Embryonic vs. Induced Pluripotent Stem Cells: A Comparative Analysis for Advanced Disease Modeling
This article provides a comparative analysis of Embryonic Stem Cells (ESCs) and Induced Pluripotent Stem Cells (iPSCs) for in vitro disease modeling, tailored for researchers and drug development professionals.
Embryonic vs. Induced Pluripotent Stem Cells: A Comparative Analysis for Advanced Disease Modeling
Abstract
This article provides a comparative analysis of Embryonic Stem Cells (ESCs) and Induced Pluripotent Stem Cells (iPSCs) for in vitro disease modeling, tailored for researchers and drug development professionals. It explores the foundational biology and ethical considerations of both cell types, details methodological advances in reprogramming and differentiation, and examines their application in modeling neurological, cardiovascular, and metabolic disorders. The content addresses key challenges including genomic instability, tumorigenicity, and protocol standardization, while evaluating the comparative efficacy of each platform for phenotypic recapitulation, drug screening, and clinical translation. The synthesis aims to guide the selection of the optimal stem cell platform for specific research and therapeutic objectives.
Understanding Stem Cell Biology: From Pluripotency to Ethical Foundations
The advent of pluripotent stem cells has revolutionized biomedical research, offering unprecedented opportunities for disease modeling, drug discovery, and regenerative medicine. Embryonic Stem Cells (ESCs), derived from the inner cell mass of blastocysts, have long served as the gold standard for pluripotency [1]. The development of Induced Pluripotent Stem Cells (iPSCs) through somatic cell reprogramming provided an alternative that bypasses ethical concerns associated with embryo destruction [2]. While both cell types share defining characteristics of pluripotency—unlimited self-renewal capacity and the ability to differentiate into derivatives of all three germ layers—ongoing scientific debate questions whether these cell types are functionally equivalent [3] [4]. This guide provides an objective comparison of ESCs and iPSCs, highlighting key similarities and differences relevant to research applications.
Core Characteristics and Pluripotency: A Comparative Analysis
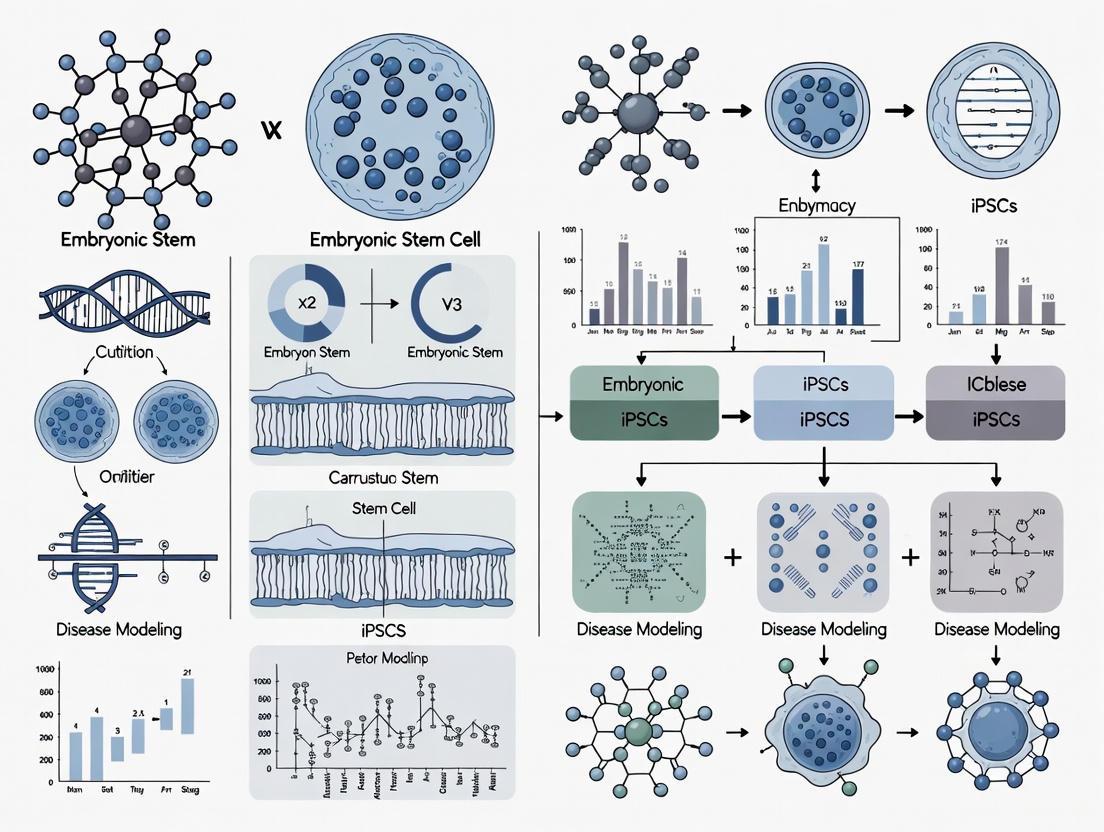
The following tables summarize the fundamental properties, molecular features, and functional applications of ESCs and iPSCs based on current research findings.
Table 1: Fundamental Characteristics of ESCs and iPSCs
| Characteristic | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Origin | Inner cell mass of blastocyst-stage embryos [1] | Reprogrammed somatic cells (e.g., fibroblasts, blood cells) [2] |
| Derivation Process | Isolation from donated embryos [1] | Introduction of reprogramming factors (e.g., OSKM) into somatic cells [1] [5] |
| Ethical Considerations | Involves embryo destruction [3] | Avoids embryo destruction, fewer ethical barriers [3] |
| Immunogenicity | Risk of allogeneic immune rejection [6] | Potential for autologous transplantation, reduced rejection risk [2] |
| Key Advantages | Represent "native" pluripotent state; gold standard for comparison [4] | Patient-specific; enable disease modeling without genetic manipulation [3] [2] |
| Key Limitations | Ethical restrictions; limited genetic diversity [3] | Potential for genomic instability; epigenetic memory [3] [2] |
Table 2: Molecular and Functional Comparison
| Parameter | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) | Experimental Evidence |
|---|---|---|---|
| Pluripotency Gene Network | Express core pluripotency factors (OCT4, SOX2, NANOG) [7] | Re-activates core pluripotency network; may show subtle gene expression differences [7] [4] | Gene expression analysis, immunostaining [6] |
| Epigenetic Landscape | Characteristic hyperdynamic chromatin structure; specific DNA methylation patterns [7] | Epigenetic reprogramming occurs; may retain residual epigenetic memory of cell of origin [3] [7] | DNA methylation analysis, chromatin immunoprecipitation [7] |
| Proteomic Profile | Reference proteome for pluripotent state [8] | Highly similar to ESCs, but shows increased levels of cytoplasmic, mitochondrial, and secreted proteins [8] | Quantitative mass spectrometry [8] |
| Trilineage Differentiation | Can differentiate into ectoderm, mesoderm, and endoderm derivatives [1] | Demonstrated capacity for trilineage differentiation; efficiency may vary between lines [2] [6] | Embryoid body formation, directed differentiation, teratoma assays [6] |
| Metabolic Activity | Reference metabolic state [8] | Higher protein content, mitochondrial potential, and metabolic rates in some studies [8] | High-resolution respirometry, metabolic flux analysis [8] |
| Disease Modeling Applications | Ideal for early embryonic lethality (e.g., Turner syndrome) [3] | Superior for patient-specific disorders (e.g., Parkinson's, ALS) and drug screening [3] [2] | Directed differentiation into disease-relevant cell types [3] [2] |
Experimental Approaches for Characterization
Standardized experimental protocols are essential for rigorous comparison between ESCs and iPSCs. Key methodologies include:
1. Reprogramming and Pluripotency Induction
- Somatic Cell Reprogramming: Dermal fibroblasts or peripheral blood mononuclear cells are transfected with reprogramming factors (typically OCT4, SOX2, KLF4, and c-MYC) using non-integrating methods such as Sendai virus or episomal vectors [2] [6]. The process involves global epigenetic remodeling, including DNA demethylation and chromatin reorganization, over several weeks [1] [7].
- Pluripotency Validation: Quality control assays confirm successful reprogramming. These include PCR and immunocytochemistry for pluripotency markers (OCT4, NANOG, SSEA-4), genomic integrity analysis via karyotyping, and functional assessment of differentiation potential through embryoid body formation and teratoma assays [2] [6].
2. Molecular and Functional Characterization
- Proteomic Analysis: Quantitative mass spectrometry using Tandem Mass Tag (TMT) labeling enables precise protein quantification. Data normalization with the "proteomic ruler" method reveals differences in absolute protein content, which may be masked by standard median normalization approaches [8].
- Raman Spectroscopy: This label-free technique detects biochemical differences based on inelastic light scattering. Studies have identified enriched nucleic acid content in iPSCs compared to ESCs, providing a non-biological method for discrimination [6].
- Directed Differentiation: Protocols using specific growth factors and small molecules guide ESCs and iPSCs toward defined lineages (e.g., neurons, cardiomyocytes). The efficiency and maturity of resulting cells are compared using lineage-specific markers and functional assays [3] [2].
Experimental Workflow for Pluripotency Studies
Key Signaling Pathways and Molecular Mechanisms
The maintenance of pluripotency and execution of differentiation programs are governed by complex molecular networks.
Molecular Regulation of Pluripotency
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Pluripotent Stem Cell Research
| Reagent Category | Specific Examples | Function in Research |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM); OCT4, SOX2, NANOG, LIN28 (OSNL) [1] [5] | Induction of pluripotency in somatic cells; different combinations affect efficiency and iPSC quality |
| Culture Matrices | Matrigel, Laminin-521 [2] | Provides extracellular matrix support for feeder-free cell culture and maintenance of pluripotency |
| Culture Media | mTeSR1, Essential 8 (E8) medium [2] | Chemically defined formulations containing essential growth factors (e.g., FGF2) for maintaining pluripotent state |
| Pluripotency Markers | Antibodies against OCT4, SOX2, NANOG, SSEA-4, TRA-1-60 [6] | Validation of pluripotent state through immunocytochemistry, flow cytometry |
| Differentiation Inducers | Growth factors (BMP4, Activin A, FGFs), Small molecules (CHIR99021, SB431542) [3] [2] | Direct differentiation toward specific lineages (ectoderm, mesoderm, endoderm) |
| Quality Control Assays | PluriTest, Karyotyping, Mycoplasma testing [2] [6] | Assessment of genomic integrity, pluripotency, and absence of contamination |
ESCs and iPSCs represent two sides of the pluripotency coin, each with distinct advantages and limitations. ESCs remain the gold standard reference for the pluripotent state, particularly valuable for studying early embryonic development and disorders involving embryonic lethality [3]. iPSCs offer unprecedented flexibility for patient-specific disease modeling, drug screening, and developing autologous cell therapies, though concerns regarding genomic stability and epigenetic memory warrant careful consideration [3] [2]. The choice between ESC and iPSC models should be guided by specific research objectives, with ESCs providing a foundational benchmark and iPSCs enabling personalized medical applications. As reprogramming technologies advance and our understanding of molecular differences deepens, both cell types will continue to be indispensable tools for unraveling developmental biology and developing novel therapeutics.
Biological Origins and Derivation Methods
Embryonic Stem Cells (ESCs) are pluripotent stem cells derived from the inner cell mass (ICM) of blastocyst-stage embryos [9] [10]. During mammalian development, the totipotent zygote undergoes multiple divisions to form a blastocyst, within which the first cell fate bifurcation occurs: the trophectoderm (TE) that will form extra-embryonic tissues, and the ICM that contains the pluripotent cells destined to form the embryo proper [9]. The ICM further segregates into primitive endoderm (PE) and epiblast (EPI) lineages, with EPI cells representing the primary source of true pluripotent cells [9]. The isolation of human ESCs (hESCs) was first achieved by James Thomson and colleagues in 1998, opening new avenues for studying human development and disease [1].
The derivation of ESCs requires precise methodological considerations to maintain the pluripotent state. Historically, the first ESCs were derived using culture conditions based on media for teratocarcinoma-derived embryonal carcinoma cells, including feeder layers and fetal calf serum [9]. Subsequent research revealed that these components could be substituted with leukemia inhibitory factor (LIF) and bone morphogenetic protein 4 (Bmp4) [9]. More recent advances utilize basic fibroblast growth factor (bFGF) to promote human ESC self-renewal [10]. Additional components required to maintain stem cell characteristics include cytokines (e.g., TGF-β, WNT3A), human serum albumin or serum replacement, and extracellular matrix components such as matrigel, fibronectin, or laminin [10].
ICM Isolation Techniques
The following diagram illustrates the primary methodological approaches for isolating the inner cell mass from blastocysts:
Two primary techniques have been developed for ICM isolation:
1. Immunosurgery: This traditional method involves removing the zona pellucida, then incubating blastocysts with antibodies that bind to trophectoderm cells, followed by complement-mediated lysis to selectively destroy the trophectoderm while leaving the ICM intact [11]. Although effective, this approach is time-consuming and carries a risk of contaminating ES cells with animal materials when used for therapeutic applications [11].
2. Microsurgical Technique: This improved mechanical method uses micromanipulators under an inverted microscope to physically separate the ICM [11]. The procedure involves: (1) anchoring the embryo on the ICM side with a holding needle using suction from a micrometer syringe; (2) cutting off the zona pellucida; and (3) tearing off the trophoblastic layer from the nudity blastocyst [11]. Comparative studies demonstrate that this microsurgical approach increases successful derivation rates compared to immunosurgery while eliminating potential animal material contamination [11].
Research Reagent Solutions for ESC Derivation
Table: Essential Research Reagents for ESC Derivation and Culture
| Reagent Category | Specific Examples | Function in ESC Biology |
|---|---|---|
| Cytokines & Growth Factors | bFGF (FGF-2), LIF, TGF-β, WNT3A | Support self-renewal and maintenance of pluripotent state; bFGF particularly important for hESC self-renewal [10]. |
| Culture Supplements | Human serum albumin, Serum replacement | Provide essential nutrients and attachment factors while maintaining defined culture conditions [10]. |
| Extracellular Matrix | Matrigel, Fibronectin, Laminin | Provide structural support and signaling cues for cell attachment and proliferation [10]. |
| Signaling Inhibitors | MEK/ERK inhibitors, GSK3 inhibitors | Help maintain naive pluripotency states in combination with other factors [10]. |
| Metabolic Components | Glutamine, Lipid supplements | Support high metabolic demands of rapidly proliferating pluripotent cells [8]. |
Comparative Analysis: ESCs vs. iPSCs in Disease Modeling
The development of induced pluripotent stem cells (iPSCs) in 2006 by Shinya Yamanaka's lab provided an alternative pluripotent cell source [12] [1]. iPSCs are generated by reprogramming somatic cells through the overexpression of key transcription factors (OCT4, SOX2, KLF4, c-MYC - OSKM factors) [1]. While both ESCs and iPSCs share the fundamental properties of pluripotency and self-renewal, significant functional differences impact their utility in disease modeling research.
Molecular and Functional Comparisons
Table: Experimental Comparison of ESCs and iPSCs in Disease Modeling
| Parameter | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Origin | Inner cell mass of blastocyst-stage embryos [9] [10] | Reprogrammed somatic cells (e.g., fibroblasts, blood cells) [12] [1] |
| Reprogramming Method | Natural embryonic development | Viral vectors (retrovirus, Sendai virus) or non-integrating methods (episomal vectors) [13] |
| Ethical Considerations | Controversial due to embryo destruction [3] | Non-controversial, no embryos required [3] |
| Genetic Background | Wild-type or specific mutations via PGD embryos [3] | Patient-specific, including disease-associated mutations [3] |
| Transcriptional Profile | Gold standard for pluripotency [14] | Near-identical to ESCs but with subtle differences [14] |
| DNA Methylation | Characteristic pluripotency signature [13] | Epigenetic memory of somatic cell origin; aberrant methylation patterns [14] [13] |
| Differentiation Propensity | Consistent across lines [14] | Variable yield of neural, cardiovascular progeny [14] |
| Disease Modeling Applications | Early embryonic lethality (e.g., Turner syndrome) [3] | Patient-specific diseases, late-onset disorders [3] |
Proteomic analyses reveal that while ESCs and iPSCs express a nearly identical set of proteins, they show consistent quantitative differences in expression levels [8]. iPSCs demonstrate increased total protein content (over 50% higher than ESCs), with significantly increased abundance of cytoplasmic and mitochondrial proteins required to sustain high growth rates, including nutrient transporters and metabolic proteins [8]. These molecular differences correlate with functional phenotypes, as iPSCs show increased glutamine uptake, enhanced lipid droplet formation, and elevated mitochondrial potential compared to ESCs [8].
Signaling Pathways Governing Pluripotency
The maintenance of pluripotency in ESCs is regulated by complex signaling networks that differ between species. The following diagram illustrates the key signaling pathways involved in maintaining human ESCs:
The core pluripotency network in ESCs is governed by transcription factors including OCT4, NANOG, and SOX2 [9]. In mouse ESCs, LIF/Stat3 signaling is critical for maintaining pluripotency, while human ESCs rely more heavily on FGF signaling and TGF-β pathways [9] [10]. Inhibition of MEK/ERK and glycogen synthase kinase-3 (GSK3) signaling, combined with activation of Stat3 by LIF, was previously thought sufficient to promote the pluripotent ground state [10]. However, culture with basic fibroblast growth factor (bFGF) has proven more effective for promoting human ESC self-renewal [10].
Experimental Workflows in Disease Modeling
ESC-Based Disease Modeling Workflow
The following diagram outlines the generalized experimental workflow for creating and validating ESC-based disease models:
ESC-based disease models are generated through two primary approaches: (1) derivation from preimplantation genetic diagnosis (PGD)-identified mutant embryos, or (2) genetic manipulation of existing wild-type ESC lines using genome editing technologies [3]. The ICM is isolated via microsurgical techniques or immunosurgery, followed by ESC derivation under appropriate culture conditions [11]. Resulting lines must be validated for pluripotency through teratoma formation assays and marker expression analysis before directed differentiation into disease-relevant cell types [3].
Advantages and Limitations in Research Applications
Each cell type offers distinct advantages for specific research applications:
ESC-Based Models Excel For:
- Studying early embryonic lethal disorders (e.g., Turner syndrome) where ESCs better model embryonic phenotypes than iPSCs from surviving patients [3]
- Investigating placental development defects underlying early miscarriage [3]
- Research requiring consistent differentiation propensity across cell lines [14]
- Studies where epigenetic memory from somatic cells would confound results [3]
iPSC-Based Models Excel For:
- Patient-specific disease modeling with complete genetic background [3]
- Studying late-onset disorders and age-related diseases [1]
- Drug screening platforms using patient-specific cells [12]
- Applications where ethical considerations limit ESC use [3]
Notably, some disease phenotypes manifest differently in ESC versus iPSC models. For example, in Turner syndrome (XO karyotype), ESCs derived by screening for spontaneous X chromosome loss revealed significant effects on placental gene expression, suggesting abnormal placental development as the cause of early embryonic lethality [3]. In contrast, iPSCs derived from Turner syndrome patients showed minimal effects on placental gene expression, representing the rare surviving cases rather than the typical embryonic lethal phenotype [3].
Similarly, in Huntington's disease, an ESC-based model expressing mutant huntingtin with expanded polyglutamine repeats demonstrated protein aggregation, while iPSC-based models from patients did not consistently show this phenotype, suggesting differential vulnerability to proteostasis disruption between these cell types [3].
Both ESCs and iPSCs provide powerful platforms for disease modeling, each with distinct advantages and limitations. ESCs, derived from the ICM of blastocysts, remain the gold standard for pluripotency and are particularly valuable for studying early developmental disorders and establishing baseline molecular profiles. iPSCs offer unprecedented access to patient-specific genetic backgrounds and avoid ethical concerns associated with ESCs. The choice between ESC and iPSC models should be guided by the specific research question, with ESCs preferred for studies of early embryonic development and disorders causing embryonic lethality, and iPSCs optimal for modeling patient-specific diseases and developing personalized therapeutic approaches. Understanding the molecular and functional differences between these cell types enables researchers to select the most appropriate model system for their specific disease modeling applications.
The field of regenerative medicine and disease modeling was fundamentally reshaped by the advent of techniques to derive human pluripotent stem cells (hPSCs), which possess an unlimited self-renewal capacity and can differentiate into virtually any adult cell type [3] [15]. For decades, human Embryonic Stem Cells (ESCs), isolated from the inner cell mass of blastocysts, served as the primary source of pluripotent cells for research [15]. However, their use is accompanied by ethical concerns and immunological rejection risks [16] [17]. A paradigm shift occurred with the discovery of induced Pluripotent Stem Cells (iPSCs), somatic cells reprogrammed to a pluripotent state through the introduction of specific transcription factors, most notably the Yamanaka factors (OCT4, SOX2, KLF4, and c-MYC) [18] [19]. This breakthrough offered a path to generate patient-specific cell lines without the ethical constraints of ESCs [17]. While theoretically similar in pluripotency, ESCs and iPSCs exhibit fundamental biological and practical differences that critically impact their efficacy in disease modeling, making the choice between them a strategic decision for researchers [3] [20]. This guide provides an objective comparison of their performance, supported by experimental data and methodologies.
Core Technology Comparison: Derivation and Practical Considerations
The fundamental distinction between ESCs and iPSCs lies in their origin and derivation process, which directly translates into specific advantages and limitations for each system. The following table summarizes the core differentiators.
Table 1: Core Technology and Practical Considerations of ESCs vs. iPSCs
| Feature | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Origin | Inner cell mass of a blastocyst [15] | Reprogrammed somatic cells (e.g., skin fibroblasts, blood cells) [3] [19] |
| Key Derivation Method | Isolation via microsurgery or immunological targeting of trophoblast cells from donated embryos [15] | Viral (retrovirus, lentivirus) or non-viral delivery of reprogramming factors (OCT4, SOX2, KLF4, c-MYC) [3] [21] |
| Ethical Status | Contentious; involves destruction of human embryos [3] [17] | Avoids ethical concerns associated with embryo use [16] [17] |
| Immunological Compatibility | Allogeneic; risk of immune rejection upon transplantation [16] | Autologous; potential for patient-specific cells, minimizing rejection [16] |
| Genetic Context | Wild-type or specific mutations via PGD; requires genetic manipulation for disease modeling [3] | Endogenously contains the patient's complete genetic background, including disease-causing mutations [3] [21] |
| Accessibility & Scalability | Limited to available embryos and associated with IVF units; restricted/banned in some countries [3] [16] | High; somatic cells are easily accessible from patients, enabling large-scale production of disease-specific lines [3] |
The derivation of mutated ESCs for disease modeling typically requires inefficient genome editing or derivation from affected embryos identified via Preimplantation Genetic Diagnosis (PGD), which is limited to a small number of diseases [3] [20]. In contrast, iPSCs are derived by reprogramming a patient's somatic cells, inherently capturing the full genetic complexity of the disease and obviating the need for complex genetic engineering [21].
Comparative Efficacy in Disease Modeling: Experimental Evidence
While both cell types are pluripotent, their utility in accurately recapitulating disease phenotypes can vary significantly based on the specific disorder. The following experimental data highlights these nuances.
Table 2: Comparative Analysis of ESC and iPSC Models in Specific Genetic Disorders
| Disease | ESC-Based Model Findings | iPSC-Based Model Findings | Comparative Efficacy Conclusion |
|---|---|---|---|
| Turner Syndrome (XO Karyotype) | XO ESCs showed significant dysregulation of placental genes, suggesting a cause for the high rate of early embryonic lethality [3] [20]. | iPSCs from surviving patients showed minimal effect on placental gene expression, representing the rare surviving cases [3] [20]. | ESCs > iPSCs for studying early developmental lethality; iPSCs are suitable for studying postnatal phenotypes [3]. |
| Spinal Muscular Atrophy | Knockdown of SMN in ESCs successfully modeled the disease [3]. | iPSCs derived from patients recapitulated disease phenotypes [3]. | ESCs ≈ iPSCs; both systems effectively modeled the disorder [3]. |
| Fanconi Anemia | Gene targeting (e.g., TALEN) or knockdown of FANCA/FANCD2 used to create models [3]. | Reprogramming itself is challenging due to genomic instability; successful models have been generated [3]. | Context-dependent; the reprogramming process can be a hurdle for diseases with genomic instability [3]. |
| Long QT Syndrome | Gene targeting in ESCs successfully created disease models [3]. | Patient-specific iPSCs effectively modeled the cardiac electrical abnormality [3]. | ESCs ≈ iPSCs; both systems are effective for modeling this cardiac channelopathy [3]. |
| Huntington’s Disease | Overexpression of mutant HTT in ESCs led to the appearance of protein aggregates [3]. | Consortium studies generated iPSC models, but one study showed aggregates formed in the ESC model [3]. | ESCs > iPSCs in one study; potential differences in phenotypic penetrance [3]. |
Detailed Experimental Protocol: Modeling Liver Disease from Pluripotent Stem Cells
A key application of hPSCs is generating disease-relevant cell types, such as hepatocytes for liver disease modeling. The following workflow, derived from a detailed differentiation roadmap, outlines the signals and markers for efficient liver progenitor generation from both ESCs and iPSCs [22].
Diagram 1: Directed Differentiation to Liver Cell Types.
This protocol emphasizes that liver commitment is executed by a temporally dynamic sequence of signaling events that suppress alternate fates (e.g., pancreas, intestines) across six consecutive lineage choices [22]. The efficiency of this process can be quantitatively tracked using cell-surface markers (e.g., CD99+CD184−CD10− for liver progenitors) [22].
Key Limitations of iPSC-Based Models
Despite their advantages, iPSCs have several documented limitations that can affect disease modeling fidelity:
- Incomplete Reprogramming and Epigenetic Memory: iPSCs may retain an epigenetic memory of their somatic cell origin, which can bias their differentiation potential [3] [20].
- Genomic Instability: The reprogramming process itself can introduce mutations or cause chromosomal instability, potentially confounding disease phenotypes [3] [20].
- Variable Reprogramming Efficiency: Certain genetic aberrations can significantly decrease the efficiency of generating iPSCs, creating a selection bias [3].
The Research Toolkit for Pluripotent Stem Cell Disease Modeling
A standardized set of reagents and tools is essential for the derivation, maintenance, and differentiation of hPSCs for disease modeling.
Table 3: Essential Research Reagent Solutions for hPSC Work
| Reagent / Solution | Function | Key Examples & Notes |
|---|---|---|
| Reprogramming Factors | Resets somatic cell identity to pluripotency. | OCT4, SOX2, KLF4, c-MYC (Yamanaka factors); delivered via retrovirus, lentivirus, or Sendai virus [19] [21]. |
| Base Medium & Supplements | Supports hPSC self-renewal and expansion in culture. | Feeder-free media (e.g., mTeSR1); often contains FGF2 (bFGF) to maintain pluripotency [22]. |
| Inductive Growth Factors & Small Molecules | Directs differentiation toward specific lineages. | ACTIVIN/TGF-β (definitive endoderm), BMP4 & FGF (liver progenitors), Retinoic Acid (patterning), small molecule inhibitors (e.g., TGF-β inhibitor SB431542) [22]. |
| Characterization Antibodies | Confirms pluripotency and lineage-specific differentiation. | Pluripotency: OCT4, SOX2, NANOG; Endoderm: SOX17, FOXA2; Liver: HNF4A, TBX3, FAH, Albumin [22]. |
| Gene Editing Tools | Introduces or corrects mutations in ESCs or isogenic iPSC lines. | CRISPR-Cas9, TALENs; used for creating knockout models or generating genetically corrected controls [3] [15]. |
Emerging Trends and Regulatory Landscape
The field of hPSC research is rapidly evolving, with several key trends shaping its future. Artificial Intelligence (AI) and Machine Learning (ML) are now being integrated to enhance iPSC technology, improving reprogramming efficiency, predicting optimal differentiation conditions, and automating quality control by analyzing colony morphology and multi-omics data [19]. Furthermore, the regulatory frameworks governing the clinical translation of these therapies vary significantly across leading research nations, influencing the pace of development [16]. The United States and Japan, with more flexible guidelines, are leading in the number of clinical trials, while the European Union maintains rigorous regulations that prioritize safety and ethics [16]. The number of clinical trials involving iPSCs has seen significant global growth since 2008, particularly targeting conditions of the cardiovascular and nervous systems [16].
Both ESCs and iPSCs are powerful and complementary tools for disease modeling. The choice between them is not a matter of superiority but of strategic alignment with the research goal. iPSCs excel in modeling patient-specific, post-natal disease pathologies, drug screening, and personalized therapeutic discovery while avoiding ethical and immunological hurdles. In contrast, ESCs can be more effective for studying early embryonic lethal disorders, due to the potential selection bias in iPSCs derived from surviving patients, and in contexts where the genetic instability of the reprogramming process is a concern. The ongoing integration of AI and refined differentiation protocols promises to further enhance the precision and scalability of both systems, solidifying their role in advancing regenerative medicine and drug development.
The field of regenerative medicine has been profoundly shaped by two cornerstone cell types: Embryonic Stem Cells (ESCs) and Induced Pluripotent Stem Cells (iPSCs). ESCs, isolated from the inner cell mass of blastocysts, represent the gold standard for pluripotency but entail ethical controversies and allogeneic immune rejection concerns [23] [1]. In contrast, iPSCs, generated through the reprogramming of somatic cells, offer an autologous alternative while maintaining comparable differentiation potential [2] [1]. Understanding the nuanced molecular similarities and differences between these cell types is paramount for evaluating their comparative efficacy in disease modeling and therapeutic development. This guide provides a systematic comparison of the transcriptional networks and epigenetic landscapes that define ESCs and iPSCs, equipping researchers with the necessary framework to select the most appropriate cell type for specific biomedical applications.
Core Molecular Characteristics
Transcriptional Networks Governing Pluripotency
The pluripotent state in both ESCs and iPSCs is maintained by a core transcriptional network centered on key transcription factors. The canonical Yamanaka factors (OCT4, SOX2, KLF4, c-MYC) form the foundation of iPSC induction, while ESCs endogenously express these and other critical regulators such as NANOG [2] [1] [24]. OCT4 (POU5F1) and SOX2 operate in a cooperative manner to activate pluripotency-associated genes while simultaneously repressing lineage-specific differentiation programs [1]. The stabilization of this network occurs through the endogenous reactivation of the OCT4 promoter, which serves as a central mechanism for establishing and maintaining the pluripotent state [2].
Recent investigations have revealed that while the core transcriptional circuitry is largely shared, subtle differences in gene expression profiles can persist in iPSCs compared to ESCs. These variations may stem from incomplete epigenetic resetting or the retention of a somatic memory reflective of the donor cell type [2] [25]. The transcriptional dynamics during reprogramming follow a biphasic pattern: an initial stochastic phase where somatic genes are silenced and early pluripotency genes are activated, followed by a more deterministic phase where late pluripotency-associated genes are established [1].
Table 1: Core Pluripotency Transcription Factors in ESCs and iPSCs
| Transcription Factor | Role in Pluripotency | Expression in ESCs | Expression in iPSCs | Functional Notes |
|---|---|---|---|---|
| OCT4 (POU5F1) | Master regulator of pluripotency | High endogenous expression | Reactivated during reprogramming | Essential for establishment and maintenance of pluripotency; central stabilizer of pluripotent state [2] [1] |
| SOX2 | Partners with OCT4 in transcriptional regulation | High endogenous expression | Reactivated during reprogramming | Forms heterodimers with OCT4; regulates expression of multiple pluripotency genes [1] |
| NANOG | Stabilizes pluripotent state | High endogenous expression | Variable reactivation | Critical for preventing spontaneous differentiation; often included in alternative reprogramming factor cocktails [1] [24] |
| KLF4 | Promotes self-renewal | Expressed | Overexpressed during reprogramming | Can be substituted by KLF2 or KLF5 with reduced efficiency [24] |
| c-MYC | Enhances proliferation | Expressed | Overexpressed during reprogramming | Not strictly essential but significantly increases reprogramming efficiency; considered oncogenic [2] [24] |
| LIN28 | RNA-binding protein | Expressed | Used in alternative reprogramming (OSNL) | Promotes reprogramming through miRNA regulation; alternative to c-MYC [1] [24] |
Epigenetic Landscapes
The epigenetic landscape represents a crucial differentiator between ESCs and iPSCs. While both cell types share fundamental pluripotency features, iPSCs frequently retain epigenetic memories of their somatic cell origin, which can manifest as differential DNA methylation patterns and chromatin accessibility profiles [2] [25]. Research indicates that the relationship between genetic variation and epigenetic variation is most pronounced at the iPSC stage, with this association weakening following differentiation [25].
Reprogramming to pluripotency requires comprehensive epigenetic remodeling, including chromatin restructuring and DNA methylation resetting [2] [1]. However, this process is often incomplete, leading to aberrant epigenetic signatures in iPSCs. A comparative analysis has revealed that iPSCs generated through transcription factor overexpression harbor more epigenetic abnormalities compared to those produced via somatic cell nuclear transfer (SCNT), suggesting that the reprogramming methodology itself significantly influences the resulting epigenetic landscape [26].
Notably, studies utilizing multiomics approaches have demonstrated that donor-specific epigenetic patterns are maintained in iPSCs, with lines from the same donor clustering together in principal component analyses of DNA methylation data [25]. This donor-specific epigenetic signature underscores the persistent influence of the original somatic epigenome, even after extensive reprogramming and passaging.
Table 2: Epigenetic Features of ESCs versus iPSCs
| Epigenetic Feature | ESCs | iPSCs | Functional Consequences |
|---|---|---|---|
| DNA Methylation Patterns | Established during embryonic development | Often retain somatic memory signatures | Can influence differentiation potential and disease modeling fidelity [25] |
| Chromatin Accessibility | Characteristic of native pluripotency | Resembles ESCs but with somatic cell-type specific variations | Affects transcription factor binding and gene expression profiles [1] [25] |
| Histone Modification Landscape | H3K4me3 at promoters of active genes; H3K27me3 at bivalent domains | Generally similar but may show variations at specific loci | Can create aberrant differentiation propensities in iPSCs [2] |
| X-Chromosome Inactivation | Inactivated in female lines | Variable reactivation and silencing patterns | Incomplete X-reactivation observed in female iPSC lines [27] |
| Imprinting Status | Normal parental-specific methylation | Frequent loss of imprinting (LOI) during reprogramming | Can affect growth and differentiation properties [27] |
| Relationship to Genetic Variation | Not applicable | Strong association in iPSCs, weakens after differentiation | Donor-specific patterns maintained despite reprogramming [25] |
Experimental Modeling and Data Generation
Methodologies for Molecular Profiling
Comprehensive molecular profiling of ESCs and iPSCs requires the integration of multiple experimental approaches to capture the complexity of their transcriptional and epigenetic states. The following protocols represent standardized methodologies for generating comparative data.
Protocol 1: Genome-Wide Epigenetic Analysis of Pluripotent Cells
- Objective: To assess and compare the DNA methylation and chromatin accessibility landscapes of ESCs and iPSCs.
- Sample Preparation: Culture ESCs and iPSCs under identical conditions using defined media (e.g., mTeSR1 or E8) on recombinant laminin or Matrigel substrates. Maintain cells for a consistent number of passages (e.g., 10-20) to minimize culture-induced artifacts [2] [27].
- DNA Methylation Profiling (Whole Genome Bisulfite Sequencing):
- Extract high-molecular-weight genomic DNA using a commercial kit.
- Treat DNA with bisulfite to convert unmethylated cytosines to uracils.
- Prepare sequencing libraries and perform whole-genome sequencing on an Illumina platform to a recommended coverage of >30x.
- Align sequences to a reference genome and calculate methylation ratios for all cytosine positions [25].
- Chromatin Accessibility Profiling (ATAC-Seq):
- Harvest 50,000 viable cells per sample.
- Perform tagmentation reaction using hyperactive Tn5 transposase.
- Purify and amplify the tagmented DNA.
- Sequence libraries and map reads to the reference genome to identify regions of open chromatin [25].
- Data Analysis: Identify differentially methylated regions (DMRs) and differentially accessible peaks between ESC and iPSC lines. Integrate data with transcriptomic profiles to correlate epigenetic states with gene expression [25].
Protocol 2: Single-Cell Multiomics for Lineage Propensity Assessment
- Objective: To evaluate cellular heterogeneity and lineage-specific transcriptional and epigenetic states at single-cell resolution.
- Sample Preparation: Culture ESCs and iPSCs as described in Protocol 1. Include both undifferentiated populations and cells directed toward early differentiation (e.g., via embryoid body formation for 3-5 days) [27].
- Single-Cell RNA Sequencing (scRNA-seq):
- Prepare single-cell suspensions with high viability (>90%).
- Partition cells into nanoliter-scale droplets using a platform such as the 10x Genomics Chromium Controller.
- Generate barcoded cDNA libraries and sequence to a depth of >50,000 reads per cell.
- Perform clustering analysis to identify distinct cell populations and lineage trajectories [27].
- Single-Cell ATAC Sequencing (scATAC-seq):
- Process cells in parallel using a commercial scATAC-seq kit.
- Sequence libraries and analyze fragment insert sizes to map nucleosome positions and transcription factor accessibility.
- Integrate with scRNA-seq data to link regulatory element activity with transcriptional outputs [27].
- Data Analysis: Compare the diversity of cell states and the frequency of spontaneous differentiation between ESC and iPSC cultures. Identify any residual somatic gene expression programs in iPSCs [25] [27].
Signaling Pathway Diagrams
The molecular pathways that govern pluripotency and reprogramming are complex. The following diagrams illustrate the core signaling networks and experimental workflows central to understanding ESC and iPSC biology.
Diagram 1: Key Pathways in Pluripotency and Reprogramming. The top section illustrates the multi-stage process of somatic cell reprogramming to iPSCs. The bottom section shows the core autoregulatory transcriptional network that maintains pluripotency in both ESCs and established iPSCs [2] [1].
Diagram 2: Experimental Workflow for Comparative Molecular Profiling. This diagram outlines the integrated multi-omics approach for generating comprehensive molecular data from ESCs and iPSCs, from sample preparation through data integration and analysis [25] [27].
Applications in Disease Modeling
The application of ESCs and iPSCs in disease modeling represents one of the most transformative advances in biomedical research. iPSCs offer a unique advantage through their ability to be derived from patients with specific genetic backgrounds, creating in vitro models that recapitulate disease pathophysiology [2] [1]. This has been particularly valuable for studying neurological disorders, cardiovascular diseases, and metabolic conditions.
Neurological Disease Models
iPSC-derived neuronal models have provided unprecedented insights into the pathogenesis of Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS). Patient-specific neurons enable the analysis of pathogenic mechanisms and the evaluation of pharmacological interventions [2]. For ALS, iPSC-derived motor neurons (iPSC-MNs) reproduce disease-specific pathology, including TDP-43 protein aggregation, and provide a platform for investigating molecular mechanisms and screening therapeutic compounds [24]. In PD models, iPSC-derived dopaminergic neurons recapitulate the degeneration characteristic of the substantia nigra and have elucidated the role of α-synuclein aggregation in both sporadic and familial forms of the disease [2].
Cardiovascular and Metabolic Disease Models
iPSCs differentiated into cardiomyocytes enable the study of arrhythmogenic disorders, heart failure, and myocardial injury. Models of congenital arrhythmias linked to mutations in genes such as KCNQ1 provide a foundation for precision cardiology [2]. In the realm of metabolic diseases, iPSCs preserve the patient's genotype in vitro, making them powerful tools for investigating conditions like cystic fibrosis, Duchenne muscular dystrophy (DMD), and Wilson's disease [2]. For type 2 diabetes and insulin resistance, iPSC-derived hepatocytes, myocytes, and adipocytes allow researchers to study tissue-specific mechanisms of insulin resistance and screen for potential therapeutics [28].
Table 3: Disease Modeling Applications of ESCs and iPSCs
| Disease Category | Model System | Key Findings/Applications | Advantages of iPSCs |
|---|---|---|---|
| Neurodegenerative (ALS) | iPSC-derived motor neurons | Recapitulate TDP-43 pathology; platform for drug screening [24] | Patient-specific genetic background; enable study of sporadic and familial forms |
| Neurodegenerative (PD) | iPSC-derived dopaminergic neurons | Model α-synuclein aggregation; study dopaminergic neuron vulnerability [2] | Capture full genetic complexity of disease; useful for personalized therapeutic testing |
| Cardiovascular | iPSC-derived cardiomyocytes | Model channelopathies (e.g., KCNQ1); test drug-induced arrhythmogenesis [2] | Source of human cardiomyocytes for disease modeling and safety pharmacology |
| Metabolic (T2D/IR) | iPSC-derived hepatocytes, adipocytes, myocytes | Study tissue-specific insulin resistance mechanisms; drug screening [28] | Generate otherwise inaccessible human metabolic cell types with disease genotypes |
| Autoimmune (SLE) | iPSC-derived B and T lymphocytes | Recapitulate dysregulated signaling and autoantibody production [2] | Model complex immune cell interactions in a patient-specific context |
| Genetic (Cystic Fibrosis) | iPSC-derived airway epithelial cells | Reproduce defective chloride transport; evaluate CFTR correctors [2] | Platform for evaluating patient-specific responses to targeted therapies (e.g., ivacaftor) |
Research Reagent Solutions
Successful molecular profiling and disease modeling require access to high-quality, well-characterized reagents and cellular tools. The following table outlines essential materials for research in this field.
Table 4: Essential Research Reagents for Pluripotent Stem Cell Research
| Reagent Category | Specific Examples | Function/Application | Considerations for ESC vs. iPSC Work |
|---|---|---|---|
| Reprogramming Factors | OSKM factors (OCT4, SOX2, KLF4, c-MYC); OSNL factors (OCT4, SOX2, NANOG, LIN28) | Induction of pluripotency in somatic cells | Delivery method (viral vs. non-viral) affects genomic integrity and safety profile [2] [24] |
| Culture Media | mTeSR1, E8 media, iPSC-Brew | Maintenance of undifferentiated pluripotent stem cells | Chemically defined media enhance reproducibility and minimize lot-to-lot variability [2] [27] |
| Culture Substrates | Matrigel, recombinant laminin-521, vitronectin | Extracellular matrix for feeder-free culture | Xeno-free substrates are preferred for clinical translation [2] |
| Differentiation Kits | Commercially available kits for cardiomyocytes, neurons, hepatocytes | Directed differentiation into specific lineages | Efficiency and purity of differentiation can vary between ESC and iPSC lines |
| Genome Editing Tools | CRISPR-Cas9 systems, PiggyBac transposon | Genetic modification for disease modeling or gene correction | Isogenic controls are critical for confirming phenotype-genotype relationships |
| Quality Control Assays | Pluripotency marker antibodies (OCT4, SOX2, NANOG), karyotyping kits, mycoplasma tests | Validation of pluripotent state and genomic integrity | Regular monitoring is essential due to genomic instability risks in culture [2] [27] |
| iPSC Lines | Commercially available control lines (e.g., from FUJIFILM CDI, REPROCELL) | Standardized reference materials for assay development | Well-characterized lines reduce experimental variability [29] [12] |
The comparative analysis of transcriptional networks and epigenetic landscapes reveals both remarkable similarities and important distinctions between ESCs and iPSCs. While ESCs continue to serve as a fundamental reference for the pluripotent state, iPSCs offer unparalleled opportunities for patient-specific disease modeling and drug development. The persistent epigenetic memory observed in some iPSC lines, rather than being solely a limitation, also provides a window into the mechanisms of cellular identity and reprogramming. As reprogramming methodologies continue to advance—with improvements in non-integrating delivery systems, chemical induction protocols, and epigenetic resetting techniques—the functional equivalence between iPSCs and ESCs is expected to increase further. The choice between these cell types for specific research applications should be guided by the experimental question at hand, weighing the standardized properties of ESCs against the patient-specific relevance and ethical advantages of iPSCs. The ongoing development of comprehensive molecular datasets and standardized profiling protocols, as outlined in this guide, will continue to refine our understanding and utilization of these powerful tools in biomedical research.
The field of regenerative medicine and disease modeling is profoundly shaped by two cornerstone cell types: Embryonic Stem Cells (ESCs) and Induced Pluripotent Stem Cells (iPSCs). ESCs, derived from the inner cell mass of a blastocyst, represent the gold standard for pluripotency—the ability to differentiate into any cell type in the body [30]. Their discovery opened unprecedented avenues for studying human development and disease. In 2006, a paradigm shift occurred with the discovery of iPSCs—adult somatic cells reprogrammed back to an embryonic-like pluripotent state through the introduction of specific transcription factors [1] [2]. This breakthrough, earning Shinya Yamanaka the Nobel Prize in 2012, provided a powerful alternative that bypassed the primary ethical controversy associated with ESCs [31] [32]. For researchers and drug development professionals, the critical question is how these two cell types compare in practical application, particularly in the context of disease modeling research. This guide provides an objective, data-driven comparison of their efficacy, focusing on scientific capabilities while acknowledging the ethical framework that underpins their use.
Ethical and Practical Foundations
The fundamental distinction between ESCs and iPSCs lies at the intersection of science and ethics.
The Ethical Divide
The derivation of ESCs requires the destruction of a human embryo, raising significant ethical concerns and debates about the moral status of the embryo [31] [32]. This has resulted in complex and varied regulatory landscapes across the globe, which can impact research funding and scope [32]. In contrast, iPSCs are derived from adult tissues, such as skin fibroblasts or peripheral blood cells, and do not involve the use of embryos, thus circumventing this primary ethical hurdle [31] [2]. However, iPSCs are not without their own ethical considerations, which include concerns about consent for tissue donation and the long-term safety of their clinical application, particularly the potential for tumor formation [31] [32].
Origin and Derivation
The following diagram illustrates the distinct origins and reprogramming pathways of ESCs and iPSCs.
Comparative Efficacy in Disease Modeling
For a researcher, the choice between ESCs and iPSCs often hinges on their functional performance in modeling diseases. The following table summarizes key comparative aspects based on current scientific evidence.
Table 1: Functional Comparison for Disease Modeling and Research Applications
| Aspect | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Pluripotency | Gold standard; proven ability to differentiate into all three germ layers [30]. | Considered functionally equivalent to ESCs in their potential [4]. |
| Genetic Background | Heterogeneous; represents a unique genetic blueprint. | Patient-specific; can be derived from individuals with specific genetic diseases, enabling personalized disease modeling [33] [2]. |
| Disease Modeling Utility | Ideal for studying early human development and fundamental biology. | Superior for modeling genetically complex diseases, drug screening on patient-specific cells, and studying sporadic disease forms [33] [1] [2]. |
| Genomic Stability | Generally high stability. | Prone to genomic and epigenetic instability due to the reprogramming process and prolonged culture; requires rigorous monitoring [33] [2]. |
| Immunogenicity | Allogeneic; potential for immune rejection upon transplantation. | Autologous potential; derived from the patient's own cells, minimizing rejection risk [2]. |
| Differentiation Efficiency | Robust and well-established protocols. | Can be variable, influenced by the somatic cell source and reprogramming method [2]. |
Key Insights from Comparative Studies
A pivotal study from the Harvard Stem Cell Institute directly addressed the question of functional equivalence. Researchers used an experimental "trick" by first differentiating human ESCs into skin cells and then reprogramming those skin cells into iPSCs. This created genetically identical lines for a direct comparison. The study found that the gene expression profiles between the original ESCs and the newly created iPSCs were remarkably similar, with only about 50 differentially expressed genes out of thousands—a difference that may be negligible "transcriptional noise" [4]. Functionally, the ESCs and iPSCs demonstrated equivalent potential to differentiate into neural cells and other specialized lineages, leading the researchers to conclude that, within the parameters of their study, the two cell types are functionally equivalent [4].
Experimental Protocols for Equivalence and Disease Modeling
To ensure the reliable application of ESCs and iPSCs in research, standardized protocols for their evaluation are critical.
Protocol 1: Direct Functional Equivalence Testing
This protocol is based on the methodology used in the Harvard Stem Cell Institute study [4].
- Establish Baseline: Begin with a well-characterized human ESC line.
- In Vitro Differentiation: Differentiate the ESCs into a target somatic cell type (e.g., dermal fibroblasts or keratinocytes).
- Reprogramming: Reprogram the ESC-derived somatic cells into iPSCs using a non-integrating method, such as Sendai virus or episomal vectors expressing the Yamanaka factors (OCT4, SOX2, KLF4, c-MYC).
- Molecular Characterization:
- RNA Sequencing: Perform whole-transcriptome RNA sequencing on the original ESC line and the derived iPSC line.
- Data Analysis: Compare gene expression profiles to identify differentially expressed genes. Functional equivalence is supported by minimal, biologically insignificant differences.
- Functional Validation:
- Directed Differentiation: Differentiate both the original ESCs and the derived iPSCs into a variety of lineages (e.g., neural ectoderm, mesoderm, endoderm).
- Assessment: Use immunocytochemistry and functional assays to compare the efficiency and maturity of the differentiated cells.
Protocol 2: Patient-Specific Disease Modeling with iPSCs
This is a generalized workflow for creating a disease model using iPSCs, applicable to conditions like Parkinson's disease or amyotrophic lateral sclerosis (ALS) [33] [2].
- Somatic Cell Collection: Obtain somatic cells from a patient with the disease of interest and a healthy matched control. Common sources include:
- Reprogramming to iPSCs: Reprogram the somatic cells using integration-free methods (e.g., mRNA, Sendai virus) to generate patient-specific and control iPSC lines.
- Quality Control: Rigorously characterize iPSC lines for pluripotency (e.g., expression of OCT4, NANOG via immunocytochemistry or PCR) and genomic integrity (e.g., karyotyping) [2].
- Directed Differentiation: Differentiate the patient and control iPSCs into the relevant cell type(s) for the disease (e.g., dopaminergic neurons for Parkinson's disease).
- Phenotypic Screening: Analyze the diseased cells for known pathological hallmarks, such as protein aggregation, electrophysiological abnormalities, or metabolic dysfunction, and compare them to healthy controls.
- Drug Screening: Use the diseased cell model to test the efficacy and toxicity of potential therapeutic compounds.
The logical flow of this modeling and drug discovery process is depicted below.
The Scientist's Toolkit: Essential Reagents and Solutions
Successful experimentation with ESCs and iPSCs relies on a suite of specialized reagents. The following table details key solutions used in the featured protocols.
Table 2: Essential Research Reagents for Stem Cell Research
| Research Reagent | Function in Protocol | Specific Examples & Notes |
|---|---|---|
| Reprogramming Vectors | Deliver transcription factors to somatic cells to induce pluripotency [2]. | Non-Integrating Methods (Preferred): Sendai virus, episomal plasmids, synthetic mRNA. Integrating Methods: Retroviruses, lentiviruses (higher risk of insertional mutagenesis). |
| Chemically Defined Medium | Supports the growth and maintenance of pluripotent stem cells [2]. | mTeSR1, Essential 8 (E8) medium. These standardized, xeno-free formulations support feeder-free culture and enhance reproducibility. |
| Extracellular Matrix (ECM) | Coats culture surfaces to support pluripotent cell adhesion and growth. | Matrigel, recombinant human laminin-521. Essential for feeder-free culture systems. |
| Pluripotency Markers | Used in quality control to confirm the pluripotent state of ESCs and iPSCs. | Antibodies against OCT4, SOX2, NANOG for immunocytochemistry; PCR kits for pluripotency gene analysis. |
| Differentiation Kits & Reagents | Directs pluripotent stem cells toward specific somatic cell fates. | Commercial kits available for neurons, cardiomyocytes, hepatocytes, etc. Often use specific growth factors and small molecule inhibitors (e.g., TGF-β inhibitors, FGF2). |
| Genomic Integrity Assays | Monitors for chromosomal abnormalities acquired during reprogramming or culture. | Karyotyping (G-banding), Comparative Genomic Hybridization (CGH) arrays. Regular monitoring is crucial for iPSCs [2]. |
The objective comparison of ESCs and iPSCs reveals a landscape of functional equivalence tempered by distinct practical advantages. While ESCs remain a critical biological reference, iPSCs offer an unparalleled capacity for patient-specific disease modeling, which is accelerating research into complex neurological, cardiovascular, and metabolic disorders [33] [2]. The ethical simplicity of iPSCs further solidifies their role as the forefront technology for personalized medicine and drug discovery.
The future of the field lies in standardization and enhanced safety. Ongoing research focuses on addressing the challenges of genomic instability in iPSCs and developing more robust, chemically defined differentiation protocols [33] [34]. Furthermore, international consortia, like the one recently launched by the ISSCR, are working to establish guidelines for the widespread and responsible adoption of these powerful stem cell-derived models [34]. For the research scientist, the choice is no longer about which cell type is inherently "better," but which is the most fit-for-purpose for their specific scientific question, with iPSCs providing a powerful and ethically sound alternative that continues to close the gap with its embryonic counterpart.
Modeling Human Diseases: Techniques and Translational Applications
The advent of induced pluripotent stem cells (iPSCs) has fundamentally transformed regenerative medicine and disease modeling research. This breakthrough, first achieved by Takahashi and Yamanaka in 2006, demonstrated that somatic cells could be reprogrammed into pluripotent stem cells through the ectopic expression of specific transcription factors [1]. The original methodology utilized retroviral vectors to deliver the reprogramming factors Oct4, Sox2, Klf4, and c-Myc (OSKM) [35]. However, these pioneering methods raised significant safety concerns regarding insertional mutagenesis and transgene reactivation, particularly concerning the oncogenic potential of factors like c-Myc [36]. In response, the field has progressively evolved toward integration-free systems that minimize genomic alteration risks while maintaining reprogramming efficiency.
Within the broader context of comparing embryonic stem cells (ESCs) and iPSCs for disease modeling research, the choice of reprogramming methodology critically influences the validity and safety of the resulting cellular models. While ESCs historically provided the gold standard for pluripotency, they face ethical limitations and immunocompatibility challenges that iPSCs inherently overcome [35]. The progressive refinement of reprogramming methods has significantly enhanced the fidelity of iPSC disease models, positioning them as a powerful alternative to ESC-based systems for investigating disease mechanisms and screening therapeutic compounds.
Historical Development and Key Reprogramming Methods
Retroviral and Lentiviral Vector Systems
The first iPSC generation method employed retroviral vectors, which offered high transduction efficiency and stable transgene expression necessary for successful reprogramming. These vectors integrate into the host genome, enabling persistent expression of the OSKM factors throughout the reprogramming process [1]. A key limitation of simple retroviral vectors is their inability to transduce non-dividing cells, which constrained their application to certain cell types [36].
Lentiviral vectors, derived from HIV-1, emerged as an improvement, capable of infecting both dividing and non-dividing cells [37]. Scientists commonly used pantropic retroviral vectors pseudotyped with VSV-G protein to enhance transduction efficiency across diverse cell types [36]. The development of doxycycline-inducible systems represented another advancement, allowing temporal control of transgene expression after reprogramming was complete [35]. Despite these improvements, integrated vectors still posed risks of insertional mutagenesis and potential reactivation of oncogenic transgenes, particularly c-Myc, which was implicated in tumor formation in iPSC chimeric mice [36].
Table 1: Evolution of Viral Vector-Based Reprogramming Methods
| Vector Type | Key Features | Advantages | Limitations |
|---|---|---|---|
| Retroviral Vectors | Integrates into host genome; requires cell division for transduction | High efficiency for dividing cells; stable expression | Limited to dividing cells; insertional mutagenesis; transgene reactivation |
| Lentiviral Vectors | HIV-1 derived; integrates into host genome; transduces non-dividing cells | Broader cell type applicability; higher transduction efficiency | Insertional mutagenesis; complex vector design |
| Inducible Systems | Doxycycline-controlled transgene expression | Temporal control over reprogramming;可以减少持续性表达风险 | Leaky expression; incomplete silencing |
Integration-Free Reprogramming Systems
The recognition of risks associated with viral integration spurred development of non-integrating delivery systems. These methods aim to transiently express reprogramming factors without permanent genomic modification, generating footprint-free iPSCs more suitable for clinical applications [36].
Sendai virus, an RNA virus-based system, replicates in the cytoplasm without nuclear integration and is gradually diluted through cell divisions. Comparative studies show Sendai virus provides high reprogramming efficiency but may require extended culture periods to become vector-free [38]. Episomal plasmids are another non-integrating approach utilizing engineered DNA elements that replicate extrachromosomally. While these avoid integration, studies indicate they may confer a slightly higher incidence of karyotypic instability compared to other non-integrating methods [38].
Self-replicating RNA vectors and synthetic mRNA represent the most advanced non-integrating approaches. These systems enable high-efficiency reprogramming without nuclear entry and can be rapidly cleared from cells. However, RNA-based methods require careful optimization to minimize innate immune responses and can have lower overall success rates despite higher efficiency when successful [38] [36]. The RNA replicon system, based on a self-replicating RNA virus, has also been successfully employed to generate iPSCs without genomic integration [36].
Table 2: Comparison of Key Integration-Free Reprogramming Methods
| Method | Mechanism | Reprogramming Efficiency | Genomic Integration | Key Applications |
|---|---|---|---|---|
| Sendai Virus | Cytoplasmic RNA virus; diluted through cell divisions | Moderate to High | No | Broad cell type applications; clinical grade iPSC generation |
| Episomal Plasmids | Extrachromosomal replication; transient expression | Moderate | Low frequency | Patient-specific iPSC generation; disease modeling |
| Synthetic mRNA | Direct delivery of reprogramming factor mRNAs; daily transfections | High when successful | No | Clinical applications; high-quality iPSC lines |
| Protein Transduction | Cell-penetrating reprogramming proteins | Low | No | Proof-of-concept studies; mechanistic research |
Comparative Analysis of Reprogramming Method Efficacies
Efficiency and Kinetics Across Methodologies
Reprogramming efficiency varies substantially across different methodologies. Retroviral approaches typically achieve efficiencies ranging from 0.01% to 0.1% for human fibroblasts, with kinetics spanning 3-4 weeks for iPSC colony emergence [35]. The stochastic nature of early reprogramming events contributes to this relative inefficiency, with only a small fraction of transfected cells completing the full reprogramming process [1].
RNA-based reprogramming demonstrates the highest efficiency among non-integrating methods, potentially exceeding 1% under optimized conditions, though with variable success rates between cell types and laboratories [38]. Sendai virus systems offer more consistent results with efficiencies typically around 0.1%, while episomal plasmids generally yield lower efficiencies of approximately 0.001% [38] [36]. The reprogramming kinetics also differ, with RNA-based methods often producing colonies within 2-3 weeks, while episomal approaches may require 4-5 weeks.
Notably, the cell type being reprogrammed significantly influences efficiency. For instance, neural stem cells (NSCs) endogenously express high levels of Sox2 and c-Myc, enabling reprogramming with just a single factor (Oct4) [35]. Similarly, melanocytes express endogenous Sox2 and can be reprogrammed without this factor, though with reduced efficiency compared to using all four Yamanaka factors [35].
Molecular Mechanisms and Trajectories
The molecular journey from somatic cell to pluripotency involves profound epigenetic remodeling, metabolic reprogramming, and sequential activation of pluripotency networks [1]. Reprogramming occurs in two broad phases: an early, stochastic phase where somatic genes are silenced and early pluripotency-associated genes activate, followed by a late, deterministic phase where late pluripotency genes become established [1].
During the early phase, the mesenchymal-to-epithelial transition (MET) represents a critical bottleneck, particularly for fibroblast reprogramming [1]. The chromatin state of the starting somatic cell significantly influences reprogramming efficiency, with more open chromatin configurations generally facilitating faster reprogramming. The process also involves global DNA demethylation, histone modification changes, and X chromosome reactivation in female cells [1].
Different reprogramming methods engage these molecular pathways with varying efficiencies. Viral methods providing sustained transgene expression may more effectively navigate epigenetic barriers, while transient methods like mRNA may require more precise timing to coordinate the complex molecular transitions.
Applications in Disease Modeling and Clinical Translation
Impact on Disease Modeling Research
The evolution of reprogramming methodologies has directly enhanced the utility of iPSCs in disease modeling and drug development. Early models utilizing integrating vectors faced concerns about genomic alterations confounding disease phenotypes, whereas modern integration-free systems generate more physiologically relevant models [33]. The ability to create patient-specific iPSCs from individuals with genetic disorders enables researchers to study disease mechanisms in human cells bearing the exact genetic background of interest [1].
iPSC-based disease models span diverse conditions including neurological disorders (Parkinson's disease, ALS), cardiac conditions (cardiomyopathies, channelopathies), ocular diseases, and metabolic disorders [39]. The development of three-dimensional organoid systems from iPSCs has been particularly transformative, enabling modeling of tissue-level architecture and cell-cell interactions not possible with traditional two-dimensional cultures [33]. For example, kidney organoids carrying PKD1 or PKD2 mutations recapitulate cyst formation seen in polycystic kidney disease, providing robust platforms for mechanistic studies and therapeutic screening [33].
Clinical Translation and Regulatory Landscape
The clinical application of iPSCs requires methods that meet regulatory standards for safety and quality. Current Good Manufacturing Practice (cGMP)-compliant reprogramming methods have been developed to support clinical trials [29]. As of 2025, systematic reviews identify 22 ongoing registered clinical trials utilizing iPSCs to treat conditions including cardiac disease, ocular disorders, cancer, and graft-versus-host disease [39].
Notable advancements in clinical translation include Fertilo, the first iPSC-based therapy to enter U.S. Phase III trials for supporting ex vivo oocyte maturation, and OpCT-001, an iPSC-derived therapy for retinal degeneration that received FDA IND clearance in 2024 [29]. Additionally, iPSC-derived dopaminergic neural progenitors for Parkinson's disease and iPSC-derived CD19-directed CAR natural killer cells for B-cell lymphoma have entered clinical testing [39].
The safety profile of iPSC-based therapies from early clinical trials appears encouraging, with a major review of global clinical trials identifying no class-wide safety concerns among over 1,200 patients dosed with PSC-derived products [29]. However, long-term monitoring continues to assess potential risks including tumorigenicity from residual undifferentiated cells or genetic abnormalities acquired during reprogramming [39].
Table 3: Essential Research Reagents for iPSC Generation and Characterization
| Reagent Category | Specific Examples | Function in Reprogramming | Considerations for Selection |
|---|---|---|---|
| Reprogramming Factors | Oct4, Sox2, Klf4, c-Myc (OSKM); Oct4, Sox2, Nanog, Lin28 | Core transcription factors inducing pluripotency | Species-specific variants; alternative factor combinations for different cell types |
| Delivery Vectors | Retroviral/lentiviral particles; Sendai virus; episomal plasmids; synthetic mRNAs | Vehicle for introducing reprogramming factors into somatic cells | Integration vs. non-integrating; efficiency vs. safety; cell type compatibility |
| Culture Media | Fibroblast medium; OPC medium; pluripotent stem cell media | Support cell viability and growth during and after reprogramming | Stage-specific formulations; xeno-free requirements for clinical applications |
| Surface Coatings | Poly-L-ornithine/Laminin; Matrigel; recombinant vitronectin | Provide extracellular matrix support for cell attachment and growth | Defined vs. undefined matrices; compatibility with different cell types |
| Characterization Antibodies | Anti-Nanog, Oct4, SSEA-4, Tra-1-60 (pluripotency); lineage-specific markers | Verification of pluripotent state and differentiation potential | Species reactivity; validation for flow cytometry vs. immunocytochemistry |
| Small Molecule Enhancers | Valproic acid; CHIR99021; PD0325901; ascorbic acid | Improve reprogramming efficiency and kinetics | Concentration optimization; potential synergistic effects |
The progression from retroviral vectors to integration-free systems represents a paradigm shift in cellular reprogramming methodologies. Each technological advancement has addressed specific limitations while introducing new considerations for researchers. The current landscape offers a diverse toolkit of reprogramming approaches, enabling selection based on specific research needs, from basic mechanistic studies to clinical-grade iPSC generation.
For disease modeling research, the choice of reprogramming method directly impacts the physiological relevance and safety of the resulting iPSC models. Integration-free methods now provide robust alternatives to ESCs without the ethical concerns, while generating genetically stable models that faithfully recapitulate disease phenotypes. As the field continues to mature, standardization of reprogramming protocols and characterization criteria will further enhance reproducibility and accelerate the therapeutic application of iPSC technology.
The ongoing clinical trials utilizing iPSCs derived through advanced reprogramming methods herald a new era in regenerative medicine, offering promising avenues for treating conditions that have previously proven intractable to conventional therapies.
The capacity of human pluripotent stem cells (hPSCs), encompassing both human embryonic stem cells (hESCs) and human induced pluripotent stem cells (hiPSCs), to differentiate into any cell type in the human body forms the cornerstone of modern regenerative medicine and disease modeling [40] [33]. The comparative efficacy of hESCs versus hiPSCs in generating functional somatic cells is a central question in biomedical research, with significant implications for both basic science and clinical translation. Directed differentiation protocols—sequential manipulation of culture conditions to mimic developmental signaling pathways—enable researchers to guide these pluripotent cells through specific lineage commitment steps into functional cell types [40] [41]. These protocols typically progress through defined stages, beginning with the induction of primitive germ layers (endoderm, mesoderm, or ectoderm), followed by lineage specification and terminal maturation into functional somatic cells such as cardiomyocytes, hepatocytes, neurons, and retinal pigment epithelial cells [40].
The fundamental thesis underlying this comparative analysis is that while both hESC and hiPSC platforms demonstrate remarkable differentiation capacity, the choice of cell source, reprogramming method, and specific protocol optimization can significantly impact the efficiency, purity, and functional maturity of the resulting cell populations. This review systematically compares the performance of hESC and hiPSC differentiation across multiple lineages, providing experimental data and methodological details to inform researchers' decisions in disease modeling and drug development.
Comparative Efficacy of hESCs and hiPSCs in Lineage Specification
Experimental Evidence Across Multiple Lineages
A comprehensive study directly compared the differentiation potentials of three hESC lines, four retrovirally derived hiPSC lines, and one hiPSC line derived with non-integrating Sendai virus technology across four independent differentiation protocols: hepatocyte, cardiomyocyte, neuronal, and retinal pigment epithelial (RPE) cell differentiation [40]. The findings revealed both significant functional similarities and crucial line-to-line variations.
Table 1: Comparative Differentiation Efficiency of hPSC Lines Across Lineages
| Cell Line Type | Hepatocyte Differentiation | Cardiomyocyte Differentiation | Neural Differentiation | RPE Differentiation |
|---|---|---|---|---|
| hESC Lines | Efficient definitive endoderm induction (CXCR4+ cells); Albumin secretion detected [40] | Beating cardiomyocytes observed; Expression of α-actinin, Troponin T, connexin-43 [40] | Active neuronal networks formed; Expression of MAP-2, GFAP [40] | Highly pigmented mature cells; Expression of BEST1, RLBP1 [40] |
| Retroviral hiPSC Lines | Variable efficiency; One line failed to produce hepatocytes [40] | Generally efficient; Similar gene expression patterns to hESCs [40] | Functional similarities observed; Comparable neuronal network activity [40] | Reactivation of transgenic OCT4 affected outcome in some lines [40] |
| Sendai Virus hiPSC Line | No transgene expression detected; Performance comparable to best hESC lines [40] | No transgene expression; Efficient cardiac differentiation [40] | No transgene-related issues detected [40] | Stable differentiation without transgene interference [40] |
The data indicate that overall, cells differentiated from hESCs and hiPSCs showed functional similarities and similar expression of genes characteristic of specific cell types [40]. However, critical differences emerged related to the reprogramming method, with residual transgene activity and epigenetic memory affecting some retrovirally derived hiPSC lines [40]. Specifically, reactivation of transgenic OCT4 was detected during RPE differentiation in retrovirally derived lines, potentially compromising differentiation outcomes [40]. One hiPSC line with incomplete silencing of exogenous KLF4 proved inferior across all differentiation directions and failed entirely to produce hepatocytes [40].
Quantitative Assessment of Differentiation Outcomes
Researchers employ multiple analytical methods to quantify differentiation efficiency and functional maturity of hPSC-derived cells. These include flow cytometry for surface markers (e.g., CXCR4+ for definitive endoderm), quantitative PCR for lineage-specific genes, immunocytochemistry for protein expression, and functional assays such as albumin secretion for hepatocytes, microelectrode array measurements for cardiomyocyte and neuronal activity, and morphological analysis of pigmentation for RPE cells [40].
Table 2: Characterization Methods for hPSC-Derived Cell Types
| Cell Type | Key Markers Analyzed | Functional Assays | Assessment Timepoints |
|---|---|---|---|
| Hepatocyte-like Cells | SOX17, FOXA2, AFP, Albumin [40] | Albumin secretion (ELISA), Cytochrome P450 activity [40] | Day 7, 14, 21 of differentiation [40] |
| Cardiomyocytes | Brachyury T, NKX2.5, α-actinin, Troponin T [40] | Beating areas counting, Microelectrode array [40] | Day 0, 3, 6, 13, 30 [40] |
| Neural Cells | Musashi, NF-68, MAP-2, GFAP [40] | Time-lapse imaging, Microelectrode array for network activity [40] | 4 and 8 weeks [40] |
| RPE Cells | MITF, BEST1, RLBP1 [40] | Pigmentation monitoring, Morphological analysis [40] | Day 28, 52, 82, 116 [40] |
Molecular Mechanisms of Directed Differentiation
Signaling Pathways Governing Lineage Specification
The directed differentiation of hPSCs recapitulates embryonic development through the coordinated manipulation of key signaling pathways. The following diagram illustrates the major signaling pathways and their roles in guiding lineage specification:
Figure 1: Signaling pathways guiding hPSC differentiation. Directed differentiation protocols manipulate key developmental pathways to steer pluripotent cells through germ layer specification into terminal cell fates. Endoderm induction typically requires activation of TGFβ/Activin A and WNT signaling; mesoderm formation involves BMP and WNT pathways; ectoderm commitment necessitates inhibition of SMAD signaling alongside FGF activation [40] [41].
Experimental Workflows for Differentiation Studies
The following diagram outlines a generalized experimental workflow for comparative differentiation studies between hESCs and hiPSCs:
Figure 2: Experimental workflow for differentiation studies. Comparative studies follow a systematic approach from cell source selection through functional validation, employing multiple characterization methods to assess differentiation efficiency and functional maturity [40] [41].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful differentiation of hPSCs requires carefully selected reagents and materials. The following table details key solutions used in the featured experiments and their specific functions:
Table 3: Essential Research Reagents for hPSC Differentiation Studies
| Reagent Category | Specific Examples | Function in Differentiation | Application Notes |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) or OCT4, SOX2, NANOG, LIN28 [40] [1] | Somatic cell reprogramming to pluripotency | Retroviral vectors show transgene reactivation; Non-integrating methods (Sendai virus) preferred [40] |
| Growth Factors & Cytokines | Activin A, BMP4, FGF2, VEGF, WNT3A [40] [41] | Manipulation of signaling pathways for germ layer specification and lineage commitment | Concentration and timing critically affect outcomes; Often used in sequential combinations [41] |
| Small Molecule Inhibitors/Activators | CHIR99021 (WNT activator), SB431542 (TGF-β inhibitor), Dorsomorphin (BMP inhibitor) [41] | Precise control of signaling pathways with temporal resolution | Offer advantages in cost, stability, and reproducibility compared to recombinant proteins [41] |
| Extracellular Matrix Substrates | Matrigel, Laminin, Vitronectin, Fibronectin [41] | Provide structural support and biochemical cues for cell attachment and polarization | Different coatings may favor specific lineages; Batch-to-batch variability can affect reproducibility [41] |
| Characterization Reagents | Antibodies against lineage-specific markers (SOX17, FOXA2, α-actinin, MAP-2) [40] | Assessment of differentiation efficiency and purity | Validation for specific applications is essential; Panel-based approaches recommended for comprehensive characterization [40] |
Critical Considerations in Experimental Design
Impact of Reprogramming Methods on Differentiation Potential
The method used to generate hiPSCs significantly influences their subsequent differentiation behavior. Retrovirally derived hiPSC lines demonstrate a higher risk of transgene reactivation, particularly during extended differentiation protocols such as RPE differentiation which takes over 80 days [40]. This reactivation can alter differentiation outcomes and confound experimental results. In contrast, hiPSC lines generated using non-integrating methods such as Sendai virus technology show no detectable transgene expression and performance comparable to the best hESC lines [40]. Additionally, some retrovirally derived hiPSC lines exhibit incomplete silencing of exogenous transcription factors, particularly KLF4, which can render them inferior across multiple differentiation directions [40].
These findings highlight the importance of selecting appropriate cell sources for disease modeling research. For critical applications where transgene interference must be minimized, integration-free hiPSCs or well-characterized hESCs provide more reliable platforms. The field is increasingly moving toward non-integrating reprogramming methods and comprehensive characterization of iPSC lines before their use in differentiation studies [40] [1].
Statistical and Design of Experiments (DOE) Approaches
Optimizing differentiation protocols requires testing numerous variables including growth factor combinations, timing, seeding density, and small molecule concentrations. Traditional one-factor-at-a-time (OFAT) approaches are inefficient for such multifactorial optimization [41]. Statistical design of experiments (DOE) methodologies enable researchers to systematically explore these complex parameter spaces with reduced experimental runs [41].
Several DOE approaches are particularly valuable for differentiation protocol optimization:
- Fractional factorial designs: Identify the most influential factors among many candidates with minimal experimental runs [41]
- Response surface methodology (RSM): Model complex relationships between factors and responses to identify optimal conditions [41]
- Definitive screening design (DSD): Efficiently estimate main effects and quadratic effects with small experimental runs [41]
These statistical approaches not only enhance experimental efficiency but also improve the reliability and reproducibility of differentiation protocols, addressing a significant challenge in stem cell research [41].
The comparative analysis of hESC and hiPSC differentiation protocols reveals a complex landscape with significant implications for disease modeling research. Both platforms can generate functional somatic cells across all germ layers, but careful attention to cell line selection, reprogramming method, and protocol optimization is essential for reproducible results [40]. The emerging promise of iPSCs in clinical studies is tempered by challenges in standardization, with current clinical trials characterized by small sample sizes, uncontrolled designs, and heterogeneity in cell products and medical conditions examined [39].
Future directions in the field include the development of more sophisticated organoid and assembloid systems that better recapitulate tissue-level complexity [33], the integration of CRISPR-Cas9 gene editing to create isogenic control lines for disease modeling [33] [1], and the implementation of Quality by Design (QbD) principles guided by DOE approaches to enhance protocol robustness and manufacturing reproducibility [41]. As standardization improves and our understanding of the molecular mechanisms governing cell fate decisions deepens, both hESC and hiPSC technologies will continue to transform disease modeling, drug discovery, and regenerative medicine.
The field of biomedical research is witnessing a paradigm shift with the emergence of three-dimensional (3D) organoid technology. Organoids are sophisticated, self-organizing 3D structures derived from stem cells that remarkably mimic the architecture and functionality of native human organs [42] [43]. This advancement addresses a critical limitation in traditional drug discovery: the poor predictive value of conventional two-dimensional (2D) cell cultures and animal models, which often fail to faithfully recapitulate human-specific pathophysiology [42]. The ability of organoids to preserve patient-specific genetic and phenotypic features has revolutionized in vitro modeling, offering unprecedented opportunities for studying human development, disease mechanisms, and for screening potential therapeutics [44] [45].
Framed within the broader thesis comparing the efficacy of embryonic stem cells (ESCs) versus induced pluripotent stem cells (iPSCs), this guide objectively explores how organoids derived from these cell sources are employed in disease modeling research. While both cell types are pluripotent, iPSCs offer the distinct advantage of being derived from a patient's own somatic cells, enabling the creation of personalized disease models that retain the individual's complete genetic background [42]. This technological evolution is pushing the boundaries of our understanding of tissue biology and accelerating the path to precision medicine [44] [42].
Core Technologies: Building Complexity from Stem Cells
Foundation and Culture of Organoids
Organoids can be derived from various sources, primarily tissue-specific adult stem cells (AdSCs) and pluripotent stem cells (PSCs), which include both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) [45] [43]. The foundational work by Sato and Clevers demonstrated that Lgr5+ intestinal stem cells could generate long-term expanding intestinal organoids, establishing a new paradigm for in vitro tissue modeling [43]. The derivation process involves embedding stem cells within a 3D environment that supports their self-organization and differentiation.
Two primary technological approaches are employed to establish the 3D culture system: scaffold-based and scaffold-free methods [45]. Scaffold-based systems use an extracellular matrix (ECM), such as Matrigel, to provide a structural and biochemical niche that guides cell organization and signaling. Conversely, scaffold-free systems rely on the innate ability of cells to aggregate and self-organize in suspension cultures, often using low-adhesion plates [45] [46]. Both methods aim to avoid the direct contact between cells and plastic culture vessels that is characteristic of 2D cultures, thereby enabling the emergence of complex tissue-like structures.
Key Signaling Pathways in Organoid Development
The successful generation of organoids requires precise manipulation of key developmental signaling pathways to guide stem cells toward specific organ fates. The following diagram illustrates the core signaling pathways involved in the differentiation of pluripotent stem cells into various organoid types, highlighting the critical morphogens and growth factors.
The directed differentiation of PSCs into specific organoid types is controlled by the temporal and spatial application of specific morphogens and growth factors [47]. For example, the generation of midbrain organoids for Parkinson's disease research relies heavily on Sonic Hedgehog (SHH) and WNT pathway activators to induce a floor-plate-like identity, which is crucial for the development of midbrain dopaminergic neurons [47]. Further maturation is often enhanced by neurotrophic factors like BDNF and GDNF [47]. In contrast, the development of intestinal organoids involves the coordinated action of WNT signals, FGFs, and TGF-β/BMP pathway modulators to establish the characteristic crypt-villus architecture [43]. Kidney organoid differentiation similarly utilizes WNT and FGF signaling, but also incorporates retinoic acid at specific stages to guide nephron patterning [43].
Comparative Analysis: hESCs vs. hiPSCs in Organoid Generation
The choice between human embryonic stem cells (hESCs) and human induced pluripotent stem cells (hiPSCs) as a starting material for organoid generation involves a careful consideration of their respective advantages and limitations. The following table provides a structured comparison of their core characteristics in the context of disease modeling and organoid research.
Table 1: Comparative analysis of hESC-derived and hiPSC-derived organoids for disease modeling
| Feature | hESC-Derived Organoids | hiPSC-Derived Organoids |
|---|---|---|
| Cell Source | Derived from the inner cell mass of blastocyst-stage embryos [42] | Reprogrammed from adult somatic cells (e.g., skin fibroblasts, blood cells) [42] |
| Genetic Background | Representative of the donor embryo; may not match the patient | Captures the complete genetic background of the somatic cell donor, enabling patient-specific modeling [42] [48] |
| Ethical Considerations | Involves the destruction of human embryos, raising ethical concerns [42] | Bypasses ethical issues associated with embryos; considered more ethically sound [42] |
| Immunocompatibility | Not genetically matched to the patient, risk of immune rejection in transplantation | Potential for autologous transplantation, minimizing immune rejection [48] |
| Primary Application | Study of normal human development, toxicology screening, as a genetic "blank slate" | Personalized disease modeling, drug screening, and study of complex genetic disorders [48] [47] |
| Key Advantage | Established, stable pluripotent cell lines | Patient-specificity and ability to model a wide range of genetic diseases without embryo use |
| Key Limitation | Ethical restrictions and limited genetic diversity | Potential variability in reprogramming and differentiation efficiency [42] |
The advent of hiPSC technology, pioneered by Takahashi and Yamanaka, marked a paradigm shift by enabling the reprogramming of adult somatic cells into a pluripotent state using defined factors [42]. This breakthrough provided a critical tool for precision medicine, as hiPSCs can be generated from patients with specific diseases, capturing the full genetic complexity of the condition in a dish [42] [47]. This is particularly valuable for modeling late-onset neurodegenerative disorders like Parkinson's disease, where patient-derived midbrain organoids can recapitulate key pathological hallmarks such as α-synuclein aggregation and dopaminergic neuron loss [47].
Disease Modeling Applications: A Comparative Showcase
Parkinson's Disease Modeling Using Midbrain Organoids
Parkinson's disease (PD) modeling exemplifies the powerful application of organoid technology, particularly hiPSC-derived organoids. Midbrain organoids (MOs) are 3D stem cell-derived structures that mimic the midbrain's architecture, a region central to PD pathology due to the loss of dopaminergic neurons in the substantia nigra [47]. The following workflow details the protocol for generating and utilizing MOs for PD research, highlighting the experimental timeline and key analyses.
This workflow enables the study of PD mechanisms and drug responses in a human-relevant system. A key study by Kim et al. (2019) utilized isogenic MOs with the LRRK2 G2019S PD-linked mutation to identify the thiol-oxidoreductase TXNIP as a novel mediator in the pathogenic protein interaction network [47]. Another study by Jo et al. (2021) demonstrated that MOs with GBA1 deficiency and α-syn overexpression accumulated detergent-resistant, β-sheet–rich α-syn aggregates, forming Lewy body–like inclusions [47]. These findings underscore the value of MOs in identifying novel pathogenic mechanisms and therapeutic targets.
Comparative Experimental Data from Organoid Models
The utility of organoid models is validated by quantitative data demonstrating their ability to recapitulate disease-specific phenotypes. The following table summarizes key experimental findings from different organoid disease models, providing a comparison of the measured parameters and outcomes.
Table 2: Quantitative experimental data from selected disease-specific organoid models
| Organoid Model / Disease | Key Experimental Readouts & Parameters | Quantitative Findings / Outcomes |
|---|---|---|
| Midbrain Organoid (PD)LRRK2 G2019S Mutation [47] | - Dopaminergic neuron loss- α-synuclein aggregation- TXNIP expression levels | - Recapitulated progressive neurodegeneration- Identified TXNIP as a key mediator in mutant organoids |
| Midbrain Organoid (PD)GBA1 Deficiency + α-syn overexpression [47] | - Formation of Lewy body-like inclusions- Detergent-resistant α-syn aggregates | - Accumulation of β-sheet–rich α-syn aggregates- Phenocopied in SNCA triplication organoids with inhibitor |
| Patient-Derived Tumor Organoid (PDTO)e.g., Colorectal, Pancreatic Cancers [42] | - Drug sensitivity/resistance profiling- Retention of original tumor histology & genomics | - Predictive of individual patient responses to chemotherapy/targeted therapy- Used clinically to inform treatment decisions |
| General Drug ScreeninghPSC-derived cells & Organoids [42] | - Drug efficacy- Toxicity assessment (e.g., hepatotoxicity) | - More accurate prediction of human-specific efficacy and toxicity compared to 2D models or animal systems |
The data show that organoids, particularly those derived from hiPSCs, provide a robust platform for modeling disease-specific phenotypes, from neurodegeneration to tumor drug response. Their ability to retain patient-specific genetic features enables personalized therapeutic strategies and improves the predictive power of preclinical drug testing [42] [47].
The Scientist's Toolkit: Essential Reagents for Organoid Research
The successful generation, maintenance, and analysis of organoids rely on a suite of specialized research reagents and materials. The following table details key solutions and their functions, forming an essential toolkit for scientists in this field.
Table 3: Key research reagent solutions for organoid generation and analysis
| Reagent / Material Category | Specific Examples | Function & Application in Workflow |
|---|---|---|
| Validated Cell Sources | - Patient-derived iPSCs- iPSCs frozen- Immortalized cell lines- Primary cell lines [49] [50] | Foundation for building disease-specific models; patient-derived iPSCs are crucial for personalized disease modeling [42]. |
| Culture & Differentiation Media | - Specialized media for iPSC maintenance- High-purity growth factors (e.g., SHH, FGFs, BDNF, GDNF) [49] [47] | Directs stem cell fate and controls differentiation into target tissues during the patterning and maturation phases [47]. |
| 3D Culture Scaffolds | - Extracellular matrix (e.g., Matrigel)- Synthetic hydrogels- Atelocollagen- Organoid recovery solution [45] [49] | Provides the 3D structural and biochemical support for organoid formation and growth, mimicking the native stem cell niche. |
| Genome Editing Tools | - CRISPR/Cas9 systems [42] [50] | Introduces or corrects disease-associated mutations in stem cells to create isogenic controls or study specific genetic effects. |
| Analysis & Validation Kits | - Antibodies for immunostaining (e.g., Tyrosine Hydroxylase for dopaminergic neurons)- scRNA-seq kits- ELISA kits [49] [47] | Enables phenotypic characterization, functional assessment, and validation of organoid models and experimental outcomes. |
Advanced 3D organoid models represent a transformative tool in biomedical research, offering a superior ability to recapitulate human tissue complexity compared to traditional 2D cultures. Within the context of comparing ESCs and iPSCs for disease modeling, hiPSC-derived organoids have emerged as a particularly powerful platform for personalized disease modeling and drug development, as they capture the patient's unique genetic background [42] [47]. This technology has demonstrated significant potential across diverse applications, from modeling neurodegenerative diseases like Parkinson's to predicting individual responses to cancer therapies [42] [47].
Despite their promise, challenges remain, including batch-to-batch variability, limited vascularization, and the need for greater maturation and complexity [42] [47]. Future directions are focused on integrating vascular networks, microglia, and other cell types to create "assembloids," as well as incorporating organoids into microfluidic organ-on-chip systems to enhance their physiological relevance and translational potential [48] [42] [47]. As these technologies continue to evolve, organoids are poised to substantially reduce the reliance on animal models and accelerate the discovery of novel therapeutics for a wide range of human diseases [42] [43].
The discovery of induced pluripotent stem cells (iPSCs) by Shinya Yamanaka in 2006 represented a paradigm shift in biomedical research, offering an ethically acceptable alternative to embryonic stem cells (ESCs) with comparable differentiation potential [2] [1]. This breakthrough enabled the generation of patient-specific pluripotent stem cells through the reprogramming of somatic cells using defined transcription factors, circumventing both the ethical concerns associated with ESCs and the risk of immune rejection in therapeutic applications [51] [52]. In the realm of neurodegenerative disease research, iPSC technology has proven particularly transformative, providing unprecedented access to live human neurons and glial cells for studying pathological mechanisms [2] [53]. The ability to differentiate iPSCs into disease-relevant cell types, including cortical neurons, dopaminergic neurons, and motor neurons, has established them as indispensable tools for modeling Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS) in vitro [2] [54] [55]. This review comprehensively examines the application of iPSC-based models for these major neurodegenerative disorders, objectively comparing their efficacy with alternative modeling approaches and highlighting the experimental data supporting their utility in both basic research and drug development.
Comparative Analysis: iPSCs versus Embryonic Stem Cells
Technical and Ethical Considerations
The debate regarding the relative merits of iPSCs and ESCs centers on technical capabilities, ethical considerations, and practical research applications. While both cell types share fundamental characteristics of pluripotency and self-renewal, their origins impart distinct advantages and limitations for disease modeling. ESCs, isolated from the inner cell mass of blastocysts, represent the "gold standard" for pluripotency but necessitate the destruction of human embryos, raising significant ethical concerns that restrict their use in many jurisdictions [52]. Additionally, the derivation of patient-specific ESC lines is not feasible, and their allogeneic nature poses immune compatibility challenges for therapeutic applications [51] [52]. In contrast, iPSCs can be generated from a patient's own somatic cells through reprogramming, eliminating ethical controversies while enabling the creation of genetically matched cell lines for autologous transplantation [51] [52]. This patient-specific approach facilitates the study of sporadic disease forms that constitute the majority of neurodegenerative cases and allows for the investigation of individual therapeutic responses [54].
Genomic Integrity and Functional Characteristics
Concerns regarding the genomic integrity of iPSCs have been raised due to potential mutations introduced during reprogramming. Early studies suggested that the reprogramming process itself might cause genomic alterations, with forced expression of transcription factors potentially inducing replicative stress and DNA damage [52]. However, comprehensive analyses have revealed that the incidence of karyotype abnormalities is similar between iPSCs (12.5%) and ESCs (12.9%), indicating that reprogramming does not significantly increase this risk [52]. Whole-genome sequencing studies of iPSC lines have further demonstrated that many observed genetic variations reflect pre-existing somatic mosaicism in parental cell populations rather than reprogramming-induced mutations [52]. Functionally, both cell types can differentiate into the neural lineages relevant for modeling neurodegenerative diseases, though some studies suggest epigenetic differences may persist between iPSCs and ESCs [52] [25]. Importantly, the ability to derive iPSCs from patients with specific genetic backgrounds provides a unique advantage for modeling polygenic and sporadic diseases that cannot be recapitulated using ESCs [54].
Table 1: Comparative Analysis of iPSCs and ESCs for Neurodegenerative Disease Modeling
| Feature | iPSCs | ESCs | Implications for Disease Modeling |
|---|---|---|---|
| Origin | Reprogrammed somatic cells | Inner cell mass of blastocyst | iPSCs enable patient-specific models; ESCs are allogeneic |
| Ethical Considerations | Minimal ethical concerns | Significant ethical controversies | iPSC research faces fewer restrictions |
| Immune Compatibility | Autologous possible | Allogeneic | iPSCs avoid immune rejection in transplantation |
| Genetic Diversity | Can model diverse genetic backgrounds | Limited genetic diversity | iPSCs better for sporadic disease modeling |
| Genomic Stability | ~12.5% karyotype abnormalities | ~12.9% karyotype abnormalities | Comparable stability between both platforms |
| Differentiation Capacity | Can differentiate into all neural cell types | Can differentiate into all neural cell types | Equivalent utility for neural differentiation |
| Disease Modeling Applications | Ideal for monogenic and sporadic diseases | Limited to generic disease mechanisms | iPSCs superior for patient-specific modeling |
iPSC-Based Disease Modeling: Methodologies and Applications
The generation of iPSCs involves reprogramming somatic cells to a pluripotent state through the restoration of transcriptional and epigenetic programs characteristic of ESCs [2]. The original method employed retroviral vectors to deliver four transcription factors—OCT4, SOX2, KLF4, and c-MYC (OSKM)—which remain the most widely used reprogramming factors [2] [1]. These factors perform distinct yet complementary roles: OCT4, SOX2, and KLF4 maintain pluripotency and inhibit differentiation, while c-MYC enhances reprogramming efficiency and promotes cell proliferation [53]. Peripheral blood mononuclear cells (PBMCs) and urinary epithelial cells have emerged as preferred somatic cell sources due to their minimally invasive collection procedures and robust reprogramming capacity [2]. To address safety concerns associated with viral integration, non-integrating methods have been developed, including episomal plasmids, Sendai virus, synthetic mRNA, and recombinant protein delivery [2] [53]. These integration-free approaches significantly reduce the risk of insertional mutagenesis while maintaining acceptable reprogramming efficiency, making them particularly suitable for clinical applications [53].
Neural Differentiation and Characterization
Following reprogramming and quality control, iPSCs are differentiated into disease-relevant neural cell types using established protocols [2] [54]. For motor neuron diseases like ALS, a five-stage differentiation protocol generates high-purity cultures of spinal motor neurons (92.44% ± 1.66% purity) expressing characteristic markers including choline acetyltransferase (ChAT), motor neuron and pancreas homeobox 1 (MNX1/HB9), and β-tubulin III (Tuj1) [54]. Similarly, protocols for dopaminergic neurons relevant to PD and cortical neurons for AD have been optimized to produce cultures that recapitulate key aspects of native neuronal populations [2]. Quality control measures include PCR-based assays, immunocytochemistry, and flow cytometry to verify pluripotency marker expression in undifferentiated iPSCs, while functional pluripotency is confirmed through directed differentiation into all three germ layers [2]. Genomic integrity must be regularly evaluated throughout the culture process, as reprogramming and extended passaging can introduce chromosomal abnormalities or epigenetic alterations that may compromise differentiation efficiency or predispose cells to malignant transformation [2] [52].
Disease-Specific Applications and Experimental Data
Amyotrophic Lateral Sclerosis (ALS)
iPSC technology has demonstrated exceptional utility in modeling ALS, particularly for the sporadic form (SALS) that constitutes approximately 90% of cases [54]. A landmark study involving iPSCs derived from 100 SALS patients established a robust model that recapitulated key disease features, including reduced motor neuron survival, accelerated neurite degeneration, and transcriptional dysregulation [54]. Importantly, the severity of in vitro phenotypes correlated with donor survival, providing face validity for the model [54]. This platform enabled large-scale drug screening of compounds previously tested in ALS clinical trials, revealing that 97% failed to mitigate neurodegeneration—a finding that mirrors clinical trial outcomes and validates the physiological relevance of the model [54]. Combination testing identified baricitinib, memantine, and riluzole as a promising therapeutic cocktail, demonstrating the potential of iPSC-based systems for identifying effective treatment strategies [54].
Parkinson's Disease (PD)
iPSC-based models of PD have successfully recapitulated the degeneration of dopaminergic neurons in the substantia nigra and revealed the pathogenic role of α-synuclein aggregation [2]. Patient-specific neurons generated from individuals with both sporadic and familial PD forms have enabled the investigation of disease mechanisms and the evaluation of pharmacological interventions [2] [55]. These models have proven particularly valuable for studying the contribution of specific genetic variants to PD pathogenesis through isogenic control lines generated using CRISPR/Cas9 genome editing [53]. The ability to generate midbrain organoids from PD patient-derived iPSCs has further advanced modeling capabilities by incorporating three-dimensional architecture and multiple cell types, better recapitulating the tissue microenvironment [53].
Alzheimer's Disease (AD)
iPSC-derived neuronal models of AD have been instrumental in elucidating disease mechanisms and screening potential therapeutics [2] [55]. Neurons and glial cells generated from AD patients reproduce hallmark pathological features, including tau hyperphosphorylation and β-amyloid deposition, providing a platform for targeted therapeutic development [2]. The integration of cerebral organoid technology with CRISPR/Cas9 genome editing has further enhanced AD modeling, enabling the investigation of complex interactions between different cell types in a three-dimensional context that more closely resembles the native brain environment [53]. These advanced models have facilitated the study of cell-type-specific contributions to AD pathogenesis and provided insights into the sequence of pathological events leading to neurodegeneration [53].
Table 2: Key Experimental Findings from iPSC-Based Neurodegenerative Disease Modeling
| Disease | iPSC Model Characteristics | Key Phenotypes Recapitulated | Drug Screening Insights |
|---|---|---|---|
| ALS | Motor neurons from 100 sporadic ALS patients [54] | Reduced survival, accelerated neurite degeneration, transcriptional dysregulation [54] | 97% of clinically tested drugs failed; combination therapy identified [54] |
| PD | Dopaminergic neurons from sporadic and familial PD patients [2] | Dopaminergic neuron degeneration, α-synuclein aggregation [2] | Platforms established for mechanistic studies and drug evaluation [2] |
| AD | Cortical neurons and glial cells from AD patients [2] | Tau hyperphosphorylation, β-amyloid deposition [2] | Models enable testing of targeted therapies against hallmark pathologies [2] |
Experimental Workflows and Methodologies
Standardized iPSC Generation and Differentiation
The experimental workflow for iPSC-based disease modeling begins with somatic cell isolation from patient samples, typically skin fibroblasts, peripheral blood mononuclear cells, or urinary epithelial cells [2]. Reprogramming employs non-integrating methods such as episomal plasmids or Sendai virus to deliver the OSKM factors, followed by culture in defined media such as mTeSR1 or E8 to establish stable iPSC lines [2] [53]. Rigorous quality control measures are implemented, including assessment of pluripotency marker expression, karyotyping, and genomic integrity analyses [2]. For neural differentiation, iPSCs are subjected to specific patterning protocols using small molecules and growth factors to direct them toward regional-specific neuronal fates—motor neurons for ALS, dopaminergic neurons for PD, and cortical neurons for AD [54]. The resulting cultures are characterized through immunocytochemistry for cell-type-specific markers, functional assessments including electrophysiology, and transcriptomic analyses to verify their identity and maturity [54].
Phenotypic Screening and Validation
A critical advantage of iPSC-based models is their compatibility with longitudinal phenotypic screening using live-cell imaging and high-content analysis [54]. For ALS research, motor neuron health is assessed through daily monitoring of survival and neurite integrity, enabling the quantification of degenerative processes [54]. In AD models, amyloid secretion and tau phosphorylation can be measured using immunoassays, while PD models may focus on mitochondrial function and α-synuclein aggregation [2]. Transcriptional profiling through RNA sequencing provides insights into disease-associated gene expression changes and can be used to validate the physiological relevance of the models by comparing them to postmortem patient tissues [54]. Pharmacological validation using known therapeutics such as riluzole for ALS establishes the responsiveness of the models and their utility for drug discovery [54].
Diagram 1: Experimental workflow for iPSC-based modeling of neurodegenerative diseases, showing the progression from somatic cell reprogramming to disease-specific applications and therapeutic development.
The Scientist's Toolkit: Essential Research Reagents
Core Reprogramming and Culture Components
Successful iPSC generation and maintenance require carefully selected reagents and culture systems. Feeder-free culture systems using extracellular matrix coatings such as Matrigel or recombinant laminin provide a defined environment for iPSC expansion while minimizing variability [2]. Chemically defined media formulations including mTeSR1 and Essential 8 (E8) maintain pluripotency while supporting robust cell growth [2]. For reprogramming, non-integrating methods such as Sendai viral vectors or episomal plasmids offer favorable balance between efficiency and safety [53]. Small molecule enhancers of reprogramming efficiency, including CHIR99021 (a GSK3β inhibitor), PD0325901 (a MEK inhibitor), and A-83-01 (a TGF-β receptor inhibitor), can significantly improve iPSC generation rates, particularly from challenging cell sources [53]. Quality control reagents for validating pluripotency include antibodies against canonical markers (OCT4, NANOG, SOX2, TRA-1-60) and differentiation kits for assessing trilineage potential [2].
Neural Differentiation and Characterization Tools
Neural induction employs dual SMAD inhibition using small molecules such as LDN-193189 (a BMP inhibitor) and SB431542 (a TGF-β inhibitor) to efficiently direct iPSCs toward neural fates [54]. Region-specific patterning factors including retinoic acid (for spinal motor neurons), SHH agonists (for ventralization), and FGFs guide the acquisition of specific neuronal subtypes relevant to different diseases [54]. Maturation media supplemented with neurotrophic factors (BDNF, GDNF, CNTF) support long-term neuronal survival and functional development [54]. Cell-type-specific markers for characterization include Tuj1 (pan-neuronal), MAP2 (mature neurons), ChAT (cholinergic neurons), and TH (dopaminergic neurons) [54]. Functional assessment employs calcium imaging dyes, electrophysiology systems, and live-cell imaging compatible reporters for longitudinal analysis of neuronal health [54].
Table 3: Essential Research Reagents for iPSC-Based Neurodegenerative Disease Modeling
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Systems | Sendai virus, episomal plasmids [53] | Deliver reprogramming factors without genomic integration | Preferred for clinical applications due to safety profile |
| Culture Media | mTeSR1, Essential 8 [2] | Maintain pluripotency and support iPSC expansion | Chemically defined formulations enhance reproducibility |
| Neural Induction | LDN-193189, SB431542 [54] | Direct differentiation toward neural lineages | Dual SMAD inhibition protocol provides high efficiency |
| Neural Patterning | Retinoic acid, SHH agonists [54] | Specify regional identity of neurons | Critical for generating disease-relevant neuronal subtypes |
| Characterization Tools | Pluripotency antibodies, neuronal markers [2] [54] | Validate cell identity and differentiation status | Essential for quality control throughout workflow |
| Phenotypic Assays | Live-cell imaging dyes, viability assays [54] | Quantify disease-relevant phenotypes | Enable high-content screening and longitudinal monitoring |
iPSC-based models have unequivocally demonstrated their value for modeling neurodegenerative diseases, offering patient-specific insights that cannot be obtained through other experimental systems. The ability to recapitulate key disease phenotypes, including motor neuron degeneration in ALS, dopaminergic neuron loss in PD, and amyloid pathology in AD, provides physiologically relevant platforms for mechanistic studies and drug discovery [2] [54]. The correlation between in vitro phenotypes and clinical outcomes, particularly in ALS, underscores the predictive validity of these models and their potential to de-risk drug development [54]. However, challenges remain regarding standardization, maturation, and model complexity. Technical variations in reprogramming methods, differentiation protocols, and culture conditions can introduce variability that complicates data interpretation and cross-study comparisons [2] [25]. Additionally, the relative immaturity of iPSC-derived neurons compared to their adult counterparts may limit their ability to fully recapitulate late-onset neurodegenerative processes [53]. Future advances will likely focus on enhancing model complexity through organoid systems, improving neuronal maturation, and incorporating non-cell autonomous contributors to disease, such as neuroinflammation [53] [56]. As the technology continues to evolve, iPSC-based models are poised to play an increasingly central role in both fundamental neurobiological research and the development of effective therapies for these devastating disorders.
ESC and iPSC Applications in Cardiovascular and Metabolic Disorders
The study of human cardiovascular and metabolic disorders has been transformed by the use of pluripotent stem cells, which possess the unique capacity to differentiate into any cell type in the body. Embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) represent two powerful platforms for disease modeling, drug screening, and regenerative medicine applications [20] [57]. ESCs are derived from the inner cell mass of blastocysts, while iPSCs are generated through the reprogramming of somatic cells back to a pluripotent state [1] [57]. Both cell types offer unprecedented access to human cardiomyocytes, hepatocytes, and other metabolically active cells that were previously difficult to study in vitro.
The fundamental distinction between these cell sources carries significant implications for research applications. ESC research involves the destruction of human embryos, raising ethical considerations that have limited their use in some countries [20]. In contrast, iPSCs can be derived from readily accessible somatic tissues such as skin fibroblasts, peripheral blood mononuclear cells, or urinary epithelial cells without ethical concerns [2]. For cardiovascular and metabolic disorder research, both systems enable the generation of patient-specific disease models, though they differ in their genetic backgrounds, epigenetic signatures, and differentiation efficiencies [58] [20].
Comparative Analysis of ESC and iPSC Properties
Biological and Technical Characteristics
Understanding the fundamental differences between ESCs and iPSCs is crucial for selecting the appropriate model system for cardiovascular and metabolic research.
Table 1: Fundamental Characteristics of ESCs and iPSCs
| Characteristic | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Origin | Inner cell mass of blastocysts [57] | Reprogrammed somatic cells [2] |
| Reprogramming Method | Not applicable | Viral (retroviral, lentiviral) or non-viral (episomal, mRNA, Sendai virus) delivery of transcription factors [2] |
| Key Transcription Factors | Endogenous pluripotency network | OCT4, SOX2, KLF4, c-MYC (OSKM) or OCT4, SOX2, NANOG, LIN28 [2] [1] |
| Ethical Considerations | Controversial due to embryo destruction [20] | Ethically non-controversial [20] |
| Genetic Background | Limited diversity | Potentially unlimited diversity from various donors [20] |
| Immunogenicity | Allogeneic potential | Potential for autologous transplantation [2] |
Differentiation Efficiency to Cardiovascular Lineages
The capacity to generate functional cardiomyocytes is a critical metric for evaluating stem cell utility in cardiovascular research. Studies have directly compared the cardiomyogenic potential of various ESC and iPSC lines.
Table 2: Cardiomyogenic Differentiation Efficiency of ESC and iPSC Lines
| Cell Line | Cell Type | Differentiation Markers | Functional Characteristics | Study |
|---|---|---|---|---|
| H1 hESC | Embryonic stem cell | MESP1, ISL1, NKX2-5 | Widespread striations and rhythmic contractility | Sepac et al., 2012 [58] |
| H9 hESC | Embryonic stem cell | MESP1, ISL1, NKX2-5 | Widespread striations and rhythmic contractility | Sepac et al., 2012 [58] |
| C2a hiPSC | Induced pluripotent stem cell | MESP1, ISL1, NKX2-5 | Poor terminal differentiation with limited contractility | Sepac et al., 2012 [58] |
| C6a hiPSC | Induced pluripotent stem cell | MESP1, ISL1, NKX2-5 | Poor terminal differentiation with limited contractility | Sepac et al., 2012 [58] |
| iPS 3.4 | Induced pluripotent stem cell | Cardiac troponin I, VCAM | Functional responses to simulated ischemia/reperfusion injury | Földes et al., 2020 [59] |
| iPS 4.1 | Induced pluripotent stem cell | Cardiac troponin I, VCAM | Protected against oxidative stress; served as testing platform for cardiocytoprotection | Földes et al., 2020 [59] |
The comparative data reveals that while both ESCs and iPSCs can be directed toward the cardiomyogenic lineage based on marker expression, functional maturation may vary significantly between cell lines. The H1 and H9 ESC lines demonstrated superior terminal differentiation with widespread striations and rhythmic contractility compared to the C2a and C6a iPSC lines, which showed poor terminal differentiation despite expressing early cardiomyogenic markers [58]. However, specific iPSC lines such as the iPS 4.1 have demonstrated sufficient functionality to serve as testing platforms for cardiocytoprotective compounds [59], indicating that line-to-line variation is a significant factor in both ESC and iPSC populations.
Applications in Cardiovascular Disorders
Disease Modeling and Drug Screening
iPSC technology has enabled the generation of patient-specific cardiomyocytes for modeling arrhythmogenic disorders, heart failure, and myocardial injury [2]. For example, models of congenital arrhythmias linked to KCNQ1 mutations provide a basis for precision cardiology, allowing researchers to study disease mechanisms and screen potential therapeutics in a human-relevant system [2]. Similarly, ESCs have been used to model cardiac disorders, though with less genetic diversity unless derived from specifically selected embryos.
The systematic analysis of different pluripotent stem cell-derived cardiac myocytes as potential testing models for cardiocytoprotection has demonstrated their utility in studying ischemia/reperfusion injury, a critical phenomenon in myocardial infarction [59]. In these studies, researchers subjected stem cell-derived cardiomyocytes to simulated ischemia/reperfusion (SI/R) injury and tested the protective effects of known cardiocytoprotective compounds. The iPS 4.1 cell line demonstrated significant SI/R-induced cell death and responded to protective interventions, establishing it as a valid testing platform [59].
Experimental Protocols for Cardiac Differentiation
Cardiomyocyte Differentiation Protocol (Adapted from Sepac et al. [58] and Földes et al. [59]):
- Pluripotent Stem Cell Culture: Maintain ESCs or iPSCs in defined medium such as mTeSR1 or E8 on Matrigel or laminin-coated plates in feeder-free conditions [2].
- Embryoid Body (EB) Formation: Harvest cells using enzymatic (dispase) or non-enzymatic (EDTA) methods and form cell clumps or EBs in suspension culture.
- Cardiac Induction: Treat EBs with activin-A and BMP4 in defined medium for 5 days to induce mesodermal and cardiac progenitor commitment.
- Cardiac Specification: Culture cells in basal medium without growth factors for 3-4 weeks to allow spontaneous differentiation into cardiomyocytes.
- Characterization: Assess differentiation efficiency through:
- Morphological observation of rhythmic contraction
- Immunostaining for cardiac markers (cardiac troponin I, VCAM, α-actinin)
- Gene expression analysis of cardiomyogenic markers (MESP1, ISL1, NKX2-5)
- Functional assessment using electrophysiology or calcium imaging
This protocol typically yields rhythmically contracting cardiomyocytes within 3-4 weeks, though efficiency varies between cell lines [58]. The resulting cardiomyocytes exhibit molecular and functional characteristics of human cardiac cells, including appropriate ion channel expression, calcium handling, and contractile properties.
Figure 1: Experimental workflow for cardiomyocyte differentiation from pluripotent stem cells, adapted from established protocols [58] [59].
Applications in Metabolic Disorders
Disease Modeling with iPSCs
iPSC technology has enabled the creation of patient-specific models for various metabolic disorders, preserving the patient's genotype in vitro [2]. These models have been particularly valuable for studying monogenic metabolic diseases where the genetic defect is known and can be investigated in differentiated cell types.
For cystic fibrosis, iPSC-derived airway epithelial cells reproduce the defective chloride transport and excessive mucus secretion caused by CFTR mutations [2]. These models have facilitated the evaluation of targeted drugs such as ivacaftor and lumacaftor, demonstrating the utility of iPSC technology in personalized medicine approaches. Similarly, in Wilson's disease, iPSC-derived hepatocytes replicate copper accumulation and oxidative stress, providing a platform for preclinical drug testing [2].
In Duchenne muscular dystrophy (DMD), iPSC-derived myocytes allow mechanistic studies of muscle degeneration, and gene editing has successfully restored dystrophin expression in vitro, highlighting the therapeutic potential of combining iPSC technology with genome editing tools [2]. These applications demonstrate how iPSCs can model both the pathological features of metabolic diseases and serve as platforms for therapeutic development.
Experimental Protocols for Metabolic Cell Differentiation
Hepatocyte Differentiation Protocol (Adapted from disease modeling studies [2]):
- Definitive Endoderm Induction: Differentiate pluripotent stem cells in RPMI 1640 medium supplemented with Activin A (100 ng/mL) and Wnt3a (50 ng/mL) for 5 days.
- Hepatic Specification: Culture cells in hepatocyte culture medium (HCM) supplemented with BMP4 (20 ng/mL) and FGF2 (10 ng/mL) for 5 days to induce hepatic progenitor cells.
- Hepatocyte Maturation: Maintain cells in HCM supplemented with HGF (20 ng/mL) and Oncostatin M (20 ng/mL) for 10-15 days to promote functional maturation.
- Characterization: Assess hepatocyte functionality through:
- Albumin secretion (ELISA)
- Urea production
- Cytochrome P450 activity
- Glycogen storage (PAS staining)
- Disease-specific functional assays (e.g., copper accumulation in Wilson's disease)
This protocol typically generates hepatocyte-like cells with functional characteristics of primary hepatocytes, though complete maturation to adult phenotypes remains challenging. The resulting cells express key hepatocyte markers including albumin, alpha-1-antitrypsin, and asialoglycoprotein receptor.
The Scientist's Toolkit: Essential Research Reagents
Successful differentiation and characterization of cardiovascular and metabolic cells from pluripotent stem cells requires specific reagents and culture systems.
Table 3: Essential Research Reagents for Pluripotent Stem Cell Differentiation
| Reagent Category | Specific Examples | Function | Application Context |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) [2] | Somatic cell reprogramming to pluripotency | iPSC generation from patient somatic cells |
| Basal Culture Media | mTeSR1, E8 medium [2] | Maintenance of pluripotent stem cells | ESC and iPSC culture in defined conditions |
| Extracellular Matrices | Matrigel, recombinant laminin [2] | Substrate for cell attachment and signaling | Feeder-free culture of pluripotent stem cells |
| Cardiac Induction Factors | Activin A, BMP4 [58] | Mesoderm induction and cardiac specification | Cardiomyocyte differentiation from ESCs/iPSCs |
| Hepatic Induction Factors | Activin A, BMP4, FGF2, HGF, Oncostatin M [2] | Endoderm induction and hepatic specification | Hepatocyte differentiation from ESCs/iPSCs |
| Characterization Antibodies | Cardiac troponin I, VCAM, NKX2-5 [58] [59] | Identification of differentiated cell types | Immunostaining and flow cytometry of cardiomyocytes |
| Functional Assay Kits | Calcium imaging dyes, electrophysiology systems | Assessment of functional maturity | Characterization of cardiomyocyte electrophysiology |
Strategic Considerations for Model Selection
Advantages and Limitations of Each System
Choosing between ESC and iPSC models requires careful consideration of their respective advantages and limitations for specific research applications.
ESC-Based Models offer several advantages: they typically demonstrate robust differentiation potential, as evidenced by superior cardiomyocyte terminal differentiation in comparative studies [58]. They avoid the reprogramming variability associated with iPSCs and lack the epigenetic memory that can influence iPSC differentiation potential [20]. However, ESCs face ethical restrictions in some countries, limiting their use [20]. Their genetic diversity is also more constrained compared to the potentially unlimited donor sources for iPSCs, and they present immunocompatibility challenges for potential therapeutic applications [57].
iPSC-Based Models provide compelling advantages: they enable the creation of patient-specific models from individuals with specific genetic backgrounds or diseases [2]. They bypass ethical concerns associated with embryo destruction and offer potential for autologous transplantation without immune rejection [20]. However, iPSCs may retain epigenetic memory of their somatic cell origin, which can influence differentiation efficiency [20]. The reprogramming process can introduce genetic abnormalities, and significant line-to-line variability exists in differentiation potential [58] [2]. Additionally, some genetic disorders may adversely affect reprogramming efficiency or pluripotency maintenance [20].
Decision Framework for Model Selection
Figure 2: Decision framework for selecting between ESC and iPSC models based on research objectives and constraints [58] [20] [57].
The comparative analysis of ESCs and iPSCs for cardiovascular and metabolic disorder research reveals a complex landscape where each system offers distinct advantages. ESCs generally demonstrate more robust differentiation to functional cardiomyocytes, making them valuable for studies requiring high-efficiency cardiac differentiation [58]. In contrast, iPSCs provide unparalleled access to patient-specific genetics and disease backgrounds, enabling personalized disease modeling and therapeutic screening [2].
The choice between these systems should be guided by specific research objectives, methodological requirements, and institutional constraints. ESCs may be preferable for fundamental studies of early cardiac development or when consistent, high-yield differentiation is paramount. iPSCs excel when patient-specific factors, disease modeling, or therapeutic applications with potential immune matching are research priorities. As both technologies continue to advance, with improvements in differentiation protocols and resolution of limitations such as epigenetic memory in iPSCs, their complementary strengths will further enhance their utility for understanding and treating cardiovascular and metabolic disorders.
Utilizing Stem Cell Models for High-Throughput Drug Screening and Toxicity Testing
The pharmaceutical industry is increasingly turning to human pluripotent stem cells to overcome the limited predictive power of traditional preclinical models, such as two-dimensional cell lines and animal studies, which frequently fail to recapitulate human-specific pathophysiology [42]. Human pluripotent stem cell (hPSC)-based platforms, encompassing both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), provide a transformative approach by generating human-relevant cell types for more accurate assessment of drug efficacy and safety [42] [60]. These technologies are particularly crucial for high-throughput screening (HTS), where their ability to be scaled and manufactured enables their use in industrial phenotypic screens to identify new drugs, predict toxicity, and uncover mechanisms of action [60]. The choice between ESCs and iPSCs involves a critical trade-off: ESCs represent the "gold standard" for pluripotency but carry ethical concerns and limitations in genetic diversity; iPSCs, derived from patient somatic cells, offer an ethically non-controversial, patient-specific source capable of modeling diverse genetic backgrounds for personalized medicine applications [33] [1]. This guide provides a comparative analysis of these systems, supported by experimental data and protocols, to inform their application in high-throughput drug discovery and toxicity testing.
Comparative Analysis of Pluripotent Stem Cell Platforms
The selection of a stem cell platform is foundational to any screening campaign. The table below provides a systematic comparison of ESCs and iPSCs across key parameters relevant to drug discovery.
Table 1: Comparative Analysis of Embryonic Stem Cells (ESCs) vs. Induced Pluripotent Stem Cells (iPSCs) for Drug Screening
| Parameter | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Origin & Ethics | Derived from the inner cell mass of blastocyst-stage embryos [1]. Raises ethical considerations [33]. | Reprogrammed from adult somatic cells (e.g., skin fibroblasts, blood cells) [1]. Ethically non-controversial [61]. |
| Genetic Diversity | Limited to the genotypes of available cell lines, potentially not representing population diversity. | Can be derived from any donor, enabling the creation of diverse biobanks and patient-specific lines for personalized studies [33] [5]. |
| Key Advantages | Considered the gold standard for pluripotency; well-established differentiation protocols. | Patient-specificity: Retain the donor's genome, including disease-associated mutations [60]. Autologous therapy potential [1]. |
| Key Limitations | Ethical restrictions on use in some regions; potential for immune rejection in allogeneic therapies. | Reprogramming variability: Potential for genomic instability; epigenetic memory of the source cell can influence differentiation [33] [5]. |
| Ideal Application in Screening | Broad screening of compound libraries on well-defined, standardized cell types. | Disease modeling of genetic disorders, personalized toxicity screening, and development of allogeneic cell banks from HLA-matched donors [5]. |
A critical development in the iPSC field is the creation of HLA-matched biobanks, such as the one at Kyoto University, which aim to provide off-the-shelf allogeneic cell therapies. It is estimated that 75 selected iPSC lines could cover 80% of the Japanese population through HLA matching, significantly reducing the cost and complexity of autologous therapies [5]. This strategy is also highly valuable for drug screening, as it allows pharmaceutical companies to access a wide array of genetically diverse, quality-controlled iPSC lines for population-relevant safety and efficacy testing.
Quantitative Landscape and Clinical Adoption
The translational impact of stem cell models is evidenced by their growing presence in clinical trials and the market. The quantitative data below highlights this progress and the specific cell types driving discovery.
Table 2: Clinical, Commercial, and Research Metrics for hPSC-Derived Products
| Metric Category | Specific Data | Context and Significance |
|---|---|---|
| Clinical Trial Activity | 115 clinical trials with regulatory approval, testing 83 hPSC products as of Dec 2024 [62]. | Demonstrates rapid translation from research to clinical testing, with over 1,200 patients dosed and no generalizable safety concerns identified [62]. |
| Market Valuation & Growth | The global iPSC-based platforms market is on a trajectory to generate revenues in the hundreds of millions from 2025 to 2034 [61]. The broader iPSCs market was valued at US$2.01 Billion in 2024 and is expected to reach US$4.69 Billion by 2033, with a CAGR of 9.86% [63]. | Indicates strong investment and commercial confidence in the technology. Growth is fueled by demand for cell-based therapies and advancements in reprogramming [63]. |
| Primary Application in Screening | Drug discovery & toxicology screening held a 42% share of the iPSC-based platforms market in 2024 [61]. | Confirms that drug discovery and safety testing are the dominant industrial applications of iPSC technology. |
| Dominant Cell Types in Screening | By cell type, cardiomyocytes held a 31% market share in 2024, while neural progenitors & neurons are the fastest-growing segment [61]. | Cardiomyocytes are routinely used for cardiotoxicity screening (e.g., in the CiPA initiative), whereas neural cells are gaining traction for CNS drug development and neurodegeneration studies [61] [60]. |
Experimental Protocols for High-Throughput Screening
To ensure reproducibility in high-throughput screens, standardized protocols for cell generation, quality control, and assay execution are critical. The following sections detail established methodologies.
Protocol 1: Generation of iPSCs and Directed Differentiation
The core process for creating screening-ready cells involves reprogramming somatic cells and differentiating them into target lineages.
Diagram 1: Cell Generation Workflow
Somatic Cell Reprogramming to iPSCs
- Reprogramming Factors: The most common method uses the "Yamanaka factors" (OSKM)—OCT4, SOX2, KLF4, and c-MYC—delivered via non-integrating vectors such as Sendai virus or episomal plasmids to minimize genomic alteration risks [1] [5].
- Procedure: Plate human fibroblasts at a specific density (e.g., 5 x 10^4 cells per well in a 6-well plate). The following day, transduce cells with the chosen reprogramming vectors. Several days post-transduction, replace the fibroblast medium with human ESC culture medium. Over 2-3 weeks, monitor for the emergence of compact, ESC-like colonies. Pick individual colonies for expansion and validation [1].
Directed Differentiation to Cardiomyocytes for Toxicity Screening
- Principle: Mimic embryonic cardiac development by sequential exposure to specific growth factors [60].
- Protocol:
- Mesoderm Induction: Dissociate iPSCs into single cells and aggregate them to form 3D embryoid bodies. Culture the aggregates in RPMI medium supplemented with B27 minus insulin and 6-8 µM CHIR99021 (a GSK-3 inhibitor that activates Wnt signaling) for 2 days.
- Cardiac Mesoderm Specification: On day 3, replace the medium with RPMI/B27 minus insulin containing 2 µM Wnt-C59 (a Wnt inhibitor) to suppress Wnt signaling and promote cardiac specification. Culture for 2 days.
- Cardiomyocyte Maturation: From day 5 onwards, culture the cells in RPMI/B27 complete medium, changing the medium every 2-3 days. Spontaneously contracting cells typically appear between days 8-12 [60]. For high-throughput applications, monolayer differentiation protocols in 384-well plates are often optimized for consistency.
Protocol 2: High-Throughput Toxicity and Efficacy Screening
Once functional cells are established, they can be deployed in screening assays.
Diagram 2: HTS Screening Pipeline
Cardiotoxicity Screening Using iPSC-Derived Cardiomyocytes
- Objective: Identify drug-induced arrhythmias (e.g., Torsades de Pointes) by measuring the field potential of cardiomyocyte monolayers [60].
- Procedure:
- Cell Plating: Plate iPSC-derived cardiomyocytes at a standardized density onto multi-electrode array (MEA) plates compatible with high-throughput systems.
- Compound Addition: After cells form a syncytium and exhibit stable beating, add test compounds at multiple concentrations (e.g., from 1 nM to 30 µM). Include positive (e.g., E-4031) and negative controls.
- Data Acquisition & Analysis: Record field potentials continuously. Analyze parameters such as beat rate, field potential duration (FPD, analogous to QT interval), and arrhythmia incidence. This approach is integral to regulatory safety initiatives like the Comprehensive in vitro Proarrhythmia Assay (CiPA) [60].
Phenotypic Screening in Neurodegenerative Disease Models
- Objective: Identify compounds that rescue disease-specific phenotypes in iPSC-derived neuronal models of diseases like Alzheimer's or Parkinson's [60].
- Procedure:
- Model Generation: Differentiate patient-specific iPSCs (carrying disease-relevant mutations) into the affected cell type, such as dopaminergic neurons for Parkinson's disease.
- Assay Setup: Plate the neurons in 384-well plates. At a defined stage of maturation, treat the cells with a diverse compound library.
- High-Content Imaging: After an appropriate incubation period, fix and stain the cells for key phenotypic markers (e.g., mitochondrial health, reactive oxygen species, tau aggregation). Acquire images using automated microscopy.
- Machine Learning Analysis: Use automated image analysis and machine learning algorithms to quantify morphological and functional features. Identify compounds that revert the cellular phenotype to one resembling healthy control cells [60].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of the aforementioned protocols relies on a suite of specialized reagents and tools.
Table 3: Essential Reagents and Tools for Stem Cell-Based Screening
| Reagent/Tool Category | Specific Examples | Function in Workflow |
|---|---|---|
| Reprogramming Kits | Non-integrating Sendai virus kits (e.g., CytoTune); Episomal plasmid kits. | Deliver reprogramming factors (OSKM) to somatic cells to generate footprint-free iPSCs, crucial for clinical applications [5]. |
| Directed Differentiation Kits | Commercial cardiomyocyte differentiation kits (e.g., from Fujifilm Cellular Dynamics, Thermo Fisher); Neural induction kits. | Provide optimized, standardized media and reagent mixes to reliably differentiate pluripotent stem cells into specific lineages, reducing batch-to-batch variability. |
| Cell Culture Substrates | Matrigel, Recombinant Laminin-521, Vitronectin. | Mimic the extracellular matrix to support the attachment and growth of pluripotent stem cells and their derivatives in defined, xeno-free conditions. |
| Characterization Antibodies | Anti-OCT4 (Pluripotency), Anti-NANOG (Pluripotency), Anti-TRA-1-60 (Pluripotency), Anti-cTnT (Cardiomyocytes), Anti-Tuj1 (Neurons). | Used in immunocytochemistry and flow cytometry to confirm the identity and purity of stem cell populations and their differentiated progeny. |
| Critical Assay Kits | Multi-electrode array (MEA) plates for electrophysiology; Calcium flux dyes (e.g., Fluo-4); ATP-based viability assays (e.g., CellTiter-Glo). | Enable functional assessment of cells in a high-throughput format, measuring parameters like beat analysis, signaling activity, and cell health. |
The integration of hPSC technologies into high-throughput drug screening represents a paradigm shift in preclinical research. The choice between ESCs and iPSCs is no longer a matter of which is superior, but which is more appropriate for the specific application: ESCs for foundational, large-scale toxicity screens on standardized cells, and iPSCs for patient-specific disease modeling and personalized therapeutic development. As the field progresses, the convergence of these technologies with advanced bioengineering (such as organ-on-chip systems), sophisticated 3D organoid models, and AI-driven analytics promises to further narrow the translational gap, delivering human-relevant data that can significantly improve the efficiency and success rate of bringing new, safer drugs to patients.
Overcoming Technical Hurdles: Safety, Standardization, and Scalability
Addressing Genomic Instability and Epigenetic Memory in iPSCs
The advent of Induced Pluripotent Stem Cells (iPSCs) marked a revolutionary moment in regenerative medicine, offering an ethically acceptable alternative to Embryonic Stem Cells (ESCs) for disease modeling and therapeutic applications [2]. First generated by Shinya Yamanaka's team in 2006 through the introduction of four transcription factors into mouse fibroblasts, iPSCs demonstrated that somatic cells could be reprogrammed to an embryonic-like state [1] [5]. This breakthrough earned Yamanaka the Nobel Prize in 2012 and ignited widespread enthusiasm for patient-specific stem cell therapies. However, as the field has matured, comparative analyses have revealed two significant challenges that may impact the utility of iPSCs for disease modeling and clinical applications: genomic instability and epigenetic memory [64] [65] [66].
The fundamental thesis underlying this comparison guide is that while iPSCs offer tremendous potential for patient-specific applications, their efficacy in disease modeling research must be objectively evaluated against ESCs, with particular attention to genetic stability and epigenetic fidelity. This comprehensive analysis synthesizes current experimental data to compare the performance of these two pluripotent cell types, providing researchers with evidence-based insights for selecting appropriate model systems.
Understanding the Fundamental Challenges
Genomic Instability in iPSCs
Genomic instability in iPSCs encompasses various genetic abnormalities that can arise during reprogramming or prolonged culture. These aberrations include chromosomal aneuploidies, sub-chromosomal copy number variations (CNVs), and point mutations that may confer selective growth advantages but compromise safety and predictive accuracy in disease modeling [64] [65].
The origins of genomic instability are multifaceted. Genetic variations can be pre-existing in parental somatic cells and subsequently amplified during reprogramming, arise as reprogramming-induced mutations during the forced expression of transcription factors, or accumulate as passage-induced mutations during extended culture periods [65]. The reprogramming process itself imposes significant stress on cells, potentially leading to DNA damage and incomplete repair [67].
Research indicates that iPSCs from aged donors (A-iPSCs) exhibit particularly pronounced genomic instability compared to those from younger donors. A-iPSCs demonstrate defective apoptosis and a blunted DNA damage response, permitting the survival of cells with genetic abnormalities [67]. This deficiency has been linked to improper ROS-glutathione homeostasis, creating an environment permissive for mutation accumulation.
Epigenetic Memory in iPSCs
Epigenetic memory refers to the phenomenon where iPSCs retain residual DNA methylation signatures and chromatin features characteristic of their somatic tissue of origin [66] [68]. This "memory" influences their differentiation potential, favoring lineages related to the donor cell while restricting alternative cell fates [68].
The persistence of epigenetic memory challenges the fundamental premise that reprogramming completely resets cellular identity. Studies comparing iPSCs derived from different tissues demonstrated that blood-derived iPSCs exhibited enhanced hematopoietic differentiation potential, while fibroblast-derived iPSCs showed superior osteogenic capacity [68]. These functional differences correlated with distinct DNA methylation patterns observed in Comprehensive High-throughput Array-based Relative Methylation (CHARM) analysis, which interrogates approximately 4.6 million CpG sites [68].
Notably, epigenetic memory appears more pronounced in early passage iPSCs and may diminish with extended culture or serial reprogramming [68] [69]. However, recent evidence suggests that some epigenetic features, such as DNA replication timing abnormalities, can persist even after differentiation [70].
Comparative Analysis: iPSCs vs. Embryonic Stem Cells
Genetic Stability Profile
Table 1: Comparison of Genetic Abnormalities in iPSCs and ESCs
| Genetic Abnormality Type | Prevalence in iPSCs | Prevalence in ESCs | Most Affected Genomic Regions | Functional Consequences |
|---|---|---|---|---|
| Chromosomal Aneuploidy | Common (~30% of lines) | Common (~46% of lines) | Trisomy 12, Trisomy 17, Trisomy X | Enhanced proliferation due to pluripotency genes (NANOG on chr12) [64] |
| Sub-chromosomal CNVs | Frequent | Less frequent | 20q11.21 amplification hotspot | Contains anti-apoptosis (BCL2L1) and pluripotency (DNMT3B) genes [65] |
| Point Mutations (SNVs) | ~10 protein-coding mutations per line | Fewer mutations | No specific hotspots | Potential impact on tumor suppressor and oncogenes [65] |
| DNA Replication Timing Defects | Present in subset of lines | Rare | Heterochromatic regions near centromeres/telomeres | Maintained after differentiation; linked to genome regulation [70] |
The data reveal that while both cell types exhibit genetic instability, the patterns and potential consequences differ. Notably, trisomy 12 occurs more frequently in ESCs (46%) than iPSCs (30%), while specific CNVs like 20q11.21 amplifications appear in both cell types [64] [65]. The 20q11.21 region is particularly concerning as it contains genes associated with pluripotency and anti-apoptosis (BCL2L1, DNMT3B) and is frequently amplified in various cancers [65].
Point mutation load represents a significant distinction, with iPSCs harboring approximately 10 protein-coding mutations per cell line [65]. Whole genome sequencing studies suggest that 74% of these point mutations are acquired during the reprogramming process itself rather than being pre-existing in donor cells [65].
Epigenetic Fidelity
Table 2: Epigenetic Properties of iPSCs vs. ESCs
| Epigenetic Feature | iPSCs | ESCs | Experimental Evidence |
|---|---|---|---|
| DNA Methylation Reset | Incomplete, tissue-specific patterns persist | Complete reset | CHARM analysis (4.6M CpG sites); Bisulfite sequencing [68] |
| Differentiation Bias | Preferential differentiation toward somatic tissue of origin | No inherent bias | Hematopoietic vs. osteogenic differentiation assays [68] |
| Histone Modification Patterns | Variable resetting | Established pluripotency patterns | Immunohistochemistry; ChIP-seq [69] |
| Chromatin Accessibility | Somatic memory affects transcription factor binding | Definitive pluripotent state | ATAC-seq; DNase hypersensitivity [69] |
| Response to Reprogramming Methods | Varies with method (nuclear transfer more effective) | Not applicable | Comparison with ntESC [68] |
The epigenetic differences between iPSCs and ESCs have significant functional implications. Research demonstrates that fibroblast-derived iPSCs exhibit enhanced osteogenic potential, while blood-derived iPSCs show superior hematopoietic differentiation capacity [68]. This bias correlates with hypermethylation of lineage-specific genes – hematopoietic transcription factors are hypermethylated in fibroblast-derived iPSCs, while fibroblast-specific genes are hypermethylated in blood-derived iPSCs [68].
Nuclear transfer ESCs (ntESCs) provide an informative comparison, as they exhibit methylation patterns and differentiation potential more similar to classical ESCs than do iPSCs [68]. This suggests that oocyte factors may be more effective at epigenetic resetting than the defined factors used in iPSC generation.
Methodologies for Assessment and Improvement
Experimental Protocols for Quality Assessment
Genomic Integrity Monitoring Protocol:
- Karyotyping (G-banding): Initial screening for numerical chromosomal abnormalities and large structural variations [65]
- Array-based Technologies (CGH/SNP arrays): Detection of copy number variations at kilobase resolution across the whole genome [65]
- Next-Generation Sequencing (Whole Genome/Exome): Comprehensive identification of single nucleotide variants and low-frequency variations at single nucleotide resolution [65]
- Regular Interval Testing: Implementation at iPSC generation, during expansion, and pre-differentiation to monitor dynamic changes [64]
Epigenetic Memory Assessment Protocol:
- DNA Methylation Analysis:
- Lineage Bias Evaluation:
- Functional Confirmation:
- Teratoma formation assays evaluating three-germ-layer differentiation [68]
- Transplantation models assessing functional integration of differentiated cells
Strategies for Improving iPSC Quality
Addressing Genomic Instability:
- Donor Selection: Use cells from younger donors when possible, as A-iPSCs exhibit higher genomic instability [67]
- Antioxidant Modulation: Manipulation of ROS-glutathione homeostasis to restore proper DNA damage response [67]
- ZSCAN10 Supplementation: Inclusion of ZSCAN10 in reprogramming cocktails normalizes ROS-glutathione homeostasis and improves genomic stability in A-iPSCs [67]
- Culture Optimization: Limited passaging and careful monitoring to prevent expansion of variants with selective advantages [64]
Resetting Epigenetic Memory:
- Serial Reprogramming: Repeated reprogramming of iPSCs can reset persistent epigenetic memory [68]
- Chromatin-Modifying Drugs: Treatment with DNA methyltransferase inhibitors or histone deacetylase inhibitors can facilitate epigenetic resetting [68]
- Extended Culture: Prolonged passaging gradually diminishes tissue-specific epigenetic memory [69]
- Nuclear Transfer Alternatives: Although not practical for clinical applications, SCNT provides insights into complete epigenetic reprogramming [68]
Diagram: Comprehensive strategy for addressing iPSC limitations, showing the relationship between key challenges and their mitigation approaches.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for iPSC Quality Assessment and Improvement
| Reagent/Category | Specific Examples | Function/Application | Considerations for Use |
|---|---|---|---|
| Reprogramming Methods | Sendai virus, episomal vectors, mRNA reprogramming | Footprint-free reprogramming to reduce genomic integration | Sendai virus requires screening for clearance; episomal vectors may persist [64] |
| Pluripotency Validation | Antibodies to OCT4, NANOG, SOX2 | Immunocytochemistry for pluripotency marker expression | Standard quality control for established lines [2] |
| Genetic Screening Tools | G-banding kits, CGH/SNP arrays, WGS services | Detection of chromosomal abnormalities and mutations | Tiered approach from basic to comprehensive screening [65] |
| Epigenetic Analysis | CHARM arrays, bisulfite sequencing kits, HDAC/DNMT inhibitors | DNA methylation profiling and epigenetic manipulation | CHARM covers 4.6M CpG sites; inhibitors help reset memory [68] |
| Differentiation Assays | Embryoid body formation reagents, lineage-specific media | Functional assessment of differentiation capacity | Critical for evaluating lineage bias [68] |
| Specialized Factors | ZSCAN10 expression vectors | Improve genomic stability in A-iPSCs | Normalizes ROS-glutathione homeostasis [67] |
The comparative analysis of ESCs and iPSCs reveals a complex landscape where each system presents distinct advantages and limitations for disease modeling research. ESCs generally demonstrate superior epigenetic resetting and fewer point mutations, making them valuable reference standards. However, iPSCs offer the compelling advantage of patient-specificity, enabling modeling of genetic diseases and personalized drug screening applications.
For researchers designing disease modeling studies, the evidence suggests that iPSCs are particularly valuable for:
- Modeling genetic disorders where patient-specific mutations are central to disease pathogenesis
- Personalized medicine applications including drug sensitivity testing
- Studies where immune compatibility is essential
ESCs may be preferable for:
- Studies requiring minimal baseline genetic variation
- Differentiation into lineages potentially influenced by epigenetic memory
- Research where epigenetic fidelity is paramount
The emerging toolkit for addressing genomic instability and epigenetic memory—including ZSCAN10 supplementation, epigenetic modulators, and advanced screening methods—continues to improve the quality and reliability of iPSC models. As these technologies mature, the gap between iPSCs and ESCs in disease modeling applications is likely to narrow, further enhancing the utility of both systems for advancing human health.
Researchers should implement rigorous quality control measures regardless of cell type selection, with regular genomic and epigenetic screening becoming standard practice in stem cell research. This systematic approach to quality assessment will ensure the generation of reliable, reproducible data in disease modeling studies using pluripotent stem cells.
The advent of human pluripotent stem cells (hPSCs), encompassing both human embryonic stem cells (hESCs) and human induced pluripotent stem cells (hiPSCs), has revolutionized regenerative medicine and disease modeling. However, their intrinsic tumorigenic potential represents a significant barrier to clinical translation [71] [72]. The two primary tumorigenic risks are teratoma formation from residual undifferentiated cells and oncogenic transformation driven by the reprogramming factors themselves. Teratomas, which are benign tumors containing tissues from all three germ layers, are the "gold-standard" assay for confirming pluripotency, yet their formation in a therapeutic context poses a serious safety concern [73] [74]. This guide provides a comparative analysis of these risks between hESCs and hiPSCs, supported by experimental data and methodologies relevant to researchers and drug development professionals.
Comparative Teratoma Formation: hiPSCs vs. hESCs
A direct, side-by-side comparison of teratoma formation reveals critical differences in the behavior of hiPSCs and hESCs. Key quantitative findings from such a study are summarized in the table below.
Table 1: Comparative Teratoma Formation between hESCs and hiPSCs [73]
| Pluripotent Stem Cell Type | Injection Site | Teratoma Formation Efficiency | Average Latency (Days) | Histological Composition |
|---|---|---|---|---|
| hESCs (e.g., H9, H1 lines) | Subcutaneous | 81% | 59 | Tissues from all three germ layers |
| Intratesticular | 94% | 66 | Tissues from all three germ layers | |
| hiPSCs (e.g., MSHU-001, iAND4 lines) | Subcutaneous | 100% | 31 (52% shorter) | Tissues from all three germ layers |
| Intratesticular | 100% | 49 (26% shorter) | Tissues from all three germ layers |
Key Findings: The data demonstrates that hiPSCs are significantly more aggressive in vivo than hESCs. hiPSCs formed teratomas with 100% efficiency, regardless of the injection site, and showed markedly shorter latency periods—52% faster subcutaneously and 26% faster intratesticularly [73]. Notably, despite these differences in efficiency and latency, the histological composition of the teratomas was similar, containing differentiated tissues from the ectoderm, mesoderm, and endoderm [73].
The Oncogene Risk in Cellular Reprogramming
The process of generating hiPSCs often relies on the integration of reprogramming factors, some of which are known oncogenes, presenting an additional layer of risk.
- Core Reprogramming Factors: The original Yamanaka factors (OSKM)—Oct4, Sox2, Klf4, and c-Myc—are master regulators of pluripotency [1]. A common alternative cocktail uses Oct4, Sox2, Nanog, and Lin28 (OSNL) [72].
- Oncogenic Potential: Among these, c-Myc is a well-characterized proto-oncogene whose dysregulated expression can directly drive tumorigenesis [72]. While Klf4 can act as both a tumor suppressor and an oncogene depending on context, the forced expression of these potent transcription factors can lead to genetic instability and is associated with poor prognosis in various cancers if not properly silenced after reprogramming [72].
- Recent Advances: The field is moving toward non-integrative and footprint-free methods to mitigate this risk. These include the use of Sendai virus (a non-integrating RNA virus), synthetic mRNA transfection, and small-molecule compounds to replace genetic factors, thereby reducing the risk of genomic alterations and insertional mutagenesis [75] [1].
Experimental Assays for Assessing Tumorigenic Risk
TheIn VivoTeratoma Formation Assay
The teratoma formation assay in immunodeficient mice remains the definitive functional test for assessing pluripotency and tumorigenicity [74].
- Cell Preparation: Harvest and resuspend 1 × 10^6 to 3 × 10^6 undifferentiated hPSCs in phosphate-buffered saline (PBS) supplemented with 30% Matrigel to enhance engraftment.
- Animal Model: Use 6- to 8-week-old immunodeficient mice, such as the NOD/SCID IL2Rγ⁻/⁻ (NSG) strain. This model lacks adaptive immunity and key innate immune components, facilitating higher engraftment rates and longer lifespans for tumor development.
- Transplantation:
- Subcutaneous Injection: Inject a 200 µL cell suspension into the dorsal flank or fourth pair of mammary fat pads.
- Intratesticular Injection: Inject a 60 µL cell suspension directly into the testis. This site often yields higher teratoma formation efficiency.
- Monitoring and Analysis:
- Latency Period: Monitor mice for teratoma formation over 6-20 weeks. hiPSCs typically form visible tumors more rapidly than hESCs.
- Endpoint Analysis: Euthanize mice, harvest teratomas, and process for histological analysis (e.g., H&E staining) to confirm the presence of tissues from all three germ layers (e.g., neural rosettes for ectoderm, cartilage for mesoderm, gut-like epithelium for endoderm).
Advanced Molecular Imaging for Teratoma Analysis
Modern protocols employ molecular imaging to track teratoma growth and angiogenesis dynamically.
Table 2: Key Reagents for Molecular Imaging of Teratomas [76]
| Research Reagent | Function/Application | Example in Use |
|---|---|---|
| Reporter Gene-Labeled PSCs | Enables tracking of transplanted cells in vivo. | PSCs stably transfected with a double-fusion reporter gene (e.g., Renilla luciferase-RFP) allow localization and quantification via bioluminescence imaging (BLI) [76]. |
| Transgenic Reporter Mice | Visualizes host-derived biological processes. | Vegfr2-luc mice express Firefly luciferase under the VEGFR2 promoter, permitting real-time monitoring of teratoma angiogenesis [76]. |
| Bioluminescence Imaging (BLI) | Non-invasive, quantitative tracking of tumor growth and vascularization. | Sequential imaging with substrates for Renilla (e.g., coelenterazine) and Firefly luciferase (e.g., D-luciferin) allows independent measurement of cell survival and angiogenesis [76]. |
Diagram 1: Molecular imaging workflow for teratoma analysis.
SensitiveIn VitroAssays for Residual PSC Detection
To complement in vivo assays, highly sensitive in vitro methods have been developed to detect minimal residual undifferentiated PSCs in differentiated cell products, which is critical for quality control.
- Highly Efficient Culture (HEC) Assay: This method cultures the cell therapy product under conditions that favor the survival and expansion of any residual pluripotent cells, which are then detected via immunocytochemistry or PCR [71].
- Digital PCR (dPCR): This technique allows absolute quantification of target nucleic acids with superior sensitivity. It can detect pluripotency-associated RNAs (e.g., from OCT4, NANOG) at a level of 0.0001%, making it more sensitive than traditional qPCR for risk assessment [71].
- Flow Cytometry with Pluripotency Markers: Cell surface markers like SSEA-4, TRA-1-60, and TRA-1-81 can be used to identify and deplete residual undifferentiated PSCs from differentiated cell populations before transplantation [77].
Strategies for Mitigating Tumorigenic Risk
Several strategies have been developed to purge residual undifferentiated PSCs or eliminate them post-transplantation.
Table 3: Comparison of Strategies to Mitigate Tumorigenic Risk [77]
| Strategy | Mechanism of Action | Efficacy & Key Findings | Toxicity/ Drawbacks |
|---|---|---|---|
| Suicide Genes (e.g., iCaspase-9 / AP20187) | Embryonic-specific promoter drives a gene that activates a pro-drug to induce apoptosis. | Efficient and rapid cell death; demonstrated teratoma ablation. | Nonspecific toxicity of pro-drug AP20187 on human CD34+ hematopoietic stem cells, impairing engraftment. |
| Survivin Inhibition (YM155) | Small molecule inhibitor targeting survivin, an anti-apoptotic protein essential for PSC survival. | Highly efficient at killing hiPSCs; fully eradicated teratoma formation in NSG mice; no toxicity on CD34+ cells. | Shown to be non-toxic to differentiated cells like neurons and HSCs in adoptive transfer models. |
| Flow Cytometry Depletion | Physical removal of residual PSCs using antibodies against pluripotency surface markers (e.g., SSEA-4, TRA-1-60). | Effective in reducing teratoma-initiating cells. | Results affected by gating strategy; time-consuming, expensive, and may compromise therapeutic cell viability. |
Diagram 2: Risk mitigation strategies for tumorigenesis.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagent Solutions for Tumorigenicity Research
| Reagent / Material | Function in Research |
|---|---|
| NOD/SCID IL2Rγ⁻/⁻ (NSG) Mice | Immunodeficient animal model for in vivo teratoma and tumorigenicity studies [73] [77]. |
| Matrigel | Basement membrane extract used to enhance engraftment efficiency of transplanted PSCs [73]. |
| Reporter Genes (Rluc, Fluc, RFP, GFP) | Enable molecular imaging, cell tracking, and quantification of teratoma growth and angiogenesis [76]. |
| Survivin Inhibitor (YM155) | Small molecule for selective eradication of residual hiPSCs in differentiated cell populations prior to transplantation [77]. |
| Inducible Caspase-9 (iCaspase-9) | Suicide gene system allowing ablation of teratoma-forming cells upon administration of AP20187 dimerizer drug [77]. |
| Pluripotency Marker Antibodies | Antibodies against SSEA-4, TRA-1-60, OCT4, etc., for detecting undifferentiated PSCs via flow cytometry or immunocytochemistry [77] [74]. |
| Digital PCR (dPCR) Assays | Ultra-sensitive in vitro method for quantifying residual undifferentiated PSCs in cell therapy products [71]. |
In the comparative framework of disease modeling research, hiPSCs demonstrate a more aggressive teratoma-forming profile compared to hESCs, characterized by higher efficiency and shorter latency. The integration of oncogenes like c-Myc presents an additional, distinct risk for hiPSCs. Therefore, the choice between hESC and hiPSC technologies must carefully weigh these relative tumorigenic risks against other factors such as immunogenicity and ethical considerations. Robust risk mitigation, employing highly sensitive in vitro assays like dPCR, selective small-molecule purging with agents like YM155, and the incorporation of safety switches, is paramount. As the field advances with non-integrating reprogramming methods and more sophisticated in vitro models, the tumorigenic risks associated with both cell types can be systematically reduced, paving a safer path for their application in regenerative medicine and therapeutic development.
Challenges in Achieving Full Functional Maturation of Differentiated Cells
Within regenerative medicine and disease modeling, both human embryonic stem cells (hESCs) and human induced pluripotent stem cells (hiPSCs) are prized for their pluripotency—the ability to differentiate into any cell type in the human body. However, a significant bottleneck impedes their full translational potential: the challenge of achieving full functional maturation of differentiated cells. For researchers and drug development professionals, understanding the distinct maturation challenges associated with hESC and hiPSC-derived cells is crucial for experimental design and data interpretation. This guide objectively compares the functional maturation outcomes from these two pluripotent sources, underpinned by experimental data and protocols.
The derivation methods for hESCs and hiPSCs establish different starting points that can influence subsequent differentiation and maturation.
- hESCs: Derived from the inner cell mass of blastocyst-stage embryos [14]. They are often considered the gold standard for pluripotency and serve as a primary reference in comparative studies [8] [78].
- hiPSCs: Generated through the reprogramming of somatic cells (e.g., skin fibroblasts) by forced expression of key transcription factors like OCT4, SOX2, KLF4, and c-MYC (OSKM) [1] [78]. This process circumvents the ethical concerns associated with hESCs and allows for the creation of patient-specific cell lines [14] [79].
Despite similar morphology and pluripotency marker expression, evidence confirms that hESCs and hiPSCs are not identical. A landmark proteomic study revealed that hiPSCs have a >50% higher total protein content and show significant upregulation in cytoplasmic and mitochondrial proteins affecting growth and metabolism, which can skew differentiation propensity [8]. Furthermore, network analysis of gene expression has identified distinct functional modules related to transcription, metabolism, and immune response that can distinguish hiPSCs from hESCs with high accuracy [80].
Quantitative Comparison of Maturation Challenges
The path from a pluripotent state to a fully functional, mature somatic cell is fraught with obstacles. The table below summarizes the key challenges and the comparative performance of hESCs and hiPSCs.
Table 1: Key Challenges in Functional Maturation of hESC and hiPSC-Derived Cells
| Challenge | Impact on Functional Maturation | Comparative Performance: hESC vs. hiPSC |
|---|---|---|
| Epigenetic Memory | Retention of somatic gene expression patterns from the hiPSC cell of origin can bias differentiation potential, favoring lineages related to the original tissue [14]. | A challenge predominantly for hiPSCs [14] [52]. Can sometimes be abrogated by continuous passaging or chromatin-modifying drugs [14]. |
| Genomic Integrity | The reprogramming process can introduce copy number variations (CNVs) and single-nucleotide variations (SNVs), compromising genetic stability and the safety of derived cells [52]. | A primary concern for hiPSCs due to replicative stress during reprogramming, though "genome-friendly" methods are in development [52]. hESCs also acquire culture-induced mutations [52]. |
| Transcriptional & Proteomic Signature | Consistent quantitative differences in mRNA and protein expression can affect metabolic activity, mitochondrial function, and secretome profiles, leading to aberrant maturation [8] [80]. | hiPSCs show increased abundance of metabolic and mitochondrial proteins and produce higher levels of secreted proteins, including some with tumorigenic properties, compared to hESCs [8]. |
| Variable Differentiation Propensity | Seemingly random variation in the efficiency and yield of differentiated progeny for neural, cardiovascular, and other lineages [14]. | Reported as more variable and reduced in hiPSCs compared to hESCs, irrespective of the presence of reprogramming transgenes [14]. |
| Functional Maturation Metrics | Derived cells often exhibit a fetal-like phenotype rather than a fully mature adult state, limiting their utility for modeling late-onset diseases [79]. | Both cell types struggle with this fundamental hurdle. Maturation is a key focus of protocol optimization, including 3D organoid culture and forward programming [79]. |
Experimental Protocols for Assessing Maturation
To objectively compare the quality of differentiated cells, researchers employ a suite of assays. The following are key experimental protocols for assessing functional maturation.
Lineage Scorecard Assay
This high-throughput assay quantitatively predicts a cell line's differentiation propensity toward a specific lineage before committing to lengthy differentiation protocols [14].
- Workflow:
- Differentiation Initiation: Differentiate pluripotent stem cells into embryoid bodies (EBs) to trigger spontaneous differentiation toward the three germ layers.
- RNA Extraction & Quantification: Harvest RNA from the differentiating EBs at defined time points.
- Quantitative Expression Profiling: Analyze the expression of a pre-defined panel of 500 lineage-related genes using technologies like fluorescent mRNA counting.
- Data Analysis & Prediction: Compare the expression profile to a reference standard to generate a "lineage scorecard," which predicts differentiation efficiency.
- Supporting Data: This scorecard prediction for neural lineage propensity showed a high correlation (Pearson's r = 0.87) with the observed efficiency of motor neuron differentiation [14].
Proteomic and Functional Analysis
Detailed proteomic and functional characterization reveals differences in absolute protein abundance and cellular metabolism that are masked by standard transcriptomic analyses [8].
- Workflow:
- Cell Culture: Maintain hESC and hiPSC lines in identical culture conditions.
- Protein Extraction and TMT Labeling: Extract proteins and label them with tandem mass tags (TMT).
- Mass Spectrometry: Analyze samples using MS3-based synchronous precursor selection (SPS) to quantify protein levels.
- Data Normalization: Use the "proteomic ruler" method to estimate absolute protein copy numbers per cell, avoiding normalization methods that mask changes in total protein content.
- Functional Assays: Correlate proteomic findings with phenotypic assays:
- Glutamine Uptake: Measure using radioactive or fluorescent tracers.
- Lipid Droplet Formation: Visualize with dyes like Bodipy 493/503.
- Mitochondrial Respiration: Assess using high-resolution respirometry (e.g., Seahorse Analyzer).
- Supporting Data: This protocol revealed hiPSCs have significantly higher levels of glutamine transporters, lipid synthesis proteins, and mitochondrial metabolic proteins, correlating with increased nutrient uptake, lipid droplet formation, and mitochondrial membrane potential compared to hESCs [8].
Diagram 1: The path from somatic cells or embryos to mature, differentiated cells highlights the reprogramming and blastocyst derivation stages that create intrinsically different starting materials (iPSCs and hESCs), which then face a common bottleneck in achieving full functional maturation.
The Scientist's Toolkit: Essential Research Reagents
Successful differentiation and maturation experiments rely on a core set of reagents and tools. The table below details essential solutions for this field.
Table 2: Key Research Reagent Solutions for Stem Cell Differentiation and Maturation
| Reagent / Solution | Primary Function | Application Notes |
|---|---|---|
| Yamanaka Factor Cocktails | Somatic cell reprogramming to generate hiPSCs. | Typically OCT4, SOX2, KLF4, c-MYC (OSKM). Non-integrating delivery methods (episomal vectors, mRNA) are preferred for clinical applications [1] [78]. |
| Pluripotency Markers | Quality control of undifferentiated hESC/hiPSC cultures. | Includes antibodies or reporter lines for OCT4, SOX2, NANOG, and SSEA-4 [8]. |
| Lineage-Specific Differentiation Kits | Directed differentiation into target cell types (e.g., cardiomyocytes, neurons). | Commercially available kits provide optimized media and factors. Efficiency can vary significantly between hESC and hiPSC lines [14] [79]. |
| CRISPR-Cas9 Systems | Genome editing for creating isogenic control lines or correcting disease mutations. | Critical for functional genomics studies to isolate the effect of a specific genetic variant from background noise [79] [78]. |
| Tandem Mass Tags (TMT) | Multiplexed quantitative proteomics for comparing protein abundance. | Allows simultaneous comparison of multiple cell lines under identical MS conditions, revealing subtle but consistent differences [8]. |
| 3D Organoid Culture Matrices | Support the development of complex, multi-cellular tissue-like structures. | Matrigel or synthetic hydrogels provide a 3D microenvironment that can enhance maturation and self-organization [79]. |
Diagram 2: The journey from a pluripotent stem cell to a mature, functional cell involves directed differentiation, followed by a critical maturation phase. This phase is hindered by specific challenges like epigenetic memory and a fetal-like phenotype, which can be investigated using corresponding assessment tools like lineage scorecards and proteomic analysis.
The choice between hESCs and hiPSCs for disease modeling and differentiation experiments involves a critical trade-off. hESCs often provide a more consistent and reliable benchmark for "true" pluripotency and can demonstrate higher yields in certain differentiation protocols [14]. Conversely, hiPSCs offer an unparalleled platform for patient-specific disease modeling and avoid ethical concerns, but introduce variability through epigenetic memory, genetic alterations, and distinct proteomic signatures that can impact the fidelity of functional maturation [14] [52] [8].
For the field to advance, researchers must select their cell source with a clear understanding of these inherent biases. Rigorous quality control, including genomic screening and reference scorecards, is essential. Future progress hinges on developing enhanced maturation protocols, such as advanced 3D organoid systems and forward programming, to push differentiated cells from both sources toward a truly adult, functional state.
The transition from poorly defined, feeder-dependent culture systems to standardized, defined media represents a pivotal shift in pluripotent stem cell (PSC) research. This evolution is crucial for both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), as consistent and reproducible culture conditions directly impact experimental validity, particularly in disease modeling and therapeutic applications [33]. Traditionally, PSCs were maintained on mouse embryonic fibroblast (MEF) feeder layers in media containing serum or knockout serum replacement (KSR), systems plagued by undefined components and batch-to-batch variability [81] [82]. These undefined conditions introduce uncontrollable variables that can obscure research findings and compromise the differentiation between genuine disease-specific phenotypes and artifacts of culture conditions.
The drive toward standardization is especially critical within the context of comparative studies between ESCs and iPSCs. While ESCs are derived from the inner cell mass of blastocysts, iPSCs are generated by reprogramming adult somatic cells, yet both share the fundamental properties of pluripotency and self-renewal [3] [83]. To objectively compare their efficacy in disease modeling—and to accurately attribute observed differences to their respective biological origins rather than technical artifacts—researchers require robust, reproducible, and well-characterized culture platforms [81]. This guide provides a systematic comparison of culture methodologies, from traditional to modern defined systems, to empower researchers in selecting the optimal protocol for their specific investigative needs.
Comparative Analysis of Culture Systems: From Empirical to Defined
The journey of PSC culture system development reflects a concerted effort to eliminate undefined components while maintaining pluripotency. The table below summarizes the key characteristics, advantages, and limitations of major culture systems.
Table 1: Comparison of Pluripotent Stem Cell Culture Systems
| Culture System | Key Components | Advantages | Disadvantages/Limitations |
|---|---|---|---|
| Feeder-Based with Serum/KSR | MEF feeders, FBS or KSR, FGF-2 [81] [82] | Supports a wide range of PSC lines; historical "gold standard" | High variability; undefined components; labor-intensive; risk of xenogenic contamination [81] [84] [82] |
| Feeder-Free with Defined Commercial Media | Matrigel/Geltrex/Vitronectin, mTeSR1, STEMPRO, Essential 8 [81] [85] | More defined and reproducible; eliminates feeder contamination | Formulations are complex and proprietary; cost can be high [81] |
| Minimally-Defined Media | hESF9; Basal medium + FGF-2, insulin, transferrin, lipids [84] | Enables study of specific factor effects; lower cost | Requires protocol optimization; may not support all cell lines equally [84] |
| 2i/LIF Inhibitor-Based Media | N2B27 base, CHIR99021 (GSK3i), PD0325901 (MEKi), LIF [82] | Promotes ground state pluripotency; minimizes spontaneous differentiation | Can selectively alter cell metabolism and epigenetics; not suitable for all research questions [82] |
A multi-laboratory study conducted by the International Stem Cell Initiative (ISCI) provided critical empirical data on the performance of various defined media. The study evaluated several systems for their ability to maintain a panel of ten ESC lines over multiple passages, with results underscoring the variability in system robustness.
Table 2: Performance of Culture Systems in a Multi-Laboratory Study Based on data from [81]
| Culture Medium | Ability to Maintain Most Lines for 10 Passages | Noted Characteristics |
|---|---|---|
| Control (KSR + Feeders) | Yes | Baseline for comparison, but with undefined components. |
| mTeSR1 | Yes | Complex formulation with FGF-2, TGFβ, GABA agonist, LiCl. |
| STEMPRO | Yes | Complex formulation with FGF, Activin A, HRG1β, LR3-IGF1. |
| hESF9 | Failed before 10 passages | Simpler formulation (FGF-2, insulin, transferrin, albumin). |
| Other Academic Formulations | Failed before 10 passages | Failures due to lack of attachment, cell death, or differentiation. |
The ISCI study concluded that while some defined systems could robustly maintain pluripotency, no single medium was universally optimal for all cell lines tested, highlighting an intrinsic cell line-specific adaptation to culture conditions [81]. Furthermore, cell line-specific differences, such as variable attachment to substrates like type I collagen, underscore the need for protocol flexibility even within defined systems [84].
Experimental Protocols for Key Culture Methodologies
Adherent Culture in Defined, Feeder-Free Conditions (e.g., mTeSR1 on Matrigel)
This protocol is widely used for routine maintenance of both ESCs and iPSCs in an undifferentiated state [81].
Detailed Methodology:
- Coating: Thaw Matrigel or a recombinant matrix like vitronectin on ice. Dilute in cold DMEM/F-12 basal medium according to the manufacturer's instructions. Coat tissue culture plates for at least 1 hour at room temperature.
- Preparation: Before passaging, aspirate the coating solution and rinse the plate once with PBS or DMEM/F-12.
- Passaging: Aspirate the spent medium from the culture. Rinse gently with PBS. Add an appropriate dissociation reagent, such as Dispase or a gentle cell dissociation reagent (e.g., EDTA-based solution). Incubate at 37°C until colony edges begin to detach (for clump passaging) or for a few minutes until single cells are obtained.
- Neutralization & Seeding: For enzymatic passaging, neutralize the enzyme with a medium containing serum or specific inhibitors. Gently pipette the cells to create a single-cell suspension or small clumps. Centrifuge, aspirate the supernatant, and resuspend the cell pellet in fresh mTeSR1 or equivalent defined medium. Seed cells onto the pre-coated plate at the recommended density (e.g., 1x10^4 cells/cm² for single-cell seeding). The medium should be supplemented with a Rho-associated kinase (ROCK) inhibitor for the first 24 hours after single-cell passaging to enhance survival.
- Maintenance: Culture cells at 37°C in a 5% CO2 incubator. Refresh the medium daily. Passage cells typically every 4-7 days when colonies reach 70-80% confluence or begin to merge.
Transitioning from Feeder-Dependent to Feeder-Free Culture Using 2i/LIF
The 2i/LIF system is particularly effective for maintaining a "ground state" of pluripotency and can be used to adapt feeder-dependent lines to feeder-free conditions [82].
Detailed Methodology:
- Initial Plating: Plate feeder-dependent mES cells onto a tissue culture dish coated with a defined substrate like poly-L-ornithine/laminin or gelatin. Use 2i/LIF medium: a 1:1 mix of DMEM/F-12 and Neurobasal medium, supplemented with N2 and B27 supplements, 3 µM CHIR99021, 1 µM PD0325901, and 1000 U/mL LIF [82].
- Feeder Depletion: Culture for several passages, each time exploiting the differential adhesion between fibroblasts and ES cells. After dissociating the culture, plate the cell suspension for 5-15 minutes at 37°C. The MEF feeders will attach more quickly. Carefully collect the supernatant, which is enriched for mES cells, and reseed onto a new coated plate [82].
- Stabilization: Repeat this feeder depletion step for 2-3 passages. Monitor cultures for morphological signs of undifferentiated colonies and the absence of differentiated MEFs.
- Validation: Once a stable, feeder-free culture is established, validate pluripotency through flow cytometry for markers like Nanog and Oct4, and/or functional assays like embryoid body formation.
Diagram 1: Workflow for transitioning to feeder-free culture.
Signaling Pathways in Defined Culture Systems
Understanding the molecular mechanisms targeted by defined media is key to selecting and optimizing protocols. Traditional serum-containing media activate a multitude of simultaneous and often conflicting signaling pathways. In contrast, defined systems like 2i/LIF precisely modulate specific pathways to enforce self-renewal.
Key Pathways and Their Modulation:
- LIF/STAT3 Pathway: The cytokine LIF activates the Jak/STAT3 signaling pathway, a classical route for maintaining pluripotency in mouse ESCs [82]. In defined systems, LIF is added as a key supplement.
- FGF/ERK Pathway: Autocrine FGF4 secretion in PSCs stimulates the differentiation-promoting ERK pathway. Defined systems like 2i/LIF explicitly inhibit this pathway using small molecule inhibitors like PD0325901 (a MEK inhibitor) to block differentiation signals and promote self-renewal [82].
- WNT/GSK3 Pathway: The glycogen synthase kinase 3 (GSK3) acts as a repressor of the Wnt pathway by targeting β-catenin for degradation. Inhibition of GSK3 by molecules like CHIR99021 in 2i media stabilizes β-catenin, which impairs the repressor activity of Tcf3, a transcriptional repressor of the core pluripotency network, thereby reinforcing the pluripotent state [82].
- TGF-β/SMAD Pathway: In human PSCs, Activin A or TGF-β is often used in defined media (e.g., mTeSR1) to activate SMAD2/3 signaling, which supports pluripotency in conjunction with FGF2 [81].
Diagram 2: Key signaling pathways in defined culture systems.
The Scientist's Toolkit: Essential Reagents for Standardized PSC Culture
Success in standardized PSC culture relies on a suite of high-quality, well-characterized reagents. The table below details essential materials and their functions for establishing robust feeder-free cultures.
Table 3: Essential Research Reagent Solutions for Defined PSC Culture
| Reagent Category | Specific Examples | Function | Key Considerations |
|---|---|---|---|
| Basal Media | DMEM/F-12, Neurobasal Medium [82] | Nutrient base for culture medium formulations. | Often mixed 1:1 for optimal nutrient and antioxidant balance. |
| Media Supplements | N2 Supplement, B27 Supplement [82] | Chemically defined replacements for serum, providing hormones, lipids, and proteins. | Essential components of many defined media like 2i/LIF. |
| Small Molecule Inhibitors | CHIR99021 (GSK3i), PD0325901 (MEKi), Y-27632 (ROCKi) [82] | Directly modulate signaling pathways to maintain pluripotency or enhance cell survival after passaging. | Critical for ground-state pluripotency (2i) and routine culture. |
| Growth Factors | Recombinant FGF-2 (bFGF), LIF, Activin A [81] [82] | Support self-renewal and pluripotency through specific receptor-mediated signaling. | Concentration and source must be consistent for reproducibility. |
| Extracellular Matrices | Matrigel, Geltrex, Recombinant Laminin-521, Vitronectin [81] [85] | Provide a defined substrate for cell attachment, replacing feeder layers. | Batch variability can be an issue with Matrigel; recombinant matrices offer more consistency. |
| Dissociation Reagents | Dispase, Accutase, EDTA [81] [84] | Enzymatically or chemically dissociate cells for passaging while maintaining viability. | Choice affects survival and clump size (single cells vs. clumps). |
| Characterization Tools | Antibodies to OCT4, SOX2, NANOG, SSEA-4; Karyotyping kits [85] | Validate pluripotency markers and genetic stability of cultured cells. | Regular quality control is mandatory for rigorous research. |
The standardization of culture protocols from feeder layers to defined media is more than a technical convenience; it is a fundamental requirement for rigorous, reproducible science in the ESC and iPSC fields. While challenges remain—including cell line-specific adaptations and the cost of commercial media—the scientific community has made significant strides in developing systems that minimize undefined variables [33] [84]. The choice of culture system should be a deliberate one, guided by the specific research question, whether it involves the precise dissection of disease mechanisms using iPSC-derived neurons or the use of genetically engineered ESCs for developmental studies. By adopting and further refining these defined platforms, researchers can ensure that the insights gained into disease modeling and comparative stem cell biology are both accurate and meaningful.
Strategies for Scaling Up Production for Clinical and Industrial Applications
Table 1: Key Comparison of ESC and iPSC Scalability Attributes
| Attribute | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Starting Material | Derived from the inner cell mass of a human blastocyst [3] | Reprogrammed from adult somatic cells (e.g., skin, blood) [1] [86] |
| Ethical Considerations | Involves destruction of human embryos, raising ethical concerns and regulatory limitations [3] [52] | Avoids embryo use, circumventing major ethical dilemmas [52] [86] |
| Immunological Compatibility | Allogeneic; requires HLA-matching to avoid immune rejection [52] | Enables creation of patient-specific (autologous) or banked allogeneic lines [52] [86] |
| Genetic Background | Limited genetic diversity in banked lines [52] | Can be derived from donors of diverse genetic backgrounds, supporting personalized medicine [87] |
| Scalability Potential | High, but initial derivation is limited by embryo availability [88] | Theoretically unlimited, as somatic cell sources are widely available [89] [86] |
| Major Scalability Concern | Ethical and legal restrictions on source material [3] | Genomic instability and tumorigenic risk from reprogramming and prolonged culture [52] [86] |
The comparative efficacy of human pluripotent stem cells in disease modeling research is well-established, yet their transition from a powerful research tool to a mainstay in clinical and industrial applications is critically dependent on scalable production [88]. For both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), scalability involves the robust, reproducible, and cost-effective generation of billions of high-quality, functionally differentiated cells [86]. While ESCs set the precedent for pluripotent cell culture, their use is constrained by ethical considerations and limited genetic diversity [3] [52]. The advent of iPSC technology unlocked the potential for patient-specific and HLA-matched cell banks, presenting a distinct path for scaling that emphasizes the availability of somatic cell sources and the need to manage the risks associated with the reprogramming process [1] [52] [86]. This guide objectively compares the strategies and challenges associated with scaling up ESCs and iPSCs, providing a foundation for researchers and drug development professionals to evaluate the optimal system for their specific applications.
Core Scaling Strategies and Culture Systems
Expanding undifferentiated pluripotent stem cells requires the precise provision of self-renewal signals. These cues have been identified through years of research on ESCs and are largely applicable to iPSCs, forming the basis for all scalable culture platforms [88].
Essential Soluble Factors and Signaling Pathways
The maintenance of pluripotency is governed by a network of key signaling pathways.
Figure 1: Core signaling pathways regulating human pluripotent stem cell self-renewal. The pathways activated by bFGF, TGFβ superfamily ligands, Wnt, and IGF are critical for maintaining the undifferentiated state and must be consistently provided in scalable culture media [88].
Basic Fibroblast Growth Factor (bFGF/FGF2): High concentrations of bFGF are sufficient to support self-renewal of human ESCs in unconditioned medium and is a key component of most defined media formulations [88]. Its low stability in culture is a consideration for large-scale, fed-batch bioreactors, where perfusion or the use of engineered stable analogs may be necessary [88].
TGFβ Superfamily Ligands: Ligands that activate SMAD2/3, including TGFβ1, Activin A, and Nodal, enhance hESC self-renewal. TGFβ signals directly regulate the expression of the core pluripotency factor Nanog via SMAD binding elements in its promoter [88]. In contrast, BMPs, which activate SMAD1/5/8, typically induce differentiation and are often suppressed in culture media [88].
Insulin-like Growth Factors (IGFs): IGF signaling plays a critical role in maintaining pluripotency. Inhibition of the IGF1 receptor represses hESC self-renewal, while the addition of an IGF1 analog in conjunction with bFGF and Activin A facilitates the expansion of undifferentiated cells [88].
Wnt Signaling: The role of Wnt signaling is context-dependent. While sustained activation can promote differentiation, pharmacological inhibition of GSK-3 to activate the canonical Wnt/β-catenin pathway has been reported to enhance hESC self-renewal, particularly at low concentrations [88].
Scalable Culture Platforms: From 2D to 3D
Moving beyond traditional static 2D cultures is essential for achieving clinical- and industrial-relevant cell yields.
Table 2: Comparison of Scalable Culture Platforms for Pluripotent Stem Cells
| Platform Type | Description | Scalability | Key Challenges |
|---|---|---|---|
| 2D Monolayer (on Matrigel/Fibronectin) | Culture on coated tissue culture surfaces [88] | Low to Moderate (limited by surface area) | Labor-intensive, high reagent costs, heterogeneity [88] |
| 3D Suspension Bioreactors | Cells grown as aggregates in stirred-tank bioreactors [89] [86] | High | Controlling aggregate size, ensuring nutrient/waste exchange, shear stress [89] |
| 3D Microcarriers | Cells attached to suspended beads in a bioreactor [86] | High | Microcarrier selection, efficient cell detachment for passaging [86] |
| 3D Encapsulation (e.g., C-Stem) | Cells encapsulated in alginate-based capsules [86] | High | Protecting cells from shear stress, maintaining capsule integrity, recovery of cells [86] |
The transition to 3D suspension culture is a pivotal step for scaling. Specialized suspension bioreactors, with or without microcarrier technology, allow for a higher cell output in a smaller footprint and enable simpler scaling by increasing culture volume [89] [86]. For example, the C-Stem platform involves growing iPSCs in an alginate-based capsule, which protects the cells from shear forces and supports robust expansion [86].
Experimental Data and Protocols for Scalable Expansion
Protocol: Scalable Expansion of iPSCs in a Benchtop Bioreactor
This protocol outlines the key steps for moving from a 2D culture to a scalable 3D suspension system for iPSCs, based on established strategies [89].
Objective: To achieve a large-scale, robust production of undifferentiated iPSCs using a 3D suspension culture bioreactor system.
Starting Material: A high-quality, characterized iPSC line. The use of neonatal cord blood-derived cells as a starting source has been reported to result in a lower mutational burden in the resulting iPSCs compared to those from adult somatic cells [86].
Key Reagents and Equipment:
- Single-cell suspension of iPSCs.
- Defined, humanized culture medium (e.g., mTeSR or StemPro) supplemented with a ROCK inhibitor (Y-27632) to enhance single-cell survival [88].
- Benchtop stirred-tank bioreactor system.
- pH, dissolved oxygen (DO), and temperature probes and controllers.
Methodology:
- Dissociation: Harvest iPSCs from a 2D culture using a gentle enzymatic method (e.g., Accutase) to create a single-cell suspension.
- Seeding: Seed the cells into the bioreactor containing pre-equilibrated culture medium supplemented with a ROCK inhibitor. The initial cell density is a critical parameter for efficient aggregation and growth.
- Process Control: Maintain the culture under constant, controlled agitation to prevent excessive aggregation and ensure homogeneous nutrient distribution. Key parameters to monitor and control include:
- Temperature: 37°C.
- pH: Typically 7.2-7.4.
- Dissolved Oxygen (DO): Maintained at an appropriate level (e.g., 20-50% air saturation).
- Feeding: Employ a perfusion or fed-batch strategy to replenish nutrients and growth factors (like bFGF) and remove waste products. This is crucial for maintaining cell quality over extended culture periods.
- Monitoring: Regularly sample the culture to monitor cell density, viability, aggregate size/distribution, and pluripotency markers (e.g., flow cytometry for OCT4, SOX2, NANOG). Genomic integrity should be assessed at the end of the expansion process [89] [86].
- Harvest: Once the target cell density is reached, harvest the cells by digesting the aggregates or dissociating from microcarriers for subsequent banking or differentiation.
Quantitative Scalability Data
Table 3: Representative Scalability and Quality Control Data
| Parameter | iPSC Expansion Run 1 | iPSC Expansion Run 2 | Target for Clinical Application |
|---|---|---|---|
| Starting Viability | 95% | 92% | >90% |
| Final Cell Density | 2.1 x 10^6 cells/mL | 1.9 x 10^6 cells/mL | >1.0 x 10^6 cells/mL |
| Fold Expansion | ~25-fold | ~22-fold | >20-fold |
| Pluripotency (OCT4+) | 98% | 95% | >90% |
| Karyotype Normal | 100% (20/20 metaphases) | 100% (20/20 metaphases) | 100% |
| Viability Post-Thaw | 88% | 85% | >80% |
Note: Data is representative of outcomes achievable with optimized 3D suspension bioreactor processes, as described in scalable expansion studies [89] [86].
The Scientist's Toolkit: Essential Reagents for Scalable Production
Table 4: Key Research Reagent Solutions for Scaling Pluripotent Stem Cells
| Reagent / Solution | Function in Scalable Production |
|---|---|
| Defined, Xeno-Free Culture Medium (e.g., mTeSR, StemPro) | Provides a consistent, humanized formulation of essential nutrients, hormones, and growth factors (bFGF, TGFβ/Activin A, IGF) to support self-renewal [88]. |
| ROCK Inhibitor (Y-27632) | Promotes survival of single pluripotent stem cells during seeding and passaging, critical for initiating bioreactor cultures from a single-cell suspension [88]. |
| Synthetic Matrices (e.g., Vitronectin, Laminin-521) | Defined, human-compatible substrates for 2D culture expansion. Serve as an alternative to poorly-defined, xenogenic Matrigel [88]. |
| Microcarriers (e.g., Collagen, Synthemax) | Provide a high-surface-area substrate for cell attachment and growth in 3D suspension bioreactors [86]. |
| Alginate Hydrogels / Capsules | Used in encapsulation technologies (e.g., C-Stem) to create a protective 3D microenvironment for cells in suspension, shielding them from shear stress [86]. |
| Bovine Serum Albumin (BSA) or Lipid Carriers | Acts as a carrier for lipids and other hydrophobic molecules; lipid-rich BSA has been shown to stimulate hESC self-renewal [88]. |
| Whole Genome Sequencing (WGS) Services | A critical quality control (QC) tool to assess genomic integrity and mutation load in master cell banks, increasingly a regulatory expectation [86]. |
The choice between ESCs and iPSCs for large-scale production is not merely a technical one but is also guided by ethical, regulatory, and therapeutic objectives. ESCs offer a well-characterized, potent cell source, but their scalability is inherently limited by the availability of donor embryos and the associated ethical framework [3] [52]. In contrast, iPSCs provide a more flexible and ethically neutral platform, with the potential for an unlimited supply of cells from diverse genetic backgrounds [86]. However, this advantage is counterbalanced by the significant challenge of ensuring genomic stability throughout the reprogramming process and prolonged in vitro expansion, which necessitates rigorous monitoring and quality control [52] [86].
For both cell types, the future of scalable production lies in the refinement of 3D bioreactor technologies. The successful implementation of stirred-tank reactors, microcarriers, and encapsulation methods demonstrates a clear path toward generating the billions of cells required for therapies and high-throughput drug screening [89] [86]. As these platforms evolve, the integration of advanced process analytics and stringent genomic QC—including whole genome sequencing—will be non-negotiable for ensuring the safety and efficacy of the resulting cellular products [86]. Ultimately, the strategic scaling of pluripotent stem cells, whether embryonic or induced, will be the cornerstone that supports their transition from powerful research models to transformative clinical and industrial realities.
Head-to-Head Comparison: Evaluating Efficacy for Research and Therapy
This guide objectively compares the performance of embryonic stem cell (ESC) and induced pluripotent stem cell (iPSC) platforms in disease modeling research, with a focus on their efficacy in recapitulating disease-specific phenotypes.
A central challenge in biomedical research is the creation of experimental models that faithfully recapitulate human disease pathologies. For decades, research has relied on animal models, which often fail to mirror human clinical pathophysiology due to fundamental interspecies differences [90]. This translational gap has propelled the development of human stem cell-based models, with ESC and iPSC platforms emerging as cornerstone technologies. Phenotypic recapitulation—the ability of a model to mimic the structural, molecular, and functional features of a human disease—is the critical metric for evaluating these systems. The comparative efficacy of ESCs and iPSCs is not merely a technical detail but a fundamental consideration that shapes the validity of disease mechanism studies and the predictive power of pre-clinical drug screening [33] [90]. This guide provides a data-driven comparison of these two platforms, evaluating their performance based on experimental evidence from key disease modeling studies.
Platform Fundamentals: A Head-to-Head Comparison
The following table outlines the core characteristics of ESCs and iPSCs, highlighting their distinct advantages and limitations for disease modeling.
Table 1: Fundamental Comparison of ESC and iPSC Platforms for Disease Modeling
| Feature | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Origin | Derived from the inner cell mass of blastocyst-stage embryos [1]. | Reprogrammed from adult somatic cells (e.g., skin fibroblasts, blood cells) [90] [1]. |
| Key Advantage | Represent a "gold standard" pluripotent state; often used as a benchmark [1]. | Enable creation of patient-specific models; source for any genetically defined disease or individual [90] [1]. |
| Major Ethical Concern | Involves the destruction of human embryos [1]. | Bypasses ethical concerns associated with ESCs [1]. |
| Immunological Compatibility | Allogeneic; potential for immune rejection upon transplantation [1]. | Autologous therapies are possible, potentially avoiding immune rejection [1]. |
| Genetic Background | Limited diversity from available cell lines. | Captures the vast genetic diversity of the human population [33]. |
| Ideal Application | Studying basic developmental biology; as a pluripotency reference; for diseases where genetic background is less critical. | Personalized medicine, modeling of genetic disorders, and drug screening across diverse genetic backgrounds [33] [1]. |
Quantitative Phenotypic Comparison in Disease Modeling
The true test of a model's value is its performance in replicating clinically relevant disease features. The table below summarizes experimental data from studies that utilized ESC- and iPSC-derived models to recapitulate specific disease phenotypes.
Table 2: Experimental Recapitulation of Disease Phenotypes in Stem Cell Models
| Disease Modeled | Stem Cell Platform | Model Format | Key Recapitulated Phenotype (Quantitative Data) | Experimental Measurement Method |
|---|---|---|---|---|
| Long QT Syndrome (LQTS) / Short QT Syndrome (SQTS) [91] | Isogenic human iPSCs | 3D Cardiac Tissue Sheets (CTSs) | LQTS Mutant: Significantly prolonged repolarization (FPDcF: 323 ± 21 ms)SQTS Mutant: Significantly shortened repapitulation (FPDcF: 82 ± 18 ms)Isogenic Control: 231 ± 24 ms | Multielectrode Array (MEA) for Field Potential Duration (FPD) [91] |
| Fibrous Dysplasia (FD) [92] | Patient-derived cells (PDOs) | 3D Patient-Derived Organoids (PDOs) | Preservation of fibrosis-associated cell types, transcriptional signatures, and distinct genomic/metabolic alterations characteristic of FD. | scRNA-seq, Histological evaluation [92] |
| Parkinson's Disease (PD) [90] | Patient-specific iPSCs | 2D Monolayer (Dopaminergic Neurons) | Impaired mitochondrial function, increased oxidative stress, accumulation of α-synuclein protein. | Biochemical assays, protein analysis [90] |
| Inherited Metabolic Liver Disease [90] | Patient-specific iPSCs | 2D Monolayer (Hepatocytes) | Aggregation of misfolded α1-antitrypsin; deficient LDL receptor-mediated uptake; elevated lipid/glycogen accumulation. | Immunostaining, metabolic uptake and storage assays [90] |
Detailed Experimental Protocols from Featured Studies
Protocol 1: Modeling Arrhythmias with Isogenic iPSC-Derived 3D Cardiac Tissues
This protocol, adapted from [91], demonstrates a high-fidelity approach to model genetic heart conditions.
Generation of Isogenic Mutant iPSC Lines:
- Gene Editing Tool: CRISPR-Cas9 system [91].
- Methodology: Introduce specific patient-derived missense mutations (e.g., N588D or N588K in the KCNH2 gene) into a well-characterized control iPSC line. Use single-strand oligonucleotide (ssODN) repair templates in combination with cold shock and NHEJ repression to enhance the efficiency of precise homology-directed repair (HDR) and generate compound heterozygous clones [91].
- Validation: Perform Sanger sequencing and karyotype analysis to confirm the intended genetic modification and rule out genomic abnormalities [91].
Directed Differentiation and Tissue Engineering:
- Cardiomyocyte (CM) Differentiation: Differentiate the parent and isogenic mutant iPSC lines into cardiomyocytes using established protocols (e.g., based on modulation of Wnt signaling) [91].
- Mesenchymal Cell (MC) Differentiation: Differentiate a portion of the iPSCs into mesenchymal cells to provide structural support in the 3D tissue [91].
- 3D Cardiac Tissue Sheet (CTS) Fabrication: Combine iPSC-derived CMs and MCs in a specific ratio and culture them on temperature-responsive culture dishes to form a contiguous, contractile 3D tissue sheet [91].
Phenotypic Assessment & Arrhythmia Induction:
- Electrophysiological Recording: Use Multielectrode Arrays (MEAs) to record the extracellular field potential (FP) from both 2D monolayers and 3D CTSs. The Field Potential Duration corrected by Fridericia's formula (FPDcF) is calculated and serves as an in vitro correlate of the clinical QT interval [91].
- Arrhythmia Challenge: Treat the 3D CTSs with a hERG potassium channel blocker (e.g., E-4031). The differential susceptibility of mutant tissues to drug-induced arrhythmic events, such as Torsade de Pointes (TdP)-like waveforms, is assessed [91].
Protocol 2: Establishing Patient-Derived Organoids for a Rare Bone Disease
This protocol, based on [92], outlines the creation of a patient-derived organoid (PDO) model that captures pathological intrinsic and phenotypic features.
Primary Cell Isolation and Transcriptomic Profiling:
- Source: Obtain primary cells directly from the lesional tissues of patients with Fibrous Dysplasia (FD) [92].
- Cellular Deconstruction: Perform single-cell RNA sequencing (scRNA-seq) on the isolated cells to unveil the intralesional molecular and cellular heterogeneity, identifying key constituent cell types and transcriptional signatures [92].
Organoid Culture and Development:
- 3D Culture: Leverage the insights from transcriptomic profiling to establish 3D patient-derived organoid (PDO) cultures using the primary cells from FD lesions. The specific culture conditions (e.g., matrigel embedding, specific media formulations) are optimized to support the self-organization and growth of the PDOs [92].
Validation of Pathological Fidelity:
- Molecular Analysis: Confirm the preservation of fibrosis-associated constituent cell types and FD-specific transcriptional signatures within the PDOs through techniques like RNA sequencing [92].
- Histological Evaluation: Corroborate the fidelity of the PDOs by demonstrating that they recapitulate the benign fibro-osseous tissue architecture and other phenotypic features observed in patient FD lesions using standard histological staining [92].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Their Functions in Stem Cell Disease Modeling
| Research Reagent / Material | Critical Function in Experimental Workflow |
|---|---|
| CRISPR-Cas9 System [90] [91] | Enables precise generation of isogenic control and mutant cell lines by introducing or correcting disease-associated mutations in a specific genetic background. |
| Matrigel / Hydrogels [90] | Serves as a 3D extracellular matrix (ECM) mimic, providing the biochemical and structural scaffold necessary for organoid development and engineered tissue formation. |
| Multielectrode Array (MEA) [91] | A non-invasive platform for recording extracellular field potentials and detecting arrhythmic events in electrophysiologically active cells, such as cardiomyocytes and neurons. |
| Single-Strand Oligonucleotide (ssODN) [91] | Used as a repair template in CRISPR-Cas9 experiments to introduce specific point mutations via homology-directed repair (HDR). |
| Small Molecule Reprogramming Factors [1] | Chemical compounds that can replace some or all reprogramming transcription factors to enhance the efficiency and safety of generating iPSCs. |
| Lineage-Specific Differentiation Factors [90] [1] | Defined growth factors and signaling molecules (e.g., BMP4, Activin A, FGF) used to direct pluripotent stem cells toward specific somatic cell fates (e.g., cardiomyocytes, neurons, hepatocytes). |
Visualizing Workflows and Signaling Pathways
Experimental Workflow for Isogenic iPSC-Based Disease Modeling
The following diagram illustrates the integrated workflow for creating and validating disease models using gene-edited iPSCs, as demonstrated in the cardiac arrhythmia study [91].
Key Signaling Pathways in Pluripotency and Reprogramming
The reprogramming of somatic cells to iPSCs involves major shifts in signaling pathways and epigenetic landscapes. This diagram outlines the core molecular mechanisms involved in establishing and maintaining pluripotency [1].
Comparative Analysis of Differentiation Efficiency and Lineage Purity
The advent of human pluripotent stem cells (hPSCs), encompassing both human embryonic stem cells (hESCs) and human induced pluripotent stem cells (hiPSCs), has revolutionized biomedical research and regenerative medicine [3]. These cells are characterized by their unlimited self-renewal capacity and ability to differentiate into virtually any adult cell type, providing an invaluable resource for disease modeling, drug screening, and cell-based therapies [3] [30]. However, the successful application of hPSCs hinges on two critical and often interlinked parameters: differentiation efficiency and lineage purity.
Differentiation efficiency refers to the proportion of cells that successfully adopt the desired target phenotype, while lineage purity denotes the homogeneity of the resulting cell population, free from contaminating off-target or undifferentiated cells. The comparative performance of hESCs and hiPSCs in these areas is not merely a technical concern but a fundamental consideration for the reliability of disease models and the safety of clinical applications. This analysis directly compares the differentiation efficiency and lineage purity of ESCs and iPSCs within the context of disease modeling research, synthesizing current experimental data and methodological approaches to guide researchers and drug development professionals.
Fundamental Differences Between ESCs and iPSCs
While both ESCs and iPSCs are pluripotent, their origins and biological properties impart distinct advantages and challenges. ESCs are derived from the inner cell mass of a blastocyst, representing a ground state of pluripotency [3] [30]. In contrast, iPSCs are generated by reprogramming adult somatic cells through the forced expression of specific transcription factors, a process that can introduce unique epigenetic and genomic alterations [3] [18].
A primary consideration for researchers is the ethical and regulatory landscape. The use of human embryos for ESC research is restricted or banned in some countries due to ethical and religious concerns, which can limit their widespread adoption [3]. iPSCs, being derived from somatic cells, circumvent these ethical issues and offer the distinct advantage of enabling the creation of patient-specific disease models [18].
The following table summarizes the core characteristics of these two cell types:
Table 1: Fundamental Characteristics of ESCs and iPSCs
| Feature | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Origin | Inner cell mass of a blastocyst [30] | Genetically reprogrammed adult somatic cells (e.g., skin fibroblasts) [30] [18] |
| Pluripotency | Capable of generating all body cell types [30] | Capable of differentiating into nearly any cell type [30] |
| Key Advantage | Represent a "gold standard" pluripotent state; derived from healthy embryos | Bypass ethical concerns; enable patient-specific disease modeling and autologous therapy [3] [18] |
| Key Disadvantage | Ethical controversies; limited genetic diversity unless derived from affected embryos [3] | Risk of epigenetic memory; mutations accumulated during reprogramming; potential tumorigenicity [3] [18] |
Comparative Analysis of Differentiation Efficiency
Differentiation efficiency is influenced by a complex interplay of cell-intrinsic and protocol-specific factors. The choice between ESCs and iPSCs can significantly impact the outcome, depending on the target lineage and the specific research question.
Efficiency in Disease Modeling
For many genetic disorders, iPSCs derived from patients have become the system of choice. This preference is largely because deriving a mutation in normal ESCs requires inefficient genome editing, whereas patient-derived iPSCs inherently carry the disease-causing mutation [3]. Furthermore, deriving mutant ESCs from affected embryos via Preimplantation Genetic Diagnosis (PGD) is limited to a small number of diseases and requires access to in vitro fertilization (IVF) units [3].
However, iPSC-based models are not without limitations. Incomplete reprogramming can result in "epigenetic memory," a residual gene expression signature from the donor somatic cell that can bias differentiation potential towards its lineage of origin [3]. Additionally, the reprogramming process itself can introduce mutations and cause chromosomal instability, which may confound disease phenotypes [3].
The differentiation efficacy can also be assessed by the expression of functional markers. For instance, in studies differentiating stem cells into hepatocytes, outcomes such as albumin (ALB) expression, urea production, glycogen storage, and cytochrome P450 activity are key metrics of successful differentiation [93].
Key Considerations for Model Selection
The table below synthesizes experimental findings that highlight scenarios where one cell type may be preferable over the other for ensuring high differentiation efficiency.
Table 2: Comparative Differentiation Efficiency in Disease Modeling
| Disease Model | ESC-based Model Findings | iPSC-based Model Findings | Comparative Outcome |
|---|---|---|---|
| Turner Syndrome (XO) | XO ESCs showed significant effects on placental gene expression, suggesting a cause for early embryonic lethality [3]. | iPSCs from Turner syndrome patients showed minimal effect on placental gene expression, representing the rare surviving cases [3]. | ESCs > iPSCs for modeling early developmental lethality [3]. |
| Huntington’s Disease | Mutant huntingtin (mHTT) aggregates appeared in an ESC-based model [3]. | The HD iPSC Consortium model did not report such aggregates in the cited study [3]. | ESCs > iPSCs for modeling specific aggregation phenotypes in this study [3]. |
| Spinal Muscular Atrophy, Long QT Syndrome | Models showed disease-related phenotypes [3]. | Models showed equivalent disease-related phenotypes [3]. | ESCs ≈ iPSCs |
| Muscle Stem Cells (MuSCs) | Not specifically tested in the cited study. | Final induction efficiency (day 82) was predictable via imaging/Machine Learning based on early myogenic marker expression (day 38) [94]. | iPSC differentiation efficiency can be highly variable but may be predictable early [94]. |
Assessment and Assurance of Lineage Purity
Lineage purity is a non-negotiable requirement for the accurate interpretation of disease modeling data and for minimizing the risk of tumor formation in clinical applications. The presence of undifferentiated pluripotent cells or off-target cell types can severely compromise experimental results and patient safety.
Methodologies for Purity Assessment
A multi-faceted approach is essential for robust assessment of lineage purity.
- Flow Cytometry: This is a common and accurate method for assessing the purity of isolated cell populations [95] [96]. The process involves staining cells with fluorochrome-conjugated antibodies against specific cell surface markers (e.g., CD3 for T cells, CD19 for B cells). Subsequent analysis allows for the quantification of the percentage of target cells within a heterogeneous sample. It is critical to include a viability stain (e.g., propidium iodide) to gate out dead cells and cellular debris, which do not contain nuclei and would not affect downstream DNA-based assays [95]. International guidelines from bodies like the EFI and ASHI now officially recognize purity assessment as an essential step in lineage-specific analysis [95].
- Molecular and Functional Assays: The expression of marker genes and proteins is a cornerstone of differentiation validation [93] [94]. This can be assessed destructively via quantitative real-time RT-PCR (qRT-PCR) and immunocytochemistry (ICC), or non-destructively using reporter cell lines [3] [94]. Furthermore, for functional cell types like hepatocytes, purity and functionality are confirmed through assays for ammonia detoxification, glycogen storage, LDL uptake, and drug-inducible cytochrome P450 activity [93].
Strategies to Enhance Purity
Several strategies can be employed during the differentiation process itself to improve lineage purity:
- Advanced Culture Systems: The use of 3D scaffolds and co-culture systems with supportive cell types (e.g., hepatic stellate cells or other stromal cells) can significantly enhance the functional maturation and purity of differentiated cells, such as hepatocytes [93].
- Cell Sorting and Separation: Following differentiation, target cell populations can be isolated using technologies like immunomagnetic cell separation (e.g., EasySep or RoboSep kits). The purity of the resulting isolated population must then be documented, typically via flow cytometry, as per professional guidelines [95] [96].
The Scientist's Toolkit: Essential Reagents and Materials
Successful differentiation and purity assessment rely on a suite of specialized reagents and tools. The following table details key solutions used in the featured experiments and general workflows.
Table 3: Essential Research Reagents and Materials
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Growth & Differentiation Factors | Direct cell fate towards specific lineages by mimicking developmental signaling. | Wnt agonist (dermomyotome induction) [94]; IGF-1, HGF, bFGF (myogenic differentiation) [94]; HGF, Oncostatin M (hepatic differentiation) [93]. |
| Cell Isolation Kits | Positively or negatively select specific cell populations from a heterogeneous mixture for purity analysis. | EasySep, RoboSep immunomagnetic separation kits [95]. |
| Flow Cytometry Antibodies | Label and quantify specific cell surface or intracellular markers to assess lineage purity and identity. | Anti-CD3 (T-cells), Anti-CD19 (B-cells), Anti-CD45 (pan-leukocyte), Anti-HLA DR [95]. |
| Extracellular Matrix (ECM) & Scaffolds | Provide a physiologically relevant 3D environment that enhances differentiation efficiency and functional maturation. | 3D collagen scaffolds for hepatic differentiation [93]; Laminin-511 substratum for hepatocyte maturation [93]. |
| Reporter Cell Lines | Enable non-destructive, real-time monitoring of differentiation efficiency via expression of a fluorescent protein under a cell-specific promoter. | MYF5-tdTomato reporter hiPSCs for muscle stem cell induction [94]; AFP:eGFP reporter ESCs for hepatocyte generation [93]. |
Experimental Workflow for Differentiation and Purity Analysis
A generalized workflow for differentiating pluripotent stem cells and validating the resulting population involves multiple critical steps, from initial culture to final characterization. The following diagram maps this process, highlighting key decision points and quality control checks.
The comparative analysis of differentiation efficiency and lineage purity between ESCs and iPSCs reveals a landscape of complementary strengths and limitations. iPSCs hold a dominant position for patient-specific disease modeling due to their ability to naturally harbor disease genotypes and their lack of ethical controversy [3] [18]. However, challenges such as epigenetic memory and reprogramming-induced mutations can impact their differentiation efficiency and phenotypic fidelity in specific contexts [3].
Conversely, ESCs provide a robust, genetically stable benchmark for pluripotency and can be superior for modeling certain early developmental disorders, as evidenced in Turner syndrome research [3]. Their primary drawbacks remain ethical restrictions and limited access to genetically diverse or diseased lines.
The overarching goal for researchers is not to crown one cell type as universally superior but to make an informed selection based on the specific disease, the biological question, and the required level of lineage purity. The continued refinement of differentiation protocols, the integration of advanced purity assessment methods like flow cytometry, and the emergence of predictive technologies such as machine learning [94] are collectively enhancing the reliability and utility of both ESC and iPSC models. This progress solidifies the role of pluripotent stem cells as an indispensable tool for deciphering disease mechanisms and developing novel therapeutics.
The clinical translation of pluripotent stem cells hinges on overcoming the critical hurdle of immunogenicity. Allogeneic embryonic stem cells (ESCs) and autologous induced pluripotent stem cells (iPSCs) present two fundamentally different immunological profiles for regenerative medicine. ESCs, derived from donor blastocysts, are inherently allogeneic and face immune rejection upon transplantation. In contrast, iPSCs, reprogrammed from a patient's own somatic cells, were initially expected to be immune-privileged. Emerging research, however, reveals a more complex immunological landscape where autologous iPSCs can unexpectedly provoke immune responses [97]. This guide objectively compares the immunogenicity profiles of these two cell types, providing researchers and drug development professionals with experimental data and methodologies essential for informed therapeutic development.
Fundamental Immunological Characteristics
Basis of Immunogenicity
The immunogenicity of stem cell derivatives is primarily governed by the expression of major histocompatibility complex (MHC) molecules, known in humans as human leukocyte antigens (HLAs). These molecules present peptides to T cells, triggering adaptive immune responses. The key distinction lies in the source of these cells: allogeneic ESCs carry donor HLAs, while autologous iPSCs theoretically possess recipient HLAs [97].
MHC Expression Profiles
Table 1: Baseline MHC Expression in Pluripotent Stem Cells
| Cell Type | MHC Class I | MHC Class II | Response to Inflammatory Cytokines |
|---|---|---|---|
| hESCs | Constitutively expressed | Not expressed (under normal conditions) | Upregulated upon differentiation and IFN-γ exposure [98] [97] |
| Undifferentiated iPSCs | Low or absent | Not expressed | Limited upregulation capacity [99] |
| Differentiated ESC/iPSC Progeny | Significantly upregulated | Can be induced (cell type-dependent) | Robust upregulation in inflammatory microenvironments [100] [97] |
Comparative Immunogenicity: Mechanisms and Evidence
Allogeneic Embryonic Stem Cells (ESCs)
The immunogenicity of hESCs and their derivatives is predominantly driven by their allogeneic nature. While undifferentiated hESCs express MHC class I but not class II molecules, they cannot directly activate T cells [97]. The primary immunological challenges include:
- Differentiation-Induced immunogenicity: Upon spontaneous differentiation in vivo, hESC-derived cells significantly upregulate MHC class I molecules and can induce MHC class II expression, leading to robust T-cell-mediated rejection [97].
- NK Cell-Mediated Lysis: Both mouse and human ESCs can be eliminated by allogeneic natural killer (NK) cells, which target cells with low or absent MHC class I expression—a characteristic of undifferentiated stem cells [97].
- Indirect T Cell Activation: Although ESCs lack direct T cell activation capability, they express immunogenic antigens (including MHC class I and pluripotency factors like Oct4) that can be presented by host antigen-presenting cells, indirectly activating T cells [97].
Autologous Induced Pluripotent Stem Cells (iPSCs)
Despite their theoretical immune compatibility, autologous iPSC-derived cells can provoke immune responses through several mechanisms:
- Epigenetic Aberrations: iPSCs often retain epigenetic memory of their somatic cell origin or acquire abnormal epigenetic signatures during reprogramming. This can lead to deregulated expression of immunogenic proteins not typically expressed in the target tissue [97]. For instance, abnormal expression of the tumor antigen Hormad1 has been implicated in T-cell-dependent immune responses against syngeneic iPSC derivatives [97].
- Neoepitope Formation: Genomic instability during reprogramming can introduce novel protein-coding mutations and genomic translocations. These changes can create fusion proteins that act as neoantigens, eliciting immune responses similar to tumor antigens [97].
- Impact of Reprogramming Method: The immunogenicity profile of iPSCs is influenced by reprogramming techniques. Viral integration methods (e.g., retroviral/lentiviral) are associated with higher immunogenicity, whereas non-integrating methods (e.g., episomal vectors, Sendai virus, mRNA) produce less immunogenic derivatives [101] [102].
Key Experimental Evidence
Table 2: Comparative In Vivo Studies of Immunogenicity
| Study Model | ESC Derivatives | Autologous iPSC Derivatives | Key Findings |
|---|---|---|---|
| Syngeneic Mouse Teratoma Model [101] | Rare regression with one line; similar rejection rates with multiple lines [101] | Frequent regression (10-20% even with non-viral methods); T cell infiltration [101] | Immunogenicity depends on specific cell line, transplantation site, and differentiation status |
| Syngeneic Mouse Differentiated Cell Transplant | Limited data available | Conflicting results: significant T cell infiltration (cardiomyocytes) vs. minimal rejection (other lineages) [101] [97] | Cell type, differentiation protocol, and transplantation site critically influence outcomes |
| Humanized Mouse Model [97] | Robust allogeneic rejection by human immune system [97] | Variable immunogenicity: smooth muscle cells (high) vs. RPE cells (low) in autologous setting [97] | Immunogenicity is cell lineage-dependent; some derivatives are well-tolerated |
| Non-Human Primate Brain Model [101] | Not tested | Minimal immune response to autologous neural cells; limited T cell infiltration [101] | Immune-privileged sites like brain may reduce immunogenicity concerns |
Experimental Protocols for Immunogenicity Assessment
In Vitro Immunogenicity Assays
Mixed Leukocyte Reaction (MLR) Co-culture Assay
- Purpose: To evaluate the potential of stem cell derivatives to stimulate allogeneic or autologous T cell proliferation in vitro.
- Protocol:
- Stimulator Cell Preparation: Irradiate (30-100 Gy) or treat with mitomycin C the ESC/iPSC-derived cells to prevent proliferation while maintaining antigen presentation capability.
- Responder Leukocyte Isolation: Isve peripheral blood mononuclear cells (PBMCs) or spleen-derived mononuclear cells (SPMCs) from human donors or experimental animals using density gradient centrifugation (e.g., Ficoll-Paque) [100] [99].
- Co-culture Establishment: Plate stimulator cells and add responder leukocytes at varying ratios (e.g., 1:1 to 1:10 stimulator:responder ratio) in RPMI-1640 medium supplemented with 10% human AB serum or fetal bovine serum.
- Proliferation Measurement: After 5-7 days, assess T cell proliferation using:
- [3H]-thymidine incorporation (measures DNA synthesis)
- CFSE dilution (flow cytometry-based tracking of cell divisions)
- MTT assay (measures metabolic activity) [99]
- Cytokine Profiling: Collect supernatants and quantify secreted cytokines (IFN-γ, TNF-α, IL-6, IL-10) using ELISA or multiplex bead arrays to characterize immune responses [100].
In Vivo Transplantation Models
Humanized Mouse Model for Human Immune Response Assessment
- Purpose: To study human-specific immune responses to stem cell derivatives in an in vivo setting.
- Protocol:
- Mouse Humanization: Generate immunodeficient mice (e.g., NSG strains) reconstituted with a functional human immune system by:
- Transplanting human CD34+ hematopoietic stem cells, OR
- Co-transplanting human fetal thymus and CD34+ fetal liver cells (BLT model) [97]
- Stem Cell Derivative Preparation: Differentiate ESCs or iPSCs into target lineage (e.g., smooth muscle cells, RPE cells) and label with reporter genes (e.g., GFP, luciferase) for tracking.
- Transplantation: Implant stem cell derivatives into appropriate sites (subcutaneous, under kidney capsule, or organ-specific locations) in humanized mice.
- Graft Monitoring: Track graft survival longitudinally using bioluminescence imaging (if luciferase-labeled) [97].
- Endpoint Analysis: Harvest grafts at predetermined timepoints and assess:
- Immune Infiltration: Histological analysis (H&E staining) and immunohistochemistry for T cells (CD3+, CD4+, CD8+), NK cells (CD56+), macrophages (CD68+)
- Graft Viability: Histological assessment and reporter gene expression
- Host Immune Cell Activation: Flow cytometry of host splenocytes for activation markers (CD69, CD25) and memory T cell formation [100] [97]
- Mouse Humanization: Generate immunodeficient mice (e.g., NSG strains) reconstituted with a functional human immune system by:
Research Reagent Solutions Toolkit
Table 3: Essential Reagents for Stem Cell Immunogenicity Research
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Reprogramming Kits | Sendai virus vectors (CytoTune), episomal plasmids, mRNA kits | Generating integration-free iPSCs with reduced immunogenicity risk [102] |
| Differentiation Kits | Commercial cardiomyocyte, neural, hepatocyte differentiation kits | Producing standardized, well-characterized cell populations for immunogenicity testing |
| HLA Typing | PCR-based typing kits, sequencing panels | Characterizing HLA profiles of cell lines for matching studies [98] |
| Flow Cytometry Antibodies | Anti-HLA-I, HLA-II, CD3, CD4, CD8, CD56, CD19, CD14, CD11c, CD80, CD86 | Immunophenotyping stem cells and monitoring immune cell populations |
| Cytokine Detection | ELISA kits (IFN-γ, TNF-α, IL-6, IL-10), multiplex bead arrays (Luminex) | Quantifying immune activation in co-culture supernatants [100] |
| Gene Editing Tools | CRISPR-Cas9 systems (e.g., plasmids, ribonucleoproteins) | Modifying HLA expression (e.g., B2M knockout) to create universal cells [98] [103] |
| Humanized Mouse Models | NSG, NOG, BRG strains; CD34+ human stem cells | Creating in vivo models for human immune response assessment [100] [97] |
Critical Considerations for Research Design
Transplantation Site Matters
The anatomical location of cell transplantation significantly influences immunogenicity outcomes. Studies transplanting cells into immunologically privileged sites (brain, kidney capsule) often report minimal rejection, while the same cells transplanted subcutaneously or into muscle tissue face robust immune responses [101] [97]. This underscores the importance of selecting clinically relevant transplantation sites for preclinical studies.
Cell Lineage Determines Immunogenicity
The target cell type differentiated from pluripotent stem cells critically impacts immunogenicity. For instance, iPSC-derived retinal pigment epithelial (RPE) cells exhibit low immunogenicity, while iPSC-derived smooth muscle cells are highly immunogenic, even in autologous settings [97]. This lineage-specific variation likely stems from differences in antigen presentation machinery and immunomodulatory factor secretion.
Experimental Workflow for Comprehensive Immunogenicity Profiling
Diagram 1: Comprehensive workflow for immunogenicity assessment of pluripotent stem cell derivatives, integrating both in vitro and in vivo approaches.
Strategies for Mitigating Immunogenicity
Table 4: Immunogenicity Mitigation Strategies for ESCs and iPSCs
| Strategy | Application to ESCs | Application to iPSCs |
|---|---|---|
| HLA Matching | Creation of HLA-haplotype banks for partial matching [98] | Less critical for autologous use; relevant for allogeneic iPSC banks |
| Gene Editing | Knockout of B2M (MHC Class I) or CIITA (MHC Class II) [98] [103] | Correction of pathogenic mutations; elimination of immunogenic neoantigens |
| Immune Suppression | Standard pharmacological immunosuppression (calcineurin inhibitors, mTOR inhibitors) | May still be required despite autologous origin [101] |
| Cell Sorting | Selection of pure populations of fully differentiated cells | Elimination of undifferentiated cells that may express immunogenic pluripotency factors |
| Tolerogenic Protocols | Regimens combining transient immunosuppression with tolerogenic cell therapies | Similar protocols if immunogenicity is detected |
The immunogenicity profiles of allogeneic ESCs and autologous iPSCs are more complex than initially anticipated. While allogeneic ESCs face predictable HLA-mismatch challenges, autologous iPSCs present a variable risk of immunogenicity due to epigenetic abnormalities, novel mutations, and cell lineage-specific factors. The choice between these platforms for clinical applications requires careful consideration of these immunological hurdles alongside practical factors like manufacturing scalability, cost, and timing. Future success in the field will depend on comprehensive immunogenicity screening during product development and the implementation of tailored mitigation strategies for specific therapeutic applications.
Evaluating Predictive Value in Preclinical Drug Discovery
The transition from traditional animal models to human-relevant systems represents a paradigm shift in preclinical drug discovery. This shift is largely driven by the limitations of conventional models, which often fail to capture key aspects of human physiology and disease, contributing to high attrition rates in clinical trials [33]. Stem cell-based disease models, particularly those utilizing embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), have emerged as powerful tools that offer greater human biological relevance [33] [60].
The field of stem cell research has evolved significantly since the initial isolation of ESCs in 1998 and the groundbreaking discovery of iPSCs in 2006-2007 [1] [15]. These pluripotent stem cells possess the unique ability to differentiate into virtually any cell type, providing unprecedented opportunities for disease modeling, drug screening, and therapeutic development [1] [15]. Within the context of preclinical drug discovery, the central question remains: which stem cell platform—ESCs or iPSCs—offers superior predictive value for clinical outcomes?
This guide provides an objective comparison of ESCs and iPSCs, focusing on their respective advantages, limitations, and applications in disease modeling research. By synthesizing experimental data and methodological approaches, we aim to equip researchers and drug development professionals with evidence-based insights for selecting the most appropriate platform for their specific preclinical applications.
Biological Foundations: ESCs vs. iPSCs
Origin and Characteristics
Embryonic Stem Cells (ESCs) are pluripotent cells derived from the inner cell mass of blastocysts. First isolated from mice in 1981 and humans in 1998, ESCs are characterized by their unlimited self-renewal capacity and ability to differentiate into all somatic cell types [1] [15]. Their pluripotency is governed by core transcription factors including OCT4, SOX2, and NANOG, which maintain the cells in an undifferentiated state while preserving their differentiation potential [1].
Induced Pluripotent Stem Cells (iPSCs) are reprogrammed somatic cells that acquire pluripotent characteristics similar to ESCs. The iPSC technology was pioneered by Shinya Yamanaka, who demonstrated in 2006 that mouse fibroblasts could be reprogrammed into pluripotent stem cells using four transcription factors: OCT4, SOX2, KLF4, and c-MYC (OSKM) [1]. A year later, human iPSCs were independently generated by Yamanaka using the same factors and by James Thomson using OCT4, SOX2, NANOG, and LIN28 [1]. The reprogramming process involves profound remodeling of the chromatin structure and epigenome, effectively reversing the developmental clock of somatic cells [1].
Key Technical Differences
The fundamental distinction between these platforms lies in their origin: ESCs are derived from embryos, while iPSCs are generated by reprogramming adult somatic cells. This difference has important implications for their research applications. ESCs represent a "naive" pluripotent state, while iPSCs may retain epigenetic memory of their somatic cell origin, potentially influencing their differentiation efficiency toward specific lineages [104]. Additionally, iPSC generation methods have evolved beyond the original viral vectors to include non-integrating methods, such as Sendai virus, episomal plasmids, and fully chemical reprogramming, addressing early safety concerns [1] [28].
Table 1: Fundamental Characteristics of ESCs and iPSCs
| Characteristic | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Cell Origin | Inner cell mass of blastocysts | Reprogrammed somatic cells (e.g., fibroblasts, blood cells) |
| Reprogramming Factors | Endogenous pluripotency network | Ectopic expression of OSKM or other factor combinations |
| Ethical Considerations | Involves embryo destruction | Ethically neutral |
| Genetic Background | Limited diversity | Can capture diverse genetic backgrounds, including patient-specific mutations |
| Immunological Compatibility | Allogeneic, potential immune rejection | Can be autologous, minimal immune rejection |
| Epigenetic Memory | None | May retain memory of tissue of origin |
| Tumorigenic Risk | Teratoma formation | Teratoma formation, potential insertional mutagenesis with viral methods |
Comparative Analysis: Application in Disease Modeling
Predictive Value for Clinical Outcomes
The predictive validity of stem cell models is paramount for their utility in preclinical drug discovery. Both ESC and iPSC platforms offer advantages over traditional cell lines and animal models by more accurately recapitulating human biology [60].
iPSCs demonstrate particular strength in patient-specific disease modeling. By deriving iPSCs from patients with genetic disorders, researchers can generate disease-relevant cell types that carry the complete genetic background of the condition being studied [1] [33]. This approach has been successfully applied to neurological disorders, cardiovascular diseases, and metabolic conditions, often revealing disease phenotypes not observable in animal models [1] [28]. For example, iPSC-derived neurons from Alzheimer's and Parkinson's patients have been used to model disease-specific phenotypes like tau aggregation and mitochondrial dysfunction, enabling compound screening that has identified neuroprotective agents [60].
ESC-derived models provide a standardized platform for disease modeling, particularly when combined with genome editing techniques. The isogenic background of ESCs facilitates the introduction of specific disease-associated mutations while maintaining consistent genetic context, strengthening causal inference in disease mechanism studies [33]. This approach has been valuable for modeling monogenic disorders and conducting controlled investigations of pathological mechanisms.
Functional Comparison in Directed Differentiation
Several studies have directly compared the differentiation potential and functionality of ESC-derived and iPSC-derived cells. While both platforms can generate the three germ layers, functional differences may emerge in specific lineages.
A 2014 study directly compared iPSC-derived mesenchymal stem cell-like cells (iMPCs) with their originating parental bone marrow stromal cells (BMSCs) [104]. The iMPCs exhibited typical MSC morphology and surface marker profiles and were capable of trilineage differentiation, but displayed unique gene expression patterns and were less responsive to traditional BMSC differentiation protocols compared to the parental BMSCs [104]. This suggests that while iPSC-derived cells can resemble their primary counterparts, functional equivalence cannot be assumed and must be validated for each application.
Table 2: Performance Comparison in Disease Modeling Applications
| Parameter | ESC-Derived Models | iPSC-Derived Models |
|---|---|---|
| Genetic Diversity | Limited | High, including patient-specific mutations |
| Differentiation Efficiency | Generally robust and consistent | Variable between lines and donors |
| Physiological Relevance | Human biology but limited disease relevance | Captures full genetic complexity of diseases |
| Reproducibility | High between batches | Moderate, requires careful quality control |
| Scalability for HTS | Excellent | Excellent once protocols are established |
| Regulatory Acceptance | Well-established in cardiotoxicity screening | Increasing acceptance, particularly in CiPA initiative |
| Modeling Complex Diseases | Limited to edited mutations | Strong for polygenic and sporadic diseases |
| Cost Considerations | Moderate | Higher due to reprogramming and validation |
Experimental Data and Case Studies
Neurological Disease Modeling
In neurodegenerative disease research, iPSC-derived neurons have demonstrated significant predictive value. Alzheimer's disease models using patient-derived neurons have recapitulated key pathological features including amyloid-beta accumulation and hyperphosphorylated tau, enabling screens for compounds that reduce pathological protein aggregation [60]. Similarly, iPSC-derived dopaminergic neurons from Parkinson's patients have been used to model disease-specific phenotypes and identify compounds that protect against mitochondrial dysfunction, a key disease mechanism [60].
ESC-derived neural progenitors provide a standardized platform for neurological disease modeling, particularly when genetically modified to carry specific mutations. This approach allows for controlled studies of mutation-specific effects while minimizing confounding genetic factors.
Cardiovascular Disease and Cardiotoxicity Screening
iPSC-derived cardiomyocytes have become a standard tool for cardiotoxicity screening, with regulatory acceptance through the Comprehensive in vitro Proarrhythmia Assay (CiPA) initiative [60]. These cells exhibit spontaneous contraction and express appropriate ion channels, enabling detection of drug-induced arrhythmias with human relevance [60]. Companies including Roche and Takeda have integrated iPSC-derived cardiomyocytes into their preclinical cardiac safety profiling pipelines [60].
ESC-derived cardiomyocytes show similar functional properties and have been used interchangeably with iPSC-derived cardiomyocytes for many applications. The choice between platforms often depends on specific project requirements regarding genetic background and scalability.
Metabolic Disease Modeling
In metabolic disease research, iPSC-derived hepatocyte-like cells have been used to model familial hypercholesterolemia and identify potential therapies [60]. A notable example includes a drug repurposing screen that identified cardiac glycosides as potential treatments for hypercholesterolemia based on their ability to reduce ApoB secretion in iPSC-derived hepatocytes [60]. Similarly, iPSC-derived insulin target cells (hepatocytes, skeletal muscle cells, adipocytes) are being applied to study insulin resistance in type 2 diabetes, enabling investigation of tissue-specific mechanisms and screening of insulin-sensitizing compounds [28].
Methodological Approaches: Protocols and Workflows
Experimental Workflow for iPSC-Based Disease Modeling
The following diagram illustrates the generalized workflow for establishing iPSC-based disease models, from somatic cell reprogramming to phenotypic analysis:
Signaling Pathways in Directed Differentiation
The differentiation of pluripotent stem cells toward specific lineages requires precise activation of developmental signaling pathways. The following diagram illustrates key pathways involved in definitive endoderm differentiation, a critical first step in generating liver, pancreatic, and other endodermal lineages:
Detailed Differentiation Protocol: iPSC to Hepatocytes
Stage 1: Definitive Endoderm Induction (Duration: 5 days)
- Basal Medium: RPMI 1640
- Key Factors: Activin A (100 ng/mL) to activate Nodal/TGF-β signaling
- Small Molecules: CHIR99021 (Wnt activator) to enhance endoderm commitment
- Supplement: Fetal Bovine Serum (0-2% gradient)
- Validation Markers: SOX17 and FOXA2 expression (≥80% positive cells) [28]
Stage 2: Hepatic Specification (Duration: 7-10 days)
- Basal Medium: Hepatocyte Culture Medium
- Key Factors: BMP4 (10-20 ng/mL) and FGF2 (10-20 ng/mL) to promote hepatic fate
- Supplement: HGF (10-20 ng/mL) for hepatoblast expansion
- Validation Markers: HNF4α and GATA4 expression [28]
Stage 3: Hepatic Maturation (Duration: 14-21 days)
- Basal Medium: Hepatocyte Culture Medium
- Key Factors: Oncostatin M (10-20 ng/mL) with Dexamethasone (0.1-1 μM) to promote functional maturation
- Validation Markers: Albumin secretion, CYP450 activity, glycogen storage [28]
Alternative protocols using fully defined small molecule cocktails have also been developed, replacing costly cytokines with small molecules like CHIR99021, dimethyl sulfoxide (DMSO), sodium butyrate, A83-01, and FPH1 to drive hepatocyte differentiation [28].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for Pluripotent Stem Cell Disease Modeling
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) | Somatic cell reprogramming | Lentiviral, Sendai virus, or mRNA methods available |
| Pluripotency Maintenance | mTeSR1, Essential 8 media | Maintain undifferentiated state | Feeder-free culture systems |
| Definitive Endoderm Induction | Activin A, CHIR99021, BMP4 | Direct differentiation toward endoderm | High Activin A concentrations (100 ng/mL) optimal |
| Hepatic Differentiation | HGF, FGF2, Oncostatin M, Dexamethasone | Hepatocyte specification and maturation | Synergistic action of HGF with other factors enhances maturation |
| Cardiac Differentiation | BMP4, Activin A, CHIR99021 | Cardiomyocyte differentiation | Protocol duration typically 12-14 days |
| Neural Differentiation | Dual-SMAD inhibition (Noggin, SB431542) | Neural induction | Can be combined with patterning factors for specific neuronal subtypes |
| Extracellular Matrix | Matrigel, Geltrex, Laminin-521 | Cell attachment and survival | Critical for single-cell passaging of pluripotent stem cells |
| Quality Control Assays | Flow cytometry for SSEA-4, TRA-1-60, Pluripotency markers | Characterize pluripotent state | Essential for validating new lines and differentiations |
| Functional Assay Kits | CYP450 activity, Albumin ELISA, Electrophysiology platforms | Assess differentiated cell function | Required for confirming physiological relevance |
Emerging Technologies and Future Directions
Advanced Modeling Approaches
The field is rapidly advancing beyond two-dimensional monocultures to more complex modeling systems. Organoid technologies enable the generation of 3D tissue structures that better recapitulate tissue architecture and cellular heterogeneity [33]. These systems have proven particularly valuable for modeling neurological disorders, congenital heart disease, polycystic kidney disease, and cancer [33]. Assembloids that combine multiple organoid types further enable modeling of inter-organ interactions, such as brain-muscle or brain-vascular connectivity [33].
Integration with Computational Approaches
In silico modeling of stem cell differentiation represents a promising approach to optimize protocols and reduce experimental costs. Mathematical models using differential equations have been developed to predict population dynamics during directed differentiation, with demonstrated ability to identify optimal differentiation timeframes and seeding densities [105]. For example, one model predicting iPSC differentiation to definitive endoderm achieved prediction errors of 26.4% and identified an optimal differentiation period of 1.9-2.4 days with plating densities near 300,000 cells per well [105].
The integration of artificial intelligence and machine learning with stem cell platforms is accelerating biomarker discovery and compound screening. AI-driven analysis of high-content imaging data from iPSC-based assays can identify subtle disease phenotypes and predict compound efficacy [106]. These approaches are particularly powerful when applied to large-scale iPSC cohorts that capture human genetic diversity.
The comparative analysis of ESCs and iPSCs reveals distinct advantages for specific applications in preclinical drug discovery. ESCs offer consistency and standardization for foundational studies and toxicity screening, while iPSCs provide unparalleled access to human genetic diversity and patient-specific disease mechanisms.
For most disease modeling applications, particularly those investigating complex polygenic disorders or requiring patient-specific contexts, iPSCs offer superior predictive value. Their ability to capture the complete genetic background of human diseases makes them invaluable for understanding disease mechanisms and identifying therapeutic candidates likely to succeed in clinical trials. However, this advantage must be balanced against their higher variability and more extensive validation requirements.
ESC-based models remain preferred for applications requiring high consistency and controlled genetic backgrounds, such as initial protocol development, mechanistic studies of specific pathways, and large-scale toxicity screening where genetic diversity may introduce confounding variables.
The future of preclinical drug discovery lies in strategic deployment of both platforms, leveraging their complementary strengths to build more predictive models of human disease. As both technologies continue to mature—with advances in differentiation protocols, organoid complexity, and computational integration—their collective impact on reducing clinical attrition rates and delivering effective therapies to patients will continue to grow.
Regulatory and Manufacturing Considerations for Clinical Translation
The clinical translation of pluripotent stem cell-based therapies presents a complex landscape of regulatory and manufacturing challenges. Within regenerative medicine, two primary cell sources—embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs)—offer distinct advantages and limitations for disease modeling and therapeutic development [14] [1]. ESCs, derived from the inner cell mass of blastocyst-stage embryos, represent the gold standard for pluripotency but involve ethical controversies and allogeneic immune rejection concerns [14] [32]. In contrast, iPSCs, generated by reprogramming adult somatic cells, provide opportunities for patient-specific autologous therapies while circumventing ethical barriers associated with embryo destruction [2] [1] [32]. This review systematically compares the regulatory pathways and manufacturing considerations critical for the successful clinical translation of both platforms, focusing on their implications for researchers, scientists, and drug development professionals.
Regulatory Frameworks for Stem Cell-Based Products
United States Food and Drug Administration (FDA) Oversight
In the United States, the FDA regulates stem cell-based products as biological products subject to strict Current Good Manufacturing Practice (CGMP) regulations [107] [108] [32]. The regulatory pathway depends on the nature and manipulation of the cells. Human cells, tissues, and cellular and tissue-based products (HCT/Ps) that are minimally manipulated, intended for homologous use, and not combined with another article (except water, crystalloids, or sterilizing/preserving agents) are regulated primarily under Section 361 of the Public Health Service Act and 21 CFR Part 1271 [32]. However, most ESC and iPSC-derived products undergo more than minimal manipulation and are intended for non-homologous use, thus qualifying as drugs or biologics requiring rigorous FDA oversight [32].
These advanced therapy products require an Investigational New Drug (IND) application before initiating clinical trials, followed by a Biologics License Application (BLA) for market approval [29] [32]. The FDA's CGMP regulations for drugs are detailed in Title 21 of the Code of Federal Regulations (CFR), encompassing parts 210 and 211 for finished pharmaceuticals, and part 600 for biological products [107] [108]. These regulations establish minimum requirements for methods, facilities, and controls used in manufacturing, processing, and packing to ensure product safety, identity, strength, quality, and purity [107].
Table 1: Key FDA Regulations for Stem Cell-Based Products
| CFR Part | Scope | Key Requirements |
|---|---|---|
| 21 CFR 210 | Current Good Manufacturing Practice in Manufacturing, Processing, Packing, or Holding of Drugs | General CGMP requirements for drug manufacturing |
| 21 CFR 211 | Current Good Manufacturing Practice for Finished Pharmaceuticals | Detailed requirements for organization, facilities, equipment, components, production controls, packaging, labeling, and distribution |
| 21 CFR 600 | Biological Products: General | Additional establishment standards for biological products including personnel, equipment, records, and reporting |
| 21 CFR 1271 | Human Cells, Tissues, and Cellular and Tissue-Based Products (HCT/Ps) | Regulatory framework for HCT/Ps, including donor eligibility, current good tissue practice, and application of regulations |
Special Regulatory Designations and Pathways
The FDA offers several expedited programs to facilitate the development of regenerative medicine therapies. The Regenerative Medicine Advanced Therapy (RMAT) designation, established under the 21st Century Cures Act, provides intensive FDA guidance throughout drug development and potential accelerated approval [29] [32]. Additional designations like Fast Track further support the efficient advancement of promising stem cell therapies [29]. As of 2025, the FDA has granted RMAT designation to several iPSC-derived products, including FT819, an off-the-shelf CAR T-cell therapy for systemic lupus erythematosus [29].
The regulatory landscape continues to evolve with increasing numbers of pluripotent stem cell clinical trials. Globally, over 115 clinical trials involving 83 distinct pluripotent stem cell-derived products have been documented, targeting indications in ophthalmology, neurology, and oncology [29]. More than 1,200 patients have been dosed with significant cell quantities (over 10¹¹ cells), with no class-wide safety concerns reported to date [29].
Figure 1: FDA Regulatory Pathway Decision Tree for Stem Cell-Based Products
Manufacturing Considerations for Clinical Translation
CGMP Compliance and Quality Systems
Strict adherence to CGMP regulations is fundamental for manufacturing stem cell-based products for clinical use. CGMP encompasses all aspects of production, including organization and personnel qualifications, facility and equipment design and maintenance, control of components and containers, production and process controls, packaging and labeling, laboratory controls, and comprehensive records and reports [107] [108]. These requirements ensure that products are consistently produced and controlled according to quality standards appropriate for their intended use [107].
For pluripotent stem cell products, maintaining genomic stability during reprogramming and long-term culture presents a particular challenge [2]. Small fluctuations in culture conditions can trigger spontaneous differentiation or loss of stem cell properties, significantly limiting downstream applications [2]. Rigorous quality control measures are essential, including regular assessment of pluripotency markers (e.g., Oct4, Nanog) via PCR, immunocytochemistry, or flow cytometry, and evaluation of genomic integrity to detect chromosomal abnormalities or epigenetic alterations that may compromise differentiation efficiency or predispose cells to malignant transformation [2].
iPSC-Specific Manufacturing Challenges
iPSC culture remains technically demanding, requiring tightly controlled microenvironmental conditions to maintain viability and pluripotency [2]. Early culture protocols employed feeder layers of mitotically inactivated mouse embryonic fibroblasts, but feeder-free systems using extracellular matrix coatings (e.g., Matrigel or recombinant human laminin) are increasingly preferred to enhance reproducibility and minimize xenogeneic contamination [2]. Chemically defined media formulations such as mTeSR1 or E8, supplemented with essential growth factors (e.g., FGF2) and differentiation pathway inhibitors (e.g., TGF-β/activin A), enable greater standardization for clinical applications [2].
The reprogramming process itself introduces manufacturing challenges. While early approaches relied on integrating viral vectors (retroviruses/lentiviruses) with associated tumorigenesis risks, integration-free methods have been developed including episomal DNA vectors, synthetic mRNA, recombinant protein delivery, and Sendai virus-based systems [2]. Although less efficient, these strategies significantly enhance biosafety profiles for clinical products [2].
Table 2: Comparison of Key Reprogramming Methods for iPSC Generation
| Reprogramming Method | Mechanism | Efficiency | Genomic Integration | Clinical Applicability |
|---|---|---|---|---|
| Retroviral/Lentiviral Vectors | Integration of reprogramming factors | High | Yes | Limited due to insertional mutagenesis risk |
| Sendai Virus | RNA-based viral vector | High | No | Suitable with careful clearance validation |
| Episomal Vectors | Non-viral plasmid DNA | Moderate | No | High suitability with transient expression |
| Synthetic mRNA | Direct delivery of reprogramming mRNAs | Moderate | No | High suitability with precise control |
| Recombinant Proteins | Direct protein transduction | Low | No | High suitability with technical challenges |
Comparative Analysis in Disease Modeling Research
Functional and Molecular Equivalence
While iPSCs and ESCs share fundamental properties of self-renewal and pluripotency, accumulating evidence reveals important functional and molecular differences that impact their utility in disease modeling and therapeutic applications [14]. Both cell types exhibit similar morphology, feeder dependence, surface marker expression, and in vivo teratoma formation capacity [14]. However, reports describe variability in the in vitro differentiation propensity of iPSCs compared to ESCs, with reduced and more variable yields of neural, cardiovascular, and hemangioblastic lineages [14].
Gene expression analyses reveal that although global profiles of iPSCs and ESCs are largely similar, subtle but consistent differences exist [14]. Some variations appear related to epigenetic memory—persisting epigenetic marks from the somatic cell type of origin that continue to affect gene expression in the resulting iPSCs [14]. This memory has been demonstrated in iPSCs derived from fibroblasts, adipose tissue, and keratinocytes, though continuous passaging or treatment with chromatin-modifying drugs appears to abrogate these transcriptional differences [14]. Additionally, comparisons of DNA methylomes have identified differentially methylated regions, with approximately 45% attributable to failure to fully reprogram the somatic cell epigenome (epigenetic memory), while 55% represent iPSC-specific aberrant methylation patterns not found in the somatic cell origin or ESCs [14].
Lineage-Specific Differentiation Efficacy
The functional implications of molecular differences between ESCs and iPSCs become apparent in lineage-specific differentiation protocols. For example, in a study comparing osteogenic differentiation potential, bone marrow-derived mesenchymal stem cells (MSCs) demonstrated significantly higher expression of osteogenic markers (osteocalcin and osteopontin) compared to iPSCs, despite iPSCs showing higher expression of core pluripotency factors Oct4 and c-Myc [109]. This suggests that factors beyond core pluripotency network expression influence differentiation efficiency.
Advancements in differentiation protocols have improved functional outcomes for both cell types. Three-dimensional culture systems and co-culture approaches enhance maturation of iPSC-derived cells, which frequently exhibit immature, fetal-like phenotypes upon initial differentiation [110]. For example, when iPSC-derived cardiomyocytes are co-cultured with iPSC-derived cardiac fibroblasts in 2D micropatterned extracellular matrix environments, they demonstrate significantly improved contractile function compared to monocultures [110]. Similarly, combining 3D hydrogel culture with endothelial cell co-culture further enhances cardiomyocyte maturation markers and reduces oxidative stress [110].
Figure 2: Comparative Workflow for ESC and iPSC Differentiation into Functional Cell Types
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Pluripotent Stem Cell Research
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM); NANOG, LIN28 | Key transcription factors for somatic cell reprogramming to pluripotency [2] [1] |
| Culture Media | mTeSR1, E8 medium | Chemically defined, xeno-free media for maintenance of pluripotent stem cells [2] |
| Culture Substrates | Matrigel, recombinant laminin-521 | Feeder-free extracellular matrix coatings for pluripotent stem cell attachment and growth [2] |
| Differentiation Factors | FGF2, TGF-β/activin A, BMP4, retinoic acid | Growth factors and small molecules directing differentiation toward specific lineages [2] [110] |
| Quality Control Assays | PCR/RT-PCR, immunocytochemistry, flow cytometry, karyotyping | Assessment of pluripotency markers, differentiation efficiency, and genomic integrity [2] [109] |
| Gene Editing Tools | CRISPR-Cas9, TALENs, ZFNs | Genetic modification of stem cells for disease modeling or therapeutic enhancement [2] |
The clinical translation of both ESCs and iPSCs requires navigating complex regulatory pathways and addressing significant manufacturing challenges. While iPSCs offer distinct advantages in circumventing ethical concerns and enabling patient-specific autologous therapies, they present unique manufacturing hurdles related to reprogramming efficiency, genomic stability, and functional maturation. ESCs remain an important reference standard and therapeutic platform, particularly for allogeneic applications. Regulatory frameworks continue to evolve alongside scientific advancements, with the FDA providing structured pathways through CGMP regulations, IND requirements, and expedited programs like RMAT. For researchers and drug development professionals, successful translation will depend on rigorous attention to quality systems, comprehensive characterization of cell products, and strategic regulatory planning that acknowledges both the similarities and distinct considerations for these powerful pluripotent stem cell platforms.
The advent of pluripotent stem cell technologies has revolutionized biomedical research, providing unprecedented opportunities for in vitro disease modeling, drug screening, and therapeutic development. Two principal platforms dominate this landscape: embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs). ESCs, first isolated from human embryos in 1998, represent the gold standard for pluripotency but are entangled with ethical considerations regarding embryo destruction [1] [111]. In contrast, iPSCs, first generated in 2006 by Shinya Yamanaka's team through somatic cell reprogramming, offer a genetically programmable alternative that circumvents these ethical concerns [1] [2]. This guide provides an objective comparison of these platforms' efficacy in disease modeling research, presenting a structured framework to aid researchers, scientists, and drug development professionals in selecting the optimal system for their specific investigative needs.
The core distinction between these technologies lies in their origins: ESCs are derived from the inner cell mass of blastocysts, while iPSCs are generated by reprogramming adult somatic cells through the introduction of specific transcription factors, most commonly Oct4, Sox2, Klf4, and c-Myc (OSKM) [1] [2]. Both cell types possess the defining characteristics of pluripotency—the ability to differentiate into derivatives of all three germ layers and virtually unlimited self-renewal capacity [2] [111]. However, as this analysis will demonstrate, significant differences in genetic stability, epigenetic memory, disease relevance, and regulatory considerations create a complex decision matrix for researchers.
Technical Comparison of Platform Characteristics
Fundamental Biological Properties
The biological properties of ESCs and iPSCs directly influence their suitability for specific research applications. The following table provides a systematic comparison of their core characteristics.
Table 1: Comparative Biological Properties of ESCs and iPSCs
| Characteristic | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Origin | Inner cell mass of blastocyst [1] | Reprogrammed somatic cells (e.g., fibroblasts, blood cells) [2] |
| Reprogramming Method | Natural embryonic development | Viral (retroviral/lentiviral) or non-viral (episomal, mRNA, Sendai virus) delivery of transcription factors [2] |
| Key Pluripotency Factors | Endogenous expression of pluripotency network | Ectopic expression of OSKM (Oct4, Sox2, Klf4, c-Myc) or alternative combinations [1] [2] |
| Genetic Background | Wild-type (unless genetically modified) | Can carry patient-specific disease-associated mutations [112] [2] |
| Ethical Considerations | Controversial due to embryo destruction [111] | Minimal ethical concerns [112] [111] |
| Immunological Compatibility | Allogeneic - potential immune rejection [112] | Potential for autologous transplantation [2] |
Experimental Performance Metrics
When evaluated for disease modeling applications, each platform demonstrates distinct strengths and limitations across key performance metrics essential for rigorous scientific research.
Table 2: Experimental Performance Metrics for Disease Modeling
| Performance Metric | ESCs | iPSCs |
|---|---|---|
| Differentiation Efficiency | Consistent, well-established protocols [111] | Variable, influenced by epigenetic memory and cell source [111] |
| Genetic Stability | High karyotypic stability [111] | Prone to genomic alterations during reprogramming [2] |
| Tumorigenic Risk | Teratoma formation in vivo (pluripotency marker) | Potential for enhanced tumorigenicity with c-Myc [111] |
| Disease Relevance | Limited to genetically modified models | Native disease-associated genotypes without genetic manipulation [2] |
| Inter-Donor Variability | Low | High - reflects genetic diversity of source population [16] |
| Protocol Standardization | Highly standardized culture systems [111] | Evolving toward standardization [2] |
Experimental Methodologies for Platform Evaluation
Core Protocols for Pluripotency Induction and Validation
iPSC Generation Protocol
The standard methodology for iPSC generation involves a multi-step reprogramming process of somatic cells [2]:
Somatic Cell Isolation and Culture: Obtain donor cells through minimally invasive procedures. Common sources include:
- Skin fibroblasts: Obtained via punch biopsy (3-4mm), cultured in DMEM with 10% FBS [2].
- Peripheral blood mononuclear cells (PBMCs): Isolated from blood samples using Ficoll density gradient centrifugation [2].
- Urinary epithelial cells: Collected from urine samples, a completely non-invasive method [2]. Culture cells until sufficient expansion (typically 2-3 weeks).
Reprogramming Factor Delivery: Introduce pluripotency factors using various methods:
- Viral Integration Methods: Use retroviral or lentiviral vectors encoding OSKM factors. High efficiency but risk of insertional mutagenesis [2].
- Integration-Free Methods:
- Episomal plasmids: DNA vectors that replicate independently of host genome [112] [2].
- Sendai virus: RNA-based virus that does not integrate into host genome [2].
- Synthetic mRNA: Daily transfection of in vitro transcribed mRNA encoding reprogramming factors [112] [2].
- Recombinant proteins: Protein-based delivery avoiding genetic material [112].
iPSC Colony Selection and Expansion: Between days 21-30 post-reprogramming, manually pick colonies with compact, ESC-like morphology using sterile techniques. Transfer to feeder layers (mouse embryonic fibroblasts) or feeder-free systems (Matrigel, laminin-521) [2]. Maintain in defined culture media such as mTeSR1 or E8 medium [2].
ESC Derivation and Culture Protocol
The established methodology for ESC derivation and maintenance [1] [111]:
Blastocyst Acquisition: Obtain donated embryos from IVF clinics with informed consent under IRB oversight.
Inner Cell Mass Isolation: Using immunosurgery or mechanical dissection, isolate the inner cell mass from the blastocyst (typically day 5-6 post-fertilization).
Plating and Initial Outgrowth: Plate the intact inner cell mass on feeder layers of mitotically inactivated mouse embryonic fibroblasts or human feeders in specialized hESC medium containing FGF2.
Colony Expansion and Passaging: After 5-7 days, mechanically dissect or enzymatically treat (collagenase/dispase) the outgrowth to generate smaller clumps for passage. Maintain cultures through repeated passaging every 5-7 days.
Cryopreservation: Use slow-freezing protocols with cryoprotectants (10% DMSO) for long-term storage [2].
Pluripotency Validation Assays
Both ESCs and iPSCs must undergo rigorous quality control to confirm pluripotent status [2]:
Molecular Characterization:
- Immunocytochemistry: Detect pluripotency proteins (Oct4, Nanog, SSEA-4, TRA-1-60, TRA-1-81).
- RT-PCR/qPCR: Analyze expression of endogenous pluripotency genes (OCT4, SOX2, NANOG).
- Flow Cytometry: Quantify percentage of cells expressing pluripotency markers.
Functional Pluripotency Assays:
- In Vitro Differentiation: Form embryoid bodies in suspension culture, then assess differentiation into three germ layers via immunostaining for β-tubulin III (ectoderm), α-smooth muscle actin (mesoderm), and α-fetoprotein (endoderm) [2].
- In Vivo Teratoma Formation: Inject 1-5 million cells into immunodeficient mice (NSG or SCID strains). Harvest tumors after 8-12 weeks, section, and stain for tissues representing all three germ layers [2].
Genomic Integrity Assessment:
- Karyotyping: Perform G-banding chromosome analysis at passage 5 and every 10 passages thereafter.
- CNV Analysis: Use SNP arrays or next-generation sequencing to detect copy number variations.
Disease Modeling Workflows
The application of pluripotent stem cells to disease modeling follows a structured pathway from cell line establishment to phenotypic analysis, with variations depending on the specific disease context.
Figure 1: Disease Modeling Workflow Comparison
Application-Specific Efficacy Analysis
Disease Modeling Capabilities Across Tissue Types
The relative performance of ESCs and iPSCs varies significantly across different disease modeling contexts, with each platform offering distinct advantages depending on the research objectives.
Table 3: Disease Modeling Applications and Platform Performance
| Disease Category | ESC-Based Models | iPSC-Based Models | Key Advantages of iPSCs |
|---|---|---|---|
| Neurological Disorders (Alzheimer's, Parkinson's, ALS) [112] [2] | Genetically modified lines | Patient-specific neurons and glia | Native genetic background reveals sporadic disease mechanisms [2] |
| Cardiovascular Diseases (Arrhythmias, cardiomyopathy) [112] [2] | Directed differentiation to cardiomyocytes | Patient-specific cardiomyocytes with disease mutations | Model congenital disorders like long QT syndrome [112] |
| Metabolic Disorders (Cystic fibrosis, Duchenne muscular dystrophy) [2] | Limited disease relevance | Airway epithelia, myocytes with native CFTR/dystrophin mutations | Preserve patient genotype for drug testing [2] |
| Autoimmune Diseases (Lupus, type 1 diabetes) [2] | Limited immune component modeling | Patient-specific immune cells and target tissues | Recapitulate immune dysfunction in native context [2] |
| Rare Genetic Disorders | Require genetic modification | Native mutation context without engineering | Access to diverse genetic backgrounds [2] |
Drug Screening and Toxicity Testing Applications
In pharmaceutical development, both platforms serve critical roles in compound screening and safety assessment, though with different implementation considerations.
Table 4: Drug Screening Applications
| Application | ESC Platform | iPSC Platform | Implementation Considerations |
|---|---|---|---|
| High-Throughput Compound Screening | Consistent genetic background reduces variability | Patient-specific lines enable personalized medicine approaches | ESC consistency advantageous for initial screens; iPSCs valuable for population-wide response assessment |
| Cardiotoxicity Testing | Standardized cardiomyocyte differentiation | Patient-specific cardiomyocytes with genetic diversity | iPSCs may better predict population-level adverse events [112] |
| Neurotoxicity Assessment | Reproducible neuronal differentiation | Disease-specific neurons (e.g., Parkinson's, ALS) | iPSCs enable disease-specific vulnerability testing [2] |
| Metabolic Toxicity | Hepatocyte differentiation possible | Patient-specific hepatocytes with native metabolic profiles | iPSCs better model polymorphic drug metabolism [2] |
| Preclinical Efficacy Testing | Isogenic controls possible via genetic engineering | Native human genetic diversity incorporated | iPSCs may improve translational predictability [112] |
Research Reagent Solutions Toolkit
Successful implementation of ESC or iPSC-based disease models requires specific reagents and materials optimized for each platform. The following table details essential components of the research toolkit.
Table 5: Essential Research Reagents for Pluripotent Stem Cell Disease Modeling
| Reagent Category | Specific Examples | Function | Platform-Specific Considerations |
|---|---|---|---|
| Reprogramming Factors | OSKM transcription factors (Oct4, Sox2, Klf4, c-Myc) [1] [2] | Induce pluripotency in somatic cells | iPSC-specific; delivery method (viral, mRNA, protein) affects safety profile [2] |
| Culture Matrices | Matrigel, laminin-521, vitronectin [2] | Provide substrate for pluripotent cell attachment and growth | Critical for feeder-free culture of both ESCs and iPSCs |
| Defined Culture Media | mTeSR1, Essential 8 (E8) medium [2] | Support pluripotent state maintenance | Both platforms benefit from defined, xeno-free formulations |
| Differentiation Kits | Commercial cardiomyocyte, neuronal differentiation kits | Direct differentiation to specific lineages | Both platforms use similar differentiation principles |
| Pluripotency Markers | Antibodies against Oct4, Nanog, SSEA-4, TRA-1-60 | Validate pluripotent status | Quality control for both ESCs and iPSCs [2] |
| Genomic Stability Assays | Karyotyping, CNV analysis by SNP sequencing [2] | Monitor genetic integrity | Particularly critical for iPSCs due to reprogramming-associated instability |
| Cell Sourcing Reagents | Fibroblast culture media, Ficoll for PBMC isolation [2] | Obtain and expand somatic cells | iPSC-specific initial requirements |
Decision Framework for Platform Selection
The choice between ESC and iPSC platforms depends on multiple factors related to the specific research goals, technical capabilities, and regulatory considerations. The following diagram outlines key decision points in platform selection.
Figure 2: Platform Selection Decision Framework
Integrated Assessment Matrix
To further guide researchers in platform selection, the following matrix synthesizes key decision criteria with corresponding platform recommendations.
Table 6: Platform Selection Decision Matrix
| Decision Factor | ESC Recommendation | iPSC Recommendation | Rationale |
|---|---|---|---|
| Genetic Disease Modeling | Limited application | Strong preference | Native disease context without genetic engineering [2] |
| High-Throughput Screening | Preferred for initial screens | Secondary validation | Reduced variability improves statistical power [112] |
| Personalized Medicine Applications | Not applicable | Exclusive capability | Autologous models enable patient-specific predictions [2] |
| Ethical Restrictions | Problematic | Preferred solution | Avoids embryo destruction concerns [112] [111] |
| Technical Expertise | Established protocols | Requires specialized reprogramming skills | iPSC generation remains technically demanding [2] |
| Regulatory Pathway | Established but ethically complicated | Evolving regulatory framework | Varies by jurisdiction; EU more restrictive, US more flexible [16] |
| Budget Constraints | Lower per-line costs | Higher initial development costs | iPSC generation requires significant investment [111] |
| Immune Compatibility Needs | Allogeneic - immune mismatch | Potential for autologous | iPSCs enable immunologically matched models [2] |
The comparative analysis presented in this framework demonstrates that both ESC and iPSC platforms offer distinct advantages for disease modeling research, with the optimal choice being highly context-dependent. ESCs provide methodological consistency and avoid reprogramming-associated artifacts, making them valuable for fundamental biology studies and initial drug screening applications where genetic uniformity is advantageous. In contrast, iPSCs offer unparalleled access to native human genetic diversity and disease-specific contexts, enabling patient-specific modeling and personalized medicine approaches that were previously impossible.
For research groups establishing new disease modeling programs, a hybrid strategy often provides the most robust approach: utilizing ESCs for protocol development and initial standardization, while incorporating iPSCs for disease-specific investigations and translational applications. As the field advances, ongoing efforts to address iPSC limitations—including reprogramming efficiency, epigenetic memory, and genomic instability—continue to enhance their reliability and expand their applications [2] [111]. Similarly, emerging technologies such as gene editing in ESCs and organoid development from both platforms present new opportunities for increasingly sophisticated disease models [111].
Ultimately, the strategic selection between ESC and iPSC platforms should align with the specific research objectives, technical capabilities, ethical considerations, and translational goals of each project. By applying the decision framework presented herein, researchers can systematically evaluate these critical factors to implement the most appropriate platform for their specific disease modeling requirements.
Conclusion
The comparative analysis reveals that both ESCs and iPSCs are powerful, yet distinct, tools for disease modeling. ESCs remain a gold standard for pluripotency, while iPSCs offer an ethically uncontested and patient-specific platform. The choice between them involves a critical trade-off: ESCs provide a robust, well-characterized system, whereas iPSCs enable personalized disease modeling but face challenges related to genomic stability and functional maturation. Future progress hinges on overcoming these technical bottlenecks through improved reprogramming and differentiation protocols, the development of complex organoid and assembloid systems, and the establishment of universal biobanks. A synergistic, rather than competing, application of both platforms, guided by the specific research question, will most effectively accelerate drug discovery and pave the way for safe, effective regenerative therapies.
References
- 1. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 2. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590075/]
- 3. Comparing ESC and iPSC—Based Models for Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4470175/]
- 4. Are embryonic stem cells and artificial stem cells equivalent? [https://www.hsci.harvard.edu/news/are-embryonic-stem-cells-and-artificial-stem-cells-equivalent]
- 5. A comprehensive analysis of induced pluripotent stem cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1593207/full]
- 6. Two sides of the same coin? Unraveling subtle differences ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-017-0720-1]
- 7. Embryonic stem cell and induced pluripotent stem cell [https://www.nature.com/articles/cr2012175]
- 8. Proteomic and functional comparison between human ... [https://elifesciences.org/reviewed-preprints/92025v1/pdf]
- 9. Transition of inner cell mass to embryonic stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC11105545/]
- 10. A closer look at Embryonic Stem Cells (ESCs) – biological ... [https://www.ptglab.com/news/blog/a-closer-look-at-embryonic-stem-cells-escs-biological-concepts/?srsltid=AfmBOor-kr3Xw_CCIuvkPwq10IDqUa71Fk8Sr9OGU82l-7JIgok4SxhN]
- 11. Efficient isolation inner cell mass from blastocysts by ... [https://www.nature.com/articles/cr2008129]
- 12. Induced Pluripotent Stem Cell (iPSC) Industry Trends for ... [https://bioinformant.com/ipsc-industry-trends/]
- 13. Epigenetic-scale comparison of human iPSCs generated ... [https://www.sciencedirect.com/science/article/pii/S2352320418300324]
- 14. Comparison of Human Induced Pluripotent and Embryonic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3070108/]
- 15. recent developments and future prospects in stem-cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634165/]
- 16. focusing on induced pluripotent stem cell (iPSC)-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11583560/]
- 17. Experts explore the future of iPSC-based cell therapies [https://regmedfoundation.org/2025/03/03/experts-explore-the-future-of-ipsc-based-cell-therapies/]
- 18. Global research dynamics in the induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12272591/]
- 19. Smarter stem cells: how AI is supercharging iPSC technology [https://link.springer.com/article/10.1007/s00441-025-03999-7]
- 20. Comparing ESC and iPSC—Based Models for Human ... [https://www.mdpi.com/2077-0383/3/4/1146]
- 21. Patient and Disease–Specific Induced Pluripotent Stem ... [https://www.sciencedirect.com/science/article/pii/S0031699724009451]
- 22. A Roadmap for Human Liver Differentiation from Pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5854481/]
- 23. Natural vs. Induced Pluripotent Stem Cell Therapies [https://esmed.org/natural-vs-induced-pluripotent-stem-cell-therapies/]
- 24. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 25. iPSCs and iPSC-derived cells as a model of human ... [https://www.nature.com/articles/s41467-025-56569-4]
- 26. The rebirth of iPSCs: Towards a healthier epigenetic ... [https://www.sciencedirect.com/science/article/pii/S2352304214000142]
- 27. Longitudinal analysis of genetic and epigenetic changes in ... [https://www.nature.com/articles/s12276-024-01334-8]
- 28. Human-Induced Pluripotent Stem Cells (iPSCs) for ... [https://www.mdpi.com/2073-4409/14/15/1188]
- 29. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 30. Types of Stem Cells: Explained (2025) [https://www.dvcstem.com/post/different-types-of-stem-cells-and-their-functions]
- 31. Stem Cell Research Controversy: A Deep Dive (2025) [https://www.dvcstem.com/post/stem-cell-research-controversy]
- 32. Ethical and Regulatory Considerations Related to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398464/]
- 33. Human Stem Cells in Disease Modelling and Treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467989/]
- 34. The ISSCR Launches Consortium to Support Adoption of ... [https://www.isscr.org/isscr-news/isscr-launches-consortium-to-support-adoption-of-stem-cell-derived-disease-models-for-drug-discovery-and-development]
- 35. Induced Pluripotent Stem Cells: Problems and Advantages ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3347549/]
- 36. All Roads Lead to Induced Pluripotent Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC4046204/]
- 37. Viral vector platforms within the gene therapy landscape [https://www.nature.com/articles/s41392-021-00487-6]
- 38. Reprogramming methods compared [https://www.nature.com/articles/nmeth.3265]
- 39. The emerging promise of induced pluripotent stem cells in ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925008461]
- 40. Comparative Analysis of Targeted Differentiation of Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3659749/]
- 41. Clever Experimental Designs: Shortcuts for Better iPSC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8700474/]
- 42. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 43. Human organoids: model systems for human biology and ... [https://www.nature.com/articles/s41580-020-0259-3]
- 44. Organoids: modelling organ development and disease in 3D [https://www.embl.org/about/info/course-and-conference-office/events/ees25-10/]
- 45. Recent progress on the organoids: Techniques ... [https://www.sciencedirect.com/science/article/pii/S0753332225001362]
- 46. Stem cells and organoids for disease-modeling and drug ... [https://sites.psu.edu/stemcellhershey/2025/05/19/stem-cell-and-organoids-for-disease-modeling-and-drug-development/]
- 47. Three-dimensional midbrain organoids: a next-generation tool ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04660-4]
- 48. hiPSC disease modeling with 3D organoids [https://www.sciencedirect.com/science/article/abs/pii/B9780323998925000219]
- 49. From iPSC to in vivo: Build more predictive disease models [https://lab-a-porter.com/2025/11/from-ipsc-to-in-vivo-build-more-predictive-disease-models/]
- 50. Disease modeling using induced pluripotent stem cells ... [https://www.uu.se/en/department/immunology-genetics-and-pathology/study/student-project/disease-modeling-using-induced-pluripotent-stem-cells-ipsc-and-organoids-for-future-drug-development]
- 51. Current Challenges of iPSC-Based Disease Modeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6562607/]
- 52. Embryonic stem cells or induced pluripotent ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3947934/]
- 53. Current Development of iPSC-Based Modeling in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027653/]
- 54. Large-scale drug screening in iPSC-derived motor neurons ... [https://www.nature.com/articles/s41593-025-02118-7]
- 55. Stem Cell Clinical Trials and Promise of Engineered Exosomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409071/]
- 56. Induced pluripotent stem cell-based modelling of disease ... [https://www.sciencedirect.com/science/article/abs/pii/S2212492625000466]
- 57. The march of pluripotent stem cells in cardiovascular ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-018-0947-5]
- 58. Comparison of cardiomyogenic potential among human ESC ... [https://pubmed.ncbi.nlm.nih.gov/22863088/]
- 59. Systematic analysis of different pluripotent stem cell ... [https://www.sciencedirect.com/science/article/pii/S1537189120302561]
- 60. Stem cell disease modeling: A new era for drug discovery [https://www.abcam.com/en-us/stories/articles/stem-cell-disease-modeling]
- 61. iPSC-based Platforms Market 2025 Report and Trends [https://www.towardshealthcare.com/insights/ipsc-based-platforms-market-sizing]
- 62. Review Pluripotent stem-cell-derived therapies in clinical trial [https://www.sciencedirect.com/science/article/pii/S1934590924004454]
- 63. Trends & Strategies Shaping the $4.6+ Billion Induced ... [https://finance.yahoo.com/news/trends-strategies-shaping-4-6-145400149.html]
- 64. Human Induced Pluripotent Stem Cells: From Cell Origin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9216482/]
- 65. Genomic Instability of iPSCs: Challenges Towards Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5346115/]
- 66. Epigenetic memory in induced pluripotent stem cells [https://www.nature.com/articles/nature09342]
- 67. ZSCAN10 expression corrects the genomic instability of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5843481/]
- 68. Epigenetic memory in induced pluripotent stem cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3150836/]
- 69. Their Role in iPSC Reprogramming and Differentiation [https://www.reprocell.com/blog/epigenetic-modifications-their-role-in-ipsc-reprogramming-and-differentiation]
- 70. Incomplete reprogramming of DNA replication timing in ... [https://www.sciencedirect.com/science/article/pii/S2211124723016753]
- 71. Evaluating teratoma formation risk of pluripotent stem cell- ... [https://www.sciencedirect.com/science/article/pii/S146532492500684X]
- 72. Prevention of tumor risk associated with the reprogramming of ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-020-01584-0]
- 73. Human Induced Pluripotent Stem Cells Develop Teratoma More Efficiently and Faster Than Human Embryonic Stem Cells Regardless the Site of Injection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2996086/]
- 74. Teratoma Formation Assay for Assessing Pluripotency and Tumorigenicity of Pluripotent Stem Cells - PubMed [https://pubmed.ncbi.nlm.nih.gov/34541178/]
- 75. Pluripotent Stem Cells: Recent Advances and Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025069/]
- 76. Comparison of Teratoma Formation between Embryonic Stem Cells and Parthenogenetic Embryonic Stem Cells by Molecular Imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5889892/]
- 77. Preventing Pluripotent Cell Teratoma in Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5442801/]
- 78. Stem cell therapy: a revolutionary cure or a pandora's box - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12096755/]
- 79. Functional genomics and the future of iPSCs in disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9133703/]
- 80. Functional Modules Distinguish Human Induced Pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3202894/]
- 81. Comparison of defined culture systems for feeder cell free ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2855804/]
- 82. A Comparative Study of Protocols for Mouse Embryonic Stem ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0081156]
- 83. Induced pluripotent stem - Wikipedia cell [https://en.wikipedia.org/wiki/Induced_pluripotent_stem_cell]
- 84. Advantages and difficulties in culturing human pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2899013/]
- 85. Induced pluripotent stem : An overview | Abcam cells [https://www.abcam.com/en-us/knowledge-center/stem-cells/induced-pluripotent-stem-cells]
- 86. Experts explore the future of iPSC-based cell therapies [https://www.drugtargetreview.com/article/156139/experts-explore-the-future-of-ipsc-based-cell-therapies/]
- 87. Exploring the promising potential of induced pluripotent ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01873-0]
- 88. Development of Scalable Culture Systems for Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2821101/]
- 89. Scalable expansion of iPSC and their derivatives across ... [https://pubmed.ncbi.nlm.nih.gov/35595152/]
- 90. Modeling human diseases with induced pluripotent stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC5868991/]
- 91. Modeling mutation-specific arrhythmogenic phenotypes in ... [https://www.nature.com/articles/s41598-024-52871-1]
- 92. Patient-Derived Organoids Recapitulate Pathological ... [https://pubmed.ncbi.nlm.nih.gov/38727265/]
- 93. The Efficiency of Stem Cells (SCs) Differentiation into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9851781/]
- 94. Early and non-destructive prediction of the differentiation ... [https://www.nature.com/articles/s41598-025-11108-5]
- 95. Purity Assessment by Flow Cytometry for Lineage-Specific ... [https://www.stemcell.com/purity-assessment-by-flow-cytometry-lineage-specific-chimerism-analysis-lp.html]
- 96. Assessment of the purity of isolated cell populations for ... [https://pubmed.ncbi.nlm.nih.gov/24461006/]
- 97. The Immunogenicity and Immune Tolerance of Pluripotent ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2017.00645/full]
- 98. Addressing the challenges of immunogenicity ... [https://pubmed.ncbi.nlm.nih.gov/41291912/]
- 99. Induced pluripotent stem cells have similar immunogenic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4352342/]
- 100. Immunogenicity of autologous and allogeneic human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12281383/]
- 101. The Potential for Immunogenicity of Autologous Induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3931018/]
- 102. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 103. Progress and challenges in developing allogeneic cell ... [https://www.sciencedirect.com/science/article/pii/S1934590925000943]
- 104. Functional Comparison of Human-Induced Pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4086513/]
- 105. In silico modeling of directed differentiation of induced ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013407]
- 106. Bridging the Gap: Translating Preclinical Biomarkers to ... [https://blog.crownbio.com/bridging-the-gap-translating-preclinical-biomarkers-to-clinical-success]
- 107. Current Good Manufacturing Practice (CGMP) Regulations [https://www.fda.gov/drugs/pharmaceutical-quality-resources/current-good-manufacturing-practice-cgmp-regulations]
- 108. Current Good Manufacturing Practice [https://www.aabb.org/regulatory-and-advocacy/regulatory-affairs/regulatory-for-cellular-therapies/biological-products/current-good-manufacturing-practice]
- 109. Comparison of Differentiation of Induced Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5396057/]
- 110. Editorial: Role of induced pluripotent stem cells (iPSCs) in ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1734717/full]
- 111. Stem cell therapy: a revolutionary cure or a pandora's box [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04334-1]
- 112. Induced Pluripotent Stem Cells as a Disease Modeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3343213/]