Stem Cell Transplantation for Myocardial Infarction: Techniques, Efficacy, and Future Directions in Regenerative Cardiology
This article provides a comprehensive analysis of stem cell transplantation techniques for myocardial infarction (MI), tailored for researchers, scientists, and drug development professionals.
Stem Cell Transplantation for Myocardial Infarction: Techniques, Efficacy, and Future Directions in Regenerative Cardiology
Abstract
This article provides a comprehensive analysis of stem cell transplantation techniques for myocardial infarction (MI), tailored for researchers, scientists, and drug development professionals. It explores the foundational science behind cardiac regeneration, details various methodological approaches and cell types—including mesenchymal stem cells (MSCs), induced pluripotent stem cells (iPSCs), and cardiac stem cells (CSCs). The content examines the primary challenges in the field, such as low cell survival and retention, and synthesizes the latest optimization strategies from recent preclinical and clinical studies. Furthermore, it presents a critical evaluation of clinical efficacy and safety data, including long-term outcomes from meta-analyses of randomized controlled trials. By integrating current evidence with emerging technologies, this review serves as a strategic resource for guiding future research and clinical translation in cardiovascular regenerative medicine.
The Science of Cardiac Repair: Stem Cell Types and Regenerative Mechanisms
Pathophysiology of Myocardial Infarction and the Need for Regeneration
Acute myocardial infarction (AMI) remains a leading cause of global mortality, responsible for approximately 18.6 million deaths annually worldwide [1]. Despite advances in reperfusion therapies and pharmacological interventions, contemporary treatments fail to regenerate lost cardiomyocytes, leaving behind noncontractile scar tissue that predisposes patients to heart failure [1] [2]. The adult human heart has limited regenerative capacity, with cardiomyocyte turnover rates declining from 1% at age 25 to 0.45% by age 75 [3]. This fundamental limitation has spurred significant research into stem cell transplantation techniques to replenish lost myocardium and restore cardiac function. This application note examines the molecular pathogenesis of AMI and details experimental protocols for stem cell-based regenerative approaches, providing researchers with methodologies to investigate cardiac repair mechanisms.
Pathophysiological Mechanisms of Myocardial Infarction
Molecular Pathways in Acute Myocardial Infarction
The pathophysiology of AMI involves a complex cascade of molecular events beginning with coronary artery occlusion and culminating in irreversible cardiomyocyte death. Key mechanisms include oxidative stress, mitochondrial dysfunction, inflammatory activation, and programmed cell death pathways [4].
Oxidative Stress and Mitochondrial Dysfunction: During ischemia, interrupted oxygen supply disrupts the mitochondrial electron transport chain, generating excessive superoxide anions and reactive oxygen species (ROS) [4]. The sudden reintroduction of oxygen during reperfusion triggers a dramatic ROS burst through reverse electron transport at mitochondrial complex I, establishing a vicious cycle of oxidative damage [4]. Concurrent calcium overload promotes sustained opening of mitochondrial permeability transition pores (mPTP), exacerbating mitochondrial impairment and cardiomyocyte death [4].
Inflammatory Cascade: Necrotic cardiomyocytes release damage-associated molecular patterns (DAMPs), including HMGB1, HSP, and S100A8/A9, which activate pattern recognition receptors (TLRs, NLRP3 inflammasome, RAGE) [4]. This interaction triggers pro-inflammatory cytokine release (IL-1β, IL-6, TNF-α) and recruits Ly6Chi monocytes and neutrophils to the infarct zone, initiating a robust inflammatory response [4].
Programmed Cell Death: Multiple cell death pathways, including apoptosis, necroptosis, and pyroptosis, are activated during AMI, collectively contributing to the substantial loss of cardiomyocytes [4]. These pathways are modulated by epigenetic regulators that influence gene expression throughout the infarction and repair process.
Table 1: Key Molecular Mediators in AMI Pathogenesis
| Molecular Category | Key Mediators | Biological Function | Experimental Detection Methods |
|---|---|---|---|
| Oxidative Stress Markers | ROS, NOX, NOS, SOD, CAT, GPX | Redox balance regulation | Fluorescent probes (DCFDA), ELISA, Western blot |
| Inflammatory DAMPs | HMGB1, HSP, S100A8/A9 | Immune cell activation | ELISA, immunohistochemistry, flow cytometry |
| Cell Death Executors | Caspases, RIPK1/RIPK3, MLKL | Programmed cell death | TUNEL assay, caspase activity assays, Western blot |
| Mitochondrial Components | mPTP, ETC complexes, mtDNA | Energy production, apoptosis regulation | Seahorse analyzer, JC-1 staining, mitochondrial isolation |
Ventricular Remodeling Post-Infarction
Following AMI, the heart undergoes structural and functional changes known as ventricular remodeling, characterized by infarct expansion, hypertrophy of non-infarcted myocardium, and progressive chamber dilation [4]. This process is driven by persistent neurohormonal activation, sustained inflammation, and fibrotic replacement of contractile tissue, ultimately leading to decreased cardiac output and heart failure development. Epidemiological data indicate that approximately 20% of AMI patients develop heart failure within 5 years after the initial event [1].
Stem Cell-Based Regenerative Approaches
Stem Cell Types and Mechanisms of Action
Several stem cell populations have been investigated for cardiac regeneration, each with distinct advantages and limitations for myocardial repair.
Table 2: Stem Cell Types for Myocardial Regeneration
| Stem Cell Type | Sources | Key Advantages | Major Limitations | Primary Mechanisms |
|---|---|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Bone marrow, adipose tissue, umbilical cord | Strong immunomodulation, abundant paracrine function, low immunogenicity | Low survival post-transplantation (<10%), functional heterogeneity | Paracrine signaling, immune regulation, homing effects |
| Induced Pluripotent Stem Cells (iPSCs) | Reprogrammed somatic cells | ESC differentiation potential, autologous transplantation, high cardiomyocyte purity (95%) | Tumorigenic risk, residual epigenetic memory, ectopic differentiation | Direct differentiation into cardiomyocytes |
| Embryonic Stem Cells (ESCs) | Inner cell mass of blastocyst | High differentiation efficiency (70-85%), secrete angiogenic factors | Ethical concerns, tumorigenic risk, immune rejection | Direct differentiation |
| Cardiac Stem Cells (CSCs) | Adult heart | Direct transplantation to damaged heart, tissue-specific | Limited studies, mechanisms not fully elucidated | Exosome secretion, angiogenesis, anti-apoptosis |
Mesenchymal Stem Cells (MSCs): MSCs primarily exert therapeutic effects through paracrine signaling rather than direct differentiation [1]. They secrete exosomes containing microRNAs (miR-21, miR-210) that regulate cardiomyocyte apoptosis and fibrosis, along with growth factors (VEGF, HGF, FGF) that promote angiogenesis [1]. MSC recruitment of endogenous progenitor cells occurs via the CCL2/CCR2 axis, enhancing tissue repair [1].
Induced Pluripotent Stem Cells (iPSCs): iPSCs are generated by reprogramming somatic cells with transcription factors (Oct4, Sox2, Klf4, c-Myc) and can differentiate into functional cardiomyocytes with approximately 95% purity using directed differentiation protocols [1]. The first iPSC-derived myocardial cell sheet transplantation trial in Japan (jRCT2052190081) demonstrated significant improvement in myocardial perfusion in 4 of 5 heart failure patients [1].
Extracellular Vesicles (EVs): Stem cell-derived extracellular vesicles (Stem-EVs) have emerged as promising cell-free alternatives for cardiac regeneration [3]. These nano-sized vesicles carry therapeutic cargo (miRNAs, mRNAs, proteins) and demonstrate anti-inflammatory, antiapoptotic, and angiogenic benefits when administered in animal models of AMI, resulting in reduced infarct size and improved cardiac function [3].
Key Signaling Pathways in Cardiac Repair
Stem cell therapies activate multiple signaling pathways to promote cardiac repair:
- Paracrine Signaling: MSC-secreted factors (VEGF, FGF, HGF) activate PI3K/Akt and MAPK pathways, promoting angiogenesis and cell survival [1].
- Immune Modulation: MSCs shift macrophage polarization from pro-inflammatory M1 to anti-inflammatory M2 phenotype via TSG-6 and PGE2 secretion [1].
- Direct Differentiation: iPSCs and ESCs differentiate into cardiomyocytes through sequential activation of Wnt, BMP, and Notch signaling pathways [1] [3].
- In Vivo Reprogramming: Cardiac fibroblasts can be directly reprogrammed to induced cardiomyocyte-like cells (iCMs) via forced expression of GMT (GATA4, Mef2C, Tbx5) or GHMT (GATA4, Hand2, Mef2C, Tbx5) transcription factors [3].
Experimental Protocols for Myocardial Regeneration Research
Protocol: MSC Transplantation in Murine Myocardial Infarction Model
Objective: To evaluate the therapeutic efficacy of mesenchymal stem cells in a murine model of myocardial infarction.
Materials and Equipment:
- 8-12 week old C57BL/6 mice
- Human bone marrow-derived MSCs (commercially available)
- LAD ligation surgical instruments
- Isoflurane anesthesia system
- Echocardiography system (Vevo 2100)
- Flow cytometry reagents for immune profiling
- Histology supplies (formalin, paraffin, sectioning equipment)
Procedure:
Myocardial Infarction Induction:
- Anesthetize mice with 2% isoflurane and maintain with 1.5% during surgery.
- Perform endotracheal intubation and connect to mechanical ventilation.
- Make left thoracotomy between 3rd and 4th ribs to expose the heart.
- Identify the left anterior descending (LAD) coronary artery and permanently ligate with 7-0 silk suture.
- Confirm successful infarction by visual observation of myocardial blanching.
Stem Cell Preparation and Transplantation:
- Culture MSCs in complete DMEM medium supplemented with 10% FBS until 80% confluent.
- Label cells with GFP or DIR dye for tracking (optional).
- Harvest cells using trypsin/EDTA and resuspend in PBS at 1×10^6 cells/50µL.
- Immediately following LAD ligation, intramyocardially inject cell suspension at 3-4 sites around the infarct border zone.
- For control group, inject equivalent volume of PBS only.
Functional Assessment:
- Perform transthoracic echocardiography at days 0, 7, 14, and 28 post-MI.
- Measure left ventricular ejection fraction (LVEF), left ventricular end-systolic volume (LVESV), and left ventricular end-diastolic volume (LVEDV).
- Conduct hemodynamic measurements using pressure-volume loops at endpoint.
Histological Analysis:
- Euthanize animals at study endpoint and perfuse with PBS followed by 4% PFA.
- Excise hearts, post-fix in 4% PFA for 24h, then embed in paraffin.
- Section hearts at 5µm thickness for staining.
- Perform Masson's trichrome staining to quantify fibrotic area.
- Immunostain for CD31 to assess capillary density.
- Use TUNEL assay to quantify apoptotic cells.
Molecular Analysis:
- Extract RNA from infarct border zone tissue using TRIzol method.
- Perform RT-qPCR for angiogenesis markers (VEGF, Ang1), inflammation markers (IL-1β, TNF-α, IL-10), and fibrotic markers (TGF-β, collagen I/III).
- Analyze macrophage polarization via flow cytometry using CD86 (M1) and CD206 (M2) markers.
Expected Outcomes: MSC-treated animals should demonstrate significantly improved LVEF (approximately 3.8% increase), reduced infarct size, enhanced capillary density, and modulated inflammatory response compared to PBS controls [1] [2].
Protocol: iPSC-Derived Cardiomyocyte Differentiation and Transplantation
Objective: To generate functional cardiomyocytes from induced pluripotent stem cells and assess their therapeutic potential in myocardial infarction models.
Materials:
- Human iPSCs (commercially available or patient-derived)
- Cardiomyocyte differentiation kit (or individual components)
- RPMI 1640 medium, B-27 supplements
- Growth factors: Activin A, BMP4, CHIR99021, IWP2
- Immunocytochemistry antibodies: cardiac troponin T, α-actinin, MLC2v
- Multi-electrode array system for electrophysiological assessment
Procedure:
Cardiomyocyte Differentiation:
- Culture iPSCs in mTeSR1 medium on Matrigel-coated plates until 80-90% confluent.
- Initiate differentiation by switching to RPMI/B-27 minus insulin medium containing 6µM CHIR99021 (GSK3β inhibitor).
- After 24h, replace medium with RPMI/B-27 minus insulin alone.
- At day 3, add RPMI/B-27 minus insulin containing 5µM IWP2 (Wnt inhibitor).
- On day 5, replace with RPMI/B-27 minus insulin.
- On day 7, switch to RPMI/B-27 complete medium and maintain with medium changes every 2-3 days.
- Spontaneous contracting cells should appear between days 8-12.
Cardiomyocyte Purification:
- At day 12-15, replace medium with glucose-free RPMI supplemented with 4mM lactate for metabolic selection.
- Maintain lactate medium for 4-6 days to eliminate non-cardiomyocytes.
- Return to normal RPMI/B-27 complete medium.
Characterization:
- Fix cells and immunostain for cardiac markers: cardiac troponin T, α-actinin, MLC2v.
- Analyze sarcomeric organization via confocal microscopy.
- Assess electrophysiological properties using multi-electrode array.
- Perform flow cytometry to quantify cardiomyocyte purity.
Transplantation:
- Dissociate cardiomyocytes using collagenase-based cell dissociation reagent.
- Resuspend in PBS at 1×10^7 cells/100µL for transplantation.
- Transplant into immunodeficient mice or immunosuppressed large animal models of myocardial infarction using intramyocardial injection.
- Monitor for arrhythmias via continuous ECG monitoring post-transplantation.
Expected Outcomes: Successful differentiation should yield >90% pure cardiomyocytes with typical sarcomeric organization and spontaneous contraction [1]. Transplantation studies should demonstrate improved myocardial function and electrical integration, though arrhythmogenic risk remains a concern [3].
Research Reagent Solutions
Table 3: Essential Research Reagents for Cardiac Regeneration Studies
| Reagent Category | Specific Products | Research Application | Key Function |
|---|---|---|---|
| Stem Cell Culture | MesenCult MSC Medium, mTeSR Plus, Matrigel | MSC and iPSC maintenance | Provides optimal growth conditions for stem cell expansion |
| Differentiation Kits | STEMdiff Cardiomyocyte Kit, Gibco PSC Cardiomyocyte Kit | Cardiac differentiation from pluripotent stem cells | Directed differentiation into functional cardiomyocytes |
| Cell Tracking | DIR dye, GFP/Lentivirus, CM-Dil | Cell fate mapping | Enables tracking of transplanted cells in vivo |
| Functional Assessment | Vevo 2100 Imaging System, Pressure-Volume Catheter | Cardiac function analysis | Measures hemodynamic parameters and ejection fraction |
| Molecular Analysis | TaqMan assays for cardiac markers, RNA-seq kits | Gene expression profiling | Quantifies molecular changes in response to therapy |
| Histology | Cardiac troponin T antibodies, Masson's trichrome kit | Tissue characterization | Identifies cardiomyocytes and quantifies fibrosis |
Challenges and Future Perspectives
Despite promising preclinical results, stem cell therapy for myocardial infarction faces significant translational challenges. The low survival rate of transplanted stem cells (less than 5% within 72 hours for MSCs) remains a major bottleneck [1]. Additionally, uncontrolled differentiation, potential tumorigenicity (particularly with iPSCs and ESCs), and arrhythmogenic risk present substantial hurdles [1] [3].
Future directions include the development of combinatorial approaches using biomaterial scaffolds to enhance cell retention and survival. Smart hydrogel scaffolds and 3D bioprinting technology show promise for creating functional cardiac tissue constructs [1]. Engineered extracellular vesicles with enhanced cardiac targeting and recombinant therapeutic cargo represent another emerging strategy [3]. Gene editing technologies like CRISPR-Cas9 offer opportunities to precisely regulate stem cell lineage commitment and improve therapeutic efficacy [1].
As research progresses, multidisciplinary approaches integrating stem cell biology, biomaterials engineering, and gene editing are expected to drive the development of precise, intelligent, and systematic stem cell therapies for myocardial infarction and atherosclerosis [1].
The pursuit of effective stem cell-based therapies for myocardial infarction (MI) represents a cornerstone of modern cardiovascular regenerative medicine. The irreversible loss of cardiomyocytes following ischemic injury is a primary driver of heart failure, a condition with a post-diagnosis 5-year survival rate of merely 50% [3]. Conventional pharmacological and device-based treatments manage symptoms but fail to address the fundamental loss of contractile heart tissue [3]. Stem cell transplantation has emerged as a promising strategy to repopulate damaged myocardium, improve cardiac function, and alter the progression towards heart failure. Among the diverse cell types investigated, Mesenchymal Stem Cells (MSCs), Induced Pluripotent Stem Cells (iPSCs), Cardiac Stem Cells (CSCs), and Skeletal Myoblasts have been identified as major candidates, each with distinct advantages and challenges. This application note details the experimental protocols, functional outcomes, and key reagents for utilizing these cells in MI research, providing a framework for preclinical investigation.
Comparative Analysis of Stem Cell Candidates
The following tables summarize the key characteristics, therapeutic mechanisms, and functional outcomes of the four major stem cell candidates in MI research.
Table 1: Characteristics and Therapeutic Mechanisms of Stem Cell Candidates
| Stem Cell Type | Source | Key Markers | Major Proposed Mechanisms of Action in MI |
|---|---|---|---|
| MSCs | Bone Marrow, Adipose Tissue, Umbilical Cord | CD73+, CD90+, CD105+; CD45-, CD34- [5] | - Paracrine secretion of anti-inflammatory, anti-apoptotic, and pro-angiogenic factors [6] [3].- Stimulation and proliferation of endogenous CSCs [7].- Immunomodulation [8]. |
| iPSCs | Reprogrammed Somatic Cells (e.g., Fibroblasts) | Oct3/4, Sox2, c-Myc, Klf4 (during reprogramming) [9] | - In vitro differentiation into cardiomyocytes (iPSC-CMs) for transplantation [10] [9].- Source for deriving induced MSCs (iMSCs) with enhanced proliferative capacity [5]. |
| CSCs | Cardiac Tissue (e.g., atrial appendages) | c-kit+, GATA-4+ [7] | - Direct differentiation into cardiomyocytes and vascular endothelial cells [11].- Activation of endogenous repair pathways (e.g., Wnt/β-catenin, Notch) [11]. |
| Skeletal Myoblasts | Skeletal Muscle | Desmin+ [12] | - Differentiation into myotubes that provide contractile force [12].- High resistance to ischemia. |
Table 2: Summary of Efficacy and Safety Outcomes from Preclinical and Clinical Studies
| Stem Cell Type | Reported Efficacy Outcomes | Reported Safety Risks | Clinical Trial Status |
|---|---|---|---|
| MSCs | - ↑ LVEF; ↓ infarct size (e.g., from 24.9% to 10.9% LV mass in swine) [7].- Improved remodeling, angiogenesis [6]. | - Low long-term cell retention [6] [3].- Variable outcomes in clinical trials [8]. | Multiple clinical trials completed (e.g., TAC-HFT, POSEIDON) showing safety and variable functional improvement [13] [3]. |
| iPSC-CMs | - ↑ LVEF (MD +8.23%) and ↑ Fractional Shortening (MD +5.16%) in meta-analysis [9].- Reduced fibrosis (MD -7.62%) [9]. | - Risk of teratoma from undifferentiated cells [9].- Arrhythmogenesis post-transplantation [9] [3]. | Preclinical stage; no human trials identified in meta-analysis [9]. |
| CSCs | - 20-fold increase in endogenous c-kit+ CSCs after MSC-mediated stimulation [7].- Promoted cardiomyocyte regeneration in models [11]. | - Limited cell number in adult heart, making isolation difficult [11]. | Early-stage clinical trials; outcomes have been mixed [3]. |
| Skeletal Myoblasts | - Improved regional contractility in infarcted area [12]. | - High incidence of ventricular arrhythmia [12]. | Clinical trials (e.g., MAGIC) showed arrhythmic risk, limiting application [12]. |
Experimental Protocols for Key Investigations
Protocol: Assessing MSC-Mediated Endogenous CSC StimulationIn Vivo
This protocol is based on a porcine model of MI designed to investigate the paracrine-mediated effects of MSCs on host cardiac stem cells [7].
Workflow: MSC Mediated Endogenous CSC Stimulation
Materials:
- Animals: Female Yorkshire swine (25-35 kg) [7].
- MSCs: Allogeneic male porcine bone marrow-derived MSCs, transduced with GFP for tracking [7].
- Control Injectates: Placebo (e.g., Plasmalyte) or concentrated conditioned medium (CCM) [7].
Methodology:
- Myocardial Infarction (MI) Induction: Subject animals to experimental MI followed by reperfusion [7].
- Cell Preparation and Delivery:
- Functional and Tissue Analysis:
- Cardiac MRI: Conduct serial cMRI at baseline, post-MI, and at 2 and 8 weeks post-injection to assess ejection fraction, infarct size, and ventricular volumes [7].
- Tissue Harvesting: Sacrifice animals at predetermined time points (e.g., 2 weeks, 8 weeks). Collect tissue samples from the infarct core, border zone, and remote healthy myocardium [7].
- Histological Analysis:
- Perform immunofluorescence staining for specific markers.
- Quantify c-kit+ CSCs and GATA-4+ CSCs in the border zones.
- Identify mitotic myocytes to assess endogenous cardiomyocyte proliferation [7].
- Use Y-chromosome (e.g., FISH) or GFP staining to track the fate of injected male or GFP-labeled MSCs [7].
Protocol:In VivoTransplantation and Assessment of iPSC-Derived Cardiomyocytes
This protocol outlines the key steps for evaluating the safety and efficacy of iPSC-CMs in small and large animal models of ischemic heart disease, as synthesized from a recent meta-analysis [9].
Workflow: iPSC-CM Transplantation and Assessment
Materials:
- iPSC-CMs: Human iPSC-CMs differentiated and purified using established protocols (e.g., metabolic selection) [10] [9]. Purity must be confirmed to minimize teratoma risk.
- Animal Models: Murine or porcine models of IHD, typically induced by permanent ligation of the left anterior descending (LAD) artery [9].
- Delivery System: Catheter-based system for intramyocardial injection; consider using bioengineered tissue patches for some studies [9].
Methodology:
- Cell Preparation: Culture and prepare a single-cell suspension of iPSC-CMs. Doses in animal studies have ranged from 2 × 10^5 to 4 × 10^8 cells [9].
- IHD Model and Transplantation:
- Induce MI in the animal model.
- At the time of injection (acute or sub-acute phase), perform intramyocardial injections of iPSC-CMs directly into the infarct and border zones. Control groups should receive a vehicle solution [9].
- Outcome Assessment:
- Efficacy: Measure Left Ventricular Ejection Fraction (LVEF) and Fractional Shortening (FS) via echocardiography or cMRI at baseline and periodically during the follow-up (1-12 weeks). Quantify fibrosis percentage in histological sections at endpoint [9].
- Safety: Monitor and record all-cause mortality throughout the study. Perform continuous electrocardiography (ECG) monitoring to detect and quantify episodes of arrhythmia, particularly sustained ventricular tachycardia [9].
- Histology: Examine heart sections for graft survival, integration with host tissue (e.g., presence of gap junctions), and evidence of tumor formation.
Protocol: Direct Reprogramming of Fibroblasts to Cardiomyocytes (In Vivo)
This protocol describes a cell-free alternative for cardiac regeneration by directly reprogramming endogenous cardiac fibroblasts into induced cardiomyocyte-like cells (iCMs) in vivo [3].
Materials:
- Reprogramming Factors: Genes for cardiac transcription factors, typically GMT (GATA4, Mef2C, Tbx5) or GHMT (plus Hand2) [3].
- Delivery Vector: A non-integrating viral vector (e.g., sendai virus, adenovirus) or non-viral nanoparticles for in vivo delivery, ideally with a fibroblast-specific promoter (e.g., FSP1) to target cell specificity [3].
Methodology:
- Vector Construction: Clone the reprogramming factor cocktail (e.g., GHMT) into the chosen delivery vector.
- MI Model and Injection: Induce MI in the animal model. Immediately or shortly after, administer the viral vector/nanoparticles directly into the myocardial wall surrounding the infarct zone.
- Validation and Analysis:
- Lineage Tracing: Use transgenic mice (e.g., Postn or Tcf21 reporter lines) to label fibroblasts and confirm their conversion into iCMs.
- Functional Assessment: Evaluate cardiac function by cMRI/echocardiography. Assess electrophysiological stability by ECG.
- Molecular Phenotyping: Analyze iCMs for the expression of mature cardiac markers (e.g., α-MHC, cTnI) and the downregulation of fibroblast markers (e.g., Vimentin). Evaluate sarcomere structure via immunofluorescence.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Stem Cell-Based Myocardial Repair
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Cell Surface Markers | CD73, CD90, CD105 (MSCs); c-kit (CSCs); SSEA-4 (iPSCs) [5] [7] | Identification, isolation, and purity assessment of specific stem cell populations via flow cytometry or immunostaining. |
| Reprogramming Factors | Oct3/4, Sox2, Klf4, c-Myc (iPSCs); GMT/GHMT (iCMs) [9] [3] | Induction of pluripotency in somatic cells or direct transdifferentiation of fibroblasts into cardiomyocytes. |
| Culture & Differentiation Supplements | bFGF, BMP, Activin A, PDGF-AB [5] [10] | Promoting mesodermal commitment and maintenance of MSCs during in vitro culture and differentiation. |
| Critical Animal Models | Yorkshire swine MI model; Murine LAD ligation model [7] [9] | Preclinical in vivo testing of cell safety, efficacy, and mechanisms of action. |
| Cell Delivery Devices | Transendocardial injection catheters (e.g., Stiletto) [7] | Precise, fluoroscopically-guided delivery of cell therapies to the infarct and border zones. |
| Functional Assessment Tools | Cardiac MRI (cMRI); Echocardiography; Electrocardiography (ECG) [7] [9] | Longitudinal, non-invasive measurement of functional outcomes (LVEF, volumes) and safety (arrhythmia). |
| Capsorubin | Capsorubin | Natural Apocarotenoid | For Research Use | Capsorubin is a natural red pigment and potent antioxidant for plant biology and nutrition research. For Research Use Only. Not for human consumption. |
| Beta-Asarone | Beta-Asarone, CAS:5273-86-9, MF:C12H16O3, MW:208.25 g/mol | Chemical Reagent |
Key Signaling Pathways in Cardiac Stem Cell Biology
The therapeutic action of stem cells, particularly the stimulation of endogenous repair mechanisms, involves a complex interplay of multiple signaling pathways.
Signaling Pathways in Cardiac Stem Cell Biology
Pathway Notes:
- Wnt/β-catenin: This pathway is crucial for CSC proliferation and self-renewal. Its activation leads to β-catenin stabilization and translocation to the nucleus, where it initiates the transcription of proliferation-related genes [11].
- Notch Signaling: Regulates cell fate decisions. Activation of Notch signaling in CSCs promotes their commitment and differentiation into cardiomyocytes while inhibiting alternative lineage differentiation [11].
- PI3K/Akt Pathway: A key pro-survival pathway. Its activation by MSC-secreted factors inhibits apoptosis and promotes the survival and proliferation of both endogenous CSCs and cardiomyocytes in the hostile post-infarct microenvironment [11].
Stem cell therapy has emerged as a transformative paradigm for myocardial infarction (MI) treatment, aiming to repair damaged heart tissue through core mechanistic actions: paracrine signaling, direct differentiation, and immune modulation [1] [14]. Despite advancements in conventional treatments, MI remains a leading cause of death worldwide, with approximately 15 million annual cases and about 20% of patients developing heart failure within five years post-onset [14]. Contemporary interventions often fail to achieve full functional regeneration of myocardial tissue, creating an urgent need for regenerative approaches [1]. Stem cells address this need through multifaceted mechanisms that promote tissue repair, angiogenesis, and immunomodulation, working synergistically to counteract the pathological processes driving post-infarction heart failure [15]. This document delineates the specific applications, experimental protocols, and reagent solutions underpinning these core mechanisms within myocardial infarction research contexts.
Paracrine Signaling
Mechanisms and Biological Significance
The paracrine effect represents a principal mechanism whereby stem cells secrete bioactive molecules that exert therapeutic effects on neighboring cells within damaged tissues [16]. This signaling encompasses the secretion of growth factors, cytokines, chemokines, and extracellular vesicles (including exosomes) that modulate the local cellular environment, promote angiogenesis, enhance cell survival, and exert anti-inflammatory effects [17] [18]. In the context of myocardial infarction, paracrine signaling ameliorates the ischemic microenvironment, attenuates cardiomyocyte apoptosis, and promotes functional recovery without requiring direct differentiation of the administered cells [1] [14].
Mesenchymal stem cells (MSCs) predominantly mediate their therapeutic benefits through paracrine actions [14] [18]. Their secretome includes vascular endothelial growth factor (VEGF) and hepatocyte growth factor (HGF), which significantly promote angiogenesis [1]. Other critical paracrine mediators include stromal cell-derived factor-1α (SDF-1α) and insulin-like growth factor-1 (IGF-1), which enhance neovascularization and reduce cardiomyocyte apoptosis in preclinical MI models [1]. Additionally, exosomes derived from MSCs carry regulatory microRNAs (e.g., miR-21, miR-210) that modulate cardiomyocyte apoptosis and fibrosis, while the CCL2/CCR2 axis facilitates the recruitment of endogenous progenitor cells to promote angiogenesis [1].
Table 1: Key Paracrine Factors in Stem Cell Therapy for Myocardial Infarction
| Paracrine Factor | Cell Source | Primary Function | Experimental Evidence |
|---|---|---|---|
| VEGF | MSCs | Promotes angiogenesis and ameliorates ischemic microenvironment | Preclinical MI models show enhanced neovascularization [1] |
| HGF | MSCs | Promotes angiogenesis and tissue repair | Preclinical models demonstrate significant tissue repair [1] |
| SDF-1α | MSCs | Enhances neovascularization, attenuates cardiomyocyte apoptosis | Promotes functional recovery in preclinical MI models [1] |
| IGF-1 | MSCs | Attenuates cardiomyocyte apoptosis | Promotes functional recovery in preclinical MI models [1] |
| Exosomes (miR-21, miR-210) | MSCs | Regulates cardiomyocyte apoptosis and fibrosis | MSC-derived exosomes carry microRNAs that regulate apoptosis [1] |
| CCL2/CCR2 | MSCs | Recruits endogenous progenitor cells to promote angiogenesis | Clinical phase III trials confirm functional improvement [1] |
Experimental Protocol: Analyzing MSC Paracrine Secretion
Objective: To isolate and characterize the paracrine factors secreted by MSCs and evaluate their effects on cardiomyocyte survival and angiogenesis.
Materials:
- Human bone marrow-derived MSCs (commercially available)
- MSC growth medium (e.g., DMEM/F12 supplemented with 10% FBS and 1% penicillin/streptomycin)
- Serum-free collection medium
- Centrifugation equipment
- Ultracentrifugation equipment for exosome isolation
- Enzyme-linked immunosorbent assay (ELISA) kits for VEGF, HGF, SDF-1α, IGF-1
- Angiogenesis assay kit (e.g., tube formation assay with HUVECs)
- Hypoxia chamber to simulate ischemic conditions
- Cardiomyocyte cell line (e.g., H9c2) or human pluripotent stem cell-derived cardiomyocytes
Methodology:
- MSC Culture and Conditioning:
- Culture MSCs in growth medium until 80% confluent.
- Wash cells with PBS and replace with serum-free medium.
- Place cells in normoxic (21% Oâ‚‚) or hypoxic (1% Oâ‚‚) conditions for 24-48 hours to simulate ischemic environments.
- Collect conditioned medium after 24 hours for analysis.
Fractionation of Conditioned Medium:
- Centrifuge conditioned medium at 2,000 × g for 30 minutes to remove cells and debris.
- Further centrifuge at 10,000 × g for 30 minutes to remove apoptotic bodies and large vesicles.
- Isolate exosomes by ultracentrifugation at 100,000 × g for 70 minutes.
- Resolve exosome pellet in PBS for downstream applications.
Analysis of Secreted Factors:
- Quantify VEGF, HGF, SDF-1α, and IGF-1 concentrations in conditioned medium using ELISA according to manufacturer protocols.
- Characterize exosomal markers (CD9, CD63, CD81) by western blotting.
- Extract and quantify exosomal miRNAs (e.g., miR-21, miR-210) using qRT-PCR.
Functional Assays:
- Cardiomyocyte Protection Assay: Culture cardiomyocytes under hypoxic conditions with MSC-conditioned medium or isolated exosomes. Assess cell viability using MTT assay and apoptosis via TUNEL staining after 24-48 hours.
- Angiogenesis Assay: Seed HUVECs on Matrigel and treat with MSC-conditioned medium or exosomes. Quantify tube formation by measuring total tube length and branch points after 6-18 hours.
Direct Differentiation
Mechanisms and Biological Significance
Direct differentiation involves the capacity of stem cells to differentiate into functional cardiomyocytes that can directly replace lost or damaged myocardial tissue post-infarction [1]. This mechanism is particularly relevant for induced pluripotent stem cells (iPSCs), which can be differentiated into cardiomyocytes with high purity (up to 95%) for potential transplantation therapies [1]. The world's first iPSC-derived myocardial cell sheet transplantation trial in Japan (jRCT2052190081) demonstrated significant improvement in myocardial perfusion in 4 of 5 heart failure patients [1].
Cardiac lineage commitment from pluripotent stem cells follows developmental principles, recapitulating embryonic heart development stages [19]. Key regulatory factors include ZNF711, which acts as a critical switch and safeguard for cardiomyocyte commitment, and retinoic acid (RA) signaling, which promotes atrial cardiomyocyte differentiation [19]. The differentiation process progresses through distinct stages: mesodermal progenitors (marked by EOMES), cardiac progenitors (marked by ISL1+/NKX2-5+), and finally functional cardiomyocytes expressing structural markers such as TNNT2 (cardiac troponin T) and MYL7 (myosin light chain 7) [19] [20].
Table 2: Stem Cell Types for Direct Differentiation in Cardiac Therapy
| Stem Cell Type | Source | Advantages | Limitations | Differentiation Efficiency |
|---|---|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | Reprogrammed somatic cells | Differentiation potential of ESCs with autologous transplantation advantages; can generate high-purity cardiomyocytes | Residual reprogramming epigenetic memory may cause differentiation bias; tumorigenic risk | Up to 95% purity with directed differentiation systems [1] |
| Embryonic Stem Cells (ESCs) | Inner cell mass of blastocyst | High differentiation efficiency (70-85%); secretes angiogenic factors | Ethical controversies; tumorigenic risk; immune rejection | 70-85% efficiency [1] |
| Cardiac Stem Cells (CSCs) | Adult heart | Can be transplanted directly to damaged heart; exosomes promote function recovery | Limited studies; mechanisms need further clarification | Secreted exosomes (e.g., miR-146a) promote regeneration [1] |
| Mesenchymal Stem Cells (MSCs) | Bone marrow, adipose tissue, umbilical cord | Strong immunomodulation; abundant paracrine function | Low survival rate post-transplantation (<10%); functional heterogeneity | Primarily via paracrine effects rather than direct differentiation [1] |
Experimental Protocol: Directed Differentiation of iPSCs to Cardiomyocytes
Objective: To efficiently differentiate iPSCs into functional cardiomyocytes using a small molecule-based approach with high purity and reproducibility.
Materials:
- Human iPSCs (maintained in feeder-free conditions)
- Essential 8 or mTeSR1 medium for pluripotent stem cell maintenance
- RPMI 1640 medium
- B-27 supplements (with and without insulin)
- CHIR99021 (GSK-3 inhibitor)
- IWP2 or IWP4 (Wnt inhibitor)
- Matrigel or defined extracellular matrices (fibronectin, vitronectin, laminin-111)
- Accutase or EDTA solution for cell detachment
- Cardiac troponin T (cTnT) antibody for flow cytometry
- Field stimulation system for metabolic purification (optional)
Methodology:
- Maintenance of Pluripotent Stem Cells:
- Culture iPSCs on Matrigel-coated plates in Essential 8 medium.
- Passage cells every 4-5 days at 70-80% confluence using EDTA solution.
- Ensure cells maintain typical pluripotent morphology with high nuclear-to-cytoplasmic ratio.
Cardiac Differentiation via GiWi Protocol:
- Day 0: Detach iPSCs and seed as single cells at optimal density (e.g., 1.5-2.0 × 10^5 cells/cm²) in Matrigel-coated plates with 10 μM Y-27632 ROCK inhibitor.
- Day 1: Replace medium with RPMI 1640 supplemented with B-27 without insulin. Add CHIR99021 (optimized concentration, typically 6-12 μM) to activate Wnt signaling and induce mesoderm formation.
- Day 3: Replace medium with RPMI/B-27 without insulin without CHIR99021.
- Day 5: Add IWP2 (2-5 μM) to inhibit Wnt signaling and promote cardiac mesoderm specification.
- Day 7: Replace medium with RPMI/B-27 without insulin without IWP2.
- Days 9-11: Begin metabolic selection by switching to RPMI 1640 containing glucose-free B-27 supplement and 4 mM lactate to enrich for cardiomyocytes.
Progenitor Reseeding Strategy (for Enhanced Purity):
- At day 3-4 (EOMES+ mesoderm stage) or day 5-6 (ISL1+/NKX2-5+ cardiac progenitor stage), detach cells using Accutase.
- Reseed cells at lower density (1:2.5 to 1:5 ratio by surface area) in fresh Matrigel-coated plates or defined matrices (fibronectin, vitronectin).
- Continue differentiation protocol from appropriate stage.
Characterization of Differentiated Cardiomyocytes:
- Flow Cytometry: Harvest cells at day 12-16, fix and permeabilize, then stain with anti-cTnT antibody to quantify cardiomyocyte purity.
- Functional Assessment: Record spontaneous contraction rates and analyze contractile properties using video-based analysis (e.g., MUSCLEMOTION software).
- Immunocytochemistry: Stain for cardiac-specific markers (cTnT, α-actinin, MYL2, MYL7) and assess sarcomeric organization.
- Gene Expression Analysis: Perform qRT-PCR for atrial (NR2F2, KCNA5) and ventricular (MYL2, MYH7) markers.
Immune Modulation
Mechanisms and Biological Significance
Immune modulation represents a critical mechanism whereby stem cells, particularly MSCs, suppress detrimental inflammatory responses and promote a regenerative microenvironment following myocardial infarction [1] [14] [18]. MSCs interact with various immune cells—including T cells, B cells, dendritic cells, and macrophages—through both direct cell-cell contact and secretion of immunoregulatory molecules [18]. This immunomodulatory capacity helps mitigate the excessive inflammation that contributes to adverse remodeling and heart failure progression post-MI.
MSCs modulate immune responses through multiple pathways: they suppress T cell activation and proliferation, reduce pro-inflammatory cytokine release (particularly TNF-α and IL-6), induce regulatory T cell (Treg) formation, and promote macrophage polarization toward the anti-inflammatory M2 phenotype [14] [18]. The immunomodulatory functions of MSCs are activated by inflammatory cytokines (e.g., IFN-γ, TNF-α) in the microenvironment, leading to increased expression of immunomodulatory factors such as prostaglandin E2 (PGE2), indoleamine 2,3-dioxygenase (IDO), and transforming growth factor-β (TGF-β) [18]. This dynamic responsiveness enables MSCs to exert context-dependent immunomodulation precisely where needed.
Experimental Protocol: Assessing Immunomodulatory Properties of MSCs
Objective: To evaluate the immunomodulatory effects of MSCs on T cell responses and macrophage polarization relevant to myocardial infarction recovery.
Materials:
- Human MSCs (bone marrow or umbilical cord derived)
- Peripheral blood mononuclear cells (PBMCs) from healthy donors
- T cell activation reagents (anti-CD3/CD28 beads)
- Macrophage differentiation factors (M-CSF)
- Polarizing cytokines (IFN-γ, LPS for M1; IL-4 for M2)
- Flow cytometry antibodies (CD4, CD25, FoxP3, CD86, CD206)
- ELISA kits for TNF-α, IL-6, IL-10, TGF-β
- Transwell co-culture systems (for cell-cell contact experiments)
- Conditioned medium collection equipment
Methodology:
- T Cell Suppression Assay:
- Isolate PBMCs from healthy donor blood using density gradient centrifugation.
- Activate T cells using anti-CD3/CD28 beads according to manufacturer's protocol.
- Co-culture activated PBMCs with MSCs at various ratios (e.g., 1:1 to 10:1 PBMCs:MSCs) in direct contact or using transwell systems.
- After 72-96 hours, analyze T cell proliferation via CFSE dilution or BrdU incorporation.
- Assess Treg induction by flow cytometry staining for CD4, CD25, and FoxP3.
- Quantify cytokine levels (TNF-α, IL-6, IL-10) in supernatant using ELISA.
Macrophage Polarization Assay:
- Differentiate monocytes from PBMCs using M-CSF (50 ng/mL) for 6 days.
- Polarize macrophages toward M1 phenotype with IFN-γ (20 ng/mL) and LPS (100 ng/mL) or toward M2 phenotype with IL-4 (20 ng/mL).
- Treat polarized macrophages with MSC-conditioned medium or co-culture with MSCs.
- After 48 hours, analyze macrophage surface markers by flow cytometry (CD86 for M1, CD206 for M2).
- Quantify secretion of phenotype-specific cytokines (TNF-α for M1; IL-10 for M2) using ELISA.
- Assess phagocytic activity using pHrodo-labeled E. coli particles.
Mechanistic Studies:
- Inhibit specific immunomodulatory pathways (IDO with 1-MT, PGE2 with indomethacin, TGF-β with neutralizing antibodies) to determine contribution to observed effects.
- Analyze MSC immunomodulatory gene expression (IDO, COX-2, TGF-β) by qRT-PCR following inflammatory priming with IFN-γ.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Stem Cell Mechanisms in Myocardial Infarction
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Stem Cell Sources | Bone marrow MSCs, iPSCs, Cardiac stem cells | Provide cellular material for therapy development | Consider differentiation potential, availability, and ethical implications [1] [18] |
| Small Molecule Inhibitors/Activators | CHIR99021 (Wnt activator), IWP2/IWP4 (Wnt inhibitors), Retinoic acid | Direct stem cell differentiation toward cardiac lineages | Concentration and timing critically affect efficiency [1] [19] |
| Extracellular Matrices | Matrigel, Fibronectin, Vitronectin, Laminin-111 | Support stem cell attachment, growth, and differentiation | Defined matrices reduce batch variability [20] |
| Characterization Antibodies | Anti-cTnT, Anti-α-actinin, Anti-NKX2-5, Anti-CD90/CD105/CD73 | Identify and purify specific cell types | Validate for flow cytometry vs. immunocytochemistry [1] [18] |
| Cytokine/Chemokine Analysis | VEGF, HGF, SDF-1α, IGF-1 ELISA kits | Quantify paracrine factor secretion | Measure both constitutive and induced secretion [1] |
| Exosome Isolation Tools | Ultracentrifugation equipment, Precipitation kits, Size-exclusion chromatography | Isolate and purify extracellular vesicles | Method affects exosome yield and quality [16] |
| Thioquinapiperifil dihydrochloride | Thioquinapiperifil dihydrochloride|High-Purity RUO | Thioquinapiperifil dihydrochloride, a phosphodiesterase inhibitor for neurology research. For Research Use Only. Not for diagnostic or personal use. | Bench Chemicals |
| 3-Bromo-7-Nitroindazole | 3-Bromo-7-nitroindazole | Building Block | RUO | 3-Bromo-7-nitroindazole, a key intermediate for kinase & cancer research. High-purity, For Research Use Only. Not for human consumption. | Bench Chemicals |
Integrated Experimental Workflow
This application note details the core molecular pathways activated during stem cell-based therapy for myocardial infarction (MI). It provides a structured analysis of three interconnected processes—angiogenesis, anti-apoptosis, and extracellular matrix (ECM) remodeling—which are critical for cardiac repair. The protocols and data presented are designed to assist researchers in quantifying these pathways to evaluate the efficacy of regenerative therapies, thereby supporting drug development and preclinical research.
Angiogenic Signaling Pathways in Cardiac Repair
Angiogenesis, the formation of new blood vessels from pre-existing vasculature, is essential for supplying oxygen and nutrients to the ischemic myocardium post-MI. Stem cells, particularly mesenchymal stem cells (MSCs), promote angiogenesis primarily through paracrine signaling.
Key Pathways and Quantitative Data
The table below summarizes the primary angiogenic factors and their measured effects in stem cell therapy for MI.
Table 1: Key Angiogenic Factors and Their Effects in Stem Cell Therapy for MI
| Factor / Pathway | Biological Effect | Measured Outcome in MI Models | Citation |
|---|---|---|---|
| VEGF/VEGFR2 | Promotes endothelial cell proliferation, migration, and survival; increases vascular permeability. | Increased vessel density; improved perfusion of ischemic tissue. | [21] [22] |
| Paracrine Secretion (VEGF, FGF, HGF) | MSCs release growth factors that promote angiogenesis and ameliorate the ischemic microenvironment. | Increased left ventricular ejection fraction (LVEF) by 3.8% in clinical trials. | [14] |
| SDF-1α | Chemokine that recruits endothelial progenitor cells (EPCs) to the site of injury. | Enhanced neovascularization and attenuated cardiomyocyte apoptosis. | [14] |
| Exosomal microRNAs (e.g., miR-21, miR-210) | Carried by MSC-derived exosomes; regulate cardiomyocyte apoptosis and fibrosis. | Reduction in infarct size; improved cardiac function. | [14] |
Experimental Protocol: Quantifying Angiogenesis
Objective: To assess the pro-angiogenic potential of stem cell-conditioned medium or transplanted cells in a murine MI model.
Materials:
- Matrigel: Basement membrane matrix for in vitro tube formation assays.
- Human Umbilical Vein Endothelial Cells (HUVECs): Standard cell model for studying angiogenesis in vitro.
- Recombinant VEGF and Anti-VEGF Antibody: Positive and negative controls, respectively.
- CD31 Antibody: For immunohistochemical staining of endothelial cells to quantify vessel density in tissue sections.
Methodology:
- In Vitro Tube Formation Assay:
- Coat a 96-well plate with growth factor-reduced Matrigel (50 µL/well) and allow it to polymerize.
- Seed HUVECs (1x10^4 cells/well) in conditioned medium from cultured MSCs.
- Include control wells with basal medium supplemented with recombinant VEGF (50 ng/mL) or an anti-VEGF antibody (10 µg/mL).
- Incubate for 6-18 hours at 37°C.
- Image the formed capillary-like structures using an inverted microscope.
- Quantify the total tube length and number of master junctions per field of view using image analysis software (e.g., ImageJ with the Angiogenesis Analyzer plugin).
- In Vivo Vessel Density Analysis:
- Induce MI in mice via permanent ligation of the left anterior descending (LAD) coronary artery.
- Administer stem cells (e.g., 1x10^6 MSCs) via intramyocardial injection into the border zone.
- After 28 days, euthanize the animals and harvest the hearts.
- Fix hearts in 4% paraformaldehyde, embed in paraffin, and section (5 µm thickness).
- Perform immunohistochemical staining with an anti-CD31 antibody to label endothelial cells.
- Count the number of CD31-positive vessels in five random high-power fields (HPF, 200x magnification) from the infarct and border zones.
Data Interpretation: A significant increase in tube length in vitro and vessel density in vivo in treatment groups compared to controls indicates a potent pro-angiogenic effect.
Angiogenesis Signaling Pathway Diagram
Title: Core Angiogenesis Pathway in Stem Cell Therapy
Anti-apoptotic Pathways Activated by Stem Cells
Inhibition of cardiomyocyte apoptosis is a major mechanism by which stem cell therapy preserves cardiac function post-MI. This occurs primarily via paracrine factors that activate pro-survival signaling cascades.
Key Pathways and Quantitative Data
The table below outlines the primary anti-apoptotic mechanisms and their documented effects.
Table 2: Anti-apoptotic Mechanisms of Stem Cells in MI
| Mechanism / Pathway | Biological Effect | Measured Outcome | Citation |
|---|---|---|---|
| Paracrine Factors (IGF-1, SDF-1α) | Activate PI3K/AKT pathway, inhibiting pro-apoptotic proteins like BAD and Caspase-9. | Attenuated cardiomyocyte apoptosis; improved functional recovery. | [14] |
| Exosomal microRNAs | miR-21 and miR-210 target pro-apoptotic genes, reducing cell death. | Reduced fibrosis and cardiomyocyte apoptosis in preclinical models. | [14] |
| Akt Overexpression | Genetically engineered MSCs overexpressing Akt enhance cell survival and protective paracrine effects. | Protected myocardium for 72 hours post-transplantation. | [23] |
| Intercellular Material Transport | Stem cells transfer healthy mitochondria to damaged cardiomyocytes via tunneling nanotubes. | Provides bioenergetic support and enhances survival of stressed cells. | [14] |
Experimental Protocol: Assessing Anti-apoptotic Effects
Objective: To evaluate the anti-apoptotic effect of stem cell-derived factors on cardiomyocytes in vitro.
Materials:
- H9c2 Cardiomyoblasts or Primary Neonatal Rat Ventricular Myocytes (NRVMs): Representative cell lines for in vitro apoptosis studies.
- Serum-Free Medium: To simulate ischemic stress.
- Recombinant IGF-1: Positive control for anti-apoptotic signaling.
- Caspase-3/7 Activity Assay Kit: (Luminescent or fluorescent) for quantifying apoptosis.
- TUNEL Assay Kit: For direct labeling of DNA fragmentation in apoptotic cells.
- Phospho-AKT (Ser473) Antibody: For detecting activation of the AKT pathway via Western Blot.
Methodology:
- Induction of Apoptosis and Treatment:
- Culture H9c2 cells or NRVMs in full-growth medium until 70-80% confluent.
- Induce apoptosis by switching to serum-free medium for 24 hours.
- Treat experimental groups with conditioned medium from MSCs. Include controls: negative control (serum-free medium only) and positive control (serum-free medium + 100 ng/mL IGF-1).
- Caspase Activity Measurement:
- After treatment, lyse cells and assay for caspase-3/7 activity according to the manufacturer's protocol.
- Measure luminescence/fluorescence with a plate reader. A decrease in signal indicates inhibition of apoptosis.
- TUNEL Staining:
- After treatment, fix cells with 4% paraformaldehyde and permeabilize with 0.1% Triton X-100.
- Perform TUNEL staining according to the kit instructions. Counterstain nuclei with DAPI.
- Image five random fields per well using a fluorescence microscope. Calculate the percentage of TUNEL-positive nuclei.
- Western Blot Analysis for AKT Pathway:
- Harvest cells in RIPA buffer. Separate proteins (30 µg per lane) by SDS-PAGE and transfer to a PVDF membrane.
- Probe the membrane with anti-phospho-AKT (Ser473) and total AKT antibodies.
- A significant increase in the ratio of phospho-AKT to total AKT in treated groups indicates pathway activation.
Data Interpretation: A statistically significant reduction in caspase activity and TUNEL-positive cells, coupled with increased AKT phosphorylation, confirms an anti-apoptotic effect.
Anti-apoptosis Signaling Pathway Diagram
Title: Stem Cell Paracrine Anti-apoptotic Signaling
Extracellular Matrix Remodeling in Myocardial Repair
The ECM is not a passive scaffold but a dynamic entity. Post-MI, maladaptive ECM remodeling leads to fibrosis and stiffening, impairing cardiac function. Stem cells contribute to ECM "normalization," which can mitigate adverse remodeling and support repair.
Key Components and Enzymes in ECM Remodeling
The table below catalogues the primary ECM components and remodeling enzymes relevant to the cardiac environment post-MI.
Table 3: Key ECM Components and Remodeling Enzymes in Cardiac Repair
| ECM Component/Enzyme | Role in Normal Heart | Change Post-MI / Role in Remodeling | Citation |
|---|---|---|---|
| Collagen I & III | Provides structural integrity and tensile strength. | Increased deposition and cross-linking, leading to fibrosis and increased stiffness. | [24] [25] |
| Matrix Metalloproteinases (MMPs: MMP-2, MMP-9, MMP-14) | Maintain ECM homeostasis via controlled degradation. | Overexpressed; degrade basement membrane (Collagen IV) facilitating adverse remodeling; activity correlates with malignant progression. | [24] |
| Lysyl Oxidase (LOX) | Catalyzes collagen cross-linking for mechanical stability. | Upregulated in hypoxia; increases ECM stiffness, promoting fibrosis and tumor progression. | [24] |
| Fibronectin | Glycoprotein involved in cell adhesion and migration. | Overproduced, contributing to increased ECM rigidity and cell migration. | [25] |
| Hyaluronic Acid | Proteoglycan that maintains tissue hydration and volume. | Accumulates, contributing to desmoplasia and increased stiffness. | [25] |
Experimental Protocol: Analyzing ECM Composition and Stiffness
Objective: To evaluate the impact of stem cell therapy on ECM composition, organization, and stiffness in a mouse MI model.
Materials:
- Picrosirius Red Stain: Specifically stains collagen fibers. When viewed under polarized light, it can differentiate between thin (green/yellow) and thick (orange/red) collagen fibers.
- Masson's Trichrome Stain: Differentiates collagen (blue) from muscle (red).
- Anti-LOX Antibody / Anti-MMP-9 Antibody: For immunohistochemical staining of remodeling enzymes.
- Atomic Force Microscopy (AFM) Cantilevers: For direct measurement of tissue stiffness on tissue sections.
Methodology:
- Tissue Preparation:
- Following the in vivo MI model described in Section 2.2, harvest hearts at the study endpoint (e.g., 28 days post-MI).
- Fix a portion of the heart in 4% paraformaldehyde for paraffin embedding and sectioning (5 µm). Flash-freeze another portion for protein analysis.
- Histological Staining and Analysis:
- Picrosirius Red Staining:
- Deparaffinize and hydrate sections. Stain with Picrosirius Red solution for 60 minutes.
- Rinse, dehydrate, and mount. Image under both brightfield and polarized light.
- Quantify the total collagen volume fraction (%) in the infarct area using image analysis software.
- Immunohistochemistry for LOX/MMPs:
- Perform antigen retrieval on deparaffinized sections.
- Incubate with primary antibodies against LOX or MMP-9 overnight at 4°C.
- Use appropriate secondary antibodies and DAB development. Counterstain with hematoxylin.
- Score the staining intensity (0-3) and percentage of positive cells in the infarct and border zones.
- Picrosirius Red Staining:
- Atomic Force Microscopy (AFM) for Stiffness:
- Use fresh or optimally preserved tissue sections.
- Use an AFM with a spherical tip cantilever to perform force mapping on the infarct border zone.
- Calculate the Young's modulus (a measure of stiffness) from the force-distance curves. Compare stiffness between treatment and control groups.
Data Interpretation: Successful ECM "normalization" is indicated by a more organized collagen structure, reduced total collagen deposition, decreased expression of pro-fibrotic enzymes (LOX), and a measured reduction in tissue stiffness toward normal values.
ECM Remodeling Pathway Diagram
Title: ECM Remodeling Pathway Post-Myocardial Infarction
The Scientist's Toolkit: Essential Research Reagents
The table below lists critical reagents for investigating the molecular pathways discussed in this application note.
Table 4: Essential Research Reagents for Key Pathway Analysis
| Reagent / Tool | Specific Example | Primary Function in Experiments | Citation |
|---|---|---|---|
| Anti-CD31 Antibody | Monoclonal anti-mouse CD31 (PECAM-1) | Immunohistochemical staining to identify and quantify endothelial cells and blood vessels. | [21] |
| Recombinant Growth Factors | Recombinant Human VEGF165, Recombinant Human IGF-1 | Used as positive controls in angiogenesis and anti-apoptosis assays to validate experimental systems. | [14] [21] |
| Matrix for Tube Formation | Growth Factor-Reduced Matrigel | Basement membrane extract used as a substrate for in vitro endothelial tube formation assays. | [21] |
| Activity Assay Kits | Caspase-Glo 3/7 Assay | Luminescent assay for sensitive quantification of caspase-3/7 activity as a marker of apoptosis. | [14] |
| Histological Stains | Picrosirius Red | Specific stain for collagen; allows for quantification of fibrosis and analysis of collagen fiber organization under polarized light. | [24] [25] |
| Enzyme Antibodies | Anti-LOX Antibody, Anti-MMP-9 Antibody | Detection and localization of key ECM remodeling enzymes in tissue sections via IHC. | [24] |
| 1-Deoxynojirimycin hydrochloride | 1-Deoxynojirimycin hydrochloride|1-DNJ | Bench Chemicals | |
| Migalastat Hydrochloride | Migalastat Hydrochloride | Research Compound | Migalastat hydrochloride is a pharmacological chaperone for enzyme research. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals |
Translational Techniques: From Cell Harvesting to Clinical Delivery
In the field of regenerative medicine for myocardial infarction (MI), the choice between autologous (using the patient's own cells) and allogeneic (using donor-derived cells) stem cell transplantation is a fundamental consideration for researchers and therapy developers [26]. Each strategy presents a distinct profile of advantages and logistical challenges, impacting therapeutic efficacy, timing, and clinical applicability [1] [26]. Autologous therapies mitigate immune rejection risks but are often limited by the patient's age and health status, which can compromise cell potency and delay treatment [26]. In contrast, allogeneic cells, particularly mesenchymal stem cells (MSCs) from sources like umbilical cord tissue, offer an "off-the-shelf" solution with consistent quality and viability, enabling administration during the critical acute or subacute phases of MI recovery [27] [26]. However, they carry a inherent risk of immune complications such as Graft-versus-Host Disease (GVHD) [28] [26]. This document details the standardized protocols for both approaches, providing a framework for preclinical and clinical research in cardiac repair.
Comparative Analysis: Autologous vs. Allogeneic Approaches
The decision between autologous and allogeneic cell sourcing involves balancing critical factors such as immune compatibility, cell viability, production timelines, and suitability for acute treatment windows. The table below summarizes the core characteristics of each approach.
Table 1: Core Characteristics of Autologous and Allogeneic Cell Therapies for MI Research
| Characteristic | Autologous Approach | Allogeneic Approach |
|---|---|---|
| Immune Rejection Risk | Negligible; uses patient's own cells [27] | Present; requires HLA typing and matching to minimize risk of GVHD [28] [26] |
| Therapeutic Potential | Limited by patient's age and comorbidities; cell potency may be reduced [26] | High; cells can be screened for optimal viability and potency [26] |
| Cell Sources | Bone marrow, adipose tissue [27] | Donor bone marrow, umbilical cord tissue, umbilical cord blood [28] [27] |
| Production & Readiness | Requires weeks for cell harvesting and expansion; not suitable for acute-phase treatment [26] | "Off-the-shelf" availability; enables treatment in acute/subacute phase [27] [26] |
| Key Challenge | Time-consuming ex vivo expansion; variable cell quality [26] | Risk of immune rejection and GVHD [28] [26] |
| Ideal For | Research on chronic phase MI or personalized medicine approaches [26] | Research requiring standardized, readily available cells for acute MI models [26] |
Quantitative Outcomes in Myocardial Infarction
Clinical and preclinical studies have evaluated the efficacy of stem cell therapy through key cardiac function parameters. The quantitative outcomes, primarily improvements in Left Ventricular Ejection Fraction (LVEF), provide critical evidence for researchers assessing therapeutic potential.
Table 2: Quantitative Outcomes of Stem Cell Therapy in Myocardial Infarction
| Outcome Measure | Reported Improvement | Notes & Context |
|---|---|---|
| LVEF (Echocardiography) | Mean Difference (MD): 2.53% at study end; MD: 3.89% from baseline [29] | High heterogeneity observed (I² = 76%) [29] |
| LVEF (MRI) | MD: 0.83% at study end (not significant); MD: 1.37% from baseline [29] | Considered a more precise imaging modality [29] |
| LVEF (Long-Term) | 2.21% at 12 and 24 months [30] | Data from a meta-analysis of 83 studies (n=7307 patients) [30] |
| Infarct Size | MD: 1.80% at 6 months; MD: 0.70% at 12 months [30] | Measured as a percentage [30] |
| Major Adverse Cardiovascular Events (MACE) | Favorable trend at 6 months (Odds Ratio: -0.89); no significant improvement at 12, 24, or 36 months [30] | Composite endpoint including death, reinfarction, stroke [30] |
Experimental Protocols
Protocol 1: Autologous Bone Marrow-Derived Mononuclear Cell (BMMNC) Preparation and Intracoronary Delivery
This protocol is widely used in clinical trials for AMI and involves harvesting the patient's own bone marrow, processing it to isolate mononuclear cells, and delivering them via the intracoronary route [29].
Materials:
- Sterile Bone Marrow Aspiration Kit: Including needles and heparinized collection bags.
- Ficoll-Paque PREMIUM: Density gradient medium for cell separation.
- Cell Culture Media: X-VIVO 10 or equivalent serum-free media [29].
- Heparinized Saline: For cell washing and suspension [29].
- Cell Counter and Flow Cytometer: For cell quantification and viability assessment (e.g., CD34+ count) [29].
Procedure:
- Bone Marrow Harvest: Under aseptic conditions and local anesthesia, aspirate approximately 50-100 mL of bone marrow from the patient's iliac crest into a heparinized container to prevent coagulation [29].
- Cell Isolation:
- Dilute the bone marrow sample with phosphate-buffered saline (PBS).
- Carefully layer the diluted marrow over Ficoll-Paque in a centrifuge tube.
- Centrifuge at 400-500 × g for 30-40 minutes at room temperature with the brake disengaged.
- After centrifugation, aspirate the mononuclear cell layer from the plasma-Ficoll interface.
- Wash the harvested cells 2-3 times with heparinized saline or culture media by centrifugation to remove platelets and residual Ficoll [29].
- Cell Characterization & Formulation:
- Resuspend the cell pellet and perform a cell count and viability assay (e.g., Trypan Blue exclusion).
- Optional: Use flow cytometry to quantify the population of progenitor cells (e.g., CD34+). Doses in clinical trials often range from 50 to 600 million total cells, with CD34+ cell counts around 1-2 million [29].
- Formulate the final product in 10-20 mL of 0.9% normal saline or the patient's own serum for infusion [29].
- Intracoronary Delivery:
- Post-PCI, deliver the cell suspension via an intracoronary balloon catheter.
- Use the stop-flow technique: inflate the balloon to briefly obstruct blood flow and facilitate cell migration into the infarcted tissue.
- The typical infusion time is several minutes, after which the balloon is deflated to restore flow [29].
Protocol 2: Allogeneic Umbilical Cord-Derived Mesenchymal Stem Cell (UC-MSC) Preparation and Intravenous Delivery
This protocol outlines the use of an "off-the-shelf" allogeneic MSC product, which is particularly relevant for acute phase research due to its immediate availability [27] [26].
Materials:
- Cryopreserved UC-MSC Vial: Obtained from a certified cell bank, typically containing 10-100 million cells per vial.
- Water Bath: Set to 37°C for rapid thawing.
- Complete Culture Media: Dulbecco's Modified Eagle Medium (DMEM) supplemented with fetal bovine serum (FBS) or human platelet lysate.
- Infusion Solution: Plasmalyte A or 0.9% normal saline for final cell formulation [27].
Procedure:
- Cell Thawing and Activation:
- Retrieve a cryopreserved vial of UC-MSCs from liquid nitrogen storage.
- Rapidly thaw the vial by gently agitating it in a 37°C water bath until only a small ice crystal remains.
- Immediately transfer the cell suspension into a pre-filled tube containing warm complete culture media to dilute the cryoprotectant (e.g., DMSO).
- Cell Washing and Formulation:
- Centrifuge the cell suspension at 300 × g for 5-10 minutes to form a pellet.
- Carefully aspirate the supernatant to remove the cryoprotectant.
- Resuspend the cell pellet in the desired infusion solution (e.g., Plasmalyte A). Clinical studies often use doses around 2 million cells per kilogram of body weight [27].
- Perform a final cell count and viability check. Viability should exceed 70-80% for administration.
- Intravenous Infusion:
- Administer the cell suspension via a peripheral intravenous (IV) drip.
- The infusion is typically performed slowly, at a controlled rate (e.g., 1 cc per minute), and is usually completed within 2-3 hours [27].
- Monitor the subject closely during and after infusion for any adverse reactions.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Stem Cell Research in MI
| Research Reagent/Material | Function/Application | Example Use in Protocol |
|---|---|---|
| Ficoll-Paque | Density gradient medium for isolating mononuclear cells from bone marrow or blood [29] | Separation of BMMNCs from other bone marrow components during autologous cell processing [29] |
| Heparinized Saline | Prevents coagulation of blood and bone marrow aspirates during collection and processing [29] | Used as a wash and suspension solution for BMMNCs in intracoronary delivery [29] |
| X-VIVO 10 Media | Serum-free cell culture medium designed for clinical-grade cell expansion [29] | Used as the suspension media for BMMNCs in clinical trials [29] |
| CRISPR-Cas9 System | Gene-editing technology to precisely modify stem cell genomes [1] | Enhancing stem cell properties (e.g., overexpressing CXCR4 to improve myocardial homing) [1] |
| Hydrogel Scaffolds | Biomaterial matrices that provide a 3D support structure for cells [1] [26] | Improving stem cell survival and retention after transplantation into the heart [1] |
| Flow Cytometry Antibodies | Kits for cell surface marker identification (e.g., CD34, CD45, CD105) for cell population characterization [29] | Quantifying the percentage of CD34+ progenitor cells in a BMMNC preparation pre-infusion [29] |
| 1-Deoxymannojirimycin hydrochloride | 1-Deoxymannojirimycin hydrochloride, CAS:73465-43-7, MF:C6H14ClNO4, MW:199.63 g/mol | Chemical Reagent |
| 2,4-Diacetylphloroglucinol | 2,4-Diacetylphloroglucinol | High Purity | RUO | 2,4-Diacetylphloroglucinol, a key Pseudomonas metabolite. For antimicrobial & anticancer research. For Research Use Only. Not for human consumption. |
Visualizing the Workflows
The following diagrams illustrate the key experimental workflows for autologous and allogeneic stem cell preparation, highlighting the divergent paths and timeframes.
Diagram 1: Autologous Cell Therapy Workflow. This process is patient-specific and involves a significant ex vivo expansion phase, delaying treatment.
Diagram 2: Allogeneic Cell Therapy Workflow. This 'off-the-shelf' process allows for rapid administration, making it suitable for acute phase research.
The selection between autologous and allogeneic cell sourcing strategies is a critical determinant in the design of myocardial infarction research and therapy development. Autologous transplantation offers immune compatibility but is constrained by logistical delays and variable cell quality from the patient. Allogeneic approaches, particularly using UC-MSCs, provide a standardized, readily available product conducive to treating acute MI, albeit with inherent immunogenic risks that require careful management through HLA-matching [28] [26]. The quantitative data from clinical trials indicate modest but significant improvements in LVEF, affirming the biological activity of cell therapy while highlighting the need for further optimization [30] [29]. Future progress will likely hinge on combining these cellular approaches with advanced biomaterials and gene-editing technologies to enhance cell survival, retention, and reparative function, ultimately improving clinical outcomes for heart failure patients.
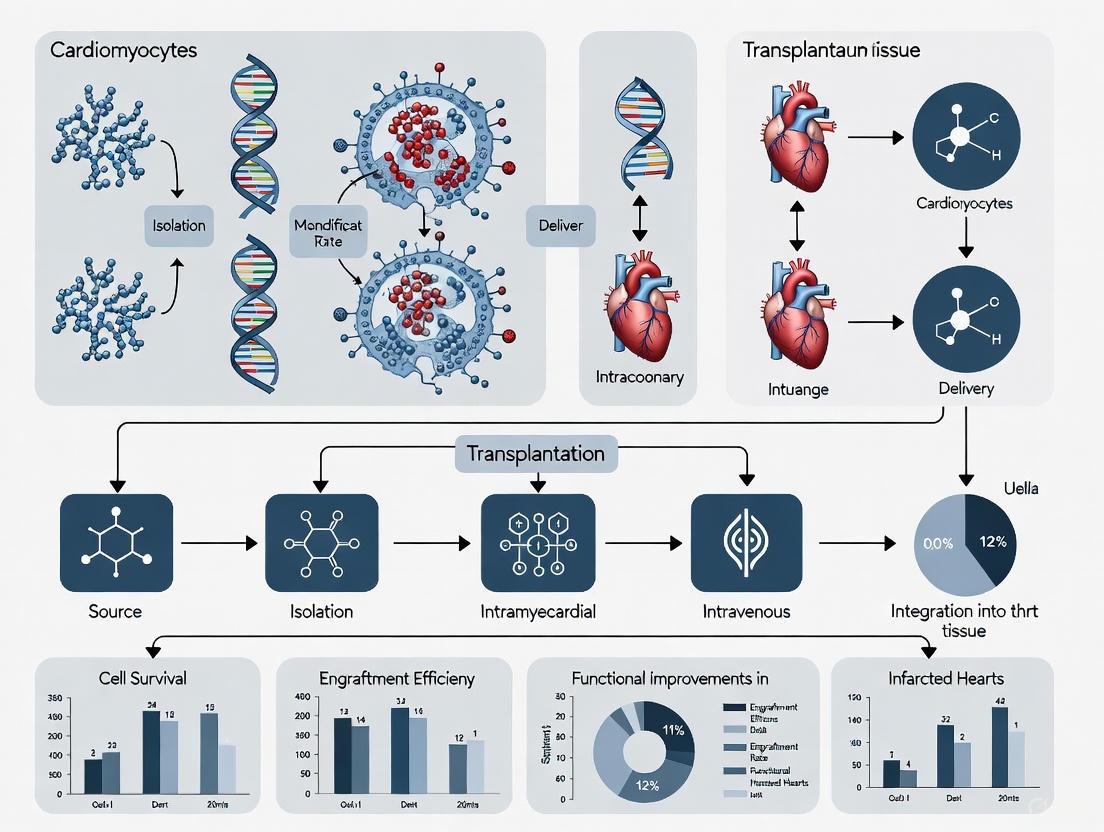
Within the paradigm of stem cell transplantation for myocardial infarction (MI) research, the route of cell delivery is a critical determinant of therapeutic efficacy. The chosen method directly influences cell retention, distribution, and functional integration within the infarcted myocardium [31]. While the therapeutic potential of various stem cells, including mesenchymal stem cells (MSCs) and induced pluripotent stem cells (iPSCs), is well-documented, their benefits are contingent upon effective targeting to the site of injury [14] [15]. This document delineates the three established delivery methods—intracoronary, intravenous, and intramyocardial injection—providing a structured comparison, detailed experimental protocols, and supporting technical data to inform preclinical and clinical research design.
Comparative Analysis of Delivery Methods
The selection of a delivery method involves balancing factors such as invasiveness, cell retention efficiency, and applicability to acute or chronic MI phases. The table below summarizes the core characteristics of each technique.
Table 1: Comparative Overview of Stem Cell Delivery Methods for Myocardial Infarction
| Feature | Intracoronary | Intravenous | Intramyocardial |
|---|---|---|---|
| Core Principle | Infusion via the coronary artery supplying the infarct zone [32] | Systemic infusion through a peripheral vein [32] | Direct injection into the infarct or border zone [33] [31] |
| Invasiveness | Moderately invasive (requires coronary access) | Minimally invasive | Highly invasive (requires percutaneous or surgical access) |
| Theoretical Cell Retention | Moderate | Low (<5% in some cases [14]) | High [31] |
| Key Advantage | Utilizes existing cardiac catheterization protocols; targets the coronary bed | Simplicity and safety of administration [32] | High local cell concentration; bypasses coronary circulation limitations |
| Primary Limitation | Risk of microvascular occlusion; requires a patent coronary artery [31] | Significant "first-pass" sequestration in lungs/spleen; low cardiac uptake | Potential for procedure-related arrhythmias or perforation; localized injury from needle [31] |
| Typical Clinical Context | Acute MI, post-PCI [34] [32] | Acute MI [32] | Chronic MI/Ischemic Heart Failure [15] [31] |
Method-Specific Application Notes & Protocols
Intracoronary Infusion
Application Notes: This method is most suitable in the acute phase of MI, following reperfusion via primary percutaneous coronary intervention (PCI) [34] [32]. It leverages the existing coronary vasculature to achieve widespread distribution of cells within the infarct territory. The success of this method depends on a patent infarct-related artery and careful control of infusion pressure and volume to minimize the risk of microvascular obstruction, a noted concern with larger cells like MSCs [31].
Detailed Experimental Protocol:
- Cell Preparation: Resuspend the stem cell product (e.g., Bone Marrow Mononuclear Cells - BMMNCs) in a sterile, isotonic solution such as heparinized saline or 0.9% normal saline supplemented with human serum albumin. A typical final volume is 10-20 mL [32].
- Catheterization: Engage the infarct-related coronary artery using a standard guiding catheter.
- Infusion: Position an infusion catheter or an over-the-wire balloon within the target coronary artery. The balloon is inflated at low pressure to occlude blood flow transiently. The cell suspension is slowly infused through the central lumen of the balloon catheter, typically over 2-5 minutes, to allow for capillary transit [32].
- Post-Infusion: After infusion, the balloon is deflated, restoring coronary flow. Monitor the electrocardiogram and the patient for signs of ischemia or arrhythmias during and after the procedure.
Intravenous Infusion
Application Notes: As the least invasive route, intravenous infusion offers a straightforward approach for systemic cell delivery. However, its major drawback is the exceedingly low retention of cells in the heart due to entrapment in the pulmonary capillary bed and other organs [14]. This makes it less efficacious for functional improvement, though it may be suitable for harnessing systemic paracrine effects [14].
Detailed Experimental Protocol:
- Cell Preparation: Prepare cells in a suitable injectable medium like 0.9% normal saline. The final volume can be adapted to standard intravenous infusion bags (e.g., 50-100 mL) [32].
- Infusion: Administer the cell suspension through a peripheral venous line. A standard intravenous infusion set with an in-line filter is used.
- Administration: The infusion is typically conducted slowly, over 30-60 minutes, with continuous monitoring of vital signs.
Intramyocardial Injection
Application Notes: This method is particularly advantageous for treating chronic, ischemic myocardial segments where the coronary vasculature may be compromised, or for delivering larger tissue-engineered constructs [15] [31]. It allows for high local cell density precisely at the site of injury or its border zone. It can be performed surgically (epicardial) or percutaneously (endocardial) using electromechanical mapping systems to guide injections [31].
Detailed Experimental Protocol (Percutaneous):
- Cell Preparation: Concentrate cells in a small volume (e.g., 2.5-5.0 mL) of isotonic buffer with human serum albumin or autologous serum [31].
- Mapping: Using the NOGA XP or a similar system, create a real-time, three-dimensional electromechanical map of the left ventricle to identify the infarct core (characterized by low voltage and poor mechanical function) and the viable border zone [31].
- Injection: Replace the mapping catheter with an injection catheter (e.g., MyoStar). Navigate the injection catheter to the target sites within the border zone. Administer multiple (e.g., 8-12) injections of approximately 0.2-0.5 mL each [31]. The procedure is often guided by a combination of electromechanical and fluoroscopic data.
- Post-Procedural Care: Monitor for complications such as pericardial effusion or ventricular arrhythmias. Echocardiography is recommended post-procedure to rule out pericardial effusion [31].
Diagram 1: Decision workflow for selecting a stem cell delivery method based on the clinical context of myocardial infarction.
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful execution of stem cell therapy experiments requires standardized reagents and specialized equipment. The following table details key materials used across the featured methodologies.
Table 2: Key Research Reagent Solutions for Stem Cell Delivery Experiments
| Item | Function/Application | Example from Literature |
|---|---|---|
| Bone Marrow Aspirate | Source for autologous stem cells (BMMNCs, MSCs) [31] | Aspirated from the iliac crest under local anesthesia [31] |
| Ficoll Density Gradient | Isolation of mononuclear cells from bone marrow or blood [31] | Used for density gradient centrifugation of bone marrow aspirate [31] |
| Culture Media (ex vivo expansion) | Expansion and maintenance of MSCs [31] | Dulbecco’s Modified Eagle’s low-glucose medium supplemented with Fetal Bovine Serum [31] |
| Trypsin-EDTA Solution | Detachment of adherent cells (e.g., MSCs) from culture flasks [33] | 0.25% trypsin-EDTA solution used to recover MSCs [33] |
| Cell Suspension Media | Final formulation for cell injection to ensure viability and isotonicity [32] [31] | Heparinized saline, 0.9% normal saline, or isotonic buffer with human serum albumin [32] [31] |
| NOGA Electromechanical Mapping System | Percutaneous, real-time 3D mapping of the left ventricle to guide intramyocardial injections [31] | Used to generate LV map and guide MyoStar injection catheter to infarct border zone [31] |
| Transforming Growth Factor-α (TGF-α) | Pretreatment agent to enhance MSC paracrine function [33] | MSCs pretreated with 250 ng/mL for 24 hours before injection [33] |
| 3,3-Dimethyl-1-butanol | 3,3-Dimethyl-1-butanol | High-Purity Reagent | High-purity 3,3-Dimethyl-1-butanol, a sterically hindered primary alcohol for chemical & materials science research. For Research Use Only. |
| 1,2,3,4,7,8-Hexachlorodibenzofuran | 1,2,3,4,7,8-Hexachlorodibenzofuran, CAS:70648-26-9, MF:C12H2Cl6O, MW:374.9 g/mol | Chemical Reagent |
Quantitative Outcomes and Efficacy Data
The long-term efficacy of stem cell therapy, often measured by Left Ventricular Ejection Fraction (LVEF) improvement and major adverse cardiac events (MACE), can be influenced by the delivery strategy. Meta-analyses of clinical trials provide the following insights.
Table 3: Long-Term Efficacy Outcomes from Meta-Analyses of Clinical Trials
| Outcome Measure | Reported Effect of Stem Cell Therapy | Notes & Context |
|---|---|---|
| Left Ventricular Ejection Fraction (LVEF) | Significant long-term improvement (Mean Difference: 2.63% [34]; MD: 2.53% at study end [32]) | Improvement observed over 12-36 months; high heterogeneity between studies [34] [35] [32] |
| Major Adverse Cardiac Events (MACE) | A trend towards reduced occurrence in intervention groups [35] | MACE is a composite of cardiovascular death, reinfarction, and stroke [35] |
| Infarct Size | Significant long-term reduction in relative infarct size, but not absolute size in most analyses [34] [35] | Effect on relative infarct size was significant only after exclusion of an outlier study [34] |
| Safety Profile | Fewer adverse events vs. controls (OR 0.66) [34]; No cardiac-related cancers reported [34] | Supports short-to-mid-term safety; longer follow-up is needed [34] |
Diagram 2: Key paracrine mechanisms of action for Mesenchymal Stem Cells (MSCs) in myocardial repair, which underpin the therapeutic effect regardless of delivery route.
Ischemic heart disease, a leading cause of global mortality, often results in myocardial infarction (MI) where infarcted tissue is replaced by non-functional scar tissue, leading to cardiac dysfunction and heart failure [36] [37]. Conventional treatments alleviate symptoms but cannot restore lost cardiac tissue, creating an urgent need for innovative regenerative strategies [37] [38]. Stem cell transplantation has emerged as a promising therapeutic avenue, yet challenges with cell retention, survival, and functional integration have limited its clinical translation [36] [38]. This document details three advanced engineering strategies—cell sheets, hydrogels, and 3D-bioprinted patches—developed to overcome these limitations within the broader context of stem cell transplantation for myocardial repair. These scaffold-based and scaffold-free platforms provide structural support, enhance cell viability, and promote functional tissue regeneration, offering new hope for treating MI [39] [36] [40].
Cell Sheet Technology
Cell sheet technology represents a scaffold-free approach for myocardial regeneration using temperature-responsive culture surfaces. This platform preserves critical cell-cell connections and endogenous extracellular matrix (ECM), overcoming limitations of enzymatic digestion that damage these essential structures [38]. The technology enables the creation of intact, connective tissue layers that can be transplanted directly onto the epicardial surface of damaged hearts.
- Key Advantages: Avoids scaffold-related inflammation and foreign body reactions; preserves native ECM and cell junctions; enables creation of layered, thickened tissues through multiple sheet stacking [38].
- Therapeutic Mechanisms: Attenuates cardiac remodeling; improves systolic function and vascularization; reduces fibrosis through paracrine signaling and direct mechanical support [38].
- Clinical Relevance: Has demonstrated safety and efficacy in improving ejection fraction and clinical outcomes in heart failure patients; can be combined with omentopexy to enhance vascularization and graft survival [38].
Experimental Protocol: Fabrication and Transplantation of Stem Cell-Derived Cell Sheets
Objective: To generate and implant a functional stem cell-derived cell sheet for cardiac tissue repair in a murine MI model.
Materials Required:
- Temperature-responsive culture dishes (e.g., grafted with poly-N-isopropylacrylamide)
- Selected stem cells (e.g., skeletal myoblasts, mesenchymal stem cells, or iPSC-derived cardiomyocytes)
- Appropriate cell culture media and supplements
- Animal model (e.g., rat or murine MI model)
- Surgical instruments for thoracotomy
Methodology:
- Cell Culture: Seed stem cells onto temperature-responsive culture dishes and culture at 37°C until reaching confluence [38].
- Sheet Harvesting: Lower the culture temperature to below 32°C for approximately 1 hour. This causes the grafted polymer to hydrate and expand, prompting the intact cell sheet to detach from the surface [38].
- MI Model Creation: Anesthetize the animal and perform left thoracotomy. Ligate the left anterior descending coronary artery to induce MI [38].
- Sheet Transplantation: Immediately or within a defined post-MI window, place the harvested cell sheet directly onto the epicardial surface of the infarcted area [38].
- Assessment: Monitor cardiac function via echocardiography at regular intervals post-operation (e.g., 2, 4, and 8 weeks). Perform histological analysis to assess graft integration, vascularization, and fibrosis [38].
Variations and Optimization:
- Cell Source Selection: The choice of cell source (see Table 1) influences therapeutic outcomes. Skeletal myoblasts offer autologous transplantation advantages, while iPSC-derived sheets show superior potential for forming vascularized, thickened human cardiac tissue [38].
- Combination Therapy: For enhanced vascularization, combine cell sheet transplantation with omentopexy. This technique leverages the omentum's natural revascularization and anti-inflammatory properties, upregulating key angiogenic factors like VEGF-A, Akt-1, and Ang-1 [38].
Table 1: Comparison of primary cell sources used in cell sheet engineering for myocardial infarction research.
| Cell Source | Key Advantages | Limitations | Key Therapeutic Outcomes |
|---|---|---|---|
| Skeletal Myoblasts (SMs) | Autologous source; resistant to ischemia; high proliferative potential [38]. | Potential for arrhythmia; non-myocyte lineage [38]. | Improved systolic function; reduced fibrosis; enhanced neovascularization [38]. |
| Mesenchymal Stem Cells (MSCs) | Extensive clinical safety data; multi-potent differentiation; strong paracrine activity [38]. | Ethical issues with allogeneic use; moderate regenerative capacity [38]. | Angiogenesis; immunomodulation; improved cardiac function [38]. |
| iPSC-Derived Cardiomyocytes | Avoids ethical issues; unlimited source; can form vascularized, functional myocardium [38]. | Requires optimization for large-scale production; risk of teratoma formation [38]. | Long-term therapeutic effect; formation of vascularized human cardiac tissue [38]. |
Hydrogel-Based Delivery Systems
Hydrogels are three-dimensional, swollen polymer networks that share high water content and flexibility similar to natural tissues, making them ideal biomaterials for cardiac regenerative medicine [36]. They serve as injectable carriers or epicardial patches for delivering cells, drugs, genetic materials, and growth factors directly to the infarcted heart, addressing issues of low retention and short half-lives associated with standalone therapies [36].
- Key Features: Biocompatibility; tunable biodegradability; injectability; excellent water absorptivity [36].
- Therapeutic Mechanisms: Provides a temporary ECM-mimetic scaffold for cell migration and proliferation; sustains the release of therapeutic agents; provides mechanical support to the infarcted wall to prevent adverse remodeling [36].
- Clinical Relevance: Injectable hydrogels can be delivered via minimally invasive intracoronary or intramyocardial routes; natural hydrogels like alginate and collagen have shown promise in improving cardiac function and reducing fibrosis in animal models [36].
Experimental Protocol: Intramyocardial Injection of a Therapeutic Hydrogel
Objective: To assess the efficacy of a natural hydrogel (e.g., collagen) in improving cardiac function and reducing fibrosis in a murine MI model.
Materials Required:
- Natural hydrogel (e.g., Collagen Type I)
- Therapeutic agent (e.g., stem cells, growth factors)
- Insulin syringes (29-30 gauge)
- Animal model (e.g., murine MI model)
- Echocardiography system
- Histology equipment
Methodology:
- MI Model Creation: As previously described in Section 2.2.
- Hydrogel Preparation: Prepare the collagen hydrogel according to manufacturer specifications. If combining with cells, gently mix them into the hydrogel precursor solution at the desired density. Maintain the solution on ice to prevent premature gelling [36].
- Hydrogel Injection: Post-MI, use an insulin syringe to perform multiple intramyocardial injections (e.g., 3-4 injections of 10-15 μL each) into the border zone of the infarcted area [36].
- In Vivo Gelation: The collagen hydrogel solidifies in situ at body temperature and physiological pH, forming a stable scaffold [36].
- Functional Assessment: Conduct echocardiography at 2, 4, and 8 weeks post-injection to measure left ventricular ejection fraction (LVEF), end-systolic volume (ESV), and end-diastolic volume (EDV) [36].
- Histological Analysis: Harvest hearts at study endpoint. Use Masson's Trichrome staining to quantify fibrosis area and immunohistochemistry (e.g., CD31 staining) to assess neovascularization [36].
Variations and Optimization:
- Hydrogel Type: Both natural (alginate, fibrin) and synthetic hydrogels can be used. Alginate is injectable and crosslinks with divalent cations, while fibrin, derived from fibrinogen, is a natural biopolymer that supports cell adhesion [36].
- Delivery Route: Hydrogels can also be applied as an epicardial patch during open-chest surgery or via intracoronary injection for a less invasive approach [36].
Classification and Properties of Hydrogels for Cardiac Repair
Table 2: Characteristics of common hydrogels used in cardiac regeneration strategies.
| Hydrogel Type | Origin | Key Properties | Cross-linking Method | Delivery Route |
|---|---|---|---|---|
| Alginate | Natural (Seaweed) | Biocompatible; similar to ECM; low thrombogenicity [36]. | Divalent cations (e.g., Ca²âº) [36]. | Intramyocardial/Intracoronary injection; Epicardial patch [36]. |
| Collagen | Natural (Mammals) | Excellent biocompatibility; low immunogenicity; major component of cardiac ECM [36]. | Chemical cross-linkers; pH/ temperature-induced assembly [36]. | Injectable; Epicardial patch [36]. |
| Fibrin | Natural (Blood) | Biopolymer; supports cell adhesion and proliferation [36]. | Thrombin-mediated fibrinogen conversion [40]. | Injectable; Incorporated in bioinks for 3D bioprinting [40]. |
| PEG | Synthetic | Tunable mechanical properties; high stability; functionalizable [36]. | Photo-polymerization; chemical cross-linking [36]. | Injectable; Epicardial patch [36]. |
3D-Bioprinted Cardiac Patches
3D bioprinting is an additive manufacturing technology that precisely deposits cells and biomaterials (bioinks) into predefined 3D architectures, offering unprecedented control over the recapitulation of native myocardial tissue microarchitecture [39] [37]. This strategy programs cellular alignment, tissue stiffness, vascular pathways, and electrical coupling, facilitating the creation of mature, functional engineered heart tissues (EHTs) [39].
- Key Advantages: Overcomes limitations of conventional 3D casting such as heterogeneous cellularization and slow electromechanical maturation; enables creation of patient-specific constructs; allows for integration of nanoengineered components (e.g., conductive particles) [39] [37].
- Therapeutic Mechanisms: Provides mechanical support to the infarcted area; promotes electromechanical integration with host tissue; enhances vascularization through pre-formed microchannels; enables sustained release of bioactive factors from nano-composites [39] [40].
- Clinical Relevance: Recent breakthroughs have demonstrated the generation of bioprinted myocardial patches that survive, beat correctly, and integrate with the host circulatory system for at least one month in animal models, marking a significant step toward clinical application [40].
Experimental Protocol: Bioprinting and Implantation of a Multi-Layered Cardiac Patch
Objective: To fabricate a vascularized, multi-layered cardiac patch via 3D bioprinting and evaluate its long-term survival and function in an animal MI model.
Materials Required:
- Extrusion-based 3D bioprinter
- Bioink components: Gelatin, Fibrinogen, Hyaluronic acid, microbial Transglutaminase (mTG) [40]
- Cells: Cardiomyocytes derived from induced pluripotent stem cells (iPSC-CMs); vascular microfragments from host adipose tissue [40]
- Animal MI model
- In vivo imaging system (e.g., ultrasound, electrophysiology)
Methodology:
- Bioink Preparation:
- Patch Bioprinting: Using the bioprinter, deposit the bioinks in a pre-defined, multi-layered structure. A proven configuration involves stacking three layers of muscle bioink between two layers of vascular bioink [40]. The mTG enzyme facilitates strong bonding between the layers.
- Maturation: Culture the printed patch in vitro for a brief period to allow for tissue maturation.
- Surgical Implantation: Induce MI in the animal model and suture the bioprinted patch directly onto the epicardial surface of the infarcted area [40].
- Functional Assessment:
- Monitor patch survival and contractile function for at least one month using in vivo microscopy and electrophysiological recording [40].
- At endpoint, perform histology to confirm integration with the host circulatory system (evidenced by perfused blood vessels within the patch) and assess structural organization [40].
Research Reagent Solutions for 3D Bioprinting
Table 3: Essential materials and their functions in 3D-bioprinting of cardiac patches.
| Research Reagent | Function/Application in Cardiac Bioprinting |
|---|---|
| Gelatin | Provides the primary consistency and plasticity for printability [40]. |
| Fibrinogen | Upon cross-linking, forms fibrin, which provides structural integrity and supports cell adhesion and remodeling, mimicking a key part of the natural ECM [40]. |
| Hyaluronic Acid | Another ECM-mimetic component that provides flexibility, hydration, and cell attachment sites [40]. |
| microbial Transglutaminase (mTG) | A critical enzyme that acts as a cross-linker, creating strong bonds between the different layers of bioink to ensure patch stability after implantation [40]. |
| iPSC-Derived Cardiomyocytes | The primary functional cell type responsible for generating contractile force in the engineered tissue [40]. |
| Vascular Microfragments | Micro-vessels derived from host tissue that serve as building blocks for creating a pervasive vascular network within the patch, enabling rapid perfusion and long-term survival in vivo [40]. |
| Conductive Nanoparticles | Nano-engineered materials (e.g., gold nanowires, graphene oxide) that can be incorporated into bioinks to enhance electrical conductivity between cells, improving synchronous tissue contraction [37]. |
Comparative Workflow and Strategic Integration
The following diagram synthesizes the information from the previous sections, illustrating the distinct workflows for creating each engineered construct and their shared therapeutic goal of myocardial repair.
Stem cell transplantation represents a promising therapeutic strategy for myocardial infarction (MI), aiming to regenerate damaged cardiac tissue and restore heart function. Within this emerging field, optimizing administration protocols is equally crucial as selecting appropriate cell types. The temporal window for intervention and the quantity of delivered cells significantly influence therapeutic outcomes, as demonstrated by numerous clinical trials. Research indicates that the post-infarction myocardial environment undergoes dynamic changes that can either support or inhibit engrafted cell survival and functionality [41]. Furthermore, the therapeutic dosage must balance sufficient cell numbers to exert meaningful effects against practical constraints of safety and feasibility. This application note synthesizes evidence from key clinical trials to provide researchers and drug development professionals with evidence-based protocols for timing and dosage considerations in stem cell transplantation for MI research, framed within the broader context of refining transplantation techniques.
Quantitative Evidence: Clinical Trial Findings on Timing and Dosage
Table 1: Summary of Clinical Trial Evidence on Cell Therapy Timing and Dosage
| Trial/Study | Cell Type | Optimal Timing | Optimal Dose | Primary Outcome | Key Findings |
|---|---|---|---|---|---|
| TIME [41] | Bone Marrow Mononuclear Cells (BMC) | Day 3 vs Day 7 post-PCI | 150 million cells | LVEF change at 6 months | No significant improvement in LVEF at 2-year follow-up regardless of timing |
| Meta-analysis of MSC Trials [42] | Mesenchymal Stromal Cells (MSC) | Within 1 week post-PCI | <10â· cells | LVEF improvement | LVEF increased by 3.22% with early transplantation; significant improvement (3.32%) with <10â· MSCs within 1 week |
| Prevent-TAHA8 [43] | Wharton's Jelly MSCs | 3-7 days post-AMI | 10â· cells | HF incidence reduction | Phase III trial protocol for HF prevention after AMI (results expected 2024) |
| BAMI [43] | Bone Marrow Mononuclear Cells | 2-8 days post-PPCI | Not specified | All-cause mortality | Lower HF hospitalization (2.7% vs 8.1%) with cell therapy vs. control |
Table 2: Differential Effects Based on Transplantation Parameters
| Parameter | Subgroup | LVEF Improvement | Evidence Level |
|---|---|---|---|
| Timing | Within 1 week | +3.22% (95% CI: 1.31 to 5.14) [42] | Meta-analysis of RCTs |
| After 1 week | -0.35% (95% CI: -10.22 to 9.52) [42] | Meta-analysis of RCTs | |
| Dose | <10â· MSCs | +2.25% (95% CI: 0.56 to 3.93) [42] | Meta-analysis of RCTs |
| >10â· MSCs | No significant improvement [42] | Meta-analysis of RCTs | |
| Combination | <10â· MSCs within 1 week | +3.32% (95% CI: 1.14 to 5.50) [42] | Meta-analysis of RCTs |
Experimental Protocols and Methodologies
Standardized Protocol for Intracoronary Cell Delivery in AMI
The following methodology outlines the procedure for intracoronary stem cell delivery in acute myocardial infarction patients, synthesized from multiple clinical trial protocols [41] [43]:
Patient Selection Criteria:
- Adults aged 18-65 years with acute ST-elevation MI (STEMI)
- Successful primary percutaneous coronary intervention (PCI) with stenting within 12 hours of symptom onset
- Left ventricular ejection fraction (LVEF) ≤40-45% by echocardiography post-PCI
- Absence of cardiogenic shock, severe arrhythmias, or comorbidities limiting life expectancy
Cell Preparation Protocol:
- Source: Bone marrow aspiration (100-120 mL) from iliac crest or umbilical cord-derived Wharton's jelly
- Processing: Density gradient centrifugation for BMC isolation; explant culture method for MSCs
- Quality Control: Cell viability >95% by trypan blue exclusion; flow cytometry for CD34+ (BMC) or CD73+, CD90+, CD105+ (MSC); endotoxin testing
- Formulation: Suspension in saline with 1-5% human serum albumin at recommended concentration
Administration Procedure:
- Timing: 3-7 days post-PCI to leverage inflammatory resolution phase
- Route: Intracoronary infusion via balloon catheter
- Technique: Low-pressure balloon inflation with 3-4 intermittent infusions lasting 2-3 minutes each
- Monitoring: Continuous ECG and hemodynamic monitoring during procedure
Endpoint Assessment:
- Primary: Change in LVEF by cardiac MRI at 6 months
- Secondary: Left ventricular volumes, infarct size, major adverse cardiac events
- Clinical: Heart failure hospitalization, mortality
Workflow for Determining Optimal Timing and Dosage
The following diagram illustrates the decision pathway for establishing timing and dosage parameters in stem cell therapy clinical trials:
Key Signaling Pathways and Biological Mechanisms
Temporal Dynamics of Post-Infarction Myocardial Environment
The therapeutic efficacy of stem cell transplantation is heavily influenced by the dynamically changing myocardial environment following infarction. The following diagram illustrates key signaling pathways and biological processes that define optimal windows for intervention:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Cardiac Cell Therapy Studies
| Category | Specific Reagents/Materials | Research Application | Protocol Considerations |
|---|---|---|---|
| Cell Isolation | Ficoll-Paque density gradient medium; Collagenase/dispase digestion enzymes; CD34+/CD133+ magnetic beads | Isolation of mononuclear cells from bone marrow or Wharton's jelly | Maintain sterile conditions; process within 8-9 hours of collection [41] |
| Cell Characterization | Flow cytometry antibodies (CD34, CD45, CD73, CD90, CD105); Tri-lineage differentiation kits; Colony-forming unit assays | Quality control and potency assessment | Follow ISCT criteria for MSCs; viability >95% required for transplantation [42] |
| In Vivo Modeling | Permanent LAD ligation surgery supplies; Ischemia-reperfusion equipment; High-field MRI systems (≥1.5T) | Preclinical efficacy testing in animal models | Standardize infarct size; use cardiac MRI for accurate functional assessment [41] |
| Molecular Analysis | qPCR kits for cardiac markers (GATA4, Nkx2.5, MEF2C); ELISA for inflammatory cytokines; Histology reagents (Masson's trichrome, H&E) | Mechanism of action studies | Analyze paracrine factors; assess engraftment and differentiation [3] |
| 3,5-Dimethoxybenzoic Acid | 3,5-Dimethoxybenzoic Acid, CAS:1132-21-4, MF:C9H10O4, MW:182.17 g/mol | Chemical Reagent | Bench Chemicals |
| Octamethylcyclotetrasiloxane | Octamethylcyclotetrasiloxane | High-Purity D4 Silicone | Octamethylcyclotetrasiloxane (D4), a high-purity volatile silicone fluid for materials science & research. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
The optimization of timing and dosage parameters represents a critical step toward realizing the clinical potential of stem cell therapy for myocardial infarction. Current evidence suggests that early intervention (within 3-7 days post-MI) with moderate cell doses (approximately 10â· cells) provides the most favorable risk-benefit profile for most cell types. The emerging understanding of the post-infarction molecular landscape explains why this temporal window coincides with the transition from inflammatory to proliferative phases, creating a microenvironment more conducive to cell survival and paracrine signaling.
Future research directions should focus on personalized protocols based on patient-specific factors such as infarct characteristics, microvascular obstruction status [41], and age-related regenerative capacity. Furthermore, the growing interest in extracellular vesicles as cell-free therapeutics may redefine optimal timing and "dosing" parameters [3]. As the field progresses, standardized protocols incorporating these evidence-based timing and dosage considerations will enhance both preclinical research and clinical translation in cardiac regenerative medicine.
Overcoming Translational Hurdles: Strategies for Enhanced Efficacy
Addressing Low Cell Survival and Engraftment in the Ischemic Milieu
The therapeutic potential of stem cell transplantation for cardiac repair following myocardial infarction (MI) is significantly hampered by the harsh ischemic microenvironment of the infarcted heart. Poor cell survival and engraftment drastically limit the efficacy and translational potential of this regenerative approach [44]. This application note provides a detailed analysis of the central challenges and evidence-based protocols designed to overcome them, framed within the context of advancing myocardial infarction research.
Quantitative studies reveal a rapid and dramatic loss of transplanted cells. After intracoronary infusion, only about 5% of bone marrow-derived mononuclear cells are detected in the myocardium within 2 hours, dropping to a mere 1% by 18 hours post-transplantation [44]. Similarly, cells delivered via intramyocardial injection show a decline from 34–80% initially to just 0.3–3.5% at 6 weeks [44]. This massive cell death is primarily driven by a combination of factors present in the ischemic milieu, including serum deprivation, hypoxia, inflammatory cytokines, and mechanical stress [44] [45].
Quantitative Assessment of the Challenge
The table below summarizes key quantitative evidence on the scale of cell loss and its impact on therapeutic efficacy.
Table 1: Documented Cell Survival Rates and Functional Outcomes Post-Transplantation
| Cell Type | Delivery Route | Timeline | Survival/Retention Rate | Functional Outcome | Source |
|---|---|---|---|---|---|
| Bone Marrow Mononuclear Cells | Intracoronary | 2 hours | ~5% | Moderate improvement in LVEF (∼3%) | [44] |
| Bone Marrow Mononuclear Cells | Intracoronary | 18 hours | ~1% | Meta-analysis showed limited functional benefit | [44] |
| Various (e.g., MSCs) | Intramyocardial | Time of injection | 34-80% | Efficacy limited by massive early cell death | [44] |
| Various (e.g., MSCs) | Intramyocardial | 6 weeks | 0.3-3.5% | Long-term engraftment is exceptionally low | [44] |
| MSCs | Intravenous (to Kidney) | 1 hour | <1% | Challenge is universal across organs and diseases | [46] |
| Cardiomyocytes | Intramyocardial | 1-4 days | ~68% (32% apoptotic) | High apoptosis even for muscle cells | [46] |
Strategic Solutions to Enhance Survival and Engraftment
A multifaceted strategy is required to combat the multifactorial problem of poor cell survival. The following section outlines proven experimental approaches.
Cell Preconditioning
Preconditioning involves exposing cells to sublethal stress in vitro to enhance their resilience upon transplantation in vivo.
- Hypoxic Preconditioning: Culturing cells in low oxygen conditions (e.g., 0.5-2% O₂ for 12-24 hours) before transplantation can upregulate pro-survival genes (e.g., HIF-1α, Akt) and enhance resistance to subsequent ischemic stress [45].
- Heat Shock Preconditioning: Brief exposure to elevated temperature (e.g., 42°C for 30-60 minutes) induces the expression of heat shock proteins (HSP27, HSP70, HSP90), which act as molecular chaperones to inhibit apoptosis [45].
- Pharmacological Preconditioning: Incubating cells with specific small molecules or cytokines prior to transplantation.
- Lysophosphatidic acid (LPA): An endogenous lipid mediator that can prevent apoptotic death and has been shown to increase cell survival two-fold within one week after injection [44].
- Growth Factors: Exposure to IGF-1, TGF-β, or bFGF can activate pro-survival signaling pathways like the PI3K/Akt pathway [45].
Genetic Modification of Donor Cells
Engineering cells to overexpress specific genes can directly combat the hostile microenvironment.
- Pro-Survival Genes: Overexpression of Akt (Protein Kinase B) profoundly inhibits mitochondrial-dependent apoptosis and has been shown to reduce caspase-3 activation in transplanted cells [45]. Similarly, overexpression of Bcl-2 can enhance graft survival.
- Angiogenic Factors: Modifying cells to express VEGF (Vascular Endothelial Growth Factor) or Angiopoietin-1 promotes local angiogenesis, improving nutrient and oxygen supply to the graft [46].
- MicroRNA Regulation: Modulating specific microRNAs, such as miR-210—a key miRNA involved in the cellular response to hypoxia—can promote transplanted cell survival in an acute MI model [44].
Bioengineering and Delivery Strategies
Optimizing how and where cells are delivered is crucial for retention and integration.
- Biomaterial Scaffolds: Using injectable fibrin or other hydrogel-based scaffolds creates a protective, three-dimensional microenvironment for the cells. This shields them from mechanical stress and washout, and can be tailored to provide sustained release of trophic factors [44] [45].
- Cell Microencapsulation: Encapsulating individual cells or clusters in microcapsules (150-250 μm) made of alginate or other biocompatible materials physically prevents their dispersion from the injection site and can improve retention [44].
- Optimized Cell Isolation Protocols: The protocol for isolating cells significantly impacts their subsequent function. For instance, storing bone marrow mononuclear cells in saline and plasma (ASTAMI protocol) was found to drastically reduce cell migration capacity and blunted blood-flow recovery in a hindlimb ischemia model by nearly 50% compared to storage in a defined medium with serum (REPAIR-AMI protocol) [47].
- Host Tissue Preconditioning: Preparing the host myocardium to better receive the graft can be as important as preparing the cells themselves. Low-level laser irradiation (LLLI) applied to the infarcted myocardium before cell delivery has been shown to augment the expression of local growth factors and antioxidant enzymes like superoxide dismutase, markedly enhancing early survival of transplanted MSCs [44].
The logical workflow for implementing these strategies and their primary molecular targets is summarized in the diagram below.
Detailed Experimental Protocol: Combining Preconditioning and Scaffold Delivery
This protocol provides a step-by-step methodology for testing a combined strategy to enhance MSC survival in a rodent model of myocardial infarction.
Objective: To assess the synergistic effect of hypoxic preconditioning and delivery within a fibrin scaffold on the survival and engraftment of Mesenchymal Stem Cells (MSCs) in a rat model of myocardial infarction.
Materials:
- Primary MSCs (e.g., rat or human bone marrow-derived).
- Cell culture reagents: Dulbecco's Modified Eagle Medium (DMEM), Fetal Bovine Serum (FBS), Penicillin-Streptomycin, Trypsin-EDTA.
- Preconditioning chamber or modular incubator for hypoxic culture (1% Oâ‚‚, 5% COâ‚‚, balance Nâ‚‚).
- Fibrin scaffold components: Fibrinogen (e.g., 10 mg/mL), Thrombin (e.g., 5 U/mL), Aprotinin (to slow degradation).
- Animal model: Adult Sprague-Dawley rats with surgically induced MI (e.g., LAD ligation).
- Cell tracking agent: e.g., DiI fluorescent dye or Lentivirus expressing GFP/Luciferase.
Procedure:
Cell Culture and Expansion:
- Culture MSCs in standard growth medium (DMEM + 10% FBS + 1% P/S) at 37°C in a normoxic incubator (21% O₂, 5% CO₂) until 80% confluent.
- Use cells at passage 3-5 for all experiments to maintain potency.
Hypoxic Preconditioning:
- Once cells are 80% confluent, replace the medium with fresh growth medium.
- Place the culture flasks/plates into the hypoxic chamber set to 1% O₂, 5% CO₂, at 37°C for 24 hours.
- Control cells should be maintained in the normoxic incubator for the same duration.
Cell-Scaffold Preparation:
- After preconditioning, trypsinize, count, and resuspend the MSCs at a high density (e.g., 5 x 10ⶠcells/50 µL).
- Prepare the fibrinogen solution (containing the cells) and thrombin solution on ice.
- Mix the cell-fibrinogen suspension with the thrombin solution at a 1:1 ratio immediately before injection. The final concentration should yield a polymerizable fibrin gel containing the cells.
In Vivo Delivery:
- Two weeks post-MI induction, re-anesthetize the rats and perform a re-thoracotomy to expose the heart.
- Using a Hamilton syringe with a 30-gauge needle, inject a total of 50 µL of the cell-scaffold construct at 3-4 sites in the border zone of the infarct.
- Control groups should include: 1) Non-preconditioned cells in scaffold, 2) Preconditioned cells in saline, and 3) Scaffold only.
Assessment and Analysis:
- In Vivo Cell Tracking: Use bioluminescent imaging (BLI) weekly for 4-6 weeks to monitor cell survival quantitatively if luciferase-expressing cells are used.
- Histological Analysis: At the study endpoint (e.g., 4 weeks post-transplantation), harvest hearts.
- Perform cryosectioning and stain for TUNEL to assess apoptosis within the graft.
- Immunostain for cardiac markers (e.g., α-actinin, cTnT) and human-specific markers (if using human MSCs) to assess engraftment and integration.
- Stain for CD31 to assess neovascularization in and around the graft.
- Functional Assessment: Perform echocardiography pre-transplantation and at the endpoint to measure changes in left ventricular ejection fraction (LVEF), end-systolic volume, and end-diastolic volume.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Investigating Cell Survival and Engraftment
| Reagent / Material | Primary Function | Example Application in Protocol |
|---|---|---|
| Hypoxic Chamber | Creates a controlled low-oxygen environment for cell preconditioning. | Essential for implementing the hypoxic preconditioning protocol (Step 2). |
| Lysophosphatidic Acid (LPA) | Small molecule lipid mediator that activates anti-apoptotic pathways. | Used in pharmacological preconditioning of cells prior to transplantation [44]. |
| Fibrinogen / Thrombin Kit | Components for forming an injectable, biocompatible fibrin hydrogel scaffold. | Used to create the protective 3D scaffold for cell delivery (Step 3) [45]. |
| Aprotinin | Serine protease inhibitor that slows the degradation of fibrin scaffolds. | Added to the fibrinogen solution to extend the scaffold's persistence in vivo. |
| Lentivirus (e.g., GFP-Luciferase) | Genetic tool for stable labeling of cells to enable tracking and quantification. | Used to transduce cells for bioluminescent imaging (BLI) to track survival (Assessment). |
| Bioluminescent Imager (IVIS) | Non-invasive optical imaging system for quantitative tracking of luciferase-expressing cells. | Critical for longitudinal monitoring of cell survival in the same animal over time (Assessment). |
| TUNEL Assay Kit | Fluorescence-based method to detect DNA fragmentation in apoptotic cells. | Used on tissue sections to quantify levels of apoptosis within the cell graft (Assessment). |
| Anti-CD31 Antibody | Immunohistochemical marker for identifying vascular endothelial cells. | Used to stain tissue sections to quantify angiogenesis promoted by the graft (Assessment). |
Addressing the critical barrier of low cell survival is paramount for realizing the clinical promise of stem cell therapy for myocardial infarction. As outlined in this note, a multimodal strategy that combines cell preconditioning, genetic engineering, and advanced bioengineering delivery systems offers the most robust solution. The provided data, strategic framework, and detailed protocol serve as a foundation for researchers to design and optimize more effective and reliable experiments, ultimately accelerating the translation of cardiac regenerative therapies from the bench to the bedside.
Myocardial infarction (MI) triggers a complex pathological cascade resulting in cardiomyocyte death, fibrotic scar formation, and adverse cardiac remodeling, which can ultimately lead to heart failure [1] [48] [3]. Despite advances in medical and interventional therapies, none address the fundamental issue of replenishing lost cardiomyocytes, making heart transplantation the only definitive cure for end-stage heart failure [3]. Stem cell transplantation has emerged as a promising strategy for cardiac regeneration, with mesenchymal stem cells (MSCs) being extensively investigated due to their multipotent differentiation capacity, paracrine activity, and immunomodulatory properties [1] [49].
However, cell-based therapies face significant challenges, including poor cell survival post-transplantation, low engraftment rates, and limited functional integration within the hostile ischemic myocardial microenvironment [1] [50] [3]. To overcome these limitations, combinatorial approaches utilizing stem cells with exosomes and growth factors have gained considerable attention. These strategies leverage the synergistic effects of cellular therapy with the potent paracrine signaling of exosomes and targeted activity of growth factors to enhance therapeutic outcomes in myocardial infarction research [50].
Table 1: Challenges of Stem Cell Therapy and Combinatorial Solutions
| Challenge | Impact on Therapy | Combinatorial Approach |
|---|---|---|
| Low cell survival post-transplantation | <5% of MSCs survive 72 hours after coronary delivery [1] | Preconditioning with exosomes to improve microenvironment [50] |
| Poor engraftment and retention | Limited functional improvement in clinical trials [3] | Sequential delivery with SDF-1 enhancing exosomes [50] |
| Harsh ischemic microenvironment | High oxidative stress and inflammation [50] | Combination with antioxidant and anti-inflammatory exosomes [51] [3] |
| Inadequate cardiomyocyte replenishment | Adult human cardiomyocyte turnover <1% per year [3] | Supplementation with cardioprotective exosomal miRNAs [1] |
Scientific Rationale and Mechanisms of Action
Stem Cell Types and Characteristics for Cardiac Applications
Multiple stem cell types have been investigated for cardiac repair, each with distinct advantages and limitations. Mesenchymal stem cells (MSCs) remain the most widely utilized due to their availability from various tissues (bone marrow, adipose tissue, umbilical cord), strong paracrine functions, and immunomodulatory properties [1] [49]. MSCs primarily exert therapeutic effects through paracrine signaling rather than direct differentiation, secreting vesicles and factors that modulate the immune response, reduce fibrosis, and promote angiogenesis [49]. Induced pluripotent stem cells (iPSCs) offer the advantage of patient-specific autologous therapy and can differentiate into functional cardiomyocytes, though concerns regarding teratoma formation and immature phenotype of derived cardiomyocytes remain [1] [48].
Exosome Biogenesis and Function
Exosomes are nano-sized extracellular vesicles (30-150 nm in diameter) delimited by a lipid bilayer and unable to replicate, serving as critical information transporters between tissues [51] [52]. Their biogenesis follows an endosomal pathway: initial invagination of the cell membrane forms early endosomes, which mature into late endosomes and subsequently generate intraluminal vesicles within multivesicular bodies (MVBs). These MVBs fuse with the plasma membrane, releasing exosomes into the extracellular space [53] [52] [54].
Exosomes contain diverse cargo including proteins, lipids, mRNA, miRNA, and other bioactive molecules that reflect their cellular origin and mediate intercellular communication [52]. Upon release, exosomes interact with recipient cells through three primary mechanisms: (1) complete endocytosis by the recipient cell; (2) direct membrane fusion; or (3) receptor-ligand interaction with surface molecules on recipient cells [53] [54]. Stem cell-derived exosomes (SC-Exos) have demonstrated comparable therapeutic benefits to their parent cells, including anti-inflammatory, anti-apoptotic, and pro-angiogenic effects, while offering advantages of lower immunogenicity and no risk of tumorigenesis [52].
Key Signaling Pathways in Cardiac Repair
The therapeutic effects of combinatorial approaches are mediated through multiple molecular pathways. MSC-derived exosomes carry microRNAs such as miR-21 and miR-210, which regulate cardiomyocyte apoptosis and fibrosis [1]. The stromal cell-derived factor-1 (SDF-1) and its receptor CXC chemokine receptor 4 (CXCR4) axis plays a vital role in stem cell recruitment to ischemic myocardium [50]. Additionally, exosomes from hypoxia-preconditioned MSCs show increased HIF-1α content, enhancing pro-angiogenic effects in spinal cord injury through VEGF overexpression—a mechanism likely applicable to cardiac repair [53].
Application Notes: Protocol for Sequential Exosome and MSC Delivery in MI
Experimental Workflow for Combinatorial Therapy
This protocol outlines a sequential delivery approach of MSC-derived exosomes followed by MSC transplantation in a rat model of acute myocardial infarction, demonstrating enhanced cardiac function through improved cell recruitment and survival [50].
Materials and Reagents
Table 2: Research Reagent Solutions for Combinatorial Therapy
| Reagent/Category | Specification/Function | Experimental Notes |
|---|---|---|
| Mesenchymal Stem Cells | Bone marrow-derived MSCs (passage 3-4); Positive for CD73, CD90, CD105; Negative for CD14, CD34, CD45 [50] [49] | Pretreat with 1μM atorvastatin for 12h to enhance CXCR4 expression and homing [50] |
| Exosome Isolation | Differential centrifugation: 300g (10min), 2,000g (20min), 13,500g (30min), 120,000g (70min) [50] | Use exosome-free FBS; Confirm by TEM, NTA, and Western blot for CD63, CD81, TSG101, Alix [50] |
| Animal Model | Female SD rats (200-220g); LAD ligation for AMI induction [50] | Verify AMI by color change in myocardial region below ligation [50] |
| Therapeutic Administration | Intramyocardial injection (exosomes); Tail vein infusion (MSCs) [50] | Optimal timing: Exosomes at 30min post-MI, MSCs at day 3 post-MI [50] |
Detailed Methodologies
Exosome Isolation and Characterization
Protocol:
- Culture MSCs in Iscove's Modified Dulbecco's Medium (IMDM) with 10% exosome-depleted FBS for 48 hours. Prepare exosome-free FBS by ultracentrifugation at 120,000g for 18 hours prior to use [50].
- Collect conditioned supernatant and perform sequential centrifugation: 300g for 10 minutes (remove cells), 2,000g for 20 minutes (remove debris), 13,500g for 30 minutes (remove macrovesicles) [50].
- Perform final ultracentrifugation at 120,000g for 70 minutes to obtain exosome pellet. Resuspend in PBS and store at -80°C [50].
- Characterize exosomes using:
- Nanoparticle Tracking Analysis (NTA) for size distribution (30-150 nm expected)
- Transmission Electron Microscopy (TEM) for morphology
- Western blot for markers CD63, CD81, TSG101, and Alix [50]
MSC Culture and Preconditioning
Protocol:
- Isolate MSCs from bone marrow of male Sprague-Dawley rats (60-80g) by flushing femurs and tibias with IMDM containing 10% FBS and penicillin/streptomycin [50].
- Culture at 37°C with 5% CO2, change medium after 24 hours to remove non-adherent cells [50].
- Passage at 90% confluence using standard trypsinization at 1:3 ratio. Use passages 3-4 for experiments [50].
- Precondition MSCs before transplantation by treating with 1μM atorvastatin for 12 hours to enhance CXCR4 expression and improve homing to ischemic myocardium [50].
Myocardial Infarction Model and Therapeutic Administration
Protocol:
- Anesthetize female Sprague-Dawley rats (200-220g) with intraperitoneal ketamine (100mg/kg) and xylazine (10mg/kg) [50].
- Perform endotracheal intubation and connect to rodent ventilator [50].
- Perform left thoracotomy to expose heart and ligate left anterior descending coronary artery with 6-0 silk suture [50].
- Verify AMI induction by observation of color change (pale region) in myocardial tissue distal to ligation [50].
- For treatment groups:
- Exosome alone: Intramyocardial injection of 10μg exosomes in border zone at 30min post-MI
- MSC alone: Intravenous infusion of 1×10^6 atorvastatin-pretreated MSCs via tail vein at day 1, 3, or 7 post-MI
- Combinatorial: Intramyocardial exosomes (30min post-MI) + intravenous MSCs (day 3 post-MI) [50]
Assessment Parameters
Functional Assessment:
- Echocardiography: Perform at baseline and 4 weeks post-treatment to measure left ventricular ejection fraction (LVEF), left ventricular end-systolic diameter (LVESD), and left ventricular end-diastolic diameter (LVEDD) [50].
- Histological Analysis:
- Collect heart tissue at sacrifice (4 weeks post-treatment)
- Measure infarct size using Masson's trichrome staining
- Assess capillary density using CD31 immunohistochemistry in infarct border zone [50]
- Molecular Analysis:
- ELISA for SDF-1 expression levels in infarct border zone
- Measurement of inflammatory factors (TNF-α, IL-6)
- TUNEL assay for apoptosis in infarct area [50]
Table 3: Quantitative Outcomes of Combinatorial vs. Individual Therapies
| Therapeutic Parameter | Exosomes Alone | MSCs Alone | Combinatorial Approach |
|---|---|---|---|
| Left Ventricular Ejection Fraction (LVEF) | Moderate improvement | 3.8% increase in LVEF [1] | Significant further improvement vs. either alone [50] |
| Infarct Size Reduction | Moderate reduction | ~20% reduction | ~40% additional reduction vs. controls [50] |
| Neovascularization | Increased capillary density | Improved angiogenesis | Significantly enhanced vs. monotherapies [50] |
| Stem Cell Retention | N/A | <5% survival at 72h [1] | Enhanced MSC survival and retention [50] |
| Inflammatory Response | Reduced TNF-α, IL-6 | Moderate anti-inflammatory effect | Significantly reduced inflammatory markers [50] |
| Optimal Timing | 30min post-MI | Day 3 post-MI | Exosomes (30min) + MSCs (Day 3) [50] |
Technical Optimization Strategies
Enhancing Exosome Production and Potency
The low yield of exosomes represents a significant bottleneck for clinical translation. Several strategies can enhance production:
Genetic Modulation:
- Knockdown of Rab4 increases exosome biogenesis and secretion by regulating multivesicular body formation, achieving up to 14-fold increase in yield without sacrificing cargo loading efficiency [55].
- Target Rab27 to modulate docking and fusion of MVBs with plasma membrane [55].
Culture Condition Optimization:
- Implement 3D culture systems using microcarriers to increase exosome production 20-fold compared to 2D culture [53].
- Apply hypoxic preconditioning (1% O2) to upregulate HIF-1α and enhance pro-angiogenic content of exosomes [53].
- Supplement culture medium with red cell membrane particles (RCMPs) to provide lipid components for enhanced exosome biogenesis [55].
Engineering Strategies:
- Modify parental cells through genetic engineering to overexpress therapeutic genes (e.g., VEGF, SDF-1) that will be packaged into exosomes [53] [52].
- Directly load exosomes with therapeutic miRNAs or mRNAs using electroporation, sonication, or incubation methods [54].
Biomaterial-Assisted Delivery
To address poor retention in cardiac tissue, consider incorporating combinatorial therapies into delivery systems:
- Hydrogel encapsulation: Provides sustained release of exosomes and protects them from rapid clearance [53].
- Cardiac patches: Incorporate exosomes and MSCs into biomaterial scaffolds for localized, prolonged delivery [48].
- Injectable hydrogels: Form in situ to retain therapeutics in the myocardial tissue [51].
Combinatorial approaches utilizing stem cells with exosomes and growth factors represent a promising strategy to enhance cardiac repair following myocardial infarction. The sequential delivery of exosomes followed by MSC transplantation leverages the synergistic effects of preconditioning the ischemic microenvironment to improve subsequent cell engraftment and survival [50]. This protocol provides a standardized methodology for investigating these combinatorial therapies, with particular emphasis on timing optimization, proper characterization of biologics, and comprehensive functional assessment.
Future directions in this field should focus on development of engineered exosomes with enhanced cardiac targeting capabilities, standardization of large-scale production methods under Good Manufacturing Practice (GMP) conditions, and exploration of patient-specific approaches using iPSC-derived products [52] [3]. As research progresses, these combinatorial strategies hold significant potential for translation into clinical therapies that effectively address the limitations of current treatments for myocardial infarction and heart failure.
Genetic Engineering and Preconditioning to Boost Potency and Homing
The promise of stem cell transplantation for myocardial infarction (MI) is fundamentally constrained by two critical biological limitations: the low survival rate of transplanted cells within the harsh, ischemic myocardial microenvironment and their inefficient homing to the infarcted region [1]. Clinical studies reveal that less than 10% of transplanted mesenchymal stem cells (MSCs) survive beyond the first week post-transplantation [1]. Furthermore, without enhancement, stem cells lack the targeted migratory capacity necessary for effective engraftment. This application note details protocols for genetic engineering and preconditioning—two powerful strategies to overcome these barriers by boosting cellular potency and directing homing, thereby maximizing the therapeutic potential of stem cell transplantation for cardiac repair.
Technological Approaches and Quantitative Comparisons
Genetic Engineering Strategies
Genetic engineering directly modifies stem cells to overexpress specific genes that enhance survival, paracrine activity, and homing.
- CXCR4 Overexpression: Engineering MSCs to overexpress the C-X-C chemokine receptor type 4 (CXCR4) improves myocardial homing efficiency by 5.2-fold by enhancing responsiveness to the SDF-1α gradient present in the infarcted heart [1].
- Akt Overexpression: MSCs engineered to overexpress the survival-promoting factor Akt demonstrate significantly enhanced protection of the myocardium and improved cell survival 72 hours post-transplantation [23].
- Transcription Factor Reprogramming: For induced pluripotent stem cell (iPSC)-derived cardiomyocytes, the forced expression of cardiac-specific transcription factors (e.g., GATA4, Mef2C, Tbx5, Hand2) directs differentiation and maturation. Machine learning-assisted epigenetic editing (EpiCRISPR) can reduce inter-batch variation in gene expression to as low as 6.4% [1].
Table 1: Key Genetic Engineering Targets for Enhancing Stem Cell Therapy
| Target Gene/Factor | Therapeutic Function | Mechanism of Action | Reported Efficacy |
|---|---|---|---|
| CXCR4 | Enhances Homing | Increases migration toward SDF-1α chemokine gradient in infarcted tissue [1] | 5.2-fold improvement in myocardial homing [1] |
| Akt | Boosts Survival & Potency | Activates pro-survival and anti-apoptotic signaling pathways [23] | Protects myocardium 72h post-transplant [23] |
| GHMT Factors | Promotes Cardiac Reprogramming | Directs non-cardiac cells (e.g., fibroblasts) into cardiomyocyte-like cells (iCMs) [3] | Generates iCMs with adult-like molecular phenotypes [3] |
Preconditioning Strategies
Preconditioning exposes stem cells to sublethal stress or specific bioactive molecules to activate intrinsic protective and regenerative pathways.
- Myocardial Infarction Serum Preconditioning: Pre-treating bone marrow MSCs with serum collected from rats after MI yields exosomes (MIS-EXO) with superior therapeutic capacity. Compared to exosomes from standard culture (CON-EXO), MIS-EXO demonstrate enhanced effects in reducing fibrosis, improving left ventricular function, and attenuating inflammation [56].
- Hypoxic Preconditioning: Mimicking the ischemic microenvironment by culturing cells under low oxygen tension can upregulate hypoxia-inducible factors (HIFs), which in turn promote the secretion of pro-survival and angiogenic factors.
- Pharmacological Preconditioning: Incubation with specific cytokines or small molecules (e.g., TGF-β, melatonin) can prime cells for enhanced paracrine secretion and stress resistance without genetic modification.
Table 2: Comparative Analysis of Preconditioning vs. Genetic Engineering
| Characteristic | Preconditioning | Genetic Engineering |
|---|---|---|
| Mechanism | Epigenetic & metabolic modulation via sublethal stress/cytokines [56] | Direct genomic modification to overexpress therapeutic genes [1] |
| Key Advantage | Non-genetic, transiently activates endogenous protective pathways [56] | Potent, stable, and targeted enhancement of specific functions [1] |
| Primary Risk | Effect may be transient and require optimization of timing/dose [56] | Risks associated with viral vectors and potential tumorigenicity [1] |
| Therapeutic Output | Enhanced paracrine secretion (e.g., exosomes with anti-fibrotic miRNAs) [56] | Enhanced homing (via CXCR4), survival (via Akt), or direct reprogramming [1] [23] |
| Clinical Translation | Perceived as lower regulatory hurdle | Requires stringent safety and efficacy profiling |
Detailed Experimental Protocols
Protocol 1: Myocardial Infarction Serum Preconditioning of MSCs
This protocol describes the generation of preconditioned exosomes with enhanced anti-fibrotic potency, as validated in a rat MI model [56].
Workflow Overview:
Materials:
- Animals: Adult Sprague-Dawley rats [56]
- Cell Culture: Rat bone marrow-derived MSCs, standard culture media [56]
- Reagents: PBS, exosome-depleted FBS, ultracentrifugation tubes [56]
Procedure:
- MI Serum Collection:
- Induce MI in rats via permanent ligation of the left anterior descending coronary artery [56].
- Under anesthesia, collect blood from the abdominal aorta 1-3 days post-MI.
- Allow blood to clot at room temperature for 30 minutes, then centrifuge at 2,000 × g for 20 minutes at 4°C.
- Collect the supernatant (serum), aliquot, and store at -80°C.
- MSC Preconditioning:
- Culture rat bone marrow MSCs to 70-80% confluence in standard medium.
- Replace the medium with culture medium containing 10% v/v collected MI serum.
- Incubate cells for 48-72 hours under normal culture conditions (37°C, 5% CO₂) [56].
- Exosome Isolation:
- Collect the conditioned medium and centrifuge at 2,000 × g for 30 minutes to remove dead cells and debris.
- Transfer the supernatant to ultracentrifugation tubes and centrifuge at 100,000 × g for 70 minutes at 4°C to pellet exosomes.
- Wash the pellet in PBS and repeat ultracentrifugation.
- Resuspend the final exosome pellet (MIS-EXO) in PBS and quantify protein content via BCA assay. Store at -80°C.
- In Vivo Administration:
- In the rat MI model, perform intramyocardial injection of MIS-EXO (e.g., 100 µg in PBS) 30 minutes after permanent ligation [56].
- Evaluate cardiac function and fibrosis at predetermined endpoints (e.g., 4 weeks).
Protocol 2: Genetic Engineering of MSCs for Enhanced Homing
This protocol outlines the genetic modification of MSCs to overexpress CXCR4 for improved targeted migration [1].
Workflow Overview:
Materials:
- Cells: Early passage human or rodent MSCs.
- Genetic Construct: Lentiviral vector encoding human CXCR4 and a selectable marker (e.g., puromycin resistance).
- Reagents: Polybrene (hexadimethrine bromide), puromycin, culture media.
- Equipment: Flow cytometer, PCR system, transwell migration plates.
Procedure:
- Viral Transduction:
- Culture MSCs to 40-50% confluence in a 6-well plate.
- Replace medium with fresh medium containing the lentiviral vector (MOI of 50-100) and 8 µg/mL Polybrene to enhance transduction efficiency.
- Centrifuge the plate at 800 × g for 30 minutes (optional, to boost infection).
- Incubate for 24 hours at 37°C, then replace with fresh complete medium.
- Selection and Expansion:
- 48 hours post-transduction, begin selection with culture medium containing puromycin (e.g., 1-2 µg/mL). Determine the optimal lethal concentration beforehand on non-transduced cells.
- Maintain selection pressure for 5-7 days, replacing the puromycin-containing medium every 2-3 days until all control (non-transduced) cells are dead.
- Expand the resistant, CXCR4-overexpressing cell population.
- Validation of CXCR4 Expression:
- Flow Cytometry: Harvest engineered MSCs and stain with a fluorescently labeled anti-CXCR4 antibody. Use isotype antibody-stained cells as a control. Analyze on a flow cytometer to confirm high CXCR4 surface expression.
- qPCR: Isolve RNA and perform qPCR with primers specific for CXCR4 to confirm transcriptional upregulation relative to non-transduced MSCs.
- Functional Homing Assay (In Vitro):
- Seed serum-starved CXCR4-MSCs in the upper chamber of a transwell insert.
- Add medium containing 100 ng/mL SDF-1α to the lower chamber.
- Incubate for 6-12 hours. Migrated cells on the lower membrane surface are fixed, stained, and counted. CXCR4-MSCs should show significantly higher migration compared to control MSCs.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Genetic Engineering and Preconditioning Protocols
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Lentiviral Vectors | Stable gene delivery for long-term expression of transgenes (e.g., CXCR4, Akt) in stem cells [1]. | Creating a stable MSC line with enhanced homing potential. |
| CRISPR-Cas9 System | Gene editing for knockout of inhibitory genes or precise insertion of therapeutic transgenes [1]. | Knocking out pluripotency genes in iPSCs to enhance cardiac differentiation efficiency. |
| Myocardial Infarction Serum | Biologically relevant preconditioning stimulus containing a complex mix of injury-related factors [56]. | Priming MSCs to secrete exosomes with enhanced anti-fibrotic and anti-inflammatory cargo. |
| SDF-1α (CXCL12) | Key chemokine for validating homing efficiency in vitro; creates a gradient in transwell assays [1]. | Testing the functional migration capacity of CXCR4-overexpressing MSCs. |
| Ultracentrifuge | Essential equipment for isolating and purifying exosomes from conditioned cell culture media [56]. | Preparing MIS-EXO for therapeutic application in animal models. |
| Flow Cytometer | Instrument for quantifying surface marker expression (e.g., CXCR4) and assessing cell purity [1]. | Validating the success of CXCR4 genetic engineering in MSCs. |
Integrating genetic engineering and preconditioning strategies provides a powerful, multi-faceted approach to surmount the primary obstacles in stem cell therapy for myocardial infarction. By systematically employing the protocols and reagents outlined in this application note, researchers can robustly enhance the survival, homing, and paracrine potency of therapeutic cells, paving the way for more effective and predictable regenerative outcomes in pre-clinical and clinical settings.
Novel Biomaterial Scaffolds and Tissue Engineering for Improved Retention
Stem cell transplantation represents a transformative approach for myocardial infarction (MI) treatment by potentially regenerating lost cardiomyocytes and restoring cardiac function. However, a fundamental limitation plaguing this therapeutic strategy is the extremely low retention and survival rates of transplanted cells within the harsh, ischemic myocardial environment. Clinical studies reveal that less than 10% of transplanted mesenchymal stem cells (MSCs) remain viable shortly after implantation, with coronary MSC survival falling to a critical <5% within 72 hours of transplantation [1]. This massive cell loss severely compromises therapeutic efficacy and clinical translation potential.
Biomaterial scaffolds have emerged as a promising solution to this retention challenge by providing three-dimensional microenvironments that mimic native cardiac tissue architecture. These engineered constructs serve as temporary mechanical and biological support systems, enhancing cell engraftment, survival, and functional integration at the infarction site. Advanced scaffolds act not merely as passive carriers but as active participants in the regenerative process, delivering bioactive cues that modulate host tissue response and guide appropriate tissue remodeling [57]. This application note details the composition, fabrication, and implementation of novel biomaterial scaffolds designed specifically to overcome the critical retention barrier in stem cell therapy for myocardial infarction.
Stem Cell Types and Their Therapeutic Mechanisms
The selection of appropriate cell sources is fundamental to designing effective scaffold-based therapies. Different stem cell categories offer distinct advantages and limitations for cardiac repair, operating through diverse mechanistic pathways.
Table 1: Characteristics of Stem Cell Types for Cardiac Repair
| Stem Cell Type | Sources | Key Advantages | Major Limitations | Primary Mechanisms |
|---|---|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Bone marrow, adipose tissue, umbilical cord | Strong immunomodulation; abundant paracrine function; homing characteristics | Low post-transplantation survival (<10%); functional heterogeneity | Paracrine signaling; immunomodulation; angiogenesis promotion [1] |
| Induced Pluripotent Stem Cells (iPSCs) | Reprogrammed somatic cells | ESC differentiation potential with autologous transplantation advantages; high-purity cardiomyocyte preparation (95% purity) | Tumorigenic risk; residual reprogramming epigenetic memory | Direct differentiation into functional cardiomyocytes [1] |
| Embryonic Stem Cells (ESCs) | Inner cell mass of blastocyst | High differentiation efficiency (70-85%); secretion of angiogenic factors (VEGF, HGF) | Ethical concerns; tumorigenic risk; immune rejection | Direct differentiation into multiple cardiac cell types [1] [13] |
| Cardiac Stem Cells (CSCs) | Adult heart | Tissue-specific differentiation; exosomes promote functional recovery (e.g., miR-146a) | Limited quantity; mechanism requires further elucidation | Exosome-mediated repair; angiogenesis; anti-apoptosis [1] |
The therapeutic effects of these cells are mediated through multiple interconnected pathways. The paracrine effect represents a predominant mechanism, particularly for MSCs, which secrete growth factors like VEGF, FGF, and HGF through exosomes to promote angiogenesis and tissue repair [1]. These exosomes carry regulatory molecules such as miR-21 and miR-210, which modulate cardiomyocyte apoptosis and fibrosis [1]. Additionally, direct differentiation enables iPSCs and ESCs to become functional cardiomyocytes within the infarcted region, while immune regulation and homing effects further contribute to the overall therapeutic response [1].
Biomaterial Scaffold Design and Composition
The ideal cardiac scaffold must replicate the complex physicochemical properties of native myocardial extracellular matrix (ECM) while providing tailored mechanical support and bioactive signaling. Several biomaterial classes have been investigated for this purpose, each offering distinct advantages.
Natural Polymer-Based Scaffolds
Decellularized extracellular matrix (dECM) has emerged as a particularly promising scaffold material due to its preservation of native tissue-specific biochemical composition and ultrastructural architecture. The decellularization process removes cellular components while retaining essential ECM components like glycosaminoglycans (GAGs), adhesive glycoproteins, and fibrous proteins including collagen and elastin [57]. These intact biological motifs provide innate cellular recognition sites that support cell adhesion, proliferation, and differentiation. Preclinical studies demonstrate that acellular cardiac ECM scaffolds can activate endogenous repair mechanisms; implantation of decellularized porcine cardiac ECM patches in rodent MI models stimulated cardiomyocyte regeneration after scar formation, improved myocardial contractility, and enhanced cardiac remodeling [57].
Hydrogel-based scaffolds represent another prominent natural polymer approach, consisting of three-dimensional, cross-linked hydrophilic polymers that closely mimic the natural ECM of cardiac tissue [57]. Their high water content and tunable physical properties make them ideal for supporting cell growth and proliferation essential for tissue regeneration. Hydrogels can be fabricated from various natural polymers including collagen, fibrin, and alginate, with their properties fundamentally determined by the biomaterials employed in their fabrication [57]. These materials influence critical parameters such as conductivity, cross-linking density, degradation rates, and interactions with therapeutic agents.
Synthetic and Composite Scaffolds
Synthetic polymers offer enhanced control over mechanical properties, degradation kinetics, and structural features compared to natural materials. Polyethylene glycol (PEG), polylactic acid (PLA), and polyglycolic acid (PGA) are commonly used synthetic options that can be processed into porous scaffolds with defined architectures. However, synthetic materials often lack the innate bioactivity of natural polymers, leading to the development of composite scaffolds that combine synthetic and natural materials to harness the advantages of both approaches.
The incorporation of conductive materials represents a significant advancement in cardiac scaffold design. Materials such as carbon nanotubes (CNTs), graphene, and conductive polymers can be integrated within cardiac patches to improve electrical signal transmission across the damaged area, restoring proper heart rhythm and function [57]. These conductive components facilitate synchronous electrical impulses between the engineered patch and native cardiac tissue, addressing the critical need for electromechanical integration in regenerating functional myocardium.
Table 2: Biomaterial Scaffold Types for Cardiac Tissue Engineering
| Scaffold Type | Key Components | Advantages | Limitations |
|---|---|---|---|
| dECM Scaffolds | Decellularized heart tissue; preserved vascular architecture | Native biochemical composition; tissue-specific bioactivity; natural mechanical properties | Batch-to-batch variability; potential immune response; processing complexity |
| Hydrogel Scaffolds | Collagen, fibrin, alginate, hyaluronic acid | High water content; excellent cell encapsulation; injectable delivery | Limited mechanical strength; rapid degradation; potential volume changes |
| Conductive Composite Scaffolds | CNTs, graphene, conductive polymers integrated with natural/synthetic polymers | Enhanced electrical conductivity; improved signal propagation; synchronous contraction | Potential nanomaterial toxicity; complex fabrication; regulatory challenges |
| 3D-Printed Scaffolds | Synthetic polymers (PLA, PGA) with biological functionalization | Precise architectural control; patient-specific design; vascular network integration | Limited resolution for microvasculature; material constraints; equipment cost |
Experimental Protocols and Methodologies
Decellularized ECM Cardiac Patch Fabrication
Objective: To create a biocompatible cardiac patch from decellularized porcine myocardial tissue that supports stem cell retention and function.
Materials:
- Porcine myocardial tissue
- Sodium dodecyl sulfate (SDS) solution (0.5-1%)
- DNase and RNase solutions
- Sterile phosphate-buffered saline (PBS)
- Antibiotic-antimycotic solution
- Lyophilizer
- Bioreactor system
Procedure:
- Tissue Preparation: Obtain fresh porcine hearts and dissect left ventricular myocardium into 0.5 cm thick sections.
- Decellularization:
- Incubate tissue sections in 1% SDS solution with continuous agitation for 24-48 hours.
- Replace SDS solution every 12 hours until tissue becomes translucent.
- Treat with DNase solution (50 U/mL) and RNase solution (1 U/mL) for 6 hours at 37°C to remove residual nucleic acids.
- Washing: Rinse thoroughly with PBS for 72 hours with solution changes every 12 hours to remove detergent residues.
- Sterilization: Immerse in antibiotic-antimycotic solution for 24 hours at 4°C.
- Characterization: Verify decellularization through H&E staining (no nuclear material), DNA quantification (<50 ng/mg tissue), and ECM composition analysis.
- Lyophilization: Freeze at -80°C and lyophilize for 48 hours to create porous scaffolds.
- Cellularization: Seed MSCs or iPSC-derived cardiomyocytes at 5-10 × 10^6 cells/cm^2 density using a bioreactor system with perfusion culture.
Quality Control:
- Confirm preservation of collagen, elastin, and GAGs through biochemical assays.
- Verify absence of nuclear material with DAPI staining.
- Assess mechanical properties matching native myocardium (elastic modulus 10-20 kPa).
Conductive Hydrogel Preparation for Cell Encapsulation
Objective: To fabricate a conductive hydrogel scaffold that enhances electrical coupling between stem cells and host myocardium.
Materials:
- Gelatin methacryloyl (GelMA)
- Carbon nanotubes (CNTs) or graphene oxide
- Photoinitiator (Irgacure 2959)
- UV crosslinking system
- MSCs or iPSC-derived cardiomyocytes
Procedure:
- GelMA Synthesis: Prepare GelMA according to established protocols with degree of functionalization ~80%.
- Conductive Component Integration:
- Disperse CNTs (0.5-1 mg/mL) in PBS using sonication.
- Mix CNT suspension with GelMA solution (5-10% w/v) containing 0.5% photoinitiator.
- Cell Encapsulation:
- Resuspend stem cells in GelMA-CNT mixture at 5-10 × 10^6 cells/mL.
- Pipette mixture into custom molds (1-2 mm thickness).
- Crosslinking: Expose to UV light (365 nm, 5-10 mW/cm^2) for 60-120 seconds.
- Culture: Transfer hydrogels to culture media and maintain in bioreactor with electrical stimulation (1-2 Hz, 5V/cm).
Quality Control:
- Measure electrical conductivity (target: 0.05-0.1 S/m).
- Assess cell viability post-encapsulation (>90%).
- Evaluate mechanical properties (compressive modulus 5-15 kPa).
Diagram 1: Scaffold Fabrication and Quality Control Workflow. This workflow outlines the key steps in producing functional cardiac patches, with essential quality control checkpoints ensuring scaffold safety and efficacy.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of scaffold-based stem cell therapy requires carefully selected reagents and materials that support cell viability, function, and integration.
Table 3: Essential Research Reagents for Cardiac Scaffold Development
| Reagent/Material | Function | Example Applications | Considerations |
|---|---|---|---|
| Mesenchymal Stem Cells | Primary therapeutic cell source; paracrine signaling | Bone marrow-derived MSCs for immunomodulation and angiogenesis | Passage number effects functionality; donor variability |
| iPSC-Derived Cardiomyocytes | Contractile cell generation; myocardial regeneration | Creating beating cardiac patches; disease modeling | Maturation state critical; potential arrhythmogenicity |
| Decellularization Reagents | Remove cellular components while preserving ECM | SDS, Triton X-100 for tissue decellularization | Concentration and exposure time optimization required |
| Conductive Nanomaterials | Enhance electrical signal propagation | CNTs, graphene in composite hydrogels | Biocompatibility assessment; dispersion optimization |
| Photoinitiators | Enable UV-mediated crosslinking of hydrogels | Irgacure 2959 for GelMA hydrogels | Cytotoxicity screening; concentration optimization |
| Vascularization Factors | Promote blood vessel formation in constructs | VEGF, FGF, angiopoietin supplementation | Spatiotemporal release kinetics; concentration gradients |
| Bioreactor Systems | Provide mechanical and electrical conditioning | Perfusion systems; electrical stimulation platforms | Mimicking physiological heart environment |
Assessment and Evaluation Techniques
Rigorous evaluation of scaffold performance and stem cell retention is essential for optimizing therapeutic outcomes. Both invasive and non-invasive methodologies provide complementary data on construct viability and functionality.
Non-Invasive Imaging Modalities
Ultrasound imaging offers a non-destructive approach for longitudinal assessment of scaffold integration and cardiac function. Techniques include:
- Backscattering Imaging: Characterizes tissue microstructural properties through spectral analysis of ultrasound signals, monitoring changes in cell density and ECM elaboration [58].
- Doppler Imaging: Visualizes blood flow and vascularization within engineered constructs, with microbubble contrast agents enhancing sensitivity for microvasculature detection [58].
- Ultrasound Elasticity Imaging: Assesses mechanical properties of scaffolds and their integration with host tissue through compressional and shear wave techniques [58].
Photoacoustic Imaging combines optical contrast with ultrasound resolution, enabling visualization of vascularization, cell tracking, and scaffold degradation without ionizing radiation [58].
Functional Assessment Protocols
Electrical Integration Analysis:
- Perform multielectrode array (MEA) mapping of scaffold-host interface.
- Measure conduction velocity and action potential propagation.
- Assess synchronization between scaffold and native tissue contractions.
Mechanical Property Evaluation:
- Determine tensile and compressive modulus using Instron testing.
- Assess contractile force generation using force transducers.
- Evaluate pressure-volume relationships in Langendorff heart preparations.
Histological and Immunochemical Analysis:
- Process explanted heart sections for standard (H&E, Masson's trichrome) and immunohistochemical staining.
- Quantify angiogenesis (CD31+ vessels), cell retention (CM-Dil labeling), and differentiation (cardiac troponin T+ cells).
- Assess apoptosis (TUNEL assay) and proliferation (Ki-67) indices.
Diagram 2: Therapeutic Mechanisms of Engineered Scaffolds. Engineered biomaterial scaffolds enhance stem cell therapy through multiple synergistic mechanisms including structural support, bioactive cue delivery, and electrical coupling, collectively improving cardiac outcomes.
Biomaterial scaffolds represent a paradigm shift in stem cell therapy for myocardial infarction by directly addressing the critical limitation of poor cell retention. The integration of advanced materials science with stem cell biology has yielded sophisticated constructs that provide tailored microenvironments supporting cell survival, differentiation, and functional integration. Current evidence suggests that optimal outcomes require a multimodal approach combining appropriate cell sources, biomimetic scaffold design, and strategic bioactive cue presentation.
Future developments will likely focus on personalized scaffold designs utilizing patient-specific iPSCs and 3D-printing technologies to create custom-tailored constructs [59]. The incorporation of multiple conductive materials and advanced maturation protocols will further enhance the electromechanical integration of engineered tissues. Additionally, the emergence of cell-free approaches utilizing scaffold-released extracellular vesicles and other paracrine factors may offer alternative strategies that circumvent cell survival challenges entirely [3].
As these technologies mature, standardized protocols for scaffold fabrication, characterization, and implantation will be essential for clinical translation. The systematic implementation of the application notes and methodologies detailed herein provides a robust foundation for advancing the field of scaffold-enhanced stem cell therapy toward meaningful clinical applications in myocardial infarction treatment.
Clinical Evidence and Comparative Outcomes: Analyzing the Trial Data
Application Note: Quantitative Efficacy Outcomes
This application note synthesizes key quantitative findings from recent meta-analyses on stem cell therapy for myocardial infarction, focusing on left ventricular ejection fraction (LVEF) improvement and scar size reduction.
Table 1: Summary of Meta-Analysis Efficacy Outcomes for Stem Cell Therapy
| Outcome Measure | Follow-up Period | Weighted Mean Difference (WMD) or Mean Difference (MD) | 95% Confidence Interval (CI) | Heterogeneity (I²) | Source Meta-Analysis |
|---|---|---|---|---|---|
| Left Ventricular Ejection Fraction (LVEF) | 6 months | WMD: 0.44% [60] | 0.13 to 0.75 [60] | 85% [60] | [60] |
| 12 months | WMD: 0.64% [60] | 0.14 to 1.14 [60] | 85% [60] | [60] | |
| 24-36 months | Significantly improved trend [35] | Reported, specific values not extracted | Not specified | [35] | |
| Scar Size Reduction | 6 months | MD: -0.36 [60] | -0.63 to -0.10 [60] | 71% [60] | [60] |
| 12 months | MD: -0.62 [60] | -1.03 to -0.21 [60] | 78% [60] | [60] | |
| Major Adverse Cardiac Events (MACE) | Mid- to long-term | Trend toward reduction [35] | Risk composite outcome | Not specified | [35] |
| Quality of Life (MLHFQ Score) | 6-12 months | MD: -0.38 to -0.49 [60] | -0.71 to -0.05 / -0.74 to -0.25 [60] | 69-72% [60] | [60] |
Experimental Protocols for Efficacy Assessment
Core Meta-Analysis Protocol
Objective: To systematically evaluate the mid- to long-term efficacy and safety of stem cell therapy in patients with acute myocardial infarction.
Primary Endpoints:
- Change in Left Ventricular Ejection Fraction (LVEF)
- Change in Myocardial Scar Size
- Incidence of Major Adverse Cardiac Events (MACE)
Methodology Overview:
- Data Sources & Search Strategy:
- Conduct systematic searches across major databases (e.g., MEDLINE, EMBASE, Cochrane Library) [35].
- Utilize search terms: "myocardial infarction," "stem cells," "bone marrow cells," "mesenchymal stem cells," "mononuclear cells," combined with "LVEF" and "scar size" [60] [35].
- Apply filters for randomized controlled trials (RCTs) and English language [35].
Study Selection:
- Inclusion Criteria: RCTs involving patients with AMI receiving stem cell therapy via intracoronary, intramyocardial, or intravenous injection post-PCI [35].
- Exclusion Criteria: Non-human studies, non-original articles, duplicate publications [60] [35].
- Follow PRISMA guidelines and register the protocol on PROSPERO [60] [35].
Data Extraction & Quality Assessment:
Statistical Analysis:
Protocol for Assessing the Impact of Cell Processing Factors
Objective: To determine the influence of cell culture duration and injected cell quantity on therapeutic efficacy [35].
Methodology:
- Subgroup Analysis Definitions:
- Outcome Measurement:
- Analyze the association of these parameters with significant improvements in LVEF [35].
Signaling Pathways and Experimental Workflow
Stem Cell Therapeutic Mechanisms
Efficacy Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Stem Cell Myocardial Regeneration Research
| Reagent/Material | Function/Application | Key Characteristics & Notes |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) [1] | Primary cell source for therapy; mediates paracrine effects and immune modulation. | Sourced from bone marrow, adipose tissue, or umbilical cord. Secretes VEGF, HGF, exosomes containing miR-21, miR-210. Low post-transplant survival (<10%) is a key challenge [1]. |
| Induced Pluripotent Stem Cells (iPSCs) [1] | Source for generating autologous cardiomyocytes; avoids ethical issues of ESCs. | Reprogrammed from somatic cells. Can achieve high-purity cardiomyocytes (∼95%). Requires careful management of tumorigenic risk and epigenetic memory [1]. |
| Cardiac Stem Cells (CSCs) / Cardiosphere-Derived Cells (CDCs) [60] [1] | Heart-derived cells with inherent cardiac repair potential. | Isolated from adult heart tissue. Secretes exosomes (e.g., containing miR-146a) that promote endothelial tube formation and reduce apoptosis [1]. |
| Ex Vivo Culture Media & Supplements [35] | Expansion and maintenance of stem cells prior to transplantation. | Critical for achieving high cell quantities (≥10â¸). Culture duration exceeding one week is associated with significant LVEF improvement [35]. |
| CRISPR-Cas9 System [1] | Gene-editing tool to enhance stem cell efficacy and direct differentiation. | Used to knock out pluripotency genes or activate cardiomyocyte-specific transcription factors, improving differentiation efficiency [1]. |
| Smart Hydrogel Scaffolds / 3D Bioprinting Matrices [1] | Biomaterial supports to improve cell retention and survival post-transplantation. | Addresses the challenge of low cell survival in the harsh infarct microenvironment. Aids in constructing complex cardiac tissue structures [1]. |
Within the broader scope of developing stem cell transplantation techniques for myocardial infarction (MI) research, a rigorous and standardized safety profile assessment is paramount. The therapeutic potential of various stem cell types to regenerate damaged myocardium is promising, yet their association with Major Adverse Cardiac Events (MACE) and specific arrhythmogenic risks necessitates comprehensive evaluation [1] [23]. This document provides detailed application notes and experimental protocols to aid researchers, scientists, and drug development professionals in systematically quantifying these risks, thereby facilitating the development of safer regenerative therapies.
Safety Profile of Stem Cell Therapies: MACE and Mortality
The composite endpoint of MACE, typically including cardiovascular death, reinfarction, and stroke, is a critical metric for evaluating the safety and efficacy of new treatments for acute coronary syndrome [35]. Evidence from recent meta-analyses on stem cell therapy for acute MI and chronic heart failure provides a encouraging initial safety profile.
Table 1: Clinical Outcomes of Stem Cell Therapy in Cardiovascular Disease
| Outcome Measure | Therapy Type | Patient Population | Effect Estimate [95% CI] | Conclusion | Source |
|---|---|---|---|---|---|
| All-Cause Mortality | MSC Transplantation | Chronic Heart Failure | RR 0.78 [0.62, 0.99] | Significant reduction | [61] |
| All-Cause Mortality | General Stem Cell Therapy | Acute Myocardial Infarction | RR 0.73 [NR] | No significant difference | [29] |
| MACE Occurrence | General Stem Cell Therapy | Acute Myocardial Infarction | Trend toward reduction | Potential risk reduction | [35] |
| Heart Failure Hospitalization | MSC Transplantation | Chronic Heart Failure | RR 0.85 [0.71, 1.01] | Non-significant reduction | [61] |
| Severe Adverse Events (SAEs) | General Stem Cell Therapy | Acute Myocardial Infarction | RR 0.93 [NR] | No significant difference | [29] |
A 2024 meta-analysis of 17 randomized controlled trials (RCTs) concluded that MSC transplantation for chronic heart failure significantly reduced all-cause mortality [61]. Similarly, a large 2024 meta-analysis of 79 RCTs with 7,103 AMI patients suggested a trend toward reduced MACE occurrence in groups receiving stem cell therapy, indicating its potential to lower the risk of composite cardiovascular death, reinfarction, and stroke [35]. Another 2025 meta-analysis focusing on AMI found no notable differences in all-cause mortality, severe adverse events, or other clinical endpoints like recurrent MI and stroke between stem cell therapy and control groups [29].
Protocol 1: Assessment of MACE in Preclinical and Clinical Studies
- Objective: To systematically evaluate the incidence of Major Adverse Cardiac Events (MACE) in subjects receiving stem cell therapy for myocardial infarction.
- Endpoint Definition: MACE is a composite endpoint. In clinical studies, clearly define and adjudicate each component:
- Cardiovascular Death: Death due to cardiac causes (e.g., MI, heart failure, arrhythmia).
- Non-fatal Myocardial Reinfarction: Based on universal definitions (e.g., elevated cardiac biomarkers with ischemic symptoms or ECG changes).
- Stroke: Acute neurological deficit of vascular origin, confirmed by imaging.
- Data Collection (Clinical Trials):
- Establish an independent clinical events committee (CEC) blinded to treatment allocation to adjudicate all potential MACE.
- Collect data at pre-specified follow-up intervals (e.g., 30 days, 3, 6, 12, 24, and 36 months).
- Record the timing, severity, and relatedness of each event to the investigational therapy.
- Preclinical Correlates (Animal Studies):
- While MACE is a clinical endpoint, surrogate measures in large animal models (e.g., swine, non-human primates) can include:
- Sudden death.
- Histopathological assessment of reinfarction or new ischemic areas at terminal study.
- Evidence of thromboembolic events in vital organs upon necropsy.
- While MACE is a clinical endpoint, surrogate measures in large animal models (e.g., swine, non-human primates) can include:
Arrhythmogenic Risk Assessment
The risk of arrhythmia is a significant concern in cardiac stem cell therapy, with the specific risk profile varying considerably depending on the cell type used. The underlying mechanisms often relate to the electrophysiological immaturity of derived cardiomyocytes and their imperfect integration with the host myocardium [62] [63].
Table 2: Arrhythmogenic Risk Profile by Stem Cell Type
| Cell Type | Reported Arrhythmogenic Risk | Postulated Mechanisms | Key Evidence |
|---|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Lower | Predominantly paracrine-mediated effects; limited direct electromechanical coupling. Pre-clinical models suggest no major safety signals for acute arrhythmia. | Systematic reviews report no association with acute adverse events [64]. |
| Pluripotent Stem Cell-Derived Cardiomyocytes (hESC-CMs/iPSC-CMs) | Higher | Electrophysiological immaturity (spontaneous automaticity, depolarized resting potential, prolonged action potential) [63]; formation of ectopic pacemakers; conduction block [62]. | Non-human primate studies show graft-induced arrhythmias from pacemaker-like activity [62]. |
| Skeletal Myoblasts (SkMs) | Higher (Clinically observed) | Failure to form gap junctions with host cardiomyocytes, leading to electrical heterogeneity and re-entrant circuits. | Early clinical trials reported increased frequency of arrhythmias in patients [23]. |
The arrhythmogenic potential is most prominently associated with pluripotent stem cell-derived cardiomyocytes (PSC-CMs), including both embryonic (ESC) and induced pluripotent (iPSC) sources. Key factors contributing to this risk include:
- Cellular Immaturity: iPSC-CMs exhibit a fetal-like electrophysiological phenotype, characterized by spontaneous automaticity, a depolarized resting membrane potential, and prolonged action potential duration [63]. This is partly due to low expression of the inward rectifier potassium current (IK1).
- Calcium Handling Abnormalities: Immature sarcoplasmic reticulum function and aberrant calcium cycling can promote delayed afterdepolarizations (DADs), which are triggers for arrhythmias [63].
- Cellular Heterogeneity: The differentiation process often yields a mixed population of ventricular-, atrial-, and nodal-like cells. This heterogeneity can create electrical dispersion and anisotropic conduction, fostering a substrate for re-entrant arrhythmias [63].
- Host-Graft Integration: The coupling between transplanted cells and the host myocardium is critical. Incomplete integration can result in areas of slow conduction or conduction block, creating an arrhythmogenic substrate [62].
Diagram 1: Arrhythmogenic Risk Pathways in PSC-CM Transplantation. This diagram illustrates how key risk factors (yellow) lead to specific electrophysiological abnormalities (red), which manifest as pro-arrhythmic triggers and substrates (green), ultimately culminating in clinical arrhythmias (blue).
Protocol 2: In Vitro and In Vivo Arrhythmogenic Risk Assessment
- Objective: To characterize the proarrhythmic potential of stem cell-derived cardiomyocytes prior to in vivo transplantation.
- In Vitro Electrophysiology:
- Platform: Use human induced pluripotent stem cell-derived cardiomyocytes (iPSC-CMs) as a baseline model.
- Key Assays:
- Patch-Clamp Electrophysiology: To quantify action potential parameters (duration, upstroke velocity, resting membrane potential) and specific ion currents (e.g., IK1, INa).
- Multi-Electrode Array (MEA): To assess field potential duration, beat rate variability, and propagation patterns in monolayer or 3D culture.
- Calcium Imaging: To evaluate calcium transient morphology and stability, and detect spontaneous calcium release events (a correlate of DADs).
- In Vivo Assessment (Large Animal Models):
- Model: Induce myocardial infarction in a translational model (e.g., swine, non-human primate).
- Intervention: Administer the candidate cell therapy into the infarct and border zones.
- Monitoring:
- Implantable telemetry devices for continuous, long-term ECG monitoring to capture episodic arrhythmias.
- Programmed electrical stimulation (PES) protocols at terminal study to assess the inducibility of sustained ventricular tachycardia (VT) or fibrillation (VF).
- High-density epicardial or non-invasive electrocardiographic mapping (ECGI) to characterize conduction velocity and identify regions of slow conduction or block.
The Scientist's Toolkit: Essential Reagents and Models
Table 3: Key Research Reagent Solutions for Safety Assessment
| Category | Item | Function/Application | Key Considerations |
|---|---|---|---|
| Cell Sources | Human iPSC-CMs | In vitro model for arrhythmia screening and disease modeling. | Assess batch-to-batch variability; use maturation protocols. |
| Mesenchymal Stem Cells (MSCs) | Safety-optimized cell type for therapy; control for comparative studies. | Define source (bone marrow, adipose, UC), passage number, and potency. | |
| Functional Assays | Patch-Clamp Electrophysiology Rig | Gold-standard for detailed characterization of ionic currents and action potentials. | Requires specialized expertise; low-throughput. |
| Multi-Electrode Array (MEA) System | Higher-throughput assessment of field potentials and network activity. | Excellent for long-term monitoring and drug screening. | |
| Calcium-Sensitive Dyes (e.g., Fluo-4) | Dynamic assessment of calcium handling and detection of instability. | Critical for identifying proarrhythmic calcium waves. | |
| In Vivo Models | Porcine MI Model | Preclinical in vivo safety and efficacy testing; cardiac size and physiology similar to human. | Infarcted heart provides the relevant pathological substrate for arrhythmia. |
| Implantable Telemetry | Continuous, ambulatory ECG monitoring in conscious animals. | Essential for capturing transient, spontaneous arrhythmias. |
A rigorous and multi-faceted safety assessment is a non-negotiable component of the development pathway for stem cell-based therapies for myocardial infarction. The current evidence indicates that MSC-based therapies appear to have a favorable safety profile with no significant increase in MACE or mortality, and may even offer prognostic benefits [64] [61]. In contrast, therapies based on pluripotent stem cell-derived cardiomyocytes carry a more substantial, though potentially manageable, arrhythmogenic risk due to issues of immaturity and integration [62] [63]. The experimental protocols and tools outlined herein provide a framework for researchers to systematically evaluate and mitigate these risks, paving the way for the translation of safer and more effective cardiac regenerative treatments. Future work must focus on optimizing cell maturation, purification, and delivery strategies to further enhance the therapeutic index.
Application Notes and Protocols Head-to-Head Comparisons of Different Cell Types and Delivery Routes
Stem cell therapy represents a promising approach for myocardial infarction (MI) treatment, aiming to regenerate damaged cardiac tissue and restore function. However, therapeutic efficacy varies significantly based on cell type selection and delivery methodology. This document provides a structured comparison of key stem cell options and administration routes, supported by quantitative data and standardized protocols for preclinical and clinical applications.
Comparative Analysis of Stem Cell Types
Stem cells investigated for MI therapy include mesenchymal stem cells (MSCs), induced pluripotent stem cells (iPSCs), cardiac stem cells (CSCs), and bone marrow-derived mononuclear cells (BMMNCs). Their mechanisms involve direct differentiation, paracrine signaling, angiogenesis promotion, and immunomodulation [15] [1] [3].
Table 1: Stem Cell Types and Functional Comparisons
| Cell Type | Sources | Advantages | Limitations | Key Efficacy Findings |
|---|---|---|---|---|
| MSCs | Bone marrow, adipose tissue, umbilical cord | Strong immunomodulation; paracrine signaling (VEGF, HGF); low immunogenicity [1] [26] | Low survival post-transplantation (<10%); functional heterogeneity [1] [65] | LVEF improvement: 2.77–4.15% (vs. controls); reduced infarct size [66] |
| iPSCs | Reprogrammed somatic cells | Autologous transplantation; high cardiomyocyte purity (95%); no ethical concerns [15] [1] | Tumorigenic risk; epigenetic memory bias [15] [3] | Improved myocardial perfusion in 4/5 patients (jRCT2052190081 trial) [1] |
| CSCs | Adult heart tissue | Direct cardiac differentiation; exosome-mediated repair (e.g., miR-146a) [15] [1] | Limited cell availability; insufficient natural repair [26] | LVEF improvement in murine models; paracrine-driven angiogenesis [26] |
| BMMNCs | Bone marrow | Ease of isolation; autologous use [15] [26] | Limited differentiation capacity; variable efficacy [15] | Marginal LVEF improvements in clinical trials [15] |
Mechanistic Insights:
- MSCs primarily act via paracrine effects, secreting exosomes containing miRNAs (e.g., miR-21, miR-210) to reduce apoptosis and fibrosis [1] [65].
- iPSCs differentiate into functional cardiomyocytes but require rigorous tumorigenicity monitoring [1] [3].
- CSCs promote endothelial tube formation and inhibit fibrosis through exosome release [1].
Delivery Routes: Efficacy and Protocols
Delivery methods directly impact cell retention, survival, and functional outcomes. The most common routes include intracoronary (IC) infusion, intramyocardial (IM) injection, and intravenous (IV) administration [26] [66].
Table 2: Delivery Route Comparisons
| Route | Procedure | Advantages | Limitations | Efficacy Data |
|---|---|---|---|---|
| Intracoronary | Infusion via catheter during angiography | High cell retention in infarcted tissue; uniform distribution [66] | Risk of microvascular occlusion; requires specialized equipment [66] | LVEF improvement: MD = 4.27% (P < 0.0001) [66] |
| Intramyocardial | Direct injection into myocardium (surgical/transendocardial) | Localized delivery; bypasses systemic circulation [26] | Invasive; risk of arrhythmias; uneven distribution [66] | Variable LVEF benefits in trials [26] |
| Intravenous | Systemic infusion via peripheral vein | Non-invasive; simple administration [66] | Low cardiac retention (<5%); entrapment in lungs/liver [66] | No significant LVEF improvement [66] |
Protocol 1: Intracoronary MSC Delivery
- Cell Preparation: Isolate and expand clinical-grade MSCs (e.g., from bone marrow or umbilical cord) under GMP conditions. Confirm surface markers (CD73+/CD90+/CD105+; CD14-/CD19-/CD34-/CD45-/HLA-DR-) via flow cytometry [65] [66].
- Administration:
- Perform coronary angiography to identify infarct-related artery.
- Dilate the artery using a balloon catheter (over-the-wire system).
- Infuse (1–2 \times 10^7) cells in 10–20 mL saline over 10–15 minutes [66].
- Post-Procedure Monitoring: Assess LVEF via cardiac MRI at 1, 6, and 12 months; monitor for MACE (e.g., arrhythmias, recurrent MI) [66].
Protocol 2: Intramyocardial iPSC-Derived Cardiomyocyte Injection
- Cell Differentiation: Differentiate iPSCs into cardiomyocytes using directed differentiation protocols (e.g., ACTIVIN-A/BMP4). Achieve >90% purity (cardiac troponin T+) [1] [3].
- Surgical Delivery:
- Use a transendocardial injection system (e.g., MyoStar) with electromapping.
- Inject (5–10 \times 10^6) cells into 10–15 peri-infarct sites [3].
- Safety Checks: Monitor for arrhythmias (telemetry); assess tumorigenicity via serial imaging [3].
Signaling Pathways and Experimental Workflows
Stem cell mechanisms involve critical pathways such as paracrine signaling, angiogenesis, and anti-apoptosis. The diagram below illustrates the workflow for comparing MSC types in MI models:
Title: Workflow for Comparing MSC Efficacy in MI Models
Key Pathways:
- Paracrine Signaling: MSCs secrete VEGF, FGF, and HGF to promote angiogenesis [1] [65].
- Anti-Apoptosis: miR-133a-transfected MSCs inhibit caspase-3/9, reducing cardiomyocyte death [67].
- Angiogenesis: UCMSCs upregulate VEGF, enhancing tube formation in HUVECs [65].
Research Reagent Solutions
Table 3: Essential Reagents for Stem Cell MI Studies
| Reagent/Cell Type | Function | Example Use |
|---|---|---|
| Clinical-Grade MSCs (UCMSCs/ADMSCs) | Cardiac repair via paracrine effects | Compare tissue-specific efficacy in murine MI models [65] |
| miR-133a Lentivirus (≥1×10^9 TU/mL) | Enhance MSC survival and anti-fibrotic effects | Transfect BM-MSCs to reduce apoptosis [67] |
| Matrigel | Assess angiogenic potential in vitro | Tube formation assays with HUVECs [65] |
| Cardiac Troponin T Antibodies | Validate iPSC-CM differentiation | Flow cytometry/purity checks [3] |
| SYBR Green qPCR Kits | Quantify gene expression (e.g., VEGF, caspase-3) | Analyze pathway activation in infarcted tissue [67] |
The selection of stem cell type and delivery route profoundly influences MI therapy outcomes. MSCs (particularly ADMSCs) excel in anti-apoptosis, while iPSCs offer long-term regeneration potential. Intracoronary delivery maximizes cell retention and functional improvement. Standardized protocols and rigorous pathway analyses are critical for translating preclinical findings into clinical applications.
Correlating Cell Culture Duration and Injected Dose with Functional Outcomes
In the field of stem cell therapy for acute myocardial infarction (AMI), optimizing technical parameters is crucial for translating preclinical promise into clinical efficacy. Among these parameters, cell culture duration and injected cell dose represent critical process variables that directly impact therapeutic outcomes. This Application Note synthesizes current evidence to establish correlations between these key technical parameters and functional outcomes, providing validated protocols for researchers developing myocardial regeneration therapies.
Evidence from a comprehensive systematic review and meta-analysis of 79 randomized controlled trials (n=7,103 patients) demonstrates that specific combinations of culture duration and cell dosage significantly enhance left ventricular ejection fraction (LVEF) at 6, 12, 24, and 36 months post-transplantation [68]. The most pronounced benefits occur with long cell culture durations exceeding one week combined with high injected cell quantities of at least 10^8 cells [68].
Quantitative Data Synthesis
Table 1: Correlation Between Cell Culture Parameters and Functional Outcomes in AMI
| Parameter | Classification | LVEF Improvement (%) | Statistical Significance | Key Findings |
|---|---|---|---|---|
| Culture Duration | >1 week | Significant | p<0.001 | Associated with most significant LVEF improvements [68] |
| ≤1 week | Variable | Not significant | Inconsistent functional outcomes | |
| Injected Cell Dose | ≥10^8 cells | Significant | p<0.001 | Synergistic effect with extended culture duration [68] |
| <10^8 cells | Modest | Variable | Dose-dependent response observed | |
| Transplantation Timing | Within first week post-AMI | 5.74% | p<0.001 [69] | Most pronounced effect when performed early after AMI |
| Beyond first week | 3.78% | p<0.001 [69] | Still significant but reduced effect | |
| Administration Protocol | Single injection | 4.54±2% (CMR) | p<0.001 [70] | Significant improvement over control |
| Double injection (10-day interval) | 7.45±2% (CMR) | p<0.001 [70] | Booster dose augments therapeutic effect |
Table 2: Efficacy by Stem Cell Type and Delivery Method
| Cell Type | LVEF Improvement | Key Advantages | Clinical Evidence |
|---|---|---|---|
| Mesenchymal Stem Cells (MSCs) | 3.78-5.74% [69] | Paracrine effects, immunomodulation, easy availability | Most widely studied; consistent efficacy |
| Wharton's Jelly MSCs | 4.54-7.45% [70] | Lower immunogenicity, higher replication rate | Superior in direct comparative assessments |
| Bone Marrow Mononuclear Cells | ~2.72% [69] | Ease of preparation, no culture required | Modest but significant improvement |
| CD133+ Cells | Significant improvement [71] | Promotes angiogenesis, reduces non-viable segments | Shown superior to mononuclear cells in some trials |
| CD34+ Cells | Not statistically significant [71] | Endothelial differentiation potential | Limited efficacy in clinical studies |
Experimental Protocols
Protocol: Optimizing Cell Culture Duration for Maximum Efficacy
Principle: Extended culture periods allow for adequate cell expansion to achieve therapeutic doses while potentially enhancing cell potency through conditioning.
Materials:
- GMP-certified cell culture facility
- Mesenchymal Stem Cells (bone marrow, adipose tissue, or Wharton's jelly-derived)
- Appropriate culture media with growth factor supplements
- Cell counting equipment (automated or manual)
- Quality control assays (flow cytometry, viability staining)
Procedure:
- Isolation and Initial Culture: Isolate MSCs from source tissue using standard enzymatic digestion or density gradient centrifugation protocols
- Culture Expansion: Maintain cells in appropriate culture conditions (37°C, 5% CO₂) with regular media changes every 2-3 days
- Extended Culture Protocol: Continue culture for >7 days (typically 10-14 days total) to achieve both adequate cell numbers and enhanced therapeutic potential [68]
- Quality Assessment: Verify MSC markers (CD73, CD90, CD105) and absence of hematopoietic markers (CD34, CD45) via flow cytometry
- Harvesting: Detach cells using gentle enzymatic treatment when target cell numbers are achieved
- Formulation: Prepare final cell product in appropriate transplantation medium (e.g., 0.9% normal saline with human serum albumin)
Validation Points:
- Cell viability >90% pre-transplantation (verified with methylene blue exclusion test) [70]
- Maintenance of MSC phenotype throughout culture period
- Absence of microbial contamination
Protocol: Intracoronary Administration with Optimized Cell Dosing
Principle: Direct coronary delivery ensures maximal engraftment in infarcted myocardium while optimized dosing balances efficacy with safety.
Materials:
- GMP-certified clinical-grade stem cells (≥10^8 cells for optimal effect) [68]
- 0.9% normal saline transplantation medium
- 6-Fr guiding catheter
- 0.014-inch soft-tipped guidewire
- Over-the-wire balloon catheter
- Standard catheterization laboratory equipment
Procedure:
- Patient Selection: Include patients 3-7 days post-AMI with successful primary PCI and LVEF <40% [70]
- Cell Preparation: Transport fresh clinical-grade cells to catheterization laboratory on day of procedure
- Coronary Access: Insert guiding catheter into left main artery under fluoroscopic guidance
- Vessel Preparation: Administer 200μg intracoronary nitroglycerin to prevent vasospasm
- Balloon Occlusion: Position and inflate over-the-wire balloon within previously stented area (2-4 bar pressure)
- Cell Infusion:
- Divide total cell dose into three equal portions
- Infuse each portion at 2.5 mL/min through infusion catheter
- Confirm arterial occlusion before each infusion via dye injection
- Assess TIMI coronary flow between infusions
- Booster Dose Consideration: For enhanced effect, repeat infusion 10 days after initial transplantation [70]
Safety Monitoring:
- Daily physical examination and vital signs during hospitalization
- Laboratory tests: FBS, CBC, urea and electrolytes, liver function tests
- Arrhythmia monitoring via telemetry
- Assessment for pulmonary embolism and coronary artery injury
Signaling Pathways and Experimental Workflows
Mechanistic Relationship Between Culture Parameters and Functional Outcomes
Experimental Workflow for Optimized Stem Cell Therapy
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Stem Cell Therapy Development
| Reagent/Category | Function | Application Notes |
|---|---|---|
| GMP-certified MSCs | Therapeutic agent | Source matters: Wharton's jelly MSCs show superior efficacy with lower immunogenicity [70] |
| Cell Culture Media | Cell expansion | Must support maintenance of MSC phenotype during extended (>7 day) culture [68] |
| Flow Cytometry Antibodies | Quality control | Verify CD73, CD90, CD105 positivity; CD34, CD45 negativity [69] |
| Viability Assays | Cell quality assessment | Methylene blue exclusion testing pre-transplantation; target >90% viability [70] |
| Transplantation Medium | Cell delivery vehicle | 0.9% normal saline with human serum albumin; prepared day of procedure [70] |
| Intracoronary Delivery System | Cell administration | Balloon occlusion catheter for targeted delivery to infarcted territory [70] |
The correlation between cell culture duration, injected dose, and functional outcomes in stem cell therapy for AMI follows a clear pattern: extended culture periods exceeding one week combined with higher cell doses (≥10^8 cells) yield the most significant improvements in LVEF [68]. Furthermore, the administration protocol—specifically the option for a booster dose 10 days after initial transplantation—can augment therapeutic effects, with repeated intervention demonstrating substantially greater efficacy (7.45% LVEF improvement vs. 4.54% for single transplantation) [70].
These findings provide a methodological framework for researchers optimizing stem cell therapies for myocardial infarction, emphasizing that precise control of technical parameters is equally important as biological selection of cell types. Future protocol development should focus on standardizing these critical parameters while maintaining flexibility for emerging evidence from clinical trials.
Conclusion
Stem cell transplantation represents a paradigm shift in the therapeutic approach to myocardial infarction, moving beyond symptomatic management toward genuine cardiac regeneration. The synthesis of evidence confirms that while stem cell therapy is generally safe and can provide sustained improvement in cardiac function, its efficacy is significantly influenced by cell type selection, delivery methodology, and treatment timing. The future of the field lies in overcoming the critical challenge of poor cell survival through innovative combinatorial strategies, such as the use of exosomes, bioengineered patches, and genetic modification. For researchers and drug developers, the priority must be standardizing protocols, personalizing cell-based treatments, and integrating these advanced regenerative strategies with evolving biomedical engineering platforms. Collaborative, multidisciplinary efforts are essential to translate these promising techniques into routine clinical applications that can fundamentally improve outcomes for MI patients.
References
- 1. Stem cell therapy for myocardial infarction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512856/]
- 2. Mesenchymal Stem Cell Therapy for Acute Myocardial ... [https://www.researchprotocols.org/2025/1/e60591]
- 3. Cardiac repair and regeneration: cell therapy, in vivo ... [https://www.nature.com/articles/s12276-025-01549-3]
- 4. Acute Myocardial Infarction: Molecular Pathogenesis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12501504/]
- 5. Induced pluripotent stem cell-derived mesenchymal stem cells [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03968-x]
- 6. 间充质干细胞治疗心肌梗æ»çš„ç ”ç©¶è¿›å±• [https://journal11.magtechjournal.com/Jwk_jcyxylc/CN/10.16352/j.issn.1001-6325.2023.01.0021]
- 7. Bone marrow mesenchymal stem cells stimulate cardiac ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3408082/]
- 8. Cardiac Repair and Mesenchymal Stem Cells [https://pubmed.ncbi.nlm.nih.gov/40760749/]
- 9. Induced Pluripotent Stem Cell-Derived Cardiomyocytes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10815661/]
- 10. Human induced pluripotent stem cell-derived ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1687840/full]
- 11. 综述:心肌梗æ»åŽå¿ƒè‚Œç»†èƒžå†ç”Ÿçš„ç ”ç©¶è¿›å±• [https://www.ebiotrade.com/newsf/2025-3/20250318051238072.htm]
- 12. 干细胞移æ¤åœ¨å¿ƒè‚Œæ¢—æ»åº”用ä¸çš„ç ”ç©¶è¿›å±• [http://dianda.cqvip.com/Qikan/Article/Detail?id=37822273]
- 13. Current status and new horizons in stem cell therapy in ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03018-z]
- 14. Stem cell therapy for myocardial infarction and atherosclerosis [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04678-8]
- 15. A comprehensive review of clinical trials and progress in ... [https://www.sciencedirect.com/science/article/pii/S2352320425001944]
- 16. Paracrine Signalling - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/paracrine-signalling]
- 17. Paracrine signaling in cancer-associated fibroblasts [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06744-4]
- 18. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 19. Cardiac differentiation roadmap for analysis of plasticity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11960529/]
- 20. Enhancing human pluripotent stem cell differentiation to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12124670/]
- 21. Angiogenic signaling pathways and anti- ... - Nature [https://www.nature.com/articles/s41392-023-01460-1]
- 22. Decoding tumor angiogenesis: pathways, mechanisms ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00779-x]
- 23. Two promising approaches in the treatment of myocardial ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1540066/full]
- 24. Extracellular matrix remodeling in tumor progression and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10007858/]
- 25. Extracellular matrix: unlocking new avenues in cancer treatment [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00757-3]
- 26. Stem Cell Therapy for Myocardial Infarction Recovery [https://www.mdpi.com/2227-9059/13/5/1209]
- 27. Stem Cell IV Therapy - A Comprehensive Guide (2025) [https://www.dvcstem.com/post/stem-cell-iv-therapy]
- 28. How to Prepare for an Allogeneic Stem Cell Transplant [https://int.livhospital.com/allogeneic-stem-cell-transplant-4/]
- 29. Efficacy & safety of stem cell therapy for treatment of acute ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550445/]
- 30. Systematic Review and Meta-Analysis of Stem Cell ... [https://www.medrxiv.org/content/10.1101/2025.08.25.25334375v1.full]
- 31. Intramyocardial Injection of Autologous Bone Marrow ... [https://link.springer.com/article/10.1007/s12265-013-9507-7]
- 32. Efficacy & safety of stem cell therapy for treatment of acute ... [https://ijmr.org.in/efficacy-safety-of-stem-cell-therapy-for-treatment-of-acute-myocardial-infarction-a-systematic-review-meta-analysis/]
- 33. Postinfarct intramyocardial injection of mesenchymal stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2904155/]
- 34. Safety and efficacy of stem cell therapy in acute myocardial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12207128/]
- 35. Mid- to long-term efficacy and safety of stem cell therapy for ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03891-1]
- 36. Application of Hydrogels in Cardiac Regeneration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10703752/]
- 37. Nanotechnology-Driven Cardiac Tissue Engineering and ... [https://www.sciencedirect.com/science/article/pii/S2666978125000844]
- 38. Stem cell-derived cell sheet transplantation for heart tissue ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-019-1536-y]
- 39. 3D Bioprinting Functional Engineered Heart Tissues [https://pubmed.ncbi.nlm.nih.gov/41226748/]
- 40. IDIBELL researchers generate heart tissue by 3D ... [https://idibell.cat/en/2025/06/idibell-researchers-generate-heart-tissue-by-3d-bioprinting-for-the-first-time/]
- 41. Effect of Timing of Stem Cell Delivery Following ST ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5805626/]
- 42. Rational transplant timing and dose of mesenchymal stromal ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-016-0450-9]
- 43. study protocol of a phase III randomized clinical trial (Prevent ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-022-06594-1]
- 44. Cell survival and redistribution after transplantation into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3822744/]
- 45. Strategies to promote donor cell survival: Combining ... [https://www.sciencedirect.com/science/article/abs/pii/S0022282808004185]
- 46. Stem Cellâ€Based Therapy for the Treatment of Ischemic Stroke [https://pmc.ncbi.nlm.nih.gov/articles/PMC6495668/]
- 47. Cell isolation procedures matter: a comparison of different ... [https://www.stemcell.com/cell-isolation-procedures-matter-a-comparison-of-different-isolation-protocols-of-bone-marrow-mononuclear-cells-used-for-cell-therapy-in-patients-with-acute-myocardial-infarction.html]
- 48. Toward Cardiac Regeneration: Combination of Pluripotent ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2020.00455/full]
- 49. Advances in mesenchymal stem cell and exosome-based ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04318-1]
- 50. Combinatorial treatment of acute myocardial infarction using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6785902/]
- 51. Regenerative topical skincare: stem cells and exosomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC11518787/]
- 52. Clinical applications of stem cell-derived exosomes [https://www.nature.com/articles/s41392-023-01704-0]
- 53. Engineering strategies and optimized delivery of exosomes for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10405842/]
- 54. Recent advances in extracellular vesicles for therapeutic ... [https://www.nature.com/articles/s12276-024-01201-6]
- 55. An optimized exosome production strategy for enhanced ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-022-01668-3]
- 56. Myocardial infarction serum preconditioning bone marrow ... [https://pubmed.ncbi.nlm.nih.gov/40169467/]
- 57. “Advancing cardiac patch viability and functionality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515126/]
- 58. Non-invasive and non-destructive characterization of tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4792694/]
- 59. A scientometric and visualization analysis of 3D printing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11585479/]
- 60. Cardiomyocyte regeneration therapy and its effect on LVEF ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12403498/]
- 61. Efficacy of mesenchymal stem cell transplantation on major ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05352-y]
- 62. Arrhythmogenic Risks of Stem Cell Replacement Therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7286806/]
- 63. Arrhythmogenic Risk in iPSC-Derived Cardiomyocytes [https://www.mdpi.com/1648-9144/61/11/2056]
- 64. Safety and Efficacy of Adult Stem Cell Therapy for Acute ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6265630/]
- 65. The therapeutic efficacy comparison of MSCs derived different ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04378-3]
- 66. Impact of mesenchymal stem cell therapy on cardiac function ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322349/]
- 67. Therapeutic potential of miR-133a-transfected bone marrow ... [https://cardiothoracicsurgery.biomedcentral.com/articles/10.1186/s13019-025-03367-0]
- 68. Mid- to long-term efficacy and safety of stem cell therapy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11389242/]
- 69. Mesenchymal stem cell transplantation after acute myocardial ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02667-1]
- 70. Effect of once versus twice intracoronary injection of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03495-1]
- 71. Factors Affecting Outcomes of Bone Marrow Stem Cell ... [https://gmr.scholasticahq.com/article/57047-factors-affecting-outcomes-of-bone-marrow-stem-cell-therapy-for-acute-myocardial-infarction]