Strategies for Managing Immune Rejection in Allogeneic Transplantation: From Mechanisms to Clinical Applications
This article provides a comprehensive analysis of the immune mechanisms and management strategies for rejection in allogeneic transplantation, tailored for researchers, scientists, and drug development professionals.
Strategies for Managing Immune Rejection in Allogeneic Transplantation: From Mechanisms to Clinical Applications
Abstract
This article provides a comprehensive analysis of the immune mechanisms and management strategies for rejection in allogeneic transplantation, tailored for researchers, scientists, and drug development professionals. It explores the foundational immunobiology of allorecognition, covering innate and adaptive immune pathways, including the roles of T cells, alloantibodies, and the recently defined 'Immunologic Constant of Rejection'. The review critically assesses current and emerging methodologies, from conventional immunosuppression to cutting-edge tolerance induction protocols, gene-editing technologies like CRISPR, and novel nanomaterial-based delivery systems. It further discusses troubleshooting for common challenges such as ischemia-reperfusion injury, drug toxicity, and resistance in non-human primate models, and evaluates validation frameworks through biomarkers, genomic profiling, and comparative clinical outcomes. The synthesis of these facets aims to inform the development of more precise and tolerable therapeutic interventions.
Decoding the Immune Response: Foundational Mechanisms of Allograft Rejection
In transplantation, the immune system recognizes and responds to genetically encoded polymorphisms between a donor and recipient, a process known as allorecognition. This immune activation primarily targets major histocompatibility complex (MHC) molecules, known in humans as human leukocyte antigens (HLAs), and is a principal driver of graft rejection. T lymphocytes play a central role in this process, recognizing alloantigens through distinct pathways—direct, indirect, and semi-direct allorecognition [1] [2]. Understanding these pathways is fundamental to developing strategies to manage immune rejection in allogeneic transplantation.
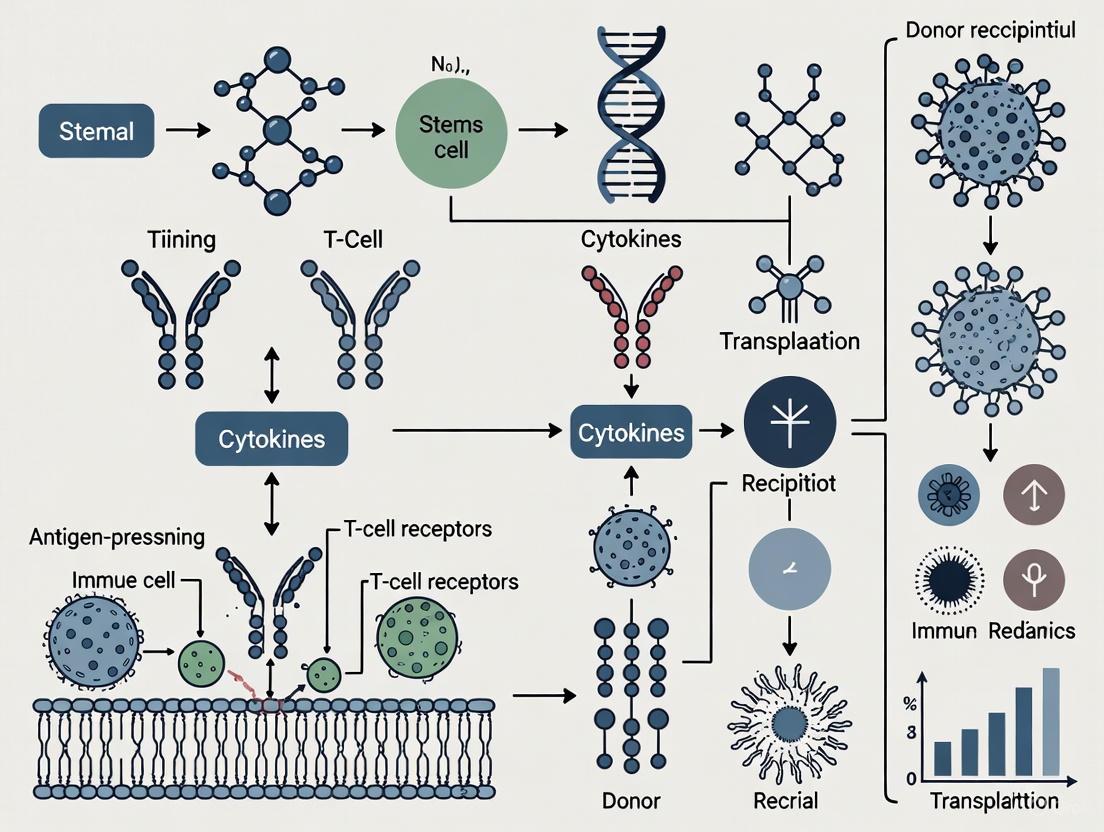
The following diagram illustrates the core cellular interactions and antigen presentation routes in the three principal allorecognition pathways.
Fundamental Concepts: Pathway Mechanisms
Direct Allorecognition
Mechanism: Recipient T cells recognize intact donor MHC molecules (complexed with peptide) presented on the surface of donor antigen-presenting cells (APCs) [1] [2]. This pathway is responsible for the remarkably high frequency of alloreactive T cells (1%-10% of the total T cell repertoire), far exceeding the frequency of T cells responding to conventional antigens [3] [2].
Two non-mutually exclusive models explain the strength of direct allorecognition:
- Multiple Binary Complex Model: The recipient T cell receptor (TCR) recognizes a specific complex of a donor MHC molecule and a particular bound peptide. As each allogeneic MHC molecule can present a vast array of different peptides, this creates numerous foreign complexes for T cells to recognize [3] [4].
- High Determinant Density Model: The TCR interacts directly with polymorphic residues on the donor MHC molecule, largely independent of the bound peptide. In this model, every MHC molecule on the donor cell is recognized as foreign, leading to a very high density of stimulatory ligands [3] [2].
Role in Rejection: The direct pathway is considered the dominant pathway in early acute rejection. Its activation is short-lived, typically lasting only a few weeks post-transplantation, as it depends on the lifespan of donor-derived passenger leukocytes within the graft [1] [4].
Indirect Allorecognition
Mechanism: Recipient APCs phagocytose donor alloantigens, process them into peptide fragments, and present these donor-derived peptides in the context of self-MHC molecules to recipient T cells [1] [2] [4]. This is the same process used for immune responses against conventional pathogens.
Role in Rejection: The indirect pathway is oligoclonal, targeting a limited number of immunodominant epitopes initially, though this can spread to other epitopes over time (epitope spreading) [1] [2]. It is critically important for chronic rejection and for responses against minor histocompatibility antigens, as it can be sustained indefinitely due to the continuous supply of recipient APCs [1] [4].
Semi-Direct Allorecognition
Mechanism: A hybrid pathway where recipient APCs acquire intact donor MHC molecules (via trogocytosis or extracellular vesicles like exosomes) and present them, without processing, to recipient T cells [1] [3] [2]. This allows a single APC to present both intact donor MHC (stimulating direct-pathway T cell clones) and processed donor peptide on self-MHC (stimulating indirect-pathway clones) [1].
Role in Rejection: The semi-direct pathway may help sustain direct-pathway T cell responses beyond the initial post-transplant period, after donor passenger leukocytes have disappeared [1] [3]. It also facilitates cross-talk between CD4+ and CD8+ T cells within a "three-cell cluster" [3].
Table 1: Comparative Features of Allorecognition Pathways
| Feature | Direct Pathway | Indirect Pathway | Semi-Direct Pathway |
|---|---|---|---|
| Antigen Presenting Cell (APC) | Donor APC | Recipient APC | Recipient APC |
| Antigen Form Recognized | Intact donor MHC | Donor peptide + Self-MHC | Intact donor MHC on recipient APC |
| Precursor T Cell Frequency | Very high (1-10%) [2] | Low (conventional) [2] | High (same as direct) [1] |
| Duration of Response | Short-lived (weeks) [1] | Long-lived (indefinite) [1] | Potentially sustained [1] |
| Primary Role in Rejection | Acute Rejection [1] [4] | Chronic Rejection [1] [4] | Acute & Chronic Rejection [1] [3] |
The Scientist's Toolkit: Key Research Reagents & Experimental Models
Successful investigation of allorecognition pathways relies on specific experimental models and reagents that allow for the isolation and manipulation of immune components.
Table 2: Essential Research Reagents and Models for Allorecognition Studies
| Reagent / Model | Function/Description | Key Application |
|---|---|---|
| TCR Transgenic T Cells | Monoclonal T cells with known specificity for a particular alloantigen [1]. | Tracking the activation, division, and fate of a defined alloreactive T cell population in vivo. |
| MHC Knockout Mice | Donor or recipient mice genetically engineered to lack specific MHC molecules [4]. | Isolating the contribution of direct vs. indirect allorecognition in graft rejection. |
| Mixed Lymphocyte Reaction (MLR) | In vitro co-culture of T cells from one individual with APCs from another [2]. | Measuring the proliferative strength of the direct alloresponse. |
| CTLA-4-Ig (Belatacept) | Fusion protein that blocks CD28-B7 costimulation [5] [6]. | Inhibiting T cell activation; used clinically and in research to promote graft survival. |
| Anti-ICOS Antibodies | Blocking antibodies against the ICOS costimulatory receptor [5]. | Studying the role of ICOS in T cell help for B cells and antibody-mediated rejection. |
| ADAM/MMP Inhibitors | Small molecule inhibitors of metalloproteases [7]. | Investigating the role of LRP1 shedding in the regulation of T cell adhesion and activation. |
Troubleshooting Guides & FAQs
FAQ 1: Why is the direct T-cell alloresponse so powerful compared to a conventional immune response?
Answer: The extraordinary strength stems from two key factors that greatly amplify the signal:
- High Frequency of Alloreactive T Cells: Between 1% and 10% of an individual's T cell repertoire can recognize a single MHC alloantigen, which is 100 to 1000 times greater than the frequency for a conventional antigen [3] [2].
- High Determinant Density: According to one model, every MHC molecule on a donor APC can be recognized as foreign, creating an immense number of stimulatory ligands on a single cell surface [1] [3].
- Multiple Binary Complexes: A single allogeneic MHC molecule can bind and present a vast array of different peptides. Each unique peptide-MHC combination can be recognized by a distinct T cell clone, massively expanding the number of T cells that can be activated [1] [2].
Troubleshooting Tip for MLR: If your Mixed Lymphocyte Reaction (MLR) shows unexpectedly low proliferation, ensure your donor stimulator APCs are healthy and metabolically active. Use irradiation or mitomycin C treatment to prevent cell division while maintaining surface MHC expression.
FAQ 2: Our in vivo model shows T-cell-mediated rejection even after donor APCs are gone. Which pathway is responsible?
Answer: This is a classic scenario implicating the indirect and/or semi-direct pathways.
- The indirect pathway is the primary suspect for late-phase and chronic rejection. Recipient APCs continuously capture donor antigens from the graft parenchyma, process them, and present donor-derived peptides to T cells indefinitely [1] [4].
- The semi-direct pathway can also contribute. Recipient APCs can acquire and display intact donor MHC molecules, allowing for the continued activation of direct-pathway T cell clones even after the original donor APCs have been cleared [1] [3] [2].
Experimental Protocol to Confirm: To dissect the contribution of each pathway in a mouse transplant model:
- Use donors that are knockout for MHC Class II, eliminating direct recognition of donor MHC II.
- Track the activation of adoptively transferred TCR transgenic CD4+ T cells specific for a donor MHC class I peptide presented by recipient (self) MHC Class II.
- The proliferation and differentiation of these T cells at late time points provide direct evidence of ongoing indirect allorecognition [1].
FAQ 3: We are blocking the CD28-B7 costimulation pathway, but rejection still occurs. What are the potential mechanisms?
Answer: Costimulation blockade can fail due to several redundant and alternative activation pathways:
- Memory T Cells: Alloreactive memory T cells, generated from prior immune challenges (e.g., infections, pregnancies), are less dependent on CD28/B7 costimulation for activation and can mediate rejection [2].
- Alternative Costimulatory Pathways: Other costimulatory molecules can compensate. Key pathways to investigate include:
- ICOS-ICOSL: Critical for T follicular helper (Tfh) cell function, germinal center formation, and alloantibody production [5].
- CD154-CD40: This receptor-ligand pair is crucial for licensing APCs and providing help for CD8+ T cell and B cell responses.
- OX40-OX40L & CD137-CD137L: Members of the TNFR family that enhance T cell survival and effector function [8] [5].
- Heterologous Immunity: Cross-reactive T cells from previous infections (e.g., CMV, EBV) can exhibit "memory" properties and bypass costimulation blockade to initiate rejection [2].
Troubleshooting Guide:
- Problem: Acute rejection despite CTLA-4-Ig treatment.
- Potential Cause 1: Strong pre-existing alloreactive memory T cell response.
- Investigation: Analyze pre-transplant blood for memory T cell markers (CD45RO) and alloreactivity.
- Potential Cause 2: Upregulation of alternative costimulatory pathways.
- Investigation: Isolate graft-infiltrating lymphocytes and analyze expression of ICOS, OX40, and CD137 via flow cytometry. Test combination therapy with anti-ICOS or anti-CD40L antibodies [5].
T-cell Co-stimulation: Beyond the Two-Signal Model
Effective T cell activation requires both an antigen-specific signal (Signal 1 via the TCR) and antigen-non-specific costimulation (Signal 2). The absence of costimulation can lead to T cell anergy or the development of regulatory T cells (Tregs) [5] [7]. The following diagram summarizes the major co-stimulatory and co-inhibitory pathways that shape the alloreactive T cell response.
Key Co-stimulatory & Co-inhibitory Receptors:
- CD28 (Stimulatory): The prototypical costimulatory receptor, constitutively expressed on T cells. Binding to CD80/86 on APCs is critical for naïve T cell activation, IL-2 production, and prevention of anergy [5].
- CTLA-4 (Inhibitory): Binds CD80/86 with higher affinity than CD28, but delivers an inhibitory signal. It functions both through intracellular phosphatase recruitment and via trans-endocytosis, physically removing CD80/86 from APCs [5]. CTLA-4-Ig (Belatacept) is used clinically to block CD28-mediated costimulation [5] [6].
- ICOS (Stimulatory): Induced upon T cell activation, it is crucial for T follicular helper (Tfh) cell differentiation, germinal center formation, and antibody responses. Blocking ICOS can prolong allograft survival in experimental models [5].
- PD-1 (Inhibitory): Expressed on activated and exhausted T cells. Engagement by PD-L1/PD-L2 inhibits T cell function, acting as a critical checkpoint for limiting immune responses [5].
Emerging Concept: An alternative perspective suggests that some forms of co-stimulation may not simply provide a second stimulatory signal. Instead, they may function by inhibiting a constitutive immunosuppressive mechanism. Recent research indicates that ligation of CD28, integrins, and CXCR4 can inhibit metalloprotease-mediated shedding of the Low-Density Lipoprotein Receptor-related Protein 1 (LRP1) from the T cell surface. The surface retention of LRP1, in collaboration with thrombospondin-1 (TSP-1), then promotes T cell adhesion and enhances TCR-induced activation [7].
In allogeneic transplantation, the innate immune system is the critical first responder that shapes subsequent adaptive immune responses. The unavoidable processes of organ procurement, preservation, and implantation generate cellular stress and tissue damage, triggering a sterile inflammatory response through the release of damage-associated molecular patterns (DAMPs) [9] [10]. These endogenous molecules are recognized by pattern recognition receptors (PRRs) on innate immune cells, initiating signaling cascades that lead to the production of proinflammatory cytokines and chemokines [11] [12]. This initial inflammation, driven particularly by ischemia-reperfusion injury (IRI), creates a local microenvironment that enhances alloantigen presentation and can predispose the graft to both acute and chronic rejection [13] [10]. Understanding these mechanisms provides crucial opportunities for therapeutic intervention to improve transplant outcomes.
FAQ: Core Concepts for Researchers
Q1: What are the key DAMPs and PRRs relevant to transplantation research? DAMPs are endogenous molecules released from stressed or dying cells that initiate and perpetuate the innate immune response. Key DAMPs in transplantation include HMGB1, HSPs, extracellular ATP, and mitochondrial DNA [12] [9]. These molecules are recognized by various PRRs, including Toll-like receptors (TLRs), RAGE, and NLRP3 inflammasome components, which are expressed on antigen-presenting cells such as dendritic cells and macrophages [11] [12].
Q2: How does ischemia-reperfusion injury initiate innate immunity? Ischemia leads to cellular metabolic changes including ATP depletion and a switch to anaerobic glycolysis [13]. Subsequent reperfusion causes a burst of reactive oxygen species (ROS) and intracellular calcium overload, resulting in mitochondrial permeability transition pore opening and various forms of regulated cell death such as necroptosis, pyroptosis, and ferroptosis [13] [9]. This cell death releases DAMPs that activate PRR-bearing innate immune cells, initiating a robust inflammatory response [9] [10].
Q3: What are the functional consequences of DAMP-PRR signaling? Engagement of PRRs by DAMPs triggers intracellular signaling pathways, predominantly leading to NF-κB activation and production of proinflammatory cytokines (IL-1β, IL-6, TNF-α) and chemokines [11] [12]. This results in increased expression of adhesion molecules, recruitment of innate immune cells (neutrophils, monocytes), and maturation of dendritic cells that can migrate to lymphoid organs to prime alloreactive T cells [11] [10].
Q4: How does innate immunity bridge to adaptive alloimmunity? DAMP-activated innate immune cells, particularly dendritic cells, upregulate costimulatory molecules (CD80, CD86) and MHC molecules, enhancing their antigen-presenting capacity [11]. The inflammatory cytokines produced during IRI promote T-cell differentiation toward proinflammatory Th1 and Th17 phenotypes while impairing regulatory T-cell function, thus shaping the subsequent adaptive immune response against the allograft [13] [10].
Troubleshooting Guide: Common Experimental Challenges
Challenge: Differentiating Between Regulated Cell Death Pathways
Problem: In vitro models of IRI show mixed cell death morphologies, making it difficult to identify the predominant pathway.
Solution: Implement a systematic approach using specific inhibitors and markers:
| Cell Death Pathway | Key Mediators | Pharmacological Inhibitors | Experimental Readouts |
|---|---|---|---|
| Necroptosis | RIPK1, RIPK3, MLKL | Necrostatin-1 (RIPK1 inhibitor) | Phospho-MLKL detection by WB, loss of membrane integrity |
| Pyroptosis | Caspase-1, GSDMD | VX-765 (caspase-1 inhibitor) | Caspase-1 activity assay, LDH release, IL-1β secretion |
| Ferroptosis | GPX4 inhibition, lipid ROS | Ferrostatin-1, Liproxstatin-1 | C11-BODIPY assay for lipid ROS, mitochondrial shrinkage |
| Apoptosis | Caspase-3, -8, -9 | Z-VAD-FMK (pan-caspase inhibitor) | Annexin V/PI staining, caspase-3 activation, TUNEL assay |
Table: Strategies for identifying regulated cell death pathways in IRI models. WB: Western blot; LDH: Lactate dehydrogenase; ROS: Reactive oxygen species. [9] [10]
Challenge: Modeling Ischemia-Reperfusion Injury In Vitro
Problem: Standard cell culture systems fail to accurately recapitulate the complex metabolic shifts of IRI.
Solution: Establish a controlled hypoxia-reoxygenation system:
- Ischemia Phase: Place cells in a modular hypoxic chamber (0.5-1% O₂, 5% CO₂, balanced N₂) with glucose-free media for 2-8 hours depending on cell type.
- Reperfusion Phase: Return cells to normoxic conditions (21% O₂) with complete culture media.
- Monitoring: Measure extracellular acidification rate (ECAR) and oxygen consumption rate (OCR) using Seahorse Analyzer to track metabolic shifts from oxidative phosphorylation to glycolysis and back [13].
- DAMP Detection: Collect supernatant for HMGB1 (ELISA), ATP (luciferase assay), and mitochondrial DNA (qPCR for mitochondrial vs. nuclear genes) at multiple time points post-reoxygenation [12].
Challenge: Assessing PRR Activation and Downstream Signaling
Problem: Difficulty in determining which PRRs are functionally relevant in specific transplant models.
Solution: Employ a combination of genetic and pharmacological approaches:
- Genetic Tools: Use siRNA knockdown or CRISPR/Cas9 gene editing in primary innate immune cells to validate receptor involvement.
- Receptor Blockade: Utilize specific antagonists:
- TLR4: TAK-242 (resatorvid) or Eritoran
- NLRP3: MCC950 or CY-09
- RAGE: FPS-ZM1 or azeliragon [12]
- Signaling Readouts: Monitor NF-κB nuclear translocation by immunofluorescence, MAPK phosphorylation by Western blot, and cytokine production by multiplex ELISA.
Key Signaling Pathways in Innate Alloimmunity
The following diagram illustrates the core signaling pathways connecting DAMPs released during IRI to innate immune activation:
DAMP-PRR Signaling Pathway in Transplant IRI. This diagram illustrates the progression from initial ischemia-reperfusion injury to priming of adaptive immunity, highlighting key points for therapeutic intervention.
The Scientist's Toolkit: Essential Research Reagents
The following table compiles key reagents for investigating innate immunity in transplantation models:
| Category | Specific Reagent | Research Application | Key Findings/Utility |
|---|---|---|---|
| DAMP Inhibitors | Glycyrrhizin | HMGB1 inhibition | Reduces IRI, decreases inflammation, improves graft survival in models [12] |
| Ferrostatin-1 | Ferroptosis inhibition | Protects renal tubular cells and islets from ferroptotic death [10] | |
| PRR Antagonists | TAK-242 (Resatorvid) | TLR4 antagonist | Reduces infarct size in MI models, inhibits proinflammatory cytokine production [12] |
| MCC950 | NLRP3 inflammasome inhibitor | Decreases infarct size, improves cardiac function in MI models [12] | |
| FPS-ZM1 | RAGE antagonist | Blocks RAGE signaling, reduces inflammation in diabetic models [12] | |
| Cell Death Modulators | Necrostatin-1 | Necroptosis inhibitor (RIPK1) | Reduces necroptosis in IRI models [9] |
| Disulfiram | Pyroptosis inhibitor (GSDMD) | Blocks pore formation, inhibits IL-1β release [9] | |
| Cytokine Targeting | Anakinra | IL-1 receptor antagonist | Reduces inflammation in autoinflammatory diseases [12] |
| Anti-TNF antibodies | TNF neutralization | Used in clinical autoimmune conditions, experimental in transplantation [12] | |
| Metabolic Modulators | 2-DG | Glycolysis inhibitor | Suppresses effector T-cell function, shifts metabolic programming [13] |
Table: Essential research reagents for investigating innate immune mechanisms in transplantation. MI: Myocardial infarction; IRI: Ischemia-reperfusion injury.
Experimental Workflow for Evaluating Innate Immunity in Transplantation Models
The following diagram outlines a comprehensive experimental approach to study innate immunity in transplantation:
Experimental Workflow for Transplant Innate Immunity Research. This workflow outlines key analytical steps from model establishment to outcome assessment, highlighting the iterative process between analysis and therapeutic intervention.
Advanced Technical Considerations
Normothermic Perfusion as an Experimental Platform
Ex vivo normothermic machine perfusion (NMP) and normothermic regional perfusion (NRP) represent advanced platforms for both assessing and modulating innate immune activation prior to transplantation [9]. These systems allow for:
- Real-time biomarker monitoring: Assessment of DAMPs (HMGB1, cell-free DNA) and metabolic parameters in the perfusate as indicators of graft injury [9].
- Therapeutic delivery: Administration of cell death inhibitors (e.g., ferrostatin-1 for ferroptosis) or DAMP-neutralizing agents directly to the organ, potentially mitigating innate immune activation before reperfusion in the recipient [9] [10].
- Gene therapy interventions: Vector delivery (e.g., adenoviral IL-10) during perfusion to modulate the graft's inflammatory profile [10].
Metabolic Reprogramming of Innate Immune Cells
Immunometabolism has emerged as a crucial regulatory layer in innate immunity. During IRI and allograft rejection, innate immune cells undergo metabolic reprogramming:
- Macrophages and DCs shift from oxidative phosphorylation to aerobic glycolysis upon TLR activation, similar to the Warburg effect in cancer cells [13].
- Metabolic inhibitors such as 2-deoxyglucose (2-DG) can suppress proinflammatory macrophage and DC activation, suggesting potential therapeutic applications [13].
- T-cell fate is influenced by the metabolic environment, with glycolytic conditions favoring Th17 differentiation while fatty acid oxidation promotes regulatory T-cell development [13].
Understanding these metabolic checkpoints provides additional opportunities for therapeutic intervention in the innate immune response to allografts.
In allogeneic transplantation, the success of engrafted cells, tissues, or organs is fundamentally governed by the immune recognition of histocompatibility antigens. These antigens are polymorphic proteins that differ between donor and recipient, triggering immune responses that can lead to graft rejection. The major histocompatibility complex (MHC), known as human leukocyte antigen (HLA) in humans, represents the most potent barrier to transplantation, while minor histocompatibility antigens (miHAs) contribute to rejection even in MHC-matched scenarios. Understanding these complex antigen systems is crucial for developing strategies to manage immune rejection in transplantation research and clinical practice.
The MHC is a large gene complex located on chromosome 6p21.3 in humans, containing the most polymorphic genes in the human genome. These genes code for cell surface proteins essential for the adaptive immune system, originally discovered through their role in transplant rejection. Beyond transplantation biology, MHC molecules play a vital physiological role in immune surveillance by presenting peptide antigens to T-cells, enabling discrimination between self and non-self or altered self structures.
MHC Antigens: Major Barriers to Transplantation
Classification and Structure of MHC Molecules
MHC molecules are divided into three main classes based on their structure, function, and genetic localization:
Table 1: Classification of Major Histocompatibility Complex Molecules
| Class | Genes | Structure | Expression | Function |
|---|---|---|---|---|
| Class I | HLA-A, HLA-B, HLA-C | α chain (45 kDa) + β₂-microglobulin (12 kDa) | All nucleated cells | Present endogenous peptides to CD8+ T-cells |
| Class II | HLA-DR, HLA-DQ, HLA-DP | α chain (32-34 kDa) + β chain (29-32 kDa) | Antigen-presenting cells | Present exogenous peptides to CD4+ T-cells |
| Class III | C2, C4, TNF, HSP | Various | Various | Immune regulation, complement proteins |
MHC class I molecules consist of a polymorphic α chain encoded within the MHC locus on chromosome 6 and a non-polymorphic β₂-microglobulin chain encoded on chromosome 15. The α1 and α2 domains form the peptide-binding groove, which accommodates peptides typically 8-11 amino acids in length. MHC class II molecules are heterodimers of α and β chains, both encoded within the MHC region, with the peptide-binding groove formed by α1 and β1 domains that bind longer peptides (13-25 amino acids).
Quantitative Analysis of MHC Polymorphism
The extreme polymorphism of MHC genes represents a significant challenge in transplantation, with thousands of alleles identified for each classical locus:
Table 2: Polymorphism of Human MHC (HLA) Genes
| HLA Locus | Number of Known Alleles | Domain of Polymorphism | Impact on Transplantation |
|---|---|---|---|
| HLA-A | > 7,000 | α1 and α2 domains | High impact for solid organ and stem cell transplantation |
| HLA-B | > 9,000 | α1 and α2 domains | Strongest immunogenicity, highest impact on rejection |
| HLA-C | > 7,000 | α1 and α2 domains | Important for NK cell regulation via KIR interactions |
| HLA-DR | > 3,000 | β1 domain | Dominant role in CD4+ T-cell activation |
| HLA-DQ | > 2,000 | α1 and β1 domains | Important for antibody-mediated rejection |
| HLA-DP | > 1,500 | β1 domain | Lesser immunogenicity but clinically relevant |
This remarkable diversity means that unrelated individuals rarely share identical HLA profiles, necessitating careful donor-recipient matching and aggressive immunosuppression to prevent rejection.
Minor Histocompatibility Antigens
Definition and Clinical Significance
Minor histocompatibility antigens (miHAs) are polymorphic peptides derived from normal cellular proteins that differ between donor and recipient. While individually less immunogenic than MHC molecules, collectively they can stimulate potent immune responses that lead to graft rejection, particularly in HLA-matched hematopoietic stem cell transplantation.
These antigens arise from genetic polymorphisms outside the HLA system, including single nucleotide polymorphisms, insertions/deletions, and gene duplications that create protein sequence differences. When processed and presented by MHC molecules, these differential peptides can be recognized as foreign by the recipient's T-cells.
Table 3: Categories and Examples of Minor Histocompatibility Antigens
| Category | Source | Example | Clinical Relevance |
|---|---|---|---|
| Y-chromosome encoded | Male-specific genes | HY antigens | Graft-versus-host disease in female to male transplants |
| Autosomal polymorphisms | Housekeeping genes | HA-1, HA-2 | Graft-versus-leukemia effects, GVHD |
| Tissue-specific | Differentiated cell proteins | Melanocyte antigens | Graft rejection in tissue-specific transplants |
| Mitochondrial | Mitochondrial proteins | MTATP6, MTND | Minor role in solid organ rejection |
Experimental Protocols for Histocompatibility Research
Protocol 1: Mixed Lymphocyte Reaction (MLR) for Alloreactivity Assessment
Purpose: To measure T-cell responses to allogeneic antigens in vitro, predicting potential graft rejection.
Materials:
- Peripheral blood mononuclear cells (PBMCs) from donor and recipient
- RPMI-1640 complete medium with 10% FBS
- 96-well U-bottom plates
- Mitomycin C or irradiation source
- [³H]-thymidine or CFSE for proliferation measurement
- ELISA kits for cytokine detection (IFN-γ, IL-2)
Procedure:
- Isolate PBMCs from donor and recipient blood using density gradient centrifugation.
- Treat stimulator cells (donor PBMCs) with mitomycin C (25-50 μg/mL for 30 minutes at 37°C) or irradiation (25-35 Gy) to prevent proliferation.
- Wash stimulator cells three times with PBS to remove mitomycin C.
- Co-culture responder cells (recipient PBMCs) with stimulator cells at a 1:1 ratio (typically 1×10⁵ cells each per well) in 96-well U-bottom plates.
- Include controls: responder cells alone, stimulator cells alone, and third-party PBMCs as positive control.
- Incubate for 5-7 days at 37°C in 5% CO₂.
- Measure proliferation by [³H]-thymidine incorporation (add 0.5-1 μCi/well for the last 18 hours) or CFSE dilution by flow cytometry.
- For cytokine analysis, collect supernatants at day 3-5 for ELISA.
Troubleshooting:
- High background in controls: Optimize mitomycin C concentration or irradiation dose; increase washing steps after treatment.
- Low proliferation response: Check cell viability; optimize cell ratios (test 2:1 or 1:2 responder:stimulator ratios); extend culture duration.
- Variable results: Use fresh PBMCs rather than frozen when possible; standardize donor selection across experiments.
Protocol 2: Cytotoxic T-Lymphocyte (CTL) Assay for miHA Responses
Purpose: To detect and quantify recipient T-cell responses against specific minor histocompatibility antigens.
Materials:
- Antigen-presenting cells (APCs) expressing target miHAs
- Candidate miHA peptides
- Recombinant human IL-2
- ⁵¹Cr sodium chromate or LDH cytotoxicity detection kit
- MHC-matched and mismatched target cells
Procedure:
- Generate miHA-specific T-cell lines by stimulating recipient PBMCs with miHA-pulsed APCs weekly for 3-4 weeks.
- Maintain T-cells in complete medium with 20-50 U/mL IL-2.
- Label target cells with ⁵¹Cr (100 μCi per 1×10⁶ cells for 1 hour) or prepare for LDH assay according to manufacturer's instructions.
- Co-culture effector T-cells with labeled target cells at various E:T ratios (40:1, 20:1, 10:1, 5:1) in triplicate.
- Incubate for 4-6 hours at 37°C.
- Measure ⁵¹Cr release in supernatant or LDH activity according to kit instructions.
- Calculate specific lysis: (Experimental release - Spontaneous release) / (Maximum release - Spontaneous release) × 100.
Troubleshooting:
- High spontaneous release: Use healthier target cells; reduce labeling time; use alternative cytotoxicity detection methods.
- Low specific lysis: Confirm MHC restriction of response; optimize T-cell priming conditions; verify miHA expression on target cells.
- Inconsistent results: Standardize target cell preparation; use multiple E:T ratios; include appropriate positive and negative controls.
Allorecognition Pathways: Mechanisms of Graft Rejection
The immune system recognizes allogeneic antigens through several distinct pathways:
Figure 1: Three pathways of allorecognition in transplantation immunology. The direct pathway involves recipient T-cells recognizing intact donor MHC molecules on donor antigen-presenting cells (APCs). The indirect pathway involves recipient APCs processing and presenting donor MHC peptides to helper T-cells. The semi-direct pathway involves recipient APCs acquiring intact donor MHC molecules through extracellular vesicles.
Recent research has revealed additional complexity in allorecognition mechanisms. The inverted direct pathway has been described where donor CD4+ T cells within the graft activate recipient B cells to produce donor-specific antibodies. Furthermore, innate allorecognition by natural killer (NK) cells and monocytes can trigger rejection through MHC-independent mechanisms, including the "missing self" recognition where NK cells activate against cells lacking self-MHC class I molecules [14] [15].
Research Reagent Solutions
Table 4: Essential Research Reagents for Histocompatibility Investigations
| Reagent Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| MHC Tetramers | HLA-A02:01/NY-ESO-1, HLA-B27:05/EBV | Detection of antigen-specific T-cells | Require precise MHC-peptide combination; validate with positive controls |
| Antibody Panels | Anti-CD3, CD4, CD8, CD45, HLA-DR, CD19, CD56 | Immune cell phenotyping | Include viability dyes to exclude dead cells; titrate for optimal signal |
| Cytokine Assays | IFN-γ ELISpot, Luminex multiplex arrays, intracellular staining | Functional T-cell analysis | Use PMA/ionomycin as positive control; establish background thresholds |
| Blocking Antibodies | Anti-MHC I (W6/32), Anti-MHC II (CR3/43), Anti-CD4, Anti-CD8 | Pathway inhibition studies | Confirm specificity with isotype controls; test multiple concentrations |
| Gene Expression | HLA sequencing primers, KIR genotyping assays | Genetic compatibility assessment | Include quality control for low-resolution and high-resolution typing |
| Antigen Presentation | TAP inhibitors, Proteasome inhibitors, Invariant chain siRNA | Antigen processing mechanism studies | Use controlled dosing with viability assays; include rescue experiments |
Frequently Asked Questions: Troubleshooting Guide
Q1: In our MLR experiments, we're consistently seeing high background proliferation in control wells containing only responder cells. What could be causing this and how can we reduce it?
A: High background proliferation often indicates suboptimal culture conditions or responder cell activation. Implement these troubleshooting steps:
- Verify that stimulator cell inactivation is complete by culturing stimulator cells alone and confirming no proliferation.
- Use fresh rather than frozen PBMCs if possible, as freeze-thaw cycles can increase background activation.
- Ensure FBS batch is thoroughly screened for low background stimulation; some serum lots contain bovine antigens that cross-react with human lymphocytes.
- Reduce culture time from 7 to 5 days to decrease background while maintaining alloresponse.
- Include additional washing steps after mitomycin C treatment to completely remove the chemical.
- Test different cell densities (0.5×10⁵ to 2×10⁵ cells/well) to find the optimal signal-to-noise ratio.
Q2: We're struggling to detect miHA-specific T-cell responses even when using donor-recipient pairs known to be mismatched for several minor antigens. What optimization strategies do you recommend?
A: Detecting miHA responses requires sensitive methods and careful optimization:
- Enhance T-cell priming by using mature dendritic cells as APCs rather than PBMCs.
- Add cytokine support (10-20 U/mL IL-2 and 5 ng/mL IL-7) after initial stimulation to promote T-cell expansion.
- Implement repeated stimulation cycles (weekly for 3-4 weeks) to expand rare miHA-specific T-cell clones.
- Use tetramer staining instead of functional assays if specific miHA epitopes are known.
- Consider the MHC restriction element - ensure your assay system includes the appropriate MHC molecule that presents the miHA.
- Try ELISpot assays which are typically more sensitive for detecting rare antigen-specific cells than proliferation or cytotoxicity assays.
Q3: Our flow cytometry analysis of HLA expression shows inconsistent results between experiments. What are the critical factors for reliable MHC quantification?
A: MHC expression measurement requires strict standardization:
- Implement calibration beads with known antibody binding capacity to standardize fluorescence quantification between experiments.
- Control for cytokine-mediated MHC modulation - ensure consistent culture conditions as IFN-γ can dramatically upregulate MHC expression.
- Use the same clone of MHC-specific antibody throughout your study as different clones recognize different epitopes with varying affinities.
- Include both positive and negative control cell lines with stable MHC expression in each experiment.
- Standardize fixation and permeabilization procedures if detecting intracellular MHC molecules.
- Ensure antibody titration for optimal signal-to-noise ratio in your specific experimental system.
Q4: We're investigating non-MHC barriers in transplantation and want to study the "missing self" hypothesis. What experimental model do you recommend?
A: Studying "missing self" recognition requires specific experimental designs:
- Implement an in vitro coculture system with purified human NK cells and allogeneic endothelial cells mismatched for MHC class I alleles [15].
- Use CRISPR/Cas9 to generate MHC class I knockout cell lines to create controlled "missing self" scenarios.
- Include KIR genotyping of NK cell donors and HLA typing of target cells to identify permissive and non-permissive interactions.
- Measure NK cell activation markers (CD107a, IFN-γ production) and target cell killing to quantify missing self responses.
- For in vivo modeling, consider F1 hybrid mouse models transplanted with parental strain grafts which naturally exhibit missing self recognition [15].
- Always include appropriate controls with MHC-matched combinations to distinguish missing self from other allorecognition pathways.
Emerging Concepts and Future Directions
Recent advances in transplantation immunology have revealed additional layers of complexity in histocompatibility. The discovery of innate allorecognition demonstrates that myeloid cells can directly recognize allogeneic non-self through mechanisms like the signal regulatory protein α-CD47 pathway [15]. This MHC-independent recognition challenges the traditional paradigm that alloimmunity is solely mediated by adaptive immunity.
Another significant development is the understanding that endogenous retrotransposable elements and antivimmune signatures can influence transplant outcomes. A 2025 study demonstrated that mouse melanoma cells capable of escaping allogeneic rejection upregulated retrotransposable elements, MHC class I, PD-L1, and Qa-1 non-classical MHC molecules [16]. Knockout of the RNA sensor RIG-I reduced expression of these immunosuppressive molecules, making tumors susceptible to rejection.
The field is also moving toward tolerance-inducing strategies rather than broad immunosuppression. Approaches including regulatory T-cell therapy, mixed chimerism induction, and thymic education are showing promise in clinical trials [17]. These strategies aim to reprogram the immune system to specifically accept donor antigens while maintaining overall immune competence, potentially eliminating the need for lifelong immunosuppression.
Core Concepts: The Basis of Humoral Rejection
What is the fundamental premise of the humoral theory of transplantation? The humoral theory of transplantation, pioneered by Professor Paul Terasaki, posits that antibodies are the primary mediators of allograft rejection. This theory challenges the historical focus on T-cells and emphasizes that antibodies can cause immediate and devastating graft destruction, from hyperacute rejection occurring within minutes to chronic rejection developing over years [18] [19].
What are the key antibodies and antigens involved in this process? The central actors are Donor-Specific Antibodies (DSA). These antibodies most commonly target donor Major Histocompatibility Complex (MHC) molecules, known in humans as Human Leukocyte Antigens (HLA)—specifically HLA class I (A, B, C) and class II (DR, DQ, DP) [18] [20]. Importantly, antibodies can also target non-HLA antigens on endothelial and epithelial cells, such as angiotensin II type 1 receptor (AT1R), endothelin-I type A receptor (ETAR), and vimentin [18].
How does antibody binding translate to physical damage in the graft? Antibody binding initiates a destructive cascade. DSA binding to donor endothelium triggers the classical complement pathway, leading to the formation of the Membrane Attack Complex (C5b-C9) that directly lyses endothelial cells [21] [22]. Complement split products (C3a, C5a) act as potent anaphylatoxins, recruiting inflammatory cells like neutrophils and monocytes. These cells, along with Natural Killer (NK) cells, further contribute to tissue damage through antibody-dependent cellular cytotoxicity (ADCC) and the release of pro-inflammatory cytokines [22]. The result is widespread endothelial injury, thrombosis, and ischemia, culminating in graft failure.
The diagram below illustrates this core mechanistic pathway of antibody-mediated graft injury.
Troubleshooting Guide: Experimental Challenges in AMR Research
Model Systems & Diagnosis
FAQ 1: How can I reliably detect and diagnose Antibody-Mediated Rejection in my experimental models? A multi-modal approach is critical for accurate AMR diagnosis. Relying on a single parameter often leads to false negatives or misinterpretation.
Table: Key Diagnostic Modalities for Experimental AMR
| Modality | Key Readouts | Experimental Significance | Common Pitfalls |
|---|---|---|---|
| Serology | Donor-Specific Antibody (DSA) detection via solid-phase assays (Luminex), C1q-binding assay to assess complement-fixing ability [18]. | Quantifies the humoral response. High Mean Fluorescence Intensity (MFI >1000) correlates with worse outcomes [18]. | DSA may be absorbed by the graft, leading to undetectable serum levels [19]. |
| Histopathology | Microvascular inflammation (glomerulitis, capillaritis), C4d deposition on peritubular capillaries (a footprint of complement activation) [21] [22]. | Provides direct evidence of tissue injury and complement activity. Considered a hallmark feature. | C4d staining can be negative in some AMR cases; injury can occur via complement-independent pathways [21]. |
| Graft Function | Serum creatinine (kidney), forced expiratory volume (lung), other organ-specific functional metrics [20] [23]. | Correlates immunological injury with clinical outcome. A persistent 20% drop in FEV1 indicates chronic lung rejection (BOS) [23]. | Functional changes are late markers; significant injury may occur before function declines. |
| Emerging Biomarkers | Donor-derived cell-free DNA (dd-cfDNA) for early graft injury [24]. | Highly sensitive for detecting early, subclinical graft injury, allowing for preemptive intervention. | Still being validated in various transplant settings; can be elevated in non-rejection injury (e.g., infection). |
FAQ 2: Our in vivo models are not consistently developing high-titer DSA. What could be limiting the humoral response? The robustness of a humoral response depends on effective T-B cell collaboration. Models using specific pathogen-free (SPF) rodents have a naïve immune system and may generate weaker responses compared to humans or "dirty" mice exposed to pathogens, which have a larger memory T-cell compartment [17]. Ensure your model has sufficient CD4+ T-cell help. The indirect pathway of allorecognition, where recipient T-cells recognize donor peptides presented by recipient Antigen-Presenting Cells (APCs), is critical for providing help to B-cells for antibody class switching and affinity maturation [20] [23]. Using donors with a greater degree of HLA/MHC mismatch can also potentiate a stronger DSA response.
Therapeutic Interventions
FAQ 3: We are testing a new B-cell targeting drug, but DSA levels are not decreasing. Why might this be? B-cell depletion strategies (e.g., anti-CD20 like Rituximab) effectively target precursor B-cells but have limited efficacy against antibody-secreting plasma cells, which are long-lived and do not express CD20 [21]. This is a common reason for therapeutic failure. To target plasma cells, you must employ proteasome inhibitors (e.g., Bortezomib), which induce endoplasmic reticulum stress and apoptosis in these specialized, high-output cells [21] [22]. For a comprehensive effect, a combination therapy targeting both the B-cell lineage (anti-CD20) and plasma cells (proteasome inhibitor) is often necessary.
FAQ 4: Our complement inhibitor is effective in vitro, but failing in our in vivo model. What are potential mechanisms of resistance? Complement activation is a powerful effector mechanism, but it is not the only one. AMR can proceed via complement-independent pathways. In these cases, DSA binding alone can activate endothelial cells, leading to increased permeability and proliferation. Furthermore, DSA can recruit NK cells and monocytes via Fc gamma receptor (FcγR) engagement, triggering antibody-dependent cellular cytotoxicity (ADCC) and pro-inflammatory cytokine release, causing significant graft injury without complement [22]. Your therapeutic strategy should account for these alternative injury pathways.
The Scientist's Toolkit: Research Reagents & Experimental Protocols
Key Research Reagent Solutions
Table: Essential Reagents for Investigating Humoral Rejection
| Research Reagent / Tool | Primary Function in AMR Research |
|---|---|
| Anti-CD20 (e.g., Rituximab) | Depletes CD20+ B-cells, interrupting the precursor pool for plasma cells and memory B-cells [21] [22]. |
| Proteasome Inhibitor (e.g., Bortezomib) | Induces apoptosis in antibody-secreting plasma cells, directly reducing DSA production [21]. |
| C5 Inhibitor (e.g., Eculizumab) | Blocks the terminal complement cascade, preventing formation of the Membrane Attack Complex (MAC) [21]. |
| Intravenous Immunoglobulin (IVIG) | Modulates immune responses via multiple mechanisms, including neutralization of autoantibodies, Fc receptor blockade, and inhibition of complement activation [21]. |
| IL-6 Receptor Inhibitor (e.g., Tocilizumab) | Blocks IL-6 signaling, a key cytokine for B-cell differentiation into plasma cells and T-follicular helper (Tfh) cell function, disrupting germinal center responses [22]. |
| Anti-Thymocyte Globulin (ATG) | Polyclonal antibody preparation that depletes T-cells, thereby reducing T-cell help for B-cell activation and antibody production [21]. |
Detailed Experimental Protocol: Assessing a Novel AMR Therapy
This protocol outlines a standard in vivo approach for evaluating the efficacy of a new therapeutic agent against established AMR.
Objective: To determine if Drug X ameliorates ongoing antibody-mediated damage and prolongs graft survival in a murine kidney transplant model.
Week 0-1: Model Establishment & Baseline Monitoring
- Induction: Perform allogeneic kidney transplantation on Day 0.
- Confirmation: On Day 7 post-transplant, collect serum and confirm DSA seropositivity via flow cytometric crossmatch or bead-based assay. Randomly enroll DSA+ animals into treatment or control groups.
Week 2: Therapeutic Intervention
- Dosing: Administer Drug X (treatment group) or Vehicle (control group) according to the planned regimen from Day 7 to Day 21.
- Monitoring: Weigh animals daily and monitor for signs of distress. Collect serial serum samples (e.g., Days 7, 14, 21) to track DSA levels and dd-cfDNA.
Week 3: Endpoint Analysis (Terminal Procedure)
- Functional Assessment: Measure serum creatinine and blood urea nitrogen (BUN) to assess graft function.
- Tissue Collection: Euthanize animals and harvest the graft.
- Perfuse one part of the graft with formalin for histology (H&E, C4d staining).
- Snap-freeze another part for RNA/protein extraction (e.g., for cytokine analysis).
- Process tissue for flow cytometry to quantify immune cell infiltration (CD45+, CD3+, CD20+, CD138+ cells).
- Histological Scoring: A pathologist blinded to the groups should score the tissue for features of AMR (e.g., Banff scores for glomerulitis (g), peritubular capillaritis (ptc), and C4d deposition).
The following workflow diagram summarizes this experimental design.
Advanced Research Frontiers
What are the emerging therapeutic targets beyond current standard-of-care? Research is moving beyond broad immunosuppression towards targeted disruption of the humoral immune response. Interleukin-6 (IL-6) is a pivotal cytokine in this context. It drives the differentiation of B-cells into plasma cells and supports the function of T-follicular helper (Tfh) cells within the germinal center, a critical site for high-affinity DSA generation [22]. Clinical trials are now investigating IL-6 receptor blockers (e.g., Tocilizumab) for treating chronic active AMR, showing promise in modulating this pathogenic axis.
Another frontier is the induction of transplant tolerance to eliminate the need for lifelong immunosuppression. Strategies include establishing donor hematopoietic chimerism, where donor stem cells engraft in the recipient, educating the immune system to accept the donor organ as "self" [17]. Alternatively, infusions of regulatory cell therapies (T-regs) are being explored to actively suppress the anti-donor immune response. While challenging, these approaches represent the ultimate goal in transplantation research [17].
Technical Support Center: FAQs & Troubleshooting Guides
Frequently Asked Questions (FAQs)
FAQ 1: What is the core molecular signature that defines the Immunologic Constant of Rejection (ICR)?
The Immunologic Constant of Rejection (ICR) describes a common, convergent effector pathway that is activated across various immune-mediated tissue destruction processes, including allograft rejection, autoimmunity, and responses to pathogens and cancer. Its core signature consists of the coordinate activation of two key element groups [25] [26]:
- Interferon-Stimulated Genes (ISGs): A consistent and prominent activation of genes regulated by interferon signaling.
- Immune Effector Functions (IEFs): The recruitment and activation of cytotoxic immune cells, leading to the expression of effector molecules like granzymes and perforin.
This pathway is often accompanied by the recruitment of immune cells via specific chemokine pathways, particularly those involving CXCR3 and CCR5 ligands [26].
FAQ 2: My gene expression data shows ISG activation in a transplant model. Does this automatically confirm the ICR and predict rejection?
Not necessarily. While the ICR hypothesis posits that ISG activation is a pillar of the rejection process, its presence must be interpreted in a broader context. You should investigate further by [26]:
- Checking for IEF Gene Co-expression: Confirm that the ISG signature is coupled with upregulated expression of immune effector function genes (e.g., granzymes A/B, perforin).
- Validating Cell Recruitment: Verify the upregulation of chemokines (e.g., CXCL9, CXCL10, CCL5) that recruit CXCR3/CCR5-expressing cytotoxic cells.
- Performing Pathway Analysis: Use tools to determine if the broader ICR network, not just isolated components, is significantly enriched.
The ICR represents a common final pathway, and its full signature provides a more reliable indicator of active rejection than any single component alone [25].
FAQ 3: What are the best practices for experimentally detecting alloreactive T cells in vivo?
Detecting rare, donor-reactive T cells is challenging. A recommended methodology is the Comprehensive Alloreactive T-cell Detection (cATD) Assay, which utilizes short-term mixed lymphocyte reaction (MLR) and flow cytometry. Below is a detailed protocol adapted from recent research [27].
Experimental Protocol: cATD Assay for Alloreactive T-Cell Detection
| Step | Specification | Purpose |
|---|---|---|
| 1. Stimulator Cell Prep | Isolate CD19+ B cells from donor spleen. Activate with CD40L (100 ng/mL) + IL-4 (10 ng/mL) for 24 hours. Irradiate (40 Gy) before co-culture. | Generates activated antigen-presenting cells from the donor to stimulate recipient T cells. |
| 2. Responder Cell Prep | Purify T cells from recipient splenocytes using negative selection. | Isbrates the recipient's T-cell population for the response assay. |
| 3. Co-culture & Staining | Co-culture stimulators and responders at a 1:1 ratio (10^6 cells each) for 18 hours. Include APC-conjugated anti-CD154 antibody in the culture medium. Add a protein transport inhibitor (e.g., monensin) for the last 4 hours. | Allows for direct antigen presentation and activation of alloreactive T cells. Anti-CD154 labels activated CD4+ T cells. |
| 4. Flow Cytometry | Stain cells for surface and intracellular markers. Identify alloreactive CD4+ T cells as CD3+CD4+CD154+. Identify alloreactive CD8+ T cells as CD3+CD8+CD137+. | Specifically labels and quantifies the activated, donor-reactive T-cell populations. |
This assay can detect alloreactive T cells as early as 7 days post-transplantation, even before visual graft rejection, and can help distinguish between rejection and tolerance models [27].
FAQ 4: How can I distinguish between acute and chronic rejection at the molecular level?
Acute and chronic rejection are driven by distinct yet sometimes overlapping immune mechanisms. The following table summarizes key differences based on clinical and experimental observations [28] [29].
Table 1: Differentiating Acute and Chronic Rejection
| Feature | Acute Rejection | Chronic Rejection |
|---|---|---|
| Typical Onset | First few months to a year post-transplant [29]. | Develops after a year or more, often a long-term problem [29]. |
| Primary Mediators | Direct T-cell allorecognition; prominent cytotoxic T-cell and innate immune activation [30]. | Involves indirect allorecognition; associated with alloantibodies and macrophage-mediated tissue fibrosis [30]. |
| ICR Signature | Often presents a strong, canonical ICR signature with clear ISG and IEF activation [26]. | The ICR signature may be less prominent or accompanied by a stronger fibrotic and antibody-mediated gene expression profile. |
| Histology | Cell-mediated attack on graft parenchyma. | Tissue remodeling, fibrosis, and vascular occlusion. |
FAQ 5: What are the major challenges in applying the ICR hypothesis to allogeneic cell therapies?
The primary challenge is immune rejection of the allogeneic cell product, which rapidly eliminates the therapy. Overcoming this requires strategies to evade the host immune system, a concept often termed "alloevasion" [31]. Key hurdles include:
- T-cell Recognition: Host CD8+ and CD4+ T cells recognize foreign HLA Class I and II molecules on the donor cells [31].
- Antibody-Mediated Rejection: Host B cells can produce alloantibodies that trigger complement-dependent cytotoxicity (CDC) and antibody-dependent cellular cytotoxicity (ADCC) [31].
- NK Cell Activation: Host NK cells attack donor cells that lack "self" HLA molecules [31].
- Immune Memory: A second dose of the therapy is often cleared more rapidly due to primed memory T and B cells [31].
The Scientist's Toolkit
Table 2: Research Reagent Solutions for ICR & Rejection Studies
| Reagent / Assay | Primary Function | Application in Rejection Research |
|---|---|---|
| cATD Assay [27] | Detects activated alloreactive T cells via CD154 (CD4+) and CD137 (CD8+) expression. | Monitoring pre- and post-transplant anti-donor T-cell responses; evaluating tolerance. |
| CXCR3/CCR5 Ligands (e.g., CXCL9, CXCL10, CCL5) [26] | Chemoattractants for T cells and NK cells. | Biomarkers for the recruitment of cytotoxic effector cells to the graft; part of the ICR signature. |
| IEF Gene Panel (Granzymes A/B, Perforin) [26] | Mediates target cell apoptosis and cytolysis. | Quantifying the effector phase of rejection; a core component of the ICR. |
| Anti-HLA Antibody Detection Assays | Measures allospecific antibody titers in serum. | Assessing humoral sensitization and risk of antibody-mediated rejection. |
| Lymphodepleting Agents (e.g., Cyclophosphamide, Fludarabine) [31] | Depletes host lymphocytes transiently. | A preconditioning regimen to reduce host-versus-graft reactivity and enhance engraftment of allogeneic therapies. |
Experimental Workflow & Pathway Visualization
The diagram below illustrates the core experimental workflow for profiling the ICR signature and the key molecular pathways involved.
The tables below consolidate key quantitative findings from recent studies to aid in experimental design and data benchmarking.
Table 3: Microbiota Diversity & Transplant Outcomes in Pediatric Allo-HSCT (n=90) [32]
| Patient Group | Overall Survival (OS) | Incidence of Grade 2-4 aGVHD | Key Microbial Features |
|---|---|---|---|
| Higher Pre-Tx Diversity | 88.9% ± 5.7% SE | Lower | Higher abundance of SCFA-producing taxa (e.g., Ruminococcaceae). |
| Lower Pre-Tx Diversity | 62.7% ± 8.2% SE | Higher | Overabundance of potential pathogens (e.g., Enterococcaceae). |
Table 4: Immune Cell Dynamics in Mouse Skin Transplant Rejection Models [27]
| Transplant Model | Immune Status | Donor-Reactive CD8+ T Cells (Day 7) | Graft Outcome |
|---|---|---|---|
| BALB/c → C57BL/6 | Rejection | Increased Proportion | Rejection |
| BALB/c → C3H/HeJ | Tolerance (with immunosuppression) | Lower Proportion | Acceptance |
FAQs: Understanding the Fundamentals of Transplant Rejection
Q1: What are the primary immunological drivers of hyperacute, acute, and chronic rejection?
The immune mechanisms differ significantly across rejection types. Hyperacute rejection is driven by pre-existing antibodies in the recipient against donor antigens (e.g., ABO blood group or HLA antigens) [33] [34]. These antibodies activate the complement cascade immediately upon revascularization, leading to widespread thrombosis and graft necrosis [35] [24].
Acute rejection primarily involves adaptive immunity. Acute T-cell-mediated rejection (TCMR) is characterized by T lymphocytes infiltrating the graft and causing damage upon recognizing foreign donor antigens [35] [33]. Acute antibody-mediated rejection (ABMR) is caused by donor-specific antibodies (DSA), often developed de novo post-transplant, which attack the vascular endothelium, triggering microvascular inflammation [35] [24].
Chronic rejection is a slow, progressive process often involving both immune and non-immune factors. Chronic active ABMR is a major cause of long-term graft loss, driven by persistent DSA leading to microvascular injury, fibrosis, and arterial intimal thickening [35] [33].
Q2: How is a definitive diagnosis of rejection established and classified?
The gold standard for diagnosis is histopathological examination of a graft biopsy, interpreted according to the international Banff Classification System [35] [33]. This system provides standardized criteria for diagnosing and grading rejection, categorizing findings based on the type and severity of tissue injury [35].
table: Banff Classification Categories for Renal Allograft Biopsy
| Category | Diagnosis | Key Pathological Features |
|---|---|---|
| Category 1 | Normal | Normal tissue or nonspecific changes [33] |
| Category 2 | Antibody-Mediated Rejection (ABMR) | Microvascular inflammation (glomerulitis, peritubular capillaritis), C4d deposition, or chronic changes like transplant glomerulopathy [35] [33] |
| Category 3 | Borderline/Suspicious for TCMR | Focal tubulitis and mild interstitial inflammation [33] |
| Category 4 | T-Cell-Mediated Rejection (TCMR) | Significant lymphocytic infiltration in tubules (tubulitis), interstitium, and/or arteries [35] [33] |
| Category 5 | Interstitial Fibrosis and Tubular Atrophy (IFTA) | Scarring indicative of chronic injury [33] |
| Category 6 | Other Changes | Lesions not considered rejection (e.g., viral infection) [33] |
Q3: What are the key risk factors for transplant rejection?
Multiple factors correlate with an increased risk of rejection [33]:
- Immunological Factors: Prior sensitization (high panel reactive antibodies), HLA mismatch, positive B-cell crossmatch, and ABO incompatibility.
- Donor/Transplant Factors: Deceased donor (vs. living donor), advanced donor age, prolonged cold or warm ischemia time.
- Recipient Factors: Younger age, Black race, non-compliance with immunosuppressive therapy, and previous rejection episodes.
Troubleshooting Guides: From Diagnostic Challenges to Research Models
Guide 1: Investigating Subclinical Rejection and Early Graft Injury
Challenge: A rise in serum creatinine is a late indicator of graft injury. Detecting rejection at an early, potentially reversible stage is critical for intervention [24].
Solution: Implement non-invasive biomarker monitoring alongside protocol biopsies.
table: Emerging Non-Invasive Biomarkers for Rejection Monitoring
| Biomarker | Substrate | Function & Application |
|---|---|---|
| Donor-Derived Cell-Free DNA (dd-cfDNA) | Blood | Highly sensitive marker for early graft injury; elevated levels indicate active cell death from rejection [24]. |
| Gene Expression Profiling (GEP) | Blood | Can exclude moderate-to-severe acute rejection; analyzes patterns of immune cell activation [24]. |
| MicroRNA (miRNA) Profiling | Blood/Urine | Enhances diagnostic specificity for precise detection of acute rejection [24]. |
| Donor-Specific Antibodies (DSA) | Blood | Diagnostic biomarker for Antibody-Mediated Rejection (ABMR); detection is a key criterion for diagnosis [35] [33]. |
Experimental Protocol: Monitoring dd-cfDNA in a Rodent Transplant Model
- Model Establishment: Induce end-stage renal disease in a recipient rodent and perform an allogeneic kidney transplant.
- Sample Collection: Collect peripheral blood (e.g., 200µL) weekly from recipient animals into EDTA tubes. Centrifuge at 1,600 x g for 10 min to separate plasma.
- cfDNA Extraction: Use a commercial cfDNA extraction kit to isolate total cfDNA from 1-4 mL of plasma.
- dd-cfDNA Quantification:
- Method A (qPCR-based): Design primers and probes for Single Nucleotide Polymorphisms (SNPs) that differ between donor and recipient. Use droplet digital PCR (ddPCR) for absolute quantification. Calculate the fraction of dd-cfDNA as (donor allele copies / total allele copies) x 100% [24].
- Method B (NGS-based): Perform shallow whole-genome sequencing of the cfDNA. Use bioinformatic algorithms to detect donor- and recipient-specific SNPs and calculate the dd-cfDNA fraction.
- Correlation: Correlate dd-cfDNA levels with simultaneous graft function tests and histology from terminal biopsies to validate its predictive value.
Guide 2: Differentiating T-Cell-Mediated vs. Antibody-Mediated Rejection in Research
Challenge: Accurately distinguishing between TCMR and ABMR in an experimental setting, as their treatments differ significantly.
Solution: A multi-modal approach combining histology, immunostaining, and serology.
Experimental Protocol: Differentiating Rejection Types in a Murine Model
- Graft Biopsy & Histology:
- Immunofluorescence/Immunohistochemistry:
- For ABMR: Stain for C4d on frozen or paraffin-embedded tissue. Linear staining in peritubular capillaries is a hallmark of classical complement activation [33].
- For Immune Cell Infiltration: Use antibodies against CD3 (T cells), CD20 (B cells), and CD68 (macrophages) to characterize the inflammatory infiltrate.
- Serological Analysis:
The Scientist's Toolkit: Key Research Reagents & Models
table: Essential Research Reagents for Investigating Transplant Rejection
| Reagent / Material | Function & Application in Rejection Research |
|---|---|
| Anti-T cell Depleting Antibodies (e.g., Anti-CD3) | Used in vivo to deplete T lymphocytes and study their critical role in acute T-cell-mediated rejection [17]. |
| Complement Inhibitors (e.g., Anti-C5) | Used to block the complement cascade, investigating its role in hyperacute and antibody-mediated rejection [35]. |
| Recombinant Cytokines & Neutralizing Antibodies | To manipulate specific immune pathways (e.g., IL-2, IFN-γ) and assess their impact on rejection or tolerance [17]. |
| MHC-Tetramers | For tracking and characterizing donor-reactive T cells in the recipient's immune system using flow cytometry. |
| Luminex Bead Arrays | High-sensitivity multiplex assay for detecting and quantifying donor-specific antibodies (DSA) in recipient serum [24]. |
| C4d Antibody | Critical immunohistochemistry reagent for diagnosing antibody-mediated rejection by detecting complement split product deposition [33]. |
| Allogeneic Mouse Strains | Research models with defined MHC mismatches (e.g., C57BL/6 to BALB/c) to study immune responses in a controlled setting. |
| CRISPR-Cas Gene Editing Tools | For generating genetically modified donor cells or organs (e.g., knocking out MHC molecules) to evade immune recognition [36] [37]. |
From Bench to Bedside: Current and Novel Intervention Strategies
Troubleshooting Guides for Common Experimental Challenges
Problem 1: Unexpectedly High Rates of Graft Rejection in Preclinical Models
Potential Cause: Inadequate therapeutic drug monitoring leading to subtherapeutic immunosuppressant levels.
- Solution: Implement rigorous therapeutic drug monitoring (TDM). For calcineurin inhibitors like tacrolimus, target trough levels of 5-15 ng/mL in the first month post-transplant, adjusting based on rejection risk [38]. For cyclosporine, monitor levels 2 hours post-dose (C2 monitoring) with targets of 1.2-1.7 μg/mL [38].
- Experimental Protocol: Collect blood samples at consistent times relative to dosing. Use validated immunoassays (ELISA) or liquid chromatography-mass spectrometry (LC-MS/MS) for precise quantification. Include dose-response curves with known standards to ensure assay accuracy.
Potential Cause: Inappropriate drug formulation or administration route affecting bioavailability.
- Solution: For oral administration in rodent models, ensure proper formulation. Tacrolimus can be suspended in 0.5% methylcellulose, while cyclosporine requires olive oil or cremophor-based vehicles due to poor aqueous solubility [38]. Confirm homogeneous suspension through visual inspection and vortexing immediately before administration.
- Experimental Protocol: Compare bioavailability between administration routes. For IV delivery in mice, dissolve tacrolimus in normal saline with 10% ethanol at 0.1 mg/mL, administering 0.1-0.3 mg/kg. For oral dosing, use 1-5 mg/kg via oral gavage after 4-hour fasting to reduce food effects.
Problem 2: Excessive Immunosuppression Leading to Infection in Experimental Models
Potential Cause: Narrow therapeutic window of conventional immunosuppressants.
- Solution: Implement combination therapy at reduced doses. The "Belatacept-Mycophenolate-Low Dose Tacrolimus" regimen allows calcineurin inhibitor minimization while maintaining efficacy [38]. In murine models, combine mycophenolate mofetil (MMF) at 30 mg/kg/day with sirolimus at 0.5 mg/kg/day rather than high-dose monotherapy.
- Experimental Protocol: Establish dose-escalation studies for combination therapies. Begin with 50% of typical monotherapy doses and titrate based on weekly flow cytometry analysis of T-cell counts (aim for CD3+ count >200 cells/μL) and monthly pathogen screening.
Potential Cause: Drug accumulation due to impaired metabolism.
- Solution: Monitor for drug-drug interactions and hepatic function. Cyclosporine and tacrolimus are metabolized by cytochrome P450 3A4; avoid co-administration with strong CYP3A4 inhibitors (e.g., ketoconazole) or inducers (e.g., rifampin) in experimental models [38].
- Experimental Protocol: Include control groups receiving CYP3A4 modulators when testing new drug combinations. Measure serum transaminases (ALT, AST) weekly and adjust dosing if levels exceed 3× upper limit of normal.
Problem 3: Drug-Related Toxicity in Primary Cell Cultures
Potential Cause: Direct cytotoxic effects at standard concentrations.
- Solution: Optimize in vitro dosing using viability assays. For calcineurin inhibitors, start with 5-10 ng/mL for tacrolimus or 50-100 ng/mL for cyclosporine in human T-cell cultures, rather than typical therapeutic ranges of 10-20 ng/mL and 100-300 ng/mL respectively [38].
- Experimental Protocol: Perform MTT or Annexin V/PI staining assays after 72-hour exposure. Calculate IC50 values for both immunosuppression (IL-2 inhibition) and cytotoxicity (viability reduction). Select concentrations where efficacy/toxicity ratio is maximized.
Potential Cause: Solvent toxicity from drug vehicles.
- Solution: Use alternative solubilization methods. Replace DMSO with cyclodextrin complexes for sirolimus (maximum 0.1% final concentration), or use ethanol-based vehicles for calcineurin inhibitors with final ethanol concentration <0.5% [38].
- Experimental Protocol: Include vehicle-only controls in all experiments. Assess cell viability and function after 24, 48, and 72 hours of exposure. Pre-test all vehicle solutions on relevant cell lines before primary cell experiments.
Frequently Asked Questions (FAQs)
Q1: What are the key mechanistic differences between calcineurin inhibitors and mTOR inhibitors?
Calcineurin inhibitors (tacrolimus, cyclosporine) and mTOR inhibitors (sirolimus, everolimus) target distinct signaling pathways in T-cell activation, as illustrated below:
Calcineurin inhibitors block the phosphatase activity of calcineurin, preventing nuclear translocation of NFAT (Nuclear Factor of Activated T-cells) and subsequent IL-2 transcription [38]. mTOR inhibitors bind to FKBP-12 and block the mammalian Target of Rapamycin (mTOR), arresting cell cycle progression at the G1-S phase by inhibiting ribosomal protein synthesis and preventing IL-2-driven T-cell proliferation [38].
Q2: How do I select the appropriate primary endpoint for evaluating novel immunosuppressant efficacy in preclinical transplantation models?
The optimal endpoints depend on your experimental timeline and research question:
- Short-term (7-14 days): Flow cytometric analysis of T-cell activation markers (CD25, CD69, HLA-DR) and mixed lymphocyte reaction (MLR) assays.
- Medium-term (2-4 weeks): Histopathological grading of allograft rejection using Banff classification for organ-specific features [39].
- Long-term (4-12 weeks): Graft survival analysis with serial monitoring of organ function (e.g., serum creatinine for kidney, bilirubin for liver) and donor-specific antibody (DSA) production.
Q3: What strategies can overcome calcineurin inhibitor nephrotoxicity in experimental models?
Three primary approaches have demonstrated efficacy:
- CNI Minimization: Combine low-dose tacrolimus (trough 3-5 ng/mL) with adjunctive agents like MMF (1-1.5 g/day equivalent) or sirolimus (trough 4-8 ng/mL) [38].
- CNI Conversion: Switch from CNI to mTOR inhibitors after 3-6 months, particularly in models with established renal dysfunction.
- Novel Formulations: Use extended-release tacrolimus formulations that produce more stable blood levels and reduce nephrotoxic peaks.
Q4: How can I distinguish between drug-induced nephrotoxicity and rejection in animal models?
Key differentiating features include:
- Timing: CNI nephrotoxicity typically develops gradually over weeks, while rejection often occurs abruptly.
- Histopathology: CNI toxicity shows arteriolar hyalinosis, striped interstitial fibrosis, and tubular atrophy; rejection demonstrates tubulitis, intimal arteritis, and inflammatory infiltrates [38].
- Biomarkers: Urinary NGAL and serum Cystatin C rise earlier in rejection than serum creatinine.
- Therapeutic Response:
- Drug Toxicity: Improves with dose reduction (improvement within 5-7 days)
- Rejection: Requires intensified immunosuppression (improvement within 2-3 days)
Q5: What are the critical in vitro assays for screening novel immunosuppressants?
Establish a tiered testing approach:
- Primary Screening: T-cell proliferation assays using CFSE dilution or 3H-thymidine incorporation with anti-CD3/CD28 stimulation.
- Mechanistic Studies: Calcium flux assays for calcineurin inhibitors; phospho-protein flow cytometry for mTOR inhibitors (pS6, p4E-BP1).
- Functional Assays: Cytokine multiplex analysis (IL-2, IFN-γ, IL-6, TNF-α) and regulatory T-cell induction assays.
- Specificity Testing: Toxicity panels on non-immune cells (hepatocytes, renal tubular cells) and antibacterial T-cell assays.
Quantitative Data Analysis
Table 1: Efficacy of Common Immunosuppressants in Preventing Acute Rejection
| Drug/Regimen | Mechanism of Action | Rejection Rate (%) | Key Toxicities | Therapeutic Monitoring Parameters |
|---|---|---|---|---|
| Tacrolimus | Calcineurin inhibitor | 10-20 [38] | Nephrotoxicity, neurotoxicity, NODAT | Trough: 5-15 ng/mL [38] |
| Cyclosporine | Calcineurin inhibitor | 15-25 [38] | Nephrotoxicity, hypertension, hyperlipidemia | C2: 1.2-1.7 μg/mL [38] |
| Mycophenolate mofetil | IMPDH inhibitor | 15-20 (monotherapy) [40] | Gastrointestinal, hematological | AUC: 30-60 mg·h/L [38] |
| Sirolimus | mTOR inhibitor | 20-30 (monotherapy) [38] | Hyperlipidemia, impaired wound healing, pneumonitis | Trough: 4-12 ng/mL [38] |
| Tacrolimus + MMF | Combination therapy | 5-12 [38] | Combined toxicities, increased infection risk | Tacrolimus: 5-10 ng/mL; MMF: AUC 30-60 mg·h/L |
Table 2: Experimental Dosing Conversion Between Species
| Drug | Human Dose | Mouse Equivalent | Rat Equivalent | Critical Administration Notes |
|---|---|---|---|---|
| Tacrolimus | 0.1-0.15 mg/kg/day [38] | 1-5 mg/kg/day oral [38] | 0.5-3 mg/kg/day oral | Administer via oral gavage; monitor weight loss >15% |
| Cyclosporine | 10-15 mg/kg/day [38] | 10-25 mg/kg/day oral [38] | 5-15 mg/kg/day oral | Formulate in olive oil; highly variable bioavailability |
| Mycophenolate mofetil | 1-1.5 g twice daily [40] | 30-60 mg/kg/day oral [40] | 20-40 mg/kg/day oral | Split dose BID; GI toxicity common at higher doses |
| Sirolimus | 2-6 mg/day loading, then 2 mg/day [38] | 0.5-1.5 mg/kg/day oral [38] | 0.3-1 mg/kg/day oral | Use fresh preparation; unstable in solution |
Signaling Pathway Visualization
T-cell Activation and Immunosuppressant Targets
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Immunosuppressant Research
| Reagent Category | Specific Products | Research Application | Key Considerations |
|---|---|---|---|
| Calcineurin Inhibitors | Tacrolimus (FK506), Cyclosporine A | T-cell activation studies, graft rejection models | Light-sensitive; requires ethanol or DMSO solubilization; monitor stability in culture media |
| mTOR Inhibitors | Sirolimus (Rapamycin), Everolimus | Cell cycle studies, cancer immunotherapy combinations | Poor aqueous solubility; use cyclodextrin complexes; short half-life in culture |
| Antimetabolites | Mycophenolate mofetil, Azathioprine | Lymphocyte proliferation assays, combination therapy studies | MMF requires conversion to active MPA form; cell-type specific sensitivity |
| Detection Assays | LC-MS/MS kits, ELISA kits (Prometheus, ThermoFisher) | Therapeutic drug monitoring, pharmacokinetic studies | LC-MS/MS gold standard for CNIs; cross-reactivity issues with some ELISAs |
| Functional Assays CFSE Cell Division, IL-2 ELISpot, Phospho-flow cytometry | Mechanism of action studies, biomarker development | Optimize stimulation conditions (anti-CD3/CD28 concentration); include activation controls | |
| Animal Models | MHC-mismatched cardiac/kidney allograft models, Humanized mice | In vivo efficacy testing, translational studies | Strain-specific responses; monitor for species-specific metabolism differences |
Troubleshooting Guides and FAQs
Common Experimental Challenges and Solutions
FAQ: Why is our tolerogenic protocol, successful in mice, failing when translated to non-human primates or human cellular models?
- Answer: A primary cause is the difference in immune system history between specific pathogen-free (SPF) laboratory mice and humans. Humans possess a substantial compartment of memory T cells generated from lifelong pathogen exposure. These memory T cells, including those generated via heterologous immunity, are highly resistant to tolerance induction protocols that are effective in naive murine immune systems. Infection of a laboratory mouse with a single pathogenic virus can render it refractory to tolerance induction [41].
- Troubleshooting Steps:
- Validate Your Model: Consider using non-SPF animal models (e.g., "dirty mice" or pet store-derived mice) whose T cell memory profile more closely resembles that of adult humans [41].
- Pre-screen for Reactivity: Implement assays to detect pre-existing donor-reactive memory T cells in your recipient subjects before protocol initiation.
- Protocol Augmentation: Enhance your conditioning regimen to more effectively target and deplete memory T cell populations.
FAQ: We successfully established mixed chimerism, but it was transient and followed by graft rejection. What went wrong?
- Answer: Transient chimerism often indicates that the level of donor engraftment was insufficient to outcompete the recovering host immune system or was effectively eliminated by a residual host-versus-graft (HvG) response. Loss of chimerism is a known precursor to solid organ graft rejection [41] [42].
- Troubleshooting Steps:
- Quantify Chimerism Rigorously: Monitor chimerism levels frequently using sensitive flow cytometric and molecular techniques. A steady decline is a key early warning sign [43] [44].
- Optimize the Cellular Product: Ensure the hematopoietic stem cell (HSC) graft contains an adequate dose of CD34+ cells for durable engraftment. The inclusion of donor T cells may be necessary to suppress the host immune system and "make space" for donor HSCs, though this increases graft-versus-host disease (GVHD) risk [41] [42].
- Review Conditioning Intensity: The non-myeloablative conditioning may have been insufficient. Evaluate if the intensity of lymphodepletion (e.g., with agents like anti-thymocyte globulin (ATG) or total lymphoid irradiation) can be safely optimized [42].
FAQ: How can we mitigate the risk of Graft-versus-Host Disease (GVHD) while still leveraging graft-versus-host reactivity for tolerance?
- Answer: GvH reactivity is a double-edged sword; it can support donor chimerism by clearing host HSCs but can also cause lethal GVHD. The challenge is to balance this effect [41].
- Troubleshooting Steps:
- T-cell Depletion (TCD): Consider sophisticated graft engineering strategies. CD34+ selection or negative depletion of TCRαβ+ T cells from the stem cell graft can significantly reduce GVHD incidence while aiming to preserve engraftment potential [41] [45].
- Precise T-cell Dosing: Some protocols use a defined, low dose of donor T cells (e.g., (1-4 \times 10^6)/kg) to facilitate engraftment without causing severe GVHD [41].
- Pharmacologic Control: Maintain a short course of post-transplant immunosuppression (e.g., tacrolimus) to control alloreactive T cells until a state of equilibrium is reached [42].
Quantitative Data from Key Clinical Studies
The table below summarizes outcomes from pivotal clinical trials investigating mixed chimerism for tolerance induction.
| Study / Protocol | Conditioning Regimen | Cellular Product | Chimerism Outcome | Immunosuppression (IS) Withdrawal Outcome | Key Adverse Events |
|---|---|---|---|---|---|
| MDR-101 (Phase 3) [42]HLA-matched kidney | rATG, low-dose TLI | CD34+ HSCs + fixed CD3+ T cells (MDR-101) | Mixed chimerism achieved in 19/20 (95%) patients | 15/20 (75%) achieved functional tolerance (off IS for 24+ months) | No GVHD or graft loss. One SAE of polyarthralgia. |
| Stanford Protocol [41]HLA-matched kidney | TLI, ATG | HSCs + low-dose donor T cells ((1 \times 10^6)/kg) | Durable chimerism in >80% of HLA-identical recipients | Successful IS withdrawal in >80% with durable chimerism | GVHD risk increased in HLA-incompatible settings. |
| Northwestern Protocol [41]HLA-mismatched kidney | TBI, fludarabine, cyclophosphamide | HSCs + donor T cells ((3.8 \times 10^6)/kg) + "facilitator" cells | High-level stable chimerism in 26/32 (~81%) patients | Successful IS withdrawal in 25/26 with stable chimerism | Fatal GVHD (n=1), chronic GVHD (n=1), severe infections (n=3) |
Detailed Experimental Protocol: MDR-101 Multicenter Trial
This protocol induces mixed chimerism for operational tolerance in 2-haplotype HLA-matched living donor kidney transplantation [42].
Objective
To establish transient mixed hematopoietic chimerism, enabling complete withdrawal of maintenance immunosuppression without graft rejection.
Materials and Reagents
- Recipient: First-time recipient of a kidney from a 2-haplotype HLA-matched, living related donor.
- Conditioning Agents:
- Rabbit anti-thymocyte globulin (rATG): Total dose of 7.5 mg/kg, administered intravenously from Day 0 to Day 4. Function: Lymphodepletion to suppress the host immune system and prevent graft rejection.
- Total Lymphoid Irradiation (TLI): 1200 cGy, delivered in 10 fractions from Day 1 to Day 11. Function: Further lymphodepletion and creation of immune space for donor cell engraftment.
- Cellular Product (MDR-101):
- Donor-derived, enriched for CD34+ hematopoietic stem cells. Function: To establish multilineage donor hematopoiesis in the recipient bone marrow.
- Contains a fixed dose of CD3+ T cells. Function: To modulate the recipient's immune response and support engraftment.
- Immunosuppression (Bridge):
- Methylprednisolone: Tapering doses from Day 0 to Day 10.
- Tacrolimus: Started on Day 0, target trough 8-11 ng/mL, later 4-6 ng/mL.
- Mycophenolate Mofetil (MMF): 1-2 g/day, started on Day 11 and discontinued on Day 39.
Experimental Workflow
The following diagram illustrates the sequential timeline of the MDR-101 clinical trial protocol.
Key Procedural Notes
- Chimerism Monitoring: The percentage of donor white blood cells (chimerism) must be monitored regularly. In the MDR-101 trial, stable mixed chimerism of ≥5% at one year post-transplant was a prerequisite for proceeding with tacrolimus withdrawal [42].
- Tapering Logic: Immunosuppression withdrawal is gradual and directly contingent upon the stability of the mixed chimerism.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Protocol | Key Considerations for Researchers |
|---|---|---|
| Anti-thymocyte globulin (ATG) | Polyclonal antibody for in vivo T-cell depletion; weakens host-versus-graft (HvG) response. | Monitor for cytokine release syndrome. Dose must be optimized to balance efficacy (preventing rejection) with over-immunosuppression (infection risk) [41] [42]. |
| CD34+ Hematopoietic Stem Cells | Foundational cell population to establish donor hematopoiesis and create a persistent source of donor-derived antigen-presenting cells. | High cell dose is critical for engraftment, especially in T-cell-depleted protocols. Purity and viability of the selected product are paramount [41] [45]. |
| Donor T cells | Facilitates engraftment by suppressing host immunity (HvG) and mediates graft-versus-leukemia (GvL) effects. | The dose is critical; too few may not support engraftment, while too many significantly increases the risk of GvHD [41] [42]. |
| Immunomagnetic Cell Sorting Systems | For positive selection of CD34+ cells or negative depletion of T cells (e.g., TCRαβ+ / CD19+) from the graft. | Performance Metrics: Aim for high T-cell depletion (>3.5-4.0 log10) and high CD34+ cell recovery (>90%) to prevent GvHD and ensure engraftment [41] [45]. |
| Tacrolimus | Calcineurin inhibitor; used as a bridge immunosuppressant to control alloreactive T cells post-transplant. | Tapering must be slow and guided by chimerism levels. Abrupt withdrawal in an unstable system can precipitate rejection [42]. |
Advanced Technical Appendix
High-Throughput T-Cell Depletion Methodology
For graft engineering, a Quadrupole Magnetic Cell Sorter (QMS) can achieve high-performance T-cell depletion. An optimized protocol using anti-CD3 Dynabeads in a "no-wash" immunomagnetic labeling process can achieve an average 3.96 ± 0.33 log10 depletion of CD3+CD45+ cells with a mean recovery of 99.43 ± 4.23% of CD34+CD45+ cells at a sorting speed of 106 cells/s [45].
Mechanisms of Central vs Peripheral Tolerance in Chimerism
The following diagram contrasts the immunological mechanisms of full donor chimerism and mixed chimerism.
FAQ: Immune Rejection in Allogeneic Transplantation
Q1: What are the primary immune mechanisms responsible for rejecting allogeneic Treg and MSC therapies?
Allogeneic cell therapies face rejection primarily through host T cell and Natural Killer (NK) cell responses. For both Tregs and MSCs, host CD8+ T cells recognize foreign HLA Class I molecules on the infused cells, leading to direct killing [46]. MSCs, while inherently less immunogenic, can upregulate HLA Class I in inflammatory environments, triggering this response [47]. NK cells contribute to rejection through "missing-self" activation; they attack cells with low or absent HLA Class I expression, a particular risk for engineered cells where B2M is knocked out to evade T cells [46] [47].
Q2: What strategies can be used to create "off-the-shelf" cell products that evade immune rejection?
Two main strategies are employed to develop universal cell products:
- HLA Matching: Using donors with stringent HLA matching to the recipient can restore cell survival and efficacy, but this is often clinically impractical [46].
- Genetic Engineering to Induce Hypoimmunogenicity: CRISPR-Cas9 gene editing is used to disrupt key genes in the HLA pathway.
- Knockout of B2M eliminates surface expression of HLA Class I, evading CD8+ T cell recognition [46] [47].
- Knockout of CIITA reduces HLA Class II expression [46].
- Insertion of a non-polymorphic HLA-E transgene inhibits NK cell-mediated killing by engaging the NKG2A inhibitory receptor on NK cells, compensating for the loss of HLA Class I [46].
Q3: How can I assess the in vivo stability and function of engineered Tregs after transplantation?
Advanced immunomonitoring technologies are critical for tracking Tregs in vivo [48].
- Single-Cell Multi-omic Profiling: Allows simultaneous analysis of transcriptome and epigenome at a single-cell level to evaluate FOXP3 stability and suppressive phenotype.
- Spatial Transcriptomics: Reveals the spatial location of infused Tregs within the graft and their interaction with host immune cells, showing enrichment of immunoregulatory programs [46].
- Epigenetic Analysis: Assessing the methylation status of the Treg-specific demethylation region (TSDR) in the FOXP3 gene is a key measure of Treg lineage stability [46].
Troubleshooting Guide: Overcoming Barriers to Engraftment
Problem: Poor In Vivo Survival of Allogeneic Tregs
Potential Cause: Rapid elimination by host alloreactive CD8+ T cells due to HLA mismatches [46].
| Solution | Experimental Methodology | Key Outcome Measures |
|---|---|---|
| CRISPR HLA Engineering | • Transfect Tregs with CRISPR machinery targeting B2M and CIITA.• Use a repair template to knock-in an HLA-E-B2M fusion gene into the B2M locus.• Validate edits via flow cytometry (loss of HLA-I/II, gain of HLA-E) and sequencing [46]. | • In vitro suppression assay: Confirm retained suppressive function against allogeneic Tconv cells.• In vivo survival: Quantify recovered engineered Tregs in a humanized mouse model via flow cytometry.• Graft survival: Monitor skin or organ allograft survival time; successful engineering should match autologous Treg efficacy [46]. |
| HLA Matching | • Screen donor-recipient pairs for matches at HLA-A, -B, -C, and -DR loci.• Use partially or fully matched Tregs for therapy [46]. | • Graft survival: Compare median survival time (MST) of grafts with matched vs. mismatched Tregs. Partially matched Tregs can achieve >100 days MST vs. 24-27 days for mismatched [46]. |
Workflow: Creating Hypoimmunogenic Tregs
Problem: Host NK Cell Killing of HLA-Engineered MSCs
Potential Cause: B2M knockout ablates HLA Class I, leading to "missing-self" recognition and activation of NK cell cytotoxicity [47].
| Solution | Experimental Methodology | Key Outcome Measures |
|---|---|---|
| Generate HLA-I Pseudo-Homozygous MSCs | Differentiate MSCs from CRISPR-edited iPSCs with disrupted HLA-A, -B, and -C alleles. This retains some HLA-I to avoid "missing-self" but reduces polymorphism [47]. | • NK Cytotoxicity Assay: Co-culture edited MSCs with allogeneic NK cells and measure lysis (e.g., LDH release).• In Vivo Engraftment: Quantify MSC persistence in immunocompetent models.• Differentiation Capacity: Confirm retained adipogenic, chondrogenic, and osteogenic potential [47]. |
Workflow: Engineering MSCs to Evade Immunity
Table 1: In Vivo Efficacy of Engineered vs. Non-Engineered Allogeneic Tregs in a Humanized Mouse Skin Graft Model [46]
| Treg Cell Type | HLA Relationship to Host | Key Genetic Modification | Median Skin Graft Survival (Days) |
|---|---|---|---|
| Autologous Tregs | Self | None | >100 |
| Allogeneic Tregs | Fully/Partially Mismatched | None | 24 - 27 |
| Partially Matched Tregs | Partially Matched | None | >100 |
| Engineered Tregs | Fully Mismatched | B2M KO + CIITA KO + HLA-E KI | Comparable to Autologous (>100) |
Table 2: Functional Validation of CRISPR-Edited Tregs and MSCs [46] [47]
| Cell Type | Editing Target | In Vitro Suppression | FOXP3/TSDR Stability | NK Cell Lysis Evasion |
|---|---|---|---|---|
| Tregs | B2M KO, CIITA KO, HLA-E KI | Retained (Equivalent to Autologous) | Stable FOXP3, Low TSDR Methylation | Yes (via HLA-E/NKG2A) |
| MSCs (iPSC-derived) | HLA-A, B, C KO | N/A (Assay not standard for MSCs) | N/A | Yes (Unlike complete B2M KO) |
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Developing Allogeneic Cellular Therapies
| Reagent / Material | Function in Experimental Protocol |
|---|---|
| CliniMACS Plus System | Clinical-grade magnetic bead-based cell separation for isolating CD4+CD127low/CD25+ Tregs from peripheral blood [48]. |
| CRISPR-Cas9 System | Precision gene editing for knocking out immunogenic genes (B2M, CIITA) or knocking in protective genes (HLA-E) [46] [47]. |
| Recombinant Human IL-2 + Rapamycin | Critical cytokines and signaling inhibitors for ex vivo polyclonal expansion of Tregs while maintaining purity and function [48]. |
| Artificial Antigen-Presenting Cells (aAPCs) | Loaded with anti-CD3/CD28 antibodies to provide stimulatory signals for Tconv-to-iTreg conversion or Treg expansion [48]. |
| Anti-human CD8 Antibody | Used for depletion studies to confirm the role of host CD8+ T cells in rejecting allogeneic cells in vivo [46]. |
| FOXP3 TSDR Methylation Assay Kit | Epigenetic analysis to confirm stable Treg lineage identity in expanded or engineered products [46]. |
Core Strategies & Technical FAQs
This section addresses frequently asked questions about the primary CRISPR-Cas strategies used to engineer immune-evasive cells for transplantation.
Q: What are the primary genetic targets for creating "immune stealth" allogeneic grafts?
A: Research focuses on disrupting the immune system's ability to recognize and activate a response against donor cells. The main strategies involve:
- Disrupting Antigen Presentation: Knocking out Beta-2 microglobulin (β2M), a critical subunit of the Major Histocompatibility Complex class I (MHC-I), significantly reduces surface expression of HLA class I molecules. This makes donor cells largely "invisible" to the host's alloreactive CD8+ T cells [49].
- Eliminating MHC Class II: Using CRISPR to target the Class II Major Histocompatibility Complex Transactivator (CIITA), a master regulator of MHC class II expression, can prevent the presentation of antigens to CD4+ T cells [49].
- Inhibiting Innate Immune Cell Killing: Overexpressing the CD47 "don't eat me" signal on the cell surface inhibits phagocytosis by host macrophages and natural killer (NK) cells [50].
- Blocking Immune Cell Adhesion: Knocking out Intercellular Adhesion Molecule-1 (ICAM-1) impairs the binding and extravasation of various immune cells (like T cells and neutrophils) to the graft, protecting it from both innate and adaptive immune responses early after transplantation [51].
Q: How can I validate that my edited grafts have reduced immunogenicity in vitro?
A: A standard validation workflow includes the following assays:
- Flow Cytometry: Confirm the successful knockout of target proteins (e.g., MHC-I, ICAM-1) on the cell surface, both at baseline and after stimulation with pro-inflammatory cytokines like TNF-α and IFN-γ [51].
- Mixed Lymphocyte Reaction (MLR): Co-culture your edited cells with allogeneic human peripheral blood mononuclear cells (PBMCs). A successful edit will result in significantly suppressed T-cell proliferation and activation compared to unedited controls [51].
- Immune Cell Adhesion Assays: Seed edited cells (e.g., stem cell-derived endothelial cells, cardiomyocytes) and stimulate them with cytokines. Then, add immune cells (e.g., monocytic cell lines like U937, or primary T cells) and measure the extent of binding. ICAM-1 knockout cells should show dramatically diminished immune cell adhesion [51].
Q: We are seeing reduced long-term persistence of our CRISPR-edited hematopoietic stem cells in mouse models. What could be the cause?
A: This is a known challenge. A 2021 meta-analysis of 15 preclinical studies found that while CRISPR-Cas9 edited hematopoietic stem and progenitor cells demonstrate equivalent early engraftment, their persistence can be reduced at later time points and in secondary transplant recipients [52]. This occurs whether homology-directed repair or non-homologous end-joining is used. The issue may be related to the fitness of the edited cells or the genotoxic stress of the editing process itself. To overcome this, the field is actively investigating improved methods to target long-term repopulating hematopoietic stem cells more efficiently [52].
Table 1: Key Genetic Targets for Immune-Evasive Grafts
| Target Gene | CRISPR System Used | Primary Immune Effect | Key Functional Outcome |
|---|---|---|---|
| B2M / CIITA | CRISPR-Cas12b [50] | Depletes HLA Class I & II; evades T-cell recognition [50] [49]. | First-in-human study showed no immune rejection for 12+ weeks without immunosuppressants [50]. |
| CD47 | CRISPR-Cas12b [50] | Overexpression inhibits macrophage and NK cell phagocytosis [50]. | Used in combination with B2M/CIITA knockout to create "hypoimmune" cells [50]. |
| ICAM-1 | CRISPR-Cas9 [51] | Diminishes binding and adhesion of T cells and neutrophils [51]. | Prolonged in vivo graft retention in humanized mouse models [51]. |
Table 2: Persistence of CRISPR-Edited Hematopoietic Cells (Preclinical Meta-Analysis)
| Outcome Measure | Finding | Implication for Research |
|---|---|---|
| Early Engraftment | Equivalent to unedited control cells [52]. | Edited cells can initially transplant successfully. |
| Long-Term Persistence | Reduced at later time points [52]. | A critical barrier for durable cures; requires improved editing protocols. |
| Performance in Secondary Transplants | Further reduced persistence [52]. | Suggests a potential fitness defect in the most primitive edited stem cells. |
Experimental Protocols
Protocol 1: Generating an ICAM-1 Knockout Pluripotent Stem Cell Line
This protocol is adapted from a 2025 Nature Communications study for creating hypoimmune human pluripotent stem cells (hPSCs) [51].
Objective: To create a clonal hPSC line with a complete knockout of ICAM-1 for use in deriving immune-evasive cellular therapies.
Materials:
- Wild-type hPSC line (e.g., H9 human embryonic stem cells).
- CRISPR-Cas9 plasmid(s) targeting early exons of the ICAM1 gene.
- Transfection reagent suitable for hPSCs.
- Antibodies for Flow Cytometry: Anti-SSEA-4, Anti-Alkaline Phosphatase, Anti-MHC-I, Anti-ICAM-1.
- Teratoma assay materials (e.g., immunodeficient mice).
Methodology:
- Design and Delivery: Design sgRNAs to target constitutive exons of the ICAM1 gene to ensure all protein isoforms are disrupted. Transfect hPSCs with the CRISPR-Cas9 construct.
- Clonal Selection and Expansion: After transfection, single cells are sorted and expanded into clonal lines.
- Genotypic Validation: Sequence the ICAM1 locus in clonal lines to identify frameshift mutations or introduction of stop codons.
- Phenotypic Validation:
- Flow Cytometry: Confirm the absence of ICAM-1 surface protein on unstimulated and cytokine-stimulated (TNF-α 10 ng/ml + IFN-γ 50 ng/ml, 48 hours) cells [51].
- Western Blot: Verify the lack of ICAM-1 protein in cell lysates.
- Pluripotency Check: Confirm the edited line maintains pluripotency via staining for markers (SSEA-4, Alkaline Phosphatase) and teratoma formation assay [51].
- Karyotyping: Perform G-banding to ensure genomic stability after editing [51].
- Off-Target Screening: Use Sanger sequencing to screen the top predicted off-target sites (e.g., from CRISPOR algorithm) [51].
Protocol 2:In VitroT-Cell Activation Assay (Mixed Lymphocyte Reaction)
Objective: To quantify the ability of edited cells to suppress allogeneic T-cell activation.
Materials:
- Test cells: ICAM-1 KO (or other edited) and wild-type hPSC-derived cardiovascular cells (e.g., endothelial cells).
- Stimulator cells: Irradiated allogeneic PBMCs.
- Responder cells: Fresh allogeneic PBMCs from a different donor, labeled with a cell proliferation dye (e.g., CFSE).
- Flow cytometer.
Methodology:
- Differentiate and Stimulate: Differentiate edited and wild-type hPSCs into the target cell type (e.g., endothelial cells). Stimulate with TNF-α (10 ng/ml) and IFN-γ (50 ng/ml) for 48 hours to mimic an inflammatory environment [51].
- Co-culture Setup: Co-culture the stimulated test cells with CFSE-labeled responder PBMCs for 5-6 days.
- Analysis by Flow Cytometry: Harvest cells and analyze by flow cytometry. Measure the dilution of CFSE in the CD3+ T-cell population as a direct indicator of proliferation.
- Expected Outcome: Co-cultures with successfully edited (e.g., ICAM-1 KO) cells will show significantly reduced T-cell proliferation and lower expression of activation markers (e.g., CD25) compared to co-cultures with wild-type cells [51].
The Scientist's Toolkit
Table 3: Essential Research Reagents for Immune Evasion Studies
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| CRISPR-Cas Systems (Cas9, Cas12b) | Precise genome editing to knockout immune-related genes or knock-in protective transgenes [50] [49]. | Creating B2M or ICAM-1 knockout lines in stem cells [50] [51]. |
| Pro-Inflammatory Cytokines (TNF-α, IFN-γ) | Mimic the post-transplantation inflammatory microenvironment to test the robustness of immune edits [51]. | Stimulating edited cells in vitro before immune co-culture assays [51]. |
| Humanized Mouse Models | In vivo platform to study human immune cell responses to edited human cell grafts [51]. | Assessing long-term graft survival and immune infiltration (e.g., in NeoThy mice) [51]. |
| Lipid Nanoparticles (LNPs) | A delivery vehicle for in vivo CRISPR therapy; does not trigger strong immune reactions like viral vectors, allowing for re-dosing [53]. | Systemic delivery of CRISPR components for in vivo gene editing (e.g., in liver-targeted therapies) [53]. |
Signaling Pathway & Experimental Workflow
Frequently Asked Questions (FAQs)
FAQ 1: What types of nanomaterials are most suitable for targeting immune cells in transplantation research? A variety of organic and inorganic nanomaterials can be engineered to target immune cells. Organic nanomaterials, such as liposomes and polymeric nanoparticles (e.g., PLGA), are prized for their biodegradability and low cytotoxicity. They can be functionalized with specific ligands to target antigen-presenting cells like dendritic cells [54] [55]. Inorganic nanomaterials, including gold nanoparticles and iron oxide nanoparticles, offer unique properties for imaging and stimuli-responsive drug release, which can be harnessed for immunomodulation [55]. The choice depends on the specific application, desired drug release profile, and compatibility with imaging techniques.
FAQ 2: How can I track the biodistribution and targeting efficiency of nanoparticles in vivo? Multimodal imaging techniques are essential for real-time, non-invasive monitoring of nanoparticles. Key modalities include:
- Magnetic Resonance Imaging (MRI): Provides high spatial resolution and excellent soft-tissue contrast, ideal for tracking magnetic nanoparticles like iron oxide NPs [56].
- Positron Emission Tomography (PET): Offers high sensitivity for quantifying the accumulation of radiolabeled nanoparticles in target tissues [56].
- Optical Imaging: Fluorescence and bioluminescence imaging allow for real-time monitoring of cellular and molecular interactions, useful for preclinical studies [56]. Hybrid systems like PET/MRI combine the strengths of multiple modalities, providing comprehensive anatomical, functional, and molecular data on nanoparticle behavior [56].
FAQ 3: My nanoparticle formulation is triggering an adverse immune response. What could be the cause? Unexpected immune activation can stem from several factors related to the nanomaterial's physicochemical properties:
- Surface Charge: Highly positive surface charges can promote non-specific interactions with immune cells, leading to inflammation and cytotoxicity [57].
- Poor Biocompatibility: The core material or degradation products may be recognized as foreign, triggering oxidative stress or an inflammatory cascade [57].
- Lack of "Stealth" Properties: Without surface modifications like PEGylation, nanoparticles can be rapidly opsonized and cleared by the mononuclear phagocyte system, causing off-target effects and immune activation [55]. Rigorous assessment of biocompatibility and nanotoxicology is crucial during the design phase [57].
FAQ 4: What strategies can enhance the stability and circulation time of nanocarriers? Surface functionalization is a primary method to improve pharmacokinetics. Coating nanoparticles with polyethylene glycol (PEG) creates a hydrophilic layer that reduces opsonin binding and uptake by immune cells, thereby prolonging circulation time—a process known as PEGylation [57] [55]. Additionally, designing bioresponsive or "smart" nanoparticles that remain stable in circulation but release their payload in response to specific pathological stimuli (e.g., pH, enzymes) at the target site can further enhance efficacy and reduce premature clearance [58].
FAQ 5: Can nanomaterials be used to modulate innate immune responses, such as NK cell activation, in transplantation? Emerging evidence suggests yes. Recent research in solid organ transplantation highlights that Natural Killer (NK) cell activation via "missing self" recognition is a key mechanism in antibody-independent rejection [15]. Nanomaterials could be engineered to deliver immunomodulatory agents that disrupt this pathway. For instance, nanoparticles could be designed to block the interaction between donor HLA class I and recipient inhibitory killer-cell immunoglobulin-like receptors (KIRs), thereby dampening NK cell-mediated damage to the graft [15].
Troubleshooting Guides
Issue 1: Poor Drug Loading or Encapsulation Efficiency
| Possible Cause | Solution | Relevant Experimental Protocol |
|---|---|---|
| Incompatibility between drug and nanocarrier material. | Modify the core material or use a different nanocarrier type (e.g., switch from polymeric NPs to liposomes for hydrophobic drugs). | For liposome preparation: Use the thin-film hydration method. Dissolve phospholipids and cholesterol in an organic solvent, evaporate to form a thin film, then hydrate with an aqueous buffer containing the drug, followed by sonication or extrusion to achieve uniform size [54] [55]. |
| Inefficient synthesis method. | Optimize critical process parameters (CPPs) like solvent ratio, stirring rate, or temperature. Implement Quality-by-Design (QbD) principles and Process Analytical Technologies (PAT) for real-time monitoring [57]. | For polymeric nanoparticles (PLGA): Use the nano-precipitation or single/double emulsion solvent evaporation method. The choice depends on the hydrophilicity of the drug. For hydrophilic drugs, a water-in-oil-in-water (w/o/w) double emulsion is typically required [55]. |
Issue 2: Low Targeting Specificity to Immune Cells
| Possible Cause | Solution | Relevant Experimental Protocol |
|---|---|---|
| Non-specific protein adsorption (protein corona). | Improve "stealth" properties via PEGylation or using biomimetic coatings. Pre-incubate NPs in relevant biological fluids (e.g., serum) to study corona formation and adjust design accordingly [55]. | Ligand Functionalization Protocol: For antibody conjugation, use carbodiimide chemistry (EDC/NHS) to form amide bonds between surface carboxyl groups on the NP and amine groups on the antibody. Purify via centrifugation or dialysis to remove unbound ligands. Characterize conjugation efficiency using spectroscopy or ELISA [54] [55]. |
| Inappropriate ligand choice or density. | Select ligands with high affinity for receptors on target immune cells (e.g., CD markers). Systematically optimize ligand density on the nanoparticle surface; too low reduces affinity, too high can cause non-specific binding. |
Issue 3: Inconsistent Sizing and Batch-to-Batch Variability
| Possible Cause | Solution | Relevant Experimental Protocol |
|---|---|---|
| Uncontrolled synthesis process. | Standardize synthesis protocols. Employ bottom-up approaches (e.g., chemical vapor deposition, self-assembly) for better control over size and monodispersity compared to top-down methods (e.g., milling) [57]. | Dynamic Light Scattering (DLS) for Characterization: Dilute the nanoparticle sample in a suitable buffer. Measure particle size, polydispersity index (PDI), and zeta potential. A PDI value below 0.2 is generally indicative of a monodisperse population. Use techniques like TEM for complementary morphological data [57]. |
| Aggregation during storage. | Use cryoprotectants (e.g., trehalose, sucrose) during lyophilization. Store nanoparticles in stable buffers at 4°C and avoid freeze-thaw cycles. |
Data Presentation Tables
Table 1: Comparison of Key Nanomaterial Platforms for Immunomodulation
| Nanomaterial Type | Core Composition | Key Advantages | Limitations | Example Application in Immune Modulation |
|---|---|---|---|---|
| Liposomes | Phospholipids, Cholesterol [54] | High biocompatibility; can encapsulate both hydrophilic/hydrophobic drugs; clinically validated [55] | Can be unstable; may trigger complement activation [55] | Delivering immunosuppressive drugs (e.g., rapamycin) to T cells or antigen-presenting cells [54] |
| Polymeric NPs | PLGA, PEG-PLA [55] | Controlled/sustained release; tunable degradation; biodegradable [55] | Complex synthesis; potential residual solvents [57] | Co-delivery of antigens and immunomodulators to dendritic cells for tolerance induction [54] |
| Dendrimers | PAMAM, PPI [55] | Monodisperse size; high drug-loading capacity; multivalent surface [55] | Toxicity concerns with higher generations; complex synthesis [55] | Cross-linking immune receptors or delivering siRNA to silence key immune genes [55] |
| Gold Nanoparticles | Gold (Au) [55] | Tunable optics (Surface Plasmon Resonance); facile surface chemistry; photothermal properties [55] | Non-biodegradable; potential long-term accumulation [57] | Photothermal ablation of alloreactive T cells; as a contrast agent for imaging graft rejection [55] |
| Mesoporous Silica NPs | Silica (SiO₂) [55] | Very high surface area; tunable pore size; stable [55] | Slow biodegradation; inflammatory potential if not engineered properly [57] | Delivery of large payloads of tolerogenic cytokines or checkpoint inhibitors [55] |
| Imaging Modality | Physical Principle | Spatial Resolution | Sensitivity | Key Applications in Tracking |
|---|---|---|---|---|
| Magnetic Resonance Imaging (MRI) | Nuclear magnetic resonance of protons (e.g., in H₂O) [56] | 10-100 µm [56] | Low to Moderate [56] | High-resolution anatomical imaging; tracking of iron oxide NPs to graft site [56] |
| Positron Emission Tomography (PET) | Detection of gamma rays from radionuclide decay [56] | 1-2 mm [56] | Very High (pico-molar) [56] | Highly sensitive quantification of radiolabeled NP biodistribution and accumulation [56] |
| Fluorescence Imaging | Detection of light emission from fluorophores [56] | 2-3 mm [56] | High (nano-molar) [56] | Real-time monitoring of cellular uptake and NP fate in preclinical models [56] |
| Computed Tomography (CT) | X-ray attenuation [56] | 50-200 µm [56] | Low [56] | Visualizing hard tissues; used with high atomic number NPs (e.g., gold) [56] |
| Multimodal (e.g., PET/MRI) | Combination of above [56] | 1-2 mm (PET) / 10-100 µm (MRI) [56] | Very High (PET) [56] | Correlating high-sensitivity biodistribution data with high-resolution anatomical context [56] |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function / Role in Experiment |
|---|---|
| Poly(lactic-co-glycolic acid) (PLGA) | A biodegradable polymer used to form nanoparticles for controlled and sustained drug release. Its degradation rate can be tuned by the lactic acid to glycolic acid ratio [55]. |
| DSPE-PEG (2000)-COOH | A phospholipid-PEG conjugate used to functionalize lipid-based and polymeric nanoparticles. The PEG extends circulation time, while the terminal carboxyl group allows for covalent attachment of targeting ligands (e.g., antibodies, peptides) [55]. |
| EDC (1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide) | A crosslinker reagent used in carbodiimide chemistry to activate carboxyl groups for conjugation to primary amines, essential for attaching targeting moieties to nanoparticles [55]. |
| Cy5.5 NHS Ester | A near-infrared fluorescent dye with an N-hydroxysuccinimide ester group that reacts with amine groups on nanoparticles or proteins, enabling tracking via fluorescence imaging [56]. |
| Anti-human CD11c Antibody | A ligand that can be conjugated to nanoparticles to specifically target dendritic cells, which express the CD11c surface marker, for precise delivery of immunomodulatory agents [54]. |
| Desferoxamine (DFO) | A chelator that can be attached to nanoparticles to complex radionuclides like Zirconium-89 (⁸⁹Zr) for labeling and tracking with PET imaging [56]. |
Experimental Protocols & Workflows
Detailed Protocol: Preparation of PLGA-PEG Nanoparticles for Targeted Delivery
This protocol describes the synthesis of PLGA-PEG-COOH nanoparticles loaded with an immunomodulatory drug (e.g., a mTOR inhibitor) and functionalized with a targeting antibody for dendritic cells [55].
Materials:
- PLGA-PEG-COOH copolymer
- Immunomodulatory drug (e.g., Rapamycin)
- Dichloromethane (DCM) or ethyl acetate
- Polyvinyl alcohol (PVA) solution (2% w/v)
- Anti-CD11c antibody
- EDC and NHS
- MES buffer (0.1 M, pH 6.0)
- Purified water
Method:
- Nanoparticle Synthesis (Double Emulsion w/o/w):
- First Emulsion: Dissolve 50 mg PLGA-PEG-COOH and 5 mg of the drug in 2 mL of DCM. Add 0.5 mL of aqueous solution (or PBS) to the organic phase and sonicate on ice using a probe sonicator at 70 W for 60 seconds to form a primary water-in-oil (w/o) emulsion.
- Second Emulsion: Immediately pour the primary emulsion into 20 mL of 2% PVA solution under vigorous stirring. Sonicate again for 90 seconds to form a stable w/o/w double emulsion.
- Solvent Evaporation: Stir the double emulsion for 4-6 hours at room temperature to allow complete evaporation of the organic solvent and nanoparticle hardening.
- Purification: Centrifuge the nanoparticle suspension at 18,000 rpm for 30 minutes at 4°C. Wash the pellet three times with purified water to remove PVA and unencapsulated drug. Resuspend in a small volume of water.
Antibody Conjugation:
- Activation: Resuspend the purified NP pellet in 1 mL of MES buffer (0.1 M, pH 6.0). Add a 10-fold molar excess of EDC and NHS to the NP suspension and react for 15 minutes at room temperature with gentle mixing.
- Conjugation: Purify the activated NPs using a centrifugal filter unit to remove excess EDC/NHS. Immediately resuspend the activated NPs in PBS (pH 7.4) and add a calculated amount of anti-CD11c antibody. React for 2 hours at room temperature.
- Purification: Purify the conjugated nanoparticles via centrifugation or dialysis against PBS for 24 hours to remove unreacted antibody. The final product can be lyophilized for storage or characterized.
Characterization:
- Determine particle size, PDI, and zeta potential by DLS.
- Determine drug loading and encapsulation efficiency using HPLC.
- Confirm antibody conjugation via BCA assay or SDS-PAGE.
Nanomaterial Design and Immune Evasion Workflow
Nanoparticle-Mediated Immunomodulation Pathways
What is the Edmonton Protocol and why was it revolutionary?
The Edmonton Protocol, established in 2000 by Shapiro et al. at the University of Alberta, represented a landmark advancement in clinical islet transplantation for Type 1 Diabetes (T1D). Its revolutionary nature stemmed from being the first glucocorticoid-free immunosuppressive regimen that achieved sustained insulin independence in seven consecutive patients [59] [60] [61]. Prior to this, only about 9% of islet transplant recipients were insulin-independent for more than one year [60]. The protocol's key innovation was eliminating corticosteroids, which are known to cause beta cell damage and insulin resistance, thereby counteracting the transplant's goals [61].
What are the core components of the original Edmonton Protocol?
The original Edmonton Protocol rested on three pillars [61]:
- Adequate Islet Mass: Transplantation of a large islet mass, typically ≥10,000 islet equivalents (IE) per kilogram of recipient body weight. This often required islets from two or more donor pancreata [59] [60].
- Steroid-Free Immunosuppression: A combination immunosuppressive regimen consisting of:
Table: Core Components of the Edmonton Protocol Immunosuppression
| Component | Mechanism of Action | Role in Protocol |
|---|---|---|
| Sirolimus | Inhibits mTOR, blocking T-cell proliferation | Maintenance immunosuppression |
| Tacrolimus | Inhibits calcineurin, reducing IL-2 production and T-cell activation | Maintenance immunosuppression |
| Daclizumab | Anti-IL-2 receptor (CD25) antibody, blocks T-cell activation | Induction therapy |
Troubleshooting Common Experimental & Clinical Challenges
How do I manage the need for multiple donors in my islet transplantation research?
The requirement for islets from multiple deceased donors (often 2-3) to achieve insulin independence was a major limitation of the early Edmonton Protocol [59]. This poses significant challenges for both clinical application and research due to donor scarcity and increased procedural variability.
Troubleshooting Guide:
- Challenge: Insufficient islet mass from a single donor.
- Solution: Focus on improving islet isolation techniques and donor selection criteria. Some centers have reported success with single-donor infusions by using potent induction immunosuppression and high-quality islets [59].
- Challenge: Low islet engraftment and survival post-transfusion.
- Solution: Investigate strategies to mitigate the instant blood-mediated inflammatory response (IBMIR). This includes co-transplantation with accessory cells (e.g., mesenchymal stem cells) or using biomaterial-based approaches to shield islets from immediate immune attack [61].
- Challenge: Islet "burnout" from constant metabolic stimulation of a marginal mass.
- Solution: Optimize metabolic support after transplantation and explore preconditioning strategies to enhance islet resilience [59].
What are the common adverse effects of the Edmonton Protocol regimen and potential alternatives?
While revolutionary, the sirolimus and tacrolimus-based regimen is associated with significant side effects, which can hinder long-term success and patient quality of life [61].
Troubleshooting Guide:
- Challenge: Drug-related toxicities (e.g., nephrotoxicity from tacrolimus, hyperlipidemia from sirolimus).
- Solution: Consider alternative, less toxic maintenance immunosuppressants. Belatacept, a CTLA4-Ig that blocks CD28/B7 T-cell costimulation, has shown promise in early trials, with some patients achieving insulin independence after a single transplant [61].
- Challenge: Daclizumab was withdrawn from the global market.
- Solution: Utilize other induction agents. Anti-thymocyte globulin (ATG) or other interleukin-2 receptor antagonists can be substituted [61].
- Challenge: Chronic immunosuppression increasing risk of infections and malignancies.
- Solution: Explore novel tolerance-inducing protocols. Recent research focuses on CD40-CD40L pathway blockade with engineered antibodies like Tegoprubart (AT-1501), which have shown efficacy in non-human primate studies when combined with other agents [61].
Table: Adverse Events and Potential Solutions in Steroid-Free Regimens
| Adverse Event / Challenge | Associated Drug(s) | Potential Solution / Alternative |
|---|---|---|
| Nephrotoxicity, Neurotoxicity | Tacrolimus | Switch to Belatacept (CTLA4-Ig) |
| Hyperlipidemia, Mouth Ulcers | Sirolimus (Rapamycin) | Dose reduction or alternative mTOR inhibitors |
| Withdrawal of drug from market | Daclizumab | Substitute with ATG or other IL-2R blockers |
| Opportunistic Infections | General immunosuppression | Tailored antimicrobial prophylaxis |
| Need for multiple donors | Protocol design | Improved islet isolation; single-donor protocols |
Current Innovations and Advanced Methodologies
What are the latest innovations to avoid systemic immunosuppression altogether?
Moving beyond the Edmonton Protocol, the field is rapidly advancing toward strategies that eliminate the need for lifelong, broad-spectrum immunosuppression.
- Genetically Modified Islets: A groundbreaking 2025 case report demonstrated the survival of transplanted allogeneic beta cells with no immunosuppression. The donor islet cells were genetically modified using CRISPR-Cas12b editing and lentiviral transduction to avoid immune recognition before transplantation into a patient's forearm muscle [36].
- Combined Hematopoietic and Islet Cell Transplantation: A novel approach in mice combines a blood stem cell transplant with an islet transplant from the same donor. This creates a hybrid immune system that accepts the donated islets without mounting an attack, effectively curing autoimmune diabetes without chronic immunosuppression [62].
- Immunoengineering and Biomaterials: Preclinical research is exploring:
- Islet Encapsulation Devices: Physical barriers to protect islets from immune cells while allowing nutrient and insulin exchange.
- Biomaterial Platforms: Scaffolds or nanoparticles that release immunomodulatory compounds locally, minimizing systemic exposure.
- Islet Surface Modification: Engineering islets to present immune-inhibitory signals on their surface [61].
The diagram below illustrates the core workflow and decision points of the original Edmonton Protocol.
How does the immunosuppressive mechanism of the Edmonton Protocol work?
The steroid-free regimen of the Edmonton Protocol was designed to synergistically inhibit T-cell activation and proliferation through multiple pathways, while avoiding the beta-cell toxicity of corticosteroids.
The Scientist's Toolkit: Essential Research Reagents & Models
Table: Key Research Reagent Solutions for Islet Transplantation Studies
| Reagent / Material | Function in Research | Example / Note |
|---|---|---|
| Anti-IL-2 Receptor Ab | Induction therapy; blocks T-cell activation | Daclizumab (original), substitute alternatives now required |
| mTOR Inhibitors | Maintenance immunosuppression; inhibits T-cell proliferation | Sirolimus (Rapamycin) |
| Calcineurin Inhibitors | Maintenance immunosuppression; inhibits T-cell signaling | Tacrolimus (low-dose) |
| CTLA4-Ig Fusion Proteins | Costimulation blockade; alternative to CNIs | Belatacept |
| Anti-CD40L Antibodies | Costimulation blockade; novel tolerance induction | Tegoprubart (AT-1501) |
| Collagenase Enzymes | Islet isolation from pancreas | Critical for high-yield, functional islets |
| Ricordi Chamber | Device for standardized islet isolation | Semi-automated process for consistent yields |
| CRISPR-Cas Systems | Genetic modification of islets to avoid rejection | Cas12b used in recent clinical case [36] |
Overcoming Clinical Hurdles: Troubleshooting and Protocol Optimization
Technical Support Center
Troubleshooting Guide: Common Toxicity Issues in Transplantation Research
Problem 1: Nephrotoxicity in models using Calcineurin Inhibitors (CNIs)
- Background & Mechanism: CNIs like Cyclosporine and Tacrolimus are cornerstone immunosuppressants but induce acute and chronic nephrotoxicity. The mechanism involves indirect hemodynamic effects and direct cellular toxicity, including increased expression of TGF-β, reduced nitric oxide, and induction of oxidative stress and apoptosis in kidney cells [63].
- Recommended Actions:
- Dose Minimization: Consider a CNI-minimization or withdrawal protocol, complemented by other agents like mycophenolic acid or mTOR inhibitors. Be aware that complete discontinuation can increase the risk of chronic rejection [63] [64].
- Therapeutic Drug Monitoring (TDM): Strictly maintain drug levels within the target therapeutic range (see Table 1) to minimize exposure-related toxicity [65].
- Switch to Non-Nephrotoxic Agents: In established nephrotoxicity, switching to a non-nephrotoxic regimen based on mTOR inhibitors (e.g., sirolimus) may be an option, though this can be associated with other side effects like impaired wound healing [63].
- Biomarker Monitoring: Move beyond serum creatinine. Investigate novel biomarkers like graft-derived circulating cell-free DNA (GcfDNA) for early detection of transplant injury ["liquid biopsy"] [65].
Problem 2: Neurotoxicity associated with CNI treatment
- Background & Mechanism: CNI-induced neurotoxicity (e.g., tremors, hallucinations, seizures) can occur in up to 59% of patients. The mechanism is linked to mitochondrial dysfunction in the brain, leading to inhibited ATP synthesis and oxygen radical formation [63].
- Recommended Actions:
Problem 3: Gastrointestinal Toxicity from Mycophenolate Mofetil (MMP)
- Background & Mechanism: MMP causes diarrhea, gastritis, and anorexia. The biochemical mechanism is not fully understood but is dose-dependent [63].
- Recommended Actions:
- Dose Adjustment/Splitting: Reduce the total daily dose or split it into more frequent, smaller doses.
- Formulation Switch: Switch from mycophenolate mofetil to enteric-coated mycophenolate sodium, which may improve upper GI tolerance [67].
Problem 4: High Risk of Opportunistic Infections
- Background & Mechanism: All immunosuppressive agents increase susceptibility to infections by dampening protective immune functions. The risk is highest during intense induction therapy [68] [69].
- Recommended Actions:
- Universal Prophylaxis: Implement protocols for antimicrobial (e.g., trimethoprim-sulfamethoxazole), antiviral (e.g., ganciclovir), and antifungal prophylaxis [68].
- Immunosuppression Minimization: Tailor immunosuppression to the lowest effective level, especially in patients who are ill or deconditioned [68].
- Immune Function Monitoring: Utilize immune cell function assays (e.g., ImmuKnow assay measuring CD4+ ATP levels) to assess overall cell-mediated immune function and guide therapy [65] [67].
Problem 5: Post-Transplant Malignancy
- Background & Mechanism: Immunosuppression impairs immune surveillance, increasing the risk of malignancies, particularly non-melanomatous skin cancers and post-transplant lymphoproliferative disorder (PTLD), often linked to Epstein-Barr virus [68].
- Recommended Actions:
- Routine Screening: Enforce rigorous and routine cancer screening (dermatological evaluation, colonoscopy, etc.) [68].
- Reduction of Immunosuppression: For PTLD, the first-line therapeutic maneuver is a prompt and aggressive reduction of immunosuppression, which is effective in about 50% of cases [68].
- Use of mTOR Inhibitors: Consider using mTOR inhibitors (sirolimus, everolimus) in patients with a history of skin cancer, as they have demonstrated anti-neoplastic properties and can lower the risk of cancer recurrence [64].
Frequently Asked Questions (FAQs) for Researchers
FAQ 1: What are the most promising strategies to completely avoid long-term immunosuppressive toxicity?
The most promising strategy is the induction of donor-specific immune tolerance, where the recipient's immune system permanently accepts the graft without ongoing immunosuppression. Current investigational approaches include:
- Hematopoietic Chimerism: Establishing donor hematopoietic stem cell engraftment to create a mixed immune system and promote central tolerance. This often requires conditioning and carries risks like graft-versus-host disease (GVHD) [17].
- Regulatory Cell Therapy: Infusing donor-specific regulatory T cells (Tregs) to suppress alloimmune responses. Innovations include genetic engineering to create CAR-redirected Tregs for enhanced precision [17].
- Thymic Education: Thymus transplantation to promote central tolerance through donor-specific education of developing T cells [17].
FAQ 2: Beyond therapeutic drug monitoring, what pharmacodynamic biomarkers can we use to assess an individual's immune response to these drugs?
Research focuses on biomarkers that reflect the biological effect of immunosuppressants on the immune system, which can help personalize therapy [67]. Key candidates include:
- Target Enzyme Activity: Measuring calcineurin activity for CNIs or IMPDH activity for mycophenolate provides a direct readout of drug effect on its molecular target [65] [67].
- Cytokine Production: Assessing the capacity of T cells to produce cytokines like IFN-γ or IL-2 can predict the risk of rejection and reflect the degree of immunosuppression [65] [67].
- Lymphocyte Activation Markers: Flow cytometry analysis of surface antigens like CD25, CD71, or CD154 can serve as biomarkers for T-cell activation and rejection risk [65] [67].
FAQ 3: Are there new immunosuppressive agents in development that have a better toxicity profile?
Yes, the field is actively developing more targeted agents. Key areas of development include:
- Costimulation Blockade: New agents block secondary signals needed for full T-cell activation. Drugs like Belatacept (already approved) target the CD80/86-CD28 pathway. Newer agents in trials include anti-CD40 and anti-CD28 monoclonal antibodies, which aim to provide effective immunosuppression with less nephrotoxicity [64].
- Antibody-Mediated Rejection (ABMR) Treatments: New agents are urgently needed for ABMR. Investigational therapies include proteasome inhibitors (e.g., Bortezomib), complement inhibitors (e.g., Eculizumab), and anti-IL-6/IL-6R agents (e.g., Tocilizumab, Clazakizumab) to target plasma cells and the inflammatory environment driving antibody production [70] [64].
FAQ 4: How does graft-versus-host disease (GVHD) relate to toxicity in transplantation research?
In hematopoietic stem cell transplantation (HSCT), GVHD is a major non-infectious complication and a direct toxicity of the therapy. It occurs when donor T cells attack host tissues. The mechanisms and management of GVHD are a critical area of study, as it represents the "flip side" of the desired graft-versus-tumor effect. Strategies to reduce GVHD risk include using matched donors, manipulating the graft to reduce T cells, and using specific conditioning regimens [69].
| Immunosuppressant | First Week | 1 Month - 3 Months | 3 - 12 Months | >1 Year |
|---|---|---|---|---|
| Tacrolimus | 12-15 ng/mL | 8-10 ng/mL | 6-8 ng/mL | 5-7 ng/mL |
| Cyclosporine | 300-350 ng/mL | 150-250 ng/mL | 100-200 ng/mL | Can tolerate <100 ng/mL |
| Complication | Associated Immunosuppressants | Key Mitigation Strategies |
|---|---|---|
| Nephrotoxicity | CNIs (Cyclosporine, Tacrolimus) | CNI minimization/withdrawal; TDM; switch to mTOR inhibitors |
| Neurotoxicity | CNIs (esp. Cyclosporine) | Dose reduction; switch to alternative CNI or regimen |
| GI Toxicity | Mycophenolate Mofetil | Dose adjustment/splitting; switch to enteric-coated formulation |
| Post-Transplant Diabetes | CNIs, Corticosteroids | Blood glucose monitoring; corticosteroid minimization |
| Hyperlipidemia | mTOR inhibitors, Corticosteroids | Lipid-lowering agents; dietary management |
| Infections | All (especially induction) | Universal antimicrobial prophylaxis; immunosuppression minimization |
| Malignancies/PTLD | All (especially T-cell depleting agents) | Routine cancer screening; reduction of immunosuppression; mTOR inhibitors |
Experimental Protocols
Protocol 1: Monitoring IMPDH Activity as a Pharmacodynamic Biomarker for Mycophenolate
Principle: Mycophenolic acid (MPA) inhibits inosine-5′-monophosphate dehydrogenase (IMPDH), a key enzyme in de novo guanosine nucleotide synthesis. Measuring IMPDH activity in peripheral blood mononuclear cells (PBMCs) provides a direct assessment of MPA's biological effect, which can help predict efficacy and toxicity [65] [67].
Methodology:
- Sample Collection: Collect whole blood in heparinized tubes. Critical: Processing should begin within 6 hours of collection.
- PBMC Isolation: Isolate PBMCs using a Ficoll density gradient centrifugation method.
- Lysate Preparation: Lyse the PBMCs to release intracellular enzymes.
- Enzyme Activity Assay:
- Incubate the lysate with the substrate inosine monophosphate (IMP) and the cofactor NAD+.
- IMPDH catalyzes the conversion of IMP to xanthosine monophosphate (XMP), which is coupled to the reduction of NAD+ to NADH.
- Monitor the increase in absorbance at 340 nm (indicating NADH production) spectrophotometrically over time.
- Data Analysis: Express IMPDH activity as the rate of NADH formation (e.g., pmol/min/mg of protein). Compare activity levels pre- and post-MPA dosing to determine the degree of inhibition.
Protocol 2: Assessing T-Cell Mediated Immunity via Intracellular ATP (ImmuKnow) Assay
Principle: This FDA-approved assay measures the increase in intracellular ATP in CD4+ T cells after mitogenic stimulation. ATP is the main energy source for immune functions, and its production correlates with cell-mediated immune function, providing a global measure of immunosuppression [65] [67].
Methodology:
- Sample Stimulation: Incubate a standardized volume of whole blood with the mitogen phytohemagglutinin (PHA) for 15-24 hours.
- Cell Selection and Lysis: Isulate CD4+ cells using magnetic beads and lyse them to release intracellular ATP.
- ATP Quantification: Add luciferase enzyme to the lysate. In the presence of ATP, luciferase catalyzes a light-producing reaction.
- Luminescence Measurement: Measure the emitted light using a luminometer. The intensity of light is directly proportional to the ATP concentration.
- Interpretation: Report results as ng ATP/mL. Clinically established zones are:
- Strong Immune Response: >525 ng/mL (may indicate under-immunosuppression)
- Moderate Immune Response: 225-525 ng/mL (target zone)
- Weak Immune Response: <225 ng/mL (may indicate over-immunosuppression and high infection risk)
The Scientist's Toolkit
Table 3: Research Reagent Solutions for Immunosuppression Studies
| Research Reagent | Primary Function in Experiments | Key Considerations |
|---|---|---|
| Anti-Thymocyte Globulin (ATG) | Polyclonal antibody for T-cell depletion; used in induction therapy and to treat rejection [66]. | Monitor for cytokine-release syndrome; depletes multiple lymphocyte lineages. |
| Belatacept | CTLA-4-Ig fusion protein; blocks CD80/86-CD28 costimulation pathway to inhibit T-cell activation [64]. | Particularly effective at inhibiting humoral responses and preventing DSA formation. |
| mTOR Inhibitors (Sirolimus/Everolimus) | Inhibits mTOR pathway, reducing cytokine-driven T-cell proliferation; used in CNI-minimization protocols [66] [64]. | Associated with delayed wound healing, hyperlipidemia, and mouth ulcers. |
| Clazakizumab | Anti-IL-6 monoclonal antibody; targets plasma cells and inflammation in antibody-mediated rejection (AMR) [64]. | Investigational therapy for late-stage AMR; blocks a key inflammatory cytokine. |
| IMPDH Activity Assay Kit | Quantifies inhibition of IMPDH enzyme for pharmacodynamic monitoring of mycophenolate efficacy [65] [67]. | Requires fresh PBMCs; activity can be affected by sample processing time. |
| Luminescence-based ATP Assay | Measures global T-cell function (CD4+ ATP levels) to assess overall immunosuppressive state [65] [67]. | Provides a functional, integrated measure of immune capacity. |
Signaling Pathways and Experimental Workflows
Calcineurin Inhibitor Toxicity Pathway
Diagram Title: Multiorgan Toxicity Pathways of Calcineurin Inhibitors
Pharmacodynamic Biomarker Workflow
Diagram Title: Experimental Workflow for Pharmacodynamic Biomarker Analysis
The Instant Blood-Mediated Inflammatory Reaction (IBMIR) is a rapid, nonspecific inflammatory and thrombotic response that occurs when transplanted islets come into contact with blood. This reaction represents a major initial barrier to successful islet engraftment and function, causing significant islet loss in both allogeneic and autologous transplantation settings [71] [72].
IBMIR is characterized by the simultaneous activation of coagulation and complement pathways, leading to thrombotic formation, complement activation, and neutrophil infiltration that collectively destroy islets shortly after transplantation. In clinical islet transplantation, IBMIR is estimated to cause loss of up to 60% of transplanted islets within the first week, dramatically reducing transplantation efficacy [71].
Mechanisms and Pathways of IBMIR
Key Pathways in IBMIR Activation
IBMIR involves multiple interconnected pathways that create a perfect storm of islet destruction. The core mechanisms include:
- Thrombin Generation: Rapid, platelet-independent thrombin generation occurs when islets express tissue factor (TF), which initiates the coagulation cascade. The addition of platelets both accelerates and exacerbates this response [71].
- Complement Activation: Platelet-independent complement activation begins as early as 30 minutes after islet exposure to plasma, with membrane attack complex (MAC) formation observed on islets within 60 minutes [71].
- Neutrophil Infiltration: Complement activation is necessary for subsequent neutrophil activation and infiltration, which causes additional inflammatory damage [71].
- Cytokine Release: Inflammatory cytokines including IL-6, IL-8, interferon-inducible protein-10, TNF-α, and MCP-1 are significantly elevated during IBMIR, amplifying the inflammatory response [72].
Table: Key Mediators in IBMIR Pathways
| Pathway | Key Components | Timeframe | Functional Impact |
|---|---|---|---|
| Coagulation | Tissue Factor, Thrombin, Platelets | Immediate (minutes) | Clot formation, islet encapsulation |
| Complement | C3a, C5a, MAC (C5b-9) | 30-60 minutes | Direct islet damage, neutrophil recruitment |
| Inflammatory Cells | Neutrophils, Monocytes | 1-3 hours | Phagocytosis, cytokine release |
| Cytokines | IL-6, IL-8, TNF-α, MCP-1 | 1-3 hours | Amplification of inflammation |
IBMIR Signaling Pathway Visualization
Diagram: IBMIR Cascade Overview - This diagram illustrates the sequential activation of coagulation, complement, and inflammatory pathways following islet transplantation that collectively contribute to islet loss.
Experimental Models for Studying IBMIR
In Vitro IBMIR Modeling
Objective: To characterize individual components of IBMIR and test potential interventions in a controlled system.
Methodology:
- Plasma Preparation: Collect whole blood from healthy volunteers into citrated tubes. Centrifuge at 150g for 10 minutes to obtain platelet-rich plasma (PRP) or at 2× 2000g for 10 minutes to obtain platelet-poor plasma (PPP) [71].
- Islet Preparation: Use 100-1000 islet equivalents (IEQ) of neonatal porcine islet cell clusters (NICC) or human islets in Hanks buffered salt solution (HBSS) with 5% human serum albumin (HSA) [71].
- Reaction Setup: Combine islets with plasma in non-tissue culture-treated plates. Incubate with agitation (120 rpm) at 37°C for predetermined timepoints (30, 60, 180 minutes) [71].
- Control Groups: Include islets alone in media and plasma alone without islets as controls.
Endpoint Measurements:
- Thrombin Generation: Measure using fluorogenic substrate (Z-GGR-AMC) with fluorescence measured at 1-minute intervals (ex. 390 nm, em. 460 nm) [71].
- Complement Activation: Quantify C3a, C4a, C5a, and soluble MAC (sMAC) using cytometric bead array or ELISA [71].
- Neutrophil Activation: Isolate neutrophils using enrichment kits, then measure CD66b, CD11b, and tissue factor expression via flow cytometry [71].
- Islet Viability Assessment: Use extracellular flux analysis to measure metabolic function and mitochondrial health post-IBMIR [71].
In Vivo Monitoring of IBMIR
Clinical Monitoring Parameters:
- Thrombin-Antithrombin III (TAT) complex: Significant rapid increase during islet infusion, persisting up to 3 hours [72].
- Platelet Count: Decreased during islet infusion indicating consumption [72].
- C-peptide: Rapid increase indicating islet destruction and insulin release [72].
- Inflammatory Markers: IL-6, IL-8, and interferon-inducible protein-10 significantly elevated [72].
Table: Key Biomarkers for IBMIR Monitoring
| Biomarker | Significance | Measurement Method | Timing |
|---|---|---|---|
| TAT Complex | Indicator of thrombin generation | ELISA | Baseline, during infusion, 1h, 3h post |
| Platelet Count | Platelet consumption | Complete blood count | Baseline, during infusion, 1h, 3h, 24h post |
| C-peptide | Islet destruction | ELISA | Baseline, during infusion, 1h, 3h post |
| C3a, C5a | Complement activation | Cytometric bead array | Baseline, 30min, 60min post |
| IL-6, IL-8 | Inflammatory response | Multiplex immunoassay | Baseline, 3h, 24h post |
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for IBMIR Research
| Reagent/Category | Specific Examples | Function/Application | Experimental Notes |
|---|---|---|---|
| Coagulation Inhibitors | Low-molecular-weight dextran sulfate, Heparin | Anticoagulation; reduces clot formation | Dextran sulfate showed significant protection of islet viability in vitro [72] |
| Complement Inhibitors | Compstatin, Anti-C5 antibodies | Blocks complement activation; reduces MAC formation | Compstatin (200 μM) effectively inhibits complement-mediated neutrophil activation [71] |
| Anti-inflammatory Agents | α1-antitrypsin, Anakinra, Etanercept | Reduces inflammatory cytokine damage | α1-antitrypsin protects islets from inflammatory damage and reduces MHC class II expression [73] |
| Enzyme Blends | Liberase HITM, Collagenase | Islet isolation; affects islet quality and IBMIR potential | Low-endotoxin enzymes (Liberase) improve islet viability and reduce inflammatory activation [74] |
| Analytical Tools | Z-GGR-AMC substrate, C5b-9 ELISA kits, Flow cytometry antibodies | Quantification of thrombin generation, MAC deposition, immune cell activation | Thrombin generation assays require careful titration of PRP to avoid spontaneous activation [71] |
Troubleshooting Guide: Frequently Asked Questions
FAQ 1: How can I differentiate IBMIR from cellular rejection in my model?
Answer: IBMIR and cellular rejection have distinct temporal and mechanistic characteristics:
- IBMIR: Occurs within minutes to hours post-transplantation. Key indicators include rapid thrombin generation (increased TAT), complement activation (elevated C3a, C5a, sMAC), platelet consumption, and immediate islet destruction. Predominantly involves innate immunity [71] [72].
- Cellular Rejection: Typically occurs days to weeks post-transplantation. Characterized by T-cell infiltration (CD4+ and CD8+ T cells), allospecific immune responses, and gradual functional decline. Unexplained hyperglycemia and C-peptide decrease are key diagnostic features [75].
Recommended Approach: Monitor early timepoints (0-24 hours) for IBMIR biomarkers and later timepoints (3-90 days) for T-cell activation markers and progressive functional loss.
FAQ 2: What strategies effectively inhibit multiple IBMIR pathways simultaneously?
Answer: Combination approaches targeting different IBMIR components show superior efficacy:
- Genetic Modification: Islets lacking galactose-α1,3-galactose (α-Gal) epitope and expressing human complement regulatory factors (CD55, CD59) show significantly reduced IBMIR in nonhuman primates [71].
- Pharmacological Combination: Simultaneous targeting of coagulation (dextran sulfate) and complement (compstatin) provides enhanced protection compared to single-pathway inhibition [71] [72].
- Anti-inflammatory Protocol: Peri-transplant use of dual anti-inflammatory therapies (anakinra plus etanercept) is an independent predictor of sustained graft survival in clinical islet transplantation [76].
FAQ 3: Why do islet transplants trigger IBMIR more severely than other cellular transplants?
Answer: Several islet-specific factors contribute to heightened IBMIR susceptibility:
- Tissue Factor Expression: Islets constitutively express high levels of tissue factor, directly activating the coagulation cascade [71].
- Transplantation Site: The intraportal site directly exposes islets to blood components, unlike encapsulated transplantation sites [74].
- Isolation Damage: Enzymatic isolation (collagenase/Liberase) disrupts islet vasculature and integrity, exposing procogulant surfaces [74].
- Low Thrombomodulin Expression: Islets have limited natural anticoagulant defense mechanisms compared to other tissues [71].
FAQ 4: How can I optimize my in vitro IBMIR model to better predict in vivo outcomes?
Answer: Enhance physiological relevance through these modifications:
- Use Platelet-Rich Plasma (PRP): While PPP simplifies interpretation, PRP (300-500 × 10⁹ cells/L) better recapitulates the acceleration of thrombin generation observed in vivo [71].
- Incorporate Flow Conditions: Static models underestimate shear stress effects. Implement perfusion systems to mimic portal vein flow conditions.
- Include Multiple Cell Types: Add peripheral blood mononuclear cells (PBMCs) or specific leukocyte populations to model cellular components of IBMIR.
- Functional Endpoints: Supplement biomarker measurements with islet function assays (glucose-stimulated insulin secretion, extracellular flux analysis) to assess metabolic consequences [71].
FAQ 5: What are the most promising emerging strategies for clinical IBMIR prevention?
Answer: Recent advances focus on multifactorial approaches:
- Stem Cell-Derived Islets: ESC or iPSC-derived islets (Vertex VX-880) offer potential for genetic manipulation to reduce immunogenicity before differentiation [77].
- Biomaterial Encapsulation: Macrodevices that provide immune isolation while allowing nutrient exchange show promise in early clinical trials [77].
- Site Modification: Localized immunomodulation of the graft microenvironment to create protective niches [77].
- Gene Editing: CRISPR-based approaches to knock out IBMIR triggers (tissue factor) or insert protective factors (complement regulators) in stem cell-derived islets [77].
Advanced Experimental Design: Comprehensive IBMIR Assessment Workflow
Diagram: Comprehensive IBMIR Assessment Workflow - This experimental workflow outlines the key timepoints and analytical approaches for thorough IBMIR evaluation in research models.
IBMIR Severity Scoring System
Based on comprehensive assessment, IBMIR responses can be categorized:
- Mild IBMIR: Isolated coagulation activation without significant complement or cellular response. <20% islet loss.
- Moderate IBMIR: Coagulation plus complement activation with partial neutrophil response. 20-50% islet loss.
- Severe IBMIR: Full activation of coagulation, complement, and cellular components with cytokine storm. >50% islet loss with significant functional impairment.
This standardized assessment enables quantitative comparison of intervention efficacy across different experimental and clinical settings.
Preventing Graft-versus-Host Disease (GvHD) in Stem Cell and Solid Organ Transplants
Troubleshooting Guide: GVHD Prophylaxis and Management
This guide addresses common challenges in preventing Graft-versus-Host Disease (GVHD) for researchers developing new transplantation protocols.
FAQ: Fundamental Concepts
What are the essential requirements for GVHD to occur? According to Billingham's criteria, three conditions must be met: (1) the graft must contain immunologically competent cells; (2) the recipient must express tissue antigens not present in the donor; and (3) the recipient must be incapable of mounting an effective response to eliminate the transplanted cells [78] [79]. T lymphocytes are the primary immunocompetent cells responsible [79].
How are acute and chronic GVHD distinguished in modern classification? The National Institutes of Health (NIH) consensus criteria classify GVHD based on clinical features rather than solely on the 100-day post-transplant timeline [80] [81]. The categories are:
- Classic Acute GVHD: Occurs within 100 days with typical acute features (maculopapular rash, GI symptoms, cholestatic hepatitis).
- Persistent, Recurrent, or Late-Onset Acute GVHD: Manifests with acute clinical features but after 100 days.
- Classic Chronic GVHD: Presents after 100 days with distinctive chronic manifestations.
- Overlap Syndrome: Features of both acute and chronic GVHD occurring at any time [80].
Which signaling pathways are critically involved in GVHD pathogenesis? The pathogenesis involves a complex cascade of immune activation. The diagram below illustrates the key pathways and cellular interactions from initial tissue damage to the final effector phase that results in target organ damage.
What are the primary risk factors for developing GVHD? The most significant risk factor is the degree of HLA mismatch between donor and recipient [82] [78]. Other important factors include older donor or recipient age, female donor with prior pregnancy, sex mismatch, stem cell source (peripheral blood stem cells carry higher risk than bone marrow or umbilical cord blood), and the specific conditioning regimen used [80] [82] [78].
FAQ: Prophylaxis and Protocol Challenges
What are the standard pharmacologic regimens for GVHD prophylaxis?
The most established prophylactic regimens involve combination immunosuppressive therapy. The table below summarizes the mechanisms and considerations for common agents.
Table 1: Standard Pharmacologic Agents for GVHD Prophylaxis
| Drug Class | Representative Agents | Mechanism of Action | Key Considerations |
|---|---|---|---|
| Calcineurin Inhibitors | Cyclosporine, Tacrolimus | Inhibits calcineurin, blocking T-cell activation and cytokine production [78] | Nephrotoxic; requires therapeutic drug monitoring [78] |
| Antimetabolites | Methotrexate (MTX) | Inhibits dihydrofolate reductase, suppressing T-cell proliferation [80] [78] | Can cause mucositis and delayed engraftment [78] |
| Inosine Monophosphate Dehydrogenase Inhibitor | Mycophenolate Mofetil (MMF) | Inhibits de novo purine synthesis, selectively blocking lymphocyte proliferation [78] | Often used with reduced-intensity conditioning [78] |
| mTOR Inhibitor | Sirolimus | Binds FKBP12 to inhibit mTOR, disrupting T-cell activation and proliferation [78] | Non-overlapping toxicity with calcineurin inhibitors [78] |
How does post-transplant cyclophosphamide (PTCy) work and when is it used?
Post-transplant cyclophosphamide is a highly effective strategy for selective T-cell depletion. It capitalizes on the differential susceptibility of highly proliferative, alloreactive T cells to cyclophosphamide-induced apoptosis during early activation, while sparing regulatory and non-dividing T cells [83] [79]. This promotes tolerance and is particularly valuable in haploidentical transplants [83]. The diagram below illustrates this mechanism and its integration into the transplant workflow.
What are the emerging strategies in GVHD prophylaxis?
Research is focused on more targeted approaches to improve the balance between GVHD prevention and preservation of the graft-versus-leukemia (GVL) effect. Key emerging strategies include [84]:
- Targeted Therapies: Janus kinase (JAK) inhibitors and costimulatory signaling blockers to specifically dampen pathogenic immune pathways.
- Cell-Based Therapies: Graft engineering with regulatory T cells (Tregs) to promote immune tolerance.
- Biomarker-Driven Approaches: Using biomarkers for early detection of GVHD or identifying high-risk patients to enable preemptive, personalized therapy.
- Optimization of PTCy: Exploring combination regimens and optimal dosing of PTCy to enhance efficacy.
The Scientist's Toolkit
Table 2: Key Research Reagent Solutions for GVHD Studies
| Research Reagent | Primary Function/Application | Experimental Notes |
|---|---|---|
| Anti-thymocyte globulin (ATG) | In vivo T-cell depletion; reduces incidence and severity of GVHD [79]. | Used in pre-transplant conditioning. The timing and dosing are critical for efficacy and minimizing side effects. |
| Ruxolitinib (JAK1/2 inhibitor) | Treatment of steroid-refractory acute and chronic GVHD [82]. | Inhibits cytokine signaling central to GVHD pathophysiology. A key agent for investigating JAK-STAT pathway inhibition. |
| Belumosudil (ROCK2 inhibitor) | Treatment of chronic GVHD after failure of ≥2 prior lines of therapy [82]. | Modulates immune responses and reduces fibrosis. Useful for studying fibrotic pathways in cGVHD. |
| Ibrutinib (BTK inhibitor) | Treatment of chronic GVHD [82]. | Targets Bruton's tyrosine kinase in B cells and IL-2-inducible T-cell kinase in T cells. A tool for dissecting B-cell involvement in cGVHD. |
| Recombinant Cytokines & Antibodies | To manipulate specific immune pathways (e.g., block TNF-α, IL-1, IL-6) in experimental models [80] [79]. | Essential for mechanistic studies to validate the role of specific cytokines and cell populations. |
| CD70 Blockers | Investigational; blocks CD27-CD70 costimulation to reduce alloreactive T-cell responses [85]. | A promising research tool for studying and targeting highly activated alloreactive T-cell clones. |
Frequently Asked Questions (FAQs)
Q1: Why do therapies that work in rodent models often fail in human clinical trials? Several interconnected factors contribute to this high failure rate, estimated to be around 95% [86]. Key reasons include:
- Pathophysiologic Heterogeneity: A single rodent model cannot recapitulate the broad spectrum of pathologies seen in a complex human disease. Animal models are best used to dissect specific cell biological responses, not to predict overall therapeutic success in humans [87].
- Publication and Funding Bias: The scientific reward system favors the publication of novel, high-magnitude positive results. This creates a biased literature filled with "cures" in mice that are often low-probability observations and do not represent the true complexity and redundancy of human biological systems [87].
- Profound Biological Differences: Despite genetic similarities, mice and humans have significant differences in their immune systems, gene expression, and physiology. For example, mouse hemoglobin has a lower oxygen affinity, and their immune systems are geared to handle different types of pathogens than humans [86].
Q2: What are the major immunological barriers to allogeneic transplantation in rodent models, and how do they differ from humans? The primary barrier is immune recognition of non-self antigens, primarily through two pathways [30] [88]:
- Direct Allorecognition: The recipient's T cells directly recognize intact Major Histocompatibility Complex (MHC) molecules on the surface of donor-derived "passenger leukocytes" or graft cells. This is a potent driver of acute rejection.
- Indirect Allorecognition: The recipient's antigen-presenting cells process donor proteins (including MHC molecules) and present them as peptides to the recipient's T cells. This pathway is particularly important for chronic rejection.
While these fundamental pathways exist in both rodents and humans, the specific MHC molecules (called HLA in humans) are highly polymorphic. The human immune system is more complex, and humanized mouse models often fail to fully replicate all aspects of human innate and adaptive immunity, limiting their predictive value [86] [88].
Q3: My autologous iPSC-derived cells are still being rejected in mouse models. Why does this happen? Even theoretically patient-specific iPSCs can trigger immune rejection due to several factors that arise during the reprogramming and differentiation process [89] [88]:
- Epigenetic Changes: The reprogramming process can introduce aberrant epigenetic marks, leading to the expression of unexpected or developmental antigens that the immune system sees as foreign.
- Genetic Mutations: The process of generating and expanding iPSCs in culture can lead to the accumulation of genetic mutations. These mutations may produce new or altered proteins that are recognized as non-self.
- Immunogenicity of Pluripotency: Pluripotent stem cells can inherently express immunogenic proteins, such as embryonic antigens, that are not present in adult tissues.
Q4: What are the limitations of "humanized" mouse models in transplantation research? While humanized mice (created by engrafting human cells or tissues into immunodeficient mice) are a valuable tool, they have significant limitations [86] [90] [91]:
- Incomplete System Reconstitution: Engrafted human immune systems often lack essential cell types, such as fully functional myeloid cells and natural killer (NK) cells, and may have limited lymph node development.
- Lack of Cross-Talk: The grafted human immune system does not fully interact with the mouse's other organ systems (e.g., gut microbiome), which is critical for a holistic immune response.
- Invasive Creation Procedures: Generating these models often requires drastic measures like genetic modification of the mouse and surgical removal of host tissues to create a niche for the human cells, which does not reflect a normal physiological state.
- Standardization Issues: A lack of standardized protocols and the common use of cells from multiple donors lead to highly variable results that are difficult to reproduce across laboratories.
Troubleshooting Common Experimental Challenges
Problem: Inconsistent Graft Rejection in Humanized Mouse Models
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Poor engraftment of human immune cells | - Flow cytometry to check levels of human CD45+ cells in mouse peripheral blood.- Compare to baseline engraftment metrics. | - Source high-quality CD34+ hematopoietic stem cells from a reliable vendor [91].- Optimize preconditioning (irradiation/chemotherapy) of host mice. |
| Missing innate immune cell populations | - Analyze for presence of human macrophages, NK cells, and myeloid cells. | - Use a newly developed humanized model variant that includes expression of key human cytokines to support innate immune development [90]. |
| Graft-versus-host disease (GvHD) | - Monitor mice for weight loss, hunching, and lethargy.- Histopathology of host tissues. | - Use cord blood-derived CD34+ cells, which carry a lower risk of GvHD compared to peripheral blood mononuclear cells (PBMCs) [91]. |
Problem: Unpredictable Immunogenicity of iPSC-Derived Cell Products
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Undetected genetic mutations | - Perform whole-genome sequencing on the iPSC line before differentiation. | - Implement rigorous genetic screening protocols and select clones with minimal mutations for therapy [89]. |
| Aberrant epigenetic memory | - Use methylation profiling and RNA sequencing to compare epigenetic landscape to target adult cell type. | - Improve reprogramming techniques using non-integrating vectors (e.g., episomal plasmids, mRNA) [89].- Apply small molecule epigenetic modifiers to reset patterns [89]. |
| Expression of immunogenic proteins | - Flow cytometry or immunocytochemistry for pluripotency markers (e.g., TRA-1-60, SSEA-3) after differentiation. | - Optimize differentiation protocols to ensure complete loss of pluripotent cells.- Use FACS sorting to purify the final cell product. |
Key Experimental Protocols
Protocol 1: Assessing T-Cell Mediated Rejection In Vivo
This protocol outlines the classic skin transplant experiment to study allograft rejection [30].
- Donor and Recipient Selection: Use two inbred mouse strains with known MHC differences (e.g., C57BL/6 and BALB/c).
- Skin Grafting:
- Harvest a full-thickness skin graft (approximately 1 cm²) from the donor mouse.
- Create a similarly sized graft bed on the flank of the recipient mouse.
- Secure the donor graft onto the recipient bed with surgical sutures or adhesive.
- Graft Monitoring:
- Monitor the graft daily for signs of rejection, defined as >90% necrosis of the graft tissue.
- A first-set rejection in a naive recipient typically occurs in 10-13 days.
- A second-set rejection in a pre-sensitized recipient occurs more rapidly, in 6-8 days.
- Mechanistic Dissection:
- To confirm T-cell dependence, repeat the experiment in T-cell deficient nude mice. Grafts will not be rejected unless T-cells are adoptively transferred [30].
Protocol 2: Non-Invasive Monitoring of Graft Rejection via Donor-Derived Cell-Free DNA (dd-cfDNA)
This advanced method can detect rejection earlier and less invasively than biopsy [92] [24].
- Sample Collection: Collect blood samples from the transplant recipient into tubes containing EDTA or a dedicated cfDNA preservative.
- Plasma Separation: Centrifuge blood samples within a few hours of collection to isolate plasma.
- DNA Extraction: Extract total cfDNA from the plasma using a commercial cfDNA extraction kit.
- Quantification of dd-cfDNA:
- Use digital droplet PCR (ddPCR) or next-generation sequencing (NGS) to detect and quantify DNA fragments that possess single-nucleotide polymorphisms (SNPs) unique to the donor.
- The result is expressed as the fraction of dd-cfDNA relative to the total cfDNA in the recipient's plasma.
- Interpretation: An elevated fraction of dd-cfDNA is a sensitive marker of active graft injury and immune-mediated rejection. This method can detect rejection weeks to months earlier than tissue biopsy [92].
Critical Signaling Pathways in Immune Rejection
The following diagram illustrates the key cellular interactions in allograft rejection, integrating both direct and indirect pathways of allorecognition.
The Scientist's Toolkit: Essential Research Reagents
| Research Reagent | Function & Application in Transplantation Research |
|---|---|
| Immunodeficient Mice (e.g., NSG, NOG) | The foundational host for creating humanized mouse models. These mice lack an intrinsic immune system, allowing for engraftment of human cells [86] [91]. |
| Human CD34+ Hematopoietic Stem Cells | Used to reconstitute a human immune system in immunodeficient mice. Sourcing from cord blood is often preferred for better engraftment and lower GvHD risk [91]. |
| CRISPR-Cas9 Gene Editing System | Used to knock out immunogenic antigens (e.g., MHC) in iPSCs to create "universal" donor cells, or to insert "immune evasion" genes like HLA-E or CD47 [89] [88]. |
| dd-cfDNA Assay Kits | Commercial kits for the extraction and quantification of donor-derived cell-free DNA from recipient blood. A non-invasive biomarker for early detection of graft injury and rejection [92] [24]. |
| Recombinant Human Cytokines (e.g., M-CSF, IL-3) | Essential for supporting the development and survival of specific human immune cell lineages (e.g., innate immune cells) in advanced humanized mouse models [90]. |
Managing Sensitized Patients and Donor-Specific Antibodies (DSA)
Troubleshooting Guides
Guide 1: Addressing Primary Graft Failure in Haploidentical HSCT
Problem: Primary graft failure in haploidentical hematopoietic stem cell transplantation (HSCT) recipients with pre-existing Donor-Specific Antibodies (DSA).
Explanation: Preformed DSA can bind to donor HLA antigens on infused stem cells, leading to complement-mediated destruction and graft failure. The risk is significantly higher with DSA Mean Fluorescence Intensity (MFI) >10,000 and positive C1q binding assays [93] [94].
Solution: Implement a pre-transplant desensitization protocol.
- Step 1: Perform DSA testing using solid-phase immunoassays (e.g., Luminex single antigen bead assay) and C1q assay to determine DSA strength and complement-fixing ability [93] [94].
- Step 2: Initiate plasma exchange (3 sessions, alternate days, 1-1.5x plasma volume) to remove circulating antibodies [93].
- Step 3: Administer Rituximab (375 mg/m²) to target B-cells and reduce antibody production [93].
- Step 4: Give IVIg (1 g/kg) to modulate immune response and neutralize remaining antibodies [93].
- Step 5: Infuse irradiated donor buffy coat on day -1 to neutralize residual DSA prior to stem cell infusion [93].
- Verification: Monitor DSA levels post-desensitization and before stem cell infusion. Patients with DSA ≤20,000 MFI who become C1q-negative after this protocol have engraftment rates comparable to non-sensitized patients [93].
Guide 2: Managing DSA-Positive Antibody-Mediated Rejection (AMR) in Kidney Transplantation
Problem: DSA-positive Antibody-Mediated Rejection in a kidney transplant recipient.
Explanation: DSA binding to donor endothelium triggers complement activation, inflammation, and microvascular damage, diagnosed as AMR on biopsy. Distinguishing this from DSA-negative microvascular inflammation is critical, as treatments differ [15] [95].
Solution: A multi-pronged therapeutic approach.
- Step 1: Confirm diagnosis via allograft biopsy using Banff classification and confirm circulating DSA [96] [97].
- Step 2: For acute AMR, initiate plasma exchange to remove DSA.
- Step 3: Administer IVIg for immunomodulation [93].
- Step 4: Consider Rituximab to deplete B-cells [97].
- Step 5: Intensify maintenance immunosuppression. Data shows that tacrolimus trough levels <7.25 ng/mL at 6 months are associated with DSA persistence and higher rejection risk [97].
- Verification: Monitor DSA levels post-treatment and perform follow-up biopsy if clinically indicated. Persistent DSA is a strong predictor of future AMR episodes and graft loss [97].
Frequently Asked Questions (FAQs)
Q1: What are the critical DSA thresholds for clinical decision-making in transplantation? The clinical relevance of DSA is concentration-dependent. The table below summarizes key MFI thresholds and their implications [93] [95] [94].
| MFI Threshold | Clinical Implication | Supporting Evidence |
|---|---|---|
| ≥ 500 MFI | Positivity threshold; associated with increased AMR risk in kidney transplantation [97]. | Scientific Reports (2025) [97] |
| ≥ 1,000 MFI | Significant risk factor for AMR and graft loss across solid organ transplants [95]. | Frontiers in Immunology (2025) Meta-Analysis [95] |
| > 5,000 MFI | High risk of engraftment failure in haploidentical HSCT; triggers desensitization [94]. | ASTCT Consensus Guidelines [94] |
| > 10,000 - 20,000 MFI | Very high risk; difficult to desensitize. Persistence post-therapy predicts graft failure [93]. | Blood Advances (2021) [93] |
Q2: How do I interpret a positive C1q assay alongside DSA MFI? The C1q assay identifies complement-fixing DSA, which are more pathogenic. A positive C1q result indicates a higher risk of antibody-mediated injury. In HSCT, patients with persistent C1q-positive DSA after desensitization have a significantly higher risk of engraftment failure and poor survival, even if the total IgG MFI is reduced [93]. Therefore, the C1q status provides a critical functional assessment of DSA danger beyond mere quantity.
Q3: What is the significance of "persistent" versus "resolved" DSA after transplantation? This is a crucial prognostic distinction. Persistent DSA (remaining at MFI >500 after transplant) is strongly associated with a higher long-term incidence of Antibody-Mediated Rejection (AMR) and graft loss. Resolved DSA (levels falling below MFI 500 post-transplant) is linked to much better outcomes, similar to those of patients who never had DSA [97]. Factors favoring DSA resolution include effective desensitization and maintaining adequate maintenance immunosuppression [97].
Q4: Beyond HLA antibodies, what other immune mechanisms contribute to rejection? Recent evidence highlights the role of innate immunity. Natural Killer (NK) cells can be activated via "missing self" when recipient inhibitory KIRs lack cognate HLA class I ligands on the donor graft. This can cause microvascular inflammation independently of DSA [15]. This explains why some rejection episodes are DSA-negative and may not respond to plasma exchange or IVIg [15].
Experimental Protocols
Protocol 1: In Vitro Model of NK Cell Alloreactivity via Missing Self
Purpose: To study the contribution of NK cells to endothelial damage in the absence of DSA [15].
Methodology:
- Cell Isolation: Isolate primary human NK cells from peripheral blood of a healthy recipient using negative selection magnetic beads.
- Endothelial Cell Culture: Culture human glomerular or umbilical vein endothelial cells in a microvascular assay plate.
- Genotyping: Perform HLA class I genotyping (HLA-A, -B, -C) and recipient inhibitory KIR genotyping to identify "missing self" combinations (e.g., recipient KIR2DL1 with donor lacking HLA-C2 group ligand) [15].
- Coculture: Coculture the purified NK cells with the endothelial cells at a specific effector-to-target ratio (e.g., 5:1) for 18-24 hours.
- Analysis:
- Cytotoxicity: Measure endothelial cell lysis using a standard 51Cr-release assay or by quantifying Lactate Dehydrogenase (LDH) release.
- Activation: Analyze NK cell activation markers (e.g., CD107a degranulation, IFN-γ production) via flow cytometry.
This model demonstrates that a single "missing self" molecule is sufficient to trigger NK cell activation and resultant endothelial damage, independent of the adaptive immune system [15].
Protocol 2: Desensitization of a Sensitized HSCT Recipient
Purpose: To reduce high-titer DSA prior to haploidentical HSCT to enable successful engraftment [93].
Workflow Diagram:
Methodology:
- Baseline Testing: Quantify DSA levels and C1q status within 30 days of transplant [93].
- Desensitization Initiation: Begin 1 week prior to admission for transplantation.
- Plasma Exchange (PE): 3 sessions on alternate days, exchanging 1-1.5x plasma volume [93].
- Rituximab Administration: Single dose (375 mg/m²) the day after PE completion [93].
- IVIg Administration: Single dose (1 g/kg) one day after rituximab [93].
- Donor Buffy Coat Infusion: On day -1, infuse irradiated buffy coat from the haploidentical donor [93].
- Final Assessment: Re-check DSA MFI and C1q on day -1. Engraftment outcomes are comparable to non-sensitized controls in patients with initial DSA ≤20,000 MFI who become C1q negative [93].
Key Signaling Pathways in Rejection
DSA-Mediated Antibody-Mediated Rejection (AMR) Pathway
This diagram illustrates the core mechanism of antibody-mediated graft injury [15] [24].
The Scientist's Toolkit: Research Reagent Solutions
Essential materials and assays for DSA and rejection research.
| Research Reagent | Primary Function / Application |
|---|---|
| Luminex Single Antigen Bead (SAB) Assay | High-sensitivity detection and semi-quantification (MFI) of anti-HLA antibodies, including DSA specificity [93] [96] [94]. |
| C1q Binding Assay | Functional assessment to identify complement-fixing, high-risk DSA [93] [94]. |
| Anti-Thymocyte Globulin (ATG) | T-cell depleting antibody used as induction therapy in highly sensitized kidney transplant recipients [97]. |
| Rituximab (anti-CD20) | Monoclonal antibody that depletes CD20+ B-cells, used in desensitization and AMR treatment protocols [93] [97]. |
| Intravenous Immunoglobulin (IVIg) | Pooled immunoglobulins used for immunomodulation, including neutralization of pathogenic antibodies [93] [97]. |
| Donor-derived cell-free DNA (dd-cfDNA) | Non-invasive biomarker for detecting early graft injury and rejection [24]. |
Optimizing Drug Delivery for Enhanced Efficacy and Reduced Off-Target Effects
Technical Support Center: FAQs & Troubleshooting Guides
Frequently Asked Questions
FAQ 1: What are the primary biological barriers that limit drug efficacy in allogeneic transplantation? The major barriers include the host's innate and adaptive immune systems, which recognize the graft as foreign and initiate rejection. Key processes involve:
- Allorecognition: The recipient's T cells recognize mismatched donor Human Leukocyte Antigens (HLAs) through direct (recognizing donor HLA on donor antigen-presenting cells) and indirect (recognizing donor HLA peptides on recipient antigen-presenting cells) pathways [30].
- Innate Immune Activation: Ischemia-reperfusion injury leads to cellular stress and the release of Damage-Associated Molecular Patterns (DAMPs). These are recognized by Pattern Recognition Receptors (PRRs) on host immune cells, triggering sterile inflammation that can exacerbate graft damage [98].
- Antibody-Mediated Rejection: Pre-existing or de novo developed donor-specific antibodies (DSAs) can cause complement-dependent damage to the graft endothelium [30].
FAQ 2: Which advanced drug delivery systems show the most promise for local immunomodulation in transplantation? Recent research highlights several promising platforms for localized drug delivery to minimize systemic side-effects [99]:
- Polymeric Nanoparticles and Microparticles: Systems based on materials like PLGA (Polylactic-co-glycolic acid) allow for controlled release of immunosuppressants.
- Hydrogels and Implants: These can be loaded with immunomodulatory agents (e.g., cytokines, monoclonal antibodies) and provide sustained, local release at the graft site.
- Liposomal Formulations: Liposomes can encapsulate drugs, protecting them from degradation and targeting them to specific cells. CPX-351, a liposomal formulation of cytarabine and daunorubicin, exemplifies this approach in pre-transplant conditioning for hematologic malignancies [100].
FAQ 3: My in vitro model shows promising immunosuppression, but efficacy is lost in my in vivo model. What could be the cause? This common issue, known as the "translational gap," can arise from several factors [99]:
- Inadequate Disease Model Complexity: The controlled environments of laboratory rodents (often specific pathogen-free) do not reflect the complex, primed immune system of adult humans, who have a large compartment of memory T cells that can resist tolerance induction [41].
- Off-Target Drug Distribution: Systemically administered drugs may not reach the graft site at therapeutic concentrations. Local delivery strategies (see FAQ 2) can help overcome this.
- Unaccounted Immune Pathways: Your in vitro system may not fully capture in vivo innate immune responses, such as "missing self" recognition by Natural Killer (NK) cells, which can cause microvascular inflammation independent of DSAs [15].
FAQ 4: How can I mitigate the risk of drug-drug interactions (DDIs) in pre-transplant conditioning regimens? A systematic medication reconciliation process is critical [101]:
- Review Concomitant Medications: Identify all pre-transplant medications (pcon-meds) and assess their potential for DDIs with conditioning agents (e.g., busulfan, cyclophosphamide).
- Discontinue or Modify Interfering Drugs: Discontinue CYP450 enzyme inducers/inhibitors according to their half-lives. For competitive inhibitors, discontinuing 5-7 elimination half-lives prior to conditioning is typically sufficient. For enzyme inducers, a longer period of ~14 days is recommended for enzyme recovery [101].
- Use Alternative Medications: When discontinuation is not feasible, switch to alternative agents with lower DDI potential. For example, certain psychiatric medications can be switched to alternatives with less impact on CYP450 enzymes [101].
FAQ 5: What are the key considerations for designing a tolerance induction protocol? The goal is to achieve donor-specific tolerance, eliminating the need for lifelong immunosuppression. Key strategies include [41]:
- Establishing Hematopoietic Chimerism: Using non-myeloablative conditioning and donor hematopoietic stem cell (HSC) infusion to create a mixed immune system that recognizes the graft as "self." This promotes central tolerance via the thymus.
- Regulatory Cell Therapy: Infusing regulatory T cells (Tregs) to suppress alloreactive responses. Innovations include genetically engineering CAR-redirected Tregs for enhanced specificity.
- IL-2 Pathway Modulation: Using low-dose IL-2 to selectively expand and sustain Treg populations.
Troubleshooting Common Experimental Challenges
Challenge 1: Poor Drug Solubility and Stability In Vitro
- Problem: The investigational immunomodulator precipitates in cell culture media, leading to inconsistent results and clogged tubing in perfusion systems.
- Solution:
- Formulate with Carriers: Use drug delivery systems to enhance solubility. For small molecules, consider encapsulation within PLGA nanoparticles or liposomes [99].
- Use Compatible Solvents: If a carrier is not an option, use the minimum necessary concentration of a biocompatible solvent like DMSO (typically <0.1% final concentration). Always include a vehicle control in your experiments.
- Confirm Stability: Perform HPLC analysis to verify drug integrity in your culture media over the intended duration of the experiment.
Challenge 2: High Systemic Toxicity in Animal Models
- Problem: The effective dose for preventing graft rejection in your rodent model causes significant off-target organ toxicity (e.g., renal, hepatic).
- Solution:
- Switch to Local Delivery: Implement a local delivery strategy. For a subcutaneous graft model, consider a drug-eluting hydrogel surrounding the graft. For solid organs, investigate intra-graft injection of sustained-release microparticles [99].
- Implement Targeted Delivery: Functionalize your nanoparticle system with ligands (e.g., antibodies, peptides) that bind to receptors upregulated on alloreactive immune cells or graft endothelium.
- Adjust Dosage Schedule: If systemic administration is mandatory, consider intermittent dosing or continuous infusion via osmotic pump to avoid peak plasma concentrations that drive toxicity.
Challenge 3: Inconsistent Graft Rejection in Control Group
- Problem: The timing and severity of graft rejection in your untreated or vehicle-control animals are highly variable, making it difficult to assess your treatment's efficacy.
- Solution:
- Standardize Transplant Technique: Ensure the surgical procedure (ischemia time, anastomosis quality) is performed consistently by a single, experienced surgeon.
- Verify Genetic Disparity: Use donor and recipient strains with well-defined and consistent MHC (e.g., fully allogeneic combinations like C57BL/6 to BALB/c). Confirm their genotypes regularly.
- Monitor Immune Competence: Check that your control animals are immunocompetent and free of underlying pathogens, which can modulate immune responses. Use animals from a specific pathogen-free (SPF) facility.
Quantitative Data for Formulation Design
Table 1: Comparison of Drug Delivery Platforms for Local Immunomodulation [99]
| Platform | Typical Size Range | Common Loaded Agents | Key Advantages | Typical Release Kinetics |
|---|---|---|---|---|
| Polymeric Nanoparticles | 50 - 300 nm | Tacrolimus, Sirolimus, monoclonal antibodies | Enhanced cellular uptake; potential for targeting | Days to a few weeks |
| Microparticles | 1 - 100 μm | Mycophenolic Acid, cytokines, steroids | High payload capacity; suitable for injection | Weeks to months |
| Hydrogels | N/A (Bulk matrix) | Proteins, growth factors, small molecules | Injectable; conforms to graft site | Tunable, from days to months |
| Liposomes | 80 - 200 nm | Cytarabine, Daunorubicin (e.g., CPX-351) [100] | Improved drug solubility and stability | Days to weeks |
Table 2: Key Immune Pathways and Potential Therapeutic Targets in Allogeneic Transplantation
| Immune Pathway | Key Effector Cells | Molecular Triggers | Experimental Targeting Approaches |
|---|---|---|---|
| T-cell Allorecognition | Alloreactive T cells | Donor MHC (HLA) molecules [30] | Calcineurin inhibitors (Tacrolimus); Co-stimulation blockade (Belatacept) |
| Antibody-Mediated Rejection | B cells, Plasma Cells, Complement | Donor-specific antibodies (DSA) [30] | Anti-CD20 (Rituximab); Proteasome inhibitors (Bortezomib); Complement inhibitors |
| "Missing Self" Recognition | Natural Killer (NK) cells | Lack of donor HLA class I inhibiting recipient KIR [15] | KIR-blocking antibodies; SIRPα-CD47 pathway modulation [15] |
| DAMP-mediated Inflammation | Monocytes/Macrophages, Dendritic Cells | HMGB1, ATP, DNA released after IRI [98] | PRR antagonists (e.g., anti-TLR4); DAMP-neutralizing antibodies |
Standard Experimental Protocol: Evaluating a Local Drug Delivery SystemIn Vivo
Title: Protocol for Evaluating a Tacrolimus-Loaded Hydrogel in a Murine Skin Allograft Model.
Objective: To assess the efficacy and local toxicity of a locally applied, sustained-release Tacrolimus formulation in preventing allograft rejection.
Materials:
- Animals: BALB/c (donor) and C57BL/6 (recipient) mice, 8-12 weeks old.
- Drug Formulation: Tacrolimus-loaded hydrogel (e.g., GelMA) and blank hydrogel control.
- Surgical Supplies: Sterile surgical instruments, sutures, anesthesia.
- Analysis: Flow cytometer, ELISA kits (IFN-γ, TNF-α), histology supplies.
Methodology:
- Skin Transplantation: Perform a full-thickness trunk skin graft from a BALB/c mouse to a C57BL/6 mouse using standard microsurgical techniques.
- Application of Hydrogel: Immediately after grafting, apply 100 μL of the Tacrolimus-loaded hydrogel to fully cover the graft bed and wound site. The control group receives blank hydrogel.
- Systemic Control Group: Include a third group that receives a daily subcutaneous injection of Tacrolimus at a known sub-therapeutic or therapeutic dose.
- Graft Monitoring: Monitor grafts daily for visual signs of rejection (erythema, edema, necrosis, eschar formation). Score rejection on a standardized scale (e.g., 0-4).
- Endpoint Analysis: On day 10-12 post-transplant, or when rejection is unequivocal in controls:
- Graft Histology: Harvest grafts for H&E staining to evaluate immune cell infiltration and tissue architecture.
- Cytokine Analysis: Harvest graft-draining lymph nodes and analyze by flow cytometry for T-cell populations and by ELISA for inflammatory cytokines.
- Systemic Drug Levels: Collect plasma to measure Tacrolimus levels via LC-MS/MS to confirm localized versus systemic drug exposure.
Signaling Pathways in Alloimmune Response
Diagram Title: Immune Recognition in Transplant Rejection
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating Transplant Immunobiology
| Reagent / Material | Primary Function | Example Application |
|---|---|---|
| PLGA Nanoparticles | Biodegradable polymer for sustained drug release. | Local delivery of Tacrolimus or Sirolimus to the graft site [99]. |
| Methacryloyl (GelMA) Hydrogel | Injectable, photopolymerizable scaffold for cell encapsulation and drug delivery. | Creating a perigraft depot for controlled release of immunomodulatory proteins [99]. |
| Anti-CD47 Monoclonal Antibody | Blocks the "don't eat me" signal on target cells. | Investigated in AML pre-transplant [100]; modulates macrophage activity in solid organ rejection via SIRPα-CD47 pathway [15]. |
| KIR-HLA Binding Assay Kit | Measures functional interaction between Killer-cell Immunoglobulin-like Receptors and HLA. | In vitro screening for "missing self" scenarios and testing KIR-blocking therapeutics [15]. |
| Anti-Human HLA Antibody (Flow) | Detects and quantifies donor-specific antibodies (DSA) in serum. | Monitoring humoral sensitization and antibody-mediated rejection in pre-clinical models [30]. |
Measuring Success: Validation Biomarkers and Comparative Outcome Analysis
Biomarkers for Acute Rejection and Operational Tolerance
Frequently Asked Questions (FAQs)
Q1: What are the primary limitations of traditional methods for monitoring transplant rejection? The current gold standard for diagnosing rejection is the tissue biopsy. However, this method is invasive, carries risks of complications (e.g., a 3.5% incidence of gross hematuria after kidney biopsy), and is subject to sampling error and inter-observer variability among pathologists [24] [102] [103]. Traditional biomarkers like serum creatinine for kidney function lack specificity for immune-mediated rejection and often only elevate after significant graft injury has occurred [24] [103].
Q2: What is an ideal biomarker in the context of transplantation? According to the NIH, a biomarker is "a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacological responses to a therapeutic intervention" [24] [103]. An ideal biomarker for transplantation should be non-invasive, and provide high sensitivity, specificity, and predictive value for diagnosing, predicting, or prognosticating graft injury [103]. It should allow for early detection, often at a subclinical stage, enabling timely intervention [24].
Q3: What are some of the most promising non-invasive biomarkers for acute rejection? Research has identified several promising blood- and urine-based biomarkers. Key candidates include:
- Donor-derived cell-free DNA (dd-cfDNA): Released into the recipient's blood during graft injury, it is highly sensitive for detecting early damage [24] [103].
- Chemokines (e.g., CXCL9, CXCL10): These proteins are involved in recruiting inflammatory cells and show elevated levels during rejection [103].
- Gene Expression Profiling: Signatures in blood or urine cells can help exclude moderate-to-severe acute rejection [24].
- MicroRNA (miRNA) Profiling: Specific miRNA patterns can enhance diagnostic specificity for precise rejection detection [24].
Q4: How is "operational tolerance" defined, and what is the challenge in identifying it? Operational tolerance describes a state where a transplant recipient maintains normal graft function and histology without any immunosuppressive therapy, while also preserving overall immune competence [17]. The major challenge is the current lack of universally validated biomarkers that can reliably identify patients who have achieved this state. This gap precludes the safe and personalized withdrawal of immunosuppression in clinical practice [17].
Q5: Besides the adaptive immune system, what other mechanisms can contribute to rejection? Emerging evidence highlights the role of innate immunity. A key concept is "missing self," where Natural Killer (NK) cells become activated if they encounter donor cells lacking the "self" HLA class I molecules that normally inhibit them. This mechanism can trigger microvascular inflammation in the graft, independent of donor-specific antibodies or T cells [15].
Performance Metrics of Key Rejection Biomarkers
The following table summarizes the diagnostic performance of several well-studied biomarkers for acute rejection in kidney transplantation, as reported in clinical studies.
Table 1: Diagnostic Performance of Selected Biomarkers for Acute Kidney Transplant Rejection
| Biomarker | Sample Type | Rejection Type | AUC | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Citation |
|---|---|---|---|---|---|---|---|---|
| Three-gene signature | Urine cell pellets | Acute TCMR | 0.74 | 71 | 72 | - | - | [103] |
| kSORT | Blood | Acute Rejection (TCMR & ABMR) | 0.94 | 83.0 | 90.6 | 93.2 | - | [103] |
| CXCL9 protein | Blood | Banff ≥1 Rejection | 0.86 | 85.2 | 80.7 | 67.6 | 92 | [103] |
| CXCL10 | Urine | ABMR | 0.70 | 73 | 61.6 | 25.7 | 92.6 | [103] |
| dd-cfDNA | Plasma | Active Rejection | 0.74 | 59 | 85 | 61 | 84 | [103] |
Abbreviations: AUC (Area Under the Curve), PPV (Positive Predictive Value), NPV (Negative Predictive Value), TCMR (T-Cell Mediated Rejection), ABMR (Antibody-Mediated Rejection).
Experimental Workflow for Biomarker Validation
A robust experimental protocol is essential for validating novel biomarkers. The following diagram outlines a generalized workflow from sample collection to clinical application.
Key Research Reagent Solutions
Successful biomarker research relies on specific reagents and tools. The table below lists essential items for a research toolkit in this field.
Table 2: Essential Research Reagents for Biomarker Investigation
| Research Reagent | Function / Application | Specific Examples / Targets |
|---|---|---|
| Anti-Human Antibodies | Flow cytometry to characterize immune cell populations in blood or tissue. | CD3 (T cells), CD4 (Helper T), CD8 (Cytotoxic T), CD19 (B cells), CD56 (NK cells) |
| ELISA Kits | Quantify soluble biomarker protein levels in serum, plasma, or urine. | CXCL9/IP-10, CXCL10/MIG, Total cfDNA, KIM-1, NGAL |
| dd-cfDNA Enrichment & Quantification Kits | Specifically isolate and measure the fraction of cell-free DNA derived from the donor organ. | PCR-based assays (e.g., for SNPs), Next-generation sequencing (NGS) kits |
| RNA Sequencing Kits | Perform transcriptomic analysis (e.g., gene expression profiling) on blood or urine cells. | Whole transcriptome kits, targeted gene panels |
| KIR & HLA Genotyping Kits | Determine recipient and donor genotypes to assess innate immune risk (e.g., "missing self"). | KIR2DL1, KIR2DL2/3, HLA-C1/C2 allotypes |
Signaling Pathways in Acute Rejection
Understanding the immune mechanisms of rejection is fundamental. The following diagram illustrates the key signaling pathways involved in T Cell-Mediated Rejection (TCMR).
In the field of allogeneic transplantation, managing immune rejection remains a significant challenge. Gene expression profiling has emerged as a powerful tool to decipher the complex molecular dialogues between donor grafts and recipient immune systems. This technical support guide provides researchers and scientists with practical frameworks for utilizing these genomic signatures to improve diagnosis and prognosis, ultimately aiding in the development of targeted therapies to enhance transplant outcomes.
Key Gene Expression Signatures in Transplantation
The following table summarizes quantitatively significant gene expression signatures identified in transplantation research, which can serve as critical biomarkers for diagnosis and prognosis.
| Gene / Signature | Expression Change | Transplant Context | Biological Association / Function | Citation |
|---|---|---|---|---|
| Gad1, Gdf10, Scg2 | Significant downregulation | HY antigen-mismatched islet grafts (Mouse model) | Protection against graft rejection; significant relationship to graft survival. | [104] |
| GPSM3, EPHX4 | Pre-transplant downregulation | Allogeneic Hematopoietic Cell Transplantation (HCT) | Protective against GVHD development; GPSM3 is an MHC-regulated gene. | [105] |
| LRG1 | Upregulated post-transplant | Allogeneic HCT | Facilitates CD34+ and myeloid progenitor growth by antagonizing TGF-beta effects; associated with GVHD. | [105] |
| IFI27, NT5C3, CCR1, LBA1 | Upregulated (IFN modules) | Allogeneic HCT | Distinct patterns predictive for GVHD development. | [105] |
| IL-1R2, Profibrotic genes | Upregulated | Chronic GVHD after HCT | Anti-inflammatory and profibrotic responses; IL-1 decoy receptor, genes in IL-4, IL-6, IL-10 pathways. | [106] |
| Inhibitory KIR / HLA Mismatch | Functional activity | Solid Organ Transplantation (e.g., Kidney) | NK cell activation via "missing self"; associated with antibody-independent microvascular inflammation. | [15] |
Experimental Protocols & Methodologies
Protocol 1: Peripheral Blood Mononuclear Cell (PBMC) Profiling for GVHD
This detailed protocol is adapted from a study that identified gene signatures associated with chronic GVHD [106].
1. Sample Collection and Preparation
- Collection: Collect whole blood (e.g., 20 mL) in heparin-containing Vacutainer tubes.
- PBMC Isolation: Isolate PBMCs within a short time frame using Ficoll gradient centrifugation.
- Cryopreservation: Aliquot 10-30 million cells into cryovials containing RPMI with 10% DMSO and 10% fetal bovine serum. Cryopreserve at -80°C until RNA extraction.
2. RNA Extraction and Quality Control
- Extraction: Use a commercial kit (e.g., RNeasy mini kit from Qiagen) to isolate total RNA from thawed PBMCs.
- Quantification: Measure RNA concentration using a spectrophotometer (e.g., NanoDrop).
- Quality Assessment: Assess RNA integrity using an instrument like the Agilent 2100 Bioanalyzer with RNA Nano Chips. Only samples with high RNA Integrity Numbers (RIN) should be processed further.
3. Microarray Hybridization (Two-Color System)
- cDNA Synthesis: Use 100 ng of total RNA for reverse transcription into cDNA. Employ a T7-promoter primer and MMLV reverse transcriptase.
- cRNA Synthesis and Labeling: Transcribe cDNA into complimentary RNA (cRNA) while incorporating fluorescent labels: Cy5-CTP for target samples and Cy3-CTP for a reference.
- Purification and Yield Check: Purify the labeled cRNA using an RNeasy kit. Determine the cRNA yield and the efficiency of Cy-dye incorporation (specific activity) using a spectrophotometer.
4. Data Acquisition and Analysis
- Hybridization: Hybridize the labeled cRNA onto a microarray platform (e.g., Agilent Whole Human Genome 4x44K oligonucleotide arrays).
- Statistical Analysis: Perform biostatistical analyses to identify differentially expressed genes. To ensure robustness, repeat analyses multiple times with random splits of the data into training and test sets.
Protocol 2: Pre-Transplant Transcriptome Fingerprint Assay (TFA) for GVHD Risk Stratification
This protocol uses high-throughput qPCR for frequent, targeted immune monitoring [105].
1. High-Frequency Blood Sampling
- Collect micro-quantities of blood (50-600 µL) from patients scheduled for allo-HCT.
- Schedule samples: pre-transplant conditioning, weekly until day 100 post-transplant, and bi-weekly until 2 years post-transplant.
2. Targeted Gene Expression Measurement
- Platform: Use a high-throughput qPCR system (e.g., Fluidigm BioMark).
- Gene Panel: Design the assay to measure the expression of a focused panel of 264 immune-related genes.
3. Computational Data Interpretation
- Modular Analysis: Interpret data using the TFA computational model, which groups genes into modules based on biological function.
- Longitudinal Modeling: Correlate gene expression data with clinical annotations. Use linear mixed models to analyze trends over time, comparing groups that do and do not develop GVHD.
Frequently Asked Questions (FAQs)
Q1: Our team is profiling mouse allogeneic islet grafts. Are there specific genes we should prioritize in our analysis?
A1: Yes. Studies in mouse models have identified several key genes. Focus on Gad1, Gdf10, and Scg2, which showed significant differential expression in HY antigen-mismatched islet grafts before rejection or tolerance phenotypes arose. These genes are suggested to have a significant relationship with protection against graft rejection and could be core components of your profiling panel [104].
Q2: We are getting inconsistent results in predicting GVHD from patient blood samples. What is a robust pre-transplant sampling and analysis strategy?
A2: For robust GVHD prediction, implement a Transcriptome Fingerprint Assay (TFA) approach.
- Timing: Collect a baseline blood sample before the start of transplant conditioning therapy [105].
- Technology: Use high-throughput qPCR (e.g., Fluidigm BioMark) for a targeted panel of immune genes. This is often more sensitive and cost-effective for clinical application than microarrays.
- Analysis: Prioritize genes like GPSM3 and EPHX4, which were significantly downregulated pre-transplant in patients who later developed GVHD. Longitudinal analysis confirms these genes distinguish GVHD cohorts over time [105].
Q3: What gene expression signature is characteristic of chronic GVHD, and how does it differ from acute GVHD?
A3: Chronic GVHD has a distinct molecular profile. The dominant gene signature in established chronic GVHD reflects compensatory anti-inflammatory and profibrotic responses. Key elements include:
- Upregulation of IL-1 receptor type II (IL-1R2), a decoy receptor that controls inflammation.
- Profibrotic genes associated with IL-4, IL-6, and IL-10 signaling pathways.
- Genes involved in extracellular matrix remodeling [106]. This signature contrasts with the more acute inflammatory and IFN-signature often seen in acute GVHD, highlighting the distinct pathophysiology of chronic GVHD [106] [105].
Q4: Can gene expression profiling explain cases of organ rejection that occur in the absence of donor-specific antibodies (DSA)?
A4: Yes. Emerging research implicates the innate immune system, particularly natural killer (NK) cells. Rejection in DSA-negative cases can be associated with "missing self" activation of NK cells [15].
- Mechanism: This occurs when donor graft cells lack the specific HLA class I molecules (e.g., C1, C2, Bw4) that are needed to engage the inhibitory receptors (KIRs) on the recipient's NK cells. The absence of this inhibitory signal triggers NK cell activation and endothelial damage, leading to microvascular inflammation [15].
- Analysis: Profiling should therefore not only focus on adaptive immune genes but also on the genetic landscape of donor-recipient KIR-HLA interactions and signatures of NK cell activity [15].
Signaling Pathways and Workflows
Chronic GVHD Profibrotic Gene Signature
The following diagram illustrates the key signaling pathways and gene upregulation involved in the pathogenesis of chronic Graft-versus-Host Disease (GVHD).
Experimental Workflow for Prognostic Gene Signature Discovery
The diagram below outlines a generalized experimental workflow for discovering prognostic gene expression signatures in transplantation research, from sample collection to clinical application.
The Scientist's Toolkit: Research Reagent Solutions
The following table lists essential reagents and materials used in gene expression profiling experiments for transplantation research.
| Research Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| Heparin Vacutainer Tubes | Anticoagulant for blood collection for PBMC isolation. | Used for collecting 20 mL whole blood samples [106]. |
| Ficoll-Paque Premium | Density gradient medium for isolation of viable PBMCs from whole blood. | Used for PBMC preparation via gradient centrifugation [106]. |
| RNeasy Mini Kit (Qiagen) | Silica-membrane based purification of high-quality total RNA from cells. | Used for total RNA isolation from PBMC samples [106]. |
| Agilent Whole Human Genome Microarray | Global profiling of transcriptome-wide gene expression. | Used for hybridization and profiling of PBMC cDNA [106]. |
| Fluidigm BioMark HD System | High-throughput nanoscale qPCR for targeted gene expression analysis. | Used in the Transcriptome Fingerprint Assay (TFA) to measure 264 immune genes [105]. |
| Cyanine (Cy) dyes (Cy3, Cy5) | Fluorescent dyes for labeling cRNA for two-color microarray hybridization. | Used to label target sample (Cy5) and reference (Cy3) cRNA [106]. |
Imaging and Non-Invasive Monitoring Techniques for Graft Health
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary non-invasive alternatives to biopsy for monitoring transplant rejection?
The field is moving beyond invasive biopsies toward several non-invasive techniques that can provide early detection of rejection.
- Molecular Imaging: Uses targeted probes to visualize specific immune cells involved in rejection, such as M1 macrophages or T cells, within the graft. For example, a near-infrared fluorescent probe (XJYZ) can target GLUT1 on M1 macrophages for in vivo imaging in kidney transplant models [107].
- Liquid Biopsy: Analyzes blood samples for biomarkers like donor-derived cell-free DNA (dd-cfDNA). Elevated levels indicate graft injury and can diagnose acute rejection with high sensitivity [24].
- Advanced Clinical Imaging: Includes techniques like strain echocardiography and cardiac magnetic resonance (CMR) with T1/T2 mapping for heart transplant monitoring. These can detect functional and inflammatory changes associated with rejection [108].
FAQ 2: How can I differentiate between antibody-mediated and T-cell-mediated rejection non-invasively?
Distinguishing between rejection types is critical and can be approached by targeting different immunological pathways.
- For Antibody-Mediated Rejection (AMR): Detection of donor-specific antibodies (DSA) in the recipient's serum is a key biomarker. Furthermore, microvascular inflammation (MVI) on biopsy can be associated with DSA. However, note that MVI can also occur in a DSA-negative context, potentially due to innate immune activation like "missing self" in Natural Killer (NK) cells [15].
- For T-Cell-Mediated Rejection (TCMR): Gene expression profiling (GEP) of blood samples can help exclude moderate-to-severe acute TCMR [24]. Molecular imaging with probes that infiltrate with T cells or associated macrophages (e.g., the M1 macrophage probe XJYZ) can also provide spatial information [107].
FAQ 3: What is the role of innate immunity in rejection, and how can it be monitored?
The innate immune system plays a significant and earlier role in rejection than previously thought.
- Key Innate Players: NK cells and monocytes/macrophages are major contributors. NK cells can be activated via "missing self" (absence of donor MHC class I molecules that recipient inhibitory receptors recognize) [15]. M1 macrophages are recruited in large numbers early in rejection [107].
- Monitoring Techniques:
FAQ 4: What are the latest technological advancements in molecular imaging for rejection?
Recent advancements focus on nanotechnology and targeted probes.
- Nanomaterials: Nanoparticles (liposomal, polymeric, metal-based) serve as versatile platforms. They can be engineered as targeted molecular probes for imaging or as "theranostic" agents that combine diagnosis and therapy [109]. Their small size allows them to pass through barriers and interact with cellular structures.
- Specific Probes: Development of near-infrared (NIR) fluorescent probes, like the XJYZ probe for M1 macrophages, enables deep-tissue imaging and real-time monitoring of cellular infiltration [107]. These probes can be conjugated with antibodies or peptides for high specificity.
Troubleshooting Guides
Issue 1: Low Signal-to-Noise Ratio in Preclinical Molecular Imaging
A low signal can hinder the accurate interpretation of imaging data.
- Potential Cause 1: Probe Specificity. The imaging probe may not be binding specifically to the target cell population.
- Solution: Validate probe specificity in vitro using flow cytometry or immunofluorescence on sorted cell populations (e.g., confirm that the XJYZ probe binds specifically to M1, not M2, macrophages) [107].
- Potential Cause 2: Suboptimal Probe Dosage or Timing. The probe concentration may be too low, or the imaging may be performed before sufficient probe accumulation.
- Solution: Perform a kinetic study to determine the optimal time post-injection for maximum target-to-background ratio. For the XJYZ probe, accumulation was monitored over days to track macrophage infiltration dynamics [107].
Issue 2: Interpreting Discordant Results Between Biopsy and Non-Invasive Tests
Conflicting results between traditional biopsy and new monitoring methods can be challenging.
- Scenario: Positive dd-cfDNA but Negative Biopsy.
- Interpretation & Action: A positive dd-cfDNA test indicates ongoing graft injury but may precede histological changes. This should be considered an early warning. It is recommended to increase surveillance frequency, check for other causes of injury (e.g., infection, drug toxicity), and consider a follow-up biopsy if clinically indicated [24].
- Scenario: DSA-Negative Microvascular Inflammation (MVI) on Biopsy.
- Interpretation & Action: This phenotype may not be explained by adaptive immunity. Investigate innate immune activation, such as "missing self" in NK cells. This requires donor and recipient genotyping for HLA class I and recipient inhibitory KIR genotype. Therapies targeting antibodies (like IVIG) are ineffective here, so the immunosuppressive strategy may need adjustment [15].
Issue 3: High Background in Liquid Biopsy Analysis
Detecting a true signal from graft injury can be complicated by non-specific noise.
- Potential Cause: Clonal Hematopoiesis (CHIP). Age-related mutations in blood cells can be detected by sensitive NGS assays and mistaken for disease-derived signals [110].
- Solution: Use a matched sequencing approach. Compare the cfDNA mutation profile with the recipient's pre-transplant germline DNA (if available) and the donor's genotype to distinguish true donor-derived mutations from recipient-specific clonal hematopoiesis [110].
The tables below summarize key performance metrics for non-invasive monitoring techniques.
Table 1: Performance of Non-Invasive Biomarkers in Detecting Acute Rejection
| Biomarker | Target/Principle | Clinical Utility | Key Performance Metrics / Findings |
|---|---|---|---|
| Donor-Derived Cell-Free DNA (dd-cfDNA) [24] | Detects DNA fragments released from injured graft cells. | Diagnosis & early detection of ACR and AMR. | Highly sensitive for early graft injury. |
| Gene Expression Profiling (GEP) [24] | Measures RNA expression patterns in peripheral blood. | Excluding moderate-to-severe ACR. | Effectively rules out active TCMR. |
| MicroRNA (miRNA) Profiling [24] | Analyzes specific miRNA patterns associated with rejection. | Enhances diagnostic specificity for AR. | Improves precision in AR detection. |
| XJYZ Fluorescent Probe [107] | NIR probe targeting GLUT1 on M1 macrophages. | Preclinical imaging of TCMR in kidney grafts. | Enabled non-invasive, dynamic monitoring of M1 macrophage infiltration in rat models. |
Table 2: Characteristics of Molecular Imaging Modalities for Rejection Monitoring
| Imaging Modality | Probe/Target Example | Key Advantages | Key Limitations |
|---|---|---|---|
| Fluorescence Imaging [107] [24] | XJYZ probe for M1 macrophages (GLUT1). | High spatiotemporal resolution; suitable for AR grading in preclinical models. | Limited tissue penetration; primarily preclinical. |
| Nuclear Imaging (PET/SPECT) [24] [108] | Radiolabeled probes for immune cells (e.g., T cells). | High sensitivity; dynamic visualization of immune responses; quantitative. | Radiation exposure; lower spatial resolution than MRI/CT. |
| Cardiac Magnetic Resonance (CMR) [108] | Native T1/T2 mapping for tissue characterization. | No radiation; excellent tissue contrast for anatomy and inflammation. | Limited specific molecular probe development. |
| Ultrasound [24] | Microbubbles functionalized with antibodies. | Real-time, portable, low-cost. | Developing targeted contrast agents. |
Experimental Protocols
Protocol 1: In Vivo Imaging of M1 Macrophage Infiltration in a Rat Renal Transplant Model
This protocol is adapted from a study using the XJYZ fluorescent probe [107].
- Objective: To non-invasively monitor the dynamics of M1 macrophage infiltration during acute TCMR.
- Materials:
- Animal Model: Allogeneic rat renal transplantation model (e.g., Wistar donor to Sprague-Dawley recipient). Syngeneic transplant serves as control.
- Imaging Probe: Near-infrared fluorescent probe XJYZ, designed to target GLUT1.
- Instrumentation: In vivo fluorescence imaging system.
- Method Steps:
- Model Establishment: Perform orthotopic kidney transplantation according to established microsurgical techniques [107].
- Probe Administration: Intravenously inject the XJYZ probe at various time points post-transplantation (e.g., days 1, 3, 5, 7).
- In Vivo Imaging: Anesthetize the recipient rat and image at predetermined time points post-injection (e.g., 24h) to determine optimal signal accumulation.
- Ex Vivo Validation: Euthanize the animal post-imaging. Harvest the transplanted kidney and native organs for:
- Ex vivo imaging to quantify fluorescence intensity.
- Histological analysis (H&E staining, immunohistochemistry for CD86/GLUT1) to correlate fluorescence with macrophage infiltration [107].
- Data Analysis: Quantify fluorescence signal in the graft region of interest and normalize to background. Correlate signal intensity with Banff rejection scores from histology.
Protocol 2: Monitoring Graft Rejection via Donor-Derived Cell-Free DNA (dd-cfDNA)
This protocol outlines the use of liquid biopsy for rejection monitoring [24].
- Objective: To detect early graft injury and acute rejection by measuring the fraction of dd-cfDNA in the recipient's blood.
- Materials:
- Patient Samples: Peripheral blood samples from transplant recipients collected in cell-free DNA blood collection tubes.
- Kits & Reagents: cfDNA extraction kits, next-generation sequencing (NGS) library preparation kits, and targeted sequencing panels (e.g., for SNP genotyping).
- Method Steps:
- Sample Collection & Processing: Collect ~10 mL of peripheral blood. Centrifuge to separate plasma from cellular components. Extract cfDNA from the plasma.
- Library Preparation & Sequencing: Prepare sequencing libraries from the extracted cfDNA. Use a targeted panel to genotype single nucleotide polymorphisms (SNPs).
- Bioinformatic Analysis: Use specialized algorithms to distinguish and quantify the proportion of cfDNA fragments originating from the donor (dd-cfDNA) versus the recipient.
- Interpretation: An elevated dd-cfDNA fraction (e.g., >1% for kidney transplants) is indicative of active graft injury and should trigger further clinical assessment for rejection [24].
Key Signaling Pathways and Immune Mechanisms in Rejection
The diagrams below illustrate core immunological concepts in transplant rejection.
Diagram 1: M1 Macrophage-Mediated Inflammation in TCMR
This diagram shows the role of M1 macrophages in T cell-mediated rejection, a key target for molecular imaging [107].
Diagram 2: Innate Immune "Missing Self" Activation in Rejection
This diagram outlines the "missing self" activation pathway of Natural Killer (NK) cells, which can cause rejection independent of donor-specific antibodies [15].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Non-Invasive Graft Monitoring Research
| Reagent / Material | Function / Application | Example / Target |
|---|---|---|
| Near-Infrared Fluorescent Probes [107] | In vivo imaging of specific immune cell populations in preclinical models. | XJYZ probe targeting GLUT1 on M1 macrophages. |
| Functionalized Nanoparticles [109] | Serve as versatile carriers for imaging agents (dyes, radionuclides) or drugs; can be targeted to specific cells. | Liposomal or polymeric nanoparticles conjugated with antibodies (e.g., anti-CD3 for T cells). |
| Anti-CD86 Antibody [107] | Immunohistochemistry marker for identifying pro-inflammatory M1 macrophages in tissue sections. | Polyclonal anti-CD86 antibody (e.g., ab220188). |
| Anti-GLUT1 Antibody [107] | Validates the expression of the imaging target GLUT1 in graft tissues. | Monoclonal anti-GLUT1 antibody (e.g., ab115730). |
| dd-cfDNA Sequencing Panel [24] | A targeted NGS panel for genotyping SNPs to quantify the proportion of donor-derived DNA in recipient plasma. | Commercially available kits (e.g., Prospera). |
| Single-Cell RNA Sequencing Kits [107] | For comprehensive analysis of the immune cell landscape within the graft to identify novel rejection targets. | 10x Genomics Chromium platform. |
Comparative Analysis of Solid Organ vs. Cellular Transplantation Outcomes
Transplantation is a cornerstone treatment for end-stage organ failure and hematologic diseases. Allogeneic transplantation—the transfer of cells, tissues, or organs from a non-identical donor—faces a major hurdle: immune rejection. The recipient's immune system recognizes the transplanted material as foreign and mounts a destructive response. This technical support content provides a framework for researchers and scientists to troubleshoot common experimental challenges in this field, framed within the broader context of managing immune rejection.
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary immune effector mechanisms responsible for graft rejection? Graft rejection is primarily an immunological response mediated by T cells and antibodies. Key mechanisms include:
- Cellular Rejection: CD8+ T cells directly lyse donor cells, while CD4+ T cells activate macrophages and other inflammatory cells, causing tissue injury [30].
- Antibody-Mediated Rejection: Pre-existing or developed alloantibodies can bind to donor endothelium, activating complement and leading to rapid graft destruction, a process known as hyperacute rejection [30].
- Allorecognition: T cells recognize donor antigens via two main pathways: direct allorecognition (recipient T cells bind directly to donor MHC molecules on graft cells) and indirect allorecognition (recipient T cells recognize processed donor peptides presented by the recipient's own antigen-presenting cells) [30].
FAQ 2: What are the key immunological differences between Solid Organ (SOT) and Hematopoietic Cell Transplantation (HCT)? While both face immune rejection, the underlying mechanisms and outcomes differ significantly, as summarized in the table below [111].
Table 1: Key Comparative Features of SOT and Allogeneic HCT
| Feature | Solid Organ Transplantation (SOT) | Allogeneic Hematopoietic Cell Transplantation (HCT) |
|---|---|---|
| Donor Status | Deceased or living donors [111] | Only living donors [111] |
| HLA Matching | Highly preferable [111] | Critical [111] |
| Recipient Conditioning | No myeloablation [111] | Myeloablative or reduced-intensity conditioning [111] |
| Primary Complication | Rejection, organ loss [111] | Graft-versus-host disease (GvHD), infections [111] |
| Desired Outcome | Organ acceptance under immunosuppression; tolerance [111] | Complete donor chimerism, off immunosuppression without GvHD [111] |
| Beneficial Immune Effect | Not typically applicable | Graft-versus-leukemia/tumor (GvL/GvT) effect [111] |
FAQ 3: What is the "Graft-versus-Leukemia" effect and why is it unique to HCT? The Graft-versus-Leukemia (GvL) effect is a powerful form of immunotherapy inherent to allogeneic HCT. Donor-derived immune cells within the graft, particularly T cells, recognize and eliminate residual malignant cells in the recipient. This provides a crucial mechanism for preventing disease relapse. A analogous effect, Graft-versus-Tumor (GvT), can also occur. This beneficial response has no direct equivalent in SOT [111].
Troubleshooting Common Experimental Challenges
Challenge 1: Poor Engraftment or Early Graft Loss
- Potential Cause: Inadequate immunosuppressive conditioning or insufficient donor-recipient matching.
- Solution: Optimize conditioning regimens. For HCT, this involves myeloablative (MAC) or reduced-intensity conditioning (RIC) protocols. Ensure rigorous HLA matching, which is critical for HCT and highly preferable for SOT [111].
Challenge 2: Difficulty in Monitoring Anti-Donor Immune Responses
- Potential Cause: Lack of sensitive and specific assays to track rare, alloreactive T-cell populations.
- Solution: Implement advanced immunomonitoring assays. The Comprehensive Alloreactive T-cell Detection (cATD) assay is a novel method that uses short-term Mixed Lymphocyte Reaction (MLR) with activation markers (CD154 for CD4+ T cells, CD137 for CD8+ T cells) to identify and characterize donor-reactive T cells. This can distinguish between tolerance and rejection states before clinical symptoms appear [27].
Table 2: Core Protocol for the cATD Assay [27]
| Step | Component | Details |
|---|---|---|
| 1. Stimulator Prep | Donor-derived B cells | Isolate and activate with CD40L + IL-4 for 24 hours. Irradiate (40 Gy) before co-culture. |
| 2. Responder Prep | Recipient T cells | Purify from splenocytes via negative selection. |
| 3. Co-culture | MLR setup | Co-culture responders and stimulators at a 1:1 ratio for 18 hours in the presence of anti-CD154 mAb. |
| 4. Analysis | Flow Cytometry | Identify alloreactive CD4+ T cells as CD3+CD4+CD154+. Identify alloreactive CD8+ T cells as CD3+CD8+CD137+. |
Challenge 3: Managing Data Complexity in Translational Studies
- Potential Cause: Reliance solely on clinical trial data, which may lack real-world diversity and long-term follow-up.
- Solution: Integrate Real-World Data (RWD). RWD, collected from sources like electronic health records, registries, and patient apps, provides insights into treatment patterns, effectiveness, and safety in diverse, real-world populations. RWD can complement clinical trials and support regulatory decision-making [112].
Experimental Protocols
Protocol 1: Assessing Alloreactive T-Cell Responses via cATD Assay
Principle: This flow cytometry-based assay rapidly detects and characterizes activated, donor-reactive T cells after a short-term Mixed Lymphocyte Reaction (MLR) [27].
Workflow: The following diagram illustrates the key steps and analysis outputs of the cATD assay protocol.
Key Materials:
- Donor and Recipient Cells: Splenocytes or purified immune cells.
- Culture Medium: Complete RPMI 1640 with supplements.
- Activation Cocktail: Recombinant CD40L and IL-4.
- Antibodies: Fluorescently-labeled anti-mouse CD3, CD4, CD8, CD154, CD137. (Note: Use anti-human antibodies for human cell applications).
- Equipment: Flow cytometer, cell culture incubator, cell separator.
Protocol 2: Utilizing Real-World Data (RWD) to Augment Clinical Trial Findings
Principle: Analyze data from routine clinical practice to understand long-term drug effectiveness, safety, and usage patterns [112].
Workflow:
- Define Research Question: e.g., "What is the real-world overall response rate (ORR) of drug X in chronic GvHD?"
- Select RWD Source: Choose from registries, electronic health records (EHR), or claims databases based on strengths and limitations.
- Data Collection & Aggregation: Extract and merge relevant data points longitudinally.
- Statistical Analysis: Compare outcomes (e.g., ORR, survival) with those from pivotal clinical trials.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Transplantation Immunology Research
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Recombinant CD40L & IL-4 | Activates B cells to become potent stimulator cells in MLR [27]. | Preparing donor-derived antigen-presenting cells for the cATD assay [27]. |
| Anti-CD154 & Anti-CD137 mAbs | Antibodies used as activation markers to identify alloreactive CD4+ and CD8+ T cells, respectively, via flow cytometry [27]. | Detection and quantification of donor-reactive T cell populations in the cATD assay [27]. |
| CFSE (Carboxyfluorescein succinimidyl ester) | A fluorescent cell dye that dilutes with each cell division, used to track T-cell proliferation [27]. | Conventional 4-day MLR to measure the precursor frequency of alloreactive T cells [27]. |
| Immunosuppressive Agents (e.g., CTLA-4 IgG, Anti-CD154) | Agents used to dampen the host immune response to prevent or treat rejection [113] [27]. | Testing tolerance induction protocols in animal models of transplantation [27]. |
| Belumosudil | A ROCK2 inhibitor used to treat steroid-refractory chronic Graft-versus-Host Disease (GvHD) [112]. | Studying second-line therapy for GvHD in both clinical trials and real-world settings [112]. |
Future Directions and Innovations
The field of transplantation is evolving to overcome current barriers. Key innovations include:
- Novel Immunomonitoring: Techniques like the cATD assay will enable earlier detection of rejection and personalized immunosuppression [27].
- Leveraging Real-World Evidence (RWE): RWD will increasingly inform clinical practice, drug development, and regulatory decisions, providing insights beyond traditional clinical trials [112].
- Digital Health Integration: mHealth platforms are being developed to improve post-transplant care, patient monitoring, and data collection, facilitating new models of integrated care [114].
- Expanding the Donor Pool: Research continues into methods like split-liver transplants, islet cell implantation, and xenotransplantation to address the critical shortage of donor organs [113].
Frequently Asked Questions (FAQs) on Tolerance Induction
Q1: What is the fundamental difference between "immune tolerance" and immunosuppression in transplantation?
A1: Immunosuppression non-specifically dampens the entire immune system, increasing risks of infections and malignancies, and requires lifelong daily treatment. In contrast, donor-specific immune tolerance is a state where the immune system is selectively unresponsive to the donor graft but remains fully competent to fight infections and other threats. This state, also called operational tolerance, is defined by normal graft function in the absence of maintenance immunosuppressive therapy [17] [115] [116].
Q2: Why do tolerance protocols that work in laboratory rodents often fail in clinical trials?
A2: A major reason is the difference in immune system history. Laboratory rodents are bred in specific pathogen-free (SPF) environments and have a immune profile similar to a human neonate, with a high ratio of naïve to memory T cells. Humans, however, are constantly exposed to pathogens, generating a large compartment of memory T cells. These memory T cells, including those generated via heterologous immunity, are more resistant to tolerance induction and can trigger rejection [17]. Even a single viral infection in a mouse can render it refractory to tolerance induction [17].
Q3: What is hematopoietic chimerism and how does it promote tolerance?
A3: Hematopoietic chimerism refers to the coexistence of donor and recipient hematopoietic (blood-forming) and immune cells within the transplant recipient. Establishing mixed chimerism (a mixture of donor and host cells) is a powerful strategy to induce tolerance. Donor-derived cells, particularly dendritic cells, can migrate to the recipient's thymus, where they participate in the education of newly developing T cells. This process, known as central tolerance, deletes T cells that are reactive to donor antigens, leading to lifelong acceptance of the graft [17] [117] [118].
Q4: What are the primary risks associated with protocols that induce full donor hematopoietic chimerism?
A4: The two major risks are:
- Graft-versus-host disease (GVHD): This occurs when donor-derived immune cells (primarily T cells) attack the recipient's tissues. GVHD can be severe and even fatal [17] [117].
- Infections: The conditioning regimens (e.g., non-myeloablative chemotherapy or irradiation) used to make space for the donor cells and the ensuing immune reconstitution can leave the patient susceptible to severe infections, which can sometimes lead to graft loss or death [17].
Q5: Are there reliable biomarkers to identify patients in whom immunosuppression can be safely withdrawn?
A5: The identification of universally validated biomarkers remains a significant challenge [17] [115]. However, in some specific protocols, the establishment of stable full donor chimerism is a reliable indicator of successful tolerance [17]. Research is actively ongoing to identify other biomarkers, such as specific gene expression signatures or ratios of immune cell subsets (e.g., dendritic cells, regulatory T cells), that can predict operational tolerance [115] [116].
Quantitative Data on Tolerance Protocols
The table below summarizes key clinical outcomes from selected tolerance induction strategies.
Table 1: Clinical Outcomes of Selected Tolerance Induction Protocols
| Protocol / Strategy | Patient Population / Context | Key Conditioning & Agents | Graft Survival & Immunosuppression (IS) Withdrawal | Major Adverse Events |
|---|---|---|---|---|
| Non-myeloablative HLA-identical HSCT & Kidney Tx [17] | HLA-identical living donors | Total lymphoid irradiation (TLI), anti-thymocyte globulin (ATG), donor T-cell infusion | >80% (24/29) achieved durable chimerism & successful IS withdrawal | Not specified in snippet |
| Intensive Conditioning & HSCT/Kidney Tx [17] | HLA-incompatible living donors | Total body irradiation, fludarabine, cyclophosphamide, donor T-cells, CD8+ facilitator cells (FCR001) | >80% (26/32) achieved high-level chimerism; majority (25/26) discontinued IS | Severe infections (graft loss n=2, death n=1); GVHD (fatal n=1, chronic n=1) |
| TCRαβ+/CD19+ Depleted HSCT [17] | Patients with Schimke immuno-osseous dysplasia (SIOD) | Reduced-intensity conditioning, TCRαβ+/CD19+ depleted grafts | 3/3 achieved full chimerism & sustained IS-free renal function | Protocol designed to mitigate GVHD risk in immunodeficient patients |
| Spontaneous Operational Tolerance [118] | General liver and kidney transplant recipients | None (occurs spontaneously) | Reported in <5% of kidney and ~20% of liver transplant recipients | N/A |
Table 2: Utility of Assays for Monitoring Transplant Tolerance
| Assay Name | What It Measures | Utility in Tolerance Monitoring | Key Limitations |
|---|---|---|---|
| Mixed Leukocyte Reaction (MLR) [115] | T-cell proliferation in response to donor antigens in vitro | Provides information on overall T-cell reactivity; lack of response may suggest tolerance. | Cannot differentiate between unresponsiveness due to deletion vs. suppression; limited predictive value alone. |
| Trans-Vivo Delayed-Type Hypersensitivity (tvDTH) [115] | In vivo inflammatory response to donor antigen; can detect T-regulatory cell function. | Can demonstrate antigen-specific suppression; used in research to identify regulatory responses. | Complex assay not routinely used in clinical practice. |
| Enzyme-Linked Immunosorbent Spot (ELISPOT) [115] | Frequency of T cells secreting IFN-γ in response to donor antigens. | Correlates with alloreactivity; higher frequencies associated with rejection risk. | Does not provide a complete picture of the tolerant state. |
| Donor-Specific Antibody (DSA) Monitoring [115] | Presence of antibodies in recipient serum that bind to donor HLA molecules. | Critical marker; presence of DSA is a strong contraindication for IS weaning and is associated with rejection. | Does not measure cellular immunity. |
Detailed Experimental Protocols
Protocol 1: Combined Bone Marrow and Kidney Transplantation for Tolerance Induction
This protocol is based on clinical trials pioneered at institutions like Massachusetts General Hospital and Northwestern University, designed to induce mixed chimerism and operational tolerance [17] [119] [117].
Objective: To achieve donor-specific immune tolerance in kidney transplant recipients, allowing for complete withdrawal of immunosuppressive drugs.
Workflow Diagram:
Methodology:
- Patient/Donor Selection: Living donor, often but not exclusively HLA-matched.
- Conditioning Regimen: The recipient undergoes a non-myeloablative or reduced-intensity conditioning regimen to create "space" in the bone marrow and partially suppress the host immune system to prevent rejection of the donor stem cells. Common agents include:
- Transplantation:
- Hematopoietic Stem Cell Transplant (HSCT): Infusion of donor bone marrow or mobilized peripheral blood stem cells.
- Solid Organ Transplant: Kidney transplantation from the same donor.
- Post-Transplant Immunosuppression: A short course of immunosuppression is used to support initial engraftment and prevent GVHD. Some protocols use a dose of post-transplant cyclophosphamide to eliminate alloreactive T cells [17].
- Monitoring & IS Weaning:
- Chimerism Analysis: Regularly monitor the level of donor hematopoietic cells in the recipient's blood (e.g., by flow cytometry or PCR). Stable mixed chimerism is a key biomarker for tolerance in these protocols [17].
- IS Tapering: If stable mixed chimerism is achieved and graft function remains normal, immunosuppressive drugs are gradually tapered and completely withdrawn over several months to a year [17] [119].
Protocol 2: In Vitro Analysis of Alloreactivity Using ELISPOT
This assay is used to monitor the recipient's immune response to donor antigens and is a key tool in tolerance research [115].
Objective: To quantify the frequency of recipient T cells that produce interferon-gamma (IFN-γ) in response to donor antigens, providing a measure of donor-specific cellular immunity.
Workflow Diagram:
Methodology:
- Plate Coating: A 96-well plate with a nitrocellulose membrane is coated with a primary antibody specific for IFN-γ.
- Cell Preparation & Plating: Peripheral blood mononuclear cells (PBMCs) are isolated from the recipient's blood. These cells are added to the wells along with different stimuli:
- Test Wells: Donor antigen (e.g., irradiated donor PBMCs, donor cell lysate, or pools of donor HLA-derived peptides).
- Control Wells: Third-party antigens (unrelated donor), a non-specific mitogen (e.g., PHA, as a positive control), and media only (negative control).
- Incubation: The plate is incubated for 24-48 hours. If a T cell in the recipient's PBMCs recognizes the donor antigen, it will be activated and secrete IFN-γ. The cytokine is captured locally by the antibody on the membrane.
- Detection: After washing, a secondary, enzyme-linked detection antibody is added, followed by a substrate. This reaction produces a colored precipitate at the site of cytokine secretion, forming a "spot."
- Analysis: The plate is read using an automated ELISPOT reader. Each spot represents a single, antigen-reactive T cell. The results are reported as spot-forming units (SFU) per million cells. A high frequency of donor-reactive spots is associated with an increased risk of rejection, while a low frequency may be consistent with a state of tolerance [115].
Key Signaling Pathways in Tolerance and Rejection
The innate immune system plays a critical role in initiating inflammation after transplantation, which can prime the adaptive immune system for rejection. Key pathways involve Pattern Recognition Receptors (PRRs) on host immune cells.
Innate Immune Signaling in Transplant Rejection
Explanation: Transplantation involves surgical trauma and ischemia-reperfusion injury, leading to cellular damage and release of endogenous Damage-Associated Molecular Patterns (DAMPs). These DAMPs (e.g., HMGB1, hyaluronan, HSPs) are recognized by Pattern Recognition Receptors (PRRs) like Toll-like receptors (TLRs) and RAGE on recipient innate immune cells [11]. This signaling triggers downstream pathways (e.g., NF-κB) leading to the production of pro-inflammatory cytokines and chemokines, and upregulation of costimulatory molecules on antigen-presenting cells (APCs). This inflammatory environment potently activates donor-reactive T cells, enhancing the adaptive immune response and increasing the risk of rejection [11].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Transplantation Tolerance Research
| Reagent / Tool | Primary Function | Example Applications in Tolerance Research |
|---|---|---|
| Anti-Thymocyte Globulin (ATG) [17] | Polyclonal antibody that depletes T lymphocytes. | Used in conditioning regimens for lymphodepletion to facilitate donor stem cell engraftment. |
| Anti-CD154 (CD40L) Antibody [116] | Blocks CD40-CD154 costimulatory pathway, critical for T cell activation. | Key component in many experimental tolerance protocols in mice; promotes deletion of alloreactive T cells and supports tolerance. |
| Cyclophosphamide [17] | Cytotoxic chemotherapeutic agent that kills rapidly dividing cells, including lymphocytes. | Used in conditioning; high-dose post-transplant cyclophosphamide selectively eliminates alloreactive T cells, mitigating GVHD and rejection. |
| Rapamycin (Sirolimus) [118] | mTOR inhibitor; suppresses T cell proliferation but is considered "tolerance-sparing" by promoting T-regulatory cell (Treg) function. | Maintenance immunosuppression that may favor the development of operational tolerance over calcineurin inhibitors. |
| CRISPR-Cas9 System [89] [31] | Gene editing technology for precise genomic modifications. | Engineering "universal" iPSCs or cell therapies by knocking out HLA genes (B2M, CIITA) and inserting inhibitory molecules (HLA-E/G) to evade immune rejection. |
| pMHC Multimers [116] | Fluorescently labeled peptide-MHC complexes used to stain and track antigen-specific T cells. | Identifying and characterizing the avidity and frequency of donor-alloreactive T cell populations in tolerant vs. rejecting hosts. |
| FOXP3 Staining Kits [118] | Antibodies for intracellular staining of the FOXP3 transcription factor. | Defining and quantifying CD4+CD25+FOXP3+ regulatory T cells (Tregs) in blood or graft tissue, a key cell population in maintaining tolerance. |
FAQs: Navigating Immune Rejection in Allogeneic Transplantation Research
Q1: What are the primary economic advantages of developing "off-the-shelf" allogeneic therapies over autologous treatments?
Allogeneic therapies offer significant economic advantages by moving from a patient-specific, service-based model to a scalable, product-based model. A single manufacturing run from a healthy donor can produce numerous cryopreserved doses for multiple patients. This reduces the high costs and complex logistics associated with individual autologous production, streamlines the supply chain, and eliminates the need for bridging therapies in patients with rapidly progressing disease [120] [121] [122].
Q2: Beyond GvHD, what is the other major immune challenge for allogeneic cell persistence, and how can it be addressed?
The other major challenge is host-versus-graft (HvG) rejection, where the recipient's immune system recognizes and eliminates the donor-derived cells. This can limit the therapy's persistence and efficacy. Strategies to overcome this include genetic engineering to create "immune-evasive" or "stealth" cells, such as knocking out β2-microglobulin (B2M) to disrupt classical HLA class I expression, or overexpressing non-classical HLA molecules like HLA-E or HLA-G to inhibit host natural killer (NK) cells [123] [124] [121].
Q3: What non-invasive biomarkers are emerging for monitoring transplant rejection, and how do they compare?
The field is rapidly advancing beyond traditional markers like serum creatinine. Key emerging biomarkers include donor-derived cell-free DNA (dd-cfDNA) and chemokines like CXCL9 and CXCL10. The table below summarizes their characteristics for easy comparison.
Table 1: Comparison of Key Non-Invasive Biomarkers for Transplant Rejection
| Biomarker | Source | Primary Utility | Key Performance Metrics | Limitations |
|---|---|---|---|---|
| dd-cfDNA | Blood or Urine | Detects graft injury from rejection (TCMR & ABMR) | AUC: ~0.80-0.87; High Negative Predictive Value (~84-95%) [125] [126] | Lacks specificity; elevated in other injuries (e.g., infection, BK nephropathy) [125] [126] |
| CXCL9/CXCL10 | Urine | Detects active T-cell mediated rejection (TCMR) | High Negative Predictive Value; levels rise before clinical rejection [125] | Confounded by BK virus infection [125] |
Q4: Which immune cell types are being investigated for allogeneic therapy to inherently reduce the risk of GvHD?
Researchers are exploring cell sources with lower inherent alloreactivity to bypass the need for extensive T-cell receptor (TCR) engineering. Natural Killer (NK) cells are a leading candidate as they do not express a TCR, eliminating the risk of TCR-mediated GvHD. Other investigated cells include γδ T cells and natural killer T (NKT) cells, which also possess favorable safety profiles regarding GvHD [123] [124] [121].
Troubleshooting Guides: Addressing Common Experimental Hurdles
Guide 1: Poor In Vivo Persistence of Allogeneic CAR-T Cells
Problem: Your engineered allogeneic CAR-T cells are being rapidly cleared in immunocompetent host models and fail to persist.
Investigation & Solutions:
- Confirm HvG Rejection: Check for infiltration of host T cells and NK cells into the graft site. High levels of host-derived cytokines (e.g., IFN-γ) can also indicate an active immune response against the donor cells.
- Enhance Immune Evasion:
- Strategy A (T-cell evasion): Implement TCR knockout (KO) using CRISPR/Cas9 or TALENs to prevent recognition by host T cells [124] [121].
- Strategy B (NK cell evasion): Consider B2M KO to reduce classical HLA I expression, but pair it with HLA-E or HLA-G overexpression to prevent "missing-self" killing by host NK cells [123] [124].
- Strategy C (Proactive defense): Engineer cells to express alloimmune defense receptors (ADR) that selectively target and eliminate alloreactive host immune cells [123].
Guide 2: Interpreting Conflicting Rejection Biomarker Data
Problem: In a kidney transplant model, dd-cfDNA levels are elevated, but a biopsy shows no signs of rejection.
Investigation & Solutions:
- Rule Out Non-Rejection Injuries: dd-cfDNA is a sensitive but non-specific marker of graft injury. Investigate other causes such as viral infections (e.g., BK nephropathy), drug toxicity, or ischemic injury [125] [126].
- Utilize a Multi-Marker Approach: Do not rely on a single biomarker.
- Test for Chemokines: Analyze urine samples for CXCL9/CXCL10. Elevation would support a diagnosis of T-cell mediated rejection despite the biopsy result, potentially indicating very early injury [125].
- Combine with Histology: The clinical value of dd-cfDNA is often highest when used as a screening tool to indicate the need for a biopsy. The results should be interpreted together with biopsy findings for accurate categorization of graft injury [125].
Guide 3: Assessing GvHD Risk of a Novel Allogeneic Cell Product In Vitro
Problem: You need to evaluate the potential of your candidate allogeneic cell product to cause GvHD before proceeding to in vivo studies.
Investigation & Solutions:
- Perform a Mixed Lymphocyte Reaction (MLR) Assay: This is a standard in vitro method to evaluate alloreactive potential [124].
- Protocol:
- Stimulator Cells: Irradiate peripheral blood mononuclear cells (PBMCs) from the intended recipient (or a representative HLA-mismatched donor) to halt their proliferation.
- Effector Cells: Use your novel allogeneic cell product as the effector population.
- Co-culture: Mix the stimulator and effector cells and culture for several days.
- Readout: Measure T-cell activation and proliferation using flow cytometry (e.g., CFSE dilution) and quantify pro-inflammatory cytokine release (e.g., IFN-γ) by ELISA [124].
- Protocol:
- Employ Advanced 3D Models: For a more physiologically relevant assessment, consider using organoid or 3D tissue culture models (e.g., intestinal organoids). These can demonstrate tissue-specific damage caused by alloreactive cells, providing a deeper insight into GvHD pathology [124].
The following workflow diagram illustrates the key steps for this in vitro GvHD risk assessment:
In Vitro GvHD Risk Assessment Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagent Solutions for Allogeneic Transplantation Research
| Reagent / Material | Function in Experimental Design | Key Considerations |
|---|---|---|
| CRISPR/Cas9 or TALEN Systems | Gene editing for TCR or B2M knockout to mitigate GvHD and HvG responses. | Critical to check for off-target effects and ensure high editing efficiency [124] [121]. |
| Anti-Human HLA Antibody Panels | Flow cytometry-based profiling to confirm knockout efficiency (e.g., loss of HLA expression post-B2M KO). | Essential for validating the success of immune-evasive engineering strategies. |
| dd-cfDNA Quantification Kits (e.g., ddPCR, NGS) | Pre-clinical and clinical monitoring of graft injury and rejection. | Choose method based on need for speed (ddPCR) or multiplexing (NGS) [125] [126]. |
| ELISA Kits for CXCL9, CXCL10, IFN-γ | Quantifying chemokine/cytokine levels in serum, urine, or culture supernatant as markers of immune activation. | Useful for both in vitro MLR assays and in vivo monitoring of rejection or GvHD [125] [124]. |
| Immune Cell Isolation Kits (e.g., for NK, γδ T cells) | Sourcing alternative effector cells for allogeneic therapy with lower inherent GvHD risk. | Purity, viability, and functional potency of the isolated cells are crucial for therapy development [123] [121]. |
| Lentiviral/Viral Transduction Systems | Stable genetic modification of cells to express CAR constructs and other transgenes (e.g., HLA-G, IL-15). | Optimizing multiplicity of infection (MOI) is key to balancing transduction efficiency and cellular toxicity [121]. |
Conclusion
The management of immune rejection in allogeneic transplantation is undergoing a profound transformation, moving from broad, non-specific immunosuppression towards precision medicine approaches that promote graft tolerance. The integration of foundational knowledge of immune pathways with innovative methodologies—such as gene editing, cellular therapies, and nanotechnology—holds immense promise for eliminating lifelong drug regimens and their associated toxicities. Future directions must focus on validating robust biomarkers in clinical trials, refining tolerance protocols for broader application across diverse patient populations, and improving the translatability of pre-clinical models. The ultimate goal is to achieve durable, drug-free graft acceptance, thereby significantly improving the quality of life and long-term survival for transplant recipients. Collaborative efforts between immunologists, clinicians, and drug development professionals are paramount to driving these next-generation therapies into clinical reality.
References
- 1. T cell Allorecognition Pathways in Solid Organ Transplantation [https://pmc.ncbi.nlm.nih.gov/articles/PMC6230624/]
- 2. Allorecognition by T Lymphocytes and Allograft Rejection [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2016.00582/full]
- 3. Allorecognition Unveiled: Integrating Recent Breakthroughs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11586167/]
- 4. Pathways of allorecognition: implications for ... [https://www.sciencedirect.com/science/article/abs/pii/S0966327402000552]
- 5. T-Cell Costimulatory Blockade in Organ Transplantation [https://pmc.ncbi.nlm.nih.gov/articles/PMC3839597/]
- 6. A New Look at Blockade of T-cell Costimulation [https://www.sciencedirect.com/science/article/pii/S160061352202665X]
- 7. T Cell Co-Stimulation: Inhibition of Immunosuppression? [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2018.00974/full]
- 8. Molecular mechanisms of T cell co-stimulation and co- ... [https://www.nature.com/articles/nri3405]
- 9. Regulated cell death and DAMPs as biomarkers ... [https://www.frontiersin.org/journals/transplantation/articles/10.3389/frtra.2025.1571516/full]
- 10. The innate immune response to allotransplants: mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6462017/]
- 11. The Innate Immune System in Allograft Rejection and Tolerance [https://pmc.ncbi.nlm.nih.gov/articles/PMC2840045/]
- 12. Damage-Associated Molecular Patterns in Myocardial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7752942/]
- 13. Exploring the Immunological Landscape of Ischemia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468464/]
- 14. Allorecognition Unveiled: Integrating Recent Breakthroughs ... [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2024.13523/full]
- 15. Sensitization in Transplantation Assessment of Risk 2025 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12331380/]
- 16. Evolution of a melanoma that escapes allogeneic rejection [https://pubmed.ncbi.nlm.nih.gov/40946314/]
- 17. Tolerance Induction Strategies in Organ Transplantation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539449/]
- 18. The Humoral Theory of Transplantation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5591932/]
- 19. Humoral Theory of Transplantation [https://www.sciencedirect.com/science/article/pii/S1600613522072215]
- 20. Acute Allograft Rejection: Cellular and Humoral Processes [https://pmc.ncbi.nlm.nih.gov/articles/PMC3089893/]
- 21. Treatment Options and Strategies for Antibody Mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3248625/]
- 22. New treatment for antibody-mediated rejection: interleukin- ... [https://www.ctrjournal.org/journal/view.html?doi=10.4285/ctr.23.0069]
- 23. Transplant rejection [https://en.wikipedia.org/wiki/Transplant_rejection]
- 24. Advancements in noninvasive techniques for transplant rejection [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05964-4]
- 25. The immunologic constant of rejection - PubMed [https://pubmed.ncbi.nlm.nih.gov/18457994/]
- 26. Gene expression profiling in acute allograft rejection: challenging the immunologic constant of rejection hypothesis - PubMed [https://pubmed.ncbi.nlm.nih.gov/21992116/]
- 27. Discrimination of Anti-Donor Response in Allogeneic ... [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.13879/full]
- 28. Rejection FAQ [https://starzlnetwork.org/resource/rejection-faq/]
- 29. Transplant Rejection [https://uvahealth.com/conditions/transplant-rejection]
- 30. Responses to alloantigens and transplant rejection - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK27163/]
- 31. The Challenge Of Immune Rejection For Allogeneic Cell ... [https://www.cellandgene.com/doc/the-challenge-of-immune-rejection-for-allogeneic-cell-therapies-0001]
- 32. Gut microbiota diversity before allogeneic hematopoietic stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10651870/]
- 33. Acute Renal Transplantation Rejection - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK553074/]
- 34. Transplant rejection: MedlinePlus Medical Encyclopedia [https://medlineplus.gov/ency/article/000815.htm]
- 35. Immune Landscape in Kidney Transplantation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12581792/]
- 36. Survival of Transplanted Beta Cells with No... Allogeneic [https://pubmed.ncbi.nlm.nih.gov/40757665/]
- 37. Progress and challenges in developing allogeneic cell ... [https://www.sciencedirect.com/science/article/pii/S1934590925000943]
- 38. Immunosuppressive Drugs - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC8987166/]
- 39. Immune Suppression in Allogeneic Hematopoietic Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9055779/]
- 40. Comparative Efficacy of Immunosuppressive Therapies in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11893482/]
- 41. Tolerance Induction Strategies in Organ Transplantation [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.14958/full]
- 42. Chimerism and Immune Tolerance: Can We Says ... [http://www.nephjc.com/news/chimera-tolerance-njqe334]
- 43. Flow cytometric cell sorting combined with molecular ... [https://www.nature.com/articles/1700800]
- 44. What if my transplant doesn't work? [https://www.anthonynolan.org/patients-and-families/recovering-a-stem-cell-transplant/what-if-my-transplant-doesnt-work]
- 45. A Novel High Throughput Immunomagnetic Cell Sorting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2094009/]
- 46. HLA matching or CRISPR editing of HLA class I/II enables ... [https://www.nature.com/articles/s41467-025-64945-3]
- 47. CRISPR-mediated engineering of mesenchymal stromal/stem ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04723-6]
- 48. Regulatory T cell therapies: from patient data to biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615433/]
- 49. CRISPR-mediated engineering of mesenchymal stromal/stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574024/]
- 50. CRISPR-Edited Beta Cells Avoid Immune Rejection ... [https://crisprmedicinenews.com/news/crispr-edited-beta-cells-avoid-immune-rejection-without-immunosuppressants-in-human-transplantation/]
- 51. Diminished immune cell adhesion in hypoimmune ICAM-1 ... [https://www.nature.com/articles/s41467-025-62568-2]
- 52. Persistence of CRISPR/Cas9 gene edited hematopoietic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8235122/]
- 53. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 54. Modulation of the immune microenvironment using ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1614640/full]
- 55. Nanomaterials in Drug Delivery: Leveraging Artificial ... [https://www.mdpi.com/1422-0067/26/22/11121]
- 56. Advances in multimodal imaging techniques in nanomedicine [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03255e]
- 57. the transformative potential of nanotechnology in medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360437/]
- 58. Bioresponsive engineered nanoparticles for immunomodulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574298/]
- 59. Edmonton Protocol - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/edmonton-protocol]
- 60. Islet cell transplantation for the treatment of type 1 diabetes [https://pmc.ncbi.nlm.nih.gov/articles/PMC4075233/]
- 61. From Edmonton to Lantidra and beyond [https://www.frontiersin.org/journals/transplantation/articles/10.3389/frtra.2025.1514956/full]
- 62. New transplant approach resets the immune system to stop ... [https://www.news-medical.net/news/20251118/New-transplant-approach-resets-the-immune-system-to-stop-Type-1-diabetes.aspx]
- 63. Biomarkers of Immunosuppressant Organ Toxicity after ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3079351/]
- 64. New immunosuppressive agents in transplantation [https://www.sciencedirect.com/science/article/abs/pii/S0755498222000355]
- 65. Biomarkers of immunosuppression - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6490196/]
- 66. Immunosuppressive drugs in organ transplantation to ... [https://www.immunologyresearchjournal.com/articles/immunosuppressive-drugs-in-organ-transplantation-to-prevent-allograft-rejection-mode-of-action-and-side-effects.html]
- 67. Biomarkers of the immunomodulatory effect ... [https://www.sciencedirect.com/science/article/abs/pii/S0955470X0900007X]
- 68. Long-Term Toxicity of Immunosuppressive Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7152453/]
- 69. The Toxicities of Allogeneic Transplantation: What Fellows ... [https://www.hematology.org/education/trainees/fellows/hematopoiesis/2022/the-toxicities-of-allogeneic-transplantation]
- 70. Cutting edge of immune response and ... [https://pubmed.ncbi.nlm.nih.gov/39346923/]
- 71. Characterizing the Mechanistic Pathways of the Instant Blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4946518/]
- 72. Evidence for Instant Blood-Mediated Inflammatory ... [https://www.sciencedirect.com/science/article/pii/S1600613522253465]
- 73. Saving islets from allograft rejection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1200297/]
- 74. A narrative review on the evolution of islet isolation techniques ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12377982/]
- 75. Diagnosis and treatment of allograft rejection in islet ... [https://www.sciencedirect.com/science/article/pii/S1600613523005233]
- 76. The Current Status of Allogenic Islet Cell Transplantation [https://pmc.ncbi.nlm.nih.gov/articles/PMC10605704/]
- 77. Allogeneic Islet Transplantation: Chronicle of a Death Foretold? [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.14598/full]
- 78. Pathogenesis and Management of Graft versus Host Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC4141413/]
- 79. Pathophysiology of GvHD and Other HSCT-Related Major ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2017.00079/full]
- 80. Graft-Versus-Host Disease - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK538235/]
- 81. Current issues in chronic graft-versus-host disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4102710/]
- 82. Graft vs. Host Disease (GvHD) [https://my.clevelandclinic.org/health/diseases/10255-graft-vs-host-disease-an-overview-in-bone-marrow-transplant]
- 83. Challenges in GVHD and GVL after hematopoietic stem ... [https://www.sciencedirect.com/science/article/pii/S000649712501420X]
- 84. Evolving GVHD Prophylaxis: Emerging Drug and Graft ... [https://www.onclive.com/view/evolving-gvhd-prophylaxis-emerging-drug-and-graft-engineering-strategies]
- 85. CD70 identifies alloreactive T cells and represents a ... [https://www.sciencedirect.com/science/article/pii/S2473952924004403]
- 86. Why Humanizing Mice Fails to Solve the Translatability Problem [https://www.scienceadvancement.org/reflections/why-humanizing-mice-fails-to-solve-the-translatability-problem/]
- 87. Why animal model studies are lost in translation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9052957/]
- 88. Immunological considerations and challenges for ... [https://www.nature.com/articles/s42003-021-02237-4]
- 89. How To Overcome Immune Rejection In iPSC-based Gene ... [https://www.cellandgene.com/doc/how-to-overcome-immune-rejection-in-ipsc-based-gene-therapy-0001]
- 90. New immune model sheds light on implant rejection [https://www.bme.jhu.edu/news-events/news/new-immune-model-sheds-light-on-implant-rejection/]
- 91. Overcoming Challenges with Animal Models in Research [https://cgt.global/overcoming-challenges-with-animal-models-in-research/]
- 92. Detecting and Fighting Transplant Rejection [https://irp.nih.gov/catalyst/29/3/detecting-and-fighting-transplant-rejection]
- 93. Treatment of allosensitized patients receiving allogeneic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8945639/]
- 94. Guideline ASTCT Consensus Recommendations on ... [https://www.sciencedirect.com/science/article/abs/pii/S2666636724006547]
- 95. A systematic review and meta-analysis of 69 studies [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1633853/full]
- 96. Early Donor-Specific HLA Antibodies Detected by Screening ... [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.14424/full]
- 97. Persistent versus resolved donor-specific antibodies ... [https://www.nature.com/articles/s41598-025-07681-4]
- 98. Activation of immune signals during organ transplantation [https://www.nature.com/articles/s41392-023-01377-9]
- 99. Drug delivery strategies for local immunomodulation in ... [https://www.sciencedirect.com/science/article/pii/S0169409X24002515]
- 100. New drugs before, during, and after hematopoietic stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9890036/]
- 101. A Guidance for Concomitant Drug Reconciliation Prior to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8326409/]
- 102. The Most Promising Biomarkers of Allogeneic Kidney Transplant Rejection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9167141/]
- 103. Non-invasive Biomarkers of Acute Rejection in Kidney Transplantation: Novel Targets and Strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6331461/]
- 104. Gene expression profiling of allogeneic islet grafts in an ... [https://pubmed.ncbi.nlm.nih.gov/23498796/]
- 105. Pre-Transplant Gene Expression May Predict Risk of Graft ... [https://www.sciencedirect.com/science/article/pii/S0006497118696259]
- 106. Identification of gene microarray expression profiles in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8166221/]
- 107. Visualizing early allograft rejection: an M1 macrophage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527843/]
- 108. New Non-Invasive Imaging Technologies in Cardiac ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10487200/]
- 109. Recent progress of nanomaterials for diagnosis and ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1703902/full]
- 110. Beyond the Biopsy: A New Blood Test Is Redefining ... [https://www.onclive.com/view/beyond-the-biopsy-a-new-blood-test-is-redefining-the-fight-against-relapsed-aml]
- 111. Similarities and Differences Between Allogeneic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525906/]
- 112. The importance of real-world data in allogeneic stem cell ... [https://gvhdhub.com/medical-information/symposium-the-importance-of-real-world-data-in-allogeneic-stem-cell-transplantation-a-focus-on-cgvhd]
- 113. Solid organ transplantation in the 21st century - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6230860/]
- 114. Feasibility of a New Model of Care for Allogeneic Stem Cell ... [https://pubmed.ncbi.nlm.nih.gov/36948273/]
- 115. “Tolerance” assays: the physician's guide to safe weaning ... [https://www.sciencedirect.com/science/article/abs/pii/S0955470X06001200]
- 116. The pursuit of transplantation tolerance: new mechanistic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6461908/]
- 117. Chimerism and immunological tolerance in solid organ ... [https://link.springer.com/article/10.1007/s00281-025-01052-x]
- 118. Harnessing Mechanisms of Immune Tolerance to Improve ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.688460/full]
- 119. Immune Tolerance in Transplantation [https://www.immunetolerance.org/for-researchers/immune-tolerance-in-transplantation?cf888914_page=2]
- 120. Autologous vs. Allogeneic Cell Therapies: Promises & ... [https://www.genedata.com/resources/learn/details/blog/autologous-allogeneic-cell-therapies]
- 121. Allogeneic CART progress: platforms, current progress and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1557157/full]
- 122. Emerging trends in clinical allogeneic CAR cell therapy [https://www.sciencedirect.com/science/article/pii/S2666634025001047]
- 123. Allogeneic CAR-engineered cellular therapy for relapsed and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12279871/]
- 124. Addressing graft-versus-host disease in allogeneic cell-based ... [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-025-00654-3]
- 125. Novel Biomarkers for Rejection in Kidney Transplantation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12347177/]
- 126. Genomic and Biomarker Innovations in Predicting Kidney ... [https://www.mdpi.com/2077-0383/14/11/3642]