Source Matters: A Comparative Analysis of Mesenchymal Stem Cell Tissue Origins for Targeted Clinical Applications
The therapeutic potential of mesenchymal stem cells (MSCs) is widely recognized, but their clinical translation is complicated by significant functional heterogeneity linked to tissue origin.
Source Matters: A Comparative Analysis of Mesenchymal Stem Cell Tissue Origins for Targeted Clinical Applications
Abstract
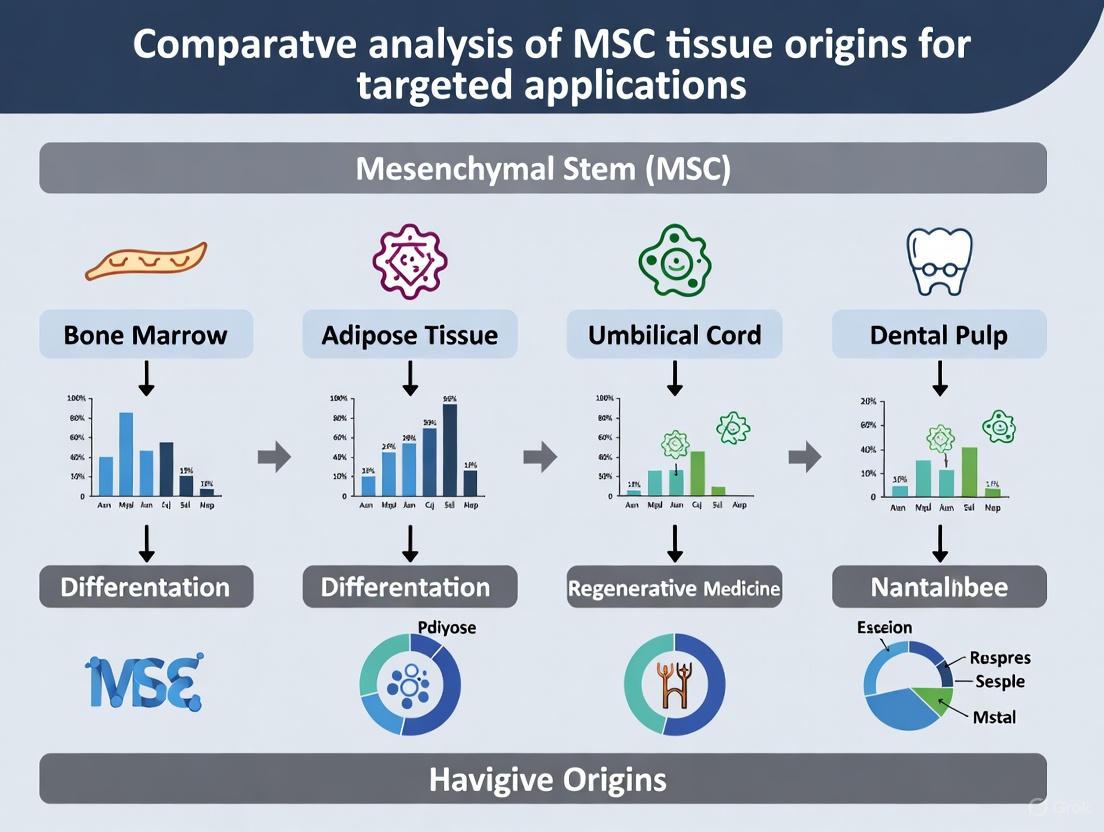
The therapeutic potential of mesenchymal stem cells (MSCs) is widely recognized, but their clinical translation is complicated by significant functional heterogeneity linked to tissue origin. This review provides a comparative analysis of MSCs derived from key sources—including bone marrow, adipose tissue, dental pulp, and umbilical cord—for researchers and drug development professionals. We synthesize foundational biology, methodological protocols, and troubleshooting strategies, emphasizing how intrinsic properties like differentiation potential, immunomodulatory capacity, and secretome profiles are dictated by ontogeny. By validating these differences through direct comparative studies and clinical trial data, this article establishes a strategic framework for selecting the optimal MSC source for specific therapeutic applications, from autoimmune diseases and orthopedic injuries to novel cell-free therapies.
Unraveling MSC Heterogeneity: Developmental Origins and Native Identities
The field of mesenchymal stromal cell (MSC) research is undergoing a significant paradigm shift, moving from a traditional focus on their stem cell characteristics toward a more nuanced understanding of their stromal and immunomodulatory functions. This evolution is reflected in recent nomenclature updates from the International Society for Cell & Gene Therapy (ISCT), which now formally recommends the term "Mesenchymal Stromal Cells" instead of "Mesenchymal Stem Cells" for the majority of clinical applications [1] [2]. This terminological refinement is not merely semantic but represents a fundamental recalibration of the scientific community's understanding of how these cells function therapeutically. The shift acknowledges that the primary mechanism of action for MSCs in most clinical settings is not long-term engraftment and differentiation but rather sophisticated paracrine signaling and immunomodulation [2] [3].
This reframing has profound implications for how researchers characterize MSCs, design potency assays, and develop cell-based therapeutics. The traditional "stem cell" narrative, which emphasized differentiation potential and tissue regeneration, is being supplemented—and in some cases supplanted—by a view of MSCs as complex immunomodulatory and trophic mediators [2]. This article examines the ongoing nomenclature debate, details the updated ISCT criteria, and explores how a more precise understanding of MSC biology is driving a more targeted approach to selecting tissue sources for specific therapeutic applications.
The Nomenclature Debate: From "Stem" to "Stromal"
Historical Context and Rationale for Change
The journey of MSC terminology began with the initial discovery of these cells in the bone marrow and the subsequent coining of the term "Mesenchymal Stem Cells" by Arnold Caplan in 1991 [4] [3]. The original classification was heavily predicated on the in vitro observations of trilineage differentiation potential (adirogenic, chondrogenic, and osteogenic) and their capacity to adhere to plastic surfaces [4]. However, as in vivo data accumulated from clinical trials, a disconnect emerged between the "stem" cell nomenclature and the observed biological effects.
Converging evidence from clinical applications, particularly in immune-mediated diseases like graft-versus-host disease (GVHD), Crohn's disease, and autoimmune disorders, consistently demonstrated that the therapeutic benefits were arising primarily from paracrine effects and immunomodulation rather than lineage-driven tissue regeneration [2]. Transplanted MSCs were found to engage with host immune cells—suppressing effector T-cell activation, expanding regulatory T cells (Tregs), and reprogramming myeloid cells toward inflammation-resolving phenotypes—through the release of bioactive molecules and extracellular vesicles [2]. This mechanistic understanding, supported by the fact that engraftment of administered MSCs is often low and transient, highlighted a misalignment between the historical name and the actual primary function [3].
The ISCT Position: A Mechanism-Aligned Terminology
In 2019, and more forcefully in 2025, the ISCT Mesenchymal Stromal Cell committee released position statements addressing this nomenclature issue [1] [2]. The core recommendation is to use the term "Mesenchymal Stromal Cells (MSCs)" to reflect the predominant in vivo mode of action. The society stipulates that researchers who wish to continue using the "stem cell" terminology must provide experimental evidence of genuine stem cell properties, such as self-renewal and multi-lineage differentiation, in their specific cellular product [1].
This shift is considered corrective, not cosmetic [2]. It aims to:
- Enhance Scientific Clarity: Aligns the cell identity with its established biological function.
- Improve Regulatory Communication: Facilitates more accurate classification and evaluation of cell therapy products.
- Mitigate Public Misunderstanding: Reduces the potential for public confusion and the misuse of the emotionally charged "stem cell" label by unregulated clinics [2].
- Refine Clinical Trial Design: Encourages the development of mechanism-aligned potency assays and clinical endpoints centered on immunomodulation rather than purely regeneration-centric outcomes.
Updated ISCT Criteria: From Minimal Definition to Comprehensive Characterization
The ISCT has substantially refined the identification and characterization criteria for MSCs, moving beyond the minimal standards established in 2006 toward a framework suited for clinical translation.
Table 1: Evolution of ISCT MSC Identification Criteria
| Standard Element | 2006 Standard | 2025 Standard |
|---|---|---|
| Cell Definition | Mesenchymal Stem Cells (MSCs) | Mesenchymal Stromal Cells (MSCs) |
| Stemness Requirement | Must demonstrate trilineage differentiation | Must provide evidence to use the term "stem" |
| Marker Detection | Qualitative (positive/negative) | Quantitative (thresholds and percentages) |
| Tissue Origin | Not emphasized | Must be specified and considered |
| Critical Quality Attributes (CQAs) | Not required | Must assess efficacy and functional properties |
| Culture Conditions | No standard reporting requirement | Detailed parameter reporting required [1] |
Key Updates in the 2025 Framework
- Clarification of Terminology: As discussed, the default nomenclature is now "Mesenchymal Stromal Cells" [1].
- Optimization of Identification Criteria: The updated standards introduce more rigorous requirements for surface marker characterization. While CD73, CD90, and CD105 are retained as basic positive markers, and CD45 is a mandatory negative marker to exclude hematopoietic contamination, reporting must now be quantitative. Researchers must specify the percentage of positive cells and the threshold used for identification via flow cytometry [1].
- Emphasis on Tissue Origin: The new standard requires explicit specification of the tissue source (e.g., bone marrow, adipose tissue, umbilical cord), acknowledging that cells from different origins exhibit distinct phenotypic and functional properties that influence their therapeutic potential [1].
- Introduction of Critical Quality Attributes (CQAs): A major advancement is the incorporation of CQAs, which moves characterization beyond basic phenotyping. CQAs compel researchers to describe the efficacy and functional properties that define the clinical functionality of their MSC product, such as immunomodulatory potency or secretome profile [1].
- Standardization of Culture and Reporting: Detailed reporting on culture conditions, including medium components, passaging methods, and environmental parameters, is now required to enhance reproducibility and transparency across studies [1].
Comparative Analysis of MSCs from Different Tissue Origins
The updated ISCT focus on tissue origin is supported by a body of evidence demonstrating that MSCs from different sources have distinct biological characteristics. This functional heterogeneity is a critical consideration for targeted therapeutic development.
Bone Marrow-Derived MSCs (BM-MSCs)
As the most historically studied type, BM-MSCs are considered the "gold standard" for comparison.
- Immunomodulation: BM-MSCs have been shown to be potent inhibitors of lymphocyte proliferation in vitro [5].
- Clinical Use: They formed the basis for the first FDA-approved MSC product for steroid-refractory pediatric acute GVHD [2]. However, a drawback is the painful isolation process and a cell yield that declines with the age of the donor [6] [3].
Adipose Tissue-Derived MSCs (AT-MSCs)
Adipose tissue is an abundant and readily accessible source of MSCs.
- Proliferation and Yield: Adipose tissue provides a 500-fold higher yield of stem cells per gram of tissue compared to bone marrow [6].
- Immunomodulation: Similar to BM-MSCs, AT-MSCs are potent inhibitors of T-cell proliferation [5]. However, studies have raised safety concerns, as AT-MSC infusions have been associated with pro-coagulant activity in vitro and, in one mouse study, with sudden death, suggesting a need for careful safety monitoring [5].
- Differentiation: They efficiently differentiate into adipogenic, osteogenic, and chondrogenic lineages [6].
Umbilical Cord-Derived MSCs (UC-MSCs)
UC-MSCs, being ontogenically primitive, offer several advantages for allogeneic therapy.
- Proliferation: They exhibit superior proliferative capacity compared to AT-MSCs and BM-MSCs, a characteristic maintained even under serum-free culture conditions [6] [7].
- Immunomodulation: Their immunomodulatory profile can differ. While they may be less potent at directly inhibiting lymphocyte proliferation than BM-MSCs, they are reported to induce a higher regulatory T-cell (Treg)/Th17 ratio, suggesting a different mode of immune regulation [5]. Like AT-MSCs, they also exhibit a higher pro-coagulant potential than BM-MSCs [5].
- Differentiation: While they show strong chondrogenic and osteogenic potential, some studies indicate their adipogenic differentiation may be less efficient than that of AT-MSCs [6] [7].
Table 2: Functional Comparison of MSCs from Different Tissue Sources
| Characteristic | Bone Marrow (BM) | Adipose Tissue (AT) | Umbilical Cord (UC) |
|---|---|---|---|
| Relative Cell Yield | Low | Very High (500-fold > BM) | High [6] |
| Proliferation Rate | Moderate | Moderate | High [6] [7] |
| In Vitro T-cell Inhibition | Potent | Potent | Less Potent [5] |
| Treg/Th17 Induction | Not Specified | Higher | Higher [5] |
| Pro-coagulant Risk | Lower | Higher | Higher [5] |
| Osteogenic Potential | High | High | High [6] [7] |
| Adipogenic Potential | High | High | Variable / Moderate [7] |
| Chondrogenic Potential | High | High | High [6] |
| Key Advantages | Established history, potent immunomodulation | High yield, easy access | High proliferation, low immunogenicity |
Experimental Data and Methodologies for Comparison
To ensure robust and reproducible comparisons between MSC sources, standardized experimental protocols are essential.
Key Experimental Workflow
The following diagram outlines a generalized workflow for the isolation, characterization, and functional comparison of MSCs from different tissues.
Detailed Methodologies
1. Isolation and Culture:
- AT-MSCs: Are typically isolated from lipoaspirate or adipose tissue fragments via enzymatic digestion (e.g., collagenase), followed by centrifugation to separate the stromal vascular fraction (SVF) containing the MSCs [6].
- UC-MSCs: Can be isolated using enzymatic methods or explant cultures, where small pieces of Wharton's jelly or cord tissue are placed in culture dishes, allowing MSCs to migrate out [5] [6]. To comply with modern standards, culture should be performed in serum-free medium (SFM) to avoid batch-to-batch variability and safety issues associated with animal serum [7].
2. Immunophenotypic Characterization by Flow Cytometry:
- Method: Cells are harvested, incubated with fluorochrome-conjugated antibodies, and analyzed using a flow cytometer.
- Positive Markers (≥95% positive): CD73, CD90, CD105.
- Negative Markers (≤2% positive): CD34, CD45, CD11b or CD14, CD19 or CD79α, and HLA-DR [4] [8]. The 2025 standards require reporting the precise percentage of positive cells for each marker [1].
3. Trilineage Differentiation Assays:
- Adipogenic Differentiation: Cells are cultured in induction medium containing corticosteroids, such as dexamethasone, and indomethacin for 2-3 weeks. Differentiation is confirmed by intracellular lipid droplet accumulation using Oil Red O staining [6] [7].
- Osteogenic Differentiation: Cells are induced with medium containing dexamethasone, ascorbate-2-phosphate, and β-glycerophosphate for 3 weeks. Calcium deposition in the extracellular matrix is visualized with Alizarin Red S staining [6] [7].
- Chondrogenic Differentiation: A pellet culture system is often used, where pellets of MSCs are spun down and cultured in a defined chondrogenic medium with TGF-β for 3 weeks. The formation of sulfated glycosaminoglycans in the cartilage matrix is detected with Alcian Blue staining [6] [7].
4. Immunomodulatory Potency Assays:
- Lymphocyte Proliferation Assay: A standard method to quantify MSC immunomodulatory capacity. MSCs are cocultured with activated peripheral blood mononuclear cells (PBMCs) or T-cells. The inhibition of T-cell proliferation is measured via techniques like 3H-thymidine incorporation or CFSE dilution assay [5]. This assay directly tests a key proposed mechanism of action for many clinical applications.
The Scientist's Toolkit: Essential Reagents for MSC Research
Table 3: Key Research Reagent Solutions for MSC Studies
| Reagent / Material | Function in Research | Application Example |
|---|---|---|
| Serum-Free Medium (SFM) | Provides defined, xeno-free culture environment; ensures reproducibility and safety for clinical translation. | Expansion of UC-MSCs under GMP-compliant conditions [7]. |
| TrypLE / Trypsin | Enzymatic detachment of adherent MSCs during subculturing. | Standard passaging of MSC cultures. |
| Flow Cytometry Antibodies | Quantitative analysis of surface markers (CD73, CD90, CD105, CD45, etc.) for phenotype validation. | Verification of MSC identity per ISCT criteria [7]. |
| Trilineage Differentiation Kits | Pre-formulated media for inducing adipogenic, osteogenic, and chondrogenic differentiation. | In vitro assessment of multilineage differentiation potential [7]. |
| Recombinant Human IFN-γ | Inflammatory priming agent; enhances MSC immunomodulatory potency by upregulating IDO and PD-L1/2. | Preconditioning MSCs before in vivo administration or in vitro co-culture assays [5]. |
| Lymphocyte Activation Reagents | Activate T-cells in co-culture systems to measure MSC-mediated immunosuppression. | Used in PBMC or T-cell proliferation assays (e.g., with PHA or anti-CD3/CD28 beads) [5]. |
The ongoing debate and subsequent refinement of MSC nomenclature and criteria by the ISCT mark the maturation of the field from exploratory research to targeted therapeutic development. The shift from "stem" to "stromal" is a pivotal correction that aligns terminology with the predominant immunomodulatory and paracrine mechanisms of action observed in clinical settings [2]. The updated 2025 standards, with their emphasis on quantitative reporting, tissue origin, and Critical Quality Attributes, provide a robust framework for developing more consistent, reproducible, and effective MSC-based therapies.
The functional comparisons between tissue sources reveal that there is no single "best" MSC type. Instead, the choice of source—be it bone marrow, adipose tissue, or umbilical cord—should be strategically aligned with the intended clinical application. The future of MSC therapy lies in a precision medicine approach, where a detailed understanding of a cell product's mechanistic profile, informed by the updated ISCT criteria, guides its selection for specific disease pathologies. This evolution in thinking, from a one-size-fits-all "stem cell" to a nuanced toolkit of functionally distinct "stromal cells," promises to unlock the full clinical potential of these remarkable therapeutic agents.
The prevailing classification of Mesenchymal Stem Cells (MSCs) often associates them primarily with a mesodermal lineage. However, emerging research reveals a critical exception: a significant population of MSCs, particularly those derived from dental tissues, originates from the ectoderm, specifically the neural crest. This ectodermal heritage endows dental MSCs with unique biological properties and functional predispositions that distinguish them from their mesodermal counterparts, such as Bone Marrow MSCs (BMMSCs) and Adipose-derived Stem Cells (ADSCs). Understanding this distinction is paramount for selecting the optimal MSC source for targeted regenerative applications. This guide provides a comparative analysis of MSCs based on their embryonic origin, consolidating key experimental data and methodologies to inform research and development strategies in regenerative medicine and drug discovery.
Embryonic Origins and Developmental Trajectories
The fundamental difference between dental MSCs and classical MSCs lies in their embryological genesis. While BMMSCs and ADSCs are derived from the mesoderm, dental MSCs originate from the cranial neural crest, an ectodermal structure that gives rise to a vast array of craniofacial tissues [9] [10].
This developmental pathway was conclusively demonstrated using double-transgenic mouse systems (e.g., P0-Cre/Rosa26EYFP and Wnt1-Cre/Rosa26EYFP), which allow for the lineage tracing of neural crest-derived cells. Studies using these models showed that approximately 90% of dental mesenchymal cells are positive for the neural crest lineage marker, whereas only about 7% are derived from the mesoderm (traced by Mesp1-Cre) [10]. This ectodermal origin is not a mere developmental footnote; it imprints a unique molecular and functional signature on dental MSCs, predisposing them toward neurogenic and odontogenic lineages and influencing their secretome and immunomodulatory functions [11] [12].
The diagram below illustrates this developmental divergence.
Comparative Analysis: Ectodermal vs. Mesodermal MSCs
The distinct embryonic origins translate into measurable differences in the biological properties and functional outputs of MSCs. The following tables provide a side-by-side comparison based on current research.
Table 1: Core Properties and Marker Expression
| Property | Ectodermal Dental MSCs (e.g., DPSCs, SHED) | Mesodermal MSCs (e.g., BMMSCs, ADSCs) |
|---|---|---|
| Embryonic Origin | Ectoderm (Cranial Neural Crest) [9] [10] | Mesoderm [11] [13] |
| Key Markers | Positive: CD29, CD44, CD73, CD90, CD105, CD146, STRO-1, Nestin [11] [9] | Positive: CD73, CD90, CD105 [14] [13] |
| Negative: CD14, CD19, CD34, CD45, HLA-DR [11] | Negative: CD34, CD45, HLA-DR [14] | |
| Proliferation & Clonogenicity | High proliferative and colony-forming capacity; SHED > DPSCs > BMMSCs [9] [15] | Moderate proliferative capacity; lower than dental MSCs [9] [13] |
| Immunogenicity | Low immunogenicity; negative for MHC-II [15] | Low immunogenicity |
Table 2: Differentiation Potential and Secretome Profile
| Characteristic | Ectodermal Dental MSCs | Mesodermal MSCs |
|---|---|---|
| Neurogenic Potential | High. Constitutive expression of Nestin, βIII-tubulin; superior neuronal differentiation in vitro [9] [12] [16] | Moderate. Can be induced toward neuronal lineage but with lower efficiency [13] [12] |
| Osteogenic Potential | Strong, primarily toward osteodentinogenesis [13] [17] | Strong, toward osteogenesis [13] |
| Adipogenic Potential | Weak or absent. DPSCs fail to differentiate into adipocytes in vitro [12] [16] | Strong. Readily form lipid droplets [13] [16] |
| Secretome Profile | Enriched in neurotrophic and angiogenic factors; microRNAs involved in oxidative stress and apoptosis pathways [16] | microRNAs more related to cell cycle and proliferation regulation [16] |
Experimental Protocols for Key Analyses
To validate the comparative properties outlined above, here are detailed methodologies for two critical experimental paradigms.
Isolation and Culture of Dental Pulp Stem Cells (DPSCs)
This protocol is adapted from established methods for isolating MSCs from human third molars [11] [9].
- Tissue Preparation: Clean the tooth surface thoroughly with disinfectants. Using sterilized dental fissure burs, cut around the cementum-enamel junction to reveal the pulp chamber.
- Pulp Extraction: Gently separate the dental pulp tissue with tweezers.
- Digestion: Rinse the pulp with a basic medium (e.g., α-MEM). Mince the tissue into small pieces (1-2 mm³) and digest in a solution of 3 mg/mL collagenase type I and 4 mg/mL dispase II for 1 hour at 37°C.
- Cell Suspension Preparation: Neutralize the digest with complete medium. Pass the cell suspension through a 70 μM cell strainer to obtain a single-cell suspension.
- Culture: Centrifuge the filtrate and resuspend the cell pellet. Seed cells in culture flasks with a standard growth medium (e.g., α-MEM supplemented with 10-15% FBS, L-ascorbic acid, L-glutamine, penicillin, and streptomycin). Incubate at 37°C in 5% CO₂.
- Expansion: Refresh the medium every 2-3 days. Passage cells upon reaching 80-90% confluence.
The workflow is summarized in the diagram below.
In Vitro Trilineage Differentiation Assay
This is a standard functional assay to confirm MSC multipotency, following ISCT guidelines [14] [16].
Osteogenic Differentiation:
- Culture Medium: Basic medium supplemented with 10% FBS, 50 µM ascorbic acid-2 phosphate, 10 mM β-glycerophosphate, and 0.1 µM dexamethasone.
- Procedure: Culture cells for 21 days, changing the medium every 3-4 days.
- Analysis: Detect mineralization by Alizarin Red S staining, which labels calcium deposits red.
Adipogenic Differentiation:
- Culture Medium: Use an adipogenic induction cocktail (typically containing insulin, indomethacin, IBMX, and dexamethasone).
- Procedure: Culture for 14-21 days.
- Analysis: Visualize lipid vacuoles by Oil Red O staining.
Chondrogenic Differentiation:
- Culture Method: Pellet culture or micromass culture in a defined chondrogenic medium containing TGF-β.
- Procedure: Culture for 21-28 days.
- Analysis: Assess cartilage matrix production (proteoglycans) by Toluidine Blue or Alcian Blue staining.
Key Consideration: A definitive outcome of this assay for dental MSCs is their consistent failure to undergo adipogenesis, a key differentiator from mesodermal MSCs [12] [16].
The Scientist's Toolkit: Essential Research Reagents
The following table lists critical reagents for working with and characterizing dental MSCs.
Table 3: Key Research Reagent Solutions
| Reagent | Function | Application Example |
|---|---|---|
| Collagenase Type I / Dispase II | Enzymatic digestion of collagen and extracellular matrix to isolate cells from dental pulp tissue [11]. | Initial isolation of DPSCs, SHED, SCAP. |
| STRO-1 Antibody | Identifies a key perivascular marker for a primitive, multipotent subpopulation of MSCs via flow cytometry or immunomagnetic sorting [9]. | Enrichment of stem cell-rich fractions from heterogeneous dental MSC populations. |
| Nestin Antibody | Detects the intermediate filament protein Nestin, a neural progenitor marker highly expressed in dental MSCs due to their neural crest origin [9] [16]. | Immunocytochemistry or flow cytometry to confirm ectodermal/neurogenic predisposition. |
| Osteo-Inductive Supplements (Ascorbate, β-Glycerophosphate, Dexamethasone) | Provides critical components to induce and support osteogenic differentiation and matrix mineralization in vitro [16]. | Trilineage differentiation assays; studying dentin regeneration. |
| Alizarin Red S | A diazo dye that binds to calcium salts, used to visualize and quantify calcium deposition in differentiated cultures [16]. | End-point analysis of successful osteogenic differentiation. |
The evidence unequivocally demonstrates that dental MSCs are not merely MSCs from a different anatomical location; they are a distinct class of MSCs shaped by their ectodermal, neural crest ancestry. This origin confers upon them a superior capacity for neurogenesis and a specific bias toward odontogenic, rather than pure osteogenic, differentiation. For researchers and drug development professionals, this knowledge is transformative. It moves the selection of an MSC source from a generic choice to a targeted, rational decision. For applications in nervous system repair, dental pulp regeneration, or leveraging a uniquely programmed secretome, ectoderm-derived dental MSCs present a compelling and powerful alternative to traditional mesodermal sources. Future research will continue to unravel the full therapeutic potential of these specialized cells, solidifying their role in the next generation of regenerative medicine.
Within the complex architecture of nearly every tissue, the perivascular niche serves as a critical in vivo reservoir for mesenchymal stem/stromal cells (MSCs). For decades, MSCs were primarily defined by their in vitro behavior, leaving their native identity and physiological functions poorly understood. Emerging research has since identified two primary perivascular cell types—pericytes and adventitial cells—as the in vivo counterparts to culture-derived MSCs. This guide provides a comparative analysis of these cellular reservoirs, detailing their anatomical positions, marker expression, functional characteristics, and experimental methodologies for their study. Understanding the distinct biological properties of these perivascular stem cells is essential for leveraging their full potential in regenerative medicine and drug development.
The concept of the "perivascular niche" has revolutionized our understanding of mesenchymal stem cell biology. Initially isolated through plastic adherence in long-term cultures, MSCs were later discovered to reside natively in perivascular locations throughout the body [18]. This discovery provided a physiological context for MSCs, linking them to specific anatomical positions and in vivo functions.
Two principal cell types constitute these in vivo reservoirs: pericytes, which envelop capillaries and microvessels, and adventitial cells, located in the outer layer (tunica adventitia) of larger arteries and veins [18]. Collectively termed perivascular stem cells (PSCs), these populations exhibit MSC characteristics in culture, including multipotency, self-renewal capacity, and expression of classic MSC surface markers [18] [19]. Their strategic positioning throughout the vascular tree makes them readily accessible for tissue repair and regeneration, with both populations contributing differentially to tissue homeostasis and pathological processes.
Defining the Cellular Reservoirs
Pericytes
Pericytes are branched, contractile cells embedded within the basement membrane of capillaries and microvessels, making direct contact with endothelial cells through cytoplasmic processes [20] [19]. First described in the 19th century by Rouget and later named "pericytes" by Zimmermann in 1923, these cells play crucial roles in vascular development, stability, and permeability [20] [19] [21].
- Morphology and Distribution: Pericytes exhibit diverse morphologies ranging from typical flat and stellate shapes in the central nervous system to more round shapes in kidneys [20]. Their density varies significantly across tissues, with the highest pericyte-to-endothelial cell ratios found in the central nervous system and retina (approximately 1:1), correlating with more stringent endothelial barrier functions [20].
- Identification Markers: No single specific marker exists for pericytes, necessitating combinatorial approaches. Common markers include PDGFR-β, NG2, CD146, CD13, RGS5, and α-SMA (though α-SMA expression is heterogeneous) [20] [19] [21].
- Developmental Origins: Pericytes originate from multiple embryonic sources, including mesoderm-derived mesenchymal stem cells, neuroectoderm-derived neural crest cells (particularly in the head and thymus), and mesothelium (in coelomic organs) [20].
Adventitial Cells
Adventitial cells reside in the outermost layer of larger blood vessels (tunica adventitia) and represent a phenotypically and anatomically distinct population from pericytes [18]. These cells function as progenitors and can give rise to bona fide MSCs in culture.
- Anatomical Position: Located in the adventitial layer of arteries and veins, these cells are not directly embedded in the capillary basement membrane like pericytes [18].
- Identification: Adventitial cells natively express typical MSC markers (CD73, CD90, CD105) and may express specific markers such as TNAP (tissue-nonspecific alkaline phosphatase) [22].
- Functional Significance: Recent lineage tracing studies demonstrate that TNAP+ adventitial cells contribute to myogenesis during fetal development, differentiating into both skeletal and smooth muscle cells [22].
Table 1: Comparative Characteristics of Perivascular Stem Cells
| Feature | Pericytes | Adventitial Cells |
|---|---|---|
| Anatomical Location | Capillaries & microvessels, embedded in basement membrane | Tunica adventitia of larger arteries & veins |
| Morphology | Branched, stellate to round shapes; cytoplasmic processes | Stromal, fibroblast-like |
| Key Identification Markers | PDGFR-β, NG2, CD146, CD13, RGS5, α-SMA (subset) | CD73, CD90, CD105, TNAP |
| Developmental Origins | Mesoderm, neural crest, mesothelium | Mesoderm |
| Primary Functions | Vascular stability, blood flow regulation, BBB maintenance | Progenitor reservoir, tissue regeneration |
Comparative Analysis of Marker Expression
The reliable identification of perivascular stem cells requires a multifaceted approach combining anatomical position with marker expression profiles. The heterogeneity of these populations necessitates using marker panels rather than relying on single antigens.
Table 2: Comprehensive Marker Expression Profiles
| Marker | Pericytes | Adventitial Cells | Also Expressed By |
|---|---|---|---|
| CD73 | + [20] | + [18] | MSCs, lymphocytes |
| CD90 | + [20] | + [18] | MSCs, hematopoietic stem cells |
| CD105 | + [20] | + [18] | MSCs, endothelial cells |
| CD146 | + [20] [19] | Not reported | Endothelial cells, smooth muscle cells |
| NG2 | + [20] [19] | Not reported | Neural cells, some progenitors |
| PDGFR-β | + [20] [19] | Not reported | Fibroblasts, smooth muscle cells |
| α-SMA | +/- (heterogeneous) [20] [19] | Not typically | Smooth muscle cells, myofibroblasts |
| TNAP | + (subset) [19] | + [22] | Osteoblasts, endothelial cells |
Marker expression can be labile and context-dependent. For instance, pericyte α-SMA expression is minimal in normal skin and brain but increases significantly after tumorigenesis or during activation states [20] [19]. Similarly, NG2 expression is associated with proliferative rather than mature pericyte phenotypes [19]. This dynamic expression underscores the importance of considering physiological and pathological contexts when identifying these cells.
Functional Comparison in Physiology and Pathology
Physiological Roles
Both pericytes and adventitial cells contribute to tissue homeostasis through related but distinct mechanisms:
- Vascular Regulation: Pericytes are essential for angiogenesis, vascular stability, and regulation of capillary diameter and blood flow [20] [19] [21]. They inhibit endothelial cell proliferation through activation of transforming growth factor beta-1 (TGF-β1), particularly during vessel maturation [19]. Adventitial cells serve as progenitors that can be recruited during vascular remodeling and tissue development [22].
- Barrier Function: Pericytes are crucial components of specialized barriers, including the blood-brain barrier (BBB) and retinal barrier [20] [21]. Pericyte deficiency increases vascular permeability, demonstrating their role in maintaining barrier integrity [19].
- Tissue Regeneration: Both cell types contribute to tissue maintenance and repair. Pericytes participate in the regeneration of white adipocytes, skeletal muscle, and dental pulp [18], while TNAP+ adventitial cells contribute to prenatal myogenesis, giving rise to skeletal and smooth muscle cells [22].
Pathological Involvement
Perivascular stem cells play dual roles in disease processes, contributing to both protective and pathogenic mechanisms:
- Fibrosis: Multiple lineage tracing studies have identified pericytes as major myofibroblast progenitors in fibrotic reactions affecting multiple organs [18]. When normal function becomes dysregulated, this differentiation contributes to pathological extracellular matrix accumulation.
- Tumor Progression: Pericytes within the tumor microenvironment modulate cancer initiation and progression, directly impacting metastatic potential and therapy resistance [19]. Specific pericyte subpopulations (type 2: Nestin-GFP+/NG2-DsRed+) are recruited during cancer angiogenesis [19].
- Cerebrovascular Diseases: CNS pericytes constrict capillaries under ischemic conditions, hindering microcirculatory reperfusion even after plaque removal in stroke [21]. They are also implicated in white matter injury, cerebral hemorrhage, and hypoxic-ischemic brain damage [21].
Experimental Protocols for Isolation and Study
Isolation Techniques
Different tissue sources require tailored isolation approaches:
- Bone Marrow-derived MSCs: Isolated from bone marrow aspirate using density gradient centrifugation to collect the mononuclear cell fraction, followed by plastic adherence [23]. Only 0.001-0.01% of cells obtained represent MSCs [23].
- Adipose Tissue-derived MSCs: Isolated from liposuction material through enzymatic digestion with collagenase, followed by centrifugation and washing [23]. Yield is approximately 5 × 10³ stem cells per gram of adipose tissue—500 times higher than equivalent bone marrow [23].
- Umbilical Cord-derived MSCs: Isolated from various umbilical cord components, including Wharton's jelly and perivascular regions, through explant culture or enzymatic digestion [23].
Functional Characterization Assays
Standardized assays evaluate the stem cell properties of isolated perivascular cells:
- Tri-lineage Differentiation: Culture in specific inductive media to assess differentiation potential:
- Osteogenic Differentiation: Cells cultured in media supplemented with β-glycerophosphate, ascorbic acid, and dexamethasone for 2-3 weeks, with mineralization detected by Alizarin Red staining [24] [25].
- Adipogenic Differentiation: Induction with insulin, indomethacin, and IBMX for 3-4 weeks, with lipid vacuoles visualized by Oil Red O staining [24] [25].
- Chondrogenic Differentiation: Pellet culture in TGF-β3-containing media for 3-4 weeks, with sulfated proteoglycans detected by Alcian Blue staining [25].
- Immunomodulatory Assays: Co-culture of MSCs with peripheral blood mononuclear cells (PBMCs) stimulated with mitogens, measuring T-cell proliferation inhibition and regulatory T-cell induction [5].
- Tube Formation Assay: Evaluation of angiogenic potential by seeding cells on Matrigel and assessing capillary-like network formation [24].
Diagram Title: Perivascular Stem Cell Isolation & Characterization Workflow
Signaling Pathways Governing Perivascular Stem Cell Function
Multiple signaling pathways coordinate the behavior of perivascular stem cells, maintaining their quiescence or activating them in response to injury:
- PDGF-B/PDGFR-β Pathway: This key signaling axis coordinates pericyte recruitment and migration during angiogenesis [19]. Endothelial cells secrete PDGF-B, attracting PDGFR-β-expressing pericytes. Disruption causes microaneurysms due to pericyte deficiency [19].
- TGF-β Pathway: Activation of TGF-β1 mediates the inhibitory effect of pericytes on endothelial cell proliferation, crucial for vessel stabilization [19]. Formation of gap junctions between endothelial cells and pericyte precursors enables production of active TGF-β [19].
- Notch Signaling: Perivascular MSCs in human dental pulp and periodontal tissue express NOTCH3, which participates in niche maintenance [26]. Notch signaling in perivascular stem cells dynamics influences their fate decisions [26].
Diagram Title: Key Signaling Pathways in Perivascular Niches
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Perivascular Stem Cell Studies
| Reagent/Category | Specific Examples | Research Application | Function |
|---|---|---|---|
| Isolation Enzymes | Collagenase | Tissue dissociation for cell isolation | Digests extracellular matrix to release perivascular cells |
| Culture Media | DMEM/F12, Alpha-MEM, MSC Serum-free Media | Cell expansion & maintenance | Provides nutrients and growth factors for cell growth |
| Induction Media | Osteo-, Adipo-, Chondro-Induction Media | Tri-lineage differentiation assessment | Directs stem cell differentiation into specific lineages |
| Flow Cytometry Antibodies | Anti-CD73, -CD90, -CD105, -CD146, -NG2, -PDGFR-β | Cell population identification & sorting | Identifies and isolates target cells based on surface markers |
| Histological Stains | Alizarin Red, Oil Red O, Alcian Blue | Detection of differentiation outcomes | Visualizes mineralized matrix, lipids, and proteoglycans |
| Cytokines/Growth Factors | PDGF-BB, TGF-β1, FGF-2 | Functional studies of signaling pathways | Activates specific receptors to study downstream effects |
Application-Oriented Recommendations for Research
Selecting appropriate perivascular stem cell sources depends on specific research objectives:
- Neurological Research: Brain-derived pericytes are optimal for blood-brain barrier studies and neurovascular unit modeling, given their high density in CNS and critical barrier functions [20] [21].
- Musculoskeletal Engineering: Umbilical cord-derived MSCs represent a preferred population with superior proliferation capacity and differentiation potential for bone and cartilage formation [23].
- Vascular Biology Studies: Adventitial cells from larger vessels or specific pericyte subpopulations (type 2: Nestin-GFP+/NG2-DsRed+) are ideal for angiogenesis research [19].
- Immunomodulation Studies: Bone marrow-derived MSCs have well-documented immunosuppressive properties, making them suitable for GVHD and autoimmune disease research [5].
When designing experiments, consider that fetal and neonatal tissue-derived MSCs (from umbilical cord, placenta) generally exhibit greater proliferative capacity and longer in vitro lifespans compared to adult tissue-derived MSCs (from bone marrow, adipose tissue) [23]. However, adult tissue sources may better represent age-related pathological processes.
Mesenchymal Stromal Cells (MSCs) represent a cornerstone of regenerative medicine, with their therapeutic potential largely dictated by their tissue of origin. While MSCs from various sources share fundamental characteristics—adherence to plastic, specific surface marker expression, and multilineage differentiation capacity—their biological properties and functional specializations vary significantly based on their anatomical niche [4]. This comparative analysis examines three prominent MSC sources: bone marrow (BM-MSCs), adipose tissue (ADSCs), and dental pulp (DPSCs), each occupying unique microenvironments that shape their distinctive regenerative profiles. Understanding these tissue-specific differences is paramount for selecting the optimal MSC source for targeted clinical applications, from orthopedic repair to neurovascular regeneration.
Defining Characteristics Across Tissue Niches
The International Society for Cellular Therapy (ISCT) establishes minimal criteria for defining MSCs, including plastic adherence, specific surface marker expression (CD73, CD90, CD105 ≥95%; CD34, CD45, CD14/CD11b, CD79α/CD19, HLA-DR ≤2%), and trilineage differentiation potential [4] [27]. However, beyond these shared characteristics, MSCs from different niches exhibit substantial heterogeneity in their differentiation bias, proliferation kinetics, and molecular signaling, reflecting adaptations to their native tissue environments.
Table 1: Core Characteristics of MSCs from Different Niches
| Feature | Bone Marrow (BM-MSCs) | Adipose Tissue (ADSCs) | Dental Pulp (DPSCs) |
|---|---|---|---|
| Tissue Origin | Bone marrow cavity [28] | Subcutaneous adipose tissue (e.g., abdomen, thighs) [27] | Dental pulp chamber [28] |
| Isolation Yield | Low (0.001-0.01% of nucleated cells) [29] | High (~500,000 stem cells/1g adipose tissue) [27] | Variable, depending on pulp volume [13] |
| Key Morphological Traits | Heterogeneous, fibroblast-like [13] | Fibroblast-like, adherent [30] | Spindle-shaped, smaller size [30] |
| Distinctive Markers | STRO-1, CD146 [13] | CD49d (high), Stro-1 (low) [29] | Nestin-positive [30] |
| Proliferation Rate | Moderate, declines with passages [13] [29] | High, stable proliferation [29] | High [30] |
Comparative Differentiation Potential
The trilineage differentiation capacity—osteogenic, adipogenic, and chondrogenic—is a hallmark of MSCs, but the efficacy with which cells from different niches execute these programs varies dramatically, revealing a clear lineage bias rooted in their tissue of origin.
Osteogenic Potential
Bone marrow MSCs, residing in the osseous environment, are considered the gold standard for osteogenesis [31]. Adipose-derived MSCs demonstrate robust but generally inferior osteogenic capability compared to BM-MSCs, with donor-matched comparisons showing BM-MSCs exhibit earlier and higher alkaline phosphatase (ALP) activity and calcium deposition [29]. Dental pulp stem cells retain a strong osteogenic/dentinogenic molecular profile, expressing genes like RUNX2, ALP, and COL1A1 even under adipogenic induction conditions, highlighting their inherent commitment to a hard tissue lineage [31].
Adipogenic Potential
Adipose tissue is, unsurprisingly, the most potent source for adipogenic differentiation. ADSCs form numerous, large lipid vesicles and significantly upregulate adipogenic genes like PPARγ2, LPL, and ADIPONECTIN [29]. In contrast, DPSCs exhibit a markedly limited adipogenic potential. When induced, they form only tiny, small lipid droplets and show minimal upregulation of late adipogenic markers [30] [31]. This represents one of the most significant functional distinctions between these MSC populations.
Chondrogenic and Neurogenic Potential
While chondrogenesis is a key defining criterion, comparative studies suggest that BM-MSCs may possess a superior chondrogenic capacity compared to ADSCs [29]. DPSCs, owing to their neural crest origin, demonstrate a pronounced neurogenic propensity. They can differentiate into functionally active neurons and glial cells and secrete neurotrophic factors that support neuroprotection and angiogenesis [28].
Table 2: Quantitative Comparison of Differentiation Potential
| Differentiation Lineage | Bone Marrow (BM-MSCs) | Adipose Tissue (ADSCs) | Dental Pulp (DPSCs) |
|---|---|---|---|
| Osteogenesis | High (Gold Standard) [31] | Moderate [29] | High (osteogenic/dentinogenic) [31] |
| Adipogenesis | Moderate [29] | High [29] | Low/Limited [30] [31] |
| Chondrogenesis | High [29] | Moderate [29] | Not fully characterized |
| Neurogenesis | Limited [13] | Possible [29] | High (Neural crest origin) [28] |
Proliferation, Secretome, and Molecular Signaling
Proliferation and Immunomodulation
ADSCs and DPSCs generally exhibit higher proliferation rates than BM-MSCs [30] [29]. This, combined with the higher yield from adipose tissue, makes ADSCs a practical choice for applications requiring large cell numbers. All MSCs possess immunomodulatory properties, interacting with T cells, B cells, dendritic cells, and macrophages through direct contact and paracrine signaling [4]. The potency of this effect can vary with source and donor health.
Secretome and Extracellular Vesicles
The therapeutic effects of MSCs are increasingly attributed to their secretome—the bioactive molecules they release, including growth factors, cytokines, and extracellular vesicles (EVs) [4] [32]. The composition of this secretome is highly source-dependent. Analysis of conditioned media shows significant variations in the profiles of anti-inflammatory and pro-inflammatory cytokines, chemokines, and growth factors between ADSCs and DPSCs [30]. While all MSC populations release a comparable number of EVs, ADSCs produce a significantly higher number of smaller exosomes than DPSCs [30]. Crucially, the microRNA (miRNA) cargo within these EVs also differs; DPSC-derived miRNAs are often involved in oxidative stress and apoptosis pathways, while ADSC-derived miRNAs play a larger role in regulating cell cycle and proliferation [30].
Underlying Molecular Pathways
The distinct differentiation biases are governed by differential regulation of key developmental signaling pathways. During adipogenic induction, BM-MSCs downregulate Wnt pathway genes and upregulate NOTCH pathway genes (NOTCH1, NOTCH3, JAGGED1) [31]. Conversely, DPSCs, which resist adipogenesis, maintain their osteogenic/dentinogenic profile (RUNX2, ALP) and upregulate Wnt-specific genes while not activating the NOTCH pathway [31]. The Wnt pathway is a known inhibitor of adipogenesis and promoter of osteogenesis, explaining these divergent commitments.
Experimental Protocols for MSC Comparison
To generate the comparative data cited in this guide, researchers employ standardized in vitro protocols. Below are detailed methodologies for key characterization experiments.
Isolation and Culture
- Bone Marrow MSCs (BM-MSCs): Bone marrow aspirate is diluted, centrifuged, and the cell pellet is resuspended and plated in a culture medium (e.g., DMEM with 10% FBS). Non-adherent cells are removed after 24 hours. Adherent MSCs are expanded and used at passages 3-6 [33] [29].
- Adipose-Derived MSCs (ADSCs): Adipose tissue is washed, minced, and digested with collagenase (e.g., 0.1% collagenase type I). The digest is centrifuged, the pellet is resuspended, and cells are plated. ADSCs are also used at passages 3-6 [30] [29].
- Dental Pulp MSCs (DPSCs): The pulp is extracted, fragmented into 1-2 mm³ pieces, and explants are placed in culture dishes. Cells growing out from the fragments are passaged and used at passages 4-6 [30].
Trilineage Differentiation Assays
- Osteogenic Differentiation: Cells are cultured in growth medium supplemented with osteogenic inducers such as 50 µM ascorbic acid-2 phosphate, 10 mM β-glycerophosphate, and 0.1 µM dexamethasone. Differentiation is assessed by alkaline phosphatase (ALP) activity and mineralized matrix staining (e.g., Alizarin Red) [30] [29].
- Adipogenic Differentiation: Cells are induced with a cocktail typically containing 0.5 mM isobutylmethylxanthine (IBMX), 1 µM dexamethasone, and 50 µM indomethacin. Differentiated adipocytes are identified by the accumulation of intracellular lipid vesicles stained with Oil Red O or Nile Red [30] [31] [29].
- Chondrogenic Differentiation: Pellet cultures or micromass cultures are maintained in a medium with TGF-β (e.g., TGF-β3) and other supplements. Chondrogenesis is confirmed by Alcian Blue or Safranin O staining for proteoglycans [29].
Secretome and Extracellular Vesicle Analysis
- Conditioned Media (CM) Collection: MSCs are cultured until sub-confluent, washed, and then incubated with a serum-free medium for 24-48 hours. The supernatant (CM) is collected, centrifuged to remove cells and debris, and concentrated or analyzed directly [30].
- Extracellular Vesicle (EV) Characterization: EVs are isolated from CM by sequential ultracentrifugation or size-exclusion chromatography. They are characterized by nanoparticle tracking analysis (NTA) for concentration and size, and Western blotting for markers like CD63, CD81, and CD9 [30].
The Scientist's Toolkit: Key Reagent Solutions
Table 3: Essential Reagents for MSC Isolation, Culture, and Characterization
| Reagent / Kit | Function / Application | Example Use in Protocol |
|---|---|---|
| Collagenase Type I | Enzymatic digestion of tissues for cell isolation. | Digestion of adipose tissue (ADSC isolation) and bone marrow (ADSC-SVF method) [30] [29]. |
| DMEM / αMEM Medium | Base culture medium for MSC expansion. | Used as the basic medium for culturing all three MSC types, supplemented with FBS [30] [33]. |
| Fetal Bovine Serum (FBS) | Essential supplement for cell growth and adhesion. | Added at 10-20% to base medium to support MSC adhesion and proliferation [30] [33]. |
| Osteogenic Induction Kit | Contains components to induce osteoblast differentiation. | Typically includes ascorbic acid, β-glycerophosphate, and dexamethasone [30]. |
| Adipogenic Induction Kit | Contains components to induce adipocyte differentiation. | Typically includes IBMX, dexamethasone, indomethacin, and insulin [31] [29]. |
| Flow Cytometry Antibody Panel | Cell surface immunophenotyping. | Antibodies against CD73, CD90, CD105 (positive) and CD34, CD45, HLA-DR (negative) for MSC definition [4] [29]. |
| Nile Red / Oil Red O | Fluorescent or colorimetric staining of intracellular lipid droplets. | Staining and quantification of adipogenic differentiation [31]. |
| Alizarin Red S | Colorimetric staining of calcium deposits. | Evaluation of mineralized matrix formation in osteogenic differentiation [29]. |
| Extracellular Vesicle Isolation Kit | Enrichment of exosomes and microvesicles from conditioned media. | Used for isolating EVs for downstream NTA and miRNA profiling [30]. |
BM-MSCs, ADSCs, and DPSCs are not interchangeable. Each possesses a unique functional profile shaped by its tissue niche: BM-MSCs are osteogenic champions, ADSCs are prolific and adipogenic, and DPSCs are neuro-vascular potent with a hard tissue commitment. The choice of MSC source should be a deliberate decision aligned with the target clinical application. Future research and clinical translation must move beyond treating MSCs as a monolithic entity and instead leverage these niche-specific specializations to develop more effective and precise regenerative therapies.
Influence of Embryonic Origin on Innate MSC Properties and Plasticity
Mesenchymal Stem Cells (MSCs) represent a cornerstone of regenerative medicine, yet their properties and therapeutic potential are profoundly influenced by their tissue of origin. This comparative analysis synthesizes current research on MSCs derived from bone marrow, adipose tissue, umbilical cord, and induced pluripotent stem cells (iPSCs), focusing on how embryonic origin dictates their phenotypic, transcriptomic, and functional characteristics. We provide structured experimental data demonstrating that origin-specific differences in differentiation capacity, immunomodulatory potential, and gene expression profiles directly impact their suitability for targeted clinical applications. By integrating quantitative comparisons, detailed methodologies, and signaling pathway visualizations, this guide equips researchers with the necessary framework to select optimal MSC sources for specific therapeutic development, ultimately advancing the rational design of MSC-based therapies.
The term "mesenchyme" originates from embryonic development, describing a loose, migratory cellular organization derived from all three germ layers—ectoderm, mesoderm, and endoderm—through epithelial-mesenchymal transitions (EMTs) [34]. This developmental history is crucial for understanding adult MSC heterogeneity. While often simplified as mesodermal derivatives, mesenchymal populations in fact have diverse embryonic origins that imprint lasting influences on their biological properties [34].
True to their embryonic nature, MSCs retain multipotent differentiation capacity, typically giving rise to mesodermal lineages like osteoblasts, chondrocytes, and adipocytes [4]. The International Society for Cellular Therapy (ISCT) establishes minimal criteria for defining MSCs: plastic adherence, specific surface marker expression (CD73+, CD90+, CD105+, CD34-, CD45-, CD11b-, CD19-, HLA-DR-), and trilineage differentiation potential [4]. However, MSCs isolated from different tissue sources demonstrate remarkable variation in their functional capabilities, proliferation rates, and molecular signatures—differences rooted in their embryonic derivation and tissue-specific niches [35].
Comparative Analysis of MSC Types by Tissue Origin
Bone Marrow-Derived MSCs (BM-MSCs)
As the most extensively studied type, BM-MSCs represent the historical "gold standard" for MSC research and applications. They originate from the mesodermal germ layer and demonstrate high differentiation potential, particularly toward osteogenic lineages, and strong immunomodulatory properties [4]. BM-MSCs have been successfully used in clinical applications since 1993, with over 950 registered clinical trials submitted to the FDA [35]. Their limitations include invasive harvesting procedures, declining cell quality and quantity with donor age, and relatively slow proliferation rates compared to alternative sources [4].
Adipose Tissue-Derived MSCs (AD-MSCs)
AD-MSCs share comparable therapeutic properties with BM-MSCs but offer practical advantages of easier harvesting and higher yields from lipoaspirate procedures [4]. These cells demonstrate robust adipogenic differentiation capacity and have shown particular promise in applications requiring enhanced angiogenesis and soft tissue regeneration. Like BM-MSCs, they originate from the mesodermal lineage but exhibit distinct gene expression profiles reflective of their adipose tissue niche, including enhanced lipid metabolism pathways [35].
Umbilical Cord-Derived MSCs (UC-MSCs)
UC-MSCs display enhanced proliferation capacity, lower immunogenicity, and distinct immunomodulatory properties compared to adult-derived MSCs, making them particularly suitable for allogeneic transplantation approaches [4]. Their fetal origin contributes to increased telomere length and enhanced replicative potential. UC-MSCs have demonstrated particular efficacy in modulating inflammatory responses and have been applied in trials for graft-versus-host disease and other immune-mediated conditions [35].
iPSC-Derived MSCs (iMSCs)
iMSCs represent a promising approach for generating standardized, high-quality cell populations for therapeutic applications [36]. However, substantial differences exist between iMSCs and primary tissue-derived MSCs. iMSCs consistently demonstrate markedly reduced chondrogenic and adipogenic propensity while maintaining efficient osteogenic differentiation [36]. Transcriptomic analyses reveal that iMSCs express very high levels of KDR and MSX2 with significantly lower PDGFRα compared to BM-MSCs, maintaining a gene expression profile more closely related to vascular progenitor cells (VPCs) than authentic MSCs [36]. This fundamental difference in cellular identity persists through culture expansion and necessitates different inductive conditions for effective differentiation.
Table 1: Functional Properties of MSCs by Tissue Source
| Property | BM-MSCs | AD-MSCs | UC-MSCs | iMSCs |
|---|---|---|---|---|
| Osteogenic Potential | High | Moderate | Moderate | High |
| Chondrogenic Potential | High | Moderate | Moderate | Low |
| Adipogenic Potential | High | High | Moderate | Low |
| Proliferation Rate | Moderate | Moderate | High | High |
| Immunomodulatory Strength | High | High | Very High | Variable |
| Transcriptomic Similarity to BM-MSCs | Reference | High | Moderate | Low |
Table 2: Surface Marker Expression Profiles Across MSC Types
| Marker | BM-MSCs | AD-MSCs | UC-MSCs | iMSCs |
|---|---|---|---|---|
| CD73 | +++ | +++ | +++ | ++ |
| CD90 | +++ | +++ | +++ | +++ |
| CD105 | +++ | +++ | +++ | + |
| CD44 | +++ | +++ | +++ | +++ |
| CD34 | - | +/- | - | - |
| CD45 | - | - | - | - |
| HLA-DR | - | - | - | - |
| KDR | + | + | + | +++ |
| MSX2 | + | + | + | +++ |
| PDGFRα | +++ | ++ | ++ | + |
Experimental Data: Quantitative Comparisons
Differentiation Capacity
Quantitative analyses of trilineage differentiation potential reveal profound differences between MSC types. In controlled differentiation experiments, BM-MSCs consistently demonstrate robust mineralization in osteogenic conditions (approximately 3-fold increase in calcium deposition), strong lipid accumulation in adipogenic conditions (approximately 80% of cells showing lipid droplets), and abundant proteoglycan production in chondrogenic conditions [4]. In contrast, iMSCs show equivalent or enhanced osteogenic capacity but significantly reduced adipogenic and chondrogenic differentiation, with adipocytes derived from iMSCs expressing significantly lower levels of lineage marker genes (PPAR-γ and ADIPOQ) and chondrocytes showing reduced expression of ACAN and COL2A1 compared to primary MSCs [36].
Gene Expression Profiles
Transcriptomic analyses using RNA sequencing have identified distinct gene expression patterns across MSC types. Hierarchical clustering demonstrates that iMSCs form a separate cluster from primary MSCs, despite similar surface marker expression [36]. BM-MSCs show elevated expression of genes related to skeletal development and hematopoiesis support, while UC-MSCs exhibit enhanced expression of genes involved in developmental processes and immune modulation. iMSCs maintain expression profiles characteristic of vascular progenitor cells, with persistent elevation of KDR and MSX2 even after extended culture [36].
DNA methylation studies further confirm these differences, with iMSCs demonstrating distinct epigenetic patterns compared to BM-MSCs, particularly in genes associated with neuronal and cardiovascular development [37]. When iPSCs were differentiated within 3D fibrin hydrogels, the resulting cells showed upregulated neural development genes rather than MSC-characteristic genes, indicating the strong influence of microenvironment on differentiation trajectory [37].
Table 3: Quantitative Differentiation Potential Across MSC Types
| Differentiation Lineage | BM-MSCs | AD-MSCs | UC-MSCs | iMSCs |
|---|---|---|---|---|
| Osteogenic Marker Expression | +++ | ++ | ++ | +++ |
| Calcium Deposition | +++ | ++ | ++ | +++ |
| Adipogenic Marker Expression | +++ | +++ | ++ | + |
| Lipid Droplet Formation | +++ | +++ | ++ | + |
| Chondrogenic Marker Expression | +++ | ++ | ++ | + |
| Proteoglycan Synthesis | +++ | ++ | ++ | + |
Methodologies: Key Experimental Protocols
Standard MSC Differentiation Protocol
The fundamental protocol for trilineage differentiation of MSCs involves specific induction cocktails and culture conditions:
Osteogenic Differentiation: Culture MSCs to 70-80% confluence in basal medium, then switch to osteogenic induction medium containing Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 10 mM β-glycerophosphate, 50 μM ascorbic acid, and 100 nM dexamethasone. Culture for 2-4 weeks with medium changes every 3-4 days. Confirm differentiation by Alizarin Red S staining of mineralized matrix [4].
Adipogenic Differentiation: Culture MSCs to complete confluence in basal medium, then switch to adipogenic induction medium containing DMEM with 10% FBS, 1 μM dexamethasone, 0.5 mM isobutylmethylxanthine (IBMX), 10 μg/mL insulin, and 200 μM indomethacin. Culture for 1-3 weeks with medium changes every 3-4 days. Confirm differentiation by Oil Red O staining of lipid droplets [4].
Chondrogenic Differentiation: Pellet 2.5 × 10^5 MSCs by centrifugation and culture in chondrogenic induction medium containing DMEM with 1% FBS, 1% insulin-transferrin-selenium (ITS), 100 nM dexamethasone, 50 μM ascorbic acid, and 10 ng/mL transforming growth factor-beta 3 (TGF-β3). Culture for 3-4 weeks with medium changes every 3-4 days. Confirm differentiation by Alcian Blue staining of proteoglycans [4].
iMSC Generation from iPSCs
Generate iMSCs using the embryoid body (EB) outgrowth method: Maintain iPSCs in suspension culture for 8 days to form EBs, then transfer to gelatin-coated plates in EB formation medium (80% KO-DMEM, 20% FBS, 1 mM L-glutamine, 14 μM β-mercaptoethanol, 1% nonessential amino acids). When outgrown cells form confluent areas, passage to new gelatin-coated flasks, removing EB clumps with a 40 μm cell strainer. Transition cells to MSC culture medium when majority display MSC-like morphology [36]. Note that resulting iMSCs require different inductive conditions for chondrogenic and adipogenic differentiation compared to primary MSCs, reflecting their vascular progenitor cell signature [36].
Directed Differentiation of MSCs into Endothelial Cells
For efficient differentiation of MSCs into functional endothelial cells, transduce MSCs with lentivirus encoding the transcription factor ER71. Culture transduced cells in endothelial differentiation medium supplemented with TGF-β inhibitor (SB431542), vascular endothelial growth factor (VEGF), and ascorbic acid for 7 days. Using this protocol, approximately 75.4 ± 4.5% of MSCs differentiate into endothelial cells as defined by double-positivity for VE-cadherin/PECAM1 [38]. The resulting cells demonstrate endothelial characteristics and functions, with potentiated immune tolerance properties mediated by IKAROS, a direct transcriptional target of ER71 [38].
Signaling Pathways and Molecular Mechanisms
The therapeutic effects of MSCs are mediated through complex signaling pathways that vary by tissue source. MSCs from all sources release bioactive molecules including growth factors, cytokines, and extracellular vesicles that modulate the local cellular environment, promote tissue repair, angiogenesis, and cell survival, and exert anti-inflammatory effects [4]. Key pathways include:
Immunomodulatory Pathways: MSCs interact with various immune cells (T cells, B cells, dendritic cells, macrophages) through direct cell-cell contacts and release of immunoregulatory molecules like prostaglandin E2 (PGE2), indoleamine 2,3-dioxygenase (IDO), and transforming growth factor-β (TGF-β) [4]. When primed with interferon-gamma (IFN-γ) and tumor necrosis factor (TNF), MSCs uniformly polarize toward a Th1 phenotype characterized by expression of immunosuppressive factors IDO, IL-10, CD274/PD-L1, and IL-4 [35].
Differentiation Pathways: Osteogenic differentiation is regulated through Wnt signaling (including CCN4/WISP-1) and BMP pathways, while adipogenesis follows PPAR-γ and C/EBPβ cascades [35]. The distinct differentiation propensities of iMSCs compared to primary MSCs result from their alternative transcriptional regulation, with maintained expression of vascular progenitor genes despite standard MSC surface marker expression [36].
The following diagram illustrates key signaling pathways that govern MSC differentiation and immunomodulation, highlighting how different MSC types vary in their activation of these pathways:
The experimental workflow for generating and characterizing MSCs from different sources involves specific processes that significantly impact the resulting cell properties:
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for MSC Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Culture Media | KO-DMEM, DMEM/F12, α-MEM | Basal media for MSC expansion and maintenance |
| Serum Supplements | Fetal Bovine Serum (FBS), Human Platelet Lysate (hPL) | Provide essential growth factors and adhesion molecules |
| Differentiation Inducers | Dexamethasone, β-glycerophosphate, IBMX, Insulin, TGF-β3 | Direct lineage-specific differentiation |
| Cytokines/Growth Factors | VEGF, FGF, EGF, IFN-γ, TNF | Modulate MSC function and priming |
| Surface Marker Antibodies | CD73, CD90, CD105, CD34, CD45, HLA-DR | Phenotypic characterization by flow cytometry |
| Transcriptional Regulators | ER71, KLF2, TAL1 (for endothelial differentiation) | Direct cell fate conversion |
| Enzymatic Dissociation Agents | Trypsin/EDTA, Collagenase, Accutase | Cell passaging and tissue dissociation |
| Matrix Scaffolds | Gelatin, Collagen I, Fibrin Hydrogels | 2D/3D culture systems for differentiation studies |
| Small Molecule Inhibitors | SB431542 (TGF-β inhibitor), ROCK inhibitor | Enhance differentiation efficiency and cell survival |
| Staining Reagents | Alizarin Red, Oil Red O, Alcian Blue | Detection of differentiated lineages |
The embryonic origin and tissue source of MSCs fundamentally determine their functional properties and therapeutic specialization. BM-MSCs remain the gold standard for skeletal regeneration, AD-MSCs excel in soft tissue and angiogenic applications, UC-MSCs offer superior immunomodulation for allogeneic settings, and iMSCs provide scalability with distinct differentiation biases. Understanding these origin-dependent differences enables researchers to select optimal MSC sources for specific therapeutic goals.
Future research directions should focus on establishing more refined molecular signatures for different MSC populations, developing precision priming protocols to enhance specific functions, and creating standardized differentiation protocols that account for source-specific requirements. As the field advances toward more targeted applications, recognizing the inherent biological differences between MSC types will be essential for developing safe, effective, and reproducible cell-based therapies.
From Bench to Bedside: Isolation, Characterization, and Therapeutic Mechanisms
Standardized Protocols for MSC Isolation from Different Tissues (BM-MSCs, AD-MSCs, UC-MSCs, DP-MSCs)
Mesenchymal Stromal Cells (MSCs) represent a cornerstone of regenerative medicine due to their multipotent differentiation capabilities, immunomodulatory properties, and relative ease of isolation from various tissue sources. The therapeutic potential of MSCs is heavily influenced by their tissue of origin, which dictates their biological characteristics, differentiation potential, and functional behavior in clinical applications. This comparative guide provides a systematic analysis of isolation methodologies, phenotypic characterization, and functional capabilities of MSCs derived from four prominent sources: bone marrow (BM-MSCs), adipose tissue (AD-MSCs), umbilical cord (UC-MSCs), and dental pulp (DP-MSCs). Understanding these distinctions enables researchers to select the most appropriate MSC source for specific therapeutic applications, thereby optimizing experimental outcomes and clinical efficacy.
Table 1: Comparative Overview of Key Characteristics Across MSC Tissue Sources
| Characteristic | BM-MSCs | AD-MSCs | UC-MSCs | DP-MSCs |
|---|---|---|---|---|
| Isolation Yield | Low (0.001-0.01% of nucleated cells) [39] | High (500,000 cells/gram tissue) [30] | High [39] | Variable [30] |
| Proliferation Capacity | Moderate, age-dependent [40] | High [30] | Very High, fetal origin [40] [41] | High, Nestin-positive [30] |
| Key Positive Markers | CD73, CD90, CD105 [4] | CD29, CD73, CD90 [30] [42] | CD73, CD90, CD105 [4] | CD73, CD90, CD105 [4] |
| Key Negative Markers | CD34, CD45, HLA-DR [4] | CD34, CD45 [42] | CD34, CD45, HLA-DR [4] | CD34, CD45, HLA-DR [4] |
| Osteogenic Potential | Strong [4] | Variable by depot [42] | Strong [4] | Strong [4] |
| Adipogenic Potential | Strong [4] | Strong, superior in perirenal vs. subcutaneous [42] | Moderate [4] | Weak/Absent [30] |
| Chondrogenic Potential | Strong [4] | Moderate [42] | Strong [4] | Strong [4] |
| Immunomodulatory Strength | Strong, well-characterized [4] | Strong [35] | Very Strong, enhanced innate immune response [41] | Moderate [30] |
| Transcriptomic Stability | Age-related decline [40] | Donor-dependent [30] | High, stable to late passage [41] | Limited data |
Table 2: Quantitative Differences in Marker Expression and Functional Capacity
| Parameter | Specific Comparison | Experimental Finding | Significance |
|---|---|---|---|
| CD105 Expression | Perirenal vs. Subcutaneous AD-MSCs (Hanwoo) | P-AMSCs: 26.3% vs. S-AMSCs: 1.2% [42] | Anatomical depot influences marker profile. |
| Proliferation Rate | UC-MSCs vs. AD-MSCs | DPSCs were consistently smaller and had a higher proliferation rate than ADSCs [30] | Source impacts expansion potential for scaling. |
| Adipogenic Outcome | DP-MSCs vs. Other MSCs | All primary cell lines possessed typical MSC characteristics, apart from the inability of DPSCs to perform adipogenesis [30] | Critical for lineage-specific application selection. |
| Transcriptomic Profile | Fetal (UC) vs. Adult (BM, AD) MSCs | 2,208 upregulated and 2,594 downregulated DEGs; enriched pathways in fetal MSCs: glycolysis, cholesterol biosynthesis, TNF-α signaling [41] | Fetal and adult MSCs are biologically distinct. |
Standardized Isolation Protocols
Bone Marrow-Derived MSCs (BM-MSCs)
Methodology: The established protocol for isolating BM-MSCs relies on density gradient centrifugation to separate mononuclear cells from other bone marrow components [39]. Bone marrow samples are diluted with Dulbecco's Phosphate-Buffered Saline (DPBS) in a 1:1 ratio and carefully layered onto a Ficoll-Paque Premium solution. This is followed by centrifugation at 400 g for 30 minutes at 20°C with the brake disengaged [41]. The resulting mononuclear cell layer is harvested, washed with DPBS to remove residual separation media, and centrifuged again. The cell pellet is then resuspended in a low-glucose Dulbecco's Modified Eagle Medium (LG-DMEM) supplemented with 10% Fetal Bovine Serum (FBS) and antibiotics. Cells are plated at a high density (1 × 10⁵ cells/cm²) and maintained in a humidified incubator at 37°C with 5% CO₂. The culture medium is replaced regularly to remove non-adherent cells, and adherent MSCs are expanded through trypsin-EDTA detachment upon reaching 80% confluency [41].
Adipose Tissue-Derived MSCs (AD-MSCs)
Methodology: Two primary methods are prevalent for isolating AD-MSCs, both beginning with tissue washing and removal of connective tissue and blood vessels.
- Enzymatic Digestion (SVF): The washed adipose tissue is subjected to digestion using collagenase (e.g., Collagenase 1A) overnight at 37°C with agitation [30]. The digested slurry is centrifuged to pellet the Stromal Vascular Fraction (SVF). The pellet is then resuspended in a basic medium (e.g., αMEM or LG-DMEM) supplemented with 10% FBS and plated on tissue culture dishes [30].
- Mechanical Fragmentation (Explant): As an alternative to enzymatic digestion, the adipose tissue can be minced into small fragments (1-2 mm³) and explanted directly onto culture dishes. These fragments are allowed to adhere, and culture medium (e.g., αMEM with 20% FBS) is added. AD-MSCs migrate out from the tissue explants over 1-2 weeks, after which they can be detached and expanded [30].
Umbilical Cord-Derived MSCs (UC-MSCs)
Methodology: The umbilical cord must be thoroughly washed with DPBS to remove blood contaminants before processing [39] [41].
- Enzymatic Digestion: The cord tissue is dissected and treated with collagenase type I (e.g., 0.1% concentration) for several hours at 37°C with gentle agitation [41]. The digested tissue is filtered through a 100-μm cell strainer to remove undigested fragments. The filtrate is centrifuged, and the cell pellet is resuspended in culture medium and plated.
- Explant Method (MCE): The Minimal Cube Explant (MCE) method involves cutting the washed umbilical cord into small 2-4 mm cubes using surgical scissors [41]. These tissue pieces are placed directly in culture dishes and allowed to adhere firmly for about an hour in an incubator. Culture medium (LG-DMEM with 10% FBS) is then gently added. MSCs that grow out from the explants are termed "smumf cells" and exhibit high proliferative capacity and genomic stability [41].
Dental Pulp-Derived MSCs (DP-MSCs)
Methodology: Sound teeth (e.g., third molars with open apex) are cleaned and cut at the amelo-cement junction using a sterile diamond disc [30]. The dental pulp is carefully extracted from the pulp chamber and radicular canals using a sterile dental instrument. The isolated pulp is then fragmented into 1-2 mm³ pieces using a scalpel. These pieces are washed, seeded onto culture plates, and maintained in a basic medium supplemented with 10% FBS [30]. Cells migrating from the pulp explants typically form a monolayer within 2-4 weeks. For comparative studies, DP-MSCs can be isolated from specific regional compartments of the pulp, such as the coronal pulp (CPSCs) and radicular pulp (RPSCs) [30].
Molecular Basis and Signaling Pathways
The functional properties of MSCs, including their stemness, proliferation, and differentiation, are governed by a complex network of intrinsic genetic regulators and extrinsic signaling pathways. Key transcription factors such as TWIST1, OCT4, SOX2, and various HOX genes play critical roles in maintaining MSC stemness and preventing senescence [40]. For instance, TWIST1 promotes proliferation and suppresses senescence by increasing EZH2, which silences senescence genes like p14 and p16 via H3K27me3 chromatin modification [40]. The distinct "HOX code" expression pattern is stable throughout life and reflects the tissue origin of MSCs, influencing their differentiation bias and functional properties [40].
Diagram 1: Key molecular regulators of MSC stemness and their functional outcomes. Transcription factors like TWIST, OCT4, SOX2, and HOX genes coordinately regulate critical processes such as proliferation, self-renewal, and differentiation, while simultaneously inhibiting senescence pathways.
Single-cell transcriptomic analyses further reveal fundamental distinctions between true stem cells and MSCs. Stem cells express critical self-renewal genes (SOX2, NANOG, POU5F1, SFRP2, DPPA4, SALL4, ZFP42, MYCN) that are absent in MSCs. Conversely, MSCs express functional markers (TMEM119, FBLN5, KCNK2, CLDN11, DKK1) not found in stem cells, highlighting their different biological identities [43].
Experimental Workflow for MSC Characterization
Diagram 2: Comprehensive MSC characterization workflow. The process begins with tissue harvest and isolation via various methods, progresses through essential in vitro characterization (immunophenotyping, proliferation, differentiation), and culminates in advanced functional analyses to determine therapeutic potential.
Trilineage Differentiation Assessment
A fundamental criterion for defining MSCs is their capacity for trilineage differentiation into osteogenic, adipogenic, and chondrogenic lineages under specific in vitro conditions [30] [4] [35].
Osteogenic Differentiation: MSCs are seeded at 3 × 10³ cells/well in 48-well plates and cultured in an osteogenic induction medium. This medium typically consists of DMEM supplemented with 10% FBS, 50 µM ascorbic acid-2 phosphate, 10 mM β-glycerophosphate, and 0.1 µM dexamethasone [30]. Successful differentiation is confirmed by alkaline phosphatase staining and Alizarin Red S staining of mineralized deposits after 2-3 weeks.
Adipogenic Differentiation: Cells are induced using a medium containing DMEM, 10% FBS, 0.5 mM isobutylmethylxanthine (IBMX), 1 µM dexamethasone, 10 µM insulin, and 200 µM indomethacin [30]. Lipid accumulation within cytoplasmic droplets, the hallmark of adipogenesis, is visualized after 2-3 weeks using Oil Red O staining. Quantitative differences can be significant, with one study showing P-AMSCs achieving 10.95% differentiation compared to 7.26% in S-AMSCs [42].
Chondrogenic Differentiation: Chondrogenesis is typically induced in a pellet culture system. Approximately 2.5 × 10⁵ MSCs are centrifuged to form a micromass pellet, which is then cultured in a serum-free chondrogenic medium. This medium is supplemented with 1% ITS (Insulin-Transferrin-Selenium), 100 nM dexamethasone, 50 µM ascorbic acid-2 phosphate, and 10 ng/mL TGF-β3 [30]. The resulting cartilage pellets are assessed after 3-4 weeks by histological staining for sulfated proteoglycans with Alcian Blue or Safranin O.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for MSC Isolation and Characterization
| Reagent/Chemical | Primary Function | Application Example | Source/Reference |
|---|---|---|---|
| Collagenase Type I | Enzymatic digestion of extracellular matrix. | Isolation of AD-MSCs (SVF) and UC-MSCs. | Sigma-Aldrich [30] [41] |
| Ficoll-Paque Premium | Density gradient medium for cell separation. | Isolation of mononuclear cells from bone marrow. | GE Healthcare [41] |
| Fetal Bovine Serum (FBS) | Critical supplement for cell culture media, providing growth factors and nutrients. | Standard component (10-20%) for MSC expansion and maintenance. | Gibco [30] [41] |
| Trypsin-EDTA | Proteolytic enzyme solution for detaching adherent cells. | Passaging and subculturing of adherent MSCs. | Sigma-Aldrich [30] [41] |
| Dexamethasone | Synthetic glucocorticoid; a potent differentiation inducer. | Component of osteogenic and adipogenic induction media. | Standard reagent [30] |
| ITS Supplement | Provides insulin, transferrin, and selenium for defined serum-free culture. | Essential for chondrogenic differentiation in pellet culture. | Standard reagent [30] |
| TGF-β3 (Transforming Growth Factor Beta 3) | Key cytokine inducing chondrocyte differentiation. | Critical component of chondrogenic induction media. | Standard reagent [30] |
| Flow Cytometry Antibodies (CD73, CD90, CD105, CD34, CD45, HLA-DR) | Cell surface marker detection for immunophenotyping. | Confirmation of MSC identity according to ISCT criteria. | Multiple suppliers [4] [42] |
The selection of an MSC tissue source is a critical determinant in the design and outcome of research and clinical applications. BM-MSCs remain the gold standard but are limited by invasive collection and age-related decline. AD-MSCs offer high yield and ease of access, though their functional properties can vary significantly based on anatomical depot. UC-MSCs offer superior proliferation, immunomodulation, and transcriptomic stability, making them a robust choice for allogeneic therapies. DP-MSCs present a unique source with high proliferative capacity but notable lineage restrictions, such as deficient adipogenesis. A deep understanding of the standardized protocols, molecular signatures, and functional distinctions outlined in this guide empowers scientists to make informed, application-driven decisions, ultimately advancing the field of regenerative medicine through the targeted use of MSCs. Future research should focus on standardizing potency assays and isolation protocols to ensure consistent and reproducible clinical translation.
Mesenchymal stem/stromal cells (MSCs) represent a cornerstone of regenerative medicine due to their capacity for self-renewal and multilineage differentiation. According to the International Society for Cellular Therapy (ISCT), the minimal criteria for defining MSCs include plastic adherence, specific surface marker expression, and trilineage differentiation potential into osteocytes, chondrocytes, and adipocytes [44]. This differentiation capacity varies significantly based on tissue source, donor characteristics, and culture conditions, creating critical implications for developing targeted therapeutic applications. Understanding these variations enables researchers to select optimal MSC sources for specific clinical applications, thereby enhancing therapeutic outcomes in areas such as bone repair, cartilage regeneration, and metabolic disease modeling.
The following comparative analysis examines key determinants of MSC differentiation efficiency, providing researchers with evidence-based guidance for cell source selection. We present consolidated experimental data, detailed methodologies, and signaling pathway analyses to inform strategic decision-making in both basic research and clinical translation.
Tissue Source-Specific Differentiation Potentials
MSCs from different tissue sources exhibit distinct differentiation biases due to their unique epigenetic programming and microenvironmental histories. These inherent predispositions significantly impact their effectiveness for specific therapeutic applications.
Table 1: Comparison of Trilineage Differentiation Potential Across MSC Sources
| Tissue Source | Osteogenic Potential | Chondrogenic Potential | Adipogenic Potential | Key Supporting Evidence |
|---|---|---|---|---|
| Bone Marrow (BMSCs) | Strong | Moderate | Lower | Hypermethylated PPARγ promoter; hypomethylated Runx2 promoter [45] |
| Adipose Tissue (ASCs) | Strong (especially with BMP9) | High (superior in 3D spheroid culture) | High | Hypomethylated PPARγ promoter; hypermethylated Runx2 promoter [46] [45] |
| Umbilical Cord | Variable (poor in spheroid models) | High | High | Success in chondrogenic and adipogenic spheroid differentiation [47] |
The epigenetic memory of MSCs significantly influences their differentiation fate. Research demonstrates that BMSCs possess hypomethylated promoters for Runx2 (a key osteogenic transcription factor), favoring osteogenesis, while ASCs show hypomethylated PPARγ promoters, predisposing them to adipogenesis [45]. This epigenetic programming creates a functional bias that persists through ex vivo expansion, making certain cell sources inherently more suitable for specific applications.
Impact of Donor Physiology and Culture Conditions
Donor physiology and culture conditions introduce significant variation in differentiation efficiency, necessitating careful consideration during experimental design.
Diabetes Status: A 2025 study revealed that adipose-derived MSCs from type 2 diabetic (T2D) donors exhibited greater chondrogenic and pro-angiogenic potential compared to those from healthy donors, despite comparable proliferation rates and marker expression under standard conditions [48]. Furthermore, when healthy AT-MSCs were cultured under diabetic-mimicking conditions (high glucose with/without insulin), they showed induced oxidative stress and enhanced pro-angiogenic effects [48]. This suggests that autologous AT-MSCs from diabetic patients remain functionally competent for specific therapeutic applications, such as treating osteoarthritis or myocardial infarction.
Culture System Advanced: Moving from traditional two-dimensional (2D) cultures to three-dimensional (3D) spheroid models under physiologically relevant conditions (e.g., hypoxia, serum-free media) significantly enhances differentiation outcomes. Spheroid culture has been demonstrated to improve matrix production, paracrine effects, stemness preservation, and cell survival post-transplantation [47]. A 2024 model using spheroid culture with hypoxia and serum-free conditions successfully supported trilineage differentiation for MSCs from most tissue sources, though umbilical cord-derived MSCs failed to undergo osteogenesis in this system [47].
Experimental Data and Methodologies
Standardized Trilineage Differentiation Protocols
Reproducible differentiation relies on standardized protocols using specific induction factors. The methodologies below are validated for human MSCs.
Table 2: Detailed Trilineage Differentiation Protocols
| Lineage | Induction Medium Components | Culture Duration & Format | Staining & Detection Methods | Key Molecular Markers |
|---|---|---|---|---|
| Osteogenesis | Dexamethasone, ascorbic acid, β-glycerophosphate [45] [49] | 12-14 days; 2D monolayer [49] | Alizarin Red S for calcium deposits [49] | Runx2, ALP activity, Col11a1 (by rt-QPCR) [50] [51] |
| Adipogenesis | Dexamethasone, isobutylmethylxanthine, indomethacin, insulin [45] [49] | 12-21 days; 2D monolayer [45] [49] | Oil Red O for lipid vacuoles [49] | PPARγ, FABP4 (by rt-QPCR) [50] [52] |
| Chondrogenesis | TGF-β3, BMP-2/6, dexamethasone, ascorbate, proline, pyruvate, ITS [50] [45] | 21 days; 3D pellet/spheroid [49] | Alcian Blue for sulfated glycosaminoglycans [49] | Sox9, ACAN (by rt-QPCR) [50] |
Key Signaling Pathways Regulating Lineage Commitment
The differentiation of MSCs is governed by complex signaling networks that often exhibit reciprocal regulation. Key pathways include TGF-β/BMP, Wnt, Hedgehog, and Notch signaling [51] [52].
This diagram illustrates the primary signaling pathways and key transcription factors governing MSC fate decisions. The reciprocal inhibition between osteogenic (Runx2) and adipogenic (PPARγ) transcription factors creates a differentiation switch, while chondrogenesis is primarily driven by Sox9 activation through TGF-β/BMP signaling [51] [52]. The Wnt/β-catenin pathway promotes osteogenesis by stabilizing β-catenin, which activates TAZ and Runx2, while simultaneously inhibiting adipogenesis [51].
The Scientist's Toolkit: Essential Research Reagents
Successful trilineage differentiation requires carefully selected reagents and materials. The following table outlines essential components for MSC differentiation research.
Table 3: Essential Research Reagents for Trilineage Differentiation Studies
| Reagent/Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Culture Media Supplements | Human Platelet Lysate (hPL), Fetal Bovine Serum (FBS) | Provides essential growth factors and adhesion proteins; hPL reduces batch variability and xenoimmunization risk [48] [47] |
| Osteogenic Inducers | Dexamethasone, Ascorbic Acid, β-glycerophosphate | Synergistically promote osteoblast differentiation and matrix mineralization [45] [49] |
| Adipogenic Inducers | IBMX, Indomethacin, Insulin | IBMX and indomethacin initiate differentiation; insulin promotes lipid accumulation [45] [49] |
| Chondrogenic Inducers | TGF-β3, BMP-2/6, ITS+Premix | Crucial for 3D chondrogenesis in pellet/spheroid culture; TGF-β3 is particularly effective [45] [52] |
| Validation Reagents | Alizarin Red S, Oil Red O, Alcian Blue | Histochemical staining for calcium deposits, lipid vacuoles, and sulfated GAGs, respectively [49] |
| Molecular Analysis Kits | rt-QPCR for ACAN, FABP4, Col11a1 | Quantitative assessment of chondrogenic, adipogenic, and osteogenic marker expression [50] |
The trilineage differentiation potential of MSCs varies significantly based on tissue origin, with bone marrow-derived MSCs exhibiting superior osteogenic capacity, while adipose-derived MSCs demonstrate robust adipogenic and chondrogenic potential, particularly in advanced 3D culture systems. These differences are rooted in epigenetic programming and are further influenced by donor physiology and culture conditions. The recognition of these source-specific attributes enables more precise cell source selection for targeted applications. For bone regeneration, BMSCs or BMP9-stimulated ASCs appear optimal [46] [45]. For cartilage repair, ASCs from diabetic donors show enhanced potential [48], while for metabolic research, ASCs provide superior adipocyte yield [45]. Future research optimizing culture conditions and leveraging epigenetic modifications will further enhance our ability to harness the full therapeutic potential of MSCs across diverse regenerative applications.
The therapeutic application of Mesenchymal Stromal Cells (MSCs) has undergone a significant paradigm shift, moving from a focus on cell differentiation and replacement toward an appreciation of their paracrine activity as the primary mechanism of action [3]. It is now widely recognized that approximately 80% of the regenerative potential of MSCs is mediated through the release of bioactive molecules, collectively known as the secretome, rather than through direct differentiation into target cells [53]. This complex mixture includes soluble factors (cytokines, chemokines, and growth factors) and extracellular vesicles (EVs) (exosomes, microvesicles) that orchestrate immunomodulation, angiogenesis, and tissue repair [4] [53]. The composition of this secretome is not universal; it varies significantly based on the tissue origin of the MSCs, influencing their therapeutic specificity and efficacy [30]. This guide provides a comparative analysis of tissue-specific secretome profiles from adipose tissue, bone marrow, and dental pulp-derived MSCs, offering researchers a data-driven foundation for selecting optimal cell sources for targeted applications in drug development and regenerative medicine.
Comparative Profiling of Tissue-Specific MSC Secretomes
The therapeutic potential of an MSC's secretome is intrinsically linked to its tissue of origin. Variations in anatomical location, ontogeny, and native function impart distinct secretory signatures that can be leveraged for different clinical applications.
Table 1: Functional Characteristics of MSCs from Different Tissues
| Tissue Origin | Key Proliferation & Morphological Traits | Distinct Secretome Features & Functional Strengths | Most Promising Therapeutic Applications |
|---|---|---|---|
| Adipose Tissue (AD-MSCs) [54] [30] | Readily isolated from liposuction waste; higher yield; larger, fibroblast-like cells. | Rich in pro-angiogenic and pro-regenerative factors; supports skin cell migration/proliferation; promotes blood vessel formation. | Wound healing, skin rejuvenation, alopecia, and inflammatory skin diseases [54]. |
| Bone Marrow (BM-MSCs) [55] [4] | The most extensively studied type; requires invasive harvest; fibroblast-like morphology. | Strong immunomodulatory effects; secretes neuroprotective factors (e.g., NGF, VEGF); high particle yield in α-MEM culture. | Retinal degenerative diseases (e.g., retinitis pigmentosa), graft-versus-host disease (GVHD) [55] [4]. |
| Dental Pulp (DPSCs) [30] | Isolated from dental pulp; high proliferation rate; smaller, Nestin-positive cells. | miRNA profiles favor oxidative stress and apoptosis pathways; enhances cell viability; reduces apoptosis. | Neuro-regenerative applications, treatments for oxidative stress-related damage. |
Beyond these inherent differences, the method of MSC isolation further influences the resulting cell population and its secretome. For instance, a comparative study showed that AD-MSCs isolated via enzymatic digestion (SVF) versus mechanical fragmentation (MF) exhibited significant variations in their secretome profiles, particularly in the sets of released microRNAs [30]. This underscores the critical need for standardized reporting and protocol transparency in MSC research.
Quantitative Secretome Analysis: Cytokines and Extracellular Vesicles
A deeper understanding of the secretome's potency requires a quantitative analysis of its components. The following table summarizes key experimental data on the protein and extracellular vesicle profiles of different MSCs.
Table 2: Quantitative Analysis of MSC Secretome Components
| MSC Source | Key Cytokines/Growth Factors | Extracellular Vesicle Characteristics | Documented Functional Outcomes |
|---|---|---|---|
| Adipose Tissue (AD-MSCs) [54] [30] [56] | Immunomodulatory, re-epithelializing, anti-fibrotic, proangiogenic factors [54]. | Produces a significantly higher number of smaller exosomes than DPSCs [30]; iMSC-EVs showed ~1.5x larger particle size than ADMSC-EVs [56]. | Increased HDF viability; reduced apoptosis in HDFs and ADMSCs; promoted skin regeneration and wound healing [54] [56]. |
| Bone Marrow (BM-MSCs) [55] | Growth factors (NGF, VEGF), immunomodulatory cytokines (IL-6, TGF-β) [55]. | Mean particle size: ~107-114 nm; yield: 3,751-4,319 particles/cell; higher yield with TFF isolation vs. UC [55]. | Increased viability of damaged ARPE-19 cells from 37.9% to 54.6%; significant reduction in apoptosis [55]. |
| Dental Pulp (DPSCs) [30] | Specific sets of cytokines and growth factors distinct from AD-MSCs [30]. | Releases a comparable number of EVs as AD-MSCs, but with a different size distribution [30]. | microRNAs involved in oxidative stress and apoptosis pathways; high proliferation rate [30]. |
The data reveals that while all MSC-EVs share common regenerative properties like enhancing viability and reducing apoptosis, their physical properties and molecular cargo are source-dependent. This influences their functional specificity, with AD-MSC secretomes being particularly potent for skin repair, while BM-MSC-sEVs show marked efficacy in retinal protection models.
Essential Experimental Workflows for Secretome Analysis
To ensure the reliability and reproducibility of secretome studies, standardized protocols for EV isolation and functional validation are paramount. The following workflows detail two critical experimental processes.
Workflow for Isolation and Characterization of Small Extracellular Vesicles (sEVs)
The isolation of pure and functional sEVs is a foundational step. The following diagram illustrates a standardized protocol based on studies optimizing sEV production from BM-MSCs [55].
Diagram 1: sEV Isolation and Characterization Workflow. This chart outlines the key steps for producing and validating mesenchymal stem cell-derived small extracellular vesicles, from cell culture to functional testing.
Key methodological notes from the literature indicate that using Alpha Minimum Essential Medium (α-MEM) supplemented with human platelet lysate may support higher cell proliferation and sEV yield compared to DMEM, although the difference was not always statistically significant [55]. For isolation, Tangential Flow Filtration (TFF) has been shown to provide a statistically higher particle yield than the traditional Ultracentrifugation (UC) method, making it more suitable for large-scale production [55]. Characterization is a multi-faceted process: NTA determines particle size and concentration, TEM confirms the classic cup-shaped morphology, and Western Blot verifies the presence of positive protein markers (CD9, CD63, TSG101) and the absence of the negative marker calnexin [55].
Workflow for Preconditioning and Functional Assays
The secretory profile of MSCs can be actively enhanced through preconditioning. The subsequent functional assays are crucial for validating therapeutic potency, as demonstrated in studies on retinal protection and skin regeneration [54] [55].
Diagram 2: Preconditioning and Functional Validation. This chart illustrates the process of enhancing the MSC secretome through environmental stimuli and testing its efficacy in relevant disease models.
For preconditioning, studies on AD-MSCs have shown that exposure to hypoxia or low-frequency electromagnetic fields can enhance the pro-regenerative capacity of their secretome for skin applications [54]. In functional assays, a classic model involves creating oxidative stress damage, such as with H₂O₂ exposure to ARPE-19 retinal pigment epithelial cells. The application of BM-MSC-sEVs (e.g., at 50 µg/mL) before or after such injury has been demonstrated to significantly increase cell viability from 37.9% to over 52.7% and reduce total apoptotic cells [55]. Similarly, the secretome from AD-MSCs can be tested for its ability to promote the proliferation and migration of skin cells like fibroblasts and keratinocytes in scratch assays [54].
The Scientist's Toolkit: Key Reagents and Materials
To implement the described experimental workflows, researchers will require a suite of specialized reagents and equipment. The following table details the essential components of the toolkit.
Table 3: Research Reagent Solutions for Secretome Studies
| Category / Item | Specific Examples & Specifications | Primary Function in Secretome Research |
|---|---|---|
| Cell Culture Media [55] [56] | Alpha Minimum Essential Medium (α-MEM); Dulbecco's Modified Eagle Medium (DMEM); Xeno-Free Human Platelet Lysate (hPL). | Supports MSC expansion and secretome collection under defined, clinically relevant conditions. |
| sEV Isolation Systems [55] | Ultracentrifugation (UC) Systems; Tangential Flow Filtration (TFF) Systems. | Isolates and concentrates small extracellular vesicles from conditioned media. |
| sEV Characterization Tools [55] [57] | Nanoparticle Tracking Analyzer (NTA); Transmission Electron Microscope (TEM); Western Blot apparatus; Antibodies (CD9, CD63, TSG101, Alix). | Physically characterizes EVs (size/concentration), visualizes morphology, and confirms identity via surface markers. |
| Functional Assay Kits [55] [56] | Cell Viability Assays (e.g., MTT); Apoptosis Detection Kits (Annexin V); Cell Migration Assays (e.g., Scratch Assay). | Quantifies the therapeutic effects of the secretome, such as promoting survival and repair. |
The comprehensive analysis of tissue-specific MSC secretomes confirms that the "one-size-fits-all" approach is obsolete in secretory cell-based therapeutics. The future of this field lies in the strategic selection of MSC sources based on their inherent molecular strengths—AD-MSCs for skin and soft tissue regeneration, BM-MSCs for immunomodulation and neuroprotection, and DPSCs for managing oxidative stress. Current research is already pushing boundaries by integrating the secretome with biomaterial scaffolds like hydrogels and 3D-printed constructs for controlled, localized delivery, thereby enhancing regenerative outcomes [53]. Furthermore, the emergence of induced MSCs (iMSCs) from iPSCs presents a promising, scalable alternative to overcome donor variability and limited expansion capacity [56]. As the field progresses, the major challenges will be the standardization of production protocols, rigorous functional characterization of secretome components, and the development of engineered EVs for targeted drug delivery. By embracing this nuanced, data-driven understanding of tissue-specific paracrine actions, researchers and drug developers can unlock the full potential of cell-free therapies for a new era of regenerative medicine.
Mesenchymal stromal cells (MSCs) are multipotent cells with potent immunomodulatory properties that make them attractive therapeutic tools for immune-related conditions. Originally identified in bone marrow, MSCs have since been isolated from various tissues, including adipose tissue (AT-MSCs), umbilical cord (UC-MSCs), placental tissue, and dental pulp [58] [4]. According to the International Society for Cellular Therapy (ISCT), MSCs must adhere to plastic under standard culture conditions; express specific surface markers (CD73, CD90, CD105); lack expression of hematopoietic markers (CD45, CD34, CD14, CD11b, CD19, HLA-DR); and differentiate into osteoblasts, adipocytes, and chondroblasts in vitro [4] [59].
The therapeutic potential of MSCs extends across a broad spectrum of applications, including graft-versus-host disease (GVHD), autoimmune disorders, tissue repair, and regenerative medicine [5] [58] [4]. While all MSCs possess immunomodulatory capabilities, they display remarkable functional heterogeneity depending on their tissue origin. Understanding these source-dependent differences is crucial for selecting the most appropriate MSC type for specific clinical applications.
Comparative Immunomodulatory Profiles of Different MSC Types
Quantitative Comparison of MSC Immunomodulatory Effects
Table 1: Comparative analysis of immunomodulatory effects across MSC tissue sources
| Immune Parameter | BM-MSCs | UC-MSCs | AT-MSCs | Experimental Context |
|---|---|---|---|---|
| T-cell proliferation inhibition | Potent suppression [5] | Moderate suppression [5] | Potent suppression [5] | In vitro lymphocyte proliferation assays |
| Treg/Th17 ratio modulation | Moderate increase [5] | High increase [5] | High increase [5] | Co-culture with PBMCs |
| Coagulation pathway activation | Low [5] | High [5] | High [5] | In vitro coagulation assays |
| B cell suppression | Moderate [58] | Moderate [58] | Strong [58] [60] | Co-culture with B cells |
| Macrophage polarization to M2 | Strong [61] [62] | Strong [61] [62] | Strong [61] [62] | Co-culture with macrophages |
| Pro-inflammatory cytokine reduction | Moderate [63] | Strong [63] | Moderate [63] | Cytokine array analysis |
Table 2: Secretory profile and functional characteristics across MSC sources
| Characteristic | BM-MSCs | UC-MSCs | AT-MSCs |
|---|---|---|---|
| Key soluble factors | PGE2, IDO, HGF [58] [59] | IDO, PGE2, TGF-β [58] | PGE2, IDO, TSG-6 [58] |
| Immunogenicity | Low [59] | Very low [58] | Low [59] |
| Pro-coagulant activity | Low [5] | High [5] | High (with safety concerns) [5] |
| Tissue source accessibility | Invasive [4] | Non-invasive [4] | Minimally invasive [4] |
| Expansion potential | Moderate [4] | High [4] | High [4] |
Safety Considerations Across MSC Types
Safety profiles vary considerably among MSC sources. AT-MSC infusions have been associated with sudden death in murine models (4 of 16 animals), potentially linked to their pro-coagulant activities [5]. Similarly, UC-MSCs demonstrate higher coagulation pathway activation compared to BM-MSCs [5]. These findings highlight the importance of considering thrombotic risks when selecting MSC products for clinical applications.
Mechanisms of T-Cell Suppression by MSCs
Experimental Approaches for Studying T-Cell Modulation
Standardized experimental protocols are essential for evaluating MSC-mediated T-cell suppression:
Mixed Lymphocyte Reaction (MLR) Protocol:
- Isolate peripheral blood mononuclear cells (PBMCs) from healthy donors using Ficoll density gradient centrifugation [5]
- Culture MSCs (1-2 × 10^4 cells) in flat-bottom 96-well plates in RPMI 1640 medium supplemented with 10% FBS and antibiotics [5]
- Activate T-cells using phytohemagglutinin (PHA), anti-CD3/CD28 antibodies, or allogeneic stimulators [59]
- Co-culture activated T-cells with MSCs at varying ratios (typically 1:1 to 1:10 MSC:T-cell) [59]
- Assess proliferation via ^3H-thymidine incorporation or CFSE dilution after 3-5 days [59]
- Analyze T-cell phenotype via flow cytometry for CD4, CD8, CD25, FoxP3, and intracellular cytokines [5] [59]
Key Research Reagents:
- Ficoll-Paque for PBMC isolation [5]
- Phytohemagglutinin (PHA) or anti-CD3/CD28 antibodies for T-cell activation [59]
- CFSE or ^3H-thymidine for proliferation assessment [59]
- Flow cytometry antibodies against CD3, CD4, CD8, CD25, FoxP3 for phenotyping [5]
Molecular Mechanisms of T-Cell Suppression
MSCs employ multiple interconnected mechanisms to suppress T-cell responses:
Diagram 1: MSC-Mediated T-Cell Suppression Mechanisms. MSCs suppress T-cells through cell contact-dependent pathways (green) and soluble factors (blue), resulting in cell cycle arrest and regulatory T-cell induction.
The immunomodulatory effects are context-dependent, influenced by the inflammatory microenvironment. MSCs require "licensing" by inflammatory cytokines like IFN-γ to exert their maximal immunosuppressive effects [58] [59]. This licensing enhances the expression of key immunomodulatory molecules including IDO, PGE2, and PD-L1.
Source-Specific Variations in T-Cell Modulation
Different MSC sources exhibit distinct T-cell modulatory patterns. BM-MSCs and AT-MSCs demonstrate more potent inhibition of lymphocyte proliferation compared to UC-MSCs [5]. However, UC-MSCs and AT-MSCs induce a higher regulatory T-cell (Treg)/T helper 17 (Th17) ratio, suggesting superior capacity to promote immune tolerance [5]. These differences likely reflect adaptations to distinct tissue microenvironments.
MSC Regulation of B-Cell Responses
Methodologies for Assessing B-Cell Modulation
B-Cell Co-Culture Protocol:
- Isolate B-cells from human PBMCs using magnetic-activated cell sorting (CD19+ selection)
- Culture MSCs to 70-80% confluence in appropriate medium
- Activate B-cells using CD40 ligand, IL-4, and B-cell receptor cross-linking
- Co-culture activated B-cells with MSCs at varying ratios (1:5 to 1:20 MSC:B-cell)
- Assess proliferation via CFSE dilution after 5-7 days
- Measure immunoglobulin production via ELISA
- Analyze regulatory B-cell (Breg) induction via flow cytometry for CD19, CD24, CD38, IL-10, and other Breg markers [60]
Key Research Reagents:
- CD19 microbeads for B-cell isolation
- CD40 ligand and IL-4 for B-cell activation
- CFSE for proliferation tracking
- ELISA kits for immunoglobulin quantification
- Antibodies for Breg phenotyping (CD19, CD24, CD38, CD1d, IL-10)
Mechanisms of B-Cell Regulation
MSCs employ diverse strategies to modulate B-cell function:
Diagram 2: MSC-Mediated B-Cell Regulation. MSCs influence B-cell function through multiple mechanisms, resulting in proliferation control, differentiation modulation, and regulatory B-cell induction.
MSCs inhibit B-cell proliferation by arresting cells in the G0/G1 phase of the cell cycle through p38 mitogen-activated protein kinase (MAPK) pathway activation [58]. They also suppress plasmablast differentiation and antibody production by downregulating the expression of Blimp-1, a critical transcription factor for plasma cell differentiation [60].
Source-Dependent B-Cell Modulation
AT-MSCs demonstrate particularly potent effects on B-cells, increasing survival of quiescent B-cells through contact-dependent mechanisms and inhibiting caspase-3-mediated apoptosis via vascular endothelial growth factor (VEGF) upregulation [58]. All MSC sources can induce regulatory B-cells (Bregs), particularly IL-10-producing B10 cells, which play crucial roles in maintaining immune tolerance in autoimmune diseases and transplantation settings [60].
MSC Modulation of Macrophage Polarization
Experimental Approaches for Studying Macrophage Plasticity
Macrophage Polarization Assay Protocol:
- Isolate human monocytes from PBMCs using CD14+ magnetic selection
- Differentiate monocytes into macrophages with M-CSF (50 ng/mL) for 5-7 days
- Polarize macrophages toward M1 phenotype with IFN-γ (20 ng/mL) and LPS (100 ng/mL)
- Co-culture polarized M1 macrophages with MSCs using transwell systems or direct contact
- Analyze macrophage phenotype via flow cytometry (CD80, CD86, CD206, CD163)
- Measure cytokine secretion via ELISA (TNF-α, IL-12, IL-10, TGF-β)
- Assess functional changes (phagocytosis, antigen presentation) [61] [62]
Key Research Reagents:
- CD14 microbeads for monocyte isolation
- M-CSF for macrophage differentiation
- Polarizing cytokines: IFN-γ, LPS (M1); IL-4, IL-13 (M2)
- Flow cytometry antibodies for M1/M2 markers (CD80, CD86, CD206, CD163)
- ELISA kits for cytokine quantification
Mechanisms of Macrophage Polarization
MSCs profoundly influence macrophage plasticity through multiple mechanisms:
Diagram 3: MSC-Mediated Macrophage Polarization. MSCs promote anti-inflammatory M2 macrophage polarization through multiple secreted factors and signaling pathways while inhibiting pro-inflammatory M1 characteristics.
MSCs promote the polarization of monocytes/macrophages toward an anti-inflammatory M2 phenotype through several mechanisms. MSC-secreted factors including PGE2, IL-1 receptor antagonist (IL-1RA), and TNF-stimulated gene 6 (TSG-6) drive this polarization [64] [63]. MSCs also modulate macrophage metabolic programming, shifting them from glycolysis to oxidative phosphorylation, which supports the M2 phenotype [63].
Source-Specific Effects on Macrophage Function
While all MSC sources promote M2 polarization, their efficiency and mechanisms may vary. BM-MSCs have been shown to enhance phagocytic activity in blood monocytes and increase alternatively activated CD163+CD206+ monocytes/macrophages in spleen tissue [64]. Interestingly, MSC phagocytosis by monocytes itself serves as a polarization signal, inducing anti-inflammatory Ly6Clow monocytes that produce IL-10 and express PD-L1 [64].
Research Reagents and Methodological Toolkit
Table 3: Essential research reagents for studying MSC immunomodulation
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Cell Isolation | Ficoll-Paque, CD4/CD8/CD19/CD14 microbeads | Immune cell purification | Purity impacts functional assays |
| Cell Culture | RPMI 1640, DMEM, FBS, antibiotic-antimycotic | MSC and immune cell culture | Serum lot variability affects results |
| Activation Reagents | PHA, anti-CD3/CD28, LPS, CD40L | Immune cell activation | Concentration optimization required |
| Detection Antibodies | CD73, CD90, CD105, HLA-DR, CD45 | MSC characterization | ISCT criteria compliance essential |
| Functional Assays | CFSE, ^3H-thymidine, ELISA kits, flow cytometry | Proliferation, cytokine measurement | Multiplex approaches recommended |
| Soluble Inhibitors | IDO, PGE2, TGF-β inhibitors | Mechanism validation | Specificity controls necessary |
The comparative analysis of MSC immunomodulation reveals tissue-specific strengths that can inform therapeutic selection. BM-MSCs demonstrate potent T-cell suppression, making them candidates for T-cell-mediated conditions. UC-MSCs show enhanced regulatory cell induction with lower immunogenicity, favorable for allogeneic applications. AT-MSCs exhibit strong B-cell modulation but require careful safety assessment due to pro-coagulant potential.
Future research should focus on standardizing isolation and culture protocols to minimize variability, developing potency assays that predict clinical efficacy, and exploring priming strategies to enhance specific immunomodulatory functions. The growing understanding of MSC-derived extracellular vesicles as alternatives to cell-based therapies also presents exciting opportunities for targeted immunomodulation without cellular risks.
Understanding these source-dependent immunomodulatory profiles enables researchers and clinicians to make informed decisions when selecting MSC types for specific therapeutic applications, ultimately advancing the field of cellular therapy for immune-mediated diseases.
In the evolving landscape of regenerative medicine, mesenchymal stem cells (MSCs) have emerged as a cornerstone for therapeutic applications due to their multipotency, immunomodulatory properties, and paracrine activity [4] [32]. The therapeutic success of MSC-based interventions is profoundly influenced by the selection of both the cell source and the delivery method. These factors collectively determine cell survival, biodistribution, engraftment, and ultimately, the clinical outcome [65] [32]. This guide provides a comparative analysis of three prominent clinical application paradigms: Cell-Assisted Lipotransfer (CAL), which enriches autologous fat grafts with stromal vascular fraction (SVF); Systemic Infusion, which delivers cells intravenously for broad distribution; and Local Injection, which precisely targets specific tissues. The objective of this comparison is to equip researchers and drug development professionals with evidence-based insights to align therapeutic strategies with specific clinical indications.
Comparative Analysis of Delivery Methods
The following tables summarize the key characteristics, efficacy data, and safety profiles of the three delivery methods, synthesizing findings from recent clinical studies and meta-analyses.
Table 1: Overview and Clinical Efficacy of MSC Delivery Methods
| Feature | Cell-Assisted Lipotransfer (CAL) | Systemic (IV) Infusion | Local Injection |
|---|---|---|---|
| Definition | Co-transplantation of lipoaspirate with enriched SVF/ADSCs [66] | Intravenous administration of MSCs for systemic circulation [65] | Direct administration of MSCs into or around a target tissue [65] |
| Primary Mechanism | Improves graft vascularization and survival via ADSCs and pro-angiogenic factors in SVF [66] [67] | Exerts immunomodulatory and anti-inflammatory effects via paracrine signaling; cells home to sites of inflammation [65] [68] | Provides concentrated local effect; promotes repair via paracrine signaling and potential differentiation [65] |
| Key Efficacy Data | Fat Survival Rate: 71% vs. 48% in non-CAL (P<0.0001) [66] | Effective for immune-mediated conditions (e.g., GvHD, Crohn's) [65] [32] | Osteoarthritis: Improved pain, function, and joint structure [65] |
| Typical Cell Dose | Varies with graft volume; involves SVF enrichment | Varies widely by indication; often requires high doses due to pulmonary entrapment [65] | Effective dose range: 50–100 million cells for intra-articular use [65] |
Table 2: Safety, Biodistribution, and Indications
| Feature | Cell-Assisted Lipotransfer (CAL) | Systemic (IV) Infusion | Local Injection |
|---|---|---|---|
| Biodistribution | Cells remain at graft site [66] | Initial trapping in lungs, then redistribution to liver, spleen, and kidneys [65] | Cells largely remain in the local tissue environment [65] |
| Common Indications | Soft tissue reconstruction (e.g., breast, face), augmentation [66] | Autoimmune diseases, inflammatory disorders (e.g., Crohn's), GvHD [65] [68] | Orthopedic injuries, osteoarthritis, focal cosmetic defects [65] |
| Safety Profile | Large-volume grafting (e.g., breast): Increased complication rate vs. traditional grafting; does not reduce need for multiple operations [66] | Generally safe; most common side effect is transient fever. No significant increase in serious adverse events [65] | Generally safe; risk profile associated with the injection procedure and target site [65] |
Experimental Protocols for Key Applications
Protocol for Cell-Assisted Lipotransfer (CAL)
The CAL technique is designed to improve the survival and volume retention of autologous fat grafts by enriching them with the Stromal Vascular Fraction (SVF), which contains ADSCs and other regenerative cells [66] [67].
- Adipose Tissue Harvesting: Subcutaneous adipose tissue is obtained via liposuction using a Coleman cannula or similar device under low-pressure aspiration to minimize cell trauma [67].
- SVF Isolation (Enzymatic):
- Washing: The lipoaspirate is washed with phosphate-buffered saline (PBS) to remove cellular debris and blood components [67].
- Digestion: The tissue is digested with collagenase (e.g., 0.075% concentration) at 37°C for 30-60 minutes with continuous agitation to break down the extracellular matrix [67].
- Centrifugation: The digest is centrifuged (e.g., 1200 g for 5-10 minutes) to separate the mixture into three layers: a top layer of mature adipocytes, a middle aqueous layer, and a pellet containing the SVF [67].
- Washing and Resuspension: The SVF pellet is resuspended in saline or PBS, passed through a filter (e.g., 100-500 µm) to remove debris, and counted for cell number and viability [67].
- Graft Preparation: The freshly isolated SVF is combined with the purified adipose tissue graft. The enriched graft is then ready for implantation [66].
- Implantation: The CAL graft is injected into the recipient site (e.g., breast, face) using a standard fat grafting technique [66].
Protocol for Systemic Infusion
This protocol outlines the intravenous administration of MSCs for systemic conditions, noting key considerations for cell preparation and patient monitoring [65] [32].
- Cell Source and Preparation: MSCs are expanded from sources like bone marrow or adipose tissue under Good Manufacturing Practice (GMP) conditions. The final cell product is washed and formulated in an infusion-ready solution, such as lactated Ringer's solution or normal saline with human serum albumin [32].
- Quality Control: Before release, the cell product undergoes rigorous testing, including viability (typically >90%), sterility (bacteria, fungi, mycoplasma), endotoxin levels (<0.25 EU/mL), and identity confirmation via flow cytometry for positive (CD73, CD90, CD105) and negative (CD34, CD45, HLA-DR) markers [32] [55].
- Pre-infusion Check: Patient vitals are recorded. Pre-medication with an antihistamine or corticosteroid may be administered per trial protocol, although it is not always necessary [65].
- Infusion: The cell suspension is administered intravenously via a peripheral line using a standard blood transfusion set. The infusion rate is typically slow initially, with monitoring for acute reactions, and can be completed over 30-60 minutes [65].
- Post-infusion Monitoring: Patients are monitored for several hours for adverse events, with transient fever being the most commonly reported side effect [65].
Signaling Pathways and Therapeutic Mechanisms
The therapeutic effects of MSCs are largely mediated through paracrine signaling and direct cellular interactions. The following diagram illustrates the key pathways involved in their immunomodulatory and tissue-reparative functions, which are central to all three delivery methods.
Diagram: MSC Immunomodulation and Tissue Repair Pathways. MSCs exert effects via paracrine factors. Green nodes show immunomodulation via T-cells, macrophages, and dendritic cells [68]. Blue nodes show B-cell suppression [68]. Red nodes show tissue repair via anti-apoptosis, angiogenesis, and proliferation [68] [32].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research and development in MSC therapies require a suite of specialized reagents and materials. The following table details key solutions used in the featured experiments and general workflows.
Table 3: Key Research Reagent Solutions
| Reagent/Material | Function/Application | Specific Examples & Notes |
|---|---|---|
| Collagenase | Enzymatic digestion of adipose tissue to isolate the Stromal Vascular Fraction (SVF) [67]. | Type I or II collagenase; concentration and incubation time (e.g., 37°C for 30-60 min) must be optimized [67]. |
| Cell Culture Media | Ex vivo expansion and maintenance of MSCs. | α-MEM and DMEM are common basal media. Supplementation with 10% Human Platelet Lysate (hPL) is a xeno-free alternative to Fetal Bovine Serum (FBS) that supports high cell proliferation [55]. |
| Flow Cytometry Antibodies | Characterization of MSC surface markers and assessment of cell purity per ISCT criteria [4] [32]. | Positive Panel: CD73, CD90, CD105. Negative Panel: CD34, CD45, HLA-DR. Viability dyes (e.g., 7-AAD) are used for live/dead discrimination [32] [55]. |
| Differentiation Kits | Functional validation of MSC trilineage differentiation potential. | Commercially available kits for inducing adiopogenic, osteogenic, and chondrogenic lineages are used with specific staining (Oil Red O, Alizarin Red, Alcian Blue) to confirm differentiation [4] [55]. |
| Tangential Flow Filtration (TFF) | Scalable, efficient isolation of small Extracellular Vesicles (sEVs/exosomes) from conditioned media [55]. | Offers higher particle yield compared to traditional ultracentrifugation (UC), making it more suitable for GMP production of MSC-derived exosomes [55]. |
The choice between Cell-Assisted Lipotransfer, Systemic Infusion, and Local Injection is not a matter of superiority but of strategic alignment with the clinical objective. CAL significantly enhances the volume retention of autologous fat grafts for soft tissue reconstruction, though its risk-benefit profile must be carefully evaluated in large-volume applications [66]. Systemic Infusion is the paradigm of choice for treating widespread inflammatory and autoimmune conditions, leveraging the body's vasculature to deliver immunomodulatory signals, albeit with an initial biodistribution skewed toward the lungs [65]. Local Injection offers targeted precision for focal defects, particularly in orthopedic and musculoskeletal applications, ensuring a high concentration of therapeutic cells is delivered directly to the site of injury [65]. Future advancements will likely come from refining cell sources, employing engineered vesicles, and developing combination therapies that maximize the synergistic potential of these powerful clinical paradigms.
Navigating Clinical Challenges: Standardization, Safety, and Potency
The therapeutic potential of Mesenchymal Stem/Stromal Cells (MSCs) spans regenerative medicine, immunomodulation, and tissue engineering, positioning them as a cornerstone of advanced therapeutic medicinal products (ATMPs) [69] [4]. However, the transition from preclinical promise to consistent clinical efficacy has been hampered by a fundamental biological reality: the profound heterogeneity of MSCs [70] [69]. This variability, stemming from donor-specific factors, tissue origins, and manufacturing processes, presents a significant obstacle to the standardization and predictability of MSC-based treatments [32]. Among these factors, donor age stands out as a particularly critical variable, systematically influencing the functional properties and regenerative capacity of MSCs [70] [71] [72]. Within the context of comparative analysis of MSC tissue origins for targeted applications, understanding and controlling for age-related decline is not merely an academic exercise but a prerequisite for developing effective, reproducible therapies. This review synthesizes current evidence on how donor age impacts MSC function across different tissue sources, providing a data-driven framework for strategic sourcing decisions in both research and clinical development.
Donor Age as a Determinant of MSC Functionality
Aging systematically impairs core MSC functionalities through a combination of cellular senescence, epigenetic drift, and accumulated molecular damage [70] [72]. The aging microenvironment contributes to a decline in the regenerative potential of endogenous MSC pools, a phenomenon recapitulated in in vitro expansions [72]. Key age-related alterations include:
- Cellular Enlargement and morphological shifts from fibroblastic to epithelial-like shapes.
- Telomere Attrition or p53/p21-mediated accumulation of DNA damage.
- Epigenetic Shifts such as impaired DNA methylation and histone acetylation.
- Oxidative Stress marked by elevated levels of reactive oxygen species (ROS) and nitric oxide (NO) [70].
These hallmarks of aging manifest functionally as reduced proliferative capacity, increased senescence, and diminished multipotency, directly impacting the therapeutic utility of MSCs isolated from older donors [70] [71] [72]. Consequently, donor age is not a mere demographic variable but a fundamental determinant of MSC product quality, necessitating careful consideration in the design and interpretation of preclinical studies and clinical trials.
Table 1: Summary of Age-Related Functional Declines in MSCs from Key Studies
| Study Model | Impact on Proliferation | Impact on Adipogenesis | Impact on Osteogenesis | Impact on Chondrogenesis | Key Findings |
|---|---|---|---|---|---|
| Human & Mouse BM-MSCs [70] | Decreased density and self-renewal with age | Not Specified | Reduced osteogenic potential with age | Not Specified | MSC content and osteogenic potential decrease with organismal aging. |
| Rabbit Model (Multi-Tissue) [71] | Impaired in BM-MSCs; unaffected in MDSCs and ASCs | Reduced in all MSC populations (BM, muscle, adipose) | Unchanged in all populations | Impaired in BM-MSCs; unaffected in MDSCs and ASCs | Aging effects are tissue-source dependent. |
| Bovine AD-MSCs [73] | High capacity in fetal/calf; reduced in adult | Higher in fetal and adult Holstein Friesian | Affected by breed, not by age | Not Specified | Donor age and breed interact to determine differentiation potential. |
Comparative Analysis of Tissue-Source Vulnerability to Aging
The detrimental effects of aging are not uniform across MSCs from different anatomical sources. A direct comparative study in rabbits revealed that Bone Marrow-derived MSCs (BM-MSCs) are the most susceptible to age-related decline, while Adipose-derived Stem Cells (ASCs) and Muscle-derived Stem Cells (MDSCs) demonstrate greater resilience [71].
- Bone Marrow-MSCs (BM-MSCs): Exhibit the most pronounced functional decline with aging, including impaired proliferation, increased senescence, and reduced chondrogenic potential [71]. In humans and mice, the density of MSCs in bone marrow decreases continuously after birth, and aging reduces both their population size and osteogenic capacity [70].
- Adipose-Derived Stem Cells (ASCs): Show notable resistance to aging effects. While age may reduce initial cell yield and adipogenic potential, key expansion properties like proliferation rates and osteogenic capacity can remain largely unaffected [71].
- Muscle-Derived Stem Cells (MDSCs): Similar to ASCs, MDSCs from aged donors can maintain robust proliferative capacity and chondrogenic response, despite a general age-related reduction in adipogenic potential [71].
This tissue-source-dependent vulnerability underscores the potential of ASCs and MDSCs as more reliable cell sources for autologous therapies in older patient populations, a critical consideration for diseases prevalent in aging populations, such as osteoarthritis and osteoporosis [71] [72].
Table 2: Tissue-Source Specific Vulnerabilities to Donor Aging
| Tissue Source | Proliferation & Expansion | Tri-Lineage Differentiation Potential | Key Clinical Implications |
|---|---|---|---|
| Bone Marrow (BM-MSCs) | Severely impaired with age [70] [71] | Osteogenesis: Reduced [70]. Chondrogenesis: Impaired [71]. Adipogenesis: Reduced [71]. | High susceptibility to donor age; less ideal for older patients. |
| Adipose Tissue (ASCs) | Largely unaffected or less impacted [71] | Osteogenesis: Unchanged [71]. Chondrogenesis: Unaffected [71]. Adipogenesis: Reduced [71]. | More reliable for autologous therapies in the aged. |
| Muscle (MDSCs) | Unaffected by age in rabbit model [71] | Osteogenesis: Unchanged [71]. Chondrogenesis: Unaffected [71]. Adipogenesis: Reduced [71]. | Robust source for musculoskeletal applications in elderly. |
| Umbilical Cord (UC-MSCs) | Enhanced proliferation, low immunogenicity [4] | Generally high potential; explicit age-effect data limited due to source. | "Off-the-shelf" product avoiding donor aging effects. |
Experimental Models and Protocols for Assessing Age-Related MSC Decline
1In VitroFunctional Assays
Standardized in vitro assays are crucial for quantifying the functional consequences of donor age on MSCs. Key methodologies include:
- Proliferation and Senescence Assays: Population doublings are tracked over successive passages to assess long-term expansion capability. Senescence is quantified using a β-galactosidase senescence assay, which detects increased activity of the enzyme senescence-associated β-gal (SA-β-gal) in aged cells [73] [71].
- Tri-Lineage Differentiation Assays: Following ISCT guidelines, MSCs are induced toward adipogenic, osteogenic, and chondrogenic fates. Differentiation efficacy is quantified using lineage-specific stains (Oil Red O for adipocytes, Alizarin Red for osteocytes, Alcian Blue for chondrocytes) and spectrophotometry of extracted dyes [73] [71].
- Immunophenotyping by Flow Cytometry: Cell surface marker expression (e.g., CD73, CD90, CD105, CD34) is analyzed using multi-color flow cytometry. This assesses phenotype purity and can reveal shifts associated with age or differentiation potential [73].
Animal Models for Aging Studies
Animal models provide a controlled system to investigate age-related MSC decline while minimizing genetic and environmental variability.
- Rabbit Model: Studies isolate BM-MSCs, MDSCs, and ASCs from the same young and old donors, enabling a direct, paired comparison of how age affects different tissue sources within a single organism [71].
- Bovine Model: Research uses cattle from distinct breeds and defined age categories to systematically dissect the impact of donor age and genetic background on AD-MSC characteristics [73].
- Primate Model: As the physiologically most relevant model for human translation, aged non-human primates are used to evaluate the systemic anti-aging effects of novel, genetically enhanced MSC populations, such as senescence-resistant cells (SRCs) [74].
Diagram 1: Signaling pathways and logical relationships of age-related impacts on MSC function. Donor factors like age, genetics, and tissue source drive molecular hallmarks of aging, which collectively lead to functional declines in proliferation, differentiation, and paracrine activity. The effect of tissue source is modulatory (dashed line).
The Scientist's Toolkit: Key Reagent Solutions for MSC Aging Research
Table 3: Essential Research Reagents for MSC Aging Studies
| Reagent / Solution | Function in Experimental Protocol | Specific Application Example |
|---|---|---|
| Liberase / Collagenase/Dispase | Enzymatic digestion of solid tissues (e.g., adipose, muscle) to isolate stromal vascular fraction containing MSCs. | Isolation of bovine AD-MSCs from subcutaneous fat [73]. |
| β-galactosidase Senescence Assay Kit | Histochemical detection of SA-β-gal activity, a biomarker for senescent cells, at pH 6.0. | Quantifying senescence levels in young vs. old rabbit MSCs [71]. |
| Tri-lineage Differentiation Media | Defined cytokine/growth factor cocktails to induce adipogenic, osteogenic, and chondrogenic differentiation. | Assessing age-related changes in multipotency per ISCT criteria [73] [71]. |
| Flow Cytometry Antibody Panels | Immunophenotyping to confirm MSC identity (CD73, CD90, CD105) and assess heterogeneity/variation (e.g., CD34). | Characterizing bovine MSC surface markers and donor/breed effects [73]. |
| FOXO3 Plasmid / Lentivirus | Genetic engineering tool to overexpress the geroprotective transcription factor FOXO3. | Generating senescence-resistant human MPCs (SRCs) for anti-aging studies [74]. |
Strategic Sourcing Recommendations and Future Directions
The evidence clearly indicates that strategic sourcing of MSCs must account for donor age to ensure product quality and experimental reproducibility. For autologous therapies targeting age-prevalent diseases, ASCs represent a more robust source due to their relative resistance to age-related functional decline compared to BM-MSCs [71]. For allogeneic "off-the-shelf" bioproducts, young donor sources such as Umbilical Cord MSCs (UC-MSCs) or perinatal tissues should be prioritized to circumvent the intrinsic aging of MSCs from adult donors [4].
Future strategies are evolving beyond donor selection to actively combat cellular aging:
- Genetic Engineering: The development of senescence-resistant cells (SRCs) by enhancing geroprotective pathways (e.g., FOXO3 overexpression) demonstrates the potential to create potent, standardized MSC products with enhanced resilience for treating age-related conditions [74].
- Cell-Free Approaches: Given the central role of paracrine secretion in MSC therapy, extracellular vesicles (EVs) and exosomes derived from MSCs are emerging as a critical, cell-free alternative. These nanovesicles can be produced from consistent, master cell banks (e.g., using iPSC-derived MSCs), mitigating issues of donor heterogeneity and age-related functional decline inherent in live-cell products [75].
In conclusion, acknowledging and systematically addressing donor heterogeneity and age-related decline is not a limitation but an opportunity to refine MSC-based therapeutic strategies. By integrating source-specific vulnerability profiles, standardized functional assessments, and innovative engineering approaches, the field can progress toward more predictable and effective clinical applications.
Mesenchymal stem cells (MSCs) are multipotent progenitor cells recognized for their intrinsic ability to home to sites of injury and inflammation, where they contribute to tissue maintenance and repair [76]. This same tropism, however, extends to developing tumors, drawing MSCs into the tumor microenvironment (TME) and placing them at the center of a significant scientific debate regarding their dual role in cancer pathogenesis [77]. Within the TME, MSCs demonstrate remarkable functional plasticity, capable of exerting both pro-tumorigenic and anti-tumorigenic effects [78]. This paradoxical nature positions MSCs as a critical but complex component of the tumor stroma, influencing cancer initiation, progression, metastasis, and therapeutic response [79] [78]. The ultimate function of MSCs appears to be dictated by a complex interplay of factors, including the specific context of the TME, the signals received from cancer cells, and the tissue source of the MSCs themselves [79]. This comparative guide objectively analyzes the experimental evidence for both sides of this dichotomy, providing researchers with a structured overview of the mechanisms, experimental data, and emerging therapeutic applications of MSCs in oncology.
Comparative Analysis of MSC Mechanisms in Cancer
The following tables synthesize quantitative and mechanistic data from key studies, illustrating the dual role of MSCs in cancer biology.
Table 1: Protumorigenic Mechanisms and Supporting Experimental Evidence of MSCs
| Mechanism | Experimental Models/Cell Lines | Key Findings/Effector Molecules | References |
|---|---|---|---|
| Immune Suppression | Breast cancer, Melanoma, Leukemia models | Suppression of T-cell proliferation & DC maturation via PGE2, IDO; Induction of T-regs; Polarization of macrophages to M2 phenotype. | [77] [78] |
| Promotion of Angiogenesis | Colorectal cancer xenografts, Breast and Prostate cancer models | Increased secretion of VEGF, IL-6, MIP-2, TGF-β; Enhanced vessel formation. | [79] [78] |
| Enhancement of Metastasis | Breast carcinoma, Melanoma models | Increased cancer cell motility and invasion; Facilitation of metastatic niche formation. | [76] |
| Chemoresistance | CML (K562, BV173 cells), AML (OCI-AML3 cells) | Protection from drug-induced apoptosis via IL-7 upregulation, Bcl-xL expression, and CXCL12/CXCR4 interaction. | [77] |
Table 2: Antitumorigenic Mechanisms and Supporting Experimental Evidence of MSCs
| Mechanism | Experimental Models/Cell Lines | Key Findings/Effector Molecules | References |
|---|---|---|---|
| Growth Inhibition | Leukemia (FBL3, P388, A20), CML (K562, BV173) | Induction of cell cycle arrest in G1 phase; Secretion of DKK-1; Activation of p38 MAPK pathway. | [77] |
| Anti-Angiogenesis | Breast cancer animal models | miR-16-mediated downregulation of VEGF via MSC-derived exosomes. | [79] |
| Pro-Apoptotic Signaling | Various cancer models (via TLR4 priming) | Polarization to MSC1 phenotype; Production of TRAIL, IL-17, GM-CSF. | [78] |
| Drug Delivery Vehicle | Pancreatic & Hepatocellular carcinoma models | Delivery of suicide genes (e.g., HSV-TK); Targeted release of oncolytic viruses. | [80] |
Experimental Protocols for Key Investigations
To ensure reproducibility and provide a clear technical framework, this section outlines standard methodologies used to generate the data cited in this guide.
Co-culture Assays for Assessing MSC-Cancer Cell Interactions
Objective: To investigate the paracrine effects of MSCs on cancer cell proliferation, apoptosis, and drug resistance in vitro.
- Cell Preparation: Isplicate and expand MSCs from a chosen source (e.g., Bone Marrow, Umbilical Cord). Culture the target cancer cell line (e.g., K562 for CML).
- Experimental Setup: Use Transwell systems or direct contact co-culture. A common MSC-to-tumor cell ratio is 1:10, though ratios from 1:1 to 1:100 are used for dose-response studies [77].
- Analysis:
- Proliferation: Perform MTT or CCK-8 assays at 24, 48, and 72 hours.
- Cell Cycle: Use flow cytometry with propidium iodide staining after 48 hours of co-culture.
- Apoptosis: Employ Annexin V/PI staining followed by flow cytometry, with or without chemotherapeutic agents (e.g., Imatinib).
- Mechanistic Investigation: Analyze conditioned media via ELISA for cytokines (e.g., IL-7, PGE2). Use Western Blot to examine apoptosis-related proteins (e.g., Bcl-xL, cleaved caspase-3) [77].
2In VivoTumor Homing and Progression Studies
Objective: To validate the tumor-tropic property of MSCs and their impact on tumor growth and metastasis in vivo.
- Animal Model: Establish immunodeficient mouse models (e.g., NOD/SCID) subcutaneously or orthotopically with human cancer cells.
- MSC Tracking: Label MSCs with a reporter gene (e.g., GFP, Luciferase) or a fluorescent dye (e.g., DiR).
- Administration: Systemically administer labeled MSCs (e.g., via intravenous or intra-arterial injection) once tumors are palpable.
- Imaging and Analysis: Track MSC homing using in vivo bioluminescent or fluorescence imaging over days to weeks. Monitor primary tumor volume with calipers and metastatic burden via imaging or histology of distant organs at endpoint [76] [80].
Signaling Pathways Governing MSC Polarization
The functional plasticity of MSCs is often determined by specific signaling pathways activated by the TME. The diagram below illustrates the key signaling that drives MSCs toward a pro-tumorigenic (MSC2) or anti-tumorigenic (MSC1) phenotype.
Therapeutic Application: MSCs as Drug Delivery Vectors
The inherent tumor-homing capability of MSCs makes them promising vehicles for targeted delivery of anticancer agents. The following workflow outlines the development and application of engineered MSCs for therapy.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating MSCs in Cancer Biology
| Reagent/Cell Type | Function/Application in Research | Specific Examples |
|---|---|---|
| Human MSC Markers | Identification and isolation of MSCs via flow cytometry or immunofluorescence. | CD105+, CD90+, CD73+, CD44+; CD45-, CD34-, CD14-, HLA-DR- [76] [78]. |
| Cancer Cell Lines | In vitro co-culture studies to assess MSC-tumor cell interactions. | K562 (CML), HL-60 (AML), Jurkat (T-ALL), MCF-7 (Breast Cancer) [77]. |
| Cytokine/Antibody Arrays | Profiling of soluble factors secreted by MSCs in the TME. | Detection of PGE2, IDO, VEGF, IL-6, TGF-β, CCL2 [77] [78]. |
| TLR Agonists | Polarization of MSCs into pro- or anti-tumorigenic phenotypes. | LPS (TLR4 agonist) for MSC1; Poly(I:C) (TLR3 agonist) for MSC2 [78]. |
| Reporter Genes | Tracking MSC migration, homing, and persistence in vivo. | GFP, Luciferase for bioluminescent imaging [80]. |
The therapeutic paradigm in regenerative medicine is shifting from whole-cell transplantation towards cell-free therapies utilizing secretions from Mesenchymal Stem Cells (MSCs). These secretions, collectively known as the secretome, include conditioned media (CM) containing soluble factors and extracellular vesicles (EVs) such as exosomes, which mediate therapeutic effects through paracrine signaling [81] [82]. This approach eliminates risks associated with live-cell transplantation, including immunogenicity and tumorigenicity, while offering superior scalability and storage capabilities [83] [82]. However, the transformative potential of secretome-based therapeutics is constrained by a critical challenge: the lack of standardized methodologies for its production, isolation, and characterization [84] [81] [83]. This comparative guide examines the impact of MSC tissue origins on secretome composition and function, providing researchers with experimental protocols and analytical frameworks to advance the standardization of these complex biologics for targeted applications.
Experimental Protocols for Secretome Production and Characterization
Standardized Production of Conditioned Media
The foundation of reproducible secretome research begins with standardized CM production. The following protocol, synthesized from current methodologies, ensures consistent collection of secretory factors while minimizing contamination [81] [83]:
- Pre-collection Culture Conditions: Culture MSCs in a standard growth medium until 80% confluence. To eliminate interference from serum proteins, thoroughly wash cells with phosphate-buffered saline (PBS) and subsequently culture in a serum-free basal medium for 24-48 hours [81] [83].
- Conditioned Media Collection: Collect the CM and perform sequential centrifugation to remove cellular debris: first at 450 × g for 5 minutes, then at 2,000 × g for 10 minutes [84].
- Processing and Storage: Concentrate the supernatant using ultrafiltration (e.g., 3 kDa cutoff filters) or lyophilization. Aliquot and store at -80°C to preserve bioactive component integrity [83].
Isolation of Extracellular Vesicles
EV isolation requires precise techniques to separate vesicles from soluble proteins and other contaminants. The following comparative methodologies are currently employed:
Table 1: Extracellular Vesicle Isolation Techniques
| Method | Principle | Advantages | Limitations |
|---|---|---|---|
| Ultracentrifugation | Sequential centrifugal forces to pellet EVs | Considered gold standard; no chemical contaminants [84] | Time-consuming; may cause vesicle damage/aggregation [83] |
| Size Exclusion Chromatography | Separates particles by size through porous matrix | High purity; preserves vesicle integrity and function [84] | Sample dilution; limited sample volume [83] |
| Tangential Flow Filtration | Uses parallel flow across membranes to separate by size | Suitable for large-volume processing; scalable for GMP [83] [82] | Membrane fouling; requires specialized equipment [83] |
| Precipitation-Based Kits | Polymers reduce EV solubility for precipitation | Simple protocol; minimal equipment needs [83] | Co-precipitation of contaminants (e.g., proteins) [84] |
Comprehensive Characterization Workflow
Rigorous characterization is essential for qualifying secretome preparations. The following integrated workflow combines orthogonal techniques to assess key physical and biochemical parameters:
Characterization Workflow for Secretome Analysis
Physical Characterization: Employ Nanoparticle Tracking Analysis (NTA) to determine particle size distribution and concentration, though note its limitation in detecting vesicles <50 nm [84]. Use Transmission Electron Microscopy (TEM) to confirm classic cup-shaped EV morphology and membrane integrity [84]. Dynamic Light Scattering (DLS) provides complementary hydrodynamic size measurements [84].
Biochemical Characterization: Quantify total protein content using BCA or Bradford assays, but interpret results cautiously as they cannot distinguish vesicular proteins from contaminants [84]. Assess sample purity via High-Performance Liquid Chromatography-Size Exclusion Chromatography (HPLC-SEC), which effectively separates EVs from soluble proteins [84]. Confirm presence of EV-specific markers (CD9, CD63, CD81, TSG101, Alix) via western blot or flow cytometry [84].
Functional Characterization: Evaluate bioactivity through cell-based assays relevant to target applications. For neuroregeneration, assess neurite outgrowth in dorsal root ganglion neurons [85]. For immunomodulation, measure suppression of peripheral blood mononuclear cell proliferation [85]. For angiogenesis, implement tube formation assays with human umbilical vein endothelial cells [82].
Impact of MSC Tissue Source on Secretome Composition
The tissue origin of MSCs significantly influences their secretory profile, creating unique molecular signatures that determine therapeutic suitability for specific applications. Understanding these source-dependent variations is essential for matching secretome products to clinical indications.
Table 2: MSC Tissue Source Impact on Secretome Composition and Function
| MSC Source | Key Secretome Components | Functional Strengths | Optimal Applications |
|---|---|---|---|
| Bone Marrow (BM-MSC) | Lower levels of neurotrophic factors; Higher immunomodulatory content [85] | Superior immunomodulation; Highest suppression of immune cell proliferation [85] | Autoimmune diseases; Graft-versus-host disease [85] [86] |
| Adipose Tissue (AT-MSC) | Wider range of angiogenic factors; Distinct exosome composition [83] | Strong pro-angiogenic potential; Enhanced tissue vascularization [83] | Ischemic conditions; Wound healing [83] |
| Wharton's Jelly (WJ-MSC) | Higher levels of neurotrophic factors; Enhanced protective molecules [85] [82] | Potent neuroregeneration; Immune-privileged phenotype; High proliferative capacity [85] [82] | Neonatal disorders (BPD, NEC); Neural repair [82] |
Comparative analysis reveals that BM-MSCs demonstrate significantly higher immunomodulatory capacity, suppressing phytohaemagglutinin-induced PBMC proliferation by 90% at 10:1 (PBMC:MSC) ratio in contact co-culture, whereas AT-MSCs and WJ-MSCs showed reduced suppression at higher ratios [85]. Conversely, WJ-MSCs secrete significantly higher levels of neurotrophic factors that stimulate neurite outgrowth in DRG neurons and reduce cell death in neural stem/progenitor cells after oxidative stress challenge [85].
Critical Signaling Pathways in Secretome-Mediated Effects
Secretome components activate conserved signaling pathways that drive functional outcomes in target tissues. Understanding these mechanistic pathways enables rational design of secretome-based therapeutics.
Signaling Pathways Activated by MSC Secretome
The therapeutic effects of MSC secretomes are mediated through specific molecular pathways:
Anti-inflammatory Signaling: Secreted factors including TNF-α-stimulated gene/protein 6 (TSG-6), interleukin-10 (IL-10), and heme oxygenase-1 (HO-1) drive macrophage polarization from pro-inflammatory M1 to anti-inflammatory M2 phenotypes and suppress NF-κB signaling, thereby resolving inflammation in conditions like bronchopulmonary dysplasia (BPD) and necrotizing enterocolitis (NEC) [82].
Angiogenic Activation: Vascular endothelial growth factor (VEGF), hepatocyte growth factor (HGF), and basic fibroblast growth factor (bFGF) activate VEGFR2 and downstream ERK signaling pathways, promoting endothelial cell proliferation and new blood vessel formation critical for tissue repair after ischemic injury [82].
Regenerative Pathways: Insulin-like growth factor-1 (IGF-1), transforming growth factor-β (TGF-β), and bFGF activate the Wnt/β-catenin pathway in dermal fibroblasts, stimulating collagen synthesis and tissue remodeling, enhancing skin elasticity by 27.07% and improving hydration by over 20% in clinical studies [87].
The Scientist's Toolkit: Essential Research Reagents
Standardized reagents and methodologies are crucial for generating reproducible secretome data. The following toolkit outlines essential materials and their applications in secretome research:
Table 3: Essential Research Reagents for Secretome Studies
| Reagent/Category | Specific Examples | Research Application | Considerations |
|---|---|---|---|
| Cell Culture Media | DMEM-F12, α-MEM, serum-free alternatives [84] [85] | MSC expansion and secretome production | Human platelet lysate preferred over FBS for clinical-grade production [85] |
| Separation Technologies | Ultracentrifugation, HPLC-SEC, TFF systems [84] [83] | EV isolation and purification | HPLC-SEC provides superior purity assessment [84] |
| Characterization Instruments | NTA (Nanosight), TEM, DLS (Zetasizer) [84] | Physical characterization of EVs | NTA limitations for particles <50nm [84] |
| Protein Analysis | BCA/Bradford assays, western blot reagents [84] | Biochemical characterization | Cannot distinguish vesicular from contaminating proteins [84] |
| Proteomic Tools | Antibody arrays, LC-MS/MS, RNA-seq [88] [89] | Comprehensive secretome profiling | Identifies novel secreted factors and tissue-specific signatures [88] |
The comparative analysis presented in this guide underscores a fundamental principle: MSC tissue origin dictates secretome composition and functional potency, enabling matching of specific secretome sources to clinical applications. However, translational progress remains hampered by methodological heterogeneity in secretome production, isolation, and characterization. Future standardization efforts must prioritize several key areas: establishing reference materials for cross-study comparisons, implementing orthogonal characterization methods to fully capture secretome complexity, developing potency assays that reliably predict in vivo efficacy, and creating computational frameworks for integrating multi-omics secretome data. As the field progresses toward clinical application, standardized approaches to secretome characterization will be essential for realizing the full potential of these sophisticated biologics in regenerative medicine, enabling reproducible, efficacious, and safe cell-free therapies across diverse medical applications.
The therapeutic efficacy of Mesenchymal Stem Cell (MSC)-based therapies is profoundly influenced by the chosen route of administration. For researchers and drug development professionals, the decision between systemic intravenous delivery and targeted local injection represents a critical juncture, balancing factors such as cell viability, systemic exposure, and targeted engraftment. Complicating this decision is the pulmonary first-pass effect, a physiological phenomenon where intravenously infused cells or therapeutics are initially sequestered in the lung capillaries before reaching the systemic circulation [90] [91]. This effect can significantly reduce the number of cells delivered to the intended target site, presenting a major hurdle for systemic administration.
This guide provides a comparative analysis of intravenous (IV) and local injection routes, with a specific focus on how the pulmonary first-pass effect impacts MSC delivery. We will summarize quantitative data from key studies, detail relevant experimental protocols, and visualize critical pathways to inform the design of pre-clinical and clinical studies for targeted applications.
Core Concepts: The Pulmonary First-Pass Effect
The first-pass effect is a pharmacological phenomenon where a medication undergoes metabolism at a specific location in the body before it reaches the systemic circulation or its site of action [90]. While traditionally associated with hepatic metabolism of orally administered drugs, a similar effect occurs in the lungs for intravenously delivered MSCs and MSC-derived Extracellular Vesicles (MSC-EVs).
Intravenously administered MSCs and MSC-EVs naturally accumulate in pulmonary tissues due to the lung’s extensive capillary network, which acts as a primary filter [92] [91]. This pulmonary first-pass filtration can sequester a significant portion of the administered dose, limiting the quantity that reaches other target organs. The biological outcome is a decrease in the active therapeutic concentration arriving at the intended site of action, which can necessitate higher initial IV dosing to achieve a therapeutic effect in non-pulmonary tissues [90].
Visualizing the Pulmonary First-Pass Effect for Intravenous Injections
The following diagram illustrates the journey of intravenously administered MSCs, highlighting the critical point of pulmonary sequestration.
Comparative Analysis: Intravenous vs. Local Injection
The choice between intravenous and local injection involves a trade-off between broad systemic distribution and high local concentration. The data below objectively compares these routes across critical parameters.
Table 1: Comparative Analysis of Intravenous vs. Local Injection Routes
| Parameter | Intravenous (IV) Injection | Local Injection (e.g., Intramuscular, Intra-articular) |
|---|---|---|
| Bioavailability at Target Site | Variable; significantly limited for non-pulmonary sites by the pulmonary first-pass effect [90] [91] | High for local targets; directly bypasses systemic circulation barriers [93] |
| Pulmonary First-Pass Effect | High; major sequestration in lung capillaries [91] | Negligible; not applicable for non-pulmonary delivery [93] |
| Systemic Exposure | Widespread; ideal for treating systemic or multi-organ conditions | Low; minimal exposure outside the local administration site |
| Therapeutic Dose Required | Often higher to compensate for pulmonary sequestration and distribution [90] [92] | Lower; direct application maximizes local dose efficiency |
| Technical Complexity | Low; standard infusion procedure | Higher; often requires imaging guidance for precision |
| Risk of Off-Target Effects | Potentially higher due to systemic distribution | Lower, confined primarily to the administration area |
| Ideal Application Context | Systemic inflammatory diseases, GVHD, multi-organ repair [94] [4] | Focal diseases, joint repair, localized wounds, direct organ injection [32] |
Table 2: Quantitative Comparison of MSC-EV Dosing by Route (Clinical Trial Data Summary) [92]
| Administration Route | Typical Effective Dose (Particles) | Key Rationale and Context |
|---|---|---|
| Intravenous Infusion | Higher doses required (e.g., >10^9 particles) | Compensates for distribution throughout the body and dilution in systemic circulation |
| Aerosolized Inhalation (Nebulization) | Lower doses effective (e.g., ~10^8 particles) | Delivers therapy directly to lung tissue, bypassing systemic filtration and minimizing loss |
Experimental Data and Protocols
Key Experimental Findings
Recent studies highlight the practical implications of the delivery route. A comprehensive review of global clinical trials for MSC-EVs found that aerosolized inhalation, a form of local pulmonary delivery, achieved therapeutic effects at doses around 10^8 particles, which was significantly lower than the doses required for the intravenous route [92]. This underscores the superior bioavailability of locally delivered therapies for lung diseases, as they avoid the dilution and sequestration inherent in IV administration.
In preclinical models, the benefit of bypassing the first-pass effect is clear. For instance, rectally administered diazepam in children with febrile seizures ensures a rapid onset of action by significantly bypassing first-pass metabolism [90]. This principle directly translates to MSC therapies, where local delivery strategies can enhance engraftment and efficacy at the target site.
Detailed Experimental Protocol: Tracking MSC Biodistribution
A critical experiment for evaluating delivery route efficiency is the quantitative assessment of cell biodistribution.
Aim: To compare the trafficking and final localization of MSCs administered via intravenous versus local injection routes. Methodology:
- Cell Labeling: MSCs are labeled with a fluorescent marker (e.g., DiR dye for in vivo imaging) or a bioluminescent marker (e.g., luciferase for bioluminescence imaging).
- Animal Model: A validated disease model (e.g., a rat model of myocardial infarction, limb ischemia, or lung injury) is used.
- Administration:
- IV Group: MSCs are injected via the tail vein.
- Local Group: MSCs are injected directly into the target tissue (e.g., myocardium, muscle, or joint space).
- In Vivo Imaging: At predetermined time points (e.g., 1 hour, 24 hours, 7 days post-injection), animals are imaged using an IVIS spectrum or similar in vivo imaging system. For luciferase-labeled cells, luciferin substrate is injected beforehand.
- Ex Vivo Analysis: At the endpoint, major organs (lungs, liver, spleen, kidneys, heart, and the target organ) are harvested and imaged ex vivo to quantify signal intensity. This step is crucial for confirming the visual data from in vivo imaging.
- Data Quantification: The fluorescent or bioluminescent signal in each organ is quantified as Total Flux (photons/second) or Radiant Efficiency. This data is used to calculate the percentage of the administered dose retained in each organ.
Expected Outcome: The IV group will show a strong initial signal in the lungs, demonstrating the pulmonary first-pass effect, which diminishes over time with subsequent signal appearing in the liver and spleen. The local injection group will show a strong, persistent signal specifically at the target site, with minimal signal in other organs.
Visualizing the Experimental Workflow for Biodistribution Studies
The flowchart below outlines the key steps in the protocol for comparing delivery routes.
The Scientist's Toolkit: Essential Research Reagents
Successful execution of delivery route optimization studies requires a suite of reliable reagents and tools.
Table 3: Key Research Reagent Solutions for Delivery Studies
| Reagent / Tool | Function in Experiment | Key Considerations |
|---|---|---|
| Lipophilic Tracers (e.g., DiD, DiR) | Fluorescently labels cell membranes for in vivo and ex vivo tracking. | Stable for short-term tracking; may dilute with cell division. |
| Lentiviral Vectors for Luciferase | Genetically engineers MSCs to stably express luciferase for highly sensitive bioluminescence imaging. | Enables long-term tracking; requires biosafety containment. |
| In Vivo Imaging System (IVIS) | Non-invasively quantifies the spatial and temporal distribution of labeled cells in live animals. | Essential for longitudinal studies within the same subject. |
| Nanoparticle Tracking Analysis (NTA) | Characterizes the size and concentration of MSC-EVs prior to administration in dosing studies. | Critical for standardizing EV-based therapeutic doses [92]. |
| Ultracentrifugation System | Isolates and purifies MSC-EVs from conditioned cell culture media. | The current gold-standard method for EV isolation, though lacking full standardization [92] [95]. |
| Flow Cytometry Antibodies (CD73, CD90, CD105, CD45, CD34) | Verifies MSC phenotype and purity according to ISCT criteria before injection [4] [32]. | Ensures that the administered population meets minimal defining standards. |
The comparative analysis unequivocally demonstrates that there is no single optimal delivery route for all MSC applications. The decision is inherently context-dependent. Intravenous injection offers a solution for systemic conditions but is hampered by the pulmonary first-pass effect, which reduces efficiency for non-pulmonary targets. In contrast, local injection provides superior target site bioavailability and is the logical choice for focal diseases, effectively bypassing systemic clearance mechanisms.
Future research must focus on standardizing protocols and developing novel engineering strategies to enhance the efficacy of both routes. For IV delivery, this includes modifying cells or EVs to evade pulmonary entrapment. For local delivery, improving retention and survival at the implantation site is paramount. By aligning the delivery strategy with the specific pathophysiology of the target disease, researchers can unlock the full therapeutic potential of MSC-based therapies.
Mesenchymal stromal cells (MSCs) have emerged as a highly promising therapeutic tool in regenerative medicine and immunotherapy due to their multipotent differentiation capacity, immunomodulatory properties, and paracrine effects [4]. However, the transition from promising preclinical results to consistent clinical efficacy has faced significant challenges, with many clinical trials failing to meet their primary endpoints despite demonstrating excellent safety profiles [32] [96]. A fundamental issue complicating MSC therapy development is substantial heterogeneity—variation exists among donors, among tissue sources, and even within individual cell populations [97]. This heterogeneity manifests in differences in differentiation potential, immunomodulatory capacity, gene expression profiles, and ultimately, therapeutic efficacy [98] [97].
The development of reliable potency assays—standardized quality control tests that predict a product's biological activity—represents one of the most critical challenges in the field of advanced therapy medicinal products (ATMPs) [99]. For cell-based therapies like MSCs, potency assays are essential not only for batch release and quality control under Good Manufacturing Practice (GMP) standards but also as potential biomarkers for predicting in vivo therapeutic efficacy [99]. Without such assays, the functional quality and consistency of MSC products cannot be guaranteed, leading to unpredictable clinical outcomes [32] [99]. This guide provides a comparative analysis of current approaches to MSC potency testing, with a specific focus on how tissue origin influences therapeutic properties and the implications for assay development.
MSCs can be isolated from multiple tissue sources, each with distinct biological characteristics and therapeutic advantages. Understanding these differences is essential for developing tissue-specific potency assays and selecting the optimal MSC source for particular clinical applications [100].
Table 1: Comparative Analysis of MSC Tissue Sources and Their Therapeutic Properties
| Tissue Source | Key Advantages | Documented Therapeutic Strengths | Limitations & Safety Considerations |
|---|---|---|---|
| Bone Marrow (BM-MSCs) | Most extensively studied; considered "gold standard" [100] | Strong immunomodulation; effective T-cell inhibition [101] | Invasive collection procedure; decline in cell quality with donor age [97] [100] |
| Adipose Tissue (AD-MSCs/ASCs) | Easily harvested via liposuction; high cell yield [4] [102] | Powerful immunomodulation comparable to BM-MSCs; anti-fibrotic effects [101] [102] | Pro-coagulant activity observed in some studies [101] |
| Umbilical Cord (UC-MSCs) | Non-invasive collection; enhanced proliferation capacity [100] [4] | Superior pro-angiogenic activity; promotes tube formation [98] | Lower inhibition of lymphocyte proliferation than BM-MSCs; pro-coagulant activity [98] [101] |
| Placenta & Amnion (P-MSCs/A-MSCs) | Fetal origin; expression of pluripotency genes [100] | Support hematopoietic stem cell expansion [100] | Limited adipogenic differentiation capacity [100] |
Beyond source-dependent variation, MSCs exhibit significant functional heterogeneity even within the same tissue source. Research has demonstrated that superficial and deep layer adipose-derived MSCs (Sup-ASCs and Deep-ASCs) show differences in proliferation and adipogenic differentiation despite similar anti-fibrotic efficacy in renal ischemia-reperfusion injury models [102]. This highlights the complex nature of MSC biology and the challenge of defining robust potency markers that remain predictive across different tissue sources and subpopulations.
Experimental Approaches for Assessing MSC Potency
In Vitro Functional Assays
A comprehensive approach to MSC potency testing requires multiple complementary assays that evaluate different aspects of cellular function. The International Society for Cellular Therapy (ISCT) has established minimal criteria for defining MSCs, including plastic adherence, specific surface marker expression (CD73, CD90, CD105), and lack of hematopoietic markers (CD34, CD45, CD14, CD19, HLA-DR), and trilineage differentiation capacity [4] [103]. However, these criteria alone are insufficient for predicting therapeutic efficacy, necessitating more sophisticated functional assays [99].
Table 2: Key Methodologies for Assessing MSC Potency and Functional Properties
| Assay Category | Specific Methods | Measured Parameters | Relevance to Therapeutic Mechanism |
|---|---|---|---|
| Immunomodulatory Capacity | Mixed lymphocyte reaction (MLR) [101]; T-cell proliferation suppression [101] | Inhibition of lymphocyte proliferation; Treg/Th17 ratio [101] | Predicts efficacy for GVHD, autoimmune diseases [101] |
| Paracrine Factor Secretion | ELISA; multiplex immunoassays [98] [102] | VEGF, HGF, PGE2, IDO, TGF-β quantification [98] [102] | Correlates with angiogenic, anti-fibrotic, anti-inflammatory effects [98] |
| Angiogenic Potential | Tube formation assay [98]; Matrigel plug assay [98] | Tubule length, junctions, nodes; vascularization in vivo [98] | Predicts efficacy for ischemic conditions (MI, stroke) [98] |
| Anti-fibrotic Activity | TGF-β/Smad signaling inhibition [102]; fibrosis models [102] | p-Smad2, α-SMA expression; collagen deposition [102] | Predicts efficacy for fibrotic diseases (renal, pulmonary, hepatic) [102] |
| Transcriptomic Analysis | RNA sequencing [98] [102]; pathway enrichment [98] | Gene expression profiles; pathway activation (angiogenesis, apoptosis) [98] | Identifies molecular mechanisms; discovers biomarker candidates [98] |
Detailed Experimental Protocols
T-cell Suppression Assay (Mixed Lymphocyte Reaction)
This widely used immunomodulatory potency assay evaluates the ability of MSCs to suppress immune cell activation [101]:
- Lymphocyte Isolation: Isolate peripheral blood mononuclear cells (PBMCs) from healthy donors by density gradient centrifugation.
- Stimulator Cell Preparation: Irradiate (30-50 Gy) or treat with mitomycin C (25-50 µg/mL for 30 minutes) allogeneic PBMCs or specific cell lines (e.g., PHA-blasts) to prevent proliferation.
- Co-culture Setup: Seed responder PBMCs (1×10^5 cells/well) with stimulator cells (1×10^5 cells/well) at a 1:1 ratio in 96-well U-bottom plates.
- MSC Addition: Add test MSCs at varying ratios (typically 1:10 to 1:100 MSC:PBMC) to the co-culture.
- Culture Conditions: Maintain cells in RPMI-1640 with 10% FBS for 5-7 days at 37°C, 5% CO₂.
- Proliferation Measurement: Add ³H-thymidine (0.5-1 µCi/well) for the final 16-18 hours of culture, then measure incorporated radioactivity using a beta counter. Alternative non-radioactive methods include CFSE dilution or WST-1 assays.
- Data Analysis: Calculate percentage suppression relative to positive control (PBMCs alone without MSCs).
Tube Formation Assay for Angiogenic Potential
This assay evaluates the pro-angiogenic capacity of MSCs through their paracrine effects on endothelial cells [98]:
- Matrigel Coating: Thaw Growth Factor Reduced Matrigel at 4°C overnight. Pipette 50 µL/well into pre-chilled 96-well plates and polymerize for 1 hour at 37°C.
- Conditioned Medium Preparation: Culture MSCs until 80% confluence, then replace with serum-free medium for 24-48 hours. Collect conditioned medium and centrifuge at 2000× g for 10 minutes to remove debris.
- Endothelial Cell Seeding: Harvest human umbilical vein endothelial cells (HUVECs) and resuspend in conditioned medium at 2×10^4 cells/mL. Seed 100 µL/well onto polymerized Matrigel.
- Incubation and Imaging: Incubate plates at 37°C, 5% CO₂ for 4-8 hours. Capture images at 4× magnification using an inverted microscope at multiple random fields.
- Quantitative Analysis: Analyze images with ImageJ software with angiogenesis plugin. Measure total tube length, number of nodes, junctions, and meshes per field.
RNA Sequencing for Comprehensive Potency Profiling
Transcriptomic analysis provides a comprehensive view of MSC functional potential [98] [102]:
- RNA Extraction: Isolate total RNA using silica membrane-based kits with DNase I treatment. Assess RNA quality (RIN > 8.0) and quantity using Bioanalyzer or TapeStation.
- Library Preparation: Use poly-A selection for mRNA enrichment or ribosomal RNA depletion. Fragment RNA, synthesize cDNA, and add platform-specific adapters.
- Sequencing: Perform high-throughput sequencing on Illumina platforms (minimum 30 million paired-end 150 bp reads per sample).
- Bioinformatic Analysis:
- Quality control with FastQC and adapter trimming.
- Alignment to reference genome (e.g., GRCh38) using STAR aligner.
- Quantify gene expression with featureCounts.
- Differential expression analysis with DESeq2 (fold change > 2, FDR < 0.05).
- Pathway enrichment analysis using KEGG, GO, and GSEA.
Signaling Pathways in MSC Therapeutic Mechanisms
The therapeutic effects of MSCs are mediated through multiple interconnected signaling pathways that modulate immune responses, promote tissue repair, and enhance cell survival. Understanding these pathways provides the scientific foundation for developing mechanism-based potency assays.
Diagram 1: Key signaling pathways mediating MSC therapeutic effects. The diagram illustrates how external stimuli (blue) trigger MSC responses (green) that lead to therapeutic outcomes (red) through specific signaling pathways (yellow).
Experimental Workflow for Comprehensive Potency Assessment
A systematic approach to potency testing integrates multiple assays to build a comprehensive picture of MSC functional capacity. The following workflow outlines the key steps in characterizing MSC potency from initial isolation to final product release.
Diagram 2: Comprehensive workflow for MSC potency assessment. The tiered approach progresses from basic characterization to advanced profiling and predictive modeling, enabling the development of robust potency signatures for product release.
The Scientist's Toolkit: Essential Research Reagent Solutions
The development and implementation of reliable potency assays requires specific research tools and reagents that enable accurate assessment of MSC functional properties. The following table details essential solutions for establishing comprehensive potency testing protocols.
Table 3: Essential Research Reagents for MSC Potency Assay Development
| Reagent Category | Specific Examples | Application in Potency Testing | Key Functional Assessment |
|---|---|---|---|
| Cell Culture Media | DMEM/F12 with 10% FBS; serum-free MSC media [98] [102] | Basic cell expansion; conditioned medium collection [98] | Proliferation capacity; paracrine factor production |
| Flow Cytometry Antibodies | CD73, CD90, CD105 (positive); CD34, CD45, HLA-DR (negative) [4] [102] | Surface marker characterization; purity assessment | Identity confirmation; contamination exclusion |
| Differentiation Kits | Adipogenic (Oil Red O); Osteogenic (Alizarin Red); Chondrogenic (Alcian Blue) [4] [102] | Trilineage differentiation capacity | Multipotency assessment; functional differentiation |
| ELISA Kits | VEGF, HGF, PGE2, TGF-β, IDO quantification [98] [102] | Secreted factor measurement in conditioned medium | Paracrine function; immunomodulatory potential |
| Extracellular Matrix | Growth Factor Reduced Matrigel [98] | Tube formation assays; cell migration studies | Angiogenic potential; microenvironment interaction |
| qPCR Reagents | Primers for angiogenesis (VEGF, Ang1); immunomodulation (IDO, TGF-β); apoptosis (Bcl-2, Bax) [98] | Gene expression profiling; pathway analysis | Molecular mechanisms; biomarker identification |
| Cell Tracking Dyes | CFSE, PKH26, CM-Dil [99] | Cell proliferation monitoring; migration tracking | In vivo persistence; biodistribution studies |
Current Challenges and Future Perspectives
Despite significant advances in MSC potency assay development, several challenges remain. The functional heterogeneity of MSCs across tissue sources and donors continues to complicate the establishment of universal potency standards [97]. Furthermore, the disconnect between in vitro potency measures and in vivo efficacy represents a significant hurdle in clinical translation [32] [99]. Most current potency assays focus on individual mechanisms, while MSC therapeutics likely function through multiple simultaneous pathways whose relative importance may vary depending on the specific clinical application [98] [4].
Future directions in potency assay development include the implementation of multi-omic approaches that integrate transcriptomic, proteomic, and secretome data to create comprehensive potency signatures [98] [102]. The development of application-specific potency assays that reflect the relevant mechanisms of action for particular clinical indications represents another critical advancement [99]. For instance, angiogenic potential may be prioritized for cardiovascular applications, while immunomodulatory capacity is essential for GvHD treatment [98] [101]. Additionally, advanced cell tracking technologies are improving our understanding of MSC biodistribution and persistence in vivo, potentially enabling the development of pharmacokinetic-pharmacodynamic (PK-PD) models for MSC therapies [103].
As the field progresses toward more precise and predictive potency testing, the integration of mechanism-based assays with product-specific biomarkers will be essential for ensuring consistent clinical efficacy of MSC-based therapies and fulfilling their promise as robust therapeutic tools in regenerative medicine and immunology [99].
Head-to-Head Comparisons: Validating Functional Differences for Targeted Therapies
The therapeutic efficacy of Mesenchymal Stem Cells (MSCs) in regenerative medicine is fundamentally constrained by the gradual decline in their functional properties during in vitro expansion. This degradation, characterized by reduced proliferation, increased senescence, and diminished multipotency, presents a significant barrier to clinical translation [40]. The choice of culture methodology is not merely a technical consideration but a critical determinant of cellular phenotype and function. This guide provides a direct comparative analysis of conventional and advanced culture systems, presenting objective experimental data on their performance in maintaining MSC proliferation capacity, mitigating senescence, and preserving long-term therapeutic potential.
Comparative Analysis of 3D Culture Systems
The limitations of two-dimensional (2D) monolayer culture have driven the development of three-dimensional (3D) systems that better mimic the native tissue microenvironment. A 2025 comparative study evaluated adipose-derived MSCs (ASCs) over a four-week period in four distinct culture environments: 2D monolayers, 3D spheroids, Matrigel, and a novel hydrogel-based Bio-Block platform [104] [105].
Table 1: Functional Outcomes of MSCs in Different 3D Culture Systems (4-Week Culture)
| Parameter | 2D Monolayer | 3D Spheroids | Matrigel | Bio-Block |
|---|---|---|---|---|
| Proliferation | Baseline | ~2-fold lower than Bio-Block | ~2-fold lower than Bio-Block | ~2-fold higher than spheroid/Matrigel |
| Senescence | Baseline | 30-37% higher than Bio-Block | 30-37% higher than Bio-Block | 30-37% reduction vs. other 3D systems |
| Apoptosis | Baseline | 2-3 fold higher than Bio-Block | 2-3 fold higher than Bio-Block | 2-3 fold decrease vs. other 3D systems |
| Secretome Protein Production | Declined 35% | Declined 47% | Declined 10% | Fully preserved |
| Extracellular Vesicle (EV) Production | Declined 30-70% | Declined 30-70% | Declined 30-70% | Increased ~44% |
| Trilineage Differentiation | Significant decline | Significant decline | Significant decline | Significantly higher |
| Stemness Markers (LIF, OCT4, IGF1) | Downregulated | Downregulated | Downregulated | Significantly higher |
The data demonstrate that the Bio-Block system consistently outperformed other platforms across all measured parameters, effectively preserving the intrinsic MSC phenotype and secretome during extended culture [104] [105]. Notably, the study also assessed the functional potency of the harvested EVs. Endothelial cells (ECs) treated with Bio-Block-derived EVs exhibited enhanced proliferation, migration, and VE-cadherin expression, whereas EVs derived from spheroids paradoxically induced senescence and apoptosis in recipient ECs, highlighting the critical influence of culture conditions on therapeutic bioactivity [105].
Alternating 2D/3D Culture Strategy
An alternative approach to mitigating culture-induced senescence involves dynamically transitioning cells between different environments. A 2025 study investigated an alternating 2D/3D protocol for placenta-derived MSCs, combining phases of adherent monolayer expansion with transient spheroid formation [106].
Table 2: Outcomes of Alternating 2D/3D Culture vs. Conventional 2D Culture
| Parameter | Conventional 2D Culture | Alternating 2D/3D Culture |
|---|---|---|
| Cell Size | Progressive enlargement | Significantly reduced |
| Replicative Lifespan | Accelerated senescence | Extended |
| Immunomodulatory Function | Declined with passage | Preserved anti-inflammatory activity |
| Proliferative Capacity | Reduced over passages | Better maintained |
| Scalability | High | Enabled via RGD-alginate hydrogel tubes (AlgTubes) |
This strategy directly addresses a critical, often overlooked consequence of in vitro expansion: cell size enlargement. Oversized MSCs face increased entrapment in lung microvasculature following systemic administration, severely limiting their homing to target tissues and raising safety concerns regarding potential microcirculation obstruction [106]. The alternating protocol successfully mitigated this enlargement while delaying senescence and preserving immunoregulatory potency, offering a scalable manufacturing solution using RGD-functionalized AlgTubes [106].
Comparative Analysis of MSC Tissue Origins
The tissue source of MSCs significantly influences their baseline characteristics and expansion potential. A 2025 comparative analysis of human MSCs from adipose tissue (ADSCs) and dental pulp (DPSCs) revealed fundamental differences [16].
Table 3: Comparison of MSC Properties by Tissue Source
| Parameter | Adipose-Derived MSCs (ADSCs) | Dental Pulp-Derived MSCs (DPSCs) |
|---|---|---|
| Proliferation Rate | Lower | Significantly higher |
| Cell Size | Larger | Consistently smaller |
| Adipogenic Differentiation | Capable | Incapable |
| Marker Expression | Standard MSC phenotype | Nestin-positive |
| Resistance to Senescence | Standard | Superior (resistant to inflammation-induced senescence) |
| Extracellular Vesicle Profile | Higher number of smaller exosomes | Comparable total EV number, different size distribution |
DPSCs demonstrated a superior proliferation rate and a smaller cell size, which is advantageous for in vivo biodistribution. Furthermore, DPSCs exhibited enhanced resistance to subculture and inflammation-induced senescence, making them particularly suitable for tissue engineering in inflammatory environments [16]. These findings underscore that, despite shared MSC characteristics, the tissue of origin is a major determinant of expansion potential and resilience.
Experimental Protocols for Key Assays
To ensure reproducibility and standardized comparison across studies, this section details the core methodologies used in the cited research.
Protocol: Long-Term Functional Comparison of 3D Systems
This protocol is adapted from the 2025 study by Hodge et al. [104] [105].
- Cell Source: Human adipose-derived MSCs (ASCs).
- Culture Groups: 2D (T-flask), 3D spheroids, Matrigel, Bio-Block hydrogel.
- Culture Duration: 4 weeks.
- Assessment Metrics:
- Proliferation: Measured via population doubling time and metabolic activity assays.
- Senescence: Quantified using Senescence-Associated β-Galactosidase (SA-β-gal) staining.
- Apoptosis: Analyzed via flow cytometry for Annexin V/propidium iodide.
- Trilineage Differentiation: Conducted using standard osteogenic, chondrogenic, and adipogenic induction media and staining (Alizarin Red, Alcian Blue, Oil Red O, respectively).
- Stemness Markers: Gene expression analysis (e.g., qPCR for LIF, OCT4, IGF1).
- Secretome Analysis: Conditioned media collected for protein quantification and EV isolation via ultracentrifugation or tangential flow filtration.
- EV Potency Assay: Isolated EVs are dosed onto endothelial cells to assess functional outcomes like proliferation and migration.
Protocol: Alternating 2D/3D Culture
This protocol is adapted from the 2025 study by Han et al. [106].
- Cell Source: Placenta-derived MSCs.
- 2D Phase: Expand MSCs as an adherent monolayer in standard culture flasks until sub-confluence.
- 3D Spheroid Phase: Detach cells and transfer to a non-adherent environment to allow spheroid formation for 24–72 hours.
- Cycle: The 2D expansion and 3D spheroid formation phases are alternated at each passage.
- Supplementation: Use of extracellular matrix supplements and chemically defined media to enhance spheroid viability.
- Scalable Format: For bioreactor compatibility, the process is implemented using RGD-functionalized alginate hydrogel tubes (AlgTubes).
- Assessment: Monitor cell size (microscopy, flow cytometry), senescence (SA-β-gal), and immunomodulatory function (e.g., T-cell suppression assay) over multiple passages.
Signaling Pathways in MSC Stemness and Senescence
The molecular basis of MSC stemness and its decline during culture is regulated by a network of key transcription factors. The following diagram illustrates the core pathways and their interactions.
Figure 1. Molecular Regulation of MSC Stemness. Key transcription factors like OCT4, SOX2, TWIST1, and HOXB7 promote stemness and proliferation [40]. TWIST1 activates EZH2, which, along with OCT4-induced DNMT1, silences critical senescence genes (p14, p16, p21) through epigenetic mechanisms (H3K27me3 modification, promoter methylation) [40]. The downregulation of these factors leads to replicative senescence.
Experimental Workflow for Culture Comparison
The following diagram outlines a standardized experimental workflow for the direct comparison of MSC culture systems, as implemented in the cited studies.
Figure 2. Workflow for MSC Culture Comparison. The process begins with cell isolation and baseline characterization, followed by seeding into different culture systems for a long-term culture period. A comprehensive suite of analyses is then performed to evaluate functional and molecular outcomes, with final data integration for comparative conclusions.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents and Materials for MSC Culture Experiments
| Item | Function/Application | Specific Examples from Research |
|---|---|---|
| Cell Culture Media | Supports MSC growth and maintenance. | RoosterNourish MSC-XF [105], α-MEM [55] [16], DMEM [55], EBM-2 [106] |
| Serum Supplements | Provides essential growth factors and adhesion proteins. | Fetal Bovine Serum (FBS) [16], Human Platelet Lysate (hPL) [55] |
| 3D Culture Matrices | Provides a biomimetic 3D environment for cell growth. | Bio-Block Hydrogel [104] [105], Matrigel [104] [105], RGD-functionalized Alginate [106] |
| Dissociation Reagents | Detaches adherent cells for subculturing and analysis. | Trypsin-EDTA [16], TrypLE Select [106] |
| Senescence Detection Kits | Histochemical detection of senescent cells. | Senescence-Associated β-Galactosidase (SA-β-gal) Staining Kit [107] |
| Extracellular Vesicle Isolation Tools | Isolates and purifies EVs from conditioned media. | Ultracentrifugation [55], Tangential Flow Filtration (TFF) [55] |
| Flow Cytometry Antibodies | Characterizes MSC surface marker expression (CD73, CD90, CD105) and detects apoptosis. | Antibodies against CD73, CD90, CD105, CD34, CD45, Annexin V [108] [16] |
| Differentiation Kits | Induces and assesses trilineage differentiation potential. | Osteogenic, Chondrogenic, and Adipogenic Induction Media [104] [16] |
The therapeutic application of Mesenchymal Stromal Cells (MSCs) has evolved significantly, shifting focus from their cell replacement potential to their powerful paracrine activity. The MSC secretome—the complete set of bioactive factors these cells secrete—is now recognized as a primary mediator of tissue repair, driving both immunomodulation and vascular regeneration [109]. This complex mixture of soluble factors and extracellular vesicles (EVs) contains growth factors, cytokines, chemokines, and genetic material that collectively orchestrate healing processes [109] [110].
The composition and potency of this secretome are not uniform; they vary dramatically based on the tissue origin of the MSCs and their pre-conditioning within specific microenvironments [109] [111]. This comparative analysis systematically evaluates the anti-inflammatory and pro-angiogenic factor release from MSCs of different sources, providing researchers and drug development professionals with objective, data-driven insights for selecting optimal secretome profiles for targeted therapeutic applications.
Quantitative Comparison of Secretome Profiles
The therapeutic potential of a secretome is defined by the concentration and diversity of its bioactive factors. Systematic proteomic analyses reveal significant differences in protein expression across MSC sources.
Table 1: Comparative Analysis of Key Angiogenic Factors in MSC Secretomes (Data from [111])
| Protein Factor | hWJSC Secretome | hBMSC Secretome | hADSC Secretome | Primary Function |
|---|---|---|---|---|
| VEGF-A | High Expression | Medium Expression | Low Expression | Blood vessel formation & permeability |
| MCP-1/CCL2 | High Expression | Medium Expression | Low Expression | Monocyte recruitment & angiogenesis |
| IL-6 | High Expression | Medium Expression | Low Expression | Pro-inflammatory & angiogenic cytokine |
| IL-8/CXCL8 | High Expression | Medium Expression | Low Expression | Neutrophil chemoattractant & angiogenesis |
| Angiogenin (ANG) | High Expression | Medium Expression | Low Expression | Ribonuclease inducing vessel formation |
| bFGF | Detected | Detected | Not Detected | Endothelial cell proliferation & migration |
| HGF | Detected | Detected | Not Detected | Mitogen for endothelial cells |
Table 2: Anti-inflammatory and Osteogenic Factor Profile Comparison
| Bioactive Factor / Effect | Cord Blood MSC [112] | iPSC-derived MSC [113] | Dental Pulp MSC [114] | Function / Experimental Outcome |
|---|---|---|---|---|
| PGE2 | Not Specified | Not Specified | Not Specified | NK cell inhibition, M2 macrophage polarization, Treg differentiation [109] |
| Galectins | Not Specified | Not Specified | Not Specified | Immune cell regulation via transmembrane signaling [109] |
| Anti-inflammatory Effect | Dynamically modulated in response to damage | Suppressed NF-κB activation & TNF-α release in monocytes | Not Specified | Response to microenvironment; crucial for tissue regeneration [113] [112] |
| Osteoinductive Potential | Not Specified | Not Specified | Exosomes > Secretome in osteogenic preconditioning | Enhanced BMSC mineralization and osteogenic gene expression [115] |
| Angiogenic Effect In Vivo | Strong blood vessel induction | Facilitated angiogenesis in zebrafish model | Enhanced endothelial cell migration (scratch assay) | Development of capillary-like structures [112] [113] [114] |
Experimental Protocols for Secretome Analysis
Standardized and robust experimental protocols are essential for the accurate collection, characterization, and functional validation of MSC secretomes.
Secretome Collection and Preparation
A standardized xenofree protocol for generating conditioned medium (CM), representative of the secretome, is critical for clinical relevance [111].
Detailed Protocol [111] [113]:
- Cell Culture: MSCs are isolated from tissues (e.g., bone marrow, Wharton's jelly, adipose tissue) and expanded under xenofree conditions using human platelet lysate (hPL) as a supplement. Cells are typically used at passages 3-4.
- Serum-Free Incubation: At ~80% confluence, cells are washed and switched to a basal, serum-free medium to eliminate interference from serum proteins. Incubation typically continues for 24 to 48 hours.
- Conditioned Medium Harvest: The medium containing the secreted factors is collected and subjected to centrifugation at 300-500 × g for 5-10 minutes to remove cellular debris [113] [116].
- Sterilization and Storage: The supernatant is sterilized by passage through a 0.22 μm filter. The resulting conditioned medium (CM) can be used immediately, concentrated, or freeze-dried for storage [116].
Key Functional Assays
The biological activity of the collected secretome is validated through specific functional assays.
Angiogenesis Assays:
- In Vitro Tube Formation: Endothelial cells (e.g., HUVECs) are seeded on a basement membrane matrix (e.g., Matrigel) and treated with the secretome. The formation of capillary-like structures is quantified, measuring network length, number of junctions, and meshes [111].
- Scratch Wound Healing/Migration: A confluent monolayer of endothelial cells is scratched to create a "wound." Secretome treatment enhances cell migration into the gap, which is quantified over 24-48 hours [114].
- In Vivo Matrigel Plug Assay: Secretome-impregnated Matrigel is injected subcutaneously into mice. After 1-2 weeks, plugs are harvested and analyzed for blood vessel infiltration via hemoglobin content or immunohistology [111].
Anti-inflammatory Assays:
- Immune Cell Coculture: Monocytes (e.g., THP-1 cells) are activated with a pro-inflammatory stimulus like LPS. The secretome is added, and the suppression of pro-inflammatory cytokines (e.g., TNF-α, IL-1β) is measured via ELISA. Flow cytometry can also assess macrophage polarization towards the anti-inflammatory M2 phenotype [109] [113].
- NF-κB Pathway Inhibition: Reporter cell lines or phosphokinome profiling are used to measure the secretome's ability to suppress the activation of the central NF-κB inflammatory pathway [113].
Signaling Pathways and Mechanisms of Action
The therapeutic effects of the MSC secretome are mediated through complex signaling pathways that regulate target cells.
Pro-angiogenic Signaling
Secretome-induced angiogenesis is a multi-factorial process involving the synergistic action of multiple growth factors and pathways [111] [110].
Key Mechanisms:
- Growth Factor Synergy: Factors like VEGF-A, bFGF, and Angiogenin act in concert, binding to receptors on endothelial cells to activate pro-survival and proliferative pathways such as PI3K/AKT and RAS-MAPK [113] [111].
- Metabolic Reprogramming: The secretome can modulate endothelial cell metabolism, increasing expression of genes involved in mitochondrial respiration to fuel the energetically demanding process of vessel sprouting [113].
- Extracellular Vesicle-Mediated Communication: Exosomes and other EVs deliver transcription factors (e.g., GATA2), mRNAs, and miRNAs into recipient endothelial cells, inducing a pro-angiogenic transcriptome and sustained protein expression [113] [110] [112].
Anti-inflammatory Signaling
The secretome polarizes the immune response towards a tolerant, reparative state by modulating key immune cells [109].
Key Mechanisms:
- Macrophage Reprogramming: Secretome factors like PGE2 and galectins drive the polarization of pro-inflammatory M1 macrophages towards an anti-inflammatory M2 phenotype, which is associated with tissue repair and regeneration [109].
- T-cell Regulation: The secretome can suppress the proliferation of pro-inflammatory T-helper cells while promoting the differentiation and activity of regulatory T-cells (Tregs), which are crucial for maintaining immune tolerance [109].
- Master Pathway Inhibition: A central mechanism is the suppression of the NF-κB signaling pathway, a master regulator of inflammation. This leads to reduced production of cytokines like TNF-α and IL-1β [113].
The Scientist's Toolkit: Essential Research Reagents
Successful secretome research requires a suite of reliable reagents and tools for cell culture, analysis, and functional testing.
Table 3: Essential Reagents for Secretome Research
| Reagent / Tool | Function & Application | Specific Examples / Notes |
|---|---|---|
| Human Platelet Lysate (hPL) | Xenofree supplement for clinical-grade MSC culture; replaces fetal bovine serum (FBS). | Essential for standardized, clinically relevant secretome production [111]. |
| Serum-Free Basal Media | Medium for secretome collection to avoid serum protein contamination. | MEM-α, DMEM/F-12 [113] [116]. |
| Extracellular Vesicle Isolation Kits | Isolate exosomes and microvesicles from conditioned medium for fractionation studies. | Based on precipitation, size-exclusion chromatography, or ultracentrifugation. |
| LC-MS/MS Proteomics | High-resolution, unbiased identification and quantification of secretome proteins. | Key for comparative analyses between MSC sources [111]. |
| ELISA Kits | Quantify specific soluble factors (e.g., VEGF, PGE2, TNF-α) in the secretome. | Used for targeted validation of proteomic data. |
| Endothelial Cell Lines | Model systems for in vitro angiogenesis assays (tube formation, migration). | HUVECs, hCMEC/D3 (brain endothelial) [113] [111]. |
| Basement Membrane Matrix | 3D substrate for endothelial tube formation assays. | Matrigel is the most widely used [111]. |
| Flow Cytometry Antibodies | Characterize MSC surface markers and analyze immune cell populations in co-cultures. | Essential panels: CD73, CD90, CD105, CD14, CD34, CD45 [111] [116]. |
Discussion and Research Implications
The comparative data indicates a clear functional specialization among MSC secretomes. Human Wharton's Jelly MSCs (hWJSCs) emerge as a superior source for applications where robust angiogenesis is desired, such as in treating ischemic diseases, due to their rich and diverse profile of pro-angiogenic factors [111]. Their secretome also demonstrates a potent ability to modulate monocytes and macrophages, making them a strong candidate for inflammation-mediated regeneration. Conversely, the osteogenic potential of secretomes can be significantly enhanced through pre-conditioning, with evidence suggesting that exosomes from preconditioned cells may be more potent than the total secretome for guiding bone regeneration [115].
The future of secretome therapy lies in advanced delivery platforms. Recent innovations, such as encapsulating the secretome within magnetically actuated micromotors, demonstrate the potential to overcome the limitation of passive diffusion, enabling active navigation and penetration into wound barriers for more effective targeted treatment [116]. This progression from raw conditioned medium to engineered delivery systems underscores the growing sophistication in the field.
For researchers, the choice of MSC source and secretome preparation protocol should be strategically aligned with the intended therapeutic outcome. This decision-making process must be informed by rigorous in vitro characterization and functional validation, as outlined in this guide, to fully harness the power of the MSC secretome for regenerative medicine.
The therapeutic potential of Mesenchymal Stem Cells (MSCs) has been extensively explored across diverse medical fields, with their efficacy being significantly influenced by their tissue of origin. Bone marrow-derived MSCs (BM-MSCs) and adipose tissue-derived MSCs (AD-MSCs) represent two of the most widely utilized sources, each demonstrating distinct advantages for specific clinical applications. BM-MSCs, the most extensively studied type, are recognized for their strong immunomodulatory effects [4] and have consequently emerged as a key candidate for treating immune-mediated conditions like graft-versus-host disease (GvHD). In contrast, AD-MSCs are easily accessible, available in abundant quantities, and exhibit notable prowess in tissue regeneration and repair, making them particularly suitable for soft tissue augmentation and plastic surgery applications [117] [27]. This guide provides a comparative analysis of clinical trial outcomes for these two cell populations in their respective flagship applications, offering researchers and drug development professionals a data-driven resource for therapeutic development.
Clinical Efficacy and Outcomes: A Comparative Analysis
BM-MSCs in Graft-versus-Host Disease (GvHD)
GvHD is a common and serious complication following allogeneic hematopoietic stem cell transplantation, where donor immune cells attack the recipient's tissues. BM-MSCs have shown significant promise in managing this condition, particularly in its steroid-refractory form.
Table 1: Efficacy Outcomes of BM-MSCs in Steroid-Refractory Acute GvHD (Meta-Analysis of 4 RCTs, n=650) [118]
| Outcome Measure | Result with BM-MSCs + Second-line Therapy | Result with Second-line Therapy Alone | Risk Ratio (RR) or Hazard Ratio (HR) [95% CI] | P-value |
|---|---|---|---|---|
| Overall Response (OR) at Day 28 | Significantly improved | Baseline | RR: 1.13 [1.03 - 1.23] | P = 0.007 |
| Complete Response (CR) at Day 28 | Significantly improved | Baseline | RR: 1.43 [1.19 - 1.70] | P < 0.001 |
| Failure-Free Survival (FFS) | Improved | Baseline | HR: 0.72 [0.54 - 0.95] | P = 0.022 |
| Incidence of Chronic GvHD | Reduced | Baseline | HR: 0.60 [0.42 - 0.86] | P = 0.005 |
| Overall Survival (OS) | No significant benefit observed | Baseline | Not Significant | - |
The meta-analysis confirmed that the addition of BM-MSCs to second-line therapy consistently improved outcomes across patient subgroups, including those with skin or gut involvement, multiorgan disease, and adults [118]. The safety profile of BM-MSCs was also found to be comparable with controls, supporting their favorable risk-benefit ratio [118] [119].
AD-MSCs in Soft Tissue and Orthopedic Applications
AD-MSCs are widely utilized in plastic and aesthetic surgeries for tissue filling and repair, such as treating facial wrinkles, skin scars, and breast reconstruction [117]. Their efficacy is often evaluated through pain and functional scores in related conditions like osteoarthritis, which provides validated metrics for their regenerative capacity.
Table 2: Efficacy Outcomes of AD-MSCs versus BM-MSCs in Knee Osteoarthritis (Meta-Analysis of 21 RCTs, n=936) [120]
| Outcome Measure | AD-MSCs Performance | BM-MSCs Performance | Clinical Implications |
|---|---|---|---|
| Visual Analog Scale (VAS) Pain at 6 months | Significant improvement (P=0.015) | Significant improvement (P=0.012) | Both sources effectively reduce pain in the medium term. |
| VAS Pain at 1 year | Significant improvement (P<0.001) | Improvement not sustained (P=0.539) | AD-MSCs demonstrate more consistent and durable pain relief. |
| WOMAC Functional Score | Significant improvement (P<0.001) | No significant improvement (P=0.541) | AD-MSCs show superior improvement in joint function. |
| Lysholm Score (Knee function) | Significant improvement (P=0.006) | No significant improvement (P=0.933) | AD-MSCs lead to better functional outcomes. |
| Safety Profile (Adverse Events) | No significant issues (P=0.673) | Significant adverse events (P=0.003) | AD-MSCs are associated with a superior safety profile. |
The meta-analysis concluded that adipose tissue is superior to bone marrow for managing knee osteoarthritis due to its safety and consistent efficacy in improving pain and functional outcomes [120]. This advantage is attributed to the easier harvesting, faster proliferation rate, and higher yield of AD-MSCs [27].
Experimental Protocols and Methodologies
Protocol for BM-MSC Therapy in Steroid-Refractory aGvHD
The following workflow outlines a typical clinical trial protocol for using BM-MSCs in GvHD, synthesized from recent RCTs [118].
Key Methodological Details:
- Patient Population: Individuals with steroid-refractory aGvHD (grades II-IV) following allogeneic hematopoietic stem cell transplantation. Steroid-refractory is typically defined as progression within 3 days, no improvement after 7 days, or failure to achieve complete response by day 14 of steroid therapy [118].
- BM-MSC Product: Culture-expanded allogeneic BM-MSCs are administered at a standard dose of 1.0 × 10^6 cells per kilogram of body weight [118]. The cells must adhere to International Society for Cell & Gene Therapy (ISCT) criteria, expressing CD105, CD73, and CD90 (≥95%), while lacking expression of hematopoietic markers CD45, CD34, CD14/CD11b, CD79α/CD19, and HLA-DR (≤2%) [4] [3].
- Administration Protocol: Intravenous infusion is the standard route, with frequencies ranging from once to twice weekly over 4 to 8 weeks, depending on patient response [118].
- Outcome Assessment: The primary endpoint is typically overall response (OR) at day 28, which includes both complete response (CR - resolution of all manifestations) and partial response (PR - improvement of at least one stage in every involved organ) [118] [119].
Protocol for AD-MSC Therapy in Soft Tissue Applications
The following diagram illustrates the standard protocol for processing and applying AD-MSCs in soft tissue regeneration.
Key Methodological Details:
- Tissue Harvesting: AD-MSCs are typically obtained from waste tissues following surgical procedures like liposuction from the abdomen and thighs, with up to 1 billion cells potentially generated from 300g of adipose tissue [27].
- Cell Processing and Characterization: The isolated stromal vascular fraction (SVF) containing AD-MSCs can be used directly or after in vitro expansion. The final product is characterized for standard MSC surface markers (CD105, CD73, CD90), viability, and the absence of microbial contamination [120] [3].
- Clinical Application: AD-MSCs are typically administered via local injection or implantation at the target site. They are often used in combination with fat grafts, hyaluronic acid, biomaterials, or platelet-rich plasma (PRP) to enhance tissue integration and survival [117].
Mechanisms of Action: Signaling Pathways and Biological Effects
Immunomodulatory Mechanisms of BM-MSCs in GvHD
BM-MSCs exert their therapeutic effects in GvHD primarily through sophisticated immunomodulation. The following diagram summarizes the key pathways involved.
Key Mechanistic Insights:
- Paracrine Signaling: In the inflammatory microenvironment of GvHD, BM-MSCs release a multitude of bioactive factors including prostaglandin E2 (PGE2), indoleamine-2,3-dioxygenase (IDO), transforming growth factor beta (TGF-β), interleukin-10 (IL-10), and hepatocyte growth factor (HGF) [4] [119] [121].
- Immune Cell Interactions: These soluble factors collectively inhibit the proliferation of effector T cells, promote the expansion of regulatory T cells (Tregs), and suppress the activity of other immune cells including B cells, dendritic cells, and natural killer cells [4] [119].
- Clinical Correlation: This broad immunomodulation translates clinically to reduced aGvHD severity, lower incidence of chronic GvHD, and improved failure-free survival, as demonstrated in randomized trials [118] [119].
Tissue Regenerative Mechanisms of AD-MSCs
AD-MSCs promote soft tissue augmentation and repair through a combination of trophic support and differentiation capacity.
Key Mechanistic Insights:
- Trophic Factor Production: AD-MSCs secrete high levels of growth factors including vascular endothelial growth factor (VEGF), fibroblast growth factor (FGF), and hepatocyte growth factor (HGF), which promote angiogenesis and tissue remodeling [121] [3].
- Direct Structural Contribution: While their primary mechanism is paracrine-mediated, AD-MSCs can differentiate into adipocytes and other mesenchymal lineages, directly contributing to tissue volume and structure in soft tissue augmentation applications [117] [27].
- Superior Secretory Profile: Compared to BM-MSCs, AD-MSCs have been shown to secrete higher levels of BDNF and VEGF, enhancing cellular survival and angiogenesis at the injury site [121].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for MSC Studies
| Reagent/Category | Specific Examples | Function in MSC Research |
|---|---|---|
| Cell Isolation Kits | CD105+ Microbeads, Stromal Vascular Fraction (SVF) Isolation Kits | Isolation and purification of specific MSC populations from tissue sources. |
| Culture Media | MesenCult, StemPro MSC SFM, DMEM/F12 with FBS | Maintenance and expansion of MSCs while preserving differentiation potential. |
| Characterization Antibodies | Anti-CD105, -CD73, -CD90, -CD45, -CD34, -HLA-DR | Verification of MSC identity per ISCT criteria via flow cytometry. |
| Differentiation Kits | Osteogenic/Chondrogenic/Adipogenic Differentiation Media | Demonstration of trilineage differentiation potential per ISCT standards. |
| Cryopreservation Media | CryoStor CS10, Bambanker | Maintenance of cell viability and functionality during frozen storage. |
| Potency Assay Kits | IDO Activity Assays, T-cell Proliferation Suppression Kits | Measurement of immunomodulatory capacity for batch consistency. |
Discussion and Future Perspectives
The comparative analysis of BM-MSCs and AD-MSCs reveals a clear principle of targeted application: the tissue source of MSCs should be matched to the therapeutic goal. BM-MSCs, with their potent immunomodulatory profile, are particularly effective for immune-mediated conditions like GvHD, where they significantly improve treatment response and reduce complications [118] [119]. Conversely, AD-MSCs, with their abundant availability, superior safety profile, and consistent tissue-regenerative capacity, are ideally suited for soft tissue augmentation and orthopedic applications [120] [117].
Future research directions should focus on standardizing product characterization and manufacturing processes to minimize heterogeneity [122] [3]. Furthermore, exploring the combination of both MSC types for conditions involving both immune dysregulation and tissue damage, such as in autoimmune diseases with tissue destruction, may unlock new therapeutic synergies. As the field progresses, the development of more refined potency assays and patient-specific biomarkers will be crucial for optimizing MSC selection for individual patients and clinical indications [119] [122].
In the evolving landscape of regenerative medicine, the selection of appropriate mesenchymal stem cell (MSC) sources represents a fundamental strategic decision that directly influences therapeutic outcomes. While MSCs can be isolated from various tissues, their developmental origins, proliferation capacities, and differentiation biases create distinct therapeutic profiles that may make them uniquely suited for specific clinical applications. This comparative analysis examines two prominent MSC sources: dental pulp stem cells (DPSCs) and adipose-derived stem cells (ADSCs), with a focused evaluation of their respective efficacies in neuro-regeneration and bone tissue engineering.
The paradigm in regenerative medicine is shifting from a one-size-fits-all approach to a targeted application-specific strategy. DPSCs, originating from the neural crest lineage, inherently possess a strong neurogenic predisposition, while ADSCs, with their mesodermal origin and robust proliferative capacity, demonstrate exceptional osteogenic potential. This review provides a structured, evidence-based comparison of these cell types through the lens of their molecular mechanisms, experimental outcomes, and practical research considerations, offering researchers a framework for selecting optimal cell sources for specific regenerative applications.
Core Biological Properties and Practical Research Considerations
Understanding the fundamental characteristics and practical handling requirements of each cell type is essential for experimental design and clinical translation.
Table 1: Fundamental Characteristics of DPSCs and ADSCs
| Characteristic | Dental Pulp Stem Cells (DPSCs) | Adipose-Derived Stem Cells (ADSCs) |
|---|---|---|
| Developmental Origin | Neural crest ectoderm [123] [124] | Mesoderm [125] [126] |
| Tissue Source Accessibility | Impacted third molars, exfoliated deciduous teeth (SHED) [123] [124] | Subcutaneous adipose tissue (minimally invasive lipoaspiration) [125] [126] |
| Key Surface Markers | STRO-1, CD44, CD90, CD105, CD73, CD166, nestin [123] [15] | CD90, CD105, CD73, CD44, CD166 [125] [126] |
| Negative Markers | CD45, CD34 [123] | CD45, CD34 (debated) [125] |
| Proliferation Rate | High (SHED > DPSCs) [124] [15] | Very high, superior to bone marrow MSCs [127] [126] |
| Senescence in Culture | Moderate | Low, better resistance than DPSCs and BMSCs [127] [125] |
| Immunogenicity | Low (negative MHC-II) [128] [15] | Low, immunomodulatory properties [125] [126] |
| Cryopreservation | Maintain properties post-thaw [15] | Compatible with cryopreservation |
Essential Research Reagents and Methodologies
Table 2: Key Research Reagents for MSC Isolation and Differentiation
| Reagent/Category | Function/Application | Specific Examples |
|---|---|---|
| Isolation Enzymes | Tissue dissociation | Collagenase (ADSCs) [125] [126]; Trypsin (DPSCs) [123] |
| Culture Media | Cell expansion | DMEM with FBS [123] [125]; Serum-free alternatives, Human Platelet Lysate [125] |
| Osteogenic Induction | Bone differentiation | BMP2, BMP9 [127] [46]; Ascorbic acid, β-glycerophosphate, dexamethasone |
| Neurogenic Induction | Neural differentiation | EGF, FGF, retinoic acid [123] [124] |
| Characterization Antibodies | Cell surface marker profiling | Anti-STRO-1, CD44, CD90, CD105, CD73, CD166 [123] [125] |
| Analysis Tools | Differentiation assessment | ALP staining, Alizarin Red S (osteogenesis); Immunocytochemistry for NFM, βIII-tubulin (neurogenesis) [128] |
Neuro-Regenerative Potential: DPSCs Demonstrate Superiority
Molecular Advantages of Neural Crest Origin
DPSCs originate from the neural crest ectoderm, which provides them with an inherent neurogenic bias that is absent in ADSCs [123] [124]. This developmental lineage equips DPSCs with higher basal expression of key neurotrophic factors including brain-derived neurotrophic factor (BDNF), nerve growth factor (NGF), glial cell line-derived neurotrophic factor (GDNF), and neurotrophin-3 (NT-3) [123] [124]. Comparative analysis reveals that DPSCs generate significantly higher levels of neurotrophic factor mRNA compared to ADSCs and other MSC types [124].
This molecular predisposition translates to functional advantages in neuronal differentiation capacity. Under appropriate induction conditions using epidermal growth factor (EGF) and fibroblast growth factor (FGF), DPSCs efficiently differentiate into functionally active neuronal cells exhibiting voltage-dependent sodium channels and the ability to generate action potentials [124]. Furthermore, DPSCs can be directed to become specific neuronal subtypes, including dopaminergic neurons, which is particularly relevant for Parkinson's disease therapeutic strategies [124].
Therapeutic Efficacy in Neurological Disease Models
The neuroregenerative capacity of DPSCs has been demonstrated across multiple neurological disease models:
Alzheimer's Disease Models: DPSC transplantation and administration of DPSC-conditioned medium (DPCM) reduce neuronal cell death induced by endoplasmic reticulum stress and oxidative stress [124]. SHED-conditioned medium (SHED-CM) shows particularly promising results due to its higher concentration of protective factors like hepatocyte growth factor (HGF) [124].
Spinal Cord Injury: Transplantation of human DPSCs into rat spinal cord injury models promotes functional recovery through secretion of neurotrophic factors that support endogenous neuron survival and induce oligodendrocyte differentiation for axon myelination [123].
Cerebral Ischemia: Intracerebral transplantation of DPSCs in rodent cerebral ischemia models significantly improves sensorimotor function, with cells migrating to various CNS regions and expressing neuronal markers [123] [124].
The therapeutic mechanism appears to be predominantly paracrine-mediated, with DPSCs secreting factors that modulate the hostile microenvironment of injured neural tissue by reducing inflammation, inhibiting microglial activation, and promoting endogenous repair mechanisms [123] [124].
Bone Regeneration Potential: ADSCs Excel in Osteogenesis
Proven Efficacy in Bone Defect Models
ADSCs demonstrate superior osteogenic capability compared to other MSC sources, including DPSCs. In direct comparative studies analyzing four mouse MSC sources, ADSCs exhibited the highest osteogenic potential upon BMP9 stimulation both in vitro and in vivo for critical-sized calvarial defect repair [46]. Transcriptomic analysis revealed that ADSCs regulate multiple osteogenesis-related signaling pathways including Wnt, TGF-β, PI3K/AKT, MAPK, Hippo, and JAK-STAT pathways during osteogenic differentiation [46].
The therapeutic efficacy of ADSCs in bone regeneration has been validated across diverse defect models:
Calvarial Defects: A clinical case study reported nearly complete calvarial continuity reconstruction in a young girl with severe head injury using autologous ADSCs combined with spongy cells from the iliac crest [125].
Femoral Head Necrosis: Direct injection of autologous ADSCs into the femoral head enhanced osteogenesis and improved microstructure in vascular deprivation-induced osteonecrotic tissue in small animal studies [125].
Critical-Sized Defects: ADSCs successfully regenerate bone in large defects resulting from trauma, multiple fractures, or tumor resection, with healing rates superior to those achieved with other MSC types [129] [46].
Practical Advantages for Clinical Translation
Beyond their superior differentiation capacity, ADSCs offer significant practical advantages for bone tissue engineering applications. ADSCs can be easily and repeatedly harvested using minimally invasive techniques with low donor site morbidity [125] [126]. The yield of MSCs from adipose tissue is substantially higher than from bone marrow aspirates, with approximately 500 times more MSCs per gram of tissue compared to bone marrow [125].
Additionally, ADSCs exhibit better senescence resistance and higher proliferation capacity in long-term culture compared to both DPSCs and bone marrow-derived MSCs [127] [125]. This expansion capability is critical for clinical applications requiring large cell quantities. Importantly, unlike bone marrow MSCs, ADSCs show no statistically significant correlation between stem cell quality, proliferation capacity, and donor age, making them reliable for treating elderly patients who represent a significant population requiring bone regeneration therapies [125].
Direct Comparative Analysis: Quantitative Experimental Data
In Vivo Performance Metrics
Table 3: Comparative In Vivo Performance in Regeneration Models
| Regeneration Model | DPSC Performance | ADSC Performance | Reference |
|---|---|---|---|
| Tooth Regeneration Success Rate | ~85% with BMP2 [127] | ~85% with BMP2; higher growth rate [127] | [127] |
| Bone Defect Repair | Limited evidence for significant bone regeneration | Superior calvarial defect repair with BMP9 [46] | [46] |
| Neuroprotection in CNS Injury | Significant functional improvement in spinal cord injury and cerebral ischemia [123] [124] | Limited neuroprotective evidence | [123] [124] |
| Proliferation Capacity | High (SHED > DPSC) [124] | Very high, superior to DPSCs [127] [125] | [127] [125] [124] |
| Senescence Resistance | Moderate | High, better than DPSCs and BMSCs [127] [125] | [127] [125] |
Experimental Differentiation Protocols
DPSC Neurogenic Differentiation Protocol [123] [124]:
- Isolation: Extract pulp from third molars using barbed broach, digest with trypsin, and culture in DMEM with FBS.
- Characterization: Verify MSC markers (STRO-1, CD44, CD105) and neural crest markers (nestin) via flow cytometry.
- Neurogenic Induction: Culture in serum-free medium supplemented with EGF (20 ng/mL), FGF (20 ng/mL), and retinoic acid (5 µM) for 14 days.
- Validation: Assess neuronal morphology and markers (NFM, βIII-tubulin) via immunocytochemistry; confirm functionality with electrophysiological measurements of voltage-dependent sodium channels.
ADSC Osteogenic Differentiation Protocol [129] [46]:
- Isolation: Digest lipoaspirate tissue with collagenase, isolate SVF via centrifugation, and culture in DMEM with FBS or human platelet lysate.
- Characterization: Confirm MSC markers (CD90, CD105, CD73) and absence of hematopoietic markers (CD45).
- Osteogenic Induction: Treat with BMP9 (10-50 ng/mL) or standard osteogenic cocktail (ascorbic acid, β-glycerophosphate, dexamethasone) for 21 days.
- Validation: Quantify mineralization via Alizarin Red S staining; measure alkaline phosphatase activity; assess osteocalcin and osteopontin expression via qPCR.
The comparative analysis of DPSCs and ADSCs reveals a clear principle in regenerative medicine: developmental origin dictates differentiation bias. DPSCs, with their neural crest lineage, demonstrate unequivocal superiority for neuro-regenerative applications, while ADSCs, of mesodermal origin, excel in bone tissue engineering.
For researchers designing studies targeting neurological disorders such as Alzheimer's disease, Parkinson's disease, spinal cord injury, or stroke, DPSCs represent the optimal cell source due to their inherent neurogenic predisposition, robust secretion of neurotrophic factors, and demonstrated efficacy across multiple neurological disease models. The use of conditioned medium from these cells may offer a cell-free therapeutic alternative while maintaining therapeutic benefits.
Conversely, for bone regeneration applications addressing critical-sized defects, femoral head necrosis, or craniofacial reconstruction, ADSCs provide superior osteogenic differentiation, practical advantages in harvesting and expansion, and proven clinical efficacy. Their resistance to senescence and age-independent quality make them particularly suitable for elderly patient populations.
Future research directions should focus on developing standardized differentiation protocols, exploring combinatorial approaches that leverage the unique strengths of each cell type, and advancing clinical trial design to validate these comparative findings in human patients. The field would benefit from more direct, side-by-side comparative studies in standardized model systems to further refine our understanding of the specific contexts where each cell type provides maximal therapeutic benefit.
The field of regenerative medicine is undergoing a significant transformation, moving from whole-cell therapies toward refined cell-free approaches centered on extracellular vesicles (EVs). Mesenchymal stem/stromal cells (MSCs) have long been recognized for their therapeutic potential in treating various diseases through immunomodulatory, anti-inflammatory, and pro-regenerative capabilities [4]. However, the understanding of how MSCs exert these effects has evolved, revealing that their paracrine secretion—rather than cell differentiation and engraftment—plays the predominant role [130] [131]. This discovery has shifted research focus toward the bioactive molecules MSCs release, particularly extracellular vesicles.
MSC-derived EVs are nanoscale lipid vesicles that carry a complex cargo of proteins, lipids, nucleic acids, and other therapeutic molecules from their parent cells [132] [131]. These EVs mediate intercellular communication by transferring functional components to recipient cells, influencing various physiological and pathological processes [133]. As therapeutic agents, EVs offer significant advantages over whole cell therapies, including reduced risk of immune rejection, tumorigenicity, and vascular occlusion; superior safety profile; ability to cross biological barriers like the blood-brain barrier; and easier storage and standardization as "off-the-shelf" products [130] [134] [131].
This comparative guide provides researchers and drug development professionals with a detailed analysis of how MSC tissue origins influence EV characteristics and therapeutic potential, supported by experimental data and methodological protocols for advancing this promising cell-free therapeutic platform.
Biological Foundations of MSC-Derived Extracellular Vesicles
Biogenesis and Composition of Extracellular Vesicles
Extracellular vesicles constitute a heterogeneous population of membrane structures released from cells into the extracellular environment. Based on their biogenesis and size, EVs are primarily categorized into: (1) exosomes (30-150 nm) that originate from the endosomal compartment through inward budding of multivesicular bodies (MVBs) and are released upon MVB fusion with the plasma membrane; (2) microvesicles (100-1000 nm) that form through direct outward budding and pinching of the plasma membrane; and (3) apoptotic bodies (100-5000 nm) that are shed during programmed cell death [132] [133].
The formation of exosomes involves sophisticated molecular machinery, including the Endosomal Sorting Complex Required for Transport (ESCRT) and ESCRT-independent pathways involving tetraspanins (CD63, CD81, CD9) and lipid microdomains [132] [131]. EVs carry diverse biomolecular cargoes that reflect their cellular origin and include:
- Proteins: Tetraspanins (CD9, CD63, CD81), ESCRT components (ALIX, TSG101), antigen presentation molecules (MHC-I/II), and membrane transport proteins [132]
- Nucleic Acids: mRNA, miRNA, other non-coding RNAs, and various DNA species [132] [131]
- Lipids: Phosphatidylserine, cholesterol, ceramides, and signaling lipids [132] [131]
Table 1: Fundamental Characteristics of Extracellular Vesicles
| EV Type | Size Range | Origin | Key Markers | Formation Mechanism |
|---|---|---|---|---|
| Exosomes | 30-150 nm | Endosomal compartment | CD63, CD81, CD9, TSG101, ALIX | Endosomal sorting, MVB fusion with plasma membrane |
| Microvesicles | 100-1000 nm | Plasma membrane | Selectins, CD40 ligand, ARF6 | Outward budding of plasma membrane |
| Apoptotic Bodies | 100-5000 nm | Disassembling apoptotic cells | Histones, fragmented DNA | Cell disassembly during apoptosis |
The following diagram illustrates the biogenesis pathways of different extracellular vesicle types:
MSCs can be isolated from various tissue sources, each imparting distinct biological properties to the cells and their secreted EVs. The primary MSC sources include:
- Bone Marrow-MSCs (BM-MSCs): The most extensively studied source, known for strong immunomodulatory effects and osteogenic potential [4] [133]
- Adipose Tissue-MSCs (AT-MSCs): Easily accessible through liposuction, with high yields and comparable therapeutic properties to BM-MSCs [135] [4]
- Umbilical Cord-MSCs (UC-MSCs): Exhibit enhanced proliferation capacity, lower immunogenicity, and superior angiogenic properties [4] [7]
- Placental/Fetal Tissue-MSCs: Including amniotic membrane (AM), chorionic plate (CP), and other placental components, offering high proliferation with minimal ethical concerns [7]
These tissue-specific differences originate from the unique microenvironment of each source, leading to variations in EV cargo composition and therapeutic efficacy [134] [133]. For instance, a comparative transcriptomic analysis of neonatal MSCs revealed distinct gene expression profiles among AM-MSCs, UC-MSCs, and CP-MSCs, which corresponded to their differential differentiation capacities and functional properties [7].
Therapeutic Efficacy Across Disease Models
Different MSC-EVs exhibit variable therapeutic effectiveness depending on the disease context, reflecting their unique molecular signatures and tissue origins.
Table 2: Comparative Therapeutic Efficacy of MSC-EVs from Different Sources
| Disease Model | BM-MSC-EVs Effects | UC-MSC-EVs Effects | AT-MSC-EVs Effects | Placental MSC-EVs Effects |
|---|---|---|---|---|
| Renal Injury/Fibrosis | Promotes kidney regeneration, reduces fibrosis [133] | Effectively ameliorates renal fibrosis [135] | N/A | N/A |
| Graft-versus-Host Disease | Prolongs survival, reduces organ damage, inhibits T-cell activation [5] [133] | Moderate efficacy with possible pro-coagulant activity [5] | Sudden death complications in murine models [5] | N/A |
| Cartilage/Osteoarthritis | Promotes cartilage regeneration, inhibits inflammation [133] | N/A | N/A | Enhanced osteogenic (AM-MSCs) and adipogenic (CP-MSCs) potential [7] |
| Liver Diseases | Significant anti-fibrotic effects in liver fibrosis [133] | N/A | N/A | N/A |
| Neurodegenerative Disorders | Improves autistic behavior in ASD models [133] | N/A | N/A | N/A |
| Cardiac Injury | Promotes cardioprotection and repair [131] | N/A | N/A | N/A |
| Immunomodulation | Induces M2 macrophage polarization, modulates T-cell responses [133] | Higher Treg/Th17 ratio induction [5] | Similar macrophage polarization and TGF-β inhibition as other sources [135] | N/A |
Molecular Mechanisms and Functional Differences
The variations in therapeutic efficacy among MSC-EVs from different sources stem from their divergent molecular cargoes and signaling pathway activation.
Immunomodulatory Properties:
- BM-MSC-EVs demonstrate potent T-cell suppression capacity, inhibiting CD4+ and CD8+ T-cell proliferation while preserving regulatory T-cell populations [133]
- UC-MSC-EVs induce a higher regulatory T-cell (Treg)/T helper 17 (Th17) ratio, promoting a more balanced immune response [5]
- AT-MSC-EVs effectively promote M2 macrophage polarization and inhibit TGF-β/Smad signaling, contributing to their anti-fibrotic effects [135]
Tissue-Specific Regenerative Capacities:
- BM-MSC-EVs exhibit strong osteogenic tendency, making them particularly suitable for bone and cartilage disorders [133]
- UC-MSC-EVs demonstrate enhanced pro-angiogenic properties and neuroregenerative potential [4]
- AM-MSC-EVs show superior osteogenic differentiation capacity, while CP-MSC-EVs display enhanced adipogenic potential under serum-free conditions [7]
Safety Profiles:
- BM-MSC-EVs have the most extensive safety data from clinical applications [133]
- UC-MSC-EVs and AT-MSC-EVs may exhibit higher pro-coagulant activity, requiring additional safety monitoring [5]
- AT-MSC-EVs administration has been associated with sudden death complications in murine GVHD models, suggesting potential source-specific risks [5]
Experimental Methodologies for MSC-EV Research
Standardized Protocols for MSC-EV Isolation and Characterization
EV Isolation Techniques:
- Ultracentrifugation: The gold standard method involving sequential centrifugation steps to separate EVs based on size and density [132]
- Size-Based Chromatography: Size-exclusion chromatography for high-purity EV separation without aggregates [132]
- Immunoaffinity Capture: Antibody-based methods for isolating specific EV subpopulations using surface markers [132]
- Polymer-Based Precipitation: Commercial kits employing polymers to precipitate EVs, though potential co-precipitation of contaminants remains a concern [132]
- Microfluidic Technologies: Emerging approaches for high-throughput, automated EV isolation with minimal sample volumes [132]
EV Characterization Methods:
- Nanoparticle Tracking Analysis (NTA): Determines EV size distribution and concentration [132]
- Transmission Electron Microscopy (TEM): Visualizes EV morphology and ultrastructure [132]
- Flow Cytometry: Detects specific surface markers using antibody staining [135] [7]
- Western Blotting: Identifies EV protein markers (CD9, CD63, CD81, TSG101, ALIX) [132] [133]
- RNA Sequencing: Profiles EV nucleic acid content and cargo composition [135] [7]
Cargo Loading and Engineering Strategies
Cell-Based Loading Methods:
- Transfection: Introducing therapeutic nucleic acids (siRNA, miRNA, mRNA) into parent MSCs using transfection reagents, resulting in engineered EVs secreted with modified cargo [136]
- Passive Incubation: Incubating MSCs with small molecule drugs (doxorubicin, curcumin) for passive incorporation into secreted EVs [136]
Non-Cell-Based Loading Methods:
- Electroporation: Applying electrical fields to create temporary pores in EV membranes for cargo incorporation [136]
- Sonication: Using ultrasound energy to disrupt EV membranes and facilitate drug loading [136]
- Freeze-Thaw Cycles: Permeabilizing EVs through repeated freezing and thawing [136]
- Direct Incubation: Simple co-incubation of isolated EVs with therapeutic compounds [136]
The following diagram illustrates the primary engineering and cargo loading strategies for MSC-EVs:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for MSC-EV Studies
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Serum-Free Media | MSC expansion under defined conditions | MSCGM-CD, chemical-defined SFM [7] |
| Isolation Reagents | EV separation and purification | Ultracentrifugation reagents, size-exclusion columns, immunoaffinity beads [132] |
| Characterization Antibodies | EV marker detection | Anti-CD63, CD81, CD9, TSG101, ALIX [135] [7] |
| Cell Culture Supplements | MSC priming to enhance EV potency | IFN-γ, TNF-α, hypoxic conditions [136] [5] |
| Transfection Reagents | Genetic modification of MSCs | Lipofectamine, electroporation systems [136] |
| Characterization Instruments | EV quantification and validation | NTA instruments, TEM, flow cytometers [132] |
The comparative analysis of MSC-derived extracellular vesicles reveals a complex landscape of therapeutic potential shaped by tissue origin. BM-MSC-EVs demonstrate particular efficacy in immune modulation and bone-related disorders, while UC-MSC-EVs show promise in regenerative applications requiring enhanced proliferation and angiogenesis. AT-MSC-EVs offer accessibility but require careful safety assessment, and placental/fetal MSC-EVs present unique differentiation capacities that may be harnessed for specific tissue engineering applications.
The future of MSC-EV therapeutics lies in strategic source selection based on target pathophysiology, combined with advanced engineering approaches to enhance specificity and potency. The development of standardized isolation protocols, comprehensive characterization standards, and rigorous safety profiling will be crucial for clinical translation. As the field progresses toward personalized medicine approaches, understanding the inherent biological differences among MSC-EVs from various tissue sources will enable researchers to design more effective, targeted cell-free therapies for specific clinical indications.
The transition from cell-based to EV-based therapeutics represents not merely a technical advancement but a conceptual evolution in regenerative medicine—one that leverages the innate therapeutic properties of MSCs while overcoming the limitations of whole-cell therapies. With continued research and methodological refinement, MSC-EVs are poised to become powerful, versatile tools in the next generation of regenerative and immunomodulatory treatments.
Conclusion
The comparative analysis of mesenchymal stem cells unequivocally demonstrates that their tissue of origin is a critical determinant of therapeutic function. Bone marrow-derived MSCs (BM-MSCs) remain the gold standard for certain immunomodulatory applications like GvHD, while adipose-derived MSCs (AD-MSCs) offer practical advantages for volume restoration in soft tissue engineering. Dental pulp and umbilical cord sources present unique profiles with enhanced proliferation and neuro-regenerative potential. Future progress hinges on moving beyond a one-size-fits-all approach. Research must focus on deeper molecular profiling to match specific MSC subtypes—or, increasingly, their purified extracellular vesicles—to patient endotypes. Standardizing isolation protocols, secretome characterization, and potency assays is paramount for advancing the field toward effective, predictable, and personalized regenerative medicines.
References
- 1. MSC Renamed? From "Stem Cells" to "Stromal Cells" [https://yoconcelltherapy.com/msc-renamed-from-stem-cells-to-stromal-cells-three-major-shifts-to-note/]
- 2. From “stem” to “stromal”: Reframing the nomenclature of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553919/]
- 3. Mesenchymal Stem Cell-Based Therapies: Challenges ... [https://link.springer.com/article/10.1007/s12013-025-01895-z]
- 4. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 5. Comparison of Mesenchymal Stromal Cells From Different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6454068/]
- 6. Comparison of human mesenchymal stem cells derived ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324912000394]
- 7. Comparative analysis of mesenchymal stem cells derived from ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-018-1104-x]
- 8. Trends in mesenchymal stem cell-derived extracellular ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1625787/full]
- 9. Stem Cells of Dental Origin: Current Research Trends and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5081960/]
- 10. Origins and Properties of Dental, Thymic, and Bone Marrow ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0046436]
- 11. Comparison of Biological Properties and Clinical Application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10276766/]
- 12. 67 mesenchymal stromal cells from different embryonic ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324921001316]
- 13. Mesenchymal Stem Cells Derived from Dental Tissues vs. ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2830488/]
- 14. Mesenchymal dental stem cells in regenerative dentistry - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3505703/]
- 15. Comparative analysis of dental-derived stem cells and ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1717849/full]
- 16. Comparative analysis of human Mesenchymal Stromal Cells ... [https://biologydirect.biomedcentral.com/articles/10.1186/s13062-025-00697-w]
- 17. An Up-To-Date Overview of Dental Tissue Regeneration ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.855396/full]
- 18. Q&A: Mesenchymal stem cells — where do they come from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4656175/]
- 19. Pericyte - an overview [https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/pericyte]
- 20. Research advances in pericyte function and their roles in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7156959/]
- 21. Pericytes in Cerebrovascular Diseases: An Emerging ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2019.00519/full]
- 22. TNAP expressing adventitial pericytes contribute to ... [https://pubmed.ncbi.nlm.nih.gov/40097085/]
- 23. A comparison of adult and neonatal tissue-derived MSC | Cell ... [https://biosignaling.biomedcentral.com/articles/10.1186/1478-811X-9-12]
- 24. Frontiers | The Perivascular and Self-Renewal of Stem Cells Niche [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2015.00367/full]
- 25. Cell origin and microenvironment: The players of ... [https://www.sciencedirect.com/science/article/abs/pii/S0040816624004105]
- 26. Editorial: Perivascular and stem cell signaling in tooth - PMC niche [https://pmc.ncbi.nlm.nih.gov/articles/PMC11825445/]
- 27. Mesenchymal stem cells: opening a new chapter in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465317/]
- 28. Stem cell-based bone and dental regeneration: a view of ... [https://www.nature.com/articles/s41368-019-0060-3]
- 29. Adipose-derived and bone marrow mesenchymal stem cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-018-0914-1]
- 30. Comparative analysis of human Mesenchymal Stromal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616983/]
- 31. Limited Adipogenic Differentiation Potential of Human ... [https://www.mdpi.com/1422-0067/25/20/11105]
- 32. Mesenchymal stromal cell therapy: Progress to date and ... [https://www.sciencedirect.com/science/article/pii/S1525001625000930]
- 33. Comparative analysis of mouse bone marrow and adipose ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-02110-x]
- 34. Embryonic mesenchyme, mesenchymal tumors and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12618774/]
- 35. Translational potential of mesenchymal stem cells in ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03885-z]
- 36. Induced Pluripotent Stem Cell‐Derived Mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6591688/]
- 37. Differentiation of Induced Pluripotent Stem Cells towards ... [https://www.nature.com/articles/s41598-019-51911-5]
- 38. Directed differentiation of human mesenchymal stromal ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961225005253]
- 39. Validated methods for isolation and qualification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12403454/]
- 40. Understanding the molecular basis of mesenchymal stem ... [https://www.nature.com/articles/s41419-025-08094-x]
- 41. Comparative Transcriptomic Profiling of Mesenchymal ... [https://link.springer.com/article/10.1007/s13770-025-00765-2]
- 42. Comparative Analysis of the Proliferation and ... [https://www.sciencedirect.com/science/article/abs/pii/S2212429225019716]
- 43. Unveiling distinctions between mesenchymal stromal cells ... [https://www.sciencedirect.com/science/article/pii/S2405844025006917]
- 44. Adipogenesis, Osteogenesis, and Chondrogenesis of Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7362937/]
- 45. Tissue source determines the differentiation potentials of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-017-0716-x]
- 46. Adipose-derived mesenchymal stem cells (MSCs) are a ... [https://www.sciencedirect.com/science/article/pii/S2452199X23003997]
- 47. Spheroid trilineage differentiation model of primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11321963/]
- 48. Comparison of biological properties of human adipose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574098/]
- 49. Trilineage Differentiation of Multipotent Human ... [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/cell-culture-and-cell-culture-analysis/primary-cell-culture/mesenchymal-stem-cell-differentiation?srsltid=AfmBOoo3YM21yDN4SqnveyO-8gutN-NrzxvnqYpldcla_XSC-KUyr4uk]
- 50. A new protocol for validation of Chondro, Adipo and Osteo ... [https://www.sciencedirect.com/science/article/abs/pii/S0040816622001951]
- 51. Fate decision of mesenchymal stem cells: adipocytes or ... [https://www.nature.com/articles/cdd2015168]
- 52. Determinants of stem cell lineage differentiation toward ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6456412/]
- 53. Mesenchymal stromal cell secretome in scaffold-based ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813025084764]
- 54. Therapeutic and Clinical Potential of Adipose-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610433/]
- 55. Comparison of production methods for mesenchymal stem ... [https://www.nature.com/articles/s41598-025-21218-9]
- 56. Comparative analysis of extracellular vesicles from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12136449/]
- 57. Proteomic profiling of plasma extracellular vesicles ... [https://www.nature.com/articles/s41598-025-06430-x]
- 58. Mesenchymal Stem Cell Immunomodulation: Mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7751844/]
- 59. Mechanisms of T-Cell Immunosuppression by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4082893/]
- 60. The Immunomodulatory Effects of Mesenchymal Stem ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.01843/full]
- 61. Macrophages in immunoregulation and therapeutics [https://www.nature.com/articles/s41392-023-01452-1]
- 62. The role and mechanisms of mesenchymal stem cells ... [https://www.sciencedirect.com/science/article/pii/S0753332223014300]
- 63. Molecular and therapeutic effects of mesenchymal stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12305160/]
- 64. Immunomodulation by Mesenchymal Stem Cells (MSCs) [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.01191/full]
- 65. Stem Cell Therapy: IV vs Injection Delivery Explained [https://adamloiacono.com/stem-cell-therapy-iv-vs-injection-delivery-explained/]
- 66. Comparison of the Efficacy and Safety of Cell-Assisted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8058798/]
- 67. Evolution of cell therapies derived from adipose tissue [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382222/]
- 68. Adipose-derived mesenchymal stem cells and their ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1617157/full]
- 69. The issue of heterogeneity of MSC-based advanced ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1400347/full]
- 70. The heterogeneity of mesenchymal stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC10734083/]
- 71. Impact of Aging on the Regenerative Properties of Bone ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0115963]
- 72. Age-related alterations and senescence of mesenchymal ... [https://www.sciencedirect.com/science/article/pii/S0047637421001111]
- 73. Donor age and breed determine mesenchymal stromal cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11871689/]
- 74. Senescence-resistant human mesenchymal progenitor ... [https://www.sciencedirect.com/science/article/abs/pii/S0092867425005719]
- 75. iPSC-, MSC- and iMSC-Derived Exosome Therapeutics [https://www.reprocell.com/blog/ipsc-msc-and-imsc-derived-exosome-therapeutics-the-cell-free-future-of-regenerative-medicine]
- 76. Mesenchymal stem cells in tumor development - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3427236/]
- 77. Mesenchymal stem cells in suppression or progression ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6756083/]
- 78. Mesenchymal stem cells in cancer progression and anticancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8570012/]
- 79. Mesenchymal stem cells in cancer therapy - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8769515/]
- 80. Targeting the tumor microenvironment with mesenchymal ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295224007263]
- 81. Method standardization of secretome production, collection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12423684/]
- 82. Exploring the therapeutic potential of MSC-derived ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04616-8]
- 83. Updated protocols for cell lysate, secretome, and exosome ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202325000568]
- 84. Limitations and challenges in the characterization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12011935/]
- 85. A Comparative Analysis of Multipotent Mesenchymal ... [https://www.nature.com/articles/s41598-020-61167-z]
- 86. Comparative computational analysis to distinguish ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10562561/]
- 87. Effectiveness of regenerative medicine for skin lightening and ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04592-z]
- 88. Comprehensive Identification and Characterization of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2019.00299/full]
- 89. Secretome analysis of in vitro aged human mesenchymal ... [https://www.nature.com/articles/s41598-018-22855-z]
- 90. First-Pass Effect - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK551679/]
- 91. Engineerable mesenchymal stem cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261791/]
- 92. Trends in mesenchymal stem cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488731/]
- 93. A roadmap to pulmonary delivery strategies for the treatment ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-022-01307-x]
- 94. Mesenchymal stem cells for lung diseases [https://www.nature.com/articles/s41420-025-02303-4]
- 95. The tiny giants of regeneration: MSC-derived extracellular ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1612589/full]
- 96. Putative microenvironmental modulators become cell therapy [https://www.sciencedirect.com/science/article/pii/S1934590921003829]
- 97. ON THE ORIGIN AND IMPACT OF MESENCHYMAL STEM ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7735381/]
- 98. The therapeutic efficacy comparison of MSCs derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077008/]
- 99. Potency assays and biomarkers for cell-based advanced ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1186224/full]
- 100. Mesenchymal Stem Cells – Sources and Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3076359/]
- 101. Comparison of Mesenchymal Stromal Cells From Different ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.00619/full]
- 102. Comparison of therapeutic effects of mesenchymal stem cells ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03350-3]
- 103. Pharmacokinetic characteristics of mesenchymal stem cells ... [https://www.nature.com/articles/s41392-024-01936-8]
- 104. Comparison of 3D culture systems on mesenchymal stem cell ... [https://pubmed.ncbi.nlm.nih.gov/41077855/]
- 105. Comparison of 3D culture systems on mesenchymal stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562725/]
- 106. Alternating 2D and 3D culture reduces cell size and ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1632810/full]
- 107. Mesenchymal Stem Cells Senescence: Mechanism and ... [https://www.medsci.org/v22p3692.htm]
- 108. Development and clinical application of human mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10784989/]
- 109. Mesenchymal Stromal Cell Secretome for the Treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8617629/]
- 110. Mesenchymal Stem Cell-Derived Extracellular Vesicles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4746282/]
- 111. Proteomic analysis of human mesenchymal stromal cell ... [https://www.nature.com/articles/s41536-019-0070-y]
- 112. Angiogenic and anti-inflammatory properties of ... [https://www.sciencedirect.com/science/article/abs/pii/S0171933516300437]
- 113. Secretome from iPSC-derived MSCs exerts proangiogenic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11287895/]
- 114. Enhancing angiogenesis through secretomes - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12167018/]
- 115. Comparison of the osteoinductive potential ... [https://pubmed.ncbi.nlm.nih.gov/41247660/]
- 116. Stem cell secretome armed magneto-actuated micromotors ... [https://www.nature.com/articles/s41467-025-61914-8]
- 117. The heterogeneity of mesenchymal stem cells: an important ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03587-y]
- 118. A meta-analysis of randomized controlled trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623177/]
- 119. Current perspectives on mesenchymal stromal cell therapy ... [https://www.nature.com/articles/s41423-023-01022-z]
- 120. Comparative effectiveness of adipose-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9850793/]
- 121. Mesenchymal stem cells in neurological disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC12636885/]
- 122. Defining minimal criteria for peer-reviewed reporting of ... [https://www.sciencedirect.com/science/article/pii/S1465324925007443]
- 123. Dental Pulp Stem Cells in Neuroregeneration - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7595495/]
- 124. Characteristics and Therapeutic Potential of Dental Pulp ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.00407/full]
- 125. Adipose Tissue-Derived Stem Cells in Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5040903/]
- 126. Adipose-derived stem cells: Sources, potency, and ... [https://www.sciencedirect.com/science/article/pii/S0753332219307346]
- 127. A comparison between adipose tissue and dental pulp as ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961211006570]
- 128. Dental pulp stem cells – A basic research and future ... [https://www.sciencedirect.com/science/article/pii/S0753332224008746]
- 129. The Role of Adipose Stem Cells in Bone Regeneration and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8143357/]
- 130. Mesenchymal Stem Cell - derived : Toward... Extracellular Vesicles [https://pubmed.ncbi.nlm.nih.gov/25868399/]
- 131. Extracellular vesicle-based therapeutics: natural versus ... [https://www.nature.com/articles/s12276-019-0223-5]
- 132. Extracellular vesicles for targeted drug delivery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12486671/]
- 133. from different sources of mesenchymal... Extracellular vesicles derived [https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-020-00427-x]
- 134. - MSC and Secreted Factors as... derived Extracellular Vesicles [https://www.frontiersin.org/research-topics/15481/msc-derived-extracellular-vesicles-and-secreted-factors-as-cell-free-therapeutic-alternatives-in-regenerative-medicine/magazine]
- 135. Comparison of therapeutic effects of mesenchymal stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10161523/]
- 136. Current Strategies and Therapeutic Applications of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11206583/]