Ensuring Safety and Efficacy: A Comprehensive Guide to Genomic Stability Assessment in Stem Cells
This article provides researchers, scientists, and drug development professionals with a detailed overview of the critical methods for assessing genomic stability in human pluripotent stem cells (hPSCs).
Ensuring Safety and Efficacy: A Comprehensive Guide to Genomic Stability Assessment in Stem Cells
Abstract
This article provides researchers, scientists, and drug development professionals with a detailed overview of the critical methods for assessing genomic stability in human pluripotent stem cells (hPSCs). It covers the foundational knowledge of why hPSCs are prone to genetic alterations, explores the full spectrum of current detection methodologies—from karyotyping to next-generation sequencing and optical genome mapping—and offers practical guidelines for their application. Furthermore, it delivers comparative analyses to inform method selection, troubleshooting strategies for common challenges in quality control, and a forward-looking perspective on integrating these techniques to ensure the safety and efficacy of clinical-grade stem cell therapies.
The Genomic Stability Imperative: Why Stem Cells Acquire Variations and the Associated Clinical Risks
Genomic instability represents one of the most significant challenges in the application of stem cell technologies for research and clinical translation. The processes of cellular reprogramming to create induced pluripotent stem cells (iPSCs) and the subsequent long-term culture necessary for their expansion and differentiation can introduce genetic alterations that compromise both the functionality and safety of these cells. For researchers, scientists, and drug development professionals, understanding the precise mechanisms behind this instability is crucial for developing robust quality control measures and safer stem cell-based therapies. This guide examines the key drivers of genomic instability by comparing the genetic alteration profiles across different stem cell technologies, with a particular focus on iPSCs and the newer conditional reprogramming (CR) technology, providing objective experimental data to inform model selection and quality assessment protocols.
Mechanisms and Origins of Genomic Instability
The genomic alterations observed in stem cells originate from multiple sources throughout the cell culture lifecycle. These variations can be categorized into three primary origins based on when they emerge during the cell processing pipeline.
Table 1: Origins of Genomic Variations in Stem Cells
| Origin Category | Description | Common Alterations |
|---|---|---|
| Pre-existing Variations [1] | Somatic mutations present in parental cells that are fixed and expanded during reprogramming due to the clonal nature of the process. | Single nucleotide variants (SNVs), Copy number variations (CNVs) |
| Reprogramming-Induced [1] [2] | Mutations acquired during the reprogramming process itself, attributed to the replicative stress and profound epigenetic remodeling involved. | Point mutations, Copy number alterations (CNAs) |
| Passage-Induced [1] [3] | Alterations that arise during extended in vitro culture, often providing a selective growth advantage that leads to their dominance in the culture. | Aneuploidy (e.g., Trisomy 12, X), Specific CNVs (e.g., 20q11.21 amplification) |
A key driver of passage-induced instability is the selective pressure that occurs during routine culture. Certain genetic abnormalities confer a growth advantage, allowing variant cells to outcompete their normal counterparts. For instance, amplifications of chromosome 20q11.21, a recurrent abnormality in pluripotent stem cells (PSCs), contain the BCL2L1 gene, an anti-apoptotic factor that enhances cell survival [3]. Similarly, trisomy 12 is frequently observed, potentially because this chromosome contains pluripotency-associated genes like NANOG that improve self-renewal [1].
Comparative Genomic Stability Across Cell Technologies
Different cell culture technologies exhibit varying propensities for genomic instability, a critical factor in model selection for research and therapy development.
Table 2: Technology Comparison of Genomic Stability and Features
| Feature | Transformed Cell Lines [4] | Induced Pluripotent Stem Cells (iPSCs) [4] [1] | Conditionally Reprogrammed (CR) Cells [4] |
|---|---|---|---|
| Success Rate | Medium | Medium | High |
| Genetic Stability | Low | Medium | High |
| Tissue Specificity | Low | Low | High |
| Heterogeneity | No | Medium | Medium |
| Tumorigenicity Risk | High | Medium (Teratoma/Tumor formation) [5] | Low (Form tumors in mice, but maintain original genetics) [4] [6] |
| Key Genetic Alterations | N/A | Trisomy 12, 20q11.21 amplification, TP53 mutations [1] [3] | Maintains original tumor genetics in early passages [6] |
The method used for reprogramming iPSCs also significantly impacts genomic stability. A systematic study comparing Sendai virus (SV) and episomal vector (Epi) methods found that all SV-iPS cell lines exhibited copy number alterations (CNAs) during reprogramming, compared to only 40% of Epi-iPS cells. Furthermore, single-nucleotide variations (SNVs) were observed exclusively in SV-derived cells during passaging and differentiation [2].
Conditional reprogramming (CR) presents an alternative with potentially higher genetic stability. This technology uses a Rho kinase inhibitor (Y-27632) and feeder cells to rapidly propagate primary epithelial cells without genetic manipulation [4]. Genomic studies have shown that early-passage CR cells from breast cancer patients maintained over 95% overlap in copy number alteration patterns with their original primary tumors and retained the same somatic mutations, demonstrating significant genomic fidelity [6].
Essential Experimental Assessment Methodologies
Rigorous and regular genomic assessment is mandatory for characterizing stem cell lines. The International Society for Stem Cell Research (ISSCR) emphasizes the need for independent oversight, accountability, and transparency at each research stage [7]. A comprehensive genomic stability workflow should be implemented at multiple critical points.
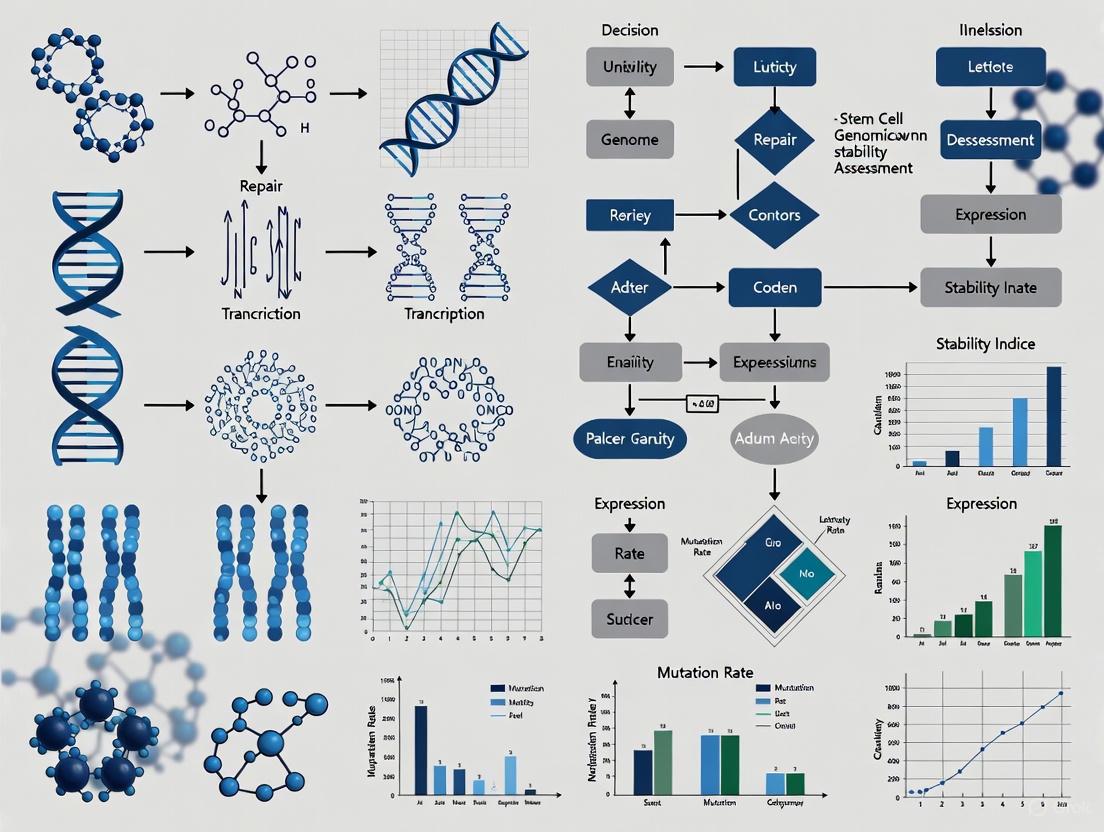
Figure: Genomic Stability Workflow. A practice-oriented testing pipeline for pluripotent stem cells, outlining key stages where genomic assessment is critical. Adapted from Stem Genomics recommendations [8].
Table 3: Key Methods for Genomic Instability Detection
| Method | Detection Capability | Resolution | Best Use Case | Protocol Summary |
|---|---|---|---|---|
| Karyotyping (G-banding) [1] [8] | Numerical and large structural chromosomal changes. | ~5-10 Mb | Initial and final cell line characterization. | Cells arrested in metaphase, dropped onto slides, Giemsa-stained, and chromosomes analyzed microscopically. |
| Digital PCR [8] | Targeted CNV detection (e.g., 20q11.21). | Single gene | High-frequency in-process monitoring and clone screening. | DNA partitioned into thousands of droplets; target amplification is measured absolutely to quantify copy number. |
| Next-Generation Sequencing (NGS) [1] [8] | Genome-wide SNVs, Indels, and CNVs. | Single nucleotide | Comprehensive profiling at acquisition, banking, and pre-clinical stages. | Fragmented DNA is adapter-ligated, clonally amplified, and sequenced in parallel; data is aligned to a reference genome for variant calling. |
For specific applications like assessing DNA strand breaks under stress conditions, novel biosensors offer sensitive alternatives. One advanced method utilizes a TdT enzyme-Endo IV-fluorescent probe biosensor, which recognizes 3'-hydroxyl ends at DNA breakpoints, extends them to form a poly-A sequence, and cleaves a fluorescent probe for signal amplification, providing a parameter called the Mean number of DNA breakpoints (MDB) [9].
The Scientist's Toolkit: Essential Research Reagents
A selection of key reagents is fundamental for conducting research in stem cell genomic stability.
Table 4: Essential Research Reagents and Kits
| Reagent/Kit Name | Primary Function | Key Application in Genomic Stability Research |
|---|---|---|
| Rho-Kinase (ROCK) Inhibitor (Y-27632) [4] | Inhibits ROCK-mediated apoptosis. | Essential for conditional reprogramming of primary cells; enhances survival of single cells. |
| Irradiated Swiss 3T3-J2 Fibroblasts [4] | Serves as feeder cells. | Provides necessary signaling and structural support for the growth of conditionally reprogrammed epithelial cells. |
| STEMdiff Mesenchymal Progenitor Kit [2] | Directed differentiation of iPSCs. | Generates iPS-derived mesenchymal stromal/stem cells (iMS cells) for studying genomic changes during differentiation. |
| TdT -Endo IV-Fluorescent Probe Biosensor [9] | Detects DNA strand breaks. | Quantifies DNA integrity in stem cells under stress (e.g., heat, cryopreservation) via a highly sensitive fluorescence signal. |
| CytoTune-iPS Sendai Reprogramming Kit [2] | Delivers reprogramming factors via non-integrating virus. | Generates iPSCs from somatic cells; used in comparative studies on reprogramming-induced genomic instability. |
The journey of a cell from its somatic state through reprogramming and prolonged culture is fraught with opportunities for genomic instability to arise, driven by factors from pre-existing mutations to culture-adapted selective advantages. A comparative analysis reveals that while no technology is immune to these changes, their nature and frequency vary significantly—iPSCs are susceptible to specific aneuploidies and mutations in genes like TP53, whereas CR cells demonstrate strong genomic fidelity to their tissue of origin, at least in early passages. For researchers and drug developers, this underscores the necessity of a rigorous, multi-stage quality control workflow that leverages complementary detection methods from karyotyping to NGS. The choice of cell technology and reprogramming method must be aligned with the application's specific needs, always balancing growth potential with genetic integrity to ensure the safety and efficacy of future stem cell-based applications.
The comprehensive assessment of genomic stability is a critical prerequisite for the clinical application of stem cells. Human induced pluripotent stem cells (hiPSCs) are susceptible to genomic instability throughout the reprogramming and extended culture processes, which poses a potential risk to the clinical application of cell-based therapies [10]. Genomic instability encompasses a spectrum of alterations, from single-nucleotide variations (SNVs) and small insertions and deletions (indels) to more complex rearrangements such as copy number variations (CNVs), structural variations (SVs), and whole-chromosome aneuploidies [10]. These alterations can originate from the initial cell state, emerge during reprogramming of somatic cells into iPSCs, or accumulate during subsequent amplification and cell banking [10].
The clinical implications of these genetic alterations are profound. Genomic instability not only affects the differentiation capacity of iPSCs but may also trigger safety issues such as tumorigenesis [10]. For example, chromosomal amplifications of oncogenes such as BCL2L1 and c-MYC, or mutation/loss of TP53, are associated with the transformation of transplanted iPSCs into tumor cells [10]. This comparison guide objectively evaluates the detection methodologies for the full spectrum of genetic alterations in stem cells, providing researchers with experimental protocols and performance data for informed technology selection.
Classification and Characterization of Genetic Alterations
Structural Variants (SVs)
Structural variants represent genomic variations that involve breakage and rejoining of DNA segments ≥50 base pairs, potentially altering gene dosage, disrupting gene regulation, or creating novel fusion genes [11]. Based on their architectural features, SVs are classified into several categories. Simple SVs include deletions, duplications, insertions, and inversions, while complex structural variants involve combinations of multiple SV types with clustered breakpoints originating from a single event [12] [11]. Catastrophic genomic events like chromothripsis (localized chromosomal shattering and random reassembly), chromoplexy (interconnected inter- and intra-chromosomal translocations), and chromoanasynthesis (replication-based complex rearrangements with copy-number gains) represent the most complex categories [11].
The mutagenesis mechanisms underlying SVs vary considerably. Non-allelic homologous recombination (NAHR) between low-copy repeats or segmental duplications leads to recurrent rearrangements with consistent breakpoints across individuals [11]. Non-homologous end joining (NHEJ) and microhomology-mediated end joining (MMEJ) repair double-strand breaks using little or short microhomologous sequences (5-25 bp), respectively [11]. Replication-based mechanisms like fork stalling and template switching (FoSTeS) and microhomology-mediated break-induced replication (MMBIR) contribute to complex rearrangements [11].
Copy Number Variations (CNVs) and Aneuploidy
CNVs are a subclass of SVs encompassing deletions or duplications/amplifications that typically range from 1 kilobase to several megabases [11]. These variants can be recurrent, with consistent size and breakpoints mediated by NAHR between segmental duplications, or non-recurrent, with varying sizes that share a minimal region of overlap encompassing dosage-sensitive genes [11].
Aneuploidy refers to the gain or loss of entire chromosomes, representing the most macroscopic form of genomic alteration. In stem cell cultures, specific recurrent aneuploidies such as gains of chromosomes 12, 17, and 20 provide selective growth advantages, leading to their overgrowth in culture conditions [10].
Single-Nucleotide Variations (SNVs) and Small Indels
SNVs and small insertions or deletions (indels) represent changes at the single-base-pair level. During iPSC culture, these mutations can accumulate over time, with some occurring in genes associated with tumors or diseases, such as CDH1 and BCOR [10]. The mutation rate and spectrum of these variations can be influenced by the reprogramming method and culture conditions [13].
Table 1: Spectrum of Genetic Alterations in Stem Cells
| Alteration Type | Size Range | Detection Methods | Common Genomic Locations | Functional Impacts |
|---|---|---|---|---|
| Aneuploidy | Entire chromosomes | Karyotyping, OGM | Chr12, 17, 20 gains | Altered gene dosage, growth advantage |
| CNVs (deletions/duplications) | 1 kb - several Mb | Microarray, OGM, WGS | Regions with segmental duplications | Gene dosage changes, gene disruption |
| Complex SVs | 50 bp - several Mb | OGM, long-read WGS | Multiple clusters | Gene fusions, regulatory rewiring |
| Simple SVs (inversions, translocations) | ≥50 bp | OGM, WGS | Genome-wide | Regulatory disruption, gene interruption |
| SNVs/Indels | 1 - 50 bp | WES, WGS | Coding regions, regulatory elements | Protein function changes, splice defects |
Detection Methodologies and Performance Comparison
Technological Platforms for Genetic Alteration Detection
Multiple technological platforms are employed for comprehensive genomic assessment, each with unique capabilities and limitations for detecting different classes of genetic alterations.
Karyotyping represents the traditional approach for identifying chromosomal anomalies in hiPSCs, yet it is limited to detecting alterations exceeding 5 Mb in size and lacks precision in pinpointing exact breakpoints [10]. The minimum mosaicism detected is 12% by routine analysis of 50 metaphase spreads [10].
Optical Genome Mapping (OGM) creates large-sized marked DNA fragments that can be assembled into whole-genome maps efficiently [10]. This technology can detect chromosomal structural variants with higher resolution than karyotyping (≥500 bp), and with higher accuracy than short-read next-generation sequencing techniques [10]. OGM effectively identifies SVs and CNVs below karyotyping resolution, particularly recurrent genome abnormalities such as gains on chr17q, chr12p, and chr20q [10].
Sequencing Technologies include whole-exome sequencing (WES) and whole-genome sequencing (WGS). WES and WGS are capable of detecting SNVs, Indels, and CNVs, though with limitations [10]. Short-read WGS has poor detection capabilities for low-frequency variants and SVs in repetitive regions, while long-read sequencing technologies (e.g., Pacific Biosciences) offer advantages for spanning complex structural variations but may have higher error rates for SNVs [14].
Table 2: Performance Comparison of Genomic Assessment Technologies
| Technology | Resolution | SV Detection Capability | Aneuploidy Detection | SNV/Indel Detection | Throughput | Cost |
|---|---|---|---|---|---|---|
| Karyotyping | >5 Mb | Limited (large balanced) | Excellent | None | Low | Low |
| Chromosomal Microarray | >50 kb | CNVs only | Yes | None | Medium | Medium |
| Optical Genome Mapping | ≥500 bp | Excellent for CNVs, SVs | Yes | Limited | Medium | Medium |
| Short-read WGS | Single base | Moderate for small SVs | Possible | Excellent | High | High |
| Long-read WGS | Single base | Excellent for complex SVs | Possible | Good (higher error rate) | Medium | Highest |
| Whole Exome Sequencing | Single base | Limited | No | Excellent (coding only) | High | Medium |
Integrated Assessment Approaches
Research demonstrates that each method has unique detection capabilities and limitations, and only integrative approaches can comprehensively identify genomic abnormalities [10]. One study established a comprehensive strategy for evaluating the genetic stability of hiPSCs by integrating karyotyping, OGM, WES, and RNA-seq, which can be applied to scenarios such as hiPSC clone screening, establishment of cell bank passages, and quality control of hiPSC-derived products [10].
For clinical applications, the selection of healthy hiPSC clones with normal chromosomes and genomes at the source is crucial for downstream cell banking [10]. Determining the maximum number of permissible passages during continuous subculturing requires accurate and sensitive detection methods that can truly reflect genetic variations [10].
Figure 1: Integrated Workflow for Comprehensive Genetic Assessment. This workflow illustrates how different detection methods contribute to identifying the full spectrum of genetic alterations in stem cells.
Experimental Protocols for Genomic Assessment
Comprehensive Genomic Stability Assessment Protocol
A comprehensive protocol for assessing stem cell genomic stability involves multiple parallel analyses. Three hiPSC lines were continually cultured in vitro for 50 passages, with genome stability evaluated every 10 passages using the following integrated methodology [10]:
Karyotyping Protocol: Before cell harvesting, colchicine is added directly to the plate of cells achieving a final concentration of 100 ng/ml for 40 minutes. Cells are then trypsinized, treated with a hypotonic solution for 20 minutes, and fixed. Metaphases are spread on microscope slides and stained using the standard G-banding technique. For chromosomal number analysis, 500 metaphases are counted, then 50 metaphases are photographed and classified in accordance with the International System for Human Cytogenetic Nomenclature [10].
Optical Genome Mapping Protocol: Ultra-high molecular weight (UHMW) genomic DNA is extracted from 1.5 × 10^6 cells using the Prep SP-G2 Blood & Cell Culture DNA Isolation Kit. DNA quantification is performed using the Qubit dsDNA BR Assay Kit. A total of 750 ng of UHMW DNA is labeled using the Bionano Prep DLS-G2 Labeling Kit. The labeled UHMW DNA is quantified and loaded onto the Saphyr Chip G2.3 at a concentration of 4 to 15 ng/μL and run on a Bionano Saphyr Gen2 instrument. A total of 2,000 GB of data are collected per sample. DNA molecules with an average mapping rate greater than 70% and a minimum length of 150 kbp are selected for subsequent analysis using the Rare Variant Analysis pipeline in Bionano Solve version 3.6.1 [10].
Whole-Exome Sequencing Protocol: While the specific protocol was not detailed in the search results, WES typically involves capture of exonic regions followed by high-throughput sequencing. This method reveals coding mutations, including germline short variants and newly acquired somatic mutations [10].
RNA Sequencing Protocol: Total RNA is extracted from 2 × 10^6 cells using TRIzol reagent. After DNase I digestion, RNA concentration and integrity are detected using Agilent 2100 Bioanalyzer. Library preparation follows standard protocols for RNA sequencing [10].
Specialized Protocol for Detecting Complex Structural Variants
For comprehensive detection of complex de novo structural variants (dnSVs), specialized bioinformatics approaches are required. One study developed a rigorous pipeline to analyze an average of 13,980 candidate variants per proband, called using the Manta caller [12]. The protocol involves:
- Variant Calling: Initial identification of candidate SVs using specialized callers like Manta [12].
- Filtering and Classification: Application of stringent filters to remove false positives and classification of complex dnSVs into subtypes based on breakpoint architecture [12].
- Visual Inspection: Manual curation and visual inspection of all high-confidence dnSVs using integrative genomics viewers [12].
- Validation: Experimental validation using orthogonal methods such as long-read sequencing or array-based comparative genomic hybridization [12].
This approach identified 1,870 dnSVs in 13,698 offspring with rare diseases, with complex dnSVs (8.4%) emerging as the third most common type following simple deletions and duplications [12].
Research Reagent Solutions and Materials
Table 3: Essential Research Reagents for Genomic Stability Assessment
| Reagent/Kit | Manufacturer | Function | Application Context |
|---|---|---|---|
| Prep SP-G2 Blood & Cell Culture DNA Isolation Kit | Bionano Genomics | UHMW DNA extraction | Optical Genome Mapping |
| Bionano Prep DLS-G2 Labeling Kit | Bionano Genomics | DNA labeling for OGM | Structural variant detection |
| Saphyr Chip G2.3 | Bionano Genomics | Platform for OGM analysis | High-resolution genome mapping |
| CytoTune-iPS 2.0 Sendai Reprogramming Kit | Thermo Fisher Scientific | iPSC generation | Stem cell reprogramming |
| Episomal iPS Cell Reprogramming Vectors | Thermo Fisher Scientific | Non-viral iPSC generation | Footprint-free reprogramming |
| STEMdiff Mesenchymal Progenitor Kit | StemCell Technologies | MSC differentiation | Stem cell differentiation studies |
| mTeSR1 Medium | StemCell Technologies | iPSC maintenance | Pluripotent stem cell culture |
| MesenCult-ACF Medium | StemCell Technologies | MSC culture | Mesenchymal stem cell expansion |
Data Interpretation and Analytical Frameworks
Analytical Considerations for Different Alteration Types
The interpretation of genetic alterations requires different analytical frameworks depending on the variant type. For CNVs and SVs, researchers should cross-reference findings with population databases like the Database of Genomic Variants (DGV) and gnomAD-SV to distinguish common polymorphisms from potentially pathogenic alterations [11]. The clinical relevance should be evaluated based on the genomic content affected, including dosage-sensitive genes, regulatory regions, and topologically associating domains (TADs) [11].
For SNVs and small indels, annotation using tools like ANNOVAR or VEP followed by filtering against population frequency databases (e.g., gnomAD) is essential. Pathogenicity prediction scores (CADD, SIFT, PolyPhen-2) help prioritize potentially functional variants [10].
Complex structural variants require special attention as they may involve multiple breakpoints and different mutation mechanisms. The analysis should characterize the architecture, identify the involved genomic elements, and infer the potential mutational mechanism (e.g., FoSTeS/MMBIR for replication-based events) [12] [11].
Quality Control Metrics and Standards
The International Society for Stem Cell Research (ISSCR) recommends establishing quality control metrics for stem cell-based model systems [15]. Key recommendations include:
- Characterization of Starting Material: Document the cell line or tissue of origin, isolation procedure, and culture conditions, as these can influence variability and reproducibility [15].
- Donor Information: Record sex, age, ethnic and genetic background, health status, and risk factors of the donor, where available and as permitted by regulations [15].
- Functional Validation: Demonstrate that cellular models are functionally and phenotypically representative of the native cell/tissue by multiple, appropriate criteria [15].
- Genetic Validation: Where assessing the impact of a known genotype, confirm the stem cell-derived disease model carries the expected genotype [15].
- Proper Controls: Use power analysis to determine sample size and include appropriate controls considering biological variability [15].
Figure 2: Structural Variant Interpretation Pipeline. This framework outlines the analytical process for classifying and determining the clinical significance of structural variants identified in stem cell genomes.
The comprehensive assessment of the genomic stability of stem cells requires a multi-technology approach, as each method offers unique capabilities and limitations. Karyotyping remains essential for detecting chromosomal-scale abnormalities, while optical genome mapping provides superior resolution for structural variants, and sequencing technologies enable base-pair level detection of small variants [10]. The integration of these methods is crucial for different applications in the stem cell pipeline, from clone selection and bank establishment to quality control of differentiated products [10].
Future directions in the field will likely focus on standardizing assessment protocols across laboratories, improving the resolution and throughput of long-read sequencing technologies, and developing better bioinformatic tools for complex variant interpretation. As the stem cell field advances toward clinical applications, robust genomic assessment will play an increasingly critical role in ensuring the safety and efficacy of stem cell-based therapies.
Chromosomal instability is a hallmark of genomic instability in cancer and a critical parameter in assessing the safety and efficacy of stem cell-based therapies. Specific recurrent abnormalities on chromosomes 1, 12, 17, and 20 serve as key markers of high-risk disease across multiple malignancies. This review systematically compares the clinical significance, frequency, and molecular pathways associated with these abnormalities, providing a comprehensive analysis of their roles in disease progression and treatment resistance. We further detail experimental methodologies for their detection and analysis, offering a standardized framework for genomic stability assessment in both clinical and research settings. Understanding these high-risk loci is paramount for developing targeted therapeutic strategies and improving risk-adapted treatment approaches.
Genomic instability represents a fundamental property of cancer cells and a significant concern in regenerative medicine, where it can compromise the safety of stem cell-based therapeutics [16]. Specific chromosomal loci are predisposed to recurrent abnormalities that drive oncogenesis, disease progression, and therapeutic resistance [17] [18]. Among these, chromosomes 1, 12, 17, and 20 harbor high-risk abnormalities that consistently emerge as markers of aggressive disease across diverse malignancies, including multiple myeloma, neuroblastoma, and various solid tumors.
The assessment of these chromosomal abnormalities provides critical insights into disease biology and patient prognosis. In multiple myeloma, for instance, cytogenetic abnormalities detected by fluorescence in situ hybridization (FISH) represent the most widely accepted predictors for poor prognosis [17]. Similarly, in neuroblastoma, gain of chromosome 17q is recognized as the strongest indicator of adverse outcome [19]. These abnormalities not only serve as prognostic markers but also represent potential therapeutic targets, making their systematic characterization essential for advancing precision medicine approaches.
This review synthesizes current understanding of high-risk loci on chromosomes 1, 12, 17, and 20, comparing their pathological significance, frequency, and clinical implications across different disease contexts. We further elaborate standardized experimental protocols for their detection and analysis, providing researchers and clinicians with comprehensive methodological guidance for genomic stability assessment.
Comparative Analysis of High-Risk Chromosomal Abnormalities
Chromosome 1 Abnormalities
Chromosome 1 abnormalities represent some of the most frequent cytogenetic alterations in cancer, particularly in multiple myeloma, where they occur in approximately 40% of newly diagnosed cases [18]. The instability of chromosome 1 manifests primarily through copy number variations (CNV) and structural changes, with gain of 1q (+1q) and deletion of 1p (del(1p)) being the most clinically significant [17] [18].
Pathogenic Mechanisms and Clinical Impact: The 1q21 region contains several genes implicated in myeloma pathogenesis, including CKS1B, MCL-1, ADAR1, and IL-6R [18]. Gain of 1q leads to overexpression of these genes, driving tumor progression through multiple pathways: CKS1B promotes cell cycle progression by activating cyclin-dependent kinases and facilitating SKP2-mediated ubiquitination of the tumor suppressor p27Kip1 [18]; MCL-1 enhances survival by inhibiting apoptosis [18]; and ADAR1 contributes to malignant transformation through RNA editing mechanisms [18]. Clinically, +1q is associated with significantly worse overall survival (HR, 1.4; 95% CI, 1.097–1.787) and progression-free survival (HR, 1.36; 95% CI, 1.16–1.58) in multiple myeloma patients [20]. The adverse prognosis is further exacerbated when +1q co-occurs with other high-risk abnormalities such as del(17p), t(14;16), or del(13q) [20].
Copy Number Considerations: The prognostic impact of +1q varies with copy number burden. Patients are categorized as having gain(1q) (three total copies) or amp(1q) (four or more total copies) [18]. While some studies report worse outcomes with increasing copy number, others found no significant differences in progression-free or overall survival between patients with three versus four or more copies [20]. This suggests that the mere presence of +1q, rather than its magnitude, may be the primary determinant of adverse outcomes.
Chromosome 12 Abnormalities
Abnormalities of chromosome 12 are prominently associated with testicular germ cell tumors (GCTs) but also play significant roles in other malignancies, including inflammatory bowel disease and select solid tumors [21].
Isochromosome 12p in Germ Cell Tumors: The pathognomonic abnormality in malignant GCTs is increased representation of genetic material on chromosome 12p, either through gene amplification or formation of an isochromosome 12p [i(12p)] [21]. This abnormality is identified in nearly 100% of invasive malignant GCTs but appears normal in pre-invasive conditions like intratubular germ cell neoplasia unclassified (ITGCN), spermatocytic seminoma, and pediatric epidermoid cysts [21]. This specific association suggests a crucial role for genes on 12p in the transition from pre-invasive to invasive disease, though the specific driver genes remain unidentified.
Other Clinical Associations: Beyond GCTs, chromosome 12 harbors susceptibility loci for inflammatory bowel disease (IBD), particularly the IBD2 locus at 12q13-14 [21]. Linkage studies have demonstrated significant association between this region and ulcerative colitis, though the specific gene responsible remains elusive despite investigation of candidates including interferon gamma (IFNG), keratin 8 (KRT8), and natural-resistance-associated macrophage protein (NRAMP2) [21].
Chromosome 17 Abnormalities
Chromosome 17 abnormalities represent critical events in multiple cancer types, with distinct pathological implications depending on the specific region affected.
17p13 Deletions in Multiple Myeloma: Deletion of 17p13 [del(17p)], which encompasses the TP53 tumor suppressor gene, occurs in 5-10% of newly diagnosed multiple myeloma cases and confers particularly poor prognosis [17]. TP53 plays a central role in cell cycle arrest, apoptosis, and DNA repair, and its loss confers resistance to conventional therapies and promotes genomic instability. The adverse impact of del(17p) is magnified when it co-occurs with other high-risk abnormalities, leading to significantly shorter survival [17].
17q Gains in Neuroblastoma: Gain of chromosome 17q is the most frequent genetic abnormality in neuroblastoma, present in 72% of cases, and represents the strongest independent indicator of adverse outcome [22] [19]. Research indicates that gain of chromosome 17 is an initial genetic event in neuroblastoma development, with additional copies of 17q acquired during clonal evolution in aggressive and metastatic disease [19]. The minimal common region of gain is 17q21-qter, and this abnormality is strongly associated with other unfavorable prognostic factors including 1p deletion, 11q deletion, and advanced disease stage [22].
Candidate Oncogenes on 17q: PPM1D (located at 17q22.3) has emerged as a strong candidate oncogene driving neuroblastoma progression [19]. PPM1D encodes a p53-inducible serine/threonine phosphatase that negatively regulates p53 activity, creating a negative feedback loop. Activation of PPM1D through segmental 17q gain, gene fusion, or gain-of-function mutations promotes tumor development and progression [19]. This makes PPM1D a promising therapeutic target in high-risk neuroblastoma.
17q12 Deletion Syndrome: Unlike the oncogenic implications of 17q gain, the recurrent 1.4-Mb heterozygous deletion at 17q12 causes a distinct multisystem disorder characterized by kidney abnormalities, maturity-onset diabetes of the young type 5 (MODY5), and neurodevelopmental conditions [23]. This condition underscores the diverse pathological consequences of chromosomal abnormalities depending on the specific genes affected.
Chromosome 20 Abnormalities
Mosaic Trisomy 20: Complete trisomy 20 is considered incompatible with life, but mosaic trisomy 20 (three chromosomes 20 in some cells) is compatible with survival and presents with highly variable phenotypes [24]. Clinical features may include craniofacial abnormalities, cutaneous manifestations, cardiovascular-pulmonary defects, gastrointestinal issues, endocrinological disturbances, reproductive anomalies, locomotor problems, and neurodevelopmental conditions [24]. Recent evidence indicates that neuropsychiatric manifestations may be more prevalent than previously recognized, with cases exhibiting complex neuropsychiatric presentations including self-injury, suicidal ideation, emotional dysregulation, and social difficulties [24].
Ring Chromosome 20 Syndrome: This rare condition results from deletion of the long arm of chromosome 20, forming a ring structure [25]. It presents with refractory epilepsy, characterized by nonconvulsive status epilepticus and brief motor seizures, typically beginning between ages 2 and 14 years [25]. Most cases are refractory to antiepileptic drugs, and patients often experience intellectual disability and behavioral regression [25].
Other Associations: Chromosome 20 also harbors the ADAM33 gene, identified as an asthma-associated gene expressed in lung fibroblasts and bronchial smooth muscle cells [25]. While its precise biological role remains unclear, ADAM33 is hypothesized to contribute to airway remodeling in asthma pathogenesis.
Table 1: Comparative Analysis of High-Risk Chromosomal Abnormalities
| Chromosome | Abnormality | Frequency | Key Genes | Associated Cancers/Conditions | Clinical Significance |
|---|---|---|---|---|---|
| 1 | Gain(1q)/Amp(1q) | 35-40% of NDMM [18] | CKS1B, MCL-1, ADAR1, IL-6R [18] | Multiple myeloma | Independent risk factor for inferior OS (HR, 1.4) and PFS (HR, 1.36) [20] |
| 1 | Del(1p) | 20-30% of NDMM [17] | FAM46C, CDKN2C, TP73 [17] | Multiple myeloma | Associated with poor prognosis; compound effect with other HRCAs [17] |
| 12 | Isochromosome 12p | Nearly 100% of malignant GCTs [21] | Not fully characterized | Testicular germ cell tumors | Marker of invasive disease; not found in pre-invasive conditions [21] |
| 12 | IBD2 locus | Varied | Not fully characterized | Inflammatory bowel disease | Greater linkage to ulcerative colitis than Crohn's disease [21] |
| 17 | Del(17p) | 5-10% of NDMM [17] | TP53 [17] | Multiple myeloma, various cancers | High-risk feature; associated with early recurrence and resistance [17] |
| 17 | Gain(17q) | 72% of neuroblastoma [22] | PPM1D [19] | Neuroblastoma | Strongest indicator of adverse outcome; early event in tumorigenesis [22] [19] |
| 17 | 17q12 deletion | Rare (exact frequency unknown) | HNF1B [23] | 17q12 deletion syndrome | Multisystem disorder: kidney disease, MODY5, neurodevelopmental issues [23] |
| 20 | Mosaic trisomy 20 | Rare (16% of all mosaicisms) [24] | Multiple genes | Trisomy 20 mosaicism syndrome | Variable phenotype; neuropsychiatric manifestations increasingly recognized [24] |
| 20 | Ring chromosome 20 | Rare | Unknown | Epilepsy syndrome | Drug-resistant epilepsy, cognitive decline, behavioral issues [25] |
Table 2: Association of Chromosome 1q Gain with Other High-Risk Cytogenetic Abnormalities in Multiple Myeloma
| Co-existing Abnormality | Impact on PFS | Impact on OS | Statistical Significance |
|---|---|---|---|
| t(14;16) | Reduced | Reduced | Significant for both PFS and OS [20] |
| del(17p) | Reduced | Reduced | Significant for both PFS and OS [20] |
| del(13q) | Reduced | Reduced | Significant for both PFS and OS [20] |
| del(1p) | Not significant | Reduced | Significant only for OS [20] |
Experimental Methodologies for Detection and Analysis
Standard Cytogenetic Techniques
Fluorescence In Situ Hybridization (FISH): FISH represents the gold standard for detecting recurrent cytogenetic abnormalities in clinical practice, particularly for malignancies like multiple myeloma where plasma cells have low proliferative rates [17] [18]. The protocol involves: (1) Preparation of metaphase chromosomes or interphase nuclei from patient samples (bone marrow aspirate); (2) Denaturation of DNA to generate single-stranded targets; (3) Hybridization with fluorochrome-labeled DNA probes specific to regions of interest (e.g., 1q21, 17p13); (4) Washing to remove non-specifically bound probes; (5) Counterstaining with DAPI and visualization using fluorescence microscopy [17] [18]. FISH allows specific detection of abnormalities like +1q, del(17p), and IGH translocations with high sensitivity and reproducibility, making it indispensable for risk stratification.
Chromosomal Microarray (CMA): CMA provides genome-wide assessment of copy number variations and is particularly valuable for detecting microdeletions/duplications beyond the resolution of conventional karyotyping [23]. The methodology involves: (1) Extraction of genomic DNA from patient and reference samples; (2) Fragmentation and labeling with different fluorescent dyes; (3) Competitive hybridization to a microarray containing thousands of oligonucleotide probes; (4) Scanning and analysis of fluorescence intensity ratios to identify copy number changes [23]. CMA is the preferred technique for diagnosing conditions like 17q12 recurrent deletion syndrome, reliably detecting the characteristic 1.4-Mb heterozygous deletion [23].
Advanced Genomic Approaches
Next-Generation Sequencing (NGS): NGS technologies, including whole-exome and whole-genome sequencing, provide comprehensive characterization of genomic alterations at base-pair resolution. These approaches enable simultaneous detection of point mutations, copy number variations, and structural variants, offering a complete genomic profile [23]. For copy number variant detection, specialized bioinformatic algorithms must be applied to NGS data [23]. In neuroblastoma research, NGS approaches have been instrumental in identifying PPM1D as a candidate oncogene on 17q and characterizing its activation through various mechanisms including gene fusion and gain-of-function mutations [19].
Comparative Genomic Hybridization (CGH): CGH allows genome-wide screening of DNA copy number variations without requiring cell culture [22]. The technique involves: (1) Extraction of test (tumor) and reference (normal) DNA; (2) Differential labeling with distinct fluorochromes; (3) Competitive hybridization to normal metaphase chromosomes or oligonucleotide arrays; (4) Quantitative analysis of fluorescence ratios along chromosomes to identify regions of gain or loss [22]. CGH has been particularly valuable in neuroblastoma research, where it first identified gain of chromosome 17q as the most frequent abnormality [22].
Single-Cell Sequencing: Emerging single-cell RNA and DNA sequencing technologies enable characterization of genomic aberrations and transcriptional patterns at single-cell resolution, allowing mapping of clonal evolution and heterogeneity within tumors [19]. In neuroblastoma, these approaches have revealed how additional copies of chromosome 17q are acquired during clonal evolution in aggressive disease [19].
Diagram 1: Experimental Workflow for Chromosomal Abnormality Detection. This diagram illustrates the integrated approaches for identifying high-risk chromosomal abnormalities, from sample processing through detection methods to clinical and research applications.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Chromosomal Abnormality Studies
| Reagent/Material | Specific Examples | Application | Function |
|---|---|---|---|
| FISH Probes | 1q21 (CKS1B), 17p13 (TP53), 13q14 (RB1), IGH breakapart | Fluorescence in situ hybridization | Targeted detection of specific chromosomal abnormalities in interphase or metaphase cells |
| Microarray Platforms | Oligonucleotide arrays, SNP genotyping arrays | Chromosomal microarray analysis | Genome-wide detection of copy number variations and loss of heterozygosity |
| Next-Generation Sequencing Kits | Whole-genome sequencing, whole-exome sequencing, targeted panels | Comprehensive genomic analysis | Detection of point mutations, structural variants, and copy number changes |
| Cell Culture Reagents | Cytokines, stromal co-culture systems | Plasma cell culture | Supporting in vitro growth of low-proliferative cells for metaphase analysis |
| DNA Extraction Kits | Phenol-chloroform, column-based methods | Nucleic acid purification | High-quality DNA preparation for microarray and sequencing applications |
| Fluorescence Microscopy Systems | Epifluorescence microscopes with filter sets | FISH visualization | Imaging of hybridized probes for abnormality detection and quantification |
| Bioinformatic Tools | CNV calling algorithms, segmentation analysis | Data analysis | Interpretation of sequencing and microarray data for abnormality identification |
High-risk chromosomal abnormalities on chromosomes 1, 12, 17, and 20 represent critical determinants of disease behavior across multiple malignancies. Their systematic identification and characterization are essential for accurate risk stratification, treatment selection, and therapeutic development. The consistent association of these abnormalities with aggressive disease phenotypes and poor clinical outcomes underscores the importance of robust detection methods and standardized reporting in both clinical and research settings.
Advancements in genomic technologies continue to refine our understanding of these high-risk loci, revealing complex pathogenic mechanisms and potential therapeutic targets. The integration of FISH, chromosomal microarray, and next-generation sequencing provides complementary approaches for comprehensive genomic assessment, enabling both targeted analysis and genome-wide discovery. As stem cell-based therapies advance, rigorous assessment of genomic stability using these methodologies will be paramount for ensuring patient safety and therapeutic efficacy.
Future directions will likely focus on developing targeted interventions for specific high-risk abnormalities, elucidating the complex interactions between co-occurring abnormalities, and translating genomic insights into improved risk-adapted treatment strategies. The continued refinement of detection methodologies and analytical frameworks will further enhance our ability to identify and characterize these critical genomic alterations across diverse disease contexts.
Genomic instability, a hallmark of cancer, is defined as an increased tendency for genomic alterations to accumulate during cell division [26] [27]. In the context of stem cell biology and tumorigenesis, this phenomenon presents a complex paradox. While genomic instability drives malignant transformation by fueling tumor evolution and heterogeneity, it can also trigger potent immune surveillance mechanisms that eliminate damaged cells [26]. The intricate relationship between genomic instability and impaired cellular differentiation represents a critical nexus in understanding cancer pathogenesis, particularly concerning cancer stem cells (CSCs) that exhibit stem-like properties including self-renewal capacity, differentiation potential, and enhanced therapy resistance [28].
Recent research has revealed that true cancer stem cells may exhibit surprising genomic stability alongside dormancy, distinguishing them from the more proliferative, genomically unstable cells that constitute the bulk of tumors [29]. This discovery highlights the sophisticated hierarchy within tumors and suggests that genomic stability in the CSC subpopulation may be a protective mechanism for long-term survival and repopulation potential. Understanding the mechanisms connecting genomic instability to disrupted differentiation programs is therefore essential for developing targeted therapeutic strategies that can effectively eradicate the root of tumorigenesis, including the elusive CSC population responsible for disease recurrence.
Molecular Mechanisms: Connecting Genomic Instability to Differentiation Failure
Forms of Genomic Instability and Their Biological Consequences
Genomic instability manifests through multiple mechanisms that collectively drive tumorigenesis by altering the normal differentiation trajectories of cells. The primary forms include DNA repair deficiencies, chromosomal instability, and telomere dysfunction, each contributing distinctly to the acquisition of malignant phenotypes.
Table 1: Forms and Consequences of Genomic Instability in Tumorigenesis
| Form of Instability | Molecular Defect | Impact on Differentiation | Associated Cancers |
|---|---|---|---|
| Mismatch Repair (MMR) Deficiency | Loss of MLH1, MSH2, MSH6, PMS2 | HyperMutation, increased neoantigens, immune activation | Colorectal, Endometrial, Gastric [26] |
| Homologous Recombination (HR) Deficiency | Mutations in BRCA1, BRCA2, ATM | Accumulation of DSBs, complex genomic rearrangements | Breast, Ovarian, Pancreatic, Prostate [26] |
| Chromosomal Instability (CIN) | Errors in chromosome segregation | Aneuploidy, gene dosage alterations, metabolic stress | >90% of solid tumors and blood cancers [30] |
| Telomere Dysfunction | Critical telomere shortening | Chromosomal end-to-end fusions, senescence bypass | Various cancers with alternative lengthening mechanisms [27] |
Chromosomal instability (CIN), particularly prevalent in human cancers, exists as both structural and numerical forms [30]. Structural CIN involves amplifications, deletions, or rearrangements of chromosomal segments, while numerical CIN entails gains or losses of entire chromosomes. Both forms disrupt the precise gene expression networks required for normal differentiation, potentially locking cells in a progenitor-like state. The resulting aneuploidy generates significant intracellular stress, including proteotoxic stress, metabolic alteration, and DNA damage, which can further impede differentiation processes [30].
Signaling Pathways Linking Instability to Differentiation Impairment
The cGAS-STING pathway represents a crucial connector between genomic instability and immune recognition, creating a double-edged sword in tumorigenesis. Chromosomal missegregation can lead to micronuclei formation, which upon nuclear envelope rupture, exposes self-DNA to the cytosol where it activates the cGAS-STING pathway [31]. This triggers type I interferon signaling and inflammatory cytokine production, potentially attracting immune cells and eliminating unstable cells. However, tumors can co-opt this pathway to promote chronic inflammation that fuels progression and impairs differentiation of tumor-infiltrating immune cells.
Beyond immune activation, genomic instability directly disrupts differentiation through p53-dependent senescence pathways, altered epigenetic landscapes, and disrupted niche signaling. The DNA damage response (DDR) can activate cell cycle checkpoints that prevent progenitor cells from entering differentiation pathways, effectively maintaining them in a stem-like state. Additionally, large-scale chromosomal alterations can disrupt the coordinated gene expression programs required for lineage commitment, particularly when master transcriptional regulators are affected by copy number alterations [30].
Experimental Approaches: Assessing Genomic Instability in Stem Cell Populations
The MAGIC Platform: Tracking De Novo Chromosomal Abnormalities
The Machine-learning-assisted Genomics and Imaging Convergence (MAGIC) platform represents a cutting-edge approach for investigating chromosomal instability dynamics in live cells [31]. This autonomously operated platform integrates live-cell imaging of micronucleated cells, machine learning on-the-fly, and single-cell genomics to systematically investigate chromosomal abnormality (CA) formation.
Table 2: MAGIC Platform Workflow and Applications
| Step | Technology | Function | Key Findings |
|---|---|---|---|
| Cell Tracking | H2B-Dendra2 photolabelling | Fluorescent nuclear labeling | Enables precise tracking of individual cells across divisions [31] |
| Phenotype Detection | Machine learning classifier (XGBoost) | Automated micronuclei identification | Achieves 90% precision, 50% recall in identifying nuclear atypia [31] |
| Cell Isolation | Fluorescence-activated cell sorting (FACS) | Target cell purification | Efficient recovery of photolabelled cells with nuclear defects [31] |
| Genomic Analysis | Single-cell template-strand sequencing (Strand-seq) | CA detection & sister cell relationship mapping | Identifies de novo CAs, reveals 5-fold enrichment in micronucleated cells [31] |
The MAGIC platform has revealed that dicentric chromosomes frequently initiate CAs, and that chromosome losses arise more frequently than gains in non-transformed cell lines. TP53-deficient cells show an approximately doubled CA mutation rate, highlighting the importance of p53 in maintaining genomic stability. Furthermore, targeted induction of DNA double-strand breaks using CRISPR-Cas9 demonstrated that break location influences the spectrum of resulting CAs, with complex rearrangements often mapping to a single homologue [31].
Identifying Dormant, Genomically Stable Cancer Stem Cells
Contrary to conventional models that might assume CSCs harbor significant genomic instability, recent research has identified a subpopulation of true cancer stem cells that exhibit both dormancy and genomic stability [29]. Using a human PDX model (Mary-X) that expresses a strong cancer stem cell phenotype, researchers employed GFP-labelled retroviral transfection and fluorescent microsphere uptake studies to distinguish proliferating from dormant cells.
The experimental approach involved:
- Retroviral GFP transfection to label proliferating cells
- Fluorescent microsphere uptake to identify dormant, non-phagocytic cells
- Array CGH to identify regions of amplifications and deletions
- FISH with derived probes on individual cells to identify genomically stable subpopulations
This methodology revealed that while 97-99% of cells expressed retroviral GFP and showed numerous gene amplifications and deletions, approximately 1-3% of cells exhibited the opposite pattern - retaining fluorescent microspheres and demonstrating genomic stability [29]. This subpopulation was significantly smaller in size than their GFP-expressing, genomically unstable counterparts and could be further enriched by sorting for established CSC markers (CD133 or ALDH positivity). These findings indicate that a truly biological cancer stem cell subpopulation exists that exhibits both dormancy and genomic stability, representing a hierarchical stem cell population capable of only unidirectional differentiation.
Comparative Analysis: Experimental Models for Studying Genomic Instability
Model Systems for Genomic Instability Research
Various model systems have been developed to study the relationship between genomic instability and tumorigenesis, each offering distinct advantages and limitations for investigating different aspects of this complex relationship.
Table 3: Experimental Models for Genomic Instability and Tumorigenesis Studies
| Model System | Key Features | Applications | Limitations |
|---|---|---|---|
| Non-Transformed Cell Lines (MCF10A, RPE-1) | Near-diploid, non-transformed | Baseline CA mutation rates, early tumorigenesis events | May not fully capture tumor microenvironment [31] |
| Bioengineered Niche Models | Recapitulate physiological ECM organization | LT-HSC maintenance, stem cell-niche interactions | Technical complexity in recreation of native niche [32] |
| Patient-Derived Xenografts (e.g., Mary-X) | Preserves tumor heterogeneity | CSC dormancy studies, therapeutic response testing | Limited human immune component, host microenvironment differences [29] |
| CIN Mouse Models | In vivo CIN investigation | Tumor progression, metastasis, therapeutic testing | Species-specific differences in cancer biology [30] |
Bioengineered niches that recreate physiological extracellular matrix organization have emerged as particularly valuable tools for studying stem cell behavior in controlled microenvironments. These systems use soft collagen type-I hydrogels to drive nestin expression in perivascular stromal cells (PerSCs), creating an environment that supports long-term haematopoietic stem cells (LT-HSCs) [32]. The induction of nestin, which is expressed by HSC-supportive bone marrow stromal cells, appears cytoprotective and regulates metabolism in PerSCs, influencing HIF-1α expression - a critical factor in maintaining LT-HSCs. Such bioengineered systems enable researchers to dissect the specific contributions of microenvironmental factors to genomic stability and differentiation potential.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Investigating the connection between genomic instability and impaired differentiation requires specialized research tools and reagents designed to detect, quantify, and manipulate genomic integrity in stem and progenitor cells.
Table 4: Essential Research Reagents for Genomic Instability Studies
| Reagent/Solution | Function | Application Examples |
|---|---|---|
| H2B-Dendra2 Protein | Photoconvertible fluorescent histone label | Live-cell tracking of nuclear morphology and cell division [31] |
| CRISPR-Cas9 Systems | Targeted DNA double-strand break induction | Studying specific CA formation processes [31] |
| Strand-seq Reagents | Single-cell template-strand sequencing | Sister chromatid exchange detection, CA mapping [31] |
| Fluorescent Microspheres | Non-dividing cell population identification | Dormant CSC isolation and characterization [29] |
| Soft Collagen Hydrogels | Physiological ECM stiffness recreation | Bioengineered stem cell niche development [32] |
| Nestin Expression Markers | Perivascular stromal cell phenotype detection | HSC-supportive niche identification and analysis [32] |
Advanced imaging dyes represent critical components of the genomic instability researcher's toolkit. The development of photo-activatable tracking dyes like DACT-1 enables cell tracking without genetic manipulation, bypassing potential artifacts associated with fluorescent protein expression [31]. Similarly, the H2B-Dendra2 system allows precise photolabelling of nuclei with a 22-fold increase in red fluorescence after illumination, facilitating automated cell sorting without detectable phototoxicity. These tools enable the precise isolation and tracking of cells with specific nuclear abnormalities, connecting morphological phenotypes with underlying genomic alterations.
Therapeutic Implications and Future Directions
The investigation into genomic instability and its relationship with impaired differentiation has yielded significant insights for therapeutic development. The paradoxical nature of CIN - where moderate levels promote tumor evolution while excessive instability leads to cell death - presents a promising therapeutic avenue known as the "just-right" model of CIN [30]. Therapeutic strategies that push tumor cells beyond their tolerable threshold of genomic instability could effectively induce lethal amounts of DNA damage and mitotic catastrophe.
Emerging approaches include:
- Centrosome declustering agents to induce multipolar divisions in cells with supernumerary centrosomes [27]
- Dual metabolic inhibition strategies targeting the metabolic plasticity of CSCs [28]
- CAR-T cells targeting CSC-specific surface markers like EpCAM to eliminate therapy-resistant subpopulations [28]
- Synthetic lethal interactions with specific DNA repair deficiencies, such as PARP inhibitors in HR-deficient tumors [26]
The discovery that true CSCs may possess relative genomic stability [29] necessitates a re-evaluation of therapeutic strategies that predominantly target rapidly dividing, genomically unstable cells. Future efforts must develop approaches to target the dormant, stable CSC subpopulation that may survive conventional genotoxic therapies and drive disease recurrence. Combining conventional therapies with agents that specifically target CSCs or force their exit from dormancy represents a promising direction for achieving more durable remissions and overcoming therapeutic resistance in advanced cancers.
The Quality Control Toolbox: From Karyotyping to NGS for Detecting Genetic Variants
In the field of stem cell research and therapeutic development, assessing genomic stability is paramount for ensuring both safety and efficacy. Karyotyping, particularly G-banding analysis, remains a cornerstone technique for visualizing chromosomal number and large-scale structural abnormalities at single-cell resolution. This methodology provides a comprehensive genome-wide view that can detect balanced structural rearrangements and mosaic abnormalities that often elude higher-resolution molecular techniques [33]. For stem cell biologists and drug development professionals, maintaining chromosomal integrity in cell lines is crucial, as acquired genetic abnormalities can compromise therapeutic utility and potentially introduce oncogenic risk [16].
While newer technologies like next-generation sequencing (NGS) and chromosomal microarray (CMA) offer enhanced resolution for specific applications, G-banding karyotyping maintains its fundamental role in the initial screening and validation of stem cell lines. Its ability to provide a simultaneous assessment of all chromosomes without prior knowledge of potential abnormalities makes it particularly valuable for detecting unexpected chromosomal changes that may occur during extended cell culture or genetic manipulation [34]. This guide provides a comprehensive comparison of G-banding with contemporary cytogenetic methods, supported by experimental data and detailed protocols relevant to stem cell genomic stability assessment.
Fundamental Principles and Technical Execution
The G-Banding Technique
G-banding (Giemsa banding) is a cytogenetic technique that produces a visible karyotype by staining condensed chromosomes with Giemsa stain after trypsin digestion. The distinct patterns of Giemsa-dark and light bands observed on chromosomes reflect regional differences in chromatin structure and composition [35]. These banding patterns are unique to each chromosome pair, enabling the identification of both numerical and structural aberrations through microscopic analysis [36]. The technique relies on the differential binding of Giemsa stain to chromosomal regions with varying base pair compositions, with constitutive heterochromatin typically staining more darkly due to its AT-rich nature.
The standard G-banding protocol involves several critical steps that must be carefully optimized for reliable results [37]:
- Specimen preparation: Cells are arrested in metaphase when chromosomes are most condensed, then subjected to hypotonic treatment and fixation.
- Slide preparation: Fixed cells are dropped onto slides and aged to achieve optimal chromosome spreading.
- Trypsin digestion: Slides are treated with trypsin (typically 0.025% at pH 7.2-7.4) for approximately 1 minute, with exact timing determined empirically based on specimen age and environmental conditions.
- Staining: Giemsa staining for 10 minutes followed by rinsing and drying.
- Microscopic examination: Banding quality is assessed under high magnification, with clear, distinct bands indicating successful processing.
The quality of G-banding is highly dependent on technical factors including trypsin concentration, digestion time, temperature, and specimen age. Older specimens generally require longer trypsin exposure, while very fresh specimens may produce fuzzy chromosomal morphology [37].
Advancements in Karyotyping Technologies
Traditional manual karyotyping has evolved significantly with the introduction of automated imaging systems and, more recently, artificial intelligence (AI)-guided analysis [35]. These systems have transformed the labor-intensive process of metaphase spread identification, chromosome segmentation, and karyogram assembly. Currently, four commercially available AI-based chromosome analysis systems (from Applied Spectral Imaging, BioView, Diagens, and MetaSystems) utilize deep learning algorithms to streamline karyotyping workflows [35] [36].
AI-guided karyotyping systems demonstrate impressive efficiency gains, reducing average analysis time from approximately 33.9 minutes with conventional methods to just 6.5 minutes for 70 metaphases [33]. Following AI analysis, technologists typically spend about 7 minutes reviewing 15 representative karyotypes, significantly accelerating turnaround times while maintaining diagnostic accuracy [33]. Clinical validation studies report that AI-assisted karyotyping with manual correction achieves 97% accuracy, 98% sensitivity, and 96% specificity compared to conventional karyotyping [33].
Comparative Performance Analysis of Cytogenetic Techniques
Technical Capabilities and Limitations
Table 1: Comparison of Key Cytogenetic Techniques for Genomic Stability Assessment
| Parameter | G-Banding Karyotyping | Chromosomal Microarray (CMA) | Next-Generation Sequencing (NGS) |
|---|---|---|---|
| Resolution | ~5-10 Mb (at 550-band level) | >100 kb (SNP arrays); >30 kb (aCGH) | >1 bp (varies with coverage) |
| Numerical Abnormalities | Excellent detection | Limited detection (except polyploidy) | Excellent detection |
| Balanced Structural Rearrangements | Excellent detection | Cannot detect | Limited detection |
| Unbalanced Structural Rearrangements | Detection >5-10 Mb | Excellent detection | Excellent detection |
| Polyploidy Detection | Excellent | Limited with some arrays | Limited |
| Single Cell Analysis | Yes | No (bulk analysis) | Limited (requires single-cell WGA) |
| Mosaicism Detection | Sensitivity ~10-20% | Sensitivity ~5-30% (depends on array) | Sensitivity ~1-5% (varies with depth) |
| Turnaround Time | 7-14 days (culture-dependent) | 3-7 days (no culture required) | 5-21 days (varies with approach) |
| Stem Cell Applications | Routine genomic stability screening, MSC characterization | Comprehensive CNV profiling, iPSC line validation | Comprehensive mutation profiling, off-target editing assessment |
Diagnostic Performance in Research Settings
Prospective comparative studies demonstrate significant differences in the diagnostic performance of various cytogenetic techniques. In the analysis of products of conception (POC), NGS-based approaches presumed the cause of miscarriage in 75.0% of cases, significantly outperforming G-banding's diagnostic rate of 42.5% [38]. This performance disparity was particularly pronounced in early gestation losses before 12 weeks, where NGS identified causal abnormalities in 73.5% of cases compared to 44.1% with G-banding [38].
A critical factor influencing this performance difference is the culture failure rate associated with G-banding. In prospective analyses, G-banding could only analyze 67.5% of submitted samples due to culture failure, while NGS successfully analyzed 100% of samples [38]. This technical limitation significantly impacts the utility of G-banding for samples with limited viability or contamination.
Table 2: Experimental Success Rates and Diagnostic Yield Across Techniques
| Performance Metric | G-Banding Karyotyping | Chromosomal Microarray | Next-Generation Sequencing |
|---|---|---|---|
| Analytical Success Rate | 67.5% (27/40 samples) [38] | >95% [39] | 100% (40/40 samples) [38] |
| Diagnostic Yield (POC Analysis) | 42.5% (17/40 cases) [38] | Not specified | 75.0% (30/40 cases) [38] |
| Early Gestation Diagnostic Yield | 44.1% (15/34 cases) [38] | Not specified | 73.5% (25/34 cases) [38] |
| Successful Analysis Among Cultured Samples | 62.9% (17/27 cases) [38] | Not specified | 70.3% (19/27 cases) [38] |
| Polyploidy Detection | Excellent [38] | Limited [39] | Limited [38] |
| Balanced Rearrangements | Excellent [33] | Cannot detect [33] | Limited [38] |
Experimental Design and Workflow Integration
G-Banding Protocol for Stem Cell Characterization
For stem cell research applications, the G-banding protocol requires specific modifications to optimize results with cultured cells [37]:
- Cell Culture and Harvesting: Grow stem cells to 60-80% confluence. Add colcemid (0.02 μg/mL) for 45-60 minutes to arrest cells in metaphase. Collect cells using trypsinization or scraping.
- Hypotonic Treatment: Resuspend cell pellet in pre-warmed 0.075M KCl solution and incubate for 20 minutes at 37°C.
- Fixation: Gradually add fresh methanol:acetic acid (3:1) fixative while gently mixing. Perform three fixation changes, each with 15-minute intervals.
- Slide Preparation: Drop cell suspension onto clean, wet slides and air dry. Age slides at 60°C overnight or at 72-75°C for 3 hours.
- Trypsinization and Staining: Treat slides with 0.025% trypsin for 30-90 seconds. Rinse in saline and stain with 2% Giemsa solution for 5-8 minutes.
- Analysis: Examine under 100x oil immersion objective. Count 15-20 metaphases and fully analyze 5-10 cells for karyotyping.
The following workflow diagram illustrates the complete G-banding procedure for stem cell genomic assessment:
Strategic Workflow Integration for Comprehensive Genomic Assessment
For comprehensive stem cell genomic stability assessment, integrating multiple complementary techniques provides the most rigorous evaluation. The following workflow demonstrates how G-banding fits within a broader analytical strategy:
Essential Research Reagents and Materials
Table 3: Essential Research Reagents for G-Banding Karyotyping
| Reagent/Material | Function | Technical Considerations |
|---|---|---|
| Colcemid | Metaphase arrest inhibitor | Concentration and exposure time optimization critical for chromosome spreading |
| Trypsin Solution | Chromosome protein digestion | Concentration (typically 0.025%) and digestion time must be empirically determined |
| Giemsa Stain | Chromosome banding pattern visualization | Standardized solution (2-4%) provides consistent G-banding patterns |
| Hypotonic Solution (KCl) | Cellular swelling and chromosome spreading | 0.075M concentration standard; temperature and timing affect spreading quality |
| Methanol:Acetic Acid Fixative | Cellular preservation and chromosome fixation | Fresh 3:1 ratio required for each experiment; multiple changes improve morphology |
| Microscopy Slides | Chromosome presentation | Pre-cleaned and chilled slides enhance chromosome spreading |
| Cell Culture Media | Stem cell maintenance and proliferation | Culture conditions must maintain stemness while allowing cell cycle progression |
G-banding karyotyping remains an essential component of comprehensive stem cell genomic assessment, providing unique capabilities for detecting balanced chromosomal rearrangements and mosaic abnormalities at single-cell resolution. While newer technologies like CMA and NGS offer superior resolution for detecting specific abnormalities, G-banding's genome-wide screening capability without prior knowledge of potential abnormalities maintains its relevance in stem cell research and characterization.
The integration of AI-guided analysis has significantly enhanced the efficiency and standardization of karyotyping, reducing turnaround times while maintaining diagnostic accuracy [35] [33]. For researchers and drug development professionals, a strategic combination of G-banding with higher-resolution techniques provides the most comprehensive approach to ensuring stem cell genomic integrity, ultimately supporting the development of safe and effective cell-based therapies.
Optical Genome Mapping (OGM) is an advanced genomic imaging technology that enables the comprehensive detection of structural variants (SVs) and copy number variants (CNVs) across the entire genome. This innovative methodology utilizes ultra-high molecular weight (UHMW) DNA to perform an unbiased assessment of genomic rearrangements with a resolution that far exceeds conventional cytogenetic approaches [40]. Unlike sequencing-based methods that infer structure from sequence data, OGM directly visualizes the physical architecture of DNA molecules by converting them into fluorescent barcode patterns that can be digitally analyzed and compared to reference genomes [41].
The application of OGM is particularly valuable in the context of stem cell genomic stability assessment, where unintended genetic modifications during differentiation and proliferation can compromise therapeutic safety and efficacy [42]. As regulatory agencies increasingly emphasize the importance of genetic stability testing for stem cell-based products, OGM offers a powerful solution for identifying cryptic rearrangements and complex variants that may escape detection by traditional methodologies [42] [43].
Fundamental Principles of OGM
The OGM workflow begins with the isolation of UHMW DNA using specialized extraction protocols that minimize DNA shearing, typically yielding fragments of 150 kilobases to megabases in size - substantially longer than conventional DNA isolation techniques [41]. This DNA is then fluorescently labeled at specific CTTAAG hexamer motifs, creating a unique labeling pattern across the genome with approximately 14-17 labels per 100kb [41]. The labeled DNA molecules are linearized in nanochannels, imaged, and digitized to generate consensus maps of 500 kb to megabase-sized segments that are computationally compared to reference genome labeling patterns [40] [41].
This imaging-based approach converts DNA into a "barcode" whose labeling profile and characteristics can sensitively and specifically resolve copy number and structural variation without requiring nucleotide-level sequence data [41]. The technology can detect a wide range of variant types including copy number gains/losses, balanced and unbalanced translocations, insertions, and inversions [41].
Performance Comparison with Conventional Cytogenetic Methods
Table 1: Comparative analysis of OGM versus conventional cytogenetic methods for structural variant detection
| Method | Resolution | SV Types Detected | Genome Coverage | Specimen Requirements | Key Limitations |
|---|---|---|---|---|---|
| Chromosome Banding Analysis | >5-10 Mb | CNVs, balanced SVs | Genome-wide | Viable cells | Low resolution, subjective interpretation [41] |
| Fluorescence In Situ Hybridization (FISH) | ~70 kb - 1 Mb | CNVs, specific SVs | Targeted | Viable or fixed cells | Limited to targeted regions, requires prior knowledge of targets [40] [41] |
| Chromosomal Microarray (CMA) | >5 kb - 200 kb | CNVs, AOH (SNP arrays) | Genome-wide | Viable or fixed cells | Cannot detect balanced SVs, provides no structural information for gains [43] [41] |
| Next-Generation Sequencing | Single nucleotide | SNVs, CNVs, some SVs | Genome-wide | Viable or fixed cells | Challenging for complex regions, specialized algorithms needed for different SV types [40] |
| Optical Genome Mapping | ~500 bp - 5 kb | CNVs, balanced SVs, AOH | Genome-wide | Viable cells (can be frozen) | Requires UHMW DNA, not suitable for fixed specimens [41] |
Table 2: Diagnostic performance of OGM in hematologic malignancies
| Study Focus | Concordance with Standard Methods | Additional SVs Detected by OGM | Clinical Impact of Additional Findings |
|---|---|---|---|
| Myelodysplastic Syndromes (MDS) [41] | >95% | 34% of cases | Changed risk assessment in 17% of patients |
| Acute Myeloid Leukemia (AML) [41] | >95% | 12-23% of cases | Altered clinical management or trial eligibility |
| Acute Leukemia (467 cases) [44] | 88.1% overall concordance with RNA-seq | 15.8% uniquely detected by OGM | Identification of cryptic, enhancer-driven events |
| B- and T-ALL [41] | Superior to combined CBA, FISH, MLPA | 20% increased detection of risk groups | Improved risk stratification |
Recent studies have demonstrated that OGM reliably detects all forms of clinically significant SVs identified by standard testing methods with greater than 95% concordance [41]. The discordances primarily involve low-level whole chromosome aneuploidies present in less than 5% of nuclei, which may fall below the reliable detection threshold of OGM [41]. Importantly, conventional diagnostic standards for SV detection fail to recognize clinically relevant aberrations at significant rates, with OGM identifying previously cryptic SVs in 34% of MDS cases and 12-23% of AML cases that would have altered clinical management [41].
Comparison with Sequencing-Based Approaches
When compared to targeted RNA sequencing in acute leukemia, OGM demonstrated complementary strengths. In a study of 467 acute leukemia cases, the overall concordance rate between a 108-gene RNA-seq panel and OGM was 88.1% for detected gene/rearrangement fusions [44]. However, significant differences emerged in their ability to detect specific variant types: OGM uniquely identified 15.8% of clinically relevant rearrangements, while RNA-seq exclusively detected 9.4% [44].
The technologies showed particularly divergent performance for specific variant categories. OGM significantly outperformed RNA-seq in detecting enhancer-hijacking lesions (including MECOM, BCL11B, and IGH rearrangements), with a markedly lower concordance of 20.6% compared to 93.1% for all other aberrations [44]. Conversely, RNA-seq slightly outperformed OGM for fusions arising from intrachromosomal deletions that were sometimes labeled by OGM as simple deletions [44]. This demonstrates that while RNA-seq is more sensitive for detecting expressed chimeric fusions, OGM is superior for identifying cryptic, enhancer-driven events that do not generate fusion transcripts [44].
Experimental Data and Validation Studies
OGM in Constitutional Disorder Diagnosis
In constitutional genetic disorder diagnosis, OGM has demonstrated significant utility in resolving complex rearrangements that challenge conventional methods. A key application is the characterization of copy-number gains, which frequently present interpretation challenges when detected by chromosomal microarray (CMA) [43]. In a comprehensive study of 4073 CMA cases, copy-number gains were significantly more likely to be classified as variants of uncertain significance (VUS) compared to losses (70.9% vs 44.1%, p<0.001) [43]. This "VUS burden" stems from CMA's inability to provide structural information about the location and orientation of multiplied regions, which is critical for determining their functional consequences [43].
When OGM was applied to 33 VUS gains involving disease-associated genes, it successfully determined the genomic structure in all cases, revealing that 26 of 33 were tandem duplications while 7 of 33 were complex rearrangements [43]. This structural information facilitated more conclusive clinical interpretation in the majority of cases, supporting benign classification for 27 of 33 gains and potentially preventing unnecessary follow-up testing and patient concern [43]. The study estimated that approximately 20% of reported VUS gains would not have been reportable if OGM data had been available initially [43].
Resolution of Complex Structural Variants
OGM has proven particularly valuable for resolving complex structural variants (cxSVs) that involve multiple breakpoints and rearrangement types. In craniosynostosis cases with large interspersed duplications, OGM successfully determined the correct structure of events ranging from 244 kb to 2.01 Mb in size [45]. The technology enabled researchers to unambiguously determine the configuration of linked interspersed duplications by analyzing multiple molecules completely spanning the duplicated segments [45].
However, the study also identified a key limitation: consistent resolution required multiple individual reads to completely span the duplicated segment, with an upper size limit of approximately 550 kb for reliable resolution using standard protocols [45]. This highlights the importance of DNA quality and molecule length for comprehensive variant characterization, particularly for the largest and most complex rearrangements.
OGM in Stem Cell Genomic Stability Assessment
Current Challenges in Stem Cell Genetic Stability
The assessment of genetic stability in stem cell-based therapeutic products presents unique challenges for conventional cytogenetic methods. During the expansion of human induced pluripotent stem cells (hiPSCs) and their differentiation into target cells like cardiomyocytes, various genetic mutations can occur that may impact therapeutic safety and efficacy [42]. Regulatory guidelines from the FDA, EMA, and ICH strongly recommend appropriate genetic stability testing methods throughout the manufacturing process [42].
Current conventional methods for assessing genetic stability, including karyotyping, FISH, and comparative genomic hybridization arrays, face significant limitations when applied to stem cell products. These include difficulties in handling large-scale cell differentiation, extended processing times, and low resolution that makes detecting small structural changes or subtle abnormalities challenging [42]. These limitations are particularly concerning given that studies have identified cancer-related mutations, such as copy number gains encompassing the ASXL1 gene on chromosome 20q11.21, in hiPSCs that persist through passaging and differentiation [42].
OGM Advantages for Stem Cell Applications
OGM addresses several key limitations of conventional methods for stem cell genomic stability assessment. The technology's genome-wide, unbiased approach enables detection of SVs and CNVs without prior knowledge of potential targets, which is particularly valuable for identifying novel or unexpected variants that may arise during stem cell culture and differentiation [40] [41]. The high resolution of OGM (~500 bp to 5 kb) far exceeds that of karyotyping (>5-10 Mb) and approaches that of CMA, while additionally providing structural context that CMA cannot deliver [41].
For stem cell applications, OGM's ability to resolve complex rearrangements and provide orientation information for duplicated segments is particularly valuable. This structural information is critical for interpreting the potential functional consequences of copy-number gains, which may represent direct or inverted duplications at the original chromosomal location or insertions into distant loci where they could disrupt critical genes [43]. In the context of stem cell genomic stability, this capability enables more accurate assessment of whether observed variants are likely to impact pluripotency, differentiation potential, or tumorigenic risk.
Research Reagent Solutions for OGM Implementation
Table 3: Essential research reagents and materials for optical genome mapping
| Reagent/Material | Function | Technical Specifications | Application Notes |
|---|---|---|---|
| Ultra-High Molecular Weight DNA | Primary analyte for OGM | Fragments >150 kb, minimum 750 ng per assay | Requires fresh or frozen viable cells; conventional fixed specimens unsuitable [41] |
| Direct Labeling and Staining Reagents | Fluorescent labeling of specific sequence motifs | CTTAAG hexamer motif labeling; ~14-17 labels/100 kb | Creates unique barcode pattern for genome-wide assessment [41] |
| Nanochannel Chips | Linearization of DNA molecules for imaging | Hundreds of thousands of parallel nanochannels | Enables uniform stretching and imaging of individual DNA molecules [40] [41] |
| Reference Genome | Bioinformatic comparison and variant calling | GRCh38/hg38 typically used | Essential for identifying deviations from normal labeling patterns [44] |
| Specialized DNA Isolation Kits | Isolation of intact UHMW DNA | Paramagnetic disk-based isolation minimizes shearing | Critical step; conventional column-based extractions yield insufficient fragment sizes [41] |
Methodological Protocols for OGM Analysis
Standard OGM Workflow
The standard OGM protocol involves several critical steps that must be carefully optimized for reliable results. The process typically requires 4 days from DNA extraction to data analysis, with the majority of time dedicated to imaging and computational analysis rather than hands-on technical work [41]. A detailed workflow is presented in the diagram below:
Data Analysis Approaches
OGM data analysis utilizes specialized algorithms tailored to different applications. For constitutional (germline) assessments, the de novo structural variant analysis pipeline is typically employed, requiring approximately 80x coverage (>400 Gbp data collection) [41]. For somatic applications such as cancer genomics, the Rare Variant Analysis (RVP) pipeline enables detection down to approximately 5% variant allele fraction, requiring higher coverage of >340x (>1500 Gbp data) [41].
The analytical process involves several key steps: (1) image processing to convert raw images into molecule maps; (2) assembly of individual molecule maps into consensus genome maps; (3) comparison of sample maps to reference genome labeling patterns; and (4) identification of deviations indicating structural variants or copy number alterations [40] [41]. Current platforms can generate up to 5000 Gigabase pairs of raw data per flow cell, providing a maximum theoretical genome-wide coverage of approximately 1250x [41].
Optical Genome Mapping represents a significant advancement in cytogenomic technology, offering unprecedented resolution for detecting structural variants and copy number alterations across the entire genome. The technology's ability to identify cryptic rearrangements and resolve complex structural variants that escape detection by conventional methods makes it particularly valuable for stem cell genomic stability assessment, where comprehensive genetic characterization is essential for ensuring therapeutic safety.
While OGM requires specialized instrumentation and bioinformatic resources, its implementation as a single assay can potentially replace the multiple complementary tests (karyotyping, FISH, CMA) currently needed for comprehensive genomic assessment. As the field of stem cell therapy continues to advance, OGM is poised to play an increasingly important role in validating the genetic integrity of therapeutic products and supporting their safe clinical translation.
Next-Generation Sequencing (NGS) has fundamentally transformed the landscape of genomic analysis, providing researchers with powerful tools to detect a wide spectrum of genetic variants. In the specific context of stem cell genomic stability assessment, understanding the capabilities and limitations of whole-exome sequencing (WES) and whole-genome sequencing (WGS) is crucial for designing robust research protocols. These technologies enable the comprehensive identification of single nucleotide variants (SNVs), insertions and deletions (indels), and copy number variations (CNVs) that may arise during stem cell culture, differentiation, or therapeutic application. The choice between WES and WGS involves careful consideration of multiple factors, including target regions, detection sensitivity, cost, and data complexity [46] [47]. This guide provides an objective comparison of WES and WGS performance based on current experimental data and offers detailed methodologies for their implementation in genomic stability studies.
Technical Foundations: WES and WGS Compared
Core Methodological Differences
Whole Exome Sequencing (WES) specifically targets the protein-coding regions of the genome (exons), which constitute approximately 1-2% of the human genome but harbor the majority of known disease-causing variants. This targeted approach utilizes hybridization-based capture (e.g., using Agilent SureSelect or similar systems) to enrich exonic regions from fragmented genomic DNA before sequencing [48] [46]. The enrichment process introduces specific technical considerations, including coverage uniformity and potential off-target effects that can influence variant detection accuracy.
Whole Genome Sequencing (WGS) employs a hypothesis-free approach by sequencing the entire genome without prior targeting. By eliminating the capture step required in WES, WGS provides more uniform coverage across both coding and non-coding regions and avoids biases introduced by probe hybridization efficiency [47]. This comprehensive approach is particularly valuable for detecting structural variants and variants in non-coding regulatory regions that may influence stem cell behavior and genomic stability.
Performance Comparison for Key Variant Types
Experimental data from recent studies enable direct comparison of WES and WGS performance across different variant classes relevant to genomic stability assessment.
Table 1: Comparative Performance of WES and WGS for Variant Detection
| Feature | Whole Exome Sequencing (WES) | Whole Genome Sequencing (WGS) |
|---|---|---|
| Analyzed Region | 1-2% of genome (protein-coding exons) [46] | Entire genome (coding + non-coding) [46] |
| Typical Sequencing Depth | ≥ 100X [47] | ≥ 30X [47] (≥ 32.5X reported in large-scale studies [49]) |
| SNV Detection | High accuracy in well-covered exonic regions [48] | Comprehensive across genome; identifies ~42x more variants than WES [49] |
| Indel Detection | Effective for small indels in exonic regions [50] | Superior due to more uniform coverage; 96.05% reliability for called indels [49] |
| Small CNV Detection | Limited, incomplete and potentially inaccurate [47] | Excellent, capable of detecting a broad size range [47] |
| Structural Variants | Limited detection [47] | Excellent detection; 1.9+ million reliable SVs identified in large cohorts [49] |
| Non-Coding Variants | Unable to detect [47] | Comprehensive detection including regulatory regions [47] |
| Typical Data Volume | 5-20 million mapped reads [46] | 600-900 million mapped reads [46] |
Table 2: Operational Considerations for Genomic Stability Studies
| Consideration | Whole Exome Sequencing (WES) | Whole Genome Sequencing (WGS) |
|---|---|---|
| Cost Efficiency | More cost-effective for focused analysis [47] | Higher upfront cost but more comprehensive [47] |
| Data Interpretation Complexity | Lower, focused on known pathogenic mutations [47] | High, requires sophisticated bioinformatics pipelines [47] |
| Turnaround Time | Faster analysis due to smaller dataset [46] | Slower analysis due to data volume [46] |
| Incidental Findings | Lower risk [46] | Higher risk [46] |
| Ideal Application | Focused studies on protein-altering variants [47] | Discovery-based research, comprehensive variant detection [47] |
Recent large-scale studies have quantified the dramatic difference in variant discovery between these approaches. The UK Biobank study comparing WES and WGS in 490,640 participants found that WGS identified approximately 42 times more variants than WES. Notably, even within coding regions, WES missed 13.7% of variants detected by WGS, with particularly poor performance in untranslated regions (UTRs) where 69.2% of 5' UTR and 89.9% of 3' UTR variants were absent from WES data [49].
Experimental Design and Workflow
Sample Preparation and Quality Control
Proper sample preparation is critical for reliable variant detection in stem cell genomic stability studies. DNA quality directly impacts sequencing library complexity and variant calling accuracy. For stem cell cultures, ensure high molecular weight DNA extraction with minimal fragmentation. Quality control metrics should include spectrophotometric assessment (A260/280 ratio ~1.8-2.0), fluorometric quantification, and evaluation of DNA integrity via agarose gel electrophoresis or automated electrophoresis systems [46] [50].
Saliva-derived gDNA has been demonstrated as a viable alternative to blood-derived DNA for both WES and WGS approaches, with studies showing high concordance (F1 scores of 0.8030-0.9998 for SNVs and 0.8883-0.9991 for indels in WGS) between sample types when using standardized protocols [50]. This option may be valuable for establishing reference samples in stem cell research.
Library Preparation and Sequencing
The library preparation process diverges significantly between WES and WGS after the initial DNA fragmentation and adapter ligation steps:
WES Library Preparation utilizes hybrid capture-based enrichment. Following library construction, exonic regions are captured using biotinylated probes complementary to the target regions (e.g., Twist Core Exome or similar systems). After capture, washing, and amplification, the enriched libraries are sequenced on platforms such as Illumina NextSeq 500 or NovaSeq series [51] [46]. The efficiency of target capture directly influences coverage uniformity and variant detection sensitivity.
WGS Library Preparation omits the enrichment step, proceeding directly to sequencing after library construction. This results in more uniform coverage but requires significantly higher sequencing output to achieve adequate depth across the entire genome. Modern WGS approaches typically utilize Illumina NovaSeq 6000 systems with an average coverage of 32.5× or higher [49].
The following workflow diagram illustrates the key procedural differences between WES and WGS:
Bioinformatics Pipelines for Variant Detection
Robust bioinformatics pipelines are essential for accurate variant identification from NGS data. For stem cell genomic stability assessment, the following pipeline components should be implemented:
Read Alignment: Map sequencing reads to the reference genome (e.g., GRCh38) using optimized aligners such as BWA-MEM or Bowtie2. For WGS data, consider using DRAGEN platforms for accelerated processing [49].
Variant Calling: Utilize specialized callers for different variant types:
- SNVs and small indels: GATK, DeepVariant, or Sentieon DNASeq [51] [52]
- CNVs: ExomeDepth (for WES) or CNVnator (for WGS) [48] [46]
- Structural variants: DRAGEN SV caller or Manta [49]
Recent benchmarks of ultra-rapid analysis pipelines demonstrate that Sentieon DNASeq and Clara Parabricks Germline provide comparable performance for germline variant calling, with cloud-based implementations offering scalable solutions for large-scale stem cell studies [51].
Essential Research Reagents and Platforms
Table 3: Research Reagent Solutions for NGS-Based Genomic Stability Studies
| Category | Specific Products/Platforms | Function in Workflow |
|---|---|---|
| Library Preparation | Agilent SureSelect, Illumina Nextera | Fragments DNA and adds platform-specific adapters for sequencing |
| Exome Enrichment | Twist Core Exome, IDT xGen Exome Panel | Captures protein-coding regions through hybridization for WES |
| Sequencing Platforms | Illumina NovaSeq X Series, PacBio Revio | Performs high-throughput DNA sequencing with various read configurations |
| Analysis Pipelines | Sentieon DNASeq, Clara Parabricks, DeepVariant | Identifies genetic variants from raw sequencing data |
| Cloud Computing | Google Cloud Platform, AWS | Provides scalable computational resources for data analysis |
| Variant Annotation | ANNOVAR, SnpEff, VEP | Functional interpretation of identified genetic variants |
Application to Stem Cell Genomic Stability Assessment
When applying WES and WGS to stem cell genomic stability assessment, researchers should consider the specific requirements of their experimental design:
For routine monitoring of known mutational hotspots in coding regions, WES provides a cost-effective solution with sufficient depth to detect low-frequency variants that may indicate emergent clonal populations in stem cell cultures [48] [46].
For comprehensive characterization of stem cell lines intended for therapeutic applications, WGS offers unparalleled ability to detect off-target effects, structural variations, and mutations in regulatory regions that might impact safety or functionality [53] [49].
For biobanking and reference standard development, WGS serves as an all-in-one test that captures the complete genomic landscape, enabling retrospective analysis as new genomic elements are discovered [49].
The integration of long-read sequencing technologies (e.g., PacBio HiFi, Oxford Nanopore) with short-read WGS provides complementary advantages for resolving complex genomic regions that are particularly relevant to stem cell biology, including repetitive elements and structural variations that may influence genomic stability [54] [55].
The selection between WES and WGS for stem cell genomic stability assessment depends primarily on the research objectives, resources, and specific variant types of interest. WES remains a powerful, cost-efficient tool for focused analysis of protein-coding regions, while WGS provides a comprehensive view of the genomic landscape with superior capability for detecting structural variants and non-coding mutations. As sequencing costs continue to decline and analytical methods improve, WGS is increasingly becoming the preferred approach for definitive genomic characterization in stem cell research and therapeutic development.
In the field of stem cell research, ensuring the genomic stability of induced pluripotent stem cells (iPSCs) is a critical challenge. Culture-acquired genetic variants, including mosaicism, can silently compromise experimental reproducibility, therapeutic safety, and efficacy [56]. While traditional karyotyping and next-generation sequencing (NGS) are established methods, digital PCR (dPCR) emerges as a powerful, rapid, and targeted tool for routine monitoring. This guide objectively compares the performance of leading dPCR platforms, providing the experimental data and protocols needed to integrate this technology into a robust genomic stability assessment strategy.
The Genomic Stability Challenge in Stem Cell Research
Induced pluripotent stem cells are prone to spontaneous chromosomal abnormalities during in vitro expansion. Studies report karyotype abnormalities in 22–23% of analyzed iPSC samples, a figure that can rise to 80% after prolonged passaging [57]. These are not random events; a pattern of recurrent anomalies shapes the iPSC genomic instability landscape. The most common recurrent aberrations include gains of chromosomes or chromosomal segments 20/20q, 1q, 12, 8, and 17, and losses of chromosomes 10 and 18 [57].
The presence of these mutations, particularly those that confer a growth advantage such as 1q gain and 20q gain, poses a direct threat to the safety and efficacy of cell therapies. These abnormalities can alter cellular behavior, leading to variability in differentiation capacity and raising the serious risk of tumorigenicity in patients post-transplantation [57] [56]. Detecting these low-frequency, mosaic variants requires a method that is not only accurate but also efficient enough for routine quality control.
Digital PCR: Principle and Advantages for Mosaicism Detection
Digital PCR (dPCR) is a third-generation PCR technology that enables absolute quantification of nucleic acids without the need for a standard curve [58] [59]. Its principle is fundamentally different from quantitative PCR (qPCR):
- Partitioning: A PCR reaction mixture is divided into thousands to millions of nanoliter-sized partitions, so that each contains zero, one, or a few target nucleic acid molecules [59] [60].
- Amplification: End-point PCR amplification is performed on all partitions in parallel.
- Detection & Quantification: Partitions are analyzed as positive (fluorescent) or negative (non-fluorescent). The absolute concentration of the target molecule is then calculated using Poisson statistics based on the ratio of positive to negative partitions [58] [59].
This workflow offers distinct advantages for detecting mosaic genetic variants in iPSCs, as outlined in the following diagram.
For genomic stability monitoring, dPCR's key advantages include:
- Absolute Quantification: Provides the exact number of target molecules per input sample, eliminating reliance on external standards and improving reproducibility across labs [59] [60].
- Superior Sensitivity: Capable of detecting rare sequence variants present at very low frequencies (e.g., below 1%) in a background of wild-type sequences, which is essential for identifying emerging mosaic clones [61] [58].
- High Tolerance to Inhibitors: The partitioning process dilutes PCR inhibitors present in the sample, making dPCR more robust than qPCR when working with complex sample types [62] [60].
- Rapid Turnaround: The workflow is faster than sequencing-based methods, providing results in hours, which facilitates frequent monitoring [58].
Comparative Performance of Leading dPCR Platforms
Two major dPCR technologies dominate the market: droplet-based dPCR (ddPCR) and nanoplate-based dPCR. The QX200 Droplet Digital PCR System from Bio-Rad is a leading ddPCR platform, while the QIAcuity Digital PCR System from Qiagen is a prominent nanoplate-based system. Independent studies have directly compared their performance for precise nucleic acid quantification.
The table below summarizes key performance metrics from a comparative study that analyzed gene copy number variations using synthetic oligonucleotides and ciliate DNA [63].
Table 1: Performance comparison of nanoplate-based and droplet-based dPCR platforms
| Performance Metric | QIAcuity (Nanoplate-based) | QX200 (Droplet-based) |
|---|---|---|
| Limit of Detection (LOD) | 0.39 copies/µL input [63] | 0.17 copies/µL input [63] |
| Limit of Quantification (LOQ) | 1.35 copies/µL input [63] | 4.26 copies/µL input [63] |
| Precision (CV Range) | 7% to 11% (with synthetic DNA) [63] | 6% to 13% (with synthetic DNA) [63] |
| Precision with Restriction Enzymes | Less affected by enzyme choice (CV: 0.6%-27.7%) [63] | Improved precision with HaeIII vs. EcoRI (CV: <5%) [63] |
| Dynamic Range | Up to 3,000 copies/µL input (demonstrated) [63] | Up to 3,000 copies/µL input (demonstrated) [63] |
| Partition Number | ~8,500 partitions per well [64] | ~20,000 droplets per sample [64] |
| Reaction Volume | 12-40 µL [64] [63] | 20 µL [64] [63] |
Another study comparing these platforms for DNA methylation analysis of the CDH13 gene in 141 breast cancer samples further confirmed their analytical performance [64].
Table 2: Diagnostic performance in methylation analysis (CDH13 gene)
| Diagnostic Metric | QIAcuity (Nanoplate-based) | QX200 (Droplet-based) |
|---|---|---|
| Sensitivity | 99.08% [64] | 98.03% [64] |
| Specificity | 99.62% [64] | 100% [64] |
| Correlation | A strong correlation between methylation levels was observed (r = 0.954) [64] |
Platform Selection: Key Differentiators
The data shows that both platforms deliver high sensitivity, specificity, and precision. The choice between them often depends on practical workflow considerations:
- Throughput and Workflow: The QIAcuity's nanoplate-based system offers a more automated, integrated workflow that minimizes hands-on time and reduces the risk of contamination, making it suitable for higher-throughput labs [64] [59].
- Partition Number and Precision: The QX200 typically generates a higher number of partitions (~20,000), which can, in theory, provide better precision, especially at very low target concentrations [64] [63].
- Ease of Use: The nanoplate-based system eliminates the need for manual droplet generation, simplifying the process and improving reproducibility for routine testing [64].
Experimental Protocol: Detecting a Recurrent 1q Gain in iPSCs
To effectively implement dPCR for routine monitoring, a validated and detailed experimental protocol is essential. The following protocol is adapted from published dPCR methodologies and tailored for detecting a recurrent gain of chromosome 1q in iPSC cultures [64] [63].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key research reagent solutions for dPCR analysis
| Reagent/Material | Function | Example |
|---|---|---|
| dPCR Master Mix | Provides optimized buffer, nucleotides, and polymerase for the PCR reaction. | QIAcuity 4x Probe PCR Master Mix [64] or ddPCR Supermix for Probes [64] |
| FAM-labeled Probe & Primers | Specifically targets and detects the sequence of interest on the aneuploid region (e.g., 1q). | Custom-designed assay for a gene on 1q [64] |
| HEX/VIC-labeled Probe & Primers | Targets a stable reference gene on a different, non-polysomic chromosome for normalization. | Custom-designed assay for a reference gene [64] |
| Restriction Enzyme | Digests genomic DNA to improve access to the target sequence and partitioning efficiency. | HaeIII or EcoRI [63] |
| Nuclease-free Water | Adjusts the reaction volume without introducing contaminants. | N/A |
| dPCR Plates or Cartridges | The physical substrate for generating thousands of partitions. | QIAcuity Nanoplate [64] or DG8 Cartridge for QX200 [64] |
Step-by-Step Workflow
Sample Preparation
- Extract genomic DNA from a small sample of iPSCs (e.g., using the DNeasy Blood and Tissue Kit [64]).
- Quantify DNA precisely using a fluorometer (e.g., Qubit 3.0 [64]).
- Digest 10-50 ng of genomic DNA with a restriction enzyme (e.g., HaeIII) for 15-30 minutes to fragment the DNA. This step has been shown to significantly improve precision, especially in droplet-based systems [63].
Reaction Setup
- Prepare the probe-based dPCR reaction mix according to Table 4. The reaction uses a duplex assay to co-amplify the target (1q) and reference genes in the same well.
Table 4: Reaction setup for a duplex dPCR assay (volumes based on QIAcuity)
Component Final Concentration/Volume 4x dPCR Master Mix 1x (3 µL for a 12 µL reaction) Forward/Reverse Primer (Target 1q) Optimized concentration (e.g., 200 nM each) FAM-labeled Probe (Target 1q) Optimized concentration (e.g., 100 nM) Forward/Reverse Primer (Reference) Optimized concentration (e.g., 200 nM each) HEX-labeled Probe (Reference) Optimized concentration (e.g., 100 nM) Restriction Enzyme-digested DNA Template 10-50 ng total Nuclease-free Water To final volume - Pipette the reaction mix into the dPCR nanoplate or cartridge.
Partitioning and Amplification
- Load the plate or cartridge into the instrument.
- The instrument automatically performs partitioning, followed by endpoint PCR amplification. A typical cycling protocol is [64]:
- Enzyme activation: 95°C for 2-10 minutes.
- 40 cycles of:
- Denaturation: 95°C for 15-30 seconds.
- Annealing/Extension: 57-60°C for 1 minute.
Data Analysis
- After the run, the instrument software automatically analyzes the fluorescence in each partition.
- Set appropriate fluorescence thresholds to distinguish positive and negative clusters for both FAM and HEX channels.
- The software calculates the absolute copy number per µL for both the target (1q) and reference assays using Poisson correction.
- Calculate the Copy Number Variation (CNV) or ratio:
CNV = (Copies/µL of Target 1q Assay) / (Copies/µL of Reference Assay)A ratio of approximately 1.5 would suggest a mosaic gain of 1q in a significant portion of the cell population, while a ratio of 1.0 indicates a normal diploid state.
Strategic Implementation in a Genomic Stability Workflow
For comprehensive iPSC genomic assessment, dPCR is most powerful when integrated with other technologies. The following diagram illustrates a risk-stratified, stage-appropriate testing strategy.
- Low-Resolution Screening: Use traditional G-banding karyotyping as an initial, broad screen for large chromosomal abnormalities during early line establishment [56].
- High-Resolution Risk Profiling: Employ NGS-based methods (e.g., whole-genome sequencing or targeted oncogenetic panels) to comprehensively characterize the cell line and identify specific mutations at base resolution. This provides a baseline and identifies which recurrent variants to monitor [56].
- Routine Monitoring with dPCR: Implement targeted dPCR assays for specific, high-risk recurrent aberrations (like 1q gain, 20q gain, or Trisomy 12) identified in the risk profile. dPCR's speed, sensitivity, and lower cost make it ideal for frequent monitoring of banked cell lines and during extended culture expansion [57].
This integrated approach balances comprehensiveness with practicality, ensuring that critical genetic defects are detected early and reliably throughout the product lifecycle.
Digital PCR represents a significant advancement in the toolkit for stem cell genomic stability assessment. As the data shows, modern platforms like the QIAcuity and QX200 offer high precision, sensitivity, and specificity for absolute quantification of nucleic acids. While NGS provides unparalleled breadth in variant discovery, dPCR offers unmatched speed, simplicity, and cost-effectiveness for targeting known, high-risk mosaic variants like recurrent aneuploidies. By integrating targeted dPCR into a layered quality control strategy—alongside low-resolution karyotyping and high-resolution NGS—researchers and therapy developers can achieve a practical, powerful, and proactive system for safeguarding the genetic integrity of iPSC cultures, thereby ensuring the safety and efficacy of stem cell-based therapies.
Understanding the relationship between genomic alterations and transcriptional changes is fundamental to both stem cell research and oncology. In the context of stem cell genomic stability assessment, unintended genetic modifications during differentiation and proliferation can lead to tumorigenicity, presenting significant safety concerns for stem cell-based therapies [42]. Similarly, cancer cells undergo dynamic reprogramming of gene regulatory controls, resulting in distinct transcriptional patterns that drive tumor progression [65]. RNA sequencing (RNA-Seq) has emerged as a powerful technological bridge connecting these domains, enabling researchers to comprehensively quantify transcriptomes at a genome-wide scale and directly correlate genomic alterations with their functional transcriptional outcomes [66].
The integration of DNA and RNA analysis provides crucial insights into how mutational processes and epigenetic alterations interact to establish tumorigenic states [67]. Transcription factors (TFs) play a pivotal role as master regulators of gene expression, and their dysregulation creates cascading effects including uncontrolled proliferation, loss of cellular identity, and genomic instability—the essential hallmarks of malignant transformation [67]. Recent advances in single-cell RNA sequencing (scRNA-seq) and spatial transcriptomics have further refined our understanding of brain cell states during ageing and disease, revealing cell-type-specific changes that were previously obscured in bulk analyses [68]. This review compares the performance of various RNA-Seq methodologies in detecting these crucial relationships, with particular emphasis on their applications in stem cell safety assessment and oncogene research.
RNA-Seq Methodologies: Technical Comparisons and Performance Metrics
Bulk RNA-Seq Versus Single-Cell and Spatial Approaches
Table 1: Comparison of RNA Sequencing Technologies and Applications
| Methodology | Resolution | Key Applications | Detection Capabilities | Technical Considerations |
|---|---|---|---|---|
| Bulk RNA-Seq | Tissue-level average expression | Differential gene expression analysis, transcriptome quantification | Genome-wide expression changes, splicing variants | Requires 20-30 million reads/sample; 3+ biological replicates recommended [66] |
| Single-Cell RNA-Seq | Individual cell resolution | Cell heterogeneity, rare cell populations, developmental trajectories | Cell-type-specific expression patterns, novel cell states | High technical variability; specialized bioinformatics pipelines needed [68] [69] |
| Spatial Transcriptomics | Tissue localization with single-molecule resolution | Tissue architecture, spatial gene expression patterns, cell-cell interactions | Gene expression within morphological context | Combines histological with transcriptomic data; computationally intensive [68] |
| Single-Nucleus RNA-Seq | Nuclear transcriptome of individual cells | Archived tissues, complex tissues difficult to dissociate | Gene expression in hard-to-isolate cells | Captures nuclear transcripts; works well with frozen samples [68] |
Bulk RNA-Seq provides a population-average view of gene expression, making it suitable for detecting major transcriptional shifts in response to experimental conditions or disease states [66]. However, this approach masks cell-to-cell heterogeneity, which can be crucial for understanding cancer evolution and stem cell differentiation. Single-cell RNA sequencing (scRNA-seq) technologies overcome this limitation by resolving transcriptional profiles at individual cell resolution, enabling identification of rare cell populations and distinct cell states within seemingly homogeneous tissues [68] [69]. Spatial transcriptomics adds another dimension by preserving geographical context, allowing researchers to correlate transcriptional patterns with tissue morphology—particularly valuable for understanding the tumor microenvironment [68].
Experimental Design Considerations for Robust Detection
The reliability of RNA-Seq data depends heavily on appropriate experimental design. Key parameters include sequencing depth, replicate number, and quality control measures. For standard differential expression analysis in bulk RNA-Seq, approximately 20-30 million reads per sample is often sufficient, though this requirement increases for detecting low-abundance transcripts or alternatively spliced isoforms [66]. Biological replication is critical for statistical power, with three replicates per condition generally considered the minimum standard, though more replicates provide greater power to detect subtle differences, especially when biological variability is high [66].
Quality control must be integrated throughout the RNA-Seq workflow, beginning with raw read assessment using tools like FastQC to identify adapter contamination, unusual base composition, or duplicated reads [66] [70]. Subsequent steps including read trimming, alignment, and post-alignment filtration ensure that only high-confidence mappings contribute to expression quantification [66]. The entire process, from FASTQ files to differential expression analysis, can be implemented through structured computational pipelines combining command-line tools for preprocessing with R-based packages for statistical analysis and visualization [70].
Correlating Genomic Alterations with Transcriptional Profiles
Machine Learning Approaches for Pattern Recognition
Advanced computational methods have significantly enhanced our ability to detect subtle transcriptional patterns associated with specific genomic alterations. Random forest models have successfully identified transcriptional signatures associated with loss of wild-type activity in cancer-related genes across various tumour types [71]. For example, genes like TP53 and CDKN2A exhibit unique pan-cancer transcriptional patterns, while others including ATRX, BRAF, and NRAS show tumour-type-specific expression patterns [71]. The performance of these classification models improves substantially when combining single-nucleotide variant data with copy number alterations, increasing F1 scores by approximately 19.3% on average compared to using SNVs/INDELs alone [71].
Table 2: Transcriptional Patterns Associated with Genetic Alterations in Cancer and Stem Cells
| Genetic Context | Transcriptional Alterations | Functional Consequences | Detection Methods |
|---|---|---|---|
| Ageing Human Brain [68] | Downregulation of housekeeping genes; Increased transcriptional variability in IN-SST neurons | Compromised inhibitory signaling; Impaired cellular homeostasis | snRNA-seq, scWGS, Spatial transcriptomics |
| Cancer Driver Mutations [71] | Gene-specific patterns (TP53, CDKN2A); Tumour-type specific signatures (BRAF, ATRX) | Uncontrolled proliferation; Evasion of growth suppression | Random forest models, RNA-Seq classification |
| Stem Cell Genetic Instability [42] | Persistent expression of oncogenic variants (KMT2C, BCOR); Cancer-related gene expression | Increased tumorigenic potential; Safety concerns for therapies | Whole-exome sequencing, Targeted sequencing, ddPCR |
| Transcription Factor Dysregulation [67] | Dysregulation of proliferative, differentiation, and DNA repair programs | Genomic instability; Oncogenic transformation | Transcriptional regulatory network analysis |
The integration of multi-omic data types enables more accurate classification of tumors based on their underlying molecular alterations. For instance, analysis of transcriptional patterns in primary and metastatic tumors has revealed that certain genes like DRG2 emerge as top contributors in classifying ATRX alterations in lower-grade gliomas, while features important in classifying PTEN aberrations include genes such as CDCA8, AURKA, and CDC20, which are closely related to PTEN function [71]. These approaches demonstrate how transcriptomic data can reflect the functional status of specific cancer genes, providing insights into active cellular pathways that may represent therapeutic targets.
Transcription Factors as Master Regulators of Oncogenic Programs
Transcription factors (TFs) serve as critical intermediaries between genomic alterations and transcriptional changes in cancer. Dysregulation of TFs initiates a cascade of biochemical events that disrupt normal cellular homeostasis, leading to uncontrolled proliferation and genomic instability [67]. Through in silico analysis of promoters from 622 cancer-driving genes, researchers have identified five distinct DNA motifs significantly overrepresented in oncogene promoters, linked to a network of 128 transcription factors that function as master regulators of carcinogenesis [67]. This finding suggests that despite the vast genetic heterogeneity of cancer, a core set of transcriptional programs is recurrently co-opted to drive oncogenic expression.
Notable examples include the MYC proto-oncogene, which accelerates the cell cycle and increases replication stress, and STAT5, which promotes cell survival and proliferation [67]. The tumor suppressor p53 activates genes involved in DNA damage repair and cell cycle arrest, with its inactivation leading to mutation accumulation and evasion of apoptotic processes [67]. Additionally, mutations in the TERT gene promoter create binding sites for ETS family TFs, leading to constitutive TERT activation and replicative immortality in cancers such as melanoma, glioblastoma, and urothelial carcinoma [67].
Experimental Protocols for Integrated Genomic-Transcriptomic Analysis
RNA-Seq Wet-Lab Workflow
The standard RNA-Seq protocol begins with RNA extraction from cells or tissues, followed by conversion to complementary DNA (cDNA) using reverse transcriptase [66]. For transcriptomic RNA-Seq, the mRNA content is specifically selected through poly(A) tail capture or ribosomal RNA depletion [70]. The resulting cDNA fragments are sequenced using high-throughput platforms, generating millions of short reads that represent the transcriptome composition at the time of sequencing [66]. For single-cell approaches, additional steps for cell isolation, barcoding, and library preparation are required before sequencing [68] [69].
Computational Analysis Pipeline
Following sequencing, the computational analysis of RNA-Seq data involves multiple steps to transform raw sequencing reads into biologically interpretable results [66] [70]. The process begins with quality control of FASTQ files using tools like FastQC to identify potential technical artifacts [66] [70]. Reads are then trimmed to remove adapter sequences and low-quality bases using programs such as Trimmomatic or Cutadapt [66] [70]. The cleaned reads are aligned to a reference genome or transcriptome using aligners like HISAT2, STAR, or through pseudoalignment with Kallisto or Salmon [66] [70]. Post-alignment processing includes quantification of reads mapping to genes or transcripts, typically performed with featureCounts or HTSeq-count, generating a count matrix for downstream analysis [66] [70].
Specialized Approaches for Stem Cell Genomic Stability Assessment
In stem cell research, assessing genetic stability requires specialized approaches to detect potentially tumorigenic mutations. Conventional methods like karyotyping and chromosomal microarray analysis can detect large chromosomal abnormalities but lack resolution for subtle changes [42]. More sensitive techniques include whole-exome sequencing (WES) to identify coding variants and targeted sequencing of cancer-related genes [42]. Droplet digital PCR (ddPCR) provides highly sensitive validation of specific mutations identified through sequencing approaches, offering superior sensitivity and accuracy compared to conventional qPCR [42]. This multi-method approach is essential for comprehensive safety assessment of stem cell-based therapeutics, as recommended by regulatory agencies including the FDA and EMA [42] [72].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents for RNA-Seq and Genomic Alteration Studies
| Reagent/Tool Category | Specific Examples | Function | Application Context |
|---|---|---|---|
| Quality Control Tools | FastQC, MultiQC | Assess sequence quality, adapter contamination, GC bias | Initial QC of raw sequencing data [66] [70] |
| Read Processing Tools | Trimmomatic, Cutadapt, fastp | Remove adapter sequences, trim low-quality bases | Pre-alignment data cleaning [66] [70] |
| Alignment Software | HISAT2, STAR, TopHat2 | Map reads to reference genome/transcriptome | Read alignment for bulk RNA-Seq [66] [70] |
| Quantification Tools | featureCounts, HTSeq-count, Salmon | Generate count matrices from aligned reads | Gene expression quantification [66] [70] |
| Differential Expression | DESeq2, edgeR | Identify statistically significant expression changes | Statistical analysis of expression data [66] [70] |
| Visualization Packages | ggplot2, pheatmap, Volcano plots | Create publication-quality graphics | Data visualization and interpretation [70] |
| Single-Cell Analysis | Seurat, Scanpy | Process and analyze scRNA-seq data | Single-cell transcriptomics [68] [69] |
| Mutation Validation | Droplet digital PCR | Validate mutations with high sensitivity | Stem cell safety assessment [42] |
Signaling Pathways in Transcriptional Dysregulation
The relationship between genomic alterations and transcriptional changes is mediated through several key signaling pathways. Transcription factors such as ELK1 and ETS from the MAPK pathway become dysregulated, leading to increased expression of proliferation genes [67]. Similarly, the PI3K/AKT/mTOR pathway, when hyperactivated, promotes uncontrolled cell proliferation and survival by acting on TFs like FOXO, which normally regulates cell cycle arrest and apoptosis [67]. E2F transcription factors regulate the G1-to-S phase transition by controlling cyclin and CDK expression, with dysregulation leading to accelerated proliferation and mutation accumulation [67].
RNA modifications represent an additional layer of gene expression regulation in cancer, with genes like NSUN2, DNMT3B, and CBP20 showing increased expression in cancer tissues and association with poor survival across multiple cancer types [65]. CBP20, an N7-methylguanosine binding protein, has emerged as a key candidate, with its knockdown leading to reduced cancer cell viability, apoptosis induction, and G1-S cell cycle arrest [65]. RNA sequencing following CBP20 depletion confirmed downregulation of cell-cycle-related pathways, highlighting how transcriptional analysis can reveal critical dependencies in cancer cells [65].
RNA sequencing technologies provide powerful approaches for correlating genomic alterations with transcriptional changes in both stem cell research and cancer biology. The continuing evolution of these methods—from bulk to single-cell and spatial approaches—offers increasingly refined insights into how genetic changes manifest as transcriptional dysregulation. For stem cell research, these capabilities are essential for comprehensive safety assessment, particularly in detecting tumorigenic transformations during differentiation and expansion [42] [72]. In cancer biology, transcriptomic profiling enables identification of active oncogenic pathways and potential therapeutic targets, moving beyond what DNA sequencing alone can reveal [71] [65].
The integration of machine learning approaches with multi-omic data represents a promising frontier for both fields, enhancing our ability to detect subtle patterns predictive of malignant transformation or therapeutic response. As these technologies continue to advance, they will undoubtedly strengthen both the safety assessment of stem cell therapies and our fundamental understanding of oncogene dysregulation, ultimately supporting the development of more effective and safer regenerative medicines and cancer treatments.
The translational potential of stem cell-based therapies in regenerative medicine is profoundly dependent on the genomic integrity of the cellular starting material. Spontaneous genetic alterations during cell culture expansion pose significant risks, including tumorigenic potential and altered functionality, which can compromise both patient safety and therapeutic efficacy [16]. Consequently, a rigorously structured testing framework implemented prior to cell bank establishment is indispensable for ensuring the reliability of downstream applications. This guide objectively compares the methodological approaches and performance metrics for genomic stability assessment within a stage-gated pathway, providing researchers with a standardized workflow from cell line acquisition to pre-banking.
The biosafety of cell therapy products hinges on a comprehensive evaluation of critical quality attributes, with genetic stability forming a cornerstone of this assessment [73]. A systematic, stage-gated strategy serves as a risk mitigation tool, enabling early detection of genomic anomalies and ensuring that only well-characterized, stable cell lines progress to Master Cell Bank (MCB) generation. This approach aligns with regulatory expectations for cell-based medicinal products and integrates quality-by-design principles directly into the initial development phases [16] [74].
The progression from an acquired cell line to a pre-bank candidate involves multiple discrete stages of evaluation, each serving as a critical decision point. The following workflow delineates the sequential stages and key assessments required at each gate.
Comparative Analysis of Genomic Stability Assessment Methods
Selecting appropriate analytical techniques for genomic stability assessment requires careful consideration of resolution, sensitivity, and throughput. The following table provides a comparative overview of established and emerging methodologies, highlighting their performance characteristics and practical implementation requirements.
Table 1: Performance Comparison of Genomic Stability Assessment Methods
| Method | Resolution | Key Performance Metrics | Throughput | Detection Capabilities | Experimental Requirements |
|---|---|---|---|---|---|
| Karyotyping (G-banding) | ~5-10 Mb | Detects numerical abnormalities and large structural variations | Low | Aneuploidy, translocations, large deletions/insertions | Metaphase cells, experienced cytogeneticist |
| Fluorescence In Situ Hybridization (FISH) | 50 kb - 2 Mb | >95% sensitivity for targeted anomalies | Medium | Specific chromosomal rearrangements, aneuploidy | Target-specific probes, fluorescence microscopy |
| Comparative Genomic Hybridization (CGH) Array | ~50-100 kb | >98% sensitivity for copy number variations | Medium-High | Genome-wide copy number variations | DNA extraction, reference sample, specialized platform |
| Next-Generation Sequencing (NGS) | Single nucleotide | >99.9% sensitivity for single nucleotide variants | High | Point mutations, indels, copy number variations, structural variants | High-quality DNA, bioinformatics expertise |
| Short Tandem Repeat (STR) Profiling | Multiple loci | 100% identity matching accuracy | High | Cross-contamination, misidentification | DNA extraction, multiplex PCR capability |
The integration of artificial intelligence into genomic analysis presents emerging opportunities for enhancing detection capabilities. AI techniques, particularly deep learning models, have demonstrated groundbreaking advances in analyzing complex biological data, enabling unprecedented insights into genomic alterations and their functional implications [75]. These approaches can significantly improve the efficiency and accuracy of genomic stability assessment, with some models achieving robust single-cell modeling (AvgBIO 0.82) and sensitive detection capabilities (Area Under Curve 0.93) in related biological applications [75].
Detailed Experimental Protocols for Key Assessments
Cell Identity Verification via Short Tandem Repeat (STR) Profiling
Purpose: To authenticate cell lines and exclude cross-contamination prior to pre-banking. Methodology:
- Extract genomic DNA using a commercial kit, ensuring DNA concentration >10 ng/μL and A260/A280 ratio between 1.8-2.0.
- Amplify 8-16 core STR loci using a commercially available multiplex PCR kit according to manufacturer specifications.
- Separate amplification products by capillary electrophoresis and analyze fragment sizes against reference databases.
- Compare STR profiles with known cell line references or early passage stocks; ≥80% match is required for authentication [76]. Acceptance Criteria: Complete STR profile match with reference material with no unexplained alleles.
Karyotypic Analysis by G-Banding
Purpose: To detect gross chromosomal abnormalities at a resolution of 5-10 megabases. Methodology:
- Culture cells to 60-70% confluence and add colcemid (0.1 μg/mL) for 45-60 minutes to arrest cells in metaphase.
- Harvest cells using trypsinization, subject to hypotonic treatment (0.075 M KCl), and fix in 3:1 methanol:acetic acid.
- Drop cell suspension onto clean slides and age overnight at 60°C.
- Treat with trypsin and stain with Giemsa to produce characteristic banding patterns.
- Analyze 20-50 metaphase spreads per sample using automated karyotyping system [16] [73]. Acceptance Criteria: ≥90% of analyzed metaphases with normal karyotype for the species.
Comprehensive Adventitious Agent Testing
Purpose: To ensure cell stocks are free from viral, bacterial, fungal, and mycoplasmal contaminants. Methodology:
- Test for mycoplasma using PCR-based methods targeting 16S rRNA genes and culture-based methods as a complement.
- Perform in vitro adventitious virus assay by inoculating cell culture supernatants onto indicator cell lines (e.g., Vero, MRC-5).
- Conduct in vivo virus testing by inoculating samples into embryonated eggs and adult mice.
- Implement molecular assays for specific viruses (e.g., retroviruses, calicivirus) based on cell type and history [76] [74]. Acceptance Criteria: All tests negative for adventitious agents with appropriate assay controls validated.
Advanced Monitoring: Detecting Oncogenic Transformation Pathways
For stem cell-based therapies, particularly those utilizing pluripotent stem cells, monitoring molecular pathways associated with oncogenic transformation is critical for comprehensive risk assessment. The following diagram illustrates key signaling nodes and pathways that require surveillance during the pre-banking phase.
The assessment of oncogenicity and tumorigenicity typically employs a combination of in vitro methods and in vivo models in immunocompromised animals [16]. Advanced AI-driven approaches are increasingly being applied to predict potential transformation risks by analyzing multi-omics data and identifying subtle patterns that may elude conventional analysis [75] [77]. These computational methods can integrate transcriptomic, proteomic, and epigenomic data to generate predictive models of cellular behavior, achieving high protein design success rates (up to 92%) in related biological applications [75].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of a stage-gated testing approach requires access to high-quality, well-characterized reagents and platforms. The following table details essential research solutions for establishing a robust pre-banking assessment pipeline.
Table 2: Essential Research Reagent Solutions for Pre-Banking Assessment
| Reagent/Category | Specific Examples | Function & Application | Performance Considerations |
|---|---|---|---|
| Cell Culture Media Systems | mTeSR1, StemFlex, DMEM/F-12 with supplements | Maintain stem cell pluripotency and genomic stability during expansion | Lot-to-lot consistency, growth promotion testing, performance qualification |
| Genomic DNA Extraction Kits | DNeasy Blood & Tissue Kit, MagMAX DNA Multi-Sample Kit | High-quality DNA for STR profiling, CGH array, and NGS analyses | Yield, purity (A260/280), fragment size, removal of PCR inhibitors |
| STR Profiling Panels | ATCC Human STR PCR Kit, GenePrint 10 System | Cell line authentication using standardized loci | Discrimination power, sensitivity, compatibility with database references |
| Karyotyping Systems | Giemsa stain, Trypsin-EDTA, Automated Karyotyping Platform | Chromosomal analysis and detection of gross abnormalities | Banding resolution, metaphase spread quality, analysis software capability |
| Mycoplasma Detection Kits | MycoAlert, VenorGeM Mycoplasma Detection | Sensitive detection of mycoplasma contamination | Detection limit (<10 CFU/mL), time to result, specificity |
| NGS Library Prep Kits | Illumina DNA Prep, KAPA HyperPrep Kit | Preparation of sequencing libraries for comprehensive genomic analysis | Coverage uniformity, GC bias, input DNA requirements, complexity |
| Bioinformatics Platforms | CellRanger, Partek Flow, CLC Genomics Workbench | Analysis of NGS data for genomic stability assessment | Variant calling accuracy, user interface, computational requirements |
The implementation of a systematic, stage-gated testing strategy from cell line acquisition through pre-banking provides a critical framework for ensuring genomic stability in stem cell research. By establishing clear acceptance criteria at each decision point and employing a complementary suite of analytical techniques—from traditional karyotyping to advanced NGS approaches—researchers can significantly mitigate the risks associated with genomic instability. This rigorous assessment directly supports the broader thesis that comprehensive genomic evaluation is fundamental to stem cell research quality.
The evolving integration of AI-driven analytical methods promises to further enhance this assessment paradigm, enabling more sophisticated pattern recognition in complex genomic data and predictive modeling of long-term stability [75] [77]. As the field advances, the stage-gated framework provides a flexible structure for incorporating these technological innovations while maintaining foundational scientific rigor. For researchers and drug development professionals, this systematic approach offers a standardized pathway for generating high-quality, well-characterized cell stocks that meet both scientific and regulatory expectations for downstream therapeutic applications.
Navigating Practical Challenges: Strategies for Robust Genomic Quality Control
The transition of stem cell therapies from research to clinical application hinges on ensuring the genomic integrity of the final product. Human induced pluripotent stem cells (hiPSCs) possess remarkable self-renewal and differentiation capabilities, making them attractive starting materials for cell therapy [42]. However, the very process of long-term in vitro culture necessary for expansion and biomanufacturing places selective pressures on cells, leading to accumulated genetic and epigenetic changes not present in vivo [78]. These unintended genetic modifications pose a critical safety concern, primarily the risk of tumorigenicity, which represents a significant barrier to clinical translation [42]. This article examines the scientific and regulatory rationale behind implementing critical testing intervals, specifically every 5-10 passages, as a essential strategy for monitoring genetic stability throughout the stem cell culture process.
The Scientific Basis for Passage-Dependent Genetic Instability
Accumulation of Genetic Variants in Culture
Prolonged cell culture creates an environment where cells with adaptive advantages, such as faster growth rates, can overtake the population. Studies systematically examining genetic variations during hiPSC expansion and differentiation have identified specific, concerning mutations. Research involving three batches of hiPSCs differentiated into cardiomyocytes at different passages identified a persistent copy number variant (CNV) at chromosome 20q11.21, encompassing the cancer-related gene ASXL1 [42]. This CNV was detected across all groups regardless of cell passage or differentiation status, indicating its early appearance and persistence.
Furthermore, whole-exome sequencing (WES) identified tier 1 variants (with known cancer links) in genes like KMT2C and MUC4, which were consistently detected in both early and intermediate passages and persisted throughout differentiation [42]. Targeted sequencing of 344 solid tumor-related genes revealed additional variants, including missense, nonsense, and frame-shift mutations, with some consistently appearing even after passaging or differentiation [42].
Impact of Culture Duration on Genetic Stability
The relationship between passage number and genetic instability is demonstrated by practical experimental challenges. In one study, late-batch (LB) hiPSCs could not be successfully differentiated into cardiomyocytes, as cells detached from the plate before reaching 2 weeks of differentiation [42]. This indicates that prolonged culture not only introduces genetic abnormalities but can also compromise fundamental cellular functions and differentiation capacity, rendering the cells unsuitable for therapeutic use.
Table 1: Genetic Abnormalities Identified at Different Culture Stages
| Genetic Abnormality | Detection Method | Persistence Across Passages | Potential Clinical Risk |
|---|---|---|---|
| CNV at 20q11.21 (ASXL1) | CytoScanHD chip analysis | All groups (early, intermediate) | Association with cancer pathways |
| KMT2C c.2263C>T p.(Gln755*) | Whole-exome sequencing | Early & intermediate passages | Tier 1 variant (known cancer links) |
| MUC4 c.8032_8033insA p.(Pro2678fs) | Whole-exome sequencing | Early & intermediate passages | Tier 1 variant (known cancer links) |
| BCOR mutations | Targeted sequencing + ddPCR validation | Consistent appearance with passaging | Tumor-related gene |
| Multiple missense/nonsense mutations | Targeted sequencing (344 genes) | Persisted with passaging/differentiation | Various oncogenic potentials |
Establishing the 5-10 Passage Testing Interval: Biological and Regulatory Rationale
The Balance Between Practical Manufacturing and Risk Mitigation
The recommendation for testing every 5-10 passages represents a consensus balancing practical manufacturing constraints with essential safety monitoring. From a biological perspective, this interval is sufficient to allow potential genetic abnormalities to accumulate to detectable levels while preventing extensive culture of compromised cells. Regulatory guidelines from the FDA, EMA, and MFDS strongly recommend using appropriate testing methods to ensure genetic stability throughout manufacturing [42]. The proliferative capacity of stem cells that enables large-scale manufacturing simultaneously carries risks that necessitate regular monitoring [78].
Phase-Appropriate Implementation in Biomanufacturing
The implementation of passage-based testing intervals should align with the phase of product development. In early-stage clinical trials, Good Manufacturing Practices (GMPs) may be introduced in a phase-appropriate manner [78]. Similarly, genetic stability testing frequency can be adapted to the specific stage of product development, with more frequent intervals (e.g., every 5 passages) for master cell banks and later intervals (e.g., every 10 passages) for well-characterized cells in advanced development phases.
Methodological Approaches for Genetic Stability Assessment
Comparison of Conventional and Advanced Monitoring Technologies
Effective passage-interval testing requires sensitive methodologies capable of detecting various genetic abnormalities. Conventional methods like karyotyping and fluorescence in situ hybridization (FISH) have significant limitations, including difficulties with large-scale cell differentiation, extended processing times, and low resolution that makes detecting small structural changes challenging [42].
Advanced technologies offer superior sensitivity and resolution. Droplet digital PCR (ddPCR) has demonstrated high sensitivity and accuracy for quantitatively detecting specific gene mutations, while conventional qPCR could not avoid false positives [42]. Next-generation sequencing methods, including whole-exome sequencing (WES) and targeted sequencing, provide higher resolution and enable efficient analysis of large genomes [42]. Chromosomal microarray analysis, such as CytoScanHD chip analysis, can identify subtle structural abnormalities that karyotyping might miss [42].
Table 2: Comparison of Genetic Stability Assessment Methods
| Method | Detection Capability | Sensitivity/LOD | Throughput | Suitability for Routine Testing |
|---|---|---|---|---|
| Karyotyping (G-banding) | Large chromosomal abnormalities | ~5-10 Mbps | Low | Moderate (established but low resolution) |
| CytoScanHD Chip | Subtle CNVs, B-allele frequency changes | ~1.7 Mbps (as demonstrated) | Medium | High for specific CNV detection |
| Whole-Exome Sequencing | Single base-pair variants, small indels | ~100x coverage depth | High | Moderate (cost, analysis complexity) |
| Targeted Sequencing | Variants in specific gene panels | ~300x coverage depth | High | High for focused analysis |
| Droplet Digital PCR | Specific known mutations | High sensitivity/accuracy for quantitative detection | Medium | High for validation/monitoring known variants |
| TdT-Endo IV-Fluorescent Probe | DNA strand breaks, mean breakpoints | High sensitivity for DNA damage | Medium | Potential for non-invasive assessment |
Workflow for Passage-Based Genetic Stability Assessment
The following diagram illustrates a comprehensive experimental workflow for assessing genetic stability at predetermined passage intervals:
Experimental Protocols for Critical Interval Testing
Comprehensive Genetic Stability Assessment Protocol
This protocol outlines the methodology for assessing genetic stability at 5-10 passage intervals, based on approaches validated in recent studies [42]:
Cell Culture and Sampling:
- Culture hiPSCs under standardized conditions across three or more batches
- Sample cells at early (e.g., passage 5), intermediate (e.g., passage 10), and late (e.g., passage 15) stages
- Include both undifferentiated cells and cells differentiated into target lineages (e.g., cardiomyocytes)
- Maintain detailed records of passage history, population doubling times, and morphological changes
Genetic Analysis Methods:
- Perform karyotyping using G-banding to detect chromosomal variations and large structural abnormalities
- Conduct chromosomal microarray analysis (e.g., CytoScanHD chip) to identify subtle copy number variations
- Implement whole-exome sequencing at approximately 100× coverage depth to identify single base-pair variants
- Perform targeted sequencing of cancer-related gene panels (e.g., 344 solid tumor-related genes) at 300× coverage depth
- Validate identified mutations using droplet digital PCR with appropriate controls
Quality Control Measures:
- Confirm successful differentiation through RT-qPCR analysis of lineage-specific markers
- Assess cell viability and proliferation rates using standardized methods
- Document all procedures according to GMP guidelines where applicable
Non-Invasive DNA Integrity Monitoring Protocol
For more frequent monitoring between the 5-10 passage comprehensive assessments, a non-invasive approach can be implemented [9]:
Culture Supernatant Collection:
- Collect conditioned media from stem cell cultures at each passage
- Centrifuge at 1200 rpm to remove cells and debris
- Store supernatant at -80°C until analysis
DNA Breakpoint Detection:
- Extract cell-free DNA from culture supernatants using commercial kits
- Apply TdT-Endo IV-fluorescent probe biosensor technology
- Quantify DNA strand breaks by measuring fluorescence signal intensity
- Calculate Mean number of DNA Breakpoints (MDB) using standard curves
- Compare MDB values across passages to track DNA integrity trends
Stress Exposure Modeling (Optional):
- Establish heat stress models (e.g., 43°C for 15-45 minutes)
- Implement cryopreservation protocols with varying cryoprotectant concentrations
- Assess DNA damage response under different stress conditions
- Evaluate protective compounds (e.g., LBP at 0.1-4 mg/mL concentrations)
Essential Research Reagent Solutions
Table 3: Key Reagents for Genetic Stability Assessment
| Reagent/Category | Specific Examples | Function in Genetic Stability Assessment |
|---|---|---|
| Cell Culture Media | hiPSC maintenance media, differentiation kits | Maintain cell viability and directed differentiation during long-term culture |
| DNA Extraction Kits | Commercial DNA extraction kits (e.g., TIANGEN DP304) | High-quality DNA extraction for sensitive genetic analyses |
| Sequencing Kits | WES kits, targeted sequencing panels | Comprehensive variant identification across exome or specific genes |
| PCR Reagents | ddPCR supermixes, primer-probe sets | Quantitative validation of identified mutations with high sensitivity |
| DNA Damage Detection | TdT-Endo IV-fluorescent probe biosensor | Sensitive detection of DNA strand breaks and mean breakpoints |
| Cytogenetic Kits | G-banding kits, FISH probes | Detection of chromosomal abnormalities and large structural variations |
| Microarray Solutions | CytoScanHD chips, processing reagents | Genome-wide copy number variation and B-allele frequency analysis |
| Quality Control Assays | CCK-8 viability kits, flow cytometry antibodies | Assessment of cell health, proliferation, and identity markers |
Comparative Analysis of Testing Strategies
Implementing a strategic testing regimen that combines different methodologies at appropriate intervals provides comprehensive genomic surveillance while managing resource constraints. The following diagram compares the application frequency and detection sensitivity of various methods within a tiered testing strategy:
The establishment of critical testing intervals every 5-10 passages represents a essential strategy in balancing stem cell biomanufacturing practicalities with rigorous safety monitoring. The evidence clearly demonstrates that prolonged in vitro culture introduces genetic abnormalities that may compromise product safety and efficacy. By implementing a tiered testing approach that combines conventional cytogenetic methods with advanced sequencing technologies and non-invasive monitoring, researchers can effectively track genomic stability throughout the manufacturing process. This systematic approach to genetic quality control aligns with regulatory expectations and provides the comprehensive safety data needed to advance stem cell therapies toward clinical application. As the field progresses, standardization of these testing intervals and methodologies across the industry will be crucial for comparing results between studies and ensuring the reliable development of safe, effective stem cell-based therapeutics.
Genetic mosaicism, the presence of multiple genetically distinct cell populations within a single culture, presents a significant challenge in stem cell research and therapeutic development. While conventional cytogenetic methods like G-banded karyotyping have served as gold standards, their detection thresholds typically fail to identify mosaicism below 5-20% [3] [79]. This limitation is particularly concerning for human pluripotent stem cells (hPSCs), which show a propensity for acquiring recurrent genetic abnormalities during culture that resemble cancer-associated mutations [3] [80]. This comprehensive review compares emerging methodologies that are pushing detection boundaries, enabling researchers to identify low-level mosaicism with unprecedented sensitivity. We evaluate orthogonal approaches including advanced sequencing technologies, digital PCR, and innovative bioinformatics tools that are transforming our ability to safeguard genomic integrity in stem cell cultures.
The detection of low-level mosaicism has emerged as a critical frontier in quality control for stem cell research and therapy development. Traditional karyotyping, while comprehensive for detecting large chromosomal abnormalities at the single-cell level, has a fundamental detection limit of approximately 5-20% mosaicism [3] [79]. This means cultures deemed "normal" by conventional analysis may harbor significant populations of genetically aberrant cells with potential tumorigenic properties [3]. The acquisition of these abnormalities is not random; hPSCs frequently show recurrent abnormalities on chromosomes 1, 8, 10, 12, 17, 18, 20, and X, regions often associated with cancer genes [3] [80]. One study of 506 hiPSC lines found that 29% had acquired copy number variations (CNVs) during culture, with recurrent regions overlapping cancer-associated genes like BCL2L1 on chromosome 20q11.21 [80]. This evidence underscores the critical need for sensitive detection methods that can identify low-level mosaicism before aberrant cells expand and compromise research validity or patient safety.
Comparative Analysis of Detection Methods
Table 1: Detection Capabilities of Mosaicism Analysis Methods
| Method | Detection Limit | Resolution | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| G-banded Karyotyping | 5-20% mosaicism [3] [79] | >5-10 Mb [79] | Comprehensive chromosomal view; detects unknown abnormalities [79] | Requires cell culture; labor-intensive; low resolution [79] |
| Chromosomal Microarray Analysis (CMA/SNP) | 10-20% mosaicism [81] | 10-200 kb [81] | Genome-wide coverage; no cell culture required | Cannot detect balanced rearrangements [81] |
| Whole Exome Sequencing (100x depth) | ~5% mosaicism [82] | Single nucleotide | Focused on coding regions; cost-effective vs. WGS [82] | Limited to exonic regions; lower resolution than targeted approaches [82] |
| Targeted Sequencing (300x depth) | 1-5% mosaicism [82] | Single nucleotide | High depth enables low-variant detection [82] | Restricted to predefined genomic regions [82] |
| Droplet Digital PCR (ddPCR) | 0.1-0.01% [82] [83] | Single nucleotide | Absolute quantification; high precision; minimal false positives [82] | Limited to known targets; cannot discover novel variants [82] |
| SAM (Sensitive Assay for Mosaicism) | 0.005% [83] | Single nucleotide | Ultra-sensitive; incorporates UMIs for accuracy [83] | Complex workflow; requires specialized design [83] |
| RetroNet (Image-based DNA sequencing) | As few as 2 supporting reads [84] | Mobile element insertions | Detects low-frequency somatic MEIs; eliminates manual inspection [84] | Specific to mobile element insertions [84] |
Table 2: Applications of Detection Methods Across Research Scenarios
| Research Scenario | Recommended Methods | Expected Outcome | Data Output |
|---|---|---|---|
| Routine stem cell quality control | Karyotyping + targeted sequencing [82] [79] | Detection of major abnormalities & known recurrent mutations | Karyogram with CNV profiles [79] |
| Pre-clinical safety assessment | WES + ddPCR validation [82] | Comprehensive variant identification with sensitive confirmation | Variant list with validated allele frequencies [82] |
| Ultra-sensitive detection of known variants | SAM or ddPCR [82] [83] | Quantification of extremely rare variants (0.005%-0.1%) | Absolute mutant copies per sample [82] |
| Analysis of mobile element insertions | RetroNet [84] | Identification of somatic MEIs with low mosaicism | Precision: 0.885, Recall: 0.579 for cancer cell line [84] |
| Prenatal diagnosis of mosaicism | CMA-seq/CMA-SNP [81] | Detection of mosaic aneuploidies and CNVs | Mosaicism level and classification [81] |
Advanced Methodologies for Enhanced Detection
Next-Generation Sequencing Platforms
Next-generation sequencing (NGS) technologies have dramatically improved our capacity to detect low-level mosaicism through enhanced resolution and depth of coverage. Targeted NGS panels achieve significantly higher sequencing depth (300× or more) in specific genomic regions of interest, enabling the identification of low-frequency variants that would be missed by whole-genome sequencing at standard depths [82] [85]. Two primary approaches dominate: capture-based sequencing, which uses probes to enrich specific genomic regions and is ideal for larger target areas, and amplicon-based sequencing, which employs PCR amplification and works well for smaller panels [85]. The exceptional depth achievable with targeted NGS (300× compared to 30-60× for standard WGS) provides the statistical power necessary to distinguish true low-frequency variants from sequencing artifacts [82] [85].
Digital PCR Technologies
Droplet digital PCR (ddPCR) represents a revolutionary approach for quantifying rare genetic variants with exceptional sensitivity and precision. Unlike traditional quantitative PCR, ddPCR partitions samples into thousands of nanodroplets, enabling absolute quantification of target sequences without the need for standard curves [82]. This technology has demonstrated particular utility in stem cell research, where it has been validated for detecting mutations with tumorigenic potential with significantly higher sensitivity and accuracy compared to conventional qPCR [82]. In one study focused on hiPSC-derived cardiomyocytes, ddPCR effectively quantified mutations in KMT2C and BCOR genes that were identified through whole-exome and targeted sequencing, demonstrating its value as an orthogonal validation method [82]. The technology's ability to detect variant alleles at frequencies as low as 0.1% without false positives makes it indispensable for safety assessment in stem cell-based therapeutic development [82].
Specialized Ultra-Sensitive Assays
The most recent innovations in mosaicism detection incorporate unique molecular identifiers (UMIs) and advanced bioinformatics to achieve unprecedented sensitivity. The Sensitive Assay for Mosaicism (SAM) employs a two-phase approach that combines deep sequencing using UMIs with CLIA-validated Sanger sequencing [83]. This method achieves a remarkable detection limit of approximately 0.005% while maintaining clinical-grade accuracy [83]. The UMI strategy improves sequencing accuracy on next-generation sequencing platforms from 99.9% to >99.999% by effectively distinguishing true biological variants from sequencing errors [83].
Similarly, RetroNet represents a novel deep learning algorithm that encodes sequencing reads into images to identify somatic mobile element insertions (MEIs) with as few as two supporting reads [84]. This approach significantly outperforms previous methods, achieving high precision (0.885) and recall (0.579) in detecting insertions present in just 1.79% of cells in a cancer cell line [84]. By transforming sequencing data into visual representations that can be processed by convolutional neural networks, RetroNet eliminates the need for biased manual inspection while extending detection capabilities to SVA elements that were previously challenging to identify [84].
Experimental Protocols for Optimal Detection
Integrated Workflow for Comprehensive Genomic Assessment
Diagram 1: Progressive workflow for mosaicism detection showing method sensitivity thresholds. Researchers can implement this cascade approach to balance comprehensiveness with sensitivity.
Implementation Guidelines for Stem Cell Laboratories
Establish Baseline Characterization: Begin with karyotyping to detect gross chromosomal abnormalities, as this method provides a comprehensive view of the entire chromosome complement and can identify abnormalities such as inversions, duplications, deletions, translocations, and aneuploidies at a single-cell level [79]. This should be performed at critical points including acquisition of new cell lines, initial biobanking, and every 10 passages during culture [79].
Intermediate Depth Analysis: Implement whole exome sequencing (100× coverage) or chromosomal microarray analysis to identify smaller structural variations that karyotyping cannot detect. One effective strategy is CytoScanHD chip analysis, which can uncover subtle abnormalities like the 1.7 Mbps gain in genomic copy numbers at chromosome 20q11.21 that encompasses the cancer-related gene ASXL1 [82].
Targeted Deep Sequencing: Focus on genomic regions of high relevance using targeted sequencing panels (achieving 300× coverage) to detect low-frequency variants. Design panels to include recurrently aberrant regions in hPSCs, particularly chromosomes 1, 12, 17, and 20, which harbor genes like BCL2L1 that provide selective growth advantages [82] [3].
Orthogonal Validation: Confirm identified mutations using ddPCR for absolute quantification. This step is crucial for validating variants with potential tumorigenic implications before finalizing reports or making decisions about cell line utility [82]. The International Council for Harmonisation (ICH) guidelines recommend validation including specificity, precision, robustness, and limit of detection assessments [82].
The Researcher's Toolkit: Essential Reagents and Technologies
Table 3: Key Research Reagent Solutions for Mosaicism Detection
| Reagent/Technology | Function | Application Notes |
|---|---|---|
| CytoScanHD Chip [82] | Genome-wide copy number and CNV analysis | Detects subtle structural abnormalities; identifies cancer-related genes in aberrant regions |
| Targeted Sequencing Panels [82] [85] | Deep sequencing of specific genomic regions | 300× coverage enables low-frequency variant detection; focus on recurrent aberrant regions in hPSCs |
| Droplet Digital PCR Systems [82] | Absolute quantification of rare variants | Validates mutations identified by NGS; avoids false positives common in qPCR |
| Unique Molecular Identifiers (UMIs) [83] | Distinguishing true biological variants from errors | Improves NGS accuracy from 99.9% to >99.999%; essential for ultra-rare variant detection |
| TdT-Endo IV-Fluorescent Probe Biosensor [9] | Quantifying DNA strand breaks in stem cells | Non-invasive assessment of DNA integrity; measures extracellular DNA fragments in culture supernatants |
| RetroNet Deep Learning Algorithm [84] | Image-based detection of mobile element insertions | Encodes sequencing reads into images; identifies somatic MEIs with as few as two supporting reads |
Overcoming the detection limits of traditional cytogenetic methods requires a multifaceted approach that strategically integrates orthogonal technologies. While karyotyping remains valuable for detecting large chromosomal abnormalities, its limitations in identifying low-level mosaicism necessitate complementary methods with greater sensitivity. The emerging paradigm employs sequential screening, beginning with traditional methods to identify gross abnormalities, progressing to NGS-based approaches for higher resolution, and culminating with ultra-sensitive techniques like ddPCR or specialized assays for quantifying rare variants of high clinical significance. This comprehensive strategy enables researchers to address the full spectrum of genetic abnormalities that may compromise stem cell quality, ultimately enhancing the safety profile of stem cell-based therapies and strengthening the validity of research findings. As technologies continue to advance, the field moves closer to routine detection of even the rarest mosaic events, bringing us nearer to the goal of complete genomic characterization in stem cell cultures.
In the field of stem cell research and therapy development, maintaining genomic stability is not merely a regulatory checkbox but a fundamental requirement for patient safety and therapeutic efficacy. Unintended genetic modifications during cell differentiation and proliferation can lead to tumorigenicity, presenting a crucial safety concern for stem cell-based therapies [42]. At the heart of this challenge lies the consistent quality of GMP-grade reagents and media, which form the foundational environment for cell cultivation and expansion.
The growing stem cell therapy market, projected to exhibit a compound annual growth rate (CAGR) of 28.9% for GMP cell therapy consumables between 2025 and 2035, underscores the urgency of establishing robust raw material management systems [86]. Similarly, the broader laboratory reagents market, valued at $8.69 billion in 2024 and expected to reach $13.27 billion by 2031, reflects the expanding ecosystem within which stem cell research operates [87]. This growth brings increased attention to the quality systems supporting therapeutic development, particularly as regulatory agencies worldwide strengthen their focus on the entire manufacturing process, from source materials to final cell products [16] [42].
The integrity of the nuclear architecture and genome stability in stem cells has been shown to depend on precise regulation of chromatin modifiers and their connection to the nuclear lamina [88]. Any inconsistency in culture media composition can disrupt these delicate regulatory networks, potentially leading to reduced heterochromatin content, increased DNA damage, and premature stem cell activation—all compromising the safety profile of the final therapeutic product [88]. This article examines the critical relationship between raw material consistency and genomic integrity, providing researchers with comparative data and methodologies to enhance their material qualification strategies.
Comparative Analysis of GMP-Grade Media Supplements
Performance Metrics Across Supplement Categories
The selection of appropriate media supplements represents one of the most significant decisions in stem cell manufacturing, with direct implications for both cell growth and genetic stability. A 2025 systematic comparison of thirteen culture media supplements, including seven serum-free media (SFM), five human platelet lysate (hPL) preparations, and fetal bovine serum (FBS), revealed critical differences in composition and functional performance [89].
Table 1: Growth Factor Composition Across Media Supplement Categories [89]
| Supplement Category | IGF-1 (ng/mL) | PDGF-AB (ng/mL) | TGF-β1 (ng/mL) | VEGF (pg/mL) | Fibrinogen (μg/mL) |
|---|---|---|---|---|---|
| FBS (Reference) | 110-125 | 35-45 | 2500-3500 | 5-15 | 5-25 |
| hPL Preparations | 40-75 | 75-120 | 150-550 | 850-2200 | 550-1200 |
| Serum-Free Media | 15-60 | 5-30 | 5-100 | 5-100 | 5-50 (2/7 samples >200) |
This comprehensive analysis demonstrated that terminology used by manufacturers often fails to accurately reflect actual composition. Notably, two out of seven commercially marketed "serum-free" media contained significant levels of human blood-derived components, including myeloperoxidase, glycocalicin, and fibrinogen, essentially reclassifying them as human platelet lysates rather than truly defined formulations [89]. This finding highlights the critical need for independent compositional verification rather than reliance on manufacturer classifications alone.
Functionally, the study found that all hPL preparations consistently supported mesenchymal stem cell (MSC) expansion, while some serum-free media failed to adequately support growth despite their theoretical advantages [89]. Interestingly, growth factor content did not directly correlate with MSC growth kinetics or maximal cell yield, suggesting that undisclosed components or specific factor ratios may play a more significant role than absolute concentrations.
Impact on Cell Phenotype and Cost Considerations
Beyond growth performance, media composition significantly influenced cell phenotype. Mesenchymal stem cells cultured in the two SFM that contained human blood components exhibited a CD44 phenotype similar to cells grown in hPL, rather than the phenotype typically associated with serum-free conditions [89]. This finding is particularly relevant for genomic stability, as surface marker profiles can indicate underlying cellular states with different proliferative capacities and differentiation potentials.
The cost-performance analysis revealed that hPL preparations generally offered the most favorable balance, with significantly lower costs than specialized serum-free media while delivering consistent growth support [89]. This economic consideration is non-trivial in scaling operations, as the study noted that "culture medium and the actual cell culture practice often are the most expensive part of cell therapy manufacturing" [89].
Essential Methodologies for Genetic Stability Assessment
Comprehensive Genetic Stability Testing Workflow
Ensuring genomic integrity requires a multi-faceted testing approach that transcends traditional karyotyping. Research on human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs) has demonstrated the necessity of employing complementary techniques to detect genetic variations across different scales and types [42].
Table 2: Genetic Stability Assessment Method Comparison [42]
| Method | Resolution | Key Applications | Limitations | Detectable Anomalies |
|---|---|---|---|---|
| Karyotyping (G-banding) | ~5-10 Mbps | Large chromosomal abnormalities | Low resolution, cannot detect subtle structural changes | Aneuploidy, large translocations |
| CytoScanHD Chip | ~200 Kbps | Copy number variations | Cannot detect balanced rearrangements | CNVs, uniparental disomy |
| Whole-Exome Sequencing | 1 bp | Single nucleotide variants | Limited to exonic regions | Point mutations, small indels |
| Targeted Sequencing | 1 bp | Known cancer-related genes | Targeted scope requires prior gene selection | Mutations in specific gene panels |
| Droplet Digital PCR | <1 bp | Validation of specific variants | Low throughput, not suitable for discovery | Absolute quantification of known mutations |
The hiPSC-CM study implemented a systematic approach where cells were differentiated at three different passages (early, intermediate, and late) and across three batches for each passage to evaluate both passage-dependent and batch-dependent genetic variations [42]. This rigorous design allowed researchers to distinguish between random mutations and consistent genetic drift patterns, providing a more comprehensive safety assessment.
Advanced Detection Techniques: ddPCR Validation
When researchers identified specific mutations in KMT2C and BCOR genes from the 17 variants detected through whole-exome and targeted sequencing, they employed droplet digital PCR (ddPCR) for validation [42]. This method demonstrated superior sensitivity and accuracy compared to conventional qPCR, which could not avoid false positives.
The ddPCR validation followed International Council for Harmonisation (ICH) guidelines, establishing specificity, precision, robustness, and limit of detection parameters [42]. This approach proved particularly valuable for quantitatively detecting mutations with tumorigenic potential, offering a highly sensitive and precise method for critical quality control checkpoints in stem cell therapeutic development.
Diagram 1: Media Impact on Genomic Stability Pathway. Inconsistent media components can disrupt nuclear architecture, ultimately leading to genomic instability and impaired stem cell function [88].
Emerging Technologies and Regulatory Framework
Innovative Media Formulations for Advanced Applications
The GMP-grade cell culture media market has responded to the stringent demands of stem cell research with increasingly sophisticated formulations. The global GMP grade cell culture media market, valued at USD 7.89 billion in 2024 and projected to reach USD 17.30 billion by 2032, reflects this rapid innovation [90]. Several specialized media have emerged as standards for specific applications:
- mTeSR Plus: This stabilized, serum-free medium enables "skip-day" feeding schedules for human induced pluripotent stem cells through enhanced FGF2 stability, maintaining pluripotency while offering workflow flexibility [91].
- TheraPEAK 293-GT Medium: A 2025 introduction specifically optimized for viral vector production in suspension HEK293 cells, featuring chemically defined, animal-origin-free formulation to support gene therapy applications [91].
- High-Intensity Perfusion (HIP) CHO Medium: Engineered for continuous bioprocessing, this media supports cell densities exceeding 100 million cells/mL, addressing scalability challenges in biomanufacturing [91].
The industry-wide shift toward chemically defined and animal-component-free media represents a significant advancement for ensuring consistency and reducing variability attributed to undefined biological components [90]. This transition is particularly crucial for stem cell applications, where subtle environmental changes can influence differentiation trajectories and genetic stability.
Regulatory Expectations and Quality Standards
Regulatory agencies worldwide have established clear expectations for raw material quality in cell therapy manufacturing. The International Society for Stem Cell Research (ISSCR) guidelines emphasize that "the quality and manufacturing of the experimental product fulfills the standards expected for safe human administration" [7]. These guidelines build on fundamental ethical principles that prioritize patient welfare and scientific rigor throughout the development process.
The biosafety assessment of stem cell-based therapies requires rigorous evaluation of multiple parameters, including toxicity, oncogenicity/tumorigenicity/teratogenicity, immunogenicity, biodistribution, and overall cell product quality [16]. Each of these safety dimensions can be influenced by the consistency and composition of culture media and reagents used throughout manufacturing.
Regulatory frameworks increasingly advocate for Quality by Design (QbD) principles and Process Analytical Technology (PAT) implementations, which align with technological advancements in sensor networks and AI-driven process control algorithms [90]. These approaches enable predictive optimization of critical parameters such as pH, dissolved oxygen, and nutrient feed rates in real time, reducing manual interventions while enhancing process consistency and documentation.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key GMP-Grade Reagents for Genomic Stability Research
| Product Category | Specific Examples | Key Function | Genomic Stability Relevance |
|---|---|---|---|
| Stem Cell Media | mTeSR Plus, TheraPEAK 293-GT | Maintain pluripotency, support specific cell types | Prevents spontaneous differentiation & genetic drift |
| Genetic Stability Assays | ddPCR, CytoScanHD, WES | Detect mutations & chromosomal abnormalities | Essential for safety profiling |
| Cell Separation | CD44-based magnetic beads | Isolate specific cell populations | Ensures population homogeneity |
| Cryopreservation Media | DMSO-containing formulations | Long-term cell storage | Maintains viability & genetic integrity |
| Growth Factor Supplements | Recombinant FGF2, TGF-β1 | Direct cell proliferation & differentiation | Provides consistent signaling environment |
Diagram 2: Genetic Stability Workflow. Systematic workflow integrating raw material qualification with genetic stability monitoring throughout stem cell culture processes [42] [89].
Managing raw materials for GMP-grade reagents and media requires a systematic, evidence-based approach that prioritizes consistency and comprehensive quality control. The comparative data presented in this analysis demonstrates that assumptions about media composition based solely on manufacturer classifications can be misleading, necessitating independent verification of critical supplements [89]. Furthermore, genetic stability assessment must employ multiple complementary techniques to detect variations across different genomic scales, with emerging technologies like ddPCR providing superior sensitivity for quantifying mutations with tumorigenic potential [42].
The connection between culture environment and genomic integrity extends beyond simple nutrient provision to encompass fundamental regulatory networks governing nuclear architecture, heterochromatin maintenance, and DNA damage response pathways [88]. As the stem cell therapy field continues its rapid expansion, implementing robust raw material management systems supported by rigorous testing protocols will be essential for ensuring the safety and efficacy of resulting therapies. By adopting the methodologies and comparative frameworks outlined in this guide, researchers and therapy developers can establish scientifically sound approaches to raw material qualification that support both regulatory compliance and therapeutic success.
The shift towards precision oncology and advanced cell-based therapies hinges on a critical, yet complex, task: robustly distinguishing harmless genetic variation from mutations that drive tumorigenesis. Establishing risk-based thresholds for tumorigenic mutations is not merely a technical procedure but a fundamental prerequisite for ensuring patient safety, particularly in the development of stem cell-based interventions where genomic instability poses a significant threat. This process requires the integration of diverse methodologies, from computational mutational signature analysis to clinical validity frameworks. A risk-based threshold is the calculated point at which the probability of a variant being pathogenic, or the level of mutational burden, becomes sufficient to warrant a change in clinical management or to deem a cellular product unsafe for use. The clinical appropriateness of genomic testing is guided by the principle that the testing must be reasonably targeted and that its results must meaningfully impact clinical management and likely improve net health outcomes [92]. This guide provides a comparative analysis of the experimental and computational frameworks central to establishing these vital thresholds, contextualized within the rigorous demands of stem cell genomic stability assessment.
Comparative Analysis of Threshold Establishment Methods
Multiple methodological frameworks exist for determining risk thresholds, each with distinct applications, strengths, and limitations. The following table summarizes the core approaches used in the field.
Table 1: Comparison of Methods for Establishing Risk-Based Thresholds
| Method | Core Application | Key Experimental/Computational Output | Regulatory/Clinical Consideration |
|---|---|---|---|
| Mutational Signature Analysis (e.g., RESOLVE) [93] | Decomposing tumor mutational landscape into etiological patterns (e.g., SBS, DBS). | Number of signatures (K), Exposure matrix (E), Signature matrix (S). Minimizes overfitting via LASSO regularization. | Focuses on dominant, biologically relevant processes; links signatures to prognosis and therapy response. |
| Tumor Mutational Burden (TMB) Risk Modeling [94] | Prognostic stratification and immunotherapy response prediction based on total mutation load. | TMB score (mutations per megabase), TMBrisk gene signature (e.g., CBWD1, ST7L, RFX5-AS1). | TMB cutpoints are cancer-type specific; requires validation for each clinical context. |
| Statistical Decision Frameworks (e.g., MRS, DCA) [95] [96] | Identifying cost-effective risk thresholds for screening and intervention. | Optimal risk-threshold, Incremental Net Benefit (INB), Mean Risk Stratification (MRS). | Incorporates costs, effectiveness, and willingness-to-pay; bridges statistical metrics and decision-making. |
| Point of Departure (PoD) for Genotoxicity [97] | Quantitative risk assessment for genotoxic compounds. | Benchmark Dose (BMD), No-Observed-Adverse-Effect-Level (NOAEL). | Moves away from binary classification to quantitative dose-response assessment for defining acceptable exposure. |
A critical application of these methods is the development of prognostic models, such as the TMB-related risk model (TMBrisk) for ovarian cancer. This model was constructed by first calculating TMB scores from whole-exome sequencing data and then correlating these scores with patient survival outcomes. Researchers then used weighted gene co-expression network analysis (WGCNA) to identify genes whose expression was correlated with TMB. A multi-gene signature was developed via Cox regression and validated in independent datasets, proving its ability to stratify patients into high- and low-risk groups with significant differences in overall survival [94]. This demonstrates a direct translational path from mutational data to a clinically actionable risk threshold.
Experimental Protocols for Key Methodologies
Protocol: Constructing a TMB-Based Prognostic Risk Model
This protocol is adapted from the study by Huang et al. (2022) that established a novel TMBrisk model for ovarian cancer [94].
Data Acquisition and Processing:
- Source: Obtain transcriptome profiles, somatic mutation data, and corresponding clinical data (e.g., overall survival, disease stage) from public repositories such as The Cancer Genome Atlas (TCGA).
- Processing: Map gene identifiers to official symbols. Remove genes with zero expression in over 50% of samples. Normalize data.
TMB Calculation:
- Extract somatic mutation information using a Perl or Python script.
- Calculate the TMB score for each sample using the formula: TMB = (Total Number of Variants) / (Size of Exon Target Region in megabases).
Differential Expression and Co-expression Analysis:
- Identify Differentially Expressed Genes (DEGs) between tumor and normal samples using the
limmaR package (criteria: fold change > 2, false discovery rate < 0.05). - Perform Weighted Gene Co-expression Network Analysis (WGCNA) to identify modules of highly correlated genes. Correlate module eigengenes with TMB scores to select the TMB-related module.
- Identify Differentially Expressed Genes (DEGs) between tumor and normal samples using the
Risk Model Construction:
- Perform univariate Cox regression on genes within the TMB-related module to identify genes with significant prognostic value.
- Use multivariate Cox regression or machine learning algorithms (e.g., Lasso-Cox) to build a parsimonious multi-gene signature.
- Calculate a risk score for each patient: Risk Score = Σ (Expression of Genei * Cox Regression Coefficienti).
Validation:
- Stratify patients into high- and low-risk groups based on the median risk score or an optimized cut-off.
- Validate the model's prognostic performance using Kaplan-Meier survival analysis and time-dependent Receiver Operating Characteristic (ROC) curves in independent datasets (e.g., from the Gene Expression Omnibus, GEO).
Protocol: Differentiating Germline from Somatic Variants in Tumor Profiling
With the expansion of tumor molecular profiling, identifying likely germline variants is a crucial step in risk assessment. The following workflow, based on Jaber et al. (2025), outlines this critical process [98].
Diagram 1: Workflow for Identifying Likely Germline Variants from Tumor Sequencing. This process is essential for identifying hereditary cancer risk and therapy biomarkers like PARP inhibitor eligibility [98].
Signaling Pathways Linking Germline Variants to Tumorigenesis
Germline variants in cancer susceptibility genes drive tumorigenesis by disrupting key cellular maintenance pathways. The following diagram illustrates the primary mechanisms and their clinical implications.
Diagram 2: Mechanisms of Germline Variant-Driven Tumorigenesis and Clinical Biomarkers. Defects in HRD and MMR pathways create specific genomic instabilities that serve as predictive biomarkers for targeted therapies [98].
Table 2: Key Research Reagent Solutions for Genomic Stability and Risk Assessment
| Reagent/Resource | Function | Application Example |
|---|---|---|
| TdT-Endo IV-Fluorescent Probe Biosensor [9] | Sensitive, non-invasive quantification of DNA strand breaks. | Assessing DNA integrity in spermatogonial stem cells (SSCs) under heat or cryopreservation stress. |
| CIBERSORT Algorithm [94] | Computational deconvolution of immune cell populations from bulk transcriptome data. | Correlating TMB and TMBrisk scores with tumor immune infiltration profiles (e.g., CD8+ T cells, Tregs). |
| COSMIC Mutational Signatures Catalogue [93] | Reference database of validated mutational patterns (SBS, DBS, ID). | Decomposing tumor mutation profiles into etiological processes using tools like RESOLVE. |
| ESTIMATE Algorithm [94] | Inference of tumor purity and stromal/immune content from expression data. | Analyzing the tumor microenvironment as a confounder or contributor in TMB-risk models. |
| GDSC Database [94] | Repository of drug sensitivity and genomic data for cancer cell lines. | Inferring potential therapeutic regimens sensitive to high-TMB or high-risk score profiles. |
| Perl/Python Scripts for MAF Processing [94] | Custom scripts for variant annotation and filtering from Mutation Annotation Format (MAF) files. | Pre-processing somatic mutation data for TMB calculation and downstream signature analysis. |
Establishing robust, risk-based thresholds for tumorigenic mutations is a multidisciplinary endeavor, integrating computational biology, high-throughput genomics, and clinical decision science. As the field of regenerative medicine advances, applying these rigorous frameworks to stem cell-based products is non-negotiable for patient safety. The methods compared here—from the RESOLVE framework's robust signature extraction to the clinical pragmatism of decision curve analysis—provide a powerful toolkit. Future progress will depend on the continued refinement of these quantitative approaches, the generation of larger, well-annotated genomic datasets, and the explicit integration of genomic stability metrics into the regulatory pathways for advanced therapies. This will ensure that the immense promise of precision medicine and regenerative therapies is realized with a firm commitment to safety and efficacy.
For researchers and drug development professionals, the maintenance of genomic stability in pluripotent stem cells (PSCs) is a critical determinant in the validity of research and the safety of future clinical applications. The shift from traditional, feeder-dependent culture systems to more defined, feeder-free systems utilizing single-cell passaging represents a significant advancement for scalability and workflow simplification. However, this transition introduces specific pressures that can impact the genetic integrity of stem cells. This guide objectively compares how different culture conditions affect genomic stability, providing supporting experimental data to inform protocol decisions within stem cell genomic stability assessment research.
Table 1: Comparative Performance of Culture Systems on Genomic Stability
Table summarizing key experimental findings on how feeder-free and single-cell passaging conditions impact culture stability.
| Culture Condition | Key Experimental Findings | Impact on Genomic Stability | Source/Model |
|---|---|---|---|
| Feeder-Free with Small Molecule Cocktail (SMC4) | Enabled high-throughput derivation; >20 FF single-cell passages with maintained pluripotency and genomic stability per karyotype/CNV analysis [99]. | Promotes stability in single-cell culture when using supportive additives [99]. | Human iPSCs [99] |
| Feeder-Free with Commercial Media (eTeSR) | After 20 weeks (30 passages) of automated single-cell passaging, 4% of clones developed common abnormalities vs. 50% in media for aggregate passaging [100]. | Significantly reduces the rate of recurrent genetic abnormalities during long-term single-cell culture [100]. | Human iPSCs (H1, H9 lines) [100] |
| Single-Cell Passaging (General) | Associated with a higher chance of cytogenetic changes vs. clump passaging; variant cells bypass post-dissociation bottlenecks that restrict karyotypically normal cells [101]. | Increases risk of genetic and epigenetic instability; selective pressure for variant cells [101]. | Human ESCs & iPSCs [101] |
| Feeder-Free Naïve-State Conversion | Feeder-free dome-shaped iPSCs (FFDS-iPSCs) maintained normal karyotype and pluripotency over 22 passages [102]. | Supports stability in naïve-state PSCs, avoiding risks associated with feeder cells [102]. | Human iPSCs [102] |
Detailed Experimental Data and Protocols
High-Throughput Platform Using a Small Molecule Cocktail
Experimental Protocol:
- Cell Lines & Culture: Established feeder-derived human induced pluripotent stem cells (hiPSCs) were adapted to feeder-free, single-cell culture on Matrigel-coated plates [99].
- Test Condition: Culture medium was supplemented with a small molecule cocktail (SMC4) containing SB431542 (TGFβi), PD0325901 (MEKi), CHIR99021 (GSKi), and Thiazovivin (ROCKi) [99].
- Control Condition: Conventional culture medium without SMC4 additives [99].
- Key Assays:
- Viability & Pluripotency: Cell survival, plating efficiency, and expression of markers (Tra181, SSEA4) were assessed [99]. -Genomic Stability: Karyotype analysis and copy number variation (CNV) were performed after multiple single-cell passages [99]. -Functional Potency: In vitro trilineage differentiation and in vivo teratoma formation assays were conducted [99].
Findings: The SMC4 cocktail was critical for promoting cell survival and self-renewal after single-cell dissociation, preventing the significant cell death and differentiation observed in conventional medium. hiPSCs maintained in SMC4-supplemented medium for over 20 feeder-free, single-cell passages retained a normal karyotype, showed no major CNVs, and demonstrated pluripotency [99].
Commercial Media Formulated for Single-Cell Passaging
Experimental Protocol:
- Cell Lines & Culture: Individual clonal sub-lines were derived from H1 and H9 hPSCs via single-cell deposition and cultured long-term on an automated platform [100].
- Test Condition: Cells maintained in eTeSR medium [100].
- Control Condition: Cells maintained in media originally developed and optimized for aggregate passaging [100].
- Key Assays: After 20 weeks (30 passages), clonal lines were screened for recurrent genetic abnormalities using the hPSC Genetic Analysis Kit and confirmed by FISH [100].
Findings: hPSCs undergoing routine single-cell passaging in eTeSR showed a dramatically lower incidence (4%) of common abnormalities (e.g., on 20q11.21) compared to the control media (50%), underscoring that media formulation is a key factor in mitigating culture-induced genomic stress [100].
Key Signaling Pathways and Experimental Workflows
Signaling Pathways in a Supportive Small Molecule Cocktail
The SMC4 cocktail targets specific signaling pathways to enhance survival and maintain pluripotency in stressful culture conditions [99]. The following diagram illustrates the mechanistic role of each component.
High-Throughput Derivation and Characterization Workflow
The platform below outlines the integrated workflow for generating and validating genomically stable, feeder-free hiPSC clones using single-cell methodologies [99].
The Scientist's Toolkit: Essential Research Reagents
Table of key reagents and their functions for optimizing feeder-free, single-cell cultures.
| Reagent Category | Example Products | Function in Culture System |
|---|---|---|
| Specialized Culture Media | eTeSR [100], StemFlex Medium [103], SMC4-supplemented medium [99] | Formulated to reduce cellular stress, enhance cloning efficiency, and maintain pluripotency under single-cell passaging and high-density culture. |
| ROCK Inhibitors | Thiazovivin [99], Y-27632 [102] | Critical for improving cell survival following single-cell dissociation by inhibiting apoptosis. |
| Defined Substrates | Recombinant Vitronectin (VTN-N) [103], Recombinant Laminin-521 [103], Matrigel [99] | Provide a defined, xeno-free surface for feeder-free cell adhesion and growth. Laminin-521 is noted for high performance in stressful applications [103]. |
| Dissociation Reagents | TrypLE Select [103], Accutase [102] | Enzymes used for gentle, single-cell passaging to replace clump-based mechanical passaging. |
| Pathway Modulators | CHIR99021 (GSK3i), PD0325901 (MEKi), SB431542 (TGFβi) [99], DBZ, iDOT1L [102] | Small molecules used to modulate key signaling pathways (Wnt, MEK/ERK, TGF-β, Notch) to support self-renewal or enable specific pluripotent states. |
The move towards feeder-free cultures and single-cell passaging is essential for the scalability and standardization required for industrial and clinical applications of PSCs. While these conditions inherently increase selective pressure and the risk of genomic instability, the data demonstrates that the risk can be effectively mitigated. The key lies in employing a supportive system: utilizing chemically defined media specifically formulated for single-cell stress, incorporating strategic small molecule cocktails, and adhering to rigorous genomic quality control measures. For researchers assessing genomic stability, the choice of culture system is not merely a matter of convenience but a critical variable that must be optimized and consistently monitored to ensure the quality and safety of PSCs and their derivatives.
Benchmarking Detection Methods: A Comparative Analysis of Sensitivity, Resolution, and Workflow Integration
Genomic stability is a critical quality attribute for stem cell research and therapy development. Genetic alterations can arise during cell culture and expansion, potentially affecting the safety and efficacy of stem cell-based products. This guide provides an objective comparison of four key technologies—karyotyping, optical genome mapping (OGM), next-generation sequencing (NGS), and digital PCR—for assessing genomic stability, enabling researchers to select the most appropriate methods for their specific applications in stem cell research and drug development.
Technology Comparison at a Glance
The table below summarizes the core performance characteristics of each technology based on current literature and technical specifications.
Table 1: Key Performance Metrics of Genomic Analysis Technologies
| Technology | Resolution | Variant Detection Sensitivity | Key Strengths | Primary Limitations |
|---|---|---|---|---|
| Karyotyping | ~5-10 Mb [104] | High for clones >20% [104] | Detects balanced rearrangements; single-cell resolution [105] [104] | Low resolution; requires cell culture [106] [104] |
| Optical Genome Mapping (OGM) | 500 bp - 150 kb [107] [104] | ~5-20% VAF [104] | Genome-wide detection of balanced/unbalanced SVs; no amplification bias [107] [108] | Cannot detect single nucleotide variants (SNVs) [107] |
| Next-Generation Sequencing (NGS) | Single nucleotide [104] | ~1-5% VAF (varies by approach) [104] | Detects SNVs, indels, CNVs, SVs; high multiplexing capability [107] [105] | Complex data analysis; poor detection of balanced SVs with short-read [105] |
| Digital PCR (dPCR) | Single nucleotide (for known variants) | <0.1% for known variants [104] | Absolute quantification; ultra-sensitive for low-frequency variants [104] | Targeted analysis only; requires prior knowledge of variant [104] |
Abbreviations: VAF: Variant Allele Frequency; SV: Structural Variant; CNV: Copy Number Variant; SNV: Single Nucleotide Variant; indel: insertion/deletion.
Detailed Methodologies and Experimental Protocols
Karyotyping (G-banding Analysis)
Protocol Overview: Karyotyping remains a frontline method for detecting large-scale chromosomal abnormalities in stem cell cultures [109]. The standard protocol involves:
- Cell Culture and Metaphase Arrest: Actively dividing cells (e.g., stem cells) are cultured and arrested in metaphase using colcemid, which inhibits spindle fiber formation.
- Hypotonic Treatment and Fixation: Cells are treated with a hypotonic solution (e.g., potassium chloride) to swell them, then fixed with Carnoy's solution (3:1 methanol:acetic acid).
- Slide Preparation and Staining: Cells are dropped onto slides to release chromosomes. Slides are treated with trypsin and stained with Giemsa stain to create a characteristic G-banding pattern.
- Microscopy and Analysis: A minimum of 20 metaphase cells are typically analyzed under a light microscope at 1000x magnification. Karyotypes are described according to the International System for Human Cytogenomic Nomenclature (ISCN).
Performance Data: A 2025 large-scale retrospective analysis of 38,652 amniotic fluid samples demonstrated karyotyping's utility in detecting structural abnormalities like translocations, inversions, and aneuploidy [109]. However, a separate 2025 study found that when compared to molecular genetic methods, the breakpoints of chromosomal rearrangements identified by OGM were located within the chromosomal bands identified by karyotyping in only 39.32% of cases, indicating a real resolution of approximately 9.01 Mb and an accuracy rate of 18.07% for breakpoint calling [106].
Optical Genome Mapping (OGM)
Protocol Overview: OGM is a high-resolution, genome-wide technique for detecting structural variants (SVs) and copy number variations (CNVs) without the need for cell culture or amplification [104] [108].
- DNA Extraction: Ultra-high molecular weight (uHMW) DNA is isolated from ~1.5 million nuclei using specialized kits to preserve DNA integrity (e.g., Blood and Cell Culture DNA Isolation Kit).
- Fluorescent Labeling: DNA is labeled at a specific 6-bp sequence motif (CTTAAG) throughout the genome.
- Data Acquisition: Labeled DNA molecules are linearized in nanochannel arrays on the Bionano Saphyr chip and imaged automatically.
- Bioinformatic Analysis: Images are processed to extract molecule length and label pattern, which are assembled de novo and compared to a reference genome (GRCh38) to identify SVs and CNVs.
Performance Data: In a 2025 study on hematologic malignancies, OGM demonstrated superior performance compared to conventional cytogenetics. It identified clinically significant cryptic alterations missed by karyotyping or FISH, such as NUP98::NSD1 fusions and KMT2A partial tandem duplications (PTDs), with a theoretical resolution as high as 500 bp [107]. Another 2025 study in preconception genetic counseling reported a 96.3% concordance between OGM and the combined results of karyotyping and chromosomal microarray analysis (CMA), with OGM improving the diagnostic yield by 5.4% by detecting cryptic translocations and small deletions [108].
Next-Generation Sequencing (NGS)
Protocol Overview: NGS encompasses various approaches, from targeted panels to whole-genome sequencing (WGS), for detecting a broad spectrum of genetic variants.
- Library Preparation: DNA is fragmented, and platform-specific adapters are ligated to the fragments. For targeted sequencing, hybrid capture or amplicon-based enrichment is used.
- Sequencing: Libraries are loaded onto a sequencer (e.g., Illumina, PacBio). Short-read sequencing is common for SNV/indel detection, while long-read sequencing is emerging for resolving complex SVs.
- Bioinformatic Analysis: Reads are aligned to a reference genome. Different algorithms are used to call SNVs, indels, CNVs, and SVs. The pipeline must be specifically validated for each variant type [105] [104].
Performance Data: NGS is indispensable for detecting single nucleotide variants (SNVs) and small insertions/deletions (indels) with high sensitivity [107] [104]. In myeloid neoplasms, for example, NGS identifies mutations in genes like TP53, U2AF1, and BCOR, which are crucial for diagnosis and risk stratification [107] [105]. While WGS can theoretically detect all variant types, the bioinformatic challenges and cost remain higher than targeted approaches. NGS can also be used to validate findings from other technologies, such as confirming the variant allele frequency of a KMT2A-PTD first detected by OGM [107].
Digital PCR (dPCR)
Protocol Overview: dPCR is a highly sensitive, targeted method for absolute quantification of known genetic variants, useful for monitoring specific genomic changes in stem cell lines.
- Sample Partitioning: The PCR reaction mixture, containing DNA sample, primers, probes, and master mix, is partitioned into thousands of individual nanoliter-sized reactions.
- Endpoint PCR Amplification: PCR is run to completion. Each partition acts as an individual PCR reaction.
- Fluorescence Reading and Quantification: Partitions are analyzed for fluorescence. The number of positive and negative partitions is counted, and the absolute concentration of the target sequence is calculated using Poisson statistics.
Performance Data: dPCR is not a discovery tool but excels in sensitivity for validating and monitoring known variants. It can detect rare mutations down to a variant allele frequency of <0.1%, making it suitable for tracking low-level mosaicism or specific oncogenic mutations in heterogeneous stem cell populations [104]. Its high precision also makes it ideal for assessing copy number variations of specific genes.
Workflow Integration for Stem Cell Genomic Assessment
The following diagram illustrates a potential integrated workflow for comprehensive genomic stability assessment of stem cells, leveraging the strengths of each technology.
Essential Research Reagent Solutions
The table below lists key reagents and materials required for implementing these genomic assessment technologies.
Table 2: Key Research Reagents and Materials for Genomic Stability Assays
| Technology | Essential Reagents & Kits | Primary Function |
|---|---|---|
| Karyotyping | Colcemid, Giemsa stain, Trypsin-EDTA, Cell culture media | Metaphase arrest, chromosome banding, cell processing |
| Optical Genome Mapping (OGM) | Bionano Prep Blood & Cell Culture DNA Isolation Kit, Bionano Prep DLS Kit, Bionano Saphyr Chip | uHMW DNA extraction, DNA labeling/repair, sample loading & imaging |
| Next-Generation Sequencing (NGS) | Library Prep Kits (e.g., Illumina DNA Prep), Hybridization Capture Kits, Sequencing Reagents (e.g., SBS chemistry) | DNA fragmentation & adapter ligation, target enrichment, base calling |
| Digital PCR (dPCR) | dPCR Supermix, TaqMan Assays (FAM/VIC), dPCR Plates/Chips | Partitioning & amplification, target-specific detection, reaction vessel |
The optimal choice for stem cell genomic stability assessment depends on the specific research or development objective. No single technology provides a complete picture; an integrated approach is often necessary.
- Karyotyping provides a low-cost, foundational screen for large, clonal chromosomal abnormalities.
- OGM offers a powerful, single-assay alternative to traditional cytogenetics for genome-wide detection of structural variants with high resolution, effectively bridging the gap between karyotyping and NGS.
- NGS is essential for comprehensive profiling, including the detection of single nucleotide variants and small indels that drive functional changes.
- Digital PCR delivers ultra-sensitive, absolute quantification for validating and monitoring specific known variants.
For a comprehensive stability assessment, a strategy beginning with karyotyping or OGM for structural integrity, followed by NGS for sequence-level variation, and employing dPCR for sensitive validation, is recommended. Adherence to international stem cell research guidelines, which emphasize rigorous assessment of genetic stability for cell therapies, is paramount [16] [7] [78].
For researchers and drug development professionals, selecting a method for assessing genomic stability in stem cells is a critical strategic decision. This choice directly impacts data reliability, regulatory compliance, and resource allocation. Genomic integrity is a fundamental Critical Quality Attribute (CQA) for stem cell-based therapies, as genetic alterations can compromise therapeutic efficacy and pose significant safety risks, including tumorigenicity [72]. The landscape of assessment technologies spans traditional cytogenetic analyses, molecular techniques, and emerging artificial intelligence (AI)-driven approaches, each with distinct performance profiles.
This guide provides an objective, data-driven comparison of current methodologies, framing them within the practical constraints of cost, time, and technical complexity faced in research and development settings. We synthesize experimental data and protocols to inform method selection for ensuring the safety of regenerative medicine applications.
Comparative Analysis of Assessment Methods
The following table summarizes the key quantitative and qualitative parameters of prevalent genomic stability assessment techniques.
Table 1: Comparison of Genomic Stability Assessment Methods for Stem Cells
| Method | Key Performance Metrics (Sensitivity/Resolution) | Approximate Cost | Typical Turnaround Time | Technical Complexity & Required Expertise | Primary Applications & Limitations |
|---|---|---|---|---|---|
| Karyotyping (G-banding) | ~5-10 Mbps [42] | Low | 1-2 weeks [42] | Medium: Expertise in cell culture, metaphase preparation, and chromosomal analysis. | Application: Detection of large chromosomal abnormalities and aneuploidy. Limitation: Low resolution; cannot detect small structural variants. |
| Chromosomal Microarray (CMA) / CGH | 50-200 kbps [42] | Medium | 3-5 days [42] | Medium: DNA extraction, hybridization, and data analysis skills. | Application: Genome-wide detection of copy number variants (CNVs) and loss of heterozygosity (LOH). Limitation: Cannot detect balanced rearrangements (e.g., inversions, translocations). |
| Whole Exome Sequencing (WES) | Single nucleotide variants (SNVs) in exons [42] | High | 1-2 weeks | High: Library preparation, next-generation sequencing (NGS) operation, and advanced bioinformatics. | Application: Comprehensive identification of single-base mutations and small indels in protein-coding regions. Limitation: Covers only ~1-2% of the genome; misses non-coding and regulatory regions. |
| Droplet Digital PCR (ddPCR) | Able to detect mutant allelic fractions <1% for specific targets [42] | Low (per assay) | 1-2 days | Low-Medium: Standard PCR skills; no need for standard curves. Highly sensitive and reproducible. | Application: High-sensitivity validation and quantification of specific pre-identified mutations (e.g., in KMT2C, BCOR) [42]. Limitation: Not a discovery tool; requires prior knowledge of the target sequence. |
| AI-Driven Image Analysis | Can detect early morphological changes predictive of genomic instability [110] | High (initial setup) | Real-time to minutes [110] | Very High: Integration of live-cell imaging, computational resources, and machine learning expertise. | Application: Non-invasive, real-time monitoring of cell cultures; predicts instability from morphology. Limitation: "Black box" models; requires extensive training datasets; indirect measure of genetics. |
Detailed Experimental Protocols
To ensure reproducibility and provide a clear understanding of methodological demands, we outline two protocols representing different ends of the technological spectrum: a targeted molecular method (ddPCR) and a non-invasive, AI-driven approach.
Protocol 1: Targeted Mutation Validation using Droplet Digital PCR (ddPCR)
This protocol is adapted from a study assessing genetic stability in human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs) [42]. It is used for the absolute quantification of specific mutations identified from broader screening methods like WES.
Workflow Overview:
Step-by-Step Methodology:
- DNA Extraction: Extract high-quality genomic DNA from hiPSCs or hiPSC-CMs using a commercial kit (e.g., QIAamp DNA Mini Kit). Quantify DNA concentration and purity using spectrophotometry (e.g., Nanodrop). Dilute DNA to a working concentration (e.g., 10-50 ng/μL) [42].
- Assay Design: Design and validate two sets of TaqMan probe-based assays:
- Mutant Assay: Probe and primers specific to the identified mutation (e.g., KMT2C c.2263C>T).
- Reference Assay: A probe/primer set for a wild-type sequence in a stable genomic region, used for normalization.
- Reaction Setup: Prepare a 20μL ddPCR reaction mix for each sample and assay. The mix typically contains:
- ddPCR Supermix for Probes (1X).
- Target assay (FAM-labeled, e.g., mutant probe) (900 nM primers, 250 nM probe).
- Reference assay (HEX-labeled) (900 nM primers, 250 nM probe).
- DNA template (~10-100 ng).
- Nuclease-free water.
- Droplet Generation: Load the reaction mix into a droplet generator. This instrument partitions the sample into approximately 20,000 nanoliter-sized water-in-oil droplets, effectively creating individual micro-reactors.
- Endpoint PCR: Transfer the droplet emulsion to a 96-well PCR plate. Seal the plate and perform PCR amplification in a thermal cycler using optimized cycling conditions.
- Droplet Reading: After PCR, place the plate in a droplet reader. This instrument flows droplets one by one past a two-color optical detection system. Each droplet is classified as FAM-positive (mutant), HEX-positive (reference), positive for both, or negative.
- Data Analysis: Use the instrument's software to analyze the data. The concentration (copies/μL) of the mutant and wild-type targets is calculated using Poisson statistics. The results are expressed as a mutant allelic frequency, crucial for assessing the clonal expansion of specific genetic variants [42].
Protocol 2: Non-Invasive Monitoring via AI-Driven Live-Cell Imaging
This protocol leverages convolutional neural networks (CNNs) to assess cell state in real-time, predicting genomic instability based on morphological features [110].
Workflow Overview:
Step-by-Step Methodology:
- System Setup:
- Equipment: An automated live-cell imaging microscope system (e.g., Incucyte or equivalent) housed within a standard cell culture incubator (37°C, 5% CO₂).
- Culture: Plate stem cells (e.g., hiPSCs or MSCs) in multi-well plates under defined culture conditions.
- Model Training (Pre-requisite):
- Data Collection: Acquire a large dataset of high-resolution phase-contrast or fluorescence images of cell cultures. These images must be linked to ground-truth data on genomic stability obtained from parallel assays (e.g., karyotyping, WES).
- Algorithm Training: Train a Convolutional Neural Network (CNN) to identify correlations between morphological features (e.g., colony texture, nucleus-to-cytoplasm ratio, cell density, irregular growth patterns) and genomic instability endpoints. This step is computationally intensive and requires significant expertise in machine learning [110].
- Image Acquisition: Program the live-cell imaging system to capture images of the cell cultures at regular intervals (e.g., every 30-60 minutes) over several days without disturbing the culture environment.
- Real-Time Analysis: Feed the acquired images in real-time into the pre-trained CNN model. The model analyzes the images to extract morphological features and classifies the cellular state.
- Output and Alerting: The system provides outputs such as:
- Phenotype Predictions: Classification of cells as "normal" or "aberrant" based on learned features associated with genetic instability.
- Anomaly Detection: Alerts for sudden morphological shifts indicative of stress, contamination, or differentiation, which can be precursors to genomic instability [110]. This allows for proactive intervention.
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful implementation of genomic stability assessments relies on a suite of specialized reagents and tools. The following table details key solutions for the featured experiments.
Table 2: Key Research Reagent Solutions for Genomic Stability Assays
| Item Name | Function & Application | Experimental Context |
|---|---|---|
| TaqMan ddPCR Assays | Sequence-specific probe-based chemistry for absolute quantification of mutant and wild-type alleles in a digital PCR format. | Essential for the validation of specific mutations (e.g., in KMT2C or BCOR) identified via NGS with high sensitivity and precision [42]. |
| Cell Culture Media & Supplements | Provides nutrients and growth factors for the maintenance and expansion of stem cells. Specific formulations are critical for maintaining pluripotency and genomic integrity. | Used across all protocols for culturing hiPSCs or MSCs prior to analysis. Inconsistent media quality is a major source of genomic instability [110] [72]. |
| DNA Extraction Kits | Isolation of high-quality, high-molecular-weight genomic DNA from cell samples with minimal shearing and contamination. | A critical first step for all molecular genetic stability tests (karyotyping, CMA, WES, ddPCR). Inadequate DNA quality can lead to false positives/negatives [42]. |
| NGS Library Prep Kits | Preparation of sequencing-ready libraries from fragmented genomic DNA, including adapter ligation and amplification. | Required for Whole Exome Sequencing (WES) to comprehensively identify single-nucleotide variants and small insertions/deletions across the exome [42]. |
| PCR & ddPCR Supermix | Optimized buffer systems containing DNA polymerase, dNTPs, and stabilizers for efficient and specific amplification in droplet digital PCR. | Forms the core reaction mix for the ddPCR protocol, ensuring robust amplification within each droplet for accurate binary endpoint detection [42]. |
| AI/Machine Learning Software | Platforms (e.g., TensorFlow, PyTorch) and custom scripts for developing, training, and deploying convolutional neural network models. | Core to the AI-driven imaging protocol for analyzing time-lapse image data, extracting features, and classifying cell states based on morphology [110]. |
The optimal method for assessing stem cell genomic stability is not universal but depends on the specific stage of research and the critical questions being asked. Karyotyping and CMA offer cost-effective, broad screening for large-scale abnormalities and are often employed as first-line quality control checks. For a more comprehensive, hypothesis-free discovery of point mutations, WES is powerful but comes with higher costs, longer analysis times, and significant bioinformatics demands. Once specific mutations of concern are identified, ddPCR provides an unparalleled solution for sensitive, quantitative, and affordable longitudinal monitoring across cell batches. Finally, AI-driven imaging represents a paradigm shift towards non-invasive, real-time prediction, though it requires substantial upfront investment in model development and validation.
A tiered strategy—using broader, cheaper methods for routine screening and reserving more complex, expensive technologies for targeted, in-depth investigation—often provides the most effective balance of cost, time, and technical complexity in the journey toward clinically safe stem cell therapies.
Comprehensive Genomic Profiling (CGP) represents a transformative approach in modern biomedical research and clinical diagnostics, enabling simultaneous analysis of hundreds of cancer-related genes and genomic biomarkers through next-generation sequencing (NGS) technologies. Unlike traditional single-gene tests or limited panels, CGP detects multiple classes of genomic alterations—including base substitutions, insertions and deletions, copy number alterations, and rearrangements—within a single assay [111] [112]. This comprehensive approach has proven particularly valuable in oncology, where it identifies actionable genomic alterations that inform targeted treatment strategies and clinical trial eligibility for patients with advanced cancers.
The integration of multiple methodological approaches significantly enhances the diagnostic power of genomic profiling, especially in complex fields like stem cell research and cancer biology. By combining various sequencing technologies, analytical frameworks, and data integration methods, researchers can achieve a more complete understanding of genomic instability and biological systems [113]. The evolution from single-analyte tests to multiparameter genomic profiling reflects the growing recognition that complex biological questions require multidimensional solutions. This article explores the technical frameworks, experimental applications, and practical implementations of integrated genomic profiling methods, with specific emphasis on their relevance to stem cell genomic stability assessment and cancer research.
Technical Frameworks for Integrated Genomic Analysis
Core Components of Comprehensive Genomic Profiling
Comprehensive Genomic Profiling employs a targeted NGS approach designed to maximize genomic information while optimizing sequencing resources and costs. The core components of CGP include large gene panels that cover hundreds of cancer-related genes, with the capability to detect all major variant types and genomic signatures such as tumor mutational burden (TMB) and microsatellite instability (MSI) [112]. Leading CGP assays typically analyze 300+ genes, providing extensive coverage of clinically relevant genomic regions while avoiding the inefficiencies of whole-exome or whole-genome sequencing for routine diagnostic applications [111] [112].
The technological foundation of CGP relies on hybrid capture-based NGS methods that provide nucleotide-level resolution across the genomic regions of interest. This approach offers several advantages over other sequencing methods: compared to single-gene assays, CGP provides a much broader genomic landscape; versus targeted panels, it offers more complete gene coverage; and relative to exome sequencing, it delivers superior coverage depth for detecting low-frequency variants [112]. The comprehensive nature of these assays makes them particularly suitable for identifying rare genomic alterations that might be missed by traditional testing approaches. For instance, in non-small cell lung cancer (NSCLC), CGP has demonstrated the ability to detect actionable genomic alterations in cases that tested negative using other genomic testing methods [112].
Multi-Omics Integration Approaches
The integration of multiple molecular data types, known as multi-omics, represents a powerful extension of genomic profiling that combines information from various biological layers including genomics, transcriptomics, proteomics, and epigenomics [113]. This integrative approach provides a more comprehensive view of biological systems by linking genetic information with functional molecular outcomes and phenotypic manifestations. In cancer research, multi-omics helps dissect complex microenvironments and reveals interactions between cancer cells and their surroundings that would remain invisible when examining single data types alone [113].
The practical implementation of multi-omics integration is exemplified by approaches that combine DNA sequencing with whole transcriptome RNA sequencing. This combined method enables a more complete understanding of clinically actionable fusions and altered splicing events. Empirical data demonstrates that the addition of RNA sequencing to DNA analysis identifies 29% more patients with unique, clinically actionable fusions that match to targeted therapies compared to DNA sequencing alone [114]. Similarly, integrating solid tumor and liquid biopsy profiling reveals complementary information, with a metastatic pan-cancer analysis showing that 9% of patients had unique actionable alterations detected in liquid biopsy that were not identified in solid tumor testing alone [114].
Table 1: Advantages of Multi-Method Integration in Genomic Profiling
| Integrated Method | Technical Advantage | Clinical/Research Benefit |
|---|---|---|
| DNA + RNA Sequencing | Detects fusion genes and altered splicing | Identifies 29% more patients with actionable fusions [114] |
| Solid + Liquid Biopsy | Reveals complementary tumor heterogeneity | Finds unique actionable alterations in 9% of patients [114] |
| Tumor + Normal Matching | Distinguishes somatic from germline variants | Reduces false-positive calls by 28% [114] |
| Multi-Omics Approaches | Links genetic variation with functional molecular outcomes | Provides comprehensive biological insights for complex diseases [113] |
Case Studies in Stem Cell Genomic Stability Assessment
Genomic Instability Tracking in Induced Pluripotent Stem Cells
A systematic investigation of genomic alterations throughout the process of generating induced pluripotent stem (iPS) cells and differentiating them into induced mesenchymal stromal/stem cells (iMS cells) provides a compelling case study in integrated genomic profiling [2]. This research employed a comprehensive approach to monitor genomic instability from reprogramming through differentiation and passaging phases, utilizing multiple techniques including chromosome analysis, chromosomal microarray, short tandem repeat analysis, and next-generation sequencing. The study design enabled researchers to identify both copy number alterations (CNAs) and single-nucleotide variations (SNVs) accumulating at different stages of stem cell generation and differentiation.
The findings revealed significant differences in genomic stability based on reprogramming methodology. Sendai virus (SV)-reprogrammed iPS cells showed higher frequencies of both CNAs and SNVs compared to those generated using episomal vectors (Epi) [2]. Specifically, all SV-iPS cell lines exhibited CNAs during the reprogramming phase, while only 40% of Epi-iPS cells showed such alterations. Furthermore, SNVs were observed exclusively in SV-derived cells during passaging and differentiation, with no SNVs detected in Epi-derived lines. Gene expression analysis further confirmed upregulation of chromosomal instability-related genes in late-passage SV-iPSCs, and notably identified TP53 mutations, highlighting the vulnerability of this critical tumor suppressor gene during stem cell reprogramming and culture [2]. These findings underscore the critical importance of careful genomic monitoring when preparing iPS cells and their derivatives for research or clinical applications.
Experimental Framework for Stem Cell Genomic Assessment
The stem cell genomic stability study implemented a comprehensive experimental workflow that integrated multiple assessment modalities at critical process points. The methodology began with fibroblast reprogramming using both Sendai virus and episomal vector approaches, followed by comprehensive characterization of resulting iPS cells through alkaline phosphatase staining, immunocytochemistry for pluripotency markers, three-germ layer differentiation assays, and teratoma formation studies [2]. The iPS cells were then differentiated into iMS cells using a standardized mesenchymal progenitor differentiation kit, with continuous monitoring throughout the process.
Genomic assessment employed a multi-technology approach: chromosome analysis provided a gross structural overview, chromosomal microarray detected copy number variations, short tandem repeat analysis monitored genetic stability, and next-generation sequencing identified single-nucleotide variations and smaller genetic alterations [2]. This integrated methodological framework allowed researchers to capture a wide spectrum of genomic abnormalities that might be missed by any single technique alone. The experimental design highlights the power of combining complementary genomic assessment methods to obtain a comprehensive understanding of genomic instability in stem cell systems, providing a model approach for similar investigations in regenerative medicine.
Diagram 1: Stem Cell Genomic Stability Assessment Workflow
Advanced Computational Integration Methods
Deep Learning Approaches for Single-Cell Data Integration
Recent advancements in deep learning have revolutionized the integration of single-cell genomic data, addressing significant challenges in batch effect correction and biological conservation. A comprehensive benchmarking study evaluated 16 different integration methods within a unified variational autoencoder framework, systematically comparing loss functions and integration performance [115]. These methods were designed to remove unwanted technical variations while preserving biologically meaningful information, utilizing batch labels and cell-type annotations as proxies for technical and biological factors respectively. The research revealed that conventional benchmarking metrics often fail to adequately capture intra-cell-type biological conservation, leading to the development of enhanced evaluation frameworks.
The study implemented a multi-level strategy for single-cell data integration: Level-1 methods focused exclusively on batch effect removal using batch labels; Level-2 approaches incorporated cell-type labels to preserve biological information; and Level-3 methods integrated both batch and cell-type information for simultaneous batch-effect removal and biological conservation [115]. This systematic comparison demonstrated that appropriate loss function design critically impacts integration quality. To address limitations in existing metrics, the researchers introduced a correlation-based loss function and refined benchmarking approaches that better capture biological conservation at both inter-cell-type and intra-cell-type levels. The resulting framework, scIB-E, provides deeper insights into the integration process and offers guidance for developing more effective methods for complex multimodal and spatiotemporal single-cell data [115].
Implementation of Computational Integration Frameworks
The practical implementation of these deep learning methods involves sophisticated computational frameworks built on variational autoencoders, which learn biologically conserved gene expression representations from high-dimensional single-cell data. Methods like single-cell Variational Inference (scVI) employ a fully probabilistic framework that accounts for both biological and technical noise in scRNA-seq data, while single-cell ANnotation using Variational Inference (scANVI) extends this approach by incorporating pre-existing cell state annotations in a semi-supervised manner [115]. These methods leverage multiple loss function types including adversarial learning, information-constraining techniques, supervised domain adaptation, and deep metric learning to balance batch effect removal with biological information preservation.
The benchmarking process utilized diverse single-cell RNA-seq datasets from immune cells, pancreas cells, and bone marrow mononuclear cells to evaluate performance across different biological contexts [115]. Performance assessment employed both quantitative metrics and visualization approaches like Uniform Manifold Approximation and Projection (UMAP) to examine cell distributions across batches and cell types. This comprehensive evaluation demonstrated that deep learning-based approaches successfully integrate large-scale single-cell data while preserving critical biological insights, providing powerful tools for atlas-level analyses that combine data from multiple experiments, studies, and platforms. These computational advances enable researchers to extract meaningful biological signals from increasingly complex and heterogeneous single-cell datasets.
Table 2: Deep Learning Integration Methods for Single-Cell Genomics
| Method Level | Primary Focus | Key Techniques | Application Context |
|---|---|---|---|
| Level-1 | Batch effect removal | GAN, HSIC, Orthogonal Projection, Mutual Information Minimization | Technical variation correction without cell-type labels [115] |
| Level-2 | Biological conservation | Supervised contrastive learning, Invariant Risk Minimization, Domain meta-learning | Known cell-type annotation integration [115] |
| Level-3 | Combined batch correction and biological conservation | Integrated loss functions from Level-1 and Level-2, Domain Class Triplet loss | Comprehensive integration with partial annotation [115] |
| scIB-E Framework | Enhanced benchmarking | Correlation-based loss, intra-cell-type conservation metrics | Refined evaluation of integration performance [115] |
Implementation in National Genomic Medicine Initiatives
The French Genomic Medicine Initiative (PFMG2025)
The 2025 French Genomic Medicine Initiative (PFMG2025) represents a large-scale implementation of integrated genomic profiling within a national healthcare system, providing valuable insights into the practical challenges and solutions for delivering genomic medicine at scale. This initiative, launched in 2016 with a government investment of €239 million, has established an operational framework for integrating genome sequencing into clinical practice with a focus on patients with rare diseases, cancer genetic predisposition, and cancers [116]. The program has developed specific infrastructures including a reference center for innovation, assessment, and transfer (CRefIX); a network of genome sequencing clinical laboratories (FMGlabs); and a national facility for secure data storage and intensive calculation (Collecteur Analyseur de Données - CAD) [116].
The PFMG2025 initiative employs distinct analysis strategies for different clinical contexts. For rare diseases and cancer genetic predisposition, short-read genome sequencing is performed, preferably including the proband with other family members (trio-based or duo-based sequencing) [116]. For cancer patients, the approach integrates genome sequencing, exome sequencing, and RNAseq from frozen patient tumor tissues in addition to germline genome sequencing, enabling detection of both hereditary and somatic variants. This integrated methodological approach has demonstrated substantial clinical utility, with data as of December 2023 showing 12,737 results returned to prescribers for rare disease/cancer genetic predisposition patients (diagnostic yield: 30.6%) and 3,109 for cancer patients [116]. The program has established a multidisciplinary genomic healthcare pathway incorporating upstream and downstream multidisciplinary meetings and molecular tumor boards to support clinical implementation.
Operational Framework and Outcomes
The operationalization of PFMG2025 highlights both the achievements and challenges of implementing integrated genomic profiling at national scale. The initiative selected two FMGlabs from 12 proposals to serve equivalent population territories, with 70 pre-indications (62 for rare diseases/cancer genetic predisposition and 8 for cancers) selected for analysis [116]. The program established national guidelines and standardized workflows for each pre-indication, defining eligibility criteria for genome sequencing and required preliminary tests. To support clinical implementation, the initiative created a network of 120 thematic upstream multidisciplinary meetings and 26 molecular tumor boards, later supplemented by 24 local non-thematic multidisciplinary meetings to improve efficiency [116].
Performance data reveals both successes and areas for improvement. The program achieved a median result delivery time of 202 days for rare diseases/cancer genetic predisposition and 45 days for cancer patients [116]. Prescription patterns show that 1,823 clinicians have created prescriber accounts, with 1,161 making at least one prescription, though 75 clinicians (6.5% of active prescribers) were responsible for 69.4% and 42.4% of prescriptions for rare diseases/cancer genetic predisposition and cancers respectively [116]. This experience demonstrates that successful implementation of integrated genomic profiling requires not only technical capabilities but also significant attention to clinical pathways, provider engagement, and operational efficiency.
Diagram 2: National Genomic Medicine Initiative Workflow
Research Reagent Solutions for Genomic Profiling
The implementation of integrated genomic profiling methods requires specialized research reagents and platforms that enable comprehensive genomic analysis. The following table details essential research reagent solutions utilized in the case studies and methodologies discussed throughout this article, providing researchers with practical guidance for establishing similar experimental approaches.
Table 3: Essential Research Reagent Solutions for Comprehensive Genomic Profiling
| Reagent Category | Specific Examples | Function/Application | Research Context |
|---|---|---|---|
| Reprogramming Systems | Sendai Virus (CytoTune-iPS 2.0), Episomal Vectors | Non-integrating reprogramming of somatic cells to iPSCs | Stem cell genomic instability studies [2] |
| Stem Cell Culture Media | mTeSR1, MesenCult-ACF Medium | Maintenance of pluripotency and directed differentiation | iPS cell culture and iMS cell differentiation [2] |
| NGS Library Preparation | TruSight Oncology Comprehensive, FoundationOne CDx | Target enrichment for comprehensive genomic profiling | Cancer biomarker detection [111] [112] |
| Single-Cell RNA-seq Kits | 10x Genomics Chromium Single Cell Immune Profiling | High-throughput single-cell transcriptomics | Immune profiling and cell heterogeneity analysis [117] |
| Cell Characterization Antibodies | Oct3/4, Nanog, Tra-1-81, SSEA markers | Pluripotency verification and lineage tracing | Stem cell quality assessment [2] |
| Genomic Analysis Software | scVI, scANVI, Cell Ranger | Bioinformatics analysis of sequencing data | Single-cell data integration [115] [117] |
The integration of multiple genomic profiling methods represents a paradigm shift in biomedical research, enabling comprehensive understanding of complex biological systems that cannot be achieved through single-method approaches. The case studies examined in this article—spanning stem cell genomic stability assessment, single-cell data integration, and national genomic medicine implementation—demonstrate the power of combined methodological frameworks to generate insights with basic research and clinical applications.
As genomic technologies continue to evolve, further innovation in integration methodologies will be essential for addressing increasingly complex research questions and clinical challenges. The ongoing development of multi-omics approaches, advanced computational integration frameworks, and standardized implementation pathways will enhance our ability to extract meaningful biological insights from complex genomic datasets. These integrated approaches will play an increasingly critical role in advancing precision medicine, regenerative medicine, and our fundamental understanding of biological systems, ultimately supporting improved diagnostic capabilities and therapeutic outcomes across a broad spectrum of human diseases.
The International Society for Stem Cell Research (ISSCR) maintains the international benchmark for scientific and ethical rigor in stem cell research, providing trusted guidance for oversight and transparency [118]. Adherence to these guidelines ensures that research is conducted with integrity and that new therapies are safe, effective, and evidence-based [7] [118]. For researchers, scientists, and drug development professionals, aligning with these standards is not merely about regulatory compliance; it is a fundamental requirement for producing reproducible, quantifiable, and clinically relevant data.
A significant challenge in the field has been the lack of standardization, particularly in quantifying stem cells. Currently, much of stem cell science and medicine operates as a non-quantitative discipline, with researchers often working without knowing the precise number of stem cells in their samples [119]. This limitation undermines the reproducibility of experiments and the efficacy of clinical applications, such as blood stem-cell transplants, which can fail as much as 20% of the time due to uncertainties in stem cell-specific dosing [119]. The ISSCR explicitly recommends that researchers, industry, and regulators collaborate on developing and implementing standards for the design, conduct, interpretation, and reporting of research [120]. This article compares current genomic stability assessment methodologies against this framework of evolving standards, providing a guide for ensuring scientific rigor and regulatory alignment.
The ISSCR Guidelines and Regulatory Framework
The ISSCR Guidelines for Stem Cell Research and Clinical Translation were comprehensively updated in 2021 and underwent a targeted update in 2025 to address advances in stem cell-based embryo models (SCBEMs) [7] [118]. These guidelines provide a comprehensive framework for the entire lifecycle of stem cell research, from basic laboratory studies to clinical translation.
Key Principles for Laboratory Research and Clinical Translation
The ISSCR outlines several fundamental ethical principles that underpin all stem cell research. These include the integrity of the research enterprise, the primacy of patient/participant welfare, respect for patients and research subjects, transparency, and social and distributive justice [7]. In practice, these principles translate into specific requirements for research conduct:
- Rigor and Oversight: All research, particularly involving sensitive materials like human embryos or SCBEMs, must have a clear scientific rationale, a defined endpoint, and be subject to appropriate oversight mechanisms [7] [118].
- Manufacturing Quality: Cell processing and manufacturing must be conducted under rigorous, expert, and independent review. The use of Good Manufacturing Practice (GMP) conditions is emphasized, though phase-appropriate implementation is recognized for early-stage clinical trials [78].
- Donor Consent and Screening: For allogeneic therapies, donors must provide written, informed consent, and donors and resulting cell banks must be screened for infectious diseases to prevent pathogen transmission [78].
The 2025 Update: Focus on Stem Cell-Based Embryo Models
The 2025 targeted update refined oversight recommendations for rapidly evolving SCBEM technologies [118]. Key revisions include:
- Retiring the classification of models as "integrated" or "non-integrated" in favor of the inclusive term "SCBEMs" [7] [118].
- Proposing that all 3D SCBEMs require appropriate oversight [7] [118].
- Reiterating the prohibition on transplanting any SCBEM into a uterus [7] [118].
- Introducing a new recommendation against culturing SCBEMs to the point of potential viability (ectogenesis) [7] [118].
Genomic Stability Assessment Methods: Aligning with Standards
Genomic stability is a critical quality attribute for stem cells, especially those destined for clinical use. Prolonged culture can subject cells to selective pressures, leading to genetic and epigenetic changes that alter differentiation behavior, function, and potentially lead to malignancy [78]. The following section compares current assessment methods, their alignment with ISSCR expectations for rigor and transparency, and their application in a regulatory context.
Comparative Analysis of Genomic Stability Assessment Methods
Table 1: Comparison of Key Genomic Stability Assessment Methods
| Method | Key Measured Parameters | Throughput | Sensitivity | Regulatory Recognition | Key Applications in Stem Cell Research |
|---|---|---|---|---|---|
| Karyotyping (G-banding) | Gross chromosomal abnormalities, ploidy. | Low | ~5-10 Mb | Well-established; often required for cell banking. | Identity testing, master cell bank characterization. |
| Fluorescence In Situ Hybridization (FISH) | Specific chromosomal rearrangements, aneuploidy. | Medium | 50 kb - 1 Mb | Recognized for specific applications. | Monitoring known, culture-associated abnormalities (e.g., 20q11.21 amplification in hPSCs). |
| Comparative Genomic Hybridization (Array CGH/SNP array) | Copy number variations (CNVs), loss of heterozygosity (LOH). | High | 50 kb - 100 kb | Increasingly accepted by regulators. | In-depth characterization of working cell banks and pre-clinical cell products. |
| Next-Generation Sequencing (NGS) | SNVs, indels, CNVs, structural variants. | High | Single nucleotide | Used under FDA RMAT, Fast Track designations [121]. | Comprehensive profiling of clonal master cell lines (e.g., hiPSC lines for off-the-shelf therapies) [121]. |
Experimental Protocols for Genomic Stability Assessment
To ensure data comparability and reliability, standardized experimental protocols are essential. The following are detailed methodologies for key assays.
Protocol for Cumulative Population Doubling Analysis (ASTM F3716)
The ASTM F3716 standard provides a reliable test method for assessing and comparing the quality of cell-expansion processes, addressing the need for quantitative proliferation data [119].
Methodology:
- Cell Seeding: Plate a known number of cells (P0) into culture vessels under standardized conditions.
- Harvesting: Once cells reach a predetermined sub-confluence (e.g., 70-80%), dissociate and count them accurately to determine the harvested cell number (P1).
- Calculation: Calculate the Population Doubling (PD) for the passage using the formula: PD = log₂(P1 harvested / P0 seeded).
- Re-seeding and Repetition: Re-seed a known number of cells to initiate the next passage cycle. Repeat steps 2 and 3 for multiple passages.
- Cumulative Calculation: The Cumulative Population Doubling (CPD) is the sum of PDs from all previous passages. Plotting CPD against time provides a proliferation curve that reveals growth rate changes and the onset of senescence.
Alignment with Standards: This method directly supports ISSCR's emphasis on quality control and standardization in cell manufacture [78]. It provides a quantitative foundation for comparing cell expansion processes across different laboratories and production batches, fulfilling the call for universal standards in stem cell research [120] [119].
Protocol for Next-Generation Sequencing (NGS)-Based Genomic Analysis
NGS has become a foundational tool for comprehensive genomic assessment, enabling whole-genome sequencing to identify single nucleotide variants (SNVs), insertions/deletions (indels), and copy number variations (CNVs) [113].
Methodology:
- DNA Extraction: Extract high-molecular-weight genomic DNA from stem cell samples using a validated method to ensure purity and integrity.
- Library Preparation: Fragment the DNA and ligate platform-specific adapters. For targeted panels, hybridize and capture genes associated with cancer or genomic instability.
- Sequencing: Perform sequencing on a platform such as Illumina's NovaSeq X, which offers high throughput and accuracy [113].
- Bioinformatic Analysis:
- Alignment: Map sequencing reads to a reference genome (e.g., GRCh38).
- Variant Calling: Use AI-powered tools like DeepVariant to identify SNVs and indels with high accuracy [113].
- CNV Calling: Determine genomic regions with abnormal read depths to identify amplifications or deletions.
- Annotation and Reporting: Annotate variants for their functional impact and filter them against population databases. Report potentially oncogenic mutations and large-scale anomalies.
Alignment with Standards: The use of AI in genomic analysis supports the ISSCR's principle of rigor by improving the trustworthiness and reliability of data [7] [113]. Furthermore, the application of NGS in clinical trials for PSC-derived products, which have dosed over 1,200 patients with no class-wide safety concerns, demonstrates its value in ensuring patient welfare [121].
Visualization of Experimental and Regulatory Workflows
The following diagrams illustrate the logical relationship between research activities and the ISSCR guidelines, as well as a standardized experimental workflow for genomic stability assessment.
Diagram 1: The logical relationship between core ISSCR principles and specific research activities, showing how guidelines directly govern practice.
Diagram 2: A standardized experimental workflow for genomic stability assessment, integrating multiple methods to ensure comprehensive analysis aligned with quality control requirements.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and solutions essential for conducting rigorous genomic stability assessments in alignment with ISSCR guidelines and regulatory expectations.
Table 2: Key Research Reagent Solutions for Genomic Stability Assessment
| Reagent/Material | Function | Application Example | Considerations for Standards Alignment |
|---|---|---|---|
| GMP-grade Cell Culture Media | Supports stem cell growth and maintenance while minimizing batch-to-batch variability. | Expansion of clinical-grade iPSCs. | Use of GMP-grade reagents is mandated for cell manufacturing under ISSCR guidelines and regulatory oversight [78]. |
| KaryoMAX Colcemid Solution | Arrests cells in metaphase for chromosomal analysis. | Preparation of samples for G-banding karyotyping. | A critical reagent for a well-established, regulatorily-recognized identity and stability test. |
| Cell Dissociation Reagents (e.g., Accutase) | Enzymatically dissociates adherent stem cells into single-cell suspensions. | Cell passaging and preparation for flow cytometry or seeding for proliferation assays. | Standardized dissociation protocols are vital for accurate cell counting and population doubling calculations per ASTM F3716 [119]. |
| QIAamp DNA Mini Kit | Isolates high-purity, high-molecular-weight genomic DNA. | DNA extraction for aCGH, SNP-array, or NGS. | DNA quality directly impacts the sensitivity and accuracy of downstream genomic analyses. |
| Illumina DNA PCR-Free Library Prep Kit | Prepares sequencing libraries for whole-genome sequencing without amplification bias. | NGS-based genomic screening for SNVs and indels. | Enables comprehensive variant profiling as recommended for advanced therapeutic products [121] [113]. |
| CytoScan HD Array | Provides high-resolution genome-wide detection of CNVs and LOH. | High-resolution analysis of genomic integrity in stem cell banks. | Offers a balance of high throughput and resolution for routine quality control of cell banks. |
| DeepVariant AI Tool | A deep learning-based variant caller for NGS data that improves accuracy. | Identifying true genetic variants versus sequencing artifacts in stem cell lines [113]. | Employs AI to enhance data rigor and reliability, supporting the ISSCR principle of integrity [7]. |
The path from basic stem cell research to clinically approved therapies is paved with rigorous standards designed to ensure safety, efficacy, and ethical integrity. As the field advances with an increasing number of clinical trials and approved products [121], the importance of quantitative, standardized methods for assessing genomic stability cannot be overstated. Methods like the ASTM F3716 proliferation standard and comprehensive NGS profiling are not merely technical exercises; they are essential practices for aligning with ISSCR guidelines and regulatory expectations. By adopting these standardized, quantitative approaches, researchers and drug developers can build the robust evidence base required for regulatory approval, ultimately accelerating the delivery of safe and effective stem cell therapies to patients in need.
The promise of human pluripotent stem cell (hPSC)-derived therapies in regenerative medicine is tempered by a significant safety concern: tumorigenicity. This risk primarily arises from residual undifferentiated PSCs that may persist in the final cell therapy product, capable of forming teratomas or other tumors upon transplantation [122]. The self-renewal and pluripotent properties that make these cells therapeutically valuable also render them potentially tumorigenic if not completely removed during the differentiation process [122]. Multiple studies have reported the presence of stem cell-derived tumors in animal models and clinical administrations, highlighting the very real nature of this risk [122]. In one documented case, a patient who received induced pluripotent stem cell (iPSC)-derived beta cells developed a mass with enlarged lymph nodes at the injection site within two months, with most cells in the mass testing positive for pluripotency markers OCT3/4 and SOX2 [122].
This article provides a comprehensive comparison of current assay methodologies for detecting residual pluripotent stem cells, focusing on their sensitivity, specificity, and applicability in quality control for clinical-grade cell therapy products. As the field moves toward broader clinical application, establishing standardized, sensitive, and reproducible detection methods becomes paramount for ensuring patient safety and regulatory compliance [123].
Tumorigenicity Risk and Detection Thresholds
Understanding the Risk Profile
The tumorigenic risk of PSC-derived products primarily originates from two sources: (1) residual undifferentiated PSCs that may persist in the differentiated cell population, and (2) genetically abnormal cells that may arise during cell culture and expansion [122] [3]. hPSCs in culture frequently acquire recurrent, non-random genetic abnormalities that resemble those found in human cancers, particularly affecting chromosomes 1, 8, 10, 12, 17, 18, 20, and X [3]. These genetically variant cells often possess a selective growth advantage, allowing them to overtake cultures over time [3].
Studies have identified that specific recurrent abnormalities, such as a gain of genomic material at chromosome 20q11.21, can encompass cancer-related genes like ASXL1 and may persist in PSCs under various culture conditions and through differentiation processes [82]. Additionally, genomic analyses have revealed recurrent mutations in tumor suppressor genes like P53 in hPSC lines, further emphasizing the need for careful genetic characterization before clinical use [3].
Establishing Detection Sensitivity Requirements
A critical question in safety testing is determining the threshold cell number required for tumor formation. Research indicates that the threshold for ESC-derived teratoma formation ranges from approximately 100 to 10,000 undifferentiated cells per million administered cells [122]. Importantly, studies have shown that as few as 10 embryonic stem cells spiked in Matrigel resulted in 0% tumorigenicity risk in immunocompromised animals, suggesting that a single stem cell is unlikely to form a tumor [122]. This is consistent with the observation that PSCs typically grow in colonies and single cells have difficulty surviving and expanding independently.
Based on this evidence, a stem cell tumorigenicity assay does not require single-cell resolution but should achieve a reasonable sensitivity of at least 0.001% (equivalent to 100 cells per million) [122]. Regulatory perspectives, however, often err on the side of caution, with the FDA recommending in vivo tumorigenicity monitoring for 4 to 7 months during assay development [122]. This extended timeframe presents practical challenges for manufacturing, where typical turnaround times for stem cell-derived products are about 1 to 3 months [122], highlighting the need for rapid, sensitive in vitro assays.
Table 1: Tumorigenicity Thresholds and Detection Requirements
| Parameter | Finding | Implication for Detection |
|---|---|---|
| Minimum tumorigenic cell number | 100-10,000 cells [122] | Assay must detect below this threshold |
| Single-cell tumorigenicity | No evidence [122] | Single-cell resolution not required |
| Recommended sensitivity | 0.001% (100 cells/million) [122] | Target for assay validation |
| Current detection limit (conventional methods) | 5-20% mosaicism [3] | Insufficient for safety testing |
Comparative Analysis of Detection Methodologies
Established and Emerging Detection Platforms
Various approaches have been developed to assess the tumorigenic potential of stem cell products, each with distinct advantages and limitations. The selection of an appropriate assay depends on the specific needs of the study and the stage of product development [122].
Animal models, particularly using immunocompromised NSG mice, remain the gold standard for tumorigenicity assessment [122]. In this procedure, stem cell-derived products are xenografted subcutaneously or intramuscularly, and animals are monitored for tumor formation over extended periods. While providing biologically relevant data, these models are time-consuming (typically requiring 10-36 weeks), expensive, and raise ethical concerns regarding animal use [122].
Molecular detection methods offer faster, more cost-effective alternatives suitable for quality control in manufacturing. These include:
- Polymerase chain reaction (PCR)-based methods
- Flow cytometry for surface marker detection
- Microfluidics-based approaches
- Soft agar culture for detecting anchorage-independent growth
Each method varies in sensitivity, throughput, cost, and technical requirements, making them differentially suitable for various applications [122].
Direct Comparison of Key Analytical Methods
Recent studies have directly compared the performance of different in vitro methods for detecting residual pluripotent stem cells. A comprehensive analysis evaluated three analytical methods—qPCR, droplet digital PCR (ddPCR), and RT-LAMP—for detecting the PSC marker LIN28A [124].
Table 2: Performance Comparison of Residual PSC Detection Methods
| Method | Sensitivity | Key Advantages | Limitations |
|---|---|---|---|
| Animal Models | Not quantified | Biologically relevant, gold standard [122] | Time-consuming (10-36 weeks), expensive, ethical concerns [122] |
| qPCR | Lower than ddPCR | Established technology, quantitative [124] | Potential for false positives, less sensitive [82] [124] |
| Droplet Digital PCR (ddPCR) | 10 cells/million (0.001%) [124] | High sensitivity and accuracy, absolute quantification [82] [124] | Requires specialized equipment, optimization needed |
| RT-LAMP | Lower than ddPCR | Rapid, isothermal amplification [124] | Less sensitive than ddPCR [124] |
| Conventional Karyotyping | 5-20% mosaicism [3] | Detects large chromosomal abnormalities | Low resolution, cannot detect small changes [82] |
| Next-Generation Sequencing (NGS) | Varies with coverage | Hypothesis-free, detects multiple variant types [85] | Data-intensive, requires bioinformatics expertise |
The results demonstrated that while all three methods exhibited consistent results across different cell lines, ddPCR showed the highest sensitivity, capable of confidently detecting 10 residual PSCs in a million fibroblasts [124]. This superior performance aligns with findings from other studies that have validated ddPCR for detecting residual undifferentiated cells in PSC-derived therapy products [123].
Advanced Genetic Stability Assessment Methods
Beyond detecting residual undifferentiated cells, comprehensive safety assessment also requires monitoring genetic stability throughout the manufacturing process. Conventional methods like karyotyping, fluorescence in situ hybridization (FISH), and comparative genomic hybridization (CGH) arrays have limitations in resolution and sensitivity, making detection of subtle genetic abnormalities challenging [82].
Next-generation sequencing (NGS) technologies offer higher resolution for genetic stability assessment [82]. Targeted NGS panels enable cost-effective, deep sequencing of specific genomic regions associated with tumorigenicity, achieving lower limits of detection for enhanced sensitivity in variant identification [85]. Two main NGS approaches are used:
- Capture sequencing: Uses specific probes to capture target sequences from DNA samples, ideal for sequencing large numbers of genes or exons [85]
- Amplicon sequencing: Uses PCR to amplify target regions, suitable for smaller regions or gene panels under 500 kb [85]
Capture sequencing has emerged as a preferred approach for many applications due to its higher testing accuracy and reduced susceptibility to artifacts compared to amplicon methods [85].
Experimental Validation and Protocol Details
Experimental Design for Assay Validation
Robust validation of detection assays requires carefully designed experiments that assess sensitivity, specificity, and reproducibility across relevant conditions. A comprehensive approach to validation should include:
Spike-in experiments: Known numbers of PSCs are mixed with differentiated cells (e.g., primary fibroblasts) across a range of concentrations to establish detection limits and create standard curves [124]. These experiments should utilize multiple independent PSC lines to account for biological variability [124].
Cross-platform comparison: The same spike-in samples should be tested across different detection platforms (e.g., qPCR, ddPCR, RT-LAMP) to enable direct performance comparisons [124].
International multisite studies: Collaborative studies across multiple laboratories help establish reproducibility and inter-laboratory variability, providing data to support standardization [123]. The Health and Environmental Sciences Institute (HESI) Cell Therapy-TRAcking, Circulation & Safety (CT-TRACS) committee has conducted such international multisite evaluations for ddPCR detection of residual PSCs [123].
Detailed ddPCR Methodology for LIN28A Detection
Based on published studies demonstrating superior sensitivity, here we detail a protocol for detecting residual PSCs using ddPCR for the LIN28A marker:
Sample Preparation:
- Prepare spike-in samples by mixing known numbers of PSCs (e.g., PSC1, NH50191, WA09/H9) into a background of primary fibroblasts (e.g., Hs68) [124]
- Use a range of concentrations from 100,000 PSCs/million down to 10 PSCs/million to establish detection limits
- Include triplicate samples for each concentration to assess technical variability
RNA Extraction and Reverse Transcription:
- Extract total RNA using column-based methods with DNase treatment to eliminate genomic DNA contamination
- Quantify RNA using spectrophotometry or fluorometry
- Perform reverse transcription using random hexamers and Moloney Murine Leukemia Virus reverse transcriptase
Droplet Digital PCR Setup:
- Prepare reaction mix containing cDNA template, LIN28A-specific primers and probe, and ddPCR supermix
- Generate droplets using a droplet generator (e.g., Bio-Rad QX200 Droplet Generator)
- Transfer emulsified samples to a 96-well PCR plate and seal properly
PCR Amplification:
- Run thermal cycling with the following conditions:
- 95°C for 10 minutes (enzyme activation)
- 40 cycles of:
- 94°C for 30 seconds (denaturation)
- 60°C for 60 seconds (annealing/extension)
- 98°C for 10 minutes (enzyme deactivation)
- 4°C hold
Droplet Reading and Analysis:
- Read droplets using a droplet reader (e.g., Bio-Rad QX200 Droplet Reader)
- Analyze data using companion software to quantify positive and negative droplets
- Apply Poisson statistics to calculate absolute copy numbers of LIN28A mRNA in the original sample
Validation Parameters:
- Specificity: Verify absence of signal in negative controls (fibroblasts alone)
- Precision: Assess coefficient of variation across replicate samples
- Limit of Detection (LOD): Determine the lowest concentration reliably detected above background
- Limit of Quantification (LOQ): Determine the lowest concentration that can be accurately quantified
This methodology has demonstrated sensitivity to detect 10 residual PSCs in a million fibroblasts, representing a significantly higher sensitivity than conventional qPCR and RT-LAMP methods [124].
Visualization of Experimental Workflows and Signaling Pathways
Tumorigenicity Risk Pathway in Stem Cell Therapies
The following diagram illustrates the primary pathways through which tumorigenicity can arise in PSC-derived therapies, highlighting key detection points for quality control:
Diagram 1: Tumorigenicity Risk Pathways and Detection Methods in Stem Cell Therapies. This diagram illustrates how tumorigenicity arises from residual undifferentiated PSCs or genetically abnormal cells, and the corresponding detection methods used to mitigate these risks.
ddPCR Workflow for Residual PSC Detection
The following diagram details the experimental workflow for detecting residual pluripotent stem cells using droplet digital PCR:
Diagram 2: Droplet Digital PCR Workflow for Residual Pluripotent Stem Cell Detection. This diagram outlines the key steps in the ddPCR methodology for sensitive detection of residual undifferentiated cells using the LIN28A marker.
Research Reagent Solutions for Tumorigenicity Assessment
Table 3: Essential Research Reagents for Residual PSC Detection
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Cell Markers | LIN28A, OCT3/4, SOX2, NANOG | Detection of undifferentiated PSCs [124] |
| PCR Reagents | ddPCR Supermix, Primers/Probes for pluripotency markers | Amplification and detection of PSC-specific transcripts [124] |
| Reference Materials | PSC lines (WA09/H9, NH50191), Primary fibroblasts (Hs68) | Positive controls and background cells for spike-in experiments [124] |
| NGS Platforms | Targeted panels, Whole exome sequencing, Capture sequencing | Comprehensive genetic stability assessment [82] [85] |
| Cell Culture Reagents | Defined culture media, Matrigel, Passaging reagents | Maintenance of PSCs and differentiated cells [3] |
| Biosensors | TdT enzyme-Endo IV-fluorescent probe | Detection of DNA strand breaks for genomic integrity assessment [9] |
The advancing clinical application of PSC-derived therapies necessitates robust, sensitive, and standardized methods for detecting residual pluripotent cells. Comparative analyses consistently demonstrate that droplet digital PCR offers superior sensitivity for detecting residual PSCs compared to conventional qPCR and other molecular methods, with the ability to detect as few as 10 PSCs in a million differentiated cells [124]. This sensitivity meets or exceeds the theoretical tumorigenicity threshold and provides a practical tool for quality control in manufacturing.
International collaborative efforts through organizations like HESI's CGT-TRACS committee are driving standardization in this field, with multisite studies demonstrating the reproducibility of ddPCR across laboratories [123]. These efforts are crucial for establishing universally accepted safety standards for stem cell-based therapies.
For comprehensive safety assessment, a combination of approaches is recommended—using highly sensitive molecular methods like ddPCR for routine batch testing of residual undifferentiated cells, supplemented with NGS-based methods for periodic genetic stability assessment throughout the manufacturing process. As the field evolves, continued refinement of these assays and their integration into regulatory frameworks will be essential for realizing the full therapeutic potential of pluripotent stem cells while ensuring patient safety.
Conclusion
The path to clinically safe stem cell therapies is inextricably linked to rigorous genomic stability assessment. No single method is sufficient; a comprehensive, integrated approach that leverages the complementary strengths of karyotyping, OGM, NGS, and digital PCR is essential for a complete picture of a cell line's genomic integrity. This multi-faceted strategy must be embedded throughout the entire development workflow—from cell line establishment and routine culture to final product release. As the field advances, future directions must focus on the standardization of potency assays, the establishment of global reference materials, the validation of rapid, in-process monitoring tools, and clearer regulatory harmonization. By adopting these robust quality control frameworks, the scientific community can confidently de-risk stem cell-based applications, paving the way for their successful translation from promising research into mainstream, life-changing medicines.
References
- 1. Genomic Instability of iPSCs: Challenges Towards Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5346115/]
- 2. Tracing genomic instability in induced mesenchymal ... [https://www.nature.com/articles/s12276-025-01439-8]
- 3. PSC Genomic Integrity and Stability | Cell Quality [https://www.stemcell.com/psc-cell-quality/genomic-integrity]
- 4. Conditionally Reprogrammed Cells as Preclinical Model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427407/]
- 5. Current advances and future prospects of cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1546423/full]
- 6. Genomic comparison of early-passage conditionally ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0186190]
- 7. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 8. Stem Genomics publishes latest genomic stability QC for ... [https://www.stemgenomics.com/blog/genomic-stability-workflow-for-pluripotent-stem-cells-psc-introducing-practical-guidelines-for-regular-in-process-testing-of-psc-lines/]
- 9. Non-invasive assessment of stem cell DNA integrity in ... [https://www.nature.com/articles/s41598-025-00701-3]
- 10. Comprehensive Assessment of the Genomic ... | Research Square [https://www.researchsquare.com/article/rs-7522863/v1]
- 11. Structural Variants: Mechanisms, Mapping, and Interpretation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12385565/]
- 12. Complex de novo structural variants are an underestimated ... [https://www.nature.com/articles/s41467-025-64722-2]
- 13. Tracing genomic instability in induced mesenchymal stromal cell ... [https://www.nature.com/articles/s12276-025-01439-8?error=cookies_not_supported&code=3e45b7ff-ff7f-4d56-956b-a53fe2492556]
- 14. New approaches for characterization of the genetic stability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5512780/]
- 15. Section 4: Stem -based Model Systems — International Society for... Cell [https://www.isscr.org/basic-research-standards/stem-cell-based-model-systems]
- 16. Safety Assessment of Stem Cell-Based Therapies [https://pubmed.ncbi.nlm.nih.gov/41227306/]
- 17. Multiple myeloma with high-risk cytogenetics and its treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9160142/]
- 18. Chromosome 1q21 abnormalities in multiple myeloma [https://www.nature.com/articles/s41408-021-00474-8]
- 19. Gain of chromosome 17 is an early genetic abnormality in ... [https://www.sciencedirect.com/science/article/pii/S0304383525003350]
- 20. Risk stratification of newly diagnosed ... [https://multiplemyelomahub.com/medical-information/risk-stratification-of-newly-diagnosed-multiple-myeloma-using-chromosome-1]
- 21. Chromosome 12 - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/chromosome-12]
- 22. Gain of chromosome 17 is the most frequent abnormality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1858505/]
- 23. 17q12 Recurrent Deletion Syndrome - GeneReviews - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK401562/]
- 24. Additional Evidence for Neuropsychiatric Manifestations in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8622498/]
- 25. Chromosome 20 - an overview [https://www.sciencedirect.com/topics/neuroscience/chromosome-20]
- 26. Genomic instability as a driver and suppressor of anti- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11562473/]
- 27. Genomic instability in human cancer: Molecular insights ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4600419/]
- 28. Cancer stem cells: landscape, challenges and emerging ... [https://www.nature.com/articles/s41392-025-02360-2]
- 29. True cancer stem cells exhibit relative degrees of ... [https://pubmed.ncbi.nlm.nih.gov/39847828/]
- 30. The two sides of chromosomal instability: drivers and ... [https://www.nature.com/articles/s41392-024-01767-7]
- 31. Origins of chromosome instability unveiled by coupled ... [https://www.nature.com/articles/s41586-025-09632-5]
- 32. Bioengineered niches that recreate physiological ... [https://www.nature.com/articles/s41467-024-50054-0]
- 33. Clinical validation of artificial intelligence-assisted ... [https://link.springer.com/article/10.1007/s00439-025-02789-z]
- 34. Karyotyping Service 2025-2033 Trends: Unveiling Growth ... [https://www.archivemarketresearch.com/reports/karyotyping-service-52612]
- 35. The Emergence of Artificial Intelligence-Guided Karyotyping [https://pmc.ncbi.nlm.nih.gov/articles/PMC12192041/]
- 36. The Emergence of Artificial Intelligence-Guided Karyotyping [https://www.mdpi.com/2073-4425/16/6/685]
- 37. Chromosome G Banding Technology Protocol [https://www.creative-bioarray.com/support/chromosome-g-banding-technology-protocol.htm]
- 38. Comparative prospective study on the clinical utility of G‐ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12044132/]
- 39. Choosing a genetic analysis method for your research ... [https://www.thermofisher.com/blog/behindthebench/choosing-a-genetic-analysis-method-for-your-research-laboratory/]
- 40. Optical Genome Mapping: A New Tool for Cytogenomic ... [https://www.mdpi.com/2073-4425/16/8/924]
- 41. Optical Genome Mapping: A 'Tool' with Significant Potential ... [https://www.cap.org/member-resources/articles/optical-genome-mapping-a-tool-with-significant-potential-from-discovery-to-diagnostics]
- 42. Assessment of Genetic Stability in Human Induced ... [https://www.mdpi.com/1422-0067/25/2/1101]
- 43. Optical genome mapping improves clinical interpretation of ... [https://www.sciencedirect.com/science/article/abs/pii/S1098360025000991]
- 44. Comparative Analysis of Targeted RNA-Seq and Optical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12608001/]
- 45. Exploring the size limits of Bionano optical genome mapping ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01571-0]
- 46. NGS Approaches in Clinical Diagnostics: From Workflow to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524640/]
- 47. Whole Exome vs. Whole Genome Sequencing [https://www.cd-genomics.com/resource-wes-and-wgs.html]
- 48. Comprehensive Outline of Whole Exome Sequencing Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6895801/]
- 49. Whole-genome sequencing of 490640 UK Biobank ... [https://www.nature.com/articles/s41586-025-09272-9]
- 50. Validated WGS and WES protocols proved saliva-derived ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10080-0]
- 51. Rapid NGS Analysis on Google Cloud Platform [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627752/]
- 52. Top 10 AI Genetic Analysis Tools in 2025: Features, Pros ... [https://www.devopsschool.com/blog/top-10-ai-genetic-analysis-tools-in-2025-features-pros-cons-comparison/]
- 53. Whole-genome sequencing improves diagnostic yield in ... [https://www.sciencedirect.com/science/article/pii/S2666247725000727]
- 54. A Primer on NGS Technologies and Their Specs (2025) [https://blog.latch.bio/p/a-primer-on-ngs-technologies-and]
- 55. DNA Sequencing: How to Choose the Right Technology [https://frontlinegenomics.com/dna-sequencing-how-to-choose-the-right-technology/]
- 56. Why Early Genetic Variant Detection in iPSC Cultures Is ... [https://www.reprocell.com/blog/why-early-genetic-variant-detection-in-ipsc-cultures-is-critical-for-safe-and-regulatory-compliant-cell-therapies]
- 57. Chromosomal Aberrations in Induced Pluripotent Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12387029/]
- 58. Digital PCR: from early developments to its future application ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00055f]
- 59. Fundamentals of digital PCR [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/pcr/digital-pcr/what-is-digital-pcr]
- 60. What Is Digital PCR? – Learn About the Advantages of dPCR [https://www.thermofisher.com/blog/behindthebench/what-is-digital-pcr/]
- 61. What is digital PCR? | IDT [https://sg.idtdna.com/page/support-and-education/decoded-plus/digital-pcr-is-it-worth-the-extra-cost/]
- 62. qPCR, dPCR, NGS – A journey - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4822211/]
- 63. Comparing the precision of two digital PCR applications for ... [https://www.nature.com/articles/s41598-025-13143-8]
- 64. Comparative Analysis of Two Digital PCR Platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361875/]
- 65. Comprehensive profiling of RNA modification-related ... [https://www.nature.com/articles/s12276-025-01531-z]
- 66. From bench to bytes: a practical guide to RNA sequencing ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1697922/full]
- 67. From Transcription Factors Dysregulation to Malignancy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562326/]
- 68. Single-cell transcriptomic and genomic changes in the ... [https://www.nature.com/articles/s41586-025-09435-8]
- 69. INFOGRAPHIC: The Science of RNA-Seq Data Visualization [https://www.rna-seqblog.com/infographic-the-science-of-rna-seq-data-visualization/]
- 70. A Guide to Basic RNA Sequencing Data Processing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12067304/]
- 71. Transcriptional patterns of cancer-related genes in primary ... [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-025-02339-z]
- 72. Safety Assessment of Stem Cell-Based Therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609812/]
- 73. Safety Assessment of Stem Cell-Based Therapies [https://www.mdpi.com/2073-4409/14/21/1660]
- 74. Cell bank system, establishment, and application in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409320/]
- 75. Artificial intelligence in bioinformatics: a survey - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12596291/]
- 76. 6 Key Questions to Cover When Selecting Your Cell ... [https://advancedtherapies.com/6-key-questions-to-cover-when-selecting-your-cell-banking-manufacturing-partner/]
- 77. How did we get there? AI applications to biological ... [https://www.sciencedirect.com/science/article/pii/S0010482525004159]
- 78. 3. Clinical Translation of Stem Cell-based Interventions [https://www.isscr.org/guidelines/clinical-translation-of-stem-cell-based-interventions]
- 79. The Barcode of Genetic Health: Karyotyping in Stem Cell ... [https://www.wicell.org/blog/the-barcode-of-genetic-health-karyotyping-in-stem-cell-cultures/]
- 80. Genomic integrity of human induced pluripotent stem cells ... [https://www.sciencedirect.com/science/article/pii/S1873506120301057]
- 81. Prenatal diagnosis and pregnancy outcomes of mosaicism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12403500/]
- 82. Assessment of Genetic Stability in Human Induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10815998/]
- 83. Development of a Clinically Applicable High-Resolution ... [https://www.sciencedirect.com/science/article/abs/pii/S1525157825000789]
- 84. Image-based DNA sequencing encoding for detecting low ... [https://www.nature.com/articles/s41467-025-64237-w]
- 85. NGS-based assays to assess genomic stability in stem cells [https://www.stemgenomics.com/about/technologies-stemcell-characterization/ngs-based-assay-genomic-testing-stem-cells/]
- 86. GMP Cell Therapy Consumables Market Growth, Analysis of ... [https://www.pharmiweb.com/press-release/2025-08-01/gmp-cell-therapy-consumables-market-growth-analysis-of-key-players-trends-drivers]
- 87. Laboratory Reagents Market Outlook 2025-2032 [https://www.intelmarketresearch.com/laboratory-reagents-2025-2032-93-6230]
- 88. Regulation of NSL by TAF4A is critical for genome stability ... [https://www.nature.com/articles/s41467-025-64402-1]
- 89. Comparison of culture media supplements identifies serum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382287/]
- 90. GMP Grade Cell Culture Media Market Size & Share 2025- ... [https://www.360iresearch.com/library/intelligence/gmp-grade-cell-culture-media]
- 91. The Best Cell Culture Media and Reagents of 2026 [https://www.labx.com/resources/the-best-cell-culture-media-and-reagents-of-2026/4823]
- 92. Somatic Tumor Testing 2025-11-15 | Carelon Clinical Guidelines and Pathways [https://guidelines.carelonmedicalbenefitsmanagement.com/somatic-tumor-testing-2025-11-15/]
- 93. Comprehensive analysis of mutational processes across 20 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12242766/]
- 94. A novel tumor mutational burden-based risk model predicts prognosis and correlates with immune infiltration in ovarian cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9393426/]
- 95. A simple framework to identify optimal cost-effective risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9190212/]
- 96. Quantifying risk stratification provided by diagnostic tests ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6827980/]
- 97. Genotoxicity in risk assessment: is it time to use a threshold ... [https://www.sciencedirect.com/science/article/abs/pii/S2468202018300664]
- 98. JCI - Detecting likely germline variants during tumor-based molecular profiling [https://www.jci.org/articles/view/190264]
- 99. A novel platform to enable the high-throughput derivation and... [https://www.nature.com/articles/srep00213?error=cookies_not_supported&code=6be1a957-af56-4c42-949d-fd11d25c9d43]
- 100. eTeSR™: Raise the Bar for Single-Cell Passaging [https://www.stemcell.com/why-etesr-for-single-cell-passaging]
- 101. PSC Genomic Integrity and Stability | Cell Quality [https://cdn.stemcell.com/psc-cell-quality/genomic-integrity]
- 102. Transcriptomic analysis of feeder-free culture system for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10122725/]
- 103. StemFlex Medium for Robust Feeder-Free PSC Culture [https://www.thermofisher.com/us/en/home/life-science/stem-cell-research/induced-pluripotent-stem-cells/medium-robust-feeder-free-psc-culture.html]
- 104. Optical Genome Mapping: A New Tool for Cytogenomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12385997/]
- 105. Genetic testing of bone marrow: the what, the when and ... [https://www.sciencedirect.com/science/article/abs/pii/S1756231725001331]
- 106. The accuracy and real resolution of karyotyping technique ... [https://pubmed.ncbi.nlm.nih.gov/40879815/]
- 107. Application of Optical Genome Mapping for the Diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12192876/]
- 108. Optical genome mapping to decipher the chromosomal ... [https://www.nature.com/articles/s41598-025-86828-9]
- 109. A retrospective analysis of 38652 amniotic fluid karyotype [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1655290/full]
- 110. AI‐Driven Quality Monitoring and Control in Stem Cell Cultures [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336434/]
- 111. Why Comprehensive Genomic Profiling? [https://www.foundationmedicine.com/resource/why-comprehensive-genomic-profiling]
- 112. Comprehensive Genomic Profiling (CGP) | Cancer ... [https://www.illumina.com/areas-of-interest/cancer/ngs-in-oncology/cgp.html]
- 113. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 114. Genomic Profiling - Oncology [https://www.tempus.com/oncology/genomic-profiling/?srsltid=AfmBOop06yUffl0d59EO8bfX6b9dosrh-V_lzjvQAwASYPThJHsrwyYa]
- 115. Benchmarking deep learning methods for ... - Genome Biology [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03869-z]
- 116. PFMG2025–integrating genomic medicine into the national ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11910791/]
- 117. Experimental Design for Immune Profiling [https://www.10xgenomics.com/support/software/cell-ranger/8.0/getting-started/cr-5p-design]
- 118. The ISSCR Releases Targeted Update to the Guidelines ... [https://www.isscr.org/isscr-news/the-isscr-releases-targeted-update-to-the-guidelines-for-stem-cell-research-and-clinical-translation]
- 119. Standards and the Future of Stem Cell Research [https://www.astm.org/news/standards-and-the-future-of-stem-cell-research]
- 120. 5. Standards in Stem Cell Research [https://www.isscr.org/guidelines/standards-in-stem-cell-research]
- 121. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 122. Assessing Tumorigenicity in Stem Cell-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376867/]
- 123. TRAcking, Circulation, & Safety (CGT-TRACS) - HESI [https://hesiglobal.org/cell-therapy-tracking-circulation-safety-ct-tracs/]
- 124. Analysis of three characterization assays reveals ddPCR ... [https://www.sciencedirect.com/science/article/pii/S1465324924007266]