Strategic Approaches to Enhance Stem Cell Engraftment: From Foundational Concepts to Clinical Translation
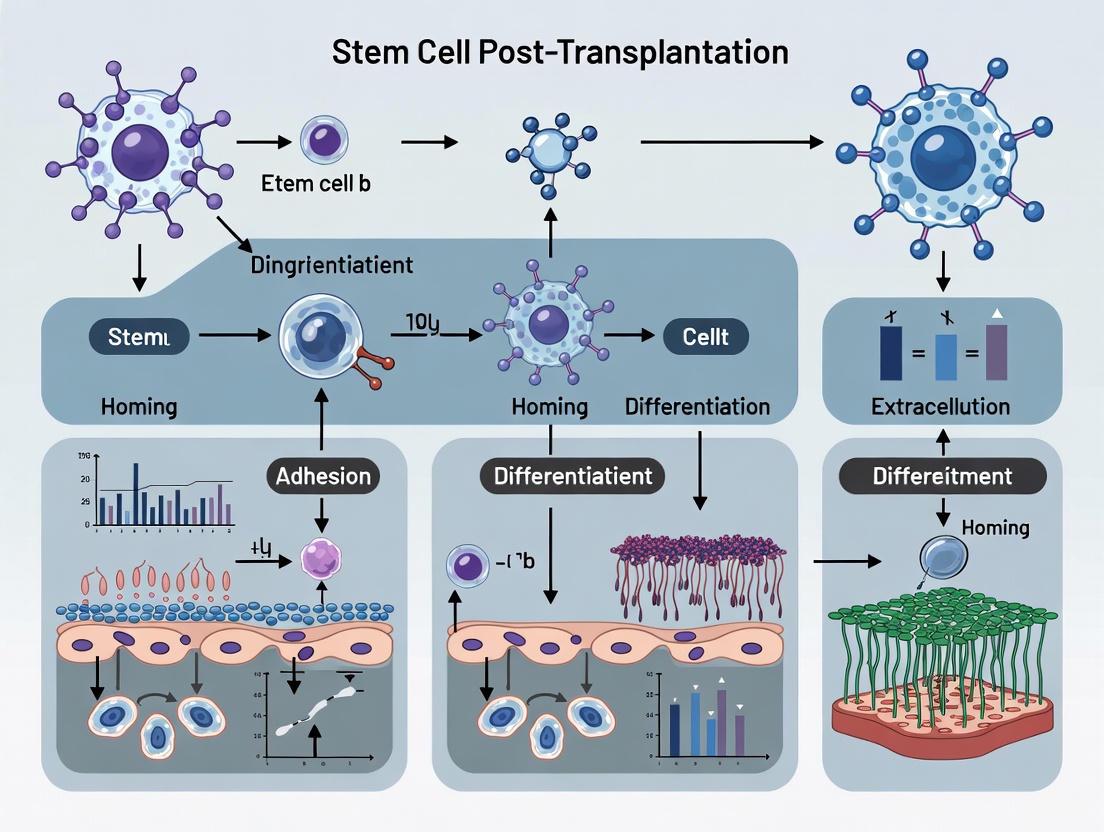
This article provides a comprehensive analysis of current strategies to improve stem cell engraftment post-transplantation, a critical determinant of therapeutic success.
Strategic Approaches to Enhance Stem Cell Engraftment: From Foundational Concepts to Clinical Translation
Abstract
This article provides a comprehensive analysis of current strategies to improve stem cell engraftment post-transplantation, a critical determinant of therapeutic success. Tailored for researchers, scientists, and drug development professionals, it synthesizes foundational biology, methodological advances, optimization protocols, and validation frameworks. The scope spans from the fundamental mechanisms of homing and survival to the application of pharmacological agents, cellular preconditioning, computational modeling, and comparative efficacy data, offering an integrated perspective on overcoming the translational barrier of low engraftment rates in regenerative medicine.
The Engraftment Challenge: Understanding the Biological Barriers to Stem Cell Survival and Integration
Core Metrics for Engraftment Success
Engraftment success is not defined by a single metric but by a combination of clinical, laboratory, and patient-reported outcomes that provide a comprehensive picture of the therapy's impact [1]. These evaluations assess both short-term and long-term benefits.
The table below summarizes the key quantitative and functional metrics used to define successful engraftment in research and clinical trials.
| Metric Category | Specific Metric | Measurement Method/Tool | Interpretation of Success |
|---|---|---|---|
| Cell Survival & Kinetics | Cell viability post-transplantation | Bioluminescence imaging, PCR-based cell tracking [2] | High percentage of cells surviving the initial hostile microenvironment; up to 90% can be lost early [2]. |
| Rate of blood cell recovery | Complete Blood Count (CBC) [3] | Sustained neutrophil and platelet count recovery to specific, predefined levels. | |
| Functional Integration | Hematopoietic recovery | Donor chimerism analysis [3] | Establishment of donor-derived hematopoiesis. |
| Tissue-specific function | Organ-specific functional tests (e.g., Echocardiogram for heart function) [4] | Improvement in the functional capacity of the target tissue or organ. | |
| Clinical Endpoints | Overall Survival | Patient follow-up over years [4] | Long-term patient survival post-transplant; e.g., 79% survival rate at 3 years for some hematopoietic transplants [4]. |
| Disease Progression | Clinical assessments, imaging (MRI, PET scans) [4] | Absence of disease recurrence or progression; e.g., reduced risk of heart attack or stroke [4]. | |
| Quality of Life (QoL) | Patient-Reported Outcomes (PROMIS surveys) [3] [4] | Patient-reported improvements in stamina, cognitive function, and social well-being [1] [4]. | |
| Biomarker & Paracrine Activity | Reduction of Inflammation | Biomarker assays (e.g., for IL-6, TNF-alpha) [1] | Significant decrease in systemic inflammatory markers. |
| Promotion of Angiogenesis | Assays for factors like VEGF [2] | Increased secretion of pro-angiogenic factors, indicating active tissue repair. |
Frequently Asked Questions: Troubleshooting Engraftment
What are the primary causes of poor cell survival post-transplantation, and how can they be mitigated?
The hostile transplantation microenvironment is a major contributor to massive cell death, with studies indicating that up to 90% of transplanted stem cells can undergo apoptosis within the first few days [2]. The primary stressors and corresponding mitigation strategies are:
Metabolic Crisis & Ischemia: The lack of immediate vascular connection leads to severe hypoxia and nutrient deprivation [2].
- Troubleshooting Strategy: Implement metabolic preconditioning, such as hypoxic preconditioning (1-5% O₂), which upregulates pro-survival genes (e.g., VEGF, GLUT-1) and antioxidant enzymes, enhancing the cells' anti-apoptotic capacity [2]. Supplementation with oxygen-releasing materials like perfluorocarbon (PFC)-hydrogel systems can also provide temporary metabolic support [2].
Oxidative Stress: The sudden shift from in vitro culture to the damaged tissue site creates a reactive oxygen species (ROS) imbalance [2].
- Troubleshooting Strategy: Use genetic modifications to boost endogenous antioxidant defenses or deliver exogenous ROS-scavenging components alongside the cells [2].
Lack of Physically Supportive Niche: Traditional 2D cell injections do not provide a structured, tissue-like environment.
- Troubleshooting Strategy: Employ 3D culture techniques, such as generating stem cell spheroids or using biomaterial scaffolds. These 3D architectures enhance cell-cell signaling and preserve differentiation potential, leading to better engraftment in vivo [2].
How is successful engraftment measured in clinical trials for different disease areas?
Success is measured through a composite of endpoints tailored to the specific disease.
For Hematological Malignancies (e.g., blood cancers):
For Regenerative Medicine (e.g., joint repair, autoimmune conditions):
For Cardiac Conditions:
- Key Metrics: Reduction in major adverse cardiac events (e.g., one trial showed a 58% reduction in heart attack or stroke risk), improvement in heart function measured by ejection fraction, and reduced hospitalization rates [4].
What patient-specific factors critically influence engraftment success, and how are they screened?
Patient selection is a critical determinant of outcomes. Key eligibility factors and pre-treatment assessments include [4]:
- Overall Health and Comorbidities: Tools like the Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI) are used. Patients with a score of 0 (no comorbidities) have significantly better survival rates.
- Inflammation Status: C-reactive protein (CRP) levels are a key biomarker. Normal CRP levels (0-9 mg/L) pre-transplant are associated with better outcomes.
- Donor Age (for allogeneic transplants): A study of 10,000 unrelated donor transplants found that younger donors consistently led to better patient outcomes due to greater regenerative potential of their cells [4].
- Pre-Treatment Workup: This involves comprehensive diagnostic tests, including advanced imaging (X-rays, CT, PET, MRI), and functional assessments of the heart, lungs, and kidneys [4].
Advanced Experimental Protocols for Enhancing Engraftment
Protocol 1: Metabolic Preconditioning of Stem Cells
This protocol aims to enhance stem cell resilience to the ischemic transplant microenvironment.
- Cell Culture: Expand human Mesenchymal Stem Cells (MSCs) in standard culture conditions.
- Hypoxic Preconditioning: Place cells in a hypoxic chamber with 1-5% O₂ for 48 hours [2].
- Mechanism: This activates Hypoxia-Inducible Factor (HIF-1α), which upregulates:
- Pro-survival genes (VEGF, GLUT-1).
- Antioxidant enzymes (e.g., SOD2).
- Induces a metabolic shift from oxidative phosphorylation to glycolysis [2].
- Validation: Preconditioned cells show twice the survival rate under serum-deprived conditions compared to normoxic (20% O₂) controls [2].
Protocol 2: Utilizing 3D Spheroids for Transplantation
3D spheroids mimic the in vivo environment more closely than single-cell suspensions.
- Spheroid Generation: Use low-attachment plates or hanging drop methods to aggregate MSCs into 3D spheroids.
- Advantages: The 3D architecture:
- Preserves multidirectional differentiation potential.
- Enhances cell-cell and cell-matrix signaling.
- Results in cellular characteristics that more closely resemble those observed in vivo, improving survival and integration post-transplantation [2].
- Transplantation: Administer the intact spheroids to the target site using specialized delivery devices.
Research Reagent Solutions for Engraftment Studies
The table below lists key reagents and materials used in advanced engraftment research.
| Reagent/Material | Function in Engraftment Research | Example Application |
|---|---|---|
| Perfluorocarbons (PFCs) | Oxygen carriers with high oxygen solubility (15-20x greater than water) to mitigate post-transplant hypoxia [2]. | Incorporated into hydrogel systems to create oxygen-releasing scaffolds that support cell survival in ischemic environments [2]. |
| Calcium Peroxide (CaO₂) | Solid peroxide for sustained oxygen generation via controlled decomposition [2]. | Embedded in PEGDA-based oxygen-producing microspheres to elevate local oxygen levels for 16-20 hours [2]. |
| Hypoxia-Inducible Factor (HIF-1α) Activators | Pharmacological agents to mimic hypoxic preconditioning and upregulate pro-survival pathways [2]. | Used in vitro to pre-condition stem cells before transplantation, enhancing their tolerance to ischemia. |
| ROS-Scavenging Nanoparticles | Mitigate oxidative stress by neutralizing excess Reactive Oxygen Species (ROS) at the transplant site [2]. | Co-delivered with stem cells to improve viability by reducing ROS-mediated cellular damage. |
| Engineered Hydrogel Scaffolds | Provide a biomimetic 3D structure that supports cell attachment, protects from physical stress, and can be loaded with biological factors [2]. | Used as a delivery vehicle for stem cells to create large-scale tissue constructs and support vascular ingrowth. |
Strategic Pathways to Enhance Engraftment
The following diagram illustrates the logical relationship between the major challenges in stem cell engraftment and the corresponding strategic solutions.
FAQs and Troubleshooting Guides
Q1: Why are my administered stem cells failing to reach the target tissue in significant numbers?
A: Low homing efficiency is a common challenge, often stemming from poor cell quality or an inadequate chemokine gradient.
- Potential Cause 1: The stem cells were damaged during harvesting or handling. Enzymatic detachment (e.g., with trypsin) can cleave crucial surface receptors like CXCR4, making cells unresponsive to homing signals [6] [7] [8].
- Solution: Use gentler cell dissociation reagents such as TrypLE, Versene, or EDTA-based solutions to preserve surface receptors [7] [8]. Perform a viability assay and check for CXCR4 expression via flow cytometry before infusion.
- Potential Cause 2: The target tissue does not emit a strong enough "homing signal." The key chemokine SDF-1 is often inactivated under normal conditions [9].
- Solution: Prime the target tissue. Strategies include direct injection of a degradation-resistant version of SDF-1 into the injury site [9] or using drugs to keep endogenous SDF-1 active [9].
Q2: My transwell migration assay results are inconsistent. What could be wrong?
A: Inconsistent results often arise from suboptimal assay conditions.
- Potential Cause 1: The cell density seeded in the upper chamber is too high or too low [6] [7].
- Solution: Titrate the cell seeding density. High densities can saturate the membrane pores, while low densities provide insufficient data points. A general starting range is 1x10^5 to 3x10^5 cells/mL [7].
- Potential Cause 2: The cells are proliferating instead of just migrating, skewing the results [7].
- Solution: Serum-starve cells (e.g., using 0.1-1% FBS media) for 24-48 hours before the assay to synchronize the cell cycle and reduce proliferation-driven movement [6] [7]. Alternatively, use a low concentration of Mitomycin C to inhibit proliferation, but be aware of its potential impact on RNA and protein synthesis [7].
- Potential Cause 3: The chemoattractant concentration or migration time is not optimized [6].
- Solution: Always include a positive control (a known potent chemoattractant) and a negative control (no chemoattractant) to benchmark your experimental results [6]. Titrate both the chemoattractant concentration and the incubation time to find the optimal window for your specific cell type.
Q3: What are the proven strategies to enhance the homing efficiency of Mesenchymal Stem Cells (MSCs)?
A: Enhancing homing is a multi-pronged approach focusing on the cell, the target, and the route.
- Strategy 1: Cell Priming and Engineering. Treat MSCs before infusion to make them more responsive. This can be done pharmacologically (e.g., with drugs that stimulate the SDF-1/CXCR4 pathway) [9] or genetically (e.g., by overexpressing CXCR4 or adhesion molecules like VLA-4) [10] [11]. Chemical modification of the cell surface, such as adding specific sugar molecules to enhance binding, is also effective [9].
- Strategy 2: Target Tissue Modification. Increase the "pull" signal from the injury site. As mentioned, this involves upregulating or stabilizing key homing chemokines like SDF-1 at the target tissue [9] [10].
- Strategy 3: Direct Administration. While systemic infusion is common, local implantation or injection of MSCs at the target site (non-systemic homing) bypasses the circulatory system and can significantly improve local cell retention [10].
Key Data and Experimental Outcomes
Table 1: Clinical Impact of MSC Infusion on Engraftment Times
This table summarizes the average engraftment times from a systematic review of 47 clinical studies on using MSCs to accelerate hematopoietic recovery after transplantation [12].
| Hematopoietic Lineage | Average Time to Engraftment (Days) with MSC Co-infusion |
|---|---|
| Neutrophils | 13.96 days |
| Platelets | 21.61 days |
Table 2: Surface Markers and Integrins Critical for MSC Homing
This table details key molecules expressed on MSCs that facilitate the homing process [10].
| Surface Marker/Integrin | Function in Homing Process | MSC Types Where Expressed |
|---|---|---|
| CD44 | Mediates initial tethering and rolling on endothelial cells | BM-MSCs, AT-MSCs |
| VLA-4 (α4β1 integrin) | Binds to VCAM-1 on endothelium; crucial for firm adhesion and transendothelial migration | BM-MSCs, AT-MSCs |
| CD90 (Thy-1) | Associated with MSC identity and immunomodulation | BM-MSCs, AT-MSCs |
| CD73 | Involved in adenosine production and immunosuppression | BM-MSCs, AT-MSCs |
| CXCR4 | Receptor for SDF-1; central for chemotactic activation | BM-MSCs, AT-MSCs |
Experimental Protocols
Protocol 1: Transwell Migration Assay for Studying Stem Cell Chemotaxis
This protocol provides a detailed methodology for assessing the migratory capacity of stem cells in response to a chemoattractant [6] [7].
Key Research Reagent Solutions:
- Transwell Permeable Supports: Cell culture inserts with a porous membrane that separates upper and lower chambers. Pore size (e.g., 8μm) must be chosen based on the cell type being studied [6].
- Chemoattractant: A chemical signal that induces cell movement (e.g., SDF-1, or media with 1-2% FBS). The concentration must be optimized [6] [7].
- Extracellular Matrix (ECM): For invasion assays, a basement membrane matrix like Corning Matrigel is used to coat the membrane, simulating the in vivo barrier a cell must degrade and invade through [6].
- Cell Dissociation Reagent: Use gentle, non-enzymatic reagents like TrypLE or EDTA to preserve cell surface receptors during harvesting [7] [8].
- Staining Solution: Crystal violet, Diff-Quik, or Calcein AM for fixing and staining migrated cells for quantification [6].
Step-by-Step Procedure:
- Preparation: Culture and maintain your stem cells, ensuring they are at 60-70% confluency before the assay. Serum-starve cells if necessary to reduce proliferation [7].
- Harvesting: Gently detach cells using a gentle dissociation reagent to preserve surface receptors. Prepare a single-cell suspension in a serum-free or low-serum medium [7].
- Assay Setup: Add the chemoattractant dissolved in medium to the lower chamber of the Transwell plate. For a negative control, use medium without chemoattractant. Seed the cell suspension into the upper chamber insert. Ensure the membrane pores are not submerged in the lower chamber fluid [6].
- Incubation: Incubate the plate at 37°C with 5% CO₂ for the optimized time (e.g., 24-48 hours for migration) [7].
- Quantification:
- For adherent cells: After incubation, gently wipe the non-migrated cells from the top of the membrane with a moist cotton swab. Fix and stain the cells that have migrated to the underside of the membrane. Image and count the stained cells using a microscope. Count multiple fields to ensure a representative average [6].
- For non-adherent cells: Collect the cells that have migrated into the lower chamber and count them using a hemocytometer or flow cytometer [6].
- Analysis: Calculate the percentage of migrated cells relative to the total number of cells seeded or as a fold-change compared to the negative control.
Protocol 2: In Vitro Priming of MSCs to Enhance Homing
This protocol outlines methods to pre-treat MSCs to increase their homing capability post-infusion [9] [10].
Step-by-Step Procedure:
- Culture MSCs: Expand MSCs (e.g., Bone Marrow-derived MSCs) in standard culture conditions until the desired passage and confluency is reached.
- Priming Treatment: Choose a priming strategy:
- Pharmacological Priming: Incubate MSCs with agents known to stimulate the SDF-1/CXCR4 pathway (e.g., certain drugs as identified in research) [9]. The concentration and duration of treatment require optimization.
- Hypoxic Priming: Culture MSCs under hypoxic conditions (e.g., 1-5% O₂) for a defined period (e.g., 24-72 hours). Hypoxia can upregulate the expression of homing receptors like CXCR4 [11].
- Cytokine Priming: Incubate MSCs with a low dose of specific cytokines (e.g., TNF-α, IFN-γ) that are known to enhance the expression of adhesion molecules and chemokine receptors [10].
- Validation: After priming, validate the success of the treatment by checking the surface expression of target receptors (e.g., CXCR4, VLA-4) using flow cytometry.
- Harvest and Infuse: Gently harvest the primed MSCs using a gentle dissociation method and proceed with systemic or local administration.
Signaling Pathways and Workflow Diagrams
Stem cell transplantation holds groundbreaking potential for treating degenerative diseases, tissue injuries, and malignancies. However, clinical outcomes often fall short of expectations, primarily due to the hostile microenvironment that transplanted cells encounter at the target site. Research indicates that up to 90% of transplanted stem cells undergo apoptosis within the initial days post-transplantation [2]. This massive cell loss stems from a complex interplay of metabolic dysfunction, immune-mediated responses, reactive oxygen species (ROS), altered biomechanical rigidity, and disrupted intercellular communication [2]. This technical support center provides targeted troubleshooting guides to help researchers overcome these critical barriers and enhance stem cell engraftment efficacy.
Troubleshooting Guide: Core Challenges and Solutions
Problem: Poor Cell Survival Due to Metabolic Crisis and Ischemia
- Question: "Why do my transplanted stem cells die so quickly, and how can I extend their viability in ischemic conditions?"
- Background: Transplanted stem cells initially lack vascular connections, leading to a severe interim phase of hypoxia and nutrient deprivation [2]. This metabolic crisis is characterized by insufficient oxygen, glucose, fatty acids, and amino acids, disrupting energy production and waste clearance [2].
- Solutions:
- Metabolic Preconditioning (Stem Cell Domestication): Pre-adapt cells to harsh conditions in vitro before transplantation. Hypoxic preconditioning (1-5% O₂) activates HIF-1α, upregulating pro-survival genes (VEGF, GLUT-1) and antioxidant enzymes. This can double the survival rate of MSCs under serum-deprived conditions compared to normoxic controls [2].
- Oxygen Supplementation: Employ advanced oxygen-delivery systems to bridge the gap until host vasculature integrates.
- Perfluorocarbons (PFCs): Use PFC-hydrogel systems for their high oxygen solubility (15-20 times greater than water) to enhance oxygen-carrying capacity and prolong release [2].
- Peroxide-based Systems: Utilize calcium peroxide (CaO₂) or H₂O₂-releasing nanoparticles for sustained oxygen generation. CaO₂ microspheres can elevate dissolved oxygen in culture media for 16-20 hours under oxygen-glucose deprivation [2].
Problem: Excessive Oxidative Stress Damaging Transplanted Cells
- Question: "How can I protect stem cells from the burst of reactive oxygen species (ROS) in the transplantation site?"
- Background: The abrupt transition from optimized in vitro conditions to the pathological oxidative environment of damaged tissues overwhelms the intrinsic antioxidant capacity of stem cells, leading to redox imbalance and death [2].
- Solutions:
- Genetic Modification: Enhance endogenous antioxidant defenses through CRISPR/Cas9 or viral vector-mediated overexpression of genes encoding for antioxidant enzymes like superoxide dismutase (SOD) [2].
- Antioxidant Administration: Deliver ROS-scavenging components directly or via engineered carriers. The use of MitoTempol, a mitochondrial-targeted antioxidant, has been shown to mitigate oxidative stress in MSCs [13].
- Nanoparticle Engineering: Utilize engineered nanoparticles like poly(ethylene glycol)-modified Zinc Oxide Nanoparticles (PZnONPs). In acidic lysosomal environments, these particles release Zn²⁺ and controlled levels of ROS, which can paradoxically enhance stem cell paracrine signaling and improve viability in the inflammatory microenvironment [14].
Problem: Hostile Immune Response and Immune Rejection
- Question: "How can I prevent allogeneic stem cells from being rejected by the host immune system?"
- Background: While MSCs have low immunogenicity, their allogeneic application can still trigger host immune recognition and rejection, primarily mediated by Major Histocompatibility Complex Class I (MHC-I) molecules and pro-inflammatory immune cells [15].
- Solutions:
- CRISPR/Cas9 for Immune Evasion: Create "immune stealth" stem cells by knocking out beta-2 microglobulin (β2M), a crucial subunit of the MHC-I complex. This significantly reduces HLA class I surface expression, evading recognition by alloreactive CD8+ T-cells and improving engraftment [15].
- Preconditioning with Inflammatory Cytokines: Prime MSCs with cytokines like Interferon-gamma (IFN-γ) to enhance their immunomodulatory potency. This upregulates the expression of anti-inflammatory mediators like indoleamine 2,3-dioxygenase (IDO), strengthening their ability to suppress T-cell proliferation [16] [15].
- Biomaterial Encapsulation: Use 3D hydrogel scaffolds or microspheres to create a physical barrier that shields cells from immediate immune attack while allowing nutrient and waste exchange [2].
Problem: Inadequate Paracrine Signaling and Therapeutic Function
- Question: "My stem cells survive but fail to exert sufficient therapeutic effects. How can I boost their paracrine function?"
- Background: The therapeutic benefits of MSCs are largely mediated by their paracrine release of bioactive molecules (growth factors, cytokines, extracellular vesicles). A hostile microenvironment can suppress this essential function [16] [17].
- Solutions:
- Disease Microenvironment Preconditioning (DMP): Precondition MSCs in vitro using serum from diseased animals, specific inflammatory cytokines (e.g., TNF-α, IL-1β), or high glucose levels to mimic the in vivo target environment. This "primes" the cells, enhancing their secretion of therapeutic paracrine factors and improving outcomes in disease models [16].
- 3D Spheroid Culture: Instead of traditional 2D monolayers, culture MSCs as 3D spheroids. This architecture preserves multidifferentiation potential and enhances cell-cell signaling, resulting in paracrine profiles that more closely resemble those observed in vivo [2].
- CRISPR Enhancement: Genetically engineer MSCs to overexpress key anti-inflammatory and reparative factors such as IL-10 or TNF-alpha stimulated gene/protein 6 (TSG-6), potentiating their innate ability to modulate inflammation and promote repair [15].
Frequently Asked Questions (FAQs)
Q1: What are the most critical factors that make the post-transplantation microenvironment hostile? The core factors form a vicious cycle: 1) Metabolic Crisis (severe hypoxia & nutrient deprivation); 2) Oxidative Stress (excessive ROS); 3) Inflammatory Immune Response (activation of T-cells and macrophages); and 4) Disrupted Cell-Matrix Interactions [2] [13] [18].
Q2: Is autologous or allogeneic stem cell source better for avoiding immune responses? Autologous cells (from the patient) generally avoid immune rejection but are more costly and time-consuming to produce. Allogeneic "off-the-shelf" cells from donors are more practical but carry a higher risk of immune rejection. CRISPR/Cas9 engineering to create hypoimmunogenic allogeneic cells is a promising solution to this dilemma [15].
Q3: Can I simply add antioxidants to the culture medium to protect against oxidative stress? While adding antioxidants to the medium can help in vitro, it offers only transient protection in vivo. More robust strategies include genetically engineering the cells to have a stronger intrinsic antioxidant system or using biomaterials that provide localized, sustained release of antioxidants at the transplantation site [2].
Q4: How long do I need to precondition MSCs for it to be effective? Preconditioning protocols vary, but for hypoxic preconditioning, a common effective duration is 24 to 48 hours [2]. For cytokine preconditioning (e.g., with IFN-γ), priming for 24-72 hours is often used. The optimal time can depend on your specific cell source and target disease [16].
The following table consolidates key quantitative data from recent research to aid in experimental design and comparison of different strategies.
Table 1: Quantitative Data on Strategies to Counteract Hostile Microenvironments
| Strategy | Key Parameter | Reported Outcome | Source/Model |
|---|---|---|---|
| Hypoxic Preconditioning | Cell Survival | 2x higher survival vs. normoxic controls under serum deprivation | MSC study [2] |
| PFC-Hydrogel System | Oxygen Solubility | 15-20 times greater than water | In vitro analysis [2] |
| CaO₂ Microspheres | Oxygen Release Duration | 16-20 hours sustained release under deprivation | SH-SY5Y cells & MSCs [2] |
| β2M Knockout (CRISPR) | T-cell Proliferation | Marked suppression of CD8+ T-cell activation and infiltration | Cardiac repair model [15] |
| PZnONPs-boosted ADSCs | Therapeutic Efficacy | Significant reduction in inflammatory markers and fibrosis in liver | Liver injury model [14] |
Essential Research Reagent Solutions
This table lists key reagents and their functions for implementing the discussed strategies.
Table 2: Key Research Reagents for Navigating Hostile Microenvironments
| Reagent / Material | Function / Application | Key Consideration |
|---|---|---|
| Perfluorocarbons (PFCs) | High-capacity oxygen carrier for incorporation into hydrogels and scaffolds. | Conjugate with hydrogels to improve retention in vivo [2]. |
| Calcium Peroxide (CaO₂) | Solid peroxide for sustained oxygen generation in oxygen-producing scaffolds. | Encapsulate to control release kinetics and local pH changes [2]. |
| Polyethylene Glycol (PEG) | Nanoparticle coating to improve dispersion, stability, and reduce toxicity. | Critical for enhancing the bioavailability of delivery systems like PZnONPs [14]. |
| CRISPR/Cas9 System | Precise gene editing for knockout (e.g., β2M) or knock-in (e.g., IL-10). | Optimize gRNA design and delivery method (lentivirus, electroporation) to MSCs [15]. |
| Interferon-gamma (IFN-γ) | Cytokine for preconditioning MSCs to enhance immunomodulatory potency. | Titrate concentration (e.g., 10-50 ng/mL) and duration (24-72h) to avoid inducing senescence [16] [15]. |
| 3D Hydrogel Scaffolds | Provides 3D architecture for spheroid culture and physical protection from immune cells. | Tune mechanical properties and incorporation of biological factors to mimic target tissue [2]. |
Visualizing the Hostile Microenvironment and Strategic Countermeasures
The following diagram illustrates the major stressors in the hostile microenvironment and the corresponding strategic approaches to enhance stem cell survival and function.
Strategic Countermeasures Against Hostile Microenvironment Stressors
Key Experimental Protocols
Protocol: Hypoxic Preconditioning of MSCs
- Objective: To enhance MSC resilience to in vivo ischemia.
- Materials: MSC culture, standard culture medium, hypoxia chamber or workstation, gas mixture (1-5% O₂, 5% CO₂, balanced N₂).
- Procedure:
- Culture MSCs to 70-80% confluence under standard conditions (37°C, 20% O₂, 5% CO₂).
- Replace the medium with fresh culture medium.
- Place the cells in a hypoxia chamber pre-equilibrated with the desired gas mixture (e.g., 1% O₂).
- Incubate for 24 to 48 hours at 37°C.
- After preconditioning, harvest the cells using standard trypsinization for immediate transplantation.
- Validation: Assess upregulation of HIF-1α via Western blot or increased expression of VEGF and GLUT-1 via qPCR [2].
Protocol: CRISPR/Cas9-Mediated β2M Knockout in MSCs
- Objective: To generate hypoimmunogenic MSCs by eliminating surface MHC-I expression.
- Materials: MSCs, sgRNA targeting the β2M gene, Cas9 expression plasmid or ribonucleoprotein (RNP) complex, transfection reagent (e.g., lipofectamine) or electroporator, flow cytometry antibodies for β2M/HLA-I.
- Procedure:
- Design: Design a sgRNA targeting an early exon of the human β2M gene.
- Delivery: Transfect MSCs with the Cas9/sgRNA construct using a high-efficiency method like nucleofection.
- Selection & Expansion: Culture transfected cells and allow them to recover for 48-72 hours.
- Clonal Selection: Use single-cell sorting or dilution cloning to isolate clonal populations.
- Screening: Screen clones for β2M knockout efficiency via flow cytometry using an anti-HLA-ABC antibody.
- Validation: Validate successful knockout by Sanger sequencing of the target site and perform functional assays to confirm evasion of CD8+ T-cell recognition [15].
### Troubleshooting Guide: Addressing Poor Engraftment in HSCT Research
Q1: How does donor age influence engraftment success and graft-versus-host disease (GvHD)?
Donor age is a critical, independent risk factor for transplantation outcomes. Utilizing younger donors is consistently associated with improved engraftment and lower rates of GvHD, primarily due to enhanced immune reconstitution and better hematopoietic stem cell fitness [19].
- Experimental Evidence: A recent 2025 analysis of European Society for Blood and Marrow Transplantation (EBMT) registry data compared outcomes for patients with acute myeloid leukemia (AML) receiving grafts from younger haploidentical donors versus older mismatched unrelated donors, and vice versa, in the context of post-transplantation cyclophosphamide (PTCy) prophylaxis [19]. The key quantitative findings are summarized below:
Table 1: Impact of Donor Age on Transplant Outcomes with PTCy Prophylaxis [19]
| Donor-Recipient Pairing Comparison | Risk of Grade II-IV Acute GvHD | Risk of Non-Relapse Mortality (NRM) | 2-Year Overall Survival |
|---|---|---|---|
| Younger Haploidentical (<35 yrs) vs. Older Mismatched Unrelated (≥35 yrs) | Significantly Lower | No Significant Difference | No Significant Difference |
| Younger Mismatched Unrelated vs. Older Haploidentical | Significantly Lower | Significantly Lower | No Significant Difference |
- Underlying Mechanism: The superior outcomes with younger donors are attributed to a higher proportion of naïve T-cells, improved functionality of donor-derived T- and NK-cells, increased hematopoietic stem cell number, and a lower risk of transferring clonal hematopoiesis [19].
- Protocol Recommendation: For researchers designing preclinical or clinical studies, donor age should be treated as a key variable. Prioritize the use of younger donor cells when comparing other intervention arms. The data suggests that the benefit of a young donor may even supersede a one-allele mismatch in HLA compatibility [19].
Q2: What conditioning regimen strategies can rescue patients from primary graft failure (PGF)?
PGF is a life-threatening complication with limited salvage options. The choice of a second conditioning regimen for a rescue transplant is crucial, as these patients are often critically ill from prolonged cytopenias [20] [21]. Recent evidence points to the efficacy of shorter, less intensive regimens containing T-cell depleting agents.
- Experimental Evidence: A 2025 retrospective study compared two conditioning regimens for second HSCT in 19 patients with PGF [20] [21]. The outcomes favored a novel 1-day regimen over a multi-day reduced-intensity regimen.
Table 2: Outcomes of Second HSCT for PGF by Conditioning Regimen [20]
| Outcome Measure | 1-Day Regimen (Fludarabine, Cyclophosphamide, Alemtuzumab, low-dose TBI) | Multi-Day RIC (Fludarabine, Busulfan, 2 Gy TBI) | P-value |
|---|---|---|---|
| Neutrophil Engraftment (Cumulative Incidence at Day +28) | 82% | 50% | P = 0.22 |
| Platelet Engraftment (by Day +28) | 70% | 54% | P = 0.61 |
| Day +100 Non-Relapse Mortality (NRM) | 30.3% | 62.5% | P = 0.12 |
| 12-Month Overall Survival (OS) | 53.3% | 37.5% | P = 0.29 |
- Protocol: 1-Day Conditioning Regimen: The successful regimen involved the administration of fludarabine, cyclophosphamide, alemtuzumab, and low-dose total body irradiation (TBI) over a single day [20]. This approach was well-tolerated and resulted in no incidents of grade III-IV acute or chronic GvHD [20].
- Research Implication: For investigators studying graft failure models, this highlights the potential of alemtuzumab-based, T-cell depleting protocols to create immune space and facilitate engraftment without the excessive toxicity of traditional regimens.
Q3: Can mesenchymal stem cell (MSC) co-infusion accelerate hematopoietic recovery, particularly platelet engraftment?
Yes, the adjunctive infusion of MSCs is a promising strategy to mitigate delayed hematopoietic recovery, a significant challenge in haploidentical and unrelated donor transplants [22]. A 2025 systematic review of 47 clinical studies (total n=1,777 patients) provides robust evidence that MSC co-transplantation is safe and effective in accelerating engraftment, with a particularly pronounced effect on platelet recovery [22].
- Mechanism of Action: MSCs support engraftment through multiple pathways:
- Secretion of Hematopoietic Cytokines: They release key factors like stem cell factor (SCF), thrombopoietin (TPO), IL-6, and TGF-β [22].
- Support of the Bone Marrow Niche: MSCs help create a more favorable microenvironment for donor HSCs to implant and proliferate [22].
- Immunomodulation: They modulate T-cell-mediated responses, which may reduce host-versus-graft reactions and support engraftment [22].
- Experimental Workflow: The typical protocol for MSC co-infusion in clinical studies involves:
- MSC Source & Expansion: MSCs are isolated from sources like bone marrow (BM), umbilical cord (UC), or Wharton's jelly (WJ) and expanded ex vivo [22].
- Dosing & Administration: A common dose is (1-2 \times 10^6) MSCs per kg of recipient body weight. The MSCs are usually infused intravenously either at the time of the HSC transplant or within a few days post-transplant [22].
- Outcome Monitoring: Key endpoints include time to neutrophil recovery (Absolute Neutrophil Count > (0.5 \times 10^9/L)), time to platelet recovery (Platelet Count > (20 \times 10^9/L) without transfusion), and incidence of GvHD [22].
### Research Reagent Solutions
Table 3: Essential Reagents for Engraftment Research
| Reagent / Material | Function in Research | Application Note |
|---|---|---|
| Post-Transplant Cyclophosphamide (PTCy) | Selective in vivo T-cell depletion; prevents GvHD and graft rejection [19]. | Central to modern HLA-mismatched transplant protocols; dosing and timing are critical variables. |
| Alemtuzumab | Anti-CD52 monoclonal antibody; causes profound T-cell depletion [20]. | Used in conditioning regimens to reduce host immunity and prevent rejection, e.g., in salvage transplants for PGF [20]. |
| Mesenchymal Stem Cells (MSCs) | Adjunct cellular therapy; supports niche function and provides immunomodulation [22]. | Source (BM, UC), passage number, and dose are key experimental parameters affecting efficacy. |
| Fludarabine | Purine analog; immunosuppressive chemotherapeutic agent [20]. | Foundation of many reduced-intensity conditioning regimens. |
| Busulfan | DNA alkylating agent; myeloablative chemotherapeutic [20]. | Used in conditioning; therapeutic drug monitoring is often required due to narrow therapeutic index. |
### Frequently Asked Questions (FAQs)
Q: Is a younger haploidentical donor preferable to an older matched sibling donor? A: Emerging evidence suggests that for patients over 50 with AML, using a younger matched unrelated donor was associated with decreased relapse risk and improved disease-free survival compared to an older matched sibling donor [19]. The field is moving towards prioritizing donor age as a key factor, sometimes even over a minor HLA mismatch [19].
Q: Why is platelet engraftment often more delayed than neutrophil recovery? A: Megakaryopoiesis (platelet production) is a complex process that is typically more protracted than myeloid lineage recovery post-transplant [22]. This prolonged thrombocytopenia is a major clinical challenge and a key reason for investigating supportive therapies like MSC co-infusion [22].
Q: Are MSCs safe to use in clinical trials? A: The 2025 systematic review concluded that MSC co-infusion is generally safe and well-tolerated, with no major safety concerns or increased risk of malignant relapse reported across 47 studies [22]. Their low immunogenicity makes them suitable for allogeneic use [22].
Practical Strategies for Improved Engraftment: Pharmacological, Cellular, and Engineering Solutions
Technical Support Center
This technical support center provides resources for researchers utilizing Thrombopoietin Receptor Agonists (TPO-RAs) in the context of stem cell transplantation and hematopoietic research. The following guides and FAQs address common experimental challenges.
Frequently Asked Questions (FAQs)
Q1: What are the key pharmacological differences between Avatrombopag and recombinant human Thrombopoietin (rh-TPO) that I should consider for my in vitro studies?
A1: The primary differences lie in their mechanism of action, molecular structure, and downstream signaling kinetics. Avatrombopag is a small, non-peptide molecule that binds to the transmembrane domain of the TPO receptor (c-Mpl), while rh-TPO is a large, glycosylated protein that mimics endogenous TPO by binding to the extracellular domain. This leads to differences in signaling duration and potential for antibody generation.
Key Differences Table:
| Feature | Avatrombopag | rh-TPO |
|---|---|---|
| Molecular Type | Small molecule, orally bioavailable | Large protein, requires parenteral administration |
| Binding Site | Transmembrane domain of c-Mpl | Extracellular domain of c-Mpl |
| Signaling Profile | Sustained, prolonged JAK2/STAT5 activation | Transient, pulsatile JAK2/STAT5 activation |
| Risk of Neutralizing Antibodies | Negligible | Possible, can cross-react with endogenous TPO |
| Half-life | ~19 hours (in vivo) | ~20-40 hours (in vivo) |
Q2: In our mouse model of hematopoietic stem cell (HSC) transplantation, we are not observing a significant improvement in platelet engraftment with Avatrombopag treatment. What could be the issue?
A2: This is a common troubleshooting point. Several factors could be at play:
- Dosing and Timing: The efficacy of TPO-RAs is highly dependent on the dosing schedule. Administration should begin after transplantation to avoid stimulating residual malignant cells in the host and continue through the nadir period. Verify your dosage against recent literature (e.g., 6 mg/kg daily via oral gavage in mice).
- Drug Formulation: Ensure the Avatrombopag is properly formulated for in vivo use, typically in a vehicle containing substances like DMSO, PEG400, and Tween-80.
- Model Specificity: The response can vary based on the transplant model (e.g., congenic vs. xenogeneic, conditioning regimen intensity). Confirm that your model is appropriate for testing platelet recovery.
- Endpoint Analysis: Ensure you are tracking platelet counts frequently enough (e.g., every 2-3 days) to capture the kinetic difference. Consider also analyzing bone marrow for megakaryocyte colony-forming units (CFU-Mk) at endpoint.
Q3: For expanding CD34+ hematopoietic stem and progenitor cells (HSPCs) in vitro, what is the recommended concentration of rh-TPO to use in a serum-free medium, and how does it compare to Avatrombopag?
A3: For rh-TPO, a concentration of 20-100 ng/mL is standard in serum-free media formulations (e.g., StemSpan SFEM) alongside other cytokines like SCF and FLT3-L. For Avatrombopag, which is cell-permeable, a typical working concentration ranges from 0.5 to 5 µM. It is critical to perform a dose-response curve for your specific cell source, as potency can vary. Note that Avatrombopag may require dissolution in DMSO (keep final concentration <0.1%).
Experimental Protocols
Protocol 1: Assessing TPO-RA Efficacy in a Mouse HSC Transplantation Model
Objective: To evaluate the impact of Avatrombopag or rh-TPO on the kinetics of platelet reconstitution post-transplantation.
Materials:
- Mice: Lethally irradiated recipient mice (e.g., C57BL/6) and donor bone marrow cells.
- TPO-RAs: Avatrombopag (or vehicle control) and/or rh-TPO (or PBS control).
- Equipment: Flow cytometer, hematology analyzer, oral gavage needles, injection supplies.
Methodology:
- Transplantation: Irradiate recipient mice (e.g., 9.5 Gy). Within 24 hours, transplant a defined number of donor bone marrow cells (e.g., 5 x 10^5) via tail vein injection.
- Drug Administration:
- Begin treatment 24 hours post-transplantation.
- Avatrombopag Group: Administer daily via oral gavage (e.g., 6 mg/kg in appropriate vehicle).
- rh-TPO Group: Administer via intraperitoneal or subcutaneous injection (e.g., 10 µg/kg daily).
- Control Group: Administer vehicle only.
- Continue treatment for 21-28 days.
- Monitoring:
- Collect peripheral blood via retro-orbital bleed or tail vein every 3-4 days.
- Analyze platelet counts using a hematology analyzer.
- At endpoint (e.g., day 28), sacrifice mice and analyze bone marrow and spleen for cellularity and progenitor cell content (e.g., by CFU assays and flow cytometry for Lin⁻Sca-1⁺c-Kit⁺ (LSK) cells).
Protocol 2: In Vitro Megakaryocyte Differentiation from Human CD34+ HSPCs
Objective: To differentiate human CD34+ cells into megakaryocytes using a cytokine cocktail including a TPO-RA.
Materials:
- Cells: Human CD34+ HSPCs (cord blood or mobilized peripheral blood).
- Media: Serum-free expansion medium (e.g., StemSpan SFEM II).
- Cytokines: SCF, IL-6, IL-9, TPO (or Avatrombopag/rh-TPO).
- Reagents: FITC-conjugated anti-CD41a and PE-conjugated anti-CD42b antibodies for flow cytometry.
Methodology:
- Culture Initiation: Seed CD34+ cells at 1-2 x 10^5 cells/mL in SFEM II.
- Cytokine Supplementation:
- Control Group: Add SCF (50 ng/mL), IL-6 (10 ng/mL), IL-9 (10 ng/mL).
- TPO-RA Groups: Add the same base cytokines plus either:
- rh-TPO (50 ng/mL)
- Avatrombopag (1 µM, from a 10 mM DMSO stock)
- Culture Maintenance: Maintain cultures at 37°C, 5% CO2 for 12-14 days. Perform half-medium changes with fresh cytokines every 3-4 days.
- Analysis:
- Flow Cytometry: Harvest cells at days 7, 10, and 14. Stain with CD41a and CD42b antibodies to identify megakaryocyte commitment (CD41a⁺CD42b⁺).
- Morphology: Prepare cytospin slides and stain with May-Grünwald Giemsa to identify large, polyploid megakaryocytes.
Signaling Pathway Visualization
Diagram 1: TPO-RA Signaling via c-Mpl
Title: TPO-RA c-Mpl Signaling Pathway
Diagram 2: HSC Engraftment Enhancement Workflow
Title: TPO-RA Enhances HSC Engraftment
The Scientist's Toolkit
Research Reagent Solutions for TPO-RA Studies
| Reagent / Material | Function / Explanation |
|---|---|
| Recombinant Human TPO (rh-TPO) | Glycosylated protein cytokine; the gold standard for activating c-Mpl in in vitro assays. Used for megakaryocyte differentiation and colony-forming unit (CFU) assays. |
| Avatrombopag (Small Molecule) | Orally bioavailable TPO-RA; useful for in vivo studies and in vitro applications where a protein-free or prolonged signaling stimulus is desired. |
| c-Mpl (TPO Receptor) Antibodies | For detecting receptor expression and phosphorylation via flow cytometry (surface) or Western blot (total). |
| Phospho-STAT5 (Tyr694) Antibodies | Critical for confirming pathway activation downstream of c-Mpl via flow cytometry or immunofluorescence. |
| Serum-Free Expansion Media (e.g., StemSpan) | Defined, serum-free media optimized for the culture and expansion of human hematopoietic stem and progenitor cells. |
| MethoCult Media | For semi-solid colony-forming unit (CFU) assays to quantify megakaryocyte progenitors (CFU-Mk). |
| CD41a / CD42b Antibodies | Flow cytometry antibodies to identify and quantify committed megakaryocytes and platelets. |
FAQs: MSC Co-Infusion for Hematopoietic Recovery
1. What is the primary clinical rationale for using MSC co-infusion in hematopoietic stem cell transplantation (HSCT)? The primary rationale is to overcome delayed hematopoietic engraftment, a significant complication of HSCT that extends neutropenia and thrombocytopenia, increasing risks of severe infections, bleeding complications, and prolonged hospitalization [22]. MSC co-infusion leverages their immunomodulatory and hematopoiesis-supporting properties to accelerate the recovery of neutrophil and platelet counts, thereby reducing these transplant-related risks [22] [23].
2. Through what key mechanisms do MSCs enhance hematopoietic recovery? MSCs enhance engraftment through multiple interconnected mechanisms:
- Secretory Function: They release a diverse array of bioactive molecules, including growth factors and cytokines such as SCF, TPO, IL-6, and TGF-β, which are crucial for supporting the survival and proliferation of hematopoietic stem cells (HSCs) [22] [17].
- Bone Marrow Niche Support: MSCs contribute to rebuilding the bone marrow microenvironment (niche) that is essential for HSC function and differentiation [22].
- Immunomodulation: They interact with various immune cells (T cells, B cells, dendritic cells) and modulate T-cell–mediated responses, creating a more favorable environment for engraftment and reducing complications like GvHD [17] [23].
- Paracrine Signaling: Much of their therapeutic effect is mediated through paracrine actions, including the release of extracellular vesicles that carry signaling molecules [17] [24].
3. Which engraftment parameter shows the most consistent improvement with MSC co-infusion? Clinical evidence most consistently demonstrates a benefit for platelet engraftment [22] [12]. A systematic review of 47 studies found that MSC co-infusion particularly benefits platelet recovery, with an average time to platelet engraftment of 21.61 days in MSC recipients [12]. This is critical as delayed platelet engraftment is traditionally more prolonged and associated with increased morbidity [22].
4. Is MSC co-infusion safe, and what are the primary safety considerations? Systematic reviews and meta-analyses conclude that MSC infusion is generally safe when quality-controlled cells are used, with no serious adverse events directly attributed to the infusion in controlled clinical trials [23] [12]. The most critical safety consideration is hemocompatibility. MSCs can express procoagulant tissue factor (TF/CD142), and its level varies with the cell source. Testing MSC products for TF/CD142 before clinical administration is recommended to mitigate the risk of thromboembolism [25]. Common, minor side effects can include transient fever, nausea, or chills, often manageable with premedication [26].
5. Does MSC source influence its efficacy in supporting engraftment? Yes, the tissue source of MSCs (e.g., bone marrow, umbilical cord, adipose tissue) can influence their functional properties and efficacy [17] [25]. Bone marrow-derived MSCs (BM-MSCs) are the most extensively studied. Umbilical cord-derived MSCs (UC-MSCs) often exhibit enhanced proliferation and lower immunogenicity [17]. The expression of procoagulant tissue factor also varies by source, impacting product safety [25]. Furthermore, donor age and manufacturing inconsistencies are sources of heterogeneity that can affect clinical outcomes [22] [27].
Troubleshooting Common Experimental Challenges
Challenge 1: Inconsistent Engraftment Outcomes in Preclinical Models
- Potential Cause: Heterogeneity in MSC batches due to donor variability, passage number, or expansion protocols.
- Solution:
- Standardize Characterization: Rigorously characterize MSCs against International Society for Cellular Therapy (ISCT) criteria (plastic adherence, surface marker expression, trilineage differentiation) [17] [25].
- Functional Potency Assays: Implement in vitro functional assays, such as a lymphocyte proliferation suppression assay (mixed lymphocyte culture), to batch-test the immunomodulatory potency of your MSC preparations before in vivo use [24].
- Control Passage Number: Use MSCs at a low passage number (e.g., before passage 5-6) to avoid senescence-related functional decline.
Challenge 2: Poor Cell Survival or Engraftment Post-Infusion
- Potential Cause: The instant blood-mediated inflammatory reaction (IBMIR) triggered upon intravenous infusion, leading to cell death and clearance.
- Solution:
- Hemocompatibility Testing: Quantify the expression of procoagulant tissue factor (TF/CD142) on your MSC product using flow cytometry or ELISA [25]. Select cell sources or batches with lower TF/CD142 expression.
- Consider Alternative Routes: While intravenous is common, investigate intra-bone marrow injection if applicable to your research question, as it may bypass IBMIR and direct cells to the niche [24].
Challenge 3: Lack of Observed Therapeutic Effect
- Potential Cause: Suboptimal dosing or timing of MSC administration.
- Solution:
- Dose Optimization: Perform a dose-escalation study. Common clinical doses range from 1-10 million cells per kilogram [25], but the optimal dose can vary based on the model and MSC source.
- Timing Optimization: The timing of MSC infusion relative to HSC transplantation is critical. Test different time points, such as co-infusion on the same day as HSCs or infusion a few days post-transplant, to identify the most effective window for your specific experimental setup [22] [23].
The table below synthesizes key clinical outcomes associated with MSC co-infusion from systematic reviews and meta-analyses.
Table 1: Clinical Outcomes of MSC Co-infusion in Allogeneic HSCT
| Outcome Measure | Impact of MSC Co-infusion | Notes & Context |
|---|---|---|
| Neutrophil Engraftment | Accelerated | Average time to engraftment: ~13.96 days [12]. Effect is significant in both RCTs and non-RCTs [23]. |
| Platelet Engraftment | Accelerated | Average time to engraftment: ~21.61 days [12]. This is the most consistently reported benefit [22] [23]. |
| Acute GvHD (aGvHD) | Trend towards reduction | Some studies show a lower incidence, particularly in HLA-mismatched settings [28], but the overall effect is not always statistically significant [23]. |
| Chronic GvHD (cGvHD) | Reduced | A significant reduction in risk has been observed in meta-analyses [23]. |
| Relapse Rate (RR) | No Significant Increase | MSC co-infusion does not appear to increase the risk of disease relapse [23]. |
| Overall Survival (OS) | Generally No Negative Impact | No significant difference in OS observed in most analyses. A reduced OS was noted in one subgroup (adults with hematological malignancies receiving HLA-identical HSCT) [23]. |
Table 2: Impact of Patient and Transplant Factors on MSC Efficacy
| Factor | Subgroup | Observed Effect of MSC Co-infusion |
|---|---|---|
| Age | Children & Adolescents | More consistent improvements in engraftment, GvHD, and non-relapse mortality [23]. |
| Adults | Less pronounced benefits; may only see reduction in cGvHD [23]. | |
| HLA Match | HLA-nonidentical | Greater benefit observed, with improvements in engraftment and GvHD incidence [23]. |
| HLA-identical | More limited benefits, primarily reduction in cGvHD [23]. | |
| Underlying Disease | Malignancies | Improvements in GvHD and non-relapse mortality [23]. |
| Non-malignancies | Accelerated hematopoietic engraftment [23]. |
Detailed Experimental Protocol: MSC Co-Infusion in an HSCT Model
Objective: To evaluate the efficacy of human bone marrow-derived MSC co-infusion on the acceleration of platelet and neutrophil recovery in an immunodeficient mouse model of human hematopoietic stem cell transplantation.
Materials Required:
- MSCs: Human bone marrow-derived MSCs, characterized per ISCT criteria (CD73+, CD90+, CD105+, CD34-, CD45-, HLA-DR-), at passage 3-5 [17].
- HSCs: Human CD34+ hematopoietic stem cells (e.g., from cord blood or mobilized peripheral blood).
- Animals: NOD-scid IL2Rγ[null] (NSG) mice, 8-12 weeks old.
- Reagents: Phosphate Buffered Saline (PBS), Irradiation equipment, Flow cytometry antibodies (e.g., anti-human CD45, CD41, CD15).
Workflow:
Procedure:
- Mouse Conditioning: Subject NSG mice to sublethal irradiation (e.g., 1-2 Gy) 24 hours before transplantation to create a myelosuppressive environment and niche space.
- Cell Preparation:
- Treatment Group: Mix 1x10^5 human CD34+ HSCs with 1x10^6 human BM-MSCs (a 1:10 ratio) in 200µL of sterile PBS.
- Control Group: Prepare 1x10^5 human CD34+ HSCs in 200µL of sterile PBS.
- Transplantation: Infuse the cell suspensions intravenously via the tail vein into the conditioned mice.
- Post-Transplant Monitoring:
- Peripheral Blood Collection: Collect small blood samples from the retro-orbital sinus or tail vein three times per week for 4-5 weeks.
- Flow Cytometry Analysis: Stain samples with fluorochrome-conjugated antibodies to track engraftment:
- Human Engraftment: Anti-human CD45.
- Platelet Reconstitution: Anti-human CD41a (expressed on platelets/megakaryocytes).
- Myeloid/Neutrophil Reconstitution: Anti-human CD15.
- Endpoint Analysis: At the end of the study (e.g., 6-8 weeks), sacrifice the mice and analyze bone marrow from femurs and tibias via flow cytometry for human cell chimerism and histology to assess bone marrow cellularity and architecture.
Key Signaling Pathways in MSC-Mediated Hematopoietic Support
The following diagram illustrates the core molecular mechanisms through which MSCs support hematopoietic recovery, integrating secretory, immunomodulatory, and niche-supportive functions.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating MSC Co-Infusion
| Reagent / Material | Function in Experimental Design | Key Considerations |
|---|---|---|
| Bone Marrow-Derived MSCs | The primary therapeutic cell product. Source for paracrine factors and immunomodulation. | Verify ISCT criteria (CD73+/90+/105+; CD34-/45-). Use low passage numbers (P3-P5) to maintain potency [17] [25]. |
| CD34+ Hematopoietic Stem Cells | Target cells for transplantation and engraftment analysis. | Source (cord blood, bone marrow, mobilized PB) can influence engraftment dynamics. Purity is critical. |
| Immunodeficient Mice (e.g., NSG) | In vivo model to study human hematopoiesis and engraftment without graft rejection. | Ensure proper conditioning (irradiation) to enable niche opening. Monitor for health post-transplant. |
| Flow Cytometry Antibodies | To quantify and characterize human cell engraftment and differentiation in mouse blood and bone marrow. | Essential panels: anti-human CD45 (engraftment), CD41/61 (platelets), CD15/66b (neutrophils), CD33 (myeloid). |
| Tissue Factor (TF/CD142) ELISA Kit | To assess the procoagulant potential and hemocompatibility of the MSC product prior to in vivo use. | A critical safety assay. High TF levels may predict thrombotic risk and poor in vivo survival [25]. |
| Lymphocyte Proliferation Assay Kit | In vitro functional potency assay to test the immunomodulatory capacity of MSCs (e.g., via suppression of PHA-driven or MLR-driven T-cell proliferation). | Correlates with in vivo efficacy. Useful for batch-to-batch quality control [24]. |
Frequently Asked Questions (FAQs) on Preconditioning Strategies
Q1: What is the fundamental purpose of preconditioning stem cells before transplantation?
A1: The primary purpose of preconditioning is to enhance the survival, function, and therapeutic efficacy of stem cells after transplantation. Upon infusion, cells face a harsh microenvironment characterized by ischemia, inflammation, and oxidative stress, leading to massive cell death—often over 90% within the first week [29]. Preconditioning uses sublethal stresses or genetic modifications to activate the cells' intrinsic protective and reparative mechanisms before transplantation. This "primes" them to better withstand the hostile host environment, improve their engraftment into target tissues, and amplify their paracrine signaling, which is crucial for tissue repair and immunomodulation [30] [29].
Q2: We are considering hypoxic priming for our MSCs. What is a standard and effective protocol we can follow?
A2: A commonly used and effective protocol involves culturing MSCs at low oxygen tensions for a defined period. Based on recent studies, you can follow this workflow [31]:
- Culture Expansion: Expand your MSCs (e.g., from umbilical cord or adipose tissue) under standard culture conditions (21% O₂, 37°C, 5% CO₂) until they reach 80-90% confluence.
- Hypoxic Priming: Replace the culture medium and place the cells in a hypoxia workstation or multi-gas incubator set to 5% CO₂ and 1-5% O₂ at 37°C. The balance gas is N₂.
- Duration: Maintain the cells under these hypoxic conditions for 24 to 48 hours.
- Harvesting: After the priming period, harvest the cells using a standard enzyme like TrypLE Select for subsequent transplantation or analysis.
Studies have shown that this 5% O₂ preconditioning significantly promotes MSC proliferation and alters their transcriptional profile, enhancing their therapeutic potential without compromising safety in animal models [32] [31].
Q3: Our in vivo experiments show poor survival of transplanted MSCs. What preconditioning strategies can we use to enhance cell survival?
A3: Poor post-transplant survival is a major hurdle. You can explore these three strategy families, which can also be combined:
- Hypoxic Preconditioning: As above, this upregulates pro-survival pathways. Hypoxia-inducible factor-1α (HIF-1α) activation leads to increased expression of survival factors like Bcl-2 and survivin [30] [29].
- Pharmacological Preconditioning: Incubate MSCs with specific drugs before transplantation. Effective agents include:
- Isoflurane: A volatile anesthetic that can enhance MSC survival [30].
- Lipopolysaccharide (LPS): Pre-treatment with low-dose LPS can activate toll-like receptors, leading to a protective phenotype [30].
- Diazoxide: A mitochondrial ATP-sensitive potassium channel opener that mimicks ischemic preconditioning [30].
- Cytokine Priming: Pre-treat MSCs with pro-inflammatory cytokines like Interferon-gamma (IFN-γ) and Tumor Necrosis Factor-alpha (TNF-α). This polarizes MSCs toward a potent immunosuppressive phenotype, characterized by high expression of Indoleamine 2,3-dioxygenase (IDO) and TSG-6, which helps them modulate the local immune response and survive longer [33].
Q4: We are researching cardiac repair. What are key genetic modification targets to enhance stem cell engraftment and function for this application?
A4: For cardiac repair, genetic modifications aim to optimize key steps in the cell therapy process. The table below outlines prime targets based on preclinical studies [34]:
Table 1: Key Genetic Modification Targets for Stem Cell-based Cardiac Repair
| Target Process | Genetic Target / Transgene | Intended Effect |
|---|---|---|
| Cell Survival | Akt (a serine/threonine kinase), Survivin, Bcl-2 | Inhibits apoptosis and increases resistance to oxidative stress in the harsh ischemic myocardial environment [34] [30]. |
| Homing & Engraftment | CXCR4 (Receptor for SDF-1) | Enhances the cell's ability to migrate toward and engraft in the infarcted area, which expresses high levels of SDF-1 [34] [30]. |
| Paracrine Signaling | Vascular Endothelial Growth Factor (VEGF) | Boosts secretion of angiogenic factors, promoting the growth of new blood vessels to improve blood supply to the damaged tissue [34]. |
| Immunomodulation | Indoleamine 2,3-dioxygenase (IDO) | Increases the cell's capacity to suppress local immune activation and inflammation, creating a more favorable environment for repair [29] [33]. |
Q5: Are there any significant safety concerns associated with preconditioning strategies, particularly hypoxic priming?
A5: Overall, hypoxic MSCs from various tissues have been demonstrated to be safe in animal models regarding parameters like hematopoietic function, proinflammatory cytokine levels, and organ toxicity [32]. However, one critical safety consideration is dose-dependent thrombogenic risk. A recent comprehensive safety assessment revealed that while intravenous injection of hypoxic MSCs at a dose of 50 million cells/kg was safe in mice, injections of higher doses led to intravenous thrombosis and embolism in various organs, ultimately causing animal death [32]. Therefore, rigorous dose-optimization studies are an essential prerequisite for clinical translation.
Troubleshooting Guides
Problem 1: Inconsistent Results with Hypoxic Preconditioning
- Potential Cause: Fluctuating oxygen levels within the hypoxia incubator.
- Solution: Regularly calibrate the oxygen sensor of your hypoxia workstation. Ensure the chamber door is kept closed as much as possible to maintain a stable low-oxygen environment. Allow sufficient time for the environment to equilibrate after opening.
- Potential Cause: Variations in cell confluency at the time of preconditioning.
- Solution: Standardize the cell confluency (e.g., 80-90%) at the start of the hypoxic exposure to ensure consistent cell-to-cell contact and metabolic state.
Problem 2: Preconditioned MSCs Fail to Show Improved Efficacy In Vivo
- Potential Cause: The preconditioning stimulus is too mild or too severe.
- Solution: Conduct a dose-response curve for your preconditioning trigger. For hypoxia, test a range of O₂ concentrations (e.g., 10%, 5%, 3%) and durations (e.g., 24h, 48h) [31]. For drugs, test a range of concentrations to find the optimal "sweet spot" that provides protection without causing significant death in vitro.
- Potential Cause: The route of administration is not optimal for cell delivery to the target organ.
- Solution: Re-evaluate the delivery method. For example, in kidney transplantation, intra-arterial infusion was effective, while intravenous was not [29]. Consider local vs. systemic delivery routes.
Problem 3: Low Cell Yield or Viability After Genetic Modification
- Potential Cause: Cytotoxicity from the viral vector or transfection reagent.
- Solution: Titrate the viral multiplicity of infection (MOI) or the amount of transfection reagent to find the balance between high transduction efficiency and acceptable cell viability. Include a viability-enhancing agent like a caspase inhibitor in the culture medium during the critical post-transduction period.
Key Signaling Pathways in Preconditioning
The therapeutic benefits of preconditioning are mediated by complex signaling pathways that converge on enhanced survival and function. Hypoxic preconditioning is central, primarily mediated by the stabilization of Hypoxia-Inducible Factor-1alpha (HIF-1α). The following diagram illustrates the core pathway and its functional outcomes:
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Preconditioning and Characterization Experiments
| Reagent / Material | Function / Application | Example / Note |
|---|---|---|
| Hypoxia Workstation | Provides a controlled, low-oxygen environment for cell priming. | Essential for consistent hypoxic preconditioning; maintains set O₂ (e.g., 1-5%), CO₂, and temperature. |
| StemMACS MSC Expansion Media | Serum-free, xeno-free media for MSC culture. | Eliminates batch variability and safety concerns of fetal bovine serum (FBS) [32]. |
| TrypLE Select Enzyme | A non-animal origin reagent for cell detachment. | Gentle harvesting of MSCs, preserving cell surface markers and viability [32]. |
| Recombinant Human Cytokines | For pharmacological/cytokine preconditioning. | IFN-γ and TNF-α are used to polarize MSCs toward an immunosuppressive phenotype [33]. |
| Lentiviral/Viral Vectors | For genetic modification of stem cells. | Used to overexpress target genes (e.g., Akt, CXCR4) or for knock-down studies (e.g., GSTO1) [34] [31]. |
| Antibodies for Flow Cytometry | For characterization of MSC surface markers. | Essential kit includes CD90, CD105, CD73 (positive) and CD45/CD34/CD11b (negative) per ISCT guidelines [32] [35]. |
| ELISA Kits | To quantify secretion of paracrine factors. | Measure concentrations of VEGF, HGF, IL-10, etc., in cell culture supernatants to confirm enhanced paracrine profile. |
| CCK-8 Assay Kit | To measure cell proliferation and viability. | A colorimetric assay used to assess the effects of preconditioning on cell growth and health [31]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary biological barriers that limit effective stem cell homing to the bone marrow post-transplantation? Effective homing is limited by several barriers. The hostile bone marrow microenvironment often contains inflammatory cytokines and reactive oxygen species that can damage infused cells [36]. There is often poor migration and invasion into the target niches, and infused cells can face limited persistence due to apoptosis or immune rejection [36]. Furthermore, the loss of key homing receptors on stem cells during ex vivo expansion can reduce their ability to respond to homing signals [37].
Q2: How can bioengineering strategies improve the retention and engraftment of mesenchymal stem cells (MSCs) in hematopoietic stem cell transplantation (HSCT)? Bioengineering strategies focus on enhancing the innate properties of MSCs. Pre-conditioning MSCs with inflammatory cytokines (e.g., IFN-γ) can enhance their immunomodulatory and secretory functions [17]. Engineering MSCs to overexpress pro-survival genes (e.g., BCL-2) or specific homing ligands and chemokine receptors (e.g., CXCR4) can increase their resistance to stress and direct them to the bone marrow [37] [38]. Utilizing MSCs as delivery vehicles for therapeutic factors like cytokines (SCF, TPO, IL-6) and extracellular vesicles can directly support the hematopoietic niche and promote recovery [22] [17].
Q3: What are the clinical signs of poor engraftment, and what is Post-Engraftment Syndrome (PES)? Poor engraftment is characterized by persistent neutropenia and thrombocytopenia, leading to increased infection and bleeding risks [22]. Post-Engraftment Syndrome (PES) is a distinct, non-infectious complication that occurs around the time of neutrophil recovery. It is diagnosed using established criteria, as outlined in the table below [39].
Table 1: Diagnostic Criteria for Post-Engraftment Syndrome (PES)
| Criteria Set | Major Criteria | Minor Criteria | Diagnostic Requirement |
|---|---|---|---|
| Spitzer (2001) | Non-infectious fever (≥38.3°C); Erythematous rash involving >25% of body surface; Non-cardiogenic pulmonary edema [39] | Hepatic dysfunction; Renal dysfunction; Weight gain ≥2.5%; Transient encephalopathy [39] | ≥3 major criteria, OR 2 major + 1 minor criterion [39] |
| Maiolino (2003) | Fever (≥38°C) without identifiable infectious cause [39] | Skin rash; Pulmonary infiltrates; Diarrhea [39] | 1 major + 1 minor criterion [39] |
Q4: What troubleshooting steps can be taken if in-vitro modified cells show poor viability or function? If cell viability is poor, first review the manufacturing process. Check for apoptosis and optimize transduction protocols if genetic modification is used [36]. Assess the formulation and storage conditions of the cell product, including the cryopreservation medium and freeze-thaw cycle [40]. For functional deficits, conduct in-depth potency assays to measure secretome, immunomodulation, and differentiation capacity against predefined release criteria [17]. Consider using advanced delivery systems, such as targeted nanoparticles or hydrogels, to provide sustained release of supportive factors in vivo [41] [42].
Troubleshooting Guides
Delayed Hematopoietic Recovery
Table 2: Troubleshooting Delayed Platelet and Neutrophil Recovery
| Observation | Potential Root Cause | Recommended Investigations | Corrective & Preemptive Strategies |
|---|---|---|---|
| Persistent thrombocytopenia/neutropenia | Graft failure or poor graft quality [40]; Hostile bone marrow microenvironment [41]; Insufficient stromal support (e.g., low MSC potency) [22] | Monitor chimerism levels; Analyze bone marrow biopsy for cellularity and niche composition; Test MSC potency (e.g., cytokine secretion profile) [22] [40] | Consider MSC co-infusion (see Table 4); Use G-CSF to support neutrophil recovery [22]; Optimize cell dose and viability pre-infusion [22] |
| High infection or bleeding risk | Delayed neutrophil and platelet engraftment [22] | Monitor absolute neutrophil count (ANC) and platelet counts daily [22] | Implement rigorous supportive care (prophylactic antibiotics, platelet transfusions) [22]; Consider MSC co-infusion to accelerate recovery [22] |
Managing Post-Engraftment Syndrome (PES)
Table 3: Identification and Management of Post-Engraftment Syndrome
| Step | Action | Details |
|---|---|---|
| 1 | Differentiate from Infection | Rule out bacterial, viral, or fungal infections through blood cultures, chest imaging, and PCR testing. PES is a diagnosis of exclusion [39]. |
| 2 | Apply Diagnostic Criteria | Use Spitzer or Maiolino criteria (see Table 1) to confirm PES. The onset is typically within 96 hours of neutrophil engraftment [39]. |
| 3 | Initiate Corticosteroid Therapy | Intravenous corticosteroids (e.g., methylprednisolone 1-2 mg/kg/day) are the first-line treatment. Most patients show rapid clinical improvement within 24-48 hours [39]. |
| 4 | Provide Supportive Care | Manage specific symptoms, which may include supplemental oxygen for pulmonary involvement or topical agents for skin rash [39]. |
Experimental Protocols for Enhancing Engraftment
Protocol 1: MSC Co-Infusion to Accelerate Hematopoietic Recovery
Methodology: This protocol is based on a systematic review of clinical studies involving over 1,700 patients [22].
- MSC Source and Preparation: Isolate MSCs from a consented donor source (e.g., bone marrow, umbilical cord). Culture and expand MSCs in vitro, ensuring they meet ISCT criteria (positive for CD73, CD90, CD105; negative for CD34, CD45, HLA-DR) [17]. Passage cells no more than 4-6 times to maintain potency.
- Dosing and Timing: The typical therapeutic dose ranges from 1-5 x 10^6 MSCs per kilogram of recipient body weight [22]. The cells are typically administered via intravenous infusion either on the same day as the HSCT or at the time of engraftment (day 0) [22].
- Quality Control: Prior to infusion, perform tests for viability (should be >90%), sterility (bacterial/fungal), and mycoplasma. Potency can be assessed via a tri-lineage differentiation assay or by measuring the secretion of key cytokines (e.g., SCF, TPO, IL-6) [17].
Rationale: MSCs support hematopoiesis by secreting growth factors (SCF, TPO), promoting angiogenesis, modulating the immune response, and directly supporting the bone marrow niche [22] [17].
Protocol 2: Engineering "Armored" Cells with Enhanced Homing
Methodology: This protocol adapts strategies from CAR-T cell "armoring" for improving stem cell homing and persistence [37].
- Genetic Modification: Use lentiviral or retroviral vectors to transduce stem cells or MSCs with genes of interest.
- Key Transgenes:
- Cytokine Expression: Engineer cells to express IL-15 or IL-7 to promote autonomous survival and proliferation, preventing exhaustion [37].
- Homing Receptor Overexpression: Introduce genes for chemokine receptors like CXCR4 to enhance migration toward SDF-1 gradients in the bone marrow [37] [38].
- Dominant-Negative Receptors: Express a dominant-negative TGF-β receptor (dnTGF-βRII) to make cells resistant to the immunosuppressive effects of TGF-β in the microenvironment [37].
- Validation: Post-transduction, validate transgene expression via flow cytometry or PCR. Confirm enhanced functional capacity in vitro using transwell migration assays towards SDF-1 and cytokine secretion assays [37].
Rationale: This "armoring" approach directly counters major barriers in the transplantation microenvironment, including growth factor deprivation, poor homing, and active immunosuppression [36] [37].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Engraftment Optimization Research
| Reagent / Material | Function / Application | Specific Examples / Notes |
|---|---|---|
| Mesenchymal Stem Cells (MSCs) | Adjunct therapy to support hematopoietic recovery and modulate immunity [22] [17] | Bone marrow-derived (BM-MSC), umbilical cord-derived (UC-MSC). Must be characterized per ISCT guidelines (CD73+, CD90+, CD105+, CD34-, CD45-) [17]. |
| Homing Peptides | Small peptides used to functionalize cells or delivery systems for targeted tissue homing [38] | Can be identified via phage display. Often cyclic and rich in Cys/Arg. Can be modified (e.g., PEGylated) to enhance stability [38]. |
| Lentiviral Vectors | For stable genetic modification of stem cells to enhance persistence and homing [37] | Used to express armored transgenes (e.g., IL-15, CXCR4, dnTGF-βRII) [37]. |
| Cytokines & Growth Factors | For pre-conditioning cells or as supportive therapy in vivo [37] [17] | SCF, TPO, IL-6, G-CSF, IL-15. Used to enhance cell potency or accelerate blood count recovery [22] [37]. |
| Polymeric Nanoparticles | Advanced delivery system for controlled release of supportive drugs or biomolecules at the niche [41] | Can be functionalized with homing peptides (e.g., bone-targeting peptides) for site-specific delivery [41] [38]. |
Overcoming Translational Hurdles: Protocols for Enhancing Cell Viability and Host Receptivity
FAQ: Core Strategies to Enhance Apoptosis Resistance
What are the main causes of low stem cell survival after transplantation? Transplanted stem cells face a hostile microenvironment that triggers apoptosis. Key stressors include severe hypoxia and nutrient deprivation due to a lack of initial vascular connections [2]. This leads to metabolic crisis and the accumulation of cytotoxic waste [2]. Additionally, cells encounter excessive reactive oxygen species (ROS) that exceed their antioxidant capacity, and disruption of cell-matrix interactions can induce a specific type of apoptosis called anoikis ("homelessness") [2] [43].
How can preconditioning stem cells improve their survival? Preconditioning involves exposing stem cells to sublethal stress before transplantation to enhance their resilience. A primary method is hypoxic preconditioning (1-5% O₂ for 24-48 hours), which activates hypoxia-inducible factor (HIF-1α) and upregulates pro-survival genes (e.g., VEGF, Bcl-2) and antioxidant enzymes [2] [43]. This reprograms cell metabolism from oxidative phosphorylation to glycolysis, reducing oxygen consumption and enhancing anti-apoptotic capacity [2]. Studies show this can double survival rates under serum-deprived conditions and improve engraftment by 1.5 to 4-fold in various disease models [2] [43].
Are there strategies that target the transplantation site itself? Yes, making the target tissue more receptive is a complementary strategy. This can involve enhancing vascular reconstruction at the site through cytokine-mediated angiogenesis or using biomaterial scaffolds to support new blood vessel formation [2]. Another approach is using monoclonal antibody-based conditioning to prepare the tissue niche, which, when combined with stem cell mobilization strategies, has been shown to safely enhance donor cell engraftment in mouse models [44].
Troubleshooting Guide: Low Post-Transplantation Engraftment
| Problem | Possible Cause | Recommended Solution | Key References |
|---|---|---|---|
| Rapid Cell Death (<24 hours) | Severe hypoxia & nutrient deprivation at graft site; Anoikis (detachment-induced apoptosis). | • Metabolic Preconditioning: Use transient serum deprivation or hypoxia pre-conditioning (1% O₂, 24-48 hrs) to upregulate pro-survival genes [2] [43].• Oxygen Supplementation: Use oxygen-generating materials (e.g., calcium peroxide/PEGDA microspheres) in scaffolding [2].• Use 3D Culture Systems: Employ spheroids or hydrogel scaffolds to preserve cell-cell and cell-matrix contact [2]. | |
| Poor Long-Term Engraftment | Chronic oxidative stress; Inflammatory host immune response; Insufficient vascular integration. | • Enhance Antioxidant Defenses: Genetically modify cells to overexpress antioxidant enzymes or deliver ROS-scavenging components [2].• Promote Angiogenesis: Pre-treat cells to boost secretion of pro-angiogenic factors (e.g., VEGF); use scaffolds incorporating vascular growth factors [2] [43].• Leverage Apoptotic Immunomodulation: Note that some apoptotic cells can recruit anti-inflammatory macrophages via phosphatidylserine-MerTK signaling, paradoxically aiding repair [45]. | |
| High Variability in Engraftment Success | Inconsistent cell quality prior to transplantation; Suboptimal delivery timing or route. | • Standardize Pre-Transplant Culture: Maintain consistent confluency (passage at ~85%), use quality-controlled reagents, and avoid over-manipulation [46] [47].• Systematic Delivery Optimization: Determine the optimal time window for transplantation post-injury and compare local vs. systemic delivery routes for your specific model [43]. |
The table below summarizes experimental data from animal models on the efficacy of various preconditioning strategies for improving stem cell engraftment.
Table 1: Efficacy of Preconditioning Strategies in Animal Models
| Preconditioning Strategy | Model | Cell Type | Key Outcomes (vs. Control) | Engraftment Improvement | Tracking Method |
|---|---|---|---|---|---|
| Hypoxia (1%, 24h) [43] | Idiopathic Pulmonary Fibrosis (Mouse) | BM-MSC | ↓Collagen deposition, ↓inflammatory cytokines, ↑pulmonary function | 4 fold at 4 days | β-Galactosidase staining |
| Hypoxia (1%, 24h) [43] | Erectile Dysfunction, DMT1 (Rat) | ADSC | ↓Collagen deposition, ↑intracavernosal pressure | 1.5 fold at 1 week | DiI fluorescent dye |
| Hypoxia (1%, 24h) [43] | Myocardial Infarction (Mouse) | BM-MSC | ↓Infarct size, ↑cardiac function | 2.5 fold at 1 day | GFP transduction |
| HDL (20–200 μg/ml, 24h) [43] | Myocardial Infarction (Rat) | BM-MSC | Activation of PI3K/Akt pathway, ↑cardiac function | 3 fold at 4 days | GFP transduction |
| Curcumin (10 μM, 24h) [43] | Myocardial Ischemia-Reperfusion (Rat) | ADSC | Activation of PTEN/Akt/p53 pathway, ↑neovascularization | 2 fold at 7 days | DiI fluorescent dye |
Experimental Protocols
Protocol 1: Hypoxic Preconditioning of MSCs
Objective: To enhance MSC resistance to apoptosis and improve in vivo survival via adaptation to low oxygen.
Materials:
- Confluent flask of MSCs (Passage 3-5)
- Tri-gas incubator (capable of maintaining 1% O₂, 5% CO₂, balance N₂)
- Standard MSC growth medium
- Phosphate Buffered Saline (PBS)
- Trypsin/EDTA or other detachment reagent
- ROCK inhibitor (e.g., Y-27632, optional for enhanced survival post-passaging) [46]
Method:
- Preparation: Passage MSCs as usual and seed them at an appropriate density. Allow cells to adhere and recover in a standard (normoxic, 20% O₂) incubator for 24 hours.
- Preconditioning: Carefully move the cell culture vessel to the tri-gas incubator set to 1% O₂, 5% CO₂, at 37°C.
- Incubation: Culture the cells under hypoxic conditions for 24-48 hours. Do not change the medium immediately before or during the preconditioning period to avoid nutrient shocks.
- Harvesting: After the preconditioning period, harvest the cells using standard procedures. It is recommended to use a ROCK inhibitor in the medium during the harvesting and transplantation process to reduce anoikis [46].
- Transplantation: Resuspend the preconditioned cells in the appropriate vehicle for immediate transplantation into the animal model or recipient.
Protocol 2: Assessing Apoptosis via Phosphatidylserine Externalization
Objective: To quantify the percentage of apoptotic cells in a population before and after preconditioning treatments.
Materials:
- Stem cell population (treated and control)
- Annexin V binding buffer
- Fluorescently conjugated Annexin V
- Propidium Iodide (PI) stain
- Flow cytometer with appropriate lasers and filters
Method:
- Cell Preparation: Harvest and wash cells twice with cold PBS.
- Staining: Resuspend ~1x10⁵ cells in 100 µL of Annexin V binding buffer.
- Add fluorescently conjugated Annexin V (as per manufacturer's instructions) and incubate for 15 minutes at room temperature in the dark.
- Add PI to a final concentration (e.g., 1 µg/mL) for the last 5 minutes of incubation to distinguish late apoptotic/necrotic cells (Annexin V+/PI+) from early apoptotic cells (Annexin V+/PI-).
- Analysis: Add 400 µL of additional binding buffer to each tube and analyze by flow cytometry within 1 hour. Use untreated cells and single-stained controls to set up compensation and quadrants.
Visualizing the Strategy: A Multi-Pronged Approach
The following diagram illustrates the interconnected strategies for enhancing stem cell resistance to apoptosis, focusing on preconditioning, microenvironment engineering, and the emerging role of immunomodulation by apoptotic cells.
The Scientist's Toolkit: Key Reagents and Materials
Table 2: Essential Research Reagents for Apoptosis Resistance Studies
| Item | Function/Application | Example Use Case |
|---|---|---|
| Tri-Gas Incubator | Maintains precise, low oxygen tensions (e.g., 1-5% O₂) for hypoxic preconditioning of cells. | Essential for protocols involving metabolic preconditioning and HIF-1α pathway activation [2] [43]. |
| ROCK Inhibitor (Y-27632) | A small molecule that inhibits Rho-associated kinase, dramatically reducing anoikis in single-cell suspensions. | Add to culture medium during passaging and for 24 hours post-transplantation to enhance survival of dissociated cells [46]. |
| Hydrogel Scaffolds | Synthetic or natural 3D matrices that provide structural and biochemical support, mimicking the native extracellular matrix. | Used to create 3D spheroids or encapsulate cells for transplantation, preserving cell-matrix signaling and preventing anoikis [2]. |
| Oxygen-Generating Particles (e.g., CaO₂) | Solid peroxides that release oxygen gradually upon reaction with water, mitigating local hypoxia. | Incorporated into hydrogel scaffolds to provide sustained oxygen release at the transplantation site, supporting cell survival before vascularization [2]. |
| Annexin V Kits | Flow cytometry-based assays to detect phosphatidylserine externalization on the cell surface, a key early marker of apoptosis. | Used to quantitatively assess the level of apoptosis in cell populations before and after preconditioning treatments [45]. |
| Serum-Free Media (e.g., STEMGOLD) | Chemically defined media that eliminate variability and unknown factors from serum, supporting consistent cell growth. | Crucial for standardizing pre-transplantation cell expansion, particularly for clinical applications, to ensure reproducibility and safety [48]. |
Stem cell homing is a critical, multi-step process where transplanted stem cells navigate from the bloodstream to their target niche, such as the bone marrow or a site of injury. This journey is orchestrated by a complex interplay of chemokines, adhesion molecules, and their respective receptors. The SDF-1/CXCR4 axis is a fundamental pathway in this process, directing cell migration, retention, and engraftment. Enhancing the efficiency of this homing mechanism is a primary goal in regenerative medicine to improve the success rates of stem cell transplantation and therapies.
Frequently Asked Questions (FAQs)
Q1: Why is the SDF-1/CXCR4 axis considered so critical for stem cell homing?
The SDF-1 (Stromal Cell-Derived Factor-1, or CXCL12)/CXCR4 axis is a master regulator of stem cell trafficking. Its importance is rooted in several key functions:
- Cell Motility: SDF-1 acts as a powerful chemoattractant, guiding CXCR4-expressing cells along a concentration gradient towards the target tissue [49] [50].
- Development and Retention: Genetic studies show that deleting either the
Cxcr4orCxcl12gene in mice causes fatal developmental defects, underscoring its non-redundant role in organogenesis, hematopoiesis, and bone marrow colonization [49] [51]. - Tissue Repair: This axis is rapidly upregulated in injured tissues like the heart, liver, and skeletal muscle, where it recruits stem cells and directly promotes the survival of local cells, facilitating preservation and regeneration [49] [52].
Q2: In my double cord blood transplantation model, high CXCR4 expression on CD34+ cells did not predict unit predominance. Why might this be?
This is a clinically observed paradox. While the SDF-1/CXCR4 axis is vital for initial homing and engraftment, long-term predominance in a competitive transplant setting is influenced by additional factors.
- Research Evidence: A clinical study of double umbilical cord blood (dUCB) transplantation found that both the proportion of CD34+CXCR4+ cells and the intensity of CXCR4 expression (Mean Fluorescence Intensity, MFI) were similar between the predominant and non-predominant units. The odds ratio for unit predominance was not significantly affected by higher CXCR4 levels [53].
- Key Insight: The authors concluded that after the initial homing phase, long-term unit predominance is largely determined by T-cell content and immunologic interactions between the donor units, rather than CXCR4 expression levels alone [53]. This suggests that CXCR4 function (e.g., responsiveness to SDF-1) may be a more critical parameter than mere surface expression.
Q3: What are the primary downstream signaling pathways activated by SDF-1/CXCR4 that drive cell migration?
The binding of SDF-1 to CXCR4, a G-protein coupled receptor (GPCR), triggers multiple interconnected signaling cascades that orchestrate cytoskeletal rearrangement and cell movement. Key pathways include:
- FAK/PI3K/Akt Pathway: Critical for the formation and disassembly of focal adhesions, driving forward movement [50].
- GSK3β/β-catenin Pathway: Regulates the translocation of β-catenin to the nucleus, where it acts as a transcription factor for genes involved in migration [50].
- Cytoskeleton Remodeling: Activation of small GTPases like Rac, RhoA, and CDC42 is essential for actin polymerization, formation of membrane protrusions like filopodia, and overall cell motility [50] [54].
The diagram below illustrates the integration of these pathways following CXCR4 activation.
Q4: What strategies can I use to improve the homing efficiency of MSCs in my experiments?
Several strategies, from genetic modification to tissue preconditioning, can enhance the homing of Mesenchymal Stem Cells (MSCs).
- In vitro Priming: Pre-treating MSCs with cytokines or small molecules that activate homing-associated pathways before transplantation [10].
- Genetic Modification: Engineering MSCs to overexpress CXCR4 to increase their sensitivity to SDF-1 gradients [10].
- Cell Surface Engineering: Chemically modifying the MSC surface to enhance interactions with the endothelium. An example is attaching specific sugar molecules that act as binding sites for bone marrow homing cues [9].
- Target Tissue Modification: Increasing the "attractiveness" of the injured site by injecting a stabilized, enzymatically resistant version of SDF-1 to create a stronger and more persistent chemotactic gradient [9].
Troubleshooting Common Experimental Issues
Problem 1: Low Stem Cell Migration in Transwell Assays
Potential Causes and Solutions:
| Cause | Diagnostic Experiment | Solution |
|---|---|---|
| Low CXCR4 receptor expression on cells. | Perform flow cytometry to quantify CXCR4 surface expression. | Prime cells with cytokines (e.g., IL-2, IL-7) known to upregulate CXCR4 transcription [51] or use genetic modification. |
| Insufficient or degraded SDF-1 gradient. | Validate the SDF-1 concentration and stability in the lower chamber via ELISA. | Prepare a fresh SDF-1 stock and use a concentration within the effective range (e.g., 50-100 ng/mL) [50]. |
| Inhibition by serum components. | Run a control assay with a low serum or serum-free medium. | Reduce serum concentration in the migration medium to minimize non-specific binding protein interference. |
| Downstream signaling is blocked. | Check phosphorylation of key effectors like Akt and FAK via Western blot after SDF-1 stimulation. | Use a Gi-protein activator like cholera toxin to bypass receptor activation, confirming pathway competence. |
Problem 2: Poor Engraftment Efficiency In Vivo
Potential Causes and Solutions:
| Cause | Diagnostic Experiment | Solution |
|---|---|---|
| Failed mobilization from the injection site. Use intravital imaging to track labeled cells in real-time [9]. | Pre-treat cells with a CXCR4 agonist or a pharmacological "priming" agent to enhance responsiveness before injection [10] [9]. | |
| Rapid desensitization of CXCR4 receptor. | Analyze receptor internalization after exposure to SDF-1 in vitro. | Co-administer a molecule that delays internalization, or use a non-internalizing CXCR4 agonist. |
| Host tissue has inadequate SDF-1 expression. | Measure SDF-1 levels in the target tissue by immunohistochemistry or ELISA. | Inject a stabilized version of SDF-1 directly into the target tissue to create a powerful, sustained homing signal [9]. |
Key Experimental Protocols
Protocol 1: Evaluating SDF-1-Induced Migration via Transwell Assay
This protocol is adapted from studies on human dental pulp stem cell (hDPSC) migration [50].
Key Reagents:
- Recombinant Human SDF-1/CXCL12
- Transwell plates with permeable membrane inserts (pore size 8 μm)
- Serum-free medium and medium with serum as a chemoattractant base
- Cell staining solution (e.g., Crystal Violet or Calcein-AM)
- AMD3100 (CXCR4 antagonist) for inhibition controls
Methodology:
- Prepare Chemoattractant: Dilute SDF-1 in serum-free medium to a concentration of 50 ng/mL and add it to the lower chamber of the Transwell plate. Include a negative control (serum-free medium only).
- Cell Preparation: Harvest and wash the stem cells. Resuspend them in serum-free medium at a density of 1-5 x 10^5 cells/mL. For inhibition control, pre-treat an aliquot of cells with 10 μM AMD3100 for 30 minutes.
- Seed Cells: Carefully add the cell suspension to the upper chamber of the Transwell insert.
- Incubate and Migrate: Incubate the plate for 6-24 hours at 37°C in a 5% CO2 incubator to allow cells to migrate through the membrane towards the lower chamber.
- Quantify Migration: After incubation, remove non-migrated cells from the upper side of the membrane with a cotton swab. Fix and stain the migrated cells on the lower side with Crystal Violet. Alternatively, use Calcein-AM to stain viable migrated cells for fluorescence-based quantification. Count cells in several predefined fields under a microscope or use a plate reader.
Protocol 2: Analyzing Key Signaling Pathways by Western Blot
This protocol allows for the verification of SDF-1/CXCR4 pathway activation in your stem cells.
Key Reagents:
- Phosphoprotein-specific antibodies: p-FAK (Tyr397), p-Akt (Ser473), p-GSK3β (Ser9), total forms of these proteins, and β-catenin.
- Lysis buffer (RIPA buffer) supplemented with protease and phosphatase inhibitors.
- SDF-1α
Methodology:
- Starvation and Stimulation: Serum-starve cells for 4-6 hours to reduce background signaling. Stimulate them with 50 ng/mL SDF-1 for a time course (e.g., 0, 15, 30, 60 minutes).
- Protein Extraction: Immediately lyse cells after stimulation on ice. Centrifuge the lysates and collect the supernatant.
- Western Blot: Separate equal amounts of protein by SDS-PAGE and transfer to a PVDF membrane. Block the membrane and incubate with primary antibodies overnight at 4°C.
- Detection and Analysis: After incubation with HRP-conjugated secondary antibodies, develop the blots using enhanced chemiluminescence (ECL). Analyze the band intensity to track time-dependent phosphorylation of Akt, FAK, GSK3β, and changes in β-catenin expression [50].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for Investigating the SDF-1/CXCR4 Axis
| Reagent | Primary Function | Example Application |
|---|---|---|
| Recombinant SDF-1α (CXCL12) | Agonist; activates CXCR4 to induce chemotaxis and downstream signaling. | Creating a gradient in Transwell migration assays; stimulating cells for phosphorylation studies [50]. |
| AMD3100 (Plerixafor) | Selective CXCR4 antagonist; blocks SDF-1 binding. | Validating the specificity of SDF-1 effects in migration and signaling assays; mobilizing stem cells from bone marrow [50]. |
| LY294002 | Selective PI3K inhibitor. | Investigating the role of the PI3K/Akt branch in SDF-1-induced migration and survival [50]. |
| PF573228 | Selective FAK inhibitor. | Probing the function of focal adhesion turnover in cell migration downstream of CXCR4 [50]. |
| Anti-CXCR4 Antibody | Detecting CXCR4 receptor expression and localization. | Flow cytometric analysis of surface expression; immunofluorescence to visualize receptor distribution. |
| Phospho-Specific Antibodies (p-Akt, p-FAK) | Detecting activation of key downstream signaling nodes. | Western blot analysis to confirm pathway activation upon SDF-1 stimulation [50]. |
FAQs and Troubleshooting Guides
Q1: Why is preconditioning with irradiation necessary for successful stromal cell engraftment?
A1: Preconditioning, specifically through irradiation, is used to create "space" and disrupt the recipient's native bone marrow (BM) stroma. This damage is a critical stimulus for donor-derived Mesenchymal Stem Cells (MSCs) to engraft and proliferate. Research demonstrates that without prior damage to the recipient's BM stroma, donor MSC engraftment is minimal to non-existent. In experimental models, unirradiated recipients showed no donor cells in the BM stromal subpopulation. Successful engraftment of donor stromal progenitor cells was only observed in recipients whose BM stroma was pre-damaged with high-dose irradiation [55].
Q2: What is the relationship between irradiation dose and engraftment efficiency?
A2: Engraftment efficiency is highly dependent on the radiation dose. Higher doses that cause significant stromal damage correlate with substantially improved donor chimerism. The table below summarizes key findings from a preclinical study [55]:
| Radiation Dose | Donor Chimerism in BM Stromal Cells | Outcome Summary |
|---|---|---|
| 0 Gy (No irradiation) | 0% | No donor cells detected in any of the studied bone marrow samples. |
| 6.5 Gy | 0.16% (in one animal only) | Minimal and inconsistent engraftment of donor cells. |
| 13 Gy | 11% and 14% (in survivors) | Significant and successful engraftment of donor stromal progenitor cells. |
Q3: My experimental MSC transplant failed to engraft. What is the most likely cause?
A3: The most probable cause, based on current evidence, is an insufficiently damaged recipient stromal niche. If the recipient's native bone marrow stroma is largely intact, it prevents administered MSCs from homing, dividing, and functioning as stem cells to replenish the compartment. You should review your preconditioning protocol, particularly the irradiation dose, to ensure it is sufficient to create the necessary biological vacancy for donor cells [55].
Q4: Are there safer alternatives to high-dose irradiation for preconditioning?
A4: Yes, research is actively exploring less toxic conditioning regimens. A significant advancement is the development of antibody-based targeting. For instance, a Phase 1 clinical trial successfully used an antibody against CD117 (a protein on blood-forming stem cells) to eliminate a patient's own stem cells without using toxic chemotherapy or radiation. This approach prepared patients for a stem cell transplant effectively and safely, which is particularly beneficial for fragile patients who cannot tolerate the side effects of irradiation [56].
The following table consolidates key quantitative findings on engraftment outcomes from systematic reviews and clinical studies involving MSC co-infusion, providing a benchmark for expected results [12] [22]:
| Parameter | Average Outcome with MSC Infusion | Key Context |
|---|---|---|
| Neutrophil Engraftment Time | 13.96 days | Average time from transplantation to neutrophil recovery in patients receiving MSC co-infusion. |
| Platelet Engraftment Time | 21.61 days | Average time to platelet recovery; a key area where MSCs show a particular benefit. |
| Studies Reporting Enhanced Engraftment | ~79% | The majority of clinical studies reported a positive effect on engraftment. |
| Number of Patients Analyzed | 1,777 | Total patients across 47 clinical studies included in a systematic review (2000-2025). |
| Serious Adverse Events | None reported | No serious adverse events were directly attributed to the MSC infusion itself. |
Detailed Experimental Protocols
This protocol details the methodology for testing the hypothesis that recipient stromal damage is a prerequisite for donor MSC engraftment.
1. Animal Preparation:
- Use inbred strain B10 mice (or another suitable syngeneic strain).
- Utilize female mice as recipients and male mice as donors to enable sex-mismatched chimerism tracking via the Y chromosome.
2. Recipient Preconditioning (Irradiation):
- Subject recipient female mice to Total Body Irradiation (TBI) using a gamma radiation source (e.g., cesium-137).
- Include experimental groups irradiated at different doses (e.g., 0 Gy, 6.5 Gy, and 13 Gy) to establish a dose-response relationship. The intensity used in the cited study was 21.8 cGy/min.
3. Donor Bone Marrow Cell Isolation:
- Sacrifice donor male mice by cervical dislocation.
- Aseptically harvest femoral and tibial bones.
- Flush the bone cavities with PBS using a syringe and needle to collect bone marrow.
- Create a single-cell suspension by repeatedly passing the marrow through the needle. Count the cells and adjust the concentration with PBS for injection.
4. Cell Transplantation:
- On the same day as irradiation, intravenously inject the recipient female mice with the donor male BM cell suspension via the tail vein. A typical injection volume is 0.5 mL.
5. Analysis of Engraftment (30 days post-transplant):
- Sample Collection: Sacrifice recipients and collect bones (e.g., femurs, tibias). Clean bones externally and flush out marrow for analysis.
- CFU-F Assay: Seed BM cells at 3x10^6 cells per T25 flask in complete αMEM medium supplemented with 20% FBS and 5 ng/mL FGF2. After 3 weeks, stain with crystal violet to count Colony-Forming Unit Fibroblast (CFU-F) colonies.
- Cell Sorting: Isolate the stromal cell population (e.g., CD45- cells) using a flow cytometer sorter.
- Donor Chimerism Quantification: Isolate DNA from sorted CD45- cells and bone tissue. Use digital droplet PCR (ddPCR) with primers for a Y-chromosome-specific gene (e.g., Prssly) and an autosomal control gene (e.g., Gapdh) to calculate the precise percentage of donor-derived cells.
This clinical protocol offers a modern alternative to genotoxic irradiation.
- 1. Patient Population: The protocol was designed for patients with Fanconi anemia, a genetic disorder that creates extreme sensitivity to DNA-damaging agents like radiation and chemotherapy.
- 2. Antibody Administration: A single intravenous infusion of the anti-CD117 antibody (briquilimab) is administered 12 days prior to the scheduled stem cell transplant.
- 3. Adjunctive Immunosuppression: Closer to the transplant date, patients receive standard immune-suppressing medications, but no radiation or busulfan chemotherapy.
- 4. Stem Cell Transplant: Patients receive a stem cell transplant from a donor (e.g., a haploidentical parent). The graft is often modified by depleting alpha/beta T-cells to reduce the risk of graft-versus-host disease and enriching for CD34+ hematopoietic stem cells.
- 5. Outcome Monitoring: Monitor patients for donor cell engraftment, chimerism levels, and recovery of blood counts.
Signaling Pathways and Experimental Workflows
Diagram: Irradiation Preconditioning Workflow for Stromal Engraftment
The following diagram illustrates the logical sequence and key mechanisms of using irradiation to precondition a recipient for MSC transplantation.
The Scientist's Toolkit: Research Reagent Solutions
This table lists essential reagents and their functions for experiments in stromal preconditioning and engraftment.
| Research Reagent | Primary Function in Experiment |
|---|---|
| Anti-CD117 Antibody (e.g., Briquilimab) | A non-genotoxic conditioning agent that targets and eliminates host hematopoietic and mesenchymal stem cells by binding the CD117 receptor, making space for donor cells [56]. |
| Anti-CD45 Antibody (e.g., clone 30-F11) | Used in flow cytometry to identify and sort the hematopoietic lineage (CD45+) cells from the stromal (CD45-) population for downstream analysis like chimerism measurement [55]. |
| FGF2 (Fibroblast Growth Factor-2) | A growth factor added to culture media (e.g., at 5 ng/mL) to support the in vitro growth and colony formation of Mesenchymal Stem Cells (CFU-F assay) [55]. |
| Primers/Probes for Y-chromosome gene (e.g., Prssly) | Essential reagents for digital droplet PCR (ddPCR) to detect and quantify male donor-derived cells in a female recipient, enabling precise measurement of donor chimerism [55]. |
| Alpha/MEM Medium + 20% FBS | The standard culture medium used for the expansion and maintenance of MSCs in vitro, providing essential nutrients and growth factors [55]. |
| Crystal Violet Stain | A dye used to stain and visualize CFU-F colonies after a few weeks of culture, allowing for manual counting and assessment of stromal progenitor frequency [55]. |
This technical support center is designed to assist researchers in navigating the complex challenges associated with stem cell transplantation. A significant obstacle in the field is the massive cell death post-transplantation, with some studies indicating that up to 90% of transplanted cells may undergo apoptosis within the initial days due to a hostile microenvironment characterized by ischemia, inflammation, and oxidative stress [57]. This severely limits the therapeutic potential of stem cell therapies.
The paradigm of "Integrated Cell and Tissue-Preconditioning" addresses this challenge by employing a dual-pronged strategy. It involves preconditioning the cells themselves to enhance their resilience and functionality, while also conditioning the target tissue to create a more receptive environment, thereby synergistically maximizing engraftment efficacy. This guide provides troubleshooting and FAQs to help you implement this sophisticated approach in your research.
Troubleshooting Common Stem Cell Engraftment Challenges
FAQ: What are the primary causes of poor stem cell survival after transplantation?
The low survival rate is multifactorial, primarily due to the harsh conditions in the transplantation site, especially in ischemic tissues. Key stressors include:
- Metabolic Crisis: The lack of an immediate blood supply leads to severe hypoxia and nutrient deprivation [57].
- Oxidative Stress: An abrupt shift from in vitro culture to an in vivo injury site creates a surge of reactive oxygen species (ROS) that overwhelms the cells' antioxidant defenses [57].
- Inflammatory Response: The host's immune response and inflammatory factors can damage transplanted cells [58] [30].
- Anoikis: This is a form of programmed cell death triggered by the disruption of cell-matrix interactions during the harvesting and transplantation process [58].
FAQ: How can we quantitatively assess the success of our preconditioning protocols?
Success can be evaluated through a combination of in vitro and in vivo assays, measuring key outcome metrics as summarized in the table below.
Table 1: Key Metrics for Assessing Preconditioning Protocol Efficacy
| Assessment Category | Specific Metric | Example Experimental Result |
|---|---|---|
| Cell Survival/Viability | Viability in low-serum media (in vitro) | 80% vs 64% survival for celastrol-preconditioned vs. control hMSCs after 4 days [59] |
| Cell Survival/Engraftment | Engraftment rate in animal model (in vivo) | 2 to 3 times greater engraftment for CDH2-overexpressing hiPSC-CMs vs. wild-type [60] |
| Paracrine Function | Secretion of proangiogenic factors (e.g., VEGFa, SDF-1α) | 3.0-fold and 1.8-fold increase of VEGFa and SDF-1α, respectively, from celastrol-preconditioned MSCs [59] |
| Therapeutic Angiogenesis | Neovessel density in vivo | Significant increase in peri-implant neovessel density with celastrol-preconditioned MSCs [59] |
| Functional Recovery | Cardiac ejection fraction (EF) in MI model | EF better preserved in CDH2-cell group (50%) vs. wild-type group (40%) [60] |
Troubleshooting Guide: Low Cell Survival Post-Transplantation
Table 2: Troubleshooting Low Post-Transplantation Cell Survival
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Massive cell death within first 48 hours | Hostile microenvironment (ischemia, inflammation) | Implement hypoxic preconditioning (e.g., 1% O₂ for 24-48 hours) to activate HIF-1α pro-survival pathways [30] [57]. |
| Disrupted cell-matrix interactions leading to anoikis | Encapsulate cells in a protective biomaterial scaffold (e.g., chitosan-based hydrogel) to provide anchor points [59] [58]. | |
| Poor cell retention at injection site | Mechanical washout in beating heart or leakage | Use an injectable thermosensitive hydrogel that is liquid at room temperature but gels at body temperature, entrapping cells [59]. |
| Insufficient therapeutic effect despite some survival | Limited paracrine factor secretion | Apply pharmacological preconditioning with compounds like celastrol (1 μM for 1 hour) to boost paracrine output [59]. |
| Inadequate vascularization of graft | Lack of angiogenic signaling | Precondition cells to overexpress proangiogenic genes (e.g., VEGF) or use cells engineered to overexpress N-cadherin, which stimulates angiogenesis [60] [30]. |
Detailed Experimental Protocols for Preconditioning
Protocol: Pharmacological Preconditioning with Celastrol
This protocol is adapted from a study demonstrating enhanced MSC viability and proangiogenic function [59].
Objective: To enhance MSC resistance to stress and boost its paracrine activity prior to transplantation.
Reagents:
- Celastrol (Cayman Chemical): Prepare a 1 mM stock solution in DMSO.
- Complete MSC culture medium (e.g., alpha-MEM with 10% FBS).
- Serum-low medium (e.g., alpha-MEM with 0.2% FBS).
- Phosphate Buffered Saline (PBS).
Procedure:
- Cell Culture: Culture MSCs (human or rat) to 90% confluence.
- Preconditioning Stimulation: Replace the medium with serum-low medium (alpha-MEM 1% FBS) containing 1 μM celastrol (from the stock solution). The final DMSO concentration should be 0.1% (v/v).
- Control Setup: For vehicle control, treat cells with serum-low medium containing 0.1% DMSO only.
- Incubation: Incubate cells for 1 hour at 37°C and 5% CO₂.
- Washing: After incubation, carefully aspirate the celastrol-containing medium and rinse the cell monolayer three times with serum-low medium to remove the compound.
- Recovery: Add complete culture medium (alpha-MEM 10% FBS) and allow cells to recover for 4 hours at 37°C and 5% CO₂.
- Harvesting for Transplantation: After recovery, harvest the preconditioned MSCs using a standard method (e.g., trypsinization) for subsequent encapsulation or direct transplantation.
Validation: Assess the success of preconditioning by comparing the viability of preconditioned vs. control cells under stress (e.g., in low serum media) and by quantifying the secretion of VEGFa and SDF-1α via ELISA.
Protocol: Hypoxic Preconditioning of Stem Cells
This protocol outlines a general method to enhance stem cell tolerance to ischemia [30] [57].
Objective: To activate endogenous cytoprotective mechanisms in stem cells by exposing them to sub-lethal hypoxia.
Reagents:
- Hypoxia chamber or workstation capable of maintaining 1-5% O₂, 5% CO₂, and balance N₂.
- Complete cell culture medium.
Procedure:
- Preparation: Culture stem cells (MSCs, NSCs, etc.) to the desired confluence (typically 70-80%).
- Preconditioning: Place the culture vessels into the pre-equilibrated hypoxia chamber. Maintain the cells at 1-5% O₂ for a defined period, commonly 24-48 hours.
- Control: Maintain control cells in a standard incubator (normoxia, ~20% O₂) for the same duration.
- Harvesting: Remove cells from the hypoxic chamber and immediately harvest them for transplantation using standard procedures.
Validation: Hypoxic preconditioning can be validated by measuring the upregulation of HIF-1α and its downstream targets (e.g., VEGF, GLUT-1) via Western blot or PCR. Functional assays can include in vitro survival under oxygen-glucose deprivation (OGD) conditions.
The following diagram illustrates the core signaling pathways activated by different preconditioning strategies, which converge on enhanced cell survival and function.
The Scientist's Toolkit: Essential Reagents and Materials
This table lists key reagents and materials used in the featured preconditioning experiments and their critical functions.
Table 3: Research Reagent Solutions for Preconditioning Experiments
| Reagent / Material | Function in Preconditioning | Example Usage & Rationale |
|---|---|---|
| Celastrol | Pharmacological preconditioning agent; natural potent antioxidant that activates cytoprotective pathways. | Used at 1 μM for 1 hour to protect MSCs against hypoxia/oxidative damage and enhance paracrine function [59]. |
| Chitosan-based Thermosensitive Hydrogel | Injectable biomaterial scaffold for cell encapsulation; protects cells and improves retention. | Provides a 3D scaffold that localizes cells, protects from inflammatory milieu, and may enhance survival (90% vs 36% for rMSC) [59]. |
| Hypoxia Chamber | Equipment for creating a controlled low-oxygen environment for hypoxic preconditioning. | Used to maintain 1-5% O₂ to sub-lethally stress cells, activating HIF-1α and pro-survival pathways [30] [57]. |
| DMOG (Dimethyloxalylglycine) | Prolyl hydroxylase inhibitor; stabilizes HIF-1α, mimicking hypoxic preconditioning under normoxia. | An alternative to physical hypoxia; enhances MSC survival after serum deprivation and oxygen-glucose deprivation [30]. |
| Perfluorocarbons (PFCs) | Synthetic oxygen carriers; used to supplement oxygen at the transplantation site. | Incorporated into hydrogels or scaffolds to mitigate local hypoxia and support cell survival post-transplantation [57]. |
| SDF-1α / CXCR4 Agonists | Chemokine signaling molecules; key for stem cell homing and recruitment. | Used to precondition cells or the target tissue to enhance the homing of transplanted or endogenous stem cells [61] [30]. |
FAQ on Advanced and Emerging Concepts
FAQ: Beyond survival, how can preconditioning improve the functional integration of stem cells?
For therapies aiming to rebuild functional tissue, such as using cardiomyocytes to repair a heart, survival alone is insufficient. Preconditioning can enhance integration:
- N-Cadherin Overexpression: Genetically engineering hiPSC-derived cardiomyocytes to overexpress N-cadherin (CDH2) improves cell-cell interaction, elevates connexin 43 expression (for gap junctions), and leads to faster electrical conduction velocity, reducing arrhythmia risk [60].
- Metabolic Reprogramming: Hypoxic preconditioning can shift stem cell metabolism from oxidative phosphorylation to glycolysis, making them more adaptable to the low-oxygen environment of the injury site and preserving energy homeostasis [57].
FAQ: Are there ethical concerns or regulatory considerations for these preconditioning strategies?
Yes, the choice of cell source and genetic modification techniques require careful consideration.
- Cell Source: The use of human embryonic stem cells (hESCs) involves ethical debates concerning embryo destruction. Alternatives like induced pluripotent stem cells (iPSCs) or adult MSCs are preferred in many contexts to avoid these issues [62] [58].
- Regulatory Compliance: Any stem cell-based product, especially those involving genetic engineering (e.g., CDH2 overexpression), must undergo rigorous safety and efficacy testing following regulatory guidelines (e.g., FDA, EMA). This includes testing for tumorigenicity (teratoma formation), off-target effects, and long-term safety in preclinical models [58] [63]. All clinical applications must adhere to the principles of integrity, transparency, and primacy of patient welfare as outlined in guidelines like those from the ISSCR [63].
Evaluating Efficacy and Safety: Clinical Outcomes, Comparative Analyses, and Future Tools
Frequently Asked Questions (FAQs)
Q1: What are the key clinical factors that predict successful engraftment kinetics? Multiple patient- and product-specific factors influence engraftment. A study of 52 pediatric autologous transplants found neutrophil engraftment significantly correlated with the patient's age, body weight, diagnosis, source of stem cells, and the number of CFU-GM/kg. Platelet engraftment was significantly linked to the time from diagnosis to transplantation, source of stem cells, and the number of CD34+ cells/kg [64].
Q2: What factors influence long-term survival for patients who have survived 2 years post-transplant? For allogeneic transplant recipients who survive beyond 2 years, long-term outcomes are generally good, but life expectancy remains inferior to the general population. Key risk factors for late death include initial diagnosis of age ≥ 60 years, chronic lymphocytic leukaemia (CLL), previous blood stream- or invasive fungal infection, and chronic graft-versus-host disease (cGVHD). Optimizing management of these complications is crucial for improving survival [65].
Q3: What is Engraftment Syndrome (ES) and how is it managed? Engraftment Syndrome is a continuum of peri-engraftment complications after autologous hematopoietic stem cell transplantation. Major criteria include non-infectious fever, skin rash, and non-cardiogenic pulmonary edema. It is often managed with corticosteroids, and most cases are mild and resolve with treatment, though severe cases can be fatal. Diagnosis requires ruling out other causes, such as infection [66].
Q4: How is the success of stem cell therapy measured in clinical trials? Success is measured through a combination of clinical observations, laboratory tests, and patient-reported outcomes. This includes physical examinations, imaging studies, monitoring of specific biomarkers, and evaluations of the patient's quality of life, physical functioning, and symptom changes. Long-term follow-up is essential to assess the durability of the response [1].
Q5: In T-cell lymphoma, what are the considerations for choosing between autologous (auto-SCT) and allogeneic (allo-SCT) transplantation? Real-world data indicates that as a consolidative therapy, up-front auto-SCT demonstrates a survival benefit. For patients in complete remission (CR), auto-SCT is effective. However, for patients with relapsed/refractory disease or those only in partial remission (PR), allo-SCT may be considered as it can demonstrate better long-term progression-free survival, albeit with a higher risk of early treatment-related mortality [67].
Troubleshooting Common Experimental Challenges
Problem: Poor or Delayed Engraftment
Potential Causes and Solutions:
- Cause: Inadequate stem cell dose.
- Cause: Underlying patient factors (e.g., older age, diagnosis).
- Cause: Damage to the bone marrow niche preventing proper homing and expansion.
- Solution: Investigate niche components and signaling pathways in your model system. Techniques like single-cell RNA sequencing can help characterize the microenvironment post-transplantation [68].
Problem: High Rates of Late Mortality/Relapse in Long-Term Studies
Potential Causes and Solutions:
- Cause: Relapse of the original malignant disease.
- Solution: In the context of allogeneic transplants, consider the graft-versus-tumor effect. Research indicates that a cytomegalovirus (CMV) seronegative donor and a diagnosis of CLL were associated with later relapse [65].
- Cause: Complications like chronic Graft-versus-Host Disease (cGVHD) or late infections.
- Solution: Focus on prophylactic measures. Studies recommend optimising prophylaxis and treatment for cGVHD, blood stream, and invasive fungal infections to improve long-term survival [65].
Problem: Differentiating Engraftment Syndrome from Other Complications
Potential Causes and Solutions:
- Cause: Overlap in symptoms with infection, drug reactions, or Graft-versus-Host Disease (GVHD).
- Solution: Apply standardized diagnostic criteria, such as the Spitzer or Maiolino criteria, which are based on the timing of symptoms relative to neutrophil engraftment and the presence of specific clinical features like non-infectious fever and rash [66]. A skin or colonic biopsy can confirm histologic evidence of immune infiltration, helping to rule out other causes [66].
Table 1: Predictive Factors for Engraftment Kinetics (Autologous Transplantation)
| Factor | Impact on Neutrophil Engraftment | Impact on Platelet Engraftment | P-Value |
|---|---|---|---|
| Patient Age | Significant Correlation | Not Specified | 0.050 [64] |
| Body Weight | Significant Correlation | Not Specified | 0.021 [64] |
| Diagnosis | Significant Correlation | Not Specified | 0.023 [64] |
| Stem Cell Source | Significant Correlation | Significant Correlation | 0.001 (Neutrophil); 0.009 (Platelet) [64] |
| CFU-GM/kg | Significant Correlation | Not Specified | 0.018 [64] |
| Time from Dx to Tx | Not Specified | Significant Correlation | 0.043 [64] |
| CD34+ cells/kg | Not Specified | Significant Correlation | 0.014 [64] |
Table 2: Long-Term Survival in Allogeneic Transplant 2-Year Survivors
| Metric | Probability / Finding | Key Risk Factors for Late Death |
|---|---|---|
| 5-Year Overall Survival | 86% | Age ≥ 60 years at initial diagnosis [65] |
| 10-Year Overall Survival | 76% | Chronic Lymphocytic Leukaemia (CLL) [65] |
| 5-Year Transplant-Related Mortality | 9.0% | Previous Blood Stream or Invasive Fungal Infection [65] |
| 5-Year Relapse Incidence | 7.7% | Chronic Graft-versus-Host Disease (cGVHD) [65] |
| Life Expectancy | Inferior to age-/gender-matched general population | - [65] |
Detailed Experimental Protocols
Protocol 1: Viral Barcoding for HSPC Fate Mapping
This protocol uses lentiviral vectors to introduce unique DNA barcodes into a population of Hematopoietic Stem and Progenitor Cells (HSPCs), allowing for high-resolution tracking of individual clones and their progeny after transplantation [68].
Key Materials:
- Library of lentiviral vectors containing a diverse pool of random 20-30 nucleotide barcode sequences.
- Target HSPCs (e.g., human CD34+ cells).
- Polybrene or other transduction-enhancing reagents.
- Culture media with appropriate cytokines (SCF, TPO, FLT3-L).
- Recipient animal model (e.g., immunodeficient mice).
Methodology:
- Library Preparation: Generate or acquire a lentiviral barcode library. The library complexity (number of unique barcodes) should vastly exceed the number of cells to be transduced to ensure each cell receives a unique mark [68].
- Cell Stimulation: Pre-stimulate the HSPCs in cytokine-enriched media for 24-48 hours to promote cell cycle entry, which improves transduction efficiency.
- Viral Transduction: Transduce the HSPCs with the viral library at a low Multiplicity of Infection (MOI << 1). This is critical to minimize the chance of a single cell receiving multiple barcodes.
- Transplantation: After a short culture period, transplant the transduced HSPCs into conditioned recipient mice.
- Sample Collection and Tracking: At designated time points post-transplant, collect peripheral blood, bone marrow, and other tissues. Isolate genomic DNA and/or single cells.
- Barcode Recovery and Sequencing:
- For bulk analysis: Amplify barcodes from genomic DNA using PCR with primers flanking the barcode region. Use high-throughput sequencing to identify the relative abundance of each barcode in different samples and time points [68].
- For single-cell resolution: Use single-cell RNA sequencing (scRNA-seq) protocols that can capture the viral barcode transcript along with the cellular transcriptome, linking clonal identity to cell type [68].
Protocol 2: Assessing Engraftment Syndrome in Preclinical Models
This protocol outlines the observation and scoring of clinical parameters to identify Engraftment Syndrome in mouse models of transplantation.
Key Materials:
- Mouse model of transplantation (e.g., syngeneic or autologous setting).
- Daily monitoring sheets for clinical scoring.
- Scale for daily weight measurement.
- Thermometer for body temperature.
Methodology:
- Baseline Measurement: Record the baseline weight and general appearance of all animals prior to transplantation.
- Post-Transplant Monitoring: Beginning around the time of expected engraftment, monitor animals at least daily for:
- Weight: Record percent weight gain from baseline. Weight gain ≥2.5% is a minor criterion for ES [66].
- Temperature: Measure body temperature. A non-infectious fever (≥101°F / 38.3°C) is a major criterion [66].
- Physical Appearance: Check for signs of skin rash (erythema), hunched posture, reduced activity, and respiratory distress (a sign of pulmonary edema).
- Scoring and Diagnosis: Apply adapted diagnostic criteria (e.g., Spitzer criteria) to identify animals with ES. Diagnosis may require the presence of major criteria (e.g., fever + rash) or a combination of major and minor criteria (e.g., weight gain, hepatic dysfunction) [66].
- Intervention: For animals diagnosed with ES, corticosteroid treatment (e.g., dexamethasone) can be administered to assess therapeutic response.
Experimental Workflow and Signaling
The following diagram illustrates the core workflow for designing a study to analyze engraftment and long-term survival, integrating both clinical and molecular fate mapping approaches.
The Scientist's Toolkit: Key Research Reagents
| Reagent / Material | Function / Application | Example Context |
|---|---|---|
| Lentiviral Barcode Library | Introduces unique, heritable DNA sequences into HSPCs for high-resolution clonal tracking. | Fate mapping studies to understand repopulation kinetics and lineage bias after transplantation [68]. |
| CD34+ Cell Selection Kit | Isulates human hematopoietic stem and progenitor cells from apheresis product or bone marrow. | Preparing a defined HSPC population for transplantation or in vitro assays [64] [68]. |
| Corticosteroids (e.g., Dexamethasone) | Used to manage and treat immune-mediated complications like Engraftment Syndrome (ES). | In vivo models to assess the response of ES to anti-inflammatory therapy [66]. |
| Cytokine Cocktail (SCF, TPO, FLT3-L) | Promotes ex vivo survival and proliferation of HSPCs, essential for pre-stimulation before transduction. | Expanding or maintaining HSPCs in culture for genetic manipulation [68]. |
| Anti-thymocyte globulin (ATG) | In vivo T-cell depletion agent; used in conditioning regimens to prevent Graft rejection and GvHD. | Clinical and preclinical allogeneic transplant models to modulate immune reconstitution [65]. |
What are the primary mechanisms of action of TPO-RAs compared to conventional supportive care?
Thrombopoietin Receptor Agonists (TPO-RAs) and conventional supportive care represent two fundamentally different approaches to managing thrombocytopenia. Their mechanisms of action differ significantly:
| Feature | TPO-RAs | Conventional Supportive Care |
|---|---|---|
| Primary Mechanism | Stimulates platelet production by activating thrombopoietin receptors on megakaryocytes and hematopoietic stem cells [69]. | Replaces circulating platelets via transfusion [70]. |
| Biological Effect | Activates JAK-STAT, MAPK, and PI3K-AKT pathways, leading to megakaryocyte proliferation, maturation, and inhibition of apoptosis [69]. | Directly increases platelet count in peripheral blood. |
| Therapeutic Goal | Addresses the underlying cause of poor platelet production [70]. | Provides immediate, temporary correction of low platelet counts. |
| Duration of Effect | Sustained effect through continued stimulation of platelet production. | Transient, lasting until transfused platelets are cleared from circulation. |
The following diagram illustrates the key signaling pathways activated by TPO-RAs that lead to increased platelet production:
Efficacy Data & Comparative Analysis
What does the quantitative data show regarding the efficacy of TPO-RAs versus conventional care in promoting platelet engraftment post-transplant?
Clinical studies have yielded context-dependent results on the efficacy of TPO-RAs and related agents like recombinant human thrombopoietin (rhTPO) in the transplant setting. The table below summarizes key findings from recent investigations:
| Study Population / Context | Intervention | Key Efficacy Outcome vs. Control | Impact on Transfusions | Study Reference |
|---|---|---|---|---|
| Severe Aplastic Anemia (SAA) post-Haplo-HSCT [71] | rhTPO | Significantly faster platelet engraftment (11 vs. 14 days; P=.003). | Significantly reduced platelet transfusions (2 vs. 3 doses; P=.004). | PMC |
| Newly Diagnosed Multiple Myeloma (NDMM) post-ASCT [72] | rhTPO | No significant difference in platelet engraftment (11.5 vs. 11.36 days; P=0.776). | No significant reduction in platelet transfusions (1.615 vs. 1.5 units; P=0.721). | Sci. Rep. (2025) |
| Prolonged Thrombocytopenia post-CAR-T therapy [73] | TPO-RAs (Eltrombopag) | Lower response rate (33% vs. 80% in ITP trials); longer time to response. | Data not specified. | Blood Adv (2023) |
| General Post-HCT Thrombocytopenia [70] | TPO-RAs (multiple) | Platelet recovery in a majority of reported cases; effective in real-world settings. | A key benefit noted, reducing reliance on transfusions. | PMC Review (2024) |
Experimental Protocols
What is a detailed experimental protocol for investigating TPO-RA efficacy in a post-transplant model?
Based on reviewed literature, here is a composite protocol for evaluating a TPO-RA in a clinical or translational research setting, such as after hematopoietic cell transplantation (HCT).
Objective: To assess the efficacy and safety of [TPO-RA Name] in promoting platelet engraftment and reducing platelet transfusion requirements following HCT.
Patient Eligibility Criteria (Example):
- Diagnosis: Severe Aplastic Anemia or other indication for HCT.
- Undergoing Haploidentical HCT with Post-Transplant Cyclophosphamide (PTCy) [71].
- Adequate organ function.
Study Arms & Intervention:
- Intervention Group: Subcutaneous injection of rhTPO at 15,000 units daily [71] OR oral administration of a TPO-RA (e.g., Eltrombopag) at a standard dose (e.g., 50 mg daily) [69] [73].
- Control Group: Standard supportive care alone, including prophylactic platelet transfusions.
Dosing Schedule:
- Initiation: Start on day +1 after stem cell infusion [71].
- Duration: Continue for 14 days or until platelet engraftment is achieved (e.g., platelet count ≥ 20 × 10⁹/L for 7 consecutive days without transfusion) [72] [71].
Endpoint Monitoring & Data Collection:
- Primary Efficacy Endpoint: Time to platelet engraftment.
- Secondary Efficacy Endpoints:
- Safety Monitoring:
- Monitor for adverse events (AEs) including liver function tests (for Eltrombopag), thrombosis, and other potential complications [74].
- Long-term Reconstitution:
- Monitor neutrophil count, hemoglobin, and platelet count at set intervals (e.g., 180 days post-transplant) [72].
Troubleshooting & FAQ
Frequently Asked Questions from Researchers and Clinicians
Q1: A patient undergoing HCT has poor platelet engraftment by day +28. Should I initiate a TPO-RA? A: Evidence supports considering TPO-RAs in this context. A 2024 review of 64 studies concluded that TPO-RAs have promising effects for treating post-HCT thrombocytopenia with a good safety profile [70]. The decision should be based on the specific cause of thrombocytopenia (e.g., poor graft function vs. active GVHD) and the specific TPO-RA, as agents like avatrombopag may offer convenience due to no dietary restrictions [70].
Q2: In our trial, a patient on eltrombopag shows a suboptimal platelet response. What are the potential reasons? A: Several factors could be at play:
- Mechanism of Thrombocytopenia: TPO-RAs primarily stimulate production. If the dominant mechanism is peripheral platelet destruction (e.g., due to antibodies or microangiopathy), the response may be blunted [70].
- Bone Marrow Reserve: The effectiveness depends on the presence and health of megakaryocyte precursors. A severely hypocellular marrow may respond poorly.
- Drug Interactions: Eltrombopag chelates polyvalent cations. Concomitant administration with calcium-rich foods, antacids, or dairy products can significantly reduce its absorption [69].
- Splenectomy Status: Clinical trials in ITP have shown that splenectomized patients may have lower response rates to TPO-RAs [75].
Q3: Are there specific safety concerns when using TPO-RAs in the post-transplant population? A: While generally safe, monitor for known class effects:
- Thromboembolism: A meta-analysis of randomized trials showed a non-significantly increased risk (RR=1.92), but this remains a clinical consideration [74]. Assess individual patient risk factors.
- Liver Function: Non-peptide TPO-RAs like eltrombopag may cause elevated liver transaminases, though a meta-analysis found no significant increase versus placebo [74]. Regular monitoring is recommended.
- Bone Marrow Reticulin Formation: Initial concerns about myelofibrosis have not been widely confirmed in long-term studies; any changes are usually mild and reversible upon discontinuation [75].
The Scientist's Toolkit
Key Research Reagent Solutions for Investigating TPO-RAs
| Reagent / Material | Function / Explanation in Research |
|---|---|
| Recombinant Human TPO (rhTPO) | First-generation TPO-RA; used as a control or benchmark in experimental models to study thrombopoiesis [70]. |
| Second-Generation TPO-RAs (e.g., Eltrombopag, Romiplostim, Avatrombopag) | Investigational agents for testing in various thrombocytopenic conditions; used to compare efficacy, safety, and mechanisms [69] [70]. |
| Janus Kinase (JAK) Inhibitors (e.g., Ruxolitinib) | Tool compounds used in mechanistic studies to inhibit the JAK-STAT pathway, helping to validate it as a critical downstream pathway of TPO-RA action [69] [76]. |
| CD34+ Hematopoietic Stem Cells | Primary cells used in in vitro cultures to study the direct effects of TPO-RAs on megakaryocyte differentiation and platelet production [69]. |
| Flow Cytometry Antibodies (e.g., CD41, CD61) | Used to identify and quantify megakaryocytes and platelets in in vitro cultures or animal models treated with TPO-RAs. |
| Animal Models of Thrombocytopenia | In vivo systems (e.g., irradiated, immune-mediated, or chemotherapy-induced models) for evaluating the efficacy and pharmacokinetics of TPO-RAs [73]. |
The following workflow diagram outlines the logical process for designing an experiment to compare TPO-RAs against conventional care:
FAQs: Viral Reactivations and Complications Post-Transplant
Q1: What are the most common viral reactivations after allogeneic HSCT, and what are their key risk factors?
Viral reactivation is a frequent complication after allogeneic hematopoietic stem cell transplantation (HSCT), occurring in a majority of patients [77]. The reactivations stem from viruses that persist latently in the patient or the transplanted cells, which can flare up in the context of post-transplant immunosuppression [77] [78].
The table below summarizes the incidence and key risk factors for common viral reactivations identified in a pediatric study [77].
| Virus | Incidence in Study Cohort | Key Identified Risk Factors |
|---|---|---|
| HHV-6 | 36/107 (33.6%) | Information not specified in the study. |
| EBV | 30/107 (28.0%) | Unrelated donor, in-vivo T-cell depletion, severe acute GvHD. |
| CMV | 21/107 (19.6%) | Recipient seropositivity status. |
| Adenovirus (ADV) | 15/107 (14.0%) | Severe acute GvHD. |
| HSV | 10/107 (9.3%) | Recipient seropositivity status. |
| VZV | 6/107 (5.6%) | Higher age at time of HSCT. |
General risk factors applicable to multiple viruses include the occurrence of acute graft-versus-host disease (aGvHD) and donor type (with unrelated donors posing a higher risk than matched related donors) [77].
Q2: How does the choice of graft source influence transplant-related mortality over time?
The source of stem cells (bone marrow vs. peripheral blood) exhibits a significant time-dependent effect on mortality endpoints. Peripheral blood stem cells (PBSC) show a protective effect early after transplantation, but this effect reverses later on [79].
The table below outlines the time-dependent hazard ratios (HR) for PBSC grafts compared to bone marrow.
| Endpoint | Early Phase Effect (HR) | Late Phase Effect (HR) | Change Point |
|---|---|---|---|
| Transplant-Related Mortality | Protective (HR: 0.70) | Detrimental (HR: 1.47) | 1 year |
| Non-Relapse Mortality | Protective (HR: 0.75) | Detrimental (HR: 1.38) | 8 months |
Q3: What are the critical immune cells involved in controlling cytomegalovirus (CMV) reactivation?
Controlling CMV reactivation requires a coordinated immune response. The key players are [78]:
- Virus-specific T cells: Polyfunctional virus-specific T cells are strongly associated with protection from viral reactivation. Adoptive transfer of these cells can prevent and treat reactivation and disease.
- Natural Killer (NK) cells: These cells play a crucial role in early viral surveillance.
- Dendritic cells: These cells are essential for priming naive T cells.
- Humoral responses: Strain-specific antibodies have recently been shown to prevent early CMV reactivation in preclinical models.
Q4: What are the major safety concerns associated with stem cell therapeutics beyond infection?
While stem cell therapies hold great promise, they carry several unique safety risks that must be managed during development and clinical application [80].
- Tumorigenic Potential: This is a major concern. Risks include teratoma formation from residual undifferentiated pluripotent stem cells and post-transplant malignancy from genomic aberrations acquired during in vitro culture. Tumor formation has been reported years after transplantation of fetal neural stem cells [80].
- Immunogenic Potential: Rejection of allogeneic cells can occur due to mismatches in HLA and other antigens. While some cells like mesenchymal stem cells (MSCs) have low immunogenicity, ensuring long-term tolerance remains a challenge [80].
Troubleshooting Guides
Guide 1: Managing Suspected Viral Reactivation in a Research Model
Problem: Unexplained morbidity or mortality in immunocompromised mouse models following stem cell engraftment.
Investigation Protocol:
- Regular Monitoring: Establish a weekly monitoring protocol for the first 3 months post-transplant, using quantitative PCR (qPCR) on peripheral blood samples to detect common viruses like CMV, HHV-6, and ADV [77].
- Assess Immune Reconstitution: Flow cytometry is critical. Track the recovery of key immune cells in the peripheral blood and lymphoid organs [77]. Focus on:
- T-cell subsets: (CD3+, CD4+, CD8+)
- NK cells: (CD56+, CD16+)
- B cells: (CD19+)
- Correlate with GvHD: Clinically score mice for signs of GvHD (skin, liver, GI tract). Statistically analyze the correlation between high GvHD scores and viral reactivation incidence, as this is a major clinical risk factor [77].
- Evaluate Intervention: If a reactivation is detected, test preemptive antiviral therapy (e.g., ganciclovir for CMV) and monitor viral load. For therapeutic research, consider adoptive transfer of virus-specific T cells and assess their efficacy in controlling the virus and improving outcomes [78].
Guide 2: Investigating Time-Dependent Effects of an Experimental Intervention
Problem: An experimental conditioning regimen shows a beneficial effect on non-relapse mortality in initial analysis, but the overall effect diminishes in long-term follow-up.
Analysis Workflow:
Methodology Details:
- Statistical Test: Use the test described by Therneau and Grambsch to identify covariates that violate the proportional hazards assumption. A significant result (e.g., p < 0.01) indicates a time-dependent effect [79].
- Model Fitting: For covariates with non-proportional hazards, fit a piecewise constant Cox model. This involves identifying a specific cut-point in time that maximizes the partial likelihood. Common cut-points identified in clinical studies are 4 months, 8 months, and 1 year [79].
- Interpretation: This approach allows you to resolve effects with different vectors early and later after transplantation. For example, reduced intensity conditioning was found to protect against non-relapse mortality only in the first 4 months (HR: 0.76), with no benefit thereafter [79].
The Scientist's Toolkit: Essential Reagents for Viral & Engraftment Research
| Research Reagent | Function in Experimental Models |
|---|---|
| qPCR Kits & Probes | For quantitative monitoring of viral DNA load (e.g., CMV, EBV, HHV-6) in blood and tissue samples to detect and track reactivations [77]. |
| Flow Cytometry Antibodies | To characterize immune reconstitution (CD3, CD4, CD8, CD19, CD56) and identify specific immune cell populations post-transplant [77]. |
| Virus-Specific T-Cells | Used in adoptive transfer experiments to study their role in preventing and treating viral reactivation and disease in immunocompromised models [78]. |
| Anti-Thymocyte Globulin (ATG) | An in-vivo T-cell depletion agent used in mouse models to mimic clinical immunosuppression and study its impact on viral reactivation risk [77]. |
| Cytokine ELISA/Kits | To measure levels of inflammatory cytokines (e.g., IFN-γ, TNF-α, IL-6) in serum or supernatant, assessing the immune response and inflammation state [80]. |
| Immunosuppressants (e.g., Cyclosporine A) | To induce immunosuppression in experimental models, control GvHD, and study the resulting susceptibility to viral infections [77]. |
Research Workflow: From Risk Identification to Management
The following diagram outlines a logical pathway for a research program aimed at understanding and mitigating viral reactivation to enhance engraftment safety.
Technical Support Center: FAQs & Troubleshooting Guides
This technical support center is designed for researchers and scientists working to enhance stem cell engraftment post-transplantation. Below you will find solutions to common computational and experimental challenges, framed within the context of a broader thesis on improving engraftment outcomes.
Frequently Asked Questions
FAQ 1: What are the earliest laboratory parameters for predicting engraftment success, and how can I measure them? Answer: Traditional markers like Absolute Neutrophil Count (ANC) >500 cells/μL can be preceded by newer, earlier parameters. For myeloid (white blood cell) engraftment, a white blood cell (WBC) count over 100 cells/μL with a more than two-fold increase from the nadir post-transplantation can predict neutrophil recovery by an average of 1.7 days. For erythroid (red blood cell) engraftment, High Light Scattering Reticulocytes (HLR) >0.1 is the earliest marker, preceding a reticulocyte count >1% by an average of 3.9 days [81]. These can be measured using modern automated hematology analyzers (e.g., DxH 800, Beckman Coulter) that provide extended counting times and data fusion software optimized for leukopenic samples [81].
FAQ 2: My computational model for bioartificial pancreas device performance is inconsistent. What stochastic factors should I incorporate? Answer: Models that treat cell clusters as uniform spheres often yield biased predictions. For accurate performance simulation of devices like encapsulated islets or SC-β cells, you must account for these stochastic factors:
- Cell Cluster Size Distribution: Model diameters as random variables sampled from empirically determined probability densities (e.g., Lognormal distribution for human islets, Weibull distribution for some SC-βs) rather than using a uniform diameter [82].
- Random Spatial Localization: Simulate the non-uniform distribution of cell clusters within the hydrogel matrix post-encapsulation [82].
- Oxygen Gradients: Implement mass transfer models that solve for internal oxygen gradients, which critically influence cell survival and function. Platforms like the SHARP (Simulated Heterogeneity and Randomness Program) computational platform are built specifically for this purpose, using a stochastic finite element method and Monte Carlo simulations [82].
FAQ 3: My agent-based model of cell engraftment on a 3D scaffold is not recapitulating experimental results. What basic behavioral rules should I check? Answer: Agent-based models for systems like lung scaffold reseeding rely on simple rules governing cell behavior. Ensure your model includes rules for:
- Directed vs. Random Movement: Program cells to sense substrate concentration gradients (e.g., oxygen, extracellular matrix components). If the signal (S) from neighboring patches is strong (e.g., S > 1), the cell should move toward the strongest signal; otherwise, it should move randomly [83].
- Engraftment and Proliferation: Model engraftment as a probabilistic event. Once engrafted, cells should have parameters for lifespan (
Tlife) and proliferation time (Tprol), with proliferation only occurring into randomly selected neighboring patches that are not already occupied [83]. - Environmental Interaction: Allow engrafted cells to modify their local patch, for example, by increasing the local substrate concentration, which can influence the behavior of neighboring cells [83].
FAQ 4: Which patient-specific factors most significantly impact engraftment kinetics, and how can I control for them in my analysis? Answer: Multiple clinical factors significantly influence engraftment speed. Key factors include [84] [64] [85]:
- Graft Source: Peripheral blood stem cells (PBSC) lead to faster neutrophil and platelet recovery than bone marrow (BM) [84].
- Disease Type: Multiple myeloma (MM) and lymphoma patients typically experience faster engraftment compared to those with leukemia, myelodysplastic syndrome (MDS), or aplastic anemia (AA) [84] [85].
- Cell Dose: The number of CD34+ cells/kg is a critical factor for platelet engraftment [64].
- Conditioning Regimen Intensity: Myeloablative regimens can impact the speed of engraftment and must be considered [81] [85].
- ABO Incompatibility: This can specifically delay erythroid recovery and is a risk factor for pure red cell aplasia (PRCA) [81] [85]. When analyzing your data, these factors should be included as covariates in your statistical or machine learning models to isolate the effect of your primary variable of interest.
FAQ 5: I want to build a machine learning model to predict neutrophil recovery. What variables and model types show promise? Answer: Recent research on cord blood transplantation (CBT) demonstrates the feasibility of machine learning for this task.
- Data Source: Leverage large, real-world registry datasets with many variables (e.g., ~98 variables known at the time of transplant) [86].
- Outcome: A primary outcome can be neutrophil recovery by day 28 post-transplantation [86].
- Model Type: A competing risk regression model with lasso penalty has been successfully used, demonstrating high predictive accuracy (Area Under the Curve, AUC, of 0.74 for day 28) and outperforming legacy models [86]. Note that prediction accuracy may decrease with time post-transplantation (e.g., AUC was 0.88 for day 14 and 0.68 for day 42 in one study) [86].
Troubleshooting Common Experimental Issues
Problem: Delayed Erythroid Engraftment Post-Allogeneic HSCT
- Step 1 - Check for ABO Incompatibility: Verify the donor-recipient ABO blood group matching. Major ABO mismatch is a common cause of delayed red cell recovery and pure red cell aplasia (PRCA) [81] [85].
- Step 2 - Monitor Early Markers: Use HLR >0.1 instead of traditional reticulocyte counts to detect erythroid engraftment several days earlier [81].
- Step 3 - Investigate Chimerism: Perform donor chimerism studies on the CD33+ cell fraction. Incomplete donor chimerism at day +100 is associated with unfavorable molecular status and poorer relapse-free survival, which can be linked to graft function issues [87].
- Step 4 - Assess Graft Function: Define and screen for "poor graft function" (persistent cytopenias in ≥2 cell lines after day +100), which is a significant predictor of outcomes [87].
Problem: Poor Predictive Performance in Engraftment Machine Learning Model
- Step 1 - Feature Quality Check: Ensure you are including known influential factors such as graft source, disease type, CD34+ cell dose, and conditioning regimen intensity as baseline features [84] [64] [85].
- Step 2 - Incorporate Novel Genetic Features: Consider including genetic data. Genome-wide association studies (GWAS) have uncovered novel genomic loci correlated with transplant outcomes like GVHD and survival, which could improve model accuracy [88].
- Step 3 - Address Competing Risks: Use modeling techniques like competing risk regression to account for events that may preclude engraftment, such as early death [86].
- Step 4 - Validate on External Data: Test your model on an independent dataset from a different institution or a public registry to ensure its generalizability and avoid overfitting [86].
Structured Data for Experimental Planning
Table 1: Key Quantitative Parameters for Early Engraftment Detection
This table compares conventional and novel laboratory markers for monitoring engraftment, helping you identify successful transplantation earlier [81].
| Parameter | Definition | Average Time Advantage vs. Conventional Marker | Clinical Significance |
|---|---|---|---|
| WBC >100/μL & >2x Nadir | White blood cell count exceeding 100/μL with a two-fold increase from the lowest post-transplant count | Precedes ANC >500/μL by 1.7 days | Earliest indicator of myeloid engraftment |
| HLR >0.1 | Ratio of High Light Scattering Reticulocytes to total RBC count | Precedes Reticulocyte Count >1% by 3.9 days | Earliest indicator of erythroid engraftment; indicates presence of very young reticulocytes |
| ANC >500/μL | Absolute Neutrophil Count exceeding 500 per microliter | Conventional Benchmark for Myeloid Engraftment | Standard endpoint for neutrophil recovery |
| Reticulocyte Count >1% | Reticulocytes comprising over 1% of total red blood cells | Conventional Benchmark for Erythroid Engraftment | Standard endpoint for erythroid recovery |
Table 2: Patient and Transplant Factors Influencing Engraftment Kinetics
This table summarizes critical factors that significantly impact the speed of hematopoietic recovery, essential for designing studies and interpreting results [84] [64] [85].
| Factor | Impact on Engraftment Kinetics | Key Context or Dosing Information |
|---|---|---|
| Graft Source | PBSC → Faster engraftment vs. Bone Marph → Slowest engraftment [84] | Cord blood is associated with the highest risk of graft failure [85]. |
| Disease Type | MM, Lymphoma → Faster vs. Leukemia, SMD, AA → Slower [84] | Fewer pre-HSCT therapy cycles in early disease stages can lead to faster engraftment [85]. |
| CD34+ Cell Dose | Higher dose correlates with faster platelet engraftment [64] | A critical quality parameter for the stem cell product. |
| Conditioning Intensity | Myeloablative regimens can influence engraftment speed [81] | Reduced-intensity conditioning may be associated with a higher rate of graft failure [85]. |
| ABO Incompatibility | Can significantly delay erythroid recovery [81] | A/O (Donor/Recipient) mismatch is a major risk factor for post-transplant Pure Red Cell Aplasia (PRCA) [85]. |
Detailed Experimental Protocols
Protocol 1: Developing an Agent-Based Model for Stem Cell Engraftment on a 3D Scaffold This protocol is adapted from studies on lung scaffold reseeding [83].
- Environment Setup: Create a 3D grid (e.g., 32x32x32 patches) representing your decellularized scaffold using modeling software like NetLogo. Define the edges of the grid as the scaffold boundary.
- Define Substrate Gradient: Assign each patch a local variable
crepresenting the concentration of a key substrate (e.g., oxygen, fibronectin). Initialize the gradient using a formula likec = (sqrt(x^2 + y^2))/2to create higher concentrations at the periphery. - Seed Cells: Initialize the model with a set number of cell agents (e.g., 30,000) placed randomly on the grid. Assign a high probability of initial engraftment (e.g., 95%).
- Program Behavioral Rules:
- Movement: At each time step, a cell assesses the substrate concentration in the three patches ahead of its current direction. Calculate S = (x1c_ahead + x2cleft + x3*cright), where x# are random numbers between 0-1. If S > 1, the cell moves toward the strongest signal; otherwise, it moves randomly.
- Engraftment & Proliferation: An engrafted cell has two counters: lifespan (
Tlife, random 0-36 steps) and proliferation time (Tprol, random 33-87 steps). At each step, increments its age. If age =Tlife, the cell dies. If age =Tprol, it places a copy of itself on a suitable empty neighboring patch.
- Run Simulation & Validate: Run the model for a set number of time steps (e.g., 80). Compare the resulting geographic patterns of cell distribution to your experimental data (e.g., from histology or imaging) to validate the rules of cellular behavior.
Protocol 2: Building a Machine Learning Model to Predict Neutrophil Engraftment This protocol is based on the development of the Cord Blood Engraftment Prediction (CBEP) model [86].
- Data Curation: Assemble a large, high-quality dataset, ideally from a multi-center registry. Select variables (features) with observed values for >80% of subjects. Variables should be known at the time of transplantation and can include patient demographics, disease status, graft characteristics, and conditioning regimen.
- Outcome Definition: Define your primary outcome. For neutrophil engraftment, a common outcome is neutrophil recovery by day 28 post-transplant. Secondary outcomes can include recovery by day 14 or 42.
- Model Building - Lasso Regression:
- Split your data into training and testing sets (e.g., 70/30).
- On the training set, fit a competing risk regression model with lasso penalty. This technique performs variable selection by shrinking the coefficients of less important variables to zero, helping to prevent overfitting.
- Use cross-validation on the training set to tune the model's hyperparameter (lambda).
- Model Evaluation: Use the held-out test set to evaluate model performance. Calculate the Area Under the Receiver Operating Characteristic Curve (AUC). An AUC of 0.74 for day 28 recovery indicates a good predictive model [86].
- Model Comparison: Compare the performance of your lasso model against other legacy or simpler models to confirm its superior predictive power.
Visualization Diagrams
Dot Script for Agent-Based Model of Cell Engraftment
Title: Computational Workflow for Agent-Based Engraftment Model
Dot Script for Machine Learning Prediction of Engraftment
Title: Workflow for Building an Engraftment ML Model
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Engraftment Prediction Research
| Research Material / Tool | Function / Application | Key Consideration |
|---|---|---|
| Automated Hematology Analyzer with Reticulocyte Parameters | Measures novel early engraftment markers like HLR and IRF for superior temporal resolution of recovery [81]. | Ensure the instrument has software optimized for counting severe leukopenic samples common post-HSCT. |
| SHARP Computational Platform | A stochastic finite element method-based platform for predicting cell survival and function in bioartificial devices by modeling oxygen gradients and random cell placement [82]. | Essential for optimizing the design of encapsulation devices by accounting for the inherent stochasticity of cell cluster size and location. |
| NetLogo Software | A user-friendly, open-source platform for developing agent-based models to simulate and understand complex cellular behaviors on 2D or 3D scaffolds [83]. | Ideal for initial model prototyping and testing hypotheses about cell-niche interactions without requiring advanced coding skills. |
| Lasso Regression Model | A machine learning technique that performs variable selection and regularization to enhance the prediction accuracy and interpretability of models for outcomes like neutrophil recovery [86]. | Particularly effective for datasets with a large number of potential predictor variables, as it automatically identifies the most important ones. |
Conclusion
Enhancing stem cell engraftment requires a multi-faceted strategy that integrates pharmacological innovation, cellular engineering, and host modulation. Robust clinical evidence now supports the use of TPO-RAs like avatrombopag and MSC co-infusion to significantly accelerate platelet and neutrophil recovery. Future success hinges on the continued development of personalized preconditioning protocols, the clinical translation of gene-editing tools like CRISPR, and the widespread adoption of AI-driven computational models to predict patient-specific outcomes. Bridging these disciplines will be essential for transforming stem cell transplantation into a more reliable and universally successful treatment paradigm.
References
- 1. Stem Cell Success Rate: Evaluated (2025) [https://www.dvcstem.com/post/stem-cell-success-rate]
- 2. Modulation of Stem Cell Survival and Engraftment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439257/]
- 3. Autologous Stem Cell Transplant: A Guide for Patients & ... [https://www.mskcc.org/cancer-care/patient-education/autologous-stem-cell-transplant-guide-patients-caregivers]
- 4. Stem Cell Therapy Success Rates Hit 78%: New Research ... [https://globalrph.com/2025/03/stem-cell-therapy-success-rates-hit-78-new-research-reveals-breakthrough-results/]
- 5. Frequently Asked Questions about Stem Cells [https://www.ortho.wustl.edu/content/Research/7135/Achieving-Excellence---Research-at-Washington-University-Orthopedics/Engineering-Cartilage-for-Joint-Preservation/Frequently-Asked-Questions-about-Stem-Cells.aspx]
- 6. Transwell Cell Migration and Invasion Assay Guide [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/corning-transwell-migration-assay-ultimate-guide-from-setup-to-analysis.html]
- 7. Beginners Guide to Setting Up Migration and Invasion ... [https://bitesizebio.com/25685/beginners-guide-to-setting-up-migration-and-invasion-assays/]
- 8. A Beginner's Guide to Cell Culture: Practical Advice for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000895/]
- 9. Stem cells going home | Harvard Stem Cell Institute (HSCI) [https://www.hsci.harvard.edu/stem-cells-going-home]
- 10. Exploring mesenchymal stem cells homing mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11631218/]
- 11. Cell Homing - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/cell-homing]
- 12. Mesenchymal stem cell infusion to accelerate ... [https://pubmed.ncbi.nlm.nih.gov/40780417/]
- 13. The Myocardial Microenvironment Modulates the Biology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7335681/]
- 14. Enhanced stem cell-mediated therapeutic immune ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961225001516]
- 15. CRISPR-mediated engineering of mesenchymal stromal/stem ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04723-6]
- 16. Disease microenvironment preconditioning: An evolving ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576925006915]
- 17. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 18. DNA Damage-Induced Inflammatory Microenvironment ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.729136/full]
- 19. (Donor) age is more than just a number… | Bone Marrow ... [https://www.nature.com/articles/s41409-024-02420-1]
- 20. Conditioning Regimens for Second Allogeneic ... [https://pubmed.ncbi.nlm.nih.gov/40514014/]
- 21. Conditioning regimens for second allogeneic ... [https://www.sciencedirect.com/science/article/abs/pii/S2666636725012308]
- 22. Mesenchymal stem cell infusion to accelerate ... [https://www.sciencedirect.com/science/article/abs/pii/S104084282500263X]
- 23. Efficacy and safety of mesenchymal stem cells co-infusion in ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02304-x]
- 24. Mesenchymal Stromal Cells for Enhancing Hematopoietic ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.839844/full]
- 25. Therapeutic MSC Infusions: When more of a good thing is ... [https://parentsguidecordblood.org/en/news/therapeutic-msc-infusions-when-more-good-thing-not-always-better]
- 26. Stem Cell Infusion: What to Expect [https://bioinformant.com/stem-cell-infusion/]
- 27. Frequently asked questions | Cellcolabsclinical [https://www.cellcolabsclinical.com/about-us/faq/]
- 28. Co-infusion of mesenchymal stromal cells to prevent GVHD ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11613890/]
- 29. Preconditioning is an effective strategy for improving the ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-01721-8]
- 30. Preconditioning Strategy in Stem Cell Transplantation Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC3728897/]
- 31. Enhanced therapeutic effects of hypoxia-preconditioned ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04166-z]
- 32. Assessment of the safety of hypoxia-primed mesenchymal ... [https://www.nature.com/articles/s41598-025-20018-5]
- 33. Translational potential of mesenchymal stem cells in ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03885-z]
- 34. Genetic Enhancement of Stem Cell Engraftment, Survival and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2668244/]
- 35. Advances in stem cell-based therapeutics for acute high ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12354629/]
- 36. Strategies for Altering Delivery Technologies to Optimize ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11989270/]
- 37. Current strategies for armoring chimeric antigen receptor T ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12460333/]
- 38. Advances in Homing Peptide Targeted Therapies [https://link.springer.com/article/10.1007/s10989-024-10682-y]
- 39. Post‐Engraftment Syndrome Following Autologous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12358217/]
- 40. What if my transplant doesn't work? [https://www.anthonynolan.org/patients-and-families/recovering-a-stem-cell-transplant/what-if-my-transplant-doesnt-work]
- 41. Advances in targeted therapies and emerging strategies for ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00090d]
- 42. Strategic Advances in Targeted Delivery Carriers for ... [https://www.mdpi.com/1422-0067/26/14/6879]
- 43. Two complementary strategies to improve cell engraftment in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5308221/]
- 44. HSC engraftment is enhanced by combining mobilization ... [https://www.sciencedirect.com/science/article/pii/S1525001625005520]
- 45. A new insight for stem cell therapy: apoptotic ... [https://www.nature.com/articles/s41392-022-01066-z]
- 46. Stem Cell Culture Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/stem-cell-culture-support/stem-cell-culture-support-troubleshooting.html]
- 47. Troubleshooting Guide for hPSC Culture [https://www.stemcell.com/troubleshooting-tips-for-hpsc-culture.html]
- 48. Best Practices for Stem Cell Culture: Common Mistakes ... [https://www.atlantisbioscience.com/blog/best-practices-for-stem-cell-culture-common-mistakes-and-solutions/?srsltid=AfmBOorhuracnqpaAEForQ4UqFm9Jqmm48wpIB6qt0A0qW-EX8eqSrP-]
- 49. The Chemokine Receptor CXCR4 in Cell Proliferation and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.02109/full]
- 50. SDF-1/CXCR4 axis induces human dental pulp stem cell ... [https://www.nature.com/articles/srep40161]
- 51. Regulation of CXCR4 Signaling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1952230/]
- 52. SDF-1:CXCR4 Axis Is Fundamental for Tissue Preservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2966775/]
- 53. CXCR4 Expression in CD34+ Cells and Unit ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3668782/]
- 54. Chemokine Signaling Pathways [https://www.rndsystems.com/pathways/chemokine-signaling-pathways]
- 55. Preliminary high-dose irradiation of the recipient and ... [https://www.nature.com/articles/s41598-025-07709-9]
- 56. Stem cell transplant without toxic preparation successfully ... [https://med.stanford.edu/news/all-news/2025/07/stem-cell-transplant.html]
- 57. Modulation of Stem Cell Survival and Engraftment [https://www.thno.org/v15p8840.htm]
- 58. Insight on stem cell preconditioning and instructive ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961216300412]
- 59. Pharmacological Preconditioning Improves the Viability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8342149/]
- 60. Improving the engraftment and integration of cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7252439/]
- 61. exploring stem cell roles from injury detection to tissue repair [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04609-7]
- 62. Stem Cell Research FAQs [https://stemcell.nd.edu/research/faq/]
- 63. Guidelines — International Society for Stem Cell Research [https://www.isscr.org/guidelines]
- 64. Predictive factors for engraftment kinetics of autologous ... [https://www.sciencedirect.com/science/article/pii/S2531137924028360]
- 65. Allogeneic stem cell transplant recipients surviving at least ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10887237/]
- 66. Engraftment Syndrome following Autologous Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4639405/]
- 67. Real-world data of long-term survival in patients with T-cell ... [https://www.nature.com/articles/s41408-023-00868-w]
- 68. Mapping Hematopoietic Fate after Transplantation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504396/]
- 69. Thrombopoietin Receptor Agonists - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK599500/]
- 70. Thrombopoietin Receptor Agonists in Post-Hematopoietic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11407319/]
- 71. Recombinant Human Thrombopoietin Promotes Platelet ... [https://www.sciencedirect.com/science/article/pii/S2666636724002495]
- 72. Recombinant human thrombopoietin does not promote ... [https://www.nature.com/articles/s41598-025-89535-7]
- 73. Utility of Thrombopoietin Receptor Agonists for Prolonged ... [https://www.sciencedirect.com/science/article/abs/pii/S2666636725009157]
- 74. Safety of non‑peptide thrombopoietin receptor agonists ... [https://www.spandidos-publications.com/10.3892/etm.2023.12092]
- 75. Thrombopoietin receptor agonists: ten years later [https://haematologica.org/article/view/8925]
- 76. The Evolving Role of Hematopoietic Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523408/]
- 77. Viral reactivations following hematopoietic stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6999888/]
- 78. Immune control of cytomegalovirus reactivation in stem cell ... [https://www.sciencedirect.com/science/article/pii/S0006497121012714]
- 79. Competing-risk outcomes after hematopoietic stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6119156/]
- 80. Understanding and Assessing the Risks of Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4367503/]
- 81. New Proposed Guidelines for Early Identification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6807356/]
- 82. A predictive computational platform for optimizing the ... [https://www.nature.com/articles/s41467-022-33760-5]
- 83. A Computational Model of Cellular Engraftment on Lung ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5107660/]
- 84. Specific factors influence the success of autologous and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2763249/]
- 85. A concise review on factors influencing the hematopoietic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8103082/]
- 86. Machine Learning Prediction Model for Neutrophil ... [https://www.sciencedirect.com/science/article/pii/S2666636724001829]
- 87. Early post-transplantation factors predict survival outcomes ... [https://www.nature.com/articles/s41408-020-0302-9]
- 88. Editorial: Improving stem cell transplantation delivery using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11931077/]