Decellularized Extracellular Matrix Scaffolds: Harnessing Native Microenvironments for Advanced Stem Cell Engraftment
This article provides a comprehensive analysis of decellularized extracellular matrix (dECM) as a biological scaffold for stem cell-driven tissue engineering and regenerative medicine.
Decellularized Extracellular Matrix Scaffolds: Harnessing Native Microenvironments for Advanced Stem Cell Engraftment
Abstract
This article provides a comprehensive analysis of decellularized extracellular matrix (dECM) as a biological scaffold for stem cell-driven tissue engineering and regenerative medicine. Tailored for researchers, scientists, and drug development professionals, it explores the foundational science behind dECM, detailing how its tissue-specific composition and structure provide a unique niche for controlling stem cell fate. The content systematically reviews current decellularization and recellularization methodologies, addresses critical challenges in scaffold optimization and biocompatibility, and evaluates the efficacy of dECM through comparative analyses with synthetic alternatives. By synthesizing current research and future directions, this resource aims to bridge translational gaps and inform the development of next-generation regenerative therapies and advanced in vitro models for drug discovery.
The Biological Blueprint: How Decellularized ECM Creates an Ideal Stem Cell Niche
Decellularization represents a cornerstone bioprocessing technique in regenerative medicine and tissue engineering. It is defined as the process of removing all cellular and nuclear material from native tissues or organs while minimizing damage to the structural and functional components of the extracellular matrix (ECM) [1] [2]. The fundamental objective is to create a natural, bioactive scaffold that retains the intricate architecture and biochemical cues of the original tissue, thereby providing an optimal microenvironment for cell attachment, proliferation, and differentiation [3].
The critical goal of preserving the native ECM cannot be overstated, as this complex three-dimensional network serves not merely as a passive structural support but as a dynamic regulator of cellular behavior [1]. A successfully decellularized ECM scaffold maintains tissue-specific biochemical composition—including collagens, elastin, glycosaminoglycans (GAGs), and growth factors—and biomechanical properties that are essential for guiding tissue-specific regeneration [1] [4]. Within the context of stem cell engraftment research, these preserved elements provide the necessary topological, mechanical, and biochemical signals that direct stem cell fate, integration, and functional tissue formation [5].
This Application Note delineates the core principles of decellularization, provides standardized protocols for quality assessment, and details experimental methodologies for creating ECM scaffolds that effectively support stem cell research and engraftment applications.
Core Principles and Quantitative Assessment of Decellularization
Effective decellularization hinges on balancing complete cell removal with maximal ECM preservation. The process must eliminate immunogenic cellular components—particularly DNA and cell membrane antigens—that could trigger adverse immune responses upon implantation [4]. Concurrently, it must conserve the native ECM's structural integrity and bioactive composition to facilitate constructive remodeling and stem cell integration [1].
Quantitative Metrics for Decellularization Efficacy
Rigorous assessment is mandatory to verify decellularization success. The table below summarizes the key quantitative and qualitative metrics used to evaluate decellularized scaffolds.
Table 1: Key Assessment Metrics for Decellularized ECM Scaffolds
| Assessment Category | Specific Metric | Target Value for Effective Decellularization | Analytical Methods |
|---|---|---|---|
| Cellular Removal | Double-stranded DNA (dsDNA) content | < 50 ng per mg of dry tissue weight [5] | DNA quantification assay (e.g., DNeasy Kit) [6] |
| DNA fragment length | < 200 base pairs [5] | Gel electrophoresis | |
| Visual absence of nuclear material | No visible nuclei in stained sections [7] | H&E staining, DAPI staining [7] [8] | |
| ECM Composition Preservation | Collagen content | Maintained relative to native tissue | Hydroxyproline assay, Sirius Red staining [8] |
| Glycosaminoglycan (GAG) content | Minimized loss (varies by protocol) | Dimethylmethylene blue (DMMB) assay, Alcian blue staining [7] [8] | |
| Elastin and other structural proteins | Maintained architecture and content | Masson's Trichrome, Immunofluorescence [7] [6] | |
| Structural & Mechanical Integrity | Ultrastructure | Preserved microarchitecture (e.g., fibrillar collagen, lamellae) | Scanning Electron Microscopy (SEM), Transmission Electron Microscopy (TEM) [7] [9] |
| Mechanical properties | Matches native tissue tensile/compressive strength | Uniaxial tensile testing, compression testing [8] [6] | |
| Biocompatibility | Cytotoxicity | No cytotoxic effects on seeded cells | MTT assay, Live/Dead staining [7] [8] |
| Cell adhesion and proliferation | Supportive of cell growth | Seeding with relevant cell types (e.g., stem cells) [8] |
Decellularization Methodologies and Comparative Analysis
Decellularization protocols typically integrate chemical, biological, and physical methods. The optimal combination is highly dependent on the tissue's intrinsic properties, such as cellular density, lipid content, and ECM density [1] [2].
Classification of Primary Decellularization Methods
Table 2: Comparison of Primary Decellularization Methodologies
| Method Type | Specific Agents | Mechanism of Action | Advantages | Disadvantages & ECM Impact |
|---|---|---|---|---|
| Chemical Detergents | ||||
| Ionic (e.g., SDS, SDC) [1] [2] | Solubilizes cell membranes and nuclear material by disrupting lipid-protein bonds. | Highly effective for dense tissues; robust cell removal [8] [6]. | Can denature proteins, damage ultrastructure, and remove GAGs; difficult to rinse out completely [1] [8]. | |
| Non-ionic (e.g., Triton X-100) [1] [2] | Disrupts lipid-lipid and lipid-protein interactions. | Gentler on ECM structure; preserves collagen alignment [8] [9]. | Less effective at removing nuclear material; may require combination with other agents [7]. | |
| Zwitterionic (e.g., CHAPS, SB-10) [2] [9] | Properties of both ionic and non-ionic detergents. | Can be effective for specific tissues like nerves. | May disrupt the basement membrane [2]. | |
| Biological Agents | ||||
| Nucleases (DNase, RNase) [2] [8] | Cleaves DNA and RNA bonds to remove residual nucleic acids. | Highly effective at degrading genetic material. | Requires subsequent washing to remove enzymes; ineffective on its own without prior cell lysis [1]. | |
| Trypsin [2] [7] | Proteolytic enzyme cleaves peptide bonds, dissociating cells from ECM. | Rapidly disrupts cell-ECM adhesion. | Prolonged exposure severely damages ECM proteins and structure [1] [8]. | |
| Physical Methods | ||||
| Freeze-Thaw Cycles [2] [3] | Intracellular ice crystals form, lysing cell membranes. | Simple, cost-effective; eliminates cellular content. | Does not remove cellular debris; can damage ECM if ice crystals are too large [3]. | |
| Agitation & Perfusion [1] [6] | Mechanical force assists in detergent penetration and debris removal. | Can be applied to whole organs via vascular conduits [6] [5]. | Perfusion requires intact vasculature; agitation may damage delicate structures. |
Protocol Performance in Different Tissues
The efficacy of a decellularization agent is highly tissue-dependent. The table below synthesizes data from comparative studies across various tissues.
Table 3: Comparative Performance of Decellularization Agents Across Different Tissues
| Tissue Type | Evaluated Protocols | Key Findings on Efficacy and ECM Preservation | Source |
|---|---|---|---|
| Porcine Annulus Fibrosus | 1. Triton X-1002. SDS3. Trypsin | Triton X-100: Best overall; preserved concentric lamellar structure, collagen, highest GAG content, and mechanical properties.SDS: Removed cells but disturbed structure and decreased tensile strength.Trypsin: Disrupted tissue architecture. | [8] |
| Human Umbilical Cord | 1. Trypsin2. Triton X-1003. SDC4. Combined (Trypsin+Triton+SDC) | Combined Protocol: Most effective; removed most cellular components while retaining collagen, GAGs, and microstructure. Single-agent protocols were less effective or more damaging. | [7] |
| Rat Sciatic Nerve | 1. DN-P1 (TBP + PAA)2. DN-P2 (SB-10, Triton, SDS) | DN-P1: Better conservation of ultrastructure and ECM components; high biocompatibility.DN-P2: Caused moderate disruption of endoneurium and perineurium. | [9] |
| Human Digits | Perfusion with SDS + Triton X-100 | Successful decellularization of complex VCA; preserved vascular integrity, collagen, elastin, GAGs, and tendon mechanical strength. | [6] |
Detailed Experimental Protocols
Combined Chemical Decellularization of Human Umbilical Cord
This protocol, adapted from a 2024 study, demonstrates an effective short-term (5-hour) combined strategy for dense connective tissue [7].
Workflow Diagram: Combined Decellularization Protocol
Reagents and Materials:
- Trypsin-EDTA solution (0.025% w/v, Thermo Fisher Scientific)
- Triton X-100 (5% v/v, Macklin Inc.)
- Sodium Deoxycholate (SD) (4% w/v, Macklin Inc.)
- Phosphate-Buffered Saline (PBS)
- Deionized water
- Orbital shaker incubator capable of maintaining 37°C and 120 rpm
Procedure:
- Tissue Preparation: Slice fresh or thawed human umbilical cord tissue longitudinally into thin sections (e.g., 5 cm × 2 cm × 0.5 cm). Rinse sections in ultrapure water on a shaking bed (120 rpm) three times for 10 minutes each.
- Enzymatic Treatment (Step 1): Transfer tissue to 0.025% trypsin-EDTA solution. Agitate at 37°C and 120 rpm for 1.5 hours to dissociate cells from the ECM.
- First Detergent Wash (Step 2): Transfer tissue to a 5% v/v solution of Triton X-100. Agitate at room temperature, 120 rpm for 1.5 hours to lyse cells and solubilize membranes.
- Second Detergent Wash (Step 3): Transfer tissue to a 4% w/v solution of Sodium Deoxycholate. Agitate at room temperature, 120 rpm for 2 hours to ensure complete removal of cellular debris.
- Washing: Thoroughly rinse the decellularized tissue with copious amounts of deionized water under agitation to remove all residual chemical reagents.
- Storage/Processing: The resulting dECM can be freeze-dried for storage or processed further into hydrogels or bioinks.
Quality Control: Confirm decellularization efficacy via H&E and DAPI staining (no visible nuclei), dsDNA quantification (<50 ng/mg dry weight), and ECM preservation via Masson's Trichrome (collagen), PAS staining (GAGs), and immunofluorescence [7].
Perfusion-Based Decellularization of Composite Tissues
For whole organs or complex vascularized composite allografts (VCAs) like human digits, perfusion decellularization is the preferred method as it utilizes the native vascular network to deliver decellularization agents [6] [5].
Workflow Diagram: Perfusion Decellularization Protocol
Reagents and Materials:
- Peristaltic pump system (e.g., Masterflex L/S digital drive)
- Pressure transducer (e.g., PT-F, Living Systems Instrumentation) for real-time pressure monitoring (target 40-60 mmHg)
- Bubble trap (e.g., Radnoti) to prevent vascular embolism
- SDS solution (0.2% w/v in deionized water)
- Triton X-100 solution (1% v/v in deionized water)
- Sterile Phosphate-Buffered Saline (PBS)
Procedure:
- Cannulation and Setup: Cannulate the main artery (e.g., digital artery) of the tissue or organ and secure the catheter. Connect the cannula to the perfusion system equipped with a pressure transducer and bubble trap.
- Initial Wash: Perfuse with PBS for 1 hour at a flow rate that maintains a physiological pressure (e.g., 40-60 mmHg) to clear the vasculature of blood and debris.
- Primary Decellularization: Perfuse with 0.2% SDS solution for 120 hours. Continuously monitor vascular resistance and adjust flow rate to maintain target pressure.
- Intermediate Wash: Perfuse with deionized water for 24 hours to help remove ionic detergents and cellular debris.
- Secondary Decellularization: Perfuse with 1% Triton X-100 solution for 24 hours to remove residual cellular material and SDS.
- Final Wash: Perfuse with PBS for 48 hours to thoroughly remove all residual detergents from the scaffold.
- Sterilization (Optional): Perfusion with 0.1% Peracetic Acid (PAA) can be incorporated for simultaneous sterilization [9].
Quality Control: Assess vascular integrity via contrast-enhanced X-ray. Evaluate decellularization by quantifying DNA in various tissue components (skin, vessel, muscle, nerve, bone) and confirm ECM preservation through histology and biochemical assays for collagen, elastin, and GAGs [6].
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Key Research Reagent Solutions for Decellularization
| Reagent/Material | Primary Function | Key Considerations for Use |
|---|---|---|
| Sodium Dodecyl Sulfate (SDS) | Ionic detergent for efficient cell lysis and DNA removal in dense tissues. | Use minimal effective concentration and duration; requires extensive washing due to cytotoxicity and potential for ECM damage [1] [8]. |
| Triton X-100 | Non-ionic detergent for gentle cell membrane disruption and lipid removal. | Better preserves ECM structure than SDS but may be insufficient as a standalone agent; often used in combination protocols [7] [8]. |
| Trypsin-EDTA | Proteolytic enzyme solution for dissociating cells from the ECM. | Exposure time is critical; prolonged use severely degrades ECM proteins like collagen and fibronectin [1] [8]. |
| DNase/RNase | Enzymes for digesting residual nucleic acid fragments post-cell lysis. | Essential for reducing fragment length and removing immunogenic DNA; used after initial detergent treatment [2] [8]. |
| Tri(n-butyl) phosphate (TBP) | Organic solvent for decellularizing compact tissues like tendons and nerves. | Can penetrate dense structures effectively; shown to preserve ultrastructure in nerve grafts [9]. |
| Peracetic Acid (PAA) | Oxidizing agent used for sterilization and to enhance tissue permeability. | Can be integrated into protocols to reduce detergent concentrations and simultaneously sterilize the scaffold [1] [9]. |
| Peristaltic Pump & Pressure Transducer | Enables perfusion decellularization of whole organs/VCAs via vascular conduits. | Critical for monitoring and maintaining physiological pressures to avoid damaging the delicate vascular network [6] [5]. |
Successful decellularization for stem cell engraftment research is a deliberate balancing act. The protocols and assessment metrics detailed in this application note provide a framework for generating high-quality, reproducible dECM scaffolds. The chosen method must be tailored to the specific tissue, with the unrelenting goal of preserving the native ECM's compositional, structural, and mechanical integrity. By adhering to these principles and rigorously validating scaffold quality, researchers can create powerful, biomimetic platforms that harness the innate signaling of the ECM to direct stem cell behavior, thereby advancing the frontiers of regenerative medicine and therapeutic development.
In the field of regenerative medicine, decellularized extracellular matrix (dECM) scaffolds have emerged as a premier biomaterial platform for stem cell engraftment research. These scaffolds are produced by removing all cellular components from native tissues while preserving the intricate structural and functional proteins of the native extracellular matrix (ECM). This process creates a natural, three-dimensional microenvironment that retains tissue-specific biological cues essential for guiding stem cell adhesion, proliferation, differentiation, and functional tissue formation [1] [10]. The preserved ECM components serve not only as a structural foundation but also as a biochemical signaling reservoir that closely mimics the native stem cell niche, making dECM scaffolds particularly valuable for studying and facilitating stem cell engraftment.
The critical importance of dECM scaffolds lies in their ability to provide a biomimetic microenvironment that synthetic scaffolds cannot fully replicate. By maintaining the complex architecture and bioactive composition of native ECM, these scaffolds create an inductive environment for stem cells. The preservation of key structural proteins and glycosaminoglycans allows researchers to investigate stem cell-ECM interactions under conditions that closely resemble in vivo physiology, providing critical insights for drug development and therapeutic applications [10] [11]. This application note details the core protein composition of acellular scaffolds and provides standardized protocols for their analysis in the context of stem cell research.
Core Structural and Functional Proteins
The functionality of acellular scaffolds in stem cell engraftment research depends on the preservation and composition of four key ECM components: collagens, elastin, laminin, and glycosaminoglycans. Each component contributes distinct structural and biological properties that collectively create a hospitable microenvironment for stem cells.
Quantitative Composition of Key ECM Proteins
Table 1: Core protein composition and functions in acellular scaffolds
| ECM Component | Primary Function | Key Characteristics | Role in Stem Cell Engraftment |
|---|---|---|---|
| Collagen | Provides tensile strength and structural integrity [1] | Most abundant protein in human body (≈30% of total protein); multiple types (I, II, III, IV) with tissue-specific distribution [12] [11] | Guides cell adhesion through integrin binding; influences stem cell differentiation through mechanical signaling [1] [11] |
| Elastin | Confers elasticity and resilience to tissues [1] | Provides recoil in tissues subjected to repeated stretch (vessels, lungs, skin); extensive cross-linking via lysyl oxidase [12] [11] | Maintains tissue integrity during dynamic mechanical processes; important for vascular and pulmonary tissue engineering |
| Laminin | Basement membrane foundation; cell adhesion and signaling [12] | Cross-shaped glycoprotein; forms networks in basal laminae; essential for early embryonic development [12] [11] | Critical for epithelial and endothelial cell attachment; regulates stem cell survival, morphology, and differentiation [13] |
| Glycosaminoglycans (GAGs) | Regulation of hydration, compressive resistance, and growth factor binding [1] | Highly negatively charged polysaccharides (heparan sulfate, chondroitin sulfate, keratan sulfate, hyaluronic acid) [12] | Reservoir for growth factors and cytokines; modulates stem cell differentiation through controlled factor release [1] [10] |
Specialized ECM Components and Their Functions
Table 2: Additional ECM components with significant biological functions
| Component | Category | Function in Scaffold |
|---|---|---|
| Fibronectin | Glycoprotein | Connects cells with collagen fibers in ECM; facilitates cell movement; binds integrins and reorganizes cytoskeleton [12] [13] |
| Proteoglycans | Protein + GAGs | Control matrix hydration; establish permeability barriers; serve as reservoirs for growth factors and cytokines [1] [11] |
| Matrix-bound vesicles | Extracellular vesicles | Contain DNA, RNA, proteins, lipids; modify macrophage activation; alter cell proliferation and migration [12] |
| Growth Factors | Bioactive molecules | TGF-β, VEGF, FGF, BMPs stored in ECM; released during remodeling to guide angiogenesis and stem cell differentiation [10] |
Experimental Protocols for Scaffold Analysis
Protocol 1: DNA Quantification for Decellularization Verification
Purpose: To verify effective removal of cellular material by quantifying residual DNA content in dECM scaffolds, ensuring minimal immunogenicity for stem cell engraftment studies.
Materials and Reagents:
- DNeasy Blood & Tissue Kit
- Nanodrop spectrophotometer or equivalent
- Microbalance (0.1 mg sensitivity)
- PBS buffer (pH 7.4)
- Liquid nitrogen and mortar/pestle
Procedure:
- Obtain 25 mg biopsy samples from multiple regions of the decellularized scaffold (center and periphery)
- Homogenize tissue samples using liquid nitrogen and mortar/pestle
- Extract DNA using DNeasy Blood & Tissue Kit according to manufacturer's protocol
- Quantify purified DNA using absorbance at 260 nm with Nanodrop
- Calculate DNA content as weight of DNA per weight of wet tissue (ng/mg)
- Compare against established criteria for acellular scaffolds (<50 ng/mg) [14] [15]
Quality Control: Include positive control (native tissue) and negative control (reagent only) in each assay batch. Effective decellularization should reduce DNA content by >95% compared to native tissue.
Protocol 2: Quantitative Glycosaminoglycan (GAG) Assay
Purpose: To quantify GAG retention in dECM scaffolds, as GAGs are critical for growth factor binding and stem cell differentiation signaling.
Materials and Reagents:
- Papain digestion solution (100 mM phosphate buffer, 10 mM cysteine HCl, 10 mM EDTA, pH 6.5)
- Papain enzyme (20 μg/mL final concentration)
- Dimethylene blue dye solution
- Chondroitin sulfate standards (0-100 μg/mL)
- Spectrophotometer or microplate reader
Procedure:
- Digest 10 mg scaffold samples in papain solution at 60°C for 18 hours
- Centrifuge digested samples at 10,000 × g for 10 minutes
- Aliquot supernatant and mix with dimethylene blue dye solution
- Measure absorbance at 525 nm immediately after mixing
- Calculate GAG content from standard curve using chondroitin sulfate
- Express results as μg GAG per mg wet weight of tissue [14]
Applications: GAG content correlates with scaffold bioactivity and growth factor retention capacity, important predictors of stem cell engraftment success.
Protocol 3: Immunohistochemical Analysis of ECM Proteins
Purpose: To visualize and semi-quantitatively analyze spatial distribution of key ECM proteins in dECM scaffolds.
Materials and Reagents:
- 10% neutral buffered formalin
- Paraffin embedding system
- Microtome
- Primary antibodies: collagen I, collagen IV, elastin, laminin
- HRP-conjugated secondary antibodies
- DAB peroxidase substrate
- Hematoxylin counterstain
Procedure:
- Fix scaffold samples in 10% neutral buffered formalin for 24 hours
- Process tissues through graded ethanol series and embed in paraffin
- Section tissues at 5 μm thickness using microtome
- Deparaffinize and rehydrate sections through xylene and graded ethanol series
- Perform antigen retrieval using appropriate buffer (citrate or EDTA)
- Block endogenous peroxidase activity and nonspecific binding sites
- Incubate with primary antibodies overnight at 4°C
- Detect with HRP-conjugated secondary antibodies and DAB substrate
- Counterstain with hematoxylin, dehydrate, and mount
- Image using digital slide scanner and analyze protein distribution [14]
Signaling Pathways in Stem Cell-ECM Interactions
The interaction between stem cells and acellular scaffolds activates multiple signaling pathways that direct stem cell fate decisions. These pathways are primarily triggered through integrin-mediated recognition of ECM components and subsequent mechanotransduction events.
ECM-Stem Cell Signaling Pathways
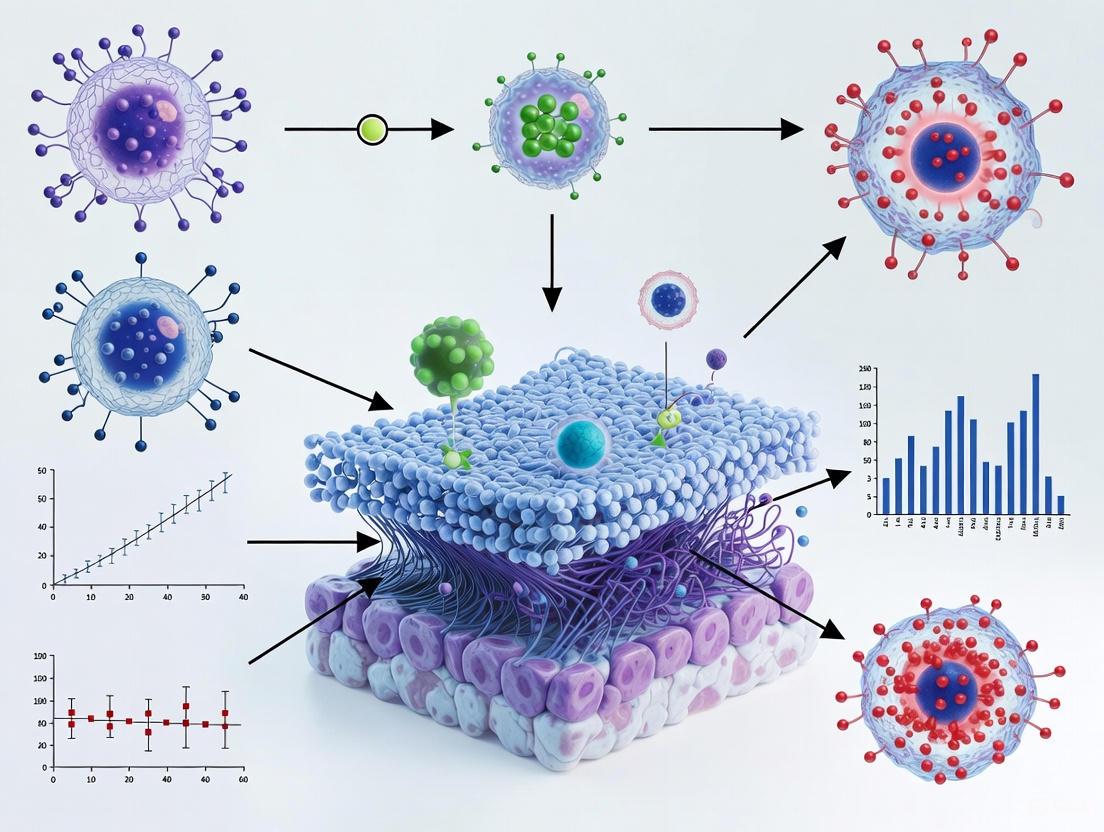
The diagram illustrates two primary mechanisms of stem cell-ECM interaction: biochemical signaling initiated when integrin receptors recognize ECM ligands such as collagen, laminin, and fibronectin, and mechanotransduction where cells sense mechanical properties of the ECM including stiffness and elasticity. These signals converge to regulate gene expression programs that ultimately determine stem cell fate decisions including proliferation, migration, and differentiation [1] [11]. The integrin-FAK signaling axis activates both MAPK and PI3K/Akt pathways, while mechanical cues influence gene expression through cytoskeletal reorganization and YAP/TAZ translocation [12] [11].
Research Reagent Solutions
Table 3: Essential research reagents for dECM scaffold analysis
| Reagent/Category | Specific Examples | Research Application | Function |
|---|---|---|---|
| Decellularization Agents | Sodium dodecyl sulfate (SDS), Triton X-100, Triton X-200, Sodium deoxycholate [1] [10] | Scaffold preparation | Remove cellular components while preserving ECM structure and bioactivity |
| DNA Quantification Kits | DNeasy Blood & Tissue Kit [14] | Quality control | Assess decellularization efficiency by measuring residual DNA content |
| Histological Stains | Hematoxylin & Eosin, Masson's Trichrome, Van Gieson's stain [14] | Structural analysis | Visualize tissue architecture, collagen distribution, and elastic fibers |
| ECM Component Assays | Total Collagen Assay Kit, Dimethylene Blue GAG Assay [14] | Quantitative analysis | Measure specific ECM component retention after decellularization |
| Growth Factor Arrays | RayBio Human Growth Factor Antibody Array [14] | Bioactivity assessment | Profile retained growth factors (VEGF, FGF, TGF-β) in dECM scaffolds |
| Cell Culture Reagents | Endothelial cells, muscle stem cells, Schwann cells [15] [16] | Functional assessment | Evaluate scaffold biocompatibility and stem cell engraftment potential |
The core structural and functional proteins preserved in acellular scaffolds—collagen, elastin, laminin, and glycosaminoglycans—collectively create a biomimetic microenvironment that is indispensable for advancing stem cell engraftment research. These components provide not only the structural foundation for tissue development but also the critical biochemical and biophysical cues that direct stem cell fate decisions. The experimental protocols outlined in this application note provide standardized methodologies for characterizing these key components, ensuring that researchers can consistently evaluate and qualify dECM scaffolds for stem cell research applications. As tissue engineering and regenerative medicine continue to evolve, understanding and optimizing the composition of acellular scaffolds will remain fundamental to developing effective stem cell-based therapies and advancing drug development platforms.
The extracellular matrix (ECM) is far more than a passive, structural scaffold for tissues; it is a dynamic, information-rich environment that actively directs stem cell fate. Within the context of regenerative medicine and decellularized tissues, understanding how matrix-bound cues guide stem cell behavior is paramount for developing effective therapies. Decellularized ECM (dECM) serves as an ideal biomimetic platform, retaining the complex biochemical composition and three-dimensional architecture of native tissue, thereby providing a multitude of physical and chemical signals. These signals are interpreted by stem cells through a process known as mechanotransduction, influencing critical cellular decisions including adhesion, proliferation, and differentiation [17] [18]. This application note details the mechanisms by which these matrix-bound cues exert their effects and provides standardized protocols for investigating these phenomena in a research setting, with a specific focus on applications within dECM scaffold technology.
The following tables consolidate key quantitative data on how specific matrix properties influence mesenchymal stem cell (MSC) behavior, serving as a critical reference for designing experiments with dECM scaffolds.
Table 1: Influence of Substrate Stiffness on MSC Lineage Specification
| Target Lineage | Substrate Stiffness Range | Key Morphological and Molecular Markers | Reference Model Tissue |
|---|---|---|---|
| Neurogenic | 0.1 - 1 kPa | Branched, filopodia-rich morphology; expression of neuronal precursors | Brain [17] [19] [20] |
| Myogenic | 8 - 17 kPa | Elongated, spindle-shaped morphology; expression of MyoD | Muscle [17] [19] |
| Chondrogenic | 20 - 25 kPa (3D) | Round cell morphology; expression of chondrogenic markers | Cartilage [20] |
| Osteogenic | 25 - 40 kPa (2D) | Spread, polygonal morphology; expression of Runx-2, alkaline phosphatase (ALP) | Collagenous bone [17] [19] [20] |
Table 2: Impact of Scaffold Biophysical Cues on MSC Behavior
| Biophysical Cue | Parameter Range | Impact on MSC Behavior |
|---|---|---|
| Cell Shape / Micropatterning | Small islands (<1600 μm²) vs. Large islands | Round shape promotes adipogenesis; spread shape promotes osteogenesis [17] |
| Cell Density | Low vs. High Density | Low density promotes osteogenesis (ALP expression); high density promotes adipogenesis [17] |
| Aspect Ratio | 1:1 vs. 4:1 (constant area) | ∼20% higher osteogenesis on 4:1 aspect ratio patterns [17] |
| Edge Curvature | High curvature (flower) vs. Straight edges (star) | High curvature promotes adipogenesis; straight edges stimulate osteogenic differentiation [17] |
Key Mechanotransduction Signaling Pathways
Cells perceive mechanical cues from the dECM through surface receptors, primarily integrins, which cluster to form focal adhesions. These structures act as bidirectional mechanical links, transmitting forces from the ECM to the intracellular cytoskeleton and vice versa. The resulting cytoskeletal tension, generated by actin-myosin contractility, activates downstream signaling pathways that ultimately lead to transcriptional changes in the nucleus.
Application Notes & Experimental Protocols
Protocol 4.1: Preparation and Characterization of Decellularized ECM (dECM) Scaffolds
This protocol outlines a standard method for preparing dECM from soft tissues (e.g., cartilage, testis) using a combination of physical and chemical decellularization, as validated in recent studies [21] [22].
Workflow Diagram:
Materials:
- Native Tissue Source: (e.g., Porcine aorta, rat testis, bovine cartilage).
- Detergents: 1% Triton X-100, 1% Sodium dodecyl sulfate (SDS), or 0.5% Sodium lauryl ether sulfate (SLES).
- Buffers: Phosphate-Buffered Saline (PBS), DNase/RNase solution.
- Equipment: Biological shaker or magnetic stirrer, -80°C freezer.
Procedure:
- Physical Pre-treatment: Rinse the tissue in PBS and puncture the capsule if present. Subject the tissue to at least three cycles of freezing at -80°C and thawing at room temperature. This process forms ice crystals that lyse cells [22].
- Chemical Decellularization:
- Washing: Wash the decellularized tissue in sterile PBS for a minimum of 3 hours, with multiple buffer changes, to thoroughly remove all residual detergents.
- Sterilization & Storage: Store the dECM scaffolds in sterile PBS at 4°C for immediate use, or freeze at -80°C for long-term storage.
Validation & Quality Control:
- Histology: Perform Hematoxylin and Eosin (H&E) and Hoechst staining to confirm the absence of visible cell nuclei [21] [22].
- DNA Quantification: Use a DNA quantification kit. A successful decellularization should show a significant reduction in DNA content compared to native tissue [22].
- ECM Composition: Use staining (e.g., Masson's Trichrome for collagen, Alcian Blue for glycosaminoglycans (GAGs)) and immunohistochemistry (e.g., for Collagen I, IV) to confirm the retention of key ECM components [21] [22].
Protocol 4.2: Functionalization of dECM with Bioactive Factors
To enhance the therapeutic potential of dECM, it can be functionalized with specific growth factors. This protocol describes a method for incorporating factors like Brain-Derived Neurotrophic Factor (BDNF) into MSC spheroid-derived dECM, leveraging its endogenous GAGs for sustained release [23].
Procedure:
- Prepare MSC Spheroid-derived dECM: Assemble MSCs into 3D spheroids and decellularize using a mild surfactant (0.5% Triton X-100) to preserve endogenous GAGs [23].
- Growth Factor Incorporation: Incubate the 3D dECM constructs in a solution containing the desired growth factor (e.g., 100 ng/mL BDNF) for 24 hours at 4°C under gentle agitation. The preserved GAGs in the gently decellularized matrix will naturally sequester the growth factors without the need for chemical crosslinkers [23].
- Washing and Use: Gently rinse the functionalized dECM with buffer to remove unbound factor before cell seeding or implantation.
Protocol 4.3: Evaluating Stem Cell Response to dECM Scaffolds
This protocol describes how to seed and culture stem cells on dECM scaffolds and assess key outcomes: adhesion, proliferation, and differentiation.
Materials:
- Stem Cells: Human Mesenchymal Stem Cells (hMSCs), induced MSCs (hiMSCs), or other relevant progenitor cells.
- Culture Medium: Appropriate basal medium (e.g., DMEM) with necessary supplements (e.g., FBS). For differentiation, use defined induction media.
- dECM Scaffolds: Prepared and sterilized as per Protocol 4.1.
Procedure:
- Cell Seeding: Seed cells onto the dECM scaffold at a desired density (e.g., 1-5 x 10⁵ cells/scaffold) using a static or dynamic seeding method. Allow 2-4 hours for initial attachment before adding culture medium.
- Culture: Maintain cell-scaffold constructs in standard culture conditions (37°C, 5% CO₂). Change the medium every 2-3 days.
Analysis and Readouts:
- Cell Viability and Proliferation:
- Live/Dead Assay: Use calcein-AM (labels live cells green) and ethidium homodimer-1 (labels dead cells red) to visualize and quantify cell viability after 1, 3, and 7 days in culture [21].
- Metabolic Activity Assays: Use AlamarBlue or MTT assays at multiple time points to track proliferative activity.
- Cell Morphology and Adhesion:
- Scanning Electron Microscopy (SEM): Fix constructs, dehydrate, and sputter-coat with gold to visualize cell morphology and attachment to the ECM fibers [22].
- Differentiation Analysis:
- Gene Expression: Use RT-qPCR to measure the expression of lineage-specific markers (e.g., Runx2 for osteogenesis, SOX9 for chondrogenesis, PPARγ for adipogenesis) after 7-21 days in culture.
- Histological Staining: For chondrogenic differentiation, fix constructs, section, and stain with Alcian Blue to detect sulfated GAG deposition, a key marker of cartilage matrix production [21].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for dECM and Stem Cell Guidance Research
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Triton X-100 (Detergent) | Mild, non-ionic detergent for gentle cell membrane solubilization. | Decellularization of cell spheroids to preserve endogenous GAGs and growth factors [23]. |
| Sodium Dodecyl Sulfate (SDS) | Strong ionic detergent for efficient nuclear and cytoplasmic material removal. | Decellularization of dense tissues; requires careful optimization to avoid ECM damage [21] [22]. |
| Gellan Gum | Biocompatible polysaccharide hydrogel for 3D bioprinting and cartilage engineering. | Used as a base bioink mixed with dECM to improve printability and provide cartilage-like environment [21]. |
| Perfluorocarbons (PFCs) | Synthetic oxygen carriers with high oxygen solubility. | Incorporated into hydrogels to enhance oxygen supply and improve stem cell survival in hypoxic transplantation sites [24]. |
| Brain-Derived Neurotrophic Factor (BDNF) | Neurotrophic growth factor crucial for neuronal survival and outgrowth. | Loaded into MSC spheroid-derived dECM to create a pro-regenerative scaffold for brain repair [23]. |
| Dolichos Biflorus Agglutinin (DBA) | Lectin that binds specifically to spermatogonial stem cells (SSCs). | Used to identify and isolate SSCs for seeding onto decellularized testicular scaffolds [22]. |
The extracellular matrix (ECM) is a complex, three-dimensional network of proteins and carbohydrates that provides not only structural support but also critical biochemical and biomechanical cues to resident cells. Decellularized ECM (dECM) represents this native architecture after cellular components have been removed, preserving tissue-specific signaling motifs that guide cell behavior, differentiation, and function. The fundamental hypothesis driving dECM research posits that the unique compositional and structural properties of ECM from different tissues—such as liver, nerve, and cardiac—create distinct microenvironments that elicit specific cellular responses crucial for tissue regeneration [25].
The therapeutic potential of dECM is particularly valuable in the context of stem cell engraftment, where the goal is to enhance cell survival, integration, and functional tissue repair. Traditional synthetic biomaterials often lack the biological complexity required to direct sophisticated cellular processes. In contrast, tissue-specific dECM bioinks and scaffolds replicate native conditions more faithfully, making them superior substrates for regenerative applications [25]. This application note details the unique properties of liver, nerve, and cardiac dECM and provides standardized protocols for their use in stem cell research.
Comparative Analysis of Tissue-Specific dECM Compositions and Effects
The compositional profile of dECM varies significantly between tissues, directly influencing its functional properties and subsequent cellular interactions. The table below summarizes key characteristics and documented cellular responses for liver, nerve, and cardiac dECM.
Table 1: Quantitative and Functional Characteristics of Tissue-Specific dECM
| Tissue dECM | Key ECM Components | Documented Stem Cell Responses | Differentiation & Functional Markers Observed | Noted Advantages in Studies |
|---|---|---|---|---|
| Liver dECM | Collagens, Glycosaminoglycans, Laminin [25] | Enhanced hepatocyte function; Stem cell differentiation into hepatocyte-like cells [25] | Increased albumin production, urea synthesis, and cytochrome P450 activity [25] | Retains tissue-specific biochemical cues; Promotes rapid and enhanced hepatic function [25] |
| Nerve dECM | Laminin, Fibronectin, Collagens [26] [27] | MSC secretion of neurotrophic factors; Enhanced axon regeneration and myelination [26] [27] [28] | Increased expression of S100, GFAP, p75 NTR (Schwann cell-like markers) [27] | Provides a supportive microenvironment for axonal growth; Enhances functional motor recovery [26] [28] |
| Cardiac dECM | (Information not explicitly covered in search results) | (Information not explicitly covered in search results) | (Information not explicitly covered in search results) | (Information not explicitly covered in search results) |
Table 2: Experimental Outcomes in Preclinical Models Using Tissue-Specific Approaches
| Tissue System | Model Used | Key Functional Outcome Measures | Results |
|---|---|---|---|
| Liver dECM Bioink | 3D cell printing of HepG2 cells and stem cells [25] | Cell viability, metabolic function (e.g., albumin secretion), and gene expression of hepatic markers [25] | Superior enhancement of hepatocyte function and stem cell differentiation compared to standard collagen bioinks [25] |
| Nerve Repair with MSC-Seeded Grafts | Rat sciatic nerve 10mm defect [26] [27] | Isometric tetanic force (ITF), compound muscle action potential (CMAP), muscle mass, histology [26] [27] | Significantly improved ITF and CMAP at 12 weeks compared to acellular allografts; Outcomes comparable to autografts by 16 weeks [26] [27] |
Experimental Protocols for dECM Utilization
Protocol: Fabrication of Liver dECM Bioink for 3D Cell Printing
This protocol outlines the process for creating a bioink from liver-derived dECM, suitable for 3D bioprinting of liver tissue constructs [25].
Step 1: Tissue Decellularization
- Obtain fresh liver tissue from an approved source (e.g., porcine or rodent).
- Rinse thoroughly with deionized water to remove blood residues.
- Treat the tissue with a series of detergent solutions (e.g., 1% sodium dodecyl sulfate, SDS) under constant agitation to lyse cells and remove cellular debris.
- Wash extensively with deionized water and phosphate-buffered saline (PBS) to eliminate all traces of detergent.
- Verify decellularization by quantifying DNA content (should be <50 ng/mg of tissue dry weight) and staining for residual nuclei (e.g., DAPI).
Step 2: dECM Digestion and Bioink Formation
- Mince the acellular dECM matrix into small pieces (< 1 mm³).
- Digest the ECM material in a 0.1% pepsin solution in 0.1M HCl under constant agitation for approximately 48-72 hours until a viscous, homogeneous solution is formed.
- Neutralize the pH to 7.4 using 1M NaOH and dilute the pre-gel solution to the desired working concentration (e.g., 3-5 mg/ml) using PBS on ice to prevent premature gelation.
- The resulting liquid is the liver dECM bioink, ready for cell mixing and printing.
Step 3: 3D Bioprinting and Gelation
- Keep the bioink on ice throughout the printing process.
- Mix the bioink with the target cell population (e.g., HepG2 cells, MSCs, or primary hepatocytes) at a concentration of 1-10 million cells/mL.
- Load the cell-bioink mixture into a sterile printing cartridge.
- Print the construct using a 3D bioprinter onto a substrate maintained at 37°C to induce thermal gelation.
- Culture the printed constructs in appropriate media for downstream application or analysis.
Protocol: Seeding MSCs onto Decellularized Nerve Allografts
This protocol describes a dynamic seeding method to adhere Mesenchymal Stem Cells (MSCs) onto decellularized nerve allografts for peripheral nerve repair [26] [27].
Step 1: Preparation of Decellularized Nerve Allografts
- Harvest nerve tissue (e.g., sciatic nerve) and decellularize using a validated protocol involving detergents, enzymes, and washes to remove immunogenic cellular material while preserving the basal lamina structure.
- Sterilize the decellularized allografts using gamma irradiation and store in PBS at 4°C until use.
Step 2: MSC Culture and Optional Differentiation
- Isolate MSCs from a relevant source (e.g., rat adipose tissue or human bone marrow).
- Culture MSCs in growth medium (e.g., α-MEM supplemented with 5% platelet lysate and 1% Penicillin/Streptomycin).
- For differentiation into Schwann cell-like cells (optional):
- Upon reaching 70-80% confluence, replace the growth medium with a differentiation cocktail containing Forskolin, bFGF, PDGF-AA, and Neuregulin-1 ß1.
- Culture the cells in this medium for approximately 10-14 days, confirming differentiation via immunocytochemistry for markers like S100, GFAP, and p75 NTR [27].
Step 3: Dynamic Seeding of MSCs onto Allografts
- Trypsinize the undifferentiated or differentiated MSCs and resuspend them in growth medium. A typical seeding density is 1 x 10^6 cells in 10 mL of medium per graft [27].
- Place a single decellularized nerve allograft into a conical tube containing the cell suspension.
- Secure the tube on a bioreactor rotator and place it in an incubator (37°C, 5% CO2) for 12 hours to allow for dynamic, uniform cell adhesion.
- After rotation, remove the seeded graft from the tube. The graft is now ready for immediate implantation.
Signaling Pathways in Tissue-Specific Stem Cell Niches
The following diagram illustrates the key signaling pathways and cellular crosstalk within a stem cell niche supported by tissue-specific dECM. The dECM provides a complex scaffold that presents specific signals to resident or transplanted stem cells, guiding their fate.
Diagram 1: Stem Cell Niche Signaling
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful experimentation with dECM requires specific reagents and materials. The following table lists key solutions used in the protocols and literature cited herein.
Table 3: Key Research Reagent Solutions for dECM and Stem Cell Work
| Reagent / Material | Function / Application | Example from Protocols / Literature |
|---|---|---|
| Sodium Dodecyl Sulfate (SDS) | Ionic detergent for effective cell lysis and removal during tissue decellularization. | Used in liver dECM protocol for decellularization [25]. |
| Pepsin | Proteolytic enzyme used to digest the solid dECM matrix into a liquid pre-gel form for bioink. | Used to solubilize liver dECM in 0.1M HCl [25]. |
| Stromal Cell-Derived Factor-1 (SDF-1/CXCL12) | Key chemokine for stem cell homing; binds to CXCR4 receptor on MSCs. | Critical for MSC homing to injured liver; its receptor CXCR4 can be overexpressed to enhance engraftment [29] [30]. |
| Differentiation Cocktail (Forskolin, bFGF, PDGF-AA, NRG-1β1) | A defined set of factors to induce MSC differentiation into a Schwann cell-like phenotype in vitro. | Used to pre-differentiate MSCs before seeding onto nerve allografts [27]. |
| Platelet Lysate | A source of growth factors and proteins used as a serum supplement for robust MSC culture. | Component of the growth medium for expanding MSCs [27]. |
| Decellularized Nerve Allograft | Provides a natural, conductive scaffold for axonal regeneration in peripheral nerve defects. | Serves as a physical scaffold and cell carrier for MSCs in rat sciatic nerve model [26] [27]. |
The evidence underscores a clear principle: tissue-specific dECM provides a uniquely advantageous microenvironment that cannot be replicated by generic or synthetic scaffolds alone. Liver dECM bioink enhances hepatocyte function and stem cell differentiation, while nerve-specific dECM scaffolds seeded with MSCs create a permissive environment for functional axonal regeneration. The provided protocols and analytical tools offer a foundation for researchers to further explore and harness the distinct biological cues of cardiac and other tissue-specific dECMs. Advancing this field requires a commitment to standardized decellularization, rigorous characterization of ECM composition, and validation in physiologically relevant models to fully unlock the potential of dECMs in regenerative medicine and drug development.
From Protocol to Practice: Decellularization Techniques and Recellularization Strategies for Functional Tissue Engineering
Within the field of regenerative medicine, decellularized extracellular matrix (ECM) has emerged as a pivotal biological scaffold for stem cell engraftment research. The process of decellularization aims to remove all cellular material from native tissues while preserving the intricate composition and three-dimensional architecture of the native ECM [31] [10]. This resulting acellular scaffold provides a biomimetic niche that is critical for supporting the survival, proliferation, and differentiation of transplanted stem cells [24] [22]. The efficacy of a decellularization protocol is therefore measured not only by its removal of immunogenic cellular components but also by its retention of the ECM's biological and mechanical properties, which are essential for creating a hospitable microenvironment for stem cell engraftment [3] [32].
Decellularization techniques are broadly categorized into physical, chemical, and enzymatic methods, each with distinct mechanisms, advantages, and drawbacks. The selection and optimization of these methods are crucial, as they directly impact the scaffold's ability to support subsequent stem cell repopulation [3] [10]. Physical methods often serve as an initial step to lyse cells, while chemical and enzymatic agents are employed to remove cellular debris and nuclear material. However, the agents used, particularly ionic detergents, can disrupt ECM integrity, thereby diminishing the scaffold's bioactivity and potential for successful stem cell therapy [31] [33]. This document provides a comparative analysis of decellularization agents and detailed protocols, framed within the context of enhancing stem cell engraftment on decellularized tissues.
Comparative Analysis of Decellularization Agents
The choice of decellularization agent significantly influences the final scaffold's properties. The following sections and tables provide a detailed comparison of the various agents used.
Physical Methods
Physical methods are frequently used as a preliminary step to disrupt cell membranes and facilitate the penetration of subsequent chemical or enzymatic agents [3] [34]. They offer the advantage of avoiding residual toxic chemicals, which is beneficial for maintaining scaffold biocompatibility [31].
Table 1: Physical Decellularization Methods
| Method | Mechanism of Action | Key Advantages | Key Limitations/Damage | Typical Parameters |
|---|---|---|---|---|
| Freeze-Thaw (Thermal Shock) | Forms intracellular ice crystals that disrupt cell membranes [3] [34]. | Maintains mechanical properties; minimizes ECM disruption; reduces immune response [31] [3]. | Incomplete decellularization alone (up to 88% DNA may remain); ice crystal size must be controlled to prevent ECM damage [3] [34]. | 8 cycles of freezing in N₂ (15 min) and thawing at 60°C (15 min) [31]. |
| Ultrasound/Sonication | Applies mechanical sound waves to lyse cell walls [31] [3]. | Even distribution; effective for cell lysis and debris removal [31] [3]. | Standardized parameters not established; potential for ECM damage if over-applied [34]. | 70% power, 20 kHz wavelength, pulsed for 45 min [31]. |
| High Hydrostatic Pressure (HHP) | Applies extreme pressure (hundreds of MPa) to disrupt cell ultrastructure [3]. | Reduces decellularization time; retains ECM structure and immunocompatibility [3]. | Can induce ice crystal damage; requires combination treatments; limited to less compact tissues [3]. | ~980 MPa for 10 min [3]. |
| Mechanical Agitation | Uses physical movement to dislodge cells and debris [34]. | Simple to implement; assists chemical and enzymatic penetration [34]. | Aggressive agitation can damage ECM architecture; speed and time are tissue-dependent [34]. | Use of orbital shakers or rollers; parameters vary [34]. |
Chemical and Enzymatic Methods
Chemical and enzymatic agents are the workhorses of decellularization, responsible for solubilizing lipid membranes and degrading nucleic acids. Their efficacy and cytotoxicity are primary considerations for stem cell viability post-recellularization.
Table 2: Chemical and Enzymatic Decellularization Agents
| Agent Category | Specific Agent | Mechanism of Action | Impact on ECM & Stem Cell Engraftment | Residual DNA Post-Treatment |
|---|---|---|---|---|
| Ionic Detergents | Sodium Dodecyl Sulfate (SDS) [10] [33] | Solubilizes lipid membranes and cytoplasmic components; disrupts DNA-protein interactions [10]. | High Disruption: Damages collagen integrity; significantly reduces GAGs and growth factors; detrimental to recellularization [31] [10] [33]. | Highly effective removal, but can leave residual nuclear cages [31]. |
| Non-Ionic Detergents | Triton X-100 [10] [33] | Disrupts lipid-lipid and lipid-protein interactions, but not protein-protein bonds [10]. | Moderate Disruption: Less effective cell lysis; tissue-dependent efficacy; better preservation of ECM structure than SDS [10]. | Less effective than SDS; may require combination with other agents [10]. |
| Zwitterionic Detergents | CHAPS [10] | Combines properties of ionic and non-ionic detergents [10]. | Lower Disruption: Better preservation of ECM structure and composition compared to ionic detergents [10]. | Effective cell removal while preserving ECM [10]. |
| Enzymes | Trypsin [31] [33] | Cleaves peptide bonds, disrupting transmembrane proteins and cell-ECM adhesion [31]. | Can damage ECM proteins like collagen and GAGs if overused; concentration and time critical [31] [33]. | Effective at removing cellular proteins, but does not degrade DNA. |
| Nucleases | DNase, RNase [33] | Degrades nucleic acids (DNA and RNA) after cell lysis. | Essential for removing immunogenic genetic material; minimal direct impact on ECM proteins [33]. | Critical for reducing DNA to negligible levels [33]. |
| Hyper/Hypotonic Solutions | Sterile Water [35], 10% NaCl [35] | Induces osmotic shock to lyse cells. | Can effectively decellularize thin membranes like anterior lens capsules with good ECM preservation [35]. | Effective for specific, thin tissues [35]. |
Detailed Decellularization Protocols
This section outlines specific, reproducible protocols that have been successfully employed for various tissues, with a focus on preserving ECM integrity for stem cell research.
This protocol highlights a chemical-free approach, ideal for generating highly biocompatible scaffolds.
- Tissue Preparation: Obtain fresh bovine tracheal cartilage. Remove adipose tissue and perichondrium, and cut into ~1 mm² fragments.
- Hypotonic Incubation: Immerse cartilage fragments in a hypotonic Tris-HCL solution (pH 8).
- Freeze-Thaw Cycles: Subject the tissues to eight cycles of freezing in liquid nitrogen for 15 minutes, followed by thawing at 60°C for 15 minutes.
- Ultrasonic Treatment: Place samples in PBS and sonicate using a homogenizer (e.g., BANDELIN SONOPULS HD 2070) at 70% power with a 20 kHz wavelength in pulse mode for 45 minutes.
- Enzymatic Wash: Immerse and agitate tissues in 0.25% trypsin for 24 hours in a shaker incubator, changing the solution every 8 hours.
- Final Wash and Storage: Wash samples thoroughly with PBS to remove debris. The decellularized scaffolds can be freeze-dried and stored at -20°C.
This protocol demonstrates the optimization of detergent and enzyme use to minimize ECM damage.
- Tissue Preparation: Acquire fresh porcine aortic or pulmonary valves.
- Detergent Wash: Treat valves with a non-ionic detergent, specifically Tergitol (a substitute for Triton X-100), for a specified duration. Note: This protocol intentionally omits harsh ionic detergents like SDS.
- Enzymatic Treatment: Incubate with a low concentration of trypsin to disrupt cell-ECM adhesion, followed by treatment with a high concentration of DNase and RNase to thoroughly degrade nucleic acids.
- Confirmation: DNA quantification should show a reduction to nearly untraceable levels. The valves should appear off-white, without shrinkage or swelling, and maintain mechanical properties equivalent to native valves.
Workflow Diagram of Decellularization Strategies
The following diagram illustrates the logical decision-making process for selecting and combining decellularization methods to create an optimal scaffold for stem cell engraftment.
The Scientist's Toolkit: Essential Research Reagents
This table lists key reagents and their critical functions in the decellularization and stem cell engraftment pipeline.
Table 3: Essential Reagents for Decellularization and Recellularization Workflows
| Reagent / Material | Function / Application | Contextual Notes |
|---|---|---|
| Tergitol | Non-ionic detergent for cell membrane disruption [33]. | An eco-friendly alternative to Triton X-100; reduces ECM damage [33]. |
| DNase & RNase | Enzymatic degradation of nucleic acids to minimize immunogenicity [33]. | High concentrations are crucial for reducing DNA to untraceable levels [33]. |
| Trypsin | Proteolytic enzyme for disrupting cell-ECM adhesion [31]. | Use lower concentrations to minimize damage to ECM proteins like collagen [31] [33]. |
| Perfluorocarbons (PFCs) | Oxygen carriers in recellularization scaffolds [24]. | Enhance stem cell survival post-transplantation by mitigating ischemic stress in the hostile microenvironment [24]. |
| Calcium Peroxide (CaO₂) | Solid peroxide for sustained oxygen release in scaffolds [24]. | Used in oxygen-generating systems to support cell viability prior to neovascularization [24]. |
| Sodium Chloride (10%) | Hypertonic solution for osmotic shock [35]. | Effective for decellularizing thin basement membranes (e.g., anterior lens capsules) with good ECM preservation [35]. |
| Tris-HCL Buffer | Common buffer for hypotonic solutions and maintaining pH [31]. | Used in physical decellularization protocols to create a hypotonic environment for cell lysis [31]. |
The strategic selection and combination of decellularization agents are paramount to producing scaffolds that are not only acellular but also functionally competent for stem cell engraftment. Physical methods provide a gentle foundation, while the careful choice of chemical and enzymatic agents—favoring non-ionic over ionic detergents and optimizing nuclease concentrations—is critical for preserving the bioactive ECM niche. The protocols and data summarized herein provide a framework for researchers to design decellularization strategies that maximize scaffold biocompatibility and bioactivity, thereby addressing a key challenge in regenerative medicine: the creation of a hospitable microenvironment for transplanted stem cells. Future efforts must focus on the standardization of these protocols and rigorous in vivo validation of the engraftment efficiency and functional outcomes of stem cells seeded on these optimized scaffolds.
In the field of regenerative medicine, decellularized extracellular matrix (dECM) has emerged as a uniquely promising scaffold for stem cell engraftment research. Unlike synthetic alternatives, dECM preserves the natural microenvironment—a complex three-dimensional architecture of structural proteins, glycosaminoglycans (GAGs), and growth factors that are essential for guiding stem cell attachment, proliferation, and differentiation [1] [2]. The process of decellularization removes cellular and immunogenic components from native tissues while aiming to preserve these critical ECM components [3] [36]. The success of this process fundamentally hinges on selecting the appropriate decellularization strategy, primarily categorized into perfusion-based and immersion-based techniques. The choice between these methods carries profound implications for the resulting scaffold's quality and its subsequent performance in stem cell engraftment studies. Perfusion decellularization, which involves circulating solutions through the native vasculature, is generally the method of choice for whole organs or thick tissues, as it achieves more uniform cell removal and better preservation of complex ECM architectures [37] [38]. In contrast, immersion decellularization, where tissues are simply submerged in detergent solutions with agitation, can be sufficient for thin or simple tissues but often struggles with scalability and completeness [14] [38]. This application note provides a structured comparison of these two foundational approaches, supported by quantitative data and detailed protocols, to guide researchers in selecting the optimal strategy for generating high-quality scaffolds conducive to stem cell research and engraftment.
Technical Comparison: Perfusion vs. Immersion Decellularization
The efficacy of a decellularization protocol is typically evaluated against three key criteria: the efficiency of cellular content removal, the preservation of essential ECM components, and the retention of mechanical and structural integrity. The table below summarizes a quantitative comparison between perfusion and immersion techniques based on these parameters.
Table 1: Quantitative Comparison of Decellularization Efficacy: Perfusion vs. Immersion
| Evaluation Parameter | Perfusion Decellularization | Immersion Decellularization | Significance for Stem Cell Engraftment |
|---|---|---|---|
| DNA Removal (Residual DNA) | < 50 ng/mg of dry tissue [38]; as low as 3.7 ng/mg in optimized gravity-fed systems [38]. | Can exceed 200 ng/mg [38]; often fails to meet the sub-50 ng/mg benchmark [37]. | Residual DNA is highly immunogenic and can trigger a host immune response, jeopardizing stem cell survival and integration [36] [2]. |
| ECM Component Preservation | Superior retention of collagen, glycosaminoglycans (GAGs), and fibronectin [37] [38]. Architecture of delicate vascular networks is maintained [14]. | Significant loss of GAGs and other core ECM proteins due to prolonged detergent exposure [37]. Structure is often disrupted. | GAGs and fibrous proteins are crucial for binding growth factors and mediating stem cell adhesion, differentiation, and tissue remodeling [1] [23]. |
| Structural & Mechanical Integrity | Maintains original 3D organ architecture and vasculature; mechanical properties (tensile strength) closely match native tissue [37] [14]. | Often results in edema, disruption of ultrastructure, and loss of mechanical strength [37]. | A biomechanically matched scaffold provides the necessary physical cues for stem cell differentiation and functional tissue formation [36] [1]. |
| Uniformity of Decellularization | High uniformity throughout the entire organ scaffold, including the core [38]. | Often incomplete and non-uniform, with cellular remnants frequently found in the tissue core [38]. | A uniform scaffold ensures predictable stem cell behavior and integration throughout the entire construct, which is vital for engineering functional tissue. |
The following workflow diagram illustrates the decisive factors and outcomes when choosing between perfusion and immersion decellularization strategies.
Diagram 1: Decision Workflow for Decellularization Strategy Selection
Detailed Experimental Protocols
Protocol 1: Gravity-Assisted Perfusion Decellularization for Whole Organs
This protocol describes a cost-effective and reproducible method for decellularizing whole organs, such as the liver, using gravity-driven flow instead of mechanical pumps. This approach has been shown to produce high-quality, acellular scaffolds with well-preserved ECM, ideal for subsequent stem cell engraftment studies [38].
Table 2: Research Reagent Solutions for Perfusion Decellularization
| Reagent/Solution | Concentration & Formula | Primary Function | Key Considerations |
|---|---|---|---|
| Heparinized Saline | 15 UI/mL in PBS [14] | Pre-clotting flush; prevents coagulation in vasculature during harvest. | Ensures vascular patency for uniform detergent distribution. |
| Sodium Dodecyl Sulfate (SDS) | 1% (w/v) in dH₂O [14] [38] | Ionic detergent; efficiently lyses cells and solubilizes nuclear & cytoplasmic membranes. | Strong detergent that can damage ECM if overused; requires thorough washing [36] [2]. |
| Triton X-100 | 1% (v/v) in dH₂O or PBS [14] | Non-ionic detergent; disrupts lipid-lipid and lipid-protein bonds; helps rinse out SDS and cellular debris. | Gentler on ECM structure than SDS but less effective at nuclear removal [36] [2]. |
| Deionized Water (dH₂O) | N/A | Wash step; creates osmotic shock to lyse remaining cells. | |
| Phosphate Buffered Saline (PBS) | 1X | Final wash; removes residual detergents and prepares scaffold for storage or sterilization. | Extensive washing is critical to eliminate cytotoxic detergent traces [2]. |
Step-by-Step Methodology:
- Organ Harvest and Cannulation: Excise the target organ (e.g., liver) with utmost care to preserve the main vascular pedicle (e.g., portal vein, inferior vena cava). Cannulate the primary artery or vein with appropriate tubing. Gently flush with 500 mL of ice-cold Heparinized Saline to remove blood and prevent clotting [14] [38].
- Gravity-Driven Perfusion Setup: Connect the cannula to a solution reservoir elevated 60-100 cm above the organ. This height provides a hydrostatic pressure of approximately 44-74 mmHg, which is sufficient for gentle perfusion without causing ECM damage [38].
- Decellularization Cycle: Perfuse the organ sequentially with the following solutions at a controlled flow rate (e.g., 5-10 mL/min) at room temperature:
- 1% SDS Solution: Perfuse for approximately 24-48 hours, or until the organ becomes translucent and no visible cellular material is flushed out. This step is responsible for the bulk of cell lysis [38].
- dH₂O Wash: Perfuse for 6-12 hours to remove SDS and induce osmotic shock.
- 1% Triton X-100 Solution: Perfuse for 12-24 hours to remove residual SDS and lipid debris.
- PBS Wash: Perfuse extensively for 24-48 hours to ensure complete removal of all detergent traces [38].
- Sterilization and Storage: The resulting acellular scaffold can be sterilized using 0.1% Peracetic Acid [1] or gamma irradiation [3]. Scaffolds should be stored in PBS at 4°C for short-term use or frozen for long-term preservation.
Protocol 2: Immersion-Based Decellularization for Simple Tissues
This protocol is suitable for thin tissues (e.g., dermis, pericardium, small intestine submucosa) or tissue slices where perfusion is not feasible. While simpler, it requires careful optimization to minimize ECM damage [14].
Step-by-Step Methodology:
- Tissue Preparation: Aseptically dissect the tissue into thin sections (e.g., 1-2 mm thick) to facilitate detergent penetration. The surface area to volume ratio is critical for success [37] [2].
- Agitation-Based Decellularization: Immerse the tissue samples in a large volume (typically 10:1 v/w) of decellularization solutions under constant agitation on an orbital shaker. Change solutions at intervals as follows:
- Hypotonic/Tris Buffer: Agitate for 24 hours.
- Detergent Solution (SDS or SDC): Agitate for 48-72 hours. Monitor tissue transparency. Agitation is crucial for forcing detergents into the tissue matrix [37] [2].
- DNase/RNase Solution (Optional): Incubate in an enzymatic solution (e.g., 100 U/mL DNase) for 6-12 hours to digest residual nucleic acid fragments [36].
- Wash Steps: Rinse repeatedly with dH₂O and PBS over 48-72 hours to remove cellular debris and detergents [37].
- Termination and Storage: Once acellular, store the scaffolds in PBS or sterilize as described in the perfusion protocol.
The Scientist's Toolkit: Essential Research Reagents
The table below expands on the key reagents used in decellularization, detailing their mechanisms and trade-offs.
Table 3: Essential Reagent Toolkit for Decellularization Protocols
| Reagent Category | Specific Examples | Mechanism of Action | Advantages & Disadvantages |
|---|---|---|---|
| Ionic Detergents | Sodium Dodecyl Sulfate (SDS), Sodium Deoxycholate (SDC) | Powerful solubilization of cell membranes and nuclear material by disrupting hydrophobic-hydrophilic bonds [36] [2]. | Adv: Highly effective for dense tissues. Disadv: Harsh; can denature ECM proteins (e.g., collagen) and deplete GAGs [36] [1]. |
| Non-Ionic Detergents | Triton X-100, Tween-20 | Disrupts lipid-lipid and lipid-protein interactions; gentler on ECM structure [37] [36]. | Adv: Better preservation of ECM ultrastructure and growth factors. Disadv: Less effective for nuclear material removal; may require combination therapies [37] [36]. |
| Zwitterionic Detergents | CHAPS | Combines properties of ionic and non-ionic detergents; effective at disrupting protein-protein interactions [37] [36]. | Adv: Can maintain structural ECM proteins. Disadv: May disrupt the basement membrane and leave cytoplasmic proteins [36]. |
| Enzymatic Agents | Trypsin, DNase, RNase | Target specific components: Trypsin cleaves peptide bonds, while nucleases digest genetic material [36] [2]. | Adv: Highly specific. Disadv: Trypsin can damage ECM if overused; typically used as a supplement to detergent methods [36]. |
| Acids & Bases | Peracetic Acid (PAA), Ammonium Hydroxide | Solubilize cytoplasmic components and degrade nucleic acids; PAA also provides sterilization [1] [2]. | Adv: Effective for sterilization and nucleic acid removal. Disadv: Can damage ECM architecture and alter mechanical properties (e.g., increase stiffness) [36] [1]. |
Strategic Application for Stem Cell Research
The ultimate success of a decellularized scaffold in stem cell engraftment research depends on its bioactivity and capacity to direct cell fate. The ECM is not a passive scaffold but an active signaling platform. The diagram below illustrates how a well-preserved dECM influences stem cell behavior through key signaling pathways.
Diagram 2: dECM-Stem Cell Crosstalk Signaling Pathways
As shown, a high-quality scaffold orchestrates stem cell behavior through multiple synchronized cues:
- Adhesion and Survival: Structural proteins like fibronectin and laminin promote stem cell adhesion via integrins, activating pro-survival pathways such as PI3K/Akt and MAPK [1].
- Differentiation: GAGs like heparan sulfate bind and present growth factors (e.g., FGF, BMP) to their receptors, activating signaling cascades that drive lineage-specific differentiation [1] [23].
- Mechanotransduction: The physical stiffness and topography of the ECM are sensed by cells through the cytoskeleton, regulating fate decisions via effectors like YAP/TAZ [1].
Therefore, the choice of decellularization method directly impacts this signaling potential. Perfusion, by better preserving the native ECM composition and 3D architecture, provides a more holistic and potent microenvironment for guiding stem cell engraftment and functional tissue formation compared to immersion [37] [38].
Within regenerative medicine and stem cell research, the scaffold serves as a critical cornerstone, providing the essential three-dimensional (3D) microenvironment that directs cell fate. For research focused on decellularized tissues for stem cell engraftment, the physical format of the scaffold is a primary determinant of its experimental utility and eventual therapeutic application. These formats—ranging from intact preserved 3D structures to versatile powders, customizable hydrogels, and advanced bioinks for 3D printing—each offer distinct advantages and limitations for directing stem cell behavior.
This document provides detailed application notes and standardized protocols for these key scaffold formats. The guidance is designed to equip researchers with the practical methodologies necessary to effectively utilize these materials in studies aimed at understanding and enhancing stem cell engraftment, proliferation, and differentiation.
The selection of an appropriate scaffold format is guided by the specific requirements of the stem cell research project, including the desired level of structural mimicry, need for customization, and the mode of delivery. The table below summarizes the core characteristics, advantages, and primary applications of each format to aid in selection.
Table 1: Comparative Analysis of Scaffold Formats for Stem Cell Research
| Scaffold Format | Key Characteristics | Advantages | Disadvantages | Typical Applications in Stem Cell Research |
|---|---|---|---|---|
| Preserved 3D Structures [39] [40] | Intact, organ-scale architecture; Native biomechanical cues. | High biological fidelity; Preserved native vasculature. | Limited customizability; Potential for immunogenicity. | Whole-organ regeneration models; Studying cell-ECM interactions in a native context. |
| Powders [41] | Lyophilized and milled dECM; Highly soluble. | Versatile application; Ease of storage and handling; Can be formed into other formats. | Lacks macroscopic structure; Requires processing for 3D culture. | Supplementation of 2D cultures; Formulation of hydrogels and bioinks; Injectable cell delivery systems. |
| Hydrogels [42] [43] | Hydrated polymer networks; Tunable mechanical properties. | High biocompatibility; Can be injected or cast in situ. | Often requires chemical cross-linking; Limited mechanical strength. | 3D stem cell encapsulation; Differentiation studies; Soft tissue regeneration models. |
| Bioinks [42] [44] | Hydrogels optimized for 3D printing; Often cell-laden. | High architectural control; Customizable, complex geometries. | Requires specialized bioprinting equipment; Can exert shear stress on cells. | Fabrication of complex, patient-specific tissue constructs; High-throughput tissue modeling. |
Detailed Protocols for Scaffold Format Application
Protocol: Preparation and Recellularization of Preserved 3D Decellularized Scaffolds
Application Note: This protocol is fundamental for leveraging the full biological complexity of native organ structures for stem cell engraftment research, such as in studies involving decellularized liver, heart, or kidney scaffolds [40].
Materials & Reagents:
- Decellularized organ scaffold (e.g., rodent liver)
- Recellularization cell suspension (e.g., stem cells)
- Bioreactor system with perfusion capabilities
- Sterile PBS
- Cell culture medium
Procedure:
- Scaffold Sterilization and Hydration: Subject the decellularized scaffold to gamma irradiation or peracetic acid treatment. Rinse thoroughly with sterile PBS and hydrate in culture medium for 24-48 hours prior to recellularization [39].
- Cell Preparation: Prepare a high-density suspension (e.g., 1-10 x 10^6 cells/mL) of the stem cell population intended for engraftment.
- Perfusion Recellularization:
- Cannulate the scaffold's primary vasculature (e.g., portal vein for liver).
- Connect the cannula to a perfusion bioreactor.
- Slowly perfuse the cell suspension through the vascular network at a low flow rate (e.g., 1-3 mL/min) to facilitate cell attachment and distribution [40].
- Gradually increase flow rates over several days to condition the cells to fluid shear stress.
- Static Maturation: Following initial perfusion seeding, the construct may be maintained under static or low-flow conditions in a bioreactor to promote further cell engraftment, proliferation, and functional maturation for up to several weeks.
- Assessment: Analyze cell viability, distribution (via histology), and markers of differentiation and function (e.g., albumin secretion for hepatocytes, contractile proteins for cardiomyocytes).
Protocol: Fabrication and Use of dECM Hydrogels
Application Note: dECM hydrogels provide a biocompatible, bioactive environment ideal for 3D stem cell culture and soft tissue engineering, balancing biological cues with practical handling [41].
Materials & Reagents:
- dECM in powder form
- Pepsin
- Dilute acidic solution (e.g., 0.1M HCl)
- Neutralizing solution (e.g., 0.1M NaOH)
- PBS and cell culture medium
- Stem cells for encapsulation
Procedure:
- Digestion: Suspend dECM powder at a concentration of 10-30 mg/mL in a pepsin solution (0.1 mg/mL in 0.1M HCl). Stir continuously at 4°C for 48-72 hours until a viscous, homogeneous solution is formed.
- Neutralization and Gelation:
- Neutralize the pre-gel solution on ice using 0.1M NaOH and pre-chilled PBS (10X concentration). The optimal ratio is typically 8:1:1 (pre-gel: PBS: NaOH). Keep the solution on ice to prevent premature gelling.
- To encapsulate cells, mix the neutralized pre-gel with a cell suspension to achieve the desired final cell density.
- Pipette the cell-pregel mixture into the desired cultureware and incubate at 37°C for 30-60 minutes to induce thermogelation into a solid hydrogel [41].
- Culture and Analysis: After gelation, carefully overlay the hydrogel with cell culture medium. Refresh the medium regularly and assess stem cell viability, morphology (e.g., via phalloidin staining), and differentiation (via immunocytochemistry for lineage-specific markers).
Protocol: 3D Bioprinting with dECM-Based Bioinks
Application Note: This protocol enables the fabrication of complex, architecturally defined constructs for creating sophisticated stem cell niche models or tissue grafts [42] [44].
Materials & Reagents:
- dECM-based bioink (prepared as in Protocol 3.2)
- Support bath or crosslinking agent (e.g., CaCl₂ for alginate-blended inks)
- Extrusion-based 3D bioprinter
- Sterile printing substrates (e.g., glass coverslips, multi-well plates)
Procedure:
- Bioink Preparation and Cell Loading: Prepare a dECM bioink as described in Protocol 3.2, ensuring viscosity is appropriate for printing. Mix the neutralized, ice-cold bioink with a stem cell suspension to create a cell-laden bioink. Maintain the bioink on ice throughout the printing process to prevent clogging.
- Printer Setup: Load the cell-laden bioink into a sterile printing cartridge. Fit the cartridge with a nozzle of appropriate diameter (e.g., 22G-27G). Calibrate the printer for the printing surface.
- Printing Parameters: Set the printing pressure and speed empirically. Typical pressures range from 20-700 kPa and speeds from 1-20 mm/s, depending on the bioink viscosity and nozzle size [45] [44]. Higher pressures and smaller nozzles increase shear stress, which can compromise cell viability.
- Cross-linking and Post-Printing Culture:
- For pure dECM bioinks, the primary cross-linking mechanism is thermal gelation at 37°C.
- For composite bioinks (e.g., with alginate), immediate post-printing immersion in a cross-linking solution (e.g., 100mM CaCl₂) may be required to stabilize the structure.
- After printing and cross-linking, transfer the constructs to an incubator and culture under standard conditions, with regular medium changes.
Table 2: Key Parameters for Extrusion-based Bioprinting of Hydrogel Bioinks
| Parameter | Typical Range | Impact on Print Outcome |
|---|---|---|
| Nozzle Diameter | 150 - 410 μm (27G - 22G) | Smaller diameter improves resolution but increases shear stress. |
| Printing Pressure | 20 - 700 kPa | Must be optimized for specific bioink viscosity to ensure continuous flow. |
| Print Speed | 1 - 20 mm/s | Must be synchronized with flow rate for consistent filament deposition. |
| Bioink Viscosity | Shear-thinning properties | High viscosity improves shape fidelity but requires higher extrusion pressure. |
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Scaffold-Based Stem Cell Research
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| Sodium Dodecyl Sulfate (SDS) [46] | Ionic detergent for decellularization. | Efficiently lyses cells and removes nuclear material from tissues; may denature ECM proteins. |
| Triton X-100 [46] | Non-ionic detergent for decellularization. | Disrupts lipid-lipid and lipid-protein bonds; gentler on ECM structure than SDS. |
| Deoxyribonuclease (DNase) [46] | Enzyme for decellularization. | Degrades residual DNA fragments within the ECM following cell lysis. |
| Methacrylic Anhydride (MA) [42] | Chemical for bioink modification. | Used to synthesize GelMA (gelatin methacryloyl), providing a photocrosslinkable bioink. |
| Polyethylene Glycol (PEG) [42] | Synthetic polymer for hydrogels. | Used to create synthetic hydrogels or modify natural hydrogels to tune mechanical properties. |
| Hyaluronic Acid (HA) [43] | Natural polymer for bioinks. | Provides excellent biocompatibility and is easily modified to create printable, cell-instructive bioinks. |
| Gamma Irradiation [39] | Method for scaffold sterilization. | Effectively sterilizes decellularized scaffolds without leaving cytotoxic chemical residues. |
Workflow and Pathway Visualizations
Scaffold Processing and Application Workflow
Bioink Formulation and Printing Pathway
Recellularization is a pivotal technology in the field of tissue engineering, representing the process of repopulating acellular organ scaffolds with patient-specific cells after decellularization [47]. The ultimate goal is to use autologous cell sources, including various stem cells, to develop functional, patient-specific tissues and organs for transplantation, thereby circumventing the need for lifelong immunosuppression regimens [47]. The success of this process critically depends on the methodology employed to introduce and culture cells within the decellularized extracellular matrix (dECM). The retained ECM provides a unique microenvironment that is instrumental for guiding recellularized cells to engraft, proliferate, and function appropriately [47]. This application note delineates three principal recellularization methodologies—Static Seeding, Dynamic Seeding using Bioreactors, and Hydrogel-Encapsulation. It provides a comparative analysis and detailed experimental protocols tailored for researchers and scientists working on stem cell engraftment in decellularized tissues.
Comparative Analysis of Recellularization Methodologies
The selection of a recellularization strategy is governed by the target tissue's complexity, the cell types involved, and the desired functional outcomes. The following table summarizes the core characteristics, applications, and performance metrics of the three primary methodologies.
Table 1: Comprehensive Comparison of Recellularization Methodologies
| Methodology | Key Principle | Optimal Cell Types | Typical Seeding Efficiency | Advantages | Limitations | Primary Tissue Applications |
|---|---|---|---|---|---|---|
| Static Seeding | Cell suspension is pipetted directly onto the scaffold and allowed to adhere without active force [48]. | Chondrocytes, Airway Epithelial Cells, Mesenchymal Stem Cells (MSCs) [48]. | ~40-60% (Highly variable and often low) [47]. | Technically simple, low-cost, minimal equipment required [47]. | Low efficiency, poor cell viability, uneven distribution, limited penetration into thick scaffolds [47]. | Thin tissues, initial proof-of-concept studies, cartilage rings in trachea [48]. |
| Dynamic (Bioreactor) Seeding | Cells are perfused through the scaffold's vascular network or agitated using bioreactors to enhance delivery [47]. | Parenchymal cells (e.g., hepatocytes, cardiomyocytes), Endothelial cells for vascular coating [47]. | ~70-90% (Can be significantly enhanced) [47]. | High seeding efficiency, superior cell viability, uniform cell distribution, enhanced nutrient/waste exchange [47]. | Requires specialized, often costly equipment; protocol complexity risk of shear stress on cells [47]. | Whole organs (heart, lung, liver, kidney), thick and complex tissues [47] [49]. |
| Hydrogel-Encapsulation | Cells are suspended within a natural or synthetic hydrogel prior to or during seeding, providing a protective 3D environment [50]. | MSCs, Induced Pluripotent Stem Cells (iPSCs), Adipose-derived stem cells [48] [50]. | >85% (High, due to protective matrix) [50]. | High cell viability, protected from immune response and shear stress, promotes uniform attachment, allows co-delivery of bioactive factors [50]. | Hydrogel mechanics can influence stem cell fate; potential for hindered nutrient diffusion if gel is too dense [51] [50]. | Injectable therapies, cartilage regeneration, corneal stroma, encapsulation for immunoisolation [50] [52]. |
Detailed Experimental Protocols
Protocol 1: Static Seeding for Tracheal Cartilage Regeneration
This protocol is designed for recellularizing decellularized tracheal rings, focusing on repopulating the cartilaginous component.
Table 2: Key Research Reagents for Static Seeding
| Reagent/Material | Function | Example & Notes |
|---|---|---|
| Decellularized Scaffold | Provides the biological, 3D structure for repopulation. | Porcine or human decellularized trachea. Ensure DNA content <50 ng/mg dry weight [47]. |
| Chondrogenic Cells | Regenerates the functional tissue of the scaffold. | Human Mesenchymal Stem Cells (hMSCs) differentiated towards chondrocytes [48]. |
| Seeding Medium | Supports cell health and function during and after seeding. | DMEM/F-12 supplemented with 10% FBS, 1% Penicillin/Streptomycin, and chondrogenic factors (e.g., TGF-β3). |
| Fibrin Glue | Acts as a biological adhesive to retain cells at the seeding site. | Fibrinogen and Thrombin solution mixed with cell suspension. |
Procedure:
- Scaffold Preparation: Hydrate the decellularized tracheal ring in sterile PBS for 24 hours. Prior to seeding, equilibrate the scaffold in the seeding medium for at least 2 hours.
- Cell Harvesting: Culture hMSCs in a standard monolayer. Induce chondrogenic differentiation for 7-14 days prior to seeding. Trypsinize the differentiated chondrocytes and resuspend in seeding medium at a high density of 5-10 x 10^6 cells/mL.
- Cell-Seeding: a. Direct Injection: Using a 27-29G insulin syringe, slowly inject 10-50 µL of the cell suspension at multiple points across the cartilaginous ring [48]. b. Fibrin Encapsulation: Mix the cell suspension with fibrinogen solution (final concentration ~20 mg/mL). Pipette this mixture onto the cartilage surface and immediately apply a drop of thrombin solution (~50 U/mL) to initiate polymerization, encapsulating the cells on the scaffold [48].
- Post-Seeding Culture: Transfer the seeded scaffold to a 6-well plate. Add seeding medium to cover the base of the well without submerging the scaffold entirely to encourage gas exchange. Incubate at 37°C and 5% CO₂.
- Medium Change: Carefully replace 50% of the medium every 48 hours. Avoid disturbing the cell-matrix construct.
- Analysis: After 7-14 days, assess cell viability (e.g., Live/Dead staining), distribution (H&E staining), and chondrogenic function (e.g., collagen type II immunostaining, sGAG quantification).
Protocol 2: Dynamic Recellularization via Perfusion Bioreactor
This protocol is optimized for whole-organ recellularization, such as a decellularized kidney, leveraging its intrinsic vascular network.
Procedure:
- Bioreactor Setup: Assemble a sterile perfusion bioreactor system. The system should include a peristaltic pump, a media reservoir with gas exchange (5% CO₂ in air), and pressure sensors. Maintain the entire system within an incubator at 37°C.
- Scaffold Cannulation: Aseptically cannulate the renal artery of the decellularized kidney scaffold. Secure the cannula and connect it to the bioreactor's perfusion circuit.
- System Priming: Perfuse the scaffold with sterile PBS at a low flow rate (2-4 mL/min) for 1 hour to remove air bubbles and ensure patency of the vascular tree.
- Cell Preparation: Trypsinize the desired cell population (e.g., human renal epithelial cells or endothelial cells for vascular coating). Resuspend the cells in perfusion medium at a concentration of 1-5 x 10^6 cells/mL. The total required volume depends on the organ size but typically ranges from 50 mL to 150 mL.
- Dynamic Seeding: a. Load the cell suspension into the media reservoir. b. Initiate perfusion in a recirculating manner. Begin with a low flow rate (2 mL/min) for the first 4 hours to facilitate initial cell adhesion. c. Gradually increase the flow rate to 5-10 mL/min over the next 24-48 hours. This step-wise increase promotes firm cell attachment and mitigates shear stress-induced detachment.
- Post-Seeding Culture: After 72 hours of recirculation, switch to a non-recirculating (throughput) perfusion mode with fresh medium to remove non-adherent cells and provide a continuous supply of nutrients.
- Monitoring and Analysis: Monitor pressure drops across the scaffold as an indicator of potential vascular blockage. After 7-14 days, harvest the construct. Analyze cell coverage via histology throughout the vascular and parenchymal regions and assess organ-specific function (e.g., albumin reabsorption for kidney) [47] [49].
Protocol 3: Hydrogel-Encapsulation for Cell Delivery
This protocol utilizes alginate-based hydrogels for the encapsulation and delivery of stem cells, offering protection and a supportive 3D microenvironment.
Table 3: Key Research Reagents for Hydrogel-Encapsulation
| Reagent/Material | Function | Example & Notes |
|---|---|---|
| Alginate | Natural polysaccharide that forms a gentle, ionic-crosslinked gel. | High G-content alginate for improved stability. Often used at 1-2% (w/v) [50]. |
| Gelatin | Enhances cell adhesion properties within the alginate matrix. | Mixed with alginate to create composite hydrogels [50]. |
| Calcium Chloride (CaCl₂) | Crosslinking agent for alginate gelation. | Typically used as a 100 mM solution. |
| Stem Cells | Therapeutic cell source for regeneration. | Human MSCs or iPSC-derived progenitor cells [48] [50]. |
Procedure:
- Hydrogel Precursor Preparation: Dissolve sodium alginate powder (1.5% w/v) in a sterile, physiological buffer (e.g., 0.9% NaCl). Gently mix overnight to ensure complete dissolution. Filter sterilize the solution.
- Cell-Hydrogel Mix Preparation: Harvest and centrifuge the desired stem cells (e.g., MSCs). Resuspend the cell pellet in the sterile alginate solution to a final density of 2-10 x 10^6 cells/mL. Gently homogenize to avoid air bubbles.
- Encapsulation & Seeding: a. Bulk Injection: Draw the cell-alginate mixture into a syringe. Using a narrow-gauge needle, slowly inject the mixture directly into the parenchymal space of the decellularized scaffold. b. Droplet Generation (Microencapsulation): Load the cell-alginate mixture into a syringe pump. Extrude the solution through a needle into a stirring bath of 100 mM CaCl₂ solution. This forms solid, cell-laden microbeads (200-500 µm in diameter) [50].
- Gelation: If using bulk injection, the gel will form in situ upon contact with divalent cations in the tissue or can be gelled by subsequently applying a mist of CaCl₂ solution. For microbeads, allow gelation to proceed for 10-15 minutes under gentle stirring.
- Washing and Culture: Collect the microbeads and wash three times with culture medium to remove excess CaCl₂. For bulk gels or injected scaffolds, transfer to a bioreactor or well plate with culture medium.
- Analysis: Assess encapsulated cell viability using fluorescent dyes (e.g., Calcein-AM for live cells). Monitor stem cell proliferation and differentiation within the hydrogel over time (e.g., 7, 14, 21 days) using immunocytochemistry and qPCR for lineage-specific markers [50].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Reagents for Recellularization Research
| Category | Item | Critical Function |
|---|---|---|
| Scaffolds | Decellularized Tissues/Organs (e.g., trachea, kidney, cornea) [48] [49] [52] | Provides the native, bioactive 3D structure for cell growth and tissue formation. |
| Cells | Mesenchymal Stem Cells (MSCs), Induced Pluripotent Stem Cells (iPSCs), Tissue-Specific Cells (e.g., chondrocytes, endothelial cells) [48] [47] | The living component that repopulates the scaffold to restore function. |
| Hydrogels | Alginate, Agarose, Fibrin, dECM-derived Hydrogels [50] [52] | Protects cells during seeding, improves retention, and provides a temporary, customizable ECM. |
| Detergents & Enzymes | Sodium Dodecyl Sulfate (SDS), Triton X-100, DNase [53] [52] | Critical for the initial decellularization process to remove cellular material and minimize immunogenicity. |
| Bioreactors | Perfusion Bioreactor Systems [47] [53] | Provides dynamic culture conditions, enhancing cell seeding efficiency, distribution, and tissue maturation. |
Workflow and Decision Pathway
The following diagram illustrates the logical decision-making process for selecting and implementing the appropriate recellularization methodology.
Tracheal Engineering with Decellularized Scaffolds
Application Note
The treatment of long-segment tracheal defects, which affect over half the trachea in adults or a third in children, remains a significant clinical challenge with no available surgical solutions [48]. Tissue engineering, particularly using decellularized extracellular matrix (dECM) scaffolds, has emerged as a promising approach to bridge this gap. Decellularized tracheal scaffolds preserve the native ECM's microarchitecture and biochemical cues while eliminating cellular antigens that trigger immune rejection [48]. These scaffolds provide the structural foundation for recellularization with patient-derived cells, creating biocompatible grafts that can regenerate functional tracheal tissue. Recent advances in decellularization techniques, including detergent-enzymatic treatment (DEM), laser microporation, and vacuum-assisted decellularization (VAD), have significantly improved scaffold quality by enhancing cell removal while minimizing ECM damage [54].
Quantitative Outcomes in Preclinical Studies
Table 1: Performance Metrics of Bioengineered Tracheal Scaffolds
| Evaluation Metric | Decellularized Native Trachea | 3D Synthetic Grafts | Hybrid Approaches |
|---|---|---|---|
| Cell Removal Efficiency | >90% nuclear material removal [48] | Not Applicable | Not Applicable |
| GAG Content Retention | 58.98 ± 2.16% protein preservation [21] | Not Applicable | Not Applicable |
| Mechanical Properties | Preservation of cartilaginous ring structure and elasticity [48] | Tunable rigidity via polymer blends (PCL/copolyamide) [54] | Intermediate damping characteristics [21] |
| In Vivo Integration | Epithelialization and partial vascularization in goat models [54] | Variable neotissue formation | Enhanced biocompatibility |
| Clinical Translation | Limited success in human cases | Preclinical optimization | Emerging as promising strategy |
Detailed Experimental Protocol: Tracheal Scaffold Decellularization and Recellularization
Part A: Detergent-Enzymatic Decellularization Method
- Tissue Acquisition: Obtain donor trachea (human or appropriate animal model) and transport in cold preservation solution.
- Initial Processing: Remove excess connective tissue and trim to desired length under sterile conditions.
- Freeze-Thaw Cycles: Subject trachea to three freeze-thaw cycles (-80°C for 2 hours followed by 37°C for 1 hour) to initiate cell lysis.
- Detergent Treatment: Immerse tissue in 0.1% sodium dodecyl sulfate (SDS) solution with continuous agitation for 48-72 hours, changing solution every 12 hours.
- Enzymatic Treatment: Transfer tissue to DNase/RNase solution (100 U/mL in PBS) and incubate for 24 hours at 37°C with agitation.
- Washing: Rinse thoroughly with PBS for 72 hours with frequent solution changes to remove all detergent residues.
- Sterilization: Treat with peracetic acid or antibiotics before final storage in PBS at 4°C [48].
Part B: Scaffold Recellularization
- Cell Source Preparation: Isolate and expand autologous mesenchymal stem cells (MSCs) from bone marrow or adipose tissue, and epithelial progenitor cells.
- Chondrogenic Differentiation: Differentiate MSCs toward chondrogenic lineage using TGF-β3 and BMP-6 supplemented media for cartilage regeneration.
- Dynamic Seeding: Utilize bioreactor systems with perfusion to seed chondrogenic cells throughout the cartilaginous portion of the scaffold.
- Epithelial Seeding: Statically seed epithelial cells onto the luminal surface with air-liquid interface culture to promote mucociliary differentiation.
- Maturation Culture: Maintain construct in specialized media for 4-6 weeks to allow tissue maturation before implantation [48].
Research Reagent Solutions
Table 2: Essential Reagents for Tracheal Engineering
| Reagent/Category | Specific Examples | Function | Key Considerations |
|---|---|---|---|
| Decellularization Agents | Sodium dodecyl sulfate (SDS), Triton X-100, DNase/RNase | Remove cellular material while preserving ECM | SDS concentration critical: high concentrations damage ECM [10] |
| Stem Cell Sources | Adipose-derived MSCs (ADSCs), Bone marrow MSCs (BM-MSCs) | Provide chondrogenic and connective tissue progenitors | ADSCs show enhanced VEGF secretion under hypoxia [24] |
| Differentiation Factors | TGF-β3, BMP-6, VEGF | Direct stem cell differentiation toward chondrogenic and vascular lineages | Hypoxic preconditioning (1-5% O₂) upregulates pro-survival genes [24] |
| Scaffold Materials | Decellularized tracheal matrix, Polycaprolactone (PCL), Thermoplastic polyurethane | Provide 3D structural support | Hybrid natural/synthetic scaffolds optimize mechanical and biological properties [54] |
| Animal Models | Goats, Rabbits | Preclinical testing | Goats preferred for translational relevance due to anatomical similarity to humans [54] |
Cardiac Repair via Engineered Tissue Constructs
Application Note
Cardiac tissue engineering aims to address the irreversible loss of cardiomyocytes following myocardial infarction, which affects millions worldwide. The field has evolved to include scaffold-free cellular approaches, cell-free biomaterial strategies, and hybrid methods combining cells with supportive matrices [55]. Decellularized ECM (dECM) from cardiac tissue provides an ideal microenvironment for stem cell engraftment, containing essential biochemical and biomechanical cues that promote cardiomyocyte maturation and function. These dECM scaffolds preserve critical cardiac-specific ECM components including collagens, glycosaminoglycans (GAGs), and sequestered growth factors like VEGF and FGF that support vascularization and tissue repair [10]. Recent advances in 3D bioprinting enable the fabrication of patient-specific cardiac patches with aligned architectures that enhance electromechanical coupling and contractile function [55].
Quantitative Outcomes in Cardiac Engineering
Table 3: Performance Metrics of Engineered Cardiac Tissues
| Evaluation Metric | Scaffold-Free Spheroids | dECM Hydrogels | 3D Bioprinted Constructs |
|---|---|---|---|
| Cell Viability | >70% in cardiac patches [55] | 97.41 ± 1.02% in GG/dECM hydrogel [21] | Varies with bioink (70-90%) |
| Contractile Function | Synchronous beating in multicellular patches [55] | Limited in hydrogel-only formats | Electromechanical coupling demonstrated |
| Vascularization | Host anastomosis in rat models [55] | Supports endothelial network formation | Perfusable channel design possible |
| Mechanical Properties | Self-supporting tissue strands [55] | Myocardial-mimetic stiffness (1-10 KPa) [55] | Tunable via polymer composition |
| Stem Cell Retention | Improved over injection methods | High retention in hydrogel matrices | Spatial control of cell placement |
Detailed Experimental Protocol: Cardiac Patch Fabrication via 3D Bioprinting
Part A: Bioink Preparation
- dECM Isolation: Decellularize ventricular tissue using perfusion with 1% SDS followed by DNase treatment, lyophilize, and digest in pepsin/HCl to create cardiac dECM hydrogel.
- Cell Sourcing: Differentiate human iPSCs to cardiomyocytes (iPSC-CMs) using established small molecule protocols (CHIR99021 followed by IWP-2 inhibition).
- Bioink Formulation: Combine cardiac dECM hydrogel (15 mg/mL) with iPSC-CMs, cardiac fibroblasts (3:1 ratio), and human umbilical vein endothelial cells at final concentration of 50-100 million cells/mL.
- Bioink Crosslinking: Adjust calcium concentration for optimal printability while maintaining cell viability.
Part B: 3D Bioprinting Process
- Design: Create digital model of cardiac patch with alternating channels (200-500 μm diameter) for enhanced nutrient diffusion.
- Printing Parameters: Use microextrusion bioprinter with maintained temperature (10-15°C) and pressure (20-40 kPa) optimized for cell viability.
- Layer-by-Layer Deposition: Print bioink in aligned pattern to promote cardiomyocyte orientation and synchronous contraction.
- Crosslinking: Immerse printed construct in calcium solution for final ionic crosslinking.
- Maturation Culture: Maintain in perfusion bioreactor with gradual increase in stimulation frequency (0.5-2 Hz over 14 days) to promote functional maturation [55].
Research Reagent Solutions
Table 4: Essential Reagents for Cardiac Tissue Engineering
| Reagent/Category | Specific Examples | Function | Key Considerations |
|---|---|---|---|
| Cell Sources | iPSC-derived cardiomyocytes, Cardiac fibroblasts, Endothelial cells | Recreate cardiac cellular microenvironment | 3:1:1 ratio (CMs:FBs:ECs) mimics native cellular composition [55] |
| Bioink Materials | Cardiac dECM hydrogel, Alginate, GelMA | Provide 3D support structure and biochemical cues | Cardiac dECM contains tissue-specific matrisome [10] |
| Bioreactor Systems | Perfusion systems, Electrical stimulation platforms | Promote tissue maturation and function | Gradual increase in pacing frequency enhances contractile force [55] |
| Characterization Tools | Multi-electrode arrays, Force transducers, Calcium imaging | Assess functional properties | Synchronous beating indicates electromechanical coupling |
| Animal Models | Rat myocardial infarction model | Preclinical efficacy testing | Patch implantation improves function in infarcted hearts [55] |
Nerve Regeneration through Innervation Strategies
Application Note
Innervation represents a critical but often overlooked component in organ engineering, with neural inputs playing essential roles in organ development, function, and homeostasis [56]. While denervated organ transplants can function temporarily through neuroendocrine signaling, bioengineered organs require intentional incorporation of neuronal networks for long-term success and proper physiological regulation. The autonomic nervous system, comprising sympathetic and parasympathetic fibers, provides essential regulatory inputs to virtually all internal organs, controlling functions from pancreatic insulin secretion to salivary production [56]. In tissue engineering, achieving proper reinnervation is particularly challenging due to the complex spatial organization required for functional neural connections. Emerging strategies focus on creating pre-innervated constructs by co-culturing organ-specific cells with neurons or incorporating neural guidance cues into biomaterial scaffolds.
Quantitative Outcomes in Innervation Engineering
Table 5: Metrics for Neural Integration in Engineered Tissues
| Evaluation Metric | Pancreatic Innervation | General Organ Engineering | Neural Scaffolds |
|---|---|---|---|
| Neural Density | Species-dependent (abundant in mice, limited in humans) [56] | Not standardized | Varies with guidance cues |
| Functional Connection | Direct β-cell association in mice; vascular alignment in humans [56] | Measured by physiological response | Electrophysiological activity |
| Developmental Timing | E12.5 in murine models; GW6 in humans [56] | Organ-specific critical periods | Dependent on neurotrophic factors |
| Neurotransmitter Specificity | Norepinephrine (sympathetic), Acetylcholine (parasympathetic) [56] | Varies by organ system | Can be guided by scaffold design |
| Regulatory Impact | Insulin/glucagon secretion modulation [56] | Homeostatic maintenance | Not fully characterized |
Detailed Experimental Protocol: Engineering Pre-innervated Pancreatic Constructs
Part A: Neural Cell Integration
- Neural Cell Source: Differentiate iPSCs to autonomic neural progenitors using dual-SMAD inhibition followed by specific patterning (BMP for sympathetic, FGF for parasympathetic).
- Pancreatic Differentiation: Generate pancreatic progenitors from iPSCs through definitive endoderm induction followed by pancreatic patterning (retinoic acid, FGF10, BMP inhibition).
- 3D Co-culture: Combine neural and pancreatic progenitors in Matrigel-based 3D culture at optimized ratio (1:5 neural:pancreatic cells).
- Neural Guidance: Incorporate graded concentrations of nerve growth factor (NGF) and artemin to direct axonal extension toward pancreatic clusters.
- Functional Maturation: Culture constructs for 4-6 weeks with gradual introduction of neuronal activity through optogenetic stimulation or potassium-induced depolarization.
Part B: Assessment of Neural-Pancreatic Connectivity
- Immunohistochemical Analysis: Stain for neural markers (Tuj1, TH, ChAT) and pancreatic markers (insulin, glucagon) to visualize spatial relationships.
- Electrophysiology: Perform patch clamp recording on insulin-positive cells to detect postsynaptic currents.
- Calcium Imaging: Monitor coordinated calcium oscillations in response to neural stimulation and glucose challenge.
- Functional Secretion Assays: Measure insulin and glucagon release under basal conditions and following neural stimulation or inhibition.
- Transcriptomic Analysis: Single-cell RNA sequencing to characterize neural and endocrine cell types and their maturation states [56].
Research Reagent Solutions
Table 6: Essential Reagents for Neural Integration
| Reagent/Category | Specific Examples | Function | Key Considerations |
|---|---|---|---|
| Neural Cell Sources | iPSC-derived neural crest, Autonomic neuron progenitors | Provide neural network foundation | Specific subtypes (sympathetic/parasympathetic) required for organ function [56] |
| Guidance Cues | NGF, Artemin, Netrins, Semaphorins | Direct axonal growth and targeting | Gradients essential for proper pathfinding [56] |
| Scaffold Materials | Matrigel, Peptide hydrogels, Decellularized neural matrix | Support 3D growth and organization | Mechanical properties influence neurite extension |
| Characterization Tools | Calcium imaging, Patch clamp electrophysiology, scRNA-seq | Assess functional connectivity | Multiple modalities needed for comprehensive assessment |
| Modulation Tools | Optogenetics, Pharmacological agents (TTX, agonists) | Test functional neural connections | Enables causal relationship establishment |
Overcoming Translational Hurdles: Challenges in Immunogenicity, Vascularization, and Functional Maturation
Decellularization is a critical bioprocessing technique that removes immunogenic cellular material from native tissues while preserving the intricate structure and bioactive composition of the extracellular matrix (ECM). The resulting acellular scaffolds serve as biomimetic templates for stem cell engraftment and tissue regeneration, making them invaluable for regenerative medicine and drug development research [1]. The fundamental challenge lies in achieving complete cell removal without compromising the ECM's structural, mechanical, and biochemical integrity, which is essential for guiding cellular behavior and functional tissue formation [32] [57].
For researchers focusing on stem cell engraftment, a successfully decellularized scaffold must achieve two primary objectives: minimize immune rejection by removing cellular antigens and provide a hospitable microenvironment that supports stem cell attachment, proliferation, and differentiation. This balance is delicate, as overly aggressive decellularization can damage the very ECM components that stem cells rely on for cues, while insufficient decellularization triggers host immune responses [1].
Quantitative Standards for DNA Removal
A cornerstone of effective decellularization is the quantitative assessment of residual DNA. The field has established specific thresholds to define successful decellularization, which are critical for ensuring the scaffold's non-immunogenicity.
Table 1: Key Quantitative Standards for Assessing Decellularization Efficacy
| Parameter | Established Threshold | Quantification Method | Significance for Scaffold Function |
|---|---|---|---|
| Residual dsDNA | < 50 ng per mg of dry ECM weight [32] | Flurometric assay (e.g., PicoGreen) | Lower residual DNA reduces immunogenic potential [1]. |
| DNA Fragment Length | < 200 base pairs [32] | Gel electrophoresis | Removal of large DNA fragments indicates effective nuclear material disruption. |
| Visual Absence of Nuclei | No visible DAPI or H&E staining [32] | Histology (DAPI/H&E staining) | Confirms absence of intact nuclear structures. |
The rationale for these stringent DNA standards is rooted in immunology. Residual nuclear material, particularly double-stranded DNA (dsDNA), can act as a Damage-Associated Molecular Pattern (DAMP), triggering innate immune responses that lead to graft rejection and fibrosis, ultimately compromising its function as a stem cell carrier [32] [1]. Furthermore, for tissues intended for clinical translation, adhering to these thresholds is often a prerequisite for regulatory approval.
Comprehensive Assessment of ECM Integrity
Beyond cell removal, a thorough evaluation of ECM preservation is paramount, as the ECM provides the critical signals for stem cell fate. The following protocols and metrics form the basis for a multi-faceted assessment of ECM integrity.
Structural and Compositional Analysis
Protocol: SEM for Ultrastructural Assessment
- Sample Preparation: Fix decellularized tissue samples in glutaraldehyde, followed by dehydration in a graded ethanol series. Critical point drying is performed to preserve structure, and samples are sputter-coated with a thin layer of gold/palladium.
- Imaging and Analysis: Image using a Scanning Electron Microscope (SEM). A well-preserved ECM should show a porous, interconnected, three-dimensional architecture with intact, aligned collagen fibrils and no visible cellular debris [1].
Protocol: Biochemical Assays for Key ECM Components
- Total Collagen Content: Use a hydroxyproline assay. Hydrolyze tissue samples and react with chloramine-T and dimethylaminobenzaldehyde. Compare against a standard curve to quantify total collagen, a primary determinant of scaffold tensile strength [1].
- Sulfated Glycosaminoglycan (GAG) Content: Employ a dimethylmethylene blue (DMMB) dye-binding assay. The concentration of sulfated GAGs is proportional to the absorbance change, which is critical for hydration and growth factor binding [1].
- Elastin Content: Quantify using a Fastin elastin assay, which relies on a specific dye-binding methodology [1].
Table 2: Key ECM Components and Their Functional Significance for Stem Cell Engraftment
| ECM Component | Primary Function in Native ECM | Impact on Stem Cell Behavior |
|---|---|---|
| Collagen | Provides tensile strength and structural integrity [1]. | Influences adhesion, migration, and mechanotransduction signaling [1]. |
| Elastin | Confers elasticity and recoil to tissues [1]. | Important for mechanosensing in dynamically stressed tissues. |
| Glycosaminoglycans (GAGs) | Regulates hydration, compressive resistance, and growth factor sequestration [1]. | Loss correlates with reduced bioactivity and impaired cell recruitment [32]. |
| Laminin & Fibronectin | Adhesive glycoproteins that mediate cell-ECM attachment [1]. | Provide critical binding sites for integrins, directly affecting stem cell survival and differentiation [1]. |
Functional and Mechanical Assessment
Protocol: In Vitro Biocompatibility and Cell Seeding Assay
- Sterilization: Sterilize decellularized scaffolds (e.g., with peracetic acid or ethanol).
- Cell Seeding: Seed scaffolds with relevant stem cells (e.g., mesenchymal stem cells) at a defined density.
- Viability Assessment: After a culture period (e.g., 3-7 days), assess cell viability using an MTT assay, which measures metabolic activity, or a live/dead staining kit visualized by fluorescence microscopy. A biocompatible scaffold will support high cell viability and infiltration [32].
Protocol: Mechanical Testing
- Method: Use a uniaxial tensile tester. Hydrate scaffolds in PBS and measure the stress-strain relationship until failure.
- Analysis: Calculate the ultimate tensile strength and elastic modulus (stiffness). The mechanical properties should be appropriate for the native target tissue to provide correct mechanobiological cues [1].
Diagram 1: Comprehensive decellularization quality assessment workflow.
Detailed Decellularization Protocol for Parenchymal Tissues
This protocol provides a generalized, optimized workflow suitable for many soft tissues, with an emphasis on balancing cell removal with ECM preservation.
Reagents and Equipment
- Decellularization Agents: 0.5-1.0% (w/v) Sodium Dodecyl Sulfate (SDS) or 1-2% (v/v) Triton X-100, 0.1% Peracetic Acid.
- Buffers: Phosphate-Buffered Saline (PBS), Tris-EDTA (TE) Buffer.
- Enzymatic Solution: DNase I (100 µg/mL) and RNase A (50 µg/mL) in Tris-buffered saline with Mg²⁺.
- Wash Solution: Antibiotic/Antimycotic solution in PBS.
- Equipment: Peristaltic pump-based bioreactor system (or orbital shaker), -80°C freezer, lyophilizer.
Step-by-Step Procedure
- Tissue Preparation: Rinse the fresh tissue in cold PBS to remove surface blood. Cut into uniform slices (2-3 mm thickness) to maximize surface area for reagent penetration.
- Freeze-Thaw Cycle (Physical Lysis): Snap-freeze tissue samples in liquid nitrogen and thaw in a 37°C water bath. Repeat 3 times to initiate cell lysis by forming ice crystals.
- Chemical Decellularization:
- Immerse tissue in 1% SDS solution. Agitate continuously on an orbital shaker (50-60 rpm) at room temperature for 24-48 hours. Alternatively, use a perfusion system for larger organs.
- Note: SDS concentration and time are tissue-dependent and must be optimized.
- Wash Cycle: Rinse tissues in copious amounts of deionized water and PBS (for 24-48 hours with multiple solution changes) to completely remove the detergent, which is cytotoxic.
- Enzymatic Treatment: Incubate tissues in DNase/RNase solution for 4-6 hours at 37°C to digest residual nucleic acid fragments.
- Sterilization and Final Wash: Treat scaffolds with 0.1% peracetic acid for 2 hours to sterilize. Perform a final extensive wash (≥24 hours) in PBS containing antibiotics.
The Scientist's Toolkit: Essential Reagents for Decellularization
Table 3: Key Research Reagent Solutions for Decellularization Protocols
| Reagent / Material | Function / Role in Protocol | Key Considerations |
|---|---|---|
| Sodium Dodecyl Sulfate (SDS) | Ionic detergent that effectively solubilizes lipid membranes and dissociates DNA from proteins [1]. | Can damage ECM ultrastructure and GAGs; requires thorough washing [32] [1]. |
| Triton X-100 | Non-ionic detergent that removes lipid membranes with less protein denaturation than SDS [1]. | Milder action may leave nuclear material; often used in combination with other agents [1]. |
| Sodium Deoxycholate (SDC) | Ionic detergent used as an alternative to SDS for certain tissue types [32]. | Efficiency and ECM impact are tissue-specific. |
| DNase I / RNase A | Enzymes that degrade residual DNA and RNA fragments to below immunogenic thresholds [1]. | Essential step after detergent treatment to remove fragmented nucleic acids. |
| Peracetic Acid | Chemical sterilant that also aids in decellularization by solubilizing organelles and degrading nucleic acids [1]. | Effective for sterilization but can damage ECM at high concentrations [1]. |
Analysis and Interpretation of Results
Post-decellularization analysis must confirm both efficacy and quality. The data should be interpreted holistically.
- Successful Decellularization: A scaffold is considered successfully decellularized when it meets all quantitative DNA criteria and shows no nuclear staining, while simultaneously retaining major structural ECM proteins (collagen, elastin) and a significant proportion of GAGs. The scaffold should further demonstrate excellent biocompatibility in cell culture assays [32] [1].
- Suboptimal Outcomes and Troubleshooting:
- High Residual DNA: Indicates insufficient decellularization. Solution: Increase detergent concentration, duration, or introduce an additional freeze-thaw cycle.
- Poor Cell Viability Post-Seeding: Often caused by residual detergent cytotoxicity. Solution: Extend the PBS wash duration or include albumin in wash buffers to absorb leftover detergent.
- Loss of Mechanical Strength: Suggests excessive collagen damage. Solution: Use a milder detergent (e.g., Triton X-100), reduce agitation speed, or shorten the decellularization time.
Diagram 2: Stem cell-ECM scaffold interactions and key signaling pathways.
Robust and standardized protocols for decellularization are the foundation of reliable research in tissue engineering and regenerative medicine. By adhering to the quantitative thresholds for DNA removal and implementing a comprehensive suite of assays to validate ECM integrity, researchers can generate high-quality, reproducible scaffolds. These acellular matrices are not merely inert structures; they are bioactive platforms that, when properly prepared, can orchestrate stem cell engraftment, support functional tissue formation, and ultimately accelerate the translation of regenerative therapies from the laboratory to the clinic. The ongoing challenge for the field lies in the continued refinement and standardization of these protocols to ensure safety and efficacy across different tissue types and applications [32] [1].
Table: Key Immune Challenges and Strategic Solutions in dECM Scaffold Development
| Immune Challenge | Underlying Cause | Strategic Solution | Expected Outcome |
|---|---|---|---|
| Innate Immune Activation | Residual DAMPs (e.g., DNA, fragmented ECM) from processing [4] | Optimization of decellularization to preserve ECM integrity; Use of apoptosis-assisted techniques [4] | Reduced neutrophil/M1 macrophage infiltration; Shift to pro-remodeling M2 phenotype [58] |
| Adaptive Immune Rejection | Presence of residual MHC and minor histocompatibility antigens [4] | Antigen removal techniques (e.g., sequential solubilization); Crosslinking to mask epitopes [4] | Minimized T-cell activation (CD4+, CD8+); Promotion of regulatory T-cell (Treg) response [4] |
| Foreign Body Response & Fibrosis | Harsh decellularization damaging ECM structure; Cytotoxic residuals [59] | Adoption of gentle physical methods (e.g., HHP); Thorough post-processing washing [60] [59] | Constructive tissue remodeling; Integration with host tissue; Neovascularization [61] [58] |
| Loss of Bioactive Cues | Destruction of ECM-bound growth factors and matrix-bound nanovesicles (MBVs) during processing [58] | Application of tailored decellularization protocols that preserve key ECM components [1] [58] | Enhanced stem cell recruitment, survival, and engraftment; Functional tissue regeneration [24] |
Within the context of advancing stem cell engraftment research, decellularized extracellular matrix (dECM) scaffolds serve as an indispensable biological platform. They provide the three-dimensional architectural and biochemical cues necessary to guide stem cell integration, differentiation, and ultimate tissue regeneration [1]. However, the clinical translation of these scaffolds is often hampered by immunogenic responses triggered by residual cellular material and alterations to the native ECM structure introduced during the decellularization process [4]. A hostile immune environment not only leads to scaffold rejection but also creates a non-conducive microenvironment for the survival and function of co-delivered or recruited stem cells [24]. Therefore, the strategic elimination of cellular remnants and the preservation of the ECM's innate immunomodulatory properties are paramount for successful stem cell-based therapies. This Application Note provides a detailed framework of protocols and analytical methods designed to mitigate immune responses, thereby creating a pro-regenerative milieu for stem cell engraftment.
Quantitative Assessment of Immune Responses to dECM
Rigorous quantification of the host immune response is critical for evaluating the success of any decellularization strategy. The following data, derived from a preclinical study on a foreskin-derived dECM scaffold, exemplifies a standard quantitative framework for assessment.
Table: Quantitative Histological Scoring of Immune Response to dECM Scaffolds in a Rat Model (5-Day vs. 30-Day Follow-Up) [61]
| Histological Parameter | Scoring Scale | Group B (5 Days) Mean ± SD | Group A (30 Days) Mean ± SD | Biological Significance |
|---|---|---|---|---|
| Neutrophil Infiltration | 0 (none) to 3 (severe) | 0.87 ± 0.35 | 1.00 ± 0.53 | Indicator of acute inflammation and tissue damage. Minimal change suggests no severe injury. |
| Eosinophil Infiltration | 0 (none) to 3 (severe) | 0.61 ± 0.51 | 0.75 ± 0.46 | Often associated with allergic responses or rejection; slight presence warrants monitoring. |
| Lymphocyte Infiltration | 0 (none) to 3 (severe) | 1.87 ± 0.35 | 1.75 ± 0.46 | Represents adaptive immune activation. Moderate level may indicate a controlled response. |
| Macrophage Presence | 0 (none) to 3 (severe) | 1.25 ± 0.46 | 1.12 ± 0.35 | Crucial for scaffold remodeling. Phenotype (M1/M2) is more critical than total number. |
| Neovascularization | 0 (none) to 3 (extensive) | 0.57 ± 0.21 | 2.00 ± 0.53* | Signifies scaffold integration and constructive remodeling. Significant increase is a positive outcome. |
| Cellular Colonization | 0 (none) to 3 (extensive) | 0.62 ± 0.32 | 2.42 ± 0.53* | Demonstrates host cell migration and repopulation, essential for tissue regeneration. |
| Encapsulation | 0 (none) to 3 (dense) | 0.87 ± 0.35 | 0.87 ± 0.35 | Mild and stable encapsulation indicates biocompatibility and absence of a chronic foreign body response. |
Note: The significant increase in neovascularization and cellular colonization at 30 days, coupled with minimal encapsulation, supports the scaffold's biocompatibility and pro-regenerative nature [61].
Protocol: Evaluation of Decellularization Efficacy and Scaffold Immunogenicity
This integrated protocol outlines the key steps for processing tissue and assessing the resulting dECM scaffold, with a focus on parameters critical for stem cell engraftment research.
Diagram Title: dECM Scaffold Production and Qualification Workflow
Materials and Reagents
Table: Research Reagent Solutions for dECM Development and Analysis
| Item | Function/Application | Specific Example |
|---|---|---|
| Sodium Dodecyl Sulfate (SDS) | Ionic detergent for efficient cell membrane lysis and nuclear material removal [59]. | 0.1-1% solution in Tris buffer for chemical decellularization [4]. |
| Triton X-100 | Non-ionic detergent for milder decellularization; helps preserve ECM structure [59]. | Often used in combination with SDS to remove residual detergent [59]. |
| Peracetic Acid (PAA) | Acidic agent for decellularization and simultaneous sterilization [1]. | 0.1% concentration recommended for thin tissues to minimize ECM damage [1]. |
| DNase/RNase | Enzymatic degradation of residual nucleic acids to reduce DAMP load [4]. | Incubation post-cell lysis (e.g., 50 U/mL DNase, 1 U/mL RNase) [60]. |
| High Hydrostatic Pressure (HHP) System | Physical decellularization method that preserves ECM ultrastructure and basement membrane [60]. | Application of 1000 MPa for 10 minutes at 30°C for porcine aorta [60]. |
| Antibodies for Flow Cytometry | Quantification of immune cell populations and phenotypes in explants. | CD68 (macrophages), CD3 (T-cells), CD4 (Helper T-cells), CD8 (Cytotoxic T-cells). |
Step-by-Step Procedure
Part A: Decellularization and Post-Processing
- Tissue Preparation: Aseptically procure and process the source tissue (e.g., human foreskin, porcine aorta) to desired dimensions. Rinse thoroughly in phosphate-buffered saline (PBS) with antibiotics (e.g., 1% gentamicin) [60].
- Decellularization Protocol Selection:
- Chemical Method (SDS-based): Immerse tissue in 0.5% SDS solution with gentle agitation for 24-48 hours at room temperature. The duration must be optimized for each tissue type to balance cell removal and ECM preservation [59].
- Physical Method (HHP-based): Place tissue in an isotonic solution within a pressure chamber. Apply hydrostatic pressure (e.g., 1000 MPa) for a defined period (e.g., 10 minutes). This physically ruptures cellular membranes [60].
- Nuclease Treatment: Following cell lysis, incubate tissue in a solution containing DNase (50 U/mL) and RNase (1 U/mL) for 4-6 hours at 37°C to digest residual nucleic acids [60] [4].
- Post-Processing Wash: Wash the decellularized tissue extensively in PBS or deionized water for a minimum of 72-96 hours with multiple solution changes to remove all cellular debris, detergents, and enzymes [59]. This step is critical to eliminate cytotoxic residuals.
- Sterilization: Utilize low-dose peracetic acid (0.1%) or ethanol washes for sterilization, as gamma irradiation can cross-link and alter the ECM mechanically [4].
Part B: Assessment of Decellularization Efficacy and Safety
- Residual DNA Quantification:
- Extract DNA from a lyophilized portion of the dECM scaffold using a commercial kit.
- Quantify the amount of DNA per mg of dry tissue weight. A threshold of <50 ng/mg dry weight is widely accepted as indicative of effective decellularization [4].
- Analyze DNA fragment size via gel electrophoresis. The absence of high-molecular-weight bands indicates successful nuclear material removal.
- ECM Composition Analysis:
- In Vitro Cytotoxicity Assay:
- Prepare an extract from the dECM scaffold by incubating it in cell culture medium.
- Apply this extract to a monolayer of representative cells (e.g., fibroblasts, mesenchymal stem cells).
- Assess cell viability after 24-72 hours using a metabolic assay (e.g., MTT, Alamar Blue). Viability should be >90% compared to control medium [59].
The Immunological Cascade in dECM Scaffold Integration
Understanding the immune mechanisms triggered upon dECM implantation is essential for developing targeted mitigation strategies. The following diagram and table outline the key pathways.
Diagram Title: Immune Pathways in dECM Integration
Table: Key Immune Players and Their Roles in dECM Scaffold Fate
| Immune Component | Role in Pro-Inflammatory/Rejection Response | Role in Pro-Remodeling/Acceptance Response |
|---|---|---|
| Macrophages | M1 Phenotype: Drives inflammation, releases proteases, contributes to scaffold degradation [58] [4]. | M2 Phenotype: Promotes ECM deposition, angiogenesis, and stem cell recruitment; resolves inflammation [58] [4]. |
| T Lymphocytes | CD4+ Th1/Th17: Secrete pro-inflammatory cytokines (IFN-γ, IL-17), sustaining M1 polarization [4]. CD8+ Cytotoxic T-cells: Directly target antigen-presenting cells. | CD4+ Tregs (Regulatory T-cells): Suppress effector T-cell function, promote immune tolerance, and support M2 polarization [58] [4]. |
| B Lymphocytes | Produce antibodies against residual antigens, activating the complement system and accelerating scaffold degradation [58]. | Can contribute to a tolerogenic humoral profile (Th2-restricted) that is compatible with constructive remodeling [58]. |
| DAMPs & Antigens | Activate innate immunity via PRRs, leading to inflammation and enhancing antigen presentation to T-cells [4]. | Well-prepared scaffolds with minimal DAMPs/antigens avoid triggering these destructive pathways. Preserved ECM bioactively promotes resolution. |
Advanced Strategies for Immunogenicity Mitigation
Beyond basic decellularization, several advanced strategies can further reduce immunogenicity and enhance scaffold compatibility for stem cell engraftment.
- Selective Antigen Removal: Techniques such as sequential antigen solubilization can be employed to specifically target and remove immunogenic molecules like α-Gal epitopes and MHC complexes from the ECM without disrupting its structural integrity [4].
- Crosslinking for Epitope Masking: Controlled crosslinking using agents like genipin or carbodiimide can mask residual antigenic epitopes on the ECM, shielding them from recognition by the host immune system. This must be optimized, as over-crosslinking can reduce biodegradability and bioactivity [4].
- Leveraging Matrix-Bound Nanovesicles (MBVs): Preserving native MBVs during decellularization is crucial. These vesicles contain non-coding RNAs and bioactive lipids that actively modulate macrophage polarization towards a pro-regenerative M2 phenotype, creating a favorable environment for stem cell survival and integration [58].
- Stem Cell Co-Implantation and Preconditioning: The immunomodulatory properties of Mesenchymal Stem Cells (MSCs) can be harnessed. Hypoxic preconditioning (1-5% O₂) of MSCs before transplantation upregulates pro-survival and angiogenic genes (e.g., VEGF, GLUT-1), enhancing their resilience and ability to survive in the initially hostile post-implantation microenvironment [24]. These MSCs can then secrete factors that suppress local inflammation and promote tolerance.
The successful clinical application of decellularized tissues in stem cell engraftment research is critically dependent on a comprehensive strategy to mitigate immune responses. This involves not only the effective elimination of cellular remnants through optimized, tissue-specific decellularization protocols but also the proactive preservation of the ECM's native immunomodulatory signals. By adhering to rigorous qualification protocols, understanding the underlying immune mechanisms, and implementing advanced mitigation strategies, researchers can produce dECM scaffolds that support stem cell survival, engraftment, and ultimately, functional tissue regeneration. The framework provided herein serves as a detailed guide for developing biocompatible dECM platforms conducive to advanced regenerative medicine applications.
A significant challenge in the field of bioengineered organs is the successful revascularization of decellularized scaffolds. The process of decellularization, which removes cellular material to leave behind a native extracellular matrix (ECM) scaffold, has shown great promise for creating transplantable organs [62]. However, the long-term functionality of these bioengineered constructs is critically dependent on re-establishing a robust, non-thrombogenic, and quiescent endothelial lining throughout the entire vascular tree [63]. This application note details the primary hurdles and provides validated protocols to address the revascularization challenge, a cornerstone for enabling stem cell engraftment in decellularized tissues.
The clinical imperative is clear: chronic lower respiratory diseases are a leading cause of death, and the demand for lung transplants far exceeds the available donor organs [63]. Decellularized organ scaffolds, potentially sourced from organs unsuitable for transplantation, offer a revolutionary solution. The ultimate success of this approach, however, hinges on overcoming the vascular barrier. Preclinical studies reveal that inadequate revascularization leads to catastrophic failure post-implantation, manifesting as hemorrhage into the airways and thrombosis within the vasculature [63].
Core Challenges in Scaffold Revascularization
Revascularization is not merely about seeding endothelial cells; it involves the complete reconstitution of a functional vascular system. The major challenges are multifaceted:
- ECM Integrity: The decellularization process itself can compromise the subendothelial basement membrane, particularly the delicate respiratory membrane in lungs, which is less than 1 μm thick in humans [63]. An intact ECM is not just a passive scaffold; it provides critical biomechanical cues and contains bioactive molecules like laminin and fibronectin that are essential for cell adhesion and function [64] [62].
- Functional Endothelium: The re-established endothelium must form a tight barrier function to prevent plasma leakage and must also exhibit quiescence to avoid inflammation and thrombosis [63]. Different vascular segments (arteries, veins, capillaries) have unique endothelial phenotypes, adding a layer of complexity to recellularization efforts [63].
- Cell Source and Seeding: Finding a clinically relevant cell source—whether primary cells, induced pluripotent stem cell (iPSC)-derived endothelial cells, or progenitor cells—and achieving homogenous cell distribution throughout the entire vascular tree, including the capillary beds, remains a significant technical hurdle [62].
Table 1: Key Challenges and Consequences in Scaffold Revascularization
| Challenge | Underlying Cause | Observed Consequence |
|---|---|---|
| Thrombogenesis | Incomplete re-endothelialization; loss of anti-thrombogenic ECM factors [64] | Clotting within the vasculature, leading to graft failure [63] |
| Hemorrhage | Damage to the capillary basement membrane and incomplete endothelial barrier [63] | Blood leakage into the parenchymal (e.g., airway) compartments [63] |
| Poor Cell Engraftment | Denaturation of adhesive ECM proteins (e.g., collagen IV, laminin) by harsh detergents [64] | Low cell adhesion and survival, resulting in incomplete vascular lining [64] |
| Inflammation | Presence of residual cellular debris from incomplete decellularization [63] | Immune rejection of the bioengineered construct [63] |
Quantitative Analysis of Decellularization Parameters
The choice of decellularization protocol directly impacts the success of subsequent revascularization. The detergent Sodium Dodecyl Sulfate (SDS) is commonly used, but its concentration must be carefully optimized to balance cell removal with ECM preservation. A 2023 study systematically compared two SDS concentrations for their effect on human endothelial cell recellularization in rat kidney scaffolds [64].
Table 2: Impact of SDS Concentration on Decellularization Efficacy and Recellularization Success
| Parameter | Low-Concentration SDS (0.66%) | High-Concentration SDS (3%) |
|---|---|---|
| SDS Concentration | 0.66% | 3% |
| Decellularization Efficacy | Complete cell removal; preservation of ECM ultrastructure and adhesive proteins (laminin, fibronectin, collagen IV) [64] | Complete cell removal; increased risk of ECM protein denaturation and GAG depletion [64] [62] |
| Relative Endothelial Cell Quantity after 5 days | 1.39 (± 0.26) | 0.62 (± 0.07) |
| Cell Distribution | Predominant distribution in the cortex, covering vascular basement membranes and glomeruli in a monolayer [64] | Poor cell density; scaffold appeared almost vacant in all anatomical areas [64] |
| Phenotype & Proliferation | Strong positivity for CD-31 (endothelial marker) and PCNA (proliferation marker); negligible apoptosis [64] | Preserved endothelial phenotype but significantly fewer proliferating cells [64] |
| Recommended Use | Preferred for revascularization and co-culture experiments [64] | Not recommended for endothelialization; may be considered for other xenogeneic cell types [64] |
Experimental Protocols
Protocol: Pressure-Controlled Decellularization of Rodent Kidneys for Optimal Revascularization
This protocol is adapted from a 2023 study that demonstrated superior endothelialization after gentle decellularization [64].
I. Materials
- Perfusion System: Pressure-controlled bioreactor or gravity-fed system.
- Decellularization Agents: Sodium dodecyl sulfate (SDS), deionized water, phosphate-buffered saline (PBS).
- Antibiotics: Penicillin-Streptomycin.
- Evaluation Reagents: 4',6-Diamidino-2-Phenylindole (DAPI), Hematoxylin and Eosin (H&E), antibodies for collagen IV, laminin, and fibronectin.
II. Method
- Organ Harvesting: Excise the rodent kidney with the renal artery, vein, and ureter intact. Cannulate the renal artery.
- Initial Perfusion: Perfuse with 1x PBS containing 1% Penicillin-Streptomycin to clear residual blood.
- Decellularization: Perfuse with 0.66% (w/v) SDS in deionized water for 48 hours under constant pressure (e.g., 30-50 mmHg).
- Rinsing: Thoroughly rinse the scaffold by perfusing with deionized water for 24 hours, followed by 1x PBS for another 24 hours to remove all detergent traces.
- Sterilization: Prior to recellularization, perfuse with 0.1% peracetic acid or use gamma irradiation.
- Quality Control:
- Histology: Stain with H&E and DAPI to confirm the absence of nuclear material.
- ECM Assessment: Perform immunohistochemical staining for collagen IV, laminin, and fibronectin to verify ECM retention.
- DNA Quantification: Measure residual DNA content to ensure it is <50 ng/mg of tissue dry weight [62].
Protocol: Dynamic Culture for Vascular Recellularization
I. Materials
- Bioreactor: A pressure- or flow-controlled bioreactor that mimics physiological vascular conditions.
- Cell Culture Media: Endothelial cell growth medium (e.g., EGM-2).
- Cells: Human immortalized endothelial cells (e.g., EA.hy 926) or iPSC-derived endothelial cells.
II. Method
- Cell Preparation: Harvest and resuspend endothelial cells at a concentration of 1-5 x 10^6 cells/mL in culture medium.
- Seeding: Slowly inject the cell suspension through the cannulated renal artery using a syringe pump. Gently rotate the scaffold to ensure even distribution.
- Dynamic Culture: Transfer the seeded scaffold to the bioreactor. Perfuse with culture medium at a low, pulsatile flow rate (e.g., 0.5-1 mL/min) for 24-48 hours to facilitate initial cell adhesion.
- Maturation: Gradually increase the flow rate and shear stress over 5-7 days to promote endothelial monolayer maturation and barrier function.
- Monitoring:
- Viability: Assess daily with glucose consumption and lactate dehydrogenase (LDH) release assays.
- Functionality: Perform perfusion with fluorescently labeled dextran or beads to assess barrier function and patency [63].
- Characterization: After 5-7 days, fix the construct and stain for CD-31, von Willebrand Factor, and PCNA to confirm endothelial phenotype and proliferation [64].
Visualizing the Revascularization Workflow
The following diagram illustrates the complete workflow from native organ to a revellularized and potentially transplantable scaffold, highlighting the critical steps for successful revascularization.
The Scientist's Toolkit: Essential Reagents for Revascularization
Table 3: Key Research Reagent Solutions for Scaffold Revascularization
| Reagent / Material | Function in Revascularization | Application Notes |
|---|---|---|
| Sodium Dodecyl Sulfate (SDS) | Ionic detergent for lysing cells and removing cellular material from the ECM [64] | Low concentrations (e.g., 0.66%) preserve ECM integrity and support endothelial cell adhesion better than high concentrations (e.g., 3%) [64] |
| Triton X-100 | Non-ionic detergent for cell lysis; often used in combination with SDS [62] | May better preserve certain ECM components like growth factors but can be less effective at complete cell removal [62] |
| Collagenase | Enzyme for tissue dissociation; can be used to isolate primary cells or assess decellularization efficacy [62] | Can degrade collagen in the ECM if exposure is not controlled; use specific types (e.g., Collagenase IV) for delicate tissues |
| Endothelial Growth Medium-2 (EGM-2) | Culture medium supplemented with growth factors (VEGF, FGF, EGF) to promote endothelial cell survival and proliferation [64] | Essential for maintaining endothelial phenotype and proliferative behavior during dynamic culture [64] |
| EA.hy 926 Cell Line | Immortalized human endothelial cell line derived from HUVEC and A549 carcinoma fusion [64] | Provides a consistent, reproducible cell source for recellularization studies, overcoming limitations of primary HUVECs [64] |
| CD-31 (PECAM-1) Antibody | Immunohistochemical marker for identifying endothelial cells and confirming phenotype post-seeding [64] | Strong positivity indicates preservation of endothelial character after recellularization [64] |
| Laminin & Collagen IV Antibodies | Staining for key basement membrane proteins to assess ECM preservation post-decellularization [64] | Critical for evaluating the retention of adhesive proteins that support endothelial cell attachment [64] [62] |
Decellularized extracellular matrix (dECM) has emerged as a foundational biomaterial in regenerative medicine, particularly for stem cell engraftment research. By removing immunogenic cellular components while preserving the native tissue's structural and biochemical composition, dECM provides a three-dimensional, non-immunogenic scaffold enriched with tissue-specific bioactive components [65]. This preserved native microenvironment offers critical biological cues that support stem cell survival, retention, and differentiation—key challenges in transplantation therapy [66]. The complex microenvironment of dECM, containing functional ECM characteristics and structural components such as collagen and proteoglycans, plays a pivotal role in maintaining tissue homeostasis and promoting angiogenesis, making it an ideal candidate for creating tissue-engineered grafts for stem cell delivery [65].
However, the decellularization process itself can compromise the structural integrity and mechanical strength of the native ECM, creating a pressing need for optimization strategies [67]. Cross-linking and functionalization with bioactive molecules represent two fundamental approaches to enhance dECM scaffold performance. Physical and chemical cross-linking methods restore biomechanical properties and degradation stability, while the incorporation of bioactive molecules further enhances the scaffold's ability to direct specific stem cell behaviors [67]. These optimization techniques aim to achieve a delicate balance between the degradation of the implanted biomaterial and the regeneration of host tissue, ultimately determining the success of stem cell engraftment outcomes [67]. This application note provides detailed protocols and methodological frameworks for optimizing dECM scaffolds to enhance stem cell integration and function in regenerative therapies.
Core Principles of dECM Biocompatibility
The Biocompatibility-Immunogenicity Balance
The fundamental premise of using dECM scaffolds lies in their inherently low immunogenic potential compared to cellular tissues. Effective decellularization removes the major histocompatibility complex (MHC) antigens and other cell-surface immunogens that trigger host rejection, while preserving the structural and functional proteins of the native ECM [68]. The immune response is a critical issue in the use of tissue engineering products such as decellularized tissues that must be considered at the time of transplantation [68]. Dendritic cells, as a component of the immune system, are responsible for recognizing implanted scaffolds, and can initiate inflammatory responses if they detect foreign agents [68].
The decellularization method must be selected to minimize disruption of the natural ECM architecture while ensuring complete removal of cellular material. Research indicates that the biocompatibility of decellularized tissues in a range of biological applications is becoming more widely acknowledged [68]. If the decellularized tissue is biocompatible, cell attachment and angiogenesis can occur effectively in the tissue [68]. This biocompatibility makes decellularized scaffolds suitable for studies in wound healing, cartilage, bone applications, and ultimately, for supporting stem cell engraftment.
Quality Control Assessment Metrics
Rigorous quality control is essential to ensure dECM scaffolds meet biocompatibility standards for stem cell research. The table below outlines key assessment metrics and their target values for optimized dECM scaffolds.
Table 1: Quality Control Metrics for dECM Scaffolds
| Assessment Category | Specific Metric | Target Value/Range | Analytical Method |
|---|---|---|---|
| Cellular Removal | DNA Content | <50 ng/mg dry weight [65] | DNA quantification |
| DNA Fragment Size | <200 bp [65] | Gel electrophoresis | |
| ECM Preservation | Collagen Content | >85% retention [65] | Hydroxyproline assay |
| GAG Content | >70% retention [65] | DMMB assay | |
| Growth Factor Retention | Variable by tissue type | ELISA/Luminex | |
| Structural Integrity | Ultrastructure Preservation | Intact fibrillar architecture [68] | SEM/TEM |
| Porosity | Tissue-specific maintenance | Micro-CT | |
| Biocompatibility | Cytotoxicity | >90% cell viability [69] | Live/Dead assay |
| Immune Response | Limited inflammatory activation [69] | Cytokine profiling |
Assessment of these parameters requires a hierarchical approach, with priority given to cellular and genetic material removal, followed by structural protein preservation [65]. A comparative analysis of the mechanical attributes and ultrastructural characteristics of tissues or organs before and after treatment is indispensable, with emphasis on the method's capacity to retain characteristics indispensable for successful tissue or organ reconstruction [65].
Cross-linking Strategies for Enhanced Mechanical Stability
Cross-linking Mechanism Classification
Cross-linking of dECM biomaterials serves to restore or improve biomechanical properties, stability, and bioactivity following decellularization treatments that can compromise native matrix integrity [67]. These methods work by creating covalent or non-covalent bonds between ECM components, primarily collagen fibrils, enhancing resistance to enzymatic degradation and improving mechanical strength. The selection of appropriate cross-linking strategies is essential to achieve a balance between degradation of the implanted biomaterial and regeneration of the host tissue [67].
The diagram below illustrates the decision pathway for selecting appropriate cross-linking methods based on specific research applications and desired material properties.
Chemical Cross-linking Protocols
Genipin Cross-linking Protocol
- Reagent Preparation: Prepare 0.5-1.0% (w/v) genipin solution in phosphate-buffered saline (PBS) or ethanol/PBS mixture (30:70 v/v). Protect from light during preparation and use due to photosensitivity.
- Cross-linking Procedure:
- Rinse dECM scaffolds thoroughly with sterile PBS to remove preservation solutions.
- Immerse scaffolds in genipin solution at a ratio of 10:1 (solution volume:scaffold volume) to ensure complete coverage.
- Incubate at 37°C for 24-48 hours with gentle agitation. The cross-linking process is evidenced by a characteristic blue-green coloration.
- Terminate reaction by removing genipin solution and washing extensively with PBS (6-8 washes over 24 hours) until the wash solution remains clear.
- Quality Control: Assess cross-linking efficiency by measuring compressive modulus increase (target: 1.5-2.5x pre-treatment value) and resistance to collagenase digestion (≥70% mass retention after 24h incubation with 1 U/mL collagenase).
EDC/NHS Cross-linking Protocol
- Reagent Preparation: Prepare cross-linking solution fresh for each use: 20 mM 1-ethyl-3-(3-dimethylaminopropyl)carbodiimide (EDC) and 10 mM N-hydroxysuccinimide (NHS) in 50 mM MES buffer (pH 5.5-6.0). Do not use PBS or other phosphate-containing buffers as they inhibit the reaction.
- Cross-linking Procedure:
- Equilibrate dECM scaffolds in MES buffer for 1-2 hours prior to cross-linking.
- Immerse scaffolds in EDC/NHS solution at 4°C for 4-6 hours with gentle agitation.
- Stop reaction by transferring scaffolds to 0.1 M Na2HPO4 buffer (pH 9.0) for 2 hours to quench unreacted esters.
- Wash extensively with PBS (4-6 changes over 24 hours) to remove byproducts.
- Quality Control: Evaluate cross-linking efficiency through amine group quantification (TNBS assay; target: 40-60% reduction in free amines) and mechanical testing.
Table 2: Comparative Analysis of Cross-linking Methods for dECM Scaffolds
| Cross-linking Method | Mechanism of Action | Advantages | Limitations | Optimal Applications |
|---|---|---|---|---|
| Genipin | Nucleophilic attack of primary amines forming heterocyclic bridges | Excellent cytocompatibility, Natural origin, Intermediate strength | Slow reaction rate, Dark blue coloration, Higher cost | Neural, Cardiovascular, Stem cell niches |
| EDC/NHS | Zero-length carbodiimide chemistry forming amide bonds between carboxyl and amine groups | No incorporation of cross-linker, Well-characterized, Tunable strength | Requires acidic pH, Potential mineral dissolution, Byproduct accumulation | Cartilage, Bone, Tendon/Ligament |
| Glutaraldehyde | Schiffs base formation between aldehyde and amine groups | High mechanical strength, Rapid reaction, Cost-effective | Cytotoxicity concerns, Calcification risk, Permanent cross-links | Heart valves, Vascular grafts (with thorough washing) |
| UV Radiation | Free radical formation leading to covalent bonds between tyrosine residues | No chemical residues, Surface-specific modification, Easy application | Potential ECM damage, Limited penetration depth, Oxidation concerns | Surface modification, Thin tissues |
| Transglutaminase | Enzyme-catalyzed acyl transfer between glutamine and lysine residues | Biological safety, Specificity, Mild conditions | High cost, Limited availability, Substrate specificity | Soft tissue engineering, Stem cell expansion |
Incorporation of Bioactive Molecules
Strategic Molecular Functionalization
The incorporation of bioactive molecules into dECM scaffolds significantly enhances their capacity to direct stem cell behavior, including adhesion, proliferation, differentiation, and engraftment. These molecules work synergistically with the native ECM components to create microenvironments that mimic native stem cell niches. Common functionalization approaches include physical adsorption, covalent conjugation, and affinity-based binding, each with specific advantages for different research applications.
For stem cell engraftment specifically, key bioactive molecules include:
- RGD Peptides: Arginine-Glycine-Aspartate sequences promote integrin-mediated cell adhesion [69]. Covalent conjugation via dopamine chemistry (RGD-dopamine) allows for stable functionalization of various scaffold surfaces, supporting large-scale cellular attachment and expansion over extended periods [69].
- Growth Factors: Molecules such as VEGF, FGF, and TGF-β can be incorporated to direct stem cell differentiation. Heparin-based binding systems protect these factors from proteolytic degradation and enable controlled release.
- Engineered Peptides: Laminin-derived and other tissue-specific peptides enhance stem cell homing and integration in specialized tissues.
The experimental workflow below outlines the key decision points and processes for effectively incorporating bioactive molecules into dECM scaffolds.
Detailed Functionalization Protocols
RGD-Dopamine Conjugation Protocol
- Reagent Preparation:
- Synthesize RGD-dopamine conjugate by reacting RGD peptide with dopamine hydrochloride in the presence of EDC/NHS in MES buffer (pH 5.5) for 12 hours at 4°C.
- Purify via dialysis against distilled water (MWCO 500 Da) and lyophilize.
- Prepare working solution at 0.5-1.0 mg/mL in Tris buffer (pH 8.5) immediately before use.
- Functionalization Procedure:
- Equilibrate dECM scaffolds in Tris buffer (pH 8.5) for 1 hour.
- Immerse scaffolds in RGD-dopamine solution with gentle agitation for 24 hours at room temperature.
- The oxidative polymerization of dopamine creates a stable coating on the ECM surface with conjugated RGD peptides.
- Rinse thoroughly with PBS to remove unbound conjugate (4-5 washes over 12 hours).
- Quality Control: Verify functionalization by X-ray photoelectron spectroscopy (nitrogen detection) and evaluate bioactivity through cell adhesion assays (target: ≥2x increase in cell attachment compared to non-functionalized controls).
Heparin-Binding Growth Factor Delivery System
- Reagent Preparation:
- Prepare heparin solution (1 mg/mL in PBS).
- Prepare EDC/NHS solution in MES buffer as described in section 3.2.
- Prepare growth factor solution at 10-50 μg/mL in PBS with 0.1% BSA.
- Functionalization Procedure:
- Covalently conjugate heparin to dECM scaffolds using EDC/NHS chemistry (follow protocol in section 3.2 with heparin addition to the reaction solution).
- Wash scaffolds extensively with PBS to remove unbound heparin.
- Incubate heparinized scaffolds with growth factor solution for 2 hours at room temperature or overnight at 4°C.
- Rinse gently with PBS to remove unbound growth factors.
- Quality Control: Quantify heparin binding via toluidine blue assay; determine growth factor loading efficiency via ELISA; assess release kinetics in physiological buffer over 14 days.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for dECM Cross-linking and Biofunctionalization
| Reagent Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Cross-linking Agents | Genipin (≥98% purity), EDC, NHS, Glutaraldehyde (25%) | Enhance mechanical properties, Reduce degradation rate | Genipin preferred for stem cell applications due to superior cytocompatibility |
| Bioactive Molecules | RGD peptides, Laminin-derived peptides, VEGF, FGF-2, BDNF | Direct stem cell behavior, Enhance engraftment | Use carrier proteins (e.g., BSA) for stock solutions of sensitive growth factors |
| Conjugation Chemistry | Dopamine hydrochloride, Sulfo-SMCC, DBCO-PEG4-NHS | Covalent attachment of bioactive molecules | Test cytotoxicity of conjugation chemistry on target stem cell population first |
| Enzymatic Assay Kits | Live/Dead viability/cytotoxicity, PicoGreen DNA quantification, Hydroxyproline assay | Quality control assessment | Establish baseline values for each new dECM batch |
| Detergents & Solutions | SDS, Triton X-100, Sodium deoxycholate, DNase/RNase solutions | Decellularization processing | Thorough washing critical to remove residual detergents [68] |
| Cell Culture Assays | AlamarBlue, Phalloidin staining, ELISA for specific markers | Functional validation | Include appropriate positive and negative controls for each assay |
Concluding Remarks and Future Perspectives
Optimizing the biocompatibility and function of dECM scaffolds through cross-linking and incorporation of bioactive molecules represents a crucial methodology in stem cell engraftment research. The techniques outlined in this application note provide researchers with standardized approaches to enhance dECM performance while maintaining the innate advantages of natural extracellular matrix. As the field progresses, emerging technologies such as spatial functionalization, smart biomaterials with responsive release mechanisms, and patient-specific ECM scaffolds will further enhance our ability to create optimal microenvironments for stem cell survival, integration, and function. By implementing these detailed protocols and maintaining rigorous quality control standards, researchers can advance the development of effective stem cell-based regenerative therapies.
{ article }
Monitoring Cell-Scaffold Interactions: Tools to Assess Stem Cell Survival, Integration, and Phenotypic Stability
In the field of regenerative medicine, decellularized tissues have emerged as a leading platform for stem cell engraftment research. These scaffolds provide a unique biomimetic niche, preserving the native extracellular matrix (ECM) architecture and bioactive cues that are crucial for guiding stem cell behavior [22]. However, the clinical success of these engineered constructs hinges on the ability to rigorously monitor and evaluate the key parameters of stem cell fate post-implantation. The hostile microenvironment at the transplantation site often leads to significant cell death, with studies indicating that up to 90% of transplanted stem cells may undergo apoptosis within the first few days [24]. This underscores the critical need for robust, standardized tools to accurately assess stem cell survival, integration into the host scaffold, and long-term phenotypic stability. This protocol details comprehensive methodologies for the quantitative assessment of these vital parameters, providing a essential framework for research aimed at reliable fertility restoration and other regenerative applications.
Assessment Tables: Key Parameters and Methods
A multi-parametric approach is essential for a complete understanding of stem cell-scaffold interactions. The following tables summarize the core assessment categories, key parameters, and corresponding analytical techniques.
Table 1: Assessing Stem Cell Survival and Viability
| Assessment Category | Key Parameter | Quantitative/Qualitative Tools | Notes and Specifications |
|---|---|---|---|
| Metabolic Activity | Oxygen consumption, Glucose utilization, Metabolic waste | Electrochemical biosensors (pH, O₂, glucose), Fluorescent probes [70] [24] | Real-time, non-invasive monitoring possible with integrated biosensors. |
| Cell Viability & Death | Live/Dead ratio, Apoptosis/Necrosis, Cytotoxicity | Live/Dead assay (Calcein-AM/Propidium Iodide), TUNEL assay, LDH release [24] [71] | End-point assays. Correlate with metabolic data for confirmation. |
| Proliferative Capacity | Cell number, DNA synthesis, Colony formation | DNA quantification (PicoGreen, DAPI), EdU/BrdU assay, CFU assays [22] [71] | Normalize DNA content to scaffold dry weight. |
Table 2: Assessing Stem Cell Integration and Phenotypic Stability
| Assessment Category | Key Parameter | Quantitative/Qualitative Tools | Notes and Specifications |
|---|---|---|---|
| Structural Integration | Cell adhesion, Migration, Spatial distribution | Histology (H&E), Immunohistochemistry (IHC) for adhesion proteins (Integrins, Vinculin), SEM [22] [72] | SEM reveals cell morphology and attachment to ECM fibers. |
| Phenotypic Stability | Lineage-specific marker expression, Undifferentiated state | Immunocytochemistry/IF, RT-qPCR, Flow Cytometry [22] [16] | Track markers like OCT4 (pluripotency) or DAZL (germ cell). |
| Functional Potency | Secretion of trophic factors, Specific differentiated function | ELISA for cytokines/VEGF, In vitro functional assays (e.g., contractility, phagocytosis) [71] [16] | Directly measures therapeutic potential of the construct. |
Experimental Protocols
This section provides detailed, step-by-step methodologies for key experiments in monitoring cell-scaffold constructs.
Protocol 1: Scaffold Recellularization and Viability Assessment
This protocol outlines the process for seeding stem cells onto a decellularized scaffold and conducting a standard viability assessment.
- 1. Scaffold Preparation: Aseptically rinse the decellularized scaffold (e.g., decellularized testis) in phosphate-buffered saline (PBS) and precondition in cell culture medium for 1-2 hours before cell seeding [22].
- 2. Cell Seeding: Resuspend the stem cell population (e.g., Spermatogonial Stem Cells - SSCs) at a high density (e.g., 1-5 x 10⁶ cells/mL). Use a dynamic seeding method: slowly pipet the cell suspension onto the scaffold and place it on an orbital shaker (50-70 RPM) in an incubator for 4-6 hours to promote uniform cell attachment. For static seeding, carefully apply multiple small droplets of cell suspension across the scaffold surface [22].
- 3. Culture: Transfer the seeded construct to a new well plate with fresh culture medium. Maintain the constructs in a standard cell culture incubator (37°C, 5% CO₂), changing the medium every 2-3 days.
- 4. Viability Staining (Live/Dead Assay)
- a. Preparation: Prepare a working solution of PBS containing 2 µM Calcein-AM and 4 µM Propidium Iodide (PI).
- b. Staining: At the desired time point, carefully wash the cell-scaffold construct with PBS. Incubate with the staining solution for 30-45 minutes at 37°C, protected from light.
- c. Imaging & Analysis: Wash the construct gently with PBS. Image immediately using a confocal microscope. Calcein-AM (green fluorescence) labels live cells, while PI (red fluorescence) labels dead cells with compromised membranes. Quantify the ratio of live to dead cells from multiple z-stack images using image analysis software (e.g., ImageJ/Fiji) [24].
Protocol 2: Quantitative PCR for Phenotypic Marker Analysis
This protocol describes RNA extraction and gene expression analysis to monitor stem cell phenotype and differentiation status.
- 1. RNA Extraction
- a. Homogenization: Lyse the entire cell-scaffold construct in a suitable lysis buffer (e.g., TRIzol). Homogenize thoroughly using a mechanical homogenizer or a pestle to disrupt the ECM.
- b. Isolation: Isolate total RNA following the standard phenol-chloroform extraction protocol or using a commercial silica-membrane column kit. Include an on-column DNase digestion step to remove genomic DNA contamination.
- 2. cDNA Synthesis: Quantify the purified RNA using a spectrophotometer (NanoDrop). Use equal amounts of RNA (e.g., 500 ng - 1 µg) for reverse transcription into cDNA using a high-capacity cDNA reverse transcription kit with random hexamer primers.
- 3. Quantitative PCR (qPCR)
- a. Reaction Setup: Prepare qPCR reactions in triplicate containing: 1X SYBR Green master mix, forward and reverse primers (e.g., for pluripotency markers like OCT4, NANOG; germ cell markers like DAZL, PIWIL2; and housekeeping genes like GAPDH, HPRT), and diluted cDNA template.
- b. Amplification: Run the plate on a real-time PCR instrument using a standard two-step amplification protocol (e.g., 95°C for 10 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 1 min).
- c. Data Analysis: Calculate the relative gene expression levels using the comparative 2^(–ΔΔCt) method, normalizing the data to the housekeeping genes and a control sample [22].
Protocol 3: Histological and Immunohistochemical Analysis
This protocol is for the structural and protein-level evaluation of cell integration and phenotype.
- 1. Fixation and Sectioning: Fix the cell-scaffold construct in 4% paraformaldehyde for 24-48 hours at 4°C. Dehydrate the samples through a graded ethanol series, clear with xylene, and embed in paraffin. Section into 5 µm thick slices using a microtome and mount onto glass slides.
- 2. Deparaffinization and Rehydration: For staining, deparaffinize the sections in xylene and rehydrate through a graded series of ethanol to water.
- 3. Staining:
- H&E Staining: Stain with Hematoxylin to label cell nuclei, followed by eosin to label proteins and the ECM. This allows for visualization of overall cell distribution and scaffold architecture [22].
- Immunohistochemistry (IHC):
- a. Antigen Retrieval: Perform heat-induced epitope retrieval by incubating the slides in a citrate-based buffer (pH 6.0) in a decloaking chamber or water bath.
- b. Blocking: Block non-specific binding by incubating with 10% normal goat serum and 1% BSA in PBS for 1 hour.
- c. Primary Antibody Incubation: Incubate with a specific primary antibody (e.g., anti-Collagen Type I to confirm ECM preservation, or anti-Ki-67 for proliferation) diluted in blocking buffer overnight at 4°C [22].
- d. Secondary Antibody & Detection: Apply an HRP-conjugated secondary antibody for 1 hour at room temperature. Visualize using a chromogen like DAB, which produces a brown precipitate. Counterstain with Hematoxylin to label nuclei.
- 4. Imaging: Analyze the stained slides under a light microscope. IHC staining allows for semi-quantitative assessment of protein expression and localization within the construct.
The Scientist's Toolkit: Research Reagent Solutions
The following table lists key reagents and materials essential for the experiments described in these application notes.
Table 3: Essential Research Reagents and Materials
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| Decellularized Tissue Scaffold | Provides a biomimetic 3D structure for cell growth. | Serves as the foundational substrate for SSC engraftment in testicular regeneration models [22]. |
| Spermatogonial Stem Cells (SSCs) | The stem cell population of interest for regenerative therapy. | Isolated via flow cytometry using DBA lectin for positive selection [22]. |
| Calcein-AM / Propidium Iodide (PI) | Fluorescent dyes for simultaneous labeling of live and dead cells. | Used in the Live/Dead assay to quantify cell viability post-seeding [24]. |
| Collagenase / Trypsin-EDTA | Enzymes for tissue dissociation and cell harvesting. | Used to isolate single cells from native tissues for subsequent culture or analysis [22]. |
| Primers for Lineage Markers | Specific oligonucleotides for gene expression analysis via RT-qPCR. | To assess phenotypic stability by measuring transcripts like DAZL and PIWI [22]. |
| Antibodies for IHC/IF | Proteins for detecting specific antigens in situ. | Anti-Collagen I verifies ECM integrity; anti-Ki-67 assesses cell proliferation [22]. |
| Extracellular Vesicles (e.g., SEVs) | Bioactive signaling particles to enhance the stem cell niche. | Supplementation of Seminal Plasma-derived EVs can improve SSC survival and function on scaffolds [22]. |
| Oxygen-Generating Nanoparticles | Materials to mitigate post-transplantation hypoxia. | Incorporation into hydrogels to provide sustained oxygen release, enhancing stem cell survival in ischemic environments [24]. |
Visualizing Workflows and Pathways
The following diagrams illustrate the core experimental workflow and the key signaling pathways involved in maintaining phenotypic stability.
Comprehensive Monitoring Workflow
Diagram Title: Comprehensive Cell-Scaffold Monitoring Workflow
Phenotypic Stability Assessment Pathway
Diagram Title: Signaling Pathways in Phenotypic Stability
{ /article }
Benchmarking dECM Performance: Efficacy, Clinical Translation, and Comparison to Synthetic Scaffolds
In vivo validation is a critical step in translating tissue engineering strategies from the laboratory to the clinic. For therapies centered on decellularized tissues and stem cell engraftment, demonstrating functional integration and regeneration in appropriate animal models is paramount. This document provides a structured framework of key metrics and detailed protocols for the comprehensive assessment of engineered tissues in orthotopic animal models, specifically within the context of a broader thesis on decellularized tissues for stem cell engraftment research. The guidance synthesizes current methodologies to ensure researchers can robustly evaluate the structural, functional, and biological outcomes of their regenerative approaches.
Key Quantitative Metrics for Assessment
A multi-faceted approach to assessment is necessary to capture the complex process of functional integration. The key quantitative metrics are summarized in the table below.
Table 1: Key Quantitative Metrics for In Vivo Validation of Engineered Tissues
| Category | Specific Metric | Measurement Technique | Interpretation & Significance |
|---|---|---|---|
| Histological & Morphological | Tissue architecture and cellularity | H&E staining | Assesses basic structure and cell distribution within the scaffold. [73] |
| Presence of specific cell lineages | Immunohistochemistry (IHC) | Identifies osteoblasts (RUNX2), chondrocytes (Collagen II), endothelial cells (CD31). [73] [74] | |
| ECM composition and deposition | Masson's Trichrome, Picrosirius Red | Evaluates collagen content and organization. [73] | |
| Radiological | Mineralized tissue formation | Micro-computed tomography (μCT) | Quantifies bone volume/total volume (BV/TV), trabecular number, and thickness. [75] [74] |
| Tissue morphology and integration | Magnetic Resonance Imaging (MRI) | Assesses soft tissue regeneration and integration with host tissue. | |
| Functional Integration | Graft perfusion and angiogenesis | Laser Doppler imaging, fluorescent microspheres | Measures blood flow and functional vascular integration. [24] |
| Mechanical properties | Tensile/compressive testing, nanoindentation | Evaluates the biomechanical competence of the regenerated tissue. | |
| Eruption and occlusion (for teeth) | Clinical observation, dental impression | Assesses the function of regenerated whole teeth in orthotopic models. [75] | |
| Cell Survival & Engraftment | Transplanted cell viability | Bioluminescence imaging (BLI), histology | Tracks the survival and location of transplanted cells over time. [24] [76] |
| Graft-mediated host cell recruitment | In situ hybridization, IHC with species-specific antibodies | Distinguishes donor from host cells to assess host cell infiltration. | |
| Molecular & Signaling | Pathway activation (e.g., BMP, Wnt) | IHC, RNA in situ hybridization, qRT-PCR | Confirms the activation of key osteogenic (e.g., RUNX2) and angiogenic pathways. [74] |
| Protein binding and drug engagement | Förster Resonance Energy Transfer (FRET) | Quantifies drug-target engagement or molecular interactions in live animals. [77] |
Detailed Experimental Protocols
Protocol: Orthotopic Implantation and Longitudinal Assessment
This protocol outlines the procedure for implanting a cell-seeded decellularized scaffold into an animal model and monitoring its integration.
Research Reagent Solutions & Essential Materials
- Decellularized Scaffold: Porcine aortic ECM [73] or other tissue-specific ECM.
- Stem Cells: Human induced pluripotent stem cell-derived MSCs (hiPSC-MSCs) [73] or adipose-derived MSCs (AD-MSCs) [78].
- Cell Culture Reagents: Matrigel, mTeSR Plus medium, DMEM supplemented with FBS, trypsin-EDTA [73].
- Animal Model: Immunodeficient mouse/rat for human cell studies, or a relevant immunocompetent species.
- Anesthesia and Analgesia: Ketamine/Xylazine or Isoflurane, Buprenorphine.
- Surgical Tools: Stereotactic frame, micro-drill, fine forceps and scissors, absorbable sutures.
- In Vivo Imaging System: IVIS or similar for bioluminescence imaging.
Procedure:
- Scaffold Seeding: Seed the decellularized scaffold (e.g., porcine aortic ECM) with hiPSC-MSCs at a density of 1-5 million cells/cm³. Culture in osteoinductive or chondrogenic medium for 7-14 days prior to implantation to promote early differentiation [73].
- Animal Preparation: Anesthetize the animal and administer pre-operative analgesia. Shave and disinfect the surgical site.
- Implantation: Create a critical-sized defect in the target tissue (e.g., femur, calvaria) or a subcutaneous pocket. Surgically implant the cell-seeded scaffold into the defect, ensuring proper fit and contact with host tissue. Secure the scaffold with sutures or bioadhesive if necessary.
- Post-operative Care: Monitor animals until fully recovered from anesthesia. Provide post-operative analgesia for 48-72 hours.
- Longitudinal Monitoring:
- Cell Survival: For cells expressing luciferase, perform weekly Bioluminescence Imaging (BLI). Administer D-luciferin substrate (150 mg/kg IP) and image under anesthesia to quantify cell viability [76].
- Tissue Formation: Conduct µCT scans every 2-4 weeks to monitor mineralized tissue formation quantitatively.
- Functional Angiogenesis: At terminal endpoints, perform perfusion with a contrast agent (e.g., Microfil) and image via µCT to reconstruct the 3D vascular network within the graft.
Protocol: Enhancing Stem Cell Survival and Potency
A major challenge is poor post-transplantation cell survival. This protocol details strategies to enhance stem cell resilience.
Research Reagent Solutions & Essential Materials
- Preconditioning Media: Low oxygen (1-5% O₂) culture chambers, serum-free media.
- Oxygen-Generating Materials: Calcium peroxide (CaO₂) or hydrogen peroxide (H₂O₂)-loaded microspheres [24].
- Hydrogel Systems: Fast-gelling hydrogels (e.g., NIPAAm-based copolymers) or PEGDA-based microspheres for oxygen delivery [24].
- Antioxidants: N-acetylcysteine (NAC), Ascorbic acid.
Procedure:
- Metabolic Preconditioning:
- Culture MSCs under hypoxic conditions (1-5% O₂) for 48 hours before transplantation. This activates HIF-1α, upregulating pro-survival genes (VEGF, GLUT-1) and enhancing anti-apoptotic capacity [24].
- Alternatively, subject cells to transient serum deprivation (e.g., 12-24 hours) to induce protective autophagy.
- Oxygen Supplementation:
- Incorporate oxygen-generating compounds directly into the delivery scaffold. For example, blend CaO₂ particles (1-2% w/w) into the hydrogel or polymer used to deliver the cells [24].
- This provides a sustained local oxygen release, mitigating ischemic stress during the critical period before host vascularization.
- Antioxidant Administration:
- Supplement the cell culture medium with antioxidants (e.g., 100 µM NAC) for 24 hours pre-transplantation to bolster the cells' defense against reactive oxygen species (ROS) [24].
- Alternatively, co-deliver ROS-scavenging nanoparticles with the transplanted cells.
Protocol: Validating Functional and Synergistic Effects
This protocol provides a framework for rigorously validating functional outcomes and claims of synergy in combination treatments.
Procedure:
- Experimental Design for Synergy:
- To test a combination therapy (e.g., drug + cell therapy), avoid the common pitfall of using only one dose level. Instead, design a full dose-response study [76].
- Include groups for: each drug/component alone at multiple doses, the combination at multiple fixed-ratio doses, and an untreated control. Use sufficiently large group sizes (n ≥ 8) to achieve statistical power [76].
- Data Acquisition & Processing:
- For tumor growth or tissue regeneration kinetics, use sensitive methods like BLI. Ensure proper normalization of each animal's signal to its own baseline (day 0) value [76].
- Apply log-transformation to the data if it follows exponential growth, and avoid carrying the last value forward for animals that die during the study, as this can bias results [76].
- Data Analysis:
- Calculate the Combination Index (CI) using established methods (e.g., Chou-Talalay) that require full dose-response curves. A CI < 1 indicates synergy, CI = 1 additivity, and CI > 1 antagonism [76].
- Use appropriate statistical tests for survival data (e.g., log-rank test) and ensure all comparisons, including between combination and single-agent groups, are reported [76].
Visualization of Workflows and Pathways
In Vivo Validation Workflow
The following diagram outlines the key stages and decision points in a comprehensive in vivo validation pipeline.
Key Signaling Pathways in Bone Regeneration
The process of stem cell-mediated bone regeneration involves the activation of several critical signaling pathways, as illustrated below.
The strategic selection of scaffolds is fundamental to advancing stem cell-based regenerative medicine. This Application Note provides a direct, data-driven comparison between decellularized extracellular matrix (dECM) and synthetic polymer scaffolds, focusing on the critical parameters of bioactivity, degradation, and mechanical properties. Framed within the context of enhancing stem cell engraftment, this document offers standardized protocols for scaffold evaluation and a curated toolkit of reagents to facilitate the replication of key experiments and support informed decision-making in research and drug development.
The failure of a significant proportion of transplanted stem cells, often due to a hostile microenvironment and lack of structural support, remains a major hurdle in regenerative medicine [24]. The scaffold serves as a temporary, artificial extracellular matrix (ECM), designed to mitigate these challenges by providing a physical and biochemical niche. The choice between biologically derived dECM and engineer-driven synthetic polymers presents a fundamental trade-off: the former excels in providing innate bioinstructive cues, while the latter offers tailored mechanical and structural consistency [79] [80]. This document dissects this dichotomy to guide researchers in selecting the optimal scaffold for specific stem cell engraftment applications.
Direct Property Comparison: dECM vs. Synthetic Polymers
The following tables provide a consolidated comparison of the core properties of dECM and synthetic polymer scaffolds, synthesizing quantitative and qualitative data from current literature.
Table 1: Bioactivity and Degradation Profile
| Property | dECM Scaffolds | Synthetic Polymer Scaffolds (e.g., PLA, PCL, PLGA) |
|---|---|---|
| Bioactivity | High; contains native signaling molecules (collagen, laminin, growth factors) that support cell adhesion, proliferation, and differentiation [79] [81]. | Low/inert; lacks innate bioactivity unless functionalized with peptides (e.g., RGD) or growth factors [80] [82]. |
| Osteoinductivity | Enhanced; MSC-dECM upregulates osteogenic markers (ALP, Osteocalcin) and calcium deposition [79]. | Requires addition of bioactive molecules (e.g., BMP-2) to become osteoinductive [80]. |
| Immunogenicity | Low if decellularized properly; risk from residual DNA or xenogeneic antigens [81]. | Low; but acidic degradation byproducts (e.g., from PLGA) can trigger inflammatory responses [80] [82]. |
| Degradation Rate | Rapid and often unpredictable; matches native tissue turnover [81] [82]. | Controllable and tunable; from months to years [80] [82]. |
| Degradation Byproducts | Natural amino acids and sugars; generally biocompatible [81]. | Acidic oligomers (e.g., lactic/glycolic acid); can cause local pH drop and inflammation [80] [82]. |
Table 2: Mechanical and Structural Properties
| Property | dECM Scaffolds | Synthetic Polymer Scaffolds (e.g., PLA, PCL, PLGA) |
|---|---|---|
| Mechanical Strength | Weak; often insufficient for load-bearing applications without reinforcement [79] [82]. | High and highly tunable; can be engineered to match bone's Young's modulus (4-15 GPa) [80] [82]. |
| Structural Integrity | Preserves native 3D architecture of source tissue; good for biomimicry [79]. | Excellent; allows for precise fabrication of complex 3D structures (e.g., via 3D printing) [83] [82]. |
| Porosity & Pore Size | Dependent on source tissue; can be difficult to control uniformly [22]. | Highly controllable and consistent porosity (e.g., 70-95% for trabecular bone mimicry) [80]. |
| Processability | Can be processed into hydrogels, powders, or sheets; challenging for complex fabrication [81]. | Highly processable; suitable for electrospinning, 3D printing, and gas foaming [80] [82]. |
Experimental Protocols for Scaffold Evaluation
To ensure consistent and reproducible research, the following protocols outline key methodologies for evaluating scaffold performance in stem cell engraftment contexts.
Protocol: In Vitro Assessment of Osteogenic Potential on Composite Scaffolds
This protocol is designed to evaluate the bioactivity of scaffolds, such as MSC-dECM/synthetic composites, by measuring their ability to support mesenchymal stem cell (MSC) differentiation into osteoblasts [79].
- Objective: To quantify the osteoinductive capacity of a test scaffold by analyzing the expression of key osteogenic markers and mineral deposition.
- Materials:
- Scaffold: MSC-dECM/PCL composite scaffold (3D-printed or electrospun) [79].
- Cells: Human Bone Marrow-derived MSCs (hBM-MSCs).
- Culture Medium: Osteogenic induction medium (e.g., DMEM supplemented with 10% FBS, 50 µM ascorbate-2-phosphate, 10 mM β-glycerophosphate, and 100 nM dexamethasone).
- Method:
- Seeding: Seed hBM-MSCs onto pre-sterilized scaffolds at a density of 5 x 10^4 cells/scaffold. Allow 4 hours for attachment before adding medium.
- Culture: Maintain constructs in osteogenic induction medium for 21-28 days, changing the medium every 2-3 days.
- Analysis (Day 21-28):
- Alkaline Phosphatase (ALP) Activity: Quantify using a colorimetric assay (e.g., pNPP substrate) and normalize to total protein content. Expected Outcome: Significantly higher ALP activity in cells on MSC-dECM composite scaffolds compared to pure PCL controls [79].
- Calcium Deposition (Alizarin Red S Staining): Fix constructs in 4% PFA, stain with 2% Alizarin Red S (pH 4.2) for 20 minutes, and extract stain for quantification or image. Expected Outcome: Extensive orange-red mineralized nodules on bioactive scaffolds [79].
- Gene Expression (qRT-PCR): Extract total RNA and analyze expression of osteogenic genes (OSTEOCALCIN, OSTEOPONTIN, RUNX2). Expected Outcome: Upregulation of all markers in test groups versus controls [79].
Protocol: In Vivo Evaluation of Bone Regeneration in a Critical-Sized Defect Model
This protocol assesses the functional performance of a scaffold in supporting stem cell engraftment and bone formation in vivo.
- Objective: To measure the bone volume regenerated by a stem cell-seeded scaffold in a calvarial defect model.
- Materials:
- Scaffold: Osteogenic MSC-dECM/HAp/Collagen composite scaffold [80].
- Cells: Luciferase-expressing hBM-MSCs for bioluminescent tracking.
- Animal Model: Immunodeficient mice or rats with a critical-sized (e.g., 5mm) calvarial defect.
- Method:
- Implantation: Anesthetize the animal and create the critical-sized defect. Implant the cell-seeded test scaffold, with an empty defect and a pure synthetic polymer scaffold as controls (n=5-8 per group).
- Longitudinal Monitoring (8-12 weeks):
- Cell Survival (IVIS Imaging): Weekly, inject animals with D-luciferin and image using an IVIS spectrum system to track the viability and persistence of the engrafted stem cells [24].
- Terminal Analysis (Week 12):
- Micro-Computed Tomography (µCT): Scan explanted calvaria to quantify new bone volume (BV) and bone mineral density (BMD) within the defect. Expected Outcome: ~2.5-fold greater bone formation in composite scaffold groups compared to controls [79].
- Histology: Process explants for H&E, Masson's Trichrome (for collagen), and immunohistochemistry (for Osteocalcin) to confirm mature, vascularized bone formation [79].
Scaffold Evaluation Workflow
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues key materials and their functions for researchers developing and testing scaffolds for stem cell engraftment.
Table 3: Key Reagents for Scaffold-Based Stem Cell Research
| Reagent / Material | Function & Application in Research |
|---|---|
| Mesenchymal Stem/Stromal Cells (MSCs) | The primary adult stem cell used for bone, cartilage, and adipose tissue regeneration; can be sourced from bone marrow (BM-MSCs) or adipose tissue (ADSCs), or derived from iPSCs (hiMSCs) for a scalable source [79] [73]. |
| Decellularized ECM (dECM) | Serves as the bioactive component of hybrid scaffolds; provides a complex, native microenvironment of structural proteins (collagen, laminin) and signaling molecules to enhance cell survival and direct differentiation [79] [81]. |
| Synthetic Polymers (PCL, PLA, PLGA) | Provide the structural and mechanical backbone of composite scaffolds; offer tunable degradation rates and high processability for creating 3D architectures [79] [80]. |
| Osteogenic Induction Medium | A defined cocktail (typically containing β-glycerophosphate, ascorbic acid, and dexamethasone) used to drive MSCs down an osteoblast lineage in vitro, allowing for quantification of scaffold osteoinductivity [79]. |
| Growth Factors (BMP-2, VEGF, FGF) | Bioactive molecules that can be encapsulated within or tethered to scaffolds to enhance vascularization (VEGF) or promote bone formation (BMP-2), mimicking staged release as in native healing [80] [84]. |
| Oxygen-Generating Materials (CaO₂, PFCs) | Incorporated into scaffolds to mitigate post-transplantation ischemia; provide localized oxygen release to enhance stem cell survival in the critical period before vascularization [24]. |
Scaffold Niche Engineering Logic
The direct comparison reveals that dECM and synthetic polymer scaffolds are not mutually exclusive but are complementary. The future of stem cell engraftment lies in advanced hybrid systems that strategically combine the bioinstructive power of dECM with the robust, tunable properties of synthetic polymers [79] [82]. The next frontier involves the development of "smart" or bioinstructive scaffolds that go beyond passive support to actively participate in regeneration through mechanisms such as the staged release of growth factors and the mitigation of post-implantation hypoxia [83] [84]. This integrative approach, leveraging the strengths of both material classes, is poised to overcome the current limitations in stem cell therapy and unlock robust, functional tissue regeneration.
Decellularized extracellular matrix (dECM) biomaterials have emerged as a cornerstone of modern regenerative medicine, representing one of the most successfully translated tissue engineering technologies. These scaffolds, created by removing cellular components from tissues while preserving the native structural and bioactive components of the extracellular matrix, provide a biomimetic microenvironment that promotes stem cell engraftment, host tissue integration, and functional regeneration [1]. The clinical success of dECM products stems from their ability to retain tissue-specific biochemical cues and mechanical properties that orchestrate cellular processes essential for regeneration, including recruitment, proliferation, and differentiation of stem and progenitor cells [85] [86]. This application note reviews the current landscape of commercially available dECM products, their documented clinical applications, and provides detailed protocols for their evaluation in stem cell engraftment research, framed within the context of advancing regenerative therapies.
Commercially Available dECM Products and Clinical Applications
The translation of dECM biomaterials from research to clinical application has resulted in several commercially available products with established therapeutic profiles. These products are derived from various tissue sources and have received regulatory approval for specific clinical indications.
Table 1: Approved dECM Products and Their Clinical Applications
| Product Name/Type | Tissue Source | Key Composition | Approved Clinical Applications | Mechanism in Stem Cell Engraftment |
|---|---|---|---|---|
| Human Dermis dECM | Human skin | Collagen I/III, elastin, GAGs, growth factors | Skin repair and regeneration, wound healing | Provides adhesion sites for mesenchymal stem cell (MSC) recruitment and angiogenic induction [1] |
| Porcine Dermis dECM | Porcine skin | Collagen I, elastin, GAGs | Hernia repair, soft tissue reinforcement | Supports fibroblast and progenitor cell infiltration with minimal immune rejection [1] |
| Porcine Small Intestinal Submucosa (SIS) | Porcine intestine | Collagen I/III/IV, fibronectin, GAGs, VEGF, FGF-2 | Rotator cuff repair, vascular grafts, body wall reconstruction | Creates chemotactic gradient for stem cell homing and modulates immune response toward regenerative phenotype [1] |
| Porcine Bladder dECM | Porcine bladder | Collagen I/IV, laminin, fibronectin | Muscle reconstruction, breast reconstruction | Promotes myogenic differentiation of stem cells and functional tissue restoration [87] [1] |
| Human Peripheral Nerve dECM | Human nerve | Collagen IV/V, laminin, fibronectin, NCAM | Peripheral nerve repair | Guides neural stem cell migration and axonal extension through retained basal lamina structures [1] |
| Fetal Bovine Dermis dECM | Fetal bovine skin | Collagen I/III, hyaluronic acid, growth factors | Wound care, burn treatment | Enhances epithelial stem cell proliferation with reduced scarring compared to adult ECM [1] |
The clinical use of these dECM biomaterials has primarily been limited to native dECM sheets or milled powder forms, though recent advances in fabrication methods including electrospinning and 3D printing are expanding their potential applications [85]. The efficacy of these products stems from their retention of tissue-specific matrisome proteins—core ECM and ECM-associated proteins that create a supportive niche for stem cell engraftment and tissue regeneration [88].
Landmark Clinical Case Studies and Efficacy Data
Several clinical studies and meta-analyses have demonstrated the efficacy of dECM-based therapies across various applications, providing evidence for their regenerative potential.
Orthopedic Applications: Cartilage Repair
A recent systematic review and meta-analysis of dECM for articular cartilage repair in osteoarthritis demonstrated significant improvement in the International Cartilage Repair Society (ICRS) score, with a weighted mean difference (WMD) of 2.45 (95% CI: 1.07 to 3.84; P-value < 0.001) compared to control treatments [89]. This analysis included 10 preclinical studies and confirmed that dECM promotes cartilage repair through provision of a tissue-like microenvironment that supports mesenchymal stem cell growth and chondrogenic differentiation [89]. The dECM hydrogel platform has shown particular promise as a delivery vehicle for therapeutic agents, exhibiting sustained-release capabilities that prolong residence time within the joint cavity [89].
Soft Tissue Reconstruction and Vascularization
In soft tissue regeneration, decellularized adipose tissue (adipoECM) has demonstrated superior host integration compared to defined collagen-based biomaterials. When implanted subcutaneously in immunocompetent BALB/c mice, adipoECM showed extensive host cell repopulation and vascularization at 60 days post-implantation, while the reference collagen-glycosaminoglycan scaffold (IntegraDRT) remained largely acellular [87]. Mass spectrometry analysis revealed that the adipoECM retained crucial matrisome components including collagen I, III, IV, V, laminin, fibrillin, fibronectin, tenascin, and elastin [87]. Immunohistochemical analysis confirmed the presence of CD31-positive cells forming functional blood vessels, plus CD90-positive mesenchymal and CD14-positive myeloid cells, indicating the recruitment of cell populations essential for soft tissue remodeling and regeneration [87].
Cardiac and Urological Applications
dECM biomaterials have shown significant clinical success in cardiac reconstruction and urological interventions [85]. In these applications, dECM scaffolds serve as inductive templates that promote site-specific tissue regeneration rather than scar tissue formation. The mechanism involves retention of angiogenic growth factors such as VEGF and FGF-2 that promote vascularization, essential for supporting engrafted stem cells and regenerating functional tissue [1].
Experimental Protocols for dECM Evaluation in Stem Cell Research
Protocol: Decellularization of Human Adipose Tissue
This protocol adapts the rapid decellularization method validated by [87] for generating adipoECM with retained bioactivity for stem cell research.
Reagents and Materials:
- Lipoaspirate samples (human)
- PBS supplemented with 100 µg/ml gentamicin
- 0.25% (w/v) bovine trypsin/EDTA
- 99.9% isopropyl alcohol (IPA)
- 1% (v/v) peracetic acid with 10% (v/v) IPA
- Sterile deionized water
- 0.9% (w/v) NaCl solution
Procedure:
- Tissue Preparation: Wash approximately 10 ml lipoaspirate in PBS with gentamicin. Remove debris and freeze tissue at -20°C.
- Additional Washes: Perform three wash cycles with PBS containing 100 µg/ml gentamicin.
- Cell Disruption: Digest tissue with 0.25% trypsin/EDTA at 37°C with orbital agitation (1000 rpm) for 60 minutes.
- Lipid Extraction: Extract lipids using 99.9% IPA at 30°C with agitation (500 rpm). Exchange IPA three times after 2, 4, and 16 hours.
- Sterilization: Incubate with 1% peracetic acid/10% IPA for 2 hours with agitation (500 rpm).
- Final Washes: Rinse with sterile water (2 times, 30 minutes each) followed by 0.9% NaCl.
- Quality Control: Assess DNA content (<50 ng/mg dry weight), sterility, and endotoxin levels (<0.25 EU/ml).
Technical Notes: This rapid protocol preserves key ECM components while effectively removing cellular material. The resulting adipoECM can be processed into hydrogel or powder forms for various experimental applications [87].
Protocol: Neural Stem Cell Culture on Decellularized Human Brain Tissue
This protocol, adapted from [88], enables investigation of neural stem cell (NSC) differentiation within region-specific human brain ECM microenvironments.
Reagents and Materials:
- Decellularized human brain tissue (DHBT) slices (200 µm thickness) from subventricular zone (SVZ), frontal cortex (FC), and white matter (WM)
- Neural stem cells (primary or cell line)
- Appropriate neural basal medium with growth factors
- 4% paraformaldehyde
- Immunostaining antibodies for astrocytic (GFAP), oligodendrocytic (O4), and neuronal (β-III-tubulin) markers
- Imaging mass cytometry setup for phenotypic analysis
Procedure:
- Scaffold Preparation: Generate DHBT using chemical-enzymatic decellularization protocol (20-min incubation with 0.5% sodium deoxycholate followed by 1-h incubation with DNase I) [88].
- Cell Seeding: Seed NSCs onto DHBT slices at density of 5×10^4 cells/cm² in appropriate neural culture medium.
- Differentiation Culture: Maintain cultures for 7-14 days, replacing medium every 2-3 days.
- Fixation and Analysis: Fix cells with 4% PFA and perform immunocytochemistry for neural lineage markers.
- Phenotypic Quantification: Use imaging mass cytometry to quantify differentiation phenotypes across different brain regions.
Expected Outcomes: NSCs cultured within WM and FC DHBT primarily acquire an astrocytic phenotype, while SVZ DHBT promotes both astrocytic and oligodendrocytic differentiation, reflecting the region-specific bioactivity of the native ECM [88].
Table 2: Research Reagent Solutions for dECM-Stem Cell Studies
| Reagent/Category | Specific Examples | Function in dECM Research | Application Notes |
|---|---|---|---|
| Decellularization Agents | Sodium dodecyl sulfate (SDS), Triton X-100, Sodium deoxycholate (SDC) | Disrupt lipid membranes and solubilize cellular components | SDS effective but can damage ECM; concentration control critical [1] |
| Enzymatic Treatments | DNase I, Trypsin/EDTA, Collagenase | Remove nuclear material and digest cellular components | DNase essential for reducing DNA content below 50 ng/mg dry weight [88] [1] |
| Sterilization Solutions | Peracetic acid, Ethanol, Antibiotic/Antimycotic | Sterilize without compromising ECM bioactivity | Peracetic acid provides sterilization while preserving structure [87] |
| Characterization Assays | DNA quantification kits, Mass spectrometry, Histology stains | Quality control of decellularization and ECM composition | DNA content <50 ng/mg and fragment length <200 bp indicate effective decellularization [1] [47] |
| Stem Cell Culture Supplements | Defined growth factors, ECM-coated plates, Serum-free media | Support stem cell maintenance and differentiation on dECM | Laminin E8 fragments support pluripotent stem cell expansion on dECM [86] |
dECM-Stem Cell Signaling Pathways in Regenerative Niches
The therapeutic efficacy of dECM biomaterials in supporting stem cell engraftment is mediated through conserved signaling pathways that are activated by cell-ECM interactions. The following diagram illustrates the principal signaling mechanisms through which dECM scaffolds influence stem cell behavior and promote tissue regeneration.
This signaling network illustrates how dECM components engage specific stem cell receptors to activate intracellular pathways that collectively promote successful engraftment and tissue regeneration. Integrin-mediated adhesion to structural and adhesive proteins activates FAK and MAPK pathways, promoting cell adhesion, proliferation, and migration [1]. Concurrently, growth factors retained within the dECM engage their cognate receptors, activating PI3K/Akt and MAPK pathways that direct lineage-specific differentiation and enhance cell survival [86] [1]. The glycosaminoglycans and proteoglycans within dECM further modulate these signals through syndecan-mediated signaling and by creating reservoirs for bioactive factors, establishing a sustained signaling microenvironment that supports stem cell maintenance and function [1].
dECM biomaterials represent a successfully translated technology with multiple approved products for clinical use across various tissue types. The continued advancement of this field requires addressing several persistent challenges, including standardization of decellularization processes, optimization of bioactivity retention, and ensuring mechanical compatibility with native tissues [85]. Future research directions should focus on refining fabrication techniques such as 3D bioprinting with dECM-based bioinks, establishing standardized criteria for dECM characterization, and developing optimized translational pathways [85] [1]. The integration of dECM scaffolds with patient-specific stem cells holds particular promise for creating personalized regenerative therapies that effectively harness the innate regenerative capacity of the body while minimizing immune rejection. As these technologies mature, dECM-based approaches are poised to expand their clinical impact, offering new solutions for tissue repair and regeneration across an increasingly broad spectrum of medical applications.
Decellularized extracellular matrix (dECM) has emerged as a foundational material in regenerative medicine, transcending its traditional role in tissue repair to become an indispensable component for creating physiologically relevant in vitro models. Derived from tissues through processes that remove cellular components while preserving the native architecture and biochemical composition, dECM provides a complex, tissue-specific microenvironment that conventional culture substrates cannot replicate [85]. This bioactive scaffold retains essential signaling molecules, structural proteins, and mechanical cues that direct cell behavior, making it particularly valuable for applications requiring high biological fidelity [21] [90].
The transition toward human-relevant in vitro systems represents a paradigm shift in biomedical research, driven by the persistent limitations of animal models and two-dimensional (2D) cell cultures. Animal models frequently fail to predict human physiological responses and drug toxicities, with approximately 90% of new drugs failing in clinical trials despite promising preclinical results [91] [92]. Similarly, conventional 2D models lack the structural complexity and cell-matrix interactions crucial for mimicking native tissue function [91]. dECM-based platforms address these limitations by providing a three-dimensional (3D) microenvironment that more accurately recapitulates the in vivo niche, enabling the development of advanced disease models and more predictive drug screening platforms [21].
This application note details experimental methodologies and applications of dECM-based systems, with a specific focus on their utility in stem cell research, disease modeling, and drug development. The protocols and data presented herein are designed to provide researchers with practical frameworks for implementing dECM technologies in their investigative workflows.
Application Notes: Functional Implementation of dECM Platforms
dECM Properties and Quantitative Performance Metrics
The efficacy of dECM biomaterials stems from their preservation of tissue-specific biochemical and biomechanical properties after decellularization. Successful decellularization is confirmed through quantitative assessments including DNA quantification (demonstrating removal of cellular material), histological analyses (verifying retention of ECM components), and scanning electron microscopy (confirming preservation of ultrastructural features) [21] [22]. The composition and bioactivity of dECM are highly dependent on the source tissue and decellularization methodology, necessitating rigorous characterization of each preparation [85].
Table 1: Quantitative Characterization of dECM Biomaterials from Various Tissues
| Tissue Source | Decellularization Method | DNA Content Reduction | Key ECM Components Retained | Mechanical Properties | Reference Application |
|---|---|---|---|---|---|
| Cartilage | Freeze-thaw cycles + SDS | ~41% protein content preserved | GAGs, collagens | Damping feature essential for cartilage | Cartilage tissue engineering [21] |
| Testis | Freeze-thaw + Triton X-100 + SLES | Significant removal (H&E confirmation) | Collagen I/IV, laminin, fibronectin | Preserved ultrastructure (SEM confirmation) | Spermatogonial stem cell niche [22] |
| Skin | Methacryloyl modification | N/A | Complex protein mixture | 30-fold increase in elastic modulus post-modification | Wound healing, skin repair [90] |
| Adipose Tissue | Not specified | N/A | Adipose-specific ECM components | Hydrogel formation capability | Adipose tissue regeneration [78] |
The biological performance of dECM scaffolds is evidenced through their support of specialized cellular functions. In testicular applications, dECM scaffolds enriched with seminal extracellular vesicles significantly enhanced spermatogonial stem cell viability and upregulated germ cell markers (DAZL, PIWI), though complete meiosis was not achieved [22]. Cartilage-derived dECM bioinks combined with gellan gum demonstrated excellent cytocompatibility (97.41 ± 1.02% cell viability) and promoted glycosaminoglycan deposition, indicating successful chondrogenic differentiation [21]. These functional outcomes underscore the capacity of dECM to provide tissue-specific inductive cues.
dECM in Advanced Disease Modeling and Drug Screening Platforms
Cardiac organoids represent a transformative application of dECM technology in disease modeling. Traditional 2D cardiac cultures lack the structural complexity and cellular interactions of native myocardium, limiting their physiological relevance [91]. Cardiac organoids cultured in dECM-based matrices exhibit higher metabolic similarities and physiological relevance, better mimicking the significant biological characteristics and functions of the normal cardiac system [91]. These 3D models recapitulate human-specific aspects of heart histogenesis, physiology, and developmental trajectory, providing superior platforms for studying cardiac biology, pathophysiology, and drug-induced cardiotoxicity [91].
The pharmaceutical industry is increasingly adopting dECM-based models to address the high attrition rates in drug development. Conventional toxicity testing using animal models and 2D cultures often fails to predict human-specific adverse effects, contributing to the 90% failure rate of new drugs in clinical trials [92]. dECM-based liver and multi-organ systems offer more physiologically relevant platforms for detecting drug-induced liver injury (DILI) and other organ-specific toxicities [92]. When integrated with microfluidic organ-on-a-chip platforms, dECM scaffolds enable the creation of sophisticated multi-tissue models that can simulate organ-organ interactions and systemic drug effects [92].
Table 2: dECM Applications in Disease Modeling and Drug Development
| Application Domain | dECM Platform | Key Advantages | Readout Parameters | Validation Status |
|---|---|---|---|---|
| Cardiovascular Research | Cardiac organoids in dECM | Mimics structural complexity, cell-cell interactions | Contractile function, electrophysiology, gene expression | Research use, disease modeling [91] |
| Hepatic Toxicology | Liver-on-chip with dECM | Human-relevant metabolism, predicts DILI | Albumin production, urea synthesis, CYP450 activity | Preclinical validation [92] |
| Musculoskeletal Repair | Cartilage GG/dECMb bioink | Supports chondrogenesis, mechanical competence | GAG deposition, collagen type II, compressive modulus | In vitro validation, in vivo testing [21] |
| Fertility Restoration | Testis dECM + SEVs | Recapitulates spermatogonial niche | SSC viability, DAZL/PIWI expression | In vitro differentiation demonstrated [22] |
| Personalized Oncology | Patient-derived organoids in dECM | Patient-specific drug response profiling | Drug sensitivity, gene expression, viability | Clinical correlation studies [93] |
The integration of machine learning with dECM-based screening platforms represents a cutting-edge approach to personalized medicine. Predictive models trained on drug response data from patient-derived cells cultured in dECM environments can accurately identify effective therapeutic options for individual patients [93]. These systems have demonstrated strong performance in recommending targeted treatments, with high correlations between predicted and actual drug activities (Rpearson = 0.873, Rspearman = 0.857 for all drugs; Rpearson = 0.781, Rspearman = 0.791 for selective drugs) [93].
Experimental Protocols
Protocol 1: Cartilage dECM Bioink Formulation and 3D Bioprinting
Principle: This protocol describes the preparation of a bioactive bioink combining cartilage-derived dECM with gellan gum for 3D bioprinting of cartilage tissue constructs. The approach leverages the biological cues of dECM with the mechanical printability of gellan gum to create scaffolds that support chondrogenic differentiation [21].
Reagents and Materials:
- Cartilage tissue (porcine or bovine sources)
- Gellan gum (Sigma-Aldrich, CAS 71010-52-1)
- Sodium dodecyl sulfate (SDS)
- Calcium chloride crosslinking solution
- Phosphate-buffered saline (PBS)
- Urea extraction buffer
- Alcian Blue staining solution
- Cell culture reagents
Procedure:
- Cartilage Decellularization:
- Subject cartilage slices to three freeze-thaw cycles (-80°C to room temperature)
- Treat with 1% SDS solution for 24-48 hours with constant agitation
- Rinse extensively with PBS to remove residual detergents
- Confirm decellularization by H&E staining and DNA quantification
dECM Processing:
- Lyophilize decellularized cartilage
- Mill into fine powder using cryogenic grinding
- Digest with urea extraction buffer to solubilize ECM components
- Centrifuge at 12,000 × g for 30 minutes to remove insoluble debris
Bioink Formulation:
- Combine 3% gellan gum with 2% dECM extract in PBS
- Sterilize by filtration or UV irradiation
- Maintain at 37°C to prevent premature gelation
3D Bioprinting:
- Load bioink into printing cartridge equipped with 22G nozzle
- Print at 18-22°C with pressure range 20-30 kPa
- Crosslink printed constructs in 100 mM CaCl₂ solution for 15 minutes
- Transfer to cell culture medium for biological assessment
Quality Control:
- Assess rheological properties (viscosity, shear-thinning behavior)
- Verify printability and shape fidelity
- Test cytocompatibility (≥95% cell viability required)
- Evaluate chondrogenic capacity (GAG deposition, collagen type II expression)
Technical Notes:
- The optimal GG/dECM ratio may require adjustment based on specific printer parameters
- Incorporation of chondrocytes or mesenchymal stem cells should occur immediately before printing
- Post-printing maturation for 4-6 weeks enhances ECM deposition and mechanical properties
Protocol 2: Testicular dECM Scaffold Preparation for Spermatogonial Stem Cell Culture
Principle: This protocol details the generation of testis-derived dECM scaffolds to support the survival and differentiation of spermatogonial stem cells (SSCs), creating a biomimetic niche for male fertility research and potential restoration [22].
Reagents and Materials:
- Rodent testicular tissue
- Triton X-100 solution
- Sodium lauryl ether sulfate (SLES)
- Protease inhibitors
- Antibiotic-antimycotic solution
- Seminal extracellular vesicles (SEVs) isolation reagents
- DBA lectin for SSC identification
Procedure:
- Testis Decellularization:
- Puncture testicular capsule with insulin needle to facilitate reagent penetration
- Perform three freeze-thaw cycles at -80°C
- Agitate in PBS on magnetic stirrer (700 RPM) for 30 minutes
- Treat with 1% Triton X-100 for 8 hours with constant agitation
- Incubate in 1% SLES for 48 hours, changing solution every 12 hours
- Rinse extensively with PBS for 3 hours to remove detergent residues
Decellularization Validation:
- Perform H&E staining to confirm nuclear material removal
- Conduct DNA quantification (≤50 ng/mg dry weight indicates successful decellularization)
- Use Masson's trichrome, Alcian blue, and immunohistochemistry to verify ECM preservation
- Analyze ultrastructure by scanning electron microscopy
SEV Isolation and Characterization:
- Collect human seminal plasma by centrifugation at 2000 × g for 20 minutes
- Ultracentrifuge supernatant at 100,000 × g for 70 minutes at 4°C
- Resuspend EV pellet in PBS and characterize by nanoparticle tracking analysis
- Confirm presence of EV markers (CD63, CD81) by western blot
Scaffold Seeding and Culture:
- Isolate whole testicular cells including DBA-positive SSCs
- Seed cells onto dECM scaffolds at density of 1×10⁶ cells/cm²
- Supplement with 50 μg/mL SEVs for enhanced bioactivity
- Maintain in stem cell culture medium at 34°C with 5% CO₂
- Assess cell viability, gene expression (DAZL, PIWI), and functional markers weekly
Technical Notes:
- Gentle agitation during decellularization preserves delicate ECM architecture
- Sterile technique is critical throughout to prevent contamination
- Optimal SSC enrichment achieved using DBA lectin magnetic sorting
- Hypoxic conditions (1-5% O₂) may better mimic testicular microenvironment
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for dECM-Based Research
| Reagent/Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Decellularization Agents | SDS, Triton X-100, SLES | Remove cellular content while preserving ECM | Concentration and exposure time must be optimized for each tissue type [21] [22] |
| Enzymatic ECM Digestants | Urea, pepsin, collagenase | Solubilize ECM for bioink formulation | Affects bioactivity; urea extraction preserves GAG content [21] |
| Crosslinkers | Methacryloyl groups, genipin, glutaraldehyde | Enhance mechanical properties of dECM hydrogels | Photo-crosslinking enables spatial control of stiffness [90] |
| dECM Modification Agents | Methacrylic anhydride, glycidyl methacrylate | Introduce polymerizable groups for mechanical tunability | Enables formation of granular hydrogels with shear-thinning properties [90] |
| Bioink Additives | Gellan gum, alginate, gelatin | Improve printability and structural integrity | Gellan gum provides native cartilage environmental resemblance [21] |
| Vesicular Signaling Cues | Seminal extracellular vesicles (SEVs) | Enhance stem cell viability and differentiation | Contains proteins, lipids, microRNAs for intercellular communication [22] |
| Characterization Tools | DNA quantification kits, rheometers, SEM | Quality assessment of dECM scaffolds | Confirm decellularization efficacy and structural preservation [21] [22] |
Visual Experimental Workflows
dECM Fabrication and Stem Cell Seeding Workflow
dECM Integration in Drug Development Pipeline
dECM-based platforms represent a significant advancement in biomedical research, providing human-relevant systems that bridge the gap between conventional cell culture and clinical applications. The methodologies outlined in this application note provide researchers with practical frameworks for implementing dECM technologies across various tissue engineering and drug discovery contexts. As these platforms continue to evolve through integration with advanced biofabrication techniques, microfluidic systems, and computational approaches, they hold immense potential to transform both fundamental biological research and therapeutic development.
Conclusion
Decellularized ECM scaffolds represent a paradigm shift in stem cell engineering, offering an unparalleled platform that recapitulates the native tissue microenvironment to direct cell behavior with high specificity. The successful translation of this technology hinges on a balanced optimization of decellularization rigor and ECM preservation, the development of robust recellularization and revascularization protocols, and rigorous validation against clinical endpoints. Future research must focus on standardizing evaluation criteria, scaling up production for whole-organ engineering, and exploiting the potential of patient-specific, autologous dECM. As these challenges are met, dECM scaffolds are poised to not only revolutionize regenerative medicine by alleviating the critical shortage of donor organs but also to provide sophisticated, human-relevant models that will accelerate and improve the drug development pipeline.
References
- 1. Acellular Extracellular Matrix Scaffolds in Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565388/]
- 2. Decellularization in Tissue Engineering and Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9081537/]
- 3. Application of decellularization methods for scaffold ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1621641/full]
- 4. Immunogenicity of decellularized extracellular matrix scaffolds [https://biomaterialsres.biomedcentral.com/articles/10.1186/s40824-023-00348-z]
- 5. Applications of Tissue Decellularization Techniques in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.802283/full]
- 6. Decellularization of Human Digits: A Step Towards Off-the- ... [https://www.mdpi.com/2306-5354/12/4/383]
- 7. Comparative Analysis of Decellularization Methods for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11276046/]
- 8. Comparison of Decellularization Protocols for Preparing a ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0086723]
- 9. Comparison of Decellularization Protocols to Generate ... [https://www.mdpi.com/1422-0067/22/5/2389]
- 10. Design and Applications of Extracellular Matrix Scaffolds in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293650/]
- 11. Biology of the Extracellular Matrix: An Overview - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4185430/]
- 12. Extracellular matrix [https://en.wikipedia.org/wiki/Extracellular_matrix]
- 13. Extracellular Matrix: Structure, Function & Medical Role [https://lifesciences.danaher.com/us/en/library/extracellular-matrix.html]
- 14. A New Method for Preparation of Decellularized Human ... [https://www.mdpi.com/1467-3045/47/4/275]
- 15. In vivo engineered extracellular matrix scaffolds with ... [https://www.nature.com/articles/s41467-019-12545-3]
- 16. Cell manufacturing for cell-based tissue engineering [https://www.frontiersin.org/journals/chemical-engineering/articles/10.3389/fceng.2025.1637075/full]
- 17. Intrinsic Mechanical Cues and Their Impact on Stem Cells and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8606660/]
- 18. Extracellular matrix elasticity and topography: material-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4258536/]
- 19. Biophysical and Biochemical Cues of Biomaterials Guide ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.640388/full]
- 20. Role of Mechanical Cues in Cell Differentiation and Proliferation [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0124529]
- 21. The introduction and evaluation of novel decellularized ... [https://www.nature.com/articles/s41598-025-11559-w]
- 22. The synergic impact of decellularized testis scaffold and ... [https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/s12938-025-01424-2]
- 23. Tailoring the therapeutic potential of stem cell spheroid- ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961225002510]
- 24. Modulation of Stem Cell Survival and Engraftment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439257/]
- 25. Development of Liver Decellularized Extracellular Matrix Bioink for... [https://pubmed.ncbi.nlm.nih.gov/28277649/]
- 26. Functional Outcomes of Nerve Allografts Seeded ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/34153019/]
- 27. Functional outcomes of nerve allografts seeded with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8373640/]
- 28. Effectiveness of Stem Cell Secretomes in the Regeneration ... [https://www.mdpi.com/2073-4409/14/7/492]
- 29. Enhancing mesenchymal stem survival and homing capability to... cell [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03476-4]
- 30. Effect of mesenchymal stem in cell regeneration and clinical... liver [https://www.oaepublish.com/articles/2394-5079.2021.07]
- 31. An update on technical method of cartilage decellularization [https://pmc.ncbi.nlm.nih.gov/articles/PMC11954751/]
- 32. Standardizing decellularization protocols for optimized ... [https://www.sciencedirect.com/science/article/pii/S2352320424002311]
- 33. Optimization of Enzymatic and Chemical Decellularization ... [https://www.mdpi.com/1422-0067/25/7/4026]
- 34. 3.2. Physical Methods for Decellularization [https://bio-protocol.org/exchange/minidetail?id=8403018&type=30]
- 35. Comparison of different decellularization methods for human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11744961/]
- 36. Decellularization Strategies for Regenerative Medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC5429943/]
- 37. Impact of various detergent-based immersion and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10544968/]
- 38. Development of Acellular Hepatic Scaffolds Through a Low ... [https://www.mdpi.com/2313-7673/10/11/777]
- 39. Application of decellularization methods for scaffold production [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213722/]
- 40. Decellularized scaffolds in regenerative medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5295461/]
- 41. Decellularized extracellular matrix scaffolds: Recent trends ... [https://www.sciencedirect.com/science/article/pii/S2452199X2100431X]
- 42. Scaffolds Bioink for Three-Dimensional (3D) Bioprinting [https://pmc.ncbi.nlm.nih.gov/articles/PMC11743847/]
- 43. 3D printed scaffolds based on hyaluronic acid bioinks for ... [https://biomaterialsres.biomedcentral.com/articles/10.1186/s40824-023-00460-0]
- 44. A Review of Bioprinting Techniques, Scaffolds, and Bioinks [https://pmc.ncbi.nlm.nih.gov/articles/PMC11447703/]
- 45. Beginner's Guide to Bioprinting [https://meow.wse.jhu.edu/protocols/beginners-guide-to-bioprinting/]
- 46. Decellularization in Tissue Engineering and Regenerative ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.805299/full]
- 47. Two Decades of Advances and Limitations in Organ ... [https://www.mdpi.com/1467-3045/46/8/543]
- 48. Decellularization techniques: unveiling the blueprint for ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1518905/full]
- 49. Current strategies on kidney regeneration using tissue ... [https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-025-03968-w]
- 50. Ad-Dressing Stem Cells: Hydrogels for Encapsulation [https://www.mdpi.com/2227-9717/9/1/11]
- 51. Moving from static to dynamic complexity in hydrogel design [https://www.nature.com/articles/ncomms2271]
- 52. The impact of decellularization methods on extracellular ... [https://www.nature.com/articles/s41598-019-49575-2]
- 53. Decellularized Scaffolds for Tissue Regeneration [https://www.intechopen.com/chapters/1195105]
- 54. Organic and Synthetic Substitutes in Tracheal Reconstruction [https://www.mdpi.com/2306-5354/12/7/704]
- 55. Engineering Functional Cardiac Tissues for Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7153535/]
- 56. The nerve center of organ engineering [https://www.nature.com/articles/s41467-025-64801-4]
- 57. Decellularized Tissue Matrix for Stem Cell and ... [https://pubmed.ncbi.nlm.nih.gov/30471032/]
- 58. Immune Response to Extracellular Matrix Bioscaffolds [https://www.mdpi.com/2673-8449/5/3/28]
- 59. Application of decellularized tissue for soft-hard ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1394714/full]
- 60. Recellularization of decellularized vascular grafts via ... [https://www.nature.com/articles/s41598-025-07458-9]
- 61. Immunogenicity and Integration of a Decellularized ... [https://www.mdpi.com/2306-5354/12/11/1186]
- 62. Frontiers | A Review of Cellularization Strategies for Tissue ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2015.00043/full]
- 63. Revascularization of decellularized lung scaffolds [https://pmc.ncbi.nlm.nih.gov/articles/PMC4669341/]
- 64. Effect of different decellularization protocols on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10022115/]
- 65. Bioactive scaffolds for tissue engineering: A review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11875452/]
- 66. Biomaterials to enhance stem cell transplantation [https://www.sciencedirect.com/science/article/pii/S1934590922001552]
- 67. Crosslinking strategies of decellularized extracellular ... [https://pubmed.ncbi.nlm.nih.gov/37990863/]
- 68. The effect of decellularization processes on the immune ... [https://www.sciencedirect.com/science/article/abs/pii/S0040816625004173]
- 69. Biocompatibility of decellularized spinach leaves [https://www.nature.com/articles/s44385-025-00028-8]
- 70. Biosensors to Monitor Cell Activity in 3D Hydrogel-Based ... [https://www.mdpi.com/1424-8220/22/4/1517]
- 71. Safety Assessment of Stem Cell-Based Therapies [https://www.mdpi.com/2073-4409/14/21/1660]
- 72. Cell–scaffold interactions in tissue engineering for oral and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9650009/]
- 73. Decellularized Porcine Aorta as a Scaffold for Human ... [https://link.springer.com/article/10.1007/s12015-025-10875-y]
- 74. Functionalized mesenchymal stem cells for enhanced bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577075/]
- 75. A systematic review of functional whole-tooth regeneration ... [https://pubmed.ncbi.nlm.nih.gov/41265151/]
- 76. Reanalysis of in vivo drug synergy validation study rules ... [https://www.nature.com/articles/s41467-025-62617-w]
- 77. Article In vivo quantitative FRET small animal imaging [https://www.sciencedirect.com/science/article/pii/S2667074723000113]
- 78. Mitochondria transplanted adipose-derived stem cells ... [https://www.sciencedirect.com/science/article/pii/S259000642500763X]
- 79. Synthetic scaffolds functionalized with mesenchymal stem/ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409398/]
- 80. Advances and Challenges in Polymer-Based Scaffolds for ... [https://www.mdpi.com/2073-4360/16/23/3303]
- 81. Utilizing decellularized extracellular matrix hydrogels for ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813024097046]
- 82. A Comparative Analysis Of Natural Vs. Synthetic Polymer ... [https://eureka.patsnap.com/report-a-comparative-analysis-of-natural-vs-synthetic-polymer-scaffolds]
- 83. Advances in smart hybrid scaffolds: A strategic approach ... [https://www.sciencedirect.com/science/article/pii/S2666138125000039]
- 84. Bioinstructive scaffolds enhance stem cell engraftment for ... [https://pubmed.ncbi.nlm.nih.gov/40247020/]
- 85. Extracellular-Matrix-Based Materials from Decellularized ... [https://pubmed.ncbi.nlm.nih.gov/41243578/]
- 86. Engineered biomaterials in stem cell-based regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11749850/]
- 87. Rapidly decellularized adipose tissue induces soft tissue ... [https://bmcbiotechnol.biomedcentral.com/articles/10.1186/s12896-025-01042-9]
- 88. Generation of decellularized human brain tissue for ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1578467/full]
- 89. Efficacy of decellularized extracellular matrix (dECM) for ... [https://josr-online.biomedcentral.com/articles/10.1186/s13018-025-05881-2]
- 90. Fabrication of granular decellularized extracellular matrix ... [https://www.sciencedirect.com/science/article/pii/S1742706125007172]
- 91. Cardiac organoids: a new tool for disease modeling and ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1537730/full]
- 92. Advanced In Vitro Models for Preclinical Drug Safety [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763796/]
- 93. Establishing predictive machine learning models for drug ... [https://www.nature.com/articles/s41698-025-00937-2]