets (parental, mutant, and revertant lines), whole-genome sequencing, and functional validation to ensure model reliability [44].
Future Directions
The field of CRISPR-iPSC neurodegenerative disease modeling is rapidly evolving toward more complex and physiologically relevant systems. Integration of microphysiological systems (MPS) and organ-on-chip technologies will enable better recapitulation of the brain's microenvironment [47]. Multi-optic characterization (transcriptomic, proteomic, metabolomic) of isogenic models will provide comprehensive signatures of disease states [44]. Automation and standardization of differentiation protocols will enhance reproducibility across laboratories [10]. Finally, the combination of CRISPR screening with iPSC-derived disease models will enable systematic functional genomics in disease-relevant human cell types [46] [45]. These advancements will continue to bridge the gap between in vitro models and clinical applications, accelerating therapeutic development for neurodegenerative diseases.
The integration of Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR-Cas9) with induced pluripotent stem cell (iPSC) technology has revolutionized the creation of advanced three-dimensional (3D) model systems. Brain and cardiac organoids derived from genetically engineered iPSCs now provide unprecedented opportunities for studying human development, disease mechanisms, and therapeutic interventions [21] [10]. These 3D structures recapitulate key aspects of human organ architecture and functionality more accurately than traditional two-dimensional cultures, offering enhanced physiological relevance for modeling complex diseases and conducting drug screening [48] [49].
The synergy between CRISPR-Cas9 gene editing and iPSC-derived organoids enables researchers to establish highly controlled isogenic models by introducing or correcting disease-specific mutations within an identical genetic background [10]. This approach has proven particularly valuable for investigating neurodegenerative disorders such as Alzheimer's disease (AD), where precise genetic manipulations in genes like APP, PSEN1, and PSEN2 have provided insights into amyloid processing and tau pathology [21]. Similarly, in cardiovascular research, self-organizing cardiac organoids (cardioids) have been developed to mimic natural cardiac characteristics, enabling studies of congenital heart diseases and drug-induced cardiotoxicity [50].
Organoid Characteristics and Applications
Comparative Analysis of Brain and Cardiac Organoids
Table 1: Key Characteristics of Brain and Cardiac Organoids
| Feature | Brain Organoids | Cardiac Organoids (Cardioids) |
|---|---|---|
| Starting Cell Source | Human pluripotent stem cells (hPSCs): embryonic stem cells (ESCs) & induced pluripotent stem cells (iPSCs) [48] [49] | Human pluripotent stem cells (hPSCs): ESCs & iPSCs [50] |
| Key Signaling Pathways | Dual SMAD inhibition, Sonic Hedgehog patterning [51] | Biphasic WNT signaling (activation/inhibition), BMP signaling axis [50] |
| Major Cell Types Generated | Neurons, astrocytes, oligodendrocytes, microglia [48] | Cardiomyocytes, endothelial cells, fibroblasts, epicardial cells [50] |
| Structural Features | Represents cortical layers, neural circuits; region-specific (cortical, midbrain, hypothalamic) [48] [51] | Chamber-like structures, beating tissue, vascular networks [50] |
| Maturation Timeline | Several months to recapitulate early human neurodevelopment [48] | 20-30 days to develop spontaneous beating and electrophysiological activity [50] |
| Primary Applications | Disease modeling (AD, Parkinson's, autism), drug screening, host-pathogen interaction studies [48] [49] [10] | Disease modeling (congenital heart disease, cardiomyopathy), drug safety/toxicity testing, regenerative medicine [50] |
| CRISPR-Cas9 Applications | Introducing/correcting mutations in AD-related genes (APP, PSEN1, PSEN2), studying amyloid pathology [21] [10] | Modeling genetic heart diseases, studying developmental pathways, drug discovery [50] |
Quantitative Assessment of Organoid Modeling Applications
Table 2: Quantitative Applications of Organoids in Disease Modeling and Drug Screening
| Application Area | Model System | Key Readouts | Reported Outcomes |
|---|---|---|---|
| Neurodegenerative Disease Modeling | iPSC-derived cortical organoids with APP/PSEN1 mutations [21] [10] | Aβ deposition, Tau phosphorylation, neuronal dysfunction | Recapitulation of early AD pathological changes; identification of oxidative stress pathways [21] |
| Cardiac Disease Modeling | Self-organizing cardioids with structural defects [50] | Contractility, electrophysiological properties, structural organization | Mimicry of 6-10 week gestational hearts; chamber-specific action potentials [50] |
| Drug Toxicity Screening | iPSC-derived brain organoids for neurotoxicity [48]; Cardioids for cardiotoxicity [50] | Cell viability, functional measurements, transcriptional changes | Detection of compound-specific toxicity patterns; more physiologically relevant than 2D models [48] [50] |
| High-Throughput Drug Screening | Cortical organoids for AD drug discovery [48]; Cardiac organoids for cardiovascular drugs [50] | High-content imaging, calcium imaging, mRNA sequencing | Identification of compounds modulating disease phenotypes; successful proof-of-concept demonstrations [48] [50] |
| Personalized Medicine | Patient-specific iPSC-derived organoids [49] [10] | Individual drug response variability, phenotype reversal | 27% higher prediction accuracy for patient-specific drug responses compared to conventional models [10] |
Experimental Protocols
Protocol 1: CRISPR-Cas9 Mediated Gene Editing in iPSCs for Organoid Generation
Purpose: To establish isogenic iPSC lines with disease-specific mutations for organoid generation [21] [10].
Materials:
- Human iPSCs (healthy donor or patient-specific)
- CRISPR-Cas9 reagents: Cas9 protein, guide RNA (gRNA) targeting gene of interest
- Single-stranded oligodeoxynucleotide (ssODN) donor template for HDR (if knock-in)
- Nucleofection system or lipofection reagent
- iPSC culture media and supplements
- Cloning disks or limited dilution plates for single-cell cloning
- Genomic DNA extraction kit
- PCR reagents and sequencing primers for validation
Procedure:
- gRNA Design and Validation: Design gRNAs flanking the target site in APP, PSEN1, PSEN2 (for AD models) or cardiac genes (for heart models). Validate cutting efficiency using Surveyor or T7E1 assay [21].
- iPSC Preparation: Culture iPSCs to 70-80% confluence in feeder-free conditions. Ensure cells are in optimal growth phase for high viability [10].
- CRISPR Complex Delivery: Form ribonucleoprotein (RNP) complexes by mixing 5μg Cas9 protein with 2μg gRNA. Incubate 10min at room temperature. Deliver RNP complexes (with 1μM ssODN donor if applicable) using nucleofection [10].
- Recovery and Selection: Plate transfected cells at appropriate density in iPSC media with 10μM ROCK inhibitor. After 48 hours, apply appropriate antibiotic selection if using a selection marker [10].
- Single-Cell Cloning: Using cloning disks or limited dilution, isolate single-cell clones and expand in 96-well plates (14-21 days) [10].
- Genotypic Validation: Extract genomic DNA from expanded clones. Perform PCR amplification of the target region and sequence to confirm precise genetic modifications. Validate selected clones for pluripotency markers and karyotypic normality [21] [10].
- Organoid Differentiation: Use validated isogenic iPSC lines for brain or cardiac organoid differentiation following established protocols [48] [50].
Protocol 2: Generation of Guided Brain Organoids for Disease Modeling
Purpose: To generate region-specific brain organoids (cortical) from CRISPR-edited iPSCs for disease modeling [48] [51].
Materials:
- Validated CRISPR-edited iPSCs
- Neural induction medium: DMEM/F-12, N2 supplement, non-essential amino acids, heparin
- Differentiation medium: Neurobasal medium, B27 supplement, BDNF, GDNF, cAMP
- Small molecules: Dual SMAD inhibitors (LDN-193189, SB431542), WNT inhibitors (IWP-2)
- Matrigel or Geltrex
- Low adhesion plates
- Spinning bioreactor or orbital shaker
Procedure:
- Embryoid Body (EB) Formation: Harvest iPSCs using gentle cell dissociation reagent. Seed 9,000 cells per well in 96-well low adhesion plates in neural induction medium with 10μM ROCK inhibitor. Centrifuge at 100g for 3min to aggregate [51].
- Neural Induction: At day 2, replace medium with neural induction medium containing 100nM LDN-193189 and 10μM SB431542. Culture for 5 days, changing medium every other day [51].
- Matrigel Embedding: At day 7, carefully transfer individual EBs to Matrigel droplets. Polymerize at 37°C for 30min. Overlay with neural induction medium [48] [51].
- Regional Patterning: From day 10, switch to differentiation medium with Dorsomorphin (2μM) and SB431542 (10μM) for forebrain specification. Culture for 10 days, changing medium every 3-4 days [51].
- Long-term Maturation: Transfer organoids to spinning bioreactor or orbital shaker at 60-70rpm. Continue culture for up to 3 months, changing medium twice weekly [48].
- Quality Assessment: At various timepoints, assess organoids for cortical layer formation (FOXG1, CTIP2, TBR1 markers), neuronal activity (calcium imaging, patch clamp), and disease-specific phenotypes [48] [51].
Protocol 3: Generation of Self-Organizing Cardiac Organoids (Cardioids)
Purpose: To generate human self-organizing cardioids from iPSCs for disease modeling and drug testing [50].
Materials:
- iPSCs with cardiac disease-associated mutations
- Cardiomyocyte differentiation medium: RPMI 1640, B27 supplement
- Small molecules: CHIR99021 (WNT activator), IWP-2 (WNT inhibitor), BMP4
- Maturation factors: Palmitate-BSA, oleate-BSA, L-carnitine, T3 hormone
- Low attachment U-bottom 96-well plates
- Poly-HEMA coated plates (optional)
Procedure:
- Mesoderm Induction: Culture iPSCs to 90% confluence. Dissociate to single cells and seed 5,000 cells per well in U-bottom low attachment plates in RPMI/B27 minus insulin with 6-12μM CHIR99021. Centrifuge at 300g for 3min to form aggregates [50].
- Cardiac Specification: At day 3, replace medium with RPMI/B27 minus insulin containing 2μM IWP-2. Culture for 48 hours [50].
- Metabolic Selection: At day 5, change to RPMI/B27 with insulin. Continue culture with medium changes every 3-4 days. Spontaneous beating typically begins around day 7-10 [50].
- Cardioid Maturation: From day 20, supplement with maturation factors: 200μM palmitate-BSA, 200μM oleate-BSA, 500μM L-carnitine, 10nM T3 hormone in RPMI/B27 with insulin for 10 days [50].
- Functional Assessment: Monitor contractility (beats per minute), electrophysiological properties (multi-electrode array), and structural characteristics (immunostaining for cardiac troponin T, α-actinin, connexin 43) [50].
- Disease Modeling and Compound Screening: Expose cardioids to pathological stimuli (hypoxia, inflammatory cytokines) or pharmaceutical compounds to model disease states or assess drug efficacy/toxicity [50].
Signaling Pathways and Experimental Workflows
Brain Organoid Patterning and Assembloid Generation
Cardiac Organoid Differentiation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for CRISPR-Organoid Research
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| CRISPR-Cas9 Systems | High-fidelity Cas9, Base editors, Prime editors [10] | Precise genome editing with reduced off-target effects; specific point mutation introduction [10] |
| Stem Cell Culture | mTeSR1, StemFlex, Essential 8 medium [52] | Maintenance of pluripotency; support of iPSC growth and expansion [52] |
| Neural Induction | Dual SMAD inhibitors (LDN-193189, SB431542), N2/B27 supplements [51] | Efficient neural conversion from pluripotent stem cells; support of neural progenitor survival [51] |
| Cardiac Differentiation | CHIR99021 (WNT activator), IWP-2/IWR-1 (WNT inhibitors), BMP4 [50] | Directed differentiation toward cardiac lineages; chamber-specific cardioid formation [50] |
| Extracellular Matrices | Matrigel, Geltrex, synthetic hydrogels [48] [49] | 3D structural support for organoid development; simulation of native extracellular environment [48] [49] |
| Patterning Molecules | Sonic Hedgehog agonists (SAG, Purmorphamine), FGF2, VEGF [51] [50] | Regional specification of organoids (dorsal/ventral brain; atrial/ventricular heart) [51] [50] |
| Maturation Factors | Thyroid hormone (T3), corticosteroids, fatty acids (palmitate, oleate) [50] | Promotion of organoid functional maturation; enhanced electrophysiological properties [50] |
| Characterization Tools | scRNA-seq, immunostaining (cell type markers), multi-electrode arrays [48] [50] | Validation of cellular composition, structural organization, and functional properties [48] [50] |
The continued refinement of brain and cardiac organoid technologies, particularly when integrated with precise CRISPR-Cas9 genome editing, represents a transformative approach in biomedical research. These advanced 3D model systems bridge the gap between traditional in vitro models and in vivo physiology, offering unprecedented opportunities for understanding human development, disease mechanisms, and therapeutic development. As these technologies mature, standardized protocols and quality control measures will be essential for maximizing their potential in both basic research and clinical applications [21] [48] [50].
The integration of human induced pluripotent stem cells (iPSCs) into high-throughput screening (HTS) platforms represents a transformative approach in modern drug discovery. iPSCs offer three distinct advantages that make them particularly powerful for early-stage drug development: patient specificity (carrying the donor's genome and disease-associated mutations), human relevance (recapitulating key functional aspects of real tissue), and scalability (can be expanded indefinitely once differentiation protocols are established) [53]. This combination addresses a critical disconnect in traditional drug discovery, where promising compounds often fail when moving from immortalized cell lines to primary cells or in vivo models [53].
When combined with CRISPR-Cas9 gene editing technology, iPSCs enable the generation of precision disease models with unprecedented genetic accuracy. CRISPR-edited iPSCs allow researchers to create isogenic cell lines that are genetically identical except for specific disease-causing mutations, providing controlled systems for studying gene function and disease mechanisms without the confounding factors associated with animal models or immortalized cell lines [6]. This integration is particularly valuable for functional genomics and precision disease modeling, where the translatability of results to human biology is paramount.
The market landscape reflects this growing importance, with the high-throughput screening market valued at approximately USD 32.0 billion in 2025 and projected to reach USD 82.9 billion by 2035, registering a compound annual growth rate (CAGR) of 10.0% [54]. Cell-based assays currently dominate the technology segment, holding 39.40% market share due to their ability to deliver physiologically relevant data and predictive accuracy in early drug discovery [54].
Quantitative Landscape of High-Throughput Screening
Market Metrics and Growth Projections
Table 1: High-Throughput Screening Market Size and Projections
| Metric | 2020-2025 Period | 2025-2035 Projection |
|---|---|---|
| Market Size | USD 19.9 billion (2020) [54] | USD 32.0 billion (2025) to USD 82.9 billion (2035) [54] |
| CAGR | 14% [54] | 10.0% [54] |
| Leading Technology Segment | Cell-based assays (39.4% share) [54] | Ultra-high-throughput screening (projected 12% CAGR) [54] |
| Leading Application Segment | Target identification (USD 7.64 billion in 2023) [55] | Target identification (projected 12% CAGR) [54] |
Regional Adoption and Key Growth Regions
Table 2: Regional Market Analysis and Growth Projections
| Region | Market Position | Projected CAGR (2025-2035) | Key Growth Drivers |
|---|---|---|---|
| North America | Dominant (50% market share) [55] | 12.6% [54] | Strong biotechnology startup ecosystem, established research infrastructure [54] |
| Asia-Pacific | Rapid growth | 13.1% (China) to 14.9% (South Korea) [54] | Expanding biopharmaceutical industry, government initiatives, increasing R&D investment [54] |
| Europe | Established market | 12.9% (UK) [54] | Drug repurposing initiatives, favorable regulatory environment [54] |
Application of CRISPR-Edited iPSCs in Disease Modeling
Neurodegenerative Disease Modeling
CRISPR-edited iPSCs have become indispensable for modeling neurodegenerative diseases such as Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS). In Alzheimer's research, CRISPR-Cas9 enables specific genetic modifications in key AD-related genes, including APP, PSEN1, PSEN2, and APOE, providing valuable insights into disease mechanisms [21]. For example, researchers have used CRISPR to generate iPSC lines with homozygous and heterozygous PSEN1 mutations, creating precision models for studying amyloid processing and tau pathology [6].
The Inducible Pluripotent Stem Cell Neurodegeneration Initiative (iNDI) represents the largest iPSC genome engineering study to date, aiming to generate hundreds of disease models for Alzheimer's Disease and Related Dementias (ADRD) [6]. Similarly, for Parkinson's disease research, studies have utilized CRISPR-Cas9 to generate fourteen isogenic iPSC lines, including homozygous and heterozygous lines for five different LRRK2 pathogenic mutations, providing valuable resources for neurological disease research [6].
Cardiotoxicity and Metabolic Disease Screening
iPSC-derived cardiomyocytes are now routinely used to screen for drug-induced arrhythmia risk and have been integrated into regulatory safety initiatives like the Comprehensive in vitro Proarrhythmia Assay (CiPA) [53]. These models are employed by pharmaceutical companies including Roche and Takeda for preclinical cardiac profiling [53].
In metabolic disease research, hepatocyte-like cells derived from iPSCs have been used to model conditions such as familial hypercholesterolemia and test potential lipid-lowering therapies [53]. A notable example includes the use of iPSC-derived hepatocytes to identify drug repurposing opportunities, where cardiac glycosides were found to reduce ApoB secretion [53].
Experimental Protocols
Protocol 1: CRISPR-Cas9 Mediated Gene Editing in iPSCs for Disease Modeling
Objective: Generate isogenic iPSC lines with specific disease-associated mutations for high-throughput screening applications.
Materials:
- Human iPSCs (from healthy donor or patients)
- CRISPR-Cas9 reagents (Cas9 protein, sgRNA, donor template)
- Electroporation system
- Flow cytometer with cell sorting capability
- PCR amplification and sequencing reagents
Procedure:
sgRNA Design and Validation:
- Design 3-5 sgRNAs targeting the genomic region of interest (e.g., APP, PSEN1, LRRK2)
- Validate sgRNA efficiency using surrogate reporter systems
- Select the most efficient sgRNA with minimal predicted off-target effects
Donor Template Construction:
- Design single-stranded DNA (ssODN) or double-stranded DNA (dsDNA) donor templates containing the desired mutation
- Include synonymous mutations to prevent re-cutting by Cas9
- Incorporate restriction sites for diagnostic screening
CRISPR-Cas9 Delivery:
- Culture iPSCs in feeder-free conditions to ~80% confluency
- Prepare ribonucleoprotein (RNP) complexes by incubating 10μg Cas9 protein with 5μg sgRNA for 10 minutes at room temperature
- Mix RNP complexes with 5μg donor template
- Electroporate using manufacturer-recommended settings for iPSCs
Clone Isolation and Screening:
- After 48 hours, dissociate cells and seed at clonal density (500-1000 cells/10cm dish)
- Allow 10-14 days for colony formation
- Pick 96 individual colonies and expand in 96-well plates
- Screen clones using PCR amplification of the targeted region followed by restriction fragment length polymorphism (RFLP) analysis or Sanger sequencing
Validation of Isogenic Clones:
- Confirm precise editing through full-length sequencing of the targeted locus
- Perform karyotype analysis to ensure genomic integrity
- Verify pluripotency markers (Nanog, Oct4, Sox2) through immunocytochemistry
- Bank validated clones for downstream differentiation
Protocol 2: High-Throughput Compound Screening Using iPSC-Derived Neurons
Objective: Identify compounds that rescue disease phenotypes in iPSC-derived neuronal models of neurodegeneration.
Materials:
- CRISPR-edited iPSC lines with disease-associated mutations
- Neural differentiation media components
- 384-well or 1536-well microplates
- Automated liquid handling systems
- High-content imaging system
- Compound libraries (1000-100,000 compounds)
Procedure:
Large-Scale Neural Differentiation:
- Differentiate iPSCs into neural progenitor cells (NPCs) using dual-SMAD inhibition
- Passage NPCs and cryopreserve in large batches to ensure consistency
- Thaw NPCs and plate in 384-well imaging microplates at 5000 cells/well
- Differentiate NPCs to mature neurons over 4-6 weeks using specific patterning factors
Compound Library Preparation:
- Prepare compound library stocks in DMSO at 10mM concentration
- Using acoustic liquid handling, transfer 10nL of compound to achieve 10μM final concentration
- Include positive controls (known efficacious compounds) and negative controls (DMSO only) on each plate
High-Content Screening:
- After 7 days of compound treatment, fix cells and immunostain for disease-relevant markers (e.g., phosphorylated tau, Aβ aggregates, TDP-43)
- Include nuclear stain (Hoechst) and neuronal marker (βIII-tubulin) for normalization
- Image plates using high-content imager with 20x objective
- Acquire 9 fields per well to ensure adequate cell sampling
Image and Data Analysis:
- Use automated image analysis algorithms to quantify disease phenotypes:
- Neurite length and branching
- Protein aggregation (puncta size, number, intensity)
- Cell viability (nuclear morphology, count)
- Normalize data to plate controls
- Calculate Z'-factor for each plate to assess assay quality (Z' > 0.5 acceptable)
- Use automated image analysis algorithms to quantify disease phenotypes:
Hit Confirmation and Validation:
- Select compounds showing >3 standard deviation improvement from mean
- Confirm hits in dose-response (8-point, 1nM-30μM) using fresh compound stocks
- Validate in multiple isogenic clones and different time points
- Assess specificity using additional disease-relevant assays
Workflow and Signaling Pathways
Integrated CRISPR-iPSC Screening Workflow
Diagram 1: Integrated CRISPR-iPSC screening workflow.
Alzheimer's Disease Signaling Pathways in iPSC-Derived Neurons
Diagram 2: Alzheimer's disease signaling pathways and CRISPR targets.
Research Reagent Solutions
Table 3: Essential Research Reagents for CRISPR-iPSC Screening
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| CRISPR-Cas9 Components | Cas9 protein, synthetic sgRNA, ssODN donor templates | Precise genome editing | RNP complexes reduce off-target effects; HPLC-purified sgRNA improves efficiency [6] |
| iPSC Culture | mTeSR1, Essential 8 medium, Y-27632 (ROCK inhibitor) | Pluripotency maintenance | Feeder-free systems enhance reproducibility; ROCK inhibitor improves single-cell survival [53] |
| Differentiation Kits | STEMdiff Neural System, Cardiomyocyte Differentiation Kit | Lineage-specific differentiation | Standardized protocols improve inter-lab reproducibility; quality control via flow cytometry [53] |
| HTS Assay Reagents | CellTiter-Glo, Calcium-sensitive dyes, Immunostaining antibodies | Viability, functional, and phenotypic assays | Miniaturization to 1536-well format reduces costs; validated antibodies essential for content imaging [54] |
| Automation Consumables | 384-well microplates, acoustic dispensing tips, robotic liquid handlers | Screening infrastructure | Black-walled plates with optical bottoms required for high-content imaging [55] |
The integration of CRISPR-edited iPSC models into high-throughput screening campaigns represents a paradigm shift in drug discovery, moving away from traditional immortalized cell lines toward more physiologically relevant human systems. The combination of patient-specific genomic backgrounds with precise genetic engineering enables modeling of complex diseases with unprecedented accuracy [53] [6].
Current clinical applications demonstrate the translational potential of this approach, with several candidates identified through iPSC-based screening advancing to clinical trials. These include bosutinib, ropinirole, and ezogabine for ALS, and WVE-004 and BII078 for ALS/FTD [28]. The continued evolution of these technologies, particularly through incorporation of artificial intelligence for data analysis and 3D organoid systems for more complex tissue modeling, promises to further enhance the predictive power of iPSC-based screening platforms [28] [21].
Despite challenges including differentiation variability, cost considerations, and standardization requirements, the field is rapidly addressing these limitations through commercial QC-verified cell batches, bioreactor technologies, and regulatory initiatives [53]. As these technologies mature, CRISPR-edited iPSC models are poised to become indispensable tools for identifying and validating novel therapeutic candidates across a spectrum of human diseases.
Navigating Technical Hurdles: Strategies for Enhancing Efficiency and Safety
In the field of CRISPR-Cas9 gene editing for creating sophisticated disease models using human induced pluripotent stem cells (iPSCs), achieving efficient homology-directed repair (HDR) remains a significant challenge. While non-homologous end joining (NHEJ) mediates relatively efficient gene knock-outs, HDR enables precise genetic modifications, including specific nucleotide substitutions, gene insertions, and corrections that are essential for accurately modeling human genetic diseases [56] [57]. However, HDR efficiency is inherently limited by its confinement to the S and G2 phases of the cell cycle and competition from the more active NHEJ pathway [57] [58]. This application note details validated methodologies, combining cell cycle synchronization and alternative editor approaches, to significantly enhance HDR rates in iPSCs, thereby supporting more reliable and efficient disease modeling and drug development research.
Understanding the HDR Efficiency Challenge
The core challenge in precise genome editing stems from the fundamental biology of DNA repair pathways in mammalian cells. When CRISPR-Cas9 induces a double-strand break (DSB), the cell can repair it through several competing mechanisms. The table below summarizes the key characteristics of these primary pathways.
Table 1: Key DNA Repair Pathways in CRISPR-Cas9 Genome Editing
| Pathway | Repair Mechanism | Cell Cycle Phase Activity | Editing Outcome | Relative Efficiency in iPSCs |
|---|---|---|---|---|
| Non-Homologous End Joining (NHEJ) | Ligates broken ends without a template | Active throughout all phases [57] | Small insertions or deletions (Indels); gene knock-out | High [18] |
| Homology-Directed Repair (HDR) | Uses homologous donor template for precise repair | Primarily restricted to S and G2 phases [57] [58] | Precise nucleotide changes, gene corrections, knock-ins | Low [18] |
| Microhomology-Mediated End Joining (MMEJ) | Uses microhomologous sequences for end joining | - | Predictable deletions [59] | Variable |
The competition between these pathways, combined with the fact that HDR is only active in a limited window of the cell cycle, results in low rates of precise editing, making subsequent selection and clonal screening labor-intensive and time-consuming [59].
Strategic Approach 1: Cell Cycle Synchronization
Synchronizing iPSCs in HDR-permissive phases (S/G2) is a powerful strategy to enhance precise editing outcomes. Research demonstrates that modulating the cell cycle can synergistically improve HDR efficiency when combined with other interventions [59].
Protocol: Cell Cycle Synchronization for Enhanced HDR
This protocol outlines two methods for synchronizing iPSCs to improve HDR efficiency, adapted from recent studies [60] [59].
Materials
- Human iPSCs: Maintained in feeder-free culture conditions.
- Essential 8 (E8) Medium: Pre-warmed to room temperature.
- Accutase: For cell dissociation.
- Small Molecule Inhibitors:
- Nocodazole: Microtubule polymerization inhibitor.
- XL413: CDC7 inhibitor.
- DMSO: Vehicle control.
- CRISPR-Cas9 Components: Cas9 ribonucleoprotein (RNP) complexes and single-stranded oligodeoxynucleotide (ssODN) donor template.
Procedure
- Cell Preparation: Harvest and count iPSCs. Seed 5 x 10⁴ cells per well in a 96-well plate and culture for 24 hours to reach 70-80% confluence [60].
- Synchronization (Choose One Method):
- G2/M Enrichment with Nocodazole: Treat cells with 100 ng/mL Nocodazole for 18 hours prior to transfection [60]. Release cells from arrest immediately after electroporation. Note: This method may reduce cell viability; optimize for your cell line [60].
- G1/S Arrest with XL413: Treat cells with 10 µM XL413 for 24 hours following electroporation. Pretreatment before editing is not effective [59].
- CRISPR Delivery: Transfect synchronized cells with pre-complexed Cas9 RNP and ssODN donor template via nucleofection. The Amaxa 4D-Nucleofector with program DZ-100 has been shown effective [60].
- Post-Transfection Culture: After transfection and synchronization, return cells to standard culture conditions (37°C, 5% CO₂) in Essential 8 medium. Refresh medium daily.
- Analysis: Allow 72-96 hours for recovery and expression of edits before analyzing editing efficiency via flow cytometry or sequencing.
Key Considerations
- Cold Shock: As an alternative, incubating cells at 32°C for 48 hours post-electroporation can slow the cell cycle and has been shown to increase HDR frequency by 1.4-fold and enrich the G2/M population from 6.0% to 25.5% [59].
- Viability Monitoring: Cell cycle synchronization can be stressful. Always include a viability assay post-treatment.
Diagram 1: Cell Cycle Synchronization Workflow for Enhanced HDR
Strategic Approach 2: Small Molecule Enhancers
An alternative approach involves using small molecule compounds to modulate DNA repair pathway choices, favoring HDR over NHEJ. The table below summarizes the performance of key enhancers.
Table 2: Small Molecule Enhancers of HDR Efficiency
| Small Molecule | Target/Mechanism | Reported HDR Increase | Key Considerations |
|---|---|---|---|
| Nedisertib | DNA-PKcs inhibitor [60] | Up to 24% increase (0.25 µM) [60] | Optimal concentration critical; 0.25 µM provided best balance of efficiency (73%) and viability (74%) [60] |
| NU7441 | DNA-PKcs inhibitor [60] [59] | 11% increase [60] | Shows synergistic effects when combined with cell cycle modulation [59] |
| SCR-7 | DNA Ligase IV inhibitor [60] [59] | Variable effects reported | Inconsistent performance across cell types; did not increase HDR in BEL-A cells [60] |
| Alt-R HDR Enhancer | Proprietary formulation | No significant increase | Negative impact on cell viability observed [60] |
Protocol: HDR Enhancement Using Small Molecules
This protocol describes the use of Nedisertib, one of the most effective DNA-PKcs inhibitors for boosting HDR [60].
Materials
- Nedisertib Stock Solution: Prepare a 10 mM stock in DMSO; store at -20°C.
- CRISPR-Cas9 Components: Cas9 RNP complex and ssODN donor template.
- Pre-warmed iPSC Culture Medium.
Procedure
- CRISPR Transfection: Perform nucleofection of iPSCs with Cas9 RNP and donor template using optimized parameters (e.g., 3 µg Cas9, gRNA:Cas9 ratio of 1:2.5, 100 pmol ssODN, 5x10⁴ cells) [60].
- Compound Treatment: Immediately after transfection, add Nedisertib to the culture medium at a final concentration of 0.25 µM. This concentration optimizes the trade-off between editing efficiency and cell viability [60].
- Incubation: Culture cells in the presence of Nedisertib for 48-72 hours.
- Compound Removal: Replace medium with standard culture medium without the inhibitor.
- Analysis: Assess editing efficiency and cell viability 5-7 days post-transfection.
Safety Note
Recent studies indicate that DNA-PKcs inhibitors, while effective at boosting HDR, can promote large-scale structural variations (SVs), including chromosomal deletions and translocations [61]. These aberrations may pose safety concerns for clinical applications and can lead to overestimation of HDR efficiency in standard short-read sequencing assays [61]. Researchers must carefully weigh the efficiency benefits against potential genomic integrity risks for their specific application.
The Scientist's Toolkit: Essential Reagents for HDR Enhancement
Table 3: Key Research Reagent Solutions for Enhancing HDR in iPSCs
| Reagent / Tool | Function | Example Application |
|---|---|---|
| Cas9 RNP Complex | Pre-complexed Cas9 protein and guide RNA; reduces off-target effects and enables rapid degradation [60] [62] | Direct delivery via nucleofection into iPSCs [60] |
| ssODN Donor Template | Single-stranded oligodeoxynucleotide repair template; contains desired edit and homology arms [60] | Introducing point mutations or small inserts; 100 nt ssODN with asymmetric homology arms (36 nt/91 nt) shown effective [60] |
| Tube Electroporation Device | Specialized electroporator minimizing surface warping; enables high efficiency RNP delivery with low cytotoxicity [62] | Transfecting hard-to-transfect cells like iPSCs and primary cells; achieved up to 42.1% HDR in iPSCs [62] |
| Cell Cycle Modulators | Small molecules synchronizing cells in HDR-permissive phases | Nocodazole (G2/M arrest) or XL413 (G1/S arrest) [60] [59] |
| DNA Repair Inhibitors | Small molecules inhibiting key NHEJ pathway proteins | Nedisertib, NU7441 (DNA-PKcs inhibitors) [60] |
Diagram 2: Strategic Modulation of DNA Repair Pathway Choice
Overcoming the challenge of low HDR efficiency is paramount for advancing iPSC-based disease modeling and drug development. The integrated application of cell cycle synchronization and small molecule enhancers provides a robust framework for significantly improving precise genome editing outcomes. However, researchers must remain cognizant of the potential genomic instability risks associated with some HDR-enhancing strategies, particularly DNA-PKcs inhibitors [61]. The optimal approach will depend on the specific research goals, balancing the need for high editing efficiency with the imperative to maintain genomic integrity in the resulting iPSC disease models.
The application of CRISPR-Cas9 in induced pluripotent stem cells (iPSCs) has revolutionized disease modeling by enabling precise genetic modifications that recapitulate human disease pathogenesis. However, off-target effects remain a significant concern that can compromise experimental validity and therapeutic applications. These unintended genomic alterations occur when the CRISPR-Cas9 complex cleaves at sites other than the intended target, primarily due to tolerance for mismatches between the guide RNA (gRNA) and genomic DNA. In iPSC-based disease modeling, where genetic integrity is paramount for accurate phenotype interpretation, mitigating off-target effects becomes crucial for generating reliable experimental models. The persistence of CRISPR components in cells can extend the window for off-target activity, making careful gRNA design and comprehensive validation essential components of any iPSC gene editing workflow [63].
Strategies for High-Fidelity gRNA Design
Computational Design and Selection
Effective gRNA design begins with comprehensive computational analysis to maximize on-target efficiency while minimizing potential off-target activity. Bioinformatic tools leverage machine learning algorithms trained on large datasets to predict gRNA performance based on sequence characteristics, genomic context, and mismatch tolerance.
Sequence-Specific Considerations: Optimal gRNAs typically exhibit high GC content (40-60%) which stabilizes the DNA:RNA duplex, and should be designed to target genomic regions with minimal homology to other sites in the genome. Guides of 20 nucleotides or less generally demonstrate reduced off-target risk while maintaining on-target activity [63].
Tool Selection: Multiple validated algorithms are available for gRNA design, each with distinct strengths. CRISPOR, CHOPCHOP, and sgRNA Scorer 2.0 incorporate comprehensive on-target and off-target prediction scores, while Rule Set 2 and CFD scores provide specialized metrics for activity prediction and off-target potential, respectively [64] [65].
Table 1: Key Computational Tools for gRNA Design and Their Applications
| Tool Name | Primary Function | Off-Target Prediction | Species Compatibility |
|---|---|---|---|
| CRISPOR | Comprehensive gRNA design | CFD score | Multiple |
| CHOPCHOP | gRNA identification & selection | Yes | Multiple |
| sgRNA Scorer 2.0 | On-target efficiency prediction | Guidescan score | Human, Mouse |
| Rule Set 2 | Activity prediction | Incorporated | Human, Mouse |
| DeepCRISPR | Deep learning-based prediction | Genome-wide off-target effects | Human |
Leveraging Experimentally Validated gRNAs
Whenever possible, utilizing previously validated gRNAs can significantly reduce off-target risks and experimental optimization time. The dbGuide database represents the largest collection of functionally validated guide RNA sequences for CRISPR/Cas9-mediated knockout experiments in human or mouse cells, containing over 4,000 manually curated sequences from peer-reviewed publications [65]. Addgene's validated gRNA repository also provides experimentally confirmed sequences with documented efficiency [66]. When using validated gRNAs, it remains essential to confirm exact sequence matching to your specific genomic target, as even single-nucleotide differences can significantly impact editing efficiency and specificity.
Chemical Modifications and High-Fidelity Nucleases
Chemical modifications to synthetic gRNAs can enhance stability and reduce off-target effects. The incorporation of 2'-O-methyl analogs (2'-O-Me) and 3' phosphorothioate bonds (PS) at specific positions in the gRNA sequence has been shown to reduce off-target editing while maintaining or even improving on-target efficiency [63].
The selection of Cas nuclease variants significantly influences off-target profiles. While wild-type SpCas9 can tolerate between three and five base pair mismatches, high-fidelity variants such as SpCas9-HF1 and eSpCas9(1.1) have been engineered to reduce non-specific cleavage. Alternative Cas proteins like Cas12a present different mismatch tolerance patterns that may be advantageous for specific applications. For precise editing without double-strand breaks, catalytically dead Cas9 (dCas9) or Cas9 nickase (nCas9) systems can be employed, with the latter requiring paired gRNAs for double-strand break generation, dramatically increasing specificity [63].
Experimental Validation of Off-Target Effects
Detection and Analysis Methods
After implementing careful gRNA design strategies, comprehensive experimental validation of editing outcomes is essential. Multiple methods exist for detecting off-target effects, each with distinct advantages and limitations.
Table 2: Comparison of Off-Target Detection Methods
| Method | Principle | Sensitivity | Throughput | Key Applications |
|---|---|---|---|---|
| Candidate Site Sequencing | Sanger or NGS of predicted off-target sites | Moderate | Low to Medium | Validation of computational predictions |
| GUIDE-seq | Integration of oligo tags at DSB sites | High | Medium | Unbiased genome-wide detection |
| CIRCLE-seq | In vitro circularization & sequencing of Cas9-cut sites | Very High | High | Comprehensive in vitro profiling |
| DISCOVER-seq | Detection of MRE11 recruitment to DSBs | High | Medium | In situ detection in living cells |
| Whole Genome Sequencing | Comprehensive sequencing of entire genome | Ultimate | Low | Gold standard for clinical applications |
For most iPSC disease modeling applications, a combination of in silico prediction followed by candidate site sequencing provides a practical balance between comprehensiveness and resource requirements. The Inference of CRISPR Edits (ICE) tool offers accessible analysis of editing efficiencies from Sanger sequencing data and is compatible with any species and CRISPR edit type [63].
Protocol: Off-Target Assessment in iPSCs Using Candidate Site Sequencing
This protocol outlines a standardized approach for validating off-target effects in CRISPR-edited iPSCs, with procedures optimized for stem cell viability and accurate detection.
Materials and Reagents
- Human iPSCs (maintained in mTeSR Plus or Stemflex medium on Matrigel)
- Accutase dissociation solution
- Nucleofection system and appropriate reagents
- Cas9 protein (Alt-R S.p. HiFi Cas9 Nuclease V3) and synthetic gRNAs
- PCR reagents and primers for candidate off-target sites
- Sanger sequencing or NGS platform
- HDR enhancer (optional; IDT)
- Pro-survival supplements (e.g., CloneR, STEMCELL Technologies; RevitaCell, Gibco)
Procedure
gRNA Selection and Off-Target Prediction
- Design gRNAs using at least two computational tools (e.g., CRISPOR and CHOPCHOP)
- Select the top 5-10 predicted off-target sites for each gRNA based on CFD scores and sequence similarity
- Design PCR primers flanking each candidate off-target site (amplicon size: 300-500 bp)
iPSC Culture and Nucleofection
- Maintain iPSCs in feeder-free conditions, passage with ReLeSR when 80-90% confluent
- One hour before nucleofection, change to cloning media (Stemflex with 1% RevitaCell and 10% CloneR) [37]
- Dissociate cells with Accutase for 4-5 minutes
- Prepare RNP complex by combining 0.6 µM gRNA with 0.85 µg/µL Cas9 protein, incubate 20-30 minutes at room temperature
- Add 0.5 µg pmaxGFP plasmid to monitor transfection efficiency
- Nucleofect using appropriate program and reagents for human iPSCs
Post-Transfection Culture and Clone Isolation
- Return cells to pre-warmed cloning media and culture for 48 hours
- Passage cells at lower density to support single-cell survival
- After 7-10 days, pick individual clones for expansion and analysis
- Maintain parallel bulk-edited population for initial screening
Genomic DNA Extraction and Amplification
- Extract genomic DNA from bulk population and individual clones
- Perform PCR amplification of all candidate off-target sites and the on-target locus
- Purify PCR products and prepare for sequencing
Sequence Analysis and Interpretation
- Perform Sanger sequencing or NGS on all amplicons
- Analyze sequencing data using ICE tool or similar analysis software
- Calculate indel percentages at each locus
- Confirm absence of mutations at off-target sites in individual clones
Expected Results and Interpretation Successful validation demonstrates high editing efficiency at the on-target locus (>70% by ICE analysis) with minimal (<0.1%) or undetectable indels at off-target sites. Clones with the desired on-target edit and clean off-target profile should be selected for further expansion and characterization [37].
Advanced Strategies for Enhanced Specificity in iPSCs
High-Efficiency Editing with Reduced Toxicity
Recent advances have demonstrated that combining p53 inhibition with pro-survival small molecules can achieve homologous recombination rates exceeding 90% in human iPSCs while reducing cell death associated with double-stranded breaks. This approach significantly improves the recovery of correctly edited clones, reducing the time required to generate isogenic lines to as little as 8 weeks [37]. The protocol involves co-transfection of a plasmid encoding shRNA against p53 along with the CRISPR components, supplemented with HDR enhancers and viability supplements such as CloneR. This method has been successfully applied to multiple genetic loci and iPSC lines, demonstrating broad applicability while maintaining karyotypic stability [37].
Novel Systems to Overcome Silencing
A significant challenge in iPSC gene editing is the silencing of Cas9 expression during directed differentiation, even when integrated into safe harbor loci like AAVS1. Emerging technologies such as SLEEK (Selection by Essential Gene Exon Knocking) bypass this limitation by inserting Cas9-EGFP into exon 9 of the essential GAPDH gene, where editing is linked to cell survival [39]. This approach ensures sustained Cas9 expression throughout differentiation, maintaining editing capability in downstream cell types derived from iPSCs—a critical advantage for disease modeling applications that require genetic manipulation in differentiated cells.
Artificial Intelligence-Driven Optimization
The integration of artificial intelligence (AI) and machine learning (ML) represents a transformative approach to enhancing CRISPR specificity. AI-driven models such as DeepCRISPR and CRISPRon analyze large-scale datasets to predict gRNA activity and off-target effects with higher accuracy than traditional methods [64]. These models can identify subtle sequence features that influence editing outcomes, enabling more precise gRNA selection. As these tools continue to evolve, they offer the potential to dramatically reduce experimental optimization time and improve the success rates of iPSC gene editing projects.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for High-Fidelity iPSC Gene Editing
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| High-Fidelity Cas9 Variants | Alt-R S.p. HiFi Cas9 V3, SpCas9-HF1 | Reduced off-target cleavage while maintaining on-target activity | Ideal for iPSC editing where specificity is critical |
| Chemical Modifications | 2'-O-Me, 3' phosphorothioate bonds | Enhanced gRNA stability and reduced off-target effects | Synthego and IDT offer modified synthetic gRNAs |
| HDR Enhancers | Alt-R HDR Enhancer, IDT | Boost homology-directed repair efficiency | Particularly valuable for point mutation knock-ins in iPSCs |
| Cell Survival Supplements | CloneR, RevitaCell, ROCK inhibitor | Improve single-cell survival post-nucleofection | Essential for clonal isolation of edited iPSCs |
| Validated gRNA Databases | dbGuide, Addgene validated gRNAs | Access to previously functional gRNA sequences | Cross-reference with your target sequence before use |
| Analysis Tools | ICE, CRISPResso2 | Quantify editing efficiency and specificity | Free, web-based tools for accessible data analysis |
The reliability of iPSC-based disease models is fundamentally dependent on the precision of the genetic modifications introduced. By implementing a comprehensive strategy that integrates computational gRNA design, high-fidelity editing systems, rigorous validation methodologies, and emerging AI technologies, researchers can significantly mitigate off-target effects while maintaining high editing efficiency. The protocols and reagents outlined here provide a roadmap for establishing robust genome editing workflows that yield genetically precise iPSC models, thereby enhancing the validity of functional studies and accelerating the development of therapeutic applications.
The integration of CRISPR-Cas9 gene editing with induced pluripotent stem cell (iPSC) technology has revolutionized the creation of human disease models for research and therapeutic development [67] [20]. However, the clinical translation of these edited cells hinges on ensuring genomic stability throughout the entire workflow—from reprogramming and editing to differentiation and expansion. Genomic instability in iPSCs can manifest as copy number variations (CNVs), single nucleotide variations (SNVs), chromosomal abnormalities, and oncogenic mutations that compromise both research validity and clinical safety [68] [69]. This application note provides detailed protocols and quality control (QC) frameworks to maintain genomic integrity in CRISPR-edited iPSC lines, specifically contextualized for disease modeling research.
The vulnerability of iPSCs to genomic alterations is exacerbated by extended in vitro culture, reprogramming stress, and the cellular response to CRISPR-induced double-strand breaks [18] [20]. Furthermore, the selective pressure during clonal expansion can favor mutations that confer survival advantages but introduce unintended functional consequences. Therefore, a multi-tiered QC strategy is indispensable for generating reliable, clinically relevant disease models.
Quality Control Framework: Critical Quality Attributes and Monitoring Technologies
A robust QC framework for CRISPR-edited iPSCs must continuously monitor defined Critical Quality Attributes (CQAs) throughout the biomanufacturing process [69]. These CQAs encompass cellular characteristics, environmental conditions, and genetic parameters that collectively determine the fitness and stability of the final cell product.
Table 1: Critical Quality Attributes (CQAs) for Genomic Stability in iPSCs
| Critical Quality Attribute (CQA) | Traditional Assessment Method | Advanced AI-Driven Monitoring | Acceptance Criteria for Clinical-Grade |
|---|---|---|---|
| Genetic Stability | Karyotyping (low-resolution), Microarrays | Deep learning on multi-omics data; Whole Genome Sequencing (WGS) [69] | Normal karyotype; No deleterious SNVs/CNVs |
| Cell Morphology & Viability | Manual microscopy, Flow cytometry | Convolutional Neural Networks (CNN) on live-cell imaging (>90% accuracy) [69] | Consistent pluripotent morphology; >85% viability |
| Differentiation Potential | Immunostaining for pluripotency markers (e.g., Oct4, Nanog) | SVM classifiers for lineage commitment (88-90% accuracy) [69] | Tri-lineage differentiation potential (ecto-, meso-, endoderm) |
| Contamination Risk | Microbial culture, Mycoplasma tests | Anomaly detection via random forest classifiers on sensor data [69] | Sterile; No mycoplasma, bacterial, or fungal contamination |
| Environmental Conditions | Offline sampling (pH, O2) | Predictive modeling from IoT sensor data; Reinforcement Learning for control [69] | Maintained optimal pH, dissolved O2, and nutrient levels |
The integration of Artificial Intelligence (AI) and machine learning significantly enhances the sensitivity and scalability of these monitoring processes. For instance, AI-driven systems can dynamically track morphological changes and predict colony formation with over 90% accuracy, enabling non-invasive, real-time assessment without destructive sampling [69]. Predictive models can also forecast deviations in oxygen saturation hours in advance, allowing for proactive intervention [69].
Experimental Protocols for Genomic Stability Assessment
Protocol: Comprehensive Genetic Analysis of CRISPR-Edited iPSC Clones
This protocol details the steps for validating the genomic integrity of single-cell-derived iPSC clones after CRISPR-Cas9 editing.
Materials & Reagents:
- QIAamp DNA Mini Kit (Qiagen) or equivalent for high-quality gDNA extraction.
- RNase A
- G-band karyotyping kit
- Illumina Infinium Global Screening Array or equivalent SNP array platform.
- PCR reagents for on-target and off-target amplification.
- Next-generation sequencing library prep kit (e.g., Illumina Nextera Flex).
Procedure:
- gDNA Extraction: Harvest edited iPSCs at ~80% confluency. Extract gDNA using the QIAamp DNA Mini Kit according to the manufacturer's instructions. Treat samples with RNase A. Quantify DNA using a fluorometer. Critical Step: Ensure DNA integrity by gel electrophoresis (sharp, high-molecular-weight band).
- Karyotype Analysis (Passage 5 and 15):
- Treat cells with colcemid (0.1 µg/mL) for 45-60 minutes.
- Harvest cells, subject to hypotonic solution (0.075 M KCl), and fix with Carnoy's solution (3:1 methanol:acetic acid).
- Prepare metaphase spreads on glass slides and perform G-banding.
- Analyze at least 20 metaphase spreads per clone for chromosomal abnormalities [20].
- Copy Number Variation (CNV) Analysis:
- Using 200 ng of gDNA, process samples with the Illumina SNP array platform following the manufacturer's protocol.
- Analyze data using dedicated software (e.g., BlueFuse Multi) to identify CNVs larger than 1-2 Mb [20].
- Whole Genome Sequencing (WGS) for Master Cell Banks:
- For final candidate clones destined for banking, perform WGS (minimum 30x coverage).
- Analyze data against a human reference genome (e.g., GRCh38) to identify single nucleotide variants (SNVs), small indels, and structural variants. Compare against databases of common genomic variants in hPSCs to filter out benign polymorphisms.
- On-target and Off-target Analysis:
- Perform PCR amplification of the on-target site and potential off-target sites predicted by tools like GUIDE-seq or CIRCLE-seq [20].
- Subject amplicons to NGS. Analyze sequencing data for precise on-target editing and indels at off-target sites. An acceptable clone should show no indels at top-predicted off-target sites.
Protocol: Pluripotency and Differentiation Potential Verification
This protocol confirms the functional quality of the edited clones beyond genetic integrity.
Materials & Reagents:
- Pluripotency Marker Antibodies: Anti-OCT4, SOX2, NANOG, SSEA-4, TRA-1-60.
- Trilineage Differentiation Kit (e.g., STEMdiff Trilineage Differentiation Kit).
- qPCR reagents and primers for lineage-specific markers.
- Flow cytometer.
Procedure:
- Immunocytochemistry (ICC) for Pluripotency Markers:
- Culture edited iPSC clones on glass coverslips in a 12-well plate.
- At ~70% confluency, fix cells with 4% paraformaldehyde for 15 minutes.
- Permeabilize with 0.1% Triton X-100, block with 5% BSA, and incubate with primary antibodies (e.g., OCT4, NANOG) overnight at 4°C.
- The next day, incubate with fluorescently-labeled secondary antibodies for 1 hour at room temperature. Mount and image. >95% of the population should express core pluripotency markers.
- Flow Cytometry Analysis:
- Dissociate a single-cell suspension of edited iPSCs and fix with 4% PFA.
- Stain with antibodies against surface markers (e.g., SSEA-4, TRA-1-60) and analyze on a flow cytometer. A clinically acceptable clone should show >90% positive staining for these markers.
- In Vitro Trilineage Differentiation:
- Using a commercial kit or established protocols, direct the edited iPSCs to differentiate into ectoderm, mesoderm, and endoderm lineages.
- After 7-10 days of differentiation, harvest cells and analyze the expression of lineage-specific genes (e.g., SOX17 for endoderm, BRACHYURY for mesoderm, PAX6 for ectoderm) via qPCR. Successful differentiation is confirmed by significant upregulation of these markers compared to undifferentiated cells.
The workflow below summarizes the key stages of the quality control process for ensuring genomic stability in CRISPR-edited iPSCs.
The Scientist's Toolkit: Essential Reagents and Solutions
Successful production of genomically stable, CRISPR-edited iPSCs relies on a suite of specialized reagents and tools.
Table 2: Essential Research Reagents for QC of CRISPR-Edited iPSCs
| Research Reagent / Solution | Function / Application | Key Considerations |
|---|---|---|
| High-Fidelity Cas9 (HiFi-Cas9) | CRISPR nuclease with reduced off-target effects [20] | Essential for improving editing specificity in repair strategies. |
| GMP-Grade Reprogramming Vectors | Non-integrating vectors (e.g., Sendai virus, episomal) for footprint-free iPSC generation [68] | Minimizes risk of insertional mutagenesis and supports clinical compliance. |
| Karyostat Assay Kit | qPCR-based assay for rapid detection of common hPSC aneuploidies [69] | Faster and more scalable than traditional karyotyping for routine checks. |
| GUIDE-seq Kit | Genome-wide unbiased identification of CRISPR off-target sites [20] | Critical for comprehensive off-target profiling during gRNA validation. |
| StemFlex Medium | Advanced culture medium for sustained iPSC pluripotency and genomic stability [18] | Reduces spontaneous differentiation and supports single-cell cloning. |
| iPSC Neurodifferentiation Kit | Directed differentiation of iPSCs into neuronal lineages for disease modeling [67] [6] | Ensures reproducible generation of relevant cell types for functional studies. |
The path to clinically relevant disease models using CRISPR-edited iPSCs is paved with rigorous and multi-faceted quality control. By implementing the detailed protocols and frameworks outlined in this application note—from high-resolution genetic screening and AI-enhanced monitoring to the use of high-fidelity editing tools—researchers can significantly enhance the genomic stability, reliability, and safety of their iPSC lines. This diligence is the foundation for generating robust, reproducible data in disease modeling and for the eventual successful translation of iPSC-based therapies from the laboratory to the clinic.
The application of human induced pluripotent stem cells (iPSCs) in disease modeling and regenerative medicine represents a frontier in biomedical research. However, a significant barrier to their clinical translation is the inherent risk of tumorigenicity posed by residual undifferentiated cells in the final cell product. These cells can form teratomas or more malignant tumors upon transplantation. Within the broader context of a thesis on CRISPR-Cas9 gene editing in iPSCs for disease modeling, this application note addresses the critical challenge of purification. We detail specific CRISPR-Cas9-based strategies and provide validated protocols for the efficient and safe purging of undifferentiated cells, thereby enhancing the safety profile of iPSC-derived therapies for research and drug development.
CRISPR-Cas9 Strategies for Purging Undifferentiated Cells
CRISPR-Cas9 technology enables the precise targeting of essential genes or cell-surface markers specific to the undifferentiated state. Below, we summarize two primary strategic approaches for eliminating residual iPSCs.
Table 1: CRISPR-Cas9 Strategies for Purging Undifferentiated Cells
| Strategy | Molecular Target | Mechanism of Action | Key Advantage |
|---|---|---|---|
| Suicide Gene Insertion | Safe harbor locus (e.g., AAVS1) or pluripotency-associated gene |
Integration of an inducible "suicide" gene (e.g., herpes simplex virus thymidine kinase) that confers sensitivity to a prodrug (e.g., ganciclovir). | Allows for temporal control; can be activated post-differentiation to eliminate any remaining undifferentiated cells. |
| Targeted Knockout of Pluripotency Genes | Core pluripotency transcription factors (e.g., OCT4, NANOG) |
Disruption of genes essential for maintaining self-renewal and pluripotency, inducing spontaneous differentiation or cell death. | Directly targets the molecular machinery of pluripotency; no external drugs required. |
| Targeted Knockout of Survival Genes | Essential genes for cell survival (e.g., GAPDH via SLEEK technology) |
Integration of a selectable marker (e.g., Cas9-EGFP) into an essential gene exon. Only edited cells survive, enabling selection for stable, engineered lines and against unedited, potentially tumorigenic cells [39]. |
Provides a powerful positive selection system to ensure a uniformly edited cell population, reducing heterogeneity. |
Detailed Experimental Protocols
Protocol 1: Generation of a Suicide Gene-Expressing iPSC Line
This protocol outlines the steps for creating an iPSC line with an inducible suicide gene integrated into a safe harbor locus, providing a fail-safe mechanism against tumorigenicity.
1. Vector Design and sgRNA Selection:
- Vector Construction: Clone an inducible promoter (e.g., Tet-On 3G system) driving the expression of a suicide gene (e.g., HSV-TK) into a donor vector containing homology arms for a safe harbor locus like
AAVS1(also known asPPP1R12C). Include a puromycin resistance cassette for selection [70]. - sgRNA Design: Design a sgRNA with high on-target efficiency and minimal off-target risk targeting the
AAVS1locus. Use algorithms like CCTop or Benchling for design and validation [70]. Benchling has been shown to provide the most accurate predictions for sgRNA efficiency [70].
2. iPSC Culture and Preparation:
- Culture iPSCs in Pluripotency Growth Medium (e.g., PGM1) on Matrigel-coated plates at 37°C with 5% CO₂ [70].
- For nucleofection, dissociate cells using 0.5 mM EDTA when they reach 80-90% confluency. Pellet cells by centrifugation at 250 g for 5 minutes [70].
3. Nucleofection and Selection:
- Co-electroporate the donor vector and the sgRNA/Cas9 plasmid (e.g., from Addgene) at a 1:1 weight ratio into the iPSC pellet using a 4D-Nucleofector system with program CA-137 and a P3 Primary Cell kit [70].
- Forty-eight hours post-nucleofection, begin selection with 0.5 μg/mL puromycin. Maintain selection for approximately one week until distinct, resistant colonies form [70].
4. Clonal Isolation and Validation:
- Pick surviving colonies and expand them clonally.
- Validate successful integration by junction PCR using primers designed outside the 5' and 3' homology arms [39]. Sequences for primers (e.g., p1-p5) should be designed using tools like Primer3 or NCBI Primer-BLAST [39].
- Confirm pluripotency of the validated clone through teratoma assay or expression of pluripotency hallmarks [70].
Protocol 2: Positive Selection via Essential Gene Knock-in
This protocol leverages the SLEEK (Selection by Essential Gene Exon Knocking) technology to bypass common issues of transgene silencing and ensure a pure population of engineered cells [39].
1. Plasmid Construction for SLEEK Integration:
- Use Gibson Assembly to generate a
Cas9-EGFP SLEEKplasmid. Design primers with 15-25 bp overlaps for seamless cloning. - The donor template contains a recoded exon 9 of the
GAPDHgene (without altering the amino acid sequence) into which theCas9-EGFPtransgene is inserted. The endogenousGAPDHpromoter drives robust, sustained expression [39].
2. iPSC Nucleofection and Selection:
- Prepare and nucleofect iPSCs as described in Protocol 1, using the
SLEEKdonor plasmid and a sgRNA targetingGAPDHexon 9. - Following nucleofection, culture cells without antibiotic selection. Only cells that undergo homology-directed repair (HDR) will restore the essential
GAPDHgene and survive. Cells that repair via non-homologous end joining (NHEJ) will be negatively selected due toGAPDHdisruption [39].
3. Validation of Knock-in:
- The resulting iPSC-Cas9-EGFP cells can be validated for
Cas9function through editing assays. - This cell line maintains normal pluripotency and karyotype and can be used as a base for further genetic modifications, with the constant
EGFPserving as a marker for the successfully engineered population [39].
Validation and Safety Assessment
Rigorous testing is mandatory to confirm the efficacy of the purging strategy and the safety of the final differentiated product.
Table 2: Key Validation Assays for Tumorigenicity Purging
| Assay Type | Method | Expected Outcome |
|---|---|---|
| In Vitro Pluripotency Marker Analysis | Flow cytometry or immunocytochemistry for markers like OCT4, NANOG, and SSEA-4 on the final cell product. | Significant reduction or absence of marker-positive cells. |
| Functional Tumorigenicity Assay (Gold Standard) | Injection of a high dose (e.g., 1-2 million cells) of the final product into immunodeficient mice (e.g., NSG mice). | No teratoma or tumor formation observed over a minimum of 16 weeks. |
| Genomic Safety Profiling | Whole-genome sequencing or targeted amplicon sequencing (e.g., using DISCOVER Seq [71]) to assess CRISPR-Cas9 on-target efficiency and potential off-target edits. |
High on-target editing efficiency with minimal to no detectable off-target effects. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for CRISPR-Cas9 Mediated Purging in iPSCs
| Reagent / Tool | Function | Example & Notes |
|---|---|---|
| Inducible Cas9 iPSC Line | Provides a tunable, highly efficient nuclease source for gene editing. | hPSCs-iCas9 line with spCas9 integrated into the AAVS1 locus [70]. Enables INDEL efficiencies of 82-93%. |
| Chemically Modified sgRNA | Enhances sgRNA stability within cells, improving editing efficiency. | CSM-sgRNA with 2'-O-methyl-3'-thiophosphonoacetate modifications at both ends [70]. |
| Nucleofection System | Enables highly efficient delivery of CRISPR components into hard-to-transfect iPSCs. | 4D-Nucleofector X Unit (Lonza) with program CA-137 and P3 Primary Cell Kit [70]. |
| Off-Target Prediction Algorithm | In silico design of sgRNAs with high on-target and low off-target activity. | CCTop [70] and Benchling [70] are widely used; Benchling showed superior predictive accuracy. |
| Editing Analysis Software | Quantifies CRISPR editing efficiency (INDEL%) from Sanger sequencing data. | ICE (Inference of CRISPR Edits) by Synthego [70]. Validated to be highly accurate compared to TIDE and T7EI assay. |
Visualizing the Experimental Workflow
The following diagram outlines the core logical pathway for implementing a CRISPR-based safety strategy in iPSCs, from engineering to final validation.
Figure 1. Overall Strategy for Preventing Tumorigenicity. This workflow integrates CRISPR engineering early in the process to create a fail-safe mechanism, which is activated after differentiation to eliminate any residual undifferentiated cells.
The specific method for eliminating undifferentiated cells can follow one of two main approaches, as visualized below.
Figure 2. Molecular Purging Mechanisms. This chart details the two primary CRISPR-based strategies for inducing cell death specifically in undifferentiated iPSCs, leading to a purified final product.
The fusion of induced pluripotent stem cell (iPSC) technology with CRISPR-Cas9 gene editing has revolutionized the creation of physiologically relevant human disease models for drug discovery and developmental research. The foundational step determining the success of all downstream applications is the establishment of robust, standardized culture protocols that consistently maintain pluripotency while enabling scalable manufacturing. This application note provides detailed methodologies and strategic considerations for mastering iPSC culture, specifically framed within the context of generating precise, CRISPR-edited disease models. Achieving this requires meticulous attention to culture conditions, quality control, and scalable bioprocessing to ensure that edited cells retain their genetic integrity and differentiation potential [72] [7].
Core Principles of Pluripotency Maintenance
Maintaining iPSCs in a pristine, pluripotent state is critical for ensuring the reliability of subsequent gene editing and differentiation experiments. Key to this is the meticulous control of the cellular microenvironment and routine monitoring of pluripotency markers.
Signaling Pathways Regulating Pluripotency
The maintenance of pluripotency is governed by a core transcriptional network and several key signaling pathways. The diagram below illustrates the primary signaling pathways and their cross-talk in maintaining iPSC pluripotency.
Figure 1: Core Pluripotency Signaling Network. This diagram illustrates the key exogenous signaling inputs (LIF, BMP4, FGF2, TGFB, WNT) and their interplay with the core transcriptional network (Oct4, Klf4, Sox2, c-Myc) to balance self-renewal and differentiation in iPSCs.
Essential Culture Parameters
Consistent maintenance of pluripotency requires optimization of several interdependent physical and chemical parameters. The following table summarizes the critical culture conditions and their optimal ranges.
Table 1: Essential Culture Parameters for Maintaining iPSC Pluripotency
| Parameter | Optimal Condition | Impact on Pluripotency |
|---|---|---|
| Base Medium | Essential 8, StemFlex, mTeSR1 | Chemically defined, xeno-free media supporting self-renewal and minimizing spontaneous differentiation [73]. |
| Matrix | Geltrex, Matrigel, Vitronectin | Provides extracellular matrix support for cell adhesion, survival, and undifferentiated growth [73]. |
| Passaging Method | Enzymatic (e.g., Accutase) or EDTA-based | Maintains cell viability and pluripotency; enzymatic passaging is preferred for large-scale cultures [73] [7]. |
| Passaging Ratio | 1:10 to 1:20 every 4-7 days | Preents over-confluence, which can trigger spontaneous differentiation and increases genomic instability risk [7]. |
| CO₂ & Temperature | 5% CO₂, 37°C | Standard physiological conditions for consistent cell growth and metabolism. |
| Quality Assessment | Pluripotency marker expression (Oct4, Nanog, SSEA-4) | Regular verification via immunocytochemistry or flow cytometry is non-negotiable for confirming pluripotent state [73]. |
Strategies for Scalable Manufacturing of iPSCs
Transitioning from laboratory-scale culture to manufacturing-scale production is a pivotal challenge in utilizing iPSCs for disease modeling and therapeutic applications. Scalable processes are necessary to generate the billions of high-quality cells required for CRISPR screening, drug discovery campaigns, and potential clinical translation [72] [7].
Scalable Manufacturing Workflow
The transition from research-scale to manufacturing-scale iPSC culture involves a systematic, integrated workflow. The following diagram outlines the key stages and their connections in a scalable bioprocessing pipeline.
Figure 2: Scalable iPSC Manufacturing Workflow. This workflow illustrates the integrated stages of scalable iPSC production, highlighting the critical roles of automation and Process Analytical Technology (PAT) in ensuring quality and efficiency from master bank creation to final harvest.
Comparison of Scalable Culture Technologies
Selecting the appropriate platform for scaling iPSC culture is determined by the specific application, required scale, and available resources. The table below provides a comparative analysis of the primary technologies.
Table 2: Comparison of Technologies for Scalable iPSC Manufacturing
| Technology | Principle | Scalability | Relative Cost | Key Applications |
|---|---|---|---|---|
| Multi-layer Flasks (e.g., Cell Stacks, HYPERFlask) | Stacked 2D surfaces | Medium (up to ~10⁹ cells) | Low | Ideal for: Process development, small-scale CRISPR screens, pre-master cell bank expansion [7]. |
| Suspension Bioreactors (e.g., Stirred-Tank) | 3D culture as cell aggregates or on microcarriers | High (up to ~10¹¹ cells) | Medium | Ideal for: Large-scale manufacturing for high-throughput drug screening, allogeneic therapy cell banks [72] [7]. |
| Automated Hollow-Fiber Bioreactors | Continuous perfusion in a high-surface-area cartridge | High | High | Ideal for: High-density culture for consistent, high-quality iPSC production with minimal manual handling [74]. |
| Fixed-Bed Bioreactors | Cells attached to packed-bed within bioreactor | Medium-High | Medium | Ideal for: Scalable, high-density culture with perfusion, minimizing shear stress on cells [7]. |
The integration of Process Analytical Technology (PAT) and process automation is no longer a luxury but a necessity for scalable manufacturing. Automated, closed-system bioreactors enable real-time monitoring of critical process parameters (CPPs) like dissolved oxygen, pH, and metabolite levels (e.g., glucose, lactate). This allows for adaptive process control to maintain critical quality attributes (CQAs) and ensures batch-to-batch consistency—a non-negotiable requirement for reproducible CRISPR editing and disease modeling [72] [7].
Integration with CRISPR-Cas9 Gene Editing Workflow
The true power of iPSCs in disease modeling is unlocked through precise genetic manipulation via CRISPR-Cas9. The quality of the starting iPSC population directly influences the efficiency of gene editing and the validity of the resulting model.
CRISPR-iPSC Workflow Integration
A successful CRISPR editing project in iPSCs requires careful planning and execution across a multi-stage workflow. The diagram below maps the key stages from guide design to clone validation, highlighting critical checkpoints.
Figure 3: CRISPR-iPSC Workflow and Key Checkpoints. This workflow outlines the sequential stages for generating gene-edited iPSC lines, emphasizing critical quality checkpoints for pluripotency, genomic integrity, and functional validation.
Protocol: CRISPR-Cas9 Knock-in in iPSCs for Disease Modeling
This protocol is designed for the precise introduction of a disease-relevant mutation into high-quality iPSCs using ribonucleoprotein (RNP) electroporation, a method favored for its high efficiency and reduced off-target effects.
Objective: To generate a clonal, genetically defined iPSC line carrying a specific point mutation (e.g., in PSEN1 for Alzheimer's disease modeling) via CRISPR-Cas9-mediated HDR.
Materials:
- Starting Material: One vial of high-quality, pluripotent iPSCs from a master cell bank, ideally at low passage number [7].
- CRISPR Components: Synthetic sgRNA, purified high-fidelity Cas9 protein, and single-stranded oligodeoxynucleotide (ssODN) HDR template with homology arms (>100 bp each) [6].
- Culture Reagents: Pre-qualified Geltrex matrix and Essential 8 Flex Medium [73].
- Electroporation System: Neon Transfection System or similar.
- Clonal Isolation: Defined, feeder-free conditions or automated cell picker.
Method:
- Pre-validation and Culture: Thaw and expand iPSCs for at least two passages in Essential 8 medium on Geltrex-coated plates. Confirm pluripotency (>95% expression of Oct4/Nanog) via flow cytometry before proceeding [73].
- RNP Complex Formation: Complex 10 µg of high-fidelity Cas9 protein with 5 µg of synthetic sgRNA to form the RNP complex. Incubate at room temperature for 10-20 minutes.
- Cell Preparation and Electroporation:
- Dissociate iPSCs into a single-cell suspension using Accutase.
- Wash cells and resuspend them in the appropriate electroporation buffer.
- Mix the cell suspension with the pre-formed RNP complex and HDR template (ssODN). Electroporate using a pre-optimized program (e.g., Neon System: 1400V, 10ms, 3 pulses) [6].
- Post-Electroporation Recovery: Plate the electroporated cells at a high density in Essential 8 medium supplemented with a Rho-associated kinase (ROCK) inhibitor. Allow the cells to recover for 48-72 hours.
- Clonal Isolation and Expansion:
- After recovery, dissociate and plate cells at a very low density (e.g., 10 cells/cm²) to facilitate the formation of distinct, clonal colonies.
- After 7-10 days, manually pick or use an automated cell picker to isolate individual colonies into 96-well plates for expansion.
- Genomic DNA Screening: Screen expanded clonal lines for the desired edit using a combination of PCR and Sanger sequencing or next-generation sequencing.
Critical Considerations for Disease Modeling:
- Isogenic Controls: The ultimate goal is to generate a mutated line and a corrected control line from the same parental clone. This isogenic pair is essential for attributing phenotypic differences directly to the edited mutation, controlling for genetic background variability [21] [6].
- Comprehensive Genomic Validation: Beyond confirming the intended edit, employ amplicon sequencing or NGS to rule out off-target edits at predicted sites. Karyotype analysis is also recommended to ensure genomic stability post-editing [72] [21].
- Functional Validation: The final step is to differentiate the validated, edited iPSC clone into the relevant cell type (e.g., neurons for neurodegenerative disease models) and confirm the expected disease-relevant phenotype, such as altered amyloid-beta processing in Alzheimer's models [21] [75].
The Scientist's Toolkit: Essential Reagents and Technologies
Success in iPSC culture and CRISPR editing is dependent on a suite of reliable, high-quality reagents and tools. The following table catalogs the essential components for a successful iPSC and CRISPR workflow.
Table 3: Essential Research Reagent Solutions for iPSC Culture and CRISPR Editing
| Category | Product Examples | Function & Importance |
|---|---|---|
| Reprogramming | CytoTune-iPS Sendai Reprogramming Kit (non-integrating) | Generates footprint-free iPSCs from somatic cells (e.g., fibroblasts, PBMCs) for a clean starting genetic background [73]. |
| Culture Medium | Essential 8, StemFlex, mTeSR1 | Chemically defined, xeno-free media that support robust iPSC self-renewal and maintain pluripotency [73]. |
| Culture Surface | Geltrex, Vitronectin, Synthemax | Recombinant or defined extracellular matrix proteins that support feeder-free attachment and growth of iPSCs. |
| Passaging | Accutase, ReLeSR, EDTA | Enzymatic or non-enzymatic reagents for gentle and effective dissociation of iPSCs for routine passaging or seeding for experiments. |
| CRISPR Delivery | Lipofectamine Stem Transfection Reagent, Neon Transfection System | High-efficiency methods for delivering CRISPR machinery (plasmid, RNA, or RNP) into hard-to-transfect iPSCs [73] [6]. |
| Genomic Analysis | Guide-it Genomic Cleavage Detection Kit, RESOURCE HTE System | Kits and systems for validating CRISPR editing efficiency and detecting on-target and potential off-target effects. |
| Characterization | TaqMan hPSC Scorecard Panel, Pluripotency Antibody Panels | Automated, quantitative tools and validated antibodies for assessing pluripotency and trilineage differentiation potential [73]. |
Mastering iPSC culture is the critical foundation upon which reliable and scalable CRISPR-based disease models are built. This requires a dual focus: unwavering commitment to maintaining pluripotency through standardized, quality-controlled culture systems, and the strategic implementation of scalable manufacturing technologies to produce the necessary quantity and quality of cells. As the field progresses towards more complex disease models, including 3D organoids, the principles outlined here—rigorous quality control, process automation, and the use of well-defined reagents—will be paramount. By adhering to these detailed protocols and strategic considerations, researchers can robustly engineer iPSCs to illuminate disease mechanisms and accelerate the drug discovery pipeline.
Proving Efficacy: Functional Assays, Preclinical Data, and Clinical Translation
The integration of CRISPR-Cas9 gene editing with human induced pluripotent stem cell (iPSC) technology has revolutionized the creation of human-relevant disease models for drug discovery. This approach enables precise introduction of pathogenic mutations into controlled genetic backgrounds, generating in vitro models that recapitulate key aspects of human disease pathology [21]. However, the translational value of these engineered models depends entirely on rigorous benchmarking of their phenotypic and functional relevance to the human disease state. Establishing this relevance requires a multi-faceted benchmarking approach that validates models across molecular, cellular, and functional domains.
The critical need for such benchmarking is underscored by the persistently high attrition rates in drug development, particularly for central nervous system disorders, where failure rates approach 90% in clinical trials [76]. This high failure rate often stems from inadequate preclinical models that fail to predict human responses. CRISPR-iPSC models bridge this translational gap by providing human-derived cellular systems with disease-relevant genetics, but their utility must be established through comprehensive characterization against defined benchmarking criteria [21] [76]. This application note provides detailed protocols and benchmarking frameworks for establishing the disease relevance of CRISPR-iPSC models, with a focus on practical implementation for research and drug development applications.
Benchmarking Framework and Key Assay Categories
Core Principles of Model Benchmarking
Effective benchmarking of CRISPR-iPSC disease models requires assessment across multiple analytical dimensions. The process should evaluate: (1) recapitulation of disease-associated endophenotypes (measurable components of the disease pathway), (2) reproducibility across differentiations and cell lines, (3) predictive validity through response to known modulators, and (4) technical robustness for reliable implementation across laboratories [77] [76]. This multi-parameter approach ensures models not only display disease-relevant phenotypes but do so consistently and in a manner that translates to therapeutic discovery.
Benchmarking should be tiered, beginning with core cellular phenotypes then progressing to more complex functional assays. This staged approach efficiently allocates resources by first establishing fundamental disease relevance before investing in higher-complexity assays. The benchmarking framework should also align with the proposed context of use, with more stringent requirements for models intended for lead optimization versus early target discovery [77].
Table: Key Assay Categories for Benchmarking iPSC-CRISPR Disease Models
| Assay Category | Measured Parameters | Disease Relevance | Common Readouts |
|---|---|---|---|
| Electrophysiological Functional Assays | Neuronal firing, network synchronization, ion channel function | Neurodegenerative diseases, channelopathies, cardiac arrhythmias | Multi-electrode array (MEA), patch clamp, impedance sensing [76] |
| Calcium Imaging & Signaling | Calcium flux, oscillatory patterns, signal propagation | Neuronal connectivity, cardiotoxicity, neuroinflammation | Fluorescent dyes, GECIs, FLIPR platforms [76] |
| Metabolic & Mitochondrial Function | OXPHOS capacity, glycolytic rate, mitochondrial membrane potential | Neurodegeneration, metabolic disorders, drug-induced toxicity | Seahorse XF Analyzer, TMRE staining, ATP assays [76] |
| High-Content Imaging & Morphological Analysis | Neurite outgrowth, soma size, synaptic density, complexity metrics | Neurodevelopmental disorders, neurodegenerative diseases | Automated microscopy, image analysis algorithms [76] |
| Secretory & Inflammatory Profiles | Cytokine/chemokine release, phagocytic activity, protein secretion | Neuroinflammation, autoimmune disorders, infection responses | ELISA, MSD, flow cytometry, functional uptake assays [76] |
Detailed Experimental Protocols
Protocol 1: Multi-Electrode Array (MEA) for Network-Level Functional Benchmarking
Purpose: To characterize and benchmark neuronal network formation and function in CRISPR-iPSC-derived neuronal models, particularly relevant for neurodegenerative and neuropsychiatric diseases.
Materials:
- CRISPR-iPSC-derived neurons (e.g., ioGlutamatergic Neurons [76])
- 48-well or 24-well MEA plates
- MEA recording system with environmental control
- Neural maintenance media
- Positive/negative control compounds (e.g., synaptic blockers)
Procedure:
- Cell Plating: Plate CRISPR-iPSC-derived neurons at optimized density (e.g., 50,000-100,000 cells per well of 48-well MEA plate) in complete neural maintenance media.
- Maturation: Culture neurons for 4-6 weeks, with half-media changes every 2-3 days, to allow synaptic maturation and network development.
- Baseline Recording: Record spontaneous electrical activity for 10 minutes per well under controlled conditions (37°C, 5% CO₂). Parameters: sampling rate ≥10 kHz, bandpass filter 0.1-3 kHz.
- Pharmacological Challenge: Apply disease-relevant compounds (e.g., synaptic receptor agonists/antagonitors) to assess network perturbation responses.
- Data Analysis: Extract parameters including mean firing rate (MFR), burst frequency, burst duration, and network bursting pattern using manufacturer's software and custom algorithms.
Benchmarking Application: Compare isogenic disease and control lines to identify disease-relevant network phenotypes. For example, TDP-43 mutant ALS models show significantly reduced mean firing rates and burst frequencies compared to isogenic controls [76].
Protocol 2: High-Content Analysis of Neuronal Morphology
Purpose: To quantitatively assess disease-relevant morphological phenotypes in CRISPR-iPSC-derived neuronal models, including neurite outgrowth, branching complexity, and synaptic density.
Materials:
- CRISPR-iPSC-derived neurons
- 96-well imaging plates
- High-content imaging system
- Fixation solution (4% PFA)
- Permeabilization buffer (0.1% Triton X-100)
- Blocking buffer (5% normal serum)
- Primary antibodies (e.g., MAP2, Tau, Synapsin)
- Fluorescent secondary antibodies
- Nuclear stain (Hoechst or DAPI)
Procedure:
- Cell Culture: Plate CRISPR-iPSC-derived neurons in 96-well imaging plates at optimized density for morphological analysis.
- Fixation: At predetermined timepoints (e.g., days 7, 14, 21), fix cells with 4% PFA for 15 minutes at room temperature.
- Immunostaining: Permeabilize with 0.1% Triton X-100 (10 minutes), block with 5% serum (1 hour), incubate with primary antibodies overnight at 4°C, then with fluorescent secondary antibodies for 1 hour at room temperature.
- Image Acquisition: Acquire images using 10x or 20x objective on high-content imager, capturing multiple fields per well to ensure statistical robustness.
- Image Analysis: Use specialized software to quantify somal size, neurite length, branching points, and synaptic puncta density.
Benchmarking Application: In Huntington's disease models, benchmark mitochondrial dysfunction via morphological analysis and Seahorse assays [76]. Compare isogenic pairs to isolate mutation-specific effects from background genetic variation.
Protocol 3: Functional Benchmarking of iPSC-Derived Microglia in Neuroinflammatory Models
Purpose: To characterize microglial immune functions relevant to neuroinflammatory and neurodegenerative diseases using CRISPR-engineered iPSC-derived microglia.
Materials:
- CRISPR-ready ioMicroglia [76]
- Microglia maintenance media
- Chemotaxis chamber
- Phagocytosis cargo (e.g., pH-sensitive E. coli particles)
- Cytokine measurement platform (ELISA/MSD)
- LPS and other immune stimuli
Procedure:
- Cell Culture: Maintain ioMicroglia in specified maintenance media according to manufacturer protocols.
- Phagocytosis Assay: Incubate microglia with pHrodo-labeled E. coli bioparticles for 2-4 hours. Measure fluorescence increase (indicates phagocytosis) using plate reader or imaging system.
- Chemotaxis Assay: Seed microglia in top chamber of transwell system with chemoattractant (e.g., C5a) in bottom chamber. After 4-6 hours, fix and count migrated cells.
- Cytokine Release: Stimulate microglia with LPS (100 ng/mL) or other TLR agonists for 24 hours. Measure TNF-α, IL-6, and IL-1β in supernatant using multiplex immunoassay.
- CRISPR Screening: For CRISPRko-Ready ioMicroglia, perform pooled screens to identify regulators of immune activation pathways [76].
Benchmarking Application: Establish consistent, reproducible human microglial models for neuroinflammatory studies, replacing rodent primary cells with human-relevant systems [76].
The Scientist's Toolkit: Essential Research Reagents
Table: Key Research Reagent Solutions for CRISPR-iPSC Model Benchmarking
| Reagent/Cell Type | Function in Benchmarking | Application Example |
|---|---|---|
| CRISPR-Ready ioCells [76] | Provides consistent, defined human cell types with engineered Cas9 expression for efficient genetic modification | Enables pooled CRISPR knockout screens in microglia to identify immune regulators |
| Isogenic iPSC Pairs [21] | Gold standard controls with identical genetic background except for specific disease mutations | Isolation of mutation-specific phenotypes in Alzheimer's (APP, PSEN1/2) or ALS-related genes |
| opti-ox Enabled Cells [76] | Ensures uniform cell differentiation through deterministic programming | Generates highly consistent neuronal cultures for reproducible electrophysiology and screening |
| ioGlutamatergic Neurons [76] | Defined, pure population of excitatory neurons for network studies | Modeling ALS-related network dysfunction in MEA assays |
| ioMicroglia [76] | Consistent human microglia for neuroimmune studies | Chemotaxis, phagocytosis, and cytokine release assays in neuroinflammation models |
| ioHepatocytes [76] | Metabolically active liver cells for toxicity and metabolism studies | Drug-induced liver injury (DILI) assessment and metabolic profiling |
Workflow Visualization
Diagram: Comprehensive Benchmarking Workflow for CRISPR-iPSC Disease Models
Data Analysis and Interpretation Framework
Establishing Benchmarking Criteria and Success Metrics
Effective benchmarking requires pre-established criteria for model validation. Key success metrics include: (1) statistically significant difference between isogenic disease and control lines in disease-relevant phenotypes, (2) effect sizes sufficient for robust detection in screening contexts (typically Z' > 0.4), (3) reproducibility across differentiations (CV < 20-30%), and (4) concordance with known disease biology [77] [76]. The specific thresholds should be established based on the model's intended application, with more stringent requirements for models advancing to lead optimization.
Data normalization is critical for meaningful cross-experiment comparisons. Recommended approaches include: (1) within-plate controls (isogenic controls on every plate), (2) reference compound normalization for functional assays, and (3) multiparametric scoring that combines readouts into a unified disease relevance score. For example, a neurodegenerative disease model might integrate metrics of neuronal activity, mitochondrial function, and stress pathway activation into a composite validation score.
Table: Quantitative Benchmarking Standards for Key Assay Types
| Assay Type | Key Parameters | Minimum Effect Size | Acceptable CV | Z' Factor Target |
|---|---|---|---|---|
| Neuronal MEA | Mean firing rate, burst frequency, synchrony index | >30% difference | <25% | >0.4 |
| Calcium Imaging | Oscillation frequency, spike amplitude, propagation | >40% difference | <30% | >0.3 |
| Mitochondrial Stress Test | Basal respiration, ATP production, max capacity | >35% difference | <20% | >0.5 |
| High-content Morphology | Neurite length, branch points, synaptic density | >50% difference | <15% | >0.4 |
| Phagocytosis Assay | Particle uptake, fluorescence intensity | >60% difference | <20% | >0.5 |
| Cytokine Release | TNF-α, IL-6 secretion (fold-change) | >3-fold change | <25% | >0.3 |
Troubleshooting and Quality Control
Common challenges in benchmarking CRISPR-iPSC models include differentiation variability, assay robustness issues, and inadequate effect sizes. To address differentiation variability, implement strict quality control checks for cell identity markers before functional assessment. For assay robustness, conduct pilot studies to optimize key parameters (cell density, timing, reagent concentrations) before full benchmarking. When effect sizes are inadequate, consider whether alternative phenotypic endpoints might better capture disease biology.
Essential quality control measures include: (1) regular karyotyping to ensure genomic stability, (2) mycoplasma testing, (3) validation of CRISPR editing through multiple methods (Sanger sequencing, NGS, functional validation), and (4) assessment of off-target effects through targeted sequencing of predicted off-target sites [21]. Additionally, establish standardized documentation practices to track cell culture passage numbers, differentiation lots, and assay conditions, as these variables significantly impact reproducibility.
Robust benchmarking of phenotypic and functional assays is fundamental to realizing the potential of CRISPR-iPSC disease models in therapeutic discovery. The frameworks and protocols outlined here provide a structured approach to establishing disease relevance, technical robustness, and predictive validity. As the field advances, benchmarking practices will increasingly incorporate multiparametric assessment strategies, complex co-culture systems, and standardized reference datasets to enable cross-laboratory model validation.
The growing regulatory emphasis on human-based systems—exemplified by the FDA's roadmap to reduce animal testing—underscores the importance of well-characterized iPSC-derived models [76]. By implementing comprehensive benchmarking strategies, researchers can generate CRISPR-iPSC models with enhanced predictive validity, ultimately accelerating the development of effective therapies for complex human diseases.
The integration of induced pluripotent stem cells (iPSCs) with CRISPR-Cas9 gene editing is revolutionizing biomedical research by creating human-specific disease models that overcome critical limitations of traditional animal and immortalized cell line models. This paradigm shift enables the generation of isogenic cell lines with precise genetic modifications, supporting more accurate disease modeling and drug screening. iPSC-derived models, particularly three-dimensional (3D) organoids, recapitulate human-specific pathophysiology with greater fidelity than previous approaches. This application note details the comparative advantages, provides protocols for implementing CRISPR-iPSC technology, and outlines key reagent solutions for researchers developing advanced disease models.
Comparative Analysis of Model Systems
The table below provides a quantitative and qualitative comparison of the key characteristics of traditional models versus CRISPR-iPSC-derived models.
Table 1: Model System Comparison for Disease Research and Drug Development
| Feature | Traditional Animal Models | Immortalized Cell Lines | CRISPR-iPSC-Derived Models |
|---|---|---|---|
| Biological Relevance & Physiological Concordance | Moderate; limited by species differences in anatomy, physiology, and drug metabolism [19] [78] [79] | Low; often cancer-derived, with non-physiological proliferation and altered signaling pathways [80] [81] | High; human-specific, can be differentiated into target cell types, and support 3D organoid structures [19] [10] |
| Genetic Background Control | Variable; requires extensive backcrossing; genetic background can confound results [78] | Fixed but often abnormal and poorly defined; prone to genetic drift [81] | Excellent; enables creation of isogenic pairs (genetically identical except for the disease-causing mutation) [19] [10] |
| Model Development Timeline | Months to years (e.g., breeding cycles) [78] | Days to weeks [80] | Weeks to months (reprogramming, editing, differentiation) [18] [81] |
| Reproducibility & Scalability | Low to moderate; high pre-analytical variability, expensive housing [78] [81] | High; easy to culture and scale for high-throughput assays [80] [81] | Moderate to high; improving with automated differentiation and deterministic programming (e.g., opti-ox technology) [81] [10] |
| Ethical Considerations | High; significant ethical concerns and regulatory restrictions [78] | Low (for human lines) [18] | Low; sourced from consenting donors, non-invasive procedures [18] [6] |
| Typical Use Case | Studying complex systemic interactions, pre-clinical safety/efficacy [78] [79] | High-throughput preliminary screening, functional genomics [81] [10] | Precision disease modeling, mechanism-of-action studies, high-content drug screening, personalized medicine [19] [43] [10] |
Application in Disease Modeling and Drug Development
Establishing Isogenic iPSC Lines for Neurodegenerative Disease Research
A primary application of CRISPR-iPSC technology is generating isogenic controls, which are critical for attributing phenotypic changes directly to a specific genetic mutation.
Protocol 1: Generation of an Isogenic iPSC Line for Alzheimer's Disease Modeling
This protocol outlines the steps to introduce a familial AD point mutation (e.g., E280A in PSEN1) into a healthy control iPSC line [6] [10].
gRNA Design and RNP Complex Formation:
- Design a target-specific gRNA with high on-target efficiency and minimal predicted off-target effects. The gRNA should be directed to the genomic locus where the PSEN1 E280A mutation will be introduced [10].
- Form the Ribonucleoprotein (RNP) complex by pre-incubating purified Cas9 protein with the synthesized gRNA. Using RNP complexes, rather than plasmid-based expression, reduces off-target effects and improves editing efficiency [18].
Donor Template Design:
- Synthesize a single-stranded oligodeoxynucleotide (ssODN) donor template. This template should contain the desired E280A point mutation, flanked by homologous arms (typically 60-90 base pairs each) matching the target sequence [10].
iPSC Transfection and HDR Enrichment:
- Culture a healthy, pluripotent iPSC line in a log phase of growth. Maintaining cells in this phase is critical as homology-directed repair (HDR) is most efficient during the S/G2 phases of the cell cycle [18].
- Transfect the cells with the RNP complex and the ssODN donor template using a high-efficiency method such as electroporation [18].
- To enrich for HDR-edited cells, you can treat the transfected cell population with a small molecule (e.g., a p53 inhibitor) temporarily to enhance the survival of edited cells [18].
Single-Cell Cloning and Screening:
- Isolate single cells via fluorescence-activated cell sorting (FACS) or limited dilution into 96-well plates.
- Expand individual clones for 3-4 weeks to obtain sufficient cell numbers for genomic DNA extraction [10].
- Screen clones first via PCR amplification of the target locus followed by Sanger sequencing to identify correctly edited heterozygous and homozygous clones [6].
Quality Control and Validation:
The following workflow diagram illustrates the key steps in this protocol.
Differentiation into 3D Organoids for Phenotypic Analysis
After obtaining the isogenic iPSC line, the next step is to differentiate the cells into a relevant tissue model, such as brain organoids, to study disease phenotypes.
Protocol 2: Differentiation of Edited iPSCs into Cortical Brain Organoids
This protocol enables the study of AD-related pathologies like Aβ deposition and tau phosphorylation in a 3D context that mimics the human brain [43] [10].
Embryoid Body (EB) Formation:
- Harvest the validated isogenic iPSCs (wild-type and PSEN1 mutant) using gentle cell dissociation reagent.
- Aggregate 9,000 cells per well into a 96-well U-bottom low-attachment plate in iPSC medium supplemented with small molecule inhibitors (e.g., SMAD inhibitors) to induce neural ectoderm differentiation [10].
Matrigel Embedding and Neuroepithelium Expansion:
- On day 5, embed individual EBs in droplets of growth factor-reduced Matrigel.
- Transfer the Matrigel-embedded EBs to a 6-well low-attachment plate with neural induction medium. Over the next 10-15 days, the EBs will develop neuroepithelial buds [10].
Organoid Maturation and Terminal Differentiation:
- Maintain the organoids on an orbital shaker in differentiation medium to improve nutrient and oxygen exchange.
- Culture the organoids for up to 3 months to allow for the development of complex cortical structures, including different neuronal layers and glial cells [10].
Phenotypic Analysis and Drug Screening:
- Fix and section a subset of organoids for immunohistochemical analysis of AD markers: Aβ plaques (e.g., 6E10 antibody), hyperphosphorylated tau (e.g., AT8 antibody), and synaptic markers [43].
- Dissociate another subset of organoids to isolate neurons for functional assays, such as electrophysiology (Multi-Electrode Array) to measure network activity [10].
- Treat mutant and wild-type organoids with drug candidates (e.g., γ-secretase modulators) for 2-4 weeks. Measure the reduction in Aβ42/Aβ40 ratio via ELISA and assess recovery of electrophysiological deficits [43] [10].
The workflow for generating and analyzing brain organoids is summarized below.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of CRISPR-iPSC workflows relies on a suite of specialized reagents and tools. The following table details essential components.
Table 2: Essential Reagents and Tools for CRISPR-iPSC Workflows
| Reagent/Tool Category | Specific Examples | Function & Application Note |
|---|---|---|
| Reprogramming & Pluripotency | Yamanaka Factors (OKSM: Oct4, Klf4, Sox2, c-Myc), Sendai virus or mRNA kits [18] [6] | Non-integrating methods are preferred for clinical translation. Used to reprogram patient somatic cells (e.g., fibroblasts) into iPSCs. |
| CRISPR Machinery Delivery | Alt-R S.p. Cas9 Nuclease V3, high-fidelity Cas9 variants (e.g., HiFi Cas9), synthetic sgRNA [18] [10] | Formulation of RNP complexes for highly efficient and specific editing with reduced off-target effects compared to plasmid DNA. |
| Donor Template for HDR | Ultramer DNA Oligos (ssODNs), dsDNA donors with homology arms [10] | ssODNs are ideal for single nucleotide changes and small insertions. Purified, long oligonucleotides ensure high HDR efficiency. |
| iPSC Culture & Maintenance | mTeSR Plus, Vitronectin (VTN-N)-coated plates, ReLeSR passaging reagent [18] | Defined, feeder-free culture systems maintain iPSCs in a robust, undifferentiated state, ensuring consistency during editing and expansion. |
| Directed Differentiation | STEMdiff Cerebral Organoid Kit, Patterning small molecules (e.g., SMAD inhibitors, Retinoic Acid) [10] | Kits and defined cytokine cocktails provide standardized protocols for generating reproducible neuronal and organoid models. |
| Characterization & QC | Flow Cytometry Antibodies (e.g., TRA-1-60, SSEA4 for pluripotency), Karyostat assays, Off-target prediction software [18] [10] | Critical for validating the quality of edited iPSC lines pre- and post-differentiation, ensuring genetic integrity and identity. |
The synergistic combination of CRISPR-Cas9 and iPSC technology provides a powerful and transformative platform for disease modeling that surpasses the limitations of traditional animal and cell line models. By enabling the precise engineering of human cells in a physiologically relevant context, this approach accelerates the path from basic research to clinical application, offering new hope for the development of effective therapies for complex human diseases.
The preclinical prediction of drug-induced cardiac and hepatic adverse effects remains a significant challenge, contributing to high attrition rates in drug development programs and post-market withdrawals [82] [83]. The predictive failures of current animal models, which often fail to replicate human-specific drug effects, have driven the adoption of human-induced pluripotent stem cell (iPSC)-derived cardiomyocytes (iPSC-CMs) and hepatocytes (iPSC-hepatocytes) [82] [21]. These cells offer a human-specific platform that can harbor genetically determined characteristics underlying inter-individual variations in drug response.
The convergence of iPSC technology with CRISPR/Cas9 gene editing has revolutionized this field, enabling the creation of highly precise, patient-specific disease models for toxicological screening [21] [43]. CRISPR/Cas9 allows for the introduction or correction of mutations in genes associated with drug sensitivity and disease, such as those involved in cardiac ion channel function or hepatic drug metabolism [21]. This is particularly powerful for modeling complex genetic backgrounds and polygenic disorders, moving beyond traditional isogenic lines to study how a mutation functions across a spectrum of human genetic diversity [22]. However, the clinical predictivity of these models hinges on the maturity and physiological relevance of the differentiated cells, which often exhibit fetal-like properties [82]. This application note details protocols and best practices for leveraging CRISPR-edited iPSC-derived cardiomyocytes and hepatocytes to enhance the accuracy of safety pharmacology assessments.
iPSC-Derived Cardiomyocytes in Cardiotoxicity Testing
Cardiotoxicity is a leading cause of drug attrition post-market release, with manifestations including arrhythmias and contractile dysfunction [83]. iPSC-CMs provide a human-relevant model for assessing compound effects on key cardiac functional parameters.
Functional Properties and Maturation Strategies
iPSC-CMs recapitulate the fundamental electrophysiology of adult human cardiomyocytes, expressing critical ionic currents (INa, IKr, IKs, ICa) and generating action potentials [83]. However, key differences exist, such as a less negative resting membrane potential and slower upstroke velocity, indicative of a less mature phenotype [83]. To enhance their predictive power, maturation protocols are essential. These include:
- Prolonged Culture Time: Extending culture duration to promote structural and functional maturation.
- Metabolic Manipulation: Shifting substrate availability from glucose to fatty acids to drive adult-like metabolic energetics [83].
- 3D Engineered Tissues: Culturing cells in three-dimensional engineered heart tissues (EHTs) that provide electromechanical stimulation, enhancing sarcomeric organization and contractile force [82].
- Co-culture Systems: Incorporating non-myocyte cells such as cardiac fibroblasts and endothelial cells to better mimic the native cardiac microenvironment and improve cellular maturity [82] [83].
Application Note: Proarrhythmic Risk Assessment
Background: A primary application of iPSC-CMs is the identification of compounds that prolong the action potential duration (APD) and QT interval, a known risk factor for lethal arrhythmias like Torsades de Pointes.
CRISPR/Cas9 Integration: To model inherited Long QT syndrome and investigate mutation-specific drug sensitivities, CRISPR/Cas9 can be used to introduce pathogenic variants (e.g., in KCNH2 or KCNQ1) into control iPSC lines. Alternatively, the technology can be used to correct disease-causing mutations in patient-derived iPSCs to create isogenic controls, confirming phenotype-genotype relationships [21] [43].
Protocol 1.1: Contractility and Calcium Transient Analysis in iPSC-CMs This protocol assesses drug effects on cardiomyocyte contraction and intracellular calcium handling, key markers of contractile function and cardiotoxicity.
- Cell Culture: Plate matured iPSC-CMs (ventricular-like subtype preferred) on a suitable substrate (e.g., fibronectin) at a density of ~100,000 cells/cm² in a multi-well plate compatible with high-speed imaging. Use a defined maturation medium for at least 2 weeks prior to assay [83].
- Dye Loading:
- For calcium imaging, incubate cells with a fluorescent calcium indicator (e.g., Cal-520 AM, 2-4 µM) in assay buffer for 30-45 minutes at 37°C.
- For simultaneous contractility measurement, no additional dye is needed if using bright-field imaging.
- Experimental Setup: Place the plate on a live-cell imaging system equipped with an environmental chamber (37°C, 5% CO₂). Use a high-speed camera (>100 frames per second) and a 20x objective.
- Baseline Recording: Record at least 30 seconds of baseline activity for both calcium transients and contractile motion.
- Compound Addition: Add the test compound at the desired concentration(s) directly to the well. Include a positive control (e.g., E-4031 for IKr blockade) and vehicle control.
- Data Acquisition: Record calcium and contractility data for 5-15 minutes post-compound addition. For long-term effects, measurements can be taken at 24-hour intervals.
- Data Analysis:
- Calcium Transient Parameters: Analyze fluorescence traces to determine amplitude, time to peak (TTP), and decay time (tau, τ).
- Contractility Parameters: Use motion-tracking software to analyze cell shortening (amplitude), contraction, and relaxation velocities.
Table 1: Key Functional Parameters of iPSC-CMs for Toxicity Assessment
| Parameter | Measurement | Significance in Toxicology | Technology for Assessment |
|---|---|---|---|
| Action Potential Duration (APD) | Duration of cardiomyocyte depolarization/repolarization cycle. | Prolonged APD (e.g., APD90) indicates pro-arrhythmic risk (QT prolongation). | Patch clamp, voltage-sensitive dyes, multi-electrode arrays (MEA). |
| Calcium Handling | Kinetics (time to peak, decay constant) and amplitude of intracellular Ca²⁺ transients. | Disrupted Ca²⁺ cycling indicates impaired contractility and arrhythmogenesis. | Fluorescent Ca²⁺ indicators (e.g., Fluo-4, Cal-520). |
| Contractility | Cell shortening magnitude and velocity. | Reduced contractility indicates negative inotropic effects. | Video-based motion tracking, traction force microscopy. |
| Ion Channel Function | Current density and kinetics of specific ion channels (e.g., IKr, INa, ICa). | Direct assessment of compound interaction with specific cardiac ion channels. | Automated patch clamp. |
| Beat Rate | Contractions per minute (BPM). | Tachycardia or bradycardia can indicate autonomic or direct pacemaker toxicity. | Impedance-based systems (xCELLigence), MEA. |
Diagram 1: iPSC-CM cardiotoxicity assessment workflow.
iPSC-Derived Hepatocytes in Hepatotoxicity Testing
Drug-induced liver injury (DILI) is another major cause of drug failure. The physiological relevance of iPSC-hepatocytes is critical, as their fetal-like profile, including low expression of cytochrome P450 (CYP) enzymes and drug transporters, limits predictive accuracy [82].
Enhancing Hepatic Maturity through Microenvironment Engineering
Advanced culture systems are employed to drive iPSC-hepatocytes toward a more adult-like phenotype:
- 3D Spheroid and Organoid Cultures: Promoting cell polarity, formation of functional bile canaliculi, and enhancing cell-cell interactions [82] [4].
- Co-culture with Non-Parenchymal Cells: Incorporating Kupffer cells (liver macrophages), endothelial cells, and stellate cells to better model the liver's architecture and inflammatory responses, which are key drivers of DILI [82].
- Microfluidic Dynamic Flow: Exposing cells to fluid shear stress in liver-on-a-chip devices, which improves nutrient/waste exchange and enhances CYP enzyme activity and albumin production [82].
- CRISPR/Cas9 Integration: Gene editing can be utilized to introduce polymorphisms in genes critical for drug metabolism (e.g., CYP2D6, CYP2C9) to model population-wide variations in drug response and susceptibility to toxicity [21] [4]. It can also be used to create reporter lines where fluorescent proteins are knocked into genes like CYP3A4, allowing for real-time monitoring of enzyme induction and inhibition.
Application Note: CYP450 Induction and Toxicity Screening
Background: The induction or inhibition of CYP450 enzymes is a common source of drug-drug interactions and can lead to hepatotoxicity. iPSC-hepatocytes model these human-specific pathways.
Protocol 2.1: High-Content Imaging for Hepatotoxicity in 3D Spheroids This protocol uses 3D spheroids for multiplexed toxicity endpoint analysis.
- Spheroid Formation:
- Using matured iPSC-hepatocytes (cultured with aforementioned methods), seed 1,000-2,000 cells per well in an ultra-low attachment round-bottom 96-well plate.
- Centrifuge the plate at low speed (e.g., 300 x g for 3 minutes) to promote aggregate formation.
- Culture for 3-5 days, allowing spheroids to compact and form bile canaliculi structures.
- Compound Treatment: Treat spheroids with the test article, a vehicle control, and a positive control for toxicity (e.g., 100 µM acetaminophen) for 24-72 hours. Refresh medium with compounds daily.
- Staining:
- Prepare a staining solution containing a cell-permeable nuclear dye (e.g., Hoechst 33342, 5 µg/mL), a mitochondrial membrane potential dye (e.g., TMRM, 100 nM), and a cell death indicator (e.g., propidium iodide, 2 µM).
- Replace the culture medium with the staining solution and incubate for 45-60 minutes at 37°C.
- Image Acquisition: Image spheroids using an automated high-content imaging system with a confocal or spinning-disk confocal microscope equipped with a 10x or 20x water immersion objective. Acquire z-stacks to capture the entire 3D structure.
- Image Analysis:
- Use analysis software to segment individual spheroids and individual nuclei.
- Quantify: Viability (ratio of propidium iodide-negative cells to total nuclei), Mitochondrial Health (TMRM intensity per cell), and Steatosis (using a lipophilic dye like BODIPY 493/503 if included).
Table 2: Key Functional Markers of iPSC-Hepatocytes for Toxicity Assessment
| Parameter | Measurement | Significance in Toxicology | Technology for Assessment |
|---|---|---|---|
| CYP450 Metabolism | Enzyme activity (e.g., CYP3A4, CYP2C9). | Induction/inhibition indicates drug-drug interaction potential; bioactivation of toxins. | LC-MS/MS of metabolite formation, luminogenic assays, fluorescent reporters. |
| Albumin/Urea Production | Synthesis and secretion of key hepatic proteins. | Marker of overall synthetic liver function; decrease indicates toxicity. | ELISA, colorimetric assays. |
| Bile Canaliculi Formation | Formation and functionality of polarized structures for bile excretion. | Disruption indicates cholestatic liver injury. | Live staining with cholyl-lysyl-fluorescein (CLF), microscopy. |
| ATP Content | Intracellular ATP levels. | General marker of cellular health and metabolic competence. | Luminescent cell viability assays. |
| Lipid Accumulation | Intracellular lipid droplet content. | Marker for steatotic (fatty liver) toxicity. | High-content imaging (e.g., Oil Red O, BODIPY staining). |
Diagram 2: iPSC-hepatocyte maturation and toxicity assessment workflow.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for iPSC Toxicology
| Item | Function | Example Application |
|---|---|---|
| iPSC Lines (CRISPR-edited) | Genetically defined basis for differentiation. | Isogenic pairs with mutations in cardiac (e.g., KCNH2) or hepatic (e.g., CYP2D6) genes for controlled toxicity studies [21] [22]. |
| Defined Differentiation Kits | Robust, reproducible differentiation of iPSCs to cardiomyocytes or hepatocytes. | Generating consistent batches of cells for high-throughput screening (HTS) campaigns [4]. |
| Maturation Media Supplements | Promote adult-like cell phenotype. | Fatty acids for metabolic maturation of iPSC-CMs; cytokine cocktails for enhanced function of iPSC-hepatocytes [82] [83]. |
| Functional Dyes & Assays | Probe live-cell physiology and toxicity endpoints. | Calcium-sensitive dyes (Fluo-4), mitochondrial potential dyes (TMRM), and viability/cytotoxicity assay kits (MTT, ATP-lite) [84] [83]. |
| High-Content Imaging Systems | Automated, multiplexed quantification of morphological and functional changes. | Analyzing nuclear condensation, mitochondrial health, and lipid accumulation in 3D spheroids [84]. |
| Multi-Electrode Array (MEA) Systems | Non-invasive, label-free recording of extracellular field potentials from beating cardiomyocytes. | Screening for compound-induced arrhythmias (e.g., changes in firing rate, field potential duration) in monolayer cultures [83]. |
| Liver Microenvironment Kits | Co-culture systems with non-parenchymal cells. | Modeling immune-mediated DILI by including Kupffer cells in hepatocyte cultures [82]. |
Data Presentation and Statistical Analysis
Robust data analysis is fundamental for reliable toxicology assessment. Adhere to the following guidelines:
- Replicates: Clearly define and report both biological replicates (cells from at least 3 independent differentiations) and technical replicates [85] [84].
- Data Transparency: Present data using scatter plots showing individual data points superimposed on bar graphs (e.g., SuperPlots) to visualize the distribution and variability of the data, rather than bar graphs with mean ± standard error (SEM) alone [85] [84].
- Error Bars: Use standard deviation (SD) to represent the variability of the data [85].
- Statistical Testing: Precisely describe statistical tests used. Report exact p-values for all comparisons. For comparisons of more than two groups, use appropriate ANOVA with defined post-hoc tests [85].
- Excluded Data: State explicitly if any data were excluded from analysis and provide the rationale and criteria for exclusion [85].
The convergence of CRISPR-Cas9 gene editing with induced pluripotent stem cell (iPSC) technology has established a powerful platform for modeling human diseases and developing transformative therapies. This integrated approach enables researchers to recapitulate patient-specific genetic pathologies in vitro, elucidate disease mechanisms, and translate these findings into clinical applications. The pipeline from preclinical discovery to human trials leverages the precision of CRISPR for creating targeted genetic modifications in iPSCs derived from patients, which can then be differentiated into disease-relevant cell types for therapeutic screening and validation [21] [18]. This application note examines the current clinical pipeline, highlighting successful transitions from preclinical research to ongoing human trials, with detailed methodologies supporting this rapidly advancing field.
The therapeutic potential of this combined technology is particularly valuable for neurological disorders, where primary human tissue is difficult to obtain. iPSC-derived neurons, astrocytes, microglia, and increasingly complex 3D organoids can recapitulate key aspects of human pathology, providing biologically relevant systems for drug screening and mechanism investigation [21] [22]. Furthermore, CRISPR-edited iPSCs enable the generation of isogenic control lines that are genetically identical except for a specific mutation, allowing researchers to isolate the functional consequences of disease-associated variants against a constant genetic background [22] [18].
Current Clinical Trial Landscape
The clinical translation of CRISPR-based therapies has achieved significant milestones, with the first FDA approval of a CRISPR therapy (Casgevy for sickle cell disease and transfusion-dependent beta-thalassemia) marking a new era in genetic medicine [86] [16]. As of 2025, the clinical pipeline continues to expand across diverse disease areas, with both ex vivo and in vivo approaches showing promising results.
Table 1: Selected CRISPR-Based Clinical Trials with Relevance to iPSC Disease Modeling
| Disease Area | Therapeutic Strategy | Delivery Method | Clinical Phase | Key Outcomes/Objectives |
|---|---|---|---|---|
| Hereditary Transthyretin Amyloidosis (hATTR) [16] | Knockout of TTR gene to reduce disease-related protein | Lipid Nanoparticles (LNP), systemic IV | Phase III | ~90% sustained reduction in TTR protein levels; functional improvement |
| Hereditary Angioedema (HAE) [16] | Knockout of KLKB1 gene to reduce kallikrein protein | LNP, systemic IV | Phase I/II | 86% reduction in kallikrein; significant reduction in attacks |
| Alzheimer's Disease & Related Dementias [21] [18] | Disease modeling using CRISPR-edited iPSCs | Ex vivo editing | Preclinical | Generation of precision models for drug screening (iNDI project) |
| CPS1 Deficiency [16] | Personalized in vivo correction | LNP, systemic IV | Case Study | First personalized in vivo CRISPR therapy; symptom improvement |
| Cancers (Various) [87] | CAR-T cell engineering with improved persistence | Ex vivo editing of T cells | Multiple trials | Enhanced anti-tumor activity through immune checkpoint disruption |
The clinical landscape demonstrates a trend toward in vivo delivery using non-viral vectors, particularly lipid nanoparticles (LNPs), which enable redosing and have favorable safety profiles compared to viral vectors [16]. The successful application of multiple LNP doses in patients with hATTR and CPS1 deficiency represents a significant advancement in delivery technology, addressing one of the major historical challenges in gene therapy [16].
Detailed Experimental Protocols
Protocol for Generating CRISPR-Edited iPSCs Using SLEEK Technology
A significant technical challenge in iPSC gene editing is the silencing of Cas9 expression during differentiation, even when Cas9 is inserted into established safe harbor loci [39]. The following protocol outlines the SLEEK (Selection by Essential Gene Exon KnocK-in) technology, which enables high-efficiency generation of iPSCs with stable Cas9-EGFP expression.
Table 2: Key Research Reagents for SLEEK Technology Implementation
| Reagent/Category | Specific Example | Function/Application |
|---|---|---|
| Vector System | SLEEK backbone with Cas9-EGFP | Donor template for targeted integration |
| Cell Culture Matrix | Matrigel, diluted 1:400 in cold DMEM | Provides extracellular matrix for iPSC attachment and growth |
| Selection Elements | GAPDH exon 9 homology arms | Enables positive selection through restoration of essential gene |
| Validation Primers | p1-p5 primer sets | PCR verification of correct 5' and 3' integration |
| Assembly Method | Gibson Assembly | Seamless cloning of Cas9-EGFP into SLEEK backbone |
Procedure:
Plasmid Construction:
- Design primers with appropriate overlaps (25 bp from vector end + 25 bp from insert end) for Gibson Assembly.
- Generate the Cas9-EGFP SLEEK plasmid using Gibson Assembly method, which utilizes overlapping regions at the ends of DNA fragments.
- Validate the assembly product using Sanger sequencing with multiple primers covering the entire Cas9 sequence (divide 4,101 bp Cas9 sequence into ~650 bp segments for complete coverage) [39].
iPSC Culture Preparation:
- Prepare Matrigel-coated plates by diluting 100 μL Matrigel into 40 mL cold basic DMEM medium (final concentration ~25.8-26.5 μg/mL).
- Add 2 mL coating medium per well of a 6-well plate and incubate at 4°C for 12 hours.
- Culture iPSCs in essential 8 medium or similar defined maintenance medium, passaging every 4-5 days to maintain log-phase growth.
- Image cells daily to identify and remove differentiated areas, maintaining pluripotency through careful culture management [39] [18].
Electroporation and Selection:
- Electroporate the Cas9-EGFP SLEEK construct and sgRNA targeting GAPDH exon 9 into iPSCs using appropriate parameters.
- The donor template contains a recoded exon 9 without changing the GAPDH amino acid sequence, allowing only genome-edited cells that undergo homology-directed repair (HDR) to restore GAPDH function and survive.
- Cells that repair through non-homologous end joining (NHEJ) will undergo negative selection due to disruption of GAPDH, an essential housekeeping gene [39].
Validation of Knock-in:
- Design PCR primers located outside both the 5' and 3' homology arms to validate successful HDR events.
- Use primer combinations: outside 5' arm F1/F2 with Reverse-1 for the 5' junction, and Poly A F with outside 3' arm R1 for the 3' junction.
- Confirm Cas9 functionality through EGFP expression and editing efficiency assays in the validated iPSC-Cas9-EGFP cells [39].
Protocol for "Village Editing" to Study Genetic Background Effects
Complex disorders often show variable penetrance due to modifier genes and polygenic risk factors. The "village editing" approach enables efficient parallel generation of isogenic lines across multiple genetic backgrounds to dissect these interactions.
Procedure:
Donor iPSC Selection:
- Select iPSC lines from 15+ donors with varying polygenic risk scores or different genetic backgrounds relevant to the disease of interest.
- Ensure all lines have been thoroughly characterized for pluripotency and genomic stability [22].
Parallel CRISPR Editing:
- Culture all selected iPSC lines together in a "cell village" format, enabling simultaneous CRISPR-Cas9 editing across multiple genetic backgrounds.
- Transfer the pooled village to neuronal differentiation conditions after achieving high editing efficiency.
- After differentiation, use lentiviral barcoding or single-cell RNA sequencing to assign cells to their original genetic background based on natural genetic variation [22].
Phenotypic Analysis:
- Differentiate edited iPSCs to relevant cell types (e.g., cortical excitatory neurons using 28-day protocol with mouse glia).
- Perform RNA sequencing to determine the effect of genetic perturbations on transcriptomes across different backgrounds.
- Analyze how genetic background influences gene expression changes in response to the introduced mutation [22].
Data Integration:
- Correlate editing outcomes with donor polygenic risk scores or specific genetic variants.
- Identify genetic modifiers that ameliorate or exacerbate the primary mutation's effects.
- Validate top candidates through follow-up experiments in isogenic lines [22].
Visualization of Workflows and Pathways
CRISPR-iPSC Therapeutic Development Workflow
CRISPR-Cas9 Mechanism and DNA Repair Pathways
Key Research Reagents and Solutions
Successful implementation of CRISPR-iPSC workflows requires specialized reagents and systems optimized for stem cell biology and precise genome engineering.
Table 3: Essential Research Reagents for CRISPR-iPSC Disease Modeling
| Reagent Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| CRISPR Delivery Systems | RNP complexes, Cas9 mRNA + sgRNA, All-in-one lentiviral vectors | Introduction of editing components into iPSCs | RNP complexes reduce off-target effects; optimize for each iPSC line [18] |
| iPSC Culture Matrices | Matrigel, Vitronectin, Laminin-521 | Extracellular matrix for pluripotency maintenance | Test multiple matrices for optimal attachment and growth [39] |
| Genome Editing Enhancers | HDR enhancers (e.g., Rad51 stimulators), NHEJ inhibitors | Increase precise editing efficiency | Cell cycle synchronization improves HDR rates [18] |
| Selection Systems | Puromycin, Hygromycin, Fluorescent reporters, SLEEK technology | Enrichment for successfully edited cells | Essential gene knock-in provides efficient positive selection [39] |
| Differentiation Kits | Commercial neuronal, cardiac, pancreatic differentiation kits | Generation of disease-relevant cell types | Optimize protocols for specific genetic backgrounds [22] [88] |
| Quality Control Tools | Karyotyping, Pluripotency tests, Off-target analysis assays | Ensure genomic integrity and editing specificity | Regular monitoring essential for maintaining iPSC quality [18] |
The clinical pipeline for CRISPR-iPSC based therapies continues to advance, with promising transitions from preclinical models to human trials. Key developments include improved delivery systems such as lipid nanoparticles that enable in vivo administration and redosing capabilities, more efficient and stable editing approaches like the SLEEK technology that address Cas9 silencing, and sophisticated modeling strategies such as "village editing" that account for genetic background effects [39] [16] [22]. These methodological advances are accelerating the pace at which CRISPR-iPSC research translates to clinical applications.
Future directions in the field include the development of more sophisticated base editing and prime editing approaches that minimize off-target effects, the creation of increasingly complex multi-tissue organoid and organ-on-a-chip systems that better recapitulate human physiology, and the implementation of standardized protocols for clinical-grade iPSC generation and editing [89] [87] [11]. As regulatory frameworks evolve to accommodate these advanced technologies, including recent FDA guidelines that no longer require animal testing for all new drugs, the path from CRISPR-iPSC disease models to clinical applications is expected to become more efficient and direct [11]. The continued integration of CRISPR-iPSC platforms into therapeutic development pipelines promises to accelerate the creation of personalized treatments for a wide range of genetic disorders.
The application of CRISPR-Cas9 gene editing in induced pluripotent stem cells (iPSCs) represents a transformative approach for developing sophisticated human disease models and therapeutic candidates. This technological synergy enables researchers to create genetically precise, patient-specific cellular models that accurately recapitulate disease pathophysiology. However, navigating the regulatory pathway for these complex biologic products requires careful attention to evolving Food and Drug Administration (FDA) frameworks and strict adherence to Good Manufacturing Practice (GMP) standards.
The regulatory landscape for cellular and gene therapy products is dynamic, with recent FDA initiatives aimed at modernizing review processes while ensuring product safety and efficacy. Key developments include updated guidance documents specifically addressing cellular and gene therapy products, new office structures within the Center for Biologics Evaluation and Research (CBER), and innovative approaches to clinical trial design for small population studies [90]. Simultaneously, the FDA has begun implementing modernization efforts that include phasing out animal testing requirements in favor of New Approach Methodologies (NAMs) for certain products, representing a significant shift in regulatory science [91].
This application note provides a comprehensive framework for researchers utilizing CRISPR-Cas9 in iPSCs to navigate this evolving regulatory environment, with specific focus on compliance strategies from preclinical development through clinical trial design.
Current FDA Regulatory Framework for Cell and Gene Therapy Products
Key Guidance Documents
The FDA has issued numerous guidance documents specifically addressing cellular and gene therapy products. The most recent relevant guidances for CRISPR-edited iPSCs include:
Table: Key FDA Guidance Documents for Cellular and Gene Therapy Products (2023-2025)
| Guidance Document Title | Release Date | Status | Relevance to CRISPR-iPSC Research |
|---|---|---|---|
| Innovative Designs for Clinical Trials of Cellular and Gene Therapy Products in Small Populations | 09/2025 | Draft | Provides recommendations for clinical trial designs in rare diseases [92] |
| Human Gene Therapy Products Incorporating Human Genome Editing | 01/2024 | Final | Offers recommendations on IND requirements for genome editing products [93] |
| Considerations for the Development of Chimeric Antigen Receptor (CAR) T Cell Products | 01/2024 | Final | Broadly applicable to gene-edited cell therapies including iPSC-derived products [90] |
| Potency Assurance for Cellular and Gene Therapy Products | 12/2023 | Draft | Critical for demonstrating product quality and biological activity [93] |
| Manufacturing Changes and Comparability for Human Cellular and Gene Therapy Products | 07/2023 | Draft | Guides manufacturing process changes and comparability studies [93] |
| Studying Multiple Versions of a Cellular or Gene Therapy Product in an Early-Phase Clinical Trial | 11/2022 | Final | Allows umbrella trials for evaluating multiple product versions simultaneously [90] |
The FDA's Office of Therapeutic Products (OTP), which replaced the former Office of Tissues and Advanced Therapies (OTAT), now oversees the regulation of these complex biologics. This reorganization has expanded review capabilities and specialized expertise in cell and gene therapy products, with the FDA staffing approximately 75-80% of planned new positions as of early 2024 to address the growing pipeline of these therapies [90].
FDA Modernization and Animal Testing Alternatives
In a significant regulatory shift, the FDA has announced plans to phase out animal testing requirements for monoclonal antibodies and other drugs, instead promoting New Approach Methodologies (NAMs) including AI-based computational models, cell lines, and organoid toxicity testing [91]. This initiative reflects a broader movement toward human-relevant testing systems that may offer better predictive value for human responses.
For CRISPR-edited iPSC products, this modernization presents opportunities to leverage advanced human cell-based systems during development. iPSC-derived organoids and tissue chips can serve as clinically relevant test platforms that may satisfy regulatory requirements while potentially providing superior human toxicity prediction compared to traditional animal models. The FDA encourages developers to submit strong safety data from these non-animal tests, which may qualify for streamlined review processes [91].
FDA Modernization: Traditional vs. Updated Pathways
GMP Compliance for CRISPR-Edited iPSC Products
Essential GMP Reagents and Materials
Current Good Manufacturing Practice (cGMP) compliance is fundamental for CRISPR-edited iPSC products intended for clinical use. GMP regulations ensure that these complex biologic products maintain consistent safety, purity, and potency profiles. The core components requiring GMP-grade quality include:
Table: Essential GMP Reagents for CRISPR-Edited iPSC Products
| Reagent/Material | GMP Requirement | Function | Critical Quality Attributes |
|---|---|---|---|
| CRISPR Nucleases (e.g., Cas9) | Required for clinical use | Creates targeted double-strand breaks in DNA | Purity, sterility, endotoxin levels, nuclease activity [94] |
| Guide RNAs (gRNAs) | Required for clinical use | Directs nuclease to specific genomic loci | Purity, sequence accuracy, sterility, absence of contaminants [94] |
| Donor DNA Templates | Required for HDR-mediated editing | Provides template for precise gene correction | Sequence accuracy, purity, endotoxin levels [94] |
| iPSC Starting Material | Required for clinical use | Foundation for edited cell products | Karyotypic normalcy, pluripotency, viability, identity [93] |
| Cell Culture Media/Supplements | Required for clinical use | Supports cell growth and maintenance | Composition consistency, sterility, endotoxin levels [93] |
| Differentiation Reagents | Required for clinical use | Directs differentiation to target cell types | Potency, purity, composition consistency [93] |
A significant challenge in the field is the procurement of true GMP-grade reagents, particularly gRNAs and nucleases, with demand currently outstripping supply. Researchers must verify that suppliers provide authentically GMP-grade materials rather than "GMP-like" research-grade reagents, as vendor changes during development can introduce variability that compromises product consistency and complicates regulatory approval [94].
Manufacturing and Comparability
The "Manufacturing Changes and Comparability for Human Cellular and Gene Therapy Products" draft guidance provides critical framework for managing process changes during development [93]. For CRISPR-edited iPSCs, maintaining comparability after manufacturing changes requires rigorous assessment of:
- Critical Quality Attributes (CQAs): Genomic stability, pluripotency markers, differentiation potential, and genetic editing accuracy
- Product Potency: Functional assessment of the edited iPSCs and their differentiated progeny
- Purity and Identity: Verification of target edit and absence of unintended modifications
- Safety: Comprehensive evaluation including off-target editing analysis and tumorigenicity potential
Documentation of manufacturing processes and changes is essential, with the FDA recommending a risk-based approach to determining when comparability studies are required [93].
Application Notes: CRISPR-iPSC Editing for Disease Modeling
Experimental Protocol: CRISPR Genome Editing in iPSCs
The following detailed protocol outlines a GMP-compliant workflow for CRISPR-Cas9 editing of iPSCs for disease modeling applications, incorporating regulatory considerations at each stage.
Pre-Editing Phase: Cell Line Establishment and Quality Control
Day 1-7: iPSC Culture Expansion and Quality Control
- Begin with characterized iPSC lines from GMP-compliant sources or establish new lines under GMP conditions using FDA-guidance on cellular derivation [93].
- Culture iPSCs in GMP-grade maintenance medium on approved substrate (e.g., recombinant laminin-521).
- Daily monitoring and removal of spontaneously differentiated areas to maintain pluripotency [18].
- Passage cells during log-phase growth (typically 70-80% confluence) using GMP-grade dissociation reagent.
- Quality Control Assessments:
- Karyotype analysis (G-banding)
- Pluripotency marker confirmation (Flow cytometry for TRA-1-60, SSEA4, OCT4, SOX2, NANOG)
- Mycoplasma testing
- Short tandem repeat (STR) profiling for identity confirmation
Editing Phase: CRISPR Delivery and Selection
Day 8: Cell Preparation and Transfection
- Synchronize cell cycle to improve HDR efficiency by treating with GMP-grade cell cycle synchronization agents (e.g., thymidine, nocodazole) [18].
- Prepare CRISPR editing components using GMP-grade Cas nuclease and guide RNA. For precise editing, include HDR template with appropriate homology arms.
- Use clinically translatable delivery method (electroporation for ribonucleoprotein complexes preferred over viral delivery for reduced regulatory burden).
- Critical Parameters:
- Cell viability post-electroporation (>70% acceptable)
- Editing component concentrations (typically 50-100μg/mL Cas9, 100-200μg/mL gRNA)
- Electroporation conditions optimized for specific iPSC line
Day 9-21: Recovery, Selection, and Clone Isolation
- Culture transfected cells in GMP-grade recovery medium supplemented with Rho-associated kinase (ROCK) inhibitor for 24 hours.
- Implement selection strategy (antibiotic selection, FACS, or single-cell sorting) using GMP-grade reagents.
- Isolate single-cell clones into 96-well plates using limited dilution or automated cell sorting.
- Expand clones for 2-3 weeks with regular medium changes and monitoring.
Post-Editing Phase: Characterization and Banking
Day 22-35: Clone Screening and Characterization
- Screen clones for desired edit using PCR-based genotyping and Sanger sequencing.
- Expand positively identified clones for comprehensive characterization.
- Comprehensive Quality Control Panel:
- Off-target analysis: NGS-based screening of predicted off-target sites
- Genomic stability: Karyotyping or CNV analysis
- Pluripotency confirmation: Flow cytometry and differentiation potential
- Identity testing: STR profiling comparison to parental line
- Mycoplasma testing: Sterility confirmation
Day 36-42: Master Cell Bank Preparation
- Prepare Master Cell Bank (MCB) of validated edited iPSC clones using GMP-grade cryopreservation medium.
- Cryopreserve in validated controlled-rate freezer with documentation of freezing parameters.
- Perform full characterization on MCB vials, including viability post-thaw and all QC parameters above.
CRISPR-iPSC Editing Workflow
Case Study: Neurodegenerative Disease Modeling with Regulatory Compliance
An exemplary application of CRISPR-edited iPSCs in disease modeling is the 2021 Inducible Pluripotent Stem Cell Neurodegeneration Initiative (iNDI), a collaboration between Synthego and the National Institutes of Health that generated 250 CRISPR-iPSC clones for Alzheimer's Disease and Related Dementias (ADRD) modeling [18]. This project demonstrates scalability while addressing regulatory considerations:
Study Design and Regulatory Alignment:
- Genetic Background Diversity: Included multiple donor backgrounds to address human genetic variability, enhancing clinical translatability
- Isogenic Controls: Created patient-derived iPSCs with corrected disease mutations using CRISPR, providing ideal matched controls
- Comprehensive Characterization: Implemented rigorous QC protocols aligned with FDA guidance on preclinical assessment [93]
- Documentation: Maintained complete chain of custody and editing documentation for regulatory compliance
Differentiation and Functional Assessment:
- Differentiated edited iPSCs to cortical excitatory neurons using GMP-compatible differentiation protocols
- Performed RNA sequencing to transcriptomically validate disease phenotypes
- Assessed functional neuronal properties using electrophysiology and calcium imaging
- Documented differentiation efficiency and cellular composition for product characterization
This approach exemplifies how disease modeling research can be conducted with attention to regulatory requirements, facilitating potential transition to therapeutic development.
Clinical Trial Design Strategies for CRISPR-Edited iPSC Products
Innovative Trial Designs for Small Populations
For CRISPR-edited iPSC products targeting rare diseases, the FDA's draft guidance "Innovative Designs for Clinical Trials of Cellular and Gene Therapy Products in Small Populations" (September 2025) provides flexible approaches to demonstrate effectiveness despite limited patient numbers [92]. Key considerations include:
- Umbrella Trial Designs: Master protocols allowing simultaneous evaluation of multiple edited iPSC product versions, efficiently comparing safety and efficacy profiles [90]
- Adaptive Designs: Pre-specified modifications to trial design based on interim data, maximizing information gain from limited subjects
- Bayesian Approaches: Incorporating external data and prior knowledge to enhance statistical power in small populations
- Novel Endpoint Development: Identifying and validating biomarkers, physiological measures, or performance outcomes that can serve as surrogate endpoints
Regulatory Interactions and Submission Strategies
Early and strategic engagement with FDA through pre-IND meetings is critical for CRISPR-edited iPSC products. Recommended approach includes:
- Pre-IND Package: Comprehensive data package including editing strategy, off-target analysis, manufacturing process, and preclinical proof-of-concept
- Clinical Trial Design Discussion: Specific alignment on patient population, endpoints, and statistical approach, particularly for rare diseases
- CMC Strategy: Clear description of manufacturing process, testing strategy, and comparability approach
- Advisory Meetings: Utilization of FDA internship programs like START (Support for clinical Trials Advancing Rare disease Therapeutics) for complex rare disease programs [90]
The Scientist's Toolkit: Essential Research Reagent Solutions
Table: Essential Research Tools for CRISPR-iPSC Disease Modeling
| Tool/Reagent Category | Specific Examples | Function | Regulatory Considerations |
|---|---|---|---|
| CRISPR Editing Systems | High-fidelity Cas9, Prime editors, Base editors | Precision genome editing | Document nuclease source and quality; GMP-grade required for clinical use [94] |
| iPSC Culture Systems | GMP-grade media, Recombinant substrates, ROCK inhibitors | Pluripotency maintenance and expansion | Quality documentation; absence of animal-derived components preferred [93] |
| Differentiation Kits | Neural, cardiac, hepatic differentiation systems | Lineage-specific differentiation | Lot consistency; defined composition; performance qualification [28] |
| Analytical Tools | NGS for off-target analysis, Flow cytometry, Pluripotency assays | Product characterization | Validated methods; standardization across batches [93] |
| Cell Banking Systems | Cryopreservation media, Controlled-rate freezers, Inventory systems | Long-term storage and stability | Documentation; stability data; container closure integrity [93] |
Navigating the regulatory landscape for CRISPR-edited iPSC products requires proactive integration of FDA guidance and GMP principles throughout the research and development continuum. Success in this rapidly evolving field depends on:
- Early Regulatory Engagement: Utilizing FDA feedback mechanisms during product development
- Investment in GMP-Compliant Processes: Establishing manufacturing workflows that can transition from research to clinical production
- Comprehensive Characterization: Implementing rigorous analytical methods to demonstrate product consistency and safety
- Adaptive Clinical Development: Employing innovative trial designs appropriate for target patient populations
As regulatory science continues to evolve alongside technological advances, researchers developing CRISPR-edited iPSC disease models must maintain vigilance in monitoring updated FDA guidance while building quality systems that ensure both scientific rigor and regulatory compliance.
Conclusion
The integration of CRISPR-Cas9 with iPSC technology has fundamentally transformed disease modeling, enabling the creation of genetically precise, patient-specific human cell systems that recapitulate complex disease pathologies. This powerful synergy accelerates the identification of novel therapeutic targets, enhances the predictive accuracy of preclinical drug safety and efficacy testing, and paves the way for personalized regenerative medicines. Future progress hinges on overcoming key challenges in manufacturing scalability, ensuring long-term safety of edited cells, and refining the predictive power of complex 3D model systems like organoids. As these technologies mature, they promise to de-risk drug development pipelines, reduce reliance on animal models, and usher in a new era of targeted, effective therapies for a wide spectrum of human diseases.
References
- 1. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 2. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 3. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 4. Induced Pluripotent Stem Cell (iPSC) Industry Trends for ... [https://bioinformant.com/ipsc-industry-trends/]
- 5. Comprehensive protocols for CRISPR/Cas9-based gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4988528/]
- 6. CRISPR Editing in iPSCs [https://www.synthego.com/ipsc-crispr/]
- 7. Scaling up pluripotent stem cell-based therapies [https://www.sciencedirect.com/science/article/pii/S1465324925006784]
- 8. Induced Pluripotent Stem Cells Production Market 2025 [https://www.custommarketinsights.com/report/induced-pluripotent-stem-cells-production-market/]
- 9. Challenges and Opportunities in the Application of CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503735/]
- 10. CRISPR And iPSC Disease Modeling And Drug Screening [https://www.cellandgene.com/doc/crispr-and-ipsc-disease-modeling-and-drug-screening-0001]
- 11. Advances in CRISPR Disease Modeling: Cells, Organoids, ... [https://www.synthego.com/blog/crispr-disease-modeling-trends/]
- 12. Characterizing and controlling CRISPR repair outcomes in ... [https://www.nature.com/articles/s41467-025-66058-3]
- 13. Design of highly functional genome editors by modelling ... [https://www.nature.com/articles/s41586-025-09298-z]
- 14. Neurons repair CRISPR damage with unique timing [https://crisprmedicinenews.com/news/neurons-repair-crispr-damage-with-unique-timing/]
- 15. The hidden risks of CRISPR/Cas: structural variations and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325979/]
- 16. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 17. Genome Editing in iPSC-Based Neural Systems [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2021.630600/full]
- 18. Overcoming Barriers of CRISPR Gene Editing in iPS Cells [https://www.synthego.com/blog/ipsc-crispr-editing/]
- 19. CRISPR and iPSCs: Recent Developments and Future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9428373/]
- 20. Application Of CRISPR Technology In iPSC Gene Correction [https://www.cellandgene.com/doc/application-of-crispr-technology-in-ipsc-gene-correction-0001]
- 21. CRISPR/Cas9 and iPSC-Based Therapeutic Approaches in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291668/]
- 22. Modeling Human Neural Development and Disease with ... [https://www.isscr.org/upcoming-programs/poster-award-webinar]
- 23. Induced pluripotent stem cell technology: a decade of progress [https://pmc.ncbi.nlm.nih.gov/articles/PMC6416143/]
- 24. Induced pluripotency: history, mechanisms, and applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC2956203/]
- 25. Induction of pluripotent stem cells from mouse embryonic ... [https://pubmed.ncbi.nlm.nih.gov/16904174/]
- 26. Publications | Shinya Yamanaka (Director Emeritus & ... [https://www.cira.kyoto-u.ac.jp/e/research/yamanaka_results.html]
- 27. Considerations for the development of iPSC-derived cell ... [https://www.sciencedirect.com/science/article/pii/S1465324924007308]
- 28. Drug discovery research with the iPSC models of ... [https://www.sciencedirect.com/science/article/pii/S0168010225001683]
- 29. Induced Pluripotent Stem Cells and CRISPR-Cas9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11201389/]
- 30. Different iPSC-derived neural stem cells shows various ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10186475/]
- 31. Sequential factor delivery enables efficient workflow for ... [https://www.nature.com/articles/s41598-025-17876-4]
- 32. Methods for Optimizing CRISPR-Cas9 Genome Editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4976696/]
- 33. Precise measurement of CRISPR genome editing ... [https://www.sciencedirect.com/science/article/pii/S2329050125000440]
- 34. Editing the genome of hiPSC with CRISPR/Cas9: disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5569153/]
- 35. Modeling mutation-specific arrhythmogenic phenotypes in ... [https://www.nature.com/articles/s41598-024-52871-1]
- 36. Generation of three isogenic control lines from patient- ... [https://www.sciencedirect.com/science/article/pii/S1873506123001551]
- 37. A high efficiency precision genome editing method with ... [https://www.nature.com/articles/s41598-024-60766-4]
- 38. Quantitative analysis of CRISPR/Cas9-mediated provirus ... [https://www.nature.com/articles/s41598-022-19861-7]
- 39. Protocol for high-efficiency generation of iPSCs stably ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12272859/]
- 40. CRISPR Guide [https://www.addgene.org/guides/crispr/]
- 41. qEva-CRISPR: a method for quantitative evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6158505/]
- 42. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590075/]
- 43. Stem cell and CRISPR/Cas9 gene editing technology in ... [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1612868/full]
- 44. CRISPR-Based Gene Editing Standardizes Stem Cell ... [https://www.synthego.com/blog/nih-indi-alzheimers-ipscs/]
- 45. CRISPR in Parkinson's Disease: Research, Gene Therapy, ... [https://www.synthego.com/blog/crispr-parkinson-research/]
- 46. CRISPR in Amyotrophic Lateral Sclerosis: Disease ... [https://www.synthego.com/blog/crispr-als-gene-therapy/]
- 47. Harnessing CRISPR technology for next-generation ... [https://www.sciencedirect.com/science/article/pii/S0165993625000329]
- 48. Human brain organoids: an innovative model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417440/]
- 49. Modeling neurodegenerative diseases with brain organoids [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1663286/full]
- 50. Technologies and applications of current human cardiac ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12648008/]
- 51. Application of brain organoids in neurodevelopmental ... [https://www.sciencedirect.com/science/article/abs/pii/S0006291X25011209]
- 52. A comprehensive analysis of induced pluripotent stem cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1593207/full]
- 53. Stem cell disease modeling: A new era for drug discovery [https://www.abcam.com/en-us/stories/articles/stem-cell-disease-modeling]
- 54. High Throughput Screening Market [https://www.futuremarketinsights.com/reports/high-throughput-screening-market]
- 55. High Throughput Screening (HTS) Market Size 2025-2029 [https://www.technavio.com/report/high-throughput-screening-market-industry-analysis]
- 56. CRISPR-Cas9-mediated homology-directed repair for ... [https://www.sciencedirect.com/science/article/pii/S2162253124002312]
- 57. Fine-Tuning Homology-Directed Repair (HDR) for Precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071731/]
- 58. Current Strategies for Increasing Knock-In Efficiency in ... [https://www.mdpi.com/1422-0067/25/5/2456]
- 59. Synergistic gene editing in human iPS cells via cell cycle ... [https://www.nature.com/articles/s41467-020-16643-5]
- 60. Optimizing CRISPR methodology for precise gene editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580712/]
- 61. The hidden risks of CRISPR/Cas: structural variations and ... [https://www.nature.com/articles/s41467-025-62606-z]
- 62. Efficient homology-directed gene editing by CRISPR/Cas9 ... [https://www.nature.com/articles/s41598-018-30227-w]
- 63. CRISPR Off-Target Editing: Prediction, Analysis, and More [https://www.synthego.com/blog/crispr-off-target-editing/]
- 64. Revolutionizing CRISPR technology with artificial intelligence [https://www.nature.com/articles/s12276-025-01462-9]
- 65. dbGuide: a database of functionally validated guide RNAs for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7779039/]
- 66. Validated gRNA Sequences [https://www.addgene.org/crispr/reference/grna-sequence/]
- 67. Stem cell and CRISPR/Cas9 gene editing technology in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417523/]
- 68. Human iPSCs and Genome Editing Technologies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8273765/]
- 69. AI‐Driven Quality Monitoring and Control in Stem Cell Cultures [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336434/]
- 70. Optimization of gene knockout approaches and sgRNA ... [https://www.nature.com/articles/s41598-025-24184-4]
- 71. CMN Weekly (31 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-31-october-2025-your-weekly-crispr-medicine-news/]
- 72. From nascent to mainstream: Overcoming barriers in iPSC ... [https://ct.catapult.org.uk/news/from-nascent-to-mainstream-overcoming-barriers-in-ipsc-therapy-development]
- 73. Pluripotent Stem Cell (PSC) Protocols [https://www.thermofisher.com/us/en/home/references/protocols/cell-culture/stem-cell-protocols/ipsc-protocols.html]
- 74. 2025 cell and gene challenges: Scalability, supply chain ... [https://www.cellgenetherapyreview.com/3975-Featured-Articles/617533-2025-cell-and-gene-challenges-Scalability-supply-chain-and-manufacturing/]
- 75. Next-generation CRISPR gene editing tools in the ... [https://www.sciencedirect.com/science/article/abs/pii/S1568163725001977]
- 76. Cell-based drug discovery: Why human iPSC-derived ... [https://www.bit.bio/blog/cell-based-drug-discovery-with-human-ipsc-models]
- 77. The importance of benchmarking in biomarker discovery ... [https://www.projectguru.in/benchmarking-biomarker/]
- 78. Replacing Animal Testing with Stem Cell-Organoids [https://pmc.ncbi.nlm.nih.gov/articles/PMC11319430/]
- 79. In Vitro vs In Vivo: A History of Modern Cell Culture [https://emulatebio.com/in-vitro-vs-in-vivo-cell-culture/]
- 80. 2D and 3D cell cultures – a comparison of different types of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6040128/]
- 81. Primary cells vs. cell lines: Is it not time for something better? [https://www.bit.bio/blog/primary-cells-vs-cell-lines]
- 82. Microengineered systems with iPSC-derived cardiac and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7859673/]
- 83. iPSC-cardiomyocytes in the preclinical prediction of ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1308217/full]
- 84. Practical considerations for data exploration in quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12045597/]
- 85. Collecting and presenting data - JBC Author Resources [https://jbcresources.asbmb.org/collecting-and-presenting-data]
- 86. Advancing CRISPR genome editing into gene therapy clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094669/]
- 87. CRISPR-Cas System: The Current and Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10136740/]
- 88. Global research dynamics in the induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12272591/]
- 89. CRISPR/Cas9 therapeutics: progress and prospects [https://www.nature.com/articles/s41392-023-01309-7]
- 90. Understanding FDA Cell and Gene Therapy Guidance [https://www.synthego.com/blog/fda-cell-and-gene-therapy-guidance/]
- 91. FDA Announces Plan to Phase Out Animal Testing ... [https://www.fda.gov/news-events/press-announcements/fda-announces-plan-phase-out-animal-testing-requirement-monoclonal-antibodies-and-other-drugs]
- 92. Innovative Designs for Clinical Trials of Cellular and Gene ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/innovative-designs-clinical-trials-cellular-and-gene-therapy-products-small-populations]
- 93. Cellular & Gene Therapy Guidances [https://www.fda.gov/vaccines-blood-biologics/biologics-guidances/cellular-gene-therapy-guidances]
- 94. CRISPR Cell and Gene Therapies: Key Challenges in ... [https://www.synthego.com/blog/crispr-cell-gene-therapy-obstacles/]