Disease Modeling with Induced Pluripotent Stem Cells: From Fundamentals to Future Therapies
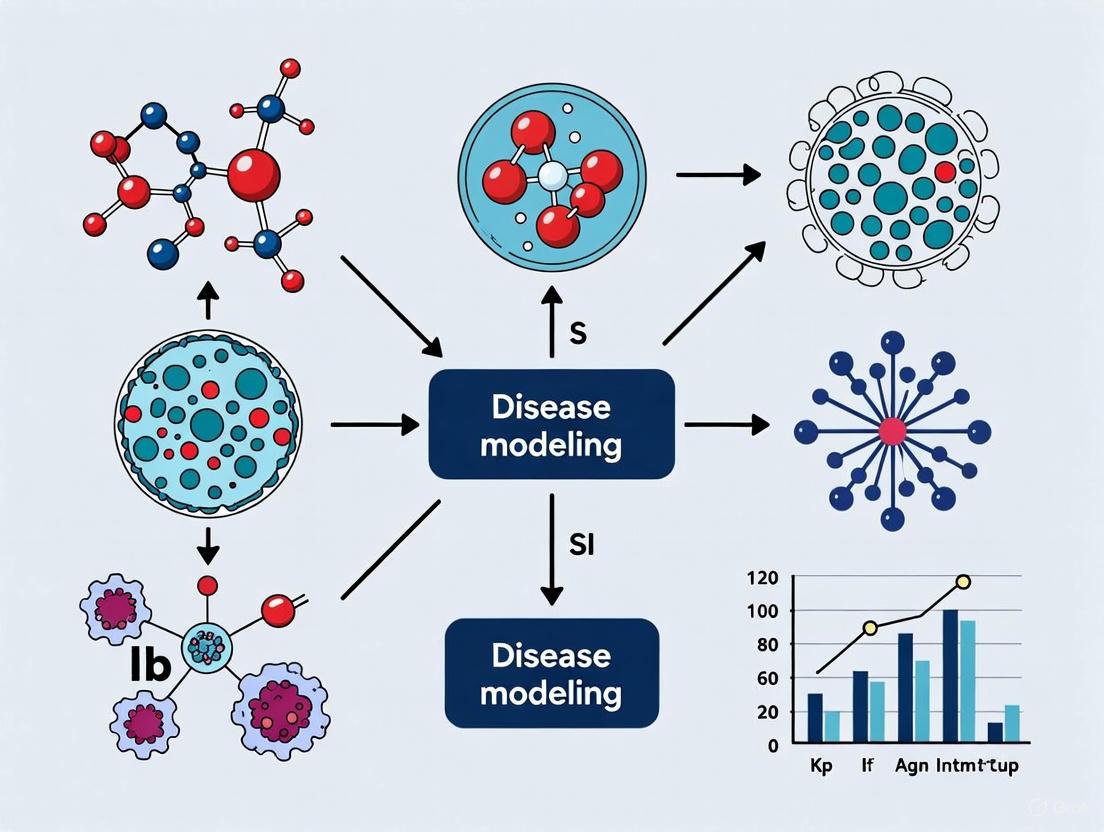
This article provides a comprehensive overview of how induced pluripotent stem cells (iPSCs) are revolutionizing disease modeling and drug discovery.
Disease Modeling with Induced Pluripotent Stem Cells: From Fundamentals to Future Therapies
Abstract
This article provides a comprehensive overview of how induced pluripotent stem cells (iPSCs) are revolutionizing disease modeling and drug discovery. Tailored for researchers and drug development professionals, it explores the foundational principles of iPSC technology, details advanced methodological applications from 2D cultures to 3D organoids, addresses key challenges such as cellular immaturity and technical variability, and validates the platform through comparisons with traditional models. By synthesizing the latest research, this review highlights the transformative potential of iPSCs in creating patient-specific disease models, enhancing drug screening accuracy, and paving the way for personalized regenerative therapies.
The iPSC Revolution: From Somatic Cells to Patient-Specific Disease Models
Induced pluripotent stem cells (iPSCs) represent one of the most significant breakthroughs in modern regenerative medicine and biomedical research. These cells are generated by reprogramming adult somatic cells back to a pluripotent state, mimicking the key characteristics of embryonic stem cells (ESCs), including unlimited self-renewal and the capacity to differentiate into any cell type in the body [1]. The development of iPSC technology has provided researchers with an unprecedented tool for disease modeling, drug discovery, and the development of cell-based therapies, all within a patient-specific context [2] [3].
Framed within a broader thesis on disease modeling, the ability to reprogram somatic cells to pluripotency enables the creation of human-specific disease models that recapitulate pathological processes in vitro. This technical guide explores the core principles, molecular mechanisms, and methodologies underlying somatic cell reprogramming, providing researchers and drug development professionals with a comprehensive foundation for applying iPSC technology to human disease research.
Historical Foundations and Key Discoveries
The conceptual foundation for cellular reprogramming was established through pioneering work in the mid-20th century. In 1962, John Gurdon demonstrated that the nucleus from a differentiated somatic cell of Xenopus laevis could be reprogrammed to a totipotent state when transplanted into an enucleated egg, giving rise to germline-competent organisms [1] [4]. This seminal somatic cell nuclear transfer (SCNT) experiment proved that the genetic material in differentiated cells remains intact and can be reset to an embryonic state, challenging the prevailing view that cell differentiation was irreversible [5] [1].
The subsequent isolation of mouse embryonic stem cells (ESCs) in 1981 by Evans and Kaufman and human ESCs by James Thomson in 1998 provided critical reference points for understanding pluripotency [5] [1]. Cell fusion experiments between ESCs and somatic cells further demonstrated that pluripotent cells contain factors capable of reprogramming somatic nuclei [5] [1].
The direct reprogramming breakthrough came in 2006 when Shinya Yamanaka and Kazutoshi Takahashi identified a combination of four transcription factors—Oct4, Sox2, Klf4, and c-Myc (OSKM)—that could reprogram mouse fibroblasts into induced pluripotent stem cells [3] [1]. This discovery, for which Yamanaka received the Nobel Prize in 2012, demonstrated that pluripotency could be induced without eggs or embryos, opening new avenues for patient-specific stem cell generation [3].
Molecular Mechanisms of Reprogramming
The Core Pluripotency Network
Reprogramming somatic cells to pluripotency involves reactivating the endogenous network of pluripotency genes while silencing somatic cell programs. At the heart of this network are key transcription factors that form an interconnected autoregulatory circuit:
- OCT4 (POU5F1): A POU-domain transcription factor essential for establishing and maintaining pluripotent identity [6] [1].
- SOX2: A high-mobility group (HMG) box transcription factor that partners with OCT4 to regulate many pluripotency-associated genes [6].
- NANOG: A homeodomain transcription factor that helps stabilize the pluripotent state by activating self-renewal genes and repressing differentiation pathways [6].
These core factors bind to and activate each other's promoters, creating a self-sustaining regulatory loop that maintains cells in a pluripotent state [6]. Additional ancillary factors including KLF4, c-MYC, LIN28, and REX1 further support and stabilize the pluripotency network [6] [1].
Epigenetic Remodeling During Reprogramming
Reprogramming requires extensive epigenetic remodeling to erase somatic cell memory and establish a pluripotent epigenome. This process involves:
- DNA demethylation: Active and passive removal of methylation marks from promoter regions of pluripotency genes like OCT4, SOX2, and NANOG [4].
- Histone modification: Changes in histone marks including increased H3K4me3 and H3K27ac at enhancers and promoters of pluripotency genes, and decreased H3K9me3 and H3K27me3 repressive marks [4].
- Chromatin reorganization: Transition from closed, heterochromatic regions to more open, accessible chromatin configurations permissive for transcription [1] [4].
- X chromosome reactivation: In female cells, reactivation of the somatically silenced X chromosome [4].
Recent research has identified factors such as Activation-induced cytidine deaminase (AID) that may facilitate active DNA demethylation during reprogramming [5].
Phased Reprogramming Process
Reprogramming follows a sequential, multi-phase process characterized by distinct molecular and cellular events:
Figure 1: The phased process of somatic cell reprogramming showing transition from stochastic early events to deterministic late-phase events.
- Initiation Phase: Characterized by rapid proliferation, metabolic changes, and mesenchymal-to-epithelial transition (MET), during which somatic genes are silenced and early pluripotency-associated genes show stochastic activation [1] [4].
- Maturation Phase: Progressive activation of pluripotency factors with ongoing epigenetic remodeling; cells begin to resemble ESCs morphologically but remain dependent on transgene expression [4].
- Stabilization Phase: Establishment of a self-sustaining pluripotency network with endogenous OCT4 and NANOG expression; cells become independent of exogenous factors and acquire stable pluripotency [4].
Single-cell analyses have revealed that the early phase is highly stochastic, with only a small fraction of cells successfully transitioning to the later, more deterministic phases where the core pluripotency network becomes stabilized [4].
Reprogramming Methodologies
Transcription Factor-Based Approaches
Various methods have been developed to deliver reprogramming factors to somatic cells, each with distinct advantages and limitations for research and clinical applications:
Table 1: Comparison of primary reprogramming methodologies
| Method | Mechanism | Efficiency | Genomic Integration | Key Applications |
|---|---|---|---|---|
| Retroviral/Lentiviral | Integrates OSKM genes into host genome | 0.1-1% | Yes (permanent) | Basic research, proof-of-concept studies [3] [1] |
| Sendai Virus | RNA virus replicating in cytoplasm | 0.1-1% | No (transient) | Clinical applications, disease modeling [3] |
| Episomal Vectors | Non-integrating plasmid DNA | 0.001-0.1% | No | Clinical-grade iPSC generation [3] |
| Synthetic mRNA | Direct delivery of reprogramming factor mRNA | 1-4% | No | Clinical applications, high efficiency requirements [3] |
| Protein Transduction | Cell-penetrating reprogramming proteins | <0.001% | No | Applications requiring minimal genetic manipulation [3] |
Chemical Reprogramming
Small-molecule approaches offer a promising alternative to genetic reprogramming methods. Fully chemical reprogramming of murine fibroblasts using seven small-molecule compounds was first achieved in 2013, and similar approaches for human cells were subsequently developed [7] [1]. Chemical reprogramming involves three key molecular events:
- Erasure of somatic cell identity through disruption of fibroblast-specific programs
- Induction of an intermediate plastic state with similarities to regenerative progenitor cells
- Establishment of pluripotency through activation of the core pluripotency network [7]
This approach provides advantages including temporal control, reduced safety concerns, and potential for standardization, making it particularly attractive for clinical applications [7].
Alternative Nuclear Reprogramming Strategies
Beyond factor-based reprogramming, two historical methods demonstrate alternative approaches to resetting cellular identity:
- Somatic Cell Nuclear Transfer (SCNT): Transfer of a somatic nucleus into an enucleated oocyte, utilizing the oocyte's cytoplasmic factors to reprogram the somatic genome to totipotency [5] [1].
- Cell Fusion: Fusion of somatic cells with pluripotent stem cells (ESCs, EGCs, or ECs) generates hybrid cells where somatic nuclei are reprogrammed by trans-acting factors from the pluripotent partner [5].
While these methods have been instrumental in demonstrating nuclear plasticity, they present technical and ethical challenges that limit their application in disease modeling and regenerative medicine [5].
Experimental Protocols for iPSC Generation
Standard Fibroblast Reprogramming Protocol
The following protocol outlines a standard method for generating iPSCs from human dermal fibroblasts using non-integrating episomal vectors:
Day 0: Plating Fibroblasts
- Plate early-passage (P3-P6) human dermal fibroblasts at 5×10^4 cells per well in a 6-well plate in fibroblast medium (DMEM + 10% FBS + 1% GlutaMAX + 1% NEAA)
- Ensure cells are 70-80% confluent at time of transfection [3]
Day 1: Transfection
- Transfect fibroblasts with 1-2 μg of episomal vectors encoding OCT4, SOX2, KLF4, L-MYC, LIN28, and p53 shRNA using an appropriate transfection reagent
- Include fluorescent marker plasmid to monitor transfection efficiency [3]
Day 2: Medium Change
- Replace transfection medium with fresh fibroblast medium
Days 3-6: Transition to Pluripotency Medium
- Gradually transition cells to essential 8 (E8) medium or mTeSR1 pluripotency medium
- Continue daily medium changes [3]
Days 7-21: Emergence of iPSC Colonies
- Continue daily changes with pluripotency medium
- iPSC colonies typically begin to appear between days 14-28
- Monitor for colonies with sharp borders, high nucleus-to-cytoplasm ratio, and prominent nucleoli [3]
Days 21-28: Colony Picking
- Manually pick well-defined iPSC colonies using a pipette tip or sterile needle
- Transfer colonies to Matrigel or laminin-521-coated plates with mTeSR1 medium containing 10 μM Y-27632 ROCK inhibitor [3]
Peripheral Blood Mononuclear Cell (PBMC) Reprogramming
For PBMC reprogramming, a less invasive somatic cell source:
Day -4: PBMC Isolation and Activation
- Isolate PBMCs from whole blood using Ficoll density gradient centrifugation
- Culture PBMCs in ImmunoCult T Cell Activator medium for 3 days to stimulate proliferation [3]
Day 0: Transfection
- Transfect 1×10^5 activated PBMCs with synthetic mRNA encoding OSKM factors using lipid-based transfection reagent
- Repeat transfections daily for 12-16 days to maintain reprogramming factor expression [3]
Days 5-20: Colony Formation
- Transfer transfected cells to Matrigel-coated plates between days 5-7
- Continue daily mRNA transfections until colonies emerge
- Change medium daily with mTeSR1 supplemented with 100 ng/mL B18R protein to enhance mRNA transfection efficiency [3]
Advanced Genome Engineering in iPSCs
Recent advances in prime editing technology enable precise genetic modifications in iPSCs with reduced off-target effects compared to conventional CRISPR-Cas9 systems. Optimized prime editing in hPSCs involves:
- Stable genomic integration of prime editors via piggyBac transposon system for sustained expression
- Use of enhanced promoters (CAG) for high-level expression of prime editor components
- Lentiviral delivery of pegRNAs (prime editing guide RNAs) ensuring robust, ubiquitous expression [8]
This optimized system has achieved editing efficiencies of up to 50% in human pluripotent stem cells in both primed and naïve states, enabling precise disease modeling through introduction of patient-specific mutations [8].
Table 2: Essential research reagents for somatic cell reprogramming and iPSC culture
| Category | Specific Reagents | Function | Example Applications |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) | Core transcription factors inducing pluripotency | Initial fibroblast reprogramming [3] [1] |
| Alternative Factors | NANOG, LIN28 | Enhance reprogramming efficiency | Human iPSC generation [1] |
| Culture Matrices | Matrigel, Laminin-521, Vitronectin | Extracellular matrix supporting pluripotency | Feeder-free iPSC culture [3] |
| Pluripotency Media | mTeSR1, Essential 8 (E8), StemFlex | Chemically defined media formulations | Maintenance of undifferentiated iPSCs [3] |
| Small Molecules | Y-27632 (ROCK inhibitor), SB431542, PD0325901 | Enhance survival and reprogramming efficiency | Improving clone recovery, supporting reprogramming [9] [3] |
| Characterization Antibodies | Anti-OCT4, Anti-NANOG, Anti-SSEA-4, Anti-TRA-1-60 | Detect pluripotency markers | Immunocytochemistry, flow cytometry [3] |
| Gene Editing Tools | CRISPR-Cas9, Prime Editors, piggyBac transposon | Genetic modification of iPSCs | Disease modeling, gene correction [8] |
Quality Control and Characterization
Rigorous quality control is essential to confirm successful reprogramming and pluripotent status:
- Pluripotency Marker Expression: Assess by immunocytochemistry (OCT4, NANOG, SSEA-4, TRA-1-60) and flow cytometry (>85% positive for pluripotency markers) [3]
- Trilineage Differentiation Potential: Demonstrate in vitro differentiation into ectoderm (neurons, glia), mesoderm (cardiomyocytes, adipocytes), and endoderm (hepatocytes, pancreatic cells) [3]
- Karyotype Analysis: Verify genomic integrity through G-band karyotyping or SNP arrays [3]
- Pluripotency Gene Expression: Confirm by RT-PCR analysis of endogenous OCT4, SOX2, and NANOG expression [3]
- Teratoma Formation: Assess in vivo differentiation potential by subcutaneous injection into immunodeficient mice, with subsequent histological confirmation of three germ layers [3]
Applications in Disease Modeling and Drug Development
The reprogramming of somatic cells to pluripotency has revolutionized approaches to studying human diseases. iPSC-based disease models offer several key advantages:
- Patient-Specific Models: iPSCs derived from patients with genetic disorders retain the disease-causing mutations, enabling modeling of monogenic and complex diseases in a human genetic background [3] [1]
- Differentiation into Affected Cell Types: Disease-specific iPSCs can be differentiated into cell types affected in the disorder, including neurons, cardiomyocytes, hepatocytes, and others [3]
- Platform for Drug Screening: iPSC-derived cells provide human-relevant platforms for compound screening, toxicity testing, and drug development [3] [1]
- Pathogenesis Studies: Enable investigation of disease mechanisms and progression through isogenic pairs (patient-specific vs. gene-corrected iPSCs) [3]
Key signaling pathways and transcriptional networks are reactivated during the reprogramming process, which can be visualized through the following pathway diagram:
Figure 2: Key molecular and cellular events in somatic cell reprogramming, showing how OSKM factors trigger multiple parallel processes that converge on pluripotency establishment.
Neurodegenerative Disease Modeling
iPSCs have been particularly valuable for modeling neurodegenerative disorders, which are often challenging to study due to limited access to affected human tissues:
- Alzheimer's Disease: Patient-specific iPSCs differentiated into neurons and glia recapitulate disease hallmarks including tau hyperphosphorylation and β-amyloid deposition [3]
- Parkinson's Disease: iPSC-derived dopaminergic neurons model degeneration of substantia nigra neurons and reveal the pathogenic role of α-synuclein aggregation [3]
- Amyotrophic Lateral Sclerosis (ALS): iPSC-derived motor neurons enable identification of disease biomarkers and screening of therapeutic compounds [3]
Cardiovascular Disease Modeling
iPSC-derived cardiomyocytes have advanced the study of cardiac disorders:
- Arrhythmogenic Disorders: Modeling of congenital arrhythmias linked to ion channel mutations (e.g., KCNQ1 mutations) [3]
- Heart Failure: Patient-specific cardiomyocytes enable drug screening and mechanistic studies [3]
- Myocardial Injury: iPSC-derived cardiomyocytes, fibroblasts, and endothelial cells explored for regenerative transplantation strategies [3]
The reprogramming of somatic cells to pluripotency represents a transformative technology with profound implications for disease modeling and therapeutic development. The core principles outlined in this technical guide—from molecular mechanisms to practical methodologies—provide researchers with the foundation needed to leverage iPSC technology effectively. As reprogramming methods continue to advance, with improvements in efficiency, safety, and standardization, iPSC-based disease models will play an increasingly central role in elucidating disease mechanisms, screening therapeutic compounds, and developing personalized medicine approaches. The integration of precise genome editing technologies with increasingly complex differentiation protocols promises to further enhance the fidelity of iPSC-based disease models, accelerating the translation of basic research findings into clinical applications.
Induced pluripotent stem cell (iPSC) technology represents a paradigm shift in biomedical research by enabling the development of human-specific disease models that overcome fundamental limitations inherent in traditional animal models. While animal studies have provided valuable insights, critical physiological differences between species often hinder their ability to accurately recapitulate human disease pathophysiology and predict drug responses. iPSCs, generated by reprogramming adult human somatic cells to a pluripotent state, provide unprecedented access to patient-specific human cells for disease modeling, drug screening, and therapeutic development. This whitepaper examines the key scientific advantages of iPSC-based models over traditional approaches, details experimental methodologies for implementing these systems, and discusses how this technology is transforming preclinical research and drug development pipelines.
Traditional animal models have long served as the cornerstone of biomedical research, yet they present significant challenges for accurately modeling human diseases and predicting clinical outcomes. These limitations stem from fundamental biological differences between species that can profoundly impact disease manifestation and therapeutic responses.
Physiological and Genetic Disparities: Numerous species-specific differences limit the translational relevance of animal models. For example, murine models of Fanconi anemia fail to develop the spontaneous bone marrow failure that is the hallmark of the human disease, despite carrying the same genetic deficiencies [10]. The heart rates of humans and mice differ by approximately ten-fold, which can lead to significantly different consequences from similar arrhythmias [10]. Additionally, mice engineered to be trisomic for genome sections orthologous to the human Down syndrome critical region failed to recapitulate human cranial abnormalities or neurodegeneration commonly associated with Down syndrome [10].
Drug Development Challenges: These species-specific differences contribute directly to the high failure rates of drugs in clinical development. It is estimated that 27%, 14%, and 7% of drugs fail in clinical trials due to adverse effects on the heart, liver, and central/peripheral nervous systems, respectively [11]. These failures often result from the inability of animal models to fully predict human-specific toxicities and efficacies.
Table 1: Fundamental Limitations of Traditional Animal Models
| Limitation Category | Specific Examples | Impact on Research |
|---|---|---|
| Physiological Differences | Ten-fold difference in heart rate between humans and mice; Different drug metabolism pathways | Poor prediction of human drug responses and toxicity |
| Genetic & Genomic Differences | Lack of conservation of gene order; Different gene expression patterns; Inbred genetic backgrounds | Failure to recapitulate human disease phenotypes |
| Developmental Differences | Different brain architecture; Varied tissue composition | Limited relevance for neurodevelopmental disorders and tissue engineering |
| Disease Manifestation | Fanconi anemia models don't develop bone marrow failure; Down syndrome models lack characteristic neurodegeneration | Incomplete disease modeling missing key pathological features |
Fundamental Advantages of iPSC-Based Disease Models
Human Biological Context
iPSC technology enables researchers to study disease mechanisms and test therapeutic interventions within an authentically human cellular context. By reprogramming somatic cells from patients, iPSCs retain the complete genetic background of the donor, including all polymorphisms, epigenetic modifications, and disease-associated mutations [1]. This human origin eliminates the confounding variables introduced by cross-species differences when extrapolating from animal models to human patients.
The capacity of iPSCs to differentiate into virtually any cell type provides access to otherwise inaccessible human tissues, particularly for diseases affecting internal organs like the brain and heart [11]. For neurological disorders, this advantage is particularly significant as human brain development, architecture, and function differ substantially from even our closest primate relatives. iPSC-derived neurons and glial cells maintain human-specific characteristics in culture, enabling researchers to study disease processes in relevant cell types [1].
Genetic Fidelity and Patient Specificity
iPSCs capture the complete genetic identity of the donor, enabling the creation of disease models with unprecedented genetic accuracy. This includes not only the primary genetic lesion responsible for a disease but also the complete genetic background that modifies disease expression and progression [10]. This genetic fidelity enables two complementary approaches to disease modeling:
- Forward genetics: Starting with patients exhibiting a disease phenotype, then generating iPSCs to identify genetic contributors [10]
- Reverse genetics: Introducing specific, predefined mutations into well-characterized iPSC lines to study their functional consequences [10]
This patient-specific approach is particularly valuable for studying complex diseases where multiple genetic factors contribute to pathogenesis, as well as for understanding the variable expressivity of monogenic disorders [1]. Additionally, iPSCs enable research on human-specific aspects of biology that cannot be modeled in other species, such as unique gene isoforms, non-coding RNAs, and epigenetic regulation mechanisms.
Table 2: Comparative Analysis of Disease Modeling Platforms
| Characteristic | Traditional Animal Models | iPSC-Based Human Models |
|---|---|---|
| Genetic Context | Species-specific genome with limited human gene orthology | Complete human genetic background with patient-specific variations |
| Physiological Relevance | Limited by cross-species differences in physiology and metabolism | Human-specific cellular physiology and signaling pathways |
| Experimental Accessibility | Limited access to disease-relevant tissues, especially for neurological disorders | Unlimited access to any cell type through directed differentiation |
| Personalization Potential | Low - requires genetic engineering for each variant | High - naturally captures individual genetic diversity |
| Throughput for Drug Screening | Moderate to low throughput, high cost | High throughput, scalable format |
| Temporal Resolution | Limited ability to observe cellular dynamics in real-time | Real-time monitoring of disease processes in live cells |
Developmental Modeling Capability
iPSC differentiation protocols recapitulate key aspects of human development, enabling researchers to study disease processes across the developmental timeline [1]. This "disease in a dish" approach allows observation of pathological changes as they unfold, from early cellular dysfunction to late-stage degeneration. For neurodevelopmental disorders like autism spectrum disorders and early-onset schizophrenia, this provides unprecedented access to the initial stages of disease manifestation that would be impossible to observe in human patients [1].
The ability to generate three-dimensional organoids from iPSCs further enhances their developmental modeling capabilities. These self-organizing structures mimic the complex architecture and cellular diversity of developing human tissues, enabling more sophisticated studies of cell-cell interactions, tissue patterning, and organ-level dysfunction [1]. Cerebral organoids, for instance, have been used to model microcephaly and other developmental brain disorders, revealing disease-specific alterations in progenitor cell populations and cortical organization that could not be observed in animal models [1].
Experimental Implementation: Methodologies and Protocols
iPSC Generation and Characterization
Reprogramming Methodologies: The foundational step in establishing iPSC-based disease models is the reprogramming of somatic cells to pluripotency. Several well-established methods exist, each with distinct advantages and limitations:
Sendai Virus Reprogramming: This non-integrating RNA virus method is widely applied due to its high efficiency (approximately 0.1% for both fibroblasts and peripheral blood mononuclear cells) and safety profile, as the virus does not enter the nucleus or integrate into the host genome [11]. The protocol involves transducing somatic cells with Sendai virus vectors carrying the reprogramming factors (typically OCT4, SOX2, KLF4, and c-MYC), followed by culture in pluripotent stem cell conditions until iPSC colonies emerge (typically 3-4 weeks for human cells) [11].
Integration-Free Methods: For clinical applications, non-viral methods such as episomal plasmids, synthesized RNAs, and recombinant proteins offer alternatives that eliminate potential viral vector concerns [11]. The mRNA reprogramming method involves repeated transfections of synthetic mRNAs encoding reprogramming factors, typically over a 2-3 week period, resulting in footprint-free iPSCs [11].
Comprehensive Characterization: Newly established iPSC lines must undergo rigorous quality control assessment to confirm pluripotency and genomic integrity before use in disease modeling. Standard characterization includes:
- Pluripotency Marker Expression: Immunofluorescence staining and flow cytometry for surface markers (TRA-1-60, TRA-1-81) and intracellular transcription factors (OCT4, NANOG, SOX2) [11]
- Trilineage Differentiation Potential: In vitro embryoid body formation followed by assessment of derivatives from all three germ layers, or in vivo teratoma formation in immunocompromised mice [11]
- Karyotype Analysis: G-band karyotyping or comparative genomic hybridization to detect chromosomal abnormalities acquired during reprogramming [11]
- Identity Confirmation: Short tandem repeat profiling to verify match with donor somatic cells [11]
- Microbiological Testing: Screening for mycoplasma and other potential contaminants [11]
Directed Differentiation to Relevant Cell Types
A critical advantage of iPSC technology is the ability to differentiate pluripotent cells into specific somatic cell types affected by disease. The following examples illustrate robust differentiation protocols for generating disease-relevant cells:
Cardiac Differentiation Protocol: iPSC-derived cardiomyocytes (iPSC-CMs) have become invaluable for modeling cardiac disorders and screening for cardiotoxicity. A standardized protocol involves:
- Mesoderm Induction: Treat iPSCs with 6-8 μM CHIR99021 (a GSK3β inhibitor) in RPMI 1640 medium supplemented with B-27 without insulin for 2 days [2]
- Cardiac Specification: Following mesoderm induction, add 2 μM Wnt-C59 (a Wnt inhibitor) in the same medium for 2 additional days to promote cardiac lineage specification [2]
- Metabolic Selection: From day 7 onward, switch to RPMI 1640 medium with B-27 complete supplement to support cardiomyocyte maturation [2]
- Functional Maturation Enhancement: To address the characteristic immature, fetal-like phenotype of iPSC-CMs, implement advanced maturation strategies:
- Co-culture Systems: Co-culture iPSC-CMs with iPSC-derived cardiac fibroblasts (iPSC-CFs) in a 2:1 ratio on micropatterned extracellular matrix substrates [2]
- 3D Hydrogel Culture: Encapsulate iPSC-CMs with human coronary artery endothelial cells in 3D gelatin methacryloyl hydrogels to better mimic cardiac tissue architecture [2]
Blood-Brain Barrier (BBB) Model Differentiation: iPSC-derived BBB models enable study of neurovascular disorders and drug penetration. A standardized protocol includes:
- Dual-SMAD Inhibition: Differentiate iPSCs using dual SMAD inhibition (10 μM SB431542 and 100 nM LDN193189) to induce neural and endothelial lineages simultaneously [12]
- Purification and Seeding: Purify endothelial cells and seed on collagen IV/fibronectin-coated transwell inserts (1×10^5 cells/cm²) [12]
- Barrier Maturation: Culture cells for at least 5 days in endothelial growth medium to establish tight junctions and mature barrier properties [12]
- Functional Validation: Measure transendothelial electrical resistance (TEER) using an epithelial voltohmmeter, with values >1000 Ω×cm² indicating competent barrier function [12]
Figure 1: Experimental workflow for establishing human iPSC-based disease models, from somatic cell reprogramming to functional characterization.
Advanced Maturation and Microenvironment Engineering
A significant challenge in iPSC-based modeling is the characteristic immature phenotype of many differentiated cell types. Advanced culture systems have been developed to enhance functional maturation:
Cardiac Maturation via Co-culture: Research demonstrates that iPSC-derived cardiac fibroblasts (iPSC-CFs) significantly enhance the functional maturity of iPSC-derived cardiomyocytes (iPSC-CMs) through both paracrine signaling and direct cell-cell interactions [2]. In co-culture systems, iPSC-CMs exhibit:
- Larger contractile strain amplitude compared to monocultures
- Increased spontaneous contraction rates with faster kinetics
- Enhanced contractile anisotropy and myofibril alignment
- Improved calcium handling and electrophysiological properties
Three-Dimensional Microenvironment Engineering: 3D culture systems more accurately mimic native tissue architecture and significantly enhance cellular maturation:
- Hydrogel-Based Cultures: iPSC-CMs co-cultured with human coronary artery endothelial cells in 3D gelatin methacryloyl hydrogels show upregulated expression of cardiac maturation markers and reduced oxidative stress compared to 2D monocultures [2]
- Organoid Systems: Self-organizing 3D structures that recapitulate aspects of tissue development and organization, enabling study of complex cell-cell interactions and tissue-level phenotypes [1]
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful implementation of iPSC-based disease modeling requires carefully selected reagents and specialized materials. The following table details essential components for establishing robust experimental systems:
Table 3: Essential Research Reagents for iPSC-Based Disease Modeling
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| Reprogramming Systems | Sendai virus vectors (CytoTune); Episomal plasmids; mRNA kits | Non-integrating delivery of reprogramming factors (OCT4, SOX2, KLF4, c-MYC) to somatic cells |
| Pluripotency Maintenance | mTeSR1; StemFlex; Essential 8 Medium | Chemically defined media supporting iPSC self-renewal and genomic stability |
| Differentiation Inducers | CHIR99021 (GSK3 inhibitor); SB431542 (TGF-β inhibitor); Retinoic acid | Small molecules directing lineage specification through targeted pathway modulation |
| Extracellular Matrices | Matrigel; Geltrex; Laminin-521; Collagen IV/Fibronectin | Substrates mimicking native basement membrane to support cell attachment and polarization |
| Characterization Antibodies | Anti-OCT4, SOX2, NANOG; TRA-1-60, TRA-1-81; Lineage-specific markers | Validation of pluripotency and differentiation efficiency through immunocytochemistry |
| Functional Assay Kits | Calcium imaging dyes; MEA plates; TEER measurement systems | Assessment of functional maturation in neuronal, cardiac, and barrier models |
Technological Integration: Enhancing iPSC Models with Artificial Intelligence
The convergence of iPSC technology with artificial intelligence (AI) represents a transformative advancement in disease modeling and drug discovery. AI-based approaches are being deployed to address key challenges in iPSC research:
Image-Based Classification and Quality Control: Machine learning algorithms, particularly convolutional neural networks (CNNs), can automatically identify and classify iPSC colonies based on morphology, predicting optimal colonies for expansion and differentiation [13] [14]. These systems can:
- Distinguish fully reprogrammed iPSCs from partially reprogrammed cells with >90% accuracy [14]
- Predict differentiation propensity based on colony morphology features [14]
- Identify subtle morphological changes indicative of genomic instability or culture adaptation [13]
Predictive Modeling of Differentiation Outcomes: AI approaches analyze high-content imaging data to forecast differentiation efficiency and functional maturation [13] [14]. For example:
- Morphological Descriptor Analysis: Quantitative analysis of cytoskeletal and nuclear features provides "barcode-like" identity to single cells, enabling prediction of lineage commitment [15]
- Time-Series Prediction Models: Hidden Markov Models can identify optimal time windows for colony selection and passage based on growth dynamics [14]
High-Content Phenotypic Screening: AI-enabled analysis of iPSC-derived cells facilitates high-throughput drug screening and toxicity assessment:
- Automated classification of cardiomyocyte beating patterns in response to pharmacological agents [13]
- Quantitative analysis of neurite outgrowth and synaptic connectivity in neuronal models [14]
- Prediction of complex disease phenotypes from simple morphological features [15]
Figure 2: Integration of artificial intelligence with iPSC technology enhances quality control, phenotypic analysis, and predictive modeling.
iPSC-based disease models represent a transformative approach that effectively overcomes the species-specific limitations inherent in traditional animal models. By providing a genetically accurate, human-specific experimental platform, iPSC technology enables researchers to study disease mechanisms, screen therapeutic compounds, and develop personalized treatment strategies with unprecedented relevance to human physiology and pathology. While challenges remain in achieving full functional maturation of some differentiated cell types, advanced culture systems and AI-enabled quality control are rapidly addressing these limitations.
The continued refinement of iPSC-based models, coupled with emerging technologies in genome editing, tissue engineering, and computational analysis, promises to further enhance their predictive validity and translational impact. As these human-specific models become increasingly sophisticated and accessible, they are positioned to significantly accelerate drug development, reduce reliance on animal studies, and ultimately enable more effective, personalized therapeutic interventions for complex human diseases.
The discovery of induced pluripotent stem cell (iPSC) technology by Shinya Yamanaka in 2006 represents a watershed moment in regenerative medicine and disease modeling. This whitepaper traces the scientific journey from the initial reprogramming of mouse fibroblasts using defined factors to current innovations accelerating iPSC applications in pharmaceutical development and disease research. We examine the evolution of reprogramming methodologies, molecular mechanisms underlying somatic cell reprogramming, and the expanding toolkit for generating clinically relevant disease models. Within the context of disease modeling, we highlight how iPSC technology has enabled researchers to create patient-specific cellular models that recapitulate pathological features, facilitating drug discovery and therapeutic development. The integration of advanced gene editing, bioengineering, and computational approaches continues to address early challenges in reprogramming efficiency, safety, and standardization, positioning iPSC-based models as indispensable assets for researchers and drug development professionals.
The development of induced pluripotent stem cell (iPSC) technology has fundamentally transformed biomedical research and regenerative medicine prospects. iPSCs are laboratory-generated pluripotent stem cells produced by reprogramming somatic cells through the forced expression of specific pluripotency genes, effectively reversing the developmental clock without the ethical concerns associated with embryonic stem cells (ESCs) [16]. This breakthrough has created unprecedented opportunities for patient-specific disease modeling, drug screening platforms, and cell therapy development [1]. For researchers and drug development professionals, iPSC technology provides a human-derived system to study disease mechanisms, test therapeutic candidates, and develop personalized medicine approaches, particularly for conditions where animal models fail to recapitulate human pathology [17] [1]. The capacity to differentiate iPSCs into virtually any somatic cell type enables the creation of human-relevant experimental models that mirror in vivo physiology and disease states with greater accuracy than traditional cell lines [18].
Historical Foundations
The conceptual foundation for iPSC technology extends back decades before its actualization. In 1962, John Gurdon's seminal somatic cell nuclear transfer (SCNT) experiments in Xenopus laevis frogs demonstrated that a nucleus from a terminally differentiated somatic cell contained all genetic information needed to generate entire organisms when transplanted into an enucleated egg [1]. This landmark discovery refuted the prevailing notion that cell differentiation involved irreversible genetic changes, suggesting instead that epigenetic factors governed cellular specialization. The isolation of mouse embryonic stem cells (ESCs) by Martin Evans, Matthew Kaufman, and Gail Martin in 1981, followed by James Thomson's derivation of human ESCs in 1998, established pluripotent cells as powerful research tools [1]. Subsequent cell fusion experiments between ESCs and somatic cells revealed that ESC factors could reprogram somatic nuclei toward pluripotency, hinting at the potential for factor-based reprogramming [1].
The pivotal breakthrough came in 2006 when Shinya Yamanaka and Kazutoshi Takahashi systematically tested 24 candidate genes important for ESC function in mouse embryonic fibroblasts (MEFs) [19] [1]. Through iterative testing, they identified four transcription factors—Oct4, Sox2, Klf4, and c-Myc (collectively termed OSKM or Yamanaka factors)—sufficient to reprogram MEFs into pluripotent stem cells [19]. These mouse iPSCs exhibited morphology, growth properties, and marker gene expression similar to ESCs, could form teratomas containing tissues from all three germ layers, and contributed to embryonic development after blastocyst injection [19]. Just one year later, Yamanaka and James Thomson independently reported successful reprogramming of human fibroblasts, with Thomson's group using an alternative factor combination (OCT4, SOX2, NANOG, and LIN28) [1] [20]. These discoveries demonstrated that pluripotent stem cells could be generated directly from somatic cells without embryos, earning Gurdon and Yamanaka the 2012 Nobel Prize in Physiology or Medicine.
Table 1: Key Historical Developments in iPSC Technology
| Year | Discovery | Researchers | Significance |
|---|---|---|---|
| 1962 | Somatic cell nuclear transfer in frogs | John Gurdon | Demonstrated reversibility of cellular differentiation |
| 1981 | Isolation of mouse embryonic stem cells | Martin Evans, Matthew Kaufman | Established pluripotent cell culture |
| 1998 | Derivation of human embryonic stem cells | James Thomson | Enabled human pluripotent cell research |
| 2006 | First induced pluripotent stem cells from mouse fibroblasts | Shinya Yamanaka | Proof-of-concept for factor-based reprogramming |
| 2007 | Generation of human iPSCs | Yamanaka and Thomson groups | Extended technology to human cells |
| 2013 | First iPSC-derived cell transplantation in humans | Masayo Takahashi | Initiated clinical applications |
| 2016 | First formal clinical trial of allogeneic iPSC-derived product | Cynata Therapeutics | Advanced regulated clinical development |
Molecular Mechanisms of Reprogramming
The process of reprogramming somatic cells to pluripotency involves profound remodeling of cellular identity through specific molecular mechanisms. When pluripotent stem cells differentiate into somatic cells, they acquire stable epigenetic memory and undergo global chromatin changes that silence pluripotency genes while activating lineage-specific genes [1]. Reprogramming effectively reverses this process, erasing somatic epigenetic signatures and reestablishing the pluripotent state.
Reprogramming occurs in two broad phases: an early, stochastic phase followed by a late, deterministic phase [1]. During the early phase, somatic genes are silenced while early pluripotency-associated genes become activated in a heterogeneous, inefficient manner, likely due to variable accessibility of closed chromatin regions to the reprogramming factors [1]. The late phase involves more synchronized activation of the core pluripotency network, including establishment of autoregulatory loops that stabilize the pluripotent state. Throughout this process, cells undergo mesenchymal-to-epithelial transition (MET), a critical step particularly when reprogramming fibroblasts [1].
The reprogramming factors each play distinct but complementary roles. Oct4 and Sox2 function as pioneer factors that bind condensed chromatin and initiate epigenetic remodeling, while Klf4 assists in chromatin opening and c-Myc promotes global transcriptional activation and proliferation [18] [1]. The process involves comprehensive rewiring of epigenetic landscapes, including DNA demethylation at pluripotency gene promoters, histone modification changes, and three-dimensional chromatin restructuring [1]. Additionally, reprogramming triggers profound shifts in cellular metabolism from oxidative phosphorylation toward glycolysis, mirroring metabolic changes in normal pluripotent cells [1].
Diagram 1: Molecular reprogramming process from somatic cell to iPSC showing key transitional phases
Evolution of iPSC Reprogramming Methods
Since the original viral transduction method, iPSC generation techniques have evolved significantly to address safety concerns and improve efficiency. The table below summarizes major reprogramming methodologies that have been developed.
Table 2: Comparison of iPSC Reprogramming Methods
| Method | Key Features | Reprogramming Efficiency | Safety Concerns | Primary Applications |
|---|---|---|---|---|
| Retroviral Vectors (Original) | Stable integration, persistent transgene expression | Low (~0.01-0.1%) | High (insertional mutagenesis) | Basic research, proof-of-concept |
| Sendai Virus | Non-integrating, viral RNA-based | Moderate (~0.1%) | Low (cleared over passages) | Clinical applications, disease modeling |
| mRNA Transfection | Non-integrating, defined timing | High (~1-4%) | Low (immune response) | Clinical-grade iPSCs, GMP manufacturing |
| Episomal Vectors | Non-integrating, plasmid-based | Low (~0.001-0.01%) | Low (potential integration) | Clinical applications, biobanking |
| Small Molecules | Non-genetic, chemical-based | Variable (up to 0.1-1%) | Low (off-target effects) | Research, screening platforms |
Early reprogramming approaches relied on integrating retroviral vectors that posed significant safety risks due to potential insertional mutagenesis and reactivation of oncogenes like c-Myc [19] [1]. Subsequent advancements focused on non-integrating methods including Sendai virus (a cytoplasmic RNA virus that doesn't integrate into the host genome), mRNA transfection (introducing in vitro transcribed mRNAs encoding reprogramming factors), and episomal vectors [18]. More recently, small molecule-based reprogramming has emerged as a promising approach that eliminates the need for genetic manipulation entirely [18] [1]. These improved methods have enabled the generation of clinical-grade iPSCs while maintaining genomic integrity, a critical consideration for therapeutic applications.
Current innovations continue to refine reprogramming techniques. Machine learning algorithms now assist in quality control and colony selection, improving reproducibility [18]. The development of 3D reprogramming systems and the identification of more specific small molecule enhancers continue to increase efficiency while reducing heterogeneity in the resulting iPSC lines [18]. These advances collectively address earlier limitations and facilitate the reliable production of iPSCs suitable for disease modeling and drug screening applications.
Current Innovations in iPSC Technology
Gene Editing and iPSC Engineering
The convergence of iPSC technology with precise gene editing tools, particularly CRISPR-Cas9, has revolutionized disease modeling and therapeutic development [18]. Researchers can now introduce or correct disease-associated mutations in iPSCs from healthy donors, creating isogenic pairs that differ only at the locus of interest, thereby controlling for genetic background variability [18]. This approach enables more precise attribution of phenotypic differences to specific genetic changes in disease models. Newer CRISPR systems including base editors and prime editors allow even more precise genetic modifications without creating double-strand DNA breaks, reducing unintended mutations [18].
Gene-edited iPSCs serve multiple purposes in pharmaceutical development: creating humanized disease models for drug screening, correcting genetic defects in patient-derived iPSCs for autologous cell therapy, and introducing reporter genes for tracking differentiation efficiency or compound screening [18]. For example, Parkinson's disease-specific neurons derived from iPSCs can be genetically edited to investigate disease progression mechanisms and identify potential therapeutic targets [18]. Similarly, dystrophin gene correction in iPSCs from Duchenne muscular dystrophy patients represents a promising autologous cell therapy approach [18].
Advanced Differentiation and Disease Modeling
Innovations in differentiation protocols have significantly enhanced the efficiency and reproducibility of generating functionally mature cell types from iPSCs. Key signaling pathways—including BMP, Wnt, and TGF-β—are precisely manipulated through optimized timing and concentration of specific growth factors and small molecules to direct differentiation toward specific lineages [18]. These advances have enabled the routine production of cardiomyocytes, neurons, pancreatic β-cells, and hepatocytes with improved functional maturity [18].
The development of three-dimensional organoids represents a major advancement in disease modeling, creating complex tissue-like structures that better mimic human physiology than traditional two-dimensional cultures [18] [1]. These self-organizing structures contain multiple cell types and exhibit primitive tissue architecture, enabling modeling of higher-order cell-cell interactions and disease processes [1]. iPSC-derived organoids have been developed for brain, liver, kidney, and gastrointestinal tissues, providing powerful platforms for studying development, disease mechanisms, and drug responses [18].
Diagram 2: iPSC differentiation pathways showing 2D versus 3D modeling approaches
Immune Evasion Strategies
A significant challenge for allogeneic iPSC-based therapies is immune rejection, which has prompted the development of innovative immune evasion strategies. Researchers are employing CRISPR-Cas9 to engineer hypoimmunogenic iPSCs by deleting HLA class I and II molecules to reduce immune surveillance while adding immune modulators like PD-L1 to create universal cell products [18]. These approaches aim to develop "off-the-shelf" iPSC lines that can be transplanted without matching or intensive immunosuppression, potentially revolutionizing cell therapy scalability and accessibility [18].
Additional strategies include cell encapsulation in immune-protective materials and genetic modifications to enhance expression of immune suppressive molecules [18]. These innovations are particularly relevant for diseases like diabetes, where iPSC-derived β-cells could restore normal insulin production but face immune destruction in type 1 diabetes patients [21]. By combining immune evasion with precise differentiation protocols, researchers are moving closer to effective cell replacement therapies for multiple conditions.
The Scientist's Toolkit: Essential Reagents and Methods
Table 3: Key Research Reagent Solutions for iPSC Research
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | Oct4, Sox2, Klf4, c-Myc | Initiate and maintain pluripotent state | Multiple factor combinations available; lab-specific optimization often required |
| Delivery Systems | Sendai virus, mRNA transfection, episomal plasmids | Introduce reprogramming factors | Choice depends on safety requirements and efficiency needs |
| Culture Media | mTeSR, E8, StemFlex | Support iPSC growth and maintenance | Defined, xeno-free formulations preferred for clinical applications |
| Differentiation Kits | Cardiomyocyte, neural, pancreatic β-cell kits | Direct lineage-specific differentiation | Protocol standardization enhances reproducibility across labs |
| Quality Control Assays | Pluritest, flow cytometry, karyotyping | Verify pluripotency and genomic integrity | Essential for confirming iPSC quality before downstream applications |
| Gene Editing Tools | CRISPR-Cas9, base editors, prime editors | Introduce precise genetic modifications | Enables creation of disease models and correction of mutations |
The iPSC research workflow requires specialized reagents and methods at each stage. For reprogramming, Sendai virus systems and mRNA transfection kits are commercially available from suppliers like Thermo Fisher Scientific and Takara Bio, providing non-integrating options for clinical-grade iPSC generation [18] [16]. Culture systems have evolved from feeder-dependent setups to defined, xeno-free media like mTeSR and E8, which improve reproducibility and reduce variability [18].
For differentiation, numerous specialized kits and protocols are available for generating specific cell types, with companies like FUJIFILM CDI, REPROCELL, and Ncardia providing iPSC-derived cardiomyocytes, neurons, and other lineages [16]. Quality control remains essential, with assays ranging from simple immunostaining for pluripotency markers (Oct4, Nanog, SSEA-4) to comprehensive genomic analyses to ensure genetic integrity [18] [22]. Advanced quality control methods include machine learning-based approaches for automated colony selection and DNA methylation profiling to verify complete reprogramming [18] [22].
Applications in Disease Modeling and Drug Development
iPSC technology has enabled unprecedented advances in disease modeling and pharmaceutical development. The ability to generate patient-specific cell types has facilitated the creation of "disease-in-a-dish" models for conditions ranging from neurological disorders to cardiovascular diseases [17] [1]. For neurological conditions like Parkinson's and Alzheimer's disease, iPSC-derived neurons recapitulate key pathological features and enable screening of neuroprotective compounds [18] [1]. In cardiovascular research, iPSC-derived cardiomyocytes allow modeling of inherited arrhythmias and testing of drug cardiotoxicity [23]. Metabolic disorders like diabetes have been modeled using iPSC-derived pancreatic β-cells, enabling studies of β-cell dysfunction and survival [21].
The pharmaceutical industry has incorporated iPSC-derived cells into drug screening platforms, leveraging their human relevance for more predictive toxicity and efficacy assessment [17] [16]. The FDA Modernization Act 2.0, which permits cell-based assays as alternatives to animal testing for drug applications, has further accelerated adoption of iPSC-based screening platforms [16]. Companies like Evotec and BrainXell have developed industrialized iPSC platforms for high-throughput drug screening, providing specialized neural and cardiac cells to pharmaceutical companies [16].
iPSCs also enable personalized medicine approaches, where patient-specific cells can be used to predict individual drug responses or develop autologous therapies [16]. Clinical trials utilizing iPSC-derived cells are underway for conditions including macular degeneration, graft-versus-host disease, heart failure, and Parkinson's disease [17] [16]. While most current trials are early-phase investigations assessing safety, they represent critical steps toward realizing the clinical potential of iPSC technology.
The journey from Yamanaka's initial discovery to current innovations illustrates how iPSC technology has matured from a fundamental biological breakthrough to an indispensable tool for disease modeling and drug development. Current research focuses on enhancing the safety, efficiency, and scalability of iPSC generation and differentiation, while addressing challenges such as functional maturity of differentiated cells and standardization across laboratories [17] [18]. The integration of gene editing, bioengineering, and computational approaches continues to expand the capabilities of iPSC-based models.
For researchers and drug development professionals, iPSCs offer a uniquely versatile platform that bridges the gap between traditional cell lines and human physiology. The ability to model diseases in human cells with relevant genetic backgrounds, combined with advances in organoid and tissue engineering technologies, provides unprecedented opportunities for understanding disease mechanisms and developing novel therapeutics. As the field addresses remaining challenges in standardization and safety assessment, iPSC-based approaches are poised to become increasingly central to biomedical research and therapeutic development, ultimately fulfilling the promise of personalized regenerative medicine.
Induced pluripotent stem cells (iPSCs) represent one of the most transformative breakthroughs in modern biomedical research, offering unprecedented opportunities for disease modeling, drug discovery, and regenerative medicine. The utility of iPSCs fundamentally rests upon two defining biological characteristics: self-renewal—the ability to undergo numerous cell divisions while maintaining an undifferentiated state—and differentiation capacity—the potential to give rise to specialized cell types representing all three embryonic germ layers [3] [1]. These twin properties enable researchers to generate patient-specific cellular models that recapitulate disease pathophysiology in vitro, providing powerful platforms for investigating molecular mechanisms of disease pathogenesis and performing high-throughput drug screening [3] [2]. For researchers and drug development professionals, understanding the molecular underpinnings and technical requirements for maintaining these essential characteristics is critical for exploiting the full potential of iPSC technology in both basic and translational research contexts.
The revolutionary discovery by Shinya Yamanaka and colleagues in 2006 demonstrated that somatic cells could be reprogrammed to a pluripotent state through the introduction of just four transcription factors: Oct4, Sox2, Klf4, and c-Myc (OSKM) [3] [1]. This groundbreaking achievement, which earned Yamanaka the Nobel Prize in Physiology or Medicine in 2012, effectively bypassed the ethical concerns associated with embryonic stem cells while providing an unlimited source of patient-specific pluripotent cells [3]. Subsequent research has refined our understanding of the molecular mechanisms governing iPSC self-renewal and differentiation, leading to more robust protocols for maintaining these essential characteristics in vitro [24] [1].
Table 1: Core Characteristics of Induced Pluripotent Stem Cells
| Characteristic | Definition | Functional Significance | Key Molecular Regulators |
|---|---|---|---|
| Self-Renewal | Capacity for extensive proliferation while maintaining undifferentiated state | Enables unlimited expansion and maintenance of pluripotent cell banks | OCT4, SOX2, NANOG, KLF4, c-MYC [3] [1] |
| Pluripotency | Potential to differentiate into derivatives of all three germ layers | Forms basis for generating diverse disease-relevant cell types | Endogenous reactivation of OCT4 promoter, chromatin remodeling [3] |
| Genetic Stability | Maintenance of genomic integrity during culture | Critical for reliable disease modeling and clinical applications | Requires continuous genomic monitoring [3] |
| Epigenetic Memory | Retention of somatic cell epigenetic signatures | May influence differentiation efficiency; erased in fully reprogrammed iPSCs | DNA methylation resetting during reprogramming [1] |
Molecular Mechanisms Governing Self-Renewal
Transcriptional Networks and Epigenetic Regulation
The self-renewal capacity of iPSCs is maintained through an intricate network of transcriptional and epigenetic regulators that function cooperatively to sustain the pluripotent state. Core transcription factors, including OCT4, SOX2, and NANOG, form a central autoregulatory loop that activates pluripotency-associated genes while simultaneously repressing differentiation genes [1]. OCT4 (encoded by POU5F1) serves as a master regulator of pluripotency, with precise expression levels critical for maintaining self-renewal—both deficiency and overexpression can trigger differentiation [3]. SOX2 cooperates with OCT4 to regulate numerous pluripotency genes, while NANOG provides stabilization to the network, enabling cytokine-independent self-renewal [1].
The reprogramming process involves profound epigenetic remodeling, including chromatin modification and DNA methylation resetting, which establishes the pluripotent state [3]. During the early phase of reprogramming, somatic genes are silenced while early pluripotency-associated genes are activated through predominantly stochastic mechanisms. The late phase involves more deterministic activation of the core pluripotency network and establishment of stable epigenetic patterns characteristic of embryonic stem cells [1]. This epigenetic reprogramming includes global DNA demethylation at pluripotency loci with concomitant increased methylation at somatic gene promoters, histone modifications that establish an open chromatin configuration at pluripotency genes, and reorganization of higher-order chromatin structure [3] [1].
The Stem Cell Niche: Microenvironmental Regulation of Self-Renewal
Self-renewal is profoundly influenced by the stem cell niche—a specialized microenvironment comprising supporting cells, extracellular matrix (ECM), and signaling molecules that collectively regulate stem cell behavior [25] [26]. The niche concept, first proposed by Schofield in 1978, posits that stem cell fate decisions are largely determined by extrinsic cues from their immediate microenvironment [25]. For iPSCs in culture, recreation of appropriate niche conditions is essential for maintaining self-renewal and pluripotency.
Early iPSC culture protocols employed feeder layers of mitotically inactivated mouse embryonic fibroblasts, which provided essential support through cell-cell contacts and secretion of supportive factors [3]. However, for enhanced reproducibility and clinical applications, feeder-free systems using defined extracellular matrix coatings such as Matrigel or recombinant human laminin have been developed [3]. These matrices provide not only structural support but also critical biochemical signaling through integrin-mediated pathways that regulate self-renewal [25]. The composition of the culture medium further contributes to niche recreation, with chemically defined formulations like mTeSR1 and E8 containing precise combinations of growth factors (e.g., FGF2) and pathway inhibitors (e.g., TGF-β/activin A) that maintain pluripotency while suppressing spontaneous differentiation [3].
Diagram 1: Regulatory Network Governing iPSC Self-Renewal. The stem cell niche provides critical extrinsic signals that interact with intrinsic transcriptional networks to maintain pluripotency.
Mechanisms of Differentiation Capacity
Developmental Principles and Directed Differentiation
The differentiation capacity of iPSCs mirrors that of embryonic stem cells, encompassing the potential to generate derivatives of all three germ layers: ectoderm, mesoderm, and endoderm [3]. This developmental potential is harnessed through directed differentiation protocols that recapitulate key aspects of embryonic development in vitro, activating evolutionarily conserved signaling pathways in a precise temporal sequence to guide cells toward specific lineages [27]. Understanding the signaling pathways that orchestrate normal development has been instrumental in developing robust differentiation protocols, particularly for disease modeling applications where mature, functionally competent cell types are required [27].
Cardiac differentiation protocols, for example, have been informed by extensive research into heart development, which involves sequentially activated signaling pathways including Wnt, TGF-β, IGF, and retinoic acid [27]. Similarly, neural differentiation strategies often employ dual SMAD inhibition to promote ectodermal specification, followed by patterning factors that regionalize the neural tissue into specific neuronal subtypes [3]. The efficiency of differentiation protocols varies considerably depending on the target cell type, with some lineages (e.g., cardiomyocytes) achieving high efficiency (>80%) while others remain challenging [3] [27].
Mathematical Modeling of Differentiation Dynamics
Recent advances in the field include the development of mathematical models to predict and optimize differentiation protocols, reducing the need for extensive empirical experimentation [28]. These in silico approaches model population dynamics during differentiation, accounting for processes such as proliferation, differentiation, and cell death [28]. For example, modeling definitive endoderm differentiation from iPSCs has revealed that space-limited growth models (logistic and Gompertz) outperform exponential growth models in predicting cell population dynamics, with differentiation outpacing proliferation as the main driver of population changes during the initial differentiation period [28]. Such models can predict optimal differentiation timeframes (e.g., 1.9-2.4 days for definitive endoderm induction) and ideal seeding densities (e.g., 300,000 cells per well for endoderm differentiation), significantly accelerating protocol optimization [28].
Diagram 2: iPSC Differentiation Capacity and Disease Modeling Applications. iPSCs undergo germ layer specification followed by terminal differentiation into disease-relevant cell types for modeling human disorders.
Quantitative Analysis of Self-Renewal and Differentiation
Table 2: Quantitative Parameters of iPSC Self-Renewal and Differentiation
| Parameter | Typical Range/Value | Measurement Methods | Influence on Disease Modeling |
|---|---|---|---|
| Reprogramming Efficiency | 0.1% to several percent [3] | Colony counting, pluripotency marker expression | Affects feasibility of generating patient-specific lines |
| Population Doubling Time | 15-24 hours [3] | Cell counting, metabolic assays | Determines expansion capability for large-scale studies |
| Karyotype Stability | Variable; requires monitoring every 10 passages [3] | Karyotyping, FISH, aCGH | Critical for genotype-phenotype correlations in disease models |
| Cardiac Differentiation Efficiency | Up to 80% for some protocols [27] | Flow cytometry for cardiac troponins | Determines yield of cardiomyocytes for disease modeling |
| Neural Differentiation Timeline | 30-60 days for mature neurons [3] | Immunostaining for neuronal markers | Impacts experimental planning for neurodegenerative disease models |
| Endoderm Differentiation Efficiency | ~70% CD117+CD184+ cells [28] | Flow cytometry for definitive endoderm markers | Affects yield of hepatic and pancreatic lineages |
Experimental Methodologies for Characterization
Assessing Pluripotency and Self-Renewal Capacity
Rigorous quality control is essential to verify the pluripotent state of iPSCs before their application in disease modeling. Standard characterization includes multiple complementary approaches to confirm both molecular and functional features of pluripotency [3]. Molecular analyses typically include PCR-based detection of endogenous pluripotency gene expression (OCT4, SOX2, NANOG), immunocytochemistry for pluripotency-associated proteins, and flow cytometry for surface markers such as TRA-1-60, TRA-1-81, and SSEA-4 [3]. Global gene expression profiling through microarray or RNA sequencing can further confirm similarity to reference embryonic stem cell lines.
Functional assessment of pluripotency represents the gold standard for confirming differentiation capacity. In vitro differentiation via embryoid body formation or directed differentiation followed by immunostaining for representatives of all three germ layers (e.g., β-III-tubulin for ectoderm, α-smooth muscle actin for mesoderm, and α-fetoprotein for endoderm) provides evidence of multilineage potential [3]. For the most stringent validation, teratoma formation assays involve injecting iPSCs into immunocompromised mice and subsequently examining the resulting tumors for the presence of differentiated tissues from all three germ layers [3]. Additionally, genomic integrity must be regularly evaluated through G-banding karyotyping or comparative genomic hybridization to detect chromosomal abnormalities that may compromise differentiation efficiency or predispose cells to malignant transformation [3].
Evaluating Differentiation Potential and Lineage Specification
The assessment of differentiation capacity requires specialized methodologies tailored to specific lineages of interest. For disease modeling applications, it is particularly important to confirm not only the presence of lineage-specific markers but also functional maturity of the differentiated cells [2]. Cardiac differentiation efficiency is typically quantified by flow cytometry analysis for cardiac troponins (cTnT) or myosin heavy chain (MHC), supplemented with functional assessments of spontaneous contraction, calcium transients, and electrophysiological properties using multi-electrode arrays [27]. Similarly, neuronal differentiation success is evaluated through a combination of morphological analysis (neurite outgrowth), immunostaining for neuronal markers (MAP2, NeuN), synaptic proteins (synapsin, PSD95), and functional assessments of electrophysiological activity using patch clamping or multi-electrode arrays [3].
Recent advances in differentiation protocol development have emphasized the importance of achieving not just lineage specification but functional maturation, as iPSC-derived cells often exhibit an immature, fetal-like phenotype [2]. Strategies to enhance maturation include extending culture duration, incorporating mechanical stimulation (e.g., cyclic stretch for cardiomyocytes), implementing three-dimensional culture systems, and developing co-culture models that better recapitulate the native tissue microenvironment [2]. For example, co-culture of iPSC-derived cardiomyocytes with cardiac fibroblasts has been shown to improve contractile function, increase spontaneous contraction rates, and enhance structural organization [2]. Similarly, three-dimensional gelatin methacryloyl hydrogel cultures promote cardiac maturation marker expression and reduce oxidative stress compared to traditional two-dimensional monocultures [2].
Table 3: Research Reagent Solutions for iPSC Characterization
| Reagent/Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Reprogramming Vectors | Episomal plasmids, Sendai virus, mRNA [3] | Delivery of reprogramming factors | Non-integrating methods preferred for clinical applications |
| Culture Matrices | Matrigel, recombinant laminin-521 [3] | Provide structural support and signaling cues | Defined matrices reduce batch variability |
| Culture Media | mTeSR1, Essential 8 (E8) [3] | Maintain pluripotency and support self-renewal | Chemically defined formulations enhance reproducibility |
| Pluripotency Markers | Antibodies against OCT4, SOX2, NANOG, TRA-1-60 [3] | Characterization of undifferentiated state | Multiple verification methods recommended |
| Differentiation Kits | STEMdiff Definitive Endoderm Kit [28] | Directed differentiation to specific lineages | Improve protocol standardization across laboratories |
| Cell Dissociation Reagents | GCDR, dispase, EDTA [3] [28] | Passaging and harvesting of cells | Impact cell viability and recovery |
| Cryopreservation Reagents | DMSO-containing solutions [3] | Long-term storage of iPSC lines | Controlled-rate freezing improves post-thaw viability |
Applications in Disease Modeling and Drug Development
The dual capacities of self-renewal and differentiation make iPSCs uniquely powerful for disease modeling and drug development applications. Patient-specific iPSCs can be differentiated into disease-relevant cell types that recapitulate pathological features in vitro, enabling investigation of disease mechanisms and high-throughput compound screening [3]. For neurodegenerative diseases such as Alzheimer's disease and Parkinson's disease, iPSC-derived neuronal models have provided new insights into pathogenic mechanisms, including tau hyperphosphorylation, β-amyloid deposition, and α-synuclein aggregation [3]. Similarly, iPSC-derived cardiomyocytes have enabled the study of arrhythmogenic disorders and heart failure, with models of congenital arrhythmias linked to KCNQ1 mutations providing a basis for precision cardiology [3].
In metabolic disease modeling, iPSCs have been particularly valuable for studying genetic disorders such as cystic fibrosis, where iPSC-derived airway epithelial cells reproduce defective chloride transport caused by CFTR mutations, facilitating evaluation of targeted therapeutics like ivacaftor and lumacaftor [3]. For Duchenne muscular dystrophy, iPSC-derived myocytes enable mechanistic studies of muscle degeneration, while gene editing approaches have successfully restored dystrophin expression in vitro, highlighting the therapeutic potential of combining iPSC technology with genome editing [3].
The self-renewal capacity of iPSCs is especially important for drug discovery applications, as it enables the generation of virtually unlimited quantities of uniform, patient-specific cells for high-throughput screening [2]. This capability addresses a major limitation of primary human cells—their limited expansion potential—while providing human-relevant models that may more accurately predict drug efficacy and toxicity compared to animal models or transformed cell lines [3] [2]. Additionally, iPSC-based models support the development of personalized medicine approaches, as panels of iPSCs from patients with varying drug responses can be used to identify genetic determinants of treatment efficacy and toxicity [3].
The essential characteristics of self-renewal and differentiation capacity establish iPSCs as an indispensable platform for disease modeling and drug development. The molecular machinery governing these properties—including core pluripotency transcription factors, epigenetic regulators, and niche-derived signals—must be carefully maintained through optimized culture conditions and rigorous quality control. As differentiation protocols continue to improve through the application of developmental principles and mathematical modeling, and as culture systems evolve to better recapitulate native tissue microenvironments, iPSC-based disease models will become increasingly sophisticated and physiologically relevant. For researchers and drug development professionals, mastering the technical requirements for maintaining iPSC self-renewal while directing differentiation into functionally mature cell types is fundamental to harnessing the full potential of this transformative technology for understanding disease mechanisms and developing novel therapeutics.
The advent of induced pluripotent stem cell (iPSC) technology has fundamentally transformed the landscape of biomedical research, providing an unprecedented platform for studying human diseases in vitro. By enabling the generation of patient-specific pluripotent stem cells from somatic tissues, this technology offers a powerful pathway to bridge the gap between clinical phenotypes and molecular pathophysiology [2] [29]. The disease modeling pipeline, which encompasses the journey from patient biopsy to functionally differentiated cells, provides researchers with a system to elucidate disease mechanisms, screen potential therapeutic compounds, and develop personalized treatment strategies. This technical guide details the comprehensive pipeline, providing detailed methodologies, quantitative benchmarks, and standardized resources essential for establishing robust and reproducible patient-specific disease models.
The iPSC Generation Process: From Skin Biopsy to Pluripotency
Patient Biopsy and Fibroblast Derivation
The initial phase of establishing a patient-specific disease model involves obtaining somatic cells and reprogramming them into a pluripotent state. A common and minimally invasive approach is the skin biopsy procedure.
Materials for Skin Biopsy Procedure [29]:
- Biopsy Collect Medium: RPMI1640, 1× Anti-Anti.
- Disposable Biopsy Punches: Diameter 4 mm.
- Anesthetic: Xylocaine (lidocaine HCL and epinephrine injection, USP).
- Disinfectant: Povidone-iodine, USP swab stick.
- Suture: 5-0 VICRYL coated suture.
- Other Supplies: Sterile fenestrated towel, sterile gauze pad, autoclaved forceps, needle holder, scissors, 15 ml conical tube, Band-Aid.
Detailed Biopsy Protocol [29]:
- Site Preparation: The biopsy site, typically on the upper arm or thigh, is disinfected with 5% povidone-iodine twice using a circular motion from the center outward and allowed to air-dry.
- Anesthesia: The skin is anesthetized locally by subcutaneous injection of 1% lidocaine.
- Tissue Extraction: Using a sterile 4 mm skin punch, a full-thickness skin sample is obtained and cut at the base with sterile scissors.
- Collection: The tissue is immediately transferred using sterile forceps into a 15 ml tube containing 10 ml of biopsy collection medium and maintained at room temperature during transport.
- Wound Closure: The edges of the wound are sutured with dissolvable suture, and the site is covered with a Band-Aid.
Fibroblast Culture from Skin Biopsy [29]: The minced biopsy tissue is explanted onto a culture dish and secured under a sterile coverslip with silicone grease. It is cultured in biopsy plating medium (DMEM, 10% fetal bovine serum (FBS), 1× nucleosides, 1× L-glutamine, 1× non-essential amino acids, 1× Anti-Anti, 0.1 mM β-mercaptoethanol). Fibroblasts typically migrate out from the tissue explants over 2-3 weeks. Upon reaching confluency, fibroblasts are harvested using trypsin-EDTA and expanded for reprogramming.
Reprogramming to Pluripotency
The critical step of converting patient-specific fibroblasts into iPSCs requires the introduction of reprogramming factors.
Reprogramming Materials [29]:
- Reprogramming Vector: CytoTune-iPS Sendai Virus Reprogramming Kit (footprint-free RNA virus).
- Reprogramming Medium: KO-DMEM, 15% KnockOut Serum Replacement, 1× L-glutamine, 1× non-essential amino acids, 1× penicillin-streptomycin, 0.1 mM β-Mercaptoethanol, basic fibroblast growth factor (bFGF) 10 ng/ml.
- Support Cells: Mitomycin-C treated mouse embryonic fibroblasts (MEFs) as feeders.
- ROCK Inhibitor: Y-27632, to enhance cell survival after passaging.
Detailed Reprogramming Protocol [29]:
- Cell Seeding: Plate patient-derived fibroblasts at an appropriate density (e.g., 5x10^4 cells per well of a 12-well plate).
- Viral Transduction: Infect fibroblasts with the CytoTune-iPS Sendai Virus vectors expressing OCT4, SOX2, KLF4, and c-MYC.
- Culture and Monitoring: Replace the virus-containing medium with fresh fibroblast medium after 24 hours. Culture the cells for 7 days, then passage onto MEF feeder layers and switch to reprogramming medium.
- iPSC Colony Picking: Between days 21-28, distinct iPSC colonies with embryonic stem cell-like morphology become visible. These colonies are manually picked and transferred to new feeder layers for expansion.
Table 1: Key Research Reagent Solutions for iPSC Generation and Culture
| Reagent Category | Specific Product/Component | Function in the Pipeline |
|---|---|---|
| Reprogramming Vector | CytoTune-iPS Sendai Virus (SeV) | Delivers reprogramming factors (OCT4, SOX2, KLF4, c-MYC) without genomic integration [29]. |
| Base Culture Medium | KO-DMEM | A specialized, low-osmolarity medium that serves as the base for iPSC culture [29]. |
| Critical Medium Supplement | KnockOut Serum Replacement (KSR) | A defined, serum-free formulation that supports the growth and maintenance of pluripotent stem cells [29]. |
| Essential Growth Factor | basic Fibroblast Growth Factor (bFGF) | A key signaling molecule that promotes self-renewal and inhibits spontaneous differentiation of iPSCs [29]. |
| Pro-Survival Reagent | Y-27632 (ROCK inhibitor) | Enhances the survival of iPSCs after single-cell passaging and during cryopreservation [29]. |
| Extracellular Matrix | 0.1% Gelatin Solution | Provides a substrate for coating culture vessels used for feeder cells or direct iPSC attachment [29]. |
| Dissociation Enzyme | TrypLE Express | A gentle, animal-origin-free enzyme solution for passaging and dissociating iPSC colonies [29]. |
Figure 1: The core workflow for generating patient-specific induced pluripotent stem cell (iPSC) lines from a skin biopsy, involving fibroblast derivation and reprogramming.
Quality Control and Experimental Design
Characterization of iPSC Lines
Newly generated iPSC lines must be rigorously characterized to confirm their identity, pluripotency, and genomic integrity.
- Pluripotency Marker Validation: Immunofluorescence staining confirms the expression of key pluripotency-associated proteins, including OCT4, SOX2, NANOG, TRA-1-60, and SSEA4 [29].
- Trilineage Differentiation Potential: The gold-standard test for pluripotency is the teratoma assay, where iPSCs are injected into immunodeficient (SCID) mice. Successful formation of a teratoma containing differentiated tissues from all three germ layers (ectoderm, mesoderm, and endoderm) confirms functional pluripotency [29].
Determining the Number of Lines Needed
A critical consideration for robust disease modeling is the number of independent iPSC lines required to distinguish disease-specific phenotypes from background biological and technical noise. A 2025 study using RNA sequencing (RNAseq) to model Lesch-Nyhan disease provided empirical guidance on this key design parameter [30].
Table 2: Empirical Recommendations for iPSC Line Numbers in Disease Modeling [30]
| Experimental Design Factor | Prior Common Practice | Empirically Recommended Practice | Impact on Result Robustness |
|---|---|---|---|
| Number of Unique Individuals | Often 1-2 per group | 3-4 unique individuals per group (e.g., 3 patients, 3 controls) | Maximizes the capture of biological disease variance while controlling for individual genetic background. |
| Number of Lines Per Individual | Often 1 | 2 independent iPSC lines per individual | Helps control for technical and clonal variability introduced during the reprogramming process. |
| Statistical Handling | Variable | In the optimized design, results were improved without statistical corrections for multiple lines from the same individual. | Suggests that when lines are produced in parallel using consistent methods, most variance is technical rather than individual-specific. |
Directed Differentiation and Functional Maturation
A significant challenge in the field is that iPSC-derived cells often exhibit an immature, fetal-like phenotype upon initial differentiation [2]. Achieving adult-like functional maturity is crucial for accurately modeling late-onset diseases.
Strategies for Enhanced Cellular Maturity
Recent research highlights advanced co-culture and 3D culture systems as effective strategies to drive maturation.
- Cardiac Fibroblast Co-culture: Co-culturing hiPSC-derived cardiomyocytes (hiPSC-CMs) with hiPSC-derived cardiac fibroblasts (hiPSC-CFs) on a 2D micropatterned substrate significantly improves multiple contractile properties, including strain amplitude, contraction rate, and kinetics. This effect is mediated by a combination of paracrine signaling and direct cell-cell contact [2].
- 3D Hydrogel Microenvironments: Combining hiPSC-CMs with human coronary artery endothelial cells within a 3D gelatin methacryloyl (GelMA) hydrogel mimics the native cardiac tissue architecture. This system upregulates cardiac maturation markers, improves cell viability, and reduces oxidative stress compared to standard 2D monocultures [2].
Figure 2: Overcoming the challenge of cellular immaturity in iPSC-derived cells through advanced culture strategies like co-culture and 3D hydrogels.
Disease Modeling Applications and Therapeutic Testing
The final output of the pipeline is a physiologically relevant in vitro model that can be used for mechanistic investigation and therapeutic screening.
In Vitro Disease Phenotyping
Patient-specific iPSC-derived cells carrying disease-causing mutations allow for the dissection of pathological mechanisms. For example, in Lesch-Nyhan disease, iPSC-derived neural cells with HPRT1 mutations enable the study of disease-relevant changes in gene expression and neuronal function [30]. These models help bridge the critical knowledge gap between a known genetic mutation and the resulting cellular pathophysiology [29].
Drug Discovery and Cell-Free Therapies
iPSC-based models provide a human-specific platform for preclinical drug screening and development.
- Drug Screening: Patient-specific disease cells can be used to test novel therapeutic agents or to repurpose existing drugs, potentially bypassing the need for expensive animal studies in the initial phases [29].
- Extracellular Vesicle (EV) Therapies: A promising cell-free alternative involves using EVs derived from iPSC-derived mesenchymal stem cells (iPSC-MSCs). These EVs exhibit potent anti-inflammatory properties and, compared to EVs from conventional MSCs, maintain their function for a longer duration during long-term cell expansion. However, batch-to-batch variability remains a challenge for clinical translation [2].
- In Vivo Tracking: The therapeutic potential of iPSC-derived cells can be evaluated in animal models. Using bright bioluminescence reporters like Antares 2 allows for sensitive, long-term tracking of injected cells (e.g., iPSC-MSCs in arthritic rat joints) to monitor localization, persistence, and mechanism of action [2].
The disease modeling pipeline, from patient biopsy to functionally mature differentiated cells, represents a cornerstone of modern personalized medicine. While challenges such as ensuring cellular maturity and managing experimental variability persist, the standardized protocols, quantitative design principles, and advanced maturation strategies detailed in this guide provide a robust framework for their mitigation. As these technologies continue to evolve and integrate with other advanced computational and omics approaches, they will undoubtedly accelerate the pace of discovery for a wide spectrum of human genetic diseases and the development of effective, personalized therapeutics.
Advanced iPSC Methodologies: From 2D Cultures to 3D Organoid Systems
The advent of induced pluripotent stem cell (iPSC) technology has revolutionized biomedical research by providing a versatile platform for disease modeling, drug discovery, and potential cell-based therapies. Directed differentiation, the process of guiding iPSCs toward specific somatic cell fates through defined culture conditions, lies at the heart of this revolution. This technical guide provides an in-depth examination of current protocols for generating three therapeutically vital cell types—cardiomyocytes, neurons, and hepatocytes—within the context of disease modeling research. We synthesize recent advances that enhance differentiation efficiency, maturity, and functionality, empowering researchers and drug development professionals to implement these methods in their investigative workflows.
Core Principles of Directed Differentiation
Directed differentiation of iPSCs recapitulates key aspects of embryonic development in vitro by sequential activation and inhibition of evolutionarily conserved signaling pathways. This process is typically achieved through the timed administration of specific growth factors, small molecules, and manipulation of culture conditions. The resulting cells can be used for disease modeling either through derivation from patients with specific genetic conditions or through gene editing to introduce disease-relevant mutations in healthy iPSC lines [31]. The fidelity of the differentiation protocol directly impacts the physiological relevance of these models for pharmaceutical research and toxicology studies.
Cardiomyocyte Differentiation
Current Advances in Cardiac Differentiation
Recent innovations in cardiomyocyte differentiation have focused on improving purity, maturity, and scalability while reducing batch-to-batch variability. Suspension culture systems have emerged as a robust alternative to traditional monolayer differentiation, offering superior scalability and consistency. One optimized bioreactor protocol differentiates iPSCs into cardiomyocytes with approximately 94% purity, yielding ~1.21 million cells per milliliter and generating about 2.4 cardiomyocytes per input iPSC [32]. These bioreactor-differentiated cardiomyocytes (bCMs) exhibit ventricular-specific markers (MYH7, MYL2, MYL3) and demonstrate functional properties with contractions beginning as early as differentiation day 5 [32].
A separate methodological adaptation demonstrated that detaching and reseeding cardiac progenitor cells at optimal densities during differentiation can significantly enhance cardiomyocyte purity. Reseeding at a 1:2.5 surface area ratio increased cardiomyocyte purity by approximately 12% (absolute), while a 1:5 ratio increased purity by about 15%, without negatively impacting cardiomyocyte number, sarcomere structure, or contractile function [33]. This approach also enables cryopreservation of intermediate progenitor populations (EOMES+ mesoderm and ISL1+/NKX2-5+ cardiac progenitor cells), facilitating quality control and on-demand cardiomyocyte production [33].
Table 1: Quantitative Outcomes of Advanced Cardiomyocyte Differentiation Protocols
| Protocol Feature | Bioreactor Suspension Protocol [32] | Progenitor Reseeding Protocol [33] |
|---|---|---|
| Average Purity | ~94% TNNT2+ cells | 10-20% absolute increase in cTnT+ purity |
| Yield | ~1.21 million cells/mL; ~2.4 CMs/input iPSC | Maintained CM number at 1:2.5 reseeding ratio |
| Key Markers | TNNT2, ACTN2, MYH7, MYL2, MYL3 | cTnT+ |
| Functional Assessment | Contraction from day 5; ventricular identity | Maintained contractility; sarcomere structure |
| Scalability | High (suspension culture) | Moderate (adaptable to multiple formats) |
| Cryopreservation | >90% viability after cryo-recovery | Progenitor stage cryopreservation possible |
Detailed Cardiomyocyte Differentiation Methodology
The following protocol describes a small molecule-based approach for cardiomyocyte differentiation in stirred suspension systems:
Initial Cell Quality Control: Begin with quality-controlled iPSC master cell banks characterized for pluripotency marker expression (SSEA4 >70% by FACS), karyotypic normality, and absence of mycoplasma contamination [32].
Embryoid Body Formation: Dissociate iPSCs to single cells and transfer to stirred bioreactor systems. Allow cells to spontaneously aggregate into embryoid bodies (EBs), monitoring size distribution. Target an average EB diameter of 100μm at the time of induction [32].
Mesoderm Induction: Initiate differentiation by adding 7μM CHIR99021 (a GSK-3 inhibitor that activates Wnt signaling) when EBs reach the target size. Incubate with CHIR99021 for 24 hours [32].
Cardiac Mesoderm Specification: Following a 24-hour gap without small molecules, add 5μM IWR-1 (a Wnt inhibitor that promotes cardiac specification) for 48 hours to direct differentiation toward cardiac lineages [32].
Terminal Differentiation and Maturation: Maintain cells in suspension culture with regular medium changes. Spontaneous contractions typically emerge by differentiation day 5. Cells can be harvested for analysis or experimentation by differentiation day 15 [32].
Cryopreservation: For progenitor cryopreservation, harvest EOMES+ mesoderm or ISL1+/NKX2-5+ cardiac progenitor cells, resuspend in cryoprotective medium, and freeze using controlled-rate freezing. Upon thawing, reseed at optimized densities (1:2.5 to 1:5 surface area ratio) to continue differentiation [33].
Neuronal Differentiation
Efficient Generation of Neurons via NGN2 Induction
For neuronal differentiation, the neurogenin 2 (NGN2) induction system has emerged as a highly efficient method for large-scale production of glutamatergic neurons. This protocol enables rapid generation of mature neurons within 5 days, achieving scales of billions of cells suitable for high-throughput screening and disease modeling applications [34].
The key innovation involves engineering iPSCs with a doxycycline-inducible NGN2 cassette targeted to the AAVS1 safe harbor locus, ensuring consistent and controlled neurogenesis across different cell lines. This system bypasses multi-stage intermediate states to directly convert iPSCs into neurons, minimizing heterogeneity and improving reproducibility [34].
Table 2: Neuronal Differentiation Protocol Outcomes Using NGN2 Induction
| Protocol Parameter | Performance Metric |
|---|---|
| Differentiation Timeline | 5 days to functional neurons |
| Scalability | Billions of neurons produced |
| Key Genetic Component | Doxycycline-inducible NGN2 in AAVS1 locus |
| Cell Engineering Method | CRISPR ribonucleoprotein and donor plasmid |
| Selection Method | Homology-directed repair enhancement, antibiotic selection, fluorescence |
| Long-term Maintenance | Neurons can be maintained for months or cryopreserved |
Detailed Neuronal Differentiation Methodology
iPSC Engineering: Electroporate iPSCs with CRISPR/Cas9 ribonucleoprotein complex and donor plasmid containing doxycycline-inducible NGN2 cassette targeted to the AAVS1 locus. Enhance homology-directed repair using small molecule additives [34].
Selection and Validation: Select successfully engineered clones using antibiotic selection and fluorescence screening. Expand validated clones and verify targeted integration through genomic analysis [34].
Neuronal Differentiation: To initiate differentiation, add doxycycline to culture medium to induce NGN2 expression. Within 24 hours, cells begin extending neuronal processes. By day 5, cultures consist of functional neurons expressing characteristic markers [34].
Maturation and Maintenance: Culture neurons with appropriate trophic support (BDNF, NT-3) for several weeks to enhance maturity. Cells can be cryopreserved at various stages or maintained in long-term culture for chronic studies [34].
Hepatocyte Differentiation
Enhanced Hepatic Differentiation through EMT Inhibition
Hepatocyte differentiation from iPSCs has been significantly improved through strategies that suppress epithelial-mesenchymal transition (EMT), a process that otherwise limits functional maturity and long-term culture stability. Inhibition of EMT during hepatic differentiation extends the in vitro culture period from 24 to 60 days and enhances expression of functional hepatic markers, including albumin secretion, urea acid metabolism, glycogen storage, and lipid accumulation [35].
The resulting iPSC-induced hepatocytes (iHeps) with EMT suppression (iHeps EMTi) demonstrate molecular profiles more closely resembling primary human hepatocytes and show improved engraftment efficiency in chimeric mouse models, making them particularly valuable for disease modeling and cell therapy applications [35].
Detailed Hepatocyte Differentiation Methodology
Definitive Endoderm Induction: Differentiate iPSCs into definitive endoderm using Activin A and Wnt signaling activation in a time-dependent manner, typically over 3-5 days. Monitor expression of SOX17 and FOXA2 markers [36] [37].
Hepatic Specification: Direct definitive endoderm toward hepatic fate using BMP-4 and FGF signaling pathway activation, generating hepatoblast intermediates that express AFP and HNF4α [36].
Hepatocyte Maturation with EMT Inhibition: Promote functional maturation using HGF, Oncostatin M, and glucocorticoids while adding small molecule inhibitors of EMT pathways. This combination significantly enhances hepatic functionality and extends culture stability [35].
Functional Assessment: Evaluate hepatocyte functionality through albumin and urea production, cytochrome P450 activity, indocyanine green uptake and release, and glycogen storage. iHeps with EMT inhibition should demonstrate superior performance across these parameters compared to conventional differentiations [35].
Experimental Workflows and Signaling Pathways
The directed differentiation processes for cardiomyocytes, neurons, and hepatocytes follow conserved developmental principles but utilize distinct signaling pathway modulations at specific timepoints. The following diagrams illustrate the key workflows and regulatory pathways for each lineage.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Directed Differentiation Protocols
| Reagent Category | Specific Examples | Function in Differentiation |
|---|---|---|
| Wnt Pathway Modulators | CHIR99021, IWP2, IWR-1 | Sequential activation/inhibition directs cardiac mesoderm formation [33] [32] |
| Transcription Factors | NGN2 (neurogenin 2) | Master regulator for neuronal commitment [34] |
| Growth Factors | Activin A, BMP4, FGF, HGF, Oncostatin M | Direct endoderm patterning and hepatic maturation [35] [36] |
| EMT Inhibitors | Small molecule EMT inhibitors | Enhance hepatocyte maturity and longevity [35] |
| Extracellular Matrices | Fibronectin, Matrigel, Laminin-111, Vitronectin | Provide structural support and biochemical cues [38] [33] |
| Selection Agents | Antibiotics, Fluorescent reporters | Enrich for successfully engineered clones [34] |
| Cryopreservation Media | DMSO-based formulations | Enable storage of progenitors and mature cells [33] [32] |
The directed differentiation protocols detailed in this technical guide represent current state-of-the-art methodologies for generating cardiomyocytes, neurons, and hepatocytes from human iPSCs. By implementing these refined approaches—incorporating bioreactor suspension culture for cardiomyocytes, NGN2 induction for neurons, and EMT inhibition for hepatocytes—researchers can achieve superior cell yields, purity, and functionality. These advances directly enhance the physiological relevance of iPSC-based disease models, enabling more predictive drug screening and deeper understanding of disease mechanisms. As these protocols continue to evolve, they will further bridge the gap between in vitro models and human pathophysiology, accelerating the development of novel therapeutics for a wide range of human diseases.
Induced pluripotent stem cell (iPSC) technology has fundamentally transformed the landscape of monogenic disease modeling, enabling researchers to recapitulate patient-specific genotypes and phenotypes in vitro. By reprogramming somatic cells into pluripotent stem cells, scientists can generate an unlimited supply of disease-relevant cell types for investigating pathological mechanisms and screening therapeutic candidates. This technical guide examines the application of iPSC-derived models for two distinct monogenic disorders: Long QT Syndrome (LQTS), a cardiac channelopathy, and Parkinson's disease (PD), a neurodegenerative disorder. The convergence of iPSC technology with advanced differentiation protocols, 3D culture systems, and gene editing tools has created unprecedented opportunities for precision medicine, allowing for the development of genetically tailored therapeutic approaches that address the root causes of these conditions rather than merely managing their symptoms.
Long QT Syndrome Modeling
Disease Background and Genetic Basis
Long QT Syndrome is an inherited cardiac arrhythmia disorder characterized by delayed myocardial repolarization that predisposes patients to ventricular arrhythmias and sudden cardiac death. With an estimated prevalence of 1:2500, LQTS represents a major cause of sudden cardiac death in young individuals (<35 years) [39]. The syndrome encompasses two hereditary forms: Romano-Ward syndrome (autosomal dominant) and Jervell and Lange-Nielsen syndrome (autosomal recessive with concomitant congenital deafness) [39]. Genetic testing in LQTS index patients has a yield of approximately 75%, with 90% of genotype-positive cases harboring variants in three core genes: KCNQ1 (LQT1, 40-55%), KCNH2 (LQT2, 30-35%), and SCN5A (LQT3, 5-10%) [39]. These genetic subtypes manifest distinct molecular mechanisms: LQT1 and LQT2 involve loss-of-function variants in potassium channels (Kv7.1 conducting IKs current and Kv11.1 conducting IKr current, respectively), while LQT3 is caused by gain-of-function variants in the sodium channel Nav1.5 leading to persistent late INa current [39].
Table 1: Genetic Subtypes of Long QT Syndrome
| Subtype | Gene | Prevalence | Channel Affected | Functional Effect | Primary Arrhythmia Triggers |
|---|---|---|---|---|---|
| LQT1 | KCNQ1 | 40-55% | Kv7.1 (IKs) | Loss-of-function | Exercise, emotional stress |
| LQT2 | KCNH2 | 30-35% | Kv11.1 (IKr) | Loss-of-function | Sudden auditory stimuli |
| LQT3 | SCN5A | 5-10% | Nav1.5 (INa) | Gain-of-function | Rest, sleep |
iPSC-Derived Cardiomyocyte Models
The generation of human iPSC-derived cardiomyocytes (hiPSC-CMs) has provided a revolutionary platform for modeling LQTS in vitro. Patient-specific hiPSC-CMs recapitulate the electrophysiological hallmarks of LQTS, including prolonged action potential duration and abnormal calcium handling, providing a human-relevant system for investigating disease mechanisms and testing therapeutic interventions [40]. However, a significant challenge in utilizing these models is the inherent immaturity of hiPSC-CMs compared to adult human cardiomyocytes. Immature hiPSC-CMs exhibit rounded morphology, poorly organized sarcomeres, absent T-tubules, and fetal-like metabolic and electrophysiological properties, which can limit their predictive value for adult-onset disease [40].
Table 2: Characteristics of hiPSC-CMs vs. Adult Cardiomyocytes
| Parameter | hiPSC-Cardiomyocytes | Adult Cardiomyocytes |
|---|---|---|
| Cell Morphology | Rounded, 3000-6000 μm³ volume | Cylindrical, ~40,000 μm³ volume |
| Sarcomere Organization | Poorly organized, random orientation | Highly organized, parallel myofibrils |
| T-tubules | Largely absent | Well-developed regular network |
| Sarcomere Length | 1.7-2.0 μm | 1.9-2.2 μm |
| Primary Metabolism | Glycolysis | Fatty acid oxidation |
| Sarcomere Protein Isoforms | αMHC, MLC2a, ssTnI, N2BA titin, EH-myomesin | βMHC, MLC2v, cardiac TnI, N2B titin, Myomesin-2 |
Advanced maturation strategies are being developed to address these limitations, including prolonged culture, electrical stimulation, biomechanical loading, and 3D tissue engineering approaches. These methods promote structural and functional maturation, resulting in improved sarcomeric organization, enhanced calcium handling, and more adult-like electrophysiological properties [40].
Experimental Protocols for LQTS Modeling
Cardiomyocyte Differentiation Protocol
Efficient differentiation of hiPSCs into cardiomyocytes employs staged activation of key developmental signaling pathways. The process begins with mesodermal induction using BMP4 and Activin A, followed by cardiac specification through Wnt pathway modulation (initial activation followed by inhibition using small molecules like CHIR99021 and IWP-2/IWR-1). Spontaneously contracting cardiomyocytes typically emerge between days 8-12, with purification achieved via lactate selection or fluorescence-activated cell sorting using cardiac-specific markers such as VCAM1 or SIRPA [40].
Functional Characterization Assays
Comprehensive electrophysiological assessment of hiPSC-CMs is essential for LQTS modeling. Patch clamp techniques (both conventional and automated) quantify action potential duration and specific ion currents (IKr, IKs, INa). Calcium imaging using fluorescent indicators (e.g., Fluo-4) evaluates calcium handling properties. Multi-electrode arrays (MEAs) provide non-invasive field potential recordings from monolayer cultures, allowing quantification of field potential duration as a surrogate for QT interval [40]. Pharmacological challenge with channel-specific blockers (E-4031 for IKr, JNJ-303 for IKs, mexiletine for late INa) further characterizes the functional impact of specific mutations.
Therapeutic Applications and Precision Medicine
iPSC-based LQTS models have enabled the development of genotype-specific therapeutic strategies. β-blockers represent the cornerstone treatment for LQTS, with non-selective variants (propranolol, nadolol) demonstrating superior efficacy due to additional Na+ channel blocking effects [39]. However, the response to β-blockers varies by genotype, with LQT3 patients showing reduced efficacy because bradycardia may exacerbate arrhythmias in this subtype [39]. Mexiletine, a late INa blocker, has emerged as a precision therapy for LQT3, shortening QTc by approximately 90ms and reducing arrhythmia risk [39]. Interestingly, recent evidence suggests mexiletine may also benefit LQT2 patients, particularly those with baseline QTc >500ms, potentially due to secondary enhancement of late INa in this genetic background [39]. Emerging therapeutic approaches include polyunsaturated fatty acids (PUFAs), which modulate voltage-gated ion channels and activate IKs currents, representing a promising investigational strategy for LQT1 [39].
Parkinson's Disease Modeling
Disease Background and Genetic Subsets
Parkinson's disease is the second most common neurodegenerative disorder, characterized by the loss of dopaminergic neurons in the substantia nigra, leading to motor symptoms including bradykinesia, rigidity, and resting tremor. While most PD cases are sporadic, monogenic forms provide valuable insights into disease mechanisms. iPSC-based models have been particularly instrumental in studying both familial and sporadic forms of PD, enabling researchers to investigate disease pathogenesis in human neurons and glial cells [41].
iPSC-Derived Neural Models
iPSC-based PD modeling employs both 2D cultures and 3D organoid systems to recapitulate key aspects of the disease. Two-dimensional cultures allow for detailed molecular and functional analysis of specific cell types, including dopaminergic neurons, glial cells, and their interactions [41]. Co-culture systems of iPSC-derived neurons and glial cells provide particular insights into cell-cell interactions in PD pathogenesis [41]. More recently, 3D brain region-specific organoids have enhanced understanding of interregional disease processes, offering a more physiologically relevant microenvironment [41]. These systems can model complex features such as neuroinflammation, protein aggregation, and selective vulnerability of neuronal populations.
Advanced neural models now include assembloids that combine multiple brain region-specific organoids to study circuit-level dysfunction. For example, dorsal-ventral forebrain assembloids have been used to model interneuron migration, revealing that human cortical interneuron migration continues postnatally—a finding with implications for neurodevelopmental disorders [42]. Such models demonstrate how iPSC technology can capture unique features of human brain development and disease.
Experimental Protocols for PD Modeling
Dopaminergic Neuron Differentiation
The generation of midbrain dopaminergic neurons from iPSCs follows a developmental principles-based approach, recapitulating floor plate patterning. Initial neural induction using dual SMAD inhibition (SB431542 and LDN193189) is followed by midbrain patterning with SHH and FGF8b. Subsequent maturation yields dopaminergic neurons expressing characteristic markers such as tyrosine hydroxylase (TH), NURR1, and FOXA2 [43]. For transplantation applications, CORIN+ floor plate cells can be sorted on days 11-13 to enrich for dopaminergic progenitors, achieving final products comprising approximately 60% DA progenitors and 40% DA neurons [43] [44].
Cerebral Organoid and Assembloid Generation
3D neural models are generated through embryonic body formation from iPSCs, followed by neural induction in defined media. For regional patterning, small molecules and growth factors are added to specify particular brain identities (e.g., SHH for ventral, FGF for dorsal). Mature organoids are maintained in spinning bioreactors or agitated cultures to enhance nutrient exchange. To create assembloids, separately patterned organoids are brought together at specific timepoints, allowing for natural migration and connectivity between regions [42].
Cell Therapy Applications
iPSC technology has progressed beyond disease modeling to therapeutic applications in PD. A recent phase I/II trial demonstrated the safety and potential efficacy of allogeneic iPSC-derived dopaminergic progenitors in seven PD patients [43]. In this trial, patients received bilateral transplantation of CORIN-sorted dopaminergic progenitors into the putamen, with cell doses ranging from 2.1-2.6 × 10⁶ cells (low-dose) to 5.3-5.5 × 10⁶ cells (high-dose) per hemisphere [43]. The primary safety outcomes were favorable, with no serious adverse events or tumor formation observed over 24 months of follow-up [43]. Efficacy assessments showed that among six patients evaluated, four showed improvements in MDS-UPDRS part III OFF scores (average improvement of 9.5 points or 20.4%), and five showed improvements in ON scores (average improvement of 4.3 points or 35.7%) [43]. Fluorine-18-L-DOPA PET imaging demonstrated a 44.7% increase in dopamine synthesis capacity in the putamen, with higher increases in the high-dose group, providing objective evidence of graft survival and function [43].
Table 3: Clinical Trial Outcomes of iPSC-Derived Dopaminergic Progenitors in Parkinson's Disease
| Outcome Measure | Baseline | 24-Month Follow-up | Change | Notes |
|---|---|---|---|---|
| MDS-UPDRS III OFF | - | - | -9.5 points (-20.4%) | 4 of 6 patients improved |
| MDS-UPDRS III ON | - | - | -4.3 points (-35.7%) | 5 of 6 patients improved |
| ¹⁸F-DOPA PET Ki | - | - | +44.7% | Greater increase in high-dose group |
| Hoehn & Yahr Stage | - | - | Improved in 4 patients | PD02 improved by 2 stages |
| Serious Adverse Events | None reported | None reported | - | 73 mild-moderate events |
| Graft Overgrowth | None | None detected on MRI | - | Gradual volume increase without tumor formation |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for iPSC-Based Disease Modeling
| Reagent Category | Specific Examples | Function/Application | Related Diseases |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) | Somatic cell reprogramming to pluripotency | All iPSC-based models |
| Neural Induction | SB431542, LDN193189, Noggin | Dual SMAD inhibition for neural specification | Parkinson's disease, neurodevelopmental disorders |
| Cardiac Differentiation | BMP4, Activin A, CHIR99021, IWP-2 | Directed differentiation to cardiomyocytes | Long QT Syndrome, cardiomyopathy |
| Neural Patterning | SHH, FGF8b, Purmorphamine | Midbrain dopaminergic neuron specification | Parkinson's disease |
| Gene Editing | CRISPR/Cas9, gRNAs, HDR templates | Generation of isogenic controls, disease mutations | All monogenic diseases |
| Cell Sorting Markers | CORIN, VCAM1, SIRPA antibodies | Enrichment of specific progenitor populations | Parkinson's disease, cardiac disorders |
| Functional Assays | Fluo-4 AM, Voltage-sensitive dyes | Calcium imaging, electrophysiological assessment | Long QT Syndrome, arrhythmia models |
| Maturation Factors | T3 thyroid hormone, IGF-1, Dexamethasone | Enhanced cellular maturation | All disease models requiring adult phenotypes |
iPSC-based modeling of monogenic diseases represents a paradigm shift in biomedical research, enabling the investigation of disease mechanisms in human-specific contexts and the development of genetically tailored therapeutic approaches. The case studies of Long QT Syndrome and Parkinson's disease illustrate how this technology platform supports both fundamental research and clinical translation. For LQTS, iPSC-cardiomyocyte models have elucidated genotype-phenotype correlations and facilitated the testing of gene-specific therapies such as mexiletine for LQT3 and investigational approaches like PUFAs for LQT1. For PD, iPSC-derived dopaminergic neurons have not only provided insights into disease pathogenesis but have also advanced to clinical-stage cell replacement therapy with demonstrated safety and preliminary efficacy. As the field progresses, addressing challenges related to cellular maturity, model complexity, and standardization will further enhance the predictive validity of these systems. The integration of multi-omics technologies, advanced bioengineering, and machine learning with iPSC-based disease models promises to accelerate the development of precision medicine for monogenic disorders.
The advent of induced pluripotent stem cell (iPSC) technology has fundamentally transformed the landscape of biomedical research, providing an unprecedented platform for disease modeling, drug discovery, and regenerative medicine. By enabling the generation of patient-specific cells, iPSCs have paved the way for highly personalized disease modeling and therapeutic strategies [2]. Within this paradigm, three-dimensional (3D) culture systems represent a revolutionary advance beyond traditional two-dimensional (2D) models, which often fail to accurately recapitulate the intricate tissue microenvironments and cell-cell interactions found in vivo, potentially leading to misleading results in mechanistic studies and translational applications [45] [46].
This whitepaper explores the cutting-edge fields of engineered heart tissues and cerebral organoids, highlighting their synergistic roles within iPSC-based disease modeling research. By providing more physiologically relevant microenvironments, these 3D models are accelerating our understanding of disease mechanisms and creating new opportunities for therapeutic development.
3D Cardiovascular Tissue Engineering
Limitations of Conventional Models and Advantages of 3D Systems
Traditional cardiovascular research has heavily relied on monolayer (2D) cell cultures, which introduce significant limitations due to their substantially different microenvironment compared to in vivo conditions. These models often yield false positive or negative results in mechanistic studies and translational applications because they cannot replicate the native cardiovascular cellular and extracellular matrix (ECM) organizations [45]. The transition to 3D culture systems addresses these shortcomings by enabling closer recapitulation of in vivo features, including cell heterogeneity, ECM composition, cell signaling, proliferation, maturation, and response to stimuli [45].
Engineered heart tissues, cardiovascular spheroids, and cardiac organoids have emerged as powerful tools that bridge this gap between conventional models and human physiology. These advanced systems show particular promise in modeling familial cardiomyopathies, cardiovascular toxicity assessment, drug discovery, and in vivo cardiac regeneration through applications such as cardiac patches [45].
Key Biofabrication Technologies for Cardiovascular Tissues
Multiple biofabrication technologies have been developed to create physiologically relevant 3D cardiovascular models:
Hydrogel-based scaffolds: Natural polymers like fibrin, alginate, and gelatin methacryloyl (GelMA) provide tunable, biomimetic environments that support cardiomyocyte function and maturation [46]. One study demonstrated that a 3D gelatin methacryloyl hydrogel co-culture system significantly enhanced the expression of cardiac maturation markers in hiPSC-derived cardiomyocytes compared to 2D monocultures [2].
3D bioprinting: This technology enables precise spatial patterning of multiple cell types and biomaterials to create complex cardiac tissue architectures. Bioprinting has been used to fabricate endothelialized myocardium and heart-on-a-chip models that better replicate the native heart structure [46].
Bioreactor systems: Dynamic culture conditions using perfusion bioreactors promote nutrient exchange and mechanical stimulation, enhancing the maturation and functionality of engineered cardiovascular tissues [45] [46].
Methodologies for Engineering 3D Cardiac Tissues
Protocol for Generating Engineered Heart Tissue from hiPSCs:
Cardiac Differentiation: Differentiate hiPSCs into cardiomyocytes using established protocols involving sequential modulation of Wnt/β-catenin signaling with small molecules like CHIR99021 and IWP-2 [2].
Fibroblast Co-culture: Combine hiPSC-derived cardiomyocytes with hiPSC-derived cardiac fibroblasts at optimized ratios (typically 3:1 to 5:1 cardiomyocytes:fibroblasts) to enhance functional maturation through paracrine signaling and direct cell-cell interactions [2].
3D Hydrogel Encapsulation: Suspend the cell mixture in a biocompatible hydrogel such as GelMA (5-10% w/v) or fibrin (5 mg/mL) supplemented with matrigel (10-20%) [2] [46].
Mechanical Conditioning: Culture the constructs in dynamic bioreactor systems that provide uniaxial stretch or electrical stimulation to promote structural and functional maturation over 2-4 weeks [45].
Functional Assessment: Evaluate contractile function, force generation, calcium handling, and electrophysiological properties to validate the engineered tissue functionality [2].
Table 1: Quantitative Comparison of 3D Culture Systems for Mesenchymal Stem/Stromal Cells (MSCs)
| Culture System | Proliferation | Senescence | Apoptosis | Secretome Protein Production | EV Production |
|---|---|---|---|---|---|
| 2D Culture | Baseline | Baseline | Baseline | Declined by 35% | Declined by 30-70% |
| Spheroids | ~2-fold lower than Bio-Blocks | 30-37% higher than Bio-Blocks | 2-3-fold higher than Bio-Blocks | Declined by 47% | Declined by 30-70% |
| Matrigel | ~2-fold lower than Bio-Blocks | 30-37% higher than Bio-Blocks | 2-3-fold higher than Bio-Blocks | Declined by 10% | Declined by 30-70% |
| Bio-Block Hydrogel | Highest (~2-fold higher than others) | Reduced 30-37% | Decreased 2-3-fold | Preserved | Increased by ~44% |
Data adapted from comparative study of MSC culture systems [47]
Cerebral Organoids: Modeling Brain Development and Disease
Evolution from 2D Models to Complex 3D Systems
The human brain's extraordinary structural and functional complexity has presented significant challenges for neuroscience research, particularly given the limitations of existing model systems. Traditional 2D neuronal cell lines (such as SH-SY5Y, IMR-32, and LUHMES cells) lack the necessary neural maturity and cannot mimic the human brain's three-dimensional spatial architecture, complex intercellular communication networks, and dynamic microenvironmental regulatory mechanisms [48]. Similarly, animal models are constrained by interspecies biological differences and inadequate simulation of human pathological phenotypes [48].
Brain organoids have emerged as a transformative technology that addresses these limitations. These three-dimensional, self-organizing, miniaturized in vitro culture models recapitulate key aspects of human brain development, generating diverse cell types, including neurons and glia relevant to specific brain regions [48]. The 3D architecture mimics the complex cellular composition, spatial organization, and cell-cell interactions found in the developing brain to a degree unattainable in traditional 2D cell cultures [48].
Cerebral Organoid Generation Protocols
Standard Protocol for Generating Unguided Whole-Brain Organoids:
Embryoid Body Formation: Aggregate approximately 500 fluorescently labeled hiPSCs per well in low-adhesion U-bottom 96-well plates to form uniform embryoid bodies [49].
Neural Induction: Transfer embryoid bodies to neural induction medium (NIM) containing DMEM/F-12, N2 supplement, non-essential amino acids, and heparin on day 4. Embed in Matrigel droplets to support neuroepithelial formation [49].
Differentiation and Maturation: Culture organoids in differentiation medium containing Neurobasal, B27 without vitamin A, L-glutamine, and insulin. On day 15, supplement with vitamin A to support further maturation [49].
Long-term Culture: Maintain organoids in spinning bioreactors or on orbital shakers (60-85 rpm) to enhance nutrient exchange and prevent necrosis, with media changes twice weekly [48].
Region-Specific Brain Organoid Generation:
Region-specific protocols incorporate precise timing of patterning factors to direct regional identity:
- Cortical Organoids: Use dual SMAD inhibition (dorsomorphin and SB431542) with Wnt inhibition (IWR-1) to promote forebrain fate [48].
- Midbrain Organoids: Add FGF8 and SHH at specific timepoints to induce midbrain patterning [48].
- Hypothalamic Organoids: Employ SHH and BMP signaling modulation [48].
Advanced Assemblage Models: Assembloids and Vascularization
To overcome the limitation of studying isolated brain regions, researchers have developed "assembloids" - complex multi-region organoid assemblies that model interactions between different brain areas. This technology has enabled the creation of cortical-striatal, cortical-thalamic, and midline assembloids to simulate long-range axonal connections and neural circuit formation [48].
Vascularization remains a critical challenge in brain organoid development, as traditional models exhibit significant vascularization defects that lead to necrotic cores and limit growth and maturation. Recent advances have addressed this limitation through:
- Vascularized Organoids: Fusion of brain organoids with induced vascular organoids to create functional blood-brain barrier (BBB) structures [48].
- Microfluidic Integration: Use of organ-on-a-chip technologies to promote vascular network formation and enable real-time monitoring [48] [50].
- In Vivo Transplantation: Transplantation of human brain organoids into rodent brains, resulting in functional vascularization and enhanced maturation [48].
Diagram 1: Cerebral Organoid Generation Workflow. This flowchart illustrates the key stages in brain organoid development from iPSCs to mature, potentially vascularized organoids and assembloids.
Key Signaling Pathways in 3D Tissue Morphogenesis
The development and maturation of both cardiac tissues and cerebral organoids are governed by complex signaling pathways that regulate tissue patterning, morphogenesis, and functional specialization.
WNT and Hippo Signaling in Brain Regionalization
Recent research using live imaging of brain organoids has revealed that extracellular matrix (ECM)-induced regional guidance and lumen morphogenesis are linked to the WNT and Hippo signaling pathways [49]. Specifically, matrix exposure modulates tissue morphogenesis by inducing cell polarization and neuroepithelial formation, fostering lumen enlargement through fusions. These processes are associated with spatially restricted induction of the WNT ligand secretion mediator (WLS) that marks the earliest emergence of non-telencephalic brain regions [49].
The Hippo pathway effector YAP (Yes-associated protein) plays a crucial role in mechanosensing and regulating organoid patterning in response to ECM cues. YAP translocates to the nucleus in response to mechanical signals, where it interacts with transcriptional partners to regulate genes involved in cell proliferation, survival, and differentiation [49].
Cardiac Maturation Signaling Pathways
In engineered heart tissues, several signaling pathways are critical for promoting structural and functional maturation:
- Wnt/β-catenin signaling: Sequential activation and inhibition drive initial cardiac differentiation from hiPSCs [2].
- Notch signaling: Regulates cardiomyocyte proliferation and maturation during later stages of development.
- IGF1 and LIF pathways: Upregulated in 3D culture systems, enhancing stem-like properties and maturation potential [47].
Diagram 2: ECM-Driven Brain Patterning Signaling. This diagram illustrates how extracellular matrix cues activate mechanosensing pathways that ultimately drive lumen expansion and brain regionalization in cerebral organoids.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Research Reagents and Solutions for 3D Tissue Engineering
| Reagent/Solution | Function | Example Applications |
|---|---|---|
| Matrigel | Basement membrane extract providing ECM proteins for 3D support | Neuroepithelial formation in brain organoids; cardiac tissue engineering [49] |
| Gelatin Methacryloyl (GelMA) | Tunable photopolymerizable hydrogel for 3D encapsulation | 3D cardiac tissue models; cardiomyocyte maturation [2] [46] |
| RoosterNourish MSC-XF Medium | Chemically defined, xeno-free medium for MSC expansion | Maintenance of stem cell properties in 3D culture [47] |
| DMEM/F-12 with N2/B27 Supplements | Neural induction and differentiation medium | Cerebral organoid generation [49] |
| Small Molecule Inhibitors/Activators | Modulate key signaling pathways (Wnt, SMAD, SHH) | Region-specific patterning of organoids [48] |
| Fibrin/Alginate Hydrogels | Natural polymer hydrogels for 3D scaffolding | Engineered heart tissue construction [46] |
| Microfluidic Devices | Enable vascularization, perfusion, and real-time monitoring | Vascularized organoid models; organ-on-a-chip systems [48] [50] |
Applications in Disease Modeling and Drug Development
Cardiovascular Disease Modeling
Engineered 3D cardiac tissues have enabled significant advances in modeling both inherited and acquired cardiovascular diseases:
- Familial Cardiomyopathies: Patient-specific iPSC-derived engineered heart tissues recapitulate key pathological features of hypertrophic and dilated cardiomyopathies, enabling mechanistic studies and drug screening [45].
- Cardiotoxicity Screening: 3D cardiac spheroids and tissues provide more predictive platforms for assessing drug-induced cardiotoxicity compared to traditional 2D models, potentially reducing late-stage drug failures [45] [46].
- Ischemic Heart Disease Modeling: Engineered cardiac tissues subjected to ischemic conditions mimic the pathophysiology of myocardial infarction, enabling studies of cardioprotective compounds and regenerative therapies [45].
Neurological Disease Modeling
Cerebral organoids have created new opportunities for studying a wide spectrum of neurological and psychiatric disorders:
- Neurodevelopmental Disorders: Organoids derived from patients with autism spectrum disorder, epilepsy, and intellectual disability reveal altered neurogenesis, neuronal migration, and synaptogenesis [48] [50].
- Neurodegenerative Diseases: Alzheimer's and Parkinson's disease models exhibit protein aggregation, neuronal death, and circuit dysfunction relevant to human pathology [48].
- Psychiatric Disorders: Although more challenging to model, organoids from patients with schizophrenia and bipolar disorder show alterations in neuronal connectivity and gene expression patterns [48].
- Infectious Diseases: COVID-19 research has utilized brain organoids to investigate mechanisms of neuroinvasion and neurological sequelae [48].
Current Challenges and Future Directions
Despite remarkable progress, several significant challenges remain in the field of 3D tissue engineering:
Technical Limitations
- Vascularization: While recent advances have been made, current vascularized organoid models still cannot fully replicate in vivo conditions, particularly the blood-brain barrier in neural tissues [48] [50].
- Functional Maturation: iPSC-derived cells in 3D cultures often exhibit an immature, fetal-like phenotype, limiting their utility for modeling late-onset diseases [2].
- Standardization and Reproducibility: Issues of organoid variability, batch effects, and lack of standardized protocols persist across both cardiac and neural models [50] [2].
Emerging Solutions and Future Perspectives
The convergence of 3D culture with cutting-edge bioengineering technologies is creating new opportunities to address these challenges:
- Advanced Biofabrication: 3D bioprinting, microfluidics, and organ-on-a-chip technologies enable more precise control over tissue architecture and microenvironmental cues [45] [46].
- Multi-omics Integration: Combining organoid technology with single-cell transcriptomics, proteomics, and high-content imaging provides unprecedented resolution in characterizing disease mechanisms [45] [49].
- Assembloid Technologies: The development of more complex multi-tissue systems, such as brain-gut assembloids, creates opportunities to study inter-organ communication in disease states [48].
- High-Content Screening: Automated platforms for organoid culture and analysis are enabling larger-scale drug screening campaigns using 3D tissue models [45] [46].
As these technologies continue to mature, 3D engineered heart tissues and cerebral organoids are poised to become increasingly central to disease modeling, drug discovery, and the development of personalized medicine approaches, ultimately bridging the gap between traditional models and human pathophysiology.
Organ-on-a-Chip (OoC) technology represents a revolutionary approach in biomedical research, employing microfluidic devices to create miniature models of human organs that recapitulate tissue-specific functions and pathological responses in vitro [51]. A critical advancement in this field is the integration of dynamic vascular perfusion and key physiological forces, which are essential for generating truly physiologically relevant microenvironments, especially for disease modeling using induced pluripotent stem cells (iPSCs) [52] [53]. These systems bridge the critical gap between traditional static 2D cell cultures, which lack physiological context, and animal models, which often poorly mimic human disease and drug responses [54] [51].
For iPSC-based disease modeling, the inclusion of a functional vascular component is particularly transformative. It enables the study of complex, non-cell-autonomous disease mechanisms by facilitating interactions between patient-derived parenchymal cells, vascular cells, and immune cells under flow conditions [53]. Furthermore, vascular perfusion is key to sustaining the viability and promoting the maturation of complex iPSC-derived tissues, such as organoids, by overcoming diffusion limitations that often lead to necrotic core formation [52]. This guide provides a technical deep-dive into the engineering principles, methodologies, and applications of vascularized and mechanically active OoC systems within an iPSC research framework.
Core Engineering Principles
The Role of Microfluidics
Microfluidics is the foundational technology enabling OoC systems. It involves the precise manipulation of small fluid volumes (typically between 10⁻⁹ and 10⁻¹⁸ liters) within channels with dimensions ranging from ten to several hundred micrometers [55]. The physics of fluid flow at this scale is characterized by a low Reynolds number, which results in predictable, laminar (non-turbulent) flow [55]. This laminar flow is essential for recreating the predictable shear stresses experienced by cells in blood vessels and for establishing stable chemical gradients that guide cell behavior, such as angiogenesis and immune cell migration [55] [51].
Recapitulating Physiological Forces
The functional superiority of OoCs over traditional models stems from their ability to mimic the biomechanical and biochemical microenvironment of human tissues. Key physiological forces integrated into these systems include:
- Fluidic Shear Stress: Generated by the flow of culture medium, shear stress is a critical cue for vascular endothelial cells, influencing their morphology, alignment, and physiological function [56] [51]. The ability to precisely control flow rates allows researchers to apply physiological levels of shear stress, which is crucial for applications like immune cell recruitment studies [57].
- Cyclic Mechanical Strain: Many organs, such as the lung and intestine, undergo rhythmic movements. OoC devices can incorporate flexible membranes that are mechanically actuated to apply cyclic stretch, mimicking peristalsis in the gut or breathing motions in the alveoli [54] [51]. This strain has been shown to enhance tissue differentiation and function.
- Biochemical Gradients: The laminar flow properties in microchannels allow for the generation of stable, spatially defined concentration gradients of oxygen, nutrients, drugs, or signaling molecules. These gradients are vital for studying processes like inflammation, cancer metastasis, and morphogenesis [51].
Table 1: Key Physiological Forces and Their Biological Roles in OoC Systems
| Physiological Force | Typical Implementation in OoC | Primary Biological Role & Impact |
|---|---|---|
| Fluidic Shear Stress | Perfusion of medium using syringe or peristaltic pumps [51]. | Endothelial cell activation & quiescence; regulation of vascular tone; immune cell adhesion [56]. |
| Cyclic Mechanical Strain | Computer-controlled vacuum application to side chambers to stretch a porous membrane [54]. | Enhances epithelial barrier function; promotes alveolar and intestinal tissue maturation [51]. |
| Biochemical Gradients | Controlled infusion of molecules from adjacent microchannels under laminar flow [51]. | Guides cell migration (e.g., angiogenesis, metastasis); directs stem cell differentiation [55]. |
Fabrication and Design Methodologies
Materials and Fabrication Techniques
The choice of material is paramount for OoC device fabrication, impacting biocompatibility, optical properties for imaging, and drug absorption characteristics.
- Polydimethylsiloxane (PDMS): This elastomer remains the most widely used material due to its gas permeability, optical transparency, and flexibility, which facilitates the integration of mechanical stretching [55] [58]. A significant drawback, however, is its tendency to absorb small hydrophobic drugs and molecules, which can skew pharmacokinetic data [57] [55].
- Alternative Materials: To address PDMS limitations, new materials are being adopted. These include rigid plastics (e.g., Chip-R1) engineered for minimal drug absorption, making them superior for toxicology and ADME studies [57]. Other materials like styrene ethylene butylene styrene (SEBS) and polycarbonate (PC) are also being explored for their reduced drug-binding properties and improved mechanical stability [55].
The standard fabrication method is soft lithography, a replica molding process using a master template, often produced via high-resolution 3D printing [56] [55]. 3D bioprinting is an emerging technique that can directly integrate microfluidic channels and living cells, allowing for the creation of more complex, patient-specific tissue geometries [55].
Gravitational Lumen Patterning for Complex Vasculature
A recent unifying technique for engineering intricate, three-dimensional vascular structures is Gravitational Lumen Patterning (GLP). This method addresses the limitation of previous models that were restricted to simple, tubular structures [56].
Experimental Protocol Overview [56]:
- Device Fabrication: Microfluidic channels are designed using CAD software to mimic pathological architectures (e.g., stenosis, aneurysms, bifurcations). Molds are 3D printed and used to create PDMS devices via soft lithography.
- Surface Treatment: The PDMS channels are chemically pretreated with APTES and glutaraldehyde to enhance the bonding of the subsequent collagen matrix.
- Collagen Injection: A cold, viscous collagen type I solution (5-7.5 mg/mL, pH 7.5) is injected into the pretreated microchannel and allowed to gelify, typically at 37°C.
- Lumen Patterning: After gelation, a PBS solution is injected through the collagen-filled channel. The interplay of surface tension, pressure-driven forces, and gravity (acting axially) patterns a cylindrical lumen within the collagen matrix. The final architecture of the lumen is dictated by the original microchannel geometry.
- Endothelialization: The engineered lumen is seeded with human endothelial cells, which adhere to the inner surface, forming a living, perfusable blood vessel surrogate.
This GLP technique enables the creation of in vivo-like vessels with varying diameters, bifurcations, tortuous paths, stenoses, and aneurysms, which can be perfused with whole blood to study associated hemodynamics and endothelial dysfunction [56].
The Scientist's Toolkit: Essential Research Reagents and Materials
Success in developing and operating vascularized OoCs relies on a suite of specialized reagents and materials.
Table 2: Essential Research Reagents and Materials for Vascularized OoC
| Category / Item | Specific Examples | Function & Application |
|---|---|---|
| Chip Materials | Polydimethylsiloxane (PDMS), Chip-R1 Rigid Polymer [57], SEBS [55] | Device fabrication; PDMS for gas exchange & flexibility; rigid plastics for low drug absorption. |
| Extracellular Matrices | Collagen Type I [56], Fibrin, Matrigel, Gelatin Methacrylate (GelMA) [55] | Provides 3D structural scaffold for tissue formation; critical for embedding cells and patterning lumens. |
| Cell Sources | iPSC-derived Endothelial Cells, iPSC-derived Organ-Specific Cells (e.g., neurons, hepatocytes) [53], Primary Human Cells [56] | Forms the vascular and tissue components; patient-derived iPSCs enable personalized disease modeling. |
| Surface Modifiers | 3-Aminopropyltriethoxysilane (APTES) [56], Pluronic Acid [55] | APTES enhances ECM-PDMS bonding; Pluronic acid passivates surfaces to prevent unwanted cell adhesion. |
| Culture Perfusion | Syringe Pumps, Peristaltic Pumps [51] | Generates controlled, continuous medium flow to deliver nutrients and apply physiological shear stress. |
iPSC Integration and Experimental Workflows
The synergy between iPSC technology and advanced OoCs opens new frontiers for modeling human diseases. The general workflow involves deriving both the parenchymal (organ-specific) cells and the vascular endothelial cells from the same iPSC donor, enabling the creation of a genetically matched, personalized human-on-a-chip.
Case Study: Modeling Sporadic ALS with a Spinal-Cord-Chip
Objective: To model sporadic Amyotrophic Lateral Sclerosis (ALS) using patient-derived iPSCs in a perfused microfluidic platform that includes a blood-brain-barrier (BBB) equivalent [53].
Detailed Protocol:
- iPSC Derivation and Differentiation: Generate iPSCs from fibroblasts of patients with sporadic ALS and healthy controls. Differentiate these iPSCs into spinal motor neurons (in the tissue chamber) and induced brain microvascular endothelial cells (iBMECs, in the vascular channel).
- Chip Assembly and Seeding: Use a two-channel microfluidic device separated by a porous membrane. Seed the iBMECs on one side of the membrane to form a confluent, perfusable vascular tube. Seed the iPSC-derived motor neurons in the adjacent channel, often within a 3D matrix like Matrigel.
- On-Chip Maturation and Perfusion: Culture the assembled chip under continuous, low-flow perfusion for several weeks to promote tissue maturation. The flow applies physiological shear stress on the endothelial cells and ensures optimal nutrient exchange.
- Perturbation and Analysis: Expose the model to potential therapeutic compounds via the vascular channel. Monitor motor neuron survival, morphology, and synaptic activity in real-time. Conduct post-experiment transcriptomic analysis (bulk and single-cell RNA-seq) to identify disease-associated pathways.
Key Findings: The spinal-cord-chip supported enhanced maturation of motor neurons and revealed early, patient-specific disease phenotypes—such as disrupted glutamatergic signaling and neurofilament accumulation—that were not detectable in standard 2D cultures [53]. This underscores how the vascularized, perfused microenvironment is critical for unmasking complex pathophysiology.
Quantitative Data and Performance Metrics
The efficacy of vascularized OoC models is validated through quantitative assessments of barrier function, transport, and tissue activity.
Table 3: Quantitative Performance Metrics of Vascularized OoC Models
| Model Type | Key Measured Parameters | Reported Values / Ranges | Significance |
|---|---|---|---|
| Generic Vascular Barrier | Transendothelial Electrical Resistance (TEER) | > 1000 Ω·cm² (for BBB models) [58] | Quantifies integrity and tight junction formation of the endothelial barrier. |
| Blood-Brain Barrier (BBB) | Apparent Permeability (Papp) | Papp for small molecules can be 1-10 x 10⁻⁶ cm/s [58] | Measures the rate of compound passage across the endothelial barrier; critical for CNS drug development. |
| Bone Marrow-on-a-Chip | Hematopoietic Cell Output | Maintained for over 4 weeks [53] | Demonstrates long-term functional viability of the model for studying hematopoiesis and toxicity. |
| Vascular Architecture-on-Chip | Lumen Diameter | 100 - 500 μm (controllable) [56] | Shows precise engineering control over vessel size and morphology. |
| Liver-on-a-Chip | Albumin & Urea Production | Sustained for multiple weeks [51] | Indicates functional maturation and longevity of hepatocytes in the model. |
The integration of vascular perfusion and physiological forces into Organ-on-a-Chip systems marks a significant leap toward creating physiologically faithful in vitro models. For disease modeling with iPSCs, this technology provides a powerful platform to study patient-specific pathologies in a controlled yet complex environment, uncovering phenotypes invisible in simpler systems [54] [53]. As the field progresses, key future directions include the development of multi-organ "human-on-a-chip" systems linked by a common vascular network to study systemic disease and drug pharmacokinetics [54] [51]. Furthermore, ongoing efforts to standardize device fabrication, culture protocols, and analytical readouts are essential for the broader adoption of OoCs in pharmaceutical development and regulatory decision-making, ultimately accelerating the path to personalized medicine.
The integration of high-throughput screening (HTS) and high-content analysis (HCA) has revolutionized modern drug discovery, enabling rapid and reliable assessment of compound toxicity and efficacy. These approaches allow researchers to test numerous materials at different concentrations across multiple cell types, substantially reducing inter-experimental variation while achieving significant savings in time and cost [59]. The growing numbers of nanomaterials (NMs) and pharmaceutical compounds have created unprecedented demand for efficient safety testing methodologies, preferably using in vitro approaches to address ethical concerns associated with animal research [59]. This technical guide explores the current landscape of HTS technologies and their application in toxicity and efficacy testing, with particular emphasis on advanced disease modeling using induced pluripotent stem cells (iPSCs).
The fundamental challenge in modern pharmaceutical development lies in the need to deliver safe and effective medicines while minimizing significant toxicity and severe side effects [60]. System-based drug discovery has emerged as a powerful paradigm that integrates chemical, molecular, and systematic information to design small molecules with controlled toxicity profiles [60]. Within this framework, HTS/HCA approaches facilitate the classification of key biological indicators of nanomaterial-cell interactions and drug effects, providing critical data for developing intelligent testing strategies based on grouping and read-across approaches [59].
High-Throughput Screening Technologies and Methodologies
Core HTS/HCA Platforms and Their Applications
Table 1: High-Throughput Screening Technologies for Toxicity and Efficacy Assessment
| Technology | Key Advantages | Primary Applications | Technical Limitations |
|---|---|---|---|
| HTS Flow Cytometry | Multiplexing capabilities; detects side scatter signals from NMs; analyzes cellular heterogeneity [59] | Specific cellular uptake studies; cell viability testing; ROS detection [59] | Potential interference with NMs; requires proper controls and validation [59] |
| Impedance-Based Monitoring (xCELLigence) | Label-free, non-invasive, biophysical assay; real-time dynamic response detection [59] | Dynamic cytotoxicity screening; 384-well plate format [59] | Restricted to adherent cells; difficult to differentiate ions from particulate matter [59] |
| High-Content Analysis (HCA) | Multiparametric analysis; quantitative and qualitative data; 384-well format [59] | Imaging and quantitative screening of NMs; subcellular localization [59] | Moderately high costs despite multiparametric capabilities [59] |
| Multiplex Analysis of Secreted Products | Quantification of up to 500 analytes simultaneously; reduced reagent volumes [59] | Cytokine profiling; biomarker discovery; secretory phenotype analysis [59] | Moderately high assay costs; requires specialized equipment [59] |
| High-Throughput Omics | 96-1536 well formats; label-free; 50-1500 parallel gene expression measurements [59] | Transcriptomic profiling; toxicogenomics; pathway analysis [59] | Not a substitute for phenotypic assays; requires computational expertise [59] |
Advanced HTS Assays for Genotoxicity Assessment
Genotoxicity evaluation represents a critical component of comprehensive safety profiling. Advanced HTS methodologies have been developed to address this need, including the High-Throughput Comet Assay, which enables simultaneous testing of multiple nanomaterials with automated scoring systems [59]. The 'CometChip' innovation utilizes microarray platforms on agarose-coated plates to enhance throughput, though long-term sample storage remains a challenge requiring further optimization [59]. Similarly, High-Content Screening (HCS) approaches to the In Vitro Micronucleus (IVMN) assay have demonstrated high sensitivity and specificity, particularly for polystyrene and iron oxide nanomaterials [59]. The γH2AX assay—focusing on foci formation—provides exceptional sensitivity for DNA damage detection, measuring several orders of magnitude beyond conventional protein level assessments, though automated scoring systems continue to require refinement and validation [59].
iPSC-Based Disease Models for Drug Screening Applications
Fundamentals of iPSC Technology in Disease Modeling
The development of induced pluripotent stem cell (iPSC) technology has created unprecedented opportunities for human disease modeling and drug screening applications. Since the initial reports of somatic cell reprogramming in 2006-2007, iPSCs have been widely applied to model human development and diseases in vitro, screen drug candidates, and develop cell therapies [1]. The molecular mechanisms underlying iPSC induction involve profound remodeling of chromatin structure and the epigenome, accompanied by comprehensive changes in cell metabolism, signaling, intracellular transport, and proteostasis [1]. Modern reprogramming methods have significantly improved safety profiles by reducing genomic alterations through non-integrative approaches including messenger RNA (mRNA) transfection, Sendai virus delivery, and small molecule-based reprogramming [18].
The exceptional value of iPSCs in drug discovery stems from their capacity for virtually unlimited expansion, amenability to genetic engineering, and ability to differentiate into most somatic cell types [1]. iPSC-based cellular models reveal human-specific phenotypes and molecular mechanisms that frequently do not manifest in conventional animal models, addressing a critical translational gap in pharmaceutical development [61]. The ability to generate patient-specific iPSCs with disease-relevant genetic backgrounds further enhances their utility for personalized drug screening and toxicity assessment [1].
Application of iPSC Models in Specific Disease Contexts
Table 2: iPSC-Based Disease Models for Drug Screening Applications
| Disease Area | iPSC-Derived Cell Types | Key Screening Applications | Notable Advances |
|---|---|---|---|
| Neurodegenerative Disorders | Neurons (including dopaminergic), glial cells [18] [62] | Modeling Parkinson's disease; detection of ER stress; neurodegenerative disease mechanisms [18] [62] | Preclinical studies showing encouraging results for Parkinson's disease; detection of ER stress in GBA1 mutation models [18] |
| Cardiovascular Disease | Cardiomyocytes, endothelial cells, vascular smooth muscle cells [63] | Drug-induced cardiotoxicity screening; disease modeling for dilated cardiomyopathy, hypertrophic cardiomyopathy [62] [63] | Isogenic models of dilated cardiomyopathy; personalized cardiovascular drug discovery [62] [63] |
| Renal Disorders | Kidney organoids with specialized nephron segments [61] | Polycystic kidney disease modeling; nephrotoxicity screening [61] | Organoids carrying PKD1 or PKD2 mutations display cyst formation reminiscent of patient pathology [61] |
The creation of 3D organoid models has significantly expanded the potential of iPSCs beyond traditional differentiation methods, generating sophisticated human tissue analogs that recapitulate structural and functional aspects of native organs [18]. These advanced models enable researchers to examine disease mechanisms, test novel therapeutic compounds, and develop regenerative medical treatments with enhanced physiological relevance [18]. For neurological applications, iPSC-derived neurons permit the investigation of disease-specific phenotypes, including the detection of endoplasmic reticulum stress in neurons carrying the p.N370S mutation in the GBA1 gene, relevant to Parkinson's disease pathology [18]. In cardiovascular research, iPSC-derived cardiomyocytes enable the assessment of drug-induced cardiotoxicity and the modeling of inherited cardiac conditions using patient-specific cells [63].
Experimental Workflows and Methodologies
Integrated Workflow for iPSC-Based Drug Screening
The following diagram illustrates the comprehensive workflow for implementing iPSC-based models in high-throughput drug screening and toxicity assessment:
Key Signaling Pathways in iPSC Differentiation and Disease Modeling
The efficient differentiation of iPSCs into relevant somatic cell types requires precise manipulation of key developmental signaling pathways. The following diagram illustrates the primary signaling networks involved in this process:
The Scientist's Toolkit: Essential Research Reagents and Solutions
Critical Reagents for iPSC-Based Screening Platforms
Table 3: Essential Research Reagents for iPSC-Based Drug Screening Applications
| Reagent Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM); OCT4, SOX2, NANOG, LIN28 [1] | Somatic cell reprogramming to pluripotency | Non-integrative methods (mRNA transfection, Sendai virus) preferred for clinical-grade iPSCs [18] |
| CRISPR-Cas9 Systems | Cas9 nuclease, base editors, prime editors [18] | Precision genome editing for disease modeling | Enables creation of isogenic control lines; corrects genetic errors in patient-derived iPSCs [18] [61] |
| Differentiation Factors | BMP, Wnt, TGF-β pathway modulators [18] | Directed differentiation to target cell types | Enhanced efficiency and reproducibility of cardiomyocyte, neuron, and pancreatic β-cell generation [18] |
| Cell Culture Matrices | 3D organoid culture systems; synthetic scaffolds [18] | Support for complex tissue models | Enables development of brain, liver, and gastrointestinal tissue models for disease modeling [18] |
| HTS Detection Reagents | Fluorescent probes, impedance sensors, secreted protein assays [59] | Multiparameter readouts for toxicity/efficacy | Must be validated for compatibility with nanomaterials and iPSC-derived cells [59] |
The integration of high-throughput screening methodologies with iPSC-based disease models represents a transformative approach in modern drug discovery and development. This powerful combination enables researchers to assess compound efficacy and toxicity using physiologically relevant human cellular models that recapitulate key aspects of disease pathology. Recent advances in CRISPR-Cas9 gene editing, 3D organoid culture systems, and multiparameter screening technologies have further enhanced the predictive validity of these platforms, accelerating the identification of promising therapeutic candidates while mitigating safety risks [18] [61].
Looking forward, several emerging technologies promise to additional refine iPSC-based drug screening capabilities. Machine learning applications for automated iPSC colony detection and quality assessment are already demonstrating potential to enhance selection consistency and improve differentiation outcomes [18]. Similarly, the development of universal hypoimmune iPSC lines through genetic engineering approaches addresses critical challenges related to immune rejection, potentially enabling the creation of standardized cell sources for screening applications [18]. As these technologies continue to mature, iPSC-based HTS/HCA platforms are poised to become increasingly indispensable tools for de-risking pharmaceutical development and delivering safer, more effective therapeutics to patients.
The integration of CRISPR/Cas9 genome editing with induced pluripotent stem cell (iPSC) technology has revolutionized disease modeling by enabling the precise generation of isogenic controls. These genetically matched cell lines, which differ only at specific disease-relevant loci, provide a powerful experimental system for distinguishing pathogenic mutations from confounding genetic background effects. This technical guide details comprehensive methodologies for creating and validating isogenic control lines in iPSC-based disease models, featuring optimized protocols, quantitative analysis frameworks, and specialized tools for researchers pursuing robust phenotypic characterization in neurodegenerative disorders, cardiovascular diseases, and cancer research.
The derivation of human induced pluripotent stem cells (iPSCs) has transformed our ability to model human diseases in vitro, providing an unlimited source of patient-specific cells for investigation of disease mechanisms and therapeutic development [64]. However, a significant challenge in utilizing patient-derived iPSCs has been the genetic variability between individuals, which can obscure disease-specific phenotypes and complicate data interpretation [65]. The emergence of CRISPR/Cas9 genome editing has provided an elegant solution to this problem through the generation of isogenic controls [66].
Isogenic controls are genetically matched cell lines that differ only at specific, targeted loci, serving as perfect genetic backgrounds against which to compare disease-associated phenotypes [67]. In the context of iPSC-based disease modeling, there are two primary strategies for creating these controls: (1) introducing disease-causing mutations into healthy control iPSCs, or (2) correcting disease-causing mutations in patient-derived iPSCs back to wild-type sequences [64]. The resulting isogenic pairs enable researchers to attribute observed phenotypic differences directly to the specific genetic alteration, rather than to the broader genetic variation between individuals [65] [66].
The applications of CRISPR-iPSC-based disease modeling span a broad spectrum of human maladies, with particular impact in neurodegenerative diseases such as Alzheimer's disease, Parkinson's disease, Huntington's disease, and Amyotrophic Lateral Sclerosis [65]. The flexibility of CRISPR/Cas9 technology allows researchers to seamlessly target and introduce precise modifications in the genomic DNA of human iPSCs, recapitulating the pathological aspects of neurodegenerative processes and investigating the role of pathological gene variants in otherwise healthy non-patient cell lines [65].
CRISPR/Cas9 System Fundamentals
Molecular Mechanism of CRISPR/Cas9
The CRISPR/Cas9 system operates as an adaptive immune mechanism in prokaryotes that has been repurposed for precise genome editing in eukaryotic cells [65]. The core components include the Cas9 nuclease and a single guide RNA (sgRNA) that directs Cas9 to specific genomic loci. The system's functionality depends on recognition of a protospacer adjacent motif (PAM) sequence adjacent to the target site, which for the commonly used Streptococcus pyogenes Cas9 is 5'-NGG-3' [65] [68].
When CRISPR components are introduced into target cells, the sgRNA directs Cas9 to create double-strand breaks (DSBs) approximately 3 base pairs upstream from the PAM sequence [68]. These breaks are subsequently repaired by one of two primary cellular mechanisms: non-homologous end joining (NHEJ) or homology-directed repair (HDR) [68]. The error-prone NHEJ pathway often results in small insertions or deletions (indels) that can disrupt gene function, while HDR uses a DNA repair template to enable precise edits, including specific point mutations or insertions [68].
Advanced CRISPR/Cas9 Toolbox
Beyond the standard CRISPR/Cas9 system, several modified versions have been developed to expand editing capabilities:
- Cas9 Nickases: Engineered Cas9 variants with a single functional catalytic domain (D10A or H840A for SpCas9) that cleave only one DNA strand, reducing off-target effects [65].
- dead Cas9 (dCas9): A catalytically inactive Cas9 that retains DNA binding capability but lacks nuclease activity, serving as a platform for CRISPR interference (CRISPRi) and CRISPR activation (CRISPRa) when fused to repressor or activator domains [65].
- Cpf1 (Cas12a) Endonucleases: Alternative CRISPR systems from Prevotella and Francisella that recognize different PAM sequences and create staggered DNA cuts with 5' overhangs, unlike the blunt ends generated by Cas9 [65].
Experimental Design and Workflow
The process of generating isogenic controls in iPSCs requires careful planning and execution across multiple stages, from sgRNA design to thorough validation of edited clones. The following workflow visualization outlines the key steps in this process:
Editing Strategy Selection
The first critical decision involves choosing between corrective or mutational approaches. For monogenic diseases where patient-derived iPSCs are available, the corrective approach involves repairing the disease-causing mutation to create an isogenic wild-type control [67]. Conversely, when studying specific mutations in otherwise healthy iPSCs, researchers introduce the pathogenic variant into the normal genetic background [67]. Each strategy offers distinct advantages depending on the research question and available starting materials.
sgRNA Design and Selection
Effective sgRNA design is paramount for successful genome editing. Key considerations include:
- Target proximity: Positioning the cut site close to the intended edit (typically within 10 bp) [68]
- On-target efficiency: Selecting guides with predicted high editing efficiency using established algorithms [68]
- Off-target potential: Minimizing similarity to other genomic sequences to reduce off-target effects [68]
- PAM availability: Identifying suitable PAM sequences near the target site [65]
Online tools such as CRISPOR, CHOPCHOP, and Synthego's guide design tools can facilitate this process by providing efficiency scores and off-target predictions.
Repair Template Design for HDR
For precise edits requiring HDR, single-stranded oligodeoxynucleotides (ssODNs) or double-stranded DNA donors serve as repair templates. Optimal design includes:
- Homology arm length: 30-90 nucleotides on each side of the edit for ssODNs [67]
- Silent mutations: Incorporating silent restriction sites or other detectable markers to facilitate screening
- Modification strategy: Using synonymous codons where possible to avoid unintended amino acid changes
- Strand selection: Designing the ssODN to correspond to the Cas9-cut strand for improved efficiency
Quantitative Methods for Editing Efficiency Analysis
Accurate quantification of editing efficiency is essential for evaluating CRISPR experiment success. The table below compares common analysis methods:
Table 1: Comparison of CRISPR Editing Analysis Methods
| Method | Detection Principle | Sensitivity | Multiplex Capability | Key Limitations |
|---|---|---|---|---|
| T7 Endonuclease I (T7E1) | Mismatch cleavage | ~80% | No | Preferential detection of some mutation types; cannot detect homozygous mutations [68] |
| Restriction Fragment Length Polymorphism (RFLP) | Loss/gain of restriction site | ~80% | No | Requires naturally occurring or introduced restriction site [68] |
| Sanger Sequencing with ICE | Decomposition of sequencing traces | >95% | Limited | Requires high-quality sequencing data [69] |
| qEva-CRISPR | Multiplex ligation-based probe amplification | >95% | Yes (up to 60 targets) | Requires specialized probe design [68] |
| Next-Generation Sequencing (NGS) | Direct sequencing of amplicons | >99% | Yes (highly multiplexed) | Higher cost and computational requirements [69] |
ICE (Inference of CRISPR Edits) Analysis
The ICE tool from Synthego provides a robust platform for analyzing CRISPR editing efficiency from Sanger sequencing data [69]. The method offers several advantages:
- Cost-effectiveness: Provides NGS-quality analysis at approximately 1/100th the cost of NGS [69]
- Quantitative precision: Delivers accurate indel percentage calculations and knockout scores [69]
- Versatility: Compatible with various nucleases including SpCas9, Cas12a, and MAD7 [69]
- Complex edit analysis: Capable of characterizing edits from multiple gRNAs simultaneously [69]
The ICE workflow involves extracting genomic DNA from edited cells, PCR-amplifying the target region, Sanger sequencing, and uploading the resulting chromatogram files to the ICE platform along with the gRNA sequence. The algorithm then compares edited traces to control traces to determine editing efficiency and characterize the specific indel profiles [69].
qEva-CRISPR for Multiplexed Analysis
qEva-CRISPR represents a ligation-based, dosage-sensitive method that enables parallel quantitative analysis of multiple targets, including both on-target and off-target sites [68]. This technique adapts the established Multipiece Ligation-dependent Probe Amplification (MLPA) strategy for CRISPR efficiency assessment, offering several distinctive advantages:
- Comprehensive mutation detection: Identifies all mutation types, including point mutations and large deletions [68]
- Multiplex capability: Simultaneously analyzes up to 60 different genomic targets [68]
- Sensitivity to difficult regions: Successfully analyzes targets in challenging genomic contexts, such as areas flanking microsatellite repeats [68]
- Repair mechanism discrimination: Distinguishes between HDR and NHEJ repair outcomes [68]
The qEva-CRISPR protocol involves designing specific oligonucleotide probes for each target, hybridizing these probes to genomic DNA, ligation, PCR amplification, and fragment analysis with capillary electrophoresis [68].
Advanced iPSC Culture and Editing Protocols
iPSC Culture Considerations for Genome Editing
Maintaining optimal iPSC health and pluripotency throughout the editing process is essential for successful isogenic control generation. Key considerations include:
- Culture conditions: Utilizing feeder-free, defined culture systems to minimize variability
- Cell state: Ensuring cells are in log-phase growth with >90% viability before editing
- Mycoplasma testing: Regularly screening for contamination that can compromise editing efficiency
- Karyotype stability: Monitoring chromosomal integrity, particularly after extended culture
CRISPR Component Delivery Methods
The following table compares common delivery methods for introducing CRISPR components into iPSCs:
Table 2: CRISPR Delivery Methods for iPSCs
| Method | Efficiency | Cell Viability | Technical Complexity | Best Use Cases |
|---|---|---|---|---|
| Electroporation | High (up to 80%) | Moderate | Intermediate | Plasmid or RNP delivery; high-throughput applications [68] |
| Lipofection | Moderate (40-60%) | High | Low | Rapid screening of multiple gRNAs [68] |
| Nucleofection | Very high (up to 90%) | Moderate to low | High | Difficult-to-transfect cells; RNP delivery [68] |
| Viral Transduction | High (60-90%) | Variable | Intermediate | Stable cell line generation; in vivo applications |
For most iPSC editing applications, ribonucleoprotein (RNP) complex delivery via electroporation offers optimal results by minimizing off-target effects and reducing the time components remain active in cells [67].
Clone Isolation and Expansion
Following CRISPR delivery, single-cell cloning is essential for establishing pure isogenic lines. Critical steps include:
- Density optimization: Seeding cells at appropriate densities (0.5-1 cell/well) in 96-well or 384-well plates
- Conditioned media: Using media conditioned by feeder cells or supplemented with ROCK inhibitor to enhance single-cell survival
- Clonal tracking: Maintaining meticulous records of clone origins throughout expansion
- Expansion strategy: Implementing a standardized passage protocol to generate adequate biomass for banking and validation
Quality Control and Validation
Comprehensive validation of isogenic iPSC lines is essential to ensure experimental integrity. The quality control workflow encompasses multiple assessment levels:
Genotypic Validation
Comprehensive genotyping confirms the presence of intended edits and absence of unintended modifications:
- Sanger sequencing: Full-length sequencing of the edited region to verify the specific genetic change
- Off-target assessment: Evaluation of predicted off-target sites using targeted sequencing or whole-genome approaches
- Karyotype analysis: G-banding or SNP microarray to detect chromosomal abnormalities
- Identity confirmation: Short tandem repeat (STR) profiling to verify cell line identity
Pluripotency and Differentiation Capacity
Ensuring edited iPSCs retain full developmental potential is critical for downstream applications:
- Pluripotency markers: Immunostaining for OCT4, SOX2, NANOG, and SSEA-4
- Trilineage differentiation: Directed differentiation into ectodermal, mesodermal, and endodermal lineages with marker analysis
- Functional assays: Teratoma formation or embryoid body development for comprehensive pluripotency assessment
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for CRISPR-iPSC Isogenic Control Generation
| Reagent Category | Specific Examples | Function | Technical Notes |
|---|---|---|---|
| CRISPR Nucleases | SpCas9, AsCas12a, MAD7 | DNA cleavage at target sites | Cas9 is most established; Cas12a recognizes different PAM sequences [65] |
| Delivery Tools | Neon Transfection System, Lipofectamine Stem | Introduction of CRISPR components into iPSCs | Electroporation generally provides highest efficiency [68] |
| Editing Assessment | ICE Software, T7E1, Surveyor Mutation Detection | Quantification of editing efficiency | ICE provides NGS-quality data from Sanger sequencing [69] |
| Cell Quality Assessment | CloneSelect Imager, Flow Cytometry | Cell viability, pluripotency confirmation | Regular monitoring maintains culture quality [67] |
| iPSC Culture | mTeSR Plus, Essential 8, Y-27632 (ROCK inhibitor) | Maintenance of pluripotent state | Defined, feeder-free systems recommended [66] |
| Single-Cell Cloning | Accutase, RevitaCell | Dissociation and survival of single cells | ROCK inhibitor improves single-cell survival [67] |
Applications in Disease Modeling
Neurodegenerative Disease Modeling
The combination of CRISPR and iPSC technology has proven particularly valuable for modeling neurodegenerative diseases, which are often challenging to recapitulate in animal models due to species-specific differences in brain anatomy, physiology, and lifespan [65]. Isogenic iPSC lines have been successfully employed to model Alzheimer's disease, Parkinson's disease, Huntington's disease, and amyotrophic lateral sclerosis [65]. For example, patient-derived iPSCs with Huntington's disease-associated mutations in the HTT gene have been corrected to create isogenic controls, enabling precise dissection of mutation-specific phenotypes in differentiated neuronal cells [68].
3D Organoid and Tissue Modeling
Moving beyond traditional 2D cultures, researchers are increasingly employing CRISPR-edited iPSCs to generate complex 3D organoid models that better recapitulate tissue-level architecture and pathophysiology [66] [64]. These advanced models enable investigation of non-cell autonomous disease mechanisms and tissue-level phenotypes that may be absent in monolayer cultures [66]. For instance, CRISPR-edited intestinal organoids carrying CFTR mutations have been instrumental in cystic fibrosis research, allowing scientists to test small-molecule correctors and modulators in physiologically relevant systems [67].
Drug Discovery and Development
Isogenic iPSC pairs provide robust platforms for high-throughput drug screening and therapeutic development [67]. By comparing compound effects across isogenic disease and control lines, researchers can identify mutation-specific responders while controlling for background genetic effects [64]. This approach has been successfully applied to conditions including long QT syndrome, familial dysautonomia, and alpha-1-antitrypsin deficiency, where iPSC-derived cardiomyocytes, neurons, and hepatocytes respectively enable disease-relevant drug testing [64] [67].
Troubleshooting Common Challenges
Even with optimized protocols, researchers may encounter specific challenges when generating isogenic controls:
- Low HDR efficiency: Strategies include synchronizing cells in S-phase, using chemical enhancers such as RS-1 or SCR7, and optimizing repair template design
- Low single-cell survival: Incorporating ROCK inhibitor at appropriate concentrations, using conditioned media, and ensuring optimal seeding densities
- Off-target effects: Employing high-fidelity Cas9 variants, RNP delivery instead of plasmids, and careful sgRNA design to minimize off-target potential
- Unintended genomic abnormalities: Regular karyotyping and SNP analysis to detect chromosomal changes, with particular attention after single-cell cloning
The strategic integration of CRISPR/Cas9 genome editing with iPSC technology represents a transformative approach for creating genetically precise isogenic controls that empower robust disease modeling and therapeutic development. By implementing the comprehensive methodologies, quality control frameworks, and specialized tools detailed in this technical guide, researchers can generate high-quality isogenic iPSC lines that eliminate genetic background confounding and enable unambiguous attribution of phenotypes to specific genetic variants. As the CRISPR toolbox continues to expand with novel editors, delivery methods, and screening technologies, the precision and efficiency of isogenic control generation will further accelerate our understanding of disease mechanisms and development of targeted therapeutics.
Navigating iPSC Challenges: Immaturity, Variability, and Scalability
The advent of human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs) has revolutionized cardiovascular research, offering an unprecedented platform for disease modeling, drug discovery, and regenerative medicine. These cells provide a patient-specific, ethically acceptable, and theoretically unlimited source of human cardiomyocytes, overcoming critical limitations associated with primary human cardiomyocytes and animal models [70] [40]. However, a significant challenge persists: hiPSC-CMs consistently exhibit a functionally and structurally immature phenotype that more closely resembles fetal cardiomyocytes than adult human cardiomyocytes (AdCMs) [70] [40] [71]. This immaturity hurdle fundamentally limits their translational relevance and predictive accuracy in pharmaceutical testing and disease modeling.
Within the broader context of induced pluripotent stem cell research for disease modeling, the immaturity of hiPSC-CMs represents a critical bottleneck. While patient-specific hiPSC-CMs can theoretically recapitulate inherited cardiomyopathies—including hypertrophic, dilated, and arrhythmogenic cardiomyopathies that affect substantial portions of the population—their fetal-like characteristics impede accurate modeling of adult-onset cardiac conditions [70] [72]. This technical guide provides a comprehensive comparison between hiPSC-CMs and AdCMs, detailing the specific aspects of immaturity, current maturation strategies, and standardized assessment methodologies essential for advancing the field toward more physiologically relevant in vitro cardiac models.
Fundamental Disparities: hiPSC-CMs versus Adult Cardiomyocytes
Structural and Morphological Differences
The structural differences between hiPSC-CMs and AdCMs are profound and fundamentally impact their functional capabilities. AdCMs exhibit an elongated, rod-shaped morphology with dimensions of approximately 140 μm in length and 20 μm in width, yielding a cell volume of about 40,000 μm³ [40]. In stark contrast, hiPSC-CMs are typically smaller and rounded, with volumes ranging between 3,000-6,000 μm³ [40]. This morphological disparity extends to their internal architecture, particularly the organization of sarcomeres, the fundamental contractile units of cardiomyocytes.
Table 1: Structural and Morphological Comparison
| Feature | hiPSC-CMs | Adult Cardiomyocytes |
|---|---|---|
| Cell Morphology | Small, rounded, irregular shape | Rod-shaped, elongated |
| Cell Volume | 3,000-6,000 μm³ | ~40,000 μm³ |
| Sarcomere Organization | Disorganized, random orientation | Highly organized, parallel myofibrils |
| Sarcomere Length | 1.7-2.0 μm | 1.9-2.2 μm |
| T-Tubule Network | Largely absent | Highly developed, regular network |
| Nuclearity | Predominantly mononucleated | Often binucleated |
| Mitochondrial Localization | Diffuse | Localized near sarcomeres |
AdCMs contain well-organized myofibrils aligned parallel to the cell's long axis, whereas hiPSC-CMs display randomly oriented sarcomeres with poor registration [40] [71]. This disorganized structure directly compromises contractile force generation and efficiency. Furthermore, hiPSC-CMs notably lack a developed T-tubule network—specialized invaginations of the sarcolemma that are crucial for synchronous calcium-induced calcium release (CICR) in mature cardiomyocytes [40] [71]. The absence of T-tubules results in spatial uncoupling between L-type calcium channels (LTCC) on the surface membrane and ryanodine receptors (RYR2) on the sarcoplasmic reticulum, leading to delayed and dyssynchronous calcium release [40].
Electrophysiological and Calcium Handling Properties
The electrophysiological profile of hiPSC-CMs markedly differs from AdCMs, with significant implications for drug testing and disease modeling. AdCMs maintain a stable resting membrane potential of approximately -90 mV, while hiPSC-CMs typically exhibit a depolarized resting potential, often above -80 mV [70] [71]. This difference primarily stems from reduced inward-rectifier potassium current (Iₖ₁) density in hiPSC-CMs, which is essential for maintaining stable resting potential in adult cells [71].
Table 2: Electrophysiological and Functional Comparison
| Parameter | hiPSC-CMs | Adult Cardiomyocytes |
|---|---|---|
| Resting Membrane Potential | -80 to -60 mV | ~-90 mV |
| Action Potential Amplitude | Reduced | 100-110 mV |
| Upstroke Velocity | Slower | 250-300 V/s |
| Conduction Velocity | <40 cm/s | 30-100 cm/s |
| Spontaneous Beating | Present | Absent (in ventricular CMs) |
| Calcium Transient Kinetics | Slow, dyssynchronous | Rapid, synchronous |
| Force Generation | Lower (few achieve >30 mN/mm²) | 25-44 mN/mm² |
| Force-Frequency Relationship | Negative or flat | Positive |
| Energy Metabolism | Primarily glycolysis | >70% fatty acid oxidation |
Calcium handling represents another area of significant immaturity. In AdCMs, coordinated activation of LTCC and RYR2 through the T-tubule system enables rapid, synchronous calcium release throughout the cell, resulting in fast calcium transient kinetics that support efficient contraction-relaxation cycles [40] [71]. In hiPSC-CMs, the lack of T-tubules and poor colocalization of calcium handling proteins leads to slow, propagating calcium waves that begin in peripheral regions and move toward the cell center [71]. This dyssynchronous calcium release contributes to impaired contractile function and negative force-frequency relationships—a hallmark of immature cardiomyocytes that contrasts sharply with the positive force-frequency relationship observed in AdCMs [70] [71].
Metabolic Characteristics
The metabolic profile of hiPSC-CMs reflects their fetal-like state, with predominant reliance on glycolysis for energy production, despite the presence of functional mitochondria [70] [40]. This contrasts with AdCMs, which primarily utilize oxidative phosphorylation, metabolizing fatty acids to generate ATP with significantly higher efficiency [70]. The transition from glycolytic to oxidative metabolism during normal cardiac maturation is accompanied by mitochondrial proliferation and structural development, with mitochondria eventually occupying approximately 30% of the cell volume in AdCMs and becoming strategically localized near sarcomeres to fuel contraction [70].
Methodologies for Enhancing hiPSC-CM Maturation
Prolonged Culture and Biochemical Manipulation
Simply extending the culture duration of hiPSC-CMs beyond the initial differentiation period promotes some aspects of maturation. Studies have demonstrated that maintaining hiPSC-CMs for extended periods (80-120 days) leads to improvements in sarcomeric organization, electrophysiological properties, and calcium handling [70]. This basal maturation can be enhanced through biochemical manipulation, including supplementation with thyroid hormone (T3) and glucocorticoids such as dexamethasone, which activate transcriptional programs associated with postnatal cardiac maturation [73].
The fundamental differentiation protocol for generating hiPSC-CMs relies on precise temporal modulation of the Wnt/β-catenin signaling pathway [73] [74]. This process typically begins with activation using GSK3 inhibitors such as CHIR99021, followed by inhibition using compounds like IWP-2 or IWR-1 [74]. The efficiency of this protocol has been refined to yield populations with >90% cardiomyocytes, as confirmed by flow cytometry for cardiac troponin T (cTnT) [74].
3D Tissue Engineering and Biomaterial Approaches
Three-dimensional (3D) culture systems significantly enhance hiPSC-CM maturation compared to traditional 2D monolayers. Engineered cardiac tissues (ECTs) recapitulate critical aspects of the native myocardial microenvironment, including cell-cell and cell-matrix interactions that promote structural and functional maturation [75]. These 3D platforms facilitate the development of elongated cell morphology, improved sarcomeric organization, and enhanced electromechanical coupling [75].
Biomaterials play a crucial role in supporting 3D tissue formation. Nanofibrous scaffolds fabricated from polymers such as polycaprolactone (PCL) and polyurethane (PU) mimic the topology and mechanical properties of the native cardiac extracellular matrix (ECM) [74]. These scaffolds are typically fabricated using techniques like solution blow spinning (SBS) or electrospinning, with fiber alignment and surface modification through oxygen plasma treatment or protein coating (e.g., gelatin) to enhance biocompatibility and cell adhesion [74]. When hiPSC-CMs are cultured on these nanofibrous mats for extended periods (10+ days), they exhibit improved structural alignment, increased expression of mature sarcomeric proteins, and enhanced gene expression profiles indicative of greater maturity [74].
Mechanical and Electrical Stimulation
Physical cues are essential drivers of cardiac maturation during postnatal development. Incorporating mechanical loading—particularly static strain or cyclic stretch—promotes hypertrophic growth, sarcomeric alignment, and improves contractile force generation in hiPSC-CMs [75]. Similarly, electrical stimulation regimens that mimic the rhythmic pacing of the native heart enhance structural and electrophysiological maturity. Application of electrical field stimulation at increasing frequencies (0.5-6 Hz) over 7-14 days promotes the development of elongated morphology, T-tubule-like structures, and more adult-like calcium handling properties [75].
Micropatterning and Structural Confinement
Micropatterning techniques constrain hiPSC-CMs to specific geometries, particularly rod-shaped patterns that mimic the native aspect ratio of AdCMs. Confining hiPSC-CMs to rectangles of 120 μm × 30 μm forces morphological alignment similar to adult cells, which in turn promotes organization of internal structures [76]. This structural confinement leads to the development of more organized sarcomeres with improved registration, enhanced density of myofibrils, and electrophysiological maturation characterized by more hyperpolarized resting membrane potentials and increased sodium current density [76].
Experimental Assessment of hiPSC-CM Maturity
Functional Electrophysiological Assessment
Multi-electrode array (MEA) systems provide a non-invasive, label-free platform for assessing the electrophysiological maturity of hiPSC-CMs through continuous recording of field potentials [73]. This technology enables quantification of key parameters including field potential duration (FPD—analogous to QT interval in ECG), beat rate, and conduction velocity [73]. MEA systems are particularly valuable for assessing drug responses, detecting arrhythmogenic potential, and evaluating disease phenotypes such as long QT syndrome [73].
Patch clamp electrophysiology remains the gold standard for detailed characterization of action potential morphology and specific ion currents. For mature hiPSC-CMs, researchers should target a resting membrane potential ≤-80 mV, action potential amplitude ≥100 mV, and upstroke velocity ≥150 V/s [70]. These parameters can be optimized through the maturation strategies outlined in Section 3.
Calcium Handling and Contractility Analysis
Calcium handling is typically assessed using fluorescent indicators (e.g., Fluo-4, Fura-2) coupled with high-speed imaging systems. Key maturity metrics include calcium transient amplitude, rise time, decay time, and synchronization across the cell [71]. For contractility assessment, traction force microscopy or video-based analysis of contractile motion can quantify contraction velocity, relaxation velocity, and sarcomere shortening [70]. More sophisticated systems including muscular thin films and cantilever-based technologies provide direct measurements of contractile force generation, with mature hiPSC-CM constructs ideally achieving >30 mN/mm² [70].
Structural and Molecular Characterization
Immunocytochemistry for sarcomeric proteins (α-actinin, cardiac troponin I, troponin T) reveals the degree of sarcomeric organization and Z-disc alignment [74]. Mature hiPSC-CMs should exhibit clear, aligned striations throughout the cytoplasm with defined H-zones and I-bands. Transmission electron microscopy provides ultrastructural assessment of sarcomere length (target: 1.9-2.2 μm), mitochondrial density and localization, and presence of T-tubule-like structures [40] [71].
Gene expression profiling through qRT-PCR or RNA sequencing should demonstrate a shift from fetal to adult isoforms, including increased expression of adult myosin heavy chain (MYH7 vs. MYH6), cardiac troponin I (vs. slow skeletal troponin I), and the N2B titin isoform (vs. N2BA) [40]. Metabolic maturity can be assessed by measuring the relative contribution of fatty acid oxidation versus glycolysis to ATP production, with mature cells deriving >70% of energy from oxidative metabolism [70].
Table 3: Key Research Reagents for hiPSC-CM Maturation Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Small Molecule Inducers | CHIR99021, IWP-2, IWR-1 | Wnt pathway modulation for cardiac differentiation |
| Hormones/Signaling Molecules | Triiodo-L-thyronine (T3), Dexamethasone | Promote metabolic and structural maturation |
| Biomaterial Scaffolds | PCL, PU nanofibrous mats | Mimic cardiac ECM topology and mechanics |
| Surface Patterning | Micropatterned substrates with cell-repellent areas | Force rod-shaped morphology and alignment |
| Electrophysiology Tools | Multi-electrode array systems, Voltage-sensitive dyes | Assess action potential parameters and conduction |
| Calcium Indicators | Fluo-4 AM, Fura-2 AM | Visualize and quantify calcium transients |
| Cell Separation Markers | Mitochondrial dyes, Surface marker antibodies | Purify cardiomyocyte populations |
| Critical Antibodies | Anti-cardiac Troponin T, Anti-α-actinin | Identify cardiomyocytes and assess sarcomere structure |
Implications for Disease Modeling and Drug Development
The immaturity of hiPSC-CMs presents significant challenges for disease modeling and drug development. While these cells express the major cardiac ion channels and contractile proteins, their fetal-like electrophysiology and calcium handling properties can mask or alter disease phenotypes [71]. For example, modeling arrhythmogenic disorders such as long QT syndrome or catecholaminergic polymorphic ventricular tachycardia in immature hiPSC-CMs may not fully recapitulate the clinical manifestations observed in patients [73] [71].
Similarly, drug responses can differ substantially between immature hiPSC-CMs and AdCMs. The negative force-frequency relationship in hiPSC-CMs contrasts with the positive relationship in AdCMs, potentially leading to misleading conclusions about inotropic drug effects [70]. Differences in ion channel expression and calcium handling may also affect the prediction of proarrhythmic potential, though hiPSC-CMs still demonstrate value for detecting hERG channel blockade and associated QT prolongation [73].
Despite these limitations, patient-specific hiPSC-CMs have provided valuable insights into inherited cardiomyopathies when combined with advanced maturation techniques. Studies of hypertrophic cardiomyopathy, dilated cardiomyopathy, and arrhythmogenic cardiomyopathy using hiPSC-CMs have revealed disease-specific abnormalities in contractile function, calcium handling, and electrophysiology [70] [72]. The integration of CRISPR/Cas9 gene editing further enables the creation of isogenic controls that confirm genotype-phenotype relationships [70] [77].
The immaturity of hiPSC-CMs represents a significant but addressable challenge in the field of cardiovascular disease modeling. While current hiPSC-CMs recapitulate many aspects of fetal rather than adult cardiomyocytes, ongoing advances in maturation strategies are steadily closing this phenotypic gap. The integration of 3D tissue engineering, biomaterial science, and physiologically relevant biophysical stimulation holds particular promise for generating more adult-like cardiomyocytes in vitro.
For researchers pursuing disease modeling applications, a combinatorial approach incorporating multiple maturation techniques—prolonged culture on biomimetic scaffolds with defined mechanical and electrical stimulation—currently provides the most pathophysiologically relevant platform. Standardized assessment of structural, functional, and metabolic parameters remains essential for benchmarking progress across different laboratories and protocols. As maturation protocols continue to improve, hiPSC-CMs will increasingly fulfill their potential as transformative tools for modeling cardiovascular diseases, screening drug efficacy and toxicity, and ultimately advancing regenerative therapies for heart disease.
The advent of human induced pluripotent stem cells (iPSCs) has fundamentally transformed biomedical research, offering an unprecedented platform for disease modeling, drug screening, and regenerative medicine. By reprogramming somatic cells to a pluripotent state, researchers can generate patient-specific cardiomyocytes (iPSC-CMs) that recapitulate genetic backgrounds of various cardiac conditions [2] [3]. However, a significant limitation impedes their full translational potential: iPSC-derived cardiomyocytes consistently exhibit immature structural, functional, and metabolic properties that more closely resemble fetal or neonatal cardiomyocytes rather than adult human heart cells [78] [79]. This immaturity manifests across multiple domains, including disorganized contractile machinery, underdeveloped calcium handling systems, depolarized resting membrane potentials, and a primarily glycolytic metabolic phenotype [78] [80].
The functional consequences of this immaturity are profound for disease modeling and drug development. Immature iPSC-CMs fail to fully recapitulate adult disease phenotypes and demonstrate altered pharmacological responses that can compromise drug safety and efficacy predictions [81]. For instance, their inability to accurately predict pro-arrhythmic drug responses or model adult-onset cardiovascular diseases underscores the critical need for effective maturation strategies [81] [82]. This technical guide comprehensively examines the current methodologies for promoting iPSC-CM maturation across metabolic, structural, and electrophysiological domains, providing researchers with evidence-based protocols to enhance the physiological relevance of their in vitro models for more accurate disease modeling and drug development applications.
Metabolic Maturation Strategies
The Metabolic Switch from Glycolysis to Fatty Acid Oxidation
The metabolic maturation of cardiomyocytes represents a crucial transition in postnatal development. Fetal cardiomyocytes primarily rely on glycolysis for ATP production, even in oxygen-rich environments—a phenomenon known as the Warburg effect [80]. In contrast, adult cardiomyocytes derive approximately 70-80% of their ATP from fatty acid β-oxidation, with the remainder coming from glucose, lactate, and ketone bodies [80]. This metabolic switch is essential for supporting the continuous contractile activity of the adult heart, as fatty acid oxidation yields significantly more ATP per molecule than glycolysis.
iPSC-CMs typically retain a fetal-like metabolic profile characterized by high glycolytic flux, low mitochondrial oxidative capacity, and limited fatty acid utilization [80]. This metabolic immaturity directly impacts their contractile function and electrophysiological stability. Promoting metabolic maturation therefore requires strategies that induce mitochondrial biogenesis and encourage the transition to oxidative metabolism.
Experimentally Inducing Metabolic Maturation
Table 1: Metabolic Maturation Media Components and Functions
| Component | Concentration Range | Primary Function | Experimental Evidence |
|---|---|---|---|
| Fatty Acids (Palmitate, Oleate) | 100-500 μM | Substrate for β-oxidation; induces metabolic enzyme expression | Increases oxygen consumption rate (OCR) and fatty acid utilization [81] [80] |
| L-Carnitine | 0.5-2 mM | Facilitates fatty acid transport into mitochondria | Enhances fatty acid oxidation capacity [80] |
| Triiodothyronine (T3) | 1-100 nM | Thyroid hormone; regulates mitochondrial biogenesis | Promotes metabolic switch and improves contractile function [82] [80] |
| Creatine | 1-5 mM | Phosphocreatine system for energy buffering | Improves ATP transfer efficiency and contractile reserve [79] |
| Insulin | Reduced (0.1-1 nM) | Limits anabolic signaling to promote oxidative metabolism | Enhances fatty acid oxidation and reduces glycolytic dependence [78] |
| Lactate | 4-10 mM | Selection pressure; forces oxidative metabolism | Enriches CM population and promotes mitochondrial maturation [79] |
Detailed Protocol: Metabolic Maturation Medium Formulation
- Base Medium Preparation: Begin with a standard cardiomyocyte maintenance medium (e.g., RPMI 1640 or DMEM without glucose).
- Supplement Addition:
- Add fatty acids (palmitate conjugated with BSA at 2:1 molar ratio) to a final concentration of 200 μM.
- Supplement with 1 mM L-carnitine, 5 mM creatine, and 10 nM triiodothyronine (T3).
- Include 5 mM lactate for metabolic selection during the initial 3-5 days of maturation.
- Reduce insulin concentration to 0.5 nM to minimize glycolytic stimulation.
- Culture Conditions: Maintain cells in maturation medium for 14-28 days, with medium changes every 2-3 days.
- Quality Control Assessment:
- Measure oxygen consumption rate (OCR) using extracellular flux analyzers.
- Quantify fatty acid oxidation rates using radiolabeled palmitate or seahorse metabolic assays.
- Assess mitochondrial density and morphology via electron microscopy and MitoTracker staining.
The efficacy of metabolic maturation can be validated through transcriptional upregulation of key genes including PPARα, PGC-1α, and CPT1B, which orchestrate fatty acid metabolism and mitochondrial biogenesis [80]. Additionally, mature iPSC-CMs should demonstrate increased mitochondrial mass, enhanced oxidative phosphorylation capacity, and a corresponding reduction in glycolytic flux [79] [80].
Structural Maturation Approaches
Recapitulating Adult Cardiomyocyte Architecture
Structural maturation encompasses the development of organized contractile machinery, proper cell shape and alignment, and the formation of specialized structures including T-tubules and intercalated discs. Adult cardiomyocytes are characterized by their rod-shaped morphology, highly organized sarcomeres with clearly defined A-, I-, and Z-bands, and aligned myofibrils that run parallel to the long axis of the cell [78] [79]. In stark contrast, immature iPSC-CMs typically exhibit random sarcomere organization, rounded morphology, and absent T-tubules, significantly limiting their contractile force generation and calcium handling capabilities [78].
Experimental Strategies for Structural Maturation
Table 2: Quantitative Assessment of Structural Maturation Parameters
| Structural Parameter | Immature iPSC-CMs | Mature iPSC-CMs | Measurement Technique |
|---|---|---|---|
| Cell Shape | Round/oval (10-20 μm diameter) | Rod-shaped (100-150 μm length) | Phase-contrast microscopy, immunostaining |
| Sarcomere Organization | Random myofibril arrangement | Aligned, continuous myofibrils | α-actinin immunostaining |
| Sarcomere Length | 1.6-1.7 μm | 1.8-2.2 μm | α-actinin staining with morphometric analysis |
| Nuclear Number | Primarily mononucleated | Binucleated (≈25%) | DAPI staining, flow cytometry |
| T-tubules | Absent | Present (in highly mature cells) | Di-8-ANEPPS staining, electron microscopy |
| Connexin 43 Localization | Circumferential/perinuclear | Polarized to cell ends | Immunofluorescence, confocal microscopy |
Detailed Protocol: Nanopatterning for Structural Alignment
- Substrate Fabrication:
- Create nanopatterned surfaces using electron beam lithography or nanoimprinting.
- Generate parallel ridge-groove patterns with 800 nm width and 800 nm pitch.
- Coat patterns with extracellular matrix proteins (laminin-521 or fibronectin) at 10-20 μg/cm².
- Cell Seeding:
- Seed dissociated iPSC-CMs at a density of 50,000-100,000 cells/cm².
- Allow attachment for 24-48 hours before initiating electrical stimulation.
- Culture Duration: Maintain cells on patterned surfaces for 14-21 days with regular medium changes.
- Assessment Methods:
- Immunostaining for α-actinin to quantify sarcomere organization and Z-band alignment.
- Measurement of sarcomere length using image analysis software.
- Analysis of cell orientation relative to patterning direction.
The integration of nanopatterning with 3D hydrogel cultures has demonstrated synergistic effects on structural maturation. Gisone et al. reported that iPSC-CMs co-cultured with human coronary artery endothelial cells in 3D gelatin methacryloyl (GelMA) hydrogels showed significantly increased expression of cardiac maturation markers compared to 2D monocultures [2]. Similarly, Josvia et al. demonstrated that cardiac fibroblasts enhance cardiomyocyte structural maturation through a combination of paracrine signaling and direct cellular interactions, leading to improved myofibril alignment and contractile anisotropy [2].
Electrophysiological Maturation Methods
Acquiring Adult-like Electrical Properties
Electrophysiological maturation encompasses the development of appropriate ion channel expression, density, and distribution; establishment of a negative resting membrane potential; and functional coupling through gap junctions. Adult ventricular cardiomyocytes exhibit stable resting membrane potentials of approximately -80 mV to -90 mV, rapid action potential upstroke velocities (>200 V/s), and coordinated calcium-induced calcium release from well-developed sarcoplasmic reticulum [78] [81]. Immature iPSC-CMs, in contrast, display depolarized resting potentials (-30 mV to -60 mV), slow upstroke velocities (2-20 V/s), and reliance on trans-sarcolemmal calcium influx rather than sarcoplasmic reticulum calcium release [78].
Experimental Approaches for Electrophysiological Maturation
Detailed Protocol: Combined Maturation with Electrostimulation
- Setup Configuration:
- Utilize a C-Pace EP culture stimulator or similar system.
- Employ carbon electrodes placed in culture medium or use commercially available stimulation plates.
- Stimulation Parameters:
- Begin with 2 Hz frequency (120 bpm) for the first 3-5 days.
- Gradually increase to 4-6 Hz (240-360 bpm) over 2-3 weeks.
- Use monophasic pulses of 2-5 ms duration and field strengths of 5-10 V/cm.
- Apply continuous stimulation for 10-14 days minimum.
- Combination with Other Cues:
- Implement concurrent metabolic maturation medium supplementation.
- Combine with nanopatterned substrates for synergistic effects.
- Maintain elevated calcium concentration (1.8-2.5 mM) in culture medium.
- Functional Assessment:
- Patch clamp electrophysiology for action potential parameters.
- Multi-electrode array (MEA) recording for conduction velocity.
- Calcium imaging for transient kinetics and sarcoplasmic reticulum function.
Table 3: Electrophysiological Parameters Before and After Maturation
| Parameter | Immature iPSC-CMs | Mature iPSC-CMs | Measurement Technique |
|---|---|---|---|
| Resting Membrane Potential | -30 to -60 mV | -65 to -80 mV | Patch clamp (current clamp) |
| Action Potential Amplitude | 80-100 mV | 100-120 mV | Patch clamp (current clamp) |
| Maximal Upstroke Velocity (Vmax) | 2-20 V/s | 50-200 V/s | Patch clamp (current clamp) |
| Action Potential Duration (APD90) | Highly variable | Shorter, more reproducible | Patch clamp (current clamp) |
| Conduction Velocity | 10-15 cm/s | 20-30 cm/s | Multi-electrode array (MEA) |
| Ito Density | Low | Significantly increased | Patch clamp (voltage clamp) |
| Force-Frequency Relationship | Negative | Positive | Contractility measurement |
Recent research has demonstrated that electrical stimulation serves as the primary driver for enhancing mitochondrial development and metabolic maturation, which subsequently improves electrophysiological properties [81]. In a systematic analysis of multiple maturation cues, electrostimulation emerged as the most significant factor for promoting electrophysiological maturation, while increased calcium concentration strongly promoted action potential maturation, and nanopatterning primarily facilitated structural organization with minimal direct effects on electrophysiology [81].
A critical outcome of successful electrophysiological maturation is the development of a positive force-frequency relationship (FFR), which is characteristic of adult myocardium but typically absent in immature iPSC-CMs [78]. The emergence of a positive FFR indicates functional maturation of calcium handling proteins, including SERCA2a, phospholamban, and ryanodine receptors, enabling frequency-dependent acceleration of relaxation—a hallmark of adult cardiac electromechanical coupling.
Integrated Maturation Workflows and Experimental Design
Combined Approach for Maximal Maturation
While individual maturation strategies provide incremental improvements, the most significant advances occur through integrated approaches that simultaneously address metabolic, structural, and electrophysiological maturation. A recent groundbreaking study demonstrated that combining lipid-enriched metabolic medium with nanopatterning and chronic electrostimulation generated iPSC-CMs with advanced maturation across all domains [81]. This combined protocol resulted in the appearance of a distinctive "notch-and-dome" action potential morphology characteristic of adult ventricular cardiomyocytes, which was not observed with any individual intervention alone [81].
Experimental Workflow for Comprehensive Maturation
The Scientist's Toolkit: Essential Research Reagents and Platforms
| Category | Specific Products/Platforms | Primary Application | Key Features |
|---|---|---|---|
| iPSC-CM Differentiation | STEMdiff Ventricular Cardiomyocyte Kit (Stemcell Technologies) | Cardiac differentiation | Defined, serum-free system for ventricular CM generation |
| Metabolic Maturation | Fatty acid-supplemented media (e.g., MM-1) [79] | Metabolic switch induction | Contains palmitate, carnitine, creatine for oxidative metabolism |
| Structural Maturation | Nanopatterned surfaces (e.g., Nanosurface plates) | Cell alignment and sarcomere organization | 800 nm ridge-groove patterns for contact guidance |
| Electrophysiological Maturation | C-Pace EP Culture Stimulator (IonOptix) | Chronic electrical pacing | Programmable stimulation parameters for multiple cultures |
| Functional Assessment | Multi-electrode array systems (Axion Biosystems) | Conduction velocity measurement | Non-invasive, long-term electrophysiological monitoring |
| Calcium Handling | FLIPR Tetra High-Throughput Cellular Screening System (Molecular Devices) | Calcium transient kinetics | High-throughput screening of calcium handling properties |
| Metabolic Analysis | Seahorse XF Analyzer (Agilent Technologies) | Metabolic flux analysis | Simultaneous measurement of OCR and ECAR |
Timeline and Expected Outcomes
A comprehensive maturation protocol typically spans 3-6 weeks post-cardiac differentiation. Key milestones include:
- Week 1: Initiation of metabolic maturation medium and nanopatterning; visible cell elongation and alignment.
- Week 2: Beginning of electrical stimulation; measurable improvements in resting membrane potential and upstroke velocity.
- Weeks 3-4: Development of organized sarcomeres with adult-like length (≥1.8 μm); emergence of positive force-frequency relationship.
- Weeks 5-6: Maximum expression of adult-specific isoforms (cTnI, MYH7); appearance of notch-and-dome action potential morphology.
Throughout this process, regular functional assessment is critical for validating maturation progression. Researchers should employ a combination of patch clamp electrophysiology, calcium imaging, contractility analysis, and molecular characterization to quantify maturation status across multiple parameters.
Implications for Disease Modeling and Drug Development
The maturation status of iPSC-CMs directly influences their utility in disease modeling and drug development applications. Immature cells fail to recapitulate key aspects of adult cardiac pathophysiology, including adult-onset disease phenotypes, proper drug responses, and disease-specific structural remodeling [81] [82]. Comprehensive maturation protocols enable more accurate modeling of genetic cardiomyopathies, arrhythmia syndromes, and metabolic cardiac disorders.
In pharmaceutical applications, matured iPSC-CMs demonstrate improved predictive accuracy for drug-induced cardiotoxicity and pro-arrhythmic potential. For instance, mature iPSC-CMs show appropriate responses to multichannel blockers like verapamil, which often abolishes beating in immature cells at clinically relevant concentrations due to differences in ion channel expression and calcium handling properties [81]. The implementation of matured iPSC-CMs in the Comprehensive in vitro Proarrhythmia Assay (CiPA) initiative represents a significant advance in cardiac safety pharmacology.
Furthermore, the enhanced structural organization and metabolic capacity of matured iPSC-CMs better replicate the pathological remodeling observed in heart failure, hypertrophy, and metabolic syndrome. This enables more clinically relevant investigation of disease mechanisms and identification of novel therapeutic targets. As maturation protocols continue to advance, iPSC-based disease models will play an increasingly central role in personalized medicine approaches and drug development pipelines.
The maturation of iPSC-derived cardiomyocytes represents a critical frontier in cardiovascular research with profound implications for disease modeling, drug discovery, and regenerative medicine. By implementing integrated strategies that simultaneously target metabolic, structural, and electrophysiological maturation, researchers can generate in vitro models that more faithfully recapitulate adult human cardiac biology. The protocols and methodologies outlined in this technical guide provide a framework for achieving comprehensive iPSC-CM maturation, enabling more physiologically relevant investigation of cardiac disease mechanisms and more accurate prediction of drug efficacy and safety. As these approaches continue to evolve and standardize, matured iPSC-CMs will increasingly serve as indispensable tools for advancing our understanding and treatment of cardiovascular disease.
The capacity of induced pluripotent stem cells (iPSCs) to generate patient-specific disease models has fundamentally transformed biomedical research, particularly for rare genetic disorders where traditional study cohorts are challenging to assemble [83]. However, a significant challenge complicates their reliable application: inherent line-to-line variability. This variability manifests as considerable experimental differences not only between iPSC lines derived from different individuals but also among different sub-lines originating from the same donor [83]. This heterogeneity poses a major barrier to obtaining robust, reproducible results, which are the cornerstone of scientific discovery and preclinical drug development.
This technical guide outlines the sources of this variability and provides a strategic framework of evidence-based methods to mitigate its effects. By adopting rigorous standards from cell line generation through experimental design and data analysis, researchers can enhance the reliability of their iPSC-based disease models.
Line-to-line variability in iPSC experiments arises from a complex interplay of biological and technical factors. A comprehensive understanding of these sources is the first step toward effective mitigation.
- Genetic and Epigenetic Background: Each donor carries a unique genetic and epigenetic background. While this is essential for modeling population diversity, it introduces variance that can obscure disease-specific phenotypes, especially in small sample sizes [83].
- Reprogramming and Culture-Induced Instabilities: The process of reprogramming somatic cells is inherently inefficient and can introduce genomic and epigenetic instabilities [3]. Furthermore, prolonged culture exerts selective pressures, potentially allowing subpopulations with accumulated mutations or epigenetic alterations to outcompete others, a significant concern for clinical applications [84].
- Differentiation Bias and Immaturity: iPSC lines can exhibit a variable propensity to differentiate into specific lineages. Moreover, iPSC-derived cells frequently display an immature, fetal-like phenotype, which may not accurately recapitulate the adult disease state. The maturity of derived cells can be enhanced by using more complex, biomimetic culture systems, such as co-cultures and 3D hydrogels [2].
Strategic Framework for Mitigation
A multi-pronged strategy, addressing every stage from cell line establishment to data analysis, is required to ensure reproducibility.
Optimal iPSC Line Establishment and Quality Control
The foundation of a reproducible experiment is a well-characterized and high-quality set of iPSC lines.
Table 1: Somatic Cell Sources for iPSC Generation
| Cell Source | Reprogramming Efficiency | Invasiveness of Collection | Key Advantages | Considerations |
|---|---|---|---|---|
| Dermal Fibroblasts | High | Moderate (skin biopsy) | High genomic stability; reliable and widely used [3] | Invasive procedure |
| Peripheral Blood Mononuclear Cells (PBMCs) | Comparable to fibroblasts | Low (blood draw) | Minimally invasive; favored for translational studies [3] | |
| Urinary Epithelial Cells | Robust | Non-invasive | Completely non-invasive and easily repeatable [3] | |
| Keratinocytes | Higher than fibroblasts | Low (hair follicle) | High reprogramming efficiency [3] | Yields fewer cells |
Essential Quality Control (QC) Measures:
- Pluripotency Verification: Confirm expression of canonical markers (OCT4, NANOG) via PCR, immunocytochemistry, or flow cytometry. Assess functional potential through trilineage differentiation assays [3].
- Genomic Integrity Monitoring: Regularly evaluate chromosomal stability using karyotyping. More sophisticated methods like population balance equation (PBE) modeling can quantify the distribution of physiological states, such as OCT4 synthesis rates, within a culture, providing a deeper view of population heterogeneity [85].
- Standardized Culture Protocols: Utilize feeder-free, chemically defined media (e.g., mTeSR1, E8) to minimize xenogeneic components and improve reproducibility [3]. The adoption of common standards is crucial for ensuring the reliability and translatability of stem cell models [86].
Robust Experimental Design and Power Analysis
Perhaps the most critical step in mitigating variability is designing experiments with sufficient statistical power.
Empirical Recommendations for Sample Size: Recent empirical research using iPSCs to model Lesch-Nyhan disease (LND) provides concrete guidance. The study, which controlled for technical variance by generating all lines in parallel, concluded that the optimal strategy involves using:
- 3-4 unique individuals per experimental group (e.g., disease vs. control).
- 2 independent iPSC lines per individual [83].
This design proved more effective for detecting disease-relevant gene expression changes than using a single line from more individuals, at least in the context of this controlled, monogenic disease study. When using multiple lines from one individual, it is often necessary to apply statistical corrections to account for the non-independence of these technical replicates [83].
Advanced Analytical and Technological Approaches
Emerging technologies offer powerful new tools to quantify and control for variability.
- AI and Deep Learning for Quality Assessment: Artificial intelligence can objectively identify high-quality models. For example, StembryoNet, a deep-learning model based on ResNet18 architecture, was able to classify mouse stem cell-derived embryo models into "normal" and "abnormal" categories with 88% accuracy by analyzing morphological features from live imaging. Such tools can standardize the selection of high-quality structures for downstream experiments [87].
- Quantitative Modeling of Cell Populations: Moving beyond population-average measurements, Population Balance Equation (PBE) modeling can derive Physiological State Functions (PSFs). These functions describe the distributions of critical cellular properties, such as the rates of division, protein synthesis (e.g., OCT4), and differentiation across a population. This framework captures the inherent heterogeneity of isogenic stem cell populations and provides a more rigorous, quantitative basis for biomanufacturing and experimental analysis [85].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Research Reagent Solutions for Reproducible iPSC Work
| Reagent/Material | Function | Application Note |
|---|---|---|
| Chemically Defined Media (e.g., mTeSR1, E8) | Maintains pluripotency and supports growth in a defined, xeno-free environment. | Essential for standardizing culture conditions and minimizing batch-to-batch variability [3]. |
| Extracellular Matrix (e.g., Matrigel, Laminin) | Provides a scaffold for cell attachment and growth in feeder-free systems. | Coating consistency is critical for reproducible cell behavior [3]. |
| ROCK Inhibitor (Y-27632) | Enhances cell survival after passaging and cryopreservation. | Used as a supplement in the first 24-48 hours after thawing or splitting cells [85]. |
| Enzymatic Passaging Reagents (e.g., Dispase, Accutase) | Gently dissociates iPSC colonies for sub-culturing. | Preferable to mechanical passaging for scalability and consistency [3] [85]. |
| Cryopreservation Medium (with DMSO) | Enables long-term storage of iPSC lines. | Typically contains 10% DMSO; controlled-rate freezing is vital for high post-thaw viability [3]. |
| Lactate Supplement | A metabolic stressor used to study cell line response and physiological resilience. | Exogenous lactate can decelerate growth and suppress the range of PSFs, revealing line-specific differences [85]. |
Visualizing Workflows and Relationships
Strategic Framework for Reproducible iPSC Research
The following diagram outlines the core strategic workflow for minimizing variability, from initial planning to final data interpretation.
Quantitative Framework for Monitoring Cell Population Heterogeneity
Advanced modeling techniques shift the analysis from population averages to a more nuanced view of rate distributions within a culture.
Addressing line-to-line variability is not about eliminating biological diversity, but rather about understanding, controlling, and accounting for it through rigorous science. By implementing the strategies outlined—adopting optimal experimental designs, enforcing stringent QC, leveraging standardized protocols, and utilizing advanced analytical tools like AI and PBE modeling—researchers can significantly enhance the reproducibility and predictive power of their iPSC-based disease models. This rigor is paramount for fulfilling the promise of iPSCs in elucidating disease mechanisms and advancing effective therapies into the clinic.
Optimizing Differentiation Efficiency for Chamber-Specific Cardiomyocytes
The derivation of induced pluripotent stem cells (iPSCs) has revolutionized cardiovascular research by providing a patient-specific platform for disease modeling, drug discovery, and potential regenerative therapies [88] [1]. Cardiomyocytes derived from human iPSCs have proven invaluable for studying inherited arrhythmias, cardiomyopathies, and drug-induced cardiotoxicity [89] [90]. However, a significant limitation persists: most differentiation protocols yield a mixed population of atrial-, ventricular-, and pacemaker-like cardiomyocytes, which can confound disease phenotypes and compromise therapeutic outcomes [90]. The human heart consists of functionally distinct chambers with specialized cardiomyocyte subtypes that exhibit unique structural, electrophysiological, and contractile properties. Recapitulating this diversity in vitro is essential for precise disease modeling and drug development [90]. This technical guide examines current strategies for optimizing the generation of chamber-specific cardiomyocytes, with particular emphasis on protocol efficiency, reproducibility, and maturation within the context of iPSC-based disease modeling research.
Developmental Principles Informing Protocol Optimization
Embryonic Origins of Chamber-Specific Cardiomyocytes
During mammalian cardiogenesis, the precursors of subtype-specific cardiomyocytes originate from distinct cellular populations in the first heart field (FHF) and second heart field (SHF) [90]. The FHF primarily gives rise to the left ventricle and parts of the atria, while the SHF contributes to the right ventricle, outflow tract, and portions of the atria [90]. This lineage specification is governed by precisely timed signaling events and transcriptional networks:
- Cardiac Mesoderm Induction: Initiated by BMP4 and Nodal signaling, leading to expression of key transcription factors including NKX2.5 and MESP1 [90].
- Myocardial Patterning: NOTCH signaling from the endocardium and retinoic acid (RA) signaling from the epicardium critically regulate chamber-specific differentiation and myocardial proliferation [90].
- Transcriptional Regulation: Core cardiac transcription factors including NKX2.5, GATA4, MEF2C, TBX5, and HAND2 interact in complex networks to establish and maintain subtype identity [90].
Key Signaling Pathways for Subtype Specification
NOTCH Signaling: NOTCH receptor-ligand interactions trigger proteolytic cleavage and release of the NOTCH intracellular domain (NICD), which translocates to the nucleus and activates target genes including HEY1/2 and HES1/5 [90]. NOTCH signaling modulates cardiomyocyte proliferation and differentiation and is required for ventricular chamber formation [90].
Retinoic Acid (RA) Signaling: RA from the epicardium regulates myocardial proliferation by inducing FGF signaling and plays essential roles in ventricular trabeculation and cardiac outflow tract morphogenesis [90]. RA signaling levels influence the atrial-ventricular specification balance, with higher RA signaling promoting atrial fate [90].
Figure 1: Signaling pathways and transcriptional regulation in cardiomyocyte subtype specification. Key developmental signals (WNT, BMP4, FGF, RA, NOTCH) activate transcription factor networks that guide progenitor cells from the first and second heart fields toward distinct ventricular, atrial, and nodal cardiomyocyte fates.
Advanced Differentiation Methodologies for Chamber-Specific Cardiomyocytes
Suspension Culture Systems for Enhanced Efficiency and Maturity
Recent advances in stirred suspension systems have demonstrated significant improvements in differentiation efficiency, reproducibility, and functional maturation compared to traditional monolayer approaches [32]. The optimized bioreactor protocol yields approximately 1.21 million cells per mL with ~94% cardiomyocyte purity (TNNT2+ cells) across multiple iPSC lines [32]. Key advantages of suspension systems include:
- Superior Scalability: Culture volumes from 2.5 to 1000 mL enable production of clinically relevant cardiomyocyte numbers [32].
- Reduced Batch Variability: Continuous monitoring and adjustment of temperature, O2, CO2, and pH parameters minimizes microenvironmental heterogeneity [32].
- Enhanced Functional Properties: Bioreactor-derived cardiomyocytes (bCMs) exhibit more mature functional properties compared to monolayer-derived counterparts, including earlier onset of contraction (differentiation day 5 vs. day 7) and higher expression of ventricular markers (MYH7, MYL2, MYL3) [32].
- Cardiac Organoid Generation: Modified suspension protocols enable generation of 3D cardiac organoids that model ventricular wall and chamber formation [32].
Stage-Specific Protocol Modifications for Subtype Specification
Ventricular Specification: Lower retinoic acid signaling during the cardiac progenitor stage promotes ventricular fate, resulting in 83.4% of cardiomyocytes staining positive for ventricular myosin light chain (MLC2v) [32]. Combined WNT activation followed by inhibition remains the foundational approach, with precise timing critical for ventricular outcomes [32] [89].
Atrial Specification: Higher retinoic acid exposure during cardiac progenitor specification drives atrial differentiation, upregulating atrial markers including MYL4 and MYL7 [32]. NOTCH signaling modulation provides additional control over atrial-ventricular patterning [90].
Progenitor Cell Reseeding for Enhanced Purity: Recent methodology demonstrates that detaching and reseeding cardiac progenitors at specific stages (EOMES+ mesoderm and ISL1+/NKX2-5+ cardiac progenitor cells) improves terminal cardiomyocyte purity by 10-20% without negatively impacting contractility, sarcomere structure, or junctional Cx43 expression [33].
Figure 2: Optimized workflow for chamber-specific cardiomyocyte differentiation. The process begins with iPSC aggregation and proceeds through mesoderm and cardiac progenitor stages, with key decision points for progenitor reseeding (to improve purity) and signaling modulation (to direct subtype specification).
Quantitative Comparison of Differentiation Platforms
Table 1: Performance Metrics of Cardiomyocyte Differentiation Platforms
| Parameter | Traditional Monolayer | Stirred Suspension System | Cardiac Progenitor Reseeding |
|---|---|---|---|
| Average Purity (% TNNT2+) | 50-70% [33] | ~94% [32] | 10-20% improvement over baseline [33] |
| Yield (cells/mL) | Variable, scale-limited | ~1.21 million [32] | Similar to baseline protocol [33] |
| Onset of Contraction | Differentiation day 7 [32] | Differentiation day 5 [32] | Similar to baseline protocol [33] |
| Batch-to-Batch Variability | Higher [32] | Significantly reduced [32] | Reduced via cryopreservation of progenitors [33] |
| Ventricular Subtype (% MLC2v+) | Lower, more variable [32] | 83.4% [32] | Unchanged or improved maturity [33] |
| Scalability | Limited by surface area | High (up to 1000mL demonstrated) [32] | Limited by surface area |
| Cryopreservation Recovery | <90% viability, functional impact [32] | >90% viability [32] | High recovery of progenitors [33] |
Table 2: Subtype Specification Efficiency Using Developmental Cues
| Specification Approach | Key Signaling Modulators | Marker Expression | Purity Reported |
|---|---|---|---|
| Ventricular | Low RA, NOTCH activation [90] | ↑ MYH7, MYL2, MYL3 [32] | 83.4% MLC2v+ [32] |
| Atrial | High RA, specific NOTCH inhibition [90] | ↑ MYL4, MYL7 [32] | Varies by protocol |
| Nodal | WNT inhibition, specific FGF signaling [90] | ↑ TBX18, SHOX2, HCN4 | Not quantified in results |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Chamber-Specific Cardiomyocyte Differentiation
| Reagent Category | Specific Examples | Function in Differentiation | Application Notes |
|---|---|---|---|
| Small Molecule Inducers | CHIR99021 (WNT activator) [32] [33] | Induces mesoderm formation | Concentration optimization critical for each cell line [32] |
| Small Molecule Inhibitors | IWP2, IWR-1 (WNT inhibitors) [32] [33] | Promotes cardiac mesoderm specification | Timing critical for efficiency [32] |
| Signaling Modulators | Retinoic Acid [90] | Directs atrial vs. ventricular specification | Concentration and timing determine subtype fate [90] |
| Extracellular Matrices | Matrigel, Vitronectin, Laminin-111 [89] [33] | Supports cell attachment and signaling | Defined matrices improve reproducibility [89] [33] |
| Cell Culture Media | RPMI/B27 [89], Essential-8, HiDef B8 [89] | Maintains pluripotency or supports differentiation | Chemically defined media reduce variability [89] |
| Characterization Antibodies | Anti-TNNT2, Anti-MLC2v, Anti-ACTN2 [32] | Cardiomyocyte identification and subtype validation | Flow cytometry, immunocytochemistry standard [32] |
Applications in Disease Modeling and Drug Development
The generation of chamber-specific cardiomyocytes has profound implications for cardiovascular disease modeling and drug development. Patient-specific atrial cardiomyocytes enable precise investigation of atrial fibrillation mechanisms, while ventricular cardiomyocytes derived from patients with hypertrophic or dilated cardiomyopathy provide authentic models of these conditions [90]. In pharmaceutical applications, the ability to test compound effects on specific cardiomyocyte subtypes enhances drug safety profiling, particularly for agents with known subtype-specific electrophysiological effects [90]. The CiPA (Comprehensive In Vitro Proarrhythmia Assay) initiative has highlighted the importance of using human iPSC-derived cardiomyocytes for evaluating drug-induced arrhythmic effects [90]. Furthermore, disease-specific cardiomyocyte subtypes serve as valuable platforms for high-throughput drug screening and personalized medicine approaches, allowing for the identification of patient-specific therapeutic responses [88] [90].
Optimizing differentiation efficiency for chamber-specific cardiomyocytes requires careful attention to developmental principles, protocol standardization, and quality control measures. The integration of suspension culture systems, stage-specific progenitor manipulation, and targeted signaling modulation enables generation of highly pure, functional cardiomyocyte subtypes suitable for disease modeling, drug screening, and therapeutic applications. Continued refinement of these methodologies will further enhance the fidelity of in vitro cardiac models and accelerate the translation of iPSC technology to clinical applications in precision cardiovascular medicine.
The field of induced pluripotent stem cell (iPSC) research has fundamentally transformed biomedical science by providing a virtually unlimited supply of patient-specific cells for disease modeling, drug discovery, and regenerative medicine [2]. Since their landmark discovery in 2006, iPSCs have enabled remarkable advances in personalized medicine by allowing researchers to reprogram somatic cells to a pluripotent state [2] [91]. However, a critical barrier persists: the consistent production of high-purity, functionally mature cells at scales necessary for robust scientific research and therapeutic applications. Frequently, iPSC-derived cells exhibit an immature, fetal-like phenotype upon differentiation, creating significant challenges for accurate disease modeling and drug screening [2]. The growing demand for stem cell technologies is reflected in market projections, with the global stem cell manufacturing market expected to grow from $16.23 billion in 2024 to $40.40 billion by 2032, representing a compound annual growth rate of 11.5% [92]. This exponential growth underscores the urgent need for advanced manufacturing technologies that can ensure the production of high-purity cells with consistent quality and functionality, particularly within the context of sophisticated disease modeling platforms that require precise cellular phenotypes.
Key Challenges in Scaling iPSC Production
Functional Immaturity of Differentiated Cells
A persistent challenge in iPSC technology is the tendency of differentiated cells to exhibit immature, fetal-like characteristics rather than adult phenotypes required for accurate disease modeling [2]. This functional immaturity limits the physiological relevance of in vitro models, particularly for late-onset diseases. Research indicates that overcoming this limitation requires more than simple differentiation protocols; it necessitates the recreation of complex tissue microenvironments through advanced co-culture systems and three-dimensional architectures that better mimic native tissue composition and organization [2].
Genomic and Epigenetic Instability
iPSC culture remains technically demanding due to the inherent genomic and epigenetic instability of pluripotent cells during prolonged expansion [91]. This instability can lead to batch-to-batch variability that compromises experimental reproducibility and reliability—particularly problematic for drug discovery applications where consistency is paramount. Rigorous quality control, including PCR-based assays and genomic integrity analyses, is essential but adds complexity to scaled production processes [91].
Manufacturing Cost and Complexity
The high costs associated with stem cell production present a significant barrier to widespread adoption, with expenses often surpassing traditional pharmaceutical manufacturing due to complex processes, specialized equipment, and stringent quality control requirements [92]. Stem cell therapy costs can range from $5,000 to $50,000, with manufacturing costs for human mesenchymal stem cells ranging from $1 to $5 per million cells at large scales using optimized processes [92]. These economic challenges are compounded by lengthy regulatory approval timelines and ethical considerations that vary across jurisdictions, further complicating scale-up initiatives [93] [94].
Table: Key Challenges in Scaling iPSC Production for Disease Modeling
| Challenge | Impact on Disease Modeling | Current Limitations |
|---|---|---|
| Functional Immaturity | Limited physiological relevance for adult-onset diseases | Fetal-like phenotypes in differentiated cells [2] |
| Genomic Instability | Reduced reproducibility and reliability | Batch-to-batch variability in differentiation outcomes [91] [93] |
| High Production Costs | Limited accessibility for research | Manufacturing costs of $1-5 per million cells [92] |
| Quality Control | Inconsistent experimental results | Lack of standardized culture protocols [91] |
Advanced Bioprocessing Technologies for Scale-Up
Automated Bioreactor Systems
The development of sophisticated bioreactor systems represents a cornerstone technology for large-scale iPSC production, enabling automated monitoring and adjustment of critical environmental parameters including pH, temperature, and oxygen levels [92]. These systems facilitate large-scale production under controlled conditions, reducing human error and variability while ensuring optimal growth conditions [92]. Advanced bioreactors maintain homogeneity throughout the culture vessel, providing consistent nutrient delivery and waste removal that is impossible to achieve with traditional flask-based culture systems. The integration of sensors and feedback control mechanisms allows for real-time process adjustments that maintain cells within optimal physiological ranges, dramatically improving yield, viability, and functional maturity of the resulting cells [92].
Three-Dimensional Culture Platforms
Three-dimensional culture systems have emerged as transformative technologies for enhancing the functional maturity of iPSC-derived cells. Research demonstrates that iPSC-derived cardiomyocytes (iPSC-CMs) exhibit higher expression of cardiac maturation markers when co-cultured with human coronary artery endothelial cells in a 3D gelatin methacryloyl hydrogel compared to classic 2D monocultures [2]. Omics analyses confirm the superiority of 3D environments, showing upregulation of pathways for cardiac differentiation and contraction in 3D systems [2]. These platforms better mimic the native tissue architecture, providing mechanical and biochemical cues that drive cells toward more mature phenotypes—a critical advantage for disease modeling applications requiring adult-like cellular characteristics. Additionally, 3D systems offer increased surface-to-volume ratios for enhanced production scalability compared to traditional 2D culture.
Integration of Artificial Intelligence
Artificial intelligence is revolutionizing stem cell manufacturing by enhancing process efficiency, precision, and scalability through advanced data analytics and machine learning algorithms [94]. AI enables real-time monitoring and optimization of stem cell culture conditions, ensuring consistent quality and yield while accelerating cell line development by predicting cell behavior and identifying optimal culture parameters [94]. The partnership between Invetech and AiCella exemplifies this trend, combining automation expertise with predictive AI models to identify critical process parameters, reduce variability, and support personalized therapies [94]. AI-powered automation reduces manual intervention, minimizing human error and contamination risks while facilitating predictive maintenance for manufacturing equipment and streamlining regulatory compliance through ensured data integrity and traceability [94].
Table: Advanced Bioprocessing Technologies for iPSC Scale-Up
| Technology | Key Features | Benefits for iPSC Production |
|---|---|---|
| Automated Bioreactors | Parameter monitoring (pH, O₂, temperature), feedback control | Reduced variability, higher yields [92] |
| 3D Culture Systems | Hydrogels, scaffold-based cultures, organoid generation | Enhanced functional maturity [2] |
| AI and Machine Learning | Predictive modeling, process optimization | Improved efficiency and quality [94] |
| Closed System Automation | Reduced human intervention, sterile processing | Lower contamination risk [92] [94] |
Quality Control and Analytics for High-Purity Cells
Molecular Characterization Techniques
Ensuring cell purity and functionality requires sophisticated analytical approaches, including the innovative "molecular bridge" technology that connects genetic barcode tracking with single-cell RNA sequencing [95]. This system enables researchers to simultaneously quantify in vivo lineage output and gene expression at the single-cell level by creating a directory that links genetic tracking barcodes with cellular cDNA barcodes [95]. Such approaches allow for unprecedented correlation between stem cell gene expression patterns and functional outcomes, providing critical insights for quality assessment. Additionally, omics analyses—including transcriptomics, proteomics, and metabolomics—provide comprehensive characterization of cell populations, verifying differentiation efficiency and identifying potential impurities or aberrant cell states that might compromise disease modeling accuracy [2].
Functional Maturation Assessment
Beyond molecular markers, functional assessment is essential for validating iPSC-derived cells, particularly for disease modeling applications. Research demonstrates that co-cultures of iPSC-derived cardiomyocytes (iPSC-CMs) and iPSC-derived cardiac fibroblasts (iPSC-CFs) exhibit significantly improved contractile function compared to monocultures, with larger contractile strain, increased rate of spontaneous contraction, faster kinetics, and enhanced contractile anisotropy and myofibril alignment [2]. These functional improvements require both paracrine signaling and direct cellular interactions, highlighting the importance of complex culture environments for achieving physiological relevance [2]. Such functional assessments provide critical quality metrics beyond simple purity measurements, ensuring that cells possess the appropriate physiological characteristics for disease modeling and drug screening applications.
Cryopreservation and Cold Chain Management
Maintaining cell viability and function during storage and transportation presents significant challenges for scaled production. Research indicates that temperature fluctuations above the glass transition temperature of cryoprotectants like dimethyl sulfoxide (-120°C) trigger a cascade of events culminating in cell death, beginning with disrupted mitochondrial cytochrome signaling and membrane potential rather than immediate loss of membrane integrity [2]. Understanding these cellular responses to temperature variations enables the development of quality control strategies incorporating precise temperature controls and cell-specific assays to preserve viability and function throughout the cold chain [2]. Advanced cryopreservation methods enhance long-term storage and viability, ensuring that cells maintain functionality after thawing and expanding their availability for research and therapeutic use [92].
Experimental Protocols for High-Purity Cell Production
3D Hydrogel Co-Culture System for Cardiac Cell Maturation
Objective: Enhance functional maturation of iPSC-derived cardiomyocytes through 3D co-culture with endothelial cells.
Methodology:
- Differentiation: Generate iPSC-derived cardiomyocytes (iPSC-CMs) using established directed differentiation protocols.
- Hydrogel Preparation: Prepare a 3D gelatin methacryloyl (GelMA) hydrogel solution at a concentration of 5-10% (w/v) in culture medium.
- Cell Encapsulation: Mix iPSC-CMs with human coronary artery endothelial cells at a ratio of 2:1 and suspend in the GelMA solution at a density of 10-20 million cells/mL.
- Crosslinking: Add photoinitiator (0.05% w/v LAP) and expose to UV light (365 nm, 5-10 mW/cm²) for 30-60 seconds to form a stable hydrogel.
- Culture Maintenance: Culture the constructs in cardiac maturation medium, changing every 48-72 hours for 14-28 days.
- Functional Assessment: Measure expression of cardiac maturation markers (TNNT2, MYL2, MYH7) via qPCR and immunostaining. Evaluate contractile function using video-based analysis systems [2].
Quality Control:
- Perform flow cytometry to quantify cardiomyocyte purity (typically >90% TNNT2+ cells).
- Assess viability using LIVE/DEAD staining (>85% viability expected).
- Monitor metabolic activity via mitochondrial function assays.
Molecular Bridge Technology for Single-Cell Lineage Tracking
Objective: Correlate single-cell gene expression with lineage output using genetic barcoding.
Methodology:
- Barcode Library Construction: Generate a lentiviral library containing >100,000 unique genetic barcodes.
- Cell Labeling: Transduce iPSCs at low MOI (<0.3) to ensure single barcode integration. Select with puromycin for 7 days.
- Transplantation/Differentiation: Differentiate barcoded iPSCs toward desired lineage or transplant into animal models.
- Single-Cell RNA Sequencing: Prepare single-cell suspensions and process using 10x Genomics Chromium system.
- Molecular Bridge Amplification: From cDNA, perform PCR using primers specific to genetic barcodes and cellular barcodes to create "molecular bridge" library.
- Sequencing and Analysis: Sequence both cDNA and molecular bridge libraries. Use molecular bridges to link single-cell transcriptomes with lineage outputs quantified through barcode abundance [95].
Data Analysis:
- Map quantitative associations between gene expression and lineage output across individual cells.
- Identify genes whose expression correlates with specific differentiation efficiencies.
- Construct differentiation trajectory maps based on lineage potential [95].
Diagram: Molecular Bridge Workflow for Linking Gene Expression and Lineage Output
Essential Research Reagent Solutions
Table: Key Research Reagents for iPSC Scale-Up and Differentiation
| Reagent Category | Specific Examples | Function in Scale-Up |
|---|---|---|
| Reprogramming Factors | Oct4, Sox2, Klf4, c-Myc | Induce pluripotency in somatic cells [91] |
| Culture Matrices | Gelatin methacryloyl (GelMA), Matrigel | Provide 3D scaffolding for maturation [2] |
| Differentiation Media | Cardiomyocyte, neuronal, hepatocyte kits | Direct lineage-specific differentiation [93] |
| Cell Separation | FACS antibodies, magnetic beads | Isulate specific cell populations [95] |
| Cryopreservation | DMSO-containing solutions | Maintain viability during storage [2] |
| Quality Control | PCR primers, flow cytometry antibodies | Assess purity and functionality [91] |
Signaling Pathways in iPSC Maturation
The functional maturation of iPSC-derived cells involves coordinated activation of multiple signaling pathways that mimic developmental processes. Research using 3D co-culture systems has demonstrated upregulation of pathways for cardiac differentiation and contraction, including Wnt/β-catenin signaling, TGF-β superfamily pathways (BMP and Activin/Nodal), and Notch signaling [2]. In cardiac maturation, these pathways drive structural and functional development through precise temporal activation and inhibition patterns. Similarly, successful differentiation to other lineages requires stage-specific manipulation of relevant signaling cascades to replicate in vivo development and achieve adult-like phenotypes suitable for disease modeling.
Diagram: Signaling Pathways Driving Functional Maturation of iPSC-Derived Cells
The scalable production of high-purity, functionally mature cells from iPSCs represents a critical enabling technology for advancing disease modeling and drug discovery. While significant challenges remain in achieving consistent adult-like phenotypes at industrial scales, integrated technological approaches combining advanced bioreactor systems, 3D culture platforms, artificial intelligence, and rigorous quality control show tremendous promise. The continued refinement of these technologies will accelerate the development of more physiologically relevant in vitro models that better recapitulate human disease, ultimately enhancing drug screening accuracy and enabling personalized medicine approaches. As these scalable production methodologies mature, they will dramatically expand the accessibility and applicability of iPSC technology across biomedical research and therapeutic development.
Validating iPSC Models: From Cellular Phenotypes to Regulatory Frameworks
The field of drug development has long been hampered by a significant translational gap, where promising interventions frequently fail in human clinical trials after showing efficacy in traditional animal models. This disconnect often stems from species-specific differences in genetics, immune responses, and organ physiology that limit the predictive power of even the most sophisticated animal studies [61]. The advent of induced pluripotent stem cell (iPSC) technology has fundamentally transformed this landscape by providing unprecedented access to patient-specific, pluripotent cell sources capable of differentiating into virtually any human cell type [61]. Phenotypic validation—the process of confirming that in vitro disease models accurately recapitulate key pathological hallmarks—serves as the critical bridge between stem cell biology and clinically meaningful applications. This whitepaper provides a comprehensive technical framework for researchers and drug development professionals to design, execute, and interpret phenotypic validation studies using iPSC-derived models, thereby enabling more predictive disease modeling and therapeutic screening.
Core Principles of Phenotypic Validation
Phenotypic validation requires a multi-parameter approach that moves beyond single-marker analysis to capture the complex pathophysiology of human diseases. The core objective is to demonstrate that an in vitro system faithfully reproduces the essential cellular and molecular features observed in human patients.
Foundational Requirements for Robust Validation
- Patient-Derived Specificity: Utilize iPSCs from genetically characterized patients to maintain authentic disease genotypes and phenotypes throughout differentiation protocols. This preserves the natural genetic diversity and modifier backgrounds present in human populations, which often significantly influence disease expression and therapeutic response [61].
- Isogenic Control Engineering: Employ CRISPR-Cas9 gene editing to create genetically matched control lines by correcting or introducing specific disease-associated mutations in otherwise identical genetic backgrounds. This powerful approach strengthens causal inference by isolating the effects of specific genetic variants from general background genetic variation [61].
- Multi-modal Assessment: Implement complementary analytical techniques that evaluate molecular, structural, functional, and metabolic disease hallmarks across multiple scales—from subcellular components to tissue-level organization. This comprehensive approach ensures that validated models capture the multifaceted nature of human pathologies.
Hierarchical Validation Framework
A tiered validation strategy ensures systematic assessment across biological organization levels. The most compelling disease models demonstrate concordance across multiple validation tiers, with higher-level functional deficits emerging from more fundamental molecular and cellular perturbations.
Technical Workflow for Comprehensive Phenotypic Validation
Establishing a robust phenotypic validation pipeline requires meticulous attention to protocol standardization, quality control checkpoints, and analytical rigor throughout the process from iPSC culture to final phenotypic analysis.
iPSC Differentiation and Quality Control
The foundation of any successful phenotypic validation study begins with reproducible and high-quality differentiation of iPSCs into relevant cell types.
Multi-parameter Phenotypic Assessment
Following successful differentiation, comprehensive phenotypic assessment evaluates disease hallmarks across multiple biological dimensions using integrated analytical approaches.
Table 1: Phenotypic Validation Parameters and Assessment Methodologies
| Validation Tier | Key Parameters | Assessment Methodologies | Validation Criteria |
|---|---|---|---|
| Genetic/Molecular | Gene expression patterns, protein localization, epigenetic modifications | RNA-seq, Western blot, immunocytochemistry, qPCR | Differential expression of disease-relevant genes, correct protein localization |
| Cellular/Morphological | Cell size, shape, organelle structure, neurite length (neuronal models) | High-content imaging, transmission electron microscopy, morphometric analysis | Presence of pathological cellular inclusions, organelle abnormalities |
| Structural/Tissue | Tissue architecture, cell-cell interactions, polarization | Confocal microscopy, histology, 3D reconstruction | Disrupted tissue organization, aberrant cell layering |
| Functional/Physiological | Electrical activity, calcium handling, contractile force, metabolic activity | Multi-electrode arrays, patch clamping, calcium imaging, Seahorse analyzer | Pathological electrophysiology, metabolic dysfunction |
Experimental Protocols for Key Validation Methodologies
This section provides detailed technical protocols for essential phenotypic validation methodologies, with emphasis on critical optimization parameters and quality control measures.
Immunofluorescence Validation of Protein Expression and Localization
This protocol enables simultaneous assessment of protein expression levels, subcellular localization, and cellular morphology in iPSC-derived cultures.
- Cell Fixation and Permeabilization: Aspirate culture medium and wash cells once with pre-warmed PBS. Fix with 4% paraformaldehyde in PBS for 15 minutes at room temperature. Permeabilize with 0.1% Triton X-100 in PBS for 10 minutes. Include appropriate positive and negative control samples with each experiment to validate antibody specificity and establish background signal levels [61].
- Antibody Staining: Block with 5% normal serum from secondary antibody host species for 1 hour. Incubate with primary antibodies diluted in blocking solution overnight at 4°C. Include isotype controls to distinguish specific from non-specific binding. Wash three times with PBS containing 0.05% Tween-20 (5 minutes per wash). Incubate with fluorophore-conjugated secondary antibodies (1:500) and nuclear counterstain (e.g., Hoechst 33342) for 1 hour at room temperature protected from light.
- Imaging and Analysis: Acquire images using a high-content imaging system or confocal microscope with consistent exposure settings across experimental groups. Quantify fluorescence intensity, subcellular distribution patterns, and co-localization coefficients using ImageJ or specialized image analysis software. Analyze a minimum of 10 random fields per condition with appropriate statistical testing between disease and control groups.
Functional Calcium Imaging in iPSC-Derived Cardiomyocytes
This protocol assesses calcium handling properties, which are frequently disrupted in cardiac disease models, using fluorometric indicators.
- Cell Loading with Calcium Indicator: Culture iPSC-derived cardiomyocytes on glass-bottom dishes optimized for live-cell imaging. Replace culture medium with recording buffer containing 2-5 μM Cal-520 AM or Fluo-4 AM calcium indicator dye. Include 0.02% Pluronic F-127 to facilitate dye loading. Incubate for 30 minutes at 37°C followed by a 30-minute de-esterification period in dye-free buffer.
- Image Acquisition and Stimulation: Place cells on a temperature-controlled stage (37°C) with continuous perfusion of oxygenated recording buffer. Field stimulate cardiomyocytes at 1 Hz frequency using parallel platinum electrodes. Acquire images at 100-200 frames per second using a high-speed CCD camera and appropriate excitation/emission filters. Record baseline activity for 2 minutes followed by experimental interventions.
- Data Analysis and Interpretation: Analyze calcium transients using specialized software (e.g., IonOptix, SoftEdge). Quantify amplitude, time-to-peak, decay kinetics (tau), and spontaneous events. Compare a minimum of 30 single cells per condition from at least three independent differentiations. Abnormal calcium handling is indicated by prolonged decay kinetics, reduced amplitude, or increased frequency of spontaneous calcium release events.
Multi-Electrode Array (MEA) Analysis of Neuronal Network Activity
This protocol enables non-invasive, long-term monitoring of electrophysiological activity in iPSC-derived neuronal cultures, particularly relevant for neurological disease modeling.
- Culture Preparation and Baseline Recording: Plate iPSC-derived neurons directly on MEA plates pre-coated with poly-D-lysine and laminin. Maintain cultures for 4-8 weeks to establish mature synaptic networks. For recording, replace culture medium with pre-warmed artificial cerebrospinal fluid recording solution. Allow the MEA plate to equilibrate for 10 minutes in the recording setup before beginning acquisition.
- Signal Acquisition and Parameter Extraction: Acquire signals at 25-50 kHz sampling rate with appropriate band-pass filtering (typically 1-5000 Hz). Record baseline activity for 15 minutes to establish network properties. Extract key parameters including mean firing rate, burst frequency, burst duration, number of spikes per burst, and network synchronization index. Include positive controls such as GABAergic or glutamatergic receptor modulators to confirm appropriate network responses.
- Pharmacological Challenge and Data Interpretation: Apply disease-relevant pharmacological challenges during recording (e.g., pro-epileptogenic compounds for seizure disorders, dopamine receptor agonists for Parkinson's disease models). Analyze changes in network activity patterns compared to baseline and isogenic control lines. Conduct experiments using a minimum of three independent differentiations with multiple technical replicates (different MEA wells) per differentiation.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful phenotypic validation requires carefully selected reagents, tools, and platforms that ensure reproducibility, specificity, and physiological relevance.
Table 2: Essential Research Reagents and Platforms for Phenotypic Validation
| Category | Specific Examples | Key Function | Technical Considerations |
|---|---|---|---|
| Stem Cell Culture | mTeSR Plus, StemFlex, Essential 8 Medium | Maintain pluripotency and support expansion | Use defined, xeno-free formulations to reduce batch variability |
| Differentiation Kits | Cardiomyocyte differentiation kits (e.g., Gibco, STEMCELL Technologies) | Directed differentiation into specific lineages | Optimize protocol timing for specific iPSC lines; include quality control checkpoints |
| Gene Editing Tools | CRISPR-Cas9 systems, ribonucleoprotein complexes | Create isogenic controls and introduce disease mutations | Validate editing efficiency and screen for off-target effects |
| Cell Characterization | Flow cytometry antibodies, ICC validated antibodies, lineage-specific markers | Assess differentiation efficiency and purity | Use validated, species-appropriate antibodies with relevant controls |
| Functional Assays | FLIPR calcium assays, multi-electrode arrays, Seahorse XF analyzers | Measure physiological responses and metabolic activity | Establish baseline parameters using control lines for comparison |
| Advanced Imaging | High-content imaging systems, confocal microscopes, live-cell imaging chambers | Quantify morphological and structural phenotypes | Standardize imaging parameters across experimental conditions |
Data Presentation and Analysis Framework
Effective presentation of phenotypic validation data is essential for clear scientific communication and rigorous interpretation. Proper table design significantly enhances the clarity and interpretability of complex datasets.
Guidelines for Effective Data Presentation in Tables
- Structural Optimization for Comparison: Organize tables to facilitate vertical comparison of numerical data by implementing right-flush alignment for numeric columns and their headers. This approach leverages the natural reading direction of numbers, which increase in size from right to left [96]. Use tabular fonts (e.g., Lato, Roboto, Source Sans Pro) where each character has equal width to ensure proper vertical alignment of place values across all data points [96].
- Visual Clarity and Readability Enhancement: Reduce visual clutter by eliminating heavy grid lines and removing unit repetition within cells [97] [96]. Ensure headers stand out from the table body through subtle formatting distinctions such as bold typeface or different background coloring [97]. Maintain consistent precision levels within columns by rounding to the same number of decimal places and using commas to group thousands where appropriate [96].
- Context and Interpretation Support: Use clear, active titles that immediately convey the table's purpose and content [97]. Highlight statistical significance and outliers through consistent symbol systems explained in a key or legend [97] [96]. For complex datasets, consider using alternating row shading (zebra striping) to improve readability while maintaining sufficient color contrast between text and background [97].
Framework for Statistical Analysis and Interpretation
Robust statistical analysis is fundamental to meaningful phenotypic validation. The following framework ensures appropriate interpretation of validation data:
- Experimental Design Principles: Implement blinding during data acquisition and analysis to prevent unconscious bias. Include appropriate sample sizes based on power calculations from pilot studies. Utilize balanced experimental designs that distribute potential confounding factors (e.g., differentiation batch effects) across comparison groups.
- Multi-level Analysis Approach: For imaging-based data, analyze both at the single-cell level and well/population level to capture both cell-autonomous and population-level phenotypes. For functional data (e.g., MEA, calcium imaging), employ time-series appropriate statistical methods that account for autocorrelation and multiple comparisons.
- Validation Metrics and Thresholds: Establish pre-defined validation criteria for each disease hallmark before beginning experiments. Determine effect size thresholds that are biologically meaningful rather than relying solely on statistical significance. Implement multiple hypothesis testing corrections when evaluating numerous parameters simultaneously.
Phenotypic validation represents the critical foundation for establishing the relevance and predictive power of iPSC-based disease models. The comprehensive framework presented here—encompassing multi-parameter assessment, rigorous experimental protocols, and clear data presentation—enables researchers to build robust bridges between in vitro observations and human pathophysiology. As the field advances, emerging technologies in single-cell omics, high-content imaging, and bioengineered microenvironments will further enhance our validation capabilities. However, the core principles of methodological rigor, appropriate controls, and transparent reporting will remain essential for generating disease models that truly recapitulate pathological hallmarks in a dish and ultimately accelerate the development of effective therapeutics for human diseases.
The predictive validity of preclinical models is a cornerstone of biomedical research and drug development. For decades, animal models have served as the primary system for evaluating drug efficacy and safety. However, the persistent high attrition rates in clinical trials have revealed critical limitations in the translational relevance of these traditional models. The emergence of induced pluripotent stem cell (iPSC) technology represents a paradigm shift in disease modeling and drug discovery. This whitepaper provides a comprehensive technical comparison between iPSC-based human models and conventional animal models, analyzing their respective predictive capabilities, applications, and limitations within the context of modern disease modeling and drug development pipelines.
The fundamental challenge driving this comparison is the translational gap between preclinical results and clinical outcomes. Despite widespread use of animal models, approximately 90% of drugs that enter clinical trials fail to gain regulatory approval, often due to unexpected lack of efficacy or safety issues in humans that were not predicted by animal studies [98]. This discrepancy arises from inherent species-specific differences in physiology, genetics, and disease mechanisms that limit the predictive value of animal data for human outcomes.
iPSC technology, pioneered by Yamanaka and colleagues, enables the reprogramming of adult somatic cells into a pluripotent state through the introduction of specific transcription factors [1]. These patient-derived cells can then be differentiated into various human cell types, including neurons, cardiomyocytes, and hepatocytes, providing genetically relevant human systems for disease modeling and drug testing. The convergence of iPSC technology with advanced 3D culture systems has further accelerated the development of human organoids that recapitulate complex tissue architecture and functionality, offering unprecedented opportunities for human-specific disease modeling and therapeutic development.
Fundamental Biological Differences
Genetic and Evolutionary Considerations
The genetic divergence between humans and commonly used animal models introduces significant limitations in translational predictability. While rodent models share approximately 85-90% genetic homology with humans, critical differences exist in gene regulation, splicing patterns, and non-coding regions that substantially impact disease manifestations and drug responses [99]. For neurodevelopmental disorders specifically, the dramatically increased cortical expansion and circuit complexity in humans means that many aspects of human brain development and function cannot be adequately modeled in rodents [99].
iPSC technology fundamentally addresses this limitation by preserving the complete genetic background of human donors, including:
- Patient-specific genetic variations that influence disease susceptibility and treatment response
- Human-specific gene regulatory elements and epigenetic markers
- Complete human transcriptional and splicing patterns that affect protein function and drug targets
- Mitochondrial genetic variants that can influence metabolic functions and drug metabolism
The preservation of the human genetic context in iPSC models enables researchers to study diseases within their native genomic environment, eliminating the need to infer human relevance from evolutionarily distant species.
Physiological and Metabolic Disparities
Beyond genetic differences, significant physiological variations between species impact drug pharmacokinetics, pharmacodynamics, and toxicity profiles. Key differences include:
- Drug metabolism enzymes with varying expression levels and substrate specificities
- Ion channel distributions and properties that affect cardiotoxicity predictions
- Blood-brain barrier characteristics that influence central nervous system drug penetration
- Immune system components and inflammatory responses that modify therapeutic outcomes
- Cellular repair mechanisms and stress responses that affect toxicology assessments
Animal models often fail to predict human-specific toxicities, as demonstrated by the case of the drug fialuridine, which caused severe liver failure in humans despite showing minimal toxicity in animal models [98]. Similarly, many compounds demonstrating efficacy in animal models of neurological diseases have failed in human trials, partly due to fundamental differences in neuronal circuitry and neurotransmitter systems [99].
iPSC-derived human cells maintain species-specific physiological properties, including:
- Human-specific metabolic enzyme profiles in hepatocytes
- Native human cardiac ion channel compositions in cardiomyocytes
- Authentic human neuronal subtypes and receptor distributions
- Human-specific cell signaling pathways and second messenger systems
Technical Comparison of Model Systems
iPSC Technology: Methods and Applications
The core technology of iPSC generation involves reprogramming somatic cells (typically skin fibroblasts or blood cells) to a pluripotent state through the introduction of defined transcription factors. The original method utilized retroviral delivery of OCT4, SOX2, KLF4, and c-MYC (OSKM), but the field has evolved to include non-integrating methods such as Sendai virus, episomal plasmids, mRNA transfection, and small molecule approaches [1].
Key Technical Protocols:
Somatic Cell Reprogramming
- Source cells: Dermal fibroblasts, peripheral blood mononuclear cells, or keratinocytes
- Reprogramming method: Non-integrating Sendai virus containing OSKM factors
- Culture conditions: Feeder-free or feeder-dependent systems using mouse embryonic fibroblasts
- Timeline: 3-4 weeks for iPSC colony emergence and expansion
iPSC Characterization and Quality Control
- Pluripotency marker analysis: Immunofluorescence for OCT4, SOX2, NANOG, SSEA-4
- Trilineage differentiation potential: Embryoid body formation and differentiation
- Karyotype analysis: G-banding or spectral karyotyping to ensure genetic stability
- Identity verification: Short tandem repeat profiling to confirm donor origin
Directed Differentiation to Relevant Cell Types
- Cardiomyocytes: Based on Wnt pathway modulation using small molecules
- Neurons: Dual SMAD inhibition to induce neural precursor cells
- Hepatocytes: Sequential exposure to activin A, FGF, and BMP factors
- Intestinal organoids: Wnt activation and EGF treatment to induce crypt-villus structures
The development of automated iPSC production systems has significantly improved reproducibility and scalability, addressing earlier challenges with batch-to-batch variability [100]. Modern platforms can generate thousands of standardized, quality-controlled iPSC lines, enabling large-scale studies that would be impossible with manual methods [101].
Animal Models: Traditional Approaches and Modern Innovations
Traditional animal models range from invertebrates (C. elegans, Drosophila) to vertebrates (zebrafish, rodents, and larger mammals). Each offers distinct advantages and limitations based on their evolutionary proximity to humans, physiological complexity, and experimental tractability.
Key Animal Model Protocols:
Genetically Engineered Mouse Models
- Transgenic approaches: Random integration of human transgenes
- Knock-in/Knock-out models: Homologous recombination for targeted genetic modifications
- CRISPR/Cas9 systems: Direct embryonic manipulation for efficient gene editing
- Humanized models: Incorporation of human genes, cells, or tissues
Disease Induction Methods
- Chemical induction: Carcinogens, toxins, or diet manipulations
- Surgical modifications: Vessel occlusion, organ resection, or shunt procedures
- Cell line implantation: Xenograft models using human cancer cells
- Microbiome manipulation: Antibiotic treatment and fecal transplantation
Phenotypic Characterization Standards
- Behavioral testing: Morris water maze, open field, rotarod, social interaction tests
- Physiological monitoring: Telemetry, metabolic cages, echocardiography
- Molecular analyses: Tissue harvesting for transcriptomics, proteomics, and histology
- Imaging modalities: MRI, CT, PET, and bioluminescent imaging
Recent advances in genetic engineering, particularly CRISPR-Cas9 technology, have enhanced the precision and efficiency of animal model generation, enabling more accurate recapitulation of human genetic variations [102]. The market for genetically engineered animal models is projected to grow significantly, with the mice segment accounting for approximately 65% market share due to their genetic tractability and well-characterized biology [102].
Quantitative Comparison of Predictive Capabilities
Table 1: Direct Comparison of Predictive Capabilities Between iPSC Models and Animal Models
| Parameter | iPSC-Derived Models | Animal Models | Clinical Correlation |
|---|---|---|---|
| Cardiotoxicity Prediction | 85-90% concordance with clinical outcomes [98] | 70-75% concordance, species-specific ion channel differences [98] | iPSC-cardiomyocytes detect human-relevant proarrhythmic effects |
| Hepatotoxicity Assessment | Human-specific metabolic profiles; detects species-specific toxicities [98] | Limited by divergent drug metabolism pathways | Improved prediction of human-relevant liver toxicity with iPSC-hepatocytes |
| Neurotoxicity Testing | Human neuronal subtypes with authentic receptor expression | Limited by blood-brain barrier differences and neuronal circuitry disparities | Human-specific neurotoxic effects better modeled with iPSC-derived neurons |
| Drug Efficacy Screening | Preserves patient-specific genetic background; enables personalized medicine approaches [100] | Limited by species differences in drug targets and signaling pathways | iPSC models show superior correlation with patient-specific drug responses |
| Metabolic Disease Modeling | Maintains human-specific metabolic regulation | Limited by fundamental metabolic pathway differences | Human iPSC models better replicate inherited metabolic disorders |
| Complex Disease Modeling | Emerging via 3D organoid systems; captures some human disease pathology | Established for phenotypic screening but limited by species barriers | Organoids show promise for modeling human-specific disease features |
Table 2: Technical and Practical Considerations for Research Applications
| Consideration | iPSC-Derived Models | Animal Models |
|---|---|---|
| Development Timeline | 2-3 months for differentiation; faster with automation [100] | 6-12 months for breeding and validation; longer for complex genetic models |
| Cost Factors | High initial reprogramming costs; moderate maintenance expenses | Varies by species; genetically engineered models require significant investment |
| Throughput Capability | High-throughput screening compatible; scalable automation available [100] | Lower throughput; limited by housing capacity and ethical considerations |
| Genetic Control | Precise genetic manipulation via CRISPR; patient-specific mutations [1] | Established genetic engineering; but human transgenes may not function identically |
| Regulatory Acceptance | Evolving frameworks for toxicity testing; increasing adoption | Well-established regulatory pathways for preclinical data |
| Species Relevance | Human genetic background and cellular physiology | Species-specific differences limit human extrapolation |
| Complexity Level | Developing improved organoid systems but lack full organismal context | Intact physiological systems with organ-organ interactions |
| Standardization Status | Improving with automation but batch-to-batch variability remains a challenge [98] | Well-standardized protocols with established phenotypic benchmarks |
Experimental Design and Workflows
iPSC-Based Disease Modeling Workflow
iPSC Disease Modeling Workflow
The standardized workflow for iPSC-based disease modeling and drug screening begins with patient recruitment and somatic cell collection, typically through minimally invasive methods such as skin punch biopsies or blood draws. Sample collection must include appropriate controls (healthy individuals, family members, or isogenic corrected lines) and comply with ethical guidelines for human subject research.
Critical quality control checkpoints include:
- Comprehensive pluripotency assessment through immunocytochemistry, flow cytometry, and qPCR analysis of marker expression
- Genetic stability monitoring via karyotyping and whole-genome sequencing to detect chromosomal abnormalities
- Line identity verification through STR profiling to prevent cross-contamination
- Microbiological testing to ensure absence of mycoplasma and other contaminants
Differentiation protocols have become increasingly efficient and reproducible, with many available as commercial kits. However, researchers must validate differentiation efficiency for each batch using cell-type specific markers and functional assays. For neuronal differentiations, this includes immunostaining for TUJ1, MAP2, and cell-type specific markers, combined with electrophysiological measurements of neuronal activity. For cardiomyocyte differentiations, validation includes staining for cardiac troponin and α-actinin, along with measurement of spontaneous beating and response to pharmacological agents.
Animal Model Experimental Workflow
Animal Model Experimental Workflow
The animal model workflow begins with careful experimental design and model selection, considering factors such as species relevance, genetic background, age, and sex. Researchers must obtain Institutional Animal Care and Use Committee (IACUC) approval, which requires justification of animal numbers through power analysis and implementation of the 3Rs principles (Replacement, Reduction, Refinement).
Key considerations in animal model studies include:
- Proper acclimatization periods to minimize stress-related artifacts
- Randomization procedures to eliminate cage placement and handling biases
- Blinded assessment of outcomes to prevent observer bias
- Appropriate sample sizes determined by power analysis rather than tradition
- Environmental standardization of lighting, temperature, and circadian rhythms
Modern animal research incorporates advanced in vivo monitoring technologies including:
- Non-invasive imaging (MRI, CT, PET) for longitudinal assessment
- Telemetric monitoring of physiological parameters in conscious animals
- Automated behavioral analysis systems for objective quantification
- Biosensor implantation for continuous biomarker monitoring
Endpoint analyses typically involve comprehensive histological examination, molecular profiling, and correlation with functional measurements. The translation of findings to human contexts requires careful consideration of species differences in anatomy, physiology, and disease mechanisms.
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Platforms for iPSC and Animal Research
| Category | Specific Products/Systems | Key Applications | Technical Considerations |
|---|---|---|---|
| iPSC Reprogramming Systems | CytoTune Sendai Virus, Episomal Vectors, mRNA Kits | Footprint-free reprogramming of somatic cells | Integration-free methods preferred for clinical applications; efficiency varies by cell type |
| iPSC Culture Media | mTeSR, StemFlex, Essential 8 | Maintenance of pluripotency | Feeder-free systems improve reproducibility; xeno-free formulations needed for therapies |
| Differentiation Kits | Cardiomyocyte, Neural, Hepatic Differentiation Kits | Directed differentiation to specific lineages | Protocol optimization often required for different iPSC lines; quality varies between vendors |
| Characterization Tools | Pluripotency Antibody Panels, Flow Cytometry Kits | Quality control of iPSCs and differentiated cells | Standardized panels enable cross-study comparisons; mandatory for regulatory submissions |
| Animal Model Sources | Charles River, Jackson Laboratory, Taconic Biosciences | Sourcing of genetically defined models | Genetic background significantly impacts phenotypes; health status critical for reproducibility |
| Genome Editing Tools | CRISPR-Cas9 Systems, Transgenic Core Services | Genetic modification of iPSCs and animals | Off-target effects must be thoroughly assessed; verification of modifications essential |
| Automated Platforms | CompacT Select, CellXpress.ai | Large-scale iPSC production and differentiation | Reduce manual labor and variability; require significant capital investment |
| Analytical Instruments | Multi-electrode Arrays, High-content Imagers, Metabolic Assays | Functional characterization of models | Standardized protocols enable data comparison across laboratories |
Applications in Disease Research and Drug Development
Neurodevelopmental and Neurological Disorders
The application of iPSC technology to neurological disorders highlights both the capabilities and current limitations of this approach. For neurodevelopmental disorders (NDDs) such as autism spectrum disorder and intellectual disability, iPSC models have revealed disease-specific phenotypes in neuronal differentiation, migration, synapse formation, and neural network activity that correlate with clinical manifestations [99]. These human-specific cellular phenotypes often differ from those observed in rodent models of the same genetic disorders, explaining some of the translational failures of therapeutics developed in animal models.
In one representative study, iPSCs from patients with Rett syndrome demonstrated impaired neuronal maturation and synaptic defects that were reversible with experimental therapeutics, providing insights into potential intervention strategies [99]. Similarly, iPSC-derived neurons from Alzheimer's disease patients with presenilin mutations showed increased production of amyloid-beta isoforms and enhanced tau phosphorylation, replicating key pathological features of the human disease [98].
However, current 2D neuronal cultures lack the complexity of human brain circuitry, limiting their utility for studying higher-order network dysfunction. The development of 3D brain organoids addresses some of these limitations by enabling the formation of layered cortical structures and more complex cell-cell interactions. These advanced models have demonstrated utility in studying Zika virus-induced microcephaly and mechanisms of neurodevelopmental diseases [98].
Cardiovascular and Metabolic Diseases
iPSC-derived cardiomyocytes have become the standard model for preclinical cardiotoxicity screening, significantly outperforming animal models in predicting drug-induced arrhythmias [98]. The comprehensive in vitro proarrhythmia assay (CiPA) initiative has formally validated iPSC-cardiomyocytes for drug safety assessment, recognizing their superior predictive value for human cardiac responses compared to animal models.
In disease modeling, patient-specific iPSC-cardiomyocytes have successfully recapitulated the electrophysiological features of hereditary channelopathies such as long QT syndrome, including the characteristic prolonged action potential duration and increased arrhythmia susceptibility. These models have enabled drug screening campaigns that identified compounds capable of correcting the underlying electrophysiological defects, several of which have advanced to clinical trials [98].
For metabolic diseases, iPSC-derived hepatocytes provide human-relevant systems for studying drug metabolism and liver toxicity. While these cells typically exhibit fetal-like characteristics, recent advances in 3D culture and co-culture systems have improved hepatocyte maturation, enhancing their utility for modeling human-specific drug-induced liver injury.
Cancer and Personalized Medicine
Patient-derived tumor organoids (PDTOs) represent a powerful application of iPSC technology in oncology. These models preserve the genomic heterogeneity of the original tumors and have demonstrated remarkable concordance with patient responses to chemotherapy, targeted therapies, and radiation [98]. In several clinical studies, PDTOs have successfully predicted individual patient responses to anticancer regimens, highlighting their potential for personalized treatment selection.
The integration of iPSC technology with precision medicine approaches enables:
- Patient-specific drug sensitivity testing to guide treatment decisions
- Identification of predictive biomarkers for therapy response
- Modeling of resistance mechanisms to optimize drug combinations
- Development of autologous cell therapies for cancer treatment
The ability to generate immune cells from iPSCs further enables the development of engineered CAR-T and CAR-NK cells for cancer immunotherapy, providing off-the-shelf allogeneic approaches that overcome limitations of patient-derived cell therapies.
Current Limitations and Future Directions
Technical Challenges and Evolving Solutions
Despite significant advances, both iPSC and animal models face technical challenges that impact their predictive value. For iPSC technology, key limitations include:
Maturation Deficiencies: iPSC-derived cells often maintain fetal-like characteristics rather than achieving full adult maturity. Current solutions include:
- Extended culture periods (90-120 days for neurons)
- 3D culture systems that enhance structural complexity
- Co-culture with other cell types to provide maturation signals
- Metabolic manipulation to promote age-related characteristics
- Introduction of genetic maturation factors
Batch-to-Batch Variability: Differences between iPSC lines and differentiations can complicate data interpretation. Addressing strategies include:
- Automated production systems to improve reproducibility [100]
- Comprehensive quality control benchmarks
- Reference iPSC lines with well-characterized behavior [101]
- Isogenic controls generated through CRISPR correction
Limited Complexity: Simplified models may miss critical aspects of human physiology. Emerging solutions involve:
- Multi-tissue organ-on-chip systems that interconnect different tissue types
- Vascularized organoids that improve nutrient exchange and mimic angiogenesis
- Immune cell incorporation to model neuroimmune and other interactions
- Sensor integration for continuous monitoring of physiological parameters
For animal models, persistent challenges include:
- Species divergence in drug metabolism, target expression, and disease mechanisms
- Genetic compensation in knockout models that can mask phenotypes
- Limited representation of human genetic diversity and environmental factors
- Inability to model complex human behaviors and cognitive functions
Integrated Approaches and Future Outlook
The most powerful approach to predictive disease modeling may involve strategic integration of both human iPSC-based systems and appropriately selected animal models. This complementary strategy leverages the human relevance of iPSC derivatives while acknowledging the current limitations of in vitro systems in replicating whole-organism physiology.
Future directions in the field include:
- Multi-omics integration to comprehensively characterize models and improve human relevance
- Microphysiological systems that combine multiple human tissue types with physiological connectivity
- Humanized animal models incorporating human iPSC-derived cells or tissues
- Machine learning approaches to extract maximal information from complex model systems
- Standardized validation frameworks to assess predictive value across model types
The iPSC market is projected to grow at 9.86% CAGR, reaching US$4.69 Billion by 2033, reflecting increasing adoption and investment in this technology [93] [103]. Similarly, the animal model market continues to expand, particularly for genetically engineered models, with an expected value of USD 3.6 billion by 2035 [102]. This parallel growth underscores the complementary roles both systems will play in future biomedical research.
The comparative analysis of iPSCs and animal models reveals a nuanced landscape where each system offers distinct advantages and limitations for predictive disease modeling and drug development. iPSC-based models provide unprecedented access to human-specific biology, genetic relevance, and personalized medicine applications, while animal models continue to offer essential insights into whole-organism physiology and complex disease interactions.
The optimal approach for specific research applications depends on multiple factors, including the biological question being addressed, the level of complexity required, and the specific endpoints being measured. For human-specific toxicities, drug metabolism studies, and genetic diseases, iPSC models frequently demonstrate superior predictive value. For complex physiological interactions, systemic effects, and behavioral outcomes, animal models remain necessary despite their limitations.
The future of predictive disease modeling lies not in choosing one system over the other, but in developing strategic integrated approaches that leverage the complementary strengths of both human iPSC-based systems and appropriately selected animal models. As both technologies continue to advance—with improvements in iPSC maturation, organoid complexity, and genetically precise animal models—their combined power to predict human disease mechanisms and treatment responses will continue to increase, ultimately accelerating the development of effective therapies for human diseases.
The Role of Isogenic Controls in Validating Genotype-Phenotype Links
In the field of disease modeling using induced pluripotent stem cells (iPSCs), establishing robust causal relationships between genetic mutations and their resulting cellular phenotypes presents a significant scientific challenge. Isogenic controls—genetically identical cell lines that differ only at a specific locus of interest—have emerged as an indispensable tool for addressing this challenge. These controls provide a critical solution to the confounding effects of genetic background variability, enabling researchers to attribute observed phenotypic differences directly to the introduced or corrected mutation with high confidence [104] [105].
The importance of isogenic controls is particularly pronounced in the context of rare disease research, where approximately 80% of diseases have a genetic origin [104] [106]. With less than 10% of rare diseases having approved therapies, patient-derived iPSCs with their isogenic counterparts offer unique model systems for mechanistic studies and therapeutic development [104]. This technical guide examines the fundamental role of isogenic controls in validating genotype-phenotype relationships, detailing experimental methodologies, and presenting applications across various disease contexts.
The Scientific Rationale for Isogenic Controls
Limitations of Traditional Control Strategies
Traditional approaches in iPSC-based disease modeling often utilize patient-derived cell lines with unaffected, often familial, controls. While valuable, these controls suffer from substantial limitations due to the extensive genetic variation between individuals. Genetic background noise from millions of single nucleotide polymorphisms (SNPs), copy number variations, and other structural genetic differences can obscure subtle phenotypic effects caused by a single disease-relevant mutation [107] [108]. This is particularly problematic for late-onset disorders where in vitro phenotypes are often subtle and susceptible to significant effects of genetic background variations [108].
The fundamental problem lies in the challenge of distinguishing phenotypic consequences of a specific mutation from the natural genetic variation present across different human genomes. Without isogenic controls, researchers cannot definitively attribute observed phenotypes to the disease-causing mutation, potentially leading to false positives or negatives in phenotypic assays [105] [107].
The Isogenic Solution
Isogenic control lines address these limitations by providing a genetically matched reference where the only difference is the specific genetic modification under investigation. The term "isogenic" derives from Greek roots meaning "same origin," reflecting their genetic identity to the parental line except for the engineered change [108]. This controlled genetic environment enables:
- Precise attribution of phenotypic differences to the introduced mutation
- Enhanced signal-to-noise ratio for detecting subtle phenotypes
- Reduced experimental variability leading to more reproducible results
- Simplified interpretation of molecular profiling data
The utility of isogenic controls extends across multiple research applications, including disease mechanism elucidation, drug discovery, and toxicity studies [104]. Recent policy changes such as the FDA Modernization Act 2.0, which allows therapeutics to be tested in cell-based assays without animal testing for clinical trial graduation, have further increased the value of well-controlled iPSC-based models [104].
Generation of Isogenic iPSC Lines: Methodological Approaches
Genome Editing Technologies
The creation of isogenic iPSC lines relies on precise genome editing technologies that enable targeted genetic modifications. Several approaches have been successfully implemented:
Table 1: Genome Editing Technologies for Isogenic Line Generation
| Technology | Mechanism | Key Features | Applications |
|---|---|---|---|
| Zinc Finger Nucleases (ZFNs) | Programmable DNA-binding domains fused to FokI nuclease | First engineered nucleases; high specificity; complex design | Safe harbor (AAVS1) integration; point mutation correction [105] [108] |
| CRISPR-Cas9 | RNA-guided DNA cleavage | Simpler design; high efficiency; versatile | Gene knockout; point mutations; large deletions [107] |
| Base Editing | DNA base conversion without double-strand breaks | Reduced indel formation; high precision | Transition mutations (C→T, A→G) [107] |
| Prime Editing | Search-and-replace editing without double-strand breaks | Versatile; all possible base transitions | Point mutations; small insertions/deletions [107] |
Experimental Workflow for Isogenic Line Generation
The generation of isogenic iPSC lines follows a systematic workflow that can be adapted based on the specific research objectives—whether creating disease models through mutation introduction or generating corrected controls from patient-derived lines.
The workflow for generating compound heterozygous mutations requires additional considerations. As demonstrated in a study modeling arrhythmogenic disorders, researchers used a combination of ssODN repair templates carrying either the patient missense mutation (ssODN M) or a silent PAM-blocking mutation (ssODN B) to prevent Cas9-mediated re-cleavage after editing [107]. This approach successfully generated several compound heterozygous clones for KCNH2 mutations associated with long and short QT syndromes.
Quality Control and Validation
Rigorous quality control is essential to ensure the integrity of isogenic iPSC lines. Key validation steps include:
- Genomic integrity assessment: Karyotyping to confirm absence of chromosomal abnormalities [107]
- Pluripotency verification: Expression of canonical markers (Oct4, Nanog) via PCR, immunocytochemistry, or flow cytometry [3]
- Off-target analysis: Genotyping of putative off-target sites to ensure editing specificity [105]
- Functional pluripotency: Directed differentiation into all three germ layers [3]
- Identity confirmation: STR profiling to verify genetic match to parental line
Applications in Disease Modeling
Neurological Disorders
Isogenic controls have proven particularly valuable in modeling neurodegenerative diseases. In Parkinson's disease research, isogenic iPSC lines differing exclusively at two susceptibility variants (A53T and other mutations) in the α-synuclein gene have enabled precise dissection of disease mechanisms [108]. The robust capability to genetically correct disease-causing point mutations in patient-derived hiPSCs represents significant progress for basic biomedical research and advances toward hiPSC-based cell replacement therapies [108].
Cardiac Channelopathies
The combination of precision gene editing and bioengineered 3D tissue models has established advanced isogenic hiPSC-derived cardiac disease models. In one study, researchers generated isogenic KCNH2 N588D and N588K compound heterozygous variants in a fixed hiPSC genomic background to model long QT syndrome (LQTS) and short QT syndrome (SQTS) respectively [107].
Table 2: Electrophysiological Phenotypes in Isogenic Cardiac Models
| Cell Line | Mutation | Condition | Field Potential Duration (FPDcF) | Phenotype | Arrhythmic Response |
|---|---|---|---|---|---|
| 409B2 Parent | None | Control | 231 ± 24 ms | Normal | Baseline |
| LQT26 | N588D | LQTS Model | 323 ± 21 ms | Prolonged | Increased susceptibility |
| SQT22 | N588K | SQTS Model | 82 ± 18 ms | Shortened | Differential susceptibility |
| CTL Clones | L589L (silent) | Control | Similar to parent | Normal | Similar to parent |
Electrophysiological analysis with multielectrode arrays showed that the field potential duration (FPDcF) was significantly shortened for the SQT mutants and significantly prolonged for the LQT mutants compared to the isogenic control [107]. When pharmacologically inhibiting the hERG channels, mutant 3D cardiac tissue sheets showed differential susceptibility to arrhythmic events compared to the isogenic controls, demonstrating the capability of these models to reproduce clinically relevant phenotypes [107].
Rare Genetic Diseases
Isogenic controls have advanced rare disease research by enabling the study of conditions that were previously difficult to model. For Juvenile Nephronophthisis (NPH), a genetic kidney disease without effective treatments, researchers developed the first human disease models using patient-derived iPSCs and isogenic controls [104] [106]. They demonstrated that NPHP1-deficient iPSCs exhibit abnormal cell proliferation, abnormalities in primary cilia, and renal cyst formation in iPSC-derived kidney organoids—phenotypes that were reversed upon reintroduction of NPHP1 expression [104].
Similarly, in modeling a rare form of autosomal dominant retinitis pigmentosa (RDH12-AD), isogenic retinal organoids exhibited a reduction in photoreceptor number and shortened photoreceptor length at week 37, reflecting the late-onset, milder disease course seen in patients [106]. These studies demonstrate how isogenic controls provide novel insights into disease mechanisms and potential therapeutic targets for rare diseases.
The Scientist's Toolkit: Essential Research Reagents
Successful generation and application of isogenic iPSC lines requires a comprehensive set of research tools and reagents. The following table summarizes essential components:
Table 3: Essential Research Reagents for Isogenic iPSC Studies
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) | Somatic cell reprogramming to pluripotency | Integration-free methods (episomal, mRNA) preferred [3] |
| Genome Editing Tools | CRISPR-Cas9, ZFNs, donor templates | Introduction or correction of mutations | PAM-blocking mutations prevent re-cleavage [107] |
| Cell Culture Matrix | Matrigel, recombinant laminin | Extracellular matrix for cell attachment | Defined matrices reduce variability [3] |
| Culture Media | mTeSR1, E8 medium | Maintenance of pluripotency | Chemically defined formulations preferred [3] |
| Differentiation Reagents | Growth factors, small molecules | Directed differentiation to target cell types | Protocol optimization required for each lineage |
| Characterization Tools | Pluripotency markers, lineage-specific antibodies | Quality control and validation | Functional assays complement molecular markers |
| Analytical Tools | MEA, patch clamp, calcium imaging | Functional phenotyping | 3D models often show enhanced phenotypes [107] |
Advanced Applications and Integration with Other Technologies
Multi-Omics Integration
The combination of isogenic controls with multi-omics technologies represents a powerful approach for elucidating comprehensive genotype-phenotype relationships. Methods that integrate genotype data with transcriptomic, proteomic, and epigenomic profiles can reveal the molecular pathways connecting genetic variations to cellular phenotypes [109]. However, such analyses face challenges including the large feature set of SNPs necessitating large sample sizes, and difficulties in obtaining multi-omics data from a single sample set [109].
Novel computational approaches have been developed to address these challenges, such as the GSPLS method which combines group lasso and SPLS models to establish genotype-phenotype associations from multi-omics data with small sample sizes [109]. These methods consider intra-omics associations to improve prediction accuracy and analyze biological pathway associations across omics layers to clarify biological significance [109].
Three-Dimensional Tissue Models
While 2D cellular models have proven valuable, they often fail to exhibit authentic disease phenotypes, resulting in poor validation in vitro [107]. The integration of isogenic controls with 3D tissue engineering approaches has significantly enhanced phenotypic relevance. As demonstrated in cardiac disease modeling, 3D cardiac tissue sheets consisting of 5-6 cell layers show greater complexity and relevance for clinical disease phenotypes compared to 2D cultures [107].
The enhanced performance of 3D models is attributed to better reproduction of native tissue architecture, inclusion of multiple cell types, and more physiologically relevant cell-cell interactions. These advanced models enable reproduction of complex clinical phenotypes such as Torsade de Pointes-like waveforms that are not typically observed in 2D systems [107].
Isogenic controls represent a critical methodological advancement in iPSC-based disease modeling, providing an essential tool for rigorous validation of genotype-phenotype relationships. By controlling for genetic background variability, these systems enable precise attribution of phenotypic effects to specific genetic modifications, enhancing the reproducibility and clinical translatability of research findings. As genome editing technologies continue to evolve and integrate with sophisticated tissue engineering approaches, isogenic iPSC models will play an increasingly central role in elucidating disease mechanisms, screening therapeutic compounds, and developing personalized cell-based treatments. The ongoing refinement of these approaches promises to accelerate the pace of discovery across a broad spectrum of human genetic disorders.
Global Regulatory Landscapes for iPSC-Based Therapies and Products
The field of induced pluripotent stem cell (iPSC) research has revolutionized regenerative medicine by enabling the reprogramming of somatic cells into a pluripotent state, creating unprecedented opportunities for disease modeling, drug discovery, and cell-based therapies [1]. Patient-specific iPSCs can be differentiated into various disease-relevant cell types, providing powerful models for elucidating disease mechanisms and screening potential therapeutics [66] [110]. However, the clinical translation of iPSC-based products is governed by complex regulatory frameworks that vary significantly across regions, reflecting different risk-benefit balances between accelerating innovation and ensuring patient safety [111]. This technical guide provides a comprehensive analysis of the global regulatory landscapes for iPSC-based therapies and products, with specific focus on their application in disease modeling research, to assist researchers and drug development professionals in navigating these complex pathways.
Global Regulatory Frameworks: A Comparative Analysis
Regional Regulatory Approaches
The regulatory frameworks for iPSC-based products typically operate at three levels: (1) legislation enacted by parliament/congress, (2) regulations adopted by the executive branch, and (3) guidelines and guidance notes published by regulatory entities as "soft law" [111]. Major regulatory regions have developed distinct approaches to overseeing stem cell therapies, creating a varied global landscape.
Table 1: Comparative Analysis of Regulatory Frameworks for iPSC-Based Products
| Region | Regulatory Authority | Key Legislation/Guidance | Clinical Trial Approval Model | Manufacturing Requirements | Special Provisions |
|---|---|---|---|---|---|
| United States | FDA Center for Biologics Evaluation and Research (CBER) [112] | 21 CFR Parts 210, 211, 312, 1271; Public Health Service Act [112] [111] | Prior notification model (IND application) [111] | No specific manufacturing license required; cGMP compliance [112] | Accelerated Approval pathways; Flexible stance on germline modification [111] |
| European Union | European Medicines Agency (EMA) [111] | Advanced Therapy Medicinal Products (ATMP) Regulation; European Biopatent Directive [111] | Prior authorization model [111] | Manufacturing license required [111] | Prohibits patents on human embryo use; Germline modification banned [111] |
| Japan | Ministry of Health, Labour and Welfare (MHLW) [111] | Act on the Safety of Regenerative Medicine; Pharmaceuticals and Medical Devices Act [111] | Conditional/time-limited approval system [111] | Specific certification for regenerative medicine manufacturers [111] | Fast-track approval for regenerative medicine products; Balanced approach [111] |
| South Korea | Ministry of Food and Drug Safety (MFDS) [111] | Pharmaceutical Affairs Act; Guidelines on Stem Cell Therapeutics [111] | Prior authorization model with expedited pathways [111] | Manufacturing license required [111] | Government-supported stem cell banks; Balanced approach [111] |
| Switzerland | Swissmedic [111] | Therapeutic Products Act; Ordinance on Licenses for Human Therapy [111] | Prior authorization model [111] | Manufacturing license required [111] | Ratified Oviedo Convention; Prohibits germline modification [111] |
Regulatory Trends and Clinical Trial Landscape
The global regulatory landscape for iPSC-based therapies is rapidly evolving, with a noticeable growth in clinical trials since 2008 [111]. The United States and Japan have emerged as leaders in clinical trial numbers, attributed to their more flexible regulatory guidelines, while the European Union trails behind with more rigorous regulations [111]. As of 2024, there were over 100 active clinical trials using iPSC-derived products, targeting conditions including Parkinson's disease, age-related macular degeneration, and cardiac repair [113].
Therapeutic studies involving iPSCs predominantly target conditions affecting the cardiovascular and nervous systems, reflecting the urgent medical needs in these areas and the relative accessibility of these cell types for transplantation [111]. The increasing number of trials underscores the importance of safety monitoring and the need for harmonized global standards to facilitate international collaboration in iPSC research.
iPSC-Based Disease Modeling: Technical Foundations
Molecular Mechanisms of iPSC Induction
The fundamental breakthrough in iPSC technology came from understanding that somatic cell reprogramming reverses developmental processes through epigenetic remodeling [1]. The original reprogramming method developed by Takahashi and Yamanaka utilized four transcription factors (OCT4, SOX2, KLF4, and c-MYC) delivered via retroviral vectors to reprogram mouse embryonic fibroblasts into pluripotent stem cells [1]. Thomson's alternative approach used OCT4, SOX2, NANOG, and LIN28 for human cell reprogramming [1].
Reprogramming occurs in two phases: an early stochastic phase where somatic genes are silenced and early pluripotency-associated genes are activated, followed by a more deterministic late phase where late pluripotency-associated genes are activated [1]. This process involves profound remodeling of chromatin structure and the epigenome, accompanied by changes in metabolism, cell signaling, and mesenchymal-to-epithelial transition (MET) [1].
Advanced Disease Modeling Platforms
From 2D to 3D Modeling Systems
Early iPSC disease modeling relied on two-dimensional (2D) monolayer cultures of differentiated cells, which successfully uncovered disease phenotypes for various monogenic and polygenic disorders [66]. For example, iPSC-derived dopaminergic neurons from Parkinson's disease patients have demonstrated impaired mitochondrial function, increased oxidative stress, and α-synuclein accumulation [66]. Similarly, iPSC-derived hepatocytes from patients with inherited metabolic disorders recapitulate disease-specific phenotypes including protein aggregation and lipid accumulation [66].
However, 2D systems lack the complex three-dimensional (3D) environment where cells normally reside, missing essential cell-cell communications, cell-matrix mechanics, and niche interactions [66]. To address these limitations, researchers have developed three primary 3D modeling approaches:
- Engineered Tissue Constructs: Utilizing porous 3D scaffolds made of ECM-mimicking materials (e.g., collagen, fibrin, Matrigel) to create organized tissue structures [66]
- Organ-on-Chip Systems: Microfluidic devices that incorporate vascular perfusion and physical forces (e.g., shear stress, tension) to better mimic organ physiology [66]
- Organoids: Self-organizing 3D cell masses that recapitulate some aspects of tissue architecture and function through developmental cues [66]
These 3D models demonstrate improved maturity and physiological relevance compared to 2D cultures, better modeling adult-onset diseases and complex tissue-level pathologies [66].
Disease-Specific Modeling Applications
Neurological Disorders: iPSC models have been particularly valuable for studying neurological conditions like Parkinson's disease (PD) and Alzheimer's disease (AD) [114]. PD-specific iPSCs differentiated into dopaminergic neurons exhibit key disease phenotypes, including Lewy body-like aggregates and impaired neuronal function [114]. For AD research, specialized protocols have been developed to generate entorhinal cortex stellate cells, which are among the first to accumulate amyloid beta [110].
Cardiovascular Diseases: iPSC-derived cardiomyocytes (iPSC-CMs) have enabled modeling of various cardiac conditions, including hypertrophic cardiomyopathy (HCM) [114]. Using CRISPR-Cas9, researchers have introduced specific mutations (e.g., in troponin T) into iPSCs, generating cardiomyocytes that show characteristic HCM features including myofibrillar disarray, enhanced contraction, and impaired relaxation [114]. However, challenges remain in achieving full maturation of iPSC-CMs to adult-like phenotypes [110].
COVID-19 Modeling: iPSC-derived cells have provided valuable platforms for studying SARS-CoV-2 infection mechanisms and screening FDA-approved drugs against viral infection [110].
The following diagram illustrates the workflow for developing iPSC-based disease models:
Regulatory Pathways for iPSC-Based Products
Investigational New Drug (IND) Application Process
In the United States, iPSC-based products are regulated as biological products requiring an Investigational New Drug (IND) application before clinical trials can commence [112]. The IND pathway involves several critical components:
Chemistry, Manufacturing, and Controls (CMC)
- Detailed description of manufacturing site, equipment, and quality control procedures [112]
- Comprehensive manufacturing workflow with list of reagents, testing specifications, and final formulation [112]
- Documentation of process development, optimization, and protocol repeatability [112]
- Storage and shipping conditions for the final product [112]
Non-Clinical Information
- Proof-of-concept and efficacy studies in relevant preclinical models [112]
- Good Laboratory Practice (GLP) toxicology and tumorigenicity studies [112]
- Pharmacokinetic profiles including absorption, distribution, metabolism, and excretion [112]
Clinical Study Plan
- Study objectives, design, and target population [112]
- Dosage, route of administration, and treatment duration [112]
- Primary and secondary endpoints with statistical methods [112]
Table 2: Essential Components for Phase I IND Application for Autologous iPSC-Based Therapy
| CMC Requirements | Non-Clinical Requirements | Clinical Protocol Requirements |
|---|---|---|
| Manufacturing site information with QC and sterility SOPs [112] | Proof-of-concept/efficacy studies in preclinical models [112] | Clinical phase and treatment indication [112] |
| Drug product and drug substance description [112] | GLP toxicology and tumorigenicity studies (single-dose, repeat-dose, genotoxicity) [112] | Study objectives and design [112] |
| Detailed manufacturing workflow diagram [112] | Pharmacokinetics: method of administration, absorption, distribution, metabolism, excretion [112] | Study population with inclusion/exclusion criteria [112] |
| List of reagents with testing specifications [112] | Analytical methods and validation reports [112] | Dosage, route of administration, treatment duration [112] |
| Process development and optimization data [112] | Organ distribution studies [112] | Primary and secondary endpoints [112] |
| Storage and shipping conditions [112] | Reproductive and developmental toxicity studies [112] | Study assessments and statistical methods [112] |
Autologous vs. Allogeneic iPSC Therapy Regulation
The regulatory considerations differ significantly between autologous (patient-specific) and allogeneic (off-the-shelf) iPSC therapies. Autologous therapies present unique manufacturing challenges, including donor tissue source variability, reprogramming method consistency, heterogeneity of differentiated cells, and controls for the manufacturing process [112]. Each autologous product batch requires a new manufacturing cycle, increasing logistical complexity and costs [112].
Allogeneic therapies offer advantages in standardization and scalability but raise different regulatory considerations regarding immune compatibility and potential for rejection [115]. Both approaches must address the inherent risk of tumorigenicity from residual undifferentiated iPSCs or the reprogramming process itself [115].
Technical Protocols for iPSC-Based Disease Modeling
iPSC Generation and Characterization Protocol
Reprogramming Methodology
- Somatic Cell Source Selection: Obtain patient somatic cells (typically skin fibroblasts or blood cells) through biopsy or blood draw [1]
- Reprogramming Factor Delivery: Introduce reprogramming factors (OCT4, SOX2, KLF4, c-MYC or alternative combinations) using non-integrating methods such as Sendai virus, episomal vectors, or mRNA transfection to minimize genomic alterations [112] [113]
- Pluripotency Stabilization: Culture transfected cells on feeder layers or in defined matrices until iPSC colonies emerge (typically 3-4 weeks) [1]
- Colony Expansion: Manually pick and expand individual colonies demonstrating embryonic stem cell-like morphology [1]
Quality Control and Characterization
- Pluripotency Marker Validation: Confirm expression of OCT4, SOX2, NANOG, SSEA-4, TRA-1-60 via immunocytochemistry and flow cytometry [112]
- Genetic Stability Assessment: Perform karyotyping, STR analysis, and whole-genome sequencing to verify genomic integrity [112]
- Differentiation Potential Verification: Demonstrate trilineage differentiation capability (ectoderm, mesoderm, endoderm) via embryoid body formation or directed differentiation [112]
- Microbiological Testing: Screen for mycoplasma, bacteria, fungi, and viruses according to cGMP standards [112]
Disease Modeling Experimental Workflow
2D Monolayer Disease Modeling
- Directed Differentiation: Differentiate iPSCs into target cell types using lineage-specific morphogens and small molecules [66]
- Phenotypic Characterization: Assess disease-specific phenotypes using functional assays (e.g., electrophysiology, calcium imaging, contractility measurements) [66]
- Molecular Analysis: Perform transcriptomic, proteomic, and metabolomic profiling to identify disease-associated pathways [66]
3D Organoid Development
- Protocol Optimization: Establish differentiation conditions that promote self-organization and tissue-like development [66] [110]
- Multiple Cell Type Incorporation: Co-culture target cell types with supporting cells (e.g., fibroblasts, endothelial cells) to better recapitulate tissue microenvironment [66]
- Maturation Enhancement: Implement extended culture periods, mechanical stimulation, or vascularization strategies to improve functional maturity [66]
The following diagram illustrates the regulatory decision pathway for iPSC-based therapy development:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for iPSC-Based Disease Modeling
| Reagent Category | Specific Examples | Function in iPSC Research |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (Yamanaka factors); OCT4, SOX2, NANOG, LIN28 (Thomson factors) [1] | Induction of pluripotency in somatic cells through epigenetic reprogramming [1] |
| Delivery Systems | Sendai virus vectors, episomal plasmids, synthetic mRNA, non-integrating lentivirus [112] [113] | Safe and efficient introduction of reprogramming factors without genomic integration [112] |
| Cell Culture Matrices | Matrigel, recombinant laminin, vitronectin, synthetic polymers [66] | Provide structural support and biochemical cues for iPSC attachment, growth, and differentiation [66] |
| Differentiation Inducers | Morphogens (BMP, WNT, FGF), small molecules (CHIR99021, SB431542), growth factors [66] [110] | Direct lineage-specific differentiation of iPSCs into target cell types through developmental pathway activation [66] |
| Gene Editing Tools | CRISPR-Cas9 systems, TALENs, zinc finger nucleases [66] [114] | Introduction or correction of disease-specific mutations in iPSCs for isogenic control generation [66] |
| Characterization Antibodies | Anti-OCT4, SOX2, NANOG (pluripotency); lineage-specific markers (TUJ1, α-actinin, AFP) [114] | Validation of pluripotency and differentiation efficiency through immunocytochemistry and flow cytometry [114] |
| 3D Culture Scaffolds | Collagen, fibrin, hyaluronic acid, PEG-based hydrogels, decellularized tissue extracts [66] | Support three-dimensional tissue organization in organoid and engineered tissue models [66] |
Emerging Trends and Future Directions
Technological Advancements
The iPSC field is rapidly evolving with several key technological advancements:
- Automation and AI Integration: Automated bioreactors and artificial intelligence-based analysis tools are being adapted for iPSC-based therapies to improve reproducibility and scalability [112] [113]. AI algorithms guide reprogramming optimization, reduce errors, and enhance reproducibility [113] [116].
- Gene Editing Innovations: CRISPR-Cas9 technology has revolutionized the generation of isogenic iPSC lines that differ only at specific disease-relevant loci, enabling precise correlation of genotypes with phenotypes [66] [114].
- Complex Model Development: Researchers are progressing from simple monocultures to multi-organ systems that combine different 3D organoid types into integrated "4D multi-organ systems" or "body-on-chip" platforms [66].
Market Evolution and Regulatory Adaptation
The global iPSC market is experiencing significant growth, with the overall iPSC market projected to reach approximately USD 5.12 billion by 2034, expanding at a CAGR of 10.25% from 2025 [113]. This growth is driving regulatory adaptation in key regions:
- North America: Maintains leadership through well-developed infrastructure, substantial research funding, and regulatory clarity from the FDA, particularly regarding non-integrating reprogramming technologies and autologous cell therapies [113].
- Asia-Pacific: Emerging as the fastest-growing region, driven by increased government investments, growing prevalence of chronic diseases, and regulatory reforms in South Korea, Australia, and Singapore that have improved approval timelines for stem cell-based therapies [113] [111].
- Europe: Facing challenges due to more rigorous regulations that prioritize safety and ethical considerations, potentially hindering innovation pace compared to more flexible regulatory regions [111].
The continuing evolution of global regulatory frameworks will play a pivotal role in determining how quickly promising iPSC-based disease models can transition from research tools to clinically applicable therapies, ultimately realizing the potential of personalized regenerative medicine.
The discovery of induced pluripotent stem cells (iPSCs) by Shinya Yamanaka in 2006 represented a paradigm shift in regenerative medicine, offering an ethically acceptable alternative to embryonic stem cells with vast therapeutic potential [3]. These reprogrammed somatic cells, capable of differentiating into any cell type in the body, have since become indispensable tools for disease modeling, drug screening, and cell-based therapies [3] [2]. The clinical translation of iPSC technology has progressed significantly, with a growing number of interventional trials now assessing the safety and efficacy of iPSC-derived cellular therapeutics across diverse medical conditions [117] [118]. This technical guide examines current trends in iPSC-based clinical trials, analyzes the evolving therapeutic applications, details critical methodological protocols, and assesses both the challenges and future directions for realizing the full translational potential of iPSC models.
The global iPSC market, valued at US$2.01 billion in 2024, is projected to reach US$4.69 billion by 2033, reflecting a compound annual growth rate of 9.86% [119]. This growth is fueled by advancing reprogramming technologies, increasing demand for human-relevant disease models, and the pressing need for personalized cellular therapeutics [119]. As the field transitions from preliminary research to clinical application, understanding the current trial landscape and technical requirements becomes essential for researchers and drug development professionals working to advance iPSC-based therapies.
Current State of iPSC Clinical Trials
Global Distribution and Trial Characteristics
A systematic scoping review of registered clinical trials and published studies in early 2025 identified 10 published clinical studies and 22 ongoing registered trials utilizing iPSCs for a wide range of diseases [117]. These include investigations for cardiac conditions, ocular disorders, cancer, graft-versus-host disease, and iPSC-derived platelets for transfusion [117]. The published studies have been predominantly small and uncontrolled, with only two studies reporting on more than four patients, resulting in a total of approximately 115 patients treated with iPSC-derived therapies worldwide as of early 2025 [117].
Earlier data from 2021 provides additional context for the evolution of therapeutic trials. Analysis of global registries revealed that Japan emerged as the frontrunner in therapeutic trials, while the United States conducted the majority of nontherapeutic studies [118]. Therapeutic trials featured a much smaller average number of participants (approximately 29) compared to nontherapeutic studies (average 187 participants) [118]. Disorders of the circulatory, nervous, and visual systems were studied in roughly equal measure in these therapeutic trials [118].
Table 1: Global Distribution of iPSC Clinical Trials (2021 Data)
| Country/Region | Therapeutic Trials | Nontherapeutic Trials | Primary Focus Areas |
|---|---|---|---|
| Japan | Leader in therapeutic applications | 3 trials (4.8%) | Circulatory, nervous, and visual systems |
| United States | Limited therapeutic focus | 21 trials (33.3%) | Disease modeling, drug screening |
| France | Moderate involvement | 13 trials (20.6%) | Not specified |
| Other EU Nations | Variable participation | 13 trials combined | Various specialized applications |
| Other Regions | Limited presence | 12 trials combined | Emerging research applications |
Table 2: Characteristics of iPSC Clinical Trials Based on 2025 Analysis
| Trial Characteristic | Published Studies | Ongoing Registered Trials |
|---|---|---|
| Total Identified | 10 studies | 22 trials |
| Total Patients Treated | ~115 patients | Data not yet available |
| Typical Study Design | Predominantly small, uncontrolled | Varied, including controlled designs |
| Largest Studies | Only 2 studies enrolled >4 patients | Larger cohorts anticipated |
| Primary Applications | Cardiac conditions, ocular disorders, cancer, GvHD, platelet transfusion | Similar range with expanded indications |
Key Therapeutic Areas in iPSC Clinical Applications
Ophthalmic Applications
The first cellular therapy involving transplant of iPSCs into humans was initiated in 2013 at the RIKEN Center in Kobe, Japan, investigating the safety of iPSC-derived cell sheets for patients with macular degeneration [16]. This pioneering trial established the foundation for ocular applications of iPSC technology and demonstrated the feasibility of iPSC-derived retinal pigment epithelial (RPE) cell transplantation. Subsequent studies have continued to explore iPSC-based interventions for various retinal degenerative conditions, leveraging the immune-privileged status of the eye and the relative simplicity of transplanting monolayer RPE cells.
Cardiovascular Diseases
iPSC-derived cardiomyocytes enable the study of arrhythmogenic disorders, heart failure, and myocardial injury [3]. Early-phase clinical trials are exploring the safety and efficacy of iPSC-derived cardiac cells for treating ischemic heart disease and heart failure. For example, models of congenital arrhythmias linked to KCNQ1 mutations provide a basis for precision cardiology [3]. In myocardial damage, iPSC-derived cardiomyocytes, fibroblasts, vascular smooth muscle cells, and endothelial cells have been investigated for regenerative transplantation strategies, with promising improvements in cardiac function reported in preclinical models [3].
Hematological and Immunological Applications
Cynata Therapeutics received approval in 2016 to launch the first formal clinical trial of an allogeneic iPSC-derived cell product (CYP-001) for treating GvHD [16]. In this historic trial, CYP-001 met its clinical endpoints and produced positive safety and efficacy data for steroid-resistant acute GvHD. Based on this success, Cynata has advanced its iPSC-derived mesenchymal stem cells (MSCs) into Phase 2 trials for severe complications associated with COVID-19, GvHD, and critical limb ischemia [16]. The company has also initiated a Phase 3 trial utilizing its iPSC-derived MSC product (CYP-004) in 440 patients with osteoarthritis, representing the world's first Phase 3 clinical trial involving an iPSC-derived cell therapeutic product [16].
Neurological Disorders
While clinical applications in neurology are still emerging, iPSC-derived neuronal models have provided new insights into Alzheimer's disease, Parkinson's disease, and amyotrophic lateral sclerosis [3]. Patient-specific neurons allow analysis of pathogenic mechanisms and evaluation of pharmacological interventions. PD models have recapitulated dopaminergic neuron degeneration in the substantia nigra and revealed the pathogenic role of α-synuclein aggregation, advancing understanding of both sporadic and familial PD [3]. These models form the foundation for developing cell replacement therapies for neurodegenerative conditions.
Technical and Methodological Considerations
iPSC Generation and Reprogramming Methodologies
The initial step in generating iPSCs is the isolation of somatic cells from donors. The choice of cell source critically influences reprogramming efficiency, quality of resulting iPSC lines, and their subsequent applications [3].
Table 3: Somatic Cell Sources for iPSC Generation
| Cell Source | Reprogramming Efficiency | Invasiveness of Collection | Key Advantages | Common Applications |
|---|---|---|---|---|
| Dermal Fibroblasts | Moderate | High (skin biopsy required) | High genomic stability; reliable reprogramming | Foundational research; disease modeling |
| Peripheral Blood Mononuclear Cells (PBMCs) | Comparable to fibroblasts | Low (minimally invasive) | Easy repeat sampling; suitable for translational studies | Large-scale cohort studies; clinical applications |
| Urinary Epithelial Cells | Robust | None (completely non-invasive) | Easily repeatable; suitable for serial sampling | Pediatric studies; longitudinal monitoring |
| Keratinocytes | Higher than fibroblasts | Moderate (hair plucking) | Higher reprogramming efficiency | Dermatological applications; genetic disorders |
| Dental Pulp/Synovial Cells | Variable | Moderate to high | Tissue-specific properties | Specialized tissue engineering |
The generation of iPSCs is achieved by reprogramming somatic cells through restoration of transcriptional and epigenetic programs characteristic of embryonic stem cells [3]. The introduction of four transcription factors (Oct4, Sox2, Klf4, and c-Myc) has been shown to be sufficient to revert fibroblasts to a pluripotent state in both murine and human cells [3]. Early approaches relied on integrating retroviral and lentiviral vectors, which carried risks of insertional mutagenesis and tumorigenesis. Integration-free methods have since been developed, including:
- Episomal DNA Vectors: Non-integrating plasmid-based systems that are gradually lost during cell division
- Synthetic mRNA: Transient delivery of reprogramming factor mRNAs
- Recombinant Protein Delivery: Direct introduction of reprogramming proteins
- Sendai Virus-Based Systems: Non-integrating viral vectors that are diluted with cell divisions
Reprogramming involves two principal mechanisms: chromatin remodeling and DNA methylation resetting [3]. The process typically requires several days to weeks and maintains low efficiency (<0.1% to several percent), depending on technical factors (vector type, transfection method) and biological factors (donor age, cell type, epigenetic profile) [3].
iPSC Culture and Quality Control Protocols
Following successful reprogramming, maintaining iPSCs under in vitro culture conditions is essential for preserving proliferative capacity and pluripotency [3]. Early iPSC culture protocols employed feeder layers of mitotically inactivated mouse embryonic fibroblasts, but feeder-free systems are increasingly used to enhance reproducibility and minimize xenogeneic contamination [3]. These rely on extracellular matrix coatings such as Matrigel or recombinant human proteins like laminin [3].
Culture media typically consist of chemically defined formulations such as mTeSR1 or E8, supplemented with essential growth factors (e.g., FGF2) and inhibitors of differentiation pathways (e.g., TGF-β/activin A) [3]. These media enable greater standardization and are considered more suitable for translational and clinical applications [3].
Rigorous quality control is essential to verify the pluripotent state of iPSCs. Key assessments include:
- Pluripotency Marker Expression: Analysis of canonical markers (Oct4, Nanog) via PCR, immunocytochemistry, or flow cytometry [3]
- Functional Pluripotency: Directed differentiation assays into all three germ layers (ectoderm, mesoderm, endoderm) [3]
- Genomic Integrity Evaluation: Regular assessment for chromosomal abnormalities or epigenetic alterations that may compromise differentiation efficiency or predispose to malignant transformation [3]
- Microbiological Testing: Screening for mycoplasma, endotoxins, and other contaminants [120]
Differentiation Protocols for Therapeutic Cell Types
Cardiomyocyte Differentiation
Protocols for differentiating iPSCs to cardiomyocytes typically follow a sequential approach mimicking embryonic heart development. The process involves:
- Mesoderm Induction: Using activin A, BMP4, and FGF2 to direct cells toward cardiac mesoderm
- Cardiac Specification: Employing Wnt inhibitors (IWP2/IWR1) during specific time windows
- Cardiomyocyte Maturation: Extended culture with metabolic substrates (fatty acids) and electrical stimulation
A critical challenge is the inherent immaturity of iPSC-derived cardiomyocytes, which typically exhibit fetal-like characteristics [2]. Recent approaches to enhance maturation include:
- 3D Culture Systems: Engineered heart tissues and hydrogel-based constructs
- Metabolic Manipulation: Switching from glycolytic to oxidative metabolism
- Mechanical Stimulation: Applying physiological stretch and stress
- Co-culture Systems: Incorporating endothelial cells and cardiac fibroblasts [2]
Neural Differentiation
Neural differentiation protocols vary based on the specific neuronal or glial subtype required:
- Forebrain Neurons: Dual SMAD inhibition using Noggin and SB431542
- Midbrain Dopaminergic Neurons: SHH activation combined with FGF8 and WNT1 signaling
- Motor Neurons: Retinoic acid and SHH agonist treatment
- Astrocytes: Extended culture with CNTF and BMP4
- Oligodendrocytes: SHH activation followed by PDGF and T3 treatment
Hepatocyte Differentiation
Hepatic differentiation typically employs a three-stage protocol:
- Definitive Endoderm Induction: Activin A and Wnt3a treatment
- Hepatoblast Specification: BMP4, FGF2, and FGF4 application
- Hepatocyte Maturation: HGF, Oncostatin M, and glucocorticoid exposure
Research Reagent Solutions for iPSC Applications
Table 4: Essential Research Reagents for iPSC Technology
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Systems | Sendai virus vectors, episomal plasmids, mRNA kits | Deliver reprogramming factors to somatic cells | Non-integrating systems preferred for clinical applications |
| Culture Media | mTeSR1, Essential 8, StemFit | Maintain pluripotency and support expansion | Chemically defined media enhance reproducibility |
| Extracellular Matrices | Matrigel, recombinant laminin-521, vitronectin | Provide substrate for feeder-free culture | Xeno-free matrices required for clinical applications |
| Differentiation Kits | Commercial cardiomyocyte, neuronal, hepatocyte kits | Direct differentiation to specific lineages | Quality control between lots is essential |
| Cell Survival Enhancers | CultureSure CEPT cocktail [120] | Improve cell viability and cloning efficiency | Particularly valuable during single-cell cloning |
| Gene Editing Tools | CRISPR/Cas9 systems, TALENs, Zinc Finger Nucleases | Introduce or correct disease-relevant mutations | Essential for isogenic control generation |
| Characterization Reagents | Flow cytometry antibodies, PCR arrays, karyotyping kits | Assess pluripotency and genomic stability | Multifactorial assessment required for QC |
Analysis of Challenges and Translational Barriers
Technical and Manufacturing Hurdles
The translational pathway for iPSC-based therapies faces several significant technical challenges:
Genomic and Epigenomic Instability Reprogramming somatic cells to pluripotency can introduce genetic and epigenetic abnormalities that may compromise safety [3]. The forced expression of transcription factors can induce mutations and DNA damage, necessitating continuous genomic monitoring throughout the reprogramming and culture process [3]. Additionally, extended in vitro culture increases the risk of karyotypic abnormalities, particularly gains of chromosomes 1, 12, 17, and 20 [3].
Tumorigenicity Risk The risk of tumor formation represents a primary safety concern for iPSC-based therapies. This risk arises from two main sources: (1) potential transformation of iPSC-derived cells due to reprogramming-induced genetic changes, and (2) transplantation of residual undifferentiated iPSCs that could lead to teratoma formation [17]. Appropriate tests to assess tumorigenicity risk require further development and regulatory clarification [17].
Manufacturing Complexity and Standardization Manufacturing iPSC-derived cells is a multi-step process involving donor cell procurement, reprogramming, expansion, differentiation, and formulation [17]. Each step introduces variability, and the lack of standardized protocols across laboratories complicates comparability between studies [117]. Furthermore, the transition from research-scale to clinical-scale production requires sophisticated bioreactor systems and rigorous quality control measures.
Regulatory and Standardization Challenges
The regulatory landscape for iPSC-based therapies continues to evolve, presenting several challenges:
Characterization Standards While iPSC characterization in published studies is generally aligned with criteria established by the International Society for Stem Cell Research, considerable variability exists in terms of study design, medical conditions examined, and cell source used for iPSC generation [117]. Moreover, a broad range of iPSC-derived cell products have been administered, further complicating cross-study comparisons [117].
Regulatory Pathways The complex, multi-step manufacturing process for iPSC-based products challenges traditional regulatory frameworks designed for simpler biological products. Regulatory agencies require extensive characterization, safety testing, and potency assays, but standardized approaches for these assessments are still emerging [17]. Alignment between regulatory bodies is needed to facilitate international trials [17].
Product Variability Differences in donor genetics, reprogramming techniques, differentiation protocols, and final product composition contribute to variability in clinical outcomes [117]. This heterogeneity complicates the determination of safety and efficacy profiles for iPSC-based therapies.
Emerging Trends and Future Directions
Technological Innovations
Gene Editing Integration The combination of iPSC technology with precise gene editing tools like CRISPR-Cas9 enables creation of genetically corrected autologous therapies and sophisticated disease models [16]. This approach is particularly valuable for monogenic disorders such as Duchenne muscular dystrophy, where gene editing has restored dystrophin expression in iPSC-derived myocytes in vitro [3].
Advanced Maturation Strategies Novel approaches to enhance the functional maturity of iPSC-derived cells include:
- 3D Bioprinting: Creating spatially organized tissue constructs with multiple cell types
- Organoid Systems: Self-organizing 3D structures that better recapitulate tissue architecture
- Biomimetic Scaffolds: Engineering substrates with tissue-specific mechanical properties
- Microphysiological Systems: "Organs-on-chips" that incorporate fluid flow and mechanical cues
Extracellular Vesicle Therapies iPSC-derived extracellular vesicles (EVs) represent a promising cell-free alternative that may offer similar therapeutic benefits with improved safety profiles [2]. EVs derived from iPSC-MSCs maintain their anti-inflammatory properties for longer durations than those from conventional MSCs, suggesting a wider therapeutic window [2].
Evolving Clinical Trial Designs
Future clinical trials will likely incorporate several key developments:
- Standardized Outcome Measures: Alignment around consistent endpoints to enhance comparability between studies
- Adaptive Trial Designs: Flexible protocols that allow modification based on interim results
- Combination Products: Integration of iPSC-derived cells with biomaterial scaffolds and controlled-release systems
- Personalized Dosing Strategies: Patient-specific dosing based on in vitro potency assays
Commercialization and Market Evolution
The iPSC landscape is witnessing increasing involvement from pharmaceutical companies and biotechnology firms [16] [119]. Key players include FUJIFILM Cellular Dynamics, Evotec, Ncardia, and Cynata Therapeutics [16] [119]. These companies are developing specialized platforms for iPSC-based drug screening and therapeutic development, contributing to the growing commercialization of the technology.
The transition from animal models to iPSC-based platforms signifies a broader move toward human-relevant, ethically responsible research [120] [121]. Recent legislative changes, including the FDA Modernization Act 2.0, permit cell-based assays as alternatives to animal testing for drug and biological product applications [16]. This regulatory shift is accelerating the adoption of iPSC-based models in early drug discovery.
The clinical translation of iPSC technology has progressed substantially since the first human trial in 2013, with a growing number of interventional studies now assessing the safety and efficacy of iPSC-derived cellular therapeutics. The field is rapidly evolving from small, uncontrolled safety studies to larger, controlled trials across multiple therapeutic areas, including ophthalmic, cardiovascular, hematological, and neurological applications.
Significant challenges remain, particularly regarding genomic stability, tumorigenicity risk, manufacturing standardization, and regulatory alignment. However, continuous technological improvements in reprogramming, differentiation, gene editing, and maturation protocols are addressing these limitations. The emergence of allogeneic iPSC-based products represents a promising approach for scaling up production and reducing costs.
As the field matures, alignment around standardized characterization criteria, outcome measures, and reporting standards will be essential for accelerating clinical adoption. With ongoing innovations and increasing collaboration between academic researchers, biotechnology companies, and regulatory agencies, iPSC-based therapies are poised to make significant contributions to regenerative medicine and personalized healthcare in the coming decade. The projected growth of the iPSC market to US$4.69 billion by 2033 reflects the considerable potential and increasing investment in this transformative technology [119].
Conclusion
Induced pluripotent stem cells have undeniably transformed the landscape of disease modeling, offering an unprecedented window into human pathology. The progression from simple 2D cultures to complex, multi-cellular 3D organoids has significantly enhanced our ability to recapitulate tissue- and organ-level diseases in vitro. While challenges remain—particularly concerning the functional immaturity of differentiated cells and technical variability—ongoing innovations in maturation protocols, genome editing, and bioengineering are providing robust solutions. The validation of these models against clinical phenotypes and their integration within evolving regulatory frameworks solidifies their critical role in the future of biomedical research. The continued advancement of iPSC technology promises to accelerate the discovery of novel therapeutics and ultimately enable the realization of personalized, regenerative medicine for a broad spectrum of human diseases.
References
- 1. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 2. Editorial: Role of induced pluripotent stem cells (iPSCs) in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1734717/full]
- 3. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590075/]
- 4. Mechanisms and models of somatic cell reprogramming - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4060150/]
- 5. Reprogrammed Pluripotent Stem Cells from Somatic Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3840974/]
- 6. Pluripotency genes of mammals: a network at work [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1578499/full]
- 7. Decoding human chemical reprogramming: mechanisms and principles - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0968000425000532]
- 8. Systematic optimization of prime editing for enhanced ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1589034/full]
- 9. The exit from naive pluripotency: a platform for the study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12493175/]
- 10. Technical challenges in using human induced pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2921621/]
- 11. Human iPSC banking: barriers and opportunities [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-019-0578-x]
- 12. Challenges and opportunities in the use of transcriptomic ... [https://www.sciencedirect.com/science/article/abs/pii/S0887233322001229]
- 13. The use of artificial intelligence in induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11108174/]
- 14. Moving Towards Induced Pluripotent Stem Cell-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8930923/]
- 15. Imaging and Tracking Stem Cells: A High Content ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3960299/]
- 16. Induced Pluripotent Stem Cell (iPSC) Industry Trends for ... [https://bioinformant.com/ipsc-industry-trends/]
- 17. The emerging promise of induced pluripotent stem cells in ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925008461]
- 18. Pluripotent Stem Cells: Recent Advances and Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025069/]
- 19. Induction of pluripotent stem cells from mouse embryonic ... [https://pubmed.ncbi.nlm.nih.gov/16904174/]
- 20. Induction of pluripotent stem cells from adult human ... [https://pubmed.ncbi.nlm.nih.gov/18035408/]
- 21. Global research dynamics in the induced pluripotent stem ... [https://www.sciencedirect.com/science/article/pii/S2352320425001488]
- 22. A Quantitative System for Discriminating Induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3572019/]
- 23. Applications, challenges, and prospects of induced ... [https://www.sciencedirect.com/science/article/pii/S101684782400102X]
- 24. A comprehensive analysis of induced pluripotent stem cell ... [https://pubmed.ncbi.nlm.nih.gov/40406420/]
- 25. Modulating the stem cell niche for tissue regeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4422171/]
- 26. The impact of the limbal niche interactions on the self- ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1667309/full]
- 27. Differentiation of Pluripotent Stem Cells for Disease Modeling [https://www.mdpi.com/1424-8247/17/3/337]
- 28. In silico modeling of directed differentiation of induced ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013407]
- 29. Skin Biopsy and Patient-Specific Stem Cell Lines - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4836060/]
- 30. Modeling rare genetic disease with patient-derived induced ... [https://pubmed.ncbi.nlm.nih.gov/40751518/]
- 31. of PSC & Directed - Tips... Differentiation Disease Modeling [https://www.stemcell.com/technical-resources/area-of-interest/pluripotent-stem-cell-research/directed-differentiation-and-disease-modeling/tech-tips-protocols.html]
- 32. Efficient and reproducible generation of human iPSC ... [https://www.nature.com/articles/s41467-024-50224-0]
- 33. Enhancing human pluripotent stem cell differentiation to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12124670/]
- 34. Protocol for generating NGN2 iPSC lines and large-scale ... [https://pubmed.ncbi.nlm.nih.gov/40022736/]
- 35. Enhancement of hepatic differentiation from induced ... [https://pubmed.ncbi.nlm.nih.gov/40377485/]
- 36. of human Directed ... differentiation induced pluripotent stem cells [https://www.nature.com/articles/nprot.2017.011?error=cookies_not_supported&code=1ee5cf3c-c2a9-4860-87c8-00d08c126e35]
- 37. for Protocol of Human Directed ... Differentiation Induced Pluripotent [https://link.springer.com/protocol/10.1007/978-1-4939-7163-3_15]
- 38. Enhanced cardiomyocyte differentiation and repair through ... [https://www.sciencedirect.com/science/article/pii/S0753332225008364]
- 39. Current and future precision therapy approaches in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12268256/]
- 40. Human induced pluripotent stem cell-derived ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1687840/full]
- 41. Induced Pluripotent Stem Cells Derived Cellular Models for ... [https://pubmed.ncbi.nlm.nih.gov/40587046/]
- 42. Modeling Human Neural Development and Disease with ... [https://www.isscr.org/upcoming-programs/poster-award-webinar]
- 43. Phase I/II trial of iPS-cell-derived dopaminergic cells for ... [https://www.nature.com/articles/s41586-025-08700-0]
- 44. Allogenic transplantation therapy of iPS cell-derived ... [https://www.sciencedirect.com/science/article/pii/S1353802025005747]
- 45. 3D Cell Culture Systems for Cardiovascular Tissue ... [https://www.frontiersin.org/research-topics/12897/3d-cell-culture-systems-for-cardiovascular-tissue-engineering-in-vitro-modelling-and-in-vivo-regenerative-therapies/magazine]
- 46. A comprehensive review on 3D tissue models [https://www.sciencedirect.com/science/article/abs/pii/S0142961223004167]
- 47. Comparison of 3D culture systems on mesenchymal stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562725/]
- 48. Brain organoids: a new paradigm for studying human ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1699814/full]
- 49. Morphodynamics of human early brain organoid ... [https://www.nature.com/articles/s41586-025-09151-3]
- 50. Emerging brain organoids: 3D models to decipher, identify ... [https://www.sciencedirect.com/science/article/pii/S2452199X25000258]
- 51. Exploring Organ-on-a-Chip Technology: A comprehensive ... [https://elveflow.com/microfluidic-reviews/exploring-organ-on-a-chip-technology-a-comprehensive-review/]
- 52. Organoids-on-a-chip: microfluidic technology enables ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1515340/full]
- 53. Using Organ-on-a-Chip Technology to Unlock Patient ... [https://emulatebio.com/using-organ-on-a-chip-technology-to-unlock-patient-derived-precision-medicine/]
- 54. Human organs-on-chips for disease modelling, drug ... [https://www.nature.com/articles/s41576-022-00466-9]
- 55. A Comprehensive Review of Organ-on-a-Chip Technology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11118005/]
- 56. Vascular architecture-on-chip: engineering complex blood ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d4lc00968a]
- 57. Expanding the Frontiers of Human Biology with Organ-on-a ... [https://emulatebio.com/expanding-the-frontiers-of-human-biology-with-organ-on-a-chip-technology-highlights-from-the-2025-mps-world-summit/]
- 58. A guide to the organ-on-a-chip [https://www.nature.com/articles/s43586-022-00118-6]
- 59. High throughput toxicity screening and intracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5215403/]
- 60. Quantitative Methods in System-Based Drug Discovery [https://www.intechopen.com/chapters/53186]
- 61. Human Stem Cells in Disease Modelling and Treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467989/]
- 62. Disease Modeling | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/disease-modeling.html]
- 63. Patient and Disease–Specific Induced Pluripotent Stem ... [https://www.sciencedirect.com/science/article/pii/S0031699724009451]
- 64. Induced pluripotent stem cells in disease modelling and ... [https://www.nature.com/articles/s41576-019-0100-z]
- 65. and iPSCs: Recent Developments and Future Perspectives in... CRISPR [https://pmc.ncbi.nlm.nih.gov/articles/PMC9428373/]
- 66. Modeling human diseases with induced pluripotent stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC5868991/]
- 67. | Molecular Devices CRISPR Genome Editing Disease Modeling [https://www.moleculardevices.com/lab-notes/clone-screening/crispr-genome-editing-disease-modeling]
- 68. qEva-CRISPR: a method for quantitative evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6158505/]
- 69. How To Use ICE: A Detailed Guide for Analyzing CRISPR ... [https://www.synthego.com/guide/how-to-use-crispr/ice-analysis-guide/]
- 70. Induced pluripotent stem cell-derived cardiomyocyte in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12376733/]
- 71. Structural Immaturity of Human iPSC-Derived Cardiomyocytes [https://pmc.ncbi.nlm.nih.gov/articles/PMC5808345/]
- 72. Advances in arrhythmogenic cardiomyopathy modeling ... [https://www.sciencedirect.com/science/article/pii/S1547527125027535]
- 73. Human induced pluripotent stem cell-cardiomyocytes for ... [https://www.kjpp.net/journal/view.html?doi=10.4196/kjpp.24.413]
- 74. Maturation of human cardiomyocytes derived from induced ... [https://www.nature.com/articles/s41598-024-63905-z]
- 75. Progress in engineering functional cardiac tissues from ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706125006762]
- 76. Article Rod-shaped micropatterning enhances the ... [https://www.sciencedirect.com/science/article/pii/S2213671124002431]
- 77. Cardiac disease mechanobiology: advances using hiPSC-CMs [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515892/]
- 78. Developmental cues for the maturation of metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4055054/]
- 79. Metabolic Culture Medium Enhances Maturation of Human ... [https://www.mdpi.com/1422-0067/26/15/7248]
- 80. Metabolic Maturation in hiPSC-Derived Cardiomyocytes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389403/]
- 81. Comprehensive promotion of iPSC-CM maturation by ... [https://www.nature.com/articles/s41467-025-58044-6]
- 82. Recent advances in regulating the proliferation or maturation ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03470-w]
- 83. Modeling rare genetic disease with patient-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317316/]
- 84. 3. Clinical Translation of Stem Cell-based Interventions [https://www.isscr.org/guidelines/clinical-translation-of-stem-cell-based-interventions]
- 85. Quantifying human pluripotent stem cell attributes with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12522491/]
- 86. Promoting the adoption of best practices and standards to ... [https://www.sciencedirect.com/science/article/pii/S2213671125001353]
- 87. AI-based approach to dissect the variability of mouse stem ... [https://www.nature.com/articles/s41467-025-56908-5]
- 88. Induced pluripotent stem cells in disease modelling and drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6584039/]
- 89. A review of protocols for human iPSC culture, cardiac ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405110/]
- 90. Subtype-specific cardiomyocytes for precision medicine: where are we now? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7529810/]
- 91. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pubmed.ncbi.nlm.nih.gov/41210051/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=00_a9J4PwqFAZZwfUHk-JsWGFsVnNNH2GKS5Nngxeig&fc=None&ff=20251111090443&v=2.18.0.post22+67771e2]
- 92. Stem Cell Manufacturing Market Growth Rate, Industry ... [https://www.datamintelligence.com/research-report/stem-cell-manufacturing-market]
- 93. Induced Pluripotent Stem Cells (iPSCs) Market Prospects ... [https://www.businesswire.com/news/home/20251111238841/en/Induced-Pluripotent-Stem-Cells-iPSCs-Market-Prospects-2025-2033-Industry-Gains-Traction-with-Rising-Investments-and-Collaborations---ResearchAndMarkets.com]
- 94. Stem Cell Manufacturing Market Size 2024 To 2034 [https://www.novaoneadvisor.com/report/stem-cell-manufacturing-market]
- 95. Quantitative association between gene expression and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10816716/]
- 96. Design of tables for the presentation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10346464/]
- 97. Understanding the anatomy and proper construction of tables [https://www.decisionfoundry.com/misc/articles/understanding-the-anatomy-and-proper-construction-of-tables/]
- 98. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 99. Transition from Animal-Based to Human Induced ... [https://www.mdpi.com/2073-4409/12/4/538]
- 100. Induced Pluripotent Stem Cells Production Market 2025 [https://www.custommarketinsights.com/report/induced-pluripotent-stem-cells-production-market/]
- 101. Reprogramming biology: iPSCs and the future of predictive ... [https://www.jax.org/news-and-insights/2025/november/reprogramming-biology-ipscs-and-the-future-of-predictive-research]
- 102. Animal Model Market Size, Share & Growth 2025-2035 [https://www.futuremarketinsights.com/reports/animal-model-market]
- 103. Trends & Strategies Shaping the $4.6+ Billion Induced ... [https://uk.finance.yahoo.com/news/trends-strategies-shaping-4-6-145400594.html]
- 104. Editorial: Studying rare diseases using induced pluripotent ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1686438/full]
- 105. Genome Editing of Isogenic Human Induced Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4149735/]
- 106. Studying rare diseases using induced pluripotent stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12450901/]
- 107. Modeling mutation-specific arrhythmogenic phenotypes in ... [https://www.nature.com/articles/s41598-024-52871-1]
- 108. Generation of Isogenic Pluripotent Stem Cells Differing ... [https://www.sciencedirect.com/science/article/pii/S0092867411006611]
- 109. Linking genotype to phenotype in multi-omics data of small ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-021-07867-w]
- 110. Editorial: Advances in iPSC technology for disease ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2023.1261279/full]
- 111. Comparative analysis of regulations and studies on stem cell ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04065-9]
- 112. Regulatory considerations for developing a phase I ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7848308/]
- 113. Induced Pluripotent Stem Cells Market Size 2025 to 2034 [https://www.precedenceresearch.com/induced-pluripotent-stem-cells-market]
- 114. Disease Modeling Using Induced Pluripotent Stem Cells [https://www.thermofisher.com/blog/behindthebench/disease-modeling-using-induced-pluripotent-stem-cells/]
- 115. Induced Pluripotent Stem Cell (iPSC) Therapy Market Size, ... [https://www.precedenceresearch.com/induced-pluripotent-stem-cell-therapy-market]
- 116. iPSC-based Platforms Market 2025 Report and Trends [https://www.towardshealthcare.com/insights/ipsc-based-platforms-market-sizing]
- 117. The emerging promise of induced pluripotent stem cells in ... [https://pubmed.ncbi.nlm.nih.gov/41160002/]
- 118. Review of the Current Trends in Clinical Trials Involving ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8445612/]
- 119. Trends & Strategies Shaping the $4.6+ Billion Induced ... [https://finance.yahoo.com/news/trends-strategies-shaping-4-6-145400149.html]
- 120. Moving Beyond Animal Models with iPSC-based Models [https://fujifilmbiosciences.fujifilm.com/us/blog/moving-beyond-animal-models-with-ipsc-based-models-shifts-and-new-challenges.html]
- 121. The Rise of iPSCs in Drug Discovery: Regulatory and ... [https://www.ncardia.com/insights/news/the-rise-of-ipscs-in-drug-discovery]