GMP Cleanroom Classification for Cell Therapy: Standards, Implementation & Validation Guide 2024
This definitive guide for researchers, scientists, and drug development professionals explores the critical role of GMP cleanroom classification in cell therapy manufacturing.
GMP Cleanroom Classification for Cell Therapy: Standards, Implementation & Validation Guide 2024
Abstract
This definitive guide for researchers, scientists, and drug development professionals explores the critical role of GMP cleanroom classification in cell therapy manufacturing. Covering foundational ISO standards and regulatory frameworks, the article details practical methodologies for achieving and maintaining classified environments. It provides actionable troubleshooting strategies for common contamination and compliance challenges, and compares global validation approaches. The guide synthesizes key principles for ensuring product safety, efficacy, and regulatory approval in advanced therapeutic medicinal product (ATMP) production.
Understanding GMP Cleanroom Basics: ISO Standards and Regulatory Frameworks for Cell Therapy
In the field of cell therapy research, the production of Advanced Therapy Medicinal Products (ATMPs) demands an environment of unparalleled control to ensure product safety, efficacy, and consistency. Contamination, whether from particulate or microbial sources, can compromise cellular products, leading to patient risk and trial failure. The foundation of this environmental control is the cleanroom, a space with defined limits for the introduction, generation, and retention of airborne particulates. The international standard ISO 14644-1, "Classification of air cleanliness by particle concentration," provides the definitive framework for classifying these critical environments. This guide details the ISO 14644-1 classes (specifically A, B, C, and D as adopted by GMP) and their profound significance in the context of Good Manufacturing Practice (GMP) for cell therapy research and drug development.
ISO 14644-1 Classification System: Core Principles
ISO 14644-1 classifies cleanrooms based on the concentration of airborne particles equal to and larger than a specified size (e.g., ≥0.5 µm). The classification is designated by an "ISO Class" number, where a lower number signifies a cleaner environment (fewer allowable particles). The standard outlines statistical methods for sampling and testing to verify compliance. For GMP applications, particularly in sterile manufacturing for pharmaceuticals and biologics, the European Union GMP Annex 1 and other regulatory documents map these ISO classes to grades (A, B, C, D) for operational clarity.
Detailed Class Specifications & GMP Correlation
The following table summarizes the maximum permitted particle concentrations per cubic meter for key ISO classes and their corresponding GMP grades, which are critical for cell therapy operations.
Table 1: ISO 14644-1 Particle Concentration Limits and GMP Grade Equivalents
| ISO 14644-1 Class | ≥0.5 µm particles / m³ | ≥5.0 µm particles / m³ | Equivalent EU GMP Grade (Operational State) | Typical Applications in Cell Therapy |
|---|---|---|---|---|
| ISO 5 | 3,520 | 29 | Grade A | Critical processing zone (e.g., cell manipulation, filling, open connections). |
| ISO 7 | 352,000 | 2,930 | Grade B | Background environment for a Grade A zone (e.g., cleanroom suite for aseptic processing). |
| ISO 8 | 3,520,000 | 29,300 | Grade C | Preparation of less critical solutions, background for Grade A/B areas, gowning. |
| ISO 9 | 35,200,000 | 293,000 | Grade D | Component and material staging, basic background for cleaner areas. |
Note: Limits are derived from the formula: *particle concentration = 10^N × (0.1/D)^2.08, where N is the ISO class number and D is the particle size in µm. The GMP grades (A-D) define not only particle limits but also microbial action levels and operational conditions (at-rest, in-operation).*
Experimental Protocol: Cleanroom Classification Testing (ISO 14644-1)
The verification of a cleanroom's ISO class requires a standardized testing protocol. Below is the core methodology.
4.1. Objective: To determine the concentration of airborne particles in a cleanroom or clean zone and verify compliance with the specified ISO class.
4.2. Key Equipment & Materials (The Scientist's Toolkit):
Table 2: Key Research Reagent Solutions & Materials for Classification Testing
| Item | Function |
|---|---|
| Discrete Particle Counter (DPC) | Primary instrument for sampling and sizing airborne particles. Must be calibrated and have a suitable flow rate (e.g., 1 CFM or 28.3 L/min). |
| Isopropyl Alcohol (IPA), 70% | Used for cleaning sampling probes and external surfaces of the DPC before entering the cleanroom. |
| Particle-Free Wipes | For general cleaning of equipment and surfaces to prevent sample contamination. |
| Validation Kit (Optional) | Aerosolizer and certified reference particles (e.g., polystyrene latex spheres) for challenging the DPC for performance checks. |
| Sampling Probe & Tubing | Connects the DPC intake to the specific location being sampled. Must be particle-shedding resistant and of appropriate length. |
| Tripod & Adjustable Arm | To position the sampling probe at the correct, stable height for testing. |
4.3. Methodology:
- Preparation: Clean the DPC and sampling accessories with IPA wipes outside the cleanroom. Allow the DPC to complete its self-check and zero-count procedure.
- Determine Sampling Locations: Calculate the minimum number of sampling locations (Nₗ) using the formula: Nₗ = √A, where A is the area of the cleanroom in m². Distribute locations evenly across the room.
- Set Test Parameters: Program the DPC with the relevant particle size thresholds (e.g., 0.5 µm and 5.0 µm).
- Perform Particle Counting: At each location, position the sampling probe at the specified work height (e.g., 0.8-1.2 m). Take a sample volume of air sufficient to count at least 20 particles for the target size. Per ISO, the minimum single sample volume is 1 liter for ISO 5, and 2 liters for others.
- Data Analysis: For each location, calculate the average particle concentration per cubic meter for each particle size. Calculate the overall mean and 95% upper confidence limit (UCL) from all locations. The cleanroom meets the classification if the UCL is at or below the class limit.
Significance in Cell Therapy GMP
The classification is not an end in itself but a cornerstone of contamination control strategy (CCS). For cell therapies:
- Grade A/ISO 5: Mandatory for all aseptic handling of open product containers. Protects the sterile product directly from particulate and microbial contamination.
- Grade B/ISO 7: Provides a controlled background that protects the Grade A zone from adjacent areas, ensuring its performance.
- Grades C & D/ISO 8 & 9: Serve as progressively less critical buffers, controlling the flow of personnel, materials, and air to prevent ingress of contamination into higher-grade areas.
This cascading pressure and classification system is fundamental to managing the inherent risks of aseptic processing for products that cannot be terminally sterilized, such as living cell therapies.
Logical Relationship: From Classification to Contamination Control
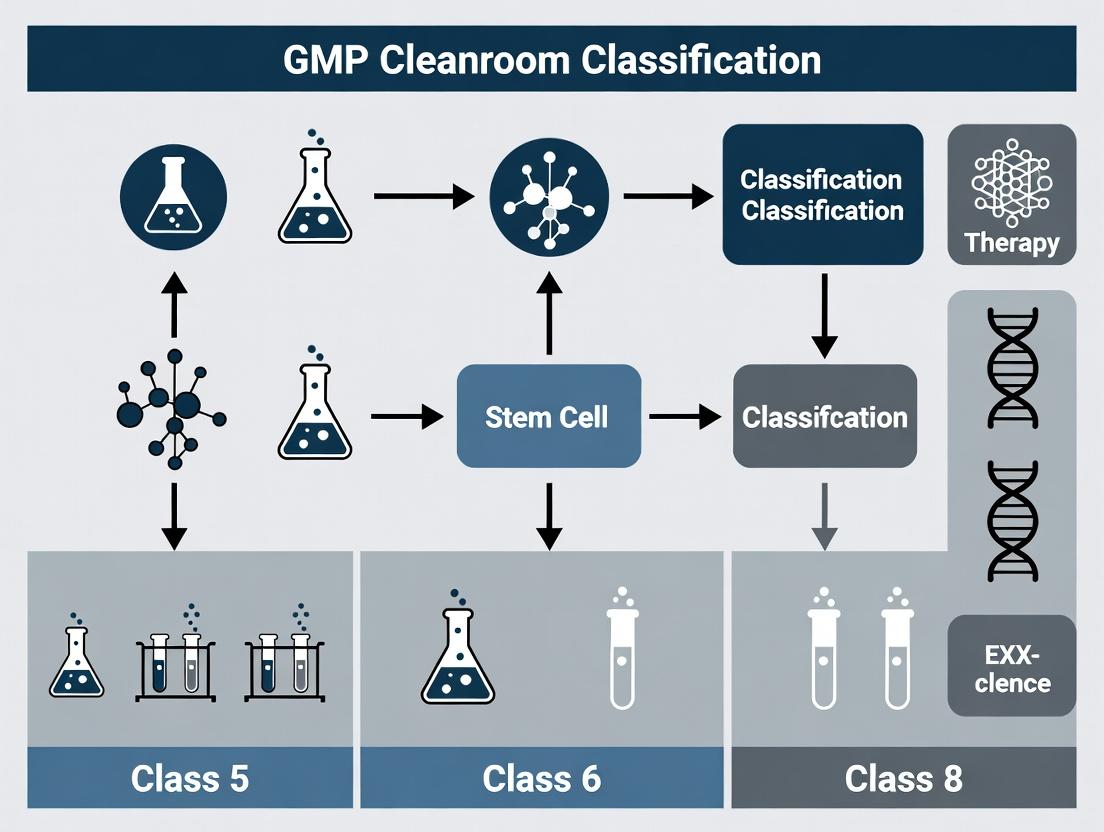
The following diagram illustrates the logical flow from the core ISO classification standard to the ultimate goal of patient safety in cell therapy.
Diagram 1: Cleanroom Class to Product Safety Flow
The ISO 14644-1 classification system, as enacted through GMP grades A-D, provides the quantitative, science-based backbone for designing, verifying, and operating cleanrooms for cell therapy research and manufacturing. Understanding the specific particle limits, testing methodologies, and operational significance of each class is non-negotiable for scientists and professionals developing these life-changing therapies. It ensures that the controlled environment is a reliable tool—not a variable—in the quest for consistent, safe, and efficacious advanced medicinal products.
Why Cleanroom Classification is Non-Negotiable for Cell Therapy Product Safety and Efficacy
In the advanced therapeutic medicinal product (ATMP) landscape, cell therapies represent a paradigm shift in treating degenerative and oncological diseases. The intrinsic biological nature of these products—living cells—renders them uniquely vulnerable to contamination and environmental stressors. Unlike traditional pharmaceuticals, they cannot undergo terminal sterilization. Consequently, their safety and efficacy are irrevocably tied to the aseptic conditions of their manufacturing environment. This whitepaper establishes cleanroom classification, as defined by ISO 14644 and EU GMP Annex 1, as the foundational pillar of Current Good Manufacturing Practice (cGMP) for cell therapy. It argues that rigorous classification is non-negotiable for controlling critical parameters like airborne particulate and microbial contamination, directly impacting product purity, patient safety, and regulatory approval.
The Science of Contamination Risk in Cell Therapy
Cell therapy products, including chimeric antigen receptor T-cells (CAR-T) and mesenchymal stem cells (MSCs), are cultured over days or weeks, providing an extended window for contamination. Microbial ingress (bacteria, fungi, mycoplasma) can outcompete or toxify cell cultures, while non-viable particulates can introduce endotoxins or act as carriers for viable contaminants. Most critically, a single contaminant introduced during manufacturing can proliferate to dangerous levels in the final infusion bag, posing severe risks of sepsis or death to the immunocompromised recipient.
Table 1: Impact of Environmental Contaminants on Cell Therapy Products
| Contaminant Type | Direct Impact on Product | Risk to Patient |
|---|---|---|
| Bacteria | Culture overgrowth, nutrient depletion, toxin release. | Sepsis, endotoxic shock. |
| Fungi/Molds | Mycotoxin production, hyphal overgrowth. | Systemic fungal infection. |
| Mycoplasma | Alters cell metabolism, function, and viability; difficult to detect. | Immune modulation, unclear pathological consequences. |
| Endotoxins (from Gram- bacteria) | Binds to cell surfaces, induces inflammatory cytokine release, alters cell phenotype. | Pyrogenic reaction, multi-organ failure. |
| Airborne Particles | Acts as carrier for viable contaminants, introduces foreign materials. | Immune reactions, granuloma formation. |
Cleanroom Classification Standards: ISO and GMP
Cleanroom classification provides a quantifiable framework for contamination control. ISO 14644-1 defines classes based on the maximum allowable concentration of airborne particles of specified sizes. EU GMP Annex 1 (2022) integrates these with additional, stricter requirements for aseptic manufacturing, including microbial monitoring grades (A, B, C, D).
Table 2: Key Cleanroom Class Limits for Aseptic Processing (ISO 14644-1 & EU GMP Annex 1)
| ISO Class | GMP Grade | ≥0.5 µm particles/m³ | ≥5.0 µm particles/m³ | Typical Operations for Cell Therapy |
|---|---|---|---|---|
| ISO 5 | A | 3,520 | 20 | Critical open manipulations (e.g., vial thaw, vector addition, final fill) within a unidirectional airflow cabinet (UDAF) or isolator. |
| ISO 5 | B | 3,520 | 20 | Background environment for a Grade A zone. Gowning for entry into Grade A/B areas. |
| ISO 7 | C | 352,000 | 2,930 | Less-critical closed processing steps (e.g., closed-system centrifugation, incubation). |
| ISO 8 | D | 3,520,000 | 29,300 | Background for Grade C areas. Non-critical support areas. |
Experimental Protocol: Environmental Monitoring (EM) for Classification & Control
Verification and ongoing monitoring of cleanroom classification are mandated. The following protocol details a standard particle count and microbial air sampling procedure.
Protocol: Routine Non-Viable and Viable Particle Monitoring in a Grade B (ISO 5) Cleanroom
Objective: To verify the airborne particulate and microbial counts comply with ISO 5 / Grade B limits at the point of use during simulated critical processing.
Materials: (See Scientist's Toolkit) Method:
- Pre-Sampling: Decontaminate all monitoring equipment with sterile 70% IPA and allow to dry. Transport to the sampling location (e.g., beside the open processing area of a biosafety cabinet).
- Non-Viable Particle Counting:
- Place the airborne particle counter probe at the designated sample location, 9-12 inches from the critical site.
- Set the counter to sample a minimum volume of 1 cubic meter per location as per ISO 14644-1.
- Initiate sampling for the required duration. Record the cumulative counts for particles ≥0.5µm and ≥5.0µm.
- Repeat sampling at a minimum of 3-5 locations within the room/zone.
- Viable Air Monitoring (Active Air Sampling):
- Load a sterile contact plate containing appropriate agar (e.g., TSA for bacteria, SDA for fungi) into the air sampler.
- Position the sampler inlet at the same critical location.
- Set the sampler to draw a calibrated volume of air (typically 1 cubic meter) over the plate.
- After sampling, seal and label the plate. Incubate TSA at 30-35°C for 3-5 days and SDA at 20-25°C for 5-7 days.
- Count resulting colony-forming units (CFUs).
- Data Analysis: Compare average particle counts and CFU results against the alert and action limits derived from ISO and GMP standards. Any excursion triggers an investigation and corrective action.
Title: Cleanroom Environmental Monitoring Workflow
The Scientist's Toolkit: Essential Reagents & Materials for EM
Table 3: Key Research Reagent Solutions for Cleanroom Monitoring
| Item | Function / Role in EM |
|---|---|
| Airborne Particle Counter | Measures the concentration of non-viable airborne particles (≥0.5µm, ≥5.0µm) to verify ISO classification compliance. |
| Active Air Sampler | Draws a calibrated volume of air onto a microbial growth medium for quantifiable CFU analysis. |
| Tryptic Soy Agar (TSA) Plates | General-purpose growth medium for detecting a wide spectrum of bacteria and fungi. |
| Sabouraud Dextrose Agar (SDA) Plates | Selective medium optimized for detecting yeasts and molds. |
| 70% Isopropyl Alcohol (IPA) | Standard cleanroom disinfectant for decontaminating equipment and surfaces prior to monitoring. |
| Contact Plates (RODAC) | For surface microbial monitoring on equipment and operator gloves. Contains neutralizing agents. |
| Particulate Matter Standards | Calibration standards (e.g., polystyrene latex spheres) for verifying particle counter accuracy. |
The Logical Chain: From Classification to Product Success
Cleanroom classification is not an isolated compliance exercise but the first link in a causal chain determining product success. It is the primary engineering control that enables all subsequent process controls to be effective.
Title: Cleanroom Impact on Cell Therapy Success
For cell therapy, the manufacturing environment is an extension of the product itself. Cleanroom classification provides the essential, quantifiable standard for that environment. It is the non-negotiable prerequisite that bridges the gap between promising preclinical science and a safe, effective, and commercially viable clinical product. Investing in rigorous classification, monitoring, and control is ultimately an investment in patient safety and the future of the therapy.
This technical guide examines the key regulatory drivers for Advanced Therapy Medicinal Product (ATMP) manufacturing, with a specific focus on cleanroom classification requirements. Framed within a broader thesis on GMP cleanroom standards for cell therapy research, it provides a comparative analysis of guidelines from the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), and the Pharmaceutical Inspection Co-operation Scheme (PIC/S). The convergence and divergence in these regulatory approaches directly impact facility design, environmental monitoring, and contamination control strategies essential for autologous and allogeneic cell therapy production.
Regulatory Landscape: Comparative Analysis
The following table summarizes the core regulatory documents and their primary focus concerning ATMP manufacturing environments.
| Regulatory Body | Key Guideline / Directive | Title / Reference | Primary Focus for ATMP Manufacturing |
|---|---|---|---|
| FDA (U.S.) | 21 CFR Parts 210, 211, 1271 | Current Good Manufacturing Practice | Integrated approach for drugs and HCT/Ps. Emphasis on prevention of contamination, cross-contamination. Risk-based controls. |
| FDA (U.S.) | Guidance for Industry (2020) | Sterile Drug Products Produced by Aseptic Processing | Aseptic processing fundamentals, cleanroom classification (ISO equivalent), monitoring. Core reference for environmental standards. |
| EMA (EU) | Regulation (EC) No 1394/2007, Directive 2001/83/EC | Advanced Therapy Medicinal Products | Legal framework for ATMPs. Requires GMP compliance per EudraLex Volume 4. Specific considerations for patient-specific products. |
| EMA (EU) | EudraLex Volume 4, Annex 1 (2022) | Manufacture of Sterile Medicinal Products | Legally enforceable GMP. Detailed cleanroom classification (A/B/C/D), contamination control strategy (CCS), isolator/RABS guidance. |
| PIC/S (International) | PI 007-6 (2021) | Recommendation on the Validation of Aseptic Processes | Harmonized guide for aseptic processes. Cleanroom classification aligned with ISO 14644-1 and EU GMP. Promotes global harmonization. |
| PIC/S (International) | PI 045-1 (2022) | Guidance on ATMPs GMP | Dedicated ATMP GMP guide. Flexible, risk-based approach to cleanroom standards, especially for open steps in autologous therapies. |
Quantitative Cleanroom Classification Standards
Cleanroom classification based on airborne particulate concentration is a foundational requirement. The following table compares the maximum permitted particle counts per cubic meter (≥0.5 μm) for each grade/class.
| Grade / Class (EU GMP / ISO) | At Rest (≥0.5 μm particles/m³) | In Operation (≥0.5 μm particles/m³) | Typical Application in ATMPs |
|---|---|---|---|
| Grade A (ISO 5) | 3,520 | 3,520 | Critical aseptic operations (e.g., vial filling, open manipulation of cells). |
| Grade B (ISO 7) | 3,520 | 352,000 | Background environment for Grade A zones (e.g., cleanroom housing a closed isolator). |
| Grade C (ISO 8) | 352,000 | 3,520,000 | Preparation of less critical solutions, background for closed processing steps. |
| Grade D (ISO 8) | 3,520,000 | Not formally defined | Gowning, background for non-critical processing steps. |
Note: FDA aseptic guidance references ISO 14644-1 standards (ISO 5, 7, 8), which are numerically aligned with the "in operation" limits above. EMA Annex 1 (2022) formally adopts the ISO nomenclature alongside Grades A-D.
Experimental Protocol: Viable Environmental Monitoring (EM) for Grade A Zones
A robust EM program is mandated to demonstrate continuous control of the aseptic core.
Title: Settle Plate Exposure for Viable Airborne Contamination Monitoring in a Grade A Laminar Airflow Hood.
Objective: To actively monitor the prevalence of viable, settling microorganisms in a Grade A zone during a simulated cell thawing and feeding operation.
Materials & Equipment:
- Pre-poured Tryptic Soy Agar (TSA) settle plates (90mm diameter).
- Incubator (set at 20-25°C for fungal growth and 30-35°C for bacterial growth).
- Ethanol (70%) and sterile wipes for plate decontamination.
- Timer.
- GMP Grade A zone (Laminar Airflow Hood/Workbench).
Methodology:
- Preparation: Decontaminate the external surface of the settle plate containers with 70% ethanol and allow them to dry. Perform the experiment during a simulated production run ("in operation").
- Placement: Remove the lid from a settle plate. Place the open plate at a predetermined, risk-assessed location within the Grade A zone where product or open containers are exposed (e.g., next to the processing rack). Ensure the plate does not obstruct airflow or the critical process.
- Exposure: Expose the plate for the duration of the critical open step (e.g., 4 hours), as defined in the CCS. Record the start and end times.
- Recovery & Incubation: After exposure, replace the lid. Collect the plate and incubate it according to a dual-incubation regimen:
- First at 30-35°C for 48-72 hours to promote bacterial growth.
- Then at 20-25°C for a further 72-96 hours to promote fungal growth.
- Analysis: Count all colony-forming units (CFUs) after each incubation phase. The acceptance criterion for Grade A per EMA Annex 1 is <1 CFU per plate for a 4-hour exposure. Any deviation must be investigated as a potential breach of aseptic conditions.
- Documentation: Record all data, including plate location, exposure time, incubator details, CFU counts, and any identification of recovered organisms.
The Scientist's Toolkit: Key Reagent Solutions for Process Validation
Essential materials for conducting sterility assurance and process validation studies in ATMP cleanrooms.
| Item / Reagent | Function / Purpose in Context |
|---|---|
| Tryptic Soy Agar (TSA) Plates | General-purpose growth medium for environmental monitoring (settle plates, contact plates, air samplers) to capture a broad spectrum of viable bacteria and fungi. |
| Sabouraud Dextrose Agar (SDA) Plates | Selective medium optimized for isolating and enumerating fungi and yeasts, used as a complementary method to TSA in EM programs. |
| LAL (Limulus Amebocyte Lysate) Reagent | Detect and quantify bacterial endotoxins (pyrogens) in final product samples or critical process water (WFI). Essential for product safety testing. |
| Cell Culture Media (Serum-free, GMP-grade) | Defined, xeno-free formulation for the expansion of therapeutic cells. Minimizes contamination risk and supports regulatory compliance. |
| Process Residual Detection Kits (e.g., for antibiotics, cytokines) | ELISA or PCR-based kits to quantify the clearance of process residuals (like induction agents) during manufacturing, demonstrating process robustness. |
| Mycoplasma Detection Kit (PCR-based) | Rapid, highly sensitive method to test master/working cell banks, harvests, and final products for Mycoplasma contamination, a critical quality attribute. |
| Closed System Processing Assemblies (Tubes, Connectors) | Sterile, functionally closed fluid pathways that maintain asepsis, reducing the classification requirement for the surrounding environment per risk-based guidelines. |
Visualizing the Contamination Control Strategy (CCS) Logic
A holistic CCS is mandated by EMA Annex 1 and expected by FDA and PIC/S.
Title: ATMP Contamination Control Strategy Logic Flow
Visualizing a Risk-Based Aseptic Processing Workflow
Decision-making for environmental controls based on process closure.
Title: Risk-Based Aseptic Processing Decision Tree
The regulatory landscape for ATMP cleanroom manufacturing is defined by the detailed, legally binding requirements of EMA Annex 1, the risk-based framework of the FDA, and the harmonization efforts of PIC/S. A successful compliance strategy hinges on implementing a dynamic, science- and risk-based Contamination Control Strategy (CCS). This CCS must integrate qualified facility design (leveraging ISO 5-8/Grade A-D classifications), validated closed systems where possible, rigorous environmental monitoring, and robust process validation (media fills). For researchers, understanding these interlocking drivers is critical to designing facilities and processes that ensure patient safety, product quality, and regulatory approval across major global markets.
Within the context of Good Manufacturing Practice (GMP) cleanroom classification for cell therapy research, environmental control is non-negotiable. The efficacy and safety of cell-based therapeutics are intrinsically linked to the environment in which they are manufactured. This technical guide details the critical parameters of non-viable particle counts, viable microbial limits, and the essentials of a robust environmental monitoring (EM) program, which together form the cornerstone of contamination control strategies essential for aseptic processing.
Particle Counts: The Foundation of Cleanroom Classification
Non-viable particle monitoring provides the primary data for cleanroom classification per ISO 14644-1 and EU GMP Annex 1. For cell therapy, where products are often minimally manipulated and cannot be terminally sterilized, controlling particulate matter is critical to prevent pyrogenic reactions, physical occlusion upon administration, and potential vector contamination.
Classification Limits and Measurement Protocol
Cleanroom classification is based on the concentration of airborne particles equal to and larger than 0.5 µm and 5.0 µm. The following table summarizes the maximum permitted concentrations for key classifications relevant to cell therapy.
Table 1: ISO 14644-1 Cleanroom Classification Limits (particles/m³ of air)
| ISO Class | ≥0.5 µm Particles | ≥5.0 µm Particles | Typical Application in Cell Therapy |
|---|---|---|---|
| ISO 5 (Class 100) | 3,520 | 29 | Critical processing (e.g., vial filling, open manipulations) within a Grade A zone. |
| ISO 7 (Class 10,000) | 352,000 | 2,930 | Background environment for Grade B aseptic preparation and filling areas. |
| ISO 8 (Class 100,000) | 3,520,000 | 29,300 | Background for Grade C areas (e.g., solution preparation, wash rooms). |
Protocol for Particle Counting:
- Instrument Calibration: Use a calibrated airborne particle counter with a suitable sample flow rate (e.g., 1 cfm or 28.3 L/min).
- Sample Volume & Locations: Determine minimum sample volume per location as per ISO 14644-1. For certification, sample locations are based on the area of the cleanroom. For routine monitoring, place samplers at sites representing worst-case conditions (e.g., near operator, product exposure points).
- Sampling Method: Conduct sampling with the cleanroom in the "at-rest" state (equipment running, no personnel) for classification, and in the "operational" state for routine monitoring.
- Data Analysis: Compare the average concentration at each location to the class limit. The room meets the classification if all locations comply.
Microbial Limits: Controlling Viable Contaminants
Microbial monitoring assesses the bioburden from personnel, materials, and equipment. For cell therapies, microbial contamination can lead to product loss, patient infection, and compromised therapeutic efficacy.
Action and Alert Limits
Microbiological monitoring employs both alert (warning level) and action (investigation/remediation level) limits. Limits are typically established based on historical data, regulatory guidance, and process capability.
Table 2: Example Microbial Monitoring Limits for Different Cleanroom Grades
| Grade | Air Sample (CFU/m³) | Settle Plates (Ø90mm, 4hr, CFU) | Surface Contact (Ø55mm, CFU/plate) | Glove Print (CFU/glove) |
|---|---|---|---|---|
| A | <1 | <1 | <1 | <1 |
| B | 10 | 5 | 5 | 5 |
| C | 100 | 50 | 25 | - |
| D | 200 | 100 | 50 | - |
CFU: Colony Forming Unit
Experimental Protocols for Viable Monitoring
Protocol for Active Air Sampling:
- Use a calibrated volumetric air sampler (e.g., slit-to-agar or centrifugal).
- Load with appropriate growth media (e.g., Tryptic Soy Agar for total aerobic count).
- Sample a defined volume (typically 1 m³) at critical locations.
- Incubate plates: 20-25°C for 5-7 days (fungi) and 30-35°C for 3-5 days (bacteria).
- Count CFUs and identify isolates to species level following aberrant results.
Protocol for Surface Monitoring (Contact Plates):
- Use pre-filled contact plates with neutralizing agar (e.g., D/E Neutralizing Agar) for disinfectant residue neutralization.
- Press the agar surface evenly against a flat test surface for ~5 seconds.
- Cover and incubate as above.
- Report results as CFU/plate.
Environmental Monitoring Program Essentials
An EM program is a holistic system integrating particle, microbial, and physical parameter data to ensure continuous environmental control.
Key Components of an EM Program
- Risk-Based Site Selection: Locations based on a risk assessment (e.g., product exposure points, high-activity areas, transfer routes).
- Frequency and Sample Volume: Defined based on process criticality, historical data, and classification.
- Data Management and Trend Analysis: Use statistical process control to identify adverse trends before action limits are breached.
- Incident Investigation: A clear procedure for out-of-specification (OOS) and out-of-trend (OOT) results, including impact assessment on product quality and corrective actions.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials for Environmental Monitoring
| Item | Function |
|---|---|
| Particle Counter | Measures and sizes non-viable airborne particles for cleanroom classification and routine monitoring. |
| Volumetric Air Sampler | Actively draws a known volume of air onto growth media for quantitative assessment of airborne microbial load. |
| Settle Plates | Passive monitoring method using open agar plates to assess fallout of viable particles over time. |
| Contact Plates (RODAC) | Contain solid culture media with a raised agar surface for sampling flat surfaces for microbial contamination. |
| Tryptic Soy Agar (TSA) | General-purpose growth medium for the cultivation of a wide variety of bacteria and fungi. |
| Sabouraud Dextrose Agar (SDA) | Selective medium optimized for the isolation and cultivation of fungi and yeasts. |
| D/E Neutralizing Agar | Contains neutralizers (e.g., lecithin, polysorbate) to inactivate residual disinfectants on sampled surfaces. |
| Incubators (Dual-Temp) | Required for incubation at both 20-25°C (mold recovery) and 30-35°C (bacteria recovery). |
| Microbial Identification System | Used for spectral, biochemical, or genetic identification of microbial isolates from EM. |
Visualization of Core Concepts
Diagram 1: GMP EM Decision Pathway
Diagram 2: EM Site Selection Workflow
The Direct Link Between Air Quality, Aseptic Processing, and Final Product Viability
Abstract: This technical guide elucidates the causal chain linking cleanroom air quality, aseptic processing integrity, and the viability of cell therapy products. Framed within a thesis on Good Manufacturing Practice (GMP) cleanroom classification, we present a data-driven analysis of how airborne particle and microbial counts directly influence process contamination rates and critical quality attributes of the final cellular drug product.
In advanced therapeutic medicinal product (ATMP) manufacturing, the production environment is a direct critical process parameter (CPP). The classification of a cleanroom (ISO 14644-1 / EU GMP Annex 1) defines the permissible concentrations of airborne particulates, which serve as vectors for microbial contamination. This establishes an unbreakable link between the measured air quality, the ability to execute processes aseptically, and the purity, potency, and viability of the final cell therapy.
Quantitative Foundations: Air Quality Standards and Measured Outcomes
Table 1: Cleanroom Classification Limits (ISO 14644-1:2015) and Associated Microbial Risk
| ISO Class | ≥0.5 µm particles/m³ | ≥5.0 µm particles/m³ | Typical Microbial Action Limit (CFU/m³) | Recommended Process for Cell Therapies |
|---|---|---|---|---|
| ISO 5 (Grade A) | 3,520 | 20 | <1 | Final product formulation, filling, open manipulations |
| ISO 7 (Grade B) | 352,000 | 2,930 | 10 | Background for ISO 5 zone, critical processing steps |
| ISO 8 (Grade C) | 3,520,000 | 29,300 | 100 | Less critical processing steps, buffer preparation |
Table 2: Correlation Between In-Process Air Quality Deviations and Product Impact
| Contaminant Type | Threshold Deviation | Observed Impact on Cell Product (from cited studies) | Corrective Action Required |
|---|---|---|---|
| Viable Airborne (CFU) | > Action Limit in Grade A | Increased probability of sterility test failure; potential for endotoxin/pyrogen presence | Halt process, investigate source, decontaminate, assess product impact. |
| Non-Viable Particles (≥0.5µm) | > ISO Class limit for 5 min | Direct physical incorporation into product; risk of immunogenic response in patient. | Review gowning, material flow, equipment. Filter integrity test. |
| Specific Organism | Detection of Staphylococcus spp., Bacillus spp. | Indicator of human shedding or environmental ingress. Compromised aseptic technique. | Review personnel practices and material transfer procedures. |
Experimental Protocols for Validating the Link
Protocol 1: Concurrent Monitoring of Viable Particles and Process Contamination
Objective: To statistically correlate real-time airborne microbial counts with contamination rates in media exchanges. Materials: Active viable air sampler (e.g., slit-to-agar or centrifugal), particle counter, sterile cell culture media, T-flasks. Method:
- Place active air sampler and particle counter within 1 ft of the open processing area (e.g., biosafety cabinet).
- Perform 30 identical media exchange operations on seeded cell culture flasks under normal conditions.
- For each operation, run the air sampler for the duration of the open manipulation (typically 5-10 minutes). Record particle counts.
- After media exchange, incubate the processed cell cultures for 14 days at 32.5°C, observing for turbidity (microbial growth).
- Culture the air sampler plates at 20-25°C for 5-7 days and 30-35°C for 2-3 days. Count CFUs.
- Perform regression analysis comparing CFU/m³ during each manipulation with the sterility outcome of the corresponding culture flask.
Protocol 2: Assessing Product Viability Impact from Particle Ingress
Objective: To measure the effect of introduced non-viable particles on critical quality attributes (CQAs) like cell viability and function. Materials: Standardized latex spheres (0.5µm, 5µm), flow cytometer, cell viability assay (e.g., Annexin V/PI), functional assay (e.g., cytokine secretion ELISpot). Method:
- Culture therapeutic T-cells under ISO 5 conditions to 80% confluence.
- Divide cells into three groups: Control (no particles), Low Particle (10 particles/cell), High Particle (100 particles/cell). Introduce particles during a simulated "open" step.
- Incubate cells for 24 hours post-exposure.
- Analyze:
- Viability: Use flow cytometry with Annexin V/PI staining.
- Apoptosis/Necrosis: Caspase-3/7 activity assay.
- Function: Stimulate cells with antigen-presenting cells; measure IFN-γ secretion via ELISpot.
- Compare CQAs between groups using ANOVA; establish a dose-response relationship between particle load and functional attenuation.
Visualizing the Contaminant Pathway and Control Strategy
Title: Contaminant Pathway from Air to Cell Therapy Product
Title: CPP-CQA Link: Air & Asepsis to Product Viability
The Scientist's Toolkit: Essential Reagent Solutions
| Research Reagent / Material | Primary Function in Air Quality/Viability Studies |
|---|---|
| Tryptic Soy Agar (TSA) Plates | For active air sampling; supports growth of aerobic mesophilic bacteria and fungi for viable particle counting. |
| Sabouraud Dextrose Agar (SDA) Plates | Selective for yeasts and molds; used for comprehensive environmental monitoring (EM) in humid processing steps. |
| Latex Microsphere Standards (0.5µm, 5.0µm) | Calibration and challenge particles for optical particle counters and for spiking studies to assess product impact. |
| Annexin V / Propidium Iodide (PI) Kit | Flow cytometry-based assay to quantify early apoptosis (Annexin V+) and late apoptosis/necrosis (PI+) in cells post-particle exposure. |
| LAL Endotoxin Assay Kit | Quantifies bacterial endotoxins (from Gram-negative bacteria) that can be introduced via air/particles and cause pyrogenic responses. |
| ATP Surface Swabs & Luminometer | Rapid hygiene monitoring of surfaces and gloves to prevent indirect contamination transfer; correlates with aseptic technique quality. |
| Closed System Processing Assemblies | Pre-sterilized, welded tubing and connectors that eliminate open manipulations, directly decoupling the process from air quality. |
| Real-Time Particle Counter with Data Logging | Provides continuous ISO classification verification and trend analysis to identify process events that generate particles. |
The viability and success of a cell therapy product are irrevocably determined by the air quality in which it is processed and the robustness of the aseptic techniques employed. Cleanroom classification is not a bureaucratic exercise but a foundational scientific control. By rigorously monitoring air quality parameters as CPPs and understanding their mechanistic link to CQAs, researchers and drug developers can design processes that inherently protect product viability, ensuring both patient safety and therapeutic efficacy.
Implementing and Maintaining a Compliant Cleanroom: A Step-by-Step Operational Guide
Within the broader thesis on GMP cleanroom classification for cell therapy research, the physical facility design is paramount for ensuring product safety, efficacy, and regulatory compliance. This whitepaper provides an in-depth technical guide to three foundational design principles: zoning, airlocks, and pressure cascades. These elements collectively control contamination and cross-contamination risks inherent in manufacturing advanced therapy medicinal products (ATMPs).
Facility Zoning Strategy
Zoning segregates operations based on criticality and contamination risk. A unidirectional flow of personnel, materials, and product is enforced to protect the aseptic core.
Table 1: Typical Cleanroom Classification & Zoning for Cell Therapy
| Zone / Room Function | Target ISO Class (ISO 14644-1) | Equivalent EU GMP Grade (Annex 1) | Primary Contamination Control Rationale |
|---|---|---|---|
| Cell Expansion & Manipulation | ISO 5 | Grade A | Direct open processing of product; highest protection required. |
| Background to Grade A Area | ISO 7 | Grade B | Provides a protected environment for the Grade A zone. |
| Critical Raw Material Prep (e.g., media) | ISO 7 | Grade B | Prevents introduction of contaminants into product contact materials. |
| Non-Viral Vector Production | ISO 7 | Grade B | Controlled environment for biological agents. |
| Viral Vector Production (Contained) | ISO 7 with negative pressure | Grade B (Contained) | Physical containment of genetically modified organisms. |
| Fill/Finish | ISO 5 (with ISO 7 background) | Grade A (with Grade B background) | Aseptic filling of final product. |
| QC Laboratories (e.g., sterility) | ISO 7 | Grade B | Testing requires aseptic conditions. |
| Warehouse & Quarantine | Unclassified | Unclassified | Storage with separation of released and non-released materials. |
Airlock Design and Function
Airlocks are transitional spaces that separate zones of different cleanliness classes. They use interlocks to prevent simultaneous door opening, allowing for controlled decontamination procedures.
Types and Protocols:
Personnel Airlocks (PAL): Used for gowning.
- Protocol: An individual enters from a corridor (ISO 8/unclassified) into the PAL. The outer door closes and locks. The individual performs a defined gowning sequence (e.g., don sterile gloves, hair cover, face mask, and gown). A visual indicator signals when it is safe to open the inner door into the higher-grade zone (e.g., ISO 7).
Material Airlocks (MAL): Used for transferring equipment and supplies.
- Protocol (Double-Door Autoclave/Pass-Through): Materials are loaded from the lower-grade side. The autoclave cycle (e.g., 121°C, 20 minutes) or vaporized hydrogen peroxide (VHP) decontamination cycle is initiated. Once cycle parameters are met and verified, the inner door can be unlocked from the clean side for retrieval.
- Protocol (Dynamic MAL with VHP): Materials are placed on racks, the outer door seals, a VHP cycle decontaminates the chamber and materials' surfaces, an aeration phase removes residual VHP, and then the inner door is unlocked.
Sample Airlocks: Often small pass-throughs for QC samples.
- Protocol: Similar to MAL but may use UV light and disinfection wiping as a transfer method for sealed containers.
Pressure Cascade Strategy
A differential pressure cascade is the primary engineering control to prevent airborne cross-contamination. Air flows from cleanest to less clean areas.
Table 2: Pressure Differential Design Standards
| Zone / Room | Typical Pressure Differential (Pascals, Pa) | Airflow Direction | Rationale |
|---|---|---|---|
| Grade A (ISO 5) Laminar Flow Hood | +45 to +55 Pa relative to Grade B | Outward from hood | Protects open product from immediate background. |
| Grade B (ISO 7) Core Rooms | +20 to +30 Pa relative to corridor | Outward from room | Maintains integrity of the aseptic processing suite. |
| Grade C (ISO 8) Corridor | +15 Pa relative to airlocks | Outward from corridor | Creates a buffer to unclassified areas. |
| Personnel Airlock (to corridor) | +10 to +15 Pa | From corridor into airlock | Prevents ingress of contamination during entry. |
| Personnel Airlock (to Grade B) | +5 to +10 Pa | From airlock into Grade B | Ensures outward flow at final entry point. |
| Contained Virus/Vector Suite | -20 to -30 Pa relative to adjacent areas | Inward to the suite | Contains biological hazards within the suite. |
| QC Microbiology Lab | -10 to -15 Pa relative to corridor | Inward to the lab | Contains testing microorganisms. |
Experimental Protocol: Pressure Cascade Verification
- Objective: To verify the designed pressure differentials between adjacent rooms are maintained under static and dynamic conditions.
- Equipment: Calibrated digital manometer, data logger, door open/close sensors.
- Method:
- Static Test: With all doors closed and HVAC in normal operation, record the pressure differential across each designated door for a minimum of 24 hours. Data logging intervals should be ≤5 minutes.
- Dynamic Test: Simulate worst-case personnel traffic. Have trained personnel move through a defined route, opening and closing doors per SOP. Record pressure differentials during these events, noting the maximum drop and recovery time to setpoint.
- Acceptance Criteria: All measured differentials must remain ≥ the minimum specified design value (e.g., +15 Pa) under static conditions. During dynamic testing, temporary drops below setpoint are permitted only if they recover to the minimum within a specified time (e.g., 3-5 seconds) and do not fall to or below 0 Pa.
Facility Pressure Cascade & Airflow Diagram
The Scientist's Toolkit: Critical Reagents & Materials for Process Validation
Table 3: Key Reagent Solutions for Cleanroom Performance Qualification
| Item | Function in Design Validation | Example/Note |
|---|---|---|
| Viable Particle Counter | Quantifies airborne microbial and particulate contamination per cubic meter in each ISO class zone. | Calibrated to sample at 1 CFM (28.3 LPM); used with agar strips for active air sampling. |
| Non-Viable Particle Counter | Measures and classifies cleanroom air by counting particles ≥0.5 μm and ≥5.0 μm. | Essential for formal ISO 14644-1 classification testing. |
| Anemometer / Balometer | Measures air velocity at HEPA filter faces and air volume changes per hour (ACH). | Verifies unidirectional laminar flow and room turnover rates. |
| Contact Plates (RODAC) | Surface monitoring for microbial contamination on floors, walls, and equipment. | Filled with tryptic soy agar (TSA) for bacterial growth. |
| Settle Plates | Passive air sampling to assess microbial fallout over a defined exposure time (e.g., 4 hours). | TSA plates for bacteria; Sabouraud dextrose agar (SDA) for fungi. |
| Vaporized Hydrogen Peroxide (VHP) Indicator | Biological or chemical indicators to validate decontamination cycles in MALs and isolators. | Geobacillus stearothermophilus spore strips are commonly used. |
| Digital Manometer | Validates the pressure differential cascade between all adjacent zones with logging capability. | Must have a resolution of at least 1 Pa and be calibrated traceably. |
| Neutralizing Broth | Used in disinfectant efficacy studies to stop the chemical action at the end of a specified contact time. | Validates that cleaning SOPs are effective. |
Selecting and Qualifying HVAC and Filtration Systems for ISO Class 5 (Grade A) Environments
Within the stringent framework of Good Manufacturing Practice (GMP) for cell therapy research, the cleanroom environment is a critical component for ensuring product sterility and patient safety. ISO Class 5 (equivalent to EU GMP Grade A) environments represent the highest air cleanliness standard for critical zones where high-risk operations, such as cell manipulation, fill-finish, and open-container processing, occur. This guide details the technical selection, design, and qualification of Heating, Ventilation, and Air Conditioning (HVAC) and filtration systems to achieve and maintain this classification, which is fundamental to preventing contamination in advanced therapy medicinal products (ATMPs).
Core System Requirements & Quantitative Specifications
Air Change Rates (ACRs) and Airflow
A unidirectional (laminar) airflow with a velocity of 0.45 m/s ±20% (90 ft/min ±20%) is mandated for ISO Class 5 zones to provide consistent particle sweeping action. For entire cleanrooms classified at ISO 5, very high air change rates (ACRs) are required.
| Parameter | ISO Class 5 / Grade A Specification | Typical Operational Range | Justification / Standard |
|---|---|---|---|
| Airflow Velocity | 0.36 - 0.54 m/s | 0.45 m/s (mean) | ISO 14644-3, EU GMP Annex 1 |
| Air Changes per Hour (ACR) | Not less than 600* | 600 - 800+ | *Derived from velocity & room volume; EU GMP Annex 1 states airflow should be "visible" |
| Airflow Pattern | Unidirectional (Laminar) | Vertical or Horizontal | Essential for particle control in critical zone |
| Room Pressurization | Positive pressure gradient relative to adjacent lower-grade areas | +10 to +15 Pa minimum | Prevents ingress of contamination (ISO 14644-4) |
Filtration Performance Specifications
Filtration is the final barrier for air quality. The system typically employs a multi-stage approach.
| Filtration Stage | Minimum Efficiency | Standard/Test Method | Typical Location & Function |
|---|---|---|---|
| Pre-filters (G4/F5) | 40-60% on 4µm particles | ISO 16890 | AHU intake; protects coils and subsequent filters from large particles. |
| Intermediate filters (F8/F9) | 80-95% on 0.4µm particles | ISO 16890/EN 779 | Downstream of conditioning coils; protects final HEPA from finer particles and moisture. |
| Final HEPA Filters (H13/H14) | ≥99.995% on 0.3µm particles (H14) | EN 1822 | At terminal point (ceiling or wall of cleanroom); ensures ISO Class 5 air. |
| ULPA Filters (U15) | ≥99.9995% on 0.12µm particles | EN 1822 | Used where enhanced viral containment is a concern. |
Detailed Qualification Methodologies (Experimental Protocols)
The qualification of the HVAC system follows a structured approach: Installation Qualification (IQ), Operational Qualification (OQ), and Performance Qualification (PQ), aligning with GMP principles.
Protocol 1: HEPA Filter Integrity Testing (DOP/PAO Scan)
Objective: To verify the integrity of each installed HEPA filter and its seal, ensuring no bypass leakage. Materials: Aerosol generator (producing Di-Octyl Phthalate (DOP) or Poly-Alpha Olefin (PAO)), photometer, aerosol probe, scanning nozzle. Procedure:
- Establish upstream challenge aerosol concentration of 10-100 µg/L of air upstream of the filter.
- Use a calibrated photometer to measure downstream background.
- Scan the entire filter face, perimeter frame, and seal interface with the scanning nozzle held 1-2 cm from the surface.
- Move the nozzle in overlapping strokes at a linear rate not exceeding 5 cm/s.
- Any leakage reading exceeding 0.01% of the upstream challenge indicates a failure.
- Document all findings; failures require repair and re-test.
Protocol 2: Airflow Velocity and Uniformity Test
Objective: To confirm unidirectional airflow meets the specified velocity and uniformity across the entire critical zone. Materials: Calibrated anemometer (thermoelectric or ultrasonic), measuring grid. Procedure:
- Define a measurement plane parallel to the filter face, typically 15-30 cm below the filter for vertical flow.
- Divide the filter bank/ceiling area into a grid of equal sections (e.g., 1m x 1m or as per risk assessment).
- Measure the velocity at the center of each grid cell.
- Calculate the average velocity and the standard deviation. The average must be 0.45 m/s ±20%, and uniformity (relative standard deviation) should be within ±20% of the mean.
- Record all data points and generate a velocity map.
Protocol 3: Non-Viable Particle Count Qualification
Objective: To certify the room/zone meets ISO Class 5 particle count limits at "as-built," "at-rest," and "in-operation" states. Materials: Calibrated discrete particle counter with appropriate sample flow rate (e.g., 1 CFM or 50 L/min), isokinetic probe. Procedure:
- Determine sample locations based on room area (ISO 14644-1 formula: NL = √A, where A is area in m²).
- For each location, sample a minimum volume of air (as per ISO 14644-1, e.g., 1 m³ for ISO 5).
- Measure particles at sizes ≥0.5µm and ≥5µm.
- Compare the average concentration per location to the limit: ≤3,520 particles/m³ for ≥0.5µm and ≤29 particles/m³ for ≥5µm.
- The environment is compliant if all locations meet these limits.
Protocol 4: Recovery Test (Clean-up Rate)
Objective: To demonstrate the system's ability to recover from a simulated contamination event, confirming robust dynamic performance. Materials: Aerosol generator, particle counter. Procedure:
- Challenge the room with an aerosol to raise the ≥0.5µm particle count to 100x the ISO Class 5 limit.
- Stop aerosol generation and immediately start measuring particle counts at a defined critical location.
- Record the time taken for the particle count to reduce to 10% of the initial challenge (100:1 clean-up) or to the ISO Class 5 limit.
- The recovery time should be short (typically 2-4 minutes), demonstrating system efficacy.
System Design Logic and Qualification Workflow
Multi-Stage Filtration and Air Handling Process
The Scientist's & Engineer's Toolkit: Key Qualification and Monitoring Materials
| Item / Reagent Solution | Primary Function in Qualification/Monitoring | Technical Notes |
|---|---|---|
| PAO (Poly-Alpha Olefin) Aerosol | Challenge agent for HEPA filter integrity testing. | Non-toxic, chemically inert, replaces carcinogenic DOP. Used at 4-20 mg/m³ concentration. |
| Photometer (Forward Light Scatter) | Measures aerosol concentration upstream and downstream of HEPA during leak testing. | Must be calibrated with specific challenge aerosol. Provides real-time leak detection. |
| Discrete Particle Counter (DPC) | Counts and sizes non-viable particles for ISO classification. | Requires calibration to ISO 21501-4. Sample flow rates of 1 CFM (28.3 L/min) or 50 L/min are standard. |
| Thermo-Anemometer / Ultrasonic Anemometer | Measures air velocity and temperature for unidirectional airflow verification. | Must have appropriate range (0-1 m/s) and resolution (±0.01 m/s). Calibration traceable to national standards. |
| Microbial Air Sampler (Active) | Quantifies viable airborne particulate (CFU/m³) for microbiological monitoring. | Types: Sieve impactors (e.g., MAS-100), centrifugal samplers. Use appropriate culture media (e.g., TSA, SDA). |
| Contact Plates (RODAC) | Monitors surface microbial contamination on floors, walls, and equipment. | Filled with neutralizing culture media (e.g., TSA+LE). Incubated at appropriate temperatures (e.g., 20-25°C and 30-35°C). |
| Digital Manometer / Pressure Gauge | Measures room pressure differentials between adjacent zones. | High sensitivity (0.1 Pa resolution). Used for continuous monitoring and alarm systems. |
| Data Loggers (Temp/RH) | For mapping temperature and relative humidity uniformity across the cleanroom. | Should be calibrated and capable of synchronous data recording over a defined period (e.g., 7 days). |
The selection and rigorous qualification of HVAC and filtration systems are foundational to establishing and maintaining an ISO Class 5 environment compliant with GMP for cell therapy research. The process requires a systematic, science-based approach from design through to ongoing verification. By adhering to the specified quantitative parameters, executing detailed qualification protocols, and implementing continuous environmental monitoring with appropriate tools, facilities can ensure the aseptic conditions necessary to safeguard the sterility, efficacy, and safety of life-changing cell therapies.
Developing Robust SOPs for Gowning, Material Transfer, and Personnel Flow
1. Introduction and Thesis Context Within the framework of Good Manufacturing Practice (GMP) for cell therapy research, the cleanroom is the cornerstone of product safety and efficacy. The broader thesis posits that cleanroom classification (ISO 5/Class A to ISO 8/Class D) defines environmental limits, but it is the stringency of Standard Operating Procedures (SOPs) that controls the dynamic variables—people and materials—to maintain those limits. This guide details the technical development of robust SOPs for gowning, material transfer, and personnel flow, which are critical for minimizing particulate and microbiological contamination in aseptic cell processing.
2. Foundational Principles and Regulatory Basis SOPs must be built on the principles of contamination control, segregation, and unidirectional flow. Key regulatory and guidance documents include:
- EU GMP Annex 1: Manufacture of Sterile Medicinal Products (2022)
- USP <797> Pharmaceutical Compounding—Sterile Preparations
- FDA Guidance for Industry: Sterile Drug Products Produced by Aseptic Processing. A risk-based approach, aligned with ICH Q9, is mandatory, focusing on process critical control points.
3. Quantitative Data on Contamination Sources Effective SOPs target the primary sources of contamination. Data is summarized in Table 1.
Table 1: Primary Sources of Cleanroom Contamination
| Contamination Source | Particle Release Rate (≥0.5 μm/min) | Relative Risk in Cell Therapy | Primary Control SOP |
|---|---|---|---|
| Personnel (Gowned, in motion) | 100,000 - 1,000,000 | Very High | Gowning & Personnel Flow |
| Packaging Materials | Variable (1,000 - 10,000 per ft²) | High | Material Transfer & Decontamination |
| Stationary Personnel | ~100,000 | Moderate | Personnel Flow & Aseptic Technique |
| Equipment Transfer | Not Quantified (Situational) | High | Material Transfer & Sanitization |
4. SOP Development: Gowning Procedure The gowning SOP is a controlled sequence to encapsulate the operator as a contamination source.
4.1 Experimental Protocol for Gowning Qualification
- Objective: Quantify the effectiveness of the gowning SOP in reducing particle shedding.
- Methodology (Operator Gowning Qualification):
- The operator performs the gowning procedure in a designated gowning room (ISO 7 or better).
- Particle counters (remote and portable) are placed in the gowning room and adjacent cleaner area.
- Baseline particle counts are recorded.
- The operator performs standardized movements (arm raising, leg lifts, sitting/standing) for 10 minutes post-gowning.
- Particle counts (0.5 μm and 5.0 μm) are measured in real-time during the movement period.
- Microbial settle plates may be placed in the gowning area to assess bioburden reduction.
- The operator enters the main cleanroom, and particle counts are monitored to assess transfer.
- Acceptance Criteria: Particle counts must remain within the target cleanroom classification limits during and after the procedure.
4.2 Gowning Sequence Diagram
Diagram Title: Sequential Gowning Procedure for ISO 5/7 Cleanrooms
5. SOP Development: Material Transfer Material transfer SOPs define methods for introducing items without compromising cleanroom integrity.
5.1 Experimental Protocol for Transfer Validation
- Objective: Validate that a material transfer method (e.g., dynamic pass-through) maintains differential pressure and does not introduce contamination.
- Methodology:
- Place particle counters inside the cleanroom near the pass-through chamber (PTC) and in the PTC itself.
- Place microbial air samplers in the same locations.
- Execute the transfer SOP (e.g., wipe outer container, place in PTC, close outer door, sanitize interior, wait for purge cycle, retrieve from inner side).
- Monitor and log real-time particle counts (0.5 μm) and differential pressure across the PTC during the entire cycle.
- After transfer, sample surfaces of the transferred item and interior PTC surfaces for viable organisms using contact plates.
- Repeat for worst-case scenarios (largest, most irregular items).
- Acceptance Criteria: No loss of differential pressure > 1 Pa, particle counts return to baseline within minutes, and contact plates show no growth or within action limits.
5.2 Material Transfer Decision Workflow
Diagram Title: Material Transfer Method Decision Tree
6. SOP Development: Personnel Flow Personnel flow SOPs enforce unidirectional movement and minimize cross-contamination between zones of different classifications.
6.1 Core Principles & Logical Flow The primary rule is movement from lower to higher classification only after proper gowning. Reverse flow requires re-gowning. A clear mapping of zones and airlocks is essential.
6.2 Personnel Flow Pathway Diagram
Diagram Title: Unidirectional Personnel Flow for Cell Therapy Suite
7. The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Materials for Contamination Control & SOP Validation
| Item Category | Specific Example/Product | Function in SOP Development/Execution |
|---|---|---|
| Environmental Monitoring | Portable Laser Particle Counter, Microbial Air Sampler, Contact Plates (TSA, SDA) | Provides quantitative data for SOP validation, routine monitoring, and media fills. |
| Surface Decontamination | Sporicidal Wipes (e.g., hydrogen peroxide, peracetic acid based), Sterile 70% IPA Wipes | Validated agents for decontaminating materials, surfaces, and gloves during transfers and operations. |
| Gowning Materials | Sterile, Low-Linting Gowns; Sterile Nitrile Gloves; Face Masks with Full Coverage | Barrier materials that meet ASTM standards for particulate and microbial shedding. |
| Material Transfer | Validated Double-Bag Assemblies, Pass-Through Chambers with Interlocks, Rapid Transfer Ports (RTPs) | Engineered systems that enable the controlled, aseptic introduction of materials. |
| Hand Hygiene | Validated Surgical Hand Scrub, Alcohol-Based Hand Sanitizer (with persistent effect) | Critical for reducing resident and transient flora before gowning and gloving. |
8. Conclusion Robust SOPs for gowning, material transfer, and personnel flow are not administrative documents but are dynamic, validated protocols that physically enforce the principles of GMP. For cell therapy research, where the product is often both the drug and the patient's own cells, these SOPs constitute the primary defense against adventitious agent contamination, directly impacting patient safety and product viability. Their development must be evidence-based, continuously monitored, and ingrained in the quality culture of the organization.
Within the context of Good Manufacturing Practice (GMP) for cell therapy research, the maintenance of designated cleanroom classifications (ISO 5/Class A to ISO 8/Class D) is non-negotiable. The product—often autologous or allogeneic living cells—is uniquely susceptible to both viable and non-viable particulate contamination, which can compromise patient safety and therapeutic efficacy. Routine and periodic environmental monitoring (EM) forms the cornerstone of contamination control strategy, providing the data to demonstrate state of control, identify trends, and trigger corrective actions. This whitepaper provides an in-depth technical guide to the three principal tools for airborne monitoring: particle counters, microbial air samplers, and settle plates.
Particle Counters: Quantifying Non-Viable Contamination
Optical particle counters (OPCs) operate on light scattering principles. A vacuum pump draws air at a controlled rate (e.g., 1.0 cubic foot per minute, 28.3 liters per minute, or 50 liters per minute) through a laser-illuminated sensing zone. Particles scatter light, with the intensity proportional to particle size, which is then counted and sorted into size channels (typically ≥0.5 µm and ≥5.0 µm for ISO classifications).
Key Experimental Protocol for Routine Monitoring
- Apparatus: Calibrated isokinetic probe, portable or remote particle counter with ≥0.5 µm and ≥5.0 µm channels, data logging software.
- Procedure:
- Perform pre-operation checks (flow rate verification, zero count check).
- For static (at-rest) classification, sample for 1 minute per location. For dynamic (in-operation) monitoring, sample continuously or at frequent intervals.
- Position the isokinetic probe in the airflow (vertical for unidirectional, strategic for non-unidirectional).
- Sample at pre-defined, risk-assessed locations: workbench height, near critical sites (e.g., vial fill, open processing), and room background.
- Record counts per cubic meter for each channel. Calculate mean from multiple locations for classification compliance.
Data Presentation: ISO 14644-1 Classification Limits (Particles/m³)
| ISO Class | ≥0.5 µm | ≥5.0 µm |
|---|---|---|
| ISO 5 (Class 100) | 3,520 | 29 |
| ISO 6 (Class 1,000) | 35,200 | 293 |
| ISO 7 (Class 10,000) | 352,000 | 2,930 |
| ISO 8 (Class 100,000) | 3,520,000 | 29,300 |
Microbial Air Samplers: Capturing Viable Contaminants
Active Air Sampling Methods
Active samplers draw a known volume of air onto or into a collection medium.
- Impaction (Slit-to-Agar, Sieve): Air is accelerated through small jets (sieve) or a slit and directed onto a 55-60mm agar plate (e.g., TSA, SDA). Microbes are physically impacted onto the surface.
- Centrifugal: A rotating impeller draws air inward and deposits particles onto a dedicated agar strip via centrifugal force.
- Filtration: Air passes through a membrane filter, which is then placed on agar or immersed in broth for incubation.
- Impinger: Air is bubbled through a liquid collection medium.
Key Experimental Protocol for Viable Air Sampling
- Apparatus: Calibrated microbial air sampler (sieve impactor recommended), pre-poured agar plates (TSA for bacteria, SDA for fungi), incubators.
- Procedure:
- Decontaminate sampler intake.
- Aseptically load sterile agar plate into sampler.
- Program sample volume (typically 1 m³ for ISO 5/6, lower volumes for dirtier areas to avoid overloading).
- Sample at critical locations. Ensure sampling head is oriented correctly per manufacturer (often facing upwards).
- Incubate plates: TSA at 30-35°C for 48-72 hours; SDA at 20-25°C for 5-7 days.
- Count Colony Forming Units (CFU) and calculate CFU/m³.
Data Presentation: Example Alert/Action Limits for Viable Air (CFU/m³)
| Cleanroom Grade (Dynamic) | Recommended Action Limit (CFU/m³) |
|---|---|
| ISO 5 (Class A) | <1 |
| ISO 6 (Class B) | 10 |
| ISO 7 (Class C) | 100 |
| ISO 8 (Class D) | 200 |
Settle Plates: Passive Air Monitoring
Principle and Rationale
Settle plates (typically 90mm agar plates) measure the deposition rate of viable, airborne particles under gravity over a defined exposure time (usually 4 hours for critical operations). This method is particularly relevant for assessing contamination risk to open product containers.
Key Experimental Protocol
- Apparatus: Pre-poured agar plates, sterile tripods/stands, timing device.
- Procedure:
- Remove lid from plate and place on a stand at a defined working height (e.g., bench level, near open processing).
- Expose for a validated duration (e.g., ≤4 hours to avoid desiccation).
- Replace lid, incubate as per active air samples.
- Count CFU per plate, report as CFU/4 hours.
Integration into a GMP Contamination Control Strategy
Effective EM programs integrate all three methods at frequencies defined by risk assessment. Data from particle counters provide real-time feedback on HVAC performance, while viable methods offer retrospective but critical biological data. Trend analysis is essential.
Cleanroom EM Data Flow for GMP Compliance
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Cleanroom Monitoring |
|---|---|
| Tryptic Soy Agar (TSA) Plates | General-purpose medium for the recovery of aerobic bacteria and fungi. Used in active air samplers and settle plates. |
| Sabouraud Dextrose Agar (SDA) Plates | Selective medium optimized for fungi and yeasts. Used for monitoring in areas prone to mold contamination. |
| Neutralizing Agar (e.g., with Lecithin & Polysorbate) | Contains agents to inactivate residual disinfectants (e.g., sporicides) that could inhibit microbial growth, ensuring accurate counts. |
| Particle Counter Calibration Kit | Contains size-calibrated polystyrene latex spheres (e.g., 0.5µm, 5.0µm) and a flow meter to verify instrument accuracy per ISO 21501-4. |
| Microbial Air Sampler Calibration Equipment | A primary standard (e.g., bubble meter, mass flow meter) to certify the sampler's air intake volume is accurate. |
| Incubators (Dual-Temperature) | Required for incubation of plates at both 20-25°C (for fungi) and 30-35°C (for bacteria) to capture the full spectrum of viable contaminants. |
Integrating Cleanroom Data with QMS (Quality Management System) for Real-Time Compliance
Within the stringent framework of GMP (Good Manufacturing Practice) for cell therapy research, the cleanroom is the nexus of product quality. Its classification—defined by parameters like airborne particle counts, pressure differentials, temperature, and humidity—directly impacts the safety and efficacy of living cellular products. Traditional compliance models rely on periodic data review, a reactive approach fraught with latency. This guide details the technical integration of continuous cleanroom environmental monitoring (EM) data directly into a modern electronic Quality Management System (eQMS) to achieve real-time compliance, enabling proactive deviation management and ensuring data integrity within the critical manufacturing environment.
Core Data Architecture & Integration Protocol
The integration requires a robust, layered architecture to facilitate seamless, bi-directional data flow between cleanroom sensors and the eQMS.
Integration Methodology
Protocol: Establishment of a Unified Data Pipeline
- Sensor Layer: Deploy validated, networked particle counters (e.g., 0.5 µm and 5.0 µm sizing), microbial air samplers, and physicochemical sensors (pressure, temp, RH). Each device must be calibrated per a traceable schedule.
- Data Acquisition & Aggregation: Utilize an Environmental Monitoring Software (EMS) or a custom middleware (e.g., built on MQTT/Sparkplug or OPC UA protocols) to collect raw data streams from all sensors. This layer performs initial data cleansing and time-synchronization.
- Translation & Normalization Layer: Implement a secure API gateway (RESTful or SOAP) to map EMS data fields to the specific input requirements of the target eQMS. This includes normalizing units, aligning sensor IDs with equipment master records, and applying data formats (ISO 8601 for timestamps).
- eQMS Ingestion: Configure the eQMS (e.g., Veeva Vault QMS, SAP QM, or MasterControl) to accept incoming data via API as Potential Deviations or Quality Events. Business rules within the eQMS are pre-configured to trigger automated workflows based on alert (e.g., > ISO Class 5 limit) or action level breaches.
Logical Workflow Diagram
Title: Cleanroom-to-QMS Real-Time Data Workflow
Key Cleanroom Parameters & Alert Thresholds
For cell therapy GMP manufacturing, cleanrooms are typically classified as ISO Class 5 (Grade A) for critical aseptic processing and ISO Class 7 (Grade B) as background. The following table summarizes key quantitative limits and their QMS impact.
Table 1: Critical Cleanroom Parameters & Integration Triggers for Cell Therapy
| Parameter | ISO Class 5 (Grade A) Limit (at rest) | ISO Class 7 (Grade B) Limit (at rest) | Typical Sampling Frequency | QMS Event Trigger Level |
|---|---|---|---|---|
| Airborne Particles (≥0.5 µm) | 3,520 per m³ | 352,000 per m³ | Continuous | Alert: 80% of limit; Action: 100% of limit |
| Airborne Particles (≥5.0 µm) | 20 per m³ | 2,930 per m³ | Continuous | Alert: 80% of limit; Action: 100% of limit |
| Microbial Viable Air (CFU/m³) | <1 | 10 | Daily/Session | Action: Any growth in Grade A; >Limit in Grade B |
| Pressure Differential | ≥10-15 Pa | ≥10-15 Pa | Continuous | Alert: Deviation > ±2 Pa from setpoint |
| Temperature | Controlled per SOP (e.g., 20±2°C) | Controlled per SOP | Continuous | Alert: Deviation > ±1°C from setpoint |
| Relative Humidity | Controlled per SOP (e.g., 45±10%) | Controlled per SOP | Continuous | Alert: Deviation > ±5% from setpoint |
Experimental Protocol for System Validation
Any integration must be validated to ensure data integrity, accuracy, and reliability. The following protocol outlines the core validation exercise.
Protocol: Validation of the Cleanroom Data-to-QMS Integration Loop
- Objective: To demonstrate that a simulated cleanroom excursion detected by the EMS is accurately, completely, and timely transmitted to the eQMS, triggering the correct quality workflow.
- Materials: See "The Scientist's Toolkit" below.
- Method:
- Baseline Configuration: Confirm all sensors are calibrated and the API connection between the EMS and eQMS is active. In the eQMS, configure a test Quality Event workflow that culminates in a specific test-CAPA form.
- Excursion Simulation: Using a calibrated particle counter calibrator or a non-shedding source, introduce a controlled concentration of particles (≥0.5 µm) into the sampling line of a single ISO Class 5 particle counter to simulate a breach of the "Action Level."
- Data Trace Monitoring: In the EMS interface, verify the excursion is recorded. Simultaneously, monitor the API traffic using a network protocol analyzer (e.g., Wireshark) to confirm data transmission.
- eQMS Event Verification: Log into the eQMS and check for the automatic creation of a new Quality Event record. Verify that all metadata (sensor ID, timestamp, location, exact particle count) is correctly populated.
- Workflow Trigger Confirmation: Manually progress the test Event to confirm the subsequent workflow steps (e.g., notification to QA, initiation of investigation form) are triggered as designed.
- Data Integrity Check: Perform an audit trail review in both the EMS and eQMS for the test record. Ensure the trace is unbroken, timestamped, and attributable.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Cleanroom Monitoring & Integration Validation
| Item | Function in Context |
|---|---|
| Calibrated Particle Counter (e.g., with 0.5µm & 5.0µm channels) | Primary device for continuous monitoring of airborne particulate contamination against ISO classification standards. |
| Aerosol Generator & Diluter | Used in validation protocols to generate known concentrations of polystyrene latex spheres (PSL) for sensor challenge testing and excursion simulation. |
| Microbial Air Sampler (e.g., viable impactor) | Active air monitoring to quantify viable (CFU) contamination, critical for aseptic processing assurance. |
| Environmental Monitoring Software (EMS) | Centralized platform for real-time data collection, visualization, and alarm management from all cleanroom sensors. |
| API Testing & Simulation Tool (e.g., Postman, SoapUI) | Validates the data structure, security, and reliability of the connection between the EMS and the eQMS. |
| Network Protocol Analyzer (e.g., Wireshark) | Captures and analyzes API traffic to verify data completeness and timing during integration validation. |
| Electronic QMS Sandbox/Test Instance | A non-production replica of the QMS used to develop, test, and validate integration workflows without impacting live quality records. |
Signaling Pathway for Real-Time Deviation Management
The integrated system creates an automated, logical pathway for managing deviations, transforming raw data into quality actions.
Title: Real-Time Deviation Management Pathway
Solving Common Cleanroom Challenges: Contamination Control and Deviation Management
Root Cause Analysis for Excursions in Particle and Microbial Monitoring Data
Within the context of Good Manufacturing Practice (GMP) cleanroom classification for cell therapy research, environmental monitoring (EM) is a critical quality attribute. Cell therapy products, particularly those involving autologous or allogeneic live cells, are highly susceptible to contamination. Excursions—data points exceeding established alert or action limits for airborne particulates or viable microorganisms—represent potential threats to product sterility, patient safety, and data integrity. A systematic Root Cause Analysis (RCA) is therefore not merely a regulatory expectation but a fundamental component of a robust quality culture. This guide details a structured RCA methodology tailored for the cell therapy research environment.
A Structured RCA Framework
A systematic, cross-functional approach is essential. The following framework provides a logical progression from identification to closure.
Diagram Title: RCA Process Workflow for EM Excursions
Quantitative Data Analysis and Trend Review
Isolated excursions must be viewed against historical data and room dynamics. Key metrics should be compiled for analysis.
Table 1: Critical EM Data for RCA Baseline
| Data Category | Specific Parameter | Typical Acceptable Range (ISO 5 / Grade A) | Relevance to RCA |
|---|---|---|---|
| Particle (≥0.5µm) | Average Count (per m³) | ≤3,520 | Baseline performance of HEPA filtration. |
| Peak Count (per m³) | Dynamic, but must not compromise classification. | Correlates with specific personnel or equipment activity. | |
| Viable Air | Colony Forming Units (CFU) per m³ | <1 | Direct sterility risk indicator. |
| Viable Surface | CFU per contact plate (e.g., 55cm²) | <1 | Integrity of disinfection protocols and aseptic technique. |
| Personnel | CFU per glove print (per hand) | <1 | Primary source of microbial contamination. |
| Facility | Pressure Differential (Pa) | ≥10-15 Pa (cascading) | Identifies airflow reversal risks. |
| Air Change per Hour (ACH) | ≥300-600 (unidirectional) | Assesses contamination dilution rate. |
Common Root Causes & Investigative Protocols
Personnel-Related Causes
- Root Cause: Improper aseptic gowning, technique, or high personnel density.
- Investigation Protocol:
- Review gowning qualification records of involved personnel.
- Simulate the operation using smoke studies or particle counters placed near personnel to visualize airflow disruption.
- Re-enact the activity with intensified EM (e.g., settle plates, active air samplers at the point of operation) to confirm the correlation.
Equipment & Process-Induced Turbulence
- Root Cause: Introduction of non-sanitized materials, equipment-generated particles, or improper setup disrupting unidirectional airflow.
- Investigation Protocol:
- Perform non-viable particle monitoring during equipment operation outside and inside the critical zone.
- Conduct surface sampling on equipment pre- and post-introduction into the cleanroom.
- Execute a media simulation (media fill) that incorporates the specific equipment operation to challenge microbial risk.
Facility & Engineering Controls Failure
- Root Cause: HVAC system malfunction, HEPA filter leak, loss of room pressure differential.
- Investigation Protocol:
- Immediately review Building Management System (BMS) logs for pressure, temperature, and humidity deviations.
- Perform a full integrity test (DOP/PAO challenge) on the HEPA filters serving the affected zone.
- Measure air change rates and airflow visualization studies (smoke tests) to confirm unidirectional airflow patterns.
Procedural & Training Deficiencies
- Root Cause: Inadequate or outdated SOPs, insufficient training on contamination control.
- Investigation Protocol:
- Conduct a document audit of relevant SOPs (sanitization, gowning, EM, equipment operation).
- Interview personnel to assess comprehension and adherence to procedures (knowledge vs. practice gap).
- Analyze training records for completeness and frequency.
The Scientist's Toolkit: Key Reagents & Materials for EM Investigations
Table 2: Essential Research Reagents for EM Root Cause Analysis
| Item | Function in RCA |
|---|---|
| Tryptic Soy Agar (TSA) Contact Plates & Air Samplers | Standard for total aerobic microbial count from surfaces and air. Incubation at 30-35°C for 3-5 days. |
| Sabouraud Dextrose Agar (SDA) Plates | Selective for molds and yeasts. Used when fungal contamination is suspected. Incubation at 20-25°C for 5-7 days. |
| Neutralizing Agents (e.g., Lecithin, Polysorbate) | Incorporated into agar to inactivate residual disinfectants (e.g., sporicides) on sampled surfaces, ensuring accurate microbial recovery. |
| Particle Counter Calibration Standards | Traceable latex spheres or other standards (e.g., 0.5µm, 5.0µm) required for periodic calibration of airborne particle counters, ensuring data accuracy. |
| PAO (Poly-Alpha-Olefin) / DOP (Dioctyl Phthalate) Oil | Challenge aerosol used for HEPA filter integrity leak testing. A photometer measures downstream penetration. |
| Microbial Identification System (e.g., MALDI-TOF, DNA sequencing kits) | Critical for tracing contamination sources. Identifies isolated microorganisms to genus/species level, enabling comparison with isolates from personnel or environments. |
The Path to Corrective and Preventive Action (CAPA)
Identified root causes must lead to meaningful actions.
Diagram Title: CAPA Development Path from Root Cause
Conclusion: For cell therapy research, where the product is often the patient's own cells, the tolerance for environmental control failures is minimal. A rigorous, evidence-based RCA process transforms an excursion from a compliance event into a catalyst for strengthening the contamination control strategy, ultimately ensuring the safety and efficacy of advanced therapeutic products.
Within GMP cleanroom classification for cell therapy research, human operators represent the predominant contamination source, contributing up to 75-90% of airborne particulate and microbial load. This whitepaper details an integrated framework of enhanced personnel gowning protocols and evidence-based behavioral training to mitigate this risk. Implementation of these programs is critical for maintaining ISO 5-7 classified environments required for aseptic processing of Advanced Therapy Medicinal Products (ATMPs).
The success of autologous and allogeneic cell therapies hinges on the aseptic manufacture of sterile, potent, and safe products. GMP cleanrooms (typically ISO 5-7) are engineered to control environmental parameters; however, personnel remain the most significant variable. Shedding from skin, hair, and respiratory tracts, amplified by improper gowning or behavior, introduces viable (microbial) and non-viable particulates that can compromise product sterility and patient safety.
Quantitative Analysis of Human-Borne Contamination
The following table summarizes key data on human emission rates and the efficacy of control measures.
Table 1: Human Particulate and Microbial Emission Rates Under Various Conditions
| Condition / Activity | Avg. Particle Emission (≥0.5µm/min) | Avg. Microbial Colony Forming Units (CFU/hr) | Primary Source |
|---|---|---|---|
| Seated, motionless | 100,000 - 1,000,000 | 100 - 1,000 | Skin, Clothing |
| Slow walking | 5,000,000 - 10,000,000 | 5,000 - 10,000 | Friction of Gown |
| Arm movement | 1,000,000 - 5,000,000 | 1,000 - 7,000 | Cuffs, Neck |
| Speaking (normal) | 500,000 - 1,000,000 | 10 - 50 per word spoken | Respiratory Tract |
| Cough/Sneeze | > 10,000,000 | > 10,000 per event | Respiratory Tract |
| With Enhanced Gowning | Reduction vs. Baseline | Reduction vs. Baseline | |
| Standard Polyester Gown | 30-50% | 40-60% | Barrier |
| Sterile, Single-Use Coverall (ISO 5) | 60-70% | 70-85% | Full-body Barrier |
| Plus Behavioral Training | Additional Reduction | Additional Reduction | |
| Trained, deliberate motion | +15-20% overall efficacy | +20-25% overall efficacy | Reduced shedding |
Enhanced Gowning Protocol: A Layered Defense System
Protocol: Sequential Gowning for ISO 5 Cleanroom Entry
This methodology must be performed in a controlled gowning room (ISO 7 or better).
- Pre-Gowning Hygiene: Wash hands and forearms with a surgical-grade antimicrobial scrub (e.g., chlorhexidine gluconate) for 3 minutes. Dry with sterile, lint-free towels.
- Base Layer: Don a low-linting, snap-front coverall and bouffant cap. All personal clothing must be fully covered.
- Sterile Gowning in Anteroom: a. Perform hand hygiene with sterile alcohol-based rub (70% Isopropyl Alcohol). b. Open sterile gown pack on bench. Don sterile boot covers first. c. Don sterile gown using aseptic "touchless" technique, ensuring sleeves cover wrists. d. Don sterile gloves, tucking gown cuffs securely inside glove gauntlet. e. Apply sterile facemask and safety goggles. f. Verify integrity in mirror. No skin or hair should be visible.
Experimental Protocol: Gowning Efficacy Validation (Glove Fingertip Test)
- Objective: Quantify microbial transfer after gowning.
- Materials: Sterile contact plates (TSA), timer, incubator.
- Method:
- After gowning, press fingertips of both gloved hands onto separate contact plates for 10 seconds.
- Repeat simulation of a core cleanroom task (e.g., assembling tubing set) for 30 minutes.
- Post-task, repeat fingertip sampling on new plates.
- Incubate plates at 30-35°C for 3-5 days. Count CFUs.
- Acceptance Criteria: ≤1 CFU per plate post-gowning; ≤3 CFU post-simulation (based on EMA Annex 1 draft guidelines).
Behavioral Training Program: Engineering Human Factors
Core Training Modules
- Aseptic Technique Drills: Repeated practice of core manipulations using media fills or simulation kits.
- Contamination Awareness: Use of fluorescent gels (e.g., Glo Germ) under UV light to visualize contamination spread from simulated breaches.
- Zonal Discipline: Training on unidirectional workflows, "first air" principle (keeping critical sites between HEPA airflow and operator), and slow, deliberate movements.
- Communication Protocols: Instruction on clear, concise verbal coordination and minimizing conversation near critical zones.
Experimental Protocol: Assessing Training Efficacy via Airborne Particle Count
- Objective: Measure real-time particle generation during a standard activity pre- and post-training.
- Materials: Portable airborne particle counter (0.5µm & 5.0µm), simulated biosafety cabinet (BSC), stopwatch.
- Method:
- Place particle counter probe inside BSC, sampling air.
- A trained operator performs a serial dilution simulation for 10 minutes. Record particle count per minute (≥0.5µm).
- The same operator undergoes behavioral training.
- Repeat the simulation post-training under identical conditions.
- Compare average and peak particle counts.
- Expected Outcome: A minimum 50% reduction in average particle count post-training.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Contamination Control Studies
| Item / Reagent | Function in Research/Validation |
|---|---|
| Tryptic Soy Agar (TSA) Contact Plates | For microbial surface monitoring of gloves, gowns, and equipment. |
| Settle Plates (TSA) | For passive air monitoring of viable, settling particles. |
| Fluorescent Tracing Gel (Glo Germ) | Visually simulates microbial contamination under UV light for training efficacy assessment. |
| Portable Airborne Particle Counter | Quantifies non-viable particulate contamination (≥0.3µm, ≥0.5µm, ≥5.0µm) in real-time. |
| Microbial Air Sampler (e.g., MAS-100) | Active volumetric air sampling for viable microorganisms. |
| Sterile, Alcohol-Based Hand Rub (70% IPA) | Standard for surgical hand hygiene; used in gowning protocols. |
| Media Fill Kit (Simulated Product) | Validates the entire aseptic process, including operator technique, without using actual product. |
System Integration and Continuous Monitoring
Enhanced gowning and training are not standalone events. They must be integrated with a robust Environmental Monitoring (EM) program providing feedback. Data from EM (viable and non-viable) should be trended and used for targeted retraining.
Contamination Control Feedback Loop
Enhanced Gowning Sequence for ISO 5
Managing Static and Dynamic State Discrepancies During Active Cell Manipulation
Within the stringent environment of a Grade B (ISO 7) GMP cleanroom, the physical containment of particulates is meticulously controlled. However, a more subtle form of "contamination" jeopardizes cell therapy research: state discrepancies in cellular systems. This guide examines the critical challenge of managing discrepancies between static classification (e.g., a cell's molecular snapshot at t=0) and its dynamic state (real-time physiological and signaling activity) during active manipulation such as transduction, gene editing, or bioreactor expansion. Ensuring that dynamic cellular behavior aligns with statically defined quality release criteria (potency, identity, purity) is paramount for regulatory compliance and therapeutic efficacy in Advanced Therapy Medicinal Products (ATMPs).
Core Concepts and Quantitative Data Framework
Static state refers to endpoint or snapshot measurements: genomic sequencing, surface marker expression via flow cytometry, or viability counts. Dynamic state encompasses real-time metabolic fluxes, signaling pathway activity, and transient phenotypic changes during stress. The discrepancy arises when static assays fail to capture critical dynamic deviations that impact final product quality.
Table 1: Comparative Analysis of Static vs. Dynamic Assessment Modalities
| Parameter | Static Assessment Method | Dynamic Assessment Method | Typical Discrepancy Impact |
|---|---|---|---|
| Metabolic State | Endpoint ATP assay, Metabolomics (LC-MS) | Seahorse XF Analyzer (OCR, ECAR), FRET-based metabolite sensors | Failure to detect transient metabolic crisis post-transduction, leading to later apoptosis. |
| Signaling Activity | Phospho-protein immunoblot (Western) | Live-cell kinase activity reporters (e.g., AKAR), Ca²⁺ imaging | Over/under-estimation of pathway activation critical for differentiation or expansion. |
| Cell Cycle Status | Fixed-cell PI staining & flow cytometry | FUCCI (Fluorescent Ubiquitination-based Cell Cycle Indicator) probes | Misidentification of synchronized, manipulation-induced arrest as a uniform population state. |
| Viability / Stress | Trypan Blue exclusion at endpoint | Real-time impedance monitoring (xCELLigence), caspase-3/7 fluorescence reporters | Undetected acute stress during manipulation resulting in compromised batch potency. |
Experimental Protocols for Discrepancy Monitoring
Protocol 1: Integrated Dynamic Metabolic Profiling During Viral Transduction
- Objective: To capture transient metabolic shifts undetected by endpoint assays.
- Materials: HEK 293T or primary T-cells, lentiviral vector, Seahorse XFp Analyzer, pre-coated cell culture microplates.
- Method:
- Seed cells in a Seahorse microplate at 5x10⁴ cells/well in a Class II BSC within the cleanroom.
- 24h post-seeding, initiate transduction in the presence of Polybrene (8 µg/mL).
- Immediately load the microplate into the Seahorse Analyzer (instrument placed in an adjacent controlled environment, ISO 8).
- Run a Mitochondrial Stress Test (Oligomycin, FCCP, Rotenone/Antimycin A) at 0, 6, 12, and 24h post-transduction.
- Correlate Oxygen Consumption Rate (OCR) and Extracellular Acidification Rate (ECAR) trajectories with parallel, static endpoint measurements of transduction efficiency (flow cytometry) and viability.
- Outcome: Identification of a critical 6-8h post-transduction metabolic bottleneck, informing optimized feeding schedules.
Protocol 2: Live-Cell Tracking of Signaling Dynamics During Cytokine Stimulation
- Objective: To visualize heterogeneity in signaling responses masked by population-averaged static data.
- Materials: Jurkat or primary CAR-T cells expressing an NF-κB-GFP live-cell reporter, recombinant human IL-15, live-cell imaging system equipped with environmental control.
- Method:
- Transfer reporter cells into a glass-bottom 96-well imaging plate.
- Mount plate in the imaging system, maintaining 37°C, 5% CO₂.
- Acquire baseline images (10min intervals). Automatically administer IL-15 (final 50 ng/mL) using integrated microfluidics.
- Continue time-lapse imaging for 12-16h, tracking nuclear translocation of GFP in single cells.
- Analyze data for response latency, amplitude, and duration. Compare with endpoint static phospho-p65 Western blot from parallel wells.
- Outcome: Quantification of responder vs. non-responder subpopulations, guiding criteria for pre-stimulation cell selection.
Visualization of Key Concepts and Workflows
Diagram 1: State Discrepancy during Cell Manipulation
Diagram 2: Key Stress Signaling Pathway Post-Manipulation
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for Dynamic State Monitoring
| Reagent / Tool | Function / Purpose | Example in Discrepancy Management |
|---|---|---|
| Genetically-Encoded FRET Biosensors | Live-cell, real-time reporting of specific ion concentrations (Ca²⁺, H⁺), metabolite levels (ATP, cAMP), or kinase activity (PKA, ERK). | Tracking immediate-early signaling dynamics post-stimulation, revealing heterogeneity invisible to endpoint ELISA. |
| Fluorescent Dyes for ROS & Viability | Cell-permeable dyes (e.g., CellROX, Annexin V early apoptosis markers) for live-cell imaging or flow cytometry. | Identifying the subset of cells experiencing acute oxidative stress during manipulation before commitment to death. |
| Seahorse XF Assay Kits | Measure mitochondrial respiration (OCR) and glycolysis (ECAR) in live cells in a microplate. | Detecting acute metabolic perturbation post-transduction, enabling timely media supplementation to prevent viability loss. |
| Real-Time Cell Analysis (RTCA) Systems | Label-free, impedance-based monitoring of cell proliferation, viability, and morphological changes. | Providing continuous readout of cell health during extended manipulations (e.g., differentiation), flagging deviations from expected growth curves. |
| CRISPR/dCas9-Based Transcriptional Reporters | Engineered cells with fluorescent reporters under control of endogenous promoters of key stress genes (e.g., CHOP, p21). | Visualizing heterogeneity in transcriptional stress responses at single-cell level in real time. |
Within the stringent environment of a GMP cleanroom for cell therapy research, the control of microbial contamination, including resilient bacterial endospores, is non-negotiable. Effective cleaning and disinfection (C&D) are critical operational pillars to maintain the required ISO classification (e.g., ISO 5/Class A for critical operations) and ensure product safety. This technical guide provides a data-driven framework for optimizing sporicidal agent selection and rotation schedules to prevent microbial resistance, mitigate biofilm formation, and comply with regulatory expectations for Advanced Therapy Medicinal Products (ATMPs).
Sporicidal Agents: Mechanisms and Quantitative Comparison
Sporicidal agents inactivate bacterial spores through distinct biochemical mechanisms, primarily oxidative damage or alkylation. The following table summarizes key performance data for common agents, based on current efficacy standards (e.g., EN 13704, ASTM E2197).
Table 1: Comparative Analysis of Common Sporicidal Agents
| Agent (Active Ingredient) | Typical Use Concentration | Recommended Contact Time (minutes) | Primary Mode of Action | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Hydrogen Peroxide (H₂O₂) | 3-10% (w/v) | 5-30 | Oxidative damage: Generates hydroxyl radicals that destroy spore coat, DNA, and core enzymes. | Leaves no residue; breaks down into water and oxygen; excellent material compatibility. | Can be deactivated by catalase; efficacy reduced by organic load; requires proper vapor distribution for VHP. |
| Peracetic Acid (PAA) | 0.2-0.5% (v/v) | 5-10 | Oxidation & Acetylation: Oxidizes spore components and acetylates proteins, disrupting metabolism. | Highly effective at low concentrations and temperatures; works in presence of some organic soil. | Pungent odor; corrosive to some metals (copper, brass); can degrade plastic over time. |
| Sodium Hypochlorite (NaOCl) | 0.5-1.0% (avail. Cl₂) | 10-20 | Chlorination & Oxidation: Chlorinates proteins and oxidizes cellular components, disrupting spore integrity. | Broad-spectrum, rapid kill; low cost. | Highly corrosive; reacts with organics to form hazardous by-products; unstable in solution. |
| Accelerated Hydrogen Peroxide (AHP) | 3-7% (w/v) | 5-10 | Chelation-enhanced Oxidation: H₂O₂ stabilized with surfactants & chelators, improving penetration and stability. | Good material compatibility; low toxicity; synergistic effect with detergents. | Newer technology with longer-term compatibility data still being accrued. |
Rationale for Rotation Schedules
A rotational schedule uses two or more sporicides with differing modes of action. The primary goals are to:
- Prevent Adaptive Resistance: Microbes may develop tolerance to repeated sub-lethal exposure of a single agent.
- Disrupt Biofilms: Different chemistries can target various components of the extracellular polymeric substance (EPS).
- Comprehensive Coverage: Ensures efficacy against a broader range of potential contaminants.
- Material Compatibility: Allows for periodic use of a less corrosive agent on sensitive equipment.
Experimental Protocol for Validation of Regimes
Validation is required per USP <1072> and EU GMP Annex 1 principles to demonstrate a 3-4 log₁₀ reduction of suitable spore-forming indicators (e.g., Bacillus atrophaeus, Geobacillus stearothermophilus).
Protocol: Carrier-Based Quantitative Suspension Test for Sporicide Efficacy
Objective: To determine the log reduction of bacterial spores by a sporicidal agent under cleanroom-relevant conditions.
Materials (The Scientist's Toolkit):
Table 2: Key Research Reagent Solutions for Sporicidal Validation
| Item | Function/Explanation |
|---|---|
| B. atrophaeus spore suspension (ATCC 9372) | Standard test organism for dry-surface and vaporized agents. Known resistance profile. |
| G. stearothermophilus spore strips (ATCC 7953) | Standard biological indicator for steam and vaporized hydrogen peroxide sterilization. |
| Porcelain Penicylinders or Stainless Steel Coupons | Non-porous, standardized carriers to simulate cleanroom surfaces. |
| Neutralizing Broth (e.g., D/E Neutralizing Broth) | Critical to halt sporicidal action immediately after contact time for accurate recovery counts. |
| Tryptic Soy Agar (TSA) plates | For viable count enumeration of recovered spores. |
| Organic Soil Load (3% BSA or 5% serum) | To simulate "dirty" conditions and test efficacy under challenge. |
| Vortex Mixer & Serial Dilution Tubes | For homogenizing recovered spores and performing decimal dilutions. |
Methodology:
- Carrier Inoculation: Apply a known volume (e.g., 10 µL) of spore suspension (≈1 x 10⁶ CFU) onto the center of each sterile carrier. Dry in a laminar flow hood for 1 hour.
- Application of Agent: Apply the sporicidal solution to cover the carrier surface completely. For wipe-based transfer, use a standardized wiping pattern and pressure.
- Contact Time: Maintain the agent on the carrier for the manufacturer's claimed contact time at controlled room temperature (20-25°C). Perform tests in triplicate.
- Neutralization: Immediately transfer the carrier to a tube containing 10 mL of neutralizing broth. Vortex vigorously for 30-60 seconds to neutralize the agent and suspend spores.
- Viable Count & Calculation: Perform serial decimal dilutions of the neutralized suspension in sterile saline or broth. Plate in duplicate on TSA. Incubate plates at 30-37°C for up to 7 days. Count colonies and calculate log reduction: Log Reduction = log₁₀(Initial CFU/Carrier) - log₁₀(Recovered CFU/Carrier)
- Controls: Include positive controls (carriers neutralized immediately after inoculation) and neutralizer toxicity controls.
Recommended Rotation Framework for Cell Therapy Cleanrooms
A typical monthly rotation schedule might alternate between an oxidizing agent and an alkylating/chelating agent.
Title: Monthly Sporicide Rotation Schedule Logic
Workflow for Implementing and Monitoring a Regime
A systematic approach ensures consistent execution and environmental control.
Title: Sporicidal Regime Implementation and Monitoring Workflow
An optimized cleaning and disinfection regime, grounded in the mechanistic understanding of sporicidal agents and validated through robust experimental protocols, is fundamental to maintaining the aseptic state of a GMP cleanroom for cell therapy. A scheduled rotation between chemistries with divergent modes of action, coupled with rigorous environmental monitoring, provides a proactive defense against contamination, directly supporting the product quality and patient safety mandates of ATMP development.
Strategies for Handling Facility Modifications and Maintaining Control During Maintenance
Thesis Context: This guide is framed within a broader thesis on maintaining GMP cleanroom classification integrity during operational changes, specifically for cell therapy research where product viability and patient safety are paramount.
Facility modifications and maintenance in a cell therapy GMP cleanroom present a critical paradox: the need to perform intrusive work while maintaining the validated state of a classified environment. Uncontrolled changes directly risk particle and microbial contamination, compromising critical research and production batches. This document outlines a risk-based, phase-gated strategy for executing modifications without losing environmental control.
Quantitative Impact of Modifications on Cleanroom Performance
Data from recent industry studies and regulatory audit findings highlight the tangible risks of modifications. The following table summarizes key quantitative impacts on cleanroom classification parameters during maintenance activities.
Table 1: Impact of Common Maintenance Activities on Cleanroom Performance Metrics
| Activity Type | Avg. Particle Count Increase (≥0.5µm/m³) | Avg. Pressure Differential Loss (%) | Recovery Time to ISO 5/Class A (min) | Microbial Risk Level |
|---|---|---|---|---|
| Panel Removal in Return Air Grid | 35,000 - 100,000 | 15-30 | 45-90 | High (Direct ingress from plenum) |
| Lighting Fixture Replacement | 10,000 - 25,000 | 5-10 | 20-40 | Medium |
| Pass-Through Chamber Service | 50,000 - 200,000 | 50-100 | 60-120 | Very High (Boundary breach) |
| Small Tool Use (Wired) | 5,000 - 15,000 | 2-5 | 15-30 | Low-Medium |
| HEPA Filter Integrity Scan (Local) | 1,000 - 5,000 | <2 | 5-15 | Very Low (Controlled) |
Data synthesized from recent PDA Technical Reports, EU GMP Annex 1 case studies, and FDA 483 observations (2022-2024).
A Phase-Gated Protocol for Controlled Modifications
The following detailed protocol ensures systematic control from planning to hand-back of the cleanroom.
Phase 1: Risk Assessment & Planning (Pre-Modification)
Objective: To classify the modification, define control strategies, and secure approvals without impacting ongoing operations.
Methodology:
- Modification Classification: Categorize the work as Minor (e.g., sensor calibration), Major (e.g., replacing a small equipment item), or Significant (e.g., altering room layout or HVAC components). Use a formal change control (CC) system.
- Impact Assessment: Conduct a cross-functional risk assessment (FMEA model) focusing on:
- Direct breach of room envelope.
- Generation of particulate or microbial load.
- Impact on adjacent critical zones.
- Utility interruptions (power, gases, HVAC).
- Interim Control Plan (ICP) Development: The ICP is the core control document. It must specify:
- Work Zone Demarcation: Use of portable soft-wall enclosures with negative pressure and independent HEPA filtration.
- Containment & Containment Verification: Protocol for smoke testing local containment before work begins.
- Environmental Monitoring (EM) Escalation: Increased non-viable and viable particle monitoring at the work zone boundary and in adjacent critical areas.
- Personnel & Material Flow: Dedicated entry/exit procedures, tool decontamination stations, and material airlocks.
- Fallback & Abort Criteria: Clear thresholds for particle counts or pressure loss that trigger work stoppage.
Phase 2: Execution with Enhanced Controls (During Modification)
Objective: To execute the modification while actively protecting the cleanroom environment.
Methodology:
- Pre-Work Clearance: Halt adjacent critical operations. Execute the ICP, including setting up containment and verifying its integrity.
- Dynamic Monitoring: Implement the escalated EM plan. Use real-time particle counters with alarms set at levels stricter than the room classification limit (e.g., alarm at 50% of ISO 5 limit for ≥0.5µm particles).
- Staged Material Introduction: All tools and parts must be introduced through a formal decontamination process (e.g., wipe-down with sporicidal agent in an airlock, followed by a defined holding time).
- Waste Containment: All waste must be sealed in bags within the containment zone before removal.
Phase 3: Decontamination & Re-qualification (Post-Modification)
Objective: To restore the area to its fully validated, operational state.
Methodology:
- Initial Clean-down: Perform a thorough decontamination of the work area and all affected surfaces using approved sporicidal agents, starting from the innermost part of the containment moving outward.
- Containment Dismantling & Final Clean: Dismantle temporary enclosures carefully, followed by a final full-room cleaning per SOP.
- Performance Re-qualification: The area must not return to service until:
- At-Rest Tests: Full particle count scan and pressure differentials meet classification specs.
- Recovery Test: Aerosol challenge test demonstrating recovery time to specified limits (refer to Table 1 for benchmarks).
- Viable Monitoring: Settle plates and contact plates show a return to baseline microbial levels for at least one full monitoring cycle.
- Documentation & CC Closure: Compile all data (ICP, EM data, re-qualification reports) and close the change control. Update room and facility documentation as required.
Diagram 1: Phase-Gated Protocol for Cleanroom Modifications
The Scientist's Toolkit: Essential Research Reagent Solutions for Contamination Control
During modifications, specific reagents and materials are critical for monitoring and maintaining microbiological control.
Table 2: Key Research Reagent Solutions for Contamination Control During Modifications
| Item | Function & Rationale |
|---|---|
| Non-Viable Particle Counter (Portable, Real-time) | Provides immediate feedback on air quality breaches during work. Essential for monitoring containment integrity and triggering abort actions. |
| Rapid Microbial Identification System | If a deviation occurs, rapid genotypic (e.g., PCR-based) or phenotypic identification helps determine if the isolate is related to construction personnel or materials, guiding corrective actions. |
| High-Efficiency Sporicidal Disinfectant | Required for pre- and post-work decontamination. Must be effective against resistant spores which may be introduced from building materials or external environments. |
| Viable Particle Sampler (Active Air Sampler) | Used for escalated EM during work. Allows for volumetric sampling to quantify microbial air contamination in real-time at the boundary of the work zone. |
| Neutralizing Agar & Broth | Used in contact plates and for surface sampling. Contains neutralizers to inactivate residual sporicidal agents, ensuring microbial recovery data is accurate post-decontamination. |
| ATP Bioluminescence Assay Kits | Provides a rapid, though non-specific, assessment of cleaning effectiveness on surfaces after the initial clean-down, before formal microbial sampling. |
Diagram 2: Risk Mitigation Layers During Modifications
For cell therapy research, where the product is often the patient's own cells, the cost of an environmental control failure is unacceptably high. Adherence to a structured, phase-gated strategy for modifications—underpinned by rigorous risk assessment, dynamic physical containment, and real-time monitoring—is not merely a regulatory expectation but a fundamental component of product quality and patient safety. By integrating these protocols into the facility's quality management system, organizations can ensure operational agility without compromising the sanctity of the GMP cleanroom environment.
Validation, Auditing, and Global Standards Comparison for Cell Therapy Cleanrooms
1. Introduction In the advanced field of cell therapy research, the cleanroom is a critical component for ensuring product purity, patient safety, and regulatory compliance. Within a broader thesis on GMP cleanroom classification, this guide details the fundamental qualification lifecycle: Installation Qualification (IQ), Operational Qualification (OQ), Performance Qualification (PQ), and the crucial phase of Ongoing Re-qualification. This structured approach is mandated by global Good Manufacturing Practice (GMP) regulations to provide documented evidence that the cleanroom environment is consistently fit for its intended use in manufacturing aseptic cell-based products.
2. The Qualification Lifecycle Phases: A Technical Deep Dive
2.1 Installation Qualification (IQ): Verification of Correct Installation IQ establishes that the cleanroom and all associated equipment have been received, installed, and configured correctly according to approved design specifications (URS - User Requirement Specification) and manufacturer recommendations.
- Objective: To verify "as-built" conditions.
- Key Activities:
- Verification of received components against purchase orders.
- Certification of critical HVAC system components (filters, fans, ducting).
- Verification of material finishes (non-shedding, cleanable surfaces).
- Installation check of ancillary systems (pressure differential monitors, environmental monitoring systems, intercoms, pass-throughs).
- Documentation of utility connections (power, gases).
- Collection of supplier documentation (manuals, material certificates, filter integrity test reports).
2.2 Operational Qualification (OQ): Verification of Operational Performance OQ demonstrates that the installed cleanroom system operates consistently across its entire declared operating range under dynamic, but unladen (at-rest), conditions.
- Objective: To verify "as-installed" systems function as specified.
- Key Experimental Protocols & Data:
- Airflow Velocity & Uniformity Test: Measure airflow at multiple points across each HEPA/ULPA filter face using a calibrated anemometer. Demonstrate uniformity (typically ±20% of average velocity).
- Air Change Rate (ACH) Calculation: ACH = (Total Airflow [m³/hr] / Room Volume [m³]). Critical for contamination control.
- Room Pressurization Cascade Test: Using a calibrated micromanometer, verify the pressure differential between adjacent areas meets specification (e.g., +10 to +15 Pa for Grade B into Grade C).
- HEPA/ULPA Filter Integrity Test (DOP/PAO Challenge): A polydisperse aerosol (e.g., Poly-Alpha-Olefin) is introduced upstream of filters. A photometer or particle counter scans the filter face, gaskets, and frame. Any leak >0.01% indicates failure.
- Recovery Test: Introduce an aerosol to achieve a particle count 100x above the class limit. Measure the time for the room to recover to the acceptable limit upon cessation of aerosol generation.
Table 1: Typical OQ Test Acceptance Criteria (ISO 14644-1:2015 / EU GMP Annex 1 Alignment)
| Test Parameter | Grade A (ISO 5) | Grade B (ISO 7) | Grade C (ISO 8) | Test Method & Instrument |
|---|---|---|---|---|
| Particle Count (≥0.5 µm) (at-rest) | ≤3,520 / m³ | ≤352,000 / m³ | ≤3,520,000 / m³ | ISO 14644-1; Light Scattering Airborne Particle Counter |
| Airflow Velocity | 0.36 - 0.54 m/s (guideline) | NA | NA | Anemometer |
| Air Change Rate | NA | Typically ≥25/hr | Typically ≥15/hr | Calculated |
| Pressure Differential | Min. +10-15 Pa between zones | Min. +10-15 Pa between zones | Min. +10-15 Pa between zones | Micromanometer |
| Filter Integrity | ≤0.01% leak (local standard) | ≤0.01% leak (local standard) | ≤0.01% leak (local standard) | Photometer Scan (PAO Challenge) |
| Temperature & Humidity | Per URS (e.g., 20±2°C, 45±15%RH) | Per URS | Per URS | Calibrated Data Logger |
Diagram 1: Cleanroom qualification lifecycle sequence.
2.3 Performance Qualification (PQ): Verification of Operational Performance Under Load PQ provides documented evidence that the cleanroom, under normal production conditions (in-operation), consistently performs to meet all predefined quality attributes.
- Objective: To verify "as-used" performance.
- Key Experimental Protocols:
- Dynamic Particle Monitoring: Particle counts are taken during simulated or actual processing with personnel present and equipment in operation. Sampling locations are risk-based, focusing at sites of greatest contamination risk (e.g., open product containers, filling lines).
- Microbial Environmental Monitoring (EM): Active (air samplers) and passive (settle plates) methods are used to quantify viable particulate.
- Process Simulation (Media Fill): While not strictly a PQ test of the room, a media fill run under PQ conditions validates the aseptic process within the qualified environment.
Table 2: Example PQ Viable Monitoring Alert/Action Limits (EU GMP Annex 1)
| Location / Sample Type | Grade A | Grade B | Grade C | Grade D |
|---|---|---|---|---|
| Active Air (CFU/m³) | <1 | 5 | 50 | 100 |
| Settle Plates (Ø 90mm, CFU/4 hours) | <1 | 2 | 10 | 50 |
| Contact Plates (Ø 55mm, CFU/plate) | NA | 2 | 10 | 25 |
| Glove Fingertips (CFU/glove) | NA | 2 | 10 | NA |
Diagram 2: PQ test execution workflow.
2.4 Ongoing Re-qualification: Ensuring a State of Control Post-PQ, the cleanroom enters a phase of continuous verification. Ongoing re-qualification is a periodic, scheduled repetition of key OQ/PQ tests to confirm the system remains in a validated state.
- Frequency: Typically every 6-12 months for major tests (filter integrity, full particle count), aligned with a risk assessment.
- Triggers: May also be event-driven (e.g., after major maintenance, facility modifications, or adverse trend in routine EM data).
- Link to Routine Monitoring: Re-qualification data is analyzed alongside daily/weekly EM, pressure, and temperature data to form a complete quality picture.
3. The Scientist's Toolkit: Key Reagent & Material Solutions for Cleanroom EM
Table 3: Essential Materials for Environmental Monitoring Program
| Item | Function/Explanation |
|---|---|
| Tryptic Soy Agar (TSA) Plates | General-purpose growth medium for aerobic bacteria and fungi. Used in settle plates, contact plates, and air samplers. |
| Sabouraud Dextrose Agar (SDA) Plates | Selective medium for fungi (yeasts and molds). Often used in parallel with TSA for comprehensive viable monitoring. |
| Neutralizing Agar | Contains agents (e.g., lecithin, polysorbate) to inactivate residual disinfectants (sporicides) on surfaces, ensuring accurate microbial recovery from contact plates. |
| Poly-Alpha-Olefin (PAO) Aerosol | A chemically inert, non-toxic liquid aerosol used for challenge testing of HEPA/ULPA filter integrity. |
| Particle Counter Calibration Standard | A suspension of traceable, monodisperse polystyrene latex (PSL) spheres used to calibrate and verify the accuracy of airborne particle counters. |
| Sterile Diluents & Neutralizers | Buffered solutions used to dilute and neutralize samples from EM activities before microbiological analysis. |
| Viable Air Sampler Calibration Kit | Used to verify the volumetric flow rate of microbial air samplers, ensuring accurate CFU/m³ calculations. |
4. Conclusion The cleanroom qualification lifecycle is a foundational pillar of GMP compliance for cell therapy research and production. A rigorous, data-driven approach to IQ, OQ, and PQ establishes the initial control state, while a robust ongoing re-qualification program, integrated with routine monitoring, ensures its permanence. This lifecycle provides the documented evidence required by regulators and, more importantly, instills confidence that the critical processing environment is effectively safeguarding the integrity of advanced therapeutic products and the patients who depend on them.
In cell therapy research, product safety and efficacy are intrinsically linked to environmental control within Good Manufacturing Practice (GMP) cleanrooms. The classification of these spaces (ISO 5/Class A to ISO 8/Class D) is maintained through rigorous particulate and microbial monitoring. However, raw data from viable air sampling, surface monitoring, and particle counts are meaningless without robust statistical analysis and trend reporting. This guide details the methodologies for transforming monitoring results into actionable intelligence for quality assurance and regulatory compliance in advanced therapy medicinal product (ATMP) development.
Core Statistical Methods for Environmental Monitoring Data
Environmental monitoring (EM) data is typically non-normal, zero-inflated (many "zero" colony-forming unit counts), and autocorrelated. Key analytical approaches include:
- Descriptive Statistics & Control Charts: For continuous data like particle counts.
- Non-parametric Analysis: For colony-forming unit (CFU) counts, utilizing methods like the Poisson or Negative Binomial distribution for modeling.
- Trend Analysis: Using statistical process control (SPC) and time-series analysis to identify deviations from a state of control.
Table 1: Statistical Methods for Cleanroom Data Types
| Data Type | Example (Cleanroom) | Key Distribution | Primary Analysis Method | Trend Tool |
|---|---|---|---|---|
| Continuous | Non-viable particle counts (0.5µm, 5.0µm) | Often Log-normal | Individual-Moving Range (I-MR) Control Charts | CUSUM (CUmulative SUM) chart |
| Discrete (Count) | Viable air sample CFUs, surface contact plate CFUs | Poisson / Negative Binomial | U-charts (for area samples), Shewhart Control Charts with transformed data | Time-ordered Pareto analysis |
| Attribute | Presence/Absence of specific organisms (e.g., Staphylococcus spp.) | Binomial | P-charts (Proportion charts) | Rolling rate calculation |
Experimental Protocols for Key Monitoring Activities
Protocol A: Viable Air Sampling via Volumetric Impaction
- Objective: Quantify viable airborne particulate (CFU/m³) within a classified zone.
- Apparatus: Active air sampler (e.g., MAS-100NT), soybean-casein digest agar plates.
- Method:
- Decontaminate sampler intake prior to entry into the controlled zone.
- Calibrate sampler to the standard volume (e.g., 1 m³).
- Place agar plate in the sampler head.
- Position sampler at critical location (e.g., near filling aperture in ISO 5 hood).
- Run sampler for the prescribed time to achieve target volume.
- Incubate plates at 20-25°C for 3-5 days, then at 30-35°C for 2-3 days.
- Count CFUs, apply positive hole correction factor if necessary, and calculate CFU/m³.
- Identify predominant morphotypes.
Protocol B: Non-Viable Particle Counting for Classification
- Objective: Verify cleanroom classification per ISO 14644-1:2015.
- Apparatus: Discrete particle counter with isokinetic probe, calibrated for 0.5µm and 5.0µm thresholds.
- Method:
- Perform the test "as-built" (at rest) or "operational" per protocol.
- Divide the cleanroom area into a grid of equal sampling locations.
- Determine minimum number of sampling points (NL) from ISO 14644-1 Table A.1.
- Position probe at sample location (at working height).
- Sample a minimum volume per location (as per ISO standard) to achieve a statistically significant count.
- Record particle concentration for each size at each location.
- Calculate the mean concentration per location and the overall 95% upper confidence limit (UCL). The area meets classification if the UCL is below the class limit.
The Scientist's Toolkit: Research Reagent & Material Solutions
Table 2: Essential Materials for EM & Analysis
| Item | Function | Application Example |
|---|---|---|
| Soybean-Casein Digest Agar (TSA) | General-purpose microbial growth medium. | Viable air and surface monitoring for total aerobic count. |
| Sabouraud Dextrose Agar (SDA) | Selective for fungi (yeasts and molds). | Routine monitoring for contamination by fungi. |
| Neutralizing Agents (e.g., Lecithin, Polysorbate) | Inactivates residual disinfectants (sporicides, etc.) on contact plates. | Surface monitoring in areas cleaned with halogen-based disinfectants. |
| Statistical Software (e.g., JMP, Minitab, R) | Performs SPC, non-parametric analysis, and generates control charts. | Trend analysis of monthly summary EM data, alert/action limit calculation. |
| Environmental Monitoring Database | Centralized repository for all EM data, with audit trail. | Long-term trend reporting, investigation support, and regulatory submission data mining. |
Visualizing the Data Analysis & Trend Reporting Workflow
Title: EM Data Analysis and Reporting Workflow
Signaling Pathway for EM Data-Driven Decision Making
Title: Cleanroom EM Data Decision Pathway
Advanced Trend Analysis & Reporting
Moving beyond single-point excursions, trend reporting analyzes data over time (e.g., quarterly) to detect subtle process shifts. Key elements include:
- Rolling Rates: Calculation of recovery rates for specific organisms.
- Pareto Analysis: Identification of the most frequent contaminant types or worst-performing locations.
- Correlation Analysis: Relating EM data to operational parameters (e.g., personnel count, interventions).
A comprehensive Trend Report must include:
- Executive Summary.
- Data Summary Tables (see Table 3 below).
- Control Charts with annotated excursions.
- Pareto Charts of isolate identification.
- Analysis of trends and correlations.
- Conclusions and recommended CAPAs.
Table 3: Example Quarterly EM Trend Summary Table
| Location/Test | ISO Class | Data Points (n) | Mean | Alert Limit | Action Limit | % ≥ Alert | Status |
|---|---|---|---|---|---|---|---|
| Viable Air (CFU/m³) | ISO 5 | 120 | 0.1 | 3 | 5 | 0.0% | In Control |
| Viable Air (CFU/m³) | ISO 7 | 180 | 2.3 | 10 | 20 | 1.1% | In Control |
| Surface Contact (CFU/plate) | ISO 5 Work Surface | 150 | 0.5 | 5 | 10 | 0.7% | In Control |
| 0.5µm Particle Count (cumulative) | ISO 5 | 120 | 1,200 | 3,520 | 3,520* | 0.0% | In Control |
*ISO 14644-1 limit for ISO 5.
Within the context of GMP cleanroom classification for cell therapy research, maintaining an audit-ready state is not merely a compliance exercise but a fundamental cornerstone of product quality, patient safety, and scientific integrity. For researchers and drug development professionals, this translates into a culture of meticulous documentation, rigorous environmental control, and robust data governance. This guide details the technical practices required to prepare for and successfully navigate inspections by regulators (e.g., FDA, EMA) and clients, ensuring that every facet of cleanroom operation and associated research stands up to scrutiny.
Foundational Principles of Cleanroom Classification & Monitoring
The classification of a GMP cleanroom (e.g., ISO 5/Class A, ISO 7/Class 10,000) defines the permissible limits for airborne particulate concentration, which is critical for aseptic processing in cell therapy. An audit-ready program relies on continuous verification and documented evidence of compliance.
Key Quantitative Standards for Classification
Table 1: ISO 14644-1 Cleanroom Classification Standards (Selected Classes)
| ISO Classification | Maximum Particles/m³ (≥0.5 µm) | Maximum Particles/m³ (≥5.0 µm) | FED STD 209E Equivalent |
|---|---|---|---|
| ISO 5 | 3,520 | 29 | Class 100 |
| ISO 7 | 352,000 | 2,930 | Class 10,000 |
| ISO 8 | 3,520,000 | 29,300 | Class 100,000 |
Core Monitoring Protocols
Protocol: Viable (Microbial) Air Monitoring (Active Sampling)
- Objective: Quantify colony-forming units (CFU) per cubic meter of air.
- Equipment: Volumetric air sampler (e.g., MAS-100NT), soy casein digest agar (SCDA) contact plates or strips.
- Methodology:
- Calibrate the air sampler according to manufacturer specifications prior to use.
- Under aseptic conditions, load a sterile agar plate into the sampler head.
- Place the sampler at a predetermined, critical location within the cleanroom (e.g., near open product containers).
- Sample a defined volume of air (typically 1 m³) at a flow rate specified for the sampler.
- Incubate plates at 20-25°C for 5-7 days followed by 30-35°C for 2-3 days (per EU GMP Annex 1).
- Count CFUs, calculate CFU/m³, and compare to established alert and action limits.
Protocol: Non-Viable Particle Counting
- Objective: Continuously monitor airborne particulate levels per ISO 14644-1.
- Equipment: Calibrated, remote particle counter with isokinetic sampling probe.
- Methodology:
- Establish a documented sampling plan with fixed locations representative of the aseptic processing zone.
- Conduct sampling at rest (room complete, equipment installed, no personnel) and in operation (normal processing conditions).
- For each location, sample a minimum volume (as per ISO 14644-1) to achieve statistically significant data.
- Record particle counts for thresholds (e.g., ≥0.5µm and ≥5.0µm) in real-time.
- Automatically log all data to a validated system with audit trail.
The Scientist's Toolkit: Critical Research Reagent & Material Solutions
Table 2: Essential Materials for Audit-Ready Cell Therapy Research
| Item | Function & Audit-Ready Consideration |
|---|---|
| Master & Working Cell Banks | Fully characterized (identity, viability, sterility, mycoplasma) starting material. Traceable from donor/lineage to final product. Certificate of Analysis (CoA) must be available. |
| GMP-Grade Growth Media & Cytokines | Defined, xeno-free formulations with documented origin and full traceability. Requires vendor audits and CoA for each lot, including endotoxin testing. |
| Closed-System Processing Units (e.g., bioreactors) | Enable aseptic processing while minimizing environmental exposure. Installation Qualification (IQ)/Operational Qualification (OQ) and cleaning validation records are critical. |
| Environmental Monitoring Kits | Pre-poured, irradiated contact plates and air sampler agar strips. Use-by dates must be valid, and growth promotion testing records available. |
| Single-Use, Sterile Assemblies | Tubing sets, connectors, and bags. Lot-controlled, ethylene oxide or gamma irradiation sterilization certificates must be on file. |
| Critical Process Data Loggers | For monitoring temperature, CO2, and other critical parameters during cell culture and storage. Must be calibrated at defined intervals with certificates. |
Diagram: Audit-Readiness Data Flow for Cleanroom Environmental Monitoring
Title: Data Workflow for Environmental Monitoring
Critical Documentation Systems
Audit readiness hinges on immediate document accessibility and integrity.
- Standard Operating Procedures (SOPs): Current, approved, and trained versions for all activities (monitoring, gowning, cleaning, investigation).
- Batch Records & Logbooks: Electronic or paper-based, completed in real-time with no blanks. All discrepancies must be explained via deviation reports.
- Training Records: Documented evidence that all personnel are qualified for assigned tasks, including cleanroom behavior and aseptic techniques.
- Change Control: A formal system to assess, approve, and implement any change to equipment, processes, or systems.
- Calibration & Maintenance Records: Scheduled and documented proof that all critical equipment (e.g., balances, incubators, particle counters) is in a controlled state.
Preparing for the Inspection: A Proactive Workflow
Title: Inspection Preparation and Execution Workflow
For cell therapy researchers operating within classified GMP environments, achieving and maintaining an audit-ready state is a dynamic, integrated process. It requires the seamless alignment of rigorous scientific protocols, controlled engineering parameters, and uncompromising quality systems. By embedding the practices outlined—from foundational cleanroom monitoring to robust data and document management—into daily operations, research teams can confidently demonstrate the integrity of their science and the safety of their therapies during any regulatory or client inspection.
This whitepaper provides a comparative analysis of the current Good Manufacturing Practice (cGMP) requirements as enforced by the U.S. Food and Drug Administration (FDA) and the European Union's GMP Annex 1 (August 2022) with a specific focus on implications for Advanced Therapy Medicinal Products (ATMPs), including cell and gene therapies. The analysis is framed within the critical context of cleanroom classification and environmental monitoring, which forms a cornerstone of the broader thesis on GMP compliance for cell therapy research.
ATMPs represent a transformative class of medicines, including somatic cell therapy, gene therapy, and tissue-engineered products. Their inherently complex, often patient-specific, and live biological nature necessitates stringent manufacturing controls. Two primary regulatory frameworks govern their production: the FDA's cGMP (21 CFR Parts 210, 211, 1271) and the EU's GMP, specifically the revised Annex 1 "Manufacture of Sterile Medicinal Products." While not exclusively for ATMPs, Annex 1's principles are directly applicable to their aseptic processing. This guide dissects the alignment and divergence between these frameworks.
Core Comparative Analysis: Key Requirements
Cleanroom Classification and Monitoring
The classification of air cleanliness by particle concentration is a fundamental divergence.
Table 1: Cleanroom Classification Comparison
| Parameter | FDA cGMP (As per guidance for sterile products & 21 CFR 211) | EU GMP Annex 1 (2022) | Implication for ATMPs |
|---|---|---|---|
| Classification System | References ISO 14644-1 (e.g., Class 5, 6, 7, 8). Primarily relies on in-operation (dynamic) limits. | Mandates ISO 14644-1 classification (Grade A, B, C, D) with clear at-rest and in-operation states. | Annex 1 is more prescriptive. ATMP facilities must now validate and monitor both operational states. |
| Grade A/ISO 5 Particle Limits (≥0.5 µm) | 3,520 particles/m³ (in-operation). | At-rest: 3,520 particles/m³. In-operation: 3,520 particles/m³. | Alignment on the critical processing zone limit. |
| Grade B/ISO 7 Particle Limits (≥0.5 µm) | No explicit "at-rest" definition. In-operation limit: 352,000 particles/m³. | At-rest: 352,000 particles/m³. In-operation: 3,520,000 particles/m³. | Annex 1 explicitly defines higher allowable particle count during dynamic conditions in the background environment. |
| Microbial Monitoring (Active Air) | Action limits based on area classification and process risk. Less prescriptive on frequency. | Grade A: <1 CFU/m³. Grade B: 10 CFU/m³. Grade C: 100 CFU/m³. Grade D: 200 CFU/m³. Specifies frequency and duration of sampling. | Annex 1 provides definitive numeric action limits. ATMP processes with open steps must adhere to Grade A limits for that zone. |
| Monitoring Frequency | Based on risk assessment and historical data. | Strongly recommends continuous monitoring for Grade A areas during critical processing. | For lengthy cell manipulation, continuous monitoring may be required, impacting facility design. |
Contamination Control Strategy (CCS)
A pivotal introduction in Annex 1 2022, absent as a formal requirement in FDA cGMP.
Table 2: Contamination Control Strategy Elements
| CCS Component | FDA cGMP Approach | EU GMP Annex 1 (2022) Requirement |
|---|---|---|
| Holistic Plan | Implicit through various regulations on quality systems, facility design, and process validation. | Explicitly mandated. A documented, proactive, and holistic CCS is required for the entire manufacturing process. |
| Scope | Covered in multiple documents (e.g., Environmental Monitoring Program, Process Validation). | Single, comprehensive document covering facilities, equipment, utilities, personnel, processes, and monitoring. |
| Lifecycle | Implied in change control and ongoing monitoring. | Stresses lifecycle management with regular review and updates based on new risks and data. |
| Risk Management | Quality Risk Management (ICH Q9) is endorsed. | QRM is the foundation of the CCS. Requires formal tools (e.g., FMEA) to identify and control risks. |
Experimental Protocol 1: Establishing a CCS for an Autologous Cell Therapy Process
- Objective: To develop and document a CCS for the open manipulation of a patient's T-cells during a CAR-T manufacturing process.
- Methodology:
- System Definition: Map the entire manufacturing process flow from apheresis receipt to final cryopreservation. Identify all open steps, transfer points, and critical control points.
- Risk Identification (using FMEA): For each step, assemble a cross-functional team to assess potential failure modes (e.g., vial breakage, operator error, incubator contamination), their causes, and effects.
- Risk Analysis: Score each failure mode for Severity (S), Occurrence (O), and Detectability (D). Calculate Risk Priority Number (RPN = S x O x D).
- Control Establishment: For high RPN steps, define controls. Example: For open manipulation in a Biosafety Cabinet (BSC):
- Engineering Control: BSC certified to NSF/ANSI 49, placed in ISO 7 room with positive pressure cascade.
- Procedural Control: Aseptic technique qualification for all operators, defined disinfection regimen.
- Monitoring Control: Continuous particle monitoring in the BSC (Grade A), settle plates during each operation, finger dabs of operators post-gowning.
- Knowledge Management: Document all data from EM, media fills, and incidents. Set alert/action limits using statistical tools.
- Review & Update: Quarterly review of all EM and deviation data. Annual formal review and update of the CCS document.
Closed Systems and Barrier Technology
Both frameworks acknowledge the value of closed systems but differ in emphasis.
Table 3: Approach to Isolation and Closure
| Aspect | FDA cGMP | EU GMP Annex 1 (2022) |
|---|---|---|
| Primary Objective | Prevent contamination and cross-contamination. | Strong preference for closed systems and RABS/isolators. Open processing is the exception requiring justification. |
| Environmental Requirements for Closed Systems | Reduced monitoring may be justified if closure is validated. | If a process step is truly closed, the background environment can be of a lower grade (justification required). |
| Validation of Closure | Expected to demonstrate integrity throughout the process. | Requires rigorous validation, including worst-case challenge studies (e.g., during transfers, connections). |
Experimental Protocol 2: Validating a "Closed" Tubing Welding System for Cell Transfer
- Objective: To validate that sterile tubing welds maintain a closed, sterile boundary during cell product transfer from one bag to another.
- Methodology:
- Integrity Testing (Physical): Use a helium leak detector or pressure decay test on a sample of welded tubing segments. Establish acceptance criteria (e.g., no detectable leak at 5 psi over 5 minutes).
- Microbial Challenge Test:
- Setup: Create a mock transfer system with two bags connected by a weld. Fill the source bag with sterile culture medium.
- Challenge: Submerge the weld joint in a high-titer suspension of Brevundimonas diminuta (≥10⁷ CFU/mL), a small-size challenge organism.
- Process: Activate the transfer pump to move medium across the challenged weld into the receiving bag.
- Analysis: Incubate the receiving bag fluid in tryptic soy broth for 14 days. Perform membrane filtration and plate on agar.
- Acceptance Criterion: No growth in the receiving bag fluid.
- Process Simulation (Media Fill): Incorporate the welding step into a full aseptic process simulation (media fill) using soybean-casein digest broth, executing a statistically significant number of runs.
Visualizing the Regulatory and Operational Framework
Diagram 1: ATMP GMP Compliance Framework.
Diagram 2: Cleanroom Monitoring Decision Flow.
The Scientist's Toolkit: Essential Reagents & Materials for ATMP GMP Compliance
Table 4: Key Research Reagent Solutions for Environmental Monitoring & Process Control
| Item / Reagent | Primary Function in ATMP GMP Context |
|---|---|
| Tryptic Soy Agar (TSA) Plates | Standard for general aerobic microbial monitoring via settle plates, contact plates, and air sampling. Detects a broad range of environmental isolates. |
| Soybean-Casein Digest Broth | Liquid growth medium used in Process Simulation Tests ("Media Fills") to validate the aseptic manufacturing process. |
| Sabouraud Dextrose Agar (SDA) Plates | Used for monitoring yeast and mold contamination in cleanrooms. Often used in parallel with TSA. |
| Neutralizing Agar | Contains agents (e.g., lecithin, polysorbate) to inactivate residual disinfectants (sporicides, alcohols) on contact plates for accurate microbial recovery. |
| Particle Count Calibration Standard | NIST-traceable polystyrene latex spheres (e.g., 0.5 µm, 5.0 µm) for calibrating and qualifying airborne particle counters, a regulatory requirement. |
| Rapid Microbiology Methods (RMM) Kits | ATP bioluminescence or nucleic acid-based kits for faster detection of microbial contamination on surfaces, though validation against traditional methods is required. |
| Cell Culture Media (GMP-grade) | Specifically formulated, endotoxin-tested, and quality-controlled media for the expansion and differentiation of therapeutic cells. The raw material of the ATMP. |
| GMP-grade Cytokines/Growth Factors | Critical process reagents for directing cell fate. Must be sourced with full traceability, Certificates of Analysis, and appropriate viral safety data. |
| Validated Cleaning & Disinfection Agents | Sporicidal (e.g., hydrogen peroxide-based) and non-sporicidal (e.g., alcohol) agents with proven efficacy against standard organisms, used on a validated rotation schedule. |
| Closed System Processing Sets | Single-use, sterile, functionally closed bags, tubing sets, and connectors that enable aseptic transfer and processing without exposure to the environment. |
The manufacturing of cell and gene therapies (CGTs) necessitates stringent environmental controls to ensure product sterility, safety, and efficacy. Good Manufacturing Practice (GMP) cleanroom classification is a cornerstone of this control. However, the distinct manufacturing paradigms for autologous (patient-specific) and allogeneic (off-the-shelf) therapies drive fundamentally different approaches to cleanroom design and classification. This whitepaper delineates these approaches, providing a technical guide for researchers and development professionals within a broader thesis on GMP standards for cell therapy research.
Foundational Principles: EU GMP Annex 1 & ISO 14644
The classification of airborne particulate cleanliness for medicinal products is defined in the EU GMP Annex 1 (2022) and ISO 14644-1 standards. Cleanrooms are classified from ISO 5 (Grade A) to ISO 9 (Grade D) based on the maximum permitted concentration of airborne particles per cubic meter by particle size (≥0.5 µm and ≥5.0 µm).
Table 1: Cleanroom Classification per EU GMP Annex 1 & ISO 14644-1
| Grade | ISO Class | Maximum permitted number of particles/m³ | Microbiological Active Air Action Limit (cfu/m³) | |
|---|---|---|---|---|
| ≥0.5 µm | ≥5.0 µm | |||
| A | ISO 5 | 3,520 | 20 | <1 |
| B | ISO 7 | 352,000 | 2,930 | 10 |
| C | ISO 8 | 3,520,000 | 29,300 | 100 |
| D | ISO 9 | Not defined (typically based on Good Housekeeping) | 200 |
Autologous Therapy: Closed System-Centric Approach
Autologous therapies involve a patient's own cells, which are harvested, manipulated (often expanded and/or genetically modified), and re-infused. Manufacturing is typically small-scale, batch-specific, and cannot tolerate cross-contamination.
Key Characteristics & Classification Strategy
- Scale: Small batch (single patient).
- Process: Often utilizes functionally closed processing systems (e.g., bioreactors, connected sets).
- Risk: High risk of cross-contamination between patient batches if open processing occurs.
- Strategy: The cleanroom classification can be de-emphasized in favor of robust process closure. The primary cleanroom (e.g., ISO 7/Class B) may serve as a background for placing multiple closed systems. Open manipulations (e.g., cell seeding, final formulation) for a single batch are performed within an ISO 5/Class A biosafety cabinet (BSC) or isolator located within this background environment.
Experimental Protocol: Viable Airborne Particle Count (VAPC) Monitoring
- Objective: To validate and routinely monitor the microbial quality of the Grade A zone (BSC/Isolator) and Grade B background.
- Methodology:
- Sampling Plan: Define fixed locations for active air samplers based on a risk assessment (e.g., near critical processing points, room corners).
- Equipment: Use a validated microbiological air sampler (e.g., impaction-based sampler like a sieve-to-agar impactor).
- Media: Use appropriate growth media (e.g., Tryptic Soy Agar for total aerobic count, Sabouraud Dextrose Agar for yeasts and molds).
- Procedure: During simulated processing or actual production, run the sampler for a specified volume (typically 1m³). Expose agar plates for <4 hours in BSC/Isolator as per Annex 1.
- Incubation: Incubate TSA plates at 20-25°C for 5-7 days and at 30-35°C for 2-3 days. Incubate SDA plates at 20-25°C for 5-7 days.
- Analysis: Count colony-forming units (cfu) and calculate cfu/m³. Compare against action limits in Table 1.
Allogeneic Therapy: Open Process-Centric Approach
Allogeneic therapies are derived from donor cells and manufactured as large, scalable batches intended for many patients. Processes often involve more open steps and larger equipment.
Key Characteristics & Classification Strategy
- Scale: Large batch (hundreds to thousands of patients).
- Process: Frequently involves open processing steps (e.g., centrifugation, open transfer) to achieve scale, though closed systems are adopted where possible.
- Risk: Lower risk of cross-contamination between products from the same batch, but higher risk of batch loss due to microbial ingress.
- Strategy: The cleanroom classification itself becomes the primary barrier. A traditional, multi-suite classification approach is used, with rooms of increasing stringency (e.g., ISO 8/Class C -> ISO 7/Class B -> ISO 5/Class A at open processing points). The entire process flow must occur within the appropriately classified environment.
Experimental Protocol: Non-Viable Particle Count (NVPC) Certification
- Objective: To certify that a cleanroom or clean zone meets the specified ISO class per ISO 14644-1.
- Methodology:
- Sampling Points: Calculate minimum number of points (NL) = √A, where A is the area in m² of the room. Distribute points evenly.
- Equipment: Use a calibrated, remote particle counter with a sample flow rate of 1.0 cfm (28.3 L/min) or higher.
- Procedure: Sample at each location at a height of 0.8-1.2m (work height). For each point, sample a volume sufficient to detect at least 20 particles at the target class limit. For ISO 5, sample at least 1m³ per point.
- Analysis: Record particle counts for ≥0.5µm and ≥5.0µm at each location. Calculate the mean concentration per point and the overall mean. The room meets the class if the overall mean and the mean at each point are below the class limit from Table 1.
Comparative Analysis
Table 2: Cleanroom Strategy Comparison for Autologous vs. Allogeneic Therapies
| Aspect | Autologous Therapy | Allogeneic Therapy |
|---|---|---|
| Primary Control Strategy | Process Closure | Environmental Classification |
| Typical Core Process Area | ISO 7 (Grade B) with multiple closed systems | ISO 5 (Grade A) open processing room with ISO 7 (Grade B) background |
| Air Change Rate (ACR) | Lower ACR may be acceptable (e.g., 20-40/hr) due to closure | Higher ACR required (e.g., 40-60/hr for ISO 5) to maintain particle counts |
| Pressure Cascades | Critical, but may be simpler (e.g., single positive pressure suite) | Complex, multi-room cascades essential to protect open processes |
| Gowning Requirements | Less stringent for closed system operators (e.g., ISO 8 gowning in ISO 7) | Full, stringent gowning per room grade (ISO 5 requires full sterile gowning) |
| Facility Footprint | Often smaller, modular, or multi-product suite | Larger, dedicated suites with clear material/patient flow separation |
| Batch Failure Impact | Impacts one patient | Impacts hundreds to thousands of patients |
| Cost Driver | Cost of single-use, closed processing sets | Cost of high-grade facility construction and validation |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Cleanroom Environmental Monitoring
| Item | Function/Brief Explanation |
|---|---|
| Particle Counter | Calibrated instrument for quantifying non-viable airborne particles of specific sizes (e.g., ≥0.5µm). Critical for room certification. |
| Microbial Air Sampler | Active air sampler (e.g., MAS-100 NT) that draws a known air volume onto growth media for viable particle (cfu) enumeration. |
| Contact Plates (RODAC) | Filled with agar (e.g., TSA) for monitoring microbial contamination on flat surfaces (walls, floors, equipment). |
| Finger Dabs/Glove Prints | Agar plates used specifically to assess the microbiological quality of operators' gloves post-gowning and during work. |
| Tryptic Soy Agar (TSA) | General-purpose growth medium for total aerobic microbial count recovery. |
| Sabouraud Dextrose Agar (SDA) | Selective medium for the recovery of yeasts and molds. |
| Neutralizing Agar | Contains inactivators (e.g., lecithin, polysorbate 80) to neutralize residual disinfectants on surfaces for accurate microbial recovery. |
| Particle Count Standard | Calibration standard (e.g., polystyrene latex spheres) for verifying the accuracy of particle counters. |
| Viable Particle Control Strain | Known concentration of a non-pathogenic organism (e.g., Bacillus atrophaeus spores) for validating microbial air sampler recovery efficiency. |
Decision and Validation Pathways
Figure 1: Cleanroom Strategy Selection Logic Flow (Max 100 chars)
The selection of a cleanroom classification strategy is not a one-size-fits-all decision but a direct function of the therapy's modality. Autologous therapies, enabled by advanced closed processing, allow for a leaner, product-centric quality model that can reduce facility burden. Allogeneic therapies, due to their scale and often more open processes, necessitate a traditional, facility-centric model where the classified environment is the primary control. Both approaches, when correctly implemented and validated, can achieve the fundamental GMP objective of assuring aseptic conditions for these life-saving advanced therapies.
Conclusion
Mastering GMP cleanroom classification is a cornerstone of successful and compliant cell therapy manufacturing. This guide has underscored that adherence to foundational ISO standards and regulatory expectations is merely the starting point. Effective implementation requires meticulous design, procedural rigor, and continuous environmental monitoring. Proactive troubleshooting and a deep understanding of validation principles are essential for mitigating the unique risks of aseptic cell processing. As therapies advance towards automation and closed systems, cleanroom strategies must evolve in parallel. Ultimately, a robustly classified and controlled environment is not just a regulatory checkbox but a fundamental determinant of product quality, patient safety, and the successful translation of groundbreaking cell therapies from bench to bedside.