Patient-Specific Disease Modeling with Stem Cells: Bridging the Gap Between Bench and Bedside
Patient-specific disease modeling, particularly using induced pluripotent stem cells (iPSCs), is revolutionizing biomedical research and drug development.
Patient-Specific Disease Modeling with Stem Cells: Bridging the Gap Between Bench and Bedside
Abstract
Patient-specific disease modeling, particularly using induced pluripotent stem cells (iPSCs), is revolutionizing biomedical research and drug development. This article provides a comprehensive overview for researchers and drug development professionals, exploring the foundational principles of stem cell-based models and their advantages over traditional systems. It delves into advanced methodological applications across neurology, cardiology, and metabolic diseases, while addressing key challenges in model maturity, standardization, and scalability. The content further examines rigorous validation frameworks and comparative analyses with animal models and immortalized cell lines, offering insights into how these human-relevant systems are accelerating therapeutic discovery and paving the way for personalized medicine.
The New Paradigm: Foundations of Stem Cell-Based Disease Modeling
Historical Foundations and Core Concepts
The field of pluripotent stem cells is built upon the fundamental principle that most somatic cells retain a complete genetic blueprint, with cellular diversity arising from reversible epigenetic mechanisms rather than irreversible genetic changes [1]. The conceptual journey began with John Gurdon's seminal somatic cell nuclear transfer (SCNT) experiments in 1962, which demonstrated that a nucleus from a differentiated frog cell could generate entire tadpoles when transplanted into an enucleated egg [1]. This pivotal work established that cellular differentiation does not involve irreversible loss of genetic potential.
The isolation of mouse embryonic stem cells (ESCs) in 1981 by Evans and Kaufman and later human ESCs (hESCs) by James Thomson in 1998 provided the first in vitro platforms for studying pluripotency [2] [1]. However, the ethical concerns surrounding embryo destruction for hESC derivation prompted the search for alternatives. The field transformed in 2006 when Takahashi and Yamanaka discovered that introducing four transcription factors—Oct4, Sox2, Klf4, and c-Myc (OSKM)—could reprogram mouse fibroblasts into induced pluripotent stem cells (iPSCs) [3] [1]. This breakthrough was successfully replicated with human cells in 2007 by both Yamanaka's group (using OSKM) and Thomson's group (using OCT4, SOX2, NANOG, and LIN28) [4] [1], establishing iPSCs as a revolutionary tool that bypassed ethical concerns while enabling patient-specific disease modeling.
Pluripotent stem cells are defined by two essential properties: self-renewal, the capacity for unlimited division while maintaining the undifferentiated state, and pluripotency, the ability to differentiate into derivatives of all three embryonic germ layers (ectoderm, mesoderm, and endoderm) [2]. These properties make them indispensable for studying human development, disease mechanisms, and regenerative medicine.
Technical Comparison of Pluripotent Stem Cell Types
Embryonic Stem Cells (ESCs)
ESCs are derived from the inner cell mass of pre-implantation blastocysts [2]. They represent the gold standard for pluripotency and possess extensive self-renewal capacity [2]. Their isolation typically involves microsurgical dissection or immunological targeting of trophoblast cells to separate the inner cell mass [2]. ESCs have been instrumental in foundational studies of early human development and differentiation pathways. However, their clinical application faces significant hurdles, including ethical controversies related to embryo destruction, potential for immune rejection upon transplantation since they are genetically distinct from recipients, and strict regulatory constraints governing their use [2] [5].
Induced Pluripotent Stem Cells (iPSCs)
iPSCs are generated by reprogramming somatic cells through the forced expression of specific transcription factors, effectively returning them to an embryonic-like pluripotent state [5] [1]. The core advantage of iPSC technology lies in its ability to create patient-specific cell lines that reflect the individual's genetic background, making them invaluable for personalized disease modeling and potentially avoiding immune rejection in autologous transplantation [5] [6]. Additionally, they circumvent the major ethical issues associated with ESCs [5].
Despite these advantages, iPSC technology faces its own challenges. The reprogramming process can introduce genetic abnormalities and carries a potential tumorigenic risk, particularly when using oncogenic factors like c-Myc or if partially reprogrammed cells remain in the final population [3] [5]. iPSCs may also retain epigenetic memory of their tissue of origin, which can influence their differentiation potential [5]. Furthermore, the reprogramming process has historically been inefficient, though methods have improved significantly [5].
Table 1: Comparison of Embryonic and Induced Pluripotent Stem Cells
| Feature | Embryonic Stem Cells (ESCs) | Induced Pluripotent Stem Cells (iPSCs) |
|---|---|---|
| Origin | Inner cell mass of blastocyst [2] | Reprogrammed somatic cells (e.g., skin, blood) [5] |
| Reprogramming Factors | N/A (naturally occurring) | OCT4, SOX2, KLF4, c-MYC (OSKM) or OCT4, SOX2, NANOG, LIN28 (OSNL) [4] [3] [1] |
| Key Advantages | Gold standard for pluripotency [5] | Patient-specific; avoids ethical concerns of ESCs; suitable for autologous therapy [5] [6] |
| Major Challenges | Ethical controversies; immune rejection in recipients; tumorigenesis [2] [5] | Genetic instability; tumorigenic risk; epigenetic memory; lower efficiency in some protocols [3] [5] |
| Primary Applications | Early development studies; differentiation paradigm [2] | Disease modeling; drug screening; personalized regenerative medicine [5] [6] |
The Molecular Machinery of Reprogramming
Core Mechanisms and Dynamics
The reprogramming of somatic cells to iPSCs is not a simple reversal of development but involves profound remodeling of the epigenetic landscape and gene expression networks [1]. The process typically occurs in two broad phases: an early, stochastic phase where somatic genes are silenced and early pluripotency genes activated, followed by a late, more deterministic phase where the core pluripotency network is stabilized [1]. The Yamanaka factors (OSKM) function as pioneer transcription factors that can bind to condensed chromatin and initiate its opening, allowing access to other transcriptional regulators [1].
During reprogramming, cells undergo mesenchymal-to-epithelial transition (MET), a critical step involving cadherin switching and cytoskeletal reorganization [1]. The process also involves global epigenetic changes, including DNA demethylation at pluripotency gene promoters and histone modification shifts that favor an open chromatin state [1]. Metabolic reprogramming from oxidative phosphorylation to glycolysis also occurs, mirroring the metabolic state of ESCs [1]. Additionally, somatic cell identity factors must be silenced while the endogenous pluripotency network (including OCT4, SOX2, and NANOG) becomes autonomously activated [1].
Reprogramming Methodologies and Delivery Systems
Significant progress has been made in developing safer and more efficient reprogramming methods. Early approaches used integrating retroviral and lentiviral vectors, which posed risks of insertional mutagenesis and oncogene activation [4] [3]. Current non-integrating methods include:
- Sendai Virus: A replication-deficient RNA virus that does not integrate into the host genome [4].
- Synthetic mRNA: Transient delivery of modified mRNA encoding reprogramming factors [4].
- Episomal Plasmids: DNA vectors that replicate extrachromosomally and are gradually diluted through cell divisions [3].
- Proteins: Direct delivery of recombinant reprogramming transcription factors [3].
- Small Molecules: Chemical compounds that can replace some transcription factors and enhance reprogramming efficiency [3] [1].
Table 2: Key Reprogramming Delivery Systems
| Delivery System | Genetic Material | Genomic Integration | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Retrovirus | RNA | Yes | High efficiency [3] | Integration; silencing; tumorigenesis risk [3] |
| Lentivirus | RNA | Yes | Can infect non-dividing cells [3] | Integration; potential insertional mutagenesis [3] |
| Sendai Virus | RNA | No | High efficiency; no integration [4] | Require clearance; immunogenic potential [4] |
| Synthetic mRNA | RNA | No | High safety; controlled timing [4] | Requires multiple transfections; immunogenic [4] |
| Episomal Plasmid | DNA | No | Simple delivery; low cost [3] | Low efficiency; potential integration [3] |
| Recombinant Protein | Protein | No | Highest safety; no genetic material [3] | Very low efficiency; challenging delivery [3] |
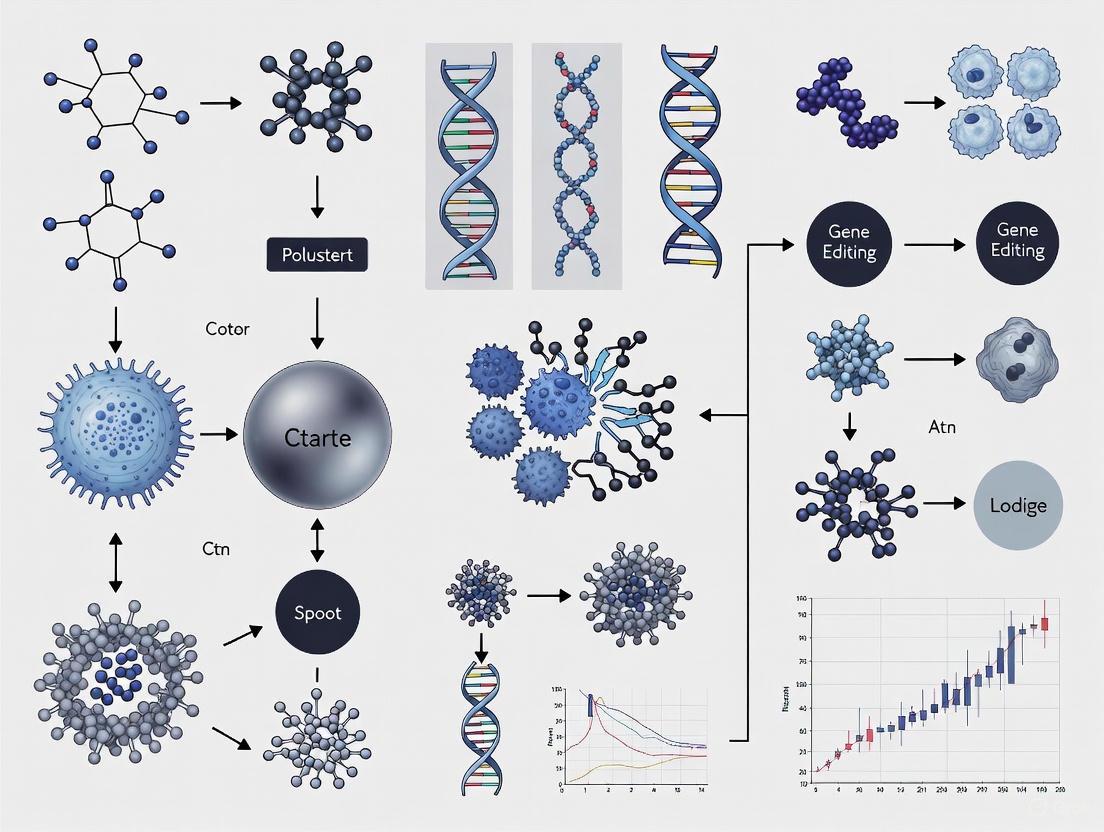
Reprogramming Mechanism Overview
The Scientist's Toolkit: Essential Reagents and Protocols
Key Research Reagent Solutions
Table 3: Essential Reagents for iPSC Research
| Reagent Category | Specific Examples | Function/Purpose |
|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (OSKM) [3] [1] | Core transcription factors inducing pluripotency |
| Reprogramming Enhancers | Valproic acid (VPA), Sodium butyrate, 5-aza-cytidine [3] | Epigenetic modifiers that increase reprogramming efficiency |
| Culture Matrices | Matrigel, Vitronectin, Laminin-521 [7] | Synthetic or purified extracellular matrix for feeder-free culture |
| Pluripotency Media | mTeSR, StemFlex, Essential 8 [4] | Defined, xeno-free media for maintaining pluripotent state |
| Differentiation Inducers | BMP4, Activin A, CHIR99021, Retinoic Acid [4] [6] | Small molecules and growth factors directing lineage specification |
| Gene Editing Tools | CRISPR-Cas9, Base Editors [4] [5] | Precision genome engineering for creating isogenic controls |
Experimental Workflow for iPSC Generation and Characterization
A standard protocol for generating iPSCs involves the following key steps:
Somatic Cell Source Selection and Preparation: Obtain starting cells (typically dermal fibroblasts or peripheral blood mononuclear cells) and culture in appropriate media to achieve optimal density and viability [3].
Reprogramming Factor Delivery: Transduce cells with non-integrating vectors (e.g., Sendai virus or mRNA) encoding the OSKM factors. The choice of delivery system depends on the balance between efficiency and safety requirements [4] [3].
Culture and Colony Expansion: Transfer transduced cells to feeder-free conditions on defined matrices approximately 4-7 days post-transduction. Replace media with defined pluripotency-supporting medium (e.g., mTeSR). Monitor for emergence of compact, ESC-like colonies with defined borders between days 14-28 [4].
Colony Picking and Expansion: Mechanically pick or dissociate distinct iPSC colonies and transfer to new culture vessels for expansion. Clonally expanded lines should be banked at early passages [4].
Quality Control and Characterization:
- Pluripotency Marker Validation: Confirm expression of key proteins (OCT4, SOX2, NANOG, SSEA-4) via immunocytochemistry and/or flow cytometry [1].
- Trilineage Differentiation Potential: Demonstrate differentiation into ectoderm, mesoderm, and endoderm derivatives in vitro (embryoid body formation) or in vivo (teratoma assay) [1].
- Karyotype Analysis: Perform G-banding or spectral karyotyping to ensure genomic integrity [5].
- Short Tandem Repeat (STR) Profiling: Authenticate cell line identity and confirm match to donor somatic cells [8].
- Microbiological Testing: Screen for mycoplasma and other contaminants [8].
Applications in Patient-Specific Disease Modeling
The ability to generate iPSCs from patients with genetic diseases has revolutionized biomedical research by providing unprecedented access to human-specific disease models. These models retain the patient's complete genetic background, enabling investigation of disease mechanisms and drug responses in a personalized context [9] [6].
Advanced Modeling Platforms
Two-Dimensional (2D) Models represent the foundational approach, where iPSCs are differentiated into specific cell types (e.g., neurons, cardiomyocytes) as monolayers [7]. These systems have successfully modeled monogenic disorders like Parkinson's disease and Long QT syndrome, revealing disease-specific phenotypes such as impaired mitochondrial function and electrophysiological abnormalities [7]. However, 2D models lack the tissue-level complexity and cell-cell interactions present in native organs [7].
Three-Dimensional Organoids are self-organizing structures that more accurately recapitulate tissue architecture and cellular heterogeneity [9] [7]. These complex models have been developed for brain, kidney, liver, and heart tissues, enabling the study of cell-cell interactions and tissue-level disease phenotypes not observable in 2D cultures [9] [7]. For example, brain organoids have been used to model neurodevelopmental disorders, while kidney organoids have replicated cyst formation in polycystic kidney disease [9].
Microphysiological Systems (Organ-on-a-Chip) integrate iPSC-derived tissues with microfluidic platforms to incorporate physiological cues such as fluid flow, mechanical strain, and tissue-tissue interfaces [7]. These systems enable real-time monitoring of functional parameters and have been applied to model the blood-brain barrier, cardiac function, and drug-induced organ toxicity [7].
Disease Modeling Pipeline
Integration with Gene Editing for Disease Modeling
The combination of iPSC technology with CRISPR-Cas9 gene editing has become particularly powerful for disease modeling [9] [7]. Isogenic controls—where disease-causing mutations are corrected in patient-derived iPSCs or introduced into healthy iPSCs—enable researchers to study the specific effects of a mutation without confounding genetic background effects [7]. This approach has been successfully applied to model cardiac channelopathies, neurodegenerative diseases, and cystic fibrosis, allowing precise correlation between genetic lesions and cellular phenotypes [7].
Clinical Translation and Regulatory Landscape
Current Clinical Trial Landscape
The clinical application of pluripotent stem cell-based therapies has gained significant momentum. As of December 2024, a comprehensive review identified 115 global clinical trials involving 83 distinct PSC-derived products, with over 1,200 patients dosed and more than 10¹¹ cells administered without significant class-wide safety concerns [8]. These trials primarily target three therapeutic areas:
Ophthalmology: The eye represents a leading target due to its immune-privileged status, ease of surgical access, and precise functional assessment. OpCT-001, an iPSC-derived therapy for retinal degeneration, received FDA IND clearance in 2024 [8].
Neurology: Multiple iPSC-derived neural progenitor cell therapies for Parkinson's disease, spinal cord injury, and ALS have received FDA IND clearance [8]. These off-the-shelf products aim to provide scalable cell sources for neurodegenerative conditions.
Oncology: iPSC-derived immune cells, particularly natural killer (NK) cells and CAR-T cells, are being developed as allogeneic cancer immunotherapies [8]. FT819, an off-the-shelf iPSC-derived CAR T-cell therapy for systemic lupus erythematosus, received FDA RMAT designation in 2025 [8].
Table 4: Select FDA-Authorized Stem Cell Clinical Trials (2023-2025)
| Therapy Name | Cell Type | Indication | Development Stage | Key Details |
|---|---|---|---|---|
| Fertilo | iPSC-derived ovarian support cells | Infertility | Phase III (FDA IND cleared) | First iPSC-based therapy in U.S. Phase III; supports ex vivo oocyte maturation [8] |
| OpCT-001 | iPSC-derived photoreceptor cells | Retinal degeneration | Phase I/IIa | First iPSC-based therapy for primary photoreceptor diseases [8] |
| FT819 | iPSC-derived CAR T-cells | Systemic lupus erythematosus | Phase I (RMAT designation) | Off-the-shelf allogeneic approach [8] |
| iPSC-derived NPCs | Neural progenitor cells | Parkinson's disease, SCI, ALS | Phase I (FDA IND cleared) | Multiple off-the-shelf products [8] |
| MyoPAXon | iPSC-derived muscle progenitors | Duchenne muscular dystrophy | Phase I | Allogeneic muscle progenitor cells [8] |
Regulatory Pathways and Approved Therapies
The transition from research to clinically approved therapies requires navigating rigorous regulatory pathways. The U.S. Food and Drug Administration (FDA) distinguishes between Investigational New Drug (IND) authorization, which permits clinical trials, and full Biologics License Application (BLA) approval for marketing [8]. Recent FDA-approved stem cell products include:
Omisirge (omidubicel-onlv): Approved in 2023 for hematologic malignancies, this cord blood-derived hematopoietic progenitor cell product accelerates neutrophil recovery after transplantation [8].
Lyfgenia (lovotibeglogene autotemcel): Approved in 2023 for sickle cell disease, this autologous cell-based gene therapy modifies patient hematopoietic stem cells to produce anti-sickling hemoglobin [8].
Ryoncil (remestemcel-L): Approved in 2024 as the first MSC therapy for pediatric steroid-refractory acute graft-versus-host disease [8].
The FDA's Regenerative Medicine Advanced Therapy (RMAT) designation provides expedited development pathways for promising therapies, reflecting the agency's commitment to advancing the field [8].
Future Perspectives and Challenges
The future of pluripotent stem cell research will be shaped by several key developments. Precision medicine integration will leverage patient-specific iPSCs to tailor drug therapies to individual genetic backgrounds, potentially revolutionizing treatment personalization [2] [6]. Advanced bioengineering approaches, including better organoid vascularization, maturation, and the creation of multi-organ systems ("body-on-a-chip"), will enhance physiological relevance [9] [7]. Immune evasion strategies, such as CRISPR-mediated deletion of HLA genes and induction of hypoimmunogenic cells, will facilitate allogeneic transplantation without immunosuppression [4].
Despite remarkable progress, significant challenges remain. Tumorigenicity risks associated with residual undifferentiated cells or genetic abnormalities necessitate stringent safety monitoring [5]. Manufacturing scalability must be addressed through automated, cost-effective Good Manufacturing Practice (GMP) processes to enable widespread clinical application [9]. Functional maturity of iPSC-derived cells often remains fetal-like, requiring improved maturation protocols to accurately model adult-onset diseases [7]. Standardization and reproducibility across different laboratories and cell lines continue to present hurdles that the field must overcome through established benchmarking and quality control measures [9] [10].
As these challenges are addressed, pluripotent stem cell technologies will increasingly transform biomedical research, drug development, and clinical practice, ultimately fulfilling their potential to provide personalized regenerative therapies for a wide range of debilitating conditions.
Patient-specific induced pluripotent stem cells (iPSCs) are catalyzing a paradigm shift in biomedical research and drug discovery. By enabling the generation of patient-specific somatic cells, iPSC technology directly addresses the critical limitations of traditional animal models and primary cell cultures. This whitepaper details the three core advantages of iPSC-based platforms: (1) patient specificity for modeling genetic diseases and personalizing therapeutic interventions; (2) human relevance for superior predictive power in pharmacology and toxicology; and (3) unlimited scalability for high-throughput drug screening and regenerative medicine. We provide a technical overview of the experimental methodologies, signaling pathways, and reagent solutions that underpin these advantages, offering researchers a framework for implementing these transformative technologies.
Patient Specificity: Modeling the Individual in a Dish
The ability to derive iPSCs from any individual imbues disease models with the unique genetic and epigenetic makeup of the patient. This patient specificity is foundational for precision medicine, allowing for the study of disease mechanisms in a genetically relevant context and the tailoring of drug therapies [11].
Technical Implementation and Workflow
The core process involves reprogramming a patient's somatic cells (e.g., dermal fibroblasts or blood cells) into pluripotent stem cells, which are then differentiated into the target cell types affected by the disease.
Diagram 1: Workflow for generating patient-specific disease models from iPSCs.
Key Methodologies and Validation
Initial reprogramming often uses the Yamanaka factors (Oct4, Sox2, Klf4, c-Myc) delivered via non-integrating methods (e.g., Sendai virus, mRNA) to minimize genomic alteration risks [12]. The resulting iPSCs are characterized for pluripotency markers (OCT3/4, NANOG) before directed differentiation. Disease phenotypes are validated through functional assays (e.g., electrophysiology for cardiomyocytes, cytochrome P450 activity for hepatocytes) and genetic correction to confirm causality of identified variants [11] [12].
Human Relevance: Bridging the Translational Gap
Traditional drug development relies heavily on animal studies, which suffer from interspecies differences in physiology, genetics, and disease pathogenesis, contributing to a >90% failure rate in clinical trials [13]. iPSC-derived human cells offer a biologically relevant alternative.
Quantitative Superiority of Human-Relevant Models
The table below summarizes the comparative performance of traditional models versus human iPSC-based systems.
| Model Characteristic | Animal Models | Primary Human Cells | iPSC-Derived Cells |
|---|---|---|---|
| Physiological Relevance | Low (e.g., mouse heart rate: 500 bpm vs. human: 60-100 bpm) [11] | High | High |
| Genetic Diversity | Limited (inbred strains) [13] | High, but limited availability | Can capture population diversity |
| Predictive Value for Drug Toxicity | Poor (false positives/negatives) [13] | Good, but limited lifespan | High (e.g., Liver Chips outperform animals) [14] |
| Scalability for HTS | Low | Very Low | High [11] |
| Cost and Timeline | High cost, long duration [14] | High cost, limited supply | Cost-effective after initial setup |
Advanced Human-Relevant Model Systems
To enhance physiological accuracy, iPSCs are being integrated into complex in vitro systems:
- Organ-on-Chips (OoCs): Microfluidic devices lined with iPSC-derived cells that emulate tissue-tissue interfaces, mechanical forces, and vascular perfusion. For example, Liver Chips have demonstrated superior prediction of drug-induced liver injury compared to animal models [14] [13].
- 3D Organoids: Self-organizing, three-dimensional structures that recapitulate key aspects of organ development and cellular complexity, such as the presence of multiple cell types and spatial organization [15] [13].
Unlimited Scalability: Enabling High-Throughput Science
The self-renewal capacity of iPSCs provides a limitless source of specific cell types, overcoming the critical bottleneck of cell sourcing that has plagued primary cell research [11] [12].
Scalable Differentiation Protocols
Modern cardiac differentiation protocols, for instance, achieve efficiencies >90% using a chemically defined, small-molecule-directed approach in monolayer cultures, enabling mass production of cardiomyocytes [11]. The process is orchestrated by manipulating key developmental signaling pathways.
Diagram 2: Signaling pathway control in scalable cardiomyocyte differentiation.
Applications in Drug Discovery and Screening
The scalable production of human cells enables applications previously deemed impractical:
- High-Throughput Toxicity Screening: iPSC-derived cardiomyocytes are used to screen compounds for cardiotoxic effects, such as QT interval prolongation, on a large scale [11].
- Phenotypic Drug Screens: Large libraries of compounds can be tested on patient-specific disease models (e.g., for Long QT syndrome, hypertrophic cardiomyopathy) to identify novel therapeutics [11].
- Clinical Trial in a Dish: Using a diverse bank of iPSC lines, researchers can pre-test drug efficacy and safety across a genetically varied human population, potentially de-risking clinical trials [11].
The Scientist's Toolkit: Essential Reagents and Solutions
A successful iPSC-based research program relies on a suite of core reagents and tools, as detailed below.
| Research Reagent | Function and Application | Example |
|---|---|---|
| Reprogramming Factors | Induce pluripotency in somatic cells. | Oct4, Sox2, Klf4, c-Myc (OSKM) [12]. |
| Small Molecule Inducers | Direct lineage-specific differentiation by modulating key signaling pathways. | GSK-3β inhibitor (CHIR99021) for mesoderm induction; WNT inhibitors (IWR-1) for cardiac specification [11]. |
| Chemically Defined Media | Provide a controlled, reproducible environment for differentiation and maintenance. | Essential for robust, high-efficiency generation of cells like cardiomyocytes and hepatocytes [11] [12]. |
| Extracellular Matrix (ECM) | Provides the physical scaffold for 3D cell culture and organoid formation. | Matrigel or synthetic hydrogels used for organoid generation and OoC seeding [13]. |
| Characterization Antibodies | Validate pluripotency and differentiation efficiency via immunostaining or flow cytometry. | Antibodies against OCT3/4, NANOG (pluripotency); TNNT2 (cardiomyocytes) [11]. |
Overcoming Ethical and Practical Limitations of Traditional Models
Traditional preclinical models, particularly animal systems, have long been the cornerstone of biomedical research. However, a significant translational gap persists, with a high proportion of drug candidates failing in human clinical trials due to unpredicted toxicities or inefficacies not predicted by animal studies [9]. This disconnect stems from fundamental species-specific differences in genetics, immune responses, and organ physiology [9]. The field is now undergoing a paradigm shift toward patient-specific disease modeling using human stem cells, which offers unprecedented access to human-specific biology and a path to overcome both the ethical and practical limitations of traditional models.
The advent of human induced pluripotent stem cells (iPSCs) has been particularly transformative. These cells, generated by reprogramming adult somatic cells, bypass the ethical controversies associated with embryonic stem cells while providing a patient-specific pluripotent cell source [16]. This breakthrough, coupled with advances in organoid culture and genome editing, has positioned stem cell-based approaches as a cornerstone for ethical and clinically predictive research [9].
The Limitations of Traditional Animal Models
The reliance on animal models has created a bottleneck in the drug development pipeline. Their limitations can be categorized into practical and ethical concerns.
Practical and Translational Shortcomings
The primary practical limitation is the poor predictive power for human outcomes. Rodents, despite their utility, often fail to capture key aspects of human physiology and disease pathogenesis [9]. This species disconnect contributes to high dropout rates in drug development, where promising interventions fail in human clinical trials. Furthermore, immortalized cell lines (e.g., HeLa, SH-SY5Y), while easy to culture, are often derived from cancers and display unpredictable or non-physiological behaviors, making them poor models for human disease [17].
Ethical Considerations
The use of animal models raises significant welfare concerns, which are subject to increasing public scrutiny and regulatory pressure. While the "3Rs" (Replacement, Reduction, Refinement) have been a guiding principle, the ultimate goal for many researchers is the complete replacement of animal models where scientifically possible. Stem cell-based human models represent the most promising path toward achieving this goal, aligning with ethical principles of social justice and minimizing harm [18].
Stem Cell-Based Models: A Paradigm Shift
Stem cell technologies offer a revolutionary toolbox for creating human-relevant systems. The key cell types and their characteristics are summarized in the table below.
Table 1: Key Human Stem Cell Types for Disease Modeling
| Stem Cell Type | Source | Differentiation Potential | Key Advantages | Primary Ethical Considerations |
|---|---|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | Reprogrammed somatic cells (e.g., skin, blood) [16] | Pluripotent | Patient-specific; avoids embryo destruction; suitable for autologous therapy [16] | Donor consent; potential misuse [16] |
| Embryonic Stem Cells (ESCs) | Inner cell mass of blastocysts [16] | Pluripotent | Gold standard for pluripotency; robust differentiation protocols | Destruction of human embryos [16] |
| Mesenchymal Stem Cells (MSCs) | Adult tissues (e.g., bone marrow, adipose) [9] | Multipotent | Immunomodulatory effects; lower ethical concerns; readily accessible | Tissue procurement and handling affect quality [9] |
| Organoids | Self-organizing stem cells (PSCs or adult) [9] | Varies (tissue-specific) | 3D architecture; recapitulates tissue heterogeneity; models cell-cell interactions [9] | Complexity of oversight for sensitive models (e.g., neural) [18] |
Core Technological Advantages
The superiority of stem cell models is built on three pillars:
- Patient Specificity: iPSCs carry the donor's genome, including disease-associated mutations, enabling direct modeling of rare or complex genetic diseases in a human cellular context [17].
- Human Relevance: Differentiated iPSC-derived cells (e.g., neurons, cardiomyocytes) recapitulate key functional aspects of real human tissue, such as synaptic activity and contractility, providing a physiologically accurate platform for study [17].
- Scalability and Throughput: Once a differentiation protocol is established, iPSC lines can be expanded indefinitely and manufactured at a scale required for high-throughput drug screening, including in 384- or 1536-well formats [17].
Experimental Protocols for Patient-Specific Disease Modeling
This section provides a detailed methodology for establishing a patient-specific disease model using iPSCs, from somatic cell reprogramming to phenotypic analysis.
Protocol 1: Generating and Validating an iPSC-Based Disease Model
Goal: To create a patient-specific iPSC line, differentiate it into relevant target cells, and model a disease phenotype.
Workflow Overview:
Step-by-Step Methodology:
Somatic Cell Source and Reprogramming:
- Obtain patient somatic cells (e.g., skin fibroblasts or peripheral blood mononuclear cells) with appropriate informed consent and ethical approval [18].
- Reprogram cells using a non-integrating method, such as Sendai virus or synthetic mRNA delivery of the Yamanaka factors (OCT4, SOX2, KLF4, c-MYC). This avoids genomic integration, a critical safety consideration.
- Culture emerging iPSC colonies on feeder layers or in defined, feeder-free conditions. Manually pick and expand clonal lines based on characteristic embryonic stem cell-like morphology.
iPSC Line Validation:
- Pluripotency Validation: Confirm the expression of key pluripotency markers (OCT4, SOX2, NANOG) via immunocytochemistry and flow cytometry. Perform in vitro trilineage differentiation (ectoderm, mesoderm, endoderm) to confirm differentiation potential.
- Genetic Integrity: Perform karyotype analysis (G-banding) or higher-resolution CNV analysis to ensure genomic stability acquired during reprogramming [9].
- Identity Confirmation: Use STR profiling to confirm the line matches the original donor.
In Vitro Disease Modeling:
- Differentiate validated iPSCs into the relevant cell type(s) using established, published protocols. For example:
- For complex tissue modeling, generate 3D organoids that self-organize to recapitulate tissue architecture and cellular heterogeneity [9]. For kidney disease, organoids carrying PKD1 or PKD2 mutations form cysts, mimicking polycystic kidney disease pathology [9].
Phenotypic and Functional Analysis:
- Characterization: Use immunostaining and single-cell RNA sequencing (scRNA-seq) to validate cell types and maturity. Compare disease lines to isogenic controls or healthy lines.
- Functional Assays: Perform assays relevant to the disease, such as:
- Multi-electrode arrays (MEA) for neuronal or cardiac electrophysiology.
- Calcium imaging for neuronal or cardiomyocyte functional analysis.
- High-content imaging to quantify disease-relevant phenotypes (e.g., tau aggregation in neurons, lipid accumulation in hepatocytes) [17].
Creating Isogenic Controls (Optional but Recommended):
- Use CRISPR-Cas9 genome editing to correct the disease-causing mutation in the patient iPSC line, creating a perfect genetic control [9].
- Alternatively, introduce the disease mutation into a healthy control line. This step strengthens causal inference by isolating the effect of the specific genetic variant from the patient's background genetic variation.
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for iPSC-Based Disease Modeling
| Reagent/Category | Specific Examples | Function in Protocol |
|---|---|---|
| Reprogramming Kits | CytoTune (Sendai Virus), mRNA Reprogramming Kits | Deliver transcription factors to convert somatic cells into iPSCs without genomic integration. |
| Culture Media | mTeSR1, StemFlex, Essential 8 | Maintain iPSCs in a defined, pluripotent state. |
| Differentiation Kits & Reagents | Small molecules (CHIR99021, SB431542), GMP-grade cytokines (BMP4, FGF2) | Direct lineage-specific differentiation into target cells (e.g., neurons, cardiomyocytes). |
| Characterization Antibodies | Anti-OCT4, SOX2, NANOG; Cell-type specific markers (e.g., TUJ1 for neurons, cTnT for cardiomyocytes) | Validate pluripotency and differentiation efficiency via immunocytochemistry and flow cytometry. |
| Genome Editing Tools | CRISPR-Cas9 systems (e.g., ribonucleoprotein complexes), HDR donors | Create isogenic control lines via precise gene correction or mutation. |
| Analysis Tools | Multi-electrode Arrays (MEA), High-Content Imagers, scRNA-seq kits | Perform functional and phenotypic analysis of derived cells and tissues. |
Data Presentation: Quantitative Advantages of Stem Cell Models
The quantitative benefits of stem cell models are evident across applications, from disease modeling to drug screening.
Table 3: Applications and Performance of Stem Cell-Derived Models in Drug Discovery
| Application Area | Stem Cell Model Used | Key Findings and Advantages | References |
|---|---|---|---|
| Cardiotoxicity Screening | iPSC-derived cardiomyocytes | Routinely used to screen for drug-induced arrhythmia risk; integrated into regulatory safety initiatives (CiPA). Used by pharmaceutical companies (Roche, Takeda) for preclinical cardiac profiling. [17] | [17] |
| Neurodegenerative Disease | iPSC-derived neurons from Alzheimer's, Parkinson's, and ALS patients | Model disease phenotypes (tau aggregation, mitochondrial dysfunction). Support phenotypic screens identifying compounds that rescue neuronal function in vitro. [17] | [17] |
| Metabolic Disease | Hepatocyte-like cells from iPSCs of Familial Hypercholesterolemia patients | Revealed drug repurposing opportunity: cardiac glycosides reduced ApoB secretion. Provided a human-relevant system for testing lipid-lowering therapies. [17] | [17] |
| Kidney Disease | Kidney organoids with PKD1 or PKD2 mutations | Displayed cyst formation reminiscent of patient pathology, providing a robust system for mechanistic studies and therapeutic screening. [9] | [9] |
Addressing Remaining Challenges and Future Directions
Despite the promise, the field must overcome several hurdles to fully realize its potential. Key challenges and developing solutions are outlined below.
- Challenge: Functional Immaturity. iPSC-derived cells often exhibit a fetal-like gene expression profile and electrophysiological activity, limiting their ability to model late-onset diseases [9] [17].
Solution: Advanced maturation strategies are under development, including prolonged culture, biomechanical stimulation, electrical pacing for cardiomyocytes, co-culture with supporting cell types, and the introduction of vascularization to improve nutrient exchange and mimic the in vivo environment more closely [9].
Challenge: Lack of Standardization. Differentiation protocols vary significantly between laboratories, leading to inconsistent results and limiting reproducibility [9].
Solution: The field is moving toward harmonized quality standards. This includes benchmarking efforts using high-dimensional molecular profiling (e.g., scRNA-seq) and the use of commercial, QC-verified cell batches to improve cross-study comparability [9] [17].
Challenge: Scalability and Manufacturing. Translating laboratory protocols into robust, cost-effective, and cGMP-compliant production systems remains difficult [9].
Solution: Implementation of automation, closed culture systems, and high-throughput bioprocessing in bioreactors is key to bringing down costs and ensuring reproducible, large-scale production of cells for therapies and screening [9] [17].
Challenge: Evolving Ethical Oversight. As models increase in complexity (e.g., stem cell-based embryo models - SCBEMs, neural organoids), new ethical questions emerge [18].
- Solution: Adherence to updated international guidelines, such as those from the International Society for Stem Cell Research (ISSCR). These guidelines provide frameworks for oversight, mandate a clear scientific rationale and defined endpoint for research, and prohibit the culture of SCBEMs to the point of potential viability [18].
The adoption of patient-specific stem cell models marks a critical evolution in biomedical research, directly addressing the ethical and practical limitations of traditional animal models. By providing a human-relevant, scalable, and genetically defined platform, iPSCs and organoids are bridging the long-standing translational gap in drug discovery. While challenges in standardization and functional maturation persist, they are being actively addressed through bioengineering and international collaboration. As the field moves forward, guided by rigorous science and thoughtful ethics, these technologies promise to accelerate the development of safer, more effective therapies for a wide range of debilitating human diseases.
Stem cell research has fundamentally transformed the landscape of biomedical science, providing unprecedented tools for modeling human diseases and developing regenerative therapies. This technical guide examines the current state and methodologies of patient-specific disease modeling across three key therapeutic areas: cardiovascular, neurological, and metabolic disorders. The advent of induced pluripotent stem cells (iPSCs) has been particularly revolutionary, enabling the generation of patient-specific cellular models that recapitulate disease phenotypes in vitro. These models serve as powerful platforms for deciphering disease mechanisms, screening therapeutic compounds, and developing personalized treatment approaches. While significant progress has been made, challenges remain in achieving full cellular maturation, standardization of protocols, and clinical translation. This document provides researchers with a comprehensive technical resource covering experimental protocols, key reagents, and analytical frameworks for advancing stem cell-based disease modeling and therapeutic development.
Patient-specific disease modeling using stem cells represents a paradigm shift in biomedical research, addressing critical limitations of traditional animal models. The ability to generate human iPSCs from somatic cells through genetic reprogramming has created unprecedented opportunities to study human diseases in genetically relevant human cellular systems [9]. These models more accurately reflect human pathophysiology and species-specific biology, thereby enhancing the predictive validity of preclinical research [9].
The fundamental workflow involves reprogramming patient somatic cells (typically dermal fibroblasts or blood cells) to pluripotency, differentiating these iPSCs into disease-relevant cell types, and utilizing the resulting cellular models for mechanistic studies or drug screening. The integration of CRISPR-Cas9 gene editing allows for creation of isogenic control lines, strengthening causal inference between genetic variants and disease phenotypes [9]. For neurological disorders, stem cell models have enabled researchers to "reconstitute events of human brain development that occur after birth," providing unprecedented access to previously inaccessible developmental processes [19].
Cardiovascular Disease Modeling
Current Landscape and Challenges
Cardiovascular diseases (CVDs) remain the leading cause of death globally, accounting for approximately 18.6 million deaths annually [20]. Myocardial infarction (MI) and atherosclerosis represent particularly devastating manifestations, with conventional treatments unable to fully regenerate damaged myocardial or vascular tissues [20]. The adult mammalian heart exhibits very limited regenerative capacity, making stem cell-based approaches particularly promising for cardiac regeneration [21].
Stem Cell Platforms and Methodologies
Multiple stem cell types are being investigated for cardiovascular disease modeling and therapy:
Table: Stem Cell Types for Cardiovascular Applications
| Stem Cell Type | Sources | Key Advantages | Major Limitations | Primary Mechanisms |
|---|---|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Bone marrow, adipose tissue, umbilical cord [20] | Strong immunomodulatory capacity; abundant paracrine function [20] | Low survival post-transplantation (<10%); functional heterogeneity [20] | Paracrine effects; immunomodulation; homing [20] |
| Induced Pluripotent Stem Cells (iPSCs) | Reprogrammed somatic cells [20] | Patient-specific; differentiation potential of embryonic stem cells [20] | Tumorigenic risk; residual epigenetic memory [20] | Direct differentiation; tissue replacement [20] |
| Cardiac Stem Cells (CSCs) | Adult heart [20] | Tissue-specific; can be transplanted directly to damaged heart [20] | Limited studies; mechanisms not fully elucidated [20] | Exosome secretion; anti-apoptosis; angiogenesis [20] |
| Embryonic Stem Cells (ESCs) | Inner cell mass of blastocyst [20] | High differentiation efficiency (70-85%) [20] | Ethical concerns; tumorigenic risk; immune rejection [20] | Direct differentiation [20] |
Key Experimental Protocols
iPSC-Derived Cardiomyocyte Differentiation
The directed differentiation of iPSCs into cardiomyocytes has been optimized using stage-specific signaling pathway modulation:
- Mesoderm Induction (Days 0-3): Culture iPSCs in RPMI/B27 medium supplemented with 6-8 µM CHIR99021 (GSK-3β inhibitor) to activate Wnt signaling [20].
- Cardiac Mesoderm Specification (Days 3-5): Replace medium with RPMI/B27 containing 2-5 µM IWP2 (Wnt inhibitor) to suppress Wnt signaling and promote cardiac commitment.
- Cardiomyocyte Maturation (Days 5-30+): Maintain cells in RPMI/B27 with occasional metabolic selection (lactate-containing media) to enrich for cardiomyocytes, achieving up to 95% purity [20].
Cardiovascular Organoid Generation
Three-dimensional cardiovascular organoids provide more physiologically relevant models for disease modeling:
- Aggregation Phase: Harvest iPSC-derived cardiac progenitors and aggregate in U-bottom plates via centrifugation (500 × g, 3 min).
- Organoid Maturation: Culture in suspension with rotational orbital shaking (60-80 rpm) for 30-60 days with defined maturation factors [9].
- Functional Assessment: Evaluate contractile function via video-based analysis, electrophysiology by microelectrode array, and structure by immunostaining for cardiac troponins, α-actinin, and connexin-43.
Technical Workflow: Cardiovascular Disease Modeling
The following diagram illustrates the integrated workflow for creating patient-specific cardiovascular disease models using stem cells:
Neurological Disease Modeling
Current Landscape and Challenges
Neurological disorders represent a diverse set of conditions with limited treatment options and complex underlying pathophysiology. Stem cell models have emerged as essential tools for investigating disease mechanisms in human-relevant systems, particularly for disorders affecting the central nervous system [19] [22].
Advanced Modeling Platforms
Cerebral Organoids and Assembloids
Three-dimensional models have revolutionized neurological disease modeling:
- Extended Maturation Timelines: Unlike traditional 2D cultures, 3D assembloid models require extended culture periods (up to 390 days) to recapitulate postnatal developmental processes [19].
- Chain Migration of Interneurons: Advanced models demonstrate that "newly born migratory interneurons arrange themselves into connected chains that are surrounded by astrocytes," essentially recapitulating early postnatal migration patterns [19].
- Cell Biological Analysis: These models enable genetic and cell biological analysis of human-specific developmental processes previously only observable in postmortem tissue [19].
Disease-Specific Modeling Approaches
Table: Neurological Disorder Modeling Strategies
| Disorder | Stem Cell Approach | Key Phenotypes Modeled | Therapeutic Mechanisms |
|---|---|---|---|
| Parkinson's Disease | iPSC-derived dopaminergic neurons [22] | Loss of dopaminergic neurons; motor deficits | Cell replacement; neuroprotection via BDNF/GDNF secretion [22] |
| Multiple Sclerosis | iPSC-derived oligodendrocytes [22] | Demyelination; immune activation | Immunomodulation; remyelination promotion [22] |
| Alzheimer's Disease | iPSC-derived cortical neurons [22] | Amyloid-beta accumulation; tau pathology; cognitive decline | Reduction of amyloid plaques; enhanced neurogenesis [22] |
| Spinal Cord Injury | Neural stem cell transplantation [22] | Axonal damage; glial scar formation | Axon regeneration; glial scar modulation via MMP secretion [22] |
| Schizophrenia | Village editing in iPSC-derived neurons [19] | Transcriptional changes influenced by genetic background | NRXN1 knockout models across donors with varying polygenic risk [19] |
Key Experimental Protocols
Dorsal-Ventral Forebrain Assembloid Generation
This protocol models interneuron migration, critical for understanding neurological disorders:
- Dorsal Organoid Differentiation: Pattern iPSCs toward cortical fates using dual SMAD inhibition (LDN193189, SB431542) and Wnt activation (CHIR99021).
- Ventral Organoid Differentiation: Generate medial ganglionic eminence identities using SHH pathway activation (SAG, Purmorphamine).
- Assemblage and Maturation: Fuse dorsal and ventral organoids at day 120 and maintain for extended culture (200+ days) to observe chain migration of interneurons [19].
- Analysis: Employ time-lapse imaging, single-cell spatial transcriptomics, and mathematical modeling to quantify migration dynamics.
DRG Organoid Modeling for Pain Disorders
For Hereditary Sensory and Autonomic Neuropathy Type IV (HSAN IV):
- iPSC Differentiation: Generate dorsal root ganglion (DRG) organoids from patient-specific iPSCs carrying NTRK1 mutations.
- Isogenic Control Creation: Correct patient mutations using CRISPR/Cas9 to establish genetically matched controls.
- Phenotypic Analysis: Assess neuronal-glial differentiation balance, focusing on ISLET+/BRN3A+ sensory neuron reduction and premature gliogenesis marked by FABP7 upregulation [19].
Technical Workflow: Neurological Disease Modeling
The following diagram illustrates the workflow for creating sophisticated neural models using stem cell technologies:
Metabolic Disease Modeling
Current Landscape and Challenges
Metabolic disorders, including metabolic dysfunction-associated steatotic liver disease (MASLD) and diabetes, represent growing global health challenges. Stem cell-derived somatic cells offer promising avenues for both disease modeling and cell replacement therapies [23].
Key Cell Types and Applications
- Hepatocyte-like Cells (HLCs): iPSC-derived HLCs model liver-specific metabolic functions and pathologies, including lipid accumulation and inflammatory responses characteristic of MASLD [23].
- Pancreatic β-like Cells: Glucose-responsive insulin-producing cells generated from stem cells hold potential for diabetes treatment, though full functional maturation remains challenging [23].
- Disease Modeling Applications: These cell types enable investigation of disease mechanisms and screening for therapeutic compounds that modulate metabolic pathways [23].
Experimental Challenges and Solutions
The field continues to address significant technical hurdles:
- Functional Maturation: Stem cell-derived hepatocyte-like and β-cells often exhibit fetal-like characteristics rather than fully mature adult phenotypes [23].
- Protocol Standardization: Differentiation protocols vary significantly between laboratories, complicating comparison of results [9].
- Metabolic Function: Achieving full metabolic capacity comparable to primary cells remains challenging, with current models showing reduced cytochrome P450 activity in HLCs and suboptimal glucose-stimulated insulin secretion in β-cells [23].
Research Reagent Solutions Toolkit
Table: Essential Research Reagents for Stem Cell Disease Modeling
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC [20] | iPSC generation | Somatic cell reprogramming to pluripotency |
| Gene Editing Tools | CRISPR/Cas9 systems [9] | Isogenic control creation | Precise genetic modification |
| Small Molecule Inhibitors/Activators | CHIR99021 (Wnt activator), IWP2 (Wnt inhibitor), LDN193189 (BMP inhibitor) [20] | Directed differentiation | Lineage specification |
| Extracellular Matrix | Matrigel, laminin-521, synthetic hydrogels [20] | 3D culture systems | Structural support for organoids |
| Characterization Antibodies | CD73, CD90, CD105 (MSC markers); TRA-1-60 (pluripotency); cardiac troponins [24] | Cell type validation | Lineage confirmation |
| Secreted Factor Assays | VEGF, HGF, FGF ELISA kits [20] | Paracrine effect analysis | Quantification of secretory profiles |
| Functional Assay Kits | Microelectrode arrays, calcium imaging dyes, Seahorse metabolic kits | Physiological assessment | Functional characterization |
Technical Challenges and Future Directions
Current Limitations
Despite significant advances, stem cell disease modeling faces several persistent challenges:
- Cellular Immaturity: Stem cell-derived tissues frequently exhibit fetal-like characteristics rather than adult phenotypes, limiting their utility for modeling late-onset diseases [9].
- Protocol Variability: Lack of standardization in differentiation protocols across laboratories compromises reproducibility and comparability [9].
- Tumorigenic Risk: Residual undifferentiated pluripotent cells in therapeutic products pose potential safety concerns [20].
- Immune Compatibility: Even autologous iPSC derivatives can trigger immune responses under certain conditions [9].
- Scalability: Current manufacturing workflows are often labor-intensive and difficult to scale for widespread clinical application [9].
Innovative Solutions
The field is rapidly developing solutions to address these challenges:
- Village Editing: "CRISPR/Cas9 gene editing in a cell village format" enables parallel analysis of genetic variants across multiple donor backgrounds, revealing how genetic context influences phenotype [19].
- Lysosomal Reprogramming: Targeting lysosomal dysfunction can reverse aging in blood stem cells, with potential applications for improving stem cell function in age-related diseases [25].
- Bioengineering Approaches: Smart hydrogel scaffolds and 3D bioprinting technologies improve stem cell survival and enable construction of complex tissue architectures [20].
- Machine Learning-Assisted Differentiation: EpiCRISPR technology reduces inter-batch variation in gene expression to 6.4%, significantly improving differentiation consistency [20].
Signaling Pathways in Stem Cell-Based Therapy
The following diagram summarizes the key molecular mechanisms through which stem cells exert their therapeutic effects:
Patient-specific disease modeling using stem cells has emerged as a transformative approach across cardiovascular, neurological, and metabolic disorders. The integration of iPSC technology with advanced gene editing, 3D culture systems, and multi-omics analyses has created unprecedented opportunities for understanding disease mechanisms and developing targeted therapies. While challenges remain in achieving full cellular maturation, protocol standardization, and clinical translation, ongoing innovations in bioengineering, computational biology, and manufacturing processes continue to advance the field. As these technologies mature, stem cell-based disease models will play an increasingly central role in drug discovery, personalized medicine, and regenerative therapies, ultimately enabling more effective and precise interventions for complex human diseases.
The Shift from Animal Models to Human-Relevant Systems
The field of biomedical research has long depended on animal models to investigate disease mechanisms and test therapeutic candidates. However, the translational gap between preclinical models and human clinical trials has become increasingly evident, with a significant proportion of drug candidates failing due to unpredicted toxicities or inefficacies in humans [9]. This disconnect stems from fundamental species-specific differences in genetics, immune responses, and organ physiology that limit the predictive power of traditional animal models [9]. In response to these challenges, human stem cell research has undergone a remarkable transformation over the last two decades, transitioning from pioneering discoveries in developmental biology to clinical applications that now shape the future of regenerative medicine and drug development [9].
The advent of human induced pluripotent stem cells (iPSCs), followed by advanced organoid culture systems and genome editing technologies, has provided unprecedented access to patient-specific and pluripotent cell sources capable of differentiating into virtually any cell type [9]. These technological advances have positioned stem cell-based approaches as a cornerstone for disease modeling, drug development, and therapeutic innovation, offering a transformative opportunity to improve translational fidelity, increase therapeutic success rates, and reduce the reliance on animal models [9]. This whitepaper examines the scientific foundations, current applications, and methodological considerations underlying this paradigm shift toward human-relevant systems in biomedical research.
The Limitations of Traditional Animal Models
Traditional animal models, particularly rodents, have been the mainstay of biomedical research for decades. However, their limitations in predicting human responses have become increasingly apparent throughout the drug development pipeline. The fundamental biological differences between species contribute to high dropout rates for drug candidates, as promising interventions frequently fail in human clinical trials despite showing efficacy in animal models [9].
The disconnect between animal models and human biology manifests in several critical areas:
- Genetic and metabolic differences that alter drug metabolism and pharmacokinetics
- Divergent immune system responses to pathogens and therapeutic interventions
- Structural and functional variations in organ systems and tissue architecture
- Species-specific disease mechanisms that do not fully recapitulate human pathology
These limitations are particularly problematic for complex human-specific diseases, including many neurological disorders, autoimmune conditions, and metabolic diseases, where animal models often fail to capture essential aspects of disease pathophysiology and progression [9]. The inability of traditional models to accurately predict human responses has driven the search for more relevant experimental systems that better mirror human biology.
Human Stem Cell-Based Model Systems: Technological Foundations
Induced Pluripotent Stem Cells (iPSCs)
The development of human induced pluripotent stem cells (iPSCs) represents a watershed moment in biomedical research. iPSCs are generated by reprogramming adult somatic cells to a pluripotent state, capable of differentiating into virtually any cell type in the human body [9]. This breakthrough technology provides three distinct advantages that make it a powerful tool across research and early-stage drug development [17]:
Table 1: Key Advantages of iPSC-Based Disease Models
| Advantage | Description | Research Application |
|---|---|---|
| Patient Specificity | iPSCs carry the donor's genome, including disease-associated mutations | Direct modeling of rare or complex genetic diseases in human cells [17] |
| Human Relevance | Differentiated cells recapitulate key functional aspects of real tissue | Study of synaptic activity, contractility, metabolic capacity in human context [17] |
| Scalability | Indefinite expansion potential with locked-in differentiation protocols | Manufacturing at scale required for high-throughput screening [17] |
iPSCs have moved from niche innovation to mainstream application, becoming a go-to tool for building more predictive, human-relevant assays in drug discovery workflows [17]. Their ability to maintain the donor's genotype and demonstrate complex functional behaviors that immortalized cell lines cannot replicate makes them particularly valuable for disease modeling and drug screening [17].
Organoid and Assembloid Technologies
The ability to generate organoids—self-organizing, three-dimensional tissue structures derived from stem cells—has been especially transformative for disease modeling [9]. Organoids recapitulate aspects of tissue architecture and function, and their emergence has opened new frontiers in disease modeling for neurological disorders, congenital heart disease, polycystic kidney disease, and cancer [9].
Complementing organoid technology, assembloids represent a more advanced approach that combines multiple organoid types or tissue lineages. These complex systems have allowed the modeling of inter-organ interactions, such as brain–muscle or brain–vascular connectivity, providing unprecedented opportunities to study human physiology and disease in a more integrated manner [9].
When provided with the proper 3D scaffold and biochemical factors, stem cells can differentiate and self-organize to form tissue-specific organoids like the optic cup, brain, intestine, liver, and kidney [26]. The homeostasis of these tissues is maintained through self-renewal and differentiation mechanisms similar to those observed in vivo, making organoids particularly valuable for studying tissue development, disease mechanisms, and drug responses [26].
Genome Editing Technologies
The combination of stem cell technologies with CRISPR-Cas9 gene editing has revolutionized disease modeling by allowing for precise manipulation of disease-associated mutations in human cells [9]. This approach enables researchers to create isogenic control lines that differ only at specific disease-relevant loci, strengthening causal inference in disease modeling studies [9].
Genome editing has already been successfully used to model monogenic conditions such as cystic fibrosis, amyotrophic lateral sclerosis, and Duchenne muscular dystrophy, providing robust platforms for mechanistic studies and therapeutic screening [9]. The precision of these editing technologies, combined with the human relevance of iPSC-derived models, exemplifies the maturation of human stem cell platforms into predictive disease models that bridge the gap between traditional cell culture and clinical research.
Applications in Disease Modeling and Drug Development
Neurodegenerative Disorders
iPSC-based models have shown particular promise in modeling neurodegenerative diseases, which have been notoriously difficult to recapitulate in animal models. iPSC-derived neurons from patients with Alzheimer's, Parkinson's, and ALS are used to model disease phenotypes like tau aggregation, mitochondrial dysfunction, and motor neuron degeneration [17]. These cultures support phenotypic screens that have identified compounds capable of rescuing neuronal function in vitro [17].
For Parkinson's disease specifically, recent advances have included the generation of dopaminergic neurons from unconventional sources such as ovarian cortical-derived progenitors, which demonstrate electrophysiological activity and point to new avenues for autologous therapies [9]. Additionally, MSC-based approaches have shown therapeutic potential for spinocerebellar ataxia (SCA), with preclinical studies suggesting that MSCs can enhance Purkinje cell survival and motor coordination through immunomodulatory and neurotrophic effects [9].
Cardiovascular Disease and Cardiotoxicity
iPSC-derived cardiomyocytes have become a standard tool in cardiac safety screening and are gaining regulatory acceptance. These cells are now used routinely to screen for drug-induced arrhythmia risk and have been integrated into regulatory safety initiatives like CiPA (Comprehensive in Vitro Proarrhythmia Assay) [17]. Companies including Roche and Takeda utilize iPSC-derived cardiomyocytes for preclinical cardiac profiling, reflecting the growing acceptance of these human-relevant systems in pharmaceutical development [17].
Cardiovascular organoids derived from pluripotent stem cells provide valuable insights into cardiac development, congenital heart disease, and drug-induced cardiotoxicity [9]. These models enable the study of cardiomyocyte maturation and tissue-level electrophysiology in a human-relevant context, though challenges remain in achieving full vascularization and structural maturation comparable to adult heart tissue [9].
Metabolic and Renal Diseases
In metabolic disease research, hepatocyte-like cells derived from iPSCs have been used to model conditions such as familial hypercholesterolemia and test potential lipid-lowering therapies [17]. In one notable example, an iPSC-based drug screen revealed a drug repurposing opportunity when cardiac glycosides were found to reduce ApoB secretion [17].
Kidney organoids have demonstrated significant utility for modeling renal diseases, particularly autosomal dominant polycystic kidney disease (ADPKD) [9]. Organoids carrying PKD1 or PKD2 mutations display cyst formation reminiscent of patient pathology, providing a robust system for mechanistic studies and therapeutic screening for a condition with limited treatment options [9].
Table 2: Stem Cell Applications Across Disease Areas
| Disease Area | Stem Cell Model | Key Applications | Notable Findings |
|---|---|---|---|
| Neurodegeneration | iPSC-derived neurons, MSC therapies | Disease modeling, phenotypic screening, cell therapy | Compounds rescuing neuronal function; Enhanced Purkinje cell survival with MSCs [9] [17] |
| Cardiovascular | iPSC-derived cardiomyocytes, cardiovascular organoids | Cardiotoxicity screening, disease modeling, developmental studies | Integration into CiPA safety initiative; Identification of arrhythmia risks [9] [17] |
| Metabolic | iPSC-derived hepatocyte-like cells | Disease modeling, drug screening | Cardiac glycosides reduce ApoB secretion [17] |
| Renal | Kidney organoids | Disease modeling, mechanism studies | Cyst formation in ADPKD models [9] |
| Reproductive | Ovarian stem cells (OSCs) | Infertility treatment | Differentiation into oocyte-like cells for premature ovarian failure [9] |
High-Throughput Screening and Drug Discovery
iPSC-derived cells are not just biologically relevant—they are also compatible with high-throughput screening methodologies essential for modern drug discovery. These cells can be plated in 384- or 1536-well formats, imaged automatically, and used to extract rich phenotypic data at scale [17].
iPSC-based models are increasingly being used in industrial phenotypic screens to identify new drugs, predict toxicity, and uncover mechanisms of action. Using high-content imaging, researchers can quantify changes in cell morphology, protein localization, or organelle health across thousands of wells. When combined with machine learning approaches, this data can be analyzed in bulk to identify compounds that reverse disease features, even when the molecular target isn't known beforehand [17].
This compatibility with automated screening platforms makes iPSC technology particularly valuable for early drug discovery, where the ability to test large compound libraries against human-relevant disease models can significantly improve the efficiency of identifying promising therapeutic candidates.
Experimental Protocols and Methodologies
iPSC Differentiation Workflows
The successful implementation of stem cell-based disease models requires robust and reproducible differentiation protocols. While specific methods vary by cell type and application, general principles underlie most iPSC differentiation workflows:
Cardiomyocyte Differentiation Protocol
- iPSC Maintenance: Culture iPSCs in essential 8 medium on vitronectin-coated plates until 80-85% confluent
- Mesoderm Induction: Treat with CHIR99021 (GSK-3β inhibitor) in RPMI/B27-insulin medium for 24-48 hours
- Cardiac Specification: Switch to RPMI/B27-insulin medium without CHIR99021 for 48 hours
- Metabolic Selection: Replace medium with RPMI/B27-complete (containing insulin) for 10-15 days with regular feeding
- Functional Validation: Assess beating behavior, cardiac troponin expression, and electrophysiological properties
Neuronal Differentiation Protocol
- Neural Induction: Treat iPSCs with dual SMAD signaling inhibitors (dorsomorphin and SB431542) in neural induction medium for 10-14 days
- Neural Progenitor Expansion: Passage neural rosettes and expand in neural expansion medium containing FGF2 and EGF
- Terminal Differentiation: Withdraw mitogens and culture in neuronal differentiation medium containing BDNF, GDNF, and cAMP
- Functional Maturation: Maintain cultures for 4-8 weeks with regular feeding, assess synaptic activity and neuronal marker expression
These protocols highlight the importance of precise temporal control of signaling pathways and growth factors to direct stem cell differentiation toward specific lineages. However, variability between laboratories remains a challenge, underscoring the need for standardized approaches and rigorous quality control [9].
Organoid Generation and Maintenance
The generation of complex 3D organoids requires additional considerations beyond 2D differentiation protocols:
Essential Components for Organoid Culture
- Extracellular Matrix: Matrigel or synthetic hydrogels to provide 3D scaffold
- Patterning Factors: Small molecules and growth factors to establish regional identity
- Maturation Factors: Hormones, nutrients, and mechanical stimuli to promote functional maturation
Recent advances have incorporated bioengineering strategies such as microfluidic platforms, electrical stimulation, and mechanical loading to improve the physiological fidelity of organoid models [9]. These approaches address limitations in vascularization and structural maturation that often constrain the utility of stem cell-derived tissues [9].
Diagram 1: Stem Cell Disease Modeling Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of stem cell-based disease models requires careful selection of research reagents and materials. The following table details essential components and their functions in establishing robust experimental systems:
Table 3: Essential Research Reagents for Stem Cell Disease Modeling
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Reprogramming Factors | OSKM factors (OCT4, SOX2, KLF4, c-MYC) | Reprogram somatic cells to pluripotency | Integration-free methods preferred for clinical applications |
| Extracellular Matrices | Matrigel, vitronectin, laminin, synthetic hydrogels | Provide structural support and biochemical cues | Batch variability; defined synthetic alternatives reducing variability |
| Small Molecule Inhibitors/Activators | CHIR99021 (GSK-3β inhibitor), SB431542 (TGF-β inhibitor), dorsomorphin | Direct differentiation by modulating signaling pathways | Concentration and timing critical for specific lineage commitment |
| Growth Factors & Cytokines | FGF2, EGF, BDNF, GDNF, BMPs, WNTs | Promote survival, proliferation, and differentiation | Cost considerations for large-scale applications; recombinant human proteins preferred |
| Culture Media Formulations | mTeSR, Essential 8, neural induction medium, cardiac differentiation medium | Provide nutrients and maintain specific cell states | Xeno-free formulations important for clinical translation |
| Genome Editing Tools | CRISPR-Cas9 systems, base editors, prime editors | Introduce disease-associated mutations or correct genetic defects | Off-target effects monitoring; isogenic control generation |
| Characterization Tools | Flow cytometry antibodies, PCR primers, electrophysiology systems | Validate cell identity, purity, and function | Multimodal characterization recommended for comprehensive assessment |
Current Challenges and Future Directions
Technical and Standardization Challenges
Despite the promising advances in human stem cell-based models, several significant challenges remain that must be addressed for the field to realize its full potential:
Standardization and Reproducibility The lack of standardization in differentiation protocols represents a major hurdle. Even for the same lineage, methods can vary significantly between laboratories, leading to inconsistent results and limiting reproducibility [9]. Recent benchmarking efforts using high-dimensional molecular profiling have highlighted the extent of this variability and underscored the need for harmonized quality standards across laboratories [9].
Functional Maturation Stem cell-derived systems frequently display developmental immaturity, maintaining fetal-like gene expression profiles, electrophysiological activity, or metabolic states [9]. This immaturity affects both their structural and functional fidelity and their ability to respond to stimuli in a manner comparable to adult tissues. Addressing this limitation requires the development of advanced maturation strategies, including prolonged culture, biomechanical stimulation, vascularization, and co-culture with supporting cell types that more closely approximate the adult in vivo environment [9].
Scalability and Manufacturing Translating stem cell technologies into widely available research tools and clinical therapies requires robust, cost-effective, and cGMP-compliant production systems [9]. Current workflows are often labor-intensive and difficult to scale, raising concerns about feasibility for widespread use [9]. Advances in automation, closed culture systems, and high-throughput bioprocessing will be critical to overcoming these barriers.
Diagram 2: Challenges and Solutions in Stem Cell Models
Safety and Ethical Considerations
Safety remains a central concern for the clinical translation of stem cell-based technologies. The risks of genomic instability, acquired during prolonged culture or as a consequence of reprogramming, pose significant barriers to clinical application [9]. Furthermore, while iPSCs were initially thought to be immunologically inert, subsequent studies revealed that even autologous iPSC derivatives can trigger immune responses under certain conditions [9]. Addressing these safety issues requires stringent quality control and regulatory oversight, including comprehensive potency assays, long-term biodistribution monitoring of transplanted cells, and careful assessment of tumorigenic potential.
Ethical considerations also remain at the forefront of stem cell research. The field continues to navigate questions related to the use of embryonic stem cells, gene editing, and the commercialization of stem cell therapies [9]. The International Society for Stem Cell Research (ISSCR) has established updated guidelines to address these challenges, promoting an ethical, practical, and sustainable approach to stem cell research and the development of cell therapies [18]. These guidelines emphasize fundamental principles including integrity of the research enterprise, primacy of patient welfare, respect for research subjects, transparency, and social justice [18].
Future Perspectives
Looking forward, several key developments are poised to advance the field of human stem cell-based disease modeling:
Multi-system Integration The development of more sophisticated assembloid systems that combine multiple tissue types will enable researchers to study inter-organ communication and systemic disease processes in ways that have not been previously possible. These integrated approaches may help bridge the gap between isolated tissue models and whole-organism physiology.
Advanced Analytics and AI The integration of high-content screening data with machine learning approaches will enhance the predictive power of stem cell-based assays. These computational methods can identify subtle patterns in complex datasets that may not be apparent through traditional analysis, potentially revealing new disease mechanisms and therapeutic opportunities.
Personalized Medicine Applications As protocols become more standardized and efficient, the use of patient-specific iPSCs for personalized drug screening may become clinically feasible. This approach could help identify optimal treatment strategies for individual patients, particularly for complex or rare genetic disorders where response to conventional therapies is variable.
The continued evolution of human stem cell-based models represents a paradigm shift in biomedical research, offering unprecedented opportunities to study human disease in relevant systems and accelerate the development of safer, more effective therapies. By addressing current challenges through collaborative science and technological innovation, these approaches promise to transform both basic research and clinical medicine in the coming years.
From Cells to Complex Systems: Methodologies and Translational Applications
The advent of induced pluripotent stem cell (iPSC) technology represents a paradigm shift in biomedical research, creating unprecedented opportunities for patient-specific disease modeling. Since the seminal discovery by Takahashi and Yamanaka that somatic cells could be reprogrammed to a pluripotent state using defined factors, the field has evolved rapidly with significant refinements in technique, safety, and efficiency [3] [1]. This technology now serves as a cornerstone for generating patient-specific cellular models that recapitulate disease pathology in vitro, enabling mechanistic studies of pathogenesis and high-throughput drug screening without the ethical concerns associated with embryonic stem cells [27] [5]. The ability to derive iPSCs from individuals with genetic disorders has transformed our approach to studying human diseases, particularly for neurological conditions, cardiovascular disorders, and rare genetic syndromes where animal models often fail to fully capture human pathophysiology [28] [17]. This technical guide comprehensively outlines the current methodologies, molecular mechanisms, and applications of iPSC derivation, with a specific focus on their utility in disease modeling platforms that support both basic research and therapeutic development.
Historical Foundations and Conceptual Framework
The conceptual foundation for cellular reprogramming was established through decades of pioneering research that challenged the dogma of irreversible cell fate determination. In 1962, John Gurdon demonstrated that the nucleus from a differentiated somatic cell could be reprogrammed to a totipotent state when transferred into an enucleated egg, leading to the generation of cloned tadpoles [29] [1]. This seminal work in somatic cell nuclear transfer (SCNT) provided the first experimental evidence that the genome of differentiated cells retains the information necessary to generate an entire organism, and that factors in the oocyte cytoplasm could reverse epigenetic modifications to restore developmental potential.
Nearly half a century later, Shinya Yamanaka and colleagues identified a specific combination of transcription factors - Oct4, Sox2, Klf4, and c-Myc (OSKM) - that could reprogram mouse fibroblasts to an embryonic stem cell-like state, creating the first induced pluripotent stem cells in 2006 [3] [1]. The following year, this approach was successfully replicated in human fibroblasts, simultaneously by Yamanaka's group using the OSKM factors and by James Thomson's laboratory using an alternative combination (OCT4, SOX2, NANOG, LIN28) [27] [29]. These discoveries demonstrated that pluripotency could be induced without embryo destruction or nuclear transfer, overcoming significant ethical barriers and creating new possibilities for patient-specific cell therapies.
The theoretical framework for these achievements builds upon Waddington's epigenetic landscape model, which conceptualized cell differentiation as a ball rolling downhill through branching valleys toward increasingly restricted developmental endpoints [1]. Cellular reprogramming effectively reverses this process, pushing cells backward along the developmental continuum through forced expression of key regulatory factors that remodel the epigenetic landscape to restore pluripotency. This paradigm shift has positioned iPSC technology as an indispensable platform for disease modeling, drug screening, and regenerative medicine applications.
Molecular Mechanisms of Somatic Cell Reprogramming
The process of reprogramming somatic cells to iPSCs involves profound molecular restructuring that occurs in a stepwise manner through defined mechanistic phases. At the most fundamental level, reprogramming requires the silencing of somatic cell transcriptional programs and the concomitant activation of the pluripotency network, accompanied by comprehensive epigenetic remodeling [29] [1].
Transcriptional and Epigenetic Remodeling
The reprogramming process initiates with the suppression of somatic genes, followed by activation of early pluripotency-associated genes, and culminates in the establishment of a stable self-renewing pluripotent state [1]. During the early phase, exogenous transcription factors bind to their target sequences and initiate widespread chromatin changes, making previously inaccessible genomic regions available for activation [29]. The OSKM factors function cooperatively in this process: c-Myc associates with histone acetyltransferase complexes to induce global histone acetylation, facilitating binding of Oct4 and Sox2 to their target loci [29]. Meanwhile, Klf4 suppresses expression of somatic genes while simultaneously activating pluripotency-associated genes [29].
The late phase of reprogramming is characterized by activation of the endogenous pluripotency network, particularly the reactivation of the OCT4 promoter, which serves as a central stabilizing mechanism for the pluripotent state [27]. This phase involves more deterministic events including DNA demethylation at pluripotency gene promoters, further chromatin remodeling, and establishment of the transcriptional and epigenetic signatures that define pluripotent stem cells [1]. The process also involves mesenchymal-to-epithelial transition (MET), which is critical for establishing the characteristic epithelial morphology of pluripotent stem cells [1].
Metabolic Reprogramming
Reprogramming induces fundamental changes in cellular metabolism, shifting from oxidative phosphorylation toward glycolysis, which is characteristic of pluripotent stem cells [1]. This metabolic transition supports the biosynthetic demands of rapidly dividing cells and helps maintain the pluripotent state through regulation of epigenetic modifiers that are sensitive to metabolic intermediates.
Timeline and Efficiency
The complete reprogramming process typically requires several weeks, with efficiency remaining generally low (often <0.1-1%) across most methods [27] [29]. Efficiency is influenced by multiple factors including the somatic cell source, donor age, specific reprogramming factors used, and culture conditions [27]. The stochastic nature of early reprogramming events contributes to this inefficiency, as the initial chromatin opening by exogenous factors occurs infrequently in individual cells [1].
Reprogramming Factor Combinations
The specific combination of reprogramming factors significantly influences the efficiency, quality, and safety of the resulting iPSCs. While the original OSKM combination remains widely used, numerous alternatives and optimizations have been developed to address limitations related to tumorigenic potential and efficiency.
Table 1: Key Transcription Factor Combinations for iPSC Reprogramming
| Factor Combination | Components | Key Features | References |
|---|---|---|---|
| OSKM | OCT4, SOX2, KLF4, c-MYC | Original Yamanaka factors; high efficiency but tumorigenic risk from c-MYC | [3] [29] |
| OSNL | OCT4, SOX2, NANOG, LIN28 | Thomson's alternative; avoids c-MYC but may have lower efficiency | [27] [29] |
| OSK | OCT4, SOX2, KLF4 | Avoids c-MYC; significantly reduced tumorigenic risk | [3] |
| OSKMNL | All six factors from OSKM and OSNL | Enhanced efficiency, especially with difficult cell sources | [29] |
Factor Substitutions and Enhancements
Substantial research has focused on identifying alternative factors that can replace or supplement the original reprogramming factors to enhance safety profiles. L-Myc and N-Myc can substitute for c-Myc with reduced tumorigenic potential [3]. Similarly, KLF2 and KLF5 can replace KLF4, while SOX1 and SOX3 can substitute for SOX2 [3]. Non-transcription factor genes can also enhance reprogramming; for example, microRNAs (particularly miR-302/367 and miR-372) and genes regulating miRNA biogenesis (such as Lin28) significantly improve reprogramming efficiency [3].
Notably, certain cell types with endogenous expression of reprogramming factors may require fewer exogenous factors. For example, neural stem cells endogenously express SOX2 and c-MYC, allowing reprogramming with OCT4 alone [3]. Small molecules also play an increasingly important role, with compounds like RepSox (a TGF-β inhibitor that can replace SOX2) and epigenetic modulators significantly enhancing reprogramming efficiency and enabling completely non-genetic approaches [3].
Delivery Systems for Reprogramming Factors
The method used to deliver reprogramming factors significantly impacts the genomic integrity and clinical applicability of resulting iPSCs. Early methods relied heavily on integrating viral vectors, but the field has progressively shifted toward non-integrating approaches to enhance safety profiles.
Table 2: Comparison of Reprogramming Factor Delivery Systems
| Delivery Method | Genetic Integration | Key Advantages | Key Limitations | Typical Efficiency |
|---|---|---|---|---|
| Retrovirus | Yes | High efficiency; stable expression | Silencing issues; insertional mutagenesis | Moderate to High |
| Lentivirus | Yes | Can infect non-dividing cells; stable expression | Insertional mutagenesis; residual expression | Moderate to High |
| Sendai Virus | No | High efficiency; no genomic integration | Viral persistence requires dilution; immunogenic | High [30] |
| Episomal Vectors | No | Non-viral; no integration | Low efficiency; requires repeated transfections | Low to Moderate [30] |
| Synthetic mRNA | No | Non-viral; high control over timing | Requires multiple transfections; immunogenic | Moderate |
| Recombinant Protein | No | Completely non-genetic; maximum safety | Very low efficiency; technically challenging | Very Low |
Non-Integrating Methods
Non-integrating reprogramming methods have become the standard for most applications, particularly those with potential clinical implications. Sendai virus, an RNA virus that replicates in the cytoplasm without genomic integration, has gained popularity due to high efficiency rates while avoiding genomic modification [27] [30]. Episomal vectors based on OriP/EBNA1 sequences from Epstein-Barr virus offer a completely non-viral approach, though with typically lower efficiency compared to viral methods [30]. A comparative analysis of these predominant non-integrating methods found that Sendai virus reprogramming yields significantly higher success rates relative to episomal methods, while the source material (fibroblasts, PBMCs, or LCLs) does not significantly impact success rates [30].
More recently, chemically defined methods using small molecules alone have been developed, representing the ultimate in safety as they involve no genetic manipulation [3] [1]. These chemical reprogramming approaches typically employ combinations of compounds that modulate epigenetic status, signaling pathways, and metabolic processes to induce pluripotency.
The choice of starting somatic cell population influences reprogramming efficiency, quality of resulting iPSCs, and practical considerations for sample collection. Multiple somatic cell types have been successfully reprogrammed to pluripotency, each with distinct advantages and limitations.
Table 3: Comparison of Somatic Cell Sources for iPSC Generation
| Cell Source | Collection Method | Reprogramming Efficiency | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Dermal Fibroblasts | Skin biopsy | Moderate | High genomic stability; well-established protocols | Invasive collection; requires expansion |
| Peripheral Blood Mononuclear Cells (PBMCs) | Blood draw | Moderate | Minimally invasive; readily available | Lower cell numbers may require expansion |
| Urinary Epithelial Cells | Urine sample | Moderate | Completely non-invasive; easily repeatable | Limited cell numbers; potential contamination |
| Keratinocytes | Hair follicle or skin biopsy | High | Higher efficiency than fibroblasts | Limited cell numbers from follicles |
| Dental Pulp Stem Cells | Tooth extraction | Moderate | Multipotenent cells may reprogram more efficiently | Limited availability |
Fibroblasts derived from skin biopsies were the first cell type used for iPSC generation and remain widely utilized due to their robustness in culture, high genomic stability, and well-established protocols [27] [31]. However, the invasiveness of skin biopsy collection has driven the development of less invasive alternatives.
Peripheral blood mononuclear cells (PBMCs) offer a minimally invasive source material with reprogramming efficiency comparable to fibroblasts [27]. Blood collection is routine in clinical settings, making PBMCs particularly suitable for large-scale studies and biobanking initiatives. Urinary epithelial cells represent the least invasive source, obtainable through simple urine collection, with demonstrated robust reprogramming capacity and excellent donor compliance for repeat sampling [27].
Keratinocytes from plucked hair follicles or skin biopsies demonstrate higher reprogramming efficiency compared to fibroblasts, though the limited cell numbers from follicles can be challenging [27]. Other specialized cell types including mesenchymal stromal cells from dental pulp, synovial tissue, and hepatocytes have also been successfully reprogrammed, though their application remains more restricted to specific research contexts [27].
Step-by-Step Experimental Protocols
Sendai Virus Reprogramming Protocol
The Sendai virus (SeV) system represents one of the most efficient non-integrating reprogramming methods, particularly suitable for blood-derived cells and fibroblasts [30].
Materials Required:
- CytoTune Sendai Reprogramming Kit (containing SeV vectors for OCT4, SOX2, KLF4, and c-MYC)
- Source cells (PBMCs, fibroblasts, or other somatic cells)
- Appropriate culture media for source cells
- iPSC culture medium (e.g., mTeSR1)
- Matrigel or feeder cells
- Rock inhibitor (Y-27632)
Procedure:
- Source Cell Preparation: Culture and expand source cells to obtain adequate numbers (typically 0.5-1 × 10^5 cells for reprogramming). For PBMCs, isolate using Ficoll density gradient centrifugation and stimulate with appropriate mitogens for 3-5 days.
- Viral Transduction: Plate source cells at appropriate density. On day 0, thaw SeV vectors and add to cells at recommended MOI (typically 3-5 for each vector). Centrifuge plates to enhance infection (2000 × g, 90 minutes at 32°C).
- Post-Transduction Culture: Refresh medium 24 hours post-transduction. Continue culture with medium changes every other day for approximately 6 days.
- Harvest and Replate: Approximately 7 days post-transduction, harvest transduced cells using appropriate dissociation reagent and replate onto Matrigel-coated plates or feeder layers at high density (2-5 × 10^4 cells/cm²) in source cell medium supplemented with Rock inhibitor.
- Medium Transition: Gradually transition to iPSC culture medium over 3-5 days, with daily medium changes.
- Colony Selection and Expansion: After 2-3 weeks, identify and manually pick emerging iPSC colonies based on characteristic morphology (tightly packed cells with high nucleus-to-cytoplasm ratio, distinct borders). Transfer to new plates for expansion.
- Quality Control: At passage 10 or later, perform comprehensive quality control assessments including pluripotency marker expression, karyotyping, and Sendai virus clearance testing.
Episomal Reprogramming Protocol
Episomal reprogramming offers a completely non-viral approach, though with typically lower efficiency compared to Sendai virus methods [30].
Materials Required:
- Episomal plasmids expressing OCT4, SOX2, KLF4, L-MYC, LIN28, and shRNA for p53
- Nucleofector device and appropriate kits
- Source cells (fibroblasts or LCLs)
- iPSC culture medium
- Matrigel-coated plates
Procedure:
- Source Cell Preparation: Culture and expand source cells to obtain 1-2 × 10^5 cells for nucleofection.
- Nucleofection: Harvest cells and resuspend in nucleofection solution with episomal plasmids (typically 1-2 μg of each plasmid). Perform nucleofection using appropriate program (e.g., U-023 for fibroblasts, U-015 for LCLs).
- Post-Nucleofection Culture: Immediately transfer nucleofected cells to pre-warmed culture medium and plate onto Matrigel-coated plates. Culture at 37°C, 5% CO2, and 5% O2 for enhanced efficiency.
- Medium Changes: Change medium every other day post-nucleofection. Monitor GFP-positive cells if using fluorescent reporter constructs to assess transfection efficiency.
- Replating: On days 6-7 post-nucleofection, harvest and replate transfected cells at appropriate density.
- Colony Selection: After 1-2 additional weeks, manually pick at least 24 clones for further expansion based on iPSC morphology.
- Expansion and Banking: Expand selected clones through enzymatic passaging until sufficient numbers for master banking (typically 9-12 wells of a 6-well plate). Cryopreserve using standardized freezing protocols.
Quality Control and Characterization
Rigorous quality control is essential to confirm successful reprogramming and ensure genomic integrity of iPSC lines, particularly for disease modeling applications.
Essential Quality Control Measures:
- Pluripotency Marker Expression: Assess expression of canonical pluripotency markers (OCT4, NANOG, SOX2, SSEA-4, TRA-1-60) via immunocytochemistry, flow cytometry, or PCR [27] [30].
- Trilineage Differentiation Potential: Demonstrate differentiation capacity into derivatives of all three germ layers through embryoid body formation or directed differentiation protocols, followed by germ layer-specific marker analysis [27].
- Genomic Integrity: Perform karyotyping to detect chromosomal abnormalities, and additional genomic analyses such as CNV arrays or SNP genotyping to identify more subtle variations [27] [30].
- Identity Verification: Confirm donor matching through STR profiling or SNP analysis [30].
- Microbiological Testing: Ensure absence of mycoplasma and other contaminants through standardized testing protocols [30].
- Vector Clearance: For viral methods, confirm clearance of reprogramming vectors through PCR-based detection [30].
Additional specialized assays may include teratoma formation in immunocompromised mice (though this is becoming less common due to animal use concerns), PluriTest for molecular verification of pluripotency, and scorecard assays for quantitative assessment of differentiation potential [31] [30].
Applications in Disease Modeling
iPSC technology has revolutionized disease modeling by enabling the generation of patient-specific cellular models that recapitulate pathological features in vitro. This approach is particularly valuable for studying human-specific disease mechanisms and for disorders where animal models inadequately mimic human pathology.
Neurodegenerative Diseases
iPSC-derived neuronal models have provided unprecedented insights into the pathogenesis of Alzheimer's disease, Parkinson's disease, and amyotrophic lateral sclerosis (ALS) [3] [27]. For ALS, patient-specific iPSC-derived motor neurons recapitulate disease-specific pathology including TDP-43 proteinopathy, axonal transport defects, and increased susceptibility to excitotoxicity, providing platforms for investigating molecular mechanisms and screening therapeutic compounds [3] [17]. Similarly, iPSC-derived dopaminergic neurons from Parkinson's patients replicate key pathological features such as α-synuclein aggregation and mitochondrial dysfunction [27].
Rare Genetic Disorders
iPSCs have become indispensable tools for studying rare genetic diseases, which collectively affect millions worldwide but individually receive limited research attention [28]. Approximately 80% of rare diseases have genetic origins, making patient-derived iPSCs uniquely suited for their study [28]. Successful models have been established for diverse conditions including Juvenile Nephronophthisis (using kidney organoids) [28], Usher syndrome (using auditory and retinal models) [28], Marfan syndrome [28], and various forms of retinitis pigmentosa [28]. These models enable not only mechanistic studies but also drug screening and toxicity assessments on patient-specific genetic backgrounds.
Cardiovascular and Metabolic Disorders
iPSC-derived cardiomyocytes enable the study of inherited arrhythmogenic disorders, heart failure, and drug-induced cardiotoxicity [27] [17]. Similarly, hepatocyte-like cells derived from iPSCs have been used to model metabolic diseases including familial hypercholesterolemia and Wilson's disease, reproducing disease phenotypes such as defective lipid metabolism and copper accumulation [27].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for iPSC Derivation and Culture
| Reagent Category | Specific Examples | Function | Notes |
|---|---|---|---|
| Reprogramming Factors | CytoTune Sendai Kit, Episomal plasmids | Deliver key transcription factors to somatic cells | Choice depends on integration concerns and efficiency needs |
| Culture Media | mTeSR1, E8 medium | Support iPSC growth and maintenance | Chemically defined media enhance reproducibility |
| Extracellular Matrix | Matrigel, Laminin-521, Vitronectin | Provide substrate for iPSC attachment and growth | Defined matrices reduce batch variability |
| Passaging Reagents | Versene, ReLeSR, Dispase | Dissociate iPSC colonies for passaging | Choice affects viability and single-cell survival |
| Rho Kinase Inhibitor | Y-27632 | Enhance survival after passaging or thawing | Critical for single-cell cloning |
| Quality Control Assays | Alkaline Phosphatase staining kits, Pluripotency antibodies | Verify pluripotent state | Multimodal assessment recommended |
| Cryopreservation Media | mFreSR, CryoStor | Maintain viability during freezing | Standardized formulations improve recovery |
Workflow Visualization
Diagram 1: Comprehensive iPSC Derivation Workflow from Somatic Cell Source to Final Application
Diagram 2: Key Molecular Events in Somatic Cell Reprogramming to Pluripotency
iPSC derivation through somatic cell reprogramming has evolved from a groundbreaking discovery to an established methodology that supports diverse research applications, with particular significance for patient-specific disease modeling. Current techniques offer multiple pathways to pluripotency, each with distinct advantages in terms of efficiency, safety, and practical implementation. The continuing refinement of reprogramming strategies—including the development of non-integrating delivery methods, chemical reprogramming approaches, and optimized culture conditions—has enhanced the utility and safety of iPSC technology. When integrated with advanced differentiation protocols that generate specific cell types and complex organoid models, iPSCs provide unprecedented opportunities to model human diseases in vitro, identify pathological mechanisms, and screen potential therapeutic compounds. As the field progresses, standardization of protocols and rigorous quality control will be essential to ensure reproducibility and reliability in disease modeling applications, ultimately accelerating the translation of basic research findings into clinical therapies for diverse human disorders.
The advent of patient-specific human induced pluripotent stem cells (iPSCs) has positioned stem cell-based disease modeling as a cornerstone of modern translational research. This approach provides unprecedented access to patient-specific and pluripotent cell sources capable of differentiating into virtually any cell type, overcoming the significant limitations of traditional animal models [9]. Directed differentiation of iPSCs into functional cardiomyocytes, neurons, and hepatocytes enables the recapitulation of patient-specific genotypes and phenotypes, creating human-relevant systems for investigating disease mechanisms, conducting drug screening, and developing personalized therapeutic strategies [9]. This technical guide details current methodologies, challenges, and applications for generating these functionally mature cell types within the context of patient-specific disease modeling.
Directed Differentiation to Cardiomyocytes
Protocol for Enhanced Cardiac Differentiation and Purity
Recent advances in cardiac differentiation have focused on improving the efficiency and purity of human pluripotent stem cell-derived cardiomyocytes (hPSC-CMs), which are critical for reliable disease modeling and therapeutic applications. An optimized method involves detaching and reseeding progenitor cells at specific developmental stages to improve final CM purity by 10–20% without negatively affecting contractility, sarcomere structure, or cellular function [32].
The stepwise protocol begins with mesoderm induction using a WNT activator (e.g., 12 µM CHIR 99,021) in RPMI 1640 medium supplemented with B-27 minus insulin for 24 hours [33]. This is followed by cardiac mesoderm formation using a cocktail of small molecules including a WNT antagonist, a sonic hedgehog agonist, and an inhibitor of transforming growth factor-β superfamily type I activin receptor-like kinase receptors [34]. The key innovation lies in the progenitor reseeding phase at either the EOMES+ mesoderm stage or the ISL1+/NKX2-5+ cardiac progenitor cell (CPC) stage, which significantly enhances population purity [32]. Finally, cardiomyocyte maturation occurs, with beating cardiospheres typically appearing by day 7-12 of differentiation [34].
This protocol also enables transition to defined extracellular matrices, including fibronectin, vitronectin, and laminin-111, all of which support progenitor differentiation into cardiomyocytes [32]. Furthermore, researchers have demonstrated that EOMES+ mesoderm and ISL1+/NKX2-5+ cardiac progenitors are cryopreservable, facilitating the storage of large batches for on-demand CM production [32].
Chamber-Specific Cardiomyocyte Differentiation
For disease modeling of conditions affecting specific heart chambers, methodologies have been developed to generate chamber-specific cardiomyocytes. The standard GiWi protocol (GSK3β inhibition followed by Wnt inhibition) predominantly produces first heart field (FHF)-like progenitor cells that give rise to left ventricular (LV)-like cardiomyocytes [33].
To generate right ventricular (RV)-like cardiomyocytes, inhibition of endogenous BMP signaling during mesoderm induction using insulin or BMP antagonists reduces expression of FHF markers and increases expression of second heart field (SHF) markers [33]. hPSC-CMs arising from these SHF-like progenitor cells show an RV-like gene expression pattern and exhibit phenotypic differences in spontaneous contraction rate, Ca2+ transients, and cell size compared to LV-like cardiomyocytes [33].
Table 1: Key Markers for Cardiac Progenitor Populations and Differentiated Cardiomyocytes
| Developmental Stage | Key Markers | Chamber Specificity |
|---|---|---|
| First Heart Field (FHF) Progenitors | TBX5+, NKX2-5+ [33] | Left Ventricle, Atria |
| Second Heart Field (SHF) Progenitors | TBX5-/NKX2-5+ (anterior); TBX5+/NKX2-5+ (posterior) [33] | Right Ventricle, Atria |
| Differentiated LV-like CMs | MYH6, TNNT2, TBX5 [34] [33] | Left Ventricle |
| Differentiated RV-like CMs | MYH6, TNNT2, lower TBX5 [33] | Right Ventricle |
Proteomic Insights into Cardiomyocyte Differentiation
Dynamic proteome profiling of differentiating human embryonic stem cells towards cardiomyocytes has provided valuable insights into the molecular mechanisms underlying heart development. Quantitative analysis via multiplexed tandem mass tag-based mass spectrometry at mesendoderm (ME), cardiac mesoderm (CME), cardiac progenitor cell (CPC), and cardiomyocyte (C) stages revealed six main protein clusters corresponding to key biological processes at each differentiation stage [34].
Pathway enrichment analysis identified ferroptosis as a key process in CME specification, while sirtuin signaling was implicated in driving cardiomyocyte fate [34]. The most significant proteome reorganization occurs at the CME stage, with 325 differentially expressed transitional-specific proteins (TSPs) identified through pairwise comparisons of consecutive stages [34]. This proteomic data provides potential biomarkers for each developmental stage toward cardiomyocyte specification, enabling better purification and characterization of stage-specific populations.
Directed Differentiation to Neurons
Direct Conversion and Enhanced Functional Maturity
Two advanced approaches for generating functional neurons have emerged: direct conversion from somatic cells and enhanced maturation of iPSC-derived neurons. MIT engineers have developed a highly efficient process for converting skin cells directly into neurons, bypassing the pluripotent stem cell stage [35]. This method uses just three transcription factors (NGN2, ISL1, and LHX3) delivered via a single modified virus, combined with genes encoding p53DD and a mutated version of HRAS to drive proliferation before conversion [35]. This approach achieves yields of more than 10 neurons from a single skin cell (approximately 1,100% yield) in mouse cells, with human cell conversion achieving 10-30% efficiency [35].
For enhancing the functional maturity of iPSC-derived neurons, a deep-proteomics-based "receptor-ligand matching" (RLM) strategy has been developed. This involves inventorying surface receptors on differentiated cells and adjusting culture conditions accordingly [36]. Application to NGN2-induced neurons (iNs) identified 3,934 membrane proteins, including the complete GDNF receptor family (GFRA1, GFRA2, and GFRA3). Supplementing culture media with selected ligands enhanced neuronal health, neurite density, synaptogenesis, and electrophysiological function [36].
Experimental Workflow for Neuronal Differentiation
The following diagram illustrates the two principal approaches for generating functional neurons from somatic cells:
Directed Differentiation to Hepatocytes
Enhanced Hepatic Differentiation via EMT Suppression
The generation of functional hepatocytes from induced pluripotent stem cells (iPSCs) faces challenges related to immaturity and limited long-term maintenance in vitro. An optimized differentiation protocol addresses this by incorporating small molecules to inhibit epithelial-mesenchymal transition (EMT) during hepatic differentiation [37].
This method generates iHeps with EMT inhibition (iHeps EMTi) that exhibit significantly extended in vitro culture periods (from day 24 to day 60) compared to conventional protocols [37]. The resulting hepatocytes show enhanced functional characteristics, including higher expression of hepatic functional markers, improved lipid accumulation, glycogen storage, albumin secretion, and urea acid metabolism [37]. Molecular profiling confirmed that iHeps EMTi more closely resemble primary human hepatocytes, addressing the critical limitation of immaturity in stem cell-derived hepatocytes.
Functional Assessment and In Vivo Engraftment
Comprehensive characterization of the functionally enhanced hepatocytes includes both in vitro and in vivo analyses. In vitro assessment demonstrates significantly improved metabolic functions critical for disease modeling and drug screening applications [37].
Perhaps more importantly for translational applications, the in vivo engraftment efficiency of iHeps EMTi in chimeric mouse models showed substantial improvement compared to conventional iHeps [37]. This enhanced engraftment capability is critical for cell therapy applications, particularly for treating liver diseases where functional integration with host tissue is essential for therapeutic efficacy.
Table 2: Functional Comparison of Conventional vs. EMT-Inhibited iPSC-Derived Hepatocytes
| Functional Parameter | Conventional iHeps | iHeps with EMT Inhibition |
|---|---|---|
| In Vitro Culture Period | Up to day 24 [37] | Up to day 60 [37] |
| Hepatic Marker Expression | Lower [37] | Significantly higher [37] |
| Albumin Secretion | Moderate [37] | Enhanced [37] |
| Urea Acid Metabolism | Moderate [37] | Enhanced [37] |
| Molecular Profile | Less similar to primary hepatocytes [37] | Closer to primary human hepatocytes [37] |
| In Vivo Engraftment | Lower efficiency [37] | Improved efficiency [37] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Directed Differentiation Protocols
| Reagent Category | Specific Examples | Function in Differentiation |
|---|---|---|
| Small Molecule Inducers | CHIR 99,021 (GSK3β inhibitor) [33], WNT antagonists [34], BMP antagonists [33], EMT inhibitors [37] | Directs cell fate through specific signaling pathway modulation |
| Transcription Factors | NGN2, ISL1, LHX3 (neuronal) [35] | Drives direct cell reprogramming and lineage specification |
| Extracellular Matrices | iMatrix-511 [33], Matrigel [33], Fibronectin, Vitronectin, Laminin-111 [32] | Provides structural support and biochemical signals for cell attachment and differentiation |
| Culture Media Supplements | B-27 Supplement (with/without insulin) [33], Growth Factors (bFGF, GDNF family ligands) [36] [33] | Supplies essential nutrients and specific differentiation signals |
| Cell Surface Marker Labels | TBX5, NKX2-5 [33], CXCR4 [33], ISL1 [32] | Identifies and isolates specific progenitor populations |
Signaling Pathways in Directed Differentiation
The following diagram summarizes the key signaling pathways and their manipulation to direct cell fate toward specific lineages:
Directed differentiation of human pluripotent stem cells to functional cardiomyocytes, neurons, and hepatocytes has reached unprecedented levels of efficiency and maturity. The protocols detailed in this guide—incorporating progenitor reseeding, chamber-specific cardiac induction, EMT suppression in hepatic differentiation, and receptor-ligand matching for neuronal maturation—represent the current state-of-the-art in the field. These advanced methodologies enable the generation of more physiologically relevant human cell models that closely mimic native tissue function, significantly enhancing their utility for patient-specific disease modeling, drug screening, and the development of novel cell therapies. As standardization and validation efforts progress through initiatives like the Consortium on Advanced Stem Cell-Based Models in Drug Discovery and Development [10], these differentiation platforms are poised to become indispensable tools for bridging the gap between preclinical research and clinical application.
The field of cardiovascular research is undergoing a significant transformation, moving away from traditional two-dimensional (2D) cell culture systems toward more physiologically relevant three-dimensional (3D) models. This shift is driven by the recognition that 3D models—including organoids, spheroids, and engineered heart tissues—better replicate the intricate cellular microenvironments found in vivo. For researchers and drug development professionals focused on patient-specific disease modeling, these advanced systems provide unprecedented opportunities to study disease mechanisms, screen drug candidates, and develop personalized therapeutic strategies with greater predictive accuracy than ever before [38]. The fundamental limitation of 2D cultures lies in their inability to fully recapitulate essential cell-cell and cell-extracellular matrix (ECM) interactions that regulate critical biological functions, including cell morphology, polarity, differentiation, migration, proliferation, and survival [38]. Consequently, data obtained from 2D cultures often demonstrate poor correlation with outcomes observed in animal studies and clinical trials, creating a translational gap that 3D models are uniquely positioned to bridge [38].
The emergence of human induced pluripotent stem cell (iPSC) technology has been particularly transformative for cardiovascular precision medicine. iPSCs allow for the production of a limitless supply of patient-specific somatic cells, enabling researchers to create disease models that carry the exact genetic background of individual patients [11]. When combined with 3D culture techniques, these patient-specific iPSCs give rise to sophisticated model systems that exhibit native tissue-like architecture, gradient-dependent physiological responses, and pathologically relevant signaling pathways [15]. This review provides an in-depth technical examination of current 3D model systems, with a specific focus on their application within stem cell research for patient-specific disease modeling and drug development.
Core 3D Model Systems: Technical Specifications and Applications
Defining Characteristics and Comparative Analysis
Three-dimensional model systems encompass a spectrum of technologies, each with distinct characteristics and applications. Scaffold-free 3D cellular spheroid cultures promote more intricate cell-cell and cell-ECM interactions than traditional 2D systems, better replicating the in vivo cellular microenvironments of complex tissues [38]. Cardiac spheroids (CSs), often referred to as "mini hearts," model molecular, cellular, and extracellular features typical of the myocardium and have become invaluable tools for disease modelling, drug and toxicity screening, and personalised therapeutics in cardiac regenerative medicine [39].
Table 1: Fundamental Differences Between 2D and 3D Culture Systems
| Property | 2D Cell Culture | 3D Spheroid Culture | References |
|---|---|---|---|
| Cell Morphology | Does not mimic in vivo tissue structure; altered cell morphology | Replicates in vivo-like tissue structure and cell morphology due to 3D organization | [38] |
| Cell Organization | Cellular monolayer | Three distinct cell layers: central necrotic core, inner quiescent layer, outer proliferating layer | [38] |
| Cell-Cell Interactions | Interactions only between horizontal neighbors | Multidirectional interactions among heterogeneous cell populations | [38] |
| Predictive Accuracy | Overestimation of drug sensitivity due to uniform nutrient access | Physiological nutrient/oxygen gradients yield in vivo-like drug responses | [38] |
| Disease Fidelity | Limited pathophysiological signaling due to lack of tissue architecture | Better preservation of pathological cell-cell and cell-ECM interactions | [38] |
Cardiac Spheroids and Organoids
Cardiac spheroids are spherical microtissues generated via 3D culture of cardiac cells, which can include primary- or induced pluripotent stem cell-derived cardiomyocytes (iPSC-CMs) alone or in combination with other cardiac resident cells [39]. These systems contrast with 2D cultures by providing superior accuracy in emulating cellular functions and signaling pathways of target tissues through their ability to form authentic cell-cell and cell-matrix interactions [39]. Spheroid formation occurs through spontaneous cell aggregation and binding of cell surface integrin receptors with ECM components (laminin, fibronectin, and collagen) to promote cell-cell contact and E-cadherin accumulation on the cell surface [39].
The cellular composition of cardiac spheroids significantly influences their functionality and physiological relevance. For instance, CSs generated using a 2:1:1 tri-culture ratio of human primary adult cardiomyocytes or iPSC-derived cardiomyocytes (iCells), with iPSC-derived cardiac fibroblasts (iCFs) and coronary artery endothelial cells (HCAECs) exhibit syncytial contraction and transcriptomic regulation that mimic the physiology of native myocardial tissue [39]. Similarly, in two-cell type cultures, researchers often use a 4:1 ratio of hiPSC-CMs: CFs to mimic healthy tissue void of fibrosis [39]. This cellular complexity allows for the modeling of multi-systemic interactions that influence cells in the body, addressing a significant limitation of traditional iPSC-derivatives utilized in monocultures [15].
Engineered Heart Tissues
Engineered heart tissues (EHTs) represent a more advanced approach to 3D cardiac modeling, typically involving the incorporation of cardiac cells within scaffold-based systems or using tissue-engineering principles to create functional myocardial patches. EHTs exhibit superior structural organization and mechanical properties compared to spheroids, often requiring the use of biological or synthetic-derived biomaterials like Matrigel or Poly(ethylene glycol) (PEG) to provide structural support and biochemical cues [39]. These systems are particularly valuable for studying cardiac contractility, mechanical stress responses, and for potential applications in cardiac regeneration through the creation of implantable tissue constructs.
Generation Methods for 3D Cardiac Models
Scaffold-Free Generation Techniques
Scaffold-free methods enable cells to self-assemble into tissue-like structures without synthetic material support, leveraging the natural self-adhesion properties of cells to form spheroids [39].
Hanging Drop (HD) Cultures: This widely used approach involves pipetting cells in suspension onto the underside of a petri dish lid, which is then inverted to promote cell accumulation to the center of each drop through surface tension and gravitational force [39]. As an open culture system, HD allows optimal gas exchange during incubation while avoiding bubble formation. Several specialized HD plates have been developed for generating spheroids, including Perfecta 3D 96-well HD plates (3D Biomatrix, MI, USA) and 384-well HD plates for higher throughput applications [39]. HD cultures offer advantages including low cost, short generation time, scaffold-independent generation, and low cell volume requirement per spheroid [38] [39]. However, challenges include labor intensiveness without robotic equipment, difficult media changes, and high cross-contamination risks [39].
Forced Floating (Low-Adhesive Surfaces): Liquid overlay on ultra-low attachment (ULA) plates utilizes a pre-coating technique with an ultra-hydrophilic polymer that creates conditions where adhesive forces between cells are stronger than the surface they're cultured on [39]. This enables free-floating cells to form aggregates of consistent size uniformity across multiple wells. Commercially available ULA-pre-treated plates include ULA-PrimeSurface Cell Culture Plates (Sumitomo Bakelite) and Nunclon Sphera 96-Well Microplates (Thermo Fisher Scientific) [39]. Similarly, microwell-based options like AggreWell plates (STEMCELL Technologies) feature 400 or 800 μm sized microwells in 6- or 24-well options, providing vessel-based size control of the spheroids [39].
Rotary Culture Systems: Spinner flasks and rotating wall vessels maintain cells in constant suspension, promoting aggregation through continuous gentle mixing [38] [39]. These systems enable large-scale production of spheroids but offer less control over individual spheroid size and uniformity compared to other methods.
Table 2: Technical Comparison of Primary Spheroid Generation Methods
| Method | Uniformity | Throughput | Cell Viability | Specialized Equipment | Key Applications |
|---|---|---|---|---|---|
| Hanging Drop | Relatively uniform based on droplet size/cell number | Scalable but labor-intensive | >92% live cells for ≤2 weeks | No | Short-term culture, drug screening, tumor & cardiovascular modeling [38] |
| Low-attachment Plates | Single, uniformly sized and shaped spheroids | High (compatible with multi-well formats) | High viability up to 7 days (declines by 21 days) | No | Affordable simple method; drug screening; tumor & cardiovascular modeling [38] |
| Liquid Overlay | Moderately reproducible; longer formation time | High (multi-well formats) | Stable for 14 days; tends to form larger necrotic core | Yes (agarose-coated plates) | Large-scale experiments [38] |
| Microfluidics | High uniformity | Medium to high | High viability due to controlled environment | Yes | Precume control of microenvironment; high-precision studies [38] |
Scaffold-Based and Advanced Engineering Approaches
Scaffold-based methods involve culturing cells within synthetic biomaterials that provide mechanical support and spatial cues [38]. These include:
Hydrogel Scaffolds: Natural hydrogels (e.g., Matrigel, collagen, alginate) or synthetic hydrogels (e.g., PEG, polyacrylamide) provide a 3D environment that mimics the native extracellular matrix [39].
Bioprinting: This advanced technique enables precise spatial patterning of multiple cell types and biomaterials to create complex tissue architectures [39]. Common approaches include extrusion-based, inkjet, and laser-assisted bioprinting.
Microfluidic Systems: Organ-on-a-chip platforms incorporate 3D tissues within microfluidic devices to better control fluid flow, mechanical forces, and tissue-tissue interfaces [15]. These systems allow for the creation of humanized animal systems for more predictive drug testing [15].
Diagram 1: Comprehensive workflow for generating cardiac spheroids from iPSCs, showing key methodological decision points and applications.
iPSC Technology for Patient-Specific Disease Modeling
iPSC Differentiation into Cardiovascular Lineages
The groundbreaking discovery by Shinya Yamanaka that a set of four transcription factors (Oct4/Sox2/c-Myc/Klf4) can reprogram somatic cells to induced pluripotent stem cells (iPSCs) has revolutionized biomedical research, providing an accessible and versatile platform for precision medicine [11]. iPSCs generated from an individual can be differentiated into a wide variety of functional somatic cells, enabling patient-specific disease modeling, drug testing, toxicity screening, and 3D organ/organoid construction [11].
Cardiac differentiation from iPSCs is induced by manipulating specific signaling pathways essential for cardiac development, recapitulating the embryonic cardiac differentiation process: from pluripotent stage (OCT3/4+, NANOG+), to mesodermal lineage (T+, MIXL1+), to cardiac progenitor lineage (MESP1+, NKX2.5+), and finally to relatively immature beating cardiomyocytes (TNNT2+, MYH6+) [11]. Modern protocols use chemically defined medium and small-molecule compounds to induce CM differentiation from a monolayer of iPSCs [11]. The process typically begins with the small-molecule glycogen synthase kinase (GSK)-3β inhibitor CHIR99021 to promote differentiation of iPSCs to mesodermal lineage, followed by treatment with canonical Wnt inhibitors (IWR-1, IWR-4, XAV939, or C59) to direct differentiation of mesodermal cells to the cardiac lineage [11]. These differentiation methods yield robustly beating troponin T+ iPSC-CMs with high efficiency (>90%) at manageable cost [11].
Chamber-Specific Cardiomyocyte Generation
Because cardiovascular diseases affect distinct heart chambers, methods have been developed to generate chamber-specific iPSC-CM subtypes. Recent studies have described how to modulate retinoic acid signaling during CM differentiation to derive atrial- and ventricular-like CMs, as well as sinoatrial nodal pacemaker cells [11]. This specificity is crucial for accurate disease modeling, as atrial CMs are required to assess mechanisms underlying atrial fibrillation, nodal CMs for conduction disorders, and ventricular CMs for ventricular tachycardia [11].
Diagram 2: Key signaling pathway manipulation for directing iPSC differentiation into chamber-specific cardiomyocytes.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for 3D Cardiac Model Generation
| Reagent/Material | Function | Application Examples |
|---|---|---|
| CHIR99021 | GSK-3β inhibitor; promotes mesodermal lineage differentiation | Initial step in cardiac differentiation protocols [11] |
| IWR-1, XAV939, C59 | Canonical Wnt inhibitors; direct cardiac lineage specification | Second step in cardiac differentiation [11] |
| Retinoic Acid | Signaling modulator for chamber-specific differentiation | Generation of atrial vs. ventricular cardiomyocytes [11] |
| Methylcellulose | Increases medium viscosity; enhances spheroid circularity and compaction | Forms tighter spheres; reduces motion-induced image blur [39] |
| Matrigel | Natural hydrogel scaffold; provides ECM support | Scaffold-based 3D culture; bioprinting applications [39] |
| Poly(ethylene glycol) (PEG) | Synthetic hydrogel scaffold; tunable mechanical properties | Engineered heart tissues; customizable 3D environments [39] |
| Ultra-Low Attachment Plates | Prevents cell adhesion; promotes 3D aggregation | Spheroid formation via forced floating method [38] [39] |
| Perfecta3D Hanging Drop Plates | Facilitates hanging drop culture | High-throughput spheroid generation [38] |
| AggreWell Plates | Microwell plates for size-controlled spheroid formation | Uniform spheroid production [39] |
Applications in Disease Modeling and Drug Development
Patient-Specific Cardiovascular Disease Modeling
iPSC-derived cardiovascular cells provide a powerful platform for effectively studying patient- and disease-specific heart disease conditions in vitro [11]. These models have been successfully applied to numerous cardiovascular conditions, including:
- Long QT Syndromes: Using patient-specific iPSC-CMs to model cardiac channelopathies and test anti-arrhythmic drugs [11].
- Hypertrophic Cardiomyopathy: Disease modeling using iPSCs from patients with genetic mutations associated with hypertrophic cardiomyopathy [11].
- Dilated Cardiomyopathy: Creating in vitro models of dilated cardiomyopathy to study disease mechanisms and screen potential therapeutics [11].
- Brugada Syndrome, Arrhythmogenic Right Ventricular Dysplasia, and Other Inherited Disorders: Modeling various inherited cardiac conditions using patient-specific iPSCs [11].
Notably, iPSCs have been used to assess whether genetic variants in individual patients are pathogenic or benign, and have proven useful in patient-specific drug screening and drug toxicity testing [11]. This approach allows for unprecedented opportunities to discover new drug targets and screen compounds for cardiovascular disease imbued with the genetic information of a specific individual [11].
Drug Screening and Toxicity Testing
The pharmaceutical industry has faced significant challenges in cardiovascular drug development, with many promising compounds failing in clinical trials due to inadequate preclinical models. 3D cardiac models address several key limitations of traditional systems:
Enhanced Predictive Accuracy: 3D systems create gradients of oxygen, nutrients, and waste, resulting in heterogeneous cell populations and responses that more closely reflect in vivo conditions [38]. These gradients influence cellular metabolism and drug susceptibility, providing a more predictive platform for evaluating drug efficacy and therapeutic resistance [38].
Overcoming Species-Specific Limitations: Animal models are inherently limited due to fundamental species differences in physiology, reproducibility, ethical concerns, and poor correlation with human clinical trial data [11]. For example, mouse hearts beat at 500 beats per minute, whereas human hearts normally range between 60 and 100 beats per minute, limiting the utility of mice for studying anti-arrhythmic drugs [11].
Patient-Specific Drug Response Profiling: iPSC-based models allow for the identification and tailoring of drugs designed for specific individual patients, moving away from the assumption that all individuals with a disease will respond identically to therapy [11].
Diagram 3: Comprehensive drug screening workflow using patient-specific 3D cardiac models, from iPSC generation to multi-parameter outcome assessment.
Current Challenges and Future Directions
Despite significant advances, several challenges remain in the field of 3D cardiac model systems. A primary limitation is the immature phenotype of iPSC-derived cardiovascular cells, which resemble fetal cardiomyocytes in morphology, size, electrophysiology, and contractile and metabolic functions [11]. This necessitates the development of improved methodologies to achieve adult cell-like phenotype. Additionally, iPSC-derived cardiovascular cells generated with current methodologies exhibit a high level of unresolved functional and transcriptomic heterogeneity [11].
Technical challenges include optimizing spheroid size to control biophysical properties like pH, oxygen, nutrients, and waste removal, as these factors significantly influence biological profiles at transcriptomic and metabolic levels [39]. For instance, smaller spheroids in diameter exhibit reduced Hif-1α expression, suggesting reduced hypoxic core formation [39]. The microenvironment in which spheroids are cultivated also requires careful optimization, as altering media composition through additives like methylcellulose or collagen can positively impact spheroid circularity and compaction [39].
Future directions include improving vascularization of 3D models to enhance nutrient perfusion and enable larger tissue constructs, developing more sophisticated multi-lineage systems that incorporate immune cells and neural elements, and creating integrated multi-organ platforms to study systemic drug effects [15]. As these technologies continue to evolve, they will undoubtedly augment the biomedical researcher's toolkit and enable more realistic models of human tissue function, ultimately accelerating the development of novel therapeutics for cardiovascular diseases [15].
CRISPR-Cas9 Genome Editing for Creating Isogenic Controls and Disease Mutations
The convergence of CRISPR-Cas9 genome editing with human induced pluripotent stem cell (hiPSC) technology has revolutionized patient-specific disease modeling. This technical guide details methodologies for generating isogenic cell pairs—genetically identical lines differing only at a specific locus of interest—which provide powerful experimental systems for elucidating disease mechanisms and advancing therapeutic development. We present comprehensive protocols, quantitative data analyses, and essential research tools that enable researchers to precisely introduce disease-associated mutations or correct genetic lesions in patient-derived hiPSCs. These approaches allow for the rigorous attribution of cellular phenotypes to specific genetic variations while controlling for background genetic variation, addressing a fundamental challenge in human genetics research.
The development of isogenic cell pairs represents a critical advancement for establishing causality in disease modeling studies. Before the advent of precise genome editing, researchers relied on comparing cell lines from different donors with and without a disease, making it difficult to distinguish phenotypic differences caused by the disease-causing mutation from those resulting from the vast genetic variability between individuals [40]. Isogenic controls overcome this limitation by providing genetically identical cells that differ only in the specific genetic modification of interest, enabling unambiguous determination of genotype-phenotype relationships [40] [41].
The combination of hiPSC technology and CRISPR-Cas9 has proven particularly powerful for creating these matched cellular models. hiPSCs can be generated from patient somatic cells and differentiated into relevant cell types affected by disease, while CRISPR-Cas9 enables precise genetic manipulation to either correct disease-causing mutations in patient-derived cells or introduce them into healthy control lines [40]. This approach has been successfully applied to model numerous neurological, cardiac, and metabolic disorders, providing unprecedented insight into disease mechanisms and creating platforms for drug screening and therapeutic development [41].
CRISPR-Cas9 Systems for Genome Editing
Core Editing Platforms
The CRISPR-Cas9 system has evolved from a bacterial adaptive immune mechanism into a versatile genome engineering tool. The fundamental system consists of two key components: the Cas9 nuclease, which creates double-strand breaks in DNA, and a guide RNA (gRNA), which directs Cas9 to specific genomic sequences through complementary base pairing [42] [43]. The recognition process requires the presence of a protospacer adjacent motif (PAM), typically 5'-NGG for the most commonly used Streptococcus pyogenes Cas9 [43].
Following DNA cleavage, cellular repair mechanisms are harnessed to achieve different editing outcomes. Non-homologous end joining (NHEJ) often results in small insertions or deletions (indels) that disrupt gene function, while homology-directed repair (HDR) can be used to introduce precise sequence changes when a donor DNA template is provided [42] [44]. The efficiency and precision of CRISPR-Cas9 have led to its widespread adoption over earlier technologies like zinc finger nucleases (ZFNs) and transcription activator-like effector nucleases (TALENs), which required more complex protein engineering for each new target site [42] [43].
Advanced CRISPR Tool variants
The core CRISPR-Cas9 system has been extensively engineered to expand its capabilities beyond simple gene knockout:
CRISPR Interference (CRISPRi): Catalytically dead Cas9 (dCas9) is fused to repressive domains like the Krüppel-associated box (KRAB) to block transcription without altering DNA sequence [45]. When targeted to gene promoters or enhancers, dCas9-KRAB recruits factors that deposit repressive H3K9 trimethylation marks, leading to reversible gene silencing [45].
CRISPR Activation (CRISPRa): Fusion of dCas9 to transcriptional activation domains like the p300 core domain enables targeted gene upregulation [45]. The dCas9-p300 fusion acetylates histone H3 at lysine 27, creating an open chromatin state permissive for transcription [45].
Base Editing: Fusion of Cas9 nickase with cytidine or adenine deaminase enzymes enables direct conversion of C•G to T•A base pairs or A•T to G•C base pairs without requiring double-strand breaks or donor templates [44] [43].
Prime Editing: A more recent development that uses a Cas9 nickase-reverse transcriptase fusion and a specialized guide RNA to directly write new genetic information into a target DNA site, enabling all possible base-to-base conversions as well as small insertions and deletions [43].
Experimental Workflows for Generating Isogenic Cell Lines
The process of creating and validating isogenic hiPSC lines involves multiple critical stages, from designing the editing strategy to thoroughly characterizing the resulting clones. The workflow below outlines the key steps in this process.
gRNA and Donor Design
The success of any genome editing experiment depends heavily on careful design of the gRNA and donor templates. For creating point mutations or making precise gene corrections, the following design principles apply:
gRNA Selection: Design gRNAs to target the genomic region of interest with high efficiency and minimal off-target potential. The gRNA should be located as close as possible to the intended edit site while considering PAM availability. Multiple online tools are available for gRNA design and off-target prediction.
Donor Template Design for HDR: For precise editing, design a single-stranded oligodeoxynucleotide (ssODN) or double-stranded DNA donor template containing the desired mutation flanked by homology arms. The optimal length of homology arms typically ranges from 60-90 nucleotides on each side for ssODNs. Incorporate silent mutations in the PAM sequence or the gRNA binding site when possible to prevent re-cutting of successfully edited alleles [40].
Delivery Methods and Experimental Protocols
The following table compares the primary methods for delivering CRISPR components into hiPSCs, each with distinct advantages and limitations.
Table 1: Comparison of CRISPR Delivery Methods for hiPSCs
| Method | Mechanism | Editing Efficiency | Advantages | Disadvantages |
|---|---|---|---|---|
| Electroporation | Electrical pulses create temporary pores in cell membrane [44] | Moderate to High | Suitable for RNPs; minimal off-target effects; no size limitations [44] | Higher cell mortality; requires optimization |
| Lipid Nanoparticles | Lipid-based vesicles fuse with cell membrane [44] [43] | Moderate | High viability; applicable to various cargo types; clinically relevant [43] | Potential cytotoxicity; optimization required |
| Viral Vectors | Lentiviral/AAV transduction [44] [43] | High | High efficiency; stable expression | Size limitations (AAV); immunogenicity; insertional mutagenesis risk [43] |
Detailed Protocol: RNP Electroporation in hiPSCs
This protocol describes the delivery of CRISPR-Cas9 as a ribonucleoprotein (RNP) complex via electroporation, which minimizes off-target effects and enables rapid editing.
Materials:
- Healthy control or patient-derived hiPSCs
- Cas9 protein and synthetic gRNA
- ssODN donor template (for HDR-mediated editing)
- Electroporation system
- mTeSR or equivalent hiPSC culture medium
- Rock inhibitor (Y-27632)
Procedure:
- Culture Preparation: Culture hiPSCs in essential 8 medium or mTeSR on Matrigel-coated plates until 70-80% confluent.
- Cell Dissociation: Harvest hiPSCs using Accutase or EDTA to create a single-cell suspension. Count cells and resuspend in appropriate electroporation buffer.
- RNP Complex Formation: Combine 10 µg Cas9 protein with 5 µg gRNA in a 1:2 molar ratio. Incubate at room temperature for 10-20 minutes to form RNP complexes.
- Electroporation Mixture: For HDR editing, mix 2-5 µL of RNP complex with 2 µL of 100 µM ssODN donor template and 1×10^5 hiPSCs in electroporation cuvette.
- Electroporation: Apply manufacturer-recommended electrical pulse parameters for hiPSCs.
- Recovery: Immediately transfer electroporated cells to Matrigel-coated plates pre-filled with recovery medium containing 10 µM Rock inhibitor.
- Selection and Cloning: After 48-72 hours, begin antibiotic selection if using a reporter system. For isolation of single-cell clones, plate cells at low density and manually pick individual colonies after 7-14 days [44].
Screening and Validation
Comprehensive characterization of edited hiPSC clones is essential to confirm the desired genetic modification while ensuring genomic integrity.
Primary Screening: Use PCR amplification of the target region followed by restriction fragment length polymorphism (RFLP) analysis if the edit creates or disrupts a restriction site. Alternatively, use mismatch detection assays (T7E1 or Surveyor) to identify modified clones.
Sequence Verification: Sanger sequencing of the targeted locus in potential positive clones to confirm the precise edit and check for unintended mutations.
Karyotype Analysis: Perform G-banding karyotyping to ensure no major chromosomal abnormalities were introduced during the editing process.
Pluripotency Validation: Confirm that edited hiPSCs maintain expression of pluripotency markers (OCT4, NANOG, SOX2) and differentiation capacity.
Off-Target Assessment: Use targeted sequencing of predicted off-target sites or whole-genome sequencing for critical applications to rule off unintended modifications.
The Scientist's Toolkit: Essential Research Reagents
Successful generation of isogenic hiPSC lines requires a comprehensive set of specialized reagents and tools. The following table details essential components for CRISPR-based genome editing workflows.
Table 2: Essential Research Reagents for CRISPR-Cas9 Genome Editing in hiPSCs
| Reagent Category | Specific Examples | Function/Purpose |
|---|---|---|
| CRISPR Components | Cas9 protein, Synthetic gRNA, Donor templates (ssODN) | Core editing machinery; directs specificity and edit type |
| Cell Culture Reagents | mTeSR medium, Matrigel, Rock inhibitor (Y-27632) | Maintain pluripotency; enhance single-cell survival |
| Delivery Tools | Electroporation kits, Lipid nanoparticles | Introduce CRISPR components into cells |
| Selection Markers | Puromycin, G418, Fluorescent reporters | Enrich for successfully transfected cells |
| Validation Tools | PCR reagents, Sequencing primers, Antibodies for pluripotency markers | Confirm genetic edits and maintain stem cell quality |
Applications in Disease Modeling and Current Clinical Trials
The combination of hiPSC technology and CRISPR-Cas9 has enabled the development of sophisticated models for numerous genetic disorders. These isogenic cell pairs have become invaluable tools for understanding disease mechanisms and developing therapeutic interventions.
Neurological Disorders
In neurological research, isogenic hiPSCs have been used to model conditions including Alzheimer's disease, Parkinson's disease, and various neurodevelopmental disorders [41]. The ability to differentiate hiPSCs into neurons, glial cells, and increasingly complex brain organoids has enabled the study of disease processes in relevant cell types that were previously inaccessible [41] [46]. For example, CRISPR-edited cerebral organoids have been used to model microcephaly, revealing insights into the developmental mechanisms underlying this condition [46].
Monogenic and Complex Diseases
Beyond neurological disorders, this approach has been applied to monogenic diseases such as β-thalassemia and sickle cell anemia, where isogenic hiPSCs have helped elucidate the molecular consequences of disease-causing mutations and provided platforms for testing therapeutic interventions [40] [44]. The methodology has also been extended to more complex polygenic disorders, where the introduction or correction of multiple alleles in a controlled genetic background can help dissect the contribution of individual genetic variants to disease risk [40].
Clinical Translation
The therapeutic potential of CRISPR-based approaches is already being realized in clinical trials, particularly for hematological diseases:
CTX001 for β-thalassemia and sickle cell disease: This autologous therapy uses CRISPR-Cas9 to edit hematopoietic stem and progenitor cells to reactivate fetal hemoglobin production by targeting the BCL11A gene. Clinical trials have shown promising results, with patients achieving transfusion independence [44].
CEP290-related retinal dystrophies: The EDIT-101 therapy uses CRISPR-Cas9 to correct a mutation in the CEP290 gene that causes Leber congenital amaurosis, demonstrating the application of this technology to inherited blindness disorders [44] [47].
These clinical advances highlight the rapid translation of CRISPR-based technologies from basic research tools to potentially transformative therapies for genetic diseases.
CRISPR-Cas9 genome editing has fundamentally transformed our approach to creating isogenic controls and introducing disease-relevant mutations in hiPSCs. The methodologies outlined in this technical guide provide a roadmap for researchers to establish rigorous, physiologically relevant models of human disease that control for genetic background variability. As the technology continues to evolve with the development of more precise editing tools and more complex differentiation protocols, these approaches will further enhance our ability to model human diseases and develop targeted interventions. The integration of isogenic hiPSC models with advanced tissue engineering approaches, including 3D organoid systems, promises to yield even more sophisticated models that better recapitulate the complexity of human tissues and organs in health and disease.
Applications in Drug Screening, Safety Pharmacology, and Personalized Therapy Development
The field of drug development is undergoing a profound transformation, driven by the integration of patient-specific stem cell technologies. Traditional preclinical models, particularly animal studies, increasingly demonstrate limited translational fidelity due to interspecies physiological differences, contributing to high failure rates in clinical trials [9]. Human stem cell-based models, especially induced pluripotent stem cells (iPSCs) and organoid systems, have emerged as powerful alternatives that recapitulate human-specific biology with unprecedented accuracy [9] [6]. These models provide unprecedented access to patient-specific human tissues for investigating disease mechanisms, screening compound libraries, and assessing cardiac and neurological safety profiles during drug development.
This technical guide examines the integration of stem cell technologies across three critical pharmaceutical applications: drug screening, safety pharmacology, and personalized therapy development. We provide detailed experimental methodologies, quantitative data summaries, and visualization of key workflows to support implementation of these technologies in research and development pipelines. By framing these applications within the broader context of patient-specific disease modeling, we highlight how stem cell platforms are advancing precision medicine and transforming therapeutic development.
Stem Cell Platforms for Disease Modeling
Stem Cell Types and Characteristics
The utility of stem cells in drug development derives from their dual capacity for self-renewal and differentiation into specialized cell types. Different stem cell classes offer complementary advantages for pharmaceutical applications.
Table 1: Stem Cell Types and Their Research Applications
| Stem Cell Type | Key Features | Differentiation Potential | Primary Research Applications |
|---|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | Patient-derived; reprogrammed somatic cells; avoid ethical concerns | Multipotent (all germ layers) | Patient-specific disease modeling; personalized drug screening; toxicity testing |
| Embryonic Stem Cells (ESCs) | Derived from blastocyst-stage embryos; controversial ethically | Pluripotent (all germ layers) | Developmental biology; mechanistic studies |
| Mesenchymal Stem Cells (MSCs) | Tissue-derived (bone marrow, adipose); immunomodulatory properties | Multipotent (mesenchymal lineages) | Immunomodulation; inflammatory disease modeling; regenerative therapy |
| Organoids | 3D stem cell-derived structures | Self-organizing; tissue-specific | Complex disease modeling; host-pathogen interactions; tissue development |
The advent of iPSC technology has been particularly transformative, enabling generation of patient-specific models that imbue in vitro systems with the genetic information of individual patients or specific disease populations [6]. When combined with CRISPR-Cas9 gene editing, researchers can create isogenic control lines that strengthen causal inference in disease modeling [9]. Meanwhile, organoid systems recapitulate aspects of tissue architecture and function that are absent in two-dimensional cultures, making them invaluable for modeling complex tissue-level pathologies [9].
Technical Considerations for Model Validation
Despite their promise, stem cell-based models face challenges in standardization and maturation. Differentiation protocols can vary significantly between laboratories, leading to inconsistent results and limiting reproducibility [9]. Furthermore, stem cell-derived tissues frequently exhibit fetal-like gene expression profiles and functional immaturity that may limit their ability to model adult-onset diseases or predict adult-specific pharmacological responses [9].
Addressing these limitations requires implementation of rigorous characterization standards and maturation strategies. The Consortium on Advanced Stem Cell-Based Models in Drug Discovery and Development, a global organization of industry and academic scientists, is working to establish harmonized validation frameworks for stem cell-based models [10]. Their efforts focus on establishing robust, transparent, and reproducible evaluation criteria that ensure biological relevance and reliability across different research settings.
Application in Drug Screening
Experimental Workflow for Compound Screening
Stem cell-based platforms have revolutionized early drug discovery by providing human-relevant systems for compound screening. The general workflow begins with patient recruitment and biopsy collection (typically skin fibroblasts or blood cells), followed by reprogramming to generate iPSCs. These iPSCs are then genetically engineered using CRISPR-Cas9 to introduce or correct disease-relevant mutations, creating isogenic pairs for controlled experiments. The edited iPSCs are differentiated into target cell types or organoids, which are then utilized in high-content screening platforms with automated imaging and analysis [6].
Figure 1: Stem Cell-Based Drug Screening Workflow. HTS: High-Throughput Screening.
Protocol: Cardiac Organoid Differentiation for Compound Screening
Purpose: Generate functional cardiovascular organoids from iPSCs for drug efficacy and toxicity screening [9].
Materials:
- Human iPSCs: Maintained in mTeSR1 or equivalent medium
- Small molecules: CHIR99021 (GSK-3 inhibitor), IWP-2 (Wnt inhibitor)
- Basal medium: RPMI 1640 supplemented with B-27
- Extracellular matrix: Matrigel for 3D culture support
- Characterization antibodies: Anti-cTnT (cardiac troponin T), Anti-α-actinin
Method:
- Maintenance: Culture iPSCs in essential 8 medium on vitronectin-coated plates until 80-90% confluent.
- Mesoderm induction: Dissociate iPSCs to single cells and plate in ultra-low attachment plates at 1×10^6 cells/mL in RPMI/B-27 medium supplemented with 6-12 µM CHIR99021 for 24 hours.
- Cardiac specification: On day 3, replace medium with RPMI/B-27 containing 5 µM IWP-2.
- Metabolic selection: From day 5 onwards, maintain organoids in RPMI/B-27 without glucose, supplemented with 4 mM lactate to enrich for cardiomyocytes.
- Maturation: Culture organoids for 30-60 days with gradual electrical stimulation (beginning at 0.5 Hz, increasing to 2 Hz) to promote structural and functional maturation.
- Characterization: Analyze contractile function via video microscopy, electrophysiology using multi-electrode arrays, and structural maturity via immunostaining for sarcomeric proteins.
Applications: Cardiovascular organoids model congenital heart disease, cardiotoxicity, and cardiomyopathies, providing human-relevant systems for drug discovery [9].
Quantitative Applications in Drug Screening
Table 2: Stem Cell Applications in Drug Screening and Safety Assessment
| Application Area | Stem Cell Model | Key Readouts | Reported Impact |
|---|---|---|---|
| Cardiotoxicity Screening | iPSC-derived cardiomyocytes | Field potential, beat rate, contraction strength | Up to 94% sensitivity in detecting drug-induced arrhythmias [6] |
| Neurological Toxicity | iPSC-derived neurons | Neurite outgrowth, synaptic activity, cytotoxicity | Detection of compound-specific neurotoxic patterns |
| Hepatotoxicity Screening | iPSC-derived hepatocytes | Albumin secretion, CYP450 activity, bile transport | Prediction of drug-induced liver injury with 85% accuracy |
| Kidney Toxicity | Kidney organoids | Cyst formation, biomarker release (KIM-1, NGAL) | Modeling of polycystic kidney disease for therapeutic screening [9] |
| Oncology Drug Screening | Cancer organoids | Tumor growth inhibition, apoptosis markers | Patient-specific therapy prediction for personalized oncology |
Application in Safety Pharmacology
The Evolving Regulatory Landscape
Safety pharmacology has traditionally relied on animal models and transformed cell lines for predictive toxicology. However, regulatory shifts are accelerating adoption of human-based models. The FDA Modernization Act 3.0 formally positions human-relevant alternative models—including organ-on-chip systems and computational approaches—as viable substitutes for traditional animal testing [48]. This regulatory evolution aligns with growing recognition of species-specific differences in drug metabolism, target specificity, and immune responses that limit animal model predictivity [9].
Stem cell-based safety models address these limitations by providing human-specific toxicology platforms that more accurately predict clinical responses. The Consortium on Advanced Stem Cell-Based Models specifically focuses on advancing stem cell-derived in vitro models for safety assessment, working to integrate these technologies with mechanistic toxicology and metabolic profiling [10].
Protocol: HERG Channel Assay Using iPSC-Derived Cardiomyocytes
Purpose: Assess compound effects on the human Ether-à-go-go-Related Gene (hERG) potassium channel to predict pro-arrhythmic risk [6].
Materials:
- iPSC-derived cardiomyocytes: Commercially available or differentiated in-house
- Patch clamp equipment: Automated or manual patch clamp system
- Extracellular solution: NaCl 140 mM, KCl 4 mM, CaCl₂ 1 mM, MgCl₂ 1 mM, Glucose 10 mM, HEPES 10 mM (pH 7.4)
- Intracellular solution: KCl 130 mM, MgCl₂ 1 mM, EGTA 5 mM, MgATP 5 mM, HEPES 10 mM (pH 7.2)
- Reference compounds: E-4031 (positive control), DMSO (vehicle control)
Method:
- Cell preparation: Plate iPSC-derived cardiomyocytes on appropriate substrates (e.g., fibronectin-coated coverslips) 24-48 hours before experimentation.
- Voltage protocol: Using whole-cell patch clamp configuration, hold cells at -80 mV, apply depolarizing pulse to +20 mV for 4 seconds, then repolarize to -50 mV for 6 seconds to record tail currents.
- Baseline recording: Record hERG current (I_Kr) amplitude under control conditions.
- Compound application: Perfuse with test compound at multiple concentrations (typically 3-5 concentrations in half-log increments), allowing 3-5 minutes equilibration at each concentration.
- Data analysis: Normalize current amplitudes to baseline, fit concentration-response relationship with Hill equation to calculate IC₅₀ values.
- Validation: Compare results to known hERG blockers (e.g., E-4031) to confirm assay sensitivity.
Interpretation: Compounds with IC₅₀ values <1 μM typically represent significant hERG blockade and require further investigation for torsadogenic risk.
Advanced Safety Assessment Platforms
Beyond standard cardiotoxicity screening, stem cell platforms enable sophisticated safety assessment across multiple organ systems. Multi-organ microphysiological systems (organ-on-a-chip platforms) connect stem cell-derived tissues to model interdependent toxicities and metabolite-mediated effects [49]. For immunotoxicity assessment, mesenchymal stem cells (MSCs) provide platforms for evaluating immunomodulatory drug effects, though their clinical translation requires careful characterization of critical quality attributes (CQAs) that correlate with biological potency [50].
The integration of artificial intelligence with stem cell-based safety data further enhances predictive capabilities. AI algorithms can identify complex toxicity patterns across large chemical libraries, improving prediction of organ-specific toxicities and enabling earlier exclusion of high-risk compounds [51] [48].
Application in Personalized Therapy Development
Patient-Specific Therapy Optimization
Personalized therapy development represents the most transformative application of stem cell technology in pharmaceutical research. Patient-derived iPSCs provide a platform for individualized drug response profiling, creating in vitro models that mirror patient genetics before treatment initiation [6]. This approach is particularly valuable for neurological disorders, cardiovascular diseases, and cancer, where inter-individual variability in treatment response significantly impacts therapeutic outcomes.
Figure 2: Personalized Therapy Development Pipeline Using Patient-Specific iPSCs.
Protocol: Patient-Specific Drug Response Profiling for Cardiomyopathy
Purpose: Identify optimal therapeutics for genetic cardiomyopathies using patient-specific iPSC-derived cardiomyocytes [6].
Materials:
- Patient-specific iPSCs: From individuals with characterized cardiomyopathy mutations (e.g., MYH7, TNNT2)
- Control iPSCs: Isogenic controls generated via CRISPR-Cas9 gene correction
- Cardiomyocyte differentiation reagents: As in Section 3.2
- Therapeutic compounds: Beta-blockers, calcium channel blockers, myosin inhibitors
- Functional assessment equipment: Multi-electrode array, calcium imaging setup, contractility measurement system
Method:
- Line generation: Establish iPSCs from patient fibroblasts or peripheral blood mononuclear cells using Sendai virus or episomal reprogramming.
- Isogenic control creation: Using CRISPR-Cas9, correct the disease-causing mutation in patient iPSCs to create matched controls.
- Cardiomyocyte differentiation: Differentiate patient and corrected iPSCs to cardiomyocytes using specified protocols.
- Compound treatment: Treat cardiomyocytes with clinically relevant drugs across concentration ranges reflecting therapeutic plasma levels.
- Phenotypic assessment:
- Electrophysiology: Record field potentials using multi-electrode arrays to detect arrhythmic events
- Calcium handling: Measure calcium transient properties using Fluo-4 AM dye
- Contractility: Quantify contraction dynamics using video-based analysis
- Viability: Assess cell death using high-content imaging with caspase and necrosis markers
- Data integration: Compare drug responses between patient and corrected lines to identify compounds that normalize disease phenotypes.
Applications: This approach successfully identifies patient-specific responses to heart failure medications, enabling therapy optimization before clinical prescription [6].
Quantitative Systems Pharmacology Integration
The combination of stem cell data with quantitative systems pharmacology (QSP) models creates powerful platforms for predicting individual treatment responses. For example, in immuno-oncology, QSP models integrate in vitro CAR-T cell kinetics with patient tumor characteristics to simulate individual treatment outcomes and optimize dosing strategies [52]. Similarly, QSP platforms for bispecific antibodies incorporate multi-scale experimental data to model patient-specific immune responses and optimize target combination designs [53].
These computational-experimental hybrids address a fundamental challenge in personalized therapy: extrapolating from in vitro stem cell data to in vivo patient responses. By creating digital twins of patient physiology, researchers can simulate how drug responses observed in stem cell models might manifest in whole organisms, accelerating translation from bench to bedside [48].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Stem Cell-Based Drug Development
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reprogramming Factors | OCT4, SOX2, KLF4, c-MYC (Yamanaka factors) | Somatic cell reprogramming to iPSCs | Sendai virus system preferred for integration-free approach |
| Differentiation Inducers | CHIR99021 (Wnt activator), BMP4, Activin A | Direct lineage-specific differentiation | Concentrations must be optimized for each iPSC line |
| Characterization Antibodies | Anti-Nanog (pluripotency), Anti-cTnT (cardiomyocytes), Anti-MAP2 (neurons) | Cell type validation via immunocytochemistry | Essential for quality control of differentiated populations |
| Gene Editing Tools | CRISPR-Cas9 components, donor template vectors | Introduction or correction of disease mutations | Isogenic controls are critical for disease modeling studies |
| Functional Assay Kits | Calcium-sensitive dyes, multi-electrode arrays, Seahorse assay kits | Assessment of cellular functionality | More predictive of drug response than viability assays alone |
Stem cell-based models have evolved from research tools to essential platforms advancing all phases of drug development. In drug screening, they provide human-relevant systems that complement traditional animal models, improving translational predictivity. In safety pharmacology, they enable detection of human-specific toxicities that might be missed in conventional species. Most transformatively, in personalized therapy development, they create windows into individual patient biology, enabling truly precision medicine approaches.
Despite remarkable progress, challenges remain in standardization, maturation, and scalability. Ongoing efforts by consortia and regulatory agencies aim to establish robust validation frameworks that will support broader adoption of these technologies [10]. As stem cell methods continue to advance and integrate with computational approaches like AI and QSP, they promise to accelerate the development of safer, more effective therapeutics tailored to individual patient needs.
Navigating Challenges: Optimization Strategies for Enhanced Model Fidelity
The immaturity of human induced pluripotent stem cell-derived cardiomyocytes (iPSC-CMs) remains a significant bottleneck in patient-specific disease modeling, drug development, and regenerative medicine. While stem cell-derived cells offer an unprecedented opportunity to study diseases using patient-specific genetic backgrounds, these cells typically exhibit fetal-like characteristics rather than adult phenotypes, limiting their translational predictive power [9] [54]. This technical guide comprehensively examines the three primary maturation strategies—electrical, mechanical, and metabolic stimulation—that researchers are employing to bridge this critical maturity gap, with particular focus on their application in cardiovascular disease modeling.
The challenge is substantial: iPSC-CMs demonstrate considerable differences from adult cardiomyocytes in morphology, gene expression patterns, metabolism, calcium handling, and electrophysiological functionality [54]. These differences can lead to inaccurate predictions in drug screening assays and failure to recapitulate clinical disease phenotypes. For instance, while the Comprehensive in vitro Proarrhythmia Assay (CiPA) has shown good correlation with clinical risk assessment, discrepancies have been reported for some multichannel blockers like verapamil, which abolishes beating activity in iPSC-CMs at clinically relevant concentrations despite its good safety profile in patients [54].
Recent advances in maturation protocols have demonstrated that combining multiple approaches can yield synergistic effects, driving stem cell-derived cells toward more adult-like states. This whitepaper provides researchers and drug development professionals with detailed methodologies, quantitative comparisons, and implementation frameworks for deploying these maturation strategies in their own patient-specific disease modeling workflows.
Electrical Stimulation Strategies
Biological Effects and Applications
Exogenous electrical stimulation has emerged as a powerful driver of structural and functional maturation in iPSC-CMs, particularly in three-dimensional (3D) culture systems. Electrical pacing mimics the physiological excitation patterns that cardiomyocytes experience in vivo, promoting organization and adult-like characteristics across multiple biological domains [55] [56].
The maturation effects observed with electrical stimulation are comprehensive, including enhanced sarcomere organization with the appearance of I-, H-, A-, M-bands, and Z-discs—structures that are typically absent or poorly organized in immature iPSC-CMs [55]. These structural improvements are accompanied by functional gains, including increased conduction velocity (from 10 cm/s to 25 cm/s in EHT models), more negative resting membrane potential (from -55 mV to -70 mV), enhanced calcium handling with faster release and decay rates, and improved contractile force (0.083 mN vs. 0.056 mN in non-stimulated controls) [56]. Additionally, electrical stimulation promotes the development of critical subcellular structures including T-tubules, desmosomes, and properly organized mitochondria positioned adjacent to the contractile apparatus [55].
Table 1: Maturation Outcomes from Electrical Stimulation in 3D Cardiac Tissues
| Maturation Domain | Specific Improvements | Experimental Model | Quantitative Changes |
|---|---|---|---|
| Structural Maturation | Sarcomere organization, Z-disc alignment, myofibrillar arrangement | EHT, Biowire, Spheroid | Appearance of I-, A-, M-, Z-bands; Increased sarcomere length |
| Electrophysiological Properties | Resting membrane potential, conduction velocity, action potential morphology | EHT, EB, Spheroid | RMP: -70 mV vs -55 mV; CV: 25 cm/s vs 10 cm/s; "Notch-and-dome" AP morphology |
| Calcium Handling | Transient amplitude, release and decay kinetics, sarcoplasmic reticulum function | Biowire, EB, EHT | Faster rising slope and time to peak; Faster tau decay; MCR: 4 Hz vs 3 Hz |
| Subcellular Structures | T-tubules, desmosomes, mitochondrial organization | EHT, Biowire | Presence of T-tubules colocalized with BIN1, RYR2, Cav1.2; Increased desmosomes |
| Gene & Protein Expression | Ion channels, gap junctions, contractile proteins | Spheroid, EHT, EB | ↑Cx43, ↑N-cadherin, ↑MLC2v, ↑SERCA, ↑RYR2; Altered MYL2/MYL2a ratio |
Technical Parameters and Implementation
Implementing effective electrical stimulation protocols requires careful optimization of multiple technical parameters. The electric field voltage (EFV) typically ranges from 1.5-6 V/cm, with specific thresholds varying based on 3D construct size and electrode configuration [55] [56]. Pulse duration generally falls between 1-10 ms, with monophasic or biphasic rectangular waveforms being most common. The stimulation frequency is typically set at 1-2 Hz (60-120 bpm) to mimic physiological heart rates, though some protocols employ progressively increasing frequencies [56].
Electrode material selection critically impacts performance and biocompatibility. Common materials include carbon rods, platinum wires, and indium tin oxide (ITO) coated surfaces, each offering different charge injection capacities and biocompatibility profiles [55]. The stimulation duration varies from days to weeks, with many protocols implementing gradual ramping of intensity to avoid damaging the developing tissues.
For 3D systems, specialized bioreactors and bioprinted scaffolds are often required, as the larger dimensions and volumes alter electrical field distribution and current density compared to 2D cultures [55]. This necessitates re-optimization of parameters previously established for 2D systems. Recent advances include the development of high-throughput, miniaturized platforms that enable parallel testing of multiple stimulation paradigms, accelerating protocol optimization [55] [56].
Diagram 1: Electrical stimulation workflow for cardiomyocyte maturation. The diagram illustrates how specific technical parameters applied through specialized bioreactors drive distinct maturation outcomes in stem cell-derived cardiomyocytes.
Mechanical and Structural Maturation Strategies
Nanoscale Patterning and Substrate Engineering
Mechanical cues through engineered substrates provide powerful stimuli for structural maturation of iPSC-CMs. Nanoscale patterning (NP) of culture surfaces induces cell alignment and organization reminiscent of native myocardial tissue [54]. This approach primarily drives structural maturation with more limited effects on electrophysiological properties alone.
The implementation of nanopatterning involves creating grooves or ridges on culture surfaces with dimensions typically ranging from 500-800 nm in width and 150-300 nm in depth [54]. These physical patterns guide cell orientation and intracellular organization, resulting in highly organized sarcomeres with well-defined striations aligned into long, continuous myofibrils that run the length of the cell. Quantitative analysis demonstrates that the majority of iPSC-CMs cultured on nanopatterned surfaces show sarcomere patterns at specific angles (typically 90° to the NP direction) with elongated nuclei along the NP direction, in contrast to random orientations observed on standard surfaces [54].
The mechanical advantages of nanopatterning include significantly longer sarcomere length and improved localization of key proteins including connexin 43 (Cx43) at cell membranes and enhanced colocalization of α-actinin and cardiac ryanodine receptor (RYR2) [54]. These structural improvements create the foundation for more coordinated contraction and efficient force generation.
Three-Dimensional Tissue Engineering
Three-dimensional culture systems significantly advance maturation beyond what is achievable in two-dimensional formats by better mimicking the physiological environment of the myocardium [55]. These systems allow organized cell-cell and cell-extracellular matrix (ECM) interactions in all three dimensions, processes that are significantly restricted in flat 2D monolayers [55].
Multiple 3D configurations have been developed, each with distinct advantages. Scaffold-free systems like embryoid bodies (EBs) and spheroids are cost-effective and straightforward to generate using standard multiwell platforms, making them suitable for higher-throughput applications like drug screening [55]. Scaffolded systems such as engineered heart tissues (EHTs) provide enhanced cell alignment due to guided tissue organization and enable direct measurement of contractile force, a key functional readout [55].
The incorporation of supporting cell types further enhances maturation in 3D systems. Co-culturing with cardiac fibroblasts (typically in 75:25 CM:fibroblast ratios) improves electrophysiological characteristics, cellular organization, and force generation [55]. More complex co-culture models incorporating smooth muscle and endothelial cells have demonstrated further enhancement of contractile performance and electrophysiological properties, with tri-cellular crosstalk between cardiomyocytes, fibroblasts, and endothelial cells through cAMP signaling driving additional maturation [55].
Table 2: Comparison of 3D Culture Systems for Cardiac Maturation
| System Type | Examples | Advantages | Limitations | Maturation Outcomes |
|---|---|---|---|---|
| Scaffold-Free | Embryoid bodies, Spheroids | Cost-effective, simple generation using standard platforms, suitable for drug screening | Limited structural organization, no direct force measurement | Improved cell-cell interactions, metabolic maturation |
| Scaffold-Based | Engineered Heart Tissues (EHTs), Biowires | Enhanced cell alignment, direct contractile force measurement, better structural organization | Custom fabrication required, more complex setup, lower throughput | Superior sarcomere organization, T-tubule development, force generation |
| Co-Culture Systems | EHTs with fibroblasts, endothelial cells | More physiological cellular composition, enhanced maturation through paracrine signaling | Increased complexity, potential batch-to-batch variability | Improved electrophysiological properties, contractile performance, structural maturity |
Metabolic Maturation Approaches
Metabolic Medium Formulation
Metabolic maturation is essential for generating adult-like iPSC-CMs, as adult cardiomyocytes primarily rely on oxidative phosphorylation for energy production, while immature cells depend more on glycolysis [54]. Strategic medium formulation drives this metabolic shift and supports overall maturation.
Lipid-enriched maturation media typically include fatty acid supplements (such as palmitic, oleic, and linoleic acids) often combined with carnitine to enhance fatty acid oxidation [54]. These compositions force cells to utilize mitochondrial β-oxidation as an energy source, promoting mitochondrial biogenesis and functional maturation. Additionally, increased calcium concentrations (typically 1.8-2.4 mM compared to standard 1.0-1.2 mM) in the medium strongly promote electrophysiological maturation, enhancing calcium handling and contractile function [54].
Hormone supplementation represents another key strategy, with thyroid hormone (T3), cortisol, and insulin-like growth factor (IGF-1) commonly included to mimic the hormonal environment that drives cardiac maturation during postnatal development [54]. These components activate signaling pathways that regulate metabolic gene expression, hypertrophy, and structural organization.
The systematic testing of maturation media components has revealed that metabolic maturation significantly enhances mitochondrial development and function, but has more limited effects on structural organization when applied alone [54]. This underscores the importance of combining metabolic approaches with other maturation strategies.
Mitochondrial Maturation Assessment
Evaluating mitochondrial development provides critical insights into metabolic maturation progress. Key assessment methods include measuring oxygen consumption rates (OCR) to quantify oxidative phosphorylation capacity, imaging mitochondrial network morphology and density, and analyzing expression of mitochondrial genes and proteins [54].
Electron microscopy reveals that metabolically matured iPSC-CMs exhibit mitochondria positioned closer to the contractile apparatus with more developed cristae structures, resembling the organization seen in adult cardiomyocytes [55]. Functional assessments typically show increased basal and maximal respiration rates, enhanced ATP-linked respiration, and greater spare respiratory capacity in metabolically matured cells [54].
Gene expression analyses demonstrate upregulation of critical mitochondrial biogenesis regulators including PPARγ, PPARα, PGC1α, and TFAM in response to metabolic maturation protocols [54]. These transcriptional changes correlate with enhanced fatty acid oxidation capacity and reduced glycolytic dependence, marking the metabolic shift characteristic of adult cardiomyocytes.
Integrated Maturation Platforms and Quantitative Assessment
Combined Maturation Strategies
Emerging evidence strongly supports integrated approaches that combine electrical, mechanical, and metabolic maturation strategies to achieve synergistic effects. A systematic investigation revealed that while nanopatterning primarily promoted structural maturation and elevated calcium concentrations strongly influenced electrophysiological properties, electrical stimulation emerged as the key driver of enhanced mitochondrial development and metabolic maturation [54].
The combination of lipid-enriched maturation medium with high calcium concentration, nanopatterning, and electrical stimulation generated iPSC-CMs with advanced electrophysiological, structural, and metabolic phenotypes [54]. This integrated approach produced cells with more negative resting membrane potential (progressing from -44.1 ± 9.8 mV to -65.6 ± 8.5 mV), increased maximum AP upstroke velocity (from 4.2 ± 1.4 V/s to 11.0 ± 7.4 V/s), and enhanced conduction velocity (from 12.5 ± 5.8 cm/s to 27.8 ± 7.3 cm/s) compared to standard culture conditions [54].
Transcriptome analysis of cells subjected to combined maturation strategies revealed activation of HMCES and TFAM targets contributing to mitochondrial development, while downregulation of MAPK/PI3K and SRF targets was associated with polyploidy, providing mechanistic insights into the maturation process [54]. Critically, this combined approach led to significant changes in drug sensitivity, yielding pharmacological responses that more closely resemble those of adult cardiomyocytes [54].
Diagram 2: Synergistic integration of maturation strategies. The diagram shows how combined electrical, mechanical, and metabolic approaches interact to drive comprehensive maturation, with each strategy contributing primarily to specific maturation domains while supporting others.
Quantitative Maturity Assessment Protocols
Accurately quantifying maturation status remains challenging but essential for comparing protocols across studies. Several computational and molecular approaches have been developed to address this need.
The "entropy score" represents a single-cell RNA sequencing-based metric that quantifies maturation levels of PSC-CMs by analyzing gene expression patterns inspired by Shannon Entropy [57]. This approach requires high-quality single-cell RNA sequencing data with a minimum of 2000 counts per cell depth and involves careful quality control to filter out poor-quality cells, particularly regarding mitochondrial read percentages which vary during maturation [57]. The protocol utilizes customized R code and specific R workspace files available through public repositories to generate reproducible entropy scores that remain consistent for the same developmental stage across datasets [57].
Organ-specific similarity scores provide another quantitative framework. The Web-based Similarity Analytics System (W-SAS) calculates percentage similarity between hPSC-derived cells and human reference tissues using organ-specific gene expression panels (Organ-GEPs) [58]. For cardiac maturation assessment, the Heart-specific Gene Expression Panel (HtGEP) includes 144 genes selected through a multi-step process comparing heart tissue to 42 other tissues in the GTEx database [58]. This system enables researchers to obtain quantitative similarity scores and gene expression pattern information for direct comparison to human heart tissue.
Functional maturity assessment incorporates multiple parameters including contractile force measurement, conduction velocity, action potential characteristics, calcium transient kinetics, and drug responsiveness profiles [56] [54]. Standardized assessment protocols are critical for comparing results across laboratories and establishing benchmarks for mature iPSC-CMs suitable for drug development and disease modeling applications.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for Cardiomyocyte Maturation Studies
| Category | Specific Items | Function/Purpose | Implementation Notes |
|---|---|---|---|
| Electrical Stimulation Systems | Carbon rod electrodes, Platinum wire electrodes, ITO-coated plates, Specialized bioreactors | Delivery of controlled electrical pulses to mimic physiological pacing | Compatibility with 3D constructs critical; Parameter optimization required for each system |
| Engineered Substrates | Nanofabricated surfaces (500-800 nm grooves), 3D scaffold materials (fibrin, collagen, synthetic polymers) | Provide structural cues for cell alignment and tissue organization | Pattern dimensions affect alignment efficiency; Stiffness matching native tissue improves outcomes |
| Metabolic Media Components | Fatty acid supplements (palmitate, oleate, linoleate), L-carnitine, Thyroid hormone (T3), Cortisol | Drive metabolic shift from glycolysis to oxidative phosphorylation | Albumin conjugation often required for fatty acid delivery; Concentration optimization needed |
| 3D Culture Components | Fibrinogen, Thrombin, Collagen I, Matrigel, Customizable synthetic hydrogels | Create 3D extracellular matrix environment for tissue formation | Matrix stiffness significantly impacts maturation; Composition affects contractile function |
| Assessment Tools | Entropy score R package, W-SAS platform, Multi-electrode arrays, Contractile force sensors | Quantitative evaluation of maturation status across multiple parameters | Standardized protocols essential for cross-study comparisons; Multi-parameter assessment recommended |
The strategic integration of electrical, mechanical, and metabolic maturation approaches represents the most promising path forward for generating iPSC-CMs with adult-like characteristics suitable for patient-specific disease modeling and predictive drug screening. While each strategy individually drives specific aspects of maturation, their combination produces synergistic effects that more comprehensively address the immaturity challenge.
Electrical stimulation emerges as particularly powerful for promoting structural and functional maturation, especially when applied to 3D tissue constructs. Mechanical cues through nanopatterning and 3D culture environments provide the structural foundation for organization, while metabolic manipulation drives the essential shift in energy metabolism characteristic of adult cardiomyocytes. The development of quantitative assessment tools like entropy scoring and organ similarity panels enables more standardized evaluation and comparison across protocols and laboratories.
For researchers implementing these strategies, a phased approach is recommended, beginning with establishing robust baseline differentiation protocols before systematically incorporating maturation techniques. The optimal combination and specific parameters will depend on the intended application, with disease modeling potentially requiring different maturity thresholds than drug safety screening. As the field advances, continued refinement of these approaches, along with development of increasingly sophisticated assessment methodologies, will further enhance the utility of patient-specific stem cell models in both basic research and clinical translation.
Overcoming Differentiation Variability and Batch Effects
The promise of patient-specific disease modeling using induced pluripotent stem cells (iPSCs) is fundamentally constrained by two major technical challenges: differentiation variability and batch effects. Differentiation variability refers to the inconsistent ability of iPSC lines to differentiate into specific, functionally mature somatic cell types, even when derived from the same genetic background [59]. Batch effects are non-biological variations introduced by technical differences in laboratory processes, including reagent lots, personnel, and culture conditions, which can confound experimental results and compromise reproducibility [60]. Within the context of a broader thesis on patient-specific disease modeling, overcoming these hurdles is paramount for generating reliable, clinically relevant data for drug discovery and development. This guide details the sources of these challenges and provides actionable, technical strategies to mitigate them.
Understanding the scale and impact of variability is the first step toward its mitigation. The following table summarizes key quantitative findings from recent studies on how differentiation variability and batch effects influence experimental outcomes in iPSC-based research.
Table 1: Quantitative Impact of Differentiation Variability and Batch Effects
| Aspect of Variability | Quantitative Finding | Experimental Context | Source |
|---|---|---|---|
| Optimal Donor Number | Best results with iPSCs from 3-4 unique individuals per group. | Gene expression profiling in Lesch-Nyhan disease model. | [60] |
| Optimal Sublines per Donor | Results improved with 2 lines per individual, without statistical corrections for relatedness. | RNAseq analysis when all lines were produced in parallel using identical methods. | [60] |
| Source of Variance | Most variance in gene expression came from technical factors unrelated to the individual donor. | Controlled study where all iPSC lines were prepared and processed with the same methods. | [60] |
| Senescence Impact | Long-term expansion of primary MSCs resulted in cellular senescence and reduced differentiation capacity by passage five (P5). | Comparison of primary MSCs and iPSC-derived MSCs (iMSCs) in xeno-free medium. | [59] |
| Batch Variability | iMSCs exhibited batch-to-batch variability in differentiation and extracellular vesicle (EV) biological properties. | Generation of three iMSC batches (SD1, SD2, SD3) from a single iPSC line. | [59] |
Core Experimental Protocols for Mitigation
Implementing robust and standardized protocols is critical for minimizing technical noise. Below are detailed methodologies for key experimental procedures cited in the context of reducing variability.
Protocol for iPSC Generation and Quality Control
This protocol, derived from a controlled study on Lesch-Nyhan disease, ensures the generation of high-quality, consistent iPSC lines [60].
- Reprogramming Method: Reprogram cultured fibroblasts using a microRNA/mRNA method (e.g., Stemgent) to avoid insertional mutagenesis or enduring effects of viral vectors.
- Quality Control Measures:
- Karyotyping: A minimum of 20 metaphase cells at a minimum of 400 band resolution to confirm the absence of relevant abnormalities.
- Pluripotency Validation:
- Immunostaining: Assess expression of pluripotency markers (SSEA3, SSEA4, TRA1-60, TRA1-81, NANOG).
- Trilineage Differentiation: Differentiate each line into the three major germ cell layers using a commercial kit (e.g., STEMdiff Trilineage Differentiation Kit). Validate with immunostaining for ectoderm (PAX6, NESTIN), endoderm (SOX17, FOXA2), and mesoderm (brachyury, NCAM) markers.
- Gene Expression: Profile pluripotency genes via RNA sequencing (RNAseq).
- Genetic Validation: Confirm the starting genetic variant (e.g., HPRT1 mutation for LND) by RT-PCR and visualize in RNAseq read alignments using the Integrative Genomics Viewer (IGV).
- Functional Assays: Confirm disease-relevant functional deficits, such as enzymatic activity (e.g., HGprt activity via a radiometric assay).
Protocol for Generating iMSCs from iPSCs
This protocol for deriving mesenchymal stromal cells from iPSCs highlights strategies to manage batch-to-batch variability [59].
- Mesoderm Induction: Plate and maintain an iPSC line (e.g., ChiPS 22) in DEF-CS medium for 2 days. Switch to a specialized mesoderm induction medium (e.g., STEMdiff mesoderm induction medium) with daily medium changes for 4 days.
- MSC Specification and Expansion:
- Switch culture medium to a xeno-free MSC medium (e.g., Alpha-MEM-GlutaMAX supplemented with a xeno-free supplement like Purstem XFS).
- Maintain culture for 2 days, then re-plate onto fibronectin-coated cell culture plastic in the MSC medium.
- After 2-3 subsequent passages, the cells will attain a fibroblastic-like appearance and no longer require fibronectin coating.
- Batch Characterization: At passage 4-5, rigorously characterize each batch of iMSCs (e.g., SD1, SD2, SD3).
- Surface Marker Analysis: Use flow cytometry with an MSC phenotyping cocktail (e.g., from Miltenyi Biosciences) to confirm typical marker expression.
- Trilineage Differentiation: Test adipogenic, osteogenic, and chondrogenic differentiation potential.
- Senescence Assay: Perform senescence-associated β-galactosidase staining at various passages (e.g., P8, P12, P16) to monitor replicative senescence.
Protocol for Bulk RNA Sequencing to Minimize Batch Effects
Standardizing transcriptomic analysis is vital for reproducible data interpretation [60].
- Sample Preparation: All samples must be grown and collected by the same individual using identical methods.
- Library Preparation and Sequencing:
- Process all samples for bulk RNAseq in a single batch to mitigate technical batch effects.
- Sequence to a depth of at least 50 million paired-end, 100bp reads.
- Use a standardized RNA extraction kit and library preparation kit across all samples.
- Quality Control:
- Assess raw read quality using FastQC.
- Verify that read counts and quality metrics are consistent across all samples and subgroups.
Visualizing the Strategic Workflow for Mitigation
The following diagram illustrates a comprehensive, integrated workflow that combines experimental and computational strategies to overcome differentiation variability and batch effects.
The Scientist's Toolkit: Essential Research Reagents
Successfully navigating the challenges of iPSC-based modeling requires a carefully selected set of tools and reagents. The following table details key solutions used in the featured studies.
Table 2: Key Research Reagent Solutions for iPSC-Based Disease Modeling
| Reagent / Kit | Function | Application Context | Source |
|---|---|---|---|
| microRNA/mRNA Reprogramming Kit (e.g., Stemgent) | Non-viral, non-integrating reprogramming of somatic cells to iPSCs. | Mitigates risks of insertional mutagenesis; generates footprint-free iPSCs. | [60] |
| STEMdiff Trilineage Differentiation Kit | Directed differentiation of iPSCs into ectoderm, mesoderm, and endoderm lineages. | Standardized validation of pluripotency for quality control of all iPSC lines. | [60] |
| Xeno-Free Supplement (XFS) (e.g., Purstem) | Chemically defined, animal-free supplement for cell culture media. | Redines batch-to-batch variability from serum; enhances anti-inflammatory properties of MSCs/iMSCs. | [59] |
| STEMdiff Mesoderm Induction Medium | Directs differentiation of iPSCs toward mesodermal lineage. | Critical first step in generating iPSC-derived mesenchymal stromal cells (iMSCs). | [59] |
| CRISPR-Cas9 Genome Editing System | Precise genetic engineering to introduce or correct mutations. | Generation of isogenic control lines, which are genetically identical except for the disease-causing mutation. | [61] |
| MSC Phenotyping Cocktail Kit | Antibody panel for flow cytometry analysis of MSC surface markers. | Phenotypic characterization and validation of iMSC batches to ensure identity and purity. | [59] |
| Senescence β-Galactosidase Staining Kit | Histochemical detection of β-galactosidase activity at pH 6.0, a marker of senescent cells. | Monitoring cellular senescence during long-term expansion of MSCs and iMSCs. | [59] |
The journey toward reliable and predictive patient-specific disease models is paved with the challenges of biological and technical variability. However, as outlined in this guide, a multi-pronged strategy that combines rigorous experimental design—including the use of multiple donors, isogenic controls, and standardized protocols—with advanced computational analytics provides a robust framework for overcoming these hurdles. By systematically implementing these practices, researchers can significantly enhance the fidelity of their iPSC models, thereby accelerating the discovery of novel therapeutic targets and the development of personalized medicines.
Standardization and Quality Control in iPSC Culture and Differentiation
The application of induced pluripotent stem cells (iPSCs) in patient-specific disease modeling and therapeutic development represents a cornerstone of modern regenerative medicine. The transition of iPSC technology from basic research to clinical applications hinges on the implementation of robust standardization and rigorous quality control measures throughout the culture and differentiation pipeline. This technical guide provides a comprehensive framework for establishing standardized methodologies essential for ensuring the safety, reproducibility, and efficacy of iPSC-based models and therapies, with particular emphasis on their application in disease modeling research.
Table 1: Key Challenges in iPSC Standardization for Disease Modeling
| Challenge Area | Specific Issues | Impact on Disease Modeling |
|---|---|---|
| Process Variability | Inconsistent differentiation protocols between laboratories [9] | Limits reproducibility and cross-study comparisons |
| Product Characterization | Lack of harmonized quality standards and potency assays [9] [62] | Compromises therapeutic safety and functional validation |
| Manufacturing Scalability | Labor-intensive workflows difficult to scale [9] | Restricts patient-specific model generation for large cohorts |
| Genomic Integrity | Instability during prolonged culture/reprogramming [9] | Affects model reliability and therapeutic safety |
| Maturation State | Fetal-like gene expression profiles in derived cells [9] | May not fully recapitulate late-onset disease phenotypes |
Core Principles of iPSC Culture Standardization
Defined Culture Systems and Reagents
Standardization begins with implementing defined culture systems that eliminate variability from undefined components. Current best practices utilize xeno-free materials and chemically defined media to ensure reproducibility and regulatory compliance [63]. The integration of small molecule cocktails such as CEPT (combination of Chroman 1, Emricasan, Polyamine supplement, and trans-ISRIB) has demonstrated significant improvement in iPSC survival and genomic stability, particularly during critical phases like single-cell passaging and freezing [64].
Automated Monitoring and Quality Control
Advanced process analytical technologies are emerging as essential tools for non-invasive, quantitative monitoring of iPSC cultures. AI-driven imaging pipelines can segment and track tens of thousands of individual iPSCs and their progeny over multiple divisions, providing unprecedented resolution into pluripotency stability and differentiation propensity [65]. These systems achieve high accuracy (F1 score ≈0.96) in identifying pluripotent nuclei in phase contrast images, enabling real-time assessment of culture quality without manual intervention [65].
Table 2: Quantitative Metrics for iPSC Quality Control
| Quality Parameter | Measurement Technology | Acceptance Criteria | Reference |
|---|---|---|---|
| Pluripotency Marker Expression | Immunofluorescence, Flow Cytometry | >95% positive for OCT4, SOX2, NANOG | [64] |
| Viability Post-Thaw | Trypan Blue Exclusion | >80% viability | [64] |
| Cell Morphology | AI-Based Image Analysis | F1 score ≈0.96 for pluripotent nuclei | [65] |
| Mitosis Rate | Time-Lapse Tracking | Line-specific baseline established | [65] |
| Karyotypic Normalcy | G-Banding, SNP Analysis | No detectable abnormalities | [9] |
| Lineage Differentiation Potential | Embryoid Body Formation | Tri-lineage differentiation confirmed | [66] |
Standardized Culture Protocols
Matrix Coating and Passaging Procedures
A standardized Matrigel coating protocol is fundamental for reproducible iPSC culture. The recommended approach involves thawing frozen stock at 4°C overnight, diluting 1:1 with cold DMEM to create stock solutions, then further diluting 1:35 with cold DMEM to prepare working stock solution [64]. Coated vessels should be incubated for at least 1 hour at 37°C before use, with the following volumes recommended:
- 6-well plate: 1 mL per well
- 12-well plate: 500 µL per well
- 24-well plate: 250 µL per well
- 96-well plate: 50 µL per well [64]
For passaging, two primary methods are recommended based on application needs. Accutase is preferred for generating single-cell suspensions when counting cells or collecting pellets for molecular analyses, while ReLeSR is recommended for standard passaging as it reduces the need for physical removal of differentiated cells [64]. For both methods, washing iPSCs with DPBS to completely remove medium before adding dissociative reagent is critical to avoid interference with enzymatic activity.
Feeding Schedule and Environmental Optimization
A consistent feeding schedule is vital for maintaining pluripotency and preventing spontaneous differentiation. The recommended protocol involves feeding with specialized medium (e.g., iPS-Brew) every other day with "double feeding" (1.5x volume) on Fridays to avoid weekend feeding [64]. Critical parameters include:
- Medium change after 24-48 hours post-passaging to remove CEPT/polyamines
- Passage ratios of 1:20 to 1:40 when using advanced media formulations
- Vigorous plate shaking (3 times up/down, 3 times left/right) to ensure even cell distribution [64]
Quality Control in Differentiation Protocols
Monitoring Differentiation Efficiency and Purity
Robust differentiation protocols require comprehensive characterization of resulting cell populations to ensure faithful representation of target lineages. In disease modeling, particularly for neurological disorders like leukodystrophies, iPSC-derived microglia have demonstrated lineage-specific gene expression profiles and functional responses to diverse inflammatory stimuli [66] [67]. Transcriptome profiling reveals selective upregulation of microglial signature genes and enrichment of microglia/macrophage-related gene sets, providing validation of differentiation efficiency [67].
Functional Validation of Differentiated Cells
Functional assessment is crucial for confirming the physiological relevance of iPSC-derived models. For microglial models, this includes evaluating responses to specific inflammogens through cytokine secretion profiling, NFκB and JAK-STAT signaling pathway activation, and the capacity for intercellular signaling such as microglia-astrocyte crosstalk [67]. These functional assays provide critical validation of disease models beyond mere marker expression.
Scaling and Manufacturing Considerations
Bioreactor Systems for Scalable Production
The transition to large-scale production requires specialized bioreactor systems capable of maintaining cell quality while achieving necessary yields. Recent advances in single-use bioreactor technology have demonstrated expansion of hiPSCs under serum-free conditions, with the Xpansion 10 multiplate and Ascent 1 m² fixed-bed bioreactors producing nearly 5 × 10⁹ viable cells within 5 days while maintaining pluripotency and differentiation potential [68]. These systems operate within defined parameters that limit wall shear stress to ≤8.2 × 10⁻⁵ N cm⁻² to prevent impairment of cell quality [68].
Automation and Artificial Intelligence
Automated production platforms and AI-driven monitoring are becoming increasingly critical for standardization at scale. Modern facilities incorporate machine learning technologies to optimize production protocols, predict cell behavior, and improve quality control processes [69]. These systems enable predictive maintenance, process optimization, and automated decision-making that enhance production efficiency while reducing variability in iPSC generation and differentiation [69] [65].
Table 3: Scalable Bioreactor Parameters for iPSC Expansion
| Bioreactor Parameter | Xpansion 10 Multiplate | Ascent 1 m² Fixed-Bed | Impact on Cell Quality |
|---|---|---|---|
| Max Wall Shear Stress | ≤8.2 × 10⁻⁵ N cm⁻² | ≤8.2 × 10⁻⁵ N cm⁻² | Preserves viability & pluripotency [68] |
| Expansion Factor | Up to 35-fold | Up to 35-fold | Achieved within 5 days [68] |
| Viable Cell Yield | ~5 × 10⁹ cells | ~5 × 10⁹ cells | Maintains differentiation potential [68] |
| Oxygen Transfer | Optimized kLa | Optimized kLa | Prevents hypoxic stress [68] |
| Mixing Time | Characterized θM | Characterized θM | Ensures homogeneity [68] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Research Reagent Solutions for Standardized iPSC Culture
| Reagent Category | Specific Examples | Function in iPSC Workflow | Application Notes |
|---|---|---|---|
| Culture Medium | StemMACS iPS-Brew XF [64] | Defined, xeno-free maintenance medium | Supports pluripotency; used with CEPT |
| Extracellular Matrix | Corning Matrigel hESC-Qualified [64] [67] | Substrate for adherent culture | Quality-controlled for pluripotent cells |
| Dissociation Reagents | Accutase [64]; ReLeSR [64] | Cell passaging | Accutase for single cells; ReLeSR for clusters |
| Cryopreservation Medium | MFreSR [64] | Cell freezing | Serum-free formulation |
| Small Molecule Cocktails | CEPT [64] | Enhanced cell survival | Reduces apoptosis in single-cell culture |
| Reprogramming Factors | Yamanaka factors (Oct3/4, Sox2, Klf4, c-Myc) [66] | iPSC generation | Delivered via Sendai virus, mRNA, etc. |
| Characterization Kits | Zymo Quick-RNA Microprep [64]; Alkaline phosphatase live staining [63] | Quality assessment | Molecular analysis & pluripotency verification |
The establishment of comprehensive standardization frameworks and rigorous quality control systems is fundamentally required for advancing iPSC-based disease modeling and therapeutic development. Through implementation of defined culture systems, automated monitoring technologies, scalable manufacturing processes, and robust characterization assays, researchers can significantly enhance the reproducibility, reliability, and translational potential of patient-specific iPSC models. As the field progresses toward clinical applications, continued refinement of these standards will be essential for realizing the full potential of iPSC technology in personalized medicine and drug development.
The field of patient-specific disease modeling using stem cells is undergoing a profound transformation, driven by the integration of advanced bioreactor technologies and sophisticated automation systems. The ability to generate induced pluripotent stem cells (iPSCs) from adult somatic cells has provided unprecedented access to patient-specific pluripotent cell sources capable of differentiating into virtually any cell type [9]. However, a significant challenge persists: translating this potential into robust, standardized, and scalable processes capable of supporting high-throughput screening (HTS) for drug discovery and disease modeling [9] [10].
Traditional two-dimensional cell culture systems and manual handling techniques are inadequate for producing the quantities of cells required for large-scale screening campaigns while maintaining consistency and physiological relevance. These limitations become particularly critical when working with complex three-dimensional structures like organoids, which better recapitulate tissue architecture and function but demand precise, controlled culture conditions [9]. The translational gap between conventional research models and human clinical trials remains stark, with a significant proportion of drug candidates failing due to unpredicted toxicities or inefficacies [9].
This technical guide examines how modern high-throughput micro-bioreactors and automated workflows are addressing these challenges. By enabling the parallel culture of hundreds of standardized, miniature bioreactor systems, these technologies provide the necessary scalability and data richness to advance stem cell-based disease models from foundational research to practical drug development tools. The integration of artificial intelligence (AI) and machine learning with these automated systems further enhances their predictive power, creating a closed-loop environment for optimizing culture parameters and accelerating discovery timelines [70] [71].
High-Throughput Bioreactor Technologies for Stem Cell Expansion
Fundamental Design Principles and Operational Characteristics
High-throughput micro-bioreactors are small-scale bioreactors specifically engineered for rapid, parallel experimentation, typically ranging from microliter volumes to 100 mL [72]. Their core advantage lies in enabling high-volume screening of cell cultures under varied conditions, drastically reducing time and resource consumption compared to traditional flask-based culture systems. These systems are designed with several key principles in mind: creating homogeneous culture conditions through precise mixing and aeration, maintaining critical process parameters like temperature and pH within narrow ranges, and enabling real-time monitoring of cell growth and metabolism [72] [73].
These miniature bioreactors serve as a crucial bridge between laboratory research and full-scale production, providing critical insights with minimal resource expenditure. By testing dozens or even hundreds of conditions simultaneously, researchers can optimize variables such as nutrient formulations, pH levels, or temperature settings across multiple bioreactors in a single run [72]. The data generated helps identify optimal conditions for producing specific cell types or tissue structures from stem cells, ultimately enhancing the efficiency and predictive power of disease modeling efforts.
Advanced Bioreactor Systems for Stem Cell Applications
Recent technological advances have yielded specialized bioreactor systems specifically designed to address the unique requirements of stem cell culture, particularly for iPSCs and their derivatives.
Table 1: Advanced Bioreactor Systems for Stem Cell Applications
| System Name/Type | Key Features | Stem Cell Application | Scalability | Reference |
|---|---|---|---|---|
| SUSI Bioreactor (Fraunhofer) | Dynamic incubator; Impeller for mixing/aeration; Real-time sensor monitoring; Automated fluid management | Long-term hiPSC culture (up to 3 months maintained differentiation potential) | Glass vessel scalable with consistent design | [73] |
| SwRI 3D-Printed Bioreactor | 3D-printed matrix; Larger surface-to-volume ratio; Automated perfusion method; Prevents cell clustering | iPSC replication; Differentiation into neural progenitors | Larger surface area vs. traditional 2D culture | [74] |
| MO:BOT Platform (mo:re) | Fully automated 3D cell culture; Automated seeding, media exchange, quality control | Standardized organoid production for screening | Scales from 6-well to 96-well formats (12x more data) | [71] |
| High-Throughput Micro-Bioreactors (Commercial Systems) | Parallel experimentation; 10 mL to 100 mL capacity; Integrated automation and data collection | Bioprocess optimization; Scale-down models | Bridge between lab research and production | [72] |
The Fraunhofer SUSI bioreactor exemplifies the integrated approach required for robust stem cell culture. Its impeller system performs the crucial tasks of mixing, aeration, and heat and mass transfer inside the glass vessel to create homogeneous conditions within the cell suspension, enabling reproducible cell propagation [73]. Researchers successfully maintained cells in the prototype for three months without reducing their differentiation potential, demonstrating the system's capability for long-term culture needs in chronic disease modeling [73].
Similarly, the Southwest Research Institute's (SwRI) 3D-printed bioreactor addresses a critical challenge in iPSC culture—the risk of spontaneous differentiation. The bioreactor's matrix boasts a larger surface-to-volume ratio compared to traditional 2D cell culture devices and can grow more cells using an automated perfusion method [74]. Due to the exceptional geometry of SwRI's bioreactor, cells maintain a monolayer without forming clusters during the cultivation process, minimizing the risk of differentiation into unwanted cell types [74].
Automated Workflows and Integration Strategies
Laboratory Automation Systems for High-Throughput Screening
The full potential of high-throughput bioreactors can only be realized when they are integrated within comprehensive automated workflows. These systems address significant bottlenecks in stem cell research by reducing labor-intensive methods and minimizing human variability across a wide range of analytical platforms [75] [76].
Modern laboratory automation for clone screening and cell culture encompasses everything from individual automated instruments to fully integrated robotic systems. The current market offers solutions ranging from simple, accessible benchtop systems to large, unattended multi-robot workflows [71]. This flexibility allows facilities to implement automation that matches their specific throughput requirements and available infrastructure.
A key development in this space is the focus on ergonomics and usability. Companies like Eppendorf have designed automated pipetting systems with features such as lighter frames, shorter travel distances, and larger plungers to distribute pressure, all informed by extensive surveys of working scientists [71]. These human-centered design principles encourage adoption and reduce strain during operation, which is particularly important for lengthy protocols common in stem cell work.
Strategic Implementation and Specialized Applications
The implementation of high-throughput experimentation at organizations like AstraZeneca provides a compelling case study in the strategic deployment of automation. Over a 20-year journey, they established five key goals: delivering high-quality reactions, screening twenty catalytic reactions per week within three years, developing a catalyst library, achieving comprehensive reaction understanding rather than just "hits," and employing principal component analysis to accelerate reaction mechanism knowledge [76].
This systematic approach highlights the importance of clear objectives when implementing automated systems. Their experience also underscores the value of specialized equipment for specific tasks. For instance, they utilized CHRONECT XPR workstations for automated powder dosing, capable of handling a wide range of solids including transition metal complexes and organic starting materials [76]. The system demonstrated less than 10% deviation from target mass at low masses (sub-mg to low single-mg) and less than 1% deviation at higher masses (>50 mg), while significantly reducing weighing time compared to manual operations [76].
For stem cell research specifically, companies like SPT Labtech have developed integrated platforms that combine pipetting, dispensing, mixing, and thermocycling within single compact units designed to simplify complex genomic workflows [71]. Such specialized systems are increasingly important for handling the sophisticated protocols required for organoid culture and genetic analysis of stem cell derivatives.
Experimental Protocols for Automated Stem Cell Culture
Automated Expansion of Induced Pluripotent Stem Cells
Protocol Objective: To achieve automated, large-scale expansion of induced pluripotent stem cells (iPSCs) in a 3D bioreactor system while maintaining pluripotency and minimizing spontaneous differentiation.
Materials and Equipment:
- SwRI-developed 3D-printed bioreactor or equivalent system [74]
- Completely defined, xeno-free iPSC culture medium
- Matrigel or equivalent extracellular matrix coating (for initial cell establishment)
- Single-use bioreactor vessels (if using disposable system)
- Automated perfusion system with integrated pH and dissolved oxygen sensors
- In-line microscope for automated cell monitoring [73]
Methodology:
- Bioreactor Preparation: Sterilize the bioreactor system according to manufacturer specifications. For reusable systems, validate sterility through microbial culture tests. Coat the bioreactor surface with extracellular matrix if required for initial cell attachment.
- Cell Inoculation: Harvest iPSCs from conventional 2D culture using standard enzymatic dissociation. Determine cell viability and concentration using automated cell counters. Inoculate the bioreactor at a density of 1-2 × 10^5 cells/mL in complete culture medium.
- Parameter Establishment: Set initial culture parameters to 37°C, 5% CO2, and 85-95% humidity. Establish impeller agitation rate at 50-60 rpm to maintain homogeneous suspension while minimizing shear stress on cells [73].
- Automated Perfusion: Initiate automated perfusion system once cell density reaches 5 × 10^5 cells/mL. Set medium exchange rate to 50-75% of vessel volume daily, adjusting based on glucose consumption rates.
- Monitoring and Sampling: Program in-line microscope for automated imaging every 6-8 hours to monitor cell morphology and detect early signs of differentiation or excessive aggregation [73]. Collect 1-2 mL samples daily for offline analysis of cell count, viability, and pluripotency markers.
- Harvesting: When cells reach target density (typically 1-2 × 10^6 cells/mL), initiate automated harvesting sequence. For the SwRI system, this involves stopping agitation, allowing cells to settle, and automatically transferring cell suspension to collection vessels [74].
Quality Control Measures:
- Daily monitoring of key pluripotency markers (OCT4, SOX2, NANOG) via flow cytometry of sampled cells
- Regular karyotype analysis to ensure genetic stability
- Endpoint differentiation potential assessment through spontaneous differentiation into all three germ layers
High-Throughput Screening of Disease-Specific Organoids
Protocol Objective: To implement an automated workflow for production, maintenance, and screening of patient-specific stem cell-derived organoids in multi-well micro-bioreactor formats.
Materials and Equipment:
- MO:BOT platform or equivalent automated 3D culture system [71]
- 96-well micro-bioreactor array plates
- Defined organoid differentiation media
- Automated liquid handling system with 96-channel head
- High-content imaging system
- Patient-specific iPSCs with disease-relevant mutations
Methodology:
- Organoid Initiation:
- Program automated system to plate single-cell suspension of iPSCs in 96-well ultra-low attachment plates at 5,000-10,000 cells per well in 100μL of organoid initiation medium.
- Centrifuge plates at 300 × g for 2 minutes to encourage aggregate formation.
- Transfer plates to automated culture system maintaining 37°C and 5% CO2.
Automated Differentiation and Maintenance:
- Schedule media exchanges according to differentiation protocol (typically every 2-3 days) using automated liquid handling system.
- For multi-lineage organoids, program medium composition changes according to established differentiation timelines.
- Implement automated quality control checks using integrated imaging to identify and exclude wells with aberrant organoid formation [71].
Compound Screening:
- At organoid maturity (protocol-dependent, typically 21-35 days), program automated drug addition using pre-diluted compound libraries in 96-well format.
- Include appropriate controls (vehicle-only and reference compounds) in each screening plate.
- Set up staggered screening schedules to accommodate time-point analyses.
Endpoint Analysis:
- Fix a subset of organoids automatically at predetermined time points using integrated fixation protocols.
- Program automated immunostaining procedures for relevant markers of disease pathology.
- Acquire high-content imaging data using automated microscopy.
- Implement automated image analysis algorithms to quantify morphological features, cell viability, and marker expression.
Troubleshooting Notes:
- For organoid cultures showing excessive size variation, implement automated size-based selection during media exchanges.
- When using polarized epithelial organoids, establish automated transepithelial electrical resistance (TEER) measurements if applicable.
- For nutrient-sensitive organoids, implement automated glucose/lactate monitoring to adjust feeding schedules.
Data Management, AI Integration, and Analytical Frameworks
Computational Infrastructure for High-Throughput Screening Data
The implementation of high-throughput screening technologies generates massive, multi-modal datasets that require sophisticated management and analytical approaches. As noted by experts at the ELRIG Drug Discovery 2025 conference, "If AI is to mean anything, we need to capture more than results. Every condition and state must be recorded, so models have quality data to learn from" [71].
Effective data management begins with comprehensive metadata capture, including detailed information about cell line origins, culture conditions, experimental parameters, and analytical measurements. Companies like Cenevo have developed integrated platforms that unite sample management software with digital R&D tools to help laboratories connect their data, instruments, and processes [71]. This approach enables AI to be applied to meaningful, well-structured information rather than fragmented data silos.
The application of artificial intelligence in stem cell-based screening takes multiple forms. Foundation models are now being applied to extract features from imaging data, using large-scale AI models trained on thousands of histopathology and multiplex imaging slides to identify new biomarkers and link them to clinical outcomes [71]. Simultaneously, AI and machine learning are being used to optimize bioprocess parameters in micro-bioreactors, enabling predictive modeling and adaptive control strategies that enhance yield and productivity [70].
Visualization of Integrated Workflow
The following diagram illustrates the comprehensive integration of bioreactor systems, automation, and data management in a high-throughput stem cell screening workflow:
This integrated workflow demonstrates how automation creates a virtuous cycle of improvement, where data from each experimental phase informs and optimizes earlier stages through AI-driven analysis.
Essential Research Reagent Solutions
Successful implementation of high-throughput screening for stem cell-based disease modeling requires carefully selected reagents and materials designed for compatibility with automated systems.
Table 2: Essential Research Reagent Solutions for Automated Stem Cell Screening
| Reagent/Material | Function | Automation-Compatible Features | Application Notes |
|---|---|---|---|
| Chemically Defined Media | Cell nutrition and maintenance | Pre-mixed liquid formulations; Stable at room temperature; Standardized compositions | Essential for reproducibility; Reduces batch variations [9] |
| Vitro-Gel Hydrogel | 3D scaffold for organoid culture | Pre-defined mechanical properties; Temperature-responsive gelling | Supports automated dispensing in liquid state at 4°C [71] |
| Extracellular Matrix Proteins | Surface coating for cell attachment | Ready-to-use solutions; Consistent protein concentrations | Enables standardized coating protocols across plates |
| Cryopreservation Media | Long-term cell storage | Formulated for automated freezing protocols; High post-thaw viability | Critical for biobanking patient-specific lines |
| Cell Dissociation Reagents | Harvesting cells from bioreactors | Enzymatic activity optimized for automation timing; Neutralization not required | Maintains high cell viability for subsequent seeding |
| Viability Assay Kits | Assessment of cell health | Homogeneous format (add-mix-measure); Compatible with HTS readers | Enables automated screening readouts |
| Genome Editing Tools | Introduction of disease mutations | Pre-complexed ribonucleoproteins; High efficiency | CRISPR/Cas9 for isogenic control lines [9] |
Implementation Challenges and Future Directions
Addressing Current Limitations in High-Throughput Stem Cell Culture
Despite significant advances, several challenges persist in the full implementation of high-throughput screening for stem cell-based disease modeling. A primary concern is the maintenance of developmental maturity in stem cell-derived cultures. These systems frequently display fetal-like gene expression profiles, electrophysiological activity, or metabolic states, which may limit their ability to accurately model late-onset degenerative conditions [9]. Addressing this limitation requires the development of advanced maturation strategies, such as prolonged culture, biomechanical stimulation, vascularization, and co-culture with supporting cell types that more closely approximate the adult in vivo environment.
Standardization remains another significant hurdle. The lack of uniform differentiation protocols across laboratories leads to inconsistent results and limits reproducibility [9]. Recent benchmarking efforts using high-dimensional molecular profiling have highlighted the extent of this variability and underscored the need for harmonized quality standards across laboratories [9]. Initiatives like the Consortium on Advanced Stem Cell-Based Models in Drug Discovery and Development are working to establish robust, transparent, and reproducible validation frameworks for stem cell-based models used in biomedical research and drug development [10].
From a technical perspective, the high initial investment costs for automated bioreactor systems can be prohibitive for some organizations [77]. Additionally, the operation and maintenance of these sophisticated systems require specialized technical expertise, creating workforce training needs [77]. The large volumes of data generated by high-throughput systems also present challenges in management, analysis, and interpretation, necessitating investments in bioinformatics infrastructure and personnel [77].
Emerging Trends and Future Developments
The field of high-throughput screening for stem cell research is rapidly evolving, with several promising trends shaping its future trajectory. The integration of artificial intelligence and machine learning for process optimization is accelerating, enabling predictive modeling of culture outcomes and adaptive control of bioreactor parameters [70] [71]. As expressed by experts at ELRIG Drug Discovery 2025, transparency in AI workflows is becoming increasingly important, with completely open processes using trusted and tested tools so clients can verify exactly what goes in and what comes out [71].
The development of more sophisticated multi-tissue systems represents another frontier. While current organoid models excel at representing individual tissues, the emergence of assembloid technology—complex systems that combine multiple organoid types or tissue lineages—allows for the modeling of inter-organ interactions, such as brain-muscle or brain-vascular connectivity [9]. These advanced models will likely require corresponding innovations in bioreactor design to support the co-culture of multiple tissue types with distinct environmental requirements.
Finally, the push toward continuous manufacturing in biopharmaceutical production is influencing stem cell culture systems [77]. The adoption of continuous processing approaches for cell production could significantly enhance efficiency and reduce costs associated with patient-specific disease modeling. This transition will likely be facilitated by further advancements in automated monitoring and control systems capable of maintaining culture stability over extended periods.
As these technologies mature and converge, they promise to transform patient-specific stem cell models from research tools into robust, reproducible platforms for drug discovery and personalized medicine, ultimately bridging the translational gap between preclinical research and clinical application.
Mitigating Tumorigenic Risk and Ensuring Genomic Stability
The application of human induced pluripotent stem cells (iPSCs) in patient-specific disease modeling represents a transformative approach for understanding disease mechanisms and accelerating drug discovery. These cells, generated by reprogramming adult somatic cells back to a pluripotent state, carry the patient's complete genetic background and can be differentiated into virtually any cell type [78] [17]. This technology enables researchers to create patient-specific in vitro models of neurodegenerative disorders, cardiac conditions, and other diseases using neurons, cardiomyocytes, and other clinically relevant cell types derived from iPSCs [78]. The field has advanced significantly through automated stem-cell production and the creation of large-scale biobanks, such as the NYSCF Array, which provide standardized, patient-derived iPSC lines for research communities [78].
Despite their considerable promise, the clinical application of iPSC-based models faces a significant hurdle: tumorigenic risk. This risk manifests primarily through three mechanisms: (1) the inherent potential of residual undifferentiated pluripotent cells to form teratomas; (2) the oncogenic potential of reprogramming factors themselves, particularly c-MYC and KLF4; and (3) the acquisition of genomic instability during reprogramming and long-term culture [79]. The core transcription factors used for reprogramming—OCT4, SOX2, KLF4, and c-MYC (OSKM)—are not only essential for establishing pluripotency but are also frequently overexpressed in human cancers [79]. Furthermore, the suppression of tumor suppressor pathways, such as p53, to enhance reprogramming efficiency simultaneously increases tumorigenicity, creating a fundamental safety challenge for therapeutic applications [79]. This technical guide provides a comprehensive framework for identifying, quantifying, and mitigating these risks to ensure genomic stability in stem cell-based disease models.
Understanding Mechanisms of Genomic Instability
Genomic instability in iPSCs arises from multiple sources, ranging from initial reprogramming stress to long-term culture adaptations. Understanding these sources is crucial for developing effective mitigation strategies.
Reprogramming Stress: The process of epigenetic reprogramming creates significant cellular stress, potentially leading to DNA damage accumulation and chromosomal aberrations [79]. This stress can activate DNA damage response pathways, and cells with compromised p53 function may bypass apoptosis, allowing propagation of damaged DNA.
Oncogenic Reprogramming Factors: The forced expression of reprogramming factors, particularly c-MYC, can directly promote genomic instability. c-MYC is a known oncogene constitutively expressed in over 70% of human cancers and can activate MYC-dependent cancer enhancers that drive genetic mutations [79].
Culture-Induced Instabilities: Long-term in vitro culture can lead to the selection of genetically abnormal subpopulations. Accumulation of DNA lesions—estimated at up to 70,000 per cell per day from spontaneous and environmental sources—can overwhelm repair mechanisms, leading to mutations that provide growth advantages in culture conditions [80].
Protein Mislocalization: Overexpression and mislocalization of key proteins can disrupt chromosomal segregation. For example, overexpression of CENP-A, a protein essential for chromosomal stability, leads to its mislocalization to non-centromeric regions, resulting in uneven chromosome distribution during cell division [81]. Recent research has identified that the absence of DNAJC9, a protein involved in proper histone H3 and H4 folding, facilitates this CENP-A mislocalization, potentially through compromised chromatin assembly [81].
Shared Pathways of Genomic Instability in Aging and Cancer
Genomic instability serves as a connecting pathway between aging, cancer, and stem cell biology. Both aging and cancer involve the accumulation of DNA damage, but with different outcomes: functional decline in aging versus clonal expansion in cancer [82]. In iPSC systems, similar mechanisms can drive cells toward tumorigenic states.
Table 1: Comparative Analysis of Genomic Instability in Aging, Cancer, and iPSC Models
| Aspect | Aging | Cancer | iPSC Models |
|---|---|---|---|
| Primary Outcome | Functional decline, cellular senescence | Uncontrolled proliferation, malignant formation | Teratoma formation, malignant transformation |
| DNA Damage Response | Attenuated repair, accumulation of damage | Dysregulated repair, evasion of checkpoints | Variable depending on p53 status, culture stress |
| Telomere Dynamics | Progressive shortening | Reactivation of telomerase | Reprogramming resets telomere length |
| Epigenetic Alterations | Drift and accumulation of errors | Global reprogramming | Extensive remodeling during reprogramming |
| Oxidative Stress | Increased ROS, mitochondrial dysfunction | Metabolic reprogramming, ROS signaling | Culture-induced oxidative stress |
The diagram below illustrates the core pathway through which genomic instability can lead to tumorigenic outcomes in stem cell models, highlighting key risk points and cellular decision nodes.
Quantitative Assessment of Genomic Stability
Rigorous assessment of genomic stability is essential for validating iPSC lines destined for disease modeling and therapeutic development. The following methodologies provide comprehensive evaluation of genomic integrity.
Biomarkers and Assays for Genomic Instability
Table 2: Analytical Methods for Assessing Genomic Stability in iPSCs
| Method Category | Specific Assay | Measured Parameters | Tumorigenic Risk Indicator |
|---|---|---|---|
| Karyotyping | G-banding karyotype | Chromosomal number, large structural variations | Aneuploidy, translocations |
| Molecular Cytogenetics | FISH, SKY, aCGH | Submicroscopic deletions/duplications | Copy number variations (CNVs) |
| DNA Damage Focus Assay | γH2AX/53BP1 immunofluorescence | DNA double-strand break foci | Persistent DNA damage |
| Telomere Analysis | Q-FISH, TRF assay | Telomere length and integrity | Telomere dysfunction |
| Sequencing-Based | Whole genome sequencing | Single nucleotide variants, indels, CNVs | Mutation load in cancer genes |
| Centromere/CIN Assay | CENP-A immunofluorescence, mitotic spread | CENP-A mislocalization, lagging chromosomes | Chromosomal instability (CIN) |
| Functional DNA Repair | Host cell reactivation assay | DNA repair capacity | Deficient repair pathways |
Experimental Protocol: Comprehensive Genomic Stability Assessment
Objective: Systematically evaluate genomic stability in patient-derived iPSC lines throughout culture expansion and differentiation.
Materials:
- Cell Lines: Patient-specific iPSC lines (passage 10-50)
- Controls: Reference iPSC line (e.g., KOLF2.1J [78]), parental somatic cells
- Culture Reagents: Essential 8 or mTeSR1 medium, Matrigel or vitronectin
- Molecular Kits: Karyostat+ kit (or equivalent), Telomere Length Assay kit
- Antibodies: Anti-γH2AX (DNA damage), anti-53BP1 (DNA damage), anti-CENP-A (centromere integrity)
- Equipment: Next-generation sequencer, metaphase spread setup, high-content imager
Procedure:
Sample Collection:
- Harvest iPSCs at specific passages (e.g., P15, P25, P35, P50) at 70-80% confluence
- Collect 1×10^6 cells for DNA/RNA extraction, 5×10^5 for karyotyping, 2×10^5 for immunostaining
- Preserve aliquots in liquid nitrogen for retrospective analysis
Karyotyping and Chromosomal Analysis:
- Treat cells with 0.1 µg/mL colcemid for 4 hours to arrest in metaphase
- Hypotonic treatment with 0.075 M KCl for 20 minutes at 37°C
- Fix with 3:1 methanol:acetic acid, drop onto slides
- Perform G-banding using trypsin-Giemsa protocol
- Analyze 20 metaphase spreads per cell line for chromosomal abnormalities
DNA Damage Assessment:
- Plate iPSCs on glass coverslips at 5×10^4 cells/cm²
- Fix with 4% PFA after 48 hours, permeabilize with 0.5% Triton X-100
- Co-stain with anti-γH2AX and anti-53BP1 antibodies (1:500 dilution)
- Counterstain with DAPI and mount with antifade medium
- Image using high-content or confocal microscope (≥10 fields per replicate)
- Quantify foci per nucleus using image analysis software (e.g., CellProfiler)
Copy Number Variation Analysis:
- Extract high-quality DNA using silica-column method
- Process using Karyostat+ kit or equivalent for CNV detection
- Hybridize to microarray or prepare libraries for whole-genome sequencing
- Analyze data using analytical software (e.g., Nexus CNV, Partek)
- Focus on regions containing cancer-associated genes (e.g., TP53, PTEN, MYC)
Telomere Length Measurement:
- Isolate genomic DNA and quantify precisely
- Perform quantitative PCR with telomere-specific and single-copy gene primers
- Calculate T/S ratio relative to reference DNA
- Compare across passages to monitor telomere maintenance
Validation Criteria:
- Normal karyotype in ≥90% of metaphases
- <5% of nuclei with >10 γH2AX/53BP1 foci
- No recurrent CNVs in oncogenes or tumor suppressors
- Stable telomere length across passages (CV <15%)
Strategies for Risk Mitigation
Reprogramming Methodologies with Reduced Tumorigenic Potential
The choice of reprogramming methodology significantly influences the genomic integrity of resulting iPSCs. Integration-free methods substantially reduce the risk of insertional mutagenesis and offer greater safety profiles.
Table 3: Comparison of Reprogramming Methods by Tumorigenic Risk Profile
| Method | Reprogramming Efficiency | Genomic Integration | Key Advantages | Tumorigenic Concerns |
|---|---|---|---|---|
| Retroviral/Lentiviral | 0.1-1% | Yes (random) | High efficiency, well-established | Insertional mutagenesis, transgene reactivation |
| Non-Integrating Viral | 0.001-0.1% | No | No genomic integration, good efficiency | Immunogenicity (adenovirus), persistence (Sendai) |
| Episomal Vectors | 0.001-0.01% | No (rare) | DNA-free, clinically applicable | Low efficiency, potential rare integration |
| Sendai Virus | ~0.1% | No | Cytoplasmic replication, high efficiency | Viral persistence requires clearance steps |
| mRNA Transfection | 0.1-1% | No | Defined components, high efficiency | Complex delivery, innate immune activation |
| Chemical Reprogramming | <0.001% | No | No genetic material, promising for clinics | Very low efficiency, protocol optimization ongoing |
The following workflow illustrates a recommended strategy for generating low-risk iPSC lines using integration-free methods, incorporating critical quality control checkpoints.
The Scientist's Toolkit: Essential Reagents for Risk Mitigation
Table 4: Research Reagent Solutions for Tumorigenic Risk Mitigation
| Reagent Category | Specific Product/Method | Function in Risk Mitigation | Application Notes |
|---|---|---|---|
| Reprogramming Kit | CytoTune-iPS Sendai Virus | Non-integrating delivery of OSKM factors | Temperature-sensitive mutant allows clearance |
| CRISPR Tools | Cas9-gRNA ribonucleoprotein | Generation of isogenic controls | Enables precise correction without vectors |
| Cell Sorting | FACS with pluripotency markers | Removal of partially reprogrammed cells | SSEA-4/TRA-1-60 positive selection |
| Quality Control | Karyostat+ CNV detection | Identification of chromosomal abnormalities | Early detection of genomic instability |
| Culture System | Defined, xeno-free media | Reduced culture-induced adaptations | Eliminates batch-to-batch variability |
| Differentiation Kit | Directed differentiation protocols | Reduced heterogeneity in target cells | Minimizes residual pluripotent cells |
| Cell Banking | Controlled rate freezing system | Maintains genetic integrity across passages | Prevents culture-induced drift |
Advanced Monitoring and Machine Learning Approaches
Emerging technologies, particularly artificial intelligence (AI) and machine learning (ML), are revolutionizing how researchers monitor and predict genomic stability in stem cell systems. These approaches enable proactive identification of at-risk cultures before overt abnormalities manifest.
Predictive Modeling: Machine learning algorithms can analyze high-content imaging data to identify subtle morphological patterns predictive of genomic instability. A recent study demonstrated that a Random Forest model achieved an AUC of 0.787 in predicting stem cell therapy outcomes based on clinical and cellular parameters [83]. Similar approaches can be adapted to predict genomic instability risk factors.
Automated Quality Control: AI-driven image analysis systems can continuously monitor iPSC cultures for early signs of differentiation or abnormal colony morphology—potential indicators of emerging instability. These systems can process thousands of images automatically, flagging cultures for further analysis [84].
Multi-Omics Integration: Machine learning approaches can integrate genomic, transcriptomic, and proteomic data to identify complex signatures predictive of tumorigenic potential. This is particularly valuable for detecting epigenetic instability that may not be evident from DNA sequencing alone [82].
Validation and Quality Control Frameworks
Standardized Validation Protocols for Disease Modeling
Ensuring the safety and genomic stability of iPSC-derived models requires implementation of comprehensive validation frameworks as outlined by international standards organizations like the International Society for Stem Cell Research (ISSCR) [85].
Recommendation 4.1.1: Document the cell line or tissue of origin, including the specific cell type, anatomical location, isolation procedure, and culture conditions, as these factors significantly influence variability and reproducibility [85].
Recommendation 4.1.2: Consider and document donor metadata including sex, age, ethnic and genetic background, health status, and risk factors, as these can influence experimental outcomes and generalizability of findings [85].
Recommendation 4.3.1: Validate that cellular models are functionally and phenotypically representative of native cells/tissues using multiple appropriate criteria, including morphology, function, and expression of cellular markers [85].
Recommendation 4.3.4: For disease models with known genotypes, confirm that the stem cell-derived disease model carries the expected genotype, as genetic instability and mosaicism in donor tissue may contribute to mixed genotypes [85].
Experimental Protocol: Validating Tumorigenic Risk Mitigation
Objective: Systematically validate the reduction of tumorigenic risk in iPSC lines and their differentiated progeny.
In Vitro Tumorigenicity Assay:
Teratoma Formation Assay:
- Inject 1×10^6 iPSCs into immunodeficient mice (e.g., NSG) intramuscularly or under the testis capsule
- Monitor for 8-12 weeks for tumor formation
- Harvest and analyze tumors histologically for all three germ layers
- Compare tumor incidence and latency period with positive control (known tumorigenic line)
Pluripotent Cell Elimination Test:
- Differentiate iPSCs using validated protocols for target cell type (e.g., cardiomyocytes)
- Analyze by flow cytometry for pluripotency markers (OCT4, NANOG, SSEA-4) at multiple time points
- Establish threshold of <0.1% pluripotent marker-positive cells in final product
Oncogenic Transformation Potential:
- Perform soft agar colony formation assay to assess anchorage-independent growth
- Plate 5×10^3 cells in 0.4% agarose over 0.8% base layer
- Culture for 3-4 weeks, score for colony formation (>50 cells)
- Compare with positive (HeLa) and negative (primary fibroblasts) controls
Genetic Stability Monitoring:
- Perform whole-genome sequencing at key manufacturing milestones
- Focus on cancer-related genes and structural variations
- Utilize bioinformatic tools to calculate mutational burden and signature
Acceptance Criteria:
- No teratoma formation within 12 weeks in immunodeficient mice
- <0.1% residual pluripotent cells in differentiated populations
- No colony formation in soft agar assays
- No mutations in critical cancer driver genes
- Stable karyotype across at least 10 passages
Mitigating tumorigenic risk and ensuring genomic stability in patient-specific stem cell models requires a multi-faceted approach spanning reprogramming methodologies, culture conditions, and rigorous quality control. The field is advancing toward increasingly safe systems through non-integrating reprogramming methods, defined culture environments, and enhanced genomic monitoring technologies. Emerging opportunities include the development of next-generation gene editing tools with enhanced specificity, improved bioreactor systems that minimize culture stress, and advanced biosensors for real-time monitoring of genomic integrity. Furthermore, the integration of AI and machine learning into quality control pipelines promises to transform how researchers detect and predict instability patterns before they compromise experimental results or therapeutic applications [83] [84] [82]. As these technologies mature, they will enable researchers to harness the full potential of patient-specific iPSC models while maintaining the genomic integrity essential for both basic research and clinical translation.
Establishing Credibility: Validation Frameworks and Model Comparisons
The integration of computational modeling and simulation (CM&S) into biomedical research represents a paradigm shift in how scientists develop therapies and understand disease. Within the critical field of patient-specific disease modeling using stem cells, establishing trust in model predictions is not merely an academic exercise but a fundamental prerequisite for clinical translation and regulatory acceptance. The ASME V&V 40-2018 standard, titled "Assessing Credibility of Computational Modeling through Verification and Validation: Application to Medical Devices," provides a risk-informed framework specifically designed to establish this necessary trust in computational models used in medical applications [86] [87]. This technical guide explores the core principles of the ASME V&V40 standard and its vital role in strengthening the scientific rigor of stem cell-based disease models.
As regulatory agencies increasingly accept in silico evidence, the need for standardized credibility assessment has become paramount. The U.S. Food and Drug Administration (FDA) has incorporated principles from ASME V&V40 into its guidance documents, including recent drafts on artificial intelligence in regulatory submissions [88]. This adoption signals a broader recognition that credibility frameworks are essential not only for traditional medical devices but also for the complex computational models underpinning advanced therapies, including those derived from stem cell research. The framework's flexibility allows application across diverse domains, from predicting medical device durability to assessing patient-specific biomechanical responses [89] [87].
Core Principles of the ASME V&V40 Standard
Risk-Based Credibility Assessment
The foundational innovation of ASME V&V40 is its risk-informed approach to credibility assessment. Unlike one-size-fits-all validation standards, V&V40 recognizes that the rigor required for model evaluation should be proportional to the decision consequence associated with the model's use [89] [87]. This principle is particularly relevant to stem cell research, where models may inform decisions ranging from early therapeutic discovery to clinical trial design.
The standard establishes a systematic process for determining the appropriate level of validation effort:
- Context of Use (COU) Definition: Precisely specifying the role and scope of the computational model within the decision-making process
- Model Risk Assessment: Evaluating both the influence of the model on the decision and the potential consequence of an incorrect decision
- Credibility Goal Establishment: Defining acceptance criteria for model accuracy based on the risk assessment
- Validation Planning: Designing activities to demonstrate the model satisfies credibility goals [87] [88]
This framework provides researchers with a structured methodology for allocating resources efficiently while ensuring sufficient evidence supports model predictions for their intended use.
Key Components of Credibility Establishment
The ASME V&V40 standard identifies several core activities essential for establishing model credibility:
- Verification: The process of determining that a computational model accurately represents the underlying mathematical model and its solution [90] [91]. This includes code verification (ensuring the numerical algorithms are implemented correctly) and calculation verification (ensuring the numerical solution is accurate).
- Validation: The process of determining the degree to which a model is an accurate representation of the real world from the perspective of the intended uses of the model [91].
- Uncertainty Quantification (UQ): The systematic characterization and propagation of uncertainties in model inputs to determine their impact on model outputs [90] [91].
- Applicability Evaluation: Assessing whether the model is appropriate for the intended Context of Use, particularly when full validation under identical conditions is not feasible [87].
For patient-specific stem cell models, each component presents unique challenges and considerations that must be addressed through careful experimental design and systematic documentation.
Application to Patient-Specific Disease Modeling with Stem Cells
Integration with Stem Cell Disease Models
The emergence of sophisticated stem cell-based disease models, particularly those utilizing induced pluripotent stem cells (iPSCs) and organoid technologies, has created unprecedented opportunities for understanding disease mechanisms and developing personalized therapies [9] [92]. These models enable researchers to create patient-specific cellular systems that recapitulate key aspects of human diseases, overcoming significant limitations of traditional animal models [9]. However, as these experimental systems grow in complexity, computational approaches become increasingly necessary to interpret results, predict outcomes, and optimize therapeutic interventions.
The ASME V&V40 framework provides essential guardrails for ensuring the predictive accuracy of these computational models when informed by stem cell data. For example, when using iPSC-derived cardiomyocytes to model cardiac arrhythmias, computational models might be employed to predict drug effects. The V&V40 standard would require researchers to define the specific context of use (e.g., "predicting pro-arrhythmic potential of compound X"), assess the risk associated with incorrect predictions, and establish corresponding credibility goals through appropriate validation activities [9] [87].
Addressing Unique Challenges in Stem Cell Research
Stem cell-based disease models present distinctive challenges for credibility assessment that require adaptations of the V&V40 framework:
- Cellular Heterogeneity: Patient-derived iPSCs and their differentiated progeny exhibit considerable biological variability, creating significant uncertainty in model inputs [9] [5].
- Model Maturity Limitations: Current stem cell differentiation protocols often yield developmentally immature cells, potentially limiting their relevance to adult-onset diseases [9].
- Scalability and Reproducibility: Reproducibility challenges in stem cell differentiation protocols can complicate model validation across laboratories [9] [5].
- Multiscale Complexity: Stem cell models often span molecular, cellular, and tissue levels, requiring integrated computational approaches with validation at each scale [92].
Successful application of V&V40 in this context requires careful consideration of these domain-specific challenges when planning verification, validation, and uncertainty quantification activities.
Implementation Framework and Experimental Protocols
Step-by-Step Credibility Assessment Protocol
Implementing ASME V&V40 for patient-specific stem cell models involves a systematic process:
Define the Question of Interest (QoI)
- Formulate a precise, actionable question that the model will address
- Example: "Can the model predict the contractile force deficit in iPSC-derived cardiomyocytes from patients with hypertrophic cardiomyopathy under β-adrenergic stimulation?"
Establish Context of Use (COU)
Conduct Risk Assessment
Establish Credibility Goals
Execute Verification, Validation, and UQ Activities
Document and Report Results
Workflow Visualization
The following diagram illustrates the integrated workflow for applying ASME V&V40 to stem cell-based disease models, showing how experimental and computational components interact throughout the credibility assessment process:
Quantitative Assessment Methods and Acceptance Criteria
Credibility Factors and Acceptance Thresholds
The ASME V&V40 framework employs specific quantitative metrics to evaluate model credibility. The table below summarizes key assessment methods and typical acceptance criteria derived from published applications in biomedical modeling:
Table 1: Credibility Assessment Methods and Acceptance Criteria
| Credibility Factor | Assessment Method | Acceptance Criteria | Example from Literature |
|---|---|---|---|
| Verification Accuracy | Grid Convergence Index (GCI) | Relative Error < 1% [91] | Patient-specific ATAA model verification achieved RE < 1% for material parameters and hemodynamic variables [91] |
| Validation Accuracy | Area Metric | Area Metric ≤ 5% [90] [91] | TAVI model validation showed device diameter predictions with area metric ≤ 5% in majority of cases [90] |
| Uncertainty Propagation | Sensitivity Indices | Pareto analysis of influential parameters [90] | TAVI model identified balloon expansion volume and stent material as most influential parameters (29.3-48% effect) [90] |
| Comparator Quality | Clinical vs. Experimental Data | Hierarchical classification based on relevance [89] | Patient-specific models using clinical imaging as primary comparator [91] |
| Numerical Accuracy | Residual Analysis | Convergence to predefined tolerance [89] | Code verification demonstrating solver convergence [89] |
Uncertainty Quantification Framework
For patient-specific stem cell models, comprehensive uncertainty quantification is essential. The following table outlines common uncertainty sources and recommended quantification approaches:
Table 2: Uncertainty Sources and Quantification Methods in Stem Cell Models
| Uncertainty Category | Specific Sources | Recommended UQ Methods | Impact on Credibility |
|---|---|---|---|
| Parametric Uncertainty | Variability in material properties, kinetic parameters | Probabilistic analysis using Latin Hypercube Sampling [90] | High impact; can dominate output variance in biomechanical models [91] |
| Biological Variability | Donor-to-donor differences in iPSC differentiation efficiency | Population-based sampling, mixed-effects modeling | Critical for patient-specific predictions; requires isogenic controls when possible [9] [92] |
| Model Structure Uncertainty | Alternative mathematical representations of biological processes | Bayesian model averaging, model selection criteria | Affects extrapolation beyond validation domain; requires careful applicability assessment [87] |
| Experimental Measurement Uncertainty | Noise in experimental readouts, assay variability | Error propagation analysis, Bayesian calibration | Impacts validation comparisons; must be characterized for proper validation [90] |
| Numerical Approximation Uncertainty | Discretization errors, solver tolerances | Grid convergence studies, residual analysis | Controlled through verification activities; typically minimized to <1% error [91] |
Regulatory Landscape and Future Developments
Integration with Regulatory Standards
The ASME V&V40 standard has gained significant traction within regulatory frameworks globally. The U.S. FDA has referenced its principles in various guidance documents, establishing it as a recognized consensus standard for demonstrating model credibility in regulatory submissions [89] [88]. This regulatory acceptance is particularly relevant for stem cell researchers aiming to translate computational models into clinically impactful tools.
Recent developments indicate expanding applications of the V&V40 framework:
- FDA Draft Guidance on AI: The February 2025 FDA draft guidance on AI in regulatory submissions adapts the V&V40 risk-based credibility framework for AI/ML models, demonstrating its flexibility beyond traditional computational models [88].
- Extension to Patient-Specific Models: Technical reports from the ASME VVUQ40 subcommittee are addressing specialized applications, including patient-specific modeling for fracture prediction and durability assessment [89].
- In Silico Trial Applications: Regulatory acceptance of in silico clinical trials creates opportunities for using validated computational models to augment or replace certain human trials, particularly for rare diseases where patient recruitment is challenging [89] [92].
Essential Research Tools for Credibility Assessment
The successful implementation of credibility assessment requires specific methodological tools and reagents. The following table summarizes key resources mentioned in the search results:
Table 3: Essential Research Reagent Solutions for Credibility Assessment
| Tool/Category | Specific Examples | Function in Credibility Assessment | Relevance to Stem Cell Models |
|---|---|---|---|
| Computational Modeling Platforms | Finite-element solvers (Abaqus, Ansys) [91] | Core simulation capability for computational models | Modeling biomechanical properties of stem cell-derived tissues [91] |
| Uncertainty Quantification Tools | Gaussian process regression, Latin Hypercube Sampling [90] | Surrogate modeling and probabilistic analysis | Quantifying effects of biological variability in iPSC differentiation [90] |
| Validation Comparators | Clinical imaging (CTA), experimental measurements [91] | Gold-standard data for model validation | Comparing model predictions to experimental measurements from organoids [9] |
| Stem Cell Characterization Tools | scRNA-Seq, flow cytometry, electrophysiology [9] | Quantitative assessment of stem cell phenotypes | Providing validation data for models of stem cell behavior [9] |
| Gene Editing Technologies | CRISPR-Cas9 [9] [5] | Creation of isogenic controls for disease modeling | Controlling for genetic background in patient-specific models [92] |
| Organoid Culture Systems | 3D matrix embeddings, bioreactors [9] | Physiologically relevant experimental models | Providing more relevant validation data compared to 2D cultures [9] |
The ASME V&V40 standard provides an essential systematic framework for establishing credibility in computational models used in stem cell research and regenerative medicine. Its risk-informed approach offers appropriate flexibility while ensuring sufficient rigor for the intended context of use. As patient-specific disease modeling using stem cells continues to advance, the integration of formal credibility assessment methodologies will be crucial for regulatory acceptance and clinical translation.
Future developments in the field will likely include increased automation of credibility assessment workflows, standardized benchmarking datasets for stem cell models, and harmonized international standards for in silico evidence. Furthermore, the integration of AI and machine learning with traditional computational models will create new challenges and opportunities for credibility assessment that will require ongoing evolution of the V&V40 framework [89] [88].
For researchers in the stem cell field, early adoption of these credibility assessment principles will not only strengthen the scientific rigor of their computational models but also accelerate the translation of groundbreaking discoveries into transformative therapies for patients. The framework provides a common language for collaboration between computational scientists, stem cell biologists, and regulatory professionals, ultimately supporting the responsible advancement of personalized medicine based on patient-specific disease models.
Quantitative Validation Against Clinical and Experimental Data
Within the paradigm of patient-specific disease modeling, quantitative validation serves as the critical bridge between innovative in vitro models and their clinical translation. The advent of human pluripotent stem cells (hPSCs), including induced pluripotent stem cells (iPSCs), has revolutionized biomedical research by enabling the generation of limitless, genetically-defined human cell types for disease modeling and drug screening [93] [6]. These patient-derived models, particularly three-dimensional organoids, outperform traditional two-dimensional cultures and animal models by more accurately recapitulating human-specific pathophysiology and genetic variability [93]. However, the true utility of these models hinges on rigorous, quantitative benchmarking against clinical and experimental data to ensure their predictive validity for therapeutic efficacy and safety. This guide details the methodologies and frameworks for establishing this essential validation, focusing on applications in precision medicine and drug development.
Foundational Models: hPSCs and Organoids
Human Pluripotent Stem Cells (hPSCs)
Human Pluripotent Stem Cells, encompassing both embryonic stem cells (hESCs) and induced pluripotent stem cells (iPSCs), are defined by their capacity for indefinite self-renewal and differentiation into any cell type of the human body [93]. The iPSC technology, pioneered by Takahashi and Yamanaka, allows for the reprogramming of adult somatic cells into a pluripotent state using defined transcription factors [93]. This breakthrough enables the creation of patient-specific cell lines that retain the individual’s complete genetic background, making them powerful tools for modeling genetic diseases and studying individual drug responses [93] [6].
Organoids as Advanced Physiological Models
Organoids are three-dimensional, self-organizing structures derived from stem cells that mimic the cytoarchitecture and functional characteristics of native human organs [93]. They preserve patient-specific genetic and phenotypic features, offering enhanced physiological relevance for pharmaceutical testing [93]. Protocols exist for generating organoids from a wide range of tissues, including brain, liver, pancreas, kidney, and patient-derived tumor organoids (PDTOs) [93].
Quantitative Validation Frameworks and Metrics
The predictive power of stem cell-based models is established through systematic validation against known clinical and experimental benchmarks. The table below summarizes the core quantitative metrics used for validation across different tissue types.
Table 1: Key Quantitative Metrics for Model Validation
| Tissue/Model Type | Functional Assays | Molecular Profiling | Pharmacological Response |
|---|---|---|---|
| iPSC-Derived Cardiomyocytes (iPSC-CMs) | Field potential / contraction analysis (Multi-electrode arrays); Calcium handling | RNA-seq; Proteomics for cardiac markers (cTnI, TNNT2) | Response to cardiotoxic drugs (e.g., Doxorubicin); hERG channel blockade |
| Hepatic Organoids | Albumin/Urea secretion; CYP450 enzyme activity; Bile canaliculi function | Transcriptomics for hepatocyte markers | Hepatotoxicity assessment (e.g., Acetaminophen); Drug metabolism studies |
| Patient-Derived Tumor Organoids (PDTOs) | Cell viability / proliferation assays; Apoptosis markers | Genomics (retention of tumor mutations); Histology | Correlation with patient clinical response to chemo/targeted therapies |
| Brain Organoids | Electrophysiology (Multi-electrode arrays); Neuronal network activity | Single-cell RNA-seq; Immunostaining for neuronal/glial markers | Neurotoxicity screening; Efficacy of neuroactive compounds |
Workflow for Quantitative Validation
The following diagram outlines the standard workflow for generating and validating patient-specific models, from biological sample to quantitative analysis.
Protocol for Validating iPSC-Derived Cardiomyocytes Against Clinical Cardiotoxicity Data
Objective: To quantitatively validate the response of iPSC-derived cardiomyocytes (iPSC-CMs) to known cardiotoxic compounds, using clinical data as a benchmark.
Materials:
- Cell Source: Patient-specific iPSC-derived cardiomyocytes [6].
- Control Cells: Isogenic control iPSC-CMs (e.g., corrected via CRISPR/Cas9) or commercially available iPSC-CM lines.
- Test Article: Doxorubicin (a known clinical cardiotoxin) and a negative control compound [93] [6].
- Equipment: Multi-electrode array (MEA) system, fluorescent plate reader for calcium flux assays, high-content imaging system.
Methodology:
- Cell Culture and Plating: Differentiate iPSCs into cardiomyocytes using established protocols. Plate mature iPSC-CMs onto MEA plates or assay-ready microplates at a standardized density.
- Compound Treatment: Treat cells with a concentration range of Doxorubicin (e.g., 0.1 nM - 10 µM) and negative control. Include replicates (n≥3) for each concentration.
- Functional Endpoint Measurement:
- Electrophysiology: Using MEA, record field potentials pre- and post-treatment. Quantify changes in beat rate, field potential duration (FPD), and arrhythmic events.
- Calcium Handling: Using fluorescent dyes (e.g., Fluo-4), measure calcium transient amplitude, duration, and decay kinetics.
- Viability & Cytotoxicity: Measure ATP content (cell viability) and release of lactate dehydrogenase (cytotoxicity) at 24-72 hours.
- Data Analysis:
- Calculate IC50 values for functional and viability parameters.
- Compare the dose-response curve of patient-specific cells to isogenic controls and established clinical cardiotoxicity thresholds.
- Statistically correlate the in vitro FPD prolongation with the known clinical risk of Torsades de Pointes.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and their applications in developing and validating patient-specific models.
Table 2: Essential Research Reagents for Patient-Specific Disease Modeling
| Reagent / Tool | Function | Application Example |
|---|---|---|
| Yamanaka Factor Reprogramming Kit | Delivers OSKM transcription factors to reprogram somatic cells into iPSCs. | Generating patient-specific iPSC lines from skin fibroblasts or blood cells [93]. |
| CRISPR/Cas9 Genome Editing System | Enables precise genetic modifications for creating isogenic controls or introducing disease mutations. | Correcting a pathogenic variant in a patient iPSC line to confirm genotype-phenotype relationships [93]. |
| Directed Differentiation Kit | Provides optimized growth factors and small molecules to guide iPSC differentiation. | Differentiating iPSCs into cardiomyocytes, neurons, or hepatocytes using lineage-specific protocols [93] [6]. |
| 3D Extracellular Matrix (e.g., Matrigel) | Provides a scaffold that supports the self-organization and polarization of cells into organoids. | Generation of intestinal, cerebral, or hepatic organoids from iPSCs or adult stem cells [93]. |
| Multi-Electrode Array (MEA) | Non-invasively records extracellular field potentials from electrically active cells. | Functional validation of iPSC-derived cardiomyocytes and neurons for drug safety pharmacology [6]. |
Data Integration and Computational Modeling
The integration of quantitative data from these models with computational approaches is increasingly vital. In silico technologies, including mechanistic models and machine learning, can generate insights from limited datasets and simulate biological processes across scales [94]. A closed-loop workflow is envisioned where patient-derived organoids generate standardized, quantitative datasets that are used to parameterize digital twins or quantitative systems pharmacology (QSP) models. Predictions from these computational models can then inform subsequent experiments, making optimal use of scarce patient materials [94]. The following diagram illustrates this integrative feedback loop.
The landscape of preclinical research is undergoing a fundamental transformation, driven by the limitations of traditional models and advanced by the emergence of human-relevant systems. This shift is particularly critical in patient-specific disease modeling, where the translational gap in drug development—exemplified by attrition rates exceeding 90% for central nervous system (CNS) drug candidates—demands more predictive tools [95] [96]. While immortalized cell lines and animal models have long been research workhorses, their physiological disconnect from human biology often undermines their predictive value. In contrast, induced pluripotent stem cell (iPSC) technology represents a paradigm shift, enabling the generation of patient-specific human cells for disease modeling, drug screening, and therapeutic development. This whitepaper provides a technical comparison of these model systems, focusing on their applications, methodologies, and relative merits in modern biomedical research.
The choice of preclinical model is a critical determinant in the success of translational research. Traditional models, including immortalized cell lines and animal systems, have provided valuable insights but possess inherent limitations in recapitulating human physiology.
- Immortalized Cell Lines, such as HeLa, SH-SY5Y, and MCF-7, are derived from tissues (often cancerous) and genetically altered to proliferate indefinitely. They are prized for their robustness, scalability, and ease of use in high-throughput assays. However, they frequently exhibit non-physiological profiles, with altered genetics and metabolism that poorly mirror native human cells [95] [97].
- Animal Models (e.g., rodents, zebrafish) offer a complex, systemic context for studying disease mechanisms and drug effects in vivo. They have been indispensable for historical research. Nonetheless, they are hampered by significant species differences in gene expression, regulation, and immune function, leading to poor prediction of human responses. Additional challenges include high costs, ethical concerns, and lengthy experimental timelines [98] [99].
- Induced Pluripotent Stem Cell (iPSC) Models are generated by reprogramming adult human somatic cells (e.g., from skin or blood) back to a pluripotent state. These cells can then be differentiated into virtually any cell type in the body. iPSCs provide a human-specific, genetically relevant platform that is particularly powerful for patient-specific disease modeling and for studying developmental processes inaccessible in human subjects [93] [1].
Technical Comparison of Model Systems
The table below provides a quantitative and qualitative comparison of the core characteristics of these three model systems, highlighting their distinct advantages and drawbacks for specific research applications.
Table 1: Comprehensive Technical Comparison of Preclinical Model Systems
| Feature | Immortalized Cell Lines | Animal Models | iPSC-Derived Models |
|---|---|---|---|
| Physiological Relevance | Low (often cancer-derived, non-physiological) [95] | Moderate (systemic biology but with species differences) [98] [99] | High (human-specific, can model native cell biology) [95] [93] |
| Human Specificity | No (often of non-human origin) [95] | No (rodent, etc.) [95] | Yes (derived from human somatic cells) [1] |
| Reproducibility & Scalability | High (easily scalable, but prone to genetic drift) [95] | Low to Moderate (high individual variability, complex breeding) [99] | Moderate to High (new protocols improving consistency; scalable production possible) [95] [100] |
| Genetic Manipulability | High (amenable to CRISPR and other editing techniques) [97] | Moderate (technically complex and time-consuming) | High (highly amenable to CRISPR for isogenic controls and disease modeling) [96] [101] |
| Time to Assay | Short (days) [95] | Long (months to years) | Moderate (weeks for differentiation) [95] [97] |
| Cost Efficiency | Low cost [99] | High cost (housing, care) [99] | Moderate cost [99] |
| Throughput | High (suitable for HTS) [95] | Low | Growing (increasingly used for HTS) [93] |
| Key Limitations | Poor predictive validity, genomic instability [95] [97] | Species mismatch, ethical concerns, low throughput [98] [99] | Protocol variability, maturation level of cells, batch-to-batch inconsistency [98] [96] [100] |
| Ideal Applications | Preliminary screening, mechanistic studies, protein production [95] [97] | Studies of systemic physiology, complex behavior, whole-organism pharmacology [99] | Disease modeling, personalized medicine, drug toxicity testing, developmental biology [96] [93] [101] |
Methodologies and Experimental Protocols
Generation of Patient-Specific iPSCs
The foundation of iPSC-based disease modeling is the reprogramming of patient-specific cells.
Diagram 1: iPSC Generation Workflow
- Somatic Cell Isolation: Obtain and culture patient-derived cells, typically dermal fibroblasts from a skin punch biopsy or peripheral blood mononuclear cells (PBMCs) [1] [101].
- Reprogramming Factor Delivery:
- iPSC Colony Culture and Isolation: Transfer transduced cells onto feeder layers (e.g., mouse embryonic fibroblasts) or in feeder-free conditions. Colonies with embryonic stem cell-like morphology emerge in 2-4 weeks and are manually or mechanically picked for expansion [1].
- Pluripotency Validation: Confirm successful reprogramming through:
- Immunocytochemistry: Detection of pluripotency markers (OCT4, SOX2, NANOG, SSEA-4).
- RT-qPCR: Analysis of endogenous pluripotency gene expression.
- In vitro or in vivo differentiation to demonstrate potential to form all three germ layers [1].
Differentiation into Target Cell Types
iPSCs can be directed to differentiate into disease-relevant cells, such as neurons, cardiomyocytes, or hepatocytes.
Table 2: Key Reagents for iPSC Differentiation
| Research Reagent Solution | Function in Protocol |
|---|---|
| Small Molecule Inhibitors/Activators (e.g., SB431542, CHIR99021) | Precisely modulate key developmental signaling pathways (e.g., TGF-β, WNT) to guide cell fate [98]. |
| Recombinant Growth Factors & Proteins (e.g., BDNF, GDNF, Activin A) | Mimic the native tissue microenvironment to promote survival, growth, and maturation of specific cell lineages [98]. |
| Chemically Defined Media | Provide a consistent, xeno-free base medium formulation tailored to support the metabolic needs of the target cell type. |
| CultureSure CEPT Cocktail | Enhances cell survival and cloning efficiency, reduces genomic instability, and improves the robustness of differentiation protocols [98]. |
| Synthetic Matrices (e.g., Geltrex, MatrigeI) | Provide a 3D scaffold that supports complex cell morphology and cell-cell interactions, crucial for functional maturation. |
Advanced Modeling: Organoids and Assembloids
For more complex modeling, 3D organoids can be generated.
- Guidance: Use growth factors and morphogens to pattern iPSC aggregates toward specific regional identities (e.g., forebrain, midbrain, hippocampus) [19] [93].
- Maturation: Culture aggregates in 3D suspension or embedded in matrices for extended periods (months) to allow self-organization and the development of complex, multi-cellular structures [19] [100].
- Fusion (Assembloids): Different region-specific organoids (e.g., cortical glutamatergic neurons and striatal GABAergic neurons) can be fused to model circuit-level interactions and long-range migration, as demonstrated in studies of interneuron migration [19].
Applications in Disease Modeling and Drug Development
Elucidating Disease Mechanisms
iPSC models have uncovered novel disease mechanisms by providing a human-specific context.
- Neurological Disorders: In a study of Hereditary Sensory and Autonomic Neuropathy Type IV (HSAN IV), patient iPSC-derived dorsal root ganglion (DRG) organoids revealed that NTRK1 mutations disrupt the balance between sensory neuron and glial cell differentiation during development, a phenotype not observed in animal models [19].
- Psychiatric Disorders: "Village editing" was used to create NRXN1 knockouts in iPSCs from 15 donors with varying genetic risk for schizophrenia. Differentiated cortical neurons showed that the genetic background profoundly influences transcriptional responses to the mutation, highlighting the importance of polygenic context in complex disorders [19].
Enhancing Drug Discovery Pipelines
iPSCs are being integrated across all stages of drug discovery to improve predictivity.
- Target Identification & Validation: CRISPR-Ready iPSC-derived cells (e.g., ioMicroglia) enable genome-wide knockout screens to identify novel regulators of disease-relevant pathways in a human cellular context [96].
- Hit-to-Lead and Lead Optimization: iPSC-derived sensory neurons are used in multi-electrode array (MEA) assays to model pain pathways and evaluate compound effects on neuronal firing. The reproducibility of cells like ioGlutamatergic Neurons allows for robust comparison of drug candidates over time [96].
- Safety and Toxicology: iPSC-derived cardiomyocytes are now a standard tool for assessing pro-arrhythmic risk, endorsed by the CiPA (Comprehensive in vitro Proarrhythmia Assay) initiative. Similarly, iPSC-derived hepatocytes are being advanced for predicting drug-induced liver injury (DILI) [96] [93].
Diagram 2: iPSCs in Drug Discovery Pipeline
Current Challenges and Future Directions
Despite their promise, iPSC technologies face hurdles that require continued innovation.
- Challenge 1: Reproducibility and Scalability. Conventional directed differentiation protocols can be variable, leading to batch-to-batch heterogeneity that compromises data quality and scalability for high-throughput screening [96] [100].
- Solution: Deterministic cell programming technologies, such as bit.bio's opti-ox, enable the precise and consistent conversion of iPSCs into defined cell types, resulting in <2% gene expression variability across lots [95] [96]. Automation and standardized, quality-controlled reagents are also key to improving reproducibility [98] [93].
- Challenge 2: Functional Maturation. iPSC-derived cells often resemble a fetal or immature state, which may not fully capture the pathophysiology of late-onset adult diseases [93].
- Challenge 3: Regulatory and Industry Adoption.
- Solution: Regulatory frameworks are evolving to accommodate these new models. The U.S. FDA Modernization Act 2.0 has eliminated the mandatory requirement for animal testing for drug approvals, paving the way for the use of human-based models like iPSCs [96] [99] [101]. Collaborative efforts to generate robust validation data will be essential for widespread regulatory acceptance.
The comparative analysis reveals a clear trajectory in preclinical research toward human-specific, patient-centric models. While immortalized cell lines offer practicality for initial screens and animal models provide systemic context, their limitations in predicting human outcomes are significant. iPSC-based models directly address this translational gap by providing a virtually unlimited source of human cells that capture patient-specific genetics for disease modeling and drug testing. Despite ongoing challenges with protocol standardization and functional maturation, innovations in deterministic programming, organoid engineering, and high-throughput screening are rapidly advancing the field. As regulatory agencies increasingly endorse these human-relevant approaches, iPSC models are poised to become a central pillar in the future of biomedical research, driving the development of more effective and personalized therapeutics.
The advancement of personalized medicine hinges on the development of predictive, patient-specific disease models. For researchers and drug development professionals, establishing model credibility—the belief in a model's predictive capability for a specific intended use—is paramount for clinical translation [102]. This is particularly true for complex, multi-scale physiological systems like the heart and brain, where traditional modeling approaches often fall short. Validation is the cornerstone of this process, requiring rigorous comparison of model predictions to experimental or clinical data [102]. This whitepaper examines validated modeling approaches in cardiac electrophysiology and neurological disorders, framing them within the transformative context of patient-specific stem cell research. We explore how these integrated methodologies are overcoming the limitations of traditional animal models, which frequently fail to capture key aspects of human physiology and contribute to high dropout rates in drug development pipelines [9].
The emergence of human induced pluripotent stem cell (iPSC) technology has been a game-changer, providing unprecedented access to patient-specific human cells for constructing more physiologically relevant models. These models are increasingly judged by three core validity criteria: construct validity (the model reflects human disease etiology), face validity (the model resembles human phenotype), and predictive validity (the model informs human treatments) [103] [104]. The following case studies detail how these principles are applied across disciplines, providing a roadmap for developing robust, clinically informative disease models.
Case Study 1: Patient-Specific Models in Cardiac Electrophysiology
Model Personalization and Calibration Techniques
Computational models of cardiac electrophysiology have matured significantly, now enabling patient-specific personalization to guide therapy, particularly for arrhythmias like atrial fibrillation (AF). Creating a personalized model requires a multi-step process that integrates anatomy, tissue properties, and electrophysiology [105]. The workflow begins with generating a personalized geometry from 3D imaging (CT, MRI) or electroanatomical mapping (EAM) data, creating monolayer, bilayer, or 3D volumetric models of the cardiac anatomy. These anatomies are often augmented with specialized structures like the sino-atrial node, Bachmann's bundle, and fiber orientations using rule-based or atlas-based methods [105].
A critical next step is the personalization of the electrophysiological substrate. Here, clinical EAM data is used to characterize the patient's pathophysiology. Key techniques include:
- Fibrosis Imaging and Bipolar Voltage Mapping: Fibrotic regions, identified via late gadolinium enhancement (L&E) MRI or low bipolar voltage mapping, are incorporated into computational models. This is achieved by reducing cell-to-cell coupling, increasing anisotropy ratios, or using percolation methods that probabilistically decouple elements based on LGE-MRI intensity [105].
- Local Activation Time (LAT) Annotation: The accurate annotation of activation times on electrograms (EGMs) is fundamental. Advanced techniques like spatiotemporal, probabilistic, and hybrid methods have been developed to improve annotation accuracy in the presence of clinical noise and far-field signals [105].
Table 1: Advanced Local Activation Time (LAT) Annotation Methods for Model Personalization.
| Annotation Type | EGM Type | Methodology | Advantage for Personalization |
|---|---|---|---|
| Spatiotemporal [105] | Unipolar | Incorporates temporal EGM deflection and spatial gradients. | Effective with noisy or fractionated signals. |
| Probabilistic [105] | Bipolar | Uses Gaussian processes and cumulative signal area to bracket LAT. | Provides uncertainty estimates; suitable for sparse data. |
| Hybrid [105] | Unipolar & Bipolar | Uses bipolar complex to window unipolar maximal negative slope. | Effective for fractionated signals where legacy methods fail. |
| DELTA [105] | Bipolar (from Unipolar) | Calculates bipolars from amplitude-normalized unipolar pairs. | Counters unipolar/bipolar recording artefacts. |
Validation and Credibility of Cardiac Electrophysiology Models
For cardiac electrophysiological (CEP) models to be trusted for clinical applications, their credibility must be established through a body of evidence. This goes beyond a single validation step and includes various types of credibility evidence [102]. The complexity of multi-scale CEP models, which integrate subcellular, cellular, tissue, and organ-level dynamics, makes traditional validation methodologies challenging. Consequently, trustworthiness is often founded on a combination of factors, including validation results from multiple scales (ion channel to whole organ), the underlying biophysical theory, and evidence gathered during model calibration [102].
A key advancement is the move towards cell-specific cardiac electrophysiology models. Traditional models were often composite constructs tuned manually to fit a simple action potential. A novel approach uses rich electrophysiology protocols—such as stochastic current-clamp stimulation and multi-step voltage clamping—applied to single cardiac myocytes. The resulting data is then used to automatically tune model parameters via a global optimization method like a genetic algorithm (GA). This process generates cell-specific models that simulate complex electrophysiological dynamics, such as arrhythmias, significantly better than traditional models [106]. This approach allows for well-controlled studies of cellular and subject-level heterogeneity in disease propensity and therapy response [106].
Figure 1: Workflow for Developing and Validating Patient-Specific Cardiac Electrophysiology Models. The process integrates clinical data to build, calibrate, and validate models for clinical decision support.
Case Study 2: Stem Cell-Derived Models for Neurological Disorders
A Framework for Validating iPSC-Based Neural Models
Human iPSC technology has revolutionized the modeling of neurological disorders by allowing the generation of patient-specific brain cells, including neurons, glia, and complex 3D brain organoids. To ensure these models are clinically predictive, a rigorous validity framework must be applied, adapting criteria traditionally used for animal models [103].
- Construct Validity: This ensures the model contains the appropriate genetic and cellular context. For monogenic disorders like Timothy syndrome or Rett syndrome, this involves introducing the disease-causing mutation into iPSCs. The challenge is greater for polygenic disorders like schizophrenia, where multiple genetic risk factors are involved. Construct validity also requires the generation of relevant cell types (e.g., dopaminergic neurons for Parkinson's disease) [103].
- Face Validity: This assesses whether the model exhibits disease-relevant phenotypes. Since behavioral symptoms define many psychiatric disorders, researchers identify molecular, cellular, and functional correlates. For example, iPSC-derived neurons from patients with schizophrenia spectrum disorders have shown altered neuronal activity patterns measured by microelectrode arrays, mirroring electrophysiological abnormalities observed in patients [103].
- Predictive Validity: This represents the most clinically relevant criterion, evaluating a model's accuracy in forecasting patient treatment responses. compelling examples include iPSC-derived neurons from lithium-responsive and non-responsive bipolar disorder patients, which showed differential drug effects that matched the clinical outcomes in the patients from whom the cells were derived. This demonstrates the potential for using patient-specific models to guide precision psychiatry [103].
Technical Hurdles and Innovative Validation Approaches
Creating valid iPSC-based neural models requires navigating several technical challenges. Genomic instability during iPSC reprogramming must be monitored to avoid confounding results. The developmental immaturity of iPSC-derived neurons, which often resemble fetal brain tissue, poses a challenge for modeling late-onset adult disorders. Furthermore, selecting the appropriate cell type and capturing the complex cellular interactions within the brain are non-trivial tasks [103].
Innovative studies are successfully addressing these challenges. For 22q11.2 deletion syndrome, a major genetic risk factor for schizophrenia, researchers combined patient brain imaging data with iPSC-derived dopaminergic neurons to reveal a direct link between the genetic deletion and altered dopamine metabolism [103]. In another example, brain organoids from Rett syndrome patients exhibited epileptiform activity, a clinical feature of the disorder. This phenotype was suppressed by therapeutic compounds, demonstrating the model's utility for drug discovery [103]. These multi-level validation approaches, which bridge genetics, cellular models, and clinical data, significantly strengthen confidence in the model's relevance.
Table 2: Key Validity Criteria for Stem Cell-Derived Neurological Disease Models.
| Validity Type | Definition | Application Example | Key Challenge |
|---|---|---|---|
| Construct Validity | Model contains appropriate genetic/cellular context. | Introducing Timothy syndrome-associated mutation into iPSCs. | Modeling polygenic disorders with many contributing variants. |
| Face Validity | Model exhibits disease-relevant phenotypes. | Rett syndrome organoids show epileptiform activity. | Identifying cellular biomarkers for behavioral symptoms. |
| Predictive Validity | Model predicts patient treatment response. | iPSC neurons from lithium-respondent vs. non-respondent bipolar patients. | Requires robust clinical data and patient outcome matching. |
The Scientist's Toolkit: Research Reagent Solutions
The development and validation of these advanced models rely on a suite of critical reagents and tools. The following table details essential solutions for researchers in this field.
Table 3: Research Reagent Solutions for Advanced Disease Modeling.
| Research Reagent / Tool | Function | Application Context |
|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) [9] [103] | Patient-specific, pluripotent cell source for generating any human cell type. | Foundation for all patient-specific disease models in cardiac and neurological research. |
| StemRNA Clinical iPSC Seed Clones [8] | GMP-compliant, master iPSC cell lines with filed Drug Master File (DMF). | Provides a standardized, regulatory-friendly starting point for consistent therapy development. |
| CRISPR-Cas9 Gene Editing [9] | Precise manipulation of disease-associated genes in stem cells. | Creating isogenic control lines; introducing or correcting mutations for construct validity. |
| Cleveland Clinic Multiple Sclerosis Performance Test [107] | A validated tool to assess lower/upper extremity function and cognition. | Used as a clinical endpoint in neurological trials (e.g., Bryostatin-1 Phase I trial for MS). |
| Microelectrode Arrays (MEAs) [103] | Measures neuronal activity and network-level electrophysiology in 2D or 3D cultures. | Assessing face validity in neural models by detecting disease-relevant activity patterns. |
| 7 Tesla (7T) MRI Scanner [107] | High-field magnetic resonance imaging for detailed structural and functional brain analysis. | A biomarker tool in clinical trials to measure changes in lesion volume, brain volume, and connectivity. |
Figure 2: Three-Pillar Validity Framework for Stem Cell-Derived Neurological Disease Models. This framework ensures models are biologically relevant, exhibit key disease features, and can predict clinical therapeutic outcomes.
Convergence for Patient-Specific Therapy
The fields of cardiac and neurological disease modeling are converging on a shared paradigm: the integration of patient-specific data, advanced cellular models, and rigorous computational analysis to predict clinical outcomes. In cardiology, this is exemplified by the personalization of cardiac electrophysiology models using EAM data to guide ablation therapy [105]. In neurology, iPSC-based platforms are being used to stratify patients based on their predicted drug response, moving towards precision psychiatry [103].
This convergence is accelerated by global consortia, such as the ISSCR's Consortium on Advanced Stem Cell-Based Models, which brings together industry, academia, and regulatory experts to establish standards and tools for integrating stem cell-derived models into drug development [10]. The ultimate goal is a future where therapies are tested first on a patient's own cellular avatars, ensuring that the treatments they receive are the most likely to be safe and effective for their specific disease biology.
Uncertainty Quantification and Population-Based Validation Approaches
Patient-specific disease modeling using human induced pluripotent stem cells (iPSCs) has emerged as a transformative platform for drug discovery and therapeutic development. These models provide unprecedented access to human-specific disease pathophysiology by carrying the patient's complete genetic background, including disease-associated mutations [17]. However, the inherent biological variability of iPSC lines, combined with technical challenges in differentiation protocols, introduces significant uncertainty into experimental outcomes and predictive validity. Immature physiological characteristics of iPSC-derived cells compared to their adult human counterparts present particular challenges for quantitative predictions of drug responses [108] [11]. Uncertainty quantification and population-based validation approaches address these limitations by providing rigorous mathematical frameworks to translate observations from stem cell models into accurate predictions of human physiological and therapeutic responses.
Foundational Concepts in Uncertainty Quantification
iPSC-based disease models exhibit multiple layers of uncertainty that must be characterized and quantified. Biological uncertainty arises from genetic and epigenetic heterogeneity across different iPSC lines, even when derived from the same donor [17]. Technical uncertainty stems from variability in differentiation protocols, which can yield cells with varying maturity levels and functional properties [17]. Experimental uncertainty encompasses measurement errors and environmental fluctuations during assay execution. Finally, model structure uncertainty relates to the fundamental physiological differences between iPSC-derived cells and native human cells, particularly their fetal-like characteristics [11].
Mathematical Frameworks for Uncertainty Quantification
Population-based mechanistic modeling combines mathematical modeling with statistical analyses to address variability in stem cell systems [108]. This approach involves generating heterogeneous populations of in silico models that reflect physiological variability through parameter randomization. These populations capture the natural biological variation expected across individuals, enabling researchers to quantify how uncertainties propagate through experimental systems and affect predictions [108]. Statistical emulators built from these populations can then map relationships between stem cell observations and adult human physiology, effectively translating quantitative measurements across model systems.
Population-Based Validation Methodologies
Core Principles and Workflow
Population-based validation employs in silico populations of models to create mapping functions between experimental systems. The fundamental workflow begins with generating diverse in silico populations that reflect physiological variability in both stem cell-derived and adult human cells [108]. Multivariable regression techniques are then applied to identify quantitative relationships between systems, accounting for their inherent differences. Finally, cross-system predictions are validated against independent datasets to assess predictive accuracy [108].
The diagram below illustrates the conceptual workflow for cross-cell type prediction modeling:
Experimental Design for Predictive Strength
Strategic experimental design significantly enhances the predictive power of population-based approaches. Research demonstrates that altering extracellular ion concentrations provides particularly effective perturbations for improving predictive accuracy [108]. Specifically, increasing extracellular calcium ([Ca²⁺]o high), decreasing extracellular sodium ([Na⁺]o low), and increasing extracellular sodium ([Na⁺]o high) have been identified as the three most informative experimental conditions for building robust cross-cell type prediction models [108]. In contrast, simple pacing protocols and decreased extracellular calcium provide comparatively less predictive value.
Table 1: Informative Experimental Conditions for Population-Based Modeling
| Experimental Condition | Predictive Value | Key Application |
|---|---|---|
| Increased extracellular Ca²⁺ | Highest | Enhances calcium handling phenotype discrimination |
| Decreased extracellular Na⁺ | High | Reveals Na+/Ca²+ exchanger dependencies |
| Increased extracellular Na⁺ | High | Challenges sodium channel function |
| 2 Hz pacing | Moderate | Provides physiological rate stress |
| 1 Hz pacing | Low | Limited discriminatory power |
| 0.5 Hz pacing | Low | Minimal additional information |
| Decreased extracellular Ca²⁺ | Low | Reduces signal fidelity |
Quantitative Framework for Cross-System Prediction
Regression Modeling Approach
Multivariable regression forms the mathematical backbone of cross-system prediction. Partial least squares regression (PLSR) has been successfully applied to translate drug responses from iPSC-derived cardiomyocytes (iPSC-CMs) to adult human cardiomyocytes [108]. This approach uses features extracted from action potential and calcium transient waveforms—including action potential duration at multiple repolarization levels, diastolic and peak voltages, calcium transient amplitude and duration, and spontaneous beating rate—to construct predictive models [108]. When properly calibrated, these models can achieve high prediction accuracy, with R² values of 0.906 for action potential duration and 0.964 for calcium transient amplitude in cross-validation studies [108].
Protocol Optimization for Efficient Prediction
Comprehensive protocol testing enables efficient experimental design by identifying the most informative conditions. One systematic evaluation constructed 56 different regression models incorporating various combinations of 3 protocols from a total of 8 possible experimental conditions [108]. The analysis revealed that models incorporating two or more of the most informative protocols (ionic concentration manipulations) achieved significantly higher predictive accuracy than those relying on less informative conditions such as pacing frequency variations. This approach allows researchers to prioritize experimental efforts toward conditions that provide maximal information for model building.
Table 2: Performance Metrics for Cross-Cell Type Prediction
| Output Metric | Cross-Validation R² | Key Predicting Features | Optimal Protocol Combination |
|---|---|---|---|
| APD90 | 0.906 | Repolarization timing, diastolic voltage | [Ca²⁺]o high, [Na⁺]o low, [Na⁺]o high |
| Calcium Transient Amplitude | 0.964 | Peak systolic [Ca²⁺], transient kinetics | [Ca²⁺]o high, [Na⁺]o low, [Na⁺]o high |
| Spontaneous Rate | 0.872 | Pacemaker current activity | [Na⁺]o low, 2 Hz pacing |
| Drug-Induced ΔAPD90 | 0.891 | Baseline APD90, drug response in iPSC-CMs | [Ca²⁺]o high, [Na⁺]o low |
| Drug-Induced ΔCaTA | 0.928 | Baseline CaTA, drug response in iPSC-CMs | [Ca²⁺]o high, [Na⁺]o low |
Applications in Disease Modeling and Drug Development
Cardiac Safety and Efficacy Testing
iPSC-derived cardiomyocytes have become a standard tool for cardiac safety assessment, particularly for evaluating drug-induced arrhythmia risk [17]. The Comprehensive in vitro Proarrhythmia Assay (CiPA) initiative has incorporated iPSC-CMs into regulatory safety frameworks, with adoption by pharmaceutical companies including Roche and Takeda for preclinical cardiac profiling [17]. Population-based validation approaches enhance these applications by enabling quantitative prediction of adult cardiac responses from stem cell observations, addressing the maturation gap between iPSC-derived and adult cardiomyocytes [108].
Neurodegenerative Disease Modeling
In neurodegenerative disease research, iPSC-derived neurons from patients with Alzheimer's, Parkinson's, and ALS model key disease phenotypes including tau aggregation, mitochondrial dysfunction, and motor neuron degeneration [17]. Patient-specific iPSC models of Parkinson's disease have successfully recapitulated endogenous alpha-synuclein aggregation, a hallmark pathological feature [109]. These systems support phenotypic screens that identify compounds capable of rescuing neuronal function in vitro, with population-based approaches providing crucial validation of predictive relevance for human therapeutic responses [17].
Implementation Tools and Reagent Solutions
Essential Research Reagents
Successful implementation of uncertainty quantification and population-based validation requires specific research tools and reagents. The table below details essential components for establishing these approaches in stem cell disease modeling.
Table 3: Research Reagent Solutions for Population-Based Validation
| Reagent/Category | Specific Examples | Function in Validation Workflow |
|---|---|---|
| iPSC Lines | Patient-specific iPSCs, isogenic controls | Provide genetically-defined substrate for disease modeling |
| Cardiomyocyte Differentiation Reagents | CHIR99021 (GSK-3β inhibitor), IWR-1/Wnt inhibitors | Generate iPSC-derived cardiomyocytes with defined protocols |
| Neural Differentiation Reagents | SMAD inhibitors, patterning factors | Produce disease-relevant neuronal subtypes |
| Ion Channel Modifiers | E-4031 (IKr blocker), nifedipine (ICaL blocker) | Validate predictive model accuracy for known compounds |
| Extracellular Ion Manipulations | High-Ca²⁺, High-Na⁺, Low-Na⁺ solutions | Provide informative perturbations for regression modeling |
| Functional Assay Reagents | Voltage-sensitive dyes, calcium indicators | Quantify action potentials and calcium handling |
| Data Analysis Platforms | MATLAB, Python with scikit-learn, R | Implement regression modeling and uncertainty quantification |
Experimental Workflow Implementation
The diagram below illustrates the complete experimental workflow for population-based validation in stem cell disease modeling:
Challenges and Future Directions
Despite significant advances, population-based validation approaches face several technical challenges. Differentiation variability remains a concern, as not all iPSC lines behave identically, and protocols often yield cells with fetal-like phenotypes [17]. Cost and throughput limitations can constrain the scale of population-based experiments, particularly for high-content screening applications [17]. Protocol standardization efforts continue to address inter-laboratory variability in iPSC culture and differentiation [17]. Future developments will likely incorporate more sophisticated machine learning approaches, enhanced maturation protocols to bridge the phenotype gap between stem cell-derived and adult cells, and increased integration of multi-omics data to refine predictive models [108] [110]. As these methodologies mature, population-based validation will increasingly enable researchers to confidently translate findings from patient-specific stem cell models to clinically relevant predictions, accelerating the development of safer, more effective therapeutics.
Conclusion
Patient-specific stem cell models represent a transformative platform that is steadily bridging the translational gap between preclinical research and clinical application. By providing human-relevant, genetically defined systems, these models offer unprecedented opportunities for mechanistic disease investigation and therapeutic discovery. While challenges in cellular maturity, standardization, and scalability persist, ongoing advancements in bioengineering, genome editing, and computational validation are rapidly addressing these limitations. The integration of rigorous credibility frameworks ensures these models meet the stringent requirements for regulatory and clinical decision-making. As the field evolves, the convergence of patient-specific iPSCs, sophisticated 3D culture systems, and AI-driven analysis promises to unlock a new era of precision medicine, enabling more predictive drug development and truly personalized therapeutic strategies for patients worldwide.
References
- 1. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 2. recent developments and future prospects in stem-cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634165/]
- 3. Advances in Induced Pluripotent Stem Cell Reprogramming ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577567/]
- 4. Pluripotent Stem Cells: Recent Advances and Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025069/]
- 5. Stem cell therapy: a revolutionary cure or a pandora's box [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04334-1]
- 6. Patient and Disease–Specific Induced Pluripotent Stem ... [https://www.sciencedirect.com/science/article/pii/S0031699724009451]
- 7. Modeling human diseases with induced pluripotent stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC5868991/]
- 8. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 9. Human Stem Cells in Disease Modelling and Treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467989/]
- 10. Consortium on Advanced Stem Cell-Based Models in ... [https://www.isscr.org/stem-cell-models-consortium]
- 11. Patient and Disease–Specific Induced Pluripotent Stem Cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6934989/]
- 12. Applications of Patient-Specific Induced Pluripotent Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3005346/]
- 13. Human disease models in drug development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10173243/]
- 14. Beyond Animals: Revolutionizing Drug Discovery with Human ... [https://wyss.harvard.edu/news/beyond-animals-revolutionizing-drug-discovery-with-human-relevant-models/]
- 15. Multi-lineage Human iPSC-Derived Platforms for Disease ... [https://www.sciencedirect.com/science/article/pii/S1934590920300643]
- 16. Stem Cell Research Controversy: A Deep Dive (2025) [https://www.dvcstem.com/post/stem-cell-research-controversy]
- 17. Stem cell disease modeling: A new era for drug discovery [https://www.abcam.com/en-us/stories/articles/stem-cell-disease-modeling]
- 18. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 19. Modeling Human Neural Development and Disease with ... [https://www.isscr.org/upcoming-programs/poster-award-webinar]
- 20. Stem cell therapy for myocardial infarction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512856/]
- 21. Current status and new horizons in stem cell therapy in ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03018-z]
- 22. Stem Cell Therapy for Neurological Disorders (2025) [https://www.dvcstem.com/post/stem-cell-therapy-for-neurological-disorders]
- 23. Therapeutic potential of stem cell-derived somatic cells to ... [https://pubmed.ncbi.nlm.nih.gov/39861937/]
- 24. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 25. Mount Sinai Scientists Reverse Aging in Blood Stem Cells ... [https://www.mountsinai.org/about/newsroom/2025/mount-sinai-scientists-reverse-aging-in-blood-stem-cells-by-targeting-lysosomal-dysfunction]
- 26. Stem cells and organoids for disease-modeling and drug ... [https://sites.psu.edu/stemcellhershey/2025/05/19/stem-cell-and-organoids-for-disease-modeling-and-drug-development/]
- 27. Induced Pluripotent Stem Cells (iPSC) and Their Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590075/]
- 28. Editorial: Studying rare diseases using induced pluripotent ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1686438/full]
- 29. A comprehensive analysis of induced pluripotent stem cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1593207/full]
- 30. Human iPSC Reprogramming Success: The Impact of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11756937/]
- 31. iPSC Reprogramming - Sampled [https://sampled.com/services/cellular-services/ipsc-services/ipsc-reprogramming/]
- 32. Enhancing human pluripotent stem cell differentiation to ... [https://www.sciencedirect.com/science/article/pii/S2589004225007138]
- 33. Specific induction of right ventricular-like cardiomyocytes from ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04656-0]
- 34. Dynamic proteome profiling of differentiating human ... [https://www.nature.com/articles/s41598-025-24649-6]
- 35. MIT engineers turn skin cells directly into neurons for ... [https://news.mit.edu/2025/mit-engineers-turn-skin-cells-into-neurons-for-cell-therapy-0313]
- 36. Proteomics-based receptor-ligand matching enhances ... [https://pubmed.ncbi.nlm.nih.gov/40845849/]
- 37. Enhancement of hepatic differentiation from induced ... [https://pubmed.ncbi.nlm.nih.gov/40377485/]
- 38. Three-dimensional spheroid models for cardiovascular biology and pathology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12270648/]
- 39. Generation and applications of cardiac spheroids | npj Biomedical Innovations [https://www.nature.com/articles/s44385-025-00024-y]
- 40. Editing the genome of hiPSC with CRISPR/Cas9: disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5569153/]
- 41. Genome Editing in iPSC-Based Neural Systems [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2021.630600/full]
- 42. CRISPR/Cas system: An emerging technology in stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6851009/]
- 43. CRISPR/Cas9 therapeutics: progress and prospects [https://www.nature.com/articles/s41392-023-01309-7]
- 44. Clinical applications of the CRISPR/Cas9 genome-editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10425811/]
- 45. CRISPR–Cas9 epigenome editing enables high-throughput ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5462860/]
- 46. Exploiting CRISPR Cas9 in Three-Dimensional Stem Cell ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2020.00692/full]
- 47. CRISPR/Cas9-mediated generation of two isogenic ... [https://www.sciencedirect.com/science/article/pii/S187350612500131X]
- 48. Integrating artificial intelligence into small molecule ... [https://www.nature.com/articles/s44386-025-00029-y]
- 49. North America Drug Safety Testing Market By Application [https://www.linkedin.com/pulse/north-america-drug-safety-testing-market-application-tjcqc]
- 50. Hallmarks of MSCs: Key quality attributes for pharmacology ... [https://www.sciencedirect.com/science/article/abs/pii/S1934590925001882]
- 51. Transformative Role of Artificial Intelligence in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406033/]
- 52. Mechanistic data-informed multiscale quantitative systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12516987/]
- 53. A mechanistic quantitative systems pharmacology model ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1571844/full]
- 54. Comprehensive promotion of iPSC-CM maturation by ... [https://www.nature.com/articles/s41467-025-58044-6]
- 55. Electrical stimulation: a missing key to promote maturation ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1686342/full]
- 56. Electrical stimulation: a missing key to promote maturation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547514/]
- 57. Protocol for quantifying stem-cell-derived cardiomyocyte ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11145390/]
- 58. Development of a quantitative prediction algorithm for ... [https://www.nature.com/articles/s41467-021-24746-w]
- 59. Batch variability and anti-inflammatory effects of iPSC ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1536843/full]
- 60. Modeling rare genetic disease with patient-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317316/]
- 61. Disease Modeling | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/disease-modeling.html]
- 62. Scaling up pluripotent stem cell-based therapies [https://www.sciencedirect.com/science/article/pii/S1465324925006784]
- 63. Development of Standardized Methods and Analytical Tools [https://pubmed.ncbi.nlm.nih.gov/41136850/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1taFIjEhLwOV_vcj2BxtdLFQIjq8EFUdayGUNCUEoVKsWP2gIF&fc=None&ff=20251101122128&v=2.18.0.post22+67771e2]
- 64. Protocol for Maintaining iPSC Cultures [https://www.protocols.io/view/protocol-for-maintaining-ipsc-cultures-g788bzrzx.html]
- 65. Building an expert system for quantitative monitoring of ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925005511]
- 66. A scoping review of stem cell models of leukodystrophies [https://www.nature.com/articles/s41525-025-00533-0]
- 67. Differential Responses of Human iPSC-Derived Microglia ... [https://www.mdpi.com/2073-4409/14/21/1687]
- 68. Expansion of induced pluripotent stem cells under ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11802622/]
- 69. Induced Pluripotent Stem Cells Production Market Analysis [https://www.futuremarketinsights.com/reports/induced-pluripotent-stem-cells-production-market]
- 70. high-throughput technologies and automated workflows to ... [https://www.sciencedirect.com/science/article/pii/S0958166925000643]
- 71. Inside ELRIG's Drug Discovery 2025 [https://www.drugtargetreview.com/article/190237/inside-elrigs-drug-discovery-2025/]
- 72. - High Micro- Throughput in the Real World: 5 Uses You'll... Bioreactors [https://www.linkedin.com/pulse/high-throughput-micro-bioreactors-real-world-w1ubc]
- 73. Bioreactor Allows Automated Long-Term Culturing of Stem ... [https://www.fraunhofer.de/en/press/research-news/2025/january-2025/bioreactor-allows-automated-long-term-culturing-of-stem-cells.html]
- 74. SwRI-developed bioreactor replicates versatile induced ... [https://www.swri.org/newsroom/press-releases/swri-developed-bioreactor-replicates-versatile-induced-pluripotent-stem-cells]
- 75. Lab Automation for High Clone Throughput Screening [https://www.moleculardevices.com/service-support/lab-automation-solutions/lab-automation-for-high-throughput-clone-screening]
- 76. Automation Revolutionizes High Throughput ... [https://chronect.trajanscimed.com/news/high-throughput-experimentation-hte]
- 77. - High Micro- Throughput Market’s Consumer Landscape... Bioreactors [https://www.datainsightsmarket.com/reports/high-throughput-micro-bioreactors-1570080]
- 78. Reprogramming biology: iPSCs and the future of predictive research [https://www.jax.org/news-and-insights/2025/november/reprogramming-biology-ipscs-and-the-future-of-predictive-research]
- 79. Possible Strategies to Reduce the Tumorigenic Risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11120835/]
- 80. Genome Stability Program [https://hillmanresearch.upmc.edu/research/programs/ccsg/genome-stability]
- 81. New research identifies a protein essential to maintaining ... [https://ccr.cancer.gov/news/article/new-research-identifies-a-protein-essential-to-maintaining-chromosomal-stability]
- 82. Cancer and Aging Biomarkers: Classification, Early ... [https://www.mdpi.com/2079-6374/15/11/737]
- 83. A Machine Learning-Based Predictive Model for Stem Cell ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1683758/full]
- 84. Applications of artificial intelligence in stem cell therapy [https://pubmed.ncbi.nlm.nih.gov/40951704/]
- 85. Section 4: Stem -based Cell Systems — International Society for... Model [https://www.isscr.org/basic-research-standards/stem-cell-based-model-systems]
- 86. VV 40 - Assessing Credibility of Computational Modeling ... [https://www.asme.org/codes-standards/find-codes-standards/assessing-credibility-of-computational-modeling-through-verification-and-validation-application-to-medical-devices]
- 87. Credibility assessment of computational models according ... [https://www.sciencedirect.com/science/article/pii/S0169260723003930]
- 88. North America Legal and Regulatory Affairs Watchdog ... [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/04/09/north-america-legal-and-regulatory-affairs-watchdo]
- 89. Current Applications and Future Developments of the ASME ... [https://dmd.umn.edu/2025/vv40]
- 90. Credibility assessment of patient-specific modeling in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471805/]
- 91. Credibility Assessment of the Patient-Specific Modeling ... [https://link.springer.com/article/10.1007/s13239-025-00801-1]
- 92. Studying Rare Diseases Using induced Pluripotent Stem ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1686438/abstract]
- 93. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 94. Advancing the frontier of rare disease modeling: a critical ... [https://www.nature.com/articles/s41746-025-02068-1]
- 95. Primary cells vs. cell lines: Is it not time for something better? [https://www.bit.bio/blog/primary-cells-vs-cell-lines]
- 96. Cell-based drug discovery: Why human iPSC-derived ... [https://www.bit.bio/blog/cell-based-drug-discovery-with-human-ipsc-models]
- 97. Stop Sabotaging Your Science With the Wrong Cell Type [https://www.synthego.com/blog/crispr-cell-type-model/]
- 98. Moving Beyond Animal Models with iPSC-based Models [https://fujifilmbiosciences.fujifilm.com/us/blog/moving-beyond-animal-models-with-ipsc-based-models-shifts-and-new-challenges.html]
- 99. Replacing Animal Testing with Stem Cell-Organoids [https://pmc.ncbi.nlm.nih.gov/articles/PMC11319430/]
- 100. iPSC-derived and Patient-Derived Organoids: Applications ... [https://www.sciencedirect.com/science/article/pii/S2666027X24000501]
- 101. Induced Pluripotent Stem Cell (iPSC) Industry Trends for ... [https://bioinformant.com/ipsc-industry-trends/]
- 102. Validation and Trustworthiness of Multiscale Models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5818422/]
- 103. Study validates stem cell models for neurological diseases [https://www.news-medical.net/news/20250715/Study-validates-stem-cell-models-for-neurological-diseases.aspx]
- 104. Neurological disease models made clear [https://www.nature.com/articles/nm.3945]
- 105. A Review of Personalised Cardiac Computational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11131150/]
- 106. Cell-Specific Cardiac Electrophysiology Models [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1004242]
- 107. A Case Study in Neurotherapeutic Clinical Trial Design [https://consultqd.clevelandclinic.org/a-case-study-in-neurotherapeutic-clinical-trial-design-and-conduct]
- 108. Population-based mechanistic modeling allows for ... [https://www.nature.com/articles/s41540-018-0047-2]
- 109. - Patient pluripotent specific -based Parkinson's stem ... cell disease [https://pubmed.ncbi.nlm.nih.gov/31186086/]
- 110. JMIR AI - Machine-Learning Predictive Tool for the Individualized... [https://ai.jmir.org/2025/1/e64519]