Preventing Anoikis in Transplanted Stem Cells: Strategies for Enhancing Engraftment and Therapeutic Efficacy
This article provides a comprehensive analysis of anoikis, a form of detachment-induced apoptosis, as a critical barrier to successful stem cell transplantation.
Preventing Anoikis in Transplanted Stem Cells: Strategies for Enhancing Engraftment and Therapeutic Efficacy
Abstract
This article provides a comprehensive analysis of anoikis, a form of detachment-induced apoptosis, as a critical barrier to successful stem cell transplantation. Tailored for researchers, scientists, and drug development professionals, it explores the foundational mechanisms of anoikis, evaluates advanced methodological strategies like biomaterial scaffolds and growth factor delivery to circumvent cell death, and discusses optimization through preconditioning and genetic engineering. The content further covers validation techniques for assessing anoikis resistance and compares the efficacy of different therapeutic approaches, synthesizing key insights to guide the development of more effective and viable cell-based regenerative therapies.
Understanding Anoikis: The Fundamental Barrier to Stem Cell Engraftment
Anoikis is a specific form of programmed cell death (PCD) that is induced by inadequate or inappropriate cell-matrix interactions [1] [2]. The term, derived from the Greek word meaning "homelessness," was first defined in the early 1990s [2]. This process acts as a critical defense mechanism, ensuring tissue homeostasis by eliminating cells that detach from their native extracellular matrix (ECM), thereby preventing them from adhering to and growing in an ectopic location [3] [4]. In the context of stem cell transplantation, anoikis is a significant barrier, as donor cells are inevitably detached and placed into a new, unfamiliar microenvironment, triggering this form of cell death and limiting therapeutic efficacy [5].
Frequently Asked Questions (FAQs)
1. What is the fundamental role of anoikis in physiology and disease? Anoikis is essential for maintaining tissue homeostasis during development and in adult tissues [4]. It is a natural tumor-suppressing mechanism that clears displaced cells, thereby preventing colonization in distant organs [6] [7]. Consequently, resistance to anoikis is a hallmark of metastatic cancer cells, enabling their survival during systemic circulation [3] [7].
2. Why is understanding anoikis critical for stem cell transplantation research? In stem cell therapies, such as photoreceptor precursor cell (PRPC) transplantation for retinal degeneration, a substantial loss of donor cells occurs within the first week post-transplantation [5]. This early cell death significantly limits the pool of cells available for integration and functional restoration. While the immune response is a factor, research indicates that metabolic stress and anoikis are key drivers of this initial cell loss, highlighting the need for strategies to enhance anoikis resistance in therapeutic cells [5].
3. What are the primary molecular pathways that execute anoikis? Anoikis proceeds through classic apoptotic pathways, both intrinsic and extrinsic [7]. The intrinsic (mitochondrial) pathway is triggered by cellular stress from detachment, leading to increased mitochondrial membrane permeability and the release of cytochrome c, which activates caspase-9 and the downstream executioner caspases [7]. The extrinsic pathway is initiated by the activation of death receptors (e.g., Fas, TNFR) at the cell surface, leading to the formation of the death-inducing signaling complex (DISC) and activation of caspase-8 [7].
4. Besides apoptosis, what other forms of programmed cell death can be triggered by cell detachment? While anoikis specifically refers to apoptosis from loss of adhesion, other forms of PCD can also be initiated. Recent research focuses on the regulatory roles of non-coding RNAs (ncRNAs), including microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), which can fine-tune stem cell fate by modulating various PCD processes, including apoptosis, autophagy, and necroptosis [8].
Troubleshooting Guides
Problem: Poor Survival of Transplanted Stem Cells Post-Transplantation
Potential Cause: Activation of anoikis due to loss of integrin-mediated survival signaling and subsequent metabolic stress.
Investigation and Solution Pathway:
Step 1: Confirm Anoikis as the Primary Cause
- Objective: Verify that cell death is due to detachment and not other factors like immune rejection or nutrient deprivation.
- Protocol: In Vitro Anoikis Assay
- Culture Control: Maintain a portion of your stem cells in standard adherent culture conditions.
- Induce Detachment: Harvest the remaining cells using a gentle cell dissociation reagent. After washing, plate the cells onto poly-HEMA-coated culture dishes. Poly-HEMA prevents cell adhesion, forcing them into suspension.
- Incubation: Culture both adherent and suspension cells for 3-24 hours (time may vary by cell type).
- Analysis: Quantify cell death.
- Viability Staining: Use trypan blue exclusion or propidium iodide staining for a simple viability count.
- Apoptosis Assay: The gold standard is to use Annexin V/propidium iodide (PI) flow cytometry. Annexin V binds to phosphatidylserine, which is externalized in early apoptosis, while PI stains cells in late apoptosis or necrosis.
- Caspase Activity: Measure the activity of executioner caspases (e.g., caspase-3/7) using luminescent or fluorescent assay kits.
Step 2: Implement Strategies to Overcome Anoikis
Based on your confirmation, apply one or more of the following interventions.
Strategy A: Enhance Pro-Survival Signaling
- Rationale: Integrin engagement activates focal adhesion kinase (FAK) and downstream pathways like PI3K/Akt and ERK, which suppress pro-apoptotic proteins like BIM and promote survival [6] [4] [2].
- Protocol:
- Genetic Modulation: Transduce your stem cells with a lentivirus encoding a constitutively active form of Akt or FAK.
- Small Molecule Inhibition: Treat cells with a selective inhibitor of pro-apoptotic signaling. For example, if your cells show high levels of BIM phosphorylation/degradation via ERK, you could test the effect of a MEK/ERK pathway activator (e.g., synthetic ligand).
- Functional Validation: After intervention, repeat the in vitro anoikis assay (Step 1) to confirm increased survival in suspension.
Strategy B: Modulate Cell-Cell and Cell-Matrix Interactions
- Rationale: Transplanting cells as small aggregates, rather than single-cell suspensions, can preserve intercellular adhesion (e.g., E-cadherin), which provides survival signals that counteract anoikis [5] [4].
- Protocol: Aggregate Transplantation
- Preparation: Do not triturate your stem cell cultures into a single-cell suspension. Instead, gently mechanically dissociate them into small clusters of 50-500 cells.
- Delivery: Use a transplantation injector with a larger bore tip to avoid shearing these aggregates during the procedure [5].
- Assessment: Use non-invasive imaging (e.g., OCT) post-transplantation to monitor the initial size and integrity of the graft.
Strategy C: Target Metabolic Stress Pathways
- Rationale: Recent single-cell RNA sequencing data reveals that metabolic stress, characterized by dysregulation of mitochondrial function and oxidative phosphorylation, is a key driver of early donor cell death post-transplantation [5].
- Protocol: Enhancing Metabolic Resilience
- Pre-conditioning: Prior to transplantation, culture your stem cells with metabolites or compounds that boost oxidative metabolism, such as acetyl-L-carnitine or coenzyme Q10.
- Media Supplementation: Include these metabolites in the transplantation suspension medium and the immediate post-transplantation culture media in vivo (if applicable).
- Outcome Measurement: Assess the mitochondrial membrane potential (using dyes like JC-1 or TMRM) and cellular ATP levels in pre-conditioned vs. control cells after detachment to confirm improved metabolic health.
Problem: Acquired Anoikis Resistance Leading to Potential Safety Concerns
Potential Cause: Inadvertent selection or induction of stem cells with hyperactive pro-survival pathways, which could pose a tumorigenic risk.
Investigation and Solution Pathway:
Step 1: Characterize the Anoikis-Resistant Phenotype
- Objective: Identify the molecular alterations conferring anoikis resistance.
- Protocol: Molecular Profiling
- Western Blot Analysis: Compare the phosphorylation (activation) status of key survival proteins (e.g., p-FAK, p-Akt, p-ERK) between your anoikis-resistant cells and normal parental cells, under both adherent and suspension conditions.
- EMT Marker Analysis: Anoikis resistance is often linked to the Epithelial-Mesenchymal Transition (EMT). Check for a loss of epithelial markers (e.g., E-cadherin) and a gain of mesenchymal markers (e.g., N-cadherin, Vimentin, SNAIL, TWIST) via immunostaining or qPCR [2].
- Functional Assay: Perform a soft agar colony formation assay to assess anchorage-independent growth, a hallmark of transformation.
Step 2: Implement Safety Measures
- Strategy: Use Inducible Expression Systems
- Rationale: To avoid permanent, constitutive activation of oncogenic pathways.
- Protocol: If genetic modification is used to enhance survival, employ a doxycycline-inducible gene expression system. This allows you to turn on the pro-survival gene (e.g., Akt) only during the critical window of transplantation, and turn it off once cells have integrated and the risk of anoikis has passed.
Table 1: Key Signaling Pathways and Molecules Regulating Anoikis
| Pathway/Molecule | Role in Anoikis | Experimental Modulation | Effect on Cell Survival |
|---|---|---|---|
| FAK/PI3K/Akt [6] [4] | Pro-survival; inactivated upon detachment. | Overexpression of constitutively active Akt. | Induces anoikis resistance. |
| EGFR/HER2 [6] | Pro-survival; often overexpressed in resistant cells. | Treatment with inhibitors (e.g., WZ4002, AST1306). | Sensitizes cells to anoikis. |
| BCL-2 Family [7] | Balances pro- and anti-apoptotic signals. | Overexpression of BCL-xL (anti-apoptotic). | Inhibits anoikis. |
| SNAIL/SIP1 [2] | Transcriptional repressors; induce EMT and resistance. | E-cadherin promoter hypermethylation. | Promotes anoikis resistance and metastasis. |
| Reactive Oxygen Species (ROS) [7] | Detachment can alter ROS levels, inducing stress. | Scavenging ROS with antioxidants. | Outcome is context-dependent. |
Table 2: Summary of Key Research Reagents for Anoikis Studies
| Reagent / Material | Function / Application | Example in Context |
|---|---|---|
| Poly-HEMA [2] | Coating for culture surfaces to prevent cell adhesion; essential for in vitro anoikis assays. | Used to simulate detachment and induce anoikis in cultured stem cells. |
| Annexin V / Propidium Iodide (PI) | Flow cytometry staining to distinguish early apoptotic (Annexin V+/PI-), late apoptotic (Annexin V+/PI+), and necrotic (Annexin V-/PI+) cells. | Standard method to quantify the percentage of cells undergoing apoptosis after transplantation or suspension culture. |
| Caspase-3/7 Activity Assay Kits | Luminescent or fluorescent-based measurement of executioner caspase activity, a direct marker of apoptosis. | Provides a quantitative readout of anoikis activation in cell populations. |
| FAK Inhibitor (e.g., PF-562271) | Small molecule inhibitor of Focal Adhesion Kinase; used to block integrin-mediated survival signaling. | Used in control experiments to confirm the role of FAK in promoting survival of adherent cells. |
| AZD6244 (Selumetinib) | Small molecule inhibitor of MEK, a kinase in the ERK survival pathway. | Used to study the contribution of the MEK/ERK pathway to anoikis resistance. |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Investigating Anoikis in Stem Cell Transplantation
| Category | Reagent/Material | Brief Function/Explanation |
|---|---|---|
| Culture & Assay | Poly-HEMA | Creates a non-adherent surface to experimentally induce anoikis in vitro. |
| Laminin / Fibronectin | ECM proteins used to coat surfaces and restore integrin signaling, testing its sufficiency for survival. | |
| Detection & Analysis | Annexin V / PI Kit | Gold-standard kit for detecting apoptosis via flow cytometry. |
| Caspase-3/7 Activity Assay | Provides a direct, quantitative measure of apoptosis execution. | |
| Phospho-Specific Antibodies | For Western Blot (e.g., p-FAK, p-Akt, p-ERK) to assess activity of survival pathways. | |
| Genetic Modulation | Lentiviral Vectors | For stable overexpression (e.g., of BCL-2, Akt) or shRNA knockdown (e.g., of BIM) of anoikis regulators. |
| Doxycycline-Inducible System | Allows temporal control over transgene expression, enhancing safety in therapeutic contexts. | |
| Small Molecule Modulators | FAK Inhibitor (e.g., PF-562271) | Tool to block pro-survival integrin signaling. |
| MEK/ERK Pathway Activators/Inhibitors | Tools to manipulate this critical survival pathway. | |
| Metabolic Compounds (e.g., Acetyl-L-carnitine) | Used to pre-condition cells and enhance their metabolic resilience to detachment stress [5]. |
The Critical Role of Integrin and ECM Signaling in Cell Survival
Troubleshooting FAQs: Integrin and Anoikis Research
Q1: My transplanted stem cells are showing low survival rates in suspension culture. What could be the cause? Low survival in suspension is often due to anoikis—a form of apoptosis triggered by detachment from the extracellular matrix (ECM) [9]. This indicates your cells lack essential survival signals normally provided by integrin-ECM binding. To address this, ensure you are providing a provisional ECM scaffold or activating key integrin-mediated survival pathways like FAK/Src and PI3K/Akt [10].
Q2: Which integrin subtypes are most critical for promoting survival in stem cells? While the specific profile can vary by cell type, integrins that bind to collagen (e.g., via α2β1) and laminin (e.g., via α6β1) are often crucial for epithelial and stem cell survival [11]. In research models, α3β1 and α11β1 have been implicated in activating pro-survival Src kinase signaling, which can circumvent anoikis [11].
Q3: How can I confirm that integrin signaling is active in my culture system? You can confirm active integrin signaling by detecting the phosphorylation of key downstream effectors like Focal Adhesion Kinase (FAK) at Tyr397 or Src at Tyr418 using western blotting or specific antibodies [10]. The formation of focal adhesions, visible through vinculin staining, is another key indicator of functional integrin-ECM connections [10].
Q4: What are the common molecular changes in cells that have become resistant to anoikis? Anoikis-resistant cells often exhibit dysregulation of apoptotic signaling pathways (both intrinsic and extrinsic), undergo epithelial-mesenchymal transition (EMT), and display metabolic reprogramming towards glycolysis to sustain energy production without matrix attachment [9] [12]. They may also show altered expression of specific integrins that sustain survival signals even in detachment [11].
Key Quantitative Data in Integrin-Mediated Survival
Table 1: Integrin Subunits and Their Roles in Cell Survival and Anoikis Resistance
| Integrin Subunit | Primary Ligands | Role in Survival & Anoikis Resistance |
|---|---|---|
| α3β1 [11] | Laminin, Fibronectin [11] | Mediates resistance to targeted therapy in melanoma via Src kinase activation; potential role in evading anoikis [11]. |
| α11β1 [11] | Collagen [11] | Works alongside α3β1 to drive pro-survival signaling and therapy resistance [11]. |
| α6β4 [11] | Laminin [11] | Promotes aggressive tumor behavior and is involved in metastasis [11]. |
| αvβ3 [11] | Fibronectin, Vitronectin (RGD-motif) [11] | Recognizes RGD motif; implicated in angiogenesis and cell survival [11]. |
Table 2: Core Components of Anoikis Resistance Pathways
| Molecular Component | Function | Effect on Anoikis |
|---|---|---|
| FAK (Focal Adhesion Kinase) [10] | Autophosphorylates at Tyr397 upon integrin clustering, recruits Src [10] | Promotes survival; inhibition induces anoikis. |
| Src [10] | Phosphorylates FAK, p130CAS, and paxillin [10] | Activates multiple downstream pro-survival and motility pathways. |
| PI3K/Akt [10] | Key survival pathway activated by integrins and growth factors [10] | Inactivates pro-apoptotic proteins like Bad, suppressing cell death. |
| Bim / Bax [9] | Pro-apoptotic BH3-only protein [9] | Directly triggers apoptosis; often downregulated in anoikis-resistant cells. |
Detailed Experimental Protocols
Protocol 1: Assessing Anoikis in Non-Adherent Conditions
Purpose: To quantify the rate of cell death specifically due to loss of cell-ECM attachment.
Methodology:
- Prepare Cells: Harvest your stem cells using a gentle method like Accutase to preserve membrane integrity.
- Create Suspension: Seed cells onto ultra-low attachment plates or plates coated with a non-adhesive polymer (e.g., poly-HEMA) to prevent adhesion. Use standard adhesion culture as a control.
- Incubate: Culture cells for 6-72 hours, depending on your cell type's sensitivity.
- Analyze Cell Death:
- Flow Cytometry: Use Annexin V/PI staining to distinguish apoptotic (Annexin V+/PI-) and late apoptotic/necrotic (Annexin V+/PI+) populations.
- Western Blotting: Analyze cleavage of executioner caspases (e.g., Caspase-3) and key survival pathway proteins like phosphorylated Akt.
Protocol 2: Validating Integrin-Mediated Survival Signaling
Purpose: To confirm the activation of specific integrin downstream pathways in your survival-promoting conditions.
Methodology:
- Stimulate or Inhibit: Treat cells with (a) ECM components like fibronectin or laminin, (b) function-blocking anti-integrin antibodies, or (c) pharmacological inhibitors (e.g., FAK inhibitor PF-562271).
- Lyse Cells: Harvest cell lysates after appropriate treatment times.
- Western Blot Analysis: Probe lysates with the following antibodies to detect key signaling nodes [10]:
- Phospho-FAK (Tyr397): Indicator of initial integrin-mediated FAK activation.
- Phospho-Src (Tyr418): Indicator of Src kinase activity.
- Phospho-Akt (Ser473): Indicator of PI3K/Akt survival pathway activity.
- Total protein antibodies for each to ensure equal loading.
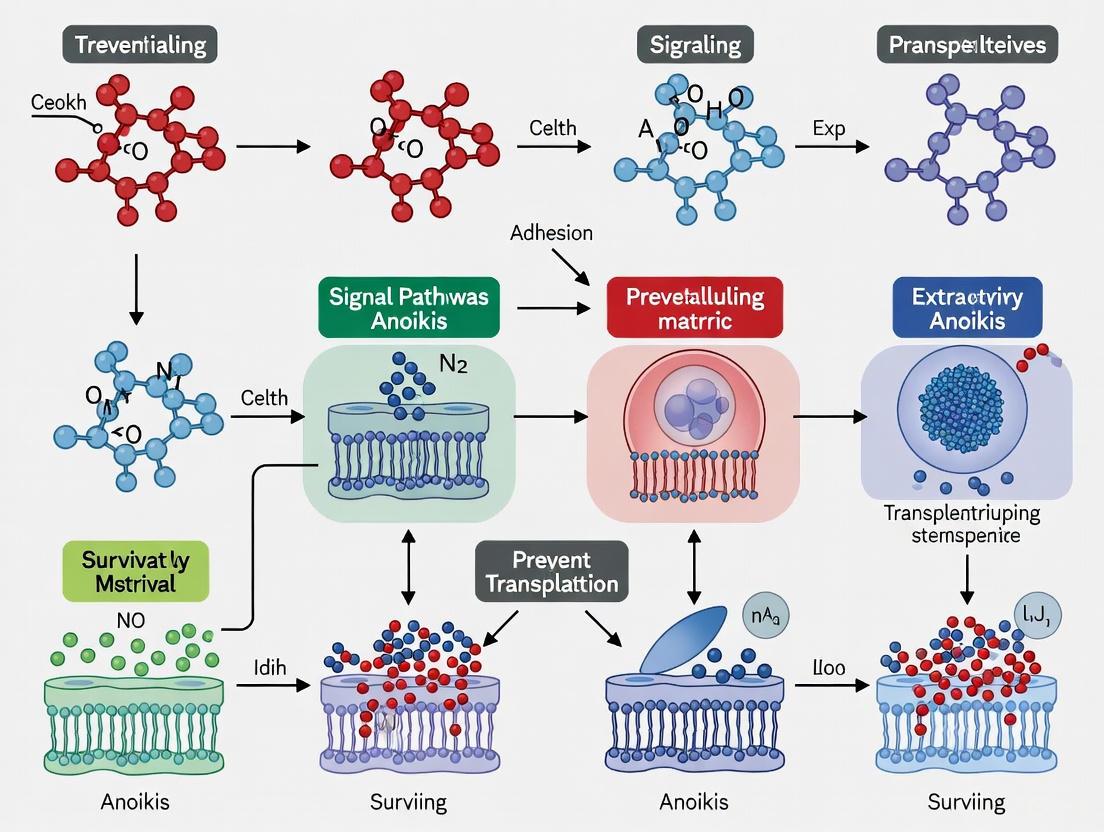
Signaling Pathway Visualizations
Integrin Survival Signaling Pathway
Experimental Workflow for Anoikis Assay
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Studying Integrin Signaling and Anoikis
| Reagent / Material | Specific Example (Catalog Number) | Function in Experiment |
|---|---|---|
| Function-Blocking Anti-Integrin Antibody | N/A - Target specific α or β subunits | Blocks ligand binding to specific integrin heterodimers to test their necessity in survival. |
| Recombinant ECM Proteins | Fibronectin, Laminin, Collagen I/IV | Coats culture surfaces to provide specific survival signals via corresponding integrins. |
| FAK Inhibitor | PF-562271 (Research compound) | Pharmacologically inhibits FAK tyrosine kinase activity to probe its role in survival. |
| Phospho-Specific Antibodies | Phospho-FAK (Tyr397) #44624G [10], Phospho-Src (Tyr418) #44660G [10] | Detects activation of key integrin downstream signaling nodes via Western Blot or IF. |
| Anoikis Induction Plates | Commercially available Ultra-Low Attachment plates | Prevents cell adhesion to any substrate, creating a controlled environment to study detachment-induced death. |
| Apoptosis Detection Kit | Annexin V-FITC / PI Kit | Quantifies the percentage of apoptotic cells via flow cytometry in suspension cultures. |
| Caveolin-1 Antibody | Caveolin 1 Antibody PA1064 [10] | Investigates the role of caveolae-mediated integrin signaling, an alternative MAPK activation pathway. |
FAQs and Troubleshooting Guides
Fundamental Mechanisms
What are the intrinsic and extrinsic pathways of apoptosis in the context of anoikis? Anoikis is a specific form of programmed cell death triggered by the loss of correct cell-ECM adhesion. It is executed through classical apoptotic pathways [13].
- Intrinsic Pathway: Also known as the mitochondrial pathway, it is initiated by internal cellular stress. In anoikis, the lack of survival signals from integrin binding leads to an imbalance in Bcl-2 family proteins. This promotes mitochondrial outer membrane permeabilization (MOMP), resulting in cytochrome c release and apoptosome formation, which activates caspase-9 [14] [15].
- Extrinsic Pathway: This pathway is initiated by the activation of transmembrane death receptors (e.g., Fas) upon ligand binding. This leads to the formation of the Death-Inducing Signaling Complex (DISC), which activates caspase-8 [16] [14]. Caspase-8 can then directly cleave and activate executioner caspases or amplify the death signal by cleaving Bid, which feeds into the intrinsic pathway [15].
Why is understanding anoikis crucial for stem cell transplantation therapy? Substantial early donor cell loss remains a major challenge in stem cell-based therapies for retinal degenerative diseases [5]. Recent research indicates that a key driver of this early cell death is metabolic stress, characterized by dysregulation of mitochondrial function and oxidative phosphorylation pathways [5]. This metabolic stress directly engages the intrinsic apoptotic pathway, leading to caspase activation and cell death, even in the presence of effective immunosuppression [5]. Therefore, inhibiting anoikis and related stress-induced apoptosis is critical for improving transplant survival.
Experimental Challenges
My transplanted stem cells are dying despite immunosuppression. What could be the cause? Your observations are consistent with recent findings. While immune rejection is a concern, early cell death can occur via non-immune mechanisms. As highlighted in photoreceptor precursor cell transplantation studies, metabolic stress is a critical barrier to cell survival post-transplantation [5]. This stress activates the intrinsic apoptosis pathway. Furthermore, cellular damage during the transplantation procedure or anoikis due to loss of adhesion can also contribute to caspase activation and early cell loss [5] [13].
I need to detect early apoptosis in my 3D stem cell cultures. What is the best method? For detecting early apoptosis, especially where membrane integrity is initially maintained, the following combination is recommended:
- Annexin V Staining: Detects the externalization of phosphatidylserine on the outer leaflet of the cell membrane, a hallmark of early apoptosis [15].
- Propidium Iodide (PI) Exclusion: Serves as a viability marker. PI is excluded from live, healthy cells and early apoptotic cells. Its uptake indicates late apoptosis or necrosis due to membrane compromise [15]. Using Annexin V+/PI- staining allows for the specific identification of cells in the early stages of apoptosis before loss of membrane integrity.
How can I differentiate between the intrinsic and extrinsic pathways in my anoikis model? You can dissect the pathway involvement by targeting specific components and observing the effect on cell survival. The table below outlines key strategies.
Table: Experimental Strategies to Differentiate Apoptotic Pathways in Anoikis
| Target | Experimental Tool | Mechanism of Action | Expected Outcome if Pathway is Critical |
|---|---|---|---|
| Caspase-8 | siRNA, Z-IETD-FMK (inhibitor) | Inhibits initiator caspase of the extrinsic pathway [16]. | Increased cell survival under anoikis conditions. |
| Caspase-9 | siRNA, Z-LEHD-FMK (inhibitor) | Inhibits initiator caspase of the intrinsic apoptosome pathway [16] [17]. | Increased cell survival under anoikis conditions. |
| Bcl-2 Family | BH3 mimetics (e.g., Venetoclax) | Inhibits anti-apoptotic proteins (e.g., Bcl-2, Bcl-xL), promoting intrinsic pathway activation [15]. | Decreased cell survival under anoikis conditions. |
| Death Receptors | Neutralizing antibodies (e.g., anti-Fas) | Blocks ligand binding and activation of the extrinsic pathway [14]. | Increased cell survival, implicating extrinsic signaling. |
Pathway Optimization
What strategies can I use to enhance stem cell survival by inhibiting anoikis?
- Target Metabolic Stress: Pre-condition stem cells to enhance their metabolic resilience prior to transplantation. This could involve adapting them to specific nutrient conditions or mild stress to upregulate protective pathways, countering the mitochondrial dysregulation observed post-transplant [5].
- Modulate Anti-apoptotic Proteins: Overexpress anti-apoptotic members of the Bcl-2 family (e.g., Bcl-2, Bcl-xL) to prevent MOMP and cytochrome c release, thereby inhibiting the intrinsic pathway [15].
- Engineer Anoikis Resistance: Investigate mechanisms used by metastatic cancer cells, such as upregulation of pro-survival signaling (e.g., PI3K/Akt, NF-κB) or alterations in cytoskeletal dynamics that generate pro-survival signals like blebs, to inform strategies for protecting stem cells [13].
- Utilize Non-coding RNAs: Explore the role of microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs) as they are pivotal regulators of programmed cell death in stem cells. For example, miR-302/367 can inhibit apoptosis by down-regulating the pro-apoptotic protein BNIP3L and up-regulating the anti-apoptotic BCL-xL [8].
Experimental Protocols
Protocol 1: Differentiating Apoptosis Pathways via Caspase Inhibition
Objective: To determine the relative contribution of intrinsic versus extrinsic caspase pathways to anoikis in your stem cell model.
Materials:
- Caspase-8 inhibitor (e.g., Z-IETD-FMK)
- Caspase-9 inhibitor (e.g., Z-LEHD-FMK)
- Pan-caspase inhibitor (e.g., Z-VAD-FMK) as a positive control
- Soluble death receptor ligands (e.g., FasL) - optional, for extrinsic pathway activation
- Annexin V / PI Apoptosis Detection Kit
- Equipment: Flow cytometer, cell culture facilities for suspension (e.g., poly-HEMA coated plates)
Method:
- Induce Anoikis: Harvest your stem cells and plate them onto ultra-low attachment or poly-HEMA coated plates to prevent adhesion. Maintain control cells in normal adherent culture.
- Apply Inhibitors: Simultaneously with plating, treat the cells with the following:
- Condition A: Vehicle control (DMSO)
- Condition B: Caspase-8 inhibitor (e.g., 20 µM Z-IETD-FMK)
- Condition C: Caspase-9 inhibitor (e.g., 20 µM Z-LEHD-FMK)
- Condition D: Pan-caspase inhibitor (e.g., 20 µM Z-VAD-FMK)
- Incubate: Culture the cells for 16-24 hours.
- Assess Apoptosis: Harvest the cells and stain with Annexin V and PI according to the kit protocol. Analyze by flow cytometry.
- Interpret Results:
- A significant reduction in Annexin V+ cells in the caspase-9 inhibited group points to a dominant intrinsic pathway.
- A significant reduction in the caspase-8 inhibited group suggests a dominant extrinsic pathway.
- Protection in both conditions indicates both pathways are active.
Protocol 2: Assessing Mitochondrial Involvement via Cytochrome c Release
Objective: To visualize the key event of the intrinsic pathway—cytochrome c release from mitochondria—during anoikis.
Materials:
- Cells undergoing anoikis and adherent controls
- Fixative (e.g., 4% PFA)
- Permeabilization buffer (e.g., 0.1% Triton X-100)
- Blocking solution (e.g., 5% BSA in PBS)
- Primary antibody: Mouse anti-cytochrome c
- Primary antibody: Rabbit anti-COX IV (mitochondrial marker)
- Fluorescently-labeled secondary antibodies (e.g., anti-mouse IgG-Alexa Fluor 488, anti-rabbit IgG-Alexa Fluor 568)
- Hoechst or DAPI nuclear stain
- Equipment: Confocal microscope
Method:
- Culture and Fix: Plate cells for anoikis induction and adherent controls. After an appropriate time point (e.g., 6-12 hours), fix the cells with 4% PFA for 15 minutes.
- Permeabilize and Block: Permeabilize cells with 0.1% Triton X-100 for 10 minutes, then block with 5% BSA for 1 hour.
- Stain: Incubate with primary antibodies (anti-cytochrome c and anti-COX IV) diluted in blocking buffer overnight at 4°C. Wash, then incubate with appropriate secondary antibodies for 1 hour at room temperature. Finally, stain nuclei with Hoechst/DAPI.
- Image and Analyze: Acquire high-resolution images using a confocal microscope.
- In healthy/adherent cells: Cytochrome c staining (green) should perfectly overlap with the mitochondrial marker COX IV (red), appearing as yellow in merged images.
- In cells undergoing intrinsic apoptosis: Cytochrome c will be released from the mitochondria, resulting in a diffuse green signal throughout the cell that no longer co-localizes with the red mitochondrial signal.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for Studying Caspase Pathways and Anoikis
| Reagent / Assay | Function / Target | Key Application in Anoikis Research |
|---|---|---|
| Z-VAD-FMK | Pan-caspase inhibitor | To confirm caspase-dependent cell death is occurring [17]. |
| Z-IETD-FMK (Caspase-8 Inh.) | Caspase-8 inhibitor | To probe the role of the extrinsic death receptor pathway [16]. |
| Z-LEHD-FMK (Caspase-9 Inh.) | Caspase-9 inhibitor | To probe the role of the intrinsic mitochondrial pathway [16] [17]. |
| Annexin V Detection Kits | Phosphatidylserine exposure | To detect early-stage apoptosis by flow cytometry or microscopy [15]. |
| TMRE / JC-1 Dyes | Mitochondrial membrane potential (ΔΨm) | To assess mitochondrial health and early intrinsic pathway activation; loss of signal indicates depolarization [15]. |
| TUNEL Assay | DNA fragmentation | To detect late-stage apoptosis; confirms cell death but is not pathway-specific [15]. |
| Antibody: Cleaved Caspase-3 | Activated executioner caspase | A definitive marker that apoptosis is executing, downstream of both intrinsic and extrinsic pathways [15]. |
| Antibody: Cytochrome c | Mitochondrial protein | Used in immunofluorescence to visualize its release into the cytosol, a key intrinsic pathway event [14] [15]. |
| BH3 Mimetics (e.g., Venetoclax) | Bcl-2 family inhibitors | To experimentally induce or sensitize cells to the intrinsic apoptotic pathway [15]. |
| Poly-HEMA | Non-adhesive coating | To create a reliable in vitro model for inducing anoikis by preventing cell adhesion [13]. |
Caspase Activation Pathways in Apoptosis and Anoikis
The following diagrams illustrate the core caspase activation cascades, which are central to executing anoikis.
Intrinsic and Extrinsic Apoptosis Pathways
Caspase Activation Hierarchy in the Intrinsic Pathway
Stem cell transplantation represents a frontier in regenerative medicine, offering potential treatments for conditions ranging from genetic diseases to organ failure. However, a critical vulnerability threatens the success of these procedures: anoikis, a form of programmed cell death triggered when cells detach from their native extracellular matrix (ECM). This technical support center provides researchers with targeted guidance for understanding and preventing anoikis in transplanted stem cells, framed within the broader research context of enhancing transplantation efficacy.
Understanding the Vulnerability: FAQs on Stem Cells and Anoikis
What is anoikis and why does it threaten transplanted stem cells?
Anoikis (from the Greek meaning "homelessness") is a specific type of programmed cell death induced by disruption of cell-ECM interactions [18]. It serves as a crucial physiological mechanism to eliminate misplaced cells and maintain tissue homeostasis [12]. During transplantation procedures, stem cells are deliberately detached from their native microenvironment, potentially triggering this apoptotic pathway and significantly reducing engraftment efficiency.
How does the transplantation process specifically induce anoikis?
The transplantation workflow inherently creates multiple stress points where anoikis can be initiated:
- Isolation Phase: Enzymatic or mechanical dissociation severs stem cell-ECM connections
- Processing & Expansion: Cells lack proper adhesion signals during ex vivo culture and manipulation
- Transport/Infusion: Cells remain in suspension without matrix contact
- Pre-Engraftment Period: Time lag before new host matrix connections establish
Are all stem cell types equally vulnerable to anoikis?
No – susceptibility varies significantly by stem cell origin and differentiation status. Research indicates that epithelial-derived stem cells and certain primed pluripotent states demonstrate higher anoikis sensitivity compared to mesenchymal stem cells, which naturally exhibit greater motility and matrix independence. Cancer stem cells (CSCs) demonstrate particularly effective anoikis resistance mechanisms, providing valuable insights for protective strategies [19] [12].
What intracellular signaling pathways mediate anoikis in stem cells?
Anoikis execution involves multiple interconnected pathways that converge on apoptosis effectors:
Table: Key Signaling Pathways in Stem Cell Anoikis
| Pathway | Role in Anoikis | Key Components |
|---|---|---|
| Integrin-FAK | Primary survival signal from ECM | Integrins, FAK, SRC, PI3K |
| Metabolic Reprogramming | Adaptation to detachment | AMPK, mTOR, glucose metabolism |
| EMT Pathways | Stemness and survival regulation | TGF-β, Wnt/β-catenin, Notch |
| Mitochondrial (Intrinsic) Apoptosis | Cell death execution | BCL-2 family, cytochrome c, caspase-9 |
| Death Receptor (Extrinsic) Apoptosis | Alternative activation | Caspase-8, FADD |
Troubleshooting Guides: Preventing Anoikis in Research Protocols
Problem: Poor post-transplantation stem cell survival rates
Potential Causes and Solutions:
- Insufficient matrix-mimicking support during cell processing
- Solution: Implement temporary ECM-mimetic hydrogels in transplantation media
- Protocol: Blend RGD-sequence peptides (1-2 mM) or laminin-derived fragments (0.5-1 mg/mL) in carrier solution for cell suspension
Overly prolonged detachment during pre-transplantation processing
- Solution: Optimize workflow to minimize time between harvesting and transplantation
- Protocol: Establish strict timeline benchmarks with checkpoints at each processing stage
Lack of pro-survival signaling during critical window
- Solution:
- Pre-condition cells with anoikis inhibitors (e.g., caspase inhibitors, 20-50 µM)
- Implement metabolic priming (cyclic AMP signaling enhancers)
- Experimental Validation: Measure activated caspase-3/7 levels at 6-hour post-detachment as anoikis indicator
- Solution:
Problem: Inconsistent anoikis resistance across stem cell batches
Standardization Protocol:
- Pre-conditioning regimen (implement 48 hours pre-harvest):
- Culture cells on collagen IV-coated surfaces (5-10 µg/cm²)
- Add FAK pathway enhancers (e.g., 10-25 nM NSC228155)
- Include metabolic modulators (1-2 mM metformin for AMPK activation)
Quality control checkpoint (assess pre-transplantation):
- Perform anoikis susceptibility assay: plate cells on ultra-low attachment plates
- Measure viability at 4-hour intervals using real-time apoptosis markers
- Establish acceptance threshold: >70% viability at 12 hours suspension
Molecular verification:
- Validate EMT marker upregulation (N-cadherin, vimentin)
- Confirm metabolic adaptation (increased glycolysis capacity)
- Verify antioxidant defense elevation (GPx, SOD activity)
Experimental Protocols: Key Methodologies
Protocol 1: Quantitative Anoikis Susceptibility Assessment
Purpose: Standardize measurement of stem cell vulnerability to detachment-induced death.
Materials:
- Ultra-low attachment multiwell plates (Corning Costar)
- Anoikis assay buffer (standard culture medium + 0.5% methylcellulose)
- Real-time apoptosis detection reagent (Annexin V-Cy5 conjugate, 1:200 dilution)
- Metabolic viability probe (PrestoBlue, 10% v/v)
- Flow cytometer with 96-well plate adapter
Procedure:
- Harvest test stem cells using standard detachment protocol
- Resuspend in anoikis assay buffer at 1×10⁵ cells/mL
- Distribute 200 µL/well into ultra-low attachment plates
- At t=0, 4, 8, 12, 24 hours:
- Transfer 50 µL aliquots to analysis plates
- Add Annexin V-Cy5 and incubate 15 minutes protected from light
- Add PrestoBlue and incubate additional 45 minutes
- Analyze via flow cytometry (Annexin V+ = apoptotic; metabolic activity = viability)
- Calculate anoikis index: (Annexin V+ cells at 12h)/(total cells at t=0) × 100
Interpretation: Anoikis index <15% indicates high resistance; 15-30% moderate; >30% high susceptibility.
Protocol 2: Matrix-Mimetic Protection Screening
Purpose: Identify optimal ECM components for specific stem cell types.
Materials Screening Array:
- Fibronectin-derived RGD peptides (0.1-2.0 mM)
- Laminin-511 E8 fragments (0.1-1.0 mg/mL)
- Collagen I/IV-derived peptides (0.5-2.0 mg/mL)
- Hyaluronic acid derivatives (0.1-0.5% w/v)
- Synthetic integrin-binding polymers (PHSRN-grafted polyacrylamide)
Procedure:
- Prepare test matrix components in carrier solution at varying concentrations
- Mix with cell suspension immediately post-detachment (final volume ratio 1:10)
- Maintain in suspension culture with gentle rotation ( prevents settling)
- Assess viability and apoptosis markers at 6, 12, 24 hours
- Identify optimal component and concentration yielding >80% viability at 12 hours
Signaling Pathways and Molecular Mechanisms
The diagram below illustrates the key signaling pathways involved in anoikis regulation in stem cells, highlighting potential therapeutic intervention points.
Research Reagent Solutions
Table: Essential Reagents for Anoikis Prevention Research
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| Anoikis Inducers | Ultra-low attachment platesAnti-integrin β1 antibodiesRGD competitive inhibitors | Experimental induction of detachmentBlocking integrin signalingCompetitive disruption of adhesion |
| Anoikis Inhibitors | Caspase inhibitors (Z-VAD-FMK)FAK pathway activators (NSC228155)RGD-sequence peptidesRecombinant laminin fragments | Direct apoptosis blockadeEnhanced survival signalingMatrix mimicry in suspensionNatural ligand replacement |
| Detection Assays Real-time Annexin V probesCaspase-3/7 activity assaysMetabolic viability indicators (PrestoBlue, MTT)EMT marker antibodies | Early apoptosis detectionExecution phase monitoringViability assessmentStemness state evaluation | |
| Matrix Components | Recombinant laminin-511 E8Fibronectin-derived peptidesCollagen IV fragmentsSynthetic polymer scaffolds | High-potency natural matrixIntegrin-binding sequencesBasement membrane componentTunable artificial microenvironment |
| Pathway Modulators | PI3K/AKT activators (SC79)Metabolic reprogramming agents (Metformin)ROS scavengers (N-acetylcysteine)Hedgehog pathway agonists (SAG) | Survival pathway enhancementEnergy stress adaptationOxidative damage protectionStemness maintenance |
Advanced Research Applications
Clinical Translation: Insights from Recent Trials
A 2025 Phase 1 clinical trial demonstrated the feasibility of targeting the vulnerability window in stem cell transplantation [20]. Researchers successfully used an antibody against CD117 (briquilimab) to prepare patients for stem cell transplantation without toxic chemotherapy or radiation, achieving nearly 100% donor cell engraftment in three pediatric patients with Fanconi anemia. This approach specifically targets the stem cell vulnerability window while avoiding conventional genotoxic preparation methods.
Single-Cell Analysis Applications
Recent advances enable unprecedented resolution in studying anoikis resistance. Single-cell RNA sequencing can identify subpopulations with innate resistance properties, while spatial transcriptomics maps protective niche interactions [21]. Implement these technologies to:
- Identify transcriptional programs in anoikis-resistant stem cell subsets
- Map ligand-receptor interactions between stem cells and protective niche cells
- Discover novel resistance biomarkers for stem cell quality control
Biomarker Development for Transplantation Readiness
Quantitative parameters predicting transplantation success include:
- EMT marker ratio (N-cadherin:E-cadherin >2.5)
- Metabolic flexibility index (glycolytic capacity:OXPHOS capacity >1.8)
- Antioxidant capacity (GPx activity >25 mU/10⁶ cells)
- Surface integrin profiling (α6β1 integrin density >5000 molecules/µm²)
Establish laboratory-specific thresholds through correlation with engraftment efficiency in model systems.
The vulnerability of stem cells to detachment-induced death during transplantation represents a significant but addressable challenge. By understanding the molecular mechanisms of anoikis and implementing the targeted strategies outlined in this technical resource, researchers can significantly improve stem cell survival and engraftment efficiency. The continued integration of mechanistic insights from cancer stem cell biology [19] [12], advanced bioinformatics approaches [21], and innovative clinical protocols [20] will further enhance our ability to protect these valuable cells throughout the transplantation process, ultimately improving outcomes in regenerative medicine applications.
Anoikis is a form of programmed cell death triggered when cells detach from their native extracellular matrix (ECM) [22]. For adherent cells, including many stem cells, interaction with the ECM via integrins transmits vital survival signals; disruption of this interaction initiates caspase-mediated apoptotic pathways [22] [23]. In the context of cell transplantation, this is a critical challenge. The very process of harvesting cells for therapy—using enzymes to detach them from culture surfaces—inevitably induces anoikis [23]. Subsequently, these cells are injected into a hostile in vivo environment where they may fail to re-establish proper matrix contacts, leading to widespread death of the transplanted graft [24] [23]. Understanding and quantifying this problem is a fundamental prerequisite for developing effective cell-based regenerative therapies.
Quantifying Transplanted Cell Death: Key Data
The high mortality rate of transplanted cells is a major bottleneck in regenerative medicine. The data below summarizes the scale of attrition attributed to a combination of factors, including anoikis, ischemia, and inflammation.
Table 1: Quantified Survival Rates of Transplanted Cells In Vivo
| Cell Type | Transplantation Model | Time Post-Transplantation | Reported Survival Rate | Key Stress Factors |
|---|---|---|---|---|
| Neonatal Cardiomyocytes [24] | Normal rat heart | 1 week | 28% | Ischemia, Anoikis |
| Skeletal Myoblasts [24] | Infarcted mouse heart | 3 days | 7% | Harsh microenvironment, Inflammation |
| Smooth Muscle Cells [24] | Infarcted rat heart | 1 week | 15% | Ischemia, Anoikis |
| Unfractionated Bone Marrow [24] | Infarcted rat heart | 3 days | 6% | Ischemia, Inflammation |
| Mesenchymal Stem Cells (MSCs) [24] | Infarcted porcine heart | Not Specified | ~5% | Anoikis, Oxidative stress |
| MSCs (General) [23] | Various injured tissues | A few days | Poor viability | Anoikis, Inflammation, Nutrient deprivation |
The timing of cell death is just as critical as the overall numbers. Research indicates that the majority of cell death occurs within the first few days after transplantation [24]. One study quantifying transplanted cardiomyocytes showed that 32% of graft cells were TUNEL-positive (a marker of cell death) just 24 hours after injection [24]. This number fell to 10% at 4 days and to only 1% after one week, highlighting the critical first days as the most vulnerable period for the graft [24].
Table 2: Critical Stressors Leading to Anoikis and Cell Death Post-Transplantation
| Stress Factor | Impact on Transplanted Cells | Consequence |
|---|---|---|
| Loss of ECM Attachment (Anoikis) [23] | Disruption of integrin signaling, leading to caspase activation. | Initiation of apoptotic pathways before cells are even transplanted. |
| Ischemia [24] | Avascular cell clumps create diffusion-limited cores, causing ATP depletion and acidosis. | Necrotic and apoptotic death, particularly in the center of cell aggregates. |
| Inflammation [24] [23] | Exposure to reactive oxygen species (ROS) and inflammatory cytokines from host immune cells. | Direct cell membrane damage and potentiation of caspase activation pathways. |
| Oxidative Stress [23] | Imbalance between ROS generation and antioxidant mechanisms in the damaged tissue. | Inactivation of cytoprotective nitric oxide (NO) and increased apoptosis. |
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: My transplanted cell viability is extremely low within the first 24 hours. What is the most likely cause and how can I address it?
A1: Rapid death immediately post-transplantation is highly indicative of anoikis. Since cells are kept in suspension during preparation and injection, they are deprived of survival signals [24] [23].
- Troubleshooting Steps:
- Pre-conditioning: Pre-treat your cells before transplantation with pro-survival factors. This can include growth factors (e.g., VEGF, IGF-1), cytokines, or free radical scavengers to prime them for stress [24] [23].
- Genetic Modification: Consider overexpressing anti-apoptotic proteins (e.g., Bcl-2) or knocking out pro-apoptotic genes in your cell line to enhance innate resistance to detachment-induced death [23].
- Co-delivery with ECM: Mix your cells with ECM molecules or synthetic adhesion peptides (e.g., RGD peptides) at the time of injection. This provides immediate provisional matrix contacts, mitigating the anoikis trigger [24].
Q2: How can I specifically distinguish anoikis from other forms of cell death, like necrosis, in my in vivo model?
A2: Distinguishing apoptosis from necrosis in vivo is challenging but can be achieved by assaying for specific hallmarks of caspase-mediated apoptosis.
- Troubleshooting Steps:
- Caspase Activity Assay: Quantify the activity of executioner caspases (e.g., Caspase-3/7) in homogenates of the graft tissue. A significant increase is a hallmark of apoptotic death, including anoikis [22].
- TUNEL Staining & Immunofluorescence: Combine TUNEL staining (labels DNA fragmentation) with immunofluorescence for activated caspase-3 on tissue sections. Co-localization strongly indicates anoikis/apoptosis. The lack of caspase activation alongside positive TUNEL staining may suggest necrosis [24] [25].
- Cell Viability Dye Retention: Use cell viability dyes that are retained in live cells but leak out of dying cells. When used in conjunction with caspase probes, you can differentiate between healthy, apoptotic (caspase+, dye-retaining), and necrotic (caspase-, dye-negative) populations [22].
Q3: My in vitro anoikis assays do not seem to translate to improved in vivo survival. What could be wrong with my experimental model?
A3: This is a common issue, as in vitro models often oversimplify the complex in vivo milieu.
- Troubleshooting Steps:
- Mimic the Hostile Niche: Move beyond simple suspension culture. Use a 3D spheroid culture system to better model the avascular, aggregated state of transplanted cells, which incorporates nutrient and oxygen gradients [26].
- Add Pathological Stressors: Challenge your cells with combined stressors in vitro. After inducing detachment, expose them to hypoxia and inflammatory cytokines (e.g., TNF-α) to more accurately simulate the post-transplantation environment [23].
- Use a Multi-Faceted Survival Strategy: Since cell death in vivo is multi-factorial, a single intervention is often insufficient. Implement a combinatorial approach, for example, using both heat shock (to counter ischemia) and anti-apoptotic genetic modification (to counter anoikis), which have been shown to have additive pro-survival effects [24].
Essential Experimental Protocols
Protocol: Detecting Anoikis via Cell Viability and Caspase Activation
This is a foundational method for quantifying anoikis in vitro, directly applicable to pre-screening potential pro-survival interventions [22].
1. Principle: Induce anoikis by forcing adherent cells into suspension, then simultaneously measure overall cell death and the activation of executioner caspases, which is a hallmark of apoptosis.
2. Materials:
- Cell Viability Dye: e.g., Calcein AM or propidium iodide (PI).
- Caspase Activity Assay Kit: A luminescent or fluorescent kit for Caspase-3/7.
- Low-Adhesion Plates: To prevent cell re-attachment during the assay.
- Poly-HEMA: A hydrogel coating used to create non-adherent culture surfaces.
3. Step-by-Step Method: 1. Prepare Non-Adherent Surfaces: Coat standard culture plates with a 1% (w/v) solution of Poly-HEMA in 95% ethanol and let them dry completely under a sterile hood. 2. Induce Anoikis: Harvest the cells of interest (e.g., MSCs) using standard trypsinization. Wash and reseed them onto the Poly-HEMA-coated plates in serum-free medium to deprive them of matrix and survival factors. Maintain them in suspension for 4-24 hours. 3. Measure Caspase Activity: Collect the suspended cells by gentle centrifugation. Lyse a portion of the cell pellet and incubate the lysate with a caspase-specific substrate. The cleavage of the substrate generates a luminescent or fluorescent signal proportional to the caspase activity. Measure the signal using a plate reader [22]. 4. Assess Cell Viability: In parallel, incubate another portion of the suspended cells with a cell viability dye. Calcein AM is metabolized to a green fluorescent product in live cells, while PI only enters dead cells with compromised membranes, staining the nucleus red. Analyze using a fluorescence microscope or flow cytometer [22]. 5. Quantify and Analyze: Calculate the percentage of viable (Calcein AM+/PI-), apoptotic (Caspase-3/7 high, Calcein AM low), and necrotic (Caspase-3/7 low, PI+) cells. Compare to adherent control cells to determine the specific increase in death due to detachment.
Protocol: Biochemical Assessment of Graft Cell Survival In Vivo
This protocol describes a higher-throughput biochemical method to assess graft size in animal hearts, reducing reliance on time-consuming histology [24].
1. Principle: Use species-specific molecular markers to quantify the amount of human graft DNA or protein remaining in the host mouse tissue at various time points post-transplantation.
2. Materials:
- Tissue Homogenizer
- qPCR System
- Primers for Human-Specific Repetitive Elements (Alu sequences) or Anti-LacZ Antibody if using LacZ-expressing cells.
- LacZ Substrate (e.g., for CPRG or ONPG assays) if applicable.
3. Step-by-Step Method: 1. Transplant and Recover Tissue: Transplant your cells (e.g., human cardiomyocytes) into the target organ (e.g., mouse heart). After a set period (e.g., 3 days), excise the entire organ and homogenize it. 2. DNA-based Quantification (Alu qPCR): - Extract genomic DNA from the tissue homogenate. - Perform qPCR using primers specific to the human Alu repetitive elements, which are present in high copy numbers in the human genome but absent in mice. - Generate a standard curve by spiking known numbers of human cells into untransplanted mouse heart tissue and extracting DNA alongside your samples. This allows you to back-calculate the number of surviving human cells in your experimental samples [24]. 3. Protein-based Quantification (LacZ Activity): - If using LacZ-expressing cells, clarify the tissue homogenate by centrifugation. - Incubate the supernatant with a LacZ substrate (e.g., CPRG) and measure the resulting colorimetric or luminescent product. - Similarly, use a standard curve from spiked samples to correlate enzymatic activity with the number of grafted cells [24]. 4. Correction for Signal Lag: Note that biochemical signals can persist for a short time after cell death. Optimize the assay to ensure it can detect as few as 1 graft cell in 40,000 host cells, and use early time points (e.g., 3 days) that have been shown to predict long-term engraftment success [24].
Key Signaling Pathways in Anoikis Resistance
The following diagram summarizes the core molecular pathway of anoikis and known resistance mechanisms that can be experimentally targeted.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Investigating Anoikis in Transplantation
| Reagent / Material | Function / Application | Specific Examples |
|---|---|---|
| Poly-HEMA [22] | Creates a non-adherent coating for culture plates to induce anoikis by preventing cell attachment. | 1-2% (w/v) solution in 95% ethanol. |
| Caspase Activity Assays [22] [25] | Quantifies the activation of executioner caspases, a key biochemical marker of anoikis. | Luminescent Caspase-Glo 3/7 assay. |
| Cell Viability Dyes [22] | Differentiates live, apoptotic, and necrotic cell populations in suspension. | Calcein AM (live), Propidium Iodide (dead), Annexin V (apoptotic). |
| 3D Spheroid Culture Systems [26] | Models the avascular, aggregated state of transplanted cells, combining anoikis and ischemia stress. | Ultra-low attachment U-plates; Hanging drop methods. |
| Human-Specific qPCR Probes [24] | Enables quantification of human cell survival in a mouse xenograft model via DNA analysis. | Primers for Alu repetitive elements. |
| RGD Peptides [23] | Synthetic peptides that mimic ECM; co-delivered with cells to provide immediate survival signals. | Cyclo(RGDfK). |
| Carbamylated EPO (CEPO) [24] | A pro-survival cytokine identified as additive to heat shock; enhances graft cell survival. | Non-erythropoietic erythropoietin derivative. |
Engineering Survival: Biomaterial and Molecular Strategies to Combat Anoikis
This technical support center is designed for researchers working at the intersection of biomaterial science and stem cell transplantation. A significant challenge in this field is anoikis—a form of programmed cell death that occurs when adherent cells detach from their native extracellular matrix (ECM). This is a major contributor to the poor survival rates of transplanted stem cells, with some studies indicating that only 5-10% of dopaminergic neurons survive the transplantation process in therapies for conditions like Parkinson's disease [27]. Biomaterial scaffolds, specifically cryogel microcarriers and hydrogels, are engineered to mimic the native ECM and provide an adherent surface, thereby combating anoikis and improving transplantation outcomes. This guide provides targeted troubleshooting and FAQs to support your experiments in this critical area.
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary mechanistic advantage of using biomaterial scaffolds to prevent anoikis in stem cell transplantation?
Biomaterial scaffolds function as synthetic ECM, providing essential biophysiochemical cues and cell-adhesive ligands. This support system counteracts anoikis by enabling cell attachment, which is a fundamental survival signal for adherent cells. The provision of an adherent surface alone has been shown to dramatically improve cell survival; one study reported a change from no surviving cells in a control group to 76% cell survival when cells were transplanted on an adherent substrate [27]. Beyond preventing detachment-induced death, these scaffolds can be functionalized to deliver growth factors and enhance cell-matrix interactions, further promoting survival and integration [27] [28].
FAQ 2: My cells are dying post-transplantation despite using a hydrogel. Could anoikis still be the cause?
Yes. While in situ forming hydrogels can modulate the host immune response, they may not prevent anoikis if cells are added in a trypsinized, single-cell suspension. Anoikis is triggered by the lack of attachment, and cells in a hydrogel precursor may not have immediate access to adhesive ligands. In contrast, pre-culturing cells on microcarriers (like cryogels or coated beads) before transplantation allows them to establish attachments prior to injection, thereby directly ameliorating anoikis [27]. Ensure your cells are adherent to a scaffold before transplantation to mitigate this risk.
FAQ 3: Why are my cell-loaded cryogel microcarriers clogging the injection cannula?
This is often a issue of size mismatch. While the average diameter of cryogel microcarriers may be around 299 µm, the inner diameter of fine-gauge cannulas used for brain injections is typically smaller (e.g., 160–210 µm for a 27–30 gauge needle) [27]. The solution lies in the unique shape-memory and compressibility of cryogels. Their macroporous, spongy structure (with pores ~72 µm and struts ~10 µm wide) allows them to withstand temporary deformation. They can be collapsed under shear stress within the needle and will re-expand to their original shape upon ejection, protecting the encapsulated cells [27]. Verify that your cryogels possess these elastic, macroporous properties.
FAQ 4: How can I control the release kinetics of growth factors from my heparin-containing cryogel microcarriers?
Growth factors like GDNF and NGF can be loaded onto heparin-containing cryogels via electrostatic interactions [27]. The release profile is influenced by the loading concentration and the inherent affinity between the growth factor and heparin. Research shows that higher loading concentrations result in a higher total amount released. Furthermore, different growth factors exhibit varying affinities; for instance, NGF typically demonstrates a higher binding affinity and slower release rate compared to GDNF when loaded under similar conditions [27]. This system can achieve near zero-order release kinetics, avoiding the significant initial burst release common in other delivery systems [27].
FAQ 5: What are the key differences between implantable and injectable biomaterial scaffolds for cell delivery?
The choice between implantable and injectable scaffolds depends on the application and required properties.
| Feature | Injectable Biomaterials | Implantable Biomaterials |
|---|---|---|
| Invasiveness | Minimally invasive [28] | More invasive, surgical placement |
| Primary Forms | Hydrogels, microcarriers, microcapsules [28] | Pre-formed porous scaffolds, patches |
| Mechanical Stress on Cells | Can be high (shear & extensional stress during injection) [28] | Lower, as cells are not forced through a needle |
| Cell Retention | Can be challenging; improved by shear-thinning hydrogels [28] | Generally high at the implant site |
| Typical Materials | Alginate, Hyaluronic Acid, PEG-based, peptides [28] | Often stiffer, more structured polymers |
Troubleshooting Guides
Problem: Poor Cell Survival and Function Post-Transplantation
Potential Causes and Solutions:
- Cause 1: Anoikis due to lack of cell adhesion.
- Solution: Ensure your biomaterial presents adequate cell-adhesive motifs. For synthetic materials like starPEG-heparin cryogels, this is inherent in the design [27]. For other hydrogels, incorporate RGD peptides or other ECM-derived adhesion proteins. Pre-culture cells on the scaffold to establish attachments before transplantation [27] [29].
- Cause 2: Harsh transplantation microenvironment (oxidative stress, inflammation).
- Solution: Precondition your stem cells before transplantation. This can include:
- Cytokine Preconditioning: Treating with IL-1β to enhance migration or IFN-γ/TNF-α to improve immunomodulation [30].
- Hypoxic Preconditioning: Culturing cells under low oxygen to enhance their resistance to the ischemic transplant site [30].
- Pharmacological Preconditioning: Using compounds like α-ketoglutarate or caffeic acid to boost antioxidant defenses and pro-survival signaling [30].
- Solution: Precondition your stem cells before transplantation. This can include:
- Cause 3: Mechanical stress during injection.
- Solution: For injectable systems, optimize delivery parameters. Use shear-thinning hydrogels (e.g., alginate, hyaluronic acid) that exhibit plug flow to protect cells [28]. One study identified that using a 26G needle at a flow rate of 5 µL/min improved neuronal differentiation and viability of neural stem cells [28].
Problem: Inconsistent or Inadequate Growth Factor Release from Scaffold
Potential Causes and Solutions:
- Cause 1: Uncontrolled burst release.
- Solution: Utilize a scaffold with high binding affinity for your target factor. Heparin-based cryogels are excellent for binding and providing sustained, near zero-order release of heparin-binding growth factors like GDNF and NGF [27]. The high surface area of the cryogel struts, as opposed to a solid sphere, also contributes to more controlled release kinetics [27].
- Cause 2: Incorrect loading concentration.
- Solution: Titrate the loading concentration of your growth factor. Research on cryogel microcarriers shows that different loading concentrations (e.g., 50, 100, and 500 ng/mL) yield distinct release rates and total amounts delivered [27]. Establish a standard curve for your specific system.
Problem: Low Cell Seeding Efficiency or Poor Cell Distribution on Microcarriers
Potential Causes and Solutions:
- Cause: Ineffective cell-carrier contact during seeding.
- Solution: Use a dynamic seeding method. A common and effective protocol is to use a spinner flask. Seed cells with the cryogel microcarriers and stir at a low speed (e.g., 30 rpm) using an on/off interval cycle (e.g., 2 minutes stirring, 30 minutes still) over several days (3-7 days). This protocol encourages cells to attach evenly to the outer and inner pore surfaces of the carriers [27].
Data and Protocol Summaries
| Parameter | Value / Measurement | Experimental Significance |
|---|---|---|
| Average Diameter (Dry) | 299 µm | Must be designed to be compressible for injection through smaller-gauge needles [27]. |
| Swelling Ratio (Wet vs. Dry) | 2.1x (diameter), 8.8x (volume) | Indicates high water content and sponge-like nature, important for nutrient diffusion [27]. |
| Average Pore Size | 72 µm | Macroporous structure allows for cell migration, vascularization, and protects cells during injection [27]. |
| Strut Width | ~10 µm | Demonstrates the fine, robust structure of the cryogel network [27]. |
| Growth Factor Release | Near zero-order kinetics for GDNF/NGF | Avoids burst release, enabling sustained trophic support for grafted cells [27]. |
| Injection Capability | Through 27-gauge needle without cell damage | Confirms mechanical robustness and injectability for minimally invasive delivery [27]. |
Table 2: Essential Reagent Solutions for Cryogel and Hydrogel Experiments
| Research Reagent | Function / Explanation | Example Application |
|---|---|---|
| starPEG (Polyethylene Glycol) | Synthetic polymer backbone; provides a tunable, bio-inert base for hydrogel formation that can be functionalized [27]. | Core component of synthetic cryogel microcarriers crosslinked with heparin [27]. |
| Heparin | Sulfated GAG; provides binding sites for growth factors and enhances bioactivity [27] [31]. | Key component in cryogels for controlled delivery of GDNF, NGF, etc. [27] |
| GelMA (Gelatin Methacryloyl) | Modified natural polymer containing RGD sequences; provides cell-adhesive motifs and enables photo-crosslinking [29]. | Used in composite bioinspired hydrogels (e.g., GHP4a) for 3D cell culture and anoikis resistance studies [29]. |
| HAMA (Hyaluronic Acid Methacryloyl) | Modified GAG; contributes to hydrogel structure, mimics ECM, and is involved in cell proliferation and migration [29]. | Component of biomimetic composite hydrogels for 3D cancer models [29]. |
| Photo-initiator (e.g., LAP) | Initiates radical polymerization upon light exposure for crosslinking methacryloyl-modified polymers [29]. | Essential for the formation of photopolymerized hydrogels like GelMA-HAMA-PEGDA composites [29]. |
| APS/TEMED | Redox initiator system for free radical polymerization at low temperatures, crucial for cryogelation [31]. | Commonly used initiation system for polymerizing GAG-based cryogels [31]. |
Detailed Experimental Protocols
Protocol 1: Synthesis and Cell Seeding of starPEG-Heparin Cryogel Microcarriers
This protocol is adapted from research on creating injectable cryogel microcarriers for cell transplantation [27].
Workflow Overview:
Materials:
- Amino-terminated starPEG.
- Heparin (e.g., Alexa 647 labeled for visualization).
- Crosslinkers: EDC (1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide) and Sulfo-NHS (N-Hydroxysulfosuccinimide).
- Organic phase for emulsion (e.g., oil).
- Lyophilizer.
- Spinner flask system.
Step-by-Step Method:
- Crosslinking Reaction: Dissolve amino-terminated starPEG and heparin in an aqueous solution. Activate the carboxylic acid groups of heparin using EDC and Sulfo-NHS chemistry [27].
- Emulsion Formation: Add the reaction mixture to an organic phase under rapid stirring to form a water-in-oil emulsion, creating small aqueous droplets that will become the microcarriers [27].
- Cryogelation: Submerge the reaction vessel in an ethanol bath at -20°C for several hours to allow ice crystals to form and the crosslinking reaction to complete in the non-frozen micro-domains [27].
- Lyophilization: Transfer the frozen microcarriers to a lyophilizer to remove both the organic solvent and the ice crystals, resulting in a dry, macroporous powder [27].
- Hydration and Sterilization: Hydrate the cryogel microcarriers in PBS or culture medium and sterilize (e.g., ethanol wash, UV, or antibiotic treatment).
- Cell Seeding: Suspend the sterile microcarriers and your cells (e.g., MSCs) in culture medium within a spinner flask. Stir at 30 rpm using an intermittent cycle (e.g., 2 minutes on, 30 minutes off) for 3-7 days to promote cell attachment [27].
- Harvesting: After confirming cell attachment and growth (e.g., via microscopy), the cell-loaded microcarriers can be concentrated and loaded into a syringe for injection.
Protocol 2: Assessing Anoikis Resistance in a 3D Biomimetic Hydrogel
This protocol is based on using composite hydrogels like GHP4a to study anoikis resistance in cancer cells, a principle applicable to stem cell survival [29].
Workflow Overview:
Materials:
- GelMA, HAMA, and 4-arm-PEGDA.
- Photo-initiator: Lithium phenyl (2,4,6-trimethylbenzoyl) phosphinate (LAP).
- LED light source (405 nm, 3W).
- Cells of interest (e.g., Caco-2 for cancer models or stem cells).
Step-by-Step Method:
- Polymer Synthesis: Synthesize or acquire GelMA and HAMA according to established protocols [29].
- Precursor Solution: Dissolve GelMA, HAMA, and 4-arm-PEGDA in PBS containing 0.25% (w/v) LAP photo-initiator. Gently mix your cell suspension into this polymer precursor solution to create a homogenous cell-polymer mix [29].
- 3D Encapsulation: Transfer the solution into a mold (e.g., PTFE) and expose it to 405 nm LED light for a defined period (e.g., seconds to minutes) to photo-crosslink the hydrogel and encapsulate the cells in 3D [29].
- Culture: Add culture medium and maintain the 3D constructs in an incubator.
- Viability and Anoikis Assessment:
- Perform Live/Dead staining to quantify overall cell viability.
- Use TUNEL assay or caspase-3/7 activity assays to specifically quantify apoptosis.
- Compare against controls: cells in traditional 2D culture and cells in ultra-low attachment plates (which induce anoikis).
- Mechanistic Analysis: Perform Western Blotting or immunofluorescence on the recovered constructs to analyze the activation of pro-survival pathways like FAK and PI3K/Akt, which are key mediators of anoikis resistance [29].
Harnessing Heparin-Based Systems for Controlled Growth Factor Release
This technical support centre is designed for researchers working at the intersection of biomaterials and regenerative medicine, specifically for those employing heparin-based systems to deliver growth factors (GFs) to transplanted stem cells. A primary challenge in this field is anoikis—a form of programmed cell death induced when cells detach from their native extracellular matrix (ECM). For transplanted stem cells, this can occur due to a lack of proper survival signals in the host microenvironment. Heparin, a highly sulfated glycosaminoglycan, is a powerful tool to address this because it can bind, stabilize, and provide controlled release of a wide range of heparin-binding GFs, thereby mimicking the natural ECM and providing crucial pro-survival signals to engrafted cells [32] [33]. This guide provides targeted troubleshooting and protocols to help you successfully implement these systems in your research on preventing anoikis in transplanted stem cells.
Frequently Asked Questions (FAQs)
Q1: Why is heparin such an effective component in growth factor delivery systems for cell transplantation?
A1: Heparin's effectiveness stems from its fundamental biological and chemical properties:
- High Affinity for GFs: Heparin has an exceptional affinity for a multitude of heparin-binding GFs (e.g., VEGF, FGF, BMPs) due to its high negative charge density from sulfate and carboxylate groups [32] [33]. This binding is crucial as it:
- Stabilizes and Protects GFs: It protects GFs from proteolytic degradation and thermal denaturation, significantly extending their functional half-life. For instance, free bFGF has a half-life of only 3 minutes in vivo, but heparin binding can stabilize it for extended periods [34] [35].
- Enhances Bioactivity: For many GFs, like FGF-2, heparin facilitates the formation of a active signaling complex with its cell surface receptor, thereby enhancing cellular response and potency [35].
- Intrinsic Bioactive Properties: Heparin itself possesses anti-inflammatory and anticoagulant properties, which can be beneficial in modulating the transplantation site environment [32].
Q2: How can I control the release kinetics of a growth factor from a heparin-based delivery system?
A2: The release kinetics are primarily controlled by the design of the heparin-carrier interaction. The following strategies allow for precise tuning from burst release to sustained delivery over weeks [32]:
- Interaction Strength: Using stronger covalent bonds or denser crosslinking within the carrier matrix will result in slower release.
- Carrier Degradation: Designing the polymer matrix (e.g., PLGA) to degrade hydrolytically or enzymatically allows release to be coupled to the degradation rate of the material itself.
- Polycation Molecular Weight: In self-assembled [polycation:heparin] complexes, using a higher molecular weight polycation leads to a more stable matrix and a slower release profile for the GF [35].
Q3: My transplanted stem cells are still undergoing high rates of cell death despite using a heparin-GF system. What could be the issue?
A3: This is a complex problem often related to the temporal mismatch between GF release and the critical window for anoikis prevention. Most transplanted cell death occurs within the first few days post-transplantation [36]. Consider the following:
- Insufficient Initial GF Dose: The initial burst release may not provide a high enough local concentration to activate pro-survival pathways (e.g., PI3K/Akt) in a sufficient number of cells.
- Release Rate is Too Slow: If the system is too tightly controlled, the release rate might be slower than the rate at which GFs are consumed or inactivated at the transplantation site, failing to reach the therapeutic threshold.
- Lack of Combinatorial Signals: Anoikis is a multi-factorial process. Relying on a single GF may be insufficient. Consider co-delivering multiple GFs (e.g., VEGF with FGF) or combining GF delivery with other pro-survival interventions like cell preconditioning (e.g., heat shock) or co-delivery of ECM proteins [36].
Troubleshooting Guide: Common Experimental Issues
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Low Growth Factor Loading Efficiency | Incorrect heparin-to-GF ratio; insufficient binding sites. | Titrate the heparin and GF concentrations. Use a mass ratio of polycation to heparin of 35:1 for [polycation:heparin] complexes, which has been shown to yield high loading efficiency [35]. |
| Rapid, Uncontrolled Burst Release | Growth factors are physically adsorbed, not stably incorporated; weak electrostatic interactions. | Shift from physical blending/adsorption to covalent grafting or network crosslinking strategies for greater stability [32] [34]. |
| Loss of Growth Factor Bioactivity | Harsh chemical reactions during immobilization; denaturation during encapsulation. | Use milder conjugation chemistries. Employ a self-assembled [polycation:heparin] complex, which has been shown to release FGF-2 that is as bioactive as fresh heparin-stabilized GF [35]. |
| Inconsistent Release Profiles Between Experiments | Inconsistent polymer batch quality; variable mixing/gelation conditions. | Standardize synthesis protocols. Use commercially available, well-characterized heparin and polymers. Ensure precise control over temperature, pH, and mixing speeds during matrix formation. |
| Poor Cell Viability or Function on the Scaffold | Cytotoxicity from polycations; failure to present GF in a bioactive manner. | Ensure thorough washing of the delivery system to remove any unreacted toxic crosslinkers. Confirm that the heparin-based system presents the GF in a way that allows it to bind to cell surface receptors. |
Featured Experimental Protocols
Protocol 1: Fabricating a Self-Assembled [Polycation:Heparin:GF] Complex for Sustained Release
This protocol describes the creation of a simple yet effective delivery matrix based on the ionic complexation of a polycation with a heparin-GF complex [35]. It is highly adaptable for various heparin-binding GFs.
Key Materials:
- Heparin sodium salt (from porcine or bovine intestinal mucosa)
- Polycation: e.g., Poly(argininate glyceryl succinate) - PAGS, or other biocompatible polycations like poly-L-lysine.
- Growth Factor of interest: e.g., FGF-2, VEGF.
- Buffers: Phosphate Buffered Saline (PBS), pH 7.4.
Methodology:
- Preparation of Solutions: Dissolve heparin in PBS to a concentration of 1 mg/mL. Dissolve your polycation in PBS to a concentration of 10 mg/mL. Prepare a solution of your GF in a suitable buffer with a carrier protein (e.g., 0.1% BSA).
- Form [Heparin:GF] Complex: Mix the heparin solution with the GF solution. The typical mass ratio for the final complex is 35:1 (PAGS:Heparin), so scale volumes accordingly. Allow to incubate for 15-30 minutes at room temperature to form the complex.
- Initiate Self-Assembly: Slowly add the polycation solution to the [heparin:GF] complex solution under gentle vortexing or stirring. A white precipitate will form immediately.
- Incubation and Harvest: Allow the suspension to incubate for 1 hour at room temperature to ensure complete complex formation.
- Washing and Storage: Centrifuge the suspension (e.g., 5000 rpm for 5 min) to pellet the complex. Carefully remove the supernatant and wash the pellet with PBS to remove any unbound GF. The complex can be stored at 4°C for immediate use or lyophilized for long-term storage.
Visual Workflow:
Protocol 2: Evaluating Growth Factor Release Kinetics and Bioactivity
Methodology:
- In Vitro Release Study:
- Place the fabricated [polycation:heparin:GF] complex (from Protocol 1) into a tube with a release medium (e.g., PBS, possibly with 0.1% BSA) at 37°C under gentle agitation.
- At predetermined time points, centrifuge the tube, collect a sample of the supernatant, and replace it with fresh pre-warmed medium.
- Quantify the amount of GF released in the collected samples using an ELISA or a bioactivity assay.
- Bioactivity Assay (Cell-Based):
- Use a cell line that is dependent on the GF for proliferation (e.g., BaF3 cells for FGF-2).
- Seed cells in 96-well plates and treat them with:
- Group A: Fresh, bolus GF solution (standard control).
- Group B: GF released from your heparin-complex at a specific time point.
- Group C: Control medium with no GF.
- After 48-72 hours, measure cell proliferation using a standard assay like MTT or AlamarBlue. The bioactivity of the released GF is confirmed if Group B shows proliferation comparable to or greater than Group A [35].
The Scientist's Toolkit: Key Research Reagents
| Research Reagent | Function & Role in the System |
|---|---|
| Heparin (unfractionated) | The core component; binds and stabilizes growth factors via strong electrostatic interactions, protecting them from degradation [32] [35]. |
| Biocompatible Polycations (e.g., PAGS, Poly-L-lysine, Chitosan) | Used to crosslink or complex with heparin to form the delivery matrix; molecular weight controls release kinetics [35]. |
| Heparin-Binding Growth Factors (e.g., FGF-2, VEGF165, BMP-2) | The therapeutic cargo; delivered to cells to promote survival, proliferation, and differentiation, thereby countering anoikis. |
| Synthetic Polymers (e.g., PLGA, PEG) | Form the structural scaffold (microspheres, hydrogels) into which the heparin-GF complex is incorporated; degradation rate controls long-term release [32] [34]. |
| Chromogenic Anti-Xa Assay Kit | A critical analytical tool not for anticoagulation, but to quantitatively measure heparin concentration and its release from a material system in vitro, providing key data on carrier behavior [37]. |
Core Signaling Pathways: Heparin-Stabilized GF Preventing Anoikis
The diagram below illustrates how a controlled release system delivers a heparin-stabilized GF to activate key intracellular pro-survival pathways in a transplanted stem cell, thereby inhibiting the anoikis cascade.
This technical support center provides targeted guidance for researchers working to enhance the survival and engraftment of transplanted stem cells. A critical challenge in this field is anoikis, a form of programmed cell death triggered when cells detach from their native extracellular matrix (ECM) [23] [38]. The strategic integration of cell-adhesive motifs, such as the RGD peptide, into biomaterial scaffolds is a primary strategy to counteract anoikis by providing essential survival signals. This resource offers troubleshooting guides and detailed protocols to help you effectively employ these peptides in your experiments, ensuring reliable and reproducible results in your pursuit of improving regenerative therapies.
Frequently Asked Questions (FAQs)
FAQ 1: Why is the RGD peptide so widely used to promote cell adhesion, and what are its key advantages?
The RGD (Arg-Gly-Asp) sequence is the primary integrin-binding domain found in many ECM proteins, such as fibronectin, vitronectin, and osteopontin [39] [40]. Its widespread use stems from several key advantages over full-length proteins:
- Proteolytic Stability: Its functionality is typically maintained during biomaterial processing and sterilization, which can denature sensitive proteins [39].
- Reduced Risk: It minimizes the risk of immune reactivity or pathogen transfer that can be associated with animal or human-derived proteins [39].
- Synthetic Simplicity: It is relatively simple and inexpensive to synthesize, facilitating clinical translation [39].
- Control over Presentation: It can be coupled to material surfaces in controlled densities and spatial orientations, which is difficult to achieve with native proteins [39].
FAQ 2: My in vitro results with RGD are excellent, but my in vivo outcomes are variable. Why?
This common problem often arises from the difference between a controlled culture environment and the complex in vivo milieu. In vitro assays are often performed in serum-depleted media on pristine surfaces. In vivo, however, your biomaterial will rapidly adsorb a complex mixture of proteins from blood and other body fluids (e.g., fibronectin, vitronectin, albumin) [39]. The cell's perception of the synthetic RGD is therefore altered within this background of native proteins. Furthermore, native ECM proteins stimulate more robust integrin signaling than the isolated RGD motif because they contain additional synergistic domains (e.g., the PHSRN sequence in fibronectin) [39]. This surface remodeling in vivo can lead to variable and sometimes inhibitory effects, explaining the discrepancy with your in vitro data [39].
FAQ 3: What is the relationship between cell adhesion and anoikis in transplanted stem cells?
Anoikis is a major limitation to the success of transplanted mesenchymal stem cells (MSCs) and other anchorage-dependent cells. Upon detachment from the culture dish and injection into the harsh microenvironment of a wound site, the loss of matrix anchorage triggers apoptotic signaling, leading to poor cell viability and low engraftment efficiency [23] [41]. Enhancing initial cell adhesion to a delivery scaffold or the host tissue is a fundamental strategy to inhibit this anoikis-driven death, thereby improving the survival and therapeutic potential of the transplanted cells [23].
FAQ 4: Are there peptide alternatives to RGD for specific applications?
Yes, other adhesive peptides can be used to target different cellular responses. A key example is the DGEA peptide, derived from collagen I. Interestingly, while RGD can sometimes inhibit bone formation in certain contexts, DGEA peptides have been shown to stimulate the osteoblastic differentiation of MSCs, making it a promising alternative for bone tissue engineering [39]. Other motifs, like KRSR, can promote osteoblast-selective adhesion by binding to cell surface heparan sulfate proteoglycans [42].
FAQ 5: How can I improve the performance of RGD in my biomaterial system?
Advanced material designs that more closely mimic the native ECM are showing great promise. Research indicates that cell adhesion and function are optimized when materials present RGD in multiple ways simultaneously. Specifically, allowing cells to engage with both mobile adhesion sites (which can dynamically cluster) and force-resistant anchoring points (which withstand cellular traction forces) can maximize adhesion formation and downstream signaling, independent of the matrix's bulk viscoelasticity [43].
Troubleshooting Guides
Guide 1: Addressing Poor Cell Adhesion on RGD-Functionalized Surfaces
| Symptom | Potential Cause | Recommended Solution |
|---|---|---|
| Low cell attachment and spreading | RGD density is too low. | Systematically increase the concentration of RGD coupled to the surface. Use a range of 0.1 to 10.0 fmol/cm² as a starting point for optimization [39]. |
| The RGD peptide is inaccessible to cells. | Ensure the peptide is presented with a flexible spacer arm (e.g., a PEG chain) to project it away from the material surface and allow integrin binding. | |
| The surface is highly protein-adsorptive (fouling). | Pre-adsorb the surface with serum proteins or use a non-fouling background (e.g., PEG) to prevent denatured proteins from masking the RGD signal [39]. | |
| Incorrect integrin targeting for your cell type. | Confirm the integrin expression profile of your cells. Consider using dual-ligand systems (e.g., RGD + KRSR) to engage multiple adhesion mechanisms [42]. | |
| High initial attachment, but poor long-term survival or function | The RGD density is too high, leading to inhibitory signaling. | Reduce the RGD density. High concentrations of synthetic RGD can compete with adsorbed native proteins and attenuate integrin signaling, leading to increased caspase activation and poor survival [39]. |
| Lack of synergistic signaling motifs. | Incorporate a second motif, such as PHSRN for fibronectin-mimetic synergy, or use a different adhesive peptide like DGEA to drive a desired differentiation outcome [39]. |
Guide 2: Preventing Anoikis in Transplanted Stem Cells
| Challenge | Strategy | Experimental Protocol Notes |
|---|---|---|
| Low engraftment efficiency due to cell death post-transplantation. | Genetic Modification: Overexpression of anti-apoptotic proteins or adhesion-enhancing receptors. | Transduce MSCs with a lentiviral vector encoding a gene like TLR4 or Akt. Confirm overexpression via qPCR and Western blot before in vivo transplantation [23]. |
| Biomaterial Scaffolds: Use of RGD-functionalized hydrogels or polymers. | Incorporate RGD into a dual-network hydrogel that provides both stable and mobile ligand presentations [43]. Encapsulate MSCs at a density of 1-5 million cells/mL and measure viability (Live/Dead assay) and apoptosis (caspase-3/7 activity) over 3-7 days in culture. | |
| Preconditioning: Treating cells before transplantation. | Pre-treat MSCs with growth factors (e.g., HGF, IGF-1) or under hypoxic conditions (1-2% O₂) for 24-48 hours to upregulate endogenous survival pathways [23]. | |
| Rapid degradation of adhesive peptides in vivo. | Use of stable synthetic biomimetics. | Replace traditional RGD peptides with proteolytically stable β-amino acid polymers (e.g., DM50CO50). These polymers mimic the dual charge-based and integrin-binding functions of natural peptides and show excellent in vivo stability [42]. |
Research Reagent Solutions
The table below summarizes key reagents and their functions for experiments in this field.
| Reagent / Material | Function / Explanation | Key Considerations |
|---|---|---|
| RGD Peptide | The gold-standard synthetic motif for promoting integrin-mediated cell adhesion [40]. | Use a spacer (e.g., PEG) for accessibility. Optimal density is cell-type specific and must be empirically determined to avoid inhibition [39]. |
| DGEA Peptide | A collagen-derived adhesive peptide that can stimulate osteoblastic differentiation of MSCs [39]. | A powerful alternative to RGD for bone tissue engineering applications where RGD may perform suboptimally. |
| KRSR Peptide | A heparin-binding peptide that promotes selective adhesion of osteoblasts and other specific cell types [42]. | Functions through a charge-based mechanism, independent of integrins. Effective in dual-ligand systems with RGD. |
| β-amino acid Polymer (e.g., DM50CO50) | A proteolytically stable, synthetic polymer that mimics the dual adhesive mechanisms of RGD and KRSR [42]. | Offers a cost-effective, stable alternative to natural peptides for in vivo applications. Promotes cell adhesion and proliferation comparable to RGD. |
| Dual-Network Hydrogel | A biomaterial platform allowing independent control of mechanical properties and ligand mobility [43]. | Enables study of the effects of mobile vs. immobile RGD presentations. Ideal for creating advanced, physiologically relevant cell culture environments. |
Experimental Pathway & Workflow Diagrams
Anoikis Prevention Pathway
The following diagram illustrates the key molecular pathways through which cell-adhesive motifs like RGD can prevent anoikis in transplanted stem cells, integrating integrin signaling and apoptotic machinery.
Biomaterial Optimization Workflow
This workflow outlines a systematic approach for developing and testing a biomaterial scaffold functionalized with cell-adhesive motifs to prevent anoikis.
Technical Support Center: Troubleshooting Guides and FAQs
This technical support center is designed for researchers working to prevent anoikis in transplanted stem cells. The guides below address common experimental challenges related to the trophic factors bFGF, GDNF, and IGF2, with a focus on practical troubleshooting and protocol optimization.
Troubleshooting Guide: Anoikis in Stem Cell Cultures
Problem: High rates of cell death following stem cell detachment or transplantation. Question: My cultured human pluripotent stem cells (hPSCs) show high mortality after detachment. How can I improve their survival?
Diagnosis and Solution: This is a classic sign of anoikis, a programmed cell death induced by detachment from the extracellular matrix. Basic Fibroblast Growth Factor (bFGF) is a critical signaling molecule for inhibiting this process in human pluripotent stem cells.
- Root Cause: Withdrawal of bFGF from the culture medium escalates anoikis. The anoikis is dependent on caspase activation and is mediated by the ERK and AKT signaling pathways [44].
- Recommended Action:
- Ensure adequate bFGF concentration: For feeder-free cultures in defined media like mTeSR1, maintain bFGF at a concentration of 100 ng/mL [44]. Lower concentrations (e.g., 4-40 ng/mL) may be insufficient and are associated with increased anoikis [44].
- Use a caspase inhibitor: The pan-caspase inhibitor z-VAD-FMK can markedly prevent the effects of bFGF withdrawal and the associated anoikis [44]. This can be used as a rescue agent or to validate the caspase-dependent mechanism of cell death in your system.
- Confirm pathway activity: Verify the activation of pro-survival pathways downstream of bFGF, specifically ERK and AKT, through western blotting for their phosphorylated forms [44].
Problem: Differentiating stem cells fail to adopt desired neuronal fates. Question: When attempting to direct hippocampal neural progenitors toward a neuronal lineage, I observe impaired maturation. Could my factor concentrations be counterproductive?
Diagnosis and Solution: Elevated levels of FGF-2 (bFGF) can paradoxically inhibit neuronal determination and maturation, despite enhancing progenitor cell division [45].
- Root Cause: High concentrations of bFGF can suppress neurogenesis in neural progenitor cultures [45].
- Recommended Action:
- Counteract with other trophic factors: Introduce GDNF or IGF2 to your differentiation protocol. These factors have been shown to counteract the inhibitory effects of elevated bFGF and promote neuronal lineage determination [45].
- Titrate your bFGF: Systematically test a range of bFGF concentrations to find the optimal level that supports progenitor health without inhibiting differentiation. The inhibitory effect is specifically linked to "elevated" levels [45].
- Consider combination treatments: Peptidergic drugs containing a mix of neurotrophic activities (e.g., Cerebrolysin) can mimic the combined effect of these trophic factors and promote neurogenesis without inhibiting proliferation [45].
Table 1: Experimentally Validated Concentrations and Functions of Key Trophic Factors
| Trophic Factor | Experimental Context | Effective Concentration | Primary Documented Effect on Anoikis/Neurogenesis | Key Signaling Pathways |
|---|---|---|---|---|
| bFGF (FGF2) | Human PS cell culture in mTeSR1 medium [44] | 100 ng/mL | Inhibits caspase-mediated anoikis; Prevents differentiation [44] | ERK, AKT [44] |
| bFGF (FGF2) | Preconditioning T2DM Adipose-derived Stem Cells (ASCs) [46] | 10 ng/mL for 9 days | Rescues proliferation & migration capacity; enhances neovessel formation [46] | Modulates miRNA profile [46] |
| GDNF | Counteracting elevated FGF-2 in adult rat hippocampal progenitors [45] | Context-dependent with other factors | Counteracts FGF-2-induced inhibition of neuronal lineage determination [45] | Preferentially binds GFRα1, activating RET → Ras/MAPK, PI3K/AKT, PLCγ [47] |
| IGF2 | Counteracting elevated FGF-2 in adult rat hippocampal progenitors [45] | Context-dependent with other factors | Counteracts FGF-2-induced inhibition of neuronal lineage determination [45] | Activates IGF1 receptor; downstream signaling supports self-renewal [44] |
Table 2: Key Reagents for Experimental Rescue or Pathway Inhibition
| Reagent | Function | Example Use Case | Reported Outcome |
|---|---|---|---|
| z-VAD-FMK | Pan-caspase inhibitor [44] | Rescue agent in bFGF-withdrawal models [44] | Markedly prevents bFGF withdrawal effects and anoikis [44] |
| PD173074 / SU5402 | FGF receptor inhibitors [44] | To validate FGF pathway specificity [44] | Decreases ERK phosphorylation and induces differentiation [44] |
| U0126 | Inhibitor of MEK/ERK pathway [44] | To inhibit ERK downstream of bFGF [44] | Causes loss of self-renewal capacity [44] |
| Anti-IGF1R Antibody | Blocks IGF1 and IGF2 binding to receptor [44] | To probe necessity of endogenous IGF signaling [44] | Impairs self-renewal of human ES cells [44] |
Detailed Experimental Protocols
Protocol 1: Testing bFGF's Role in Preventing Anoikis in hPSCs This protocol is adapted from studies on human embryonic stem (ES) and induced pluripotent stem (iPS) cells [44].
Cell Culture and Adaptation:
- Culture human PS cells (e.g., H14 ES cells or YK26 iPS cells) on Matrigel-coated plates.
- Adapt cells to a defined medium like mTeSR1 for at least one passage before the experiment.
Experimental Medium Preparation:
- Control Group: Customized mTeSR1 containing 100 ng/mL bFGF.
- Treatment Group: Customized mTeSR1 containing 0 ng/mL bFGF (withdrawal group).
- Optional Rescue Group: bFGF-deficient mTeSR1 supplemented with 20-50 µM caspase inhibitor z-VAD-FMK.
Cell Proliferation and Viability Assay:
- Collect both freshly detached (floating) cells and the remaining adherent cells at 24h and 48h post-medium change.
- Harvest attached cells using Accutase.
- Combine cell fractions and stain with ViaCount reagent.
- Analyze cell count and viability using flow cytometry (e.g., Guava EasyCyte system).
- Calculate the floating cell ratio:
[Floating cell number / (Floating + Attached cell number)] * 100.
Flow Cytometry for Apoptosis and Pluripotency:
- Dissociate cells with Accutase, then fix and permeabilize.
- Stain cells with anti-OCT4 (pluripotency marker) and anti-active Caspase-3 (apoptosis marker) antibodies.
- Analyze using flow cytometry to determine the percentage of OCT4+/aCasp3+ cells.
Protocol 2: Preconditioning Stem Cells with bFGF to Enhance Therapeutic Potential This protocol is based on rescuing dysfunctional adipose-derived stem cells (ASCs) from individuals with type 2 diabetes [46].
Cell Culture and Treatment:
- Isolate and culture ASCs in standard growth medium (e.g., DMEM low glucose with 10% FBS).
- At approximately 70% confluence, treat experimental groups with ASC medium supplemented with 10 ng/mL bFGF.
- Maintain treatment for 9 days, changing the medium every 2-3 days.
- Include an untreated control group cultured in standard ASC medium only.
Functional Validation Assays:
- Proliferation: Use an MTS assay at days 3, 6, and 9 to quantify cell proliferation.
- Migration: Perform a transwell migration assay to assess the enhanced migratory capacity of preconditioned cells.
- In Vivo Angiogenesis: Use a Matrigel plug assay in nude mice to evaluate the contribution of preconditioned ASCs to neovessel formation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Investigating Trophic Factors in Anoikis
| Item / Reagent | Function / Explanation | Example Product / Vendor |
|---|---|---|
| Defined Culture Medium | Serum-free, animal-free medium to provide a controlled environment for studying specific factors. | mTeSR1 (Stem Cell Technologies) [44] |
| Recombinant Human bFGF | The primary trophic factor to be tested for its anti-anoikis effects. | R&D Systems (233-FB) [46] |
| Caspase Inhibitor | Tool to confirm the mechanism of cell death is apoptosis-dependent. | z-VAD-FMK (Biomol International) [44] |
| Matrigel | Basement membrane matrix to provide a physiological substrate for cell adhesion, preventing anoikis in control groups. | BD Matrigel (BD Biosciences) [44] |
| FGF Receptor Inhibitors | Chemical tools to validate the specificity of bFGF signaling. | PD173074 (Stemgent), SU5402 (Pharmacia & Upjohn) [44] |
| Anti-active Caspase-3 Antibody | Flow cytometry antibody to detect and quantify cells undergoing apoptosis. | BD Bioscience [44] |
| Anti-OCT4 Antibody | Flow cytometry antibody to monitor the pluripotent state of stem cells. | BD Bioscience (conjugated with allophycocyanin) [44] |
Signaling Pathway and Experimental Workflow Diagrams
Frequently Asked Questions (FAQs)
What is the primary cause of early cell death in stem cell transplantation, and how can it be countered? A significant challenge is anoikis, a form of programmed cell death triggered when cells detach from their native extracellular matrix (ECM), losing essential survival signals [38]. Co-transplantation with supporting cells like Mesenchymal Stem Cells (MSCs) is a primary strategy to inhibit anoikis. MSCs secrete anti-apoptotic factors and provide direct cell-to-cell contact, enhancing the survival of the transplanted therapeutic cells [48].
Which supporting cells are most effective for co-transplantation to prevent anoikis? Mesenchymal Stem Cells (MSCs) are the most extensively studied and used supporting cells. They are effective due to their multi-functional properties, which include:
- Anti-apoptotic activity: Secreting factors that protect against cell death. MSCs can even transfer mitochondria to stressed cells, enhancing their energy production and survival [48].
- Immunomodulation: Altering the activity of host immune cells (T cells, dendritic cells, etc.) to reduce rejection of the transplanted graft [48].
- Angiogenic potential: Releasing factors like Vascular Endothelial Growth Factor (VEGF) to promote the formation of new blood vessels, ensuring long-term nutrient and oxygen supply to the graft [48].
Beyond supporting cells, what other materials can be used to enhance graft survival? The inclusion of specific extracellular matrix (ECM) proteins in the transplant formulation is a highly effective strategy. Experimental data shows that these proteins can directly enhance the survival and function of transplanted cells by providing critical adhesion signals that prevent anoikis.
Table: Functional Impact of ECM Proteins on Transplanted Cells
| ECM Protein | Experimental Impact on Transplanted Cells | Proposed Mechanism of Action |
|---|---|---|
| Fibronectin | Enhanced cell survival by 1.7-fold [49] | Provides integrin-mediated adhesion signals, countering detachment-induced death. |
| Vitronectin | Improved cell proliferation by 1.8-fold [49] | Promoves cell spreading and division through specific integrin binding (e.g., αvβ5). |
How can researchers experimentally validate the suppression of anoikis in a co-transplantation model? Validation involves a combination of in vitro and in vivo approaches:
- In vitro: Culture cells in suspension (e.g., on ultra-low attachment plates) to simulate detachment. Cells protected from anoikis (e.g., by genetic modification or conditioned media from MSCs) will show significantly lower apoptosis rates, measurable by assays like PI staining [50].
- In vivo: After co-transplantation, graft survival can be quantified using methods like scintigraphy (if cells are pre-labeled) or quantitative PCR (qPCR) of species-specific or gender-specific DNA (e.g., human Y-chromosome DNA in a mouse host) [49] [51]. Reduced expression of pro-apoptotic genes like FADD and Bit1 or overexpression of anti-apoptotic protein Bcl-2 are established markers of successful anoikis inhibition [49].
Troubleshooting Guides
Problem: Poor Graft Survival and Engraftment Post-Transplantation
Potential Cause: The transplanted cells are undergoing anoikis due to a lack of proper ECM attachment and are vulnerable to the hostile inflammatory environment at the transplant site.
Solution Checklist:
- Optimize Co-culture Pre-transplantation:
- Prior to transplantation, pre-mix your primary cells (e.g., pancreatic islets, myoblasts) with MSCs and culture them together for a period [48]. This allows for the formation of composite aggregates where MSCs can directly transfer mitochondria and upregulate pro-survival pathways in the therapeutic cells [48].
- Protocol: Isolate primary cells and expand MSCs. Combine them at an optimized ratio (e.g., 1:1 to 1:5 islet-to-MSC ratio has been used in diabetes research) on a non-adherent surface or in suspension culture for 24-48 hours before transplantation [48].
Supplement with ECM Proteins:
- Directly add ECM proteins like Fibronectin or Vitronectin to the cell suspension immediately before transplantation [49]. This provides immediate integrin-mediated survival signals.
Utilize Genetically Modified Cells:
- Consider using donor cells that overexpress anti-apoptotic proteins like Bcl-2, which has been shown to completely abolish anoikis in vitro and enhance in vivo survival by over 3-fold [49]. Alternatively, knocking down pro-apoptotic mediators like FADD or Bit1 can also significantly reduce anoikis [49].
Problem: Inconsistent Results with Co-culture and MSC Preparation
Potential Cause: Variability in MSC source, quality, or activation state leads to inconsistent protective effects.
Solution Checklist:
- Standardize MSC Source and Quality:
- Source MSCs from reliable providers or internal banks that adhere to International Society for Cellular Therapy criteria [48]. Use MSCs at low passage numbers to prevent senescence-related functional loss.
Pre-activate MSCs:
- "Prime" or pre-activate MSCs before co-transplantation by treating them with a cytokine cocktail (e.g., IFN-γ, TNF-α, IL-1β). This enhances their immunomodulatory function, increasing the secretion of protective factors like prostaglandin E2, which improves graft survival [48].
Ensure Proper Cell-Cell Contact:
- Verify that your co-culture conditions promote physical interaction. The protective effect is partly mediated by adhesion molecules like N-cadherin [48]. Use rotational culture systems if necessary to promote the formation of uniform, mixed cell aggregates.
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Reagents for Anoikis and Co-transplantation Research
| Reagent / Material | Function in Research | Key Examples / Notes |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Primary supporting cell for co-transplantation; provides anti-apoptotic, immunomodulatory, and angiogenic support. | Bone marrow, umbilical cord, or adipose tissue-derived; ensure they meet ISCT criteria [48]. |
| ECM Proteins | Provides critical adhesion signals to inhibit anoikis; used in culture or mixed with cells pre-transplantation. | Fibronectin, Vitronectin, Laminin; concentration and combination should be optimized for specific cell types [49]. |
| Anoikis-Induction Plates | To simulate detachment and study anoikis mechanisms in vitro; a critical control for validation experiments. | Ultra-low attachment plates or poly-HEMA coated plates prevent cell adhesion. |
| Pro-Survival Factors | Chemical or biological molecules that enhance cell survival post-transplantation. | Carbamylated EPO (CEPO); effects are additive to heat shock treatment [51]. |
| qPCR Assays for Graft Tracking | To quantitatively track and validate survival of transplanted human cells in an animal model. | qPCR for human-specific Alu sequences or Y-chromosome genes [51]. |
| siRNA/shRNA for Pro-Apoptotic Genes | To genetically validate key anoikis pathways and enhance graft survival. | Targets include FADD, Bit1; knockdown reduces anoikis [49]. |
| Anti-Apoptotic Expression Vectors | To genetically engineer cells for enhanced resistance to detachment-induced death. | Overexpression of Bcl-2 family proteins [49]. |
Key Signaling Pathways in Anoikis and Co-Transplantation Protection
The following diagram illustrates the core signaling pathways that lead to anoikis and the protective mechanisms activated through MSC co-transplantation.
Anoikis Signaling and Protective Pathways. This diagram outlines the process where cell detachment triggers pro-apoptotic pathways (red), leading to cell death. The protective mechanisms (green) afforded by MSC co-transplantation, such as mitochondrial transfer and secretion of survival factors, act to counteract these signals and promote graft survival. Genetic strategies like Bcl-2 overexpression also directly inhibit the apoptosis execution step.
Optimizing Protocols: Preconditioning, Delivery, and Host-Modification Strategies
Essential Knowledge: Caspase Inhibitors in Stem Cell Research
What is the primary role of caspase inhibitors like z-VAD-FMK in preventing anoikis in stem cell transplantation?
Anoikis is a specific form of programmed cell death (apoptosis) induced when cells detach from their native extracellular matrix (ECM). For stem cells undergoing transplantation—a process that inherently involves detachment—anoikis is a major cause of early cell loss [12]. Caspase inhibitors like z-VAD-FMK play a critical role by blocking the activity of caspases, a family of cysteine-dependent proteases that are the central executioners of apoptosis [52] [53] [54].
Research on human pluripotent stem cells (including embryonic and induced pluripotent stem cells) has demonstrated that they are subject to constant anoikis in culture. The cytokine basic Fibroblast Growth Factor (bFGF) represses this anoikis via inhibition of caspase activation. Withdrawing bFGF escalates anoikis, an effect that can be markedly prevented by the addition of the pan-caspase inhibitor z-VAD-FMK [44]. This confirms that caspase-mediated signaling is a key pathway in detachment-induced death.
How does preconditioning with z-VAD-FMK work at a molecular level?
Preconditioning involves treating stem cells with an agent before transplantation to equip them to survive the stressful post-transplantation environment. z-VAD-FMK is a broad-spectrum, irreversible caspase inhibitor that covalently binds to the catalytic cysteine residue in the active site of most caspases, effectively blocking their proteolytic activity [52] [53].
The molecular mechanisms and outcomes of preconditioning with z-VAD-FMK are summarized in the diagram below:
A specific study on preconditioning mesenchymal stem cells (MSCs) with 20 µM Z-VAD-FMK for 24 hours prior to hypoxia exposure resulted in a significant decrease in apoptosis, as measured by TUNEL assay and Annexin V analysis. This was accompanied by a marked down-regulation in the gene and protein expression of caspases 1, 3, 6, 7, and 9, and a significant increase in the survival markers Akt1, NF-κB, and Bcl-2 [55].
Troubleshooting Guides
Problem: Preconditioned cells are still dying after transplantation, or death is only delayed.
Potential Causes and Solutions:
Cause: Activation of alternative, non-apoptotic cell death pathways.
- Explanation: Caspase inhibition can sometimes lead to the activation of backup cell death programs. The broad-spectrum caspase inhibitor z-VAD-FMK is known to modulate all three major types of cell death: it blocks apoptosis but can sensitize cells to necrotic death and induce autophagic cell death [56].
- Solution: Investigate the presence of necrotic (e.g., loss of membrane integrity) or autophagic markers (e.g., LC3-I to LC3-II conversion) in dying cells. Consider combining z-VAD-FMK with inhibitors of other death pathways, such as necroptosis inhibitors (e.g., Necrostatin-1), while carefully optimizing concentrations to avoid toxicity.
Cause: Insufficient protection against metabolic stress.
- Explanation: The post-transplantation environment involves severe metabolic challenges beyond just anoikis. A recent 2025 study on transplanted photoreceptor precursor cells identified metabolic stress, characterized by dysregulation of mitochondrial function and oxidative phosphorylation, as a critical driver of early donor cell death, independent of immune rejection [5].
- Solution: Precondition cells not only with a caspase inhibitor but also with strategies to enhance metabolic resilience. This could include preconditioning under mild metabolic stress to induce adaptive responses or using media supplements that promote mitochondrial health.
Cause: Suboptimal preconditioning protocol.
- Explanation: The timing and concentration of z-VAD-FMK are critical. Paradoxically, while lower concentrations (1-30 µM) inhibit TNFα-stimulated apoptosis in neutrophils, higher concentrations (>100 µM) have been shown to enhance it, indicating a cell type- and context-specific effect [57].
- Solution: Perform a dose-response and time-course experiment to identify the optimal window for your specific stem cell type. A typical effective protocol for MSCs uses 20 µM for 24 hours [55].
Problem: The caspase inhibitor is showing unexpected toxicity or off-target effects.
Potential Causes and Solutions:
Cause: Inhibition of non-apoptotic caspase functions.
- Explanation: Caspases are involved in vital cellular processes beyond apoptosis, including proliferation, differentiation, and inflammatory response. Indiscriminate inhibition can disrupt these functions [52] [53].
- Solution: Consider switching to a more specific caspase inhibitor instead of a pan-caspase inhibitor like z-VAD-FMK. If anoikis is primarily executed by caspase-3, a more specific caspase-3 inhibitor might be sufficient and cause fewer side effects.
Cause: Compound-specific toxicity.
- Explanation: The pro-apoptotic effects of high-dose z-VAD-FMK in some cell types like neutrophils are considered a compound-specific effect, not a general feature of caspase inhibition [57]. Furthermore, FMK-based inhibitors like z-VAD-FMK have been associated with high toxicity in vivo, which has limited their clinical translation [52] [53].
- Solution: Evaluate alternative, next-generation caspase inhibitors such as Q-VD-OPh. Q-VD-OPh is a broad-spectrum caspase inhibitor that has demonstrated enhanced efficacy, better cell permeability, and, crucially, significantly reduced non-specific toxicity in vitro, even at high concentrations (up to 500-1000 µM) [52] [53].
Frequently Asked Questions (FAQs)
Besides z-VAD-FMK, what are the main alternative caspase inhibitors available?
Caspase inhibitors can be categorized based on their origin and structure. The table below summarizes the key types and examples.
Table 1: Caspase Inhibitor Classes and Examples
| Class | Example(s) | Key Characteristics | Primary Target(s) |
|---|---|---|---|
| Peptide-based Inhibitors | z-VAD-FMK | Broad-spectrum, irreversible, FMK group. Common in research. | Caspase-2, -3, -8, -9 [52] |
| Boc-D-FMK | Broad-spectrum, irreversible. | Caspase-3, -7, -8, -9 (poor for -2, -5, -6, -10) [52] | |
| Q-VD-OPh | Broad-spectrum, irreversible. Less toxic than FMK-based inhibitors. | Caspase-1, -2, -3, -6, -8, -9 [52] | |
| Ac-DEVD-CHO | Reversible, aldehyde group. Higher selectivity for executioner caspases. | Caspase-3 [52] | |
| Peptidomimetic Inhibitors | VX-765 (Belnacasan), IDN-6556 (Emricasan) | Designed for better drug-like properties (stability, potency). Several have entered clinical trials for liver and inflammatory diseases. | Caspase-1 (VX-765); Caspase-3, -7, -8 (IDN-6556) [52] [53] |
| Natural Inhibitors | XIAP, cIAP1/2 | Cellular proteins that directly bind and inhibit caspases. | Caspase-3, -7, -9 (XIAP) [52] [53] |
What are the key experimental steps for preconditioning stem cells with z-VAD-FMK?
The following workflow outlines a standard protocol, based on a study using mesenchymal stem cells, which you can adapt for your specific cell type [55].
Why have caspase inhibitors struggled in clinical trials, and what does this mean for transplantation research?
Despite promising preclinical results, the clinical development of caspase inhibitors for diseases like liver failure and rheumatoid arthritis has faced challenges. Key reasons include:
- Inadequate Efficacy & Poor Target Specificity: It has been difficult to achieve sufficient inhibition of the intended caspases without affecting other physiologically important caspases, leading to a lack of robust clinical benefit [52] [53].
- Adverse Safety Profiles: Some inhibitors, like VX-740 (pralnacasan), showed promise but were terminated due to liver toxicity in animal models at high doses. The toxicity of FMK-based inhibitors like z-VAD-FMK also limits their clinical use [52] [53].
- Activation of Alternative Cell Death Pathways: As noted in the troubleshooting guide, inhibiting apoptosis can sometimes trigger other forms of cell death, such as necroptosis or pyroptosis, undermining the therapeutic goal [56] [52].
Implication for Transplantation Research: For the field of stem cell transplantation, these challenges highlight that while caspase preconditioning is a powerful research tool to enhance survival in vitro and in animal models, the path to clinical translation requires next-generation inhibitors with better safety profiles, such as Q-VD-OPh, or highly localized delivery to minimize systemic side effects.
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Materials for Caspase Preconditioning Experiments
| Item | Function/Description | Example |
|---|---|---|
| Pan-Caspase Inhibitor | Irreversibly binds active site of a broad range of caspases to block apoptosis. | z-VAD-FMK (e.g., [44] [55]) |
| Alternative Broad-Spectrum Inhibitor | A less toxic, broad-spectrum alternative to FMK-based inhibitors. | Q-VD-OPh (e.g., [52]) |
| Specific Caspase Inhibitors | Used to identify the contribution of specific caspases (e.g., initiator vs. executioner). | Ac-DEVD-CHO (Caspase-3), Ac-IETD-CHO (Caspase-8) (e.g., [52]) |
| Apoptosis Detection Kit | To quantify the efficacy of preconditioning by measuring apoptosis levels. | TUNEL Assay Kit, Annexin V/Propidium Iodide Staining (e.g., [55]) |
| Caspase Activity Assay | To directly measure caspase activity, confirming inhibitor efficacy. | Fluorometric or Colorimetric Caspase Assay Kits (e.g., [54]) |
| Western Blot Antibodies | To analyze protein levels of caspases, cleaved caspases, and survival markers (e.g., Bcl-2, p-Akt). | Antibodies against Caspase-3, Cleaved Caspase-3, Bcl-2, etc. (e.g., [55] [54]) |
Genetic and Metabolic Engineering to Enhance Anoikis Resistance
FAQs and Troubleshooting Guides
Frequently Asked Questions
Q1: What is the primary cause of low survival in transplanted stem cells, and how does anoikis contribute to this? A1: The primary limitation is poor cell viability at the transplantation site, where a significant percentage of cells die within the first few days. Anoikis, a form of programmed cell death triggered by loss of cell adhesion to the extracellular matrix (ECM), is a major driver of this low survival. When stem cells are detached for transplantation and fail to adhere properly to the host tissue, they undergo anoikis, drastically reducing engraftment efficiency [23].
Q2: What are the key genetic engineering strategies to enhance anoikis resistance in stem cells? A2: Key strategies include:
- Overexpression of Adhesion Molecules: Engineering stem cells to overexpress integrins (e.g., ITGA5B1) enhances their adhesion to the host ECM, suppressing anoikis and promoting survival and nitric oxide production [58].
- Modulation of Anti-Apoptotic Pathways: Genetic modifications to overexpress anti-apoptotic proteins (e.g., Bcl-2) or components of pro-survival pathways (e.g., PI3K/Akt) can inhibit the caspase cascade responsible for anoikis [23] [59].
- Knockout of Pro-Apoptotic Signals: Targeting genes that promote detachment-induced death, such as Toll-Like Receptor 4 (TLR4), has been shown to improve mesenchymal stem cell survival [23].
Q3: How can metabolic reprogramming be used to combat anoikis? A3: Detached cells often face metabolic crises. Metabolic engineering can address this by:
- Enhancing Antioxidant Defenses: Engineering cells to manage reactive oxygen species (ROS) buildup upon detachment prevents oxidative stress-induced death [7].
- Promoting Alternative Energy Pathways: Reprogramming cells to utilize nutrients like amino acids and fatty acids more efficiently under detachment stress can supply crucial energy for survival, thereby fostering anoikis resistance [7] [12] [60].
Q4: What are the critical signaling pathways to target for inducing anoikis resistance? A4: The most critical pathways include:
- Integrin-Mediated Signaling: Enhancing signaling through integrins like α5β1, αvβ3, and β1 activates downstream pro-survival mediators [59].
- PI3K/Akt Pathway: This is a central survival pathway. Its activation, often downstream of integrins or growth factors, strongly inhibits anoikis [59] [61].
- FAK and Src Signaling: Focal Adhesion Kinase (FAK) and Src kinase are pivotal in transducing adhesion signals into cell survival responses. Their activation is a common strategy to confer resistance [59] [61].
Q5: What are the functional consequences of successfully engineering anoikis resistance? A5: Successfully engineered anoikis resistance leads to:
- Improved Cell Survival and Engraftment: Significantly higher rates of cell viability post-transplantation.
- Enhanced Paracrine Function: Increased secretion of therapeutic growth factors and cytokines from the surviving cells.
- Better Structural Integration: Improved adhesion and physical incorporation into the host tissue, providing structural support [23] [58].
Troubleshooting Common Experimental Issues
Problem: Low efficiency in achieving stable genetic modification of stem cells.
- Potential Cause: Low titer or inefficient lentiviral transduction.
- Solution:
- Concentrate your viral supernatant to achieve a higher titer.
- Optimize the Multiplicity of Infection (MOI) for your specific stem cell type.
- Use polybrene or other transduction enhancers at a non-toxic concentration.
- Implement a robust selection protocol (e.g., puromycin) to eliminate non-transduced cells.
Problem: Engineered cells show resistance in vitro but fail to survive in vivo.
- Potential Cause: The harsh transplantation microenvironment (e.g., inflammation, ischemia) is overwhelming the engineered resistance.
- Solution:
- Combinatorial Preconditioning: Combine genetic engineering with hypoxic preconditioning to better prepare cells for the ischemic environment [23].
- Biomaterial Support: Co-deliver cells with an ECM-derived hydrogel or scaffold to provide immediate physical adhesion cues and protect cells from anoikis during the critical initial phase [23].
- Anti-inflammatory Treatment: Consider short-term, localized anti-inflammatory therapy to mitigate the host immune response that can kill transplanted cells [51].
Problem: Inconsistent results in the CytoSelect Anoikis Assay.
- Potential Cause: Variation in cell preparation or assay conditions.
- Solution:
- Ensure consistent cell detachment using a gentle, non-enzymatic cell dissociation buffer to avoid receptor damage.
- Use poly-HEMA coated plates that are properly prepared and dried to prevent any well-to-well variability in cell attachment.
- Include a positive control (e.g., adherent cells on a standard plate) and a negative control (e.g., cells treated with a pro-apoptotic agent) in every experiment.
- Standardize the duration of the suspension culture based on the sensitivity of your cell line.
Problem: Concern that engineered anoikis resistance could promote tumorigenicity.
- Potential Cause: The same pathways that confer resistance (e.g., PI3K/Akt) are often dysregulated in cancer.
- Solution:
- Use Inducible Systems: Employ inducible promoters (e.g., tetracycline-regulated systems) to transiently express the resistance gene only around the time of transplantation.
- Select Safe Targets: Prioritize targets that enhance adhesion and metabolic fitness (e.g., integrins) over strongly oncogenic drivers.
- Rigorous Safety Testing: Perform long-term studies in immunocompromised mice to assess the potential for uncontrolled growth of the engineered cells before clinical translation.
Experimental Protocols & Data
Detailed Protocol: Assessing Anoikis via Caspase-3/7 Activity
Principle: This protocol measures the activation of effector caspases-3 and -7, which are key executioners of anoikis, in cells placed in suspension.
Materials:
- Caspase-Glo 3/7 Assay System (or equivalent)
- Poly-HEMA coated plates (or ultra-low attachment plates)
- Cell culture medium
- Luminescence plate reader
Method:
- Prepare Suspension Culture: Seed cells into poly-HEMA coated 96-well plates at a density of 1x10^4 cells per well in 100µL of medium. For the adherent control, seed cells in a standard tissue culture-treated plate.
- Incubation: Incubate the plates for 6-24 hours (time may vary by cell type) at 37°C, 5% CO₂.
- Equilibrate Reagents: Thaw and equilibrate the Caspase-Glo 3/7 reagents to room temperature.
- Add Reagent: Add 100µL of the Caspase-Glo 3/7 reagent directly to each well containing 100µL of cell culture medium.
- Mix and Incubate: Mix the contents gently using a plate shaker for 30 seconds. Incubate the plate at room temperature for 1 hour to allow the luminescent signal to develop.
- Measurement: Measure the luminescence of each well using a plate reader. The signal is proportional to the amount of caspase activity present.
Troubleshooting: High background in suspended samples can indicate rapid cell death. Reduce the incubation time in suspension. Consistently low signal may suggest low caspase activity; confirm with an alternative apoptosis assay (e.g., Annexin V staining).
Key Experimental Data and Reagents
Table 1: Quantitative Data on Strategies to Enhance Cell Survival
| Strategy | Experimental Model | Key Outcome | Reference |
|---|---|---|---|
| ITGA5B1 Overexpression | Rat Bone Marrow MSCs (rBMSCs) | Suppressed anoikis, enhanced cell adhesion and NO production [58]. | |
| TLR4 Knockout | Murine MSCs | Improved survival of transplanted cells [23]. | |
| Heat Shock Preconditioning | Human Embryonic Stem Cell-Derived Cardiomyocytes | Enhanced graft cell survival; effects were additive with pro-survival factors like CEPO [51]. | |
| Carbamylated EPO (CEPO) | Human Embryonic Stem Cell-Derived Cardiomyocytes | Identified as a pro-survival factor; effects additive to heat shock [51]. |
Table 2: Research Reagent Solutions for Anoikis Studies
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Poly-HEMA | Creates a non-adherent surface to force cells into suspension. | Inducing anoikis in vitro for assay validation [58]. |
| Lentiviral Vectors (e.g., pLVX) | Stable gene delivery for overexpression or knockdown. | Engineering rBMSCs to overexpress ITGA5 and ITGB1 [58]. |
| CytoSelect Anoikis Assay | Colorimetric quantification of cell death in suspension. | Directly measuring anoikis sensitivity after genetic modification [58]. |
| Recombinant Growth Factors (e.g., HGF, FGF-2) | Pre-treatment to activate pro-survival pathways ex vivo. | Priming MSCs before transplantation to enhance viability [23]. |
| Caspase-Glo 3/7 Assay | Luminescent measurement of caspase activity, a key anoikis marker. | Quantifying the level of apoptosis in detached cell populations. |
Signaling Pathways and Workflows
Anoikis Resistance Signaling Network
Anoikis Resistance Signaling Network Diagram: This diagram illustrates the key molecular pathways that can be genetically and metabolically engineered to promote anoikis resistance. Enhanced signaling from integrins and growth factor receptors converges on central hubs like FAK/Src and PI3K, leading to Akt activation. Akt then drives both metabolic reprogramming and the upregulation of anti-apoptotic proteins like Bcl-2, which collectively inhibit the mitochondrial release of cytochrome C and the subsequent activation of the caspase cascade, thereby blocking anoikis [23] [7] [59].
Experimental Workflow for Engineering Resistance
Stem Cell Engineering Workflow: This workflow outlines the critical steps for developing anoikis-resistant stem cells for transplantation. The process begins with the selection of a genetic or metabolic target (e.g., ITGA5B1, Akt). Stem cells are then engineered using methods like lentiviral transduction. The modified cells must be rigorously validated in vitro using anoikis, adhesion, and metabolic assays before proceeding to in vivo transplantation. Finally, the functional outcome is assessed through measures of engraftment efficiency, paracrine activity, and restoration of tissue function [23] [58].
Troubleshooting Guide: Common Injection Issues and Solutions
| Problem Symptom | Potential Cause | Recommended Solution | Underlying Principle |
|---|---|---|---|
| Low post-injection cell viability | High shear stress in syringe needle | Use larger needle diameter (e.g., 27G+), reduce injection speed [62] | Lower shear forces reduce acute membrane damage and apoptotic signaling [62] |
| High rates of early anoikis | Cells delivered as single-cell suspensions | Transplant small cell aggregates/fragments instead [5] | Maintains cell-ECM and cell-cell contacts, providing survival signals [5] |
| Acute cell necrosis during delivery | Severe, irreversible membrane damage from fluid stretching | Utilize piezoelectric hydrogel carriers that activate endogenous repair via Ca2+ influx [62] | Electrical stimulation triggers rapid plasma membrane resealing mechanisms [62] |
| Poor long-term engraftment | Combined mechanical stress & lack of metabolic resilience | Pre-condition cells to enhance metabolic fitness; optimize medium viscosity [5] [62] | Mitigates post-transplantation metabolic stress and supports survival in new microenvironment [5] |
| Inconsistent delivery outcomes | Uncontrolled flow parameters and variable shear | Implement finite element modeling (e.g., CFD+FEA) to simulate and optimize flow [62] | Predicts shear stress distribution to establish reproducible, gentle injection protocols [62] |
Frequently Asked Questions (FAQs)
Q1: What is the direct link between mechanical shear stress and anoikis in transplanted stem cells?
Mechanical shear stress during injection directly causes physical damage to the cell membrane. Even mild damage can trigger intracellular apoptotic signaling pathways, which are a direct precursor to anoikis—the programmed cell death that occurs upon detachment from the extracellular matrix (ECM) [62]. Furthermore, the dissociation of cells into single-cell suspensions for injection inherently disrupts their natural cell-ECM and cell-cell adhesions, making them profoundly susceptible to anoikis. Transplanting cells as small aggregates or fragments, rather than single cells, has been shown to help mitigate this by preserving critical survival signals [5].
Q2: What are the optimal quantitative parameters for needle-based cell delivery?
Research utilizing finite element modeling and experimental validation has provided the following quantitative guidance for minimizing shear stress [62]:
| Parameter | Optimal Range / Value | Impact on Cell Survival |
|---|---|---|
| Needle Gauge | 27-gauge or larger (e.g., 0.45 mm inner diameter) | A 0.45 mm diameter needle was shown to significantly reduce fluid shear stress and fluid stretching compared to smaller diameters, directly increasing survival from ~30% to much higher levels [62]. |
| Injection Speed | Slow, controlled rate | High injection speeds generate turbulent flow and peak shear forces, causing immediate membrane damage and necrosis [62]. |
| Cell Carrier Viscosity | Tuned to match the shear-thinning properties of the hydrogel used (e.g., RGD-OSA/HA-ADH) | A medium with appropriate viscosity can cushion cells against abnormal stress. The BTO/RGD-OSA/HA-ADH piezoelectric hydrogel is a prime example [62]. |
Q3: How can I experimentally measure and validate the shear stress my cells experience during injection?
A robust protocol involves a combination of computational modeling and direct biological validation:
- Protocol Title: Integrated Fluid Dynamics and Cell Viability Assessment of Injection Parameters.
- Step 1 - Computational Modeling (CFD): Model your specific syringe and needle setup (e.g., a 0.45 mm × 12.7 mm needle) using a one-way fluid-structure interaction method. Integrate a Computational Fluid Dynamics (CFD) solver like STAR-CCM+ with a Finite Element Analysis (FEA) solver like ABAQUS. This simulation will predict the distribution and magnitude of shear stress and fluid stretching forces throughout the injection process [62].
- Step 2 - In Vitro Viability Testing: Perform the injection using the parameters you modeled. Immediately after injection, assess cell viability using a live/dead assay (e.g., calcein-AM/propidium iodide staining) and flow cytometry. Quantify the percentage of viable, apoptotic, and necrotic cells.
- Step 3 - Functional Integration Assay: For a more relevant endpoint in the context of anoikis prevention, culture the injected cells under low-adhesion conditions for 24-72 hours and measure the rate of apoptosis (e.g., via caspase-3 activation or Annexin V staining). This assesses the cells' ability to resist anoikis after the mechanical insult of injection.
Q4: Are there any "smart" materials that can actively protect cells from shear stress?
Yes, recent advances include the development of piezoelectric hydrogels. An example is the BTO/RGD-OSA/HA-ADH hydrogel [62].
- Mechanism of Action: When this hydrogel experiences mechanical stress during injection, the embedded Barium Titanate (BTO) nanoparticles deform and generate a protective piezoelectric potential (an internal electric field). This electrical stimulation directly activates mechanosensitive Piezo1 channels on the stem cell membrane [62].
- Protective Effect: Piezo1 activation causes a rapid influx of calcium (Ca2+). This Ca2+ surge serves two critical functions:
- It immediately triggers endogenous membrane repair mechanisms (e.g., "lipid-patch" and "endocytic removal" models) to reseal any shear-induced membrane damage.
- It promotes actin polymerization, increasing cellular stiffness and resistance to deformation [62]. This "electrical protection" strategy has been shown to significantly enhance stem cell survival during delivery in a rat model of intervertebral disc degeneration [62].
Key Signaling Pathways
Mechanostress to Anoikis Pathway
This diagram illustrates the primary signaling pathway through which mechanical shear stress during injection can lead to anoikis.
Experimental Optimization Workflow
This diagram outlines a logical workflow for designing experiments to optimize injection parameters and validate their effectiveness.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function/Benefit | Application Context |
|---|---|---|
| Piezoelectric BTO Nanoparticles | Converts injection shear stress into protective electrical signals to activate cell repair via Piezo1 [62]. | Integrated into hydrogels for creating "smart" cell delivery systems that actively protect cells. |
| RGD-OSA/HA-ADH Hydrogel | An injectable, biocompatible scaffold that forms via Schiff base reaction; RGD peptide enhances cell adhesion [62]. | Serves as a tunable viscosity cell carrier that can be enhanced with piezoelectric particles. |
| Poly-HEMA Coated Plates | Prevents cell attachment, creating a suspension culture to model detachment and study anoikis [63]. | In vitro assay for quantifying anoikis resistance of cells after the injection process. |
| Piezo1 Ion Channel Agonists | Chemically activates the Piezo1 channel to mimic protective electrical stimulation [62]. | Pre-conditioning strategy to potentially boost cell resilience before transplantation. |
| Computational Fluid Dynamics (CFD) Software | Models fluid flow and predicts shear stress distribution within specific needle geometries [62]. | Essential for in silico prediction and optimization of injection parameters before wet-lab experiments. |
Host Tissue Preconditioning to Improve the Implantation Niche
Host Tissue Preconditioning refers to strategies that modify the recipient site before stem cell transplantation to create a more hospitable microenvironment, thereby countering the primary cause of cell death post-transplantation. In the context of preventing anoikis—the programmed cell death triggered by inadequate or inappropriate cell-matrix contact—preconditioning the host tissue is a critical intervention. The hostile environment of a damaged tissue, characterized by ischemia, inflammation, oxidative stress, and degraded extracellular matrix (ECM), promotes anoikis and leads to the catastrophic loss of up to 99% of transplanted cells within hours [64]. By preparing the host niche to better support transplanted cells, researchers can significantly enhance cell survival, retention, and ultimately, the therapeutic efficacy of regenerative procedures [65] [64].
Core Concepts and Signaling Pathways
The Problem: A Hostile Implantation Niche
The success of stem cell transplantation is severely limited by the harsh conditions at the implantation site. Key detrimental factors include:
- Anoikis: Loss of cell-ECM interactions upon delivery leads to immediate apoptotic signaling [64].
- Ischemia and Nutrient Deprivation: Poorly vascularized transplant sites lack oxygen and nutrients. Oxygen diffusion is limited to about 200 microns from its source, creating central necrosis in injected cell clumps [64].
- Oxidative Stress: Inflammation and reduced blood supply create a pro-oxidant environment [64].
- Host Immune Response: Innate immune reactions, including instant blood-mediated inflammatory reactions (IBMIR) and complement activation, can lyse transplanted cells [64].
The Preconditioning Strategy: Mimicking Hormesis
The biological principle underpinning host preconditioning is hormesis, where brief, sublethal exposure to stress can activate protective and reparative mechanisms, leading to increased resistance to subsequent, more severe stress [65]. The goal of preconditioning is not to cause further damage, but to gently perturb the host tissue to upregulate pro-survival pathways and improve the local microenvironment before the cells arrive.
The following diagram illustrates the logical workflow connecting the problem of the hostile niche to the application and ultimate benefits of host tissue preconditioning.
Frequently Asked Questions (FAQs)
Q1: Why can't we just deliver more cells to compensate for the high death rate? A: This is not a scalable or effective solution. The primary issue is the microenvironment's inadequacy, not the initial cell number. Injecting more cells can exacerbate the problem by creating larger, poorly oxygenated cell clumps, leading to even greater central necrosis and potentially amplifying the local inflammatory response [64]. The focus should be on improving the quality of the niche, not just the quantity of cells.
Q2: How does host preconditioning differ from stem cell preconditioning? A: While both aim to improve transplantation outcomes, their targets are different. Stem cell preconditioning (e.g., hypoxia, heat shock) modifies the cells themselves ex vivo to enhance their inherent resistance to stress [65]. Host tissue preconditioning modifies the in vivo environment where the cells will be delivered, making it more supportive and less hostile. These strategies are complementary and can be used in combination.
Q3: Is host preconditioning safe, given it involves intentionally stressing the tissue? A: Safety is a paramount concern. The key is the sublethal, controlled nature of the preconditioning stimulus. The doses of radiation, drugs, or mechanical stimuli used are designed to be low enough to avoid significant additional damage but sufficient to trigger a protective hormetic response. Clinical models, such as the gentle pre-conditioning used in stem cell transplants for Type 1 diabetes, demonstrate the feasibility of this approach in a medical setting [66].
Q4: Can host preconditioning prevent anoikis entirely? A: It can significantly reduce it, but likely not eliminate it entirely. Anoikis is a multi-factorial process. Host preconditioning primarily addresses the niche-related factors, such as providing a better matrix for attachment and reducing inflammatory triggers. For comprehensive protection, it should be combined with strategies that directly target the cells, such as biomaterial encapsulation (which provides an artificial ECM) or genetic modification of the cells to overexpress anti-apoptotic proteins [65] [64] [28].
Troubleshooting Common Experimental Challenges
| Challenge | Potential Cause | Solution |
|---|---|---|
| Preconditioning causes further tissue damage | Stimulus intensity is too high. | Titrate the preconditioning stimulus (e.g., drug dose, radiation level) to find the minimal effective dose that triggers a protective response without causing significant damage. |
| No improvement in cell survival | Preconditioning method is mismatched to the injury model or cell type. | Re-evaluate the molecular pathways activated by your preconditioning. Ensure they counter the specific stresses of your model (e.g., use pro-angiogenic factors for ischemic sites). |
| High variability in engraftment results | Inconsistent application of the preconditioning stimulus. | Standardize the delivery method (e.g., precise coordinates for injection, calibrated radiation source). Include positive controls in your experiments. |
| Strong immune rejection despite preconditioning | Preconditioning may not adequately modulate the adaptive immune response. | Consider combining host preconditioning with transient immunosuppressive drugs or using stem cells with inherent immunomodulatory properties, like MSCs [64]. |
Experimental Protocols & Data Presentation
Protocol: Pharmacological Preconditioning with Pro-Angiogenic Cytokines
This protocol aims to enhance the vascularization of the host niche prior to stem cell transplantation.
Materials:
- Recombinant growth factors (e.g., VEGF, FGF)
- Sterile saline or PBS (for dilution)
- Appropriate syringes and needles (e.g., 26G-30G)
- Animal model of tissue injury (e.g., myocardial infarction, stroke)
Step-by-Step Method:
- Solution Preparation: Reconstitute the lyophilized growth factor according to the manufacturer's instructions. Prepare working aliquots in sterile saline on ice to prevent degradation.
- Dosage Determination: Refer to established literature for your specific injury model. A typical starting range for VEGF is 0.5-2.0 µg per injection site.
- Administration: At a predetermined time before cell transplantation (e.g., 24-72 hours), anesthetize the animal.
- Stereotactic/Localized Injection: Using a precision syringe, slowly inject the preconditioning cytokine solution directly into the target tissue or the peri-infarct region.
- CRITICAL STEP: Control the flow rate (e.g., 1-2 µL/min) to minimize mechanical damage and backflow [28].
- Post-Procedure Care: Monitor animals until they recover from anesthesia.
- Transplantation: Proceed with your standard stem cell transplantation procedure at the chosen time point.
Quantitative Data from Key Studies
The table below summarizes data from seminal studies demonstrating the efficacy of various preconditioning methods in different disease models.
Table: Efficacy of Host and Donor Cell Preconditioning in Animal Models
| Preconditioning Method | Cell Type & Animal Model | Key Performance Outcomes | Reference |
|---|---|---|---|
| Hypoxic Preconditioning (0.5% O₂, 24h) | Bone marrow–derived MSCs in Rat Stroke Model | Increased cell survival and improved brain functional recovery and motor functions compared to normoxic groups. | [65] |
| Hypoxic Preconditioning (0.1% O₂, 6h) | Cardiac Progenitor Cells (CPCs) in Mouse MI Model | Increased survival and heart functions: increased left ventricular systolic function (LVS) and reduced infarct size. | [65] |
| Oxidative Preconditioning (100 µM H₂O₂, 2 days) | CPCs in Rat MI Model | Increased survival and improved heart functions: improved left ventricular cardiac function and reduced scar. | [65] |
| Gentle Immune Preconditioning (Antibodies + low-dose radiation) | Blood Stem Cells & Islets in Mouse Type 1 Diabetes | Cured established autoimmune diabetes in 9/9 mice; prevented disease in 19/19 mice. No graft-versus-host disease. | [66] |
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for Host Tissue Preconditioning Research
| Reagent / Material | Function / Application in Preconditioning |
|---|---|
| Recombinant VEGF | A key cytokine for pharmacological preconditioning; induces angiogenesis to improve blood supply to the niche. |
| Low-Dose Radiation Source | Used in clinically-relevant models to create space in the bone marrow and modulate the host immune system for engraftment [66]. |
| Small Molecule AKT Agonists | Activates the PI3K/Akt pathway, a critical pro-survival signal that can protect against anoikis and other stresses. |
| Biomaterial Scaffolds | Injectable hydrogels (e.g., alginate, hyaluronic acid) can be used to pre-treat the niche, providing immediate ECM support to prevent anoikis upon cell delivery [28]. |
| Damage-Associated Molecular Pattern (DAMP) Analogs | Molecules like HMGB1 or ATP can be used to simulate sterile injury and precondition the immune and regenerative response [67]. |
Signaling Pathways in Anoikis and Preconditioning
Understanding the molecular pathways of anoikis is essential for developing effective preconditioning strategies. Anoikis is mediated through classic apoptotic pathways, both intrinsic and extrinsic. The diagram below integrates the mechanisms of anoikis with potential points of intervention for host preconditioning.
Diagram Legend:
- Red Nodes/Arrows: Represent key steps in the progression of anoikis.
- Yellow Nodes: Represent initiating events.
- Green Nodes/Arrows: Illustrate how host preconditioning strategies can intervene to block pro-death signals and reinforce pro-survival pathways, thereby creating a protective niche for transplanted cells.
Combating Hypoxic and Nutrient Stress Post-Transplantation
This technical support center provides troubleshooting guides and FAQs for researchers addressing hypoxic and nutrient stress in transplanted stem cells, with a specific focus on preventing anoikis.
Troubleshooting Guides and FAQs
Why do a significant number of my stem cell-derived grafts fail within the first week post-transplantation, even with immunosuppression?
Extensive early cell loss following transplantation is a common challenge. Evidence suggests this can occur independently of immune rejection and is frequently driven by metabolic stress.
- Primary Cause: Metabolic stress triggered by the harsh post-transplantation microenvironment is a critical barrier to cell survival. Transcriptomic analysis of transplanted photoreceptor precursor cells identified dysregulation of mitochondrial function and oxidative phosphorylation pathways as a key driver of early donor cell death [68].
- Anoikis Context: This metabolic stress is compounded by the loss of cellular adhesion post-transplantation, a process known as anoikis. Anoikis is a form of programmed cell death triggered by detachment from the native extracellular matrix and neighboring cells, which is an inherent part of the transplantation process [69] [70].
How does hypoxia specifically impact the function and identity of stem cell-derived islets (SC-islets)?
Hypoxia directly induces a progressive loss of cellular identity and metabolic function in insulin-producing β-cells within SC-islets.
The table below summarizes the quantitative effects of oxygen levels on SC-β cells over time, based on recent research [71].
| Oxygen Level | Duration of Exposure | Effect on SC-β Cell Population (C-peptide+/NKX6.1+) | Functional Consequence |
|---|---|---|---|
| 21% (Normoxia) | 6 weeks | Population remained stable (~55%) | Normal glucose-stimulated insulin secretion (GSIS) |
| 5% (Hypoxia) | 6 weeks | Gradual decline to ~10% | Impaired GSIS after 1 week; exacerbated after 2 weeks |
| 2% (Severe Hypoxia) | 1 week | Significant population decline | Complete loss of GSIS function |
Key Molecular Findings: Single-cell RNA sequencing revealed that under hypoxia, SC-β cells show a significant reduction in the expression of mature insulin (INS). This is linked to reduced expression of immediate early genes (EGR1, FOS, JUN), which subsequently downregulates key β-cell transcription factors, leading to a loss of identity [71].
What are the primary molecular pathways activated in stem cells under hypoxic conditions?
The cellular response to hypoxia is primarily mediated by Hypoxia-Inducible Factors (HIFs). The following diagram illustrates the core hypoxia response pathway in stem cells.
This pathway activation can have dual effects. In various stem cells, including ESCs and NSCs, hypoxia and HIF signaling promote pluripotency, self-renewal, and proliferation [72]. However, in the context of transplanted SC-islets, sustained hypoxia leads to the loss of β-cell identity and function, as described above [71].
What detailed experimental protocol can I use to investigate anoikis resistance relevant to transplantation?
The following workflow, adapted from metastasis research, provides a robust method to study anoikis sensitivity. It is highly relevant for understanding the detachment-induced cell death that occurs during stem cell transplantation [69] [70].
Detailed Protocol: Detachment-Induced Anoikis Assay [69]
- Cell Preparation: Culture your chosen cell line (e.g., A549 or stem cell-derived progenitors) in standard flasks. Upon reaching 70-80% confluence, wash with PBS and detach using a trypsin-EDTA solution.
- Neutralization and Suspension: Neutralize trypsin with culture medium containing serum. Centrifuge and resuspend the cell pellet in fresh medium at a density of 1 × 10^5 cells/mL.
- Induction of Anoikis: Transfer 5 × 10^4 cells in 500 μL of medium into an ultra-low attachment 24-well plate. Prepare replicate wells for cell counting and cell death detection. Incubate at 37°C in a CO2 incubator for desired time intervals (e.g., 0, 24, 48, 72 hours).
- Evaluation of Anoikis:
- Cell Death Detection ELISA: Use a commercial kit to detect histone-associated DNA fragments, a marker of apoptosis. Follow the manufacturer's instructions to prepare immunoreagents and quantify cell death.
- Flow Cytometry: Use an Annexin V-FITC apoptosis detection kit. Resuspend cells in Annexin V Binding Buffer, add Annexin V-FITC and Propidium Iodide (PI), incubate, and analyze by flow cytometry to distinguish live (Annexin V-/PI-), early apoptotic (Annexin V+/PI-), and late apoptotic/necrotic (Annexin V+/PI+) cells.
The Scientist's Toolkit
Essential Research Reagent Solutions
The table below lists key reagents and their functions for investigating hypoxic stress and anoikis in transplantation models.
| Research Reagent / Tool | Primary Function in Experimental Context |
|---|---|
| Ultra-Low Attachment Plates | Prevents cell attachment, inducing anoikis for in vitro modeling of transplantation-induced detachment [69]. |
| Annexin V-FITC Apoptosis Kit | Flow cytometry-based detection and quantification of apoptotic cells, including those undergoing anoikis [69]. |
| Cell Death Detection ELISA PLUS | Photometric enzyme immunoassay for quantifying histone-associated DNA fragments during apoptotic cell death [69]. |
| Anti-HLA Antibodies | Detects HLA expression; critical for assessing immunogenicity of transplanted cells [73]. |
| EDN3 (Endothelin 3) | A potent player identified to help preserve β-cell identity and function under hypoxic conditions when overexpressed [71]. |
| HIF-1α Antibodies | Western blot or immunofluorescence detection to confirm stabilization of the key hypoxia response protein [72]. |
Promising Intervention Strategies
- Genetic Engineering to Enhance Fitness: Overexpression of EDN3 has been shown to preserve β-cell identity in hypoxia by modulating genes involved in glucose sensing and insulin expression [71].
- Stem Cell Preconditioning: This promising method involves pre-treating stem cells with pharmacological, biological, or physical inducers to improve their resistance to the harsh host environment, enhancing survival, paracrine effects, and angiogenesis post-transplantation [74].
- Engineering Hypoimmune Cells: To mitigate immune-related stress, strategies include genetically downregulating HLA class I and II molecules while overexpressing immune-modulating ligands like PD-L1, HLA-G, and CD47 to evade host immune rejection [73].
Assessing Efficacy: Validation Models and Comparative Analysis of Therapeutic Platforms
Anoikis is a specific form of programmed cell death induced by the loss of cell contact with the extracellular matrix (ECM) and other cells [61]. For transplanted stem cells, resisting anoikis is a critical first step towards successful engraftment and tissue regeneration. The development of an anoikis-resistant phenotype allows cells to survive the detachment from their native microenvironment, a process essential for both metastatic cancer progression and the survival of therapeutic stem cells [9] [61].
Traditional two-dimensional (2D) cell culture systems, while simple and cost-effective, fail to mimic the physiological three-dimensional (3D) environment in which cells reside in vivo [75] [76]. Cells cultured in 2D often exhibit altered morphology, gene expression, and signaling pathways, leading to irrelevant predictions of cellular behavior, including responses to drugs and survival signals [75] [77]. To bridge this gap, three-dimensional (3D) cell culture systems have emerged as a powerful tool. These systems provide a more physiologically relevant context, promoting enhanced cell-cell and cell-ECM interactions that closely resemble the in vivo architecture of tissues [78] [79]. Within 3D cultures, such as spheroids, cells can establish gradients of nutrients, oxygen, and signaling molecules, creating heterogeneous zones of proliferating, quiescent, and necrotic cells, much like real tissues [75] [76]. This review will focus on the use of spinner flask systems and other 3D culture techniques as essential platforms for studying and promoting anoikis resistance in the context of regenerative stem cell research.
Key 3D Culture Systems for Studying Anoikis Resistance
Various 3D culture systems are employed to investigate the mechanisms of anoikis resistance. The table below summarizes the main types, their principles, and relevance to anoikis research.
Table 1: Key 3D Culture Systems for Modeling Anoikis Resistance
| Model System | Principle and Methodology | Advantages for Anoikis Research | Limitations |
|---|---|---|---|
| Scaffold-Free Spheroids (Liquid Overlay, Pellet Cultures) | Cells self-aggregate into 3D structures on non-adherent surfaces or through forced aggregation (e.g., centrifugation) [79]. | • Simple and cost-effective.• Mimics cellular heterogeneity with core and surface layers [75].• Directly tests a cell's innate ability to resist anoikis via cell-cell adhesion. | • Limited control over size and uniformity.• Lacks a defined ECM for studying integrin-mediated survival signaling. |
| Spinner Flask Bioreactors | Cells are maintained in suspension by constant, gentle stirring via a magnetic impeller, preventing adhesion and promoting spheroid formation [80]. | • Enables large-scale production of spheroids.• Improves nutrient and gas exchange throughout the culture [80].• Ideal for long-term studies of anchorage-independent survival. | • Shear stress from stirring can damage some cell types.• Requires specialized equipment and optimization of stirring speed. |
| Scaffold-Based Cultures (Hydrogels, ECM Matrices) | Cells are embedded within a 3D matrix of natural (e.g., Matrigel, collagen) or synthetic polymers that mimic the ECM [75]. | • Provides physiological, integrin-binding cues that can promote anoikis resistance [77].• Highly tunable biochemical and mechanical properties. | • Can be expensive.• Matrix composition may vary between batches (natural hydrogels).• Can complicate cell retrieval for downstream analysis. |
| Organoids | Complex 3D structures derived from tissue-specific adult stem cells or induced pluripotent stem cells (iPSCs) that self-organize into organ-like tissues [76] [79]. | • Highest physiological relevance; contains multiple cell types and architecture of the native tissue [79].• Powerful for patient-specific studies of stem cell behavior and survival. | • Technically challenging and time-consuming to establish.• High variability between organoid lines. |
Experimental Protocols for Establishing 3D Anoikis Models
Protocol: Generating Anoikis-Resistant Spheroids Using a Spinner Flask System
This protocol is adapted from methods used to establish anchorage-independent osteosarcoma cultures for studying chemoresistance [80].
Objective: To generate uniform, large-scale 3D spheroids for investigating anoikis resistance in stem cells.
Materials:
- Single-cell suspension of stem cells of interest
- Complete cell culture medium
- Spinner flask (e.g., 100 mL working volume)
- Magnetic stir plate
- 70% ethanol for sterilization
- Hemocytometer or automated cell counter
Method:
- Preparation: Autoclave the spinner flask and its components. Inside a biological safety cabinet, assemble the sterile spinner flask and add the complete culture medium to the desired working volume (e.g., 50-70% of total flask capacity).
- Seeding: Create a single-cell suspension and determine cell viability and concentration. Seed cells into the spinner flask at an optimal density, which must be determined empirically. A common starting density is 0.5 - 1.0 x 10^6 cells/mL [80].
- Initiating Culture: Place the spinner flask on the magnetic stir plate inside a standard cell culture incubator (37°C, 5% CO₂). Begin stirring at a low speed, typically 50-80 rpm, to keep cells in suspension without subjecting them to damaging shear forces.
- Maintenance: Monitor spheroid formation and growth daily. The culture medium can be partially refreshed every 2-3 days. To do this, allow spheroids to settle briefly, remove 50-70% of the spent medium, and replace it with fresh, pre-warmed complete medium.
- Harvesting: Spheroids are typically ready for experimentation within 3-7 days. They can be harvested by simply pouring out the contents of the spinner flask and allowing the spheroids to settle under gravity or by using a low-speed centrifugation step.
Protocol: Anchorage-Independent Growth Assay in Ultra-Low Attachment Plates
This is a standard, small-scale method to quantitatively assess a cell population's capacity for anoikis resistance [80].
Objective: To measure the ability of stem cells to form spheroids and survive in an anchorage-independent environment.
Materials:
- Single-cell suspension of stem cells
- Complete cell culture medium
- Ultra-Low Attachment (ULA) multi-well plates (e.g., 96-well round-bottom plates)
- Multichannel pipettes
Method:
- Preparation: Create a single-cell suspension with high viability.
- Seeding: Seed cells into the ULA plates. For a 96-well format, a common seeding density is 5,000 - 20,000 cells per well in 100-200 µL of medium. The optimal density should be determined for your specific cell type.
- Culture and Monitoring: Place the plates in the cell culture incubator. Do not disturb the plates for the first 24-48 hours to allow for initial spheroid aggregation.
- Analysis: After 4-7 days, spheroid formation can be analyzed. Common endpoints include:
- Imaging: Capture brightfield images to assess spheroid size, shape, and integrity.
- Viability Assay: Perform assays like CellTiter-Glo 3D, which is optimized for quantifying ATP in 3D cultures as a marker of viable cells.
- Size Quantification: Use image analysis software to measure the diameter and area of the formed spheroids.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for 3D Anoikis Studies
| Reagent/Material | Function and Application | Example Use in Anoikis Research |
|---|---|---|
| Ultra-Low Attachment (ULA) Plates | Surface-treated plastic that inhibits cell attachment, forcing cells to aggregate into spheroids. | The foundational tool for scaffold-free spheroid formation and anchorage-independent growth assays [80]. |
| Basement Membrane Extracts (e.g., Matrigel) | A natural, complex hydrogel derived from mouse tumors, rich in ECM proteins like laminin and collagen. | Used in scaffold-based 3D cultures to provide pro-survival, integrin-mediated signaling that can inhibit anoikis [77]. |
| Spinner Flasks & Bioreactors | Systems that use constant agitation to maintain cells in suspension for large-scale 3D culture. | Essential for generating large quantities of uniform spheroids for molecular biology analyses (e.g., RNA sequencing, protein extraction) [80]. |
| Viability Assays (e.g., CellTiter-Glo 3D) | Luminescent assays that measure ATP content, correlating with the number of metabolically active cells in a 3D structure. | Quantifying the survival and proliferation of cells within spheroids under test conditions [80]. |
| Histone Deacetylase (HDAC) Inhibitors (e.g., Vorinostat) | Compounds that induce hyperacetylation of histones, altering gene expression. | Used experimentally to reverse epigenetic adaptations that confer anoikis resistance; shown to mitigate anchorage-independent growth [80]. |
Signaling Pathways in Anoikis and Resistance: A Visual Guide
The following diagram illustrates the key signaling pathways that regulate anoikis and how they are modulated in resistant cells within a 3D environment.
Diagram 1: Key signaling pathways regulating anoikis. In anoikis-sensitive cells (left), ECM detachment leads to the deactivation of integrins and growth factor receptors, causing the downregulation of pro-survival pathways (PI3K/Akt, Mek/Erk). This allows the accumulation of pro-apoptotic proteins like Bim, triggering caspase activation and cell death. Anoikis-resistant cells (right) maintain activation of these survival pathways through alternative mechanisms, suppressing apoptosis [7] [61].
Troubleshooting Guides and FAQs
Spinner Flask-Specific Issues
Q1: My cells are not forming spheroids and are instead dying. What could be the cause? A: This indicates a failure to overcome anoikis. Potential causes and solutions include:
- Cause 1: Incorrect Stirring Speed. Too high a speed causes destructive shear stress; too low allows cells to settle and form clumps.
- Solution: Optimize the agitation rate. Start between 50-80 rpm and adjust based on microscopic observation of spheroid formation and cell viability.
- Cause 2: Poor Cell Viability at Seeding.
- Solution: Ensure a high-viability (>90%) single-cell suspension is used at seeding. Pre-conditioning cells in other 3D cultures (e.g., ULA plates) may enhance their survival in spinner flasks.
- Cause 3: Inadequate Culture Medium.
- Solution: Supplement the medium with survival-promoting factors. Consider adding Rho-associated protein kinase (ROCK) inhibitor Y-27632 (at 10 µM) to reduce initial anoikis, or include specific growth factors that activate pro-survival pathways like PI3K/Akt [7].
Q2: My spheroids are highly variable in size. How can I improve uniformity? A: Heterogeneous spheroid size can affect experimental reproducibility.
- Cause 1: Inconsistent Seeding.
- Solution: Ensure the cell suspension is perfectly homogeneous when seeding into the flask. Using a well-mixed, single-cell suspension is critical.
- Cause 2: Aggregation at Inoculation.
- Solution: Increase the stirring speed slightly immediately after seeding to prevent initial clumping, then reduce to the standard maintenance speed after a few hours.
- Cause 3: Overly Long Culture Duration.
- Solution: Spheroids can coalesce over time. Harvest spheroids at a consistent time point before significant fusion occurs, or use a perfusion bioreactor system for better long-term control.
General 3D Culture and Assay Challenges
Q3: How can I effectively distinguish between true anoikis resistance and general prosurvival signaling in my 3D model? A: This requires careful experimental design with appropriate controls.
- Solution: Include a 2D adherent culture control and a 3D suspension culture treated with a known inducer of apoptosis (e.g., a death receptor agonist). True anoikis resistance is demonstrated when cells in 3D suspension show significantly higher survival than the apoptotic control, and their survival is not merely due to generalized upregulation of survival pathways that also occur in 2D. Confirming the downregulation of key apoptotic executers (e.g., cleaved caspases) in your 3D spheroids compared to a positive control for death is essential [61].
Q4: I am having difficulty analyzing gene expression in cells recovered from my 3D spheroids. The results are noisy and inconsistent. A: This is a common challenge due to the cellular heterogeneity within spheroids.
- Cause: Heterogeneous Cell Populations.
- Solution: The outer proliferating layer and inner quiescent/core cells of a spheroid have vastly different transcriptomes [75]. For more consistent results, use methods to isolate specific spheroid regions (e.g., laser capture microdissection) or use early-stage spheroids that are less heterogeneous. Furthermore, ensure spheroids are thoroughly dissociated into a single-cell suspension before RNA extraction. Protocols for 3D cultures often require longer digestion times with enzymes like accutase or trypsin-EDTA compared to 2D cultures.
Q5: My 3D cultures, while surviving, show altered differentiation potential. Is this related to anoikis resistance? A: Yes, the mechanisms are often linked. The pathways that confer anoikis resistance, such as the upregulation of Sox2 and c-Myc, are also associated with the maintenance of a stem-like, undifferentiated state [80]. This is a critical consideration for stem cell transplantation, as promoting survival must be balanced with the ultimate goal of differentiation into functional tissue.
Low cell retention and engraftment following transplantation is a major obstacle limiting the successful application of cell therapy, including for cardiac repair and other regenerative applications. Accurate methods for tracking cell fate and quantifying cell survival are essential for developing strategies to improve engraftment. A key challenge during this process is anoikis, a specialized type of programmed cell death that is activated upon cell detachment from the native extracellular matrix. For stem cells to successfully engraft, they must resist anoikis after transplantation until they can re-adhere within the host tissue. Research into molecular pathways such as the FOXM1/SQLE axis, which mediates glycolysis to suppress anoikis in cancer cells, provides valuable insights that can be applied to promote stem cell survival in translational research. [59] [81] [82]
► FAQs on Engraftment Assessment and Anoikis Prevention
Q1: What are the primary causes of poor cell engraftment in animal models? Poor engraftment is typically caused by a combination of factors, including significant physical cell loss during or immediately after injection, acute cell death triggered by ischemia or inflammation in the host tissue, and the activation of anoikis due to loss of survival signals from the extracellular matrix. [81]
Q2: How can I determine if my transplanted cells are dying from anoikis? Anoikis shares molecular pathways with apoptosis. You can look for the activation of hallmark apoptotic signals, such as the cleavage of caspase-3 and caspase-9. Furthermore, detecting the presence of pro-apoptotic proteins like Bax and a decrease in anti-apoptotic proteins like Bcl-2 or Bcl-xL in the retrieved cells can indicate anoikis. Strategies that overexpress pro-survival signals have been shown to mitigate these effects. [59]
Q3: Why should I consider using a ROCK inhibitor in my transplantation protocol? ROCK inhibitor (e.g., Y-27632) is widely recommended to enhance initial cell survival post-transplantation. It is particularly effective at reducing anoikis by modulating the actin cytoskeleton and decreasing membrane blebbing and apoptosis that occur after single-cell dissociation and injection. It is often added to the transplantation medium and for the first 24 hours post-transplantation. [83]
Q4: My genetically labeled cells are not detected after engraftment. Does this always mean they have died? Not necessarily. While cell death is a likely cause, the absence of signal could also be due to technical limitations such as transgene silencing. If using non-integrating vectors or certain viral vectors, the reporter gene expression may be lost over time, even if the cells are alive. Using stable genetic markers, such as lentiviral vectors or transgenic donor animals, and validating your detection system with positive controls is crucial. [81]
Q5: What is the advantage of using a dual-reporter system for tracking cell fate? A dual-reporter or recombination-based system (e.g., Cre-Lox) is more sophisticated and can help rule out false positives from phagocytosis. Macrophages can ingest labeled debris from dead cells and appear as false-positive signals, suggesting a viable transplanted cell. A dual system makes this artifact much less likely and provides higher fidelity data. [81]
► Troubleshooting Common Experimental Issues
Problem: Low cell viability and retention immediately after intramyocardial injection.
- Potential Cause: High shear stress during injection, inflammation, and loss of adhesion leading to anoikis.
- Solution:
- Precondition Cells: Treat cells before transplantation with a ROCK inhibitor (Y27632) or small molecules that enhance resistance to detachment-induced death. [83]
- Optimize Delivery: Use a smaller-gauge needle and slower injection rate to minimize shear forces. Mixing cells with a biocompatible hydrogel can provide temporary ECM support, mitigating anoikis.
- Genetic Modification: Consider engineering cells to overexpress anti-apoptotic proteins (e.g., Bcl-2) or key survival factors identified in anoikis-resistance pathways, such as components of the integrin-FAK signaling axis. [59] [81]
Problem: Inconsistent engraftment quantification between technical replicates.
- Potential Cause: Sampling error from histological methods or variable transgene expression.
- Solution:
- Use Non-Histological Methods: Correlate histological counts with a quantitative method like qPCR for a species- or sex-specific gene (e.g., Alu repeats for human cells in mice) to get a whole-organ assessment. [81]
- Standardize Sampling: If using histology, ensure systematic random sampling of the entire organ and analyze multiple sections and optical fields.
- Validate Reporter Stability: Perform in vitro studies to confirm your reporter label (e.g., eGFP) remains stable and bright through multiple cell divisions. [81]
Problem: High background autofluorescence obscures detection of labeled cells in host tissue.
- Potential Cause: Myocardial tissue is notorious for autofluorescence, which can mask specific signals.
- Solution:
- Use Far-Red Reporters: Label cells with quantum dots or fluorescent proteins (e.g., mCherry, tdTomato) that emit in the red or near-infrared spectrum, where tissue autofluorescence is lower. [81]
- Confocal Microscopy: Always use confocal microscopy instead of widefield fluorescence to achieve optical sectioning and reduce out-of-focus light.
- Immunohistochemical Detection: Use an antibody against your reporter protein (e.g., anti-GFP) with a enzymatic detection system (e.g., DAB) that is not susceptible to fluorescence bleed-through. [81]
Problem: Failure to track cell fate longitudinally in the same animal.
- Potential Cause: Histological methods require sacrificing the animal, preventing repeated measurements.
- Solution:
- Implement In Vivo Imaging: Use bioluminescence imaging (BLI) by transducing cells with a luciferase reporter gene. Inject the substrate (e.g., D-luciferin) and image photons emitted by living cells over weeks. This allows for direct, longitudinal tracking of cell survival. [81]
- Magnetic Resonance Imaging (MRI): If cells are labeled with iron oxide particles, use MRI to monitor their location and persistence non-invasively. [81]
► Methodologies for Key Engraftment Experiments
Protocol 1: Longitudinal Cell Tracking Using Bioluminescence Imaging (BLI)
Objective: To non-invasively monitor the survival and persistence of transplanted stem cells in a single animal over time.
Materials:
- Firefly luciferase-expressing stem cells
- IVIS Spectrum Imaging System (or similar)
- D-luciferin, potassium salt (15 mg/mL in PBS)
- Isoflurane anesthesia system
Procedure:
- Cell Preparation: Stably transduce your stem cells with a lentiviral vector expressing firefly luciferase (Fluc) and a fluorescent marker (e.g., eGFP) for post-mortem validation.
- Transplantation: Inject luciferase-positive cells into the target tissue of an anesthetized animal (e.g., mouse).
- Image Acquisition:
- At each time point (e.g., day 1, 3, 7, 14, etc.), inject D-luciferin intraperitoneally (150 mg/kg body weight).
- Five minutes post-injection, anesthetize the animal with isoflurane and place it in the imaging chamber.
- Acquire a series of images with exposure times ranging from 1 second to 5 minutes.
- Quantification:
- Use the imaging software (e.g., Living Image) to draw regions of interest (ROIs) around the signal and measure the total flux (photons/second).
- Normalize the data to the signal from the first day post-transplantation to plot survival kinetics. [81]
Protocol 2: Validating Engraftment and Fate with Immunohistochemistry
Objective: To confirm the presence, location, and phenotype of transplanted cells at the study endpoint.
Materials:
- Cryostat or microtome
- Primary antibodies: anti-GFP (for transplanted cells), anti-Troponin I (for cardiomyocyte fate), anti-Ki67 (for proliferation)
- Species-appropriate fluorescent secondary antibodies
- Hoechst 33342 or DAPI nuclear stain
- Confocal microscope
Procedure:
- Tissue Harvest & Sectioning: At the experimental endpoint, perfuse the animal, harvest the heart, and prepare cryosections (5-10 µm thick).
- Immunostaining:
- Fix sections in 4% PFA for 15 minutes, permeabilize with 0.1% Triton X-100, and block with 5% serum for 1 hour.
- Incubate with primary antibody cocktail overnight at 4°C.
- The next day, wash and incubate with secondary antibodies for 1 hour at room temperature.
- Counterstain nuclei with DAPI and mount with an anti-fade medium.
- Imaging & Analysis:
- Image sections using a confocal microscope. Acquire Z-stacks to ensure accurate cell identification.
- Identify transplanted cells as GFP-positive. Co-localization of GFP with Troponin I indicates differentiation into a cardiomyocyte lineage. Co-localization with Ki67 suggests proliferation. [81]
► Comparison of Cell Engraftment Assessment Methods
Table 1: Strengths and limitations of key techniques for tracking cell engraftment.
| Method | Key Principle | Key Strengths | Major Limitations |
|---|---|---|---|
| Histology & Microscopy | Direct visual identification of labeled cells in tissue sections. | Widely available; provides data on cell location and fate; can be quantitative with rigorous design. [81] | Requires animal sacrifice (no longitudinal data); susceptible to sampling error and artifacts (e.g., phagocytosis). [81] |
| Bioluminescence Imaging (BLI) | Detection of light from luciferase-expressing cells after substrate injection. | Highly sensitive; enables longitudinal tracking in the same animal; provides quantitative kinetic data on cell survival. [81] | Low spatial resolution; signal depth/attenuation can be an issue; requires genetic modification of cells. [81] |
| Quantitative PCR (qPCR) | Amplification of species- or sex-specific DNA sequences. | Highly sensitive and quantitative; not susceptible to transgene silencing; provides a whole-organ assessment. [81] | Requires animal sacrifice; does not provide information on cell location or viability state. [81] |
| Magnetic Resonance Imaging (MRI) | Detection of iron oxide-labeled cells to alter local magnetic fields. | High spatial resolution; non-invasive; allows for longitudinal tracking; clinically translatable. [81] | Low sensitivity; requires large numbers of labeled cells for detection; ambiguous signal if label is phagocytosed. [81] |
| Fluorescent In Situ Hybridization (FISH) | Uses fluorescent probes to detect species-specific genomic sequences. | Does not require pre-labeling; target is stable genomic DNA; high specificity. [81] | Labor-intensive; low throughput; requires animal sacrifice; technically challenging to optimize. [81] |
► The Scientist's Toolkit: Essential Research Reagents
Table 2: Key reagents and materials for engraftment and anoikis studies.
| Reagent / Material | Function / Application |
|---|---|
| ROCK Inhibitor (Y-27632) | Significantly improves survival of dissociated stem cells after transplantation by reducing anoikis and apoptosis. Used in pre-treatment and post-transplantation media. [83] |
| Lentiviral Vectors | For stable genetic modification of stem cells to express reporter genes (eGFP, Luciferase) or pro-survival genes (e.g., Bcl-2, constitutively active AKT) to combat anoikis. [81] |
| Quantum Dots | Robust, photostable nanoparticles for cell labeling. Their emission in the red/NIR spectrum reduces interference from tissue autofluorescence for improved histological detection. [81] |
| D-Luciferin | The substrate for firefly luciferase, injected into animals for non-invasive bioluminescence imaging to track cell survival over time. [81] |
| Anti-GFP Antibody | Used for highly sensitive immunohistochemical detection of GFP-positive transplanted cells, often providing a clearer signal than native GFP fluorescence. [81] |
| Matrigel / Geltrex | Basement membrane extracts. Can be co-injected with cells to provide temporary extracellular matrix support, mitigating anoikis and improving initial retention. [83] |
| Anoikis Pathway Antibodies | Antibodies against cleaved Caspase-3, Bax, Bcl-2, p-FAK, etc., to monitor activation of cell death or survival pathways in retrieved grafts via western blot or IHC. [59] |
► Signaling Pathways in Anoikis and Cell Survival
The diagram below illustrates the core signaling pathways that regulate anoikis, a key challenge in cell engraftment. Integrin-mediated adhesion normally activates pro-survival signals, while detachment triggers cell death.
Anoikis Regulation Pathways: This diagram shows how cell-matrix adhesion via integrins activates survival signals (FAK/Src, PI3K/Akt), while detachment triggers the caspase-mediated apoptotic cascade leading to anoikis. [59]
► Experimental Workflow for Engraftment Studies
The following diagram outlines a comprehensive experimental workflow for assessing cell engraftment, integrating multiple methods from pre-transplantation to final analysis.
Engraftment Assessment Workflow: This workflow combines non-invasive BLI for longitudinal survival data with endpoint histological and molecular analyses for validation and fate determination, providing a robust assessment of engraftment success. [81]
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What is the primary cause of low stem cell survival after transplantation in pre-clinical models? A major cause is anoikis, a form of cell apoptosis triggered by the lack of proper cell adhesion to the extracellular matrix (ECM). When stem cells are injected in a suspension, they lack the necessary adhesive ligands from their surroundings, leading to rapid cell death and poor engraftment rates [28] [84].
Q2: How do biomaterial scaffolds functionally prevent anoikis? Scaffolds prevent anoikis by mimicking the native extracellular matrix (ECM). They provide essential adhesion sites (e.g., via integrin binding) that activate pro-survival signaling pathways within the cell. Furthermore, they can shield cells from mechanical stress during injection and create a protective microenvironment against hypoxic and inflammatory conditions at the transplant site [28] [85] [84].
Q3: My team is debating scaffold-based vs. scaffold-free approaches. What are the key trade-offs? The core trade-off lies between microenvironmental control and structural simplicity.
| Feature | Scaffold-Based Approaches | Scaffold-Free Approaches |
|---|---|---|
| Anoikis Prevention | Excellent, provides direct adhesion sites | Variable; relies on strong cell-cell contacts |
| Microenvironment Control | High (biochemical, mechanical) | Low |
| Structural Complexity | High, can mimic native tissue | Low, often limited to simpler tissues |
| Invasiveness | Can require surgical implantation | Often minimally invasive (e.g., injectable) |
| Reproducibility | Can vary with scaffold batch | Generally high |
| Typical Applications | Complex tissue regeneration (heart, bone) | Tubular tissues, layered structures (cornea) [86] [87] |
Q4: We are using PLA-based scaffolds but see poor cell adhesion. What is a potential solution? A common issue is the inherent hydrophobicity of PLA, which limits cell attachment. A proven solution is to coat the PLA with a hydrophilic, bioactive polymer. For instance, coating PLA particles with Carboxymethyl Cellulose (CMC) has been shown to significantly enhance human Mesenchymal Stem Cell (hMSC) adhesion, viability, and secretion of growth factors, even under hypoxic conditions [85].
Q5: What is a key alternative to scaffolds that still prevents anoikis during transplantation? Cell Sheet Technology is a prominent scaffold-free alternative. This technique uses temperature-responsive culture dishes to harvest intact, confluent layers of cells along with their own naturally deposited ECM. This preserved ECM is rich in adhesion proteins and signaling molecules, which protects the cells from anoikis upon transplantation [86].
Troubleshooting Common Experimental Issues
Problem: Low Cell Retention After Injection
- Potential Cause #1: High shear and extensional stress during ejection from the syringe.
- Solution: Optimize injection parameters. Use shear-thinning hydrogels (e.g., alginate, hyaluronic acid) as delivery vehicles and consider a larger needle gauge (e.g., 26G) with a lower flow rate (e.g., 5 μL/min) to reduce cell death [28].
- Potential Cause #2: Lack of immediate adhesion sites at the transplantation site.
- Solution: Co-transplant cells with an injectable biomaterial carrier. Use microcarriers or microcapsules that offer a large surface area for cell attachment and protect them from the hostile in vivo environment [28] [85].
Problem: Inconsistent Results with 3D Culture Models
- Potential Cause: Using 2D cultures to model 3D biological processes, which fails to recapitulate key cell-matrix interactions and the heterogeneous microenvironment.
- Solution: Transition to 3D culture systems. For scaffold-based methods, use hydrogels like chitosan or synthetic polymers to provide a 3D ECM-like structure. For scaffold-free methods, use spheroids or organoids. 3D systems maintain better stem cell potential and are more predictive of in vivo drug responses [88] [84].
Problem: Scaffold Triggers Unwanted Immune Response
- Potential Cause: The scaffold material or its degradation products are immunogenic.
- Solution: Select biocompatible and biodegradable materials with known low immunogenicity, such as certain types of hyaluronic acid or polylactic acid (PLA). Using a patient's own ECM components or incorporating immune-modulating factors into the scaffold design can also help mitigate immune rejection [84].
Table 1: Quantitative Comparison of Scaffold-Based Formulations
| Biomaterial Formulation | Key Functional Property | Cell Type Tested | Key Quantitative Outcome | Reference |
|---|---|---|---|---|
| CMC-coated PLA Particles | Provides attachment surface | hMSCs | Enhanced cell viability under severe hypoxia; Improved collagen synthesis and wound closure in vivo. | [85] |
| Thermosensitive Chitosan Hydrogel | Injectable; liquid at room temp, gels at 37°C | MSCs | Serves as an ideal 3D injectable scaffold, improving cell delivery and supporting tissue repair. | [84] |
| Shear-Thinning Hydrogels (Alginate, HA) | Plug flow behavior reduces shear stress | RSCs, MSCs, ASCs | Prevents mechanical stress during injection, improving retention and viability. | [28] |
| Poly(N-isopropylacrylamide) (PIPAAm) | Temperature-responsive surface | Various (Cardiomyocytes, etc.) | Enables harvest of intact cell sheets with ECM, preventing anoikis and improving engraftment. | [86] |
Detailed Experimental Protocols
Protocol 1: Evaluating Anoikis Prevention Using CMC-PLA Particles
This protocol is adapted from a 2025 study that synthesized CMC-PLA particles to inhibit anoikis in hMSCs [85].
1. Synthesis of CMC-PLA Particles
- Dissolve PLA in Dimethyl Sulfoxide (DMSO) to create a 7% (w/v) solution.
- Spray the PLA solution into cooled hexane under constant agitation to form PLA particles.
- Wash the resulting particles in an aqueous NaCl solution to remove residual DMSO.
- Mix the washed PLA particles with a CMC solution.
- Freeze-dry the mixture to obtain the final CMC-PLA particles.
- Sieve the particles through a 100 μm mesh to ensure uniform size.
2. In Vitro Anoikis Assay
- Coat a 24-well plate with poly-HEMA to create a non-adherent surface.
- Suspend hMSCs in serum-free DMEM at a density of 2 x 10^4 cells per well.
- Add CMC-PLA particles to the cell suspension at a concentration of 1 mg/mL.
- Incubate the plate under hypoxic conditions (1% O2) for 72 hours to mimic the wound microenvironment.
- After incubation, use a Cell Counting Kit-8 (CCK-8) to assess cell viability. Filter the medium through a 40 μm strainer before absorbance reading to separate cells attached to particles from dead, floating cells.
- For visualization, stain hMSCs with a fluorescent dye (e.g., DiI) before the assay and observe adhesion to particles using fluorescence microscopy.
3. In Vivo Validation for Wound Healing
- Create wound models (e.g., in mice).
- Divide subjects into groups: control, hMSCs alone, hMSCs with PLA particles, and hMSCs with CMC-PLA particles.
- Inject treatments directly into the wound site.
- Monitor and quantify wound closure over time.
- Harvest tissue samples for histological analysis (e.g., H&E staining for collagen synthesis, CD31 staining for angiogenesis).
Protocol 2: Cell Sheet Engineering for Transplantation
This protocol details the use of temperature-responsive surfaces to create scaffold-free cell sheets for transplantation, effectively preventing anoikis [86].
1. Preparation of Temperature-Responsive Surfaces
- Covalently graft Poly(N-isopropylacrylamide) (PIPAAm) onto standard tissue culture polystyrene dishes using electron beam irradiation. The optimal polymer density is between 0.8–2.2 μg cm−2.
2. Cell Seeding and Sheet Formation
- Seed the target cells (e.g., cardiomyocytes, oral mucosal epithelial cells) onto the PIPAAm-grafted dishes.
- Culture the cells at 37°C (hydrophobic surface state) in a standard CO2 incubator until they reach confluence and form strong cell-cell connections and their own ECM.
3. Sheet Harvesting
- After confluence, reduce the culture temperature to below 32°C (typically 20°C) for about 30-60 minutes.
- The PIPAAm surface becomes hydrophilic and hydrated, causing the intact cell sheet to spontaneously detach without the need for enzymatic digestion.
- Carefully transfer the floating cell sheet, along with its underlying ECM, using a pipette or a supportive membrane.
4. Transplantation
- The cell sheet can be directly applied to the target tissue (e.g., heart, cornea).
- To create 3D structures, multiple sheets can be layered on top of one another.
Signaling Pathways and Experimental Workflows
Diagram 1: Anoikis Prevention Signaling Pathway
Anoikis Prevention Pathway: This diagram illustrates how biomaterial scaffolds provide integrin-binding sites that activate intracellular pro-survival signaling pathways, thereby inhibiting the activation of caspase-3 and anoikis.
Diagram 2: Cell Sheet Engineering Workflow
Cell Sheet Engineering Workflow: This workflow outlines the key steps in creating scaffold-free cell sheets using temperature-responsive culture surfaces, preserving the native ECM to prevent anoikis upon transplantation.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Anoikis Prevention Research
| Item | Function in Research | Key Consideration |
|---|---|---|
| Temperature-Responsive Culture Dishes (PIPAAm) | Enables harvest of intact, ECM-preserved cell sheets without enzymatic digestion, preventing anoikis. | Optimal polymer density (0.8-2.2 µg cm⁻²) is critical; culture conditions may vary by cell type. [86] |
| Carboxymethyl Cellulose (CMC) | A hydrophilic polymer used to coat materials (e.g., PLA) to enhance cell attachment and moisture retention. | Improves the biocompatibility and cell-adhesive properties of hydrophobic biomaterials. [85] |
| Polylactic Acid (PLA) | A biodegradable polymer used to create scaffolds and particles for cell delivery. | Its hydrophobicity can limit cell adhesion, often requiring surface modification. [85] |
| Shear-Thinning Hydrogels (Alginate, Hyaluronic Acid) | Injectable biomaterials that protect cells from mechanical stress during transplantation, improving viability and retention. | Their plug flow behavior minimizes shear forces on cells during injection. [28] |
| Poly-HEMA | Used to coat cultureware to create a non-adherent surface for in vitro anoikis induction assays. | Essential for creating a control environment where cells cannot attach, triggering anoikis. [85] |
| CCK-8 Assay Kit | A colorimetric method for quantifying cell viability and proliferation in the presence of biomaterials. | Provides a sensitive and easy-to-use alternative to MTT assays. [85] |
Troubleshooting Guide: Improving Transplanted Stem Cell Survival and Function
This guide addresses common challenges in achieving therapeutic benefit from stem cell transplants, focusing on moving beyond mere cell survival to functional integration.
Problem 1: Poor Survival of Transplanted Cells at the Injury Site
- Potential Cause: Transplanted cells undergo anoikis, a form of programmed cell death triggered by detachment from the extracellular matrix, and face a harsh microenvironment (hypoxia, inflammation, nutrient deprivation) [23] [89].
- Solutions:
- Use Pro-Survival Cocktails: Pretreat cells with a combination of agents before transplantation. A proven example includes Matrigel (to provide substrate and prevent anoikis), a pan-caspase inhibitor (e.g., ZVAD), an anti-apoptotic protein (e.g., BCL-XL BH4), and growth factors like IGF-1 [89].
- Genetic Modification: Engineer cells to overexpress pro-survival or pro-proliferation genes (e.g., CCND2) to enhance their resilience and engraftment [89].
- Hypoxic Preconditioning: Precondition cells in low-oxygen environments before transplantation to enhance their tolerance to the ischemic conditions of the injury site [23].
Problem 2: Excessive Differentiation in Stem Cell Cultures Prior to Transplant
- Potential Cause: Suboptimal culture conditions, including old culture medium, overgrown colonies, or excessive time outside the incubator during handling, can spur spontaneous differentiation, reducing the pool of viable cells for therapy [90].
- Solutions:
- Ensure complete culture medium is fresh (e.g., less than 2 weeks old when stored at 2-8°C) [90].
- Passage cultures when colonies are large and dense, but before they overgrow. Remove any areas of differentiation prior to passaging [90].
- Minimize the time the culture plate is out of the incubator to less than 15 minutes [90].
Problem 3: Low Cell Attachment or Suboptimal Aggregate Formation After Passaging
- Potential Cause: Inconsistent cell aggregate size and low attachment efficiency after passaging can lead to poor yields and unhealthy cultures [90] [83].
- Solutions:
- For low attachment, initially plate a higher number of cell aggregates (2-3 times higher) to maintain a densely confluent culture [90].
- If aggregates are too large, increase incubation time with the dissociation reagent by 1-2 minutes and increase pipetting to break them up [90].
- Work quickly after cells are treated with passaging reagents to minimize the time aggregates spend in suspension [90].
- Ensure you are using the correct culture plate type (tissue culture-treated or non-treated) for the specific coating matrix (e.g., Matrigel or Vitronectin XF) [90].
Problem 4: Inadequate Functional Integration Leading to Arrhythmias (for Cardiac Cell Therapy)
- Potential Cause: Upon transplantation, iPSC-derived cardiomyocytes (iPSC-CMs) may not electromechanically couple properly with the host myocardium, leading to arrhythmias [89].
- Solutions:
- Tissue Engineering: Instead of injecting single-cell suspensions, use pre-formed 3D cardiac tissues or patches that promote better cell alignment and maturation before and after transplantation [89].
- Improving Host-Graft Coupling: Research is focused on genetic modifications and pharmacological treatments to enhance the formation of gap junctions between graft and host cells.
Problem 5: Immune Rejection of Transplanted Cells
- Potential Cause: Allogeneic stem cell transplants are recognized as foreign by the host's immune system, leading to graft rejection [73] [89].
- Solutions:
- Use Hypoimmune Cells: Genetically engineer stem cells to evade immune detection. Strategies include knocking out Major Histocompatibility Complex (MHC) genes to reduce immunogenicity and overexpressing "don't-eat-me" signals like CD47 [73].
- Co-transplantation with Immunomodulatory Cells: Co-transplant with accessory cells like mesenchymal stem cells (MSCs) or regulatory T cells (Tregs) that can suppress the local immune response [73].
Frequently Asked Questions
Q1: Why is preventing anoikis critical for stem cell therapy success? Anoikis is a major cause of early cell death post-transplantation. Since cell adhesion to the extracellular matrix is crucial for survival signals, preventing anoikis is a primary strategy for enhancing initial engraftment and increasing the number of functional cells that can contribute to tissue repair [23].
Q2: What is a key difference between measuring cell survival and therapeutic benefit? Cell survival is a short-term metric indicating whether transplanted cells remain alive. Therapeutic benefit is a long-term, functional outcome that depends not only on survival but also on proper integration, differentiation, and physiological function of the cells within the host tissue. For example, in heart repair, benefit is measured by improved ejection fraction, not just the presence of grafted cells [89].
Q3: How can I test the functional response of cells to a therapy before in vivo transplantation? Functional precision medicine tests, such as the 3D Predict Glioma test, expose a patient's tumor cells to chemotherapeutic agents ex vivo to measure response. This approach can predict whether a patient's cells will respond to a specific drug, allowing for therapy personalization and improved outcomes before treatment even begins [91].
Q4: Should I use primary cells or cell lines for my transplantation research? For physiologically relevant results, primary cells are generally recommended. Data from primary cells have increased physiological relevance compared to cell lines, as they are isolated directly from tissues and are more representative of the in vivo state [92].
Q5: What strategies can improve the survival of iPSC-derived cardiomyocytes in an infarcted heart? Key strategies include [89]:
- Pretreatment with a pro-survival cocktail to inhibit anoikis and apoptosis.
- Genetic manipulation to enhance proliferation (e.g., CCND2 overexpression).
- Using cardiac patches or 3D tissues instead of single-cell suspensions to provide structural support.
- Overexpressing specific microRNAs (e.g., miR-21, miR-24) to promote cell survival.
Experimental Data & Strategies for Enhancing Therapeutic Outcomes
The table below summarizes quantitative findings and strategic approaches from key studies for improving functional outcomes in stem cell therapy.
Table 1: Documented Improvements in Survival and Function from Pre-clinical and Clinical Studies
| Therapeutic Area | Intervention / Strategy | Key Functional Outcome Measured | Reported Improvement | Reference |
|---|---|---|---|---|
| High-Grade Glioma | Functional drug testing with 3D Predict Glioma test to identify TMZ responders | Progression-Free Survival (PFS) | 5.8 months longer median PFS in test-predicted responders vs non-responders | [91] |
| High-Grade Glioma | Functional drug testing with 3D Predict Glioma test to identify TMZ responders | Overall Survival (OS) | 7.6 months longer median OS in test-predicted responders vs non-responders | [91] |
| Ischemic Heart Disease | Transplantation of hiPSC-CMs overexpressing CCND2 | Cardiac Function (Ejection Fraction) | Improved ejection fraction and reduced scar size in a porcine model | [89] |
| Stem Cell Therapy (General) | Pretreatment with pro-survival cocktails & genetic modification | Cell Engraftment & Survival | Significantly enhanced cell survival in the hostile infarct environment | [23] [89] |
| Type 1 Diabetes | Engineering hypoimmune stem cell-derived beta cells | Immune Evasion & Graft Acceptance | Protected from immune rejection without systemic immunosuppression | [73] |
Table 2: Essential Research Reagent Solutions for Anoikis and Survival Studies
| Reagent / Material | Function / Application | Specific Examples / Notes |
|---|---|---|
| ROCK Inhibitor (Y-27632) | Improves cell survival after passaging and thawing by reducing apoptosis; critical for single-cell cloning. | Often used in hPSC culture; can be added to media during passaging [90] [83]. |
| Pro-Survival Cocktail Components | Prevents anoikis and apoptosis in cells post-transplantation. | Combination of Matrigel, ZVAD (caspase inhibitor), BCL-XL BH4, Cyclosporine A, IGF-1, Pinacidil [89]. |
| Extracellular Matrix (ECM) Coatings | Provides a physiological substrate for cell adhesion, mimicking the native environment and preventing anoikis. | Geltrex, Matrigel, Vitronectin XF, Laminin, Fibronectin [90] [83]. |
| Gentle Cell Dissociation Reagents | Passages cells as small aggregates, preserving cell-cell contacts and reducing stress compared to single-cell dissociation. | ReLeSR, Gentle Cell Dissociation Reagent; incubation time can be adjusted for ideal aggregate size [90]. |
| Hypoimmune Genetic Modification Tools | CRISPR-Cas9 or viral vectors for creating immune-evasive cells. Used to knock out MHC genes and/or overexpress immune checkpoint proteins like PD-L1 and CD47 [73]. |
Experimental Protocols for Key Assays
Protocol 1: Assessing Anoikis Sensitivity in Transplantable Stem Cells
Objective: To quantify the rate of anoikis in stem cell populations following detachment, simulating the transplantation process.
Materials:
- Stem cell culture (e.g., MSCs or iPSCs)
- Ultra-low attachment plate
- Standard culture medium
- ROCK inhibitor (Y-27632)
- Annexin V / Propidium Iodide (PI) apoptosis detection kit
- Flow cytometer
Methodology:
- Cell Detachment: Harvest cells using a standard method (e.g., enzymatic digestion with trypsin or accutase) to create a single-cell suspension.
- Induction of Anoikis: Seed the detached cells into an ultra-low attachment plate in standard culture medium. This prevents re-attachment and induces anoikis.
- Control Setup: In parallel, seed cells into a tissue culture-treated plate that allows for re-attachment. This serves as the negative control for anoikis.
- Optional Treatment: To test protective compounds, add the candidate agent (e.g., 10 µM ROCK inhibitor) to the medium in the ultra-low attachment plate.
- Incubation: Incubate cells for 6-24 hours.
- Analysis: Collect floating and adherent (from control plate) cells. Stain with Annexin V and PI according to the kit protocol and analyze by flow cytometry to distinguish live (Annexin V-/PI-), early apoptotic (Annexin V+/PI-), and late apoptotic/necrotic (Annexin V+/PI+) cells.
Protocol 2: Evaluating In Vivo Engraftment and Functional Benefit in a Myocardial Infarction Model
Objective: To determine the survival, integration, and functional impact of transplanted iPSC-CMs in an immunodeficient murine model of myocardial infarction.
Materials:
- hiPSC-CMs
- Pro-survival cocktail
- Immunodeficient mice (e.g., SCID mice)
- Ligation sutures for coronary artery occlusion
- Echocardiography system
- Histology reagents (fixatives, antibodies for human-specific markers)
Methodology:
- Cell Preparation: Pre-treat hiPSC-CMs with the pro-survival cocktail for 30-60 minutes prior to transplantation [89].
- Myocardial Infarction Model: Anesthetize mice and perform a left thoracotomy to expose the heart. Permanently ligate the left anterior descending (LAD) coronary artery to induce a myocardial infarction.
- Cell Transplantation: Immediately after infarction, inject the pre-treated hiPSC-CMs (e.g., 1-5 million cells in a small volume) directly into the border zone of the infarct. Inject the control group with an equivalent volume of carrier solution alone.
- Functional Assessment (Weeks 4-8 post-op):
- Perform echocardiography to measure functional parameters such as Left Ventricular Ejection Fraction (LVEF), Left Ventricular End-Systolic Dimension (LVESD), and Left Ventricular End-Diastolic Dimension (LVEDD). Compare these metrics between the treatment and control groups to assess functional improvement [89].
- Histological Analysis (Endpoint):
- Harvest hearts, section them, and perform immunohistochemistry.
- Use human-specific antibodies (e.g., anti-human mitochondrial antibody) to identify and quantify the number of surviving engrafted human cells.
- Co-stain for cardiac markers (e.g., cTnT) and gap junction proteins (e.g., Cx43) to assess differentiation and electromechanical coupling with host tissue.
Signaling Pathways and Experimental Workflows
Anoikis Signaling Pathway in Detached Stem Cells
Workflow for Evaluating Functional Stem Cell Therapy
Safety and Immunogenicity Profiling of Anoikis-Resistant Cell Products
Core Concepts and Definitions
Anoikis and Its Role in Cell Transplantation Anoikis is a form of programmed cell death triggered when cells detach from their native extracellular matrix (ECM). In the context of cell transplantation, this process poses a significant challenge. Transplanted cells, including mesenchymal stem cells (MSCs), often face detachment from their natural matrix environment, leading to anoikis and poor engraftment rates at the transplantation site. This is particularly problematic in regenerative medicine applications where cell survival is crucial for therapeutic success [23] [38].
Anoikis Resistance in Therapeutic Applications Anoikis resistance describes the ability of cells to survive despite detachment from the ECM. While this phenomenon is potentially harmful in cancer metastasis, it can be beneficial in cell transplantation therapies. Researchers can engineer therapeutic cells with enhanced anoikis resistance to improve survival post-transplantation. However, this approach must be carefully balanced with safety considerations, as induced anoikis resistance may potentially alter immunogenic properties or lead to unintended proliferation [23] [38].
Troubleshooting FAQs: Common Experimental Challenges
Q1: Our transplanted anoikis-resistant MSCs show unexpectedly low viability despite genetic modifications for enhanced survival. What might be causing this?
A1: Poor viability of transplanted anoikis-resistant cells can result from multiple factors:
- Harsh Microenvironment: The transplant site often presents nutrient and oxygen deprivation, inflammatory responses, and oxidative stress that collectively overwhelm survival mechanisms [23].
- Insufficient Adhesion: Even with anoikis resistance, weak adhesion to host tissue ECM can limit long-term survival and integration. Consider co-delivering ECM molecules or using hydrogel scaffolds to provide temporary structural support [23].
- Incomplete Pathway Activation: Single genetic modifications may be insufficient against multiple cell death pathways. Combinatorial approaches targeting different survival mechanisms often yield better results [36].
Q2: How can we distinguish true anoikis resistance from general apoptosis resistance in our modified cell products?
A2: Several experimental approaches can help make this distinction:
- Detachment-Specific Assays: Use controlled detachment protocols with ultra-low attachment plates while maintaining constant nutrient conditions to isolate matrix detachment effects from other variables [69].
- Pathway-Specific Markers: Monitor caspase-8 and caspase-9 activation specifically in detached conditions, as these are key initiators of anoikis pathways [59].
- Integrin Signaling Analysis: Assess integrin β1 and focal adhesion kinase (FAK) phosphorylation status, as these are specifically involved in anchorage-dependent survival signaling [38] [59].
Q3: We're concerned about potential immunogenic changes in our anoikis-resistant cell products. How can we systematically profile this?
A3: Immunogenicity profiling should include multiple dimensions:
- Immune Cell Infiltration Analysis: Use techniques like ssGSEA (single-sample Gene Set Enrichment Analysis) to characterize immune cell populations that interact with your anoikis-resistant cells, similar to approaches used in cancer studies [93].
- Checkpoint Molecule Expression: Monitor PD-L1, CTLA-4, and other immune checkpoint molecules that may be altered in anoikis-resistant cells [93].
- Cytokine Secretion Profiling: Analyze the secretome of modified cells, particularly looking for changes in pro-inflammatory cytokines that might trigger host immune responses [23].
Q4: What are the key molecular markers we should monitor to validate successful anoikis resistance without malignant transformation?
A4: Essential markers include:
- Pro-Survival Pathways: Phospho-Akt, phospho-ERK, and Bcl-2 family proteins indicate successful activation of survival signaling [23] [59].
- Anoikis-Specific Indicators: Monitor TXNIP and AMPK activation, which are involved in detachment stress response [94].
- Safety Markers: Regularly check for absence of cancer-associated markers such as NRAGE/TBX2 complex formation and p14ARF downregulation, which are associated with undesirable transformation [13].
Experimental Protocols for Safety and Immunogenicity Assessment
Protocol 1: Detachment-Induced Anoikis Assay
This protocol provides a standardized method to quantify anoikis sensitivity in engineered cell products [69].
- Cell Preparation: Culture test cells in appropriate medium until 70-80% confluence.
- Detachment: Wash with PBS and detach using trypsin-EDTA solution.
- Neutralization: Add culture medium with FBS to neutralize trypsin.
- Centrifugation: Spin at 200 × g for 5 minutes and resuspend in fresh medium.
- Experimental Setup: Seed 5×10⁴ cells/mL in 500 μL medium into ultra-low attachment 24-well plates. Include standard attachment plates as control.
- Incubation: Maintain at 37°C in CO₂ incubator for desired timepoints (0, 24, 48, 72 hours).
- Assessment: Use Cell Death Detection ELISA PLUS kit per manufacturer's instructions with modifications as needed.
- Validation: Confirm results with Annexin V-FITC apoptosis detection via flow cytometry.
Key Considerations:
- Include positive controls (known anoikis-sensitive cells) and negative controls (known anoikis-resistant cells).
- Optimize seeding density for each cell type based on doubling time and growth characteristics.
- Perform pilot tests to determine optimal timepoints for detection [69].
Protocol 2: Immunogenicity Profiling Co-culture System
This method assesses how anoikis-resistant cells interact with immune components [93].
- Isolate Peripheral Blood Mononuclear Cells (PBMCs): Freshly isolate from human blood samples using Ficoll gradient.
- Culture Anoikis-Resistant Cells: Maintain test cells in suspension culture for 24-48 hours to mimic post-transplantation detachment.
- Setup Co-culture: Combine anoikis-resistant cells with PBMCs at varying ratios (1:5 to 1:20) in ultra-low attachment plates.
- Time Course: Maintain co-cultures for 24-96 hours with sampling at multiple timepoints.
- Analysis:
- Flow cytometry for T-cell activation markers (CD69, CD25)
- Multiplex cytokine analysis of supernatant (IL-2, IFN-γ, IL-10, TGF-β)
- Mixed lymphocyte reaction to assess allogeneic responses
- Validation: Compare response to non-modified control cells under identical conditions.
Quantitative Assessment Data
Table 1: Survival Enhancement Strategies for Transplanted Anoikis-Resistant Cells
| Strategy | Mechanism of Action | Reported Efficacy | Potential Immunogenicity Concerns |
|---|---|---|---|
| Heat Shock Preconditioning | Upregulates heat shock proteins, enhances stress resistance | 2.1-3.5x improvement in early survival [36] | Low; may slightly increase MHC expression |
| Genetic Modification (Akt overexpression) | Activates PI3K/Akt survival pathway, suppresses pro-apoptotic signals | 3.8x increase in engraftment efficiency [23] | Moderate; requires viral vectors, potential insertional mutagenesis |
| Hypoxic Preconditioning | Mimics transplant microenvironment, induces metabolic adaptation | 2.5x improvement in cell viability [23] | Low; transient effects post-engraftment |
| ECM Molecule Co-delivery | Provides immediate adhesion sites, reduces anoikis trigger | 4.2x increase in retained cells at day 7 [36] | Variable; depends on ECM source and purity |
| Anti-apoptotic Protein Treatment | Direct inhibition of caspase cascades | 2.8x reduction in apoptosis markers [23] | Low to moderate; depends on delivery method |
Table 2: Key Molecular Markers for Anoikis Resistance Safety Profiling
| Marker Category | Specific Targets | Expected Change in Safe Anoikis Resistance | Warning Sign (Potential Malignant Transformation) |
|---|---|---|---|
| Survival Signaling | p-Akt, p-ERK, Bcl-2, Bcl-xL | Moderate increase (2-4x baseline) | Sustained high activation (>5x baseline) |
| Detachment Stress Response | AMPK, TXNIP, LC3B | Transient activation, normalizes by 24-48h | Persistent activation beyond 72h |
| Integrin Signaling | Integrin β1, FAK, Src | Initial decrease, recovery after re-attachment | Constitutive activation in suspension |
| Cell Cycle Regulation | Cyclin D1, p21, p27 | G0/G1 arrest in suspension | Continued proliferation in suspension |
| Immunomodulatory Factors | PD-L1, HLA-G, CD47 | Moderate upregulation (2-3x) | Extreme upregulation (>5x) or significant downregulation |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Anoikis Resistance Studies
| Reagent/Category | Specific Examples | Primary Function | Considerations for Safety/Immunogenicity Studies |
|---|---|---|---|
| Anoikis Assay Systems | CytoSelect 96-Well Anoikis Assay [95] | Quantify anoikis in pre-coated plates with colorimetric/fluorometric detection | Allows medium-throughput screening of multiple modified cell lines |
| Detachment Cultureware | Ultra-low attachment plates (Corning) [69] | Prevents cell adhesion to induce anoikis in controlled conditions | Essential for standardized assessment across experimental batches |
| Cell Death Detection Kits | Cell Death Detection ELISA PLUS (Roche) [69] | Specific detection of histone-associated DNA fragments in apoptotic cells | Provides quantitative, reproducible data on anoikis levels |
| Flow Cytometry Reagents | Annexin V-FITC kits, TruStain FcX [69] | Distinguish apoptotic cells and block nonspecific antibody binding | Critical for immunophenotyping and assessing immune cell interactions |
| Extracellular Matrix Proteins | Matrigel, laminin, fibronectin [69] | Study re-attachment capacity and integrin signaling | Test different ECM components to assess integrin expression changes |
| Metabolic Assays | ATP quantification, Seahorse kits [94] | Monitor bioenergetic stress during detachment | Detached cells show marked ATP reduction; key safety parameter |
Signaling Pathways and Experimental Workflows
Anoikis-Resistant Cell Product Safety and Immunogenicity Profiling Workflow
Molecular Mechanisms of Anoikis Resistance in Transplanted Cells
Conclusion
Overcoming anoikis is not merely about enhancing short-term cell survival; it is a fundamental prerequisite for unlocking the full therapeutic potential of stem cell transplantation. The integration of biomaterial science, molecular biology, and clinical protocol optimization offers a multi-faceted arsenal to protect cells through the critical transplantation phase. Promising strategies, such as injectable cryogel microcarriers that provide mechanical support and trophic factor delivery, alongside targeted caspase inhibition and host microenvironment modulation, show significant potential to improve engraftment rates. Future research must focus on translating these combinatorial approaches into clinically viable, scalable, and safe therapies. The ongoing expansion of pluripotent stem cell-derived therapies in clinical trials underscores the urgency of solving the anoikis challenge, paving the way for more effective treatments for a wide range of degenerative diseases and injuries.
References
- 1. Anoikis mechanisms [https://pubmed.ncbi.nlm.nih.gov/11544023/]
- 2. The Sensors and Regulators of Cell-Matrix Surveillance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3292620/]
- 3. understanding of anoikis resistance mechanisms and ... [https://pubmed.ncbi.nlm.nih.gov/22024283/]
- 4. Understanding of anoikis resistance mechanisms and ... [https://www.sciencedirect.com/science/article/abs/pii/S0898656811003330]
- 5. Metabolic stress and early cell death in photoreceptor ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04509-w]
- 6. Anoikis - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/anoikis]
- 7. Mechanisms for Modulating Anoikis Resistance in Cancer and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8039382/]
- 8. The role of non-coding RNA regulates stem cell programmed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12123353/]
- 9. Anoikis resistance in Cancer: Mechanisms, therapeutic ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383525003167]
- 10. Integrin Cell Signaling Pathway [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/signaling-pathways/integrin/integrin-overview.html]
- 11. Therapeutic Use of Integrin Signaling in Melanoma Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468206/]
- 12. Metabolic reprogramming and signaling adaptations in ... [https://pubmed.ncbi.nlm.nih.gov/39821582/]
- 13. Anoikis resistance and cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619527/]
- 14. Intrinsic and Extrinsic Pathways of Apoptosis [https://www.thermofisher.com/us/en/home/life-science/antibodies/antibodies-learning-center/antibodies-resource-library/cell-signaling-pathways/cellular-apoptosis-pathway.html]
- 15. Mechanisms of Cell Death: Apoptosis | Intrinsic & Extrinsic ... [https://blog.cellsignal.com/mechanisms-of-cell-death-apoptosis]
- 16. Caspase Activation Pathways: an Overview - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK14011/]
- 17. Caspase activation pathways: some recent progress [https://www.nature.com/articles/cdd200959]
- 18. Targeting anoikis resistance as a strategy for cancer therapy [https://www.sciencedirect.com/science/article/abs/pii/S1368764624000578]
- 19. Cancer Stem Cells Protect Non-Stem Cells From Anoikis: Bystander Effects - PubMed [https://pubmed.ncbi.nlm.nih.gov/26918647/]
- 20. Stem cell transplant without toxic preparation successfully ... [https://med.stanford.edu/news/all-news/2025/07/stem-cell-transplant.html]
- 21. Cancer stem cells and tumor-associated macrophages as mates in tumor progression: mechanisms of crosstalk and advanced bioinformatic tools to dissect their phenotypes and interaction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11839637/]
- 22. Detection of Anoikis Using Cell Viability Dye and Quantitation of Caspase Activity - PubMed [https://pubmed.ncbi.nlm.nih.gov/34033095/]
- 23. Cell Adhesion and Long-Term Survival of Transplanted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4333334/]
- 24. Systems Approaches to Preventing Transplanted Cell Death ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2587485/]
- 25. Methods for Assessing Apoptosis and Anoikis in Normal Intestine/Colon and Colorectal Cancer - PubMed [https://pubmed.ncbi.nlm.nih.gov/29589304/]
- 26. An experimental workflow for investigating anoikis resistance in cancer metastasis [https://polscientific.com/journal/JBM/12/3/10.14440/jbm.2024.0140]
- 27. an injectable, shape memory cryogel microcarrier platform ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5656175/]
- 28. Biomaterials to enhance stem cell transplantation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10169090/]
- 29. Bioinspired 3D hydrogel scaffold to mimic tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12281143/]
- 30. Engineering strategies to enhance the research progress of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04471-7]
- 31. Glycosaminoglycan-Based Cryogels as Scaffolds for Cell ... [https://www.mdpi.com/1420-3049/26/18/5597]
- 32. Heparin-Based Growth Factor Delivery Platforms: A Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472959/]
- 33. Recent advances in the design and immobilization of ... [https://www.sciencedirect.com/science/article/pii/S0141813024015472]
- 34. Novel biomaterial strategies for controlled growth factor ... [https://www.nature.com/articles/am2017171]
- 35. Control Growth Factor Release Using a Self-Assembled ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0011017]
- 36. Systems approaches to preventing transplanted cell death ... [https://providence.elsevierpure.com/en/publications/systems-approaches-to-preventing-transplanted-cell-death-in-cardi/]
- 37. Troubleshooting heparin resistance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11665620/]
- 38. Anoikis in cell fate, physiopathology, and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11401975/]
- 39. Advantages of RGD peptides for directing cell association with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3091033/]
- 40. Arginylglycylaspartic acid [https://en.wikipedia.org/wiki/Arginylglycylaspartic_acid]
- 41. Loss of cell anchorage triggers apoptosis (anoikis) in ... [https://www.sciencedirect.com/science/article/abs/pii/S1096719202000045]
- 42. Dual mechanism β-amino acid polymers promoting cell ... [https://www.nature.com/articles/s41467-020-20858-x]
- 43. Hydrogels with multiple RGD presentations increase cell ... [https://www.sciencedirect.com/science/article/pii/S1742706125002880]
- 44. Inhibition of Caspase-mediated Anoikis Is Critical for Basic ... Fibroblast [https://pmc.ncbi.nlm.nih.gov/articles/PMC2797176/]
- 45. Trophic factors counteract elevated FGF-2-induced inhibition of adult... [https://pubmed.ncbi.nlm.nih.gov/16859812/]
- 46. bFGF rescues dysfunctional properties of adipose-derived ... [https://link.springer.com/article/10.1007/s00125-025-06533-0]
- 47. Frontiers | Exploring the diversity of biological processes regulated by... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1618330/full]
- 48. Strategy for Clinical Setting of Co-transplantation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11179456/]
- 49. Induction of Anoikis Following Myoblast Transplantation ... [https://www.sciencedirect.com/science/article/pii/S1600613522027599]
- 50. CTTN overexpression in HNSCC inhibits Anoikis-apoptosis [https://www.nature.com/articles/s41598-025-21891-w]
- 51. Systems Approaches to Preventing Transplanted Cell Death ... [https://pubmed.ncbi.nlm.nih.gov/18466917/]
- 52. A long way to go: caspase inhibitors in clinical use - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8519909/]
- 53. A long way to go: caspase inhibitors in clinical use [https://www.nature.com/articles/s41419-021-04240-3]
- 54. A Comprehensive Exploration of Caspase Detection Methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC11121653/]
- 55. Preconditioning Mesenchymal Stem Cells With Caspase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4017598/]
- 56. Caspase inhibitors promote alternative cell death pathways [https://pubmed.ncbi.nlm.nih.gov/17062895/]
- 57. z-VAD-fmk augmentation of TNFα-stimulated neutrophil ... [https://www.sciencedirect.com/science/article/pii/S0006497120457003]
- 58. Integrin alpha5beta1 suppresses rBMSCs anoikis and ... [https://www.sciencedirect.com/science/article/pii/S0753332217344062]
- 59. Anoikis resistance in gastric cancer: a comprehensive review [https://www.nature.com/articles/s41419-025-07860-1]
- 60. Mechanisms for Modulating Anoikis Resistance in Cancer ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.626577/full]
- 61. Anoikis resistance––protagonists of breast cancer cells ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-023-01183-4]
- 62. Endogenous stem cell repair strategy via ... [https://www.sciencedirect.com/science/article/abs/pii/S1385894725013968]
- 63. NY-ESO-1 facilitates anoikis resistance and tumor ... [https://www.nature.com/articles/s41419-025-08017-w]
- 64. Challenges and Strategies for Improving the Regenerative ... [https://www.mdpi.com/1422-0067/18/10/2087]
- 65. Preconditioning Stem Cells for In Vivo Delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4120806/]
- 66. Type 1 diabetes cured in mice with gentle blood stem-cell and ... [https://med.stanford.edu/news/all-news/2025/11/type-1-diabetes-cure.html]
- 67. The regenerative journey: exploring stem cell roles from injury ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502613/]
- 68. Metabolic stress and early cell death in photoreceptor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291488/]
- 69. An experimental workflow for investigating anoikis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12422110/]
- 70. An experimental workflow for investigating anoikis ... [https://pubmed.ncbi.nlm.nih.gov/40937375/]
- 71. Improving cellular fitness of human stem cell-derived islets ... [https://www.nature.com/articles/s41467-025-59924-7]
- 72. The role of hypoxia in stem cell regulation of the central ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8611781/]
- 73. Engineering hypoimmune stem cell-derived beta cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04745-0]
- 74. Translational insights into stem cell preconditioning [https://www.sciencedirect.com/science/article/pii/S075333222100809X]
- 75. Three-dimensional cell culture systems as an in vitro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6904866/]
- 76. Three-dimensional in vitro culture models in oncology research [https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-022-00887-3]
- 77. Three-Dimensional in Vitro Cell Culture Models in Drug ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2018.00006/full]
- 78. Emerging roles of 3D-culture systems in tackling tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10804388/]
- 79. Three-Dimensional Cell Cultures: The Bridge between In Vitro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10419178/]
- 80. Anoikis-resistant subpopulations of human osteosarcoma ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-015-0466-4]
- 81. Assessment and Optimization of Cell Engraftment after ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2826722/]
- 82. FOXM1 boosts glycolysis by upregulating SQLE to inhibit ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12075401/]
- 83. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 84. Constructing a cell microenvironment with biomaterial ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02650-w]
- 85. Carboxymethyl cellulose‐polylactic acid particles for inhibiting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284428/]
- 86. Scaffold-Free 3-D Cell Sheet Technique Bridges the Gap ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6801996/]
- 87. The ECM: To Scaffold, or Not to Scaffold, That Is the Question [https://www.mdpi.com/1422-0067/22/23/12690]
- 88. Cellular Systems for Colorectal Stem Cancer Cell Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC11817814/]
- 89. Exploring hiPSC-CM replacement therapy in ischemic hearts [https://link.springer.com/article/10.1007/s00395-025-01117-w]
- 90. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 91. Functional prediction of response to therapy prior ... [https://www.nature.com/articles/s41598-024-68801-0]
- 92. Frequently Asked Questions on Primary Cells [https://www.stemcell.com/primary-cells-faq.html]
- 93. Anoikis resistance regulates immune infiltration and drug ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1427475/full]
- 94. Elucidating cellular signaling mechanisms of anoikis resistance [https://open.library.ubc.ca/soa/cIRcle/collections/ubctheses/24/items/1.0103433]
- 95. 96-Well Anoikis Assay [https://www.cellbiolabs.com/96-well-anoikis-assay]