Ensuring Clinical Safety: GMP Strategies for Tumor-Free Pluripotent Stem Cell Manufacturing
This article provides a comprehensive guide to Good Manufacturing Practice (GMP) processes specifically designed to eliminate tumorigenic risk in pluripotent stem cell (PSC) therapies.
Ensuring Clinical Safety: GMP Strategies for Tumor-Free Pluripotent Stem Cell Manufacturing
Abstract
This article provides a comprehensive guide to Good Manufacturing Practice (GMP) processes specifically designed to eliminate tumorigenic risk in pluripotent stem cell (PSC) therapies. Targeting researchers and drug development professionals, it explores the biological origins of tumorigenicity, details current GMP-compliant methodologies for prevention and removal, addresses critical troubleshooting and process optimization, and evaluates analytical validation strategies. The content synthesizes the latest regulatory expectations and technological advances to outline a robust framework for translating safe PSC-based therapies from the lab to the clinic.
Understanding the Tumorigenicity Challenge in PSC Therapies: Biology, Risks, and Regulatory Imperatives
Within the rigorous framework of GMP manufacturing for pluripotent stem cell (PSC)-based therapies, two critical, interrelated sources of tumorigenic risk dominate the safety assessment paradigm: (1) Residual Undifferentiated Cells (RUCs) and (2) Genetic Instability (GI). RUCs, persisting post-differentiation, retain the capacity for teratoma formation and uncontrolled proliferation. Concurrently, GI, arising from pre-existing mutations, culture adaptation, or reprogramming artifacts, can lead to oncogenic transformation, even in differentiated cell populations. This application note details standardized protocols for quantifying these risks, ensuring comprehensive product characterization for regulatory filings and clinical translation.
Quantitative Risk Assessment: Data Tables
Table 1: Comparison of Assay Sensitivities for Residual Undifferentiated Cell Detection
| Assay Method | Target | Sensitivity (Detection Limit) | Throughput | Key Advantage | Key Limitation |
|---|---|---|---|---|---|
| Flow Cytometry | Surface markers (e.g., SSEA-4, TRA-1-60) | 0.1 - 0.5% | High | Quantitative, single-cell | Requires specific antibodies; misses low-expressing cells. |
| qRT-PCR | Pluripotency transcripts (e.g., NANOG, POUSF1) | 0.01 - 0.1% | Medium-High | Highly sensitive, no live cells needed | Does not confirm protein expression or functional pluripotency. |
| Teratoma Assay (In Vivo) | Functional pluripotency | 1x10^4 - 1x10^6 cells (empirical) | Very Low | Gold-standard functional readout | 8-20 week duration, variable, semi-quantitative, ethical burden. |
| Microscopy (ICC/IF) | Intracellular/ surface markers | 0.5 - 1% | Low-Medium | Morphological context, co-localization | Subjective, lower sensitivity, not high-throughput. |
Table 2: Assays for Monitoring Genetic Instability in PSC Manufacturing
| Assay Category | Specific Assay | Resolution | Key Outputs | Relevance to Tumorigenicity |
|---|---|---|---|---|
| Karyotyping | G-banding | ~5-10 Mb | Aneuploidy, large translocations | Detects gross abnormalities (e.g., trisomy 12, 17). |
| Molecular Karyotyping | SNP/array-CGH | 10-100 Kb | Copy Number Variations (CNVs), loss of heterozygosity (LOH) | Identifies sub-chromosomal CNVs in oncogenic loci. |
| Targeted Sequencing | NGS Panels (e.g., cancer genes) | Single nucleotide | Mutations in specific oncogenes/tumor suppressors | Interrogates known high-risk drivers (e.g., TP53, PIK3CA). |
| Whole Genome Sequencing | WGS | Single nucleotide | Comprehensive variant profile (SNVs, indels, CNVs, SVs) | Gold standard for exhaustive genomic characterization. |
Detailed Experimental Protocols
Protocol 2.1: High-Sensitivity Flow Cytometry for Residual Undifferentiated Cell Quantification
Objective: To quantitatively detect and quantify RUCs in a final PSC-derived cell product down to a sensitivity of ≤0.1%.
Materials (Research Reagent Solutions):
- Single-cell suspension of final differentiated cell product.
- Flow Cytometry Staining Buffer: PBS + 2% FBS + 1 mM EDTA. Function: Maintains cell viability and prevents clumping.
- Viability Dye (e.g., 7-AAD or DAPI): Function: Distinguishes live from dead cells for accurate analysis.
- Fluorochrome-conjugated Antibodies: Anti-SSEA-4 (APC), Anti-TRA-1-60 (FITC), and corresponding isotype controls.
- Fixation Buffer (1-4% PFA): Function: Optional post-staining cell fixation for biosafety.
Procedure:
- Cell Preparation: Generate a single-cell suspension using gentle enzymatic dissociation. Pass cells through a 35-40 µm cell strainer. Count and adjust concentration to 1-5 x 10^6 cells/mL in staining buffer.
- Viability Staining: Add viability dye to the cell suspension, incubate for 5-10 minutes on ice, protected from light.
- Surface Marker Staining: Aliquot cells. Add predetermined optimal concentrations of anti-SSEA-4, anti-TRA-1-60, and isotype control antibodies to respective tubes. Incubate for 30 minutes on ice in the dark.
- Washing: Wash cells twice with 2 mL of cold staining buffer, centrifuging at 300 x g for 5 minutes.
- Fixation (Optional): Resuspend cells in 200-500 µL of fixation buffer if required by biosafety protocol.
- Acquisition: Analyze on a flow cytometer calibrated with compensation beads. Acquire a minimum of 1 x 10^5 events per sample. For rare event detection, consider acquiring >1 x 10^6 events.
- Analysis: Gate sequentially on live cells, single cells (FSC-A vs. FSC-H), and then analyze fluorescence. The percentage of dual-positive (SSEA-4+/TRA-1-60+) cells is reported as the RUC content.
Protocol 2.2: Genomic DNA Isolation and Array-CGH for CNV Profiling
Objective: To detect acquired copy number variations (CNVs) in PSC master cell banks and end-of-production cells.
Materials (Research Reagent Solutions):
- PSC pellet (≥1 x 10^6 cells).
- Commercial gDNA Isolation Kit (e.g., Qiagen DNeasy): Function: Provides high-purity, high-molecular-weight genomic DNA.
- NanoDrop or Qubit Fluorometer: Function: Accurately quantifies DNA concentration and assesses purity (A260/A280).
- Array-CGH Kit/Service (e.g., Agilent or Illumina): Function: Platform for competitive hybridization to detect CNVs.
- Bioanalyzer or TapeStation: Function: Assesses DNA integrity prior to labeling.
Procedure:
- DNA Extraction: Isolate genomic DNA from test (PSC sample) and sex-matched reference (commercial human genomic DNA) samples using the recommended protocol. Elute in nuclease-free water or TE buffer.
- DNA QC: Quantify DNA using a fluorometric method. Verify DNA integrity via Bioanalyzer; ensure DNA Integrity Number (DIN) > 7.5.
- Enzymatic Labeling: Digest 500 ng – 1 µg of test and reference DNA with appropriate restriction enzymes. Label test DNA with Cy5-dUTP and reference DNA with Cy3-dUTP using a random priming method.
- Purification & Hybridization: Purify labeled products using columns or beads. Combine equal amounts of labeled test and reference DNA, add blocking agents (Cot-1 DNA, blocking oligos), and hybridize onto the array slide for 24-40 hours at 65°C with rotation.
- Washing & Scanning: Perform stringent post-hybridization washes. Scan the array slide using a dual-laser scanner to capture fluorescence intensities.
- Data Analysis: Use vendor software (e.g., Agilent CytoGenomics) to calculate log2 ratios, perform aberration detection (ADM-2 algorithm), and visualize CNVs. Report all aberrations >100 Kb and focus on known oncogenic loci.
Signaling Pathways & Experimental Workflows
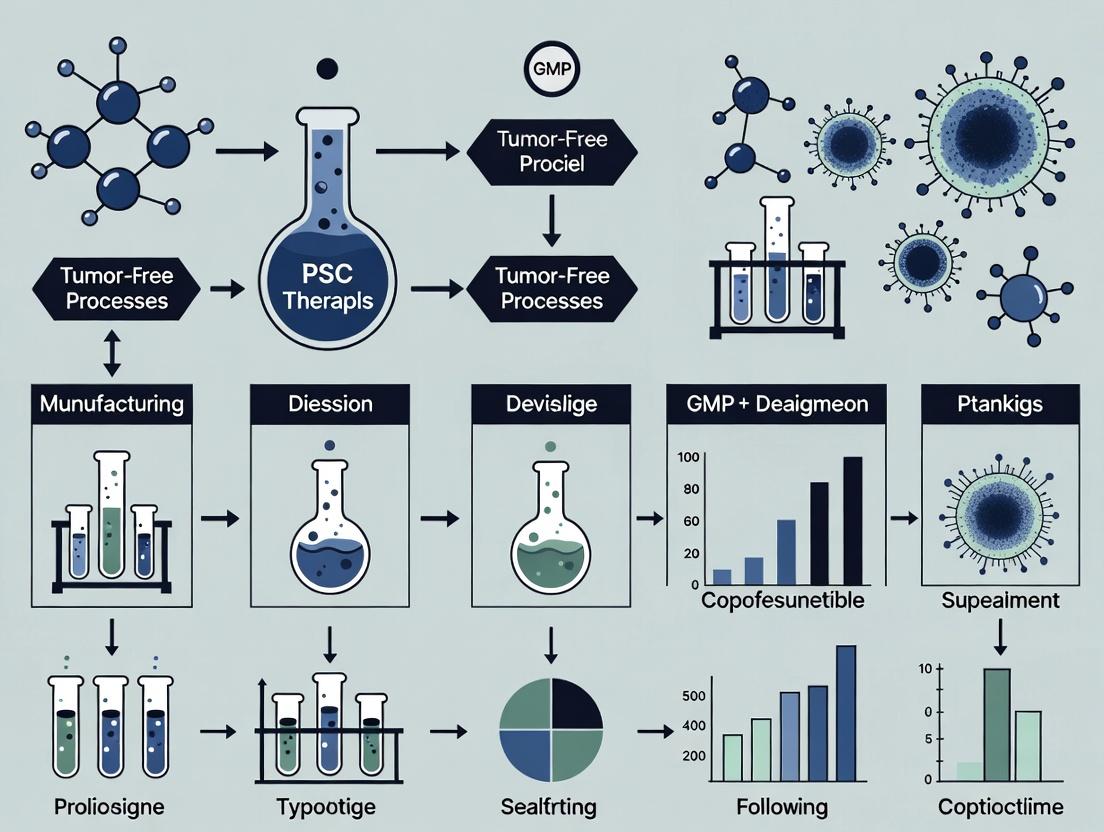
Diagram 1: Tumorigenic Risk Sources and Outcomes
Diagram 2: Integrated Safety Testing Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item/Category | Example Product/Code | Function in Risk Assessment |
|---|---|---|
| Pluripotency Surface Marker Antibodies | Anti-human SSEA-4, TRA-1-60, TRA-1-81 | Direct detection and quantification of residual undifferentiated cells via flow cytometry or ICC. |
| gDNA Isolation Kit | Qiagen DNeasy Blood & Tissue Kit | High-yield, pure genomic DNA extraction for downstream genetic stability assays (qPCR, CGH, NGS). |
| Viability Stain for Flow | 7-Aminoactinomycin D (7-AAD) | Exclusion of dead cells from flow analysis to prevent false-positive RUC signals from permeable cells. |
| NGS Panels for PSCs | Illumina TruSight Oncology 500 or custom panels | Targeted sequencing for known cancer-associated mutations acquired during culture or reprogramming. |
| Karyotyping Dyes/Reagents | Giemsa Stain (for G-banding) | Visualization of chromosomes for the detection of gross numerical and structural abnormalities. |
| Reference Genomic DNA | Coriell Institute Human Genomic DNA | Sex-matched control DNA for comparative genomic hybridization (CGH) experiments. |
| Cell Dissociation Reagent | Accutase or gentle cell dissociation reagent | Generation of high-viability single-cell suspensions critical for accurate flow cytometry and clonal assays. |
| qRT-PCR Master Mix | TaqMan Gene Expression Master Mix | Sensitive, specific quantification of pluripotency gene expression for low-level RUC detection. |
For GMP manufacturing of Pluripotent Stem Cell (PSC) therapies, the primary risk is the inadvertent introduction or selection of cells with oncogenic potential into the final product. The molecular convergence of core pluripotency networks (e.g., OCT4, SOX2, NANOG) with classic oncogenic pathways (e.g., PI3K/AKT, MYC, Wnt/β-catenin) underlies this risk. Understanding and monitoring these shared mechanisms is not merely a biological curiosity but a critical Quality Control (QC) imperative. This document provides application notes and detailed protocols for investigating these convergent nodes to develop safety assays for tumor-free PSC therapies.
The table below summarizes the core pluripotency factors, their convergent oncogenic pathways, shared downstream targets, and associated risks in PSC manufacturing.
Table 1: Core Pluripotency Factors and Their Oncogenic Convergence
| Pluripotency Factor/Network | Convergent Oncogenic Pathway | Key Shared Target/Effector | Functional Outcome of Convergence | Risk in PSC Therapy |
|---|---|---|---|---|
| OCT4 (POU5F1) | PI3K/AKT/mTOR | c-MYC expression | Enhanced self-renewal & metabolic reprogramming (glycolysis). | Teratoma formation; somatic cell reprogramming to induced pluripotent stem cells (iPSCs). |
| NANOG | TGF-β/Activin/Nodal | SMAD2/3 signaling | Maintenance of undifferentiated state; inhibition of differentiation. | Propagation of partially differentiated or aberrant cells. |
| SOX2 | Receptor Tyrosine Kinase (RTK) / RAS-RAF | ERK1/2 activity | Regulation of proliferation vs. differentiation decisions. | Clonal expansion of genetically unstable cells. |
| Wnt/β-catenin (Pluripotency modulator) | Wnt/β-catenin (Oncogenic) | β-catenin/TCF complex | Promotion of self-renewal; inhibition of mesendodermal differentiation. | Somatic mutation-driven overactivation leading to unchecked growth. |
| c-MYC (Pluripotency enhancer) | MYC (Master oncogene) | Global transcriptional amplification | Increases biomass production, ribosomal biogenesis, and cell cycle progression. | Genomic instability; dramatically increased tumorigenic potential. |
Table 2: Quantitative Assay Metrics for Convergence Monitoring
| Assay Target | Technique | Normal Range in Undifferentiated hPSCs | Alert/Threshold Level ( Indicative of Risk) | GMP-Ready Alternative |
|---|---|---|---|---|
| p-AKT (S473) | Phospho-flow cytometry | MFI: 1,000 - 3,000 (assay dependent) | >150% of process-validated baseline | ELISA on cell lysates. |
| Nuclear β-catenin | High-content imaging | % positive nuclei: 10-25% | >40% positive nuclei | qPCR for AXIN2, a canonical Wnt target. |
| c-MYC mRNA | RT-qPCR | ΔΔCt relative to housekeeper: 0.5 - 2.0 | >5-fold increase over validated control | ddPCR for absolute quantification. |
| Residual Undifferentiated Cells (via OCT4) | Flow cytometry | <0.1% in final product | >0.5% | PCR-based detection of pluripotency-associated transcripts. |
Experimental Protocols
Protocol 3.1: Phospho-Flow Cytometry for PI3K/AKT/mTOR & ERK Signaling Dynamics
Purpose: To quantitatively measure the activity of convergent oncogenic signaling pathways at the single-cell level in a PSC culture. Reagents: See "The Scientist's Toolkit" (Section 5). Procedure:
- Cell Harvest & Fixation: Gently dissociate a single well of a 6-well PSC culture using EDTA-based dissociation reagent (e.g., 0.5 mM EDTA in PBS). Do not use trypsin, which can artificially activate signaling. Quench with 2% FBS/PBS. Count cells.
- Stimulation (Optional): To assay pathway responsiveness, split cell suspension. Treat one aliquot with 100 ng/mL IGF-1 or bFGF for 15 minutes at 37°C. Keep another aliquot unstimulated as a baseline control.
- Fixation: Add an equal volume of pre-warmed (37°C) 4% PFA to the cell suspension (final 2% PFA). Incubate for 10 minutes at 37°C.
- Permeabilization: Pellet cells (300 x g, 5 min). Resuspend in 1 mL of ice-cold 100% methanol. Vortex gently and incubate at -20°C for at least 30 minutes. Cells can be stored at -20°C for weeks.
- Staining: Pellet methanol-fixed cells (600 x g, 5 min). Wash twice with 2 mL FACS Buffer (2% FBS, 0.1% NaN3 in PBS). Resuspend pellet (~1x10^6 cells) in 100 µL FACS Buffer containing predetermined optimal dilutions of conjugated antibodies: Anti-p-AKT (S473)-Alexa Fluor 488 and Anti-p-ERK1/2 (T202/Y204)-PE/Cyanine7. Include isotype controls.
- Acquisition & Analysis: Incubate for 1 hour at RT in the dark. Wash twice with FACS Buffer. Resuspend in 300 µL FACS Buffer. Acquire data on a flow cytometer capable of detecting the fluorophores. Analyze median fluorescence intensity (MFI) for each phospho-protein in the live cell gate. Compare stimulated vs. unstimulated and monitor baseline drift over passages.
Protocol 3.2: High-Content Imaging for Nuclear β-catenin Localization
Purpose: To assess aberrant activation of the Wnt/β-catenin pathway, a key convergent node. Procedure:
- Cell Seeding: Seed PSCs as single cells in a Geltrex-coated 96-well imaging plate at a density of 15,000 cells/well. Culture for 48 hours to reach ~70% confluence.
- Treatment: Treat wells with either: a) Control medium, b) 3 µM CHIR99021 (GSK-3β inhibitor, positive control for β-catenin nuclear localization) for 6 hours.
- Fixation & Permeabilization: Aspirate medium. Wash once with PBS. Fix with 4% PFA for 15 minutes at RT. Permeabilize with 0.5% Triton X-100 in PBS for 15 minutes.
- Immunostaining: Block with 5% BSA in PBS for 1 hour. Incubate with primary antibody Mouse anti-β-catenin (1:400 in blocking buffer) overnight at 4°C.
- Wash & Secondary Stain: Wash 3x with PBS. Incubate with Donkey anti-mouse IgG-Alexa Fluor 555 (1:500) and Hoechst 33342 (1:2000) for 1 hour at RT in the dark.
- Image Acquisition & Analysis: Image on a high-content imager (e.g., ImageXpress) using DAPI and TRITC filters. Use analysis software to identify nuclei (Hoechst) and measure the mean intensity of β-catenin staining within the nuclear mask. Calculate the Nuclear to Cytoplasmic (N:C) Ratio of β-catenin. A significant increase in the N:C ratio indicates pathway activation.
Signaling Pathway & Workflow Diagrams
Diagram 1: Pluripotency and oncogenic pathway convergence network.
Diagram 2: Phospho-flow cytometry workflow for GMP monitoring.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Convergence Research & Safety Assays
| Reagent / Material | Function / Target | Example Product (Research-Use) | GMP-Compatible Alternative Consideration |
|---|---|---|---|
| Phospho-Specific Antibodies (p-AKT, p-ERK, p-mTOR) | Detect activated kinases in convergent pathways. | Cell Signaling Technology #4060 (p-AKT Ser473, XP Rabbit mAb) | In-house validated ELISA kits with animal component-free antibodies. |
| Small Molecule Pathway Inhibitors/Activators | Experimental modulation of pathways (e.g., for threshold testing). | Tocris CHIR99021 (GSK-3β inhibitor), LY294002 (PI3K inhibitor) | Not for product manufacturing. Used for process characterization/assay development only. |
| Flow Cytometry Antibodies (OCT4, SSEA-4, TRA-1-60) | Quantify residual undifferentiated PSCs. | BD Biosciences 560794 (OCT3/4 Alexa Fluor 647) | Clinical-grade, fluorochrome-conjugated antibodies manufactured under GMP. |
| LIVE/DEAD Fixable Viability Dyes | Exclude dead cells from phospho-signaling analysis. | Thermo Fisher Scientific L34957 (Aqua Dead Cell Stain) | Defined, serum-free viability dyes with DMF/CE-mark. |
| EDTA-based Dissociation Reagents | Gentle cell harvesting without trypsin-induced signaling artifacts. | Thermo Fisher Scientific 13151014 (Gentle Cell Dissociation Reagent) | Defined, xeno-free, recombinant enzyme dissociation cocktails. |
| qPCR/ddPCR Assays | Quantify oncogenic (MYC) or pluripotency (POU5F1) transcripts. | Thermo Fisher Scientific Hs00153408_m1 (MYC) | Custom-designed, master mix kits for IVD use. |
| Geltrex/Laminin-521 | Defined, xeno-free extracellular matrix for consistent PSC growth. | Thermo Fisher Scientific A1413302 (Geltrex, LDEV-Free) | Clinical-grade, human recombinant laminin-511/521. |
Within the research thesis on GMP manufacturing for tumor-free pluripotent stem cell (PSC) therapies, the regulatory framework is a critical design constraint. This Application Note details the key FDA, EMA, and ICH guidelines governing cell therapy safety, with a focus on tumorigenicity risk assessment. Adherence to these guidelines directly informs the experimental protocols required to advance a PSC-derived product from research to clinical application.
Comparative Analysis of Regulatory Guidelines
The following table summarizes the core safety guidelines from the FDA (United States), EMA (Europe), and the harmonizing ICH, with emphasis on tumorigenicity and safety testing.
Table 1: Key Regulatory Guidelines for Cell Therapy Safety Assessment
| Agency/Guideline | Code/Ref | Focus Area | Key Safety Requirements (Tumorigenicity Focus) | Recommended Testing Paradigm |
|---|---|---|---|---|
| FDA (CBER) | Guidance for Industry: CGT for Rare Diseases (2025) | Preclinical Safety | Assessment of tumorigenicity, biodistribution, and long-term persistence. | In vitro transformation assays, in vivo tumorigenicity studies in immunocompromised animals, vector integration site analysis for genetically modified cells. |
| FDA (CBER) | Content and Review of CMC Information for IND (2022) | Chemistry, Manufacturing, Controls (CMC) | Safety linked to product impurities, residual undifferentiated PSCs, and process consistency. | Quantification of undifferentiated PSCs (e.g., flow cytometry for pluripotency markers), testing for adventitious agents, endotoxin, and mycoplasma. |
| EMA (CAT/CHMP) | Guideline on Safety & Efficacy Follow-up & Risk Management for ATMPs (2021) | Risk Management | Comprehensive Risk Management Plan (RMP) and Pharmacovigilance. Mandates long-term follow-up (LTFU) for tumorigenicity risk. | Minimum 15-year LTFU for PSC-derived products. RMP must include specific strategies for monitoring unanticipated tumor formation. |
| ICH | ICH S12: Nonclinical Biodistribution Considerations for Gene Therapy Products (2023) | Biodistribution | Biodistribution (BD) studies to understand organ/tissue exposure and inform tumorigenicity risk. | BD assessments using validated methods (e.g., qPCR, imaging). Data used to select tissues for histopathology in toxicology studies and define LTFU obligations. |
| ICH | ICH Q5A(R2): Viral Safety Evaluation of Biotechnology Products (2023) | Viral Safety | Testing for viruses in cell banks and unprocessed bulk harvest. | In vitro and in vivo virus assays, PCR-based testing for specific viruses, and validation of viral clearance in the manufacturing process. |
Experimental Protocols for Tumorigenicity Risk Assessment
The following detailed protocols are essential for addressing regulatory expectations regarding residual pluripotent cells and tumorigenic potential.
Protocol 2.1: Quantitative Flow Cytometry for Residual Undifferentiated PSCs Objective: To quantify the percentage of SSEA-4/TRA-1-60 positive cells in a final PSC-derived cell product. Materials: See "The Scientist's Toolkit" below. Method:
- Single-Cell Suspension: Dissociate the final cell product to a single-cell suspension using a validated enzyme-free method. Pass cells through a 35 µm strainer.
- Staining: Aliquot 1x10^6 cells per tube. For the test sample, incubate cells with fluorochrome-conjugated anti-SSEA-4 and anti-TRA-1-60 antibodies (or appropriate isotype controls) for 30 minutes at 4°C in the dark.
- Washing & Analysis: Wash cells twice with PBS containing 2% FBS. Resuspend in buffer containing a viability dye (e.g., 7-AAD). Acquire data on a flow cytometer calibrated with compensation beads.
- Gating Strategy: Exclude debris and doublets. Gate on live, single cells. Quantify the percentage of cells positive for both SSEA-4 and TRA-1-60.
- Acceptance Criteria: Establish a product-specific specification limit (e.g., ≤ 0.001% positive cells) based on risk assessment and process capability.
Protocol 2.2: In Vivo Tumorigenicity Assay in Immunocompromised Mice Objective: To assess the tumor-forming potential of the final PSC-derived product compared to positive (undifferentiated PSCs) and negative (vehicle) controls. Method:
- Cell Preparation: Prepare test article (final product), positive control (undifferentiated PSCs), and vehicle control under aseptic conditions.
- Animal Model: Use NOD.Cg-PrkdcscidIl2rgtm1Wjl*/SzJ (NSG) mice, 8-10 weeks old (n=10 per group). House in sterile, ventilated caging.
- Administration: Administer cells via a clinically relevant route (e.g., intramuscular, subcutaneous). Dose escalation is recommended. A typical high dose is 1x10^7 cells/site for the test article and 1x10^6 cells/site for the positive control.
- Observation & Endpoints: Monitor animals twice weekly for 26-52 weeks for palpable mass formation, clinical signs, and body weight. Terminate animals with tumors reaching a humane endpoint.
- Necropsy & Histopathology: Perform a full necropsy on all animals. Weigh organs and preserve injection sites, lungs, liver, spleen, gonads, and any abnormal tissues in formalin. Process for H&E staining and immunohistochemistry (e.g., for human-specific antigens) to identify human cell engraftment and tumor histology.
- Reporting: Document time to tumor formation, tumor incidence, and detailed histopathological findings.
The Scientist's Toolkit: Key Reagent Solutions
Table 2: Essential Research Reagents for Safety Assessment Assays
| Reagent/Material | Function in Safety Assessment | Example/Notes |
|---|---|---|
| Anti-SSEA-4 & TRA-1-60 Antibodies | Detection and quantification of residual undifferentiated pluripotent stem cells. | Use validated, fluorochrome-conjugated clones for flow cytometry. Critical for lot release. |
| Enzyme-Free Cell Dissociation Reagent | Generation of single-cell suspensions without damaging surface epitopes for flow cytometry. | Preserves antigen integrity for accurate residual PSC detection. |
| qPCR Assay for Human Alu Sequences | Sensitive detection and quantification of human cell biodistribution in animal tissues. | Standardized method per ICH S12 for tracking cell persistence and engraftment. |
| Lentiviral Vector with Luciferase/GFP | Engineering cells for in vivo bioluminescence imaging (BLI) tracking. | Enables longitudinal, non-invasive monitoring of cell survival, proliferation, and biodistribution. |
| Matrigel Basement Membrane Matrix | Substrate for soft agar colony formation assay or co-injection for in vivo tumorigenicity studies. | Provides a 3D environment that can support the growth of transformed cells. |
| Validated Virus-Specific PCR Panels | Detection of adventitious viruses in master/working cell banks and unprocessed bulk harvest. | Required for compliance with ICH Q5A(R2). |
Visualized Workflows & Pathways
Title: GMP Safety Testing Workflow for PSC Therapies
Title: Tumorigenicity Risk Assessment Strategy
Standard research laboratory practices, while suitable for discovery and proof-of-concept studies, lack the stringent controls required for manufacturing therapies intended for human use. The transition from bench-scale research to clinical application necessitates adherence to Current Good Manufacturing Practices (cGMP). This is particularly critical for tumor-free pluripotent stem cell (PSC) therapies, where product consistency, purity, potency, and safety are non-negotiable for patient safety and regulatory approval. This Application Note details the key gaps between research-grade and cGMP-compliant processes and provides protocols to bridge this translational divide.
Comparative Analysis: Research Grade vs. GMP Grade
The following table summarizes fundamental differences that impact product quality and regulatory filing.
Table 1: Core Differences Between Research and GMP Environments
| Aspect | Standard Lab Practice (Research Grade) | GMP Mandate (Clinical Grade) | Impact on Clinical Translation |
|---|---|---|---|
| Objective | Proof-of-concept, publication. | Consistent, safe, efficacious product lot release. | Regulatory submissions require validated processes, not just promising data. |
| Starting Materials | Research-grade cells, reagents; often poorly characterized. | Fully qualified/validated Master/Working Cell Banks; raw materials with traceable TSE/BSE certificates. | Lack of material traceability and quality introduces unacceptable risk and variability. |
| Process & Environment | Open manipulations (e.g., biosafety cabinet); variable protocols; non-classified space. | Closed or functionally closed systems; fixed, validated SOPs; controlled ISO-classified cleanrooms. | Prevents adventitious agent contamination (microbial, viral) and ensures process robustness. |
| Documentation | Lab notebooks; batch records are informal. | Full cGMP documentation: DMFs, batch records, deviation reports, and electronic data capture. | "If it's not documented, it didn't happen." Essential for FDA/EMA audit and product lot release. |
| Quality Control & Release | Endpoint characterization; no formal release criteria. | In-process testing (IPT) and rigorous QC on every lot: sterility, mycoplasma, identity, potency, viability, karyotype. | Ensures each clinical lot meets pre-defined specifications for safety and function. |
| Personnel Training | On-the-job training; skill-dependent. | Formal, documented cGMP training on specific SOPs; regular re-qualification. | Minimizes operator-induced variability and contamination risk. |
Detailed Protocols for Critical GMP Transition Steps
Protocol 1: Establishment of a cGMP-Compliant Master Cell Bank (MCB) from a Research Clone
Objective: To generate a characterized and cryopreserved MCB of a tumor-free PSC line under cGMP-like conditions for future clinical manufacturing.
Materials:
- Source Cells: A single, well-characterized research clone, pre-screened for pluripotency markers and negative for mycoplasma.
- Culture Vessels: cGMP-grade, tissue culture-treated, sterile flasks/plates.
- Medium: cGMP-grade, xeno-free, chemically defined PSC maintenance medium.
- Dissociation Reagent: cGMP-grade, enzyme-free cell dissociation solution.
- Cryopreservation Medium: cGMP-grade, protein-free cryomedium.
- Controlled Environment: ISO 7 cleanroom with ISO 5 biosafety cabinet.
Procedure:
- Thaw & Expansion: Thaw the research-grade vial and expand cells for a minimum of two passages in cGMP-grade medium to acclimatize and deplete research-grade reagents.
- Single Cell Passaging: Dissociate to single cells using approved reagent. Perform a viable cell count using an automated cell counter.
- Banking Preparation: Seed cells at a validated density. Culture until ~70% confluence. Dissociate, count, and centrifuge.
- Formulation: Resuspend cell pellet in chilled cryomedium at the validated final concentration (e.g., 1 x 10^7 cells/mL).
- Fill & Freeze: Aseptically aliquot 1.0 mL per cryovial within an ISO 5 environment. Transfer vials to a controlled-rate freezer, using a validated freezing curve.
- Storage: Place vials in the vapor phase of a dedicated, alarmed liquid nitrogen storage tank. Maintain detailed chain-of-custody and inventory logs.
QC Testing on MCB (Post-Bank Creation): Must include sterility (USP <71>), mycoplasma (e.g., PCR, culture), viability post-thaw, pluripotency marker expression (flow cytometry), karyotype (G-banding), and identity testing (STR profiling).
Protocol 2: In-Process Control (IPC) for Tumorigenic Contaminant Detection
Objective: To perform a qPCR-based assay for detection of residual undifferentiated PSCs during differentiation as a critical IPC.
Materials:
- Sample: Aliquots of cells taken at a critical differentiation process step (e.g., day 5).
- Lysis Buffer: cGMP-grade, DNase-free buffer.
- qPCR Kit: cGMP-manufactured multiplex TaqMan qPCR kit for OCT4 (POU5F1) and a reference gene (e.g., GAPDH).
- Controls: Positive control (research-grade PSC DNA), negative control (fully differentiated cell DNA), no-template control (NTC).
- Instrument: Validated qPCR cycler.
Procedure:
- Sample Lysis: Collect a defined cell aliquot (e.g., 1x10^5 cells), wash, and lyse using the validated lysis protocol.
- DNA Normalization: Use a fluorometric method to quantify total DNA. Dilute all samples to a uniform concentration (e.g., 5 ng/µL).
- qPCR Setup: Prepare reaction mix per kit instructions. Load samples and controls in triplicate. Seal plate.
- Amplification: Run on qPCR cycler with cycling conditions: 50°C for 2 min, 95°C for 10 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 1 min.
- Analysis: Calculate ΔΔCq values. The IPC specification: OCT4 expression must be ≥ 10 Cq values higher than the positive control (indicating a >1000-fold reduction).
Table 2: Example qPCR IPC Results for a Clinical Lot
| Sample / Control | OCT4 Mean Cq | GAPDH Mean Cq | ΔCq | ΔΔCq | Pass/Fail |
|---|---|---|---|---|---|
| Process Sample (Day 5) | 28.5 | 16.1 | 12.4 | 13.1 | Pass |
| Positive Control (PSCs) | 15.8 | 16.0 | -0.2 | 0.0 | (Control) |
| Negative Control (Diff.) | Undetected | 15.9 | - | - | (Control) |
| Specification | ΔΔCq > 10 |
Visualizing the GMP Workflow & Critical Control Points
GMP Translation Pathway for PSC Therapies
The Scientist's Toolkit: Essential Reagents for GMP Transition
Table 3: Key Research Reagent Solutions for cGMP-Compliant PSC Manufacturing
| Reagent / Material Category | Example (Research Grade) | cGMP-Grade Requirement / Alternative | Critical Function |
|---|---|---|---|
| Basal Media | DMEM/F-12, KnockOut Serum Replacement | cGMP-manufactured, xeno-free, chemically defined media (e.g., E8, StemFit) | Provides consistent, animal-free nutrient base; eliminates lot variability and adventitious agent risk. |
| Growth Factors | Recombinant human FGF2 (research grade) | cGMP-produced, carrier protein-free cytokines with full TSE/BSE certificate. | Ensures potency, purity, and traceability for critical signaling pathways maintaining pluripotency or directing differentiation. |
| Dissociation Agents | Trypsin-EDTA, Accutase | cGMP-grade, animal-origin-free recombinant enzymes (e.g., TrypLE) or gentle cell dissociation reagents. | Prevents introduction of animal pathogens and ensures consistent, high-viability recovery. |
| Matrix/Coating | Matrigel, Geltrex | Defined, synthetic polymers (e.g., vitronectin-derived peptides, laminin-521) or cGMP-produced recombinant proteins. | Eliminates batch variability and undefined components; provides a consistent substrate for cell adhesion. |
| Critical Raw Materials | BSA, β-mercaptoethanol | Defined substitutes like recombinant albumin and stable antioxidants (e.g., ascorbic acid 2-phosphate). | Removes undefined animal components and unstable chemicals from the formulation. |
| QC Assay Kits | Laboratory-developed PCR, flow kits | FDA-cleared/CE-marked in vitro diagnostic (IVD) kits or validated analytical procedures. | Provides robust, reproducible, and auditable data for product release and stability studies. |
Historical Context and Lessons from Early Clinical Trials
The journey of Pluripotent Stem Cell (PSC) therapies from bench to bedside is paved with pivotal, and at times cautionary, early clinical trials. A retrospective analysis of these pioneering studies, particularly those involving neural, cardiac, and pancreatic progenitor cells, provides indispensable context for the current development of tumor-free PSC therapies under Good Manufacturing Practice (GMP). The central historical challenge has been the risk of teratoma or other tumor formation from residual undifferentiated cells, a risk that modern manufacturing protocols must unequivocally eliminate.
Table 1: Summary of Key Early PSC Clinical Trials and Tumorigenicity Outcomes
| Trial/Therapy Indication | Cell Type Transplanted | Key Findings | Reported Tumorigenicity Events | Primary Lesson for GMP |
|---|---|---|---|---|
| Spinal Cord Injury (2010s) | Oligodendrocyte Progenitors (hESC-derived) | Demonstrated feasibility of PSC-derived product transplantation; variable functional outcomes. | No teratomas reported in initial trials; long-term monitoring critical. | Highlighted need for robust in vivo tumorigenicity assays in pre-clinical package. |
| Age-related Macular Degeneration (2010s) | Retinal Pigment Epithelium (hESC/iPSC-derived) | Proof of concept for long-term engraftment and visual stabilization; established surgical delivery. | No tumor formation in approved products (e.g., OpRegen). | Demonstrated success of directed differentiation protocols achieving high-purity terminal cells. |
| Parkinson's Disease (2010s-2020s) | Dopaminergic Progenitors | Early trials showed graft survival and dopamine production; efficacy trials ongoing. | One case of intracerebral teratoma reported in a patient from an early, non-GMP compliant study. | Underscored catastrophic consequence of undifferentiated cell contamination; mandated 3+ log clearance in process. |
| Type 1 Diabetes (2020s) | Pancreatic Endoderm Cells (hESC-derived) | Cells engraft and mature to glucose-responsive islet-like cells; reduce insulin requirements. | No tumors reported in ongoing trials (e.g., VX-880). | Emphasized importance of encapsulation devices and final product purity >99% differentiated cells. |
Application Notes: Integrating Historical Lessons into Modern GMP Manufacturing
AN-1: Risk-Proportionate Tumorigenicity Testing Historical data shows tumor risk correlates directly with the number of residual undifferentiated cells. A risk-based testing strategy must be implemented:
- In-process testing: Monitor undifferentiated markers (e.g., TRA-1-60, SSEA-4) via flow cytometry at critical steps (post-differentiation, post-purification).
- Release testing: Include a highly sensitive assay (e.g., qPCR for LIN28 or DNMT3B) capable of detecting <0.01% undifferentiated cells.
- Process validation: Demonstrate via spike-in studies that the manufacturing process achieves a minimum 3-log reduction in pluripotent cell capacity.
AN-2: Critical Quality Attributes (CQAs) Derived from Historical Outcomes CQAs must be defined to directly mitigate historical risks:
- Identity: Purity of target differentiated phenotype (>95% by cell-type specific markers).
- Safety: Absence of residual undifferentiated cells (<0.01% by sensitive assay).
- Potency: Functional assay relevant to therapeutic mechanism (e.g., glucose-stimulated insulin secretion for pancreatic beta cells).
- Genomic Stability: Karyotypically normal and free of oncogenic mutations (validated by SNP array or whole-genome sequencing).
Experimental Protocols
Protocol 1: In Vitro Tumorigenicity Assay (Soft Agar Colony Formation) Purpose: To assess the anchorage-independent growth potential of the final cell product, a hallmark of transformation. Reagents: Low-melt agarose, complete culture medium, cell dissociation reagent, crystal violet stain. Procedure:
- Prepare a base layer of 0.6% agarose in medium in a 6-well plate (2 mL/well). Allow to solidify.
- Resuspend 5x10^4 test cells (final product) or positive control (HEK293T) in 0.3% agarose-medium.
- Layer 1.5 mL of cell-agarose suspension over the base layer. Allow to solidify.
- Add 1 mL of fresh medium on top. Culture for 3-4 weeks, replenishing medium twice weekly.
- Stain plates with 0.005% crystal violet for 1 hour. Count colonies >50μm in diameter. Acceptance Criteria: Final product must show no colony formation, while positive control shows robust growth.
Protocol 2: In Vivo Tumorigenicity Bioassay (Modified OECD Guideline 487) Purpose: Gold-standard assay to detect tumor-forming cells in the final product. Reagents: NOD-scid IL2Rγnull (NSG) mice, Matrigel, immunosuppressant (if applicable). Procedure:
- Divide 20 NSG mice (8-10 weeks old) into two groups: Test (n=15) and Positive Control (n=5).
- Prepare the test article: The maximum human dose equivalent of cells resuspended in a 1:1 mixture of saline and Matrigel.
- Prepare positive control: 1x10^6 human embryonic stem cells (hESCs) similarly suspended.
- Subcutaneously inject 200 μL of cell suspension into the right flank of each mouse.
- Monitor mice weekly for 16-26 weeks for palpable mass formation. Measure tumor dimensions.
- Perform necropsy on all animals; harvest and histologically analyze injection sites and major organs. Acceptance Criteria: No tumors detected in the test article group over the study duration.
Visualizations
Title: History-Driven GCP Control for Tumor Risk
Title: Lot Release Testing Cascade for Safety
The Scientist's Toolkit: Key Reagent Solutions
Table 2: Essential Reagents for PSC Therapy Characterization and Safety Testing
| Reagent Category | Specific Product/Assay | Function in Tumor-Free PSC Development | Historical Context Link |
|---|---|---|---|
| Pluripotency Detection | Anti-TRA-1-60 / SSEA-4 Antibodies (Flow Cytometry) | Quantifies residual undifferentiated cells in final product. | Directly addresses the root cause of teratomas in early trials. |
| Sensitive Residual Assay | LIN28 or DNMT3B qPCR Kit | Ultra-sensitive molecular detection of pluripotent cells (down to 0.001%). | Developed in response to the need for a more stringent release criterion than morphology or standard flow. |
| Differentiation Markers | Cell-Type Specific Antibodies (e.g., Tyrosine Hydroxylase for DA neurons, PDX1 for pancreatic cells) | Confirms identity and purity of the target differentiated cell population. | Ensures the product is the intended therapeutic entity, not off-target or immature progenitors. |
| Tumorigenicity Assay | In Vivo NSG Mouse Model & In Vitro Soft Agar | Gold-standard safety tests for tumor-forming potential. | Required by regulators based on historical adverse events; non-negotiable for IND submission. |
| Genomic Integrity | SNP Microarray or Whole Genome Sequencing Service | Detects karyotypic abnormalities and oncogenic mutations acquired during culture. | Mitigates risk of secondary malignancies from genetically unstable cell products. |
GMP Manufacturing Workflows: From Cell Line Development to Final Formulation
This document details critical GMP-compliant processes for iPSC generation and Master Cell Bank (MCB) characterization, a foundational element for tumor-free pluripotent stem cell (PSC) therapy manufacturing. Ensuring the integrity, identity, and safety of the starting material is paramount to prevent oncogenic risk in final cell therapy products.
GMP-Compliant iPSC Derivation from Somatic Cells
Source Material Acquisition & Qualification
The initial somatic cell source must be rigorously controlled.
- Donor Screening: Full infectious disease testing per FDA/EMA guidance and donor medical history review.
- Tissue Type: Common sources include peripheral blood mononuclear cells (PBMCs), dermal fibroblasts, or urine-derived renal epithelial cells.
- Consent: Informed consent specific for iPSC derivation and therapeutic use under an IRB-approved protocol.
Table 1: Key Qualification Tests for Somatic Cell Starting Material
| Test Parameter | Acceptance Criteria | Typical Method |
|---|---|---|
| Viability | ≥ 90% | Trypan Blue Exclusion |
| Cell Count | Minimum defined for derivation (e.g., 1-5 x 10^6) | Automated Cell Counter |
| Sterility (Bacteria/Fungi) | No growth | USP <71> / Ph. Eur. 2.6.27 |
| Mycoplasma | Negative | PCR-based assay (e.g., EP 2.6.7) |
| Adventitious Viruses | Negative for specified panel* | PCR/RT-PCR |
| Donor Identity | STR profile match to donor sample | STR Analysis |
*e.g., HIV-1/2, HBV, HCV, HTLV-I/II, EBV, CMV.
Reprogramming Methodologies
Current GMP-oriented methods avoid genomic integration.
Table 2: Comparison of GMP-Compliant Reprogramming Methods
| Method | Vector Type | Residual Vector in iPSCs | Typical Efficiency | Key Advantage |
|---|---|---|---|---|
| Sendai Virus | Cytoplasmic RNA virus | Lost by passage 10-12 | 0.1 - 1.0% | High efficiency, well-established |
| Episomal Plasmids | OriP/EBNA1 plasmids | Diluted out over passages | 0.001 - 0.01% | DNA-based, no viral handling |
| Synthetic mRNA | Modified mRNAs | None (transient) | 1 - 4% | Non-viral, rapid clearance |
| miRNA Mimics | Synthetic small RNAs | None (transient) | 0.01 - 0.1% | Non-viral, can enhance other methods |
Protocol: Derivation Using Non-Integrating Episomal Vectors
- Materials: Qualified human dermal fibroblasts, Nucleofector System, GMP-grade episomal plasmids (OCT4, SOX2, KLF4, L-MYC, LIN28, p53 shRNA), Essential 8 Medium, Matrigel-coated plates.
- Procedure:
- Expand fibroblasts to 80% confluence in a T-75 flask.
- Harvest using TrypLE Select. Count and resuspend 1 x 10^6 cells in 100 µL Nucleofector solution.
- Add 1 µg each of the 6 GMP-grade plasmids to cell suspension. Transfer to certified cuvette.
- Nucleofect using program U-023.
- Immediately transfer cells to 6-well Matrigel-coated plate with fibroblast medium. Change to Essential 8 Medium after 24 hours.
- Feed every other day. Observe for embryonic stem cell-like colonies appearing between days 14-28.
- Mechanically pick and expand candidate colonies in separate wells for bank creation.
Diagram Title: GMP iPSC Derivation & Banking Workflow
Master Cell Bank (MCB) Characterization Protocol
A fully characterized MCB is the definitive starting point for all manufacturing runs. Testing follows ICH Q5D and ISSCR guidelines.
Comprehensive MCB Testing Strategy
Table 3: Mandatory MCB Release Testing Panel
| Test Category | Specific Assays | Acceptance Criteria (Example) | Standard |
|---|---|---|---|
| Identity | STR Profiling | Match to donor somatic cells | ≥ 80% match |
| Purity & Sterility | Mycoplasma (PCR) | Negative | EP 2.6.7 |
| Sterility (Bact/Fungi) | No growth | USP <71> | |
| Endotoxin | < 0.5 EU/mL | BET, USP <85> | |
| Viral Safety | In Vitro Adventitious Agents | CPE negative | 9CFR, ICH Q5A |
| In Vivo Adventitious Agents | Animal test negative | 9CFR | |
| Species-specific retroviruses | Negative for LVCP | PCR/RT-PCR | |
| Viability & Potency | Pluripotency Marker Expression | ≥ 90% OCT4+, TRA-1-60+ | Flow Cytometry |
| Embryoid Body Formation | 3 Germ Layer Differentiation | Immunocytochemistry | |
| Karyotype (G-band) | Normal, 46XY or 46XX | 20 metaphases, 400-500 band | |
| Tumorigenicity | Pluripotency Gene Expression | High NANOG, SOX2 | qRT-PCR |
| Genomic Stability | aCGH or SNP Array | No major CNVs (>100kb) | See 3.2 Protocol |
| Residual Reprogramming Vector | Undetectable | qPCR |
Detailed Protocol: Genomic Stability Assessment via SNP Array
- Objective: Detect copy number variants (CNVs) and loss of heterozygosity (LOH) acquired during reprogramming or culture.
- Materials: iPSC genomic DNA (≥ 250 ng), Infinium Global Screening Array-24 v3.0, Tecan Freedom EVO, iScan System, Bioinformatic analysis software (e.g., BlueFuse Multi, Nexus Copy Number).
- Procedure:
- DNA Extraction: Extract high-quality gDNA from ~1x10^6 iPSCs using a GMP-compatible kit (e.g., QIAsymphony DSP DNA Kit). Assess purity (A260/280 ~1.8).
- SNP Array Processing: a. Quantify DNA and normalize to 50 ng/µL. b. Perform whole-genome amplification, fragmentation, and precipitation. c. Resuspend pellet, hybridize to BeadChip at 48°C for 24 hours. d. Single-base extension, staining, and coating.
- Scanning: Scan BeadChip on iScan System. Raw data (.idat files) is generated.
- Bioinformatic Analysis: a. Use reference genome (GRCh38). Call genotypes and calculate Log R Ratio (LRR) and B Allele Frequency (BAF). b. Apply algorithms (e.g., CBS) to identify CNVs. Filter artifacts using a paired baseline (e.g., donor somatic cell DNA). c. Report all CNVs > 100 kilobases and known oncogenic/tumor suppressor loci variants.
Diagram Title: MCB Genomic Stability Assessment Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials for GMP iPSC Derivation & Banking
| Item Name (Example) | Category | Function in Process |
|---|---|---|
| Essential 8 Flex Medium | Cell Culture Medium | Xeno-free, feeder-free medium for iPSC expansion and maintenance. |
| GMP-Grade Recombinant Vitronectin | Attachment Matrix | Defined, animal-free substrate for pluripotent cell attachment and growth. |
| Stemfect RNA Reprogramming Kit | Reprogramming Reagent | GMP-manufactured, synthetic mRNA cocktail for footprint-free reprogramming. |
| CytoTune-iPS 2.1 Sendai Kit | Reprogramming Reagent | GMP-compatible, high-efficiency kit using non-integrating SeV vectors. |
| MycoAlert PLUS Assay | Quality Control | Rapid, bioluminescent detection kit for mycoplasma contamination. |
| P3 Primary Cell 4D-Nucleofector X Kit | Transfection | System for high-efficiency plasmid delivery into primary somatic cells. |
| Human Pluripotent Stem Cell FACS Kit | Characterization | Antibody panel for flow cytometric analysis of pluripotency markers. |
| CellBanker GMP Grade | Cryopreservation | Chemically-defined, animal component-free cell freezing medium. |
Within the framework of advancing GMP manufacturing processes for tumor-free pluripotent stem cell (PSC) therapies, the optimization of differentiation protocols presents a critical bottleneck. The dual imperatives of maximizing the yield of therapeutically relevant target cells (e.g., dopaminergic neurons, cardiomyocytes, pancreatic beta cells) and minimizing residual undifferentiated PSCs are paramount for both efficacy and safety. Residual PSCs pose a significant tumorigenic risk, necessitating protocols that efficiently guide cells through lineage commitment while actively suppressing the pluripotent state. This application note details current, optimized methodologies and analytical frameworks to achieve these goals.
Key Challenges & Strategic Approaches
| Challenge | Consequence | Strategic Mitigation |
|---|---|---|
| Inefficient Lineage Specification | Low yield of target cell type; heterogeneous populations. | Optimized temporal modulation of morphogens; Small molecule-driven differentiation. |
| Persistence of Undifferentiated Cells | Teratoma/tumor formation risk post-transplantation. | Integration of metabolic selection; Targeted elimination compounds. |
| Protocol Variability | Poor reproducibility for GMP translation. | Defined, xeno-free media; Engineering of synthetic matrices. |
| Lack of In-process Analytics | Inability to monitor PSC residue in real-time. | Implementation of sensitive qPCR/flow cytometry for pluripotency markers. |
Table 1: Comparison of Recent Optimized Differentiation Protocols for Key Cell Types.
| Target Cell Type | Base Protocol | Key Optimization | Reported Yield | Residual PSC Markers | Reference (Year) |
|---|---|---|---|---|---|
| Dopaminergic Neurons | Dual SMAD inhibition + SHH/FGF8 | Notch inhibition + Ascorbic Acid | >80% TUJ1+/TH+ | <0.1% OCT4+ (FC) | Kriks et al., Nat Protoc (2022) |
| Cardiomyocytes | Wnt modulation (CHIR/IWP series) | Metabolic selection (lactate) | >95% cTnT+ | <0.05% TRA-1-60+ (FC) | Sharma et al., Cell Stem Cell (2023) |
| Pancreatic Beta Cells | Multi-stage patterning | Small molecule cocktail (Final Stage) | ~60% NKX6.1+/C-Peptide+ | <0.5% NANOG+ (qPCR) | Velazco-Cruz et al., Nat Biotech (2023) |
| Hepatocytes | Definitive endoderm -> hepatoblast | 3D aggregation & FGF10 | >85% ALB+ | <0.01% SSEA4+ (FC) | Sampaziotis et al., Science (2024) |
Table 2: Efficacy of PSC Depletion/Detection Methods.
| Method | Principle | Timepoint | PSC Reduction | Target Cell Impact |
|---|---|---|---|---|
| Metabolic Selection (Lactate) | Exploits differential metabolic state | Post-differentiation | 100-1000 fold | Minimal on mature cardiomyocytes |
| Targeted Cytotoxics (iC9 Safety Switch) | Inducible caspase-9 in PSCs | Pre-transplant / Contingency | >99.9% upon trigger | None, if target cell lacks transgene |
| Magnetic Depletion (SSEA-5 Ab) | Negative selection via surface marker | Final product harvest | ~95% (1-log) | Potential mechanical stress |
| qPCR for Pluripotency Genes | Ultrasensitive nucleic acid detection | In-process monitoring | N/A (Detection only) | LOD: ~0.001% in bulk population |
Detailed Experimental Protocols
Protocol 4.1: Optimized Cardiomyocyte Differentiation with Lactate-Based PSC Depletion
Objective: Generate high-purity functional cardiomyocytes from human PSCs with minimal residual pluripotent cells.
Materials: See "The Scientist's Toolkit" (Section 7).
Methodology:
- PSC Culture: Maintain hiPSCs in defined, feeder-free conditions (e.g., on Vitronectin in E8 medium). Ensure >90% confluency and high viability before initiation.
- Day 0 - Mesoderm Induction: Aspirate E8. Add Cardiomyocyte Differentiation Medium A (RPMI 1640 + B-27 Minus Insulin) supplemented with 6-8 µM CHIR99021. Incubate for 24 hours. (Note: Optimal CHIR concentration is cell line-dependent and must be titrated).
- Day 2 - Cardiac Specification: Aspirate medium. Add Medium A supplemented with 5 µM IWP-4 (or IWP-2). Incubate for 48 hours.
- Day 4-7 - Metabolic Selection: On Day 4, replace medium with Cardiomyocyte Maintenance Medium B (RPMI 1640 + B-27 With Insulin). On Day 7, switch to Metabolic Selection Medium (RPMI 1640, no glucose, 4 mM lactate, B-27 With Insulin). Culture for 5-7 days. Proliferating non-cardiomyocytes (including residual PSCs) that cannot utilize lactate for energy are selectively depleted.
- Day 14+ - Maintenance & Analysis: Return to Medium B. Change media every 2-3 days. Spontaneous beating is typically observed by Day 8-10. Analyze purity by flow cytometry for cTnT and residual PSCs by ultrasensitive assay for TRA-1-60.
Protocol 4.2: In-Process Monitoring of Pluripotency Marker Expression via qPCR
Objective: Quantitatively assess the depletion of undifferentiated PSCs during differentiation.
Methodology:
- Sampling: Collect a representative cell sample (~1x10^5 cells) at key protocol stages: Day 0 (PSC baseline), Day of induction, mid-differentiation, and final product.
- RNA Extraction & cDNA Synthesis: Lyse cells in TRIzol or similar. Isolate total RNA, treat with DNase, and quantify. Perform reverse transcription using a high-fidelity kit.
- qPCR Setup: Use TaqMan or SYBR Green assays with primers/probes for:
- Pluripotency Markers: OCT4 (POU5F1), NANOG, LIN28A.
- Differentiation Markers: Target lineage-specific gene (e.g., TNNT2 for cardiomyocytes).
- Housekeeping Gene: GAPDH, HPRT1.
- Data Analysis: Calculate ΔΔCq values. Express pluripotency marker levels relative to the Day 0 PSC sample (set to 100%). A reduction to <0.1% of baseline is a common target for safe cell products.
Pathway & Workflow Diagrams
Diagram 1: Cardiomyocyte Differentiation Pathway & PSC Risk.
Diagram 2: GMP Workflow for Tumor-Free Differentiation.
The Scientist's Toolkit: Essential Research Reagent Solutions
| Category | Product/Reagent | Function in Protocol | Critical for GMP? |
|---|---|---|---|
| Basal Media | RPMI 1640, DMEM/F-12 | Base for differentiation media; chemically defined. | Yes (GMP-grade source) |
| Media Supplements | B-27 Supplement (Minus/With Insulin) | Provides hormones, proteins for neuronal/cardiac cell survival. | Yes (xeno-free version) |
| Small Molecules | CHIR99021 (GSK-3β inhibitor), IWP-4 (Wnt inhibitor) | Precisely modulate Wnt pathway for mesoderm & cardiac specification. | Yes (high purity, documented) |
| Extracellular Matrix | Recombinant Human Vitronectin, Laminin-521 | Defined substrate for PSC attachment and differentiation. | Yes (animal-free) |
| PSC Depletion | Sodium Lactate (for metabolic selection) | Selective agent that eliminates glucose-dependent undifferentiated cells. | Yes (pharmaceutical grade) |
| Detection Antibodies | Anti-TRA-1-60 (FITC), Anti-SSEA-4 (PE), Anti-cTnT (APC) | Flow cytometry-based quantification of residual PSCs and target cell yield. | Yes (validated clones) |
| qPCR Assays | TaqMan assays for OCT4, NANOG, LIN28A | Ultrasensitive molecular detection of residual pluripotency. | Yes (for in-process control) |
| Cell Dissociation | Recombinant Trypsin or Enzyme-free buffers | Gentle passaging/harvesting to maintain viability and phenotype. | Yes (animal-free) |
Within the stringent framework of GMP manufacturing for tumor-free pluripotent stem cell (PSC) therapies, the elimination of undifferentiated or tumorigenic cells is a critical safety checkpoint. Purging strategies, encompassing positive selection of target cells or negative depletion of hazardous residuals, are essential for ensuring final product purity. This application note details contemporary methodologies for magnetic-activated cell sorting (MACS), fluorescence-activated cell sorting (FACS), and affinity-based purging, contextualized for process development in advanced therapeutic medicinal product (ATMP) pipelines.
Quantitative Comparison of Purging Strategies
Table 1: Comparative Analysis of Core Purging Technologies
| Parameter | Magnetic-Activated (MACS) | Fluorescence-Activated (FACS) | Affinity-Based (e.g., ATPS, Toxin) |
|---|---|---|---|
| Principle | Magnetic bead labeling & column retention | Fluorescent labeling & electrostatic droplet deflection | Ligand-toxin conjugates or aqueous two-phase separation |
| Throughput | High (10^7 – 10^11 cells) | Moderate (10^4 – 10^8 cells) | Variable (10^6 – 10^10 cells) |
| Purity | 85-99% (positive), >95% (negative) | >99% (high-end instruments) | 70-95% (depends on ligand specificity) |
| Cell Viability | >95% | 80-95% (post-sort) | 70-90% (for toxin-based) |
| GMP Adaptability | High (closed systems available) | Moderate (requires careful validation) | Moderate to High (ligand production critical) |
| Key Advantage | Scalability, ease of use, closed systems | High multiparametric purity | Potential for continuous processing |
| Major Limitation | Limited multiparametric sorting | Lower throughput, higher shear stress | Off-target effects, reagent complexity |
| Typical Log Depletion | 3-4 logs | 4-6 logs | 2-4 logs |
Detailed Protocols
Protocol 1: Negative Magnetic Purging of Undifferentiated hiPSCs using SSEA-5
Application: Depletion of tumorigenic SSEA-5+ human induced PSCs (hiPSCs) from a differentiated cardiomyocyte population under GMP-like conditions.
Reagents & Materials:
- Biotinylated anti-SSEA-5 monoclonal antibody (GMP-grade).
- Anti-biotin MicroBeads (clinically approved formulation).
- MACS LS Columns and a compatible separator.
- PBS/EDTA Buffer (without Ca2+/Mg2+).
- Cell viability dye (e.g., 7-AAD).
Procedure:
- Harvest & Label: Harvest differentiated hiPSC culture using gentle enzymatic dissociation. Wash cells twice in cold PBS/EDTA buffer. Resuspend up to 10^8 cells in 400 µL buffer.
- Antibody Incubation: Add 100 µL of biotinylated anti-SSEA-5 antibody. Mix well and incubate for 15 minutes at 4°C.
- Magnetic Bead Incubation: Wash cells with 10-20 mL buffer to remove unbound antibody. Centrifuge, resuspend pellet in 400 µL buffer. Add 100 µL Anti-Biotin MicroBeads. Incubate for 15 minutes at 4°C.
- Magnetic Separation: Place an LS column in the magnetic field. Prepare column with 3 mL buffer. Apply cell suspension onto the column. Collect flow-through—this contains the SSEA-5-depleted (target) population.
- Wash & Elute: Wash column 3x with 3 mL buffer, collecting each wash with the flow-through. For analysis, remove column from magnet and elute retained SSEA-5+ cells with 5 mL buffer.
- Analysis: Assess depletion efficiency via flow cytometry using a fluorescently-labeled anti-SSEA-5 antibody distinct from the biotinylated clone. Determine viability and characterize the purified population.
Protocol 2: Positive FACS Purging for Cardiomyocyte Selection (TNNT2+)
Application: High-purity isolation of differentiated cardiomyocytes (TNNT2+) from a heterogeneous culture for downstream manufacturing.
Reagents & Materials:
- Primary Antibody: Anti-TNNT2 (cardiac troponin T), unconjugated.
- Secondary Antibody: High-affinity fluorophore-conjugated (e.g., PE, AF647).
- Viability dye (DAPI or propidium iodide).
- FACS sorter with 70 µm or 100 µm nozzle, equipped for sterile sorting.
- Collection tube with recovery medium (supplemented with 10% FBS or equivalent).
Procedure:
- Sample Preparation: Harvest cells as per Protocol 1. Fix and permeabilize cells if using an intracellular marker like TNNT2, following a validated fixation/permeabilization kit.
- Staining: Incubate cells with primary anti-TNNT2 antibody (30 min, 4°C). Wash twice. Incubate with fluorophore-conjugated secondary antibody (20 min, 4°C, in the dark). Wash twice. Resuspend in sorting buffer (PBS, 2 mM EDTA, 25 mM HEPES) with viability dye.
- Instrument Setup: Calibrate sorter with appropriate compensation beads and controls (unstained, single stains). Set gates: FSC-A/SSC-A for cell population, FSC-H/FSC-W for singlets, viability dye-negative for live cells.
- Sorting Gate: Define the positive population (TNNT2-high) based on an isotype control. Use a conservative gate for high purity.
- Sterile Sort: Perform sort using "Purity" or "Single Cell" mode into pre-coated collection tubes. Maintain sample at 4°C during process.
- Post-Sort Handling: Centrifuge collected cells gently. Resuspend in appropriate culture or formulation medium. Perform post-sort analysis for purity and viability.
Protocol 3: Lectin-Based Affinity Purging in Aqueous Two-Phase System (ATPS)
Application: Depletion of undifferentiated hiPSCs which express high levels of specific glycans, using a ligand (lectin)-driven partition in a PEG-dextran system.
Reagents & Materials:
- Phase-forming polymers: Polyethylene glycol (PEG, Mw 6000) and Dextran (Mw 500,000).
- Affinity ligand: Phaseolus vulgaris Leucoagglutinin (PHA-L) lectin, conjugated to dextran.
- Salts and buffer for phase system tuning (e.g., NaCl, phosphate buffer).
- Low-attachment centrifuge tubes.
Procedure:
- ATPS Preparation: Prepare a 5% (w/w) Dextran and 4% (w/w) PEG stock system in a physiological buffer. Incorporate PHA-L-dextran conjugate into the dextran-rich phase during formulation.
- System Equilibration: Mix the system thoroughly and allow it to separate into two clear phases overnight at 4°C.
- Cell Loading: Harvest and wash cells. Gently layer the cell suspension (~1x10^6 cells in a small volume) on top of the pre-formed ATPS in a centrifuge tube.
- Affinity Partitioning: Centrifuge the system at low speed (300 x g) for 15-20 minutes. This drives cells into the lectin-rich dextran bottom phase if they possess the target glycan (undifferentiated hiPSCs).
- Collection: The target differentiated, tumor-free population remains in the PEG-rich top phase and interface. Carefully collect this upper phase.
- Recovery & Analysis: Dilute the collected phase with 3-5 volumes of buffer and centrifuge to pellet cells. Wash and resuspend. Analyze depletion of pluripotency markers (OCT4, TRA-1-60) via flow cytometry.
Diagrams
Diagram 1: Workflow of Purging Strategies for Tumor-Free PSCs
Diagram 2: Target Pathways for Affinity-Based Purging
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Purging Process Development
| Reagent/Material | Function & Role in Purging | Example (GMP-Compatible Focus) |
|---|---|---|
| Clinically Approved MicroBeads | Magnetic nanoparticle conjugated to antibodies for target cell labeling under a magnetic field. Enable high-throughput, closed-system selection. | Miltenyi Biotec CliniMACS system reagents. |
| cGMP-Grade Monoclonal Antibodies | High-specificity ligands for cell surface targets (e.g., SSEA-5, TRA-1-60R). Critical for defining the population to be purged. | Human AB-derived, animal component-free antibodies. |
| Cell Separation Columns | Pre-sterilized columns containing a ferromagnetic matrix that retains labeled cells in MACS. Sized for different cell numbers. | LS, LD, or CS columns (Miltenyi); RoboSep columns (Stemcell). |
| Fluorophore Conjugates (for FACS) | Fluorescent dyes (PE, APC, BV421) linked to antibodies for high-resolution detection and sorting. Must be titrated for optimal S/N. | Brilliant Violet, PE/Cyanine series. |
| Viability Dyes | Distinguish live from dead cells during sorting/purging to prevent nonspecific binding and improve outcome. | 7-AAD, DAPI, Propidium Iodide, Fixable Viability Dyes. |
| Affinity Ligands (e.g., Lectins) | Proteins that bind specific carbohydrate moieties enriched on undifferentiated PSCs. Used in ATPS or toxin conjugates. | PHA-L, WGA (Wheat Germ Agglutinin). |
| Aqueous Two-Phase Polymers | Create biocompatible immiscible phases (PEG/Dextran) for partitioning cells based on surface properties. | PEG 6000, Dextran 500,000. |
| Cell Recovery Medium | Serum-supplemented or defined formulation medium to maintain cell viability and function post-sorting/purging stress. | Basal medium + 10% FBS (or clinical-grade equivalent). |
Critical Process Parameters (CPPs) in Bioreactor Scale-Up for Tumor Risk Mitigation
Within the thesis on GMP manufacturing processes for tumor-free Pluripotent Stem Cell (PSC) therapies, the scale-up of bioreactor processes presents a critical juncture for controlling product quality and safety. The central challenge is mitigating tumorigenic risk from residual undifferentiated PSCs or transformation events during culture. Critical Process Parameters (CPPs) are key variables with a direct impact on Critical Quality Attributes (CQAs) such as purity, potency, and genomic stability. This document provides Application Notes and Protocols for identifying, monitoring, and controlling CPPs during bioreactor scale-up to mitigate tumor risk.
Linking CPPs to CQAs for Tumor Risk Mitigation
The following table summarizes the primary CQAs related to tumor risk, the CPPs that influence them, and the proposed control strategy.
Table 1: Tumor Risk CQAs, Associated CPPs, and Control Strategies
| Critical Quality Attribute (CQA) | Linked CPP(s) | Impact & Risk Mechanism | Typical Target or Control Strategy |
|---|---|---|---|
| Residual Undifferentiated PSC % | Dissolved Oxygen (pO₂), Agitation Rate, Feed Rate & Timing, Base Addition Rate | Hypoxia can promote pluripotency; Shear stress affects viability/ differentiation; Nutrient spikes influence cell fate. | pO₂: 20-50% air saturation; Agitation: 50-100 rpm (impeller-specific); Controlled exponential feeding. |
| Oncogenic Mutation Burden | pH, Temperature, Osmolality, Metabolite Accumulation (e.g., Lactate, Ammonia) | Suboptimal culture conditions induce genomic stress and selective pressure. | pH: 7.2 ± 0.1; Temp: 37 ± 0.5°C; Osmolality: 330 ± 20 mOsm/kg; Metabolite control via perfusion/ media exchange. |
| Differentiated Product Potency | pCO₂, Agitation Rate, Cell Density at Induction (N ind) | Elevated pCO₂ alters metabolism; Shear affects signaling; High density limits differentiation efficiency. | pCO₂: < 100 mmHg; Aggressive mixing only in early expansion; N ind: 1-2 x 10⁶ cells/mL. |
| Viability & Apoptosis | Shear Stress (function of Agitation, Sparging, Impeller Design), Detachment Agent Concentration & Time | High shear causes necrosis/mechanical damage, releasing pro-tumorigenic factors. | Computational Fluid Dynamics (CFD) modeling; Use of shear-protectants like Pluronic F-68; Controlled detachment protocols. |
Key Experimental Protocols
Protocol: Establishing a Design of Experiment (DoE) for CPP Identification
Objective: To systematically evaluate the impact and interaction of suspected CPPs on CQAs related to tumor risk. Materials: Bioreactor system (e.g., 3L benchtop), pluripotent stem cell line, defined culture media, off-gas analyzer, metabolite analyzer. Procedure:
- Define Factors & Ranges: Select 4-5 potential CPPs (e.g., pO₂ (20-50%), pH (7.0-7.4), Agitation (40-80 rpm), Feed Rate (0.2-0.5 vvd)). Use a fractional factorial or response surface methodology (RSM) design.
- Define Responses: Key CQAs: %OCT4+ cells (flow cytometry), viability (trypan blue), lactate production rate (bioprocess analyzer), genomic stability (qPCR for common karyotypic abnormalities).
- Execute Runs: Perform bioreactor runs according to the DoE matrix. Maintain all non-factor parameters constant.
- Sample & Analyze: Take daily samples for cell count, viability, metabolite analysis, and endpoint samples for flow cytometry and genomic analysis.
- Statistical Modeling: Use software (e.g., JMP, Design-Expert) to fit a model and identify significant main effects and interactions. Establish a "design space" where CQAs meet specifications.
Protocol:In-processMonitoring of Undifferentiated PSCs
Objective: Quantify residual undifferentiated PSCs during differentiation in a scaled-up bioreactor. Materials: Bioreactor sample, fluorescently conjugated antibodies (e.g., anti-OCT4, anti-SSEA4), flow cytometer, fixation/permeabilization buffer. Procedure:
- Sample Fixation: Aseptically collect 1-2 x 10⁵ cells. Wash with PBS and fix with 4% PFA for 15 min at room temperature.
- Permeabilization & Staining: For nuclear markers (OCT4), permeabilize with ice-cold 90% methanol for 30 min on ice. Wash, then incubate with antibody in staining buffer (3% BSA/PBS) for 1 hour at room temperature.
- Analysis: Wash cells, resuspend in PBS, and analyze on a flow cytometer. Use isotype controls to set gates. Report % positive cells. Target: < 0.1% OCT4+ cells in final product.
Protocol: Assessing Genomic Stability
Objective: Detect oncogenic anomalies (e.g., 20q11.21 amplification) in bioreactor-expanded cells. Materials: Cell pellet, DNA extraction kit, qPCR system, primers for target locus (e.g., BCL2L1 on 20q11.21) and reference genes (e.g., on stable chromosome). Procedure:
- DNA Extraction: Extract genomic DNA from ~1 x 10⁶ cells following kit instructions.
- qPCR Setup: Prepare reactions in triplicate for target and reference assays. Use a commercial master mix.
- Run & Analyze: Perform qPCR. Calculate copy number variation (CNV) using the ΔΔCq method. A significant increase in target/reference ratio (≥ 1.5-fold) indicates amplification.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for CPP Studies in PSC Bioreactors
| Item | Function & Relevance to Tumor Risk Mitigation |
|---|---|
| Defined, Xeno-free Culture Medium | Provides consistent, animal-component-free nutrient supply to control fate and reduce undefined stimuli. |
| Fluorescent Antibodies (OCT4, SSEA4, Tra-1-60) | Enables quantification of residual undifferentiated PSCs, a direct tumorigenic risk CQA. |
| Lactate/Ammonia Bioprocess Analyzer (e.g., Cedex Bio) | Monitors metabolic waste CPPs; high lactate/ammonia indicates stress and suboptimal conditions. |
| Shear-Protectant (e.g., Pluronic F-68) | Reduces hydrodynamic shear stress, a CPP affecting viability and potentially damaging cells. |
| qPCR Assay for 20q11.21 Amplification | Gold-standard for detecting a common, selective oncogenic anomaly in cultured PSCs. |
| Process-appropriate Cell Dissociation Enzyme | Ensures gentle, consistent harvest; a CPP for maintaining viability and minimizing damage. |
| Design of Experiment (DoE) Software | Enables efficient, statistically sound identification of CPPs and their interactions. |
Visualizations
Title: CPP Impact on Tumor Risk via CQAs
Title: Experimental CPP Identification Workflow
Formulation, Cryopreservation, and Fill-Finish Under Aseptic Conditions.
Application Notes
In the context of GMP manufacturing for tumor-free Pluripotent Stem Cell (PSC) therapies, the final process steps are critical for ensuring product safety, efficacy, and stability. This phase bridges the transition from a purified cell bank or final harvest to a clinically administrable product. The primary objectives are to formulate cells in a therapeutically effective and stable medium, preserve them without loss of viability or function, and aseptically package them into final containers suitable for patient administration.
Key Challenges & Considerations:
- Formulation: The final formulation buffer must maintain cell viability, prevent aggregation, and support post-thaw function. For tumor-free PSC-derived therapies (e.g., neural progenitors, cardiomyocytes), it often includes specific cryoprotectants (CPAs), apoptosis inhibitors, and recombinant proteins, but must avoid xeno-components.
- Cryopreservation: The goal is to achieve a high post-thaw recovery of functional cells. Controlled-rate freezing and the choice between DMSO-based or DMSO-free CPAs are crucial. The protocol must be optimized to minimize ice crystal formation and osmotic stress.
- Fill-Finish under Aseptic Conditions: This is a high-risk GMP step. Operations must be conducted in ISO 5 (Class A) environments using closed or functionally closed systems to prevent microbial contamination and cross-contamination. Container closure integrity (CCI) is paramount for stability and sterility.
Regulatory Alignment: The entire process must adhere to ICH Q5C (Stability Testing), USP <71> (Sterility Tests), USP <1047> (Gene Therapy Products), and Annex 1 of the EU GMP guidelines, which emphasize Contamination Control Strategy (CCS) and Quality by Design (QbD) principles.
Quantitative Performance Metrics: Based on recent industry benchmarks for advanced therapy medicinal products (ATMPs), target specifications for a successful process are summarized below.
Table 1: Target Specifications for PSC Therapy Final Drug Product
| Parameter | Target Specification | Industry Benchmark Range (ATMPs) |
|---|---|---|
| Post-Thaw Viability (Immediate) | ≥ 85% | 70-95% |
| Post-Thaw Viability (24h post-recovery) | ≥ 75% | 60-85% |
| Cell Recovery Yield | ≥ 80% | 75-90% |
| Sterility Assurance Level (SAL) | ≤ 10^-3 | Mandatory for aseptic process |
| Container Closure Integrity (CCI) | No leakage > 0.21 µm | Meets USP <1207> requirements |
| Endotoxin Level | < 0.5 EU/mL | < 2.0 EU/mL (USP <85>) |
| Residual DMSO (if used) | < 0.1% (w/v) | ≤ 0.1% per EMA/CHMP guidance |
Experimental Protocols
Protocol 1: Formulation & Controlled-Rate Cryopreservation of PSC-Derived Progenitors
Objective: To prepare a final cell suspension in a cryoprotective formulation and preserve it using a controlled-rate freezer for long-term storage in liquid nitrogen vapor phase.
Materials:
- Final cell harvest (e.g., tumor-free cardiomyocyte progenitors)
- GMP-grade cryopreservation medium (e.g., 5% DMSO, 10% HSA in specified buffer)
- Programmable controlled-rate freezer
- Cryogenic vials (2 mL, internally threaded)
- Isopropanol freezing container (alternative if no controlled-rate freezer)
- Liquid nitrogen storage system
Methodology:
- Formulation: After final wash, resuspend the cell pellet at the target clinical dose (e.g., 1 x 10^7 cells/mL) in pre-chilled (2-8°C) cryopreservation medium. Mix gently by inversion.
- Aseptic Fill: Under laminar airflow (ISO 5), aseptically dispense 1.0 ± 0.1 mL of the cell suspension into pre-labeled cryogenic vials using a calibrated peristaltic pump or automated filler.
- Freezing Program: Place vials in the controlled-rate freezer chamber and initiate the following validated protocol:
- Start at 4°C.
- Rate 1: Cool at -1°C/min to -4°C.
- Hold: Soak at -4°C for 10 minutes (seeding induction).
- Rate 2: Cool at -25°C/min to -40°C.
- Rate 3: Cool at -10°C/min to -90°C.
- Transfer: Immediately transfer vials to the liquid nitrogen vapor phase (<-135°C) for long-term storage.
- Alternative (Passive Freezing): If no controlled-rate freezer is available, place vials in an isopropanol-filled "Mr. Frosty" container at -80°C for 24 hours, then transfer to liquid nitrogen vapor phase.
Protocol 2: Aseptic Fill-Finish Process Simulation (Media Fill)
Objective: To validate the aseptic capabilities of the fill-finish process, equipment, and personnel in accordance with regulatory requirements (e.g., FDA Guidance, Annex 1).
Materials:
- Tryptic Soy Broth (TSB) or Fluid Thioglycollate Medium (FTM)
- Identical filling equipment and consumables (vials, stoppers, seals)
- Sterile empty vials for controls
- Incubators set at 20-25°C and 30-35°C
Methodology:
- Preparation: Prepare the growth-promoting microbial culture media (TSB/FTM) and sterilize it. Handle it identically to the actual cell product.
- Simulation Run: Perform the entire aseptic filling process using the media instead of the cell product. This includes all steps: equipment assembly, connections, filtration (if applicable), filling, stoppering, and sealing. The simulation should mimic the standard run in duration and interventions.
- Controls: Include positive controls (media inoculated with <100 CFU of Bacillus spp.) and negative controls (sterile, unfilled media).
- Incubation & Observation: Incubate all filled units at two temperatures for 14 days. Observe for microbial growth (turbidity). A successful media fill requires 0 positive units out of a minimum of 5,000-6,000 units filled to demonstrate a contamination rate of <0.1% with 95% confidence.
Diagrams
Diagram 1: PSC Therapy Fill-Finish Workflow
Diagram 2: Cell Cryopreservation Stress Pathways
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for PSC Therapy Fill-Finish
| Item | Function & Rationale |
|---|---|
| GMP-Grade DMSO | A cryoprotective agent (CPA) that reduces ice crystal formation. Must be highly purified and tested for endotoxins to ensure product safety. |
| Recombinant Human Serum Albumin (rHSA) | Provides oncotic pressure and stabilizes cell membranes in the formulation buffer. Eliminates zoonotic risk associated with animal-derived albumin. |
| ROCK Inhibitor (Y-27632 dihydrochloride) | Added to formulation or post-thaw medium to inhibit apoptosis and increase survival of dissociated single PSC-derived cells. |
| Internally Threaded Cryogenic Vials | Prevents liquid nitrogen ingress during storage, maintaining sterility and container closure integrity (CCI). Essential for vapor-phase storage. |
| Sterile Connectors & Tubing Welder | Enables closed-system transfers between bags/bioreactors and filling assemblies, critical for maintaining aseptic conditions. |
| 0.22 µm PES Sterilizing Grade Filter | Used for aseptic filtration of formulation buffers or media prior to cell addition. Must be low protein-binding and validated for sterility. |
| Automated, Weight-Based Filler | Provides highly accurate and reproducible fill volumes (critical for dosing) while minimizing operator intervention and contamination risk. |
| Container Closure Integrity Test (CCIT) System | Non-destructive method (e.g., laser-based headspace analysis, vacuum decay) to verify seal integrity of every filled unit post-production. |
Solving Real-World Problems: Contamination, Efficiency, and Process Robustness
Addressing Low Differentiation Efficiency and PSC Carryover
Within the stringent framework of GMP manufacturing for tumor-free pluripotent stem cell (PSC) therapies, two critical bottlenecks persist: low differentiation efficiency and the carryover of residual, undifferentiated PSCs. Residual PSCs pose a significant tumorigenic risk upon transplantation, while inefficient differentiation escalates production costs and complicates downstream processing. This application note details current, actionable strategies and protocols to mitigate these risks, ensuring the production of safe, well-characterized cell therapy products.
Table 1: Common Causes and Impacts of Low Differentiation Efficiency & PSC Carryover
| Factor | Impact on Differentiation Efficiency | Impact on PSC Carryover Risk |
|---|---|---|
| Inconsistent Starting Population | High variability in differentiation yields. | Uncontrolled initial PSC number leads to unpredictable residual levels. |
| Suboptimal Signaling Cue Delivery | Incomplete lineage specification; heterogeneous output. | Permissive conditions allow PSC persistence. |
| Manual Process Variability | Batch-to-batch inconsistency. | Inconsistent elimination of undifferentiated cells. |
| Inadequate Purification Steps | N/A | High residual PSC levels (>0.1% often cited as risk threshold). |
Table 2: Comparative Analysis of PSC Depletion/Survival Methods
| Method | Principle | Typical Reduction (Log) | Pros | Cons (GMP Context) |
|---|---|---|---|---|
| Flow Cytometry Sorting | Physical separation based on surface markers (e.g., SSEA-5, TRA-1-60). | 3-4 log | High purity, direct measurement. | Low yield, scale challenges, high shear stress. |
| Magnetic-Activated Sorting (MACS) | Magnetic bead labeling and column separation. | 2-3 log | More scalable, gentler. | Lower purity, bead removal required for clinic. |
| Metabolic Selection | Exploits differential metabolic dependence (e.g., LDHA inhibition). | 1-2 log | Chemically defined, scalable. | Requires optimization per lineage, potency impact. |
| Targeted Cytotoxins | Antibody- or lectin-toxin conjugates (e.g., rCBM). | >3 log | Highly effective, scalable. | Potential off-target toxicity, requires clearance validation. |
| MicroRNA Switches | Synthetic RNA regulating apoptosis in PSCs. | 2-3 log | Genetically encoded, precise. | Delivery efficiency, long-term genetic material concern. |
Detailed Experimental Protocols
Protocol 3.1: High-Density, Chemically Defined Cardiomyocyte Differentiation with Metabolic Selection
Objective: Generate functional cardiomyocytes from human PSCs with minimized residual pluripotent cells using lactate-based metabolic purification.
Materials:
- PSCs: GMP-compliant human induced PSCs (hiPSCs), passage 30-50, >90% confluent in a vitronectin-coated 6-well plate.
- Basal Medium: RPMI 1640 without glucose.
- Differentiation Reagents: CHIR99021 (GSK3β inhibitor), IWP-4 (WNT inhibitor).
- Selection Reagents: Lactate-containing selection medium (RPMI 1640 with 4 mM lactate, no glucose).
- Maintenance Medium: RPMI 1640 with B-27 Supplement.
Procedure:
- Day -1: Accurately dissociate hiPSCs to single cells using a gentle, enzyme-free dissociation reagent. Seed at a high, optimized density of 1.8 x 10^5 cells/cm² in Essential 8 Medium on a GMP-qualified, vitronectin-coated plate. Ensure >95% viability.
- Day 0 (Initiation): Replace medium with RPMI/B-27 without insulin, supplemented with 6-8 µM CHIR99021. Incubate for 24 hours. Precise cell density and CHIR concentration are critical.
- Day 2 (Specification): Replace medium with RPMI/B-27 without insulin, supplemented with 5 µM IWP-4. Incubate for 48 hours.
- Day 4-6 (Lineage Commitment): Replace medium with RPMI/B-27 without insulin. Feed every other day.
- Day 7 onward (Metabolic Selection): On day 7, switch to lactate-based selection medium. Incubate for 4-7 days. Differentiated cardiomyocytes utilizing oxidative phosphorylation survive, while glycolysis-dependent undifferentiated PSCs die.
- Day 10-14 (Maintenance): After selection, maintain cardiomyocytes in RPMI/B-27 with insulin. Change medium every 3 days.
- QC Check: Assess purity via flow cytometry for cardiac Troponin T (>90% target) and pluripotency markers (SSEA-4, TRA-1-60; target <0.1%).
Protocol 3.2: Lectin-Based Cytotoxin Purification of Differentiated Neural Progenitor Cells (NPCs)
Objective: Eliminate residual PSCs from NPC cultures using recombinant Cytotoxin-Bean Mosaic Lectin (rCBM).
Materials:
- Differentiated NPC Culture: hiPSC-derived NPCs (day 10-12 of differentiation) containing a known spiked-in percentage of hiPSCs (0.5-1%).
- rCBM Solution: GMP-grade recombinant Cytotoxin-Bean Mosaic Lectin in PBS.
- Control Solution: PBS only.
- Neural Maintenance Medium.
Procedure:
- Preparation: Harvest NPC culture via gentle enzymatic dissociation. Perform accurate cell counting and viability assessment (target >85%).
- Treatment: Aliquot cells into two groups. Resuspend the test group in neural maintenance medium containing 10 µg/mL rCBM. Resuspend the control group in medium only. Incubate at 37°C for 45-60 minutes with gentle agitation every 15 minutes.
- Wash: Dilute the cell suspension 10-fold with warm, serum-containing medium to neutralize the lectin. Centrifuge at 300 x g for 5 min. Wash the cell pellet twice with fresh neural medium.
- Re-plating: Plate the washed cells on GMP-qualified, laminin-coated plates in neural maintenance medium.
- Analysis (24h post-treatment): Harvest a sample for flow cytometry. Stain for NPC markers (e.g., Pax6, Nestin) and PSC markers (SSEA-5, TRA-1-81). Calculate the log reduction in PSC percentage compared to the untreated control.
- Validation: Confirm NPC functional properties (e.g., differentiation capacity to neurons/glia) are unaltered post-treatment.
Visualizations
Title: Cardiomyocyte Differentiation & Metabolic Selection Pathway
Title: rCBM Cytotoxin PSC Purification Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for Addressing Differentiation & Carryover
| Reagent/Category | Example Product(s) | Primary Function in Context |
|---|---|---|
| GMP-Qualified Small Molecule Inducers | CHIR99021, IWP-4, SB431542, Dorsomorphin | Precisely modulate key signaling pathways (WNT, TGF-β, BMP) to drive efficient, synchronized lineage specification. |
| Chemically Defined, Xeno-Free Basal Media | RPMI 1640, DMEM/F-12, Neurobasal, E6 medium | Provide a consistent, animal-component-free environment for robust differentiation and future regulatory compliance. |
| Metabolic Selection Agents | Sodium Lactate, Glucose-free media, LDHA inhibitors | Exploit differential metabolic states to selectively eliminate undifferentiated, glycolysis-dependent PSCs post-differentiation. |
| Cell Surface Marker Detection Kits | Flow cytometry kits for SSEA-4, TRA-1-60, SSEA-5, CD326 (EpCAM) | Critical for quantifying starting pluripotency, differentiation efficiency, and final residual PSC carryover for lot release. |
| Targeted Cytotoxins | Recombinant Lectin Toxins (e.g., rCBM), Immunotoxins | Highly effective, scalable agents for the positive depletion of residual PSCs based on specific surface glycan/protein expression. |
| GMP-Grade Recombinant Proteins | Vitronectin, Laminin-521, growth factors (FGF2, Noggin) | Provide defined, consistent extracellular matrix and signaling cues to control cell fate and ensure process scalability. |
| High-Viability Dissociation Reagents | Enzyme-free, gentle cell dissociation buffers | Maintain high cell viability during passaging of starting PSCs and harvesting of differentiated products, crucial for yield and consistency. |
Mitigating Cell Stress and Genetic Drift During Scale-Up
Within the context of Good Manufacturing Practice (GMP) manufacturing processes for tumor-free pluripotent stem cell (PSC) therapies, successful scale-up presents a critical bottleneck. The transition from small-scale research to clinically relevant bioreactor volumes introduces significant risks of intensified cellular stress and accelerated genetic drift. This document provides detailed application notes and protocols to identify, monitor, and mitigate these challenges, ensuring the production of safe, potent, and consistent cell therapy products.
Quantitative Analysis of Scale-Up Stressors
The following table summarizes key stressors and their measurable impact on PSCs during scale-up, based on current literature and process analytics.
Table 1: Key Stressors and Observed Impacts During PSC Bioreactor Scale-Up
| Stressor Category | Parameter Measured | Typical Change from Static to Bioreactor (e.g., 1L) | Potential Consequence for PSCs |
|---|---|---|---|
| Fluid Shear Stress | Wall Shear Stress (Pa) | 0.001 - 0.01 Pa (static) to 0.05 - 0.3 Pa (stirred-tank) | Increased ER stress, altered differentiation propensity, cell detachment. |
| Metabolic Flux | Lactate Production Rate (mmol/10^6 cells/day) | Increase by 20-50% | Medium acidification, growth inhibition, shift to glycolytic metabolism. |
| Oxygen Dynamics | pO2 Fluctuations (% air saturation) | ± 5-20% variability vs. stable in incubator | Hypoxic/oxidative stress, genomic instability, altered epigenetic state. |
| Nutrient Depletion | Glucose (mM) depletion time | 2-3x faster at high cell densities | Nutrient stress, activation of AMPK pathways, spontaneous differentiation. |
| Cell-Cell Interaction | Local Cell Density (cells/mL) | Can exceed 3x10^6/mL in aggregates vs. monolayer | Autocrine signaling dysregulation, core necrosis in aggregates. |
| Genetic Drift Indicator | SNV/Indel Frequency increase | 1.5-2.5x higher after 10 passages in suboptimal bioreactor conditions | Increased risk of oncogenic or detrimental mutations. |
Protocol: Real-Time Monitoring and Feedback Control for Stress Mitigation
Objective: To implement a process analytical technology (PAT) framework for monitoring key metabolic and physiological parameters in a stirred-tank bioreactor, enabling feedback control to maintain cells within a specified "healthy process space."
Materials:
- GMP-compliant, single-use stirred-tank bioreactor (e.g., 3L working volume).
- Integrated pH, dissolved oxygen (DO), and temperature probes.
- In-line or at-line metabolite analyzer (e.g., for glucose, lactate, ammonium).
- Off-gas analyzer for O2 and CO2.
- Bioreactor control unit with feedback control capabilities.
- Tumor-free, clinically certified human iPSC line.
- GMP-grade, defined, xeno-free culture medium.
- GMP-grade recombinant human growth factors (bFGF, TGF-β1).
Procedure:
- Bioreactor Setup & Calibration: Assemble the single-use bioreactor according to manufacturer's instructions. Calibrate pH and DO probes under process temperature (37°C). Prime the metabolite sampling loop if available.
- Inoculation: Detach and dissociate PSCs from a high-quality, pre-expanded monolayer culture into a single-cell suspension using a GMP-grade enzyme. Determine viability (target >90%). Seed the bioreactor at a density of 0.5-1.0 x 10^6 viable cells/mL in pre-equilibrated medium.
- Parameter Setpoints & Control Strategy:
- pH: Maintain at 7.2 ± 0.1 via automatic CO2 gassing or base addition.
- DO: Maintain at 40% air saturation via cascade control (first adjusting stirrer speed from 40-80 rpm, then blending O2/N2 gas).
- Temperature: 37.0 ± 0.2°C.
- Stirring: Begin at minimum speed to keep cells suspended (e.g., 40 rpm), increase only as needed for DO control.
- Monitoring & Feed Regimen:
- Record pH, DO, temperature, and agitation speed continuously.
- Sample culture daily for off-line analysis: cell count & viability, metabolite (glucose, lactate) concentration, and osmolality.
- Implement a feeding strategy based on glucose consumption rate. When glucose falls below 15 mM, perfuse or bolus-feed fresh medium to restore to 25 mM. This prevents nutrient starvation and lactate buildup.
- Harvest Criteria: Harvest cells during late exponential phase, typically when viable cell density reaches 2-3 x 10^6 cells/mL and before viability drops below 85%. Rapid cooling and GMP-compliant downstream processing are critical.
Protocol: Longitudinal Genomic Stability Assessment via Targeted NGS
Objective: To periodically assess genetic drift by screening for known recurrent genetic variants in PSCs during extended bioreactor culture across multiple scales.
Materials:
- Cell samples from each passage (P) during scale-up (e.g., P+1, P+3, P+5 in bioreactor).
- DNeasy Blood & Tissue Kit (GMP-grade equivalent).
| Research Reagent Solution | Function in Protocol |
|---|---|
| Targeted NGS Panel (e.g., "PSC Stability Panel") | Probes designed to capture exons of genes like TP53, MYC, BCL2, TERT, and common copy number variant (CNV) regions (20q11.21). |
| GMP-Grade Cell Dissociation Reagent | Ensures single-cell suspension for accurate sampling without introducing animal-derived components. |
| Nuclease-Free Water (GMP) | For eluting high-quality DNA, free of contaminants that inhibit downstream sequencing. |
| DNA Quantitation Kit (fluorometric) | Accurately measures low-concentration DNA samples for precise library preparation input. |
| Multiplex PCR Master Mix | For efficient and uniform amplification of all targeted genomic regions from the sample DNA. |
| Indexing Adapters (Unique Dual Indexes) | Allows pooling of multiple samples in one sequencing run while preventing index hopping errors. |
| Sequence Analysis Software (FDA-part11 compliant) | Analyzes sequencing data for variants, aligning to a reference genome and comparing to a process-specific baseline. |
- Library preparation kit for targeted sequencing.
- Bench-top next-generation sequencer.
- Bioinformatic pipeline for variant calling (e.g., GATK, custom scripts).
Procedure:
- Sample Collection: At each pre-defined passage, aseptically remove a 5 mL cell suspension sample from the bioreactor. Pellet cells, wash with PBS, and freeze pellet at -80°C for batch DNA extraction.
- DNA Extraction: Extract genomic DNA using the GMP-grade kit. Elute in nuclease-free water. Quantify DNA using a fluorometric method; ensure integrity via gel electrophoresis or fragment analyzer.
- Library Preparation & Sequencing: Use 50 ng of gDNA per sample. Prepare sequencing libraries using the targeted panel according to manufacturer's instructions, incorporating unique dual indexes for sample multiplexing. Pool libraries at equimolar concentrations. Sequence on the NGS platform to achieve a minimum mean coverage of 500x across all targets.
- Bioinformatic Analysis:
- Align sequencing reads to the human reference genome (hg38).
- Call single nucleotide variants (SNVs), small insertions/deletions (indels), and copy number variations (CNVs) in the targeted regions.
- Filter variants against dbSNP and in-house databases of common benign polymorphisms.
- Compare variants across sequential passages. Flag any variant that: a) Appears de novo and is present in >5% of reads. b) Increases in allele frequency by >10% per passage. c) Is located in a known oncogene or tumor suppressor gene.
- Action Thresholds: Establish predefined thresholds (e.g., any oncogenic TP53 variant >15% allele frequency). If a sample exceeds thresholds, initiate an investigation and consider terminating the batch for product release.
Signaling Pathways in PSC Stress Response
PSC Stress Response Signaling Network
Experimental Workflow for Scale-Up and Monitoring
PSC Scale-Up and Genetic Monitoring Workflow
Balancing Purging Stringency with Final Product Viability and Potency
Within GMP manufacturing of Pluripotent Stem Cell (PSC)-derived therapies, a critical paradox exists: the rigorous removal of tumorigenic residual undifferentiated PSCs (purge stringency) can compromise the yield, viability, and functional potency of the desired differentiated therapeutic cell product. This application note details protocols and analytical frameworks to quantify and optimize this balance, ensuring a final product that meets both safety and efficacy release criteria.
Table 1: Efficacy and Impact of Common Purging Strategies
| Purging Modality | Mechanism | Typical Log Reduction of Undiff. PSCs | Avg. Impact on Therapeutic Cell Viability | Key Potency Metric Affected |
|---|---|---|---|---|
| Pharmacologic (e.g., CC3 inhibitor) | Induces selective apoptosis | 3.0 - 4.5 log | -15% to -30% | Mitochondrial function |
| Immunologic (MHC-I/II & Antibody) | Antibody/complement-mediated lysis | 2.5 - 4.0 log | -10% to -25% | Surface marker expression |
| Metabolic (2-DG/LDH inhibition) | Exploits glycolytic dependence | 2.0 - 3.5 log | -20% to -40% | Glucose utilization rate |
| Physical (Size/Sedimentation) | Density gradient separation | 1.5 - 2.5 log | -5% to -15% | Cell recovery yield |
| Flow Cytometry-Based Sorting | Surface marker (e.g., SSEA-5) | >4.0 log | -25% to -50% | Post-sort functional recovery |
Table 2: Correlation of Purging Residuals with Final Product Characteristics
| Residual Undiff. PSC Level | Final Product Viability (Mean ± SD) | In Vivo Teratoma Incidence (NOD/SCID) | Relative Functional Potency* |
|---|---|---|---|
| > 0.1% (1:1000) | 92% ± 3% | 100% (5/5) | 1.05 ± 0.12 |
| 0.01% (1:10,000) | 88% ± 4% | 60% (3/5) | 0.98 ± 0.10 |
| 0.001% (1:100,000) | 82% ± 6% | 20% (1/5) | 0.91 ± 0.15 |
| < 0.0001% (1:1M) | 75% ± 8% | 0% (0/5) | 0.78 ± 0.18 |
*Potency normalized to unpurified control batch (e.g., secretion rate, engraftment, electrophysiological activity).
Experimental Protocols
Protocol 1: Titrated Pharmacologic Purging & Multi-Parameter Assessment
Objective: To determine the optimal concentration and duration of a selective agent (e.g., CC3 inhibitor) that maximizes tumorigenic cell depletion while preserving therapeutic cell health.
Materials: Differentiated PSC-derived cardiomyocytes (or relevant lineage), residual undifferentiated PSCs (spiked-in), selective purging agent, cell culture medium, flow cytometer, ATP luminescence assay kit, qRT-PCR reagents.
Methodology:
- Co-culture Setup: Spike the therapeutic cell batch with 1% SSEA-4+ undifferentiated PSCs. Plate in a GMP-compliant matrix.
- Titrated Treatment: Apply the purging agent in a 6-point concentration gradient (e.g., 0nM, 50nM, 100nM, 250nM, 500nM, 1000nM) for three time points (24h, 48h, 72h).
- Harvest & Quantify Depletion: Harvest cells. Use flow cytometry (SSEA-4, TRA-1-60) to quantify remaining undifferentiated PSCs. Calculate log reduction.
- Viability & Health Assessment:
- Perform 7-AAD/Annexin V staining for apoptosis/necrosis.
- Measure ATP content (luminescence) of the total population.
- Extract RNA for lineage-specific potency gene markers (e.g., TNNT2 for cardiomyocytes, INS for beta cells).
- Data Integration: Plot log reduction vs. viability/potency to identify the "elbow" point of diminishing returns.
Protocol 2: Post-Purging Functional Potency Assay (Cardiomyocyte Example)
Objective: To assess the functional maturity and potency of PSC-derived cardiomyocytes after a purging process.
Materials: Purged cell batch, multi-electrode array (MEA) system or calcium imaging setup, β-adrenergic agonist (isoproterenol).
Methodology:
- Cell Plating: Plate purified cardiomyocytes on MEA plates or imaging dishes at standardized density.
- Electrophysiological Recording (MEA):
- Record baseline field potential duration (FPD) and beating rate for 5 minutes.
- Challenge with 1µM isoproterenol. Record response (expected: increased beating rate).
- Calculate the Fridericia-corrected FPD (FPDc) to assess repolarization maturity.
- Calcium Transient Analysis (Alternative):
- Load cells with a calcium-sensitive dye (e.g., Fluo-4 AM).
- Record calcium flux kinetics (time to peak, decay tau) under baseline and stimulated conditions.
- Potency Metric: Derive a Functional Potency Index (FPI) = (∆Beating Rate with Iso / Baseline Rate) * (1 / FPDc). Compare purged vs. control batches.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Purging Balance Studies
| Item | Function in Context | Example Product/Cat. Number* |
|---|---|---|
| Selective PSC Cytotoxins | Induces apoptosis in undiff. PSCs via targeted pathways. | CC3 Inhibitor (e.g., PluriSin#1 analogs) |
| Lineage-Specific Reporter Cell Line | Enables real-time tracking of therapeutic vs. tumorigenic cells. | PSC line with GFP under TNNT2 or PDX1 promoter. |
| High-Sensitivity Flow Cytometry Antibodies | Detects low-frequency residual undiff. PSCs (<0.001%). | Anti-SSEA-5 (BV421), anti-TRA-1-60 (PE-Cy7). |
| Metabolic Probe Set | Measures shift in oxidative phosphorylation vs. glycolysis post-purge. | Seahorse XFp Glycolysis/Oxidative Stress Test Kits |
| GMP-Grade Magnetic Sorting Beads | Physical separation based on surface marker expression. | Anti-SSEA-4 MicroBeads, LS Columns. |
| Functional Potency Assay Kit | Quantifies lineage-specific secretory or enzymatic function. | C-Peptide ELISA (beta cells), Neurotransmitter ELISA (neurons). |
| In Vivo Teratoma Assay Matrigel | Gold-standard safety test for residual tumorigenicity. | GFR Matrigel, for NOD/SCID mouse injection. |
*Examples are illustrative. Specific catalog numbers should be verified for current GMP compliance.
Visualizations
Diagram 1: Decision Workflow for Purging Strategy Selection
Diagram 2: Key Signaling Pathways in Pharmacologic Purging
Managing Adventitious Agent Contamination Risks in Complex Processes
The advancement of pluripotent stem cell (PSC)-based therapies necessitates the highest standards of safety, particularly regarding tumorigenicity and freedom from adventitious agents. Adventitious agents—viruses, mycoplasma, bacteria, and other contaminants—pose a significant risk in complex, multi-step manufacturing processes involving biological raw materials, cell culture, and viral vectors. In the context of Good Manufacturing Practice (GMP) for tumor-free PSC therapies, managing these risks is non-negotiable for patient safety and regulatory approval. This document provides application notes and detailed protocols for the detection, prevention, and control of adventitious agents.
Current Risk Landscape & Regulatory Framework
Recent guidelines from the FDA, EMA, and ICH emphasize a risk-based, lifecycle approach to viral safety. The source of PSCs (e.g., donor-screened tissues vs. established lines), the use of animal-derived components, and open processing steps are critical risk factors. The table below summarizes key quantitative data on contamination risks and detection limits.
Table 1: Adventitious Agent Contamination Risks & Detection Capabilities in PSC Processes
| Risk Factor / Agent Category | Typical Sources in PSC Processes | Estimated Incidence in Biologics* | Recommended Detection Method(s) | Typical Assay Sensitivity (Limit of Detection) |
|---|---|---|---|---|
| Endogenous Retroviruses | Inherent to certain cell substrates | High (species-specific) | PCR-based assays (qPCR, ddPCR) | ≤ 10 copies/mL |
| Mycoplasma | Cell culture reagents, operator handling | ~1-5% in cell banks | Culture-based (28 days), Indicator Cell Culture (ICC), PCR | ≤ 1 CFU/mL (Culture), ≤ 10 genome copies (PCR) |
| Bacteria & Fungi | Non-sterile reagents, environment, personnel | Varies by aseptic control | Sterility testing (USP <71>, Ph. Eur. 2.6.27) | 1 CFU per sample |
| Virus (Unknown) | Animal-derived reagents (e.g., FBS, trypsin), cell lines | Low, but high impact | Next-Generation Sequencing (NGS) | Variable; ~10^2 - 10^5 genome copies/mL |
| Murine Minute Virus (MMV) | Rodent-derived raw materials (common contaminant) | Occasional outbreaks in biopharma | qPCR for specific viruses | ≤ 10 genome copies/mL |
| Replication-Competent Lentivirus (RCL) | Lentiviral vector production for PSC modification | Very low with 3rd-gen systems | Sensitive cell-based assay (e.g., qPCR for gag after amplification) | ≤ 1 IU/mL |
*Incidence data generalized from industry surveys and regulatory reports.
Core Experimental Protocols for Detection and Control
Protocol 3.1: Comprehensive Adventitious Agent Testing of Master Cell Banks (MCBs)
Objective: To establish the viral and microbial safety of a PSC Master Cell Bank. Materials: See Scientist's Toolkit. Method:
- Sample Preparation: Thaw a vial of MCB and expand cells to obtain ≥10^7 cells and 10 mL of supernatant.
- In Vitro Assay for Viruses:
- Inoculate supernatant and cell lysate onto a panel of indicator cell lines (e.g., Vero, MRC-5, A9, Crandell-Rees Feline Kidney).
- Observe for cytopathic effect (CPE), hemadsorption, and hemagglutination over 28 days.
- Perform a blind passage at day 14 onto fresh indicator cells.
- In Vivo Assay for Viruses: Inject supernatant and lysate into suckling mice, adult mice, and embryonated eggs. Observe for illness/mortality over 28 days.
- Mycoplasma Testing:
- Perform both culture-based (28-day broth/agar) and indicator cell culture (DNA stain, e.g., Hoechst) methods.
- Confirm with a validated PCR assay targeting 16S rRNA genes.
- PCR/ qPCR for Specific Viruses: Test for a panel of relevant viruses (e.g., herpesviruses, parvoviruses, retroviruses) using validated assays.
- Sterility Testing: Follow USP <71> using fluid thioglycollate medium and soybean-casein digest broth for 14 days.
Protocol 3.2: Next-Generation Sequencing (NGS) for Unbiased Virus Detection
Objective: To identify known and novel viral sequences in process intermediates. Method:
- Nucleic Acid Extraction: Extract total nucleic acid (DNA and RNA) from 1 mL of process sample (e.g., harvest fluid) using a method that enriches for viral particles (e.g., nuclease digestion, ultracentrifugation).
- Library Preparation: Generate a sequencing library without target-specific amplification. Use reverse transcription for RNA and random amplification.
- Sequencing: Perform high-throughput sequencing (e.g., Illumina MiSeq, 10-20 million reads).
- Bioinformatics Analysis:
- Trim adapters and filter low-quality reads.
- Align non-host reads to comprehensive viral sequence databases (e.g., NCBI Virus, Virosaurus).
- Use de novo assembly for novel virus identification.
- Confirm findings with targeted PCR.
Protocol 3.3: In-Process Control: Real-Time PCR for Mycoplasma
Objective: Rapid, in-process monitoring for mycoplasma contamination. Method:
- Sample Collection: Aseptically collect 100 µL of cell culture supernatant from the bioreactor or culture vessel.
- DNA Extraction: Use a commercial microspin column kit for microbial DNA.
- qPCR Setup:
- Prepare a master mix containing primers/probes targeting the mycoplasma 16S rRNA gene (pan-mycoplasma assay).
- Include a positive control (e.g., M. orale DNA) and a no-template control.
- Run in triplicate.
- Thermocycling: Use standard cycling conditions (e.g., 95°C for 10 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 60 sec).
- Analysis: A sample is positive if it amplifies with a Ct value less than the validated cutoff (e.g., Ct < 38).
Visualizations
Title: Control Strategy for PSC Manufacturing
Title: Adventitious Agent Testing Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Adventitious Agent Risk Management
| Item / Reagent Solution | Function in Risk Management | Example (for informational purposes) |
|---|---|---|
| MycoAlert Detection Assay | A bioluminescent, rapid (20-min) assay for mycoplasma detection in cell culture. | Lonza, Cat# LT07-318 |
| ViralSEQ NGS Service | A validated, off-the-shelf NGS service for broad virus detection in biologics. | Charles River Laboratories |
| ATCC VRM Kit | Provides validated viral RNA/DNA reference materials for assay development. | ATCC, Cat# VRM-20 |
| EndoPORATOR | A system for efficient, animal-component-free transfection, reducing raw material risks. | Polyplus-transfection |
| PCR Mycoplasma Detection Kit | A highly sensitive and specific PCR-based kit for mycoplasma screening. | Minerva Biolabs, Cat# 11-9100 |
| Gibco CTS KnockOut SR | A defined, xeno-free serum replacement for PSC culture, eliminating animal serum risks. | Thermo Fisher, Cat# A3181502 |
| ViaGram Red+ Bacterial Stain | A fluorescent stain for rapid detection of bacteria and fungi in culture samples. | Thermo Fisher, Cat# V7023 |
| qScript XLT One-Step RT-qPCR ToughMix | A robust master mix for sensitive detection of viral RNA in complex samples. | Quantabio, Cat# 95132-100 |
Application Notes: Integrating Cost-Effective Strategies into Tumor-Free PSC Therapy Manufacturing
The transition from research-scale to Good Manufacturing Practice (GMP) production of tumor-free pluripotent stem cell (PSC) therapies presents profound economic hurdles. Key challenges include the high cost of GMP-grade reagents, extensive quality control (QC) testing, low-yield differentiation protocols, and the capital intensity of single-use bioreactor systems. A multi-pronged strategy focusing on process intensification, alternative cell culture media, and advanced analytics for real-time release is critical for achieving commercial viability.
Table 1: Cost Drivers and Mitigation Strategies in GMP PSC Production
| Cost Driver | Typical Cost Impact (USD) | Proposed Mitigation Strategy | Estimated Cost Reduction |
|---|---|---|---|
| GMP-grade Growth Factors (e.g., bFGF, TGF-β) | $50,000 - $200,000 per batch | Use of engineered cell lines for factor production; ligand-independent media formulations. | 40-60% |
| Closed System Bioreactor & Single-Use Consumables | $500,000 - $2M (Capital) + $100k/batch | Transition to scalable, stirred-tank reactors with reusable core components. | 30% per batch |
| Tumorigenicity Testing (In vivo assays, PCR, FACS) | $100,000 - $300,000 per lot | Implementation of in-process analytics (e.g., metabolomics) and PCR for pluripotency markers as surrogate release tests. | 50% |
| Manual Labor in 2D Culture | High (Process-dependent) | Automation of expansion and differentiation in 3D bioreactors. | 25-40% |
| QC for Adventitious Agents | $50,000 - $150,000 | Risk-based testing strategies and use of well-characterized cell banks. | 30% |
Detailed Experimental Protocols
Protocol 1: Cost-Reduced 3D Bioreactor Expansion of Undifferentiated PSCs
Objective: To scale up PSC expansion in a stirred-tank bioreactor using a defined, ligand-reduced medium to lower reagent costs while maintaining pluripotency and genomic stability.
Materials:
- GMP-grade human PSC line (master cell bank)
- Controlled, stirred-tank bioreactor (e.g., 3L working volume)
- Cost-Reduced Defined Medium (CRDM): Basal medium supplemented with recombinant insulin (replacing high-cost albumin), and low-dose engineered growth factors.
- GMP-grade recombinant human laminin-521 microcarriers.
- Metabolite analyzers (for glucose/lactate/ammonia).
- Off-gas analyzer for oxygen consumption rate (OCR).
Methodology:
- Bioreactor Preparation: Sterilize bioreactor vessel. Coat microcarriers with laminin-521 per manufacturer's protocol and load into bioreactor with CRDM.
- Inoculation: Detach PSCs from a validated 2D culture using non-enzymatic passaging. Inoculate at a density of 1 x 10^5 cells/mL.
- Process Control: Maintain at 37°C, pH 7.2, DO at 40%. Agitation is set to 60 rpm initially, increased incrementally to 120 rpm to prevent aggregate formation.
- Feeding Strategy: Employ a continuous perfusion system starting at day 2. Perfusion rate is dynamically adjusted based on real-time metabolite and OCR data to minimize medium waste.
- Monitoring: Sample daily for cell count, viability (trypan blue), and metabolite concentrations. Use daily glucose consumption rate to calculate growth kinetics.
- Harvest: At peak viability (>90%), stop agitation. Allow microcarriers to settle. Wash cells with GMP-grade buffer. Use gentle enzymatic dissociation to harvest cells.
- QC Sampling: Test harvested cells for pluripotency markers (OCT4, NANOG via flow cytometry), karyotype, and sterility.
Protocol 2: In-Process PCR Assay for Residual Pluripotency as a Surrogate Tumorigenicity Test
Objective: To establish a quantitative PCR (qPCR) assay for residual pluripotency gene expression (OCT4, LIN28) during differentiation, correlating results with the gold-standard in vivo teratoma assay to enable faster, cheaper lot release.
Materials:
- RNA from differentiated PSC-derived cardiomyocyte (or other target lineage) batches.
- GMP-compliant RNA extraction kit.
- Reverse transcription kit.
- Validated qPCR assays for OCT4, LIN28, and housekeeping genes (e.g., GAPDH, HPRT1).
- Digital PCR system (for absolute quantification, optional).
- Pre-established correlation data linking threshold cycle (Ct) values to teratoma-forming potential.
Methodology:
- Sample Collection: Collect aliquots of 1x10^6 cells at critical differentiation timepoints (e.g., day 0, 7, 14) and from the final product.
- RNA Extraction: Isolate total RNA using a column-based method. Determine concentration and purity (A260/A280 ~2.0).
- cDNA Synthesis: Convert 1 µg of total RNA to cDNA using a high-capacity reverse transcription kit.
- qPCR Setup: Perform triplicate reactions for each target gene. Use the following 10 µL reaction: 5 µL master mix, 0.5 µL each primer (10 µM), 1 µL cDNA, 3 µL nuclease-free water.
- Thermocycling Conditions: 95°C for 10 min; 40 cycles of 95°C for 15 sec, 60°C for 1 min.
- Data Analysis: Calculate ΔΔCt values relative to undifferentiated PSCs and housekeeping genes. A predefined threshold (e.g., >10^6-fold reduction in OCT4 expression vs. baseline) must be met for the batch to pass.
- Correlation & Validation: The ΔΔCt values from this in-process test are cross-referenced with historical data from the corresponding in vivo teratoma assay results for the same process to validate the surrogate model.
Visualizations
Strategy for Economically Viable GMP PSC Production
Cost-Effective 3D Bioreactor PSC Expansion Protocol
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Cost-Conscious GMP PSC Process Development
| Item & Example | Function in Process | Rationale for Cost/Scalability Benefit |
|---|---|---|
| Ligand-Indefined/Reduced Medium (e.g., E8-modified CRDM) | Supports PSC self-renewal without high-cost recombinant proteins like TGF-β. | Drastically reduces recurring material cost, increases batch consistency. |
| GMP-Grade Laminin-521 Fragments/Peptides | Synthetic or truncated versions of full-length protein for microcarrier coating. | Lower cost than full-length recombinant protein, while maintaining integrin-binding function for cell adhesion. |
| Metabolite & Off-Gas Probes (Bioreactor-integrated) | Real-time monitoring of glucose, lactate, ammonium, O₂, CO₂. | Enables dynamic feeding (perfusion), minimizing medium use and allowing early detection of process drift. |
| qPCR/dPCR Kits for Pluripotency & Lineage Markers | Quantitative nucleic acid testing for residual undifferentiated cells. | Serves as a faster, cheaper surrogate for in vivo tumorigenicity assays, accelerating lot release. |
| Closed, Automated Cell Processing System (e.g., Sepax, Cocoon) | Integrated cell washing, concentration, and formulation. | Reduces manual handling error and labor cost, maintains sterility in a closed path, suitable for scale-out. |
| Engineered Feeder/Stromal Cell Lines | Genetically modified to secrete required growth factors (e.g., FGF2). | Co-culture with these cells can replace addition of purified GMP-grade factors to the medium. |
Analytics and Release Criteria: Measuring, Comparing, and Proving Tumor-Free Status
Within the GMP manufacturing of pluripotent stem cell (PSC)-derived therapies, the detection and elimination of residual undifferentiated PSCs is a critical safety specification. These cells pose a tumorigenic risk upon transplantation. This application note details three gold-standard assays—Flow Cytometry, PCR, and Next-Generation Sequencing (NGS)—for the sensitive detection of these cells, providing protocols and comparative data to support process validation and lot release testing.
Assay Comparison & Performance Characteristics
The following table summarizes the key performance metrics for each assay in the context of detecting undifferentiated PSCs (e.g., expressing OCT4, TRA-1-60, SSEA-4) within a differentiated cell product.
Table 1: Comparative Analysis of Residual Undifferentiated Cell Detection Assays
| Assay Parameter | Flow Cytometry | PCR (qRT-PCR/ddPCR) | NGS (scRNA-seq/Bulk RNA-seq) |
|---|---|---|---|
| Primary Output | Protein expression (%) & cell count | Gene expression (Ct, copies/µL) | Transcriptomic profile & rare cell identification |
| Detection Limit | ~0.1 - 0.5% of total population | ~0.001 - 0.01% (ddPCR more sensitive) | ~0.01 - 0.1% (highly dependent on read depth) |
| Throughput | Medium-High (96-well possible) | High (384-well standard) | Low-Medium (per sample) |
| Time to Result | 1-2 days (sample prep + analysis) | 1-2 days (RNA extraction + run) | 3-7+ days (library prep + sequencing + bioinformatics) |
| Key Advantages | Single-cell, multiparametric, live cell analysis | High sensitivity, quantitative, amenable to automation | Unbiased, discovery-driven, detailed mechanistic insight |
| Key Limitations | Lower sensitivity, requires specific antibodies | Requires primer specificity, indirect detection | High cost, complex data analysis, longer turnaround |
| GMP Suitability for Release | Excellent for process monitoring & setting specifications | Excellent for sensitive, quantitative release criteria | Ideal for characterization & risk assessment, less routine for release |
| Typical Target(s) | SSEA-4, TRA-1-60, OCT4 (surface/intracellular) | POU5F1 (OCT4), NANOG, DNMT3B | Pluripotency gene expression signature |
Detailed Experimental Protocols
Protocol 3.1: Flow Cytometry for Surface Pluripotency Markers
Objective: To quantify the percentage of cells expressing undifferentiated PSC markers (SSEA-4, TRA-1-60) in a final cell therapy product.
- Cell Harvest & Preparation: Gently dissociate the cell product to a single-cell suspension using a validated enzyme (e.g., Accutase). Wash cells twice with DPBS containing 0.5% BSA (FACS Buffer). Pass through a 35-40 µm cell strainer. Perform a viable cell count using Trypan Blue.
- Staining: Aliquot 1 x 10^6 cells per test tube. Prepare master mixes of directly conjugated antibodies (e.g., SSEA-4-FITC, TRA-1-60-PE) and appropriate isotype controls diluted in FACS Buffer. Resuspend each cell pellet in 100 µL of antibody mix. Incubate for 30 minutes at 4°C in the dark.
- Wash & Fix: Wash cells twice with 2 mL FACS Buffer. Resuspend in 300-500 µL of FACS Buffer containing a viability dye (e.g., 7-AAD or DAPI). Optionally, fix cells with 1-2% PFA if analysis is not immediate.
- Acquisition & Analysis: Run samples on a calibrated flow cytometer (e.g., BD FACSDiva). Collect a minimum of 50,000 events per sample. Use unstained and isotype controls to set negative gates. Analyze data to determine the percentage of viable cells double-positive for SSEA-4 and TRA-1-60.
Protocol 3.2: Droplet Digital PCR (ddPCR) for Pluripotency Gene Expression
Objective: To achieve absolute quantification of pluripotency gene transcripts with high sensitivity for residual undifferentiated cells.
- RNA Extraction & QC: Extract total RNA from a representative sample (≥1 x 10^6 cells) using a GMP-compliant, automated magnetic bead-based system (e.g., Agencourt RNAdvance). Quantify RNA using a spectrophotometer (A260/A280) and assess integrity (RIN > 8.0 via Bioanalyzer).
- Reverse Transcription: Convert 100 ng - 1 µg of total RNA to cDNA using a high-capacity reverse transcription kit with random hexamers.
- ddPCR Reaction Setup: Prepare a 20 µL reaction mix containing:
- 10 µL of ddPCR Supermix for Probes (no dUTP)
- 1 µL of POU5F1 (OCT4) and GAPDH (reference) primer/probe assays (FAM/HEX)
- 5 µL of diluted cDNA (1:10)
- 4 µL of nuclease-free water
- Droplet Generation & PCR: Transfer the reaction mix to a DG8 cartridge for droplet generation using the QX200 Droplet Generator. Transfer emulsified samples to a 96-well PCR plate. Perform amplification: 95°C for 10 min, 40 cycles of [94°C for 30 sec, 60°C for 1 min], 98°C for 10 min (ramp rate 2°C/sec).
- Droplet Reading & Analysis: Read the plate on the QX200 Droplet Reader. Use QuantaSoft software to analyze the data. Results are reported as copies/µL of input cDNA. Calculate the normalized ratio of POU5F1 to GAPDH.
Protocol 3.3: NGS-based scRNA-seq for Rare Undifferentiated Cell Detection
Objective: To perform an unbiased assessment of cell population heterogeneity and identify rare undifferentiated cells.
- Single-Cell Suspension Preparation: Create a high-viability (>90%) single-cell suspension. Critical step: Optimize dissociation to minimize doublets and cell stress. Remove debris and dead cells using a density gradient medium or a dead cell removal kit.
- Single-Cell Partitioning & Barcoding: Use a commercial platform (e.g., 10x Genomics Chromium). Load cells, gel beads, and partitioning oil onto a Chromium Chip B to target a recovery of 5,000-10,000 cells. The controller generates nanoliter-scale droplets containing a single cell and a barcoded bead.
- Reverse Transcription & Library Prep: Inside each droplet, cells are lysed, and mRNA transcripts are barcoded during reverse transcription. Break droplets, recover cDNA, and amplify. Proceed to construct sequencing libraries following the manufacturer's protocol, including fragmentation, end-repair, A-tailing, adapter ligation, and sample indexing.
- Sequencing & Bioinformatics: Pool libraries and sequence on an Illumina NovaSeq (e.g., 150 bp paired-end, targeting ~50,000 reads/cell). Use the Cell Ranger pipeline for demultiplexing, barcode processing, and alignment. Downstream analysis in R (Seurat package): filter cells, normalize, scale data, perform PCA and UMAP clustering. Identify clusters expressing high levels of pluripotency genes (POU5F1, NANOG, SOX2) and calculate their prevalence.
Diagrams
Assay Selection Decision Workflow
Core NGS scRNA-seq Wet-Lab Process
Pluripotency Signaling Pathway Core
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Kits for Residual PSC Detection Assays
| Reagent/Kits | Provider Examples | Function in Assay |
|---|---|---|
| Anti-human SSEA-4 (e.g., Clone MC-813-70), Alexa Fluor conjugate | BD Biosciences, Thermo Fisher | Primary antibody for flow cytometric detection of undifferentiated PSC surface marker. |
| Anti-human TRA-1-60 (e.g., Clone TRA-1-60), PE conjugate | BioLegend, Miltenyi Biotec | Primary antibody for flow cytometric detection of a key PSC surface antigen. |
| Cell Viability Dye (e.g., 7-AAD, DAPI, Fixable Viability Dye eFluor 506) | Thermo Fisher, BioLegend | Distinguishes live from dead cells in flow cytometry, ensuring accuracy. |
| Agencourt RNAdvance Blood/V3 Kit | Beckman Coulter | GMP-amenable, automated magnetic bead-based total RNA isolation for PCR/NGS. |
| TaqMan ddPCR Assay for POU5F1 (OCT4), FAM-MGB | Bio-Rad Laboratories | Predesigned, highly specific primer-probe set for absolute quantification of pluripotency transcript. |
| ddPCR Supermix for Probes (no dUTP) | Bio-Rad Laboratories | Optimized master mix for droplet digital PCR reactions. |
| Chromium Next GEM Single Cell 3' Reagent Kits v3.1 | 10x Genomics | End-to-end solution for single-cell partitioning, barcoding, and library preparation for scRNA-seq. |
| NovaSeq 6000 S4 Reagent Kit (300 cycles) | Illumina | High-output sequencing flow cell and reagents for NGS library sequencing. |
| Seurat R Toolkit | Satija Lab / CRAN | Comprehensive open-source software package for scRNA-seq data analysis and visualization. |
Within the framework of developing GMP-compliant, tumor-free pluripotent stem cell (PSC) therapies, rigorous tumorigenicity testing is a critical release and safety checkpoint. Residual undifferentiated PSCs or early progenitor cells possess the potential for uncontrolled proliferation and teratoma formation in vivo. This document details standardized application notes and protocols for key assays used to assess this risk: the in vivo teratoma formation assay and the in vitro soft agar colony formation assay, supplemented by advanced mouse xenograft models.
Teratoma Formation Assay
Application Note
The teratoma assay is the gold standard for assessing the pluripotent and tumorigenic potential of PSC-derived products. For GMP manufacturing, it is used as a lot-release test for master cell banks or as a validation test for differentiation process efficacy. A successful, well-differentiated teratoma containing tissues from all three embryonic germ layers (ectoderm, mesoderm, endoderm) confirms pluripotency, while the absence of teratoma formation after implantation of the final therapeutic product indicates effective removal of tumor-initiating cells.
Protocol: Teratoma Formation in Immunodeficient Mice
Objective: To assess the tumorigenic potential of a PSC-derived cell product by subcutaneous or intramuscular injection and subsequent histological analysis.
Materials:
- Test article: ≥1x10^6 cells (PSC line or differentiated product) in a viable, single-cell suspension.
- Control: Undifferentiated PSCs (positive control), PBS/Matrigel (negative control).
- Mice: 6-8 week old, immunodeficient (e.g., NOD-scid IL2Rγnull (NSG), NOD-scid).
- Matrix: Growth factor-reduced Matrigel (optional, enhances engraftment).
- Instruments: 1mL syringe, 23-27G needle, surgical tools for dissection.
Procedure:
- Cell Preparation: Harvest cells using a gentle dissociation reagent. Wash and resuspend in cold, serum-free medium or PBS. Mix with an equal volume of cold Matrigel (if using) on ice to prevent polymerization. Final cell concentration should target 1-5x10^7 cells/mL.
- Injection: Anesthetize mouse. Load cell suspension (100 µL total volume) into a cold syringe. For subcutaneous injection, pinch the skin on the dorsal flank, insert the needle, and deliver the bolus. For intramuscular injection, target the hind limb tibialis anterior muscle.
- Monitoring: Palpate weekly for nodule formation. Monitor mice for 12-24 weeks or until the tumor reaches 1.5 cm in any dimension.
- Necropsy & Analysis: Euthanize mouse, excise tumor, and measure/weigh. Fix in 10% Neutral Buffered Formalin for 24-48 hours.
- Histopathology: Process fixed tissue for paraffin embedding, section, and stain with Hematoxylin and Eosin (H&E). A qualified pathologist should evaluate sections for the presence of tissues derived from all three germ layers.
Key Quantitative Endpoints:
- Tumor incidence (% of injection sites forming a teratoma).
- Latency period (time to palpable tumor).
- Tumor volume/weight at endpoint.
- Germ layer representation (semi-quantitative scoring).
Table 1: Example Teratoma Assay Results for a Hypothetical PSC-Derived Cardiomyocyte Product
| Cell Type Injected | Dose (cells) | Tumor Incidence (n=10) | Mean Latency (weeks) | Mean Tumor Weight (g) | Multilineage Differentiation (Y/N) |
|---|---|---|---|---|---|
| Undifferentiated PSCs | 1 x 10^6 | 10/10 (100%) | 8.2 ± 1.1 | 1.45 ± 0.3 | Yes |
| Final CM Product | 5 x 10^6 | 1/10 (10%)* | 20 | 0.08 | No (only cardiac tissue) |
| Differentiated CM (Intermediate Stage) | 5 x 10^6 | 8/10 (80%) | 15.5 ± 2.3 | 0.95 ± 0.4 | Yes |
*Presumed to be due to residual undifferentiated cells.
Soft Agar Colony Formation Assay
Application Note
This in vitro assay tests for anchorage-independent growth, a hallmark of cellular transformation. It is a sensitive, quantitative method to detect contaminating proliferative cells in a PSC-derived product. While not a direct measure of pluripotency, it is highly effective for identifying cells with oncogenic mutations or dysregulated growth pathways that could lead to tumor formation in vivo.
Protocol: Soft Agar Colony Formation
Objective: To quantify the clonogenic growth potential of cells in a semi-solid medium.
Materials:
- Base Agar: 1-2% agar in distilled water, autoclaved.
- Top Agar: 0.3-0.6% agar in complete culture medium, kept at 42°C in a water bath.
- Feeder Layer: Complete medium with 0.5-1% agar.
- 6-well or 24-well cell culture plates.
- Cell Stain: 0.005% Crystal Violet or MTT reagent.
Procedure:
- Prepare Feeder Layer: Melt base agar and cool to 60°C. Mix with 2X concentrated complete pre-warmed medium (1:1) to achieve a final 0.5-0.7% agar solution. Quickly add 1-2 mL per well to a multi-well plate. Let solidify at room temperature for 30 minutes.
- Prepare Cell Layer: Harvest test cells (PSC product) into a single-cell suspension. Count. Melt top agar (0.3-0.6%) and equilibrate to 42°C. Mix the cell suspension with the liquified top agar (1:1) to achieve the final agar concentration and a desired cell density (e.g., 5,000-50,000 cells/mL). Plate 1 mL of this mixture on top of the set feeder layer. Swirl gently to ensure even distribution.
- Solidify & Incubate: Allow the top layer to set for 20 minutes at room temperature. Carefully add 1-2 drops of complete medium on top to prevent drying. Incubate plates at 37°C, 5% CO2 for 2-4 weeks. Replenish the medium overlay twice weekly.
- Stain & Count: After 14-28 days, add MTT reagent or Crystal Violet stain to visualize colonies. Count colonies >50 µm in diameter using an automated colony counter or microscope.
Key Quantitative Endpoints:
- Colony forming efficiency (CFE) = (Number of colonies / Number of cells plated) x 100%.
- Colony size distribution.
Table 2: Typical Soft Agar Colony Formation Data
| Cell Sample | Plating Density (cells/well) | Mean Colony Count (≥50µm) | Colony Forming Efficiency (%) | Interpretation |
|---|---|---|---|---|
| Positive Control (HeLa) | 10,000 | 1250 ± 150 | 12.5% | High transformation |
| Undifferentiated PSCs | 20,000 | 45 ± 10 | 0.23% | Low but detectable |
| Final Therapeutic Product | 100,000 | 2 ± 1 | 0.002% | Passes specification (<0.01%) |
| Negative Control (Primary Fibroblasts) | 20,000 | 0 | 0% | No transformation |
Mouse Xenograft Models for Tumorigenicity
Application Note
Beyond the teratoma assay, more sensitive and disease-relevant in vivo models are employed. These include intramyocardial, intrastriatal, or intrahepatic injection models to assess tumorigenicity in the intended therapeutic organ microenvironment, which may influence cell survival and proliferation.
Protocol: Intramyocardial Injection for Cell Therapy Safety Testing
Objective: To assess the tumorigenic risk of a PSC-derived product in a clinically relevant cardiac delivery model.
Materials:
- Test cells in suspension.
- Mice: Immunodeficient (e.g., NSG) or humanized mouse models.
- Surgical microscope, heating pad.
- Ventilator (for survival surgery).
- 30µL Hamilton syringe with a 33G needle.
- Buprenorphine (analgesia).
Procedure:
- Anesthesia & Preparation: Induce and maintain surgical anesthesia. Intubate and ventilate the mouse. Perform a left thoracotomy under aseptic conditions to expose the heart.
- Injection: Load cell suspension (10-20 µL containing 1x10^5 - 1x10^6 cells) into the Hamilton syringe. Under microscopic guidance, insert the needle into the left ventricular wall and slowly inject. Withdraw needle and apply gentle pressure with a cotton swab.
- Closure & Recovery: Close the thoracic cavity and skin in layers. Administer analgesia and allow mouse to recover on a heating pad.
- Monitoring & Analysis: Monitor by echocardiography for cardiac function and mass formation. Terminate at 3-6 months. Perform detailed histopathological analysis of the heart, lungs, and other organs for ectopic growth.
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for Tumorigenicity Assays
| Reagent/Material | Function/Application | Key Considerations for GMP Context |
|---|---|---|
| Growth Factor-Reduced Matrigel | Basement membrane matrix to support cell engraftment and survival in teratoma assays. | Lot-to-lot variability is high. For GMP, consider defined, xeno-free synthetic matrices (e.g., synthetic peptides). |
| Immunodeficient Mice (NSG, NOG) | In vivo hosts lacking adaptive immunity, allowing human cell engraftment. | Maintain in specific pathogen-free (SPF) facilities. Standardize age, sex, and housing conditions for reproducible results. |
| Agar, Low Gelling Temperature | Forms the semi-solid matrix for the soft agar assay. | Use high-purity, cell culture tested grades. Concentration must be optimized for each cell type. |
| Defined, Xeno-Free Cell Dissociation Reagents | Generate single-cell suspensions from PSC cultures or 3D products for injection. | Essential for GMP. Enzymatic (e.g., recombinant trypsin) or non-enzymatic (e.g., chelation-based) options. |
| Pathology Services (GLP-compliant) | For unbiased histological processing, H&E staining, and teratoma scoring. | Outsourcing to a GLP-certified partner provides regulatory-grade data for IND submissions. |
| Luminescent Cell Viability Markers (e.g., Luciferase-expressing cells) | Enables longitudinal, non-invasive bioluminescence imaging (BLI) of cell survival and growth in mice. | Requires genetically engineered reporter cell lines. Critical for quantifying tumor cell burden over time. |
Diagrams
Title: Teratoma Formation Assay Protocol Workflow
Title: Key Pathways Leading to PSC Tumorigenicity
Within the context of Good Manufacturing Practice (GMP) for tumor-free pluripotent stem cell (PSC) therapies, comparability studies are critical after any defined process change. These studies are designed to ensure that the change does not adversely impact the safety, identity, purity, potency, or efficacy of the cellular therapy product. The process changes can range from raw material sourcing to a major manufacturing scale-up.
Regulatory guidance from agencies like the FDA (e.g., ICH Q5E) and EMA mandates a risk-based approach. The extent of the comparability study is dictated by the nature and risk level of the change.
Risk-Based Assessment for Process Changes
A preliminary risk assessment categorizes changes into Major, Moderate, or Minor, dictating the study's scope.
Table 1: Risk Categorization and Study Scope for PSC Process Changes
| Change Category | Example for PSC Therapy | Likely Study Scope |
|---|---|---|
| Major (High Risk) | Change of core reprogramming method; Introduction of a novel differentiation matrix. | Extensive in vitro and in vivo functional assays; Full panel of safety tests (tumorigenicity, genomic stability); Possible clinical bridging study. |
| Moderate (Medium Risk) | Scale-up in bioreactor; Change in a critical growth factor supplier. | Comprehensive product characterization (omics, flow cytometry); Key potency assays; Extended in vitro safety. |
| Minor (Low Risk) | Change in a non-critical raw material (e.g., a specific buffer salt); Upstream process optimization with same critical parameters. | Limited analytical testing (critical quality attributes only); Reduced lot-to-lot analysis. |
Critical Quality Attributes (CQAs) for Tumor-Free PSC Therapies
The comparability study must demonstrate equivalence for a predefined set of CQAs.
Table 2: Key CQAs and Analytical Methods for Tumor-Free PSC Comparability
| CQA Category | Specific Attribute | Standard Analytical Method | Acceptance Criterion for Equivalence |
|---|---|---|---|
| Identity & Purity | Cell Surface Marker Profile (e.g., Tra-1-60, SSEA-4 for PSCs) | Flow Cytometry | ≥ 95% positive for target population; Comparable mean fluorescence intensity. |
| Pluripotency Gene Expression (OCT4, NANOG) | qRT-PCR | No statistically significant change (p>0.05) in expression levels. | |
| Absence of Teratoma-Forming Cells | In vitro clonal assay; Residual undifferentiated cell assay (RUCA). | Below predefined limit of detection (e.g., < 0.1% tumorigenic cells). | |
| Potency | Differentiation Capacity (e.g., to cardiomyocytes, neurons) | Directed differentiation + lineage-specific marker analysis (Flow/ICC). | Equivalent efficiency and marker expression vs. pre-change product. |
| Secretome Profile (for paracrine-acting therapies) | Multiplex ELISA / Proteomics | Comparable levels of key therapeutic factors. | |
| Safety | Genomic Stability (Karyotype, CNVs) | G-band karyotyping; SNP microarray/Whole Genome Sequencing. | Normal karyotype; No new major CNVs of concern. |
| Residual Vector/Reprogramming Factor | qPCR for vector sequences (if applicable). | Below validated clearance threshold. | |
| Sterility, Endotoxin, Mycoplasma | Compendial methods (USP <71>, <85>, <63>). | Meets all pharmacopeial specifications. |
Detailed Experimental Protocols
Protocol 4.1: Residual Undifferentiated Cell Assay (RUCA)
Purpose: Quantify residual tumorigenic PSCs in a differentiated cell therapy product. Materials:
- Test and reference cell samples.
- Matrigel-coated 96-well plates.
- Essential 8 Flex or mTeSR Plus medium (for PSC growth).
- Fixation buffer (4% PFA) and Permeabilization buffer (0.1% Triton X-100).
- Primary antibodies: Anti-OCT4, Anti-NANOG.
- Fluorescent secondary antibodies, DAPI. Procedure:
- Sample Spiking & Plating: Prepare a limiting dilution series of the test product. Spike known numbers of PSCs (0, 10, 50, 100) into a background of differentiated cells for a standard curve. Plate in Matrigel-coated plates in Essential 8 medium.
- Culture: Culture for 7 days, with medium change every other day.
- Immunostaining: Fix, permeabilize, and block cells. Incubate with anti-OCT4/NANOG overnight at 4°C. Apply secondary antibodies for 1 hour at RT. Counterstain nuclei with DAPI.
- Imaging & Analysis: Image wells using a high-content imager. Count colonies positive for pluripotency markers. Use the standard curve to extrapolate the frequency of residual undifferentiated cells in the unspiked test sample.
- Acceptance: The calculated frequency in the post-change product must not exceed the pre-change product frequency and must be below the validated safety threshold.
Protocol 4.2: Directed Differentiation Potency Assay (e.g., to Cardiomyocytes)
Purpose: Demonstrate equivalent differentiation capacity. Materials:
- PSC samples (pre- and post-change).
- Cardiomyocyte differentiation kit (e.g., based on Wnt modulation).
- RPMI 1640 medium with B-27 supplements.
- Flow antibodies: cTnT, NKX2.5. Procedure:
- Differentiation: Seed PSCs as single cells in Matrigel-coated plates. Initiate differentiation when cells reach 90% confluence using specified small molecule inhibitors/activators according to the kit protocol over 10-14 days.
- Harvest: At day 15, dissociate cells to a single-cell suspension.
- Staining: Fix and permeabilize cells. Stain intracellularly with anti-cTnT and anti-NKX2.5 antibodies and appropriate isotype controls.
- Flow Cytometry: Acquire data on a flow cytometer. Gate on live, single cells. Calculate the percentage of cTnT+/NKX2.5+ double-positive cardiomyocytes.
- Analysis: Compare the differentiation efficiency (%) between pre- and post-change PSC batches using statistical tests (e.g., t-test). Equivalence is typically defined as no statistically significant difference (p>0.05) and within a pre-defined margin (e.g., ±10%).
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for PSC Comparability Studies
| Item | Function / Application | Example Vendor(s) |
|---|---|---|
| Essential 8 / mTeSR Media | Defined, xeno-free culture medium for maintaining PSC pluripotency. | Thermo Fisher, STEMCELL Technologies |
| Matrigel / Recombinant Laminin-521 | Substrate for feeder-free PSC culture. Critical for consistent attachment and growth. | Corning, Biolamina |
| Flow Cytometry Antibody Panels | Characterization of pluripotency markers (SSEA-4, Tra-1-60) and differentiation lineage markers. | BD Biosciences, BioLegend |
| Residual Undifferentiated Cell Assay Kit | Standardized kit for detecting tumorigenic PSCs in a differentiated product background. | STEMCELL Technologies (STEMdiff) |
| SNP Microarray Kit | Assessment of copy number variants (CNVs) for genomic stability. | Thermo Fisher (CytoScan), Illumina |
| Mycoplasma Detection Kit | Sensitive PCR-based detection of mycoplasma contamination. | Lonza (MycoAlert), Minerva Biolabs |
| Directed Differentiation Kits | Robust, protocolized kits for differentiating PSCs to specific lineages (neuronal, cardiac, hepatic). | Thermo Fisher, STEMCELL Technologies |
Visualizations
Diagram Title: Comparability Study Workflow for PSC Process Changes
Diagram Title: Link Between Process Change, CQAs, and Patient Risk
Setting Scientifically Justified Release Specifications for PSC Contaminants
Within the rigorous framework of Good Manufacturing Practice (GMP) for pluripotent stem cell (PSC)-based therapies, establishing release specifications for residual undifferentiated cells and other contaminants is a critical determinant of clinical safety and efficacy. The tumorigenic potential of undifferentiated PSCs necessitates their quantification as a critical quality attribute (CQA). This document provides application notes and protocols for developing and validating scientifically justified release limits for PSC-derived cellular therapy products, framed within a thesis on mitigating tumorigenicity risk in GMP manufacturing.
Critical Quality Attributes (CQAs) and Contaminant Classes
For a PSC-derived therapeutic product, release specifications must address distinct classes of process-related and product-related contaminants.
Table 1: Key Contaminant Classes and Associated Risks
| Contaminant Class | Specific Example | Primary Risk | Typical Analytical Method |
|---|---|---|---|
| Product-Related: Undifferentiated Cells | Residual hiPSCs/hESCs | Teratoma/Tumor Formation | Flow Cytometry (Pluripotency Markers), qRT-PCR |
| Product-Related: Incomplete Derivatives | Stage-specific progenitors | Off-target effects, poor engraftment | Flow Cytometry, Immunocytochemistry |
| Process-Related: Reagents | Residual Matrigel/Laminin-521 | Immunogenicity, batch variability | ELISA, LC-MS |
| Process-Related: Vectors | Residual Sendai/Viral Vectors | Insertional mutagenesis, immunogenicity | qPCR/ddPCR for vector copies |
| Process-Related: Reagents | Residual Small Molecules (e.g., CHIR99021) | Off-target toxicity | HPLC/MS |
Quantitative Risk Assessment & Setting Preliminary Limits
Release limits must be informed by a combination of process capability, analytical method capability (AMC), and patient safety risk assessment. A risk-based approach is recommended by ICH Q9 and related guidelines.
Table 2: Risk-Based Approach to Limit Setting for Residual Undifferentiated PSCs
| Risk Factor | Assessment Method | Data Input for Limit Setting |
|---|---|---|
| Patient Safety (Severity) | Preclinical tumorigenicity studies in immunocompromised mice (e.g., NOG mice). | Minimum tumorigenic dose/cell number. |
| Process Capability | Historical batch data from GMP runs (n ≥ 10). | Mean and standard deviation of residual PSC levels. |
| Analytical Method Capability | Validation of the release assay (e.g., flow cytometry for TRA-1-60). | Limit of Detection (LOD), Limit of Quantification (LOQ), precision. |
| Therapeutic Dose | Total number of cells per dose. | Converts a ppm limit to an absolute cell number per dose. |
Preliminary Limit Calculation Example: If preclinical data suggests a tumorigenic threshold of >10,000 undifferentiated cells, and the maximum therapeutic dose is 1×10^8 cells, a preliminary limit could be set at 100 ppm (0.01%), or 10,000 residual PSCs per dose. This must be tightened based on process capability.
Core Experimental Protocols
Protocol 4.1: Tumorigenicity Potency Assay for Risk Assessment
Objective: Determine the minimum tumorigenic dose of residual undifferentiated PSCs in the final product format. Materials:
- NOG (NOD/Shi-scid/IL-2Rγnull) mice, 6-8 weeks old.
- Test Article: Final product spiked with known numbers of the parental PSC line (e.g., 10, 10^2, 10^3, 10^4, 10^5 cells).
- Control: Parental PSC line alone.
- Matrigel (optional, for subcutaneous injection). Method:
- Prepare cell suspensions in the final product formulation buffer with appropriate spike levels.
- For intramuscular or subcutaneous injection, mix cells with Matrigel (1:1 v/v) on ice.
- Inject 50-100 µL total volume per site into mice (n=10 per group).
- Monitor animals for 16-26 weeks. Palpate injection sites weekly.
- Terminate and necropsy animals upon tumor detection (>1 cm diameter) or at study end.
- Isolate and weigh tumors. Perform histopathology (H&E) and confirm human origin (e.g., anti-human mitochondrial antibody staining). Data Analysis: Use probit or logistic regression to calculate the TD50 (dose inducing tumors in 50% of animals). The No-Observed-Effect-Level (NOEL) informs the safety factor.
Protocol 4.2: Multiparameter Flow Cytometry for Residual PSC Quantification
Objective: Quantify residual undifferentiated cells in a final differentiated cell product. Materials:
- Single-cell suspension of the final product.
- Fixable Viability Dye (e.g., Zombie NIR).
- Antibodies: Anti-TRA-1-60-APC, Anti-SSEA4-PE, Anti-[Lineage Marker]-FITC (e.g., CD184 for neural progenitors).
- Intracellular staining kit (if using nuclear markers like OCT4).
- Flow cytometer with 488nm, 561nm, and 640nm lasers. Method:
- Viability Staining: Wash cells, resuspend in PBS with viability dye. Incubate 15 min at RT in the dark.
- Surface Staining: Wash, then block with 5% BSA for 15 min. Add surface antibody cocktail (TRA-1-60, SSEA4, lineage marker). Incubate 30 min at 4°C. Wash.
- Fixation/Permeabilization: If detecting intracellular markers, fix and permeabilize cells per kit instructions.
- Intracellular Staining: Add anti-OCT4 antibody or isotype control. Incubate, then wash.
- Acquisition: Resuspend in staining buffer and acquire ≥100,000 events on the flow cytometer. Use a forward/side scatter gate to exclude debris, then a viability gate.
- Analysis: Plot viability-positive cells for pluripotency vs. lineage markers. Residual PSCs are defined as TRA-1-60+/SSEA4+/Lineage-. Validation: Establish LOD/LOQ using spiked samples in the product matrix. Determine precision (repeatability, intermediate precision).
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Contaminant Analysis
| Item | Function | Example Product/Catalog |
|---|---|---|
| Pluripotency Marker Antibody Panel | Specific detection of undifferentiated PSCs via flow or imaging. | Anti-TRA-1-60 (Clone TRA-1-60), Anti-SSEA4 (Clone MC813-70) |
| Droplet Digital PCR (ddPCR) System | Absolute quantification of residual viral vector genomes without a standard curve. | Bio-Rad QX200 ddPCR System |
| NOG Mice | Gold-standard immunocompromised model for assessing in vivo tumorigenicity. | Charles River, Strain Code: 6149 |
| Recombinant Laminin-521 | Xeno-free, defined substrate for PSC culture, replacing undefined Matrigel. | Biolamina, LN521 |
| Mass Spectrometry Grade Solvents | For sensitive detection of residual small molecule contaminants. | Merck, LiChrosolv LC-MS Grade |
| qRT-PCR Assay for Pluripotency Genes | Sensitive, orthogonal method for residual PSC detection. | TaqMan assays for POU5F1 (OCT4), NANOG |
Signaling Pathways & Decision Framework
Diagram 1: Framework for Setting PSC Release Specifications (99 chars)
Diagram 2: Key Signaling Pathways in PSC Self-Renewal (86 chars)
Diagram 3: Residual PSC Quantification Workflow (85 chars)
Comparative Analysis of Commercially Available Purging Technologies and Their Validation Packages
Within the development of GMP manufacturing processes for tumor-free pluripotent stem cell (PSC) therapies, the risk of teratoma formation from residual undifferentiated cells is a critical safety hurdle. Effective purging technologies are essential to remove these tumorigenic cells from differentiated therapeutic products. This application note provides a comparative analysis of current commercially available purging platforms and details standardized protocols for validating their efficacy and safety within a regulated research and development framework.
Purging strategies typically exploit biochemical or physiological differences between undifferentiated PSCs and their differentiated progeny. The table below summarizes key technologies, their mechanisms, and validation parameters.
Table 1: Comparative Analysis of Commercial Purging Platforms
| Technology Name (Vendor) | Mechanism of Action | Target | Reported Purging Efficiency (% Reduction) | Key Validation Parameters | Format |
|---|---|---|---|---|---|
| Small Molecule Inhibitors (e.g., Target-Specific) | Induces selective apoptosis in undifferentiated cells. | Pluripotency-associated kinases (e.g., PLK1, ROCK). | 95 - 99.9% (3-5 log reduction) | IC50, dose-response, exposure time, viability of target population. | Soluble reagent. |
| Immunomagnetic Depletion (e.g., Anti-SSEA-5 Microbeads) | Antibody-mediated magnetic labeling and column-based removal. | Cell surface pluripotency markers (SSEA-5, TRA-1-60). | 99 - 99.99% (2-4 log reduction) | Antibody specificity, bead-cell ratio, flow rate, post-sort purity. | Kit (Microbeads, columns). |
| Lactic Acid-Based Metabolic Selection | Exploits differential sensitivity to lactate/pH stress. | Metabolic vulnerability of undifferentiated cells. | 90 - 99% (1-2 log reduction) | Media lactate concentration, pH, exposure duration, recovery conditions. | Media supplement. |
| Cytotoxic Antibody & Complement | Antibody binds target cells, complement mediates lysis. | Cell surface pluripotency markers. | 99 - 99.9% (2-3 log reduction) | Antibody titer, complement activity, cytotoxicity assay. | Antibody + serum complement. |
Core Experimental Protocols for Purging Validation
Protocol 2.1: Standardized Purging Efficiency Assay
Objective: Quantify the reduction of undifferentiated PSCs from a spiked co-culture with differentiated cells. Materials: See "Scientist's Toolkit" (Section 4). Method:
- Spiked Sample Preparation: Label undifferentiated PSCs (e.g., with a fluorescent dye like CellTracker Red). Mix these "target" cells with your differentiated therapeutic cell population at a defined ratio (e.g., 1:10 to 1:100).
- Purging Intervention: Apply the commercial purging technology according to the manufacturer's optimized protocol (see Table 1 for key parameters).
- Post-Purging Analysis: a. Flow Cytometry: Analyze the post-treatment population for the presence of the fluorescent label or intrinsic pluripotency markers (e.g., SSEA-4). Calculate log reduction: Log Reduction = log10(% Target Pre-Treatment / % Target Post-Treatment). b. qPCR for Pluripotency Genes: Assay for OCT4, NANOG expression. Normalize to housekeeping genes and compare to pre-purging levels.
- Viability Assessment: Perform trypan blue exclusion or use a viability dye (e.g., 7-AAD) on the final product to ensure the purging process does not compromise the therapeutic population.
Protocol 2.2: Functional Validation viaIn VivoTeratoma Assay
Objective: Confirm the elimination of tumorigenic potential in the purged final product. Method:
- Cell Preparation: Generate three test articles: a) Purged final product, b) Unpurged spiked mixture (positive control), c) Differentiated cells only (negative control).
- Animal Transplantation: Inject 1x10^6 cells (or relevant dose) from each article subcutaneously into immunodeficient mice (e.g., NSG), n=5 per group.
- Observation & Endpoint: Monitor for tumor formation for 12-16 weeks. Palpate weekly for nodules.
- Histopathological Analysis: Excise any formed masses, fix, section, and stain with H&E. Confirm teratoma presence by identifying tissues from all three germ layers.
Validation Package Framework and Visualization
A comprehensive validation package must demonstrate process robustness, specificity, and suitability for GMP. The following diagram outlines the core logical flow of the validation strategy.
Diagram Title: Purging Technology Validation Workflow
The experimental workflow for the core purging efficiency assay is detailed below.
Diagram Title: Purging Efficiency Assay Protocol
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagent Solutions for Purging Validation
| Reagent/Material | Function in Validation | Example/Notes |
|---|---|---|
| Fluorescent Cell Tracker Dyes | Pre-label undifferentiated PSCs for tracking in spiked co-cultures. | CellTracker Red CMTPX; enables clear distinction from unlabeled differentiated cells. |
| Validated Anti-Pluripotency Antibodies | Detection of residual undifferentiated cells via flow cytometry or immunomagnetic selection. | Anti-SSEA-4, Anti-TRA-1-60; critical for defining pre- and post-purging populations. |
| qPCR Master Mix & Primers | Quantify residual pluripotency gene expression with high sensitivity. | TaqMan assays for OCT4/POU5F1, NANOG; requires validated reference genes (e.g., GAPDH, HPRT1). |
| Immunodeficient Mice | In vivo functional validation of tumorigenic potential. | NSG (NOD-scid IL2Rγnull) mice; gold-standard model for teratoma assay. |
| Defined Differentiation & Purging Media | Provides consistent cellular context for purging and post-purging recovery. | Vendor-specific or custom GMP-grade media; must be serum-free/xeno-free for clinical relevance. |
| Viability Assay Kit | Assess cytotoxicity of purging process on the therapeutic cell population. | 7-AAD/Annexin V flow kit or trypan blue; ensures product viability meets release criteria. |
Conclusion
The path to clinically viable, tumor-free PSC therapies is underpinned by a holistic GMP strategy that integrates rigorous biological understanding, robust manufacturing processes, and sensitive, multi-faceted analytics. Success requires moving beyond single-point purification to a quality-by-design approach where tumor risk mitigation is embedded at every stage, from cell line establishment to final product release. Future directions will be driven by advances in gene editing for built-in safety switches, continuous manufacturing, and AI-driven process analytics, ultimately enabling the reliable production of transformative cell therapies that meet the highest standards of patient safety and regulatory compliance.