Ensuring iPSC Pluripotency: A Comprehensive Guide to Quality Control for Research and Translation
This article provides a comprehensive guide to quality control (QC) measures for ensuring induced pluripotent stem cell (iPSC) pluripotency, tailored for researchers, scientists, and drug development professionals.
Ensuring iPSC Pluripotency: A Comprehensive Guide to Quality Control for Research and Translation
Abstract
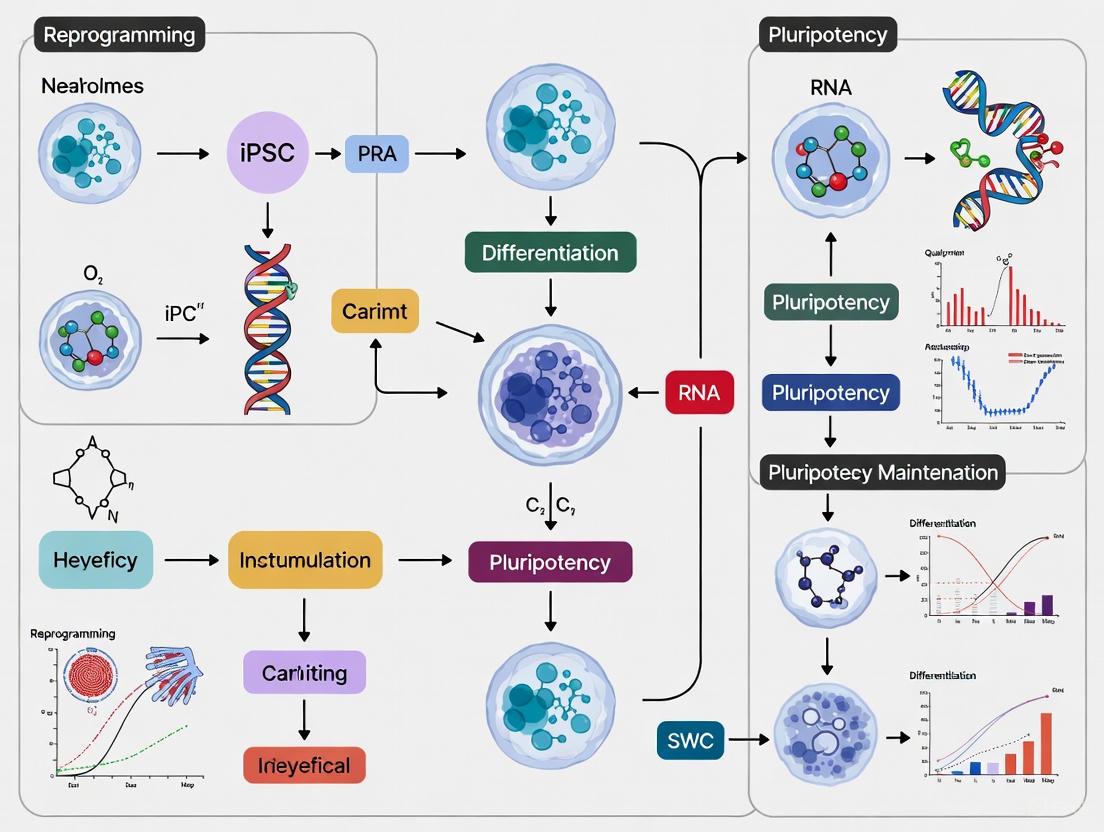
This article provides a comprehensive guide to quality control (QC) measures for ensuring induced pluripotent stem cell (iPSC) pluripotency, tailored for researchers, scientists, and drug development professionals. It covers the foundational principles of pluripotency, detailing the core molecular network and the impact of reprogramming methods on QC outcomes. The methodological section explores a multi-parameter QC toolkit, including assays for genomic integrity, pluripotency verification, and functional differentiation potential. The guide also addresses critical troubleshooting strategies for common issues like genetic instability and differentiation variability, and concludes with a comparative analysis of validation frameworks and regulatory standards essential for preclinical and clinical translation. By synthesizing the latest advances and persistent challenges, this resource aims to support the development of safe, reproducible, and high-quality iPSC lines for research and therapy.
The Foundation of Pluripotency: Core Concepts and Molecular Mechanisms
Pluripotency is the defining characteristic of stem cells that allows them to self-renew indefinitely while maintaining the potential to differentiate into derivatives of all three embryonic germ layers: ectoderm, mesoderm, and endoderm. For researchers working with induced pluripotent stem cells (iPSCs), rigorous verification of pluripotency is a critical quality control measure that ensures experimental integrity and reproducibility. This technical support center provides comprehensive guidance on key pluripotency markers, detailed experimental protocols for their analysis, and troubleshooting solutions for common challenges encountered in pluripotency assessment.
Key Pluripotency Markers: A Comprehensive Reference
Accurate assessment of pluripotency requires evaluating multiple marker categories through complementary techniques. The following tables summarize the essential markers for verifying the pluripotent state.
Table 1: Core Transcription Factors and Functional Indicators of Pluripotency
| Marker | Type | Function in Pluripotency | Detection Methods |
|---|---|---|---|
| OCT4 (POU5F1) | Transcription Factor | Maintains pluripotency by repressing differentiation pathways | qPCR, ICC, Western Blot |
| NANOG | Transcription Factor | Critical for self-renewal and suppression of differentiation | qPCR, ICC, Western Blot |
| SOX2 | Transcription Factor | Partners with OCT4 to sustain stemness | qPCR, ICC, Western Blot |
| Alkaline Phosphatase (ALP) | Functional Enzyme | High activity in undifferentiated cells | Enzymatic staining |
| Telomerase | Functional Enzyme | Maintains telomere length for self-renewal | TRAP assay, qPCR |
Table 2: Characteristic Surface Antigens of Pluripotent Stem Cells
| Marker | Type | Expression Pattern | Detection Methods |
|---|---|---|---|
| SSEA-3 | Glycolipid Surface Antigen | Expressed in pluripotent cells | Flow Cytometry, ICC |
| SSEA-4 | Glycolipid Surface Antigen | Highly expressed in undifferentiated hPSCs | Flow Cytometry, ICC |
| TRA-1-60 | Proteoglycan Surface Antigen | Specific to pluripotent state | Flow Cytometry, ICC |
| TRA-1-81 | Proteoglycan Surface Antigen | Specific to pluripotent state | Flow Cytometry, ICC |
Recent research has identified additional genes with strong potential to discriminate between undifferentiated and differentiated states of iPSCs. Long-read nanopore transcriptome sequencing has revealed 172 genes potentially associated with differentiation states not addressed in current guidelines, with validated unique markers including CNMD, NANOG, and SPP1 for pluripotency [1].
Experimental Protocols for Pluripotency Assessment
RNA Extraction and qPCR Analysis Protocol
Principle: Quantify transcriptional signatures of core pluripotency factors to confirm stem cell status at the genetic level.
Materials and Reagents:
- High-quality RNA extraction kit (RNase-free)
- cDNA synthesis kit with reverse transcriptase
- qPCR reagents: SYBR Green Master Mix
- Pluripotency-specific primers (OCT4, NANOG, SOX2)
- Housekeeping gene primers (GAPDH, ACTB)
- Nuclease-free water and consumables
Step-by-Step Methodology:
Cell Preparation: Harvest PSCs at 70-80% confluency to avoid spontaneous differentiation. Use feeder-free or feeder-dependent cultures with compact colonies displaying high nucleus-to-cytoplasm ratios [2].
RNA Extraction:
- Lyse cells using kit reagents under RNase-free conditions
- Bind RNA to purification columns
- Wash with appropriate buffers
- Elute with nuclease-free water
- Measure concentration and purity (A260/A280 ratio >1.8)
cDNA Synthesis:
- Use 0.5-1μg total RNA in reverse transcription reaction
- Follow kit protocol for reaction conditions
- Store synthesized cDNA at -20°C
qPCR Setup and Analysis:
- Prepare reaction mix: SYBR Green Master Mix, forward/reverse primers, cDNA template, nuclease-free water
- Run qPCR with appropriate cycling conditions
- Normalize results against housekeeping genes (GAPDH, ACTB)
- Interpret results: High OCT4, SOX2, and NANOG expression indicates pluripotency
Protein-Level Validation: Immunocytochemistry (ICC)
Principle: Visualize and localize pluripotency-associated proteins within cells to confirm expression and nuclear localization characteristic of undifferentiated states.
Materials and Reagents:
- Primary antibodies: Anti-OCT4, Anti-SOX2, Anti-NANOG, Anti-SSEA-4, Anti-TRA-1-60
- Fluorescently labeled secondary antibodies
- Fixative: 4% Paraformaldehyde (PFA)
- Permeabilization buffer: 0.1-0.5% Triton X-100
- Blocking solution: 1-5% BSA or serum in PBS
- Mounting medium with DAPI
- PBS buffer
Step-by-Step Methodology:
Cell Fixation:
- Aspirate culture medium from cells grown on coverslips or chamber slides
- Wash gently with PBS
- Fix with 4% PFA for 15-20 minutes at room temperature
- Wash 3 times with PBS
Permeabilization and Blocking:
- Permeabilize with 0.1-0.5% Triton X-100 for 10-15 minutes (for intracellular markers)
- Wash with PBS
- Block with 1-5% BSA or appropriate serum for 30-60 minutes
Antibody Incubation:
- Incubate with primary antibodies diluted in blocking buffer overnight at 4°C
- Wash 3 times with PBS (5 minutes each)
- Incubate with fluorescent secondary antibodies for 1 hour at room temperature (protected from light)
- Wash 3 times with PBS
Visualization and Analysis:
- Mount with DAPI-containing medium to counterstain nuclei
- Image with fluorescence or confocal microscopy
- Analyze for expected patterns: Nuclear staining for OCT4, SOX2, NANOG; cell surface for SSEA-4, TRA-1-60
Research Reagent Solutions for Pluripotency Analysis
Table 3: Essential Reagents for Pluripotency Marker Analysis
| Reagent Category | Specific Products | Function in Experiment |
|---|---|---|
| Primary Antibodies | Anti-OCT4, Anti-SOX2, Anti-NANOG, Anti-SSEA-4, Anti-TRA-1-60 | Specific binding to pluripotency markers for detection |
| Secondary Antibodies | Fluorescently labeled goat anti-mouse/anti-rabbit | Signal amplification and detection |
| Cell Culture Media | TeSR, mTeSR, ReproFF2, StemFit | Maintain pluripotent state during expansion |
| qPCR Reagents | SYBR Green Master Mix, RNA extraction kits, reverse transcriptase | Gene expression analysis at transcriptional level |
| Cell Dissociation | Gentle Cell Dissociation Reagent, Accutase | Generate single-cell suspensions for analysis |
| Fixation/Permeabilization | Paraformaldehyde, Triton X-100 | Preserve cellular architecture and enable antibody access |
Troubleshooting Guide: Common Challenges and Solutions
FAQ: Addressing Frequent Pluripotency Assessment Issues
Q: How do I distinguish between fully reprogrammed and partially reprogrammed iPSCs?
A: Fully reprogrammed iPSCs express pluripotency markers at levels comparable to human embryonic stem cells (hESCs), with consistent expression across multiple detection methods (qPCR, ICC, flow cytometry). Partial reprogramming often shows incomplete marker profiles and reduced self-renewal capacity. Validate using a combination of transcriptional and protein-level analyses [2].
Q: What sample size is required for complete pluripotency marker profiling?
A: For a full multi-platform analysis, generally 1-2 million cells are recommended. However, with optimized protocols, analysis can be performed with as few as 200,000 cells using microfluidics and high-sensitivity antibody assays [2].
Q: How often should I validate pluripotency markers in my stem cell lines?
A: Validation every 3-5 passages is recommended, before differentiation experiments, or whenever cells undergo significant environmental changes (e.g., switch of feeder system, media brand, or culture substrate) [2].
Q: My PSCs appear negative for key markers despite proper culture conditions. What could be wrong?
A: This could result from partial differentiation, stress-induced gene downregulation, or culture adaptation. Reassess culture conditions and use fresh feeder layers or optimized feeder-free matrices. Supplement with small molecules (e.g., ROCK inhibitors) to stabilize pluripotency, and reduce passage numbers to maintain original stemness [2].
Q: What are the gold standard markers for definitive pluripotency validation?
A: The most widely accepted gold-standard markers are OCT4, SOX2, and NANOG at the transcriptional level, combined with surface markers such as SSEA-3/4 and TRA-1-60/TRA-1-81. Using a combination ensures robust and reproducible validation of pluripotency [2].
Technical Issue Resolution
Table 4: Troubleshooting Common Experimental Problems
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Low-quality RNA leading to poor qPCR amplification | RNase contamination, suboptimal cell lysis, degraded samples | Use RNase-free consumables with inhibitors; confirm RNA integrity; store at -80°C [2] |
| Weak ICC staining or non-specific background | Suboptimal antibody concentration, cross-reactivity, expired antibodies | Test multiple antibody clones; optimize dilutions with titration; validate with positive controls [2] |
| Variable flow cytometry results | Poor sample preparation, dead cells, antibody aggregation | Filter cells to remove clumps; incorporate viability dyes; vortex antibody solutions before use [2] |
| Spontaneous differentiation in culture | Over-confluence, suboptimal passaging, poor quality matrices | Passage at 70-80% confluency; use appropriate matrices; remove differentiated areas before analysis [3] |
| Inconsistent results across detection methods | Method-specific limitations, sample heterogeneity | Employ orthogonal validation methods; ensure consistent sample processing; use multiple detection techniques [1] [2] |
Advanced Techniques and Emerging Markers
While traditional markers remain essential for pluripotency verification, recent advances in sequencing technologies have revealed additional genes with strong potential to discriminate between undifferentiated and differentiated states. Long-read nanopore transcriptome sequencing has identified 172 genes potentially associated with differentiation states not addressed in current guidelines, with validated unique markers for pluripotency including CNMD, NANOG, and SPP1 [1].
Machine learning-based scoring systems such as "hiPSCore" have been developed using these refined marker panels, trained on multiple iPSC lines and demonstrating accurate classification of undifferentiated and differentiated cells [1]. These approaches enhance the standardization of pluripotency assessment while reducing time, subjectivity, and resource requirements.
For comprehensive pluripotency assessment within quality control frameworks, researchers should integrate both established marker analysis and emerging technologies to ensure robust characterization of iPSC lines for research and therapeutic applications.
The core pluripotency network, orchestrated by the transcription factors OCT4, SOX2, and NANOG, governs the remarkable capacity of pluripotent stem cells to self-renew and differentiate into any cell type in the body. This regulatory circuitry is fundamental to embryonic development and serves as the cornerstone for generating induced pluripotent stem cells (iPSCs) [4] [5]. In iPSC research, stringent quality control measures are essential to ensure the faithful reprogramming of somatic cells and the maintenance of authentic pluripotent states. Understanding the precise roles, expression levels, and interactions of these core factors is therefore not merely of biological interest but a critical practical requirement for generating reliable, clinically relevant cell models [6] [7]. This technical support center provides targeted troubleshooting guides and FAQs to help researchers navigate the specific experimental challenges associated with assessing and maintaining this core network.
Key Research Reagent Solutions
The following table catalogs essential reagents used in the study and manipulation of the core pluripotency network, with explanations of their primary functions in an experimental context.
Table 1: Key Research Reagents for Pluripotency Network Analysis
| Research Reagent | Function and Application in Pluripotency Research |
|---|---|
| Yamanaka Factors (OSKM) | A set of four transcription factors (OCT4, SOX2, KLF4, c-MYC) used for somatic cell reprogramming to generate iPSCs [6] [7]. |
| bFGF (Basic Fibroblast Growth Factor) | A critical growth factor for maintaining pluripotency in human ESCs and iPSCs, primarily through activation of the MAPK signaling pathway [8]. |
| LIF (Leukemia Inhibitory Factor) | A cytokine used to maintain pluripotency in mouse ESCs through activation of the Jak/Stat3 signaling pathway; not typically required for human ESCs [4]. |
| 2i Inhibitors (ERK1/2 + GSK3β) | A combination of small-molecule inhibitors that safeguard mouse ESCs in a "ground state" of pluripotency by suppressing differentiation signals [4]. |
| BMP4 (Bone Morphogenetic Protein 4) | A signaling molecule that, in combination with LIF, helps maintain mouse ESC pluripotency by inducing Id genes. Its role is complex and context-dependent in human ESCs [4] [9]. |
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: What are the distinct functional roles of OCT4, SOX2, and NANOG in human pluripotent stem cells?
While OCT4, SOX2, and NANOG form a core cooperative network, each factor has unique, non-overlapping functions in lineage specification. Understanding these distinct roles is crucial for interpreting differentiation outcomes.
- OCT4's Role in Lineage Specification: OCT4 level is a critical determinant of cell fate and interacts with external signaling pathways like BMP4. Research shows that high OCT4 levels enable self-renewal in the absence of BMP4 but specify mesendoderm in its presence. Conversely, low OCT4 levels induce embryonic ectoderm differentiation without BMP4 but specify extraembryonic lineages with BMP4 [9].
- NANOG as a Specific Repressor: NANOG primarily functions as a repressor of neuroectoderm and neural crest lineages. It does not act as a pan-repressor of all differentiation pathways but is specifically critical for preventing this particular fate [9].
- SOX2/SOX3 Redundancy in Repression: SOX2, along with its family member SOX3, functions redundantly to repress primitive streak differentiation and mesendoderm specification [9].
FAQ 2: How can we experimentally assess the protein interaction and genomic binding of the core pluripotency factors?
A common experimental workflow involves Chromatin Immunoprecipitation (ChIP) followed by sequencing (ChIP-seq) to map the genomic binding sites of these factors and identify their target genes.
Experimental Protocol: ChIP-seq for Core Pluripotency Factors
- Cross-linking: Fix cells (e.g., iPSCs) with formaldehyde to covalently link transcription factors like OCT4, SOX2, and NANOG to their DNA binding sites.
- Cell Lysis and Chromatin Shearing: Lyse cells and fragment the chromatin into small pieces (200–500 bp) using sonication.
- Immunoprecipitation: Incubate the sheared chromatin with a specific, validated antibody against your target protein (e.g., anti-OCT4). Use Protein A/G beads to pull down the antibody-protein-DNA complexes.
- Washing and Elution: Wash the beads stringently to remove non-specifically bound chromatin. Elute the bound complexes from the beads and reverse the cross-links to free the DNA.
- DNA Purification: Purify the immunoprecipitated DNA.
- Library Prep and Sequencing: Prepare a sequencing library from the purified DNA and perform high-throughput sequencing (ChIP-seq).
- Data Analysis: Map the sequenced reads to the reference genome to identify peaks of enrichment, which represent genomic regions bound by the transcription factor. Co-occupancy of OCT4, SOX2, and NANOG on target gene promoters is a hallmark of the core pluripotency network [4] [5].
FAQ 3: Our iPSCs show spontaneous differentiation. How do we troubleshoot issues with the core pluripotency network?
Spontaneous differentiation often indicates a failure to maintain the core pluripotency network. The table below outlines common problems and their solutions.
Table 2: Troubleshooting Spontaneous Differentiation in iPSC Cultures
| Symptom | Potential Cause | Recommended Solution |
|---|---|---|
| Heterogeneous expression of OCT4/NANOG, with patches of differentiated cells. | Inconsistent culture conditions: Fluctuations in key signaling pathways (e.g., FGF, TGF-β). | Standardize feeding schedules. Use fresh, pre-warmed media. For human cells, ensure consistent high concentration of bFGF (e.g., 100 ng/mL) to maintain MAPK signaling [8]. |
| Rapid loss of pluripotency markers after passaging. | Passaging-induced stress leading to apoptosis or initiation of differentiation. | Use a Rho-associated kinase (ROCK) inhibitor (e.g., Y-27632) for 24 hours post-passaging to improve cell survival [8]. Optimize passaging method and frequency. |
| Uniform differentiation toward a specific lineage. | Imbalanced core factor expression. Low OCT4 can drive neuroectoderm differentiation; high OCT4 with BMP4 can push mesendoderm. | Monitor and control OCT4 expression levels. Review differentiation protocols to ensure no inducing factors are present in the maintenance medium. Check for adequate NANOG expression to repress neuroectoderm [9]. |
| Failure to silence exogenous reprogramming factors in established iPSCs. | Incomplete reprogramming or use of integrating vectors that remain active. | Use non-integrating reprogramming methods (e.g., Sendai virus, episomal plasmids, mRNA) [7]. Perform qRT-PCR to confirm silencing of exogenous transgenes and activation of endogenous pluripotency genes. |
FAQ 4: What signaling pathways are critical for maintaining the core pluripotency network, and how do they interact with it?
The core transcription factors are regulated by and interact with specific external signaling pathways to maintain pluripotency. The required pathways differ between species.
- Mouse ESC Signaling: Relies on LIF (activating Jak/Stat3) and BMP4 (inducing Id genes) signaling. Pluripotency can also be maintained in a "ground state" using small-molecule inhibitors ("2i") against ERK1/2 and GSK3β [4].
- Human ESC/iPSC Signaling: Depends on FGF (particularly bFGF) and TGF-β/Activin/Nodal signaling pathways [4] [8]. Withdrawing bFGF leads to downregulation of OCT4, SOX2, and NANOG and initiates differentiation, primarily toward the ectoderm lineage, accompanied by a decrease in MAPK pathway activity [8].
FAQ 5: What are the key quality control checks for the core pluripotency network in a new iPSC line?
Rigorous quality control is mandatory for any newly derived or acquired iPSC line. The assessment should include multiple layers of validation.
- Expression Analysis: Confirm the expression of endogenous OCT4, SOX2, and NANOG at the mRNA level (via qRT-PCR) and protein level (via immunocytochemistry). Ensure that transgenes used for reprogramming have been silenced in integration-free lines [7].
- Functional Genomic Assessment: Perform ChIP-seq to validate that the core factors bind to their known target genomic sites, confirming a properly wired regulatory network [4] [5].
- Pluripotency Validation: Demonstrate the capacity for in vitro differentiation into cell types of all three germ layers (ectoderm, mesoderm, endoderm) via directed differentiation or teratoma formation assays.
- Karyotyping and Genetic Stability: Perform G-banding karyotyping or higher-resolution genetic analysis to ensure the cell line has a normal, stable karyotype, as prolonged culture can lead to chromosomal abnormalities.
- Mycoplasma Testing: Routinely test for mycoplasma contamination, which can alter cell physiology and differentiation potential without causing overt turbidity in the culture medium.
The choice of reprogramming method is a critical initial step in induced pluripotent stem cell (iPSC) generation, with significant implications for quality control (QC), downstream applications, and clinical translation. The table below summarizes the core characteristics of major integrating and non-integrating approaches.
Table 1: Characteristics of Major iPSC Reprogramming Methods
| Method Type | Specific Method | Genetic Integration | Reprogramming Efficiency | Key Safety Considerations | Primary Research Applications |
|---|---|---|---|---|---|
| Integrating | Retroviral/Lentiviral Vectors | Yes (Random) | High (e.g., ~0.01% for retroviral [10]) | Insertional mutagenesis, transgene reactivation [11] [12] | Basic research, disease modeling [12] |
| Non-Integrating | Sendai Virus (SeV) | No (Cytoplasmic) | High (e.g., ~0.05% [10]) | Requires dilution over passages to clear viral vectors [11] | Disease modeling, drug screening, clinical applications [13] [10] |
| Non-Integrating | Episomal Vectors | No | Low to Moderate (e.g., ~0.05% [10]; ~0.0006% [11]) | Rapid transgene clearance (typically 17-21 days) [11] | Clinical-grade iPSC generation, biobanking [11] [13] |
| Non-Integrating | Synthetic mRNA | No | High (with repeated transfections) | Labor-intensive; potential interferon response [11] [14] | Clinical-grade iPSC generation [14] |
The following workflow outlines the key decision points when selecting a reprogramming method based on research goals and QC priorities.
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: What is the single most important QC differentiator between integrating and non-integrating methods?
The most critical differentiator is genomic integration and the associated risk of insertional mutagenesis. Integrating methods, such as those using retroviruses, permanently insert the reprogramming transgenes into the host cell's genome. This can disrupt tumor suppressor genes or activate oncogenes, posing a significant tumorigenicity risk for clinical applications [11] [12]. Non-integrating methods avoid this risk by ensuring transient expression of the reprogramming factors.
FAQ 2: Our lab uses Sendai virus reprogramming. A QC check shows residual viral vectors at passage 5. Is this normal?
Yes, this is an expected finding. Sendai virus vectors are cytoplasmic and are gradually diluted out as cells divide. However, their clearance requires a sufficient number of cell passages. It is recommended to perform passaging until the vectors are undetectable by PCR. One study notes that a "far greater number of cell divisions are required to dilute the cell line free of contaminating viral proteins and the vector" [11]. You should establish a QC protocol to routinely test for viral clearance at later passages (e.g., passage 10 or beyond) before using the iPSC line for critical experiments.
FAQ 3: We are struggling with the low efficiency of episomal reprogramming. How can we improve our success rate without compromising safety?
The low efficiency of episomal reprogramming is a known challenge [11]. You can consider these troubleshooting strategies without reverting to integrating methods:
- Optimize your starting cell type. Fibroblasts, peripheral blood mononuclear cells (PBMCs), and cord blood cells have been successfully reprogrammed with episomal vectors [11] [13].
- Use small molecules. Supplementing the culture with small molecules like RepSox, valproic acid (VPA), or sodium butyrate can enhance reprogramming efficiency significantly [15] [12]. For instance, one study found that combining 8-Br-cAMP with VPA increased efficiency by up to 6.5-fold [15].
- Validate your nucleofection protocol. For episomal vectors, efficient delivery via nucleofection is crucial. Ensure you are using the correct program and conditions for your specific cell type [13].
FAQ 4: Do different reprogramming methods create inherent functional differences in the final iPSC line?
Evidence suggests that once fully reprogrammed and quality-controlled, iPSCs exhibit similar pluripotency profiles regardless of the reprogramming method used. A comparative study that analyzed the gene expression profiles of iPSCs derived via retroviral, Sendai virus, and episomal methods found no significant differences attributable to the reprogramming technique [10]. The critical factor is that the lines are fully reprogrammed to a bona fide pluripotent state. Variability is more likely due to the genetic background of the donor or technical handling.
Essential Experimental Protocols for QC
Protocol: Confirming Absence of Reprogramming Transgenes in Non-Integrating iPSC Lines
Purpose: To ensure that iPSC lines generated with non-integrating methods (e.g., Sendai virus, episomal vectors) are free of residual reprogramming vectors, a key safety QC test.
Materials:
- iPSC genomic DNA (minimally 100 ng)
- PCR primers specific for the reprogramming factors (e.g., OCT4, SOX2, KLF4, c-MYC) and the specific vector backbone (e.g., SeV genome, Epstein-Barr virus OriP/EBNA1 for episomes)
- Positive control (e.g., DNA from the original transfected/transduced cells)
- Negative control (e.g., DNA from a known negative cell line or nuclease-free water)
- PCR Master Mix
- Thermo-cycler and gel electrophoresis equipment
Procedure:
- Sample Collection: Extract high-quality genomic DNA from the candidate iPSC line at a minimum of passage 10. Earlier passages are likely to yield positive results and are not conclusive [11].
- PCR Setup: Set up PCR reactions for each reprogramming factor/vector-specific primer set. Include positive and negative controls in every run.
- Amplification: Run the PCR using optimized cycling conditions for your primers.
- Analysis: Resolve the PCR products on an agarose gel. A line is considered clear of vectors if no PCR product is amplified with the vector-specific primers, while the positive control shows a clear band.
Troubleshooting: If the result is positive, continue passaging the cells and re-test at a later passage. For Sendai virus, specific kits are available (e.g., CytoTune Sendai Virus Detection Kit) to facilitate this QC step.
Protocol: Validating Pluripotency via Embryoid Body (EB) Formation
Purpose: This in vitro assay tests the differentiation capacity of iPSCs into derivatives of all three germ layers, a core QC metric for pluripotency [10].
Materials:
- Confluent well of iPSCs in a 6-well plate
- Dispase or Collagenase IV solution
- iPSC medium without bFGF
- Low-attachment 6-well plate or Petri dish
- Cultureware coated with Poly-L-Ornithine/Laminin or Gelatin for EB plating
- RT-PCR reagents and primers for germ layer markers
Procedure:
- EB Formation: Harvest iPSCs by enzymatic digestion to create small clumps. Resuspend the cell clumps in iPSC medium without bFGF and transfer to a low-attachment plate to prevent adhesion. Culture for 7-10 days, allowing EBs (3D spherical structures) to form.
- EB Plating: After 7-10 days, transfer the EBs to a standard culture plate coated with Poly-L-Ornithine/Laminin or Gelatin. Continue culture for an additional 7-14 days in the same medium, allowing cells to migrate and differentiate out of the EBs.
- Analysis: After the differentiation period, analyze the outgrowths.
- Immunofluorescence: Stain for specific protein markers: ECTODERM (β-III-Tubulin), MESODERM (α-Smooth Muscle Actin), and ENDODERM (Alpha-Fetoprotein).
- qRT-PCR: Analyze the expression of key genes: ECTODERM (PAX6), MESODERM (MSX1), and ENDODERM (SOX17) [10].
Troubleshooting: If spontaneous differentiation is inefficient, consider adding differentiation-inducing agents like retinoic acid to the medium.
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for iPSC Reprogramming and QC
| Reagent/Category | Specific Examples | Function in Reprogramming/QC |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM); OCT4, SOX2, NANOG, LIN28 (OSNL) [15] [16] | Core transcription factors that induce pluripotency in somatic cells. |
| Small Molecule Enhancers | Valproic Acid (VPA), Sodium Butyrate, RepSox, 8-Br-cAMP [15] [12] | Improve reprogramming efficiency by modulating epigenetic marks and signaling pathways. |
| Non-Integrating Vectors | CytoTune Sendai Virus Kit, Episomal plasmids (e.g., pCE-epi vector system) [11] [13] | Delivery systems for transient expression of reprogramming factors, enhancing safety profile. |
| Pluripotency Markers | Antibodies against OCT4, SOX2, NANOG, SSEA4, TRA-1-60 [13] [10] | Used in immunostaining and flow cytometry to confirm the undifferentiated state of iPSCs. |
| Germ Layer Markers | Antibodies against β-III-Tubulin, α-SMA, AFP; PCR primers for PAX6, MSX1, SOX17 [10] | Critical for validating pluripotency via EB assays, confirming trilineage differentiation potential. |
The following diagram summarizes the multi-stage quality control pipeline for validating iPSC lines, from the initial reprogramming event to final confirmation of pluripotency and safety.
The Role of Epigenetic Remodeling in Establishing Pluripotency
Core Concepts: Epigenetic Reprogramming to Pluripotency
What is the fundamental role of epigenetic remodeling in establishing pluripotency? Reprogramming somatic cells into induced pluripotent stem cells (iPSCs) requires profound alterations in the epigenetic landscape to reset gene expression and stabilize self-renewal. This process reverses the epigenetic modifications that occur during cellular differentiation, transforming a specialized cell with restricted potential into a pluripotent one with broad developmental capacity [17] [6].
What are the key epigenetic changes during this process?
- DNA Methylation: Somatic cells exhibit stable, tissue-specific DNA methylation patterns that must be reset. During reprogramming, pluripotency gene promoters (like OCT4 and NANOG) undergo demethylation to become active again, while somatic cell-specific genes are silenced through hypermethylation [17].
- Histone Modifications: Pluripotent stem cells possess a unique epigenetic profile enriched for open, active chromatin modifications (H3K4me3, H3K36me3, histone acetylation). Reprogramming establishes these marks at pluripotency genes and creates bivalent domains (H3K4me3 and H3K27me3) at differentiation-related genes, keeping them in a "poised" state for future development [17].
Troubleshooting Guide: Epigenetic Barriers in iPSC Generation
Problem 1: Low Reprogramming Efficiency
Potential Cause: Epigenetic barriers are hindering the reprogramming process. Solutions:
- Utilize epigenetic modifiers: Treatment with DNA methyltransferase inhibitors (e.g., 5-aza-cytidine) or histone deacetylase inhibitors (e.g., Valproic Acid, Sodium butyrate, Trichostatin A) can increase reprogramming efficiency by opening condensed chromatin [15] [17].
- Target specific epigenetic enzymes: Knockdown of Dot1l (H3K79 methyltransferase) or Suv39H1/2 (H3K9 methyltransferases) facilitates reprogramming by reducing repressive heterochromatin [15] [17].
- Enhance activating marks: Overexpression of Jhdm1b (H3K36me demethylase) or Ezh2 (PRC2 component for H3K27 methylation) has been shown to enhance reprogramming efficiency [17].
Problem 2: Incomplete Reprogramming (Partially Reprogrammed Cells)
Potential Cause: Failure to fully reset the epigenetic landscape, particularly at key pluripotency loci. Solutions:
- Demethylation agents: Treatment with agents like 5-aza-cytidine facilitates the transition of partially reprogrammed cells into a full state of pluripotency [17].
- Activate specific factors: Overexpression of Kdm4b (H3K9 demethylase) promotes conversion from pre-iPSCs to iPSCs [17].
- Ensure complete MET: The Mesenchymal-to-Epithelial Transition is a critical early event; optimize culture conditions to support this process [6].
Problem 3: Genomic Instability and Aberrant Karyotypes
Potential Cause: Epigenetic dysregulation during reprogramming and in vitro culture can lead to chromosomal abnormalities. Solutions:
- Implement rigorous quality control: Regularly monitor chromosomal stability using G-banding karyotyping (detects larger structural abnormalities >5-10 Mb) and SNP array analysis (detects smaller copy number variations >350 kb and loss of heterozygosity) [18].
- Monitor common anomalies: Pay particular attention to common hPSC abnormalities involving chromosomes 12, 17, 20 (especially 20q11.21 amplification), and X [18].
- Maintain reference standards: Compare iPSC epigenetic profiles (DNA methylation patterns, histone marks) to embryonic stem cells as a reference for complete reprogramming [17].
Epigenetic Modifiers in Reprogramming
Table 1: Key Epigenetic Modifiers That Influence Reprogramming Efficiency
| Epigenetic Modifier | Function | Effect on Reprogramming | Mechanism |
|---|---|---|---|
| Hdac inhibitors (VPA, Sodium butyrate) | Histone deacetylase inhibitor | Increases efficiency [17] | Opens chromatin structure |
| 5-aza-cytidine | DNA methyltransferase inhibitor | Increases efficiency [17] | Demethylates pluripotency gene promoters |
| Dot1l | H3K79 methyltransferase | Silencing facilitates reprogramming [15] [17] | Reduces repressive histone methylation |
| Suv39H1/2 | H3K9 methyltransferase | Downregulation increases reprogramming [15] [17] | Decreases heterochromatin formation |
| Ezh2 (PRC2) | H3K27 methyltransferase | Overexpression enhances reprogramming [17] | Establishes repressive marks on somatic genes |
| Kdm4b | H3K9 demethylase | Overexpression promotes conversion from pre-iPSCs [17] | Removes repressive histone marks |
| Wdr5 (Set/Mll complex) | H3K4 methyltransferase complex | Knockdown decreases reprogramming [17] | Reduces active chromatin marks |
| Mbd3 (NuRD complex) | Chromatin remodeling | Conflicting reports; may be indispensable [17] | Complex role in chromatin regulation |
Experimental Protocols for Quality Control
Protocol 1: Assessing DNA Methylation Reprogramming
Purpose: Verify complete epigenetic resetting at pluripotency gene promoters. Methodology:
- Bisulfite Sequencing: Treat DNA with bisulfite to convert unmethylated cytosines to uracils, then sequence key pluripotency gene promoters (e.g., OCT4, NANOG).
- Global Methylation Analysis: Use methods like MethylC-Seq for genome-wide DNA methylation profiling at single-base resolution.
- Comparison to ESCs: Compare iPSC methylation patterns with embryonic stem cells as a reference standard [17].
Expected Results: Successfully reprogrammed iPSCs should show hypomethylation at pluripotency gene promoters similar to ESCs, with establishment of non-CG methylation patterns characteristic of pluripotent cells [17].
Protocol 2: Monitoring Histone Modification Patterns
Purpose: Confirm establishment of pluripotent-appropriate chromatin state. Methodology:
- Chromatin Immunoprecipitation (ChIP): Use antibodies specific for histone modifications (H3K4me3, H3K27me3, H3K9me3) followed by sequencing.
- Focus on Key Loci: Assess bivalent domains at developmental gene promoters and active marks at pluripotency genes.
- Validate with Functional Assays: Correlate epigenetic patterns with gene expression (RNA-seq) and functional pluripotency assays [17].
Protocol 3: Chromosomal Integrity Assessment
Purpose: Ensure genomic stability after reprogramming. Methodology:
- G-banding Karyotyping: Analyze at least 20 metaphases with 300-500 band resolution to detect larger structural abnormalities (>5-10 Mb).
- SNP Array Analysis: Use platforms like Illumina's Global Screening Array to detect smaller copy number variations (>350 kb) and copy-neutral loss of heterozygosity.
- Regular Monitoring: Perform these assessments every 10-15 passages, as abnormal clones can overtake a culture in less than five passages [18].
Epigenetic Reprogramming Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Epigenetic Quality Control
| Reagent/Category | Specific Examples | Function in Quality Control |
|---|---|---|
| DNA Methylation Inhibitors | 5-aza-cytidine, RG108 | Improve reprogramming efficiency; verify methylation role [15] [17] |
| Histone Deacetylase Inhibitors | Valproic Acid, Sodium butyrate, Trichostatin A | Enhance reprogramming; modulate chromatin accessibility [15] [17] |
| Chromatin Remodeling Modulators | RepSox, Neplanocin A | Improve reprogramming robustness; study chromatin dynamics [15] |
| Pluripotency Media | mTeSR Plus, mTeSR1 | Maintain pluripotent state; ensure consistent culture conditions [19] |
| Passaging Reagents | ReLeSR, Gentle Cell Dissociation Reagent | Maintain epigenetic state during subculture; minimize stress [19] |
| Extracellular Matrices | Vitronectin XF, Corning Matrigel | Provide appropriate signaling context for pluripotency maintenance [19] |
| SNP Array Platforms | Illumina Global Screening Array | Detect chromosomal abnormalities and copy number variations [18] |
| Epigenetic Editing Tools | CRISPR-dCas9 fusion systems | Precisely manipulate specific epigenetic marks for functional studies [15] |
Frequently Asked Questions
How can we distinguish complete versus partial epigenetic reprogramming? Complete reprogramming is characterized by: (1) Global DNA methylation patterns resembling embryonic stem cells, including establishment of non-CG methylation; (2) Demethylation of pluripotency gene promoters (OCT4, NANOG); (3) Appropriate histone modification patterns including bivalent domains at developmental genes; and (4) Stable expression of pluripotency markers without spontaneous differentiation [17].
Why do we observe donor-specific epigenetic variation in iPSCs? iPSCs maintain some donor-specific epigenetic patterns even after reprogramming due to underlying genetic variation. Studies show that epigenetic variation is most strongly associated with genetic variation at the iPSC stage, though this relationship weakens after differentiation. This reflects the complex interaction between genotype and epigenome that persists through reprogramming [20].
What are the most critical quality control checkpoints for epigenetically stable iPSCs?
- Regular karyotyping (every 10-15 passages) to detect chromosomal abnormalities [18]
- DNA methylation profiling at key pluripotency loci to confirm complete reprogramming [17]
- Expression analysis of pluripotency markers and spontaneous differentiation potential [19]
- Epigenetic stability monitoring across passages to ensure maintenance of pluripotent state [20]
How does partial reprogramming for rejuvenation differ from complete reprogramming? Partial reprogramming involves transient expression of Yamanaka factors (OSKM) long enough to produce epigenetic rejuvenation (restoration of youthful gene expression patterns) but not long enough to fully dedifferentiate cells into iPSCs. This approach aims to refresh cellular function while maintaining cell identity, though it requires precise control to avoid tumor formation or loss of cellular identity [21].
The Pillars of Pluripotency QC
Robust quality control (QC) for induced pluripotent stem cell (iPSC) research extends beyond routine checks; it requires a deep understanding of the molecular foundations of pluripotency. The core properties defining pluripotent stem cells are self-renewal, the ability to divide indefinitely, and potency, the capacity to differentiate into all cells derived from the three germ layers (ectoderm, endoderm, and mesoderm) [22]. Effective QC verifies that your iPSC lines consistently demonstrate these two traits. The following table outlines the essential pillars of pluripotency QC.
| QC Pillar | Key Indicators | Purpose |
|---|---|---|
| Self-Renewal | Consistent expression of pluripotency factors (e.g., OCT4, SOX2, NANOG); Stable karyotype and proliferation rate | Confirms genetic stability and unlimited expansion capacity in culture [22]. |
| Pluripotency | In vitro: Spontaneous differentiation via embryoid body formation; In vivo: Teratoma formation with tissues from three germ layers | Provides functional evidence of the ability to differentiate into any somatic cell type [22]. |
| Epigenetic State | Specific epigenetic landscape (e.g., open chromatin, DNA methylation patterns); Reactivation of endogenous pluripotency genes | Validates complete reprogramming and a stable, ESC-like epigenetic signature [6]. |
Troubleshooting Common iPSC QC Challenges
Q1: Our iPSC colonies appear heterogeneous, with some cells spontaneously differentiating. What is the cause, and how can we achieve a more homogeneous culture?
This indicates your cells are in a "metastable" state. The solution often lies in refining your culture conditions to promote a "ground state" of pluripotency.
- Root Cause: Standard culture media containing serum introduces undefined factors that can prod cells toward differentiation. Fluctuations in the expression of pluripotency and lineage-specific factors lead to heterogeneity [22].
- QC Solution: Transition to a defined, serum-free culture system using small-molecule inhibitors. The "2i" system, comprising PD0325901 (a MEK inhibitor) and CHIR99021 (a GSK3 inhibitor), blocks prodifferentiation signals. This promotes a uniform "ground state" of pluripotency, resulting in morphologically homogeneous colonies and a more consistent gene expression profile [22].
- Protocol:
- Passage your iPSCs into pre-coated culture vessels.
- Replace the standard medium with a defined base medium (e.g., N2B27) supplemented with 1 µM PD0325901 and 3 µM CHIR99021.
- Change the medium daily and passage cells every 3-4 days.
- Monitor colony morphology for a more uniform, compact appearance.
Q2: We confirmed the expression of key pluripotency markers, but the cells fail to form robust teratomas in vivo. What might be wrong?
This suggests incomplete or unstable reprogramming.
- Root Cause: The reprogramming process is inefficient and occurs in distinct phases. An early, stochastic phase can yield cells that express core pluripotency markers but have not fully stabilized their epigenetic landscape, preventing robust multi-lineage differentiation [6].
- QC Solution: Do not rely on a single QC assay. Your QC workflow must be multi-faceted. Combine pluripotency marker analysis (e.g., immunostaining for OCT4) with functional assays like embryoid body (EB) formation in vitro and the gold-standard teratoma assay in vivo. Furthermore, assess the epigenetic status, such as the methylation state of pluripotency gene promoters, to ensure complete epigenetic reprogramming [6] [22].
- Protocol: Embryoid Body (EB) Formation for In Vitro Differentiation
- Harvest iPSCs using gentle enzymatic dissociation to create small clumps.
- Transfer cell clumps to a low-attachment culture plate in a medium that does not contain pluripotency-sustaining factors (e.g., no bFGF or 2i).
- Allow EBs to form over 3-5 days, changing the medium every other day.
- Plate EBs onto gelatin-coated tissue culture dishes and continue culture for another 10-14 days.
- Analyze the outgrowths for markers of the three germ layers (e.g., β-III tubulin for ectoderm, α-fetoprotein for endoderm, and smooth muscle actin for mesoderm) via immunocytochemistry.
Foundational Signaling Pathways in Pluripotency
A deep understanding of the signaling pathways that maintain or disrupt pluripotency is non-negotiable for effective QC. The following diagrams map the critical networks you must monitor.
LIF/Stat3 Signaling for Self-Renewal
FGF4-Driven Differentiation Pathway
Research Reagent Solutions for Pluripotency QC
A consistent and well-defined set of reagents is the bedrock of reproducible QC. The table below details essential materials for foundational pluripotency experiments.
| Reagent / Material | Function in QC | Example & Notes |
|---|---|---|
| Small-Molecule Inhibitors (2i) | Maintains "ground state" pluripotency by suppressing differentiation signals. | PD0325901 (MEK inhibitor) and CHIR99021 (GSK3 inhibitor). Used in serum-free media for homogeneous, naive pluripotent cultures [22]. |
| Cytokines for Self-Renewal | Supports pluripotency in mouse iPSC cultures via specific signaling pathways. | Leukemia Inhibitory Factor (LIF). Activates the JAK/STAT3 pathway. Often used with Serum or BMP4 in traditional mouse iPSC culture [22]. |
| Feeder Cells | Provides a supportive extracellular matrix and factors for cell growth. | Mouse Embryonic Fibroblasts (MEFs). Mitotically inactivated. Can introduce variability; feeder-free cultures on defined substrates (e.g., Geltrex) are preferred for consistency [22]. |
| Pluripotency Marker Antibodies | Detects the presence and intracellular location of key pluripotency transcription factors. | Anti-OCT4, Anti-SOX2, Anti-NANOG. Critical for immunocytochemistry and confirming the molecular signature of pluripotency. |
| Karyotyping Kits | Monitors genomic integrity after reprogramming and long-term culture. | G-banding analysis or SKY FISH kits. Aneuploidy can occur in culture; regular screening is essential for credible research [22]. |
| In Vivo Teratoma Assay Components | The gold-standard functional test for pluripotency. | Immunodeficient Mice (e.g., NOD/SCID). Subcutaneous injection of iPSCs should yield a tumor with tissues from the three germ layers within 8-12 weeks [22]. |
The iPSC QC Toolkit: Essential Assays and Analytical Methods
Regular visual inspection of induced pluripotent stem cell (iPSC) colonies is a fundamental and rapid quality control method for any pluripotency research program. Morphology serves as a sensitive, real-time indicator of cellular health and pluripotent status. Careful daily monitoring under a phase-contrast microscope allows researchers to identify early signs of differentiation or culture decline, often before these changes are detected by molecular assays. This non-invasive assessment is crucial for maintaining the integrity of experiments and ensuring the reproducibility of results, forming the first line of defense in a comprehensive quality control strategy.
Key Morphological Features of Undifferentiated iPSCs
The table below summarizes the core characteristics of high-quality, undifferentiated iPSC colonies and contrasts them with features indicating poor cell quality.
Table 1: Morphological Features of Undifferentiated vs. Differentiating iPSC Colonies
| Feature | High-Quality, Undifferentiated Colonies | Poor Quality or Differentiating Colonies |
|---|---|---|
| Colony Shape | Relatively round and symmetrical [23] | Irregular, asymmetric, or loss of border integrity [23] |
| Cell Packing | Tightly packed cells with a high nucleus-to-cytoplasm ratio; very dense colony centers [23] | Loosely packed cells with visible phase-bright gaps between them [23] |
| Nucleoli | Prominent nucleoli [23] | Not specified in search results |
| Phase Brightness | Colony centers appear phase-bright under phase contrast [23] | Phase-brightness that appears "mottled," sporadic, and not localized to the center [23] |
| Spontaneous Differentiation | Low levels (5-10%) are normal [23] | Increased areas (>10%) of spontaneous differentiation [23] |
Diagram 1: Visual Assessment Workflow for iPSC Morphology.
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: My colonies have developed "spiky" or irregular edges a few days after passaging. Does this indicate differentiation? Not necessarily. For the first few days after passaging (up to 4 days), colonies may exhibit looser packing and "spiky" edges as they spread out and become established. This is often a normal variation. The density and robustness of the colonies should increase rapidly after this timepoint. If the spiky edges and loose packing persist or worsen as the colonies grow, it may then indicate a decrease in cell quality [23].
Q2: What does it mean if the centers of my colonies appear very phase-bright? Phase-bright colony centers are a characteristic of high-quality, densely packed human pluripotent stem cells (hPSCs) and are typically observed near the optimal time for passaging. This is a sign of healthy, proliferative cells. However, you should be concerned if the phase-brightness appears "mottled," sporadic, and is not localized to the center of the colony, as this can be an indicator of poor cell quality [23].
Q3: Is it normal for colonies to merge, and what is the impact? Yes, it is normal for colonies to merge, especially as they expand and toward the time of passaging. This can also occur if aggregates are seeded at a low density and are not well-dispersed. Merging itself is not typically a cause for concern. However, very large, merged colonies may begin to spontaneously differentiate in the center due to nutrient gradients or contact inhibition. Maintaining an appropriate seeding density to achieve well-separated colonies is considered best practice [23].
Q4: How does the culture substrate affect colony morphology? The physical and chemical properties of the culture substrate can significantly influence colony morphology. Studies have shown that groove-ridge structures with submicrometer periodicity can induce elongation of iPSC colonies, guide the orientation of apical actin fibers, and direct the plane of cell division [24]. Furthermore, the symmetry of colonies can vary between different extracellular matrices (e.g., Vitronectin XF vs. Matrigel) [23].
Essential Protocols for Morphological Assessment
Daily Observation Protocol
Objective: To routinely monitor the health, density, and undifferentiated status of iPSC cultures. Materials: Phase-contrast microscope, cell culture vessel. Procedure:
- Frequency: Examine cultures daily using a phase-contrast microscope, both before and after feeding [23] [25].
- Assessment: Systematically scan the entire surface of the culture vessel. Evaluate the following:
- Colony Density and Distribution: Determine if the culture is ready to be passaged.
- Morphology: Check for the key features of undifferentiated colonies listed in Table 1.
- Differentiation: Identify and estimate the percentage of the culture surface showing signs of spontaneous differentiation (e.g., changes in cell morphology, loose packing). A low amount (5-10%) is normal, but an increase indicates a need for action [23].
- Contamination: Look for any signs of microbial contamination.
Documentation Protocol
Objective: To maintain a visual record of culture status over time for tracking quality and experimental reproducibility. Materials: Phase-contrast microscope with a digital camera. Procedure:
- Image Capture: Take representative, high-resolution images of colonies at regular intervals (e.g., daily or at each passage) using consistent magnification and lighting.
- Annotation: Label each image with the cell line name, passage number, date, and any relevant culture conditions.
- Storage: Archive images in a structured database for future reference and comparison.
Research Reagent Solutions
The table below lists essential materials used in the culture and quality assessment of iPSCs.
Table 2: Essential Reagents for iPSC Culture and Quality Control
| Reagent/Category | Function | Example Use-Case |
|---|---|---|
| Defined Culture Medium | Provides essential nutrients, growth factors, and signals to maintain self-renewal and pluripotency. | mTeSR Plus, mTeSR1 [23] |
| Cell Culture Substrate | A defined extracellular matrix that supports iPSC attachment, colony formation, and expansion. | Vitronectin XF, Corning Matrigel [23] |
| Passaging Reagent | Enzymatic or non-enzymatic solution used to dissociate colonies for sub-culturing. | Accutase, ReLeSR (for clump passaging) [25] |
| ROCK Inhibitor | A small molecule that increases single-cell survival and cloning efficiency post-passage by inhibiting apoptosis. | Y-27632, used when passaging as single cells [25] |
| Pluripotency Markers | Antibodies for key transcription factors and cell surface antigens to confirm undifferentiated status. | Antibodies against Oct3/4, Nanog, SSEA-4, TRA-1-60, TRA-1-81 [26] |
Diagram 2: Simplified Mechanotransduction Pathway in iPSCs.
Within the framework of a thesis on quality control for induced pluripotent stem cell (iPSC) research, rigorous validation of pluripotency markers is non-negotiable. This technical support center addresses common pitfalls in Immunocytochemistry (ICC), Flow Cytometry, and quantitative Reverse Transcription PCR (qRT-PCR), providing targeted solutions to ensure data integrity and reproducibility.
Troubleshooting Guides & FAQs
Immunocytochemistry (ICC)
Q1: My ICC staining for OCT4 shows high background noise, obscuring the nuclear signal. What can I do? A: High background is often due to non-specific antibody binding or inadequate blocking.
- Solution: Increase the concentration of your blocking serum (e.g., from 5% to 10%) and extend the blocking time to 1 hour at room temperature. Include a detergent like 0.1% Triton X-100 in your blocking and antibody dilution buffers to reduce non-specific hydrophobic interactions. Re-titrate your primary antibody to find the lowest effective concentration.
Q2: I am not detecting any signal for my pluripotency marker NANOG. My positive control works. What is wrong? A: This typically indicates an issue with antibody penetration or antigen accessibility.
- Solution: Ensure your permeabilization step is sufficient. For nuclear markers like NANOG, use a stronger permeabilization agent (e.g., 0.5% Triton X-100 for 20 minutes) or consider a methanol fixation step (-20°C methanol for 10 minutes), which simultaneously fixes and permeabilizes cells. Verify that your primary antibody is validated for ICC.
Flow Cytometry
Q3: My flow cytometry data for SOX2 shows a large spread in fluorescence intensity and poor separation between the positive and negative populations. A: This can be caused by cell clumping, improper voltage settings, or high background.
- Solution:
- Cell Preparation: Filter cells through a 35-40 µm cell strainer immediately before analysis to remove clumps.
- Voltage/Gain: Use an unstained control and a single-color control (e.g., IgG isotype control) to set the voltage on the relevant detector. Adjust the voltage so that the negative population is in the first decade of the log scale.
- Gating: Use a sequential gating strategy: first, gate on FSC-A vs. SSC-A to select live, single cells; then, gate on FSC-A vs. FSC-H to exclude doublets.
Q4: What is an acceptable percentage of positive cells for a core pluripotency marker in a high-quality iPSC line? A: For a well-characterized iPSC line, the expression of core transcription factors (OCT4, SOX2, NANOG) should be highly homogeneous.
Table 1: Expected Pluripotency Marker Expression in a High-Quality iPSC Line via Flow Cytometry
| Pluripotency Marker | Expected % Positive Cells | Acceptable Threshold |
|---|---|---|
| OCT3/4 | >90% | >85% |
| SOX2 | >90% | >85% |
| NANOG | >85% | >80% |
| SSEA-4 | >95% | >90% |
qRT-PCR
Q5: My qRT-PCR results show high Ct values for the housekeeping gene GAPDH in my iPSC samples. What does this indicate? A: High Ct values for a stable housekeeping gene suggest poor RNA quality or quantity.
- Solution: Check RNA integrity using an instrument like a Bioanalyzer. A RNA Integrity Number (RIN) >9.5 is ideal for iPSCs. Ensure you are using a minimum of 50-100 ng of high-quality RNA per reaction. Re-evaluate your choice of housekeeping gene; β-actin or GAPDH are commonly used, but 18S rRNA or TBP may be more stable in some stem cell contexts.
Q6: How do I calculate the relative fold-change in gene expression for my pluripotency markers? A: The most common method is the 2^(-ΔΔCt) method.
- Solution:
- Calculate ΔCt: ΔCt = Ct(Target Gene) - Ct(Housekeeping Gene) for each sample.
- Calculate ΔΔCt: ΔΔCt = ΔCt(Test Sample) - ΔCt(Calibrator Sample). The calibrator is often the undifferentiated iPSC control.
- Calculate Fold-Change: Fold-change = 2^(-ΔΔCt).
Table 2: Example qRT-PCR Data Analysis for Pluripotency Markers
| Sample | Gene | Ct Value | ΔCt | ΔΔCt | Fold-Change vs. Control |
|---|---|---|---|---|---|
| iPSC Control | OCT4 | 24.5 | 24.5 - 18.0 = 6.5 | 6.5 - 6.5 = 0.0 | 2^0 = 1.0 |
| GAPDH | 18.0 | ||||
| Differentiated Cells | OCT4 | 29.0 | 29.0 - 18.2 = 10.8 | 10.8 - 6.5 = 4.3 | 2^(-4.3) ≈ 0.05 |
| GAPDH | 18.2 |
Experimental Protocols
Protocol 1: Immunocytochemistry for Pluripotency Markers
- Culture & Fixation: Culture iPSCs on Matrigel-coated coverslips. At ~70% confluence, aspirate media and fix with 4% Paraformaldehyde (PFA) for 15 minutes at room temperature (RT).
- Permeabilization & Blocking: Wash 3x with PBS. Permeabilize and block with a solution of 5% normal serum (e.g., goat serum) and 0.3% Triton X-100 in PBS for 1 hour at RT.
- Primary Antibody Incubation: Incubate with primary antibody (e.g., Anti-OCT4, 1:200) diluted in blocking solution overnight at 4°C.
- Secondary Antibody Incubation: Wash 3x with PBS. Incubate with fluorophore-conjugated secondary antibody (1:500) diluted in blocking solution for 1 hour at RT in the dark.
- Counterstaining & Mounting: Wash 3x with PBS. Incubate with DAPI (1 µg/mL) for 5 minutes. Wash and mount coverslip onto a slide using an anti-fade mounting medium.
Protocol 2: Flow Cytometry Analysis of Pluripotency Markers
- Cell Harvest & Fixation: Dissociate iPSCs into a single-cell suspension using Accutase. Centrifuge and resuspend ~1x10^6 cells in 4% PFA. Fix for 20 minutes at RT.
- Permeabilization: Centrifuge, wash with PBS, and resuspend in ice-cold 90% methanol for 30 minutes on ice. (This step is crucial for intracellular markers like OCT4 and NANOG).
- Staining: Centrifuge and wash with FACS Buffer (PBS + 2% FBS). Resuspend cell pellet in 100 µL FACS Buffer containing the primary antibody or isotype control. Incubate for 1 hour at RT in the dark.
- Analysis: Wash cells twice with FACS Buffer. If using a directly conjugated antibody, resuspend in FACS Buffer and analyze immediately on a flow cytometer. If using an unconjugated primary, perform a secondary antibody incubation step first.
Protocol 3: RNA Extraction and qRT-PCR for Pluripotency Markers
- RNA Extraction: Lyse cells directly in a culture plate using TRIzol reagent or a commercial silica-membrane column kit. Include a DNase I digestion step to remove genomic DNA contamination.
- cDNA Synthesis: Quantify RNA concentration. Use 1 µg of total RNA for reverse transcription with a kit using random hexamers and M-MLV Reverse Transcriptase.
- qPCR Setup: Prepare a master mix containing SYBR Green PCR Master Mix, forward and reverse primers (e.g., for OCT4, SOX2, NANOG, and a housekeeping gene), and nuclease-free water. Add cDNA template. Run in triplicate on a real-time PCR instrument.
- Data Analysis: Use the instrument software to determine Ct values. Export data and calculate relative fold-change using the 2^(-ΔΔCt) method.
Visualizations
Title: ICC Experimental Workflow
Title: Flow Cytometry Gating Strategy
Title: qRT-PCR Fold-Change Calculation
The Scientist's Toolkit
Table 3: Essential Research Reagents for Pluripotency Marker Analysis
| Reagent / Material | Function / Purpose |
|---|---|
| 4% Paraformaldehyde (PFA) | Cross-linking fixative that preserves cellular architecture for ICC and Flow Cytometry. |
| Triton X-100 | Non-ionic detergent used to permeabilize cell membranes, allowing antibodies to access intracellular targets. |
| Normal Serum (e.g., Goat Serum) | Used for blocking to prevent non-specific binding of antibodies to cells or tissue. |
| Fluorophore-Conjugated Antibodies | Antibodies tagged with a fluorescent dye (e.g., Alexa Fluor 488) for detection in ICC and Flow Cytometry. |
| SYBR Green Master Mix | A reagent used in qRT-PCR that fluoresces when bound to double-stranded DNA, allowing for quantification of amplified PCR products. |
| DNase I | Enzyme that degrades genomic DNA during RNA preparation to prevent false-positive signals in qRT-PCR. |
| Matrigel | Basement membrane matrix used to coat culture surfaces, providing a substrate that supports iPSC attachment and pluripotency. |
The teratoma formation assay is a critical in vivo functional test used to confirm the pluripotency of human pluripotent stem cells (hPSCs), including both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs). This assay provides the most stringent validation of a cell line's capacity to differentiate into derivatives of all three embryonic germ layers—ectoderm, mesoderm, and endoderm—within an in vivo environment [27] [28].
For researchers in the field of iPSC quality control, this assay serves a dual purpose: it not only confirms developmental potential but also provides crucial safety data by assessing tumorigenic risk. The same pluripotent characteristic that makes hPSCs powerful tools in regenerative medicine also creates major clinical hurdles, highlighting the fine line that both separates and connects pluripotency and tumorigenicity [27]. Despite being time-consuming and requiring animal models, it remains the gold standard for pluripotency assessment, particularly for pre-clinical safety evaluation of hPSC-derived cell therapy products [29] [30].
Key Principles and Biological Basis
What is a Teratoma?
Teratomas are benign tumors characterized by rapid growth in vivo and their haphazard mixture of tissues, often containing semi-semblances of organs, teeth, hair, muscle, cartilage, and bone [27]. The presence of multiple tissue types derived from all three germ layers provides definitive evidence of robust pluripotency [27] [31].
When these tumors contain undifferentiated "embryonal carcinoma elements," they are classified as teratocarcinomas, indicating malignant potential [29]. The distinction is critical for safety assessment, as the presence of undifferentiated cells in a therapeutic product poses significant tumorigenicity risks [29] [30].
Why Use the Teratoma Assay?
While in vitro alternatives exist—such as embryoid body formation, directed differentiation, and bioinformatic tools like PluriTest—the teratoma assay offers unique advantages [28] [31]:
- Provides a more physiologically relevant environment compared to artificial petri dish conditions
- Allows assessment of both pluripotency and malignant potential simultaneously
- Remains the preferred method for detecting undifferentiated cells in differentiated cell products intended for transplantation
- Is generally required by regulatory authorities for pre-clinical safety assessment of hPSC-derived therapies [29] [30]
Experimental Design and Protocols
Essential Materials and Reagents
The following research reagents are fundamental for executing a proper teratoma formation assay:
Table: Essential Research Reagent Solutions for Teratoma Formation Assays
| Reagent/Category | Specific Examples & Details | Primary Function |
|---|---|---|
| hPSC Lines | H7, H9 (WA07, WA09), or validated iPSC lines; optionally with reporter genes (Fluc, mRFP, HSVtk) | Starting cellular material for implantation [27] |
| Cell Culture | Gelatin, Matrigel, mTESR-1 hES Growth Medium, Collagenase Type IV | Maintenance and preparation of undifferentiated hPSCs [27] |
| Animal Models | Immunodeficient mice (Nu/Nu nude, SCID, NOD/SCID, NSG) | Host organisms that allow hPSC engraftment without rejection [27] [30] |
| Injection Supplies | 28.5 gauge insulin syringes, Matrigel for cell suspension | Delivery of cells to implantation site [27] |
| Anesthesia & Support | Isoflurane vapor system, 37°C heat pad | Animal comfort and physiological support during procedures [27] |
Critical Experimental Parameters
Multiple factors significantly influence teratoma formation efficiency and must be carefully controlled:
Table: Key Experimental Parameters Affecting Teratoma Formation
| Parameter | Options/Recommended Values | Impact on Assay Outcome |
|---|---|---|
| Injection Site | Subcutaneous, intramuscular, kidney capsule, intratesticular | Affects teratoma formation efficiency and differentiation patterns [27] [32] |
| Cell Number | 1×10^4 to 1×10^6 cells (site-dependent); ~1×10^5 for intramyocardial | Must exceed critical threshold for teratoma formation; too high increases malignancy risk [27] |
| Animal Strain | Immunocompromised strains (Nu/Nu, SCID, NOD/SCID, NSG) | Prevents xenogeneic rejection of human cells [27] [30] |
| Assay Duration | 6-20 weeks (cell line and site dependent) | Must allow sufficient time for teratoma development and tissue differentiation [29] |
Standardized Workflow Protocol
The following diagram illustrates the core experimental workflow for conducting a teratoma formation assay:
Detailed Methodological Steps
Cell Preparation and Injection
- Culture hPSCs: Maintain undifferentiated hPSCs on feeder layers or in feeder-free conditions using validated media [27].
- Harvest cells: Use collagenase Type IV or manual scraping to create cell aggregates or single-cell suspensions [27].
- Prepare injection sample: Resuspend cells in an appropriate buffer, often mixed with Matrigel (approximately 1:1 ratio) to enhance cell survival and engraftment [27].
- Load syringes: Use 28.5 gauge insulin syringes for precise delivery while maintaining cell viability [27].
Animal Procedures and Monitoring
- Anesthetize mice: Use isoflurane vapor in oxygen for safe and reversible anesthesia [27].
- Inject cells: Administer cell suspension to selected site (subcutaneous, intramuscular, or kidney capsule) [27].
- Post-operative care: Provide analgesic if needed and monitor recovery on a 37°C heat pad [27].
- Longitudinal monitoring: Palpate weekly for tumor formation; utilize non-invasive imaging (BLI, MRI) if cells express reporter genes [27].
Tissue Harvest and Analysis
- Harvest tumors: Euthanize mice at predetermined endpoints (typically 8-20 weeks) or when tumors reach 1-2 cm in diameter [27] [32].
- Process tissue: Fix teratomas in formalin, embed in paraffin, and section for staining [27].
- Histological analysis: Stain sections with H&E and examine for tissues representing all three germ layers [27] [31].
Troubleshooting Common Experimental Issues
FAQ 1: What should I do if no teratoma forms after injection?
Potential Causes and Solutions:
- Insufficient cell number: Ensure you're injecting at or above the critical threshold (typically >10,000 cells, depending on site) [27]. Consider creating a cell number titration series.
- Suboptimal injection site: Test multiple sites (subcutaneous, intramuscular, kidney capsule) as efficiency varies [27] [32].
- Cell quality: Verify pluripotency status prior to injection using flow cytometry for markers (OCT4, SOX2, NANOG, TRA-1-60) [33].
- Animal model issues: Confirm immunodeficient status of mice and use younger animals (6-8 weeks) for better engraftment [27] [32].
FAQ 2: Why does my teratoma show incomplete differentiation or lacks all three germ layers?
Potential Causes and Solutions:
- Insufficient growth time: Allow more time for differentiation (extend to 12-20 weeks) as different lineages appear at different rates [29].
- Excessive cell number: Very high cell numbers can sometimes lead to poor differentiation; try reducing cell number by 50% [27].
- Sampling error: Ensure thorough sectioning and sampling of the entire teratoma, as germ layer distribution can be heterogeneous [31].
- Cell line variability: Acknowledge that different hPSC lines have varying differentiation biases [27] [28].
FAQ 3: How can I distinguish between a benign teratoma and a malignant teratocarcinoma?
Key Distinguishing Features:
- Benign teratomas contain only well-differentiated tissues from the three germ layers without undifferentiated components [29] [32].
- Teratocarcinomas contain undifferentiated "embryonal carcinoma" cells in addition to differentiated tissues, indicating malignant potential [29] [32].
- Histopathological analysis by an experienced pathologist is essential for accurate classification [29].
- Additional indicators of malignancy include invasive growth, high proliferation index (Ki67 staining), and metastasis [32].
FAQ 4: What are the ethical considerations and alternatives to reduce animal use?
Ethical Framework and Alternatives:
- Follow 3Rs principles: Replacement, Reduction, and Refinement as outlined in EU Directive 2010/63/EU [32].
- Implement humane endpoints: Establish clear tumor size limits (typically 1-2 cm diameter or 10% body weight) to prevent suffering [32].
- Consider in vitro alternatives: For initial screening, use embryoid body formation, directed differentiation, or bioinformatic tools (PluriTest, ScoreCard) [28] [31] [32].
- Maximize data obtained: Combine endpoints where possible and share data to avoid duplication of experiments [32].
Data Interpretation and Analysis
Histopathological Assessment
Proper analysis requires systematic examination of hematoxylin and eosin (H&E) stained sections for well-differentiated tissues representing:
- Ectoderm: Neural tissue (rosettes, pigment epithelium), stratified squamous epithelium, glial cells [27] [31]
- Mesoderm: Cartilage, bone, muscle (skeletal, smooth), adipose tissue, connective tissue [27] [31]
- Endoderm: Respiratory epithelium, intestinal epithelium, glandular structures [27] [31]
Documentation should include high-quality photomicrographs with scale bars and clear tissue identification.
Quantitative and Semi-Quantitative Approaches
While traditional teratoma assessment is qualitative, newer approaches provide more objective measures:
- TeratoScore: A computational method that quantifies differential gene expression in teratoma tissue to provide quantitative assessment of differentiation capacity [28].
- Scoring systems: Some laboratories implement semi-quantitative scoring based on tissue diversity, organization, and maturity [31].
The following decision diagram guides the interpretation of teratoma assay results:
Current Methodological Innovations and Future Directions
The field continues to evolve with several important developments:
- Enhanced sensitivity assays: Digital PCR and highly efficient culture (HEC) assays now offer superior detection sensitivity for residual undifferentiated hPSCs in differentiated products [30].
- Standardization efforts: Recent consensus recommendations from the Health and Environmental Sciences Institute's International Cell Therapy Committee aim to harmonize evaluation procedures globally [30].
- Imaging advancements: Non-invasive longitudinal imaging with reporter gene-expressing cells allows monitoring of teratoma development without sacrificing animals at multiple timepoints [27].
- In vitro alternatives: While not yet replacing teratoma assays for safety assessment, improved 3D culture systems and organoid technologies show promise for reducing animal use in the future [31] [32].
For drug development professionals and researchers, understanding both the power and limitations of the teratoma assay remains essential for proper preclinical assessment of hPSC-based therapies. While the assay continues to be required by regulatory authorities for clinical applications, employing complementary in vitro methods during early development can enhance efficiency and reduce animal use [30] [32].
Troubleshooting FAQ: Common Issues in Directed Differentiation
FAQ 1: What are the most common causes of low differentiation efficiency across all three germ layers?
Low differentiation efficiency often stems from issues with starting cell quality, inappropriate signaling molecule concentration, or suboptimal culture conditions. Ensure your iPSCs are fully pluripotent and undifferentiated before beginning, with >75% expression of key markers like NANOG, OCT4, SSEA4, TRA-1-60, and TRA-1-81 [33] [34]. Other factors include incorrect timing of growth factor addition, poor cell density optimization, and variability between cell lines. Always include positive controls and validate with multiple pluripotency markers to confirm starting cell quality [35] [34].
FAQ 2: How can I troubleshoot high background staining during immunocytochemical analysis of germ layer markers?
High background staining in immunocytochemistry can result from multiple factors. To reduce nonspecific background: quench endogenous peroxidases with 3% H₂O₂ in methanol, block endogenous biotin using avidin/biotin blocking solutions, optimize primary antibody concentration to prevent nonspecific binding, and add NaCl (0.15-0.6 M) to antibody diluents to reduce ionic interactions [36]. For fluorescent detection, address autofluorescence by testing different fixatives or using near-infrared fluorescent dyes that don't compete with tissue autofluorescence [36].
FAQ 3: What quality control standards should be implemented for clinical-grade iPSC differentiation?
For clinical-grade applications, implement rigorous quality control tests validated under Good Manufacturing Practice (GMP) standards. These include: residual episomal vector screening (minimum 20,000 cells/120 ng genomic DNA), pluripotency marker assessment (>75% expression of at least three markers), and differentiation potential verification (positive for at least two lineage-specific markers per germ layer) [34] [37]. Testing should occur between passages 8-10 to avoid unnecessary rejection of lines still losing reprogramming vectors [34].
FAQ 4: How does extracellular matrix affect definitive endoderm differentiation efficiency?
Substrate properties significantly influence definitive endoderm differentiation. Research demonstrates that synthetic PEG-based hydrogels presenting cyclic RGD peptides support efficient DE differentiation when combined with appropriate soluble factors [38]. Increasing substrate stiffness (G' = 1.0-4.0 kPa) produces a linear increase in DE differentiation efficiency, with focal adhesion kinase activity regulating both iPSC growth and DE differentiation outcomes [38]. This fully defined synthetic matrix offers a clinically translatable alternative to poorly-defined xenogeneic substrates like Matrigel [38].
FAQ 5: What are the key signaling pathways to manipulate for specific germ layer specification?
Germ layer specification requires precise manipulation of evolutionarily conserved signaling pathways. For mesendoderm (precursor to both mesoderm and endoderm), TGF-β family signals (particularly Nodal/Activin) are crucial [39] [40]. For ectoderm specification, TGF-β signaling must be attenuated, a process mediated by factors like Ectodermin, a Smad4 ubiquitin ligase that restricts mesoderm-inducing signals [40]. Mesoderm formation requires synergistic activity of FGF signaling with TGF-β signals, while definitive endoderm specification relies on high levels of Activin/Nodal signaling [39] [38].
Quantitative Standards for Germ Layer Differentiation Validation
Table 1: Minimum Acceptance Criteria for Successful Germ Layer Differentiation [34]
| Parameter | Minimum Acceptance Criteria | Testing Method |
|---|---|---|
| Pluripotency Starting Population | ≥75% expression of at least 3 pluripotency markers | Flow cytometry, immunocytochemistry |
| Ectoderm Confirmation | Positive for ≥2 of: PAX6, SOX1, Nestin, βIII-tubulin | Immunocytochemistry, qRT-PCR |
| Mesoderm Confirmation | Positive for ≥2 of: Brachyury, SMA, Desmin, CD31 | Immunocytochemistry, qRT-PCR |
| Endoderm Confirmation | Positive for ≥2 of: SOX17, FOXA2, CXCR4, AFP | Immunocytochemistry, qRT-PCR |
| Genetic Stability | Normal karyotype maintained post-differentiation | Karyotype analysis, SNP array |
Table 2: Differentiation Efficiency Based on Pre-culture Medium Composition [41]
| Pre-culture Medium Type | Cardiac Troponin T (cTnT) Positivity | Germ Layer Efficiency |
|---|---|---|
| StemFit AK03 medium (standard) | 84% | Baseline mesodermal differentiation |
| Similar to E8 medium (Type 2) | 91% | Enhanced mesodermal/ectodermal differentiation |
| Similar to E8 medium (Type 3) | 89% | Enhanced mesodermal differentiation |
| Similar to EB Formation medium | 95% | Highest mesodermal differentiation |
Experimental Protocols for Germ Layer Differentiation
Protocol 1: Standardized Three-Germ Layer Differentiation Workflow
This protocol adapts International Stem Cell Banking Initiative (ISCBI) recommendations for quality-controlled differentiation [33] [34].
Starting Material Requirements:
- Fully characterized iPSC line (passage 8-15)
- ≥75% expression of pluripotency markers (OCT4, NANOG, SSEA4, TRA-1-60)
- Normal karyotype verified
- Confirmed absence of residual episomal vectors (for reprogrammed lines)
Differentiation Workflow:
- Pluripotent State Confirmation: Validate starting population via flow cytometry for pluripotency markers and ensure absence of spontaneous differentiation [33] [34].
- Embryoid Body Formation: Harvest iPSCs using gentle dissociation reagents and aggregate in low-adhesion plates in EB formation medium (77% DMEM + 20% KOSR + 1% NEAA + 0.1% β-mercaptoethanol + 1% GlutaMAX) [41].
- Germ Layer Specification: Plate EBs on appropriate substrate and expose to germ layer-specific induction factors:
- Definitive Endoderm: Activin A (100 ng/mL) for 5 days in serum-free conditions [38]
- Mesoderm: BMP4 (10-50 ng/mL) with FGF2 (20 ng/mL) for 7-10 days
- Ectoderm: Dual SMAD inhibition (SB431542 + LDN193189) in neural induction medium
- Lineage Validation: Assess differentiation efficiency at day 10-14 using immunocytochemistry and qRT-PCR for germ layer-specific markers.
Protocol 2: Defined Matrix for Definitive Endoderm Differentiation
This protocol utilizes fully-defined synthetic substrates for clinically-translatable definitive endoderm differentiation [38].
Materials:
- PEG-based hydrogel presenting cyclic RGD peptide
- Stiffness range: 1.0-4.0 kPa (optimally 4.0 kPa)
- Serum-free definitive endoderm differentiation medium
- Recombinant human Activin A
Procedure:
- Substrate Preparation: Coat culture vessels with PEG-based hydrogel functionalized with cyclic RGD peptide at optimal stiffness (4.0 kPa) [38].
- iPSC Seeding: Seed undifferentiated iPSCs as single cells at 1.5-2.0×10⁵ cells/cm² in mTeSR or Essential 8 medium with ROCK inhibitor.
- Definitive Endoderm Induction: Once cells reach 80-90% confluence, switch to serum-free definitive endoderm differentiation medium containing 100 ng/mL Activin A.
- Medium Refreshment: Change differentiation medium daily for 5 days.
- Efficiency Assessment: Analyze for definitive endoderm markers SOX17, FOXA2, and CXCR4 via flow cytometry. Expect >85% SOX17+ cells with optimal conditions [38].
Critical Notes:
- Monitor integrin and syndecan receptor expression temporally during differentiation
- Focal adhesion kinase (FAK) activity regulates growth and DE differentiation efficiency
- Higher substrate stiffness within the 1.0-4.0 kPa range linearly increases differentiation efficiency
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Germ Layer Differentiation and Characterization
| Reagent/Category | Specific Examples | Function in Differentiation |
|---|---|---|
| Pluripotency Maintenance Media | StemFit AK03, Essential 8, mTeSR Plus | Maintain undifferentiated state prior to differentiation initiation [41] |
| Extracellular Matrices | iMatrix-511, Synthemax, PEG-based hydrogels | Provide adhesion signals and mechanical cues for lineage specification [41] [38] |
| Germ Layer Inducers | Activin A, BMP4, FGF2, CHIR99021, Retinoic Acid | Activate signaling pathways for specific germ layer commitment [35] [39] |
| Signaling Inhibitors | SB431542, LDN193189, XAV939 | Block alternative lineage differentiation (e.g., dual SMAD inhibition for ectoderm) [35] |
| Characterization Antibodies | OCT4, NANOG, SOX17, Brachyury, PAX6 | Validate pluripotency and differentiation efficiency via immunostaining [33] [34] |
| Cell Dissociation Reagents | TrypLE Select, Accutase, EDTA solutions | Gentle dissociation for embryoid body formation and subculturing [41] |
Experimental Workflows and Signaling Pathways
Directed Differentiation Experimental Workflow
Signaling Pathways in Germ Layer Specification
Frequently Asked Questions (FAQs)
1. What are the most common chromosomal aberrations found in iPSC cultures, and why should I be concerned about them? Studies have shown that iPSC lines frequently acquire chromosomal abnormalities during reprogramming and long-term in vitro cultivation [42]. Common recurrent anomalies include trisomy of chromosome 12, trisomy 17, and amplification of regions like 20q11.21 [18] [43]. These aberrations are a major concern because they can compromise the utility of iPSCs by affecting their differentiation potential, altering the functionality of differentiated cells, and posing a significant tumorigenic risk for future therapeutic applications [42] [18]. Genetically abnormal clones can rapidly overtake a culture, sometimes in less than five passages, underscoring the need for vigilant monitoring [18].
2. When should I use G-banding karyotyping versus higher-resolution methods like SNP array? The choice of method depends on your specific quality control needs. G-banding karyotyping is the gold standard for a genome-wide overview and is the only method among the three that can detect balanced structural aberrations like translocations [18]. However, its resolution is limited to alterations larger than 5-10 Mb [18]. SNP arrays offer a much higher resolution, capable of detecting copy number variations (CNVs) and copy-neutral loss of heterozygosity (CN-LOH) as small as 350 kb to 100 kb [18] [43]. Therefore, for a comprehensive analysis that detects both large structural changes and smaller sub-chromosomal variants, a combination of G-banding and a higher-resolution method is recommended.
3. My SNP array data shows a "waviness factor." What does this indicate, and should I be worried? The waviness factor (WF) is a quality metric computed by analysis software like PennCNV that measures the amount of dispersion in signal intensity across the genome [44]. A high WF is a good indicator of poor DNA quality [44]. While the specific threshold can be platform-dependent, PennCNV uses a default exclusion criterion of WF > 0.05, meaning samples with a waviness factor exceeding this value are considered of poor quality and should be excluded from further analysis [44].
4. Can the reprogramming method influence the genetic stability of my iPSC lines? Yes, the reprogramming method can be a factor. One large-scale study found that both integrating (retroviral) and non-integrating (Sendai virus) methods resulted in iPSC lines with somatic CNVs, with similar frequencies observed (69.4% in RiPSCs vs. 73.9% in SiPSCs) [43]. The key finding was that the number of somatic single nucleotide variants (SNVs) was independent of the reprogramming method, cell type, and passage number [43]. This highlights that genetic instability is a universal challenge in iPSC generation, regardless of the technique used.
5. What are the critical quality control metrics for SNP array data, and what are the acceptable thresholds? For reliable SNP array results, several key quality metrics should be checked. The call rate represents the percentage of SNPs successfully genotyped; a call rate between 95% and 98% is generally considered acceptable [18]. For the signal intensity data, the standard deviation of the Log R Ratio (LRR_SD) should typically be below 0.3, and the B Allele Frequency (BAF) drift should be less than 0.01 [44]. Samples failing these thresholds may yield unreliable CNV calls.
Troubleshooting Guides
Problem: Inconclusive or Failed G-banding Karyotyping Potential Cause and Solution: A common issue is the failure to obtain a sufficient number of metaphase cells for analysis, which accounted for 10.8% of cases in one study [42]. This can often be traced to suboptimal cell culture conditions at the time of harvest.
- Solution: Ensure the iPSC culture is healthy and actively dividing. The ideal confluence for cytogenetic harvest is between 60% and 80% [42]. Avoid harvesting from over-confluent or poorly differentiating cultures. Optimize the concentration and incubation time with colcemid to arrest a sufficient number of cells in metaphase.
Problem: High Rate of Sub-chromosomal Aberrations Detected by SNP Array Potential Cause and Solution: The appearance of CNVs, particularly in later passages, is a recognized sign of culture-induced genetic instability [42] [43].
- Solution: Review your cell culture practices. The frequency of chromosomal aberrations increases with higher passage numbers [42]. Implement a rigorous schedule for routine genetic quality control and establish a bank of low-passage master cell lines. Avoid prolonged culture periods and minimize stress to the cells during passaging.
Problem: Poor Quality Signals in SNP Array Analysis Potential Cause and Solution: Poor data quality, indicated by high LRRSD or BAFdrift, often originates from the sample preparation stage.
- Solution:
- DNA Quality: Use high-quality, high-molecular-weight genomic DNA. Assess concentration and purity using spectrophotometry and confirm the absence of degradation [45].
- Probe Filtering: Remove probes that cannot be uniquely mapped to the genome, as they can generate noisy data. This can be done using resources like the UCSC Genome Browser's liftover tool [44].
- Parameter Files: Ensure you are using the correct Population Frequency of B allele (PFB) and GC-model files that match your specific genotyping array and reference genome build [44].
Comparison of Genomic Integrity Screening Methods
The table below summarizes the core characteristics, strengths, and limitations of the three primary techniques for genomic screening in iPSCs.
Table 1: Method Comparison for Genomic Integrity Screening
| Feature | G-banding Karyotyping | SNP Microarray | CNV Analysis (from SNP Array) |
|---|---|---|---|
| Resolution | 5 - 10 Mb [18] | Single nucleotide (for SNPs) | ~350 kb to 100 kb [18] [43] |
| Key Detectable Aberrations | Aneuploidy, large structural rearrangements (translocations, inversions), polyploidies [42] | Single Nucleotide Polymorphisms (SNPs), Loss of Heterozygosity (LOH) | Copy Number Variations (CNVs), Copy-Neutral LOH (CN-LOH) [18] |
| Primary Limitations | Low resolution; requires metaphase cells; cannot detect CN-LOH or small CNVs [18] | Cannot detect balanced translocations; limited to known SNP loci [18] [45] | Constrained by known SNP information; cannot detect balanced translocations [45] |
| Key Quality Metrics | Number of metaphases analyzed (≥20), banding resolution [42] | Call Rate (≥95-98%) [18], LRRSD (<0.3), BAFdrift (<0.01) [44] | Waviness Factor (<0.05) [44] |
| Throughput | Low (manual, expert-dependent) | High (automated) | High (automated) |
Detailed Experimental Protocols
Protocol 1: G-banded Karyotyping for iPSCs This protocol is based on established methods used for iPSCs derived from peripheral blood or Wharton's jelly [42].
- Cell Culture and Harvest:
- Hypotonic Treatment:
- Suspend the cell pellet in 6 ml of a pre-warmed hypotonic solution (0.075 M KCl with HEPES) to swell the cells [42].
- Incubate at 37°C for one hour.
- Fixation:
- Gently add a cold methanol-acetic acid solution (3:1 ratio) to the cell suspension for fixation [42].
- Repeat the fixation step 2-3 times with fresh fixative.
- Slide Preparation and Staining:
- Drop the fixed cell suspension onto clean microscope slides.
- Age the slides and subject them to the G-banding technique using trypsin and Giemsa stain [42].
- Analysis:
- Capture metaphase images digitally using a microscope.
- Analyze at least 20 metaphases per sample using specialized software [42]. A clonal aberration is typically defined as the same structural change or gain of the same chromosome present in at least two cells, or the loss of a chromosome in at least three cells [42].
Protocol 2: Detecting CNVs from Illumina SNP Array Data using PennCNV This protocol outlines the steps for using PennCNV software to identify CNVs from intensity data [44].
- Data Export:
- Generate a signal intensity file from Illumina's GenomeStudio or BeadStudio software. The file must contain SNP identifiers and the Log R Ratio (LRR) and B Allele Frequency (BAF) values for each sample [44].
- Data Preprocessing:
- Remove SNPs that cannot be uniquely mapped to the reference genome to reduce noise [44].
- Obtain the appropriate Population Frequency of B allele (PFB) and GC-model files for your specific array platform and reference genome build.
- CNV Calling:
- Run PennCNV with a command that specifies the input files and model files. Example command:
detect_cnv.pl --test --hmm hhall.hmm --pfb hh660.hg19.pfb --gcmodel hh660.hg19.gcmodel lrr_baf.split1 --output lrr_baf_1.rawcnv --log lrr_baf_1.log[44].
- Run PennCNV with a command that specifies the input files and model files. Example command:
- Quality Control and Filtration:
- Run PennCNV's
filter_cnv.plscript to generate a quality control summary. - Exclude samples of poor quality based on the following default criteria: LRRSD > 0.3, BAFdrift > 0.01, and WF > 0.05 [44].
- Run PennCNV's
The workflow for this protocol is summarized in the following diagram:
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Kits for Genomic Integrity Screening
| Item | Function/Brief Explanation | Example/Note |
|---|---|---|
| Colcemid | Inhibits microtubule polymerization, arresting cells in metaphase for karyotyping. | Used at 0.04-0.1 µg/ml for 1-2 hours on iPSC cultures [42] [18]. |
| Sendai Reprogramming Kit | Non-integrating viral vector system for generating iPSCs. | Reduces risk of insertional mutagenesis; contains OCT-3/4, Klf4, Sox2, cMyc factors [42]. |
| QIAamp DNA Blood Mini Kit | For extraction of high-quality, high-purity genomic DNA from cell cultures. | Pure DNA is critical for success in SNP array and other molecular analyses [18]. |
| CytoScan HD Array | A high-density SNP-based chromosomal microarray for CNV and LOH detection. | Provides high-resolution data; used in routine diagnostics and research [43]. |
| Illumina Global Screening Array | A modern SNP array platform for genotyping and CNV analysis. | Can be analyzed with Illumina's GenomeStudio software and cnvPartition plug-in [18]. |
| cnvPartition Plug-in | Algorithm within GenomeStudio that automates CNV calling from SNP array data. | Provides a user-friendly option for researchers with minimal bioinformatics expertise [18]. |
In induced pluripotent stem cell (iPSC) research, microbiological safety is not merely a regulatory formality but a fundamental prerequisite for data integrity and experimental reproducibility. Microbiological contaminants, particularly mycoplasma, can profoundly alter key characteristics of iPSCs, including their proliferation rate, metabolic activity, differentiation potential, and global gene expression profiles [46] [26]. Because mycoplasma contamination does not typically cause turbidity in culture media and is invisible under a standard light microscope, it can persist undetected for extended periods, compromising every experiment that utilizes the contaminated cell line [47] [46]. For research aimed at understanding the mechanisms of pluripotency or developing drug screening platforms, undetected contamination can lead to the publication of erroneous conclusions and the wasteful expenditure of resources. Therefore, integrating rigorous, routine sterility and mycoplasma testing is an indispensable component of a robust quality control framework for iPSC pluripotency research.
Understanding Mycoplasma Contamination
Mycoplasma species are the smallest self-replicating prokaryotes, and their lack of a cell wall makes them resistant to many common antibiotics like penicillin and allows them to pass through standard filtration pores [47] [26]. The prevalence of mycoplasma contamination in cell cultures is estimated to be between 15% and 35% globally [47] [46]. Contamination primarily originates from laboratory personnel, contaminated culture reagents (especially animal sera), or cross-contamination from other infected cell lines [47] [46].
Table: Common Mycoplasma Species in Cell Culture and Their Sources
| Mycoplasma Species | Primary Source |
|---|---|
| M. orale, M. fermentans, M. hominis | Human oropharyngeal tract (laboratory personnel) |
| M. arginini, Acholeplasma laidlawii | Fetal Bovine Serum (FBS) |
| M. hyorhinis | Porcine-derived trypsin |
Consequences for iPSC Research
The impact of mycoplasma contamination on iPSC cultures is extensive and detrimental to research quality:
- Genetic and Epigenetic Alterations: Contamination can induce chromosomal aberrations and karyotype abnormalities, directly confounding studies on genomic stability [46] [26].
- Disruption of Cell Physiology: Mycoplasmas compete with host cells for nutrients and can disrupt nucleic acid synthesis, inhibit cell proliferation, and alter cellular metabolism [47] [46].
- Compromised Pluripotency and Differentiation: By altering the host cell's gene expression profile and metabolism, mycoplasma can affect the expression of pluripotency markers and skew differentiation outcomes, rendering studies on lineage specification unreliable [26] [48].
Detection Methodologies: Protocols and Comparisons
Routine testing is the cornerstone of mycoplasma prevention. The following are standard detection methods.
Direct Culture Method
This is the historical gold standard method.
- Protocol: The sample supernatant is inoculated onto specialized agar plates and into broth medium. The plates are incubated under microaerophilic conditions for up to 4-5 weeks and periodically examined for the development of characteristic "fried-egg" colonies [46].
- Advantages: Highly sensitive and specific.
- Disadvantages: Extremely long turnaround time, requires expertise in mycoplasma culture.
Indirect Staining (DNA Fluorochrome) Method
This method is faster than direct culture and is widely used.
- Protocol:
- Inoculate the test sample onto an indicator cell line (e.g., Vero cells) grown on a cover slip.
- After 3-5 days of co-culture, fix the cells and stain them with a DNA-binding fluorochrome like Hoechst 33258.
- Examine the cells under a fluorescence microscope. A positive result is indicated by extranuclear filamentous or speckled staining in the cytoplasm of the indicator cells, representing the mycoplasma DNA [46].
- Advantages: Faster than direct culture (results in about 1 week) and can detect non-cultivable species.
- Disadvantages: Requires a cell culture step and subjective interpretation.
PCR-Based Detection
This is the most common method used in modern research due to its speed and sensitivity.
- Protocol:
- Extract DNA from the cell culture supernatant.
- Perform PCR using universal primers targeted to the 16S rRNA gene conserved across mycoplasma species. A touchdown PCR protocol is often used to increase sensitivity and specificity [46].
- Analyze the PCR products by gel electrophoresis. The presence of a band at the expected size indicates contamination.
- Advantages: Rapid (results in hours to a day), highly sensitive, can detect a wide range of species, and can be automated for high-throughput screening.
- Disadvantages: Does not distinguish between viable and non-viable organisms; risk of false positives from contamination.
Table: Comparison of Major Mycoplasma Detection Methods
| Method | Duration | Sensitivity | Key Advantage | Key Limitation |
|---|---|---|---|---|
| Direct Culture | 4-5 weeks | High (~100 CFU) | Gold standard, specific | Very slow, requires specialized culture |
| Indirect Staining | ~1 week | Moderate | Detects non-cultivable species | Subjective, requires cell culture |
| PCR-Based | < 1 day | High (≤ 100 CFU) | Fast, highly sensitive, specific | Cannot confirm viability |
The experimental workflow for managing mycoplasma risk, from prevention to final verification, is outlined below.
Frequently Asked Questions (FAQs) and Troubleshooting
Q1: Can't I just use antibiotics in my culture media to prevent mycoplasma contamination? No, this is not a reliable strategy. Mycoplasmas lack a cell wall, rendering common antibiotics like penicillin completely ineffective. While some strains may be inhibited by certain antibiotics (e.g., streptomycin inhibits about half), many are resistant to the concentrations routinely used in cell culture [46]. Furthermore, the continuous use of antibiotics can itself alter the gene expression profile of your iPSCs, introducing an unwanted variable into your research [26]. Best practice is to maintain cultures without routine antibiotics and rely on strict aseptic technique.
Q2: My iPSC cultures look healthy and are proliferating normally. Do I still need to test for mycoplasma? Absolutely. This is a common and dangerous misconception. Mycoplasma contamination often persists as a "silent" infection without obvious cell death or turbidity [47] [46]. The contaminants can chronically affect cell physiology and gene expression without overt signs, meaning your cells can appear healthy while generating fundamentally flawed and irreproducible data.
Q3: I've identified a mycoplasma-positive culture. What should I do? The most universally recommended and safest course of action for research iPSC lines is to immediately discard the contaminated culture [47] [48]. Autoclave all flasks and media that came into contact with it. Decontaminate the work area and equipment used. Then, revive a new vial of cells from your mycoplasma-free master cell bank. This approach prevents the spread of contamination to other cultures in your laboratory. While eradication protocols exist (e.g., using specific antibiotics like BM-cyclin or quinolones), they are not always effective, can induce selective pressure, and there is no guarantee that the "cured" line will retain its original genetic and phenotypic properties [47].
Q4: How often should I test my cultures for mycoplasma? Testing should be performed on a regular schedule. A good practice is to test when a new cell line is received (during the initial quarantine period), when a new master bank is created, and routinely on working stocks (e.g., every 1-2 months or with every other passage). Cultures should also be tested immediately before starting critical experiments, such as a long-term differentiation study or before banking cells for future use [26] [49].
Detailed Experimental Protocol: PCR-Based Mycoplasma Detection
The following protocol provides a generalized procedure for detecting mycoplasma via PCR, consistent with methods described by major biological repositories [46].
Principle: Universal primers amplify a conserved region of the 16S rRNA gene present in most common mycoplasma contaminants.
Materials:
- Template DNA: Cell culture supernatant, centrifuged to pellet cells and debris. The resulting supernatant can be used directly or further concentrated.
- Positive Control DNA: Genomic DNA from a known mycoplasma species (e.g., M. pneumoniae or M. hominis).
- Negative Control: Nuclease-free water or medium from a known mycoplasma-free culture.
- PCR Master Mix: Containing Taq polymerase, dNTPs, and reaction buffer.
- Universal Primers: Forward and reverse primers targeting the mycoplasma 16S rRNA gene.
- Agarose Gel Electrophoresis equipment.
Procedure:
- Sample Preparation: Collect ~500 µL of cell culture supernatant (from cultures at least 3 days post-passage, without antibiotics). Centrifuge at 12,000 × g for 5-10 minutes to remove cells and large debris. Use the supernatant as the template. Alternatively, commercial DNA extraction kits can be used.
- PCR Reaction Setup:
- Prepare a master mix for the number of reactions (samples, positive control, negative control) plus one extra. For each reaction, combine:
- 12.5 µL of 2X PCR Master Mix
- 1 µL of Forward Primer (10 µM)
- 1 µL of Reverse Primer (10 µM)
- 9.5 µL of Nuclease-Free Water
- Aliquot 24 µL of the master mix into each PCR tube.
- Add 1 µL of the respective template DNA (sample, positive control, negative control) to each tube. Mix gently.
- Prepare a master mix for the number of reactions (samples, positive control, negative control) plus one extra. For each reaction, combine:
- PCR Amplification: Run the PCR using a thermocycler with the following typical protocol:
- Initial Denaturation: 95°C for 5 minutes
- 35-40 Cycles of:
- Denaturation: 95°C for 30 seconds
- Annealing: 55-60°C for 45 seconds (temperature may be optimized)
- Extension: 72°C for 1 minute
- Final Extension: 72°C for 7 minutes
- Hold: 4°C
- Analysis of Products:
- Prepare a 1.5-2% agarose gel in 1X TAE or TBE buffer.
- Mix 10 µL of each PCR product with a DNA loading dye and load onto the gel. Include a DNA molecular weight ladder.
- Run the gel at 100-120 V until bands are sufficiently separated.
- Visualize the gel under UV light. A positive result is indicated by a band of the expected size (e.g., ~500 bp, depending on the primer set). The positive control should show a band, while the negative control should not.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table: Key Reagents for Microbiological Safety in iPSC Culture
| Reagent / Tool | Function / Application | Key Considerations |
|---|---|---|
| Mycoplasma Detection Kit (PCR) | Rapid, sensitive detection of mycoplasma contamination. | Choose a kit that detects a broad panel of species common in cell culture. |
| Hoechst 33258 Stain | DNA-binding dye used in the indirect staining method for mycoplasma. | Requires a fluorescence microscope and an indicator cell line. |
| DNase/Rnase-Free Water | Used as a negative control and for preparing reagents in PCR testing. | Essential for preventing false positives in PCR assays. |
| Certified Mycoplasma-Free FBS | Critical cell culture supplement sourced to minimize contamination risk. | Always source from reputable suppliers who provide testing certification. |
| Animal Component-Free Growth Factors | Supports cell growth while reducing contamination risk from animal sources. | Enhances experimental consistency and reduces variable outcomes [48]. |
| ROCK Inhibitor (Y-27632) | Improves survival of iPSCs after passaging and freezing. | Not a microbiological reagent, but critical for maintaining healthy, robust cultures for reliable testing [48]. |
Maintaining microbiological safety through rigorous sterility and mycoplasma testing is a non-negotiable aspect of quality control in iPSC pluripotency research. The integrity of data on pluripotency marker expression, genomic stability, and differentiation potential is entirely dependent on the health and purity of the underlying cell cultures. By integrating the preventative measures, routine testing schedules, and robust detection protocols outlined in this guide, researchers can safeguard their experiments, ensure the reproducibility of their findings, and make meaningful contributions to the advancement of stem cell science and its therapeutic applications.
Navigating QC Challenges: Troubleshooting and Process Optimization
Identifying and Eliminating Differentiation in Culture
Troubleshooting Guide: Common Questions on Managing iPSC Differentiation
Why is there excessive differentiation (>20%) in my cultures?
Excessive differentiation often results from suboptimal culture conditions or handling techniques. Key factors to check include:
- Culture Medium: Ensure your complete cell culture medium (e.g., mTeSR Plus or mTeSR1) has been stored at 2-8°C and is less than 2 weeks old [19].
- Handling Time: Avoid keeping culture plates out of the incubator for more than 15 minutes at a time [19].
- Passaging Timing: Passage cultures when colonies are large and compact with dense centers, before they overgrow [19].
- Colony Density: Decrease colony density by plating fewer cell aggregates during passaging [19].
- Targeted Removal: Physically remove differentiated areas before passaging [19].
How can I improve cell attachment after passaging?
Poor attachment can be addressed through several technical adjustments:
- Initial Plating Density: Plate 2-3 times more cell aggregates initially and maintain a more densely confluent culture [19].
- Work Quickly: Minimize the time cell aggregates spend in suspension after treatment with passaging reagents [19].
- Pipetting Technique: Avoid excessive pipetting that breaks up cell aggregates; instead, increase incubation time with passaging reagent by 1-2 minutes [19].
- Surface Coating: Verify you're using the correct plate type—non-tissue culture-treated plates for Vitronectin XF coating and tissue culture-treated plates for Corning Matrigel coating [19].
What causes differentiated cells to detach with colonies when using ReLeSR?
This issue typically stems from over-digestion and can be resolved by:
- Reduced Incubation: Decrease incubation time with ReLeSR by 1-2 minutes [19].
- Temperature Adjustment: Lower the incubation temperature to room temperature (15-25°C) [19].
How do I achieve ideal cell aggregate sizes during passaging?
The table below summarizes adjustments for optimizing aggregate size:
| Problem | Target Size | Solution |
|---|---|---|
| Aggregates too large | >200 μm | • Increase pipetting• Increase incubation time 1-2 minutes [19] |
| Aggregates too small | <50 μm | • Minimize manipulation• Decrease incubation time 1-2 minutes [19] |
| Colonies remain attached | N/A | • Increase incubation time 1-2 minutes [19] |
Quality Control Framework for iPSC Pluripotency
Essential Quality Control Testing
Implementing robust quality control measures is crucial for maintaining pluripotent iPSC cultures and ensuring experimental reproducibility [26] [50].
Pluripotency Marker Assessment: Regularly verify expression of hallmark pluripotency genes including Nanog, Oct3/4, SSEA-4, TRA-1-60, and TRA-1-81 using immunofluorescence staining, flow cytometry, RT-PCR, or Western blotting [26].
Trilineage Differentiation Potential: Functionally confirm pluripotency by demonstrating capacity to differentiate into all three germ layers—ectoderm, mesoderm, and endoderm—via teratoma formation assays or directed differentiation protocols [26].
Genomic Stability Monitoring: Conduct regular karyotyping using G-banding supplemented with digital PCR and array CGH to detect chromosomal abnormalities and mutations that may accumulate over passages [26] [50].
Sterility Testing: Perform comprehensive sterility assessment through direct inoculation or membrane filtration methods, as routine antibiotic use is discouraged due to potential alterations in gene expression profiles [26].
Research Reagent Solutions for Quality Control
| Reagent/Category | Function | Examples/Notes |
|---|---|---|
| Pluripotency Markers | Verify stem cell state | Antibodies against Nanog, Oct3/4, SSEA-4, TRA-1-60, TRA-1-81 [26] |
| Differentiation Media | Assess trilineage potential | Formulations for directed differentiation into ectoderm, mesoderm, endoderm [26] |
| Karyotyping Reagents | Monitor genomic stability | G-banding materials, digital PCR kits, array CGH platforms [26] [50] |
| Sterility Testing Kits | Detect microbial contamination | Bacterial/fungal culture systems, PCR-based detection kits [26] |
| Mycoplasma Detection | Identify mycoplasma contamination | PCR kits, indirect staining assays, agar and broth cultures [26] |
Advanced iPSC Quality Control Protocols
Comprehensive Pluripotency Verification Workflow
Mycoplasma Testing Protocol
Mycoplasma contamination represents a significant concern in iPSC culture as these organisms can remain undetected while altering gene expression and inducing karyotype abnormalities [26].
Testing Methodologies:
- PCR-Based Detection: Most common method; ensures detection of multiple mycoplasma species
- Indirect Staining: Alternative method using DNA-binding dyes
- Agar and Broth Culture: Traditional culture method requiring longer incubation
Frequency: Test cultures regularly, especially when introducing new cell lines or reagents [26].
Clinical-Grade Considerations for iPSC Research
As iPSC technologies advance toward clinical applications, quality control measures must align with regulatory standards. Current clinical trials utilize iPSCs for conditions including cardiac diseases, ocular disorders, cancer, and graft-versus-host disease [51]. The field is progressing toward standardized characterization criteria to enhance comparability between studies and accelerate development of safe, effective iPSC-derived therapies [51].
For advanced differentiation challenges or persistent quality issues, consider that iPSC-derived cells may exhibit immature, fetal-like phenotypes rather than adult cell characteristics, which could limit their relevance for modeling late-onset diseases [14]. Specialized differentiation protocols or alternative iPSC clones may be necessary for specific research applications.
For researchers in pluripotency research, the genomic instability of induced pluripotent stem cells (iPSCs) presents a significant challenge to data reproducibility, reliable differentiation, and safe clinical translation. Genetic variations can arise from pre-existing mutations in somatic cells, be induced during the reprogramming process itself, or accumulate during prolonged culture [52] [53]. This technical support center provides a structured guide to understanding, troubleshooting, and mitigating these instability issues, framed within the essential context of quality control for iPSC-based research and drug development.
Understanding Genetic Instability in iPSCs
Origins and Types of Genetic Variations
Genetic variations in iPSCs have at least three distinct origins, each with characteristic profiles [52] [53]:
dot source_origins {
- graph [bgcolor="#F1F3F4" fontcolor="#202124" fontname="Helvetica"]*
- node [shape=rectangle style=filled fontname="Helvetica" fontcolor="#202124"]*
- edge [color="#5F6368"]*
- "Parental Somatic Cells" [fillcolor="#FBBC05" fontcolor="#202124"]*
- "Reprogramming Process" [fillcolor="#EA4335" fontcolor="#FFFFFF"]*
- "Prolonged In Vitro Culture" [fillcolor="#34A853" fontcolor="#FFFFFF"]*
- "iPSC Line" [fillcolor="#4285F4" fontcolor="#FFFFFF"]*
-
- "Parental Somatic Cells" -> "iPSC Line" [label=" Pre-existing variations\nare fixed by cloning"]*
- "Reprogramming Process" -> "iPSC Line" [label=" Introduces new\nmutations"]*
- "Prolonged In Vitro Culture" -> "iPSC Line" [label=" Culture-induced\nmutations accumulate"]* }
Table: Primary Types of Genetic Variations in iPSCs
| Variation Type | Detection Method | Common Examples & Functional Impact |
|---|---|---|
| Chromosomal Aberrations (Aneuploidy, Translocations) | G-banding Karyotyping [52] [26] | Trisomy 12, 8, and X are recurrent. They can confer a selective growth advantage but compromise differentiation potential and raise tumorigenicity concerns [52]. |
| Copy Number Variations (CNVs) (Duplications, Deletions) | SNP Array, Array CGH, Whole Genome Sequencing [52] | Amplification of 20q11.21 is a known hotspot, containing genes like BCL2L1 (anti-apoptosis) and DNMT3B, potentially enhancing survival under culture stress [52]. |
| Single Nucleotide Variants (SNVs) | Whole Genome Sequencing, Whole Exome Sequencing [52] | An average of ~10 protein-coding mutations per human iPSC line. The functional impact depends on the specific gene affected, with mutations in cancer-related genes being a primary concern [52]. |
Impact of Reprogramming Methods on Genomic Integrity
The choice of reprogramming method significantly influences the initial genetic load of an iPSC line. A shift from integrating to non-integrating methods is critical for minimizing genomic alterations [13].
Table: Comparison of Common Non-Integrating Reprogramming Methods
| Method | Key Features | Reported Success Rates | Advantages | Disadvantages/Limitations |
|---|---|---|---|---|
| Sendai Virus (SeV) | Non-integrating, RNA virus-based vector. | Significantly higher success rates relative to the episomal method [13]. | High efficiency; viral genome remains in cytoplasm and is gradually diluted out [13]. | Requires biosafety level 1 precautions; potential for persistent viral detection. |
| Episomal Vectors | Non-integrating, OriP/EBNA1-based plasmid. | Lower success rates compared to SeV [13]. | Non-viral, simple manipulation; no special biosafety requirements [13]. | Lower efficiency; requires nucleofection for transfection [13]. |
Troubleshooting Guide: Common Scenarios & Solutions
FAQ 1: My iPSC line has been in culture for over 20 passages and is now differentiating poorly. Could genetic instability be the cause?
- Likely Cause: Accumulation of passage-induced mutations, potentially in genes critical for pluripotency or the specific differentiation pathway. CNVs like amplifications of 20q11.21 or trisomy 12 can provide a growth advantage to undifferentiated cells while impairing directed differentiation [52] [53].
- Recommended Actions:
- Karyotyping: Perform G-banding analysis to check for gross chromosomal abnormalities [52] [26].
- High-Resolution CNV Analysis: Use SNP array or array CGH to identify smaller amplifications or deletions that karyotyping might miss [52] [53].
- Return to Low-Passage Stock: If genetic anomalies are confirmed, thaw a low-passage vial from your master cell bank that has been fully characterized. Always bank iPSCs early (e.g., before passage 20) and perform quality control on the banked stocks [54].
FAQ 2: I've just generated new iPSC clones and need to select the best one for banking. What key quality control checks should I prioritize?
- Essential QC Checklist for New Clones:
- Pluripotency Confirmation:
- Immunofluorescence/Flow Cytometry: Confirm expression of hallmark pluripotency markers (e.g., Nanog, Oct3/4, SSEA-4, TRA-1-60, TRA-1-81) [26].
- Functional Test: Perform a trilineage differentiation assay in vitro to confirm potential to differentiate into ectoderm, mesoderm, and endoderm derivatives [26].
- Genomic Integrity Assessment:
- Identity and Sterility:
- Short Tandem Repeat (STR) Analysis: Authenticate the cell line against the donor source material [13] [26].
- Mycoplasma Testing: Use PCR or indirect staining to ensure culture is free of this common, insidious contaminant that can alter gene expression [26].
- Sterility Testing: Ensure the culture is free of bacterial and fungal contaminants [26].
- Pluripotency Confirmation:
FAQ 3: My cultures are becoming heterogeneous, with varying growth rates and morphologies. Is this genetic instability?
- Likely Cause: While spontaneous differentiation can cause heterogeneity, genetic instability is a prime suspect. The development of a heterogeneous population with different functional characteristics and growth rates is a classic consequence of accumulating genetic variations [53].
- Recommended Actions:
- Re-cloning: Manually pick well-defined, morphologically pristine colonies to re-establish a homogeneous culture [13].
- Optimize Culture Conditions: Ensure you are using high-quality, defined media and matrices. Avoid overgrowth and passaging cells at the correct density to minimize selective pressure [19] [55].
- Monitor Passaging Technique: Excessive scraping or enzymatic digestion time can be stressful. Use gentle dissociation reagents and minimize the time cells are in suspension [19] [56].
- Routine Monitoring: Implement a schedule for periodic genomic assessment (e.g., every 10-15 passages) to catch instability early [26].
The Scientist's Toolkit: Key Reagents & Protocols
Research Reagent Solutions
Table: Essential Materials for iPSC Culture and Quality Control
| Reagent Category | Example Products | Critical Function |
|---|---|---|
| Feeder-Free Culture Media | mTeSR Plus, mTeSR1, StemFlex, HiDef B8 Growth Medium [19] [54] [55] | Chemically defined media that support robust expansion and maintenance of pluripotency while minimizing spontaneous differentiation. |
| Basement Membrane Matrices | Geltrex, Matrigel, Laminin-521 [56] | Provide a scaffold that mimics the extracellular matrix, supporting attachment and growth of iPSCs in feeder-free conditions. |
| Passaging Reagents | ReLeSR, Gentle Cell Dissociation Reagent, Versene [13] [19] | Non-enzymatic or mild enzymatic reagents for dissociating iPSC colonies into small aggregates for passaging, minimizing damage. |
| Cryopreservation Solutions | CryoStor CS10, 90% FBS + 10% DMSO [13] [56] | Specialized solutions that enhance post-thaw viability and recovery of iPSCs. |
| ROCK Inhibitor | Y-27632 [13] [56] | Significantly improves cell survival after passaging, thawing, or single-cell dissociation by inhibiting apoptosis. |
Core Quality Control Workflow
A robust QC protocol is not a one-time event but a dynamic process integrated throughout the iPSC lifecycle [26].
dot source_qc_workflow {
- graph [bgcolor="#F1F3F4" fontcolor="#202124" fontname="Helvetica"]*
- node [shape=rectangle style=filled fontname="Helvetica" fontcolor="#202124"]*
- edge [color="#5F6368"]* *
- "New iPSC Clone" [fillcolor="#4285F4" fontcolor="#FFFFFF"]*
- "Pluripotency Verification" [fillcolor="#FBBC05" fontcolor="#202124"]*
- "Genomic Integrity Check" [fillcolor="#EA4335" fontcolor="#FFFFFF"]*
- "Identity & Sterility Test" [fillcolor="#34A853" fontcolor="#FFFFFF"]*
- "Master Cell Bank" [fillcolor="#4285F4" fontcolor="#FFFFFF"]*
- "Ongoing Culture & Differentiation" [fillcolor="#5F6368" fontcolor="#FFFFFF"]*
- "Routine Monitoring (q10-15 passages)" [fillcolor="#5F6368" fontcolor="#FFFFFF"]* *
- "New iPSC Clone" -> "Pluripotency Verification"*
- "New iPSC Clone" -> "Genomic Integrity Check"*
- "New iPSC Clone" -> "Identity & Sterility Test"*
- "Pluripotency Verification" -> "Master Cell Bank"*
- "Genomic Integrity Check" -> "Master Cell Bank"*
- "Identity & Sterility Test" -> "Master Cell Bank"*
- "Master Cell Bank" -> "Ongoing Culture & Differentiation"*
- "Ongoing Culture & Differentiation" -> "Routine Monitoring (q10-15 passages)" [label=" Feedback loop"]* }
For researchers and drug development professionals working with induced pluripotent stem cells (iPSCs), potency testing represents a critical quality control measure required for clinical translation. Potency is defined as the therapeutic activity of a drug product measured by appropriate laboratory tests, serving as a legal requirement for lot release testing of biologics [57]. In the context of iPSC-derived therapies, these assays provide a quantitative measure of the product's intended biological activity and mechanism of action. However, the inherent variability of biological systems presents significant challenges for achieving reproducible results. This technical support center addresses the specific issues you might encounter during potency experiments and provides actionable strategies to enhance data reliability and consistency.
Understanding Potency Assays and Variability
What are the main types of potency assays used in iPSC research?
Several potency assay formats are employed to measure the biological activity of iPSC-derived products, each with specific applications and variability considerations [57]:
- Immunoassays: Measure drug-target binding using recombinant proteins (non-cell-based) or cell surface targets (cell-based)
- Enzymatic assays: Quantify reaction rates when the drug or target has mechanism-of-action (MoA) relevant enzymatic activity
- Functional cell-based assays: Assess downstream effects of drug-target interaction, such as pathway activation/inhibition using reporter systems
- Animal assays: Measure organism-level responses (increasingly rare due to ethical concerns and high variability)
Why is relative potency (%RP) used instead of absolute quantification?
Most potency assays report results as % Relative Potency (%RP) rather than absolute values because biological activity is often difficult to quantify in absolute terms [57]. Relative measurement involves pairwise comparison of dose-dependent responses between a reference standard (well-characterized drug lot) and test samples. The fundamental assumption of parallelism must be met, where the curve shapes of reference and test samples are similar, allowing horizontal shift (EC50) to measure potency changes.
Multiple factors contribute to potency assay variability, which is typically higher than in physicochemical methods [57]:
Table 1: Key Sources of Potency Assay Variability
| Variability Source | Impact Level | Description |
|---|---|---|
| Biological System | High | Inherent variability of cellular responses, passage effects, and differentiation status |
| Reagent Quality | Medium-High | Lot-to-lot variations in growth factors, antibodies, and media components |
| Operator Technique | Medium | Differences in pipetting, cell handling, and protocol execution |
| Instrumentation | Medium | Calibration differences between plate readers, flow cytometers, and other equipment |
| Assay Design | Medium-Low | Insufficient replication, suboptimal dilution schemes, or inadequate controls |
Troubleshooting Guides
FAQ: Addressing High Variability in Potency Measurements
Q: Our potency assays show unacceptably high CV (%) values (>20%). What systematic approach should we take to identify the root cause?
A: Begin with a structured investigation focusing on these key areas:
Assess reagent quality and consistency: Variability in growth factors, media, and critical reagents significantly compromises assay reproducibility [58]. Implement rigorous raw material qualification by testing multiple batches in parallel and selecting lots with minimal performance variation. Maintain adequate inventory of qualified batches to ensure long-term consistency.
Evaluate cell culture processes: In iPSC-derived products, variability often originates from differences in differentiation efficiency and cellular heterogeneity [58]. Standardize passage procedures, seeding densities, and differentiation protocols. Monitor pluripotency markers and differentiation status consistently across batches.
Review assay execution techniques:
- Pipetting accuracy: Calibrate pipettes regularly and use reverse pipetting for viscous reagents
- Plate washing: Avoid aggressive washing that disrupts antigen-antibody complexes [59]. Use consistent washing pressure and duration across all wells
- Incubation times: Standardize time between reagent additions and plate reading
- Environmental control: Maintain consistent temperature and CO₂ levels during cell-based assays
Validate instrument performance: For plate-based assays, run system suitability tests using established controls. Implement dual-wavelength readings (e.g., 450nm/650nm for HRP-TMB) to correct for background interference [59]. Regularly maintain and calibrate instrumentation according to manufacturer specifications.
Q: How can we demonstrate assay robustness for regulatory submissions?
A: Implement a comprehensive validation strategy based on ICH and FDA guidelines [59]:
Precision Studies: Determine both intra-assay (within-run) and inter-assay (between-run) precision using multiple concentrations covering the assay range. Acceptable CV% is typically <15-20%, depending on the assay type and stage of development [59].
Accuracy/Recovery: Spike known amounts of analyte into relevant matrices and calculate percentage recovery.
Linearity and Range: Demonstrate the assay produces results proportional to analyte concentration across the specified range.
Specificity: Confirm the assay measures only the intended analyte without interference from similar molecules or matrix components.
FAQ: Managing Reagent and Supply Chain Challenges
Q: We're experiencing significant batch-to-batch variability in critical reagents. What procurement and qualification strategy should we implement?
A: Develop a comprehensive reagent management system:
Supplier Qualification: Select suppliers who provide comprehensive characterization data, including specificity testing, batch-to-batch performance metrics, and detailed documentation [60] [61].
Enhanced Verification: Implement orthogonal verification methods for critical reagents:
- Genetic strategies: Use knockout/knockdown cells to confirm antibody specificity [61]
- Orthogonal validation: Compare protein detection results with mRNA expression data from the same samples [61]
- Independent antibody validation: Test multiple antibodies against non-overlapping epitopes of the same target [61]
Bridging Studies: When new reagent batches are introduced, perform parallel testing with the previous qualified batch across multiple assay runs. Establish predefined acceptance criteria for performance equivalence (e.g., ±15% difference in potency values) [60].
Inventory Management: Maintain sufficient stock of qualified reagent batches to support ongoing studies and avoid unplanned transitions.
FAQ: Addressing Regulatory Concerns
Q: What specific potency assay challenges do regulators focus on for iPSC-derived therapies?
A: Regulatory agencies emphasize several key aspects during potency assay review [58] [37]:
Link to Mechanism of Action: The assay must measure biological activity relevant to the proposed therapeutic effect, not just a surrogate marker.
Demonstration of Assay Precision and Robustness: Provide comprehensive data on assay variability and its impact on reportable results.
Control Strategy for Allogeneic Products: For off-the-shelf iPSC therapies, demonstrate consistent potency across multiple manufacturing batches [62].
Phase-Appropriate Validation: Early-stage trials may use less-validated assays, but progressively tighten validation criteria as products approach commercialization [57].
Experimental Protocols and Methodologies
Standard Operating Procedure: Establishing a Qualified Potency Assay
Purpose: To develop and qualify a robust potency assay for iPSC-derived cell therapies with acceptable variability for lot-release decisions.
Materials:
- Well-characterized reference standard
- Test samples covering expected potency range
- Qualified critical reagents (antibodies, growth factors, detection substrates)
- Validated instrumentation (plate reader, flow cytometer, etc.)
Procedure:
Assay Development Phase:
- Optimize critical parameters using Design of Experiments (DoE) approaches
- Identify key sources of variability through preliminary testing
- Establish system suitability criteria and controls
Pre-qualification:
- Conduct at least 6 independent runs over multiple days
- Include multiple analysts and equipment when possible
- Test samples across the specification range (50-150% of target potency)
Data Analysis:
- Calculate intra-assay and inter-assay CV% for each concentration level
- Determine reportable result variability based on different numbers of assay runs
- Establish preliminary specifications based on process capability and method variability
Documentation:
- Record all deviations and their impact on results
- Maintain complete records of reagent lots, cell passages, and instrumentation used
The workflow below illustrates the key stages in developing a robust potency method.
Protocol: ELISA-Based Potency Assay Validation
For immunoassays measuring specific biomarkers in iPSC-derived products, follow this validation protocol:
Sample Preparation:
- Prepare minimum of 3 concentrations covering assay range (e.g., 50%, 100%, 150% of target)
- Include positive and negative controls with known reactivity
- Use standardized cell lysis and protein normalization methods [60]
Assay Execution:
- Run triplicate wells for each sample concentration
- Include standard curve with at least 6 points in duplicate
- Implement randomized plate layouts to minimize positional effects
- Use consistent incubation times and temperatures across runs
Data Analysis and Acceptance Criteria:
Table 2: ELISA Validation Acceptance Criteria [60] [59]
| Parameter | Acceptance Criteria | Regulatory Guidance |
|---|---|---|
| Signal/Blank Ratio | >5.0 at highest point | CST Standards [60] |
| Intra-assay CV% | <15% for all concentrations | EMA/FDA [59] |
| Inter-assay CV% | <15-20% for all concentrations | EMA/FDA [59] |
| Accuracy/Recovery | 80-120% of expected value | ICH Q2(R1) [59] |
| Linearity | R² > 0.95 across range | Industry Standard |
Research Reagent Solutions
Table 3: Essential Materials for Robust Potency Testing
| Reagent Category | Specific Examples | Function | Quality Considerations |
|---|---|---|---|
| Detection Antibodies | Phospho-SMAD2/SMAD3 ELISA kits [60] | Measure specific pathway activation | Verify specificity using knockout controls [61] |
| Cell Culture Media | Defined, xeno-free formulations [58] | Support iPSC differentiation | Batch testing for consistent performance |
| Reference Standards | Well-characterized iPSC lines [57] | Calibrate potency measurements | Extensive banking and characterization |
| Critical Assay Reagents | Recombinant proteins, growth factors [58] | Stimulate specific responses | Rigorous qualification and vendor audits |
| gRNA for Engineering | Synthego INDe solutions [59] | Genetic modification of iPSCs | "GMP-like" process controls |
Advanced Strategies for Variability Reduction
Implementing a Tiered Analytics Approach
For complex iPSC-derived products, a single potency assay may be insufficient to fully characterize biological activity. Implement a tiered approach [58]:
- Identity and Purity Tests: Flow cytometry for specific surface markers (quick, low variability)
- Mechanism-Based Potency Assays: Functional assays measuring relevant biological responses
- Characterization Assays: Extensive testing (genomic, proteomic) not used for lot release
Statistical Approaches for Variability Management
Use statistical models to estimate different sources of variability and determine the optimal number of assay runs needed for reportable results [57]. Linear mixed models can partition variability into components (e.g., between-run, within-run, analyst-to-analyst) to guide improvement efforts.
The diagram below illustrates the relationship between assay runs and reportable results in variability management.
Emerging Technologies for Standardization
Novel approaches are being developed to overcome traditional variability challenges:
- CRISPR-Cas9 Gene Editing: Create precisely engineered iPSC lines with reporter systems for specific differentiation pathways [63]
- AI and Machine Learning: Automated colony morphology classification and differentiation outcome prediction to enhance standardization [63]
- Digital Twins: Computational models of bioprocesses to predict outcomes and optimize parameters [58]
Successfully overcoming assay variability in iPSC potency testing requires a systematic approach addressing reagent quality, procedural consistency, statistical understanding of variability sources, and phase-appropriate validation strategies. By implementing the troubleshooting guides, experimental protocols, and reagent management strategies outlined in this technical support resource, research scientists and drug development professionals can generate more reproducible potency data to advance iPSC-based therapies through the development pipeline. Continued attention to standardization and emerging technologies will further enhance the reliability of these critical quality control measures.
Optimizing Culture Conditions to Maintain Genomic and Epigenetic Stability
Troubleshooting Guide: Common iPSC Culture Challenges
This guide addresses frequent issues encountered when culturing human pluripotent stem cells to help you maintain genomic and epigenetic stability in your iPSC lines.
Problem 1: Excessive Differentiation (>20%) in Cultures
Potential Solutions:
- Ensure your complete cell culture medium has been kept at 2-8°C and is less than 2 weeks old [19].
- Remove differentiated areas manually prior to passaging [19].
- Limit time culture plates are out of the incubator to less than 15 minutes at a time [19].
- Ensure cell aggregates after passaging are evenly sized and passage cultures before overgrowth occurs [19].
- Decrease colony density by plating fewer cell aggregates during passaging [19].
Problem 2: Poor Cell Attachment After Passaging
Potential Solutions:
- Plate 2-3 times more cell aggregates initially and maintain a more densely confluent culture [19].
- Work quickly after cells are treated with passaging reagents to minimize time aggregates spend in suspension [19].
- Reduce incubation time with passaging reagents if your cell line is particularly sensitive [19].
- Ensure you're using the correct plate type for your coating matrix [19].
Problem 3: Suboptimal Cell Aggregate Size
Potential Solutions:
- For larger aggregates (>200 μm): Increase pipetting of the cell aggregate mixture and increase incubation time by 1-2 minutes [19].
- For smaller aggregates (<50 μm): Minimize manipulation of aggregates after dissociation and decrease incubation time by 1-2 minutes [19].
Problem 4: Failure in Neural Differentiation
Potential Solutions:
- Remove differentiated and partially differentiated hPSC cells before neural induction [64].
- Plate cell clumps (not single cell suspensions) at recommended density of 2-2.5 × 10⁴ cells/cm² [64].
- Use overnight treatment with 10 μM ROCK inhibitor Y27632 when splitting hPSCs to prevent extensive cell death [64].
Quantitative Data Tables for Culture Optimization
Table 1: Epigenetic Modifiers for Enhancing Reprogramming Efficiency
| Modifier Type | Specific Agent | Function in Reprogramming | Effect on Efficiency |
|---|---|---|---|
| Histone Deacetylase Inhibitors | Valproic Acid (VPA) | Increases chromatin accessibility | Up to 6.5-fold increase when combined with 8-Br-cAMP [15] |
| DNA Methyltransferase Inhibitors | 5-Aza-cytidine, RG108 | Reduces DNA methylation | Enhances robustness of reprogramming [15] |
| Histone Methylation Regulators | Neplanocin A (DZNep) | Modifies histone methylation patterns | Improves reprogramming robustness [15] |
| cAMP Analogs | 8-Br-cAMP | Activates cAMP signaling pathways | 2-fold improvement in human fibroblast reprogramming [15] |
Table 2: Quality Control Parameters for iPSC Characterization
| Quality Attribute | Assessment Method | Acceptance Criteria |
|---|---|---|
| Genomic Integrity | Karyotype analysis | Normal euploid karyotype [54] |
| Pluripotency | Trilineage differentiation | Differentiation into all three germ layers [54] |
| Vector Clearance | PCR-based detection | Confirmed absence of reprogramming vectors [54] |
| Identity | STR profiling | Match to donor material [54] |
Detailed Experimental Protocols
Protocol 1: Enhancing Reprogramming with Epigenetic Modulators
Materials Required:
- Valproic Acid (VPA) stock solution
- 8-Br-cAMP
- Base reprogramming media
- Fibroblast or PBMC culture
Methodology:
- Initiate reprogramming with OSKM or OSNL factors using your preferred delivery system
- At 24 hours post-initiation, add VPA at optimized concentration (typically 0.5-2 mM)
- Simultaneously supplement with 8-Br-cAMP at recommended concentration
- Maintain epigenetic modifier treatment for 7-10 days during critical reprogramming phase
- Monitor for emerging iPSC colonies with characteristic morphology
- Isolate and expand colonies for quality control assessment [15]
Protocol 2: Clearance of Sendai Reprogramming Vectors
Materials Required:
- Temperature-controlled incubator (capable of maintaining 38-39°C)
- RT-PCR reagents for Sendai vector detection
Methodology:
- Culture iPSCs for minimum of 10 passages post-reprogramming
- Perform RT-PCR to confirm absence of Klf4 vector
- If only c-Myc and KOS vectors remain, shift culture temperature to 38-39°C
- Maintain elevated temperature for 5 consecutive days
- Verify vector clearance via RT-PCR testing
- Return to standard culture conditions (37°C) [64]
Signaling Pathways and Workflow Diagrams
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Maintaining Genomic and Epigenetic Stability
| Reagent Category | Specific Products | Function in iPSC Culture |
|---|---|---|
| Reprogramming Enhancers | Valproic Acid (VPA), 8-Br-cAMP | Improve reprogramming efficiency through epigenetic modulation [15] |
| Quality Control Markers | H3K4me3, H3K27me3 antibodies | Assess bivalent chromatin state for pluripotency [65] |
| Culture Media Systems | mTeSR Plus, Essential 8 Medium | Provide defined conditions for stable expansion [19] [64] |
| Passaging Reagents | ReLeSR, Gentle Cell Dissociation Reagent | Enable controlled dissociation while preserving cell integrity [19] |
| ROCK Inhibitors | Y-27632 | Enhance cell survival after passaging and freezing [64] |
| Vector Clearance Tools | Temperature shift protocols, PCR detection | Ensure complete removal of reprogramming vectors [64] |
Leveraging AI and Machine Learning for Automated Colony Selection and QC
Frequently Asked Questions (FAQs)
1. How can AI perform non-invasive, label-free quality control for iPSC colonies? AI systems use convolutional neural networks (CNNs) to analyze high-resolution bright-field or phase-contrast microscopy images. These models are trained to identify key morphological features of healthy iPSC colonies, such as specific textures and compact structures, without the need for fluorescent labels or disruptive staining. This allows for real-time, non-invasive monitoring of colony health and pluripotency potential [66] [67].
2. What specific colony features can AI detect and quantify? AI-driven image analysis can automatically quantify multiple critical quality attributes (CQAs), including:
- Colony Confluency: The total area covered by cells.
- Colony Size Distribution: The range and average size of colonies.
- Morphological Phenotypes: Distinct cell shapes and structures indicative of health or differentiation.
- Differentiation Patches: Areas within a colony that have begun to spontaneously differentiate, which are often visually distinct from the uniform texture of pluripotent cells [68].
3. Can AI predict the best time to passage iPSC colonies? Yes. By continuously monitoring cultures, AI systems can trigger automated passaging protocols based on user-defined rules. A common parameter is colony confluency; for instance, the system can be programmed to initiate passaging automatically when confluency reaches a specific threshold (e.g., 70%), ensuring cells are never overgrown, which can lead to unwanted differentiation [68].
4. How does AI improve the accuracy of colony selection during reprogramming? Traditional manual selection relies on subjective human judgment. AI classifiers, trained on thousands of images of positive and negative colonies, provide a consistent, quantitative standard. This reduces human error and batch-to-batch variation. Studies have shown a high correlation (Pearson Coefficient r > 0.877) between AI-selected colonies and those verified by gold-standard biological methods like OCT4-GFP reporter expression [66].
5. What are the data requirements for implementing an AI-based QC system? Implementing a robust AI system requires a substantial dataset of annotated images for training the machine learning models. The precision of these models improves with more data, creating a foundation for reliable iPSC analysis. The required datasets include images of colonies labeled by experts or verified with biological assays to indicate pluripotency status [69].
Troubleshooting Guides
Problem 1: Poor Reprogramming Efficiency or Colony Formation
Potential Causes and Recommended Actions:
| Potential Cause | Recommended Action |
|---|---|
| Low-quality starting somatic cells. | Ensure somatic cells are healthy, proliferating, and at a low passage number before reprogramming initiation [56]. |
| Suboptimal reprogramming parameters. | Use AI-driven analysis of historical data to identify and predict ideal conditions, such as transcription factor ratios and timing [67]. |
| Inaccurate identification of early-stage colonies. | Implement an AI time-lapse imaging system to detect subtle, early morphological changes (as early as day 7 in a 20-24 day process) that precede classical colony formation [66]. |
Problem 2: Excessive Spontaneous Differentiation in Cultures
Potential Causes and Recommended Actions:
| Potential Cause | Recommended Action |
|---|---|
| Overgrown colonies. | Use automated monitoring to passage colonies at the optimal confluency (e.g., 70-80%), preventing overgrowth which triggers differentiation [19] [68]. |
| Inconsistent colony size after passaging. | Ensure cell aggregates are evenly sized during passaging. Automated systems can standardize this process to improve uniformity [19]. |
| Undetected differentiated patches. | Employ AI models trained to identify and quantify differentiated areas (often marked in analysis outputs) so they can be manually removed or used to discard a culture well [68]. |
Problem 3: Low Cell Survival After Passaging
Potential Causes and Recommended Actions:
| Potential Cause | Recommended Action |
|---|---|
| Harsh mechanical dissociation. | Automated liquid handlers can be programmed for gentle, consistent pipetting to break colonies into optimally-sized clusters [68]. |
| Passaging from overly confluent cultures. | AI-driven confluency monitoring prevents cultures from becoming too dense before passaging, which can compromise cell health [64]. |
| Absence of protective reagents. | Supplement culture medium with a ROCK inhibitor (e.g., Y-27632) for 18-24 hours post-passaging to increase cell survival, especially when working with single cells [56] [64]. |
Experimental Protocols & Data
AI-Assisted iPSC Colony Detection and Analysis Protocol
This protocol outlines a label-free method for detecting and predicting iPSC colony formation using time-lapse imaging and machine learning [66].
Key Materials:
- Cell Culture System: Human somatic cells (e.g., urinal cells) undergoing reprogramming in a 6-well plate format.
- Imaging System: Time-lapse bright-field microscope.
- Analysis Software: Capable of running machine learning models for classification and segmentation (e.g., CNNs, Hidden Markov Models).
Methodology:
- Image Acquisition: Capture time-lapse bright-field images of the reprogramming culture at regular intervals (e.g., every 12 hours) over the entire process (e.g., 20-24 days).
- Model Training: Train a convolutional neural network (CNN) classifier using a dataset of manually annotated images. These images should be cropped into small patches and labeled as either "positive iPSC colony texture" or "negative."
- Colony Detection:
- Sliding Window Classification: Scan entire well images using the trained CNN to identify patches with iPSC colony features.
- Segmentation and Post-processing: Generate a binary mask of detected colony areas, then apply post-processing to discard small, fragmented areas based on size and location.
- Growth Tracking and Prediction:
- Register and digitally tag each detected colony feature across the time-lapse series.
- Train a Hidden Markov Model (HMM) on this time-series data to estimate the growth phase and statistically predict the optimal maturation time window for colony selection.
Performance Metrics: The algorithm-detected colonies showed no significant biological differences compared to manually selected colonies when verified with standard molecular approaches (Immunofluorescence, QPCR, RNA-Seq) [66].
Table: Quantitative Performance of AI-Based Colony Detection
| Metric | Description | Reported Performance |
|---|---|---|
| Detection Correlation | Correlation (Pearson's Coefficient) with OCT4-GFP reporter expression in mouse models. | r = 0.877 [66] |
| Early Detection | Timepoint when earliest cellular texture changes can be detected. | Day 7 of a 20-24 day process [66] |
| Prediction Capability | Ability to model growth and predict optimal selection phase. | Statistically independent prediction achieved [66] |
Automated iPSC Culture and Passaging Protocol
This protocol describes the use of an integrated automated system (e.g., CellXpress.ai) for maintaining iPSC cultures [68].
Key Materials:
- Automated System: Cell culture system with integrated incubator, liquid handler, and automated imager.
- Cell Line: Human iPSCs.
- Reagents: mTeSR media, Vitronectin, ReLeSR passaging reagent, PBS.
Methodology:
- Seeding and Culture: Plate iPSCs onto vitronectin-coated 6-well plates in mTeSR medium.
- Automated Monitoring: The system performs scheduled media exchanges every 24 hours and acquires transmitted-light images every 12 hours.
- AI Analysis: Acquired images are analyzed in real-time using pre-trained deep learning models to segment iPSC colonies and detect differentiation.
- Decision Making: The software uses rules based on analysis data (e.g., confluency, differentiation percentage) to make decisions.
- Example Rule: IF confluency >70% in >90% of wells AND differentiated area <5%, THEN trigger passaging protocol.
- Automated Passaging: When triggered, the system executes a cluster-based passaging method using ReLeSR to dissociate colonies and re-seed them into new plates.
Visual Workflows
Diagram: AI-Driven iPSC Quality Control Workflow
Diagram: AI-Based Colony Selection during Reprogramming
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Materials for Automated iPSC Culture and AI-QC
| Item | Function | Example Use Case |
|---|---|---|
| ROCK Inhibitor (Y-27632) | Increases survival of dissociated iPSCs by inhibiting apoptosis. | Added to plating medium after passaging to improve cell attachment and viability [56] [64]. |
| Gentle Cell Dissociation Reagent | Enzyme-free solution that promotes the dissociation of iPSCs into small clusters. | Used for passaging to generate uniform, optimally-sized cell aggregates for reproducible results [3]. |
| Defined Culture Matrix (e.g., Vitronectin, Geltrex) | Provides a consistent, feeder-free substrate for iPSC attachment and growth. | Coats cultureware to support the maintenance of pluripotency in defined media; essential for standardized automated workflows [68] [64]. |
| Chemically Defined Medium (e.g., mTeSR, Essential 8) | Provides a consistent, xeno-free nutrient environment for iPSC growth. | Used as the basal medium for routine culture and expansion; its consistency is critical for automated feeding schedules [68] [64]. |
| Reprogramming Kit (e.g., CytoTune -iPS Sendai) | Delivers reprogramming factors to somatic cells to generate iPSCs. | Used for the initial generation of iPSC lines; non-integrating vectors are preferred for clinical applications [64]. |
From Bench to Bedside: Validation Frameworks and Regulatory Standards
Establishing a Phase-Appropriate QC Strategy for Research vs. Clinical Applications
What is a phase-appropriate Quality Control (QC) strategy? A phase-appropriate QC strategy is a quality management approach that evolves with your product's development stage. For induced pluripotent stem cells (iPSCs), this means implementing increasingly rigorous controls as you transition from basic research to clinical applications. In early research, the focus is on fundamental characterization and proof-of-concept, whereas clinical applications require stringent safety and quality standards compliant with regulatory bodies like the FDA and EMA [58] [14].
Why is it crucial for iPSC-based research and therapies? Implementing a phase-appropriate strategy is essential because it ensures patient safety and product efficacy in clinical applications while avoiding unnecessary costs and complexity during research phases. The regulatory environment for iPSC-derived therapies remains fragmented globally, making strategic planning critical for successful translation [58]. A well-defined QC roadmap helps researchers allocate resources efficiently, meet regulatory expectations, and accelerate the path to clinical implementation.
Core Quality Control Assays for iPSCs
Standard QC Testing Panels
All iPSC lines require thorough characterization, though the stringency and specific requirements vary between research and clinical applications.
Table 1: Standard vs. Optional QC Tests for iPSCs
| Test Category | Standard QC Tests | Further Optional QC Tests |
|---|---|---|
| Sterility & Viability | Sterility testing, Mycoplasma testing, Cell viability [49] | - |
| Pluripotency Verification | Stem cell marker FACS, Alkaline phosphatase staining [49] | Embryoid body formation, Pluritest array [49] |
| Genetic Integrity | - | Karyotyping, Sendai persistence testing [49] |
Pluripotency Assessment Methods
What are the key markers for confirming pluripotency? Pluripotency is typically confirmed through a combination of methods:
- Protein Marker Expression: Flow cytometry or immunocytochemistry for key pluripotency markers including Oct4, Nanog, Sox2, SSEA4, Tra-1-60, and Tra-1-81 [70].
- Functional Assays: Alkaline phosphatase staining provides a simple, inexpensive initial assessment [49]. Embryoid body formation demonstrates differentiation potential into all three germ layers [49].
- In Vivo Validation: The teratoma formation assay in immunocompromised mice remains a gold standard for demonstrating developmental potential, though it's time-consuming and not feasible for routine clinical lot release [71].
Research-Grade QC Strategy
Minimum Essential QC for Research
What are the absolute minimum QC requirements for research-use iPSCs? For research applications, a minimal QC panel should include:
- Sterility Testing: Ensure cells are free from mycoplasma and microbial contamination [49].
- Pluripotency Verification: Confirm expression of key pluripotency markers (Oct4, Nanog, Sox2) via flow cytometry or immunostaining [49] [70].
- Identity Confirmation: Short tandem repeat (STR) profiling to verify cell line identity [13].
- Viability Assessment: Document population doubling time and morphological characteristics [49].
Common Research Pitfalls and Solutions
Why do my iPSCs show inconsistent differentiation results? Inconsistent differentiation often stems from:
- Undetected Genetic Variations: Low-level genetic abnormalities that accumulate during reprogramming or culture expansion can alter differentiation potential [58].
- Epigenetic Memory: Residual epigenetic signatures from the somatic cell source may bias differentiation toward related lineages [71].
- Solution: Implement more rigorous clone selection and perform genetic screening (karyotyping) on master cell banks. Consider using multiple iPSC clones for critical differentiation experiments to control for clonal variation [14].
How can I improve the reproducibility of my iPSC experiments?
- Document Culture Conditions: Maintain detailed records of passage methods, split ratios, and media batches [13].
- Standardize Banking Procedures: Create structured cell banks with consistent freezing protocols [13].
- Quality Raw Materials: Use research-grade reagents from qualified suppliers and document all lots [58].
Clinical-Grade QC Strategy
Enhanced QC Requirements for Clinical Applications
What additional QC measures are required for clinical applications? Clinical-grade iPSCs require significantly enhanced characterization:
- Comprehensive Genetic Analysis: Whole genome sequencing to identify sequence variations, plus targeted analysis of common mutation hotspots [14] [70].
- Tumorigenicity Risk Assessment: Enhanced safety testing for residual undifferentiated cells and evaluation of tumor-forming potential [58].
- Process Validation: Rigorous demonstration that your manufacturing process consistently produces iPSCs meeting all quality attributes [58].
Table 2: Clinical-Grade vs. Research-Grade QC Requirements
| QC Parameter | Research Grade | Clinical Grade |
|---|---|---|
| Reprogramming Method | Integrating or non-integrating methods [13] | Non-integrating only (mRNA, Sendai, episomal) [14] [72] |
| Genetic Stability | Karyotyping (optional) [49] | Whole genome sequencing, CNV analysis [14] [70] |
| Manufacturing Environment | Research laboratory | Current Good Manufacturing Practice (cGMP) [14] [70] |
| Documentation | Laboratory notebooks | Full traceability, electronic batch records [58] |
| Raw Materials | Research grade | GMP-grade, qualified for clinical use [58] |
Addressing Clinical Translation Challenges
How do I manage the high cost of clinical-grade QC?
- Phase-appropriate Validation: Implement the most critical safety tests early, then add progressively more comprehensive characterization as you advance toward clinical trials [58].
- Leverage Core Facilities: Utilize specialized GMP facilities and qualified service providers for specific assays rather than building all capabilities in-house [14].
- Strategic Assay Selection: Focus on potency assays with clinical relevance and implement modern, scalable alternatives to traditional cumbersome assays [58].
What are the critical safety concerns for clinical application?
- Tumorigenic Risk: The potential for residual undifferentiated cells to form tumors requires robust processes to eliminate these cells from final products and sensitive detection methods for quality control [58].
- Genetic Stability: iPSCs can acquire mutations during reprogramming and expansion that may impact safety [58]. Comprehensive genomic assessment is essential.
- Solution: Implement orthogonal safety testing approaches that combine multiple methods to build a comprehensive safety profile [58].
Scaling Challenges and Advanced Technologies
QC for Scalable Manufacturing
How does QC change when scaling iPSC manufacturing? Transitioning from small-scale to large-scale manufacturing introduces several QC challenges:
- 3D Bioreactor Systems: Suspension culture in Vertical-Wheel bioreactors can achieve 93.8-fold expansion over 5 days compared to 19.1-fold in 2D culture, but requires new QC parameters to monitor cell quality in dynamic conditions [70].
- Automated Quality Control: Implement in-process monitoring and automated imaging systems to maintain consistency across larger batches [58].
- Advanced Analytics: Use digital twins and process analytical technology (PAT) to model processes and detect deviations in real-time [58].
Emerging Technologies for Enhanced QC
What new technologies are improving iPSC QC?
- Chromatin Accessibility Mapping: ATAC-seq analysis reveals chromatin dynamics during reprogramming, providing deeper quality assessment beyond surface markers [73] [74].
- Machine Learning: Automated image analysis of iPSC colonies can enhance quality assessment and selection consistency [72].
- Lineage Scorecards: Molecular reference standards that predict differentiation propensity toward specific lineages, enabling more targeted QC for specific applications [71].
Troubleshooting Common QC Issues
Research to Clinical Transition
Why does my research-grade iPSC line fail to meet clinical standards? Common issues when transitioning research lines to clinical applications include:
- Incomplete Documentation: Lack of complete traceability for reagents and processes used during initial line derivation [58].
- Unqualified Reprogramming Methods: Use of integrating vectors that are unacceptable for clinical applications [13] [72].
- Solution: Plan for clinical translation early by using non-integrating reprogramming methods and documenting all processes according to GMP standards from the beginning [14].
Genetic Stability Problems
How can I prevent genetic instability in long-term iPSC culture?
- Monitor Common Mutations: Regularly screen for recurrent genetic abnormalities in known hotspot regions (e.g., TP53) [58] [70].
- Control Culture Conditions: Avoid excessive passaging and minimize stress during routine culture [13].
- Bank Early: Create extensive early-passage master cell banks to preserve genetically stable stocks [58].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for iPSC QC
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Sendai Virus Vectors | Non-integrating reprogramming | Higher success rates vs. episomal methods; requires clearance testing [13] |
| mRNA Reprogramming | Non-integrating reprogramming | Avoids vector persistence concerns; suitable for clinical applications [14] [72] |
| Vitronectin | Defined culture substrate | Xeno-free alternative to Matrigel for clinical applications [70] |
| Flow Cytometry Panels | Pluripotency verification | Quantify Oct4, Sox2, Nanog, SSEA4, Tra-1-60, Tra-1-81 expression [70] |
| GMP-grade Media | Cell culture | Chemically defined, xeno-free formulations for clinical manufacturing [58] |
Experimental Workflows and Signaling Pathways
iPSC QC Workflow Diagram
IPSC QC Workflow: From reprogramming to application, showing divergent QC paths for research versus clinical use.
Chromatin Dynamics in Reprogramming
Chromatin Dynamics: OSKM factors remodel chromatin, opening pluripotency loci while closing somatic genes—a key QC checkpoint.
Frequently Asked Questions
What is the most critical difference between research and clinical QC? The most significant difference is the requirement for comprehensive safety testing in clinical applications, particularly regarding genetic stability and tumorigenic potential. While research QC focuses on fundamental characterization, clinical QC must provide absolute confidence in product safety for human use [58] [14].
Can I convert my research-grade iPSC line to clinical grade? While theoretically possible, it is often more efficient to derive new lines using clinical-grade processes from the beginning. Converting research lines requires complete re-derivation under GMP conditions, requalification of all raw materials, and extensive documentation that may not exist for the original line [14].
How many clones should I characterize for clinical applications? For clinical applications, it is recommended to characterize multiple clones (at least 3-5) to select the optimal candidate based on genetic integrity, differentiation potential, and growth characteristics. This provides a backup option if your primary clone fails to meet all requirements during advanced characterization [13].
What are the key indicators of poor iPSC quality? Key red flags include: spontaneous differentiation in culture, abnormal morphology (heterogeneous cell size, irregular colony borders), slow growth rates, failure to differentiate into target lineages, and genetic abnormalities detected in routine screening [58] [49].
Establishing a phase-appropriate QC strategy is essential for successful iPSC research and clinical translation. By implementing the right level of quality control at each development stage—from basic research characterization to comprehensive clinical safety testing—researchers can advance their programs efficiently while maintaining scientific rigor and regulatory compliance. The frameworks and troubleshooting guides provided here offer a practical foundation for developing robust QC protocols tailored to specific application needs.
For researchers and drug development professionals working with induced pluripotent stem cells (iPSCs), robust potency assays are indispensable. They are critical quality attributes (CQAs) that confirm your therapeutic product possesses the specific biological activity required for its intended clinical effect, directly linking to its mechanism of action (MoA) [75]. This guide provides a technical foundation for navigating the complexities of potency assay development, offering troubleshooting support and detailed protocols to ensure the quality and efficacy of your iPSC-based therapies.
Understanding Potency Assays: Key Concepts and Challenges
Frequently Asked Questions
What defines a potency assay for an iPSC-derived therapy? The FDA defines potency as "the specific ability or capacity of the product... to effect a given result" [75]. For an iPSC-derived cell therapy, this translates to an assay (or a series of assays) that measures the biological activity reflective of the product's intended therapeutic mechanism of action, such as differentiation capacity, secretory function, or specific enzymatic activity.
Why is a single potency assay often insufficient for complex cell therapies? Cell therapies, especially iPSC-derived products, often have multiple, complex modes of action. A "matrix approach," which involves using two or more complementary assays to capture different aspects of the product's key biological functions, is widely recommended and often required by regulators [75] [76]. This strategy provides a collective conclusion on potency, offering a more comprehensive safety and efficacy profile than any single test could.
What are the most significant hurdles in developing a potency assay for clinical use? Key challenges include:
- Inherent Product Variability: Especially for autologous therapies, the starting biological material can vary [76].
- Lack of Reference Standards: Unlike protein biologics, cell therapies often lack a well-characterized reference standard for direct comparison [76].
- Need for Rapid Release: The short shelf-life of live cell products demands quick turnaround times for quality control testing [76].
- Defining Critical Quality Attributes (CQAs): A limited understanding of which product characteristics truly predict clinical efficacy can make it difficult to define and validate robust potency assays [58].
Troubleshooting Common Potency Assay Issues
| Problem Area | Potential Cause | Recommended Solution |
|---|---|---|
| High Background Staining (IHC/IF) | Endogenous enzyme activity (e.g., peroxidases) | Quench with 3% H2O2 in methanol or use a commercial peroxidase suppressor [36]. |
| High Background Staining (IHC/IF) | Endogenous biotin | Block samples using an avidin/biotin blocking solution prior to adding the detection complex [36]. |
| High Background Staining (IHC/IF) | Nonspecific antibody binding | Optimize primary antibody concentration; add NaCl (0.15-0.6 M) to the antibody diluent to reduce ionic interactions [36]. |
| Weak Target Staining | Loss of primary antibody potency | Test antibody on a known positive control; ensure proper storage conditions and avoid repeated freeze-thaw cycles by aliquoting [36]. |
| Weak Target Staining | Inhibitory secondary antibody concentration | Test decreasing concentrations of the secondary antibody; excessively high concentrations can paradoxically reduce signal [36]. |
| High Assay Variability | Uncontrolled cell culture conditions | Implement real-time, in-process monitoring of metabolites and differentiation markers to catch deviations early [58]. |
| Poor Scalability | Reliance on lengthy animal models | Transition to robust, reproducible in vitro assays for GMP validation, using animal models primarily for proof-of-concept [75]. |
Comparative Analysis of Major Potency Assay Modalities
A strategic selection of assay types is crucial for balancing predictive value with practical constraints in a development pipeline.
Quantitative Comparison of Assay Types
Table: Key Characteristics of Common Potency Assay Modalities
| Assay Modality | Measured Endpoint | Typical Assay Duration | Key Strengths | Key Limitations |
|---|---|---|---|---|
| Embryonic Stem Cell Test (EST) | Inhibition of differentiation (e.g., cardiopoiesis) [77] | 10+ days | High relevance to developmental toxicity; covers a range of pathways [77] | Lengthy duration; may not capture all organ-specific vulnerabilities [77] |
| Flow Cytometry | Cell surface and intracellular marker expression [76] | 1-2 days | High-throughput; quantitative; multiparametric | Requires predefined markers; may not directly measure function [76] |
| Cell-Based Functional Assay | Functional output (e.g., cytokine release, cytotoxic killing) [76] | 2-7 days | Directly measures a relevant biological activity; high predictive value | Can be highly variable and lengthy; poor performance for rapid QC release [76] |
| Genomic Assay | Genomic stability / genetic integrity | 3-5 days | Provides deep data on genetic CQAs; can be automated | Requires expert interpretation; unclear thresholds for acceptable risk [58] |
Experimental Protocol: Embryonic Stem Cell Test (EST)
The following protocol outlines a standardized mouse Embryonic Stem Cell Test (mEST), which can be adapted for human iPSC lines to assess developmental toxicity potential [77].
Methodology:
- Cell Culture: Maintain mouse embryonic stem cells (mESCs) in an undifferentiated, pluripotent state using standard culture conditions.
- Compound Exposure: Prepare a concentration range of the test compound. Include a positive control (e.g., 5-fluorouracil) and a negative control (e.g., caffeine) [77].
- Differentiation Induction: Seed mESCs into differentiation-permissive media to form embryoid bodies (EBs). Expose the developing EBs to the test compounds for the entire differentiation period.
- Endpoint Analysis (10-12 days):
- Apical Readout: Score the inhibition of cardiac differentiation by visually counting the number of contracting EBs under a light microscope [77].
- Molecular Readout: Fix EBs and use immunohistochemistry (IHC) or flow cytometry for specific differentiation markers (e.g., cardiac troponins) for a more quantitative assessment [77].
- Data Analysis: Calculate the IC50 for the inhibition of differentiation. The assay's predictive model classifies compounds as toxic or non-toxic based on the concentration that inhibits differentiation by 50%.
Experimental Protocol: Matrix Potency Assay for iPSC-Derived Cardiomyocytes
This protocol exemplifies the "matrix approach" for characterizing a hypothetic iPSC-derived cardiomyocyte product.
Methodology:
- Cell Viability and Quantity (Day 1):
- Perform a cell count using an automated cell counter with trypan blue exclusion to determine viable cell number and total population.
- Purity Assessment via Flow Cytometry (Day 1-2):
- Prepare a single-cell suspension.
- Stain cells with fluorochrome-conjugated antibodies against key cardiomyocyte markers (e.g., cTnT, NKX2-5).
- Include appropriate isotype and fluorescence-minus-one (FMO) controls to ensure gating accuracy and specificity [58].
- Analyze on a flow cytometer; report the percentage of positively stained cells in the viable population.
- Functional Assessment via Metabolic Activity (Day 1-5):
- Plate a defined number of cells in a multi-well plate.
- After cell attachment, measure metabolic activity using a resazurin-based assay (e.g., Alamar Blue) daily for 4 days to generate a growth and metabolic activity profile.
- Data Integration:
- The potency is not a single number but a profile combining the viability, purity (% cTnT+), and functional metabolic activity. Establish acceptance criteria for each parameter based on characterization lots and correlation with in vivo function.
Visualizing Workflows and Signaling
iPSC Potency Assay Development Pathway
Key Signaling in Pluripotency and Differentiation
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for iPSC Potency Assay Development
| Research Reagent | Function in Potency Assays |
|---|---|
| Pluripotency Markers (e.g., Antibodies against Oct4, Sox2, Nanog) | Confirm the undifferentiated state of the starting iPSC population, a foundational CQA [58]. |
| Differentiation Markers (e.g., Antibodies against cTnT, β-III-tubulin, AFP) | Assess the successful and specific differentiation into target lineages (e.g., cardiomyocytes, neurons, hepatocytes) [77] [76]. |
| Validated iPSC Line | Serves as a well-characterized biological reference material for assay development and system qualification [58]. |
| GMP-Grade Cell Culture Media | Provides a consistent, defined, and reproducible environment for the maintenance and differentiation of iPSCs, reducing batch-to-batch variability [58]. |
| Advanced Verification Antibodies | Antibodies that have undergone additional specificity testing provide higher confidence in IHC and flow cytometry results for critical marker expression [36]. |
Defining Critical Quality Attributes (CQAs) for iPSC-Derived Therapeutics
Frequently Asked Questions (FAQs)
Q1: What are Critical Quality Attributes (CQAs) for iPSC-based therapies, and why are they essential? Critical Quality Attributes (CQAs) are biological, chemical, or physical properties that must be within an appropriate limit, range, or distribution to ensure the desired product quality, safety, and efficacy [78]. For iPSC-derived therapeutics, establishing CQAs is fundamental for the industrialization of these products. They are integral to a "Quality by Design" (QbD) approach, helping to define a robust and commercially viable Good Manufacturing Practice (cGMP) compliant process by linking Critical Process Parameters (CPPs) to the CQAs [79]. Monitoring CQAs throughout development and manufacturing is critical for ensuring the final cell therapy product is safe, pure, potent, and consistent from batch to batch [78] [80].
Q2: What are the major categories of CQAs for the starting iPSC material? For the iPSC master cell banks themselves, which act as the starting material, the key CQA categories are Identity, Purity, Viability, Potency, and Safety [79]. The tests for these attributes confirm that the cells are indeed pluripotent stem cells (Identity), free of unintended differentiation or contaminants (Purity, Safety), alive and quantifiable (Viability), and capable of differentiating into the target cell type (Potency) [79].
Q3: My iPSC cultures show high levels of spontaneous differentiation. What could be the cause? Excessive differentiation (>20%) is a common problem that can compromise the quality of your starting material. Potential causes and solutions include [19]:
- Old or Inefficient Culture Medium: Ensure complete cell culture medium is fresh (e.g., kept at 2-8°C for less than two weeks).
- Improper Passaging: Colonies should be passaged when they are large and dense, but before they overgrow. Ensure cell aggregates after passaging are evenly sized.
- Prolonged Exposure Outside Incubator: Avoid having culture plates out of the incubator for more than 15 minutes at a time.
- High Colony Density: Decrease the colony density by plating fewer cell aggregates during passaging.
Q4: How can I ensure the genomic stability of my iPSC lines? Genomic instability is a well-known risk in hPSC cultures, with specific aberrations (like gains on chromosome 20q11.21) conferring a selective growth advantage [18]. A robust quality control panel must include methods to monitor chromosomal integrity.
- Karyotyping by G-banding is the gold-standard for a genome-wide overview and can detect large structural abnormalities (>5-10 Mb) like translocations [18].
- SNP array analysis offers higher resolution, capable of detecting smaller copy number variations (CNVs) and copy-neutral loss of heterozygosity (CN-LOH) that G-banding might miss [18]. A practical guide for using SNP arrays in hPSC quality control is available for researchers with minimal bioinformatics expertise [18].
Q5: What are the key considerations for developing analytical methods to measure CQAs? As therapies move toward commercialization, the analytical methods used to measure CQAs must be rigorously developed. Key parameters for assay validation include [79]:
- Specificity: The ability to distinguish between positive and negative controls.
- Linearity, Accuracy, and Precision: These determine the quantitative range (LLOQ/ULOQ), recovery rate, and variability (e.g., %CV) of the assay.
- Automation: Automating analytical methods can reduce hands-on time, decrease operator-to-operator variability, and improve reliability and precision for more consistent results [79] [80].
Q6: How can process automation help in managing CQAs? Automation is a key technology for improving the development of iPSC-derived therapies. It addresses several challenges [78] [80]:
- Reduces Variability: Automated systems minimize operator-to-operator variability in both manufacturing and analytics.
- Enhances Robustness: Increases the reliability and reproducibility of processes and assays.
- Increases Throughput and Scalability: Allows for faster process optimization and production of the large cell quantities needed for clinical use.
- Reduces Contamination Risk: Minimizes hands-on time and the associated risk of cell culture infections.
Troubleshooting Common iPSC Workflow Issues
Problem 1: Low Cell Attachment After Passaging Low cell attachment can significantly slow down research progress. Consider these solutions [19]:
- Initial Plating Density: Plate a higher number of cell aggregates initially (e.g., 2-3 times higher) to establish a more densely confluent culture.
- Work Quickly: Minimize the time that cell aggregates are in suspension after being treated with passaging reagents.
- Optimize Passaging Sensitivity: Reduce the incubation time with passaging reagents if your cell line is particularly sensitive.
- Correct Cultureware: A common error is using the wrong plate type. Ensure you use non-tissue culture-treated plates when coating with Vitronectin XF and tissue culture-treated plates when coating with Corning Matrigel.
Problem 2: Challenges with CRISPR Gene Editing in iPSCs iPSCs are notoriously difficult to genetically manipulate. A major challenge is the low frequency of Homology-Directed Repair (HDR), which is necessary for precise gene knock-ins or mutation corrections [81].
- Proposed Solution: Improve HDR efficiency by synchronizing the cell cycle of your iPSC population. Since HDR is most active in specific cell cycle phases (S/G2), creating a synchronized culture can increase the proportion of cells capable of undergoing the desired precise edit [81].
Problem 3: Managing High Costs and Long Timelines for Therapy Development The high Cost of Goods (COGs) and lengthy development processes are significant hurdles for the commercialization of iPSC therapies [78].
- Proposed Solutions: Strategies to address this include [78] [80]:
- Implementing advanced, automated manufacturing systems to improve efficiency and consistency.
- Establishing well-designed testing strategies early in development to avoid costly late-stage failures.
- Focusing on process optimization and scale-up to reduce manual labor and increase output.
CQA Testing Framework and Specifications
The following table summarizes the key assays used for the release and characterization of iPSC master cell banks, categorizing them by the quality attribute they measure [79].
Table 1: Standard Tests for iPSC Master Cell Bank Characterization and Release
| Test | Purpose | Typical Use | Key Specifications / Notes |
|---|---|---|---|
| Sterility/Mycoplasma | Safety/Sterility | Release | Ensures absence of microbial and mycoplasma contamination [79]. |
| Endotoxin | Safety/Sterility | Release | Confirms low levels of pyrogenic substances [79]. |
| Flow Cytometry | Identity/Purity | Release | Measures surface marker expression (e.g., Tra-1-60, SSEA-4) to confirm pluripotency and purity [79]. |
| Cell Count & Viability (CCV) | Content | Release | Determines total live cell count and viability percentage [79]. |
| Karyotype (G-banding) | Safety/Genomic | Release | Gold-standard for detecting large-scale chromosomal abnormalities (>5-10 Mb) [18]. |
| SNP Array Analysis | Safety/Genomic | Characterization/Release | High-resolution method for detecting CNVs and CN-LOH; recommended for comprehensive QC [18]. |
| EB Formation | Potency | Characterization | Tests spontaneous differentiation potential into all three germ layers (Embryoid Body formation) [79]. |
| Directed Differentiation | Product-Specific Potency | Characterization | Assesses ability to differentiate into the specific cell lineage required for the therapy [79]. |
| Alkaline Phosphatase | Identity/Use | Characterization | A common enzymatic marker for pluripotent stem cells [79]. |
| Telomere Analysis | Safety/Use | Characterization | Checks for maintenance of telomere length, indicative of cellular "health" [79]. |
For advanced characterization and process understanding, the relationship between CPPs and CQAs must be monitored. The following table outlines key parameters and attributes for the iPSC expansion process.
Table 2: Example Critical Process Parameters (CPPs) and Linked CQAs for iPSC Expansion
| Process Step | Critical Process Parameter (CPP) | Linked Critical Quality Attribute (CQA) | Impact & Rationale |
|---|---|---|---|
| Passaging | Seeding Density | Pluripotency Marker Expression, Genomic Stability | Incorrect density can promote spontaneous differentiation or select for aberrant clones [19] [18]. |
| Passaging | Aggregate Size After Dissociation | Pluripotency Marker Expression, Viability | Overly large aggregates can lead to central necrosis and differentiation; overly small aggregates may not survive [19]. |
| Culture | Time Between Passages | Genomic Stability, Pluripotency | Over-confluent cultures are stressed and more prone to acquiring karyotypic abnormalities [19] [18]. |
| Media Feeding | Media Age & Feeding Frequency | Pluripotency Marker Expression, Viability | Depletion of nutrients and growth factors or accumulation of waste products can induce stress and differentiation [19]. |
Experimental Protocols for Key CQA Assessments
Protocol 1: Assessing Genomic Stability via SNP Array Analysis This protocol provides a practical guide for detecting chromosomal aberrations using SNP arrays, a high-resolution complement to traditional karyotyping [18].
- Genomic DNA Extraction: Extract high-quality genomic DNA from iPSCs using a commercial kit (e.g., QIAamp DNA Blood Mini Kit). Ensure DNA concentration and purity (A260/280 ratio) meet standard requirements for array processing.
- SNP Array Processing: Process the DNA on a selected SNP array platform (e.g., Illumina's Global Screening Array). This step is typically performed by a specialized core facility or service provider.
- Data Analysis with GenomeStudio:
- Load the data into Illumina's GenomeStudio software with the cnvPartition plug-in.
- Check the Call Rate, which should typically be >95% as a key quality metric. This represents the percentage of SNPs successfully genotyped.
- Analyze the B-allele Frequency (BAF) and Log R Ratio (LRR) plots to identify chromosomal aberrations. Deviations from the expected patterns indicate copy number variations (CNVs) or loss of heterozygosity (LOH).
- Interpretation: Common abnormalities in hPSCs include gains of chromosomes 1, 12, 17, 20, and X. The gain of 20q11.21 is a frequent anomaly that confers a growth advantage.
Protocol 2: Validating Pluripotency via Flow Cytometry This method quantitatively assesses the expression of key pluripotency-associated surface markers, providing a readout for the Identity and Purity CQAs.
- Cell Harvesting: Gently dissociate iPSC colonies into a single-cell suspension using a cell dissociation reagent (e.g., Accutase). Quench the reaction with culture medium.
- Staining: Aliquot cells into staining tubes. Incubate with fluorochrome-conjugated antibodies against key markers (e.g., Tra-1-60 and SSEA-4) and appropriate isotype controls for 20-30 minutes on ice, protected from light.
- Washing and Fixation: Wash cells twice with a cold buffer (e.g., PBS with 1% BSA) to remove unbound antibody. Cells can be fixed with a 1-4% paraformaldehyde solution if analysis is not immediate.
- Flow Cytometry Analysis: Resuspend cells in buffer and analyze on a flow cytometer. Collect a minimum of 10,000 events per sample.
- Data Analysis: Gate on live, single cells. The percentage of cells positive for Tra-1-60 and SSEA-4 should be very high (typically >90%) for a high-quality, undifferentiated iPSC culture. Compare to isotype controls to set positive gates accurately.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for iPSC Generation, Culture, and Quality Control
| Reagent Category | Example Products / Methods | Function |
|---|---|---|
| Reprogramming | Sendai virus vectors, episomal vectors [82] | Non-integrating methods to safely reprogram somatic cells into iPSCs. |
| Cell Culture Media | mTeSR Plus, mTeSR1 [19] | Serum-free, defined media formulated to maintain iPSCs in a pluripotent state. |
| Passaging Reagents | ReLeSR, Gentle Cell Dissociation Reagent [19] | Non-enzymatic reagents for gentle dissociation of iPSC colonies into aggregates for passaging. |
| Culture Substrates | Vitronectin XF, Corning Matrigel [19] | Defined extracellular matrix coatings that support the attachment and growth of iPSCs in feeder-free conditions. |
| Gene Editing | CRISPR/Cas9 systems [81] [83] | Tools for introducing precise genetic modifications in iPSCs for disease modeling or therapy development. |
| Differentiation | High-quality GMP-grade growth factors & cytokines [80] | Proteins that direct the differentiation of iPSCs into specific target cell types (e.g., neurons, cardiomyocytes). |
| Cell Analysis - Flow Cytometry | Antibodies against OCT4, NANOG, SOX2, Tra-1-60, SSEA-4 [79] [82] | Key reagents for validating pluripotency (Identity) and purity by detecting specific markers. |
| Cell Analysis - Genomic QC | SNP Arrays (e.g., Illumina Global Screening Array) [18] | Platform for high-resolution detection of chromosomal aberrations as part of safety testing. |
Quality Control Workflow and Testing Strategy
The following diagram illustrates the logical workflow for applying a CQA-based quality control strategy from the establishment of an iPSC line through to its use in manufacturing a therapeutic product.
Quality Control Workflow for iPSC Line Release
CQA Testing Strategy Throughout Development
The strategy for testing CQAs evolves as an iPSC-based product moves from research toward commercialization. The following diagram outlines the testing focus at different stages.
iPSC Testing Strategy Across Development Stages
What are the core regulatory principles for iPSC-based therapies in the US, EU, and Japan?
A risk-based approach is a foundational principle for regulating iPSC-based products across the FDA (US), EMA (EU), and PMDA (Japan). This means the level of regulatory scrutiny is tailored to the product's specific risks, considering factors like the degree of cell manipulation, route of administration, and target patient population [84]. The following table summarizes the key regulatory frameworks and guidelines for each region.
Table 1: Core Regulatory Frameworks for iPSC-Based Products
| Region / Agency | Product Classification | Key Guidelines & Laws | Governing Principles |
|---|---|---|---|
| USA (FDA) | Biological Products (351 HCT/Ps) under the Public Health Service Act [84] | - Preclinical Assessment of Investigational Cellular and Gene Therapy Products [84]- Considerations for the Design of Early-Phase Clinical Trials [84] | Risk-based approach; Case-by-case evaluation based on product properties [84] |
| European Union (EMA) | Advanced Therapy Medicinal Products (ATMPs) [84] | - Guideline on Human Cell-Based Medicinal Products [85] [84]- Reflection Paper on Stem Cell-Based Medicinal Products [84] | Risk-based approach according to Annex I, part IV of Directive 2001/83/EC [84] |
| Japan (PMDA) | Regenerative Medical Products [84] | - Guidelines on Ensuring Quality and Safety of iPS Cell-Derived Products (Allogeneic & Autologous) [84]- Points to Consider for Tumorigenicity Tests and Genomic Stability [84] | Risk-based approach; Specific guidelines for different iPS cell applications (e.g., retinal, articular cartilage) [84] |
What are the critical quality control checkpoints for iPSC lines?
Maintaining genetic integrity and pluripotency from the starting material through to the final product is paramount. A phase-appropriate, risk-based testing strategy should be implemented, with rigorous checks at each stage of development [85] [58]. Key checkpoints include the donor tissue, the master cell bank (MCB), working cell banks (WCB), and the final drug product.
Diagram: iPSC Product Development and QC Workflow. QC testing must be integrated at every stage, from donor tissue to final product release.
How do regulatory expectations for genetic stability testing differ?
Regulators universally require genetic stability testing, but the specific methodologies and acceptance criteria are part of a risk-based strategy [85] [84]. There is a growing emphasis on using high-resolution methods like Next-Generation Sequencing (NGS) to complement traditional karyotyping.
Table 2: Genetic Stability Testing Expectations Across Regions
| Testing Method | Detection Capability | Regulatory Standing & Application |
|---|---|---|
| G-band Karyotyping | A low-resolution method for detecting large-scale chromosomal abnormalities (e.g., aneuploidies, translocations) [85]. | Considered the gold standard and widely accepted for detecting major cytogenetic abnormalities [26]. |
| Array CGH / Digital PCR | A higher-resolution technique for identifying submicroscopic copy number variations (CNVs) and regional amplifications/deletions [26]. | Often used to supplement karyotyping data. Its use is encouraged for a more comprehensive view of genomic integrity [26]. |
| Next-Generation Sequencing (NGS) | Can detect single nucleotide variants (SNVs), small insertions/deletions (indels), and CNVs in a single assay. Can be focused on cancer-related gene panels or whole genomes [85]. | Recommended for a deeper molecular insight. There is a push towards NGS-based oncogenetic profiling to rule out critical mutations in genes like TP53 and KRAS [85]. |
How should we manage culture-acquired genetic variants in our iPSC lines?
Culture-acquired genetic variants are a major safety concern in iPSC therapy development, as they can confer a growth advantage to certain clones and potentially lead to tumorigenicity or altered differentiation potential [85]. A proactive, risk-stratified management strategy is required by regulators [85] [58].
- Establish a Risk Stratification Model: Profile your iPSC clones early based on factors like reprogramming method, donor characteristics, passage number, and results from genetic testing. This allows you to prioritize low-risk clones for clinical development and exclude high-risk ones [85].
- Implement Stage-Appropriate Testing: The frequency and extent of genetic testing should align with the product's development phase. Banking DNA at key manufacturing stages enables retrospective analysis as new knowledge emerges [58].
- Focus on Clinically Relevant Mutations: Adopt NGS-based oncogenetic profiling to screen for mutations in a curated panel of well-established driver genes (e.g., TP53, KRAS, BCOR) linked to cancer, rather than just generating long lists of variants of unknown significance [85].
What are the best practices for demonstrating pluripotency and differentiation potential?
A combination of analytical and functional assays is required to fully characterize pluripotency and differentiation potential, moving beyond a single marker [26].
- Analytical Assays for Pluripotency Markers: Use techniques like immunofluorescence staining or flow cytometry to confirm the expression of hallmark pluripotency-associated transcription factors and surface markers. Key markers include OCT3/4, NANOG, SOX2, SSEA-4, TRA-1-60, and TRA-1-81 [26].
- Functional Assay: Trilineage Differentiation: As the definitive test, demonstrate the iPSC line's ability to differentiate into cell types of the three primary germ layers—ectoderm, mesoderm, and endoderm. This can be achieved in vivo via the teratoma formation assay in immunocompromised mice or in vitro via directed differentiation or serum-based spontaneous differentiation protocols [26]. The resulting cells should be analyzed for germ layer-specific markers using immunohistochemistry, immunofluorescence, or RT-PCR.
What are common pitfalls in raw material selection and quality control?
Variability in raw materials is a significant source of inconsistency in iPSC cultures. A rigorous qualification process is essential [58].
- Misunderstanding "GMP-Grade" Terminology: The term "GMP-grade" indicates that a material was manufactured according to Good Manufacturing Practice standards but does not, by itself, guarantee it is suitable for your specific clinical application. You must still assess the material's origin, purity, and safety data [58].
- Inadequate Qualification and Testing: Always request comprehensive data sheets from suppliers detailing component origins, testing (e.g., sterility, endotoxin), and release criteria. Perform your own identity, purity, and potency tests to ensure raw materials meet your specifications before use in GMP manufacturing [58].
- Lack of Contingency Planning: Qualify multiple batches of critical raw materials (e.g., growth factors, matrices) or secure a single, large, well-characterized batch to ensure consistency throughout clinical development and avoid supply chain disruptions [58].
The Scientist's Toolkit: Essential Reagents for iPSC Quality Control
Table 3: Key Reagents and Materials for iPSC Quality Control
| Reagent / Material | Function in QC | Key Considerations |
|---|---|---|
| Pluripotency Marker Antibodies | Detection of core pluripotency factors (OCT4, SOX2, NANOG) and surface markers (SSEA-4, TRA-1-60) via immunofluorescence or flow cytometry [26]. | Validate antibodies for specificity and performance in your specific assay. Prefer antibodies that are well-documented in the literature. |
| Trilineage Differentiation Kits | Directed in vitro differentiation into ectoderm, mesoderm, and endoderm lineages for functional pluripotency assessment [26]. | Use standardized, serum-free protocols to ensure reproducibility and minimize batch-to-batch variability. |
| Karyotyping Kits | G-band analysis for detecting gross chromosomal abnormalities [26]. | A standard, widely accepted method. Should be supplemented with higher-resolution techniques for a complete picture. |
| NGS Oncogenetic Panels | Targeted sequencing to identify mutations in hundreds of cancer-associated genes, providing a deep molecular safety profile [85]. | Select panels that cover genes most relevant to iPSC biology and tumorigenic risk (e.g., TP53, P13K, RAS pathway genes). |
| Mycoplasma Detection Kits | Essential for routine screening of mycoplasma contamination, which can alter gene expression and cell health [26]. | Use highly sensitive methods like PCR. Test regularly and maintain a culture policy that avoids routine antibiotics to prevent hidden contamination [26]. |
| STR Profiling Kits | Short Tandem Repeat (STR) analysis for authenticating cell line identity and matching iPSCs to their donor source [26]. | A mandatory test to prevent cross-contamination and misidentification. Profile the source tissue and the resulting iPSC clones. |
FAQs: Addressing Common Challenges in iPSC Biobanking
FAQ 1: What are the most critical factors to ensure the long-term reliability of iPSC lines in a biobank? Long-term reliability is anchored in three pillars: the use of non-integrating reprogramming methods, a robust Quality Management System (QMS) compliant with international standards like ISO 20387, and comprehensive pre-analytical quality control.
- Reprogramming Methods: Non-integrating methods, such as Sendai virus (SeV) vectors, are preferred as they minimize the risk of genomic alterations like insertional mutagenesis, thereby enhancing the safety and reliability of hiPSCs for therapeutic applications [13].
- Quality Management System (QMS): Implementing a QMS defines the policies, procedures, and resources for consistent operations. It is essential for complying with international biobanking standards and demonstrating competence to stakeholders [86].
- Pre-analytical QC: This involves rigorous measures during sample collection, including proper labeling, documentation, and handling to minimize variability introduced by factors like ischemia time, temperature, and contamination [86].
FAQ 2: Our iPSC cultures frequently show excessive differentiation (>20%). What are the primary causes and solutions? Excessive differentiation often stems from suboptimal culture conditions and handling. Key corrective actions include [19]:
- Monitor Medium Age: Ensure complete cell culture medium (e.g., mTeSR Plus) is less than two weeks old.
- Manage Passage Timing: Passage cultures when colonies are large and compact but before they overgrow. Actively remove differentiated areas prior to passaging.
- Optimize Passaging: Ensure cell aggregates after passaging are evenly sized and reduce incubation time with dissociation reagents like ReLeSR if the cell line is sensitive.
- Control Environment: Minimize the time culture plates are outside the incubator (aim for less than 15 minutes).
FAQ 3: How does the choice of starting material and reprogramming method impact the success rate of iPSC generation? While the source material (e.g., fibroblasts, PBMCs, LCLs) may not significantly impact success rates, the reprogramming method does. A comparative analysis found that the Sendai virus (SeV) reprogramming method yields significantly higher success rates compared to the episomal reprogramming method [13]. This makes SeV a preferred choice for biobanking where maximizing efficiency and consistency is crucial.
FAQ 4: What ethical and legal considerations are paramount when establishing an iPSC biobank? Ethical and legal compliance is non-negotiable. Key considerations include [87] [88]:
- Informed Consent: Obtain explicit consent confirming that donated samples can be used to generate iPSC lines, which may be shared worldwide with commercial and non-profit organizations for future research, including genomic characterization [87].
- Data Protection: Comply with data protection laws such as the EU's General Data Protection Regulation (GDPR) to ensure the privacy and confidentiality of donor data [88].
- Legal Frameworks: Adhere to national regulations governing human tissue use, such as the UK Human Tissue Act (2004) or the US Common Rule (45 CFR 46) [88].
FAQ 5: What are the recommended quality control measures for a new iPSC line? A tiered QC approach is recommended to ensure pluripotency, genetic integrity, and identity [13] [87].
- Pluripotency Verification: Tests include alkaline phosphatase (AP) staining.
- Genetic Integrity: Perform karyotyping to check for chromosomal abnormalities, and utilize more sensitive techniques like CNV (Copy Number Variation) and SNP (Single Nucleotide Polymorphism) analysis to identify genomic alterations [13].
- Identity Testing: Use Short Tandem Repeat (STR) profiling to confirm cell line identity and exclude cross-contamination [13].
- Sterility Testing: Test for mycoplasma and other microbial contaminants.
Troubleshooting Guides for iPSC Culture
Problem: Low Cell Attachment After Passaging
Potential Causes and Solutions [19]:
- Cause: Initial cell density is too low.
- Solution: Plate 2-3 times the usual number of cell aggregates and maintain a more densely confluent culture.
- Cause: Over-manipulation of cell aggregates during passaging.
- Solution: Work quickly to minimize the time aggregates are in suspension and avoid excessive pipetting. If colonies are dense, increase incubation time with the passaging reagent by 1-2 minutes instead of vigorous pipetting.
- Cause: Incorrect cultureware.
- Solution: Ensure you are using non-tissue culture-treated plates when coating with Vitronectin XF and tissue culture-treated plates when coating with Corning Matrigel.
Problem: Inconsistent Cell Aggregate Size During Passaging
Managing aggregate size is critical for uniform growth [19].
- If aggregates are too large (>200 µm):
- Gently pipette the mixture up and down (without creating a single-cell suspension).
- Increase incubation time with the passaging reagent by 1-2 minutes.
- If aggregates are too small (<50 µm):
- Minimize manipulation after dissociation.
- Decrease incubation time by 1-2 minutes.
Data Presentation: Comparative Analysis of Reprogramming Methods
The table below summarizes findings from a study comparing non-integrating reprogramming methods, highlighting their impact on key quality metrics [13].
Table 1: Impact of Reprogramming Method on iPSC Quality
| Reprogramming Method | Genomic Integration Risk | Relative Success Rate | Key Genomic Integrity Findings |
|---|---|---|---|
| Sendai Virus (SeV) | Non-integrating | Significantly higher than episomal method | Fewer CNVs and SNPs compared to integrating methods [13] |
| Episomal Vectors | Non-integrating | Lower than SeV method | Fewer CNVs and SNPs compared to integrating methods [13] |
| Lentiviral (Historical) | Integrating | Not recommended for biobanking | Higher number of CNVs, SNPs, and chromosomal mosaicism [13] |
Experimental Protocols for Key Biobanking Procedures
- Culture Starting Cells: Maintain fibroblasts or Lymphoblastoid Cell Lines (LCLs) in standard conditions.
- Nucleofection: Use the Amaxa Nucleofector II device with program U-023 (fibroblasts) or U-015 (LCLs) to introduce OriP/EBNA1 episomal vectors.
- Post-Transfection Culture: Maintain transfected cells at 37°C, 5% CO2, and 5% O2. Feed every other day.
- Monitor Efficiency: Assess nucleofection efficiency by monitoring GFP-positive cells.
- Replate and Expand: On days 6-7, replate transfected cells. After 1-2 weeks, manually pick at least 24 clones for expansion and banking.
- Transduction: Transduce fibroblasts or Peripheral Blood Mononuclear Cells (PBMCs) using the CytoTune Sendai Reprogramming Kit.
- Post-Transduction Culture: Refresh medium 24 hours post-transduction. Culture for ~6 more days, exchanging medium every other day.
- Monitor Efficiency: Estimate transduction efficiency by examining GFP-positive cells.
- Replate and Pick Colonies: Harvest and replate cells approximately 7 days (fibroblasts) or 3 days (PBMCs) after transduction. After 2-3 weeks, manually pick at least 24 colonies for expansion.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for iPSC Generation and Culture
| Reagent / Kit Name | Function in Workflow |
|---|---|
| CytoTune Sendai Reprogramming Kit | A non-integrating method for reprogramming somatic cells into iPSCs using Sendai virus vectors [13]. |
| OriP/EBNA1 Episomal Vectors | A non-integrating DNA-based method for delivering reprogramming factors to somatic cells [13]. |
| mTeSR1 / mTeSR Plus Medium | A defined, complete culture medium for the maintenance of human pluripotent stem cells [19]. |
| ReLeSR | A non-enzymatic passaging reagent used for the gentle dissociation of hPSC colonies into cell aggregates [19]. |
| Y-27632 (ROCK inhibitor) | A small molecule that increases cell survival after passaging and thawing by inhibiting apoptosis [13]. |
| Vitronectin XF / Corning Matrigel | Extracellular matrix coatings used for feeder-free culture of iPSCs, providing a substrate for cell attachment and growth [19]. |
Workflow and Relationship Diagrams
iPSC Biobank QC Workflow
Biobank QMS Pillars
Conclusion
Robust quality control is the non-negotiable foundation upon which the entire promise of iPSC technology rests, bridging the gap between basic research and clinical translation. A multi-parametric approach—combining morphological, molecular, functional, and genomic analyses—is essential for comprehensively validating pluripotency and ensuring safety. While significant progress has been made with safer reprogramming methods and advanced analytical tools, challenges in standardization, tumorigenicity risk assessment, and scalable potency assays remain. The future of iPSC QC will be shaped by the integration of AI-driven analytics, the establishment of globally harmonized regulatory standards, and the development of more predictive in vitro safety models. By adhering to rigorous and evolving QC frameworks, researchers and developers can fully leverage the transformative potential of iPSCs to advance regenerative medicine, disease modeling, and drug discovery.
References
- 1. Reassessment of marker genes in human induced ... [https://www.nature.com/articles/s41467-024-52922-1]
- 2. Pluripotent Cell Markers Expression Analysis of Stem Cells [https://www.creative-biolabs.com/stem-cell-therapy/pluripotent-cell-markers-expression-analysis.htm]
- 3. Troubleshooting Guide for STEMdiff™ Cardiomyocyte Kits [https://www.stemcell.com/troubleshooting-guide-for-human-pluripotent-stem-cell-derived-cardiomyocytes.html]
- 4. Decoding the Pluripotency Network: The Emergence of New ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5423462/]
- 5. The transcriptional regulation of pluripotency | Cell Research [https://www.nature.com/articles/cr2012172]
- 6. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 7. Induced pluripotent stem cells: opportunities and challenges [https://pmc.ncbi.nlm.nih.gov/articles/PMC3130417/]
- 8. bFGF-mediated pluripotency maintenance in human induced ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-018-0307-1]
- 9. Distinct Lineage Specification Roles for NANOG, OCT4 ... [https://www.sciencedirect.com/science/article/pii/S1934590912000756]
- 10. Reprogramming Methods Do Not Affect Gene Expression ... [https://www.mdpi.com/1422-0067/18/1/206]
- 11. The Challenges to Advancing Induced Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10768945/]
- 12. Research and therapy with induced pluripotent stem cells ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-019-1455-y]
- 13. Human iPSC Reprogramming Success: The Impact of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11756937/]
- 14. Key Challenges in Clinical iPSC Applications [https://www.reprocell.com/blog/key-challenges-in-clinical-ipsc-applications-how-reprocell-helps-you-succeed]
- 15. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 16. A comprehensive analysis of induced pluripotent stem cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1593207/full]
- 17. Epigenetic mechanisms of induced pluripotency - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4322530/]
- 18. Chromosomal quality control in hPSCs: A practical guide to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12259632/]
- 19. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 20. iPSCs and iPSC-derived cells as a model of human ... [https://www.nature.com/articles/s41467-025-56569-4]
- 21. A Review of the Present State of Epigenetic ... [https://www.fightaging.org/archives/2025/10/a-review-of-the-present-state-of-epigenetic-reprogramming-to-treat-aging/]
- 22. Pluripotent Stem Cells: Current Understanding and Future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4699068/]
- 23. Assessing Morphology of hPSCs Passaged As Aggregates [https://www.stemcell.com/assessing-morphology-of-hpscs.html]
- 24. Surface Topography Guides Morphology and Spatial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5550028/]
- 25. Assess and Maintain Human Pluripotent Stem Cell Quality [https://www.stemcell.com/psc-cell-quality]
- 26. Quality Control: What is really in your hiPSC culture? [https://www.reprocell.com/blog/key-quality-controls-of-human-induced-pluripotent-stem-cells]
- 27. Teratoma formation: A tool for monitoring pluripotency in stem ... [https://www.ncbi.nlm.nih.gov/books/NBK133287/]
- 28. Assessment of established techniques to determine ... [https://www.nature.com/articles/s41467-018-04011-3]
- 29. Teratoma Assay for Testing Pluripotency and Malignancy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9967860/]
- 30. Evaluating teratoma formation risk of pluripotent stem cell- ... [https://www.sciencedirect.com/science/article/pii/S146532492500684X]
- 31. A Review, Analysis and Call for Innovation | Stem Cell ... [https://link.springer.com/article/10.1007/s12015-024-10793-5]
- 32. Reconsidering pluripotency tests: Do we still need teratoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7615844/]
- 33. Methods for Pluripotent Stem Cell Characterization [https://pmc.ncbi.nlm.nih.gov/articles/PMC11815987/]
- 34. Validating human induced pluripotent stem cell-specific ... [https://www.sciencedirect.com/science/article/pii/S1465324924006108]
- 35. Common pitfalls of stem cell differentiation - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5002043/]
- 36. IHC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 37. Quality and Regulatory Requirements for the Manufacture ... [https://pubmed.ncbi.nlm.nih.gov/39821060/]
- 38. Synthetic hydrogel substrate for human induced pluripotent ... [https://pubmed.ncbi.nlm.nih.gov/39504708/]
- 39. Molecular specification of germ layers in vertebrate embryos [https://pmc.ncbi.nlm.nih.gov/articles/PMC4744249/]
- 40. Germ-Layer Specification and Control of Cell Growth by ... [https://www.sciencedirect.com/science/article/pii/S0092867405001078]
- 41. Effect of iPS cell culture medium on the differentiation ... [https://www.nature.com/articles/s41598-025-13259-x]
- 42. Chromosomal aberrations after induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8425414/]
- 43. Need for high-resolution Genetic Analysis in iPSC [https://www.nature.com/articles/s41598-018-35506-0]
- 44. Analyzing Copy Number Variation using SNP Array Data [https://pmc.ncbi.nlm.nih.gov/articles/PMC4015338/]
- 45. The Principles and Workflow of SNP Microarray [https://www.cd-genomics.com/the-principles-and-workflow-of-snp-microarray.html]
- 46. Mycoplasma Contamination [https://www.atcc.org/the-science/authentication/mycoplasma-contamination]
- 47. Prevention and Detection of Mycoplasma Contamination in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3584481/]
- 48. Tips and tricks for iPSC culture [https://www.ptglab.com/news/blog/tips-and-tricks-for-ipsc-culture/?srsltid=AfmBOoo37zAmEc1kD7DPDX1KPsHrCCT1LDB3JUdBkYWVQxDyASPsrV56]
- 49. iPSC Quality Control - Sampled [https://sampled.com/services/cellular-services/ipsc-services/ipsc-quality-control/]
- 50. iPSC Quality Control: 4 Important Reasons for Robust Control [https://sampled.com/ipsc-quality-control-4-reasons/]
- 51. The emerging promise of induced pluripotent stem cells in ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925008461]
- 52. Genomic Instability of iPSCs: Challenges Towards Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5346115/]
- 53. Genetic instability of iPSCs: Why does it matter? [https://www.cellgs.com/blog/genetic-instability-of-ipscs-why-does-it-matter.html]
- 54. Frequently Asked Questions on iPSCs [https://www.stemcell.com/ipsc-faq.html]
- 55. iPSC Maintenance Challenges and How to Overcome Them [https://definedbioscience.com/blogs/news/ipsc-maintenance-challenges-and-how-to-overcome-them?srsltid=AfmBOorGHbz6y5FF1JMaSGA5b9gt9W4nrQ0GuZRo45RURqFW6yIPgti0]
- 56. Tips and tricks for successfully culturing and adapting human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8640166/]
- 57. Potency Assay Variability Estimation in Practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11788244/]
- 58. From nascent to mainstream: Overcoming barriers in iPSC ... [https://ct.catapult.org.uk/news/from-nascent-to-mainstream-overcoming-barriers-in-ipsc-therapy-development]
- 59. 北京西美杰科技有限公司 [http://www.xmjsci.com/]
- 60. ELISA 试剂盒批间可重复性:保障数据的质量 - CST 博客 [https://blog.cellsignal.cn/elisa-kit-lot-to-lot-reproducibility]
- 61. 增强抗体验证 [https://www.sigmaaldrich.com/HK/zh/technical-documents/technical-article/protein-biology/immunohistochemistry/antibody-enhanced-validation?srsltid=AfmBOopBWQhcXWN_tUrSQIov7zfxfHt5oV3oWDgcK1Zt2WELGozlN5y_]
- 62. Engineering the next generation of allogeneic CAR cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277817/]
- 63. Clinical translation of human iPSC technologies: advances ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1627149/full]
- 64. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 65. Epigenetic regulation of reprogramming and pluripotency [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1559183/full]
- 66. A Machine Learning Assisted, Label-free, Non-invasive Approach for... [https://www.nature.com/articles/s41598-017-13680-x?error=cookies_not_supported]
- 67. Smarter stem cells: how AI is supercharging iPSC technology [https://link.springer.com/article/10.1007/s00441-025-03999-7]
- 68. of Automation culture, passaging, and expansion with... iPSC [https://www.moleculardevices.com/en/assets/app-note/dd/3d-biology/automation-of-ipsc-culture-passaging-and-expansion-with-cellxpress-ai-automated-cell-culture-system]
- 69. The use of artificial intelligence in induced pluripotent stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11108174/]
- 70. Suspension culture improves iPSC expansion and ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03382-9]
- 71. Comparison of Human Induced Pluripotent and Embryonic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3070108/]
- 72. Pluripotent Stem Cells: Recent Advances and Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025069/]
- 73. Chromatin accessibility dynamics during cell fate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7857421/]
- 74. Chromatin landscape dynamics during reprogramming ... [https://www.nature.com/articles/s41420-024-02230-w]
- 75. How To Overcome Potency Assay Development ... [https://www.cellandgene.com/doc/how-to-overcome-potency-assay-development-challenges-for-gene-therapies-0001]
- 76. Navigating Challenges in Cell Therapy Potency Assays [https://www.biopharminternational.com/view/navigating-challenges-in-cell-therapy-potency-assays]
- 77. Pluripotent stem cell assays: Modalities and applications for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9130094/]
- 78. a review of key challenges by the JSRM-ISCT iPSC Committee [https://pubmed.ncbi.nlm.nih.gov/38958627/]
- 79. Characterization of human induced pluripotent stems cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC9929203/]
- 80. Key tips and technologies for the development of iPSC- ... [https://www.biotechniques.com/drug-discovery-development/sartorius_ipsccgt_key-tips-and-technologies-for-the-development-of-ipsc-derived-cell-therapies/]
- 81. Overcoming Barriers of CRISPR Gene Editing in iPS Cells [https://www.synthego.com/blog/ipsc-crispr-editing/]
- 82. Unlocking the Power of iPSCs: iPSC Product Categories ... [https://bioinformant.com/ipsc-product-categories/]
- 83. CRISPR and iPSCs: Recent Developments and Future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9428373/]
- 84. Country-specific regulation and international ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10444560/]
- 85. Why Early Genetic Variant Detection in iPSC Cultures Is ... [https://www.reprocell.com/blog/why-early-genetic-variant-detection-in-ipsc-cultures-is-critical-for-safe-and-regulatory-compliant-cell-therapies]
- 86. Quality control- Backbone of Human Biorepositories [https://www.cureline.com/news/quality-control-backbone-of-human-biorepositories-1693999788.html]
- 87. EBiSC best practice: How to ensure optimal generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8365092/]
- 88. ISO 20387 and Other Biobanking Quality Standards [https://biosamplehub.org/iso-20387/]