Engineering Regeneration: Integrating Stem Cells and Biomaterial Scaffolds for Advanced Tissue Repair
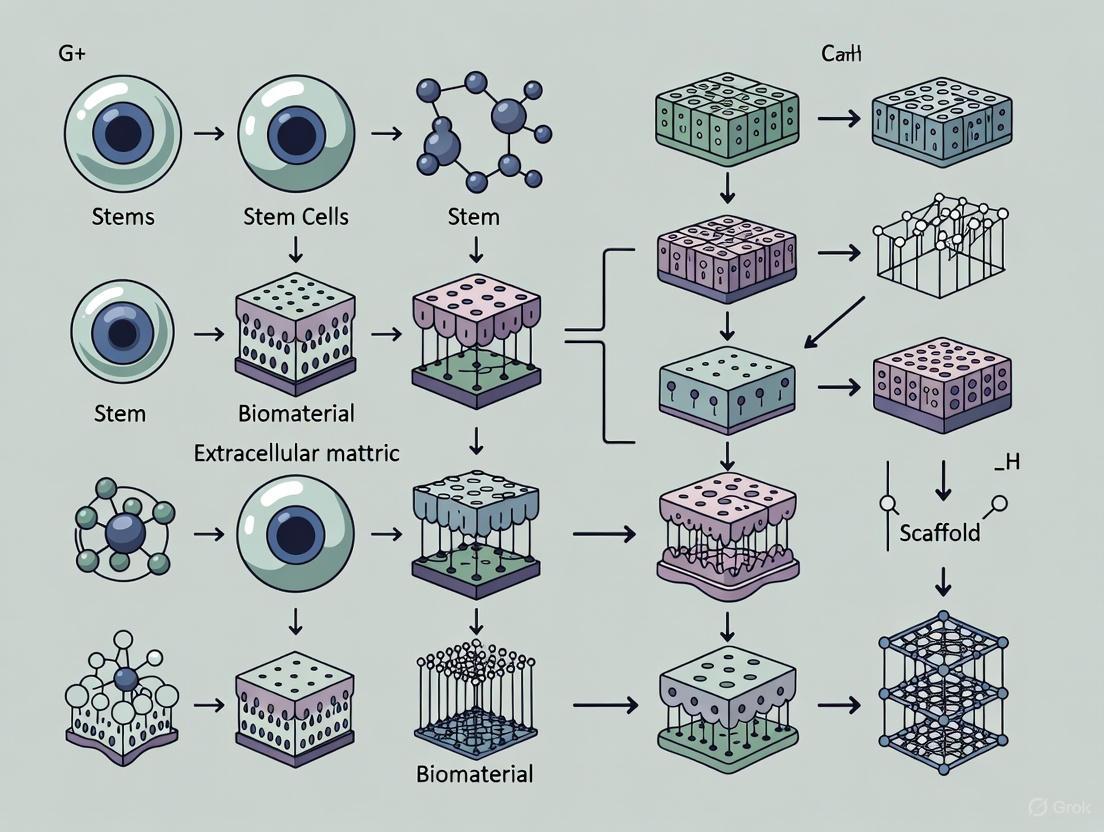
This article provides a comprehensive overview of the latest strategies in tissue engineering that combine stem cells with advanced biomaterial scaffolds.
Engineering Regeneration: Integrating Stem Cells and Biomaterial Scaffolds for Advanced Tissue Repair
Abstract
This article provides a comprehensive overview of the latest strategies in tissue engineering that combine stem cells with advanced biomaterial scaffolds. Tailored for researchers, scientists, and drug development professionals, it explores the foundational biology of stem cells and biomaterials, details cutting-edge methodological applications from 3D bioprinting to organoid development, addresses key challenges in cell viability and manufacturing, and evaluates the current regulatory and clinical trial landscape. By synthesizing information from recent market analyses and peer-reviewed studies (2024-2025), this review aims to serve as a critical resource for advancing therapeutic development and translational research in regenerative medicine.
The Biological and Material Foundation of Regenerative Engineering
Stem cells represent the foundational building blocks of regenerative medicine, offering unprecedented potential for repairing and regenerating damaged tissues and organs. These remarkable cells are defined by two fundamental characteristics: the capacity for self-renewal, allowing them to produce identical copies of themselves, and differentiation, enabling them to develop into specialized cell types [1] [2]. Within the context of tissue engineering, stem cells are increasingly combined with advanced biomaterial scaffolds to create powerful therapeutic strategies that address the limitations of traditional transplantation approaches. The integration of stem cell biology with biomaterial science has accelerated the development of innovative solutions for conditions ranging from neurodegenerative diseases to cardiovascular disorders and orthopedic injuries [3] [4].
The therapeutic application of stem cells extends beyond simple cell replacement, harnessing complex biological mechanisms including developmental signaling pathways, paracrine signaling, and metabolic reprogramming [1] [5]. By understanding and manipulating these mechanisms, researchers can optimize stem cell behavior for specific clinical applications. This document provides detailed application notes and experimental protocols for harnessing two key stem cell properties—pluripotency and paracrine signaling—within biomaterial-assisted tissue engineering frameworks, offering researchers standardized methodologies for advancing regenerative medicine applications.
Stem Cell Classification and Properties
Stem cells are classified based on their origin, differentiation potential (potency), and functional characteristics. Understanding these classifications is essential for selecting appropriate cell sources for specific tissue engineering applications.
Classification by Potency
The differentiation capacity of stem cells, referred to as potency, determines their therapeutic potential and application scope [1] [2].
Table 1: Classification of Stem Cells by Potency
| Potency Type | Differentiation Potential | Representative Examples |
|---|---|---|
| Totipotent | Can differentiate into all cell types, including extraembryonic tissues | Zygote (fertilized egg) |
| Pluripotent | Can differentiate into nearly all cell types derived from the three germ layers | Embryonic Stem Cells (ESCs), Induced Pluripotent Stem Cells (iPSCs) |
| Multipotent | Can differentiate into a limited range of closely related cell types | Hematopoietic Stem Cells (HSCs), Mesenchymal Stem Cells (MSCs) |
| Oligopotent | Can differentiate into only a few cell types | Lymphoid or myeloid stem cells |
| Unipotent | Can produce only one cell type but retain self-renewal capacity | Muscle stem cells |
Classification by Origin
Stem cells are also categorized based on their tissue source, which influences their availability, ethical considerations, and therapeutic properties [1] [4].
Table 2: Classification of Stem Cells by Origin
| Cell Type | Definition | Key Characteristics |
|---|---|---|
| Embryonic Stem Cells (ESCs) | Pluripotent cells derived from the inner cell mass of a 4-5 day-old blastocyst | • Pluripotent differentiation capacity• Ethical controversies• Tumorigenic risk (teratoma formation) |
| Adult Stem Cells (ASCs) | Multipotent or unipotent cells found in various adult tissues | • Tissue-specific differentiation• Lower tumorigenic risk• Examples: HSCs, MSCs, neural stem cells |
| Induced Pluripotent Stem Cells (iPSCs) | Somatic cells reprogrammed into a pluripotent state via genetic manipulation | • Patient-specific (autologous)• Bypasses ethical concerns• Retain epigenetic "memory" of original tissue |
Mesenchymal Stem Cells: A Key Therapeutic Player
Among adult stem cells, Mesenchymal Stem Cells (MSCs) have emerged as particularly valuable for regenerative applications due to their multipotency, immunomodulatory properties, and relative ease of isolation [6]. According to the International Society for Cellular Therapy (ISCT), MSCs are defined by three key criteria: (1) adherence to plastic under standard culture conditions; (2) expression of specific surface markers (CD73, CD90, CD105 ≥95%) while lacking hematopoietic markers (CD34, CD45, CD14 or CD11b, CD79α or CD19, HLA-DR ≤2%); and (3) capacity to differentiate into osteogenic, chondrogenic, and adipogenic lineages in vitro [6].
MSCs can be isolated from multiple tissue sources, each with distinctive properties:
- Bone Marrow-derived MSCs (BM-MSCs): Most extensively studied, high differentiation potential, strong immunomodulatory effects [6]
- Adipose-derived MSCs (AD-MSCs): Easier to harvest in high yields, comparable therapeutic properties to BM-MSCs [6]
- Umbilical Cord-derived MSCs (UC-MSCs): Enhanced proliferation capacity, lower immunogenicity, suitable for allogeneic transplantation [2] [6]
The following diagram illustrates the relationships between different stem cell types and their key characteristics:
Pluripotency: Mechanisms and Experimental Manipulation
Molecular Regulation of Pluripotency
Pluripotency is maintained through complex transcriptional networks, epigenetic regulation, and signaling pathways. The core pluripotency network centers around transcription factors including Oct4, Sox2, Klf4, and c-Myc (collectively known as OSKM), which maintain the undifferentiated state and self-renewal capacity [4]. These factors work in concert with epigenetic modifiers that establish permissive chromatin states, allowing broad developmental potential while preventing uncontrolled differentiation.
Key signaling pathways regulating pluripotency include:
- TGF-β/Activin/Nodal signaling: Supports self-renewal through SMAD2/3 activation
- Wnt/β-catenin pathway: Balanced activity maintains pluripotency; hyperactivation promotes differentiation
- FGF signaling: Regulates multiple aspects of pluripotent stem cell biology
- Hippo pathway: Influences cell proliferation and pluripotency through YAP/TAZ regulation
- BMP signaling: Promotes differentiation in human ESCs but supports self-renewal in mouse ESCs
External mechanical cues from the microenvironment also influence pluripotent stem cell fate through mechanotransduction pathways that ultimately converge on the transcriptional regulation of pluripotency factors [5].
Experimental Protocol: Biomaterial-Assisted Maintenance of Pluripotency
Title: Culture of Human Pluripotent Stem Cells (hPSCs) on Synthetic Thermoresponsive Scaffolds
Purpose: To maintain hPSCs in a pluripotent state using customizable synthetic terpolymer scaffolds, enabling robust expansion and subsequent differentiation.
Materials:
- Cell Source: Human induced pluripotent stem cells (hiPSCs) or human embryonic stem cells (hESCs)
- Synthetic Terpolymer Scaffold: Composed of N-isopropylacrylamide (NiPAAm), vinylphenylboronic acid (VPBA), and polyethylene glycol monomethyl ether monomethacrylate (PEGMMA) synthesized via free-radical polymerization [7]
- Functionalization Reagents: RGD peptides, vitronectin, fibronectin
- Culture Media: Commercially available defined hPSC maintenance medium
- Supplement: Appropriate growth factors for pluripotency maintenance
- Characterization Reagents: Antibodies for flow cytometry (e.g., against OCT4, SOX2, NANOG), immunofluorescence staining reagents
Methodology:
- Scaffold Preparation:
- Synthesize terpolymer via free-radical polymerization with varying molar ratios of NiPAAm, VPBA, and PEGMMA to optimize properties
- Functionalize polymer with bioactive molecules (RGD peptides, vitronectin, or fibronectin) by incorporating during synthesis or through post-synthesis conjugation
- Characterize scaffold properties: lower critical solution temperature (LCST ~37°C), mechanical stiffness (0.5-18 kPa), and transparency
Cell Seeding and Culture:
- Seed hPSCs at appropriate density (e.g., 10,000-50,000 cells/cm²) onto functionalized terpolymer scaffolds in both 2D and 3D configurations
- Maintain cultures in defined hPSC medium at 37°C with 5% CO₂
- Change medium daily and monitor cell morphology and confluence
Passaging:
- Utilize thermoresponsive properties of scaffold for gentle cell harvesting: reduce temperature below LCST to dissolve polymer-cell interactions
- Collect cells and reseed at appropriate splitting ratio onto fresh functionalized scaffolds
Pluripotency Assessment:
- Analyze pluripotency marker expression (OCT4, SOX2, NANOG) via flow cytometry and immunofluorescence after multiple passages
- Evaluate genomic stability through karyotyping after long-term culture (e.g., 9 months)
- Assess in vitro differentiation potential by forming embryoid bodies and evaluating three-germ layer marker expression
Quality Control:
- Compare expansion rates and pluripotency maintenance against traditional matrices (Matrigel, Cultrex)
- Ensure >90% expression of pluripotency markers in cultured population
- Confirm absence of spontaneous differentiation in maintenance culture
The following diagram illustrates the regulatory network that maintains pluripotency in stem cells:
Paracrine Signaling: Mechanisms and Therapeutic Exploitation
The Paracrine Mechanism of Stem Cell Action
Rather than solely differentiating to replace damaged cells, stem cells—particularly MSCs—exert significant therapeutic effects through paracrine signaling, releasing bioactive molecules that modulate the local microenvironment and promote tissue repair [6]. This secretome includes growth factors, cytokines, chemokines, and extracellular vesicles (exosomes) that collectively influence processes such as angiogenesis, immunomodulation, cell survival, and endogenous stem cell recruitment.
Key components of the MSC secretome include:
- Growth factors: VEGF (angiogenesis), HGF (anti-fibrotic, mitogenic), FGF2 (tissue repair), IGF-1 (cell survival)
- Immunomodulatory factors: PGE2, IDO, TGF-β, IL-10 (suppress excessive inflammation)
- Extracellular vesicles (exosomes): Carry proteins, lipids, mRNA, miRNA that influence recipient cell behavior
The paracrine activity of MSCs is not static but can be enhanced through preconditioning strategies including hypoxia, inflammatory cytokine exposure, 3D culture, and photobiomodulation [8].
Experimental Protocol: Enhancing MSC Paracrine Function via Photobiomodulation
Title: Photobiomodulation (PBM) Preconditioning of MSCs to Enhance Paracrine Secretion
Purpose: To augment the therapeutic potential of MSCs by using non-invasive photobiomodulation to enhance their paracrine functions, particularly for bone tissue engineering applications.
Materials:
- Cell Source: Human MSCs (bone marrow, adipose tissue, or umbilical cord-derived)
- PBM Device: Low-level laser therapy (LLLT) system with appropriate wavelength (typically 600-900 nm)
- Culture Reagents: Standard MSC expansion medium, serum-free collection medium for conditioned media
- Analysis Reagents: ELISA kits for growth factors (VEGF, HGF, FGF2), multiplex cytokine array, materials for exosome isolation and characterization
Methodology:
- MSC Culture and Preparation:
- Culture MSCs under standard conditions (α-MEM with 10% FBS, 37°C, 5% CO₂)
- Harvest cells at 80-90% confluence using trypsin/EDTA
- Seed cells at appropriate density for PBM treatment (e.g., 10,000 cells/cm²)
Photobiomodulation Protocol:
- Determine optimal PBM parameters through dose-response studies:
- Wavelength: 630-660 nm (red light) or 810-850 nm (near-infrared)
- Energy density: 0.5-10 J/cm²
- Power density: 5-100 mW/cm²
- Irradiation time: Calculate based on energy density and power density
- Replace culture medium with serum-free medium before irradiation
- Apply PBM treatment using calibrated device at specified parameters
- Return cells to incubator following treatment
- Determine optimal PBM parameters through dose-response studies:
Conditioned Media Collection:
- Collect conditioned media at specific timepoints post-PBM (e.g., 24, 48, 72 hours)
- Concentrate conditioned media using centrifugal filters (3-10 kDa cutoff)
- Store at -80°C for subsequent analysis and functional assays
Paracrine Factor Analysis:
- Quantify secreted growth factors (VEGF, HGF, FGF2, IGF-1) using ELISA
- Analyze comprehensive cytokine/chemokine profiles using multiplex immunoassays
- Isolate and characterize exosomes via ultracentrifugation and nanoparticle tracking analysis
Functional Validation:
- Apply conditioned media to target cells (e.g., endothelial cells for angiogenesis assays, osteoblasts for bone formation assays)
- Assess functional outcomes: tube formation (angiogenesis), migration (wound healing), proliferation (MTT assay), differentiation (lineage-specific markers)
Optimization Notes:
- Conduct parameter optimization for each MSC source and specific application
- Consider multiple PBM treatments over several days for enhanced effect
- Monitor MSC viability and proliferation post-PBM to ensure non-cytotoxic parameters
The following diagram illustrates how paracrine signaling mediates therapeutic effects:
Biomaterial Integration and Tissue Engineering Applications
Biomaterial Strategies for Stem Cell Guidance
The integration of stem cells with biomaterial scaffolds represents a cornerstone of modern tissue engineering, addressing critical challenges in cell survival, integration, and functional tissue formation [4]. Biomaterials provide physical support and biochemical cues that mimic the native stem cell niche, enabling precise control over stem cell behavior.
Advanced biomaterial approaches include:
- "Bottom-up" design: Creating biomaterials based on fundamental stem cell biological needs rather than adapting cells to pre-existing materials [4]
- Mechanotransduction control: Using material stiffness, topography, and elasticity to direct stem cell fate through mechanical signaling [5]
- Dynamic scaffolds: Incorporating responsive elements (thermoresponsive, pH-sensitive, enzyme-degradable) that adapt to changing biological requirements
- Spatial patterning: Creating biomaterial gradients to establish organized tissue structures
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Stem Cell and Biomaterial Research
| Category | Specific Reagents | Function/Application |
|---|---|---|
| Stem Cell Culture | Defined hPSC medium, MSC growth medium, Essential 8, mTeSR1 | Maintenance of pluripotency and expansion |
| Biomaterial Polymers | NiPAAm-VPBA-PEGMMA terpolymer [7], PEGDA, GelMA, chitosan, collagen, hyaluronic acid | Scaffold fabrication with tunable properties |
| Biofunctionalization | RGD peptides, vitronectin, fibronectin, laminin, YIGSR peptides | Enhancing cell-material interactions |
| Characterization Antibodies | CD73, CD90, CD105 (MSC markers); OCT4, SOX2, NANOG (pluripotency) | Cell phenotype verification |
| Secretome Analysis | VEGF, HGF, FGF2 ELISA kits; multiplex cytokine arrays; exosome isolation kits | Paracrine function assessment |
| Differentiation Inducers | Osteogenic: dexamethasone, β-glycerophosphate, ascorbic acid; Cardiogenic: BMP4, activin A, Wnt modulators | Lineage-specific differentiation |
Experimental Protocol: Biomaterial-Assisted Cardiac Differentiation
Title: Directed Differentiation of hPSCs to Cardiomyocytes using Synthetic Thermoresponsive Scaffolds
Purpose: To efficiently generate functional cardiomyocytes from hPSCs using bioactive molecule-functionalized synthetic scaffolds for cardiac regenerative applications.
Materials:
- Cell Source: hPSCs (hiPSCs or hESCs) maintained in pluripotent state
- Scaffold Material: NiPAAm-VPBA-PEGMMA terpolymer functionalized with RGD peptides, vitronectin, and/or fibronectin [7]
- Differentiation Media: Cardiomyocyte differentiation kits or sequentially timed media with specific growth factors
- Characterization Reagents: Antibodies for cardiac troponin T (cTnT), cardiac troponin I (cTnI), α-actinin, MLC2v; calcium indicators for functional assessment
Methodology:
- Scaffold Preparation and Functionalization:
- Prepare terpolymer scaffolds with stiffness optimized for cardiac differentiation (∼10-15 kPa)
- Functionalize with RGD peptides (0.5-2 mM), vitronectin (0.5-1 μg/cm²), or fibronectin (1-2 μg/cm²)
- Characterize functionalization efficiency via ELISA or fluorescent tagging
Cardiac Differentiation Protocol:
- Seed hPSCs at high density (∼80% confluence) onto functionalized scaffolds
- Initiate differentiation using sequential media changes:
- Days 0-1: RPMI 1640 + B27 supplement (without insulin) + 6-8 μM CHIR99021 (Wnt activator)
- Days 2-3: RPMI 1640 + B27 supplement (without insulin) + 2-5 μM IWP2/Wnt-C59 (Wnt inhibitor)
- Days 4-7: RPMI 1640 + B27 supplement (without insulin)
- After Day 7: RPMI 1640 + complete B27 supplement (with insulin)
- Change media every 2-3 days throughout differentiation process
Functional Characterization:
- Assess cardiac-specific marker expression via flow cytometry (cTnT, cTnI) at day 15
- Evaluate structural maturation via immunofluorescence (sarcomeric organization using α-actinin)
- Measure spontaneous contraction rates and synchrony
- Assess electrophysiological properties using calcium imaging or patch clamping
Comparison with Traditional Methods:
- Compare differentiation efficiency against Matrigel, Cultrex, and VitroGel controls
- Quantify percentage of cTnT-positive cells and maturation markers
Expected Outcomes:
- ∼65% cTnT-positive cells and ∼25% cTnI-positive cells [7]
- Improved structural organization compared to traditional matrices
- Enhanced functional properties and maturation status
The strategic integration of stem cell biology with advanced biomaterial engineering represents the future of regenerative medicine. By harnessing both pluripotency and paracrine signaling mechanisms within tailored microenvironments, researchers can develop more effective and predictable therapeutic strategies. The protocols outlined herein provide standardized methodologies for manipulating these fundamental stem cell properties, offering researchers robust tools for advancing tissue engineering applications across multiple organ systems. As the field progresses, continued refinement of these approaches—particularly through the development of more sophisticated biomaterial systems that dynamically respond to biological cues—will further enhance our ability to direct stem cell fate and function for clinical applications.
The global demand for effective tissue regeneration strategies continues to rise due to the increasing burden of trauma, chronic diseases, and age-related tissue degeneration [9]. Biomaterial scaffolds, particularly hydrogels, have emerged as fundamental components in tissue engineering, serving as synthetic niches that mimic the native extracellular matrix (ECM) to direct cellular behavior and support tissue formation [9] [10]. These three-dimensional frameworks provide not only structural support but also biochemical and mechanical cues that orchestrate regenerative processes, including cell adhesion, migration, proliferation, and differentiation [9] [11]. The design of ideal scaffolds requires careful balancing of multiple properties—mechanical, structural, and biological—to create environments that precisely control cell-matrix interactions through mechanotransduction while maintaining structural integrity under physiological loads [9] [12]. This document outlines the key properties of ideal scaffolds and hydrogels, provides detailed experimental protocols for their evaluation, and presents application-specific considerations for their use in tissue engineering contexts, framed within broader research combining stem cells with biomaterial scaffolds.
Properties of Ideal Scaffolds and Hydrogels
Mechanical Properties
The mechanical properties of scaffolds are critical determinants of their success in tissue engineering, as they directly govern cell–matrix interactions through mechanotransduction [9]. The stiffness and viscoelasticity of the scaffold influence cell adhesion, migration, proliferation, and lineage commitment, while adequate compressive strength and shear resistance are required to preserve structural integrity under physiological loads [9] [12]. Precise tuning of these parameters is essential to reproduce the biomechanical milieu of native tissues and to achieve functional regeneration.
Table 1: Key Mechanical Properties of Ideal Scaffolds and Their Functional Significance
| Property | Ideal Range/Target | Functional Significance | Measurement Techniques |
|---|---|---|---|
| Compressive Modulus | Tissue-specific: 0.02–1.16 MPa (superficial cartilage) to 6.44–7.75 MPa (deep zone cartilage) [12] | Withstands physiological loads; influences chondrocyte phenotype [12] | Uniaxial compression testing, AFM |
| Elasticity/Stiffness | Matches target tissue (e.g., neural: 0.1-1 kPa; bone: 10-30 kPa) [9] | Directs stem cell lineage specification; regulates cell spreading [9] | Rheometry, tensile testing |
| Viscoelasticity | Stress relaxation timescale similar to native ECM [9] | Enhances cell migration and proliferation; dissipates energy [9] | Dynamic mechanical analysis |
| Shear Resistance | Sufficient to maintain integrity during implantation [9] | Prevents scaffold failure during handling and implantation [9] | Rheometry, shear testing |
| Degradation Rate | Synchronized with tissue regeneration rate [13] | Maintains mechanical support during healing; prevents collapse or obstruction [13] | Mass loss measurement, GPC |
Biological and Structural Properties
Beyond mechanical properties, ideal scaffolds must possess specific biological and structural characteristics that support cellular activities and tissue development. These properties ensure the scaffold functions as a temporary ECM, providing both physical support and biological cues until the new tissue is fully formed [12] [10].
Table 2: Biological and Structural Properties of Ideal Scaffolds
| Property | Requirements | Significance in Tissue Regeneration |
|---|---|---|
| Biocompatibility | No immune rejection; non-toxic degradation products [12] [13] | Prevents adverse host responses; supports cell viability and function [12] |
| Porosity | High (>80%) with interconnected pores (typically 100-400 μm, tissue-dependent) [14] | Facilitates cell migration, vascularization, nutrient diffusion, and waste removal [14] |
| Bioactivity | Capacity to deliver growth factors, drugs, or genes [12] [13] | Promotes specific cellular responses (e.g., chondrogenesis, osteogenesis) [12] |
| Biodegradability | Rate matched to tissue regeneration; non-inflammatory byproducts [12] | Provides temporary support while gradually transferring load to new tissue [12] |
| Architectural Mimicry | Replicates tissue-specific hierarchical structure [10] | Recapitulates native tissue organization and function [10] |
Experimental Protocols
Protocol 1: Fabrication and Characterization of Tunable Hydrogel Scaffolds
Objective: To synthesize hydrogel scaffolds with tunable mechanical properties and characterize their physical and biological performance.
Materials:
- Methacrylated gelatin (GelMA) or polyethylene glycol diacrylate (PEGDA)
- Photoinitiator (Irgacure 2959 or lithium phenyl-2,4,6-trimethylbenzoylphosphinate)
- Phosphate-buffered saline (PBS)
- Primary cells or cell line relevant to target tissue
- Cell culture media and supplements
Procedure:
Hydrogel Precursor Preparation:
- Prepare GelMA or PEGDA solutions at concentrations ranging from 5-15% (w/v) in PBS.
- Add photoinitiator at 0.05-0.1% (w/v) and mix thoroughly until completely dissolved.
- Filter sterilize the solution using a 0.22 μm syringe filter for cell-laden hydrogels.
Scaffold Fabrication via Photocrosslinking:
- Transfer precursor solution to molds of desired dimensions (e.g., 8mm diameter, 2mm thickness for compression testing).
- Expose to UV light (365 nm, 5-10 mW/cm²) for 30-120 seconds based on crosslinking density requirements.
- For cell-laden constructs, maintain sterile conditions and limit UV exposure time to preserve cell viability.
Mechanical Characterization:
- Perform uniaxial compression testing using a materials testing system.
- Hydrate samples in PBS for 24 hours prior to testing.
- Apply displacement rate of 0.1 mm/min until 60% strain is reached.
- Calculate compressive modulus from the linear region of the stress-strain curve (typically 10-20% strain).
Biological Performance Assessment:
- Seed cells on hydrogel surfaces or encapsulate during fabrication at density of 1-5×10⁶ cells/mL.
- Culture for 1, 3, 7, and 14 days, assessing viability (Live/Dead staining), proliferation (DNA quantification), and tissue-specific differentiation (histology, immunohistochemistry, qPCR).
Protocol 2: 3D Bioprinting of Porous Scaffolds with Controlled Architecture
Objective: To fabricate scaffolds with precisely controlled porosity and internal architecture using 3D bioprinting technology.
Materials:
- Bioink (alginate, gelatin-fibrinogen, hyaluronic acid-based, or cell-laden hydrogels)
- 3D bioprinter with temperature-controlled printheads
- Crosslinking solution (CaCl₂ for alginate, thrombin for fibrin, or UV for photopolymerizable inks)
- CAD software for scaffold design
Procedure:
Scaffold Design:
- Design porous architecture using CAD software with pore sizes of 100-400 μm and 60-90% porosity.
- Incorporate interconnected channels to enhance nutrient diffusion.
- Generate G-code for printing path following a layer-by-layer approach.
Bioink Preparation:
- Mix polymer solution with cells if creating cell-laden constructs at density not exceeding 20×10⁶ cells/mL.
- Maintain bioink at appropriate temperature to balance viscosity and cell viability.
- Load bioink into sterile printing cartridges avoiding bubble formation.
Printing Process:
- Set printing parameters: pressure 20-80 kPa, nozzle speed 5-15 mm/s, nozzle diameter 100-400 μm.
- Maintain stage temperature at 4-10°C for thermal-sensitive bioinks.
- Print layer height set at 70-90% of nozzle diameter to ensure proper layer adhesion.
Crosslinking and Post-processing:
- Apply crosslinking solution immediately after printing each layer for ionic crosslinking.
- For photopolymerizable inks, expose each layer to UV light (365 nm, 3-5 mW/cm²) for 10-30 seconds.
- Transfer printed constructs to culture media and maintain under standard cell culture conditions.
Porosity Characterization:
- Quantify pore size, distribution, and interconnectivity using micro-CT imaging.
- Calculate porosity percentage using the formula: Porosity (%) = (1 - ρscaffold/ρmaterial) × 100, where ρ represents density.
- Assess permeability using fluid flow measurements.
Signaling Pathways in Scaffold-Cell Interactions
The following diagram illustrates key integrin-mediated signaling pathways through which biomaterial scaffolds influence cell behavior, a crucial mechanism in tissue engineering strategies.
Integrin-Mediated Cell-Scaffold Signaling
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Scaffold Development and Evaluation
| Reagent/Category | Function | Examples & Applications |
|---|---|---|
| Natural Polymers | Provide biocompatibility and bioactivity | Gelatin, collagen, hyaluronic acid, chitosan, silk fibroin [12] [13] |
| Synthetic Polymers | Offer tunable mechanical properties and degradation | PEG, PLGA, PCL, PLA [9] [15] |
| Crosslinkers | Enable mechanical stabilization | Genipin, glutaraldehyde, UV initiators (Irgacure 2959) [9] |
| Bioactive Factors | Enhance biological functionality | BMP-2 for bone, TGF-β for cartilage, VEGF for vascularization [12] [13] |
| Characterization Tools | Assess physical and mechanical properties | Rheometers, mechanical testers, micro-CT, SEM [9] [14] |
Application Notes
Bone Tissue Engineering
For bone regeneration, scaffolds require robust mechanical properties with compressive modulus matching cancellous bone (0.1-2 GPa) [15] [13]. Hydrogels for osteoporotic bone defects must address the pathological microenvironment characterized by chronic inflammation, impaired vascularization, and unbalanced bone remodeling [13]. Natural hydrogels like alginate and chitosan can be reinforced with bioceramics (hydroxyapatite) to improve osteoconductivity and mechanical strength [13]. Incorporating bioactive factors such as BMP-2 promotes osteogenic differentiation of mesenchymal stem cells, while bisphosphonates can be loaded to inhibit osteoclast activity [13]. The degradation rate should be synchronized with new bone formation, typically over 4-12 weeks.
Cartilage Tissue Engineering
Articular cartilage repair demands scaffolds that withstand compressive loads while promoting chondrogenesis [12]. Ideal compressive modulus ranges from 0.02-1.16 MPa in superficial zones to 6.44-7.75 MPa in deep zones to maintain chondrocyte phenotype [12]. Natural polymer-based scaffolds (collagen, hyaluronic acid) provide excellent chondrocyte support, while composite hydrogels combining synthetic and natural polymers balance mechanical strength with bioactivity [12]. Incorporating TGF-β3 enhances chondrogenic differentiation of mesenchymal stem cells. Porosity of 80-90% with pore sizes of 100-300 μm facilitates cell migration and ECM production while maintaining structural integrity [12].
Skin Tissue Engineering
Hydrogel scaffolds for skin regeneration prioritize moisture retention, exudate absorption, and biocompatibility [9] [11]. Natural polymers like collagen, fibrin, and chitosan mimic the dermal ECM and promote fibroblast migration and angiogenesis [11]. The ideal scaffold should have moderate stiffness (5-20 kPa) to support fibroblast function while allowing epithelialization [9]. Incorporating antimicrobial agents (silver nanoparticles, antibiotics) helps prevent infection in wound environments [11]. Porous structures with gradient porosity support different cell types—denser layers for structural integrity, more porous layers for cell infiltration [11].
Advanced Fabrication Workflow
The following diagram illustrates the integrated workflow for designing, fabricating, and evaluating biomaterial scaffolds, incorporating computational modeling and experimental validation.
Scaffold Design and Fabrication Workflow
Market Dynamics and Growth Drivers in Tissue Engineering
The global tissue engineering market is experiencing transformative growth, propelled by the convergence of rising clinical demand, technological innovation, and increasing investment in regenerative medicine. This expansion is fundamentally driven by the integration of advanced biomaterial scaffolds with stem cell technologies, creating powerful therapeutic platforms for tissue regeneration. With the market projected to grow at a compound annual growth rate (CAGR) of 12.1% to 20.0%, reaching values between $28.97 billion and $103.36 billion by 2032, the field represents a pivotal shift in therapeutic strategies for chronic diseases, traumatic injuries, and age-related tissue degeneration [16] [17] [18]. This growth is underpinned by sophisticated research protocols that combine biologically active scaffolds with stem cells to recreate functional tissue constructs, offering solutions to previously untreatable medical conditions while reducing dependency on organ transplantation.
Market Analysis and Quantitative Landscape
The tissue engineering market demonstrates robust expansion across all segments and regions, characterized by increasingly diverse applications and material technologies. The following tables provide a detailed quantitative breakdown of current market dynamics and future projections.
Table 1: Global Tissue Engineering Market Size and Growth Projections
| Market Aspect | 2024/2025 Base Values | 2030/2032 Projections | CAGR (%) | Data Sources |
|---|---|---|---|---|
| Overall Market Size | $13.02B (2025) [18], $19.6B (2024) [16], $29.63B (2025) [17] | $28.97B (2032) [18], $103.31B (2032) [16], $103.36B (2032) [17] | 12.1% - 20.0% | [16] [17] [18] |
| Tissue Engineering & Regeneration Submarket | $4.8B (2024) [19] | $9.8B (2030) [19] | 12.8% | [19] |
| Cardiac Tissue Engineering | $632.10M (2024) [20] | $2,943.92M (2034) [20] | 16.65% | [20] |
Table 2: Tissue Engineering Market Share by Segment (2024 Base Year)
| Segment | Leading Category | Market Share (%) | Fastest-Growing Category | Projected CAGR (%) |
|---|---|---|---|---|
| Material Type | Synthetic Polymers [21] | 54.64% [21] | Hybrid/Composite Materials [21] | 14.61% [21] |
| Application | Orthopedic & Musculoskeletal [21] | 42.12% [21] | Cardiovascular & Vascular [21] | 14.12% [21] |
| End User | Hospitals & ASCs [21] | 63.32% [21] | Specialty Regenerative Clinics [21] | 13.92% [21] |
| Region | North America [21] | 45.53% [21] | Asia-Pacific [21] | 14.34% [21] |
Primary Market Growth Engines
Clinical Demand Drivers
The rising global prevalence of chronic diseases and traumatic injuries establishes a substantial clinical foundation for tissue engineering adoption. Cardiovascular diseases alone account for approximately 17.9 million annual deaths worldwide, creating significant demand for vascularized tissue constructs [18]. Orthopedic and musculoskeletal applications dominate current market share (42.12%), driven by the increasing incidence of bone and joint disorders and an aging global population [16] [21]. Osteoarthritis affects approximately 595 million people worldwide, generating a substantial patient cohort for cartilage repair scaffolds and regenerative interventions [21]. The demographic shift toward older populations further accelerates demand, as age-related tissue degeneration creates need for regenerative solutions in joint reconstruction, wound care, and organ function restoration [18].
Technological Innovation Catalysts
Advanced manufacturing technologies are fundamentally transforming tissue engineering capabilities. 3D bioprinting enables precise fabrication of complex tissue architectures through layer-by-layer deposition of bioinks containing cells and biomaterials [20]. Innovations such as Stanford University's vascular network algorithm and the University of Pittsburgh's CHIPS system for perfusable scaffolds have compressed design-to-clinic timelines while enhancing reproducibility [21]. Stem cell technologies, particularly induced pluripotent stem cells (iPSCs), provide ethically acceptable, patient-specific cardiomyocyte and vascular cell sources for engineered tissues [20]. Advanced scaffold materials, including smart scaffolds that respond to physiological stimuli, now provide not only structural support but also enhance cellular attachment, proliferation, and differentiation through controlled release of bioactive molecules [20].
Investment and Regulatory Landscape
Venture capital investment continues to bolster the tissue engineering ecosystem, supporting startups and biotech firms in research, product development, and commercialization initiatives [19]. Simultaneously, regulatory frameworks are evolving to accommodate innovative products, with the FDA's 2025 roadmap to phase out animal testing prioritizing organoid models and advanced computational methods that align with tissue engineering approaches [21]. Europe's ATMP regulation is gradually harmonizing dossier requirements, while Asia-Pacific regulators are clarifying product classifications to ease market entry barriers [21]. These coordinated advancements in both funding and regulatory pathways are significantly de-risking development processes and accelerating clinical translation.
Advanced Application Notes: Stem Cell-Seeded Biomaterial Scaffolds
Protocol: Fabrication of MSC-Seeded Nanofibrous Scaffolds for Skin Regeneration
Principle: This protocol details the fabrication of mesenchymal stem cell (MSC)-seeded electrospun nanofibrous scaffolds for advanced wound healing applications, combining the regenerative capacity of MSCs with the structural guidance of biomaterial scaffolds.
Materials:
- Mesenchymal stem cells (bone marrow, adipose, or umbilical cord derived)
- Polycaprolactone (PCL) or poly(lactic-co-glycolic acid) (PLGA)
- Hexafluoro-2-propanol (HFIP) or trifluoroethanol (TFE)
- Fibronectin or collagen type I solution
- Cell culture media (DMEM/F12 supplemented with FBS and growth factors)
- Trypsin-EDTA solution for cell detachment
- Electrospinning apparatus with high-voltage power supply
- Syringe pump with metal needle
- Mandrel collector
Procedure:
Scaffold Fabrication (Day 1):
- Prepare polymer solution by dissolving PCL or PLGA in HFIP at 10-15% w/v concentration
- Stir the solution for 12 hours at room temperature until completely dissolved
- Load solution into syringe and mount onto syringe pump
- Set electrospinning parameters: flow rate 1.0 mL/h, voltage 15-20 kV, needle-to-collector distance 15 cm
- Collect fibers on rotating mandrel (500-1000 rpm) for 4-6 hours to achieve 100-200 μm thickness
- Vacuum-dry scaffolds for 48 hours to remove residual solvent
Surface Functionalization (Day 3):
- Treat scaffolds with oxygen plasma (100 W, 5 minutes) to enhance surface hydrophilicity
- Immerse in fibronectin solution (10 μg/mL in PBS) for 2 hours at 37°C
- Rinse with sterile PBS and UV sterilize for 30 minutes per side
Cell Seeding and Culture (Day 4):
- Trypsinize MSCs at 80% confluence and resuspend at 2×10^6 cells/mL
- Seed cells onto scaffolds at density of 1×10^5 cells/cm² using static seeding or perfusion bioreactor
- Allow cell attachment for 6 hours before adding complete culture media
- Culture for 7-14 days with media changes every 48 hours
- For 3D bioprinting applications, encapsulate MSCs in bioink (e.g., gelatin methacryloyl) at 5×10^6 cells/mL and print using pneumatic extrusion at 15-25°C
Quality Control:
- Verify scaffold morphology by SEM imaging (fiber diameter 500-1000 nm)
- Assess porosity (>90%) and pore interconnectivity using mercury porosimetry
- Confirm cell viability >95% post-seeding via live/dead staining
- Validate sterility through microbiological testing
Diagram 1: Experimental workflow for fabricating MSC-seeded scaffolds
Mechanism of Action: Scaffold-Stem Cell Interactions in Wound Healing
The therapeutic efficacy of MSC-seeded scaffolds in wound healing operates through multiple coordinated mechanisms. MSCs secrete paracrine factors including exosomes that modulate key signaling pathways to promote tissue regeneration [22]. The scaffold serves as a temporary ECM mimic, providing mechanical support while enhancing MSC retention, viability, and directed differentiation at the wound site.
Diagram 2: Signaling mechanisms of MSC-seeded scaffolds in wound healing
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Tissue Engineering Applications
| Reagent Category | Specific Examples | Function/Application | Research Context |
|---|---|---|---|
| Stem Cell Sources | Mesenchymal Stem Cells (BM-MSCs, UC-MSCs, AT-MSCs) [23], Induced Pluripotent Stem Cells (iPSCs) [20] | Differentiation into target cell types; paracrine signaling; immunomodulation | UC-MSCs show higher proliferation and anti-inflammatory effects than other sources [23] |
| Scaffold Materials | Synthetic Polymers (PCL, PLGA) [21], Natural Polymers (Chitosan, Hyaluronic Acid, Collagen) [11] [24], Hybrid Composites [21] | 3D structural support; cell attachment; mechanical signaling; controlled degradation | Hybrid composites show fastest growth (14.61% CAGR) by merging synthetic durability with biologic cues [21] |
| Bioactive Molecules | Growth Factors (VEGF, FGF-2, TGF-β) [23], Exosomes [22], Signaling Peptides | Enhance angiogenesis; guide cell differentiation; modulate inflammation | MSC-derived exosomes activate PI3K/Akt and TGF-β/Smad pathways in skin regeneration [22] |
| 3D Bioprinting Systems | Bioprinters, Bioinks (Gelatin methacryloyl, Alginate) [16] | Fabrication of complex tissue architectures; cell encapsulation; patient-specific implants | Enables customized cardiac grafts with native tissue-like architecture [20] |
| Characterization Tools | SEM, Live/Dead Assays, ELISA, PCR | Assess scaffold morphology; cell viability; protein and gene expression | Essential for quality control and validation of tissue constructs |
Emerging Frontiers and Future Directions
The tissue engineering field continues to evolve with several emerging trends shaping its trajectory. Personalized medicine approaches are gaining prominence, leveraging patient-specific cells and 3D bioprinting technologies to create customized tissue constructs that minimize immune rejection [20]. Cell-free therapies utilizing exosomes and extracellular vesicles derived from MSCs represent a promising frontier, overcoming challenges related to cell survival and immunogenicity while maintaining therapeutic efficacy [22]. The integration of artificial intelligence in biomaterial discovery and scaffold design is accelerating R&D cycles while reducing development costs [19]. Additionally, decellularized extracellular matrix scaffolds from native tissues are emerging as biologically relevant platforms that provide innate signaling cues for enhanced tissue regeneration [21]. These innovations collectively address current limitations in scalability, functionality, and clinical translation while opening new therapeutic possibilities for complex tissue and organ regeneration.
The tissue engineering market demonstrates exceptional growth potential driven by substantive clinical needs and remarkable technological advancements. The strategic integration of stem cell biology with sophisticated biomaterial scaffolds represents the cornerstone of next-generation regenerative therapies, enabling researchers to address previously intractable medical challenges. As the field continues to mature, ongoing innovations in 3D bioprinting, smart material design, and stem cell engineering promise to further accelerate the development of functional tissue constructs that restore, maintain, or improve damaged tissue function. The convergence of increased research funding, regulatory pathway optimization, and cross-disciplinary collaboration positions tissue engineering as a transformative force in modern medicine, with the potential to fundamentally reshape therapeutic approaches across diverse clinical specialties.
The clinical translation of tissue-engineered constructs combining stem cells with biomaterial scaffolds consistently confronts a formidable obstacle: the hostile in vivo microenvironment at injury sites. This microenvironment represents a complex biological landscape that actively resists regenerative efforts through multiple synergistic mechanisms. Despite promising in vitro results demonstrating stem cell differentiation and biomaterial biocompatibility, the transition to clinical success remains limited by this biological barrier [24] [25].
The post-implantation microenvironment exhibits dynamic, multifactorial hostility characterized by oxidative stress, inflammatory signaling, pathological scarring, and excitotoxicity. These interconnected processes collectively establish a regeneration-inhibitory milieu that significantly compromises stem cell viability, integration, and functional efficacy [24]. In traumatic brain injury, for example, this microenvironment evolves through primary and secondary injury phases, creating self-perpetuating pathological cascades that actively suppress regenerative processes [24]. Understanding and addressing these barrier mechanisms is thus fundamental to advancing clinical outcomes in tissue engineering.
Key Barrier Mechanisms and Quantitative Profiling
Oxidative Stress and Mitochondrial Dysfunction
Following implantation, tissue-engineered constructs encounter elevated reactive oxygen species (ROS) that directly damage cellular components and disrupt signaling pathways. The oxidative stress microenvironment originates from mitochondrial dysfunction in compromised host tissues, where calcium ion influx triggers excessive mitochondrial calcium uptake, resulting in membrane permeabilization and electron transport chain disruption [24]. This process establishes a self-perpetuating cycle of ROS production and cellular damage.
Table 1: Quantitative Markers of Oxidative Stress in Hostile Microenvironments
| Marker Category | Specific Marker | Normal Range | Hostile Microenvironment Range | Measurement Techniques |
|---|---|---|---|---|
| ROS Species | Superoxide anion | 5-20 µM | 50-200 µM | Fluorescent probes (DHE, DCFH-DA) |
| Hydrogen peroxide | 0.1-1 µM | 5-50 µM | Amplex Red assay | |
| Hydroxyl radical | <0.1 µM | 1-10 µM | Electron spin resonance | |
| Oxidative Damage Markers | Lipid peroxidation (MDA) | 1-3 µM | 5-20 µM | TBARS assay |
| Protein carbonylation | 1-2 nmol/mg | 5-15 nmol/mg | DNPH assay | |
| 8-OHdG (DNA damage) | <5 ng/mL | 10-50 ng/mL | ELISA | |
| Antioxidant Defense | Glutathione (GSH) | 20-40 nmol/mg | 5-15 nmol/mg | Colorimetric assay |
| Superoxide dismutase | 10-30 U/mg | 3-10 U/mg | Spectrophotometric assay | |
| Catalase | 50-100 U/mg | 10-40 U/mg | Spectrophotometric assay |
Experimental Protocol 1: Quantifying Intracellular ROS in Implanted Stem Cells
Principle: This protocol measures ROS levels within stem cells after in vivo implantation using the oxidant-sensitive fluorescent probe DCFH-DA (2',7'-dichlorodihydrofluorescein diacetate), which converts to fluorescent DCF upon oxidation.
Reagents:
- DCFH-DA solution (20 µM in PBS)
- Collagenase type IV (for construct retrieval)
- DNase I (0.1 mg/mL)
- Flow cytometry buffer (PBS with 2% FBS)
- Antioxidant standards (N-acetylcysteine, 10 mM)
Procedure:
- Construct Retrieval: At designated time points post-implantation (e.g., 6h, 24h, 72h), excise the tissue-engineered construct with surrounding host tissue (5mm margin).
- Tissue Dissociation: Mechanically mince tissue into 1-2mm³ fragments using sterile scalpels. Digest with collagenase IV (2 mg/mL) and DNase I (0.1 mg/mL) for 45 minutes at 37°C with gentle agitation.
- Cell Isolation: Filter dissociated cells through 70µm cell strainer. Centrifuge at 400 × g for 5 minutes. Resuspend in flow cytometry buffer at 1×10⁶ cells/mL.
- DCFH-DA Staining: Incubate cells with 20 µM DCFH-DA for 30 minutes at 37°C in the dark.
- Flow Cytometry Analysis: Wash cells twice with PBS. Analyze using flow cytometer with excitation at 485nm and emission at 535nm. Use unstained cells and antioxidant-treated controls for baseline fluorescence.
- Data Normalization: Express results as mean fluorescence intensity (MFI) normalized to pre-implantation values or antioxidant-treated controls.
Technical Notes: Maintain samples on ice throughout processing to minimize artifactual ROS generation. Include viability dye (e.g., propidium iodide) to exclude dead cells from analysis. For spatial localization, cryosection constructs can be stained similarly for confocal microscopy imaging [24].
Figure 1: Oxidative Stress Pathway in Hostile Microenvironment. This pathway illustrates how calcium influx triggers mitochondrial dysfunction, leading to self-perpetuating ROS production that ultimately causes stem cell apoptosis.
Neuroinflammation and Glial Activation
The inflammatory component of the hostile microenvironment involves rapid activation of resident glial cells and infiltration of peripheral immune cells. Microglia transition to pro-inflammatory (M1) states, releasing cytokines including TNF-α, IL-1β, and IL-6 that create a toxic environment for implanted stem cells [24]. Astrocytes become reactive and contribute to glial scar formation through upregulation of glial fibrillary acidic protein (GFAP) and chondroitin sulfate proteoglycans (CSPGs) that physically and chemically inhibit neurite outgrowth and stem cell integration [24] [26].
Table 2: Inflammatory Mediators in Hostile Microenvironments
| Inflammatory Component | Specific Marker | Baseline Expression | Hostile Microenvironment Expression | Detection Methods |
|---|---|---|---|---|
| Pro-inflammatory Cytokines | TNF-α | 10-50 pg/mL | 200-1000 pg/mL | ELISA, multiplex immunoassay |
| IL-1β | 5-20 pg/mL | 100-500 pg/mL | ELISA, multiplex immunoassay | |
| IL-6 | 10-30 pg/mL | 150-800 pg/mL | ELISA, multiplex immunoassay | |
| Glial Activation Markers | Iba1 (microglia) | 1-2 fold | 5-15 fold | Immunohistochemistry, Western blot |
| GFAP (astrocytes) | 1-2 fold | 10-20 fold | Immunohistochemistry, Western blot | |
| CSPGs | Neurocan | 1-2 fold | 5-10 fold | Western blot, ELISA |
| Phosphacan | 1-2 fold | 5-10 fold | Western blot, ELISA | |
| NG2 | 1-2 fold | 8-15 fold | Western blot, immunohistochemistry |
Experimental Protocol 2: Flow Cytometric Analysis of Microenvironmental Inflammation
Principle: This protocol enables quantitative assessment of inflammatory cell populations and activation states within implanted tissue-engineered constructs using multiparametric flow cytometry.
Reagents:
- Fluorescently conjugated antibodies: CD45 (leukocyte marker), CD11b (microglia/macrophages), CD86 (M1 polarization), CD206 (M2 polarization), GFAP (astrocytes)
- Intracellular cytokine staining kit with brefeldin A
- Fixable viability dye eFluor 506
- Cell stimulation cocktail (PMA/ionomycin)
- Flow cytometry staining buffer (PBS with 2% FBS, 0.09% sodium azide)
- Fixation/Permeabilization solution
Procedure:
- Construct Processing: Harvest constructs at specified time points. Process immediately for single-cell suspension as described in Protocol 1.
- Viability Staining: Resuspend cells in PBS containing fixable viability dye (1:1000 dilution). Incubate 15 minutes at 4°C in the dark.
- Surface Marker Staining: Wash cells with flow cytometry buffer. Incubate with fluorochrome-conjugated surface antibodies (CD45, CD11b, CD86, CD206) for 30 minutes at 4°C in the dark.
- Fixation and Permeabilization: Wash cells, then fix and permeabilize using commercial fixation/permeabilization kit according to manufacturer instructions.
- Intracellular Staining: Incubate cells with intracellular antibodies (GFAP, cytokines) for 30 minutes at 4°C in the dark.
- Flow Cytometry Acquisition: Wash cells and resuspend in flow cytometry buffer. Acquire data using flow cytometer with appropriate laser and filter configurations. Collect at least 50,000 events per sample.
- Data Analysis: Use fluorescence minus one (FMO) controls for gating. Analyze using FlowJo software, employing sequential gating strategy: single cells → live cells → leukocytes (CD45+) → microglia/macrophages (CD11b+) → polarization states (CD86+/CD206+) [27].
Technical Notes: For cytokine detection, incubate cells with protein transport inhibitor (brefeldin A, 1µL/mL) for 4-6 hours before harvesting. Include isotype controls for each antibody to assess non-specific binding [27].
Glial Scar Formation and Physical Barriers
Reactive astrocytes form dense glial scars that create both physical and chemical barriers to regeneration. The scar tissue presents a dense meshwork of hypertrophic astrocyte processes enriched in inhibitory extracellular matrix molecules including CSPGs, which interact with neuronal receptors to collapse growth cones and inhibit stem cell migration [24]. The temporal progression of scar maturation correlates with declining regenerative capacity, creating a critical therapeutic window for intervention.
Excitotoxicity and Ionic Imbalance
The hostile microenvironment exhibits disrupted ionic homeostasis characterized by excessive glutamate release and subsequent hyperactivation of glutamate receptors. This excitotoxicity drives pathological calcium influx into cells, activating calcium-dependent proteases, phospholipases, and endonucleases that degrade cellular structures [26]. The resulting ionic imbalance further disrupts normal electrophysiological function and compromises stem cell integration and synaptic formation.
Advanced Analytical Approaches
Multiomics and Spatial Analysis of Microenvironments
Advanced analytical frameworks like MESA (multiomics and ecological spatial analysis) enable comprehensive characterization of hostile microenvironments by integrating spatial omics with single-cell multiomics data [28]. This approach adapts ecological diversity metrics to quantify cellular heterogeneity and spatial organization within tissue contexts, revealing patterns not discernible through conventional analysis.
Experimental Protocol 3: Spatial Analysis of Cellular Microenvironments Using MESA
Principle: This protocol applies ecological spatial analysis to quantify cellular diversity and organization within and around implanted tissue-engineered constructs, identifying pathological hot spots and interaction patterns.
Reagents:
- Multiplex immunohistochemistry/immunofluorescence antibody panels
- CODEX/COMET staining reagents
- Tissue clearing reagents (optional)
- Mounting medium for imaging
- DNA staining dye (DAPI, Hoechst)
Procedure:
- Tissue Preparation: Harvest construct with surrounding tissue at specified time points. Fix in 4% PFA for 24 hours at 4°C. Process for cryosectioning or paraffin embedding.
- Multiplex Staining: Perform cyclic immunofluorescence staining according to CODEX protocol or similar multiplex imaging approach. Include markers for key cell types (neurons, astrocytes, microglia, immune cells, implanted stem cells).
- Image Acquisition: Acquire whole-slide images using automated microscopy system with appropriate filter sets for each marker. Maintain consistent exposure across samples.
- Cell Segmentation and Phenotyping: Use automated cell segmentation algorithms (CellProfiler, Ilastik) to identify individual cells and assign marker expression profiles.
- Spatial Analysis Implementation:
- Apply MESA framework to calculate Multiscale Diversity Index (MDI) assessing cellular heterogeneity across spatial scales
- Compute Global Diversity Index (GDI) to evaluate whether patches of similar diversity cluster spatially
- Determine Local Diversity Index (LDI) to identify diversity "hot spots" and "cold spots"
- Calculate Diversity Proximity Index (DPI) to assess spatial relationships between identified spots
- Integration with Single-Cell Data: Map single-cell RNA sequencing data onto spatial coordinates using integration algorithms (MaxFuse) to create in silico multiomics profiles.
- Neighborhood Analysis: Define cellular neighborhoods based on local composition and multiomics profiles. Perform differential expression and ligand-receptor interaction analysis within identified neighborhoods [28].
Technical Notes: Optimal tissue thickness for spatial analysis is 5-10μm. Include controls for antibody cross-reactivity and autofluorescence. For 3D reconstruction, perform serial sectioning and alignment [28].
Figure 2: Spatial Microenvironment Analysis Workflow. This workflow integrates multiplex tissue staining with computational analysis to identify hostile cellular neighborhoods within tissue-engineered constructs.
Extracellular Vesicle Analysis from Native Microenvironments
Solid tissue-derived extracellular vesicles (ST-EVs) provide critical insights into intercellular signaling within hostile microenvironments. These vesicles carry molecular cargo that reflects the pathophysiological state of originating tissues and participate in creating regeneration-inhibitory niches [29].
Experimental Protocol 4: Isolation and Characterization of Solid Tissue-Derived Extracellular Vesicles
Principle: This protocol enables enrichment of extracellular vesicles directly from implanted tissue-engineered constructs and surrounding host tissue to analyze microenvironmental signaling molecules.
Reagents:
- Collagenase/hyaluronidase digestion cocktail
- Protease and phosphatase inhibitors
- OptiPrep density gradient medium
- PBS (calcium- and magnesium-free)
- Exosome-depleted FBS
- Antibodies for EV characterization (CD63, CD81, CD9, TSG101)
- Negative control markers (calnexin, GM130)
Procedure:
- Tissue Collection and Processing: Harvest construct with 2-3mm margin of surrounding tissue. Rinse in cold PBS to remove blood contaminants. Mince into 1mm³ pieces using sterile scalpels.
- Enzymatic Digestion: Digest tissue fragments with collagenase IV (1mg/mL) and hyaluronidase (100U/mL) for 45 minutes at 37°C with gentle agitation. Neutralize with complete media containing 10% exosome-depleted FBS.
- Differential Centrifugation:
- Centrifuge at 300 × g for 10 minutes to remove cells
- Centrifuge supernatant at 2,000 × g for 20 minutes to remove cell debris
- Centrifuge supernatant at 10,000 × g for 30 minutes to remove apoptotic bodies and large vesicles
- Ultracentrifuge supernatant at 100,000 × g for 70 minutes to pellet EVs
- Density Gradient Purification: Resuspend EV pellet in PBS. Layer onto discontinuous iodixanol density gradient (5%, 10%, 20%, 40%). Ultracentrifuge at 100,000 × g for 18 hours. Collect EV-containing fractions (density 1.10-1.18 g/mL).
- EV Characterization:
- NTA: Dilute EVs 1:1000 in PBS, analyze using Nanosight NS300 for size distribution and concentration
- TEM: Adsorb EVs to formvar/carbon-coated grids, negative stain with 2% uranyl acetate, image at 80kV
- Western Blot: Analyze EV markers (CD63, CD81, CD9, TSG101) and exclude contaminants (calnexin, GM130)
- Proteomic and RNA Analysis: Extract EV proteins and RNA for omics analysis to identify microenvironment-specific cargo [29].
Technical Notes: Process tissues immediately after collection or flash-freeze in liquid nitrogen. Include proteinase inhibitors throughout processing. Validate EV isolation efficiency using spiked-in reference particles [29].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Microenvironment Analysis
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Viability/Cytotoxicity Assays | DCFH-DA, MitoSOX, CellROX | ROS detection and quantification | Measure multiple ROS species with different probes |
| Calcein-AM/EthD-1 (Live/Dead) | Cell viability assessment | Distinguish live/apoptotic/necrotic populations | |
| LDH cytotoxicity assay | Membrane integrity assessment | Correlate with histological damage | |
| Cytokine/Chemokine Analysis | Multiplex bead arrays (Luminex) | Simultaneous quantification of multiple inflammatory mediators | Requires small sample volumes |
| ELISA kits for TNF-α, IL-1β, IL-6 | Specific cytokine quantification | High sensitivity, established protocols | |
| Extracellular Matrix Analysis | CSPG detection antibodies (NG2, neurocan) | Inhibitory matrix component quantification | Critical for assessing glial scar maturation |
| Polarized light microscopy for collagen alignment | ECM organization assessment | Reveals structural barriers | |
| Ion/Neurotransmitter Sensing | Glutamate sensors (iGluSnFR) | Excitotoxicity assessment | Real-time monitoring possible |
| Calcium indicators (Fura-2, Fluo-4) | Calcium dyshomeostasis measurement | Rationetric vs. single-wavelength probes | |
| Spatial Analysis Tools | CODEX/COMET imaging systems | Highly multiplexed tissue imaging | Requires specialized instrumentation |
| GeoMx Digital Spatial Profiler | Region-specific RNA/protein analysis | Allows selection of specific microregions | |
| Single-Cell Analysis | 10x Genomics platform | Single-cell RNA sequencing | Reveals cellular heterogeneity |
| CITE-seq (cellular indexing of transcriptomes and epitopes) | Combined protein and RNA at single-cell level | Correlates surface markers with transcriptome |
The hostile in vivo microenvironment presents multifaceted barriers to clinical success of tissue-engineered constructs through interconnected mechanisms of oxidative stress, inflammation, physical barrier formation, and excitotoxicity. Comprehensive characterization of these barriers using quantitative biochemical assays, spatial analysis frameworks, and extracellular vesicle profiling provides critical insights for developing targeted countermeasures. The experimental protocols detailed herein enable researchers to systematically dissect these microenvironmental challenges, forming a foundation for developing intervention strategies that can mitigate these barriers and enhance regenerative outcomes. Future advances will depend on integrating these analytical approaches with novel biomaterial designs and stem cell engineering strategies that collectively neutralize the hostile microenvironment while promoting regenerative processes.
Advanced Fabrication Techniques and Target Applications
Scaffold Design and 3D Bioprinting for Complex Tissue Architecture
Application Note: Integrating Vascularization in Scaffold Design
Core Challenge: The Vascularization-Osteogenesis Paradox
A primary obstacle in engineering large-segment bone defects is overcoming early ischemia and restricted nutrient diffusion, which can lead to cell apoptosis rates exceeding 60% within the scaffold core [30]. Successful regeneration hinges on dynamic crosstalk within the "vascular–osteogenic niche," where endothelial cells secrete osteogenic factors like PDGF-BB and VEGF, and nascent bone matrix releases chemokines such as SDF-1α to guide vascular ingrowth [30]. Scaffolds that provide only mechanical support without biological guidance are insufficient for complex tissue regeneration.
Strategic Solution: "Vascularization-Osteogenesis Integration" Paradigm
A transformative design paradigm involves combining 3D-printed scaffolds with vascularized bone substitutes to create a "scaffold plus vascular-pedicled flap" co-implantation system [30]. This strategy leverages microsurgery to create a functional microcirculation network ex vivo using an arteriovenous loop (AVL), bundle (AVB), flow-through (AVFT), or venous bundle (VB) within the scaffold, or by placing the graft in a muscle pouch (MP) [30]. This pre-vascularized network, when implanted, rapidly restores perfusion, establishes a co-culture microenvironment for endothelial cells and mesenchymal stem cells, and maximizes osteogenic and angiogenic efficiency, thereby accelerating defect repair [30].
Quantitative Analysis of 3D-Printing Technologies for Scaffold Fabrication
Table 1: Comparison of 3D-Printing Technologies for Bone Tissue Scaffolds [30]
| Technology | Suitable for Metal | Energy Source | Typical Materials | Mechanical Properties | Typical Applications |
|---|---|---|---|---|---|
| Selective Laser Sintering (SLS) | No | Laser | Polymers, Bioceramics | Moderate strength (non-load-bearing) | Customized bone tissue scaffolds |
| Selective Laser Melting (SLM) | Yes | Laser | Metal | High strength (load-bearing) | Load-bearing implants (e.g., hip joints) |
| Stereolithography (SLA) | No | UV Light | Photosensitive resins, Biohydrogels | Low-moderate (soft tissue) | Cartilage repair, craniofacial scaffolds |
| Fused Deposition Modeling (FDM) | No | Thermal | PLA, PCL | Tunable | Prototyping, PLA-based scaffold research |
Protocol: Fabrication and Pre-vascularization of a Bioactive Composite Scaffold
Scaffold Design and Bioink Preparation
- Design Phase: Utilize CAD software to design a scaffold with hierarchical porosity, incorporating macro-pores (≥300 μm) to facilitate vascular ingrowth and cell proliferation, alongside micro-pores (<50 μm) to enhance cell adhesion and nutrient diffusion [31]. The design should aim for a total porosity ≥80% [32].
- Bioink Formulation: Prepare a composite bioink:
- Base Hydrogel: A gelatin-alginate blend provides a biocompatible, cell-friendly environment mimicking the native extracellular matrix (ECM) [33].
- Bioactive Additives: Incorporate gelatin microspheres for the sustained release (e.g., over 7 days) of deferoxamine (DFO), a pro-angiogenic factor that activates the HIF-1α pathway [30].
- Mechanical Reinforcement: Add 1 wt% halloysite nanotubes (HNTs) to synergistically enhance osteogenic differentiation and mechanical integrity [30].
Bioprinting Process
- Printer Setup: Employ a pneumatic or piston-driven extrusion bioprinting system equipped with a cooling stage (maintained at 4-10°C) and a UV light source for cross-linking [34].
- Printing Parameters: Use a nozzle diameter between 200-400 μm to balance printing resolution and minimizing shear stress on cells. Maintain a printing pressure and speed that ensures smooth filament extrusion without discontinuity [34].
- Cross-linking: Post-deposition, cross-link the structure by immersing in a calcium chloride solution (for ionic alginate cross-linking) and/or exposing to UV light (for methacrylated gelatin), depending on the bioink composition [34].
In-vitro Pre-vascularization
- Cell Seeding: Seed the sterilized scaffold with a co-culture of Human Umbilical Vein Endothelial Cells (HUVECs) and Human Mesenchymal Stem Cells (hMSCs) at an optimized ratio (e.g., 1:1) in an appropriate endothelial cell growth medium.
- Bioreactor Maturation: Culture the cell-seeded scaffold in a perfusion bioreactor for 7-14 days. The dynamic flow conditions enhance nutrient/waste exchange and promote the self-assembly of endothelial cells into capillary-like networks throughout the scaffold structure [30].
Surgical Implantation (Vascular-Pedicled Flap Co-implantation)
- Flap Harvest: In the recipient site, carefully raise a pedicled tissue flap (e.g., a muscle or fascia flap) with its intrinsic blood supply intact.
- Scaffold Implantation: Position the pre-vascularized scaffold into the bone defect.
- Anastomosis: Surgically anastomose (connect) the pedicle artery and vein of the flap to the pre-formed vascular network within the scaffold or place the scaffold in direct contact with the vascularized flap to facilitate rapid host vessel ingrowth [30]. This establishes immediate perfusion upon implantation.
Experimental Workflow for Bioprinted Construct Validation
The following diagram illustrates the integrated in-vitro and in-silico workflow for developing and validating a bioprinted tissue construct.
Reagent and Material Solutions for Research
Table 2: Essential Research Reagents and Materials for 3D Bioprinting Complex Tissues
| Item | Function/Application | Specific Example |
|---|---|---|
| Gelatin-Alginate Hydrogel | Serves as the primary bioink matrix; provides cell adhesion sites and enables gentle ionic/thermal cross-linking. | GelMA (Methacrylated Gelatin) for UV cross-linking [33]. |
| Deferoxamine (DFO) | Pro-angiogenic small molecule; loaded into microspheres for sustained release to activate HIF-1α pathway and promote vascularization [30]. | DFO@GMs (DFO-loaded Gelatin Microspheres) [30]. |
| Halloysite Nanotubes (HNTs) | Nanoscale additive; improves the composite scaffold's mechanical strength and synergistically enhances osteogenic differentiation [30]. | 1 wt% HNTs in a PCL composite [30]. |
| Stromal Cell-Derived Factor-1α (SDF-1α) | Chemotactic cytokine; incorporated into scaffolds to actively recruit host mesenchymal stem cells (MSCs) to the defect site [30]. | H-BCP@SDF-1α/EPC composite scaffold [30]. |
| Polylactic Acid (PLA) | Thermoplastic polymer for FDM printing; used to create scaffolds with high mechanical strength and complex geometries. | Hybrid Dome Face Centered Porous Structure (HDFCPS) designs [32]. |
| Endothelial & Stem Cells | Cellular components for pre-vascularization and osteogenesis; form the co-culture microenvironment critical for "vascularization-osteogenesis integration". | Co-culture of HUVECs and hMSCs [30]. |
Signaling Pathways in the Vascular-Osteogenic Niche
The following diagram summarizes the key biochemical crosstalk between endothelial and osteogenic cells within a successful bioactive scaffold.
Within the evolving field of tissue engineering, the combination of stem cells and biomaterial scaffolds represents a frontier for regenerative medicine. A critical factor for the success of these therapies is the survival and functional efficacy of the transplanted cells. Mesenchymal stem cells (MSCs) are a cornerstone of this approach due to their multipotency, immunomodulatory properties, and pro-regenerative paracrine activity [3] [23]. However, upon transplantation, they face a hostile microenvironment characterized by inflammation, hypoxia, and oxidative stress, which severely compromises their therapeutic potential [35] [36] [37].
To address this limitation, preconditioning has emerged as a vital strategy. Preconditioning involves the in vitro exposure of MSCs to sublethal stresses or specific bioactive molecules, which "primes" the cells to better withstand the harsh in vivo conditions they will encounter post-transplantation [36]. This process acts as a form of cellular training, enhancing their resilience, improving their engraftment, and boosting their secretory profile. For tissue engineering applications, preconditioned MSCs, when integrated with supportive biomaterial scaffolds, show significantly improved outcomes in wound healing, neural repair, and organ regeneration [35] [24] [38].
This document provides detailed application notes and protocols for three core preconditioning strategies—hypoxic, cytokine, and pharmacological—framed within the context of advanced tissue engineering. It is designed to equip researchers and drug development professionals with standardized, actionable methodologies to enhance the therapeutic performance of stem cell-based constructs.
Hypoxic Preconditioning
Rationale and Mechanism
Hypoxic preconditioning moves MSCs from standard culture conditions (21% O₂) to a physiologically relevant low-oxygen environment (typically 1-5% O₂). This mimics the natural oxygen tension of stem cell niches and the ischemic conditions of damaged tissues [39]. This conditioning enhances MSC survival, paracrine function, and engraftment primarily through the hypoxia-inducible factor-1α (HIF-1α) pathway [37] [39]. Stabilization of HIF-1α triggers the upregulation of a suite of pro-survival and pro-angiogenic genes.
Key benefits of this approach include:
- Enhanced Cell Survival: Activation of Akt-dependent survival pathways reduces apoptosis [39].
- Improved Angiogenic Potential: Increased secretion of vascular endothelial growth factor (VEGF) and other pro-angiogenic factors [35] [39].
- Boosted Migration and Engraftment: Upregulation of the SDF-1/CXCR4/CXCR7 chemokine axis enhances homing to injury sites [37] [39].
Application Note: Hypoxic Preconditioning for Tissue-Engineered Constructs
In tissue engineering, hypoxic preconditioning is particularly valuable for therapies targeting ischemic tissues (e.g., myocardial infarction, diabetic wounds) or for cells destined for the interior of large, dense biomaterial scaffolds where nutrient and oxygen diffusion may be limited. Preconditioned MSCs exhibit greater resilience within these confined environments and can more effectively stimulate vascularization upon implantation, which is critical for the integration and longevity of the engineered tissue [38].
Protocol: Standardized Hypoxic Preconditioning of Adipose-Derived MSCs
Objective: To enhance the therapeutic potential of Adipose-Derived MSCs (ADSCs) through controlled hypoxic culture.
Materials:
- Cell Source: Human ADSCs (Passage 3-5)
- Base Medium: DMEM/F-12
- Supplements: 10% Fetal Bovine Serum (FBS), 1% Penicillin-Streptomycin
- Hypoxia Chamber/Workstation: A tri-gas incubator capable of maintaining 1-5% O₂, 5% CO₂, and balance N₂.
- Analytical Reagents: Antibodies for Flow Cytometry (CD73, CD90, CD105, CD34, CD45); ELISA kits for VEGF and SDF-1; RNA isolation kit for PCR analysis of HIF-1α, VEGF, and CXCR4.
Procedure:
- Cell Culture: Expand ADSCs under standard conditions (37°C, 21% O₂, 5% CO₂) in complete medium until 70-80% confluence.
- Preconditioning Setup:
- Harvest and seed ADSCs at a density of 5,000 cells/cm² in standard culture flasks or plates.
- Once cells reach 60-70% confluence, place the culture vessels into the pre-equilibrated hypoxia chamber.
- Set and maintain the oxygen concentration at 2% O₂. The culture period should be 48-72 hours [39].
- Post-Preconditioning Handling:
- After the incubation period, harvest the preconditioned ADSCs for subsequent analysis or implantation.
- For use in tissue engineering, cells can be seeded directly onto biomaterial scaffolds (e.g., collagen hydrogels, PCL nanofiber meshes) either before or after the hypoxic exposure, depending on scaffold compatibility.
Quality Control:
- Validate preconditioning efficacy by quantifying VEGF and SDF-1 secretion in the conditioned medium via ELISA.
- Confirm upregulation of HIF-1α and CXCR4 gene expression using RT-qPCR.
- Verify that the cells maintain standard MSC surface marker expression (CD73+, CD90+, CD105+, CD34-, CD45-) via flow cytometry.
Signaling Pathway
Diagram Title: Hypoxic Preconditioning Activates the HIF-1α Signaling Pathway
Cytokine Preconditioning
Rationale and Mechanism
Cytokine preconditioning involves priming MSCs with specific inflammatory cytokines or growth factors to mimic the inflammatory disease microenvironment. This process enhances the cells' immunomodulatory capacity and primes them for robust paracrine activity. The approach is guided by the concept of Disease Microenvironment Preconditioning (DMP), where exposing MSCs to disease-specific signals improves their adaptability and therapeutic function upon transplantation [36].
Commonly used cytokines include:
- TNF-α and IFN-γ: Synergistically promote immunomodulation by inducing the expression of chemokines like CCL2 and anti-inflammatory factors [35] [37].
- IL-1β: Enhances MSC migration and promotes a anti-inflammatory macrophage polarization [40] [35].
- TGF-β1: Improves cell survival, engraftment, and reduces healing time in wound models [35] [37].
Application Note: Cytokine Preconditioning for Immunomodulation
This strategy is exceptionally powerful for designing cell-biomaterial systems aimed at treating inflammatory conditions, such as chronic wounds (e.g., diabetic foot ulcers), autoimmune diseases, or neural injuries characterized by intense neuroinflammation (e.g., Traumatic Brain Injury) [24] [36]. Cytokine-preconditioned MSCs seeded within a protective hydrogel can create a local immunomodulatory "hub" that actively suppresses detrimental inflammation and promotes a regenerative tissue environment.
Protocol: TNF-α and IFN-γ Preconditioning for Enhanced Immunomodulation
Objective: To prime MSCs for heightened immunomodulatory and reparative functions using a combination of TNF-α and IFN-γ.
Materials:
- Cell Source: Bone Marrow-derived MSCs (BM-MSCs) or Umbilical Cord-derived MSCs (UC-MSCs), Passage 3-5.
- Base Medium: α-MEM or DMEM.
- Supplements: 10% FBS, 1% Penicillin-Streptomycin.
- Preconditioning Cytokines: Recombinant Human TNF-α and Recombinant Human IFN-γ.
- Analytical Reagents: Flow cytometry antibodies for IDO, TSG-6, and CCL2; ELISA kits for PGE2 and IL-6.
Procedure:
- Cell Preparation: Culture MSCs to 70% confluence in standard complete medium.
- Cytokine Treatment:
- Post-Preconditioning Processing:
- After incubation, carefully wash the cells with PBS to remove all cytokines.
- The preconditioned MSCs are now ready for harvest and subsequent use. They can be incorporated into biomaterial systems, such as injectable chitosan-based hydrogels, which provide a supportive matrix and can be delivered locally to the wound site [24] [38].
Quality Control:
- Assess the upregulation of immunomodulatory markers IDO and TSG-6 via flow cytometry or Western blot.
- Measure the secretion of PGE2 and CCL2 into the conditioned medium using ELISA.
Table 1: Cytokine Preconditioning Parameters and Outcomes
| Cytokine | Concentration | Exposure Time | Key Molecular Changes | Primary Functional Outcome |
|---|---|---|---|---|
| TNF-α | 10-20 ng/mL | 24-48 hours | ↑ miR-146a, ↑ miR-34a [40] | Enhanced immunomodulation |
| IFN-γ + TNF-α | 20 ng/mL + 10 ng/mL | 24 hours | ↑ CCL2, ↑ IL-6, ↑ IDO [35] [37] | M2 Macrophage Polarization |
| IL-1β | 10-50 ng/mL | 24-72 hours | ↑ miR-146a, ↑ MMP-3 [40] [35] | Enhanced Migration & Anti-inflammatory |
| TGF-β1 | 5-10 ng/mL | 48-72 hours | ↑ Pro-survival signals [35] | Improved Engraftment & Wound Closure |
Signaling Pathway
Diagram Title: Cytokine Preconditioning Triggers Key Signaling Pathways
Pharmacological Preconditioning
Rationale and Mechanism
Pharmacological preconditioning utilizes small molecule drugs or natural compounds to biochemically manipulate MSCs, enhancing their stress resistance and therapeutic functions. This approach offers advantages such as well-defined chemical properties, ease of application, and scalability. The mechanisms are compound-specific but often involve the activation of cytoprotective and pro-angiogenic pathways [35] [37].
Promising pharmacological agents include:
- Lipopolysaccharide (LPS): At low doses, LPS can enhance the anti-inflammatory miRNA content of MSC-derived extracellular vesicles (e.g., upregulating miR-222-3p, miR-181a-5p) [40] [37].
- Caffeic Acid: A natural antioxidant that improves MSC viability under hypoxic conditions and upregulates VEGF and SDF-1 secretion [37].
- α-Ketoglutarate: A metabolic intermediate that boosts antioxidant defenses and promotes angiogenesis via HIF-1α and VEGF [35].
Application Note: Pharmacological Priming for Harsh Microenvironments
Pharmacological preconditioning is highly suited for pre-adapting MSCs to the specific stresses of a damaged tissue. For instance, in a diabetic wound, which is characterized by high oxidative stress and impaired angiogenesis, preconditioning MSCs with caffeic acid or α-ketoglutarate before seeding them into a collagen-based scaffold can significantly improve their survival and angiogenic output, leading to faster wound closure [35].
Protocol: LPS Preconditioning to Modulate MSC-Derived EV miRNA
Objective: To enhance the anti-inflammatory and pro-regenerative properties of MSC-derived extracellular vesicles (EVs) through LPS preconditioning.
Materials:
- Cell Source: Bone Marrow-derived MSCs (BM-MSCs).
- Base Medium: DMEM.
- Supplements: 10% EV-depleted FBS (ultracentrifuged), 1% Penicillin-Streptomycin.
- Preconditioning Agent: Ultrapure Lipopolysaccharide (LPS) from E. coli.
- EV Isolation Kit: Commercial exosome isolation kit (e.g., based on size-exclusion chromatography or precipitation).
Procedure:
- Cell Culture: Grow BM-MSCs to 70% confluence in complete medium supplemented with EV-depleted FBS.
- LPS Treatment:
- Prepare a working solution of LPS in the complete medium. A dose of 0.1 μg/mL to 0.5 μg/mL is effective for miRNA modulation without inducing excessive toxicity [40].
- Treat the MSCs with the LPS-containing medium for 24 hours.
- EV Harvest and Isolation:
- After treatment, collect the conditioned medium.
- Centrifuge the medium at 2,000 × g for 10 minutes to remove dead cells and debris.
- Isolate the EVs from the supernatant using a standardized isolation kit, following the manufacturer's instructions.
- Downstream Application: The resulting miRNA-enriched EVs can be incorporated into smart wound dressings or biomaterial coatings for controlled release, providing a potent, cell-free therapeutic [40] [38].
Quality Control:
- Characterize EVs by nanoparticle tracking analysis (size ~30-150 nm) and Western blot for markers CD63, CD81, and TSG101.
- Validate miRNA cargo changes using RT-qPCR arrays for miR-222-3p and miR-181a-5p.
Table 2: Pharmacological Preconditioning Agents and Their Effects
| Pharmacological Agent | Concentration | Exposure Time | Key Molecular Changes | Primary Functional Outcome |
|---|---|---|---|---|
| LPS | 0.1 - 0.5 μg/mL | 24 hours | ↑ miR-222-3p, ↑ miR-181a-5p in EVs [40] | Enhanced anti-inflammatory effect of EVs |
| Caffeic Acid | 10 - 50 μM | 48 hours | ↑ VEGF, ↑ SDF-1 [37] | Improved angiogenesis & cell survival |
| α-Ketoglutarate | 0.5 - 2 mM | 48-72 hours | ↑ HIF-1α, ↑ VEGF [35] | Antioxidant & pro-angiogenic activity |
| Collagen | 50 - 100 μg/mL | 72 hours | ↑ Secretion of chemokines & growth factors [35] | Enhanced epidermal regeneration |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Stem Cell Preconditioning Research
| Reagent / Material | Function / Application | Example Specifications |
|---|---|---|
| Tri-Gas Hypoxia Chamber | Creates and maintains a precise low-oxygen environment for hypoxic preconditioning. | Capable of maintaining 1-5% O₂, 5% CO₂, balance N₂. |
| Recombinant Human Cytokines | Preconditioning stimuli for cytokine-based protocols. | TNF-α, IFN-γ, IL-1β, TGF-β1; >95% purity. |
| Lipopolysaccharide (LPS) | Pharmacological priming of MSCs to enhance EV miRNA content. | Ultrapure, from E. coli, suitable for cell culture. |
| EV-Depleted FBS | Provides essential growth factors while preventing contamination of isolated EVs with serum-derived vesicles. | Prepared by ultracentrifugation (100,000 × g, 16h) or commercially available. |
| Extracellular Vesicle Isolation Kit | Standardized isolation of EVs from preconditioned MSC conditioned medium. | Based on size-exclusion chromatography or polymer precipitation. |
| Chitosan Hydrogel | A natural biomaterial scaffold for delivering preconditioned MSCs, especially in wound healing. | High molecular weight, >75% deacetylation; forms injectable gel. |
| ELISA Kits | Quantification of secreted factors (VEGF, SDF-1, PGE2) to validate preconditioning efficacy. | Commercial kits specific for human antigens. |
| Flow Cytometry Antibodies | Characterization of MSC surface markers and immunomodulatory protein expression (IDO, TSG-6). | Conjugated antibodies for CD73, CD90, CD105, CD34, CD45, IDO. |
Hypoxic, cytokine, and pharmacological preconditioning are powerful and practical strategies that significantly augment the resilience and functional capacity of MSCs. When these primed cells are integrated with advanced biomaterial scaffolds, they form a synergistic therapeutic system that directly addresses the core challenges in regenerative medicine. The protocols and data outlined herein provide a robust foundation for researchers to standardize and implement these techniques, thereby accelerating the development of more effective and reliable stem cell-based therapies for tissue repair and regeneration. Future work should focus on optimizing combination strategies and establishing standardized protocols for clinical-grade manufacturing.
Diabetic foot ulcer (DFU) represents a common and severe complication of diabetes mellitus, characterized by impaired healing processes and a significant risk of amputation [41]. Effective and safe treatments are urgently needed, as traditional therapies often provide insufficient care for these intense wounds [23]. Within the broader context of tissue engineering techniques combining stem cells with biomaterial scaffolds, mesenchymal stem cells (MSCs) have demonstrated crucial roles in tissue regeneration, wound repair, and inflammation regulation [42] [41]. However, the innate therapeutic function of MSCs is often limited for direct clinical application, prompting the development of advanced engineering strategies to enhance their efficacy [23] [41].
This application note presents a comprehensive case study and supporting protocols for using genetically engineered MSCs to promote diabetic wound healing. We focus specifically on human umbilical cord-derived MSCs (hUMSCs) modified to overexpress key anti-inflammatory factors – interleukin (IL)-4, IL-10, and IL-13 – and their integration with advanced biomaterial scaffolds to create optimized tissue constructs for skin regeneration [43] [41]. The content is structured to provide researchers with detailed methodological guidance, quantitative outcomes, and practical resources for implementing these techniques in both basic research and drug development settings.
Background and Clinical Significance
The Burden of Diabetic Wounds
Diabetes mellitus affects hundreds of millions of adults worldwide, with projections indicating rising prevalence in coming decades [41]. DFU represents one of the most serious complications, with healing impaired by diabetic neuropathy, peripheral vasculopathy, and persistent inflammation [41]. The global wound care market reflects this significant clinical need, expected to reach over $29.6 billion by 2030, with advanced wound dressings representing the largest and fastest-growing segment [23].
The normal wound healing process progresses through four coordinated stages: hemostasis, inflammation, proliferation, and remodeling [23] [41]. In diabetic wounds, this process stalls, often in the inflammatory phase, due to multiple factors including dysfunctional immune cell activity, particularly impaired macrophage polarization [41].
MSCs in Wound Healing: Native and Engineered Functions
MSCs are multipotent stromal cells capable of self-renewal and differentiation into various cell types, including osteoblasts, chondrocytes, and adipocytes [42] [44]. They can be sourced from multiple tissues, including bone marrow, adipose tissue, umbilical cord, and Wharton's jelly [23] [42] [44]. Their diverse functions include immune modulation, anti-inflammatory effects, anti-apoptosis, and promotion of angiogenesis, making them ideal candidates for tissue engineering research [44].
MSCs contribute to wound healing through multiple mechanisms:
- Immunomodulation: Suppressing excessive inflammation and promoting transition to regenerative phases
- Angiogenesis: Stimulating new blood vessel formation through VEGF and FGF-2 secretion [23]
- Re-epithelialization: Enhancing keratinocyte migration and proliferation [23]
- Extracellular matrix remodeling: Guiding organized collagen deposition and tissue organization [42]
However, the innate biological functions of unmodified MSCs often prove insufficient for robust therapeutic effects in challenging environments like diabetic wounds [41]. Genetic engineering significantly enhances the biological functions of MSCs and circumvents certain limitations of MSC-based repair therapy [41].
Case Study: Genetically Modified hUMSCs for Diabetic Wound Healing
Experimental Rationale and Design
This case study details an approach using recombinant lentiviral vectors to modify hUMSCs to simultaneously overexpress three anti-inflammatory factors: IL-4, IL-10, and IL-13 (creating "MSCs-3IL") [41]. The rationale for selecting these specific cytokines stems from their complementary roles in wound healing:
- IL-4 and IL-13: Promote fibroblast chemotaxis, proliferation, collagen and ECM production, and polarize macrophages toward the anti-inflammatory M2 phenotype [41]
- IL-10: An anti-inflammatory and antifibrotic cytokine that promotes scarless regenerative wound healing [41]
The hypothesis was that co-modification of MSCs with these three cytokines would create a synergistic therapeutic effect capable of effectively driving diabetic wound repair by modulating the dysfunctional immune response characteristic of these wounds.
Key Methodology and Protocols
Isolation, Culture, and Characterization of hUMSCs
Protocol: hUMSCs Isolation and Expansion
- Source Tissue: Obtain umbilical cords (approximately 1.6 cm in diameter) from healthy full-term cesarean-delivered fetuses with appropriate ethical approvals [41]
- Processing: Remove the amniotic membrane to obtain Wharton's jelly. Dissect Wharton's jelly into 2 mm³ tissue blocks [41]
- Culture Conditions: Culture tissue blocks with Dulbecco's modified Eagle's medium/F12 (DMEM/F12) supplemented with 10% fetal bovine serum (FBS) and 1% penicillin/streptomycin at 37°C with 5% CO₂ [41]
- Passaging: The cells that migrate from the tissue blocks are considered first-passage MSCs (P0). Upon reaching approximately 80% confluency, detach cells with 0.25% trypsin solution, collect, and passage or freeze. Use cells from passages 4 to 8 (P4–P8) for experiments [41]
- Characterization: Confirm expression of MSC-positive markers (CD105, CD73, and CD90) and absence of MSC-negative markers (CD14, CD19, HLA-DR, CD34, and CD45) using flow cytometry. Verify multilineage differentiation potential by culturing in osteogenic, adipogenic, and chondrogenic differentiation media followed by staining with alizarin red S, oil red O, and alcian blue [41]
Genetic Modification of hUMSCs
Protocol: Lentiviral Vector Construction and MSC Transduction
- Vector Design: Obtain lentiviral vectors encoding IL-4, IL-10, and IL-13 from commercial sources (e.g., VectorBuilder, Inc.) [41]
- Cell Seeding: Seed hUMSCs (1.2 × 10⁵/well) in six-well plates [41]
- Virus Preparation: Dilute virus in MSC culture medium supplemented with 8 µg/mL polybrene [41]
- Transduction: Infect hUMSCs at a multiplicity of infection (MOI) of 20. Include three experimental groups: (1) MSCs (unaltered MSCs); (2) MSCs-V (MSCs infected with empty lentiviral vector); and (3) MSCs-3IL (MSCs infected simultaneously with vectors producing IL-4, IL-10, and IL-13) [41]
- Validation: Assess overexpression efficiency using flow cytometry, quantitative real-time PCR, Western blot, and enzyme-linked immunosorbent assay (ELISA) [41]
In Vitro Functional Assays
Protocol: Macrophage Polarization Assay
- Macrophage Culture: Maintain Raw264.7 macrophage cell line under standard conditions [41]
- Conditioned Media Preparation: Collect conditioned media from MSCs, MSCs-V, and MSCs-3IL cultures [41]
- Treatment: Treat macrophages with conditioned media for specified duration
- Analysis: Assess macrophage phenotype using flow cytometry for M1 (CD86) and M2 (CD206) markers, plus quantitative real-time PCR for phenotype-specific genes [41]
Protocol: Scratch Assay for Migration Assessment
- Cell Seeding: Seed relevant cells (keratinocytes, fibroblasts) in culture plates to form confluent monolayer [41]
- Wound Creation: Create a uniform scratch using a pipette tip or specialized tool
- Treatment: Apply conditioned media from experimental MSC groups
- Monitoring: Capture images at regular intervals (0, 12, 24 hours) and quantify migration rate by measuring scratch closure area [41]
In Vivo Diabetic Wound Healing Model
Protocol: Diabetic Mouse Wound Healing Study
- Animal Model: Use C57BL/6J mice (6-8 weeks old, 25 g, male) with induced diabetes [41]
- Wound Creation: Create full-thickness skin wounds on dorsal surface [41]
- Treatment Groups: Include (1) Control (vehicle), (2) MSCs, (3) MSCs-V, and (4) MSCs-3IL
- Cell Administration: Apply cells (e.g., 1×10⁶ cells/wound) in appropriate delivery vehicle directly to wounds
- Monitoring: Assess wound closure rate daily through photography and planimetry [41]
- Endpoint Analysis: At sacrifice timepoints (e.g., days 7, 14), collect tissue for histological analysis (H&E staining, Masson's trichrome), immunohistochemistry (PCNA, F4/80, CD31, CD86, CD206, IL-4, IL-10, IL-13), and gene expression analysis [41]
Key Results and Outcomes
Table 1: Quantitative Outcomes of MSC Engineering and In Vitro Performance
| Parameter | Unmodified MSCs | MSCs-V (Vector Control) | MSCs-3IL (Engineered) |
|---|---|---|---|
| IL-4 mRNA Increase | Baseline | No significant change | 15,000-fold increase |
| IL-10 mRNA Increase | Baseline | No significant change | 800,000-fold increase |
| IL-13 mRNA Increase | Baseline | No significant change | 950,000-fold increase |
| IL-4 Protein Secretion | Undetectable/low | Undetectable/low | ~400 ng/mL |
| IL-10 Protein Secretion | Undetectable/low | Undetectable/low | ~200 ng/mL |
| IL-13 Protein Secretion | Undetectable/low | Undetectable/low | ~6 ng/mL |
| M2 Macrophage Polarization | Moderate effect | Moderate effect | Strong enhancement |
| Cell Phenotype | Normal MSC markers | Normal MSC markers | Unchanged MSC markers |
Table 2: In Vivo Wound Healing Outcomes in Diabetic Mouse Model
| Healing Parameter | Control Group | MSC Group | MSC-3IL Group |
|---|---|---|---|
| Day 7 Closure Rate | ~30% | ~45% | ~75% |
| Day 14 Closure Rate | ~60% | ~80% | >96% |
| Re-epithelialization | Delayed, incomplete | Moderate | Robust, complete |
| M1 Macrophages (CD86+) | High prevalence | Moderate reduction | Significant reduction |
| M2 Macrophages (CD206+) | Low prevalence | Moderate increase | Significant increase |
| Angiogenesis (CD31+ vessels) | Sparse | Moderate | Dense, organized |
| Collagen Organization | Disorganized, thin | Moderate organization | Thick, aligned fibers |
Safety Assessment
The MSCs-3IL demonstrated favorable safety profiles in comprehensive assessments:
- Cell Phenotype: No changes in surface marker expression or differentiation potential [41]
- In Vivo Distribution: Normal dynamic distribution with no abnormal accumulation [41]
- Tumorigenicity: No karyotype variations or tumor risk observed [41]
- General Toxicity: No adverse effects noted in treated animals [41]
Integration with Biomaterial Scaffolds
PCAT Scaffold System for Enhanced Delivery
A critical advancement in applying engineered MSCs involves their integration with specialized biomaterial scaffolds that enhance cell retention, viability, and functionality. The PCAT scaffold system represents one such approach, specifically designed to provide sustained release of therapeutic factors while supporting MSC engraftment [43].
Scaffold Composition and Fabrication:
- Base Materials: Poly(ε-caprolactone) (PCL) and type I collagen at 19:1 ratio [43]
- Fabrication Method: Electrospinning with parameters: 19 kV voltage, 15 cm needle-to-collector distance, 0.6 mL/h injection volume, at room temperature with 50-55% humidity [43]
- Growth Factor Incorporation: TGF-β3 encapsulation in calcium alginate capsules immobilized within the scaffold [43]
- Structural Properties: High surface area, porosity, and fiber morphology mimicking native ECM [43]
Scaffold-Seeded MSC Constructs
The combination of MSCs-3IL with PCAT scaffolds creates synergistic tissue constructs that enhance wound healing through multiple mechanisms:
- Sustained Factor Release: PCAT enables sustained TGF-β3 release for up to seven days while maintaining bioactivity [43]
- Enhanced MSC Function: The scaffold promotes hWJ-MSCs proliferation and modulates secretion of endogenous growth factors [43]
- Improved Healing Outcomes: In vivo results show promoted epidermal graft integration with well-defined basement membrane and dermal papillae, robust granulation tissue with aligned collagen fibers, neovascularization, and reduced inflammatory cell infiltration [43]
Signaling Mechanisms and Pathways
The therapeutic effects of engineered MSCs operate through coordinated modulation of key signaling pathways that regulate the wound healing process. The following diagram illustrates the central mechanism through which MSCs-3IL promotes diabetic wound healing by driving macrophage polarization from the pro-inflammatory M1 phenotype toward the anti-inflammatory M2 phenotype.
Diagram 1: Engineered MSCs promote wound healing via macrophage polarization. This mechanism represents a key pathway through which MSCs-3IL enhances diabetic wound repair.
The following workflow diagram summarizes the complete experimental pipeline from cell isolation through in vivo validation, providing researchers with a comprehensive overview of the entire process.
Diagram 2: Complete experimental workflow for engineered MSC therapy development.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Engineered MSC Studies
| Reagent/Category | Specific Examples | Function/Application | Notes |
|---|---|---|---|
| MSC Sources | Bone marrow-derived MSCs (BM-MSCs), Adipose-derived MSCs (AT-MSCs), Umbilical cord-derived MSCs (UC-MSCs) | Provide cellular platform for engineering; different sources offer distinct advantages | UC-MSCs show higher proliferation, anti-inflammatory effects, and avoid ethical concerns [23] [41] |
| Genetic Engineering Tools | Lentiviral vectors (e.g., from VectorBuilder), Polybrene, Selection markers | Enable stable overexpression of therapeutic factors | Lentiviral systems provide efficient transduction with stable expression [41] |
| Characterization Antibodies | CD105, CD73, CD90 (positive markers); CD14, CD19, HLA-DR, CD34, CD45 (negative markers) | MSC phenotype validation via flow cytometry | Essential for confirming MSC identity per ISCT criteria [42] [41] |
| Cytokine Detection | ELISA kits for IL-4, IL-10, IL-13; Quantitative PCR reagents | Measure overexpression at protein and mRNA levels | Critical for validating engineering efficiency [41] |
| Macrophage Polarization Markers | CD86 (M1), CD206 (M2), Flow cytometry antibodies | Assess immunomodulatory capacity of engineered MSCs | Key functional assay for mechanism validation [41] |
| Scaffold Materials | Poly(ε-caprolactone), Type I collagen, Calcium alginate | Create supportive matrices for cell delivery and factor release | Electrospun scaffolds provide ECM-mimetic structure [43] |
| Animal Models | C57BL/6J diabetic mice, Wound creation tools | In vivo efficacy assessment | Standardized models enable reproducible healing assessment [41] |
| Histological Stains | H&E, Masson's trichrome, Alizarin red, Oil red O, Alcian blue | Tissue structure, collagen content, and differentiation assessment | Essential for evaluating healing quality and safety [41] |
This case study demonstrates that genetically modified hUMSCs effectively overexpress three key anti-inflammatory factors (IL-4, IL-10, IL-13) and significantly enhance diabetic wound healing with high efficiency and safety [41]. The integration of these engineered cells with advanced biomaterial scaffolds like PCAT further improves therapeutic outcomes by providing sustained factor delivery and structural support [43].
The broader implications for tissue engineering techniques combining stem cells with biomaterial scaffolds are substantial. This approach represents a shift from simple cell delivery toward sophisticated "living material" systems that actively coordinate the healing process through precise spatial and temporal control of therapeutic factor presentation. Future directions will likely focus on optimizing scaffold design for specific wound environments, developing more precise genetic control systems, and creating off-the-shelf allogeneic approaches that maintain efficacy while minimizing immunogenicity.
For researchers and drug development professionals, the protocols and data presented here provide a foundation for developing enhanced MSC-based therapies for diabetic wounds and other applications in regenerative medicine. The consistent demonstration of safety with enhanced efficacy positions these engineered approaches as promising candidates for clinical translation in addressing the significant unmet need represented by diabetic foot ulcers.
The limited regenerative capacity of the adult central nervous system (CNS) presents a significant challenge for recovering from injuries such as traumatic brain injury (TBI), spinal cord injury (SCI), and stroke, as well as neurodegenerative diseases [3] [45]. While neural progenitor cells (NPCs) hold immense therapeutic potential due to their ability to differentiate into neurons, astrocytes, and oligodendrocytes, translating this potential into effective clinical treatments has been hampered by difficulties in maintaining NPC stemness during in vitro expansion and ensuring their survival and functional integration after transplantation [46]. The traditional methods of NPC culture, such as two-dimensional (2D) monolayers and three-dimensional (3D) neurospheres, are limited by factors including surface area constraints and restricted oxygen diffusion, which can lead to necrosis and loss of stemness [46].
Biomaterial-guided strategies have emerged as a promising solution to these challenges. By mimicking key aspects of the native neural stem cell niche, engineered biomaterials can provide the necessary biochemical and biophysical cues to support NPC expansion, maintain stemness, and direct differentiation [47] [4]. This case study explores a specific biomaterial-based approach for NPC expansion and transplantation, detailing the experimental protocols, mechanistic insights, and key reagents essential for its implementation. The primary goal is to provide a reproducible methodology for generating therapeutic-grade NPCs for CNS repair applications, framed within the broader context of tissue engineering strategies that combine stem cells with advanced biomaterial scaffolds.
Materials and Methods
Fabrication of Viscoelastic Hyaluronic Acid-Elastin Like Protein (HELP) Hydrogels
The foundation of this protocol is the creation of a 3D hydrogel matrix with tunable viscoelastic and biochemical properties designed to mimic the native brain extracellular matrix (ECM) [46].
Protocol 1: Synthesis of HELP Hydrogels
- Objective: To fabricate a stress-relaxing, cell-instructive hydrogel for the 3D culture and expansion of NPCs.
- Principle: Dynamic covalent hydrazone bonds are formed between modified hyaluronic acid (HA) and a designer elastin-like protein (ELP). The stress relaxation rate is controlled by the ratio of aldehyde-functionalized HA derivatives, while the biochemical cues are provided by peptide motifs (RGD and HAVDI) incorporated into the ELP backbone [46].
- Materials:
- Hyaluronic Acid (HA), functionalized with aliphatic aldehyde, benzaldehyde, or tetrazine groups.
- Elastin-Like Protein (ELP), functionalized with hydrazine or norbornene groups, and containing cell-adhesive peptides (RGD and/or HAVDI).
- Phosphate-Buffered Saline (PBS), sterile.
- Procedure:
- Polymer Preparation: Dissolve the functionalized HA and ELP polymers separately in sterile PBS to achieve final stock concentrations of 2% (w/v). Gently vortex and incubate at room temperature until fully dissolved.
- Crosslinking Initiation: For viscoelastic gels, combine the aldehyde-modified HA (a mixture of aliphatic aldehyde and benzaldehyde-functionalized HA) with the hydrazine-modified ELP at a 1:1 volume ratio. For control elastic gels, combine the tetrazine-modified HA with the norbornene-modified ELP.
- Gelation: Pipette the polymer mixture thoroughly to ensure homogeneity. Transfer the desired volume to a cell culture plate or mold.
- Incubation: Allow the hydrogel to crosslink for 30-60 minutes at room temperature or 37°C until a solid gel forms.
- Critical Parameters:
- The stiffness of the hydrogel (target ~800 Pa) is controlled by the polymer concentration and crosslinking density [46].
- The stress relaxation rate is tuned by the ratio of aliphatic aldehyde to benzaldehyde groups in the HA component. A 50:50 ratio creates a "Dynamic Fast" gel, while a 0:100 ratio creates a "Dynamic Slow" gel [46].
- The concentration of RGD (e.g., 1 mM) and HAVDI peptides is controlled by the ELP composition.
Neural Progenitor Cell Encapsulation and 3D Culture
This protocol describes the process of embedding NPCs within the HELP hydrogel to create a 3D culture system that promotes stemness maintenance.
Protocol 2: NPC Encapsulation and Expansion
- Objective: To encapsulate NPCs within the HELP hydrogel and maintain them in a proliferative, stem-like state.
- Principle: The viscoelastic matrix allows for cell-mediated remodeling, enabling NPCs to make cell-cell contacts crucial for stemness. The HAVDI peptide directly engages N-cadherin receptors, mimicking pro-stemness signaling typically achieved through cell-contact [46].
- Materials:
- Neural Progenitor Cells (NPCs), isolated from relevant tissue or differentiated from pluripotent stem cells.
- HELP hydrogel components (as in Protocol 1).
- NPC proliferation medium (e.g., DMEM/F-12 supplemented with B27, N2, EGF, and FGF).
- Trypsin-EDTA or a non-enzymatic cell dissociation reagent.
- Procedure:
- Cell Harvest: Harvest NPCs from 2D culture or neurospheres using a standard method. Create a single-cell suspension and count the cells.
- Cell-Polymer Mixing: Centrifuge the cell suspension and resuspend the NPC pellet in the ELP polymer solution at twice the desired final cell density.
- Encapsulation: Mix the cell-polymer suspension with an equal volume of the HA polymer solution. Pipette gently but thoroughly to mix without introducing bubbles.
- Seeding and Gelation: Quickly pipette the cell-laden polymer mixture into the culture vessel and incubate to allow gelation (as in Protocol 1).
- Culture Maintenance: After gelation, carefully overlay the hydrogel with pre-warmed NPC proliferation medium. Culture at 37°C in a 5% CO₂ incubator.
- Medium Change: Replace 50-70% of the culture medium every 2-3 days.
- Cell Retrieval (for passaging or analysis): To recover encapsulated NPCs, degrade the hydrogel by adding a solution of hyaluronidase (e.g., 100 U/mL in PBS) and incubating at 37°C for 30-60 minutes. Gently pipette to dissociate the gel, collect the cells by centrifugation, and resuspend for further use.
- Critical Parameters:
- A final cell encapsulation density of 5-10 million cells/mL is recommended.
- The combination of a fast-relaxing matrix ("Dynamic Fast") and the presence of both RGD and HAVDI peptides is critical for achieving a distributed 3D network of stem NPCs, as opposed to dense neurospheres.
- Monitor cell morphology and viability daily.
Results and Data Analysis
Quantitative Analysis of NPC Stemness and Expansion
The success of the biomaterial strategy is evaluated by quantifying NPC stemness markers, proliferation, and viability compared to standard culture methods. The data below, synthesized from the referenced study, should be presented in a tabular format for clear comparison [46].
Table 1: Performance of NPCs in Different 3D Culture Conditions
| Culture Condition | Nestin+/Sox2+ Stemness (%) | EdU+ Proliferation (%) | Viability (%) | Morphology |
|---|---|---|---|---|
| Elastic Static Gel (RGD only) | ~40% | ~25% | ~70% | Limited spreading, small clusters |
| Viscoelastic Dynamic Fast Gel (RGD only) | ~75% | ~55% | ~85% | Large, dense neurospheres |
| Viscoelastic Dynamic Fast Gel (RGD + HAVDI) | ~90% | ~80% | ~95% | Distributed 3D network |
| Traditional Neurospheres | ~80% | ~60% | ~75% (core necrosis) | Large, dense spheres |
Key Findings:
- Viscoelasticity is necessary for proliferation: NPCs in elastic gels show significantly reduced proliferation and stemness compared to those in viscoelastic gels [46].
- HAVDI enables a distributed morphology: The addition of the N-cadherin mimetic (HAVDI) peptide to a viscoelastic matrix prevents the formation of diffusion-limiting neurospheres and promotes a homogeneous 3D network, which correlates with the highest metrics of viability, proliferation, and stemness [46].
- Superior performance: The combination of viscoelasticity and HAVDI signaling creates a synergistic effect, outperforming both traditional neurospheres and other 3D hydrogel conditions.
Signaling Pathways and Mechanistic Workflow
The biomaterial-guided maintenance of NPC stemness is mediated by specific biophysical and biochemical signaling events. The following diagram illustrates the key pathways and the overall experimental workflow.
Diagram 1: Stemness Signaling and Experimental Workflow. The top section outlines how matrix viscoelasticity and the HAVDI peptide synergistically activate N-cadherin/β-catenin signaling to maintain NPC stemness. The bottom section details the sequential steps from hydrogel fabrication to functional assessment in vivo.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of this biomaterial-guided strategy requires a set of key reagents, each serving a specific function in replicating the neural stem cell niche.
Table 2: Essential Research Reagents for Biomaterial-Guided NPC Culture
| Reagent Category | Specific Example | Function & Rationale |
|---|---|---|
| Base Polymer | Hyaluronic Acid (HA) | Major component of the native brain ECM; provides biocompatibility and a biomimetic foundation for the scaffold [46]. |
| Engineered Protein | Elastin-Like Protein (ELP) | A modular protein polymer that provides a backbone for crosslinking and a scaffold for presenting defined peptide signals; offers tunable properties [46]. |
| Integrin Ligand | RGD Peptide | A fibronectin-derived peptide that engages cell surface integrins (e.g., α5β1), promoting initial cell adhesion and survival within the 3D matrix [3] [46]. |
| Cadherin Mimetic | HAVDI Peptide | An N-cadherin-derived peptide that acts as an agonist for N-cadherin receptors on NPCs, directly activating intracellular signaling (via β-catenin) required for stemness maintenance [46]. |
| Crosslink Chemistry | Dynamic Hydrazone Bonds | Forms reversible crosslinks that allow the hydrogel to undergo stress relaxation (viscoelasticity), enabling cell spreading and migration critical for forming cell-cell contacts [46]. |
| NPC Culture Supplement | EGF & FGF | Growth factors included in the culture medium to support the proliferation and maintenance of NPCs in an undifferentiated state [46]. |
| Hydrogel Degrader | Hyaluronidase | An enzyme that specifically degrades HA-based hydrogels, allowing for the gentle retrieval of viable, encapsulated cells for downstream analysis or transplantation [46]. |
Discussion and Application Notes
The data and protocols presented herein demonstrate that a rationally designed biomaterial microenvironment can directly address the critical bottleneck of NPC stemness loss in vitro. The synergistic combination of matrix viscoelasticity and engineered N-cadherin signaling creates a permissive niche that not only maintains stemness but also promotes a scalable, distributed 3D culture morphology, overcoming the diffusion limitations of traditional neurospheres [46].
For researchers aiming to apply this strategy, the following points are critical:
- Material Characterization: Prior to cell culture, rigorously characterize the mechanical properties (elastic modulus, stress relaxation half-life) of the fabricated hydrogels using rheometry to ensure batch-to-batch consistency.
- Pre-screening: The optimal stiffness and relaxation rate may vary slightly depending on the NPC source (e.g., human vs. rodent). A small screening experiment is recommended.
- In Vivo Translation: For therapeutic applications, the expanded NPCs can be transplanted within a supportive biomaterial carrier (e.g., the same HELP hydrogel or an injectable hydrogel [45] [24]) to the site of CNS injury. This carrier can be further functionalized with other therapeutic agents, such as anti-inflammatory drugs [24] or other neurotrophic factors [3], to modulate the hostile injury microenvironment and enhance graft survival and integration.
- Safety Profile: The use of xenogeneic components should be minimized for clinical translation. The HELP platform, based on HA and a defined ELP, offers a path toward a defined, clinical-grade product.
In conclusion, this case study provides a detailed roadmap for leveraging advanced biomaterials to control NPC fate. This approach represents a significant advancement in neural tissue engineering, with strong potential for generating robust cell populations for regenerative therapies, disease modeling, and drug screening for a range of CNS disorders.
Liver Organoid Generation using Matrigel-Free Hydrogel Systems
Liver organoids, three-dimensional in vitro structures that recapitulate the architectural and functional characteristics of the native liver, have emerged as transformative tools for disease modeling, drug development, and regenerative medicine [48] [49]. Traditional liver organoid culture systems heavily rely on Matrigel, a tumor-derived extracellular matrix (ECM) from murine sources, which presents significant limitations for clinical translation. These limitations include batch-to-batch variability, xenogenic components, and the presence of ill-defined growth factors, which hinder experimental reproducibility and pose safety risks for therapeutic applications [50] [51]. Consequently, the development of defined, animal-free hydrogel systems is paramount for advancing liver organoid research toward clinically relevant applications. This protocol details the establishment of a robust, Matrigel-free platform for generating functional liver organoids, leveraging bioengineered hydrogels that provide a physiologically relevant microenvironment while enhancing translational potential within tissue engineering frameworks.
Hydrogel Alternatives for Liver Organoid Culture
Comparison of Matrigel-Free Hydrogel Options
The selection of an appropriate hydrogel is critical for supporting the complex processes of hepatocyte differentiation, proliferation, and self-organization. The table below summarizes the key characteristics of promising Matrigel-free hydrogels investigated for liver organoid culture.
Table 1: Characteristics of Matrigel-Free Hydrogels for Liver Organoid Culture
| Hydrogel Type | Composition | Key Advantages | Documented Performance in Liver Culture |
|---|---|---|---|
| Fibrin-Based Hydrogels | Fibrinogen polymerized with Thrombin [50] | Biocompatible, human-derived, role in angiogenesis, tunable mechanics [50] | Supports vascular network formation and endothelial sprouting; promotes hepatoblast expansion [50] |
| Vitronectin-Based Coatings | Recombinant human protein [50] | Xeno-free, defined composition, supports pluripotency and differentiation [50] | Effective for 2D hiPSC culture prior to 3D differentiation; maintains pluripotency [50] |
| Synthetic PEG-Based Hydrogels | Poly(ethylene glycol) derivatives | Highly tunable mechanical properties, defined chemical structure | Supports endothelial sprouting; concerns about clinical applicability due to potential cytotoxic impurities [50] |
| Other Natural Polymer Blends | Collagen, Chitosan, Alginate, Hyaluronan [3] | Biocompatibility, inherent bioactivity | Used in neural tissue engineering; potential for liver application requires further validation [3] |
Recommended Hydrogel System: Fibrin-Based Hydrogel
Based on current evidence, fibrin-based hydrogels represent a particularly promising candidate for liver organoid generation. Fibrin, a natural polymer formed during wound healing, exhibits excellent biocompatibility, supports cell proliferation, and possesses inherent angiogenic properties that are crucial for developing vascularized organoids [50]. Its gelation time and mechanical stiffness can be precisely controlled by adjusting the ratio of its two components, fibrinogen and thrombin, making it highly adaptable for specific organoid culture needs [50] [48] [52].
Detailed Protocols for Matrigel-Free Liver Organoid Generation
This section provides a step-by-step protocol for generating liver organoids from human induced pluripotent stem cells (hiPSCs) using a Vitronectin-Fibrin system.
Protocol 1: hiPSC Culture and Expansion on Vitronectin
Objective: To maintain and expand hiPSCs in a xeno-free, defined 2D culture system to generate a sufficient cell population for subsequent 3D organoid differentiation.
Materials:
- hiPSC line (e.g., SCV1273, UKKi032-C)
- Recombinant Human Vitronectin XF
- Essential 8 or other defined, xeno-free medium
- Dulbecco's Phosphate-Buffered Saline (DPBS), without Ca2+/Mg2+
- Gentle Cell Dissociation Reagent
- Tissue culture-treated plates
Method:
- Coating: Thaw Vitronectin on ice and dilute in DPBS to a working concentration of 5 µg/mL. Add enough solution to cover the surface of the culture vessel (e.g., 1 mL per well of a 6-well plate) and incubate at room temperature for at least 1 hour.
- Seeding: Aspirate the Vitronectin solution immediately before use. Do not allow the coating to dry. Harvest hiPSCs as single cells using a gentle dissociation reagent. Resuspend the cell pellet in Essential 8 medium supplemented with 10 µM Y-27632 (ROCK inhibitor). Seed the cells at a density of 1.5–2.0 x 10^4 cells per cm^2 onto the Vitronectin-coated plates.
- Maintenance: Culture cells at 37°C with 5% CO2. Refresh the medium daily. Monitor cells for typical pluripotent morphology (high nucleus-to-cytoplasm ratio, compact colonies with defined edges).
- Passaging: When colonies reach 70-80% confluency (typically every 5-6 days), passage cells using the gentle dissociation reagent to generate single cells. Re-seed onto fresh Vitronectin-coated plates as described in step 2. Cells cultured on Vitronectin should maintain pluripotency markers (OCT3/4, Nanog) comparable to Matrigel cultures [50].
Protocol 2: 3D Vascular Liver Organoid Differentiation in Fibrin Hydrogel
Objective: To differentiate hiPSCs into complex, vascularized liver organoids within a 3D fibrin hydrogel matrix.
Materials:
Method:
- Preparation of Hydrogel Components:
- Dissolve Fibrinogen in DPBS to a final concentration of 10 mg/mL.
- Dilute Thrombin in a suitable buffer (e.g., 40 mM CaCl2 in DPBS) to a concentration of 2 U/mL.
- hiPSC Harvest: Differentiate Vitronectin-expanded hiPSCs toward a definitive endoderm lineage using a standard protocol [53] [37]. On day 5 of differentiation, harvest the resulting progenitor cells as small clumps or single cells.
- Hydrogel-Cell Mixture and Polymerization: Mix the cell suspension with the fibrinogen solution on ice. A typical final cell density is 1-5 x 10^6 cells/mL of hydrogel. Add the appropriate volume of thrombin solution to the cell-fibrinogen mixture and pipette gently to mix. A common ratio is 1 part thrombin solution to 9 parts cell-fibrinogen mixture.
- Droplet Seeding: Quickly pipette 20-40 µL drops of the mixture onto the surface of an ultralow attachment plate.
- Gelation: Incubate the plate at 37°C for 15-30 minutes to allow complete fibrin polymerization.
- Culture: After gelation, carefully flood each well with pre-warmed Vascular Organoid Differentiation Medium. Culture the organoids for 18-21 days, with medium changes every 2-3 days. Organoids should exhibit vascular network formation and endothelial cell sprouting comparable to Matrigel-based cultures, as validated by gene expression (CD31, PDGFrβ) and immunohistochemistry [50].
- Preparation of Hydrogel Components:
The following workflow diagram illustrates the complete process from hiPSC culture to mature liver organoid.
The Scientist's Toolkit: Essential Reagents for Matrigel-Free Culture
Table 2: Key Research Reagent Solutions for Matrigel-Free Liver Organoid Generation
| Reagent Category | Specific Product Examples | Function in the Protocol |
|---|---|---|
| Xeno-Free Cell Culture Matrix | Recombinant Human Vitronectin XF [50] | Provides a defined, animal-free substrate for the attachment and expansion of hiPSCs, maintaining pluripotency. |
| Fibrin Hydrogel System | Fibrinogen from human plasma; Thrombin from human plasma [50] | Forms the 3D biodegradable scaffold for organoid differentiation, supporting vascular network formation and cell sprouting. |
| Defined Culture Medium | Essential 8 Medium; Vascular Organoid Differentiation Medium [50] [53] | Provides specific nutrients, hormones, and growth factors for cell maintenance and directed differentiation. |
| Small Molecule Inhibitors/Activators | CHIR99021 (Wnt activator), A83-01 (TGF-β inhibitor), Y-27632 (ROCK inhibitor) [52] [54] | Precisely modulates key signaling pathways (e.g., Wnt, TGF-β) to guide differentiation and improve cell survival. |
| Characterization Antibodies | Anti-OCT3/4, Anti-Nanog, Anti-CD31, Anti-PDGFRβ [50] | Validates pluripotency (OCT3/4, Nanog) and confirms vascular differentiation (CD31, PDGFRβ) via immunostaining. |
Functional Validation and Analysis of Organoids
Rigorous characterization is essential to confirm that the liver organoids generated in Matrigel-free conditions recapitulate key hepatic functions and structures.
- Gene Expression Analysis: Perform qRT-PCR to track the downregulation of pluripotency markers (e.g., OCT4) and the upregulation of hepatic and vascular lineage markers throughout the differentiation process. Key markers include:
- Early Mesoderm/Endoderm: TWIST, SNAIL
- Mature Hepatocytes: Albumin (ALB), Alpha-1-antitrypsin (A1AT)
- Mature Vasculature: CD31 (Endothelial cells), PDGFrβ (Mural cells) [50]
- Immunohistochemistry and Whole-Mount Staining: Confirm the protein-level expression of markers and the formation of complex 3D structures. Stain for CD31 to visualize endothelial networks and PDGFrβ for surrounding mural cells, demonstrating the creation of a vascular niche [50].
- Functional Assays:
- Albumin/Urea Secretion: Quantify the secretion of albumin and urea into the culture supernatant using ELISA or colorimetric assays, indicating mature hepatocyte function [48] [54].
- CYP450 Activity: Measure the metabolic activity of key cytochrome P450 enzymes (e.g., CYP3A4) using luminescent or fluorescent substrates [49].
- Bile Transport: Assess the functionality of bile canaliculi using fluorescent bile acid analogs like cholyl-lysyl-fluorescein (CLF) [49].
Molecular Mechanisms: Signaling Pathways in Hydrogel-Organoid Interaction
Understanding the molecular crosstalk between cells and the fibrin-based hydrogel is key to optimizing the system. The diagram below illustrates the proposed signaling pathways triggered by the hydrogel that support organoid development.
The fibrin hydrogel engages with cell surface integrins, initiating a critical signaling cascade. This triggers the FAK-ERK-AMPK pathway, which regulates fundamental cellular processes. ERK activation contributes to the induction of cell polarization, a hallmark of mature hepatocytes [52]. Concurrently, AMPK activation helps maintain ROS-autophagy homeostasis, suppressing excessive autophagy and thereby creating a microenvironment conducive to the efficient expansion and survival of hepatoblast organoids [52].
Overcoming Translational Hurdles: Scalability, Efficacy, and Safety
Enhancing Cell Survival and Engraftment in Hostile Microenvironments
The success of regenerative medicine and tissue engineering hinges on the effective transplantation and integration of therapeutic cells. However, hostile microenvironments at transplantation sites—characterized by inflammatory signals, oxidative stress, hypoxic conditions, and immune attacks—severely compromise cell survival and engraftment [55]. These detrimental conditions lead to massive cell death, with studies indicating that up to 90% of transplanted cells may perish within the first days post-transplantation [55]. In chronic wounds and fibrotic tissues, this problem is exacerbated by pathological processes that create particularly inhospitable conditions for cellular therapy [38].
Biomaterial-based strategies have emerged as powerful tools to shield transplanted cells and enhance their retention and function. These approaches involve engineering protective microenvironments using advanced biomaterials that can be tailored to provide structural support, biochemical cues, and physical protection. By mimicking key aspects of the native extracellular matrix, these biomaterial systems address multiple challenges simultaneously, offering a comprehensive solution to the problem of poor cell survival in hostile milieus [55] [4].
The paradigm is shifting from simply delivering cells to creating engineered microenvironments that actively support cellular function. This approach recognizes that successful regeneration depends not only on the cells themselves but also on their surrounding context. By designing biomaterials that interact dynamically with both the transplanted cells and the host tissue, researchers can tip the balance toward survival and integration even in challenging pathological environments [4].
Biomaterial Strategies for Enhanced Cell Survival
Biomaterial Classes and Their Properties
Table 1: Biomaterial Classes for Cell Protection and Delivery
| Biomaterial Class | Key Examples | Advantages | Applications in Cell Delivery |
|---|---|---|---|
| Natural Polymers | Alginate, Hyaluronic Acid (HA), Chitosan, Collagen | High biocompatibility, inherent bioactivity, often mimic native ECM components [12] | Shear-thinning hydrogels for injection [55], supportive scaffolds for direct implantation |
| Synthetic Polymers | Polyethylene Glycol (PEG), PLGA-PEG, PNIPAAm | Tunable mechanical properties, controllable degradation, design flexibility [55] | Thermoresponsive hydrogels for minimally invasive delivery [55] |
| Composite Hydrogels | HA-transglutaminase with collagen [12], peptide amphiphiles | Combine advantages of multiple materials, enhanced functionality | Creating biomimetic microenvironments for chondrogenesis [12] |
| Decellularized ECM | Tissue-derived scaffolds | Retains native tissue-specific biochemical and structural cues | Provides tissue-specific niches for enhanced differentiation and integration |
Key Biomaterial Properties for Hostile Microenvironments
Effective biomaterial scaffolds for hostile microenvironments must possess several critical properties:
Biocompatibility and Appropriate Degradation: The material must support cell viability without eliciting detrimental immune responses. Its degradation rate should match the pace of new tissue formation, and the breakdown products must be non-toxic [12]. For instance, gelatin derivatives modified with alanyl-glutamine have been designed to release beneficial metabolites during degradation, actively supporting cell metabolism in the challenging wound environment [12].
Mechanical and Structural Properties: Scaffolds must provide mechanical support that matches the target tissue, typically requiring a compressive modulus in the range of 0.02–1.16 MPa for soft tissues [12]. Optimal porosity (typically >90% for hydrogels) facilitates nutrient diffusion, waste removal, and cellular infiltration while maintaining structural integrity [55] [12].
Bioactivity and Signaling: Beyond passive support, advanced biomaterials incorporate bioactive signals such as adhesion peptides (e.g., RGD sequences), growth factors, or immunomodulatory compounds. These signals guide cellular behavior, promote integration, and actively modulate the hostile microenvironment toward a more regenerative state [55] [12].
Application Notes: Experimental Protocols
Protocol 1: MSC Delivery via Injectable, Shear-Thinning Hydrogel
This protocol details the encapsulation and delivery of Mesenchymal Stem Cells (MSCs) using a hyaluronic acid-based hydrogel designed to protect cells from mechanical stress during injection and enhance retention in hostile microenvironments.
Materials:
- Hyaluronic acid (HA) modified with methacrylate groups (MeHA)
- Photoinitiator (Lithium phenyl-2,4,6-trimethylbenzoylphosphinate, LAP)
- MSC culture expanded to passage 3-5
- Sterile phosphate-buffered saline (PBS)
- UV light source (365 nm, 5-10 mW/cm²)
- 22G-26G syringe needles
Procedure:
- Hydrogel Precursor Preparation: Dissolve MeHA in PBS to a final concentration of 2% (w/v). Add LAP photoinitiator to a concentration of 0.05% (w/v). Sterilize the solution by passing through a 0.22 µm filter.
- Cell Encapsulation: Harvest MSCs using standard trypsinization and centrifuge at 300 × g for 5 minutes. Resuspend the cell pellet in the MeHA precursor solution to a density of 5-10 × 10⁶ cells/mL. Gently mix to ensure uniform cell distribution without creating bubbles.
- Hydrogel Cross-linking: Transfer the cell-laden solution to a syringe and expose to UV light (365 nm, 5-10 mW/cm²) for 60 seconds to form a soft hydrogel.
- Injection and Final Cross-linking: Equip the syringe with a 22G-26G needle. Inject the pre-gelled construct into the target site. Apply a second, longer UV exposure (2-3 minutes) to achieve full cross-linking and stability in situ.
Validation Methods:
- Cell Viability Assessment: At 24 hours post-encapsulation, assess viability using Live/Dead staining (Calcein-AM/Ethidium homodimer-1). Expect >85% viability with optimized precursor concentration and cross-linking conditions [55].
- Retention Quantification: Label cells with a fluorescent dye (e.g., CM-DiI) prior to encapsulation. Use in vivo imaging systems (IVIS) to track retention at the implantation site over 7-14 days. Hydrogel-delivered cells typically show 3-5× higher retention compared to suspension injection [55].
Protocol 2: Biomimetic Scaffold for Pancreatic Islet Transplantation
This protocol creates a collagen-hyaluronic acid composite scaffold designed to mimic the native pancreatic extracellular matrix, providing a protective niche for islets in the hostile diabetic microenvironment.
Materials:
- Type I collagen solution (3-5 mg/mL)
- High molecular weight hyaluronic acid (1.5 MDa)
- 1-ethyl-3-(3-dimethylaminopropyl)carbodiimide (EDC) and N-hydroxysuccinimide (NHS)
- Isolation of pancreatic islets from human or porcine sources
Procedure:
- Composite Fabrication: Mix type I collagen and hyaluronic acid solutions in a 3:1 ratio (v/v). Add EDC/NHS cross-linkers at 5 mM concentration to initiate covalent bonding between the polymers.
- Scaffold Formation: Pour the mixture into cylindrical molds (5 mm diameter × 2 mm height). Incubate at 37°C for 2 hours to facilitate collagen fibrillogenesis and cross-linking.
- Islet Seeding: Place 500-1000 islet equivalents onto each scaffold. Use centrifugal force (100 × g for 2 minutes) to enhance islet incorporation into the porous structure.
- Culture and Transplantation: Maintain constructs in vitro for 24-48 hours before transplantation. For in vivo studies, implant the islet-laden scaffolds into the epididymal fat pad or under the kidney capsule.
Validation Methods:
- Functionality Assessment: Perform glucose-stimulated insulin secretion (GSIS) assays. Calculate the stimulation index (high glucose/low glucose). Scaffold-cultured islets typically maintain stimulation indices >2, compared to <1.5 in conventional culture.
- In Vivo Function: Transplant into diabetic SCID mice and monitor blood glucose levels. Functional islets in biomimetic scaffolds should reverse diabetes (blood glucose <200 mg/dL) within 7 days and maintain normoglycemia for >30 days [55].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Cell Engraftment Studies
| Reagent/Material | Function | Example Application |
|---|---|---|
| Tyrodes-albumin solution | Vehicle for cell suspension during injection | Controls for injection-induced shear stress [55] |
| RGD-modified alginate | Enhances cell-material interaction via integrin binding | Improves MSC spreading and survival in vivo [55] |
| VEGF/FGF-2-loaded microspheres | Promotes angiogenesis in ischemic environments | Co-delivery with cells to enhance vascularization [23] |
| Matrix Metalloproteinase (MMP)-degradable peptides | Allows cell-mediated scaffold remodeling | Facilitates cell migration and integration in PEG hydrogels [55] |
| IL-1Ra releasing nanoparticles | Modulates local inflammatory response | Protects cells in pro-inflammatory wound environments [38] |
Visualizing the Strategy: From Challenge to Solution
Microenvironment Challenges and Biomaterial Solutions
Biomaterial Engineering Workflow
Experimental Validation Pipeline
Integrating stem cells with advanced biomaterial systems represents a paradigm shift in addressing the fundamental challenge of cell survival in hostile microenvironments. The strategies outlined here—from injectable hydrogels that protect against mechanical stress during delivery to biomimetic scaffolds that provide essential survival signals—offer powerful tools to enhance engraftment and therapeutic efficacy. By creating protective microenvironments through rational biomaterial design, researchers can significantly improve outcomes in tissue engineering and regenerative medicine applications.
The future of this field lies in developing even smarter biomaterial systems that can dynamically respond to changes in the microenvironment, providing precisely timed cues and support throughout the entire engraftment process. As these technologies mature and undergo regulatory review, they hold tremendous promise for making cell-based therapies more reliable and effective for treating a wide range of debilitating conditions.
The field of regenerative medicine increasingly recognizes induced mesenchymal stem cells (iMSCs) derived from induced pluripotent stem cells (iPSCs) as a transformative solution to critical limitations associated with primary mesenchymal stem cells (MSCs). Traditional MSC sources—including bone marrow, adipose tissue, and umbilical cord—exhibit inherent challenges that impede standardized therapeutic development: donor-to-donor variability, limited proliferative capacity, senescence in culture, and biological heterogeneity [56]. These constraints directly impact the reproducibility of cell-based therapies and the biomaterial scaffolds they populate, creating significant bottlenecks in clinical translation.
iPSC-derived MSCs represent a paradigm shift, offering an essentially unlimited and consistent cell source that bypasses these limitations [57]. By leveraging the indefinite self-renewal capacity of iPSCs, researchers can generate large, homogeneous populations of iMSCs under defined, xeno-free conditions. This approach provides unprecedented opportunities for standardized manufacturing, precise genetic engineering, and reproducible scaffold integration—key attributes for advancing tissue engineering applications [56] [57]. Furthermore, iMSCs maintain critical MSC functionalities, including tri-lineage differentiation potential (osteogenic, chondrogenic, adipogenic) and immunomodulatory properties, while demonstrating enhanced proliferative capacity compared to their primary counterparts [58].
The integration of iMSCs with advanced biomaterial scaffolds creates powerful synergies for tissue regeneration. Biomaterials can be tailored to mimic native extracellular matrix properties, providing physical and biochemical cues that direct iMSC differentiation and function [59]. This combination enables the creation of predictive, physiologically relevant models for drug screening and disease modeling, while forming the foundation for next-generation engineered tissues [59] [60].
Comparative Analysis: iMSCs vs. Primary MSCs
Quantitative Advantages of iMSC Platforms
Table 1: Functional Comparison of Primary MSCs vs. iMSCs
| Parameter | Primary MSCs | iMSCs |
|---|---|---|
| Scalability | Limited expansion capacity; senesce after limited passages [56] | Essentially unlimited via iPSC intermediate; superior proliferation rate [57] |
| Batch Consistency | High donor-to-donor variability [56] [58] | Highly homogeneous populations from standardized differentiation protocols [57] |
| Genetic Stability | Variable with passage number; age-related changes [56] | Consistent genetic background; amenable to comprehensive QC banking [57] |
| Donor Availability | Limited by tissue source and donor age [56] | Unlimited starting material from iPSC banks [57] |
| Manufacturing Standardization | Challenging due to biological variability [58] | Highly reproducible under defined conditions [57] |
| Regenerative Performance | Variable therapeutic efficacy [56] | Superior in some disease models (e.g., osteoarthritis) [61] [56] |
| Immunomodulatory Capacity | Variable response to inflammatory stimuli [58] | Can be protocol-tuned for strong immunomodulation [58] |
Table 2: iMSC Performance in Preclinical Disease Models
| Disease Model | Therapeutic Effects | Comparison to Primary MSCs |
|---|---|---|
| Osteoarthritis | Greater therapeutic effect than synovial membrane MSCs [61] | Superior cartilage protection and regeneration [61] |
| Inflammatory Bowel Disease | Reduced inflammation, promoted tissue repair [57] | Enhanced regenerative outcomes [57] |
| Graft-versus-Host Disease | Promoted immune tolerance, supported tissue healing [57] | Consistent immunomodulatory response [57] |
| Spinal Cord Injury | Improved axonal regeneration, reduced glial scarring when combined with biomaterials [60] | More predictable integration with scaffolds [60] |
Addressing Primary MSC Limitations
Primary MSCs face substantial constraints that impact their therapeutic utility. With increasing donor age, MSC numbers significantly decline while their proliferative capacity diminishes [56]. Tissue harvesting procedures, particularly bone marrow aspiration, can be invasive and carry risks of pain and infection [56]. Perhaps most importantly, primary MSCs exhibit considerable functional heterogeneity depending on their tissue source—for instance, bone marrow contains approximately 500-fold fewer MSCs than adipose tissue [56]. This biological variability directly translates to inconsistent experimental results and clinical outcomes, complicating the development of standardized therapies [58].
iMSC technology effectively addresses these challenges by providing a renewable cell source that can be quality-controlled through comprehensive banked inventories. The isogeneic nature of iPSC-derived products ensures consistent performance across experiments and manufacturing lots [57]. Furthermore, the ability to generate iMSCs from iPSCs originating from diverse genetic backgrounds enables researchers to create more representative cellular models that better reflect population diversity while maintaining experimental reproducibility [58].
Experimental Protocols: iMSC Generation, Characterization, and Scaffold Integration
iPSC Reprogramming and iMSC Differentiation
Protocol 1: Episomal Reprogramming for Clinical-Grade iPSC Generation
This non-integrating method minimizes tumorigenicity risks while generating iPSCs suitable for downstream iMSC differentiation [62].
- Starting Material Preparation: Isolate human foreskin fibroblasts (HFF) or peripheral blood mononuclear cells (PBMCs) and culture under standard conditions.
- Reprogramming Factor Delivery: Transfect cells with episomal vectors containing OCT4, SOX2, KLF4, and small molecule reprogramming enhancers (omit c-MYC and LIN28 to reduce oncogenic risk) [62].
- iPSC Colony Selection: Culture transfected cells on Vitronectin XF-coated plates in TeSR2 medium. Monitor for embryonic stem cell-like colony emergence (typically 14-21 days post-transfection).
- iPSC Expansion and Validation: Pick and expand colonies. Characterize pluripotency through:
- Master Cell Banking: Create master and working cell banks under xeno-free conditions, confirming absence of episomal vectors through PCR [62].
Protocol 2: Directed Differentiation of iPSCs to iMSCs Using ARG and TEX Methods
Differentiation protocol selection significantly influences iMSC functional properties, enabling customization for specific applications [58].
ARG Protocol (yields iMSCs with strong immunomodulatory potential):
- Seed iPSCs at 70-80% confluence on Vitronectin XF-coated plates in TeSR2 medium.
- Initiate differentiation by switching to αMEM supplemented with 10% human platelet lysate (hPL), 1% GlutaMAX, and 1% penicillin/streptomycin.
- Culture for 14-21 days, replacing medium every 2-3 days, until adherent fibroblastic morphology emerges.
- Passage cells using TripLE and continue expansion in αMEM/10% hPL [58].
TEX Protocol (yields iMSCs with higher proliferation and differentiation capacity):
- Seed iPSCs as above in TeSR2 medium.
- Begin differentiation in DMEM/F12 supplemented with 20% KnockOut Serum Replacement, 1% non-essential amino acids, 1% GlutaMAX, and 0.1mM β-mercaptoethanol.
- At day 7, transition to αMEM with 10% hPL for additional 14 days.
- Passage and expand cells in αMEM/10% hPL [58].
Diagram 1: iMSC Generation Workflow
Comprehensive iMSC Characterization
Protocol 3: Validation of MSC Identity and Functional Potency
Surface Marker Profiling:
- Detach iMSCs with TripLE and resuspend 1×10^6 cells in PBS with 10% FBS.
- Incubate with antibodies against CD73, CD90, CD105 (positive markers) and CD34, CD45 (negative markers) for 15 minutes at room temperature [58].
- Analyze using flow cytometry; >95% positivity for CD73, CD90, CD105 and <5% for CD34, CD45 confirms phenotype [58].
Trilineage Differentiation Capacity:
- Osteogenesis: Culture iMSCs in osteogenic differentiation medium (StemPro) for 21 days. Fix and stain with Alizarin Red to detect calcium deposits [58].
- Adipogenesis: Culture in adipogenic medium for 21 days. Fix and stain with LipidTOX Green to detect lipid vacuoles [58].
- Chondrogenesis: Pellet iMSCs in chondrogenic medium for 21 days. Fix, section, and stain with Alcian Blue to detect glycosaminoglycans [58].
Functional Immunomodulatory Assessment:
iMSC Integration with Biomaterial Scaffolds
Protocol 4: Incorporation into 3D Biomaterial Constructs
Scaffold Selection and Preparation:
- Natural Polymers: Type I collagen, fibrin, hyaluronic acid (modified with RGD), chitosan/alginate composites [60].
- Synthetic Polymers: PLGA, PCL, or PEG-based hydrogels with tunable mechanical properties.
- Sterilize scaffolds according to manufacturer protocols (UV, ethanol, or ethylene oxide).
iMSC Seeding and Culture:
- 3D Hydrogel Encapsulation: Mix iMSCs with hydrogel precursors (e.g., GelMA, collagen) at 5-20×10^6 cells/mL. Crosslink under mild conditions (photoinitiation for GelMA, thermal for collagen) [60].
- Static Scaffold Seeding: Seed iMSCs onto pre-formed porous scaffolds at 0.5-2×10^6 cells/cm^3. Allow 4-6 hours for attachment before adding culture medium.
- Dynamic Culture: Use bioreactor systems (perfusion, rotating wall) to enhance nutrient/waste exchange for thick constructs (>2mm).
Construct Validation:
- Assess cell viability using Live/Dead staining at 24 hours and 7 days post-seeding.
- Evaluate cell distribution through histology (H&E, DAPI) after fixation and sectioning.
- Analyze tissue-specific matrix production (collagen, sulfated GAGs) depending on target differentiation lineage.
Diagram 2: iMSC Integration with Biomaterials
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for iMSC Generation and Application
| Reagent Category | Specific Products | Function & Application |
|---|---|---|
| Reprogramming Systems | Episomal vectors (non-integrating), Sendai virus (CytoTune), mRNA systems | Generate footprint-free iPSCs from somatic cells [62] |
| iPSC Culture | TeSR2/TeSR-E8, Vitronectin XF, Recombinant Laminin-521 | Maintain pluripotency under xeno-free conditions [58] |
| iMSC Differentiation | αMEM with human platelet lysate (hPL), DMEM/F12 with KnockOut SR | Direct iPSC differentiation toward MSC lineage [58] |
| Characterization Antibodies | CD73, CD90, CD105 (positive); CD34, CD45 (negative) | Confirm MSC surface marker profile via flow cytometry [58] |
| Differentiation Media | StemPro Osteo/Chondro/Adipogenesis kits | Validate trilineage differentiation potential [58] |
| Biomaterial Scaffolds | Collagen type I, Fibrin, GelMA, Chitosan-Alginate composites | Provide 3D microenvironment for tissue engineering [60] |
| Cytokines & Growth Factors | Interferon-γ (IFNG), TGF-β, BMP-4, FGF-2 | Modulate immunogenicity and direct differentiation [58] |
iPSC-derived MSCs represent a significant advancement in cellular therapy and tissue engineering, addressing the fundamental limitations of primary MSCs while offering enhanced standardization and scalability. The protocols outlined herein provide a framework for generating, characterizing, and implementing iMSCs in research settings, with particular emphasis on their integration with biomaterial scaffolds for tissue engineering applications.
As the field progresses, ongoing efforts to optimize differentiation protocols, enhance manufacturing standardization, and conduct rigorous safety assessments will further solidify the position of iMSCs as indispensable tools for regenerative medicine. With their proven capabilities in preclinical models and ongoing clinical evaluation, iMSCs stand poised to become a cornerstone technology for developing consistent, effective tissue engineering therapies.
Gene Editing and mRNA Technologies for Enhanced Therapeutic Potential
The field of tissue engineering is evolving beyond the traditional combination of stem cells and biomaterial scaffolds. The integration of advanced gene editing technologies, particularly CRISPR-Cas9, and mRNA-based delivery systems is creating a new paradigm for developing sophisticated therapeutic strategies. These approaches enable precise genetic modification of stem cells to enhance their inherent regenerative capabilities, control their differentiation pathways, and improve their survival and integration within engineered tissue constructs [63] [23]. This document provides detailed application notes and experimental protocols for leveraging these technologies within tissue engineering research.
The selection of the appropriate cargo form—DNA, mRNA, or Ribonucleoprotein (RNP)—is a critical determinant of experimental outcomes. Table 1 summarizes the key characteristics of these CRISPR cargo forms, while Table 2 provides a comparative analysis of the delivery vehicles used to transport them into target cells.
Table 1: Comparison of CRISPR-Cas9 Cargo Forms for Tissue Engineering Applications
| Cargo Form | Composition | Editing Onset | Duration of Activity | Off-Target Risk | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|---|
| Plasmid DNA | DNA plasmid encoding Cas9 and gRNA | Slow (24-48 hrs) | Prolonged (days-weeks) | Higher | Cost-effective; stable; sustained expression | Risk of genomic integration; cytotoxicity; variable efficiency [64] [65] |
| mRNA | mRNA for Cas9 + separate gRNA | Intermediate (12-24 hrs) | Short (days) | Moderate | No genomic integration risk; transient expression; cytoplasmic translation [65] | Immunogenicity; lower stability; requires delivery optimization [65] |
| Ribonucleoprotein (RNP) | Pre-complexed Cas9 protein and gRNA | Immediate (hours) | Very Short (hours) | Lowest | High precision; immediate activity; reduced off-target effects [64] | Manufacturing complexity; challenging in vivo delivery [64] [65] |
Table 2: Delivery Vehicles for Gene Editing Components
| Delivery Vehicle | Cargo Compatibility | Typical Efficiency | Key Advantages | Primary Limitations | Tissue Engineering Relevance |
|---|---|---|---|---|---|
| Adeno-Associated Virus (AAV) | DNA | High in permissive cells | Mild immune response; proven clinical safety [64] | Limited payload capacity (<4.7 kb) [64] [65] | Useful for in vivo targeting but size-limited for larger editors. |
| Lentivirus (LV) | DNA | High | Large cargo capacity; infects dividing/non-dividing cells [64] | Genomic integration raises safety concerns [64] [65] | Ex vivo modification of stem cells. |
| Lipid Nanoparticles (LNPs) | mRNA, RNP | Moderate to High | Low immunogenicity; scalable; tunable targeting [64] [65] | Endosomal entrapment; requires formulation optimization [64] | Promising for in vivo mRNA delivery. |
| Virus-Like Particles (VLPs) | RNP, protein | Moderate | No viral genome; improved safety; transient delivery [64] [66] | Manufacturing and stability challenges [64] | Emerging tool for precise RNP delivery. |
| Engineered Exosomes/EVs | mRNA, protein, miRNA | Moderate (improved with engineering) | Low immunogenicity; natural targeting; cross biological barriers [67] [66] [68] | Heterogeneity; standardized isolation is challenging [64] [67] | Excellent for cell-cell communication in constructs. |
Application Notes & Experimental Protocols
Protocol: Enhancing Extracellular Matrix Production in hiPSC-Derived Cardiac Fibroblasts via TALEN-Mediated Gene Editing
This protocol details the genetic enhancement of human induced pluripotent stem cell-derived cardiac fibroblast-like cells (iCFs) to produce designer human tissue-engineered matrices (hTEMs) with superior mechanical properties for cardiovascular implants [63].
Principle and Objective
The objective is to overexpress key extracellular matrix (ECM) and ECM-related proteins (e.g., Elastin - ELN, Fibulin-5 - FBLN5, Lysyl Oxidase - LOX) in iCFs using Transcription Activator-Like Effector Nuclease (TALEN)-mediated gene integration. This enhances the composition, structure, and mechanical functionality of the resulting decellularized matrices [63].
Materials and Reagents
- Cells: Human induced pluripotent stem cells (hiPSCs).
- Culture Media: mTeSR1, RPMI-1640, B27-minus insulin supplement, Cardiac Fibroblast Medium (CFBM).
- Differentiation Factors: CHIR99021 (GSK-3 inhibitor), IWR-1-endo (Wnt inhibitor), basic Fibroblast Growth Factor (bFGF).
- Plasmids: AAVS1-TALEN-L and AAVS1-TALEN-R plasmids; donor plasmid containing the gene of interest (e.g., ELN, FBLN5, LOX) with puromycin resistance, cloned into the AAVS1 safe harbor locus.
- Transfection Reagent: Neon Transfection System or equivalent electroporator.
- Selection Agent: Puromycin.
Step-by-Step Procedure
Part A: Differentiation of hiPSCs into Cardiac Fibroblast-like Cells (iCFs)
- Day 0: Culture hiPSCs to 60-70% confluency. Initiate differentiation by replacing the medium with RPMI-1640 + B27-minus insulin + 12 µM CHIR99021. Incubate for 24 hours.
- Day 1: Replace the medium with RPMI-1640 + B27-minus insulin (without CHIR99021). Incubate for 24 hours.
- Day 2: Replace the medium with RPMI-1640 + B27-minus insulin + 5 µM IWR-1. Incubate for 24 hours.
- Day 3: Switch to Cardiac Fibroblast Medium (CFBM). Continue culture, refreshing the medium every 2-3 days until Day 18.
- Day 18: Passage cells directly onto non-coated plastic plates at a 1:3 ratio. This step purifies the iCF population by selecting for adherent cells.
- Day 22: Passage the purified iCFs onto collagen type I-coated plates for expansion and subsequent experiments [63].
Part B: TALEN-Mediated Gene Editing of iCFs
- Preparation: Culture hiPSCs to 70% confluency. Pre-treat with 10 µM Rho kinase inhibitor for 2 hours before detachment.
- Electroporation: Detach and resuspend hiPSCs at a concentration of 200,000 cells in 20 µL of mTeSR1. Add AAVS1-TALEN-L, AAVS1-TALEN-R, and the donor vector plasmid in a 1:1:2 mass ratio. Electroporate using the Neon Transfection System (1100 V, 30 ms, 1 pulse).
- Recovery and Selection: Plate the electroporated cells and culture in mTeSR1 for 3-4 days. Then, initiate puromycin selection (1 µg/mL) for 3 days to eliminate non-transfected cells.
- Clonal Expansion: Pick puromycin-resistant colonies, expand them, and validate the integration of the transgene via PCR and Sanger sequencing using specific primers for the AAVS1 locus [63].
Part C: Generation and Analysis of Gene-Edited hTEMs
- Culture the validated, gene-edited iCFs on engineered tissue substrates under standard conditions to produce ECM.
- Decellularize the constructs using established protocols (e.g., using detergents like SDS or Triton X-100) to obtain acellular hTEMs.
- Analyze the resulting matrices using proteomics (e.g., for increased collagen and elastic fiber assembly proteins) and biaxial mechanical testing to confirm enhanced functional properties [63].
Protocol: Intracellular Delivery of CRISPR-Cas9 RNP Using Engineered ARMMs
This protocol describes the use of engineered Arrestin Domain-Containing Protein 1 (ARRDC1)-Mediated Microvesicles (ARMMs) as a non-viral platform for delivering CRISPR-Cas9 ribonucleoprotein (RNP) complexes to target cells, such as neurons, for gene editing applications [66].
Principle and Objective
ARMMs are a type of extracellular vesicle that bud directly from the plasma membrane. By fusing Cas9 to ARRDC1, the protein responsible for ARMMs biogenesis, Cas9 RNP can be efficiently packaged and delivered to recipient cells. This method is particularly useful for targeting hard-to-transfect cells, like neurons, for therapeutic gene knock-out (e.g., targeting the APP gene in Alzheimer's research) [66].
Materials and Reagents
- Plasmids: Plasmids encoding ARRDC1-Cas9 or sARRDC1-Cas9 (shorter variant) fusion constructs, and a plasmid for VSV-G (vesicular stomatitis virus glycoprotein).
- Cells: Producer cells (e.g., HEK293T), and target cells (e.g., U2OS reporter cells or human neuronal cells).
- Isolation Kits: Standard extracellular vesicle isolation kits or reagents for differential ultracentrifugation.
- Antibodies: Antibodies for characterization (e.g., anti-CD63, anti-Alix, anti-Cas9).
Step-by-Step Procedure
- Producer Cell Transfection: Culture HEK293T producer cells to 60-80% confluency. Co-transfect them with the ARRDC1-Cas9 (or sARRDC1-Cas9) fusion construct and the VSV-G plasmid using a standard transfection method (e.g., PEI, lipofectamine). VSV-G incorporation enhances ARMMs budding and Cas9 encapsulation [66].
- ARMMs Collection: 48-72 hours post-transfection, collect the cell culture supernatant. Centrifuge at low speed (e.g., 2,000 × g for 10 minutes) to remove cell debris.
- ARMMs Purification: Concentrate and purify the ARMMs from the clarified supernatant. This can be achieved by ultracentrifugation (e.g., 100,000 × g for 70 minutes) or using commercial EV isolation kits. Resuspend the purified ARMMs pellet in PBS.
- Characterization: Characterize the isolated ARMMs for size and concentration (e.g., by Nanoparticle Tracking Analysis) and confirm the presence of Cas9 and typical EV markers (e.g., CD63, Alix) via western blotting [66].
- Target Cell Treatment: Incubate target cells (e.g., neuronal cells) with the purified ARMMs. For neuronal cells targeting the APP gene, a typical experiment might use ARMMs derived from 5 x 10^5 producer cells per well of a 24-well plate.
- Editing Analysis: Harvest target cells 3-5 days post-treatment. Analyze gene editing efficiency using genomic DNA extraction followed by T7E1 assay or next-generation sequencing. Confirm functional outcomes, such as reduction in pathogenic amyloid-β peptides, via ELISA [66].
Protocol: Biomaterial-Assisted Exosome Delivery for Bone Regeneration
This protocol outlines a cell-free tissue engineering strategy using mesenchymal stem cell (MSC)-derived exosomes loaded into a biomaterial scaffold to promote bone regeneration in critical-sized defects [68].
Principle and Objective
MSC-derived exosomes carry pro-osteogenic miRNAs, proteins, and lipids that can stimulate osteoblast proliferation and differentiation. Loading these exosomes into a biomaterial scaffold (e.g., hyaluronic acid hydrogel) provides a protective niche, enables sustained release, and enhances retention at the defect site, overcoming the limitations of direct cell transplantation [68].
Materials and Reagents
- Exosome Source: Conditioned medium from human MSCs (e.g., BM-MSCs, UC-MSCs).
- Isolation Kits: Total Exosome Isolation Kit or reagents for differential ultracentrifugation.
- Biomaterial Scaffold: Hyaluronic acid (HA) hydrogel or other osteoconductive scaffold (e.g., collagen, tricalcium phosphate).
- Characterization Antibodies: Anti-CD9, anti-CD63, anti-CD81.
- Animal Model: Critical-sized calvarial defect model in rats.
Step-by-Step Procedure
- Exosome Isolation:
- Culture MSCs until 80% confluency. Replace with serum-free media for 48 hours to collect conditioned medium.
- Centrifuge the conditioned medium at 2,000 × g for 30 minutes to remove cells and debris.
- Further centrifuge the supernatant at 10,000 × g for 45 minutes to remove larger vesicles.
- Isolate exosomes from the resulting supernatant by ultracentrifugation at 100,000 × g for 70 minutes, or using a commercial polymer-based precipitation kit. Resuspend the pellet in PBS and filter-sterilize (0.22 µm) [68].
- Exosome Characterization:
- Nanoparticle Tracking Analysis (NTA): Determine the size distribution and concentration of particles.
- Transmission Electron Microscopy (TEM): Confirm the cup-shaped morphology of exosomes.
- Western Blotting: Verify the presence of positive markers (CD9, CD63, CD81) and the absence of negative markers (e.g., calnexin) [68].
- Scaffold Loading and Implantation:
- Mix the purified exosomes (e.g., 100-200 µg total protein) with the hydrogel precursor solution. Induce gelation according to the manufacturer's instructions to form the exosome-laden scaffold.
- In a rat calvarial defect model, implant the exosome-loaded hydrogel into the critical-sized defect.
- For controls, use an empty defect and a hydrogel-only scaffold.
- Outcome Assessment:
- Micro-Computed Tomography (µCT): Perform at 4, 8, and 12 weeks post-implantation to quantify new bone volume and bone mineral density.
- Histological and Immunohistochemical Staining: At endpoint, process explanted tissue for H&E, Masson's Trichrome, and Osteocalcin staining to visualize new bone formation and osteogenic activity [68].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Gene Editing and mRNA Delivery in Tissue Engineering
| Reagent / Solution | Function / Application | Key Considerations |
|---|---|---|
| CHIR99021 | GSK-3β inhibitor; activates Wnt signaling to initiate hiPSC differentiation [63] | Concentration and timing are critical for efficient cardiac lineage specification. |
| Puromycin Dihydrochloride | Selection antibiotic for cells with integrated resistance genes post-transfection [63] | Dose-response must be determined for each cell type to optimize kill curve. |
| Lipid Nanoparticles (LNPs) | Synthetic delivery system for mRNA and RNP in vivo [64] [65] | Formulation (ionizable lipid:PEG-lipid:helper lipid) determines efficiency and tropism. |
| VSV-G Envelope Protein | Pseudotypes lentivirus or ARMMs; broadens tropism and enhances vesicle budding [66] | Confers enhanced stability and fusion capability to delivered vesicles. |
| Hyaluronic Acid (HA) Hydrogel | Biomaterial scaffold for exosome/cell delivery; provides a hydrated 3D microenvironment [68] | Can be modified with RGD peptides to improve cell adhesion; allows controlled release. |
| Rho Kinase (ROCK) Inhibitor | Improves survival of dissociated hiPSCs after passaging or transfection [63] | Essential for maintaining viability in single-cell cloning steps. |
Workflow and Signaling Pathways
Workflow for Generating Gene-Edited Tissue Constructs
The following diagram illustrates the integrated workflow for creating enhanced tissue-engineered constructs using gene-edited stem cells.
Generation of Gene-Edited Tissue Constructs
Signaling Pathways in Bone Regeneration via MSC-Exosomes
This diagram outlines the key signaling pathways activated by MSC-derived exosomes to promote bone regeneration, a key process in exosome-based tissue engineering strategies.
Exosome-mediated Bone Regeneration Pathways
Optimizing Biomaterial Degradation Rates and Immune Compatibility
The success of tissue engineering strategies combining stem cells with biomaterial scaffolds hinges on two critical and interconnected properties: the degradation rate of the biomaterial and its compatibility with the host immune system. An ideal scaffold provides temporary mechanical support and a conducive microenvironment for stem cell proliferation and differentiation, degrading in a controlled manner as new tissue forms. Conversely, uncontrolled degradation can lead to premature structural failure or the release of harmful byproducts, while poor immune compatibility can trigger chronic inflammation, fibrous encapsulation, and ultimately, implant failure [69] [70]. This Application Note provides detailed protocols and frameworks for systematically evaluating and optimizing these essential parameters to ensure the translational success of advanced tissue engineering constructs.
Quantitative Profiling of Biomaterial Degradation
Accurately monitoring degradation is essential to ensure the scaffold maintains integrity until the new tissue can bear load and degrades completely without residue. The following protocols and table summarize key parameters and methods.
Table 1: Key Parameters and Methods for Biomaterial Degradation Assessment
| Parameter | Standard Method | Measurement Output | Inferences & Limitations |
|---|---|---|---|
| Mass Loss | Gravimetric Analysis (ASTM F1635-11) | Percentage weight loss over time; precision of 0.1% required [69]. | Infers surface erosion & bulk degradation. Limitation: Cannot distinguish dissolution from degradation [69]. |
| Molecular Weight Change | Size Exclusion Chromatography (SEC), Solution Viscosity [69] | Decrease in average molecular weight (Mw, Mn) over time. | Confirms backbone cleavage and bulk degradation. Essential for understanding mechanical decay [69]. |
| Morphological Changes | Scanning Electron Microscopy (SEM) [69] [71] | Visual assessment of surface erosion, pore structure collapse, and crack formation. | Qualitatively infers degradation mode. Limitation: Requires solid, insoluble samples; may not reflect bulk changes [69]. |
| Chemical Composition | Fourier Transform Infrared Spectroscopy (FTIR), Nuclear Magnetic Resonance (NMR) [69] | Loss of specific functional groups (e.g., ester, amide), appearance of degradation by-products. | Confirms degradation by identifying chemical bond cleavage [69]. |
Protocol: Gravimetric Analysis for Mass Loss
Objective: To quantitatively measure the mass loss of a solid biomaterial scaffold during in vitro degradation.
Materials:
- Pre-weighed dry biomaterial scaffolds (e.g., 3D-printed PCL, PLA)
- Degradation medium (e.g., Phosphate Buffered Saline (PBS), pH 7.4, with or without enzymes like Collagenase or MMPs)
- Incubator/shaker bath maintained at 37°C
- Analytical balance (precision ±0.01 mg)
- Vacuum oven or desiccator
Procedure:
- Initial Mass (M₀): Dry scaffolds to a constant weight in a vacuum oven. Record the initial dry mass (M₀) for each sample (n≥5).
- Immersion: Immerse each scaffold in a sufficient volume of degradation medium (e.g., 20 mL per 100 mg scaffold) in sealed containers.
- Incubation: Place containers in an incubator at 37°C with constant agitation (e.g., 60 rpm).
- Sampling & Medium Refreshment: At predetermined time points (e.g., days 1, 3, 7, 14, 28), remove samples from the incubation medium (n=3 per time point). Replace the degradation medium entirely to maintain pH and enzyme activity.
- Final Mass (Mₜ): Gently rinse retrieved samples with deionized water to remove salts. Dry them to a constant weight in a vacuum oven and record the final dry mass (Mₜ).
- Calculation: Calculate the percentage mass loss at each time point: Mass Loss (%) = [(M₀ - Mₜ) / M₀] × 100.
Protocol: Monitoring Molecular Weight via Size Exclusion Chromatography (SEC)
Objective: To track changes in the molecular weight of the polymeric scaffold, indicating backbone cleavage.
Materials:
- Degraded scaffold samples (from Protocol 2.1)
- Appropriate SEC solvent (e.g., Tetrahydrofuran for polyesters)
- SEC system with refractive index (RI) and light scattering detectors
- SEC columns (e.g., Phenogel columns)
Procedure:
- Sample Preparation: Dissolve a known mass (~2-5 mg) of the degraded scaffold in the SEC solvent. Filter the solution through a 0.45 μm PTFE syringe filter.
- SEC Analysis: Inject the filtered solution into the SEC system. Use narrow dispersity polymer standards to calibrate the system.
- Data Analysis: Determine the number-average (Mₙ) and weight-average (M𝓌) molecular weights for the sample at each time point. Plot Mₙ/M₀ or M𝓌/M₀ over time to visualize the degradation profile.
Assessing and Engineering Immune Compatibility
The host immune response, particularly from macrophages, is a decisive factor for integration. Smart biomaterials are now designed not to be inert but to actively modulate the immune system towards a pro-regenerative (M2) state and away a pro-inflammatory (M1) state [70] [72].
Table 2: Key Techniques for Characterizing Immune Response to Biomaterials
| Target Aspect | Characterization Technique | Key Readouts | Interpretation |
|---|---|---|---|
| Macrophage Polarization | Immunofluorescence/Flow Cytometry | Surface Markers: CD86 (M1), CD206 (M2). Cytokine Secretion: TNF-α (M1), IL-10 (M2) [70]. | Determines the phenotype of immune cells interacting with the scaffold. A high M2/M1 ratio is indicative of pro-regenerative environment. |
| Foreign Body Response (FBR) | Histology (H&E, Trichrome Staining) | Thickness of fibrous capsule, density of immune cells at material interface [70]. | A thin, non-dense capsule suggests good biocompatibility. A thick, cellular capsule indicates a chronic FBR. |
| In Vivo Integration & Angiogenesis | Immunohistochemistry | Staining for CD31 (PECAM-1) for blood vessels, α-SMA for myofibroblasts and vessels [71]. | Quantification of vascularization within and around the implant indicates successful integration and nutrient supply. |
Protocol: In Vitro Macrophage Polarization Assay
Objective: To evaluate the immunomodulatory potential of a biomaterial by assessing its ability to drive macrophage polarization towards a pro-regenerative M2 phenotype.
Materials:
- Murine macrophage cell line (e.g., RAW 264.7) or primary human monocyte-derived macrophages
- Biomaterial extract or direct contact setup (sterile material discs)
- Cell culture plates (24-well)
- Lipopolysaccharide (LPS) for M1 polarization
- IL-4 for M2 polarization
- Flow cytometry antibodies: Anti-CD86 (FITC), Anti-CD206 (PE)
- ELISA kits for TNF-α and IL-10
Procedure:
- Cell Seeding & Stimulation: Seed macrophages in a 24-well plate. Divide into groups:
- Group 1 (M1 Control): Culture with LPS (e.g., 100 ng/mL).
- Group 2 (M2 Control): Culture with IL-4 (e.g., 20 ng/mL).
- Group 3 (Test): Culture directly on biomaterial discs or with concentrated biomaterial extract.
- Group 4 (Naïve): Culture in standard medium.
- Incubation: Incubate cells for 24-48 hours.
- Analysis:
- Flow Cytometry: Harvest cells, stain with CD86 and CD206 antibodies, and analyze by flow cytometry. Calculate the ratio of CD206+ (M2) to CD86+ (M1) cells.
- Cytokine ELISA: Collect culture supernatants and measure the concentrations of TNF-α (M1 marker) and IL-10 (M2 marker) using ELISA.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Biomaterial Degradation and Immune Compatibility Studies
| Reagent/Material | Function & Application | Example & Notes |
|---|---|---|
| Polydioxanone (PDS) | A synthetic, biodegradable polymer used for sutures and scaffolds; model polymer for degradation studies [73]. | Allows study of ester bond hydrolysis; degradation rate is tunable via processing. |
| pH-Sensitive Polymers | Scaffolds that degrade or change properties in acidic environments (e.g., tumors, inflammatory sites) [70] [72]. | Polymers with hydrazone, acetal, or orthoester bonds; used for targeted drug delivery. |
| Enzyme-Responsive Materials | Scaffolds designed to degrade in response to specific enzymes (e.g., MMPs in healing wounds) [70] [72]. | Hyaluronic acid-based scaffolds cleavable by hyaluronidase; enables cell-responsive degradation. |
| LPS (Lipopolysaccharide) | A potent activator of macrophages; used as a positive control to induce the pro-inflammatory M1 phenotype in vitro [70]. | Standard quality from E. coli; used at ng/mL concentrations in cell culture. |
| Recombinant IL-4 | A cytokine that drives macrophage polarization towards the pro-regenerative M2 phenotype; used as a positive control [70]. | Essential for validating the M2 state in control groups in polarization assays. |
| Anti-CD86 & Anti-CD206 Antibodies | Key cell surface markers for identifying M1 (CD86) and M2 (CD206) macrophage populations via flow cytometry [70]. | Conjugated to different fluorophores (e.g., FITC, PE) for simultaneous staining. |
Clinical Translation, Regulatory Pathways, and Efficacy Analysis
The integration of stem cells with biomaterial scaffolds represents a foundational strategy in advanced tissue engineering, aimed at overcoming the limitations of conventional regenerative approaches. Mesenchymal stem cells (MSCs) and induced pluripotent stem cells (iPSCs) have emerged as two of the most prominent cell sources for these applications [6] [74]. MSCs, with their multipotent differentiation capacity, immunomodulatory properties, and paracrine activity, are particularly suited for repairing mesodermal tissues and modulating the immune response to engineered constructs [6] [75]. iPSCs, possessing unlimited self-renewal and the potential to differentiate into any cell type, offer a platform for generating patient-specific tissues and overcoming the scarcity of primary cells [76] [74]. The combination of these cells with biomaterial scaffolds provides a supportive, three-dimensional microenvironment that enhances cell survival, guides tissue formation, and improves the overall efficacy and translation of regenerative therapies [77] [74]. This Application Note synthesizes the most recent efficacy data from clinical trials utilizing MSCs and iPSCs, providing detailed protocols and analytical frameworks to guide researchers in the field.
Global Clinical Trial Landscape and Efficacy Data
Mesenchymal Stem Cell (MSC) Clinical Trials
MSC-based therapies have been investigated in hundreds of clinical trials across a diverse range of medical conditions. The therapeutic effects of MSCs are primarily mediated through their potent paracrine activity and immunomodulatory functions, rather than long-term engraftment and differentiation [6] [75]. They release bioactive molecules, including growth factors, cytokines, and extracellular vesicles (EVs), which play crucial roles in modulating the local cellular environment, promoting tissue repair, angiogenesis, and exerting anti-inflammatory effects [6].
Table 1: Efficacy Data from Recent MSC Clinical Trials
| Medical Indication | Trial Details (Source, Design) | Key Efficacy Outcomes | Reported Adverse Events |
|---|---|---|---|
| Knee Osteoarthritis (KOA) | Source: Bone Marrow, Adipose; 16 RCTs (N=622) [78] | Significant improvement in WOMAC and VAS pain/function scores at 3, 6, and 12 months. Repeated injections superior to single injection at 6 & 12 months. | Higher incidence of adverse events with repeated injections. |
| Inflammatory & Autoimmune Diseases | Source: Bone Marrow (e.g., Remestemcel-L); Phase 3 RCTs [75] | First FDA-approved MSC therapy for pediatric steroid-refractory acute Graft-versus-Host Disease (GVHD). Demonstrated improved response rates. | Well-documented safety profile with no significant infusion reactions or related malignancy. |
| Wound Healing | Source: Various (e.g., Placental, Umbilical Cord); 96 registered trials [37] | Promising results in diabetic foot ulcers and burns; accelerates re-epithelialization and vascularization. | Limited by harsh wound microenvironment affecting cell survival. |
| Lung Diseases (via MSC-EVs) | Source: Various; Analysis of 66 trials [79] | Nebulized MSC-EVs achieved therapeutic effects at lower doses (~10^8 particles) vs. intravenous route. | Lack of standardized dosing and reporting. |
A recent network meta-analysis of 16 randomized controlled trials for knee osteoarthritis (KOA) provides robust, quantitative efficacy data. The analysis concluded that MSC therapy significantly improves pain and functional scores compared to controls (e.g., hyaluronic acid, saline) [78]. Furthermore, it directly compared administration protocols, finding that repeated MSC injections provided greater and more durable improvements in WOMAC and VAS scores at 6 and 12 months compared to a single injection, though with a higher incidence of adverse events [78]. This highlights the critical balance between efficacy and safety in treatment regimen design.
The translation of MSC therapies has been challenging, with many trials failing to meet their efficacy endpoints despite a consistent safety record [75]. The first FDA-approved MSC therapy in the U.S., Remestemcel-L, for pediatric steroid-refractory acute GVHD, marks a significant milestone, validating the potential of MSC-based products [75].
Induced Pluripotent Stem Cell (iPSC) Clinical Trials
The clinical landscape for iPSCs is younger and more emerging than for MSCs, but it is rapidly evolving. The unique value proposition of iPSCs lies in their unlimited self-renewal and ability to be differentiated into any cell type for therapeutic use, enabling the creation of off-the-shelf, standardized cell products [76] [80].
Table 2: Emerging Clinical Trial Data for iPSC-Based Therapies
| Medical Indication | Therapeutic Product / Approach | Key Efficacy Findings | Trial Status & Challenges |
|---|---|---|---|
| Systemic Lupus Erythematosus (SLE) | FT819: Off-the-shelf, iPSC-derived CD19-targeted CAR T-cells [80] | Phase 1 data presented demonstrating safety and efficacy with a fludarabine-free conditioning regimen. | Ongoing Phase 1 trial; designed to evaluate safety and activity. |
| Ocular Disorders, Cardiac Conditions, Cancer | Various iPSC-derived cell products (e.g., retinal cells, cardiomyocytes) [76] | Early promise shown in treating a wide range of diseases. | 10 published studies (N=115 total); studies are small, uncontrolled, and highly variable. |
| Platelet Transfusion | iPSC-derived platelets [76] | Investigated as a source for transfusion. | Among 22 ongoing registered trials. |
A systematic scoping review from 2025 identified only 10 published clinical studies utilizing iPSCs, treating a total of 115 patients [76]. The studies are characterized by their small scale, lack of control groups, and significant variability in study design, medical conditions, and the specific iPSC-derived cell products administered [76]. This heterogeneity complicates the consolidation of efficacy data at this early stage.
However, promising clinical candidates are advancing. For instance, Fate Therapeutics' FT819, an off-the-shelf, iPSC-derived CAR T-cell product candidate for autoimmune diseases like SLE, has reported Phase 1 safety and efficacy data [80]. This represents a shift from patient-specific autologous therapies towards standardized, mass-produced allogeneic cell products, potentially broadening patient access [80].
Detailed Experimental Protocols
Protocol for Intra-Articular MSC Injection in Knee Osteoarthritis
This protocol is derived from the synthesis of multiple RCTs included in the 2025 network meta-analysis [78].
3.1.1 Cell Source and Preparation:
- Source Selection: Isolate MSCs from bone marrow aspirate or adipose tissue (lipoaspirate). Adherence to ISCT criteria is mandatory: plastic adherence, expression of CD73, CD90, CD105 (≥95%), and lack of hematopoietic markers (CD34, CD45, HLA-DR, etc. ≤2%), with trilineage differentiation potential [6] [78].
- Expansion and Harvesting: Culture cells in standard medium (e.g., α-MEM) supplemented with 10-20% fetal bovine serum (FBS) or platelet lysate. Use cells at passages 3-5 to maintain potency and prevent senescence. Prior to injection, detach cells using a non-enzymatic cell dissociation solution or trypsin/EDTA, and wash thoroughly to remove all traces of enzymes and serum. Re-suspend in sterile, clinical-grade normal saline or lactated Ringer's solution at the final concentration.
- Quality Control: Perform endotoxin testing, sterility testing, and viability analysis (must be >90%) immediately prior to release for injection. Characterize cell surface markers via flow cytometry for each batch.
3.1.2 Patient Preparation and Injection Technique:
- Screening: Confirm KOA diagnosis via radiographic imaging (Kellgren-Lawrence grading) and symptomatic assessment (WOMAC, VAS).
- Injection Procedure: Position the patient supine with the knee extended or slightly flexed. Under aseptic conditions, perform a lateral or medial parapatellar approach. After local anesthesia, use a 21-22 gauge needle for intra-articular injection. The typical injected volume ranges from 2-5 mL containing a cell dose of 1-100 x 10^6 MSCs, depending on the trial protocol [78].
- Post-Injection Care: Instruct the patient to rest the joint for 24-48 hours, avoiding strenuous activity for 2-4 weeks. Clinical follow-ups for efficacy (WOMAC, VAS) and safety should be scheduled at 1, 3, 6, and 12 months post-injection.
3.1.3 Protocol Variation for Repeated Injections:
- Based on the meta-analysis findings, a protocol for repeated injections can be designed with two to three injections of a lower cell dose (e.g., 10-20 x 10^6 cells), administered 3-6 months apart [78]. This regimen requires rigorous monitoring for increased incidence of adverse events, such as transient synovitis or joint pain.
Protocol for MSC-Derived Extracellular Vesicle (EV) Nebulization
This protocol outlines the production and administration of MSC-EVs for respiratory conditions, based on the analysis of clinical trials registered between 2014-2024 [79].
3.2.1 MSC-EV Isolation and Characterization:
- Cell Culture and EV Production: Culture MSCs from a selected source (e.g., Umbilical Cord) until 70-80% confluency. Replace medium with a serum-free, EV-depleted medium for 48 hours. Collect the conditioned medium.
- EV Isolation: Isolate EVs from the conditioned medium using sequential ultracentrifugation: first at 300 × g to remove cells, then 2,000 × g to remove dead cells, followed by 10,000 × g to remove cell debris, and finally ultracentrifugation at 100,000 × g for 70-120 minutes to pellet EVs. Re-suspend the EV pellet in sterile phosphate-buffered saline (PBS).
- Characterization and Quality Control: Characterize EVs using three complementary methods: 1) Nanoparticle Tracking Analysis (NTA) to determine particle size distribution and concentration (targeting 30-150 nm for exosomes); 2) Transmission Electron Microscopy (TEM) to confirm cup-shaped morphology; and 3) Flow Cytometry or Western Blot to detect positive (CD9, CD63, CD81) and negative (calnexin) surface markers [79].
- Dosing: The effective dose for nebulization is approximately 10^8 particles, significantly lower than intravenous requirements [79].
3.2.2 Nebulization Administration:
- Device Setup: Use a vibrating mesh nebulizer to minimize shear stress and preserve EV integrity. Connect the device to an oxygen source or compressor.
- Administration: Load the prepared EV suspension into the nebulizer cup. Instruct the patient to breathe normally through the mouthpiece until the solution is fully aerosolized (typically 10-15 minutes). The aerosolized particles should have a mass median aerodynamic diameter (MMAD) of 1-5 µm for optimal alveolar deposition.
Signaling Pathways and Mechanisms of Action
The therapeutic efficacy of MSCs and iPSCs is mediated through complex, overlapping signaling pathways that regulate tissue repair and immune modulation. Understanding these mechanisms is critical for rational therapy design.
Immunomodulatory Pathways of MSCs
MSCs interact with a wide array of immune cells, shifting the balance from a pro-inflammatory to an anti-inflammatory and pro-regenerative state, which is crucial for the integration of tissue-engineered constructs [6] [75].
Diagram 1: MSC Immunomodulatory Signaling Pathways. MSCs secrete factors that modulate innate and adaptive immunity. Key pathways include macrophage polarization to an anti-inflammatory M2 phenotype, inhibition of T-cell proliferation, promotion of regulatory T-cells, and enhancement of neutrophil function [6] [75] [37].
Tissue Repair and Paracrine Signaling Pathways
The primary mechanism through which MSCs facilitate tissue repair is paracrine signaling, mediated by secreted growth factors, cytokines, and extracellular vesicles (EVs) [6] [75] [37].
Diagram 2: MSC-Mediated Tissue Repair Pathways. MSCs promote repair through direct differentiation and potent paracrine activity. They secrete factors that drive angiogenesis (VEGF, FGF), re-epithelialization (EGF, KGF), and extracellular matrix (ECM) remodeling. MSC-derived extracellular vesicles (MSC-EVs) transfer regulatory miRNAs that further enhance these processes [6] [75] [74].
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of stem cell therapy protocols requires a standardized set of high-quality reagents and materials. The following table details key components for MSC and iPSC research and manufacturing.
Table 3: Essential Research Reagents for Stem Cell Therapy Development
| Reagent / Material | Function / Application | Examples & Key Characteristics |
|---|---|---|
| Cell Isolation Kits | Isolation of MSCs from tissue sources (BM, AD). | Kits for bone marrow mononuclear cell separation (e.g., Ficoll-Paque density gradient); Collagenase enzymes for adipose tissue digestion. |
| Culture Media & Supplements | In vitro expansion and maintenance of MSCs/iPSCs. | Basal media (α-MEM, DMEM); Serum supplements (FBS, Human Platelet Lysate); Essential supplements (L-glutamine, ascorbic acid). |
| Characterization Antibodies | Flow cytometry analysis of cell surface markers. | Antibody panels against positive markers (CD73, CD90, CD105) and negative markers (CD34, CD45, HLA-DR) per ISCT criteria [6]. |
| Trilineage Differentiation Kits | In vitro confirmation of MSC multipotency. | Defined, serum-free kits for osteogenic, chondrogenic, and adipogenic differentiation with specific inducers. |
| EV Isolation Reagents | Isolation and purification of extracellular vesicles. | Ultracentrifugation reagents; Size-exclusion chromatography (SEC) columns; Polymer-based precipitation kits. |
| EV Characterization Tools | Quantification and validation of isolated EVs. | Nanoparticle Tracking Analysis (NTA) systems; Antibodies for exosome markers (CD9, CD63, CD81) for WB/flow cytometry. |
| Biomaterial Scaffolds | 3D support structure for cell delivery and tissue growth. | Natural (collagen, fibrin, hyaluronic acid) and synthetic (PLA, PLGA) polymers in porous, hydrogel, or fibrous forms [77] [74] [37]. |
| iPSC Reprogramming Factors | Generation of iPSCs from somatic cells. | Sendai viral vectors, episomal plasmids, or mRNA encoding Yamanaka factors (OCT3/4, SOX2, KLF4, c-MYC) [74]. |
The global clinical trial landscape for MSC and iPSC therapies is dynamic and maturing. Robust efficacy data, particularly for MSCs in conditions like knee osteoarthritis and GVHD, is accumulating, leading to the first regulatory approvals. The field is moving beyond simple cell injection towards sophisticated protocols involving repeated dosing, optimized delivery routes like nebulization for EVs, and the use of engineered cells. While iPSC clinical applications are at an earlier stage, they hold immense promise for generating standardized, off-the-shelf cell products. The continued integration of these advanced cell therapies with biomaterial scaffolds is poised to enhance cell survival, retention, and functional integration, ultimately driving the next generation of regenerative medicine solutions. Future work must focus on standardizing protocols, establishing potency assays, and conducting large-scale, well-controlled trials to fully realize the therapeutic potential of these powerful cellular platforms.
FDA-Approved Stem Cell Products and RMAT Designations (2023-2025)
The period from 2023 to 2025 has marked a significant acceleration in the development and regulatory approval of advanced regenerative medicine products, particularly those combining stem cell technologies with sophisticated biomaterial scaffolds. These innovations represent a paradigm shift in therapeutic strategies for conditions previously considered intractable, including genetic disorders, solid tumors, and degenerative diseases [81]. The convergence of cell biology and materials science has enabled the creation of complex tissue engineering constructs that replicate native tissue microenvironments while providing the mechanical and biochemical cues necessary for functional regeneration [11] [12].
The Regenerative Medicine Advanced Therapy (RMAT) designation, established under the 21st Century Cures Act, has been instrumental in accelerating this progress by providing an expedited development pathway for products addressing unmet medical needs in serious conditions [82]. This designation, coupled with advances in biomaterial scaffold design, has created a fertile environment for translating basic research into clinically impactful therapies. These application notes detail the approved products, their technical specifications, and the experimental methodologies essential for researchers working at the intersection of stem cell biology and tissue engineering.
Tabulated Regulatory Approvals and Designations (2023-2025)
FDA-Approved Stem Cell and Combined Products
Table 1: FDA-Approved Stem Cell and Related Products (2023-2025)
| Product Name | Company/Institution | Approval Date | Technology Type | Indication |
|---|---|---|---|---|
| CASGEVY (exagamglogene autotemcel) | Vertex Pharmaceuticals | Dec 2023 [83] | Gene-edited autologous CD34+ cells | Sickle cell disease [83] |
| LYFGENIA (lovotibeglogene autotemcel) | bluebird bio, Inc. | Dec 2023 [83] | Autologous cell-based gene therapy | Sickle cell disease with history of vaso-occlusive events [83] |
| LENMELDY (atidarsagene autotemcel) | Orchard Therapeutics | Mar 2024 [83] | Autologous hematopoietic stem cell gene therapy | Metachromatic leukodystrophy (MLD) [83] |
| AMTAGVI (lifileucel) | Iovance Biotherapeutics | Feb 2024 [83] | Tumor-infiltrating lymphocytes (TIL) | Unresectable or metastatic melanoma [83] |
| RYONCIL (remestemcel-L) | Mesoblast, Inc. | Dec 2024 [84] | Allogeneic bone marrow-derived mesenchymal stem cells | Pediatric steroid-refractory acute graft versus host disease [81] |
| OMISIRGE (omidubicel-onlv) | Gamida Cell Ltd. | Apr 2023 [81] | Nicotinamide-modified umbilical cord blood-derived hematopoietic progenitor cells | Hematologic malignancies undergoing cord blood transplantation [81] |
| ZEVASKYN (prademagene zamikeracel) | Abeona Therapeutics Inc. | Apr 2025 [83] | Gene therapy | Recessive dystrophic epidermolysis bullosa (RDEB) [83] |
RMAT Designations Transitioning to Approval
Table 2: Recent RMAT Designations with Regulatory Status
| Product/Asset | Company | RMAT Date | Approval Status | Therapeutic Area |
|---|---|---|---|---|
| Obecabtagene autoleucel (obe-cel) | Autolus Therapeutics | Apr 2022 [85] | Approved Nov 2024 [83] | B-cell Acute Lymphocytic Leukemia [83] |
| Valoctocogene roxaparvovec | BioMarin Pharmaceutical | Mar 2021 [85] | Approved Jun 2023 [83] | Severe hemophilia A [83] |
| Lovo-cel (Lyfgenia) | bluebird bio | Oct 2017 [85] | Approved Dec 2023 [83] | Severe sickle cell disease [83] |
| Exagamglogene autotemcel (Casgevy) | Vertex Pharmaceuticals | N/A [84] | Approved Dec 2023 [83] | Sickle cell disease and beta thalassemia [84] |
| Rethymic | Enzyvant Therapeutics | N/A | Approved Oct 2021 [83] | Congenital athymia [83] |
Experimental Protocols for Product Characterization
Protocol: Characterization of 3D Biomaterial Scaffolds for Cell Delivery
Purpose: To evaluate the physical properties and biological compatibility of biomaterial scaffolds used in stem cell delivery systems, ensuring they meet criteria for cell viability, differentiation, and functional integration [11] [12].
Materials:
- Porous scaffold materials (collagen, hyaluronic acid, silk fibroin, chitosan, or synthetic polymers)
- Stem cell population (MSCs, iPSCs, or tissue-specific progenitors)
- Differentiation media (chondrogenic, osteogenic, or lineage-specific)
- Mechanical testing system (compression/tension capable)
- Scanning Electron Microscope (SEM)
- Live/Dead viability assay kit (calcein-AM/ethidium homodimer)
- qPCR equipment and lineage-specific primers
Procedure:
- Scaffold Fabrication: Prepare scaffolds using freeze-drying, electrospinning, or 3D bioprinting techniques to achieve porosity of 70-90% with pore sizes ranging 100-300μm [12].
- Mechanical Characterization:
- Assess compressive modulus using uniaxial compression testing at 0.1-1mm/min strain rate
- Target mechanical properties matching native tissue: 0.02-1.16 MPa for cartilage superficial zone; 6.44-7.75 MPa for deep zone [12]
- Scaffold Sterilization: Employ gamma irradiation (25-35 kGy) or ethylene oxide treatment followed by degassing for 24-48 hours
- Cell Seeding:
- Trypsinize and resuspend cells at 5-20×10^6 cells/mL in appropriate medium
- Apply cell suspension drop-wise to scaffold (50-100μL per 5mm thickness)
- Incubate 2-4 hours for initial attachment before adding culture medium
- Viability Assessment (Days 1, 3, 7, 14):
- Incubate scaffold constructs with Live/Dead stain (2μM calcein-AM, 4μM ethidium homodimer) for 45 minutes at 37°C
- Image using confocal microscopy; calculate viability percentage from 5 random fields
- Differentiation Capacity (Day 14-28):
- Maintain in lineage-specific differentiation media with biweekly changes
- Analyze gene expression (SOX9, COL2A1, ACAN for chondrogenesis; RUNX2, OPN for osteogenesis)
- Perform histological staining (Alcian Blue for proteoglycans, Alizarin Red for mineralization)
Troubleshooting:
- Poor cell infiltration: Increase scaffold porosity or incorporate channel structures
- Rapid scaffold degradation: Adjust crosslinking density (e.g., genipin concentration for natural polymers)
- Inconsistent differentiation: Pre-condition scaffolds with growth factors (TGF-β3 for chondrogenesis, BMP-2 for osteogenesis)
Protocol: Functional Validation of Stem Cell-Scaffold Constructs in Preclinical Models
Purpose: To evaluate the therapeutic efficacy and safety profile of stem cell-biomaterial constructs in relevant animal models, providing critical preclinical data for regulatory submissions including RMAT designation requests.
Materials:
- Immunocompromised rodents (NU/NU mice or similar) or large animal models (ovine, porcine)
- Surgical equipment for orthotopic implantation
- In vivo imaging system (bioluminescence/fluorescence)
- Histology processing equipment and specific antibodies for immunohistochemistry
- Behavioral/functional assessment tools (gait analysis, force plate assessment)
Procedure:
- Construct Preparation:
- Seed scaffolds with clinically-relevant cell density (5-20×10^6 cells/cm³)
- Pre-differentiate for 7-14 days if lineage commitment is required pre-implantation
- Confirm viability >80% immediately before implantation
- Surgical Implantation (Cartilage Defect Model Example):
- Create critical-sized defect (e.g., 3-6mm diameter in trochlear groove)
- Trim construct to precise defect dimensions
- Press-fit implant ensuring flush integration with native tissue
- Secure with fibrin glue if necessary
- Post-operative Monitoring:
- Assess functional recovery weekly (weight-bearing, locomotion)
- Perform in vivo imaging at 2, 4, and 8 weeks if cells are labeled
- Endpoint Analysis (8-12 weeks):
- Euthanize animals and harvest construct with surrounding native tissue
- Process for histology (fix in 4% PFA, decalcify if osseous, paraffin embed)
- Section at 5-8μm thickness for H&E, Safranin-O, and Masson's Trichrome staining
- Perform immunohistochemistry for tissue-specific markers (collagen type II, aggrecan)
- Mechanical Assessment:
- Evaluate compressive properties of regenerated tissue
- Compare to native tissue values and empty defect controls
Quality Controls:
- Include empty scaffold and cell-only controls
- Use minimum n=8-10 per group for statistical power
- Blind assessments during histological and functional analyses
Visual Workflows for Product Development and Regulation
RMAT to Approval Pathway
Figure 1: Pathway from RMAT Designation to FDA Approval
Tissue Engineering Product Development Workflow
Figure 2: Tissue Engineering Product Development
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Stem Cell-Scaffold Engineering
| Material/Reagent | Supplier Examples | Key Function | Application Notes |
|---|---|---|---|
| Type I/II Collagen | Advanced BioMatrix, Sigma-Aldrich | Natural polymer scaffold providing cell adhesion sites | Type II preferred for chondrogenic differentiation; crosslink for stability [12] |
| Hyaluronic Acid (HA) | Lifecore Biomedical, Sigma-Aldrich | Glycosaminoglycan component of native ECM | Modify with methacrylate groups for photopolymerization [12] |
| Silk Fibroin | Silk Inc., Ajinomoto | High mechanical strength natural polymer | Superior to collagen in maintaining chondrocyte phenotype [12] |
| Chitosan | Sigma-Aldrich, NovaMatrix | Crustacean-derived polysaccharide with antimicrobial properties | Used in clinical scaffolds for osteochondral lesions [12] |
| Gelatin-Methacryloyl (GelMA) | Cellink, Advanced BioMatrix | Photocrosslinkable hydrogel with RGD sequences | Tunable mechanical properties via UV crosslinking density [12] |
| Mesenchymal Stem Cells | Lonza, ATCC | Multipotent stromal cells with immunomodulatory properties | Bone marrow-derived most common; iMSCs gaining traction [81] |
| iPSC-Derived Progenitors | REPROCELL, Fujifilm | Pluripotent stem cell-derived lineage-specific cells | Enhanced consistency and scalability vs primary cells [81] |
| TGF-β3 | PeproTech, R&D Systems | Inducer of chondrogenic differentiation | Use at 10ng/mL in 3D culture; combine with BMP-6 for synergy [12] |
| Live/Dead Viability Kit | Thermo Fisher, Biotium | Dual fluorescence staining for cell viability | Calcein-AM (live, green); Ethidium homodimer (dead, red) [12] |
The integration of advanced stem cell technologies with sophisticated biomaterial scaffolds has created unprecedented opportunities for addressing complex medical conditions through regenerative medicine approaches. The regulatory landscape, particularly through the RMAT designation pathway, has adapted to facilitate the translation of these innovative technologies while maintaining rigorous safety and efficacy standards [82]. The approval of groundbreaking therapies such as CASGEVY, LYFGENIA, and RYONCIL between 2023 and 2025 demonstrates the successful convergence of biological and engineering principles in clinical practice [83] [81].
Future developments in this field will likely focus on enhancing the biofunctionality of scaffolds through incorporation of nanotechnologies, spatial control of biochemical cues, and improved mechanical compatibility with native tissues [11] [12]. The emergence of iPSC-derived therapeutic cells and the increasing use of allogeneic cell sources will further transform the landscape, potentially improving accessibility and reducing costs [81]. As these technologies mature, the continued collaboration between regulatory scientists, tissue engineers, and clinical researchers will be essential to ensure that promising innovations successfully navigate the path from laboratory discovery to clinical implementation.
Comparative Analysis of International Regulatory Frameworks
This document provides a detailed comparative analysis of the international regulatory frameworks governing tissue-engineered medical products (TEMPs), with a specific focus on combinatorial products incorporating stem cells and biomaterial scaffolds. For researchers and drug development professionals, navigating the diverse regulatory pathways across major jurisdictions is a critical step in clinical translation. This application note summarizes the core regulatory principles, classifies product types based on key characteristics, and provides a standardized experimental protocol for preclinical evaluation of scaffold-based therapies, complete with visualization tools and essential research reagents.
The field of tissue engineering, which combines scaffolds, cells, and biologically active molecules into functional tissues, holds immense promise for restoring, maintaining, or improving damaged tissues and whole organs [86]. The primary societal mission of this biomedical research and its clinical translation is to alleviate and prevent human suffering caused by illness and injury, a collective effort that depends on public support and operates within internationally coordinated ethical and regulatory frameworks [87]. These frameworks are designed to ensure that stem cell research is conducted with scientific and ethical integrity and that new therapies are evidence-based [87]. As the complexity of products increases—ranging from acellular scaffolds to advanced, cell-engineered technologies—the regulatory pathways for approval and commercialization become correspondingly more complex [86] [23]. A clear understanding of these frameworks is not merely a bureaucratic hurdle but a foundational component of responsible research and development, ensuring patient safety and the generation of robust, reliable data required for market access.
Analysis of International Regulatory Pathways
Regulatory frameworks for TEMPs vary significantly across the globe, but they share common principles of evaluating safety, efficacy, and quality. The level of regulatory scrutiny is typically determined by a product's composition, origin, processing, and intended use [86]. The following table summarizes the key regulatory pathways in the United States, a major market with a well-defined structure.
Table 1: U.S. FDA Regulatory Pathways for Tissue-Engineered Products
| Regulatory Pathway | Governing Center | Key Characteristics of Products | Data & Evidence Requirements | Example Products (from search results) |
|---|---|---|---|---|
| Biologics License Application (BLA) | Center for Biologics Evaluation and Research (CBER) | Contains live, metabolically active cells (allogeneic or autologous); more than minimally manipulated. | Requires clinical trial(s) to demonstrate safety and efficacy [86]. | Epicel (cultured epidermal autograft) [86]. |
| Premarket Approval (PMA) | Center for Devices and Radiological Health (CDRH) or CBER | High-risk (Class III) devices; often a combination product (device + biologic). | Requires scientific evidence to ensure safety and effectiveness; typically requires clinical data [86]. | Integra Dermal Regeneration Template, TransCyte [86]. |
| 510(k) Clearance | Center for Devices and Radiological Health (CDRH) | Device-based products; demonstrates substantial equivalence to a legally marketed predicate device. | Generally does not require clinical trials; performance and biocompatibility data are key [86]. | Biobrane, Oasis Wound Matrix, Novosorb BTM [86]. |
| Human Cells, Tissues, and Cellular and Tissue-Based Products (HCT/P) 361 | Center for Biologics Evaluation and Research (CBER) | Minimally manipulated; intended for homologous use only; not combined with another article. | Does not require pre-market approval; focuses on preventing disease transmission [86]. | Cadaver skin allografts, AlloDerm, EpiBurn [86]. |
Internationally, the principles of oversight are harmonized around core ethical tenets. The International Society for Stem Cell Research (ISSCR) provides guidelines that, while not legally binding, address international diversity and maintain principles of rigor, oversight, and transparency [87]. These guidelines underscore widely shared principles, including the integrity of the research enterprise, the primacy of patient welfare, respect for research subjects, and social justice [87]. Key recommendations relevant to tissue engineering include the strict prohibition of transplanting human stem cell-based embryo models (SCBEMs) into a uterus and the marketing of unproven stem cell interventions prior to rigorous independent expert review and regulatory approval [87]. Adherence to such international standards provides assurance of ethical and scientific integrity, which is crucial for global collaboration and translation.
Experimental Protocol: Preclinical Evaluation of a Scaffold in a Humanized Murine Wound Model
Preclinical in vivo testing is a critical step in evaluating the safety and efficacy of scaffold-based therapies before advancing to clinical trials. The following protocol, adapted from Gadalla et al. (2024), details a robust method for testing tissue-engineered constructs in a splinted excisional wound model that better recapitulates human-like wound healing by preventing mouse skin contracture [88].
Protocol for Scaffold Implantation in a Splinted Excisional Wound Model
Key Features: This protocol builds upon established methods to enable scaffold testing, utilizes a protective construct to prevent wound disruption, and is adaptable for a wide variety of biomaterials [88].
Experimental Workflow:
Materials and Reagents:
- Animals: Immunodeficient mice (e.g., NOD-scid), 8-12 weeks old.
- Scaffold: Sterile, pre-cut circular implant (e.g., porous polyethylene or test biomaterial).
- Splints: Donut-shaped silicone splints (thin and thick).
- Surgical Tools: Sterile biopsy punch, forceps, needle holder, sutures (e.g., 6-0 nylon), surgical scissors.
- Anesthesia: Isoflurane vaporizer and appropriate anesthetic.
- Analgesia: Buprenorphine sustained-release formulation.
- Dressing: Non-adherent wound dressing, bandage wrap, surgical tape.
Step-by-Step Procedure:
- Preoperative Preparation: Anesthetize the mouse using an isoflurane vaporizer. Administer preoperative analgesia (e.g., buprenorphine). Shave the dorsal fur and clean the skin with alternating betadine and alcohol scrubs.
- Wound Creation: Using a sterile biopsy punch, create two full-thickness, circular excisional wounds on the dorsum [88].
- Scaffold Implantation: Sutured the pre-sterilized, circular scaffold implant into the wound bed using 6-0 nylon sutures to ensure firm contact with the wound base [88].
- Splint Application:
- Place a thin, donut-shaped silicone splint around the wound and secure it to the skin with interrupted sutures. This primary splint prevents skin contracture.
- Place a second, thicker donut-shaped splint on top of the first. This "tenting" splint creates space to prevent the wound dressing from directly contacting the wound bed and disrupting the scaffold [88].
- Wound Dressing: Apply a non-adherent wound dressing over the wound. Wrap the mouse's abdomen in a bandage roll and secure it with surgical tape to protect the wound site from contamination and animal interference [88].
- Postoperative Care: Monitor animals until fully recovered from anesthesia. House them individually. Administer postoperative analgesia as per institutional guidelines. Change dressings as needed until the endpoint.
- Endpoint Analysis: Euthanize animals at predetermined time points. Harvest wound tissue for histological analysis (e.g., H&E staining for granulation tissue, Masson's trichrome for collagen, immunohistochemistry for specific cell markers like CD31 for angiogenesis) and molecular biology assays.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Scaffold-Based Wound Healing Research
| Research Reagent / Material | Function / Application |
|---|---|
| Porous Polyethylene Implant | Serves as a standardized, inert scaffold for testing; provides mechanical support and a 3D structure for cell infiltration [88]. |
| Silicone Splints | Prevents wound margin contracture in murine models, forcing healing via re-epithelialization and granulation tissue formation to mimic human healing [88]. |
| Polycaprolactone (PCL) | A synthetic, biodegradable polymer commonly used in 3D printing and electrospinning to create scaffolds with tunable mechanical properties [89]. |
| Nanocellulose Ink | A natural polymer ink for 3D printing sustainable, self-standing, and porous 3D scaffolds for in vitro cell testing [90]. |
| Optimal Cutting Temperature (O.C.T.) Compound | A water-soluble embedding medium used for cryosectioning; acts as a cryoprotectant to facilitate the sectioning of scaffold-containing tissues [89]. |
| Formalin/Paraformaldehyde (PFA) | Cross-linking fixatives used to preserve tissue and cellular morphology within scaffolds for histological analysis (e.g., FFPE sectioning) [89]. |
| Primary Antibodies (e.g., anti-CD31, anti-α-SMA) | Used in immunohistochemistry to identify specific cell types or proteins (e.g., endothelial cells for angiogenesis, myofibroblasts for contraction) [23]. |
Technical Visualization: Key Signaling Pathways in Wound Healing
Understanding the cellular and molecular mechanisms is crucial for designing effective therapies. Key cells like fibroblasts, keratinocytes, and endothelial cells orchestrate healing through specific signaling pathways. The following diagram summarizes these interactions.
Pathway Overview: Upon injury, the microenvironment becomes hypoxic, activating various cell types [23]. Fibroblasts are activated by cytokines like TGF-β and PDGF, leading to their differentiation into contractile myofibroblasts and the production of extracellular matrix (ECM) proteins, driving wound contraction and tissue remodeling [23]. Keratinocytes at the wound edge proliferate and migrate in response to growth factors like EGF and KGF, a process critical for re-epithelialization and restoring the skin barrier [23]. Endothelial cells are stimulated by VEGF and FGF-2 to proliferate and form new blood vessels (angiogenesis), supplying oxygen and nutrients essential for the healing process [23]. Dysregulation of these pathways is a hallmark of chronic wounds.
In the field of tissue engineering, the combination of stem cells with biomaterial scaffolds represents a cornerstone strategy for regenerating damaged tissues and organs. The scaffold serves as a temporary three-dimensional framework, not only providing mechanical support but also delivering critical biochemical and biomechanical cues that guide cell behavior, including adhesion, proliferation, and differentiation [91] [11]. These scaffolds are broadly categorized into synthetic and biologically-derived (or natural) materials, each with distinct advantages and limitations. Synthetic scaffolds, such as those made from Poly(lactic-co-glycolic acid) (PLGA) or Polycaprolactone (PCL), offer tunable mechanical properties and reproducible manufacturing [92]. In contrast, biologically-derived scaffolds, including those from decellularized tissues (e.g., MatriDerm) or natural polymers like collagen, provide innate biocompatibility and bioactivity that closely mimic the native extracellular matrix (ECM) [91] [93]. This application note provides a structured, data-driven benchmark of these scaffold classes and details standardized protocols for their evaluation, specifically framed within research combining them with stem cells for regenerative applications.
The performance of scaffolds is evaluated across multiple physicochemical and biological parameters. The following tables consolidate key quantitative data for direct comparison.
Table 1: Comparative Physicochemical & Mechanical Properties of Scaffold Types
| Property | Synthetic Scaffolds (e.g., PLGA, PCL) | Biological Scaffolds (e.g., Collagen, dECM) | Hybrid/Composite Scaffolds |
|---|---|---|---|
| Typical Compressive Strength | 8-50 MPa (Pure PCL: 8-10 MPa; Composite PLA: 50-200 MPa) [94] | Highly variable; often lower than synthetic counterparts [92] | Aims to balance and enhance properties [92] |
| Elastic Modulus | Highly tunable, can match cancellous bone (e.g., ~50-200 MPa) [94] | Softer matrices promote neurogenesis; stiffer favor osteogenesis [91] | Tailorable to specific tissue requirements [91] [92] |
| Porosity | Controlled via fabrication (e.g., SLS: 60-80%) [94] | Inherits native tissue porosity or created via freeze-drying [91] [93] | Can achieve high, interconnected porosity [95] |
| Degradation Rate | Predictable, from weeks to years; may produce acidic byproducts [92] | Rapid and sometimes unpredictable (collagen); plant-based (cellulose) is slow [95] [92] | Designed for synchronized degradation with tissue growth [92] |
| Batch-to-Batch Consistency | High [92] | Low for animal-derived; variable for plant-derived [95] [92] | Moderate to High [92] |
Table 2: Comparative Biological Performance & Market Analysis
| Parameter | Synthetic Scaffolds | Biological Scaffolds | Hybrid/Composite Scaffolds |
|---|---|---|---|
| Cell Adhesion | Poor without functionalization; lacks natural ligands [92] | Excellent; presents natural cell-binding sites (e.g., RGD in collagen) [93] [92] | Enhanced; combines structural support with bioactivity [92] |
| In Vivo Bioactivity | Typically bio-inert; requires bio-functionalization [92] | High; contains conserved growth factors and structural proteins [91] [93] | High; designed to be bioactive [91] [92] |
| Immune Response | Minimal initial response; acidic degradation can cause inflammation [92] | Low for human/ECM-derived; risk for animal-derived [95] [92] | Can be engineered to be immunomodulatory [23] |
| Clinical Maturity | High in orthopedics and dentistry [92] [94] | Dominant in wound care (e.g., MatriDerm) [93] [92] | Emerging, high growth potential [92] |
| Global Market Share (2023) | ~40% [92] | ~60% (Collagen-based lead) [92] | Part of the overall segments |
Experimental Protocols for Scaffold Evaluation
The following protocols are essential for benchmarking scaffold performance in the context of stem cell-based tissue engineering research.
Protocol: In Vitro Assessment of Stem Cell-Scaffold Interactions
This protocol evaluates the cytocompatibility and bioactivity of scaffolds using human Mesenchymal Stem Cells (hMSCs).
- Objective: To assess the adhesion, viability, proliferation, and osteogenic differentiation of hMSCs on synthetic and biologically-derived scaffolds.
- Materials:
- Scaffolds: Sterile 5x5mm discs of synthetic (e.g., PCL) and biological (e.g., decellularized bone ECM or MatriDerm) scaffolds.
- Cells: Human Mesenchymal Stem Cells (hMSCs), e.g., Bone Marrow-derived (BM-MSCs).
- Culture Media: Growth Medium (DMEM, 10% FBS, 1% P/S); Osteogenic Differentiation Medium (Growth Medium supplemented with 10 mM β-glycerophosphate, 50 µM ascorbic acid, and 100 nM dexamethasone).
- Procedure:
- Pre-conditioning: Hydrate all scaffolds in PBS for 1 hour, then transfer to culture media for 24 hours prior to cell seeding.
- Cell Seeding: Seed hMSCs at a density of 50,000 cells per scaffold in a low-attachment 24-well plate. Allow 2 hours for cell attachment before adding media.
- Culture: Maintain constructs in Growth Medium for 7 days, changing media every 48 hours. For differentiation groups, switch to Osteogenic Medium on day 3.
- Analysis:
- Day 3 & 7: Cell Viability/Proliferation. Use a Resazurin-based assay (e.g., AlamarBlue) to quantify metabolic activity [93]. Process scaffolds for SEM to visualize cell morphology and adhesion.
- Day 14 & 21: Osteogenic Differentiation. Fix constructs and perform staining for alkaline phosphatase (ALP) activity (early marker) and Alizarin Red S for calcium deposition (late marker). Quantify dye elution spectrophotometrically.
Protocol: Decellularization of Plant-Based Scaffolds
Plant-based scaffolds are an emerging, ethical alternative with inherent vascular structures. This protocol outlines their preparation.
- Objective: To decellularize plant tissues (e.g., apple hypanthium, spinach leaves) to create a cellulose-based scaffold for tissue engineering [95].
- Materials:
- Plant source (e.g., sterilized apple slices).
- Detergent solutions: 1% (w/v) Sodium Dodecyl Sulfate (SDS) and 1% (v/v) Triton X-100.
- Nuclease solution: e.g., DNase/RNase in buffer.
- Peracetic acid or ethanol for sterilization.
- Procedure:
- Chemical Decellularization: Immerse plant samples in 1% SDS solution under constant agitation for 48 hours to lyse and remove cellular material.
- Rinsing: Thoroughly rinse with deionized water for 72 hours to remove all SDS residues.
- Nuclease Treatment (Optional): Incubate in DNase/RNase solution for 4-6 hours to remove residual nucleic acids.
- Wash and Sterilization: Wash with 1% Triton X-100 for 24 hours, followed by extensive PBS rinsing. Sterilize using 0.1% peracetic acid or 70% ethanol.
- Functionalization (Critical for Cell Adhesion): Treat with an ECM protein solution (e.g., 50 µg/mL fibronectin or collagen) for 24 hours to enable mammalian cell attachment [95].
Signaling Pathways in Scaffold-Driven Regeneration
The following diagram illustrates the key signaling pathways through which scaffolds, particularly biologically-derived ones, influence stem cell fate and tissue regeneration. These pathways are crucial for the rationale behind combining stem cells with bioactive scaffolds.
Scaffold-Mediated Stem Cell Signaling
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Scaffold-Based Tissue Engineering Research
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Polycaprolactone (PCL) | Synthetic, biodegradable polymer for scaffold fabrication; offers good mechanical strength [92] [94]. | Fused Deposition Modeling (FDM) 3D printing of bone scaffolds [94]. |
| Decellularized ECM (dECM) | Biologically-derived scaffold; preserves native tissue's biochemical and structural complexity [91]. | Studying cell-ECM interactions; creating in vivo-like microenvironments for stem cells [91] [93]. |
| MatriDerm | Commercial biological wound matrix of bovine collagen types I, III, V, and elastin [93]. | Positive control for in vitro studies on fibroblast and macrophage interactions with natural scaffolds [93]. |
| Resazurin Sodium Salt | Cell-permeant dye used in viability and proliferation assays (e.g., AlamarBlue) [93]. | Quantifying metabolic activity of cells seeded on 3D scaffolds over time [93]. |
| Recombinant Growth Factors (VEGF, BMP-2) | Soluble signaling molecules to functionalize scaffolds or add to culture media [91] [94]. | Enhancing angiogenesis (VEGF) or osteogenic differentiation (BMP-2) of stem cells on scaffolds [94] [23]. |
| Fibronectin / Collagen I | Natural adhesion proteins for surface functionalization of synthetic or plant-based scaffolds [95]. | Coating scaffolds to improve initial cell attachment and spreading [95]. |
Conclusion
The synergy between advanced stem cell biology and sophisticated biomaterial design is fundamentally transforming the landscape of regenerative medicine. Key takeaways confirm that engineering strategies—such as preconditioning, 3D bioprinting, and the use of iPSC-derived cells—are successfully overcoming historical challenges of poor cell survival and functionality in hostile wound environments. The maturation of the field is evidenced by a robust clinical pipeline, specific FDA approvals, and a market poised for significant growth. Future progress hinges on the development of standardized, fully defined biomaterials to replace animal-derived matrices, the refinement of personalized combination products through AI-driven design, and greater global regulatory harmonization. For researchers and drug developers, the priority must now be on designing clinically relevant models that not only demonstrate functional tissue regeneration but also address the critical path of scalable, cost-effective, and reproducible manufacturing for widespread therapeutic application.
References
- 1. Pharmacological modulation of stem cells signaling pathway ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12210473/]
- 2. Different Types of Stem Cells | A 2025 Guide [https://omnistem.com/different-types-of-stem-cells/]
- 3. Exploration of biomaterial and stem cell-based strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574274/]
- 4. Bottom-up Biomaterial strategies for creating tailored stem ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1581292/full]
- 5. Engineering stem cell metabolism using biomaterial- ... [https://www.sciencedirect.com/science/article/pii/S3050562325001837]
- 6. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 7. Synthetic thermoresponsive scaffolds for the expansion and ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra04674b?page=search]
- 8. Effects on Mesenchymal Stem Cells and their Paracrine ... [https://pubmed.ncbi.nlm.nih.gov/40637970/]
- 9. Tissue engineering: Hydrogel scaffolds and mechanical ... [https://www.sciencedirect.com/science/article/abs/pii/S0001868625003021]
- 10. Biomaterials in tissue repair and regeneration: key insights ... [https://www.frontiersin.org/journals/medical-technology/articles/10.3389/fmedt.2025.1565810/full]
- 11. The role of biomaterials-based scaffolds in advancing skin ... [https://www.sciencedirect.com/science/article/pii/S0965206X25000063]
- 12. Recent advances in bionic scaffolds for cartilage tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289700/]
- 13. Innovative modification strategies and emerging ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1591896/full]
- 14. Recent Advances in 3D Bioprinting of Porous Scaffolds for ... [https://www.mdpi.com/2079-4983/16/9/328]
- 15. Mechanical and biological properties of 3D printed bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12010109/]
- 16. Tissue Engineering Market Size, Share, Growth & Forecast, ... [https://www.fortunebusinessinsights.com/tissue-engineering-market-111426]
- 17. Tissue Engineering Market Outlook 2025-2032 [https://www.intelmarketresearch.com/tissue-engineering-market-17045]
- 18. Tissue Engineering Market Size to Exceed USD 28.97 Bn ... [https://www.coherentmarketinsights.com/press-release/tissue-engineering-market-to-surpass-us-14-billion-by-2026-1150]
- 19. Tissue Engineering and Regeneration Market Set to Surge ... [https://www.bccresearch.com/pressroom/hlc/tissue-engineering-and-regeneration-market-set-to-surge-at-128-cagr?srsltid=AfmBOopbHJgDanEsaip7z2EnFs0nkZb-K1QOHKdth836hbnzkDbTl4tv]
- 20. [Latest] Global Cardiac Tissue Engineering Market Size/ ... [https://finance.yahoo.com/news/latest-global-cardiac-tissue-engineering-163000002.html]
- 21. Global Tissue Engineering Market Size & Share Analysis [https://www.mordorintelligence.com/industry-reports/tissue-engineering-market]
- 22. Potential of mesenchymal stem cells and exosomes in ... [https://pubmed.ncbi.nlm.nih.gov/41172571/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1Jgu41lFGSjVSi0g_GOn6ReFV1ZOsx1wRYCQgPUWDxEw7yEwWQ&fc=None&ff=20251111220310&v=2.18.0.post22+67771e2]
- 23. Cell-engineered technologies for wound healing and ... [https://www.nature.com/articles/s44385-025-00042-w]
- 24. Biomaterials and stem cells targeting the microenvironment for ... [https://pubs.rsc.org/en/content/articlehtml/2025/bm/d4bm01521e]
- 25. Beyond the Present Constraints That Prevent a Wide Spread ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6514054/]
- 26. Exploration of biomaterial and stem cell-based strategies for ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07266-9]
- 27. Modern experimental methods for assessing the effectiveness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318997/]
- 28. Quantitative characterization of tissue states using ... [https://www.nature.com/articles/s41588-025-02119-z]
- 29. Recommendations for Studying In Situ Extracellular Vesicles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12606037/]
- 30. 3D-printed artificial bone scaffolds: the design of materials, the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12443788/]
- 31. Advances in 3D-printed scaffold technologies for bone defect ... [https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/s12938-025-01381-w]
- 32. Design and analysis of 3D-printed PLA scaffolds [https://www.sciencedirect.com/science/article/pii/S2590123025022285]
- 33. Predicting and elucidating the post-printing behavior of 3D ... [https://www.nature.com/articles/s41598-023-28286-9]
- 34. Printability and Shape Fidelity of Bioinks in 3D Bioprinting - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7564085/]
- 35. Engineering strategies to enhance the research progress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12220656/]
- 36. Disease microenvironment preconditioning: An evolving ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576925006915]
- 37. Engineering strategies to enhance the research progress of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04471-7]
- 38. Smart integrated biomaterial systems for precision and ... [https://www.sciencedirect.com/science/article/pii/S2352320425002378]
- 39. Preconditioning of Hypoxic Culture Increases The ... [https://oamjms.eu/index.php/mjms/article/view/5870]
- 40. preconditioning strategies for MSC-derived extracellular ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1509418/full]
- 41. Preclinical study of engineering MSCs promoting diabetic ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04248-y]
- 42. Mesenchymal stromal cells in wound healing applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC8569889/]
- 43. Engineered dermal tissue constructs using mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12477933/]
- 44. Research advances in mesenchymal stem cells and ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1647909/full]
- 45. Biomaterials and Tissue Engineering in Neurosurgery [https://www.mdpi.com/2673-6284/14/3/65]
- 46. Viscoelastic N‑cadherin-like interactions maintain neural ... [https://www.nature.com/articles/s41467-025-60540-8]
- 47. Advancing models of neural development with biomaterials [https://pmc.ncbi.nlm.nih.gov/articles/PMC8612873/]
- 48. Liver organoids: established tools for disease modeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10043560/]
- 49. Hepatic organoids as a platform for liver disease modeling ... [https://www.sciencedirect.com/science/article/pii/S221074012500124X]
- 50. Animal-free alternatives for Matrigel in human iPSC- ... [https://www.nature.com/articles/s41598-025-20091-w]
- 51. Current advances and prospects in biomaterials-guided ... [https://www.sciencedirect.com/science/article/pii/S2666138125000131]
- 52. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592637/]
- 53. Cell manufacturing for cell-based tissue engineering [https://www.frontiersin.org/journals/chemical-engineering/articles/10.3389/fceng.2025.1637075/full]
- 54. Liver organoids: updates on generation strategies and ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03865-3]
- 55. Biomaterials to enhance stem cell transplantation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10169090/]
- 56. Induced Mesenchymal Stem Cells: An Emerging Source for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11943107/]
- 57. The Therapeutic Advantage of Induced Pluripotent Stem ... [https://www.reprocell.com/blog/the-therapeutic-advantage-of-induced-pluripotent-stem-cells-derived-mesenchymal-stem-cells-imscs]
- 58. Comparison of human isogeneic Wharton's jelly MSCs and ... [https://www.nature.com/articles/s41419-019-1498-0]
- 59. Biomaterials and Advanced Biofabrication Techniques in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6895005/]
- 60. Biomaterial-based regenerative therapeutic strategies for ... [https://www.nature.com/articles/s41427-023-00526-4]
- 61. iPSC-, MSC- and iMSC-Derived Exosome Therapeutics [https://www.reprocell.com/blog/ipsc-msc-and-imsc-derived-exosome-therapeutics-the-cell-free-future-of-regenerative-medicine]
- 62. The Challenges to Advancing Induced Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10768945/]
- 63. Combining genome and tissue engineering for next- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12629539/]
- 64. CRISPR Delivery Methods: Cargo, Vehicles, and Challenges [https://www.synthego.com/blog/delivery-crispr-cas9/]
- 65. Unlocking mRNA-driven CRISPR-Cas9 gene therapy via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12594903/]
- 66. Engineering ARMMs for improved intracellular delivery of ... [https://www.sciencedirect.com/science/article/pii/S2773041725000186]
- 67. Biomedical Engineering Applications of Stem -derived Cell Exosomes [https://www.dovepress.com/stem-cell-derived-exosomes-a-comprehensive-review-of-biomedical-applic-peer-reviewed-fulltext-article-IJN]
- 68. Engineering exosomes and biomaterial -assisted exosomes as... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03275-x]
- 69. A review of biomaterial degradation assessment ... [https://www.nature.com/articles/s41529-024-00487-1]
- 70. Smart biomaterials: as active immune modulators to shape ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1669399/full]
- 71. Advanced biomaterial strategies for overcoming age- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12145203/]
- 72. Smart biomaterials: as active immune modulators to shape pro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12558899/]
- 73. Biomaterials text mining: A hands-on comparative study of ... [https://www.sciencedirect.com/science/article/pii/S1871678423000444]
- 74. A review of regenerative medicine and tissue engineering with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12176865/]
- 75. Mesenchymal stromal cell therapy: Progress to date and ... [https://www.sciencedirect.com/science/article/pii/S1525001625000930]
- 76. The emerging promise of induced pluripotent stem cells in ... [https://pubmed.ncbi.nlm.nih.gov/41160002/]
- 77. Tissue Engineering and Regenerative Medicine 2025 [https://www.frontiersin.org/research-topics/73076/tissue-engineering-and-regenerative-medicine-2025---quo-vadisundefined]
- 78. Efficacy and safety of single versus repeated injections of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04638-2]
- 79. Trends in mesenchymal stem cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488731/]
- 80. Fate Therapeutics Announces Phase 1 Data Presentation of ... [https://ir.fatetherapeutics.com/news-releases/news-release-details/fate-therapeutics-announces-phase-1-data-presentation-ft819]
- 81. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 82. Regenerative Medicine Advanced Therapy Designation [https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/regenerative-medicine-advanced-therapy-designation]
- 83. CBER Regenerative Medicine Advanced Therapy (RMAT) ... [https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/cber-regenerative-medicine-advanced-therapy-rmat-approvals]
- 84. From the Editors: Cell & Gene Therapy Approvals in 2024 [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/01/16/cell-gene-therapy-approvals-in-2024]
- 85. What Is An RMAT? List of RMAT Designations (147) [https://bioinformant.com/rmat/]
- 86. Navigating the Regulatory Pathways and Requirements for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8335953/]
- 87. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 88. Protocol for the Implantation of Scaffolds in a Humanized ... [https://pubmed.ncbi.nlm.nih.gov/39346758/]
- 89. Histological Processing of Scaffolds: Challenges and ... [https://www.mdpi.com/2079-4983/16/8/279]
- 90. Protocol for the fabrication of self-standing (nano)cellulose ... [https://www.sciencedirect.com/science/article/pii/S2666166724007482]
- 91. Design and Applications of Extracellular Matrix Scaffolds in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293650/]
- 92. A Comparative Analysis Of Natural Vs. Synthetic Polymer ... [https://eureka.patsnap.com/report-a-comparative-analysis-of-natural-vs-synthetic-polymer-scaffolds]
- 93. Comparison of cell‐scaffold interactions in a biological and a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11725368/]
- 94. 3D-printed artificial bone scaffolds: the design of materials ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1614727/full]
- 95. Plant-Based Scaffolds for Tissue Engineering: A Review [https://www.mdpi.com/2073-4360/17/19/2705]