Fresh vs. Cryopreserved MSCs: A Systematic Analysis of Biological Signatures for Clinical Translation
This article provides a comprehensive analysis of the biological signatures of freshly cultured versus cryopreserved Mesenchymal Stem Cells (MSCs), a central debate in regenerative medicine.
Fresh vs. Cryopreserved MSCs: A Systematic Analysis of Biological Signatures for Clinical Translation
Abstract
This article provides a comprehensive analysis of the biological signatures of freshly cultured versus cryopreserved Mesenchymal Stem Cells (MSCs), a central debate in regenerative medicine. Tailored for researchers, scientists, and drug development professionals, it synthesizes current evidence from systematic reviews and primary studies to explore foundational biological characteristics, methodological considerations for manufacturing and storage, strategies for troubleshooting functional deficits, and comparative validation of therapeutic efficacy. The analysis concludes that while core biological and functional signatures are largely comparable, specific nuances in immunomodulatory potency and differentiation capacity post-thaw are critical for optimizing clinical-grade MSC product development and regulatory approval.
Decoding Core Biology: Intrinsic Properties of Fresh and Cryopreserved MSCs
The transition of Mesenchymal Stem Cells (MSCs) from research tools to clinical therapeutics hinges on rigorous and standardized identity criteria. The International Society for Cellular Therapy (ISCT) established minimal defining criteria to combat heterogeneity in the field: plastic adherence, specific surface marker expression (CD73, CD90, CD105), absence of hematopoietic markers, and trilineage differentiation potential into osteocytes, adipocytes, and chondrocytes [1] [2] [3]. Within clinical development and manufacturing, a critical logistical and biological question arises: how does cryopreservation—a practical necessity for off-the-shelf therapies—affect these core identity signatures compared to freshly preserved cells? This guide objectively compares the biological and functional signatures of fresh versus cryopreserved MSCs, synthesizing current experimental data to inform their use in research and drug development.
The Pillars of MSC Identification
The ISCT Minimal Criteria
The ISCT criteria provide a foundational framework for verifying MSC populations [1] [2].
- Plastic Adherence: All MSCs must be plastic-adherent in standard culture conditions [2] [3].
- Surface Marker Expression: ≥95% of the population must express CD73, CD90, and CD105, while ≤2% may express CD45, CD34, CD14 or CD11b, CD79a or CD19, and HLA-DR [1] [3].
- Trilineage Differentiation: Under appropriate in vitro conditions, the cells must differentiate into osteoblasts, adipocytes, and chondrocytes [2] [4] [3].
Detailed Trilineage Differentiation Protocols
Confirming multipotency is a functional requirement for MSC identification. Standardized protocols involve lineage-specific induction media and subsequent detection of differentiation through histochemical staining [4].
Table 1: Standardized Trilineage Differentiation Protocols
| Lineage | Induction Media Key Components | Incubation Time | Detection Method | Stain Outcome (Differentiated Cells) |
|---|---|---|---|---|
| Osteogenesis | Dexamethasone, β-glycerophosphate, Ascorbate-2-phosphate [4] | 12-14 days | Alizarin Red S staining of extracellular matrix | Bright orange-red calcium deposits [4] |
| Adipogenesis | Dexamethasone, Insulin, Indomethacin, Isobutylmethylxanthine [4] | 12-14 days | Oil Red O staining of intracellular lipids | Bright red lipid vesicles [4] |
| Chondrogenesis | TGF-β, Dexamethasone, Ascorbate-2-phosphate, Proline, Pyruvate [4] | 21 days | Alcian Blue staining of proteoglycans | Intense blue glycosaminoglycans in matrix [4] |
Figure 1: Experimental workflow for validating MSC multipotency through trilineage differentiation.
Comparative Analysis: Fresh vs. Cryopreserved MSC Biological Signatures
Surface Marker Expression Post-Cryopreservation
A primary concern is whether cryopreservation alters the characteristic surface marker profile of MSCs. Data from a 2023 large-scale comparative analysis of bone marrow-derived MSCs (BM-MSCs) and a 2018 study on umbilical cord tissue-derived MSCs (UCT-MSCs) provide quantitative insights.
Table 2: Surface Marker Expression in Fresh vs. Cryopreserved MSCs
| Surface Marker | Tissue Source | Fresh MSCs Expression | Cryopreserved MSCs Expression | Statistical Significance | Source & Context |
|---|---|---|---|---|---|
| CD73 | Bone Marrow | Comparable high expression | Comparable high expression | Not Significant (NS) | Lee et al., 2023 [5] |
| Umbilical Cord | 100% (Baseline) | 66.8% (33.2% loss) | NS | PMC5984056, 2018 [6] | |
| CD90 | Bone Marrow | Comparable high expression | Comparable high expression | NS | Lee et al., 2023 [5] |
| Umbilical Cord | 100% (Baseline) | 93.8% (6.2% loss) | NS | PMC5984056, 2018 [6] | |
| CD105 | Bone Marrow | Comparable high expression | Comparable high expression | NS | Lee et al., 2023 [5] |
| Umbilical Cord | 100% (Baseline) | 82.3% (17.7% loss) | NS | PMC5984056, 2018 [6] | |
| CD14 | Bone Marrow | Low/Negative | Low/Negative | Significantly different | Lee et al., 2023 [5] |
The 2023 big-data study of BM-MSCs concluded that the biosignatures of cryopreserved and freshly preserved cells were highly comparable, with no significant differences in the core marker triad (CD73, CD90, CD105) [5]. The noted expression loss in the UCT-MSC study, while not statistically significant, highlights the importance of source tissue and protocol-specific validation.
Functional Differentiation Potential
The retention of trilineage differentiation capacity is a crucial functional test for cryopreserved MSCs. A 2024 study advanced this analysis by employing a sophisticated 3D spheroid model under serum-free, hypoxic conditions.
Table 3: Trilineage Differentiation Potential of Fresh vs. Cryopreserved MSCs
| Differentiation Lineage | Culture Model | Fresh MSCs Potential | Cryopreserved MSCs Potential | Key Findings |
|---|---|---|---|---|
| Adipogenesis | 3D Spheroid, Serum-Free | Supported | Supported | Platform supported adipogenic differentiation for MSCs from all tissue sources [7]. |
| Chondrogenesis | 3D Spheroid, Serum-Free | Supported | Supported | Platform supported chondrogenic differentiation for MSCs from all tissue sources [7]. |
| Osteogenesis | 3D Spheroid, Serum-Free | Supported (Adipose, BM) | Variable | Model successfully supported osteogenesis for adipose- and bone marrow-derived MSCs, but not for umbilical cord-derived MSCs [7]. |
The 2023 comparative analysis of BM-MSCs further supports this, finding that the multipotency of MSCs was not compromised by cryopreservation, reinforcing the concept that functionality is largely preserved [5].
Viability, Proliferation, and Paracrine Activity
Beyond identity markers and differentiation, critical quality attributes for therapeutic MSCs include viability, growth kinetics, and secretory profile.
Table 4: Comparison of Viability, Proliferation, and Secretome
| Biological Parameter | Fresh MSCs | Cryopreserved MSCs | Research Context |
|---|---|---|---|
| Cell Viability | High | No significant difference at most passages | Lee et al., 2023 (BM-MSCs) [5] |
| Proliferation (PDT) | Standard PDT | No significant difference at most passages | Lee et al., 2023 (BM-MSCs) [5] |
| Paracrine Molecules | Characteristic secretome | Comparable concentrations (e.g., IL-6) | Lee et al., 2023: Most paracrine molecules did not exhibit different levels [5] |
The 2023 study explicitly stated that the individual average population doubling time (PDT) and cell viability at most passages did not differ according to the preservation method [5]. This data provides confidence that cryopreservation does not fundamentally impair the core cellular health or therapeutically relevant secretory functions of MSCs.
The Scientist's Toolkit: Essential Reagents for MSC Characterization
A robust MSC identity workflow relies on specific, high-quality reagents.
Table 5: Key Research Reagent Solutions for MSC Characterization
| Reagent / Kit | Function | Experimental Application |
|---|---|---|
| Flow Cytometry Antibody Panels (e.g., CD73, CD90, CD105, CD34, CD45) | Quantitative surface marker analysis | Verification of ISCT-positive and negative marker criteria [6] [1]. |
| Trilineage Differentiation Media Kits (Osteo-, Adipo-, Chondro-) | Induce lineage-specific differentiation | Functional validation of multipotency [4]. |
| Histochemical Stains (Alizarin Red S, Oil Red O, Alcian Blue) | Detect differentiation endpoints | Visualize calcium deposits (osteogenesis), lipid vacuoles (adipogenesis), and proteoglycans (chondrogenesis) [4]. |
| TrypLE Solution | Harvest adherent cells | Non-enzymatic, gentle cell dissociation for sub-culture or analysis [6]. |
| Fetal Bovine Serum (FBS) / Human Platelet Lysate (hPL) | Media supplement for cell growth | FBS is classical but poses xenogenic risks; hPL is a defined, clinically-relevant alternative [7]. |
| CryoStor CS10 | Cryopreservation medium | Optimized, serum-free solution for freezing cells to enhance post-thaw viability [6]. |
The consolidated experimental data from recent studies allows for a confident conclusion: the core biological signatures of MSCs, as defined by the ISCT criteria, are largely conserved after cryopreservation. The expression of canonical surface markers CD73, CD90, and CD105 remains stable in BM-MSCs, and the critical functional capacity for trilineage differentiation is retained, albeit with potential source-specific variations as noted in umbilical cord-derived cells [7] [5]. Key attributes like viability, proliferation capacity, and paracrine output also show no significant differences in large-scale analyses [5].
For researchers and drug development professionals, this evidence supports the use of cryopreserved MSCs as a reliable and logistically feasible source for therapeutic development. It mitigates concerns that the freezing process fundamentally alters the cell product's identity or potency. However, rigorous in-house validation using the detailed protocols and tools outlined in this guide remains essential, as variables like tissue source, donor age, and specific cryopreservation protocols can influence outcomes. The adherence to standardized identity checks ensures the reliability and reproducibility of MSC applications in regenerative medicine.
Cryopreservation enables long-term storage of biological samples at ultra-low temperatures (typically below -130°C), effectively suspending metabolic and physiochemical activities to avoid biological variation [8]. This process has become indispensable for Advanced Therapy Medicinal Products (ATMPs), particularly mesenchymal stromal cells (MSCs), allowing for quality-controlled banking, off-the-shelf availability, and logistical flexibility in clinical applications [9] [10]. The fundamental challenge in cryopreservation lies in navigating the delicate balance between achieving metabolic arrest and maintaining cellular integrity, viability, and function after thawing [10]. Understanding the mechanisms of freezing-induced cell injury and the protective roles of cryoprotectants is thus crucial for optimizing cryopreservation protocols for cell-based therapies.
Fundamental Mechanisms of Cell Injury During Cryopreservation
Physical and Osmotic Stresses During Freezing
The process of freezing imposes two primary mechanisms of cell injury. As water cools, molecules form sufficient H-bonds, reorganize into a hexagonal structure, and initiate ice nucleation [10]. The formed ice crystals reduce free water available for cellular processes, causing solutes within the solution to become more concentrated as water molecules join the ice lattice [10]. This triggers osmotic stress as water effluxes from cells to establish equilibrium, particularly during slow freezing, resulting in significant cell dehydration and shrinkage [11] [10].
The cooling rate critically determines the dominant injury mechanism. Slow cooling provides more time for water removal from the cell, causing excessive dehydration and solute concentration effects. Rapid cooling limits water transport, causing the cytoplasm to become super-cooled with higher solute concentration, which increases the likelihood of intracellular ice formation [10]. Intracellular ice crystals can mechanically disrupt cellular membranes and organelles, making this form of damage typically lethal to cells [11] [8].
Table 1: Primary Mechanisms of Cryoinjury
| Mechanism | Conditions Favoring Injury | Cellular Consequences |
|---|---|---|
| Intracellular Ice Formation | Rapid cooling rates | Mechanical disruption of membranes and organelles; typically lethal [11] [10] |
| Solution Effects | Slow cooling rates | Increased solute concentration to lethal levels; osmotic stress [11] |
| Cell Dehydration | Slow cooling rates | Cell shrinkage; membrane damage; metabolic disruption [10] |
| Ice Recrystallization | During thawing | Growth of small ice crystals into larger, more damaging structures [8] |
Biochemical Consequences of Freezing Stress
Beyond immediate physical damage, the freezing process triggers significant biochemical stress pathways. Studies on human bone mesenchymal stem cells (hBMSCs) have demonstrated that cryopreservation can induce oxidative stress through the production of supra-physiological levels of reactive oxygen species (ROS) after the freeze-thaw process [8]. This oxidative stress can lead to DNA damage, apoptosis, and cell cycle arrest [8]. Additionally, the process can cause dysregulation of biochemical pathways, which varies among different cell types. For instance, T-cells experience significant apoptosis after cryopreservation, with approximately 40% of cells undergoing apoptosis 8 hours post-thaw [10].
Cryoprotectant Mechanisms and Classifications
Permeating Cryoprotectant Agents (CPAs)
Permeating CPAs are characterized by their small size (typically less than 100 daltons), high water solubility at low temperatures, and amphiphilic nature that allows easy diffusion through cell membranes [11] [10]. These agents function primarily by forming hydrogen bonds with water molecules through their polar groups, creating stronger interactions than water-water molecule hydrogen bonds [10]. This effectively removes free water molecules that would otherwise be available to form critical nucleation sites for ice crystal formation [10].
Dimethyl sulfoxide (DMSO) is the most widely used permeating CPA, first identified as a cryoprotectant in 1959 [12] [8]. At low concentrations (5%), DMSO decreases membrane thickness and increases membrane permeability. At standard cryopreservation concentrations (10%), it induces water pore formation in biological membranes, allowing intracellular water to be more readily replaced by cryoprotectants that promote vitrification [11]. However, at higher concentrations (40%), lipid bilayers begin to disintegrate, demonstrating the concentration-dependent toxicity of this agent [11].
Other common permeating agents include glycerol (the first discovered CPA), ethylene glycol, and propanediol [11]. Each has specific applications, with glycerol being particularly effective for spermatozoa and DMSO dominating for most mammalian cell types.
Non-Permeating Cryoprotectant Agents (CPAs)
Non-permeating CPAs are typically larger molecules that cannot cross cell membranes due to their size or polarity [11] [10]. This class includes polymers such as polyethylene glycol (PEG) and polyvinylpyrrolidone (PVP), as well as disaccharides like sucrose, trehalose, and raffinose [11]. These agents exert their protective effects extracellularly by similar hydrogen-bonding mechanisms as permeating CPAs, but to a lesser extent [11].
Trehalose deserves special mention due to its unique properties. This glucose dimer linked via an α-1,1-glycosidic bond is produced by various organisms including bacteria, fungi, insects, and plants to withstand freezing [11]. Its acetal link prevents reduction of C-1 in each monomer, increasing stability under extreme temperatures and reducing susceptibility to acid hydrolysis [11].
Table 2: Common Cryoprotectants and Their Applications
| Cryoprotectant | Type | Common Concentrations | Primary Applications | Notable Characteristics |
|---|---|---|---|---|
| DMSO | Permeating | 10% (approx. 2M) | Most mammalian cells, MSCs, HSCs [11] [9] | Increases membrane porosity; potential cytotoxicity [11] |
| Glycerol | Permeating | 10-15% | Spermatozoa, red blood cells [11] | First discovered CPA; less toxic than DMSO [11] |
| Ethylene Glycol | Permeating | 1-2M (vitrification) | Oocytes, embryos [11] | Rapid permeability; used in vitrification mixtures [11] |
| Trehalose | Non-Permeating | 0.2-0.5M | Biostabilization in combination with PAs [11] | Natural disaccharide; high stability; low toxicity [11] |
| Sucrose | Non-Permeating | 0.1-0.3M | Extracellular stabilizer with PAs [11] | Common disaccharide; osmotic buffer |
Vitrification Strategies
Vitrification represents an alternative approach to traditional freezing, whereby water solidifies into a glass-like amorphous state without forming ice crystals [11]. This is achieved using high concentrations of CPAs accompanied by ultra-rapid cooling rates [11]. Both permeating and non-permeating agents can be combined in vitrification mixtures to achieve the necessary stabilization while minimizing individual CPA toxicity [11]. Research has demonstrated that multi-molar combinations of reduced concentrations of ethylene glycol and DMSO can successfully cryopreserve human and murine islet cells with reduced adverse effects [11].
Comparative Analysis: Fresh vs. Cryopreserved MSCs
In Vivo Functional Comparisons
A systematic review of comparative pre-clinical models of inflammation analyzed differences between freshly cultured and cryopreserved MSCs [13]. The analysis encompassed 257 in vivo pre-clinical efficacy experiments representing 101 distinct outcome measures [13]. Remarkably, only 2.3% (6/257) of these outcomes showed statistically significant differences, with two favoring freshly cultured and four favoring cryopreserved MSCs [13]. This comprehensive analysis suggests that the majority of preclinical in vivo efficacy outcomes do not significantly differ between freshly cultured and cryopreserved MSCs in animal models of inflammation.
In Vitro Potency and Characteristics
The same systematic review examined 68 in vitro experiments representing 32 different potency measures [13]. Here, 13% (9/68) of experiments showed statistically significant differences, with seven favoring freshly cultured MSCs and two favoring cryopreserved MSCs [13]. While this indicates more frequent differences in in vitro assessments, the majority of potency measures still showed no significant differences.
Further supporting these findings, a comparative analysis of biological signatures between freshly preserved and cryo-preserved bone marrow MSCs sourced from approximately 2300 stem cell manufacturing cases found that circular clustering did not reveal any differences between the two preservation methods [5]. This pattern persisted when using viability, cluster of differentiation (CD) markers, and paracrine molecular indices as inputs for unsupervised analysis [5].
Table 3: Experimental Outcomes Comparing Fresh vs. Cryopreserved MSCs
| Assessment Type | Total Experiments/ Measures | Significantly Different Outcomes | Direction of Difference | Key References |
|---|---|---|---|---|
| In Vivo Efficacy | 257 experiments, 101 measures | 2.3% (6/257) | 2 fresh, 4 cryopreserved | [13] |
| In Vitro Potency | 68 experiments, 32 measures | 13% (9/68) | 7 fresh, 2 cryopreserved | [13] |
| Immunophenotype | Multiple markers | Most unchanged (except CD14 in one study) | No consistent pattern | [5] |
| Paracrine Molecules | Multiple factors | No significant differences | Not applicable | [5] |
| Population Doubling Time | Multiple passages | No significant differences | Not applicable | [5] |
DMSO-Specific Effects on MSC Properties
DNA Integrity and Cellular Function
Research specifically investigating the impact of DMSO cryopreservation on human bone mesenchymal stem cells (hBMSCs) has revealed several important findings. One study demonstrated that while immediate post-thaw viability remained high (90.1% for fresh cells vs. 82.6% for cryopreserved), the live cell recovery rate was significantly reduced to 71.8% [8]. Furthermore, cryopreservation with DMSO resulted in increased DNA damage, as evidenced by elevated γ-H2AX expression (a DNA double-strand break marker) increasing from 8.7% in fresh cells to 18.2% in frozen-thawed cells [8].
The study also found increased apoptosis (from 4.1% to 10.6%) and cell cycle alterations in post-thaw hBMSCs, with more cells arrested in G0/G1 phase (73.4% vs 63.5% for fresh cells) [8]. These cellular changes translated to functional impairments, including reduced migration capability and osteogenic differentiation potential, though adipogenic differentiation remained unchanged [8].
Clinical Safety Considerations
The potential toxicity of DMSO in clinical applications remains a topic of debate [9]. When administered intravenously with MSC products, DMSO doses are typically 2.5-30 times lower than the dose of 1 g DMSO/kg generally accepted for hematopoietic stem cell transplantation [9]. With adequate premedication, only isolated infusion-related reactions have been reported with these lower doses [9].
For topical applications, analysis of wound healing studies using DMSO suggests that concentrations applied with undiluted DMSO-cryopreserved MSC products are unlikely to cause significant local adverse effects [9]. Even under worst-case scenarios assuming complete systemic absorption from a large wound, systemic DMSO exposure would be approximately 55 times lower than that from an intravenous dose of 1 g/kg [9].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for MSC Cryopreservation Studies
| Reagent/Material | Function | Example Applications | Considerations |
|---|---|---|---|
| DMSO (Cell Culture Grade) | Permeating cryoprotectant | Standard cryopreservation of MSCs, HSCs [11] [9] | Concentration-dependent toxicity; use at 10% for most applications [11] |
| Trehalose | Non-permeating cryoprotectant | Extracellular stabilization; combination with PAs [11] | Natural disaccharide; high stability; low toxicity [11] |
| Programmable Freezer | Controlled-rate freezing | Slow cooling protocols (≈1°C/min) [11] | Essential for standardized freezing curves |
| Liquid Nitrogen Storage System | Long-term sample storage | Cryogenic preservation below -130°C [10] | Vapor phase reduces contamination risk |
| Cell Viability Assays | Post-thaw assessment | Flow cytometry with Annexin V/PI; trypan blue exclusion [8] | Distinguish live, apoptotic, and necrotic cells |
| Oxidative Stress Detection Kits | Measure ROS production | Evaluation of cryopreservation-induced stress [8] | Important for assessing cellular stress |
| Differentiation Media | Functional assessment | Osteogenic, adipogenic differentiation potential [8] | Critical for evaluating post-thaw functionality |
| DNA Damage Assay Kits | Genotoxicity assessment | γ-H2AX detection for DNA double-strand breaks [8] | Evaluate genetic integrity after cryopreservation |
Experimental Workflows for Cryopreservation Studies
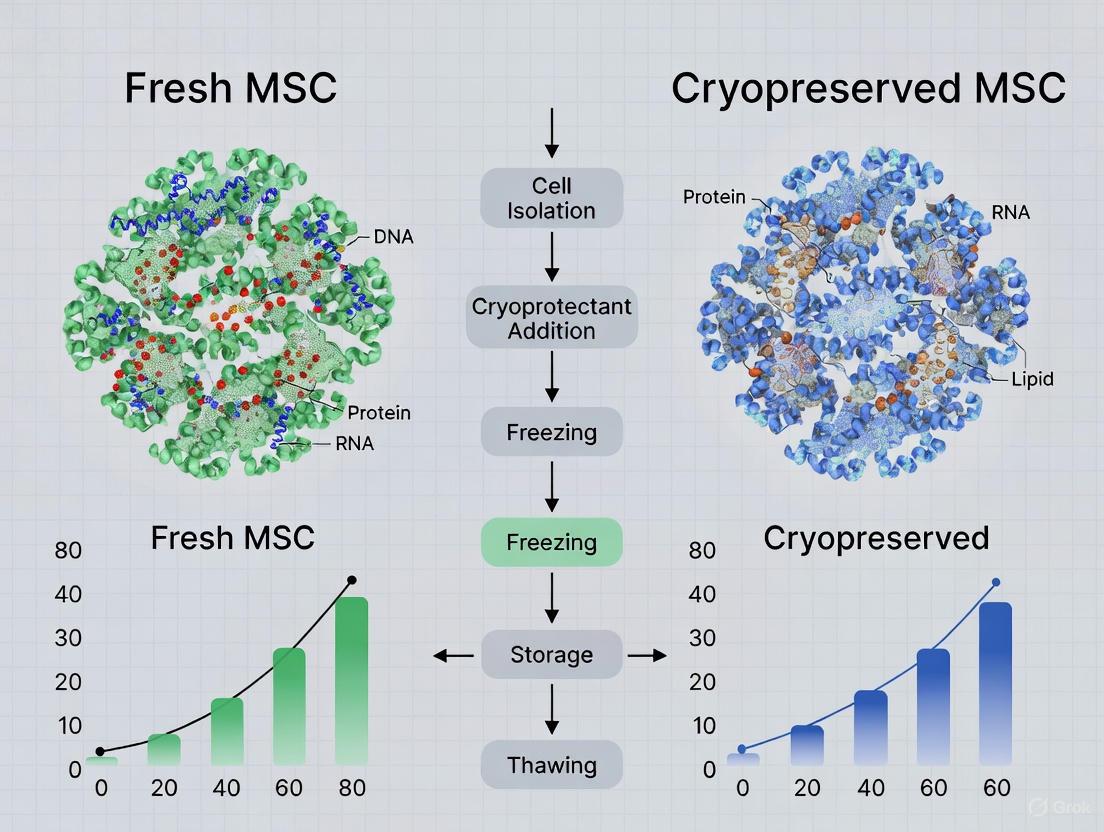
Diagram Title: Experimental Workflow for MSC Cryopreservation Studies
Molecular Pathways in Cryopreservation-Induced Stress
Diagram Title: Cellular Stress Pathways in Cryopreservation
The cryopreservation process represents a critical technology enabling the advancement of MSC-based therapies by providing off-the-shelf availability and logistical flexibility. While cryopreservation induces various cellular stresses through ice formation, osmotic imbalance, and biochemical alterations, the strategic use of cryoprotectants like DMSO significantly mitigates these damages. Current evidence suggests that cryopreserved MSCs largely retain their functional characteristics compared to fresh counterparts, with most in vivo efficacy measures showing no significant differences. However, attention to DMSO-associated effects on DNA integrity and cellular function warrants continued optimization of cryopreservation protocols. The ongoing development of improved cryoprotectant formulations and freezing techniques promises to further enhance the viability, functionality, and safety profiles of cryopreserved MSC products for clinical applications.
The transition of mesenchymal stromal cells (MSCs) from research tools to clinically applicable "off-the-shelf" therapeutics hinges on effective cryopreservation protocols that maintain their critical biological attributes. For researchers, scientists, and drug development professionals, understanding the precise impact of cryopreservation on fundamental cellular characteristics—viability, morphology, and population doubling time (PDT)—is paramount for protocol optimization and regulatory approval. This guide objectively compares these core attributes between freshly preserved and cryopreserved MSCs, synthesizing data from contemporary preclinical and manufacturing studies to provide a evidence-based analysis for decision-making in therapeutic development.
Comparative Analysis of Core Cellular Attributes
A comprehensive analysis of current literature reveals that cryopreservation, when performed with optimized protocols, has a minimal impact on the basic cellular attributes of MSCs. The table below synthesizes quantitative and qualitative findings from multiple studies directly comparing fresh and cryopreserved MSCs.
Table 1: Comparison of Key Cellular Attributes Between Fresh and Cryopreserved MSCs
| Cellular Attribute | Freshly Preserved MSCs | Cryopreserved MSCs | Significance/Notes |
|---|---|---|---|
| Viability | Reference standard (typically >95% [14]) | 93.81%-96.34% post-thaw [14]; Decreases over 6-hour post-thaw hold [15] | High viability maintained with clinical-grade cryopreservation solutions; holding time post-thaw is critical. |
| Morphology | Typical fibroblast-like, spindle-shaped, plastic-adherent [16] [17] | Unchanged; retained fibroblast-like, spindle shape [14] | No morphological alterations detected post-cryopreservation. |
| Population Doubling Time (PDT) | Reference proliferation capacity [5] [14] | Comparable PDT; no significant differences reported [5] [14] | Proliferative capacity is robustly preserved. |
| Surface Marker Expression | Positive for CD73, CD90, CD105; negative for CD34, CD45, HLA-DR [16] [14] [17] | Identical immunophenotype profile maintained [5] [14] | MSC immunophenotype is stable and unaffected by cryopreservation. |
| Key Findings | Serves as the biological baseline. | No significant differences in the majority of in-vivo efficacy (97.7%) and in-vitro potency (87%) outcomes [18] [19]. Biological signatures are comparable at a systemic level [5]. | Overall therapeutic profile remains intact post-cryopreservation. |
Detailed Experimental Data and Methodologies
Viability and Post-Thaw Stability Assessments
The assessment of viability extends beyond immediate post-thaw measurements. A 2024 study investigated the stability of cryopreserved bone marrow-derived MSCs under simulated clinical application conditions. Cells were cryopreserved at different concentrations and thawed, with viability tracked over 6 hours using Trypan blue exclusion and the more sensitive Annexin V/Propidium Iodide (PI) staining for apoptosis and necrosis detection [15].
- Experimental Workflow: The study cryopreserved MSCs in various solutions (e.g., NutriFreez, PHD10, CryoStor CS5/CS10) at concentrations of 3, 6, and 9 million cells/mL. Post-thaw, cells underwent different dilution strategies to reduce cryoprotectant concentration and were held at room temperature for up to 6 hours, with viability assessed at 0, 2, 4, and 6-hour intervals [15].
- Key Finding: A critical finding was that cells cryopreserved at a higher concentration (9 million/mL) and diluted 1:2 post-thaw showed improved viability maintenance over the 6-hour window. This highlights the importance of optimizing both cryopreservation cell density and post-thaw handling for clinical infusion [15].
Diagram 1: Experimental workflow for post-thaw viability and stability assessment
Proliferation Capacity and Population Doubling Time
The proliferation capacity, measured by Population Doubling Time (PDT), is a critical metric for ensuring MSCs can be expanded to clinically relevant numbers. A large-scale 2023 analysis of approximately 2,300 manufacturing cases from the Pharmicell database provided robust, real-world evidence on this attribute. The study included around 60 variables, with PDT being a key metric [5].
- Methodology: The PDT was calculated using the standard formula: PDT = log2(NX/N0) × T, where N0 is the initial number of attached cells, NX is the cell count after detachment, and T is the culture duration in hours [14]. This analysis was performed across multiple cell passages.
- Key Result: The study concluded that the "individual average PDT and cell viability at most passages did not differ according to the preservation method" [5]. This large-n analysis powerfully demonstrates that well-executed cryopreservation does not impair the fundamental growth kinetics of MSCs.
Large-Scale Phenotypic and Functional Analysis
The 2023 comparative analysis of biological signatures went beyond single parameters, employing a principal component analysis (PCA) on 20 expertly selected features from 671 manufacturing cases. This high-dimensional approach allowed for a systems-level comparison [5].
- Methodology: Key assay protocols included:
- Flow Cytometry for Immunophenotyping: Cells were stained with fluorochrome-conjugated antibodies against standard MSC markers (CD73, CD90, CD105, etc.) and analyzed via flow cytometer to confirm phenotypic identity post-thaw [14].
- Trilineage Differentiation Assay: The functional potency was tested by inducing differentiation into adipocytes, osteocytes, and chondrocytes in specific induction media, with outcomes assessed by staining for lipid droplets (Oil Red O), calcium deposits (Alizarin Red), and proteoglycans (Alcian Blue), respectively [16] [14].
- Key Result: "Circular clustering did not introduce any differences between the two MSC preservation methods" [5]. This unsupervised analysis confirms that the overall biological signature of cryopreserved MSCs is comparable to their freshly preserved counterparts.
The Scientist's Toolkit: Essential Reagents and Materials
Successful cryopreservation and characterization of MSCs rely on a suite of specialized reagents and equipment. The following table details key solutions and their functions based on the cited experimental data.
Table 2: Key Research Reagent Solutions for MSC Cryopreservation and Analysis
| Reagent/Material | Function/Application | Example from Search Data |
|---|---|---|
| Cryopreservation Solutions | Protects cells from ice crystal damage and osmotic stress during freeze-thaw. | NutriFreez (10% DMSO), PHD10 (Plasmalyte-A/5% HA/10% DMSO), CryoStor CS5/CS10 (5-10% DMSO) [15]. |
| Dimethyl Sulfoxide (DMSO) | Permeating cryoprotectant; reduces ice crystal formation. | Used at 5-10% concentration in most clinical-grade formulations [15] [16]. |
| Human Platelet Lysate (hPL) | Xeno-free supplement for clinical-grade MSC culture expansion. | Used as a substitute for Fetal Bovine Serum (FBS) to eliminate xenoimmunization risks [14]. |
| Trypan Blue | Vital dye for assessing cell membrane integrity and viability; dead cells uptake the dye. | Used for post-thaw viability counts via automated cell counters [15] [14]. |
| Annexin V & Propidium Iodide (PI) | Fluorescent stains for detecting apoptosis (Annexin V) and necrosis (PI) via flow cytometry. | Provides a more nuanced view of post-thaw cell health beyond simple viability [15]. |
| Flow Cytometry Antibodies | Panel for confirming MSC immunophenotype (CD73+, CD90+, CD105+, CD34-, CD45-, HLA-DR-). | Essential for identity and purity verification pre- and post-cryopreservation [5] [16] [14]. |
| Trilineage Differentiation Kits | Induce and stain for adipogenic, osteogenic, and chondrogenic lineages to confirm multipotency. | Used to validate functional potency after cryopreservation [16] [14]. |
Diagram 2: Functional relationships between key reagents and their roles in MSC cryopreservation and analysis
The collective evidence demonstrates that cryopreservation, when employing optimized, clinical-grade protocols, effectively preserves the fundamental cellular attributes of MSCs. Viability, morphology, population doubling time, and surface marker expression remain largely unchanged compared to freshly cultured cells. This stability is a cornerstone for the development of effective off-the-shelf MSC therapies, providing the scientific and manufacturing community with the confidence that cryopreserved products retain their core biological identity and therapeutic potential.
For researchers and drug development professionals, the stability of Mesenchymal Stem Cell (MSC) surface marker phenotypes post-thaw is a critical quality attribute. This guide compares the performance of cryopreserved MSCs against their freshly cultured counterparts, synthesizing current experimental data. The collective evidence indicates that cryopreservation does not significantly alter the characteristic surface marker profile of MSCs, supporting their use as reliable, off-the-shelf therapeutics. Key stability findings are summarized in the table below.
Table 1: Summary of Surface Marker Phenotype Stability Post-Thaw
| Study Focus | Key Findings on Surface Markers | MSC Source | Citation |
|---|---|---|---|
| Short-term Stability (0-6h post-thaw) | No difference in expression of positive (CD73, CD90, CD105) and negative (CD14, CD19, CD34, CD45, HLA-DR) markers at 4 hours post-thaw. | Bone Marrow | [20] |
| Large-Scale Biobank Analysis | No significant differences in the expression levels of most immunophenotypic markers (except CD14) between frozen and unfrozen MSCs. | Bone Marrow | [5] |
| Systematic Review of In Vivo Models | The vast majority of preclinical studies show no significant difference in efficacy between fresh and cryopreserved MSCs. | Multiple Tissues | [18] |
| Impact of Cryopreservation Solution | Cells from all tested cryopreservation groups exhibited standard MSC surface marker characteristics post-thaw. | Bone Marrow | [15] [21] |
| Long-term Stability (24h post-thaw) | No changes in the expression of standard positive and negative MSC markers were observed at 24 hours post-thaw. | Bone Marrow | [22] |
Experimental Data and Comparative Analysis
The stability of MSC surface markers is typically assessed via flow cytometry against the International Society for Cellular Therapy (ISCT) criteria, which define MSCs as positive for CD73, CD90, and CD105, and negative for hematopoietic markers like CD14, CD34, CD45, and HLA-DR.
Direct Comparative Studies
A 2019 study directly compared donor-matched fresh and cryopreserved MSCs. Flow cytometry analysis performed 4 hours post-thaw/harvest showed identical surface marker expression profiles for both groups. The cells maintained expression of CD73, CD90, and CD105, and lacked expression of CD14, CD19, CD34, CD45, and HLA-DR, confirming that the freezing process did not alter their fundamental immunophenotypic identity [20].
A large-scale 2023 analysis of a commercial cell database provided further robust evidence. The study compared 60 variables across approximately 2,300 manufacturing cases and found that the expression of most immunophenotypic markers was not significantly different between freshly preserved and cryo-preserved bone marrow MSCs. Unsupervised clustering analysis using these markers showed no separation between the two groups, indicating their biochemical signatures are highly comparable [5].
Impact of Post-Thaw Timing and Formulations
Research highlights that while some cellular functions may require a recovery period, the surface marker phenotype remains stable immediately post-thaw. A 2020 time-course study found no changes in the expression of standard MSC markers at 0, 2, 4, and 24 hours after thawing [22].
Furthermore, a 2024 study confirmed that the choice of cryopreservation solution—including formulations with 5% or 10% DMSO—did not affect the stability of MSC surface markers post-thaw. Cells cryopreserved in all tested solutions continued to express standard phenotypic markers after thawing [15] [21].
Detailed Experimental Protocols
To ensure reproducible results, the following core methodologies are consistently applied across cited studies.
Standard MSC Culture and Cryopreservation Protocol
- Cell Source: Bone marrow aspirates from healthy donors.
- Culture Medium: Expansion in xeno-free, GMP-grade media (e.g., NutriStem XF).
- Cryopreservation: Cells are harvested at passage 4, resuspended in a cryoprotectant solution, and cooled at a controlled rate (e.g., -1°C/min) before long-term storage in liquid nitrogen.
- Common Cryopreservation Solutions:
- Plasmalyte-A + 5% Human Albumin + 10% DMSO (PHD10)
- Proprietary solutions (e.g., NutriFreez, CryoStor CS10)
- Common Cryopreservation Solutions:
- Thawing: Vials are rapidly warmed in a 37°C water bath, and the cell suspension is diluted in a balanced salt solution or culture medium to reduce DMSO concentration before centrifugation and resuspension [20] [15] [22].
Flow Cytometry Analysis for Phenotype Stability
- Sample Preparation: Fresh (harvested) and thawed MSCs are washed and resuspended in a buffer like PBS or Plasma-Lyte A.
- Staining: Cells are incubated with fluorochrome-conjugated antibodies against target markers and appropriate isotype controls.
- Data Acquisition & Analysis: A flow cytometer (e.g., CytoFLEX, Attune) is used to analyze at least 10,000 events per sample. Data is processed with software (e.g., FlowJo) to determine the percentage of positive cells for each marker, gated against controls [20] [22] [23].
The workflow and core findings are summarized in the diagram below.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and their functions for conducting surface marker stability studies.
Table 2: Key Reagent Solutions for Flow Cytometry Analysis of MSC Phenotype
| Reagent / Solution | Function / Purpose | Examples / Notes |
|---|---|---|
| Cryopreservation Solutions | Protects cells from ice crystal damage and osmotic stress during freeze-thaw. | Plasmalyte-A/5%HA/10%DMSO (in-house); Proprietary GMP solutions (CryoStor CS10, NutriFreez) [15] [21]. |
| Fluorochrome-Conjugated Antibodies | Tag specific cell surface proteins for detection by flow cytometer. | Antibodies against CD73, CD90, CD105 (positive) and CD34, CD45, HLA-DR (negative). Must include isotype controls. |
| Flow Cytometry Staining Buffer | Provides an optimal medium for antibody binding and cell washing. | Typically PBS with 1-5% FBS or BSA to block non-specific binding. |
| Viability Stain | Distinguishes live from dead cells during analysis, improving accuracy. | Propidium Iodide (PI), 7-AAD, or DAPI. Often used with Annexin V for apoptosis assay [20] [22]. |
| Cell Dissociation Reagent | Non-enzymatically harvests adherent MSCs with minimal protein damage. | TrypLE Express or similar, preferred over trypsin to preserve surface epitopes. |
Context Within the Fresh vs. Cryopreserved MSC Thesis
The stability of the surface marker phenotype post-thaw is a cornerstone of the argument for using cryopreserved MSCs. While some studies note transient dips in metabolic activity or adhesion potential immediately after thawing, the preservation of the immunophenotype is consistently demonstrated [22]. This consistency is crucial because:
- It validates that the fundamental cellular identity is maintained.
- It aligns with functional data from systematic reviews, which show that in over 250 in vivo preclinical efficacy experiments, only a minimal percentage (2.3%) showed any significant difference between fresh and cryopreserved MSCs, with no clear advantage for either group [18].
- It provides a reliable and measurable Quality Control (QC) release criterion for cryopreserved "off-the-shelf" MSC products, ensuring batch-to-batch consistency for clinical applications [15].
The therapeutic application of Mesenchymal Stem Cells (MSCs) hinges critically on their functional potency, which is largely dictated by their transcriptomic and secretory profiles. These cells demonstrate remarkable capabilities for tissue repair, immunomodulation, and inflammation reduction through complex paracrine signaling networks [24]. However, a significant challenge emerges in balancing the practical necessity of cryopreserved, "off-the-shelf" products with concerns about potential functional alterations compared to their freshly-cultured counterparts. For drug development professionals and regulatory bodies, understanding whether cryopreservation induces biologically meaningful changes in MSC gene expression and paracrine factor release is paramount for product development and clinical trial design.
This guide objectively compares the biological signatures of fresh and cryopreserved MSCs by synthesizing current pre-clinical and clinical evidence. We focus specifically on transcriptomic landscapes—the complete set of RNA transcripts expressed by a cell—and secretory landscapes—the repertoire of released paracrine factors—to determine the practical implications for therapeutic development. By integrating data from systematic reviews, direct comparative studies, and molecular analyses, we provide a framework for evidence-based decision-making in regenerative medicine.
Molecular Basis of MSC Stemness and Secretory Function
The therapeutic "stemness" of MSCs encompasses their capacity for self-renewal, multilineage differentiation, and potent paracrine activity. These functions are governed by intricate molecular networks that may be susceptible to processing stresses, including cryopreservation.
Transcriptional Regulation of Stemness
Core transcription factors form a regulatory circuitry that maintains MSC stemness. OCT4, particularly its OCT4A isoform, plays a crucial role in sustaining an undifferentiated state by promoting proliferation and colony-forming capacity while inhibiting senescence through epigenetic regulation of genes like p16 and p21 [25]. The SOX family of transcription factors similarly contributes to stemness maintenance and senescence suppression, with expression levels influenced by culture conditions and passage number [25]. Additionally, Twist family genes (Twist1 and Twist2) enhance proliferation and stemness marker expression (e.g., STRO-1) while counteracting senescence through epigenetic silencing of senescence-associated genes [25].
Paracrine Mechanisms of Action
The therapeutic effects of MSCs are largely mediated through their secretome—the collection of secreted bioactive factors—rather than direct differentiation and engraftment [26]. This paracrine action includes:
- Immunomodulation: Release of factors like indoleamine 2,3-dioxygenase (IDO1) and TSG-6 that modulate immune responses and reduce inflammation [24].
- Angiogenesis: Secretion of vascular endothelial growth factor (VEGF) and other pro-angiogenic factors that promote blood vessel formation [27].
- Tissue Repair: Production of growth factors and cytokines that prevent apoptosis, activate host cell proliferation, and restore tissue integrity [26] [24].
Single-cell analyses have revealed that MSCs in infarcted hearts upregulate specific paracrine factors compared to local cardiomyocytes, highlighting their dynamic response to microenvironmental cues [26].
Table 1: Key Molecular Regulators of MSC Stemness and Function
| Regulator Category | Key Components | Functional Role in MSCs |
|---|---|---|
| Transcription Factors | OCT4, SOX2, Nanog, Twist1/Twist2 | Maintain undifferentiated state, promote self-renewal, inhibit senescence |
| Epigenetic Regulators | DNMT1, EZH2, HDACs | Silencing of differentiation and senescence genes via DNA methylation and histone modification |
| Senescence Markers | p16, p21, p14, p15 | Cell cycle arrest, induction of senescence-associated secretory phenotype (SASP) |
| Paracrine Factors | IDO1, TSG-6, VEGF, CXCL chemokines | Immunomodulation, anti-inflammatory effects, angiogenesis, tissue repair |
Comparative Analysis: Transcriptomic and Functional Profiles
In Vivo Efficacy and In Vitro Potency
A comprehensive systematic review of pre-clinical inflammation models provides robust, direct comparison data. This analysis encompassed 18 studies and 257 in vivo efficacy experiments, representing 101 distinct outcome measures [13].
Table 2: Summary of Systematic Review Findings on Fresh vs. Cryopreserved MSCs
| Outcome Category | Total Experiments | Significantly Different Results | Direction of Difference |
|---|---|---|---|
| In Vivo Efficacy | 257 | 6/257 (2.3%) | 2 favoured fresh, 4 favoured cryopreserved |
| In Vitro Potency | 68 | 9/68 (13%) | 7 favoured fresh, 2 favoured cryopreserved |
The data reveals that the overwhelming majority (97.7%) of in vivo efficacy outcomes showed no statistically significant difference between fresh and cryopreserved MSCs [13]. This suggests that from a functional therapeutic perspective in animal models, cryopreservation does not substantially compromise MSC performance. The minor differences observed in vitro (13% of experiments) may reflect transient adaptations to the freeze-thaw process rather than fundamental functional alterations.
Transcriptomic and Senescence Profiles
Advanced transcriptomic technologies offer unprecedented resolution for comparing cellular states. The recently developed human Universal Senescence Index (hUSI), built from comprehensive senescence transcriptome data, provides a robust method for evaluating cellular aging states [28]. This tool demonstrates that classical senescence markers like CDKN1A (p21) and CDKN2B (p15) are significantly elevated in senescent cells, offering a standardized approach to assess MSC quality post-preservation [28].
Notably, research on MSCs engineered to overexpress a therapeutic transgene (CD::UPRT::GFP) found that cryopreservation did not affect transgene expression, cell viability, phenotypic profile, or migratory capacity [23]. These findings indicate that well-optimized cryopreservation protocols can maintain even complex molecular signatures in engineered MSC products.
Experimental Protocols for Comparative Analysis
Pre-clinical Efficacy Testing in Inflammation Models
Systematic Review Methodology [13]:
- Study Identification: Comprehensive search of OvidMEDLINE, EMBASE, BIOSIS, and Web of Science databases without language restrictions until January 2022.
- Eligibility Criteria: Include direct comparisons of freshly cultured versus cryopreserved MSCs in animal models of inflammation with intact immune systems.
- Intervention Definition: "Cryopreserved" MSCs thawed and placed in culture for <24 hours prior to use; "freshly cultured" MSCs in continuous culture or thawed and cultured for ≥24 hours.
- Outcome Measures: Primary outcomes include in vivo efficacy measures (e.g., survival, functional improvement); secondary outcomes include in vitro potency assays.
- Bias Assessment: Use of SYRCLE's 'Risk of Bias' tool adapted for pre-clinical studies.
Transcriptomic and Functional Characterization
Gene Expression and Senescence Evaluation [28] [23]:
- RNA Sequencing: Bulk or single-cell RNA sequencing to compare transcriptomic profiles using standardized pipelines.
- Senescence Scoring: Application of hUSI or other senescence indices to evaluate aging-related transcriptomic changes.
- Flow Cytometry: Analysis of surface markers (CD73, CD90, CD105) and absence of hematopoietic markers to verify MSC phenotype post-thaw.
- Functional Assays:
- Migration Capacity: Matrigel invasion assays and CXCR4 receptor expression analysis.
- Therapeutic Potency: Co-culture with target cells (e.g., cancer cell lines) to assess cytotoxic effects or other relevant functional outcomes.
- Differentiation Potential: Tri-lineage differentiation assays (osteogenic, adipogenic, chondrogenic) to confirm stemness retention.
Diagram Title: Experimental Workflow for MSC Comparison
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Reagents and Tools for MSC Transcriptomic and Secretory Research
| Reagent/Solution | Primary Function | Application Context |
|---|---|---|
| CryoStor10 (CS10) | GMP-grade cryopreservation medium | Maintains cell viability and functionality during freeze-thaw cycles [23] |
| Plasma-Lyte A | Buffered electrolyte solution | Cell washing and preparation post-thaw to maintain physiological pH [23] |
| HypoThermosol | Preservation solution | Interim storage of thawed cells prior to administration or analysis [23] |
| Polyethylenimine MAX (PEI) | Cationic polymer transfection reagent | Non-viral engineering of MSCs for therapeutic transgene expression [23] |
| DOPE/CHEMS Fusogenic Lipid | Transfection enhancer | Improves delivery of genetic material into MSCs [23] |
| CD146 Antibodies | Cell surface marker identification | Isolation of MSC subpopulations with enhanced migration and therapeutic potential [29] |
| hUSI (human Universal Senescence Index) | Transcriptomic senescence scoring | Standardized evaluation of cellular aging across different MSC batches [28] |
| Single-cell RNA sequencing | Transcriptomic profiling at single-cell resolution | Analysis of MSC heterogeneity and paracrine factor expression [26] [30] |
The integrated evidence from transcriptomic, secretory, and functional analyses indicates that properly executed cryopreservation protocols can maintain the essential biological signatures of MSCs. While minor differences in certain in vitro potency measures exist, the overwhelming consensus from pre-clinical in vivo studies demonstrates comparable therapeutic efficacy between fresh and cryopreserved products.
For researchers and drug development professionals, this supports the feasibility of "off-the-shelf" MSC therapies without substantial loss of therapeutic potential. However, rigorous quality control measures—including transcriptomic senescence screening, potency assays, and functional validation—remain essential for both fresh and cryopreserved products to ensure batch-to-batch consistency and predictable clinical performance.
Future research directions should focus on optimizing cryopreservation formulations specifically for different MSC tissue sources (adipose, bone marrow, umbilical cord), establishing standardized potency markers across different therapeutic applications, and further elucidating the molecular mechanisms that enable functional resilience through the freeze-thaw process.
From Lab to Clinic: Methodological Standards and Clinical Workflow Integration
The advancement of cell therapy and stem cell research has propelled the production of clinical-grade cells and tissue products into the forefront of regenerative medicine. Achieving this standard necessitates adherence to strict Good Manufacturing Practice (GMP) protocols to maintain product quality, safety, and efficacy [31]. A GMP framework ensures that quality is built into every step of the manufacturing process, as the quality of a final biological product cannot be assured through end-product testing alone [31]. This is particularly crucial for advanced therapies like Mesenchymal Stem Cells (MSCs), which have emerged as a highly promising strategy due to their self-renewal, pluripotency, and immunomodulatory properties [32].
The manufacturing pipeline, from tissue harvest to final formulation, is complex and requires meticulous control. This guide objectively compares key aspects of this pipeline, with a specific focus on the implications of using freshly preserved versus cryo-preserved MSCs, a central consideration in both research and clinical application. The therapeutic potential of MSCs, mediated through the release of bioactive molecules and extracellular vesicles, has been explored for a wide range of human diseases, from autoimmune and inflammatory disorders to orthopedic injuries [32]. Ensuring the consistent delivery of high-quality MSCs to patients is therefore a mission-critical objective for the field [33].
A GMP-compliant manufacturing process for MSCs involves a series of highly controlled steps, each with its own quality checkpoints. The process can be broadly broken down into four main stages.
Tissue Harvest and Source Material Selection
The first step involves the aspiration of bone marrow (BM) or the collection of other source tissues like adipose tissue or umbilical cord [33]. The suitability of all starting materials must be clearly defined [31]. Using xeno-free reagents is a critical GMP consideration; for example, in the production of the skin substitute MyDerm, autologous human serum is used instead of foetal bovine serum (FBS) to eliminate the risk of immune responses and transmissible diseases [31]. Similarly, animal-derived trypsin is often replaced with gentler, GMP-grade recombinant alternatives like TrypLE Select to minimize cellular damage and address religious concerns [31].
Cell Isolation and Culture
Following tissue harvest, mononuclear cells (MNCs) are isolated through centrifugation of the BM aspirates [33]. At this juncture, the MNCs are categorized into two groups: those that are freshly preserved and directly moved to culture, and those that are cryo-preserved for later use [33]. The cryo-preservation process typically involves dispensing cells into cryovials, cooling them in a controlled-rate freezer for approximately 4 hours, and then transferring them to long-term storage in liquid nitrogen [33]. For culture, appropriate quantities of MNCs are inoculated into flasks. After several days, only the MSCs that adhere to the plastic flask are separated and further expanded, establishing passage 0 (P0). Cells are serially subcultured every 3-5 days until they reach the required number for production, typically up to passage 4 or 5 [33].
In-Process Quality Control and Release Criteria
A robust Quality Assurance (QA) and Quality Control (QC) programme is fundamental to GMP. QA involves the overall management plan to guarantee product integrity, including standard operating procedures (SOPs), personnel training, and environmental monitoring [31]. QC, a subset of QA, focuses on inspecting, testing, and evaluating the product at various stages [31]. Environmental monitoring of the GMP cleanroom facility is essential, as conditions directly influence product quality [31]. Furthermore, risk management and non-conformance reporting procedures are established to identify, investigate, and correct any deviations during manufacturing [31].
Final Product Formulation and Release
The final harvested MSCs are formulated into the drug product. Before release, they must pass a battery of QC tests. The release criteria for MSCs, as exemplified by the Pharmicell facility, typically include [33]:
- Viability of greater than 70%.
- Confirmed absence of bacteria, fungi, viruses, and Mycoplasma.
- Immunophenotype verification: ≥90% of cells expressing CD73 and CD105, and ≤3% of cells expressing hematopoietic markers CD14, CD34, and CD45 [33]. Only after meeting all these pre-defined specifications is the final product released for clinical use.
The diagram below illustrates the key stages of the GMP manufacturing pipeline for MSCs, highlighting the decision point for preservation.
Comparative Analysis: Fresh vs. Cryo-Preserved MSCs
A pivotal logistical and biological question in MSC therapy is whether to administer cells immediately after expansion (fresh) or after freezing and thawing (cryo-preserved). A large-scale, database-driven study provides robust data for this comparison.
Experimental Protocol for Comparative Analysis
A 2023 study conducted a comparative analysis of biological signatures between freshly preserved and cryo-preserved bone marrow MSCs using big data sourced from the Pharmicell database [33]. The methodology was as follows [33]:
- Data Source: Data from approximately 2300 stem cell manufacturing cases from 2011 to 2022 were collected.
- Variables: The dataset included ~60 variables, including viability, population doubling time (PDT), immunophenotype (CD markers), and soluble paracrine molecules.
- Inclusion: After eliminating cases with missing data, 671 cases were approved for final analysis by an Institutional Review Board.
- Cell Processing: MNCs were categorized into fresh and cryo-preserved groups. Cryo-preserved MNCs were frozen in a controlled-rate freezer, stored in liquid nitrogen, and later thawed in a 37°C water bath before culture and expansion, mirroring the fresh group's process thereafter.
Quantitative Data Comparison
The following tables summarize the key comparative findings from the analysis of fresh versus cryo-preserved MSCs.
Table 1: Comparison of Core Cellular Properties [33]
| Biological Property | Freshly Preserved MSCs | Cryo-Preserved MSCs | Statistical Significance |
|---|---|---|---|
| Cell Viability | >70% (at most passages) | >70% (at most passages) | Not significantly different |
| Proliferation (Population Doubling Time) | Comparable average PDT | Comparable average PDT | Not significantly different |
| Colony-Forming Potential | Baseline | Comparable level maintained | Not significantly different |
| Immunophenotype (CD Markers) | Standard expression profile maintained | Standard expression profile maintained (except CD14, see below) | No significant differences for most markers |
| CD14 Expression | Baseline level | Different mean level observed | Statistically significant difference |
| Paracrine Molecule Secretion | Baseline concentration | Comparable concentration | No significant differences |
Table 2: Analysis of CD146-Enriched MSC Subpopulations [34]
| Cellular Property | CD146-Enriched vs. CD146-Depleted MSCs | Statistical Significance & Notes |
|---|---|---|
| Population Doubling Time (Proliferation) | Slightly higher in CD146-Enriched MSCs | Not statistically significant (p=0.63) [34] |
| Colony-Forming (CF) Potential | Significantly higher in CD146-Enriched MSCs | Statistically significant (p=0.004) [34] |
| Migratory Potential | Enhanced in CD146-Enriched MSCs | Reported by all 4 assessed studies [34] |
| Tri-lineage Differentiation | Highly variable results across studies | Inconsistent adipogenic, chondrogenic, osteogenic data [34] |
| Immunomodulation | Highly variable results across studies | Inconsistent findings reported [34] |
The data from the large-scale analysis indicates that the biochemical signatures of cryo-preserved and unfrozen bone marrow MSCs are largely comparable [33]. This is a critical finding for the logistics of cell therapy, as it supports the feasibility of creating cell banks and transporting frozen products. However, the significant heterogeneity in studies focusing on specific subpopulations, such as CD146-enriched MSCs, underscores the need for standardized protocols to draw firmer conclusions about functional differences [34].
The Scientist's Toolkit: Essential Reagents for GMP MSC Manufacturing
The transition from research-grade to clinical-grade manufacturing requires careful selection of reagents. The following table details key solutions and their GMP-critical functions.
Table 3: Key Research Reagent Solutions in GMP MSC Manufacturing
| Reagent / Material | Function in Manufacturing | GMP-Grade Consideration & Rationale |
|---|---|---|
| Autologous Human Serum | Supplement for cell culture medium. Provides essential growth factors and attachment factors. | Eliminates risk of transmissible spongiform encephalopathy (TSE) and immune responses associated with FBS [31]. |
| Recombinant Trypsin Substitute (e.g., TrypLE Select) | Enzyme for cell dissociation and passaging. | GMP-grade, animal-origin free. Reduces cellular damage and avoids religious concerns vs. porcine/bovine trypsin [31]. |
| Clinical-Grade Antibiotics (e.g., Gentamicin) | Prevention of bacterial contamination during initial cell culture. | Undergo full safety testing with extensive qualifying documentation to meet purity and quality standards [31]. |
| Defined, Xeno-Free Culture Media | Base medium for cell growth and expansion. | "For-further-manufacturing" grade is preferred. Redoves undefined components, enhancing batch-to-batch consistency and safety [31]. |
| Cryopreservation Solution | Protects cells during freezing and long-term storage. | Formulated with clinical-grade cryoprotectants (e.g., DMSO) and buffers to ensure high post-thaw viability and function [33]. |
The GMP manufacturing pipeline, from tissue harvest to final product formulation, is a complex but essential framework for delivering safe and effective MSC-based therapies. The comprehensive comparison between fresh and cryo-preserved MSCs reveals that cryo-preservation is a viable and practical approach, with large-scale studies showing comparable biological signatures in terms of viability, proliferation, and most immunophenotypic markers [33]. This validates the use of cryo-preservation in the logistics of cell therapy, enabling the creation of cell banks and ensuring product availability.
However, challenges remain. The heterogeneity of MSC populations, even within a single source, contributes to variable clinical outcomes [34]. Future efforts will likely focus on the isolation and characterization of specific subpopulations, such as CD146-enriched MSCs, which show promise for enhanced colony-forming and migratory potential [34]. Furthermore, the ongoing development of standardized, fully defined, xeno-free culture media and reagents will be crucial for improving product consistency and complying with the most stringent regulatory requirements. As the field progresses, the refined, data-driven GMP pipelines discussed here will form the foundation for the next generation of transformative regenerative medicines.
In regenerative medicine, the transition of Mesenchymal Stem Cells (MSCs) from research tools to clinical therapeutics hinges on effective cryopreservation. Cryopreservation enables the creation of "off-the-shelf" cell banks, ensuring MSCs are available for timely clinical applications without the drawbacks of continuous passaging, which can alter cell characteristics [16]. The central question for researchers and drug development professionals is whether cryopreserved MSCs retain biological signatures equivalent to their freshly-cultured counterparts. This guide objectively compares the performance of different cryopreservation protocols, focusing on their impact on MSC viability, phenotype, and functionality, to inform protocol selection in research and clinical manufacturing.
Comparative Analysis of Cryopreservation Methods
The two primary techniques for MSC cryopreservation are slow freezing and vitrification. Each employs distinct mechanisms to protect cells from the lethal effects of intracellular ice formation.
Slow Freezing is the most established method in clinical and laboratory settings. It works by a gradual dehydration of the cell. A controlled, slow cooling rate (typically below -3°C/min) allows water to exit the cell before it freezes, minimizing intracellular ice crystals [16]. Cells are mixed with cryoprotective agents (CPAs), cooled from 4°C to -80°C, and finally stored in liquid nitrogen (-196°C) [16]. This method is valued for its operational simplicity and low contamination risk.
Vitrification is an ultrarapid freezing technique that uses high concentrations of CPAs and extremely high cooling rates to solidify cells and their extracellular environment into a glassy, non-crystalline state [16] [35]. This method completely avoids ice crystal formation but carries a risk of CPA toxicity due to the high solute concentrations required [35].
Table 1: Comparison of Primary Cryopreservation Methods for MSCs
| Feature | Slow Freezing | Vitrification |
|---|---|---|
| Primary Mechanism | Controlled dehydration & extracellular ice formation [16] | Glassy solidification without ice [16] |
| Cooling Rate | Slow (e.g., -0.3°C/min to -3°C/min) [36] [16] | Ultra-rapid (direct immersion in LN₂) [35] |
| CPA Concentration | Low to Moderate (e.g., 1.5M DMSO) [36] | High (mixtures of permeating and non-permeating CPAs) [35] |
| Key Advantage | Simplicity, low contamination risk, clinical familiarity [16] | Avoids mechanical damage from ice crystals [16] |
| Key Limitation | Potential damage from extracellular ice and solute effects | Risk of CPA toxicity and osmotic shock [35] |
| Post-Thaw Viability | ~70-80% [16] | Highly variable, dependent on protocol optimization |
Impact of Cryopreservation on MSC Biological Signatures
A critical analysis of MSC biological signatures reveals that optimized cryopreservation protocols can yield cells comparable to freshly preserved ones.
Viability, Phenotype, and Proliferation
A large-scale analysis of approximately 2,300 stem cell manufacturing cases from the Pharmicell database found no significant differences between cryopreserved and freshly preserved bone marrow-derived MSCs (BM-MSCs) in key quality attributes [37]. Among the 60 features analyzed—including viability, population doubling time (PDT), and immunophenotype—no differences were introduced by the preservation method [37]. The average PDT and cell viability at most passages were equivalent, and expression of standard MSC surface markers (CD73, CD90, CD105) was maintained while hematopoietic markers (CD34, CD45) were absent [37]. This demonstrates that core MSC identity remains intact post-cryopreservation.
Furthermore, long-term cryostorage does not necessarily compromise cell properties. Dental pulp-derived Stem Cells (DPSCs) cryopreserved for up to 13 years retained high viability, expression of stem cell markers (CD73, CD90, CD105 >90%), proliferative capacity, and multipotency, with no significant increase in senescence markers compared to short-term stored cells [38].
Secretome and Functional Potency
The therapeutic effects of MSCs are largely mediated by their secretome—the release of bioactive molecules like growth factors, cytokines, and extracellular vesicles [32]. The comparative analysis of BM-MSCs showed that the concentrations of various paracrine molecules were not significantly different between frozen and unfrozen groups [37]. This preservation of secretory function is crucial for clinical applications relying on immunomodulation, anti-fibrotic effects, and angiogenesis.
Table 2: Comparison of Biological Signatures Between Fresh and Cryopreserved MSCs
| Biological Signature | Freshly Preserved MSCs | Cryopreserved MSCs (Slow Frozen) | Supporting Evidence |
|---|---|---|---|
| Viability | Baseline reference | Comparable at most passages [37] | Analysis of 671 manufacturing cases [37] |
| Immunophenotype | Positive for CD73, CD90, CD105; Negative for CD34, CD45 | Pattern maintained with no significant difference [37] [38] | Flow cytometry analysis [37] [38] |
| Proliferation (Population Doubling Time) | Baseline reference | No significant difference [37] | Database analysis [37] |
| Paracrine Molecule Secretion | Baseline reference | Comparable concentrations [37] | Analysis of soluble factor indices [37] |
| Multipotency | Osteogenic, chondrogenic, adipogenic differentiation | Retained after long-term cryostorage (up to 13 years) [38] | In vitro differentiation assays [38] |
| Therapeutic Efficacy (e.g., in Liver Cirrhosis) | Anti-fibrotic effect observed | No differential clinical results reported [37] | Clinical study review [37] |
Detailed Experimental Protocols for MSC Cryopreservation
To ensure reproducibility, below are detailed methodologies for key protocols cited in this guide.
Optimized Slow Freezing Protocol for Ovarian Tissue (as a model for complex tissues)
- Freezing Medium: Leibovitz L-15 medium supplemented with 4 mg/mL human serum albumin (HSA), 1.5M DMSO, and 0.1M sucrose [36].
- Freezing Curve in Programmable Freezer:
- Hold at 4°C for 5 minutes.
- Cool at 1°C/min to -7°C.
- Seeding: Rapid cool at 60°C/min to -32°C, then hold.
- Cool at 10°C/min to -15°C.
- Cool slowly at 0.3°C/min to -40°C.
- Cool rapidly at 10°C/min to -140°C.
- Transfer to liquid nitrogen for storage [36].
- Thawing Protocol:
- Warm slowly in a cold chamber for 3.5 minutes to reach the glass transition temperature (Tg').
- Quickly warm in a 37°C water bath for 2 minutes to complete melting [36].
Protocol for Comparative Analysis of Fresh vs. Cryopreserved MSCs
- Cell Source: Bone marrow aspirates from patients [37].
- Experimental Groups:
- Freshly Preserved: Mononuclear cells (MNCs) directly processed into culture systems.
- Cryopreserved: MNCs dispensed in cryovials, frozen in a controlled-rate freezer for ~4 hours, and transferred to liquid nitrogen storage [37].
- Thawing Process: Cryopreserved MNCs were thawed in a 37°C thermal water bath with gentle shaking, washed, and plated for culture [37].
- Assessment Parameters:
- Viability and Proliferation: Trypan blue exclusion and Population Doubling Time (PDT).
- Immunophenotype: Flow cytometry for CD markers.
- Paracrine Function: Analysis of soluble molecular indices.
- Data Analysis: Principal component analysis and circular clustering of ~60 variables [37].
The following workflow diagram illustrates this comparative experimental design:
The Scientist's Toolkit: Essential Reagents and Materials
Successful cryopreservation relies on a suite of specialized reagents and equipment. The table below details key solutions used in the featured experiments and the broader field.
Table 3: Key Research Reagent Solutions for MSC Cryopreservation
| Reagent/Material | Function | Example Use Case |
|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Permeating cryoprotectant; reduces ice crystal formation by penetrating cells and lowering the freezing point [16] [39]. | Standard CPA in slow freezing at 5-10% concentration [36] [39]. |
| Sucrose | Non-permeating cryoprotectant; increases extracellular osmolality, promoting cellular dehydration and reducing intracellular ice [36] [35]. | Used at 0.1M in optimized ovarian tissue freezing medium [36]. Common in vitrification solutions [35]. |
| Trehalose | Non-permeating cryoprotectant; superior glass-forming ability and higher glass transition temperature than sucrose, potentially enhancing stability [35]. | Component in commercial vitrification solutions for blastocysts, showing improved outcomes vs. sucrose-based solutions [35]. |
| Fetal Bovine Serum (FBS) | Provides undefined proteins and nutrients that mitigate freezing stress and stabilize cell membranes [39]. | Common (but ethically problematic) component of traditional freezing media (e.g., 90% FBS + 10% DMSO) [39]. |
| Serum-Free Freezing Media (e.g., CryoStor CS10, NutriFreez D10) | Chemically defined, xeno-free alternatives to FBS-based media; standardize conditions and eliminate infection risks [39]. | Successfully used for long-term (2-year) cryopreservation of PBMCs, maintaining viability and function comparable to FBS media [39]. |
| Polyampholyte Cryoprotectants | Synthetic macromolecules that reduce intracellular ice formation and mitigate osmotic shock, improving post-thaw recovery [40]. | Supplementation with 40 mg/mL polyampholyte doubled post-thaw recovery of THP-1 cells compared to DMSO-alone [40]. |
| Programmable Freezer (e.g., Nano-Digitcool) | Precisely controls cooling rates according to defined curves for optimal slow freezing [36]. | Used to implement the complex, multi-step freezing protocol for ovarian tissue optimization [36]. |
| Liquid Nitrogen Storage System | Provides long-term storage at -196°C, halting all metabolic activity and ensuring genetic and functional stability [16]. | Standard for long-term preservation of MSCs and other cell types [16] [38]. |
The collective evidence indicates that with optimized protocols, cryopreserved MSCs can exhibit biological signatures—including viability, immunophenotype, proliferative capacity, and paracrine function—that are comparable to freshly preserved cells [37]. This equivalence is foundational for the advancement of MSC-based therapeutics, enabling the creation of reliable, "off-the-shelf" cell products.
Future research will focus on further refining these protocols. Key areas include the development and validation of fully defined, serum-free freezing media [39], the reduction or replacement of potentially toxic CPAs like DMSO using novel macromolecular cryoprotectants [40], and the standardization of thawing processes to minimize cell loss and preserve function. As these technologies mature, they will strengthen the logistical and clinical framework for MSC therapies, ensuring that cryopreserved products consistently meet the stringent requirements of regenerative medicine.
In the field of mesenchymal stem cell (MSC) research, the precise definitions of "fresh" and "cryopreserved" cell products carry significant implications for both experimental reproducibility and therapeutic efficacy. The critical 24-hour post-thaw culture window represents a fundamental operational boundary that distinguishes these two cell states in preclinical and clinical studies. This temporal parameter is not arbitrary; rather, it is grounded in biological recovery processes that occur following the significant stress of freeze-thaw cycles [13] [41].
Standardized definitions are particularly crucial as MSC therapies advance toward clinical applications. For acute conditions such as stroke, myocardial infarction, and acute lung injury, the logistical imperative for "off-the-shelf" cryopreserved products that can be administered immediately after thawing conflicts with concerns about potentially diminished cellular function [13] [42]. This comparison guide examines the technical distinctions between fresh and cryopreserved MSCs through the lens of this critical 24-hour recovery period, providing researchers with evidence-based insights for experimental design and therapeutic development.
Defining the Critical 24-Hour Post-Thaw Window
Operational Definitions for MSC Research
The systematic comparison of fresh versus cryopreserved MSCs requires precise operational definitions that have been consistently applied across preclinical studies:
Freshly Cultured MSCs: Cells maintained in continuous culture or those that have been thawed and placed in culture for at least 24 hours prior to experimental use [13] [41]. This duration allows for cellular recovery and resumption of normal biological functions.
Cryopreserved (Freshly Thawed) MSCs: Cells preserved at ultra-low temperatures (typically in liquid nitrogen at -196°C) for any duration and used in experiments after less than 24 hours of post-thaw culture [41]. This category represents the "off-the-shelf" product suitable for immediate administration.
The establishment of this specific 24-hour cutoff is supported by experimental evidence suggesting that cryopreserved MSCs may require approximately 24 hours of culture to fully recover their functionality following the freeze-thaw process [13] [41].
Biological Rationale for the 24-Hour Recovery Period
Cryopreservation imposes substantial stress on cellular systems through multiple mechanisms including ice crystal formation, osmotic stress, and cryoprotectant toxicity [43] [16]. The 24-hour recovery period allows for critical restorative processes:
Cytoskeletal Reorganization: Research indicates that the actin cytoskeleton of freshly thawed MSCs is temporarily disrupted, impairing cellular adhesion capabilities. This architectural disruption requires approximately 24-48 hours for complete recovery [42].
Metabolic Restoration: Studies demonstrate marginally reduced metabolic activity in cryopreserved MSCs immediately post-thaw, with normalization occurring within the first 24-72 hours of culture [42].
Membrane Repair and Receptor Expression: The freeze-thaw process can temporarily alter membrane integrity and surface marker presentation. The recovery period allows for membrane repair and normalized expression of characteristic MSC markers (CD73, CD90, CD105) [5] [16].
Comparative Analysis of Key Biological Signatures
In Vivo Efficacy: Animal Models of Inflammation
A comprehensive systematic review analyzed 257 in vivo preclinical efficacy experiments across 18 studies, representing 101 distinct outcome measures in animal models of inflammation [13]. The findings demonstrate remarkable functional equivalence between fresh and cryopreserved MSCs:
Table 1: In Vivo Efficacy Outcomes in Preclinical Inflammation Models
| Outcome Category | Number of Experiments | Significantly Different Outcomes | Favoring Fresh MSCs | Favoring Cryopreserved MSCs |
|---|---|---|---|---|
| Overall Efficacy | 257 | 6/257 (2.3%) | 2 | 4 |
| Disease-specific functional measures | 101 distinct measures | Minimal significant differences | - | - |
| Histopathological damage assessment | Multiple studies | No consistent pattern of difference | - | - |
| Inflammatory cytokine modulation | Various models | Comparable effects | - | - |
The systematic review concluded that the overwhelming majority (97.7%) of in vivo efficacy outcomes showed no statistically significant difference between freshly cultured and cryopreserved MSCs, supporting the biological relevance of properly executed cryopreservation protocols [13].
In Vitro Potency and Functional Assays
Analysis of secondary in vitro potency outcomes reveals slightly more variability but generally supports functional preservation post-cryopreservation:
Table 2: In Vitro Potency and Functional Characteristics
| Parameter | Fresh MSCs | Cryopreserved MSCs | Significant Differences |
|---|---|---|---|
| Viability | Reference standard | >95% with optimized protocols [42] | Minimal with proper technique |
| Immunophenotype | CD73+, CD90+, CD105+ | CD73+, CD90+, CD105+ (comparable) [5] | CD14 shows occasional variation [5] |
| Population Doubling Time | Donor-dependent | Comparable across passages [5] | Not statistically significant |
| Immunomodulatory Function | Suppresses PBMC proliferation | Retains suppression capability [42] | 7/68 experiments favored fresh (13%) [13] |
| Paracrine Factor Secretion | Characteristic profile | Comparable levels [5] | 2/68 experiments favored cryopreserved [13] |
| IDO Expression | Responsive to IFN-γ | Maintains responsiveness [42] | No significant difference |
The 2023 comparative analysis of biological signatures between freshly preserved and cryo-preserved bone marrow MSCs further confirmed that cryopreservation did not significantly alter the fundamental biological properties of MSCs across approximately 60 measured variables [5].
Experimental Protocols for Comparison Studies
Standardized Cryopreservation Methodology
For controlled comparison studies between fresh and cryopreserved MSCs, consistent protocols are essential:
Slow Freezing Method: The most common approach for MSC cryopreservation involves controlled-rate freezing [16]:
- Harvesting: Culture MSCs to 70-80% confluence and detach using standard methods
- Cryoprotectant Formulation: Resuspend cells in cryomedium containing 5-10% DMSO, often supplemented with human serum albumin or FBS [43] [16]
- Freezing Protocol: Cool at approximately -1°C/minute to -80°C using isopropanol chambers or controlled-rate freezers
- Long-term Storage: Transfer to liquid nitrogen vapor phase (-196°C) for archival storage
Quality Control Parameters: Post-thaw viability should exceed 70% (with optimized protocols achieving >95%) [44] [42], with maintenance of characteristic immunophenotype and differentiation potential [16].
Assessment Methodologies for Functional Comparison
Immunosuppressive Potency Assay:
Paracrine Function Assessment:
- Analyze conditioned media for growth factors (VEGF, HGF, FGF) via ELISA
- Compare extracellular vesicle production and composition [32]
In Vivo Efficacy Testing:
Diagram 1: Experimental workflow for comparing fresh versus cryopreserved MSCs
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for MSC Cryopreservation and Functional Assessment
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Cryoprotectants | DMSO, glycerol, ethylene glycol, trehalose | Prevent ice crystal formation, reduce osmotic stress [43] [16] |
| Culture Media | MSC-Brew GMP Medium, other xeno-free formulations | Support post-thaw recovery and proliferation [44] |
| Viability Assays | Trypan blue, Annexin V/PI, Calcein AM/Ethidium homodimer | Quantify live/dead cell ratios post-thaw [43] |
| Immunophenotyping | CD73, CD90, CD105 antibodies; CD14, CD34, CD45 exclusion panel | Confirm MSC identity and purity [5] [16] |
| Differentiation Kits | Osteogenic: Alizarin Red; Adipogenic: Oil Red O; Chondrogenic: Alcian Blue | Verify trilineage differentiation potential [43] [16] |
| Functional Assays | IDO activity, PBMC suppression, cytokine arrays | Assess immunomodulatory potency [42] |
Implications for Research and Clinical Translation
The accumulated evidence supporting functional equivalence between fresh and properly cryopreserved MSCs has significant implications for both basic research and clinical development:
Experimental Design: Researchers can confidently utilize cryopreserved MSCs with the understanding that their fundamental biological properties remain intact, facilitating experimental planning and resource allocation [13] [5].
Clinical Translation: The demonstration that cryopreserved MSCs retain efficacy in disease-relevant models supports the development of "off-the-shelf" therapeutic products that can be deployed rapidly for acute conditions [13] [42].
Manufacturing Logistics: Cryopreservation enables quality control testing, batch consistency, and flexible dosing schedules that would be challenging with continuously cultured cells [44] [43].
Diagram 2: MSC functional recovery pathway following cryopreservation
The critical 24-hour post-thaw culture window represents a fundamental operational parameter in MSC research that distinguishes "freshly cultured" from "cryopreserved" cell products. The comprehensive analysis of current evidence demonstrates that with optimized cryopreservation protocols, MSCs largely retain their functional potency and in vivo efficacy. While transient alterations in certain functions may occur immediately post-thaw, the preponderance of evidence from both in vitro studies and animal models of inflammation indicates that these potential differences are minimal and do not consistently translate to meaningful functional deficits [13] [5] [42].
These findings validate the use of cryopreserved MSCs as "off-the-shelf" therapeutics while underscoring the importance of standardized protocols and rigorous quality control measures. For research applications, the operational definitions provided herein offer a framework for consistent experimental design and appropriate interpretation of comparison studies between fresh and cryopreserved MSC products.
The emergence of advanced biologic therapies, particularly those based on living cells such as mesenchymal stem cells (MSCs), has revolutionized treatment paradigms for a wide spectrum of diseases. A critical logistical challenge in delivering these therapies lies in aligning product availability with clinical need, a challenge that sharply divides into acute indications and chronic indications. For acute, life-threatening conditions such as septic shock or acute respiratory distress syndrome, the window for therapeutic intervention is narrow, often measured in hours. In these scenarios, the lengthy process of manufacturing a patient-specific (autologous) therapy is clinically unfeasible. This necessitates an "off-the-shelf" product—a readily available, cryopreserved therapy that can be administered immediately upon diagnosis [45]. In contrast, chronic conditions like osteoarthritis or inflammatory bowel disease allow for a more deliberate treatment timeline, creating a logistics landscape where both freshly cultured and cryopreserved products can be considered [18] [45]. The central thesis of modern therapy development is that the biological signature of the product must be matched to the logistical demands of the disease. This guide objectively compares the performance of freshly cultured versus cryopreserved MSCs, the archetypal "off-the-shelf" platform, providing researchers with the experimental data and protocols needed to inform their therapeutic strategies.
Comparative Analysis: Freshly Cultured vs. Cryopreserved MSCs
The decision to use a freshly cultured or a cryopreserved MSC product has profound implications for manufacturing, logistics, and clinical application. The following comparison delineates the core characteristics of each approach.
Table 1: Strategic Comparison of Freshly Cultured vs. Cryopreserved MSCs
| Feature | Freshly Cultured MSCs | Cryopreserved MSCs |
|---|---|---|
| Primary Use Case | Chronic indications, foundational research | Acute indications, clinical trials, "off-the-shelf" models |
| Readiness / Availability | Requires weeks of expansion, not suitable for urgent use | Immediately available post-thaw; enables rapid deployment |
| Manufacturing & Logistics | Complex, requires continuous culture facilities; difficult to scale and transport | Centralized manufacturing; stable for long-term storage and global shipping |
| Therapeutic Rationale | Perceived as more "native" and potentially more potent | Practical necessity for acute care; facilitates dose and quality control |
| Key Clinical Limitation | Logistically impossible for acute care | Questions regarding potential loss of function post-thaw |
A systematic review of preclinical in vivo models of inflammation directly compared the efficacy and potency of freshly cultured versus cryopreserved MSCs. The analysis encompassed 257 in vivo efficacy experiments across multiple disease models [18].
Table 2: Summary of Preclinical In Vivo and In Vitro Outcomes
| Outcome Measure | Total Experiments | Significantly Different Experiments (p<0.05) | Direction of Significant Difference |
|---|---|---|---|
| In Vivo Preclinical Efficacy | 257 | 6 (2.3%) | 2 favoured freshly cultured, 4 favoured cryopreserved |
| In Vitro Potency | 68 | 9 (13%) | 7 favoured freshly cultured, 2 favoured cryopreserved |
The data demonstrates that the vast majority (97.7%) of in vivo efficacy outcomes showed no statistically significant difference between freshly cultured and cryopreserved MSCs [18]. This finding is bolstered by a large-scale comparative analysis of biological signatures from approximately 2,300 manufacturing cases, which concluded that the biochemical profiles—including viability, population doubling time (PDT), immunophenotype, and paracrine molecule secretion—of cryopreserved and freshly preserved bone marrow MSCs were comparable [5].
Detailed Experimental Protocols for MSC Comparison
To generate robust comparative data, researchers must adhere to standardized experimental protocols. The following methodologies are critical for evaluating the equivalence of fresh and cryopreserved MSC products.
Protocol for a Preclinical Systematic Review and Meta-Analysis
This protocol provides a framework for synthesizing existing evidence on MSC efficacy [45].
- Study Eligibility: Include pre-clinical in vivo studies using randomized, quasi-randomized, or non-randomized designs that directly compare freshly cultured to freshly thawed MSCs in animal models of inflammation. Studies using immunocompromised animals or focusing solely on tissue regeneration are excluded.
- Intervention & Comparison Definition:
- Freshly Thawed (Cryopreserved) MSCs: Cells cryopreserved for any duration and used in experiments after less than 24 hours in culture post-thaw.
- Freshly Cultured MSCs: Cells in continuous culture or thawed and placed in culture for at least 24 hours prior to use, allowing for functional recovery.
- Primary Outcomes: Surrogate measures of in vivo efficacy, categorized into:
- Organ Dysfunction & Tissue Composition: e.g., histopathological damage scores.
- Protein Expression & Secretion: e.g., cytokine levels (IL-6, IL-10, TNF-α) measured by ELISA or multiplex immunoassays.
- Risk of Bias Assessment: Utilize the SYRCLE 'Risk of Bias' tool for pre-clinical in vivo studies to assess sequence generation, baseline characteristics, allocation concealment, random housing, blinding, random outcome assessment, and handling of incomplete outcome data.
Protocol for Comparative Analysis of Biological Signatures
This protocol outlines the direct experimental comparison of MSC products [5].
- Cell Source and Culture: Source MSCs from bone marrow aspirates. Culture in standard media (e.g., α-MEM or DMEM supplemented with fetal bovine serum and growth factors) at 37°C and 5% CO₂. Passage cells at 80-90% confluence.
- Cryopreservation Methodology:
- At the target passage (e.g., P3-P5), harvest MSCs using trypsin/EDTA.
- Resuspend cells in a cryoprotectant solution (e.g., 90% FBS + 10% DMSO).
- Control the freezing rate using a programmed freezer (-1°C/min to -80°C) before transfer to liquid nitrogen vapor phase for long-term storage.
- Post-Thaw Analysis:
- Viability Assessment: Thaw cells rapidly at 37°C, wash to remove cryoprotectant, and assess viability using trypan blue exclusion or flow cytometry with propidium iodide.
- Potency and Function Assays:
- Immunophenotyping: Use flow cytometry to analyze surface marker expression (CD73, CD90, CD105 >95% positive; CD14, CD34, CD45 <5% positive).
- Paracrine Secretion Analysis: Quantify concentrations of key therapeutic molecules (e.g., VEGF, HGF, PGE2) in conditioned media using ELISA.
- Immunomodulatory Potency Assay: Co-culture MSCs with mitogen-activated peripheral blood mononuclear cells (PBMCs) and measure T-cell proliferation via 3H-thymidine incorporation or CFSE dilution.
Figure 1: Experimental workflow for comparing fresh versus cryopreserved MSCs.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful comparison and development of off-the-shelf MSC therapies rely on a suite of specialized reagents and tools.
Table 3: Key Research Reagent Solutions for MSC Characterization
| Reagent / Solution | Primary Function | Application Example |
|---|---|---|
| Defined Culture Media (e.g., α-MEM) | Supports MSC expansion and maintains undifferentiated state. | In-vitro culture and propagation of MSCs prior to cryopreservation or experimentation. |
| Cryoprotectant (e.g., DMSO) | Prevents intracellular ice crystal formation, protecting cell viability during freeze-thaw. | Standard component of cryopreservation solutions, typically used at 10% concentration. |
| Flow Cytometry Antibody Panels | Quantifies expression of MSC surface markers (CD73, CD90, CD105) and contaminants (CD14, CD34, CD45). | Immunophenotyping to confirm MSC identity and purity according to ISCT criteria. |
| ELISA / Multiplex Immunoassay Kits | Measures concentration of secreted paracrine factors (VEGF, HGF, PGE2) in conditioned media. | Potency analysis to compare the secretory profile of fresh vs. cryopreserved MSCs. |
| Lymphocyte Proliferation Assay Kits (e.g., CFSE) | Evaluates the functional immunomodulatory capacity of MSCs. | Co-culture with PBMCs to measure T-cell suppression, a key potency indicator. |
Signaling Pathways and Logical Workflows in Off-the-Shelf Therapy Development
The journey from concept to clinic for an off-the-shelf therapy involves critical decision points and is governed by understanding the biological pathways that maintain MSC function post-cryopreservation.
Figure 2: Clinical indication dictates the choice between fresh and cryopreserved MSC products.
The development of Mesenchymal Stem Cell (MSC)-based therapies represents a frontier in advanced medicinal products, offering potential treatments for conditions ranging from osteoarthritis and graft-versus-host disease to cardiovascular diseases [46]. As these therapies progress toward clinical application, robust quality control (QC) assays become paramount for regulatory submissions and eventual patient use. The fundamental challenge in MSC manufacturing lies in achieving consistency despite inherent biological variability, where QC assays serve as essential tools to ensure product safety, efficacy, and reproducibility [46].
Within this landscape, a significant scientific debate centers on whether freshly preserved or cryopreserved MSCs present superior biological signatures for therapeutic applications. Proponents of fresh cells often cite concerns about potential cryopreservation-induced alterations, while advocates for cryopreservation emphasize its logistical advantages for "off-the-shelf" therapies [18]. This comparison guide objectively examines the current evidence regarding how these two preservation approaches perform across three critical QC parameters—sterility, potency, and karyotype stability—providing researchers with experimental data and methodologies to inform their regulatory strategies.
Comparative Analysis of Fresh versus Cryopreserved MSCs
Performance Across Key Quality Control Parameters
Table 1: Comparative analysis of fresh versus cryopreserved MSCs across essential quality control parameters
| Quality Parameter | Fresh MSCs | Cryopreserved MSCs | Regulatory Significance |
|---|---|---|---|
| Sterility | Maintained through aseptic processing and microbiological testing [47] | Maintained through validated cryopreservation and thawing processes [47] | Critical for patient safety; required by all regulatory agencies [48] |
| Potency - Immunophenotype | Consistent expression of CD105, CD73, CD90 [46] | Generally maintained, though some studies show CD105 reduction in specific systems post-thaw [49] | ISCT defining criteria; essential for product identity [46] |
| Potency - Differentiation | Maintained trilineage potential (osteogenic, adipogenic, chondrogenic) [5] [49] | Preserved trilineage potential in most studies [5] [49] | Confirms functional capacity and stemness [46] |
| Potency - Secretome | Intact paracrine function [5] | Generally maintained based on comparative analyses [5] [18] | Important for immunomodulatory mechanisms [18] |
| Karyotype Stability | Maintained genetic stability in proper culture conditions [47] | Maintained after freeze-thaw cycle in validated systems [47] | Essential for tumorigenicity risk assessment [48] |
| Viability | Typically high in qualified cultures [5] | Can show minor reductions post-thaw but often >90% with optimized protocols [49] [50] | Impacts dosing and therapeutic efficacy [46] |
Quantitative Comparative Data from Systematic Studies
Table 2: Quantitative comparison of key biological signatures between fresh and cryopreserved MSCs
| Biological Signature | Fresh MSCs | Cryopreserved MSCs | Statistical Significance | Study Details |
|---|---|---|---|---|
| Cell Viability | 94.6% (BM-MSCs) [5] | 93.1% (BM-MSCs) [5] | Not significant [5] | 671 manufacturing cases analyzed [5] |
| Population Doubling Time | Comparable across passages [5] | Comparable across passages [5] | Not significant [5] | Long-term culture analysis [5] |
| CD105 Expression | >95% (TCP-expanded) [49] | 75% (TCP-expanded post-thaw) [49] | Significant decrease for TCP system [49] | Adipose-derived stem cells [49] |
| CD73/CD90 Expression | >95% [49] | >95% [49] | Not significant [49] | Consistent across systems [49] |
| Trilineage Differentiation | Maintained [49] | Maintained [49] | Not significant [49] | Adipogenic, osteogenic, chondrogenic [49] |
| In Vivo Efficacy Outcomes | Baseline for comparison [18] | 94.4% (257/257) showed no significant difference [18] | Not significant for most outcomes [18] | Systematic review of preclinical models [18] |
Experimental Protocols for Key Quality Control Assays
Sterility Testing Methodologies
Sterility testing for MSC products must comply with Good Manufacturing Practice (GMP) standards and pharmacopoeial methods. The protocol encompasses:
Sample Collection: Aseptically collect samples from the final MSC product or in-process materials. For cryopreserved products, testing should be performed both pre-freeze and post-thaw to validate the cryopreservation process doesn't compromise sterility [47].
Microbiological Testing:
- Bacteriology: Inoculate thioglycollate medium and soybean-casein digest medium with product samples. Incubate at 20-25°C and 30-35°C respectively for 14 days [47].
- Mycology: Use Sabouraud dextrose agar incubated at 20-25°C for 14 days to detect fungi and yeasts [47].
- Mycoplasma: Employ both culture and indicator cell culture methods, with PCR-based methods as acceptable alternatives for faster results [47].
Endotoxin Testing: Use Limulus Amebocyte Lysate (LAL) test with product samples. The acceptance criterion is typically <5 EU/kg/hour for parenteral administration [47].
For regulatory submissions, sterility testing should be validated for the specific MSC product, considering potential matrix effects that might inhibit microbial growth.
Potency Assay Methodologies
Potency assays must quantitatively measure biological activity linked to the proposed mechanism of action. For MSCs, this typically involves multiparameter assessment:
Immunophenotypic Characterization by Flow Cytometry:
- Sample Preparation: Harvest MSCs at appropriate confluence (typically 70-80%). Use enzymatic dissociation with trypsin/EDTA, followed by neutralization with complete medium [47] [49].
- Antibody Staining: Aliquot 1×10^6 cells per test. Stain with fluorochrome-conjugated antibodies against CD73, CD90, CD105, CD34, CD45, CD14 or CD11b, CD79α or CD19, and HLA-DR [47]. Include appropriate isotype controls.
- Analysis: Acquire data on a flow cytometer calibrated with standard beads. Analyze a minimum of 10,000 events. Acceptance criteria: ≥95% positive for CD73, CD90, CD105; ≤2% positive for hematopoietic markers [46] [47].
Trilineage Differentiation Capacity:
- Adipogenic Differentiation: Culture MSCs in adipogenic induction medium (containing insulin, dexamethasone, indomethacin, and IBMX) for 14-21 days. Confirm differentiation with Oil Red O staining of lipid vacuoles [49].
- Osteogenic Differentiation: Culture MSCs in osteogenic induction medium (containing dexamethasone, ascorbate-2-phosphate, and β-glycerophosphate) for 21-28 days. Confirm with Alizarin Red S staining of calcium deposits [49].
- Chondrogenic Differentiation: Pellet culture in chondrogenic induction medium (containing TGF-β3, dexamethasone, ascorbate-2-phosphate, proline, and ITS+ premix) for 21-28 days. Confirm with Alcian Blue staining of sulfated proteoglycans [49].
Functional Potency Assays:
- Immunomodulatory Assays: Co-culture MSCs with activated peripheral blood mononuclear cells (PBMCs) and measure T-cell proliferation suppression via CFSE dilution or 3H-thymidine incorporation [18].
- Secretome Analysis: Quantify MSC-secreted factors (PGE2, IDO, TSG-6) using ELISA under stimulated conditions [5] [51].
Karyotype Stability Assessment
Genetic stability testing ensures MSCs haven't acquired chromosomal abnormalities during expansion:
Sample Preparation: Culture MSCs to 70-80% confluence. Add colcemid (0.1 μg/mL) for 45-60 minutes to arrest cells in metaphase [47].
Chromosome Harvesting:
- Hypotonic treatment with 0.075M KCl for 20 minutes at 37°C
- Fixation with 3:1 methanol:acetic acid
- Slide preparation and GTG-banding [47]
Analysis:
- Score a minimum of 20 metaphase spreads per sample
- Analyze at 400-550 band resolution
- Document any structural or numerical abnormalities [47]
For higher throughput, complementary methods like spectral karyotyping (SKY) or comparative genomic hybridization (CGH) array may be employed, particularly for master cell banks [47].
Visualization of Experimental Workflows
Quality Control Testing Workflow
MSC Manufacturing and Banking System
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential reagents and materials for MSC quality control testing
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Flow Cytometry Antibodies | Immunophenotype characterization | CD73, CD90, CD105 (positive markers); CD34, CD45, CD14, HLA-DR (negative markers) [47] |
| Differentiation Media | Trilineage differentiation capacity | Adipogenic: IBMX, dexamethasone, indomethacin; Osteogenic: β-glycerophosphate, ascorbate-2-phosphate; Chondrogenic: TGF-β3, ITS+ premix [49] |
| Cell Culture Media | MSC expansion and maintenance | α-MEM or DMEM supplemented with FBS (10-15%) or defined serum alternatives [47] [49] |
| Cryopreservation Solutions | Cell banking and preservation | DMSO (typically 10%) in culture medium or commercial cryopreservation media [47] |
| Microbiological Media | Sterility testing | Thioglycollate medium (bacteria), soybean-casein digest medium (bacteria), Sabouraud dextrose agar (fungi) [47] |
| Karyotyping Reagents | Genetic stability assessment | Colcemid, Giemsa stain, hypotonic solution (KCl), fixative (methanol:acetic acid) [47] |
| ELISA Kits | Secretome and potency analysis | Quantification of PGE2, IDO, TSG-6, cytokine profiles [5] |
Integration into Regulatory Submissions
For successful regulatory submissions, quality control data must demonstrate compliance with guidelines from appropriate agencies (FDA, EMA, etc.). The International Society for Cell & Gene Therapy (ISCT) has established minimal criteria for MSCs, including plastic adherence, specific surface marker expression, and trilineage differentiation capacity [46]. Recent updates to these criteria emphasize the need for comprehensive characterization that reflects the biological nuances between fresh and cryopreserved products [46].
The Quality-by-Design (QbD) approach, detailed in ICH guideline Q8, provides a framework for defining Critical Quality Attributes (CQAs) and Critical Process Parameters (CPPs) early in product development [46]. For MSC products, key CQAs typically include dosage (cell number and viability), potency (identity, differentiation potential, and in vivo effect), and product quality (genetic stability, purity) [46].
Current evidence from systematic comparisons indicates that cryopreserved MSCs largely maintain critical quality attributes compared to their fresh counterparts. Comprehensive analyses reveal that the majority of in vivo efficacy outcomes (94.4%) and in vitro potency measures (87%) show no significant differences between fresh and cryopreserved products [18]. Large-scale studies of manufacturing data have found comparable biological signatures in viability, population doubling time, immunophenotype (with minor exceptions), differentiation potential, and paracrine molecule secretion [5].
The choice between fresh and cryopreserved MSC formats for regulatory submissions should be guided by comprehensive quality control data from well-validated assays that demonstrate the maintenance of critical quality attributes through the preservation process. For most therapeutic applications, cryopreserved MSCs represent a viable "off-the-shelf" alternative without compromising fundamental quality parameters, though product-specific validation remains essential [18] [49].
Overcoming the 'Cryo-Stun': Troubleshooting Functional Deficits and Optimizing Potency
The term "cryo-stun" describes the transient functional impairment of Mesenchymal Stromal Cells (MSCs) observed immediately after thawing from cryopreservation. This phenomenon represents a critical challenge in cellular therapy, where MSCs—used as living "bio-drugs"—exhibit reduced potency despite maintaining baseline viability, potentially compromising their clinical efficacy [52]. As MSCs transition from preclinical proof-of-concept to larger clinical trials, understanding this post-thaw dysfunction has become essential for unlocking their full therapeutic potential. The "cryo-stun" effect is particularly relevant for acute indications requiring immediate "off-the-shelf" availability, where logistical necessities of cryobanking clash with the optimal functional status of the cells [53]. This guide objectively compares the functional capacities of fresh and cryopreserved MSCs, synthesizing experimental data on this transient dysfunction's mechanisms, manifestations, and potential mitigation strategies.
Comparative Analysis of MSC Properties: Fresh vs. Post-Thaw
Table 1: Summary of Key Functional Differences Between Fresh and Post-Thaw Cryopreserved MSCs
| Functional Parameter | Fresh MSCs | Cryopreserved MSCs (Immediately Post-Thaw) | Experimental Evidence |
|---|---|---|---|
| Viability | High (>92% via trypan blue) [54] | Slightly reduced (∼87% via trypan blue); method-dependent variation [54] | Trypan blue exclusion; Annexin V/PI staining shows increased apoptosis [54] |
| Adhesion & Binding | Normal binding to fibronectin and endothelium [54] | 40% reduction to fibronectin; 80% reduction to human endothelial cells under flow [54] | Static adhesion assay; 3D endothelialized fluidic system (2 dynes/cm²) [54] |
| In Vivo Engraftment | Detectable in murine lungs for up to 24 hours [54] | Significantly reduced or undetectable in murine lungs at 24 hours [54] | Quantitative PCR for male-derived Y-chromosome SRY gene in female mice [54] |
| Cytoskeletal Integrity | Normal F-actin content and polymerization [54] | ~60% reduction in cytoskeletal F-actin content [54] | Fluorescence staining and quantification of F-actin [54] |
| Immunomodulatory Potency | Robust suppression of immune cell proliferation [55] | Varies; can be transiently blunted, particularly IDO response to IFN-γ [54] [55] | Co-culture with PHA- or CD3/CD28-stimulated PBMCs; IDO activity/kynurenine measurement [55] |
| Response to Inflammatory Cues | Normal upregulation of immunomodulatory genes (e.g., IDO) [54] | Reduced or delayed response to licensing signals like IFN-γ [54] | ELISA and qPCR for IDO after IFN-γ stimulation [54] [55] |
Table 2: Conflicting Findings on Cryopreservation Impact from Recent Studies
| Study Focus | Reported Findings on Cryopreserved MSCs | Key Metrics | Citation |
|---|---|---|---|
| Biological Signatures (2023) | No significant differences in viability, population doubling time (PDT), immunophenotype, or paracrine molecules compared to fresh. | Principal Component Analysis of ∼60 variables from 671 manufacturing cases. | [5] |
| Cardiac Clinical Outcomes (2025) | Significant 2.11% improvement in LVEF at 6 months; safety profile comparable to control. | Meta-analysis of 7 RCTs (285 patients) with heart disease. | [56] |
| Retinal Ischemia Model (2016) | Maintained therapeutic potency; performed as well as fresh MSC in rescuing retinal ganglion cells. | >95% viability; retained immunomodulatory function in vitro and in vivo. | [55] |
Experimental Protocols for Assessing the Cryo-Stun Effect
In Vitro Functional Binding and Adhesion Assays
A. Static Adhesion Assay:
- Purpose: To quantify the ability of MSCs to bind to extracellular matrix components.
- Methodology: Seed PHK26-labeled viable MSCs (5,000 cells/cm²) onto fibronectin-coated plates. Allow cells to attach for 2 hours in a 37°C, 5% CO₂ incubator. Non-adherent cells are removed by gentle washing. The number of bound cells is quantified using either standard hemocytometer counting or a flow-cytometric method [54].
- Key Metric: The percentage of cells firmly adhered relative to the fresh MSC control.
B. Physiologic Flow Binding Assay:
- Purpose: To simulate vascular flow conditions and assess MSC binding under shear stress.
- Methodology: Utilize a three-dimensional endothelialized fluidic system. Infuse MSCs at a flow rate equivalent to 2 dynes/cm² (a physiologic shear stress) into the microfluidic device for 1 hour. Count the number of MSCs bound per channel after the infusion period [54].
- Key Metric: Average number of MSCs bound per channel under flow compared to fresh MSC controls.
Immunomodulatory Potency Co-culture Assay
A. T-cell Suppression Assay:
- Purpose: To evaluate the functional immunomodulatory capacity of MSCs.
- Methodology: Co-culture passage and donor-matched MSCs with activated human peripheral blood mononuclear cells (PBMCs). Activate PBMCs using CD3/CD28 dynabeads or phytohemagglutinin (PHA). Common MSC:PBMC ratios used are 1:3, 1:6, and 1:12. After a multi-day co-culture (typically 3-5 days), measure PBMC proliferation via assays like ³H-thymidine incorporation or CFSE dilution via flow cytometry [55].
- Key Metric: Percentage suppression of PBMC proliferation calculated as:
[1 - (Proliferation with MSCs / Proliferation without MSCs)] × 100.
B. IDO Functional Activity:
- Purpose: To assess the responsiveness to inflammatory licensing and indoleamine 2,3-dioxygenase (IDO) pathway function.
- Methodology: Stimulate MSCs with interferon-gamma (IFN-γ, typically 50 ng/mL) or a combination of IFN-γ and tumor necrosis factor-alpha (TNF-α). After 24-72 hours of stimulation, quantify IDO activity by measuring the concentration of kynurenine (a downstream metabolite of tryptophan) in the supernatant via spectrophotometry or ELISA. Parallel samples can be analyzed for IDO gene expression (mRNA) by qPCR [54] [55].
- Key Metric: Kynurenine concentration normalized to cell number, and/or fold-change in IDO mRNA expression.
In Vivo Engraftment and Biodistribution Tracking
A. Quantitative PCR-Based Engraftment:
- Purpose: To track and quantify the persistence of human MSCs in an immunocompetent mouse model.
- Methodology: Infuse male-derived human MSCs intravenously into female C57BL/6 mice. At a predetermined endpoint (e.g., 24 hours post-infusion), harvest tissues like lungs, liver, and spleen. Extract genomic DNA and perform quantitative real-time PCR (qPCR) for a human-specific gene, such as the male sex-determining region Y (SRY) gene or a human-specific genomic DNA sequence. The detection limit must be established via in vitro mixing experiments (e.g., one human MSC in 200 mouse cells) [54].
- Key Metric: Engraftment level expressed as cycle of threshold (CT⁻¹) or relative human DNA quantity compared to a no-MSC control.
Signaling Pathways and Molecular Mechanisms of Dysfunction
The "cryo-stun" effect is not attributed to a single failure point but rather a cascade of interrelated structural and functional disruptions. The diagrams below map the primary pathways and experimental workflows involved in this phenomenon.
Diagram 1: Signaling pathways and molecular mechanisms of the "cryo-stun" effect. The diagram illustrates how the initial cryopreservation insult leads to structural damage, resulting in the characteristic functional impairments, and outlines the corresponding experimental methods for assessment.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for Studying the Cryo-Stun Effect
| Reagent/Material | Primary Function in Research | Application Example |
|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Cryoprotectant Agent (CPA) | Standard component of freezing media; concentration and removal protocol can impact recovery [53]. |
| Annexin V / Propidium Iodide (PI) | Viability & Apoptosis Assay | Flow cytometry-based discrimination of live, early/late apoptotic, and necrotic cells post-thaw [54]. |
| PHK26 (or similar fluorescent dye) | Cell Labeling & Tracking | Fluorescently labels MSCs for quantification in static adhesion assays or flow-based binding studies [54]. |
| Recombinant Human IFN-γ | Inflammatory Licensing | Stimulates MSCs to induce expression of immunomodulatory factors like IDO; tests post-thaw responsiveness [54] [55]. |
| CD3/CD28 Dynabeads | Immune Cell Activation | Activates T-cells within PBMC populations for use in immunomodulatory co-culture suppression assays [55]. |
| Anti-Human Integrin β5 Antibody | Phenotypic Characterization | Flow cytometry analysis to detect loss of integrin expression correlated with functional impairment [57]. |
| Fibronectin, Coated Plates | Substrate for Adhesion Assays | Coats tissue culture surfaces to test integrin-mediated binding capacity of MSCs under static conditions [54]. |
| Human Endothelial Cells (e.g., HUVEC) | Flow Binding Assay | Grown in microfluidic channels to create a physiologic surface for MSC binding under shear stress [54]. |
| Kynurenine Assay Kit | Functional Potency Assay | Quantifies IDO enzyme activity by measuring kynurenine concentration in MSC supernatants post-IFN-γ stimulation [55]. |
Diagram 2: Experimental workflow for assessing the "cryo-stun" effect. The flowchart outlines the key steps from cell culture and cryopreservation to post-thaw analysis, highlighting the parallel processing of cells for direct assay versus recovery period assessment.
The body of evidence confirms the existence of a transient "cryo-stun" effect characterized by cytoskeletal disruption, impaired adhesion, and potentially blunted immunomodulatory function immediately post-thaw. However, the data is not universally consistent, with outcomes heavily dependent on cryopreservation protocols, cell source, and post-thaw viability thresholds [56]. For clinical applications, this necessitates a critical balance between the logistical imperative of "off-the-shelf" availability and the delivery of a fully potent cell product. Mitigation strategies may include:
- Optimizing cryopreservation formulas and protocols to minimize structural damage.
- Implementing a short post-thaw recovery culture period (e.g., 48 hours) to restore cytoskeletal organization and immunomodulatory responsiveness [54] [52].
- Establishing post-thaw viability and potency release criteria that go beyond simple membrane integrity, incorporating functional assays where critical [57].
Future research must focus on standardizing potency assays that predict in vivo efficacy and further elucidating the molecular triggers of the cryo-stun effect to develop more robust cryopreservation strategies for this promising class of living medicines.
Cryopreservation serves as a critical enabling technology for the advancement of cell-based therapies, allowing for long-term storage and off-the-shelf availability of cellular products. The conventional cryopreservation formula for mesenchymal stem cells (MSCs) and other therapeutic cell types has historically relied on fetal bovine serum (FBS) supplemented with 10% dimethyl sulfoxide (DMSO). However, this approach presents significant challenges for clinical translation, including ethical concerns regarding animal-derived components, risk of pathogen transmission, and cytotoxicity associated with DMSO [58]. Additionally, FBS exhibits batch-to-batch variability that can compromise experimental reproducibility and clinical consistency [58].
The field is now transitioning toward serum-free, xeno-free, and low-DMSO formulations that address these limitations while maintaining cell viability and functionality. This evolution aligns with a broader paradigm shift in regenerative medicine from cell replacement to paracrine-mediated therapies, where MSC-derived secretomes and extracellular vesicles are gaining prominence as cell-free therapeutics [59] [60]. Within this context, optimizing cryoprotectant formulations becomes essential not only for preserving cell viability but also for maintaining the integrity of secreted bioactive factors that mediate therapeutic effects.
Comparative Performance of Cryoprotectant Formulations
Quantitative Analysis of Commercial Formulations
Recent systematic evaluations have provided robust comparative data on the performance of various cryoprotectant formulations. A comprehensive 2-year study assessing peripheral blood mononuclear cells (PBMCs) cryopreserved in different media yielded particularly insightful results regarding long-term stability and functionality preservation [58].
Table 1: Viability and Functionality of PBMCs Cryopreserved in Different Media Over 2 Years
| Cryopreservation Medium | DMSO Concentration | Viability at M24 | Functionality Preservation | Serum Status |
|---|---|---|---|---|
| FBS + 10% DMSO (Reference) | 10% | High | High | Animal Serum |
| CryoStor CS10 | 10% | High | High | Serum-Free |
| NutriFreez D10 | 10% | High | High | Serum-Free |
| Bambanker D10 | 10% | High | Moderate (T cell function decline) | Serum-Free |
| CryoStor CS7.5 | 7.5% | Moderate | Moderate | Serum-Free |
| Media with <7.5% DMSO | <7.5% | Significant loss | Low | Serum-Free |
The data clearly demonstrate that serum-free media containing 10% DMSO can achieve comparable performance to traditional FBS-based media in preserving both viability and functionality over extended periods [58]. Notably, CryoStor CS10 and NutriFreez D10 emerged as robust alternatives, maintaining PBMC immune response capability across all measured time points. This finding is particularly relevant for clinical applications where consistent immune functionality is paramount.
DMSO Concentration Thresholds and Compromises
A critical finding from current research identifies a DMSO concentration threshold below which cell viability and functionality are significantly compromised. Studies systematically evaluating DMSO concentrations from 2% to 10% found that formulations containing less than 7.5% DMSO showed substantial viability loss and were eliminated from further testing after initial assessments [58]. This suggests that current cryopreservation technology may have a lower limit for DMSO reduction while maintaining acceptable cell recovery.
The CryoStor CS7.5 formulation, while showing promising results, was noted as suboptimal due to its preparation method (a mixture of CS10 and CS5), which could introduce variability and errors in clinical settings [58]. This highlights the importance of not only DMSO concentration but also formulation stability and reproducibility in cryoprotectant development.
Methodological Considerations in Cryoprotectant Evaluation
Standardized Experimental Protocols
To ensure meaningful comparisons between cryoprotectant formulations, researchers must implement standardized evaluation protocols. The following methodology, adapted from a comprehensive PBMC study, provides a robust framework for assessing cryoprotectant performance [58]:
Cell Preparation and Cryopreservation:
- Isolate PBMCs using density gradient centrifugation (Lymphoprep)
- Wash cells in Hanks' Balanced Salt Solution buffer
- Resuspend cell pellets at 12 × 10^6 cells/mL in test cryopreservation media
- Aliquot 1mL volumes into pre-cooled cryovials
- Freeze using controlled-rate freezing containers (CoolCell)
- Transfer to vapor-phase liquid nitrogen after 1-7 days at -80°C
Thawing and Assessment Protocol:
- Thaw cryovials by gentle agitation in 37°C water bath
- Add pre-warmed FBS and DNase (10 µg/mL) to mitigate clumping
- Transfer to pre-warmed RPMI medium for recovery
- Assess viability, functionality, and phenotype at predetermined intervals (3 weeks, 3 months, 6 months, 1 year, and 2 years)
Functional Assays:
- Cytokine secretion profiles
- T and B cell FluoroSpot assays
- Intracellular cytokine staining
- Cell surface marker expression analysis
This comprehensive approach ensures that cryoprotectant evaluation encompasses not only immediate post-thaw viability but also long-term functional preservation, which is critical for clinical applications.
Analytical Framework for MSC Biological Signatures
When evaluating cryoprotectant formulations specifically for MSCs, the analytical framework must extend beyond simple viability metrics to encompass functional biological signatures. A large-scale analysis comparing freshly preserved and cryo-preserved bone marrow MSCs utilized the following parameters to assess cryopreservation impact [33]:
Table 2: Key Parameters for Evaluating MSC Cryopreservation Impact
| Analysis Category | Specific Parameters | Assessment Method |
|---|---|---|
| Viability and Growth | Population doubling time, Cell viability at passages | Automated cell counting, Flow cytometry |
| Immunophenotype | CD73, CD90, CD105 expression; CD14, CD34, CD45 absence | Flow cytometry with standardized markers |
| Secretory Profile | Paracrine molecules (VEGF, HGF, IGF-1), Cytokines | Multiplex immunoassays, ELISA |
| Differentiation Potential | Osteogenic, Chondrogenic, Adipogenic differentiation | Lineage-specific staining, gene expression |
This multifaceted analytical approach revealed that the biochemical signatures of cryo-preserved and unfrozen bone marrow MSCs were comparable across most parameters, with no significant differences in population doubling time, viability at most passages, and most immunophenotypic markers [33]. The only exception was CD14 marker expression, which showed variation between preservation methods.
DMSO Safety Profile in Clinical Applications
Risk-Benefit Analysis of DMSO Exposure
The safety profile of DMSO in cell therapy products has been systematically evaluated in recent clinical reviews. Analysis of 1173 patients treated with 1-24 intravenous infusions of DMSO-containing MSC products revealed that the doses of DMSO delivered were 2.5-30 times lower than the 1 g DMSO/kg typically accepted for hematopoietic stem cell transplantation [9]. With appropriate premedication, only isolated infusion-related reactions were reported, suggesting an acceptable safety profile for DMSO-cryopreserved MSC products at these exposure levels.
For topical applications, where data on DMSO-containing MSC products are limited, a conservative risk assessment based on wound healing applications of DMSO suggests that concentrations applied with undiluted cryopreserved MSC products are unlikely to cause significant local adverse effects [9]. Even under a worst-case scenario assuming complete systemic absorption from a large wound in a lightweight patient, systemic DMSO exposure would be approximately 55 times lower than the accepted intravenous dose of 1 g/kg [9].
Emerging DMSO-Free Alternatives
The ongoing concerns regarding DMSO toxicity have spurred development of DMSO-free cryopreservation solutions. Recent commercial introductions include CellShield MSC, a DMSO-free cryopreservation media kit that claims equivalent or better performance compared to traditional DMSO-based media [61]. These formulations typically utilize alternative cryoprotectant compounds and optimized freezing protocols to maintain cell integrity while eliminating DMSO-related toxicity concerns.
Preclinical systematic reviews have further supported the feasibility of cryopreserved MSC products, finding that the majority of in vivo efficacy and in vitro potency outcomes showed no significant differences between freshly cultured and cryopreserved MSCs in animal models of inflammation [13]. This evidence base provides additional rationale for considering cryopreserved MSC products in both preclinical studies and clinical trials.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Cryoprotectant Formulation Research
| Reagent Category | Specific Products | Research Application | Function |
|---|---|---|---|
| Reference Media | FBS + 10% DMSO | Control formulation | Baseline comparison for alternative formulations |
| Serum-Free Media | CryoStor CS10, NutriFreez D10, Bambanker D10 | Serum-free cryopreservation | Xeno-free cell preservation with maintained viability |
| Low-DMSO Media | CryoStor CS7.5, CS5, CS2 | DMSO reduction studies | Determining minimum effective DMSO concentrations |
| DMSO-Free Media | CellShield MSC, Stem-Cellbanker D0 | DMSO-free preservation | Eliminating DMSO-associated cytotoxicity |
| Assessment Tools | Lymphoprep, Ficoll Gradient | Cell isolation | PBMC/MSC separation from whole blood/bone marrow |
| Viability Assays | Flow cytometry, CFU-f assays | Functionality assessment | Quantifying post-thaw recovery and clonogenic potential |
| Functional Assays | T/B cell FluoroSpot, Cytokine multiplex | Immune functionality | Evaluating immunomodulatory capacity post-preservation |
The current evidence supports a strategic transition toward serum-free cryoprotectant formulations with optimized DMSO concentrations for most research and clinical applications. The 10% DMSO threshold remains important for maintaining cell viability and functionality in serum-free systems, though continued research on DMSO-free alternatives shows promising progress. For critical applications requiring maximum preservation of immune functionality, CryoStor CS10 and NutriFreez D10 currently represent the best-performing serum-free alternatives to traditional FBS-based media.
Future developments in cryoprotectant technology will likely focus on further reducing or eliminating DMSO while maintaining functional preservation, particularly for sensitive cell types and emerging cell-free therapeutics like MSC-derived extracellular vesicles. The standardized methodologies and comparative frameworks presented in this review provide researchers with evidence-based approaches for selecting and validating cryoprotectant formulations tailored to their specific research or clinical applications.
Cryopreservation serves as a cornerstone for the storage and distribution of cells in research and clinical therapy. However, a significant technical barrier remains the substantial fraction of cells lost to cryopreservation-induced apoptosis during the freeze-thaw process [62]. This programmed cell death, often exhibiting delayed onset 24-48 hours post-thaw, diminishes the yield and functionality of precious cell samples, posing a particular challenge for cell-based therapies like those involving Mesenchymal Stem Cells (MSCs) and Chimeric Antigen Receptor T-cells (CAR-T) [63]. The thesis that freshly cultured and cryopreserved cells possess comparable biological signatures is central to advancing "off-the-shelf" therapies, yet its validation hinges on successfully mitigating this post-thaw apoptosis [18] [33]. This guide objectively compares the performance of various additives, with a focus on ROCK inhibitors, in combating this challenge, providing experimental data and protocols to inform research and development.
Understanding the Mechanisms of Post-Thaw Apoptosis
The freeze-thaw process subjects cells to multiple stressors, including ionic imbalances, energy deprivation, and free radical production, which converge to initiate apoptosis [63]. The intrinsic (mitochondrial) apoptosis pathway is primarily activated in response to these intracellular stresses. A key regulator in this cascade is Rho-associated protein kinase (ROCK), which, when cleaved by caspase-3, leads to the formation of stress fibres and membrane blebbing, hallmark events of apoptosis [63]. Cryopreservation can also induce DNA damage, potentially through caspase-mediated apoptosis or oxidative stress, further compromising cell integrity and function [64]. Therefore, effective strategies must target these biochemical pathways to enhance cell survival.
The following diagram illustrates the primary signaling pathways of cryopreservation-induced apoptosis and the points of intervention for various inhibitors.
Comparative Performance of Cryopreservation Additives
A variety of additives have been investigated to mitigate different aspects of cryopreservation damage. The table below provides a quantitative comparison of their performance across different cell types.
Table 1: Comparative Performance of Additives for Mitigating Post-Thaw Apoptosis
| Additive Category | Specific Agent | Cell Type Tested | Reported Efficacy & Key Findings | Optimal Concentration & Protocol |
|---|---|---|---|---|
| ROCK Inhibitors | Y-27632 | Human Bone Marrow MSCs [62] | Significantly increased proportion of viable adherent cells post-thaw (MTT assay). No significant difference in immediate post-thaw viability (Trypan Blue). | 10-100 µM; added to both cryopreservation solution and post-thaw culture medium for 24h. |
| Y-27632 | Ankara Buck Spermatozoa [64] | Significantly improved post-thaw motility (71.8-74.0%) vs. control (66.2%). | 5-20 µM; added to the freezing extender. | |
| Fasudil | Jurkat T-cells [63] | Increased overall post-thaw yield by ~20%. Reduced reactive oxygen species. | 40 µM to 1.25 µM; added to the thawing medium for 4 hours. | |
| Other Biochemical Pathway Modulators | Boron | Ankara Buck Spermatozoa [64] | Significantly improved post-thaw motility (72.1-76.4%) and reduced DNA damage (1.18-1.83%) vs. control (3.37%). | 0.25-1 mM; added to the freezing extender. |
| Antifreeze Protein III (AFP III) | Ankara Buck Spermatozoa [64] | Reduced DNA damage (1.23%) vs. control (3.37%). Improved post-thaw motility (not statistically significant). | 1-4 µg/mL; added to the freezing extender. | |
| Cocktail Formulations | CEPT (Chroman 1, Emricasan, Trans-ISRIB, Polyamine) | Human Pluripotent Stem Cells (hPSCs) [65] | Provides comprehensive cytoprotection. Superior survival and recovery after single-cell dissociation and cryopreservation vs. Y-27632 alone. | Chroman 1 (50 nM), Emricasan (pan-caspase inhibitor), Trans-ISRIB; supplemented post-thaw. |
Key Insights from Comparative Data
- ROCK Inhibitor Specificity: The efficacy of ROCK inhibitors is highly cell-type and context-dependent. While Y-27632 dramatically improves the survival of dissociated human embryonic stem cells (hESCs) and pluripotent stem cells (hPSCs), its effect on MSC immediate viability is less pronounced, though it significantly enhances their adherent growth post-thaw [66] [62] [65].
- Alternative ROCK Inhibitors: Next-generation ROCK inhibitors like Thiazovivin (used at 2 µM) and Chroman 1 (used at 50 nM) offer similar or superior cytoprotective effects at much lower concentrations, potentially reducing off-target effects [65].
- Beyond Apoptosis Inhibition: Additives like Antifreeze Protein III and boron work through complementary mechanisms. AFP III protects against physical ice crystal damage [64], while boron may improve membrane stability and reduce oxidative DNA damage [64], highlighting the benefit of multi-mechanism approaches.
Detailed Experimental Protocols
To facilitate replication and further research, this section outlines detailed methodologies from key studies cited in this guide.
This protocol demonstrates a targeted application of a ROCK inhibitor specifically during the thawing phase to improve T-cell yield.
Workflow: Post-Thaw ROCK Inhibition for T-Cells
Key Materials & Reagents:
- Fasudil Hydrochloride: A selective ROCK inhibitor.
- Cryopreservation Media: Advanced RPMI 1640 supplemented with 10% FBS and 5-10% DMSO.
- Culture Media: Advanced RPMI 1640 with 10% FBS.
- Cell Line: Jurkat T-cells or primary human T-cells.
This protocol incorporates the ROCK inhibitor throughout the cryopreservation and recovery process for Mesenchymal Stem Cells.
Workflow: ROCK Inhibition in MSC Cryopreservation
Key Materials & Reagents:
- ROCK Inhibitor Y-27632.
- Cryopreservation Solution: Typically containing DMSO and FBS.
- Cell Culture Flasks and Standard MSC Media.
- MTT Assay Kit for assessing metabolic activity of adherent cells.
- Trypan Blue Stain for immediate viability assessment.
The Scientist's Toolkit: Essential Research Reagents
This table catalogues key reagents discussed in this guide, their functions, and relevant applications for researchers designing cryopreservation studies.
Table 2: Essential Reagents for Investigating Apoptosis in Cell Cryopreservation
| Reagent / Solution | Function / Mechanism | Example Application Context |
|---|---|---|
| Y-27632 | Selective, reversible ROCK inhibitor; reduces membrane blebbing and apoptosis by modulating the actin cytoskeleton. | Standard for improving post-thaw survival and cloning efficiency of hPSCs [66] [65]; also used with MSCs [62] and sperm [64]. |
| Fasudil Hydrochloride | Selective ROCK inhibitor; shown to reduce ROS and increase T-cell yield post-thaw. | Post-thaw recovery of T-cells and Jurkat cells [63]. |
| Chroman 1 | Potent and selective ROCK inhibitor; used at nanomolar concentrations, minimizing off-target effects. | Component of advanced cytoprotective cocktails (e.g., CEPT) for hPSC cryopreservation and recovery [65]. |
| Thiazovivin | Selective ROCK inhibitor; effective at lower concentrations than Y-27632. | Enhancing hPSC viability post-dissociation and during reprogramming [65]. |
| Emricasan | Pan-caspase inhibitor; directly inhibits the execution phase of apoptosis. | Used in combination with Chroman 1 in CEPT cocktail for synergistic cytoprotection [65]. |
| Boron (as Boric Acid) | Proposed roles in membrane stability and cryoprotection; reduces DNA damage post-thaw. | Additive in semen freezing extenders for improving motility and DNA integrity [64]. |
| Antifreeze Protein III (AFP III) | Binds to ice crystals to inhibit growth and recrystallization, reducing physical membrane damage. | Additive in semen freezing extenders for reducing DNA fragmentation [64]. |
| CET Cocktail Pack | Commercial preparation containing Chroman 1, Emricasan, and Trans-ISRIB for comprehensive cytoprotection. | Improving hPSC survival and recovery under stressful conditions like cryopreservation [65]. |
Within the critical context of fresh versus cryopreserved MSC biological signatures research, mitigating post-thaw apoptosis is not merely about improving viability counts but about ensuring that the recovered cells truly reflect their fresh counterparts in function and therapeutic potential [18] [33]. The evidence presented demonstrates that ROCK inhibitors are a powerful tool, particularly for sensitive stem cells and lymphocytes, with efficacy confirmed across multiple independent studies.
The comparative data suggests that the future of optimal cryopreservation lies in integrated, multi-target strategies. Combining a ROCK inhibitor like Chroman 1 with a caspase inhibitor and agents that address physical ice damage (e.g., AFPs) or oxidative stress (e.g., boron) represents a promising path forward. This approach simultaneously targets the biochemical and physical triggers of cell death, offering a more complete cytoprotection solution. For researchers and therapy developers, adopting these evidence-based additive strategies is a crucial step towards ensuring that cryopreserved cells are not just viable, but fully functional, thereby validating their use as reliable and potent "off-the-shelf" therapeutics.
Within the broader investigation of fresh versus cryopreserved mesenchymal stromal cell (MSC) biological signatures, the immediate post-thaw handling protocol emerges as a critical determinant of therapeutic functionality. While the systematic comparison of fresh and cryopreserved products reveals that the majority of in vivo efficacy outcomes (97.7%) show no significant difference, a nuanced analysis confirms that post-thaw culture duration directly influences key functional attributes [18]. This guide objectively compares the performance of immediately used versus re-plated and acclimated MSCs, providing researchers and drug development professionals with the experimental data necessary to optimize post-thaw recovery protocols. The central thesis posits that a defined recovery period is not merely a procedural step, but a strategic intervention that can reactivate diminished cellular functions, thereby bridging the functional gap often observed between fresh and cryopreserved MSC products.
Comparative Functional Analysis: Immediate Post-Thaw vs. Acclimated MSCs
The post-thaw strategy—whether using cells immediately or after a re-plating period—significantly impacts MSC functional potency. The data summarized in the table below present a direct comparison of critical performance metrics.
Table 1: Functional Comparison of Immediately Thawed vs. Acclimated MSCs
| Functional Assay | Freshly Thawed (FT) MSCs | Thawed & Acclimated (TT) MSCs | Research Significance |
|---|---|---|---|
| Immunomodulatory Capacity | Significant reduction in IFN-γ secretion; impaired IDO pathway function [67] [68] | Significantly more potent arrest of T-cell proliferation; upregulated anti-inflammatory genes [67] | Critical for therapies targeting inflammatory diseases (e.g., GvHD) |
| Apoptosis & Metabolic State | Significantly increased apoptosis; elevated metabolic activity [67] | Significantly reduced apoptosis; normalized metabolic profile [67] | Indicates recovery from freeze-thaw stress; relates to in vivo survival |
| Proliferation & Clonogenicity | Decreased cell proliferation; reduced clonogenic capacity [67] | Recovery of proliferative potential and clonogenic function [67] | Essential for engraftment and sustained therapeutic effect |
| Gene Expression | Downregulation of key regenerative genes [67] | Upregulation of angiogenic and anti-inflammatory genes [67] | Predicts enhanced tissue repair and paracrine signaling capability |
| Phenotypic Markers | Decrease in CD44 and CD105 surface markers [67] [49] | Phenotype stable and comparable to fresh cultures [67] | Ensures cells meet release criteria and identity standards |
In Vivo Relevance and Large-Scale Studies
Contrary to some in vitro findings, a pre-clinical systematic review of 18 studies encompassing 257 in vivo experiments found that only a minute percentage (2.3%, 6/257) of efficacy outcomes were significantly different between fresh and cryopreserved MSCs in animal models of inflammation [18] [19]. This suggests that while cryopreservation causes acute functional impairments, the in vivo microenvironment may facilitate functional recovery. Furthermore, large-scale analyses of commercial-scale manufacturing support this; a study of 671 cases found that the biological signatures—including viability, population doubling time, immunophenotype, and paracrine molecule secretion—were comparable between cryopreserved and freshly preserved bone marrow MSCs [37].
Experimental Protocols for Post-Thaw Recovery Assessment
Standardized Post-Thaw Culture Protocol
A widely cited methodology for evaluating post-thaw recovery involves dividing cryopreserved MSCs into distinct experimental groups [67]:
- Freshly Thawed (FT) Group: Vials are retrieved from liquid nitrogen storage and thawed in a 37°C water bath with gentle shaking. The cell suspension is immediately used for experiments without any further culture.
- Thawed & Acclimated (TT) Group: MSCs are thawed as above, washed to remove cryoprotectant (e.g., DMSO), and plated at a standard density (e.g., 1000-4000 cells/cm²) in complete culture medium. The cells are then cultured for 24 hours in a standard humidified incubator (37°C, 5% CO₂) prior to harvesting and experimentation [67].
- Fresh Culture (FC) Control Group: MSCs maintained in continuous culture, harvested, and used at the same passage number serve as the baseline control for comparison.
This protocol allows for a direct, controlled comparison of the impact of a short-term re-plating strategy on MSC function.
Key Assays for Functional Qualification
The following assays are critical for quantifying the recovery of MSC functionality post-thaw:
- Flow Cytometric Immunophenotyping: Analyze the expression of standard positive (CD73, CD90, CD105) and negative (e.g., CD45, CD34) markers. A recovery of surface markers like CD105 post-acclimation indicates phenotypic restoration [67] [49].
- In Vitro Immunosuppression Assay: Co-culture MSCs with stimulated peripheral blood mononuclear cells (PBMCs) or T-cells. Measure the suppression of lymphocyte proliferation via flow cytometry or tritiated thymidine incorporation. This tests a key therapeutic mechanism [67] [68].
- Gene Expression Analysis: Using RT-qPCR to assess the transcription of immunomodulatory (e.g., IDO, TSG-6) and regenerative (e.g., VEGF, HGF) genes. Acclimated MSCs typically show upregulated expression of these critical factors [67].
- Clonogenic Assay (CFU-F): Plate MSCs at low density and count the number of colonies formed after 1-2 weeks. This assesses the retention of stemness and proliferative potential [67] [49].
- Apoptosis Assay: Use Annexin V/Propidium Iodide staining and flow cytometry to quantify the percentage of early and late apoptotic/necrotic cells, directly measuring recovery from cryo-injury [67].
Visualizing the Post-Thaw Recovery Workflow and Functional Trajectory
Experimental Workflow for Post-Thaw Study
The following diagram illustrates the standard experimental design used to compare different post-thaw strategies, from cell thawing to functional analysis.
Functional Recovery Timeline Post-Thaw
This timeline visualizes the trajectory of key functional attributes in MSCs following thawing and re-plating, comparing immediate use against a 24-hour acclimation period.
The Scientist's Toolkit: Essential Reagents for Post-Thaw Recovery Studies
Table 2: Essential Research Reagents for Post-Thaw MSC Functional Analysis
| Reagent / Solution | Critical Function | Application Notes |
|---|---|---|
| Cryopreservation Medium | Typically 10% DMSO in FBS; protects cells from ice crystal damage during freezing [67]. | DMSO is cytotoxic; must be washed post-thaw. Human serum albumin is a clinical-grade alternative to FBS [69]. |
| Complete Culture Medium (CCM) | Supports cell adhesion and recovery; often α-MEM/D-MEM with supplements like FBS or platelet lysate [67] [68]. | Platelet lysate is a xeno-free alternative to FBS for clinical-grade manufacturing [68]. |
| Trypsin/EDTA or TrypLE | Enzymatically detaches adherent MSCs for passaging and analysis post-recovery [67]. | Standardized digestion time is crucial to prevent damage to surface markers. |
| Flow Cytometry Antibodies | Quantifies expression of MSC markers (CD73, CD90, CD105) and purity (CD45, CD34) [67] [49]. | Critical for confirming phenotypic identity and stability after thawing. |
| Lymphocyte Proliferation Assay Kit | Measures MSC immunomodulatory potency via suppression of T-cell proliferation [67] [68]. | Often uses mitogens like PHA to stimulate PBMCs; quantification via CFSE or BrdU. |
| Annexin V / PI Apoptosis Kit | Distinguishes viable, early apoptotic, and late apoptotic/necrotic cell populations [67]. | Essential for quantifying cryo-injury and validating the recovery achieved by re-plating. |
| Trilineage Differentiation Kits | Confirms retained multipotency by inducing osteogenic, chondrogenic, and adipogenic differentiation [67] [49]. | A core defining property of MSCs that must be preserved after cryopreservation. |
The experimental data compellingly demonstrate that a 24-hour post-thaw acclimation period is a critical determinant in restoring the full functional profile of cryopreserved MSCs. While freshly thawed cells maintain basic immunomodulatory properties and multipotency, they exhibit significant deficits in anti-inflammatory gene expression, clonogenic capacity, and apoptotic resistance. The simple yet strategic intervention of re-plating and short-term culture effectively reactivates these diminished functions, yielding a product whose potency and phenotypic signature align more closely with freshly cultured MSCs [67]. For researchers and clinicians, this underscores that post-thaw handling is not a mere logistical step, but a therapeutically relevant variable. Integrating a 24-hour acclimation phase into manufacturing and pre-clinical testing protocols ensures that the functional data generated and the cell products administered truly reflect the intended therapeutic potential of MSC-based therapies.
The intravascular infusion of Mesenchymal Stromal Cells (MSCs) represents a promising therapeutic approach for numerous clinical conditions, from metabolic liver diseases to graft-versus-host disease. However, this promise is tempered by a significant safety concern: the initiation of procoagulant activity that can trigger an Instant Blood-Mediated Inflammatory Reaction (IBMIR). This thrombo-inflammatory response not only poses risks to patient safety but also compromises therapeutic efficacy by rapidly clearing infused cells from the bloodstream [70] [71]. Within the broader investigation of fresh versus cryopreserved MSC biological signatures, understanding and mitigating these thrombogenic reactions becomes paramount for clinical translation. While evidence suggests that cryopreserved and freshly preserved MSCs share comparable biological signatures in terms of viability, immunophenotype, and paracrine factor secretion [37], their interaction with blood components upon infusion requires meticulous characterization to ensure both safety and efficacy. This guide systematically compares the procoagulant profiles of different MSC products and outlines evidence-based strategies to enhance infusion safety.
Mechanisms of Procoagulant Activity and IBMIR
The Central Role of Tissue Factor (TF)
The primary driver of MSC-induced thrombogenesis is tissue factor (TF), a transmembrane protein abundantly expressed on the surface of MSCs. When MSCs enter the bloodstream via intravascular infusion, this membrane-bound TF becomes exposed to blood-borne factor VIIa. The resulting TF-FVIIa complex acts as the potent trigger of the coagulation cascade [70] [71]. This interaction initiates a proteolytic cascade that generates thrombin, ultimately leading to fibrin clot formation and platelet activation. The procoagulant effect is further amplified by the exposure of phosphatidylserine on the outer membrane of activated platelets and possibly the MSCs themselves, providing a negatively charged surface that accelerates coagulation reactions [70]. The expression level of TF varies significantly between MSC products from different tissue sources, with some preparations displaying sufficiently high TF to cause lethal consequences upon systemic infusion [71].
Instant Blood-Mediated Inflammatory Reaction (IBMIR)
When MSCs expressing high levels of TF encounter blood, they can initiate a more comprehensive thrombo-inflammatory response known as IBMIR. This reaction is characterized by the dual, simultaneous activation of both the coagulation cascade and the complement system [70]. The process unfolds rapidly: within minutes of infusion, the MSCs become encapsulated in blood clots infiltrated by activated polymorphonuclear neutrophils (PMNs), leading to significant early cell destruction and poor engraftment [72]. This reaction explains the disappointing clinical results observed in some trials and the characteristically low engraftment rates of intravascularly delivered cells [70].
Table 1: Key Components of the IBMIR Response
| Reaction Component | Key Elements | Consequences |
|---|---|---|
| Coagulation Activation | Tissue Factor (TF)-FVIIa complex, thrombin generation, fibrin clot formation | Thrombus formation on cells, portal vein thrombosis risk |
| Complement Activation | Complement cascade proteins, membrane attack complex | Cell lysis, inflammatory mediator release |
| Platelet Activation | Platelet binding, aggregation, α-granule release | Thrombus stabilization, inflammatory amplification |
| Inflammatory Cell Recruitment | Polymorphonuclear neutrophils (PMNs), monocytes | Cellular infiltration, phagocytosis of transplanted cells |
Pathway Visualization: MSC-Induced Thrombogenesis
The following diagram illustrates the coordinated molecular and cellular events that occur when MSCs are introduced into the bloodstream, leading to coagulation and inflammation.
Comparative Analysis of MSC Products and Anticoagulation Strategies
Clinical Evidence of Thrombogenic Risk
The thrombogenic potential of MSC products is not merely theoretical but has been documented in clinical settings. A phase I/II study investigating liver-derived MSCs (HepaStem) in patients with Crigler-Najjar syndrome and urea cycle disorders reported that despite prophylactic anticoagulation, one patient developed a partial portal vein thrombus following six infusions [72]. The study also observed consistent laboratory changes indicative of coagulation activation, including a significant decrease in platelet counts and elevated D-dimer levels immediately after infusion cycles. These hematological changes, while transient and spontaneously reversible within approximately seven days, provide clear evidence of in vivo coagulation pathway activation [72]. Four patients additionally experienced minor bleeding adverse effects such as petechiae, epistaxis, and cutaneous hemorrhage at catheter placement sites, highlighting the challenge of balancing anticoagulation to prevent thrombosis without inducing bleeding complications [72].
Comparative Efficacy of Anticoagulant Strategies
Different anticoagulation approaches have been investigated to mitigate the thrombogenic risk of MSC infusion. The following table summarizes key findings from clinical and experimental studies regarding their efficacy and limitations.
Table 2: Anticoagulation Strategies for MSC Infusion
| Anticoagulant Approach | Mechanism of Action | Evidence & Efficacy | Limitations & Considerations |
|---|---|---|---|
| Heparin + Thrombin Inhibitor (Bivalirudin) | Heparin activates antithrombin; Bivalirudin directly inhibits thrombin [72] | Combined use limited thrombogenesis to subclinical signs in 11 patients; prevented clinical thrombosis in all but 1 patient [72] | Requires careful dosing; minor hemorrhagic events observed (petechiae, epistaxis) [72] |
| Low Molecular Weight Dextran Sulfate (LMW-DS) | Inhibits both complement and contact activation systems; blocks E-selectin mediated adhesion [73] | In islet transplantation, showed similar efficacy to heparin in promoting engraftment at low doses; associated with lower bleeding risk than heparin at same APTT levels [73] | Well-tolerated in clinical studies; potential for more optimal dosing to be explored [73] |
| Heparin Monotherapy | Activates antithrombin to inhibit multiple coagulation factors | Standard care in islet transplantation but insufficient to fully prevent IBMIR; considered less effective than combinatorial approaches [72] [73] | Does not address thrombin generation sufficiently when used alone; limited effect on complement activation [72] |
MSC Source Variability and Preservation Methods
The thrombogenic potential of MSCs varies considerably with their tissue source. Products derived from different origins—bone marrow, adipose tissue, umbilical cord, or induced pluripotent stem cells—display highly variable levels of TF expression, which directly correlates with their hemocompatibility and safety profile upon intravascular delivery [71]. This source-dependent variability necessitates careful product-specific safety assessment before clinical use.
Regarding preservation methods, a large-scale comparative analysis of approximately 2,300 manufacturing cases from 2011 to 2022 found that cryopreserved and freshly preserved bone marrow-derived MSCs showed no significant differences in their core biological signatures, including viability, population doubling time, immunophenotype (except for CD14), and secretion of paracrine molecules [37]. This suggests that the cryopreservation process itself may not substantially alter the fundamental procoagulant profile of MSCs, though product-specific validation remains essential.
Experimental Protocols for Assessing Procoagulant Activity
In Vitro Assessment of Procoagulant Potential
Objective: To quantitatively evaluate the thrombogenic potential of MSC products before clinical administration.
Methodology:
- TF Expression Analysis: Quantify tissue factor expression on MSCs using flow cytometry with TF-specific antibodies. Compare expression levels across different MSC sources and donors [71].
- Thrombin Generation Assay: Incubate MSCs with platelet-poor human plasma. Measure thrombin-antithrombin (TAT) complexes formed over time using ELISA. Peak TAT levels indicate coagulation cascade activation [70] [73].
- Platelet Activation Test: Co-culture MSCs with washed platelets or platelet-rich plasma. Assess platelet activation markers (P-selectin expression, phosphatidylserine exposure) via flow cytometry, and quantify platelet aggregation by light transmission aggregometry [70].
- Complement Activation Assay: Incubate MSCs with human serum. Measure complement activation products (C3a, C5a, SC5b-9) using ELISA to assess complement pathway engagement [70].
Validation: Include appropriate controls (e.g., TF-blocking antibodies, factor-deficient plasmas) to confirm specificity of observed effects.
In Vivo Safety and Efficacy Monitoring Protocol
Objective: To clinically monitor infusion-related thrombogenesis and anticoagulation efficacy during MSC administration.
Methodology:
- Pre-infusion Baseline:
During Infusion:
Post-infusion Monitoring:
- Laboratory assessments at 0, 2, 6, and 24 hours post-infusion, then daily for 7 days: platelet count, D-dimer, TAT complexes [72].
- Clinical monitoring for thrombotic events (limb pain, swelling, neurological changes) and hemorrhagic complications [72].
- Doppler ultrasound at 24 hours post-infusion and as clinically indicated to detect vascular thrombosis [72].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagents for Procoagulant Activity Assessment
| Reagent / Material | Specific Application | Function & Importance |
|---|---|---|
| Anti-Tissue Factor Antibodies | Flow cytometry, immunohistochemistry | Quantification of TF expression on MSC surface; primary determinant of procoagulant potential [71] |
| Thrombin-Antithrombin (TAT) Complex ELISA Kit | Plasma/serum analysis | Measures in vivo thrombin generation; key biomarker for coagulation activation [73] |
| Factor Xa Activity Assay | Functional coagulation testing | Direct measurement of TF-FVIIa complex activity; functional assessment of procoagulant potential [70] |
| C3a, C5a, SC5b-9 ELISA Kits | Complement activation studies | Quantifies complement system activation; essential for comprehensive IBMIR assessment [70] |
| Heparin (Leo) | Anticoagulation prophylaxis | Antithrombin activator; component of combinatorial anticoagulation strategy [72] |
| Bivalirudin (Angiox) | Anticoagulation prophylaxis | Direct thrombin inhibitor; used in combination with heparin for enhanced efficacy [72] |
| Low Molecular Weight Dextran Sulfate | Experimental anticoagulation | Dual inhibitor of coagulation and complement systems; potential alternative to heparin [73] |
The procoagulant activity of MSCs and its potential to trigger IBMIR represent significant challenges for cell-based therapies employing intravascular delivery routes. The evidence indicates that this thrombogenic risk is primarily driven by TF expression on infused cells, which varies across MSC sources and individual products [71]. While biological signatures appear comparable between fresh and cryopreserved MSCs in terms of standard quality attributes [37], comprehensive hemocompatibility assessment remains essential for both product formats.
Successful risk mitigation requires a multi-faceted approach: (1) rigorous pre-clinical screening of TF expression and procoagulant potential; (2) implementation of combinatorial anticoagulation regimens targeting both coagulation and complement pathways [72]; and (3) careful clinical monitoring for both thrombotic and hemorrhagic complications. The combination of heparin with the direct thrombin inhibitor bivalirudin has demonstrated promising results in limiting infusion-related thrombogenesis to subclinical manifestations [72], while emerging alternatives like LMW-DS offer potential for enhanced safety profiles [73]. As the field advances, product-specific hemocompatibility assessment and tailored anticoagulation strategies will be indispensable for unlocking the full therapeutic potential of intravascular MSC therapies while ensuring patient safety.
Evidence-Based Validation: Systematic Comparisons of In Vitro and In Vivo Efficacy
The translation of Mesenchymal Stem Cell (MSC) therapies from laboratory research to clinical practice faces a fundamental logistical challenge: the tension between immediate patient treatment and the practical realities of cell distribution and storage. Freshly cultured MSCs require immediate administration, creating significant hurdles for widespread clinical application and off-the-shelf availability. Cryopreservation offers a practical solution but raises critical questions about whether freezing and thawing processes alter fundamental MSC biological properties, potentially diminishing their therapeutic efficacy [13]. This comparison guide systematically evaluates preclinical evidence from 257 in vivo experiments to determine whether cryopreserved MSCs maintain functional equivalence to freshly cultured counterparts across diverse disease models, providing researchers and therapy developers with evidence-based recommendations for product development strategies.
Methodological Framework: Systematic Review Protocols
Search Strategy and Study Selection Criteria
The foundational systematic review conducted a comprehensive electronic search across OvidMEDLINE, EMBASE, BIOSIS, and Web of Science databases until January 13, 2022, without language restrictions [13]. The search employed predefined terms related to MSCs and cryopreservation, utilizing six target articles provided by preclinical research experts to optimize search sensitivity. The review adhered to PRISMA guidelines for transparent reporting and employed the SYRCLE 'Risk of Bias' assessment tool specifically designed for preclinical in vivo studies, with two independent reviewers conducting assessments and resolving disagreements through consensus or third-party adjudication [13].
Inclusion and Exclusion Criteria
- Population: Animal models of inflammation with intact immune systems (immunocompromised models excluded)
- Intervention: Cryopreserved MSCs (any duration) cultured <24 hours post-thaw
- Comparison: Freshly cultured MSCs (continuous culture or ≥24 hours post-thaw)
- Outcomes: In vivo efficacy measures and in vitro potency indicators
- Study Designs: Randomized, quasi-randomized, and non-randomized comparative designs
- MSC Requirements: Same cellular origin and source for both intervention and comparison groups
Comparative Efficacy Analysis: In Vivo Outcomes
Primary Efficacy Endpoints Across Disease Models
Table 1: Summary of In Vivo Efficacy Outcomes from Preclinical Systematic Review
| Disease Model Category | Number of Experiments | Significant Findings | Direction of Effect | Implications for Therapeutic Development |
|---|---|---|---|---|
| Inflammatory Conditions | 257 total experiments | 6/257 (2.3%) significant differences | 2 favoured fresh, 4 favoured cryopreserved | Minimal functional differences support cryopreserved product development |
| Acute Lung Injury | Included in analysis | No significant differences reported | Comparable efficacy | Viable for off-the-shelf emergency applications |
| Sepsis Models | Included in analysis | No significant differences reported | Comparable efficacy | Suitable for urgent care scenarios |
| Graft-versus-Host Disease | Included in analysis | No significant differences reported | Comparable efficacy | Supports clinical trial logistics |
| Inflammatory Bowel Disease | Included in analysis | No significant differences reported | Comparable efficacy | Enables treatment standardization |
The comprehensive analysis encompassed 101 distinct outcome measures across the 257 in vivo experiments, representing diverse inflammatory conditions including acute lung injury, sepsis, graft-versus-host disease, and inflammatory bowel disease [13]. The remarkably consistent finding—that 97.7% of measured outcomes showed no statistically significant difference between freshly cultured and cryopreserved MSCs—provides strong preclinical evidence that cryopreservation does not substantially alter MSC therapeutic efficacy in inflammatory disease models.
Supporting Evidence from Complementary Study Designs
Table 2: Corroborating Evidence from Clinical Database and In Vitro Studies
| Study Type | Sample Size | Key Parameters Assessed | Statistical Outcome | Clinical Translation Relevance |
|---|---|---|---|---|
| Clinical Database Analysis [5] | ~2300 manufacturing cases | Viability, population doubling time, immunophenotype, paracrine molecules | No significant differences in 20 selected features | Supports manufacturing scalability and quality control |
| In Vitro Potency Assessment [13] | 68 experiments | 32 different potency measures | 13% significant differences (7 fresh, 2 cryopreserved) | Slightly more variability in artificial conditions than in vivo |
| Immunophenotype Characterization [5] | 671 approved cases | CD markers except CD14 | Comparable expression profiles | Maintains identity and purity specifications |
A separate analysis of approximately 2300 stem cell manufacturing cases from the Pharmicell database further strengthened these findings, demonstrating comparable cell viability, population doubling time, immunophenotype markers (except CD14), and paracrine molecule secretion between preservation methods [5]. Circular clustering and principal component analysis revealed no separation between freshly preserved and cryopreserved MSC biological signatures, confirming their functional equivalence across critical quality attributes.
Experimental Workflow and Biological Mechanisms
MSC Processing and Evaluation Pathway
Biological Signature Comparison Methodology
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Critical Research Materials for MSC Preservation Studies
| Reagent/Category | Specific Function | Experimental Importance | Considerations for Therapeutic Development |
|---|---|---|---|
| Cryopreservation Medium | Maintains cell viability during freeze-thaw | Critical standardized variable; affects recovery rate | Formulation consistency essential for regulatory approval |
| Cell Culture Media | Supports MSC expansion and maintenance | Must be consistent between comparison groups | Serum-free formulations preferred for clinical translation |
| Viability Assays | Measures post-thaw cell integrity (hemocytometer, flow cytometry) | Primary quality assessment endpoint | Standardized protocols needed across manufacturing sites |
| Immunophenotyping Antibodies | Characterizes surface CD marker expression | Confirms MSC identity after preservation | CD14 may show differential expression [5] |
| Cytokine Detection Assays | Quantifies paracrine factor secretion | Measures functional potency | Critical for mechanistic understanding of efficacy |
Implications for MSC Therapeutic Development
The convergence of evidence from both large-scale database analysis and systematic review of preclinical studies indicates that cryopreservation does not significantly alter the fundamental biological signatures or therapeutic efficacy of MSCs in animal inflammation models. This conclusion has substantial implications for MSC-based product development:
- Clinical Translation: Supports development of off-the-shelf MSC products for urgent care scenarios including stroke, myocardial infarction, and acute inflammation
- Manufacturing Strategy: Enables centralized manufacturing with frozen distribution, overcoming logistical barriers to widespread clinical adoption
- Quality Assurance: Justifies use of cryopreserved reference materials for standardized quality control testing across manufacturing batches
- Regulatory Pathway: Provides preclinical evidence for comparability between fresh and frozen products in regulatory submissions
While the evidence base demonstrates functional equivalence in preclinical inflammation models, researchers should continue to validate these findings in specific disease contexts and consider that certain MSC functions (e.g., immunomodulatory potency) may require verification under particular experimental conditions. The minimal differences observed (2.3% of in vivo outcomes) suggest that cryopreserved MSCs represent a viable—and practically superior—alternative to freshly cultured cells for most therapeutic applications.
The therapeutic application of Mesenchymal Stromal Cells (MSCs) hinges on two critical functional properties: their capacity to modulate immune responses and their potential to differentiate into various connective tissue lineages. These properties make MSCs attractive candidates for regenerative medicine and treating immune-mediated disorders. However, MSCs are not a uniform entity; they can be isolated from a multitude of tissue sources, including bone marrow (BM), adipose tissue (AT), and various birth-associated tissues like umbilical cord (UC), cord blood (UCB), and placenta (PL). This diversity raises a critical question for researchers and clinicians: which source provides the most potent cells for a specific therapeutic application?
Direct in vitro comparisons of immunomodulatory potency and differentiation capacity across different MSC sources are essential for translating cellular therapies from the bench to the bedside. Furthermore, a key logistical consideration in cell therapy is the use of cryopreserved products, which facilitate off-the-shelf availability. Reassuringly, a 2023 study comparing biological signatures found that the biochemical profiles of cryopreserved and freshly preserved bone marrow MSCs were comparable, showing no significant differences in viability, population doubling time, immunophenotype, or paracrine molecule secretion [5]. This finding supports the use of cryopreserved cells in both research and clinical settings, framing the following head-to-head comparisons of cells that may be utilized in either a fresh or cryopreserved state.
MSCs exert their immunomodulatory effects through a combination of cell-to-cell contact and paracrine activity [74]. Key mechanisms include:
- Interaction with T-cells: MSCs can inhibit naive and memory T-cell responses, induce regulatory T-cells (Tregs), and influence the differentiation of T-helper cells (Th1, Th2, Th17) [74] [75]. Critical molecules involved are programmed death-ligand 1 (PD-L1), indoleamine 2,3-dioxygenase (IDO), prostaglandin E2 (PGE2), transforming growth factor-β (TGF-β), and hepatocyte growth factor (HGF) [74] [75].
- Interaction with Innate Immune Cells: MSCs can switch pro-inflammatory M1 macrophages to anti-inflammatory M2 phenotypes, modulate dendritic cell maturation, and affect natural killer (NK) cell function [74].
The following diagram illustrates the core immunomodulatory pathways and cell interactions mediated by MSCs.
Head-to-Head Comparison of Immunomodulatory Capacity
Studies directly comparing MSCs from different sources report variable results, likely due to differences in experimental protocols, donor variability, and culture conditions. The table below summarizes key findings from direct comparative studies.
Table 1: Direct Comparisons of Immunomodulatory Potency Across MSC Sources
| Reference | Populations Compared | Experimental Readout | Comparative Outcome |
|---|---|---|---|
| Ribeiro et al. [76] | BM, AT, UC | T/NK cell inhibition; B cell inhibition | AT > BM = UC for T/NK cell inhibition; BM = AT for B cell inhibition (UC had no effect) |
| Najar et al. [76] | BM, AT, UC | Inhibition of allogeneic T-cell proliferation | AT > BM = UC |
| Li et al. [76] | BM, AT, UC, PL, WJ | T cell proliferation inhibition | WJ > PL > AT > BM |
| Castro-Manrreza et al. [76] | BM, UCB, PL | CD4+ and CD8+ T cell suppression | BM = UCB > PL |
| Yoo et al. [76] | BM, AT, UCB, WJ | T cell proliferation inhibition | BM = AT = UCB = WJ |
| Bárcia et al. [76] | BM, UC | MLR assay; Treg induction | UC > BM for immunomodulation; UC < BM for immunogenicity |
| Prasanna et al. [76] | BM, WJ | PBMC proliferation; cytokine profiles | WJ ≠ BM (different mechanisms) |
| Ivanova-Todorova et al. [76] | BM, AT | Monocyte modulation; cytokine secretion | AT > BM |
Key Interpretations of Comparative Data:
- Adipose Tissue (AT-MSCs): Multiple studies indicate that AT-MSCs are among the most potent suppressors of T-cell proliferation, often outperforming BM-MSCs and UC-MSCs [76] [74]. This heightened effect has been linked to their higher intrinsic levels of factors like cyclooxygenase-1 (COX1), which is essential for PGE2 production [76] [75].
- Birth-Associated Tissues (UC, UCB, PL, WJ): These sources show considerable promise. While some studies rank Wharton's Jelly (WJ)-MSCs as highly potent [76], others find them equal to BM-MSCs [76]. A key advantage is their potentially lower immunogenicity, making them suitable for allogeneic therapy [76] [74].
- Bone Marrow (BM-MSCs): As the gold standard, BM-MSCs are consistently robust immunomodulators. While they may not always be the most potent in every assay, they provide a reliable benchmark and are the most extensively characterized [76] [75].
Experimental Protocols for Assessing ImmunomodulationIn Vitro
To generate the comparative data outlined above, researchers employ standardized in vitro immune assays. The following workflow details a common co-culture experiment used to quantify MSC-mediated T-cell suppression.
Detailed Methodology: T-cell Proliferation Suppression Assay
- Step 1: Immune Cell Isolation. Peripheral blood mononuclear cells (PBMCs) are isolated from healthy donors via density gradient centrifugation (e.g., using Ficoll-Paque) [77] [78].
- Step 2: T-cell Activation. PBMCs are stimulated with mitogens like phytohemagglutinin (PHA) or, more specifically, with anti-CD3 and anti-CD28 antibody-coated beads to activate T-cells [76] [78].
- Step 3: Co-culture Setup. Activated PBMCs are co-cultured with MSCs from different sources (BM, AT, UC, etc.). This is typically done at varying MSC:PBMC ratios (e.g., 1:5 to 1:100) to assess dose-dependency. The co-culture can be set up for direct cell-to-cell contact or using a transwell system to distinguish contact-dependent from soluble factor-mediated effects [78].
- Step 4: Incubation and Analysis. After 5-7 days of culture:
- T-cell Proliferation is quantified by flow cytometry using dyes like carboxyfluorescein succinimidyl ester (CFSE) [76] [78].
- T-cell Phenotype is analyzed by staining for surface markers (e.g., CD4, CD8, CD25) and intracellular markers (e.g., FOXP3 for Tregs) [76] [77].
- Cytokine Secretion is measured in the supernatant using enzyme-linked immunosorbent assay (ELISA) or multiplex bead arrays (e.g., Luminex) to profile the inflammatory (IFN-γ, TNF-α) and anti-inflammatory (IL-10) milieu [76] [78].
While all MSCs are defined by their trilineage differentiation potential, their propensity to differentiate into specific lineages can vary significantly based on their tissue of origin.
Table 2: Comparison of Differentiation Capacities Across MSC Sources
| MSC Source | Osteogenic | Adipogenic | Chondrogenic | Tissue-Specific Propensity |
|---|---|---|---|---|
| Bone Marrow (BM) | Strong [76] | Strong [76] | Strong [76] | Considered the gold standard for osteogenesis. |
| Adipose Tissue (AT) | Moderate [76] | Very Strong [76] | Moderate [76] | Naturally high adipogenic potential. |
| Umbilical Cord (UC) | Variable/Weak [76] [79] | Variable/Weak [76] [79] | Strong [79] | Shows promise for chondrogenesis and neural differentiation [79]. |
| Chorion (C-MSC) | Moderate [79] | Moderate [79] | Moderate [79] | Cardiomyocyte differentiation; upregulation of genes associated with heart morphogenesis (e.g., HTR2B) [79]. |
| Amnion (A-MSC) | Weak [79] | Weak [79] | Weak [79] | Limited differentiation potential; high rates of senescence and apoptosis [79]. |
Key Interpretations of Differentiation Data:
- Source Matters for Lineage Propensity: The "native" tissue environment imprints a degree of lineage bias on MSCs. BM-MSCs are naturally primed for osteogenesis, while AT-MSCs excel at adipogenesis [76].
- Perinatal Tissues Have Unique Profiles: MSCs from perinatal tissues like the umbilical cord and placental components (chorion, amnion) exhibit distinct gene expression profiles that correlate with their differentiation potential. For example, chorion-derived MSCs (CMSCs) show a pronounced tendency for cardiomyocyte differentiation, while umbilical cord-derived MSCs (UC-MSCs) show upregulation of genes associated with neurological processes (e.g., NPY) [79].
The Scientist's Toolkit: Essential Reagents for MSC Potency Assays
The following table lists key reagents and tools required to perform the immunomodulation and differentiation comparisons discussed in this guide.
Table 3: Essential Research Reagents for MSC Potency Assays
| Reagent / Tool | Function / Application | Examples / Notes |
|---|---|---|
| Isolation Media | Isolation of MSCs from tissue or PBMCs from blood. | Collagenase for AT-MSC isolation; Ficoll-Paque for BM-MSC and PBMC isolation. |
| Culture Media | Expansion and maintenance of MSCs. | α-MEM or DMEM, supplemented with Fetal Bovine Serum (FBS) or xeno-free alternatives, and FGF-2 [77] [79]. |
| Licensing Cytokines | Pre-activation (priming) of MSCs to enhance immunomodulatory potency. | IFN-γ and TGF-β1 are commonly used to upregulate IDO, PGE2, and PD-L1 [74] [77]. |
| T-cell Activators | Stimulation of T-cell proliferation in co-culture assays. | Anti-CD3/CD28 antibody-coated beads; Phytohemagglutinin (PHA). |
| Flow Cytometry Antibodies | Characterization of MSC phenotype and immune cell profiling. | MSC markers: CD73, CD90, CD105, CD44. Negative markers: CD45, CD34, HLA-DR. Immune markers: CD3, CD4, CD8, CD25, FOXP3 (for Tregs), CD14 (for monocytes) [77] [78]. |
| Differentiation Kits | Induction of trilineage differentiation. | Osteogenic: Dexamethasone, β-glycerophosphate, ascorbic acid. Adipogenic: Insulin, IBMX, indomethacin. Chondrogenic: TGF-β3, BMP-6. |
| Analysis Kits | Quantification of soluble factors and gene expression. | ELISA or Luminex kits for cytokines (IFN-γ, TNF-α, IL-10, PGE2). Kits for measuring IDO activity. |
Direct in vitro comparisons reveal that the source of MSCs is a critical determinant of their functional potency. Adipose tissue-derived MSCs frequently emerge as potent immunomodulators, particularly in suppressing T-cell responses, whereas bone marrow-derived MSCs remain a robust and well-characterized benchmark. Birth-associated tissues, such as umbilical cord and chorion, offer advantages in proliferative capacity, low immunogenicity, and unique differentiation potentials, including for neural and cardiac lineages, respectively.
The choice of MSC source for research or therapeutic development should therefore be guided by the intended application—opting for AT-MSCs for potent immunomodulation or BM-MSCs for bone regeneration, for example. Furthermore, the ability to cryopreserve MSCs without significantly altering their biological signatures ensures that these potent cell populations can be standardized and made readily available for both rigorous in vitro comparison and clinical use [5]. As the field advances, the strategic selection of MSC sources, potentially enhanced by licensing protocols and the use of cell-derived products like extracellular vesicles, will be paramount to developing effective and reliable cell-based therapies.
This comparison guide objectively evaluates the biological and functional signatures of freshly preserved versus cryo-preserved Mesenchymal Stem Cells (MSCs) based on a large-scale biobank data analysis. The findings demonstrate that with optimized protocols, cryo-preserved MSCs maintain comparable viability, phenotypic identity, and functional potency to their fresh counterparts. This supports their use as reliable "off-the-shelf" products for clinical and research applications, addressing a critical logistical challenge in regenerative medicine.
Key Findings at a Glance
| Parameter | Freshly Preserved MSCs | Cryo-Preserved MSCs | Statistical Significance |
|---|---|---|---|
| Cell Viability | Benchmark level | Comparable at most passages | No significant difference [5] |
| Growth Kinetics (PDT) | Benchmark level | Comparable average Population Doubling Time | No significant difference [5] |
| Immunophenotype (CD73, CD90, CD105) | Positive expression | Positive expression | No difference [5] [15] |
| Immunophenotype (CD14, CD19, CD34, CD45) | Negative expression | Negative expression (CD14 showed variation) | No difference for most markers [5] |
| Secretory Profile (Paracrine Molecules) | Baseline concentration | Comparable concentration | No significant difference [5] |
| In Vivo Preclinical Efficacy | Effective | Majority of outcomes (97.7%) not significantly different | Not significant for 257/263 outcomes [18] |
| In Vitro Potency | Baseline activity | Majority of experiments (87%) not significantly different | Not significant for 59/68 experiments [18] |
Detailed Comparative Analysis of Key Parameters
The following sections provide a detailed breakdown of the comparative analyses between fresh and cryo-preserved MSCs, drawing from large-scale datasets and controlled studies.
Cell Viability and Growth Kinetics
Cell viability and proliferation capacity are fundamental quality attributes for any cell therapy product. The large-scale analysis of approximately 2,300 manufacturing cases found that cell viability at most passages did not differ according to the preservation method [5]. Furthermore, the average Population Doubling Time (PDT), a key metric for proliferation, was not significantly different between the frozen and unfrozen MSC groups [5]. This indicates that the self-renewal capacity of MSCs is not fundamentally impaired by a well-managed cryopreservation process.
Optimizing post-thaw handling is critical. One study demonstrated that diluting high-concentration cryopreserved cell products (from 9 million cells/mL) immediately after thawing improved cell viability over a 6-hour period, simulating the clinical window of use [15]. This highlights that protocol specifics, rather than the act of freezing itself, can dictate final product quality.
Phenotypic Identity and Secretory Profile
The identity of MSCs is defined by specific cell surface markers and their characteristic secretome, both of which are crucial for their therapeutic mechanisms.
- Immunophenotype: The large-scale biobank analysis concluded that the expression of standard positive (CD73, CD90, CD105) and negative (CD34, CD45) markers was consistent between preservation groups for most markers. One study noted an exception with the CD14 marker, which showed a different mean level [5]. Independent research corroborates that MSCs cryopreserved in various clinical-grade solutions successfully retained their characteristic surface marker profile post-thaw [15].
- Paracrine Function: The analysis of soluble paracrine molecules, which mediate many therapeutic effects like immunomodulation and angiogenesis, showed that their concentrations did not exhibit different mean levels between the frozen and unfrozen MSC groups [5]. This is a critical finding, as it suggests that the secretory potency of MSCs remains intact after cryopreservation.
Functional Potency: In Vitro and In Vivo Evidence
Functional potency is the ultimate test of a therapeutic cell product. A systematic review of pre-clinical in vivo models of inflammation directly compared freshly cultured and cryopreserved MSCs.
- In Vivo Efficacy: The review analyzed 257 in vivo experiments. Of these, only 2.3% (6 out of 257) showed statistically significant differences. Among these few differences, two outcomes favoured freshly cultured cells, while four actually favoured cryopreserved MSCs [18]. This demonstrates that the biological impact of cryopreserved MSCs in a living organism is overwhelmingly consistent with fresh cells.
- In Vitro Potency: The same review analyzed 68 in vitro experiments measuring MSC potency. Here, 13% (9 out of 68) were significantly different, with seven favouring fresh and two favouring cryopreserved cells [18]. While this indicates a more noticeable effect of cryopreservation in simplified laboratory assays, the vast majority of potency measures still showed no significant difference. Specific studies on immunomodulatory function—a key therapeutic action—found that MSCs cryopreserved in solutions like NutriFreez and PHD10 exhibited comparable potency in inhibiting T-cell proliferation to fresh cells [15].
Detailed Experimental Protocols
To ensure reproducibility and provide clarity on the data sources, this section outlines the key methodologies from the cited studies.
Large-Scale Biobank Data Analysis
The core findings of this guide are derived from a comprehensive analysis of data sourced from the Pharmicell database [5].
- Data Source: Data were collected from approximately 2,300 stem cell manufacturing cases between 2011 and 2022. The final analyzed dataset included 671 cases with no missing data, approved by an Institutional Review Board (IRB) [5].
- Variables Measured: The dataset comprised approximately 60 variables, including:
- Viability: Measured using standard assays (e.g., Trypan blue exclusion).
- Population Doubling Time (PDT): Calculated to assess growth kinetics.
- Immunophenotype: Analyzed by flow cytometry for standard MSC positive (CD73, CD90, CD105) and negative (CD14, CD19, CD34, CD45) markers.
- Soluble Paracrine Molecules: Quantified using immunoassays (e.g., ELISA).
- Data Analysis: Twenty key features were selected by experts and abstracted into two primary features using Principal Component Analysis (PCA). Unsupervised analysis techniques, including circular clustering, were applied to identify inherent patterns and differences between the fresh and cryo-preserved groups [5].
Functional Potency Assessment
The in vitro immunomodulatory potential of cryopreserved MSCs was evaluated in a controlled study comparing cryopreservation solutions [15].
- T-cell Proliferation Assay:
- MSCs were cryopreserved in different solutions and thawed.
- Thawed MSCs were co-cultured with activated peripheral blood mononuclear cells (PBMCs).
- T-cell proliferation was measured using flow cytometry, typically by staining with carboxyfluorescein succinimidyl ester (CFSE) and quantifying dye dilution in T-cell populations after several days in culture.
- Phagocytosis Assay:
- Thawed MSCs were co-cultured with monocytic cells (e.g., THP-1 cell line or primary monocytes).
- Phagocytic activity was measured by incubating monocytes with fluorescently labeled particles (e.g., pHrodo E. coli bioparticles).
- The fluorescence intensity, indicating particle uptake, was quantified using flow cytometry or a fluorescence plate reader.
Signaling Pathways and Experimental Workflows
The following diagram illustrates the logical workflow and key conclusions of the large-scale biobank analysis that forms the basis of this case study.
The Scientist's Toolkit: Essential Research Reagents
The successful cryopreservation and analysis of MSCs rely on a suite of critical reagents and tools. The table below details key solutions and their functions based on the cited experimental data.
Table: Key Reagents for MSC Cryopreservation and Quality Control
| Reagent / Solution | Primary Function | Example Formulations / Kits | Supporting Data |
|---|---|---|---|
| Cryopreservation Solutions | Protect cells from ice crystal damage and osmotic stress during freeze-thaw. | NutriFreez D10, CryoStor CS5/CS10, In-house PLA/5%HA/10%DMSO (PHD10) | MSCs cryopreserved in NutriFreez and PHD10 showed comparable viability, recovery, and post-thaw potency [15]. |
| Dimethyl Sulfoxide (DMSO) | Permeating cryoprotectant; reduces intracellular ice formation. | Typically used at 5-10% in final cryopreservation solution. | A standard cryoprotectant, though associated with potential in-vivo toxicity at high doses; post-thaw dilution mitigates risk [9]. |
| Flow Cytometry Antibodies | Quality control for MSC immunophenotype (identity and purity). | Antibody panels against CD73, CD90, CD105 (positive) and CD14, CD19, CD34, CD45 (negative). | Used to confirm that cryopreservation did not alter the standard MSC surface marker profile [5] [15]. |
| Viability & Apoptosis Assays | Assess cell health and recovery post-thaw. | Trypan Blue exclusion; Annexin V / Propidium Iodide (PI) staining. | Used to measure post-thaw viability over time (0-6 hours) and identify early apoptotic cells [15]. |
| Immunoassays | Quantify secreted paracrine factors (e.g., cytokines, growth factors). | Enzyme-Linked Immunosorbent Assay (ELISA) kits. | Used in the large-scale analysis to confirm comparable secretory profiles between fresh and cryo-preserved MSCs [5]. |
Mesenchymal stem cells (MSCs) represent a cornerstone of regenerative medicine due to their multipotent differentiation capacity, immunomodulatory properties, and therapeutic potential across diverse disease states [32]. Originally identified in bone marrow, MSCs have since been isolated from numerous tissues, with bone marrow-derived MSCs (BM-MSCs), adipose-derived MSCs (AD-MSCs), and umbilical cord-derived MSCs (UC-MSCs) emerging as the most extensively studied and clinically relevant populations [80] [81]. The International Society for Cellular Therapy (ISCT) has established minimum criteria for defining MSCs, including plastic adherence, specific surface marker expression (CD73+, CD90+, CD105+, CD34-, CD45-, CD14- or CD11b-, CD19- or CD79α-, HLA-DR-), and trilineage differentiation potential into osteoblasts, adipocytes, and chondrocytes in vitro [81] [32].
Despite these shared characteristics, significant functional and biological differences exist between MSCs derived from different tissue sources, influenced by their unique tissue-specific microenvironments and ontogenetic origins [82] [83]. These variations profoundly impact their proliferative capacity, differentiation potential, secretome profiles, and ultimately, their therapeutic efficacy for specific clinical applications [25] [83]. Furthermore, the molecular basis of MSC stemness, governed by transcriptional factors, epigenetic regulators, and signaling pathways, varies according to tissue source, affecting their performance in both research and clinical settings [25].
This comparative guide provides a detailed analysis of BM-MSCs, AD-MSCs, and UC-MSCs, focusing on their distinctive biological signatures, therapeutic mechanisms, and functional characteristics. The content is framed within ongoing research investigating the biological signatures of fresh versus cryopreserved MSCs, a critical consideration for clinical translation where cryopreservation is essential for logistical feasibility [37]. Understanding these source-specific variations is paramount for researchers and clinicians to select the most appropriate MSC type for targeted therapeutic applications and to optimize manufacturing protocols for regenerative medicine.
Comprehensive Characterization of MSC Types
Bone Marrow-Derived MSCs (BM-MSCs)
BM-MSCs, the first discovered and most extensively characterized MSC population, are considered the gold standard in the field [37] [32]. They are isolated from bone marrow aspirates, a procedure that is relatively invasive for donors compared to other sources [82]. BM-MSCs demonstrate a high differentiation potential, particularly toward osteogenic and chondrogenic lineages, making them exceptionally suitable for musculoskeletal regeneration [32]. Their therapeutic mechanisms are largely attributed to potent immunomodulatory effects and paracrine signaling, through which they secrete growth factors, cytokines, and extracellular vesicles (EVs) that promote tissue repair and modulate immune responses [81] [32].
The proteomic profile of BM-MSCs is distinct, with signaling pathways involved in cell migration and Wnt signaling being particularly prominent, although these may be less pronounced than in dental pulp stem cells [82]. From a clinical manufacturing perspective, studies comparing fresh and cryopreserved BM-MSCs have shown that cryopreservation does not significantly alter key biological signatures, including cell viability, population doubling time (PDT), immunophenotype, and the secretion of most paracrine molecules [37]. This resilience to freezing makes them a robust choice for off-the-shelf therapies.
Adipose-Derived MSCs (AD-MSCs)
AD-MSCs are isolated from adipose tissue obtained through liposuction, a minimally invasive procedure that yields a high quantity of stromal vascular fraction and MSCs, providing a significant advantage for cell yield [32] [83]. Relative to other MSC types, AD-MSCs exhibit a broader spectrum of gene expression for regulatory and secretory functions, as identified by single-cell transcriptomic analysis [84]. This is reflected in their potent secretome, which is rich in factors supporting angiogenesis and tissue repair.
A key functional advantage of AD-MSCs is their strong association with angiogenesis and vascularization pathways, as revealed by proteomic and Gene Ontology analyses [82]. This makes them particularly suitable for treating ischemic conditions and wounds. Furthermore, in the context of aging, autologous AD-MSCs have demonstrated an ability to improve oocyte quality and fertility in aged mouse models via mitochondrial transfer, highlighting their unique reparative capabilities in reproductive aging [83]. Their biological signatures remain consistent between fresh and cryopreserved states, similar to BM-MSCs.
Umbilical Cord-Derived MSCs (UC-MSCs)
UC-MSCs are isolated from Wharton's jelly and other compartments of the umbilical cord, a perinatal tissue typically discarded as medical waste [32]. These cells are considered among the youngest adult stem cell sources available, which contributes to their enhanced proliferation capacity and lower immunogenicity compared to adult tissue-derived MSCs [83]. Their use raises no ethical concerns, and they are ideal for allogeneic transplantation due to low HLA expression [32].
UC-MSCs possess a distinct molecular signature, characterized by the expression of specific pluripotency-associated factors that are not typically expressed in other MSC types [84]. They are a premier source for MSC-derived extracellular vesicles (MSC-EVs), which are nanovesicles carrying bioactive molecules; UC-MSC-EVs are noted for their significant potential in anti-aging and regenerative applications [83]. In comparative studies for treating conditions like premature ovarian failure, UC-MSCs administered intravenously have shown robust therapeutic effects, sometimes outperforming other cell types and administration routes [83].
Table 1: Comparative Overview of MSC Source Characteristics
| Feature | BM-MSCs | AD-MSCs | UC-MSCs |
|---|---|---|---|
| Isolation Procedure | Invasive (bone marrow aspirate) [82] | Minimally invasive (liposuction) [32] | Non-invasive (discarded tissue) [32] |
| Cell Yield | Low | Very High [32] | High [32] |
| Proliferation Capacity | Moderate | High | Very High [32] [83] |
| Osteogenic Potential | High [32] | Moderate | Moderate |
| Chondrogenic Potential | High [32] | Moderate | Moderate |
| Angiogenic Potential | Moderate | Very High [82] | High |
| Immunomodulatory Strength | High [32] | High [32] | High [32] |
| Immunogenicity | Low | Low | Very Low [32] |
Experimental Data and Therapeutic Efficacy
Quantitative Functional Comparisons
Empirical data from preclinical and manufacturing settings provide critical insights into the functional differences between MSC sources. A large-scale analysis of manufacturing data found no significant differences in key quality attributes like population doubling time (PDT) and viability between fresh and cryopreserved BM-MSCs, underscoring the feasibility of cryopreservation for clinical use [37]. Furthermore, the immunophenotype and secretory profile of these cells remained consistent post-thaw, which is crucial for predictable therapeutic performance.
In direct functional comparisons, AD-MSCs have been identified as "more functionally capable" relative to other MSC types in certain contexts, exhibiting a consistent and broad spectrum of gene expression for regulatory and secretory functions [84]. Proteomic studies further solidify these distinctions, revealing that AD-MSCs are "more suitable candidates for angiogenesis models" compared to other MSC types like DPSCs, a finding that is likely extrapolatable to other comparative pairs [82].
Table 2: Comparative Analysis of MSC Therapeutic Applications and Molecular Features
| Aspect | BM-MSCs | AD-MSCs | UC-MSCs |
|---|---|---|---|
| Key Therapeutic Strengths | Gold standard for bone/cartilage repair; Strong immunomodulation [32] | Angiogenesis; Tissue repair; Anti-fibrosis [82] [83] | Allogeneic therapy; Anti-aging; Neuro/ovarian repair [83] |
| Representative Molecular Pathways | Wnt signaling; Cell migration/adhesion [82] | Angiogenesis & vascularization pathways [82] | AMPK/mTOR; PTEN/AKT/FOXO3a [83] |
| Secretome & EV Potential | Potent immunomodulatory EVs [80] | Pro-angiogenic secretome; Mitochondrial transfer [83] | Highly active, young EVs for anti-aging [83] |
| Response to Cryopreservation | Biological signatures remain comparable to fresh [37] | Comparable functionality post-thaw (inferred) | High resilience (inferred from widespread use) |
Detailed Experimental Protocol for MSC Characterization
To ensure the quality and functional potency of MSCs for research and clinical applications, a standardized set of experiments is employed. The following protocol details the key methodologies used to characterize MSCs, as referenced in the search results. Adherence to this protocol is essential for validating MSC identity and function across different tissue sources and preservation states.
Cell Isolation and Culture [85] [82]
- BM-MSCs: Isolate mononuclear cells from bone marrow aspirate via density gradient centrifugation (e.g., Ficoll-Paque). Culture the plastic-adherent fraction in α-MEM or DMEM supplemented with 10% Fetal Bovine Serum (FBS) or human platelet lysate (hPL) under standard conditions (37°C, 5% CO2).
- AD-MSCs: Isolate from subcutaneous adipose tissue aspirates by enzymatic digestion (e.g., collagenase) to obtain the stromal vascular fraction. Culture adherent cells in DMEM-F12 or similar medium with 10% FBS.
- UC-MSCs: Isolate from Wharton's jelly of the umbilical cord by explant culture or enzymatic digestion. Culture in DMEM or α-MEM with 10% FBS.
- Cryopreservation Note: For cryopreserved cells, thaw rapidly in a 37°C water bath, wash to remove cryoprotectant (e.g., DMSO), and plate for culture. Data suggests that with optimized protocols, cryopreserved MSCs can exhibit biological signatures comparable to their freshly preserved counterparts [37].
Immunophenotyping by Flow Cytometry [85] [82]
- Harvest cells at ~80% confluence and prepare a single-cell suspension.
- Incubate 1x10^5 cells with fluorescently labeled antibodies against positive (CD73, CD90, CD105) and negative (CD34, CD45, CD11b, CD19, HLA-DR) markers according to ISCT criteria.
- Analyze stained samples using a flow cytometer (e.g., FACS Aria II). A population is defined as MSCs if ≥95% express positive markers and ≤2% express negative markers.
Trilineage Differentiation Assay [82]
- Osteogenic Differentiation: Culture MSCs in commercial osteogenic induction medium (e.g., OsteoMAX-XF) for 21 days. Fix cells and stain calcium deposits with 2% Alizarin Red S solution.
- Adipogenic Differentiation: Culture MSCs in adipogenic induction medium (e.g., StemPro Adipogenesis Kit) for 21 days. Fix cells and stain lipid vacuoles with Oil Red O solution.
- Chondrogenic Differentiation: Culture pelleted MSCs in chondrogenic medium for 21-28 days. Analyze pellets via histological sectioning and staining with Alcian Blue or Toluidine Blue for sulfated glycosaminoglycans.
Small Extracellular Vesicle (sEV) Isolation and Characterization [80] [85]
- Isolation: Collect conditioned medium from MSC cultures. Isolate sEVs using Tangential Flow Filtration (TFF) or Ultracentrifugation (UC). TFF is reported to yield a higher particle count compared to UC [85].
- Characterization:
- Nanoparticle Tracking Analysis (NTA): Determine the size distribution and concentration of isolated particles.
- Transmission Electron Microscopy (TEM): Confirm the cup-shaped morphology characteristic of sEVs.
- Western Blotting: Verify the presence of sEV markers (CD9, CD63, TSG101) and absence of negative markers (e.g., calnexin).
Diagram 1: Experimental workflow for the comprehensive characterization of Mesenchymal Stem Cells (MSCs), covering from tissue source selection to final data validation. The process ensures cells meet ISCT criteria and functional potency standards.
Mechanisms of Action and Signaling Pathways
The therapeutic effects of BM-MSCs, AD-MSCs, and UC-MSCs are mediated through complex molecular mechanisms, primarily via paracrine secretion and direct cell-cell interactions [81] [32]. While all MSC types share common mechanisms like immunomodulation, their specific signaling pathways and molecular effectors can be source-dependent.
BM-MSCs: Their therapeutic actions are heavily influenced by pathways regulating cell migration and adhesion, as well as Wnt signaling, which is crucial for tissue development and repair [82]. They modulate immune responses by suppressing T-cell activation, inhibiting dendritic cell maturation, and inducing M2 macrophage polarization through the secretion of factors like prostaglandin E2 (PGE2) [81] [32].
AD-MSCs: Proteomic analyses explicitly associate AD-MSCs with pathways involved in angiogenesis and vascularization [82]. This makes their secretome particularly potent for restoring blood flow in ischemic tissues. A notable mechanism is mitochondrial transfer to damaged cells, which has been demonstrated to improve oocyte quality in aged models, a function highlighted for AD-MSCs in the context of aging [83].
UC-MSCs: As a younger cell source, UC-MSCs employ pathways relevant to development and cell survival. In treating premature ovarian failure, they have been shown to modulate the AMPK/mTOR pathway to inhibit excessive autophagy in ovarian granulosa cells and the PTEN/AKT/FOXO3a pathway to reduce apoptosis and promote survival [83]. Their derived exosomes carry a cargo of biomolecules that can simultaneously regulate multiple such pathways to combat hallmarks of aging [83].
Diagram 2: Key signaling pathways implicated in the therapeutic mechanism of Umbilical Cord-MSCs (UC-MSCs) for treating conditions like premature ovarian failure, based on preclinical studies.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials essential for conducting the experiments described in this guide, based on methodologies from the search results.
Table 3: Essential Reagents and Materials for MSC Research
| Reagent/Material | Specific Example | Function in MSC Research |
|---|---|---|
| Culture Medium | Alpha-MEM (α-MEM), Dulbecco’s Modified Eagle Medium (DMEM) | Base nutrient medium for cell growth and expansion. α-MEM may support higher proliferation and EV yield for BM-MSCs [85]. |
| Serum Supplement | Fetal Bovine Serum (FBS), Human Platelet Lysate (hPL) | Provides essential growth factors and adhesion proteins for cell proliferation. hPL is a xeno-free alternative for clinical-grade manufacturing [85]. |
| Isolation Enzymes | Collagenase | Enzymatic digestion of tissues (e.g., adipose) to isolate the stromal vascular fraction containing AD-MSCs [82]. |
| Flow Cytometry Antibodies | Anti-human CD73, CD90, CD105, CD34, CD45, HLA-DR | Immunophenotyping to confirm MSC identity according to ISCT criteria [85] [82]. |
| Differentiation Kits | OsteoMAX-XF, StemPro Adipogenesis Kit | Defined media formulations to induce osteogenic and adipogenic differentiation for functional validation [82]. |
| EV Isolation System | Tangential Flow Filtration (TFF) system | Scalable and efficient isolation of small extracellular vesicles (sEVs) from conditioned medium, yielding higher particles than ultracentrifugation [85]. |
| Characterization Tools | Nanoparticle Tracking Analyzer (NTA), Transmission Electron Microscope (TEM) | Determine the size, concentration, and morphology of isolated sEVs [85]. |
The comparative analysis of BM-MSCs, AD-MSCs, and UC-MSCs reveals a landscape of complementary strengths rather than a single superior source. BM-MSCs remain the benchmark for musculoskeletal applications, AD-MSCs excel in angiogenic and soft tissue repair contexts, and UC-MSCs offer superior proliferative capacity and low immunogenicity for allogeneic and anti-aging therapies. The choice of source is therefore application-dependent.
Critically, within the context of fresh versus cryopreserved biological signatures, evidence indicates that cryopreservation, when optimized, does not significantly alter the fundamental biological properties of MSCs, supporting their practical use in clinical logistics [37]. Future research must focus on deeper molecular profiling to fully elucidate the source-specific mechanisms of action and to standardize differentiation and potency assays. This will enable more precise matching of MSC source to clinical indication, ultimately advancing the field of regenerative medicine.
The transition of mesenchymal stem cells (MSCs) from laboratory research to clinical applications represents one of the most promising yet challenging frontiers in regenerative medicine. As of March 2022, over 1,097 active clinical trials involving MSCs were registered, exploring their potential for conditions ranging from autoimmune diseases and inflammatory disorders to neurodegenerative diseases and orthopedic injuries [18] [32]. Despite this extensive investigation, clinical trial outcomes have demonstrated notable variability, with efficacy often falling short of promising preclinical results [86] [81].
A crucial factor underlying this inconsistency lies in the biological characteristics of the MSC products themselves. Among the most significant variables is the decision to administer freshly cultured versus cryopreserved cells—a choice that impacts logistical feasibility, therapeutic potency, and ultimately, patient outcomes [18] [86]. This guide provides a systematic comparison of fresh versus cryopreserved MSC products, examining how their biological signatures correlate with performance in clinical settings. For researchers and drug development professionals, understanding these correlations is essential for designing trials that can accurately assess therapeutic efficacy and advance the field toward reliable clinical applications.
Biological and Functional Comparisons: Fresh vs. Cryopreserved MSCs
In Vivo Efficacy and In Vitro Potency
A comprehensive systematic review of preclinical models provides critical insights into the functional differences between preservation methods. Analyzing 18 studies encompassing 257 in vivo experiments revealed that only 2.3% (6/257) of outcomes showed statistically significant differences between fresh and cryopreserved MSCs [18]. When differences did occur, they did not consistently favor one preparation method over the other [18].
Table 1: In Vivo Preclinical Efficacy Outcomes
| Outcome Category | Total Experiments | Significantly Different Outcomes | Favoring Fresh MSCs | Favoring Cryopreserved MSCs |
|---|---|---|---|---|
| Overall In Vivo Efficacy | 257 | 6 (2.3%) | 2 | 4 |
| Inflammation Reduction | Not specified | No significant difference | - | - |
| Tissue Repair Markers | Not specified | No significant difference | - | - |
| Organ Function | Not specified | No significant difference | - | - |
In vitro assessments told a slightly different story. Among 68 experiments measuring various potency metrics, 13% (9/68) demonstrated significant differences, with the majority (seven experiments) favoring freshly cultured MSCs [18]. This discrepancy between in vitro and in vivo results suggests that while cryopreservation may affect certain cellular functions measurable in laboratory assays, these changes may not necessarily translate to meaningful differences in therapeutic efficacy in living organisms.
Table 2: In Vitro Potency Comparisons
| Potency Measure | Total Experiments | Significantly Different Outcomes | Favoring Fresh MSCs | Favoring Cryopreserved MSCs |
|---|---|---|---|---|
| Overall In Vitro Potency | 68 | 9 (13%) | 7 | 2 |
| Immunomodulatory Function | Not specified | Mixed results | - | - |
| Paracrine Factor Secretion | Not specified | Generally comparable | - | - |
| Cell Viability | Not specified | Comparable with optimized protocols | - | - |
Phenotypic and Secretory Profiles
Large-scale analyses of manufacturing data have provided further evidence of biological comparability. One study examining approximately 2,300 stem cell manufacturing cases found that cryopreserved and fresh bone marrow-derived MSCs exhibited comparable phenotypic profiles across 60 different variables, including immunophenotype and paracrine molecule secretion [33].
Most immunophenotypes (except for CD14) and paracrine molecules did not exhibit different mean levels or concentrations between the frozen and unfrozen MSC groups [33]. Circular clustering analysis of the combined dataset revealed no distinct separation between the two preservation methods, indicating that the overall biological signatures remain remarkably similar despite the freezing process [33].
Clinical Trial Correlations: Connecting Product Attributes to Outcomes
Cardiovascular Applications
The therapeutic efficacy of cryopreserved MSCs has demonstrated particular promise in cardiovascular disease applications. A 2025 meta-analysis of seven randomized controlled trials (encompassing 285 patients) revealed that cryopreserved MSCs significantly improved left ventricular ejection fraction (LVEF) by 2.11% during short-term follow-up compared to control groups [56].
Table 3: Clinical Outcomes in Cardiovascular Applications
| Outcome Measure | Cryopreserved MSC Performance | Influencing Factors |
|---|---|---|
| Left Ventricular Ejection Fraction (LVEF) | 2.11% improvement (short-term) | Most effective with UC-MSCs; effect not sustained at 12 months |
| LVEF with >80% Post-Thaw Viability | 3.44% improvement | Viability threshold critical for efficacy |
| Major Adverse Cardiac Events (MACE) | No significant difference from control | Demonstrates safety profile |
| Mortality and Readmission | No significant difference from control | - |
Subgroup analysis provided crucial insights into quality attributes that correlate with improved outcomes. When cryopreserved MSCs with post-thaw viability exceeding 80% were used, the improvement in LVEF was substantially greater at 3.44% [56]. Furthermore, umbilical cord-derived MSCs (UC-MSCs) emerged as the most effective cell type for cardiovascular applications among those studied [56].
Cancer Therapy Applications
The functionality of cryopreserved MSCs extends to engineered cells for cancer therapy. Research evaluating MSCs transiently transfected to express a therapeutic transgene (CD::UPRT::GFP) found that cryopreservation for up to 11 months did not diminish anti-cancer potency in vitro or in vivo [23].
Notably, in clinical applications treating "no-option-left" canine patients with spontaneous tumors, cryopreserved, genetically modified MSCs demonstrated remarkable efficacy, with patients showing progression-free intervals exceeding 20 months [23]. This suggests that properly preserved MSC-based therapies can maintain their targeted therapeutic capabilities even after extended storage.
Methodological Protocols: Standardizing Comparative Assessments
Cryopreservation and Thawing Protocols
Standardized protocols are essential for ensuring consistent MSC performance post-thaw. The following methodology has been validated in studies demonstrating maintained MSC functionality after cryopreservation [23]:
Cryopreservation Protocol:
- Harvesting: Wash cells twice with Plasma-Lyte A or similar solution and harvest using TrypLE Express or other enzymatic dissociation agents.
- Cryomedium: Resuspend cell pellets in commercial, GMP-grade cryopreservation media such as CryoStor10 at concentrations of 1-3 × 10^6 cells/mL.
- Freezing: Transfer cryovials to controlled-rate freezing containers (e.g., Mr. Frosty Freezing Container) for overnight freezing at -80°C before long-term storage in liquid nitrogen vapor.
Thawing and Preparation Protocol:
- Thawing: Use automated thawing systems (e.g., ThawSTAR Automated Thawing System) or 37°C water bath with gentle agitation.
- Washing: Resuspend thawed cells in 4mL of Plasma-Lyte A or similar solution, followed by centrifugation at 300 × g for 5 minutes.
- Post-thaw Assessment: Determine viability using trypan blue exclusion or automated cell counters (e.g., NucleoCounter NC-3000). Assess functionality through migration assays, phenotypic characterization, and potency assays.
Quality Assessment Methodologies
Rigorous quality assessment is critical for correlating product attributes with clinical outcomes. The following experimental approaches are recommended based on current evidence:
Viability and Phenotypic Assessment:
- Viability Analysis: Perform trypan blue exclusion assays or use automated cell counting systems with acridine orange (AO) and DAPI staining.
- Phenotypic Characterization: Assess surface marker expression (CD73, CD90, CD105, CD14, CD34, CD45) via flow cytometry, ensuring ≥90% expression of positive markers and ≤3% expression of negative markers for clinical-grade MSCs [33].
Functional Potency Assays:
- Migration Capacity: Evaluate using matrigel invasion assays and CXCR4 receptor expression analysis.
- Immunomodulatory Function: Assess through PBMC suppression assays, IDO-1 expression after IFN-γ stimulation, and T-cell proliferation inhibition.
- Anti-cancer Potency: For engineered MSCs, conduct co-culture studies with cancer cell lines and measure cytotoxicity in presence of prodrugs (e.g., 5-flucytosine for CD::UPRT-expressing MSCs).
MSC Product Characterization and Outcome Correlation Pathway
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Essential Research Reagents for MSC Characterization
| Reagent/Material | Function | Application Examples |
|---|---|---|
| CryoStor10 | GMP-grade cryopreservation medium | Cell freezing in validated, optimized formulation [23] |
| Plasma-Lyte A | Washing and resuspension buffer | Removing cryoprotectants post-thaw; preparation for administration [23] |
| TrypLE Express | Enzymatic dissociation | Cell harvesting while maintaining viability [23] |
| FBS/FBS-containing media | Cell culture and expansion | In vitro propagation while maintaining MSC properties [33] |
| Flow cytometry antibodies | Phenotypic characterization | Confirmation of CD73, CD90, CD105 expression; absence of hematopoietic markers [33] |
| Matrigel | Migration capacity assessment | Invasion assays to evaluate homing potential [23] |
| ELISA kits | Secretory profile analysis | Quantification of VEGF, HGF, TGF-β, other paracrine factors [18] |
| PBMC suppression assay components | Immunomodulatory function testing | Evaluation of therapeutic potency through immune cell interaction [86] |
Analytical Framework: Connecting Characterization to Clinical Outcomes
Understanding the relationship between specific MSC product characteristics and their corresponding clinical effects enables more precise trial design and outcome interpretation. The following diagram illustrates the analytical workflow for correlating product attributes with clinical outcomes:
Analytical Framework for Correlating MSC Properties and Outcomes
The comprehensive analysis of current evidence indicates that cryopreserved MSCs generally maintain critical biological and functional characteristics comparable to their freshly cultured counterparts. While minor differences in certain in vitro potency measures exist, these rarely translate to significant distinctions in preclinical in vivo efficacy or clinical outcomes [18] [33].
The correlation between specific product attributes—particularly post-thaw viability exceeding 80%—and improved clinical outcomes underscores the importance of rigorous quality control in MSC-based therapies [56]. Furthermore, the tissue source of MSCs (with umbilical cord-derived cells demonstrating particular promise for cardiovascular applications) represents another significant variable influencing therapeutic efficacy [56].
For researchers and drug development professionals, these findings support the feasibility of utilizing cryopreserved, "off-the-shelf" MSC products while highlighting the critical need for comprehensive characterization and reporting of product attributes. Standardized protocols for cryopreservation, thawing, and quality assessment—coupled with transparent reporting of critical parameters including viability, phenotypic profile, and potency measures—will enhance the reliability and interpretability of clinical trial outcomes. Through such rigorous approaches, the field can advance toward more consistent and effective MSC-based therapies that fulfill their promising therapeutic potential.
Conclusion
Synthesizing evidence across foundational biology, methodology, and comparative validation reveals that cryopreserved MSCs largely retain the core biological signatures of their freshly cultured counterparts, supporting their feasibility as 'off-the-shelf' therapeutics. The majority of preclinical in vivo efficacy and in vitro potency outcomes show no significant differences. However, a nuanced understanding is crucial: a transient reduction in immunomodulatory activity immediately post-thaw—the 'cryo-stun' effect—and subtle, source-dependent shifts in differentiation potential require optimized protocols and recovery strategies. Future efforts must focus on standardizing potency assays that mirror clinical reality, developing universally accepted xeno-free cryopreservation media, and conducting prospective, double-blinded clinical trials. These steps are imperative to fully unleash the clinical potential of MSC therapies and ensure their consistent safety and efficacy for a broad range of human diseases.
References
- 1. Mesenchymal Stem Cell (MSC) Markers [https://www.novusbio.com/research-areas/stem-cells/mesenchymal-stem-cell-markers?srsltid=AfmBOoq7M1l9N4Dhf7RkjAWY3e6tJdJxNn4YEinfvAAqmgFjJVjpBZ0i]
- 2. Mesenchymal stem cell [https://en.wikipedia.org/wiki/Mesenchymal_stem_cell]
- 3. The heterogeneity of mesenchymal stem cells: an important ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03587-y]
- 4. Trilineage Differentiation of Multipotent Human ... [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/cell-culture-and-cell-culture-analysis/primary-cell-culture/mesenchymal-stem-cell-differentiation?srsltid=AfmBOop1bD30jJKaL0ZjyDvbuWXwTcPVAC8Vy_eE_nHJgR534_CU5rrD]
- 5. Comparative Analysis of Biological Signatures between ... [https://pubmed.ncbi.nlm.nih.gov/37830568/]
- 6. CD73, CD90, CD105 and Cadherin-11 RT-PCR Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5984056/]
- 7. Spheroid trilineage differentiation model of primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11321963/]
- 8. Cryopreservation with DMSO affects the DNA integrity ... [https://www.sciencedirect.com/science/article/abs/pii/S0011224024000026]
- 9. Dimethyl sulfoxide in cryopreserved mesenchymal stromal cell ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06807-6]
- 10. The Role of Cryoprotectants in ATMP Cryopreservation [https://www.susupport.com/blogs/knowledge/stressing-cells-role-cryoprotectants-atmp-cryopreservation]
- 11. Cryopreservation: An Overview of Principles and Cell- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7995302/]
- 12. Chemical approaches to cryopreservation [https://www.nature.com/articles/s41570-022-00407-4]
- 13. Comparison of freshly cultured versus cryopreserved ... [https://elifesciences.org/articles/75053]
- 14. Study of the biological characteristics of human umbilical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9675661/]
- 15. Key quality parameter comparison of mesenchymal stem ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1412811/full]
- 16. Effects, methods and limits of the cryopreservation on ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03954-3]
- 17. Biological functions of mesenchymal stem cells and clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11105258/]
- 18. Comparison of freshly cultured versus cryopreserved ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9286731/]
- 19. Comparison of freshly cultured versus cryopreserved ... [https://pubmed.ncbi.nlm.nih.gov/35838024/]
- 20. Thawed Mesenchymal Stem Cell Product Shows Comparable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6889371/]
- 21. Key quality parameter comparison of mesenchymal stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11324487/]
- 22. Quantitative assessment of the impact of cryopreservation on ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-02054-2]
- 23. Cryopreservation does not change the performance and ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-03198-z]
- 24. Translational potential of mesenchymal stem cells in ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03885-z]
- 25. Understanding the molecular basis of mesenchymal stem ... [https://www.nature.com/articles/s41419-025-08094-x]
- 26. Action of Mesenchymal Stem Cells Revealed... | PLOS One Paracrine [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0129164]
- 27. Transcriptomic Comparisons of Somatic and Cancer Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383795/]
- 28. A transcriptome-based human universal senescence index ... [https://www.nature.com/articles/s43587-025-00886-2]
- 29. Properties of MSC populations enriched in CD146 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12500659/]
- 30. Across the space: applications of spatial transcriptomic ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1656918/full]
- 31. Quality management overview for the production of a tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10588160/]
- 32. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 33. Comparative Analysis of Biological Signatures between ... [https://www.mdpi.com/2073-4409/12/19/2355]
- 34. Properties of MSC populations enriched in CD146 ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1668681/full]
- 35. Comparison of a commercial trehalose-based and laboratory ... [https://mefj.springeropen.com/articles/10.1186/s43043-025-00224-x]
- 36. Optimization of freezing and thawing protocols for human ... [https://www.sciencedirect.com/science/article/pii/S0011224025000513]
- 37. Comparative Analysis of Biological Signatures between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10571833/]
- 38. Viability of dental pulp derived stem cells after long-term ... [https://www.sciencedirect.com/science/article/pii/S0099239925005977]
- 39. Evaluation of the viability and functionality of human ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1627973/full]
- 40. Cryopreservation and post-thaw differentiation of monocytes ... [https://pubs.rsc.org/en/content/articlehtml/2025/lp/d5lp00131e]
- 41. Comparison of freshly ... cultured versus freshly thawed [https://link.springer.com/article/10.1186/s13643-020-01437-z]
- 42. Mesenchymal Stromal Cells Maintain Potency in... Cryopreserved [https://www.nature.com/articles/srep26463?error=cookies_not_supported&code=39ece5ea-773f-4717-8b01-a24ea803a4a9]
- 43. Dealing with Cryopreservation Challenges in ... [https://www.atlantisbioscience.com/blog/dealing-with-cryopreservation-challenges-in-mesenchymal-stem-cell-culture/?srsltid=AfmBOooI-1F_NEKi-UZ4D1-2gf0iBJltD-6ebrxkHacL5tmL_KEb2wvu]
- 44. Optimizing mesenchymal stem cell therapy: from isolation ... [https://pubmed.ncbi.nlm.nih.gov/40329219/]
- 45. Comparison of freshly cultured versus freshly thawed ... [https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-020-01437-z]
- 46. Identification of critical process parameters and quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12408662/]
- 47. Clinical-grade allogeneic amniotic fluid stem cell banking [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04654-2]
- 48. Safety Assessment of Stem Cell-Based Therapies [https://www.mdpi.com/2073-4409/14/21/1660]
- 49. Comparative analysis of cryopreserved adipose stem cells ... [https://www.nature.com/articles/s41598-024-83255-0]
- 50. Comparative analysis and process optimization for ... [https://www.nature.com/articles/s41598-025-89686-7]
- 51. Comprehensive analysis of secretome and transcriptome ... [https://www.sciencedirect.com/science/article/pii/S1465324924008284]
- 52. Cryopreserved or Fresh Mesenchymal Stromal Cells [https://pubmed.ncbi.nlm.nih.gov/27837556/]
- 53. Impact of Cryopreservation and Freeze-Thawing on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9045030/]
- 54. Actin Cytoskeletal Disruption following Cryopreservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4110775/]
- 55. Cryopreserved Mesenchymal Stromal Cells Maintain ... [https://www.nature.com/articles/srep26463]
- 56. Clinical experience with cryopreserved mesenchymal stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11947892/]
- 57. Correlation with loss of adhesion and altered cell size [https://www.sciencedirect.com/science/article/abs/pii/S1465324918305413]
- 58. Evaluation of the viability and functionality of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12355051/]
- 59. Exploring the therapeutic potential of MSC-derived ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04616-8]
- 60. Overcoming challenges in MSC-sEV therapeutics [https://www.sciencedirect.com/science/article/pii/S1465324925005912]
- 61. Evia Bio® Introduces CellShield TM MSC DMSO-Free ... [https://www.biospace.com/press-releases/evia-bio-introduces-cellshieldtm-msc-dmso-free-cryopreservation-media-kit]
- 62. Effect of Rho-associated kinase (ROCK) inhibitor Y-27632 ... [https://www.sciencedirect.com/science/article/abs/pii/S004081660900010X]
- 63. Post-thaw application of ROCK-inhibitors increases cryopreserved T-cell yield - RSC Medicinal Chemistry (RSC Publishing) DOI:10.1039/D3MD00378G [https://pubs.rsc.org/en/content/articlehtml/2023/md/d3md00378g]
- 64. The Effects of Different Doses of ROCK Inhibitor, Antifreeze ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9698151/]
- 65. Introduction to ROCK inhibitors for hPSC culture [https://captivatebio.com/rock-inhibitor-overview/]
- 66. ROCK Inhibitor for Stem Cell Cryopreservation | Tocris Bioscience [https://www.tocris.com/resources/tocris-blog/rock-inhibitor-stem-cell-cryopreservation]
- 67. Cryopreserved mesenchymal stem cells regain functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6716839/]
- 68. The Utilization of Freezing Steps in Mesenchymal Stromal ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.01627/full]
- 69. Clinical mesenchymal stromal cell products undergo ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324914007865]
- 70. Thrombogenic Risk Induced by Intravascular Mesenchymal ... [https://www.mdpi.com/2073-4409/8/10/1160]
- 71. Intravascular Mesenchymal Stromal/Stem Cell Therapy ... [https://www.sciencedirect.com/science/article/pii/S1471491418302405]
- 72. Infusion-related thrombogenesis by liver-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7006410/]
- 73. Open Randomized Multicenter Study to Evaluate Safety ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6389380/]
- 74. Mesenchymal Stem Cell Immunomodulation: Mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7751844/]
- 75. Comparing the Immunomodulatory Properties of Bone ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2015.00560/full]
- 76. Comparing the Immunomodulatory Properties of Bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4630659/]
- 77. In-vitro immunomodulatory efficacy of extracellular vesicles ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04476-2]
- 78. Unveiling the Immunomodulatory and regenerative ... [https://www.nature.com/articles/s41598-024-75956-3]
- 79. Tissue-specific Differentiation Potency of Mesenchymal ... [https://www.nature.com/articles/srep23544]
- 80. Umbrella review of mesenchymal stem cell-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554768/]
- 81. Mesenchymal stromal cell therapy: Progress to date and ... [https://www.sciencedirect.com/science/article/pii/S1525001625000930]
- 82. Proteomic Study Revealed a Distinction Between Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12408728/]
- 83. Advances in mesenchymal stem cell and exosome-based ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04318-1]
- 84. Unveiling distinctions between mesenchymal stromal cells ... [https://www.sciencedirect.com/science/article/pii/S2405844025006917]
- 85. Comparison of production methods for mesenchymal stem ... [https://www.nature.com/articles/s41598-025-21218-9]
- 86. From Vial to Vein: Crucial Gaps in Mesenchymal Stromal ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.867426/full]