Stem Cell Therapy Efficacy in Randomized Clinical Trials: A 2025 Landscape Analysis for Research and Development
This article provides a comprehensive analysis of the current efficacy and safety data from randomized clinical trials (RCTs) of stem cell therapies.
Stem Cell Therapy Efficacy in Randomized Clinical Trials: A 2025 Landscape Analysis for Research and Development
Abstract
This article provides a comprehensive analysis of the current efficacy and safety data from randomized clinical trials (RCTs) of stem cell therapies. Tailored for researchers, scientists, and drug development professionals, it explores the global clinical trial landscape, mechanisms of action, and therapeutic efficacy across various disease domains, including autoimmune diseases, neurological disorders, and organ failure. It critically examines methodological challenges, optimization strategies for cell sourcing and delivery, and the role of advanced imaging in efficacy validation. The review also discusses the transition towards cell-derived products and provides a forward-looking perspective on the future of regenerative medicine, synthesizing key findings to guide future clinical research and therapeutic development.
The Global Landscape and Mechanistic Foundations of Stem Cell Therapy
Stem cell therapy has emerged as a transformative approach in regenerative medicine, offering potential solutions for some of the most challenging autoimmune, cardiovascular, and neurological conditions. The analysis of clinical trial data provides critical insights into the evolution, current status, and future direction of this dynamic field. This comprehensive analysis leverages data from Trialtrove, a premier clinical intelligence database, to examine global trends in stem cell clinical trials from 2006 to 2025. The focus centers on evaluating the efficacy profiles of these therapies across different disease areas based on evidence from randomized controlled trials (RCTs), which represent the gold standard for therapeutic validation.
Research communities have demonstrated vigorous commitment to studying potential applications across a wide range of diseases, with the past few years witnessing exponential advancement in clinical trials revolving around stem cell-based therapies [1]. By examining nearly two decades of trial data, this analysis identifies patterns in therapeutic focus, geographic distribution, methodological approaches, and efficacy outcomes that are shaping the next generation of stem cell treatments. The findings presented herein offer researchers, scientists, and drug development professionals an evidence-based perspective on the current state and future trajectory of stem cell therapeutics.
Table 1: Global Stem Cell Clinical Trial Overview (2006-2025)
| Analysis Category | Key Findings | Data Source |
|---|---|---|
| Total Trials Analyzed | 1,511 global trials screened; 244 included after eligibility assessment | Trialtrove [2] |
| Trial Phase Distribution | 83.6% in Phase I-II; 16.4% in Phase III | Trialtrove [2] |
| Leading Disease Areas | Crohn's disease (n=85), SLE (n=36), scleroderma (n=32) | Trialtrove [2] |
| Geographic Leadership | U.S. and China leading in trial numbers | Trialtrove [2] |
| Primary Funding Sources | Academic institutions (49.2% of trials) | Trialtrove [2] |
| Therapeutic Mechanisms | Immune modulation, tissue repair via growth factors, anti-infection/anti-proliferative effects | Trialtrove [2] |
The analysis of Trialtrove data reveals a field in transition, with stem cell therapies demonstrating promising efficacy in specific autoimmune and neurological conditions while showing more limited benefits in cardiovascular applications. The predominance of early-phase trials (83.6% in Phase I-II) indicates a technology still in its relative infancy regarding regulatory approval but with substantial research interest [2]. Disease-specific variations in both cell sources and administration routes highlight the tailored approach required for different therapeutic areas.
Beyond the stem cell-specific trends, the broader clinical trial landscape has shown notable shifts in 2024-2025, with a 5.5% increase in Phase I-III trial initiations and particularly strong growth in autoimmune and inflammation studies (17% surge) according to Citeline's Annual Clinical Trials Roundup [3] [4]. This growth occurs amidst changing regional patterns, including China's expanding role in rare disease trials (now representing 47% share) and Europe's rebound in trial activity post-conflict [3].
Therapeutic Area Efficacy Analysis
Autoimmune and Rheumatic Diseases
Table 2: Stem Cell Efficacy in Autoimmune Diseases (Meta-Analysis of 42 RCTs)
| Disease Area | Therapeutic Outcome | Efficacy Measures | Safety Profile |
|---|---|---|---|
| Osteoarthritis (OA) | Significant symptom improvement | VAS: Bone marrow SMD=-0.95; Umbilical cord SMD=-1.25; Adipose tissue SMD=-1.26 [5] | No increased adverse events (RR=1.23, P=0.15) [5] |
| Systemic Lupus Erythematosus (SLE) | Significant disease activity reduction | SLEDAI: SMD=-2.32, P=0.0003 [5] | No increased adverse events (RR=0.83, P=0.76) [5] |
| Inflammatory Bowel Disease | Improved clinical efficacy | RR=2.02, P<0.00001 [5] | No increased adverse events (RR=0.99, P=0.96) [5] |
| Multiple Sclerosis | Limited symptom improvement | Not significant [5] | No increased adverse events (RR=1.12, P=0.50) [5] |
| Systemic Sclerosis | Limited symptom improvement | Not significant [5] | Consistent safety profile [5] |
Mesenchymal stem cell (MSC) transplantation has demonstrated particularly promising results for several rheumatic and autoimmune conditions, according to a systematic review and meta-analysis of 42 RCTs involving 2,183 participants [5]. The analysis encompassed rheumatoid arthritis (RA), osteoarthritis (OA), spondyloarthritis, systemic sclerosis arthritis, systemic lupus erythematosus (SLE), inflammatory bowel disease, multiple sclerosis, and primary Sjögren's syndrome (PSS). The findings reveal a differential efficacy profile across conditions, with MSC transplantation demonstrating significant benefits for OA, SLE, and inflammatory bowel disease, while showing more limited impact on multiple sclerosis and systemic sclerosis.
The safety profile across these applications is notably consistent, with no significant increase in adverse events compared to control groups [5]. This safety record, coupled with the immunomodulatory properties of MSCs, positions stem cell therapy as a viable alternative treatment option for autoimmune and rheumatic immune diseases, particularly for conditions that have shown responsiveness in clinical trials. The therapeutic mechanisms primarily involve immunomodulation, tissue repair via growth factors, and anti-infection/anti-proliferative effects [2].
Cardiovascular Diseases
The efficacy profile of stem cell therapy in cardiovascular applications presents a more complex picture. A comprehensive meta-analysis of 48 RCTs examining stem cell preparations in acute myocardial infarction (AMI) found no significant benefit on clinical endpoints including all-cause mortality, recurrent myocardial infarction, severe adverse events, heart failure hospitalization, cancer incidence, or stroke [6]. The risk ratios for these endpoints were 0.73, 0.93, 0.67, 0.79, 0.82, and 0.81 respectively, with none reaching statistical significance.
Despite the lack of impact on clinical endpoints, modest functional improvements were observed in echocardiographic left ventricular ejection fraction (LVEF), which improved significantly at study end with a mean difference of 2.53% and a difference from baseline of 3.89% [6]. This improvement, however, was characterized by high heterogeneity (I² = 76%), suggesting variable responses across patient populations or methodologies. When assessed via MRI—considered a more precise imaging modality—LVEF showed no significant change at study end but demonstrated a modest improvement from baseline (MD 1.37%) [6].
For advanced heart failure, a systematic review of 27 clinical trials conducted between 2014 and 2024 noted that while various stem cell approaches (including cardiac stem cells, cardiosphere-derived cells, bone marrow-derived mononuclear cells, mesenchymal stem cells, and pluripotent stem cells) have demonstrated clinically acceptable safety profiles, their efficacy varies and has yet to be conclusively confirmed [7]. The field has seen a shift in focus toward the paracrine signaling effects of injected cells rather than direct differentiation and replacement of damaged tissue.
Neurological Applications
Stem cell therapy for ischemic stroke has demonstrated more encouraging results, particularly for long-term functional outcomes. A systematic review and meta-analysis of 13 RCTs involving 872 patients with acute/subacute ischemic stroke found that stem cell transplantation within one month of onset significantly improved functional outcomes at specific timepoints [8]. The primary outcome was measured using the modified Rankin Scale (mRS), where scores of 0-1 represent minimal or no symptoms, and 0-2 represent functional independence.
The analysis revealed that the 1-year incidence of mRS scores 0-1 was significantly higher in the cell-therapy group (45/195) compared to the control group (23/179), with a risk ratio of 1.74 [8]. At the 90-day mark, the incidence of mRS scores 0-2 was also higher in the treatment group. Importantly, stem cell therapy was not associated with increased serious adverse events or mortality, supporting its safety profile in neurological applications [8].
The timing of functional assessment appears crucial in evaluating outcomes, as differences in NIHSS scores became significant only at the 180-day mark, highlighting the importance of longer follow-up periods in stroke trials [8]. These findings suggest that stem cell therapy for acute/subacute ischemic stroke is safe and can improve long-term functional outcomes, though treatment protocols require further standardization.
Methodology and Experimental Protocols
Data Source and Retrieval Methodology
The foundation of this analysis derives from Trialtrove, a comprehensive clinical intelligence database that aggregates data from more than 60,000 trusted sources including clinical trial registries, conference presentations, scientific literature, and regulatory documents [9]. The database provides curated, real-world intelligence on trial design, enrollment timelines, patient populations, endpoints, outcomes, and geographic trends, enabling robust benchmarking and trend analysis.
For the specific analysis of autoimmune disease trials, researchers extracted clinical trial data from 2006-2025 from Trialtrove, applying strict inclusion criteria that restricted the analysis to interventional trials while excluding observational studies, non-autoimmune disease trials, and records with incomplete information [2]. From an initial identification of 1,511 global trials, 244 were included after rigorous screening and cross-referencing, with descriptive statistics used to analyze trial phases, disease types, geographic distribution, funding sources, therapeutic mechanisms, and stem cell sources.
Meta-Analysis Protocol Standards
The efficacy data presented in this analysis primarily derives from systematic reviews and meta-analyses conducted according to PRISMA guidelines and registered in international prospective registers of systematic reviews (PROSPERO) [6] [8] [5]. These analyses employed comprehensive search strategies across multiple databases including PubMed, Embase, Cochrane, Web of Science, and regional databases, without language restrictions.
Statistical analysis typically utilized RevMan software with random-effects models depending on heterogeneity [6] [5]. Measures of effect included risk ratios with 95% confidence intervals for dichotomous variables and mean differences or standardized mean differences for continuous variables. Heterogeneity was assessed using the I² statistic, with values exceeding 50% indicating substantial heterogeneity. Risk of bias was evaluated using the Cochrane Risk of Bias tool, with sensitivity analyses conducted to test the robustness of findings.
Endpoint Selection and Standardization
Across the analyzed trials, standardized endpoint selection was critical for meaningful cross-trial comparisons. For cardiovascular trials, primary outcomes typically included all-cause mortality, recurrent myocardial infarction, severe adverse events, hospitalization for heart failure, cancer incidence, and left ventricular ejection fraction [6]. Neurological trials predominantly utilized the modified Rankin Scale for functional outcomes, supplemented by NIH Stroke Scale scores and Barthel Index scores [8]. Autoimmune disease trials employed disease-specific activity indices such as SLEDAI for lupus, VAS for osteoarthritis, and clinical efficacy rates for inflammatory bowel disease [5].
The consistent application of these validated endpoints enables more reliable pooling of data across studies and enhances the statistical power to detect treatment effects in meta-analyses. This methodological standardization is particularly important in stem cell research, where variations in cell sources, preparation methods, administration routes, and patient populations can contribute to significant heterogeneity in outcomes.
Technical and Resource Requirements
Table 3: Essential Research Reagent Solutions for Stem Cell Clinical Trials
| Research Reagent | Function and Application | Experimental Context |
|---|---|---|
| Bone Marrow Aspiration Kits | Source for BMMNCs and MSCs | AMI trials; Autoimmune disease research [6] [5] |
| Cell Separation Media | Isolation of mononuclear cells via density gradient centrifugation | Preparation of BMMNCs for intracoronary administration [6] |
| X VIVO 10 Media | Serum-free cell culture medium for MSC expansion | Clinical-grade cell preparation [6] |
| CD133+ Selection Kits | Immunomagnetic selection of specific progenitor cell populations | Isolation of CD133+ cells for cardiovascular repair [6] |
| Multiple Electrolytes Injection | Vehicle solution for cell suspension and control injections | Placebo preparation in controlled trials [6] |
| Heparinized Saline | Anticoagulant solution for intracoronary cell delivery | Standardized administration in cardiovascular applications [6] |
| Flow Cytometry Antibody Panels | Characterization of cell surface markers (CD105, CD73, CD90, CD45, CD34) | Verification of MSC phenotype per ISCT criteria [5] |
| Cryopreservation Media | Maintenance of cell viability during storage and transport | Logistics management in multicenter trials [9] |
The successful implementation of stem cell clinical trials requires specialized reagents and materials that ensure cell viability, purity, and functional potency. Cell sourcing and characterization represent critical initial steps, with bone marrow aspiration, adipose tissue extraction, or umbilical cord collection serving as primary tissue sources [6] [5]. The International Society for Cellular Therapy (ISCT) defines MSCs by specific criteria including plastic adherence, expression of CD105, CD73, and CD90, and lack of expression of hematopoietic markers, necessitating standardized flow cytometry protocols [5].
The administration route and formulation vary significantly by disease application. Intracoronary injection through balloon catheters is standard for cardiovascular applications, while intravenous infusion is common for systemic autoimmune conditions [6]. Suspension media including heparinized saline, normal saline, and specialized electrolyte solutions serve as both vehicle controls and cell carriers, highlighting their importance in trial design [6]. Dose optimization remains an area of active investigation, with trials exploring ranges from millions to billions of cells depending on the application and cell type.
The analysis of Trialtrove data from 2006-2025 reveals a field characterized by continued innovation and methodological refinement. The differential efficacy profiles across disease areas highlight the importance of target selection, with particularly promising results in autoimmune conditions like SLE, OA, and inflammatory bowel disease, and functional improvement in stroke recovery [8] [5]. In contrast, cardiovascular applications have demonstrated more modest functional benefits without significant impact on major clinical endpoints [6].
Future developments in the field will likely prioritize technological innovation, international collaboration, and precision medicine approaches to address current challenges [2]. The growing trial activity in autoimmune and inflammatory conditions (17% surge according to recent data) indicates shifting research priorities [3]. Additionally, advancements in cell engineering, delivery methods, and patient selection criteria hold potential for enhancing therapeutic efficacy across applications.
The safety profile of stem cell therapies remains consistently acceptable across diverse applications, with no significant increase in adverse events compared to control groups in multiple meta-analyses [6] [8] [5]. This safety record, coupled with promising efficacy in specific indications, supports the continued investigation of stem cell therapies as potential treatment options for conditions with significant unmet medical needs. As the field matures, standardization of protocols, validation of potency assays, and clarification of mechanistic pathways will be critical for advancing from investigational use to standardized clinical application.
Stem Cell Therapy Efficacy in Randomized Clinical Trials Research
Stem cell therapy represents a revolutionary frontier in regenerative medicine, offering potential treatments for a range of debilitating diseases by harnessing the unique properties of stem cells for self-renewal, multilineage differentiation, and immunomodulation [10]. The therapeutic potential of various stem cell types, including mesenchymal stem cells (MSCs), hematopoietic stem cells (HSCs), neural stem cells (NSCs), and induced pluripotent stem cells (iPSCs), has been explored across diverse medical conditions [11]. This review systematically evaluates the efficacy of stem cell therapies for autoimmune, neurological, and metabolic conditions within the framework of randomized controlled trials (RCTs), providing evidence-based comparisons to guide researchers and drug development professionals. We synthesize quantitative data from recent meta-analyses and clinical trials, detail experimental methodologies, and visualize key mechanistic pathways to offer a comprehensive assessment of the current landscape.
Analysis of Disease Targets
Autoimmune Diseases
Autoimmune diseases, characterized by immune dysregulation and chronic inflammation, represent a major focus of stem cell therapy research. Current therapies often lack sustained efficacy and safety, necessitating alternative approaches [12].
- Clinical Trial Landscape: A systematic review of global clinical trials from 2006 to 2025 identified 244 interventional trials focusing on stem cell therapy for autoimmune diseases. The most frequently studied conditions were Crohn's disease (n=85), systemic lupus erythematosus (SLE, n=36), and scleroderma (n=32). The majority (83.6%) of these trials were in early phases (Phase I-II), with the United States and China leading in trial numbers [12].
- Efficacy of MSC Transplantation: A 2025 meta-analysis of 42 RCTs involving 2,183 participants provided robust evidence for the efficacy of MSC transplantation in specific autoimmune and rheumatic diseases [5]. The analysis demonstrated significant symptom improvement in several conditions, while revealing limited benefits in others.
Table 1: Efficacy of Mesenchymal Stem Cell (MSC) Transplantation in Autoimmune and Rheumatic Diseases (Meta-Analysis of RCTs)
| Disease | Outcome Measure | Effect Size [95% CI] | P-value | Source Tissue |
|---|---|---|---|---|
| Osteoarthritis (OA) | VAS Pain Score | SMD = -1.25 [-2.04 to -0.46] | 0.002 | Umbilical Cord [5] |
| Osteoarthritis (OA) | VAS Pain Score | SMD = -1.26 [-1.99 to -0.52] | 0.0009 | Adipose Tissue [5] |
| Osteoarthritis (OA) | VAS Pain Score | SMD = -0.95 [-1.55 to -0.36] | 0.002 | Bone Marrow [5] |
| Systemic Lupus Erythematosus (SLE) | SLEDAI Disease Activity | SMD = -2.32 [-3.59 to -1.06] | 0.0003 | Not Specified [5] |
| Inflammatory Bowel Disease (IBD) | Clinical Efficacy | RR = 2.02 [1.53 to 2.67] | < 0.00001 | Not Specified [5] |
| Multiple Sclerosis | Symptom Improvement | Not Significant | - | Not Specified [5] |
| Systemic Sclerosis | Symptom Improvement | Not Significant | - | Not Specified [5] |
Abbreviations: CI, Confidence Interval; RR, Risk Ratio; SMD, Standardized Mean Difference; SLEDAI, Systemic Lupus Erythematosus Disease Activity Index; VAS, Visual Analogue Scale.
- Safety Profile: The same meta-analysis confirmed the safety of MSC transplantation, finding no significant increase in the incidence of adverse events across studies for osteoarthritis, SLE, inflammatory bowel disease, and multiple sclerosis [5].
Neurological Diseases
Ischemic Stroke
Stem cell therapy has been investigated as a means to promote repair and regeneration following ischemic stroke, a leading cause of global disability and mortality [13].
- Efficacy on Functional Outcomes: A 2025 meta-analysis of 13 RCTs involving 872 patients with acute/subacute ischemic stroke evaluated the long-term efficacy of stem cell therapy administered within one month of onset [8]. The analysis revealed significant improvements in functional independence, particularly at long-term follow-up.
- The primary outcome, the modified Rankin Scale (mRS) score (where 0-1 indicates excellent functional outcome), showed a significantly higher incidence in the cell-therapy group at 1 year (45/195 vs. 23/179 in controls; RR=1.74, 95% CI 1.09-2.77) [8].
- At 90 days, the incidence of mRS scores 0-2 (functional independence) was also higher in the cell-therapy group (RR=1.31, 95% CI 1.01-1.70) [8].
- Safety: The therapy was not associated with an increased incidence of serious adverse events or mortality, supporting its safety profile in stroke patients [8].
Neurodegenerative Diseases
For chronic neurodegenerative diseases (NDs) like Alzheimer's disease (AD), Parkinson's disease (PD), Amyotrophic Lateral Sclerosis (ALS), and Huntington's disease (HD), stem cell therapy aims to replace lost neurons and modulate the disease environment [14].
- Clinical Trial Landscape: A systematic review identified 94 clinical trials for these four NDs. The field is predominantly in early stages, with only three Phase 3 trials identified (one each for ALS and HD completed, and one ongoing in ALS). Over 8,000 participants have been enrolled, with nearly 70% in AD-related studies [14].
- Promising Alternatives: Stem cell-derived exosomes have emerged as a promising cell-free alternative. These nanovesicles can cross the blood-brain barrier more efficiently than stem cells, deliver therapeutic molecules directly to the brain, and exhibit a reduced risk of immunological rejection and tumorigenicity. While most research is preclinical, clinical investigations are anticipated to increase [14].
Metabolic Diseases
The search results indicate a comparative lack of recent, high-level meta-analyses or systematic reviews focusing specifically on stem cell therapy for metabolic conditions like diabetes mellitus within the provided data. While one review mentions the "unprecedented therapeutic opportunities" for a range of conditions including diabetes, it does not provide specific efficacy data from clinical trials [11]. Another review on heart failure, which can have metabolic components, notes that stem cell therapies have demonstrated clinically acceptable safety profiles but that their efficacy "varies and has yet to be conclusively confirmed" [7]. This highlights a significant area for future targeted clinical research.
Experimental Protocols and Methodologies
The validity of RCT findings hinges on rigorous and standardized experimental protocols. This section details methodologies commonly employed in the cited trials.
Trial Design and Patient Selection
The highest quality evidence comes from RCTs that adhere to strict guidelines.
- Registration and Protocol: Trials should be pre-registered in databases like ClinicalTrials.gov, and follow published protocols (e.g., on PROSPERO for systematic reviews) [5] [8].
- Participants: Participants must meet recognized diagnostic criteria for the target disease (e.g., the American College of Rheumatology criteria for rheumatoid arthritis or standardized stroke diagnosis) [5] [8].
- Intervention and Control: The experimental group receives the stem cell product (e.g., MSCs from various sources), while the control group receives a placebo, conventional therapy, or standard care [5] [8].
- Outcomes: Primary and secondary outcomes are defined a priori. These are often disease-specific functional scores, such as the mRS for stroke, SLEDAI for SLE, or VAS for pain in osteoarthritis [5] [8].
Stem Cell Preparation and Characterization
The process of preparing the cellular product is critical for consistency and safety.
- Source and Isolation: MSCs are isolated from tissues like bone marrow, adipose tissue, or umbilical cord via enzymatic digestion or density gradient centrifugation. iPSCs are generated by reprogramming somatic cells [11] [10].
- Characterization: According to International Society for Cellular Therapy (ISCT) standards, MSCs must be adherent to plastic; express surface markers CD105, CD73, and CD90 (≥95%); lack expression of hematopoietic markers CD45, CD34, CD14, CD11b, CD79α, CD19, and HLA-DR (≤2%); and possess the capacity to differentiate into osteoblasts, adipocytes, and chondrocytes in vitro [10].
- Quality Control: Tests for viability, sterility (mycoplasma, bacteria, fungi), and potency are essential before clinical administration.
Administration and Follow-up
- Route of Administration: This varies by disease target. Common routes include intravenous (IV) infusion, intra-arterial injection, intrathecal injection, or direct implantation into the target tissue [13] [14].
- Dosing and Timing: Trials investigate optimal cell doses (e.g., 1-2 million cells per kg body weight) and the ideal therapeutic time window (e.g., within 36 hours for acute stroke vs. chronic phase for neurodegenerative diseases) [13] [8].
- Follow-up and Monitoring: Patients are followed for extended periods (e.g., 1-5 years) to assess both primary efficacy outcomes and long-term safety, including monitoring for adverse events and potential tumorigenicity [5] [8].
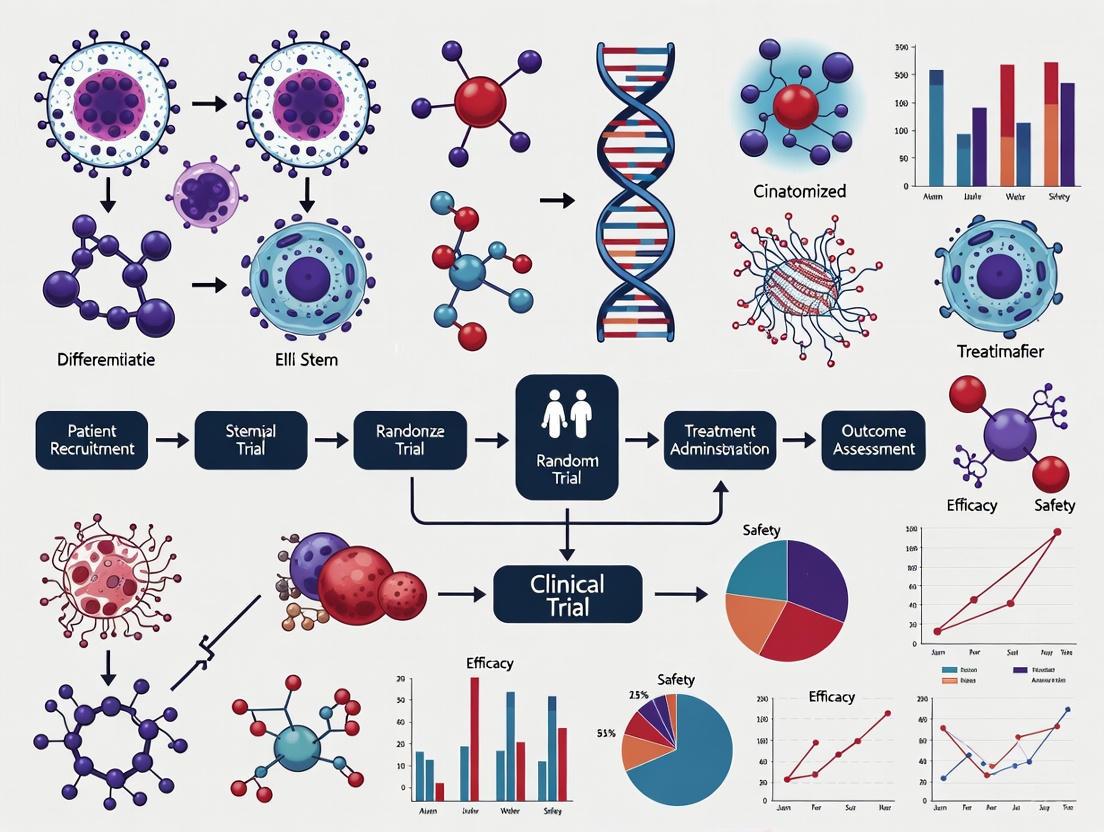
Visualization of Key Mechanisms
The therapeutic effects of stem cells, particularly MSCs, are mediated through multiple interconnected mechanisms. The following diagram illustrates the primary pathways through which MSCs exert their therapeutic effects in autoimmune and neurological diseases.
Diagram 1: Key Therapeutic Mechanisms of Mesenchymal Stem Cells (MSCs). MSCs mediate their effects primarily through paracrine signaling of bioactive molecules, immunomodulation via interactions with diverse immune cells, and direct repair mechanisms including mitochondrial transfer and differentiation. VEGF: Vascular Endothelial Growth Factor; HGF: Hepatocyte Growth Factor; Tregs: Regulatory T-cells.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials essential for conducting preclinical and clinical research in stem cell therapy.
Table 2: Essential Reagents and Materials for Stem Cell Therapy Research
| Reagent/Material | Function in Research | Specific Examples |
|---|---|---|
| Cell Culture Media | Supports the growth, expansion, and maintenance of stem cells in vitro. | Defined media (e.g., DMEM/F12) supplemented with growth factors like FGF-2 for MSC expansion; TeSR-E8 for pluripotent stem cells. |
| Characterization Antibodies | Flow cytometry analysis to confirm stem cell identity based on surface marker expression. | Anti-CD105, Anti-CD73, Anti-CD90 (positive markers); Anti-CD45, Anti-CD34, Anti-HLA-DR (negative markers for MSCs) [10]. |
| Differentiation Kits | Induces stem cell differentiation into specific lineages to confirm multipotency. | Osteogenic, adipogenic, and chondrogenic differentiation kits (e.g., containing dexamethasone, ascorbate, insulin, TGF-β3) [10]. |
| Extracellular Vesicle Isolation Kits | Isolates exosomes and other EVs from stem cell culture supernatants for mechanistic studies or therapeutic use. | Polymer-based precipitation kits, size-exclusion chromatography columns, or tangential flow filtration systems. |
| Animal Disease Models | Preclinical testing of stem cell therapy safety and efficacy. | Transgenic mouse models of AD/PD, Middle Cerebral Artery Occlusion (MCAO) model for stroke, collagen-induced arthritis model. |
| In Vivo Imaging Systems | Tracks the biodistribution, persistence, and fate of transplanted cells in live animals. | Bioluminescence (BLI) and Fluorescence (FLI) imaging systems; MRI for anatomical and functional assessment [13]. |
This comparison guide synthesizes current evidence from randomized clinical trials on stem cell therapy for autoimmune, neurological, and metabolic conditions. The data demonstrates a promising yet nuanced picture: stem cell therapy, particularly using MSCs, shows significant efficacy and a favorable safety profile in specific autoimmune diseases like SLE, OA, and IBD, as well as in improving long-term functional outcomes after ischemic stroke. In contrast, the evidence for its application in neurodegenerative diseases is still in earlier phases of clinical validation, and robust data for metabolic diseases remains limited. The field is rapidly evolving with the emergence of innovative approaches such as stem cell-derived exosomes and engineered iPSCs, which may address current challenges related to tumorigenicity and poor cell integration. Future progress will depend on standardizing treatment protocols, conducting larger Phase III trials, and leveraging advanced imaging and 'omics' technologies to better understand therapeutic mechanisms and identify responsive patient populations.
Stem cell therapies have emerged as a transformative approach in regenerative medicine, demonstrating significant potential in treating conditions ranging from degenerative diseases to hematologic disorders and organ failure. Within the clinical trial landscape, three stem cell types have garnered predominant focus: Mesenchymal Stem Cells (MSCs), valued for their immunomodulatory properties and tissue repair capabilities; Pluripotent Stem Cells (PSCs), including induced pluripotent stem cells (iPSCs) and embryonic stem cells (ESCs), prized for their unlimited differentiation potential; and Hematopoietic Stem Cells (HSCs), the workhorse of established transplant medicine for blood and immune system reconstitution [10] [15]. The therapeutic application of these cells hinges on their unique biological properties—MSCs act largely through paracrine signaling and immunomodulation, PSCs offer potential for cell replacement through their pluripotency, and HSCs provide curative potential for hematologic diseases through direct engraftment and differentiation [10] [16]. This review systematically compares the efficacy, safety, and clinical applications of these key stem cell types based on current clinical trial evidence, providing researchers and drug development professionals with a data-driven analysis of their respective positions in modern medicine.
Mesenchymal Stem Cells (MSCs): The Immunomodulatory Workhorse
Biological Properties and Clinical Mechanisms
Mesenchymal stem cells are multipotent stromal cells characterized by their capacity for self-renewal and differentiation into mesodermal lineages including osteoblasts, chondrocytes, and adipocytes [10]. According to International Society for Cellular Therapy (ISCT) standards, MSCs must express specific surface markers (CD73, CD90, and CD105 ≥95%) while lacking expression of hematopoietic markers (CD34, CD45, CD14 or CD11b, CD79α or CD19, HLA-DR ≤2%) [10]. The therapeutic effects of MSCs are mediated primarily through paracrine mechanisms rather than direct differentiation, releasing bioactive molecules including growth factors, cytokines, and extracellular vesicles that modulate the local cellular environment, promote tissue repair, angiogenesis, and exert anti-inflammatory effects [10] [7]. MSCs additionally interact with various immune cells—including T cells, B cells, dendritic cells, and macrophages—modulating immune responses through both direct cell-cell contacts and release of immunoregulatory molecules [10].
MSCs are isolated from multiple tissue sources, each with distinct functional characteristics:
- Bone Marrow-derived MSCs (BM-MSCs): The most extensively studied type, known for high differentiation potential and strong immunomodulatory effects [10]
- Adipose-derived MSCs (AD-MSCs): Easier to harvest in greater quantities with comparable therapeutic properties [10]
- Umbilical Cord-derived MSCs (UC-MSCs): Exhibit enhanced proliferation capacity and lower immunogenicity, suitable for allogeneic transplantation [10]
A 2024 meta-analysis directly compared these sources for knee osteoarthritis treatment, with functional improvement assessed via WOMAC scores and pain relief via VAS scores [17]. The following table summarizes the comparative efficacy data:
Table 1: Comparative Efficacy of MSC Sources in Knee Osteoarthritis (6-month follow-up)
| Outcome Measure | BM-MSC vs. AD-MSC (MD, 95% CI) | BM-MSC vs. UC-MSC (MD, 95% CI) |
|---|---|---|
| WOMAC Total | -20.12 (-125.24 to 42.88) | -7.81 (-158.13 to 74.99) |
| WOMAC Stiffness | -0.51 (-7.27 to 4.29) | -0.75 (-9.74 to 6.63) |
| WOMAC Functional Limitation | -12.22 (-35.05 to 18.86) | -9.31 (-44.26 to 35.27) |
| WOMAC Pain | -11.42 (-39.52 to 11.77) | -6.73 (-47.36 to 29.15) |
MD: Mean Difference; CI: Confidence Interval [17]
While most differences were not statistically significant, the meta-analysis concluded that BM-MSCs may present clinical advantages over other MSC sources for functional improvement, with BM-MSCs and UC-MSCs potentially offering superior pain relief compared to AD-MSCs [17].
Experimental Protocols in MSC Clinical Trials
Standardized protocols for MSC isolation, expansion, and characterization are critical for clinical trial reproducibility. Typical manufacturing processes include:
- Isolation: Mononuclear cell separation via density gradient centrifugation from bone marrow aspirate, adipose tissue digestion, or umbilical cord extraction
- Expansion: Culture in serum-free media supplemented with growth factors (primarily FGF-2) under strict Good Manufacturing Practice (GMP) conditions
- Characterization: Flow cytometry verification of surface marker expression (≥95% positive for CD73, CD90, CD105; ≤2% positive for hematopoietic markers) and differentiation assays into osteogenic, chondrogenic, and adipogenic lineages [10]
For osteoarthritis trials referenced in Table 1, the typical intervention involved single intra-articular injections of 10-100×10^6 MSCs, with efficacy outcomes measured at 6 and 12 months using standardized scoring systems (WOMAC, VAS) [17].
Figure 1: MSC Clinical Trial Workflow from cell isolation to outcome assessment
Pluripotent Stem Cells: The Differentiative Powerhouses
Biological Properties and Clinical Transition
Pluripotent stem cells, comprising both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), are defined by their capacity for unlimited self-renewal and ability to differentiate into derivatives of all three germ layers [15]. While ESCs originate from the inner cell mass of blastocysts, iPSCs are generated through reprogramming of somatic cells by introducing specific transcription factors (OCT4, SOX2, c-MYC, and KLF4) [18] [15]. iPSCs have emerged as particularly promising due to their avoidance of ethical concerns associated with ESCs and their potential for patient-specific therapies, though most current clinical applications favor allogeneic approaches [19] [15].
The clinical transition of PSC-based therapies has accelerated remarkably. According to the Human Pluripotent Stem Cell Registry (hPSCreg) database, since 2018 there has been a definitive switch toward iPSCs, with allogeneic approaches dominating over personalized medicines [19]. As of 2023, 109 clinical studies using PSCs were recorded, targeting 44 different diseases across 14 countries [19].
Clinical Applications and Trial Outcomes
PSC-derived therapies have diversified significantly, with 22 different cell types now used in clinical trials. The most frequent applications include:
- Retinal Pigment Epithelial Cells: Used in 22 clinical trials for degenerative eye diseases such as age-related macular degeneration
- NK Cell-like Derivatives: Employed in 18 clinical studies, predominantly initiated within the last five years, many incorporating chimeric antigen receptors (CARs) for cancer immunotherapy
- Cardiomyocyte-like Cells: Applied in 12 studies targeting heart failure through direct myocardial regeneration
- Tissue-Specific Stem Cells/MSC-like Cells: Utilized in 12 trials leveraging their immunomodulatory properties for diverse disease targets [19]
Table 2: Current Clinical Applications of PSC-Derived Cell Therapies
| Cell Type | Number of Trials | Primary Indications | Notable Characteristics |
|---|---|---|---|
| Retinal Pigment Epithelial Cells | 22 | Degenerative eye diseases | Most established application; multiple phase II/III trials |
| NK Cell-like Derivatives | 18 | Liquid and solid tumors | Often CAR-modified; predominantly industry-sponsored |
| Cardiomyocyte-like Cells | 12 | Heart failure | Addressing myocardial regeneration; safety established |
| Tissue-Specific Stem Cells | 12 | Diverse inflammatory/autoimmune conditions | Immunomodulatory properties; multiple mechanisms |
While comprehensive efficacy data from phase III trials remains limited, the safety profile of PSC-derived therapies has been generally acceptable across applications [19] [7]. Study durations range from 1 to 19 years (median 7 years), reflecting the long-term follow-up required for these novel interventions [19].
Experimental Protocols and Manufacturing
Critical to PSC clinical translation is robust differentiation protocols and manufacturing:
- Reprogramming: For iPSCs, somatic cells (typically dermal fibroblasts) are reprogrammed using non-integrating Sendai virus or episomal vectors expressing OCT4, SOX2, c-MYC, and KLF4 [18]
- Differentiation: Directed differentiation using stage-specific growth factors and small molecules—for example, retinal pigment epithelial cells via dual SMAD inhibition, cardiomyocytes through Wnt modulation
- Purification: Cell sorting for specific surface markers or metabolic selection to eliminate undifferentiated pluripotent cells
- Quality Control: Karyotyping, pluripotency confirmation, and teratoma formation assays to ensure genetic stability and prevent tumorigenicity [19] [18]
The field faces standardization challenges, with most clinical trials not publicly disclosing the specific PSC lines used—only 11 ESC lines and 1 iPSC line could be traced across all registered trials [19].
Figure 2: PSC differentiation and therapeutic application workflow
Hematopoietic Stem Cells: The Established Curative Modality
Biological Properties and Clinical Applications
Hematopoietic stem cells are multipotent stem cells responsible for lifelong production of all blood cell lineages, residing primarily in bone marrow but mobilizable to peripheral blood and present in umbilical cord blood [20] [16]. HSCs are characterized by surface markers CD34+, CD59+, CD90+, CD38-, and CD45RA-, though clinical transplantation typically uses heterogeneous populations containing HSCs [16]. Allogeneic hematopoietic stem cell transplantation (allo-HSCT) represents the most established stem cell therapy, offering curative potential for various hematologic disorders, immune deficiencies, and genetic diseases through complete reconstitution of the recipient's hematopoietic system [20] [16].
Efficacy and Safety Outcomes Across Indications
Substantial clinical trial data supports HSCT efficacy across conditions:
- Sickle Cell Disease (SCD): A 2025 meta-analysis of 58 studies (n=7,931) demonstrated 94% overall survival (OS) and 86% event-free survival (EFS) post-allo-HSCT, with graft failure (GF) at 9% and mortality at 6% [16]
- Hepatitis-Associated Aplastic Anemia (HAAA): A 2023 retrospective analysis comparing immunosuppressive therapy (IST) with HSCT showed 5-year OS of 83.7±4.9% for IST versus 93.3±6.4% for matched-sibling donor HSCT and 80.8±12.3% for haploidentical-HSCT [20]
- Hematologic Response Rates: HSCT recipients exhibited significantly more rapid and sustained hematopoiesis than IST (HR 76.92%, 96.15% and 96.15% at 3, 6 and 12 months, respectively, versus 55.71% at 6 months for IST) [20]
Table 3: Hematopoietic Stem Cell Transplantation Outcomes Across Indications
| Condition | Study Scale | Overall Survival | Event-Free Survival | Graft Failure | Key Complications |
|---|---|---|---|---|---|
| Sickle Cell Disease | 58 studies (n=7,931) | 94% | 86% | 9% | aGVHD (20%), cGVHD (14%) |
| HAAA (MSD-HSCT) | Single-center (n=26) | 93.3±6.4% (5-year) | 93.3±6.4% (5-year) | Not specified | Infection, GVHD |
| HAAA (IST) | Single-center (n=70) | 83.7±4.9% (5-year) | 64.3±6.0% (5-year) | Not applicable | Relapse, clonal evolution |
Subgroup analyses demonstrate that clinical outcomes vary significantly based on donor type (matched sibling donor vs. haploidentical), conditioning regimens (myeloablative vs. reduced intensity), and stem cell sources (bone marrow vs. peripheral blood vs. cord blood) [20] [16]. Personalized conditioning regimens and post-transplantation prophylaxis strategies are critical for minimizing graft-versus-host disease (GVHD) and graft failure issues [16].
Experimental Protocols in HSCT Trials
Standardized HSCT protocols include:
- Conditioning Regimens: Myeloablative (e.g., busulfan/cyclophosphamide) or reduced-intensity (e.g., fludarabine-based) regimens to eliminate recipient immune system and create niche space
- Stem Cell Source: Bone marrow harvest, peripheral blood apheresis after mobilization, or umbilical cord blood unit selection
- GVHD Prophylaxis: Calcineurin inhibitors (cyclosporine, tacrolimus) with methotrexate or mycophenolate mofetil
- Engraftment Monitoring: Daily complete blood counts with neutrophil engraftment defined as first of three consecutive days with ANC >500/μL, platelet engraftment as first of seven consecutive days with platelets >20,000/μL without transfusion [20]
For HAAA trials, the FAC conditioning regimen composed of fludarabine (30 mg/m²/d, days -5 to -1), cyclophosphamide (30 mg/kg/d or 37.5 mg/kg/d, days -5 to -2), and anti-thymocyte globulin has demonstrated efficacy with acceptable toxicity [20].
Comparative Analysis: Efficacy, Safety and Applications
Cross-Category Efficacy and Safety Profiles
Direct comparison of the three stem cell categories reveals distinct efficacy and safety profiles:
- Therapeutic Mechanisms: MSCs function predominantly through paracrine signaling and immunomodulation; PSCs through targeted cell replacement; HSCs through complete hematopoietic system reconstitution [10] [16] [15]
- Efficacy Timeframes: MSC effects typically manifest within months; PSC-derived therapies may require longer integration; HSCs demonstrate rapid hematologic reconstitution within weeks [17] [20] [19]
- Safety Considerations: MSCs exhibit excellent safety profiles with minimal adverse events; PSCs carry theoretical tumorigenicity risks from residual undifferentiated cells; HSCs face significant risks including GVHD, graft failure, and conditioning regimen toxicities [17] [19] [16]
Notably, MSC therapy for acute/ subacute ischemic stroke demonstrated significantly improved 1-year functional outcomes (mRS scores 0-1: 45/195 cell therapy vs. 23/179 control; RR=1.74, 95% CI=1.09-2.77) without increased serious adverse events [8]. Similarly, stem cell therapy for acute myocardial infarction showed a favourable safety profile with significant long-term improvement in left ventricular ejection fraction (mean difference 2.63%, 95% CI 0.50% to 4.76%, p=0.02) [21].
Regulatory and Manufacturing Considerations
Regulatory frameworks significantly influence stem cell therapy development globally:
- United States: Flexible approach with prior notification model for clinical trials and Accelerated Approval pathway potential [15]
- European Union & Switzerland: Rigorous regulations requiring manufacturing licenses and prior authorization for clinical trials [15]
- Japan & South Korea: Balanced approaches incorporating elements from both regulatory regimes with strong national funding programs [15]
Manufacturing challenges vary substantially—MSCs require expansion while maintaining functionality; PSCs need complex differentiation protocols and rigorous safety testing; HSCs require careful donor matching and cell processing [10] [19] [16]. The trend toward allogeneic "off-the-shelf" products is evident across all categories, though most advanced in HSCs [19].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Stem Cell Clinical Trial Research
| Reagent Category | Specific Examples | Research Function | Application Notes |
|---|---|---|---|
| Surface Marker Antibodies | CD73, CD90, CD105, CD34, CD45, CD14, CD19, HLA-DR | Cell population characterization and purity assessment | Critical for ISCT compliance for MSCs; CD34 for HSCs [10] |
| Cytokines & Growth Factors | FGF-2, SCF, TPO, IL-6, BMP-4, Activin A, VEGF | Maintenance, expansion, and directed differentiation | FGF-2 essential for MSC expansion; specific combinations for PSC differentiation [10] [18] |
| Cell Culture Media | Serum-free MSC media, mTeSR1, StemSpan | Maintenance of stemness and proliferation | Defined, xeno-free formulations required for clinical applications [18] |
| Reprogramming Factors | OCT4, SOX2, c-MYC, KLF4 | iPSC generation from somatic cells | Non-integrating delivery systems preferred for clinical applications [18] [15] |
| Characterization Assays | Teratoma formation, trilineage differentiation, karyotyping | Safety and functionality assessment | Mandatory for PSC-derived products; differentiation capacity for MSCs [19] |
The clinical trial landscape for stem cell therapies continues to evolve, with each major category finding its distinctive therapeutic niche. MSCs demonstrate robust safety and efficacy in immunomodulatory and tissue repair contexts, particularly for orthopedic, inflammatory, and neurological conditions. PSCs offer unprecedented potential for cell replacement therapies, with ongoing innovation in manufacturing and safety protocols needed to fully realize their clinical potential. HSCs remain the gold standard for curative intent in hematologic diseases, with continuing refinements in donor selection, conditioning regimens, and supportive care improving outcomes.
Future progress will depend on addressing key challenges: standardization of manufacturing protocols and potency assays, development of more predictive preclinical models, implementation of harmonized regulatory standards across jurisdictions, and execution of well-powered late-stage clinical trials with standardized endpoints. As the field matures, combination approaches leveraging the strengths of multiple stem cell types may offer synergistic benefits, potentially representing the next frontier in regenerative medicine.
Stem cell therapy has emerged as a transformative approach in regenerative medicine, with its therapeutic potential demonstrated across a spectrum of human diseases including cardiovascular, neurological, and autoimmune conditions [10]. The efficacy of these therapies in randomized clinical trials (RCTs) is fundamentally underpinned by three core biological mechanisms: immune modulation, paracrine signaling, and direct tissue repair. Rather than operating in isolation, these mechanisms function as an integrated system where stem cells respond to inflammatory cues in damaged tissues, subsequently releasing a complex portfolio of bioactive molecules that coordinate repair processes [22] [23] [10]. This guide provides a systematic comparison of these mechanisms across different stem cell types, with detailed experimental data and methodologies to inform research and drug development.
Table 1: Core Therapeutic Mechanisms of Stem Cells
| Mechanism | Key Effectors | Primary Biological Outcomes | Evidence Level |
|---|---|---|---|
| Immune Modulation | IDO, PGE2, HLA-G5, IL-10, TGF-β, TSG-6, PD-L1 [22] [10] [24] | Suppression of T-cell proliferation, macrophage polarization to anti-inflammatory phenotype, Treg induction [10] [24] | Multiple RCTs across autoimmune diseases and inflammatory disorders [10] |
| Paracrine Signaling | VEGF, HGF, FGF, Sfrp2, HASF, microRNAs, EVs [23] [10] | Angiogenesis, cardiomyocyte protection, reduced apoptosis, tissue remodeling [23] | Preclinical models and secondary outcomes in cardiovascular RCTs [21] [23] |
| Tissue Repair & Differentiation | Direct differentiation, cell-cell contact, ECM protein secretion [10] | Replacement of damaged cardiomyocytes, neurons, cartilage; structural restoration [10] | Limited human evidence; primarily preclinical observations [10] |
Immune Modulation: Mechanisms and Experimental Evidence
The immunomodulatory capabilities of stem cells, particularly mesenchymal stem/stromal cells (MSCs), represent one of the most rigorously validated mechanisms in clinical research. These cells function as "signal-responsive regulators" that sense inflammatory environments and deploy sophisticated immunosuppressive responses [22] [10].
Molecular Effectors and Mechanisms
MSCs modulate both innate and adaptive immunity through multiple molecular pathways. When licensed by pro-inflammatory cytokines like interferon-gamma (IFN-γ) and transforming growth factor-beta 1 (TGF-β1), MSCs significantly upregulate indoleamine 2,3-dioxygenase (IDO), which metabolizes tryptophan and suppresses T-cell proliferation [10] [24]. They also express prostaglandin E2 (PGE2), which inhibits macrophage production of tumor necrosis factor-alpha (TNF-α) and interleukin-1 beta (IL-1β) while enhancing IL-10 secretion [24]. Additional mediators include HLA-G5, which inhibits T-cell and antigen-presenting cell function, and programmed death-ligand 1 (PD-L1), which induces T-cell anergy and apoptosis [22] [10].
Experimental Protocols for Assessing Immune Modulation
PBMC Co-culture Assay for T-cell Modulation:
- Objective: Quantify MSC-mediated suppression of T-cell proliferation and regulatory T-cell (Treg) induction [24].
- Methodology: Isolate PBMCs from healthy donors using Ficoll density gradient centrifugation. Label PBMCs with cell proliferation dyes (e.g., CFSE). Co-culture activated PBMCs with MSCs or MSC-derived extracellular vesicles (EVs) at varying ratios (e.g., 10:1 PBMC:MSC) for 3-5 days. Assess T-cell proliferation via flow cytometry measuring CFSE dilution and quantify Treg population (CD4+CD25+FOXP3+) using specific surface and intracellular staining [24].
- Key Measurements: Percentage inhibition of T-cell proliferation, fold-increase in Treg population, cytokine profiling (IFN-γ, TNF-α, IL-10) via ELISA or multiplex assays.
Macrophage Polarization Assay:
- Objective: Evaluate MSC-induced shift from pro-inflammatory (M1) to anti-inflammatory (M2) macrophage phenotype [24].
- Methodology: Differentiate human THP-1 monocytic cells into macrophages using phorbol esters. Polarize toward M1 phenotype using lipopolysaccharide (LPS) and IFN-γ. Treat with MSC-conditioned medium or EVs for 24-48 hours. Analyze surface markers (CD80, CD86 for M1; CD206, CD163 for M2) via flow cytometry and measure cytokine secretion (TNF-α, IL-1β, IL-10) [24].
- Key Measurements: M1/M2 marker expression ratios, pro- vs anti-inflammatory cytokine ratios, nitric oxide production.
Comparative Efficacy Across Cell Types
Table 2: Immunomodulatory Efficacy Across Stem Cell Types
| Stem Cell Type | Key Strengths | Limitations | Clinical Evidence |
|---|---|---|---|
| Bone Marrow MSCs | Strong T-cell suppression, enhanced IDO expression following licensing [10] [24] | Invasive harvesting, donor age-dependent effects [10] | Phase III trials in GvHD; 85% success in autoimmune disease treatment [10] [25] |
| Adipose-Derived MSCs | Abundant tissue source, potent TSG-6 secretion, anti-fibrotic effects [26] [10] | Variable cell yields based on processing methods [10] | Advanced phase trials for Crohn's disease and rheumatoid arthritis [26] [10] |
| Umbilical Cord MSCs | High proliferation capacity, low immunogenicity, superior EV production [10] | Limited donor availability, ethical considerations in some regions [10] | Promising results in COVID-19 ARDS and neurodegenerative conditions [10] |
| Embryonic Stem Cells | Pluripotency, theoretically unlimited expansion capacity [10] | Ethical controversies, teratoma risk, requires differentiation prior to use [10] [7] | Limited clinical application due to safety and ethical concerns [10] [7] |
Paracrine Signaling: Secreted Factors as Primary Mediators
Paracrine signaling has emerged as the predominant mechanism explaining stem cell efficacy in many clinical contexts, whereby stem cells release bioactive molecules that orchestrate tissue repair without significant long-term engraftment [23] [10].
Key Paracrine Factors and Functions
Stem cells secrete a diverse array of factors with distinct therapeutic functions. Vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF) stimulate angiogenesis, creating new blood vessels to support damaged tissues [23]. Hepatocyte growth factor (HGF) promotes tissue regeneration and possesses anti-fibrotic properties [23]. The secreted frizzled-related protein 2 (Sfrp2) and hypoxic induced Akt regulated stem cell factor (HASF) provide crucial cardioprotection by reducing cardiomyocyte apoptosis through mitochondrial death pathway modulation [23]. Additionally, extracellular vesicles (EVs) containing microRNAs, proteins, and lipids mediate intercellular communication and transfer of bioactive components [10] [24].
Experimental Protocols for Paracrine Analysis
Conditioned Media Collection and Concentration:
- Objective: Generate cell-free therapeutic material for mechanistic studies [23] [24].
- Methodology: Culture MSCs to 70-80% confluence. Replace with serum-free medium to eliminate confounding factors. After 24-48 hours, collect conditioned medium and concentrate using centrifugal filter devices (e.g., 3-10 kDa cutoff). Analyze protein content via proteomic approaches or target-specific ELISAs [23].
- Key Applications: In vitro cytoprotection assays, angiogenesis assays, in vivo testing of cell-free therapeutics.
Tube Formation Assay for Angiogenic Potential:
- Objective: Quantify the pro-angiogenic effects of stem cell secretions [23].
- Methodology: Plate human umbilical vein endothelial cells (HUVECs) on Matrigel or similar basement membrane matrix. Treat with MSC-conditioned media or purified factors. Incubate for 4-18 hours and visualize tube networks. Analyze by measuring total tube length, number of branches, and junction points using image analysis software [23].
- Key Measurements: Total tube length, number of branches, junction points per field.
Clinical Translation of Paracrine Mechanisms
The paracrine hypothesis has significant clinical implications, suggesting that cell-free therapies utilizing conditioned media or isolated extracellular vesicles could potentially replicate stem cell benefits while minimizing risks associated with whole-cell transplantation [24]. This approach offers practical advantages including standardized manufacturing, extended shelf life, and reduced safety concerns related to cell viability and differentiation potential [24]. In cardiovascular clinical trials, this mechanism is supported by observations where stem cell administration improved left ventricular ejection fraction (LVEF) and reduced infarct size despite minimal long-term engraftment [21] [23]. Meta-analyses of RCTs have demonstrated significant long-term LVEF improvement (mean difference 2.63%, 95% CI 0.50% to 4.76%, p=0.02) following stem cell therapy in acute myocardial infarction patients [21].
Tissue Repair and Regeneration: Direct and Indirect Mechanisms
The capacity of stem cells to directly contribute to tissue repair encompasses both differentiation into functional somatic cells and the activation of endogenous repair programs.
Differentiation Capacity Across Stem Cell Types
Different stem cell populations exhibit varying differentiation potential. Mesenchymal stem cells demonstrate multipotent capacity, differentiating into mesodermal lineages including osteoblasts, chondrocytes, and adipocytes [10]. Embryonic stem cells and induced pluripotent stem cells offer pluripotency, with the ability to generate all somatic cell types, including cardiomyocytes and neurons [10] [7]. Tissue-resident progenitor cells, such as cardiac stem cells, exhibit more restricted differentiation potential typically limited to their tissue of origin [7].
Endogenous Regeneration Activation
Beyond direct differentiation, stem cells activate endogenous repair mechanisms by stimulating resident tissue-specific progenitor cells through paracrine signaling [23] [10]. This is particularly important in tissues with limited regenerative capacity, such as neuronal and cardiac tissue. The secretion of factors like brain-derived neurotrophic factor (BDNF) and glial cell line-derived neurotrophic factor (GDNF) by MSCs promotes neuronal survival and outgrowth, while stem cell factor (SCF) mobilizes bone marrow-derived progenitors to participate in tissue repair [23] [10].
Experimental Toolkit for Mechanism Validation
Research Reagent Solutions
Table 3: Essential Research Reagents for Stem Cell Mechanism Studies
| Reagent/Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Cell Isolation Kits | Ficoll-Paque for PBMC isolation, collagenase digestion kits for adipose MSCs, CD34+ selection kits [10] [24] | Isolation of specific stem cell and immune cell populations | Separation of mononuclear cells based on density; enzymatic tissue dissociation; magnetic bead-based cell selection |
| Cytokine Licensing Cocktails | Recombinant human IFN-γ, TGF-β1, TNF-α [24] | Enhancement of immunomodulatory potency | Pre-activation of MSCs to boost IDO, PGE2, PD-L1 expression; typically used at 20-50 ng/mL for 48-72 hours |
| EV Isolation Systems | Size-exclusion chromatography, ultracentrifugation, precipitation kits, tangential flow filtration [24] | Production of cell-free therapeutic fractions | Isolation of small EVs (30-150 nm) based on size, density, or surface markers |
| Flow Cytometry Antibodies | CD73, CD90, CD105 (MSC markers); CD45, CD34 (negative markers); CD4, CD25, FOXP3 (Treg panel) [10] [24] | Cell phenotype characterization and functional assessment | Confirmation of stem cell identity; quantification of immune cell populations; analysis of cell surface and intracellular markers |
| Differentiation Media Kits | Osteogenic (ascorbate, β-glycerophosphate, dexamethasone), adipogenic (insulin, IBMX, dexamethasone), chondrogenic (TGF-β3, BMP-6) [10] | Validation of stem cell multipotency | Induction of lineage-specific differentiation through cytokine and chemical induction |
In Vivo Model Systems
Animal models remain essential for validating stem cell mechanisms in complex physiological environments. For cardiovascular applications, rodent and porcine myocardial infarction models (induced by permanent coronary artery ligation or ischemia-reperfusion) demonstrate functional improvements following stem cell therapy, including reduced infarct size and enhanced ventricular function [23]. In neurological research, middle cerebral artery occlusion (MCAO) models for stroke show significant functional recovery with stem cell treatment, with meta-analyses reporting improved modified Rankin Scale scores at 90 days (RR=1.31, 95% CI=1.01-1.70) and 1 year (RR=1.74, 95% CI=1.09-2.77) [8]. For wound healing applications, diabetic murine models (e.g., db/db mice) demonstrate accelerated wound closure with adipose-derived MSC therapy through enhanced angiogenesis and tissue remodeling [26].
Comparative Efficacy in Randomized Clinical Trials
RCT evidence supporting stem cell mechanisms varies substantially across medical conditions, reflecting differences in therapeutic applications and trial methodologies.
Table 4: Stem Cell Efficacy Outcomes Across Medical Specialties Based on RCT Evidence
| Medical Condition | Primary Efficacy Outcomes | Safety Profile | Level of Evidence |
|---|---|---|---|
| Acute Myocardial Infarction | Long-term LVEF improvement (2.63%, p=0.02); reduced relative infarct size; no short-term benefit [21] | Fewer adverse events vs controls (OR 0.66, 95% CI 0.44-0.99); no cardiac-related cancers [21] | Meta-analysis of 15 trials (n=1,218) [21] |
| Ischemic Stroke | Improved mRS scores 0-2 at 90 days (RR=1.31, 95% CI=1.01-1.70); mRS 0-1 at 1 year (RR=1.74, 95% CI=1.09-2.77) [8] | No significant difference in serious adverse events or mortality [8] | Meta-analysis of 13 trials (n=872) [8] |
| Chronic Wounds | Complete healing in 56% vs 38% controls (p=0.0042); reduced healing time (65 vs 90 days) [26] | Similar adverse events with fewer osteomyelitis cases and amputations [26] | Multicenter RCT (n=208) with bioengineered skin substitutes [26] |
| Advanced Heart Failure | Varied efficacy across cell types; consistent safety demonstration [7] | Clinically acceptable safety across multiple cell types [7] | Systematic review of 27 clinical trials [7] |
The therapeutic efficacy of stem cells in randomized clinical trials results from the integrated operation of immune modulation, paracrine signaling, and tissue repair mechanisms rather than any single pathway. The relative contribution of each mechanism varies depending on stem cell type, tissue environment, and disease pathology. Current evidence suggests that paracrine signaling and immune modulation may deliver more immediate therapeutic effects, while direct differentiation likely contributes to longer-term tissue restoration. Future research directions should prioritize standardized protocols for cell manufacturing and delivery, development of potency assays based on mechanism-specific biomarkers, and exploration of combination therapies that enhance endogenous regenerative responses. The evolving understanding of extracellular vesicles as primary mediators of stem cell efficacy offers promising opportunities for cell-free therapeutic strategies that may overcome current challenges in stem cell transplantation while maintaining therapeutic benefits.
Clinical Trial Design and Therapeutic Application Across Indications
Autoimmune and liver diseases represent a significant global health burden, often progressing to chronic, debilitating conditions with limited treatment options. Within the evolving landscape of regenerative medicine, stem cell therapy has emerged as a promising intervention aimed at addressing the underlying pathophysiology of these conditions rather than merely alleviating symptoms. This analysis critically examines the disease-specific efficacy of stem cell therapies, with a particular focus on outcomes from randomized controlled trials (RCTs) in both autoimmune and hepatic disorders. The evaluation is structured around core therapeutic mechanisms, including immunomodulation, tissue regeneration, and anti-fibrotic effects, which are quantified through clinical, biochemical, and histological endpoints. By synthesizing current evidence from active clinical trials and published meta-analyses, this guide provides a comparative framework for researchers and drug development professionals to understand the positioning of stem cell therapies within the current therapeutic arsenal and to inform future clinical development strategies.
Comparative Efficacy of Stem Cell Therapies in Autoimmune Diseases
Stem cell therapy has shown variable efficacy across different autoimmune diseases, with the most robust evidence emerging from RCTs in Crohn's disease (CD), systemic lupus erythematosus (SLE), and scleroderma. The therapeutic effect is primarily mediated through immune modulation and tissue repair mechanisms, with outcomes highly dependent on cell source, administration route, and patient selection.
Table 1: RCT Outcomes for Stem Cell Therapies in Autoimmune Diseases
| Disease | Stem Cell Type | Primary Endpoint(s) | Key Efficacy Findings | Reported Clinical Remission Rate | Major Adverse Events |
|---|---|---|---|---|---|
| Crohn's Disease (CD) [12] | Hematopoietic Stem Cells (HSCs), Mesenchymal Stem Cells (MSCs) | Clinical remission, endoscopic improvement | Sustained drug-free remission, fistula healing | Middle to High (>50% - >75%) [12] | Infections, cytopenias (HSC-based therapy) |
| Systemic Lupus Erythematosus (SLE) [27] [12] | MSCs, CAR T-cells | Disease activity index (e.g., BILAG), serological markers | Durable drug-free remission, normalized complement, reduced anti-dsDNA titers [27] | Middle to High (>50% - >75%) [12] | Mild cytokine release syndrome (CAR-T) [27] |
| Scleroderma [12] | HSCs, MSCs | Skin score (mRSS), overall survival | Improved skin flexibility, stabilization of organ function | Middle (>50% - ≤75%) [12] | Treatment-related mortality (HSC-based therapy) |
| Rheumatoid Arthritis (RA) [12] | MSCs | ACR20/50/70 response, DAS28 score | Reduction in joint swelling, tenderness, and pain | Low to Middle (≤50% - ≤75%) [12] | Infusion-related reactions |
| Multiple Sclerosis (MS) [27] | HSCs, CAR T-cells (preclinical) | EDSS score, relapse rate | Long-term remission, reduced disability progression [27] | Information missing | Information missing |
The table illustrates that CD and SLE are the most responsive to stem cell therapy, often achieving high remission rates. A global analysis of clinical trials indicates that over 80% of stem cell trials for autoimmune diseases are in early phases (I-II), with the U.S. and China leading in trial volume [12]. The efficacy is driven by several core mechanisms. MSCs secrete soluble factors like TGF-β, PGE2, and IDO, and exosomes containing regulatory miRNAs (e.g., miR-21, miR-146a) to suppress pathogenic Th1 and Th17 cells while promoting regulatory T cell (Treg) expansion [12]. Hematopoietic stem cell transplantation (HSCT) utilizes high-dose immunosuppression to ablate the aberrant immune system and rebuild a tolerant one from the reinfused HSCs, demonstrating long-term remission potential in scleroderma and MS [12]. Emerging therapies like CD19-directed CAR T-cells achieve a profound "reset" of immune tolerance by selectively eliminating autoreactive B cells, leading to drug-free remission in refractory SLE [27].
Comparative Efficacy of Stem Cell Therapies in Liver Diseases
For liver diseases, stem cell therapy demonstrates significant promise in improving liver function and reversing fibrosis, particularly in acute-on-chronic liver failure (ACLF) and cirrhosis. The efficacy is measured through scoring systems, biochemical markers, and histological improvement.
Table 2: RCT Outcomes for Mesenchymal Stem Cell (MSC) Therapies in Liver Diseases
| Disease | Cell Source & Route | Primary Endpoint | Key Efficacy Findings | Significance (p-value) | Major Adverse Events |
|---|---|---|---|---|---|
| Acute-on-Chronic Liver Failure (ACLF) [28] | UC-MSCs, BM-MSCs; Intravenous/ Hepatic Artery | MELD score, Albumin (ALB) | Decreased MELD score, increased ALB at 4 & 24 weeks | p < 0.05 [28] | No significant increase in AEs/SAEs [28] |
| Liver Cirrhosis [29] [30] | BM-MSCs, UC-MSCs; Intravenous | Histological fibrosis, liver function tests | Reduced liver scarring, improved synthetic function | p < 0.05 in multiple trials [29] | Mild, transient post-infusion reactions |
| Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) [31] | Information missing | Liver fat content, fibrosis stage | Potential to reduce inflammation and scarring | Information missing | Information missing |
Meta-analyses of RCTs confirm that MSC infusion is effective and safe for ACLF patients, improving liver function without increasing adverse events [28]. The therapeutic potential of MSCs in liver diseases is primarily mediated through three interconnected mechanisms. MSCs create an immunosuppressive environment by secreting factors like PGE2, IDO, and HLA-G, which modulate T cells, B cells, NK cells, dendritic cells (DCs), and macrophages (MΦs), shifting them from a pro-inflammatory to an anti-inflammatory phenotype [30]. They also attenuate liver fibrosis by secreting HGF and other factors that inhibit the activation of hepatic stellate cells (HSCs)—the main collagen-producing cells—and promote the degradation of excess extracellular matrix [29] [30]. Furthermore, MSCs promote tissue repair by releasing growth factors like HGF and VEGF, which support the regeneration of endogenous hepatocytes, and can potentially differentiate into hepatocyte-like cells [29] [30]. Extracellular vesicles from MSCs (MSC-EVs) have emerged as a cell-free alternative, delivering bioactive cargo like microRNAs that regulate immune function and inhibit cell death [29].
Key Experimental Protocols in Stem Cell Clinical Trials
MSC Therapy for Acute-on-Chronic Liver Failure (ACLF)
The efficacy of MSCs in ACLF is established through rigorous RCT protocols. A recent meta-analysis followed the PRISMA statement and Cochrane guidance, sourcing data from PubMed, Web of Science, EMBASE, and the Cochrane Library [28]. The study selection adhered to the PICOS principle: Population: patients diagnosed with ACLF; Intervention: MSC infusion; Comparison: conventional medical therapy; Outcomes: MELD score, Albumin (ALB), international normalized ratio (INR), alanine aminotransferase (ALT); Study design: RCTs [28]. The quality of included studies was assessed using the Cochrane risk of bias tool. Statistically, continuous outcomes were analyzed using the standardized mean difference (SMD) with a 95% confidence interval (CI), while dichotomous data used the odds ratio (OR) with 95% CI. Heterogeneity was quantified with the I² statistic, applying a fixed-effects model if I² < 50% and p > 0.1, and a random-effects model otherwise [28]. This rigorous methodology confirmed that MSC treatment significantly improved MELD scores and ALB levels at both 4 and 24 weeks compared to the control group [28].
CAR T-Cell Therapy for Autoimmune Diseases
The protocol for adapting CAR T-cell therapy for autoimmune diseases like SLE involves a multi-step process. First, leukapheresis is performed to collect a patient's T cells [27]. These T cells are then genetically engineered ex vivo to express synthetic chimeric antigen receptors (CARs) targeting specific immune cell markers, such as CD19 on B cells or BCMA on plasma cells [27]. The engineered CAR T-cells are expanded in culture to achieve a sufficient therapeutic dose. Before infusion, patients often receive lymphodepleting chemotherapy (e.g., with cyclophosphamide and fludarabine) to enhance the engraftment and persistence of the CAR T-cells [27]. Finally, the CAR T-cells are infused back into the patient, where they initiate the targeted elimination of autoreactive B-lineage cells, leading to a "resetting" of immune tolerance. This approach has resulted in durable drug-free remission in patients with refractory SLE [27].
Visualization of Key Mechanisms and Workflows
Stem Cell Mechanisms in Liver Fibrosis
Diagram Title: MSC Mechanisms Against Liver Fibrosis
CAR T-Cell Workflow for Autoimmunity
Diagram Title: CAR T-Cell Therapy Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for Stem Cell Therapy Research
| Reagent/Material | Primary Function in R&D | Specific Application Example |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) [28] [30] [12] | Core therapeutic agent; source of immunomodulation and trophic factors. | Investigated in >50 clinical trials for liver cirrhosis; most common cell type in autoimmune trials [29] [12]. |
| Hematopoietic Stem Cells (HSCs) [12] | Core therapeutic agent for immune system reconstitution. | Used in high-dose immunosuppression/chemotherapy protocols for scleroderma and MS [12]. |
| CAR Transduction Vectors [27] | Genetic engineering of autologous T cells. | Creating CD19- or BCMA-targeting CAR T-cells for SLE and other autoimmune diseases [27]. |
| Cell Culture Media & Supplements | Ex vivo expansion and maintenance of stem cells. | Critical for growing MSCs and expanding CAR T-cells to sufficient doses for therapy [27]. |
| Hepatocyte Growth Factor (HGF) [29] [30] | Key paracrine factor; promotes liver regeneration and inhibits HSC activation. | A major mediator of the anti-fibrotic and regenerative effects observed in MSC-based liver therapies [29] [30]. |
| Extracellular Vesicles (EVs)/Exosomes [29] [12] | Cell-free therapeutic alternative; carry regulatory miRNAs and proteins. | MSC-EVs are being explored to treat liver failure and mitigate complications, mimicking MSC effects [29]. |
The therapeutic potential of stem cell therapy in regenerative medicine and for treating immune-mediated inflammatory diseases is immense, yet its clinical translation faces significant challenges [10]. The efficacy of these therapies in randomized clinical trials is not solely dependent on the type of stem cell selected but is profoundly influenced by three critical trial parameters: cell dosage, delivery routes, and timing windows. These parameters are interdependent pillars that determine the cellular fate, biodistribution, and ultimate therapeutic success [32] [33]. A comprehensive analysis of global clinical trials reveals that most (83.6%) are in early to mid-phase (Phase I-II), underscoring the ongoing efforts to optimize these fundamental aspects [34]. The absence of universal guidelines for administration, as noted in cardiac regeneration trials, exemplifies the broader challenge across therapeutic areas [32]. This guide objectively compares current strategies and supporting experimental data for these parameters, providing a framework for researchers and drug development professionals to enhance clinical trial design within the broader thesis of optimizing stem cell therapy efficacy.
Cell Dosage: Balancing Efficacy and Safety
Cell dosage is a primary determinant of therapeutic outcome, influencing both the potency of the intervention and its safety profile. Dosing strategies must account for the specific disease pathology, stem cell source, and desired mechanism of action—whether for immune modulation, tissue repair, or a combination thereof.
Dosage Ranges and Disease-Specific Considerations
The optimal cell dose varies significantly across disease areas and cell types. In advanced heart failure trials, mesenchymal stem cell (MSC) doses have ranged from 20 to 150 million cells per infusion, with higher doses often associated with more pronounced improvements in cardiac function, though not consistently across all studies [7]. For autoimmune conditions like Crohn's disease and systemic lupus erythematosus, clinical trials have employed a wide spectrum of doses, reflecting the ongoing search for an optimal range [34]. The therapeutic effect in many contexts is mediated primarily through paracrine signaling—the release of bioactive molecules such as growth factors, cytokines, and extracellular vesicles—rather than direct cell engraftment [10] [7]. This mechanism suggests that a minimum threshold dose is necessary to achieve a critical concentration of these therapeutic factors at the target site.
Table 1: Comparative Analysis of Stem Cell Dosing in Clinical Trials
| Therapeutic Area | Cell Type | Common Dosing Range | Key Efficacy Findings | Safety Considerations |
|---|---|---|---|---|
| Advanced Heart Failure [7] | Mesenchymal Stem Cells (MSCs) | 20 - 150 million cells | Promising outcomes; efficacy varies and is not yet conclusively confirmed. | Clinically acceptable safety profile across trials. |
| Autoimmune Diseases (e.g., Crohn's, SLE) [34] | MSCs, Hematopoietic Stem Cells (HSCs) | Wide spectrum reported | Disease-specific variations in clinical remission rates. | Lack of robust long-term safety data; mild immune rejection possible with allogeneic MSCs. |
| Graft-versus-Host Disease (GVHD) Prophylaxis [35] | MSCs | Context-dependent | Prophylactic administration reduces incidence. | Risks must be balanced against efficacy. |
Experimental Protocols for Dose Optimization
Dose-finding studies typically follow a phase I, dose-escalation design. A standard protocol involves administering escalating doses to sequential patient cohorts, starting from a baseline dose established in preclinical models. For example, a trial might initiate dosing at 1 million cells per kilogram of patient body weight, with subsequent cohorts receiving 2, 4, and 8 million cells/kg, respectively [36]. Patients are monitored closely for dose-limiting toxicities (DLTs) over a predefined period, often 28 days. Efficacy is measured through condition-specific endpoints—e.g., left ventricular ejection fraction for heart failure [7], or Crohn's Disease Activity Index for inflammatory bowel disease [34]—alongside biomarker analysis. A key emerging biomarker is the reduction in inflammatory markers such as Interleukin-6 (IL-6) and Tumor Necrosis Factor Alpha (TNF-α), which can indicate a systemic anti-inflammatory response to therapy [36]. This combined assessment of safety and biological activity helps identify the minimum effective dose and the maximum tolerated dose.
Delivery Routes: Determining Cellular Biodistribution and Engraftment
The route of administration directly controls the homing, distribution, and retention of stem cells, thereby defining their therapeutic potential. The choice of route is a trade-off between targeting precision, invasiveness, and cell survival.
Comparison of Primary Delivery Strategies
Clinical trials employ diverse delivery routes, each with distinct advantages and limitations. Local implantation (e.g., intramyocardial for cardiac disease, intralesional for orthopedic injuries) aims for maximal cell retention at the injury site but is inherently invasive [7]. Intravascular systemic infusion (intravenous) is minimally invasive and allows for broad distribution, making it suitable for systemic diseases like autoimmune disorders and GvHD [34] [10]. However, a significant drawback is the "first-pass effect," where a large proportion of cells are trapped in the lungs, liver, and spleen, reducing the fraction that reaches the intended target tissue [10]. Regional delivery (e.g., intra-arterial, intrathecal) seeks a middle ground, offering better targeting than intravenous routes with lower invasiveness than direct local injection. Disease-specific variations in administration routes are evident from trial data, with the optimal choice depending on the pathophysiology and location of the target tissue [34].
Table 2: Delivery Routes in Stem Cell Clinical Trials
| Delivery Route | Key Applications | Advantages | Disadvantages & Experimental Findings |
|---|---|---|---|
| Local Implantation(e.g., Intramyocardial, Intra-articular) | Cardiac repair [7], Orthopedic injuries | High local cell concentration; direct targeting of damaged tissue. | Invasive; potential for procedure-related complications; limited diffusion from injection site. |
| Systemic Infusion(Intravenous - IV) | Autoimmune diseases [34], GvHD [10] | Minimally invasive; suitable for widespread/multifocal diseases. | Significant first-pass pulmonary sequestration; low target site engraftment; risk of ectopic tissue formation. |
| Regional Delivery(e.g., Intra-arterial, Intrathecal) | Stroke, Neurological disorders | Better target specificity than IV; can bypass certain biological barriers. | Requires specialized interventional skills; variable efficacy based on catheter placement and flow dynamics. |
Methodologies for Tracking Delivery and Engraftment
Evaluating the success of a delivery route requires robust tracking methodologies. In clinical practice, this is often achieved through imaging techniques. Cells can be labeled with superparamagnetic iron oxide (SPIO) nanoparticles or radiotracers (e.g., ⁹⁹mTc, ¹⁸F-FDG) prior to administration, allowing for non-invasive tracking using Magnetic Resonance Imaging (MRI) or Positron Emission Tomography (PET) scans, respectively [7]. These imaging studies provide critical data on cell distribution, migration, and persistence in vivo. Furthermore, the homing capability of MSCs is intrinsically linked to inflammation; they are attracted to sites of injury via chemokine gradients, particularly the CXCR4/SDF-1 axis [34] [36]. Therefore, the timing of administration relative to the inflammatory state of the disease is a critical co-factor influencing the success of any delivery route.
Timing Windows: The Chronobiology of Therapeutic Success
The timing of stem cell administration, both in terms of the patient's disease stage and the specific time of day, is an emerging critical parameter that can dramatically influence clinical outcomes, including survival, relapse, and the incidence of complications.
Disease Stage and Post-Transplant Timing
The therapeutic window for intervention is highly context-dependent. In the setting of hematopoietic stem cell transplantation (HSCT) for hematologic disorders, early prophylactic or pre-emptive cellular therapy is increasingly favored. For instance, prophylactic donor lymphocyte infusion (DLI) in high-risk acute myeloid leukemia (median 190 days post-HSCT) has been shown to improve overall and relapse-free survival, albeit with an increased risk of GvHD [35]. Similarly, virus-specific T-cells are most effective when administered early (median 36 days post-HSCT) for managing viral reactivations [35]. This contrasts with therapeutic DLI for overt relapse, which shows limited efficacy. In non-malignant diseases, the optimal timing likely correlates with the acute versus chronic phase of the disease and the level of inflammation, which aids in stem cell homing [36].
Circadian Timing in Administration
Recent evidence introduces a novel dimension to timing: circadian biology. A retrospective cohort study and subsequent investigations have demonstrated that the time of day for allogeneic stem cell infusion can significantly impact patient outcomes [37]. Infusions performed during the daytime (compared to nighttime) were associated with a lower incidence of acute GvHD. The proposed mechanism involves harnessing the natural circadian rhythms of the immune system—"the circadian immune system"—to reduce alloreactivity and improve engraftment [37]. This paradigm shift highlights the potential for simple, non-invasive optimization of therapy timing to enhance safety and efficacy.
Diagram 1: Stem cell therapy timing strategies and their impacts on key clinical outcomes.
Experimental Workflow for Timing Studies
The evidence supporting timing optimization comes from rigorous clinical study designs. The workflow for establishing a circadian timing effect, for instance, involved a retrospective analytical cohort study [37]. Patient cohorts were stratified based on the time of day they received allogeneic stem cell infusions (daytime vs. nighttime). The primary outcome measured was the incidence of acute GvHD, with secondary outcomes including overall survival and relapse-free survival. Statistical models were then used to control for potential confounding variables (e.g., patient age, underlying disease, conditioning regimen) to isolate the effect of infusion timing. This methodology provides a template for prospectively validating timing windows in other therapeutic contexts.
Integrated Signaling Pathways in Stem Cell Fate
The therapeutic actions of stem cells are governed by an intricate network of conserved signaling pathways. Pharmacological modulation of these pathways—TGF-β, Wnt, Hedgehog, Notch, FGF, BMP, and Hippo—is a promising strategy to enhance stem cell survival, direct differentiation, and modulate the stem cell niche, thereby overcoming current clinical limitations [33].
Diagram 2: Key stem cell signaling pathways and their therapeutic modulation.
The Scientist's Toolkit: Essential Reagents and Materials
Advancing research in this field requires a suite of specialized reagents and tools to ensure the quality, safety, and efficacy of stem cell products.
Table 3: Key Research Reagent Solutions for Stem Cell Therapy Development
| Reagent / Material | Function | Application in Experimental Protocols |
|---|---|---|
| cGMP-grade Cell Culture Media & Supplements | Expansion and maintenance of stem cells under stringent, clinically relevant conditions. | Critical for manufacturing MSC-based drugs; ensures product quality and compliance with regulatory standards [10] [38]. |
| Flow Cytometry Antibody Panels (e.g., CD73, CD90, CD105, CD34, CD45, HLA-DR) | Characterization and quality control of stem cell populations based on ISCT criteria [10]. | Used to verify MSC phenotype prior to release for therapy, confirming positive marker expression ≥95% and negative marker expression ≤2% [10]. |
| Differentiation Induction Kits (Osteogenic, Chondrogenic, Adipogenic) | Functional validation of MSC multipotency in vitro as per ISCT definitions [10]. | A mandatory release test for MSCs to confirm their trilineage differentiation potential before clinical use. |
| Small Molecule Pathway Modulators | Pharmacological enhancement of stem cell therapy by targeting key pathways (e.g., TGF-β, Wnt, Hedgehog) [33]. | Used in R&D to direct stem cell differentiation, enhance survival, or modulate immunogenicity. |
| Extracellular Vesicle (EV) Isolation Kits | Isolation and purification of EVs, key mediators of the paracrine effects of MSCs [10]. | For studying the therapeutic mechanisms of MSCs and developing cell-free therapeutic products. |
| Cell Labeling/Tracking Reagents (e.g., SPIO nanoparticles, fluorescent dyes) | Non-invasive monitoring of administered cells in vivo. | Used in preclinical and clinical imaging studies (MRI/PET) to track cell biodistribution and persistence post-delivery [7]. |
Optimizing stem cell therapy efficacy in clinical trials demands a holistic and integrated approach to cell dosage, delivery routes, and timing windows. The experimental data summarized in this guide demonstrate that these parameters are not independent variables but are deeply interconnected. The success of a high cell dose may be negated by a suboptimal delivery route that fails to deliver cells to the target site, and the benefit of an optimally timed intervention can be lost with an insufficient cell quantity. Future efforts must prioritize the development of standardized protocols grounded in robust mechanistic understanding, leveraging pharmacological modulation and innovative delivery systems. As the field moves towards precision medicine, the systematic and simultaneous optimization of these three critical trial parameters will be paramount for unlocking the full clinical potential of stem cell therapies and achieving consistent success in late-stage randomized controlled trials.
Stem cell therapy has emerged as a transformative approach in regenerative medicine, demonstrating potential for treating conditions ranging from autoimmune diseases to cardiovascular disorders and neurological injuries [12] [39]. However, as clinical research has advanced, it has become increasingly evident that stem cells alone may not fully address the complex pathophysiology of many chronic conditions. This recognition has catalyzed the development of integrated treatment protocols that combine stem cells with established conventional and biologic therapies. The fundamental premise underlying these combination strategies is that stem cells can potentiate the effects of conventional treatments while simultaneously modulating immune responses and promoting tissue repair through multiple mechanistic pathways [12].
The therapeutic efficacy of stem cells, particularly mesenchymal stem cells (MSCs), derives from their dual capacity for immune modulation and tissue repair [12]. These cells secrete a repertoire of soluble factors, including TGF-β, PGE2, and regulatory exosomes containing miRNAs such as miR-21 and miR-146a, which collectively suppress excessive activation of Th1 and Th17 cells while promoting the expansion of regulatory T cells (Treg) [12]. When deployed alongside conventional therapies, stem cells can address the limitations of pharmacologic approaches, which often focus on symptom management rather than addressing underlying tissue damage or immune dysregulation [40].
This guide systematically compares the performance of stem cell monotherapies against combination approaches, with a specific focus on evidence from randomized clinical trials. By examining therapeutic efficacy, safety profiles, and mechanistic insights across different disease contexts, we provide a comprehensive resource for researchers and drug development professionals working to advance the field of regenerative medicine.
Global Clinical Trial Landscape and Combination Therapy Trends
Analysis of global clinical trial data reveals significant trends in the development of combination therapies involving stem cells. A systematic review of trials registered between 2006 and 2025 identified 244 interventional trials focusing on stem cell therapy for autoimmune diseases, with the majority (83.6%) in Phase I-II stages [12]. These trials demonstrate substantial variation in combination strategies based on disease type, stem cell source, and therapeutic targets.
Table 1: Global Distribution of Stem Cell Clinical Trials for Autoimmune Diseases (2006-2025)
| Characteristic | Category | Number of Trials | Percentage |
|---|---|---|---|
| Trial Phase | Phase I-II | 204 | 83.6% |
| Phase III-IV | 40 | 16.4% | |
| Leading Disease Indications | Crohn's Disease | 85 | 34.8% |
| Systemic Lupus Erythematosus | 36 | 14.8% | |
| Scleroderma | 32 | 13.1% | |
| Geographic Distribution | United States | 78 | 32.0% |
| China | 56 | 23.0% | |
| European Union | 42 | 17.2% | |
| Funding Sources | Academic Institutions | 120 | 49.2% |
| Industry | 76 | 31.1% | |
| Mixed Funding | 48 | 19.7% |
The data reveals that academic institutions serve as the primary drivers of combination therapy research, funding nearly half of all registered trials [12]. This distribution reflects the transitional nature of the field, with many approaches still in exploratory stages. Geographic analysis shows concentrated research activity in the United States and China, which collectively account for more than half of all clinical trials in this space [12]. Regulatory frameworks significantly influence this distribution, with the United States adopting a more flexible stance that facilitates rapid development of stem cell therapies compared to the more rigorous regulations in the European Union and Switzerland [15].
Table 2: Combination Therapy Approaches by Disease Category
| Disease Category | Common Conventional/Biologic Agents | Stem Cell Types | Primary Combination Rationale |
|---|---|---|---|
| Cardiovascular Diseases | Beta-blockers, ACE inhibitors, statins | MSCs, BMMNCs, CPCs | Enhance tissue repair while managing cardiovascular risk factors [40] [7] |
| Autoimmune Diseases | Immunosuppressants, biologics, glucocorticoids | MSCs, HSCs | Immune reset followed by modulation of immune response [12] |
| Neurological Disorders | Thrombolytics, rehabilitative therapies | MSCs, BM-MNCs | Neuroprotection and enhancement of endogenous repair mechanisms [41] |
| Oncological Conditions | Chemotherapy, targeted therapies, immune checkpoint inhibitors | HSCs, CAR-T cells | Myeloablation support and enhanced antitumor immunity [42] |
The selection of combination partners reflects disease-specific therapeutic requirements. In cardiovascular contexts, stem cells are typically combined with standard pharmacologic management to address both functional improvement and risk factor control [40]. For autoimmune conditions, the emphasis shifts to immune modulation, often employing hematopoietic stem cells (HSCs) to reset the immune system alongside immunosuppressive agents to maintain tolerance [12]. These disease-specific approaches highlight the precision medicine aspect of combination therapy development.
Therapeutic Mechanisms and Signaling Pathways in Combination Therapy
The mechanistic basis for combining stem cells with conventional therapies involves complementary actions on disease pathways. Stem cells exert their effects through multiple mechanisms, including direct cell replacement, paracrine signaling, and immune modulation [12] [39]. When integrated with pharmacologic agents, these effects can be synergistic, potentially allowing for dose reduction of conventional drugs while maintaining or enhancing efficacy.
The diagram above illustrates how combination therapies leverage complementary mechanisms of action. Stem cells contribute immune modulation through Treg expansion and Th1/Th17 suppression, alongside tissue repair capabilities via growth factor secretion and cellular differentiation [12]. Conventional therapies typically provide inflammation control through cytokine modulation and pathway targeting of specific molecular targets involved in disease pathogenesis. The convergence of these mechanisms creates a synergistic therapeutic effect that translates to improved clinical outcomes.
In cardiovascular applications, the paracrine effects of stem cells have garnered increasing attention. Injected cells secrete factors that activate endogenous repair mechanisms, including angiogenesis, reduced apoptosis, and modulation of inflammatory responses [7]. When combined with standard pharmacologic agents that manage hemodynamic stress and cardiovascular risk factors, this paracrine activity can lead to more substantial improvements in cardiac function than either approach alone [40].
For autoimmune conditions, combination strategies frequently employ hematopoietic stem cell transplantation (HSCT) alongside intensive immunosuppressive regimens. This approach essentially "resets" the immune system by eliminating autoreactive lymphocytes, followed by重建 of a tolerant immune repertoire [12]. The therapeutic effect is further enhanced by the immunomodulatory properties of MSCs, which create a favorable microenvironment for immune tolerance through secretion of soluble factors like TGF-β and PGE2, as well as exosomes containing regulatory miRNAs [12].
Comparative Efficacy Data: Stem Cell Monotherapy vs. Combination Approaches
Direct comparative studies provide the most compelling evidence for the superiority of combination approaches over monotherapies. Recent prospective cohort studies and randomized controlled trials have quantified these differences across multiple disease domains, with consistent patterns emerging regarding the enhanced efficacy of integrated treatment protocols.
Table 3: Efficacy Outcomes: Stem Cell Monotherapy vs. Combination Approaches
| Disease Context | Therapeutic Protocol | Primary Efficacy Endpoint | Outcome Results | Study Reference |
|---|---|---|---|---|
| Heart Disease (n=95) | Stem cell therapy (n=47) | LVEF improvement | 30.2% → 43.6% (Δ13.4%) | [40] |
| Conventional therapy (n=48) | LVEF improvement | 32.5% → 36.8% (Δ4.3%) | [40] | |
| Heart Disease (n=95) | Stem cell therapy (n=47) | 6-min walk test | +80 meters | [40] |
| Conventional therapy (n=48) | 6-min walk test | +30 meters | [40] | |
| Heart Disease (n=95) | Stem cell therapy (n=47) | MLHFQ score | 56.2 → 38.5 (Δ17.7) | [40] |
| Conventional therapy (n=48) | MLHFQ score | 54.7 → 48.6 (Δ6.1) | [40] | |
| Acute Myocardial Infarction (meta-analysis, n=1,218) | Stem cell therapy | Long-term LVEF | +2.63% (p=0.02) | [43] |
| Control | Long-term LVEF | No significant improvement | [43] | |
| Stroke (meta-analysis, 17 studies) | Stem cell therapy (non-IV) | NIHSS improvement | Significant improvement at 6-12 months | [41] |
| Standard care | NIHSS improvement | Less improvement than intervention | [41] |
The efficacy advantage of stem cell approaches is particularly evident in functional outcomes. In heart failure patients, stem cell therapy produced significantly greater improvements in left ventricular ejection fraction (LVEF) compared to conventional pharmacologic management alone (13.4% vs. 4.3% absolute improvement) [40]. Similarly, exercise capacity measured by the six-minute walk test showed dramatically better results in the stem cell group (80-meter improvement vs. 30-meter improvement with conventional therapy) [40]. These functional benefits translated to meaningful quality of life improvements, with the stem cell group demonstrating substantially greater enhancements on the Minnesota Living with Heart Failure Questionnaire [40].
In autoimmune diseases, combination strategies have demonstrated particular success in achieving sustained remission in treatment-resistant cases. The strategic deployment of stem cell therapy alongside conventional immunosuppressants addresses both the symptomatic manifestations and underlying immune dysregulation characteristic of these conditions [12]. Clinical remission rates in autoimmune trials were categorized as low (≤50%), middle (>50% and ≤75%), or high (>75%), with combination approaches frequently achieving middle to high remission rates even in refractory patient populations [12].
Safety Profile and Adverse Event Management
The safety evaluation of combination therapies must account for potential interactions between stem cells and concomitant treatments. Overall, stem cell therapies have demonstrated favorable safety profiles across multiple clinical contexts, with meta-analyses reporting fewer adverse events in stem cell recipients compared to controls (OR 0.66, 95% CI 0.44 to 0.99, p=0.05) [43].
Table 4: Safety Profiles Across Different Stem Cell Therapeutic Approaches
| Therapeutic Area | Common Adverse Events | Stem Cell-Specific Safety Concerns | Risk Mitigation Strategies |
|---|---|---|---|
| Cardiovascular | Arrhythmias, injection site reactions | Procedural complications, cell embolization | Electrophysiological monitoring, optimized delivery protocols [43] |
| Autoimmune Diseases | Infections, immune reactions | Disease flare, autoimmunity transfer | Progressive immunosuppression tapering, vigilant monitoring [12] |
| Neurological | Headache, fever, transient neurological symptoms | Seizures, inappropriate cell migration | Anticonvulsant prophylaxis, precise stereotactic delivery [41] |
| Oncological | Graft-versus-host disease, engraftment syndrome | Malignant transformation, tumor promotion | Rigorous genetic stability testing, lineage tracking [44] |
In the cardiovascular domain, a systematic review and meta-analysis of 21 trials with 1,218 participants established the short-term to mid-term safety of stem cell therapy for acute myocardial infarction [43]. Importantly, no cardiac-related cancer cases were reported in any group, though authors noted that longer follow-up periods are necessary to fully assess potential oncogenic risks [43]. The overall favorable safety profile supports further clinical development of these approaches, though continued vigilance regarding long-term outcomes remains essential.
The integration of stem cells with biologic agents requires particular attention to immune compatibility and timing of administration. Sequential dosing strategies often optimize therapeutic synergy while minimizing potential interference between cell-based and pharmacologic interventions [12]. In HSC-based multidrug therapy for autoimmune conditions, immunosuppressive agents such as cyclophosphamide, rituximab, and corticosteroids are typically administered alongside stem cell infusion to create a favorable immunologic environment for engraftment and tolerance induction [12].
Experimental Protocols and Methodological Considerations
Robust experimental design is essential for evaluating combination therapies in clinical trials. This section outlines key methodological considerations and protocols based on successful clinical trials cited in this review.
Patient Selection and Stratification
Optimal patient selection criteria vary by disease context but share common elements across indications. For cardiovascular trials, typical inclusion criteria encompass adults aged 18-75 years with confirmed diagnosis of ischemic heart disease, heart failure, or myocardial infarction, while exclusion criteria commonly include history of malignancy, presence of autoimmune diseases, severe comorbid conditions, and pregnancy or breastfeeding status [40]. Similar selection principles apply to autoimmune disease trials, with additional emphasis on documenting prior treatment resistance to establish refractory disease status [12].
Stem Cell Preparation and Characterization
Standardized protocols for stem cell processing, expansion, and quality control are fundamental to reproducible outcomes. MSC-based therapies typically involve isolation from bone marrow, adipose tissue, or umbilical cord sources, followed by expansion in culture systems that maintain differentiation potential and immunomodulatory properties [39]. Comprehensive characterization includes surface marker profiling (CD73, CD90, CD105 positivity with concomitant absence of hematopoietic markers), differentiation capacity assessment, and genetic stability testing [15].
Combination Therapy Administration Protocols
Integration of stem cells with conventional therapies requires careful attention to timing, dosing, and administration sequences. In HSC transplantation for autoimmune diseases, a typical protocol involves:
- Mobilization: G-CSF administration to mobilize hematopoietic stem cells
- Collection: Leukapheresis for HSC harvest
- Conditioning: Immunoablation with cyclophosphamide and antithymocyte globulin
- Transplantation: Infusion of purified CD34+ HSCs
- Maintenance: Progressive reintroduction of conventional immunosuppressants [12]
For cardiovascular applications, stem cells are typically delivered via intracoronary infusion or direct myocardial injection alongside continued guideline-directed medical therapy [40] [7]. The concomitant pharmacologic management generally includes beta-blockers, ACE inhibitors/ARBs, statins, and antiplatelet agents, with dosing adjustments based on individual patient tolerance and response [40].
The experimental workflow for combination therapy trials involves sequential phases from patient selection through long-term monitoring. Critical stages include stem cell preparation with rigorous quality control, appropriate conditioning regimens when applicable, precise stem cell delivery, and careful integration of conventional therapies. Each phase requires specialized expertise and infrastructure to ensure protocol adherence and patient safety.
Advancing combination therapy research requires specialized reagents and methodological approaches. The following table summarizes key resources essential for investigating integrated stem cell and conventional therapy protocols.
Table 5: Essential Research Reagents and Resources for Combination Therapy Studies
| Category | Specific Reagents/Resources | Primary Research Application | Technical Considerations |
|---|---|---|---|
| Stem Cell Characterization | CD34, CD133, CD44, CD73, CD90, CD105 antibodies | Immunophenotyping of stem cell populations | Panel design must distinguish stem cells from hematopoietic lineages [44] |
| Functional Assays | CFU-F, trilineage differentiation kits, transwell migration systems | Assessment of stem cell functional potency | Standardized protocols enable cross-study comparisons [39] |
| Cell Tracking | GFP/luciferase labeling systems, iron oxide nanoparticles, DNA barcoding | In vivo fate mapping of administered cells | Multimodal approaches enhance detection sensitivity [41] |
| Immune Monitoring | Multiplex cytokine arrays, flow cytometry panels (Treg, Th1, Th17), MLR | Evaluation of immunomodulatory effects | Longitudinal sampling captures dynamic immune responses [12] |
| Molecular Analysis | miRNA profiling arrays, single-cell RNA sequencing, epigenetic markers | Mechanistic studies of stem cell actions | Integration with functional data strengthens conclusions [12] |
The selection of appropriate characterization markers is context-dependent. For hematopoietic stem cells, CD34 and CD133 serve as primary surface markers, while mesenchymal stem cells are typically identified through CD73, CD90, and CD105 expression alongside absence of hematopoietic markers [44] [39]. Functional assays must evaluate both differentiation capacity and paracrine activity to fully characterize the therapeutic potential of stem cell populations [39].
Advanced cell tracking methodologies are particularly important in combination therapy research, as they enable researchers to determine the fate and persistence of administered cells in the context of concomitant drug treatments [41]. Similarly, comprehensive immune monitoring provides insights into how stem cells modulate responses to conventional immunomodulatory agents, potentially revealing synergistic mechanisms that underlie clinical efficacy [12].
The integration of stem cells with conventional and biologic therapies represents a promising frontier in regenerative medicine. Evidence from clinical trials across multiple disease domains indicates that combination approaches frequently outperform monotherapies, achieving superior efficacy while maintaining acceptable safety profiles [12] [40] [43]. The mechanistic basis for this advantage lies in the complementary actions of stem cells—addressing underlying tissue damage and immune dysregulation—and conventional therapies—managing symptomatic disease manifestations [12] [39].
Future progress in this field will require addressing several key challenges. Standardization of cell preparation protocols, optimization of dosing and timing sequences, and development of predictive biomarkers for patient selection represent critical priorities for the research community [15] [39]. Additionally, regulatory frameworks must continue to evolve to accommodate the unique aspects of combination product development, potentially incorporating adaptive licensing pathways that facilitate iterative evidence generation [15].
As the field advances, personalized combination regimens tailored to individual patient characteristics and disease mechanisms will likely emerge as the optimal approach. The continued elucidation of stem cell actions at molecular and cellular levels will inform these precision medicine strategies, potentially unlocking the full therapeutic potential of integrated treatment paradigms for a broad spectrum of currently intractable conditions.
Stem cell therapy represents a revolutionary frontier in modern medicine, offering unprecedented potential to address a wide range of debilitating diseases and injuries [11]. However, the clinical translation of these therapies faces significant challenges, particularly in consistently demonstrating efficacy in randomized clinical trials [13]. A principal barrier lies in the limitations of conventional assessment methods, which often fail to capture the nuanced biological effects of cellular therapeutics. Unlike pharmaceutical compounds with direct molecular targets, stem cells exert their benefits through complex mechanisms including paracrine signaling, immunomodulation, and tissue regeneration over extended timelines [13] [11]. This complexity demands more sophisticated evaluation tools that can provide objective, quantitative data on therapeutic activity at the structural, functional, and molecular levels.
Advanced assessment methodologies, particularly magnetic resonance imaging (MRI) and molecular biomarker profiling, are emerging as critical technologies for addressing these challenges. These tools enable researchers to visualize tissue repair processes, monitor functional recovery, and identify predictive indicators of treatment response [13] [45] [46]. By providing deeper insights into therapeutic mechanisms and patient stratification, these advanced assessment methods are poised to accelerate the development and validation of stem cell therapies across multiple disease domains.
MRI as a Quantitative Tool for Structural and Functional Assessment
Multimodal MRI Techniques and Applications
MRI provides a non-invasive, multi-parametric approach for serially monitoring the effects of stem cell therapy. Different MRI sequences yield complementary information about tissue structure, integrity, and function, making them invaluable for comprehensive therapeutic assessment as detailed in the table below.
Table 1: Multimodal MRI Techniques for Assessing Stem Cell Therapy Efficacy
| MRI Technique | Primary Measured Parameters | Biological Correlates | Clinical Applications |
|---|---|---|---|
| T1/T2-Weighted Structural Imaging | Lesion volume, brain atrophy, ventricular size [47] | Macroscopic morphological changes, tissue loss [13] | Ischemic stroke, multiple sclerosis [46] [47] |
| Diffusion Tensor Imaging (DTI) | Fractional Anisotropy (FA), Mean Diffusivity (MD), Axial/Radial Diffusivity [47] | White matter microstructural integrity, axonal injury, remyelination [13] [46] | Stroke recovery, MS [46] [47] |
| Functional MRI (fMRI) | Blood Oxygen Level Dependent (BOLD) signal | Functional connectivity, neural network activity [13] | Stroke, neurodegenerative diseases |
| Magnetic Resonance Spectroscopy (MRS) | Metabolite concentrations (e.g., NAA, choline, creatine) [13] | Neuronal health, cellular metabolism, viability | Stroke, metabolic disorders |
Documented Efficacy via MRI in Clinical and Preclinical Studies
Evidence from clinical trials and preclinical models demonstrates MRI's utility in detecting treatment-induced changes correlated with functional improvement.
- Multiple Sclerosis: A 2025 systematic review and meta-analysis found that MRI could detect significant treatment effects in MS patients receiving mesenchymal stem cell (MSC) therapy. The analysis showed a significant reduction in T2 lesion volume (mean difference -5.12 mm³) and a higher likelihood of no new T2 lesions (risk ratio 1.69) in MSC-treated patients compared to controls [46]. Advanced techniques like DTI further revealed microstructural repair, particularly with intrathecal MSC administration [46].
- Ischemic Stroke: In a rat model of ischemic stroke, quantitative MRI measurements correlated strongly with behavioral recovery after MSC therapy. The group receiving patient serum-cultured MSCs showed the most prominent functional improvement, which was matched by significant decreases in infarct lesion volume and reduced brain atrophy on T2-weighted imaging [47]. DTI parameters further revealed microstructural improvements, with significantly higher relative fractional anisotropy (rFA) and fiber density (rFD) values, indicating enhanced white matter integrity [47].
- Cardiac Applications: While focusing on neurological conditions, MRI's role extends to cardiovascular applications. Cardiac MRI (CMRI) serves as the gold standard for assessing infarct size and left ventricular ejection fraction in myocardial infarction trials, providing critical efficacy endpoints for stem cell therapies [21].
Experimental MRI Protocols in Preclinical Research
Standardized protocols are essential for generating reproducible, quantifiable MRI data. The following workflow visualizes a comprehensive preclinical imaging protocol from a rat stroke study.
Figure 1: Preclinical MRI Assessment Workflow for Stem Cell Therapy in Stroke
Detailed Methodology:
- Animal Model: Adult male Sprague-Dawley rats (250-300 g) subjected to 90-minute transient middle cerebral artery occlusion (tMCAO) to induce ischemic stroke [47].
- Intervention Groups: Randomized allocation to receive either PBS control, fetal bovine serum-cultured human MSCs (FBS-hMSCs), or stroke patient serum-cultured hMSCs (SS-hMSCs) via intravenous injection 24 hours post-stroke [47].
- MRI Acquisition: Conducted using a 7T small animal MR scanner. Protocol includes:
- T2-weighted imaging: For quantification of ischemic lesion volume and ventricular size.
- Diffusion Tensor Imaging (DTI): For calculating microstructural indices (FA, AD, RD) and fiber density in the ischemic recovery area [47].
- Image Analysis: Quantitative volumetric analysis of lesions and ventricles; voxel-based analysis of DTI indices; tractography for fiber density mapping [47].
- Behavioral Correlation: Functional improvement assessed using modified neurological severity score (mNSS) correlated with MRI parameters [47].
Molecular Biomarkers for Predicting and Monitoring Treatment Response
Metabolic Biomarkers as Predictive Tools
Beyond imaging, molecular biomarkers offer critical insights into treatment mechanisms and potential for predicting therapeutic responses. Metabolic profiling has emerged as a promising approach for identifying patients most likely to benefit from stem cell therapy.
In a clinical study focusing on systemic lupus erythematosus (SLE), researchers identified specific metabolic changes associated with successful MSC transplantation therapy [45]. Plasma samples from 20 SLE patients collected before and after MSCT revealed that clinical improvements at 180 days post-treatment were correlated with specific metabolite changes. Notably, increases in thiamine monophosphate (TMP) and asiaticoside levels were strongly associated with positive treatment outcomes [45]. Most significantly, a 35% increase in TMP levels was identified as a predictive biomarker for treatment success, potentially offering clinicians a valuable tool for patient stratification and outcome prediction [45].
Research Reagent Solutions for Biomarker Discovery
The following table outlines essential research tools and their applications in biomarker discovery and validation for stem cell therapy studies.
Table 2: Essential Research Reagents for Biomarker and Efficacy Studies
| Reagent / Solution | Primary Function | Application Context |
|---|---|---|
| Metabolomic Assay Kits | Quantification of metabolite changes (e.g., TMP, asiaticoside) [45] | Predictive biomarker identification in SLE clinical trials |
| ELISA Kits for Inflammatory Mediators | Measurement of cytokines (e.g., IL-6, TNF-α) and growth factors | Monitoring immunomodulatory effects of MSCs |
| Cell Culture Media Supplements | Preconditioning stem cells (e.g., with patient serum) [47] | Enhancing therapeutic potency in preclinical models |
| Flow Cytometry Antibody Panels | Characterization of stem cell surface markers and immune cell populations | Quality control and mechanism of action studies |
| MRI Contrast Agents | Enhancement of tissue visualization and lesion demarcation | Quantitative assessment of structural changes |
Integrated Assessment Frameworks and Future Directions
Synergistic Application in Clinical Trials
The most comprehensive assessment of stem cell therapy efficacy comes from integrating multiple advanced methodologies. A 2025 systematic review and meta-analysis of stem cell therapy for acute and subacute ischemic stroke exemplifies this approach, combining clinical scales with imaging and biomarker data [8]. The analysis of 13 randomized controlled trials demonstrated that stem cell therapy significantly improved long-term functional outcomes, with a 74% higher incidence of favorable mRS scores (0-1) at one year and a 31% higher incidence of mRS scores 0-2 at 90 days in the cell therapy group compared to controls, without increasing serious adverse events or mortality [8].
The synergistic relationship between MRI and biomarker assessment creates a comprehensive framework for evaluating stem cell therapy, as visualized below.
Figure 2: Integrated Framework for Efficacy Assessment
Current Challenges and Future Outlook
Despite promising advancements, several challenges remain in fully establishing MRI and biomarkers as primary endpoints in stem cell therapy trials. Methodological heterogeneity across studies, lack of standardized imaging protocols, and small sample sizes currently limit the broader application of these techniques [46]. Future efforts should focus on:
- Developing uniform imaging protocols and analytical pipelines for multi-center trials
- Validating predictive biomarker panels across diverse patient populations
- Integrating artificial intelligence and machine learning approaches for analyzing complex multimodal datasets [13]
- Establishing correlative frameworks linking imaging parameters, molecular biomarkers, and clinical outcomes
As the field progresses toward more personalized therapeutic approaches, these advanced assessment methods will play an increasingly vital role in elucidating mechanisms of action, identifying patient subgroups most likely to respond, and ultimately demonstrating the clinical efficacy of stem cell therapies across a spectrum of neurological, cardiovascular, and autoimmune conditions [13] [11] [12].
Addressing Efficacy Challenges and Optimizing Therapeutic Protocols
The therapeutic potential of stem cells, particularly mesenchymal stem cells (MSCs), is vast due to their immunomodulatory properties and capacity for tissue repair [34]. However, the translation of promising preclinical results into consistent, successful clinical outcomes has been hampered by significant heterogeneity in cell sourcing, potency, and manufacturing processes. This variability presents a critical bottleneck in stem cell therapy efficacy within randomized clinical trials (RCTs), as biological potential can be undermined by inconsistent production standards [48]. For researchers and drug development professionals, addressing these sources of heterogeneity is paramount for advancing regenerative medicine. This guide objectively compares how different sourcing, manufacturing, and assessment strategies impact therapeutic potential, providing a framework for standardizing protocols to enhance clinical trial success.
The Clinical Trial Landscape: A Mirror of Manufacturing Variability
The current state of global clinical trials reflects both the promise and the challenges of stem cell therapies. An analysis of 244 interventional trials registered between 2006 and 2025 reveals that the field is still in its translational infancy, with 83.6% of trials in Phase I or II [34]. This distribution indicates that the community is still grappling with establishing foundational manufacturing and efficacy protocols before large-scale Phase III trials can be successfully undertaken.
Table 1: Global Clinical Trial Distribution for Stem Cell Therapies in Autoimmune Diseases (2006-2025)
| Trial Characteristic | Distribution |
|---|---|
| Total Analyzed Trials | 244 |
| Most Researched Diseases | Crohn's disease (n=85), Systemic Lupus Erythematosus (n=36), Scleroderma (n=32) |
| Geographic Leadership | United States and China lead trial numbers |
| Primary Funding Source | Academic institutions (49.2% of trials) |
| Dominant Cell Type | Mesenchymal Stem Cells (MSCs) |
The predominance of academic funding highlights a crucial challenge: academic labs often employ individualized, non-standardized protocols, whereas robust, commercially viable therapies require consistent, scalable manufacturing processes [34] [48]. This reliance on varied academic protocols directly contributes to the heterogeneity observed in clinical outcomes.
Cell Sourcing: A Primary Source of Biological Variability
The tissue source from which stem cells are derived is a major determinant of their fundamental biological properties and therapeutic potential.
Table 2: Impact of Cell Source on Biological Properties and Therapeutic Potential
| Cell Source | Key Advantages | Documented Limitations & Variability |
|---|---|---|
| Bone Marrow (BM-MSCs) | - Historical gold standard [49]- Extensive published data | - Invasive, painful extraction [49]- Donor-age-dependent decline in cell quality and potency [48] |
| Adipose Tissue (AT-MSCs) | - Abundant tissue source- Less invasive harvest | - Heterogeneous cell population requiring rigorous purification- Differential secretory profiles compared to BM-MSCs |
| Umbilical Cord/Placenta (UC-MSCs) | - Non-invasive collection [49]- Immunologically naive- High proliferative capacity [49] | - Potential for microbial contamination during procurement- Donor-to-donor biological variability |
Experimental Protocol: Evaluating Source-Dependent Potency
To objectively compare the functional potency of MSCs from different sources, researchers employ standardized in vitro immunomodulation assays.
Detailed Methodology:
- Cell Sourcing and Expansion: Isolate and expand BM-MSCs, AT-MSCs, and UC-MSCs using identical culture conditions (e.g., basal medium, serum type, O2 tension, and seeding density).
- Lymphocyte Proliferation Assay: Co-culture MSCs from each source with activated peripheral blood mononuclear cells (PBMCs) from the same human donor. A common method uses phytohemagglutinin (PHA) to activate T-cells.
- Experimental Control: Include a control well of PHA-activated PBMCs without MSCs to establish baseline proliferation.
- Quantification: After 72-96 hours, measure T-cell proliferation using a calibrated method such as 3H-thymidine incorporation or CFSE dye dilution followed by flow cytometry.
- Data Analysis: Calculate the percentage suppression of proliferation:
[1 - (Proliferation in Co-culture / Proliferation in Control)] × 100%.
Expected Outcome: This protocol often reveals significant source-dependent variation in immunosuppressive capacity. For instance, some studies suggest UC-MSCs may exhibit more potent immunosuppression per cell than BM-MSCs or AT-MSCs [49]. This experimental approach provides critical, quantifiable data for selecting a cell source based on the desired therapeutic mechanism.
Manufacturing Processes: The Critical Amplifier of Variability
Perhaps the most impactful yet controllable source of heterogeneity lies in the manufacturing process itself. Inconsistencies here can fundamentally alter the cellular product, leading to failed clinical trials.
Key Manufacturing Variables and Their Impact
Table 3: Impact of Manufacturing Process Parameters on Final Cell Product
| Process Parameter | Documented Effect on Cell Product | Supporting Evidence |
|---|---|---|
| Culture Media Formulation | "The therapeutic profile of the cells changes greatly depending on the media environment in which they're grown." [48] | A study culturing identical donor cells in five different commercial media produced cells with "dramatically different" biological properties, differentiation ability, and immunomodulatory activity [48]. |
| Scale-Up System (2D vs. 3D) | Alters cell morphology, proliferation rate, and secretome. | The industry is shifting towards 3D bioreactors for scale-up. In 2024, 30% of new capacity installations were closed-system bioreactors to enhance reproducibility [50]. |
| Passage Number & Cell Density | Influences senescence, differentiation potential, and surface marker expression. | High passage numbers are linked to reduced potency and genetic instability, necessitating strict in vitro lifespan limits. |
The following diagram illustrates how these manufacturing variables introduce heterogeneity that directly impacts clinical outcomes, creating a cycle that is difficult to break without standardization.
Experimental Protocol: Quantifying Media-Induced Variability
The REMEDI group's experimental design offers a robust protocol for quantifying the specific impact of media formulation [48].
Detailed Methodology:
- Standardized Cell Source: Obtain bone marrow aspirates from a minimum of three consented human donors.
- Controlled Expansion: Isolate MSCs from each donor and expand them under identical conditions (same incubator, operator, seeding density, and passage number) with one key variable: the culture medium.
- Variable: Use five distinct, commercially available, GMP-grade MSC culture media formulations.
- Functional Output Analysis: Harvest the cells and perform a battery of analyses on each group:
- Surface Phenotype: Flow cytometry for standard positive (CD73, CD90, CD105) and negative (CD34, CD45, HLA-DR) markers.
- Differentiation Potential: Induce adipogenic, osteogenic, and chondrogenic differentiation using standardized kits. Quantify outcomes with Oil Red O, Alizarin Red, and Alcian Blue staining, respectively, using spectrophotometric or image-based quantification.
- Immunomodulatory Activity: Use the T-cell suppression assay detailed in Section 2.2.
Expected Outcome: This protocol demonstrates that while cells from all five media groups may meet the minimal ISCT criteria for MSCs (plastic adherence and surface markers), they will exhibit significant, statistically relevant differences in their functional potency, such as varying levels of T-cell suppression and differential capacity [48]. This empirically proves that current release criteria are insufficient for guaranteeing consistent therapeutic efficacy.
The Scientist's Toolkit: Essential Reagents and Solutions for Standardization
Navigating heterogeneity requires a suite of high-quality, well-characterized reagents and tools. The following table details key solutions for critical stages of R&D and manufacturing.
Table 4: Key Research Reagent Solutions for Stem Cell Manufacturing & Quality Control
| Reagent/Tool | Primary Function | Role in Mitigating Heterogeneity |
|---|---|---|
| GMP-Grade Culture Media Kits | Provides nutrients, growth factors, and cytokines for cell growth. | Prevents batch-to-batch variability associated with serum-containing media; ensures defined, consistent composition [50] [51]. |
| Closed-System Bioreactors | Scalable 3D environment for cell expansion. | Reduces contamination risk and operator-dependent variability; enables controlled, reproducible scale-up [50] [52]. |
| Flow Cytometry Panels | Quantifies surface marker expression (CD73, CD90, CD105, etc.). | Provides a quantitative identity check for the cell population, though it is insufficient for a full potency assessment [48]. |
| Cell Potency Assay Kits | Measures a specific, therapeutically relevant function (e.g., IDO activity, T-cell suppression). | Moves quality control beyond identity/purity to confirm biological function; critical for correlating with clinical efficacy [48]. |
| Automation & AI Software | Robotic handling and AI-driven process monitoring. | Reduces human error; uses predictive models to detect process deviations early and maintain optimal culture parameters [52] [53] [51]. |
The industry is increasingly adopting these tools, with consumables accounting for 47% of the stem cell manufacturing market product mix in 2024, underscoring their foundational role [50]. Furthermore, the integration of AI and automation is a major trend, with AI-powered bioprocess monitoring platforms being launched to enhance reproducibility and predictive control [53] [51].
The journey toward consistent efficacy in stem cell clinical trials hinges on the systematic reduction of heterogeneity from sourcing through manufacturing. The experimental data and comparative analyses presented here demonstrate that the current "one-size-fits-all" release criteria are inadequate. The future lies in adopting a more nuanced, process-aware approach that includes:
- Defined, Therapeutically Relevant Potency Assays: Replacing or supplementing phenotypic markers with quantitative functional assays that correlate with clinical mechanism of action.
- Process Standardization and Closed Systems: Widespread adoption of automated, closed-system bioreactors and standardized, GMP-grade consumables to minimize operator- and facility-induced variability.
- Data-Driven Manufacturing: Leveraging AI and machine learning for real-time process monitoring and predictive control, allowing for the detection of subtle deviations that foretell a loss of product quality [52] [53].
By embracing these strategies, researchers and drug developers can transform stem cell manufacturing from an artisanal craft into a robust, reproducible engineering discipline. This evolution is essential for fulfilling the promise of regenerative medicine and achieving consistent success in randomized clinical trials.
Within the broader thesis on stem cell therapy efficacy in randomized clinical trials (RCTs), the analysis of safety and tolerability profiles represents a critical pillar for translational research. As regenerative medicine advances, understanding the adverse event (AE) profiles of different stem cell types across various disease applications is paramount for researchers and drug development professionals. This guide provides an objective comparison of these safety profiles based on recent meta-analyses, presenting structured quantitative data to inform preclinical studies and clinical trial design. The analysis focuses on AEs ranging from common, transient reactions to more serious, procedure-related complications, contextualizing them within the risk-benefit framework of stem cell therapy development.
Quantitative Safety Profiles Across Medical Applications
Recent meta-analyses of RCTs provide comprehensive safety data for stem cell therapies across neurological, orthopedic, and other conditions. The tables below summarize the frequency and nature of adverse events associated with different stem cell treatments.
Table 1: Overall Adverse Event Incidence from Recent Meta-Analyses
| Medical Condition | Number of Studies & Patients | Cell Types Analyzed | Serious Adverse Event (SAE) Risk vs. Control | Most Common Non-Serious Adverse Events |
|---|---|---|---|---|
| Ischemic Stroke (Acute/Subacute) | 13 RCTs (n=872 patients) [8] | BM-MSCs, BMMNC, Progenitor Cells | No significant difference (RR 0.85, 95% CI 0.70–1.04) [8] | Nausea, fever, transient headache [8] |
| Knee Osteoarthritis | 8 RCTs (n=502 patients) [54] | BM-MSC, AD-MSC, UC-MSC | No significant difference (P > 0.05) [54] | Transient injection site pain, swelling [54] |
| Chronic Spinal Cord Injury | 45 studies (n=1,633 cases) [55] | NSC, OEC, BM-MSC, UC-MSC, ESC | No life-threatening AEs or deaths reported [55] | Transient backache (90%), meningism (90%), cord malacia (80%) [55] |
Table 2: Cell-Type Specific Adverse Event Rankings and Profiles
| Cell Type | Therapeutic Context | Noted Efficacy Ranking | Specific Safety Concerns | Incidence of Common AEs |
|---|---|---|---|---|
| Umbilical Cord MSC (UC-MSC) | Ischemic Stroke [56] | Best for neurological recovery (NIHSS) [56] | Inflammatory thromboembolism in case reports (kidney transplant patients) [57] | Low-grade fever, nausea [58] |
| Bone Marrow Mononuclear Cells (BMMNC) | Ischemic Stroke [56] | Best for motor function (FMA) and daily living (MBI) [56] | No specific serious AEs predominant in meta-analyses | Fatigue, headache [58] |
| Embryonic Stem Cells (ESC) | Spinal Cord Injury [55] | N/A in included analyses | Lowest rate of AEs in SCI trials (2.33%) [55] | Limited data in meta-analyses |
| Olfactory Ensheathing Cell (OEC) & BM-MSC Combination | Spinal Cord Injury [55] | N/A in included analyses | Highest rate of AEs in SCI trials (55%) [55] | Back pain, meningism [55] |
| Adipose-Derived MSC (AD-MSC) | Knee Osteoarthritis [54] | Significant efficacy in subgroup analysis [54] | No significant difference in AEs vs. control in OA [54] | Injection site pain, swelling [54] |
Detailed Methodologies of Cited Meta-Analyses
Search Strategy and Study Selection
The cited meta-analyses employed rigorous systematic review methodologies following PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines and Cochrane Handbook recommendations [54]. For the ischemic stroke analysis, investigators conducted a computerized search of Cochrane Library, PubMed, Web of Science, Google Scholar, CNKI, and Wanfang databases from their inception to December 2024 [56]. The osteoarthritis meta-analysis systematically searched Web of Science, PubMed, EMBASE, and Scopus up to August 1, 2024 [54]. Both used precise PICOS (Population, Intervention, Comparison, Outcome, Study design) criteria for study selection, focusing exclusively on randomized controlled trials to ensure the highest evidence quality.
Data Extraction and Quality Assessment
For each eligible study, two independent authors extracted data using standardized forms, resolving discrepancies through consensus [54]. Extracted information included: (1) baseline study characteristics (author, publication year, country); (2) patient demographics and sample sizes; (3) intervention details (cell type, dose, administration route); (4) outcome measures (primary and secondary efficacy endpoints); and (5) safety data (adverse event frequency, nature, and severity). Risk of bias assessment utilized the Cochrane Risk of Bias Tool, evaluating selection, performance, detection, attrition, reporting, and other biases. Studies were categorized as low, unclear, or high risk [54], with the stroke meta-analysis reporting five studies with low risk, six with medium risk, and two with high risk [8].
Statistical Analysis Protocol
Meta-analyses were performed using Review Manager (version 5.3) software [54]. For continuous outcomes (e.g., WOMAC, NIHSS), weighted mean differences (WMD) or standardized mean differences (SMD) with 95% confidence intervals (CI) were calculated. For dichotomous outcomes (e.g., incidence of AEs, mortality), risk ratios (RR) with 95% CI were used. Heterogeneity was assessed using I² statistics and chi-square tests, with I² > 50% indicating substantial heterogeneity requiring random-effects models. Fixed-effects models were applied when heterogeneity was low (I² < 50%) [54]. Sensitivity analyses and meta-regression were conducted where appropriate to explore heterogeneity sources [8].
Mechanisms and Pathways of Adverse Events
The safety profile of stem cell therapies is influenced by multiple factors, from cell processing to patient-specific factors. The diagram below illustrates the primary pathways through which adverse events can occur.
Diagram 1: Pathways to Adverse Events in Stem Cell Therapy. This diagram illustrates how cell processing, cell type, administration methods, and patient-specific factors contribute to different adverse event profiles, from common procedure-related events to serious complications like thromboembolism and rare malignant transformation.
Thromboembolism as a Primary Safety Concern
Thromboembolism emerges as the most significant serious adverse event across multiple meta-analyses, particularly associated with mesenchymal stromal cells (MSCs) [57]. The proposed mechanism involves the release of procoagulant tissue factor (TF) by MSCs, which activates the extrinsic coagulation pathway [57]. This risk appears dose-dependent and may be influenced by cell culture conditions and passage number. Case reports describe inflammatory-associated thromboembolism in kidney transplant patients and those with chronic kidney disease following umbilical cord MSC (hUC-MSC) infusion [57]. The delayed manifestation of these events underscores the importance of long-term safety monitoring in clinical trials.
Tumorigenicity and Malignant Transformation
The potential for tumorigenicity represents a fundamental safety consideration in stem cell therapy. While most clinical trials have not reported life-threatening tumors or malignant transformations, in vitro studies demonstrate that long-term cell culture can lead to chromosomal abnormalities and spontaneous malignant transformation [57]. One study reported approximately 46% of human MSCs underwent spontaneous malignant transformation after four weeks in culture [57]. Chromosomal abnormalities in adipose-derived MSCs significantly increase starting from passage 5 [57]. These findings highlight the critical importance of establishing standardized protocols for in vitro expansion and comprehensive genetic testing before clinical application.
Procedure-Related and Site-Specific Adverse Events
The administration route significantly influences the adverse event profile, with most events being mild to moderate and transient. The diagram below illustrates the development of chromosomal abnormalities during cell culture, a key risk factor for tumorigenicity.
Diagram 2: Culture Duration Impact on Genomic Stability. This workflow shows how increasing passage number during in vitro expansion elevates the risk of chromosomal abnormalities and malignant transformation, highlighting the importance of limiting culture duration for clinical applications.
- Intravenous administration commonly produces systemic reactions including fatigue, headache, chills, nausea, and low-grade fever, typically resolving within 24-48 hours [58].
- Local injection (e.g., intra-articular for osteoarthritis) most frequently causes injection site reactions - pain, swelling, bruising, and redness [54] [58].
- Intrathecal administration (used for neurological conditions) may result in headache, nausea, dizziness, and transient neurological symptoms [58].
- Spinal cord injury applications demonstrate unique site-specific AEs, with transient backache and meningism occurring in up to 90% of patients and cord malacia in 80% [55].
The Scientist's Toolkit: Research Reagent Solutions for Safety Monitoring
Table 3: Essential Research Reagents for Stem Cell Safety Assessment
| Reagent/Category | Primary Function in Safety Assessment | Specific Application Examples |
|---|---|---|
| Flow Cytometry Antibodies | Characterization of cell surface markers to verify identity and purity. | CD73, CD90, CD105 (positive); CD19, CD20, CD34, CD45 (negative) for MSC verification [57]. |
| Karyotyping & FISH Kits | Detection of chromosomal abnormalities and genetic stability assessment. | Monitoring chromosomal aberrations in late-passage cells (≥P5) [57]. |
| Mycoplasma Detection Kits | Screening for mycoplasma contamination in cell cultures. | Routine quality control to prevent contaminated cell administration [57]. |
| Viral PCR Panels | Detection of adventitious viral agents in cell products. | Screening for persistent viruses (B19V, TTV, EBV, MCPyV, HHV-7) in donor cells [57]. |
| Tissue Factor (TF) ELISA | Quantification of procoagulant activity in cell preparations. | Assessing thrombogenic potential of MSC batches before administration [57]. |
| Cell Counters & Viability Kits | Determination of cell dose, viability, and potency. | Standardizing doses for administration; ensuring >70% viability [54]. |
| Sterility Testing Media | Validation of sterile manufacturing processes. | Bacterial and fungal culture testing prior to clinical use [58]. |
| Tumorigenicity Assays | In vitro and in vivo assessment of tumor formation potential. | Soft agar assays; in vivo tumor formation studies in immunodeficient mice [57]. |
The comprehensive analysis of recent meta-analyses demonstrates that stem cell therapies, particularly those utilizing adult stem cells like MSCs, present acceptable safety profiles across multiple disease applications, with no significant increase in serious adverse events compared to control groups in randomized trials. The most common adverse effects are transient and procedure-related, while the most significant serious risks include thromboembolism and potential tumorigenicity associated with specific cell processing conditions. These findings support the continued clinical investigation of stem cell therapies while emphasizing the critical importance of standardized protocols, rigorous safety monitoring, and careful patient selection in both research and clinical applications.
The therapeutic potential of stem cell therapy in regenerative medicine is vast, yet its clinical efficacy is often constrained by a significant bottleneck: the inefficient homing and engraftment of administered cells to target tissues. Homing refers to the multistep process by which cells navigate the circulatory system, adhere to the endothelium near the injury site, and extravasate into the target tissue. Engraftment signifies the subsequent survival, integration, and functional persistence of these cells within the host environment. Overcoming the barriers to efficient homing and engraftment is not merely an engineering challenge; it is a fundamental prerequisite for translating promising preclinical results into consistent clinical success. Current data reveals that when administered systemically, a disappointingly low percentage of cells—often less than 5%—successfully reach the intended lesion site, with the majority becoming trapped in filter organs like the lungs, liver, and spleen [59]. This review, framed within the context of randomized clinical trial research, objectively compares the performance of emerging strategies designed to surmount these delivery barriers, providing a critical analysis of their supporting experimental data for researchers and drug development professionals.
Quantifying the Problem: The Scale of Inefficiency
The first step in addressing a problem is to measure it. A wealth of tracking studies, utilizing modalities like bioluminescence, radionuclide labeling, and magnetic resonance imaging (MRI), has quantified the stark realities of stem cell delivery post-transplantation. The table below summarizes the key biodistribution and engraftment challenges identified in the literature.
Table 1: Major Identified Barriers to Efficient Homing and Engraftment
| Barrier Category | Specific Challenge | Impact on Cell Therapy |
|---|---|---|
| Administration & Biodistribution | First-pass pulmonary entrapment | Massive initial cell loss (up to 60-80%) following intravenous injection [59]. |
| Cell-Environment Interaction | Poor directional homing | Limited expression of homing receptors (e.g., CXCR4) on cultured MSCs reduces chemotaxis toward injury signals (SDF-1) [59]. |
| Post-Engraftment Survival | Hostile microenvironment | Anoikis (detachment-induced cell death), ischemia, inflammation, and immune responses limit long-term cell survival [59]. |
| Technical & Logistical | Suboptimal delivery routes and cell sourcing | The choice of administration method and tissue source significantly influences initial engraftment efficiency and durability [59] [36]. |
The consequence of these barriers is unambiguous: a low engraftment efficiency that is generally "low and transient in nature" [59]. This directly translates to subtherapeutic cell densities at the target site, forcing the use of higher, potentially riskier cell doses in an attempt to achieve a clinical effect. Therefore, the field's focus has shifted from simply injecting more cells to developing intelligent strategies that enhance the delivery and persistence of every administered cell.
Strategic Comparisons: Analyzing Solutions for Enhanced Delivery
Researchers are tackling the delivery problem from multiple angles. The following sections compare the performance of several key strategic approaches, supported by experimental data and protocols.
Route of Administration: A Foundational Choice
The method of cell delivery is a primary determinant of initial biodistribution. The table below compares the most common routes, their performance characteristics, and typical use cases.
Table 2: Performance Comparison of Stem Cell Delivery Routes
| Delivery Route | Mechanism & Workflow | Engraftment Efficiency & Key Findings | Clinical Applications |
|---|---|---|---|
| Intravenous (IV) | Systemic infusion via peripheral or central vein; cells circulate through pulmonary capillary bed before systemic distribution. | Lowest engraftment. Study: >80% first-pass lung entrapment; engraftment generally transient [59]. | Systemic conditions (e.g., GvHD, systemic lupus) where widespread distribution is desired. |
| Intra-arterial (IA) | Direct injection into an artery supplying the target organ (e.g., hepatic, cerebral); bypasses pulmonary circulation. | Significantly higher than IV. Study: IA delivery to heart/liver resulted in 4-5x greater initial retention vs. IV [59]. | Focal diseases of organs like the heart, liver, or brain. |
| Local/Targeted Injection | Direct surgical or image-guided injection into the target tissue (e.g., myocardium, joint space, spinal cord). | Highest initial local retention. Bypasses circulation entirely. Challenge: Potential for rapid effusion and limited diffusion from injection site. | Musculoskeletal defects, myocardial infarction, localized neurological injury. |
Supporting Experimental Protocol: A classic comparative study involves administering luciferase-expressing MSCs to animal models via IV, IA, and local routes. Cells are tracked in real-time using bioluminescence imaging (BLI). Quantification of total photon flux over the target organ at various time points (e.g., 1 hour, 24 hours, 1 week post-injection) provides longitudinal data on cell retention and survival, clearly demonstrating the superiority of IA over IV for organ-specific targeting [59].
Cell Targeting and Engineering Strategies
To improve the innate homing ability of stem cells, researchers employ various pre-conditioning and genetic engineering techniques.
Table 3: Comparison of Cell-Targeting and Engineering Strategies
| Strategy | Methodology | Experimental Evidence & Efficacy |
|---|---|---|
| Genetic Modification | CXCR4 Overexpression: Lentiviral/retroviral transduction to increase receptor for SDF-1α. Other Modifications: Expression of adhesive ligands (e.g., VLA-4). | Enhanced Homing: Study: CXCR4-overexpressing MSCs showed 2-3x greater migration toward SDF-1 in vitro and significantly higher retention in ischemic myocardium in vivo [60]. |
| Chemical & Biologic Pre-conditioning | Hypoxia Pre-conditioning: Culture in low oxygen (1-5% O2) before transplantation. Cytokine Priming: Incubation with inflammatory cytokines (e.g., TNF-α, IFN-γ). | Improved Survival & Function: Study: Hypoxia pre-conditioning upregulated pro-survival genes (e.g., HIF-1α, CXCR4) and increased anti-apoptotic and angiogenic factor secretion, leading to ~50% higher engraftment in a mouse model [59]. |
| Surface Modification ("Cell Painting") | Chemical Coupling: Using biotin-streptavidin or NHS-chemistry to conjugate homing ligands (e.g., E-selectin, VCAM-1 antibodies) to the cell membrane. Lipid Coating: Incorporating targeting motifs into the cell membrane via synthetic liposomes. | Direct Organ Targeting: Study: Coating MSCs with antibodies targeting lung VCAM-1 increased lung-specific sequestration by >70% compared to naive MSCs, demonstrating proof-of-concept for directed adhesion [59]. |
Supporting Experimental Protocol: The efficacy of CXCR4 overexpression is typically validated through a tiered protocol: 1) In vitro Transwell migration assay: Modified and control MSCs are placed in the upper chamber, with SDF-1α in the lower chamber. Migration is quantified after 6-24 hours. 2) In vivo homing model: Fluorescently (e.g., DiR) or luciferase-labeled cells are injected into a disease model (e.g., myocardial infarction). Homing is quantified after 24-48 hours via fluorescence-mediated tomography (FMT) or BLI, and confirmed by ex vivo tissue analysis using qPCR for human-specific Alu sequences or histology.
Biomaterial-Based Delivery Systems
Scaffolds and hydrogels can enhance engraftment by providing a protective niche and tethering cells at the delivery site.
Table 4: Comparison of Biomaterial-Assisted Delivery Systems
| Biomaterial System | Composition & Mechanism | Performance Data |
|---|---|---|
| Hydrogel Encapsulation | Natural (e.g., hyaluronic acid, fibrin) or synthetic (e.g., PEG) polymers that form a hydrated 3D network. Cells are suspended in the polymer solution and gelation occurs in situ. | Enhanced Retention & Survival: Study: MSCs delivered in an RGD-modified PEG hydrogel to an infarcted heart showed ~40% cell retention at 1 week vs. <10% with saline injection. The hydrogel also attenuated post-infarct wall thinning [59]. |
| Injectable Microcarriers | Porous polymer (e.g., PLGA) microspheres that provide high surface area for cell attachment. Injected as a cell-carrier suspension. | Prolonged Engraftment: Study: MSCs attached to PLGA microcarriers and injected into a bone defect model maintained viability and osteogenic activity for over 4 weeks, leading to significantly more bone formation than cell-only injections. |
| Pre-formed Scaffolds | Macroporous 3D structures (e.g., for bone or cartilage repair) that are seeded with cells and surgically implanted. | Spatial Control: Provides structural guidance for tissue regeneration. Ensures 100% initial local cell placement, but requires invasive implantation and integration with host tissue. |
Visualizing Strategy Workflows and Signaling
The following diagrams, generated with DOT language and adhering to the specified color palette and contrast rules, illustrate the core concepts and workflows of the strategies discussed.
Strategic Pathways for Enhanced Homing & Engraftment
This diagram provides a consolidated overview of the three main strategic approaches to overcoming delivery barriers.
CXCR4/SDF-1α Genetic Modification Workflow
This diagram details the experimental workflow and mechanistic rationale for one of the most prominent genetic engineering strategies.
The Scientist's Toolkit: Essential Reagents for Homing & Engraftment Research
This table catalogs key reagents and materials essential for conducting experimental research in this field.
Table 5: Essential Research Reagents for Homing and Engraftment Studies
| Reagent / Material | Function & Application | Example Use Case |
|---|---|---|
| Recombinant Human SDF-1α (CXCL12) | Chemoattractant for in vitro migration assays (Transwell) and for validating CXCR4 receptor function. | Creating a concentration gradient in the lower chamber of a Transwell plate to quantify MSC migration [59]. |
| Lentiviral Vector for CXCR4 | Genetic engineering tool for stable overexpression of the CXCR4 homing receptor in stem cells. | Generating a cell population with enhanced chemotactic potential toward SDF-1α for therapy [60]. |
| Cell Tracker Dyes (e.g., CM-Dil, CFSE) | Fluorescent lipophilic or cytoplasmic dyes for short-term, non-dividing cell tracking in vivo and ex vivo. | Labeling MSCs prior to injection to allow their visualization in tissue sections via fluorescence microscopy 48 hours post-transplant. |
| Luciferase Reporter Constructs | Genetic tool for stable expression of firefly luciferase, enabling real-time in vivo bioluminescence imaging (BLI). | Longitudinal, non-invasive tracking of cell biodistribution and survival in living animals over weeks [59]. |
| Matrix Metalloproteinase (MMP)-Degradable PEG Hydrogel | A synthetic biomaterial that encapsulates cells, provides mechanical protection, and degrades in response to cell-secreted enzymes. | Studying the effect of a protective, permissive 3D environment on MSC retention and survival in a subcutaneous or myocardial implant model. |
| Anti-Human CXCR4 Antibody (for Flow Cytometry) | Antibody to detect and quantify the surface expression levels of the CXCR4 receptor on human cells. | Confirming successful CXCR4 overexpression after genetic modification and correlating receptor levels with migratory capacity. |
The journey from a cell injection to functional tissue engraftment is fraught with obstacles. No single strategy presents a perfect solution; each has its own trade-offs in terms of complexity, safety, and applicability. The current body of research, including data from randomized controlled trials, strongly suggests that the most promising path forward lies in combinatorial approaches. For instance, employing intra-arterial delivery of hypoxia-pre-conditioned MSCs encapsulated in a protective, bioactive hydrogel may synergistically address the challenges of initial retention, survival, and functional integration simultaneously.
Future clinical success will depend on the development of precision delivery protocols tailored not only to the specific disease but also to the patient's unique pathophysiology. As the field advances, the standardization of these enhanced delivery strategies will be critical for achieving the consistent, reproducible, and efficacious outcomes required to solidify stem cell therapy's role in mainstream medicine. The systematic comparison of these strategies provides a clear roadmap for researchers and drug developers aiming to navigate and overcome the critical delivery barriers that have long limited the full potential of regenerative medicine.
The field of regenerative medicine is undergoing a fundamental transformation, moving away from whole-cell therapies toward sophisticated cell-free approaches centered on extracellular vesicles (EVs) and secretomes. This paradigm shift is driven by growing recognition that the therapeutic benefits of mesenchymal stem cells (MSCs) are largely mediated through their paracrine secretions rather than cell replacement or direct engraftment [61] [62]. While stem cell therapy has demonstrated a favourable safety profile in clinical trials for conditions ranging from acute myocardial infarction to ischemic stroke [43] [8], the therapeutic landscape is rapidly evolving toward harnessing the bioactive components that MSCs naturally secrete.
This transition addresses several limitations inherent in cell-based therapies, including risks of immune rejection, tumorigenicity, and complex logistical handling requirements [62]. Secretome-based therapeutics—which encompass the complete set of bioactive factors secreted by cells, including EVs, proteins, and growth factors—offer enhanced safety profiles, superior manufacturing scalability, and more precise therapeutic targeting [62] [63]. The strategic pivot from cellular to cell-free regenerative agents represents a maturation of the field toward more controlled, standardized, and clinically translatable therapeutic modalities.
Defining the Therapeutic Agents: Exosomes, EVs, and Secretomes
The terminology in cell-free therapy can be confusing, as these biological agents exist in nested hierarchical relationships with distinct characteristics:
The secretome constitutes the complete set of molecules secreted by cells, including both soluble factors and membrane-bound vesicles [62]. Within this broader category, extracellular vesicles (EVs) represent heterogeneous populations of lipid-membrane particles released by cells, further categorized based on their biogenesis and size [63]. Exosomes (30-150 nm) are a specific subtype of EV of endocytic origin, while microvesicles (100-1000 nm) form through outward budding of the plasma membrane [63] [64]. In contrast, stem cells are undifferentiated biological entities capable of both self-renewal and differentiation into specialized cell types [65].
Table 1: Fundamental Characteristics of Cell-Based and Cell-Free Therapeutic Agents
| Therapeutic Agent | Definition | Size Range | Key Components |
|---|---|---|---|
| Stem Cells | Undifferentiated cells capable of self-renewal and differentiation | 10-20 μm (cell diameter) | Living cells with intact cellular machinery |
| Secretome | Total set of bioactive factors secreted by cells | Variable (mixed components) | Soluble proteins, growth factors, extracellular vesicles |
| Extracellular Vesicles (EVs) | Lipid-bound vesicles secreted for intercellular communication | 30-1000 nm | Proteins, lipids, nucleic acids (miRNA, mRNA) |
| Exosomes | EV subtype of endocytic origin | 30-150 nm | CD63, CD9, CD81, TSG101, ALIX, miRNA |
The therapeutic mechanism of these agents differs fundamentally. While stem cells were originally investigated for their differentiation potential and ability to replace damaged tissues, evidence now indicates that their benefits are primarily mediated through paracrine signaling [62]. Secretomes and EVs function as sophisticated communication networks, transferring complex biological information between cells through the targeted delivery of proteins, lipids, and genetic material [65] [63]. This distinction underpins the entire rationale for cell-free therapy development.
Mechanisms of Action: Comparative Therapeutic Pathways
Molecular Composition and Bioactivity
The therapeutic potential of secretomes and EVs derives from their diverse molecular cargo, which varies based on the originating cell type and culture conditions. MSC secretomes contain numerous soluble factors with demonstrated regenerative capacity, including proangiogenic factors (VEGF, IGF-1, HGF), antiapoptotic molecules (bFGF, TGF, GM-CSF), and anti-inflammatory mediators (TSG-6, IL-10, HO-1) [62]. These components work synergistically to modulate immune responses, promote tissue repair, and enhance regenerative processes.
EVs serve as protective vehicles for more labile molecular species, particularly microRNAs that regulate gene expression in recipient cells [64]. Research comparing EVs from different MSC subpopulations has revealed striking functional differences despite morphological similarities. For instance, Y201 MSC-derived EVs demonstrated significantly enriched matrix-associated proteins and RGD-containing proteins (fibronectin, MFG-E8) that enhanced their bioactivity through specific integrin-FAK-ERK1/2 signaling pathways [64]. In contrast, Y202 MSC-derived EVs from the same donor showed markedly reduced therapeutic efficacy in inflammatory disease models, highlighting how closely related MSC subtypes produce EVs with substantially different clinical potential [64].
Comparative Functional Mechanisms
The mechanisms through which cell-free therapies exert their effects differ substantially from whole-cell approaches:
Unlike stem cells that must first respond to environmental cues, secretomes and EVs deliver pre-programmed bioactive cargo directly to target cells [62]. This direct delivery mechanism enables more precise modulation of cellular processes, potentially resulting in more consistent and predictable therapeutic outcomes. The inherent homing capabilities of certain EVs allow them to navigate biological barriers, including the blood-brain barrier, enabling targeted delivery to specific tissues [63].
Clinical Evidence: Efficacy and Safety Profiles
Quantitative Clinical Outcomes
Randomized controlled trials and meta-analyses provide compelling evidence supporting the efficacy of both cell-based and cell-free therapies across various conditions:
Table 2: Clinical Outcomes of Stem Cell vs. Cell-Free Therapies in Randomized Trials
| Condition | Therapy Type | Clinical Outcomes | Safety Profile |
|---|---|---|---|
| Ischemic Stroke | Stem Cell Therapy | Significant improvement in mRS scores 0-1 at 1 year (RR=1.74, 95% CI 1.09-2.77) [8] | No significant difference in serious adverse events vs. control (RR=0.85, 95% CI 0.70-1.04) [8] |
| Systemic Lupus Erythematosus | UC-MSC Secretome | Significant reduction in MEX-SLEDAI scores (p<0.05); Increased C3 complement levels [66] | No severe adverse events; well-tolerated in 6-week trial [66] |
| Acute Myocardial Infarction | Stem Cell Therapy | Long-term improvement in LVEF (MD=2.63%, 95% CI 0.50-4.76); Reduced relative infarct size [43] | Fewer adverse events vs. controls (OR=0.66, 95% CI 0.44-0.99) [43] |
| Respiratory Diseases | MSC-EVs (Nebulization) | Therapeutic effects at approximately 10^8 particles; lower dose required vs. intravenous [67] | Aerosolized delivery well-tolerated; reduced systemic exposure [67] |
Administration and Dosing Considerations
Clinical studies reveal important differences in administration routes and dosing requirements between therapeutic formats. For EV-based therapies, administration route significantly influences the effective therapeutic dose. Nebulization therapy for respiratory diseases achieved therapeutic effects at approximately 10^8 particles, substantially lower than doses required for intravenous administration [67]. This route-dependent efficacy underscores the importance of matching delivery strategies to both the therapeutic agent and target pathology.
For whole-cell therapies, timing of administration appears critical to therapeutic success. In ischemic stroke, intervention within one month of onset resulted in significantly improved long-term functional outcomes [8]. Similarly, the source of MSCs influences therapeutic potential, with umbilical cord-derived MSCs demonstrating particularly potent immunomodulatory effects, likely due to their non-invasive harvest, immune-privileged phenotype, and high proliferative capacity compared to bone marrow-derived alternatives [62].
Technical Considerations: Production and Characterization
Isolation and Manufacturing Methods
The transition to clinical application requires robust, scalable production methods for secretomes and EVs. Current isolation techniques each present distinct advantages and limitations:
Table 3: Comparison of Extracellular Vesicle Isolation and Characterization Methods
| Method Category | Specific Techniques | Key Advantages | Technical Limitations |
|---|---|---|---|
| EV Isolation | Ultracentrifugation (UC) | Considered gold standard; high purity potential | Low yield; time-consuming; equipment intensive |
| Tangential Flow Filtration (TFF) | Higher yield vs. UC; scalable for GMP production [68] | Potential membrane fouling; lower purity | |
| Size-Exclusion Chromatography | Preserves vesicle integrity; good purity | Limited scalability; sample dilution | |
| Polymer-Based Precipitation | Simple protocol; accessible equipment | Co-precipitation of contaminants | |
| EV Characterization | Nanoparticle Tracking Analysis | Size distribution and concentration data | Limited resolution at low concentrations |
| Western Blotting | Specific marker detection (CD63, CD9, TSG101) | Qualitative rather than quantitative | |
| Transmission Electron Microscopy | Visual confirmation of morphology | Artifacts possible; sample preparation challenges | |
| Flow Cytometry | Single-particle analysis | Detection limits for smallest EVs |
Advanced manufacturing approaches are addressing scalability challenges. Hollow-fiber bioreactors enable GMP-compliant exosome production by supporting cell attachment and nutrient transport in a scalable format [63]. Similarly, tangential flow filtration systems have demonstrated superior particle yields compared to traditional ultracentrifugation while maintaining EV functionality [68].
Standardization and Quality Control
The lack of standardized protocols represents a significant barrier to clinical translation. Current EV research suffers from substantial heterogeneity in characterization methods, dose units, and outcome measures [67]. Manufacturing variability extends to culture conditions, with studies demonstrating that factors such as culture media composition (DMEM vs. α-MEM) can influence both MSC expansion and subsequent EV yield, though these differences may not achieve statistical significance [68].
The field is increasingly recognizing the need for standardized dosing frameworks, potency assays, and harmonized clinical protocols to advance reproducible therapies [67]. This is particularly important given findings that EVs from different MSC subpopulations exhibit distinct protein cargo and functional capabilities, necessitating careful characterization of source cells and their resulting products [64].
The Scientist's Toolkit: Essential Research Reagents and Methods
Successful research into cell-free therapies requires specific reagents and methodologies:
Table 4: Essential Research Tools for EV and Secretome Studies
| Reagent/Method | Specific Application | Function/Purpose |
|---|---|---|
| EV-Depleted FBS | Cell culture for EV production | Removes contaminating bovine EVs from culture system [64] |
| Ultracentrifugation | EV isolation from conditioned media | Separates EVs based on size and density; considered benchmark method [64] |
| Nanoparticle Tracking Analysis | EV characterization | Measures size distribution and concentration of particles in suspension [68] [64] |
| CD63/CD9/CD81 Antibodies | EV characterization via Western blot | Detection of tetraspanin markers to confirm EV identity [68] |
| TSG101/ALIX Antibodies | EV characterization | Detection of additional exosome markers to verify isolation [63] |
| TEM with Uranyl-Acetate | EV morphology assessment | Visualizes cup-shaped morphology of exosomes [68] [64] |
| Mass Spectrometry | Proteomic analysis of EV cargo | Identifies protein composition and potential functional mechanisms [64] |
| miRNA Screening Arrays | EV cargo analysis | Profiles miRNA content responsible for genetic regulation [64] |
| Tangential Flow Filtration | Large-scale EV production | Scalable isolation method suitable for GMP manufacturing [68] |
| Hollow-Fiber Bioreactors | Upstream EV production | Enables high-density cell culture for increased EV yield [63] |
Future Directions and Clinical Translation
The development path for cell-free therapies faces several significant challenges that must be addressed to achieve widespread clinical implementation. Manufacturing standardization remains a critical hurdle, with current processes exhibiting substantial variability in isolation techniques, characterization methods, and potency assessment [67]. The field must establish harmonized protocols and reference materials to enable comparative analyses across studies and manufacturing platforms.
Dosing optimization represents another fundamental challenge. Current clinical trials demonstrate wide variation in dosing strategies, with units ranging from particle number to protein content [67]. Future work must establish dose-response relationships and therapeutic windows for specific clinical indications, taking into account administration route and treatment frequency.
Looking ahead, engineered EVs with enhanced targeting capabilities or modified cargo represent the next frontier in cell-free therapy development [63]. Both endogenous and exogenous modification strategies are being explored to create next-generation EV-based drugs with improved therapeutic potential. As the field addresses current limitations in scalable production and quality control, cell-free therapies are poised to become increasingly important components of the regenerative medicine landscape, potentially offering more consistent, safe, and targeted therapeutic options for a wide range of conditions.
Efficacy Validation, Comparative Analysis, and Future Directions
This critical review examines the evolving body of evidence from meta-analyses of randomized controlled trials (RCTs) investigating stem cell therapy for various medical conditions. By synthesizing findings from recent systematic reviews and meta-analyses, we evaluate the efficacy, safety, and methodological rigor of stem cell interventions. The analysis focuses particularly on cardiovascular and neurological applications, where the most extensive clinical research has been conducted. This review highlights consistent patterns in functional outcomes, addresses heterogeneity in treatment protocols, and identifies key considerations for future research directions in regenerative medicine.
Stem cell therapy represents a promising frontier in regenerative medicine, with a rapidly expanding body of clinical research seeking to validate its therapeutic efficacy. Meta-analyses of randomized controlled trials (RCTs) provide the highest level of evidence for evaluating these innovative treatments by synthesizing results across multiple studies [69]. As the field matures, these quantitative syntheses have become increasingly important for distinguishing genuine therapeutic potential from inflated claims and for guiding future research directions.
The clinical application of stem cells spans numerous medical conditions, with substantial research investment in cardiovascular and neurological diseases where current treatment options remain limited. Systematic reviews and meta-analyses are essential tools in this evidence-based evaluation, using rigorous statistical methods to combine data from individual studies [69]. These methodologies enhance statistical power and provide more precise estimates of treatment effects than individual trials alone, particularly important in a field characterized by relatively small-scale initial studies.
This review critically examines recent meta-analyses of RCTs investigating stem cell therapy, with a focus on methodological quality, consistency of findings, and translation of results to clinical practice. By evaluating the strength of evidence across different medical applications, we aim to provide researchers and clinicians with a comprehensive assessment of the current state of evidence in stem cell therapeutics.
Methodological Framework for Meta-Analyses in Stem Cell Research
Fundamental Principles of Systematic Review and Meta-Analysis
Systematic reviews and meta-analyses represent the pinnacle of the evidence hierarchy in medical research, providing structured approaches to synthesizing research findings [69]. A systematic review is a type of literature review that uses systematic processes to identify, select, and critically assess all available literature on a specific research question. A meta-analysis is a statistical method that quantitatively combines the results of a systematic review, enhancing the accuracy of effect estimates and providing greater power to detect treatment effects [69].
The process begins with formulating a well-defined research question using established frameworks such as PICO (Population, Intervention, Comparator, Outcome) or its extensions [69]. Comprehensive literature searches across multiple databases are then conducted to ensure inclusion of diverse studies, with tools like EndNote and Covidence streamlining reference management and study selection. Quality assessment using validated tools such as the Cochrane Risk of Bias Tool is crucial for evaluating methodological rigor, while standardized data extraction forms ensure consistent information capture [69].
Statistical Synthesis and Interpretation
Meta-analysis employs statistical software such as R and RevMan to compute effect sizes, confidence intervals, and assess heterogeneity [69]. Visual representations including forest plots and funnel plots facilitate interpretation of results, while statistical methods like Egger regression and the trim-and-fill technique address challenges such as publication bias and heterogeneity [69]. Sensitivity analyses further validate the robustness of findings, and network meta-analyses enable indirect comparisons between interventions when head-to-head trials are limited [70] [71].
The following diagram illustrates the standard workflow for conducting a systematic review and meta-analysis in stem cell research:
Efficacy Outcomes Across Medical Applications
Cardiovascular Disease
The most extensive evidence for stem cell therapy exists for cardiovascular applications, particularly acute myocardial infarction (AMI) and chronic ischemic heart disease. A comprehensive 2024 meta-analysis of 79 RCTs with 7,103 patients demonstrated that stem cell therapy significantly improved left ventricular ejection fraction (LVEF) at 6, 12, 24, and 36 months post-transplantation compared to control values, indicating potential for long-term cardiac function enhancement [72].
A trend toward reduced major adverse cardiac events (MACE) was observed in intervention groups, suggesting potential to lower the risk of cardiovascular death, reinfarction, and stroke [72]. Significant LVEF improvements were particularly associated with long cell culture durations exceeding 1 week, especially when combined with high injected cell quantities (at least 10⁸ cells) [72]. Interestingly, no significant reduction in infarct size was observed despite functional improvements, suggesting potential mechanisms other than myocardial regeneration may contribute to clinical benefits.
Neurological Applications
Ischemic Stroke
Recent meta-analyses show promising but modest benefits for stem cell therapy in ischemic stroke. A 2025 systematic review and meta-analysis of 13 RCTs involving 872 patients found that stem cell transplantation for acute/subacute ischemic stroke within 1 month of onset significantly improved long-term functional outcomes [8].
The analysis demonstrated that the 1-year incidence of excellent functional outcome (modified Rankin Scale [mRS] scores 0-1) was significantly higher in the cell-therapy group (45/195) than in the control group (23/179), with a risk ratio (RR) of 1.74 (95% CI: 1.09-2.77) [8]. Similarly, the 90-day incidence of good functional outcome (mRS scores 0-2) was higher in the treatment group (RR = 1.31, 95% CI: 1.01-1.70) [8]. No significant differences were observed in serious adverse events or mortality, supporting the safety of stem cell therapy in this population.
An earlier 2016 meta-analysis specifically focused on stem cell therapy for brain ischemia also reported positive findings, with the stem cell transplantation group showing superior outcomes in neurologic deficit scores (NIHSS), motor function (FMA), daily life ability (Barthel index), and functional independence (FIM) compared to controls [73].
Table 1: Efficacy Outcomes of Stem Cell Therapy for Ischemic Stroke
| Outcome Measure | Time Point | Risk Ratio or Mean Difference | 95% Confidence Interval | Number of Studies |
|---|---|---|---|---|
| mRS 0-1 | 1 year | 1.74 | 1.09-2.77 | 13 |
| mRS 0-2 | 90 days | 1.31 | 1.01-1.70 | 13 |
| NIHSS | 180 days | -0.80 | -1.54 to -0.05 | 13 |
| Serious Adverse Events | Entire follow-up | 0.85 | 0.70-1.04 | 13 |
| Mortality | Entire follow-up | 0.72 | 0.49-1.08 | 13 |
Comparative Efficacy Across Conditions
The efficacy of stem cell therapy appears to vary across different medical conditions and patient populations. The most consistent benefits have been observed in cardiovascular applications, particularly for AMI, with sustained improvements in LVEF over long-term follow-up [72]. Neurological applications show more modest but statistically significant functional improvements, particularly when administered in the acute or subacute phase after injury [8] [73].
The following diagram illustrates the proposed mechanisms of action through which stem cell therapy may produce therapeutic effects across different conditions:
Methodological Considerations and Limitations
Heterogeneity in Study Design and Implementation
Substantial heterogeneity represents a significant challenge in interpreting meta-analyses of stem cell therapy. This variability manifests across multiple domains, including cell type (mesenchymal stem cells, bone marrow mononuclear cells, neural stem cells, etc.), cell dosage, delivery route (intravenous, intracoronary, intramyocardial, intrathecal), timing of administration relative to disease onset, and patient selection criteria [72] [8] [73].
This methodological diversity complicates direct comparison across studies and may contribute to the variable treatment effects observed in meta-analyses. For instance, the 2024 AMI meta-analysis found that culture duration and cell quantity significantly influenced treatment efficacy, with better outcomes associated with longer culture durations (>1 week) and higher cell quantities (≥10⁸ cells) [72]. Similarly, the optimal timing for stem cell administration after stroke remains uncertain, though most positive trials have intervened within the first month after onset [8].
Assessment of Bias and Quality
The methodological quality of included RCTs varies substantially across meta-analyses. In the stroke meta-analysis, risk of bias assessment revealed that only five of thirteen studies had low risk, six had medium risk, and two had high risk of bias [8]. Common methodological limitations included inadequate blinding, deviations from intended interventions, and selective reporting of results.
Publication bias represents another concern, as small studies with null results may remain unpublished, potentially inflating overall effect estimates in meta-analyses. While funnel plot asymmetry and statistical tests like Egger's regression can assess publication bias, these methods have limited power when meta-analyses include relatively few studies [69] [71].
The Scientist's Toolkit: Essential Methodological Elements
Table 2: Key Methodological Components in Stem Cell Meta-Analyses
| Component | Function | Examples |
|---|---|---|
| Search Databases | Identify relevant literature | MEDLINE, Embase, Cochrane Library, Google Scholar [69] |
| Quality Assessment Tools | Evaluate methodological rigor | Cochrane Risk of Bias Tool, Newcastle-Ottawa Scale [69] |
| Reference Management | Streamline study selection | EndNote, Zotero, Mendeley [69] |
| Statistical Software | Perform meta-analysis | R, RevMan, Stata [69] [71] |
| Efficacy Endpoints | Measure treatment effects | LVEF, mRS, NIHSS, Barthel Index [72] [8] [73] |
| Safety Monitoring | Assess adverse events | MACE, mortality, serious adverse events [72] [8] |
Recent meta-analyses of RCTs provide cautious optimism regarding the potential efficacy of stem cell therapy for certain medical conditions, particularly cardiovascular diseases and acute neurological injuries. The evidence suggests modest but statistically significant functional improvements across multiple outcome measures, with acceptable safety profiles in studied populations. However, substantial heterogeneity in treatment protocols and methodological limitations in individual trials necessitate cautious interpretation of these findings.
Future research should prioritize standardization of cell products, delivery methods, and patient selection criteria to reduce heterogeneity and facilitate more definitive conclusions. Larger, rigorously designed RCTs with longer follow-up durations are needed to establish optimal treatment parameters and confirm long-term benefits. Additionally, continued methodological refinement in meta-analytic approaches, including individual participant data meta-analyses and network meta-analyses comparing different stem cell types, will enhance our understanding of this promising therapeutic approach.
As the field evolves, stem cell therapy may potentially occupy an important position in the regenerative medicine arsenal, particularly for conditions with limited current treatment options. However, translating this potential into validated clinical applications will require ongoing rigorous evaluation through well-designed trials and systematic synthesis of their findings.
The choice between autologous (self-derived) and allogeneic (donor-derived) cell sources is a fundamental strategic decision in both clinical practice and trial design for stem cell-based therapies. The comparative efficacy and safety profiles of these approaches are highly context-dependent, varying significantly across disease areas, cell types, and patient populations. The table below summarizes key comparative findings from recent clinical research.
Table 1: Key Comparative Findings of Autologous vs. Allogeneic Cell Therapies
| Disease Area | Therapy Type | Key Efficacy Findings | Key Safety Findings | Clinical Context |
|---|---|---|---|---|
| Multiple Myeloma [74] | Allo- vs Auto-SCT (post-relapse) | Auto-SCT superior: Significantly longer OS and PFS vs. allo-SCT. | Allo-SCT inferior: Higher non-relapse mortality (NRM: 15-32% vs 4-12%). | Relapse after first-line auto-SCT; based on meta-analysis & registry data (n=815). |
| Alzheimer's Disease [75] [76] | Allogeneic MSC (Laromestrocel) | Positive signal: Slowed whole brain volume decline by 48.4% vs placebo. Improved cognitive/functional scores. | Favorable profile: No infusion reactions, hypersensitivities, or amyloid-related imaging abnormalities. | Mild Alzheimer's; Phase 2a RCT (n=49); allogeneic source enables immediate "off-the-shelf" use. |
| Multiple Sclerosis [77] | Autologous MSC-Neural Progenitors | Mixed efficacy: No significant difference vs placebo on primary endpoint. Improved outcomes in high-disability subgroup for walking and bladder function. | Well-tolerated: Safety profile supported through phase II RCT. | Progressive MS (non-relapsing); autologous approach avoids immunosuppression for transplantation. |
| Heart Disease [78] | Stem Cell Therapy (Type not specified) vs Conventional | Stem cell superior: Significant improvement in LVEF (30.2% to 43.6%) and quality of life vs conventional therapy. | Fewer hospitalizations: Stem cell group 10.6% vs 27.1% in conventional group. | Prospective cohort study (n=95); highlights regenerative potential irrespective of source. |
| Cancer/Autoimmunity [79] | Allogeneic CAR-T/CAR-NK | Promising efficacy: Overcomes autologous challenges (cost, manufacturing time, patient selection). | Safety engineering: Genetic strategies to reduce graft-versus-host disease risk. | Emerging "off-the-shelf" approach; uses cells from healthy donors. |
Disease-Specific Efficacy Profiles
Hematologic Malignancies
In multiple myeloma, a head-to-head comparison in the relapsed/refosed setting demonstrates a clear efficacy advantage for autologous stem cell transplantation (auto-SCT) over allogeneic transplantation (allo-SCT). A comprehensive 2025 meta-analysis and individual patient data analysis of 815 patients from two large registries found that a second auto-SCT resulted in significantly longer overall survival (OS) and progression-free survival (PFS) compared to allo-SCT. The primary driver of this efficacy discrepancy was the significantly higher non-relapse mortality (NRM) associated with allo-SCT, which ranged from 15% to 32%, compared to 4% to 12% for auto-SCT [74]. This elevated NRM is largely attributable to complications like graft-versus-host disease (GVHD) and infections post-transplant.
Neurodegenerative Diseases
Conversely, allogeneic cell sources show distinct promise in neurodegenerative conditions like Alzheimer's disease. In a 2025 randomized, double-blind, placebo-controlled phase 2a trial, allogeneic bone marrow-derived mesenchymal stem cells (laromestrocel) demonstrated potential efficacy in patients with mild Alzheimer's [75] [76].
- Efficacy Signals: The therapy slowed the decline of whole brain volume by 48.4% and left hippocampal volume by 61.9% compared to placebo at 39 weeks. This was accompanied by improvements in clinical assessments, including a composite Alzheimer's disease score and activities of daily living [76].
- Safety Advantage: Critically, the study reported no infusion-related reactions, hypersensitivities, or amyloid-related imaging abnormalities (ARIAs), which are known risks with some newer anti-amyloid monoclonal antibodies [76].
For progressive multiple sclerosis, research has focused on autologous cell products. A 2024 phase II RCT investigated intrathecal administration of autologous mesenchymal stem cell-neural progenitors (MSC-NPs). While the study did not meet its primary endpoint, exploratory analysis revealed a significant therapeutic response in a high-disability subgroup (EDSS 6.0-6.5), with improvements in timed walk tests and bladder function [77]. The autologous source is logistically feasible here without the need for immunosuppression to prevent graft rejection.
Solid Organs and Regenerative Applications
In heart disease, a 2025 prospective cohort study demonstrated that stem cell therapy could offer significant advantages over conventional treatments. The stem cell group showed a marked improvement in left ventricular ejection fraction (LVEF) from 30.2% to 43.6% after six months, far exceeding the minor improvement in the conventional therapy group. This was coupled with greater improvements in exercise capacity and quality of life, alongside lower hospitalization rates [78]. This evidence supports the regenerative potential of cell therapy, for which the autologous versus allogeneic debate remains a key research question.
Experimental Protocols and Methodologies
The divergent outcomes described above are rooted in the distinct experimental and manufacturing protocols for each cell source. The following workflow delineates the key procedural differences.
Protocol Details: Allogeneic MSC Therapy for Alzheimer's Disease
The positive signal from the allogeneic approach in Alzheimer's was generated by a rigorous clinical protocol [75] [76].
- Study Design: A randomized, double-blind, placebo-controlled, parallel-group phase 2a trial across ten US centers.
- Randomization & Dosing: 49 participants were randomized 1:1:1:1 to four groups: placebo (n=12); a single infusion of 25 million cells (n=13); four monthly infusions of 25 million cells (n=13); or four monthly infusions of 100 million cells (n=11).
- Cell Product: Laromestrocel, a bone-marrow-derived, allogeneic mesenchymal stem cell product.
- Primary Endpoint: Safety, measured by the rate of treatment-emergent serious adverse events within 4 weeks of infusion.
- Key Secondary/Exploratory Endpoints: Clinical assessments (composite AD score, MoCA, ADCS-ADL), brain volume changes via MRI, and neuroinflammation biomarkers.
Protocol Details: Autologous MSC-Neural Progenitor Therapy for Multiple Sclerosis
The phase II trial for progressive MS utilized a detailed protocol for an autologous product [77].
- Study Design: Randomized, double-blind, placebo-controlled clinical trial with a compassionate crossover design at a single site.
- Patient Stratification: Subjects were stratified by disease subtype (SPMS or PPMS) and baseline EDSS score.
- Cell Manufacturing: MSCs were isolated from a single bone marrow aspirate from each subject, expanded ex vivo, and then cultured in neural maintenance media to generate MSC-NPs. This is a patient-specific, multi-week process.
- Dosing Regimen: Six intrathecal injections of up to 10 million autologous MSC-NPs every two months.
- Primary Outcome: EDSS Plus, defined by improvement in EDSS, timed 25-foot walk, or nine-hole peg test.
Signaling Pathways and Mechanistic Insights
The therapeutic mechanisms of stem cell therapies, particularly MSCs, are mediated through a complex interplay of paracrine signaling and cell-to-cell interactions. The allogeneic MSCs used in the Alzheimer's trial are thought to exert effects via provascular, anti-inflammatory, and immunomodulatory mechanisms [76]. The diagram below illustrates the key signaling pathways involved in the therapeutic action of MSCs.
Caption: MSC Mechanisms: Key signaling pathways and biomarkers associated with Mesenchymal Stem Cell therapy, synthesized from multiple clinical studies [77] [76].
The Scientist's Toolkit: Essential Research Reagents
Successful translation of autologous and allogeneic therapies from bench to bedside relies on a suite of critical research reagents and materials. The following table details key solutions used in the featured experiments and the broader field.
Table 2: Key Research Reagent Solutions for Cell Therapy Development
| Reagent / Solution | Function in R&D | Application Context |
|---|---|---|
| Neural Maintenance Media [77] | Directs MSC differentiation toward a neural progenitor (MSC-NP) phenotype with enriched neural gene expression. | Critical for manufacturing the autologous MSC-NP product used in the progressive MS trial. |
| cGMP-Grade Cell Culture Supplements [77] [76] | Ensure consistent, reproducible, and safe ex vivo expansion of both autologous and allogeneic cell products under current Good Manufacturing Practice (cGMP). | Universal requirement for clinical-grade cell manufacturing. |
| Release Assay Reagents [77] | Quality control testing for cell viability, sterility (mycoplasma, endotoxin), potency, and identity pre-release. | Mandatory for lot release of any clinical-grade cell product. |
| Cryopreservation Media | Long-term storage of master cell banks (allogeneic) and patient-specific doses (autologous). | Enables "off-the-shelf" availability for allogeneic products and logistical management for autologous ones. |
| Immunomodulation Assay Kits (e.g., T-cell suppression) [77] [76] | Quantify a key mechanistic potency of MSCs—their ability to modulate immune responses—in vitro. | Used for product characterization and lot-to-lot consistency testing. |
| Lentiviral/Retroviral Vectors [79] | Genetic engineering for CAR expression in allogeneic CAR-T and CAR-NK cell products. | Foundational for creating the next generation of "off-the-shelf" cellular immunotherapies. |
Evolving Regulatory Frameworks and the Path to Standardization
The field of stem cell therapy stands at a pivotal crossroads, where remarkable scientific promise must be reconciled with rigorous evidentiary standards and regulatory oversight. For researchers, scientists, and drug development professionals, the path from laboratory discovery to clinically validated treatment is fraught with complexity. The central challenge lies in balancing accelerated innovation against the imperative for robust safety and efficacy demonstrations through randomized clinical trials (RCTs). Global regulatory bodies have responded with diverse frameworks aimed at streamlining development while maintaining scientific rigor [80]. Concurrently, clinical research continues to generate critical efficacy data across multiple therapeutic areas, from cardiology to neurology. This guide examines the current regulatory landscape and synthesizes the clinical evidence shaping the standardization of stem cell therapies, providing researchers with a comprehensive resource for navigating this evolving domain.
Global Regulatory Frameworks for Stem Cell Therapies
The regulatory environment for stem cell therapies represents a complex tapestry of international approaches, each attempting to reconcile rapid medical advancement with patient safety. Harmonization efforts across jurisdictions remain challenging due to differing ethical considerations, legal traditions, and healthcare infrastructures [80]. Understanding these diverse frameworks is essential for researchers designing global clinical development programs.
Table 1: Comparative Analysis of Global Regulatory Frameworks for Regenerative Medicine
| Country/Region | Primary Legislation | Regulatory Body | Key Features | Expedited Pathways |
|---|---|---|---|---|
| United States | 21st Century Cures Act | FDA/Center for Biologics Evaluation and Research (CBER) | Regulates cell therapies as biologics; requires IND approval for clinical trials | Regenerative Medicine Advanced Therapy (RMAT) designation |
| European Union | Regulation (EC) No 1394/2007 | EMA/Committee for Advanced Therapies (CAT) | Centralized marketing authorization for Advanced Therapy Medicinal Products (ATMPs) | Priority Medicines (PRIME) scheme |
| Japan | Act on the Safety of Regenerative Medicine; Pharmaceuticals and Medical Devices Act | PMDA/MHLW | Two-tiered system: conditional approval based on safety & probable efficacy followed by confirmatory studies | Conditional/time-limited approval system |
| South Korea | Pharmaceutical Affairs Act; Advanced Biomedical Regeneration Act | MFDS | Expedited review for critical therapies; detailed safety monitoring | Special approval for innovative biologics |
| Canada | Food and Drugs Act | Health Canada/Biologic and Radiopharmaceutical Drugs Directorate | Regulates stem cell products as biologics; thorough review for market approval | Advanced Therapeutic Products Pathway |
| Mexico | General Health Law | COFEPRIS | Experimental treatments restricted to clinical trials; specific NOM-260 regulation pending | Case-by-case review for innovative therapies |
The United States framework has evolved significantly with the introduction of the 21st Century Cures Act, which established the Regenerative Medicine Advanced Therapy (RMAT) designation to expedite development and review of promising therapies [80]. The FDA categorizes most stem cell products as somatic cellular therapies requiring premarket approval, with human cells, tissues, and cellular tissue-based products (HCT/Ps) regulated under 21 CFR Part 1271 [80]. This framework mandates stringent donor eligibility criteria, current good tissue practices (cGTP), and comprehensive measures to prevent communicable disease transmission.
The European Union employs a centralized authorization procedure overseen by the European Medicines Agency (EMA) and its Committee for Advanced Therapies (CAT) [80]. This pathway provides a standardized marketing authorization valid across all member states, though national differences in implementation and reimbursement persist. The EU's approach classifies stem cell therapies as Advanced Therapy Medicinal Products (ATMPs), subject to the same rigorous standards as traditional pharmaceuticals but with adapted requirements recognizing their unique characteristics.
Japan pioneered an innovative conditional approval system that permits market authorization based on demonstrated safety and probable efficacy, requiring post-marketing surveillance to confirm clinical benefit [80]. This approach aims to accelerate patient access while maintaining ongoing evaluation of therapeutic effectiveness. The system operates under two separate laws: the Act on the Safety of Regenerative Medicine governs clinical research, while the Pharmaceuticals and Medical Devices Act regulates product approval.
Figure 1: Stem Cell Therapy Development and Regulatory Pathway. This workflow illustrates the potential accelerated pathway (green) available for promising therapies alongside the traditional clinical development route.
Emerging regulatory systems in countries like Mexico illustrate the challenges faced by developing nations in establishing robust oversight. Mexico's COFEPRIS has actively shut down clinics offering unapproved stem cell treatments while simultaneously working to develop specific regulations for advanced therapies [81]. The pending Official Mexican Standard NOM-260 aims to establish comprehensive rules for stem cell procurement, processing, storage, and clinical application, though it has not yet been finalized [81].
Efficacy Evidence from Randomized Clinical Trials
Assessment of stem cell therapy efficacy requires critical evaluation of outcomes from randomized controlled trials across diverse medical conditions. Recent meta-analyses provide the most comprehensive evidence regarding therapeutic potential, though results vary significantly by clinical indication and cell type.
Cardiovascular Diseases
In cardiovascular medicine, stem cell therapy has been extensively investigated for acute myocardial infarction and heart failure. A 2025 meta-analysis of 15 trials with 1,218 participants evaluated stem cell therapy for acute myocardial infarction, with cardiac MRI as the preferred assessment method [21].
Table 2: Efficacy Outcomes of Stem Cell Therapy for Acute Myocardial Infarction [21]
| Outcome Measure | Short-Term Follow-Up | Long-Term Follow-Up | Statistical Significance |
|---|---|---|---|
| Left Ventricular Ejection Fraction (LVEF) | No significant improvement | Mean difference 2.63% (95% CI 0.50% to 4.76%) | P=0.02 |
| Absolute Infarct Size | No significant reduction | Not reported | Not significant |
| Relative Infarct Size | No significant reduction | Standardized mean difference -0.63 (95% CI -0.94 to -0.32) | P<0.0001* |
| Adverse Events | Odds ratio 0.66 (95% CI 0.44 to 0.99) | Not separately reported | P=0.05 |
Note: *Significant only after exclusion of an outlier study
The analysis demonstrated a favorable safety profile with fewer adverse events in stem cell therapy groups compared to controls (OR 0.66, 95% CI 0.44 to 0.99, p=0.05) [21]. Importantly, no cardiac-related cancer cases were reported in any group, though longer follow-up is needed to fully assess oncogenic risks. The findings suggest potential long-term benefits for LVEF and relative infarct size, though substantial heterogeneity between studies complicates interpretation.
For advanced heart failure, a systematic review of 27 clinical trials conducted between 2014 and 2024 found that all stem cell approaches demonstrated clinically acceptable safety profiles, though efficacy varied significantly [7]. Mesenchymal stem cell (MSC)-based therapy emerged as the most widely used and consistently promising approach among different cell types [7].
Neurological Applications
Ischemic stroke represents another major area of stem cell therapy investigation. A 2025 meta-analysis of 13 randomized controlled trials with 872 patients examined functional outcomes after stem cell transplantation within one month of stroke onset [8].
Table 3: Efficacy Outcomes of Stem Cell Therapy for Acute/Subacute Ischemic Stroke [8]
| Outcome Measure | Time Point | Risk Ratio or Mean Difference | Statistical Significance |
|---|---|---|---|
| mRS score 0-1 | 90 days | RR=1.15 (95% CI 0.72-1.84) | P=0.55 |
| mRS score 0-1 | 365 days | RR=1.74 (95% CI 1.09-2.77) | P=0.02 |
| mRS score 0-2 | 90 days | RR=1.31 (95% CI 1.01-1.70) | P=0.044 |
| NIHSS Score | 180 days | Mean difference -0.80 (95% CI -1.54 to -0.05) | P<0.05 |
| Serious Adverse Events | Overall | RR=0.85 (95% CI 0.70-1.04) | P=0.11 |
| Mortality | Overall | RR=0.72 (95% CI 0.49-1.08) | P=0.12 |
The meta-analysis revealed significantly improved functional outcomes in the cell therapy group, with higher rates of excellent recovery (modified Rankin Scale [mRS] scores 0-1) at 1 year (RR=1.74, 95% CI 1.09-2.77, p=0.02) [8]. The 90-day incidence of good functional outcome (mRS scores 0-2) was also significantly higher in the cell therapy group (RR=1.31, 95% CI 1.01-1.70, p=0.044). No significant differences were observed in serious adverse events or mortality, supporting the safety profile of stem cell therapy for acute and subacute ischemic stroke.
Autoimmune Diseases
The application of stem cell therapy for autoimmune diseases represents a rapidly expanding frontier. Analysis of global clinical trials from 2006 to 2025 identified 244 interventional trials, with most (83.6%) in Phase I-II [12]. The most frequently studied conditions were Crohn's disease (n=85), systemic lupus erythematosus (n=36), and scleroderma (n=32) [12].
The therapeutic mechanisms of stem cells in autoimmune conditions primarily involve immune modulation, tissue repair through growth factor secretion, and anti-inflection/anti-proliferative effects [12]. Mesenchymal stem cells (MSCs) have been extensively studied due to their potent immunomodulatory and regenerative properties, including secretion of soluble factors such as TGF-β, PGE2, and IDO, as well as exosomes containing regulatory miRNAs [12]. Hematopoietic stem cell (HSC) transplantation achieves therapeutic effects by eliminating the aberrant immune system and re-establishing immune tolerance, demonstrating long-term remission potential in conditions like scleroderma and multiple sclerosis [12].
Methodological Standards and Reporting Requirements
Clinical Trial Design Considerations
Designing rigorous clinical trials for stem cell therapies requires careful consideration of several unique aspects. The Cochroke Handbook for Systematic Reviews of Interventions provides foundational methodology, while stem cell-specific extensions have been proposed to address field-specific challenges [21]. Key considerations include optimal cell dosage, timing of administration, route of delivery, and patient selection criteria, all of which contribute significantly to trial outcomes and variability.
Recent meta-analyses have highlighted substantial heterogeneity in study designs, including variations in cell types, dosing regimens, and outcome assessment methods [21] [8]. This heterogeneity complicates cross-trial comparisons and meta-analyses, underscoring the need for more standardized approaches. The field would benefit from consensus development on core outcome sets and standardized measurement timepoints.
Essential Research Reagents and Materials
Table 4: Essential Research Reagent Solutions for Stem Cell Therapy Development
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Immunomodulation, tissue repair via paracrine signaling | Myocardial infarction, Crohn's disease, stroke |
| Cardiosphere-Derived Cells (CDCs) | Cardiac tissue regeneration, reduction of fibrosis | Advanced heart failure, myocardial infarction |
| Induced Pluripotent Stem Cells (iPSCs) | Generation of patient-specific cells; differentiation into various cell types | Disease modeling, drug screening |
| Bone Marrow-Derived Mononuclear Cells (BMMNCs) | Multiple regenerative mechanisms; source of progenitor cells | Ischemic stroke, myocardial infarction |
| Hematopoietic Stem Cells (HSCs) | Immune system reconstitution; re-establishment of immune tolerance | Scleroderma, multiple sclerosis |
| Culture Media & Differentiation Kits | Maintenance, expansion, and directed differentiation of stem cells | All in vitro processing and differentiation protocols |
| Flow Cytometry Antibodies | Characterization of cell surface markers; purity assessment | Quality control for cell products (e.g., CD34+, CD45-, CD73+) |
| cGMP-Grade Cytokines | Directed differentiation; enhancement of cell survival and engraftment | Manufacturing processes for clinical-grade cells |
Laboratory Protocols and Manufacturing Standards
Robust manufacturing protocols are essential for ensuring the consistent quality, potency, and safety of stem cell therapies. Current Good Manufacturing Practice (cGMP) requirements apply to all cellular products destined for clinical use [80] [82]. The manufacturing process must include comprehensive characterization of cell identity, purity, and viability, with rigorous testing for microbial contamination [80].
Critical protocol considerations include:
- Cell sourcing: Autologous versus allogeneic approaches with distinct manufacturing challenges
- Expansion techniques: Scale-up methods maintaining cell functionality and genetic stability
- Cryopreservation: Maintenance of cell viability and potency after thawing
- Quality control: Comprehensive testing including sterility, mycoplasma, endotoxin, and adventitious viruses
Figure 2: Stem Cell Product Manufacturing and Quality Control Workflow. This diagram outlines critical stages in cell product manufacturing, highlighting key quality assessment points (red) throughout the process.
Future Directions and Standardization Initiatives
The future evolution of stem cell therapy depends on addressing several critical challenges through international collaboration and methodological refinement. The International Society for Stem Cell Research (ISSCR) has developed comprehensive guidelines that are regularly updated to address emerging scientific advances and ethical considerations [83]. The 2025 update to the ISSCR guidelines specifically refined recommendations for stem cell-based embryo models (SCBEMs), retiring previous classifications in favor of the inclusive term "SCBEMs" and prohibiting uterine transplantation [83].
Key priorities for advancing the field include:
Protocol Harmonization: Development of standardized protocols for cell manufacturing, characterization, and potency assays to reduce variability between research centers and clinical trials [21] [8].
Long-Term Safety Assessment: Implementation of extended follow-up periods for trial participants to fully evaluate long-term safety profiles, including potential oncogenic risks [21].
Analytical Advancement: Refinement of imaging and functional assessment methodologies, with cardiac MRI emerging as the gold standard for structural outcomes in cardiovascular applications [21].
Regulatory Convergence: Increased international regulatory cooperation to streamline development pathways while maintaining rigorous safety standards, potentially leveraging existing frameworks like the FDA's RMAT designation and Japan's conditional approval system [80].
Manufacturing Innovation: Development of scalable, cost-effective manufacturing processes to address the high costs and complexity currently associated with personalized stem cell therapies [12].
The trajectory of stem cell therapy standardization will depend on continued dialogue between researchers, clinicians, regulators, and patients. As efficacy signals become more consistent across larger, well-designed trials, and regulatory frameworks evolve to accommodate the unique aspects of cellular therapies, the path to standardized clinical application becomes increasingly clear. The ongoing challenge remains balancing the imperative for rigorous evidence generation with the need to deliver promising therapies to patients with serious, unmet medical needs.
Conclusion
The current body of evidence from randomized clinical trials solidifies the therapeutic potential of stem cell therapy across a spectrum of diseases, demonstrating promising efficacy and a generally favorable safety profile. Key advancements in understanding mechanistic foundations and optimizing clinical protocols are paving the way for more reliable and effective treatments. However, significant challenges remain, including trial heterogeneity, manufacturing complexities, and the need for long-term data. The future of the field lies in addressing these hurdles through international collaboration, standardized protocols, and the strategic development of next-generation approaches like off-the-shelf allogeneic products and cell-free therapies derived from secretome. These efforts are crucial for fulfilling the promise of regenerative medicine and translating preclinical success into consistent clinical outcomes for patients.
References
- 1. Current state of stem cell-based therapies: an overview - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7367472/]
- 2. Global clinical trials on stem cell therapy for autoimmune ... [https://pubmed.ncbi.nlm.nih.gov/40777013/]
- 3. Watch the Annual Clinical Trials Roundup 2025 - Citeline [https://www.citeline.com/en/resources/the-annual-clinical-trials-roundup-2025-ondemand]
- 4. The Annual Clinical Trials Roundup, 2025 Edition - Citeline [https://www.citeline.com/en/resources/the-annual-clinical-trials-roundup-2025]
- 5. Efficacy and safety of mesenchymal stromal cell ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04184-x]
- 6. Efficacy & safety of stem cell therapy for treatment of acute ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550445/]
- 7. A comprehensive review of clinical trials and progress in ... [https://www.sciencedirect.com/science/article/pii/S2352320425001944]
- 8. Efficacy and safety of stem cell therapy for acute and ... [https://www.nature.com/articles/s41598-025-04405-6]
- 9. Trialtrove | Citeline [https://www.citeline.com/en/products-services/clinical/trialtrove]
- 10. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 11. recent developments and future prospects in stem-cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634165/]
- 12. Global clinical trials on stem cell therapy for autoimmune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1616231/full]
- 13. Clinical trials and advanced MRI techniques with stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505762/]
- 14. Stem Cell Clinical Trials and Promise of Engineered Exosomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409071/]
- 15. Comparative analysis of regulations and studies on stem cell ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04065-9]
- 16. Efficacy and Safety of Allogeneic Hematopoietic Stem Cell ... [https://www.sciencedirect.com/science/article/pii/S2666636725014472]
- 17. Comparative Analysis of Short-Term and Long ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11178400/]
- 18. Mesenchymal stem/stromal cells from human pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10916050/]
- 19. History and current status of clinical studies using human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10444540/]
- 20. Comparison of hematopoietic stem cell transplantation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10063874/]
- 21. Safety and efficacy of stem cell therapy in acute myocardial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12207128/]
- 22. Immune modulatory stem cells represent a significant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11911480/]
- 23. Paracrine mechanisms of stem cell reparative and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3021634/]
- 24. In-vitro immunomodulatory efficacy of extracellular ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04476-2]
- 25. Success Rates of Stem Cell Therapy: Evaluated (2025) [https://auragens.com/success-rates-of-stem-cell-therapy-evaluated-2025/]
- 26. The Efficacy of Stem Cells in Wound Healing: A Systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10931571/]
- 27. Innovations in immunotherapy for autoimmune diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485509/]
- 28. Efficacy and safety of mesenchymal stem cell therapy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12010635/]
- 29. From signaling pathways to clinical trials: mesenchymal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12326728/]
- 30. Mesenchymal stem cell therapy as a game-changer in liver ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04127-y]
- 31. Efforts Focused on Fatty Liver over Two Years (2023-2025) [https://pmc.ncbi.nlm.nih.gov/articles/PMC12520595/]
- 32. Navigating mesenchymal stem cells doses and delivery ... [https://www.sciencedirect.com/science/article/pii/S2352320425000483]
- 33. Pharmacological modulation of stem cells signaling pathway ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12210473/]
- 34. Global clinical trials on stem cell therapy for autoimmune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12328461/]
- 35. 399 when to start cellular therapy after hematopoietic stem ... [https://www.sciencedirect.com/science/article/pii/S2531137925018437]
- 36. Stem Cell Success Rate: Evaluated (2025) [https://www.dvcstem.com/post/stem-cell-success-rate]
- 37. Harnessing circadian timing to reduce aGVHD - The Innovation [https://www.the-innovation.org/article/doi/10.59717/j.xinn-med.2025.100165]
- 38. Current Landscape of FDA Stem Cell Approvals and Trials ... [https://www.reprocell.com/blog/current-landscape-of-fda-stem-cell-approvals-and-trials-2023-2025]
- 39. Stem cell-based therapy for human diseases [https://www.nature.com/articles/s41392-022-01134-4]
- 40. Comparison of Conventional Therapies With Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12464503/]
- 41. Stem Cell–Based Therapies via Different Administration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808770/]
- 42. UCSD Stem Cell Transplant Clinical Trials for 2025 [https://clinicaltrials.ucsd.edu/stem-cell-transplant]
- 43. Safety and efficacy of stem cell therapy in acute myocardial ... [https://pubmed.ncbi.nlm.nih.gov/40579230/]
- 44. Biomarkers and Targeted Therapy for Cancer Stem Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842814/]
- 45. New Study Identifies Potential Biomarkers for Predicting ... [https://www.lupus.org/news/new-study-identifies-potential-biomarkers-for-predicting-effectiveness-of-mesenchymal-stem]
- 46. The Role of MRI as a key evaluator of mesenchymal stem ... [https://pubmed.ncbi.nlm.nih.gov/40714636/]
- 47. Brain morphological and connectivity changes on MRI after ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0246817]
- 48. Identifying the REMEDI to problems in stem-cell research [https://www.bioprocessintl.com/upstream-downstream-processing/identifying-the-remedi-to-problems-in-stem-cell-research]
- 49. Global Stem Cells Clinical Trial Updates and Outcomes [https://stemcellthailand.org/stem-cell-clinical-trials-results/]
- 50. Stem Cell Manufacturing Market Size, Growth | Report [2034] [https://www.360researchreports.com/market-reports/stem-cell-manufacturing-market-203048]
- 51. Stem Cell Manufacturing Market Size 2024 To 2034 [https://www.novaoneadvisor.com/report/stem-cell-manufacturing-market]
- 52. Stem Cell Community Day 2025 to Focus on Process ... [https://www.biopharminternational.com/view/stem-cell-community-day-2025-to-focus-on-process-engineering-and-scale-up-innovation]
- 53. Stem Cell Manufacturing Market to Hit Valuation of US$ [https://www.globenewswire.com/news-release/2025/10/02/3160449/0/en/Stem-Cell-Manufacturing-Market-to-Hit-Valuation-of-US-65-49-Billion-by-2033-Astute-Analytica.html]
- 54. Efficacy and safety of mesenchymal stem cells in knee ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04252-2]
- 55. Adverse events of cell therapy clinical trials in human ... [https://www.sciencedirect.com/science/article/pii/S2352320424000440]
- 56. The efficacy and safety of stem cell therapy for ischemic ... [https://pubmed.ncbi.nlm.nih.gov/40450234/]
- 57. Adverse events, side effects and complications in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9659480/]
- 58. Side Effects of Stem Cell Therapy [https://www.dvcstem.com/post/stem-cell-therapy-safe]
- 59. MSCs: Delivery Routes and Engraftment, Cell-Targeting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3755386/]
- 60. Stem Cell Therapy Success Rates Hit 78%: New Research ... [https://globalrph.com/2025/03/stem-cell-therapy-success-rates-hit-78-new-research-reveals-breakthrough-results/]
- 61. Comparison of MSCs and Muse cells: the possible use for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12222320/]
- 62. Exploring the therapeutic potential of MSC-derived ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04616-8]
- 63. Clinical applications of extracellular vesicles [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1671963/full]
- 64. Extracellular vesicle bioactivity and potential for clinical ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04665-z]
- 65. Exosomes vs Stem Cells: Differences & Utility (2025) [https://www.dvcstem.com/post/exosomes-vs-stem-cells]
- 66. Umbilical cord mesenchymal stem cell-derived secretome ... [https://pubmed.ncbi.nlm.nih.gov/40352183/]
- 67. Trends in mesenchymal stem cell-derived extracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488731/]
- 68. Comparison of production methods for mesenchymal stem ... [https://www.nature.com/articles/s41598-025-21218-9]
- 69. A comprehensive guide to conduct a systematic review and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366998/]
- 70. A systematic review and meta-analysis of the efficacy and ... [https://www.nature.com/articles/s41591-025-03978-z]
- 71. A Network Meta-Analysis of Efficacy and Safety Across 22 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566755/]
- 72. Mid- to long-term efficacy and safety of stem cell therapy for ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03891-1]
- 73. Clinical Efficacy and Meta-Analysis of Stem Cell Therapies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5021879/]
- 74. Allogeneic versus autologous stem cell transplantation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057802/]
- 75. Allogeneic mesenchymal stem cell therapy with ... [https://pubmed.ncbi.nlm.nih.gov/40065171/]
- 76. Allogeneic mesenchymal stem cell therapy with ... [https://www.nature.com/articles/s41591-025-03559-0]
- 77. Efficacy of intrathecal mesenchymal stem cell-neural ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03765-6]
- 78. Comparison of Conventional Therapies With Stem Cell ... [https://pubmed.ncbi.nlm.nih.gov/41018340/]
- 79. Emerging trends in clinical allogeneic CAR cell therapy [https://www.sciencedirect.com/science/article/pii/S2666634025001047]
- 80. Brief summary of the regulatory frameworks of regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11794276/]
- 81. SCA LRA Update - April 2025: Regulatory Landscape of ... [https://www.isctglobal.org/telegrafthub/blogs/ken-ip1/2025/04/09/sca-lra-update-april-2025-regulatory-landscape-of]
- 82. Is Stem Cell Research Legal? Explained (2025) [https://www.dvcstem.com/post/is-stem-cell-research-legal]
- 83. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]